Breech Position: What It Means if Your Baby Is Breech
Medical review policy, latest update:.
Medically reviewed for accuracy.

What does it mean if a baby is breech?
What are the different types of breech positions, what causes a baby to be breech, recommended reading, how can you tell if your baby is in a breech position, what does it mean to turn a breech baby, how can you turn a breech baby, how does labor usually start with a breech baby.
If your cervix dilates too slowly, if your baby doesn’t move down the birth canal steadily or if other problems arise, you’ll likely have a C-section. Talk your options over with your practitioner now to be prepared. Remember that though you may feel disappointed things didn’t turn out exactly as you envisioned, these feelings will melt away once your bundle of joy safely enters the world.
Updates history
Jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
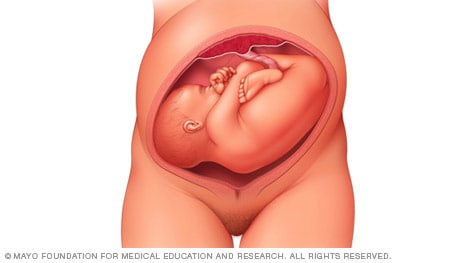
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
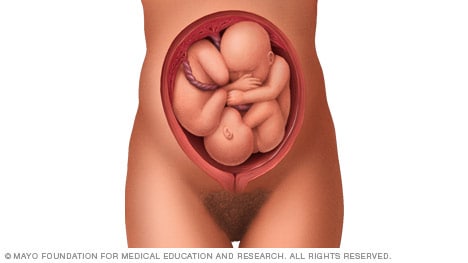
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
What to know if your baby is breech
Find out what breech position means, how to turn a breech baby, and what having a breech baby means for your labor and delivery.

What does it mean when a baby is breech?
Signs of a breech baby, why are some babies breech, how to turn a breech baby: is it possible, will i need a c-section if my baby is breech, how to turn a breech baby naturally.
Breech is a term used to describe your baby's position in the womb. Breech position means your baby is bottom-down instead of head-down.
Babies are often active in early pregnancy, moving into different positions. But by around 8 months, there's not much room in the uterus. Most babies maximize their cramped quarters by settling in head down, in what's known as a cephalic or vertex presentation. But if you have a breech baby, it means they're poised to come out buttocks and/or feet first. At 28 weeks or less, about a quarter of babies are breech, and at 32 weeks, 7 percent are breech. By the end of pregnancy, only 3 to 4 percent of babies are in breech position. At term, a baby in breech position is unlikely to turn on their own.
There are several types of breech presentations:
- Frank breech (bottom first with feet up near the head)
- Complete breech (bottom first with legs crossed)
- Incomplete or footling breech (one or both feet are poised to come out first)
(In rare cases, a baby will be sideways in the uterus with their shoulder, back, or arm presenting first – this is called a transverse lie.)
See what these breech presentations look like .
If your baby is in breech position, you may feel them kicking in your lower belly. Or you may feel pressure under your ribcage, from their head.
By the beginning of your third trimester , your practitioner may be able to tell what position your baby is in by feeling your abdomen and locating the baby's head, back, and bottom.
If your baby's position isn't clear during an abdominal exam at 36 weeks, your caregiver may do an internal exam to try to feel what part of the baby is in your pelvis. In some cases, they may use ultrasound to confirm the baby's position.
We don't usually know why some babies are breech – in most cases it seems to be chance. While sometimes a baby with certain birth defects may not turn to a head-down position, most babies in breech position are perfectly fine. Here are some things that might increase the risk of a breech presentation:
- You're carrying multiples
- You've been pregnant before
- You've had a breech presentation before
- There's too much amniotic fluid or not enough amniotic fluid
- You have placenta previa (the placenta is covering all of part of the opening of the uterus)
- Your baby is preterm
- Your uterus is shaped abnormally or has growths, such as fibroids
- The umbilical cord is short
- You were a breech delivery, or your sibling or parent was a breech delivery
- Advanced maternal age (especially age 45 and older)
- Your baby is a low weight at delivery
- You're having a girl
There is a procedure for turning a breech baby. It's called an external cephalic version (ECV). An ob/gyn turns your baby by applying pressure to your abdomen and manually manipulating the baby into a head-down position. Some women find it very uncomfortable or even painful.
An EVC has about a 58 percent success rate, and it's more likely to work if this isn't your first baby. It's not for everyone – you can't have the procedure if you're carrying multiples or if you have too little amniotic fluid or placental abruption , for example. Your provider also won't attempt to turn your breech baby if your baby has any health problems.
The procedure is done after 36 weeks and in the hospital, where your baby can be monitored and where you'll be near a delivery room should any complications arise.
It depends, and it's something you'll want to talk with your caregiver about ahead of time. Discuss your preferences, the advantages and risks of each option ( vaginal and cesarean delivery of a breech presentation), and their experience. The biggest risk of a breech delivery is when the body delivers but the head stays entrapped within the cervix.
In the United States, most breech babies are delivered via cesarean. You may wind up having a vaginal breech delivery if your labor is so rapid that you arrive at the hospital just about to deliver. Another scenario is if you have a twin pregnancy where the first baby is in the head-first position and the second baby is not. A baby who delivers head-first will make room for the breech baby.
However, the vast majority of babies who remain breech arrive by c-section. If a c-section is planned, it will usually be scheduled at 39 weeks. To make sure your baby hasn't changed position in the meantime, you'll have an ultrasound at the hospital to confirm their position just before the surgery.
If you go into labor or your water will break s before your planned c-section, be sure to call your provider right away and head for the hospital.
In rare circumstances, if you're at low risk of complications and your caregiver is experienced delivering breech babies vaginally, you may choose to have what is called a "trial of vaginal birth." This means that you can attempt to deliver vaginally but should be prepared to have a cesarean delivery if labor isn't progressing well. You and your baby will be closely monitored during labor.
In addition to ECV, there are some alternative, natural ways to try to turn your baby. There's no proof that any of them work – or that all of them are safe. Consult your practitioner before trying them.
There's no conclusive proof that the mother's position has any effect on the baby's position, but the idea is to employ gravity to help your baby somersault into a head-down position. A few tips:
- Get into one of the following positions twice a day, starting at around 32 weeks.
- Be sure to do these moves on an empty stomach, lest your lunch comes back up.
- Make sure there's someone around to help you get up if you start feeling lightheaded.
- If you find these positions uncomfortable, stop doing them.
Position 1: Lie flat on your back and raise your pelvis so that it's 9 to 12 inches off the floor. Support your hips with a pillow and stay in this position for five to 15 minutes. Position 2: Kneel down, with your forearms on the floor in front of you, so that your bottom sticks up in the air. Stay in this position for five to 15 minutes. Sleeping position
Many women wonder if there are sleeping positions to turn a breech baby. But the positions you use to try to coax your baby head down for a short time shouldn't be used while you're sleeping. (It's not safe to sleep flat on your back in late pregnancy, for example, because the weight of your baby may compress the blood vessels that provide oxygen and nutrients to them.)
The best position for sleeping during pregnancy is on your side. Placing a pillow between your legs in this position may help open your pelvis, giving your baby room to move more easily. Support your back with plenty of pillows, too. Again, there's no proof that this works, but since it's the best sleeping position for you and your baby, you may as well give it a try.
Moxibustion
This ancient Chinese technique burns herbs to stimulate key acupressure points. To help turn a breech baby, an acupuncturist or other practitioner burns mugwort near the acupressure point of your pinky toes. According to Chinese medicine, this should stimulate your baby's activity enough that they may change position on their own. Some studies show that moxibustion in combination with acupuncture and/or positioning methods may be of some benefit. Others show moxibustion to provide no help in coaxing a baby into cephalic position. If you've discussed it with your caregiver and want to give it a try, contact your state acupuncture or Chinese medicine association and ask for the names of licensed practitioners.
One small study found that women who are regularly hypnotized into a state of deep relaxation at 37 to 40 weeks are more likely to have their baby turn than other women. If you're willing to try this technique, look for a licensed hypnotherapist with experience working with pregnant women.
Chiropractic care
There's a technique – called The Webster Breech Technique – that aims to reduce stress on the pelvis by relaxing the uterus and surrounding ligaments. The idea is that a breech baby can turn more naturally in a relaxed uterus, but research is limited as to the risks and benefits of this technique. If you're interested, talk with your provider about working with a chiropractor who's experienced with the technique.
This is a safe – and again, unproven – method based on the fact that your baby can hear sounds outside the womb. Simply play music close to the lower part of your abdomen (some women use headphones) to encourage your baby to move in the direction of the sound.
Learn more:
- C-section recovery
- Third trimester pregnancy guide and checklist
- Hospital bag checklist
Was this article helpful?
Breech, posterior, transverse lie: What position is my baby in?

