The Female Reproductive System
Chapter 16: Lesson 3
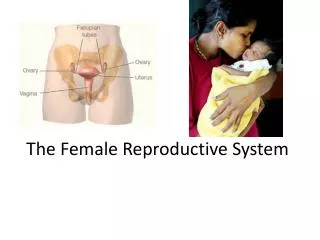
Female Reproductive Organs
The organs of the female reproductive system matures at puberty and enables pregnancy to occur with the first monthly ovulation.
The female reproductive system has several functions, including producing female sex hormones and storing the eggs .
Eggs- Female gametes or ova.
A female at birth has more than 400,000 immature ova in her ovaries.
The female sex glands that store the ova, or eggs, and produce female sex hormones- estrogen and progesterone.
The ovaries are an important part of the female reproductive system. Their job is twofold. They produce the hormones that trigger menstruation . They also release at least one egg each month for possible fertilization.
The ovaries are located on each side of the uterus .
The hollow, muscular,pear-shaped
organ that nourishes and protects a fertilized ovum until birth.
The ovaries produce the eggs that travel through the fallopian tubes. Once the egg has left the ovary it can be fertilized and implant itself in the lining of the uterus .
The process of ovulation is controlled by the release of luteinizing hormone by the pituitary gland.
The process of releasing a mature ovum into the fallopian tube each month.
A mature ovum is released from an ovary and moves into one of the two fallopian tubes .
Fallopian Tubes- A pair of tubes with fingerlike projections that draw in the ovum.
Majority of woman have two fallopian tubes, one on each side of the uterus. Women can still get pregnant if they have only one fallopian tube because an egg can still travel through the unaffected fallopian tube. However, if both tubes are completely blocked, fertility without treatment won't be possible.
Fallopian Tubes
Endometrium
The cervix is the opening of the uterus.
The uterus protects and nourishes a developing fetus.
The ovaries contain ova and produce hormones.
Ova travel to the uterus through the fallopian tubes.
Endometrium tissue lines the uterus.
The passageway from the uterus to the outside of the body.
Sperm from the male enter the female reproductive system through the vagina .
A muscular, elastic passageway that extends from the uterus to the outside of the body
Because it has muscular walls it can expand and contract. This ability to become wider or narrower allows the vagina to accommodate something as slim as a tampon and as wide as a baby.
The vagina's muscular walls are lined with mucous membranes, which keep it protected and moist.
The vagina has several functions: for sexual intercourse, as the pathway that a baby takes out of a woman's body during childbirth, and as the route for the menstrual blood to leave the body from the uterus.
- If sperm are present in the fallopian tubes, the sperm cell and ovum may unite, resulting in fertilization.
- The fertilization of an egg by a sperm produces a cell called a zygote.
- When the zygote leaves the fallopian tube, it enters the uterus and attaches itself to the uterine wall. The fetus remains in the uterus until birth.
After a female matures, the uterus prepares each month for possible pregnancy. If pregnancy doesn’t occur, menstruation occurs .
Menstruation- The shedding of the uterine lining
If pregnancy does not occur, the thickened lining of the uterus (endometrium) breaks down into blood, tissue, and fluids. This will then pass through the cervix and into the vagina.
Cervix- The opening to the uterus. This is what expands during childbirth
***NEED TO KNOW THIS***
Breast Self-Exam
Breast cancer is the most common cancer and the second leading cause of death, after lung cancer, for women in the United States.
The American Cancer Society recommends that females examine their breasts once a month, right after the menstrual period, when breasts are not tender.
Female Reproductive System Problems
Menstrual Cramps
Cramps that occur at the beginning of a menstrual period
Premenstrual Syndrome
A disorder caused by hormonal changes
Toxic Shock Syndrome
A rare but serious bacterial infection that affects the immune system and the liver
Infertility and Other Disorders
Endometriosis
Ovarian cysts
Uterine tissue grows outside the uterus
Diseases spread through sexual contact
Infection that causes discharge, odor, pain, itching, or burning
Fluid-filled sacs on the ovary
Cancer of the cervix, uterus, or ovaries
Infertility in females can have several causes.

