- Our Program Divisions
- Our Three Academies
- Government Affairs
- Statement on Diversity and Inclusion
- Our Study Process
- Conflict of Interest Policies and Procedures
- Project Comments and Information
- Read Our Expert Reports and Published Proceedings
- Explore PNAS, the Flagship Scientific Journal of NAS
- Access Transportation Research Board Publications
- Coronavirus Disease 2019 (COVID-19)
- Diversity, Equity, and Inclusion
- Economic Recovery
- Fellowships and Grants
- Publications by Division
- Division of Behavioral and Social Sciences and Education
- Division on Earth and Life Studies
- Division on Engineering and Physical Sciences
- Gulf Research Program
- Health and Medicine Division
- Policy and Global Affairs Division
- Transportation Research Board
- National Academy of Sciences
- National Academy of Engineering
- National Academy of Medicine
- Publications by Topic
- Agriculture
- Behavioral and Social Sciences
- Biography and Autobiography
- Biology and Life Sciences
- Computers and Information Technology
- Conflict and Security Issues
- Earth Sciences
- Energy and Energy Conservation
- Engineering and Technology
- Environment and Environmental Studies
- Food and Nutrition
- Health and Medicine
- Industry and Labor
- Math, Chemistry, and Physics
- Policy for Science and Technology
- Space and Aeronautics
- Surveys and Statistics
- Transportation and Infrastructure
- Searchable Collections
- New Releases
VIEW LARGER COVER

Fluoride in Drinking Water
A scientific review of epa's standards.
Most people associate fluoride with the practice of intentionally adding fluoride to public drinking water supplies for the prevention of tooth decay. However, fluoride can also enter public water systems from natural sources, including runoff from the weathering of fluoride-containing rocks and soils and leaching from soil into groundwater. Fluoride pollution from various industrial emissions can also contaminate water supplies. In a few areas of the United States fluoride concentrations in water are much higher than normal, mostly from natural sources. Fluoride is one of the drinking water contaminants regulated by the U.S. Environmental Protection Agency (EPA) because it can occur at these toxic levels. In 1986, the EPA established a maximum allowable concentration for fluoride in drinking water of 4 milligrams per liter, a guideline designed to prevent the public from being exposed to harmful levels of fluoride. Fluoride in Drinking Water reviews research on various health effects from exposure to fluoride, including studies conducted in the last 10 years.
RESOURCES AT A GLANCE
- Report Brief
- Environment and Environmental Studies — Water Quality
Suggested Citation
National Research Council. 2006. Fluoride in Drinking Water: A Scientific Review of EPA's Standards . Washington, DC: The National Academies Press. https://doi.org/10.17226/11571. Import this citation to: Bibtex EndNote Reference Manager
Publication Info
| Chapters | skim | |
|---|---|---|
| i-xxii | ||
| 1-12 | ||
| 13-22 | ||
| 23-88 | ||
| 89-102 | ||
| 103-130 | ||
| 131-180 | ||
| 181-204 | ||
| 205-223 | ||
| 224-267 | ||
| 268-303 | ||
| 304-339 | ||
| 340-353 | ||
| 354-410 | ||
| 411-415 | ||
| 416-438 | ||
| 439-441 | ||
| 442-446 | ||
| 447-508 |
What is skim?
The Chapter Skim search tool presents what we've algorithmically identified as the most significant single chunk of text within every page in the chapter. You may select key terms to highlight them within pages of each chapter.
Copyright Information
The National Academies Press (NAP) has partnered with Copyright Clearance Center's Marketplace service to offer you a variety of options for reusing NAP content. Through Marketplace, you may request permission to reprint NAP content in another publication, course pack, secure website, or other media. Marketplace allows you to instantly obtain permission, pay related fees, and print a license directly from the NAP website. The complete terms and conditions of your reuse license can be found in the license agreement that will be made available to you during the online order process. To request permission through Marketplace you are required to create an account by filling out a simple online form. The following list describes license reuses offered by the NAP through Marketplace:
- Republish text, tables, figures, or images in print
- Post on a secure Intranet/Extranet website
- Use in a PowerPoint Presentation
- Distribute via CD-ROM
Click here to obtain permission for the above reuses. If you have questions or comments concerning the Marketplace service, please contact:
Marketplace Support International +1.978.646.2600 US Toll Free +1.855.239.3415 E-mail: [email protected] marketplace.copyright.com
To request permission to distribute a PDF, please contact our Customer Service Department at [email protected] .
What is a prepublication?
An uncorrected copy, or prepublication, is an uncorrected proof of the book. We publish prepublications to facilitate timely access to the committee's findings.
What happens when I pre-order?
The final version of this book has not been published yet. You can pre-order a copy of the book and we will send it to you when it becomes available. We will not charge you for the book until it ships. Pricing for a pre-ordered book is estimated and subject to change. All backorders will be released at the final established price. As a courtesy, if the price increases by more than $3.00 we will notify you. If the price decreases, we will simply charge the lower price. Applicable discounts will be extended.
Downloading and Using eBooks from NAP
What is an ebook.
An ebook is one of two file formats that are intended to be used with e-reader devices and apps such as Amazon Kindle or Apple iBooks.
Why is an eBook better than a PDF?
A PDF is a digital representation of the print book, so while it can be loaded into most e-reader programs, it doesn't allow for resizable text or advanced, interactive functionality. The eBook is optimized for e-reader devices and apps, which means that it offers a much better digital reading experience than a PDF, including resizable text and interactive features (when available).
Where do I get eBook files?
eBook files are now available for a large number of reports on the NAP.edu website. If an eBook is available, you'll see the option to purchase it on the book page.
View more FAQ's about Ebooks
Types of Publications
Consensus Study Report: Consensus Study Reports published by the National Academies of Sciences, Engineering, and Medicine document the evidence-based consensus on the study’s statement of task by an authoring committee of experts. Reports typically include findings, conclusions, and recommendations based on information gathered by the committee and the committee’s deliberations. Each report has been subjected to a rigorous and independent peer-review process and it represents the position of the National Academies on the statement of task.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 21 January 2021
How effective and cost-effective is water fluoridation for adults? Protocol for a 10-year retrospective cohort study
- Deborah Moore ORCID: orcid.org/0000-0001-9965-9371 1 ,
- Thomas Allen 2 ,
- Stephen Birch 2 , 3 ,
- Martin Tickle 4 ,
- Tanya Walsh 5 &
- Iain A. Pretty 6
BDJ Open volume 7 , Article number: 3 ( 2021 ) Cite this article
9633 Accesses
11 Citations
62 Altmetric
Metrics details
- Dental treatments
- Fluoridation
Tooth decay can cause pain, sleepless nights and loss of productive workdays. Fluoridation of drinking water was identified in the 1940s as a cost-effective method of prevention. In the mid-1970s, fluoride toothpastes became widely available. Since then, in high-income countries the prevalence of tooth decay in children has reduced whilst natural tooth retention in older age groups has increased. Most water fluoridation research was carried out before these dramatic changes in fluoride availability and oral health. Furthermore, there is a paucity of evidence in adults. The aim of this study is to assess the clinical and cost-effectiveness of water fluoridation in preventing invasive dental treatment in adults and adolescents aged over 12.
Methods/design
Retrospective cohort study using 10 years of routinely available dental treatment data. Individuals exposed to water fluoridation will be identified by sampled water fluoride concentration linked to place of residence. Outcomes will be based on the number of invasive dental treatments received per participant (fillings, extractions, root canal treatments). A generalised linear model with clustering by local authority area will be used for analysis. The model will include area level propensity scores and individual-level covariates. The economic evaluation will focus on (1) cost-effectiveness as assessed by the water fluoridation mean cost per invasive treatment avoided and (2) a return on investment from the public sector perspective, capturing the change in cost of dental service utilisation resulting from investment in water fluoridation.
Discussions
There is a well-recognised need for contemporary evidence regarding the effectiveness and cost-effectiveness of water fluoridation, particularly for adults. The absence of such evidence for all age groups may lead to an underestimation of the potential benefits of a population-wide, rather than targeted, fluoride delivery programme. This study will utilise a pragmatic design to address the information needs of policy makers in a timely manner.
Similar content being viewed by others

Comments on recent community water fluoridation studies
A review of water fluoridation studies and the effect on dental caries and treatment costs, undertaken in Scotland

The environmental impact of community caries prevention - part 3: water fluoridation
Dental caries and fluoride.
Dental caries, or tooth decay, is the leading global cause of disease, affecting 35% of the population. 1 It a major public health problem with significant costs for both the individual and society. It can cause pain, sleepless nights, sepsis, overuse of antibiotics, embarrassment and the loss of productive workdays. 2 It’s treatment is also very costly; across the 28 European Union countries, dental care costs are higher than those for Alzheimer’s disease, cancer, and stroke, with only diabetes and cardiovascular disease costing more. 3 Despite the consistently high prevalence of dental caries globally, in high-income countries, prevalence in children has declined substantially over the past 40 years. 4 , 5 This major success has been attributed to the increased use of fluorides for prevention, particularly in toothpastes. 6
The caries-preventive effect of fluoride was first discovered in the first half of the 20th century, when a series of US studies reported that drinking water containing 1.0–1.2 mg of fluoride per litre was associated with a 50% lower caries prevalence. 7 , 8 , 9 Decay occurs when dietary sugars are metabolised by intraoral bacteria to create acid waste products which can dissolve the mineral component of tooth enamel. 10 At the earliest stage, when defects are still microscopic, fluoride promotes replacement of the lost mineral, helping to reverse the decay process. 11 , 12 Fluoride was first added to public water supplies in the 1950s and became widely available in toothpastes from the mid-1970s. 6 It has since been added to mouthwashes and professionally applied gels and varnishes. 13 Improvements to oral health in the post-fluoride era have been dramatic: In 1973 the UK child dental health survey found that 97% of 15 year olds had experienced decay, compared to 42% in 2013. 5
More than 70% of public water supplies in the US are now fluoridated, as are 89% in Australia. 14 , 15 Within the UK, only England has implemented water fluoridation and since 1995 coverage has remained at around 10% of the population. 16 Decisions on water fluoridation currently rest with Local Authorities and several areas of England are considering investing in water fluoridation to improve the dental health of their populations. 17 , 18 , 19 Current estimates of cost-effectiveness suggest that after 10 years, every £1 spent on water fluoridation will lead to a £21.98 return, with savings due to reduced dental treatment costs and societal impacts of poor dental health such as absenteeism. 20 However, as outlined below, the majority of the evidence upon which this estimate is based is more than 40 years old and does not take-into-account the dramatic improvements in dental health that have been experienced within that time frame as a result of the increased availability of topical fluoride products.
Existing literature
There have been three landmark reviews of the evidence underpinning water fluoridation in the UK. In 2000 the York Centre for Research and Dissemination, commissioned by the Department of Health, undertook the first systematic review. 21 The York review found the majority of included studies demonstrated a beneficial effect of water fluoridation for preventing caries in children, but the quality of the evidence was low. In 2002, the Department of Health requested the Medical Research Council (MRC) to make recommendations for future research priorities. 22 These included:
The impact of water fluoridation on caries reduction in children against a background of widespread topical fluoride use (for example, in toothpastes, gels and varnishes).
Economic impacts and the effects of fluoridation on health and wellbeing beyond the usual measures of decayed, missing and filled teeth.
The effect of fluoridation on social disparities in dental caries.
Effects of fluoridation on the dental health of adults.
In 2015 Cochrane Oral Health carried out a systematic review of water fluoridation. 23 The included studies were assessed as being at high-risk of bias and most had been carried out prior to the widespread introduction of fluoride toothpastes in the mid-1970s. When analysed in a separate sub-group analysis, the post-1975 studies no longer demonstrated a protective effect. Furthermore, no studies which included adults met the review’s inclusion criteria. The reviewers concluded that whilst there was historical evidence of a caries-protective effect, the lack of contemporary evidence made it difficult to determine if water fluoridation remains effective.
In response to the urgent need for more recent evidence on the effects of water fluoridation in children, the UK National Institute of Health Research (NIHR) funded ‘CATFISH’ study is currently underway in Cumbria, UK. It is hoped that this 7-year prospective cohort study will address many of the research priorities first posed by the MRC almost 20 years ago. 24 However, it will not address the effectiveness of water fluoridation for adults and no other such studies are in progress. Studies including adults are increasingly important due to changing disease patterns and demographics. Fluoride and increased access to restorative dentistry mean that most adults today can expect to retain some natural teeth for their whole lifetime. 25 Whilst this is a positive outcome, there is increasing evidence that the majority of caries-free children do not remain so as adults. 26 , 27 , 28 The highest prevalence and incidence of tooth decay in permanent teeth is now thought to occur in adolescents and older adults. 29 , 30 , 31 , 32 , 33
Dry mouth is a common side effect of many long-term medications and wearing partial dentures, dementia and dependency on others for mouthcare, can all increase an older person’s risk of tooth decay. 32 Older people are also more likely to have gingival recession, which exposes the more susceptible root surfaces to decay. 31 After a lifetime of repair, teeth can become heavily filled and fragile. Restoring new cavities or replacing old crumbling fillings in such teeth can be technically demanding and hence, costlier. Difficulties with consent and co-operation due to advanced dementia or medical complexities can mean that routine dental care is no longer possible for some older people and management is limited to pain relief and control of sepsis. 34 , 35 With the number of people aged over 65 projected to increase by 71% between 2010 and 2050 in developed countries, 36 there is an urgent need to understand the effectiveness and cost-effectiveness of different caries-preventive strategies for adults.
Challenges of studying water fluoridation in adults
There are several reasons why the recent Cochrane systematic review did not identify any studies on the effect of water fluoridation on adult dental health. 23 Firstly, the inclusion criteria specified prospective studies with a concurrent control, comparing two populations whose fluoridation status was the same at baseline and subsequently changed. The opportunity for such studies was greatest during the 1970s and 1980s, when the majority of new schemes were introduced. At that time the strategic focus was caries-prevention in children, because the norm was almost universal experience of disease by adolescence. 37 With changing disease patterns there is increasing awareness of the need to prevent caries in adults, 38 , 39 but less opportunity to study the effects of new water fluoridation schemes because coverage has either reached near-maximum levels (US and Australia), or stalled (UK). Several authors have critiqued the Cochrane review’s inclusion criteria as being unfeasibly stringent. 40 , 41 They argue that the majority of contemporary evaluations relate to surveillance of existing schemes, therefore, the most feasible and realistic study designs are well-controlled cross-sectional or cohort studies. 40 , 41
Secondly, there are logistical difficulties in recruiting large numbers of adults and following them over several years, as is required in studies of caries development. Groups of children can be recruited, examined and followed-up relatively efficiently with the support of schools and nurseries. Even with this help, the costs of repeated clinical examinations by trained and calibrated dentists are high. For example, the ongoing CATFISH study in children is funded at £1.6 million. 42 A comparable community-based setting for adults does not exist, so recruitment and follow-up would either be prohibitively time and resource intensive, or would risk significant loss to follow-up. 43
Thirdly, measuring exposure to water fluoridation is more challenging in adults than in children. Assigning water fluoridation exposure status to individuals requires some knowledge of where they have lived within specific timeframes. Obtaining an accurate residential history is more difficult in adults than children, due to the longer recall periods involved. Recent studies in adults that utilised participant recall have suffered from missing data and large numbers of exclusions. 41 , 44 , 45 , 46 , 47 , 48 , 49
Finally, measuring caries progression in older adults is also particularly challenging. Progression is usually recorded by counting the number of teeth, or tooth surfaces, affected by decay and noting any increase in the count over time. However, when new decay occurs on a previously affected tooth or tooth surface, the count does not increase. This ‘ceiling’ effect is a particular problem in older adults when many teeth and surfaces have already been affected by decay. A recent study on the effects of water fluoridation in Australian adults did not demonstrate any benefit in the age groups over 45, which the authors attributed to this measurement ceiling. 46 Studies in the UK and Australia have also shown that it is the number of extracted teeth, rather than the count of decayed teeth or surfaces, that is the best measure of oral health disparities in older adults. 50 , 51
The study design is a retrospective cohort study using anonymised, routinely collected electronic billing records of individuals who received NHS dental care in England within the last 10 years (T—10 years, with exact date ‘T’ depending on the day of data download). We will utilise these records to explore differences in the number and types of dental treatments provided for patients receiving fluoridated or non-fluoridated water.
Variation in water fluoridation coverage across England means that individuals will have differential levels of exposure, depending on where they have lived. As described in the MRC guidance on ‘natural experiments’, this type of variation offers opportunities for evaluating public health interventions, where random allocation of individuals or clusters to intervention groups is not possible. 52
A logic model is presented in Fig. 1 illustrating the steps involved in successful delivery of water fluoridation and the factors which may influence programme delivery and outcomes.
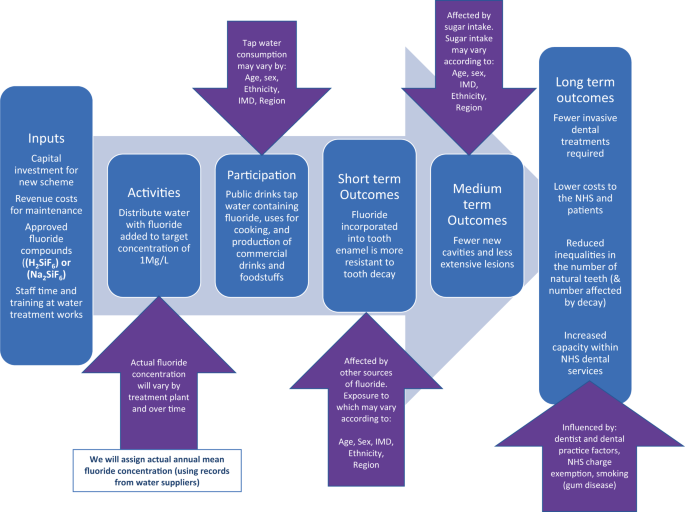
A ‘theory of change’ illustrating how programme inputs create public health outcomes (columns) and the factors that may influence this process (arrows).
Rationale for the proposed study design
Conducting research on the effects of water fluoridation in adults involves significant methodological challenges. This has resulted in a paucity of evidence and recommendations for research that have not been addressed in 20 years. 22 , 53 The present study has been designed to contribute to the evidence base, in a pragmatic and cost-efficient way, using routinely collected NHS dental treatment data.
Using routine data has several advantages over traditional designs using clinical epidemiological surveys:
The costs of using existing data are much lower than a clinical examination study that would require significant input in terms of recruitment, clinical facilities and clinician time.
The data has already been collected, avoiding the problems of loss to follow-up and long waiting times for decision makers.
To address questions on cost-effectiveness requires real-world information on treatment decisions and use of resources, which are available in NHS dental datasets.
Using dental treatment as an outcome allows us to meet the MRC recommendation that researchers study ‘the effects of fluoridation on health and wellbeing beyond the usual measures of decayed, missing and filled teeth [DMFT]’. 22 Avoiding unpleasant and costly dental treatment was seen as particularly important by the dental patients and members of the public that we spoke to during the design stage of this study.
Using dental treatment data allows for consideration of the lifetime consequences of recurrent decay, including the ‘repeat restoration cycle’. 54 This will avoid the measurement ceiling observed in older people when using the traditional count of the number of decayed, missing and filled teeth (DMFT).
Description of the data source
The National Health Service (NHS) offers state-subsidised dental care to all adults and fully-funded dental care to specific groups, including children under 18. 55 Using published literature on dental attendance and use of NHS dentistry, we estimate that ~79% of the English adult population will have attended an NHS dental practice between 2010 and 2020. 56 , 57 , 58 The NHS Business Services Authority (BSA) are an ‘arms-length’ body of the Department for Health and Social Care, responsible for processing payment claims made by dentists for the NHS treatment they provide. 59 This study will utilise the NHS BSA Dental Claims dataset for England. 60 The dental claims data is stored for a period of 10 years, and the NHS BSA are able to link together discreet courses of treatment provided for one individual by matching their patient identifier (surname, initial, gender and date of birth) to their unique 10-digit NHS number. The number and types of dental treatment received can be identified even when provided by different NHS dentists in different areas of the country.
The record also contains the unique ‘NHS performer number’ of the dentist who carried out the treatment. Using this number, it is possible for the NHS BSA to add the age, gender, place of qualification and year of qualification of the treating dentist. Information about the dental practice, such as the size and type of contracting arrangement and the financial value of the contract is also available. With regards to individual patients, the dataset includes their home address at each course of treatment, their age, gender and ethnicity. Importantly, it also includes an individual-level measure of socio-economic status, in the form of the NHS charge exemption category. The reason for any fee exemption or remission must be recorded at every course of treatment. Reasons include being in receipt of welfare payments due to low income, being out-of-work, or long-term ill health; as well as being aged 18 in full time education, being in prison, being pregnant or having had a baby in the previous 12 months. 55
Constraints of using routinely collected data
There are inevitably some constraints when using an existing dataset that was not designed for research. The NHS BSA dataset is structured around courses of dental treatments. To create a longitudinal record for an individual requires the patient’s unique NHS number. Initial scoping by the NHS BSA suggests that around 50% of the records they hold can be linked in this way, which will limit the size of the cohort available for analysis. We will investigate any potential impact on generalisability by asking the BSA to compare the demographic characteristics of those records with and without an NHS number. We expect that the recorded dental treatment will be an accurate reflection of NHS care, because the claim form is signed by the patient and claims are randomly checked for fraud by the BSA. However, any treatments provided privately are not recorded. This may occur if, for example, the dentist recommends a metal crown or filling in a molar tooth, but the patient requests a more aesthetic, tooth coloured option. Since 2017 the number of ‘decayed, missing and filled teeth (DMFT)’ has also been recorded. However, this relies on the dentist completing an accurate dental charting and keeping it up to date, which audits have shown may not always happen. 61 , 62
The NHS BSA dataset does not include diagnosis, so some treatments will have been provided for non-caries reasons, such as periodontal (gum) disease, or injury. This will not present a problem in detecting fewer treatments due to caries, because a relative difference between groups will be evident. This is true unless there is another, known or unknown reason, why non-caries treatments would vary systematically by intervention group. It is possible that dentists in fluoridated areas may perform a greater number of discretionary treatments such as replacing old or worn fillings, because of less time pressure and/or a desire to maintain income when practising in low-caries populations. More frequent replacement of old fillings would increase the likelihood of a null finding if this occurs at sufficient volume. If we do indeed fail to detect a difference between groups, systematic differences in the treatment behaviour of dentists in response to lower caries levels would need to be considered as a possible explanation.
It is well-established that dentists have different thresholds for surgical intervention when faced with the exact same scenario of caries progression. 63 Random inter-operator variation would not introduce measurement bias as it would be equally distributed between intervention and control groups. However, any variation which is associated with the patient’s likelihood of being in the fluoridated or non-fluoridated group could do so. Factors which are known to be related to the intervention threshold of dentists include age, dental school, access to continued professional development, size of practice, gender and remuneration system. 64 , 65 Some of these factors could feasibly show geographic clustering, for example, in cities or closer to dental schools. Because there are relatively few fluoridated areas in England, it could occur by chance that clusters of such dentist and dental practice factors are unequally distributed across intervention groups. We will account for any such imbalances during the analysis stage.
The dataset does not contain any information about patient behaviours which are strongly related to oral health, such as toothbrushing, sugar intake and smoking. Potential confounding due to non-random variation in these behaviours will be addressed by taking into account their underlying social determinants, such as age, gender, area-based deprivation (Index of Multiple Deprivation), ethnicity and income-related exemptions from NHS dental charges. 66 , 67 Most of these fields will be well completed as they are essential requirements on every form. The exception is ethnicity, which the patient is asked to complete. Depending on the extent of the missing data for this field, we may need to account for ethnicity using area-based measures and/or via a sensitivity analysis restricted to complete records. The wider, societal costs associated with oral health problems and their treatment, such as absenteeism and presenteeism with relation to work or school, cannot be measured from the routine data available in this study. However, it is not expected that the relationship between treatments and these costs will differ between fluoridated and non-fluoridated regions.
To pragmatically assess the clinical and cost-effectiveness of water fluoridation for preventing dental treatment and improving oral health in a contemporary population of adults, using a natural experiment design.
Primary objective
To compare the effect of 10-year exposure to fluoridated water with no exposure, on the number of invasive dental treatments, including restorations (fillings), endodontics or extractions, received by adults attending NHS dental practices.
Secondary objectives
To evaluate the cost-effectiveness of water fluoridation in reducing the amount of invasive dental treatment in an adult population with 10-year exposure to fluoridated water when compared to a population with no exposure, taking a public sector perspective.
To estimate the return on investment from a public sector perspective in terms of the change in the cost of providing dental treatments generated from an investment in water fluoridation.
To compare the impact of 10-year exposure to water fluoridation with no exposure on the oral health (number of remaining natural teeth and decay experience [DMFT]) of adults attending NHS dental practices.
To measure the impact of 10-year exposure to water fluoridation on social inequalities in oral health in adults attending NHS dentists.
Participants
Adults and adolescents aged over 12 years, attending NHS dental practices in England in the last 10 years (T—10 years). Adolescents aged over 12 were included as this is the age at which the permanent, adult teeth are usually present in the mouth (except for third molars, or ‘wisdom teeth’). 68
Inclusion criteria
1. Dental records that can be assigned to a unique individual using the combination of NHS BSA Identifier (initial, surname, gender, D.O.B) and NHS number.
Exclusion criteria
1. Individuals will be excluded from further analysis if they do not have at least two episodes of dental attendance, within the 10-year observation period (T—10 years).
Exposure definition
Determining an individual’s level of exposure to water fluoridation represents a major challenge for conducting research on its effects (Fig. 1 ). The implementation of the UK target dose of 1 Mg F/L is inconsistent both over time and at different water treatment plants. 16 , 69 Equipment failures, unexpected weather events and difficulty in obtaining the correct fluoridation chemicals mean there are some water fluoridation plants which have had periods of inactivity or have been producing water which is sub-optimally fluoridated for a number of years. 16 A recent study found that over a period of 18–35 years, the achieved mean water fluoride concentrations of eight water treatment plants in England varied from 0.53 Mg F/L (SD 0.47) to 0.93 Mg F/L (SD 0.22) Mg F/L, with a range of 0.00 Mg F/L to 1.26 Mg F/L. 69
We propose to quantify exposure to water fluoridation for individuals, for the defined 10-year exposure and observation period (T—10 years). It is accepted that we do not know where the participants have lived prior to the 10-year period or what their exposure to water fluoridation has been historically. In view of the main method of action of fluoride now being understood to be topical 70 and the fact that caries has been estimated to progresses at a rate of around 0.8–1.2 new surfaces per year in adults, 28 , 33 , 71 we would expect to see some difference in the number of dental treatments received due to new caries over a period of 10 years, even for those who moved into the fluoridated region at the start of the observation period. The advantage of this pragmatic approach is that we do not need to restrict our sample to participants who have lived in fluoridated or non-fluoridated regions since childhood. Such a criterion would make any study extremely difficult to recruit to, resulting in a small sample size 47 and would also result in a skewed sample that is unlikely to be generalisable to the wider population.
Annual water fluoride concentrations must be recorded by water companies as part of routine water quality monitoring. 72 We will obtain this information and compile a record of annual water fluoride concentrations (Mg F/L) for England that can be linked to patient place of residence. This will involve some approximation using Geographic Information System mapping, as water geographies are not aligned with standard UK geographies such as postcode areas or local authority boundaries. We will then create a 10-year exposure profile (Mg F/L) for each individual, based on how many years they lived within each region and what the annual water fluoride concentration was during that time period. We will then summarise the average 10-year water fluoridation exposure for each individual, using either mean and standard deviation, or median and IQR (depending on distribution).
For the main analysis, we will group individual participants according to their personal residential water fluoride concentration over the 10-year period (T—10 years):
Exposed : Individuals who have lived in lower super output areas (LSOAs) with an average fluoride concentration of ≥0.7 mg f/l. This is estimated to be ~10% of English population. 16
Un-exposed : Individuals who have lived in LSOAs with an average fluoride concentration of <0.7 mg f/l. This is estimated to be ~90% of English population). 16
This approach to exposure classification will not differentiate between fluoride that is in the water as a result of geology (naturally fluoridated), or as a result of a public health programme (artificially fluoridated). However, variability in implementation of water fluoridation programmes and the effect of achieved fluoride concentration is important and will be considered in ancillary analyses.
Comparator group
A key consideration in the design of this study is the selection of an appropriate comparator group, to minimise bias and to strengthen causal inference. Decisions regarding the implementation of water fluoridation are currently made by local authorities. Important factors in these decisions are population oral health, population size, the complexity of the local water system and local government politics. 17 Therefore, the likelihood of an individual receiving water fluoridation is related to such place-based factors. 73 Place-based factors may also influence the likelihood of an individual receiving different types of dental treatment. Examples include; dentist: population ratio, population oral health, proximity to a dental school, and availability of secondary care referral services. In order to ensure these place-based factors are taken into account during the analysis, we propose to compare exposed and unexposed individuals from local authority areas that are most similar to each other on a range of place-based characteristics.
Selection of the characteristics for matching of local authority areas will be undertaken in partnership with key stakeholders including clinicians, public health specialists, statisticians and policy makers. Similarity of local authorities based on these selected characteristics will be formally assessed using propensity scores. 74 , 75 Following the creation of balanced propensity scores, local authority areas will be matched using nearest neighbour matching or ‘greedy’ matching using the ‘MatchIt’ package in R. 75 , 76 Matched sets of local authority areas will be formed using one to many matching (with a ratio of no more than 1:5 of intervention local authority units to controls), based on similar values of the estimated propensity score.
A descriptive analysis will be undertaken to determine whether balance at the local authority level has been achieved. Average standardised absolute mean differences will be calculated as a global measure of successful matching. This approach is preferable to statistical significance tests which can, in large datasets, be overly sensitive to observed differences. Expert knowledge of local areas will also be used to qualitatively assess success.
Estimated sample size
We estimate that that after exclusions and matching of local authority areas, the final sample size of the study will be approximately six million individuals.
Primary outcome measure
Number of invasive dental treatments (restorations, endodontics and extractions) received by adults attending NHS dental practices over 10 years of observation (T—10 years).
Secondary outcome measures
Mean cost per episode of invasive dental treatment avoided.
Total number of natural remaining teeth (routinely recorded in NHS BSA dataset from 2017).
Total number of teeth affected by decay (DMFT) (routinely recorded from 2017).
Analysis of clinical outcomes
A generalised linear model with clustering by local authority area will be used to analyse the primary outcome of number of invasive dental treatments received during the period of observation. This model will include the area level propensity score and individual-level covariates. Given the large number of observations, clinical importance of the magnitude of the treatment effect will be preferred over statistical significance. Thresholds for minimally important differences will be defined a priori in partnership with key stakeholders including decision makers, public health professionals, patients, clinicians and the public.
Economic evaluation
The economic evaluation of water fluoridation will focus on an assessment of cost-effectiveness and calculating the return on investment.
Cost-effectiveness will be based on the primary study outcome, assessed as the mean cost per episode of invasive dental treatments avoided, from a public sector perspective, by estimating the incremental cost-effectiveness ratio (ICER). The ICER is measured by the difference in water fluoridation costs between fluoridated and non-fluoridated regions (incremental costs), divided by the difference in the number of invasive dental treatments between fluoridated or non-fluoridated regions (incremental effects). Reductions in dental service costs are not factored into the incremental costs of fluoridation (numerator in the ICER) because the reduction in treatment episodes is used as the measure of effects (denominator in the ICER). Deduction of the costs of reduced dental treatments from the costs of water fluoridation would involve ‘double counting’ this change in treatment episodes and these effects on costs are instead considered in an estimation of the financial return on investment. Sensitivity analysis will determine if cost-effectiveness is impacted by characteristics of the population or water fluoridation scheme.
To provide valuable information to policy makers, we will calculate the public sector financial return on investment in water fluoridation. The investments will be captured by the costs of providing water fluoridation, while the returns will be captured by changes in NHS costs relating to reductions in dental service utilisation.
Cost of dental treatments
In order to assess the financial return on investment associated with fewer dental treatments in fluoridated areas we will measure the following:
NHS costs : Contracts to provide NHS dentistry in England consist of an agreed annual financial payment, combined with a defined level of expected annual activity. Activity is measured in Units of Dental Activity (UDAs), which are accrued based on the complexity of care provided within each course of treatment. The financial value of UDAs varies across the country, based on historical arrangements, but the average value in 2018/9 was £27.04. 77
A Band 1 course of treatment (examination, prevention, radiographs) attracts 1 UDA (for which the NHS pays £27.04). A Band 2 course of treatment (restoration, endodontics, extractions) attracts 3 UDAs (for which the NHS pays £81.12). A Band 3 course of treatment (crowns, dentures) attracts 12 UDAs (for which the NHS pays £324.48).
Patient costs : Where patients are not exempt from NHS charges, they pay a portion of the above total NHS costs. The proportion of the full NHS cost that is paid by patients has increased in recent years. In 2018/9 the patient charges for each band is as follows: Band 1 (£22.70), Band 1 Urgent (£22.70), Band 2 (£62.10), and Band 3 (£269.30). 78 Patient costs will be allocated using the true costs for the year in question. Patient costs relating to the time and travel required for dental treatments cannot be measured using data available for this study.
Cost per item of treatment: Payment bands will also be disaggregated to extract a more precise cost of the treatment provided within each band. This will involve assigning a unit cost per item of treatment. NHS dental costs are still assigned in this way in Scotland based on the estimated mean time taken to provide different items of service, so we will utilise Scottish dental treatment costs data as a more ‘resource-based’ approach to costing.
Patient costs will be deducted from NHS costs to reflect that patient charges are recovered by the NHS and are a source of income. Each costing approach will be applied to the patient level data for patients living in fluoridated and non-fluoridated regions.
The costs of dental treatments and the number of treatments avoided will be discounted at 1.5% which is the UK National Institute for Health and Care Excellence (NICE) recommended discount rate for public health interventions. Sensitivity analysis will apply the 3.5% discount rate common for health care interventions.
Cost of fluoridation
Costs of water fluoridation involve capital expenditure for equipment, and ongoing revenue costs, which include; maintenance, training of operators, the time taken by water company staff, and the fluoride chemical supply. Public Health England, on behalf of the Secretary of State, fund capital costs. 17 Revenue costs are paid by Public Health England and subsequently recharged to Local Authorities. Capital costs will also need to consider the estimated lifetime of the plant and any major refurbishments required. Capital and revenue costs of fluoridation will be obtained by liaising with Public Health England and the appropriate water companies. Fluoridation costs will be allocated appropriately to the whole population in each fluoridated region to calculate the per capita cost. As costs do not vary by patient characteristics, the per capita cost will be applied to our patient population. We will determine the degree to which the cost of water fluoridation is driven by fixed costs and variable cost, the latter varying with the size of the population served.
Several areas of England are currently considering investing in water fluoridation to improve the dental health of their populations. 18 , 19 Water fluoridation proposals are controversial, with some groups and individuals vehemently opposed. 79 In 2007, the Nuffield Council on Bio-ethics developed an ethical framework specifically for public health, where they considered the case of water fluoridation. 80 The guidance determined that there is no ethical prohibition against adding beneficial substances to the water supply to improve health and reduce health inequalities, even when some individuals oppose it. Rather, the decision should be made through local democratic processes and should consider the balance of risks and benefits expected, the potential for alternative interventions which do not compromise autonomy to the same extent and the role of consent if there are expected harms. Legislation states that any proposal to introduce water fluoridation in the U.K. must include a 3-month public consultation period where these issues can be explored.
Whilst there are many spurious and scientifically implausible claims of harm from water fluoridation, 79 there is one well-recognised unwanted effect. Dental fluorosis is an increased porosity of tooth enamel which may be observed as brown or white flecks on the permanent teeth. It occurs as a result of fluoride ingestion during the time that the tooth enamel is forming, between birth and 8 years of age. A recent study in England estimated the prevalence of ‘aesthetically objectionable’ fluorosis to be around 10% in fluoridated cities, compared to 2% in non-fluoridated cities. 81 There is no lower ‘threshold’ dose for dental fluorosis. Instead, prevalence increases linearly with every increase in dose above 0.01 mgF/kg of bodyweight per day. 82 Prevalence is thought to have increased in recent years, due to inadvertent ingestion of topical fluorides such as toothpastes and varnishes. 46 , 81 , 83 , 84 Some countries, including Ireland and the U.S., have reduced the target dose for water fluoridation programmes as a result. 85 , 86 , 87
It has been suggested that a targeted approach, using topically applied fluoride products, may be a more feasible and acceptable strategy for caries-prevention. 79 , 88 , 89 Such an approach offers the opportunity for individuals to consent or dissent. For those who do ingest the topical fluoride products inadvertently, if they have been targeted as ‘high-risk’ for caries, the benefit: risk profile would be more favourable than in a population-wide approach. For a targeted, or high-risk approach to be efficient, the disease must have a low enough prevalence to make the extra effort involved with identifying those at risk cost-effective. 90 The most recent children’s dental health survey found that 44% of 15 year olds in England had experienced decay in their permanent teeth, which is higher than the 30% above which a targeted approach is no longer practical. 90 , 91 Recent estimates from national surveys across western Europe demonstrate that by the age of 35–44, the prevalence of decay experience is at least 92%. 92 With sufficient time, caries remains almost universal and the difficulties of accurately predicting which individuals or communities are at highest risk are well recognised. 93 , 94 Undoubtedly, population-wide interventions to prevent caries remain essential if the greatest burden of disease is to be avoided.