Raspberry leaf tea is popular during pregnancy – but possible benefits aren't proven

Too much amniotic fluid (polyhydramnios)

C-section recovery: Timeline, aftercare tips, and expectations

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
ACOG. 2019. If your baby is breech. FAQ. The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/if-your-baby-is-breech Opens a new window [Accessed November 2021]
ACOG. 2018. Mode of term singleton breech delivery. Committee opinion number 745. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/mode-of-term-singleton-breech-delivery Opens a new window [Accessed November 2021]
Brici P et al. 2019. Turning foetal breech presentation at 32-35 weeks of gestational age by acupuncture and moxibustion. Evidence-based Complementary and Alternative Medicine https://www.hindawi.com/journals/ecam/2019/8950924/ Opens a new window [Accessed November 2021]
Ekeus C et al. 2019. Vaginal breech delivery at term and neonatal morbidity and mortality — a population-based cohort study in Sweden. Journal of Maternal Fetal Neonatal Medicine 32(2):265. https://pubmed.ncbi.nlm.nih.gov/28889774/ Opens a new window [Accessed November 2021]
Fruscalzo A et al 2014. New and old predictive factors for breech presentation: our experience in 14433 singleton pregnancies and a literature review. Journal of Maternal Fetal Neonatal Medicine 27(2): 167-72. https://pubmed.ncbi.nlm.nih.gov/23688372/ Opens a new window [Accessed November 2021]
Garcia MM et al. 2019 Effectiveness and safety of acupuncture and moxibustion in pregnant women with noncephalic presentation: An overview of systematic reviews. Evidence Based Complementary Alternative Medicine 7036914. https://pubmed.ncbi.nlm.nih.gov/31885661/ Opens a new window [Accessed November 2021]
Gray C. 2021. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed November 2021]
Meaghan M et al. 2021. External cephalic version. NCBI StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482475/ Opens a new window [Accessed November 2021]
MedlinePlus. 2020. Breech - series - Types of breech presentation. https://medlineplus.gov/ency/presentations/100193_3.htm Opens a new window [Accessed November 2020]
Noli SA et al. 2019. Preterm birth, low gestational age, low birth weight, parity, and other determinants of breech presentation: Results from a large retrospective population-based study. Biomed Research International https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6766171/ Opens a new window [Accessed November 2021]
Pistolese RA. 2002. The Webster Technique: A chiropractic technique with obstetric implications. Journal of Manipulative and Physiological Therapeutics 25(6): E1-9. https://pubmed.ncbi.nlm.nih.gov/12183701/ Opens a new window [Accessed November 2021]