27.2 Anatomy and Physiology of the Female Reproductive System
Learning objectives.
By the end of this section, you will be able to:
- Describe the structure and function of the organs of the female reproductive system
- List the steps of oogenesis
- Describe the hormonal changes that occur during the ovarian and menstrual cycles
- Trace the path of an oocyte from ovary to fertilization
The female reproductive system functions to produce gametes and reproductive hormones, just like the male reproductive system; however, it also has the additional task of supporting the developing fetus and delivering it to the outside world. Unlike its male counterpart, the female reproductive system is located primarily inside the pelvic cavity ( Figure 27.9 ). Recall that the ovaries are the female gonads. The gamete they produce is called an oocyte . We’ll discuss the production of oocytes in detail shortly. First, let’s look at some of the structures of the female reproductive system.
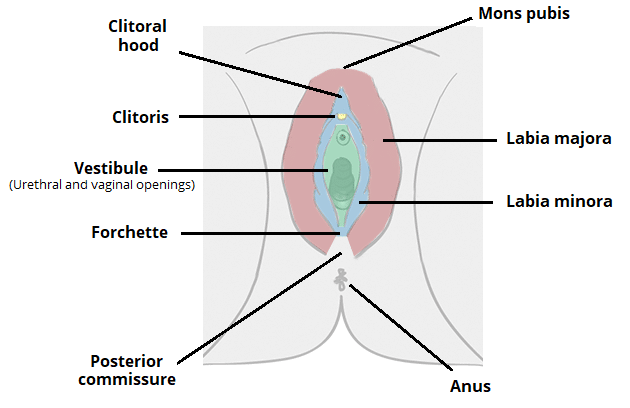
External Female Genitals
The external female reproductive structures are referred to collectively as the vulva ( Figure 27.10 ). The mons pubis is a pad of fat that is located at the anterior, over the pubic bone. After puberty, it becomes covered in pubic hair. The labia majora (labia = “lips”; majora = “larger”) are folds of hair-covered skin that begin just posterior to the mons pubis. The thinner and more pigmented labia minora (labia = “lips”; minora = “smaller”) extend medial to the labia majora. Although they naturally vary in shape and size from woman to woman, the labia minora serve to protect the female urethra and the entrance to the female reproductive tract.
The superior, anterior portions of the labia minora come together to encircle the clitoris (or glans clitoris), an organ that originates from the same cells as the glans penis and has abundant nerves that make it important in sexual sensation and orgasm. The hymen is a thin membrane that sometimes partially covers the entrance to the vagina. An intact hymen cannot be used as an indication of “virginity”; even at birth, this is only a partial membrane, as menstrual fluid and other secretions must be able to exit the body, regardless of penile–vaginal intercourse. The vaginal opening is located between the opening of the urethra and the anus. It is flanked by outlets to the Bartholin’s glands (or greater vestibular glands).
The vagina , shown at the bottom of Figure 27.9 and Figure 27.10 , is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract. It also serves as the exit from the uterus during menses and childbirth. The outer walls of the anterior and posterior vagina are formed into longitudinal columns, or ridges, and the superior portion of the vagina—called the fornix—meets the protruding uterine cervix. The walls of the vagina are lined with an outer, fibrous adventitia; a middle layer of smooth muscle; and an inner mucous membrane with transverse folds called rugae . Together, the middle and inner layers allow the expansion of the vagina to accommodate intercourse and childbirth. The thin, perforated hymen can partially surround the opening to the vaginal orifice. The hymen can be ruptured with strenuous physical exercise, penile–vaginal intercourse, and childbirth. The Bartholin’s glands and the lesser vestibular glands (located near the clitoris) secrete mucus, which keeps the vestibular area moist.
The vagina is home to a normal population of microorganisms that help to protect against infection by pathogenic bacteria, yeast, or other organisms that can enter the vagina. In a healthy woman, the most predominant type of vaginal bacteria is from the genus Lactobacillus . This family of beneficial bacterial flora secretes lactic acid, and thus protects the vagina by maintaining an acidic pH (below 4.5). Potential pathogens are less likely to survive in these acidic conditions. Lactic acid, in combination with other vaginal secretions, makes the vagina a self-cleansing organ. However, douching—or washing out the vagina with fluid—can disrupt the normal balance of healthy microorganisms, and actually increase a woman’s risk for infections and irritation. Indeed, the American College of Obstetricians and Gynecologists recommend that women do not douche, and that they allow the vagina to maintain its normal healthy population of protective microbial flora.
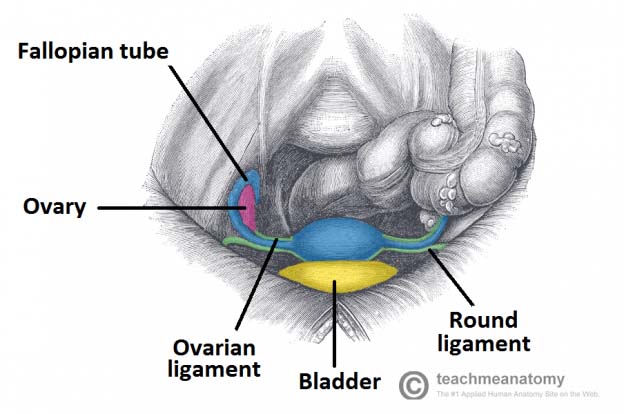
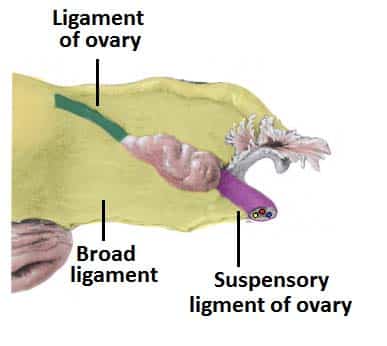
The ovaries are the female gonads (see Figure 27.9 ). Paired ovals, they are each about 2 to 3 cm in length, about the size of an almond. The ovaries are located within the pelvic cavity, and are supported by the mesovarium, an extension of the peritoneum that connects the ovaries to the broad ligament . Extending from the mesovarium itself is the suspensory ligament that contains the ovarian blood and lymph vessels. Finally, the ovary itself is attached to the uterus via the ovarian ligament.
The ovary comprises an outer covering of cuboidal epithelium called the ovarian surface epithelium that is superficial to a dense connective tissue covering called the tunica albuginea. Beneath the tunica albuginea is the cortex, or outer portion, of the organ. The cortex is composed of a tissue framework called the ovarian stroma that forms the bulk of the adult ovary. Oocytes develop within the outer layer of this stroma, each surrounded by supporting cells. This grouping of an oocyte and its supporting cells is called a follicle . The growth and development of ovarian follicles will be described shortly. Beneath the cortex lies the inner ovarian medulla, the site of blood vessels, lymph vessels, and the nerves of the ovary. You will learn more about the overall anatomy of the female reproductive system at the end of this section.
The Ovarian Cycle
The ovarian cycle is a set of predictable changes in a female’s oocytes and ovarian follicles. During a woman’s reproductive years, it is a roughly 28-day cycle that can be correlated with, but is not the same as, the menstrual cycle (discussed shortly). The cycle includes two interrelated processes: oogenesis (the production of female gametes) and folliculogenesis (the growth and development of ovarian follicles).
Gametogenesis in females is called oogenesis . The process begins with the ovarian stem cells, or oogonia ( Figure 27.11 ). Oogonia are formed during fetal development, and divide via mitosis, much like spermatogonia in the testis. Unlike spermatogonia, however, oogonia form primary oocytes in the fetal ovary prior to birth. These primary oocytes are then arrested in this stage of meiosis I, only to resume it years later, beginning at puberty and continuing until the woman is near menopause (the cessation of a woman’s reproductive functions). The number of primary oocytes present in the ovaries declines from one to two million in an infant, to approximately 400,000 at puberty, to zero by the end of menopause.
The initiation of ovulation —the release of an oocyte from the ovary—marks the transition from puberty into reproductive maturity for women. From then on, throughout a woman’s reproductive years, ovulation occurs approximately once every 28 days. Just prior to ovulation, a surge of luteinizing hormone triggers the resumption of meiosis in a primary oocyte. This initiates the transition from primary to secondary oocyte. However, as you can see in Figure 27.11 , this cell division does not result in two identical cells. Instead, the cytoplasm is divided unequally, and one daughter cell is much larger than the other. This larger cell, the secondary oocyte, eventually leaves the ovary during ovulation. The smaller cell, called the first polar body , may or may not complete meiosis and produce second polar bodies; in either case, it eventually disintegrates. Therefore, even though oogenesis produces up to four cells, only one survives.
How does the diploid secondary oocyte become an ovum —the haploid female gamete? Meiosis of a secondary oocyte is completed only if a sperm succeeds in penetrating its barriers. Meiosis II then resumes, producing one haploid ovum that, at the instant of fertilization by a (haploid) sperm, becomes the first diploid cell of the new offspring (a zygote). Thus, the ovum can be thought of as a brief, transitional, haploid stage between the diploid oocyte and diploid zygote.
The larger amount of cytoplasm contained in the female gamete is used to supply the developing zygote with nutrients during the period between fertilization and implantation into the uterus. Interestingly, sperm contribute only DNA at fertilization —not cytoplasm. Therefore, the cytoplasm and all of the cytoplasmic organelles in the developing embryo are of maternal origin. This includes mitochondria, which contain their own DNA. Scientific research in the 1980s determined that mitochondrial DNA was maternally inherited, meaning that you can trace your mitochondrial DNA directly to your mother, her mother, and so on back through your female ancestors.
Everyday Connection
Mapping human history with mitochondrial dna.
When we talk about human DNA, we’re usually referring to nuclear DNA; that is, the DNA coiled into chromosomal bundles in the nucleus of our cells. We inherit half of our nuclear DNA from our father, and half from our mother. However, mitochondrial DNA (mtDNA) comes only from the mitochondria in the cytoplasm of the fat ovum we inherit from our mother. She received her mtDNA from her mother, who got it from her mother, and so on. Each of our cells contains approximately 1700 mitochondria, with each mitochondrion packed with mtDNA containing approximately 37 genes.
Mutations (changes) in mtDNA occur spontaneously in a somewhat organized pattern at regular intervals in human history. By analyzing these mutational relationships, researchers have been able to determine that we can all trace our ancestry back to one woman who lived in Africa about 200,000 years ago. Scientists have given this woman the biblical name Eve, although she is not, of course, the first Homo sapiens female. More precisely, she is our most recent common ancestor through matrilineal descent.
This doesn’t mean that everyone’s mtDNA today looks exactly like that of our ancestral Eve. Because of the spontaneous mutations in mtDNA that have occurred over the centuries, researchers can map different “branches” off of the “main trunk” of our mtDNA family tree. Your mtDNA might have a pattern of mutations that aligns more closely with one branch, and your neighbor’s may align with another branch. Still, all branches eventually lead back to Eve.
But what happened to the mtDNA of all of the other Homo sapiens females who were living at the time of Eve? Researchers explain that, over the centuries, their female descendants died childless or with only male children, and thus, their maternal line—and its mtDNA—ended.
Folliculogenesis
Again, ovarian follicles are oocytes and their supporting cells. They grow and develop in a process called folliculogenesis , which typically leads to ovulation of one follicle approximately every 28 days, along with death to multiple other follicles. The death of ovarian follicles is called atresia, and can occur at any point during follicular development. Recall that, a female infant at birth will have one to two million oocytes within her ovarian follicles, and that this number declines throughout life until menopause, when no follicles remain. As you’ll see next, follicles progress from primordial, to primary, to secondary and tertiary stages prior to ovulation—with the oocyte inside the follicle remaining as a primary oocyte until right before ovulation.
Folliculogenesis begins with follicles in a resting state. These small primordial follicles are present in newborn females and are the prevailing follicle type in the adult ovary ( Figure 27.12 ). Primordial follicles have only a single flat layer of support cells, called granulosa cells , that surround the oocyte, and they can stay in this resting state for years—some until right before menopause.
After puberty, a few primordial follicles will respond to a recruitment signal each day, and will join a pool of immature growing follicles called primary follicles . Primary follicles start with a single layer of granulosa cells, but the granulosa cells then become active and transition from a flat or squamous shape to a rounded, cuboidal shape as they increase in size and proliferate. As the granulosa cells divide, the follicles—now called secondary follicles (see Figure 27.12 )—increase in diameter, adding a new outer layer of connective tissue, blood vessels, and theca cells —cells that work with the granulosa cells to produce estrogens.
Within the growing secondary follicle, the primary oocyte now secretes a thin acellular membrane called the zona pellucida that will play a critical role in fertilization. A thick fluid, called follicular fluid, that has formed between the granulosa cells also begins to collect into one large pool, or antrum . Follicles in which the antrum has become large and fully formed are considered tertiary follicles (or antral follicles). Several follicles reach the tertiary stage at the same time, and most of these will undergo atresia. The one that does not die will continue to grow and develop until ovulation, when it will expel its secondary oocyte surrounded by several layers of granulosa cells from the ovary. Keep in mind that most follicles don’t make it to this point. In fact, roughly 99 percent of the follicles in the ovary will undergo atresia, which can occur at any stage of folliculogenesis.
Hormonal Control of the Ovarian Cycle
The process of development that we have just described, from primordial follicle to early tertiary follicle, takes approximately two months in humans. The final stages of development of a small cohort of tertiary follicles, ending with ovulation of a secondary oocyte, occur over a course of approximately 28 days. These changes are regulated by many of the same hormones that regulate the male reproductive system, including GnRH, LH, and FSH.
As in men, the hypothalamus produces GnRH, a hormone that signals the anterior pituitary gland to produce the gonadotropins FSH and LH ( Figure 27.13 ). These gonadotropins leave the pituitary and travel through the bloodstream to the ovaries, where they bind to receptors on the granulosa and theca cells of the follicles. FSH stimulates the follicles to grow (hence its name of follicle-stimulating hormone), and the five or six tertiary follicles expand in diameter. The release of LH also stimulates the granulosa and theca cells of the follicles to produce the sex steroid hormone estradiol, a type of estrogen. This phase of the ovarian cycle, when the tertiary follicles are growing and secreting estrogen, is known as the follicular phase.
The more granulosa and theca cells a follicle has (that is, the larger and more developed it is), the more estrogen it will produce in response to LH stimulation. As a result of these large follicles producing large amounts of estrogen, systemic plasma estrogen concentrations increase. Following a classic negative feedback loop, the high concentrations of estrogen will stimulate the hypothalamus and pituitary to reduce the production of GnRH, LH, and FSH. Because the large tertiary follicles require FSH to grow and survive at this point, this decline in FSH caused by negative feedback leads most of them to die (atresia). Typically only one follicle, now called the dominant follicle, will survive this reduction in FSH, and this follicle will be the one that releases an oocyte. Scientists have studied many factors that lead to a particular follicle becoming dominant: size, the number of granulosa cells, and the number of FSH receptors on those granulosa cells all contribute to a follicle becoming the one surviving dominant follicle.
When only the one dominant follicle remains in the ovary, it again begins to secrete estrogen. It produces more estrogen than all of the developing follicles did together before the negative feedback occurred. It produces so much estrogen that the normal negative feedback doesn’t occur. Instead, these extremely high concentrations of systemic plasma estrogen trigger a regulatory switch in the anterior pituitary that responds by secreting large amounts of LH and FSH into the bloodstream (see Figure 27.13 ). The positive feedback loop by which more estrogen triggers release of more LH and FSH only occurs at this point in the cycle.
It is this large burst of LH (called the LH surge) that leads to ovulation of the dominant follicle. The LH surge induces many changes in the dominant follicle, including stimulating the resumption of meiosis of the primary oocyte to a secondary oocyte. As noted earlier, the polar body that results from unequal cell division simply degrades. The LH surge also triggers proteases (enzymes that cleave proteins) to break down structural proteins in the ovary wall on the surface of the bulging dominant follicle. This degradation of the wall, combined with pressure from the large, fluid-filled antrum, results in the expulsion of the oocyte surrounded by granulosa cells into the peritoneal cavity. This release is ovulation.
In the next section, you will follow the ovulated oocyte as it travels toward the uterus, but there is one more important event that occurs in the ovarian cycle. The surge of LH also stimulates a change in the granulosa and theca cells that remain in the follicle after the oocyte has been ovulated. This change is called luteinization (recall that the full name of LH is luteinizing hormone), and it transforms the collapsed follicle into a new endocrine structure called the corpus luteum , a term meaning “yellowish body” (see Figure 27.12 ). Instead of estrogen, the luteinized granulosa and theca cells of the corpus luteum begin to produce large amounts of the sex steroid hormone progesterone, a hormone that is critical for the establishment and maintenance of pregnancy. Progesterone triggers negative feedback at the hypothalamus and pituitary, which keeps GnRH, LH, and FSH secretions low, so no new dominant follicles develop at this time.
The post-ovulatory phase of progesterone secretion is known as the luteal phase of the ovarian cycle. If pregnancy does not occur within 10 to 12 days, the corpus luteum will stop secreting progesterone and degrade into the corpus albicans , a nonfunctional “whitish body” that will disintegrate in the ovary over a period of several months. During this time of reduced progesterone secretion, FSH and LH are once again stimulated, and the follicular phase begins again with a new cohort of early tertiary follicles beginning to grow and secrete estrogen.
The Uterine Tubes
The uterine tubes (also called fallopian tubes or oviducts) serve as the conduit of the oocyte from the ovary to the uterus ( Figure 27.14 ). Each of the two uterine tubes is close to, but not directly connected to, the ovary and divided into sections. The isthmus is the narrow medial end of each uterine tube that is connected to the uterus. The wide distal infundibulum flares out with slender, finger-like projections called fimbriae . The middle region of the tube, called the ampulla , is where fertilization often occurs. The uterine tubes also have three layers: an outer serosa, a middle smooth muscle layer, and an inner mucosal layer. In addition to its mucus-secreting cells, the inner mucosa contains ciliated cells that beat in the direction of the uterus, producing a current that will be critical to move the oocyte.
Following ovulation, the secondary oocyte surrounded by a few granulosa cells is released into the peritoneal cavity. The nearby uterine tube, either left or right, receives the oocyte. Unlike sperm, oocytes lack flagella, and therefore cannot move on their own. So how do they travel into the uterine tube and toward the uterus? High concentrations of estrogen that occur around the time of ovulation induce contractions of the smooth muscle along the length of the uterine tube. These contractions occur every 4 to 8 seconds, and the result is a coordinated movement that sweeps the surface of the ovary and the pelvic cavity. Current flowing toward the uterus is generated by coordinated beating of the cilia that line the outside and lumen of the length of the uterine tube. These cilia beat more strongly in response to the high estrogen concentrations that occur around the time of ovulation. As a result of these mechanisms, the oocyte–granulosa cell complex is pulled into the interior of the tube. Once inside, the muscular contractions and beating cilia move the oocyte slowly toward the uterus. When fertilization does occur, sperm typically meet the egg while it is still moving through the ampulla.
Interactive Link
Watch this video to observe ovulation and its initiation in response to the release of FSH and LH from the pituitary gland. What specialized structures help guide the oocyte from the ovary into the uterine tube?
If the oocyte is successfully fertilized, the resulting zygote will begin to divide into two cells, then four, and so on, as it makes its way through the uterine tube and into the uterus. There, it will implant and continue to grow. If the egg is not fertilized, it will simply degrade—either in the uterine tube or in the uterus, where it may be shed with the next menstrual period.
The open-ended structure of the uterine tubes can have significant health consequences if bacteria or other contagions enter through the vagina and move through the uterus, into the tubes, and then into the pelvic cavity. If this is left unchecked, a bacterial infection (sepsis) could quickly become life-threatening. The spread of an infection in this manner is of special concern when unskilled practitioners perform abortions in non-sterile conditions. Sepsis is also associated with sexually transmitted bacterial infections, especially gonorrhea and chlamydia. These increase a woman’s risk for pelvic inflammatory disease (PID), infection of the uterine tubes or other reproductive organs. Even when resolved, PID can leave scar tissue in the tubes, leading to infertility.
Watch this series of videos to look at the movement of the oocyte through the ovary. The cilia in the uterine tube promote movement of the oocyte. What would likely occur if the cilia were paralyzed at the time of ovulation?
The Uterus and Cervix
The uterus is the muscular organ that nourishes and supports the growing embryo (see Figure 27.14 ). Its average size is approximately 5 cm wide by 7 cm long (approximately 2 in by 3 in) when a female is not pregnant. It has three sections. The portion of the uterus superior to the opening of the uterine tubes is called the fundus . The middle section of the uterus is called the body of uterus (or corpus). The cervix is the narrow inferior portion of the uterus that projects into the vagina. The cervix produces mucus secretions that become thin and stringy under the influence of high systemic plasma estrogen concentrations, and these secretions can facilitate sperm movement through the reproductive tract.
Several ligaments maintain the position of the uterus within the abdominopelvic cavity. The broad ligament is a fold of peritoneum that serves as a primary support for the uterus, extending laterally from both sides of the uterus and attaching it to the pelvic wall. The round ligament attaches to the uterus near the uterine tubes, and extends to the labia majora. Finally, the uterosacral ligament stabilizes the uterus posteriorly by its connection from the cervix to the pelvic wall.
The wall of the uterus is made up of three layers. The most superficial layer is the serous membrane, or perimetrium , which consists of epithelial tissue that covers the exterior portion of the uterus. The middle layer, or myometrium , is a thick layer of smooth muscle responsible for uterine contractions. Most of the uterus is myometrial tissue, and the muscle fibers run horizontally, vertically, and diagonally, allowing the powerful contractions that occur during labor and the less powerful contractions (or cramps) that help to expel menstrual blood during a woman’s period. Anteriorly directed myometrial contractions also occur near the time of ovulation, and are thought to possibly facilitate the transport of sperm through the female reproductive tract.
The innermost layer of the uterus is called the endometrium . The endometrium contains a connective tissue lining, the lamina propria, which is covered by epithelial tissue that lines the lumen. Structurally, the endometrium consists of two layers: the stratum basalis and the stratum functionalis (the basal and functional layers). The stratum basalis layer is part of the lamina propria and is adjacent to the myometrium; this layer does not shed during menses. In contrast, the thicker stratum functionalis layer contains the glandular portion of the lamina propria and the endothelial tissue that lines the uterine lumen. It is the stratum functionalis that grows and thickens in response to increased levels of estrogen and progesterone. In the luteal phase of the menstrual cycle, special branches off of the uterine artery called spiral arteries supply the thickened stratum functionalis. This inner functional layer provides the proper site of implantation for the fertilized egg, and—should fertilization not occur—it is only the stratum functionalis layer of the endometrium that sheds during menstruation.
Recall that during the follicular phase of the ovarian cycle, the tertiary follicles are growing and secreting estrogen. At the same time, the stratum functionalis of the endometrium is thickening to prepare for a potential implantation. The post-ovulatory increase in progesterone, which characterizes the luteal phase, is key for maintaining a thick stratum functionalis. As long as a functional corpus luteum is present in the ovary, the endometrial lining is prepared for implantation. Indeed, if an embryo implants, signals are sent to the corpus luteum to continue secreting progesterone to maintain the endometrium, and thus maintain the pregnancy. If an embryo does not implant, no signal is sent to the corpus luteum and it degrades, ceasing progesterone production and ending the luteal phase. Without progesterone, the endometrium thins and, under the influence of prostaglandins, the spiral arteries of the endometrium constrict and rupture, preventing oxygenated blood from reaching the endometrial tissue. As a result, endometrial tissue dies and blood, pieces of the endometrial tissue, and white blood cells are shed through the vagina during menstruation, or the menses . The first menses after puberty, called menarche , can occur either before or after the first ovulation.
The Menstrual Cycle
Now that we have discussed the maturation of the cohort of tertiary follicles in the ovary, the build-up and then shedding of the endometrial lining in the uterus, and the function of the uterine tubes and vagina, we can put everything together to talk about the three phases of the menstrual cycle —the series of changes in which the uterine lining is shed, rebuilds, and prepares for implantation.
The timing of the menstrual cycle starts with the first day of menses, referred to as day one of a woman’s period. Cycle length is determined by counting the days between the onset of bleeding in two subsequent cycles. Because the average length of a woman’s menstrual cycle is 28 days, this is the time period used to identify the timing of events in the cycle. However, the length of the menstrual cycle varies among women, and even in the same woman from one cycle to the next, typically from 21 to 32 days.
Just as the hormones produced by the granulosa and theca cells of the ovary “drive” the follicular and luteal phases of the ovarian cycle, they also control the three distinct phases of the menstrual cycle. These are the menses phase, the proliferative phase, and the secretory phase.
Menses Phase
The menses phase of the menstrual cycle is the phase during which the lining is shed; that is, the days that the woman menstruates. Although it averages approximately five days, the menses phase can last from 2 to 7 days, or longer. As shown in Figure 27.15 , the menses phase occurs during the early days of the follicular phase of the ovarian cycle, when progesterone, FSH, and LH levels are low. Recall that progesterone concentrations decline as a result of the degradation of the corpus luteum, marking the end of the luteal phase. This decline in progesterone triggers the shedding of the stratum functionalis of the endometrium.
Proliferative Phase
Once menstrual flow ceases, the endometrium begins to proliferate again, marking the beginning of the proliferative phase of the menstrual cycle (see Figure 27.15 ). It occurs when the granulosa and theca cells of the tertiary follicles begin to produce increased amounts of estrogen. These rising estrogen concentrations stimulate the endometrial lining to rebuild.
Recall that the high estrogen concentrations will eventually lead to a decrease in FSH as a result of negative feedback, resulting in atresia of all but one of the developing tertiary follicles. The switch to positive feedback—which occurs with the elevated estrogen production from the dominant follicle—then stimulates the LH surge that will trigger ovulation. In a typical 28-day menstrual cycle, ovulation occurs on day 14. Ovulation marks the end of the proliferative phase as well as the end of the follicular phase.
Secretory Phase
In addition to prompting the LH surge, high estrogen levels increase the uterine tube contractions that facilitate the pick-up and transfer of the ovulated oocyte. High estrogen levels also slightly decrease the acidity of the vagina, making it more hospitable to sperm. In the ovary, the luteinization of the granulosa cells of the collapsed follicle forms the progesterone-producing corpus luteum, marking the beginning of the luteal phase of the ovarian cycle. In the uterus, progesterone from the corpus luteum begins the secretory phase of the menstrual cycle, in which the endometrial lining prepares for implantation (see Figure 27.15 ). Over the next 10 to 12 days, the endometrial glands secrete a fluid rich in glycogen. If fertilization has occurred, this fluid will nourish the ball of cells now developing from the zygote. At the same time, the spiral arteries develop to provide blood to the thickened stratum functionalis.
If no pregnancy occurs within approximately 10 to 12 days, the corpus luteum will degrade into the corpus albicans. Levels of both estrogen and progesterone will fall, and the endometrium will grow thinner. Prostaglandins will be secreted that cause constriction of the spiral arteries, reducing oxygen supply. The endometrial tissue will die, resulting in menses—or the first day of the next cycle.
Disorders of the...
Female reproductive system.
Research over many years has confirmed that cervical cancer is most often caused by a sexually transmitted infection with human papillomavirus (HPV). There are over 100 related viruses in the HPV family, and the characteristics of each strain determine the outcome of the infection. In all cases, the virus enters body cells and uses its own genetic material to take over the host cell’s metabolic machinery and produce more virus particles.
HPV infections are common in both men and women. Indeed, a recent study determined that 42.5 percent of females had HPV at the time of testing. These women ranged in age from 14 to 59 years and differed in race, ethnicity, and number of sexual partners. Of note, the prevalence of HPV infection was 53.8 percent among women aged 20 to 24 years, the age group with the highest infection rate.
HPV strains are classified as high or low risk according to their potential to cause cancer. Though most HPV infections do not cause disease, the disruption of normal cellular functions in the low-risk forms of HPV can cause the male or female human host to develop genital warts. Often, the body is able to clear an HPV infection by normal immune responses within 2 years. However, the more serious, high-risk infection by certain types of HPV can result in cancer of the cervix ( Figure 27.16 ). Infection with either of the cancer-causing variants HPV 16 or HPV 18 has been linked to more than 70 percent of all cervical cancer diagnoses. Although even these high-risk HPV strains can be cleared from the body over time, infections persist in some individuals. If this happens, the HPV infection can influence the cells of the cervix to develop precancerous changes.
Risk factors for cervical cancer include having unprotected sex; having multiple sexual partners; a first sexual experience at a younger age, when the cells of the cervix are not fully mature; failure to receive the HPV vaccine; a compromised immune system; and smoking. The risk of developing cervical cancer is doubled with cigarette smoking.
When the high-risk types of HPV enter a cell, two viral proteins are used to neutralize proteins that the host cells use as checkpoints in the cell cycle. The best studied of these proteins is p53. In a normal cell, p53 detects DNA damage in the cell’s genome and either halts the progression of the cell cycle—allowing time for DNA repair to occur—or initiates apoptosis. Both of these processes prevent the accumulation of mutations in a cell’s genome. High-risk HPV can neutralize p53, keeping the cell in a state in which fast growth is possible and impairing apoptosis, allowing mutations to accumulate in the cellular DNA.
The prevalence of cervical cancer in the United States is very low because of regular screening exams called pap smears. Pap smears sample cells of the cervix, allowing the detection of abnormal cells. If pre-cancerous cells are detected, there are several highly effective techniques that are currently in use to remove them before they pose a danger. However, women in developing countries often do not have access to regular pap smears. As a result, these women account for as many as 80 percent of the cases of cervical cancer worldwide.
In 2006, the first vaccine against the high-risk types of HPV was approved. There are now two HPV vaccines available: Gardasil ® and Cervarix ® . Whereas these vaccines were initially only targeted for women, because HPV is sexually transmitted, both men and women require vaccination for this approach to achieve its maximum efficacy. A recent study suggests that the HPV vaccine has cut the rates of HPV infection by the four targeted strains at least in half. Unfortunately, the high cost of manufacturing the vaccine is currently limiting access to many women worldwide.
The Breasts
Whereas the breasts are located far from the other female reproductive organs, they are considered accessory organs of the female reproductive system. The function of the breasts is to supply milk to an infant in a process called lactation. The external features of the breast include a nipple surrounded by a pigmented areola ( Figure 27.17 ), whose coloration may deepen during pregnancy. The areola is typically circular and can vary in size from 25 to 100 mm in diameter. The areolar region is characterized by small, raised areolar glands that secrete lubricating fluid during lactation to protect the nipple from chafing. When a baby nurses, or draws milk from the breast, the entire areolar region is taken into the mouth.
Breast milk is produced by the mammary glands , which are modified sweat glands. The milk itself exits the breast through the nipple via 15 to 20 lactiferous ducts that open on the surface of the nipple. These lactiferous ducts each extend to a lactiferous sinus that connects to a glandular lobe within the breast itself that contains groups of milk-secreting cells in clusters called alveoli (see Figure 27.17 ). The clusters can change in size depending on the amount of milk in the alveolar lumen. Once milk is made in the alveoli, stimulated myoepithelial cells that surround the alveoli contract to push the milk to the lactiferous sinuses. From here, the baby can draw milk through the lactiferous ducts by suckling. The lobes themselves are surrounded by fat tissue, which determines the size of the breast; breast size differs between individuals and does not affect the amount of milk produced. Supporting the breasts are multiple bands of connective tissue called suspensory ligaments that connect the breast tissue to the dermis of the overlying skin.
During the normal hormonal fluctuations in the menstrual cycle, breast tissue responds to changing levels of estrogen and progesterone, which can lead to swelling and breast tenderness in some individuals, especially during the secretory phase. If pregnancy occurs, the increase in hormones leads to further development of the mammary tissue and enlargement of the breasts.
Hormonal Birth Control
Birth control pills take advantage of the negative feedback system that regulates the ovarian and menstrual cycles to stop ovulation and prevent pregnancy. Typically they work by providing a constant level of both estrogen and progesterone, which negatively feeds back onto the hypothalamus and pituitary, thus preventing the release of FSH and LH. Without FSH, the follicles do not mature, and without the LH surge, ovulation does not occur. Although the estrogen in birth control pills does stimulate some thickening of the endometrial wall, it is reduced compared with a normal cycle and is less likely to support implantation.
Some birth control pills contain 21 active pills containing hormones, and 7 inactive pills (placebos). The decline in hormones during the week that the woman takes the placebo pills triggers menses, although it is typically lighter than a normal menstrual flow because of the reduced endometrial thickening. Newer types of birth control pills have been developed that deliver low-dose estrogens and progesterone for the entire cycle (these are meant to be taken 365 days a year), and menses never occurs. While some women prefer to have the proof of a lack of pregnancy that a monthly period provides, menstruation every 28 days is not required for health reasons, and there are no reported adverse effects of not having a menstrual period in an otherwise healthy individual.
Because birth control pills function by providing constant estrogen and progesterone levels and disrupting negative feedback, skipping even just one or two pills at certain points of the cycle (or even being several hours late taking the pill) can lead to an increase in FSH and LH and result in ovulation. It is important, therefore, that the woman follow the directions on the birth control pill package to successfully prevent pregnancy.
Aging and the...
Female fertility (the ability to conceive) peaks when women are in their twenties, and is slowly reduced until a women reaches 35 years of age. After that time, fertility declines more rapidly, until it ends completely at the end of menopause. Menopause is the cessation of the menstrual cycle that occurs as a result of the loss of ovarian follicles and the hormones that they produce. A woman is considered to have completed menopause if she has not menstruated in a full year. After that point, she is considered postmenopausal. The average age for this change is consistent worldwide at between 50 and 52 years of age, but it can normally occur in a woman’s forties, or later in her fifties. Poor health, including smoking, can lead to earlier loss of fertility and earlier menopause.
As a woman reaches the age of menopause, depletion of the number of viable follicles in the ovaries due to atresia affects the hormonal regulation of the menstrual cycle. During the years leading up to menopause, there is a decrease in the levels of the hormone inhibin, which normally participates in a negative feedback loop to the pituitary to control the production of FSH. The menopausal decrease in inhibin leads to an increase in FSH. The presence of FSH stimulates more follicles to grow and secrete estrogen. Because small, secondary follicles also respond to increases in FSH levels, larger numbers of follicles are stimulated to grow; however, most undergo atresia and die. Eventually, this process leads to the depletion of all follicles in the ovaries, and the production of estrogen falls off dramatically. It is primarily the lack of estrogens that leads to the symptoms of menopause.
The earliest changes occur during the menopausal transition, often referred to as peri-menopause, when a women’s cycle becomes irregular but does not stop entirely. Although the levels of estrogen are still nearly the same as before the transition, the level of progesterone produced by the corpus luteum is reduced. This decline in progesterone can lead to abnormal growth, or hyperplasia, of the endometrium. This condition is a concern because it increases the risk of developing endometrial cancer. Two harmless conditions that can develop during the transition are uterine fibroids, which are benign masses of cells, and irregular bleeding. As estrogen levels change, other symptoms that occur are hot flashes and night sweats, trouble sleeping, vaginal dryness, mood swings, difficulty focusing, and thinning of hair on the head along with the growth of more hair on the face. Depending on the individual, these symptoms can be entirely absent, moderate, or severe.
After menopause, lower amounts of estrogens can lead to other changes. Cardiovascular disease becomes as prevalent in women as in men, possibly because estrogens reduce the amount of cholesterol in the blood vessels. When estrogen is lacking, many women find that they suddenly have problems with high cholesterol and the cardiovascular issues that accompany it. Osteoporosis is another problem because bone density decreases rapidly in the first years after menopause. The reduction in bone density leads to a higher incidence of fractures.
Hormone therapy (HT), which employs medication (synthetic estrogens and progestins) to increase estrogen and progestin levels, can alleviate some of the symptoms of menopause. In 2002, the Women’s Health Initiative began a study to observe women for the long-term outcomes of hormone replacement therapy over 8.5 years. However, the study was prematurely terminated after 5.2 years because of evidence of a higher than normal risk of breast cancer in patients taking estrogen-only HT. The potential positive effects on cardiovascular disease were also not realized in the estrogen-only patients. The results of other hormone replacement studies over the last 50 years, including a 2012 study that followed over 1,000 menopausal women for 10 years, have shown cardiovascular benefits from estrogen and no increased risk for cancer. Some researchers believe that the age group tested in the 2002 trial may have been too old to benefit from the therapy, thus skewing the results. In the meantime, intense debate and study of the benefits and risks of replacement therapy is ongoing. Current guidelines approve HT for the reduction of hot flashes or flushes, but this treatment is generally only considered when women first start showing signs of menopausal changes, is used in the lowest dose possible for the shortest time possible (5 years or less), and it is suggested that women on HT have regular pelvic and breast exams.
As an Amazon Associate we earn from qualifying purchases.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction
- Authors: J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix
- Publisher/website: OpenStax
- Book title: Anatomy and Physiology
- Publication date: Apr 25, 2013
- Location: Houston, Texas
- Book URL: https://openstax.org/books/anatomy-and-physiology/pages/1-introduction
- Section URL: https://openstax.org/books/anatomy-and-physiology/pages/27-2-anatomy-and-physiology-of-the-female-reproductive-system
© Jan 27, 2022 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.
The Female Reproductive Tract
The female reproductive tract is all located within the pelvis. It is made up of the vulva, the vagina, the cervix, the uterus, the fallopian tubes and the ovaries. These organs are supported in the pelvis by ligaments.
The vulva refers to the external female genitalia. Its anatomical structure can be broken down further into the mons pubis, labia majora and minora, vestibule, Bartholin’s glands and clitoris.
The vagina is a distensible muscular tube which connects the uterus and cervix to the external vaginal orifice. It sits posteriorly to the bladder and urethra and anteriorly to the rectum and anal canal. The vagina is involved in sexual intercourse, childbirth and menstruation.
The cervix is the lower part of the uterus, just superior to the vagina. At each end is a cervical os, a narrow opening into the uterus and vagina either side. It facilitates the passage of sperm whilst maintaining a sterile environment in the upper female reproductive system.
The uterus, commonly referred to as the womb, is the location of normal implantation of an early embryo. It has a large variation of positions within the pelvis, described by its degree of anteversion or retroversion, and anteflexion or retroflexion.
The fallopian tubes connect the ovaries to the uterus, and therefore have the function of transport of the ovum towards the uterus. Their length is split into sections: the fimbriae, infundibulum, ampulla and isthmus.
The ovaries are the female gonads, and so are the site of gametogenesis. They sit laterally to the uterus, and closely adjacent to the fimbriae of the fallopian tubes.
There are many ligaments of the female reproductive tract which support the organs of the female reproductive tract and also act as a conduit for neurovascular structures supplying these.
In this section, learn more about the female reproductive tract, including the vulva, vagina, cervix, uterus, fallopian tubes, ovaries and the ligaments of the female reproductive tract.
The Fallopian (Uterine) Tubes
The Ovaries
Ligaments of the Female Reproductive Tract
Anatomy Video Lectures
START NOW FOR FREE