It is important to note that the most fundamental component of any population-wide caries-prevention strategy is sugar reduction through the use of upstream policy levers. 2 Reducing the underlying cause of disease through the restoration of normality, rather than adding a protective factor, is a more radical approach, and does not come with the risk of unwanted effects such as dental fluorosis. 95 However, with any highly prevalent chronic disease, the social and biological causal pathways involved are complex and action at multiple levels is required. 96 Fluoride is highly effective at preventing caries and its use over the last 50 years has transformed dental health. Whether it should be applied in targeted programmes or at the population level is the key question for local communities. Within these debates, it is imperative that the benefits for the whole population, including the health care system, can be articulated. We recognise our pragmatic study design comes with some limitations in terms of causal attribution and our results will need to be triangulated alongside the range of contemporary evidence for water fluoridation. At the same time, real-world data offers meaningful evidence of impact and the ability to capture the most important benefit of a population-wide approach.
Abajobir, A. A. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390 , 1211–1259 (2017).
Article Google Scholar
Watt, R. G. et al. Ending the neglect of global oral health: time for radical action. Lancet 394 , 261–272 (2019).
Article PubMed Google Scholar
FDI World Dental Federation. The Challenge of Oral Disease—A call for global action . Myriad Editions. Geneva: The Oral Health Atlas (2015). https://doi.org/10.1038/npg.els.0002133 .
Petersson, G. H. & Bratthall, D. The caries decline: a review of reviews. Eur. J. Oral. Sci. 104 , 436–443 (1996).
Murray, J. J., Vernazza, C. R. & Holmes, R. D. Forty years of national surveys: an overview of children’s dental health from 1973-2013. Br. Dent. J. 219 , 281–285 (2015).
Bratthall, D., Hänsel-Petersson, G. & Sundberg, H. Reasons for the caries decline: what do the experts believe?. Eur. J. Oral. Sci. 104 , 416–422 (1996).
Dean, H., Jay, P., Arnold, F. & Elvove, E. Domestic Water and Dental caries II. A study of 2,832 white children aged 12-14 years, of 8 suburban Chicago communities, including lactobacillus acidophilis studies of 1,761 children. Public Health Rep . 57 , 761–792 (1941).
Dean, H. The investigation of physiological effects by the epidemiological method. In Fluorine and Dental Health (ed. Moulton, F.) 23–31 (Am. Ass. Adv. Sci., 1942).
Dean, H., Arnold, F., Jay, P. & Knutson, J. Studies on mass control of dental caries through fluoridation of the public water supply. Public Health Rep. 65 , 1403–1408 (1950).
Ten Cate, J. & Featherstone, J. Mechanistic aspects of the inter- actions between fluoride and dental enamel. CRC Crit. Rev. Oral. Biol. 2 , 283–296 (1991).
Zero, D. T. Sugars—the arch criminal? Caries Res . 38 , 277–285 (2004).
Sheiham, A. & James, W. P. T. A new understanding of the relationship between sugars, dental caries and fluoride use: implications for limits on sugars consumption. Public Health Nutr. 17 , 2176–2184 (2014).
Marinho, V., Higgins, J., Logan, S. & Sheiham, A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents (Review). Cochrane Database Syst. Rev . 4 , 1–2 (2003).
Google Scholar
Centers for Disease Control and Prevention. Community water fluoridation. Fluoridation statistics. Revised 2016 (2018). https://www.cdc.gov/fluoridation/statistics/2014stats.htm . Accessed 26 Feb 2018.
Australian Government National Health and Medical Research Council. Water Fluoridation and Human Health in Australia : Questions and Answers. (2017). https://www.nhmrc.gov.au/sites/default/files/documents/attachments/water-fluoridationqa.pdf . Accessed 11 Jan. 2021.
Public Health England. Water fluoridation: Health monitoring report for England 2018. (2018). https://www.gov.uk/government/publications/water-fluoridation-health-monitoring-report-for-england-2018 . Accessed 11 Jan. 2021.
Public Health England. Improving oral health : a community water fluoridation toolkit for local authorities. (2016). https://www.gov.uk/government/publications/improving-oral-health-community-water-fluoridation-toolkit . Accessed 11 Jan. 2021.
Hull City Council. Community Water Fluoridation. (2018). http://www.hull.gov.uk/health-and-wellbeing/public-health/community-water-fluoridation . Accessed 11 Jan. 2021.
Durham County Council. Report of Amanda Healy, Director of Public Health County Durham, Adult and health Services, Durham County Council. Oral Health Update (2017). https://democracy.durham.gov.uk/documents/s83873/Agenda Item 13 - Oral Health Update.pdf . Accessed 8 Aug 2018.
York Health Economics Consortium & Public Health England. A rapid review of evidence on the cost-effectiveness of interventions to improve the oral health of children aged 0-5 years. (2016). https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/560972/Rapid_review_ROI_oral_health_5_year_old.pdf . Accessed 11 Jan 2021.
McDonagh, M. S. et al. Systematic review of water fluoridation. BMJ 321 , 855–859 (2000).
Article PubMed PubMed Central Google Scholar
Medical Research Council. Water fluoridation and health. Water Fluorid. Heal . 1–48 (2002).
Iheozor-Ejiofor, Z. et al. Water fluoridation for the prevention of dental caries. Cochrane Database Syst. Rev . https://doi.org/10.1002/14651858.CD010856.pub2 (2015).
Goodwin, M. et al. The CATFISH study protocol: an evaluation of a water fluoridation scheme. BMC Oral. Health 16 , 8 (2016).
Steele, J. G., Treasure, E. T., O’Sullivan, I., Morris, J. & Murray, J. J. Adult Dental Health Survey 2009: transformations in British oral health 1968-2009. Br. Dent. J. 213 , 523–527 (2012).
Kruger, E. et al. Dental caries and changes in dental anxiety in late adolescence. Community Dent. Oral. Epidemiol. 26 , 355–359 (1998).
Broadbent, J. M., Thomson, W. M. & Poulton, R. Progression of dental caries and tooth loss between the third and fourth decades of life: a birth cohort study. Caries Res. 40 , 459–465 (2006).
Broadbent, J. M., Thomson, W. M. & Poulton, R. Trajectory patterns of dental caries experience in the permanent dentition to the fourth decade of life. J. Dent. Res. 87 , 69–72 (2008).
Kassebaum, N. J. et al. Global burden of untreated caries: a systematic review and metaregression. J. Dent. Res. 94 , 650–658 (2015).
Luan, W., Baelum, V., Fejerskov, O. & Chen, X. Ten-year incidence of dental caries in adult and elderly Chinese. Caries Res. 34 , 205–213 (2000).
Griffin, S., Griffin, P., Zlobin, N. & Swann, J. L. Estimating rates of new root caries in older adults. J. Dent. Res. 83 , 634–638 (2004).
Chalmers, J. M., Carter, K. D. & Spencer, A. J. Caries incidence and increments in Adelaide nursing home residents. Spec. Care Dent. 25 , 96–105 (2005).
Thomson, W. M. Dental caries experience in older people over time: what can the large cohort studies tell us? Br. Dent. J. 196 , 89–92 (2004).
Pretty, I. A. et al. The Seattle Care Pathway for securing oral health in older patients. Gerodontology 31 , 77–87 (2014).
Murray, C. G. Advanced restorative dentistry—a problem for the elderly? An ethical dilemma. Aust. Dent. J. 60 , 106–113 (2015).
WHO, National Institutes of Health, National Institutes of Ageing & U.S. Department of Health and Human Services. Global Health and Ageing (World Health Organization, 2011). https://doi.org/10.1016/B978-0-12-375000-6.00006-9 .
World Health Organization. Dental Diseases and Oral Health Factsheet. World Health Organization Global Strategy on Diet, Physical Activity and Health 2 (2003). https://www.who.int/oral_health/publications/orh_fact_sheet.pdf . Accessed 15 June 2020.
Bernabé, E. & Sheiham, A. Extent of differences in dental caries in permanent teeth between childhood and adulthood in 26 countries. Int. Dent. J. 64 , 241–245 (2014).
Petersen, P. E. & Yamamoto, T. Improving the oral health of older people: The approach of the WHO Global Oral Health Programme. Community Dent. Oral. Epidemiol. 33 , 81–92 (2005).
Rugg-Gunn, A. J. et al. Critique of the review of ‘Water fluoridation for the prevention of dental caries’ published by the Cochrane Collaboration in 2015. Br. Dent. Joural 220 , 335–340 (2016).
Slade, G. D., Sanders, A. E., Do, L., Roberts-Thomson, K. & Spencer, A. J. Effects of fluoridated drinking water on dental caries in Australian adults. J. Dent. Res. 92 , 376–382 (2013).
NIHR. An evaluation of a water fluoridation scheme in Cumbria. Funding and Awards (2016). https://www.fundingawards.nihr.ac.uk/award/12/3000/40 . Accessed 15 June 2020.
Spencer, A. J., Liu, P., Armfield, J. M. & Do, L. G. Preventive benefit of access to fluoridated water for young adults. J. Public Health Dent. 77 , 263–271 (2017).
Crocombe, L. A., Brennan, D. S., Slade, G. D., Stewart, J. F. & Spencer, A. J. The effect of lifetime fluoridation exposure on dental caries experience of younger rural adults. Aust. Dent. J. 60 , 30–37 (2015).
Do, L. & Spencer, A. J. Contemporary multilevel analysis of the effectiveness of water fluoridation in Australia. Aust. N. Z. J. Public Health 39 , 44–50 (2015).
Do, L. et al. Effectiveness of water fluoridation in the prevention of dental caries across adult age groups. Community Dent. Oral Epidemiol . https://doi.org/10.1111/cdoe.12280 (2017).
Peres, M. A., Peres, K. G., Barbato, P. R. & Höfelmann, D. A. Access to fluoridated water and adult dental caries. J. Dent. Res. 95 , 868–874 (2016).
Hopcraft, M. & Morgan, M. Dental caries experience in a young adult military population. Aust. Dent. J. 48 , 125–129 (2003).
Hopcraft, M. & Morgan, M. V. Dental caries experience in Australian Army recruits 2002-2003. Aust. Dent. J. 50 , 16–20 (2005).
Steele, J. et al. The interplay between socioeconomic inequalities and clinical oral health. J. Dent. Res. 94 , 19–26 (2015).
Mejia, G., Jamieson, L. M., Ha, D. & Spencer, A. J. Greater inequalities in dental treatment than in disease experience. J. Dent. Res. 93 , 966–971 (2014).
Medical Research Council. Using natural experiments to evaluate population health interventions: guidance for producers and users of evidence. (2011). https://mrc.ukri.org/documents/pdf/natural-experiments-guidance/ . Accessed 11 Jan 2021.
McDonagh, M. et al. A systematic review of public water fluoridation. NHS Cent. Rev. Dissem. 18 , 1–125 (2000).
Elderton, R. J. Preventive (evidence-based) approach to quality general dental care. Med. Princ. Pract. 12 , 12–21 (2003).
NHS. Understanding NHS Dental Charges. (2020). https://www.nhs.uk/using-the-nhs/nhs-services/dentists/understanding-nhs-dental-charges/ . Accessed 6 Mar 2020.
The Information Centre for Health and Social Care. 8 : Access and barriers to care - a report from the Adult Dental Health Survey 2009. (2011). https://digital.nhs.uk/data-and-information/publications/statistical/adult-dental-health-survey/adult-dental-health-survey-2009-summary-report-and-thematic-series . Accessed 11 Jan 2021.
NHS England. Summary of the Dental Results from the GP Patient Survey—January to March 2018. 2019 , 1–11 (2019).
Office for National Statistics. Dataset: Estimates of the population for the UK, England and Wales, Scotland and Northern Ireland. Mid 2009: Superseded (2019). https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland . Accessed 11 Jan 2021.
The National Archives. The Functions of the National Health Service Commissioning Board and the NHS Business Services Authority (Awdurdod Gwasanaethau Busnes y GIG) (Primary Dental Services) (England) Regulations 2013/469. (2013). http://www.legislation.gov.uk/uksi/2013/469/contents/made . Accessed 18 Mar 2020.
NHS Business Services Authority. NHS Dental Services - Completion of form guidance FP17—England. (2017). https://www.nhsbsa.nhs.uk/sites/default/files/2017-07/Completion of form guidance-FP17-England %28V9%29-07 2017.pdf . Accessed 27 Mar 2019.
Morgan, R. G. Quality evaluation of clinical records of a group of general dental practitioners entering a quality assurance programme. Br. Dent. J. 191 , 436–441 (2001).
PubMed Google Scholar
Brown, N. L., Jephcote, V. E. L., Morrison, J. N. & Sutton, J. E. Inaccurate dental charting in an audit of 1128 general dental practice records. Dent. Update 44 , 254–260 (2017).
Innes, N. P. T. & Schwendicke, F. Restorative thresholds for carious lesions: systematic review and meta-analysis. J. Dent. Res. 96 , 501–508 (2017).
Gordan, V. V. et al. How dentists diagnose and treat defective restorations: evidence from the dental practice-based research network. Oper. Dent. 34 , 664–673 (2009).
Ghoneim, A. et al. What influences the clinical decision-making of dentists? A cross-sectional study. PLoS ONE 15 , 1–21 (2020).
Heilman, A., Tsakos, G. & Watt, R. Chapter 3: Oral health over the lifecourse. In A Life Course Perspective on Health Trajectories and Transitions 4 , 39–61 (Springer, 2015).
Ministry of Housing Communities and Local Government. English Indices of Deprivation 2019. (2019). https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 . Accessed 29 Sept 2020.
AlQahtani, S. J. Atlas of Tooth Development. Barts and London School of Medicine and Dentistry (2009). https://www.atlas.dentistry.qmul.ac.uk/content/english/atlas_of_tooth_development_in_English.pdf . Accessed 1 Nov 2021.
Moore, D., Goodwin, M. & Pretty, I. Long—term variability in artificially and naturally fluoridated water supplies in England. Community Dent. Oral. Epidemiol. 00 , 1–7 (2019).
Aoba, T. Solubility properties of human tooth mineral and pathogenesis of dental caries. Oral. Dis. 10 , 249–257 (2004).
Broadbent, J. M., Foster Page, L. A., Thomson, W. M. & Poulton, R. Permanent dentition caries through the first half of life. Br. Dent. J. 215 , 1–6 (2013).
The National Archives. The Water Supply (Water Quality) Regulations SI 2016/614. (2016). https://www.legislation.gov.uk/uksi/2016/614/contents/made . Accessed 11 Jan 2021.
Lankelly Chase. Historical review of place based approaches. (2017). https:// lankellychase.org.uk/resources/publications/historical-review-of-place-based-approaches/ . Accessed 12 Jan 2021.
de Vocht, F. et al. Propensity score matching for selection of local areas as controls for evaluation of effects of alcohol policies in case series and quasi case-control designs. Public Health 132 , 40–49 (2016).
Ho, D. E., King, G., Stuart, E. A. & Imai, K. MatchIt: nonparametric preprocessing for parametric causal inference. J. Stat. Softw. 42 , 1–28 (2011).
R Core Team. R: A language and environment for statistcial computing. (2018). https://www.r-project.org/ . Accessed 12 Jan 2021.
NHS Business Services Authority. NHS Payments to dentists in England 2018-19. NHS Payments to Dentists (2019). https://www.nhsbsa.nhs.uk/dental-data/nhs-payments-dentists . Accessed 6 Mar 2020.
NHS. How much will I pay for NHS dental treatment? (2017). https://www.nhs.uk/common-health-questions/dental-health/how-much-will-i-pay-for-nhs-dental-treatment/ . Accessed 29 Sept 2020.
Fluoride Action Network. 50 reasons to oppose fluoridation. (2020). https://fluoridealert.org/articles/50-reasons/ . Accessed 18 Aug 2020.
Krebs, J. et al. Public Health: ethical issues. Nuffield Council on Bioethics (2007). https://www.nuffieldbioethics.org/publications/public-health . Accessed 12 Jan 2021.
Pretty, I. A. et al. Prevalence and severity of dental fluorosis in four English cities. Community Dent. Health 33 , 292–296 (2016).
Mejàre, I. Current guidance for fluoride intake: is it appropriate? Adv. Dent. Res. 29 , 167–176 (2018).
Whelton, H., Ketley, C., Mcsweeney, F. & MullaneO. D. A review of fluorosis in the European Union: prevalence, risk factors and aesthetic issues. Community Dent. Oral. Epidemiol. 32 , 9–18 (2004).
Clark, D. C. Trends in prevalence of dental fluorosis in North America. Community Dent. Oral. Epidemiol. 22 , 148–152 (1994).
Centers for Disease Control and Prevention. U.S. Public Health Service Recommendation for Fluoride Concentration in Drinking Water for the Prevention of Dental Caries. Public Health Rep. 130 , 1–14 (2015).
Goverment of Ireland. Forum on fluoridation. Government of Ireland (2002). https://www.fluoridesandhealth.ie/download/documents/fluoridation_forum.pdf . Accessed 12 Jan 2021.
The Irish Expert Body on Fluorides and Health. FAQ on Fluoride and Water Fluoridation. (2013). https://www.fluoridesandhealth.ie/faqs/ . Accessed 12 Jan 2021.
Scientific Committee on Health and Environmental Risks (SCHER). Critical review of any new evidence on the hazard profile, health effects, and human exposure to fluoride and the fluoridating agents of drinking water. (2010). http://ec.europa.eu/health/scientific_committees/environmental_risks/docs/scher_o_139.pdf . Accessed 12 Jan 2021.
Scottish Government. Oral Health Improvement Plan. (2018). https://beta.gov.scot/publications/oral-health-improvement-plan/ . Accessed 12 Jan 2021.
Hausen, H. Caries prediction—state of the art. Community Dent. Oral. Epidemiol. 25 , 87–96 (1997).
The Health and Social Care Information Centre. Children’s Dental Health Survey 2013. Report 2: Dental disease and damage in children. England, Wales and sNorthern Ireland. (2015). https://files.digital.nhs.uk/publicationimport/pub17xxx/pub17137/cdhs2013-report2-dental-disease.pdf . Accessed 12 Jan 2021.
Carvalho, J. C. & Schiffner, U. Dental Caries in European Adults and Senior Citizens 1996-2016: ORCA Saturday Afternoon Symposium in Greifswald, Germany—Part II. Caries Res. 53 , 242–252 (2019).
Brewster, L., Sherriff, A. & Macpherson, L. Effectiveness and reach of a directed-population approach to improving dental health and reducing inequalities: a cross sectional study. BMC Public Health 13 , 1 (2013).
Tickle, M., Brown, P., Blinkhorn, A. & Jenner, T. Comparing the ability of different area measures of socio-economic status to segment a population according to caries prevalence. Community Dent. Health 17 , 138–144 (2000).
Rose, G. Strategy of prevention: lessons from cardiovascular disease. Br. Med. J. 282 , 1847–1851 (1981).
Sniehotta, F. F. et al. Complex systems and individual-level approaches to population health: a false dichotomy? Lancet Public Heal. 2 , e396–7 (2017).
Download references
Acknowledgements
We would like to thank Nikki Dodds and the NHS Business Services Authority for their help and support with scoping the utility of the dental dataset for this research question. This study/project is funded by the National Institute for Health Research (NIHR) Public Health Research (PHR) Programme (Project number: NIHR 128533). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
Dental Public Health, Division of Dentistry, Dental Health Unit, The University of Manchester, Lloyd Street North Manchester Science Park, Manchester, M15 6SE, UK
Deborah Moore
Director, Centre for the Business and Economics of Health, University of Queensland, St Lucia, Queensland, 4072, UK
Thomas Allen & Stephen Birch
Health Economics, Manchester Centre for Health Economics, The University of Manchester, Jean McFarlane Building Oxford Road, Manchester, M13 9PL, UK
Stephen Birch
Dental Public Health & Primary Care, Division of Dentistry, The University of Manchester, Coupland 3, Manchester, M13 9PL, UK
Martin Tickle
Healthcare Evaluation, Division of Dentistry, The University of Manchester, Coupland 3, Manchester, M139PL, UK
Tanya Walsh
Public Health Dentistry, Division of Dentistry, Dental Health Unit, The University of Manchester, Lloyd Street North Manchester Science Park, Manchester, M15 6SE, UK
Iain A. Pretty
You can also search for this author in PubMed Google Scholar
Contributions
D.M. contributed to the conception and development of the study design, led the funding application and the drafting and submission of this paper. T.A. led the conception and development of the health economics approach, contributed to the development of the study design, the drafting of this paper and approved the submitted version. S.B. contributed towards the conception and development of the health economics approach and study design, the drafting of this paper and approved the submitted version. M.T. contributed to the conception and development of the study design, the drafting of this paper and approved the submitted version. T.W. led the development of the approach to statistical analysis, contributed to the conception and development of the study design, the drafting of this paper and approved the submitted version. I.P. led the conception of the work, contributed to the development of the study design, the drafting of this paper and approved the submitted version.
Corresponding author
Correspondence to Deborah Moore .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval and consent to participate
The study has been externally peer reviewed and approved by the funding organisation NIHR (NIHR 128533). Ethical approval was granted by North East–Tyne and Wear South NHS Research Ethics Committee (Ref: 20/NE/0144) on 27.07.2020. Permission for NHS BSA to access identifiable NHS dental records without consent (in order to select the cohort and undertake anonymisation) was been granted by the HRA Confidentiality Advisory Group (Ref: 20/CAG/0072) on 07.07.2020.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Moore, D., Allen, T., Birch, S. et al. How effective and cost-effective is water fluoridation for adults? Protocol for a 10-year retrospective cohort study. BDJ Open 7 , 3 (2021). https://doi.org/10.1038/s41405-021-00062-9
Download citation
Received : 03 November 2020
Accepted : 04 November 2020
Published : 21 January 2021
DOI : https://doi.org/10.1038/s41405-021-00062-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Bdj open 2021 - our most successful year to date.
- Jonathan Lewney
British Dental Journal (2022)
Fluoride in the drinking water and dental caries experience by tooth surface susceptibility among adults
- Lina Stangvaltaite-Mouhat
- Alina Puriene
- Jolanta Aleksejuniene
BMC Oral Health (2021)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Election 2024
- Entertainment
- Newsletters
- Photography
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election results
- Google trends
- AP & Elections
- College football
- Auto Racing
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
US government report says fluoride at twice the recommended limit is linked to lower IQ in kids
FILE - Water flows from a water fountain in Concord, N.H., on Friday, Jan. 7, 2011. (AP Photo/Jim Cole, File)
FILE - A child rinses a toothbrush in San Francisco on June 18, 2019. (Gabrielle Lurie/San Francisco Chronicle via AP, File)
- Copy Link copied
NEW YORK (AP) — A U.S. government report expected to stir debate concluded that fluoride in drinking water at twice the recommended limit is linked with lower IQ in children.
The report, based on an analysis of previously published research, marks the first time a federal agency has determined — “with moderate confidence” — that there is a link between higher levels of fluoride exposure and lower IQ in kids. While the report was not designed to evaluate the health effects of fluoride in drinking water alone, it is a striking acknowledgment of a potential neurological risk from high levels of fluoride.
Fluoride strengthens teeth and reduces cavities by replacing minerals lost during normal wear and tear , according to the U.S. Centers for Disease Control and Prevention. The addition of low levels of fluoride to drinking water has long been considered one of the greatest public health achievements of the last century.
“I think this (report) is crucial in our understanding” of this risk, said Ashley Malin, a University of Florida researcher who has studied the effect of higher fluoride levels in pregnant women on their children. She called it the most rigorously conducted report of its kind.
The long-awaited report released Wednesday comes from the National Toxicology Program, part of the Department of Health and Human Services. It summarizes a review of studies, conducted in Canada, China, India, Iran, Pakistan, and Mexico, that concludes that drinking water containing more than 1.5 milligrams of fluoride per liter is consistently associated with lower IQs in kids.
The report did not try to quantify exactly how many IQ points might be lost at different levels of fluoride exposure. But some of the studies reviewed in the report suggested IQ was 2 to 5 points lower in children who’d had higher exposures.
Since 2015, federal health officials have recommended a fluoridation level of 0.7 milligrams per liter of water, and for five decades before the recommended upper range was 1.2. The World Health Organization has set a safe limit for fluoride in drinking water of 1.5.
The report said that about 0.6% of the U.S. population — about 1.9 million people — are on water systems with naturally occurring fluoride levels of 1.5 milligrams or higher.
“The findings from this report raise the questions about how these people can be protected and what makes the most sense,” Malin said.
The 324-page report did not reach a conclusion about the risks of lower levels of fluoride, saying more study is needed. It also did not answer what high levels of fluoride might do to adults.
The American Dental Association, which champions water fluoridation, had been critical of earlier versions of the new analysis and Malin’s research. Asked for comment, a spokeswoman late Wednesday afternoon emailed that the organization’s experts were still reviewing the report.
Fluoride is a mineral that exists naturally in water and soil. About 80 years ago, scientists discovered that people whose water supplies naturally had more fluoride also had fewer cavities, triggering a push to get more Americans to use fluoride for better dental health.
In 1945, Grand Rapids, Michigan became the first U.S. city to start adding fluoride to tap water. In 1950, federal officials endorsed water fluoridation to prevent tooth decay, and continued to promote it even after fluoride toothpaste brands hit the market several years later. Though fluoride can come from a number of sources, drinking water is the main source for Americans, researchers say.
Officials lowered their recommendation for drinking water fluoride levels in 2015 to address a tooth condition called fluorosis, that can cause splotches on teeth and was becoming more common in U.S. kids.
Separately, the Environmental Protection Agency has maintained a longstanding requirement that water systems cannot have more than 4 milligrams of fluoride per liter. That standard is designed to prevent skeletal fluorosis, a potentially crippling disorder which causes weaker bones, stiffness and pain.
But more and more studies have increasingly pointed to a different problem, suggesting a link between higher levels of fluoride and brain development. Researchers wondered about the impact on developing fetuses and very young children who might ingest water with baby formula. Studies in animals showed fluoride could impact neurochemistry cell function in brain regions responsible for learning, memory, executive function and behavior.
In 2006, the National Research Council, a private nonprofit organization in Washington, D.C., said limited evidence from China pointed to neurological effects in people exposed to high levels of fluoride. It called for more research into the effect of fluoride on intelligence.
After more research continued to raise questions, the National Toxicology Program in 2016 started working on a review of the available studies that could provide guidance on whether new fluoride-limiting measures were needed.
There were earlier drafts but the final document has repeatedly been held up. At one point, a committee of experts said available research did not support an earlier draft’s conclusions.
“Since fluoride is such an important topic to the public and to public health officials, it was imperative that we made every effort to get the science right,” said Rick Woychik, director of the National Toxicology Program, in a statement.
Malin said it makes sense for pregnant women to lower their fluoride intake, not only from water but also from certain types of tea. It might also make sense to have policy discussions about whether to require fluoride-content on beverage labels, she said.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
METHODS article
Revisiting fluoride in the twenty-first century: safety and efficacy considerations.

- 1 Shoreview Dental LLC, Keizer, OR, United States
- 2 NoDK LLC, Wilsonville, OR, United States
- 3 Oral Health Outreach LLC, Wilsonville, OR, United States
- 4 Leicester School of Pharmacy, De Montfort University, Leicester, United Kingdom
Over 100 years of scientific literature is available which describes the long relationship between dentistry and the many possible applications of fluoride anion (F − ) as successful therapeutic strategies. To date, systemic introduction of fluoride via water, milk and salt fluoridation, and fluoride-containing tablets, has been employed. Post-eruption topical fluoride products have also been introduced, such as fluoridated toothpaste, along with fluoride-containing rinses and varnishes. Importantly, a recent addition to the available armamentarium of fluoride therapeutics now exists in the form of metal ion-fluorido adducts, most especially silver(I)-diammine fluoride (SDF). In view of its high level of therapeutic success, very recently this agent was added to the World Health Authority's (WHO's) list of essential medicines available for the treatment and prevention of tooth decay. Overall, this current state of affairs merits a major review of all these fluoride-containing therapeutic compounds, together with their risks and benefits, both individually and collectively. In this study, a simple graphical tool has been developed for the rapid “on-site” evaluation of fluoride intake with respect to a range of oral healthcare products and body mass index is presented as a gauge of safety for the risk of fluoride toxicity in individual patients. This exposition commences with (a) an account of the history and value of fluoride therapeutics in clinical dentistry, including applications of monofluorophosphate and stannous fluoride; (b) an evaluation of the toxicological activities of fluoride, together with a summary of any reports, albeit very rare ones, arising from its clinically-driven overuse; (c) a history of the development, molecular structure, mechanisms of action, and therapeutic applications of SDF, including a summary of any possible toxic activities and effects arising from silver(I) ion rather than fluoride itself; and (d) the establishment of a working relationship between fluoride exposure and toxicity, with special reference to the instigation of newly-developed tabular/graphical reference guidelines for use by dental clinicians who employ fluoride-rich products in their practices. Particular attention is given to the oral care and treatment options of pediatric patients. In conclusion, applications of this unique monitoring tool may serve as a valuable toxicity guide for dental practitioners.
Introduction: Fluoride Use in Dentistry and Oral Health
In 1901, the dentist Fredrick McKay working in Colorado Springs, Colorado noticed a condition in many of his patients which he referred to as “Colorado Brown Stain” ( Figure 1B ) [ 1 ]. In order to attempt to understand this phenomenon, Dr. McKay requested the assistance of Dr. G. V. Black from Northwestern University ( Figure 1A ) to facilitate the development of an explanation for the possible cause of this clinical finding. Dr. Black identified the enamel lesions as hypomineralized areas, which he characterized as “mottled enamel” ( Figure 1C ), and which he assumed to be at a higher risk of further demineralization [ 2 , 3 ].
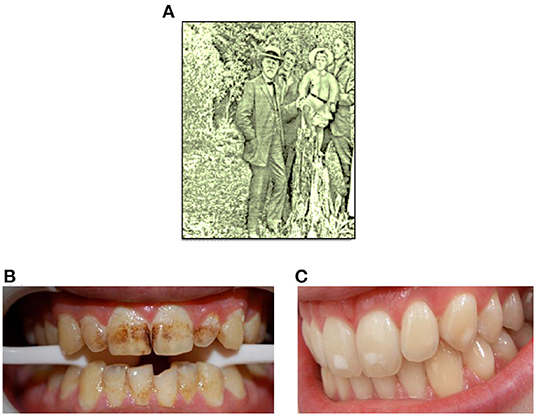
Figure 1. (A) Dr. Black in Colorado Springs, 1909. (B,C) Typical photographic representations of “Colarado brown stain” and mild mottled enamel, respectively.
However, one surprising and counter-intuitive discovery made by McKay and Black was that patients with the so-called “Colorado brown stain,” or severely mottled enamel, had a diminished rate of caries development than that of other patient groups. McKay speculated that this phenomenon might arise from some chemical agent present in local drinking water [ 4 ], and in the 1930's, systematic animal experiments and human epidemiological studies demonstrated a cause-and-effect relationship between fluoride (F − ) levels present in drinking water and mottled enamel [ 3 ].
A full outline of the history of fluoride use in dentistry and oral health is beyond the scope of this manuscript, but particularly notable are the works of H. Trendley Dean, who continued to explore relationships between water fluoride levels, mottled enamel, and tooth decay. These efforts led to the proposal that an optimal level of fluoride in drinking water may minimize the negative cosmetic effects of mottled enamel, and also maximize the protective benefits offered against dental caries. This optimized fluoride level was proposed to be 1 ppm [ 5 ]. Moreover, the performance of a carefully controlled clinical trial in 1944 (based in Michigan, USA), along with additional studies conducted both in the USA and globally [ 1 ], confirmed highly valuable and resoundingly significant reductions in caries rate when fluoride was added to drinking water. In 2001, the United States Centers for Disease Control and Prevention identified water fluoridation as one of the 10 most important public health interventions of the 20th century [ 6 ]. A detailed account of the history of the substantial public health benefits offered by fluoride in dentistry is provided in Ref. [ 7 ].
In the current study, the authors report the development of a relatively simple graphical tool for the rapid evaluation of patient fluoride intake with respect to the composition of a series of oral healthcare products, and recipient body mass index. This tool is readily employable for the purpose of monitoring the safety and potential deleterious health risks of such fluoride-containing products, particularly toward children, at patient points-of-contact. Indeed, it is proposed that its routine clinical application will serve to provide valuable toxicological guidelines for both clinical dentists and oral healthcare specialists alike, and which may be viewed and interpreted rapidly. In this context, a full consideration of working relationships between fluoride exposure and toxicity will serve as a valuable health and safety benefit to dental practice staff, including those who regularly employ 50% (w/v) silver nitrate or 38% (w/v) SDF aqueous solution therapies, both with and without the subsequent application of a 5% (w/v) fluoride varnish product. Moreover, the clinical implications for these methodological developments are discussed, along with future recommendations for fluoride therapeutics in oral health.
Uniquely for a Methods report with a predominantly clinical readership, the authors also provide valuable information regarding the precise molecular structures, the fluoride and metal ion [silver(I) and tin(II)] speciation status, potential mechanisms of action, and health and safety information for all fluoride-containing adducts considered, in addition to those of fluoride anion itself.
Fluoride Anion (F – ) as in Sodium Fluoride (Na + /F – )
Today, the use of fluoride as an additive to water supplies and by way of topical application products are common. There are two major effects of these fluoride products. The first involves the development of tooth enamel during the pre-eruption stage. When fluoride is available systemically during the maturation of enamel hydroxyapatite crystals, fluoride becomes incorporated into enamel prisms, forming a fluorapatite compound which is more resistant to acid dissolution. Secondly, an additional pathway involves the topical application of fluoride to erupted teeth. A normal cyclical process of enamel demineralization and remineralization occurs in erupted teeth, as pH levels fall and rise, respectively, in view of biofilm activity. If topical fluoride is available during the remineralization phase, fluorapatite is formed, and this, in turn, will create an acid-resistant surface. Currently, fluoridated toothpaste has become the major source of topical fluoride throughout the world [ 6 ]. The principal mechanisms of reduced caries rates in many populations around the world have been largely attributed to the application of topical fluoride via oral healthcare products such as these toothpastes [ 6 ].
A series of Cochrane reviews providing an overview of the evidence available on the abilities of fluoride therapies to prevent dental caries was reported by Marinho in 2014 [ 8 ]. Major findings from the reviews considered were that for topically-applied fluoride treatments, there were clear decreases in caries increment in permanent and primary dentitions for all forms of therapies and fluoride varnishes alone, respectively; an arrest of dental caries with topically-administered fluoride products was also revealed, this effect being independent of water fluoridation exposure level, or of other routes of fluoride delivery (their caries preventative actions was found to be enhanced in cases with elevated initial caries population degrees, notably when higher fluoride doses are applied, or when involving the supervision of children's employment of fluoride-containing toothpastes and oral rinses). Moreover, clear protective effects against dental caries and its prevalence in both children and adolescents were offered by the use of fluoride-containing toothpaste products—such products represent the commonest form of fluoride intake globally, and such effects were observed as much as those with the use of other topically-applied fluoride formulations such as oral rinses, gels and varnishes. Additionally, evidence available revealed that the use of a fluoride toothpaste, together with another class of topically-applied fluoride treatment, give rise to additive diminutions in dental caries when compared to those receiving only fluoride-containing toothpaste. Clear enhancements in preventative effects against dental caries were observed with increasing fluoride toothpaste contents when this level is ≥1,000 ppm (the actions of such products containing lower fluoride contents were unclear, however). Nevertheless, there remains some marginal evidence that commencing the application of fluoride toothpaste in children of ≤ 12 months of age may be linked to an elevated risk of fluorosis.
Reviews which considered alternative fluoride interventions and comparisons, and published in The Cochrane Library, were also evaluated in this Cochran review [ 8 ]. These included studies of the caries- preventative influences of fluoride supplements, slowly-releasing fluoride devices and fluoride milk formulas, along with sealants and fluoride varnishes.
Although fluoride-liberating monofluorophosphate (MFP) and stannous fluoride (SnF 2 ) therapies are no longer very widely used in dentistry and dentifrices, we have nevertheless considered their cariostatic activities and mechanisms of action, along with their molecular structures and biological chemistry in Sections Monofluorophosphate (MFP) and Stannous Fluoride (tin(II)-fluoride, SnF 2 ), respectively. Silver(I)-diammine fluoride (SDF) is covered in Section Silver(I)/Fluoride Ion-Containing Products and Their History: Silver(I)-Diammine Fluoride (SDF).