Where to go next

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Breech presentation.
Caron J. Gray ; Meaghan M. Shanahan .
Affiliations
Last Update: November 6, 2022 .
- Continuing Education Activity
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. This activity reviews the cause and pathophysiology of breech presentation and highlights the role of the interprofessional team in its management.
- Describe the pathophysiology of breech presentation.
- Review the physical exam of a patient with a breech presentation.
- Summarize the treatment options for breech presentation.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by breech presentation.
- Introduction
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of one or both hips extended, also known as footling (one leg extended) breech, or double footling breech (both legs extended). [1] [2] [3]
Clinical conditions associated with breech presentation include those that may increase or decrease fetal motility, or affect the vertical polarity of the uterine cavity. Prematurity, multiple gestations, aneuploidies, congenital anomalies, Mullerian anomalies, uterine leiomyoma, and placental polarity as in placenta previa are most commonly associated with a breech presentation. Also, a previous history of breech presentation at term increases the risk of repeat breech presentation at term in subsequent pregnancies. [4] [5] These are discussed in more detail in the pathophysiology section.
- Epidemiology
Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 28 weeks or less, 25% are breech.
Specifically, following one breech delivery, the recurrence rate for the second pregnancy was nearly 10%, and for a subsequent third pregnancy, it was 27%. Prior cesarean delivery has also been described by some to increase the incidence of breech presentation two-fold.
- Pathophysiology
As mentioned previously, the most common clinical conditions or disease processes that result in the breech presentation are those that affect fetal motility or the vertical polarity of the uterine cavity. [6] [7]
Conditions that change the vertical polarity or the uterine cavity, or affect the ease or ability of the fetus to turn into the vertex presentation in the third trimester include:
- Mullerian anomalies: Septate uterus, bicornuate uterus, and didelphys uterus
- Placentation: Placenta previa as the placenta is occupying the inferior portion of the uterine cavity. Therefore, the presenting part cannot engage
- Uterine leiomyoma: Mainly larger myomas located in the lower uterine segment, often intramural or submucosal, that prevent engagement of the presenting part.
- Prematurity
- Aneuploidies and fetal neuromuscular disorders commonly cause hypotonia of the fetus, inability to move effectively
- Congenital anomalies: Fetal sacrococcygeal teratoma, fetal thyroid goiter
- Polyhydramnios: Fetus is often in unstable lie, unable to engage
- Oligohydramnios: Fetus is unable to turn to vertex due to lack of fluid
- Laxity of the maternal abdominal wall: Uterus falls forward, the fetus is unable to engage in the pelvis.
The risk of cord prolapse varies depending on the type of breech. Incomplete or footling breech carries the highest risk of cord prolapse at 15% to 18%, while complete breech is lower at 4% to 6%, and frank breech is uncommon at 0.5%.
- History and Physical
During the physical exam, using the Leopold maneuvers, palpation of a hard, round, mobile structure at the fundus and the inability to palpate a presenting part in the lower abdomen superior to the pubic bone or the engaged breech in the same area, should raise suspicion of a breech presentation.
During a cervical exam, findings may include the lack of a palpable presenting part, palpation of a lower extremity, usually a foot, or for the engaged breech, palpation of the soft tissue of the fetal buttocks may be noted. If the patient has been laboring, caution is warranted as the soft tissue of the fetal buttocks may be interpreted as caput of the fetal vertex.
Any of these findings should raise suspicion and ultrasound should be performed.
Diagnosis of a breech presentation can be accomplished through abdominal exam using the Leopold maneuvers in combination with the cervical exam. Ultrasound should confirm the diagnosis.
On ultrasound, the fetal lie and presenting part should be visualized and documented. If breech presentation is diagnosed, specific information including the specific type of breech, the degree of flexion of the fetal head, estimated fetal weight, amniotic fluid volume, placental location, and fetal anatomy review (if not already done previously) should be documented.
- Treatment / Management
Expertise in the delivery of the vaginal breech baby is becoming less common due to fewer vaginal breech deliveries being offered throughout the United States and in most industrialized countries. The Term Breech Trial (TBT), a well-designed, multicenter, international, randomized controlled trial published in 2000 compared planned vaginal delivery to planned cesarean delivery for the term breech infant. The investigators reported that delivery by planned cesarean resulted in significantly lower perinatal mortality, neonatal mortality, and serious neonatal morbidity. Also, there was no significant difference in maternal morbidity or mortality between the two groups. Since that time, the rate of term breech infants delivered by planned cesarean has increased dramatically. Follow-up studies to the TBT have been published looking at maternal morbidity and outcomes of the children at two years. Although these reports did not show any significant difference in the risk of death and neurodevelopmental, these studies were felt to be underpowered. [8] [9] [10] [11]
Since the TBT, many authors since have argued that there are still some specific situations that vaginal breech delivery is a potential, safe alternative to planned cesarean. Many smaller retrospective studies have reported no difference in neonatal morbidity or mortality using these specific criteria.
The initial criteria used in these reports were similar: gestational age greater than 37 weeks, frank or complete breech presentation, no fetal anomalies on ultrasound examination, adequate maternal pelvis, and estimated fetal weight between 2500 g and 4000 g. In addition, the protocol presented by one report required documentation of fetal head flexion and adequate amniotic fluid volume, defined as a 3-cm vertical pocket. Oxytocin induction or augmentation was not offered, and strict criteria were established for normal labor progress. CT pelvimetry did determine an adequate maternal pelvis.
Despite debate on both sides, the current recommendation for the breech presentation at term includes offering external cephalic version (ECV) to those patients that meet criteria, and for those whom are not candidates or decline external cephalic version, a planned cesarean section for delivery sometime after 39 weeks.
Regarding the premature breech, gestational age will determine the mode of delivery. Before 26 weeks, there is a lack of quality clinical evidence to guide mode of delivery. One large retrospective cohort study recently concluded that from 28 to 31 6/7 weeks, there is a significant decrease in perinatal morbidity and mortality in a planned cesarean delivery versus intended vaginal delivery, while there is no difference in perinatal morbidity and mortality in gestational age 32 to 36 weeks. Of note, due to lack of recruitment, no prospective clinical trials are examining this issue.