Encyclopaedia
Anterior interosseous nerve.
by Max Bidewell and Kumail Jaffery
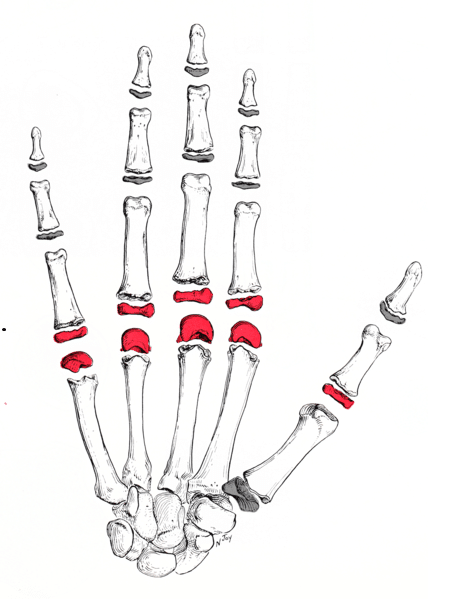
Joints of the Upper Limb
The metacarpophalangeal joint.
by Aren Mnatzakanian
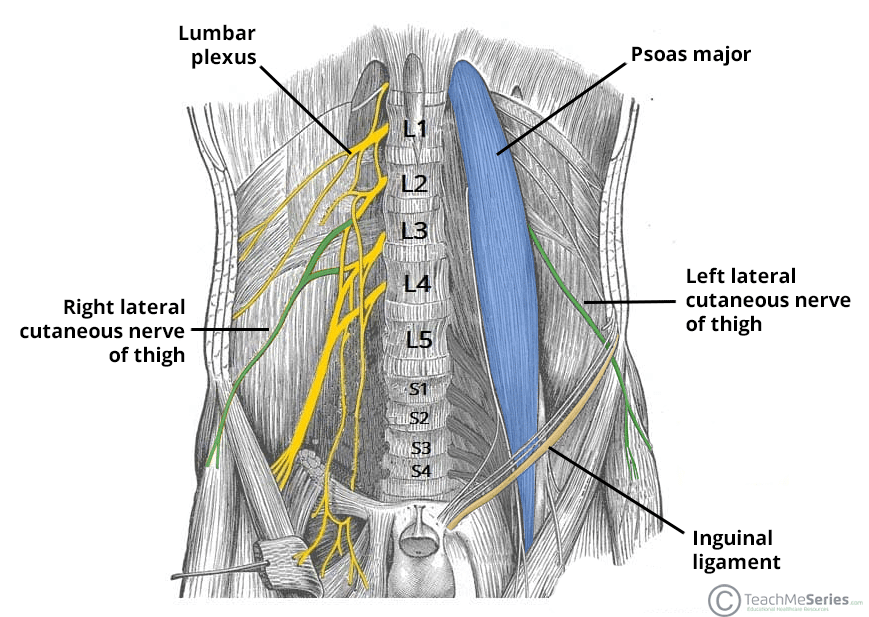
Lateral Cutaneous Nerve of the Thigh
by Mihir Himanshu Majeethia
Forgot Password
Please enter your username or email address below. You will receive a link to create a new password via emai and please check that the email hasn't been delivered into your spam folder.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
BioEd Online
Science teacher resources from baylor college of medicine.
- Log in / Register
Overview of the Female Reproductive System