Monofluorophosphate (MFP)
MFP, as its sodium salt, has previously found a considerable level of application in oral health products, usually toothpastes, in view of its now well-known cariostatic and microbicidal effects. Its molecular structure consists of tetrahedral [PO 3 F] − structural units with an intact P-F bond, which is subject to hydrolysis through the actions of phosphatase enzymes in vivo , a process liberating free fluoride anion and inorganic orthophosphate. Investigations performed in an animal model system demonstrated that although there was no such hydrolysis in the stomach, this process occurred very rapidly in both the small intestine and the liver, but more slowly in blood [ 9 ]. In both rats and humans, no evidence for direct absorption of [PO 3 F] − anion into blood circulation was obtained [ 9 ]. Hence, these observations support the low acute toxicity found for MFP, and also the lack of gastric irritation associated with its use.
In 1993, Holloway and Worthington [ 10 ] conducted a critical review of a meta-analysis to establish the relative therapeutic effectiveness of sodium MFP when evaluated against sodium fluoride. In addition to revealing some important study flaws, this investigation found that two and three studies favored sodium fluoride and sodium MFP, respectively, whereas no fewer than five of them should not have been incorporated into a meta-analysis process. However, the only two scientifically-conceived and performed investigations did not conclude with any advantages of either agent over the other.
Stannous Fluoride (Tin(II)-Fluoride, SnF 2 )
The chemical bonding in stannous fluoride (SnF 2 ), a complex with a tin(II) (Sn(II)) metal ion coordination center and fluoride ligands, has a quite a strong covalent character. This agent has been demonstrated to successfully control and avert both dental caries and gingivitis via its ability to facilitate enamel mineralization and alleviate inflammation and bleeding of the gingiva. It also potentially exerts a rather broad-spectrum microbicidal effect, and also has the capacity to significantly modify the microbial contents of dental biofilms. Its mechanism of action involves the deposition of a stable acid-resistant tooth surface coating, which comprises calcium fluoride generated via the actions of SnF 2 on apatite, and its transformation to fluorapatite, processes involving the exchange of F − ‘ligands' from Sn(II) to Ca 2+ . Both the Sn(II) center and F − ligand moieties play roles in the development of anti-erosive properties, possibly by intensifying the degree of cross-linking between salivary proteins of the absorbent layer, for example mucins [ 11 ]. This process gives rise to a layer which is more resistant against erosive attack, and it is conceivable that Sn(II) ions may form inter-protein metal ion-centered bridges through coordination to oxygen- and/or nitrogen-donor amino acid residue complexants in these biopolymers. Sn(II) has a preference for oxygen-donor atoms in ligands available in vivo , although the cumulative stability constants for its fluoride complexes are indeed quite high [ 12 ]. Notably, the value and protective effects offered by SnF 2 appear to be associated with the uptake of Sn(II) metal ion species by mineralized dentine containing a largely conserved organic component. Indeed, its ability to suppress erosion is critically dependent on the availability of a demineralized organic dentine environment [ 12 ].
Recently, Alsina and Gaillard [ 13 ] investigated the identities and structures of tin(II)-fluoride complexes in aqueous solutions via a combination of thermodynamic modeling, X-ray absorption spectroscopy, and quantum mechanical computations. Spectroscopic measurements confirmed the presence of three tin(II)-fluoride complexes in this medium (specifically [SnF] + , [SnF 2 ] and [SnF 3 ] − ). Interestingly, in addition to the fluoride ligands, the [SnF 3 ] − complex also contained weakly coordinated water, which was displaced by glycerol added to the solvent system. These results provided a confirmation of the nature of previously proposed stannous-fluoride complexes. They also served to explain why the addition of glycerol, an agent commonly present in dentifrices, protects Sn(II) against oxidation in aqueous solution.
Silver(I)/Fluoride Ion-Containing Products and Their History: Silver(I)-Diammine Fluoride (SDF)
W. D. Miller identified silver nitrate as the most effective and non-toxic antimicrobial substance effective against oral bacteria in 1890 [ 14 ]. Moreover, G.V. Black described in detail his method for arresting tooth decay using silver nitrate in his text entitled “Pathology of The Hard Tissues of The Teeth,” which was published in 1908 [ 15 ]. This practice was continued by Percy Howe at the Forsyth Institute [ 16 ]. Recent additions to the literature have revisited this approach by combining silver nitrate with fluoride varnish [ 17 ].
Silver(I)-diammine fluoride (SDF) was investigated in 1969 by Mizuho Nishino as part of her PhD thesis working in the laboratory of Yamaga [ 18 ]. This was a development from an interest in attempting to evolve a combination product, which would capture the antimicrobial properties of silver(I) cation [Ag(I)] and the enamel protectant effects of fluoride [ 18 ]. The first commercial product was Saforide, manufactured by Morita in 1970. Saforide is a 38% (w/v) concentration aqueous solution which is, by composition, 25% silver, 8% ammonia, 5% fluoride and 62% water by weight [expressed as (w/w)]. The addition of ammonia was predominantly selected in order to stabilize the product, and to circumvent silver(I) ion precipitation from solution as metallic silver [Ag(0)] or insoluble, black-colored silver(I) oxide (Ag 2 O).
SDF [38% (w/w)] was released into the US market (as Advantage Arrest) by the FDA in 2014 as a desensitization agent. However, clinicians often use this product to arrest active caries in an off-label manner [ 19 ]. Given the high fluoride concentration of this product, appropriate consideration must be made with regard to any potential toxic effects exerted by it, most notably when applied in combination with other sources of fluoride. Some authors have promoted an application technique which includes careful drying of the lesion, placement of SDF with a gentle scrubbing motion, followed by covering with a fluoride varnish product to maintain direct contact of the SDF with the treated tooth surface, prevent salivary contamination, and mask the adverse taste sensation known for this product [ 20 ].
SDF comprises a two-coordinate complex with the silver(I) ion complexed near-linearly by two ammonia ligands [[Ag(NH 3 ) 2 ] + ], apparently with a fluoride counter ion (F − ). Hence, the molar concentration of SDF in aqueous solution products containing 38% (w/v) of this complex is as high as 2.34 mol./L, with an equivalent molar concentration of fluoride, which translates to a product level of 45,215 to 51,000 ppm F − in clinical sample analyses [ 21 ].
In the solid-state, the crystal structure of diamine silver(I) complex with a sulfate counter ion in place of fluoride [[Ag(NH 3 ) 2 ] + ) 2 .SO 4 2 - ] was re-determined by Zachwieja and Jacobs in 1992 [ 22 ]. As expected, these Ag(I) cations were significantly bent, with an N-Ag-N angle of 174.3°, which was ascribable to a degree of oxygen donot atom complexation at its Ag(I) center. Intriguingly, one relevant further crystal structure report found that Ag(I)-coordinated ammonia ligands in the compound [Ag(I)(NH 3 ) 2 ]F · 2NH 3 form strong N–H ··· F hydrogen bonds to adjacent fluoride ions, in addition to weaker N–H ··· N ones to free ammonia ligands [ 23 ]. Therefore, one new conjecture from the authors is that in aqueous solution, the [Ag(I)(NH 3 ) 2 ] + species may effectively aid the delivery of cariostatic fluoride anion to optimal diseased tooth remineralization sites in vivo .
Similarly, the crystal structure of diamine silver(I) acetate ([Ag(NH 3 ) 2 ]OAc) demonstrated almost linear [Ag(NH 3 ) 2 ] + cations (bond angle 176.95°), arranged in a corrugated chain of equidistant silver atoms ( Figure 2 ) [ 24 ]. Intriguingly, in this compound, the Ag(I)–Ag(I) distance was found to be within what is described as the “argentophilic” contact range, this indicating that there may be a significant interaction between silver(I) metal ion centers in the solid-state.
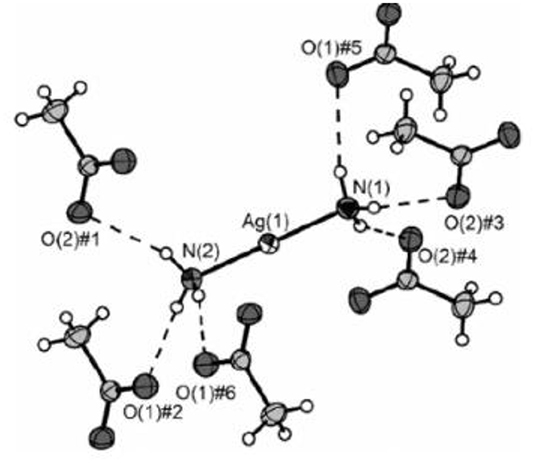
Figure 2 . X-ray crystal structure of diammine silver(I) acetate ([Ag(NH 3 ) 2 ]OAc), which has close to linear two-coordination of silver(I) by two ammonia (ammine) ligands. Reproduced from Ref. [ 22 ] with permission.
Although there are many reports available on the therapeutic properties and efficacies of SDF regarding its value in the treatment of dental caries, such reports are beyond the scope of this review. However, recently Zhao et al. [ 25 ] conducted a full and very extensive systematic review of such actions in the oral health research area, and this work primarily identified a grand total of 1,123 publications. Of the 29 peer-reviewed publications selected for further analysis, which explored the influence of SDF on dental hard tissues and cariogenic bacteria, 11 studied the bactericidal properties of SDF, and found that it acted against cariogenic bacteria, predominantly Streptococcus mutans , and also suppressed the development of cariogenic tooth biofilms; 20 investigations examined the remineralization of demineralized dentine or enamel by this agent, and found that mineral loss from these sites was retarded following SDF treatment, and that a calcium ion (Ca 2+ ) and phosphate-loaded surface was generated on carious lesions which were indeed arrested; finally, 4 reports detailed the protective role of SDF toward dentine collagen, and discovered that it inhibited the actions of collagenases and hence averted collagen degradation. Therefore, the authors of this detailed review concluded that SDF offers very favorable therapeutic effects for each of these three mechanistic considerations.
Toxicities of Fluorides and Their Excessive Use
Sodium fluoride.
The harmful effects of fluoride exposure may be placed into two main categories:
Firstly, a massive acute systemic exposure from an industrial accident, and inadvertent ingestions of large quantities of fluoride anion-containing products have been observed [ 26 ]. These events can lead to serious injury and death, but thankfully, this type of exposure is very rare. Another type is that chronic exposure to fluoride anion, which can lead to hypomineralized areas of enamel (mottled enamel), which was first recognized as “Colorado brown stain” as noted above [ 1 ]. Separate exposures to different types of fluoride compounds are, of course, considered additive, and therefore other fluoride products such as fluoride toothpastes, and the newer product SDF, should be cumulatively considered. Examples of fluoride-containing tap water and oral health products, and their fluoride contents, are provided in Table 1 . While the use of fluoridated toothpaste is intended to produce a topical effect, in some situations the toothpaste may be ingested. This is especially a problem for young children who are first learning to brush their teeth. It is therefore universally suggested that just a smear of toothpaste be placed onto the toothbrush of children aged under 6 years, and that adult supervision of tooth-brushing takes place for younger children. There have been cases reported of children eating toothpaste, a situation giving rise to nausea and vomiting.
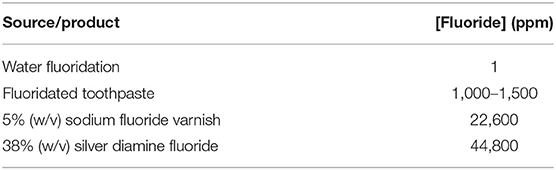
Table 1 . Fluoride contents (ppm) of fluoridated tap water and some typical oral health products.
Secondly, a mild chronic overexposure to fluoride in children over time may result in some form of fluorosis in developing teeth, and may also cause a transient gastric disturbance [ 27 ].
Tooth enamel is porous, and despite having an opacity, is quite transparent; it contains a significant content of protein. Dental fluorosis is one common concern for oral health practitioners, which represents a developmental perturbation of tooth enamel, and which commences during its formation. Unfortunately, fluorosis arises from the excessive systemic exposure of children to fluoride during their first 6 years, a period when permanent teeth crown enamel is generated. Clinical manifestations of fluorosis range from (quantitative) narrow, white horizontally-running lines, more extensive marks, or yellow- to light brown-colored regions of porous enamel, to the qualitatively-visible loss of enamel to varying extents [ 28 , 29 ]. In order to achieve the optimal therapeutic effects from the use of fluoride toothpastes, it is of much importance for consumers to pay close attention to recommended guidelines available for the employment of products containing such agents. In this manner, the likelihood of fluorosis is diminished, and fluoride's protective effects against the induction and development of dental caries are optimized [ 1 , 30 , 31 ].
The excessive use of fluoride can, however, give rise to acute toxicity, most especially with the ingestion of one or more doses of this agent during a short time duration, which then may give rise to adverse poisoning effects [ 32 ]. Primarily, the stomach is affected, and the first symptoms and signs consist of nausea, abdominal pain, bloody vomiting and diarrhea. Subsequently, collapse occurs, together with wetness, paleness, weakness, skin hypothermia, weak heart sounds, shallow breathing, dilated pupils, hypocalcaemia and hyperkalemia, and cyanosis, followed by fatality in some cases within 2–4 h. Further outcomes involve muscle paralysis, together with carpopedal and extremity spasms. From previous investigations of a series of overdose cases, the probable toxic dose (PTD) of fluoride has been stipulated to be 5 mg/kg of body mass (BM) [ 30 ]. This PTD value represents the minimal dose that may provoke serious or life-threatening signs and symptoms; such events call for immediate hospitalization and treatment [ 32 ]. As an example, a 30 kg pediatric patient would attain the PTD value for fluoride anion if they ingested 150 g ( ca . 112 mL) of a toothpaste containing 1,000 ppm (mg/kg) of this agent.
A further adverse toxiciological outcome of excessive fluoride ingestion is skeletal fluorosis. Recently, Srivastava and Flora [ 33 ] reviewed up-to-date findings focused on skeletal fluorosis and the input of oxidative stress in its progression. This study found that the human consumption of fluoride at concentrations of 1.5 ppm or greater is predominantly responsible for skeletal fluorosis. Indeed, the testing of water supplies from rural areas demonstrated that 80% of villages had water fluoride levels greater than acceptable limits set by the WHO. Indeed, those residing in such areas are afflicted by this condition. Moreover, in many Asian and African regions, endemic fluorosis affects the majority of the populations, i.e., ca . 100 million subjects. Skeletal fluorosis represents a slowly progressing disorder, and requires preventative circumvention using mitigation strategies, which indeed have been performed with defluoridation processes globally. Despite being reversible, resolution of such fluoride toxicity and its side-effects is complicated with only very limited treatment options, and these are certainly not affordable in the poverty-stricken rural areas where they are most needed. Since there are no available therapies to effectively combat fluorosis, its direct aversion serves as the best option available. Indeed, the review presented in Ref. [ 33 ] discusses the development of relatively simple and economically-viable approaches for fluoride removal from water supplies, in addition to research data available based on strategic therapies for skeletal fluorosis.
Ingested fluoride is predominantly distributed within calcified bone tissues, and is then slowly, albeit cumulatively, recycled during bone remodeling processes. In 1998, Boivin et al. [ 34 ] reported a method for the determination of fluoride retention in bone, results from which served as a valuable complement to bone histology for skeletal fluorosis diagnosis and monitoring, and putatively useful for the management of fluoride treatments administered for osteoporosis. Notably, mean fluoride levels were found to be 0.05 and 0.08% (w/w) for two large groups (n >100 each) of untreated osteoporotic patients, treatment duration-dependent 0.24–0.67% (w/w) for 166 osteoporotic patients receiving fluoride therapy, and 0.56–1.33% (w/w) for n = 96 patients with a typical skeletal fluorosis condition. The latter group values were found to be critically dependent on fluorosis etiologies, and associations with the level and duration of fluoride exposure. Overall, throughout prolonged fluoride ingestion episodes, the primary uptake of fluoride by bone is somewhat variable, and is highly linked to remodeling activity. Subsequently, fluoride uptake is enhanced more rapidly, and then attains stability at its maximal level. In order to examine the safety and efficacy of fluoride products, it is necessary to consider the body mass index (BMI) of the patient, together with the precise molecular nature of the fluorido agent applied, and where considered appropriate, a full summation of human exposure to a combination of fluoride-containing products.
Considerations of the Toxicities of Silver and Silver Ions
Separate considerations should be made for the potential toxic effects of silver and its Ag(I) cation. Essentially, silver(I) ions are very toxic to bacteria via diffusion through cell walls and cell membranes, and are either specifically or non-specifically complexed by selected amino acid residues present in intracellular or extracellular proteins, and/or by the purine and pyrimidine base moiety, or phosphate ligands, in DNA. These processes denature these biomolecular substrates, and also cause bacterial metabolism to be disrupted [ 35 ]. Ag(I) ion has quite a strong affinity for sulfur donor atoms present in the thiol function of the amino acid L-cysteine [ 36 ], and such interactions represent a key mechanistic action regarding the bactericidal properties of this metal ion.
Since humans are entirely covered by some form of epithelium (dead cells), silver ions bind to epithelial cells and do not gain access to the intracellular spaces, a process rendering them non-toxic. However, in cases of extremely high exposure to silver(I) ions, a condition known as argyria may develop. In these rare cases of silver exposure, silver is deposited throughout organ systems, and the skin will exhibit a pale blue-gray coloration [ 37 ], the case reported in this reference involving the accidental ingestion of colloidal silver. Moreover, accidental skin exposure to silver nitrate and SDF generates a temporary superficial stain similar to a “henna tattoo.” Fortunately, this stain, which appears to largely consist of metallic silver [Ag(0)], eventually disappears with normal skin cell exfoliation. Recent studies, however. have explored the possible toxic effects of silver(I) ion exposure from SDF [ 38 ]. The silver content of small amounts of SDF used to treat tooth decay results in a very low exposure, and therefore systemic silver toxicity should not represent a major concern to clinicians. However, most SDF products available are caustic (with pH values ranging from 10 to 13), and therefore could cause a chemical “burn” to the epithelial lining or conjunctiva of the eye, if indeed an inadvertent spillage were to occur. Both operators and patients should, of course, be wearing eye protection during treatment episodes.
Estimations of Fluoride Exposures and Toxicities For Differential Fluoride-Containing Oral Healthcare Products: Quantitative Problems Experienced by Dental Clinicians
The potential for various human exposures to fluoride from differential oral healthcare product sources presents a highly challenging situation for clinicians who are attempting to optimize the benefits of fluoride against its potential negative side-effects, such as gastritis and enamel mottling. In addition, the various common units available for expressing or displaying fluoride concentrations may lead to some confusion amongst dental practitioners, for example through the use of % compositions [both (w/w) and (w/v)], parts-per-million (ppm) and moles per liter (mol./L, i.e., molarity) concentration units, etc. Therefore, the diagrams and Tables provided below ( Figures 3 , 4 , and Tables 2 , 3 ) aim to provide a simple and rapid means of estimating the exposure of patients based on body mass index (BMI) and their various fluoride exposure patterns. The overall goal of this strategy is to easily inform both the clinician and patient of the likelihood of any potential toxic outcomes for the use of fluoride compounds during such dental treatments.
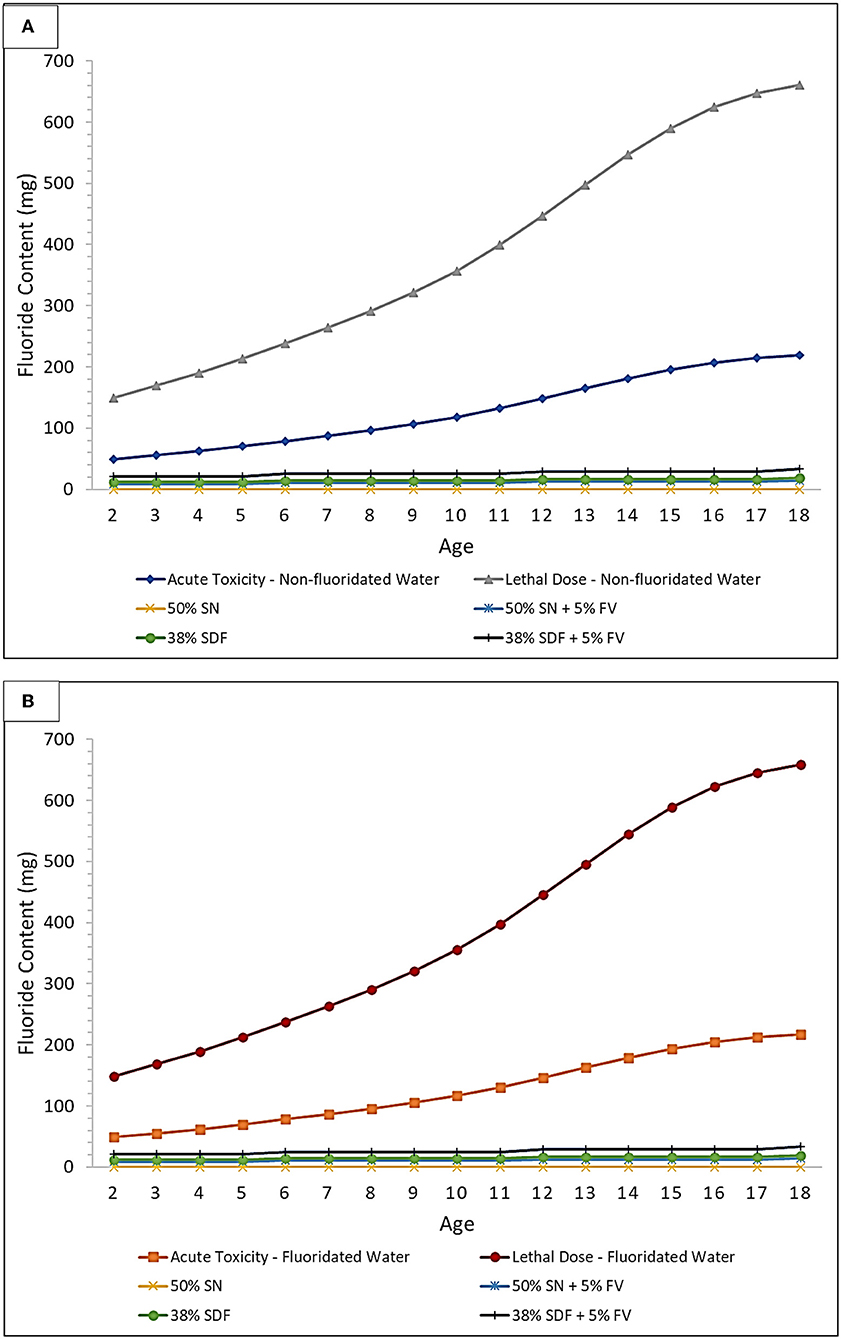
Figure 3 . Acute toxicity and CLD thresholds of fluoride for silver nitrate (SN) and SDF both with and without a sodium fluoride-containing varnish (FV) in (A) non-fluoridated and (B) fluoridated water environments. Treatment comparison against the fluoride Acute Toxicity and CLD Thresholds (including considerations for the ingestion of fluoridated water, or not, and also toothpaste up to the age of 6 years) using 10 μl of 50% (w/v) SN, or 10 μl of 38% (w/v) SDF, and both with and without the application of 20 μl of a 5% (w/v) FV. These plots were derived using the assumption that every tooth is treated for each age group considered, and all ages are within the 3% weight group, to further demonstrate the safety margin in a worst-case-scenario.
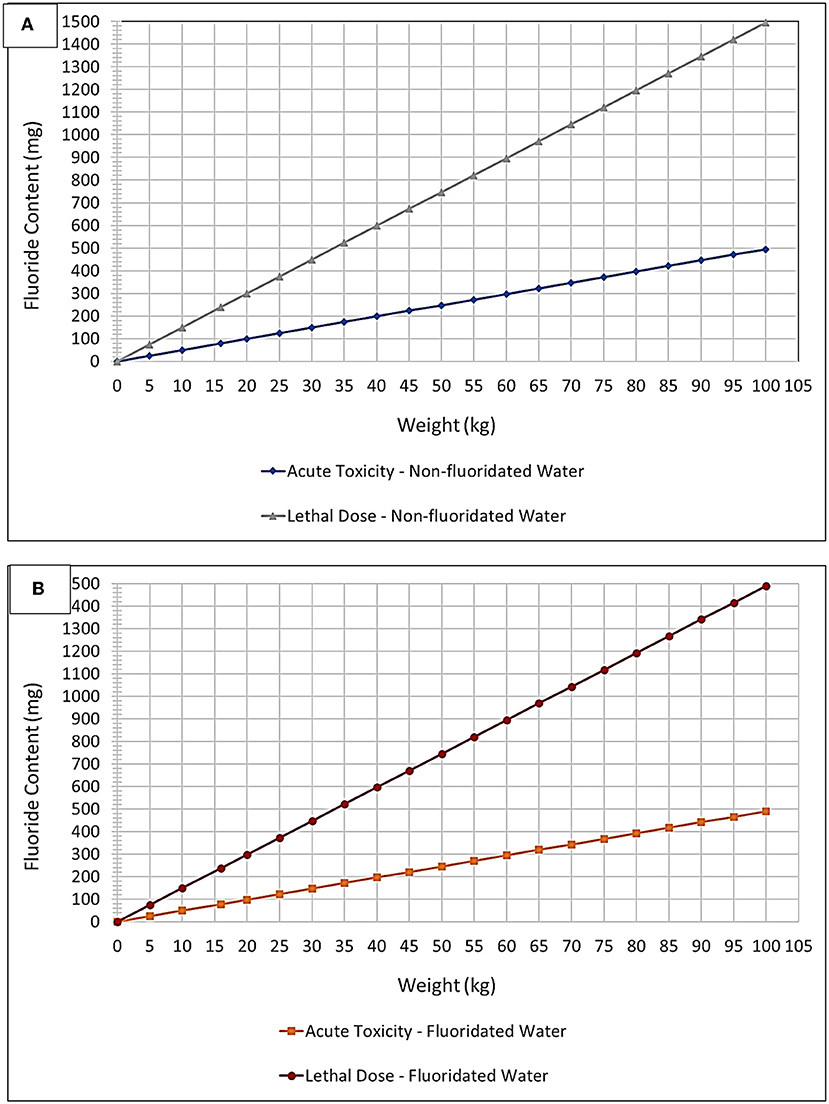
Figure 4 . “Plug and play” plot option – fluoride toxicity. Acute Fluoride Toxicity and CLD Thresholds expressed as a plot of mg of potential fluoride ingested vs. child body weight (kg) for (A) non-fluoridated and (B) fluoridated water environments. These thresholds were adjusted to account for fluoridated and non-fluoridated water environments, in addition to the ingestion of toothpaste up to an age of 6 years based on a mean weight of 16 kg (lowest 3% body weight average).
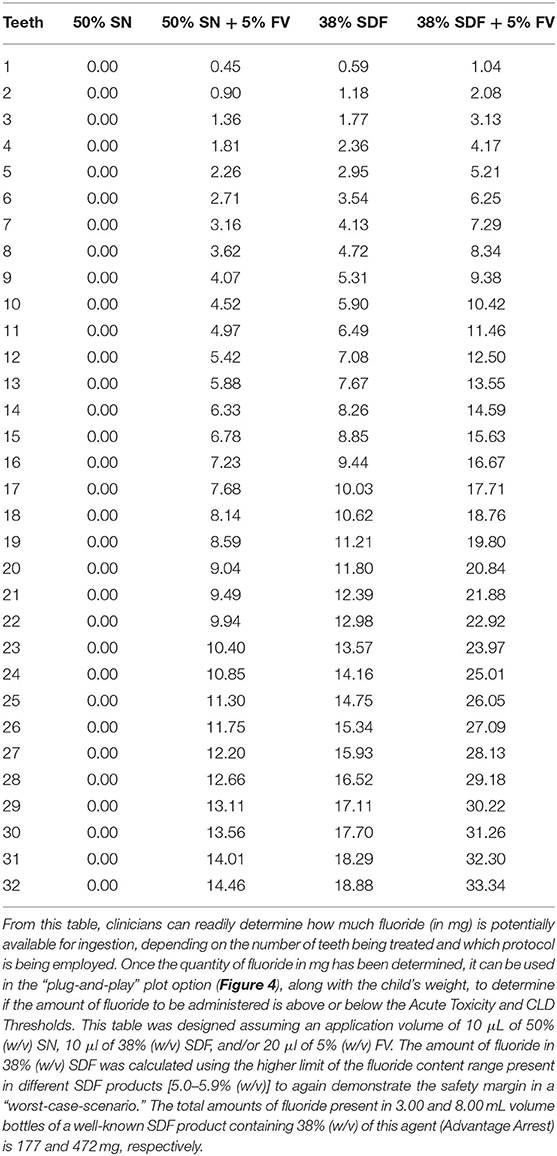
Table 2 . Fluoride content (mg) based on number of teeth treated and protocol used (SN or SDF, both with and without FV).
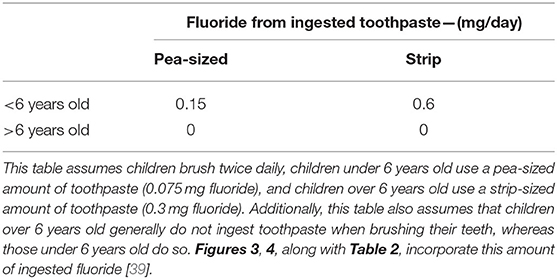
Table 3 . Amount of fluoride from toothpaste ingested by children based on age.
Working Relationship of Fluoride Exposure to Toxicity
In Figure 3 , the acute fluoride toxicity and Certainly Lethal Dose (CLD) threshold curves are demonstrated for the therapeutic application of silver nitrate and SDF treatments, both with and without the co-application of a fluoride varnish; both fluoridated and non-fluoridated water environments are considered. The lethal dose value employed was that available in Ref. [ 40 ], specifically 15 mg/kg. Childrens' weights at each age were selected to be the lowest 3% for each age group in order to provide a “worst-case-scenario” to provide an improved portrayal of the safety margin. This was then used to determine how much fluoride would have to be ingested to meet the 5 mg/kg body weight PTD acute fluoride toxicity and CLD thresholds. In addition, since different age groups have differing average numbers of teeth, this was accounted for when determining how many mg of fluoride is available for ingestion during treatments. This plot assumes that every tooth is treated using a 10 μl “drop” of 38% (w/v) SDF [ 41 ], or alternatively 50% (w/v) silver(I) nitrate (SN) and a 20 μL volume of 5% (w/v) sodium fluoride varnish (FV) [ 42 ], since these are approximately the volumes that are employed in the field. It should also be borne in mind that 38% (w/v) SDF has a fluoride content ranging from 5.0 to 5.9%, and this value is dependent on the brands and batches utilized. The calculations for Figure 3 were performed using a 5.9% fluoride content value in order to optimize a demonstration of the safety margin. Notably, however, treatment of every tooth using any of the protocols shown places all patients well within the safety margin. This safety margin obviously increases as children become older with greater body masses.
Figure 4 and Table 2 , however, offer a “plug-and-play” option for practicing clinicians who wish to know exactly how close to the acute fluoride toxicity threshold a child patient will be when undergoing such treatment, and this is critically dependent on the protocol used, the number of teeth treated, and the child's body weight. A small child with a large number of teeth, for example, may have to have only half of their teeth treated to ensure that their exposure to fluoride isn't too high during that treatment session. Taken together, they offer a tool for clinicians to facilitate the proper instigation of a safe treatment plan featuring these treatment protocols. Moreover, this plot accounts for both fluoridated and non-fluoridated water environments. By viewing the amount of fluoride received during a certain treatment protocol (derived from Table 2 ) as a function of the patients' body mass, a clinician can readily determine its safety margin expressed relative to fluoride Acute Toxicity and CLD Thresholds.
Table 3 shows exactly how much fluoride can be ingested by children depending on how old they are and what amount of toothpaste they are using during toothbrushing episodes. However, it should also be noted that children under the age of 6 years generally ingest approximately one-half of the quantity of toothpaste used, whereas children older than this generally do not swallow significant amounts of their toothpaste products [ 39 ].
Using Table 2 , a clinician can determine how many mg of fluoride is potentially ingestible based on the protocol used and the number of teeth being treated.
The relationship between the dental profession and fluoride has been long and complex. It began over 100 years ago when it was first speculated that an unknown substance in the water of communities in Colorado, USA was causing enamel staining (mottling). Subsequently, a correlation was made between mottling incidence and reduced caries rates, and careful analysis demonstrated that fluoride anion was involved in both processes. A concerted effort then proceeded to determine how to balance the protective effects of fluoride against its potential negative outcomes. Particularly notable is the addition of the novel “metallodrug”-type agent SDF to the World Health Authority's (WHO's) list of essential medicines targeted on the prevention and treatment of tooth decay [ 43 ].
Presently, we find ourselves in a situation where fluoride has been added to community water supplies, toothpaste and other therapeutics. During this period of time, no standard measurement units have been used when demonstrating the concentration of fluoride in these products. Sometimes, a percentage of net weight or volume is used, and sometimes a parts-per-million (ppm) metric has been employed. This often leads to the confusion of clinicians and the general public when they try to judge the safety and efficacy of fluoride-containing products and materials which they use during their daily working lives. There are even examples where certain groups have based their political views on fluoride supplementation. A full review of no fewer than 87 cases of toxic exposure to high levels of fluoride by children have been reported in the literature [ 44 ]. In this study, 84 out of 87 cases featured the accidental ingestion of fluoride-containing oral healthcare products, i.e., drops, rinses and tablets, etc., at home by children aged up to 6 years old. However, two children aged 8 and 9 years old were reported as becoming symptomatic following treatment with fluoride by a dental clinician. The single remaining case involved the fatal ingestion of an unknown quantity of an insecticide containing sodium fluoride by a child aged 13 months (a substantial decline in blood serum calcium concentration was observed post-mortem). Approximately one-third of the total of 87 child cases displayed gastrointestinal ( n = 25) and drowsiness ( n = 1) symptoms, the former including nausea, vomiting, abdominal pain and diarrhea; 3 of these only became symptomatic at a time-point >1 h subsequent to ingestion.
A central theme of this report is to enable clinicians to identify the margin of safety that a patient may experience based on body mass index and exposure to various fluoride-containing products. Indeed, the included graphical Figure diagrams and Tables are valuable for the rapid estimation and recognition of such margins in order to provide solutions in “on-the-spot” clinical situations at points of patient contact. Hence, this information will serve to assist clinicians with the taking of informed decisions regarding the application or prescription of fluoride-containing products. Another major objective of this study was to assist the public in the evaluation of this controversial subject through common dialogue with their dental clinicians, a process which will hopefully lead to a more complete general understanding of the subject matter.
Potential Limitations of the Study
Firstly, the local water fluoridation level is a factor which will always depend on the water intake of an individual, and which may vary based on environmental temperature, and differential between-subject water consumption levels ascribable to exercise and other requirements, etc. Notably, previous scientific reports based on this subject have often utilized group estimates rather than individual quantitative data available.
Secondly, the unintended systemic exposure to fluoride in toothpaste covers a wide range of situations. For example, are parents sufficiently educated regarding the amount of toothpaste to place on the brush, as in the well-known “smear” approach, and do children purposely swallow toothpaste because they are fond of the taste, or other explanations?
Thirdly, the fluoride content involved in the applications of SDF to caries lesions should be considered, the treatment intent being their topical administration to these locations. However, there may be some inadvertent systemic absorption of fluoride; indeed, the transient systemic presence of fluoride following SDF application has been reviewed in Ref. [ 41 ].
Finally, possible variations in exposure level should not deflect from the importance and usefulness of making realistic predictions of acceptable and safe values for this critically important parameter. However, the wide safety margins demonstrated in previous studies should provide reassurance to clinicians who wish to embrace any newly-developed fluoride therapies.
Conclusions
In this manuscript, we present a simple graphical plot/tabular tool which allows clinicians to gauge the overall exposure of their patients to fluoride-containing products with respect to both acute and chronic toxicities. This tool will undoubtedly also assist clinicians who wish to discuss these issues with adult patients, and parents of child patients, about fluoride anion, fluoride adducts, and their potential, albeit very unlikely, toxic effects.
