162 ADHD Essay Topics & Examples
Looking for ADHD topics to write about? ADHD (attention deficit hyperactivity disorder) is a very common condition nowadays. It is definitely worth analyzing.

🔝 Top 10 ADHD Research Topics
🏆 best adhd essay examples, 💡 most interesting adhd topics to write about, 🎓 exciting adhd essay topics, 🔥 hot adhd topics to write about, 👍 adhd research paper topics, ❓ research questions about adhd.
In your ADHD essay, you might want to focus on the causes or symptoms of this condition. Another idea is to concentrate on the treatments for ADHD in children and adults. Whether you are looking for an ADHD topic for an argumentative essay, a research paper, or a dissertation, our article will be helpful. We’ve collected top ADHD essay examples, research paper titles, and essay topics on ADHD.
- ADHD and its subtypes
- The most common symptoms of ADHD
- The causes of ADHD: genetics, environment, or both?
- ADHD and the changes in brain structures
- ADHD and motivation
- Treating ADHD: the new trends
- Behavioral therapy as ADHD treatment
- Natural remedies for ADHD
- ADD vs. ADHD: is there a difference?
- Living with ADHD: the main challenges
- Everything You Need to Know About ADHD The frontal hemisphere of the brain is concerned with coordination and a delay in development in this part of the brain can lead to such kind of disorder.
- Learning Disabilities: Differentiating ADHD and EBD As for the most appropriate setting, it is possible to seat the child near the teacher. It is possible to provide instructions with the help of visual aids.
- Attention Deficit Hyperactivity Disorder (ADD / ADHD) Some critics maintain that the condition is a work of fiction by the psychiatric and pharmacists who have taken advantage of distraught families’ attempts to comprehend the behaviour of their children to dramatise the condition.
- Children With Attention-Deficit Hyperactivity Disorder The purpose of the present research is to understand the correlation between the self-esteem of children with ADHD and the use of medication and the disorder’s characteristics.
- Attention Deficit Hyperactivity Disorder Awareness According to Sayal et al, ADHD is common in young boys as it is easier to identify the problem. The disorder is well-known, and there is no struggle to identify the problem.
- ADHD and Its Effects on the Development of a Child In particular, this research study’s focus is the investigation of the impact of household chaos on the development and behavior of children with ADHD.
- The History of ADHD Treatment: Drug Addiction Disorders Therefore, the gathered data would be classified by year, treatment type, and gender to better comprehend the statistical distribution of the prevalence of drug addiction.
- Attention Deficit Hyperactivity Disorder and Recommended Therapy The condition affects the motivational functioning and abnormal cognitive and behavioural components of the brain. Dysfunction of the prefrontal cortex contributed to a lack of alertness and shortened attention in the brain’s short-term memory.
- Rhetorical Modes Anthology on Attention Deficit Disorder It clearly outlines the origin and early symptoms of the disorder and the scientist who discovered attention deficit hyperactivity disorder. Summary & Validity: This article describes the causes of hyperactivity disorder and the potential factors […]
- Attention-Deficit Hyperactivity Disorder in a Young Girl The particular objective was to assist Katie in becoming more focused and capable of finishing her chores. The patient received the same amount of IR Ritalin and was required to continue taking it for an […]
- Similarities and Differences: SPD, ADHD, and ASD The three disorders, Sensory Processing Disorder, Attention Deficit Hyperactivity Disorder, and Autism Spectrum Disorder, are often confused with each other due to the connections and similarities that exist.
- Assessing the Personality Profile With ADHD Characteristics On the contrary, the study was able to understand significant changes in the emotional states and mood of the children when the observations and the tests ended.
- Aspects of ADHD Patients Well-Being This goal can be achieved through the help of mental health and behavioral counselors to enhance behavioral modification and the ability to cope with challenges calmly and healthily.
- ADHD and Problems With Sleep This is because of the activity of a person in the middle of the day and the condition around them. The downside of the study is that the study group included 52 adults with ADHD […]
- The Attention Deficit Hyperactivity Disorder Treatment It has been estimated that when medicine and therapy are applied as treatment together, the outcomes for children with ADHD are excellent.
- Attention Deficit Hyperactivity Disorder Organization’s Mission Children and Adults with Attention-Deficit/Hyperactivity Disorder is an organization that is determined to handle individuals affected by ADHD. The organization was founded in 1987 following the rampant frustration and isolation that parents experienced due to […]
- Case Conceptualization: Abuse-Mediated ADHD Patient The case provides insight into the underlying causes of James’s educational problems and the drug abuse of his parents. The case makes it evident that the assumption from the first case conceptualization about James’s ADHD […]
- Change: Dealing With Patients With ADHD In the current workplace, the most appropriate change would be the increase in the awareness of nurses regarding the methods of dealing with patients with ADHD.
- Dealing With Attention Deficit Hyperactivity Disorder Although my experience is not dramatic, it clearly shows how untreated ADHD leads to isolation and almost depression. However, the question arises of what is the norm, how to define and measure it.
- Parents’ Perception of Attending an ADHD Clinic The main principles of the clinic’s specialists should be an objective diagnosis of the neurological status of the child and the characteristics of his/her behavior, the selection of drug treatment only on the basis of […]
- ADHD: Mental Disorder Based on Symptoms The DSM-5 raised the age limit from 6 to 12 for qualifying the disorder in children and now requires five instead of six inattentive or hyperactive-impulsive symptoms.
- Understanding Attention-Deficit/Hyperactivity Disorder Thus, the smaller sizes of the reviewed brain structures associated with ADHD result in problems with attention, memory, and controlling movement and emotional responses.
- Effective Therapies for Attention Deficit Hyperactivity Disorder The problem at hand is that there is a need to determine which of the therapies administered is effective in the management of ADHD.
- Participants of “ADHD Outside the Laboratory” Study The participants in the testing group and those in the control group were matched for age within 6 months, for IQ within 15 points and finally for performance on the tasks of the study.
- Variables in “ADHD Outside the Laboratory” Study The other variables are the videogames, matching exercise and the zoo navigation exercise used to test the performance of the boys.
- Different Types of Diets and Children’s ADHD Treatment The last factor is a trigger that can lead to the development of a child’s genes’ reaction. Thus, diet is one of the factors that can help prevent the development of ADHD.
- Attention Deficit Hyperactivity Disorder in Children The consistent utilization of effective praises and social rewards indeed results in the behavioral orientation of the child following the treatment goals.
- Vyvanse – ADD and ADHD Medicine Company Analysis It is produced by Shire and New River Pharmaceuticals in its inactive form which has to undergo digestion in the stomach and through the first-pass metabolic effect in the liver into L-lysine, an amino acid […]
- Dealing With the Disruptive Behaviors of ADHD and Asperger Syndrome Students While teaching in a class that has students with ADHD and Asperger syndrome, the teacher should ensure that they give instructions that are simple and easy to follow.
- Current Issues in Psychopharmacology: Attention-Deficit Hyperactivity Disorder This is the area that is charged with the responsibility for vision control as well as a regulation of one’s brain’s ability to go to aresynchronize’ and go to rest.
- Cognitive Psychology and Attention Deficit Disorder On top of the difficulties in regulating alertness and attention, many individuals with ADD complain of inabilities to sustain effort for duties.
- Adult and Paediatric Psychology: Attention Deficit Hyperactivity Disorder To allow children to exercise their full life potential, and not have any depression-caused impairment in the social, academic, behavioral, and emotional field, it is vital to reveal this disorder as early in life, as […]
- Attention-Deficit Hyperactivity Disorder: Biological Testing The research, leading to the discovery of the Biological testing for ADHD was conducted in Thessaloniki, Greece with 65 children volunteering for the research. There is a large difference in the eye movement of a […]
- Issues in the Diagnosis of Attention-Deficit Hyperactivity Disorder in Children Concept theories concerning the nature of attention-deficit/hyperactivity disorder influence treatment, the approach to the education of children with ADHD, and the social perception of this disease.
- Attention Deficit Hyperactivity Disorder Care Controversy The objective of this study was to assess the efficacy, in terms of symptoms and function, and safety of “once-daily dose-optimized GXR compared with placebo in the treatment of children and adolescents aged 6 17 […]
- Attention Deficit Hyperactivity Interventions The authors examine a wide range of past studies that reported on the effects of peer inclusion interventions and present the overall results, showing why further research on peer inclusion interventions for children with ADHD […]
- Attention Deficit Hyperactivity Disorder (ADHD) in a Child A child counselor works with children to help them become mentally and emotionally stable. The case that is examined in this essay is a child with attention deficit hyperactivity disorder.
- Attention Deficit Hyperactivity Disorder: Drug-Free Therapy The proposed study aims to create awareness of the importance of interventions with ADHD among parents refusing to use medication. The misperceptions about ADHD diagnosis and limited use of behavioral modification strategies may be due […]
- Attention Deficit Hyperactivity Disorder: Psychosocial Interventions The mentioned components and specifically the effects of the condition on a child and his family would be the biggest challenge in the case of Derrick.
- Attention Deficit Hyperactivity Disorder: Signs and Strategies Determining the presence of Attention Deficit Hyperactivity Disorder in a child and addressing the disorder is often a rather intricate process because of the vagueness that surrounds the issue.
- Cognitive Therapy for Attention Deficit Disorder The counselor is thus expected to assist the self-reflection and guide it in the direction that promises the most favorable outcome as well as raise the client’s awareness of the effect and, by extension, enhance […]
- Bright Not Broken: Gifted Kids, ADHD, and Autism It is possible to state that the book provides rather a high-quality review of the issues about the identification, education, and upbringing of the 2e children.
- Treatment of Children With ADHD Because of the lack of sufficient evidence concerning the effects of various treatment methods for ADHD, as well as the recent Ritalin scandal, the idea of treating children with ADHD with the help of stimulant […]
- Medication and Its Role in the ADHD Treatment Similar inferences can be inferred from the findings of the research conducted by Reid, Trout and Schartz that revealed that medication is the most appropriate treatment of the symptoms associated with ADHD.
- Psychology: Attention Deficit and Hyperactivity Disorder It is important to pay attention to the development of proper self-esteem in children as it can negatively affect their development and performance in the future.
- Cognitive Behavior Therapy in Children With ADHD The study revealed that the skills acquired by the children in the sessions were relevant in the long term since the children’s behaviors were modeled entirely.
- Is Attention Deficit Hyperactivity Disorder Real? In fact, the existence of the condition, its treatment and diagnosis, have been considered controversial topics since the condition was first suggested in the medical, psychology and education.
- Is Attention Deficit Disorder a Real Disorder? When Medicine Faces Controversial Issues In addition, it is necessary to mention that some of the symptoms which the children in the case study displayed could to be considered as the ones of ADHD.
- Foods That Effect Children With ADHD/ ADD Therefore, it is the duty of parents to identify specific foods and food additives that lead to hyperactivity in their children.
- Toby Diagnosed: Attention Deficit Hyperactivity Disorder The symptoms of the disorder are usually similar to those of other disorder and this increases the risks of misdiagnosing it or missing it all together.
- Identifying, Assessing and Treating Attention Deficit Hyperactivity Disorder For these criteria to be effective in diagnosing a child with ADHD, the following symptoms have to be present so that the child can be labelled as having ADHD; the child has to have had […]
- Attention Deficit Hyperactivity Disorder Influence on the Adolescents’ Behavior That is why the investigation was developed to prove or disprove such hypotheses as the dependence of higher rates of anxiety of adolescents with ADHD on their diagnosis, the dependence of ODD and CD in […]
- Stroop Reaction Time on Adults With ADHD The model was used to investigate the effectiveness of processes used in testing interference control and task-set management in adults with ADHD disorder.
- Working Memory in Attention Deficit and Hyperactivity Disorder (ADHD) Whereas many studies have indicated the possibility of the beneficial effects of WM training on people with ADHD, critics have dismissed them on the basis of flawed research design and interpretation.
- Attention-Deficit Hyperactivity Disorder: The Basic Information in a Nutshell In the case with adults, however, the definition of the disorder will be quite different from the one which is provided for a child ADHD.
- How ADHD Develops Into Adult ADD The development of dominance is vital in processing sensations and information, storage and the subsequent use of the information. As they become teenagers, there is a change in the symptoms of ADHD.
- Medical Condition of Attention Deficit Hyperactivity Disorder A combination of impulsive and inattentive types is referred to as a full blown ADHD condition. To manage this condition, an array of medical, behavioral, counseling, and lifestyle modification is the best combination.
- Effects of Medication on Education as Related to ADHD In addition, as Rabiner argues, because of the hyperactivity and impulsivity reducing effect of ADHD drugs, most ADHD suffers are nowadays able to learn in an indistinguishable class setting, because of the reduced instances of […]
- Attention Deficit Hyperactivity Disorder: Diagnosis and Treatment Generally the results indicate that children with ADHD had a difficult time in evaluating time concepts and they seemed to be impaired in orientation of time.
- The Ritalin Fact Book: Stimulants Use in the ADHD Treatment Facts presented by each side of the critical issue The yes side of the critical issue makes it clear that the drugs being used to control ADHD are harmful as they affect the normal growth […]
- Behavior Modification in Children With Attention Deficit Hyperactivity Disorder Introduction The objective of the article is to offer a description of the process of behavior modification for a child diagnosed with ADHD.
- What Is ADHD and How Does It Affect Kids
- The Benefits of Physical Activities in Combating the Symptoms of ADHD in Students
- The Effects of Exercise and Physical Activity as Intervention for Children with ADHD
- What Are the Effects of ADHD in the Classroom
- Are Children Being Diagnosed with ADHD too Hastily
- The Effectiveness of Cognitive Behavioral Therapy on ADHD
- Understanding ADHD, Its Effects, Symptoms, and Approach to Children with ADHD
- ADHD Stimulant Medication Abuse and Misuse Among U.S. Teens
- Severity of ADHD and Anxiety Rise if Both Develop
- The Best Approach to Dealing with Attention Deficit/Herpactivity Disorder or ADHD in Children
- An Analysis of the Potential Causes and Treatment Methods for Attention Deficit Hyperactivity Disorder (ADHD) in Young Children
- The Best Way to Deal with Your Child Who Struggles with ADHD
- Response Inhibition in Children with ADHD
- Behavioral and Pharmacological Treatment of Children with ADHD
- Symptoms And Symptoms Of ADHD, Depression, And Anxiety
- Bioethics in Intervention in the Deficit Attention Hyperkinetic Disorder (ADHD)
- The Effects of Children’s ADHD on Parents’ Relationship Dissolution and Labor Supply
- The Effects of Pharmacological Treatment of ADHD on Children’s Health
- The Educational Implications Of ADHD On School Aged Children
- Differences in Perception in Children with ADHD
- The Effects Of ADHD On Children And Education System Child
- Students With ADD/ADHD and Class Placement
- The Advantage and Disadvantage of Using Psychostimulants in the Treatment of ADHD
- How to Increase Medication Compliance in Children with ADHD
- Effective Teaching Strategies for Students with ADHD
- Scientists Probe ADHD Treatment for Long Term Management of the Disease
- Should Stimulants Be Prescribed for ADHD Children
- The Rise of ADHD and the an Analysis of the Drugs Prescribed for Treatment
- The Correlation Between Smoking During Pregnancy And ADHD
- Exploring Interventions Improving Workplace Behavior In Adults With ADHD
- The Promise of Music and Art in Treating ADHD
- The Struggle Of ADHD Medication And Over Diagnosis
- The Problems of Detecting ADHD in Children
- The Harmful Effects of ADHD Medication in Children
- The Symptoms and Treatment of ADHD in Children and Teenagers
- The Impact of Adult ADD/ADHD on Education
- The Experience of Having the ADHD Disorder
- The Young Children And Children With ADHD, And Thinking Skills
- The Use of Ritalin in Treating ADD and ADHD
- The Ethics Of Giving Children ADHD Medication
- The Importance of Correctly Diagnosing ADHD in Children
- The Rise in ADHD Diagnosis and Treatment within the United States of America
- The World of ADHD Children
- The Use of Drug Therapies for Children with ADHD
- What Are the Effects of ADHD in the Classroom?
- Does ADHD Affect Essay Writing?
- What Are the Three Main Symptoms of ADHD?
- How Does ADHD Medication Affect the Brain?
- What Can ADHD Lead To?
- Is ADHD Legitimate Medical Diagnosis or Socially Constructed Disorder?
- How Does Art Help Children With ADHD?
- What Are the Four Types of ADHD?
- Can Sports Affect Impulse Control in Children With ADHD?
- What Age Does ADHD Peak?
- How Can You Tell if an Adult Has ADHD?
- Should Antihypertensive Drugs Be Used for Curing ADHD?
- How Does ADHD Affect Cognitive Development?
- Is Adult ADHD a Risk Factor for Dementia or Phenotypic Mimic?
- How Are People With ADHD Seen in Society?
- Can Additional Training Help Close the ADHD Gender Gap?
- How Does School Systems Deal With ADHD?
- Are Children With Low Working Memory and Children With ADHD Same or Different?
- How Does ADHD Affect School Performance?
- Should Children With ADHD Be Medicated?
- How Does Society View Children With ADHD?
- What Do Researches Tell Us About Students With ADHD in the Chilean Context?
- Why Should Teachers Understand ADHD?
- Does DD/ADHD Exist?
- What Are Some Challenges of ADHD?
- Why Is ADHD an Important Topic to Discuss?
- Is ADHD Born or Developed?
- Can ADHD Cause Lack of Emotion?
- Does ADHD Affect Females?
- Is ADHD on the Autism Spectrum?
- Neuropsychology Topics
- Bipolar Disorder Research Ideas
- Pathogenesis Research Ideas
- Abnormal Psychology Paper Topics
- Schizophrenia Essay Topics
- Dissociative Identity Disorder Essay Topics
- Cognitive Therapy Essay Topics
- Emotional Intelligence Paper Topics
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 20). 162 ADHD Essay Topics & Examples. https://ivypanda.com/essays/topic/adhd-essay-topics/
"162 ADHD Essay Topics & Examples." IvyPanda , 20 Feb. 2024, ivypanda.com/essays/topic/adhd-essay-topics/.
IvyPanda . (2024) '162 ADHD Essay Topics & Examples'. 20 February.
IvyPanda . 2024. "162 ADHD Essay Topics & Examples." February 20, 2024. https://ivypanda.com/essays/topic/adhd-essay-topics/.
1. IvyPanda . "162 ADHD Essay Topics & Examples." February 20, 2024. https://ivypanda.com/essays/topic/adhd-essay-topics/.
Bibliography
IvyPanda . "162 ADHD Essay Topics & Examples." February 20, 2024. https://ivypanda.com/essays/topic/adhd-essay-topics/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Expert Review
- Open access
- Published: 08 June 2024
Improving the efficacy and effectiveness of evidence-based psychosocial interventions for attention-deficit/hyperactivity disorder (ADHD) in children and adolescents
- Anil Chacko ORCID: orcid.org/0000-0002-3275-4726 1 ,
- Brittany M. Merrill 2 ,
- Michael J. Kofler ORCID: orcid.org/0000-0002-8604-3647 3 &
- Gregory A. Fabiano 2
Translational Psychiatry volume 14 , Article number: 244 ( 2024 ) Cite this article
4352 Accesses
1 Altmetric
Metrics details
- Human behaviour
Attention-deficit/hyperactivity disorder (ADHD) is a prevalent, chronic, and impairing mental health disorder of childhood. Decades of empirical research has established a strong evidence-based intervention armamentarium for ADHD; however, limitations exist in regards to efficacy and effectiveness of these interventions. We provide an overview of select evidence-based interventions for children and adolescents, highlighting potential approaches to further improving the efficacy and effectiveness of these interventions. We conclude with broader recommendations for interventions, including considerations to moderators and under-explored intervention target areas as well as avenues to improve access and availability of evidence-based interventions through leveraging underutilized workforces and leveraging technology.
Similar content being viewed by others

RETRACTED ARTICLE: Is homeopathy effective for attention deficit and hyperactivity disorder? A meta-analysis