The female reproductive system is responsible for the production, storage and release of ova. Its two main components are the ovaries and the accessory sex organs.
User Tools [+] Expand
User tools [-] collapse.
- You currently have no favorites. You may add some using the "Add to favorites" link below.
- Stored in favorites
- Add to favorites
- Send this Page
- Print this Page
Join our Mailing List
Stay up to date with news and information from BioEd Online, join our mailing list today!
- Click Here to Subscribe
Need Assistance?
If you need help or have a question please use the links below to help resolve your problem.

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
Anatomy & Physiology Of Female Reproductive System
Published by Claude Austin Modified over 8 years ago
Similar presentations
Presentation on theme: "Anatomy & Physiology Of Female Reproductive System"— Presentation transcript:

FUNCTIONS OF THE FEMALE REPRODUCTIVE SYSTEM
Anatomy of female reproductive system
Anatomy of the Female Genital Tract & Pelvic Floor
Chapter 16 The Reproductive System
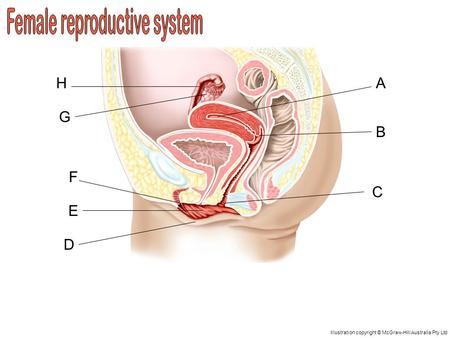
A D C B H G F E Illustration copyright © McGraw-Hill Australia Pty Ltd.
Anatomy of Female Reproductive System
MALE & FEMALE REPRODUCTIVE SYSTEMS
The Female Reproductive System
The Reproductive System
Sex can Wait- Lesson 10 – Female Reproductive System.
FEMALE REPRODUCTIVE ANATOMY
Sperm Release Pathway: The Parasympathetic Step
Question What are the responsibilities of partners who engage in sexual intercourse? List five.
Female Reproductive System
F EMALE R EPRODUCTIVE SYSTEM Chapter 32. P URPOSE OF THE FEMALE REPRODUCTIVE SYSTEM : Produce gamete Production of offspring Continuation of the genetic.
Reproductive Systems Female.
Vagina Day Female Reproduction.