After over 100 years of discovery, and the clinical application of fluoride products into clinical practice, this field continues to evolve with new knowledge and therapeutics, most especially with the design of novel fluoride-containing and -delivery compounds such as cariostatic SDF. A periodic review of this history, and current tools for clinical practice, are indicated here for the benefit of both patients and clinicians. Relevant information concerning the molecular structures, solution status and potential mechanisms of action of all fluoride derivatives employed in oral health, such as MFP, stannous fluoride and SDF is also presented, as is information on their possible, albeit very unlikely, adverse health effects. Fluoride is now commonly present in diverse sources such as community water systems, toothpastes and topical products, as well as new therapeutics, and therefore the development and use of a simple graphical tool to estimate possible fluoride-induced toxicities serves as a major benefit for practicing dental clinicians, together with oral healthcare workers in general.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
SD and MD: conceptualization, resources, writing—original draft preparation, and project administration. SD, MD, and MG: methodology, software, validation, investigation, data curation, writing—review and editing, and writing—final draft preparation. MD and MG: formal analysis and visualization. All authors have read and agreed to the published version of the manuscript.
Conflict of Interest
Authors SD and MD were employed by Shoreview Dental LLC, Oral Health Outreach LLC, and NoDK LLC.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Harris NO, García-Godoy F. Primary Preventive Dentistry . Upper Saddle River, NJ: Pearson/Prentice Hall. (2004).
Google Scholar
2. Fejerskov O. Dental Fluorosis: A Handbook for Health Workers . Copenhagen: Munksgaard (1988).
3. Fejerskov O, Kidd EAM editors. Dental Caries: The Disease and Its Clinical Management . Copenhagen: Blackwell Monksgaard (2003).
PubMed Abstract | Google Scholar
4. Murray JJ, Rugg-Gunn AJ, Jenkins GN. Fluorides in Caries Prevention . 3rd ed. Oxford: Wright/Butterworth-Heinemann (1991).
5. Elwood R, Fejerskov O, Cury JA, Clarkson B. Dental Caries - the Disease and Its Clinical Management . 2nd ed. Oxford, Malden: Blackwell (2008).
6. Horowitz HS. The 2001 CDC recommendations for using fluoride to prevent and control dental caries in the United States. J. Public Health Dent. (2003) 63:3–8. doi: 10.1111/j.1752-7325.2003.tb03467.x
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Šket T, Kukec A, Kosem R, Artnik B. The history of public health use of fluorides in caries prevention. Zdravstveno Varstvo . (2017) 56:140–6. doi: 10.1515/sjph-2017-0018
8. Marinho VCC. Cochrane fluoride reviews: an overview of the evidence on caries prevention with fluoride treatments. R Coll Surg Engl. (2014) 5:78–83. doi: 10.1308/rcsfdj.2014.5.2.78
CrossRef Full Text | Google Scholar
9. Ericsson Y, Patterson C. Studies on the hydrolysis and absorption of monofluorophosphate ions. Pharmacol Therapeut Dent. (1980) 5:47–54.
10. Holloway PJ, Worthing HV. Sodium fluoride or sodium monofluorophosphate? A critical view of a meta-analysis on their relative effectiveness in dentifrices. Am J Dent. (1993) 6:S55–8.
11. Algarni AA, Mussi MCM, Moffa EB, Lippert F, Zero DT, Siqueira WL, et al. The impact of stannous, fluoride ions and its combination on enamel pellicle proteome and dental erosion prevention. PLoS ONE. (2015) 10:e0128196. doi: 10.1371/journal.pone.0128196
12. Ganss C, Hardt M, Lussi A, Cocks A-K, Klimek J, Schlueter N. Mechanism of action of tin-containing fluoride solutions as anti-erosive agents in dentine - an in vitro tin-uptake, tissue loss, and scanning electron microscopy study. Europ J Oral Sci. (2010) 118:376–84. doi: 10.1111/j.1600-0722.2010.00742.x
13. Alsina MA, Gaillard J-F. Structural characterization of metal complexes in aqueous solutions: a XAS study of stannous fluoride. Phys Chem Chem Phys. (2018) 20:12727–35. doi: 10.1039/C8CP01461B
14. Miller WD. The Micro-Organisms of the Human Mouth . (Unaltered reprint of the original work published in 1890 in Philadelphia). X + 390 S. 128 Abb., 3 Tafeln. Basel-München-Paris-London-New York-Sydney 1973: S. Karger (1890).
15. Black GV. The Pathology of the Hard Tissues of the Teeth . 1st ed. Vol. 1. Chicago, IL: Medico-Dental Publishing Company (1908).
16. Howe PR. A Method of Sterilizing and at the Same Time Impregnating With a Metal, Affected Dentinal Tissue . 59. Philadelphia, PA: S. S. White Dental Manufacturing Company (1917).
17. Gao S, Zhao I, Duffin S, Duangthip D, Lo E, Chu C. Revitalising silver nitrate for caries management. Int J Environ Res Public Health. (2018) 15:80. doi: 10.3390/ijerph15010080
18. Yamaga R, Nishino M, Yokomizo I. Diammine silver fluoride and its clinical application. J Osaka Univ Dent School. (1972) 12:1–20.
19. Fontana M. Phase III RCT. Effectiveness of Silver Diamine Fluoride in Arresting Cavitated Caries Lesions. (2021). Available online at: https://clinicaltrials.gov/ct2/show/nct03649659 (accessed January 10, 2022).
20. Kher MS, Rao A. Contemporary Treatment Techniques in Pediatric Dentistry . 出版商 Cham: Springer International Publishing (2019).
21. Crystal YO, Rabieh S, Janal MN, Rasamimari S, Bromage TG. Silver and fluoride content and short-term stability of 38% silver diamine fluoride. J Am Dent Assoc. (2019) 150:140–6. doi: 10.1016/j.adaj.2018.10.016
22. Zachwieja U, Jacobs H. Redetermination of the crystal structure of diammine silver(I)-sulfate, [Ag(NH 3 ) 2 ] 2 SO 4 . Zeitschrift für Kristallographie Crystalline Mater. (1992) 201:207–12. doi: 10.1524/zkri.1992.201.3-4.207
23. Kraus F, Baer SA, Fichtl MB. The reactions of silver, zirconium, and hafnium fluorides with liquid ammonia: syntheses and crystal structures of Ag(NH 3 ) 2 F·2NH 3 , [M(NH 3 ) 4 F 4 ]·NH 3 (M = Zr, Hf), and (N 2 H 7 )F. Eur J Inorg Chem. (2009) 2009:441–7. doi: 10.1002/ejic.200800980
24. Woidy P, Kraus F. The diammine silver(I) acetate [Ag(NH 3 ) 2 ]OAc. Zeitschrift für Anorganische und Allgemeine Chemie. (2013) 639:2643–7. doi: 10.1002/zaac.201300338
25. Zhao IS, Gao SS, Hiraishi N, Burrow MF, Duangthip D, Mei ML, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Intern Dent J. (2017) 68:67–76. doi: 10.1111/idj.12320
26. Yagiela JA, Dowd FJ, Neidle EA. Pharmacology and Therapeutics for Dentistry . St. Louis, MO: Mosby (2004).
27. Meyer-Lueckel H, Paris S, Ekstrand KR. Caries Management: Science and Clinical Practice . Stuttgart; New York: Thieme (2013).
28. DenBesten P, Li W. Chronic fluoride toxicity: dental fluorosis. Monogr Oral Sci. (2011) 22:81–96. doi: 10.1159/000327028
29. Wong MCM, Clarkson J, Glenny A-M, Lo ECM, Marinho VCC, Tsang BWK, et al. Cochrane reviews on the benefits/risks of fluoride toothpastes. J Dent Res . (2011) 90:573–9. doi: 10.1177/0022034510393346
30. Whitford GM. Acute toxicity of ingested fluoride. Monographs Oral Sci. (2011) 22:66–80. doi: 10.1159/000325146
31. Ellenikiotis H. Pharmacokinetics of 38% Silver Diamine Fluoride in Children . UCSF (2021). Available online at: https://escholarship.org/uc/item/4nq8s2f8 (accessed November 10, 2021).
32. Toumba J, Lygidakis N, Oulis C, Parnell C, Espelid I, Poulsen S, et al. Guidelines on the use of fluoride in children: an EAPD policy document. Eur Arch Paediat Dent. (2009) 10:129–35. doi: 10.1007/BF03262673
33. Srivastava S, Flora SJS. Fluoride in drinking water and skeletal fluorosis: a review of the global impact. Curr Environ Health Rep . (2020) 7:140–6. doi: 10.1007/s40572-020-00270-9
34. Boivin G, Chapuy MC, Baud CA, Meunier PJ. Fluoride content in human iliac bone: results in controls, patients with fluorosis, and osteoporotic patients treated with fluoride. J Bone Miner Res . (1988) 3:497–502. doi: 10.1002/jbmr.5650030504
35. Seifo N, Robertson M, MacLean J, Blain K, Grosse S, Milne R, et al. The use of silver diamine fluoride (SDF) in dental practice. Br Dent J. (2020) 228:75–81. doi: 10.1038/s41415-020-1203-9
36. Leung BO, Jalilehvand F, Mah V, Parvez M, Wu Q. Silver(I) complex formation with cysteine, penicillamine, and glutathione. Inorg Chem. (2013) 52:4593–4602. doi: 10.1021/ic400192c
37. Wadhera A, Fung M. Systemic argyria associated with ingestion of colloidal silver. Dermatol Online J. (2005) 11:12. doi: 10.5070/D30832G6D3
38. Chen K-F, Milgrom P, Lin YS. Silver diamine fluoride in children using physiologically based PK modeling. J Dent Res. (2020) 99:907–913. doi: 10.1177/0022034520917368
39. Thornton-Evans G, Junger ML, Lin M, Wei L, Espinoza L, Beltran-Aguilar E. Use of toothpaste and toothbrushing patterns among children and adolescents — United States, 2013–2016. MMWR Morb Mortal Wkly Rep. (2019) 68:87–90. doi: 10.15585/mmwr.mm6804a3
40. Whitford GM. The Metabolism and Toxicity of Fluoride . Basel: Karger (1996).
41. Lin YS, Rothen ML, Milgrom P. Pharmacokinetics of 38% topical silver diamine fluoride in healthy adult volunteers. J Am Dent Assoc. (2019) 150:186–92. doi: 10.1016/j.adaj.2018.10.018
42. Milgrom P, Taves DM, Kim AS, Watson GE, Horst JA. Pharmacokinetics of fluoride in toddlers after application of 5% sodium fluoride dental varnish. Pediatrics. (2014) 134:870–4. doi: 10.1542/peds.2013-3501
43. World Health Organization. Executive Summary: The Selection and Use of Essential Medicines (2021): Report of the 23rd WHO Expert Committee on the Selection and Use of Essential Medicines. (2021). Available online at: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.01 (accessed January 20, 2022).
44. Augenstein WL, Spoerke DG, Kulig KW, Hall AH, Hall PK, Riggs BS, et al. Fluoride ingestion in children: a review of 87 cases. Pediatrics. (1991) 88:907–12. doi: 10.1542/peds.88.5.907
Keywords: fluoride, silver, silver diammine fluoride, monofluorophosphate, stannous fluoride, health and safety, toxicity, dental caries
Citation: Duffin S, Duffin M and Grootveld M (2022) Revisiting Fluoride in the Twenty-First Century: Safety and Efficacy Considerations. Front. Oral. Health 3:873157. doi: 10.3389/froh.2022.873157
Received: 10 February 2022; Accepted: 07 April 2022; Published: 04 July 2022.
Reviewed by:
Copyright © 2022 Duffin, Duffin and Grootveld. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martin Grootveld, mgrootveld@dmu.ac.uk
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Fluoride Exposure: Neurodevelopment and Cognition

Topic Overview
CASRN: 16984-48-8 Status: Evaluation completed
- Background Information
Since 1945, the use of fluoride has been a successful public health initiative for reducing dental cavities and improving general oral health of adults and children. There is a concern, however, that some pregnant women and children may be getting more fluoride than they need because they now get fluoride from many sources including treated public water, water-added foods and beverages, teas, toothpaste, floss, and mouthwash, and the combined total intake of fluoride may exceed safe amounts.
Therefore, the National Toxicology Program (NTP) conducted a systematic review of the published scientific literature on the association between fluoride exposure and neurodevelopment and cognition. The NTP released their findings in a State of the Science Monograph (available below under Documents). A corresponding meta-analysis on children’s IQ has been accepted by a scientific journal for publication later in 2024.
The NTP started this work in 2016. As with all research documents intended for publication, the NTP fluoride monograph and meta-analysis underwent rigorous scientific evaluation. The evaluation process has involved many steps. The draft fluoride monograph received critical feedback during peer-review by the National Academies of Science, Engineering and Medicine (NASEM), from other external experts, and from experts in several federal health agencies. After modifications were made, additional evaluation following a rigorous scientific framework was conducted by subject matter experts organized by the NTP Board of Scientific Counselors. This document is now complete and available for reference.
The monograph represents a thorough review of the data, and the various interpretations of the data, to accurately reflect what we know and where additional research is needed.
The NTP monograph concluded that higher levels of fluoride exposure, such as drinking water containing more than 1.5 milligrams of fluoride per liter, are associated with lower IQ in children. The NTP review was designed to evaluate total fluoride exposure from all sources and was not designed to evaluate the health effects of fluoridated drinking water alone. It is important to note, however, that there were insufficient data to determine if the low fluoride level of 0.7 mg/L currently recommended for U.S. community water supplies has a negative effect on children’s IQ.
The NTP uses 4 confidence levels - high, moderate, low, or very low - to characterize the strength of scientific evidence that associates a particular health outcome with an exposure. After evaluating studies published through October 2023, the NTP Monograph concluded there is moderate confidence in the scientific evidence that showed an association between higher levels of fluoride and lower IQ in children.
The determination about lower IQs in children was based primarily on epidemiology studies in non-U.S. countries such as Canada, China, India, Iran, Pakistan, and Mexico where some pregnant women, infants, and children received total fluoride exposure amounts higher than 1.5 mg fluoride/L of drinking water. The U.S. Public Health Service currently recommends 0.7 mg/L, and the World Health Organization has set a safe limit for fluoride in drinking water of 1.5 mg/L. The NTP found no evidence that fluoride exposure had adverse effects on adult cognition.
Application
Many substances are healthy and beneficial when taken in small doses but may cause harm at high doses. More research is needed to better understand if there are health risks associated with low fluoride exposures. This NTP monograph may provide important information to regulatory agencies that set standards for the safe use of fluoride. It does not, and was not intended to, assess the benefits of fluoride.
| Date | Document |
|---|---|
| Oct 07, 2015 | requesting information on nominated substances |
| Nov 19, 2015 | |
| Dec 02, 2015 | |
| Jul 01, 2016 | ( ) NTP (National Toxicology Program). 2016. Systematic literature review on the effects of fluoride on learning and memory in animal studies. NTP Research Report 1. Research Triangle Park, NC: National Toxicology Program. Research Report 1. |
| Jun 01, 2017 | |
| May 29, 2019 | |
| Sept 16, 2020 | |
| Sept 16, 2020 | |
| Mar 15, 2023 | |
| May 18, 2023 | |
| Aug 21, 2024 | - Final ( ) National Toxicology Program (NTP). 2024. NTP monograph on the state of the science concerning fluoride exposure and neurodevelopment and cognition: a systematic review. Research Triangle Park, NC: National Toxicology Program. NTP Monograph 08. |
| Aug 21, 2024 | |
| Aug 21, 2024 |
Meetings & Events
| Date | Event | Event Type | Materials | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| May 04, 2023 | Board of Scientific Counselors |
Board of Scientific Counselors Meeting Presentations May 4, 2023Presentation of the NTP BSC Working Group Report Oral Public Comments from Chris Neurath Oral Public Comments from David Kennedy Oral Public Comments from J. William Hirzy Oral Public Comments from Paul Connett Oral Public Comments from Bill Osmunson Oral Public Comments from Jack Kall Oral Public Comments from Howard Pollick Board of Scientific Counselors Meeting Videos May 4, 2023Some browsers may experience play back issues when accessing these videos. We are working to resolve this issue. Videos may take some minutes to display depending on the size of the video and your Internet connection. Captions are done in real-time so there may be misspellings. We cannot guarantee absolute accuracy in captioning and there may be delays in syncing captioning text with audio. If you have issues or would like an accurate version of certain sections of the videos, please let us know. Videos and Closed CaptioningMay 4, 2023, peer review of the revised ntp monograph on fluoride exposure and neurodevelopmental and cognitive health effects by the national academies of science, engineering, and medicine. Expert Panels - Other Panels Peer Review of the Revised NTP Monograph on Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects by the National Academies of Science, Engineering, and Medicine Final Documents October 19, 2020
Peer Review of the Draft NTP Monograph on Systematic Review of Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects by the National Academies of Science, Engineering, and Medicine
NTP Board of Scientific Counselors MeetingBoard of Scientific Counselors NTP Board of Scientific Counselors Meeting Meeting Materials December 1-2, 2015Supplemental materials for some events, meetings, and workshops prior to 2021 have been archived. These archived materials frequently include presentations, background materials, and public comments. Email us or use our contact form to request a list or copy of archived materials. Board of Scientific Counselors MeetingBoard of scientific counselors meeting final documents may 16, 2023. Transmittal Letter Final Version of the NTP Board of Scientific Counselors Working Group Report Federal Register Notices May 16, 2023
Board of Scientific Counselors Meeting Meeting Materials May 16, 2023Public comments.
Board of Scientific Counselors Meeting Presentations May 16, 2023Board of scientific counselors meeting videos may 16, 2023, may 16, 2023. Note on Accessibility : Persons with disabilities or using assistive technology may find some documents are not fully accessible. For assistance, email us or use our contact form and identify the documents/pages for which access is required. We will assist you in accessing the content of these files. NIEHS has helpful information on accessibility.
An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
 Save citation to fileEmail citation, add to collections.
Add to My BibliographyYour saved search, create a file for external citation management software, your rss feed, ntp research report on systematic literature review on the effects of fluoride on learning and memory in animal studies: research report 1 [internet].
Affiliation
Background: Previous systematic reviews of epidemiology studies have found support for a geographical association between high levels of naturally occurring fluoride in water (>1.5 ppm) and lower IQ in children. Most of the evidence from humans is from fluoride-endemic regions having higher background levels of fluoride compared to the fluoride concentrations historically used in community water fluoridation programs (0.7–1.2 ppm). Confidence in this body of evidence is limited, primarily due to poor reporting quality, lack of consideration of confounding (e.g., nutritional status, socioeconomic status, iodine deficiency), and concern for co-exposures to relatively high levels of other known neurotoxicants such as lead or arsenic. A systematic review of experimental animal studies could help in interpreting the human evidence. Objective: To investigate whether fluoride exposure has detrimental impacts on neurobehavior in laboratory animal studies, prioritizing assessment of learning and memory outcomes. Confidence in the body of evidence was assessed according to one of four statements: (1) High, (2) Moderate, (3) Low, or (4) Very Low/No Evidence Available. Methods: We included experimental animal studies that used mammalian species (whole organism) exposed during development or adulthood, which compared the effects of oral exposure to various fluoride concentrations to vehicle controls on neurobehavioral responses. The principal outcomes were learning and memory, but other neurobehavioral studies were included (e.g., anxiety, motor activity, aggression, sexual behavior). Studies assessing brain-related cellular, morphometric or histological endpoints were considered beyond the scope of this analysis. A literature search was performed up to January 14, 2016, using PubMed, BIOSIS, EMBASE, Scopus, Web of Science, PsycINFO, and several specialized databases. There were no date or language restrictions, and unpublished data and abstracts were excluded. Risk of bias was assessed regarding randomization, allocation concealment, blinding, exposure characterization, health outcome assessment, incomplete outcome data, selective outcome reporting, and other biases. Results: The database searches yielded 4,643 unique records and 13 records were identified from other sources. Of the 4,656 studies, we identified 68 studies using mice or rats and testing drinking water or dietary concentrations of 0.45 to 272 ppm fluoride (0.12 to 40 mg/kg-d). Most included studies were published after 2000. Forty-eight studies addressed learning and memory, 16 of which assessed exposure during development. Synthesis of results: Meta-analysis was not conducted due to the small number of studies that measured endpoints similarly based on study design, that is, dose levels, duration of treatment, lifestage at exposure, species, or differences in measurement of behavioral responses. Relatively few studies provided information on other sources of fluoride (e.g., diet, water source). Most studies were statistically underpowered to detect a <20% change from control groups for behavioral tests. Approximately 30% of the learning and memory studies were considered to have a very serious risk of bias and were excluded from the narrative analysis. Conclusions were reached based on an analysis of 32 studies. Results show low-to-moderate confidence for a pattern of findings suggestive of an effect on learning and memory based on developmental and adult exposure studies. The evidence is strongest (moderate level-of-evidence) in animals exposed as adults and weaker (low level-of-evidence) in animals exposed during development. Level-of-evidence conclusions were rated down due to concern for indirectness and risk of bias. The evidence was strongest and most abundant for adult exposure studies using the Morris water maze. In many cases, across the entire dose range tested, whether the effects were specifically related to learning and memory—versus a possible impact on motor or sensory function that could have impaired the ability of the animal to perform the learning and memory tests as measured—was not possible to discern. This was considered a form of indirectness. Additional studies are required to have higher confidence in the specificity of the responses as learning or memory impairments and in quantitative measures such as the effect sizes, point of departure, identification of no observed effect level or lowest observed effect level doses, or parameters for benchmark dose analysis. Based on control values (means and standard deviations/standard errors) and the number of animals per group, the studies appear statistically underpowered to detect a <10% or <20% change from controls for most behavioral endpoints. Conclusion: Very few studies assessed learning and memory effects in experimental animals (rats and mice) at exposure levels near 0.7 parts per million, the recommended level for community water fluoridation in the United States. At concentrations higher than 0.7 parts per million, this systematic review found a low to moderate level-of-evidence that suggests adverse effects on learning and memory in animal exposed to fluoride. The evidence is strongest (moderate level-of-evidence) in animals exposed as adults and weaker (low level-of-evidence) in animals exposed during development. Confidence in these findings was reduced primarily based on potential confounding of the learning and memory assessments by deficits in motor function or fear and risk of bias limitations. Additional research is needed, in particular to address potential effects on learning and memory following exposure during development to fluoride at levels nearer to 0.7 parts per million. NTP is conducting laboratory studies in rodents to fill data gaps identified by this systematic review of the animal studies. The findings from those studies will be included in a future systematic review to evaluate potential neurobehavioral effects from exposure to fluoride during development with consideration of human, experimental animal and mechanistic data. PubMed Disclaimer
Similar articles
Publication types
Related information
LinkOut - more resourcesFull text sources.

NCBI Literature Resources MeSH PMC Bookshelf Disclaimer The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited. Quarterly Journal of the International Society for Fluoride Research Inc. (ISFR)Conferences. the website for the 36th isfr conference in new delhi 12 to 14 november 2024 is now open.
Epublications ahead of print. These papers will be published in due course in Fluoride which will continue to be published quarterly. Papers in Fluoride will be given a year of publication, volume, and issue number but not new page numbers. They may be cited as e.g. Fluoride 2024;57(1): e254. Epub 2023 November 18. Papers should now be submitted using the template below, using only the portrait orientation and not the landscape orientation, and will generally be published as Epublications soon after acceptance.
Issues published in 2024. With the rolling publication template system now in use papers are published as Epublications within a few days of acceptance and then placed in an issue at a later date with the year of publication, volume number, issue number, Epub number and date of Epublication.
Back issues
Searching all the issues of Fluoride since 1968Information for authors and about the isfr, use of template for submitting papers to fluoride. This template in Word should be used by authors to submit papers to Fluoride from September 1, 2023. Only the portrait page orientation should be used. The landscape orientation should not be used because of the difficulites this creates in printing Fluoride which has a portrait orientaiton. Please add square brackets to the reference numbers in the reference section e.g. [1] rather than 1, to meet the requirements of CNKI, a Chinese abstractin g service which now covers Fluoride . From September 1, 2023 the practice of sending 5 free offprints was discontinued. Copies of papers may be downloaded from the website.Word files may open differently on different computers upsetting the placement of figures and you are welcome to send both a Word file and a pdf file of a paper. The pdf files open consistently.
Where to send papers, prepared using the template, for consideration of publication in FluorideAuthors should send papers to the nearest regional editor. e.g. authors in the USA and Canada should send papers to the Regional Editor for Latin America, Central America and Cuba; an Author is Australia should send it to the Regional Editor for India; an author in the UK should send it to the Regional Editor for Eastern Europe. The regional editors are: Regional Editor for Africa:
Regional Editor for Eastern Europe:
Regional Editors for India, Bangladesh, Bhutan, Indonesia, Maldives, Myanmar, Nepal, and Sri Lanka:
Regional Editor for Latin America, including Mexico, Central America, and Cuba:
Regional Editor for the Middle East:
Regional Editors for Pakistan and Afghanistan:
Regional Editors for People's Republic of China
Regional Editor for Asia in developmental biology, reproduction, embryology, and endocrinologyGeneral information on the isfr, applying for membership of the isfr, isfr conferences, subscription to fluoride in hard copy (online access if free) and manuscript submission.
Citation of articles from Fluoride and membership of the ISFR Advisory and Editorial Boards
Pro Forma Invoice information
Some information on chronic fluoride toxicity including the books Fluoridation the great dilemma and Fluoride fatigue , the thesis Education and fluoridation in New Zealand: an historical study and some information on the history of the ISFR
Impact factor
Contact information for problems
Copyright statement© Owned and published by the ISFR. Copyright 2024. All rights reserved. Aug 30 1452 Welcome to FAN’s new website! If you encounter any technical issues, email us the specifics so we can resolve them. National Research Council (2006)An overview of the NRC's groundbreaking report on fluoride toxicity, including excerpts of its key findings and recommendations, statements from the panelists, and a discussion of its relevance to water fluoridation and sulfuryl fluoride. NRC’s FindingsThe National Research Council’s report concluded that EPA’s safe drinking water standard (4 ppm) for fluoride is unsafe and “should be lowered.” The NRC based this conclusion on its finding that EPA’s 4 ppm standard places a person at increased risk for both tooth damage ( severe dental fluorosis ) and bone damage ( bone fracture ). While most of the press coverage of the NRC report focused on NRC’s concerns with teeth and bone, there are many other serious concerns expressed in the NRC report. As evident in the following excerpts, the NRC report lends credence to fluoride’s ability to affect a wide range of systems in the body, particularly the brain and endocrine system. These concerns are further amplified in the NRC’s research recommendations . FLUORIDE’S EFFECTS ON THE BRAIN: To read the NRC’s complete discussion of fluoride’s effect on the brain, click here. “On the basis of information largely derived from histological, chemical, and molecular studies, it is apparent that fluorides have the ability to interfere with the functions of the brain and the body by direct and indirect means.” p.222 “A few epidemiologic studies of Chinese populations have reported IQ deficits in children exposed to fluoride at 2.5 to 4 mg/L in drinking water. Although the studies lacked sufficient detail for the committee to fully assess their quality and relevance to U.S. populations, the consistency of the results appears significant enough to warrant additional research on the effects of fluoride on intelligence.” p.8 “histopathological changes similar to those traditionally associated with Alzheimer’s disease in people have been seen in rats chronically exposed to AlF.” p.212 “Fluorides also increase the production of free radicals in the brain through several different biological pathways. These changes have a bearing on the possibility that fluorides act to increase the risk of developing Alzheimer’s disease.” p.222 “More research is needed to clarify fluoride’s biochemical effects on the brain.” p.222 “The possibility has been raised by the studies conducted in China that fluoride can lower intellectual abilities. Thus, studies of populations exposed to different concentrations of fluoride in drinking water should include measurements of reasoning ability, problem solving, IQ, and short- and long-term memory.” p.223 “Studies of populations exposed to different concentrations of fluoride should be undertaken to evaluate neurochemical changes that may be associated with dementia. Consideration should be given to assessing effects from chronic exposure, effects that might be delayed or occur late-in-life, and individual susceptibility.” p.223 “Additional animal studies designed to evaluate reasoning are needed.” p.223 FLUORIDE’S EFFECTS ON THE ENDOCRINE SYSTEM: “In summary, evidence of several types indicates that fluoride affects normal endocrine function or response; the effects of the fluoride-induced changes vary in degree and kind in different individuals. Fluoride is therefore an endocrine disruptor in the broad sense of altering normal endocrine function or response, although probably not in the sense of mimicking a normal hormone. The mechanisms of action remain to be worked out and appear to include both direct and indirect mechanisms, for example, direct stimulation or inhibition of hormone secretion by interference with second messenger function, indirect stimulation or inhibition of hormone secretion by effects on things such as calcium balance, and inhibition of peripheral enzymes that are necessary for activation of the normal hormone.” p.266 “Some of these [endocrine] effects are associated with fluoride intake that is achievable at fluoride concentrations in drinking water of 4 mg/L or less, especially for young children or for individuals with high water intake. Many of the effects could be considered subclinical effects, meaning that they are not adverse health effects. However, recent work on borderline hormonal imbalances and endocrine-disrupting chemicals indicated that adverse health effects, or increased risks for developing adverse effects, might be associated with seemingly mild imbalances or perturbations in hormone concentrations. Further research is needed to explore these possibilities.” p.8 “Further effort is necessary to characterize the direct and indirect mechanisms of fluoride’s action on the endocrine system and the factors that determine the response, if any, in a given individual.” p.266 “The effects of fluoride on various aspects of endocrine function should be examined further, particularly with respect to a possible role in the development of several diseases or mental states in the United States.” p.267 FLUORIDE’S EFFECTS ON THE THYROID: To read the NRC’s complete discussion of fluoride’s effect on the thyroid, click here. “several lines of information indicate an effect of fluoride exposure on thyroid function.” p.234 “it is difficult to predict exactly what effects on thyroid function are likely at what concentration of fluoride exposure and under what circumstances.” p.234-5 “Fluoride exposure in humans is associated with elevated TSH concentrations, increased goiter prevalence, and altered T4 and T3 concentrations; similar effects on T4 and T3 are reported in experimental animals..” p.262 “In humans, effects on thyroid function were associated with fluoride exposures of 0.05-0.13 mg/kg/day when iodine intake was adequate and 0.01-0.03 mg/kg/day when iodine intake was inadequate.” p.262-3 “The recent decline in iodine intake in the United States (CDC 2002d; Larsen et al. 2002) could contribute to increased toxicity of fluoride for some individuals.” p.263 “Intake of nutrients such as calcium and iodine often is not reported in studies of fluoride effects. The effects of fluoride on thyroid function, for instance, might depend on whether iodine intake is low, adequate, or high, or whether dietary selenium is adequate.” p.265 FLUORidE’S EFFECTS ON THE PINEAL GLAND: “The single animal study of pineal function indicates that fluoride exposure results in altered melatonin production and altered timing of sexual maturity (Table 8-1). Whether fluoride affects pineal function in humans remains to be demonstrated. The two studies of menarcheal age in humans show the possibility of earlier menarche in some individuals exposed to fluoride, but no definitive statement can be made. Recent information on the role of the pineal organ in humans suggests that any agent that affects pineal function could affect human health in a variety of ways, including effects on sexual maturation, calcium metabolism, parathyroid function, postmenopausal osteoporosis, cancer, and psychiatric disease.” p.264 FLUORIDE’S EFFECTS ON INSULIN SECRETION/DIABETES: “The conclusion from the available studies is that sufficient fluoride exposure appears to bring about increases in blood glucose or impaired glucose tolerance in some individuals and to increase the severity of some types of diabetes. In general, impaired glucose metabolism appears to be associated with serum or plasma fluoride concentrations of about 0.1 mg/L or greater in both animals and humans. In addition, diabetic individuals will often have higher than normal water intake, and consequently, will have higher than normal fluoride intake for a given concentration of fluoride in drinking water. An estimated 16-20 million people in the U.S. have diabetes mellitus; therefore, any role of fluoride exposure in the development of impaired glucose metabolism or diabetes is potentially significant.” p.260 FLUORIDE’S EFFECTS ON THE IMMUNE SYSTEM: “Nevertheless, patients who live in either an artificially fluoridated community or a community where the drinking water naturally contains fluoride at 4 mg/L have all accumulated fluoride in their skeletal systems and potentially have very high fluoride concentrations in their bones. The bone marrow is where immune cells develop and that could affect humoral immunity and the production of antibodies to foreign chemicals.” p.293-4 “There is no question that fluoride can affect the cells involved in providing immune responses. The question is what proportion, if any, of the population consuming drinking water containing fluoride at 4.0 mg/L on a regular basis will have their immune systems compromised? Not a single epidemiologic study has investigated whether fluoride in the drinking water at 4 mg/L is associated with changes in immune function. Nor has any study examined whether a person with an immunodeficiency disease can tolerate fluoride ingestion from drinking water.” p.295 “bone concentrates fluoride and the blood-borne progenitors could be exposed to exceptionally high fluoride concentrations. Thus, more research needs to be carried out before one can state that drinking water containing fluoride at 4 mg/L has no effect on the immune system.” p.295 “it is important to consider subpopulations that accumulate large concentrations of fluoride in their bones (e.g., renal patients). When bone turnover occurs, the potential exists for immune system cells and stem cells to be exposed to concentrations of fluoride in the interstitial fluids of bone that are higher than would be found in serum. From an immunologic standpoint, individuals who are immunocompromised (e.g., AIDS, transplant, and bone-marrow-replacement patients) could be at greater risk of the immunologic effects of fluoride.” p.302 “Within 250 µm of a site of resorption, it is possible to encounter progenitor cells that give rise to bone, blood, and fat. Thus, one must assume that these cells would be exposed to high concentrations of fluoride. At this time, it is not possible to predict what effect this exposure would have on the functioning of skeletal elements, hematopoiesis, and adipose formation.” p.142 “It is paramount that careful biochemical studies be conducted to determine what fluoride concentrations occur in the bone and surrounding interstitial fluids from exposure to fluoride in drinking water at up to 4 mg/L, because bone marrow is the source of the progenitors that produce the immune system cells.” p.303 “In addition, studies could be conducted to determine what percentage of immunocompromised subjects have adverse reactions when exposed to fluoride in the range of 1-4 mg/L in drinking water.” p.303 FLUORIDE’S INTERACTIVE/SYNERGISTIC EFFECTS (w/ IODINE, ALUMINUM, ETC): “Better characterization of exposure to fluoride is needed in epidemiology studies investigating potential effects. Important exposure aspects of such studies would include the following: collecting data on general dietary status and dietary factors that could influence exposure or effects, such as calcium, iodine, and aluminum intakes.” p.88 “Available information now indicates a role for aluminum in the interaction of fluoride on the second messenger system; thus, differences in aluminum exposure might explain some of the differences in response to fluoride exposures among individuals and populations.” p.265 “With the increasing prevalence of acid rain, metal ions such as aluminum become more soluble and enter our day-to-day environment; the opportunity for bioactive forms of AlF to exist has increased in the past 100 years. Human exposure to aluminofluorides can occur when a person ingests both a fluoride source (e.g., fluoride in drinking water) and an aluminum source; sources of human exposure to aluminum include drinking water, tea, food residues, infant formula, aluminum-containing antacids or medications, deodorants, cosmetics, and glassware.” p.51 “Further research should include characterization of both the exposure conditions and the physiological conditions (for fluoride and for aluminum or beryllium) under which aluminofluoride and beryllofluoride complexes can be expected to occur in humans as well as the biological effects that could result.” p.52 “Another possible explanation for increased blood lead concentrations which has not been examined is the effect of fluoride intake on calcium metabolism; a review by Goyer (1995) indicates that higher blood and tissue concentrations of lead occur when the diet is low in calcium. Increased fluoride exposure appears to increase the dietary requirement for calcium (see Chapter 8); in addition, the substitution of tap-water based beverages (e.g., soft drinks or reconstituted juices) for dairy products would result in both increased fluoride intake and decreased calcium intake.” p.52 “[G]iven the expected presence of fluoride ion (from any fluoridation source) and silica (native to the water) in any fluoridated tap water, it would be useful to examine what happens when that tap water is used to make acidic beverages or products (commercially or in homes), especially fruit juice from concentrate, tea, and soft drinks. Although neither Urbansky (2002) nor Morris (2004) discusses such beverages, both indicate that at pH < 5, SiF6 2- would be present, so it seems reasonable to expect that some SiF6 2- would be present in acidic beverages but not in the tap water used to prepare the beverages. Consumption rates of these beverages are high for many people, and therefore the possibility of biological effects of SiF62-, as opposed to free fluoride ion, should be examined.” p.53 FLUORIDE’S EFFECTS ON THE REPRODUCTIVE SYSTEM: “A few human studies suggested that high concentrations of fluoride exposure might be associated with alterations in reproductive hormones, effects on fertility, and developmental outcomes, but design limitations make those studies insufficient for risk evaluation.” p.8 “the relationship between fertility and fluoride requires additional study.” p.193 FLUORIDE & DOWN’S SYNDROME: “The possible association of cytogenetic effects with fluoride exposure suggests that Down’s syndrome is a biologically plausible outcome of exposure.” p.197 “A reanalysis of data on Down’s syndrome and fluoride by Takahashi (1998) suggested a possible association in children born to young mothers. A case-control study of the incidence of Down’s syndrome in young women and fluoride exposure would be useful for addressing that issue. However, it may be particularly difficult to study the incidence of Down’s syndrome today given increased fetal genetic testing and concerns with confidentiality.” p.204 FLUORIDE’S EFFECTS ON THE GASTROINTESTINAL SYSTEM: “The numerous fluoridation studies in the past failed to rigorously test for changes in GI symptoms and there are no studies on drinking water containing fluoride at 4 mg/L in which GI symptoms were carefully documented.” p.269 “GI effects appear to have been rarely evaluated in the fluoride supplement studies that followed the early ones in the 1950s and 1960s.” p.274 “The table suggests that fluoride at 4 mg/L in the drinking water results in approximately 1% of the population experiencing GI symptoms.” p.274 “Whether fluoride activates G proteins in the gut epithelium at very low doses (e.g., from fluoridated water at 4.0 mg/L) and has significant effects on the gut cell chemistry must be examined in biochemical studies.” p.280 “There are a few case reports of GI upset in subjects exposed to drinking water fluoridated at 1 mg/L. Those effects were observed in only a small number of cases, which suggest hypersensitivity. However, the available data are not robust enough to determine whether that is the case.” p.295 “Studies are needed to evaluate gastric responses to fluoride from natural sources at concentrations up to 4 mg/L and from artificial sources.” p.302 FLUORIDE’S EFFECTS ON THE LIVER: “It is possible that a lifetime ingestion of 5-10 mg/day from drinking water containing 4 mg/L might turn out to have long-term effects on the liver, and this should be investigated in future epidemiologic studies.” p.293 “The effect of low doses of fluoride on kidney and liver enzyme functions in humans needs to be carefully documented in communities exposed to different concentrations of fluoride in drinking water.” p.303 FLUORIDE’S EFFECTS ON THE KIDNEY: “Human kidneys… concentrate fluoride as much as 50-fold from plasma to urine. Portions of the renal system may therefore be at higher risk of fluoride toxicity than most soft tissues.” p.280 “Early water fluoridation studies did not carefully assess changes in renal function.” p.280 “future studies should be directed toward determining whether kidney stone formation is the most sensitive end point on which to base the MCLG.” p.281 “On the basis of studies carried out on people living in regions where there is endemic fluorosis, ingestion of fluoride at 12 mg per day would increase the risk for some people to develop adverse renal effects.” p.281 FLUORIDE & CAncER: “Fluoride appears to have the potential to initiate or promote cancers, particularly of the bone, but the evidence to date is tentative and mixed (Tables 10-4 and 10-5). As noted above, osteosarcoma is of particular concern as a potential effect of fluoride because of (1) fluoride deposition in bone, (2) the mitogenic effect of fluoride on bone cells, (3) animal results described above, and (4) pre-1993 publication of some positive, as well as negative, epidemiologic reports on associations of fluoride exposure with osteosarcoma risk.“ p.336 “Because fluoride stimulates osteoblast proliferation, there is a theoretical risk that it might induce a malignant change in the expanding cell population. This has raised concerns that fluoride exposure might be an independent risk factor for new osteosarcomas.” p.134 “Osteosarcoma presents the greatest a priori plausibility as a potential cancer target site because of fluoride’s deposition in bone, the NTP animal study findings of borderline increased osteosarcomas in male rats, and the known mitogenic effect of fluoride on bone cells in culture (see Chapter 5). Principles of cell biology indicate that stimuli for rapid cell division increase the risks for some of the dividing cells to become malignant, either by inducing random transforming events or by unmasking malignant cells that previously were in nondividing states.” p.322 “Further research on a possible effect of fluoride on bladder cancer risk should be conducted.” p.338 Welcome to the soft launch of the new FAN website! In the coming weeks the site will be updated to restore all old links, content, and functionality. We appreciate your patience.