Medical conditions and Attention-Deficit/Hyperactivity Disorder symptoms from early childhood to adolescence
Perspectives on parental support of attention deficit hyperactivity disorder self-management at the transition to adulthood
Evidence-based treatments for adhd - an overview.
Multiple groups, committees, and professional organizations have provided the field with recommendations for evidence-based treatment approaches for ADHD. There is clear consensus across these recommendations that pharmacological treatments, notably stimulant medication, psychosocial treatments, and a combination of these two approaches have the strongest evidence base. Table 1 provides a brief overview of the major conclusions of each guideline for the treatment of ADHD in children. It is clearly recommended that families should receive psychoeducation regarding ADHD, and that the evidence-based psychosocial treatments are behavioral parent training (BPT), behavioral interventions in classroom and peer settings, and organizational skills training [ 1 , 2 , 3 , 4 , 5 ].
There are inconsistencies among the guidelines that make broad statements of consensus difficult. For instance, there are differences in precision in recommendations for psychosocial treatments, with some very broad in scope [ 6 ] compared to others with more precise recommendations regarding particular treatment types (e.g., BPT [ 2 ]) and particular populations (e.g., children under six; [ 5 ]). Broad suggestions of seeking “psychological” or “educational” treatment is unhelpful in some guidelines and practice parameters, as there are many approaches that fall under this category and some are clearly efficacious whereas other approaches commonly deployed do not have evidence of efficacy for ADHD [ 1 , 2 , 3 , 4 ]. There are also differences in the strength of recommendations, with more contemporary guidelines emphasizing multimodal treatments more so than older guidelines. However, perhaps most notably, there is not clear consensus among the recommendations on the best sequence or combination of treatments for ADHD, even though this is a key question for most families pursuing treatment for ADHD. It is also important to note that most guidelines focus on proximal ADHD treatment – as ADHD is now conceptualized as a life-course persistent disorder [ 7 ], treatment efforts will need to be protracted across time and appropriate for evolving developmental levels.
Efforts at improving efficacy and effectiveness of psychosocial intervention for ADHD: what do we know and where do we go?
Given the prominent role of psychosocial, primarily behavioral interventions, for ADHD, we highlight the evidence for several of these key interventions, integrating the literature on improving efficacy and effectiveness of these interventions. We also discuss digital therapeutics given the explosion in its availability and purported efficacy for children with ADHD. Following this, we close with potential broad future directions for psychosocial treatments for children with ADHD.
Behavioral parent training
Behavioral parent training (BPT) is likely the most well-studied psychosocial intervention for children’s mental health disorders, including for ADHD [ 8 ]. It serves as the first line intervention approach for younger children with ADHD and is an integral part of comprehensive intervention approaches for school-age children with ADHD. Importantly, BPT is less studied in adolescents with ADHD. Although parenting is not etiological to ADHD, there are clear reasons to focus on parenting when supporting a child with ADHD. Of primary importance is that raising a child with ADHD is stressful, and not surprisingly, elicits ineffectual parenting practices (e.g., inconsistent, harsh, lax, overreactive, less responsive). As a result, parents often have lower parenting efficacy/competence, higher levels of coercive management practices, utilize maladaptive coping strategies (e.g., increased use of alcohol), and have more negative attributions/perceptions of their child [ 8 ]. These parent-level challenges can be addressed, in part, by supporting parents to utilize more proactive and effective parenting practices which can help improve functioning for themselves and ultimately their children. Importantly, the most common comorbidities with ADHD, Oppositional Defiant Disorder [ODD] and Conduct Disorder (CD) are best treated with BPT—making BPT an essential treatment for the most common disruptive behavior disorders in childhood [ 8 ].
BPT is based on operant-conditioning and social learning theories, with techniques that focus on antecedents (e.g., effective instructions, rules) and consequences (e.g., active ignoring, time-out from positive reinforcement) of behaviors. This core content is delivered in a flexible manner with varying formats (e.g., group, individual) durations (brief vs longer), with or without child involvement, delivery (e.g., with or without video-based learning). Moreover, over the past two decades, there have been efforts at tailoring BPT to meet the needs of specific populations (e.g., single mothers, fathers; Latine; [ 9 , 10 , 11 , 12 ]). These BPT programs, often referred to as “homegrown” BPT as compared to commercialized BPT programs (those that have been more extensively developed, manualized and are commercially available; e.g., Defiant Children [ 13 ]) retain the core content of traditional BPT but have modifications to format or additional content that are based on the needs of the targeted populations. Overall, commercialized BPT and homegrown BPT have been found to be effective in improving the functioning of children with ADHD and their parents [ 14 , 15 , 16 ]. A recent meta-analysis also suggests sustained benefits of BPT over the course of a year on child ADHD symptoms, parenting behavior, parenting sense of competence and parental mental health [ 17 ]. The significance of BPT should be, however, put into a broader context to appreciate the clinical benefits of this intervention. While multiple randomized controlled trials have established the statistical significance of BPT for ADHD, the effect size for BPT ranges from small to medium effects, depending upon the outcome [ 18 ]. This means that for many outcomes, the effect sizes would be “visible to the naked eye of a careful observer” [ 19 ]. While there is limited data, only a significant minority of children are “normalized” following BPT [ 15 ]. Collectively, a more nuanced perspective on BPT for ADHD suggests that it is an evidence-based intervention that can result in visible improvements on key outcomes. There is room, however, to improve the potency of BPT. The implications of the findings reported above suggest several broad areas for further investigation. First is to increase access to BPT given the benefits of the intervention. Wolraich et al. [ 20 ] note that there is a lack of an adequate pool of behavioral and mental health specialists who are available to provide evidence-based psychosocial treatments for ADHD, including BPT. National data suggest that the majority of youth with ADHD are receiving no treatment, even when identified, and the lack of BPT treatment is most pronounced in young children with ADHD [ 21 ]. Efforts at utilizing technology to increase the workforce offers novel and promising approaches to address this issue [ 22 ].
A second area is to increase the potency of BPT. We believe there are multiple ways to achieve this goal, with the most apparent being improving the extent to which parents fully engage in BPT, given the relation between increased engagement and improved potency of outcomes [ 23 ]. It is common for families of children with ADHD, even those who have enrolled in BPT, to not initiate treatment or drop out of BPT prior to completion [ 9 , 23 ]. Given this, there have been notable efforts at improving engagement to BPT through addressing perceptual (e.g., expectations about BPT), practical (e.g., transportation) and cultural barriers to treatment prior to BPT [ 10 , 24 ] as well as during BPT [ 25 ]. Given that engagement challenges often involve practical barriers (e.g., transportation, child care, fixed appointment times), there has been efforts at increasing access through reducing these barriers such as providing BPT through mobile applications [ 26 ], web-based platforms [ 27 ] and telehealth delivery [ 28 , 29 ]. These efforts have led to improved engagement and associated outcomes for families, beyond traditional BPT [ 30 ]. Engagement with BPT remains an important area of research, particularly the extent to which these enhancements to BPT can be readily applied in routine settings [ 25 , 31 , 32 ], an understudied empirical question.
A second and meaningful line of research to improve the potency of BPT has been focused on improving specificity of BPT content by translating contemporary theories of ADHD into refinements to BPT. Van der Oord and Tripp [ 33 ]), utilizing contemporary motivational reinforcement-based theories of ADHD, suggest that given altered reinforcement sensitivity in ADHD, rewards and punishment should be judiciously provided. As an example, they note evidence that while mild negative punishment (e.g., response-cost, time-out from positive reinforcement) improves on-task behavior in children with ADHD, mild punishment can also lead to more errors on tasks, increased emotionality in children with ADHD, missed learning opportunities, and lack of task persistence [ 34 , 35 ]. These authors note caution in the use of punishment, especially positive punishment (e.g., verbal reprimands), with children with ADHD. Rather, there should be a focus on rewarding alternative adaptive behaviors to reduce the need to use punishment. These theory-driven considerations to adapting BPT are important, yet empirically understudied. As such, the extent to which these ADHD-theory-adapted BPT results in improved outcomes relative to standard BPT is not known. Importantly, however, some efforts in this area have resulted in little difference for ADHD-adapted BPT relative to standard BPT. As an example, in an RCT, the New Forest Parenting Program (NFPP), which was developed to address underlying mechanisms of ADHD (self-regulatory and cognitive problems [ 36 ] was found to be no better than a standard BPT program and in some areas less effective (e.g., parental stress, parenting behavior, parent reports of ADHD symptoms at follow-up) for preschool children with ADHD [ 37 ]. These data suggest the importance of rigorously evaluating novel approaches that are considered improvements to BPT to well-established traditional BPT for ADHD.
Overall, the efficacy of BPT suggests that this should be first-line intervention approach for children with ADHD, with significant and noticeable effects of BPT on both parent- and child-level outcomes with maintenance of gains over the course of a year. This statement comes with the caveat that there is room for improvement in the potency of BPT. As we will discuss in the future directions section below, greater attention must be given to dissemination of BPT (and all psychosocial interventions for ADHD) within routine systems of care and evaluation of the effectiveness of these interventions alone and in combination when delivered within these systems.
Behavioral classroom management
ADHD is largely defined by challenges in settings such as schools where behavioral expectations are often demanding of attention capacity and self-control, and so it is not surprising that many of the efficacious treatments for ADHD have focused on improving academic functioning and classroom behaviors. Children with ADHD are effectively treated with classroom contingency management strategies [ 38 ]. Systematic reviews [ 1 , 2 , 4 , 5 , 39 ] as well as meta-analyses [ 40 , 41 , 42 ] clearly illustrate that behavioral classroom management is an efficacious treatment for ADHD.
As noted above, behavioral classroom management is an efficacious treatment for ADHD. Before discussing evidence for efficacy and effectiveness of behavior classroom management, it is worth noting approaches that do not strongly support positive outcomes. In the United States, children with ADHD are eligible for behavioral classroom management support through Section 504 Accommodation plans administered through the Americans with Disabilities Act or through an Individualized Education Program if the committee on special education determines it is needed. These policies have provided school-based behavioral supports for students with ADHD for over 30 years. However, given that follow-up studies indicate that the long-term educational outcomes for students with ADHD are modest, at best [ 43 , 44 , 45 , 46 ], it is important to emphasize that these accommodation plans or individualized education programs are only useful if they include effective interventions and supports for the child or adolescent with ADHD.
Practically speaking, behavioral classroom management approaches that are effective will include setting clear goals and rules, ensure that the child receives clear feedback on progress toward meeting goals, and that consequences, typically rewards and privileges contingent on meeting behavioral goals and following rules, are provided liberally. It is important to note that positive behavior support strategies are interwoven into the fabric of elementary school classrooms - teachers provide rules and structure for activities, there is praise issued for appropriate behavior, and schools have standard discipline procedures including office referrals or detentions for rule violations. Feedback is provided on a regular, if infrequent basis (i.e., on quarterly report cards). For most children with ADHD this provides a reasonable baseline of behavioral classroom management, but additional strategies and supports are typically needed to make the overall approach to supporting a child with ADHD more efficacious.
Children with ADHD typically need much more frequent behavioral feedback and positive consequences for appropriate behavior in schools. For that reason, a daily report card is among the most efficacious positive behavior supports within a classroom [ 47 , 48 ]. The daily report card has long been used effectively to treat ADHD, monitor outcomes, and open a daily line of communication between teachers and the child’s parent [ 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 ], and it is a procedure aligned with a long tradition of using contingency management with children with disruptive behavior in general educational settings [ 58 ] and in special education settings [ 57 , 59 , 60 ]. In addition to being among the most efficacious classroom interventions, it is also one of the most cost effective [ 61 ].
Recent changes in the ways schools address social, emotional, and behavioral challenges may promote greater effectiveness of the implementation of classroom behavior management strategies. Multi-tiered systems of support (MTSS [ 62 ] in schools conceptualize the behavior of children as being within a continuum, and through regular screening and progress monitoring, provide more intensive intervention, when indicated and for as long as is needed. Currently MTSS efforts in schools are focused on academic achievement targets, and there is less emphasis on MTSS for behavior [ 63 ]. However, the MTSS model of screening and intervention is similar to the single case design approach to intervention that has been long-used within the ADHD treatment literature [ 4 , 5 , 47 ]. In this approach, following the collection of baseline data, behavior classroom management interventions are systematically introduced to evaluate their effectiveness. Educators also benefit from ongoing coaching, support, and monitoring of progress to promote consistent and protracted use of these behavioral interventions [ 64 ].
Supporting this approach to school-based intervention is a recent study that evaluated the effectiveness of different sequences of ADHD treatment [ 65 ]. In this study, using a sequential, multiple assignment randomized trial (SMART [ 66 ]), children were randomly assigned to begin the school year with one of the two evidence-based treatments for ADHD - a low dose of stimulant medication or an initial course of behavior therapy (eight parent training sessions and a daily report card intervention at school). Teachers provided feedback on how the child was functioning in the classroom, and if there was evidence of impaired functioning, the child was then randomly assigned to more treatment – either a greater dose of the treatment at the start of the school year, or a other modality. Thus, children could have a treatment sequence of: (1) medication followed by an increased dose of medication; (2) medication with behavior therapy added; (3) behavior therapy followed by an increased dose of behavior therapy; or (4) behavior therapy followed by medication. Results were interesting as they illustrated the best sequence of treatment for reducing discipline referrals and disruptive behaviors observed in the classroom were those that started with behavior therapy first. Further, the behavior therapy first approaches also cost less to implement across the school year than the treatment sequences that included medication [ 61 ]. Importantly, this study of the effectiveness of treatment sequencing spanned an entire school year, improving upon the research base of efficacy treatments where many studies focused on shorter time periods. While the Pelham study provides a foundation for considering combined and sequenced approaches, far less has been done on the effectiveness of behavioral classroom approaches when conducted within and supported entirely by school-staff over the course of multiple school years.
Overall, there is strong support for behavioral classroom interventions, including the Daily Report Card [ 48 , 50 , 67 ], and it is strongly recommended that this intervention be initiated for children with ADHD experiencing classroom-based impairment. For older children (e.g., middle school, high school), a behavioral contract may be used to initiated contingency management across the multiple classrooms characteristic of this grade level. Educators and parents should ensure that school-based interventions are implemented consistency and continuously, as school-based behavioral challenges are likely to extend across school years and grade levels.
Organization skills training
Related to their difficulties staying on task and following the rules in the classroom setting, children with ADHD have impaired organization, time management, and planning skills that undermine their academic abilities and potential. Homework management and organizational skills have been shown to predict concurrent GPA and later academic outcomes [ 68 , 69 ]. Organizational skills training (OST) interventions utilize behavioral methods to teach skills directly to students with ADHD. The training programs often include behavioral management procedures administered by a counselor, parent, or teacher to reinforce skill use and progress in treatment. Organizational interventions have largely targeted middle school to early high school students with ADHD (ages 10–14 [ 70 ]), with sessions focusing on materials organization, understanding time and time management, and planning larger assignments. Session frequency and length vary widely from about 10, 60-minute family sessions in a clinic [ 71 ] to 40, 2.5-hour student sessions in an after-school setting [ 72 ]. Multicomponent OST packages lead to improvements in organizational skills, planner use, and adolescent impairment [ 73 ].
Embedding OST in schools is key to enhancing the reach of these interventions. Though availability of school personnel to implement OST varies across districts, current work aims to train school counselors to implement OST with students with ADHD [ 74 ]. Langberg and colleagues [ 74 ] found that OST delivered by school staff led to improvements in organization, time management, and planning skills as performance and behavior during homework based on parent-report. Importantly, these results were found despite the school counselors receiving only 2 h of training in the intervention with no ongoing supervision. Purposefully limiting training and post-training investment allows for the examination of treatment effects in the context in which they would likely be provided—i.e., in schools, by school mental health providers with little funding for training and ongoing supervision. Toward the same goal of increasing the sustainability of OST within schools, investigators are developing online tools to assist school staff with OST implementation at low to no cost [ 75 ].
Psychosocial treatments for children with ADHD have primarily been researched in elementary-age youth, and early work in developing organizational skills interventions addressed this gap by upwardly extending treatments to middle school age youth. As the evidence accumulated that such interventions were efficacious among children with ADHD in middle school [ 1 , 2 ], further developmental extension was clearly justified [ 76 ]. adapted their OST program developed for middle schoolers to pilot with high school students with ADHD. Pilot data demonstrated feasibility and indicated that high schoolers may need about 50 sessions to benefit from the OST program. In the full-scale randomized clinical trial [ 77 ], high schoolers attended an average of 40 brief OST sessions while their caregivers attended an average of 4 behavioral parent training sessions. Compared to the control group, beneficial effects of treatment were found on parent-reported academic functioning and organizational skills, and no significant effects on grades, teacher-reported, or self-reported outcomes were found. Results are promising, and much more work is needed to support the academic functioning of older adolescents with ADHD.
Digital therapeutics
Of all the available non-medication treatments, this category is the only one that features protocols patented by the US Patent and Trademark Office (USPTO) and cleared by the U.S. Food and Drug Administration (FDA) for the treatment of ADHD. It is also the most controversial, with competing consensus statements concluding that these types of interventions have proven effective vs. proven ineffective [ 78 ], millions of dollars in fines for false advertising [ 78 ], and a perceived disconnect between benchmarks for effectiveness between the FDA and professional organizations that evaluate psychosocial treatments for children [ 79 ]. Overall, there appears to be evidence for small benefits of cognitive training on reducing inattentive symptoms, and potentially overall ADHD symptoms [ 80 ]. However, we contend that omnibus meta-analytic effect sizes are fundamentally uninterpretable in the context of cognitive training/digital therapeutics because the treatments that fall under this general umbrella feature wide variations in neurocognitive/neurological training targets, conceptual models of neurocognition that define these intended training targets, success/failure to meaningfully engage and improve the intended training target(s), and technologies employed to ‘hit’ the intended target(s). Therefore, what these treatments share are more peripheral features, rather than core mechanistic features necessary to meet meta-analytic assumptions. Even interventions given the same, more specific label (e.g., “working memory training”) vary widely in their approach, conceptual basis, and success/failure at engaging their mechanistic target as shown previously [ 81 ]. It will be important for the field to evaluate each intervention on its own merits because these protocols generally share very little with each other except for the use of a serious games approach [ 82 ] to engaging children in treatment.
Several neurocognitive training protocols have been developed and tested for children with ADHD; we briefly review three of the most prominent: EndeavorRX, CogMed, and Central Executive Training (Cenextra; an intervention developed by one of the co-authors). All three of these approaches are computerized digital therapeutics that include gaming elements and adaptive changes in difficulty. EndeavorRX trains cognitive attention abilities [ 83 ], Cenextra trains the ‘working’ components of working memory [ 84 ] and CogMed is intended to improve attention and working memory abilities [ 85 ], though clinical trial and meta-analytic evidence indicates that CogMed successfully engages short-term memory but not working memory abilities [ 81 , 86 , 87 ].
In terms of efficacy, EndeavorRX showed early promise in pilot/uncontrolled studies given generally favorable feasibility, acceptability, and engagement data [ 83 ]. In addition, EndeavorRX showed potential for reductions in parent-reported ADHD symptoms in proof-of-concept and open-label trials with children with ADHD [ 88 , 89 ]. However, the only controlled trial to date [ 83 ] demonstrated that these potential reductions were likely attributable to placebo effects – that is, Endeavor RX failed to show superior improvements in ADHD behavioral symptoms relative to a control condition (a spelling game). Evans et al. [ 79 ] concluded that “there is no evidence that using this game will result in any benefit in terms of their functioning and presenting problems.” (p. 125).
Cenextra also showed early promise in a head-to-head comparison with behavioral parent training (BPT) indicating favorable feasibility, acceptability, and engagement data. Cenextra was superior to BPT for improving working memory ( d = 1.06) and reducing objectively-assessed hyperactivity ( d = 0.74), and equivalent to BPT for reducing parent-reported ADHD symptoms at post-treatment [ 90 ]. These benefits were largely confirmed in an RCT comparing Cenextra with an active, credible digital therapeutic control called Inhibitory Control Training (ICT; [ 84 ]). Evidence suggesting improved functional outcomes is also emerging, and includes superior improvements relative to both BPT and ICT on masked teacher perceptions of organizational skills, academic success, impulse control, and academic productivity 1–2 months after treatment ended [ 91 , 92 ].
Similar to EndeavorRX and Cenextra, Cogmed showed considerable promise in early trials, and is arguably the most extensively studied neurocognitive training program. Results from meta-analytic reviews and RCTs, however, suggest that CogMed does not improve working memory, but rather improves select components of short-term memory (meta-analytic d = 0.63; [ 81 , 86 , 93 , 94 ]. This is an important limitation for at least two reasons: First, most children with ADHD do not have deficits in short term memory (20–38% impairment rates) despite the majority having impairments in working memory (75–81%; [ 95 , 96 , 97 ]). Second, short-term memory abilities are not significantly associated with ADHD symptoms in most studies [ 81 , 95 ], which suggests limited potential for downstream improvements in ADHD behavioral symptoms. Indeed, conclusions from multiple meta-analytic reviews suggest that benefits on ADHD behavioral symptoms from CogMed are generally limited to unblinded parent ratings [ 81 , 93 ]. Notably, however, a more recent meta-analysis published by the developer of CogMed suggests significant, small benefits for reducing inattention ( d = 0.37; [ 98 ]), though the extent to which this was driven by unblinded parent ratings was unclear.
A key benefit of digital therapeutics – and ‘software as medicine’ in general – is that they have the potential to continually adapt and improve based on real-time patient data. Thus, it is possible that interventions that are not showing the behavioral/functional benefits we had hoped for now could begin to do so in the future. Thus, we highlight some key areas for improvement based on conceptual models and the limited available literature on moderators of cognitive training efficacy for children with ADHD. First, there is a need to maximize dosage . In the context of digital therapeutics, ‘dosage’ refers to the quantity and quality of time spent actively engaging with the training exercises. Most existing protocols have been studied over a relatively limited time frame of 4–10 weeks of training, with a total training time of about 10–12 h across intervention protocols [ 83 , 84 , 99 ]. It is possible that this level of training is insufficient for producing large enough neurocognitive improvements to translate into meaningful – and statistically detectable – gains in downstream behavioral/functional outcomes, suggesting the need for more intensive/longer duration training.
An option closely related to maximizing dosage is increasing the specificity of the neurocognitive training target(s). Although training a variety of neurocognitive functions is appealing at face value, meta-analytic evidence indicates that such protocols produce smaller near-transfer effects than protocols that focus on a single neurocognitive training target [ 81 ]. It is presumed that the reason for this finding is that the more different cognitive ‘muscles’ that we are trying to train, the less time we can spend on any one of those ‘muscles’. Thus, it appears likely that maximizing efficacy will require separate protocols for each neurocognitive function that is impaired in ADHD, combined with a ‘personalized medicine’ approach in which each child’s neurocognitive profile is estimated at pre-treatment, and then a treatment plan is developed to target each of their identified weaknesses. We must leverage basic science to link training targets with behavioral/functional outcomes . Related to dosage and specificity issues is the idea of matching neurocognitive training targets with the specific outcome(s) of interest. Stated bluntly, neurocognitive training is not likely to be helpful if we are training neurocognitive abilities that are not robustly linked with the reason(s) a child presents for treatment. On the other hand, neurocognitive training protocols have great potential if they are able to produce robust improvements in their training target, and if that training target is robustly associated with the observable behaviors/functional outcomes we are trying to improve. A final area that shows promise for improving the efficacy of digital therapeutic interventions is augmentation: Combining them with existing treatments to (potentially) produce synergistic and/or augmentative benefits. This area of inquiry is in its infancy, and currently shows more conceptual promise than actual benefits [ 100 ].
Future directions in improving efficacy and effectiveness
This brief review of psychosocial treatments for ADHD illustrates the robust evidence in support of these interventions. Importantly, there is no panacea or magic bullet for ADHD; the interventions reviewed herein have notable limitations and response to interventions vary. As such, there continues to be efforts at refining existing approaches and developing novel approaches to treating the complex presentation of ADHD. We highlight here what we believe are key future directions, broadly speaking, in improving the effectiveness and efficacy of treatment for ADHD. These fall under two broad areas: future directions in treatments and future directions in service delivery of these treatments.
Future directions in treatment for ADHD
Moderators of treatment effects.
Much of the intervention literature has focused on static factors or social addresses (terms that describe rather than explain; e.g., marital status, child age;) as factors, largely because these are measures of convenience. Efforts toward using dynamic factors have shed light on what works for whom and can further refine an intervention to increase potency. As an example, in BPT, parent-level variables (e.g., parenting stress [ 101 ]) have been shown to moderate BPT engagement and outcomes, suggesting that future refinements to BPT that more directly address parental stress may increase the potency of BPT. Such efforts should be employed across all psychosocial interventions for ADHD. Importantly, as we have discussed elsewhere [ 8 , 102 ], efforts should go beyond variable-centered approaches (e.g., child age, parent stress) toward holistic, person- and/or family-centered approaches (the clustering of variables that more fully represent a child/parent/family). As an example, Dale et al. [ 103 ] employed a person-centered approach to create subgroups of families based on the intersection of multiple parent, child, and family factors to understand response to BPT for families of preschool children with ADHD. Three distinct family profiles emerged, with data suggesting differential response for families with high stress, elevated parental anxiety, and elevated parental depression. These typological approaches better reflect reality- people are more accurately reflected as a complex intersection of variables rather than just any one variable- and taking this approach may better result in a nuanced understanding of response to treatment and further inform treatment for types of people and families.
ADHD is complex and presentations vary. It is not uncommon for children and adolescents with ADHD to also have significant difficulties outside of core symptoms of ADHD (e.g., emotion dysregulation, sleep disturbances) that may moderate treatment response. As an example, ADHD is frequently associated with emotional regulation challenges, with studies suggesting that the vast majority of children with ADHD (i.e., 75%) have some symptoms of emotion dysregulation, with 25% having severe emotion dysregulation [ 104 ]. In fact, children with ADHD and severe emotion dysregulation are more likely to have complex presentations, cross-situational impairments and severe psychopathology [ 105 ]. Interestingly, there are few rigorous randomized controlled trials evaluating the effects of psychosocial interventions for emotion dysregulation in children with ADHD [ 106 ]. These and other moderators may best be evaluated through novel approaches such as individual participant data meta-analysis [ 107 ]. Addressing the needs of youth with ADHD and their families will require going beyond addressing core symptoms of ADHD. In fact, we have long argued that these types of functional impairments (e.g., academic, social functioning) should be the targets for ADHD treatment rather than ADHD symptoms [ 8 ].
Novel intervention targets
The presentation of ADHD at key developmental periods/tasks may pose significant challenges for affected youth and their families- necessitating novel targets of intervention. An example of this is the transition to learning to drive. Adolescents are the riskiest drivers on the roadway, overall; if an adolescent has ADHD they are significantly more at risk for negative driving outcomes including accidents, accidents that cause injury, and fatalities [ 108 , 109 ]. The period of time when individuals with ADHD are learning to drive may therefore be a critical, and also opportune time to initiate intervention. A recent RCT with adolescents with ADHD [ 110 ], evaluated a specially designed computerized simulated-driving program with feedback and found reduced problematic driving as compared with a control program. During real-world driving in the year after training, the rate of collisions and near-collisions was lower in the intervention group. These efforts highlight the potential of psychosocial interventions for addressing impairments inherent with developmental transitions for youth with ADHD. Related work suggests that intervening with adolescents at the transition to middle school and high school with intensive summer “bridge” programs may be a useful approach with high levels of engagement [ 111 ]. Future work should focus on embedding treatment efforts into other developmental tasks/transitions/tasks (e.g., start of preschool or initiation of employment).
Future directions in service delivery
ADHD is now very clearly understood to persist throughout development and into adulthood and there has rightfully been a shift toward a chronic care model [ 7 ]. Given this, attention must be given to developing integrated, consistently available and longitudinal approaches embedded in routine service systems such that children, adolescents (and even adults) with ADHD and their families can receive appropriate care. Unfortunately, availability and access to evidence-based interventions are limited. Recent studies suggest that only 31% of families of children with ADHD receive BPT [ 21 ] and just 32% receive behavioral classroom management [ 112 ]. Given this, we highlight herein issues related to increasing availability and access to evidence-based psychosocial treatment for ADHD- important goals to help close the science-to-service-gap in ADHD. More specifically, we briefly highlight efforts on (1) leveraging the existing workforce, and (2) using technology to deliver evidence-based psychosocial treatments.
Leveraging existing workforces
In light of mental health workforce shortages ( https://data.hrsa.gov/topics/health-workforce/workforce-projections ) new models of care will need to utilize and expand existing, but underdeveloped, non-professional and paraprofessional workforces [ 31 , 32 ]. One example of a sustainable, scalable model of care is the Family Peer Advocate (FPA) ADHD Model [ 25 ]. FPAs are part of a national family support model of current and former parent/caregivers of children with identified mental health needs who provide a range of services, including parenting skills training, emotional support, education about mental health services, and direct advocacy [ 30 ]. FPA-services are flexibly delivered in a variety of parent-identified settings (e.g., parent’s homes, community settings) and often connect and engage parents with key service settings/providers (e.g., schools, primary care, mental health clinics), reducing the systemic barriers associated with traditional service delivery models. Moreover, FPAs have many shared experiences with the families they serve including personal experience with providing care and navigating the service system for children with mental health challenges, often within the same community as those they serve. As a result, FPA care is associated with high acceptability ratings and increased engagement [ 113 ]. This FPA Model appears to be especially effective in reaching ethnically diverse families from socioeconomically disadvantaged backgrounds [ 30 , 113 ]. Emerging data suggest that FPAs can reliably and effectively deliver BPT for youth with ADHD [ 25 ], suggesting that this and other workforce (e.g., ADHD Coaches) should be leveraged in order to increase availability and access to evidence-based psychosocial interventions for ADHD.
The idea of leveraging the existing workforce also applies to school settings. The MTSS intervention framework, which embeds intervention in schools into universal, targeted, and indicated approaches is an example of a potential means of re-allocating professional time and expertise. Rather than waiting for school psychologists and special educators to get involved only when the child is considered for special education, a MTSS approach might utilize the expertise of these professionals to consult with the general education teacher on how to implement positive behavior supports for a child with ADHD. In this way, intervention is implemented quicker, in the setting where the initial impairment is identified, by existing school professionals [ 56 , 114 ].
Use of technology
Technology-based approaches to delivering evidence-based interventions have the potential to revolutionize mental health service access and delivery across multiple mental health disorders [ 115 ]. Online self-directed BPT approaches are potentially more feasible, affordable, and acceptable, can have significant reach to include traditionally underserved populations, and are readily scalable and sustainable [ 116 , 117 ]. Over 13 studies have recently been conducted demonstrating that online BPT can improve child behavioral outcomes. Importantly, a recently published trial compared Triple P Online (TPO; an evidence-based, commercially available, self-directed online BPT) to a face-to-face (F2F) therapist-delivered Triple P for preschool children with disruptive behavior problems [ 118 ]. This large randomized controlled trial found that TPO was non-inferior to F2F Triple P on observed and parent-reported child behavior, with clinically meaningful effect sizes. This study, combined with several other studies [ 27 , 119 , 120 ] demonstrate the effectiveness of online BPT in general and specifically for ADHD. Technology is increasingly being utilized in practice settings (e.g., ADHD Care Assistant in primary care [ 121 ]; Online Daily Report Card in schools [ 122 ]) to increase access to evidence-based psychosocial interventions. Concerted efforts and rigorous empirical investigation will be necessary to further determine the effectiveness of these approaches. Importantly, while there is high potential for such technology-delivered approaches, engagement to these formats will remain important to address [ 123 ].
Conclusions
ADHD is a prevalent, pervasive, chronic and impairing disorder that necessitates early, integrated, continuous interventions over a child’s development. Fortunately, several psychosocial interventions are available that address key functional impairments in children and adolescents with ADHD. Given the complex presentation of ADHD, novel approaches to address both underlying pathophysiological mechanisms associated with ADHD (e.g., working memory) as well as domains closely impacted in those with ADHD (e.g., emotion regulation) and key developmental tasks (e.g., driving) are emerging areas in ADHD intervention science. Efforts to improve the efficacy of psychosocial interventions remain important as the acute benefits of these interventions do not result in normalized functioning for many youth and there remains an under-appreciation for whom these interventions are most impactful. Likely most pressing is the translation of the intervention science to improve outcomes for the millions of youth affected by ADHD, the science-to-service gap is prominent; many children who can benefit from evidence-based psychosocial interventions do not receive them. Improving access and availability of evidence-based psychosocial interventions remains critical to ensure that the significant efforts made over decades in developing and evaluating interventions for ADHD result in population-level benefits for youth with ADHD.
Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2014;43:527–51.
Article PubMed Google Scholar
Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2018;47:157–98.
Pelham WE Jr, Fabiano GA. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2008;37:184–214.
Pelham WE Jr, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol. 1998;27:190–205.
Article Google Scholar
Barbaresi WJ, Campbell L, Diekroger EA, Froehlich TE, Liu YH, O’Malley, et al. Society for Developmental and Behavioral Pediatrics clinical practice guideline for the assessment and treatment of children and adolescents with complex attention-deficit/hyperactivity disorder. J Dev Behav Pediatr. 2020;41:S35–S57.
American Academy of Child and Adolescent Psychiatry. Practice parameters for assessment and treatment of children and adolescents with Attention-Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894–921.
DuPaul GJ, Evans SW, Mautone JA, Owens JS, Power TJ. Future directions for psychosocial interventions for children and adolescents with ADHD. J Clin Child Adolesc Psychol. 2020;49:134–45.
Chacko A, Alan C, Uderman J, Cornwell M, Anderson L, Chimiklis A. Ch 10. In: Barkley R, editor. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment, 4th edn. New York: Guilford Press; 2015.
Chacko A, Wymbs BT, Arnold FW, Pelham WE, Swanger-Gagne M, Girio EL, et al. Enhancing traditional behavioral parent training for single-mothers of children with ADHD. J Clin Child Adolesc Psychol. 2009;38:206–18.
Chacko A, Wymbs BT, Chimiklis A, Wymbs FA, Pelham WE. Evaluating a comprehensive strategy to improve engagement to group-based behavioral parent training for high-risk families of children with ADHD. J Abnorm Child Psychol. 2012;40:1351–62.
Gerdes AC, Kapke TL, Grace M, Castro A. Feasibility, acceptability, and preliminary outcomes of a culturally-adapted evidence-based treatment for Latino youth with ADHD. J Atten Disord. 2021;25:432–47.
Fabiano GA, Pelham WE, Cunningham CE, Yu J, Gangloff B, Buck M, et al. A waitlist-controlled trial of behavioral parent training for fathers of children with ADHD. J Clin Child Adolesc Psychol. 2012;41:337–45.
Article PubMed PubMed Central Google Scholar
Barkley RA, Benton CM. Your defiant child: eight steps to better behavior. Chicago: Guilford Press; 2013.
Leijten P, Melendez-Torres GJ, Knerr W, Gardner F. Transported versus homegrown parenting interventions for reducing disruptive child behavior: a multilevel meta-regression study. J Am Acad Child Adolesc Psychiatry. 2016;55:610–7.
Rajwan E, Chacko A, Wymbs BT, Wymbs FA. Evaluating clinically significant change in parent and child functioning: Comparison of traditional and enhanced behavioral parent training. J Abnor Chil Psychol. 2014;42:1407–12.
Marquet-Doléac J, Biotteau M, Chaix Y. Behavioral parent training for school-aged children with ADHD: a systematic review of randomized control trials. J Atten Disord. 2023;28:377–93.
Doffer DPA, Dekkers T, Hornstra R, van der Oord S, Luman M, Leijten P, et al. Sustained improvements by behavioural parent training for children with attention-deficit/hyperactivity disorder: a meta-analysis into longer-term child and parental outcomes. JCCP Adv. 2023;3:e12196.
Fabiano GA, Schatz NK, Aloe AM, Pelham WE Jr, Smyth AC, Zhao X, et al. Comprehensive meta-analysis of attention-deficit/hyperactivity disorder psychosocial treatments investigated within between group studies. Rev Educ Res. 2021;91:718–60.
Cohen J. Things I have learned (so far). In: Annual Convention of the American Psychological Association, 98th, 1990, Boston, MA, USA; Presented at the aforementioned conference. American Psychological Association; 1992.
Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2019;144:e20192528.
Danielson ML, Visser SN, Chronis-Tuscano A, DuPaul GJ. A national description of treatment among U.S. children and adolescents with ADHD. J Pediatr. 2018;192:240–6.
Ortiz C, Vidair HB, Acri M, Chacko A, Kobak K. Pilot study of an online parent-training course for disruptive behavior with live remote coaching for practitioners. Prof Psychol Res Pract. 2020;51:125–33.
Chacko A, Jensen S, Lowry LS, Cornwell M, Chimiklis A, Chan E, et al. Engagement in behavioral parent training: review of the literature and implications for practice. Clin Child Fam Psychol Rev. 2016;19:204–15.
Sanchez AL, Jent J, Aggarwal NK, Chavira D, Coxe S, Garcia D, et al. Person-centered cultural assessment can improve child mental health service engagement and outcomes. J Clin Child Adolesc Psychol. 2022;51:1–22.
Chacko A, Hopkins K, Acri M, Mendelsohn A, Dreyer B. Expanding ADHD service provision in urban socioeconomically disadvantaged communities: a pilot study. Clin Pract Pediatr Psychol. 2020;8:189–94.
Google Scholar
Chacko A, Isham A, Cleek A, Mckay M. Using mobile health technology to improve homework implementation in evidence-based parenting intervention for disruptive behavior disorders in youth. Pilot Feasibility Stud. 2016;2:1–11.
DuPaul GJ, Kern L, Belk G, Custer B, Daffner M, Hatfield A, et al. Face-to-face versus online behavioral parent training for young children at risk for ADHD: treatment engagement and outcomes. J Clin Child Adolesc Psychol. 2018;47:S369–S383.
Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2015;54:263–74.
Xie Y, Dixon JF, Yee OM, Zhang J, Chen YA, DeAngelo S, et al. A study on the effectiveness of videoconferencing on teaching parent training skills to parents of children with ADHD. Telemed J E Health. 2013;19:192–9.
Article CAS PubMed Google Scholar
Acri M, Hooley CD, Richardson N, Moaba LB. Peer models in mental health for caregivers and families. Community Ment Health J. 2017;53:241–9.
Chacko A, Scavenius C. Bending the curve: Community based behavioral parent training to address ADHD symptoms in the voluntary sector in Denmark. J Abnorm Child Psychol. 2018;46:505–17.
Chacko A, Gopalan G, Franco L, Dean-Assael K, Jackson J, Marcus S, et al. Multiple-Family Group service delivery model for the children with disruptive behavior disorders. J Emot Behav Disord. 2015;23:67–77.
Van der Oord S, Tripp G. How to improve behavioral parent and teacher training for children with ADHD: Integrating empirical research on learning and motivation into treatment. Clin Child Fam Psychol Rev. 2020;23:577–604.
Furukawa E, Alsop B, Sowerby P, Jensen S, Tripp G. Evidence for increased behavioral control by punishment in children with attention-deficit hyperactivity disorder. J Child Psychol Psychiatry. 2017;3:248–57.
Furukawa E, Alsop B, Shimabukuro S, Tripp G. Is increased sensitivity to punishment a common characteristic of attention deficit/hyperactivity disorder? An experimental study of response allocation in Japanese children. Atten Deficit Hyperact Disord. 2019;11:433–43.
Sonuga-Barke EJ, Thompson M, Abikoff H, Klein R, Brotman LM. Nonpharmacological interventions for preschoolers with ADHD: The case for specialized parent training. Infants Young Child. 2006;19:142–53.
Abikoff HB, Thompson M, Laver‐Bradbury C, Long N, Forehand RL, Miller Brotman L, et al. Parent training for preschool ADHD: a randomized controlled trial of specialized and generic programs. J Child Psychol Psychiatry. 2015;56:618–31.
DuPaul GJ. Attention deficit-hyperactivity disorder: classroom intervention strategies. Sch Psychol Int. 1991;12:85–94.
Harrison JR, Soares DA, Rudzinski S, Johnson R. Attention deficit hyperactivity disorders and classroom-based interventions: Evidence-based status, effectiveness, and moderators of effects in single-case design research. Rev Educ Res. 2019;89:569–611.
DuPaul GJ, Eckert TL. The effects of school-based interventions for attention deficit/hyperactivity disorder: a meta-analysis. Sch Psych Rev. 1997;26:5–27.
DuPaul GJ, Eckert TL, Vilardo B. The effects of school-based interventions for attention deficit hyperactivity disorder: A meta-analysis 1996–2010. Sch Psych Rev. 2012;41:387–412.
Fabiano GA, Pelham WE Jr, Coles EK, Gnagy EM, Chronis-Tuscano A, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clin Psychol Rev. 2009;29:129–40.
Arnold LE, Hodgkins P, Kahle J, Madhoo M, Kewley G. Long-term outcomes of ADHD: academic achievement and performance. J Atten Disord. 2020;24:73–85.
Kent KM, Pelham WE, Molina BS, Sibley MH, Waschbusch DA, Yu J, et al. The academic experience of male high school students with ADHD. J Abnorm Child Psychol. 2011;39:451–62.
Kuriyan AB, Pelham WE, Molina BS, Waschbusch DA, Gnagy EM, Sibley MH, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41:27–41.
Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 2009. 2009;48:484–500.
Pyle K, Fabiano GA. A meta-analysis of single-subject design studies utilizing the daily report card intervention for students with ADHD. Excep Child. 2017;83:378–95.
Volpe R, Fabiano, GA. Daily behavior report cards: an evidence-based system of assessment and intervention. New York, NY: The Guilford Press; 2013.
Kelley ML. School-home notes: promoting children’s classroom success. New York: The Guilford Press; 1990.
O’Leary KD, Pelham WE, Rosenbaum A, Price GH. Behavioral treatment of hyperkinetic children: an experimental evaluation of its usefulness. Clin Pediatr. 1976;15:510–5.
Owens JS, Holdaway AS, Zoromski AK, Evans SW, Himawan LK, Girio-Herrera E, et al. Incremental benefits of a daily report card intervention over time for youth with disruptive behavior. Behav Ther. 2012;43:848–61.
Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment for attention-deficit/hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol. 2005;34:449–76.
Pelham WE, Gnagy EM, Burrows-Maclean L, Williams A, Fabiano GA, Morrissey SM, et al. Once-a-day Concerta™ methylphenidate versus t.i.d. methylphenidate in laboratory and natural settings. Pediatrics. 2001;10:e105.
Pelham WE, Hoza B, Pillow DR, Gnagy EM, Kipp HL, Greiner AR, et al. Effects of methylphenidate and expectancy on children with ADHD: behavior, academic performance, and attributions in a summer treatment program and regular classrooms. J Consult Clin Psychol. 2002;70:320–35.
Pfiffner LJ, Mikami AY, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K. A randomized, controlled trial of integrated home-school treatment for ADHD, Primarily inattentive type. J Am Acad Child Adolesc Psychiatry. 2007;46:1040–51.
Pfiffner LJ, Villodas M, Kaiser N, Rooney M, McBurnett K. Educational outcomes of a collaborative school-home behavioral intervention for ADHD. Sch Psychol Q. 2013;28:25–36.
Vannest KJ, Davis JL, Davis CR, Mason BA, Burke MD. Effective intervention for behavior with a daily behavior report card: a meta-analysis. Sch Psych Rev. 2010;39:654–72.
Hops H, Walker HM. CLASS: contingencies for learning and academic and social skills. Seattle WA: Educational Achievement Systems; 1988.
Reid R, Maag JW, Vasa SF, Wright G. Who are the children with attention deficit-hyperactivity disorder? A school-based survey. J Spec Educ. 1994;28:117–37.
Schnoes C, Reid R, Wagner M, Marder C. ADHD among students receiving special education services: a national survey. Excep Child. 2006;72:483–96.
Page TF, Pelham WE III, Fabiano GA, Greiner AR, Gnagy EM, et al. Comparative cost analysis of sequential, adaptive, behavioral, pharmacological, and combined treatments for childhood ADHD. J Clin Child Adolesc Psychol. 2016;45:416–27.
Burns MK, Jimerson SR, VanDerHeyden AM, Deno, SL. Toward a unified response-to-intervention model: Multi-tiered systems of support. In: Handbook of response to intervention: The science and practice of multi-tiered systems of support. Boston, MA: Springer US; 2015. p. 719–32.
Briesch AM, Chafouleas SM, Nissen K, Long S. A review of state-level procedural guidance for implementing multitiered systems of support for behavior (MTSS-B). J Posit Behav Inter. 2020;23:131–44.
Owens JS, McLennan JD, Hustus CL, Haines-Saah R, Mitchell S, Mixon CS, et al. Leveraging technology to facilitate teachers’ use of a targeted classroom intervention: Evaluation of the Daily Report Card. Online (DRC. O) System. Sch Ment Health. 2019;11:665–77.
Pelham WE, Fabiano GA, Waxmonsky JG, Greiner AR, Gnagy EM, Pelham WE III, et al. Treatment sequencing for childhood ADHD: A multiple-randomization study of adaptive medication and behavioral interventions. J Clin Child Adolesc Psychol. 2016;45:396–415.
Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA. A “SMART” design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48.
Owens JS, Hustus CL, Evans SW. The daily report card intervention: Summary of the science and factors affecting implementation. In: Handbook of research on emotional and behavioral disorders. Routledge; 2020. p. 371–85.
Langberg JM, Epstein JN, Girio-Herrera E, Becker SP, Vaughn AJ, Altaye M. Materials organization, planning, and homework completion in middle-school students with ADHD: impact on academic performance. Sch Ment Health. 2011;3:93–101.
Langberg JM, Molina BSG, Arnold LE, Epstein JN, Altaye M, Hinshaw SP, et al. Patterns and predictors of adolescent academic achievement and performance in a sample of children with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2011;40:519–31.
Bikic A, Reichow B, McCauley SA, Ibrahim K, Sukhodolsky DG. Meta-analysis of organizational skills interventions for children and adolescents with Attention-Deficit/Hyperactivity Disorder. Clin Psychol Rev. 2017;52:108–23.
Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriguez L, et al. Parent–teen behavior therapy+ motivational interviewing for adolescents with ADHD. J Consult Clin Psychol. 2016;84:699.
Evans SW, Schultz BK, DeMars CE, Davis H. Effectiveness of the challenging horizons after-school program for young adolescents with ADHD. Behav Ther. 2011;42:462–74.
Chan E, Fogler JM, Hammerness P. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA. 2016;315:1997–2008.
Langberg JM, Dvorsky MR, Molitor SJ, Bourchtein E, Eddy LD, Smith ZR, et al. Overcoming the research-to-practice gap: a randomized trial with two brief homework and organization interventions for students with ADHD as implemented by school mental health providers. J Consult Clin Psychol. 2018;86:39.
Pfiffner LJ, Dvorsky MR, Friedman LM, Haack LM, Chung S, Charalel JM, et al. Development of a web-based training platform for school clinicians in evidence-based practices for ADHD. Sch Ment Health. 2023;15:49–66.
Evans SW, Schultz BK, DeMars CE. High school–based treatment for adolescents with attention-deficit/hyperactivity disorder: results from a pilot study examining outcomes and dosage. Sch Psych Rev. 2104;43:185–202.
DuPaul GJ, Evans SW, Owens JS, Cleminshaw CL, Kipperman K, Fu Q, et al. School-based intervention for adolescents with attention-deficit/hyperactivity disorder: effects on academic functioning. J Sch Psychol. 2021;87:48–63.
Simons DJ, Boot WR, Charness N, Gathercole SE, Chabris CF, Hambrick DZ, et al. Do “brain-training” programs work? Psychol Sci. 2016;17:103–86.
Evans SW, Beauchaine TP, Chronis-Tuscano A, Becker SP, Chacko A, Gallagher R, et al. The efficacy of cognitive videogame training for ADHD and What FDA clearance means for clinicians. Evid Based Pract Child Adolesc Ment Health. 2021;6:116–30.
Westwood SJ, Parlatini V, Rubia K, Cortese S, Sonuga-Barke EJ. Computerized cognitive training in attention-deficit/hyperactivity disorder (ADHD): a meta-analysis of randomized controlled trials with blinded and objective outcomes. Mol Psychiatry. 2023;28:1402–14.
Rapport MD, Orban SA, Kofler MJ, Friedman LM. Do programs designed to train working memory, other executive functions, and attention benefit children with ADHD? A meta-analytic review of cognitive, academic, and behavioral outcomes. Clin Psychol Rev. 2013;33:1237–52.
Cannon-Bowers J, Bowers C, editors. Serious game design and development: technologies for training and learning. New York: IGI Global; 2010.
Kollins SH, DeLoss DJ, Cañadas E, Lutz J, Findling RL, Keefe RS, et al. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): a randomised controlled trial. Lancet Digit Health. 2020;2:e168–e178.
Kofler MJ, Wells EL, Singh LJ, Soto EF, Irwin LN, Groves NB, et al. A randomized controlled trial of central executive training (CET) versus inhibitory control training (ICT) for ADHD. J Consult Clin Psychol. 2020;88:738–56.
Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlström K, et al. Computerized training of working memory in children with ADHD-a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2005;44:177–86.
Roberts G, Quach J, Spencer-Smith M, Anderson PJ, Gathercole S, Gold L, et al. Academic outcomes 2 years after working memory training for children with low working memory: a randomized clinical trial. JAMA Pediatr. 2016;170:e154568.
Chacko A, Bedard AC, Marks DJ, Feirsen N, Uderman JZ, Chimiklis A, et al. A randomized clinical trial of Cogmed working memory training in school‐age children with ADHD: A replication in a diverse sample using a control condition. J Child Psychol Psychiatry. 2014;55:247–55.
Davis NO, Bower J, Kollins SH. Proof-of-concept study of an at-home, engaging, digital intervention for pediatric ADHD. PLoS ONE. 2018;13:e0189749.
Kollins SH, Childress A, Heusser AC, Lutz J. Effectiveness of a digital therapeutic as adjunct to treatment with medication in pediatric ADHD. NPJ Digit Med. 2021;4:1–8.
Kofler MJ, Sarver DE, Austin KE, Schaefer HS, Holland E, Aduen PA, et al. Can working memory training work for ADHD? Development of central executive training and comparison with behavioral parent training. J Consult Clin Psychol. 2018;86:964.
Singh LJ, Gaye F, Cole AM, Chan ES, Kofler MJ. Central executive training for ADHD: effects on academic achievement, productivity, and success in the classroom. Neuropsychol. 2022;36:330–45.
Chan ESM, Gaye F, Cole AM, Singh LJ, Kofler MJ. Central executive training for ADHD: impact on organizational skills at home and school. A randomized controlled trial. Neuropsychol.
Chacko A, Feirsen N, Bedard AC, Marks D, Uderman JZ, Chimiklis A. Cogmed working memory training for youth with ADHD: a closer examination of efficacy utilizing evidence-based criteria. J Clin Child Adolesc Psychol. 2013;42:769–83.
Sala G, Gobet F. Working memory training in typically developing children: a meta-analysis of the available evidence. Dev Psychol. 2017;53:671–85.
Kofler MJ, Singh LJ, Soto EF, Chan ESM, Miller CE, Harmon SL, et al. Working memory and short-term memory deficits in ADHD: A bifactor modeling approach. Neuropsychol. 2020;34:686–98.
Fosco WD, Kofler MJ, Groves NB, Chan ESB, Raiker JS. Which ‘working’ components of working memory aren’t working in youth with ADHD? J Abnorm Child Psychol. 2020;48:647–60.
Karalunas S, Gustafsson H, Dieckmann N, Tipsord J, Mitchell SH, Nigg J. Heterogeneity in development of aspects of working memory predicts longitudinal attention deficit hyperactivity disorder symptom change. J Abnorm Child Psychol. 2017;126:774–92.
Spencer-Smith M, Klingberg T. Correction: benefits of a working memory training program for inattention in daily life: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0167373.
Klingberg T, Forssberg H, Westerberg H. Training of working memory in children with ADHD. J Clin Exp Neuropsychol. 2002;24:781–91.
Chacko A, Bedard AC, Marks D, Gopalan G, Feirsen N, Uderman J, et al. Sequenced neurocognitive and behavioral parent training for the treatment of ADHD in school-age children. Child Neuro. 2018;24:427–50.
Article CAS Google Scholar
Chacko A, Feirsen N, Rajwan E, Wymbs BT, Wymbs FA. Distinguishing never-attenders, dropouts, and completers to behavioral parent training: The importance of parental cognitions. J Child Fam Stud. 2017;26:950–60.
Vardanian MM, Ramakrishnan A, Peralta S, Siddiqui Y, Shah S, Clark-Whitney E, et al. Clinically significant and reliable change: comparing an evidence-based intervention to usual care. J Child Fam Stud. 2020;29:921–33.
Dale C, Parent J, Forehand R, DiMarzio K, Sonuga-Barke E, Long N, et al. Behavioral parent training for preschool ADHD: family-centered profiles predict changes in parenting and child outcomes. J Clin Child Adolesc Psychol. 2021;51:726–39.
Sobanski E, Banaschewski T, Asherson P, Buitelaar J, Chen W, Franke B, et al. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J Child Psychol Psychiatry. 2010;51:915–23.
Qian Y, Chang W, He X, Yang L, Liu L, Ma Q, et al. Emotional dysregulation of ADHD in childhood predicts poor early-adulthood outcomes: a prospective follow up study. Res Dev Disabil. 2016;59:428–36.
Vacher C, Goujon A, Romo L, Purper-Ouakil D. Efficacy of psychosocial interventions for children with ADHD and emotion dysregulation: a systematic review. Psychiatry Res. 2020;291:113–51.
Groenman AP, Hornstra R, Hoekstra PJ, Steenhuis L, Aghebati A, Boyer BE, et al. An individual participant data meta-analysis: behavioral treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2022;61:144–58.
Aduen PA, Cox DJ, Fabiano GA, Garner AA, Kofler MJ. Expert recommendations for improving driving safety for teens and adult drivers with ADHD. ADHD Rep. 2019;27:8.
Aduen PA, Kofler MJ, Sarver DE, Wells EL, Soto EF, Cox DJ. ADHD, depression, and motor vehicle crashes: A prospective cohort study of continuously-monitored, real-world driving. J Psychiatr Res. 2018;101:42–49.
Epstein JN, Garner AA, Kiefer AW, Peugh J, Tamm L, MacPherson RP, et al. Trial of training to reduce driver inattention in teens with ADHD. N Engl J Med. 2022;387:2056–66.
Sibley MH, Coxe SJ, Campez M, Morley C, Olson S, Hidalgo-Gato N, et al. High versus low intensity summer treatment for ADHD delivered at secondary school transitions. J Clin Child Adolesc Psychol. 2018;47:248–65.
DuPaul GJ, Chronis-Tuscano A, Danielson ML, Visser SN. Predictors of receipt of school services in a national sample of youth with attention-deficit/hyperactivity disorder. J Atten Disord. 2019;23:1303–19.
Hoagwood KE, Cavaleri MA, Serene Olin S, Burns BJ, Slaton E, et al. Family support in children’s mental health: A review and synthesis. Clin Child Fam Psychol Rev. 2010;13:1–45.
Fabiano GA, Pyle K. Best practices in school mental health for attention-deficit/hyperactivity disorder: A framework for intervention. Sch Ment Health. 2019;11:72–91.
Nieuwboer CC, Fukkink RG, Hermanns JM. Online programs as tools to improve parenting: a meta-analytic review. Child Youth Ser Rev. 2013;35:1823–9.
Tan-MacNeill KM, Smith IM, Johnson SA, Chorney J, Corkum P. A systematic review of online parent-implemented interventions for children with neurodevelopmental disorders. Child Health Care. 2021;50:239–77.
Thongseiratch T, Leijten P, Melendez-Torres GJ. Online parent programs for children’s behavioral problems: a meta-analytic review. Eur Child Adolesc Psychiatry. 2020;29:1555–68.
Prinz RJ, Metzler CW, Sanders MR, Rusby JC, Cai C. Online‐delivered parenting intervention for young children with disruptive behavior problems: a noninferiority trial focused on child and parent outcomes. J Child Psychol Psychiatry. 2022;63:199–209.
Baker S, Sanders MR, Turner KM, Morawska A. A randomized controlled trial evaluating a low-intensity interactive online parenting intervention, Triple P Online Brief, with parents of children with early onset conduct problems. Behav Res Ther. 2017;91:78–90.
Franke N, Keown LJ, Sanders MR. An RCT of an online parenting program for parents of preschool-aged children with ADHD symptoms. J Atten Disord. 2020;24:1716–26.
Power TJ, Michel J, Mayne S, Miller J, Blum NJ, Grundmeier RW, et al. Coordinating systems of care using health information technology: development of the ADHD care assistant. Adv Sch Ment Health Promot. 2016;9:201–18.
Mixon CS, Owens JS, Hustus C, Serrano VJ, Holdaway AS. Evaluating the impact of online professional development on teachers’ use of a targeted behavioral classroom intervention. Sch Ment Health. 2019;11:115–28.
Breider S, de Bildt A, Nauta MH, Hoekstra PJ, van den Hoofdakker BJ. Self-directed or therapist-led parent training for children with attention deficit hyperactivity disorder? A randomized controlled non-inferiority pilot trial. Internet Interv. 2019;18:100262.
Coghill D, Banaschewski T, Cortese S, Asherson P, Brandeis D, Buitelaar J, et al. The management of ADHD in children and adolescents: bringing evidence to the clinic: perspective from the European ADHD Guidelines Group (EAGG). Eur Child Adolesc Psychiatry. 2021;32:1337–61.
Download references
Author information
Authors and affiliations.
New York University, New York, NY, USA
Anil Chacko
Florida International University, Miami, FL, USA
Brittany M. Merrill & Gregory A. Fabiano
Florida State University, Tallahassee, FL, 32306, USA
Michael J. Kofler
You can also search for this author in PubMed Google Scholar
Contributions
AC, BM, MJK and GAF were involved in the development, writing, review, revisions and final approval of the manuscript.
Corresponding author
Correspondence to Anil Chacko .
Ethics declarations
Competing interests.
MJK holds a patent for neurocognitive interventions that target central executive working memory and inhibitory control and that were recently licensed to Sky Therapeutics, a company for which MJK provides consulting and holds equity.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Chacko, A., Merrill, B.M., Kofler, M.J. et al. Improving the efficacy and effectiveness of evidence-based psychosocial interventions for attention-deficit/hyperactivity disorder (ADHD) in children and adolescents. Transl Psychiatry 14 , 244 (2024). https://doi.org/10.1038/s41398-024-02890-3
Download citation
Received : 16 January 2023
Revised : 14 February 2024
Accepted : 22 March 2024
Published : 08 June 2024
DOI : https://doi.org/10.1038/s41398-024-02890-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