Female Reproductive System.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

22.2: Introduction to the Reproductive System
- Last updated
- Save as PDF
- Page ID 17787

- Suzanne Wakim & Mandeep Grewal
- Butte College
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
It’s All About Sex
A tiny sperm breaks through the surface of a huge egg. Voilà! In nine months, a new baby will be born. Like most other multicellular organisms, human beings reproduce sexually. In human sexual reproduction, individuals with testes produce sperm, and individuals with ovaries produce eggs, and a new offspring forms when a sperm unites with an egg. How do sperm and eggs form? And how do they arrive together at the right place and time so they can unite to form a new offspring? These are functions of the reproductive system.

What Is the Reproductive System?
The reproductive system is the human organ system responsible for the production and fertilization of gametes (sperm or eggs) and carrying of a fetus. Both both sexes gonads produce gametes. A gamete is a haploid cell that combines with another haploid gamete during fertilization, forming a single diploid cell called a zygote. Besides producing gametes, the gonads also produce sex hormones. Sex hormones are endocrine hormones that control the development of sex organs before birth, sexual maturation at puberty, and reproduction once sexual maturation has occurred. Other reproductive system organs have various functions, such as maturing gametes, delivering gametes to the site of fertilization, and providing an environment for the development and growth of offspring.
Sex Differences in the Reproductive System
The reproductive system is the only human organ system that is significantly different between males and females. Embryonic structures that will develop into the reproductive system start out the same in males and females, but by birth, the reproductive systems have differentiated. How does this happen?
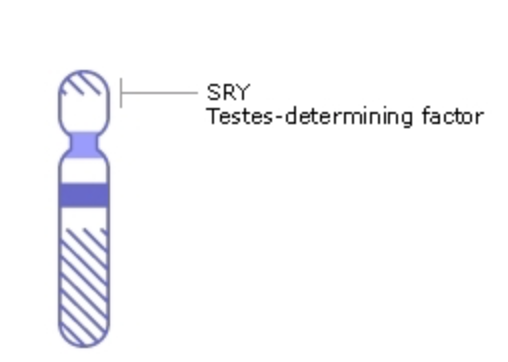
Sex Differentiation
Starting around the seventh week after conception in genetically male (XY) embryos, a gene called SRY on the Y chromosome (Figure \(\PageIndex{2}\)) initiates the production of multiple proteins. These proteins cause undifferentiated gonadal tissue to develop into testes. Testes secrete hormones — including testosterone — that trigger other changes in the developing offspring (now called a fetus), causing it to develop a complete male reproductive system. Without a Y chromosome, an embryo will develop ovaries, that will produce estrogen. Estrogen, in turn, will lead to the formation of the other organs of a female reproductive system.
Homologous Structures
Undifferentiated embryonic tissues develop into different structures in male and female fetuses. Structures that arise from the same tissues in males and females are called homologous structures . The testes and ovaries, for example, are homologous structures that develop from the undifferentiated gonads of the embryo. Likewise, the penis and clitoris are homologous structures that develop from the same embryonic tissues.
Sex Hormones and Maturation
Male and female reproductive systems are different at birth, but they are immature and incapable of producing gametes or sex hormones. Maturation of the reproductive system occurs during puberty when hormones from the hypothalamus and pituitary gland stimulate the testes or ovaries to start producing sex hormones again. The main sex hormones are testosterone and estrogen . Sex hormones, in turn, lead to the growth and maturation of the reproductive organs, rapid body growth, and the development of secondary sex characteristics , such as body and facial hair and breasts.
Role of Sex Hormones in Transgender Treatment
Feminizing or masculinizing hormone therapy is the administration of exogenous endocrine agents to induce changes in physical appearance. Since hormone therapy is inexpensive relative to surgery and highly effective in the development of secondary sex characteristics (e.g., facial and body hair in female-to-male [FTM] individuals or breast tissue in male-to-females [MTFs]), hormone therapy is often the first, and sometimes only, medical gender affirmation intervention accessed by transgender individuals looking to develop masculine or feminine characteristics consistent with their gender identity. In some cases, hormone therapy may be required before surgical interventions can be conducted. Trans-females are prescribed estrogen and anti-testosterone medication, such as cyproterone acetate and spironolactone. Trans-men are prescribed testosterone.
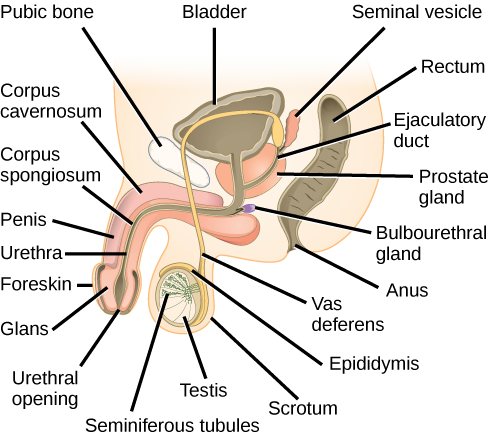
Male Reproductive System
The main structures of the male reproductive system are external to the body and illustrated in Figure \(\PageIndex{3}\). The two testes (singular, testis) hang between the thighs in a sac of skin called the scrotum. The testes produce both sperm and testosterone. Resting atop each testis is a coiled structure called the epididymis (plural, epididymes). The function of the epididymes is to mature and store sperm. The penis is a tubular organ that contains the urethra and has the ability to stiffen during sexual arousal. Sperm passes out of the body through the urethra during a sexual climax (orgasm). This release of sperm is called ejaculation.
In addition to these organs, there are several ducts and glands that are internal to the body. The ducts, which include the vas deferens (also called the ductus deferens), transport sperm from the epididymis to the urethra. The glands, which include the prostate gland and seminal vesicles, produce fluids that become part of semen. Semen is the fluid that carries sperm through the urethra and out of the body. It contains substances that control pH and provide sperm with nutrients for energy.
Female Reproductive System
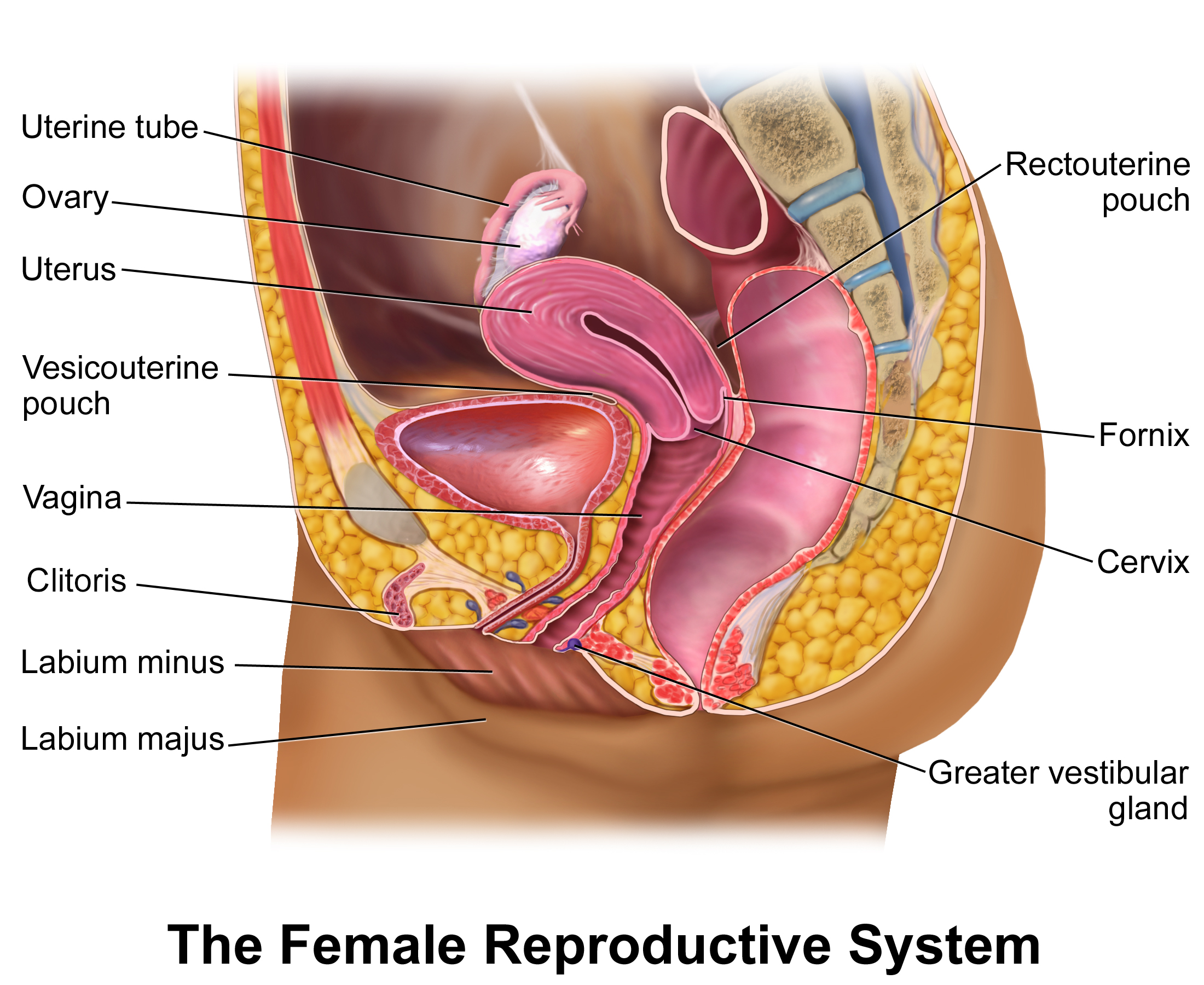
The main structures of the female reproductive system are internal to the body and shown in Figure \(\PageIndex{4}\). They include the paired ovaries, which are small, oval structures that produce eggs and secrete estrogen. The two Fallopian tubes (aka uterine tubes) start near the ovaries and end at the uterus. Their function is to transport eggs from the ovaries to the uterus. If an egg is fertilized, it usually occurs while it is traveling through a Fallopian tube. The uterus is a pear-shaped muscular organ that functions to carry a fetus until birth. It can expand greatly to accommodate a growing fetus, and its muscular walls can contract forcefully during labor to push the baby into the vagina. The vagina is a tubular tract connecting the uterus to the outside of the body. The vagina is where sperm are usually deposited during sexual intercourse and ejaculation. The vagina is also called the birth canal because a baby travels through the vagina to leave the body during birth.
The external structures of the female reproductive system are referred to collectively as the vulva. They include the clitoris, which is homologous to the male penis. They also include two pairs of labia (singular, labium), which surround and protect the openings of the urethra and vagina.
- What is the reproductive system?
- Define gonad.
- What are sex hormones? What are their general functions?
- Distinguish between male and female sex hormones.
- How does the differentiation of the reproductive system occur in males and females?
- In the context of the human male and female reproductive systems, what are homologous structures?
- When and how does the human reproductive system mature?
- List the organs of the male reproductive system.
- List the organs of the female reproductive system.
- What are female gametes called? What are male gametes called?
- True or False: The vagina is the homologous structure to the penis.
- rue or False: In the absence of a Y chromosome in humans, ovaries will develop.
- Fallopian tubes
- all of the above
- Fallopian tube
- Explain the difference between the vulva and the vagina.
Explore More
People's sense of gender identity does not always match their anatomy. Some people do not identify as either male or female, and instead, they identify as non-binary, or genderqueer. Others may identify as a gender that is the opposite of what is typically associated with their chromosomes or reproductive organs. These people are called transgender, and they may choose to transition to the opposite gender, a process that may or may not involve physical modifications. Watch the video below to learn about the use of hormones in gender transitioning.
Sex determination may be more complicated than originally thought. Check out this video to learn more:
Attributions
- Sperm-Egg ; public domain via Wikimedia Commons
- Human Y chromosome by National Center for Biotechnology Information ( NCBI ); public domain via Wikimedia Commons
- Male Reproductive System by Charles Molnar and Jane Gair; CC BY 4.0 from Concepts of Biology - 1st Canadian edition
- Female Reproductive System by Blausen.com staff (2014). " Medical gallery of Blausen Medical 2014 ". WikiJournal of Medicine 1 (2). DOI : 10.15347/wjm/2014.010 . ISSN 2002-4436 . licensed CC BY 3.0 via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0
- Some text is adapted from White Hughto JM, Reisner SL.. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals . Transgend Health. 2016;1(1):21-31 CC BY 4.0
ANATOMY OF THE FEMALE REPRODUCTIVE SYSTEM
Jul 22, 2014
710 likes | 2.98k Views
ANATOMY OF THE FEMALE REPRODUCTIVE SYSTEM. Prof . Ahmed Fathalla Ibrahim Professor of Anatomy College of Medicine King Saud University E-mail: [email protected]. OBJECTIVES. At the end of the lecture, students should: List the organs of female reproductive system.