The long battle over fluoride comes to a headBy Michael Schulson/Undark Posted on Mar 11, 2024 8:15 AM EDT This article was originally featured on Undark . In a wood-paneled federal courtroom in downtown San Francisco, experts and litigators gathered last month for hearings on an old question: Is it safe to add fluoride to drinking water? Around 210 million Americans today have access to artificially fluoridated tap water, and the policy has had a pronounced effect on oral health by reducing tooth decay. It’s widely hailed as a public health success story. In the current lawsuit, plaintiffs are taking a long-standing and, to many experts, provocative stance, arguing that water fluoridation poses a risk to human health, and that the Environmental Protection Agency is obligated to address the issue. The outcome of the case could effectively end water fluoridation in United States. A ruling from Judge Edward M. Chen is expected soon. In some circles, just entertaining questions about fluoride safety is synonymous with tinfoil-hat conspiracy theorizing. After all, some anti-fluoride activists have, over the years, made wild claims—for example, that fluoride is a form of communist mind control—that don’t have any evidence to back them up. The lawsuit, though, has put a consequential spotlight on a real scientific debate that has been roiling public health researchers for the past several years. Today, there is a modest body of evidence suggesting that fluoride, at doses considerably higher than what’s generally in the water, might be bad for human brains, in particular developing fetal brains. A few studies also suggest possible harms from the levels that many municipalities in the U.S. currently add to their drinking water. And most scientists involved agree that the uncertainty warrants more research. What to make of that uncertainty—and how it should be communicated to the public—has divided researchers. Some experts, especially among dentists, think the evidence is far too weak to be making policy prescriptions. “The best available evidence just doesn’t suggest that this is a real association at the levels to which people are exposed to fluoride in fluoridated water,” said Scott Tomar, a dentist and oral health epidemiologist at the University of Illinois Chicago. But some current and former federal scientists, as well as academic researchers in toxicology and environmental health, say there’s reason for concern. Some also suggest that something else is going on: Faced with uncomfortable data, they say, water fluoridation proponents have attacked and obstructed fluoride research. And rather than allowing the scientific debate to flourish in the open, dental groups and some public health experts have targeted researchers who study fluoride and brain development, in a pattern that some characterized as suppressing important science. “I see this as an infringement of scientific integrity, that the scientists have been prevented from getting their information out.” Central to the debate is an unpublished government report, produced by a little-known federal program, that has been subject to years of bureaucratic wrangling. In fact, that wrangling contributed to delaying the EPA lawsuit for more than two years as the judge awaited the report’s publication, before finally settling on the use of draft documents. They are now a central piece of evidence in the case. Fluoride safety is exactly the kind of issue the National Toxicology Program was designed to tackle: It’s an interagency program, housed at the National Institutes of Health, that investigates whether things like the “ forever chemicals ” PFAS and cellphone radiation are harmful to people’s health. In 2016, the NTP asked its scientists to gather all the existing scientific research on fluoride, analyze the data, and say something authoritative about whether fluoride might be damaging to human brains. After years of research and peer review, a draft of the report concluded there might be reason for concern, mostly at levels of fluoride exposure higher than most, but not all, Americans experience. In April 2022, the NTP group was ready to publish its findings. “That’s when the wheels fell off,” said Brian Berridge, a former pharmaceutical industry scientist who led NTP’s day-to-day operations at the time. Dental organizations obtained internal drafts of the report. They then began to lobby federal officials, according to documents obtained via public records requests by advocates opposed to water fluoridation. Officials from other agencies, including the Food and Drug Administration and the Centers for Disease Control and Prevention, registered concerns. The report was soon tracked into yet another round of review, blindsiding scientists who thought it was done. Berridge grew frustrated. “After 17 years in the industry, I’ve seen efforts to modify messages to fit commercial interests,” he wrote in an email to NIH colleagues that May. “I wasn’t party to that there, and I’m not game to do that here.” Today, nearly two years after NTP scientists were prepared to tell the public that pregnant women should monitor their fluoride intake, and that too much fluoride may “negatively affect children’s cognition and neurodevelopment,” the project remains in a kind of bureaucratic limbo. Berridge retired from the agency in the spring of 2023, upset by the handling of the fluoride report. “That’s not the way I want to do science,” he said. “So I decided to do something different.” Fluoride strengthens teeth because teeth are like living rocks: tissue sheathed in a mesh of crystals called enamel. Unlike bone, which grows and mends itself over a person’s lifetime, teeth don’t self-repair. When fluoride washes over tooth enamel, in a smear of toothpaste or a swish of water, some of it can be incorporated into those crystals, helping to repair and strengthen the tooth. The process helps keep damage and decay at bay. The stuff is found nearly everywhere: in the air and in the dirt; in bottles of soda and in tea leaves. A typical cup of black tea contains fluoride at a concentration of 2.5 milligrams per liter. A liter of ocean water contains around 1.2 mg of fluoride. In some places, abundant fluoride leaches from soil and rock into the local water supply. A liter of tap water in parts of Cypress, Texas, for example, contains 3.81 mg of fluoride. Meanwhile, in Portland, Oregon, the number is closer to zero. Researchers in the early 20th century noticed that people living in areas with high levels of fluoride in the drinking water had fewer cavities, and by the 1940s, a campaign was underway to add fluoride to municipal water supplies—today generally at a concentration of 0.7 mg/L. Almost immediately, some communities objected to having a chemical added to the water supply, even if it often occurred naturally. Portland, for example, has long resisted fluoridation. One of the very first U.S. towns to add fluoride to its water supply, Stevens Point, Wisconsin, did so in secret, before a planned public referendum, fueling wider opposition to the practice, according to a 1985 paper by the historian Donald R. McNeil. Over the years, the policy came to be associated with broader suspicions about government and public health authority. “The fluoridation question is almost tailor-made for endless controversy in a free-wheeling democratic society,” McNeil wrote, adding that fluoridation’s opponents included “not only the fanatics, the fearful, and the vendors of snake oil, but also a goodly proportion of those Americans who simply distrust authority, government, science.” More recently, the anti-vaccination activist and presidential candidate Robert F. Kennedy Jr. has promised to halt water fluoridation if he’s elected to the White House. There’s extensive evidence that fluoridation dramatically improved dental health. In 1999, the CDC named water fluoridation as one of the 20th century’s 10 greatest public health achievements, alongside family planning and vaccination. But since at least the 1980s, there have also been scientists—some working within the federal government—who worry that ingesting fluoride could have toxic effects. Those concerns were bolstered in the 1990s and 2000s by research coming out of China. In 1991 a team of Chinese disease researchers published a report from Biji village, in the landlocked Shanxi Province of northern China. At the time, the researchers reported, the drinking water in the village had unusually high fluoride levels of 4.55 mg/L. They administered IQ tests to 320 children there, and then compared the scores to those of children in a nearby village, Jiaobei, where fluoride levels were below 1 mg/L. The children in Jiaobei, they found, had significantly higher IQs. In the next few years, other researchers in China repeated that basic setup: high fluoride village, low fluoride village, cognitive tests. Many scientists today say those and other studies were poorly done, and that there are lots of things besides fluoride that could be affecting any reported differences in IQ. But the consistency of the results raised concerns: Again and again, the research found an association between higher fluoride exposure and lower IQ. In 2002, the EPA asked a panel of experts to review the evidence on fluoride safety. Based on the data from China, as well as studies conducted in lab rats, the panel determined that there was reason to pay attention. “More research is needed to clarify the effect of fluoride on brain chemistry and function,” they wrote in a 2006 report. It was unclear, the EPA advisers noted, whether the China data was relevant to most U.S. communities. The dose makes the poison, toxicologists say, and the study subjects in China were generally drinking water with 2.5 mg/L or more of fluoride, well above the recommended levels for U.S. tap water. Still, there are signs that some federal scientists felt concern. In a 2015 report , the U.S. Public Health Service amended its recommended level of fluoride in U.S. public water supplies, from a range of .7 to 1.2 mg/L to a standard of .7 mg/L. The stated reason was to reduce the unsightly tooth mottling that can occur from prolonged fluoride exposure. But a draft of the report, circulated among federal officials in 2014 and obtained by Undark, suggests that concerns about the possibility of neurotoxic effects had also played a role. “While additional research may address identified gaps in knowledge,” the draft said, “HHS seeks to protect health by lowering the recommended fluoride concentration.” When the report was published the next year, that paragraph had been removed. Some scientists did answer the call for more research on fluoride and brain development. Among them was Christine Till, a neuropsychologist at York University in Canada. Till was a newly tenured professor in 2016, studying the impact of chemical exposures, when she received her first grant to look at possible links between fluoride and brain development. A colleague had suggested studying the Maternal-Infant Research on Environmental Chemicals cohort, or MIREC, in Canada. Starting in 2008, researchers had collected urine and other samples from pregnant women. They had also asked the women lots of questions about their lifestyle and consumption habits. After the babies were born, and as the children aged, the scientists then tested many of the children for all sorts of things. The goal was to create a dataset scientists could use to look for associations: for example, if exposure to a certain chemical in the womb was connected with lowered IQ scores years later. Till and several colleagues successfully got permission from MIREC to analyze the urine of those women, measuring the amount of fluoride in each sample. Her team also reviewed women’s self-reported consumption patterns, to estimate how much fluoride they were taking in from tap water and other sources during their pregnancies. And they looked at the IQ scores of the children when they were 3 or 4 years old, to see if there was some kind of link between fluoride intake during pregnancy and cognitive performance. “The fluoridation question is almost tailor-made for endless controversy in a free-wheeling democratic society.” Their team included experts in environmental health and epidemiology, as well as a dental public health expert, E. Angeles Martinez Mier, a professor at the Indiana University School of Dentistry who has served on the American Dental Association’s National Fluoridation Advisory Committee. “I really was expecting not to find anything,” said Rivka Green, a lead researcher on the MIREC study who undertook the work as one of Till’s graduate students. Some of Green’s relatives are dentists, and they made fun of her for even considering the topic. She had no particular concern about fluoride, she recalled: “Everyone says it’s safe. Let’s show it safe. And that’s it. That would be great.” One day in 2017, Green, who was pregnant and driving home from an appointment with her obstetrician, got a call from Till. The statistician on their team had just run the numbers, Till told her. And something had shown up in the data—something significant. “There’s a finding,” Till told Green. There seemed to be some association in the data between higher fluoride exposure and lower IQ. In 2019, the team published their results in JAMA Pediatrics, a prestigious journal. “The decision to publish this article was not easy,” the journal editor, pediatrics researcher Dmitri Christakis, wrote in a brief note accompanying the paper. “Given the nature of the findings and their potential implications, we subjected it to additional scrutiny.” Till, Green, and their colleagues had found that women with higher self-reported fluoride exposures had, on average, children with IQs that were around 3 points lower. And higher urinary fluoride measures during pregnancy were associated with lower levels of IQ in boys, but not girls. That kind of change is small enough that it could have gone unnoticed, according to environmental health experts. But a drop of three IQ points still could have an effect. “That is the average of some people who will lose six points of IQ. And some people will only lose one or two,” said Howard Hu, a physician and epidemiologist at the University of Southern California. That kind of difference, he said, is comparable to the effect that leaded gasoline had on IQ—before its use was banned by Congress. “The effect of fluoride, from what we can see, is not that different from the effect of lead, when we look at the actual magnitude of the impact on IQ,” Hu said. Was the finding true? The study was a kind of observational study, meaning it could show a correlation between fluoride levels in the urine and slightly lower IQ, but not prove that fluoride ingestion caused the decline. Such studies are widely used to research environmental toxins, including lead. But in related fields that search for links between diet and certain outcomes—most notably nutritional epidemiology —such studies can be famously finicky, giving mixed results. And experts were quick to raise a host of pointed questions about Till and her team’s paper: How reliable were IQ tests of 3 and 4-year-olds? Could the findings be biased by differences among the people administering the IQ tests? Why did the IQ drop sometimes show up in boys but not girls? And could a few urine samples—or, for that matter, self-reports on beverage consumption—actually provide a good measure of how much fluoride makes it to a developing fetus? (Some experts say such data cannot show such a connection; others point to research suggesting that it can, including a 2020 study from scientists at the University of California San Francisco that found a link between urinary fluoride levels and levels of fluoride in amniotic fluid.) One other issue: If fluoride did affect the brain, nobody really knew how. In other words, there was no clear mechanism by which this one chemical was affecting brain development, although Till and others have proposed that an effect on thyroid function could be one mechanism behind it. “Everyone says it’s safe. Let’s show it safe. And that’s it. That would be great.” Still, some experts who were not involved in the study told Undark it was a strong piece of research. The MIREC research was some “of the very best, actually, in the field,” said Akhgar Ghassabian, an environmental epidemiologist at New York University. “It’s one study. It’s a good study. And I would say the results are relevant,” said David Eaton, an emeritus professor at the University of Washington and a past president of the Society of Toxicology. “But it’s really hard to know whether the magnitude of the effect and the reproducibility of that effect is the end of the story.” In a recent Zoom conversation, Green acknowledged that the study had limitations. But, she said, that was true of any study. “At first I was, you know, maybe this is just a standalone, it’s a fluke—which happens,” she said. “We know that happens. And that’s why we don’t rely on one study.” The NTP process is built, in part, on the insight that no single study is definitive, especially on complicated questions about environmental hazards. Instead, the goal is to do a methodical review of every single study published on a given question, and then look for patterns in that entire body of evidence . John Bucher helped pioneer those methods at NTP. The soft-spoken toxicologist joined the program in the 1980s, and eventually became its associate director in 2007. In retirement, Bucher still works on some projects for NTP, and he’s one of the lead authors of the fluoride report. In a series of conversations this winter, from his home in the forested piedmont of central North Carolina, Bucher reflected on the years he and his colleagues had spent reviewing the body of literature on fluoride—including research like the Shanxi study, as well as the work of Till and her colleagues. Compared to scientific research on other hazardous substances, he said, the fluoride literature shows a fairly clear pattern. “My impression is that the findings are generally more consistent in direction of effect,” he said. “That is, they tend to show deficiencies, at least in IQ.” “As the literature continued to accumulate we were more and more convinced that there were no single flaws that could explain the consistency in the findings.” A similar study to Till and Green’s paper, conducted in Mexico, also found an association between higher levels of fluoride in pregnant women’s urine and lower IQ. Meanwhile, recent studies on mothers and their children in Spain and Denmark, using similar methods, did not find any clear negative effects from fluoride. (Several researchers have questioned the Spanish result, which showed that higher fluoride levels increased boys’ IQ scores by as much as 15 points.) In the most recent publicly available draft, the NTP report identifies 19 studies on fluoride and children’s IQ that it rates as high-quality. Of those, 18 find some adverse effect from fluoride. Of the 53 lower-quality studies reviewed by Bucher and his colleagues, 46 suggest some negative effect from fluoride on IQ. “As the literature continued to accumulate,” Bucher said, “we were more and more convinced that there were no single flaws that could explain the consistency in the findings.” Most of those studies look at fluoride exposures higher than 1.5 mg/L—in other words, more than double the levels founds in most Americans’ drinking water. Bucher stressed that the report is not—and was never intended to be—an evaluation of the safety of adding fluoride to water. “We don’t have enough data to make any statement with any certainty about it at the lower levels,” he said. Still, even the findings at higher levels of fluoride may be relevant to some Americans. Individual fluoride exposure can vary a lot, depending on what a person drinks. And according to one recent estimate , more than 2.9 million Americans are served by water utilities that deliver tap water with levels of fluoride at or above 1.5 mg/L. According to CDC data , that includes utilities in Troy, Missouri (12,116 people served; 2.31 mg/L); Seminole, Texas (8,549 people served; 4.40 mg/L); and Abercrombie, North Dakota (258 people served; 2.29 mg/L). Such communities “are clearly in the range that we would predict would be—we would say they would be presumed neurotoxicants,” said Bucher. By April 2022, the NTP report was poised to be published. It had, by that point, undergone peer review from five external experts, and been subjected to two rounds of review by a National Academies of Sciences, Engineering, and Medicine panel. In the second round, reviewers mostly took issue with some of the report’s language, rather than the underlying science, and urged the NTP to make clearer that “little or no conclusive information can be garnered” from the report “about the effects of fluoride at low exposure concentrations.” “Overall, I feel that they have been responsive to many comments,” said Ghassabian, the NYU professor, who served on the NASEM committee. In the spring of 2022, the NTP notified other agencies that the report was coming. Soon after, some officials expressed concerns about the way the science was being communicated, seemingly worried that it could undermine community water fluoridation programs. At the same time, dental organizations had obtained the document and were raising concerns with officials at the CDC, according to emails obtained via public records requests and shared with Undark. The report looked to many dental experts like yet another assault on a public health program. According to emails and public statements from around the time, leaders in the field saw the report as issuing alarming conclusions, with too little context, based on evidence that was, at best, highly tentative. They worried that NTP had overstated the quality of some fluoride studies. “We don’t have enough data to make any statement with any certainty about it at the lower levels.” According to the internal emails, the report received scrutiny from top government officials, including the NIH’s acting principal deputy director at the time, Tara Schwetz, and assistant secretary of health Rachel Levine. In early May 2022, Rick Woychik, the director of NTP, halted publication. Instead, the report and an accompanying analysis of fluoride research would undergo another round of review, this time overseen by an independent board of scientists that advises the NTP. The entire process has struck some in the federal government as unusual. “It just seems like it’s just stretching out the scientific review process,” said one federal official with detailed knowledge of the report, who spoke on condition of anonymity because of concerns about professional repercussions. “It’s kind of hard to defend, I think, for something that’s actually slated to just be submitted to a journal for peer review,” the official added. The official also questioned the decision to allow agencies like the CDC—which has long promoted water fluoridation—to weigh in on the NTP’s research. “You’re talking about having that document reviewed by agencies who have a vested interest in the policy of fluoride,” the official said, adding that the review process now appeared entangled with various policy biases. “That, to me, is really when it crosses the boundary.” (A CDC spokesperson said that the agency routinely reviews draft reports on “emerging science” from other parts of the federal government in order “to assure that our recommendations maximize benefits while minimizing any potential harms.”) Linda Birnbaum, a toxicologist who served as director of both NTP and the National Institute of Environmental Health Sciences from 2009 until 2019, also criticized the review process. “I see this as an infringement of scientific integrity, that the scientists have been prevented from getting their information out,” she said. That information, she argued, has implications for public health: “I think the data is overwhelmingly clear that fluoride is associated with the potential for neurodeficits.” Christine Flowers, a spokesperson for the National Institute of Environmental Health Sciences, which houses the NTP, declined to make the program’s current director, Rick Woychik, available for an interview. The ongoing delay in publication, she wrote in an email, “was to ensure that we get the science right.” So far, progress on the main report appears to be stalled. According to Bucher, the authors have received no revisions to the document since September 2023. The accompanying analysis paper, though, is finally moving forward. The next step would be submission to a journal—where it will undergo yet another round of peer review. For some scientists, the NTP saga has echoes of another dispute: the response to Christine Till and her team in Canada, after their 2019 paper was published in JAMA Pediatrics. In 2021, following a series of letters to York University and other institutions criticizing the paper, a group of academics and dental leaders filed a series of misconduct complaints with the researchers’ institutions, as well as the U.S. federal government, which had funded the study. “That’s fucking mean. I mean, that’s terrible” said Hu, the physician and epidemiologist at the University of Southern California, who previously served as dean of the Dalla Lana School of Public Health at the University of Toronto. Hu was not involved with the paper, but he has collaborated with Till on other research, and he helped lead influential fluoride studies in Mexico. “You don’t do that,” he said of the complaints, “unless you actually have evidence of scientific misconduct.” Such allegations are typically reserved for cases of data fabrication and fraud, and they can bring immediate consequences, delaying research, freezing funding, and taking up large amounts of a researcher’s time. “I think the data is overwhelmingly clear that fluoride is associated with the potential for neurodeficits.” For the scientists who signed the complaints, the stakes felt high. Among them was Jennifer Meyer, an associate professor of public health at the University of Alaska, Anchorage. Meyer first became interested in fluoride when she moved to Juneau, Alaska, a number of years after the city halted water fluoridation. Dentists, she said, observed an immediate rise in tooth decay—a finding that Meyer and two colleagues backed up with hard data in later research . It was galling for Meyer to see Till’s team make public statements recommending that pregnant women limit their fluoride intake. It seemed to her that the scientists, based on what she saw as one deeply flawed study, were in effect issuing public health advisories. Such activity, she suggested, might be worth silencing: “If you’re out there terrifying the public about a well-known public health intervention on which you have you have no basis to make that claim, and yet you’re continuing to do it, then it becomes, I think, a step too far,” Meyer said. Some people may see that as academic free speech, she added. “But I can’t stand up in a theater and yell ‘Fire!’ There are limits to freedom of speech.” Meyer connected with other researchers who were concerned about the MIREC study, including Juliet Guichon, a law and ethics scholar at the University of Calgary’s medical school. Guichon had been involved with pro-fluoridation campaigns in Calgary, and she saw the research—and the subsequent statements by Till and others—as linked to a long campaign against fluoridation. The research team, she told Undark, seemed like it had cherrypicked its data in order to find an alarming-sounding result. Guichon drafted the complaints in 2021. She and Meyer recruited a group of dental and public health experts to sign it, including Howard Pollick, a dentist and clinical professor of health sciences at the University of California San Francisco, who often serves as an American Dental Association spokesperson on fluoridation; Christine Wood, the director of the Association of State and Territorial Dental Directors; William Maas, a former top dental official at the CDC; and Raman Bedi, the former Chief Dental Officer of England. Tomar, the University of Illinois Chicago professor, joined the group as well. The group fractured over how far to go. Everyone signed the complaints sent to the U.S. government and several universities. But most of the signatories did not sign the complaint to York University, which called for Christine Till to be fired, as well as one other complaint seeking a scientist’s termination. In copies of the 40-plus pages of allegations obtained by Undark, the complainants describe in detail what they see as inappropriate statistical practices by the research team—practices that, they say, amount to intentional falsification of data to produce a specific result. The document appears to contain no direct evidence of the fabrication or falsification of data, and the complaints were dismissed by all institutions, including the U.S. Department of Health and Human Service’s Office of Research Integrity. (The complaint “was not adjudicated in what anyone would regard as an independent and thorough matter,” Guichon said.) The group also unsuccessfully petitioned JAMA Pediatrics to retract the paper. Some researchers suggested that the complainants had been motivated more by a desire to defend fluoridation than by any evidence of scientific misconduct. “It’s one branch of public health, which is dental public health, in tension with another branch of public health, environmental public health,” Hu said. “And we’re supposed to be the same tribe, but we’re not. Some of these dental folks—when you look at their objections, they’re not environmental epidemiologists. Some of them were just unfamiliar with the methodology.” In interviews, Till described a kind of ongoing campaign against her work. Fluoridation proponents, she said, would email venues where she gave talks, warning against hosting her. “That’s the life of a fluoride researcher,” she said. Till has tenure, but she now warns younger researchers about studying the topic. “It’s not a place for someone who worries about their job security,” she said. Till and others have taken particular issue with one allegation: that they refused to share their data. Under MIREC policies, research teams do not own the highly sensitive personal data and may not share it. Other researchers must apply directly to MIREC if they wish to access it. In 2020, dental experts petitioned MIREC to access the data. Over the next year they were repeatedly denied. (At one point, Till and a collaborator sent a letter to MIREC encouraging an external review of the data—but only if conducted by people who had no “ideological biases.”) In a statement to Undark, Maryse Bouchard, the scientist who currently oversees the MIREC program, said the dental group “did not demonstrate sufficient expertise or methodological improvement to meet the requirements for a robust reanalysis.” “MIREC data are not being withheld,” Bouchard wrote. Those statements have not stopped many critics of Till’s work from continuing to allege that her group has blocked access to the underlying data. Guichon suggested to Undark that Till or others had exercised influence over MIREC’s decision, noting that some of the MIREC leaders had co-published papers with Till’s collaborators. Guichon did not provide any concrete evidence of collusion. But, she said, “I would ask the question, if MIREC is independent of the group of authors who wrote the paper, how would we know that?” Some of that suspicion has extended to the NTP report. In conversations with Undark, Guichon questioned whether NTP was truly independent, noting an instance in 2020 in which an NTP scientist retweeted a link shared by the Fluoride Action Network, an activist group and EPA lawsuit plaintiff. Still, the dispute over the report has mostly focused on wording—and on whether the NTP does enough to convey uncertainty about lower levels of fluoride exposure. Pollick, the UCSF dentist and fluoridation spokesperson, has made public statements questioning the NTP report; in an interview, he clarified that his concerns were mostly about how the science is communicated by the NTP team, rather than its substantive claims. Indeed, what almost everyone seems to agree on is this: There is uncertainty about whether fluoride, at the kinds of doses routinely encountered by Americans, can have neurotoxic effects. And it would be helpful to have more research. But scientists have been divided over how to proceed amid that uncertainty. For Bucher, the current evidence likely warrants a recommendation for pregnant women to exercise caution around their fluoride intake. There’s evidence of potential risk, he continued, “and there’s absolutely no documented benefit to an unborn child receiving fluoride through the mom.” To others, the evidence needs to be far clearer before issuing any kind of public health advice—especially when that advice appears to undermine a policy that has a demonstrated benefit for many people, perhaps especially those from marginalized communities, who have less access to robust dental care. Tomar, the University of Illinois Chicago dentist and epidemiologist, and one of the signatories on the general complaints about Christine Till’s paper, framed the question as, more broadly, about giving up a known good in order to prevent a possible harm. “The preponderance of evidence does not support their conclusion of public health harm in terms of lowered IQ,” he said. “But we are pretty sure that if you stopped water fluoridation tomorrow, there will be public health harm in terms of increased oral disease.” Today, the CDC advises parents to pay attention to their children’s fluoride intake (such as from swallowing large amounts of toothpaste) in order to protect against tooth mottling. No federal advisory exists for limiting fluoride intake during pregnancy. Nor are there necessarily warnings about potential neurotoxic effects given to people who live in communities where fluoride levels exceed 1.5 mg/L, creeping into the range where many researchers consider the evidence of harm to be more clear-cut. “The preponderance of evidence does not support their conclusion of public health harm in terms of lowered IQ.” Eaton, the University of Washington toxicologist, used to chair a board of expert advisers to the NTP, and he oversaw the working group that conducted the most recent external review of the fluoride report. In typical cases where there’s uncertainty about a toxin, he said during a recent interview with Undark, regulators build in a buffer, setting the allowable threshold at 10 or even 100 times lower than the amount that’s considered likely to cause harm. By that standard, “you would come to the conclusion that water fluoridation is problematic,” he said. “But what you have to consider in that is the public health benefits of water fluoridation”—as well as the potential difficulty of dealing with naturally occurring fluoride. Eaton would like to see the government convene an expert panel to weigh all of those considerations and provide guidance to the federal agencies, he said: “It really needs a good, objective look at balancing the risks and benefits from the public health perspective.” In November 2023, Woychik, the current director of both National Institute of Environmental Health Sciences and NTP, held an online townhall with institute employees. Someone asked him whether the fluoride report would come out soon, adding that it seemed that “science is being prevented from being published.” His answer seemed to gesture both to the internal pressure to move the report forward—and the veil of concerns and allegations that have come to surround the delays. “There is not a government conspiracy starting with the ASH and the director of the NIH,” he said, using an acronym for assistant secretary for health, according to a transcript of the meeting obtained by Undark. “These papers are going to be, from my point of view, the most impactful papers that are published from the NIEHS, that will impact public health,” Woychik said, noting that every word would be scrutinized by both pro- and anti-fluoridation camps. All of this back-and-forth has energized anti-fluoridation activists. Today, the cutting edge of the movement is a family affair. In 2000, environmental chemist Paul Connett became the founding director of the Fluoride Action Network, aiming to fight a policy he saw as harmful to public health. Today his son, Michael, is leading the lawsuit demanding that the EPA to reexamine the way it treats water fluoridation. The EPA, Connett’s suit alleges, has essentially failed to assess fluoride in the way it would other toxins. “Because of this interest in protecting this oral health program, you are failing to use your own risk assessment framework,” Michael Connett said in an interview with Undark shortly before the trial resumed. Several researchers testified at the trial, including Hu, the University of Southern California professor, and Berridge, the former NTP official. Both sides found broad agreement on certain issues: that fluoride at higher concentrations can pose risks, and that the NTP report had real scientific merits. “I think our scientists generally agree that the NTP monograph was a high-quality review,” said one of the EPA’s lawyers, Paul Caintic, during his opening statement. He argued that the evidence “is simply too inconsistent and too unclear to conclude that there’s been a demonstration that low-level fluoride exposure presents an unreasonable risk of neurodevelopmental harm.” For his part, Connett argued that the agency should move forward based on the evidence available. “We do not need to wait for every piece of the puzzle to fit nicely together before we take action to prevent harm,” Connett said on the final day of the hearing. During closing arguments, Judge Edward M. Chen appeared to echo concerns that the levels of fluoride in drinking water came relatively close to levels at which there was stronger evidence of harm. “What do I do with the fact that you don’t have to go much higher to find—in the words of Dr. Barone—something is going on?” he asked the EPA’s lawyers at one point during the trial’s final day, naming one of the agency’s senior scientists and key witnesses. The Fluoride Action Network has been optimistic. “Once we get the victory and the NTP report comes out—or both situations—we’re just going to have a big education campaign, ensuring that water operators, decision makers, state level decision makers all throughout the country are aware of it,” said executive director Stuart Cooper in an interview with Undark in December, shortly before the trial resumed. On its website, the organization has been describing 2024 as “the perfect storm.” That storm could stoke skepticism of public health institutions at a time when many are facing declines in public trust . Already, the case has drawn enthusiastic attention from people in the world of anti-vaccination activism. “What do I do with the fact that you don’t have to go much higher to find—in the words of Dr. Barone—something is going on?” More research is coming. Hu has a large study of fluoride effects in the United States currently under review at a journal; while he declined to say what the paper found, there are indications it shows a link between fluoride and harmful effects, bolstering the findings by Till’s team in Canada. Till has begun work on a population of mother-child pairs in New Hampshire, incorporating another way of measuring fluoride exposure—toenail analysis—in the research. Berridge, the former NTP leader who resigned over the report’s repeated delays, is frustrated that the public doesn’t have access to the most up to date information from the NTP. “We need to be transparent about the science,” he said, “so that people who need to make decisions—either individuals, regulators, or policymakers—can make those decisions based on whatever the best science of the day is.” This website uses cookies to ensure you get the best experience. Learn more about DOAJ’s privacy policy. Hide this message You are using an outdated browser. Please upgrade your browser to improve your experience and security. The Directory of Open Access JournalsQuick search, fluoride fluoride: quarterly journal of the international society for fluoride research inc.. 0015-4725 (Print) / 2253-4083 (Online)
Publishing with this journalThere are no publication fees ( article processing charges or APCs ) to publish with this journal. Look up the journal's:
Expect on average 33 weeks from submission to publication. Best practiceThis journal began publishing in open access in 1968 . What does DOAJ define as Open Accesss? This journal uses their publisher’s own license. → Look up their open access statement and their license terms . The author does not retain unrestricted copyrights and publishing rights. Journal metadataPublisher International Society for Fluoride Research Inc. , New Zealand Other organisation International Society for Fluoride Research Inc. Manuscripts accepted in Japanese, Chinese, Spanish, English LCC subjects Look up the Library of Congress Classification Outline Medicine: Dentistry Keywords fluoride toxicology fluoride biochemistry veterinary aspects of fluoride clinical aspects of fluoride agricultural aspects of fluoride dental aspects of fluoride WeChat QR code Impact of fluoride on neurological development in childrenJuly 25, 2012 — For years health experts have been unable to agree on whether fluoride in the drinking water may be toxic to the developing human brain. Extremely high levels of fluoride are known to cause neurotoxicity in adults, and negative impacts on memory and learning have been reported in rodent studies, but little is known about the substance’s impact on children’s neurodevelopment . In a meta-analysis, researchers from Harvard School of Public Health (HSPH) and China Medical University in Shenyang for the first time combined 27 studies and found strong indications that fluoride may adversely affect cognitive development in children. Based on the findings, the authors say that this risk should not be ignored, and that more research on fluoride’s impact on the developing brain is warranted. The study was published online in Environmental Health Perspectives on July 20, 2012. The researchers conducted a systematic review of studies, almost all of which are from China where risks from fluoride are well-established. Fluoride is a naturally occurring substance in groundwater, and exposures to the chemical are increased in some parts of China. Virtually no human studies in this field have been conducted in the U.S., said lead author Anna Choi , research scientist in the Department of Environmental Health at HSPH. Even though many of the studies on children in China differed in many ways or were incomplete, the authors consider the data compilation and joint analysis an important first step in evaluating the potential risk. “For the first time we have been able to do a comprehensive meta-analysis that has the potential for helping us plan better studies. We want to make sure that cognitive development is considered as a possible target for fluoride toxicity,” Choi said. Choi and senior author Philippe Grandjean , adjunct professor of environmental health at HSPH, and their colleagues collated the epidemiological studies of children exposed to fluoride from drinking water. The China National Knowledge Infrastructure database also was included to locate studies published in Chinese journals. They then analyzed possible associations with IQ measures in more than 8,000 children of school age; all but one study suggested that high fluoride content in water may negatively affect cognitive development. The average loss in IQ was reported as a standardized weighted mean difference of 0.45, which would be approximately equivalent to seven IQ points for commonly used IQ scores with a standard deviation of 15.* Some studies suggested that even slightly increased fluoride exposure could be toxic to the brain. Thus, children in high-fluoride areas had significantly lower IQ scores than those who lived in low-fluoride areas. The children studied were up to 14 years of age, but the investigators speculate that any toxic effect on brain development may have happened earlier, and that the brain may not be fully capable of compensating for the toxicity. “Fluoride seems to fit in with lead, mercury, and other poisons that cause chemical brain drain,” Grandjean says. “The effect of each toxicant may seem small, but the combined damage on a population scale can be serious, especially because the brain power of the next generation is crucial to all of us.” * This sentence was updated on September 5, 2012. Read a September 2012 statement by the authors. ** Learn more about the IQ measurements by HSPH’s Anna L. Choi and Philippe Grandjean in response to a letter to the journal published in the March 2013 (Vol. 121, No. 3) Environmental Health Perspectives. Follow-up Fluoride Study PublishedDecember 19, 2014 — As a follow-up, Philippe Grandjean , adjunct professor of environmental health at Harvard School of Public Health (HSPH), Anna Choi , research scientist in the Department of Environmental Health , and colleagues have published a pilot study of cognitive functions in Chinese children exposed to different levels of fluoride from drinking water. The new paper, entitled “Association of lifetime exposure to fluoride and cognitive functions in Chinese children: A pilot study,” has been published online and in the January-February 2015 issue of Neurotoxicology and Teratology . — Marge Dwyer