- Differential Diagnosis
- Face and brow presentation
- Fetal anomalies
- Fetal death
- Grand multiparity
- Multiple pregnancies
- Oligohydramnios
- Pelvis Anatomy
- Preterm labor
- Primigravida
- Uterine anomalies
- Pearls and Other Issues
In light of the decrease in planned vaginal breech deliveries, thus the decrease in expertise in managing this clinical scenario, it is prudent that policies requiring simulation and instruction in the delivery technique for vaginal breech birth are established to care for the emergency breech vaginal delivery.
- Enhancing Healthcare Team Outcomes
A breech delivery is usually managed by an obstetrician, labor and delivery nurse, anesthesiologist and a neonatologist. The ultimate decison rests on the obstetrician. To prevent complications, today cesarean sections are performed and experienced with vaginal deliveries of breech presentation is limited. For healthcare workers including the midwife who has no experience with a breech delivery, it is vital to communicate with an obstetrician, otherwise one risks litigation if complications arise during delivery. [12] [13] [14]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Caron Gray declares no relevant financial relationships with ineligible companies.
Disclosure: Meaghan Shanahan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Gray CJ, Shanahan MM. Breech Presentation. [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. [Z Geburtshilfe Neonatol. 1997] [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. Krause M, Fischer T, Feige A. Z Geburtshilfe Neonatol. 1997 Jul-Aug; 201(4):128-35.
- The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. [Early Hum Dev. 1993] The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. Sival DA, Prechtl HF, Sonder GH, Touwen BC. Early Hum Dev. 1993 Mar; 32(2-3):161-76.
- The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. [PLoS One. 2019] The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. Jennewein L, Allert R, Möllmann CJ, Paul B, Kielland-Kaisen U, Raimann FJ, Brüggmann D, Louwen F. PLoS One. 2019; 14(12):e0225546. Epub 2019 Dec 2.
- Review Breech vaginal delivery at or near term. [Semin Perinatol. 2003] Review Breech vaginal delivery at or near term. Tunde-Byass MO, Hannah ME. Semin Perinatol. 2003 Feb; 27(1):34-45.
- Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. [Gynecol Obstet Fertil Senol. 2...] Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. Mattuizzi A. Gynecol Obstet Fertil Senol. 2020 Jan; 48(1):70-80. Epub 2019 Nov 1.
Recent Activity
- Breech Presentation - StatPearls Breech Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Our website uses cookies
This website uses cookies as well as similar tools and technologies to understand visitors’ experiences. By continuing to use this website, you consent to Columbia University’s usage of cookies and similar technologies, in accordance with the Columbia University Website Cookie Notice. (link opens in a new window)
Skip to content
Breech Position and Breech Birth
Make an appointment.
Our team is here to help you make an appointment with the specialists that you need.
Top of the page
- Condition Basics
What is breech position?
During most of pregnancy, there is enough room in the uterus for the baby (fetus) to change position. By 36 weeks of pregnancy, most babies turn into a head-down position. This is the normal and safest fetal position for birth.
But in about 4 out of 100 births, the baby doesn't naturally turn head-down. Instead, the baby is in a breech position. footnote 1 Babies in breech position usually must be delivered by C-section .
There are three main breech positions :
The buttocks are in place to come out first during delivery. The legs are straight up in front of the body, with the feet near the head. This is the most common type of breech position.
The buttocks are down near the birth canal. The knees are bent, and the feet are near the buttocks.
One leg or both legs are stretched out below the buttocks. The leg or legs are in place to come out first during delivery.
What causes it?
Most of the time, there is no clear reason why the baby did not turn head-down.
In some cases, breech position may be linked to early labor, twins or more, problems with the uterus, or problems with the baby. footnote 2
What are the signs?
You probably won't be able to feel whether your baby is breech. But if you are 36 or more weeks pregnant and think you feel the baby's head pressing high up in your belly or you feel kicking in your lower belly, see your doctor for an exam.
How is it diagnosed?
During a routine exam late in your pregnancy, your doctor will feel your upper and lower belly and may do a fetal ultrasound to find out if your baby is breech. Your doctor may also learn that your baby is breech when he or she checks your cervix .
How is breech position treated?
Sometimes a doctor can turn a baby from a breech position to a head-down position by using a procedure called an external cephalic version. (If you are using a midwife and your baby is in breech position, your midwife will refer you to a doctor for this procedure.) If the baby can be turned head-down before labor starts, you may be able to have a vaginal birth.
You also can ask your doctor if you can try certain positions at home that may help turn your baby. This is called postural management. There is no research to prove that this works, but it's not harmful. It may work for you.
It's normal to feel disappointed and worried about a breech pregnancy, especially if the doctor has tried to turn the baby without success. But most breech babies are healthy and don't have problems after birth. Talk to your doctor if you're concerned about your baby's health.
How is a breech baby delivered safely?
In most cases, a planned cesarean delivery (C-section) is safest for the baby. If your fetus is still in a breech position near your due date, your doctor will likely schedule a cesarean. If you are using a midwife, your midwife will refer you to a doctor for a scheduled cesarean.
In rare cases, a cesarean breech birth may not be recommended or even possible. For instance, if a breech labor progresses too quickly, a vaginal birth may be the only option. During a twin birth in which the first twin is head-down and the second twin is breech, both babies may best be delivered vaginally. footnote 3
No matter what position a baby is in, every labor and delivery is unique. Even though you and your doctor have a birth plan for labor and delivery, plans can change. If something unexpected happens, your doctor may need to make some quick decisions to keep you and your baby safe.
- Related Information
- Cesarean Section
- Labor and Delivery
- Multiple Pregnancy: Twins or More
- Vaginal Birth After Cesarean (VBAC)
Citations American College of Obstetricians and Gynecologists (2000, reaffirmed 2012). External cephalic version. ACOG Practice Bulletin No. 13. Obstetrics and Gynecology , 95(2): 1–7. Cunningham FG, et al. (2010). Breech presentation and delivery. In Williams Obstetrics , 23rd ed., pp. 527–543. New York: McGraw-Hill. American College of Obstetricians and Gynecologists (2006, reaffirmed 2012). Mode of term singleton breech delivery. ACOG Committee Opinion No. 340. Obstetrics and Gynecology , 108: 235–237.
Current as of: July 10, 2023
Author: Healthwise Staff Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Author: Healthwise Staff
Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Topic Contents