Share Presentation
- transverse slit
- upper surface
- anteverted anteflexed uterus
- uterine tubes body
- birth canal

Presentation Transcript
ANATOMY OF THE FEMALE REPRODUCTIVE SYSTEM Prof. Ahmed FathallaIbrahim Professor of Anatomy College of Medicine King Saud University E-mail: [email protected]
OBJECTIVES At the end of the lecture, students should: • List the organs of female reproductive system. • Describe the pelvic peritoneum in female. • Describe the position and relations of the ovaries. • List the parts of the uterine tube. • Describe the anatomy of uterus regarding: subdivisions, cavity, relations, ligaments & main support. • Describe the anatomy of vagina regarding: structure, extent, length & relations. • Describe the supply (arteries, veins, lymph, nerves) of female reproductive system.
FEMALE REPRODUCTIVE SYSTEM UTERINE TUBE OVARY UTERUS V A G I N A POSTERIOR VIEW
PELVIC PERITONEUM IN FEMALE Rectouterine (Douglas) pouch: Reflection of peritoneum from rectum to upper part of posterior surface of vagina Uterovesical (vesicouterine) pouch: Reflection of peritoneum from uterus to upper surface of urinary bladder Broad ligament of uterus: Extension of peritoneum from lateral wall of uterus to lateral wall of pelvis, encloses the uterine tubes BROAD LIGAMENT
PELVIC PERITONEUM IN FEMALE
THE OVARIES It is an almond-shaped organ. It is attached to the back of the broad ligament by a peritoneal fold (mesovarium) Its medial end is attached to uterus by ligament of ovary. Its lateral end is related to the fimbriae of the uterine tube. BROAD LIGAMENT Female pelvic organs (Posterior view)
THE UTERINE (FALLOPIAN) TUBES 2 3 It is 10 cm long. It is enclosed in the broad ligament of uterus. It is divided into: 1) Intramural part: opening into the uterine wall 2)Isthmus: narrowest part 3)Ampulla: widest part (site of fertilization) 4)Infundibulum: funnel-shaped end, has finger-like processes (fimbriae), related to ovary 1 4 X
FUNCTION OF: OVARIES: PRIMARY SEX ORGANS IN FEMALE Production of female germ cells Secretion of female sex hormones UTERINE TUBES: Site of fertilization Transport of fertilized ovum into the uterus
2’ THE UTERUS 3’ A hollow, pear-shaped muscular organ Divided into: Fundus: no cavity Body: cavity is triangular Cervix: cavity is fusiform, divided into: *Supravaginal part *Vaginal part 1’ Fundus Body
THE UTERUS FUNDUS: The part of uterus above the level of uterine tubes BODY: The part of uterus from the level of uterine tube to the level of the isthmus of uterus CERVIX:The part of the uterus below the level of the isthmus of the uterus
THE CERVICAL CANAL INTERNAL OS: opening between cavity of body of uterus & cavity of cervix (cervical canal) EXTERNAL OS: opening between cervical canal & cavity of vagina In a nulliparous woman: external os appears circular. In a multiparous woman: external os appears as a transverse slit with an anterior & a posterior lip. Multiparous Nulliparous
RELATIONS OF UTERUS FUNDUS + BODY + SUPRAVAGINAL PART OF CERVIX: Anterior: superior surface of urinary bladder Posterior: sigmoid colon Lateral: uterine artery VAGINAL PART OF CERVIX: surrounded by vaginal fornices Anterior: anterior fornix of vagina Posterior: posterior fornix of vagina Lateral: lateral fornices of vagina
FUNCTION OF UTERUS
POSITIONS OF UTERUS ANTEFLEXED UTERUS ANTEVERTED UTERUS Long axis of body of uterus is bent forward on long axis of cervix Long axis of whole uterus is bent forward on long axis of vagina
POSITIONS OF UTERUS RETROVERTED UTERUS RETROFLEXED UTERUS Fundus & body of uterus are bent backward on the vagina and lie in rectouterine pouch Long axis of body of uterus is bent backward on long axis of cervix
USUAL POSITION OF UTERUS ANTEVERTED ANTEFLEXED UTERUS
LIGAMENTS OF UTERUS 1)Ligaments at junction between fundus & body of uterus (At the level of uterine tube) 2 Extends through inguinal canal to labium majus 1
LIGAMENTS OF UTERUS 2)Ligaments of cervix Extend from cervixto: anterior (pubocervical), lateral (transverse cervical or cardinal) posterior (uterosacral or sacrocervical) pelvic walls
LEVATOR ANI MUSCLES • FORM THE PELVIC FLOOR: separate pelvis from perineum • FORM PELVIC DIAPHRAGM: traversed by urethra, vagina & rectum • SUPPORT PELVIC ORGANS Urethra Levatorani Vagina Urethra Rectum Rectum Vagina
SUPPORT OF UTERUS • Ligaments of cervix (especially transverse cervical) • Round ligament of uterus (maintains antevertedanteflexed position) • Levatorani muscles UTERINE PROLAPSE • Downward dispalcement of uterus due to damage of: • Ligaments of uterus • Levatorani muscles
VAGINA • STRUCTURE: Fibro-muscular tube • EXTENT: From external os, along pelvis & perineum, to open in the vulva (female external genitalia), behind urethral opening • LENGTH: Its anterior wall (7.5 cm) is shorter than its posterior wall (9 cm) • FUNCTION: 1) Copulatory organ & 2) Birth canal
RELATIONS OF VAGINA • ANTERIOR: Urinary bladder (in pelvis) & urethra (in perineum) • POSTERIOR: Rectum (in pelvis) & anal canal (in perineum) • LATERAL:ureters(in pelvis)
ARTERIAL SUPPLY From abdominal aorta From internal iliac artery (Artery of pelvis)
QUESTION 1 • Which one of the following structures is related (or attached) to the lateral end of the ovary? • Fimbriae of uterine tube • Ampulla of uterine tube • Ligament of ovary • Round ligament of uterus
QUESTION 2 • Which one of the following structures is anterior to the uterus? • Urinary bladder • Ureter • Sigmoid colon • Ovary
- More by User

Anatomy of the Female Reproductive System
Xiu Xiu Jiang Email: [email protected] Ai Xia Liu Email: [email protected] Telephone (office): 87061501-1839 Women ’ s Hospital, School of Medicine, Zhejiang University . Anatomy of the Female Reproductive System. Jiang Xiu Xiu
1.28k views • 42 slides
FEMALE REPRODUCTIVE ANATOMY
FEMALE REPRODUCTIVE ANATOMY. The vulva refers to those parts that are outwardly visible The vulva includes: Mons pubis Labia majora Labia minora Clitoris Urethral opening Vaginal opening Perineum. Individual differences in: Size Coloration Shape Of external gentalia are common.
576 views • 35 slides
Anatomy of female reproductive system
Anatomy of female reproductive system. Zhao Aimin. Bony pelvis. Sacrum( 骶骨) Coccyx( 尾骨) Coxae( 髋骨) Ilium( 髂骨) Ischium( 坐骨) Pubis( 耻骨 ). Pelvis . Falase pelvis (major). True pelvis (minor). Sacrum and coccyx posteriorly Ischium and pubis bilaterally and anteriorly.
1.01k views • 22 slides
FEMALE REPRODUCTIVE ANATOMY.
572 views • 33 slides
The Female Reproductive System
The Female Reproductive System. Chapter 20 Part II. The Female Reproductive System. Female Reproductive System. Ovaries contain large number of follicles produce female gametes (eggs or ova) in ovarian cycle Fimbriae – extensions of fallopian tubes partially cover each ovary
1.25k views • 47 slides
The Female Reproductive System. By Dr D Fisher. Anatomy of Female Reproductive System. Female reproductive organs Ovaries Uterine tubes Uterus Vagina External genital organs Mammary glands. Female Reproductive Anatomy. Female Pelvis.
790 views • 25 slides
The FEMALE REPRODUCTIVE SYSTEM
The FEMALE REPRODUCTIVE SYSTEM. Ch 16 Pages 452-456. iPad Vocabulary Activity. Open iSwifter APP Open the bookmarks tab and choose “ Glencoe chapter activities ” Open: “ Student Center ” Drop Down: “ Chapter Activities ” Go to: Chapter 16 Next, Open: “Interactive Study Guides”
1.01k views • 11 slides
Female Reproductive Anatomy
Female Reproductive Anatomy. Macroscopic Female Functional Anatomy. Recognize the various structures of the female reproductive system Relate function to each structure Distinguish differences among species. Objectives:. Female Reproductive Tract. Four common layers Mucosa
665 views • 16 slides
The Female Reproductive System. Figure 26–20c The Appearance of the Endometrium during the Uterine Cycle. The Female Reproductive System. Blood Supply of the Vagina Is through vaginal branches of internal iliac (uterine) arteries and veins. The Female Reproductive System.
1.82k views • 156 slides
Female Reproductive Anatomy. Ovaries are the primary female reproductive organs Make female gametes (ova) Secrete female sex hormones (estrogen and progesterone) Accessory ducts include uterine tubes, uterus, and vagina Internal genitalia – ovaries and the internal ducts
600 views • 31 slides
Anatomy of The Reproductive System
Anatomy of The Reproductive System. 8 th grade By Leah Turner, Jennifer Golay and Kyle Boling . What is Reproduction?. On your diagram write at the top of the page or on the back what you think reproduction is in one to three sentences. Answer.
344 views • 13 slides
The Female Reproductive System . By Justine Wilson and Kim Iwanski. Main Fucntions. To produce the hormones estrogen and progesterone To reproduce It is the sight of fetal development . The Ovaries . Functions Production of Estrogen and Progesterone
363 views • 18 slides
Female Reproductive Anatomy. The reproductive organs found outside the body are called genitals. These organs are collectively called the vulva: Mons pubis Labia majora (outer lips) Labia minora (inner lips) Clitoris Vaginal opening Urinary opening. Parts of the vulva.
357 views • 19 slides
The Female Reproductive System. Female Reproductive Structures. Female Reproductive Structures. Step by Step – The life of a female. Ovaries develop in ___________ Produce sex hormones (___________ and ___________) 400 000 ___________ develop (potential eggs)
440 views • 32 slides
The Female Reproductive System. Borges, Yisel Chavez, Monica Period 5 May 9, 2013. I. Structure A. Organs of the Female Reproductive System. Vagina : a muscular hollow tube that extends from the vaginal opening to the uterus (3-5 inches long)
430 views • 9 slides
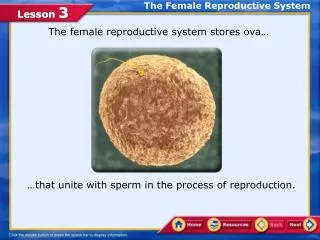
The Female Reproductive System. The female reproductive system stores ova…. …that unite with sperm in the process of reproduction. Lesson Objectives. In this lesson, you will learn to:. Describe the parts and functions of the female reproductive system
610 views • 45 slides
CHAPTER 1 The anatomy of the female reproductive system
CHAPTER 1 The anatomy of the female reproductive system. Section 1 Pelvis Section 2 External genital organs Section 3 Internal genital organs Section 4 Neighbouring organs Section 5 Vascular ,lymphatic and nervous system Section 6 Pelvic floor. Section 1 Pelvis. (一) composition
552 views • 24 slides
Reproductive System Cont. Female Anatomy & Physiology
Reproductive System Cont. Female Anatomy & Physiology. Chapter 28. FEMALE ANATOMY. Ovaries = produce eggs Ovarian follicles = contain eggs in various stages of development and the cells that surround them; surrounding cells nourish the eggs & produce estrogen
107 views • 9 slides
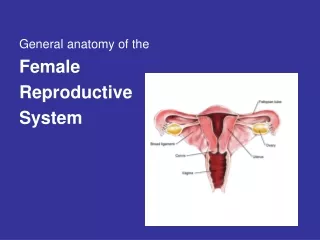
General anatomy of the Female Reproductive System
General anatomy of the Female Reproductive System. Points to Ponder. How many chromosomes do body and sex cells each have? Understand the anatomy of both the male and female. What are the 3 parts of a sperm? How do hormones play a role in the male?
467 views • 33 slides
Reproductive System Female Anatomy and Hormones
Reproductive System Female Anatomy and Hormones. Female Anatomy and Hormones. The vulva is the external opening to the urogenital tract Leads to the vagina Urine exits through the urethra into the caudal vagina and then the vuvla. Female Anatomy and Hormones.
240 views • 19 slides