Kinetics of fluoride after brushing with the no-rinse method
BMC Oral Health volume 24 , Article number: 1050 ( 2024 ) Cite this article 87 Accesses Metrics details Fluoride plays a vital role in preventing dental caries, with its addition to oral care products significantly promoting oral hygiene. A no-rinse brushing method aims to increase fluoride retention in the oral cavity, as rinsing with water decreases fluoride levels in saliva, which could affect remineralization. While the no-rinse brushing method holds promise for improving fluoride retention in the oral cavity, critical inquiries persist regarding its safety. This study investigated the kinetics of oral fluoride and potential risks to fully assess its effectiveness and implications for oral health. Ten healthy adults participated in a crossover study comparing the no-rinse with the rinse method. All subjects followed American Dental Association (ADA) brushing guidelines. Levels of fluoride in saliva (supernatant and sediment) and urine were measured over time, and plasma fluoride was measured one hour after brushing. Pharmacokinetic parameters were also calculated from the data. Participants using the no-rinse method had higher fluoride levels in supernatant immediately and up to 30 min post-brushing compared to the rinse method. Fluoride levels in sediment were higher only immediately after brushing. The total fluoride concentration in saliva remained elevated for up to 5 min with the no-rinse method. Systemic fluoride absorption showed no significant difference between the two methods based on blood and urine analysis. This research indicates that the no-rinse method can enhance fluoride retention in the oral cavity for up to 30 min after a single brushing. In addition, our findings suggest that this method does not significantly influence systemic fluoride levels or toxicity. Thai Clinical Trials Registry, TCTR ( http://thaiclinicaltrials.org ). Clinical trial registration number: TCTR20231104001 (4/11/2023). Peer Review reports IntroductionFluoride is widely recognized as a key in preventing dental caries and maintaining oral health. Toothpaste containing fluoride at 1,000 to 1,500 ppm has effectively prevented tooth decay [ 1 ]. Fluoride in the oral cavity can be absorbed by tooth enamel, forming fluorapatite, which strengthens enamel and reduces its susceptibility to acid erosion [ 2 ]. This process, known as remineralization, is crucial for preventing dental caries. Fluoride is typically ingested and absorbed in the gastrointestinal tract with an absorption half-life of 30 min and peak levels in plasma at approximately 1 h [ 3 , 4 , 5 , 6 ]. Once absorbed, fluoride primarily distributes in plasma and accumulates in mineralized tissues, particularly bones. It can be slowly released from deposit sites when plasma fluoride levels decrease. While fluoride metabolism in the liver is minimal, renal excretion is the primary elimination route, with excretion rates associated with urine pH, glomerular filtration rate (GFR), plasma fluoride levels, and urine flow rate. The Australian Dental Association has recommended teeth brushing with a no-rinse method twice daily to retain higher fluoride concentration in the oral cavity for extended periods [ 7 ]. Public Health England, the Department of Health and Social Care, NHS England, and NHS Improvement also advise spitting out excess toothpaste rather than rinsing as a guidance to promote better oral health [ 8 ]. A prior study revealed a correlation between water rinsing, saliva fluoride concentration, and dental caries with individuals who rinsed less having higher salivary fluoride levels and lower incidences of dental caries [ 9 ]. Another study found that individuals who often rinsed with water after brushing exhibited a higher incidence of caries than those who did not rinse or only occasionally rinsed during the 3-year observation period [ 10 ]. Additionally, researchers have demonstrated that water rinsing decreases the fluoride availability in saliva by 2.5 times [ 11 ], and brushing with fluoride toothpaste without rinsing significantly increases fluoride concentration in saliva up to 15 min post-brushing [ 12 ]. These findings highlight the importance of the no-rinse method in increasing salivary fluoride levels and prolonging remineralization in the oral cavity. However, the evidence supporting the recommendation of the no-rinse method remains limited, primarily focusing on the impact of fluoride quantity on salivary concentration rather than the effects and safety of this post-rinsing method. Despite the potential benefits of the no-rinse method, concerns exist regarding fluoride toxicity and accumulation, especially considering the prolonged contact time with fluoride-containing toothpaste. Children and adolescents are particularly sensitive to fluoride toxicity, but adults can also experience symptoms such as skeletal fluorosis and other systemic effects [ 13 , 14 ]. Long-term fluoride ingestion reported symptoms such as abdominal pain, vomiting, and nausea in 70% of subjects [ 15 ]. Abnormalities of histological samples collected from the gastrointestinal tract were also observed. Therefore, it is crucial to consider the potential impact of high fluoride concentration when using the no-rinse method. Nowadays, concerns about potential fluoride toxicity due to accumulation when people don’t rinse after brushing have emerged. This recent study aimed to assess the kinetics of fluoride retention within the oral cavity, its absorption into the systemic circulation, and its urinary excretion after brushing with the no-rinse method. This research aims to contribute to evidence-based guidelines for the clinical application of fluoride to ensure its effective delivery while prioritizing safety. Materials and methodsThis study is a crossover design. The study was approved by the Committee on Human Rights Related to Human Experimentation, Mahidol University, Thailand (COA. No. MU-DT/PY-IRB 2023/063.2609). The trial protocol was registered with the Thai Clinical Trials Registry (TCTR) (TCTR20231104001). Sample size calculations were performed using raw data from a prior study [ 16 ] with the G*Power program (version 3.1.9.4). The type I error was set at 0.05 with 95% power. From the power analysis, subjects of at least 9 participants were required to participate in the study. We decided to include 10 participants in this study by considering a 10% dropout rate. The participants who reached the following criteria, age between 20 and 35, resting salivary flow rate above 0.3 ml/min, having healthy teeth and gums, no history of liver and kidney disease, and did not take medications that might have affected their salivary flow rate were included in this study. Those who were unable to collect urine every 2 h were excluded. Each participant was conducted both no-rinse and rinse post brushing with at least 7 days of washing period between the rinsing techniques. The washing period refers to the interval between the experiments of the two different rinsing methods, allowing for a clear distinction in the effects of each technique. We selected a 7-day washout period in accordance with guidance from the US FDA on studying bioavailability and bioequivalence that an adequate washout period for cross-over study should be approximately ten times the elimination half-life of the drug [ 17 ]. During the washout period, we provided each participant with instructions on maintaining their oral hygiene. Participants were advised to brush their teeth using the Modified Bass technique, as recommended by the ADA, and to avoid any medications that could affect the salivary flow rate throughout the study. To ensure compliance, we contacted participants on day 3 or 4 of the washout period for a follow-up check. Brushing and rinsing procedureTo participate in the study, all participants needed to avoid high-fluoride foods for 12 h before attending each experimental visit. During the first visit, urine samples were collected to measure baseline fluoride levels, ensuring the controlled intake of low-fluoride foods didn’t affect urinary fluoride. Participants were then randomly assigned to two groups (group A underwent the rinse method on the second visit and switched to the no-rinse method after a 7-day washout period for the third visit, while Group B started with the no-rinse method on the second visit, had a 7-day washout period, and then switched to the rinse method in the third visit) (Fig. 1 ). On the days of the second and third visits, fluoride-containing toothpaste was not used in the morning. Participants were instructed to consume only the food (breakfast, lunch) and drink (low fluoride-containing water) provided during the experimental procedure. The experiments were started at least 2 h after breakfast. Each group used either no-rinse method or rinsed with 10 ml of deionized water for 10 s, applying 1 g of pre-weighed toothpaste of the no-rinse toothpaste containing 1500 ppm fluoride (Dentiste Anticavity Max Fluoride Toothpaste, Bangkok, Thailand). Our staff instructed them to follow the American Dental Association (ADA) recommended brushing method, briefly using a modified bass technique with 1 g of pre-weighed toothpaste for 2 min, covering all tooth surfaces.  Group allocation and processes from the first visit to the third visit for group A and group B Samples collectionOur staff instructed participants to collect unstimulated saliva in a 50 ml sterile tube for 2 min before and immediately, 5, 10, 15, 30, 60, and 90 min after brushing. Urine was collected before, and intervals of 30–60 min, 1–2 h, 2–4 h, and 4–6 h after brushing. Total urine was collected in a 600 ml container at each collection time point to calculate cumulative fluoride excretion. Additionally, 5 ml of blood was collected in a heparinized tube by a registered nurse at 1 h after using the no-rinse method to analyze plasma fluoride. The salivary flow rate of each individual was also determined before brushing by collecting unstimulated saliva in a 50 ml sterile tube for 2 min. The salivary flow rate was measured by calculating the total volume of saliva collected at baseline before brushing with no-rinse formula toothpaste divided by the time of collection. Fluoride measurementAll samples including saliva, blood, and urine were processed differently before evaluating fluoride concentration. Saliva was centrifuged at 3024 g for 10 min to separate supernatant and sediment. The blood sample underwent centrifugation at 240 g for 5 min to obtain plasma. Urine sample volumes were recorded before fluoride measurement. All samples were kept at -20 °C until fluoride analysis using a calibrated ion-specific sensitive electrode (Orion™ Model 9609BNWP, Thermo Fisher Scientific Cambridgeshire, UK). The flow charts below show the complete experimental protocol (Fig. 2 ).  Timeline for sample collection and the process of sample preparation for fluoride measurement Pharmacokinetic of fluorideThe area under the curve (AUC) of total fluoride levels in saliva collected from the no-rinse and rinse groups was calculated from the graph illustrating fluoride levels over time using Prism ® version 9 (Prism Software Inc., San Diego, CA, USA). This was done to assess fluoride bioavailability in the oral cavity. We measured the total urine volume at each collection point to determine the fluoride levels in urine samples. The fluoride quantity was calculated using the following equation. The cumulative fluoride amount was calculated and plotted against the time of urine collection. Additionally, the excretion rate (fluoride amount/ time) was computed and plotted on a semi-log scale against the collection time. The slope of this graph yielded the elimination rate constant (k e ). The plasma fluoride concentration at a single time point was utilized to calculate renal clearance using the following equation. Additionally, the volume of distribution (V d ) and half-life (t 1/2 ) were calculated using the following equation. Statistical analysisStatistical analysis was done using IBM SPSS Statistics version 28.0 (IBM Corporation, Armonk, NY) and Prism ® version 9 (Prism Software Inc., San Diego, CA, USA). Data are represented as mean ± standard error of the mean (SEM). Histogram and Shapiro-Wilk Test were used for the normality test. A Generalized Estimating Equation (GEE) was used for salivary and urine fluoride analysis. A Paired t-test was used for plasma fluoride analysis, the AUC of fluoride in whole saliva, and the comparison of fluoride in supernatant and sediment after tooth brushing. Demographic profile of study subjectsThe study included 4 males (40%) and 6 females (60%). The mean age, height, weight, and body mass index (BMI) of the study population were 22 ± 1.16 years, 166 ± 9.26 cm, 60.5 ± 17.91 kg, and 21.91 ± 4.48 kg/m 2 , respectively. The salivary flow rate of all subjects is in the normal range (average salivary flow rate is 0.58 ± 0.2 ml/min). All characteristics of the study subjects and the mean salivary flow rate are shown in Table 1 . Fluoride concentration in the oral cavityFluoride concentrations were determined in two compartments of saliva, including supernatant and sediment. Fluoride concentrations in supernatant after brushing following the no-rinse method showed significantly higher than those in supernatant from the rinse method immediately ( p = 0.02), and 5 min ( p < 0.001), 10 min ( p = 0.002), 15 min ( p = 0.002) and 30 min ( p = 0.006), respectively after brushing (Fig. 3 A). In the sediment compartment, fluoride concentrations in the no-rinse group displayed a significantly higher level than those in the rinse group at only the immediate time point after brushing ( p = 0.007) (Fig. 3 B). When calculated for fluoride in the whole saliva, the no-rinse method exhibited significantly higher levels than those in the rinse group immediately after brushing ( p = 0.03), and this difference remained statistically significant at 5 min ( p = 0.01) (Fig. 3 C). In addition, the AUC calculated from fluoride in saliva was more critical in the no-rinse than in the rinse technique ( p = 0.0185) (Fig. 4 ). Furthermore, we observed that after 60 min following toothbrushing, the sediment had a higher fluoride content than the supernatant in both methods. This pattern of fluoride distribution between the 2 compartments of saliva was also observed at the baseline (Fig. 5 ).  The salivary fluoride concentration of various time points after tooth brushing with no-rinse and rinse method. Fluoride concentrations in saliva were determined in supernatant ( A ), sediment ( B ), and whole saliva ( C ). Data are mean ± SEM ( n = 10). Statistical significance was determined using a Generalized Estimating Equation (ESS) represented by ** P < 0.01, *** P < 0.001  AUC of fluoride in whole saliva after tooth brushing with no-rinse and rinse method. Data are mean ± SEM ( n = 10). Statistical significance was determined using a Paired t-test represented by * P < 0.05  The fluoride concentrations in supernatant and sediment at various time points after tooth brushing with no-rinse ( A ) and rinse ( B ) method. Data are mean ± SEM ( n = 10). Statistical significance was determined using a Paired t-test represented by * P < 0.05, ** P < 0.01 Fluoride concentration in plasmaAnalysis revealed that the no-rinse method resulted in a systemic circulation fluoride concentration at 1 h after brushing of 0.0260 ± 0.12 ppm, while the rinse method exhibited a similar concentration of 0.0234 ± 0.09 ppm (Fig. 6 ). The statistical analysis revealed no significant disparity between 2 groups (p-value = 0.52).  Fluoride concentration in plasma between no rinse and rinse methods at 1 h after brushing. Data are mean ± SEM. N = 10 in both groups. Statistical significance was determined using a Paired t-test Renal fluoride excretionThe cumulative amount of fluoride was calculated and plotted against the time of urine collection (Fig. 7 A). At all time points, no statistically significant differences were observed between the groups (p-value > 0.05). Furthermore, the rate of excretion (amount of fluoride/time) was computed and plotted on a semi-log scale against the time of collection. The slope of this graph provided the elimination rate constant (k e ), which was 0.19 h − 1 for the no-rinse method and 0.23 h − 1 (Fig. 7 B) for the rinse method.  The cumulative amount of fluoride and rate of fluoride excretion of no-rinse and rinse method after brushing. Data are shown as mean ± SEM. N = 10 in both groups. Statistical significance was determined using a Generalized Estimating Equation (ESS) for the cumulative amount of fluoride ( A ). The slopes were calculated to obtain the k e for fluoride in both experimental groups ( B ) From the K e value obtained from the semi-logarithmic graph, we determined the half-life of fluoride after brushing using the no-rinse method to be approximately 3 h and 38 min. This value closely aligns with the half-life calculated from the rinse method, which was approximately 3 h. The renal clearance, estimated from urinary fluoride concentration, urine flow rate, and plasma concentration at 1 h after brushing in the no-rinse group, was 14.36 ml/ min. In contrast, the rinse method yielded an 11.85 ml/ min renal clearance. Furthermore, the volume of distribution (V d ) estimated from both methods was similar. Specifically, it was determined to be 4.53 L with the no-rinse method and 3.09 L with the rinse method. This study investigated the kinetics of fluoride in healthy adults following the use of 1500 ppm sodium fluoride toothpaste, specifically employing the no-rinse method after brushing. The research aligned with the recommendations of several dental associations, including the Australian Dental Association, British Dental Association, Nation Health Service (NHS.UK), and Canadian Dental Association, all of which advise against rinsing after brushing. However, there is currently limited data available regarding its efficacy and safety. To bridge this gap, this study compared the no-rinse and rinse methods to assess their impact on fluoride concentrations in supernatant, sediment, and whole saliva. Blood and urine samples were collected at various time points to comprehensively evaluate fluoride absorption to the systemic circulation and excretion. Our findings showed that the no-rinse method resulted in higher levels of fluoride in saliva than the rinse method, particularly immediately after brushing and up to 5 min afterward. Examining saliva components, we found that fluoride concentration peaked in the supernatant immediately after brushing and gradually moved to the sediment. Despite higher salivary fluoride, fluoride levels in plasma and urine are below those observed in patients with fluorosis, suggesting the safety of the no-rinse method after a single brushing. The no-rinse method consistently resulted in higher fluoride concentrations in both the supernatant and sediment immediately after brushing, and in the supernatant at subsequent time points, compared to the rinse method. A prior study indicated that no-rinsing after brushing with sodium fluoride resulted in higher salivary fluoride levels than the rinse method until 1 min [ 16 ]. In contrast, our study showed that using the no-rinse method with sodium fluoride toothpaste sustained greater fluoride levels in the whole saliva for up to 5 min, longer than previously reported. The duration of fluoride exposure in the oral cavity directly influences its effectiveness in promoting remineralization of enamel or dentin. Longer exposure allows fluoride to exert its protective and strengthening effects, contributing to oral health and reducing the risk of tooth decay [ 18 , 19 ]. If the no-rinse method consistently extended the level of fluoride over 5 min over a period of time, it might show significant remineralization and reduce the incidence of caries. Furthermore, we found that fluoride levels in the supernatant after using the no-rinse method reached the concentrations required to inhibit 50% demineralization (0.3 to 0.4 ppm) [ 20 ] for up to 30 min, whereas the rinse method maintained these fluoride levels for up to 15 min after brushing. Our findings align with previous studies, which demonstrated that the no-rinse method maintained salivary fluoride retention in the oral cavity better than the rinse method [ 21 ]. Additionally, increased rinsing water decreases fluoride retention in the oral cavity, leading to lower salivary fluoride levels and potentially higher dental caries incidence [ 9 , 12 ]. Thus, minimizing rinsing after brushing may enhance fluoride efficacy. This study separated whole saliva into supernatant and sediment components to examine how the rinsing methods (no-rinse Vs. rinse) impact fluoride’s kinetics in both saliva compartments. This approach is crucial as these compartments may influence the bioavailability of fluoride differently within the oral cavity. The cell-free supernatant saliva represents a complex secretion originating from the salivary glands. At the same time, the sediment comprises the bulk of the human oral microbiome, cellular constituents, proteins, and food particles [ 22 ]. At baseline (before brushing), fluoride accumulated more in the sediment. Immediately after brushing, fluoride was initially distributed in the supernatant in both methods. However, fluoride levels became more prominent in the sediment after 60 min post brushing. This pattern was observed with the no-rinse and rinse methods at 60 min, but only the no-rinse method maintained elevated fluoride levels in the sediment for up to 90 min, indicating that this effect might be more noticeable with the no-rinse method. Our findings align with previous research showing a biphasic clearance pattern, with rapid fluoride declines in the first 40–60 min followed by a slower decrease [ 23 , 24 ]. The gradual decline after 60 min may result from sustained fluoride release from the sediment reservoir, suggesting it acts as a fluoride reservoir in the oral cavity that could help prevent demineralization [ 22 , 25 ]. Besides the fluoride reservoir in the sediment, fluoride retention in the saliva is also influenced by other factors, including fluoride levels in the mouth, salivary flow rates, toothpaste fluoride content, rinse method, and fluoride clearance rates [ 16 , 21 , 26 , 27 , 28 , 29 ]. Salivary flow rate affects fluoride concentration in the oral cavity because a high salivary flow rate increases fluoride clearance and may reduce its concentration in the oral cavity [ 26 ]. In our study, the calculated salivary flow rate was 0.58 ± 0.20 ml/min, slightly higher than the typical unstimulated rate of 0.3–0.4 ml/min [ 30 ]. This higher rate could be a factor to consider, but our crossover design helps mitigate its impact. We also determined a kinetic parameter, the AUC of salivary fluoride, for both post-brushing methods since AUC measures fluoride’s oral bioavailability. Our findings revealed a notably higher AUC in the no-rinse group compared to the rinse groups. A clinical study demonstrated the impact of water rinsing on salivary fluoride AUC, showing that the AUC of salivary fluoride was 2.5 times lower when water rinsing was used [ 11 ]. Therefore, our findings suggest that the no-rinse brushing method increases fluoride retention in the oral cavity and potentially lowers the risk of caries. Absorption of high fluoride intake into the plasma is associated with the risk of dental and skeletal fluorosis. Fluoride toxicity poses serious health risks, leading to dental issues and cognitive impairment in children [ 13 , 14 , 31 , 32 , 33 ]. Dental fluorosis has been reported in individuals aged 1 to 23 years, with younger people being more susceptible [ 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 ]. While dental fluorosis is less common in adults, fluoride absorption can lead to skeletal fluorosis in adults [ 14 , 40 , 42 , 43 ]. In addition, children aged 6 to 13 years have been diagnosed with this condition [ 44 ]. These conditions arise due to the absorption of high fluoride levels into the plasma. Preventive measures and monitoring of fluoride exposure are crucial. Despite advocacy for the “spit, no-rinse” brushing method to preserve fluoride levels in the oral cavity, concerns about fluoride accumulation and the risk of fluorosis remain. Our study aims to assess fluoride concentration in plasma to validate the safety of the no-rinse method. Measuring plasma fluoride reflects systemic absorption, while urine fluoride indicates elimination. Previous studies have focused on sodium lauryl sulfate (SLS) toxicity to oral tissues [ 45 , 46 ] and assumed low SLS content in toothpaste is safe with the no-rinse method [ 47 , 48 ]. However, there is no evidence documenting systemic fluoride absorption with this approach. Our study aims to provide concrete data on fluoride absorption by including urine and blood evaluations for a comprehensive safety profile of the no-rinse method. As fluoride toxicity arises from high fluoride absorption into plasma, analyzing plasma fluoride levels is an approach to assess the safety of the no-rinse method. To minimize intrusion, we collected blood samples at a single time point, 1 h after brushing, based on fluoride’s absorption half-life of 30 min [ 49 ]. This timing allowed us to estimate peak fluoride absorption. Our study observed similar mean blood fluoride levels of approximately 0.02 ppm for both the no-rinse and rinse methods. These levels are below those reported in patients with dental and skeletal fluorosis (0.16–1.25 ppm) [ 13 , 50 ]. A study demonstrated that less water use for rinsing leads to higher fluoride absorption into the plasma [ 51 ], as well as The United States Environmental Protection Agency (EPA) states that a higher amount of fluoride exposure is linked to the severity of fluorosis [ 52 , 53 ]. Our results showed that even though the no-rinse method leads to higher fluoride exposure, the plasma fluoride levels remained within the safety limit (0.02 ppm) [ 50 ] and were similar to those observed with the rinse method. This data provides insights into the safety of the no-rinse method after a single brushing. However, further long-term studies are needed to assess the effects of repeated use of no-rinse toothpaste formulas compared to rinsing methods. Since urinary fluoride directly reflects fluoride excretion after absorption into the plasma, our study assesses fluoride levels in urine at various time points after brushing with either the no-rinse or rinse method. Our study found no significant difference in the amount of fluoride (µg) in urine samples between the no-rinse and rinse groups. In addition, the amount of fluoride in urine from 1 to 6 h after no-rinse brushing is comparable to the amount of baseline urine fluoride (32.54 ± 24.11 µg). This indicates minimal fluoride entered the bloodstream after brushing with the no-rinse method in this study. According to previous studies, patients with dental or skeletal fluorosis had urine fluoride levels ranging from 0.7 to 11.4 ppm, which tend to be higher in adults than in children [ 53 , 54 ]. In contrast to the previous study, the urine fluoride concentrations after no-rinse brushing at all time points in our study ranged from 0.23 to 0.29 ppm, which is far below the urine levels reported from the previous studies. These findings suggest that the single using of the no-rinse method has minimal impact on overall fluoride exposure in the body. The calculated half-life of fluoride in the no-rinse formula toothpaste was approximately 3 h and 19 min from the no-rinse method and 2 h and 54 min from the rinse method. This is similar to the recorded half-life reported previously in animal studies: fluoride half-life is generally 3–10 h [ 6 ]. The renal clearance of fluoride was measured at 14.36 ml/min and 11.85 ml/min in the no-rinse and rinse groups, respectively. These findings align closely with a previous study of renal fluoride clearance in healthy adults, which typically ranges from 12.4 to 71.4 ml/min [ 55 ]. Notably, renal clearances calculated from our study were lower than previous findings in children and adolescents which was 30–40 ml/min [ 56 ]. The differences in renal clearance observed between our study and previous research may be due to the underlying renal diseases present in the subjects of the prior study. In contrast, our research focused exclusively on healthy young adults. In addition, factors such as urinary pH, urine flow rate, and glomerular filtration rate variance between individuals can also influence the renal clearance of fluoride [ 56 , 57 ]. In terms of volume of distribution, it was determined to be 4.53 L with the no-rinse method and 3.09 L with the rinse method. The low volume of fluoride distribution suggests minimal distribution into other tissues or fat compartments [ 58 ]. However, fluoride remains concentrated within the bloodstream and is cleared effectively by the kidneys. This implies that urine can reflect systemic fluoride levels. Since approximately 50% of fluoride from the bloodstream can be transferred to calcified tissues [ 6 , 59 , 60 , 61 ], our study acknowledges the limitation of providing a partial representation of systemic absorption. We selected the no-rinse toothpaste to use in this study for its convenience and reduced toxicity to oral tissues. Unlike conventional toothpaste, this formulation excludes sodium lauryl sulfate (SLS), paraben, sugar, plastic microbeads, and alcohol. The absence of SLS, known to be toxic to human gingival fibroblasts [ 46 ], makes it more suitable for sensitive oral tissues. SLS in toothpaste can influence fluoride pharmacokinetics by decreasing fluoride uptake to the enamel, disrupting plaque biofilm, and increasing fluoride release from oral reservoirs into saliva [ 62 , 63 ]. By using the same toothpaste for both methods, we ensured that differences in fluoride absorption were due to the rinsing method alone. For future studies, including a conventional toothpaste with 1000–1500 ppm fluoride as a positive control could help validate our findings. We acknowledge some confounding variables in our study, such as baseline oral health status and hygiene practices, which could not be fully controlled. While we screened participants for baseline oral health conditions, variability still exists. Additionally, using other dental products such as mouthwash containing fluoride during the study could influence the no-rinse method’s effects. Future research should control for these variables for more precise data. We also recognize the limitation that our safety data is based on a single brushing with a specific no-rinse toothpaste. Further investigations are needed to evaluate the long-term use of the no-rinse method, compare different toothpaste formulations with conventional ones, and assess the safety of other ingredients in the toothpaste. Our fluoride data may not apply to all age groups, as fluoride accumulation and excretion vary with age [ 60 ]. Children’s ability to control fluoride ingestion post-brushing is also our concern, which could increase their risk of dental fluorosis with the no-rinse method. Therefore, further studies involving more diverse populations and various oral conditions, such as periodontitis, are necessary to generalize our safety results. Despite these limitations, our study provides valuable insights into optimizing fluoride toothpaste usage to maximize benefits while minimizing risks. Overall, our study investigates the safety profile of fluoride, specifically addressing concerns about systemic absorption when brushing without rinsing. This research provides critical information for clinical recommendations and guidelines to enhance oral health benefits while minimizing the risk of fluorosis. To ensure internal validity, we randomly assigned participants into two groups and used a cross-over design, allowing the same participants to test the no-rinse and rinse methods. We standardized variables by starting the experiment 2 h after breakfast, using the same amount (1 g) and type of fluoride toothpaste, and providing low-fluoride food and drinking water to minimize fluoride intake from other sources [ 64 , 65 ]. These controls strengthened our study’s internal validity. Although our findings from young adults may not apply to all age groups, however, the methodology we developed and validated for assessing fluoride toxicity can be applied to future studies involving children and other populations. Additionally, the brushing technique used in our study follows guidelines recommended by the ADA and BDA, making it relevant to various aspects of oral hygiene care. In summary, minimal fluoride entered the plasma after brushing without rinsing, indicating potential safety in a controlled experiment. ConclusionsThe no-rinse tooth brushing method demonstrated higher efficacy than the rinse method by preserving fluoride concentrations above levels necessary to prevent demineralization until 30 min after a single brushing. Sediment, particularly from the no-rinse method, acts as a reservoir for salivary fluoride, which effectively retains fluoride levels over an extended period. Analysis of fluoride levels in plasma and urine following no-rinse and rinse methods revealed no significant difference in single exposure to fluoride toothpaste formulated for no-rinse use. Within the limitation of this study, we provide information on the safety profile of fluoride after a single brushing of no-rinse formula toothpaste, particularly addressing concerns regarding potential systemic absorption when brushing without subsequent rinsing. Data availabilityThe datasets supporting the conclusions of this article are included within the article. Further enquiries can be directed to the corresponding author. AbbreviationsAmerican Dental Association Area under the curve Body mass index Environmental Protection Agency Generalized Estimating Equation Glomerular filtration rate Elimination rate constant Volume of distribution Expert Committee on Selection and Use of Essential Medicines Application Review, Fluoride toothpaste – dental caries, World Health Organization (WHO) https://cdn.who.int/media/docs/default-source/essential-medicines/2021-eml-expert-committee/expert-reviews/a14_fluoridetp_rev2.pdf?sfvrsn=c35d4123_7 (2021) Accessed 14 Feb 2024. Ten Cate JM, Buzalaf MAR. Fluoride Mode of Action: once there was an observant dentist. J Dent Res. 2019;98:725–30. https://doi.org/10.1177/0022034519831604 . Article CAS PubMed Google Scholar Ullah R, Zafar MS, Shahani N. Potential fluoride toxicity from oral medicaments: a review. Iran J Basic Med Sci. 2017;20:841–8. https://doi.org/10.22038/ijbms.2017.9104 . Article PubMed PubMed Central Google Scholar Martínez-Mier EA. Fluoride:its metabolism, toxicity, and role in Dental Health. J Evidence-Based Complement Altern Med. 2012;17:28–32. https://doi.org/10.1177/2156587211428076 . Article CAS Google Scholar National Research Council, Fluoride in Drinking Water: A Scientific Review of EPA’s Standards. (The National Academies Press, 2006). Appendix NTP. U, Pharmacokinetics and Concentrations of Fluoride Measured in Tissue, Blood, Urine, or Bone, NTP Research Report on Systematic Literature Review on the Effects of Fluoride on Learning and Memory in Animal Studies: Research Report 1 [Internet], https://www.ncbi.nlm.nih.gov/books/NBK552757 / (2016) Accessed 12 Feb 2024. Do LG. Guidelines for use of fluorides in Australia: update 2019, Australian Research Centre for Population oral, Health. Aust Dent J. 2020;65:30–8. https://doi.org/10.1111/adj.12742 . England PH., Department of Health and Social Care, NHS England, NHS Improvement, Delivering better oral health: an evidence-based toolkit for prevention, https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention (2021) Accessed 14 July 2023. Sjögren K, Birkhed D. Factors related to fluoride retention after toothbrushing and possible connection to caries activity. Caries Res. 1993;27:474–7. https://doi.org/10.1159/000261583 . Article PubMed Google Scholar Chestnutt IG, Schäfer F, Jacobson AP, Stephen KW. The influence of toothbrushing frequency and post-brushing rinsing on caries experience in a caries clinical trial. Community Dent Oral Epidemiol. 1998;26:406–11. https://doi.org/10.1111/j.1600-0528.1998.tb01979.x . Zamataro CB, Tenuta LM, Cury JA. Low-fluoride dentifrice and the effect of postbrushing rinsing on fluoride availability in saliva. Eur Arch Paediatr Dent. 2008;9:90–3. https://doi.org/10.1007/bf03262616 . Pornsri Patimanukaseam TT, Reeponmaha T. Fluoride content in saliva following tooth brushing with and without rinsing. Thai Dent Public Health J. 2012;17(2):109–16. Google Scholar Usman M, et al. Evaluation of the chronic intoxication of fluoride on human serum metabolome using untargeted metabolomics. Arab J Chem. 2022;15:103928. https://doi.org/10.1016/j.arabjc.2022.103928 . https://doi.org:. Mohammadi AA, Yousefi M, Yaseri M, Jalilzadeh M, Mahvi AH. Skeletal fluorosis in relation to drinking water in rural areas of West Azerbaijan, Iran. Sci Rep. 2017;7:17300. https://doi.org/10.1038/s41598-017-17328-8 . Article CAS PubMed PubMed Central Google Scholar Das TK, Susheela AK, Gupta IP, Dasarathy S, Tandon RK. Toxic effects of chronic fluoride ingestion on the upper gastrointestinal tract. J Clin Gastroenterol. 1994;18:194–9. https://doi.org/10.1097/00004836-199404000-00004 . Albahrani MM, Alyahya A, Qudeimat MA, Toumba KJ. Salivary fluoride concentration following toothbrushing with and without rinsing: a randomised controlled trial. BMC Oral Health. 2022;22:53. https://doi.org/10.1186/s12903-022-02086-5 . Guidance for Industry BIOEQUIVALENCE GUIDANCE. U.S. Department of Health and Human Services, Food and Drug Administration. Cent Veterinary Med (CVM) 15 (2006). Giacaman R, Fernández C, Muñoz-Sandoval C, Fuentes N. Longer Retention Time of Fluoridated Varnishes enhances Enamel Remineralisation in Vitro. Oral Health Prev Dent. 2017;15:1–5. https://doi.org/10.3290/j.ohpd.a38778 . Article Google Scholar Watson PS, et al. Penetration of fluoride into natural plaque biofilms. J Dent Res. 2005;84:451–5. https://doi.org/10.1177/154405910508400510 . Lynch RJ, Navada R, Walia R. Low-levels of fluoride in plaque and saliva and their effects on the demineralisation and remineralisation of enamel; role of fluoride toothpastes. Int Dent J. 2004;54:304–9. https://doi.org/10.1111/j.1875-595x.2004.tb00003.x . Sotthipoka K, Thanomsuk P, Prasopsuk R, Trairatvorakul C, Kasevayuth K. The effects of toothpaste amounts and post-brushing rinsing methods on salivary fluoride retention. J Health Res. 2018;32:421–31. https://doi.org/10.1108/JHR-11-2018-082 . Naumova EA, et al. Kinetics of fluoride bioavailability in supernatant saliva and salivary sediment. Arch Oral Biol. 2012;57:870–6. https://doi.org/10.1016/j.archoralbio.2012.01.011 . Talwar M, Tewari A, Chawla HS, Sachdev V, Sharma S. Fluoride concentration in Saliva following Professional Topical Application of 2% Sodium Fluoride Solution. Contemp Clin Dent. 2019;10:423–7. https://doi.org/10.4103/ccd.ccd_681_18 . Duckworth RM, Morgan SN. Oral fluoride retention after use of fluoride dentifrices. Caries Res. 1991;25:123–9. https://doi.org/10.1159/000261354 . Zero DT, et al. Studies of fluoride retention by oral soft tissues after the application of home-use topical fluorides. J Dent Res. 1992;71:1546–52. https://doi.org/10.1177/00220345920710090101 . Oliveby A, Ekstrand J, Lagerlöf F. Effect of salivary flow rate on salivary fluoride clearance after use of a fluoride-containing chewing gum. Caries Res. 1987;21:393–401. https://doi.org/10.1159/000261045 . Naumova EA, Gaengler P, Zimmer S, Arnold WH. Influence of individual saliva secretion on fluoride bioavailability. Open Dent J. 2010;4:185–90. https://doi.org/10.2174/1874210601004010185 . Duckworth RM, Stewart D. Effect of mouthwashes of variable NaF concentration but constant NaF content on oral fluoride retention. Caries Res. 1994;28:43–7. https://doi.org/10.1159/000261619 . Opydo-Szymaczek J, Pawlaczyk-Kamieńska T, Borysewicz-Lewicka M. Fluoride Intake and Salivary Fluoride Retention after using high-fluoride toothpaste followed by Post-brushing Water Rinsing and Conventional (1400–1450 ppm) fluoride toothpastes used without rinsing. Int J Environ Res Public Health. 2022;19. https://doi.org/10.3390/ijerph192013235 . Iorgulescu G. Saliva between normal and pathological. Important factors in determining systemic and oral health. J Med Life. 2009;2:303–7. PubMed PubMed Central Google Scholar Bronckers AL, Lyaruu DM, DenBesten PK. The impact of fluoride on ameloblasts and the mechanisms of enamel fluorosis. J Dent Res. 2009;88:877–93. https://doi.org/10.1177/0022034509343280 . Fejerskov O, Manji F, Baelum V. The nature and mechanisms of dental fluorosis in man. J Dent Res. 1990;69(Spec No):692–700. https://doi.org/10.1177/00220345900690s135 . discussion 721. Gopu BP, et al. The relationship between Fluoride exposure and cognitive outcomes from Gestation to Adulthood-A systematic review. Int J Environ Res Public Health. 2022;20. https://doi.org/10.3390/ijerph20010022 . Ramesh M et al. The prevalence of dental fluorosis and its associated factors in Salem district. Contemp Clin Dent 7 (2016). Marques RB, et al. Fluoridated water impact on tooth decay and fluorosis in 17-20-year-olds exposed to fluoride toothpaste. J Public Health Dent. 2022;82:385–94. https://doi.org/10.1111/jphd.12472 . Curtis AM, et al. Decline in Dental Fluorosis Severity during Adolescence: a Cohort Study. J Dent Res. 2020;99:388–94. https://doi.org/10.1177/0022034520906089 . Bårdsen A, Bjorvatn K. Risk periods in the development of dental fluorosis. Clin Oral Investig. 1998;2:155–60. https://doi.org/10.1007/s007840050063 . Nakornchai S, Hopattaraput P, Vichayanrat T, Prevalence, severity and factors associated with dental. Fluorosis among children aged 8–10 years in Bangkok, Thailand. Southeast Asian J Trop Med Public Health. 2016;47:1105–11. PubMed Google Scholar Bhagavatula P, Levy SM, Broffitt B, Weber-Gasparoni K, Warren JJ. Timing of fluoride intake and dental fluorosis on late-erupting permanent teeth. Community Dent Oral Epidemiol. 2016;44:32–45. https://doi.org/10.1111/cdoe.12187 . Choubisa SL, Choubisa L, Choubisa D. Osteo-dental fluorosis in relation to age and sex in tribal districts of Rajasthan, India. J Environ Sci Eng. 2010;52:199–204. CAS PubMed Google Scholar Franzman MR, Levy SM, Warren JJ, Broffitt B. Fluoride dentifrice ingestion and fluorosis of the permanent incisors. J Am Dent Assoc. 2006;137:645–52. https://doi.org/10.14219/jada.archive.2006.0261 . Gebretsadik HG, Skeletal Fluorosis. A risk factor of bone fractures among adults in Ethiopia: a case-control study. J Orthop Sports Med (2023). Farid H, Khan FR. Clinical management of severe fluorosis in an adult. BMJ Case Rep 2012 (2012). https://doi.org/10.1136/bcr-2012-007138 Tefera N, et al. Association between Dietary Fluoride and Calcium Intake of School-Age children with symptoms of Dental and skeletal fluorosis in Halaba, Southern Ethiopia. Front Oral Health. 2022;3. https://doi.org/10.3389/froh.2022.853719 . Chuang AH, Bordlemay J, Goodin JL, McPherson JC. Effect of Sodium Lauryl Sulfate (SLS) on primary human gingival fibroblasts in an in Vitro Wound Healing Model. Mil Med. 2019;184:97–101. https://doi.org/10.1093/milmed/usy332 . Tabatabaei MH, Mahounak FS, Asgari N, Moradi Z. Cytotoxicity of the ingredients of commonly used toothpastes and mouthwashes on human gingival fibroblasts. Front Dent. 2019;16:450–7. https://doi.org/10.18502/fid.v16i6.3444 . Krisdapong S. Spit don’t rinse -. J Health Sci Thail. 2017;26:S348–59. 7 Final Report on the Safety Assessment of Sodium Lauryl Sulfate and Ammonium Lauryl Sulfate. J Am Coll Toxicol. 1983;2:127–81. https://doi.org/10.3109/10915818309142005 . Committee on Fluoride in Drinking Water, Fluoride in Drinking Water: A Scientific Review of EPA’s Standards, National Academy of Sciences, Engineering, and Medicine, https://nap.nationalacademies.org/catalog/11571/fluoride-in-drinking-water-a-scientific-review-of-epas-standards (2006) Accessed. Susheela AK, Bhatnagar M. Reversal of fluoride induced cell injury through elimination of fluoride and consumption of diet rich in essential nutrients and antioxidants. Mol Cell Biochem. 2002;234–235:335–40. Sjögren K, Ekstrand J, Birkhed D. Effect of water rinsing after toothbrushing on fluoride ingestion and absorption. Caries Res. 1994;28:455–9. https://doi.org/10.1159/000262020 . The United States Environmental Protection Agency (EPA), Safe Drinking Water Act, Fluoride Risk Assessment and Relative Source Contribution, https://www.epa.gov/sdwa/fluoride-risk-assessment-and-relative-source-contribution (2010) Accessed 5 April 2024. Nayak B, et al. Health effects of groundwater fluoride contamination. Clin Toxicol (Phila). 2009;47:292–5. https://doi.org/10.1080/15563650802660349 . Patcharaporn Gavila SC. and Thantrira Porntaveetus. in Urinary and Water Fluoride Concentrations in Dental Fluorosis Patients in Thailand. The 19th International Scientific Conference of the Dental Faculty Consortium of Thailand (DFCT 2022). 204–209. Schiffl H, Binswanger U. Renal handling of Fluoride in Healthy Man. Ren Physiol. 2008;5:192–6. https://doi.org/10.1159/000172857 . Spak CJ, Berg U, Ekstrand J. Renal clearance of fluoride in children and adolescents. Pediatrics. 1985;75:575–9. Whitford GM, Pashley DH, Stringer GI. Fluoride renal clearance: a pH-dependent event. Am J Physiology-Legacy Content. 1976;230:527–32. https://doi.org/10.1152/ajplegacy.1976.230.2.527 . Mahabadi AMN. Volume Distribution, July 24, 2023) Accessed 31 March 2024. Thompson LJ. In: Gupta RC, editor. Veterinary toxicology (Third Edition). Academic; 2018. pp. 429–31. Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride, https://www.ncbi.nlm.nih.gov/books/NBK109832/ (1997) Accessed 23 Jan 2024. Marília AR, Buzalafa GMW. Fluoride metabolism. Monogr Oral Sci. 2011;22:20–36. Fowler CE, et al. The effect of dentifrice ingredients on enamel erosion prevention and repair. Surf Interface Anal. 2021;53:528–39. https://doi.org/10.1002/sia.6940 . Vogel GL, Schumacher GE, Chow LC, Tenuta LM. Oral fluoride levels 1 h after use of a sodium fluoride rinse: effect of sodium lauryl sulfate. Caries Res. 2015;49:291–6. https://doi.org/10.1159/000381192 . Bureau of Dental Health, Ministry of Public Health, Thailand, Report the fluoride content in bottled drinking water and mineral water as reference data for dispensing fluoride supplements for children, Survey on bottled drinking water and mineral water readily available in convenient stores in Bangkok, September - November 2016., https://dental.anamai.moph.go.th/ (2016) Accessed 1 Feb 2024. Carwile JL, Ahrens KA, Seshasayee SM, Lanphear B, Fleisch AF. Predictors of plasma fluoride concentrations in children and adolescents. Int J Environ Res Public Health. 2020;17. https://doi.org/10.3390/ijerph17249205 . Download references AcknowledgementsThe authors acknowledge the Faculty of Dentistry, Mahidol University, for their generous support, which made this research possible. We would like to express our deepest appreciation to all participants who dedicated their time and effort to this study, as their valuable contributions significantly enriched our research and advanced our understanding in this field. Additionally, we wish to acknowledge the invaluable contributions of the reviewers and editors whose insightful comments and suggestions greatly enhanced the quality and clarity of this manuscript. This research is funded by the Faculty of Dentistry, Mahidol University. Open access funding provided by Mahidol University Author informationAuthors and affiliations. Department of Pharmacology, Faculty of Dentistry, Mahidol University, Bangkok, Thailand Tipparat Parakaw, Sirada Srihirun, Pornpen Dararat & Nisarat Ruangsawasdi You can also search for this author in PubMed Google Scholar ContributionsTP contributed to the study design, conducted experiments, collected and analyzed data, interpreted the findings, and was a major contributor to manuscript writing and preparation. SS provided guidance during the experiments, assisted with data interpretation, and critically reviewed the manuscript. PD participated in subject recruitment, prepared materials, and collected data. NR contributed to the study design, provided guidance during the experiments, interpreted data, critically reviewed the manuscript, and offered revisions and advice on the manuscript. All authors have read and approved the final manuscript. Corresponding authorCorrespondence to Nisarat Ruangsawasdi . Ethics declarationsEthics approval and consent to participate. The study was approved by the Committee on Human Rights Related to Human Experimentation, Mahidol University, Thailand (COA. No. MU-DT/PY-IRB 2023/063.2609). The written informed consent was obtained from all the study participants. Consent for publicationNot applicable. Competing interestsThe authors declare no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . Reprints and permissions About this articleCite this article. Parakaw, T., Srihirun, S., Dararat, P. et al. Kinetics of fluoride after brushing with the no-rinse method. BMC Oral Health 24 , 1050 (2024). https://doi.org/10.1186/s12903-024-04807-4 Download citation Received : 15 May 2024 Accepted : 23 August 2024 Published : 08 September 2024 DOI : https://doi.org/10.1186/s12903-024-04807-4 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative BMC Oral HealthISSN: 1472-6831
Is Fluoride Bad for You? We Brushed Up on the Science of Toothpaste’s Star IngredientFluoride has recently come under fire—but what does the research say?  What is fluoride?Fluoride benefits, fluoride downsides, the bottom line, fluoride alternatives. Who hasn’t dashed into the drugstore and been stymied by the overwhelming number of toothpaste options: mint, fruity, gel, whitening, sensitive—and, increasingly, fluoride-free? Even major companies like Colgate have followed the trend, joining no-fluoride mainstays like Dr. Bronner’s and Tom’s of Maine. No wonder global sales of toothpaste sans fluoride—a mineral—are over $6 billion and projected to soar above $10 billion within a decade. But is fluoride bad for you? Meet the experts: Mark Wolff, D.D.S., Ph.D., dean of the School of Dental Medicine at the University of Pennsylvania; Dominik Nischwitz, D.D.S., a biological dentist and the author of It’s All in Your Mouth ; Howard Pollick, B.D.S., M.P.H., a spokesperson on fluoridation for the American Dental Association (ADA) There’s a reason it’s in so many products, after all. Prevention bit into years of research to find out. It’s a mineral that appears naturally in rocks, soil, and water. Fluoride was added to toothpaste, as well as many community water systems, in the 1950s after scientists realized that people whose drinking water was naturally higher in fluoride had much less tooth decay. But lately there has been growing criticism of fluoride, with some communities passing or debating legislation to remove the mineral from their water. And now the debate has reached the toothpaste aisle. To some extent, say many dentists, fluoride is a victim of its own success—it’s a key reason so many of us sport healthy smiles. We’re so unused to major tooth decay that we’ve forgotten how we got here. As Americans decades ago were all too aware, cavities are destructive holes in teeth that form when the bacteria that consume sugars in our mouths (from sweets and other carbs) produce acids. These acids can dissolve the protective enamel on a tooth’s surface, forming a cavity. Fluoride strengthens resistance to acid and can replenish some of the enamel the bacteria destroy, says Mark Wolff, D.D.S., Ph.D., dean of the School of Dental Medicine at the University of Pennsylvania. In children, fluoridated water strengthens permanent teeth as they start to come in. “We take for granted that we don’t have as much tooth decay,” says Wolff, who has consulted for toothpaste brands, but “it will return if we stop using fluoride.” Even just 50 years ago, he says, “the number of people with decay was massive.” Nearly 100 toothpaste studies back up the claim that children, teens, and adults who regularly brush with fluoridated toothpaste have much less decay, researchers with the highly regarded Cochrane Library have determined. Another sign of fluoride’s potency: When parts of Canada stopped putting the mineral in their water, more kids in these zones needed dental work, with children 5 and under most at risk, researchers reported earlier this year. “The fluoride research is very clear: Fluoride helps remineralize early and even later-stage cavities,” stopping them from forming or getting worse, says Gretchen Gibson, D.D.S., M.P.H., an associate professor at Kansas City University’s College of Dental Medicine. Even if your local water system adds fluoride (as is currently true in some 73% of the country), having fluoride in toothpaste is important because its protection is applied directly to teeth. “Not having fluoride in toothpaste increases the risk that more of your teeth will decay and need treatment,” says Howard Pollick, B.D.S., M.P.H., a spokes person on fluoridation for the American Dental Association (ADA). For people at high risk for cavities, including those with a history of decay and kids who don’t always brush well, a dentist can also apply fluoride directly to teeth. A different Cochrane Library review found fewer cavities in kids who used fluoride toothpaste and whose dentists applied a fluoride gel, varnish, or mouth rinse during cleaning appointments.  The research seems pretty reassuring, right? Well, that’s where things get a bit tricky. Despite fluoride’s well-researched benefits, there is controversy over whether it is in fact safe to consume. Over the years, water fluoridation has been called everything from government mind control to a Communist plot by people on the extreme end of the debate. That said, research does show that extremely high levels of fluoride can be dangerous. Most of the proven problems are from overconsumption, with very high doses being shown to cause mottled teeth, bone damage, and joint problems, among other issues. This research has involved areas around the world with naturally extreme levels of fluoride in their groundwater, not communities where small, controlled amounts of fluoride are added. Still, the findings have caused some to sour on fluoride. One concern researchers are still working through has to do with the idea that fluoride could be dangerous to the brain and nervous system, especially in young children, perhaps by causing inflammation and changes to brain cells. This potentially very scary issue, known as neurotoxicity, got a lot of attention when Canadian researchers found an association with slightly lower IQ levels in the preschool sons (but, oddly, not daughters) of women who’d had higher fluoride exposure while pregnant. Other researchers linked lower IQ in children in India with naturally high fluoride in their water. But there are limits to this research: Both of these studies were what is known as observational, meaning they didn’t prove that one factor caused the other. Another issue was that this research involved fluoride in drinking water, not in toothpaste, which people are not meant to swallow. Even if someone did eat a little, as children commonly do, the amount ingested would be minuscule in comparison to the levels people in these studies took in. Some anti-fluoride folks, especially those known as biological dentists who also advocate the removal of heavy metals from prior mercury fillings, say they’ll never support fluoride in toothpaste. “Even if the results are not 100% clear, I would always go the safer route and avoid fluoride,” says Dominik Nischwitz, D.D.S., a biological dentist and the author of It’s All in Your Mouth . A comprehensive assessment from the U.S. Department of Health and Human Services, performed by the National Toxicology Program (NTP), hopes to alleviate concerns about neurotoxicity, but the NTP, which first came together to study the subject in 2015, has yet to release its final report. An incomplete draft that was made public revived the controversy, with an association of biological dentists claiming that the report raised concerns “about the long-term negative health effects of fluoride exposure.” The interim draft was subsequently reviewed by a specially convened working group that made a lot of changes, citing insufficient information and lack of precision in the text. A new draft is in the works and should be published soon. Until that report comes out, people who wonder if they should be buying fluoride-free toothpastes (or the best natural toothpastes ) may be reassured by the ADA’s assessment that fluoride remains safe for children and adults. A review from German researchers also concluded that evidence “does not support” calling fluoride a neurotoxin. “In the amount people are consuming through toothpaste after spitting, I do not worry about it creating problems,” says Wolff. In fact, fluoride amounts are regulated by the U.S. Food and Drug Administration; companies can’t simply load up their pastes with astronomical levels of it. If people take proper care of their teeth, many can remain cavity-free, he adds, and fluoride toothpaste is the way to do it. “This is true for children, adults, and seniors alike,” Pollick says. If you go fluoride-free, you’ll need to severely limit sugary snacks and beverages to keep bacteria and their acids away from your teeth, Pollick says. If you’re unsure, you could use a paste with the fluoride alternative hydroxyapatite, such as Davids; small studies have shown that this ingredient also prevents cavities, but there’s less research proving its safety than there is for fluoride.  New Study Says Coffee May Help With Muscle Mass  How Hypnosis Helped One Woman in Agony With IBS  This Pillow for Neck Pain Is On Sale for Under $40  COVID-19 Symptoms to Know in 2024  20 Foods That Lower Blood Pressure Naturally  All About Wetland Virus, a New Tick-Borne Illness  Kate Middleton’s Cancer Journey  This Diabetes Medication May Lower Dementia Risk  Keep Track of Meds With These Pill Organizers  The Invincibility Fallacy  When to Get the New COVID-19 Vaccine  How to Stay Safe During the Deli Meat Recall An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
 Developmental fluoride neurotoxicity: an updated reviewPhilippe grandjean. 1 Department of Environmental Health, Harvard T.H. Chan School of Public Health, Boston, MA 02115 USA 2 Department of Public Health, University of Southern Denmark, Odense, Denmark Associated DataAfter the discovery of fluoride as a caries-preventing agent in the mid-twentieth century, fluoridation of community water has become a widespread intervention, sometimes hailed as a mainstay of modern public health. However, this practice results in elevated fluoride intake and has become controversial for two reasons. First, topical fluoride application in the oral cavity appears to be a more direct and appropriate means of preventing caries. Second, systemic fluoride uptake is suspected of causing adverse effects, in particular neurotoxicity during early development. The latter is supported by experimental neurotoxicity findings and toxicokinetic evidence of fluoride passing into the brain. An integrated literature review was conducted on fluoride exposure and intellectual disability, with a main focus on studies on children published subsequent to a meta-analysis from 2012. Fourteen recent cross-sectional studies from endemic areas with naturally high fluoride concentrations in groundwater supported the previous findings of cognitive deficits in children with elevated fluoride exposures. Three recent prospective studies from Mexico and Canada with individual exposure data showed that early-life exposures were negatively associated with children’s performance on cognitive tests. Neurotoxicity appeared to be dose-dependent, and tentative benchmark dose calculations suggest that safe exposures are likely to be below currently accepted or recommended fluoride concentrations in drinking water. The recent epidemiological results support the notion that elevated fluoride intake during early development can result in IQ deficits that may be considerable. Recognition of neurotoxic risks is necessary when determining the safety of fluoride-contaminated drinking water and fluoride uses for preventive dentistry purposes. In 2006, the U.S. National Research Council (NRC) evaluated the fluoride standards of the Environmental Protection Agency (EPA) and concluded that fluoride can adversely affect the brain through both direct and indirect means, that elevated fluoride concentrations in drinking-water may be of concern for neurotoxic effects, and that additional research was warranted [ 1 ]. At the time, and continuing through today, the EPA’s Maximum Contaminant Level Goal (MCLG) for fluoride was 4.0 mg/L that aimed at protecting against crippling skeletal fluorosis, which is still considered to be the critical adverse health effect from fluoride exposure [ 2 ]. Following the NRC review, evidence has accumulated that the developing human brain is inherently much more susceptible to injury from neurotoxic agents, such as fluoride, than is the adult brain [ 3 ]. A review and meta-analysis published in 2012 [ 4 ] assessed a total of 27 research reports, all but two of them from China, on elevated fluoride exposure and its association with cognitive deficits in children. All but one study suggested that a higher fluoride content of residential drinking water was associated with poorer IQ performance at school age. Only a couple of these studies had been considered by regulatory agencies [ 1 , 5 ]. As much additional evidence has emerged since then, it seems appropriate to update the assessment of potential human neurotoxicity associated with elevated fluoride exposure, especially during early development. The present review first outlines the importance of drinking water as a source of fluoride exposure, followed by the toxicokinetics of fluoride absorbed into the body, including passage through the placenta and the blood-brain barrier, and finally a brief summary of the experimental evidence of developmental neurotoxicity. All of this evidence supports the plausibility that elevated fluoride exposure in early life may cause adverse effects on the brain. The main part of this review addresses the epidemiological studies of fluoride neurotoxicity, with a focus on children and the dose-dependent impact of prenatal and early postnatal exposures. Potential sources of fluoride exposureFluoride occurs in many minerals and in soil [ 6 ], thus also in groundwater; the average concentration in the U.S. is 0.26 mg/L [ 7 ]. Since the mid-1940s, fluoride has been added to many community water supplies with the aim of preventing tooth decay [ 8 ]. In the U.S., fluoridation is recommended at a concentration of 0.7 mg/L [ 9 ]. Water fluoridation is applied in several other countries as well, such as Australia, Brazil, Canada, Chile, Ireland, New Zealand, and the United Kingdom. For adults in the U.S., fluoridated water and beverages contribute an average of about 80% of the daily total fluoride intake (estimated to average 2.91 mg) in fluoridated communities [ 10 ]. In a Canadian study of pregnant women [ 11 ], water fluoridation was the major predictor of urinary fluoride excretion levels, with creatinine-adjusted concentrations of 0.87 mg/L and 0.46 mg/L in fluoridated (0.6 mg/L water) and non-fluoridated (0.12 mg/L) communities. In addition to fluoridated water and other forms of caries prevention, tea is an important source of fluoride exposure, even if prepared with deionized water [ 12 , 13 ]. Additional sources of fluoride intake include certain foods (such as sardines), industrial emissions, supplements, pesticide residues, and certain pharmaceuticals that can release fluoride [ 1 ]. Few studies provide population-based data on fluoride exposure, although national data on plasma-fluoride concentrations are available from a recent NHANES study in the U.S. [ 14 ]. Uptake, distribution and retentionApproximately 75–90% of ingested fluoride is absorbed and readily distributed throughout the body, with approximately 99% of retained fluoride being bound in calcium-rich tissues such as bone and teeth [ 6 , 15 ] as well as the calcified parts of the pineal gland [ 16 ]. Fluoride also crosses the placenta and reaches the fetus [ 1 , 6 ] and the amnionic fluid [ 17 ]. The fluoride concentration in breast milk is low, generally less than 0.01 mg/L [ 1 , 18 ], and formula can therefore contribute much higher intakes, especially when prepared with high-fluoride water [ 19 – 21 ]. Children and infants retain higher proportions of absorbed fluoride compared to adults, i.e., about 80–90%, as compared to about 50–60% in adults [ 6 , 15 ]. As drinking water is usually the major source of exposure, the community water-fluoride concentration has often been used as an exposure parameter in ecological studies. For individual exposure assessment, the total fluoride intake can be calculated from daily water consumption and the intakes of other major sources, such as tea. Analyses of biological samples, i.e., urine and blood (generally in the form of plasma or serum) provide information on fluoride circulating in the body [ 22 ]. In adults, the fasting plasma-fluoride concentration, when expressed in micromoles per liter [μmol/L], is approximately equal to the concentration in the drinking water or in the urine expressed in mg/L [ 1 ]. Fluoride excretion is mainly via urine, and the concentration represents both recent absorption and releases from long-term accumulation due to continuous bone tissue remodeling [ 6 ]. Pregnant women may show lower urinary fluoride levels than non-pregnant controls, perhaps due to fetal uptake and storage in hard tissues [ 23 ], although the urinary fluoride excretion tends to increase from the first to the third trimester [ 11 , 24 ]. Children have lower urine-fluoride concentrations, most likely due to fluoride incorporation in the growing skeleton [ 1 ]. As indicator of daily intake [ 25 , 26 ], urinary fluoride excretion is often assessed in spot urine samples, although morning urine or 24-h samples may provide better precision, as may be the case with timed excretion [ 27 ]. To adjust for temporal differences in urine production, fluoride concentrations in spot samples are usually standardized according to the creatinine concentration and/or relative density. These considerations are important when evaluating the validity of exposure assessments in epidemiological studies. While the blood-brain barrier may to some extent protect the adult brain from many toxic agents, this protection is less likely in the fetus and small child with an incompletely formed barrier [ 28 ]. As indication that fluoride passes the blood-brain barrier, fluoride concentrations in human cerebrospinal fluid approach those occurring in serum [ 29 ]. Further, imaging studies of radioactive fluoride used in cancer treatment document that circulating fluoride reaches the brain [ 30 – 33 ]. Within the brain, fluoride appears to accumulate in regions responsible for memory and learning [ 34 , 35 ]. As fluoride can pass both the placental barrier and the blood-brain barrier, it reaches the fetal brain [ 36 ]. Accordingly, autopsy studies in endemic areas in China have shown elevated fluoride concentrations in aborted fetal tissues, including brain [ 37 , 38 ]. Also, fluoride concentrations in maternal and cord serum correlate well [ 39 ], cord blood showing slightly lower concentrations, apparently about 80% of the concentrations in maternal serum [ 40 ], though depending on gestational age [ 17 ]. Fetal blood sampling techniques have allowed documentation of elevated fluoride concentrations in the fetal circulation after administration of sodium fluoride to the mother [ 41 ]. Accordingly, assessment of fluoride in maternal samples during pregnancy may be used as indicator of fetal exposure. Due to a well-established dose-response relationship between early-life fluoride exposure and the degree of dental fluorosis [ 6 , 20 , 42 ], this abnormality can serve as a useful biomarker of developmental fluoride exposure. When water fluoridation was first introduced in the middle of the twentieth century, U.S. health authorities estimated that less than 10% of children in fluoridated communities (at 1 mg/L water) would develop dental fluorosis, and only in its mildest forms [ 43 ]. Subsequent epidemiological studies have demonstrated prevalence and severity of fluorosis much higher than predicted [ 9 , 44 , 45 ]. Increased occurrence of dental fluorosis has also been recorded in fluoridated areas in the United Kingdom [ 46 ]. This increase may be related to the widened use of fluoridated water for beverages and food products for general consumption and for formula preparation for infants [ 19 , 21 ], as well as increased usage (and ingestion) of fluoride-containing toothpastes among preschoolers [ 47 ]. Experimental neurotoxicityIn vitro studies have documented fluoride toxicity to brain cells, most of the studies using high fluoride concentrations, though some effects have been demonstrated at lower, more realistic levels [ 48 , 49 ]. In the low-dose studies, 0.5 μmol/L (10 μg/L) was sufficient to induce lipid peroxidation and result in biochemical changes in brain cells [ 48 ], while 3 μmol/L (57 μg/L) induced inflammatory reactions in brain cells [ 49 ]. These concentrations are similar to the upper ranges of serum-fluoride levels reported in the general population [ 6 ]. In addition, fluoride can negatively affect brain development in rats at levels below those that cause dental lesions [ 50 ]. Utilizing computerized surveillance of rat behavior, a landmark study showed signs of neurotoxicity at elevated fluoride exposure [ 51 ], and more recent studies have reported fluoride-induced neurochemical, biochemical, and anatomic changes in the brains of treated animals, although often at doses much above human exposure levels. Among possible mechanisms of developmental neurotoxicity is toxicity to the thyroid gland [ 52 ], a mechanism relevant in regard to several neurotoxicants [ 53 , 54 ]. Thus, the NRC concluded that fluoride is an endocrine disrupter that can affect thyroid function at intake levels as low as 0.01 to 0.03 mg/kg/day in individuals with iodine deficiency [ 1 ]. A 2016 review by the National Toxicology Program (NTP) focused on fluoride neurotoxicity in regard to learning and memory [ 55 ]. At water concentrations higher than 0.7 mg/L, NTP found a low-to-moderate level of evidence. The evidence was the strongest (moderate) in animals exposed as adults and weaker (low) in animals exposed during development, where fewer studies were available at relevant exposure levels. Most experimental studies had used concentrations exceeding the levels added to water in fluoridation programs, but the NTP recognized that rats require about five times more fluoride in their water to achieve the same serum-fluoride concentrations as humans [ 55 ]. Subsequently, several additional developmental studies have been published, including two that reported impaired learning/memory in rats consuming water with fairly low fluoride concentrations [ 56 , 57 ]. However, not all studies have reported adverse effects [ 58 ], perhaps due in part to strain or species-related differences in vulnerability to fluoride. In addition, most animal studies used subchronic exposure scenarios and, due to the lack of fluoride transfer into milk, neonatal exposure was not considered, thereby likely underestimating the effect from early-life exposure. Overall, the experimental evidence of developmental neurotoxicity appears to be strengthened and to provide plausibility to the potential occurrence of neurodevelopmental effects in humans. Publications on fluoride neurotoxicity in humans were identified from the PubMed data base by using “fluoride” along with search terms “neurotoxic*”, “neurologic”, and “intelligence”. The searches were narrowed by limiting to “human,” “most recent 10 Years,” and “English.” Additional searches using “fluoride” also included search terms “prenatal exposure delayed effects”[MeSH] or “neurotoxicity syndrome”[MeSH]. Secondary searches used combinations of fluoride with “maternal exposure” or “academic disorder, developmental”. Supporting literature from earlier years was obtained by using the terms “occupational exposure” or “endemic disease”. References cited in the publications and in recent review reports [ 55 , 59 – 61 ] were also retrieved, as were publications listed by PubMed under “Similar articles”. Because these articles may not represent an exhaustive list of relevant studies, separate searches included the web site of the journal Fluoride ( http://www.fluorideresearch.org/ ) and the site ( http://oversea.cnki.net/kns55/default.aspx ) that covers many Chinese-language journals not included in PubMed. Full-text copies of all relevant studies were obtained, and studies were disregarded if no more than an abstract in English was available. For the purpose of identifying safe exposure levels, regulatory agencies routinely use benchmark dose calculations [ 62 ]. While such calculations would normally require access to the original data, approximate BMD and BMDL results can be generated from descriptive data on associations between maternal urinary fluoride concentrations and the child’s IQ [ 63 ]. The benchmark dose (BMD) is the dose leading to a pre-defined change (denoted BMR) in the response (in this case, an IQ loss), when compared to comparable, but unexposed individuals. The BMR must be defined before the analysis [ 62 ], and recent practice suggests that a decrease in IQ of one point is an appropriate BMR [ 64 – 67 ]. In the above framework, the difference between the expected IQ level at the unexposed background (E [Y (0)]) and at the BMD (E [Y (BMD)]) is equal to the BMR: In a linear model (Y(d) = α + βd + ɛ), we get BMD = −BMR/β. The main result of the benchmark analysis is the benchmark dose level (BMDL), which is defined as a lower one-sided 95% confidence limit of the BMD. In the linear model where β lower is the one-sided lower 95% confidence limit for β [ 67 ]. Thus, in this model the benchmark results are a function of statistics routinely calculated in regression analysis. For a linear dose-response model, epidemiological studies that report developmental fluoride exposure in regard to IQ will allow computation of BMD and BMDL based only on the regression coefficient and its uncertainty, assuming a Gaussian distribution. Occupational and endemic area studiesThe neurotoxicity of chemicals is often first discovered from workplace exposures [ 68 ], later followed by case reports and small studies of highly-exposed children or pregnant women, then confirmed in population studies that are later complemented by prospective studies [ 69 ]. The same seems to be true of fluoride. A brief summary is therefore presented on the progress of this evidence before focusing on developmental exposures. In connection with his seminal studies of occupational fluoride poisoning in the 1930s, Kaj Roholm reported evidence of nervous system effects in the Copenhagen cryolite workers [ 70 ]: “The marked frequency of nervous disorders after employment has ceased might indicate that cryolite has a particularly harmful effect on the central nervous system.” (p. 178). Later on, the Manhattan Project in the 1940s recorded neurological effects in workers exposed to uranium hexafluoride gas (UF 6 ), and the “rather marked central nervous system effect with mental confusion, drowsiness and lassitude as the conspicuous features” was attributed to the fluoride rather than uranium [ 71 ]. Subsequent occupational health studies are somewhat harder to interpret, as fluoride exposure usually occurs as part of a mixture, e.g., in aluminum production [ 72 ]. Nonetheless, industrial fluorosis (a.k.a. osteosclerosis) was found to be associated with gradually progressive effects on the normal function and metabolism of the brain and other aspects of the nervous system [ 73 ], and a review highlighted difficulties with concentration and memory accompanied by general malaise and fatigue [ 74 ]. More recent studies have applied neuropsychological tests to assess cognitive problems associated with occupational fluoride exposures [ 75 , 76 ]. The present literature search did not reveal any recent publications on neurotoxicity from occupational fluoride exposure. While Roholm [ 70 ] described unusually serious dental fluorosis in a son of a female cryolite worker, none of the occupational studies identified referred to adverse neurobehavioral effects in the progeny of female workers. Opportunities for epidemiological studies of the general population depend on the existence of comparable groups exposed to different and stable amounts of fluoride, e.g., from drinking water. Such circumstances are difficult to find in many industrialized countries, as water-fluoride concentrations may not be well defined, residents may consume beverages from a variety of sources, and exposures are affected by residences changing over time. Multiple epidemiological studies of developmental fluoride neurotoxicity have been conducted in countries such as China where elevated water-fluoride concentrations may exceed 1 mg/L in many rural communities. In these settings, families typically remain at the same residence, with a well-defined water source that has provided fairly constant fluoride exposures. Studies from high-fluoride endemic areas in China have reported on abnormal neuropathology findings from aborted fetuses [ 37 ] and lower nerve cell numbers and volumes in fetal brain tissue at the elevated exposures [ 38 ]. Deviations observed in neurotransmitters and receptors have suggested neural dysplasia [ 77 ], as later replicated along with decreased excitatory aspartic acid and elevated inhibitory taurine in comparison to controls [ 78 ]. Although these studies are in agreement with the notion that fluoride from the mother’s circulation can pass into the fetal brain with subsequent anatomic and biochemical changes, the studies related to elevated fluoride exposure originate primarily from coal burning, which may have contributed other, undocumented contaminants. Additional community studies in adults have focused on cognitive problems and neurological symptoms in subjects with skeletal fluorosis. Using neuropsychological tests, including the Wechsler scale, 49 adult fluorosis patients were compared with controls and showed deficits in language fluency, recognition, similarities, associative learning, and working memory [ 79 ]. Further, cognitive impairment in elderly subjects from a waterborne fluorosis area was found to be much more common than in less-exposed controls [ 80 ]. Dementia diagnosis in North Carolina was more common at higher water-fluoride concentrations [ 81 ], and similar findings for fluoride (and aluminum) have recently been reported from Scotland [ 82 ]. Excess occurrence of neurological symptoms (i.e., headaches, insomnia, and lethargy) have also been recorded in both adults and children from waterborne fluorosis areas [ 83 ]. However, these studies are hard to evaluate due to uncertainty about past fluoride exposure levels and the possible influence of other risk factors. The literature search did not reveal any other recent studies that added important evidence in this regard. Cross-sectional studies of children in exposed communitiesMost studies that have investigated fluoride’s impact on childhood IQ are from locations in China with elevated exposure to fluoride, within and outside of known endemic areas [ 1 , 4 , 84 ]. When water supplies derive from springs or mountain sources, small or large pockets of increased exposures may be created near or within similar areas of lower exposures, thus representing useful epidemiology settings. The fluoride exposure from the household water would then represent the only or major difference between nearby neighborhoods. At the time, children in rural China had very little exposure to fluoridated dental products [ 85 ]. The local water-fluoride concentration can then serve as a feasible and appropriate exposure parameter, and some studies emphasized that the children were born in the particular study area, and/or had been using the same water supply since birth. Reliable exposure assessment then becomes possible when rural families remain for a long time at the same residence. Any deviation from stable exposure would result in exposure misclassification and thereby a likely underestimation of the toxicity [ 86 ]. Thus, the consistency of study findings supports the likelihood that developmental fluoride exposure causes cognitive deficits [ 4 ]. Although the study designs are technically cross-sectional, many of the settings allowed consideration of the current exposure as an indicator also of a longer-term exposure level. Most study reports have not been widely disseminated and considered in literature reviews. Four studies from China that were published in English [ 87 – 90 ] were cited in the 2006 NRC report [ 1 ], while the World Health Organization (WHO) considered only two [ 87 , 90 ] in its revised Environmental Health Criteria document on fluoride from 2002 [ 26 ]. A meta-analysis from 2007 included five studies [ 91 ], four of which were not in a subsequent review [ 84 ]. The latter review was cited by the EU Scientific Committee on Health and Environmental Risks (SCHER) working group in 2010 [ 5 ] in support of a conclusion that the evidence of neurotoxicity was insufficient. A meta-analysis from 2012 was based on a collaboration with Chinese experts on fluoride toxicity and covered 27 cross-sectional studies reporting associations between children’s intelligence and their fluoride exposure [ 4 ]. Overall, children who lived in areas with high fluoride exposure had lower IQ scores than those who lived in low exposure or control areas, the average difference being close to 7 IQ points. These findings were consistent with an earlier review [ 84 ], but included nine more studies and more systematically addressed study selection, exclusion information, and bias assessment. Two of the 27 studies that we included in the analysis were conducted in Iran [ 92 , 93 ], while all other study populations were from China. Two cohorts were exposed to fluoride from coal burning [ 94 , 95 ], but otherwise the study populations were exposed to fluoride through drinking water contaminated from soil minerals. Due to the use of different cognitive tests, normalized data were used to estimate the possible effects of fluoride exposure on intelligence. The results were materially unchanged in various sensitivity analyses, as were analyses that excluded studies with possible concerns about co-factors, such as iodine deficiency and arsenic toxicity, or non-water fluoride exposure from coal burning [ 4 ]. Among the 27 studies, all but one showed random-effect standardized mean difference (SMD) estimates that indicated an inverse association, ranging from − 0.95 to − 0.10 (one study showed a slight, non-significant effect in the opposite direction). The overall random-effects SMD estimate (and 95% confidence interval, CI) was − 0.45 (− 0.56, − 0.34). Given that the standard deviation (SD) for the IQ scale is 15, an SMD of − 0.45 corresponds to a loss of 6.75 IQ points. Although substantial heterogeneity was present among the studies, there was no clear evidence of publication bias [ 4 ]. Given the large number of studies showing cognitive deficits associated with elevated fluoride exposure under different settings, the general tendency of fluoride-associated neurotoxicity in children ( p < 0.001) seems robust. Recent cross-sectional studies of childrenThe present study presents an updated literature search that revealed 14 new studies on the association between early-life fluoride exposure and IQ in children (Table 1 ). All 14 studies reported apparent associations between elevated fluoride exposure and reduced intelligence, although one did not reach statistical significance. The several new Chinese-language studies showed similar associations between fluoride exposure and reduced IQ [ 96 , 101 – 103 , 105 , 107 , 108 ], although often published as short reports in national journals and according to the standards of science at the time. Similar findings were reported from India [ 98 , 100 , 110 ] and Africa [ 104 , 106 ]. As with the previous reports, most of these newer studies suffer from limitations of covariate reporting, which limited the opportunity to assess possible bias. Also, a variety of outcomes have been employed, such as neuropsychological tests and Raven-based intelligence scales. Of note, fluoride exposure was accompanied by other contaminants from coal burning in some studies [ 96 , 99 , 101 , 102 ]. Four studies used the degree of dental fluorosis as exposure parameter, and three of them reported a clear negative association with IQ [ 100 , 103 , 107 ], although statistical significance was not reached in one study [ 102 ]. The water-fluoride concentrations tended to be somewhat lower than in previous studies and thus more relevant to exposures occurring outside of endemic areas. Characteristics of 14 cross-sectional studies of fluoride exposure and children’s cognitive and developmental outcomes published after 2012
a Raven’s Standardized Progressive Matrices; b Wide Range Assessment of Memory and Learning; c Wechsler Intelligence Scale for Children-Revised; d Raven’s Colored Progressive Matrices; e Combined Raven’s Test-The Rural in China; f mental development index & psychomotor development index (assessed using the Standardized Scale for the Intelligence of Children formulated by the Children Development Center of China; g DAP, Draw-A-Person To ascertain the validity of the methodology used in Chinese studies of fluoride neurotoxicity, my colleagues and I carried out a small study in Sichuan using methods commonly applied in Western neurobehavioral epidemiology [ 97 ]. The 51 children examined had lived in their respective communities all their life, i.e., at least since conception. All three measures of fluoride exposure showed negative associations for cognitive function tests. One exposure parameter was the known water-fluoride concentration at the residence where the child was born, another was the child’s morning urine-fluoride after having ingested fluoride-free water the night before (neither measure reached formal statistical significance as predictor of cognitive deficits). The strongest and statistically significant association was seen with the degree of dental fluorosis that served as a marker of the child’s early-life fluoride exposure. Other recent studies (Table (Table1) 1 ) also found dental fluorosis to be a useful risk indicator. While one previous study in the U.S. failed to observe a relationship between dental fluorosis and behavior (parental assessment by the Child Behavior Checklist) [ 111 ], a dose-response relationship between urinary fluoride concentrations (range, 0.24–2.84 mg/L) and reduced IQ was reported in a population without any severe dental fluorosis [ 112 ]. A recent meta-analysis of waterborne fluoride exposures [ 60 ] covered 18 studies with water-fluoride concentrations below 4 mg/L; clear IQ reductions were observed at water-fluoride concentrations of about 1 mg/L and above. In addition, four cross-sectional studies reported linear relationships between urinary fluoride (one study also included plasma-fluoride) and IQ among children living in areas with mean water-fluoride contents of 1.4 mg/L, 1.5–2.5 mg/L, 1.4 mg/L, and 0.5–2.0 mg/L [ 99 , 107 , 109 , 113 ]. Although meta-analysis of studies has previously been carried out [ 4 , 60 ], the heterogeneity of the new studies and differences in exposure assessment and cognitive tests suggested that a joint analysis would require too many assumptions to provide useful evidence on the dose-dependence of neurotoxicity. The information summarized in Table Table1 1 therefore serves as qualitative documentation that elevated fluoride exposure during early development is associated with cognitive deficits. Although the presence of confounding bias cannot be excluded, the fairly uniform findings under different study conditions would argue against any serious bias. The largest study, by far, reported an IQ loss of 4.29 (95% CI, 0.48–8.09) and 2.67 (0.68–4.67) for each increase by 0.5 mg/L in the fluoride concentration in water and urine, respectively [ 107 ]. A recent study with individual exposure data [ 109 ] reported lower losses of 0.79 (0.28–1.30) and 0.61 (0.22–0.99) IQ points for each increase by 0.5 mg/L in fluoride in water and urine, respectively. Of note, the ranges of exposures in these studies overlap with concentrations commonly reported from regions without endemic disease. Prospective studiesMore weight must be placed on prospective studies that include assessment of individual levels of fluoride exposures in early life (Table 2 ). Two prospective studies from New Zealand explored the possible neurobehavioral consequences of community water fluoridation. The first study reported no association between behavioral problems and residence in a fluoridated community during the first 7 years of life [ 114 ]. However, like the subsequent study, the authors had no access to individual measurements of fluoride exposure, and the exposure status relied solely on residence in a fluoridated community and its duration, where age at the time of residence was apparently not considered. Characteristics of the five prospective studies of fluoride exposure and children’s cognitive and neurobehavioral, developmental and cognitive outcomes
a Rutter Behavior Rating Scales; b Connors Behavior Rating Scales; c Wechsler Abbreviated Scale of Intelligence; d McCarthy Scales of Children’s Abilities; e Wechsler Abbreviated Scale of Intelligence; f Bayley Scale of Infant Development II; g Wechsler Preschool and Primary Scale of Intelligence, 3rd edition A more comprehensive study was based on a birth cohort established in Dunedin, New Zealand from births in 1972–1973 [ 115 ]. The 1037 children were recruited at age 3 years, and IQ tests were administered at ages 7, 9, 11 and 13 years, and again at age 38; the average IQ result for 992 subjects was used for comparison between residents in areas with and without water fluoridation. No significant differences in IQ in regard to fluoridation status were noted, and this finding was independent of potential confounding variables that included sex, socioeconomic status, breastfeeding, and birth weight. Prenatal fluoride exposure was not considered. The average difference in childhood exposure between fluoridated vs. non-fluoridated areas was estimated to be 0.3 mg/day [ 117 ]. However, the 93 cohort subjects who did not live in a fluoridated area may well have received fluoride supplements, as was the case for a total of 139 children in the study, thereby impacting on the exposures [ 20 ]. A further concern is that formula may have contributed substantial fluoride exposure [ 19 , 21 ], and it is therefore interesting that breastfeeding – and thus avoidance of formula – in the fluoridated areas contributed an advantage that averaged 6.2 IQ points at age 7–13 years, while the advantage was less (4.3) in the non-fluoridated areas [ 115 ]. Subsequently, the authors estimated the average total fluoride intake up to age 5 years, including tablets, toothpastes, and dietary sources, without finding any IQ difference [ 118 ]. However, information on maternal tea consumption during pregnancy was not obtained, although tea has long been recognized as an important source of fluoride in New Zealand [ 119 ]. Lead exposure in this cohort was later reported to cause IQ deficits [ 120 ], but control for the blood-lead concentration at age 9 years showed no change in the results for fluoride [ 117 ]. Despite the shortcomings, this study has been hailed as evidence that fluoridated water is “not neurotoxic for either children or adults, and does not have a negative effect on IQ” [ 121 ]. This conclusion seems rather optimistic [ 122 ], given the fact that the exposure assessment was imprecise (especially for prenatal exposure) and that the statistical power was probably insufficient to allow identification of any important IQ deficit. More recent studies provide more robust evidence. In a prospective study from an area in Mexico with elevated levels of fluoride in drinking water, maternal pregnancy urine-fluoride (corrected for specific gravity) was examined for its association with scores on the Bayley Scales among 65 children evaluated at age 3–15 months [ 24 ]. The mothers in the study had average urine-fluoride concentrations at each of the three trimesters of pregnancy of 1.9, 2.0, and 2.7 mg/L (higher than the following study). The fluoride exposure indicators during first and second trimesters were associated with significantly lower scores on the Bayley Mental Development Index score after adjustment for covariates [ 24 ]. The existence of the ELEMENT (Early Life Exposure in Mexico to Environmental Toxicants) birth cohort allowed longitudinal measurements of urine-fluoride in pregnant mothers and their offspring and their associations with measures of cognitive performance of the children at ages 4 and 6–12 years [ 63 ]. The cohort had been followed to assess developmental lead neurotoxicity, and biobanked urine samples were available for fluoride analysis and adjustment for creatinine and density. Most of the mothers provided only one or two urine samples, thereby introducing some imprecision in the exposure estimate. Child cognitive function was determined by the General Cognitive Index (GCI) of the McCarthy Scale at age 4 years in 287 children, and IQ by an abbreviated Wechsler scale (WASI) at age 6–12 years in 211 children. Urinary fluoride (mg/L) in the mothers averaged 0.90 (s.d., 0.35) and, in the children, 0.82 (s.d., 0.38). Covariates included gestational age, birth weight, sex, parity, age at examination, and maternal characteristics, such as smoking history, marital status, age at delivery, maternal IQ, and education. After covariate adjustment, an increase in maternal urine-fluoride by 1 mg/L during pregnancy was associated with a statistically significant loss of 6.3 (95% CI, − 10.8; − 1.7) and 5.0 (95% CI, − 8.2; − 1.2) points on the GCI and IQ scores, respectively. These associations remained significant, and the effect sizes appeared to increase, in sensitivity analyses that controlled for lead, mercury, and socioeconomic status. Although adjustment could not be made for iodine deficiency or arsenic exposure, any residual confounding was judged to be small in this population. Important strengths are that the cohort was followed from birth with meticulous documentation for lead exposure and other neurobehavioral risks. This study also ascertained the childhood fluoride exposure at the time of IQ testing (6–12 years) and found no indication of adverse impact on the IQ in the cross-sectional analysis [ 63 ]. Between 2008 and 2011, 2001 pregnant women were recruited into the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort in Canada. A subset of 601 of their children were examined at age 3–4 years, slightly less than half of them residing in fluoridated communities [ 116 ]. Maternal spot urine samples were obtained from each of the three semesters of pregnancy, and results were analyzed for those 512 mother-child pairs where urine was available from all three semesters, so that the overall average urine-fluoride could be used as an exposure biomarker, with adjustment for specific gravity and creatinine. Information was obtained on food and beverage intakes, including tea (assuming a fluoride content of 0.52 mg in each cup of black tea). Intellectual abilities were assessed using the age-appropriate Wechsler scale that provided a full-scale IQ. Covariate adjustment included exposures to other neurotoxicants and other relevant covariates, such as sex, age at examination, and maternal exposure to indirect smoking, race, and education [ 116 ]. As had been shown by the same research group in a previous study of a larger population [ 11 ], women residing in fluoridated communities had higher urine-fluoride concentrations (0.69 vs 0.40 mg/L) and also higher calculated daily fluoride intakes from water and other beverages (0.93 vs. 0.30 mg/day). Regression analyses showed that an increase in urine -fluoride of 1 mg/L was associated with a statistically significant loss in IQ of 4.49 points in boys, though not in girls. An increase of 1 mg/L of fluoride in water and an increase of 1 mg/day of fluoride intake was associated with an IQ loss of 5.3 points and 3.66 points, respectively, for both boys and girls [ 116 ]. Thus, this study at somewhat lower exposures is in good agreement with the data from the two studies carried out in Mexico. In an extension of the MIREC study of prenatal fluoride exposures, the authors subsequently assessed the possible impact of fluoride exposure from reconstituted formula in fluoridated and non-fluoridated communities [ 123 ]. After adjustment for prenatal fluoride exposure and other covariates, each increase by 1 mg/L in the water fluoride concentration was found to be associated with a statistically significant decrease of 8.8 IQ points in the children who had been formula-fed in the first 6 months of life, while no such difference was seen among the exclusively breastfed children. Although the results were somewhat unstable and included only 68 formula-fed children from fluoridated communities, these results support the notion that early postnatal brain development is also likely to be vulnerable to neurotoxicant exposures, as is well documented, e.g., from arsenic exposure in infancy [ 124 ]. The substantial IQ losses associated with elevated water-fluoride concentrations are in accordance with the difference of almost 7 IQ points between exposed groups and controls in the meta-analysis from 2012 [ 4 ]. Also, the largest cross-sectional study from 2018 showed a statistically significant loss of 8.6 IQ points for each increase by 1 mg/L in the fluoride concentration in water [ 107 ], although somewhat less in another recent study [ 109 ]. Several additional reports using other cognition measures are also of relevance. Another Canadian study analyzed data from two cycles of the Canadian Health Measures Survey (CHMS) [ 125 ]. Randomly measured urine-fluoride results from children aged 3-to-12 years were linked to parental reports or self-reported learning disabilities. When the two cycles of the CHMS were combined (both including at least 1100 subjects), unadjusted urine-fluoride was significantly correlated with an increased incidence of learning disabilities. However, this effect lost its statistical significance after controlling for creatinine and specific gravity. The authors concluded that there was no robust association between fluoride exposure and reported learning disability among Canadian children at the ages studied. However, the exposure assessment probably did not reflect the time of greatest vulnerability to fluoride, and the information on learning disability was somewhat uncertain, also in regard to the time of appearance. A more recent analysis relying on the same data showed that elevated fluoride in tap water was associated with an increased risk of Attention-Deficit/Hyperactivity Disorder (ADHD) symptoms and ADHD diagnosis among Canadian youth, although the association with ADHD was not present when urine-fluoride concentrations were used as exposure indicator [ 126 ]. A related study of the ELEMENT population showed that elevated prenatal fluoride exposure was associated with higher scores on the Conners’ Rating Scale and thus with tendencies toward inattention and development of ADHD [ 127 ]. These prospective studies from North America focused on prenatal and early postnatal exposure known as a key window of neurological vulnerability [ 69 ]. All of these studies relied on individual exposure indicators, thus providing substantial support to the conclusion that elevated fluoride exposure during early development can cause neurotoxicity. Retrospective studies of fluoride neurotoxicityA few retrospective studies are available but provide only weak evidence on the possible existence of fluoride-related neurotoxicity. A Swedish study utilized the register of military conscripts who underwent neurocognitive tests [ 128 ]. The authors then estimated the water-fluoride concentrations for each of the about 80,000 subjects based on their residential history, where the geographic location of the current residence was linked to a water supply with a known fluoride content. The study found no meaningful or consistent relationship between the test results and the home water-fluoride concentration (0 to 2 mg/L). The study did identify a relationship between water-fluoride and increased income, which the authors attributed to improved dental health. However, the study did not have access to specific individual fluoride exposure data, nor was developmental exposure assessed. This study is therefore non-informative due to the likely misclassification of any causative exposure. In the U.S., parental reports on ADHD among 4-to-17-year-olds were collected from the National Survey of Children’s Health and combined with information on water fluoridation at state level [ 129 ]. The prevalence of artificial water fluoridation in 1992 predicted significantly the state prevalence of ADHD from the surveys in 2003, 2007 and 2011. After adjustment for socioeconomic status, each 1% increase in artificial fluoridation prevalence in 1992 was associated with approximately 67,000 to 131,000 additional ADHD diagnoses from 2003 to 2011. Given the state-level exposure assessment and the use of parental reports of ADHD, this ecological study has important weaknesses, although the findings are in agreement with other recent studies. However, the study has been criticized, as inclusion of mean elevation as a covariate apparently abolishes the significance of fluoridation as a predictor [ 130 ]. Overall, the retrospective studies are limited by exposure data that do not necessarily reflect early-life conditions and therefore add little weight to the information otherwise available on fluoride neurotoxicity in children. Dose-dependence and benchmark dosesThe studies reviewed show dose-dependent fluoride neurotoxicity that appears to be statistically significant at water concentrations of or below 1 mg/L, but the studies themselves do not identify a likely threshold. Regulatory agencies often use benchmark dose calculations to develop non-cancer health-based limits for dietary intakes, such as drinking water [ 62 , 131 ]. One recent report [ 132 ] used this approach to generate benchmark results from a study of more than 500 children in China [ 89 ]. The authors used a high BMR of 5 IQ points, but results were also given for a more appropriate BMR of 1 IQ point. For the latter, the BMDL was calculated to be a daily intake level of 0.27 mg/day [ 132 ]. Using the average water intake of 1.24 L/day in non-pregnant women [ 133 ], the BMDL corresponds to a water concentration of 0.22 mg/L. The report did not provide data for urine-fluoride concentrations. As described in the Methods section, the regression coefficients and their standard deviations, as provided in the published reports [ 63 , 116 ], were applied to estimate tentative BMD values. Assuming linearity and Gaussian distributions, the right-hand columns of Table 3 show the calculated results for the two prospective studies with the maternal urine-fluoride concentration as the exposure parameter in regard to the cognitive function measures (both boys and girls). For the ELEMENT study, results for the larger number of children with CGI outcomes are also shown. Overall, the BMDL results appear to be in agreement. Adjusted differences in cognitive outcomes per mg fluoride per liter maternal urine (U-fluoride) during pregnancy, and benchmark dose results (boys and girls) in regard to maternal urinary fluoride excretion (mg/L urine adjusted for creatinine)
The Table Table3 3 results also appear to be reliable, given that the studies provide ample coverage of subjects with lower-level exposures close to the BMDL. The Canadian children had lower prenatal exposures than the Mexican study subjects, and along with the apparent lack of fluoride effects in girls, the BMD results are higher than in the ELEMENT study, although the greater uncertainty results in a fairly low BMDL. The results suggest a BMDL of about 0.2 mg/L or below, a level that is similar to the result calculated from the study in China [ 89 , 132 ] and clearly below commonly occurring exposure levels, even in communities with drinking water fluoridation. Plausibility and implicationsThe present review updates the conclusions from a 2012 meta-analysis of cross-sectional studies of intellectual deficits associated with elevated fluoride exposure [ 4 ]. Subsequent epidemiological studies have strengthened the links to deficits in cognitive functions, several of them providing individual exposure levels, though most of the new studies were cross-sectional and focused on populations with fluoride exposures higher than those typically provided by fluoridated water supplies. Prospective studies from the most recent years document that adverse effects on brain development happen at elevated exposure levels that occur widely in North America and elsewhere in the world, in particular in communities supplied with fluoridated drinking water [ 24 , 63 , 116 , 123 ]. These new prospective studies are of very high quality and, given the wealth of supporting human studies and biological plausibility, leave little doubt that developmental neurotoxicity is a serious risk associated with elevated fluoride exposure, especially when this occurs during early brain development. While evidence on the neurotoxic impact of early postnatal exposure remains limited [ 21 , 123 ], other neurotoxicity evidence suggests that adverse effects are highly plausible [ 124 ]. Research on laboratory animals confirms that elevated fluoride exposure is toxic to the brain and nerve cells, as already indicated by the NRC review [ 1 ]. The evidence today is substantially more robust. The NTP review placed more confidence in fluoride impairing learning in adult animals due to fewer experimental studies being available on developmental exposure [ 55 ]. Still, not all studies are in agreement [ 58 ], perhaps due to species or strain differences in vulnerability. However, fluoride is known to pass the placental barrier and to reach the brain, and the animal studies bear out the importance of the prenatal period for fluoride neurotoxicity. Toxicant exposures in early life can have much more serious consequences than exposures occurring later in life, and the developing brain is known to be particularly vulnerable [ 69 ]. Thus, the vulnerability of early brain development supports the notion that fluoride neurotoxicity during early life is a hazard of public health concern [ 134 ]. Dental fluorosis has been dismissed as a “cosmetic” effect only [ 6 , 135 , 136 ], but the association of dental changes with intellectual deficits in children [ 95 , 97 , 100 , 103 , 107 , 112 ] suggests that dental fluorosis should no longer be ignored as non-adverse. Dental fluorosis may perhaps serve as a sensitive indicator of prenatal fluoride exposure, and information is needed to determine to which extent the time windows for dental fluorosis development in different tooth types [ 137 ] overlap with vulnerable periods for brain development. Although the adverse outcome pathway is unclear, several epidemiological studies suggest that thyroid dysfunction is a relevant risk at elevated fluoride exposures. Thus, studies in children have reported deficient thyroid functions, including elevated TSH (thyroid stimulating hormone) at elevated fluoride exposure [ 138 – 142 ], and one study linked elevated fluoride exposure to both thyroid dysfunction and IQ deficits [ 109 ]. In Canada, elevated urine-fluoride was associated with increased TSH among iodine-deficient adults, though not in the general population, after exclusion of those with known thyroid disease [ 143 ]. In England, the diagnosis of hypothyroidism was nearly twice as frequent in medical practices located in a fully fluoridated area, as compared to non-fluoridated areas [ 144 ]. These findings are highly relevant to the neurotoxicity concerns, as thyroid hormones are crucial for optimal brain development [ 53 , 54 ]. Given that fluoride is excreted only in minute amounts in human milk [ 1 , 18 ], the focus on prenatal exposure appears justified, but formula-mediated neonatal exposures represent an additional concern, as indicated by dental fluorosis studies [ 137 ] and the most recent study from Canada [ 123 ]. The human brain continues to develop postnatally, and the period of heightened vulnerability therefore extends over many months through infancy and into early childhood [ 69 ]. Fluoride exposures during infancy are of special concern in regard to formula produced with fluoride-containing water [ 21 , 145 ]. Unfortunately, current animal models do not appropriately cover neonatal fluoride exposure. Thus, future studies that focus on exposures prenatally, during infancy, and in later childhood may allow more detailed assessment of the vulnerable time windows for fluoride neurotoxicity. One prospective study suggested that boys may be more vulnerable to fluoride neurotoxicity than girls [ 116 ]. Given that endocrine disrupting mechanisms often show sex-dependent vulnerability [ 146 ], further research is needed to understand the extent that males may require additional protection against fluoride exposure. Recent studies have also identified possible genetic predisposition to fluoride neurotoxicity [ 113 , 147 ]. This means that some subgroups of the general population will be more vulnerable to fluoride exposure so that exposure limits aimed at protecting the average population may not protect those with susceptible genotypes, as has been shown, e.g., for methylmercury neurotoxicity [ 148 ]. The impact of iodine deficiency on fluoride vulnerability also needs to be considered [ 143 ]. Past studies of fluoride-exposed workers suggest possible neurotoxicity, but recent evidence rather points to possible accelerated aging in fluoride-exposed adults [ 80 – 82 ]. As has been proposed for other developmental neurotoxicity [ 134 , 149 ], early-life exposure to fluoride deserves to be examined in regard to its possible impact on the risk of adult neurodegenerative disease. Despite the growing evidence, health risks from elevated exposures to fluoride have received little attention from regulatory agencies. Thus, the EPA’s regulation of fluoride in water, most recently confirmed in 2016, is based on the assumption that crippling fluorosis is the most sensitive adverse effect [ 59 ]. The MCLG for fluoride (4 mg/L) may perhaps serve that purpose, but it is clearly not protective of adverse effects on the brain, especially in regard to early-life exposures. In its most recent review of fluoride [ 59 ], the EPA referred to the 2012 meta-analysis [ 4 ] and highlighted that IQ deficits occurred at water-fluoride concentrations “up to 11.5 mg/L”, although this level represented only the highest exposure in the 27 studies assessed. Neither the EPA nor a U.S. federal panel [ 9 , 59 ] noted that most of the studies included in the review had water-fluoride concentrations below the MCLG of 4 mg/L. Thus, out of the 18 studies that provided the water-fluoride concentrations, 13 found deficits at levels below the MCLG, with an average elevated level at 2.3 mg/L, the lowest being 0.8 mg/L [ 4 ]. The results in Table Table1 1 show that the recent cross-sectional results from different communities are in accordance with the previous review [ 4 ] and extend the documentation of cognitive deficits associated with only slightly elevated exposures. The appearance of prospective studies that offer strong evidence of prenatal neurotoxicity should inspire a revision of water-fluoride regulations. The benchmark results calculated from these new studies, though tentative only at this point, support the notion that the MCLG is much too high. Depending on the use of uncertainty factors, a protective limit for fluoride in drinking water would likely require that the MCGL be reduced by more than a 10-fold factor, i.e., below the levels currently achieved by fluoridation. The notion that fluoride is primarily a developmental neurotoxicant means that fluoride – an element like lead, mercury, and arsenic – can adversely affect brain development at exposures much below those that cause toxicity in adults. For lead and methylmercury, adverse effects in children are associated with blood concentrations as low as about 10 nmol/L. Blood-fluoride concentrations associated with elevated intakes from drinking-water may exceed 20 μg/L, or about 1 μmol/L, i.e., about 100-fold greater than the serum concentrations of the other trace elements that cause neurodevelopmental damage. Thus, although fluoride is neurotoxic, it appears to be much less potent than elements that occur at much lower concentrations in the Earth’s crust. Although substances that occur naturally in the biosphere may be thought to be innocuous, or even beneficial as in the case of fluoride, the anthropogenic elevations in human exposures may well exceed the levels that human metabolism can successfully accommodate [ 150 ]. Perhaps dentistry interests in promoting water fluoridation have affected the risk assessment and reduced the regulatory attention to fluoride toxicity. Thus, reports on fluoride toxicity have been disregarded under a heading referring to “Anti-Fluoridation Activities” [ 121 ], and our review article [ 4 ] was said to rely on “selective readings” [ 115 ], with IQ deficits occurring at high fluoride concentrations “up to 11.5 mg/L” [ 151 ], although most of the studies related to concentrations that were only slightly elevated. Further, an ecological study without individual exposure data [ 115 ] that failed to identify an association with IQ was considered as strong support of the safety of water fluoridation and more relevant to fluoridation policy than other evidence on neurotoxicity [ 121 ]. While water fluoridation continues to be recommended [ 9 ], the benefits appear to be minimal in recent studies of caries incidence [ 152 ]. Perhaps due to modern use of topical fluoride products, especially fluoridated toothpaste, countries that do not fluoridate the water have seen drops in dental cavity rates similar to those observed in fluoridated countries [ 153 ]. This finding is in agreement with the observation that fluoride’s predominant benefit to dental health comes from topical contact with the surface of the enamel, not from ingestion, as was once believed [ 154 , 155 ]. Already in 2001, the U.S. Centers for Disease Control (CDC) concluded that fluoride supplementation during pregnancy did not benefit the child’s dental health [ 156 ]. Consensus has since then been building on the lack of efficacy of water fluoridation in preventing caries [ 152 ]. It therefore appears that population-based increase of systemic fluoride exposure may be unnecessary and, according to the evidence considered in this review, counterproductive. The focus should therefore shift from population-wide provision of elevated oral fluoride intake to consideration of the risks and consequences of developmental neurotoxicity associated with elevated fluoride exposure in early life. The prospective studies suggest that prevention efforts to control human fluoride exposures should focus on pregnant women and small children. In addition to drinking water, attention must also be paid to other major sources of fluoride, such as black tea [ 13 ]. Thus, excessive tea-drinking is known to potentially cause skeletal fluorosis [ 12 ], and the possible impact of tea drinking deserves to be considered along with other possible sources that may affect pregnant women and small children. The evidence on fluoride neurotoxicity in the general population is fairly recent and unlikely to represent the full toxicological perspective, including adverse effects that may occur at a delay, as has been seen with many developmental neurotoxicants in the past [ 134 ]. While some ecological studies failed to identify clear evidence for fluoride neurotoxicity, they cannot be relied on as proof that elevated fluoride exposure is safe, in particular regarding early brain development. Recent prospective studies with individual exposure assessments provide strong evidence, and the large number of cross-sectional studies from populations with stable and well-characterized exposures provide additional support. ConclusionsPrevious assessment of neurotoxicity risks associated with elevated fluoride intake relied on cross-sectional and ecological epidemiology studies and findings from experimental studies of elevated exposures. The evidence base has greatly expanded in recent years, with 14 cross-sectional studies since 2012, and now also three prospective studies of high quality and documentation of individual exposure levels. Thus, there is little doubt that developmental neurotoxicity is a serious risk associated with elevated fluoride exposure, whether due to community water fluoridation, natural fluoride release from soil minerals, or tea consumption, especially when the exposure occurs during early development. Even the most informative epidemiological studies involve some uncertainties, but imprecision of the exposure assessment most likely results in an underestimation of the risk [ 86 ]. Thus, the evidence available today may not quite reflect the true extent of the fluoride toxicity. Given that developmental neurotoxicity is considered to cause permanent adverse effects [ 69 ], the next generation’s brain health presents a crucial issue in the risk-benefit assessment for fluoride exposure. AcknowledgmentsEsben Budtz-Jørgensen commented on the text and calculated the benchmark dose results. Howard Hu (ELEMENT study) and Christine Till (MIREC study) provided helpful comments and allowed me to publish the tentative benchmark calculations. Abbreviations
Author’s contributionsThe author read and approved the final manuscript. The author is supported by the NIEHS Superfund Research Program (P42ES027706). Availability of data and materialsEthics approval and consent to participate, consent for publication, competing interests. The author is an editor-in-chief of Environmental Health but was not involved in the editorial handling of the manuscript submitted. The author recently served as a health expert in a lawsuit in the U.S. on the protection against fluoride neurotoxicity from fluoride in drinking water. Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.  | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
IMAGES
VIDEO
COMMENTS
A comprehensive summary of studies published between 1990 and 2005 is provided in the National Research Council (NRC) report, demonstrating that developmental processes are susceptible to fluoride (NRC 2006). Four developmental toxicity studies are highlighted, because of their compliance to standard guidelines, adequate numbers of animals, and ...
The most effective way of caries prevention is the use of fluoride. Aim: The aim of our research was to review the literature about fluoride toxicity and to inform physicians, dentists and public health specialists whether fluoride use is expedient and safe. ... Williams DB. Final report of local studies on water fluoridation in Brantford. Can ...
WATER FLUORIDATION. Fluoride is naturally found in fresh water. Its concentration depends on the geographical location and source, and ranges from 0.01 ppm to a maximum of 100 ppm ().In the 1930s, several studies reported a low prevalence of dental caries among people consuming natural drinking-water with high fluoride ().Water fluoridation, in which controlled amount of fluoride is added to ...
After reviewing the scientific literature, it became clear that there were growing concerns about fluoride as a developmental neurotoxin. 4,5 In 2006, a report by the National Research Council ...
According to a report by Choi et al. (2012), neurotoxicity can occur at fluoride concentrations above 1 mg/l. ... Fluoride research is an important field of study, as fluoride is a widely used mineral with various applications in medicine, industry, and public health. In recent years, research in this field has focused on several important ...
National Research Council. 2006. Fluoride in Drinking Water: A Scientific Review of EPA's Standards. Washington, DC: The National Academies Press. doi: 10.17226/11571. ... NOTICE: The project that is the subject of this report was approved by the Governing Board of the National Research Council, whose members are drawn from the councils of the ...
Fluoride in Drinking Water reviews research on various health effects from exposure to fluoride, including studies conducted in the last 10 years. ... Consensus Study Report: Consensus Study Reports published by the National Academies of Sciences, Engineering, and Medicine document the evidence-based consensus on the study's statement of task ...
Most water fluoridation research was carried out before these dramatic changes in fluoride availability and oral health. Furthermore, there is a paucity of evidence in adults.
Updated 9:37 AM PDT, August 22, 2024. NEW YORK (AP) — A U.S. government report expected to stir debate concluded that fluoride in drinking water at twice the recommended limit is linked with lower IQ in children. The report, based on an analysis of previously published research, marks the first time a federal agency has determined — "with ...
1 Department of Toxicology, Leibniz Research Centre for Working Environment and Human Factors (IfADo), Dortmund, Germany. ... In contrast, 21 of 23 recent epidemiological studies report an association between high fluoride exposure and reduced intelligence. The discrepancy between experimental and epidemiological evidence may be reconciled with ...
Uniquely for a Methods report with a predominantly clinical readership, the authors also provide valuable information regarding the precise molecular structures, the fluoride and metal ion [silver(I) and tin(II)] speciation status, potential mechanisms of action, and health and safety information for all fluoride-containing adducts considered ...
Therefore, the National Toxicology Program (NTP) conducted a systematic review of the published scientific literature on the association between fluoride exposure and neurodevelopment and cognition. The NTP released their findings in a State of the Science Monograph (available below under Documents). A corresponding meta-analysis on children ...
This study used nonfluoridated water but supports earlier findings by Koblar et al. who report that the adequate intake of fluoride from a 70 kg adult consuming five cups of tea daily ranges from 25 to 210% depending upon tea brand and ... The National Research Council's report on the health effects of ingested fluoride in the United States ...
Additional research is needed, in particular to address potential effects on learning and memory following exposure during development to fluoride at levels nearer to 0.7 parts per million. NTP is conducting laboratory studies in rodents to fill data gaps identified by this systematic review of the animal studies.
For correspondence: 11 Pond Hollow Road, Averill Park, NY 12018, USA. Email:[email protected]. Maximum Contaminant Level Goal (MCLG) of 4 mg/L and the Secondary Maximum Contaminant Level (SMCL) of 2 mg/L of fluoride in drinking water. On March 22, 2006, NRC released its report in which it is clearly stated that the current MCLG does not ...
Aug 30 1452. ISFR is an independent non-profit organization which promotes the sharing of scientific research on all aspects of inorganic and organic fluorides by hosting international conferences on fluoride research and publishing quarterly, online and in print.
The National Research Council's report concluded that EPA's safe drinking water standard (4 ppm) for fluoride is unsafe and "should be lowered." The NRC based this conclusion on its finding that EPA's 4 ppm standard places a person at increased risk for both tooth damage (severe dental fluorosis) and bone damage (bone fracture). While most of the press coverage of the NRC report ...
"More research is needed to clarify the effect of fluoride on brain chemistry and function," they wrote in a 2006 report. It was unclear, the EPA advisers noted, whether the China data was ...
A recent comprehensive systematic review by Twetman et al. summarized literatures on "fluoride toothpaste" from 2002 to 2008 and concluded, "There was strong evidence that daily use of fluoride toothpaste has a significant caries-preventive effect in children, compared with placebo (prevented fraction 24%). The effect was boosted by ...
A peer-reviewed, open access journal in fluoride toxicology, fluoride biochemistry, veterinary aspects of fluoride, clinical aspects of fluoride, agricultural aspects of fluoride & dental aspects of fluoride. ... Quarterly Journal of the International Society for Fluoride Research Inc. 0015-4725 (Print) / 2253-4083 (Online) Website ISSN Portal ...
July 25, 2012 — For years health experts have been unable to agree on whether fluoride in the drinking water may be toxic to the developing human brain. Extremely high levels of fluoride are known to cause neurotoxicity in adults, and negative impacts on memory and learning have been reported in rodent studies, but little is known about the ...
Fluoride plays a vital role in preventing dental caries, with its addition to oral care products significantly promoting oral hygiene. A no-rinse brushing method aims to increase fluoride retention in the oral cavity, as rinsing with water decreases fluoride levels in saliva, which could affect remineralization. While the no-rinse brushing method holds promise for improving fluoride retention ...
A 2006 National Research Council report stated that it is apparent that fluorides have the ability to interfere with the functions of the brain and the body by direct and indirect means.[19,20] This finding was confirmed by a study where groups of children exposed to 8 ppm fluoride in water were found to have lower average IQs, less children ...
"The fluoride research is very clear: Fluoride helps remineralize early and even later-stage cavities," stopping them from forming or getting worse, says Gretchen Gibson, D.D.S., M.P.H., an ...
A review and meta-analysis published in 2012 assessed a total of 27 research reports, all but two of them from China, on elevated fluoride exposure and its association with cognitive deficits in children. All but one study suggested that a higher fluoride content of residential drinking water was associated with poorer IQ performance at school age.