This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use . Learn how we develop our content .

To learn more about Healthwise, visit Healthwise.org .
© 1995-2024 Healthwise, Incorporated. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.
Breech Presentation: What It Is and How It Can Affect Your Baby's Delivery

As you get close to your due date, your baby might sense she’s approaching her grand entrance and move into a head-down position in your uterus, ready to be born. However, in some cases, she might choose another position instead, such as bottom or feet down. When this happens, it’s called a breech presentation. Read on to learn how your healthcare provider checks the position of your baby, what delivery options you may have if your baby is breech, and what can cause a breech presentation.
What Is Breech?
During your pregnancy, your baby has likely taken every opportunity to let you know she means business by kicking up a storm and doing countless somersaults. It's natural for your baby to move and shift positions within the uterus. Then, usually between 32 and 36 weeks of pregnancy, your baby will likely get into a head-down position in preparation for being born.
There is a small chance — just 3 to 4 percent — that your baby may not move into this head-down position by the time your pregnancy is full term. This is called a breech presentation. The chance of a breech presentation is higher if your pregnancy is not yet full term or if you go into preterm labor .
Types of Birth Positions
There are many different types of positions, including a number of breech presentations, that your baby may take on before birth:
Frank breech presentation. Your baby's bottom is positioned downward. This is the most common type of breech presentation.
Complete breech presentation. Your baby's feet are positioned downward with her hips and knees flexed, almost cross-legged.
Incomplete breech presentation. Your baby's feet are positioned downward with only one hip or one knee flexed.
Shoulder presentation or transverse lie. This is a form of breech in which your baby is positioned horizontally in the uterus. Few babies remain this way at the time of delivery.
Footling breech. One or both of your baby's feet are pointed downward.
Cephalic or vertex presentation (occiput). Your baby is in the normal position for delivery. Her head is down and she’s facing toward your back.
Cephalic or vertex presentation (occiput posterior). In some cases, your baby may be in a downward position but with her face toward your front. If this happens in early labor, your baby may naturally turn to face your back on her own, or, later in labor, your provider may decide to manually assist the baby in getting into this position. If this doesn't work, your baby can still be delivered vaginally, but delivery may be prolonged and more painful.
The causes of your baby being in breech position aren't always clear, but it can be more common if any of the following apply to you:
You've been pregnant before
You are pregnant with twins (read on to learn more about twin breech)
The uterus has more or less amniotic fluid than usual
The uterus has an abnormal shape or has abnormal growths, such as fibroids.
You have a condition called placenta previa , which is when the placenta covers the cervix.
Your healthcare provider likely already knows whether any of these factors affect your situation, but you might want to mention it just to be sure.
Diagnosis of a Breech Presentation
At one of your prenatal visits in the lead up to your due date, your provider will check that everything is progressing as planned , and will examine your abdomen to try to find out whether your baby is in the correct head-down position. If your provider thinks there may be a breech presentation, she or he may recommend an ultrasound exam to confirm it.
Can a Breech Baby Be Turned?
If your baby is breech, your provider may consider turning your baby so that a vaginal delivery can proceed, if that’s in the cards for you anyway. Alternatively, your provider may recommend that a cesarean delivery is the safer option.
Keep in mind, your baby's position might change at some point before delivery day, so your provider may recommend waiting and seeing.
If you are 37 weeks pregnant or more, your provider may recommend turning your baby through a process called external cephalic version or ECV.
ECV involves your provider placing hands on your abdomen and applying firm pressure in order to turn the baby. This procedure will most likely be done near a delivery room. Your provider may offer an epidural block to help with any pain this procedure causes.
An ECV is about 50 percent effective and there is a small risk of complications. You and your baby will be monitored closely before, during, and after the procedure to ensure that both of you are doing well.
If the ECV procedure is successful, your baby can be delivered vaginally , if there’s no other impediment.
Delivery Options for a Breech Baby
If your baby is in a breech position, the risks associated with a vaginal delivery are much higher than with a cesarean section. Risks include the umbilical cord cutting off his blood supply or his head or shoulders becoming stuck. That’s why, in some cases, your provider may recommend a cesarean delivery .
It could be that your provider’s level of experience in delivering breech babies might also inform the discussion you have with your provider about what’s right for your situation. Ultimately, your provider will recommend the best course of action for you and your baby based on your personal situation.
Twins and Breech Presentation
It's possible for twins to be delivered vaginally if the first baby — the lower-positioned twin — is correctly positioned with the head facing down. Of course, that's if the twin pregnancy is otherwise progressing well and there are no complications. If the second twin is in a breech position, the provider may do an ECV procedure to get this baby in the correct head-down position for a vaginal delivery, too.
If the first twin baby (the one lower down) is in a breech position, the provider may recommend a cesarean section. Triplets or more will most likely require a cesarean section.
Although you might feel like the added stress of a breech baby is the last thing you need as you approach your due date, remember that your healthcare provider has seen this situation before and will know what to do to ensure your baby is delivered safely. Next thing you know, you'll be bringing your brand-new baby home , stocking up on diapers, waking up for late-night feedings, and reveling in your baby's growth .
See all sources
- Cleveland clinic: Cesarean Birth (C-Section)
- Cleveland Clinic: Fetal Positions for Birth
- Mayo Clinic: Fetal presentation before birth
- Mayo Clinic: Prenatal care: 3rd trimester visits
- Mayo Clinic: Third Trimester
- Book: Your Pregnancy and Childbirth: Month to Month, Sixth Edition Paperback – January 1, 2016 by American College of Obstetricians and Gynecologists (Author)

Review this article:
Read more about pregnancy.
- Giving Birth
- Pregnancy Announcement
- Pregnancy Calendar
- Pregnancy Symptoms
- Baby Shower & Registry
- Prenatal Health and Wellness
- Preparing For Your New Baby
- Due Date Calculator
Join a World of Support
through Pregnancy and Parenthood.

TRACK WITH TOOLS

LEARN WITH EXPERTS

GET REWARDED

Where You Already Belong
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.
Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.
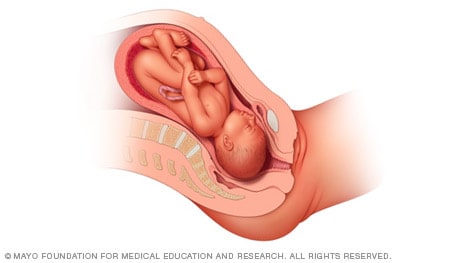
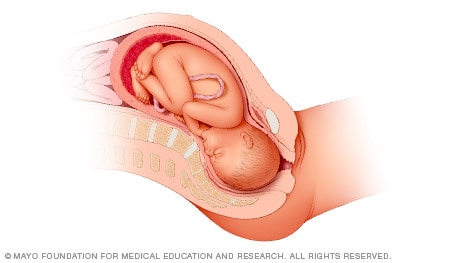
Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.
If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.
- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.