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

26.1A: Overview of the Male and Female Reproductive Systems
- Last updated
- Save as PDF
- Page ID 8233
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
The human reproductive system functions to produce human offspring, with the male providing sperm and the female providing the ovum.
Learning Objectives
- Summarize the reproductive systems of men and women
- The male reproductive system consists of external organs. The testes in the scrotum produce the male gamete, sperm, which is ejaculated in seminal fluid by the penis.
- The female reproductive system primarily consists of internal organs. The female gamete, ovum, is produced in the ovaries and is released monthly to travel to the uterus via the Fallopian tubes.
- Fertilization can occur if the penis is inserted through the vulva into the vagina and sperm is ejaculated towards the cervix. If an ovum is currently in the uterus, it can then be fertilized by sperm that manage to enter the cervix.
- Once fertilized, an ovum becomes a zygote and if all goes well, develops into a fetus in the uterus.
- Natural birth occurs when the fetus is pushed from the vagina after nine months in the uterus.
- fallopian tubes : The Fallopian tubes, also known as oviducts, uterine tubes, and salpinges (singular salpinx) are two very fine tubes lined with ciliated epithelia leading from the ovaries of female mammals into the uterus, via the utero-tubal junction.
- penis : The male sexual organ for copulation and urination; the tubular portion of the male genitalia (excluding the scrotum).
- vagina : A fibromuscular tubular tract which is the female sex organ and has two main functions: sexual intercourse and childbirth.
While the ultimate purpose of the human reproductive system is to produce offspring, the proximate purpose is to produce pleasure and induce bonding. This can be seen in our closest relatives, the bonobo chimpanzees, who have sex for a wide variety of reasons including pleasure, bonding, and alleviating tension in addition to producing offspring.
The reproductive system or genital system is a set of organs within an organism that work together to produce offspring. Many non-living substances, such as fluids, hormones, and pheromones, are important accessories to the reproductive system. Unlike most organ systems, the sexes of differentiated species often have significant differences. These differences allow for a combination of genetic material between two individuals and thus the possibility of greater genetic fitness of the offspring.
The Reproductive Process
Human reproduction takes place as internal fertilization by sexual intercourse. During this process, the erect penis of the male is inserted into the female’s vagina until the male ejaculates semen, which contains sperm, into the vagina. The sperm travels through the vagina and cervix into the uterus for potential fertilization of an ovum. Upon successful fertilization and implantation, gestation of the fetus occurs within the female’s uterus for approximately nine months (pregnancy). Gestation ends with labor resulting in birth. In labor, the uterine muscles contract, the cervix dilates, and the baby passes out through the vagina. Human babies and children are nearly helpless and require high levels of parental care for many years. One important type of parental care is the use of the mammary glands in the female breasts to nurse the baby.
The Male Reproductive System
The human male reproductive system is a series of organs located outside of the body and around the pelvic region. The primary direct function of the male reproductive system is to provide the male gamete or spermatozoa for fertilization of the ovum. The major reproductive organs of the male can be grouped into three categories. The first category is sperm production and storage. Production takes place in the testes, housed in the temperature-regulating scrotum. Immature sperm then travel to the epididymis for development and storage. The second category, the ejaculatory fluid-producing glands, includes the seminal vesicles, prostate, and vas deferens. The final category, used for copulation and deposition of the spermatozoa (sperm) within the female, includes the penis, urethra, vas deferens, and Cowper’s gland.

The Human Male Reproductive System : Cross-sectional diagram of the male reproductive organs.
Only our species has a distinctive mushroom-capped glans, which is connected to the shaft of the penis by a thin tissue of frenulum (the delicate tab of skin just beneath the urethra). One of the most significant features of the human penis is the coronal ridge underneath the gland around the circumference of the shaft. Magnetic imaging studies of heterosexual couples having sex reveal that during coitus, the typical penis expands to fill the vaginal tract, and with full penetration can even reach the woman’s cervix and lift her uterus. This combined with the fact that human ejaculate is expelled with great force and considerable distance (up to two feet if not contained), suggests that men are designed to release sperm into the uppermost portion of the vagina. This may be an evolutionary adaptation to expel the semen left by other males while at the same time increasing the possibility of fertilization with the current male’s semen.
The Female Reproductive System
The human female reproductive system is a series of organs primarily located inside the body and around the pelvic region. It contains three main parts: the vagina, which leads from the vulva, the vaginal opening, to the uterus; the uterus, which holds the developing fetus; and the ovaries, which produce the female’s ova. The breasts are also a reproductive organ during parenting, but are usually not classified as part of the female reproductive system. The vagina meets the outside at the vulva, which also includes the labia, clitoris, and urethra. During intercourse, this area is lubricated by mucus secreted by the Bartholin’s glands. The vagina is attached to the uterus through the cervix, while the uterus is attached to the ovaries via the Fallopian tubes. At certain intervals, approximately every 28 days, the ovaries release an ovum that passes through the Fallopian tube into the uterus. If the ova is fertilized by sperm, it attaches to the endometrium and the fetus develops. In months when fertilization does not occur, the lining of the uterus, called the endometrium, and unfertilized ova are shed each cycle through a process known as menstruation.

The Human Female Reproductive System : The female reproductive system is largely internal.
LICENSES AND ATTRIBUTIONS
CC LICENSED CONTENT, SHARED PREVIOUSLY
- Curation and Revision. Authored by : Boundless.com. Provided by : Boundless.com. License : CC BY-SA: Attribution-ShareAlike
CC LICENSED CONTENT, SPECIFIC ATTRIBUTION
- Reproductive system. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/Reproductive_system . License : CC BY-SA: Attribution-ShareAlike
- penis. Provided by : Wiktionary. Located at : en.wiktionary.org/wiki/penis . License : CC BY-SA: Attribution-ShareAlike
- vagina. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/vagina . License : CC BY-SA: Attribution-ShareAlike
- fallopian tubes. Provided by : Wikipedia. Located at : en.Wikipedia.org/wiki/fallopian%20tubes . License : CC BY-SA: Attribution-ShareAlike
- Female Reproductive System. Provided by : Wikimedia. Located at : upload.wikimedia.org/wikipedi...em_lateral.png . License : Public Domain: No Known Copyright
- Male Reproductive System. Provided by : Wikimedia. Located at : upload.wikimedia.org/wikipedi...le_anatomy.png . License : Public Domain: No Known Copyright
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 30, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Microfluidic organ chip models human cervix to fill key women's health gap
by Benjamin Boettner, Harvard University
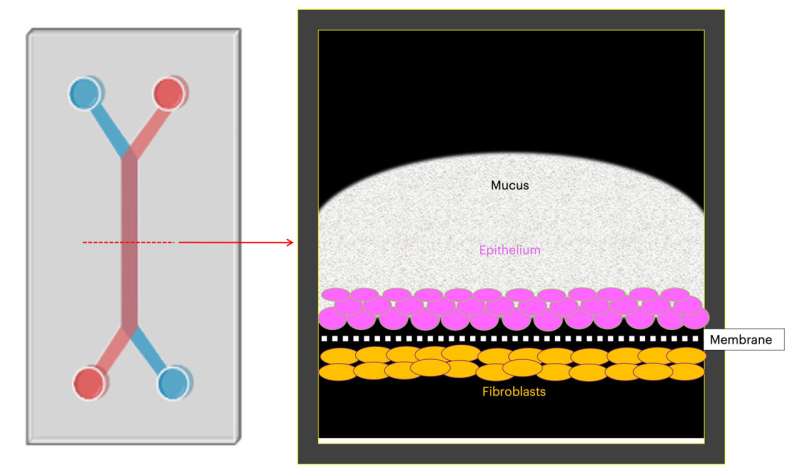
Bacterial vaginosis (BV) has been identified as one of the many unmet needs in women's health and affects more than 25% of reproductive-aged women. It is caused by pathogenic bacteria that push the healthy microbiomes in the female vagina and cervix—the small gatekeeper canal that connects the uterus and vagina—into a state of imbalance known as dysbiosis.
This dysbiosis then triggers inflammation that not only causes severe discomfort, but can also can result in a host of downstream complications, including an increased risk for infection with HIV and other sexually transmitted diseases, higher rates of spontaneous abortion and pre-term birth, as well as pelvic and endometrial inflammatory diseases.
Thus far, the only treatments for BV are antibiotics, which often fail to kill the invading bacteria in the infected vagina and cervix . Antibiotic therapies also don't prevent the recurrence of this condition in more than 60% of women. Although BV was first described more than a century ago, the pathogenic events following the initial infection remain very poorly understood, which contributes to the dearth of more effective BV treatments.
Now, filling an important gap, a collaborative team of researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University and University of California Davis, led by Wyss Founding Director Donald Ingber, M.D., Ph.D., has developed a microfluidic human in vitro model of the complex cervix tissue, a human cervix-on-a-chip (Cervix Chip), that overcomes major limitations of existing animal models and static in vitro models.
With unprecedented fidelity and detail, the Cervix Chip replicates the complex interactions between the cervical epithelial cells, the protective mucus layer they produce, and the cervical microbiome in its healthy state as well as when it is under attack from BV-causing bacteria.
These findings are published in Nature Communications .
The researchers created an organ chip model of the cervical wall by growing human cervical epithelial cells in one of two parallel channels running through a microfluidic device the size of a USB memory stick and growing cervical fibroblast cells in the adjacent channel.
The channels are separated by a porous membrane which allows the two cell types to communicate similarly as in a woman's body. Importantly, the team was able to reconstitute the two major sections of the cervical wall by identifying alternative flow-conditions used to perfuse the epithelial channel with medium, which produced region-specific mechanical cues.
Their Cervix Chip technology enabled the team to also replicate the mucus production of the cervix, and how mucus features change under the influence of sex hormones, as well as healthy and pathogenic microbial communities.
"Our engineered cervix model and the breadth and depth of analysis it allows sets a new standard in research that is well in line with existing clinical observations, while offering first new insights into cervix functionality and vulnerability," said first author Zohreh Izadifar, Ph.D., who spearheaded the project as a Postdoctoral Fellow on Ingber's team and now is a Research Faculty member at Boston Children's Hospital and Harvard Medical School (HMS).
The study's accomplishments are an important milestone. Researchers had identified highly prevalent BV in African women as an area of high priority, as it dramatically increases the risk of pre-term births and HIV infection on the continent. With the end goal of finding urgently needed treatments against BV, a research consortium was formed, including Ingber as well as co-senior author Carlito Lebrilla, Ph.D. at University of California Davis.
"In this study, we leveraged critical findings that we had made in a previously developed Vagina Chip to create a platform that now enables researchers to find answers to additional long-standing questions in women's health," said Ingber. "The Cervix Chip can be used alongside the Vagina Chip to evaluate the efficacy of potential new treatments in the form of live biotherapeutic products that other members of our ... consortium are developing for treatment of BV. We also hope to use the chip to identify new treatments for other infectious diseases of the female reproductive tract."
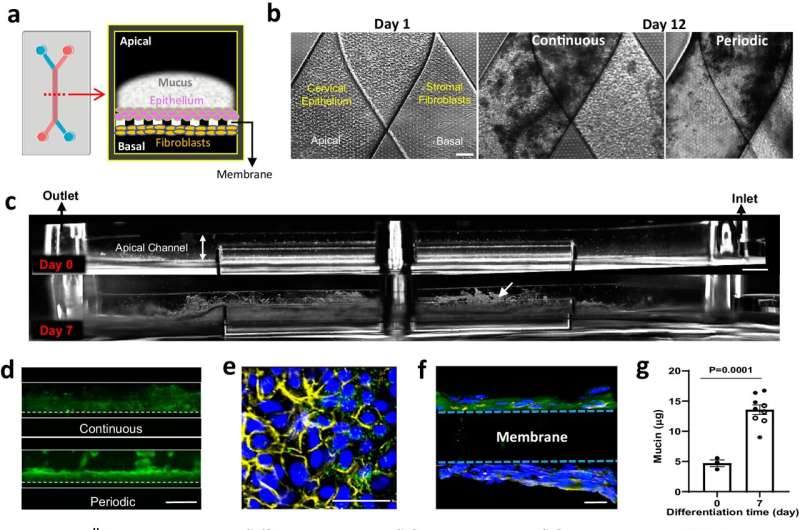
The female cervix at high resolution
The cervical canal consists of two distinct sections: the lower cervical canal, known as the ectocervix, leading into the vagina, and the upper cervical canal, known as the endocervix, which connects to the uterus. The endocervix produces most mucus in the lower female reproductive tract, periodically discharging it before it continues its journey in a more even flow through the ectocervix and vagina, both of which produce lesser amounts of additional mucus.
Mirroring this physiology, the team found that exposing the Cervix Chip only periodically to fluid flow causes it to generate a thin monolayered epithelium typical of the endocervix, while exposing it continuously to fluid flow results in the thick ectocervix-like multi-layered epithelium. On-chip, both cervical epithelia displayed their typical gene expression patterns.
Mucus is a complex substance that consists of mucin proteins that are decorated with highly branched tress of various sugar molecules. The team's collaborator Lebrilla is an expert in analytical chemistry and sugar biology, and his team undertook an in-depth "glycomics" analysis of the sugars making up the mucus produced in the Cervix Chip under different conditions. This joint effort enabled the researchers to confirm that the sugar structures of the mucus closely resembled those found in samples obtained from women.
Importantly, the modeled cervix responded to sex hormone concentrations typical of the follicular phase of the menstrual cycle by increasing the thickness, water content, and altering the sugar arrangements of the produced mucus when compared to luteal hormone conditions. It also produced a stronger inflammatory response and slightly reduced its protective barrier functions in the follicular phase.
"All of these findings closely reflect cervix physiology described from clinical observations," said Izadifar.
Studying BV in the Cervix Chip
In the development of BV, aggressive pathogenic bacteria migrate from the vagina through the cervical canal up to the cervix, which—with its mucus production and immune-modulating abilities, normally functions as a gatekeeper against infections. When they take over the local beneficial bacterial communities, dysbiosis emerges. The pathological outcomes of this invasion are closely associated with alterations in the protective mucus layer, and the pathogenic bacteria gaining access to the underlying epithelia.
To mimic healthy and pathological microbial conditions in the Cervix Chip, the researchers first populated it with Lactobacillus crispatus bacteria, which dominate healthy cervical microbiomes. The L. crispatus bacteria induced the mucus layer to thicken and improve its quality, while leaving the underlying epithelium fully intact during three days of co-culture. Moreover, their presence induced the expression of proteins in cervical epithelial cells that are involved in their normal differentiation and protection against pathogens.
When they instead populated the Cervix Chip with Gardnerella vaginalis bacteria, which cause dysbiosis, the epithelium's barrier functions became severely compromised. In addition, the expression of proteins associated with pathogenic processes, including inflammation, was significantly elevated.
"Interestingly, we identified specific mucus structural and sugar modifications that could help explain the deterioration of the mucus's quality related to BV, and indirectly could have an impact on downstream pathological processes," said Izadifar. "In the future, our bottom-up approach to reconstituting the female cervix and its in vivo-like responsiveness will allow us to comprehensively investigate the relevance of the cervix's distinct tissue and microbial components in diverse pathologies."
Additional authors on the study are Justin Cotton, Siyu Chen, Viktor Horvath, Anna Stejskalova, Aakanksha Gulati, Nina LoGrande, Bogdan Budnik, Sanjid Shahriar, Erin Doherty, Yixuan Xie, Tania To, Sarah Gilpin, Adama Sesay, and Girja Goyal.
Explore further
Feedback to editors