The impact of psychological theory on the treatment of Attention Deficit Hyperactivity Disorder (ADHD) in adults: A scoping review
Rebecca e champ, marios adamou, barry tolchard.
- Author information
- Article notes
- Copyright and License information
Competing Interests: The authors have declared that no competing interests exist.
‡ These authors also contributed equally to this work.
* E-mail: [email protected]
Contributed equally.
Received 2021 May 21; Accepted 2021 Nov 25; Collection date 2021.
This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Psychological theory and interpretation of research are key elements influencing clinical treatment development and design in Attention Deficit Hyperactivity Disorder (ADHD). Research-based treatment recommendations primarily support Cognitive Behavioural Therapy (CBT), an extension of the cognitive behavioural theory, which promotes a deficit-focused characterisation of ADHD and prioritises symptom reduction and cognitive control of self-regulation as treatment outcomes. A wide variety of approaches have developed to improve ADHD outcomes in adults, and this review aimed to map the theoretical foundations of treatment design to understand their impact. A scoping review and analysis were performed on 221 documents to compare the theoretical influences in research, treatment approach, and theoretical citations. Results showed that despite variation in the application, current treatments characterise ADHD from a single paradigm of cognitive behavioural theory. A single theoretical perspective is limiting research for effective treatments for ADHD to address ongoing issues such as accommodating context variability and heterogeneity. Research into alternative theoretical characterisations of ADHD is recommended to provide treatment design opportunities to better understand and address symptoms.
Introduction
The combination of psychological theory and interpretation of research have been highlighted as critical influencers guiding decision-making for clinical treatment design and development for Attention Deficit Hyperactivity Disorder (ADHD) [ 1 , 2 ]. ADHD is a neurodevelopmental disorder of self-regulation with symptoms negatively affecting daily functioning at work and at home, with long-term impacts in academic, occupational, social and emotional areas of functioning [ 3 – 8 ]. Effective, long-term treatment outcomes benefit both the individual with ADHD and society as a whole as undiagnosed and untreated adults with ADHD may become an economic burden due to increased health care costs and decreased productivity at work [ 9 , 10 ].
Russell Barkley [ 11 ] postulated the first unifying theory of ADHD, which places a core deficit of behavioural inhibition at the source of ADHD behaviours. Several theoretical models attribute additional and alternative cognitive sources for the development of ADHD symptoms [ 12 – 14 ]. While a variety of different interventions are available and the benefit of other forms of support is acknowledged (e.g. psychotherapy or coaching), only Cognitive Behavioural Therapy (CBT), Mindfulness, Dialectical Behavioural Therapy (DBT) and potentially Neurofeedback have the most empirical support [ 15 ]. Results of non-pharmacological intervention studies suggest these interventions have a positive effect on core behavioural symptoms of ADHD (inattention, hyperactivity/impulsivity), particularly when compared to inactive control conditions [ 15 , 16 ]. However, recent systematic reviews of non-pharmacological treatment highlight that different classes of intervention design take similar approaches; that heterogeneity in sample size, study design, quality and symptom outcome measurement makes meta-analysis difficult, and there is a high risk of bias [ 15 – 17 ]. Additionally, the National Institute for Health and Care Excellence (NICE) [ 18 ] only recommends interventions that match a similar protocol to medications: Randomised Controlled Trials (RCTs), primarily based in CBT [ 15 ], despite a growing wider evidence base.
It is hypothesised that much of current research for the characterisation of ADHD is based on a cognitive behavioural theoretical paradigm that does not account comprehensively for the broad spectrum of ADHD presentation [ 1 , 19 – 24 ]. This paradigm is deficit-focused with primary treatment outcomes of symptom reduction and control of maladaptive behaviours. Recent research in psychology suggests that this may not be the best approach to improving mental health, and it may be necessary to develop positive psychological factors and emotions that cultivate health and wellbeing [ 25 , 26 ]. This scoping review aims to map the evidence and understand the influence of current psychological theories on design and treatment recommendations in adult ADHD by answering the following questions:
Are characterisations of ADHD dominated by a cognitive behavioural paradigm?
Does that paradigm influence treatment design and outcomes?
Are there any alternative characterisations of ADHD that present a different perspective to the cognitive behavioural paradigm?
A broad approach was considered most effective to identify gaps in the literature, as data regarding supportive psychological theories would likely be identified in publications beyond specific study designs. To our knowledge, this is the first scoping review providing an overview of the theoretical characterisations of ADHD and their impact on available treatments.
Search strategy
The scoping review was carried out over three months: February, March and April 2020. The scoping review protocol was published on the Open Science Framework ( https://osf.io/ ). Search design and criteria were formulated based on guidance and recommendations by Arksey & O’Malley [ 27 ], Colquhoun et al. [ 28 ], O’Brien et al. [ 29 ] and the Joanna Briggs Institute [ 30 ]. A starting timeframe from the publication of Barkley’s [ 11 ] theory was selected as the foundation for current theoretical characterisations of ADHD. Papers were reviewed from multiple countries, including the United States, the United Kingdom, The Netherlands, Canada, Argentina, Brazil, Colombia, Iceland, Ireland, Portugal, Spain, Belgium, Germany, Switzerland, Finland, Sweden, Israel, Iran, China, Hong Kong, India and Australia, and multiple languages including English, Dutch, German, French, and Spanish.
Research evidence was identified by conducting searches across web-based databases with pre-determined search terms. Table 1 outlines the search terms and syntax used in primary and secondary searches.
Table 1. Search strategy.
Additional searches were in generic search engines Google and Google Scholar, and checks of references from guidance documents and systematic reviews for additional material. Once identified, these references were collected through additional database searches or a direct search in the specific journal or publication.
Inclusion criteria
Titles and abstracts of materials were reviewed for eligibility. Materials were considered appropriate if they met the following criteria:
Studies involving research on a pilot, efficacy, or applicability of a treatment intervention for adults with ADHD (19–65+, male and female)
Systematic reviews of treatment literature or specific approaches to treatment for adults with ADHD
Thesis, conference papers, or reports reviewing, presenting, or recommending treatment approaches for adults with ADHD
Documents, articles, books, or consensus statements presenting guidance or recommendations for treatment for adults with ADHD
Exclusion criteria
In addition to meeting the inclusion criteria, materials were excluded if they met one of the following exclusion criteria:
Treatment approaches designed for a specific subset of participants (couples, military, substance abuse)
Treatment approaches designed to treat specific comorbidities (Autism, Bi-polar, Learning Disabilities, Tourette’s, Oppositional Defiant Disorder, Personality Disorder, Traumatic Brain Injury)
Treatment approaches designed for the inclusion of younger age groups (children, adolescents) or their parents
Materials summarising and updating recent developments in the field of treatment for adult ADHD (general practice journals, nursing practice journals, medical student journals)
Characterisations of adult ADHD that were not empirically researched
A large body of literature has been published over the years which present different characterisations of adult ADHD and subsequent recommendations for treatment. Predominantly based in the US, these biopsychosocial models range from origin theories of genetic strengths [ 31 ], diversity [ 32 ] and developmental impairment of the prefrontal cortex due to issues with attachment and trauma [ 33 ], to identifying multiple presentations of ADHD diagnosed individually with SPECT imaging [ 34 ]. While these models do present alternative characterisations of ADHD, they are not empirically researched and therefore will be excluded from this review.
The following PRISMA flowchart ( Fig 1 ) presents the search process details, including the number of articles located, those eliminated and those included in the final analysis.
Fig 1. Flowchart of scoping review: Characterisation of adult ADHD.
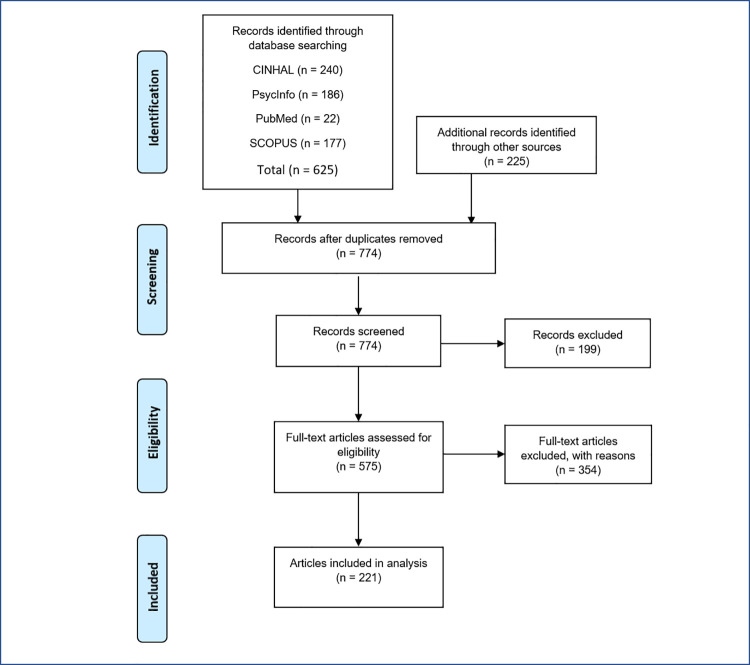
Results and analysis
The 221 articles were subdivided into the following categories according to their primary content: Cognitive Behavioural Therapy (122), Coaching (36), Psychotherapy (16), and Other (47). All articles were assessed for quality against the relevant Critical Appraisals Skills Programme (CASP) checklists. Results summary of the ADHD characterisation cited for each intervention category is displayed in a mosaic plot ( Fig 2 ).
Fig 2. ADHD characterisations cited in intervention category.
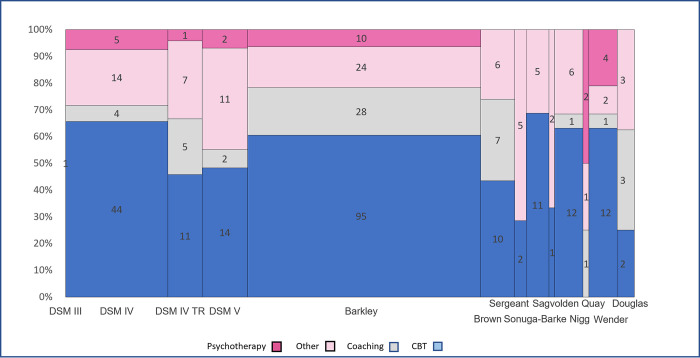
An overview of interventions published by year is displayed in a column chart ( Fig 3 ).
Fig 3. ADHD interventions published by year.
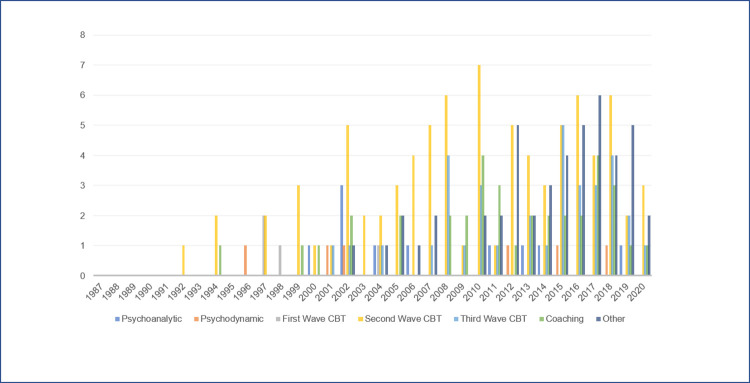
Due to the number and variety of materials, a narrative analysis was performed to review the publications’ composition. Systematic reviews were also analysed separately to see if any review of the characterisation of ADHD had been completed previously.
Systematic reviews
Over the years, several systematic reviews of treatments for adult ADHD have been published. Searches were undertaken through Joanna Briggs Institute Evidence Synthesis, The Cochrane Database of Systematic Reviews, and the Campbell Library show some of these reviews are specific to the efficacy of a particular intervention approach, such as psychodynamic therapy [ 35 ], homoeopathy [ 36 ], Cognitive Behavioural Therapy (CBT) [ 37 – 41 ], Mindfulness [ 42 , 43 ], and Meditation [ 44 , 45 ]. Others have been focused on efficacy [ 2 , 15 , 16 , 46 – 48 ], long term outcomes [ 10 , 49 ], or guidance [ 50 ]. Only one systematic review investigated the characterisation of adult ADHD but failed to find evidence of neurocognitive disfunction as a predictor of persistence [ 51 ]. Interestingly, one systematic review investigated how adults with ADHD experience and manage their symptoms [ 52 ]. Therefore, it seems that no recent attempt has reviewed the psychological theories for the characterisation of adult ADHD.
Data extraction
Articles were reviewed, and data extracted into categorised excel spreadsheets for comparison. Each document was examined for the following criteria:
Research Purpose/Outcome
Treatment Approach
ADHD Characterisation
ADHD Theory
Intervention analysis
Research studies and guidance documents present treatment approaches in various environments, contexts and skill levels of delivery. The following interventions present a wide range of delivery in clinical and non-clinical environments; therapeutic, academic, and social contexts; and professionals including psychiatrists, clinical psychologists, nurses, occupational therapists, psychotherapists, as well as counsellors, coaches, and mentors.
Cognitive Behavioural Therapy (CBT)
Due to the involvement of cognitive behavioural theory in establishing the characterisation of ADHD, the bulk of research in the field has used this intervention model. While recommended as the primary treatment modality, treatment goals and methodologies have changed over time. Due to this shift in focus, some early research references non-empirical anecdotal work. This analysis will use the delineation of “waves” as seen in the current theoretical literature to demonstrate these changes [ 53 ] ( S1 Appendix ).
First wave : Behaviourism . Before 1990, ADHD was still considered a disorder of childhood. Although considerable research exists regarding “first wave” treatments in children, the few approaches developed for adults apply pure behavioural theory and techniques. A case study of three subjects focused on improving attentional behaviour in psychiatric patients [ 54 ], and the design utilises operant theory and models used for brain injury [ 55 ]. Guidance documents for teachers, parents and counsellors [ 56 ] and psychotherapists [ 57 ] highlight the importance of behavioural skill development. The conceptualisation of ADHD in these treatment models is a disorder of attention [ 54 ] and a neurobiological disorder of self-regulation, executive function deficits and disinhibition [ 56 , 57 ]. Burgess et al. [ 54 ] exemplify the transition of the conceptualisation of attentional deficits in ADHD from mental illness to mental disorder.
The therapist’s role in these models is to assist the client in learning and practising practical behavioural strategies for task attention, organisation, listening and scheduling, and planning and organising daily activities. Treatment designs are varied, with only one specifying weekly sessions from 6–10 weeks [ 54 ]. Characterisation of ADHD aetiology highlight issues with inability to maintain vigilance (attention deficit) and distractibility [ 54 ], self-regulation, impaired inhibition, developmental delay, and deficits in executive function, referencing Barkley [ 56 , 57 ].
Rational Emotive Behaviour Therapy (REBT) . A single case study for ADHD specifically used REBT [ 58 ]. REBT approaches ADHD as a combination of neurobiological deficits [ 59 ] and developed secondary psychological personality disorders. Failure to develop cognitive structures leads to a lack of connection between thoughts, emotions and feelings, leading to deeply held distorted convictions and beliefs. The therapist’s role in this model is to assist the individual to dispute evaluative cognitions (“musts”) to develop a more rational philosophical orientation to the world. The approach incorporates independent “experiments” by clients outside of therapy, problem-solving methodology, and gentle introduction of rational self-statements for clients who lack the cognitive sophistication to engage in disputing of irrational beliefs [58, p. 95]. Treatment design has a developmental and longitudinal focus, in this case eight years. Characterisation of ADHD is described as DSM-IV core symptoms of attentional difficulties, impulsivity and hyperactivity [ 60 ] and references both Douglas’s [ 61 ] cognitive processing deficit model and Barkley’s [ 59 ] model of response inhibition and executive function deficits contributing to deficient self-regulation, impaired cross-temporal organisation of behaviour, and diminished social effectiveness and adaptation.
Second wave : Cognitive and cognitive behavioural therapy model . Cognitive and Cognitive Behavioural approaches are the primary and recommended treatment for working with ADHD and therefore make up the bulk of studies reviewed for this analysis. Considered “second wave” cognitive behavioural therapies, they consist of systematic reviews [ 2 , 37 , 38 , 41 ], randomised controlled trials (RCT) [ 62 – 80 ], group interventions [ 81 – 87 ], individual interventions [ 88 – 90 ], quantitative analysis [ 91 ], qualitative analysis [ 92 ], a cohort study [ 93 ], case-control studies [ 69 , 94 – 98 ], single case studies [ 99 – 102 ], multiple case studies [ 103 – 106 ], and psychotherapeutic treatment guidance [ 8 , 106 – 138 ]. Many of these studies deliver CBT as a standalone intervention, however multimodal treatment is recommended, and several treatment models include individual coaching or mentoring support alongside or in between CBT sessions [ 57 , 72 , 77 , 86 , 103 , 112 , 127 , 131 , 137 , 139 ]. One intervention also includes hypnosis and CBT [ 140 ].
Second wave interventions for ADHD recognise the neurobiological deficits as specific to the disorder and not brain injury. While they stress there is no “cure” for ADHD and the literature is clear that ADHD does not arise from distorted cognitions, cognitive treatment models focus primarily on improving, strengthening, or retraining cognitive abilities to increase awareness of behaviour and behavioural control. Early research identified cognitive distortions and maladaptive strategies and beliefs as interfering with skills acquisition and therefore needed support [ 104 , 136 ]. Further research shifted this view slightly to perceive the development of a negative self-concept as the core issue for maladaptive schema or “secondary symptoms” of stress, anxiety, depression, and chronic perceived failure attributed to a history of unachieved potential and negative feedback resulting from a lack of recognition of the disorder. [ 122 , 141 , 142 ]. Aims of treatment reduce deficit-based symptoms, develop environmental restructuring and accommodations, improve self-esteem and negative self-concept through disorder psychoeducation, and increase confidence in capabilities through supported skills practice and repetition. Approaches vary widely, including cognitive rehabilitation, cognitive and metacognitive remediation, and cognitive restructuring. However, most treatment approaches in this area are defined as Cognitive Behavioural Therapy (CBT) ( S1 Appendix ).
The therapists’ role in these models is more a “partner”, “expert teacher-motivator” [ 122 ] and collaborator than the traditional medical expert role [ 117 , 121 , 129 ]. Originally defined by Hallowell & Ratey [ 143 ] as “coaching”, therapists are encouraged to be active and directive in providing structure and redirection to goals or session topics [ 83 , 87 , 101 , 108 , 129 , 135 , 137 , 144 ]. Failure to initiate behavioural changes or maintain new habits and strategies, or “procrastivity”, is attributed to motivational problems due to the nature of the disorder [ 8 , 108 , 121 , 145 ]. CBT for ADHD identifies the ADHD client’s difficulty with delayed gratification and generation of positive emotions as the reason for lack of engagement or “Coping Drift”, where individuals stop implementing the skills taught in treatment [ 121 , 145 ]. Professionals are cautioned that repetition is key, and strategies must be reinforced, or relapse is likely. Therefore relapse prevention is included in practice as well as model design [ 8 , 70 , 71 , 74 , 83 , 86 , 93 , 94 , 108 , 121 , 126 , 136 , 145 , 146 ]. Recommendations for resistance or avoidance of aversive emotional states is to provide therapist support to develop tolerance [ 107 , 122 , 135 ], reframe past experiences [ 112 , 128 , 147 ], and build resilience when encountering setbacks [ 8 , 111 , 118 , 137 , 138 , 146 ]. Treatment designs are limited in length, either by the number of sessions (3 to 16) or by relevance (academic year) except for single case studies [ 99 – 102 , 104 ]. Intervention delivery methods vary from individual or group therapy and didactic teaching with therapeutic support to a computerised program and self-help manuals ( S1 Appendix ).
Characterisation of ADHD and aetiology highlight issues with attentional and behavioural control (hyperactivity, impulsivity, disorganisation) initially, but broadens to give a higher priority to executive dysfunction deficits, motivation and sustained attention, issues with emotional control and self-regulation. Guidance documents definitions of ADHD are often cited: of the 84 papers in this Second Wave analysis, 29 reference DSM-IV [ 60 ], seven reference DSM-IV-TR [ 148 ], and eight reference DSM-V [ 149 ]. Several studies reference alternative characterisations of ADHD, such as similarity to brain injury [ 117 ] and Brown’s Executive Function model [ 83 , 94 ]. However, Barkley is cited in 70 documents.
Third Wave : Mindfulness and acceptance . Third Wave cognitive behavioural interventions take a different treatment approach to traditional CBT. While they are similar in the practical application of behavioural techniques, they differ in their theoretical approach and the focus on cognitive change. Third-wave approaches explore context: the relationship between a person’s thoughts and emotions rather than content alone. This relationship includes a more holistic perspective of health beyond the reduction of disorders [ 53 ]. Therefore, this analysis will review them separately. These approaches include Metacognitive Therapy (MCT), Dialectical Behavioural Therapy (DBT), and Mindfulness Cognitive Behavioural Therapy (MCBT).
Metacognitive Therapy (MC) . Four documents used a metacognitive approach (MC), divided into group metacognitive therapy [ 5 , 76 , 150 ] and metacognitive remedial psychotherapeutic guidance [ 151 ]. Metacognitive interventions conceptualise ADHD as neurobiological dysfunction in the corticostriatal pathways, displayed as deficits in executive functions [ 151 ]. MC highlights the importance of awareness of cognitions or thinking about thinking to strengthen executive functions to enhance functioning and improve self-control. Borrowing from the psychoanalytic frame [ 152 ], treatment of this hybrid model aims to develop an “observing ego” or self-awareness, increasing the ability to be conscious of maladaptive thoughts and behaviours and confront them via self-analysis. The therapist’s role is to focus on cognitive and behavioural aspects of treatment and only address motivational or unconscious elements if they remain unexplained by neurobehavioural origins. Individual treatment plans are designed on a case-by-case basis to capture the individual’s unique problems and strengths. Analysis of authentic and emotionally charged experiences facilitates self-awareness using metaphoric problem identification, followed by strategy design and modification [ 151 ]. In group therapy, the therapist acts as an educator and facilitator, assisting with goal identification, the leading theme focused or problem assessment discussion, and offering support and encouragement [ 76 ]. Characterisation of ADHD focuses primarily on executive function deficits, followed by inattention and memory. This focus is reflected practically in treatment design as hyperactivity/impulsivity is considered less prevalent in adults [ 76 ]. Barkley is a primary citation in all four documents.
Dialectical Behavioural Therapy (DBT) . Ten studies identified an adapted model of Dialectical Behavioural Therapy (DBT) for ADHD. These consist of randomised controlled trials [ 21 , 153 – 155 ], a pragmatic open study [ 156 ], and group interventions [ 157 – 161 ]. This treatment model recognises ADHD neurobiological deficits but is grounded in a phenomenological conceptualisation, perceiving the nature of ADHD as a personality disorder. This conceptualisation is supported by similarities in symptoms and the positive response to the treatment of ADHD with comorbid Borderline Personality Disorder (BPD) [ 158 ]. Linehan [ 162 ] characterises BPD as a disorder of self-regulation from biological irregularities combined with dysfunctional environments, including their interaction and transaction. Experiences of invalidating environments impair childhood ability to learn to label experiences and emotions, modulate emotional arousal, tolerate distress, or form realistic goals and expectations, resulting in a child who invalidates their own experiences, generating a lack of self-trust. The adapted model is presented in group format of 13 weeks of 2-hour sessions. The design prioritises ADHD symptom-oriented modules, highlights non-empirically researched resources of ADHD [ 163 ], and includes DBT “mindfulness” training explicitly. The therapist’s role in the DBT adapted model for ADHD supports treatment aims of learning to “control ADHD—instead of being controlled by ADHD” through psychoeducation and provision of session structure and flexibility for individuals. A key therapist practice adopted from DBT is the dialectical balance between validating symptoms, aiming for a stabilising effect and encouragement of motivation, and skills training for behavioural change [ 158 ]. These models characterise ADHD as a deficit of attention and emotional control with hyperactive and impulsive behaviour, but later papers highlight issues with executive function and self-regulation [ 157 ]. Four studies cite Wender [ 164 ] as diagnostic criteria [ 153 , 158 – 160 ], two studies cite DSM-IV [ 154 , 155 ], and four studies cite Barkley specifically [ 21 , 156 , 157 , 161 ].
Mindfulness . Twenty-two documents included mindfulness in treatment options for ADHD. These included systematic reviews [ 42 , 165 – 167 ], randomised controlled trials [ 168 – 174 ], a pragmatic open study [ 156 ], group interventions [ 98 , 175 , 176 ], a case-control study [ 177 ], a multiple case study [ 178 ], and psychotherapeutic guidance [ 8 , 179 – 182 ]. Only two studies presented mindfulness treatment alone [ 98 , 156 ]. In Edel et al. [ 156 ], mindfulness was used as a comparator to DBT.
Mindfulness-based approaches conceptualise ADHD as a neurobiological disorder of self-regulation with deficits in executive function. Issues with sustained and selective attention are addressed by mindfulness meditation, which is presented as a self-regulatory practice recognised as mental training to strengthen and improve regulation of attention, emotions and brain function [ 167 , 175 , 177 , 181 ]. The therapist’s role is primarily to introduce and support developing the new skill set of “mindful awareness” or cognitive defusion to facilitate the ability to decrease emotional responses while continuing to act [ 8 ]. Interestingly, Zylowska’s [ 175 , 176 ] Mindfulness-Based Cognitive Therapy treatment model includes within its psychoeducation a characterisation of ADHD as a “neurobiological difference” with both evolutionary non-adaptive and potentially adaptive aspects [ 183 – 185 ]. However, within the treatment approach, the ADHD characterisation remains based on cognitive behavioural theory.
Treatment is in a group format, and length varies from 8 to 12 weeks of 2 to 3-hour sessions. The characterisation is reasonably consistent across this group, focusing primarily on poor sustained attention, inhibition and emotional dysregulation attributed to executive dysfunction, with one study highlighting impairments in performance monitoring [ 173 ]. Two papers cite DSM IV [ 42 , 168 ], two cite DSM V [ 167 , 170 ], and sixteen cite Barkley specifically [ 8 , 98 , 156 , 165 , 166 , 169 , 171 – 173 , 175 , 176 – 180 , 182 ].
Thirty-six documents presented coaching as a beneficial intervention for ADHD. These include a systematic review [ 186 ], a randomised controlled trial [ 187 ], individual interventions [ 188 – 199 ], qualitative studies [ 200 – 204 ], quantitative studies [ 205 – 207 ], and psychotherapeutic guidance [ 118 , 143 , 208 – 218 ]. It is important to note that nineteen studies were conducted at university for students, and therefore have academic goal achievement as a focus [ 187 – 195 , 197 – 199 , 201 , 204 , 206 , 208 , 212 ].
The term “coaching therapy” was coined by Hallowell and Ratey [ 143 ] to highlight the need for a therapist to take a more “active, encouraging role” with ADHD patients. The role of the “therapist-coach” was to provide a structuring force, maintaining focus and reminding patients of goals and objectives through directive interaction, as opposed to open-ended psychoanalysis. ADHD Coaching has since developed into an independent modality, which can be delivered alone or as part of a multi-modal approach. The ADHD Coaches Organisation (ACO) defines ADHD Coaching as a blending of three elements: Life Coaching, Skills Coaching, and Education [ 218 ]. Life coaching separates ADHD Coaching from therapy by highlighting the therapist-client relationship’s collaborative nature, where the coach supports client self-awareness and achievement of self-identified goals, providing structure and accountability as needed. The client is viewed as a creative and resourceful expert with individual strengths which are leveraged in skills coaching to design systems and strategies to strengthen clients’ ability to manage daily life. Education is provided through relevant ADHD research and tools, as requested by the client or as needed.
Conceptualisations of ADHD within coaching models focus almost exclusively on working with neurobiological deficits in executive function, with the primary treatment aim to set and achieve goals and develop skill sets to support practical day to day management. Some models even define themselves specifically as “Executive Function Coaching” [ 191 , 195 , 198 , 204 , 206 , 208 ]. However, some models highlight ADHD Coaching as based on or similar to CBT [ 186 , 196 , 199 , 208 ]. The role of the coach is to support clients to improve self-regulation, defined as the ability to persist in goal-directed behaviour through time [ 204 , 209 ], by modelling cognitive strategies, practising non-judgement, offering pragmatic support and guidance, and holding clients accountable by reflection in session or monitoring progress via between session check-ins. Negative emotions are addressed as barriers to goal achievement and confidence, but models are specific that ADHD coaching is practical [ 186 ], dealing with “what, when and how–never why” [ 213 ].
Six documents mention self-determination models as part of a wider ADHD Coaching treatment model [ 190 , 191 , 194 , 195 , 204 , 206 ]. These are functional theory models designed to assist students, particularly those with learning disabilities, to develop internal or dispositional characteristics of self-determined behaviour and goal acquisition [ 219 – 221 ]. Field & Hoffman’s model [ 221 ] defines self-determination as the ability to define and achieve goals grounded in knowing and valuing oneself, which can be supported or thwarted by internal variables and environmental factors. The model specifically focuses on internal controllable variables to assist individuals to adapt to environments with unpredictable support. The core theory is that to be self-determined, one must develop internal awareness and the skills and strength to act on this internal foundation. The model has five major components:
“Know Yourself”: Increase awareness of one’s preferences, strengths, weaknesses and needs by “dreaming” or overcoming barriers in socialised expectations for individuals with disabilities that limit options and perceptions of self-efficacy, building on a foundation for self-determined decision making.
“Value Yourself”: Develop affective variables of self-esteem, including identifying strengths in areas commonly perceived as weakness, supporting the self-acceptance of disability and motivation for self-advocacy, increasing the ability to be self-determined.
Plan: Learn planning skills and visual rehearsal of creative and effective actions for short-range steps leading to long term goals.
Act: Awareness of how to assertively communicate goals, desires and intentions to others and access relevant resources. Understanding persistence, negotiation, and conflict resolution around risk-taking and barriers that may result from taking action.
Experience Outcomes and Learn: Learn skills in evaluation of progress based on experience of change and comparison to expected outcomes. Recognition and celebration of successes crystallises the self-determination process.
Wehmeyer et al.’s model [ 219 , 222 ] is a teaching model to help students become causal agents. Based on cognitive behavioural theory [ 223 , 224 ], social cognitive theory [ 225 ] and research in self-management and self-control [ 226 ], this model defines self-determination as the abilities necessary to act as one’s primary causal agent and make choices and decisions about the quality of life free from external influence and interference [ 227 ]. Developed from a model designed to teach students decision making, independent performance, self-evaluation, and adjustment skills, the updated model includes defining those who are self-determined to persistently regulate problem-solving to meet self-directed personal goals using student-directed learning strategies [ 219 ]. This ability is developed through a learned problem-solving sequence of thoughts and actions to reduce the discrepancy between what students want or need and what they have or know. The sequence requires the students to 1) identify the problem; 2) identify potential solutions; 3) identify barriers to solving the problem; and 4) identify consequences to each solution, thereby enabling the student to regulate problem-solving by setting goals to meet needs, constructing plans to meet goals, and adjusting actions to complete plans [ 219 ]. A comprehensive combined curriculum of these frameworks was later developed [ 220 ]. While they provide support for client autonomy and causal agency within the design of these ADHD Coaching models, these models prioritise goal setting and identification as regulators for human behaviour and recommend student-directed learning strategies based on operant psychology, applied behavioural analysis and positive reinforcement techniques. Thus, treatment approaches for ADHD remain based on cognitive behavioural theory.
Treatment approaches in ADHD Coaching models are primarily cognitive behavioural, including reframing negative self-talk [ 228 ], continuous reinforcement [ 189 , 209 ], implementing rewards and consequences [ 188 , 189 , 192 , 196 , 212 ], and between-session assignments [ 192 , 196 , 209 , 217 ]. These models focus on the characterisation of ADHD as deficits in executive function relating to goal-directed behaviour, disorganisation and planning, motivation, and ultimately self-regulation. Citations for characterisation in ADHD Coaching models include one referencing DSM IV [ 211 ], three reference DSM-IV-TR [ 191 , 202 , 214 ], one reference to Brown’s Executive Function Model [ 195 ], and twenty-eight reference Barkley specifically [ 118 , 128 , 143 , 186 , 188 , 189 , 191 – 194 , 196 – 201 , 203 – 207 , 209 , 212 , 214 – 218 ].
Other interventions
Fourty-seven documents describe non-pharmacological interventions not based on psychotherapy. These include Neurofeedback, Transcranial Stimulation, Hypnotherapy, Light Therapy, Computer-Based, Mentoring, Self-Monitoring, Binaural Beat Auditory Stimulation, and Movement-related interventions.
Neurofeedback . Twelve documents explored Neurofeedback as an intervention for ADHD. These include randomised controlled trials [ 229 – 231 ], individual interventions [ 232 , 233 ], case-control studies [ 234 , 235 ], a single case study [ 236 ], and treatment guidance [ 118 , 237 – 239 ]. Neurofeedback (NF) treatment models focus heavily on neurocognitive deficits as being the origin of ADHD behaviours. The research uses Electroencephalography (EEG) measures to study the correspondences between intracranial electrical currents and responding voltages on the scalp. These measures indicate aspects of brain electrical function and processing, such as the electrical activity of various brain regions and their response to stimuli during cognitive tasks. EEG activity is quantified by computation of amplitude and power values for specific frequency bands of activity, source localization, and brain electrical activity mapping. Frequency refers to the number of oscillations, or waveforms, within a given time period. Analysis of waveforms, or a mixture of frequency bands, is a relational and complex process of examining frequency bands associated with both regions of the brain and cognitive or behavioural characteristics.
Characterisations of ADHD are presented as disturbances in cortical arousal, executive function, and self-regulation. Theta/beta and theta/alpha waveform ratios (TBR) are considered a measure of differences in excess, slow-wave activity and epileptiform spike and wave activity [ 240 ], interpreted as abnormal brain processes indicating cortical under arousal, insufficient inhibitory control, and maturational delay in ADHD [ 241 ]; however recent studies have challenged TBR as a marker for ADHD diagnosis [ 235 ]. Sensory-motor rhythm (SMR) or low beta waveform ratios are thought to indicate cortical hypo-arousal, interpreted as deficiencies in the early stages of information processing [ 230 ]. Decreased contingent negative variation (CNV), a steady, slow, negative-going waveform associated with cognitive energy in anticipation of task performance, is considered indicative of dysfunctional regulation of energetical resources in ADHD [ 234 ].
Based on research in children, two treatment approaches reflect changes in the conceptualisation of ADHD and, therefore, treatment aims. Traditionally, the focus of treatment has been based on a “conditioning and repair model” [ 242 ]. Treatment aims to address dysfunctions and see behavioural improvement and remediation of symptoms following NF application [ 243 ]. Skill acquisition and learning are implicit, automatic, and unconscious. Changes in activity indicate positive results: the ability to decrease slow-wave activity (theta) and/or increase fast wave EEG activity (beta) should correlate with symptom improvement; or modulation of slow cortical potentials (SCP), changes of cortical electrical activity, indicate improved cortical regulatory processes [ 244 ]. The role of the therapist is to act as a model for affect regulation [ 236 ] as well as use behavioural principles such as operant conditioning (i.e., positive reinforcement) in the training process resulting in normalisation and stable change in resting EEG, or “EEG trait” [ 245 ], and behaviour [ 231 , 233 , 234 ].
More recently, the NF treatment focus has developed into a “skills acquisition model” [ 242 ]. Rather than simply improving neuropsychological deficits, it is thought that NF may be used as a tool for enhancing or optimising specific cognitive or attentional states [ 246 , 247 ]. This model recognises the bio-psycho-social model of neurodevelopmental disorders, characterising ADHD as impairments in attention, executive functions and self-regulation [ 229 , 230 ]. In this model, self-regulation, or neuro-regulation, is defined as explicit learning of controlled cognitive processes of cortical regulation evidenced by normalised shifts in EEG amplitudes [ 242 , 248 , 249 ]. Performance optimisation is evidenced by improved skill in changing the “EEG state” via self-initiated effort during task performance [ 243 , 250 ]. The therapist’s role is to use cognitive behavioural therapy elements such as positive feedback and coaching and operant procedures as active support within treatment sessions to enhance self-efficacy and self-confidence to support neuro-regulation [ 244 , 251 ]. Citations for characterisation of ADHD in NF models include two citations for DSM-IV-TR [ 231 , 238 ], two for DSM -V [ 232 , 233 ], one for Sonuga-Barke’s Delay Aversion Model [ 237 ], three for Sergeant’s Cognitive-Energic Model [ 230 , 234 , 237 ], and four citations for Barkley [ 118 , 229 , 237 , 239 ].
Transcranial stimulation . Four documents present Transcranial Stimulation as a treatment approach for ADHD. These include a systematic review [ 252 ], two randomised controlled trials of Transcranial Direct Stimulation (tDCS) [ 253 , 254 ], and a randomised controlled trial of Transcranial Magnetic Stimulation (rTMS) [ 255 ]. Both forms of transcranial stimulation conceptualise ADHD as a neurobiological disorder with deficits in executive functions, including attention, working memory, impulsivity, and inhibitory control. The treatment aims to increase cortical excitability in the area of stimulation, leading to improved neuropsychological and cognitive functions.
Treatment approaches are non-invasive but differ in their application. Transcranial Magnetic Stimulation uses a coil placed on the subjects head to deliver brief, intense pulses of current (up to 50 Hz) to generate a sizeable electromagnetic induction field initiating neurotransmitter release in the cortex and subcortical white matter of the brain [ 255 , 256 ]. Transcranial Direct Current Stimulation uses conductive sponge electrodes applied to the scalp in specific locations to deliver a weak electrical current (1–2 mA or milliamps) for up to 20 minutes. It is hypothesised that the electrical current changes the polarisation of the neurons, affecting their average level of discharge [ 253 , 254 , 256 ]. Multiple treatments are administered daily for 3–4 weeks. Protocols suggest two applications of stimulation: “online”, or while a patient is completing a task, or “offline” where the treatment is applied before or without specific targeted tasks. Citations for characterisation of ADHD in these models include DSM-IV [ 252 ], DSM-IV-TR [ 254 ], DSM V [ 255 ] and Barkley [ 253 ].
Hypnotherapy . Two RCTs examined hypnotherapy as a treatment approach for ADHD [ 74 , 257 ]. These studies conceptualise ADHD as a developmental neurobiological disability with deficits in attention, issues with hyperactivity/impulsivity and problems in executive function, including processing speed, regulating alertness, modulating emotions, and utilizing memory. Treatment aims to improve symptoms, mood, quality of life and cognitive performance. Treatment design is based on symptoms outlined in the DSM-IV and Brown’s Executive Dysfunction Model [ 258 ]. The therapist’s role was to follow a semi-structured manual to review the previous session, present the theme for the current session, perform induction and guided hypnotherapy with a post-hypnotic suggestion, and lead discussion. Treatment length was ten weekly sessions of 40 to 60 minutes. Citations for characterisation of ADHD were the DSM-IV [ 257 ] and Brown’s Executive Dysfunction Model [ 74 ].
Light therapy . Five documents present light therapy as a treatment approach for ADHD: a systematic review [ 259 ], an individual intervention [ 260 ], a quantitative study [ 261 ], a literature review [ 262 ], and treatment guidance [ 263 ]. These documents conceptualise ADHD as a neuropsychiatric disorder with primary symptoms of impulsivity, inattention, and hyperactivity impacted by mood regulation difficulties, maintaining arousal and sleep disturbances that contribute to pathophysiology. This conceptualisation is supported by links between ADHD, seasonal affective disorder (SAD) and circadian rhythms and highlighted by similarities in symptoms between sleep deprivation and ADHD [ 261 , 263 ]. Research indicates abnormalities in circadian related physiological measures such as heart rate increase relevant to autonomic function, dysregulation in melatonin rhythm leading to delays in melatonin onset, which may affect the modulation of the sleep/wake cycle [ 263 , 264 ], as well as some evidence of low cortisol impacting wakening times [ 259 ]. Also, a later diurnal preference, or evening chronotype, is highly prevalent in the ADHD population. Its association with shorter night sleep periods is believed to generate sleep debt, delay the sleep phase, and exacerbate symptoms or potentially play a causal role in ADHD symptoms [ 262 , 263 ].
Light Therapy (LT) treatment aims to assist with phase-shifting abnormal circadian rhythms through light exposure to achieve sleep onset to improve alignment with work, academic, or social norms. Treatment outcomes are improved sleep and improved ability to maintain effort, arousal and attention [ 260 , 262 ]. The treatment has been trialled as a three-week self-administered daily dose of 10,000 lux at a distance of 24 inches using a full-spectrum fluorescent lightbox [ 260 ]. Citations for the characterisation of ADHD in these documents include DSM-IV [ 260 ], DSM-V [ 259 ], Douglas [ 262 ], Brown’s Executive Dysfunction Theory [ 261 ], and Barkley [ 261 ].
Computer-based interventions . Eight documents presented computer-based interventions as a treatment approach for ADHD. These include randomised controlled trials [ 265 – 268 ], individual interventions [ 269 , 270 ], and case-control studies [ 271 , 272 ]. These approaches characterise ADHD as a neurobiological disorder with executive function deficits, including difficulties in sustained attention, response inhibition, goal persistence, and working memory. Computer-based interventions take two approaches: supportive or training. Supportive interventions aim to target specific symptoms and facilitate functioning via supportive software. Individuals are given access to tools used independently following training for a set timeframe. In Hecker et al. [ 271 ], a software tool designed to reduce internal and external distractions aimed to reduce effort and improve engagement, resulting in increased time reading and comprehension. In Irvine [ 269 ], a smartphone app for time management aimed to reduce the discrepancy between the perception of time and actual time spent by providing immediate real-time feedback on the current status and time use, leading to adjustments of future tasks according to behavioural therapeutic principles.
Training interventions aim to strengthen cognitive skills and/or remediate deficiencies via cognitive behavioural learning strategies of repetition and positive reinforcement. Working Memory Training [ 265 , 266 , 268 ] aimed to enhance auditory-verbal and visual-space working memory through intensive training with increasing task difficulty leading to improved cognitive and academic performance and attentional self-regulation. Cognitive ability training [ 272 ] aimed to improve cognitive skills of decision making, attention, organisation and time management through simulated activities in a gaming environment, providing immediate real-time rewards. Cognitive training for executive function [ 267 , 270 ] aimed to remediate cognitive processes deficiencies by repeated and graded exposure to neutral and universal stimuli and feedback. Training is self-administered, hierarchical and adjusted to individual performance with outcomes for improvements in daily executive functioning, occupational performance, and quality of life. Treatment length varied in frequency and intensity, from 20-minute sessions 3–5 times a week for 12 weeks to 45-minute sessions five days a week for five weeks and included weekly check-ins or supportive coaching. Citations for characterisation of ADHD in these approaches include DSM-IV [ 265 , 266 , 268 , 270 ], DSM V [ 271 ], Brown’s Executive Dysfunction Model [ 267 , 270 ], Nigg’s Integrative Theory [ 267 ], and Barkley [ 266 , 267 , 269 , 270 ].
Mentoring . One study presented mentoring as an individual intervention for ADHD [ 273 ]. Based in a university environment, ADHD is characterised as deficits in basic cognitive skills, such as attention, concentration, and memory and higher-level cognitive skills or “executive functioning”, such as planning, organization, judgment, problem-solving, and cognitive flexibility. These can negatively affect the university experience, as more independent self-management and a complex skill set are required for success, particularly time management and organization, academic skills, and social skills.
The mentoring program pairs second-year master’s level occupational therapy (MSOT) students (mentors) with undergraduate college students (mentees) for one-to-one support twice weekly for 2-hour sessions in the fall and spring semesters. This mentoring is a credit-bearing course that addresses skill development in time management and organization, academic skills, and social skills for college success. Mentees are graded on attendance, professional behaviours, compliance on a weekly to-do list, a presentation on academic resources, and a 4-part written paper on an academic skill. Mentors are participating as part of a professional Occupational Therapy training programme with an overall goal to facilitate student success in college, and if factors overwhelmingly interfere with this goal, to identify an alternate, suitable plan. As part of the training, mentors meet in discussion groups to brainstorm ways to overcome the mentoring process’s challenges. The citation for the characterisation of ADHD in this intervention is primarily the DSM V [ 273 ].
Self-monitoring . One study presented individual self-monitoring as an intervention for ADHD [ 274 ]. Based in a university environment, ADHD is characterised as a neurobehavioral disorder with symptoms of inattention, hyperactivity, and impulsivity, which increases the risk of academic failure or underachievement.
A checklist tool is co-designed and supported with integrity checks and email reminders every 2–4 days, with face-to-face check-in sessions every two weeks. The self-monitoring intervention aims to teach participants to observe and record behaviours to change the behaviour in the future. Outcomes are to obtain higher grades, endorse fewer ADHD symptoms, engage in more positive study skills, further attain goals, and improve medication adherence. Citations for characterisation of ADHD is DSM IV [ 274 ].
Binaural beat auditory stimulation . Two documents present binaural beat auditory stimulation as a treatment for ADHD. These include an individual intervention [ 275 ] and a literature review [ 276 ]. These approaches characterise ADHD as a disorder with core deficits in behavioural inhibition and sustained attention, highlighting a decrease in beta wave states interfering with maintenance of attention as a contributing factor.
Binaural beat auditory stimulation generates tones of two frequencies presented separately in each ear which are synthesised by the medulla into a single low-frequency tone. The pulse frequency from this binaural beat is the difference between the two tones and generates electrical activity that EEG can record. Treatment aims to match the difference between the tones to a particular brain-wave state, such as the beta range, which will correspondingly be maintained by overall brain activity and affect cognition levels [ 277 ]. Treatment involves exposure to auditory stimulus via headphones during an active task. Citations for characterisation of ADHD only directly reference Barkley [ 275 ].
Movement-related interventions . Twelve documents present movement-related interventions as a treatment for ADHD, including a systematic review [ 278 ], a pilot study [ 279 ], case-control studies [ 280 – 285 ], and treatment guidance [ 286 – 289 ]. In these approaches, ADHD is a disorder with core issues in special working memory, attention control, response inhibition, motor control, delay aversion, emotional self-regulation, and executive dysfunction. Movement-related interventions approach treatment in two ways: passive and active.
One document presented a passive intervention. Whole Body Vibration (WBV) devices deliver sinusoidal or oscillating wave vibrations at low frequencies to enhance mechanical muscular performance [ 290 ], improve balance and proprioception [ 291 ], and increase vigilance [ 292 ], potentially by inducing muscle contractions and increasing tension through the stretch reflex. Treatment is passive, delivered while sitting still, and aims to improve attention, inhibitory control, and cognitive performance in ADHD [ 280 ].
Active movement-related interventions aim to improve neurobiological factors such as increased cerebral blood flow, enhance neuroplasticity [ 288 , 289 ], assist the development of cortical and subcortical brain regions through activity [ 287 ], reduce the impact of comorbid anxiety, depression, stress and negative affect [ 279 , 288 ], and improve cognitive function and performance [ 282 – 286 ]. There is a specific focus on hypodopominergic functioning in ADHD and the upregulation of a brain-derived neurotrophic factor (BDNF) protein in several studies. [ 281 , 283 , 286 , 288 , 289 ]. Research shows that BDNF is linked to differentiation and survival of dopaminergic neurons, and decreased levels of BDNF have been suggested as being involved in ADHD pathology [ 293 ]. As well as improved cognition, one of the benefits of acute exercise is elevated levels of BDNF, which these models argue makes exercise an important intervention for ADHD. Treatment varies both in approach and length, from vigorous physical activity for 30 minutes, such as cycling, to fine motor movement stimulation using an anti-stress ball during a task. Citations for the characterisation of ADHD in these approaches include DSM IV [ 287 ], DSM V [ 285 ], Nigg [ 281 , 286 ], Sergeant [ 282 ], Sonuga-Barke [ 282 , 286 ], and Barkley [ 278 – 280 , 283 , 284 , 286 , 288 , 289 ].
Alternative models
Psychoanalysis and Psychodynamic . There are very few studies in Psychoanalysis and Psychodynamic approaches for adult ADHD. A group intervention [ 294 ], single [ 295 , 296 ] or double case studies [ 297 – 299 ] were reviewed, as well as an evaluation study [ 300 ]. Much of the literature consists of literature reviews [ 35 , 301 – 304 ] and guidance pieces [ 152 , 305 , 306 ], which demonstrate considerable debate in the characterisation and aetiology of ADHD. Early papers reflect issues in clinical approaches by highlighting the importance of considering ADHD diagnosis as defined by DSM-IV in light of epidemiological evidence [ 301 , 307 ]. Both Psychoanalysis and Psychodynamic approaches present alternative models to Barkley, with distinct variation in characterisation.
Historically, Psychoanalysis does not recognise neurobiological deficits. Behaviours associated with ADHD are conceptualized as disturbances in the ego, identified as the organising force responsible for synthesis and integration of internal and external stimuli, internalisation of object relations and structure and development of the superego, and integral to facilitating the capacity for self-observation and self-reflection. Early presentations of these disturbances in childhood lead to attachment issues and interfere with sibling relationship development [ 301 ]. Behaviours are perceived as defence mechanisms, identified as an internal struggle for control [ 296 , 300 ]. Psychodynamic perspectives differ in that behaviours are conceptualized as a reaction to neurobiological deficits [ 152 , 302 , 306 ], facilitating engagement with Barkley’s model. Executive functioning deficits are presented as synonymous with self-regulation deficits, interfering with the development of personality structure and an internal representation of self about others. Self-regulation deficits disrupt the ability to empathise, which distorts the capacity to mentalise and develop a coherent sense of self [ 304 ].
The therapist’s role in these models is to act as the organising force for the client, assisting them to develop ego capacities via therapeutic relationship and transference. This enables the client to experience empathy, recognise mental states, and identify self in relation to others [ 35 , 301 , 304 ]. With the exception of the group intervention [ 294 ], treatment designs are intensive, up to four times a week [ 301 , 304 ] and long term, between 2 and 12 years [ 295 , 296 , 298 , 301 , 304 ]. Despite the alternative model to characterise ADHD, four studies reference international guidance [ 297 , 301 , 302 , 307 ], seven studies mention executive function or cognitive control [ 35 , 152 , 295 , 297 , 299 , 304 , 306 ], and seven reference Barkley specifically [ 35 , 294 , 295 , 297 – 299 , 304 ].
A review of 221 documents confirmed that treatment approaches for ADHD are based on a dominant cognitive behavioural paradigm for conceptualising ADHD, which attributes symptoms solely to neurobiological and developmental deficits leading to challenges with cognitive function, behavioural control, and management of self-regulation. This is reflected in descriptions of treatment aims, approaches and outcomes ( S1 Appendix ).
While this scoping review aimed for as broad a scope as possible, it is important to acknowledge the limitations of this study. First, while translation services were used as much as possible, the material identified in the results were primarily published in English. Further, the majority of the documents presented were published in the US, Canada and European countries. This may be due to documents being presented or published by journals not listed by the major search engines, and therefore not identified in the search strategies. Alternatively, there may not be a large existent body of published research in other countries, as the official diagnosis criteria for adults with ADHD was only recognised in 2013 [ 149 ]. Secondly, this scoping review was an enormous undertaking, and results are only up to date as of April 2020. However, searches did not reveal any other recent reviews of the theoretical charactarisation of ADHD, therefore it is believed this is the most current comprehensive scoping review on the topic.
This review reflects current research understanding that ADHD is complex and multidimensional in its presentation and impact. Clearly, it shows a broad, cross-disciplinary interest in developing treatment approaches to support individuals with ADHD to reduce symptoms, improve functioning and achieve a better quality of life. Critically, it highlights that a single theoretical perspective limits research into effective treatments for ADHD. Existing aetiological theories of ADHD have been challenged for their refutability [ 308 ], and other issues such as accounting for context variability, or inability to fully link or account for the full aspects of the symptomology [ 19 – 21 ], and heterogeneity [ 1 , 22 – 24 ] including specific links between domains and outcome [ 22 ] and cognition and motivation to select actions for a given context [ 309 ]. Recent recommendations for resolving challenges with heterogeneity in ADHD emphasise the importance of theoretical guidance in decision-making and recognise the critical role of beliefs, assumptions, and goals in preventing misapplication of conclusions to clinical circumstances or populations [ 1 ]. It is proposed that treatments based on approaches from a singular perspective on processes of self-regulation and a deficit-based origin of impairments in ADHD may be limited in scope and capacity to identify and support positive psychological factors for well-being and growth. Hence, the findings in this scoping review identify a gap in research and practice for alternative theoretical perspectives of ADHD.
This review concludes that further research into additional theoretical models of self-regulation would provide opportunities to develop alternative treatment approaches and benefit research and understanding of the symptomology of ADHD.
Supporting information
Data availability.
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
- 1. Nigg JT, Karalunas SL, Feczko E, Fair DA. Toward a revised nosology for attention-deficit/hyperactivity disorder heterogeneity. Biol Psychiatry Cogn Neurosci Neuroimaging [Internet]. 2020;1–12. Available from: 10.1016/j.bpsc.2020.02.005 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Toplak ME, Connors L, Shuster J, Knezevic B, Parks S. Review of cognitive, cognitive-behavioral, and neural-based interventions for Attention-Deficit/Hyperactivity Disorder (ADHD). Clin Psychol Rev. 2008;28(5):801–23. doi: 10.1016/j.cpr.2007.10.008 [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Barkley RA. Major life activity and health outcomes associated with attention-deficit/hyperactivity disorder. J Clin psychiatry Suppl. 2002;63(12):10–5. [ PubMed ] [ Google Scholar ]
- 4. Bokor G, Anderson PD. Attention-Deficit/Hyperactivity Disorder. J Pharm Pract. 2014. Aug 4;27(4):336–49. doi: 10.1177/0897190014543628 [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Solanto M V, Marks DJ, Mitchell KJ, Wasserstein J, Kofman MD. Development of a new psychosocial treatment for adult ADHD. J Atten Disord. 2008;11(6):728–36. doi: 10.1177/1087054707305100 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Barkley RA. Executive functions: What they are, how they work, and why they evolved. New York, NY: Guildford Press; 2012. [ Google Scholar ]
- 7. Brown TE. A new understanding of ADHD in children and adults: Executive function and impairments. New York, NY: Routledge; 2013. [ Google Scholar ]
- 8. Ramsay JR. Rethinking adult ADHD. Washington D.C.: American Psychological Association; 2020. [ Google Scholar ]
- 9. Kooij J, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. Updated European consensus statement on diagnosis and treatment of adult ADHD. Eur Psychiatry [Internet]. 2019;56:14–34. Available from: doi: 10.1016/j.eurpsy.2018.11.001 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, et al. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Med [Internet]. 2012;10(1):99. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3520745&tool=pmcentrez&rendertype=abstract doi: 10.1186/1741-7015-10-99 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Barkley RA. ADHD and the nature of self control. London: Guildford Press; 1997. [ Google Scholar ]
- 12. Sergeant J. The cognitive-energetic model: an empirical approach to attention-deficit hyperactivity disorder. Neurosci Biobehav Rev. 2000;24:7–12. doi: 10.1016/s0149-7634(99)00060-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Sonuga-Barke EJS. Psychological heterogenity in AD/HD—a dual pathway model of behavior and cognition. Behav Brain Res. 2002;130(1–2):29–36. doi: 10.1016/s0166-4328(01)00432-6 [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Sagvolden T, Johansen EB, Aase H, Russell VA. A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive/impulsive and combined subtypes. Behav Brain Res. 2005;28:397–468. doi: 10.1017/S0140525X05000075 [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Fullen T, Jones SL, Marie L, Adamou M. Psychological treatments in adult ADHD: a systematic review. J Psychopathol Behav Assess [Internet]. 2020; Available from: 10.1007/s10862-020-09794-8 [ DOI ] [ Google Scholar ]
- 16. Nimmo-Smith V, Merwood A, Hank D, Brandling J, Greenwood R, Skinner L, et al. Non-pharmacological interventions for adult ADHD: a systematic review. Psychol Med. 2020;1–13. doi: 10.1017/S0033291720000069 [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Bolea-Alamañac B, Nutt DJ, Adamou M, Asherson P, Bazire S, Coghill D, et al. Evidence-based guidelines for the pharmacological management of attention deficit hyperactivity disorder: update on recommendations from the British Association for Psychopharmacology. J Psychopharmacol [Internet]. 2014;28(3):179–203. Available from: doi: 10.1177/0269881113519509 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. NICE, editor. Attention deficit hyperactivity disorder: diagnosis and management. In National Institute for Health Care and Excellence; 2019. Available from: https://www.nice.org.uk/guidance/cg72 [ PubMed ] [ Google Scholar ]
- 19. Brown TE. Differential diagnosis of ADD versus ADHD in adults. In: Nadeau KG, editor. A comprehensive guide to attention deficit disorder in adults. New York: Brunner/Mazel Inc.; 1995. p. 93–108. [ Google Scholar ]
- 20. Brown TE. Smart but stuck: Emotions in teens and adults with ADHD. San Francisco: Jossey-Bass; 2014. [ Google Scholar ]
- 21. Hirvikoski T, Waaler E, Alfredsson J, Pihlgren C, Holmström A, Johnson A, et al. Reduced ADHD symptoms in adults with ADHD after structured skills training group: results from a randomized controlled trial. Behav Res Ther [Internet]. 2011;49(3):175–85. Available from: doi: 10.1016/j.brat.2011.01.001 [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Cordova M, Shada K, Demeter D V., Doyle O, Miranda-Dominguez O, Perrone A, et al. Heterogeneity of executive function revealed by a functional random forest approach across ADHD and ASD. NeuroImage Clin [Internet]. 2020;26:102245. Available from: doi: 10.1016/j.nicl.2020.102245 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Feczko E, Miranda-Dominguez O, Marr M, Graham AM, Nigg JT, Fair DA. The heterogeneity problem: approaches to identify psychiatric subtypes. Trends Cogn Sci [Internet]. 2019;23(7):584–601. Available from: doi: 10.1016/j.tics.2019.03.009 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Berger A, Posner MI. Pathologies of brain attentional networks. Neurosci Biobehav Rev. 2000;24:3–5. doi: 10.1016/s0149-7634(99)00046-9 [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Jacob K. Recovery model of mental illness: A complementary approach to psychiatric care. Indian J Psychol Med. 2015;37(2):117. doi: 10.4103/0253-7176.155605 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Liberman RP. Recovery from disability: Manual of psychiatric rehabilitation. Arlington, VA: American Psychiatric Publishing, Inc.; 2008. [ Google Scholar ]
- 27. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32. [ Google Scholar ]
- 28. Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol [Internet]. 2014;67(12):1291–4. Available from: doi: 10.1016/j.jclinepi.2014.03.013 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. O’Brien KK, Colquhoun H, Levac D, Baxter L, Tricco AC, Straus S, et al. Advancing scoping study methodology: a web-based survey and consultation of perceptions on terminology, definition and methodological steps. BMC Health Serv Res [Internet]. 2016;16(1):1–12. Available from: doi: 10.1186/s12913-016-1579-z [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Aromataris E, Munn Z. Johanna Briggs Institute reviewer’s manual. The Joanna Briggs Institute. 2017. [ Google Scholar ]
- 31. Hartmann T, Popkin M. ADHD: a hunter in a farmer’s world. Rochester, Vermont: Healing Arts Press; 2019. [ Google Scholar ]
- 32. Weiss L. Embracing ADHD: A healing perspecive. Lanham, MD: Taylor Trade Publishing; 2015. [ Google Scholar ]
- 33. Maté G. Scattered minds: The origin and healing of Attention Deficit Disorder. London, UK: Vermilion; 1999. [ Google Scholar ]
- 34. Amen D. Healing ADD: The breakthrough program that allows you to see and heal the 7 types of Attention Deficit Disorder. New York, NY: Berkley Publishing Group; 2013. [ Google Scholar ]
- 35. Conway F. Psychodynamic psychotherapy of ADHD: a review of the literature. Psychotherapy. 2012;49(3):404–17. doi: 10.1037/a0027344 [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Heirs M, Dean ME. Homeopathy for attention deficit/hyperactivity disorder or hyperkinetic disorder. Cochrane Database Syst Rev. 2007;(4). [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Auclair V, Harvey P-O, Lepage M. Cognitive behavioral therapy and the treatment of ADHD in adults TT—La thérapie cognitive-comportementale dans le traitement du TDAH chez l’adulte. Sante Ment Que [Internet]. 2016;41(1):291–311. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27570962 [ PubMed ] [ Google Scholar ]
- 38. Chandler ML. Psychotherapy for adult attention deficit/hyperactivity disorder: a comparison with cognitive behaviour therapy. J Psychiatr Ment Health Nurs. 2013;20(9):814–20. doi: 10.1111/jpm.12023 [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Jensen CM, Amdisen BL, Jørgensen KJ, Arnfred SMH. Cognitive behavioural therapy for ADHD in adults: systematic review and meta-analyses. ADHD Atten Deficit Hyperact Disord. 2016;8(1):3–11. doi: 10.1007/s12402-016-0188-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Lopez PL, Torrente FM, Ciapponi A, Lischinsky AG, Cetkovich-Bakmas M, Rojas JI, et al. Cognitive-behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2018;2018(3). doi: 10.1002/14651858.CD010840.pub2 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Young Z, Moghaddam N, Tickle A. The efficacy of cognitive behavioral therapy for adults with ADHD: a systematic review and meta-analysis of randomized controlled trials. J Atten Disord [Internet]. 2016;24(6):875–88. Available from: doi: 10.1177/1087054716664413 [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Lee CSC, Ma M ting, Ho H yui, Tsang K kei, Zheng Y yi, Wu Z yi. The effectiveness of mindfulness-based intervention in attention of individuals with ADHD: a systematic review. Hong Kong J Occup Ther [Internet]. 2017;30:33–41. Available from: doi: 10.1016/j.hkjot.2017.05.001 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Poissant H, Mendrek A, Talbot N, Khoury B, Nolan J. Behavioral and cognitive impacts of mindfulness-based interventions on adults with attention-deficit hyperactivity disorder: a systematic review. Behav Neurol. 2019;2019. doi: 10.1155/2019/5682050 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Zhang J, Díaz-Román A, Cortese S. Meditation-based therapies for attention-deficit/hyperactivity disorder in children, adolescents and adults: a systematic review and meta-analysis. Evid Based Ment Health. 2018;21(3):87–94. doi: 10.1136/ebmental-2018-300015 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Krisanaprakornkit T, Ngamjarus C, Witoonchart C, Piyavhatkul N. Meditation therapies for attention-deficit/hyperactivity disorder (ADHD). Cochrane Database Syst Rev. 2010;(6). doi: 10.1002/14651858.CD006507.pub2 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Sonuga-Barke EJ, Brandeis D, Cortese S, Daley D, Ferrin M, Holtmann M, et al. Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatry. 2013;170(3):275–89. doi: 10.1176/appi.ajp.2012.12070991 [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Vidal-Estrada R, Bosch-Munso R, Nogueira-Morais M, Casas-Brugue M, Ramos-Quiroga JA. Psychological treatment of attention deficit hyperactivity disorder in adults: a systematic review. Actas Esp Psiquiatr. 2012;40(3):147–54. [ PubMed ] [ Google Scholar ]
- 48. De Crescenzo F, Cortese S, Adamo N, Janiri L. Pharmacological and non-pharmacological treatment of adults with ADHD: a meta-review. Evid Based Ment Health. 2017;20(1):4–11. doi: 10.1136/eb-2016-102415 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Arnold LE, Hodgkins P, Caci H, Kahle J, Young S. Effect of treatment modality on long-term outcomes in attention-deficit/hyperactivity disorder: a systematic review. PLoS One [Internet]. 2015;10(2):1–19. Available from: 10.1371/journal.pone.0116407 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Seixas M, Weiss M, Müller U. Systematic review of national and international guidelines on attention-deficit hyperactivity disorder. J Psychopharmacol. 2012. Jun;26(6):753–65. doi: 10.1177/0269881111412095 [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Van Lieshout M, Luman M, Buitelaar J, Rommelse NNJ, Oosterlaan J. Does neurocognitive functioning predict future or persistence of ADHD? A systematic review. Clin Psychol Rev [Internet]. 2013;33(4):539–60. Available from: doi: 10.1016/j.cpr.2013.02.003 [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Bjerrum MB, Pedersen PU, Larsen P. Living with symptoms of attention deficit hyperactivity disorder in adulthood: a systematic review of qualitative evidence. JBI Database Syst Rev Implement Reports. 2017;15(4):1080–153. doi: 10.11124/JBISRIR-2017-003357 [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Hayes SC, Hofmann SG. The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry. 2017;16(3):245–6. doi: 10.1002/wps.20442 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 54. Burgess PW, Mitchelmore S, Giles GM. Behavioral treatment of attention deficits in mentally impaired subjects. Am J Occup Ther. 1997;3241(8):505–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Wood RL. Head trauma rehabilitation: A neurobehavioural approach. London: Croom Helm; 1987. [ Google Scholar ]
- 56. Jordan DR. Attention Deficit Disorder: ADHD and ADD syndromes. Third. Austin, TX: Pro-Ed; 1998. [ Google Scholar ]
- 57. Carpentier P. ADHD in adults: food for psychotherapists? J Psychother. 2004;30(2):83–9. [ Google Scholar ]
- 58. Yankura J, Dryden W. Using REBT with common psychological problems: A therapist’s casebook. New York: Springer Publishing Co.; 1997. [ Google Scholar ]
- 59. Barkley RA. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. New York: Guildford Press; 1990. [ Google Scholar ]
- 60. American Psychiatric Association. The diagnostic and statistical manual of mental disorders. 4th ed. Washington D.C.: American Psychiatric Association; 1994. [ Google Scholar ]
- 61. Douglas VI. Higher mental processess in hyperactive children: implications for training. In: Knights RM, Bakker DJ, editors. Treatment of hyperactive and learning disordered children. Baltimore: University Park Press; 1980. p. 65–92. [ Google Scholar ]
- 62. Stevenson CS, Whitmont S, Bornholt L, Livesey D, Stevenson RJ. A cognitive remediation programme for adults with Attention Deficit Hyperactivity Disorder. Aust N Z J Psychiatry. 2002;36(5):610–6. doi: 10.1046/j.1440-1614.2002.01052.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Safren SA, Otto MW, Sprich S, Winett CL, Wilens TE, Biederman J. Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms. Behav Res Ther. 2005;43(7):831–42. doi: 10.1016/j.brat.2004.07.001 [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Young S, Khondoker M, Emilsson B, Sigurdsson JF, Philipp-Wiegmann F, Baldursson G, et al. Cognitive-behavioural therapy in medication-treated adults with attention-deficit/hyperactivity disorder and co-morbid psychopathology: a randomized controlled trial using multi-level analysis. Psychol Med. 2015;45(13):2793–804. doi: 10.1017/S0033291715000756 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 65. In de Braek DMJM, Dijkstra JB, Ponds RW, Jolles J. Goal management training in adults with ADHD: an intervention study. J Atten Disord. 2017;21(13):1130–7. doi: 10.1177/1087054712468052 [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Pettersson R, Söderström S, Edlund-Söderström K, Nilsson KW. Internet-based cognitive behavioral therapy for adults With ADHD in outpatient psychiatric care: a randomized trial. J Atten Disord [Internet]. 2017;21(6):508–21. Available from: doi: 10.1177/1087054714539998 [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Young S, Emilsson B, Sigurdsson JF, Khondoker M, Philipp-Wiegmann F, Baldursson G, et al. A randomized controlled trial reporting functional outcomes of cognitive–behavioural therapy in medication-treated adults with ADHD and comorbid psychopathology. Eur Arch Psychiatry Clin Neurosci. 2017;267(3):267–76. doi: 10.1007/s00406-016-0735-0 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Dittner AJ, Hodsoll J, Rimes KA, Russell AJ, Chalder T. Cognitive–behavioural therapy for adult attention-deficit hyperactivity disorder: a proof of concept randomised controlled trial. Acta Psychiatr Scand. 2018;137(2):125–37. doi: 10.1111/acps.12836 [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Solanto M V., Surman CB, Alvir JMJ. The efficacy of cognitive–behavioral therapy for older adults with ADHD: a randomized controlled trial. ADHD Atten Deficit Hyperact Disord [Internet]. 2018;10(3):223–35. Available from: doi: 10.1007/s12402-018-0253-1 [ DOI ] [ PubMed ] [ Google Scholar ]
- 70. Huang F, Tang YL, Zhao M, Wang Y, Pan M, Wang Y, et al. Cognitive-behavioral therapy for adult ADHD: a randomized clinical trial in china. J Atten Disord. 2019;23(9):1035–46. doi: 10.1177/1087054717725874 [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Van der Oord S, Boyer BE, Van dyck L, Mackay KJ, De Meyer H, Baeyens D. A randomized controlled study of a cognitive behavioral planning intervention for college students with ADHD: an effectiveness study in student counseling services in Flanders. J Atten Disord. 2020;24(6):849–62. doi: 10.1177/1087054718787033 [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Cherkasova M V., French LR, Syer CA, Cousins L, Galina H, Ahmadi-Kashani Y, et al. Efficacy of cognitive behavioral therapy with and without medication for adults with ADHD: a randomized clinical trial. J Atten Disord. 2020;24(6):889–903. doi: 10.1177/1087054716671197 [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Weiss M, Hechtman L. A randomized double-blind trial of paroxetine and/or dextroamphetamine and problem-focused therapy for attention-deficit/hyperactivity disorder in adults. J Clin Psychiatry. 2006;67(4):611–9. [ PubMed ] [ Google Scholar ]
- 74. Virta M, Salakari A, Antila M, Chydenius E, Partinen M, Kaski M, et al. Hypnotherapy for adults with attention deficit hyperactivity disorder: a randomized controlled study. Contemp Hypn. 2010;27(1):5–18. [ Google Scholar ]
- 75. Safren SA, Sprich SE, Cooper-Vince C, Knouse LE, Lerner JA. Life impairments in adults with medication-treated ADHD. J Atten Disord. 2010;13(5):524–31. doi: 10.1177/1087054709332460 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 76. Solanto M V, Marks DJ, Wasserstein J, Mitchell K, Abikoff H, Alvir JMJ, et al. Efficacy of meta-cognitive therapy for adult ADHD. Am J Psychiatry. 2010;167(August):958–68. doi: 10.1176/appi.ajp.2009.09081123 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 77. Emilsson B, Gudjonsson G, Sigurdsson JF, Baldursson G, Einarsson E, Olafsdottir H, et al. Cognitive behaviour therapy in medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. BMC Psychiatry. 2011;11. doi: 10.1186/1471-244X-11-11 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 78. Weiss M, Murray C, Wasdell M, Greenfield B, Giles L, Hechtman L. A randomized controlled trial of CBT therapy for adults with ADHD with and without medication. BMC Psychiatry. 2012;12. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Vidal-Estrada R, Bosch R, Nogueira M, Gómez-Barros N, Valero S, Palomar G, et al. Psychoeducation for adults with attention deficit hyperactivity disorder vs. cognitive behavioral group therapy: a randomized controlled pilot study. J Nerv Ment Dis. 2013;201(10):894–900. doi: 10.1097/NMD.0b013e3182a5c2c5 [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Dittner AJ, Rimes KA, Russell AJ, Chalder T. Protocol for a proof of concept randomized controlled trial of cognitive-behavioural therapy for adult ADHD as a supplement to treatment as usual, compared with treatment as usual alone. BMC Psychiatry. 2014;14(1):1–11. doi: 10.1186/s12888-014-0248-1 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Wiggins D, Singh K, Getz HG, Hutchins DE. Effects of brief group intervention for adults with attention deficit/hyperactivity disorder. J Ment Heal Couns [Internet]. 1999;21(1):82–92. Available from: internal-pdf://253.226.149.212/Wiggins et al 2000 Rathlin.pdf [ Google Scholar ]
- 82. Burt KL, Parks-Charney R, Schwean VL. The AD/HD skills and strategies program: a program for AD/HD adults in postsecondary education. Can J Sch Psychol. 1997;12(2):122–34. [ Google Scholar ]
- 83. Virta M, Vedenpaa A, Gronroos N, Chydenius E, Partinen M, Vataja R, et al. Adults with ADHD benefit from cognitive-behaviourally oriented group rehabilitation. J Atten. 2008;12(13):218–26. [ DOI ] [ PubMed ] [ Google Scholar ]
- 84. Bramham J, Young S, Bickerdike A, Spain D, McCartan D, Xenitidis K. Evaluation of group cognitive behavioral therapy for adults with ADHD. J Atten Disord [Internet]. 2009. Mar [cited 2014 Nov 13];12(5):434–41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18310557 doi: 10.1177/1087054708314596 [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Holmefur M, Lidström-Holmqvist K, Roshanay AH, Arvidsson P, White S, Janeslätt G. Pilot study of let’s get organized: a group intervention for improving time management. Am J Occup Ther. 2019;73(5):1–10. doi: 10.5014/ajot.2019.032631 [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Anastopoulos AD, King KA. A cognitive-behavior therapy and mentoring program for college students with ADHD. Cogn Behav Pract. 2015;22(2):141–51. [ Google Scholar ]
- 87. LaCount PA, Hartung CM, Shelton CR, Clapp JD, Clapp TKW. Preliminary evaluation of a combined group and individual treatment for college students with attention-deficit/hyperactivity disorder. Cogn Behav Pract [Internet]. 2015;22(2):152–60. Available from: 10.1016/j.cbpra.2014.07.004 [ DOI ] [ Google Scholar ]
- 88. Rostain AL, Ramsay JR. A combined treatment approach for adults with ADHD—results of an open study of 43 patients. J Atten Disord. 2006;10(2):150–9. doi: 10.1177/1087054706288110 [ DOI ] [ PubMed ] [ Google Scholar ]
- 89. Lindstedt H, Umb-Carlsson Õ. Cognitive assistive technology and professional support in everyday life for adults with ADHD. Disabil Rehabil Assist Technol. 2013;8(5):402–8. doi: 10.3109/17483107.2013.769120 [ DOI ] [ PubMed ] [ Google Scholar ]
- 90. Luiu AL, Prada P, Perroud N, Lovis C, Ehrler F. ADHD mobile app feasibility test for adults. Stud Health Technol Inform. 2018;255:247–51. [ PubMed ] [ Google Scholar ]
- 91. Strohmeier CW, Rosenfield B, DiTomasso RA, Ramsay JR. Assessment of the relationship between self-reported cognitive distortions and adult ADHD, anxiety, depression, and hopelessness. Psychiatry Res. 2016;238:153–8. doi: 10.1016/j.psychres.2016.02.034 [ DOI ] [ PubMed ] [ Google Scholar ]
- 92. Young S, Bramham J, Gray K, Rose E. A phenomenological analysis of the experience of receiving a diagnosis and treatment of ADHD in adulthood: a partner’s perspective. J Atten Disord. 2008;12(4):299–307. doi: 10.1177/1087054707311659 [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Anastopoulos AD, King KA, Besecker LH, O’Rourke SR, Bray AC, Supple AJ. Cognitive-behavioral therapy for college students with ADHD: temporal stability of improvements in functioning following active treatment. J Atten Disord. 2020;24(6):863–74. doi: 10.1177/1087054717749932 [ DOI ] [ PubMed ] [ Google Scholar ]
- 94. Wang X, Cao Q, Wang J, Wu Z, Wang P, Sun L, et al. The effects of cognitive-behavioral therapy on intrinsic functional brain networks in adults with attention-deficit/hyperactivity disorder. Behav Res Ther [Internet]. 2016;76:32–9. Available from: doi: 10.1016/j.brat.2015.11.003 [ DOI ] [ PubMed ] [ Google Scholar ]
- 95. Salakari A, Virta M, Grönroos N, Chydenius E, Partinen M, Vat, et al. Cognitive-behaviourally-oriented group rehabilitation of adults with ADHD: results of a 6-month follow-up. J Atten Disord. 2010;13(5):516–23. doi: 10.1177/1087054709332069 [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. Torrente F, López P, Alvarez Prado D, Kichic R, Cetkovich-Bakmas M, Lischinsky A, et al. Dysfunctional cognitions and their emotional, behavioral, and functional correlates in adults with attention deficit hyperactivity disorder (ADHD): is the cognitive-behavioral model valid? J Atten Disord [Internet]. 2014;18(5):412–24. Available from: doi: 10.1177/1087054712443153 [ DOI ] [ PubMed ] [ Google Scholar ]
- 97. Young S. Coping strategies used by adults with ADHD. Pers Individ Dif. 2005;38(4):809–16. [ Google Scholar ]
- 98. Mitchell JT, McIntyre EM, English JS, Dennis MF, Beckham JC, Kollins SH. A pilot trial of mindfulness meditation training for ADHD in adulthood: impact on core symptoms, executive functioning, and emotion dysregulation. J Atten Disord [Internet]. 2013;21(13):1105–20. Available from: 10.1177/1087054713513328 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. Puente AN, Mitchell JT. Cognitive-behavioral therapy for adult ADHD: a case study of multi-method assessment of executive functioning in clinical practice and manualized treatment adaptation. Clin Case Stud. 2016;15(3):198–211. [ Google Scholar ]
- 100. Ramsay JR. “Turning intentions into actions”: CBT for adult ADHD focused on implementation. Clin Case Stud. 2016;15(3):179–97. [ Google Scholar ]
- 101. Goodwin RE, Corgiat MD. Cognitive rehabilitation of adult attention deficit disorder: a case study. J Cogn Rehabil [Internet]. 1992;10(October):28–35. Available from: http://search.proquest.com.ezp.lib.unimelb.edu.au/docview/618290820?accountid=12372 [ Google Scholar ]
- 102. Ramsay JR. “Without a net”: CBT without medications for an adult with ADHD. Clin Case Stud. 2012;11(1):48–65. [ Google Scholar ]
- 103. Weinstein C. Cognitive remediation strategies: an adjunct to the psychotherapy of adults with attention-deficit hyperativity disorder. J Psychother Pract Res. 1994;3:44–57. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 104. Wilens TE, McDermott SP, Biederman J, Abrantes A, Hahesy A, Spencer TJ. Cognitive therapy in the treatment of adults with ADHD: a systematic chart review of 26 cases. J Cogn Psychother An Int Q. 1999;13(3):215–26. [ Google Scholar ]
- 105. Yovel I, Safren SA. Measuring homework utility in psychotherapy: cognitive-behavioral therapy for adult attention-deficit hyperactivity disorder as an example. Cognit Ther Res. 2007;31(3):385–99. [ Google Scholar ]
- 106. Ramsay JR, Rostain AL. Cognitive therapy: a psychosocial treatment for ADHD in adults. ADHD Rep. 2004;12(1):1–5. [ Google Scholar ]
- 107. Safren SA, Sprich S, Chulvick S, Otto MW. Psychosocial treatments for adults with attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2004;27(2):349–60. doi: 10.1016/S0193-953X(03)00089-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 108. Safren SA, Perlman C, Sprich S, Otto M. Mastering your adult ADHD. New York: Oxford University Press; 2005. [ Google Scholar ]
- 109. Gentile JP, Atiq R, Gillig P. Psychotherapy for the patient with adult ADHD. Psychiatry (Edgmont). 2006;3(8):31–315. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 110. Ramsay JR. Current status of cognitive-behavioral therapy as a psychosocial treatment for adult attention-deficit/hyperactivity disorder. Curr Psychiatry Rep [Internet]. 2007. Oct 3;9(5):427–33. Available from: http://link.springer.com/10.1007/s11920-007-0056-0 [ DOI ] [ PubMed ] [ Google Scholar ]
- 111. Young S, Bramham J. ADHD in adults: a psychological guide to practice. Chichester, West Sussex: John Wiley & Sons, Inc; 2007. [ Google Scholar ]
- 112. Young SJ, Ross RR. R&R2 for ADHD youths and adults: a prosocial competence training program. Ottawa, Canada: Cognitive Centre of Canada; 2007. [ Google Scholar ]
- 113. Knight LA, Rooney M, Chronis-Tuscano A. Psychosocial treatments for attention-deficit /hyperactivity disorder. Curr Psychiatry Rep. 2008;10:412–8. doi: 10.1007/s11920-008-0066-6 [ DOI ] [ PubMed ] [ Google Scholar ]
- 114. Ramsay JR, Rostain AL. Cognitive behaviour therapy for college students with attention deficit/hyperactivity disorder. J College Stud Psychother. 2008;21(1):3–20. [ Google Scholar ]
- 115. Ramsay JR, Rostain AL. Adult ADHD research. J Atten Disord. 2008;11(6):624–7. doi: 10.1177/1087054708314590 [ DOI ] [ PubMed ] [ Google Scholar ]
- 116. Knouse LE, Safren SA. Current status of cognitive behavioral therapy for adult attention-deficit hyperactivity disorder. Psychiatr Clin North Am [Internet]. 2010. Sep [cited 2014 Dec 15];33(3):497–509. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2909688&tool=pmcentrez&rendertype=abstract doi: 10.1016/j.psc.2010.04.001 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 117. Sohlberg MM, Mateer CA. Improving attention and managing attentional problems. Ann N Y Acad Sci. 2001;931:359–75. [ PubMed ] [ Google Scholar ]
- 118. Ramsay JR. Nonmedication treatments for adult ADHD. Washington D.C.: American Psychological Association; 2010. [ Google Scholar ]
- 119. Ramsay JR. CBT for adult ADHD: adaptations and hypothesized mechanisms of change. J Cogn Psychother. 2010;24(1):37–45. [ Google Scholar ]
- 120. Newark PE, Stieglitz RD. Therapy-relevant factors in adult ADHD from a cognitive behavioural perspective. ADHD Atten Deficit Hyperact Disord. 2010;2(2):59–72. doi: 10.1007/s12402-010-0023-1 [ DOI ] [ PubMed ] [ Google Scholar ]
- 121. Young S, Bramham J. Cognitive-behavioural therapy for ADHD in adolescents and adults: A psychological guide to practice. 2nd ed. Chichester, West Sussex: Wiley-Blackwell; 2012. [ Google Scholar ]
- 122. Knouse LE. Cognitive behavioural therapies for ADHD. In: Barkley RA, editor. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. 4th ed. New York: Guilford Press; 2014. p. 757–94. [ Google Scholar ]
- 123. Knouse LE. Cognitive-behavioral therapy for ADHD in college: recommendations “hot off the press.” ADHD Rep. 2015;23(5):8–15. [ Google Scholar ]
- 124. Ramsay JR. The relevance of cognitive distortions in the psychosocial treatment of adult ADHD. Prof Psychol Res Pract. 2017;48(1):62–9. [ Google Scholar ]
- 125. Jeavons A, Bishop T, French B, Bastable S, Harpham-Salter A. The adult ADHD treatment handbook. Abington, Oxon: Routledge; 2018. [ Google Scholar ]
- 126. Knouse LE, Ramsay JR. Managing side effects in CBT for adult ADHD. ADHD Rep. 2018;26(2):6–10. [ Google Scholar ]
- 127. Kooij JJS, Bijlenga D, Michielsen M. Assessment and treatment of ADHD in people over 60. ADHD Rep. 2019;27(4):1–7,15–16. [ Google Scholar ]
- 128. Nadeau K. The clinician’s role in the treatment of ADHD. In: Goldstein S, Ellison AT, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 107–26. [ Google Scholar ]
- 129. Nadeau KG. Life management skills for the adult with ADHD. In: Nadeau KG, editor. A comprehensive guide to attention deficit disorder in adults. New York, NY: Brunner/Mazel Inc.; 1995. p. 191–217. [ Google Scholar ]
- 130. Murphy K. Empowering the adult with ADHD. In: Nadeau KG, editor. A comprehensive guide to attention deficit disorder in adults. New York, NY: Brunner/Mazel Inc.; 1995. p. 135–45. [ Google Scholar ]
- 131. Wender PH, Wolf LE, Wasserstein J. Adults with ADHD an overview. Ann N Y Acad Sci. 2001;931(1):1–16. [ PubMed ] [ Google Scholar ]
- 132. Mongia M, Hechtman L. Cognitive behavior therapy for adults with attention-deficit/hyperactivity disorder: a review of recent randomized controlled trials. Curr Psychiatry Rep. 2012;14(5):561–7. doi: 10.1007/s11920-012-0303-x [ DOI ] [ PubMed ] [ Google Scholar ]
- 133. Wedlake M. Cognitive remediation therapy for undergraduates with ADHD. ADHD Rep. 2002;10(5):11–6. [ Google Scholar ]
- 134. Young S. Psychological therapy for adults with attention deficit hyperactivity disorder. Couns Psychol Q. 1999;12(2):183–90. [ Google Scholar ]
- 135. Young S. A model of psychotherapy for adults with ADHD. In: Goldstein S, Ellison T, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 147–63. [ Google Scholar ]
- 136. McDermott S. Cognitive Therapy for adults with attention-deficit/hyperactivity disorder. In: Brown TE, editor. Attention-deficit disorders and comorbidities in children, adolescents, and adults. Arlington, VA: American Psychiatric Publishing, Inc.; 2000. p. 569–606. [ Google Scholar ]
- 137. Murphy K. Psychological counselling of adults with ADHD. In: Barkley RA, editor. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. 3rd ed. New York, NY: Guildford Press; 2006. [ Google Scholar ]
- 138. Brooks RB. Changing the mindset of adults with ADHD: strategies for fostering hope, optimism, and resilience. In: Goldstein S, Ellison AT, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 127–46. [ Google Scholar ]
- 139. Stevenson CS, Stevenson RJ, Whitmont S. A self-directed psychosocial intervention with minimal therapist contact for adults with attention deficit hyperactivity disorder. Clin Psychol Psychother. 2003;10(2):93–101. [ Google Scholar ]
- 140. Low CB. Attention deficit hyperactivity disorder: dissociation and adaptation (a theoretical presentation and case study). Am J Clin Hypn. 1999;41(3):253–61. doi: 10.1080/00029157.1999.10404216 [ DOI ] [ PubMed ] [ Google Scholar ]
- 141. Fleming AP, McMahon RJ. Developmental context and treatment principles for ADHD among college students. Clin Child Fam Psychol Rev. 2012;15(4):303–29. doi: 10.1007/s10567-012-0121-z [ DOI ] [ PubMed ] [ Google Scholar ]
- 142. Jackson B, Farrugia D. Diagnosis and treatment of adults with attention deficit hyperactivity disorder. J Couns Dev. 1997;75(4):312–9. [ Google Scholar ]
- 143. Hallowell E, Ratey J. Driven to distraction. New York: Touchstone; 1994. doi: 10.1080/14640749408401099 [ DOI ] [ Google Scholar ]
- 144. Ramsay JR, Rostain AL. Psychosocial treatments for attention-deficit/hyperactivity disorder in adults: current evidence and future directions. Prof Psychol Res Pract. 2007;38(4):338–46. [ Google Scholar ]
- 145. Ramsay JR, Rostain AL. The adult ADHD toolkit. New York: Routledge; 2015. [ Google Scholar ]
- 146. Ramsay JR, Rostain. A cognitive therapy approach for adult attention deficit/hyperactivity disorder. J Cogn Psychother An Int Q. 2003;17(4):319–34. [ Google Scholar ]
- 147. Young S, Bramham J, Gray K, Rose E. The experience of receiving a diagnosis and treatment of ADHD in adulthood: a qualitative study of clinically referred patients using interpretative phenomenological analysis. J Atten Disord. 2008;11(4):493–503. doi: 10.1177/1087054707305172 [ DOI ] [ PubMed ] [ Google Scholar ]
- 148. American Psychiatric Association [APA]. The diagnostic and statistical manual of mental disorders. IV-TR. Washington D.C.: American Psychiatric Publishing, Inc.; 2000. [ Google Scholar ]
- 149. American Psychiatric Association [APA]. The diagnostic and statistical manual of mental disorders. 5th ed. Washington D.C.: American Psychiatric Association; 2013. [ Google Scholar ]
- 150. Solanto M V. Cognitive-behavioural therapy for adult ADHD. New York: Guildford Press; 2010. [ Google Scholar ]
- 151. Wasserstein J, Lynn A. Metacognitive remediation in adult ADHD. Treating executive function deficits via executive functions. Ann N Y Acad Sci [Internet]. 2001;931:376–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11462754 [ PubMed ] [ Google Scholar ]
- 152. Bemporad JR. Aspects of psychotherapy with adults with attention deficit disorder. Ann N Y Acad Sci. 2001;931:302–9. doi: 10.1111/j.1749-6632.2001.tb05787.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 153. Philipsen A, Graf E, Tebartz van Elst L, Jans T, Warnke A, Hesslinger B, et al. Evaluation of the efficacy and effectiveness of a structured disorder tailored psychotherapy in ADHD in adults: study protocol of a randomized controlled multicentre trial. Atten Defic Hyperact Disord. 2010. Dec;2(4):203–12. doi: 10.1007/s12402-010-0046-7 [ DOI ] [ PubMed ] [ Google Scholar ]
- 154. Philipsen A, Jans T, Graf E, Matthies S, Borel P, Colla M, et al. Effects of group psychotherapy, individual counseling, methylphenidate, and placebo in the treatment of adult attention-deficit/hyperactivity disorder a randomized clinical trial. JAMA Psychiatry. 2015;72(12):1199–210. doi: 10.1001/jamapsychiatry.2015.2146 [ DOI ] [ PubMed ] [ Google Scholar ]
- 155. Lam AP, Matthies S, Graf E, Colla M, Jacob C, Sobanski E, et al. Long-term Effects of multimodal treatment on adult attention-deficit/hyperactivity disorder symptoms: follow-up analysis of the COMPAS trial. JAMA Netw open. 2019;2(5):e194980. doi: 10.1001/jamanetworkopen.2019.4980 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 156. Edel MA, Hölter T, Wassink K, Juckel G. A comparison of mindfulness-based group training and skills group training in adults with ADHD: an open study. J Atten Disord. 2017;21(6):533–9. doi: 10.1177/1087054714551635 [ DOI ] [ PubMed ] [ Google Scholar ]
- 157. Fleming AP, Fleming AP. Randomized controlled trial of group cognitive-behavioral therapy for ADHD among college students. University of Washington; 2013. [ Google Scholar ]
- 158. Hesslinger B, Philipsen A, Richter H, Ebert D. Psychotherapie der ADHS im Erwachsenenalter. In: Diagnostik und Therapie der ADHS im Erwachsenenalter. 2004. p. 63–80. doi: 10.1111/j.1471-4159.2004.02740.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 159. Hesslinger B, Tebartz van Elst L, Nyberg E, Dykierek P, Richter H, Berner M, et al. Psychotherapy of attention deficit hyperactivity disorder in adults: a pilot study using a structured skills training program. Eur Arch Psychiatry Clin Neurosci. 2002. Aug;252(4):177–84. doi: 10.1007/s00406-002-0379-0 [ DOI ] [ PubMed ] [ Google Scholar ]
- 160. Jacob C, Philipsen A, Ebert D, Deckert J. "Multimodale Therapie der Aufmerksamkeitsdefizit-/ Hyperaktivitätsstörung im Erwachsenenalter. Nervenarzt. 2008;79(7):801–8. doi: 10.1007/s00115-008-2510-6 [ DOI ] [ PubMed ] [ Google Scholar ]
- 161. Philipsen A, Richter H, Peters J, Alm B, Sobanski E, Colla M, et al. Structured group psychotherapy in adults with attention deficit hyperactivity disorder: results of an open multicentre study. J Nerv Ment Dis [Internet]. 2007. Dec [cited 2014 Dec 5];195(12):1013–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18091195 doi: 10.1097/NMD.0b013e31815c088b [ DOI ] [ PubMed ] [ Google Scholar ]
- 162. Linehan MM. Cognitive-behavioural treatment of borderline personality disorder. 14th ed. New York: Guildford Press; 1993. [ Google Scholar ]
- 163. Hartmann T. ADD: a different perception. Grass Valley, California: Underwood Books; 1997. [ Google Scholar ]
- 164. Wender PH. Attention deficit hyperactivity disorder in adults. New York: Oxford University Press; 1995. [ Google Scholar ]
- 165. Aadil M, Cosme RM, Chernaik J. Mindfulness-based cognitive behavioral therapy as an adjunct treatment of attention deficit hyperactivity disorder in young adults: a literature review. Cureus. 2017;9(5). doi: 10.7759/cureus.1269 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 166. Cairncross M, Miller CJ. The effectiveness of mindfulness-based therapies for ADHD. J Atten Disord [Internet]. 2016;108705471562530. Available from: doi: 10.1177/1087054715625301 [ DOI ] [ PubMed ] [ Google Scholar ]
- 167. Xue J, Zhang Y, Huang Y, Tusconi M. A meta-analytic investigation of the impact of mindfulness-based interventions on ADHD symptoms. Med (United States). 2019;98(23):1–10. doi: 10.1097/MD.0000000000015957 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 168. Janssen L, Kan CC, Carpentier PJ, Sizoo B, Hepark S, Grutters J, et al. Mindfulness based cognitive therapy versus treatment as usual in adults with attention deficit hyperactivity disorder (ADHD). BMC Psychiatry. 2015;15(1). doi: 10.1186/s12888-015-0591-x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 169. Hepark S, Janssen L, de Vries A, Schoenberg PLA, Donders R, Kan CC, et al. The efficacy of adapted MBCT on core symptoms and executive functioning in adults with ADHD: a preliminary randomized controlled trial. J Atten Disord [Internet]. 2015;23(4):351–62. Available from: doi: 10.1177/1087054715613587 [ DOI ] [ PubMed ] [ Google Scholar ]
- 170. Bachmann K, Lam AP, Sörös P, Kanat M, Hoxhaj E, Matthies S, et al. Effects of mindfulness and psychoeducation on working memory in adult ADHD: a randomised, controlled fMRI study. Behav Res Ther [Internet]. 2018;106(April):47–56. Available from: doi: 10.1016/j.brat.2018.05.002 [ DOI ] [ PubMed ] [ Google Scholar ]
- 171. Gu Y, Xu G, Zhu Y. A randomized controlled trial of mindfulness-based cognitive therapy for college students with ADHD. J Atten Disord [Internet]. 2018;22(4):388–99. Available from: doi: 10.1177/1087054716686183 [ DOI ] [ PubMed ] [ Google Scholar ]
- 172. Hoxhaj E, Sadohara C, Borel P, D’Amelio R, Sobanski E, Müller H, et al. Mindfulness vs psychoeducation in adult ADHD: a randomized controlled trial. Eur Arch Psychiatry Clin Neurosci [Internet]. 2018;268(4):321–35. Available from: doi: 10.1007/s00406-018-0868-4 [ DOI ] [ PubMed ] [ Google Scholar ]
- 173. Schoenberg PLA, Hepark S, Kan CC, Barendregt HP, Buitelaar JK, Speckens AEM. Effects of mindfulness-based cognitive therapy on neurophysiological correlates of performance monitoring in adult attention-deficit/hyperactivity disorder. Clin Neurophysiol [Internet]. 2014;125(7):1407–16. Available from: doi: 10.1016/j.clinph.2013.11.031 [ DOI ] [ PubMed ] [ Google Scholar ]
- 174. Janssen L, Kan CC, Carpentier PJ, Sizoo B, Hepark S, Schellekens MPJ, et al. Mindfulness-based cognitive therapy v. treatment as usual in adults with ADHD: a multicentre, single-blind, randomised controlled trial. Psychol Med. 2018;48(11):1920. doi: 10.1017/S0033291718000776 [ DOI ] [ PubMed ] [ Google Scholar ]
- 175. Zylowska L, Ackerman D, Yang M, Futrell J, Horton N, Hale TS, et al. Mindfulness meditation training in adults and adolescents with ADHD: a feasibility study. J Atten Disord. 2008;11(6):737–46. doi: 10.1177/1087054707308502 [ DOI ] [ PubMed ] [ Google Scholar ]
- 176. Zylowska L, Smalley SL, Schwartz JM. Mindful awareness and ADHD. Clin Handb Mindfulness. 2009;319–38. [ Google Scholar ]
- 177. Bueno VF, Kozasa EH, Da Silva MA, Alves TM, Louzã MR, Pompeiá S. Mindfulness meditation improves mood, quality of life, and attention in adults with attention deficit hyperactivity disorder. Biomed Res Int. 2015;2015. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 178. Mitchell JT, Zylowska L, Kollins SH. Mindfulness meditation training for attention-deficit/hyperactivity disorder in adulthood: current empirical support, treatment overview, and future directions. Cogn Behav Pract. 2015;22(2):172–91. doi: 10.1016/j.cbpra.2014.10.002 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 179. Baijal S, Gupta R. Meditation-based training: a possible intervention for attention deficit hyperactivity disorder. Psychiatry (Edgmont) [Internet]. 2008;5(4):48–55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19727310%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2719552 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 180. Ramsay JR, Rostain AL. Adult attention-deficit/hyperactivity disorder as an implementation problem: Clinical significance, underlying mechanisms, and psychosocial treatment. Pract Innov. 2016;1(1):36–52. [ Google Scholar ]
- 181. Bachmann K, Lam AP, Philipsen A. Mindfulness-based cognitive therapy and the adult ADHD brain: A neuropsychotherapeutic perspective. Front Psychiatry. 2016;7(JUN):1–7. doi: 10.3389/fpsyt.2016.00117 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 182. Zylowska L. The mindfulness prescription for adult ADHD. Boulder, CO: Trumpeter; 2012. [ Google Scholar ]
- 183. Jensen PS, Mrazek D, Knapp PK, Steinberg L, Pfeffer C, Schowalter J, et al. Evolution and revolution in child psychiatry: ADHD as a disorder of adaptation. J Am Acad Child Adolesc Psychiatry [Internet]. 1997;36(12):1672–81. Available from: doi: 10.1097/00004583-199712000-00015 [ DOI ] [ PubMed ] [ Google Scholar ]
- 184. Stein DJ, Fan J, Fossella J, Russell VA. Inattention and hyperactivity-impulsivity: psychobiological and evolutionary underpinnings of ADHD. CNS Spectr. 2007;12(3):190–6. doi: 10.1017/s1092852900020903 [ DOI ] [ PubMed ] [ Google Scholar ]
- 185. Smalley S. Reframing ADHD in the genomic era. Psychiatr Times [Internet]. 2008;15(7):74–8. Available from: http://www.psychiatrictimes.com/display/article/10168/1163208?pageNumber=2 [ Google Scholar ]
- 186. Ahmann E, Tuttle LJ, Saviet M, Wright S. A Descriptive review of ADHD coaching research: implications for college students. J Postsecond Educ Disabil. 2018;31(1):17–39. [ Google Scholar ]
- 187. Field S, Parker DR, Sawilowsky S, Rolands L. Assessing the impact of ADHD coaching services on university students’ learning skills, self-regulation, and well-being. J Postsecond Educ Disabil. 2013;26(1):83–101. [ Google Scholar ]
- 188. Swartz SL, Prevatt F, Proctor BE. A coaching intervention for college students with attention deficit/hyperactivity disorder. Psychol Sch. 2005;42(6):647–56. [ Google Scholar ]
- 189. Reaser AL. ADHD coaching and college students. Florida State University; 2008. doi: 10.1111/j.1863-2378.2008.01123.x [ DOI ] [ Google Scholar ]
- 190. Farmer JL, Allsopp DH, Ferron JM. Impact of the personal strengths program on self-determination levels of college students with LD and/or ADHD. Learn Disabil Q [Internet]. 2015;38(3):145–59. Available from: doi: 10.1037/neu0000189 [ DOI ] [ PubMed ] [ Google Scholar ]
- 191. Farmer JL. The development of the Personal Strengths Intervention (PSI) to improve self- determination and social-emotional levels in postsecondary students with learning disabilities and/or ADHD: A multiple baseline study. [Internet]. Available in ProQuest Dissertations and Theses database. (UMI No. 3466210). 2011. Available from: http://search.ebscohost.com.proxy-ub.rug.nl/login.aspx?direct=true&db=psyh&AN=2012-99070-067&site=ehost-live&scope=site
- 192. Prevatt F, Lampropoulos GK, Bowles V, Garrett L. The use of between session assignments in ADHD coaching with college students. J Atten Disord [Internet]. 2011;15(1):18–27. Available from: doi: 10.1177/1087054709356181 [ DOI ] [ PubMed ] [ Google Scholar ]
- 193. Parker DR, Hoffman SF, Sawilowsky S, Rolands L. An examination of the effects of ADHD coaching on university students ‘ executive functioning. J Postsecond Educ Disabil. 2011;24(2):115–32. [ Google Scholar ]
- 194. Richman EL, Rademacher KN, Maitland TL. Coaching and college success. J Postsecond Educ Disabil [Internet]. 2014;27(1):33–50. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=eric&AN=EJ1029647&site=ehost-live [ Google Scholar ]
- 195. Bomar R. The role of online academic coaching on levels of self-determination of college students with learning disabilities. Texas Woman’s University; 2017. [ Google Scholar ]
- 196. Prevatt F, Smith SM, Diers S, Marshall D, Coleman J, Valler E, et al. ADHD coaching with college students: exploring the processes involved in motivation and goal completion. J College Stud Psychother [Internet]. 2017;31(2):93–111. Available from: 10.1080/87568225.2016.1240597 [ DOI ] [ Google Scholar ]
- 197. Singley D. Effects of academic coaching on college students with learning disabilities or attention-deficit hyperactivity disorder. Theses Diss 2811 [Internet]. 2017;1–116. Available from: https://preserve.lehigh.edu/etd/2811 [ Google Scholar ]
- 198. Goudreau SB, Knight M. Executive function coaching: assisting with transitioning from secondary to postsecondary education. J Atten Disord [Internet]. 2018;22(4):379–87. Available from: doi: 10.1177/1087054715583355 [ DOI ] [ PubMed ] [ Google Scholar ]
- 199. Prevatt F, Yelland S. An empirical evaluation of ADHD coaching in college students. J Atten Disord [Internet]. 2015;19(8):666–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23509112 doi: 10.1177/1087054713480036 [ DOI ] [ PubMed ] [ Google Scholar ]
- 200. Huh J, Ackerman MS. Exploring social dimensions of personal information management with adults with AD/HD. Conf Hum Factors Comput Syst—Proc. 2010;3715–20. [ Google Scholar ]
- 201. Parker DR, Hoffman SF, Sawilowsky S, Rolands L. Self-control in postsecondary settings: students’ perceptions of ADHD college coaching. J Atten Disord. 2013;17(3):215–32. doi: 10.1177/1087054711427561 [ DOI ] [ PubMed ] [ Google Scholar ]
- 202. Schrevel SJC, Dedding C, Broerse JEW. Why do adults with ADHD choose strength-based coaching over public mental health care? A qualitative case study from the Netherlands. SAGE Open [Internet]. 2016;6(3). Available from: 10.1177/2158244016662498 [ DOI ] [ Google Scholar ]
- 203. Saviet M, Ahmann E. Communication modalities in coaching for individuals with attention-deficit/hyperactivity disorder (ADHD): a qualitative examination. Int J Evid Based Coach Mentor. 2020;18(1):103–22. [ Google Scholar ]
- 204. Parker DR, Boutelle K. Executive function coaching for college students with learning disabilities and ADHD: a new approach for fostering self-determination. Learn Disabil Res Pract [Internet]. 2009;24(4):204–15. Available from: http://doi.wiley.com/10.1111/j.1540-5826.2009.00294.x [ Google Scholar ]
- 205. Kubik J. Efficacy of ADHD coaching for adults with ADHD. J Atten Disord. 2010;13(5):442–53. doi: 10.1177/1087054708329960 [ DOI ] [ PubMed ] [ Google Scholar ]
- 206. DuPaul GJ, Dahlstrom-Hakki I, Gormley MJ, Fu Q, Pinho TD, Banerjee M. College students with ADHD and LD: effects of support services on academic performance. Learn Disabil Res Pract. 2017;32(4):246–56. [ Google Scholar ]
- 207. Ahmann E, Saviet M. Communication modalities and their perceived effectiveness in coaching for individuals with attention-deficit/hyperactivity disorder (ADHD). Int J Evid Based Coach Mentor. 2019;17(2):93–107. [ Google Scholar ]
- 208. Prevatt F. Coaching for college students with ADHD. Curr Psychiatry Rep [Internet]. 2016;18(12):1–7. Available from: doi: 10.1007/s11920-016-0751-9 [ DOI ] [ PubMed ] [ Google Scholar ]
- 209. Parker DR, Sleeper-Triplett J, Field S, Sawilowsky S. ADHD college coaching: potential adverse events. ADHD Rep. 2018;26(2):10–4. [ Google Scholar ]
- 210. Nadeau KG. Non-medication treatments for women with ADHD: working with coaches and organizers. In: Nadeau KG, Quinn P, editors. Understanding women with ADHD. Washington D.C.: Advantage Books; 2002. p. 124–32. [ Google Scholar ]
- 211. Jaksa P, Ratey N. Therapy and ADD coaching: similarities, differences, and collaboration [Internet]. 1999 [cited 2016 Feb 7]. p. http://www.nancyratey.com/adhdcoaching/therapy-add . Available from: http://www.nancyratey.com/adhdcoaching/therapy-addcoaching
- 212. Quinn P, Ratey N, Maitland TL. Coaching college students with ADHD. Silver Spring, MD: Advantage Books; 2000. [ Google Scholar ]
- 213. Ratey N. Life coaching for adult ADHD. In: Goldstein S, Ellison AT, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 261–77. [ Google Scholar ]
- 214. Weyandt LL, DuPaul GJ. ADHD in college students: developmental findings. Dev Disabil Res Rev. 2008;14(4):311–9. doi: 10.1002/ddrr.38 [ DOI ] [ PubMed ] [ Google Scholar ]
- 215. Assheton J. Coaching clients with ADHD. ADHD Pract. 2009;1(2):15–7. [ Google Scholar ]
- 216. Murphy K, Ratey N, Maynard S, Sussman S, Wright SD. Coaching for ADHD. J Atten Disord. 2010;13(5):546–52. doi: 10.1177/1087054709344186 [ DOI ] [ PubMed ] [ Google Scholar ]
- 217. Bowles VM. A survey of the methods and processes involved in interventions with ADHD clients from a psychologist and ADHD coach perspective. Florida State University; 2012. [ Google Scholar ]
- 218. Wright SD. ADHD coaching matters: the definitive guide. College Station, TX: ACO Books; 2014. [ Google Scholar ]
- 219. Wehmeyer ML, Palmer SB, Agran M, Mithaug DE, Martin JE. Promoting causal agency: The self-determined learning model of instruction. Except Child. 2000;66(4):439–53. [ Google Scholar ]
- 220. Wehmeyer ML, Field S. Self-Determination: instructional and assessment strategies. Thousand Oaks, CA: Corwin Press; 2007. [ Google Scholar ]
- 221. Field S, Hoffman A. Development of a model for self-determination. Career Dev Except Individ. 1994;17(2):159–69. [ Google Scholar ]
- 222. Mithaug DE, Wehmeyer ML, Agran M, Martin JE, Palmer S. The self-determined learning model of instruction: Engaging students to solve their learning problems. In: Wehmeyer ML, Sands DJ, editors. Making it happen: student involvement in educational planning, decision-making and instruction. Baltimore: Paul H. Brookes; 1998. p. 299–328. [ Google Scholar ]
- 223. Agran M, Martin JE. Applying a technology of self-control in community environments for individuals who are mentally retarded. In: Hersen M, Eisler RM, Miller PM, editors. Progress in behavior modification. Newbury Park, CA: SAGE; 1987. p. 108–51. [ PubMed ] [ Google Scholar ]
- 224. Kanfer R, Goldstein AP. Helping people change: A textbook of methods. New York: Pergamon Press; 1986. [ Google Scholar ]
- 225. Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986. [ Google Scholar ]
- 226. Martin JE, Burger D, Elias-Burger S, Mithaug DE. Applications of self-control strategies to facilitate independence in vocational and instructional settings. In: Bray NW, editor. International review of research in mental retardation. San Diego: Academic Press; 1988. p. 155–93. [ Google Scholar ]
- 227. Wehmeyer ML. Perceptions of self-determination and psychological empowerment of adolescents with mental retardation. Educ Train Ment Retard Dev Disabil. 1994;29(1):9–21. [ Google Scholar ]
- 228. Ratey N, Jaksa P. The ADDA guiding principles for coaching individuals with attention deficit disorder [Internet]. Attention Deficit Disorder Association. 2002. [cited 2020 Jun 13]. Available from: http://www.nancyratey.com/adhdcoaching/adda-coachingprinciples [ Google Scholar ]
- 229. Salomone S, Fleming GR, Shanahan JM, Castorina M, Bramham J, O’connell RG, et al. The effects of a self-alert training (SAT) program in adults with ADHD. Front Hum Neurosci. 2015;9(FEB):1–14. doi: 10.3389/fnhum.2015.00045 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 230. Cowley B, Holmström É, Juurmaa K, Kovarskis L, Krause CM. Computer enabled neuroplasticity treatment: a clinical trial of a novel design for neurofeedback therapy in adult ADHD. Front Hum Neurosci. 2016;10(MAY2016):1–13. doi: 10.3389/fnhum.2016.00001 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 231. Schönenberg M, Wiedemann E, Schneidt A, Scheeff J, Logemann A, Keune PM, et al. Neurofeedback, sham neurofeedback, and cognitive-behavioural group therapy in adults with attention-deficit hyperactivity disorder: a triple-blind, randomised, controlled trial. The Lancet Psychiatry. 2017;4(9):673–84. doi: 10.1016/S2215-0366(17)30291-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 232. Mayer K, Blume F, Wyckoff SN, Brokmeier LL, Strehl U. Neurofeedback of slow cortical potentials as a treatment for adults with attention deficit-/hyperactivity disorder. Clin Neurophysiol. 2016;127(2):1374–86. doi: 10.1016/j.clinph.2015.11.013 [ DOI ] [ PubMed ] [ Google Scholar ]
- 233. Barth B, Mayer K, Strehl U, Fallgatter AJ, Ehlis AC. EMG biofeedback training in adult attention-deficit/hyperactivity disorder: an active (control) training? Behav Brain Res. 2017;329(January):58–66. doi: 10.1016/j.bbr.2017.04.021 [ DOI ] [ PubMed ] [ Google Scholar ]
- 234. Mayer K, Wyckoff SN, Schulz U, Strehl U. Neurofeedback for adult attention-deficit/hyperactivity disorder: investigation of slow cortical potential neurofeedback-preliminary results. J Neurother. 2012;16(1):37–45. [ Google Scholar ]
- 235. Deiber MP, Hasler R, Colin J, Dayer A, Aubry JM, Baggio S, et al. Linking alpha oscillations, attention and inhibitory control in adult ADHD with EEG neurofeedback. NeuroImage Clin. 2020;25(December 2019). doi: 10.1016/j.nicl.2019.102145 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 236. Fisher SF. Neurofeedback, affect regulation and attachment: a case study and analysis of anti-social personality. Int J Behav Consult Ther. 2007;3(1):109–17. [ Google Scholar ]
- 237. Bidwell L, McCleron J, Kollins S. Cognitive enhancers for the treatment of ADHD. Pharmacol Biochem Behav. 2012;99(2):262–74. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 238. Fox DJ, Tharp DF, Fox LC. Neurofeedback: an alternative and efficacious treatment for attention deficit hyperactivity disorder. Appl Psychophysiol Biofeedback. 2005;30(4):365–73. doi: 10.1007/s10484-005-8422-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 239. Loo SK, Barkley RA. Clinical utility of EEG in attention deficit hyperactivity disorder. Appl Neuropsychol. 2005;12(2):64–76. doi: 10.1207/s15324826an1202_2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 240. Satterfield JH, Cantwell DP, Satterfield BT. Pathophysiology of the hyperactive child syndrome. Arch Gen Psychiatry. 1974;31(6):839–44. doi: 10.1001/archpsyc.1974.01760180079010 [ DOI ] [ PubMed ] [ Google Scholar ]
- 241. Monastra VJ, Lubar JF, Linden M. The development of a quantitative electroencephalographic scanning process for attention deficit-hyperactivity disorder: reliability and validity studies. Neuropsychology. 2001;15(1):136–44. doi: 10.1037//0894-4105.15.1.136 [ DOI ] [ PubMed ] [ Google Scholar ]
- 242. Gevensleben H, Moll GH, Rothenberger A, Heinrich H. Neurofeedback in attention-deficit/hyperactivity disorder–different models, different ways of application. Front Hum Neurosci. 2014;8(OCT):1–10. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 243. Bakhshayesh AR, Hänsch S, Wyschkon A, Rezai MJ, Esser G. Neurofeedback in ADHD: a single-blind randomized controlled trial. Eur Child Adolesc Psychiatry. 2011;20(9):481–91. doi: 10.1007/s00787-011-0208-y [ DOI ] [ PubMed ] [ Google Scholar ]
- 244. Arns M, Heinrich H, Strehl U. Evaluation of neurofeedback in ADHD: the long and winding road. Biol Psychol [Internet]. 2014;95(1):108–15. Available from: doi: 10.1016/j.biopsycho.2013.11.013 [ DOI ] [ PubMed ] [ Google Scholar ]
- 245. Lubar JF, Shouse MN. EEG and behavioral changes in a hyperkinetic child concurrent with training of the sensorimotor rhythm (SMR)—a preliminary report. Biofeedback Self Regul. 1976;1(3):293–306. doi: 10.1007/BF01001170 [ DOI ] [ PubMed ] [ Google Scholar ]
- 246. Gevensleben H, Holl B, Albrecht B, Vogel C, Schlamp D, Kratz O, et al. Is neurofeedback an efficacious treatment for ADHD? A randomised controlled clinical trial. J Child Psychol Psychiatry Allied Discip. 2009;50(7):780–9. doi: 10.1111/j.1469-7610.2008.02033.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 247. Gruzelier JH. EEG-neurofeedback for optimising performance. II: Creativity, the performing arts and ecological validity. Neurosci Biobehav Rev [Internet]. 2014;44:142–58. Available from: doi: 10.1016/j.neubiorev.2013.11.004 [ DOI ] [ PubMed ] [ Google Scholar ]
- 248. Drechsler R, Straub M, Doehnert M, Heinrich H, Steinhausen HC, Brandeis D. Controlled evaluation of a neurofeedback training of slow cortical potentials in children with attention deficit/hyperactivity disorder (ADHD). Behav Brain Funct. 2007;3:1–13. doi: 10.1186/1744-9081-3-1 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 249. Strehl U, Leins U, Goth G, Klinger C, Hinterberger T, Birbaumer N. Self-regulation of slow cortical potentials: a new treatment for children with attention-deficit/hyperactivity disorder. Pediatrics. 2006;118(5). doi: 10.1542/peds.2005-2478 [ DOI ] [ PubMed ] [ Google Scholar ]
- 250. Heinrich H, Gevensleben H, Freisleder FJ, Moll GH, Rothenberger A. Training of slow cortical potentials in attention-deficit/hyperactivity disorder: evidence for positive behavioral and neurophysiological effects. Biol Psychiatry. 2004;55(7):772–5. doi: 10.1016/j.biopsych.2003.11.013 [ DOI ] [ PubMed ] [ Google Scholar ]
- 251. Gevensleben H, Rothenberger A, Moll GH, Heinrich H. Neurofeedback in children with ADHD: validation and challenges. Expert Rev Neurother. 2012;12(4):447–60. doi: 10.1586/ern.12.22 [ DOI ] [ PubMed ] [ Google Scholar ]
- 252. Mirzaiyan M, Kunwar PS, Uzayisenga R, Rashidi S. Transcranial direct current stimulation for treatment of ADHD: a review of the mechanisms of action. Curr Psychiatry Rev. 2018;14(4):215–20. [ Google Scholar ]
- 253. Allenby C, Falcone M, Bernardo L, Wileyto EP, Rostain A, Ramsay JR, et al. Transcranial direct current brain stimulation decreases impulsivity in ADHD. Brain Stimul [Internet]. 2018;11(5):974–81. Available from: doi: 10.1016/j.brs.2018.04.016 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 254. Cosmo C, Ferreira C, Miranda JGV, do Rosário RS do, Baptista AF, Montoya P, et al. Spreading effect of tDCS in individuals with attention-deficit/hyperactivity disorder as shown by functional cortical networks: a randomized, double-blind, sham-controlled trial. Front Psychiatry. 2015;6(AUG):1–9. doi: 10.3389/fpsyt.2015.00111 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 255. Paz Y, Friedwald K, Levkovitz Y, Zangen A, Alyagon U, Nitzan U, et al. Randomised sham-controlled study of high-frequency bilateral deep transcranial magnetic stimulation (dTMS) to treat adult attention hyperactive disorder (ADHD): negative results. World J Biol Psychiatry. 2018;19(7):561–6. doi: 10.1080/15622975.2017.1282170 [ DOI ] [ PubMed ] [ Google Scholar ]
- 256. Priori A, Hallett M, Rothwell JC. Repetitive transcranial magnetic stimulation or transcranial direct current stimulation? Brain Stimul [Internet]. 2009;2(4):241–5. Available from: doi: 10.1016/j.brs.2009.02.004 [ DOI ] [ PubMed ] [ Google Scholar ]
- 257. Hiltunen S, Virta M, Salakari A, Antila M, Chydenius E, Kaski M, et al. Better long-term outcome for hypnotherapy than for CBT in adults with ADHD: Results of a six-month follow-up. Contemp Hypn Integr Ther. 2014;30(3):118–34. [ Google Scholar ]
- 258. Brown TE. Attention deficit disorder: The unfocused mind in children and adults. New Haven, CT: Yale University Press; 2005. [ Google Scholar ]
- 259. Coogan AN, McGowan NM. A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. ADHD Atten Deficit Hyperact Disord. 2017;9(3):129–47. [ DOI ] [ PubMed ] [ Google Scholar ]
- 260. Rybak YE, McNeely HE, Mackenzie BE, Jain UR, Levitan RD. An open trial of light therapy in adult attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(10):1527–35. doi: 10.4088/jcp.v67n1006 [ DOI ] [ PubMed ] [ Google Scholar ]
- 261. Rybak YE, McNeely HE, Mackenzie BE, Jain UR, Levitan RD. Seasonality and circadian preference in adult attention-deficit/hyperactivity disorder: clinical and neuropsychological correlates. Compr Psychiatry. 2007;48(6):562–71. doi: 10.1016/j.comppsych.2007.05.008 [ DOI ] [ PubMed ] [ Google Scholar ]
- 262. Korman M, Palm D, Uzoni A, Faltraco F, Tucha O, Thome J, et al. ADHD 24/7: Circadian clock genes, chronotherapy and sleep/wake cycle insufficiencies in ADHD. World J Biol Psychiatry. 2020;21(3):156–71. doi: 10.1080/15622975.2018.1523565 [ DOI ] [ PubMed ] [ Google Scholar ]
- 263. Coogan AN, Baird AL, Popa-Wagner A, Thome J. Circadian rhythms and attention deficit hyperactivity disorder: The what, the when and the why. Prog Neuro-Psychopharmacology Biol Psychiatry [Internet]. 2016;67:74–81. Available from: 10.1016/j.pnpbp.2016.01.006 [ DOI ] [ PubMed ] [ Google Scholar ]
- 264. Chesson AL, Littner M, Davila D, Anderson WMD, Grigg-Damberger M, Hartse K, et al. Practice parameters for the use of light therapy in the treatment of sleep disorders. Sleep. 1999;22(5):641–60. doi: 10.1093/sleep/22.5.641 [ DOI ] [ PubMed ] [ Google Scholar ]
- 265. Gropper RJ, Gotlieb H, Kronitz R, Tannock R. Working Memory Training in College Students With ADHD or LD. J Atten Disord [Internet]. 2014;18(4):331–45. Available from: doi: 10.1177/1087054713516490 [ DOI ] [ PubMed ] [ Google Scholar ]
- 266. Mawjee K, Woltering S, Tannock R. Working memory training in post-secondary students with ADHD: A randomized controlled study. PLoS One [Internet]. 2015;10(9):1–21. Available from: doi: 10.1371/journal.pone.0137173 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 267. Stern A, Malik E, Pollak Y, Bonne O, Maeir A. The efficacy of computerized cognitive training in adults with ADHD: a randomized controlled trial. J Atten Disord [Internet]. 2016;20(12):991–1003. Available from: doi: 10.1177/1087054714529815 [ DOI ] [ PubMed ] [ Google Scholar ]
- 268. Mawjee K, Woltering S, Lai N, Gotlieb H, Kronitz R, Tannock R. Working memory training in ADHD: controlling for engagement, motivation, and expectancy of improvement (Pilot study). J Atten Disord. 2017;21(11):956–68. doi: 10.1177/1087054714557356 [ DOI ] [ PubMed ] [ Google Scholar ]
- 269. Irvine MJD. Outcome evaluation of a time management smartphone application: a pilot study [Internet]. George Fox University; 2013. Available from: http://digitalcommons.georgefox.edu/psyd/118 [ Google Scholar ]
- 270. Stern A, Pollack Y, Yakir A, Maeir A. Pilot study of computerized cognitive training in adults with attention-deficit/hyperactivity disorder: change in executive functions and quality of life following 3 months of training using the AttenGo TM program. Isr J Occup Ther. 2012;21(4). [ Google Scholar ]
- 271. Hecker L, Burns L, Elkind J, Elkind K, Katz L. Benefits of assistive reading software for students with attention disorders. Ann Dyslexia. 2002;52(December):243–72. [ Google Scholar ]
- 272. Mancera L, Baldiris S, Fabregat R, Gomez S, Mejia C. ATenDerAH: A videogame to support e-learning students with ADHD. Proc—IEEE 17th Int Conf Adv Learn Technol ICALT 2017. 2017;438–40. [ Google Scholar ]
- 273. Schindler V. An occupational therapy-based supported education program for university students with various DSM-5 diagnoses: program description and academic outcomes. Open J Occup Ther. 2019;7(2). [ Google Scholar ]
- 274. Scheithauer MC, Kelley ML. Self-monitoring by college students with ADHD: the impact on academic performance. J Atten Disord [Internet]. 2017;21(12):1030–9. Available from: doi: 10.1177/1087054714553050 [ DOI ] [ PubMed ] [ Google Scholar ]
- 275. McMurray J. Auditory binaural beats enhance EEG-measured beta wave activity in individuals with ADHD [Internet]. The Journal -The Monroe Institute. 2004. [cited 2020 Aug 8]. Available from: http://www.monroeinstitute.org/journal/auditory-binaural-beats-enhance-eeg-measured-beta-wave-activity-in-individuals-with-adh [ Google Scholar ]
- 276. Peterson O. Rhythm as an intervention for health and mental health difficulties: a comprehensive literature review. Doctoral Thesis. Alliant International University; 2012.
- 277. Lane JD, Kasiamn SJ, Owens JE, Marsh GR. Binaural auditory beats affect vigilance performance and mood. Physiol Behav. 1998;63(2):249–52. doi: 10.1016/s0031-9384(97)00436-8 [ DOI ] [ PubMed ] [ Google Scholar ]
- 278. Den Heijer AE, Groen Y, Tucha L, Fuermaier ABM, Koerts J, Lange KW, et al. Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: a systematic literature review. J Neural Transm. 2016;124:3–26. doi: 10.1007/s00702-016-1593-7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 279. Abramovitch A, Goldzweig G, Schweiger A. Correlates of physical activity with intrusive thoughts, worry and impulsivity in adults with attention deficit/hyperactivity disorder: a cross-sectional pilot study. Isr J Psychiatry Relat Sci. 2013;50(1):47–54. [ PubMed ] [ Google Scholar ]
- 280. Fuermaier ABM, Tucha L, Koerts J, Van Heuvelen MJG, Van Der Zee EA, Lange KW, et al. Good vibrations—effects of whole body vibration on attention in healthy individuals and individuals with ADHD. PLoS One. 2014;9(2). doi: 10.1371/journal.pone.0090747 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 281. Gapin JI, Labban JD, Bohall SC, Wooten JS, Chang YK. Acute exercise is associated with specific executive functions in college students with ADHD: a preliminary study. J Sport Heal Sci [Internet]. 2015;4(1):89–96. Available from: 10.1016/j.jshs.2014.11.003 [ DOI ] [ Google Scholar ]
- 282. Kallweit C, Paucke M, Strauß M, Exner C. Adult ADHD: influence of physical activation, stimulation, and reward on cognitive performance and symptoms. J Atten Disord. 2019;108705471984505. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 283. Mehren A, Özyurt J, Thiel CM, Brandes M, Lam AP, Philipsen A. Effects of acute aerobic exercise on response inhibition in adult patients with ADHD. Sci Rep. 2019;9(1):1–13. doi: 10.1038/s41598-018-37186-2 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 284. Mehren A, Özyurt J, Lam AP, Brandes M, Müller HHO, Thiel CM, et al. Acute effects of aerobic exercise on executive function and attention in adult patients with ADHD. Front Psychiatry. 2019;10(MAR):1–15. doi: 10.3389/fpsyt.2019.00132 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 285. Rassovsky Y, Alfassi T. Attention improves during physical exercise in individuals with ADHD. Front Psychol. 2019;9(JAN):1–5. doi: 10.3389/fpsyg.2018.02747 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 286. LaCount PA, Hartung CM. Physical exercise interventions for emerging adults with attention-deficit/hyperactivity disorder (ADHD). ADHD Rep. 2018;26(5):1–11. [ Google Scholar ]
- 287. Halperin JM, Healey DM. The influences of environmental enrichment, cognitive enhancement, and physical exercise on brain development: can we alter the developmental trajectory of ADHD? Neurosci Biobehav Rev. 2011;35(3):621–34. doi: 10.1016/j.neubiorev.2010.07.006 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 288. Archer T, Kostrzewa RM. Physical exercise alleviates ADHD symptoms: regional deficits and development trajectory. Neurotox Res. 2012;21(2):195–209. doi: 10.1007/s12640-011-9260-0 [ DOI ] [ PubMed ] [ Google Scholar ]
- 289. Gapin JI, Labban JD, Etnier JL. The effects of physical activity on attention deficit hyperactivity disorder symptoms: the evidence. Prev Med (Baltim). 2011;52(SUPPL.). doi: 10.1016/j.ypmed.2011.01.022 [ DOI ] [ PubMed ] [ Google Scholar ]
- 290. Cardinale M, Bosco C. Use of vibration as an exercise intervention. Exerc Sport Sci Rev. 2003;31(1):3–7. doi: 10.1097/00003677-200301000-00002 [ DOI ] [ PubMed ] [ Google Scholar ]
- 291. Cochrane DJ, Sartor F, Winwood K, Stannard SR, Narici M V., Rittweger J. A Comparison of the physiologic effects of acute whole-body vibration exercise in young and older people. Arch Phys Med Rehabil. 2008;89(5):815–21. doi: 10.1016/j.apmr.2007.09.055 [ DOI ] [ PubMed ] [ Google Scholar ]
- 292. Poulton EC. Increased vigilance with vertical vibration at 5 Hz: an alerting mechanism. Appl Ergon. 1978;9(2):73–6. doi: 10.1016/0003-6870(78)90151-5 [ DOI ] [ PubMed ] [ Google Scholar ]
- 293. Tsai SJ. Attention-deficit hyperactivity disorder may be associated with decreased central brain-derived neurotrophic factor activity: clinical and therapeutic implications. Med Hypotheses. 2007;68(4):896–9. doi: 10.1016/j.mehy.2006.06.025 [ DOI ] [ PubMed ] [ Google Scholar ]
- 294. Shaikh A. Group therapy for improving self-esteem and social functioning of college students with ADHD. J College Stud Psychother. 2018;32(3):220–41. [ Google Scholar ]
- 295. Carney JK. Self- and interactive regulation: treating a patient with AD/HD. Psychoanal Inq. 2002;22(3):355–71. [ Google Scholar ]
- 296. Waska R. Attention deficit disorder or object detachment disorder: a brief psychoanalytic case study. Psychoanal Rev. 2014;101(3):367–83. doi: 10.1521/prev.2014.101.3.367 [ DOI ] [ PubMed ] [ Google Scholar ]
- 297. Zabarenko LM. AD/HD, psychoanalysis, and neuroscience: a survey of recent findings and their applications. Psychoanal Inq. 2002;413–32. [ Google Scholar ]
- 298. Wright JL. Psychoanalysis in conjunction with medication: a clinical research opportunity. J Am Psychoanal Assoc. 2006;54:833–55. doi: 10.1177/00030651060540031601 [ DOI ] [ PubMed ] [ Google Scholar ]
- 299. Lusk SL. A psychoanalytic approach to the complexity of understanding and treating patients with ADHD beyond childhood: the experiences of two psychoanalytic candidates. Psychoanal Study Child [Internet]. 2019;72(1):61–70. Available from: 10.1080/00797308.2019.1557476 [ DOI ] [ Google Scholar ]
- 300. de Almeida Silva V, Louza MR, de Silva MA, Nakano EY. Ego defense mechanisms and types of object relations in adults with ADHD. J Attentional Disord. 2012;20(11):979–87. doi: 10.1177/1087054712459559 [ DOI ] [ PubMed ] [ Google Scholar ]
- 301. Gilmore K. A psychoanalytic perspective on attention-deficit/hyperactivity disorder. J Am Psychoanal Assoc. 2000;(48):1259–93. doi: 10.1177/00030651000480040901 [ DOI ] [ PubMed ] [ Google Scholar ]
- 302. Rafalovich A. Psychodynamic and neurological perspectives on ADHD: exploring strategies for defining a phenomenon. J Theory Soc Behav. 2002;31(4):397–418. [ Google Scholar ]
- 303. Zabarenko L. ADHD via psychoanalysis, neuroscience, and cognitive psychology: why haven’t we fielded a team? J Infant, Child, Adolesc Psychother. 2011;10(1):5–12. [ Google Scholar ]
- 304. Conway F. Current research and future directions in psychodynamic treatment of ADHD: ss empathy the missing link? J Infant, Child, Adolesc Psychother. 2015;14:280–7. [ Google Scholar ]
- 305. Levin FM. Attention deficit disorder: a neuropsychoanalytic sketch. Psychoanal Inq. 2002;22(3):336–54. [ Google Scholar ]
- 306. Bemporad J, Zambenedetti M. Psychotherapy of adults with attention-deficit disorder. J Psychother Pract Res. 1996;5:228–37. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 307. Rothstein A. Plea for a balanced conception of AD/HD and its diagnosis and treatment. Psychoanal Inq. 2002;22(3):391–412. [ Google Scholar ]
- 308. Johnson KA, Wiersema JR, Kuntsi J. What would Karl Popper say? Are current psychological theories of ADHD falsifiable? Behav Brain Funct. 2009;5(15):1–11. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 309. Pennington BF. Toward a new neuropsychological model of attention-deficit/hyperactivity disorder: subtypes and multiple deficits. Biol Psychiatry. 2005;57:1221–3. doi: 10.1016/j.biopsych.2005.03.010 [ DOI ] [ PubMed ] [ Google Scholar ]
Decision Letter 0
Gerard hutchinson.
18 Oct 2021
PONE-D-21-16848
The Impact of Psychological Theory on the Treatment of Attention Deficit Hyperactivity Disorder (ADHD) in Adults: A Scoping Review
Dear Dr. Champ ,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
Kindly address all points raise dby the two reviewers and resubmit by November 15th, 2021. If you need more time, you can inform the journal office at [email protected] . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: https://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
We look forward to receiving your revised manuscript.
Kind regards,
Gerard Hutchinson, MD
Academic Editor
Journal requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. We note that this manuscript is a scoping review; our author guidelines therefore require that you use PRISMA guidance to help improve reporting quality and consistency for this type of study. Please include copies of the completed PRISMA checklist for scoping reviews ( http://www.prisma-statement.org/Extensions/ScopingReviews ) as Supporting Information with a file name “PRISMA checklist
Additional Editor Comments (if provided):
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Partly
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: N/A
Reviewer #2: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #1: Yes
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Authors make a very good review on characterizations of ADHD from different psychological approaches, as well as the different psychological therapies applied to patients. Description of psychological approaches and characteristics of therapies applied is detailed and sufficient. In this regard, it is an interesting article on the history of ADHD psychological treatment. However, the present manuscript is largely descriptive, and could be greatly improved by adding information that would also be useful in the discussion section, as well as to support authors´conclusions.
MAJOR ISSUES
1.- The hierarchy of ideas is not always clear, it would benefit from establishing headings and subheadings clearly. For example, at first authors talk about behavioral therapy and state that the review will address this subject in waves, and describe the first wave in page 7, line 150 (authors could use a subheading for this section). However, after first wave authors address REBT (page 8, line 167), and later return to the second wave on page 8, line 181). Are authors considering REBT a subheading of the CBT first wave? This situation repeats along the manuscript. Please add subheadings as needed.
2.- In the present version of the manuscript, a detailed description of each psychological approach is provided, along with information regarding the specific therapeutic interventions. However, authors do not state whether the interventions they mention (first wave, REBT, second wave, etc) were successful or not (except for light therapy and computer based interventions, where some treatment outcomes are mentioned), or which symptoms were treated more effectively, or if follow up studies revealed information regarding symptoms control in the long term, or if sessions could be separated for longer periods of time as treatment advanced, etc. Information regarding the effectiveness of each of the psychological therapies addressed would be necessary to understand not only how psychological approaches have changed, but also if these changes had an effect on patients´ health. Please include information regarding effectiveness of the psychological treatments described, it could be included as a paragraph at the end of each section (first wave, second wave, etc.).
Furthermore, it would be useful for discussion. In page 24, lines 633 and 634, authors say that “Critically, it highlights that a single theoretical perspective limits research into effective treatments for ADHD”, which implies first, that current psychological treatments for ADHD can be more effective, and secondly, that there are psychological approaches, currently not considered, that could improve treatment effectiveness. Therefore, this statement should be supported by at least two points in the discussion section: a) Specify how the effectiveness of psychological treatment could be improved, i.e. which outcomes could be better (improvement in more areas, observing effects after a shorter treatment, etc); and b) propose some aspects not considered in the current psychological approach, that could be useful when addressing ADHD, improving treatment effectiveness.
MINOR ISSUES
1.- Page 3, Line 65. Quebec is not a language
2.- It would be very useful if authors included a table comparing the different theoretical approaches for ADHD, outlining similitudes and differences
Reviewer #2: The main aim of this review was to consider the use of psychological theory in the development of ADHD treatment for adults. Key themes of the cognitive-behavioural approach to adult ADHD have been explored. The review is a useful contribution to the field. Whilst literature is available on the topic, I would suggest this is a timely update that explores a breadth of evidence.
The rationale for the scoping review is clear. It is written clearly and easy to follow. The review is well informed and provides the field with a useful foundation for future research directions.
I would suggest minor revisions would be beneficial to the reader, the sentence ‘characterisations of ADHD that were not empirically researched’ on line 98, page 5 could be expanded on, to let the reader understand the inclusion criteria further. Also, attention should be paid to the reference list, some information is missing/inconsistent due to formatting errors.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: No
Reviewer #2: No
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at [email protected] . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
Collection date 2021.
16 Nov 2021
I would like to thank the reviewers for their time and comments. The following details the response to requests for revisions:
Reviewer 1:
The reviewer raises excellent points about the manuscript. As requested, the hierarchy of ideas has been clarified and headings and subheadings are more specific.
However, their comments regarding efficacy and further detail in the discussion address an entirely different focus and aim than the current piece presents. I agree the request for detailed information on the efficacy of treatments throughout the manuscript would assist the reader to “understand not only how psychological approaches have changed, but also if these changes had an effect on patients´ health”, if this were an article focused on the history and development of the efficacy of treatments for ADHD as Reviewer 1 describes it. However, the focus of the manuscript is to identify, map and confirm the theoretical underpinnings of the characterisation of ADHD which informs treatment design, approaches and outcomes.
Perhaps this is less clear because the questions that prompted the research had not been included. Therefore, additional information is provided in the introduction which will clarify the aims of the research (lines 59-64). I have also addressed the question of evidence for efficacy in treatment of specific symptoms (lines 40-45).
I am very pleased to receive comments regarding requests for a comparative table of psychological theories, and information on “how the effectiveness of psychological treatments could be improved” and to “propose some aspects not considered in the current psychological approach”. This is a much larger and more in-depth question that goes beyond the current manuscript. A second manuscript directly addressing these queries has been submitted for publication and is currently under review. Therefore, I have now described issues with current treatment approaches as highlighted in recent systematic reviews (lines 45-51) but overall the current work only addresses these queries nominally (lines 52-58 and 673-678) to prepare the ground for a future discussion of the kind that Reviewer 1 has requested.
Reviewer 2:
I appreciate that some readers may not be aware of non-empirical characterisations of ADHD. Therefore, I have defined this body of literature more clearly, provided examples, and given further explanation for their exclusion (lines 113-119). I have also reviewed and updated my references.
Decision Letter 1
26 Nov 2021
PONE-D-21-16848R1
Dear Dr. Champ
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at [email protected] .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact [email protected] .
Additional Editor Comments (optional):
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: The additions on the revised version of the manuscript allow a clearer definition of its purpose, which is more focused on the theoretical aspect of ADHD characterization and, as stated in the title, its impact on ADHD treatment. In this regard, the first part of these objectives (theoretical aspect of ADHD characterization) is fully addressed along the manuscript. Moreover, what the title implies regarding the impact of psychological theory on ADHD treatment is briefly addressed at the discussion section.
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Acceptance letter
Dear Dr. Champ:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact [email protected] .
If we can help with anything else, please email us at [email protected] .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Gerard Hutchinson
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data availability statement.
- View on publisher site
- PDF (1.3 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Twenty years of research on attention-deficit/hyperactivity disorder (ADHD): looking back, looking forward
Affiliations.
- 1 Academic Unit of Psychology, Center for Innovation in Mental Health, University of Southampton, Southampton, UK.
- 2 Clinical and Experimental Sciences (CNS and Psychiatry), Faculty of Medicine, University of Southampton, Southampton, UK.
- 3 Solent NHS Trust, Southampton, UK.
- 4 New York University Child Study Center, New York City, New York, USA.
- 5 Division of Psychiatry and Applied Psychology, School of Medicine, University of Nottingham, Nottingham, UK.
- 6 Departments of Paediatrics and Psychiatry, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Melbourne, Victoria, Australia.
- 7 Murdoch Children's Research Institute, Melbourne, Victoria, Australia.
- 8 Royal Children's Hospital, Melbourne, Victoria, Australia.
- PMID: 30301823
- PMCID: PMC10270437
- DOI: 10.1136/ebmental-2018-300050
In this clinical review we summarise what in our view have been some the most important advances in the past two decades, in terms of diagnostic definition, epidemiology, genetics and environmental causes, neuroimaging/cognition and treatment of attention-deficit/hyperactivity disorder (ADHD), including: (1) the most recent changes to the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases; (2) meta-analytic evidence showing that, after accounting for diagnostic methods, the rates of ADHD are fairly consistent across Western countries; (3) the recent finding of the first genome-wide significant risk loci for ADHD; (4) the paradigm shift in the pathophysiological conceptualisation of ADHD from alterations in individual brain regions to a complex dysfunction in brain networks; (5) evidence supporting the short-term efficacy of ADHD pharmacological treatments, with a different profile of efficacy and tolerability in children/adolescents versus adults; (6) a series of meta-analyses showing that, while non-pharmacological treatment may not be effective to target ADHD core symptoms, some of them effectively address ADHD-related impairments (such as oppositional behaviours for parent training and working memory deficits for cognitive training). We also discuss key priorities for future research in each of these areas of investigation. Overall, while many research questions have been answered, many others need to be addressed. Strengthening multidisciplinary collaborations, relying on large data sets in the spirit of Open Science and supporting research in less advantaged countries will be key to face the challenges ahead.
© Author(s) (or their employer(s)) 2018. No commercial re-use. See rights and permissions. Published by BMJ.
Publication types
- Attention Deficit Disorder with Hyperactivity* / diagnosis
- Attention Deficit Disorder with Hyperactivity* / etiology
- Attention Deficit Disorder with Hyperactivity* / genetics
- Attention Deficit Disorder with Hyperactivity* / therapy
- Hyperactivity Disorder Essay Topics Topics: 93
- Disorders Essay Topics Topics: 554
- Sepsis Essay Topics Topics: 52
- Communicable Disease Research Topics Topics: 57
- Melanoma Essay Topics Topics: 60
- Myocardial Infarction Research Topics Topics: 52
- Patient Safety Topics Topics: 148
- Osteoporosis Paper Topics Topics: 56
- Heart Attack Topics Topics: 54
- Parkinson's Disease Topics Topics: 53
- Sleep Deprivation Topics Topics: 48
- Hepatitis Essay Topics Topics: 57
- Arthritis Paper Topics Topics: 58
- Chlamydia Research Topics Topics: 49
- Thrombosis Paper Topics Topics: 48
124 ADHD Research Topics & Titles
🏆 best essay topics on adhd, ✍️ adhd essay topics for college, 🧠 adhd topics for research paper, 👍 good adhd research topics & essay examples, 🤔 adhd dissertation topics, 🎓 most interesting adhd research titles, 🆚 add versus adhd, 💡 simple adhd essay ideas, ❓ adhd research questions.
- The Influence and Effects of Colour on Attention Deficit Hyperactivity Disorder Children
- ADHD & Personality
- Sugar: Does It Really Cause Hyperactivity?
- ADHD in the Classroom: John’s Interrupting Behavior Analysis
- Understanding ADHD: A Comprehensive Case Study
- ADHD Awareness
- Hidden Dangers of Attention Deficit Hyperactivity Disorder Medications
- ADHD: The Center’s for Disease Control and Prevention Webpage The Center’s for Disease Control and Prevention webpage on attention deficit hyperactivity disorder sufficiently employs ethos, pathos, and logos rhetoric allures.
- The Relation Between Attention Deficit Disorder and Colitis Patients suffering from co-occurring conditions find it hard to receive timely, quality, and safe medical support.
- Theoretical Approach to ADHD: Case Study Analysis The executive function (EF) theory by Russel Barkley applies to understanding and developing strategies to improve the child’s learning process.
- Students with Attention Deficit Hyperactivity Disorder: Academic Progress This work examines the use of stability balls in the classroom for the improvement of disciplinary and academic outcomes of students with attention deficit hyperactivity disorder.
- Attention Deficit Hyperactivity Disorder and Nursing Intervention Attention deficit hyperactivity disorder (ADHD) is one of children’s most frequent neurodevelopmental diseases.
- Increase in ADHD Diagnoses The paper includes a different approach to diagnosis, changes in populations’ attitudes toward ADHD, and the influence of social media.
- Impact of ADHD on Students ADHD (attention deficit hyperactivity disorder) are experience challenges in managing high levels of energy, controlling impulses, and maintaining attention.
- Characteristics of ADHD Attention deficit hyperactivity disorder refers to disorders of the nervous system. Neurological disorders are based on prerequisites of a neurological nature.
- The Effects of Food on ADHD The issue of ADHD and its relation to food has been a concern for a while. According to the outcomes of the study, the daily intake of food must be controlled in ADHD patients.
- Exploring ADHD: Genetics, Environment, and Brain Changes Attention deficit hyperactivity disorder is the most prevalent child behavioral disorder characterized by inattention, hyperactivity, and impulsivity.
- Is ADHD Genetically Passed Down to Family Members? Genetic correlations between such qualities as hyperactivity and inattention allowed us to define ADHD as a spectrum disorder rather than a unitary one.
- Aspects of Attention Deficit Hyperactivity Disorder The paper discusses attention deficit hyperactivity disorder. It is a neurologic and developmental illness diagnosed in childhood.
- Is Attention Deficit Hyperactivity a Real Disorder? Attention deficit hyperactivity disorder is one of the most prevalent children neurodevelopmental diseases. It is identified during childhood and frequently persists into maturity.
- ADHD in Children and Adults: Causes, Symptoms, and Solutions The paper will try to explain why ADHD is serious, how it can damage a person’s quality of life long into adulthood, and how it can interfere with one’s communication ability.
- Stimulant Therapy for Attention Deficit Hyperactivity Disorder Despite the potential for negative consequences, stimulant therapy is an effective treatment for attention deficit hyperactivity disorder signs.
- Pediatric Occupational Therapy for Attention Deficit Hyperactivity Disorder This is a systematic review of quantitative research studies and occupational therapy interventions for children with Attention Deficit Hyperactivity Disorder (ADHD).
- Attention Deficit Hyperactive Disorder Behavior Attention Deficit Hyperactive Disorder is a psychological disorder that causes a person’s brain to be abnormally hyperactive than usual behavior.
- Attention Deficit and Effective Treatment of Disorder Effective behavioral and pharmaceutical treatments help reduce the symptoms of ADHD. It can assist individuals in doing better at home, school, and in social situations.
- Attention Deficit Hyperactivity Disorder Treatment The Attention-Deficit/ Hyperactivity Disorder Therapy mechanisms include psychoeducation, where parents are encouraged to discuss the condition with their children.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Prominent Aspects, Management, and Prevention Attention-Deficit/Hyperactivity Disorder (ADHD) is characterized by a pattern of inattention or hyperactivity in a person.
- A Counseling Theory for Child with Attention Deficit Hyperactive Disorder Attention deficit hyperactive disorder (ADHD) is usually spread among children and adolescents. Proper educational counseling can help students with ADHD to cope with the problem.
- Living with Attention Deficit Hyperactivity Disorder Though ADHD is not a very dangerous illness, it is better not underrate its effects. Many patients may feel rejected by society, and this alienation is likely to worsen the situation.
- Relationship Between ADHD-Inattentive and -Hyperactive The cause and effect relationship between ADHD-inattentive and ADHD-hyperactive-impulsive is conditional upon the former’s role in the latter’s emergence.
ADHD in Women
ADHD, attention deficit hyperactivity disorder, is a neurodevelopmental condition that is different for women and men. For females, it usually involves issues with focus and inattentiveness, whereas for men, it is about impulsivity and hyperactivity. Most women also display depression and anxiety disorders as part of the symptoms associated with ADHD. Here are some research questions about ADHD in women that may guide your writing process.
Difficulty Concentrating as a Symptom of ADHD
ADHD has numerous symptoms, including difficulties in focusing, anxiety, and impulsiveness. Children diagnosed with ADHD often struggle to concentrate on one boring task for several minutes. They are forgetful, disorganized, and easily distracted. However, an exciting project might trigger a child to be hyper-focused to the point of detaching from reality. Pick one of the following ADHD research topics on concentration to speed up home task completion.
Attention Deficit Hyperactivity Disorder and Impulsivity
Impulsivity is a major symptom of ADHD. It means a person has issues with self-control and acts without thinking of the consequences. Other signs include impatience, blurting out answers, interrupting other people, engaging in reckless behavior, and temper outbursts. Treatment for ADHD impulsivity comprises behavior therapy, skills training, and psychological counseling. Looking for great ADHD essay topics linked to impulsivity? Here are some valuable suggestions to follow.
- Mental Health and ADHD in Universities The issue of mental health in university learners is rarely brought up, yet it has a tangible effect on the target audience’s health and ability to learn.
- Attention Deficit Hyperactivity Disorder Diagnosis Controversy The article provides an overview of the factors that led to an increase in the number of cases of attention deficit hyperactivity disorder.
- ADHD and Socially Constructed Impairment ADHD is responsible for many complications in the life of people suffering from it, including limited educational achievement, and low self-organizational capacity.
- Sleep Disturbance and Neuropsychological Function Within ADHD Sleep disruption is an inherent behavioral feature in childhood attention-deficit/hyperactivity disorder, known as ADHD.
- Hyperactivity Disorder Symptoms and Sleep Issues The document to be analyzed is “The moderating roles of bedtime activities and anxiety/depression in the relationship between attention-deficit/hyperactivity” by Tong
- ADHD: Treatment and Over Medication When children have ADHD, it is possible to influence their symptoms by forging a special supportive bond between them, parents, and the education system.
- The Phenomenon of the ADHD Disorder The paper analyzes the facts represented for whether or not attention-deficit/hyperactivity disorder is real.
- Childhood Mental Disorders: Attention Deficit Hyperactivity Disorder Description, causes, symptoms, discussion around possible treatment options for children with attention deficit hyperactivity disorder.
- Attention Deficit Hyperactivity Disorder Stimulants: Research Method The article that highlights the evaluation of study with regard to the Utility of illegal Attention Deficit Hyperactivity Disorder (ADHD) Stimulants among college students.
- Critique of Articles on Parenting, ADHD, Child Psychology, and Development In this work, the author criticized articles on parenting, ADHD, child psychology, early adult romantic relationships and development.
- Attention Deficit Hyperactivity Disorder Symptoms Analysis ADHD, usually starts presenting it self during childhood, and is thought to be a continual chronic condition, and there is no medical cure for this disorder.
- Diagnosis and Treatment for Attention Deficit Hyperactivity Disorder I have been having trouble coping with the fact that my son Ryan was recently diagnosed with attention deficit hyperactive disorder (ADHD).
- Attention Deficit Hyperactivity Disorder Identification The criteria for identifying students with the ADHD problem required identifying the essential patterns of attention exhibited by the patient.
- Developmental Disorder Overview: Attention Deficit Hyperactivity Disorder One of the developmental disorders often diagnosed in the middle childhood years is attention-deficit/hyperactivity disorder (ADHD).
- Attention-Deficit Hyperactivity Disorder Diagnostic Mood disorders are adjustment problems that come from stressors emanating from inside and which can be triggered by factors that cannot be controlled.
- General Features and Etiology of ADHD Attention Deficit Hyperactivity Disorder (ADHD) is a mental health disorder that is expressed by extensive impulsivity and deficient attentiveness.
- Teaching Students With Attention Deficit Hyperactivity Disorder Attention Deficit Hyperactivity Disorder is a psychiatric disorder characterized by impulsive actions that are not related proportionally to the age of the affected person.
- Child Psychiatry: Attention Deficit Hyperactivity Disorder Attention Deficit Hyperactivity Disorder is a childhood disruptive behavioral disorder that manifests in “inattention, impulsivity and hyperactivity” and can persist into adulthood.
- Attention Deficit Hyperactivity Disorder at School This work is observations of Jacob, a child with attention deficit hyperactivity disorder (ADHD), which was made at Cornell Junior Public School.
- Attention Deficit Hyperactivity Disorder in Students This paper reports the observation of a classroom with children with ADHD. It provides a brief overview of ADHD and summarizes articles regarding ADHD in children.
- Diagnostic Assessment of Children and Adolescents With ADHD The purpose of the study is to evaluate current clinical evidence on the value of different diagnostic tests of children and adolescents with ADHD in social and educational contexts.
- Attention Deficit Hyperactivity Disorder in Children: Studies Analysis This paper analyzes five scholarly articles on Attention Deficit Hyperactivity Disorder (ADHD) in children. The authors studied the effects and treatment of the disorder.
- A Special Education Plan: Grade 1 Male Student With ADHD It is important to know the needs of children with Attention Deficit Hyperactivity Disorder and make the necessary modifications to accommodate them in the classroom.
- Co-Occurrence of ADHD and Bipolar Disorder: Understanding Symptoms and Treatment The relationship between Attention Deficit Hyperactivity Disorder (ADHD) and bipolar disorder has received a lot of attention.
Here are some interesting research questions about ADHD and its impact on a person’s life.
Personal and Societal Costs of ADHD
Treating ADHD is pricey, and studies show that in the US, an estimated $31.6 billion is the total annual cost that covers healthcare for people diagnosed with ADHD, family members caring for people with ADHD, and the work absenteeism of ADHD adults and their caregivers. Finding ways to enhance the health of those with ADHD can help many individuals and families save more money and possibly lower this financial burden.
Policies Related to ADHD
Various policies govern the authorization of ADHD treatment. Such treatments are usually authorized and compensated by specific health plans or government programs. One crucial policy affecting ADHD treatment is a pre-authorization requirement by health plans before physicians can prescribe specific medications. Thus, the state program or health insurance must review the prescription request before granting the medication coverage.
Due to the rise of ADHD cases among children over the years, many state programs have improved pre-authorization policies related to ADHD medications for pediatric use. Look through the list of research topics on ADHD policies presented below.

Factors Increasing the Risk of ADHD
The causes of ADHD are yet to be established. However, research shows that genes play a significant role in facilitating ADHD and related symptoms. Some families have more prevalent cases of ADHD, while others have minimal cases. Environmental exposure might be another critical factor that contributes to ADHD despite the inconsistent evidence. Understanding the factors increasing ADHD symptoms will help public health experts act accordingly and introduce practical recommendations. Next comes a list of ADHD titles on this subtopic.
- ADHD and Its Effects on the Development of a Child‘s
- How ADHD Medication Affects the Brain?
- The Epidemiological Rates for ADHD
- ADHD and Its Impact on Mainstream Schooling
- Effective Teaching Strategies for Students With ADHD
- The Debate Over Ritalin Use by Children With ADHD
- ADHD Diagnosis, Diagnostic Tools, and Its Cultural and Ethical Implications
- Dealing With Children Suffering From Add and ADHD
- The Link Between ADHD and Electronic Stimulation
- Affordable Non-Drug Solution to ADHD
- Ten Positive Things About ADHD
- ADHD and What Causes the Childhood Behavioral Condition
- Treating ADHD Long Term Can Cause Harm by Creating Thoughts of Suicide
- The Advantage and Disadvantage of Using Psychostimulants in the Treatment of ADHD
- ADHD and Antisocial Behavior Juvenile Delinquency
- Scientists Probe ADHD Treatment for Long-Term Management of the Disease
- The Correlation Between Technology and Adolescent Mental Health Particularly ADHD
- Over Diagnosis and Medication for ADHD
- How Do School Systems Deal With ADHD?
- Resting-State Brain Signal Variability in Prefrontal Cortex Is Associated With ADHD Symptom Severity in Children
ADD means attention-deficit disorder, while ADHD is known as attention-deficit hyperactivity disorder. ADD is an initial term that was used in the 1980s to diagnose children with this condition. However, in the early 90’s, the name changed to ADHD, with the inclusion of hyperactivity.
Since the 1990s, ADHD has been associated with three types of diagnosis – inattentive, hyperactive/impulsive, and combined type. Most people still use the term ADD to identify the inattentive type since it does not have the hyperactivity aspect. Today, ADHD is commonly diagnosed according to the symptoms rather than the types. It helps avoid the confusion between ADD and ADHD.
Therefore, there is no factual difference between ADD and ADHD. ADD is an old term, while ADHD is the new abbreviation used in the medical world.
- Social-Emotional and Behavioral Difficulties Alongside ADHD Education
- The Diagnosis, Symptoms, and Treatments for ADHD or Attention Deficit Hyperactivity Disorder
- Comorbidity Between Reading Disability and ADHD
- ADHD: Parents Should Use Alternative Treatments for Illness
- Parental Income, Education and the Diagnosis of ADHD in Children and Adolescents: The Case for Germany
- The Good, the Bad, and the Ugly of Treatments of ADHD
- Twice-Exceptional Students With ADHD Characteristics and Strategies
- Psychosocial Academic Interventions for Children With ADHD
- Impact of Misdiagnosis and Overprescribing of ADHD Medications
- The Relation Between Sleep, Memory Enhancement, and Causes of Emotional Deficiency Among ADHD Patients
- How Can You Tell if an Adult Has ADHD?
- About the Controversies Between the Existence of ADHD, and the Different Viewpoints
- The Effects of ADHD Pharmacological Treatment on Teens’ Risky Behaviors
- ADHD Children and How Behavior Therapy Is Necessary With the Use of Medication
- Effective Management Techniques for Children With ADHD
- Side Effects ADHD Ritalin Symptoms
- ADHD: The Serious Public Health Problem
- Alcohol Abuse During Pregnancy and ADHD Symptoms
- Should Children Diagnosed With ADHD Be Given Medication to Address Their Symptoms
- The Young Children and Children With ADHD, and Thinking Skills
- What Are the Effects of ADHD in the Classroom?
- What Effect Does Being Identified With ADHD Have on a Child?
- What Are the Nine Symptoms of ADHD?
- What Are the Three Key Symptoms Used to Diagnose ADHD?
- What Are the Seven Types of ADHD?
- Is ADHD on the Autism Spectrum?
- At What Age Can ADHD Be Diagnosed?
- Can You Treat ADHD Without Medication?
- Is ADHD a Serious Mental Illness?
- Can You Have ADHD Without Being Hyper?
- What Is Ring of Fire ADHD?
- At What Age Does ADHD Peak?
- Do ADHD Brains Look Different?
- Is ADHD Classified as Special Needs?
- Can People With ADHD Have Special Interests?
- Can Additional Training Help Close the ADHD Gender Gap?
- Can Sports Affect Impulse Control in Children With ADHD?
- How Does ADHD Affect School Performance?
- Should Children With ADHD Be On Ritilan or Similar Drugs?
- Do People With ADHD Have Sensory Issues?
- What Is the Most Common Treatment for ADHD?
- Can ADHD Be Mistaken for Bipolar?
- Why Is ADHD Not Considered a Disability?
- Can ADHD Cause Panic Attacks?
- Why Is It So Hard to Get Tested for ADHD?
- What Foods Should Be Avoided With ADHD?
- Can ADHD Be Cured or Grown Out Of?
- Does Omega-3 Help ADHD?
- What Is the Mental Age of Someone With ADHD?
- Does ADHD Affect Intelligence?
Cite this post
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, January 16). 124 ADHD Research Topics & Titles. https://studycorgi.com/ideas/adhd-essay-topics/
"124 ADHD Research Topics & Titles." StudyCorgi , 16 Jan. 2022, studycorgi.com/ideas/adhd-essay-topics/.
StudyCorgi . (2022) '124 ADHD Research Topics & Titles'. 16 January.
1. StudyCorgi . "124 ADHD Research Topics & Titles." January 16, 2022. https://studycorgi.com/ideas/adhd-essay-topics/.
Bibliography
StudyCorgi . "124 ADHD Research Topics & Titles." January 16, 2022. https://studycorgi.com/ideas/adhd-essay-topics/.
StudyCorgi . 2022. "124 ADHD Research Topics & Titles." January 16, 2022. https://studycorgi.com/ideas/adhd-essay-topics/.
These essay examples and topics on ADHD were carefully selected by the StudyCorgi editorial team. They meet our highest standards in terms of grammar, punctuation, style, and fact accuracy. Please ensure you properly reference the materials if you’re using them to write your assignment.
This essay topic collection was updated on October 28, 2024 .
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Topic collections
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 4
- Twenty years of research on attention-deficit/hyperactivity disorder (ADHD): looking back, looking forward
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Samuele Cortese 1 , 2 , 3 , 4 , 5 ,
- David Coghill 6 , 7 , 8
- 1 Academic Unit of Psychology, Center for Innovation in Mental Health , University of Southampton , Southampton , UK
- 2 Clinical and Experimental Sciences (CNS and Psychiatry), Faculty of Medicine , University of Southampton , Southampton , UK
- 3 Solent NHS Trust , Southampton , UK
- 4 New York University Child Study Center , New York City , New York , USA
- 5 Division of Psychiatry and Applied Psychology, School of Medicine , University of Nottingham , Nottingham , UK
- 6 Departments of Paediatrics and Psychiatry, Faculty of Medicine, Dentistry and Health Sciences , University of Melbourne , Melbourne , Victoria , Australia
- 7 Murdoch Children’s Research Institute , Melbourne , Victoria , Australia
- 8 Royal Children’s Hospital , Melbourne , Victoria , Australia
- Correspondence to Dr Samuele Cortese, Academic Unit of Psychology and Clinical and Experimental Sciences (CNS and Psychiatry), University of Southampton, Southampton SO17 1BJ, UK; samuele.cortese{at}gmail.com
In this clinical review we summarise what in our view have been some the most important advances in the past two decades, in terms of diagnostic definition, epidemiology, genetics and environmental causes, neuroimaging/cognition and treatment of attention-deficit/hyperactivity disorder (ADHD), including: (1) the most recent changes to the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases; (2) meta-analytic evidence showing that, after accounting for diagnostic methods, the rates of ADHD are fairly consistent across Western countries; (3) the recent finding of the first genome-wide significant risk loci for ADHD; (4) the paradigm shift in the pathophysiological conceptualisation of ADHD from alterations in individual brain regions to a complex dysfunction in brain networks; (5) evidence supporting the short-term efficacy of ADHD pharmacological treatments, with a different profile of efficacy and tolerability in children/adolescents versus adults; (6) a series of meta-analyses showing that, while non-pharmacological treatment may not be effective to target ADHD core symptoms, some of them effectively address ADHD-related impairments (such as oppositional behaviours for parent training and working memory deficits for cognitive training). We also discuss key priorities for future research in each of these areas of investigation. Overall, while many research questions have been answered, many others need to be addressed. Strengthening multidisciplinary collaborations, relying on large data sets in the spirit of Open Science and supporting research in less advantaged countries will be key to face the challenges ahead.
https://doi.org/10.1136/ebmental-2018-300050
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder in children, with an estimated worldwide prevalence around 5%. 1 Although it has for a long time been considered a childhood disorder, it is now established that impairing ADHD symptoms persist in adulthood in a sizeable portion of cases (around 65%), 2 although there is variability in the estimate due to methodological heterogeneity across studies. 3
As for other mental health conditions there has, over the past two decades, been an increasing body of research on ADHD. Reasons for this increase include: increased recognition of the impact of ADHD on functioning; advances in research methodology and technology; and interest from pharmaceutical companies.
Here, we provide an overview of what we deem have been some the most important advances, in the past two decades, in ADHD research. We also discuss key areas for future research.
Given the large body of literature and space constraints, this review is selective rather than systematic and comprehensive. We relied mostly on meta-analyses, retrieved with a search in PubMed using the following syntax/terms (update: 8 August 2018): (ADHD OR Attention Deficit OR Hyperkinetic Disorder) AND (meta-analy* OR metaanaly).
Presentation
Diagnostic definition.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), 4 published in 2013, introduced several significant changes in relation to the DSM Fourth Edition Text Revision (DSM-IV-TR) 5 criteria. First, the threshold in the number of symptoms (criterion A) necessary for the diagnosis in older adolescents and adults was reduced from 6 to 5. This change is in keeping with the notion that, despite a reduction in the number of symptoms over development, adults with ADHD in childhood can still present with impairment. 2 The required age of onset was increased from ‘prior to 7’ to ‘prior to 12’. The purpose of these changes was well intended and designed to facilitate the diagnostic process in adults, who often have trouble pinpointing the exact age of onset, especially if early in the development. Unfortunately, neither change was based on empirical evidence, and methods used for diagnostic ascertainment in adults are still under debate. 3 Another pivotal change in DSM-5 is the removal of the veto around the dual diagnosis of ADHD and autism spectrum disorders (ASD) that was present in previous editions of the DSM. Unlike the age of onset and symptom number changes this change is supported by a significant body of research (see ref 6 ). Finally, the (sub)types of ADHD defined in the DSM-IV-(TR) were replaced by the notion of different presentations. This acknowledges the instability in the phenotypic manifestation of inattention or hyperactive/impulsive symptoms over time, 7 in contrast to the more static notion of a subtype.
With regard to the International Classification of Diseases (ICD), it appears that the veto to diagnose ASD in the presence of ADHD will be retained in the upcoming ICD 11th Revision ( https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f821852937 ).
Overall, while these changes to a degree reflect recent empirical evidence and/or practical needs in the diagnostic process, there are still issues that need to be addressed. First, current criteria still focus on the number of symptoms rather than on a more precise definition of functional impairment. This should be a priority for the field and efforts, such as the development of the International Classification of Functioning, Disability and Health: Child and Youth version, are already ongoing. 8 Second, while currently each of the symptoms listed in the DSM criterion A carries the same weight, it has been argued that inattention should be more heavily weighted than hyperactivity/impulsivity. 9 Supporting evidence, which comes from clinical samples, needs to be replicated in population-based studies. Third, from a practical standpoint, it is unclear on how to best integrate different information sources (eg, parents, teachers, etc). Addressing this challenge is pivotal. Fourth, although proposed as a separate type of ADHD or even a separate diagnostic entity, the extent to which the construct of sluggish cognitive tempo (impairment of attention in hypoactive-appearing individuals) overlaps with ADHD inattentive presentation remains still unclear. 10 11 Finally, one of the most controversial topics in the entire field of ADHD research is currently around the possibility that ADHD can emerge de novo in adulthood, in contrast to its conceptualisation as a neurodevelopmental disorder. Despite an increasing number of important studies, the controversy is far from being solved 12 and we expect it will be a major focus of research in the field in coming years.
We also expect that proposed radical, although controversial, changes in the nosographic approach to mental health conditions, such as the Research Domain Criteria will significantly influence future research on ADHD. 13
Epidemiology
One of the most controversial questions in relation to the epidemiology of ADHD has been around possible differences in the prevalence of the disorder in different countries. In particular, the differential rates of clinical diagnosis in North America and Europe are cited by detractors of ADHD, as supporting the notion that ADHD is not a ‘real’ disorder but rather a social construct. 14 However, a meta-analysis published in 2007 1 found that diagnostic criteria, source of information, requirement of impairment for diagnosis and geographic origin of the studies significantly impacted on the estimated pooled rate of ADHD (5.29%). A significant difference in prevalence emerged only between North America and both Africa and the Middle East, although evidence from non-Western countries was limited. However, as there were only a limited number of studies available for Africa and Middle East, these findings should be considered with caution. By contrast, no significant differences emerged between Europe and North America, suggesting that when using the same diagnostic approach the rates of the disorder are fairly consistent in Western countries, with variability in the prevalence accounted for primarily by methods used to diagnose ADHD. Another more recent meta-analysis 15 found no evidence to support an increase in the epidemiological prevalence of ADHD over the past three decades when standardised diagnostic procedures are followed. This implies that the trend for increased rates of diagnosis 16 are not accounted for by actual increases in prevalence. Rather, the mismatch between administrative and epidemiological rates of the disorder, which varies between the USA and Europe, is likely accounted for by cultural and social factors. 16
As the bulk of the available epidemiological studies focus on school-age children from North America and Europe, further population-based studies from other continents as well as in preschoolers and adults should be encouraged. Additionally, longitudinal epidemiological studies aimed at better understanding the developmental trajectories and predictors of remission/persistence of ADHD in adulthood will be instrumental, alongside other clinical, neuropsychological, genetic and neuroimaging studies, to inform prevention programmes. Development of a standardised definition of caseness and remission will be pivotal for this body of research to be fruitful.
Genetics and environmental causes of ADHD
Studies of twins and adopted children indicate a high heritability for ADHD (60%–90%). 17 Efforts to find the genes underpinning this heritability have been more challenging than initially anticipated. As for other mental health conditions, it became clear that ADHD aetiology is accounted for by a complex interaction of many genes each with a relatively small effect and by gene × environment interactions. 18
The first approach to finding the genes involved in ADHD was the ‘candidate gene’ approach. This approach focuses on identifying the variants in genes coding for proteins hypothesised, a priori, to be involved in the pathophysiology of ADHD. These studies identified only about 10 genes as having significant support, 19 which together accounted for only a small fraction of the total ADHD heritability. The next major approach, ‘genome-wide association studies’ (GWAS), which allows the analysis of a large number of common (ie, present at greater than 5% frequency in the population) single-nucleotide polymorphisms across the entire genome, was initially unsuccessful in ADHD, as the available sample was too small to show a meaningful effect. However, in a major breakthrough, the first 12 independent loci have been recently identified through GWAS. 20 Associations were enriched in loss-of-function intolerant genes and brain-expressed regulatory marks, paving the way for a number of novel lines of investigation on the neurobiology of ADHD.
A further recently developed approach focuses on rare (ie, a frequency in the general population below 1%) ‘copy number variants’ (CNV). These are defined as replications or deletions of the DNA with a length of at least 1 kb. CNVs over-represented in ADHD have been detected, but their contribution can so far only explain 0.2% of ADHD heritability. 21
As for environmental aetiological factors, there have been, over the past years, considerable data suggesting that prenatal and postnatal factors, such as maternal smoking and alcohol use, low birth weight, premature birth and exposure to environmental toxins, such as organophosphate pesticides, polychlorinated biphenyls and zinc, are associated with increased risk for ADHD. 17 22 However, except for preterm birth, genetics studies have implicated unmeasured familial confounding factors, which are not in line with a causal role of environmental factors. 23
Severe maternal deprivation has also been related to the development of ADHD-like symptoms. 24
The study of the causes of ADHD still has many unanswered questions. We need a better understanding of how genes interact with each other, and of the interplay between environmental factors and genes. Genetics has the potential to offer many other exciting future avenues of research in ADHD. We will only mention briefly here: (1) the use of induced pluripotent stem cell derived from peripheral tissue of patients with ADHD and used to generate brain cells with the aim to model brain circuits and responses to medications or other stressors; (2) the use of zebrafish and fruit fly models to augment currently available animal models of ADHD.
Neuroimaging and neurocognition
Initial pathophysiological models of ADHD published 20 years ago 25 were based on dysfunctions in a limited number of brain areas, namely the frontal cortex and the basal ganglia. Over the past two decades, and similar to other mental health conditions, a major paradigm shift from alterations in individual brain regions to dysfunction in brain networks has begun to reshape our understanding of the pathophysiology of ADHD. Structurally, meta-analyses and mega-analyses of the structural MRI studies conducted over the past two decades pointed to consistently replicated alterations in the basal ganglia, 26 and in a number of other subcortical areas. 27 Functionally, a comprehensive meta-analysis 28 found that the majority of the ADHD-related hypoactivated areas were related to the ventral attention and the frontoparietal networks. By contrast, the majority of ADHD-related hyperactivated areas fell within the default mode network and other hyperactivated areas were within the visual network. This is in line with the hypothesis that the attentional lapses that characterise ADHD result from an inappropriate intrusion of the default network in the activity of task-positive networks frontoparietal, ventral or dorsal attention networks, 28 according to the default network hypothesis of ADHD , 29 which has been arguably one of the most inspiring proposals in the neuroscience of ADHD over the past two decades.
While we have gained insight into the brain networks that are dysfunctional in ADHD and in the delay in cortical maturation, 30 we look forward to the next generation of neuroimaging studies which we hope will start to translate these findings into the clinical practice. The introduction of machine learning approaches, such as support vector machine, has been welcomed in the field of clinical neuroscience as a way to translate neuroscientific findings at the individual patient level, thus overcoming the main limitation of current studies that can only provide results valid at the group, rather than individual, level. 31 An increasing number of studies have used machine learning based on MRI data to validate the diagnosis of ADHD with varying degrees of success. 32 33
Neurocognitive studies have made a considerable contribution to our understanding of ADHD. In recent years, the field has moved away from linear single-cause models of ADHD towards multipathway models that emphasise the heterogeneity inherent to ADHD and provide a link between individual differences at the brain level and clinical presentation. 34 35
We believe that an interesting line of research for the future will be to combine genetics, clinical, neurocognitive and neuroimaging data to define, via machine learning approaches, response to treatment, tolerability profiles and functional trajectory of the disorder over time. This will be a crucial step towards personalised and precision approaches to treatment.
Over the past two decades, there has been a marked increase in the number of randomised controlled trials (RCT) aimed at testing the short-term efficacy and tolerability of pharmacological treatments for ADHD (both stimulant and non-stimulant medications). Most have been sponsored by Big Pharma and were designed to support the licence of the medication. In parallel, due to concerns around possible side effects of medications and lack of clarity around their long-term effects, several lines of research on non-pharmacological interventions have been developed. Recent important methodologically sound meta-analyses allow us to summarise and critically discuss this large body of evidence.
For the pharmacological interventions, a comprehensive network meta-analysis 36 of 133 double-blind RCTs demonstrated high to moderate effect sizes (in terms of efficacy) for the different medications versus placebo. Standardised mean differences (SMD) ranged from −1.02 (95% CI −1.19 to −0.85) for amphetamines to −0.56 (95% CI −0.66 to −0.45) for atomoxetine (methylphenidate: −0.78, 95% CI −0.93 to −0.62). In children/adolescents, methylphenidate was the only drug with better acceptability than placebo; in adults this was the case only for amphetamines (with no difference between placebo and other active drugs). Taking into account both efficacy and safety, evidence from this meta-analysis supported methylphenidate as preferred first-choice medication for the short-term treatment of ADHD in children/adolescents and amphetamines for adults.
As for non-pharmacological options, a comprehensive synthesis on non-pharmacological treatments for children and adolescents with ADHD has been provided in a series of meta-analyses by the European ADHD Guidelines Group (EAGG). In 2013, they published a first systematic review/meta-analysis 37 addressing the efficacy of behavioural interventions, diet interventions (restricted elimination diets, artificial food colour exclusions and free fatty acid supplementation), cognitive training and neurofeedback on ADHD core symptoms (ie, inattention, hyperactivity and impulsivity). The systematic review included only RCTs and considered two contrasting outcomes: those rated by individuals not blinded to the treatment condition (active vs control) and those rated by individuals who were probably blinded to treatment (eg, teachers in trials assessing a behavioural intervention implemented with parents). The results were strikingly different depending on the type rater. When considering not blinded ratings, all interventions resulted significantly more efficacious than the control condition in terms of reduction of ADHD core symptoms. However, when considering the more rigorous probably blinded ratings, only free fatty acid supplementation and artificial food colour exclusion remained significantly more efficacious than the control conditions, with small effect sizes (SMD=0.16 and 0.42, respectively), indicating that the clinical impact of these treatments on ADHD core symptoms is, at the group level, modest.
Subsequent EAGG meta-analyses focused on ADHD core symptoms and on ADHD-related problems. A meta-analysis 38 specifically focusing on behavioural interventions showed that, even when considering probably blinded ratings, the behavioural interventions were efficacious at improving important aspects related to ADHD, namely parenting (SMD for positive parenting 0.63; SMD for negative parenting 0.43) and conduct problems (SMD 0.31). Another updated meta-analysis 39 on cognitive training, which was found efficacious in improving verbal and visual working memory, which are impaired in a sizeable portion of children with ADHD and have been demonstrated to dissociate from ADHD symptoms. 40 These meta-analyses also suggest that training which targets several neuropsychological aspects may be more efficacious at improving ADHD symptoms, than training targeting only one aspect of cognitive functioning. The most recent meta-analysis 41 by the EAGG on neurofeedback did not provide support for the efficacy of neurofeedback on any of the neuropsychological and academic outcomes. Overall, this body of research does not provide solid evidence to routinely recommend non-pharmacological interventions as highly effective treatments for ADHD core symptoms, although some of them (eg, behavioural interventions or cognitive training) may be effective for important associated impairments (oppositional behaviours and working memory deficits, respectively). The role of fatty acid supplementation and artificial food colours exclusion as possible treatment strategies should be considered cautiously given the small effect size, with CIs close to non-significance.
Probably, the most crucial area of future treatment research in ADHD will be to gain insight into the long-term positive and negative effects of treatments, using randomised trials with withdrawn designs, as well as additional population-based studies with self-controlled methodologies and longitudinal follow-up studies. These should clarify the conclusions from the various follow-up waves of the Multimodal Treatment of ADHD (MTA) study, showing that neither the type and intensity of treatment received during the initial 15-month randomised phase of the study (treatment as usual medication (MED), behavioural therapy (BEH), medication plus behavioural therapy (COMB)) nor exposure to medication over the subsequent observational periods predicted the functional outcome at follow-up which has now extended to 16 years. Of note, in the MTA, the treatments received in the three experimental arms (MED, BEH, COMB) during initial 15-month randomised phase were carefully crafted in an attempt to achieve optimal outcomes. After this initial phase all participants were free to choose the type of treatment they received from their regular provider. As it is likely that these treatments were not as carefully optimised and monitored as the three experimental groups during the randomised phase, these longer term findings of the MTA are not easily interpretable and might be, to some extent, misleading.
Conclusions
Many questions have been successfully answered in the field of ADHD. Many others remain to be addressed. Additional multidisciplinary collaborations, use of large data sets in the spirit of Open Science and support of research activities in less advantaged countries are key to address the challenge.
- Polanczyk G ,
- de Lima MS ,
- Horta BL , et al
- Faraone SV ,
- Biederman J ,
- Sibley MH ,
- Mitchell JT ,
- 4. ↵ American Psychiatric Association . Diagnostic and statistical manual of mental disorders, DSM-5 . Fifth edn . American Psychiatric Publishing , 2013 .
- 5. ↵ American Psychiatric Association . Diagnostic and statistical manual of mental disorders . Fourth edn : American Psychiatric Publishing , 2000 .
- Visser JC ,
- Rommelse NN ,
- Greven CU , et al
- Willcutt EG ,
- Pennington BF , et al
- Coghill D , et al
- Sokolova E ,
- Claassen T , et al
- Becker SP ,
- Leopold DR ,
- Burns GL , et al
- Agnew-Blais J ,
- Arseneault L
- Peterson BS
- Sergeant J ,
- Gillberg C , et al
- Polanczyk GV ,
- Salum GA , et al
- Daley D , et al
- Asherson P ,
- Banaschewski T , et al
- Cummins TD ,
- Tong J , et al
- 20. ↵ Discovery Of The First Genome-Wide Significant Risk Loci For ADHD . https://www.biorxiv.org/content/early/2017/06/03/145581
- Hohmann S ,
- Lahey BB , et al
- Sciberras E ,
- Mulraney M ,
- Silva D , et al
- Stevens SE ,
- Sonuga-Barke EJ ,
- Kreppner JM , et al
- Castellanos FX
- Rubia K , et al
- Hoogman M ,
- Bralten J ,
- Hibar DP , et al
- Cortese S ,
- Chabernaud C , et al
- Eckstrand K ,
- Sharp W , et al
- Pettersson-Yeo W ,
- Marquand AF , et al
- Johnston BA ,
- Matthews K , et al
- Coghill DR ,
- Del Giovane C , et al
- Brandeis D ,
- Cortese S , et al
- van der Oord S ,
- Ferrin M , et al
- Brandeis D , et al
- Rhodes SM ,
Contributors SC drafted the paper. DC revised the first draft.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests SC declares reimbursement for travel and accommodation expenses from the Association for Child and Adolescent Central Health (ACAMH) in relation to lectures delivered for ACAMH, and from Healthcare Convention for educational activity on ADHD. DC declares grants and personal fees from Shire and Servier; personal fees from Eli Lilly, Novartis and Oxford University Press; and grants from Vifor.
Patient consent Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Celebrating 25 Years
- Join ADDitude
- |
- What Is ADHD?
- The ADHD Brain
- ADHD Symptoms
- ADHD in Children
- ADHD in Adults
- ADHD in Women
- Find ADHD Specialists
- Symptom Checker Tool
- Symptom Tests
- More in Mental Health
- ADHD Medications
- Medication Reviews
- Natural Approaches
- ADHD Therapies
- Managing Treatment
- Treating Your Child
- Success @ School 2024
- Behavior & Discipline
- Positive Parenting
- Schedules & Routines
- School & Learning
- Health & Nutrition
- Teens with ADHD
- More on ADHD Parenting
- Do I Have ADD?
- Getting Things Done
- Time & Productivity
- Relationships
- Organization
- Health & Nutrition
- More for ADHD Adults
- New Contest!
- Free Webinars
- Free Downloads
- Newsletters
- Guest Blogs
- eBooks + More
- Search Listings
- Add a Listing
- News & Research
- For Clinicians
- For Educators
- ADHD Directory
- Manage My Subscription
- Get Back Issues
- Digital Magazine
- Gift Subscription
- Renew My Subscription
ADHD Research Roundup: New Studies, Findings & Insights
Adhd research continues to reveal new insights about attention deficit — its relationship to trauma, race, emotional dysregulation, rejection sensitive dysphoria, and treatments ranging from medication to video games. we’ve curated the most significant news of the past year., adhd research continues to reveal new truths.
ADHD research has produced groundbreaking and impactful discoveries in the past year. Our understanding of the relationship between health care and race has deepened. Alternative treatments, like video games and neurofeedback, are showing encouraging promise while ADHD stimulant medication continues to demonstrate benefits for patients of all ages. The connections between comorbid conditions, gender, and ADHD are better understood than ever before. And we are encouraged by the ongoing work coming from the world’s leading research teams.
Read below to catch up on the most significant news and research from 2020, and stay updated on new findings as they are published by subscribing to ADDitude’s free monthly research digest .
General ADHD Research
Study: Long-Term Health Outcomes of Childhood ADHD are Chronic, Severe November 24, 2020 Childhood ADHD should be considered a chronic health problem that increases the likelihood of adverse long-term health outcomes, according to a population-based birth cohort study of children with ADHD and psychiatric disorders. Further research on the impact of treatment is needed.
Study: Living with ADHD Causes Significant Socioeconomic Burden October 21, 2020 Living with ADHD poses a significant economic burden, according to a new study of the Australian population that found the annual social and economic cost of ADHD was $12.76 billion, with per person costs of $15,664 over a lifetime.
Study: Unmedicated ADHD Increases the Risk of Contracting COVID-19 July 23, 2020 The COVID-19 infection rate is nearly 50% higher among individuals with unmedicated ADHD compared to individuals without ADHD , according to a study of 14,022 patients in Israel. The study found that ADHD treatment with stimulant medication significantly reduces the risk of virus exposure among individuals with ADHD symptoms like hyperactivity and impulsivity.
[ Does My Child Have ADHD? Take This Test to Find Out ]
Study: Poverty Increases Risk for ADHD and Learning Disabilities March 23, 2020 Children from families living below the poverty level, and those whose parents did not pursue education beyond high school, are more likely to be diagnosed with ADHD or learning disabilities, according to a new U.S. data brief that introduces more questions than it answers.
ADHD and Children
Study: Diagnosed and Subthreshold ADHD Equally Impair Educational Outcomes in Children December 21, 2020 Children with diagnosed and subthreshold ADHD both experienced impaired academic and non-academic performance compared to controls used in an Australian study examining the two community cohorts.
Study: Children with ADHD More Likely to Bully — and to Be Bullied November 23, 2020 Children with ADHD are more likely than their neurotypical peers to be the bully, the victim of bullying, or both, according to a new study.
Study: ADHD Symptoms in Girls Diminish with Extracurricular Sports Activity October 16, 2020 Consistent participation in organized sports reliably predicted improved behavior and attentiveness in girls with ADHD, according to a recent study of elementary school students active — and not active — in extracurricular activities. No such association was found for boys with ADHD.
[ Do I Have ADHD? Take This Test to Find Out ]
Study: ADHD in Toddlers May Be Predicted by Infant Attentional Behaviors August 12, 2020 Infants who exhibit behaviors such as “visually examining, acting on, or exploring nonsocial stimuli including objects, body parts, or sensory features” may be more likely to demonstrate symptoms of ADHD as a toddler, according to a new study that also found a correlation between this Nonsocial Sensory Attention and later symptoms of executive dysfunction.
Study Shows Gender Disparities in ADHD Symptoms of Hyperactivity and Poor Response Inhibition June 26, 2020 Girls with ADHD are less physically hyperactive than are boys with the condition, and experience fewer problems with inhibition and cognitive flexibility, according to a new meta-analysis that says more accurate screening tools are needed to recognize the subtler manifestations of ADHD in girls.
Study: Raising a Child with ADHD Negatively Impacts Caregivers’ Mental Wellbeing July 27, 2020 Caring for a child with ADHD negatively impacts caregivers’ quality of sleep, relationships, and satisfaction with free time, among other indicators of mental wellbeing, according to a recent study from the United Kingdom. The significant deficit in sleep and leisure satisfaction led researchers to conclude that caregivers may benefit from greater support — for example, coordinated health and social care — that focuses on these areas.
Study: ADHD, Diet, Exercise, Screen Time All Directly or Indirectly Impact Sleep July 27, 2020 A child with ADHD is more likely to experience sleep problems, in part because ADHD symptoms influence diet and physical activity — two factors that directly impact sleep. This finding comes from a new study that also shows how screen time impacts exercise, which in turn impacts sleep. Understanding these interwoven lifestyle factors may help caregivers and practitioners better treat children with ADHD.
ADHD and Adolescents
Teens with ADHD Should Be Regularly Screened for Substance Use Disorder: International Consensus Reached July 17, 2020 Adolescents with ADHD should be regularly screened for comorbid substance use disorder, and vice versa. This was one of 36 statements and recommendations regarding SUD and ADD recently published in the European Research Addiction Journal.
Study: Girls with ADHD Face Increased Risk for Teen Pregnancy February 12, 2020 Teenagers with ADHD face an increased risk for early pregnancy, according to a new study in Taiwan. However, long-term use of ADHD medications does reduce the risk for teen pregnancies. Researchers suggested that ADHD treatment reduces the risk of any pregnancy and early pregnancy both directly by reducing impulsivity and risky sexual behaviors and indirectly by lowering risk and severity of the associated comorbidities, such as disruptive behavior and substance use disorders.
Study: Teens with ADHD Face Increased Risk for Nicotine Addiction January 27, 2020 Young people with ADHD find nicotine use more pleasurable and reinforcing after just their first smoking or vaping experience, and this may lead to higher rates of dependence, according to findings from a new study published in the Journal of Neuropsychopharmacology .
Study: Adolescent Health Risks Associated with ADHD Go Unmonitored by Doctors February 27, 2020 The health risks facing adolescents with ADHD — teen pregnancy, unsafe driving, medication diversion, and more — are well documented. Yet, according to new research, primary care doctors still largely fail to address and monitor these urgent topics during their patients’ transition to young adulthood.
Study: Emotional Dysregulation Associated with Weak, Risky Romantic Relationships Among Teens with ADHD May 20, 2020 Severe emotional dysregulation increases the chances that an adolescent with ADHD will engage in shallow, short-lived romantic relationships and participate in unprotected sex, according to a new study that suggests negative patterns developed in adolescence may continue to harm the romantic relationships and health of adults with ADHD .
ADHD and Adults
Study: Discontinuing Stimulant Medication Negatively Impacts Pregnant Women with ADHD December 17, 2020 Women with ADHD experience negative impacts on mood and family functioning when they discontinue stimulant medication use during pregnancy, according to a new observational cohort study that suggests medical professionals should consider overall functioning and mental health when offering treatment guidance to expectant mothers.
New Study: Adult ADHD Diagnosis Criteria Should Include Emotional Symptoms April 21, 2020 The ADHD diagnosis criteria in the DSM-5 does not currently include emotional symptoms, despite research indicating their importance. Now, a new replication analysis has found that ADHD in adults presents in two subtypes: attentional and emotional. Researchers suggest that this system offers a more clinically relevant approach to diagnosing ADHD in adults than does the DSM-5 .
Study: Stimulant ADHD Medication Relatively Safe and Effective for Older Adults June 30, 2020 Older adults with ADHD largely experience symptom improvement when taking a low dose of stimulant medication, which is well tolerated and does not cause clinically significant cardiovascular changes. This is the finding of a recent study examining the effects of stimulant medication among adults aged 55 to 79 with ADHD, some of whom had a pre-existing cardiovascular risk profile.
ADHD, Race, and Culture
Study Explores Medication Decision Making for African American Children with ADHD June 23, 2020 In a synthesis of 14 existing studies, researchers have concluded that African American children with ADHD are significantly less likely than their White counterparts to treat their symptoms with medication for three main reasons: caregiver perspectives on ADHD and ADHD-like behaviors; beliefs regarding the risks and benefits associated with stimulant medications; and the belief that ADHD represents a form of social control.
Culturally Adapted Treatment Improves Understanding of ADHD In Latinx Families August 31, 2020 Latinx parents are more likely to recognize and understand ADHD after engaging in culturally adapted treatment (CAT) that includes parent management training sessions adapted to be more culturally appropriate and acceptable, plus home visits to practice skills. This recent review of ADHD knowledge among Latinx parents found that CAT outperformed evidence-based treatment (EBT) in terms of parent-reported knowledge of ADHD.
Treating ADHD
Study: New Parent Behavior Therapy Yields Longer ADHD Symptom Control in Children October 6, 2020 ADHD symptom relapse was significantly reduced in children of parents who participated in a new schema-enhanced parent behavior therapy, compared to those whose parents participated in standard PBT.
Research: Physical Exercise Is the Most Effective Natural Treatment for ADHD — and Severely Underutilized January 22, 2020 A new meta-analysis shows that physical exercise is the most effective natural treatment for controlling ADHD symptoms such as inhibition, attention, and working memory . At the same time, a comprehensive study reveals that children with ADHD are significantly less likely to engage in daily physical activity than are their neurotypical peers.
A Video Game Prescription for ADHD? FDA Approves First-Ever Game-Based Therapy for Attention June 18, 2020 Akili Interactive’s EndeavorRx is the first game-based digital therapeutic device approved by the FDA for the treatment of attention function in children with ADHD. The history-making FDA OK followed a limited-time release of the device during the coronavirus pandemic, and several years of testing the device in randomized controlled trials.
Study: Neurofeedback Effectively Treats ADHD April 9, 2020 Neurofeedback is an effective treatment for ADHD , according to a new quantitative review that used benchmark studies to measure efficacy and effectiveness against stimulant medication and behavior therapy. These findings relate to standard neurofeedback protocols, not “unconventional” ones, for which significant evidence was not found.
Study: Mindfulness-Enhanced Behavioral Parent Training More Beneficial for ADHD Families June 29, 2020 Behavioral parent training (BPT) enhanced with mindfulness meditation techniques provides additional benefits to parents of children with ADHD, such as improved discipline practices and parental behavioral regulation. This is the finding of a new randomized control trial conducted by researchers who compared mindfulness-enhanced to standard BPT.
Mapping the ADHD Brain: MRI Scans May Unlock Better Treatment and Even Symptom Prevention March 9, 2020 Brain MRI is a new and experimental tool in the world of ADHD research. Though brain scans cannot yet reliably diagnose ADHD, some scientists are using them to identify environmental and prenatal factors that affect symptoms, and to better understand how stimulant medications trigger symptom control vs. side effects.
New Clinical Guidelines: Holistic Treatment Is Best for Children with ADHD and Comorbidities February 3, 2020 The Society for Developmental and Behavioral Pediatrics (SDBP) says that children and teens with ADHD plus comorbidities should receive psychosocial treatment, such as classroom-based management tools, in addition to ADHD medication.
Study: Mindfulness Exercises Effectively Reduce Symptoms in Boys with ADHD and ODD May 19, 2020 Boys with both ADHD and ODD were less hyperactive and more attentive after attending a multi-week mindfulness training program, according to a new study that finds promise in this treatment as a viable complement or alternative to medication.
ADHD and Comorbid Conditions
Study: Risk for Diabetes 50% Higher for Adults with ADHD October 23, 2020 A diagnosis of ADHD increased the likelihood of diabetes by as much as 50% for adults with ADHD, according to a recent study from the National Health Interview Survey that found the strong correlation independent of BMI.
Study: ADHD Symptoms Associated with More Severe Gambling Disorder and Emotional Dysregulation January 28, 2020 Roughly one-fifth of individuals diagnosed with gambling disorder in the study also tested positive for ADHD symptoms. This population is more likely to experience severe or acute symptoms of gambling disorder, which is tied to higher emotional dysregulation, according to a new study of 98 Spanish men.
ADHD Research: Next Steps
- Read: New Insights Into Rejection Sensitive Dysphoria
- Download: The All-Time Best Books on ADHD
- Learn: What Is ADHD? Definition, Myths & Truths
ADHD News & Research: Read These Next

The Physician’s Guide for Distinguishing Bipolar Disorder and ADHD

Does Trauma Cause ADHD? And Vice Versa?

The Best of 2021: Must-Read Articles on ADHD

Is It Just ADHD? Comorbidities That Unlock an Accurate Mental Health Diagnosis
Adhd newsletter, adhd for professionals, news, research & insights straight to your inbox..
It appears JavaScript is disabled in your browser. Please enable JavaScript and refresh the page in order to complete this form.
Center for ADHD Research Projects
Research projects.
The Center for ADHD strives to find new and innovative approaches to treat children with attention deficit hyperactivity disorder.
Current Projects
Current projects and proposed research include:
- Studies Seeking Participants
- ADHD Study For Parents of Children 4 to 11 Years Old
- Study for Children 10 to 12 With Excessive Daydreaming, Mental Confusion, Fogginess, Spaciness and / or Slowed Behavior / Thinking
- ADHD Study for Children 8 to 12 Years Old
- Carboxylesterase 1 Genetic Variation and Methylphenidate in ADHD (CES1) Study Summary
- Down Syndrome and ADHD Study for Children and Teens 6 to 17 Years Old
- A Study for Black and Latino Caretakers of Children Newly Diagnosed with ADHD
- ADHD Medication Effects on Adolescents with ADHD
- Ongoing Studies
- Carboxylesterase 1 Genetic Variation and Methylphenidate in ADHD (CES1) Study Summary 18+
- Evaluating Assessment and Medication Treatment of ADHD in Children with Down Syndrome (TEAM-DS)
- Longitudinal Examination of Sluggish Cognitive Tempo and Internalizing Psychopathology in Adolescence (ALERT study)
- Longitudinal Evaluation of Sluggish Cognitive Tempo: Identifying Mechanisms of Educational Impairment (CASS-2 study)
- Mindful Awareness Practices (MAPs) in Adolescents with ADHD and Sluggish Cognitive Tempo (SCT)
- A Family Navigator Intervention to Improve ADHD- Related Treatment Adherence (I2-ART) for Minority Children
- Parsing Neurobiological Bases of Heterogeneity in ADHD
- Nationwide dissemination of a web-based quality improvement intervention to improve the quality of ADHD care among community-based pediatricians
- Improving ADHD Behavioral Care Quality in Community-Based Pediatric Settings
- Improving Medication Continuity Among Adolescents with ADHD
- Predictors of Stimulant Medication Continuity in Children with ADHD
- Teaching Academic Success Skills to Middle School Students with Autism Spectrum Disorders (ASD) with Executive Functioning Deficits – School Setting
Completed Projects
- Evaluating Assessment and Medication Treatment of ADHD in Children with Down Syndrome
- ADHD Study for Teens With Sleep Problems
- Improving ADHD Driving Study
- The Effects of ADHD Medication (TEAM) Study
- A Multi-Method Feasibility Study Investigating Reaction Time Variability in Autism Spectrum Disorder
- Children’s Attention Problems Study
- Evaluation of the Computerized Progressive Attention Training (CPAT) program for children with ADHD
- Multisite Study of School-Based Treatment Approaches for ADHD
- Evaluation of an Intervention for Improving Community-Based Pediatric ADHD Care
- Multimodal Treatment Study Follow-Up
- Developing New Technologies to Improve ADHD Medication Continuity
- Shared Decision Making to Improve Care for Children with ADHD
- Medication Continuity in Children Treated for ADHD
- Improving Self-regulation & School Readiness in Preschoolers
- Interventions for Children with ADHD and Reading Difficulties
- Sleep in Teens with ADHD
- Omega-3 fatty acid supplements on ADHD brain function
- ADHD iPAD App study
- Medication Response in Children with Predominantly Inattentive Type ADHD
- Cognitive Training Program for Children with ADHD
- ADHD Collaborative
- Disseminating a Model Intervention to Promote Improved ADHD Care in the Community
- Examining the Effects of Cell Phone Use in an ADHD Population: A Pilot Study
- Organizational Skills Intervention
- Response Variability in Children with ADHD
- A novel intervention to improve the driving performance of ADHD teens
- Impact of COVID-19 in Adolescents with and without ADHD
- Treating Sleep in Adolescents with ADHD and Co-occurring Sleep Problems
- SCT Interview Study
- Phenotypic Correlates Distinguishing Sluggish Cognitive Tempo from ADHD
- Teaching Academic Success Skills to Middle School Students with Autism Spectrum Disorders (ASD) with Executive Functioning Deficits
- Longitudinal Impact of Sleep in Teens (LIST) With and Without ADHD Study
- Concentration at School Study (CASS)

Connect With Us
3333 Burnet Avenue, Cincinnati, Ohio 45229-3026
© 1999-2024 Cincinnati Children's Hospital Medical Center. All rights reserved.

Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Attention-Deficit/Hyperactivity Disorder Diagnosis, Treatment, and Telehealth Use in Adults — National Center for Health Statistics Rapid Surveys System, United States, October–November 2023
Weekly / October 10, 2024 / 73(40);890–895
Brooke S. Staley, PhD 1 ,2 ; Lara R. Robinson, PhD 1 ; Angelika H. Claussen, PhD 1 ; Samuel M. Katz, MPH 1 ,3 ; Melissa L. Danielson, MSPH 1, *; April D. Summers, MPH 1 ; Sherry L. Farr, PhD 1 ; Stephen J. Blumberg, PhD 4 ; Sarah C. Tinker, PhD 1 ( View author affiliations )
What is already known about this topic?
Attention-deficit/hyperactivity disorder (ADHD) is a common childhood disorder that can continue into adulthood, but there is limited information about diagnosis and treatment in adults.
What is added by this report?
In 2023, an estimated 15.5 million U.S. adults had an ADHD diagnosis, approximately one half of whom received their diagnosis in adulthood. Approximately one third of adults with ADHD take stimulant medication; 71.5% had difficulty filling their prescription because the medication was unavailable. Approximately one half of adults with ADHD have ever used telehealth for ADHD services.
What are the implications for public health practice?
ADHD affects many adults. Information on diagnosis and treatment helps the development of clinical care guidelines and regulatory decision-making around medication shortages and telehealth for ADHD.
- Article PDF
- Full Issue PDF
- Clinical Implications of Attention-Deficit/Hyperactivity Disorder in Adults: What New Data on Diagnostic Trends, Treatment Barriers, and Telehealth Utilization Tell Us
- Prescription in Peril: Navigating Adult ADHD, Stimulant Shortages, and the Telehealth Lifeline

Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that develops during childhood and can last into adulthood. Data from the National Center for Health Statistics Rapid Surveys System collected during October–November 2023 were used to estimate the prevalence of ADHD diagnosis and treatment among U.S. adults. In 2023, an estimated 15.5 million U.S. adults (6.0%) had a current ADHD diagnosis based on self-report; approximately one half received the diagnosis at age ≥18 years. Approximately one third of adults with ADHD took a stimulant medication to treat their ADHD in the previous year, 71.5% of whom had difficulty getting their ADHD prescription filled because it was unavailable. Approximately one half of adults with ADHD have ever used telehealth for ADHD-related services. Telehealth might have benefits for persons with ADHD, including helping them access behavioral treatment or medication prescriptions for ADHD. This report provides national estimates of the prevalence and treatment of ADHD among U.S. adults to help guide clinical care and regulatory decision-making for ADHD among U.S. adults.
Introduction
Worldwide, approximately 2%–5% of adults experience attention-deficit/hyperactivity disorder (ADHD) symptoms such as inattention, hyperactivity, and impulsivity ( 1 , 2 ). However, recent data on ADHD diagnosis and treatment among adults in the United States are limited; no national data exist on ADHD treatment in U.S. adults, and national prevalence estimates of current ADHD in adults rely on data from 2003. † Telehealth policies implemented during the COVID-19 pandemic expanded access to ADHD diagnosis and treatment, including medication ( 3 ). Pharmacotherapy is a first-line treatment for adults with ADHD ( 2 ), and prescribing of stimulant medication has increased since the COVID-19 pandemic began ( 4 ). Shortages of stimulant medications § in the United States have affected many persons with ADHD who rely on pharmacotherapy to appropriately treat their ADHD ( 2 , 5 ). Timely data are needed to develop clinical guidelines, and guide decision-making for policies, including regulation concerning stimulant prescription and telehealth access for ADHD in U.S. adults.
Rapid Survey System: Survey Panels and Sample
The National Center for Health Statistics (NCHS) Rapid Surveys System (RSS) approximates national representation of the U.S. adult population based on self-reported health data from two commercial online survey panels: NORC at the University of Chicago’s AmeriSpeak Panel ( 1 ) and Ipsos’s KnowledgePanel ( 2 ). These cross-sectional samples are surveyed simultaneously using the same RSS questionnaire, conducted online and by telephone, and are then combined ( 6 ). To reduce coverage and nonresponse biases, responses are weighted and calibrated to the estimates from the second quarter of the 2023 National Health Interview Survey to reflect the total population of U.S. adults aged ≥18 years. The RSS Round 2 (RSS-2), fielded during October–November 2023, includes data from 7,046 completed interviews ( 6 ). More details on RSS and incorporated panels are available at https://www.cdc.gov/nchs/rss/rss-topics.html ; the RSS-2 brief technical note is available at https://www.cdc.gov/nchs/data/rss/round2/technical-notes.pdf . The cumulative response rates of the two commercial panels were 3.8% and 4.0%, and the RSS-2 overall completion rate was 37.2% ( 6 ).
Adults with current ADHD were identified using two survey questions: “Have you ever been diagnosed with attention-deficit/hyperactivity disorder, or ADHD, by a doctor or other health professional?” and, if so, “Do you currently have ADHD?” ( https://www.cdc.gov/nchs/data/rss/round2/questionnaire.pdf ). Adults reporting current ADHD received follow-up questions regarding receipt and type of treatment, type of medication use (categorized as stimulant or nonstimulant medications), difficulty obtaining prescription medication, and use of telehealth services for their ADHD care. Demographic variables included age, age at diagnosis (<18 years versus ≥18 years), gender, education, race and ethnicity, household income as a percentage of the federal poverty level, insurance status, and metropolitan status; these data were collected before the survey through panel-specific profile assessments that are harmonized for inclusion in RSS-2 data ( 6 ). SAS-callable SUDAAN (version 11.0.3; RTI International) was used to conduct all analyses. Variances were computed using the Taylor linearization method. This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy. ¶
Prevalence of ADHD Among U.S. Adults
An estimated 6.0% of adults had a current ADHD diagnosis, equivalent to one in 16, or approximately 15.5 million U.S. adults ( Table 1 ). When compared with adults who have never received a diagnosis of ADHD, those with current ADHD were more likely to be aged <50 years (84.5% versus 51.2%), less likely to have a bachelor’s degree or higher (28.1% versus 35.3%), less likely to be non-Hispanic Black or African American (7.4% versus 12.9%), more likely to be non-Hispanic White (70.4% versus 61.4%), and more likely to have a household income below the federal poverty level (22.1% versus 12.3%).
ADHD Diagnosis and Treatment
More than one half of adults with ADHD (55.9%) received their diagnosis during adulthood (age ≥18 years) ( Table 2 ). At the time of the survey, approximately one third of adults with ADHD were not receiving any treatment (36.5%), while another one third were receiving both medication and counseling or behavioral treatment (35.2%). Approximately one half of adults (50.4%) with ADHD were prescribed medication to treat their ADHD during the previous 12 months. Approximately one third of adults with current ADHD reported taking prescription stimulant ADHD medication during the previous 12 months (33.4%); nonstimulant ADHD medication use was less common (5.9%). Among adults who reported taking a stimulant medication, 71.5% reported difficulty getting their ADHD prescription filled during the previous 12 months because their medication was not available.
Telehealth Use for ADHD
Almost one half of adults with ADHD (46.0%) reported ever receiving telehealth services for their condition ( Table 3 ). Approximately one in 11 adults (8.9%) received their diagnosis via telehealth only, and an additional one in 10 (9.5%) received their diagnosis through a combination of in-person and telehealth visits. Since the start of the COVID-19 pandemic (i.e., March 2020), approximately one third of adults with current ADHD used telehealth to obtain a prescription for ADHD medication (30.5%) or to receive counseling or therapy for ADHD (30.8%).
This analysis of a nationally representative sample of U.S. adults found that in 2023, an estimated 15.5 million (6.0%) had a current ADHD diagnosis, approximately one half of whom received their diagnosis during adulthood. Results highlight the magnitude of ADHD as a public health issue across the life course. Approximately one third of adults with current ADHD are not receiving any ADHD treatment. Among those receiving stimulant pharmacotherapy, seven in 10 reported difficulty obtaining their ADHD medication because it was not available. Approximately one half of adults with current ADHD have ever used telehealth for ADHD services.
Diagnostic criteria for ADHD require evidence of symptoms before age 12 years ( 7 ), but actual diagnosis might occur years beyond symptom onset. These data suggest diagnosis in adulthood is common. Although the majority of adults with current ADHD received counseling or medication treatment for their ADHD in the previous year, approximately one third did not receive any type of treatment. ADHD pharmacotherapy is associated with reduced social and emotional impairment, unintentional injuries, substance use disorders, and risk of death due to unnatural causes ( 2 , 5 ).
The finding that 71.5% of adults who reported taking a stimulant medication had difficulty getting their ADHD prescription filled during the previous 12 months highlights the importance of ensuring an adequate supply of these medications. A 2024 CDC Health Advisory** conveyed that medication shortages and major disruptions to ADHD provider access increase concerns about risk for injury and overdose. Patients experiencing these difficulties might seek medication outside the regulated health care system, increasing their risk for overdose because of the prevalence of counterfeit pills in the illegal drug market, which might contain unexpected substances such as fentanyl.
The availability of clinical care guidelines for adults with ADHD could improve standards of care and associated health outcomes for this population ( 8 ). Reducing delays in diagnosis and treatment access could improve ADHD symptoms and long-term health risks for adults with the condition ( 2 , 3 ).
Research using health care claims data suggests that approximately one half of adults with ADHD received their ADHD care via telehealth, and that adults with ADHD use telehealth approximately twice as frequently as do those without ADHD ( 9 ). Similarly, the current data indicate that approximately one half of adults with ADHD have ever used telehealth for ADHD care. In March 2023, the Drug Enforcement Administration and the U.S. Department of Health and Human Services extended COVID-19 flexibilities regarding stimulant prescribing via telehealth †† without an initial in-person medical evaluation through December 31, 2024. Findings in this report provide information on the size of the affected population for potential rule changes, and if the exception is not extended, provide information that can help providers prepare for increased in-person health care demands.
Telepsychiatry guidelines for ADHD care acknowledge the potential benefits and risks associated with use of telehealth for ADHD care. Benefits include reduced time and effort, especially given the organizational challenges faced by persons with ADHD; increased access, especially in some geographic areas; and reduced wait times. Risks include concerns about the quality of care, such as accuracy of diagnosis and potential for misuse or diversion of prescription medication, and lack of access to technology by some populations. Experts on ADHD treatment suggest that the benefits of increased access to diagnosis and treatment via telehealth outweigh the risks of undiagnosed and untreated ADHD ( 3 ). Evaluating, monitoring, and identifying standards for quality telehealth implementation have been demonstrated to help maximize these benefits and limit risks ( 10 ).
Limitations
The findings in this report are subject to at least three limitations. First, self-reports of ADHD diagnosis might be subject to recall and reporting biases and were not validated against medical records. Second, surveys with commercial online panels have low response rates and might underrepresent certain subpopulations, increasing the potential for nonresponse bias. Nonresponse bias in RSS is reduced through innovative weighting approaches and calibration of the data to benchmark NCHS surveys, with comparisons to the National Health Interview Survey suggesting low bias for prevalence estimates of chronic health conditions ( 6 ). The data are cross-sectional and cannot be used to examine trends over time. Finally, the sociodemographic and geographic data were collected before the RSS survey administration, which could have affected the demographic distribution for some variables such as age, education, household income, and metropolitan status ( 6 ).
Implications for Public Health Practice
Public health professionals can use the findings from this report to better understand the prevalence of ADHD in adulthood, how adults obtain ADHD care, the potential gaps or delays in diagnosis, and the magnitude of treatment needs. As policies are currently developed and evaluated related to ADHD clinical care for adults, access to prescription stimulant medications, and flexibilities related to telehealth, these results can guide clinical care and regulatory decision-making.
Acknowledgments
Rebecca Bitsko, National Center on Birth Defects and Developmental Disabilities, CDC; Jonaki Bose, Amy Brown, Grace Medley, Tina Norris, Jeannine Schiller, Emily Terlizzi, Anjel Vahratian, Xun Wang, National Center for Health Statistics, CDC.
Corresponding author: Brooke S. Staley, [email protected] .
1 National Center on Birth Defects and Developmental Disabilities, CDC; 2 Epidemic Intelligence Service, CDC; 3 Oak Ridge Institute for Science and Education, Oak Ridge, Tennessee; 4 National Center for Health Statistics, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* Deceased.
† https://www.nimh.nih.gov/health/statistics/attention-deficit-hyperactivity-disorder-adhd
§ https://www.fda.gov/drugs/drug-safety-and-availability/fda-announces-shortage-adderall
¶ 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
** https://emergency.cdc.gov/han/2024/pdf/CDC_HAN_510.pdf
†† https://www.federalregister.gov/documents/2023/10/10/2023-22406/second-temporary-extension-of-covid-19-telemedicine-flexibilities-for-prescription-of-controlled
- Ayano G, Tsegay L, Gizachew Y, et al. Prevalence of attention deficit hyperactivity disorder in adults: umbrella review of evidence generated across the globe. Psychiatry Res 2023;328:115449. https://doi.org/10.1016/j.psychres.2023.115449 PMID:37708807
- Faraone SV, Bellgrove MA, Brikell I, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers 2024;10:11. https://doi.org/10.1038/s41572-024-00495-0 PMID:38388701
- Hong J, Mattingly GW, Carbray JA, et al. Expert consensus statement for telepsychiatry and attention-deficit hyperactivity disorder. CNS Spectr 2024;1–12. https://doi.org/10.1017/S1092852924000208 PMID:38764385
- Danielson ML, Bohm MK, Newsome K, et al. Trends in stimulant prescription fills among commercially insured children and adults—United States, 2016–2021. MMWR Morb Mortal Wkly Rep 2023;72:327–32. https://doi.org/10.15585/mmwr.mm7213a1 PMID:36995976
- Li L, Zhu N, Zhang L, et al. ADHD pharmacotherapy and mortality in individuals with ADHD. JAMA 2024;331:850–60. https://doi.org/10.1001/jama.2024.0851 PMID:38470385
- National Center for Health Statistics. NCHS Rapid Surveys System: survey description. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2024. https://www.cdc.gov/nchs/data/rss/round2/survey-description.pdf
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2022.
- Childress A, Sibley M, Solanto MV, Wiznitzer M, Newcorn JH. Guidelines in the United States for the diagnosis and treatment of attention-deficit/hyperactivity disorder in adults: why they are needed. Psychiatr Ann 2023;53:461–9. https://doi.org/10.3928/00485713-20230911-04
- Danielson ML, Claussen AH, Arifkhanova A, Gonzalez MG, Surman C. Who provides outpatient clinical care for adults with ADHD? Analysis of healthcare claims by types of providers among private insurance and medicaid enrollees, 2021. J Atten Disord 2024;28:1225–35. https://doi.org/10.1177/10870547241238899 PMID:38500256
- Kobeissi MM, Hickey JV. An infrastructure to provide safer, higher-quality, and more equitable telehealth. Jt Comm J Qual Patient Saf 2023;49:213–22. https://doi.org/10.1016/j.jcjq.2023.01.006 PMID:36775714
Abbreviations: ADHD = attention-deficit/hyperactivity disorder; FPL = federal poverty level. * Respondents were asked, “Have you ever been diagnosed with attention-deficit/hyperactivity disorder, or ADHD, by a doctor or other health professional?” Those who responded “yes” were then asked, “Do you currently have ADHD?” † Weighted to reflect the total population of U.S. adults aged ≥18 years, based on estimates from the second quarter of the 2023 National Health Interview Survey. § Adults who reported previous but not current ADHD diagnosis (129; 1.8%) are not included in the table. Adults who did not answer the initial diagnosis question (32) were excluded from the analysis. Row percentage is reported in the table for this variable. ¶ This information was not collected as part of the Rapid Surveys System survey but came from the panel’s profile data. Column percentages are reported in the table for these variables. ** Persons of Hispanic or Latino (Hispanic) origin might be of any race but are categorized as Hispanic; all racial groups are non-Hispanic. Only the Other group included multiple races; the other groups consisted of a single racial group. Data on race and ethnicity were missing for four respondents with a current ADHD diagnosis, and 51 respondents who have never received an ADHD diagnosis.
Abbreviation: ADHD = attention-deficit/hyperactivity disorder. * Weighted to reflect the total population of U.S. adults aged ≥18 years, based on estimates from the second quarter of the 2023 National Health Interview Survey. † Respondents who self-reported ever being diagnosed with ADHD by a doctor or health professional were asked, “How old were you when a doctor or other health professional first diagnosed you with ADHD?” Data for age at diagnosis were missing for five adults with current ADHD. § Respondents who self-reported having ADHD currently were asked, “During the past 12 months, did you receive counseling or therapy from a mental health professional to help you with your ADHD?” and “During the past 12 months, were you prescribed medication to help you with your ADHD?” Data for ADHD treatment were missing for one adult with current ADHD. ¶ Respondents who reported having ADHD currently were asked, “During the past 12 months, were you prescribed medication to help you with your ADHD?” Data on whether a medication to treat ADHD was prescribed during the previous 12 months were missing for two respondents. ** Respondents who reported having ADHD currently were asked, “During the past 12 months, what prescription medications did you take to help you with ADHD? Please do not list any medications you were prescribed but did not take.” †† Sample restricted to the 232 adults who reported that they were prescribed medication to treat their ADHD during the previous 12 months. §§ Sample restricted to the 152 adults who reported taking a stimulant medication to treat their ADHD during the previous 12 months.
Abbreviation: ADHD = attention-deficit/hyperactivity disorder. * Weighted to reflect the total population of U.S. adults aged ≥18 years, based on estimates from the second quarter of the 2023 National Health Interview Survey. † Respondents who self-reported having ADHD currently were asked, “Have you ever received any telehealth services for ADHD? That is, have you ever talked about your ADHD with a doctor, nurse, or other health professional by video or by phone?” Data for ever using telehealth services for ADHD were missing for three adults who had a current ADHD diagnosis. § Respondents who self-reported having used telehealth to receive ADHD care were asked, “Were you diagnosed with ADHD during telehealth visits, in-person visits, or a combination of both?” Missing data for two respondents and denominator was restricted to adults who reported ever using telehealth services for ADHD. ¶ Respondents could select both items; therefore, percentages are not exclusive.
Suggested citation for this article: Staley BS, Robinson LR, Claussen AH, et al. Attention-Deficit/Hyperactivity Disorder Diagnosis, Treatment, and Telehealth Use in Adults — National Center for Health Statistics Rapid Surveys System, United States, October–November 2023. MMWR Morb Mortal Wkly Rep 2024;73:890–895. DOI: http://dx.doi.org/10.15585/mmwr.mm7340a1 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Research Paper

Parents often agonize over a child’s behavior, wondering if their child is just unruly or if there might be a medical cause to problems experienced in school and other rigid settings. Increasingly, parents are finding a diagnosis—attention deficit hyperactivity disorder (ADHD)—to account for some of the behavior issues that make parenting a particularly challenging activity. According to the medical community, ADHD is a neurological disorder primarily characterized by inattentiveness, hyperactivity, and impulsivity. ADHD is generally detected in childhood, but increasing numbers of individuals are being diagnosed in adulthood. The vast majority of identified ADHD sufferers are male. A heated debate centers on the nature of the disorder, including whether a medical label is appropriate and how it should be treated.
I. Introduction
II. Three Contested Perspectives
1. ADHD as a Disease
2. the medicalization of adhd, 3. adhd as social construction.
III. Children with ADHD and Their Parents
IV. Conclusion
Introduction
ADHD has received increased attention in the professional and popular literature in recent years. Most sources agree that ADHD diagnoses are on the rise in the United States. Comparing two similar data sources illustrates this increase. According to a 1987 study, the weighted national estimate of children receiving treatment for ADHD was approximately a half million. A follow-up to this research in 1997 reported a weighted national estimate of children receiving ADHD treatment of more than 2 million. These figures can be loosely compared to the most recent data available from the Centers for Disease Control and Prevention on the number of children in the United States ever diagnosed with ADHD. According to this source, this distinction applied to 4.5 million youth in 2006 (the most recent estimate). From this illustration emerges a general idea of the rate of change surrounding ADHD diagnoses in the United States.
Three Contested Perspectives
A crucial element of the ADHD debate involves its definition. Many physicians and psychologists believe that ADHD is a medical issue with neurological implications and genetic causes. Others—those who favor a more holistic approach to life or who may not have parented—feel that ADHD is a creation of overzealous practitioners and pharmaceutical companies. Still others see the phenomenon as social in origin, arising from changing values and ideals regarding childhood. Thus, three main perspectives exist in the ADHD controversy. The first is the medical perspective that views ADHD as a physiological disease. The second perspective describes ADHD as subject to the medicalization process that transforms many behavioral issues into medical problems. The third perspective portrays ADHD as a social issue arising from changing interpretations of behavior rather than children’s physical disabilities.
The underlying assumption of a medical model of a disorder is that some recognized standard of behavior, one that is displayed by the majority of the populace, is absent in an individual. The absence of the expected behavior is attributed to an illness or disease, which, once properly diagnosed, can be treated to help bring about more desired behavior.
Many psychologists, psychiatrists, physicians, and other clinicians, as well as parents, teachers, and members of the general public, believe this model is appropriate for ADHD. The idea that inattentiveness and hyperactivity in children indicate a disorder originated near the turn of the 20th century. The condition, then termed hyperkinetic reaction of childhood, was officially recognized by the American Psychiatric Association in the second edition of its Diagnostic and Statistical Manual of Mental Disorders (DSM-II) in 1968. For the DSM-III, the label was revised to attention deficit disorder (ADD). The terminology changed again for the revision of the third addition, the DSM-III-R, when the disorder was given the more inclusive title of attention deficit hyperactivity disorder or ADHD.
The current DSM-IV lists inattentiveness, hyperactivity, and impulsivity as the three primary characteristics of ADHD. The manual also indicates that an ADHD diagnosis is not appropriate unless symptoms have been present for at least six months, these symptoms occur to a degree that is developmentally deviant, and these symptoms were developed by the time the individual was seven years old.
The medical community has been searching for a verifiable physiological cause of ADHD for some time. Although no exact biological origin has been determined, researchers and clinicians have focused their efforts on the brain for answers to the root of the disorder. Among the proposed possibilities are chemical imbalances and brain deficiencies that may arise from low birth weight or premature birth. Some notable investigation has also been done on the frontal lobe, the area of the brain responsible for behavioral and emotional regulation. As this area matures, individuals gain the ability to plan before acting and, when necessary, to ignore the desire to act. Scientists have observed a difference in the size and shape of the frontal lobe in ADHD individuals compared to non-ADHD individuals. These variations may indicate a diminished capacity for self-control in people with the disorder. Yet this research has also proven inconclusive, even leading some who accept the medical view of ADHD to admit that no irrefutable biological cause has been discovered to explain it—a point that critics and skeptics are quick to emphasize.
In addition to the argument for neurological markers of ADHD, researchers have also proposed a genetic factor for the disorder. As science learns and understands more about human DNA, the quest to locate particular genetic sources for illnesses has expanded beyond physiological disease to behavioral disorders like ADHD. No one has yet pinpointed an ADHD gene, but many believe it will be discovered eventually. Other proponents of the medical understanding of ADHD see it as more complicated than that, feeling that a single ADHD gene is not likely to be identified. Those who hold this point of view assert that science is beginning to realize that mental disorders originate from complex interactions of genes, chemicals, and other neurological components, meaning that the isolation of a specific ADHD gene is not likely.
Strong arguments asserting that ADHD is a disease come from individuals, or from the relatives of individuals, who have ADHD. According to many of these advocates, ADHD causes much pain for those it touches, especially when not diagnosed and medical treatment can bring relief. ADHD literature contains a large number of personal stories by individuals dealing with the disorder. Many of these report that they were considered stupid, lazy, and unmotivated as children. They also describe deep feelings of guilt and isolation because they were unable to meet academic and social expectations. For these individuals who found relief and understanding after being diagnosed with ADHD, the validity of the medical model is unquestionable. The stories of ADHD sufferers can often be found alongside reports from family members who describe distress over not knowing how to relate to or help their loved one with ADHD. These personal accounts available in the literature give human voices to an issue that is dismissed by some critics as a myth and others as invention.
Another perspective on ADHD is that it, like a number of other social issues, has been subjected to the process of medicalization. Prominent medicalization researchers and others cite as key elements of the medicalizing of ADHD the changing views of children in the United States, the unprecedented power of the medical profession, and the clout of pharmaceutical companies offering so-called miracle drugs to fix behavioral problems.
Prior to the Industrial Revolution, children were seen as miniature adults rather than members of a special life stage prior to adulthood. Children were considered responsible and were expected to become productive members of society at early ages, for most this meant joining the labor force or helping on the family farm. At this time, the realms of child care and management rested squarely within the family.

But with urbanization came a decreased need for child labor and a greater emphasis on education. Eventually, society came to see children’s proper place as in the classroom, and compulsory education arose. As youth were being thrust into schools, their parents were coming to view them as innocent creatures with little social power, dependent on the protection and care of adults. Over time, as people began to place more stock in the word of professionals and specialists over the teachings of folkways and tradition, parents more often sought out these specialized groups for ideas about how to properly rear children. This view of youth as innocent and dependent coupled with a loss of authority in the family is described by some as a prime contributor to the medicalization of untoward child behavior. Furthermore, because children are not considered mature enough to be culpable, their unacceptable actions cannot be labeled crimes, leaving only illness labels to explain their deviant conduct.
Before medicine gained respect as a scientific field, bad children were thought to be under the devil’s influence, morally lacking, or subject to poor parenting. Religion and the family had the main responsibility for shaping society’s views on appropriate and inappropriate behavior. However, once physicians began to make medical breakthroughs, including the advent of vaccinations, the profession began to build expert power. Over the last century or so, the medical field has acquired great authority and now has almost absolute control over how U.S. society defines disease, illness, and treatment. Thus, when physicians approach behavioral difficulties, such as those displayed with ADHD, as medical issues requiring medical treatment, most people accept this definition without question.
The makers of pharmaceuticals have also been gaining influence in society. Some now see these companies as a driving force behind the medicalization of a host of issues, including ADHD. Many people believe that if a drug exists that treats symptoms, then it proves disease is present. Such is often the case with ADHD. Psychostimulants, such as Ritalin and Adderall, have been shown to be very effective at helping children calm down and pay attention. Because of this success, despite the positive effects found for alternative treatments such as parent training programs, medications are considered the most useful method of curbing ADHD difficulties. Critics contend, however, that the efficacy of psychostimulants for adjusting the behavior of children diagnosed with ADHD is not valid evidence of a biological deficit, because these drugs produce similar results in children who do not have ADHD as well.
Following the view of some proponents, one primary reason aspects of human behavior are being increasingly tied to genetic explanations is because this is financially beneficial for drug manufacturers who are supposedly able to offer the only solutions to medical defects. Supporting this argument is the fact that, in the 1960s, pharmaceutical companies began to aggressively market psychostimulants for children with ADHD by using print advertisements in medical journals, direct mailing, and skilled representatives who promoted their products to doctors. These tactics proved effective, and more doctors and clinicians looked to psychostimulant medications as solutions for problematic behavior in children. Today, millions of people in the United States take these medications, causing some to fear that drugging children has become a new form of social control or that doctors are handing out prescriptions haphazardly to anyone claiming to have trouble concentrating or sitting still.
In addition to the perspectives of ADHD as disease and the medicalization of ADHD is the view of ADHD as social construction. According to social psychology, humans are driven by the desire to make sense of the world around them. Individuals observe one another’s behavior, interact in situations, and perform acts, all to which they constantly try to attach definitions to help them understand the world and their place in it. This process is social and varies based on situational, historical, and other factors, which means that society’s understandings can change over time. Several authors believe this has occurred with the interpretation of youthful conduct.
Ideas about desirable and undesirable child behavior vary within and between cultures. Th us, no universal definitions of good and bad conduct exist. Some claim that, in the United States, children’s actions have not changed so much as society’s interpretations of them. U.S. society used to be more understanding of variations in children’s behavior and allowed them outlets for excess energy, such as time for recess and physical education built into the school day. Recently, however, following the No Child Left Behind Act of 2001 and the thrust to improve standardized test scores, most schools have done away with these sanctioned play times.
In a scholastic atmosphere now calling for more productivity from even the youngest students, inattentiveness and hyperactivity are considered more of a problem than they were formerly. Some critics of this social development, such as Armstrong (2002), are troubled by the demands that they believe society places on children to be more like machines than human beings. Following this and some others’ views, society, with pressure from experts, no longer sees disruptive students as exuberant or eccentric but rather as sick and in need of medication to put them back on the path to success, almost as if these children are broken and in need of repair.
The emergence of the field of developmental psychology also may have engendered a change in the social definitions of childhood conduct (Timimi 2005). Developmental psychology offers standardized ideals for child development. Milestones are prescribed based on age, and deviation from these standards is considered cause for alarm and is often approached from a medical standpoint. This discipline promotes developmental markers not only for areas such as physical growth, language use, and motor skills but for maturity, ability to attend to stimuli, and social interaction.
Some argue that, due to the prescriptions of developmental psychology, parents, teachers, and physicians are now more likely to view behaviors that are not deemed age appropriate or acceptable as highly problematic. What may have once been considered simply a difficult personality is often pathologized today. Authors who hold this view seem to apply a version of the Thomas Theorem to the issue, the basic idea of which is that anything perceived as real is real in its consequences. Following this, it appears to some that people, accurately or not, view ADHD as a real disorder and thus look for symptoms confirming it, causing real consequences for children who are given the resulting pathological label.
A final illustration of society’s changing definitions surrounding this issue deals with the locus of blame for children’s misbehavior. Some researchers today support the view that poor home environments can impact children such that they display symptoms of ADHD. According to these authors, chaos, disharmony, hostility, and dysfunction at home can cause children to have trouble focusing in class or to act out irrationally. Supporters of this view, however, are in the minority. Furthermore, prior to the medical diagnosis, behavioral difficulties characterizing ADHD were frequently thought to result from poor parenting, especially by mothers. Today, however, the prevailing professional opinion is that mothering behaviors are a consequence, not a cause, of children’s behaviors. Thus, less desirable actions and reactions on the part of parents are now seen as a consequence of stress that builds up from dealing with a troubled child rather than a poorly behaved child being seen as a symptom of poor parenting. The emphasis on biology over parenting has taken responsibility away from parents and placed it on intangible sources deep within the child’s brain.
Children with ADHD and Their Parents
While the debate rages on about the proper conceptualization of ADHD behaviors, parents and children are caught in the middle. Much research has found that actions consistent with ADHD in a child have negative implications for that child’s relationship with his or her parents. In general, households with children who have ADHD are characterized by higher parental stress and distress and more parent-child conflict than households without children who have ADHD. Studies of parents’ self-reports find that mothers and fathers of these children have trouble relating to their off spring, often lack a sense of closeness with the child, and view themselves as less skilled and competent as parents. Commonly, these parents experience feelings of hopelessness and desperation to find help. In efforts to address the challenges they face, some parents display negative reactions to their children, including being excessively controlling, viewing the youths less positively, and resorting to more authoritarian discipline styles.
In addition to these joint concerns, studies have found issues unique to mothers and to fathers regarding their children with ADHD. For example, research has found a correlation between depression in mothers and parenting children with ADHD. Following a social tradition of disproportionate responsibility for rearing children, many mothers internalize the notion that they are to blame when their sons or daughters misbehave. This history of mother blaming has been somewhat relieved by the rise of the medical model for ADHD, which takes the liability away from mothers and places it on the child’s internal defects that are outside their control. Despite this, a number of mothers today are still deeply troubled when their children behave negatively, both out of concern for the quality of life of the child and for others’ potentially hurtful perceptions about their parenting.
Many fathers of children with ADHD experience their role differently from mothers. For example, one study found that fathers were much less willing than mothers to accept the medical view of their children’s difficulties. Additionally, this research noted that many fathers were not active in the diagnostic and treatment process of their children’s disorder, but they did not stand in the way of it either. Often they were sidelined during this progression, some by choice and others in an effort to avoid conflict in the marital relationship.
One notable finding by researchers, such as psychiatrist Ilina Singh, is that a number of fathers feel guilt in connection to their sons’ ADHD. The medical model for this behavioral disorder proposes a genetic linkage that passes ADHD from father to son. Due to this, some fathers blame themselves for causing their sons’ problems. One consequence of acknowledging their possible responsibility is that men think back to their own childhoods, in which they behaved similarly to their sons, and question whether they should have been given the same diagnosis.
Finally, discord can arise between a husband and wife as they struggle to deal with their child with ADHD for a number of reasons. One example is a disagreement over the true nature of their off spring’s problems. Also, trouble can emerge simply from the general stress of the environment. Partners who are feeling upset about issues with their child may take out their emotions on one another. Another source of conflict might be a husband’s opinion that his wife is at least somewhat responsible for their child’s unruly behavior because she is too indulgent, a sentiment some fathers report they have.
Critics of the medical model and of the medicalization of ADHD sometimes condemn parents for their willingness to accept such a label for their children. Some of these critics believe that parents today take the easy way out, choosing to take their children to a doctor for medication rather than altering their parenting styles to address difficult behavior. Contrary to this perception, however, many parents report experiencing great worry over the decision to seek treatment for their children. Many would likely report that these actions were a last resort. A great number of ADHD diagnoses are initiated at school. Parents are often called to school repeatedly to address a child’s unruly behavior, and eventually a teacher or administrator suggests an ADHD evaluation. If a parent is reluctant, this suggestion may continue to be made until he or she gives in. Regardless of whether they feel the ADHD label is appropriate, if a practitioner tells a parent that a son or daughter has ADHD, that parent has additional pressure to take steps to address it. Many parents, who may see themselves as grossly unqualified to determine the nature of their children’s problems, eventually defer to the opinion of the experts (teachers, doctors, psychologists) and accept the ADHD diagnosis and treatment. Despite critics’ claims, these parents would surely report that this decision is anything but easy.
ADHD is an issue touching more and more lives in the United States each day. Extensive research has been done on this topic, ranging from medical investigation to social interpretation, yet it remains an area ripe for exploration and debate. Science continues to seek definitive proof that a deficiency or imbalance in the brain, transmittable by DNA, causes recognizable unwanted behaviors that can be labeled and treated as a disease. At the same time, those opposed to this view continue to study and question the social factors surrounding this issue and disprove any biological basis. Neither side has had absolute success, so the controversy continues.
Regardless of where one stands in the debate, it is hard to deny that an increasing number of parents and children are being faced with the ADHD label. Those parents who hear competing information from various sources in the controversy often feel torn over the right thing to do and experience negative feelings, regardless of their decision. Perhaps one day an irrefutable medical discovery will be made to mark ADHD as a disease. Perhaps social opinion on children’s behavior will shift, and more rambunctious or unruly behavior will not be considered as problematic as it is today. Either of these events could result in an end to the debate surrounding ADHD. However, at this point, there is no indication that either type of solution will occur any time soon. Thus, ADHD diagnoses are sure to continue, with proponents’ blessings and critics’ curses.
Also check the list of 100 most popular argumentative research paper topics .
References:
- Armstrong, Thomas, “ADD: Does It Really Exist?” In Taking Sides: Clashing Views on Controversial Issues in Abnormal Psychology, 3d ed., ed. Richard P. Halgin. Dubuque, IA: McGraw-Hill/ Duskin, 2002.
- Barkley, Russell A., Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment, 3d ed. New York: Guilford Press, 2006.
- Conrad, Peter, and Joseph W. Schneider, Deviance and Medicalization: From Badness to Sickness. Philadelphia: Temple University Press, 1992.
- Hallowell, Edward M., “What I’ve Learned from ADD.” In Taking Sides: Clashing Views on Controversial Issues in Abnormal Psychology, 3d ed., ed. Richard P. Halgin. Dubuque, IA: McGraw- Hill/Duskin, 2002.
- McBurnett, Keith, and Linda Pfifner, eds., Attention Deficit Hyperactivity Disorder: Concepts, Controversies, New Directions. New York: Informa Healthcare, 2008.
- Singh, Ilina, “Boys Will Be Boys: Fathers’ Perspectives on ADHD Symptoms, Diagnosis, and Drug Treatment,” Harvard Review of Psychiatry 11 (2003): 308–316.
- Timimi, Sami, Naughty Boys: Anti-Social Behavior, ADHD and the Role of Culture. New York: Palgrave Macmillan, 2005.
- Wegandt, Lisa L., An ADHD Primer, 2d ed. Mahwah, NJ: Lawrence Erlbaum, 2007.
ORDER HIGH QUALITY CUSTOM PAPER

Related Posts
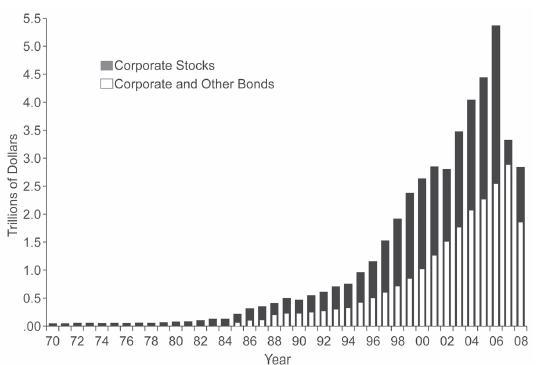
The Best Study Techniques for Students with ADHD
Effective Study Techniques for Students with ADHD
By Shazia Akoojee
Students with ADHD often face unique challenges when it comes to managing their time, staying organized, and maintaining focus in their academic journey. However, with the right strategies and tools, such as MyStudyLife , these challenges can be effectively managed. Below are some of the best study techniques specifically tailored for ADHD students, and how My Study Life can support their academic success.

Breaking Down Tasks into Manageable Steps
One of the most effective study tips for ADHD students is to break down larger tasks into smaller, manageable ones. This approach helps prevent feelings of overwhelm and makes complex assignments more achievable. For example, if a student has a research paper due, they can divide the project into steps such as selecting a topic, gathering research, drafting an outline, and writing each section. By focusing on one task at a time, students can maintain their focus and avoid frustration.
How My Study Life Helps:
My Study Life allows students to create detailed task lists and set deadlines for each step, ensuring they stay organized and on track.
To learn more about managing academic tasks effectively, check out these study tips from Harvard university.
Mastering Time Management with the Pomodoro Technique
Time management is another crucial area where ADHD students often struggle. Using techniques like time blocking and the Pomodoro Technique can be highly effective. Time blocking involves scheduling specific periods for studying, breaks, and extracurricular activities. The Pomodoro Technique, which encourages focused 25–30 minute study sessions followed by a short break, helps maintain concentration and avoid burnout.
My Study Life supports this by allowing users to schedule study blocks and set reminders, helping them stay accountable and organized throughout their sessions.
Eliminating Distractions for Better Focus
ADHD students often find it difficult to concentrate in environments filled with distractions. Creating a distraction-free study space is key to maintaining focus. This could involve turning off notifications, using noise-canceling headphones, or curating a playlist for studying.
My Study Life acts as a central hub for managing academic tasks and reminders, reducing the need to switch between multiple apps, which minimizes distractions.
Using Visual Aids for Task Tracking
Visual aids are incredibly helpful for ADHD students when it comes to organizing tasks. Keeping track of assignments and deadlines visually helps reduce anxiety and improves task prioritization. Seeing tasks laid out in a calendar format can make the workload feel more manageable.
The app provides a comprehensive calendar and task-tracking feature, giving students a clear visual overview of their assignments, exams, and deadlines. This structured layout encourages better organization and control over academic responsibilities.
Incorporating Movement Breaks
Physical activity has been shown to boost focus and cognitive function, making it a valuable tool for students with ADHD. Taking short breaks to stretch or engage in light exercise can refresh the mind and improve concentration.
While My Study Life doesn’t directly promote physical activity, the app enables students to schedule regular breaks during their study sessions, ensuring they allocate time for movement and rest.
Prioritizing Tasks
Prioritization is a skill many ADHD students find difficult. Learning to distinguish which tasks require immediate attention can greatly improve time management. Tools like the Eisenhower Matrix, which categorizes tasks by urgency and importance, can help students identify their priorities.
How My Study Life Helps:
My Study Life simplifies prioritization by allowing users to set due dates and mark tasks as “important” or “upcoming,” helping them focus on what matters most.
Centralizing Tasks with Digital Tools
Digital tools can be highly beneficial for time management, particularly for ADHD students. My Study Life is a powerful app that helps students manage schoolwork, organize study schedules, and track deadlines—all in one place.
By centralizing tasks and deadlines, the app reduces the chaos that often comes with managing multiple responsibilities.

Rewarding Progress to Stay Motivated
Rewarding oneself for completing tasks can be a great motivator. Positive reinforcement, like taking a break for a snack or watching an episode of a favorite show, encourages students to stay dedicated to their studies.
My Study Life visually tracks progress and completed tasks, providing a sense of accomplishment that can further motivate students.
Studying with ADHD doesn’t have to be overwhelming. By employing effective study techniques and using tools like My Study Life, students can take control of their academic paths. From breaking tasks into smaller steps to managing time effectively and reducing distractions, these strategies can significantly improve focus and productivity. With the right approach and resources, ADHD students can thrive and achieve their academic goals.
Related Posts

Harnessing AI for Academic Success: Tools for Students | Productivity, Focus, and Time Management

Back-to-School Checklist: Organize Your Semester with MyStudyLife

Back to School 2024: Mastering Organization for a Smooth Year Ahead
Leave a reply cancel reply.
Your email address will not be published.Required fields are marked *
Filter By Category
- Career Planning
- High School Tips and Tricks
- Productivity
- Spanish/Español
- Student News
- University Advice
- Using MyStudyLife
Hit enter to search or ESC to close

IMAGES
VIDEO
COMMENTS
Another idea is to concentrate on the treatments for ADHD in children and adults. Whether you are looking for an ADHD topic for an argumentative essay, a research paper, or a dissertation, our article will be helpful. We've collected top ADHD essay examples, research paper titles, and essay topics on ADHD.
A study using single PET-CT found that adults with ADHD had increased levels of striatal DAT compared to normal controls, which may lead to decreased availability of striatal dopamine in ADHD. 78. Research on the role of the basal ganglia in ADHD has primarily focused on the caudate. 79 The caudate has been implicated in a complex loop ...
Improving children's HRQoL is increasingly identified as a key goal of ADHD treatment alongside clinical treatment outcomes and improvement in functional outcomes (Danckaerts et al., 2010), thus, routine inclusion of a generic HRQoL measure in health interventions for children with ADHD is encouraged. Future research should also incorporate ...
This framework summarizes and visualizes information on a collection of papers on any given topic. Research weaving combines the power of two methods: systematic mapping, ... Research on ADHD over the past decades has been driven mainly by a medical model. Whereas the neurobiological correlates of ADHD are undeniable and crucial, we look ...
ADHD - attention deficit hyperactivity disorder - is a neurodevelopmental disorder that involves problems with attention, concentration and/or increased activity levels, resulting in problems ...
Long-term research into the impact of ADHD across the life span indicates that symptoms beyond the core symptoms such as functionality and anxiety become more prominent over time, yet current research does not reflect this because the majority of studies are short term and evaluating pharmacological interventions (Ingram et al., 1999).
Decades of empirical research has established a strong evidence-based intervention armamentarium for ADHD; however, limitations exist in regards to efficacy and effectiveness of these ...
Objectives: The aim of this project was to identify the ten most important research questions for attention deficit/hyperactivity disorder (ADHD) treatment as identified by people with ADHD together with personnel involved in the treatment of ADHD in school, health, and correction services. Methods: A working group consisting of consumers and personnel was established.
However, searches did not reveal any other recent reviews of the theoretical charactarisation of ADHD, therefore it is believed this is the most current comprehensive scoping review on the topic. This review reflects current research understanding that ADHD is complex and multidimensional in its presentation and impact.
Systematic Search for and Retrieval of Research Reports. The inclusion criteria (see Table 1) were defined as studies on children's and adolescents' experiences and understanding of their ADHD, whereby qualitative methods were used for collecting and analysing data.The children and adolescents, diagnosed with ADHD, had to be under 19 years of age at the time the study was conducted.
Affiliations 1 Academic Unit of Psychology, Center for Innovation in Mental Health, University of Southampton, Southampton, UK.; 2 Clinical and Experimental Sciences (CNS and Psychiatry), Faculty of Medicine, University of Southampton, Southampton, UK.; 3 Solent NHS Trust, Southampton, UK.; 4 New York University Child Study Center, New York City, New York, USA.
ADHD exists in adults, but … The syndrome now known as ADHD was originally conceptualized as a childhood disorder, and various terms were used to describe it (Barkley, Citation 2015).By the late 1970s, studies following children with the syndrome into adulthood were beginning to be published (Conrad & Potter, Citation 2000).Researchers noted that although many children "outgrew" their ...
Recent studies have demonstrated that 1) the association between ADHD and achievement difficulties is driven more by inattentive than hyperactive-impulsive symptoms, 2) deficits in working memory ...
🧠 ADHD Topics for Research Paper ADHD in Women. On-time delivery! Get your 100% customized paper done in as little as 1 hour. Let's start. ADHD, attention deficit hyperactivity disorder, is a neurodevelopmental condition that is different for women and men. For females, it usually involves issues with focus and inattentiveness, whereas for ...
Fourth, although proposed as a separate type of ADHD or even a separate diagnostic entity, the extent to which the construct of sluggish cognitive tempo (impairment of attention in hypoactive-appearing individuals) overlaps with ADHD inattentive presentation remains still unclear.10 11 Finally, one of the most controversial topics in the entire ...
Conclusion This research highlights the experiences of adults with ADHD. It is important for practitioners to be aware of the perceived positive and negative effects of the disorder, and how it ...
Read below to catch up on the most significant news and research from 2020, and stay updated on new findings as they are published by subscribing to ADDitude's free monthly research digest. General ADHD Research. Study: Long-Term Health Outcomes of Childhood ADHD are Chronic, Severe November 24, 2020
Surveillance of ADHD Among Children in the United States: Validity and Reliability of Parent Report of Provider Diagnosis. Cree RA, Bitsko RH, Danielson ML, et al. J Atten Disord. 2023;27(2):111-123. 2022. State-Level Estimates of the Prevalence of Parent-Reported ADHD Diagnosis and Treatment Among U.S. Children and Adolescents, 2016 to 2019.
Research Projects. The Center for ADHD strives to find new and innovative approaches to treat children with attention deficit hyperactivity disorder. Current Projects. Current projects and proposed research include: Studies Seeking Participants; ADHD Study For Parents of Children 4 to 11 Years Old
Reported taking a prescribed nonstimulant ADHD medication during the previous 12 mos** Yes: 27: 5.9 (3.4-9.4) No: 417: 94.1 (90.6-96.6) Reported having difficulty getting ADHD prescription filled during the previous 12 mos because their ADHD medication was not available: Among all adults who reported taking any ADHD medication †† 141: ...
A follow-up to this research in 1997 reported a weighted national estimate of children receiving ADHD treatment of more than 2 million. These figures can be loosely compared to the most recent data available from the Centers for Disease Control and Prevention on the number of children in the United States ever diagnosed with ADHD.
Students with ADHD often face unique challenges when it comes to managing their time, staying organized, and maintaining focus in their academic journey. ... For example, if a student has a research paper due, they can divide the project into steps such as selecting a topic, gathering research, drafting an outline, and writing each section. ...