What does it mean for my baby?
The birth process is often more challenging if your baby is in a breech position at the start of labour . A vaginal birth can be more risky for your baby. Your doctor or midwife may advise you to have a caesarean birth, especially if your baby is in a footling breech position.
If your baby is born in a breech position, they have a higher risk of developmental dysplasia of the hip (DDH) , when your baby’s hip doesn’t develop normally. They should have an ultrasound of their hips after six weeks of age to check for this.
Why might my baby remain in a breech position?
Often, it is unclear why a baby stays in a breech position. Some of the common causes include:
- too much or too little amniotic fluid around the baby
- a short umbilical cord
- a low-lying placenta
- many previous pregnancies, making the muscles of the uterus more floppy
- multiple pregnancy
- uterine fibroids
- an irregular size or shape of your uterus
Can my baby still turn after 36 weeks?
Some breech babies turn themselves naturally in the last month of pregnancy. The chance of this happening gets lower as time goes on.
If your baby is in a breech position at 36 weeks, your doctor or midwife might suggest you an ECV, or external cephalic version after 37 weeks . This procedure tries to turn breech babies to the head-down position, ready for a normal vaginal birth. However, ECV is not suitable for everyone, so it’s important to discuss this option with your doctor or midwife.
Is there anything else I can do to make my baby turn?
Some people think that you might be able to encourage your baby to turn by holding yourself in certain positions, such as kneeling with your bottom in the air and your head and shoulders flat to the ground. Other options you might hear include acupuncture, a Chinese herb called moxibustion and chiropractic treatment. There is no good evidence that these work.
Talk to your doctor or midwife before trying any techniques, to check if they might harm you or your baby.
What are my birth options if my baby is breech?
If your baby does not turn, you will have 2 options:
- planning an elective caesarean birth
- trying to have a vaginal breech birth
Most breech babies are born by caesarean. You may be able to have a vaginal birth with a breech baby, but you will need to go to a hospital that can offer you and your baby specialised care.
If your baby is breech, an elective (planned) caesarean is safer for your baby than a vaginal birth in the short term. However, in the longer term their health will be similar, on average, regardless of how they were born.
A vaginal birth is safer for you than an elective caesarean. However, about 4 in 10 people planning a vaginal breech birth end up needing an emergency caesarean . If this happens to you, your risk of complications will be higher.
Your obstetrician . or midwife can talk about your options with you. Whether it’s safe for you to try a vaginal birth will depend on many factors, such as how big your baby is, the exact position of your baby, where the placenta is, the structure of your pelvis and whether you’ve had a caesarean in the past.
What are the safety risks of a vaginal breech birth?
If your baby is being born bottom-first, their largest part — their head — is the last to come out. There is a chance that their head or arms may not follow easily once their body is born.
Risks to your baby can include:
- Erb’s palsy (damage the nerves in your baby’s shoulder and /or arm)
- fractures, dislocations or other injuries
- bleeding in your baby’s brain
- low Apgar scores
- their head getting stuck — this is an emergency
If your waters break when your baby is not head-first, there is a higher risk of cord prolapse . This is an emergency.
If you feel your waters break and you have been told that your baby is not head-first, seek medical help immediately.
What is involved in a vaginal breech birth?
It is important that a midwife or obstetrician with skills and experience in vaginal breech births is with you to help you birth your baby.
Your baby’s heart rate should be monitored continuously with a cardiotocograph (CTG) . You may want to ask your doctor or midwife if you can use a cordless, waterproof CTG so you can remain upright and mobile, and so you can use the bath or shower for pain management during labour.
You will be able to choose what pain relief you have.
Giving birth in an upright position is recommended with a breech baby, however you may need to give birth in a different position if your obstetrician or midwife has more experience with it.
Your obstetrician or midwife will be close by and can help guide your baby into the best position for birth if needed. If your progress during labour slows down, there are a number of techniques they can use to assist your baby to be born vaginally. However, sometimes it may be necessary to have an emergency caesarean section.
Can I have a vaginal breech birth at any hospital?
No. Not all hospitals have obstetricians and midwives on staff with the skills and experience in assisting with a vaginal breech birth. If it is important to you to have a vaginal breech birth and your doctor, midwife or hospital don’t offer this option, you can ask them to refer you to another health service.
What should I ask my doctor or midwife?
It is worth discussing whether you can have an ECV, because if this is successful, you can go on to try a vaginal birth that is safer and more straightforward.
You should also ask if:
- a vaginal birth is safe for the type of breech position your baby is in
- the health service you are planning to use can manage a vaginal breech birth
- your doctor or midwife has training and experience in managing a vaginal breech birth
What if I am planning a home birth and my baby is breech?
If you are planning a home birth , discuss options for your care with your midwife. A planned homebirth is only considered safe if your baby is head-first.
If your baby is breech when you go into labour, it is safest to give birth at a hospital with staff experienced in supporting vaginal breech births and facilities for an emergency caesarean.
Your midwife may be able to continue supporting you during your birth in hospital and after you go home. This will depend on the arrangement between your midwife and the hospital.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: September 2022
Related pages
External cephalic version (ecv), search our site for.
- Caesarean Section
- Foetal Version
Need more information?
Top results
Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

Presentation and position of baby through pregnancy and at birth
Presentation and position refer to where your baby’s head and body is in relation to your birth canal. Learn why it’s important for labour and birth.
Read more on Pregnancy, Birth & Baby website

Malpresentation
Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Breech Baby at Term Information about care options - Pregnancy and the first five years
Breech Baby at Term Information about care options
ECV is a procedure to try to move your baby from a breech position to a head-down position. This is performed by a trained doctor.
Complications of pregnancy
Read this article to learn more about possible complications in pregnancy.
Read more on Rahma Health website

Anatomy of pregnancy and birth - pelvis
Your pelvis helps to carry your growing baby and is tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

Breech Baby: What Causes it and What to Expect

Are you wondering what it means to have a breech baby and what it means for your delivery?
From very early in the pregnancy, your tiny acrobat is twisting, turning, kicking, and tumbling about, suspended in the amniotic fluid in your uterus. As they grow, it gets harder to turn around—you’ll feel lots of somersaults and karate kicks!
By the time you’re at week 36, the position your baby is in begins to matter for delivery. Most babies will have turned so their heads are down toward the birth canal, but some have not—they are in the breech position. A breech baby presents with their buttocks and/or feet first instead of their head, which is a higher risk position for vaginal birth.
But just because your baby is in a breech position doesn’t mean they will stay that way. The closer the baby gets to full term, however, the harder it is to turn around on their own.
The Importance of Fetal Position Before Delivery
The position of the baby’s head matters for delivery. During birth, the baby’s head pushes through the vaginal canal, widening it and making it possible for the rest of the body to follow more easily. If the baby’s buttocks or feet lead the way, labor can become more difficult and dangerous.
Dangers of a vaginal breech birth include cord prolapse (a rare emergency when the umbilical cord exits the cervical opening first), traumatic injury such as a dislocated shoulder, or reduced oxygen if the head cannot pass through the canal after the rest of the body quickly enough. To avoid these risks, your OBGYN may recommend turning the baby to the head down position with an external, manual manipulation called external cephalic version (ECV). If that doesn’t work or your baby remains in the breech position at week 39 gestation, your OBGYN will recommend a C-section as the safest birth option.
Breech Positions
Your baby’s position will be assessed at your 36 week visit with a small ultrasound. By this time, most babies will be positioned with their head down toward the birth canal. However, about 3-4% of them will not.
There are three types of breech baby positions:
- Frank Breech Position
The baby is in a pike position, with both feet up near the baby’s head.
- Incomplete Breech Position
One leg is up by the baby’s head.
- Complete Breech Position
Both knees are bent and the baby’s feet and bottom are closest to the birth canal.
Causes of Breech Baby
Most of the time, the position of the baby is a chance occurrence with no clear cause. In about 15% of breech cases, a uterine abnormality is the cause. Other reported risk factors include:
- A previous sibling or either parent who was in breech presentation
- Uterine abnormality (bicornuate or septate uterus, fibroid)
- Placental location (placenta previa, cornual placenta)
- Extremes of amniotic fluid volume (polyhydramnios, oligohydramnios)
- Fetal anomaly (anencephaly, hydrocephaly, sacrococcygeal teratoma, neck mass)
- Crowding from multiple gestation
- Fetal neurologic impairment
- Maternal hypothyroidism
- Older maternal age
How to Fix Breech Position Naturally
In many situations, babies move out of the breech position on their own.
Some natural solutions women use to encourage a breech baby to turn over before the 39th week include:
- Moxibustion
- Acupuncture
- Chiropractic care
While these methods do not have sufficient evidence to prove they are effective, they are not harmful if performed by a licensed professional.
Yoga and swimming are other activities that could encourage the baby to turn around by creating a sense of more space as your posture changes.
OBGYNs can perform an external cephalic version (ECV) if a baby has not shifted positions after 37 weeks gestation. To perform this procedure, the OBGYN will place their hands on the mother’s stomach and apply pressure to physically turn the baby. This can be painful and does carry some risk, which is why it is performed in the hospital. In many circumstances, a spinal anesthetic (epidural) can be offered.
Chances of C-Section with Breech Baby
If a baby is still presenting as breech by week 39 and interventions have not encouraged the baby to turn around, a C-Section will be recommended nearly 100% of the time.
In the case of twins , if the first baby is born head first and the second is in breech position, the second baby can be born breech with a vaginal delivery under certain circumstances.
Breech Births and Birth Defects
In most cases, babies who are born breech do not experience lasting harm. The most common problem associated with breech babies is hip dysplasia due to their reduced movement and position in the uterus.
All the reasons babies can end up topsy-turvy by the final weeks of pregnancy aren’t fully understood. But with regular check-ins, you and your OBGYN can be prepared for a safer, smoother delivery.