False belief in MMR vaccine-autism link endures as measles threat persists, finds survey
9 minutes ago

Pollutants and climate change contribute to millions of deaths from cardiovascular disease each year, warn scientists

Chromatin openness sheds new light on prostate cancer plasticity

AI-driven tool can detect Lewy body dementia via changes in vocal emotional expression

Scientists develop AI tool to predict how cancer patients will respond to immunotherapy
2 hours ago

Neoadjuvant immunotherapy for early stage melanoma shows positive results

Targeting leukemia's survival route: A novel approach to overcoming leukemia recurrence

Study finds timing of brain waves shapes the words we hear
3 hours ago

Study finds semaglutide associated with reduction in incidence and recurrence of alcohol-use disorder

New analytical tool can improve understanding of heritable human traits and diseases
4 hours ago
Related Stories

What to know about cervical cancer
May 6, 2024

Patient-derived and mouse endo-ectocervical organoid generation
May 13, 2022

Progesterone protects babies from preterm birth in women with a short cervix, research shows
Mar 12, 2024

4 ways to reduce risks of cervical cancer
Jan 11, 2023

Q and A: Cervical cancer and HPV screening
Jan 13, 2023

Researchers advance the understanding of preterm birth
Jan 30, 2018
Recommended for you

This self-powered sensor could make MRIs more efficient
May 31, 2024

Tackling the hurdle of tumor formation in stem cell therapies

Scientists develop visual tool to help people group foods based on their levels of processing

Prenatal testing offers a window for finding a mother's cancer risk

A multimodal approach to better predict recovery in patients with disorders of consciousness

Rewritable, recyclable 'smart skin' monitors biological signals on demand
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
The female reproductive organs are involved in sexual activity, fertility, menstruation and reproduction. Every person's reproductive organs look slightly different. Some people are born with missing or irregularly-shaped reproductive organs. This can affect the functions of your reproductive system and lead to irregular bleeding, difficulty ...
14. Uterus Pear-shaped muscular organ in the female reproductive tract. The fundus is the upper portion of the uterus where pregnancy occurs. The cervix is the lower portion of the uterus that connects with the vagina and serves as a sphincter to keep the uterus closed during pregnancy until it is time to deliver a baby. The uterus expands considerably during the reproductive process. The ...
The organs of the female reproductive system matures at puberty and enables pregnancy to occur with the first monthly ovulation. Female Reproductive Organs. The female reproductive system has several functions, including producing female sex hormones and storing the eggs. Eggs- Female gametes or ova.
1. Female genital system Dr. Mohammed Mahmoud Mosaed. 2. Female reproductive system • Female reproductive system consists of: • Internal genital organs: • Uterus • Vagina • Fallopian tubes (uterine tubes) • Ovary • External genitalia (Vulva) 3. The uterus • The uterus is a hollow, pear-shaped organ with thick muscular walls.
The external genital organs, or vulva, are held by the female perineum. These are the mons pubis, labia majora and minora, clitoris, vestibule, vestibular bulb and glands. The vagina, uterus, ovaries and uterine tubes compose the internal genital organs. Female reproductive organs undergo substantial structural and functional changes every month.
Vagina. The vagina, shown at the bottom of Figure 27.9 and Figure 27.10, is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract.It also serves as the exit from the uterus during menses and childbirth. The outer walls of the anterior and posterior vagina are formed into longitudinal columns, or ridges, and the superior portion of the vagina—called ...
The female reproductive system is a group of organs that work together to enable reproduction, pregnancy, and childbirth. It also produces female sex hormones, including estrogen and progesterone .
Female reproductive system presentation. The female reproductive system consists of internal and external organs that work together to produce eggs, facilitate fertilization and pregnancy, and nourish infants. The internal organs include the uterus, ovaries, fallopian tubes, and vagina. The ovaries produce eggs and hormones, the fallopian tubes ...
The female reproductive tract is all located within the pelvis. It is made up of the vulva, the vagina, the cervix, the uterus, the fallopian tubes and the ovaries. These organs are supported in the pelvis by ligaments. The vulva refers to the external female genitalia. Its anatomical structure can be broken down further into the mons pubis ...
The vagina, shown at the bottom of Figure 27.3.1 27.3. 1 and Figure 27.3.2 27.3. 2, is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract. It also serves as the exit from the uterus during menses and childbirth.
The female reproductive system is responsible for the production, storage and release of ova. Its two main components are the ovaries and the accessory sex organs. Overview of the Female Reproductive System (slide set).
The female reproductive system includes all of the internal and external organs that help with reproduction. The internal sex organs are the ovaries, which are the female gonads, the fallopian tubes, two muscular tubes that connect the ovaries to the uterus, and the uterus, which is the strong muscular sack that a fetus can develop in.The neck of the uterus is called the cervix, and it ...
The human female reproductive system (or female genital system) contains two main parts: Produce the anatomically female egg cells. These parts are internal; the vagina meets the external organs at the vulva, which includes the labia, clitoris, and urethra. The vagina is attached to the uterus through the cervix, while the uterus is attached to ...
The female reproductive system is made up of internal and external organs that function to produce haploid gametes called eggs (or oocytes), secrete sex hormones (such as estrogen), and carry and give birth to a fetus. As shown in Figure 11.6.2 11.6. 2, the internal reproductive organs include the vagina, uterus, Fallopian (uterine) tubes, and ...
5 External Female Structures. Mons Pubis. Labia Majora Labia Minora. Clitoris. Vestibule. Perineum. 6 Mons Pubis It is covered with varying amounts of pubic hair. Is rounded, soft fullness of subcutaneous fatty tissue, prominence over the symphysis pubis that forms the anterior border of the external reproductive organs.
The main structures of the female reproductive system are internal to the body and shown in Figure 22.2.4 22.2. 4. They include the paired ovaries, which are small, oval structures that produce eggs and secrete estrogen. The two Fallopian tubes (aka uterine tubes) start near the ovaries and end at the uterus.
Video: Female reproductive system. You are watching a preview. Go Premium to access the full video: Main organs of the female reproductive system. Female reproductive system [18:21] Main organs of the female reproductive system. Main organs of the female reproductive system. Watch the video tutorial now.
2. 3. The female reproductive system is designed to carry out several functions. 4 is the normal pH of the vagina. 40 weeks is the normal gestation period. 400 oocytes released between menarche and menopause. 400,000 oocytes present at puberty. 28 days in a normal menstrual cycle. 280 days (from last normal menstrual period) in a normal ...
Presentation Transcript. ANATOMY OF THE FEMALE REPRODUCTIVE SYSTEM Prof. Ahmed FathallaIbrahim Professor of Anatomy College of Medicine King Saud University E-mail: [email protected]. OBJECTIVES At the end of the lecture, students should: • List the organs of female reproductive system. • Describe the pelvic peritoneum in female.
The male reproductive system consists of external organs. The testes in the scrotum produce the male gamete, sperm, which is ejaculated in seminal fluid by the penis. The female reproductive system primarily consists of internal organs. The female gamete, ovum, is produced in the ovaries and is released monthly to travel to the uterus via the ...
The human female reproductive system consists of primary and secondary sex organs, external genitalia, and mammary glands. The primary sex organs are the ovaries, which produce eggs and hormones. The secondary sex organs include the fallopian tubes, uterus, cervix and vagina which make up the duct system. The external genitalia include the mons ...
Taking care of individuals with female pelvic organs from childhood through adolescence, reproductive ages and postmenopausal ages. Treating pelvic floor disorders.
We also hope to use the chip to identify new treatments for other infectious diseases of the female reproductive tract." Development and characterization of human ecto-and endo-cervix chips ...
The female reproductive system is made up of the internal and external sex organs that function in reproduction of new offspring. In humans, the female reproductive system is immature at birth and develops to maturity at puberty to be able to produce gametes, and to carry a fetes to full term. Female reproductive system