You might also like

5801 Research Park Blvd, Suite 400, Madison WI 53719
608-729-6300

This site uses cookies. By continuing to browse the site, you are agreeing to our use of cookies.
Cookie and Privacy Settings
We may request cookies to be set on your device. We use cookies to let us know when you visit our websites, how you interact with us, to enrich your user experience, and to customize your relationship with our website.
Click on the different category headings to find out more. You can also change some of your preferences. Note that blocking some types of cookies may impact your experience on our websites and the services we are able to offer.
These cookies are strictly necessary to provide you with services available through our website and to use some of its features.
Because these cookies are strictly necessary to deliver the website, refusing them will have impact how our site functions. You always can block or delete cookies by changing your browser settings and force blocking all cookies on this website. But this will always prompt you to accept/refuse cookies when revisiting our site.
We fully respect if you want to refuse cookies but to avoid asking you again and again kindly allow us to store a cookie for that. You are free to opt out any time or opt in for other cookies to get a better experience. If you refuse cookies we will remove all set cookies in our domain.
We provide you with a list of stored cookies on your computer in our domain so you can check what we stored. Due to security reasons we are not able to show or modify cookies from other domains. You can check these in your browser security settings.
These cookies collect information that is used either in aggregate form to help us understand how our website is being used or how effective our marketing campaigns are, or to help us customize our website and application for you in order to enhance your experience.
If you do not want that we track your visit to our site you can disable tracking in your browser here:
We also use different external services like Google Webfonts, Google Maps, and external Video providers. Since these providers may collect personal data like your IP address we allow you to block them here. Please be aware that this might heavily reduce the functionality and appearance of our site. Changes will take effect once you reload the page.
Google Webfont Settings:
Google Map Settings:
Google reCaptcha Settings:
Vimeo and Youtube video embeds:
The following cookies are also needed - You can choose if you want to allow them:

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Breech - series—Types of breech presentation
- Go to slide 1 out of 7
- Go to slide 2 out of 7
- Go to slide 3 out of 7
- Go to slide 4 out of 7
- Go to slide 5 out of 7
- Go to slide 6 out of 7
- Go to slide 7 out of 7
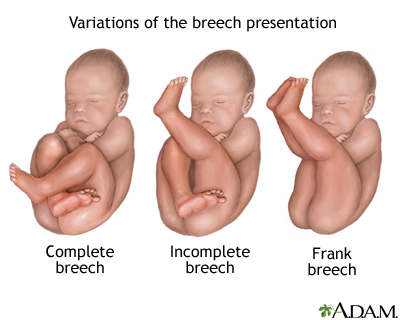
There are three types of breech presentation: complete, incomplete, and frank.
Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal.
Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Frank breech is when the baby's legs are folded flat up against his head and his bottom is closest to the birth canal.
There is also footling breech where one or both feet are presenting.
Review Date 11/21/2022
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
Intermittent Fasting

Pre-Exposure Prophylaxis (PrEP)
What can i do if my baby is breech.
Last Updated June 2023 | This article was created by familydoctor.org editorial staff and reviewed by Deepak S. Patel, MD, FAAFP, FACSM
Right before birth, most babies are in a headfirst position in the mother’s uterus. Sometimes, the baby is in a bottom-first (or feet-first) position. This is called a breech birth or breech baby. Babies can be breech early in pregnancy. Most of them turn on their own to be headfirst by the time of delivery. As you get closer to your due date, your doctor will be able to tell if your baby is breech. They can check by a physical exam, ultrasound, or both.
Breech babies are more likely in these cases:
- Early, or premature births
- Multiple births (two or more babies)
- An abnormal level of amniotic fluid
- An abnormal shaped uterus
Path to improved health
It’s important to see your doctor regularly throughout your pregnancy. Your doctor can tell if your baby is breech and help plan what to do. There are several ways to try and turn your baby. Your doctor may suggest methods to help turn the baby naturally. These could be the first attempt if it is still early and there are no health problems or concerns. Another option is to do a procedure called external cephalic version (ECV). Or your doctor may want to schedule a cesarean delivery (C-section).
External cephalic version
ECV is one way to turn a baby from breech position to head down position while it’s still in the uterus. The doctor will apply pressure to your stomach to turn the baby from the outside. Sometimes, they use ultrasound as well.
Many women who have normal pregnancies can have ECV. You should not have ECV if you have:
- Vaginal bleeding
- A placenta that is near or covering the opening of the uterus
- A low level of fluid in the sac that surrounds and protects the baby
- An abnormal fetal heart
- Premature rupture of the membranes
- Twins or other multiples pregnancy
ECV usually is done in a hospital toward the end of pregnancy, around 37 weeks. Before the procedure, the doctor will do an ultrasound to confirm that your baby is breech. They also will monitor your baby’s heart rate to make sure it is normal. The doctor may give you medicine to relax the muscles in your uterus. This can help decrease discomfort and increase the success of turning your baby. The medicine may be given as a shot or through a vein (IV). It is very safe, with no risk to your baby.
During the ECV, you will lie down and the doctor will place their hands on your stomach. After locating the baby’s head, the doctor will gently try to turn the baby to the headfirst position.
After the procedure, your doctor will monitor your baby’s heart rate again. If the procedure is successful, you shouldn’t have to stay in the hospital. Your chance of having a normal vaginal delivery is high. However, there is a chance that the baby can turn back around to the breech position. The success rate of ECV depends on several factors:
- How close you are to your due date
- The amount of fluid around your baby
- How many pregnancies you have had
- The weight of your baby
- How the placenta is positioned
- The position of your baby
If the procedure is not successful, your doctor will talk to you about delivery. They will discuss the pros and cons of having a vaginal delivery or a C- section. The doctor may suggest repeating the ECV.
The risks of ECV are small, but include:
- Early onset labor
- Minor blood loss for either the baby or the mother
- Fetal distress leading to an emergency C-section
Natural methods
Some people look to natural ways to try and turn their baby. These methods include exercise positions, certain stimulants, and alternative medicine. They may help but there is no scientific evidence that they work.
- Breech tilt, or pelvic tilt : Lie on the floor with your legs bent and your feet flat on the ground. Raise your hips and pelvis into a bridge position. Stay in the tilt for about 10 to 20 minutes. You can do this exercise three times a day. It may help to do it at a time when your baby is actively moving in your uterus.
- Inversion : There are a few moves you can do that use gravity to try and turn the baby. They help relax your pelvic muscles and uterus. One option is to rest in the child’s pose for 10 to 15 minutes. A second option is to gently rock back and forth on your hands and knees. You also can make circles with your pelvis to promote activity.
- Music: Certain sounds may appeal to your baby. Place headphones or a speaker at the bottom of your uterus to encourage them to turn.
- Temperature : Like music, your baby may respond to temperature. Try placing something cold at the top of your stomach where your baby’s head is. Then, place something warm (not hot) at the bottom of your stomach.
- Webster technique : This is a chiropractic approach. It is meant to align your pelvis and hips and relax your uterus. The goal is to encourage your baby to turn.
- Acupuncture : This is a form of Chinese medicine. It involves placing needles at pressure points to balance your body’s energy. It may help relax your uterus and stimulate your baby’s movement.
Things to consider
It is not always possible to turn your baby from being breech. Some breech babies can be safely delivered through the vagina, but usually doctors deliver them by C-section. Risks involved with a C-section include bleeding and infection. There also can be a longer hospital stay for both the mother and her baby.
Other risks can occur for breech babies who are born vaginally. These include:
- Injuries during or after delivery
- Separation of the baby’s hip socket and thigh bone
- Problems with the umbilical cord. For example, the umbilical cord can be flattened during delivery. This can cause nerve and brain damage due to a lack of oxygen.
Questions to ask your doctor
- How can I tell if my baby is breech?
- If my baby is breech, does it mean there is something wrong with them?
- What are the benefits and risks of ECV?
- What are my options for delivery if my baby remains in the breech position?
- What are the health risks to my baby and me if they are born breech?
Medline Plus: Breech Birth
Last Updated: March 10, 2023
This article was contributed by familydoctor.org editorial staff.

Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Related Articles
Natural family planning.
Natural family planning (NFP) is a form of pregnancy planning. It does not involve medicine or devices. It tracks…
Healthy Pregnancy for Women with Diabetes
Diabetes can cause problems during pregnancy. Learn how to manage your diabetes to have a healthy pregnancy.
Postpartum Depression (PPD)
Postpartum depression effects women after giving birth. It involves feelings of sadness, loneliness, worthlessness and restlessness that can last…
Advertisement

familydoctor.org is powered by

Visit our interactive symptom checker
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

IMAGES
VIDEO
COMMENTS
A breech baby (breech birth or breech presentation) ... If a baby is still breech at 37 weeks of pregnancy, your options for delivery may change. This is because there are risks to a vaginal delivery when a baby is breech. In many cases, ... Bridge position: Lie on the floor with your legs bent and your feet flat on the ground. Raise your hips ...
Very rarely, a problem with the baby's muscular or central nervous system can cause a breech presentation. Having an abnormally short umbilical cord may also limit your baby's movement. Smoking. Data shows that smoking during pregnancy may up the risk of a breech baby.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder.
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant patient's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder.
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered. ... American Pregnancy Association. Breech Presentation. Gray CJ ...
In the last weeks of pregnancy, a fetus usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation.A breech presentation occurs when the fetus's buttocks, feet, or both are in place to come out first during birth. This happens in 3-4% of full-term births.
How to turn a breech baby naturally. Get into one of the following positions twice a day, starting at around 32 weeks. Be sure to do these moves on an empty stomach, lest your lunch comes back up. Make sure there's someone around to help you get up if you start feeling lightheaded. If you find these positions uncomfortable, stop doing them.
Epidemiology. Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 28 weeks or less, 25% are breech. Specifically, following one breech delivery, the recurrence rate for the second pregnancy was nearly 10% ...
The buttocks are in place to come out first during delivery. The legs are straight up in front of the body, with the feet near the head. This is the most common type of breech position. Complete breech. The buttocks are down near the birth canal. The knees are bent, and the feet are near the buttocks. Footling breech.
Breech birth happens when a baby doesn't move into a head-first position before birth and instead stays in a bottom-down position. The cause of a breech presentation isn't fully understood, but various situations make it more likely. There are three types of breech baby positions, depending on the position of the baby in your uterus ...
Then, usually between 32 and 36 weeks of pregnancy, your baby will likely get into a head-down position in preparation for being born. There is a small chance — just 3 to 4 percent — that your baby may not move into this head-down position by the time your pregnancy is full term. This is called a breech presentation.
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
A breech birth is when a baby is born bottom first instead of head first, as is normal. Around 3-5% of pregnant women at term (37-40 weeks pregnant) have a breech baby. Due to their higher than average rate of possible complications for the baby, breech births are generally considered higher risk. Breech births also occur in many other mammals such as dogs and horses, see veterinary ...
If your baby is lying bottom-down in your uterus (womb), this is called the breech position. It is common for a baby to be in a breech position before 35 to 36 weeks of pregnancy. Most babies turn to a head-down position before the last month of pregnancy. About 3 in every 100 babies are lying in a breech position at the end of pregnancy.
Move the towel up to cover the arms and rotate the body to make the back anterior. To deliver the head, place your index and middle fingers of one hand over the fetal maxilla to flex the head, while the body rests on your palm and forearm, as shown here. With your other hand, hook 2 fingers over the neck, grasp the shoulder, and apply gentle ...
Most of the time, the position of the baby is a chance occurrence with no clear cause. In about 15% of breech cases, a uterine abnormality is the cause. Other reported risk factors include: A previous sibling or either parent who was in breech presentation. Uterine abnormality (bicornuate or septate uterus, fibroid)
Overview. There are three types of breech presentation: complete, incomplete, and frank. Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal. Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Breech tilt, or pelvic tilt: Lie on the floor with your legs bent and your feet flat on the ground. Raise your hips and pelvis into a bridge position. Stay in the tilt for about 10 to 20 minutes. You can do this exercise three times a day. It may help to do it at a time when your baby is actively moving in your uterus.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant patient's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder.