Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Center for Substance Abuse Treatment (US). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. (Treatment Improvement Protocol (TIP) Series, No. 57.)


Trauma-Informed Care in Behavioral Health Services.
- Order print copy from SAMHSA
Section 1 A Review of the Literature
- Introduction to Trauma and Traumatic Stress Reactions
Providing a comprehensive literature review on trauma, traumatic stress, trauma-informed care (TIC), and trauma-related interventions is a daunting task when considering the quantity and prolific production of research in this area in the past 20 years. To manage the volume of information, this literature review mainly focuses on reviews and meta-analyses rather than seminal work to address many of the most relevant topics.
What Is Trauma?
In this text, “trauma” refers to experiences that cause intense physical and psychological stress reactions. “Trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or threatening and that has lasting adverse effects on the individual’s functioning and physical, social, emotional, or spiritual well-being” ( Substance Abuse and Mental Health Services Administration [SAMHSA], Trauma and Justice Strategic Initiative, 2012 , p. 2). Although many individuals report a single specific traumatic event, others, especially those seeking mental health or substance abuse services, have been exposed to multiple or chronic traumatic events. According to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), trauma is defined as when an individual person is exposed “to actual or threatened death, serious injury, or sexual violence” ( American Psychiatric Association [APA], 2013 , p. 271).
The definition of psychological trauma is not limited to diagnostic criteria, however. In fact, some clinicians have moved away from considering trauma-related symptoms as indicators of a mental disorder and instead view them as part of the normal human survival instinct or as “adaptive mental processes involved in the assimilation and integration of new information with intense survival emphasis which exposure to the trauma has provided” ( Turnbull, 1998 , p. 88). These normal adaptive processes only become pathological if they are inhibited in some way ( Turnbull, 1998 ), or if they are left unacknowledged and therefore untreated ( Scott, 1990 ).
Trauma has been characterized more broadly by others. For example, Horowitz (1989) defined it as a sudden and forceful event that overwhelms a person’s ability to respond to it, recognizing that a trauma need not involve actual physical harm to oneself; an event can be traumatic if it contradicts one’s worldview and overpowers one’s ability to cope.
How Common Is Trauma?
Trauma exposure is common in the United States. However, trauma exposure varies considerably according to different demographic characteristics and is especially high among clients receiving behavioral health services (see the discussions under the headings “ Extent and Effects of Trauma and Traumatic Stress Reactions in Specific Populations ” and “ Other Disorders That May Be Related to Trauma ” for more information on relevant rates). Although the large surveys discussed here provide data on trauma exposure for the general population, published literature often provides more specific data as well, which is one reason why differences in exposure according to gender and race/ethnicity are highlighted here.
At one time, trauma was considered an abnormal experience. Contrary to this myth, the first National Comorbidity Study (NCS), a large national survey designed to study the prevalence and effects of mental disorders in the United States, established how prevalent traumas are in the lives of the general U.S. population ( Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995 ). Presented with a list of 11 types of traumatic experiences and a 12th “other” category, 60.7 percent of men and 51.2 percent of women reported experiencing at least one trauma in their lifetime ( Kessler, 2000 ; Kessler et al. 1995 ; 1999 ):
- The most common trauma was witnessing someone being badly injured or killed (cited by 35.6 percent of men and 14.5 percent of women).
- The second most common trauma was being involved in a fire, flood, or other natural disaster (cited by 18.9 percent of men and 15.2 percent of women).
- The third most common trauma was a life-threatening accident/assault, such as from an automobile accident, a gunshot, or a fall (cited by 25 percent of men and 13.8 percent of women.
The NCS also found that it was not uncommon for individuals to have experienced multiple traumatic events ( Kessler, 2000 ). Among men in the total sample, 14.5 percent reported two traumatic events, 9.5 percent reported three, 10.2 percent reported four or more, and 26.5 percent reported only one such event. Among women, 13.5 percent of the total sample reported two traumatic events, 5 percent reported three, 6.4 percent reported four or more, and 26.3 percent reported only one.
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is another large national survey of behavioral health, but it only assessed posttraumatic stress disorder (PTSD) and trauma exposure in its second wave of interviews, in which 34,653 of the original 43,093 respondents were reinterviewed ( Pietrzak, Goldstein, Southwick, & Grant, 2011a ). In the Wave 2 interview, respondents were asked about 27 different types of potentially traumatic events; the most commonly reported traumatic events were serious illness or injury to someone close (affecting 48.4 percent of those who did not have PTSD symptoms and 66.6 percent of those with PTSD), unexpected death of someone close (affecting 42.2 percent of those without PTSD and 65.9 percent of those with PTSD), and seeing someone badly injured or killed (affecting 24 percent of those without PTSD and 43.1 percent of those with PTSD; Pietrzak, Goldstein, Southwick, & Grant, 2011a ). According to the same data, 71.6 percent of the sample witnessed trauma, 30.7 percent experienced a trauma that resulted in injury, and 17.3 percent experienced a trauma that was purely psychological in nature (e.g., being threatened with a weapon; El-Gabalawy, 2011).
NESARC also found that exposure to specific traumatic events varied considerably according to race, ethnicity, or cultural group. The survey found that 83.7 percent of non-Latino White Americans reported a traumatic event, compared with 76.4 percent of African Americans, 68.2 percent of Latinos, and 66.4 of percent of Asian Americans, Native Hawaiians, or Pacific Islanders ( Roberts, Gilman, Breslau, Breslau, & Koenen, 2011 ). Exposure to specific traumas also varied considerably. White Americans were more likely to report an unexpected death of someone they knew (44.7 percent did) than were African Americans (39.9 percent), Latinos (29.6 percent), and Asian Americans, Native Hawaiians, or Pacific Islanders (25.8 percent) as well as being more likely to report having a close friend/relative who experienced a life-threatening injury. On the other hand, African Americans were the most likely to report being the victim of assaultive violence (29.7 percent), followed by White Americans (26.1 percent), Latinos (25.6 percent), and Asian Americans, Native Hawaiians, or Pacific Islanders (16.3 percent). In terms of combat trauma, White Americans and African Americans were about as likely to have been combatants (10 percent of each group reported combat trauma), and more likely than Asian Americans, Native Hawaiians, or Pacific Islanders (5.4 percent) or Latinos (4.4 percent). However, Asian Americans, Native Hawaiians, or Pacific Islanders were the most likely to have been unarmed civilians in a war zone (7.5 percent), followed by Latinos (3.8 percent), White Americans (2 percent), and African Americans (1.9 percent).
Across the world, according to data from the World Health Organization (WHO) surveys, which includes the NCS and NCS replication (NCS-R) and surveys from 20 other countries, the most commonly reported traumas are the death of a loved one (30.5 percent), witnessing violence to others (21.8 percent), and experiencing interpersonal violence (18.8 percent; Stein et al., 2010 ). As Kessler (2000) noted, trauma from assaultive violence in the United States is likely to be more common than in most other developed countries in general. However, trauma related to other traumatic events (e.g., automobile accidents, natural disasters) appear to be quite similar throughout developed countries.
A longitudinal survey from New Zealand also provides useful data on trauma exposure. In this survey, a cohort of subjects from a single town was interviewed at age 26 and again at age 32 in order to evaluate what constituted the worst trauma those individuals had experienced ( Koenen, Moffitt et al., 2008 ). The types of worst experiences reported before age 26 were:
- Sudden unexpected death by trauma of a close family member or friend (38 percent).
- Personal assault or victimization (32 percent).
- Serious accidents (14 percent).
- Hearing about or witnessing a close friend or relative experiencing an assault, serious accident, or serious injury (12 percent).
- Personal illness (3 percent).
- Natural disaster (1 percent)
How Common Are Traumatic Stress Reactions?
As with trauma rates, PTSD rates vary considerably across different demographic groups. The reader should consult the section titled “ Extent and Effects of Trauma and Traumatic Stress Reactions in Specific Populations ” for more specific information on PTSD rates. More general information from major surveys is included in this section.
The DSM-5 ( APA, 2013 ) estimates that the prevalence rate of PTSD in the U.S. adult population is about 8 percent, but studies of populations at high risk for PTSD (e.g., combat veterans, survivors of natural disasters) have found PTSD rates ranging from 3 to 58 percent. The NCS (which evaluated behavioral health disorders, including PTSD) found that, for Americans ages 15 to 54, the lifetime prevalence of PTSD (based on DSM Third Edition, text revision [DSM-III-R; APA, 1987 ] criteria) was 7.8 percent, with women more than twice as likely as men to have the disorder during their lives (10.4 percent of women and 5 percent of men; Kessler et al., 1995 ). In the NCS-R, which interviewed 9,282 individuals ages 18 and older between February 2001 and April 2003, the lifetime prevalence of PTSD was 6.8 percent, again with a much higher rate for women (9.7 percent) than for men (3.6 percent; Kessler, Berglund et al., 2005 ; NCS, 2005). The past-year prevalence rate for PTSD was 3.5 percent, with 5.2 percent of women and 1.8 percent of men having PTSD in the 12 months prior to their interviews ( Kessler, Chiu et al., 2005 ).
Kessler, Berglund et al. (2005) examined the issue of lifetime prevalence in the NCS-R to determine whether the prevalence statistics of the NCS were still valid in light of changes to the diagnostic criteria that occurred with the publication of the DSM Fourth Edition, text revision (DSM-IV-TR; APA, 2000 ). The study was divided into two parts. Part I included face-to-face diagnostic interviews of 9,282 participants who were 18 years of age or older. Part II included factors related to diagnosis (e.g., risk factors) and was completed only with participants from Part I who had a “lifetime disorder” and a probability sample from other Part I participants ( n =5,692). Data analysis in this study estimated a lifetime PTSD prevalence of 6.8 percent, but the authors also analyzed the data to determine projected lifetime risk and found that at age 75, the lifetime risk for PTSD was 28 percent higher than the lifetime prevalence estimate. However, the authors suggested that because of certain study limitations (e.g., related to sample parameters, reluctance to participate or to disclose diagnoses), these results should be considered a conservative estimate.
As noted earlier, Wave 1 of NESARC did not evaluate PTSD, but Wave 2 found that 6.4 percent of the population (8.6 percent of women and 4.1 percent of men) had PTSD at some point during their lives ( Pietrzak et al., 2011a ). NESARC researchers also evaluated lifetime prevalence of partial PTSD (defined as including at least one symptom under Criteria B, C, and D, with symptom duration of at least 1 month) and found that 6.6 percent of the total population (8.6 percent of women and 4.5 percent of men) met criteria for partial but not full PTSD at some point during their lives. It should be noted, however, that most large behavioral health surveys, such as the NCS and NESARC, rely on retrospective evaluation of symptoms, and some research indicates that they underestimate behavioral health disorders compared with prospective longitudinal studies (Moffitt et al., 2009). Differences in prevalence estimates may also be related both to changes in PTSD diagnostic criteria and to a variety of methodological differences in the research (e.g., different diagnostic instruments, procedures) on which these estimates were based ( Kessler, 2000 ; Kessler, Chiu et al., 2005 ; Kessler et al., 1995 ; Narrow, Rae, Robins, & Regier, 2002 ).
It is also worth noting that delayed PTSD may account for a considerable percentage of PTSD cases. A meta-analytic review that included studies in which individuals were assessed 1 to 6 months after trauma exposure and again at least 6 months later found that 24.8 percent of PTSD cases involved delayed trauma ( Smid, Mooren, van der Mast, Gersons, & Kleber, 2009 ). Studies included in the review found between 3.8 and 83.3 percent of their samples had delayed PTSD. Factors that were associated with significantly greater odds of having delayed rather than nondelayed PTSD included a Western (as opposed to non-Western) cultural background and military combat exposure.
More recently, Smid, van der Velden, Gersons, and Kleber (2012) conducted a study of 1,083 individuals affected by a large fireworks disaster to evaluate delayed PTSD rates at both 18 months and 4 years after the disaster. In their review of prospective studies of disaster survivors, they found that between 2 and 19 percent of survivors developed delayed PTSD, whereas in their own study, 3.8 percent ( n =24) of the total sample ( n =636) who were available for all assessments had delayed PTSD and 13.5 percent had PTSD that was not delayed.
What Is Complex Trauma?
An individual has been exposed to complex trauma when he or she has either experienced repeated instances of the same type of trauma over a period of time or experienced multiple types of trauma ( van der Kolk, McFarlane, & Weisaeth, 1996 ). Expert consensus is that people who have complex trauma will typically require more intensive and extensive treatment as well as possible adaptations to standard treatment (see the expert clinician survey in Cloitre et al., 2011 ).
This Treatment Improvement Protocol (TIP) uses a definition of complex trauma developed by the National Child Traumatic Stress Network (NCTSN; 2003), which defines complex trauma as a “dual problem” involving both “exposure to traumatic events and the impact of this exposure on immediate and long-term outcomes” (p. 5). NCTSN notes that complex trauma usually involves multiple instances of trauma (occurring either simultaneously or sequentially) and multiple forms of trauma (e.g., experiencing emotional abuse, sexual abuse, and physical abuse). Also, complex trauma, such as that experienced by children who sustain repeated abuse, typically results in emotional dysregulation and a lack of appropriate coping mechanisms, which in turn can increase the risk of further traumatic experiences. Although the NCTSN definition was developed for explaining childhood trauma, it can be adapted to fit an adult population.
Herman (1992) was among the first to highlight the inadequacy of existing diagnostic criteria for PTSD for people who have complex trauma by pointing out that these criteria were developed based on a clinical consideration of symptoms experienced by individuals who had survived relatively time-limited traumatic experiences (e.g., combat veterans, survivors of rape). Herman proposed that many individuals with a history of prolonged and repeated trauma (as opposed to trauma that is time-limited or related to a single traumatic event) present with clinical characteristics that “transcend simple PTSD” (p. 379); these characteristics include physical symptoms (including many of the symptoms listed in the diagnostic criteria for PTSD, although they may appear more “complex, diffuse, and tenacious” [p. 379]), personality changes in which the individual’s sense of identity is negatively affected and which may inhibit the individual’s ability to form relationships with others, and a propensity for vulnerability to further harm (by self or others).
In 1992, Herman published the seminal work Trauma and Recovery (revised in 1997), which discussed proposed changes to the next DSM that would include a new term for this trauma-related constellation of symptoms. Her suggestion was the term “complex post-traumatic stress disorder” (complex PTSD). However, none of the proposed changes she discussed were included in the DSM-IV ( APA, 1994 ), DSM-IV-TR ( APA, 2000 ), or DSM-5 ( APA, 2013 ). Jackson, Nissenson, and Cloitre (2010) observed that the DSM-IV classification of “associated features and disorders” ( APA, 2000 ) for PTSD is intended to cover symptoms of complex PTSD (e.g., problems with affect regulation, impaired relationships), but it does not take into account one key aspect of complex PTSD as it was originally defined, which is that such symptoms and disorders (e.g., substance abuse) are not viewed as secondary to PTSD symptoms, but rather, as equally important and directly related to traumatic experiences.
Complex trauma is typically interpersonal and generally involves situations in which the person who is traumatized cannot escape from the traumatic experiences because he or she is constrained physically, socially, or psychologically ( Herman, 1992 ). Because of this, people who have experienced complex trauma often have additional disturbances in their ability to self-regulate—beyond those seen in PTSD—that are not related to complex trauma. These include difficulties in emotional regulation, difficulties in one’s capacity for relationships, problems with attention or consciousness (e.g., dissociative experiences), a disturbed belief system, and/or somatic complaints or disorganization ( Briere & Scott, 2012 ; Cloitre et al., 2011 ; van der Kolk, McFarlane, & Van der Hart, 1996 ).
What Is Acute Stress Disorder?
Acute stress disorder (ASD), according to the DSM-5, involves a traumatic stress reaction that occurs within 1 month of trauma exposure and includes at least nine symptoms from any of the five categories (intrusion, negative mood, dissociation, avoidance, and arousal; APA, 2013 ). To receive this diagnosis, the individual also has to display a reaction that causes significant distress or impairment in social, occupational, or other important areas of functioning. ASD can occur at the time of the trauma exposure or any time within 4 weeks of that event As Roberts, Kitchiner, Kendardy, and Bisson (2010) observed, there is a large degree of overlap between ASD and PTSD symptoms, but what distinguishes them is the timing of those symptoms relative to trauma exposure. Cardeña and Carlson (2011) provided a history of the ASD diagnosis and discussed the validity of the diagnostic criteria. ASD can develop into PTSD if the symptoms extend beyond 1 month.
What Is PTSD?
PTSD is a traumatic stress reaction that develops in response to a significant trauma. It is a mental disorder, and for behavioral health providers in the United States, the currently accepted diagnostic criteria for the disorder are those provided by the DSM-5 ( APA, 2013 ). For professionals in the field of behavioral health, the definition of psychological trauma is historically and clinically tied to the diagnostic criteria for PTSD, which made their first appearance in the DSM-III ( APA, 1980 ). However, over the years, the diagnostic criteria have undergone some significant changes. These changes are important factors to consider when reading, evaluating, and especially comparing research.
Criterion A concerns the type of trauma involved; Criterion B describes symptoms of intrusion; Criterion C includes the presence of persistent avoidance of stimuli associated with the trauma; Criterion D highlights symptoms of negative alterations in cognitions and mood associated with the traumatic event(s); Criterion E includes marked alterations in arousal and reactivity as it relates to the trauma; Criterion F addresses the duration of the symptoms; and Criterion G includes clinical distress or impairment in important areas of functioning (e.g., occupational). The presenting symptoms cannot be attributable to the physiological effects of a substance, including alcohol or medications.
The first part of the evolving PTSD definition is Criterion A ( Exhibit L-1 ), which describes changes in the definition of a traumatic event from that of “a recognizable stressor,” to “an event that is outside the range of usual human experience,” to an event that is defined by two specific descriptors, to “exposure to actual or threatened death, serious injury, or sexual violence.”
Exhibit L-1
Evolution of Criterion A for PTSD in the DSM.
Criterion B has also evolved. In the DSM-III ( APA, 1980 ), it described reexperiencing a trauma through three symptoms: intrusive thoughts, recurrent dreams, or the feeling of reexperiencing the trauma as a result of some sort of stimulus. DSM-III-R ( APA, 1987 ) expanded Criterion B by adding another symptom: “intense psychological distress at exposure to events that symbolize or resemble an aspect of the traumatic event, including anniversaries of the trauma” (p. 250). It also added information regarding symptom presentations that may occur in children (e.g., repetitive play expressing aspects of the trauma). DSM-IV ( APA, 1994 ) added a fifth symptom of “physiological reactivity on exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event” (p. 428) and additional symptom presentations that may occur in children (e.g., nightmares that lack recognizable features, reenactments of the trauma). Likewise, DSM-5 (2013) became more developmentally focused in diagnostic criteria and added a separate criterion for children younger than 7 years of age. Additional changes in the DSM-5 include a more explicit definition of the stressor criterion, an additional and separate symptom cluster highlighting avoidance and persistent negative alterations in cognitions and mood, and the elimination of an individual’s subjective reaction to the traumatic event (intense fear, helplessness, or horror).
Criterion C addresses avoidance of stimuli associated with the traumatic event(s). Criterion C evolved between DSM-III and DSM-III-R ( Exhibit L-2 ), with only minimal changes in language in the DSM-IV and DSM-IV-TR ( APA, 1994 ; 2000 ). The DSM-5 dropped the terminology of numbing of general responsiveness in this criterion’s heading ( APA, 2013 ).
Exhibit L-2
Evolution of Criterion C for PTSD in the DSM.
Criterion D addresses symptoms related to negative alterations in cognitions and mood associated with the traumatic event(s). This symptom cluster is a new addition to DSM-5 and includes “irritable behavior and angry outbursts (with little or no provocation), typically expressed as verbal or physical aggression toward people or objects; reckless or self-destructive behavior; hypervigilance; exaggerated startle response; problems with concentration; sleep disturbance (e.g., difficulty falling or staying asleep or restless sleep)” ( APA, 2013 , p. 272). In prior DSM publications, criterion D related to increased arousal (e.g., difficulties with sleep and concentration). In DSM-5, this criterion has moved to Criterion E, with no other changes in symptoms. This criterion has also evolved from the description in the DSM-III to a more concise description in the DSM-III-R, and it has become even more concise in the DSM-IV, DSM-IV-TR, and DSM-5 ( Exhibit L-3 ).
Exhibit L-3
Evolution of Criterion E for PTSD in the DSM.
A time criterion was added in the DSM-III-R ( APA, 1987 ) to specify a minimum timeframe of 1 month or more for experiencing symptoms in Criteria B, C, D, and E. In the DSM-IV ( APA, 1994 ), DSM-IV-TR ( APA, 2000 ), and DSM-5 ( APA, 2013 ), this criterion was retained, with the slight change of requiring more than 1 month of symptoms ( APA, 1994 ; 2000 , 2013 ). The criterion that addresses the level of distress and functioning was not included until the publication of the DSM-IV ( APA, 1994 ) and has remained the same in the DSM-5 ( APA, 2013 ). This criterion added a new defining characteristic, which specifies that “the disturbance causes clinically significant distress or impairment in social, occupation, or other important areas of functioning” ( APA, 2013 , p. 272).
Turnbull (1998) describes the historical development of the idea of PTSD up to its inclusion in the International Statistical Classification of Diseases and Related Health Problems, 9th Revision (1979) and the DSM-III-R. The DSM-5 recognizes certain specifiers that may further characterize PTSD ( APA, 2013 ). For example, a specific case of PTSD may be with delayed expression (full criteria are not met until at least 6 months have passed since the trauma exposure, although the onset of symptoms may immediately follow the trauma; APA, 2000 ; 2013 ).
What Is Partial PTSD?
Partial PTSD is a category developed by researchers to evaluate people who have some impairment related to elevated PTSD symptoms but do not meet full criteria for the disorder. The term is commonly defined as either having at least one PTSD symptom from Criteria B, C, and D that lasts at least 1 month after a traumatic event (Criterion A) or as meeting Criterion A plus two of the other three criteria ( Mylle & Maes, 2004 ). These authors also reviewed studies about the prevalence of partial PTSD according to both criteria. Partial PTSD has been associated with several of the same negative consequences associated with full PTSD, but not to the same extent as a full PTSD diagnosis (e.g., Pietrzak et al., 2011a ).
What Is TIC?
In the past 15 years, there have been many definitions of TIC and various models for incorporating it across organizations. This TIP uses SAMHSA’s definition of TIC, which describes this type of care involving “these key elements: (1) realizing the prevalence of trauma; (2) recognizing how trauma affects all individuals involved with the program, organization, or system, including its own workforce; and (3) responding by putting this knowledge into practice” ( SAMHSA, Trauma and Justice Strategic Initiative, 2012 , p. 4). In a seminal article on the development of a trauma-informed service system, Harris and Fallot (2001) proposed that such a system is one in which administrators and staff understand how traumatic experiences negatively affect behavioral health in multiple ways and are committed to responding to those needs through universal trauma screening, staff education and training regarding trauma and its effects, and willingness to review and change policies and procedures to prevent the (re)traumatization of clients.
As part of the overall review of policies, practices, and research involving trauma-informed services for individuals who are homeless, Hopper, Bassuk, and Olivet (2010) reviewed the literature and organizational principles on TIC and found several common themes. These included an awareness of how symptoms and behaviors are related to traumatic experiences, an emphasis on safety, an opportunity for individuals to develop or regain a sense of control over their lives, and an emphasis on strengths rather than on deficiencies. They used these themes to develop the following definition of TIC ( Hopper, Bassuk, & Olivet, 2010 , p. 82):
Trauma-Informed Care is a strengths-based framework that is grounded in an understanding of and responsiveness to the impact of trauma, that emphasizes physical, psychological, and emotional safety for both providers and survivors, and that creates opportunities for survivors to rebuild a sense of control and empowerment.”
Other definitions of TIC exist, and Hopper and colleagues (2010) reviewed some of the better-known versions of these and presented them in a table (see Exhibit L-4 ) for easy comparison.
Exhibit L-4
Principles of TIC.
Elliott, Bjelajac, Fallot, Markoff, and Reed (2005) discussed TIC within the context of services for women and suggested some guiding principles for such services; they also briefly reviewed literature in support of those principles.
What Is the Relationship of Culture to Traumatic Stress Reactions?
Although cultural responses to trauma may vary, high PTSD rates have been diagnosed in a wide range of cultures following exposure to a significant traumatic event, including Ju’hoansi (i.e., Kalahari Bushmen) exposed to domestic violence, Cambodians who lived through the Khmer Rouge regime, survivors of the Rwandan genocide, and Filipinos who experienced a large-scale natural disaster ( Marques, Robinaugh, LeBlanc, & Hinton, 2011 ). Neurobiological research also indicates that affect dysregulation, changes in right hemisphere functioning, and a kindling phenomenon occurs across cultures in individuals who have PTSD or a prolonged stress reaction as the result of trauma exposure ( Wilson, 2007 ).
Marsella and Christopher (2004) observed that intrusive PTSD symptoms appear to be more common cross-culturally than symptoms of avoidance or the reexperiencing of trauma and that the occurrence of the two latter categories of symptoms may vary considerably across cultures. Other international research indicates that the presentation and occurrence of specific PTSD symptoms and the rates of other mental disorders and/or symptoms following trauma vary considerably among nations/cultural groups ( Marques et al., 2011 ). For example, research conducted with Vietnamese survivors of a typhoon found that both depression and panic disorder appeared to be more common responses to the trauma than PTSD ( Amstadter et al., 2009 ). Other studies conducted with Vietnamese ( Hinton et al., 2001 ) and Cambodian ( Hinton, Ba, Peou, & Um, 2000 ) refugees have also found high rates of panic disorder/panic attacks co-occurring with PTSD among trauma survivors.
Members of some cultural groups may also have increased risk for PTSD, or for certain PTSD symptoms, compared with members of other groups. Research from the United States suggests that Latinos have greater risk for PTSD when trauma exposure is controlled for than African Americans, White Americans, or Asian Americans (e.g., see Marshall, Schell, & Miles, 2009 ). A study conducted in the Netherlands with a diverse group of individuals affected by an airline disaster found that those who came from non-Western cultures ( n =379) experienced significantly more health-related anxieties, more severe PTSD symptoms, more fatigue, and more impaired health-related quality of life than did those from Western cultures ( n =406; Verschuur, Maric, & Spinhoven, 2010 ). Other research conducted with refugees in Finland who were survivors of torture ( N =78) found that those from southeastern European cultures had significantly more PTSD symptoms than did those from Middle Eastern, Central African, or Southern Asian cultures ( Schubert & Punamäki, 2011 ).
Marsella (2010) , as part of a review of the ethnocultural aspects of PTSD, noted that culture may affect individuals’ responses to trauma by providing meaning to symptoms (e.g., nightmares), by shaping individuals’ beliefs about traumatic events (e.g., through different concepts of destiny or fate), by affecting individuals’ beliefs about their own responsibility for the trauma and their subsequent response, by indicating what disabilities or impairments may result from the trauma, and by shaping the threshold for normal versus pathological levels of arousal (e.g., through perceptions and interpretations of stressors). He also indicated that cultural beliefs may be used to help heal maladaptive responses to trauma. Hoshmand (2007) reviewed research that suggested the importance of understanding cultural sources of strength/resilience when interpreting trauma from a cultural perspective.
Because of these differences, members of certain cultural groups may not present symptoms in a manner that can be easily identified as PTSD or another behavioral health disorder. For instance, clinicians working with Cambodian refugees have observed that traumatic memories in the form of flashbacks or nightmares may be interpreted as attacks by dead spirits, whereas hyperarousal symptoms may indicate a physical or spiritual weakness ( Hinton, Hinton, Pich, Loeum, & Pollack, 2009 ; Hinton, Park, Hsia, Hofmann, & Pollack, 2009 ). Hoshmand (2007) recommended taking an ecological approach to interpreting trauma, which means that traumatic experiences and trauma responses are interpreted within the context of the individual’s culture and with respect to other factors (e.g., gender, age) that might shape those responses.
Role of acculturation
Another relevant concern is the degree to which acculturation affects responses to trauma. Research in this area is limited, but the preponderance of evidence seems to indicate that greater acculturation is associated with lower levels of PTSD symptoms ( Dunlavy, 2010 ). This is contrary to the evidence relating acculturation, for some immigrant groups, to certain other behavioral health problems, notably substance abuse and depressive symptoms (e.g., Alegría et al., 2008 ; Gonzalez & Gonzalez, 2008 ; Grant et al., 2004 ; Xie & Greenman, 2005 ). In her own data analysis concerning African immigrants to Sweden, however, Dunlavy found no significant associations between acculturation and PTSD symptoms.
A large study in this area was conducted in the Netherlands with a group of 221 immigrants affected by a large fireworks explosion and a matched group of 127 immigrants unaffected by the disaster ( Drogendijk, van der Velden, & Kleber, 2012 ). The study found that lower acculturation (assessed with the Lowlands Acculturation Scale [LAS]) was associated with increased behavioral health problems for individuals who had experienced this trauma but not for those in the control group. Specifically, a greater need to keep the norms and values of one’s original culture (measured with a subscale of the LAS) was significantly associated with more intrusion and avoidance symptoms (indicative of PTSD), anxiety, depression, hostility, and somatic complaints for those affected by this trauma. For those unaffected, acculturation had no significant association with behavioral health measures, nor were other domains of acculturation significantly associated with PTSD symptoms, although having skills to cope with a new culture/society and feeling socially integrated into that society were associated with better outcomes in the other areas of behavioral health measures. The authors observed that their findings may indicate that, in the context of a disaster affecting large numbers of people, a lack of flexibility in terms of cultural norms and values may be a source of additional stress.
The role of acculturation vis-à-vis PTSD, however, may vary according to cultural group and the predominant culture’s relationship to that group (e.g., it may be different for immigrant and indigenous populations). For example, a study conducted in Taiwan with members of an aboriginal group affected by an earthquake ( N =196) found that lower levels of acculturation to mainstream Taiwanese culture were associated with significantly higher levels of PTSD symptoms following the disaster ( Lee et al., 2009 ). Other studies indicate that a domain from the Demographic and Post-Migration Living Difficulty Questionnaire labeled “difficulties adjusting to cultural life” in a new society was also associated with greater PTSD symptom severity among refugees in studies in Australia ( Schweitzer, Melville, Steel & Lacherez, 2006 ) and the United Kingdom ( Carswell, Blackburn, & Barker, 2011 ). This domain, which evaluates feelings of isolation, loneliness, boredom, and a lack of access to preferred foods, may also represent difficulties in acculturation, as the sense of isolation may be greater among less acculturated refugees who are not able to establish social connections in their new culture.
For immigrants/refugees, better acquisition of the language of their new country, which may also represent greater acculturation, has also been associated with significantly lower levels of PTSD symptoms among Iraqi refugees living in Sweden ( N =48) but not with significant differences in rates of PTSD diagnosis ( Söndergaard & Theorell, 2004 ). Similarly, a study of Burmese refugees living in Australia ( N =70) found a significant association between postmigration living difficulties, of which concern about communication problems was the most often-cited example, and PTSD symptoms ( Schweitzer, Brough, Vromans, & Asic-Kobe, 2011 ).
Schweitzer and colleagues (2006) , in their study of 63 Sudanese refugees in Australia, also found that support from family and others within a Sudanese community was a significant resilience factor with regard to behavioral health, whereas social support from the larger Australian society was not. The planned TIP, Improving Cultural Competence (SAMHSA, planned c), includes more information on the role of acculturation in behavioral health disorders and their treatment.
- Types of Trauma
There are numerous forms and types of trauma. In this section, the research reviewed explores a wide variety of traumas; however, the sheer volume of research available precludes a thorough review of each trauma type. In addition, the order of appearance in this document does not denote a specific trauma’s importance or prevalence, nor is a lack of relevance implied if a given trauma is not specifically addressed in this TIP. The intent of this section is to give the reader a broad science-based perspective on the types of trauma.
Adverse Childhood Experiences
Adverse childhood experiences (ACEs), often referred to as early childhood or interpersonal trauma, are childhood experiences that can have a negative effect on an individual’s well-being that often lasts into adulthood. These experiences include child abuse and neglect as well as substance abuse and mental illness in the family, having a family member incarcerated, and violence directed toward a parent (usually the mother; Dube et al., 2005 ). ACEs are associated with significant increases in a number of negative social, behavioral health, and physical health outcomes, including alcohol and drug use disorders, depression, suicidality, risky sexual behavior, sexual victimization in adulthood, domestic violence, self-harm behaviors, physical inactivity, obesity, heart disease, cancer, liver disease, sexually transmitted diseases, teen pregnancy, homelessness, unemployment, and being both a perpetrator and/or a victim of interpersonal violence ( Dietz et al., 1999 ; Felitti et al., 1998 ; Herman, Susser, Struening, & Link, 1997 ; Hillis, Anda, Felitti, Nordenberg, & Marchbanks, 2000 ; Lalor & McElvaney, 2010 ; Noll, Horowitz, Bonanno, Trickett, & Putnam, 2003 ; Roberts, McLaughlin, Conron, & Koenen, 2011 ; Tam, Zlotnick, & Robertson, 2003 ).
Childhood trauma also appears to be more likely to result in PTSD than trauma experienced in adulthood. Wrenn and colleagues (2011) , using a largely African American, inner-city sample of people who had experienced trauma ( N =767), found that childhood trauma was associated with significantly greater PTSD risk than trauma experienced in adulthood alone. Childhood abuse was associated with even greater risk than other trauma experienced in childhood.
A major study evaluating the effects of ACEs was conducted with 17,421 members of a large health maintenance organization (HMO) in California in collaboration with the Centers for Disease Control and Prevention ( Dube et al., 2005 ). Two rounds of questionnaires were given, with 7,641 respondents completing both assessments ( Edwards, Anda, Felitti, & Dube, 2004 ). In the initial assessment, 29.9 percent of men and 27 percent of women reported experiencing physical abuse as children; 24.7 percent of women and 16 percent of men, sexual abuse; and 13.1 percent of women and 7.6 percent of men, emotional abuse ( Dube et al., 2005 ). Also, 29.5 percent of women and 23.8 percent of men reported parental substance abuse, 23.3 percent of women and 14.8 percent of men reported parental mental illness, and 13.7 percent of women and 11.5 percent of men reported violence directed toward their mothers.
The NCS and NCS-R evaluated a similar group of 12 experiences, labeled childhood adversities (CAs), which included parental death, parental divorce/separation, life-threatening illness, and extreme economic hardship in addition to the experiences included in the ACE study ( Green et al., 2010 ). In this sample, 8.4 percent reported childhood physical abuse; 6 percent, sexual abuse; 5.6 percent, neglect; 14 percent, family violence; 10.3 percent, parental mental illness; 8.5 percent, parental substance abuse; and 5.8 percent, life-threatening illness ( Green et al., 2010 ).
In a multivariate model, almost all of the CAs evaluated in the NCS were associated with increased odds of having a mental disorder; the strongest associations were with parental mental illness, parental substance abuse, family violence, childhood physical abuse, childhood sexual abuse, and life-threatening illness ( Green et al., 2010 ). These data also show a significant association between certain CAs (i.e., parental mental illness, substance abuse in the family, family violence, childhood physical/sexual abuse, childhood neglect, economic hardship) and the persistence of mental disorders ( McLaughlin, Green, Gruber et al., 2010a ). The associations of single trauma to mental disorders were modest, but multiple traumas had a cumulative effect, so that exposure to multiple CAs further increased the strength of the association with both onset and persistence of mental disorders. These same CAs were also significantly associated with functional impairment related to behavioral health disorders ( McLaughlin et al., 2010b ).
Another large study, the Developmental Victimization Survey, investigated forms of childhood abuse and maltreatment in 2,030 children and adolescents ages 2 to 17. The study found that 13.8 percent had sustained some form of maltreatment in the year of the survey; 10.3 percent, psychological/emotional abuse; 3.6 percent, physical abuse; 1.4 percent, neglect; and 0.6 percent, sexual abuse ( Finkelhor, Ormord, Turner, & Hamby, 2005 ). However, some literature indicates that all these data underrepresent the extent of childhood abuse and neglect, as both research and expert opinion indicate that these traumas are generally underreported (see review by Gilbert et al., 2009 ).
Gilbert and colleagues (2009) specifically reviewed data on psychological abuse, which is not often evaluated in the literature. They found that approximately 10 percent of children in the United States and the United Kingdom experience psychological abuse in any given year, and between 4 and 9 percent sustain severe emotional abuse. Children who have sustained one type of abuse or neglect are likely to have experienced other types as well, according to research conducted with a variety of samples (see reviews by Edwards et al., 2003; Gilbert et al., 2009 ).
Research indicates that women are much more likely to sustain sexual abuse than men. Some studies have found that men are more likely than women to sustain physical abuse in childhood (e.g., Dube et al., 2005 ), whereas others did not find significant differences (e.g., Finkelhor et al., 2005 ). Although childhood sexual abuse is more common for women than for men, research evaluating outcomes for both genders has, for the most part, found similar long-term consequences for men and women ( Banyard, Williams, & Siegel, 2004 ; Dube et al., 2005 ).
Research also indicates that children living in households with yearly incomes of $20,000 or less (in 2003–2004) are significantly more likely than children from other households to experience psychological/emotional abuse, but not physical or sexual abuse ( Finkelhor et al., 2005 ). According to the same study, children from low-income families are also significantly more likely to witness domestic violence and violence in their communities, and they are significantly more likely to sustain violent assault or rape not perpetrated by a family member. Other research has also found that children who are maltreated, especially those who sustain physical abuse, are more likely to be exposed to violence in their communities and to witness domestic violence; these latter traumatic experiences have specific negative effects on children’s functioning beyond those associated with abuse/neglect ( Lynch & Cicchetti, 1998 ).
Different types of childhood abuse may have different behavioral health effects. In a study of 196 clients in treatment for alcohol dependence, a history of emotional abuse in childhood was associated with a significant increase in risk for mood disorders (especially major depression) and PTSD, physical abuse in childhood was associated with a significant increase in suicide attempts, and sexual abuse in childhood was associated with significant increases in risk for anxiety disorders, including PTSD ( Huang, Schwandt, Ramchandani, George, & Heilig, 2012 ). A study of 140 women found that those who experienced sexual abuse in childhood were significantly more likely to engage in self-harm behaviors, those who sustained emotional abuse were significantly more likely to be victims of sexual assault/rape in adulthood, and those who were neglected in childhood were significantly more likely to be victims of physical abuse in adulthood ( Noll et al., 2003 ).
More so than other ACEs, physical and sexual abuse in childhood are associated with even greater and more lasting problems, including significantly higher rates of depression, substance use disorders, and PTSD in later life (see review by Gilbert et al., 2009 ). In addition, Gilbert and colleagues (2009) found strong evidence linking childhood abuse with suicide attempts, high-risk sexual behavior, criminal behavior, and obesity. As one seminal article on the effects of childhood trauma observes, “deficits in virtually all of the major tasks of development” can result from such abuse in childhood ( Lynch & Cicchetti, 1998 , p. 238). A more recent analysis of NCS-R data that controlled for other anxiety disorders, depression, and demographic factors also found that childhood sexual abuse was associated with significantly greater risk for social anxiety disorder (SAD), panic disorder, and generalized anxiety disorder (GAD), in addition to PTSD, in adulthood ( Cougle, Timpano, Sachs-Ericsson, Keough, & Riccardi, 2010 ). Physical abuse in childhood, however, was only associated with significantly higher risk for specific phobias and PTSD.
Abuse during childhood also appears to predispose individuals to further abuse and trauma as they grow older. Sexual abuse in childhood and the severity of such abuse have been shown in a number of studies to be significantly associated with a greater risk for sexual abuse in adulthood (see review by Classen, Palesh, & Aggarwal, 2005 ). Physical abuse in childhood, to a lesser degree, is also associated with an increased risk for sexual abuse in adulthood ( Classen et al., 2005 ). Women who were physically abused as children are at greater risk for being victims of domestic violence, whereas men who were physically abused are at greater risk for being perpetrators of domestic violence ( Whitfield, Anda, Dube, & Felitti, 2003 ). This study, which used data from the ACE study described previously, did not assess the relationship of child abuse to violence perpetrated by women or sustained by men.
In addition to likely contributing to behavioral health disorders, childhood abuse may also affect behavioral health treatment outcomes. Research conducted with 146 women who were homeless and had substance use disorders found that those who had histories of childhood abuse (physical, sexual, and/or emotional) had significantly worse outcomes in terms psychological functioning (assessed with multiple instruments) and substance abuse (assessed with an instrument derived from the Addiction Severity Index [ASI]; Sacks, McKendrick, & Banks, 2008 ). More information on the relationship between childhood abuse/neglect and substance abuse in adulthood can be found in TIP 36, Substance Abuse Treatment for Persons With Child Abuse and Neglect Issues ( Center for Substance Abuse Treatment [CSAT], 2000 ).
Ford (2009) reviewed the neurobiological and development research that helps explain how trauma experienced in childhood can affect the brain and how those effects may continue throughout a person’s lifetime (see also earlier work, Anda et al., 2006 ). More recent studies confirm this research. As one example, Dannlowski and colleagues (2012) found strong associations between childhood maltreatment (assessed retrospectively using the Childhood Trauma Questionnaire) and both decreased gray-matter volume in a number of areas of the brain and increased response in the amygdala upon seeing pictures of threatening facial expressions.
Schumm, Briggs-Phillips, and Hobfoll (2006) reviewed three theories on why sexual abuse in childhood has extensive and lasting negative effects: these individuals develop a generalized fear response as a result of their inability to control or predict abuse, and this leaves them unable to emotionally engage in interpersonal relationships; they feel worthless and perceive others as disapproving of them; and/or they become easy targets for exploitative social networks, which further harm their ability to trust. The authors noted that these patterns together may contribute to problems with interpersonal relationships, which in turn affect behavioral health.
Disasters/Mass Trauma
Large-scale traumatic events like natural disasters (e.g., earthquakes, hurricanes), human disasters (e.g., chemical spills, nuclear accidents), and terrorist attacks have unique effects because of the number of people affected and the fact that whole communities/populations may experience consequences ( Norris, Friedman, & Watson, 2002 ). In addition to affecting behavioral health, such traumatic events often involve multiple losses, including the loss of lives (of friends and family), home, occupation/employment, health/physical well-being, and even one’s worldview (such events may affect one’s sense of security or beliefs about the justice of the world; Walsh, 2007 ).
Not all disasters/mass trauma incidents appear to have the same effect on people’s behavioral health. In their review of 160 studies of mass trauma events, Norris and colleagues (2002) found that rates of serious psychological impairment (measured with a number of different instruments) were significantly higher for individuals who endured trauma from mass violence (e.g., terrorist attacks) than for those who experienced a technological or natural disaster. Severe impairment was also more common if the event occurred in a developing (rather than developed) country, and, in most studies, if the individual who experienced the event was female rather than male.
DiGrande, Neria, Brackbill, Pulliam, and Galea (2010) assessed PTSD symptoms for 3,271 individuals evacuated from the World Trade Center on 9/11 by phone interview (and by face-to-face interview for 5 percent of the sample) 2 to 3 years after the event. They found that 95.6 percent had at least one PTSD symptom and 15 percent had probable PTSD according to their scores on the PTSD Checklist (PCL), Stressor-Specific Version. Specific experiences associated with significantly higher odds for PTSD included witnessing a horrific incident (e.g., the airplane hitting the towers, people falling from the building, people who were injured or killed), being injured in the attack, being exposed to the dust cloud that resulted from the building collapse, being above the impact zone when the attack occurred, and evacuating later rather than earlier.
Another study of people affected by the 9/11 attacks that used a national sample ( n =933 respondents to the 2-month follow-up assessment; n =787 respondents to the 6-month assessment) and a Web-based survey also found that 17 percent reported at least one ASD/PTSD symptom 2 months after the 9/11 attack; 5.8 percent reported at least one symptom 6 months after the attack ( Silver, Holman, McIntosh et al., 2002 ). Individuals were significantly more likely to report symptoms if they were female, were separated/divorced/widowed, had a diagnosed depressive or anxiety disorder, had a physical illness, had disengaged from coping efforts, and/or had greater exposure to the actual attacks. The authors concluded that individuals need not be directly exposed to mass trauma events for those events to have a negative effect on their behavioral health.
Norris and colleagues (2002) reviewed information on risk and protective factors associated with behavioral health disorders and symptoms for survivors of natural disasters and those caused by people drawn from 160 studies published between 1981 and 2001. For the most part, these are the same as found with other populations of trauma survivors, with possible exceptions being the presence of children, which is a risk factor for anxiety in mothers involved in disasters (fathers were not studied in the four articles reviewed), and the loss of material resources, which has been found to be a risk factor for behavioral health disorder symptoms in survivors of disasters but is rarely evaluated in studies involving other types of trauma. Such losses also appear to have a greater effect on older adults involved in disasters (see the “ People in Specific Age Groups ” section).
Domestic Violence/Intimate Partner Violence
Domestic violence or intimate partner violence, also referred as interpersonal trauma, is a major source of trauma for women (and can affect men as well) and carries with it a high risk for PTSD ( Coker, Weston, Creson, Justice, & Blakeney, 2005 ). Between 2001 and 2005, intimate partner violence accounted for 21.5 percent of nonfatal violence against women and 3.6 percent of violence against men ( Catalano, 2012 ). Rates of domestic violence are high for people with behavioral health disorders, especially people with substance use disorders.
Coker and colleagues (2005) evaluated data regarding links between intimate partner violence and PTSD taken from the National Violence Against Women Survey, a large national household survey of 8,000 women and 8,000 men conducted in the mid-1990s (see Tjaden & Thoennes [2000] for more information on the study). Among a subsample of men and women who were survivors of intimate partner violence (368 women, 185 men), PTSD rates were high, with 24 percent of the women and 20 percent of the men having moderate to severe levels of PTSD symptoms, indicating possible current PTSD (although rates of possible PTSD were higher for women, the difference between genders was not significant). The authors also found that higher socioeconomic status (SES), current marriage, and the cessation of intimate partner violence were all associated with significantly lower odds of having elevated PTSD symptoms.
Research from Spain suggests a dose–response relationship between intimate partner violence and PTSD ( Pico-Alfonso, 2005 ); although physical, sexual, and psychological abuse from partners were all significantly related to PTSD, the latter had the strongest relationship.
Political Violence/Torture
Trauma from political violence and torture varies considerably across the globe and is common among some refugee groups ( Johnson & Thompson, 2008 ). Histories of torture are also common among smaller populations, such as former prisoners of war ( Engdahl, Dikel, Eberly, & Blank, 1997 ). Accurate data on the prevalence of such trauma in the United States is difficult to obtain, because most major surveys do not inquire specifically about it.
Because of the high degree of interpersonal violence involved, political violence and torture often result in traumatic stress reactions that pose particular problems for providers in terms of treatment and assessment. In Steel and colleagues’ (2009) meta-analysis of research on trauma and traumatic stress among refugees and others exposed to mass conflict and political violence, of all the experiences evaluated, torture was associated with the greatest increase in PTSD risk (more than doubling the odds of having PTSD).
Johnson and Thompson (2008) reviewed literature on the prevalence of PTSD among survivors of political and civilian war trauma. They cited studies involving torture survivors that found PTSD rates ranging from 18 to 90 percent of study participants. They observed evidence of a dose–response relationship between torture and both initiation and maintenance of PTSD. This review suggests that protective factors for PTSD that results from torture and civilian war trauma include being prepared for torture, having strong social and family support, and having stronger religious beliefs.
Some theories hold that having redress for torture and other political violence may help survivors process their traumatic experiences and thus aid in behavioral health treatment (e.g., Roht-Arriaza, 1995 ). However, Başoğlu and colleagues (2005) found only a relatively weak association between the lack of redress for war-related trauma and PTSD symptoms among a group of 1,358 civilian war survivors in the former Yugoslavia. Fears about threats to one’s safety and beliefs about losing control over one’s life had much stronger associations with PTSD symptoms.
The role of forgiveness in the behavioral health of survivors of torture and other political violence may depend on the context of the violence and the object of forgiveness. Kira and colleagues (2009) found, among a group of 501 Iraqi refugees, that those who forgave perpetrators of violence in general as well as those who collaborated with the regime (as measured with a modified version of the Forgiveness Versus Refusal To Forgive Scale) had significantly better physical and behavioral health than did those who did not forgive those people. On the other hand, forgiveness of dictators and specific individuals who were the principal perpetrators of the violence was associated with significantly worse physical and behavioral health outcomes.
Sexual Assault/Rape
In 2010, 1.3 percent of women age 12 and older were victims of sexual assault/rape, and it was estimated that, in the general population, about 0.1 percent of men were victims—although there were not sufficient data to be certain of the accuracy of that estimate ( Truman, 2011 ). These data are based on a general population survey that excluded the institutionalized population, which sustains even higher rates of sexual assault/rape. For example, from 2008 to 2009, 4.4 percent of prison inmates were victims of sexual assault ( Beck & Harrison, 2010 ). Although women are more likely than men to be sexually assaulted even in prison, there are about 13 times as many men as women in such facilities, so a large number of incarcerated men are affected. Among prison inmates in 2008–2009, 1.9 percent of men and 4.7 percent of women reported being sexually victimized by other inmates in the prior year, whereas 2.9 percent of men and 2.1 percent of women reported being sexually victimized by staff members during that period.
Histories of sexual abuse among clinical populations are also likely to be considerably more common than in the general population (e.g., see TIP 51, Substance Abuse Treatment: Addressing the Specific Needs of Women [ CSAT, 2009b ], for a review of data on sexual assault among female clients in substance abuse treatment settings). Certain other populations, including survivors of childhood physical and/or sexual abuse, people with disabilities, and people who are homeless, also have a higher risk for sexual assault ( Luce, Schrager, & Gilchrist, 2010 ).
Accurate data on sexual assault among patients institutionalized for mental disorders are difficult to locate, but rates of sexual assault should be expected to be high in this group as well. According to a study by Teplin, McClelland, Abram, and Weiner (2005) of 936 patients with serious mental illness (SMI) attending outpatient residential day treatment at a Chicago program, participants were 17.2 times more likely to have been victims of sexual assault or rape in the prior year and 22.5 times more likely to have been victims of rape than a comparable general population sample from the National Crime Victimization Survey during the same period.
Studies have also found very high PTSD rates among survivors of sexual assault, especially survivors of rape, and data suggest that sexual assault is more likely than most other types of trauma to result in PTSD (see reviews in Ullman & Filipas, 2001 ). In addition, sexual abuse in adulthood or childhood is also associated with high levels of other behavioral health disorders. In a meta-analytic review of 37 studies providing data on 3,162,318 individuals, Chen and colleagues (2010) found that a history of sexual abuse in childhood or adulthood was associated with more than three times the risk for an anxiety disorder compared with individuals who had no such history; more than twice the risk for depression, an eating disorder, or PTSD; and more than four times the risk for suicide attempts.
Ullman and Filipas (2001) reviewed research identifying factors associated with increased risk for PTSD among victims of sexual assault/rape. These include being attacked by a stranger, being subjected to physical force or threatened with a weapon, being physically injured, having a prior history of childhood sexual abuse, being raped in a location typically considered safe, using wishful thinking as a coping strategy in response to the attack, and receiving fewer community services and/or experiencing a high degree of secondary victimization following the attack. On the other hand, the use of positive distancing (e.g., acceptance coping, optimism, cognitive distancing) was associated with lower PTSD risk.
In their own research on 332 women who had been sexually assaulted, Ullman and Filipas (2001) determined that, although positive social reactions following the assault were not significantly associated with severe PTSD symptoms, more negative responses from others were associated with more severe PTSD symptoms. In particular, being treated differently or being discriminated against showed the strongest association with more severe PTSD, and responses in which people tried to distract the victim (e.g., telling her to move on with her life) showed less severity but were still significantly linked with more severe PTSD. Positive social support was not significantly related to PTSD symptom severity, but some factors were identified as significantly associated with more positive social support—namely, lower severity of victimization and disclosing more about the assault (discussing it at greater length and/or in more detail). Greater injury severity and a greater perceived threat at the time of the assault were also associated with significantly more severe PTSD symptoms.
Combat Trauma
Because of the resources available to the military (including the ability to compile accurate data about a relatively large population), combat trauma is one of the most widely studied types of trauma in terms of behavioral health. For more information on the impact of trauma and deployment, see the planned TIP, Reintegration-Related Behavioral Health Issues in Veterans and Military Families (SAMHSA, planned f). This section summarizes information available in more detail in that TIP.
According to the largest study of PTSD among Vietnam War veterans, the National Vietnam Veterans Readjustment Study (NVVRS), 15.2 percent of male veterans had current PTSD, and 30.6 percent met criteria for PTSD at some point during their lives ( Kulka et al., 1990b ). In addition, 8.5 percent of women who were in the Vietnam theater as civilian nurses had current PTSD, and 26.9 percent had PTSD at some point during their lives. These rates were considerably higher than rates in veterans from that era who did not serve in Vietnam (of whom 2.5 percent of men and 1.1 percent of women had current PTSD) or a civilian comparison group that was also included in the study.
A later reanalysis of NVVRS data, which took into account criticisms of the initial study, provided a more conservative estimate of 9.1 percent of men having current PTSD and 18.7 percent meeting criteria for the disorder at some point during their lives ( Dohrenwend et al., 2006 , 2007 ). These authors found that, even for individuals who had substantial impairment relating to PTSD symptoms, PTSD diagnoses decreased over a 10- to 11-year period following the war; for the majority, this occurred without receiving mental health services. The NVVRS also found that war zone stress, which included combat trauma and exposure to other traumatic events, was also significantly related to major depression, dysthymia, obsessive–compulsive disorder (OCD), GAD, alcohol use disorders, and antisocial personality disorder (ASPD) for men ( Jordan et al. 1991 ). The majority (63 percent) of male veterans who had high levels of exposure to war zone stress met criteria for at least one mental disorder during their lives, and 41 percent had at least one current disorder at the time of assessment.
Studies of military personnel who served in Operation Desert Shield/Desert Storm, Operation Enduring Freedom (OEF), and/or Operation Iraqi Freedom (OIF) also found high rates of PTSD and other behavioral health disorders among those exposed to combat. For instance, the National Health Survey of Gulf War Era Veterans and Their Families, conducted 5 years after Operation Desert Storm ended, found that the PTSD rate was three times higher for deployed troops than for nondeployed troops during the same period, with 12.1 percent of deployed troops having probable current PTSD according to the PCL ( Kang, Natelson, Mahan, Lee, & Murphy, 2003 ). This study found a correlation between a greater intensity of combat exposure and greater likelihood of having PTSD.
Several major studies have evaluated behavioral health disorders among individuals deployed to OEF/OIF. For example, a review included in a RAND Center for Military Health Policy Research report found that between 5 and 15 percent of returning service members had current PTSD, and between 2 and 10 percent had current depression ( Karney, Ramchand, Osilla, Caldarone, & Burns, 2008 ). Combat duty and being wounded both significantly increased the chances that an individual would have PTSD. Although greater numbers of women were exposed to combat trauma in OEF/OIF than in prior conflicts, studies also continued to find higher PTSD rates in men than in women who had been deployed, with rates of 9.3 percent and 8.4 percent, respectively, in one large ( N =163,812) study ( Haskell et al., 2011 ).
Historical Trauma
Historical trauma refers to trauma inflicted in the past on members of a certain cultural group that may continue to have effects on the current generation. The concept was originally developed to help explain how generations descended from Holocaust survivors continued to be psychologically affected by the trauma their parents and/or grandparents had experienced ( Duran et al., 1998 ; Sotero, 2006 ). Clinicians working with other populations, such as Native Americans, observed a similar pattern with regard to how the behavioral health of more recent generations continued to be affected by violence committed against their ancestors ( Brave Heart, 2003 , 2004 ; Duran, Duran, Brave Heart, & Yellow Horse-Davis, 1998 ). Other groups who experienced large-scale and well-remembered violence, such as attempted genocide or slavery, also have to deal with historical trauma.
The phenomenon has been studied most often in the United States with Native American populations, and for many Native Americans receiving behavioral health services, historical trauma may be an important clinical issue ( Brave Heart, 2004 ; Evans-Campbell, 2008 ). Some research indicates that thinking about historical loss is associated with certain behavioral health problems, such as increased risk for alcohol use disorders ( Whitbeck et al., 2004 ). Although the exact mechanism through which historical trauma works is not known, the process may be one in which subsequent generations experience secondary trauma as the result of their parents’ PTSD. Another explanation is that traumatic experiences harm an individual’s ability to parent effectively and thus increase the abuse of children, causing those children to have traumatic stress reactions themselves ( Brave Heart, 1999 ). Some research also points to substance abuse connected to trauma as central in the perpetuation of historical trauma ( Libby, Orton, Beals, Buchwald, & Manson, 2008 ).
Sotero (2006) , who reviewed research on historical trauma across diverse populations, proposed that large-scale interpersonal trauma continues to affect communities/cultural groups through material (e.g., displacement), psychological (e.g., PTSD), economic (e.g., loss of sources of income/sustenance), and cultural (e.g., lost knowledge of traditions and beliefs) effects. These powerful effects of trauma cause the next generation to experience similar consequences, resulting in worse coping skills or attempts to self-medicate distress through substance abuse.
Cumulative Trauma
Kessler (2000) observed that large epidemiological surveys typically ask about the worst or most severe trauma an individual has endured, with the assumption that if the individual has had PTSD, it would appear after such a trauma. This approach may undercount lifetime prevalence, however, because further trauma following the worst episode of trauma exposure may have a kindling effect that results in PTSD a considerable length of time after the worst episode occurred.
Thus, repeated trauma further increases risk for PTSD, and prior trauma is recognized as a PTSD risk factor following a traumatic event (see the “ Risk and Protective Factors ” section). For example, research conducted with inner-city women ( N =777) found that women who had experienced multiple traumas significantly increased their risk for PTSD ( Schumm, Briggs-Phillips, & Hobfoll, 2006 ). Therefore, women who had experienced child abuse and also had been raped as adults were over 17 times more likely than others to be screened as probably having PTSD, whereas women who had experienced only one of those two types of trauma were about six times more likely than others to meet screening criteria for probable PTSD.
Studies conducted with other populations have also found that greater exposure to traumatic events increases risk for a number of behavioral health disorders. For example, a seminal study conducted with Cambodian refugees ( N =993) found a significant dose–response relationship between the number of traumatic events an individual had experienced and depression, PTSD symptoms (including arousal, reexperiencing, and emotional numbing, but not avoidance), and symptoms of culturally specific behavioral health disorders ( Mollica, McInnes, Poole, & Tor, 1998 ).
- Extent and Effects of Trauma and Traumatic Stress Reactions in Specific Populations
The incidence and prevalence of trauma and of behavioral health problems related to trauma vary across demographic groups. Some of the major demographic differences that may affect trauma exposure and behavioral health are discussed in this section.
Members of Specific Cultural/Ethnic/Racial Groups
Rates of trauma exposure among some samples of members of certain cultural, ethnic, and racial groups are higher than the U.S. average. To what extent this reflects socioeconomic and geographic factors is not clear, as other data indicate that people in urban areas and those with lower SES are also at greater risk for certain types of trauma (see “ People With Lower SES ”). Researchers have found that PTSD rates vary considerably among diverse cultures and that rates are high among people exposed to significant trauma, regardless of their culture of origin ( Marques et al., 2011 ).
According to data from Wave 2 of NESARC ( N =34,653), which oversampled to achieve a racially/ethnically diverse sample, non-Latino White Americans were significantly more likely to have some trauma experience during their lives compared with members of other ethnic/racial groups, with 83.7 percent of White Americans, 76.4 percent of African Americans, 66.4 percent of Asian Americans, and 68.2 percent of Latinos reporting some type of trauma exposure during their lives ( Roberts et al., 2011 ). However, this did not hold true for every type of trauma exposure. African Americans and Latinos were significantly more likely than White Americans to have been exposed to childhood maltreatment, with the largest difference being the increased likelihood of witnessing domestic violence. African Americans were significantly more likely than White Americans to have been violently assaulted. Asian Americans, who had significantly lower levels of exposure than White Americans to many kinds of trauma, were significantly more likely to have been exposed to war-related trauma (mostly as the result of being unarmed civilians in a combat zone) and to be refugees from a region where combat was occurring.
Among certain subpopulations of major ethnic/racial groups, trauma exposure may be even more common. For example, Goldmann and colleagues (2011) assessed trauma histories of 1,306 African American residents of Detroit, the majority of whom had annual incomes below $35,000 (34.6 percent below $15,000, and 27 percent between $15,000 and $35,000). They found that 87.2 percent reported at least one type of trauma during their lives; 51 percent reported experiencing assaultive violence, 64.5 percent reported another type of injury or shocking experience (e.g., witnessing someone being seriously injured or killed), and 64 percent reported learning about trauma from a loved one. Of those who reported at least one trauma, 17 percent likely had PTSD at some point during their lives, with a higher rate of likely PTSD for individuals experiencing certain types of trauma (e.g., 32.8 percent of those who had been raped and 31.2 percent of those who had been badly beaten had a lifetime PTSD diagnosis).
In Wave 2 of NESARC, African American men were significantly more likely than White American men to have PTSD at some point during their lives, but this was not the case for African American women ( Roberts et al., 2010 ). According to the same research, Asian American men and women were significantly less likely than White American men and women to meet criteria for a lifetime diagnosis of PTSD. Asnaani, Richey, Dimaite, Hinton, and Hofmann (2010) combined data from the NCS-R and two other surveys that use the same methodology (the National Study of American Life and the National Latino and Asian American Study of Mental Health) to evaluate the lifetime prevalence of PTSD. Their data indicated that, after controlling for age, gender, and SES, both White Americans and African Americans were significantly more likely than Asian Americans or Latino Americans to have PTSD at some point during their lives, whereas White Americans and African Americans did not differ from one another significantly in this regard. Latino Americans were also significantly more likely than Asian Americans to have the disorder.
As Norris and Slone (2007) observed in their chapter on the epidemiology of PTSD, data are inconclusive about whether there are significant differences in the likelihood that members of diverse racial/ethnic/cultural groups within the United States will develop PTSD, especially given differences in trauma exposure relating to both culture and SES. Marques and colleagues (2011) , in a review of cross-cultural differences in anxiety disorders, observed that the evidence is mixed regarding differences in PTSD prevalence between African Americans and White Americans. They concluded that the evidence is stronger regarding elevated levels of PTSD among Latinos compared with members of other ethnic racial groups. Another review by Pole, Gone, and Kulkarni (2008) similarly concluded that evidence fairly consistently suggests that Latinos are more likely than members of other ethnic/cultural groups to develop PTSD but that significant differences in PTSD rates observed among other ethnic/racial/cultural groups in the United States tend to disappear when other factors, such as trauma exposure, are taken into account.
Research indicating significantly higher PTSD rates among Latino populations in the United States is worth a closer look. Research conducted with Vietnam veterans, a group for whom trauma exposure can be fairly accurately determined, identified Latinos as having greater risk for PTSD, and this finding was confirmed in later analyses of the data. Ruef, Litz, and Schlenger (2000) analyzed data from the NVVRS, a large, publicly mandated study that oversampled for Latinos and African Americans. Although the NVVRS found that PTSD rates were higher among both Latino veterans (27.9 percent of whom had PTSD at the time of the study) and African American veterans (20.6 percent) than among White American or other veterans (13.7 percent), after controlling for combat exposure and significant predeployment variables that affected PTSD (e.g., childhood behavioral problems, substance use disorder symptoms prior to entering the military), only Latino veterans still had significantly higher PTSD rates.
Ruef, Litz, and Schlenger’s analysis (2000) of the extensive NVVRS data took into account issues such as linguistic competence in English, cultural differences in reporting style, experiences of racism during deployment, postdeployment adjustment problems, participation in behavioral health treatment, and co-occurring disorders. Most of these factors could not explain differences in PTSD rates between Latinos and African Americans, the latter of whom faced many of the same stressors. Latinos in the study reported experiencing less racism than did African Americans, but they may have also experienced less unit cohesion because of their smaller relative numbers (unit cohesion is also believed to be a protective factor in regard to PTSD; see the “ Risk and Protective Factors ” section). The authors did find that Latinos reported significantly fewer people in their units who they believed were concerned about their welfare than did African Americans or White Americans.
Using both NVVRS data and data from the Hawaii Vietnam Veterans Project, Schnurr, Lunney, Sengupta, and Waelde (2003) concluded that Latino male veterans had significantly higher PTSD rates compared with White men, whereas Asian American male veterans had significantly lower rates. This finding suggests that the higher PTSD rates observed in Latinos in Vietnam were not simply the result of greater identification with the Vietnamese. Also, in another analysis of NVVRS data, Ortega and Rosenheck (2001) found that acculturation did not significantly affect PTSD rates among Latinos, discounting the possible explanation that differences in acculturation were responsible for higher PTSD rates in this population. They did, however, find that in an adjusted model, Puerto Rican veterans were more likely than Mexican American veterans to have PTSD, suggesting that cultural differences among Latinos may affect PTSD. Wilcox, Briones, and Suess (1991) also found that Puerto Rican Vietnam veterans had more severe PTSD symptoms than did Mexican American veterans.
Research conducted with veterans of OIF and OEF also indicates that Latinos are at greater risk of developing PTSD than members of other ethnic/cultural groups. Researchers at the RAND Center found that, for OEF/OIF veterans, Latino ethnicity and female gender were both associated with increased risk for depression and PTSD, even after controlling for trauma exposure ( Tanielian et al., 2008 ).
Latinos have been found to have higher PTSD rates relative to members of other ethnic/racial groups in research conducted with other populations, including New York city residents who witnessed the 9/11 attack ( Galea et al., 2004 ), police officers in three major cities ( Pole et al., 2001 ; 2005 ), and hurricane survivors in Florida ( Perilla, Norris, & Lavizzo, 2002 ). However, among a group of people who were exposed to hurricanes in Florida in 2004, Latino ethnicity was only a significant PTSD risk factor for those under age 60, suggesting that age may also interact with culture in affecting PTSD ( Acierno, Ruggiero, Kilpatrick, Resnick, & Galea, 2006 ).
Pole and colleagues (2008) reviewed possible explanations for why Latinos have elevated PTSD rates. Two explanations appear to have the greatest support: culturally defined differences in coping styles (Latinos appear to engage more in self-blame coping and wishful thinking coping, generally related to religious beliefs) and increased likelihood of experiencing peritraumatic dissociation, a possible PTSD risk factor that appears to be a more common reaction to trauma for individuals with greater adherence to Latino cultural norms.
Marshall and colleagues (2009) evaluated differences in PTSD symptoms among a mostly male (77.6 percent male across the study) group of Latinos ( n =330), African Americans ( n =171), and non-Latino White Americans ( n =135) who had sustained a sudden physical injury and were treated at a trauma center in the Los Angeles area. As with other studies, these authors found that Latinos reported significantly more severe PTSD symptoms (with a difference equivalent to about a 3-point increase in PCL scores) than African Americans and non-Latino White Americans. However, they also observed that certain PTSD symptoms were responsible for this difference. Of the 17 symptoms included on the PCL, Latinos were significantly more likely than non-Latino White Americans to report 11 of the symptoms, with considerable variation in the magnitude of the differences. As Triffleman and Pole (2010) observed in a review of this study, these findings suggest that “elevated rates of PTSD diagnosis among [Latinos] may be due to differing symptoms, differing levels of symptom severity, and potentially differing relationships between symptoms” compared with non-Latino White Americans (p. 492).
Particular types of trauma may have a greater or lesser impact on members of a particular cultural group. For instance, Palinkas, Downs, Patterson, & Russell (1993) found that in the wake of the Exxon Valdez disaster, Alaska Natives exposed to the event had significantly higher PTSD and GAD rates than did White Americans who were also exposed. Lilly and Graham-Bermann (2009) evaluated PTSD in 120 mothers with low incomes who were victims of intimate partner violence, of whom 42 were African American and 78 were White American. The women in the study had experienced multiple traumas in the prior year (an average of 36 acts of sexual abuse, 10 acts of severe physical violence, and 17 acts of mild physical violence). The authors found that the African American women in the study had significantly fewer PTSD symptoms (as assessed with the Posttraumatic Stress Scale for Family Violence) than did the White American women, even though African American women had experienced more severe violence (although not significantly more so) than the White American women.
Research has also found that the relationship of different types of childhood abuse to PTSD symptoms varies by cultural group. Among a group of 669 lesbian, gay, or bisexual individuals, emotional abuse in childhood had a significantly stronger relationship to PTSD and other anxiety symptoms for African Americans compared with White Americans, whereas physical abuse in childhood had a significantly stronger relationship to PTSD and other anxiety symptoms for Latinos than for White Americans ( Balsam, Lehavot, Beadnell, & Circo, 2010 ). International research also indicates that, in Turkey and India, childhood emotional abuse and neglect have a greater effect on dissociation than physical or sexual abuse, which is contrary to what is found in the United States ( Lewis-Fernández, Martínez-Taboas, Sar, Patel, & Boatin, 2007 ).
Trauma rates vary by subpopulations within these broad cultural, racial, and ethnic classifications and may be affected more strongly by noncultural factors (e.g., amount of trauma exposure). For instance, data suggest that PTSD rates are relatively low for Asian Americans (e.g., Pietrzak et al., 2011a ), but among Cambodian refugees, PTSD rates are considerably higher. Marshall, Schell, Elliott, Berthold, and Chun (2005) , in a telephone survey of 586 Cambodian adults living in Long Beach, CA, found that 100 percent had experienced trauma, and 62 percent met criteria for a past-year diagnosis of PTSD.
As another example, the American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project (AI-SUPERPFP), which collected data from 3,084 American Indians ages 15 to 54 who were members of either a Northern Plains Tribe or a Southwest Tribe, found significant differences in some types of trauma exposure between American Indians from the two different regions ( Manson, Beals, Klein, & Croy, 2005 ). PTSD rates also varied, although the differences were not significant; the largest difference found was between men from the Southwestern Tribes (11.7 percent of whom met criteria for PTSD during their lifetime) and men from the Northern Plains Tribes (8.9 percent of whom had lifetime PTSD; Beals, Manson, Whitesell, Spicer, Mitchell et al., 2005 ). Larger, but still not significant, differences were found in lifetime PTSD rates between male American Indian Vietnam veterans from the Northern Plains Tribes ( n =305) and those from the Southwestern Tribes ( n =316), who had lifetime rates of 57 percent and 45 percent respectively ( Beals et al., 2002 ). These rates, however, were considerably higher than found in the general population sample of Beals, Manson, Whitesell, Spicer, Novins, and colleagues (2005) , indicating that factors other than cultural background (in this case, combat exposure) likely play a greater role in trauma exposure and traumatic stress reactions.
As suggested by the example of Cambodian American immigrants, rates of trauma are high among immigrants from countries where military action and political violence are occurring, regardless of their specific cultural background. Steel and colleagues (2009) conducted a meta-analysis of trauma and traumatic stress reactions among groups exposed to mass conflict and displacement. Although reported rates of PTSD and depression varied widely among the studies included in the review, the authors found that, across surveys, 30.6 percent of participants had PTSD, and 30.8 percent had depression.
Women and Men
Research generally indicates that men are more likely than women to experience a traumatic event during their lives ( Olff, Langeland, Draijer, & Gersons, 2007 ). However, data from multiple sources show that women are significantly more likely than men to experience intimate partner violence and sexual assault (both in childhood and dulthood; Pratchett, Pelcovitz, & Yehuda, 2010 ). This same review found that various research suggests that between 20 and 22 percent of women experience intimate partner violence, and approximately a quarter of all women are victims of sexual assault. Women are significantly less likely than men, however, to experience many other types of trauma, including nonsexual assault, combat, traumatic accidents, and witnessing the death or injury of another person.
Research has consistently found that women are more likely than men to have PTSD, and this holds true, albeit to a lesser extent, when controlling for trauma exposure ( Kimerling, Ouimette, & Weitlauf, 2007 ; Olff et al., 2007 ). For example, data from Wave 2 of NESARC showed that women were significantly more likely than men to have PTSD or partial PTSD at some point during their lives ( Pietrzak et al., 2011a ). Women were nearly twice as likely as men to have a lifetime PTSD diagnosis, with 8.6 percent of women and 4.1 percent of men meeting those criteria. Women were also more likely to meet criteria for a partial but not full diagnosis of PTSD during their lives (8.6 percent for women compared with 4.5 percent for men). The NCS also found that women ages 15 to 54 were about twice as likely as men in that age range to have PTSD at some point during their lives (the rates were 10.4 percent and 5 percent, respectively; Kessler et al., 1995 ). Although specific percentages differ, these relative PTSD rates among men and women are in line with findings from other large studies in the United States and some studies from other Western countries (see review by Olff et al., 2007 ).
In another analysis of NCS data, Kessler (2000) noted that a larger percentage of women exposed to trauma (20.4 percent) than men exposed to trauma (8.1 percent) had PTSD, but he did not find the difference to be significant. However, women were significantly more likely to have PTSD than men exposed to the same trauma if they had experienced a sexual assault other than rape, a physical attack, a trauma to a loved one, or threat with a weapon. Men, however, had significantly higher PTSD rates connected to combat trauma. Additionally, McLean, Asnaani, Litz, and Hofmann (2011) found a significant difference in both prior-year and lifetime PTSD rates among men and women when they combined data from the NCS-R and two other large national surveys that used the same methodology (National Study of American Life and National Latino and Asian American Study of Mental Health). According to these data, 4.3 percent of women and 1.7 percent of men met criteria for PTSD in the year prior to assessment, and 8.5 percent of women and 3.4 percent of men had the disorder at some point during their lives.
A large trauma study conducted in the Detroit metropolitan area ( N =2,181) found that although men were significantly more likely to experience trauma and to have experienced multiple traumas, women were about twice as likely to develop PTSD following a traumatic experience (13 percent of women compared with 6.2 percent of men; Breslau, 2002 ). However, this study, which evaluated the relative risk for PTSD related to particular types of trauma, also found that this difference could largely be attributed to differences in response to assaultive violence. Although PTSD rates did not differ significantly between men and women exposed to other types of trauma, women were almost six times more likely to develop PTSD in response to assaultive violence than were men (35.7 percent of women and 6 percent of men exposed to such violence developed PTSD).
In addition to research indicating that women are more likely than men to develop PTSD as a result of assaultive violence, a study conducted with 6,697 male and 554 female veterans from OIF and OEF found that women who sustained physical injury as a result of a traumatic experience were significantly more likely than men who sustained such injuries to develop PTSD ( Maguen, Luxton, Skopp, & Madden, 2011 ). In many studies that evaluate PTSD rates by gender for men and women exposed to the same specific trauma or type of trauma, women are more likely than men to develop PTSD. For example, female 9/11 survivors were significantly more likely than male survivors to have probable PTSD (DiGrande et al., 2010). In a study that compared three different international samples (American, Mexican, and Polish) of individuals who experienced a natural disaster, women in all three samples had significantly more PTSD symptoms ( North, Kaniasty, Conrad, Inman, & Murphy, 2002 ). Also, in a group of 454 college students, women who experienced the death or illness of a loved one had significantly more PTSD symptoms than did men who experienced the same ( Gold, Marx, Soler-Baillo, & Sloan, 2005 ).
According to data from the Trauma Recovery Project ( n =627), women were also found to be significantly more likely than men to develop prolonged PTSD (lasting for at least 18 months) and had significantly worse ratings of quality of life as a result of prolonged PTSD ( Holbrook, Hoyt, Stein, & Sieber, 2002 ). In addition, studies indicate that women with PTSD, compared with men with the disorder, are more likely to have co-occurring mood disorders but less likely to have co-occurring substance use disorders ( McLean & Anderson, 2009 ; McLean et al., 2011 ; Olff et al., 2007 ). Even in the absence of PTSD, trauma exposure is associated with significantly higher levels of depressive symptoms and lower levels of substance abuse among women than among men ( Maguen et al., 2011 ). Using NCS-R data, Dunn, Gilman, Willett, Slopen, and Molnar (2012) found that higher rates of rape and sexual assault among women compared with men were in part responsible for higher depression rates among women.
Research generally indicates that women are more likely than men to seek treatment for behavioral health disorders ( McLean & Anderson, 2009 ). Therefore, women are also significantly more likely to receive treatment for PTSD. According to NESARC data, women are approximately 34 percent more likely to be treated for PTSD than men ( Roberts et al., 2011 ). Women often respond differently to trauma than do men, which may contribute to higher PTSD rates among women. For example, women are more likely to report dissociation immediately after or in the few weeks following trauma exposure ( Cardeña & Carlson, 2011 ). Women also tend to report more intense emotional responses and more dissociation following trauma exposure (see review by Olff et al., 2007 ). Research conducted with survivors of serious vehicular accidents indicates that women are significantly more likely than men are to experience certain PTSD symptoms 1 month after the accident (e.g., distress in similar situations, physical reactions to memories, hypervigilance, trouble sleeping, avoidance of thoughts/feelings/activities/places, exaggerated startle response; Fullerton et al., 2001 ).
Pratchett and colleagues (2010) reviewed some of the possible explanations for why women have higher PTSD rates compared with men, even after accounting for trauma exposure. One possibility was that women are more likely to experience types of trauma (e.g., sexual assault) that have a greater propensity to lead to PTSD. Other possibilities are that, in aggregate terms, women’s cognitive appraisals of trauma may differ from those of men and that interpersonal violence, in particular, may be perceived as a greater threat to women’s core identity. In addition, following from research showing significant gender differences in emotional reactivity and/or emotional regulation, women may have more intense emotional responses than men to trauma, which in turn may increase PTSD risk. However, increased emotional reactivity does not necessarily mean that women are more affected by trauma, just that they are affected differently. Research conducted with children who have histories of sexual trauma indicates that boys are more likely to present externalizing symptoms, whereas girls more often present internalizing symptoms. Another possible explanation is that women tend to use different coping strategies following trauma exposure, which may make them more prone to developing PTSD ( Olff et al., 2007 ).
Research reviewed by Olff and colleagues (2007) also indicates that women who have peritraumatic dissociation at the time of trauma are much more likely than men who have it to develop PTSD; women are also more likely to respond to acute trauma with dissociation and less likely to respond with hyperarousal than are men ( Fullerton et al., 2001 ). Research evaluating physiological differences in male and female responses to trauma tends to confirm that such differences exist. McLean and Anderson (2009) also reviewed possible explanations for higher PTSD rates among women.
Women may also be affected differently than men by some risk and resilience factors, such as social support. Research conducted with victims (118 male and 39 female) of violent crime found that a negative response from others and a lower level of satisfaction with support from others, had a significantly greater effect on women than on men, although these factors were associated with greater PTSD symptom severity for both men and women ( Andrews, Brewin, & Rose, 2003 ). Similarly, research conducted with military personnel deployed in the Gulf War found that a lack of social support had a greater relationship to depressive symptoms for women than for men, and greater concerns about disruptions in family and personal relationships had a more pronounced connection to anxiety symptoms for women than for men ( Vogt, Pless, King, & King, 2005 ). For military personnel deployed to OIF, negative changes in intimate relationships (according to self-report) following deployment were significantly related to PTSD for women but not men, but only when there was a high level of combat exposure ( Skopp et al., 2011 ).
Another PTSD risk factor that has been found to have a stronger relationship to PTSD for women than for men includes childhood abuse history ( Brewin, Andrews, & Valentine, 2000 ). Conversely, both antisocial behavior in childhood and younger age at the time of the traumatic event appear to have stronger relationships to PTSD for men than for women ( King, King, Foy, & Gudanowski, 1996 ). In addition, culture appears to play a role in the higher PTSD rates observed in women, and culture can also moderate these differences ( Kimerling et al., 2007 ). Research by Norris, Perilla, Ibanez, and Murphy (2001) that compared PTSD rates for men and women from either the United States or Mexico who were exposed to a natural disaster found that the magnitude of gender differences in PTSD rates were significantly greater for Mexicans than for Americans.
People With Lower SES
Although it is not possible to say whether lower SES is associated with increased risk for all types of trauma, studies have found that lower SES is linked to significantly greater risk for accidents ( Cubbin & Smith, 2002 ), criminal victimization ( Rand & Robinson, 2012 ; Truman, 2011 ), combat trauma ( Prigerson, Maciejewski, & Rosenheck, 2002 ), and domestic violence ( Mouton et al., 2004 ; Vest, Catlin, Chen, & Brownson, 2002 ). Research from around the world, similarly, has found that lower SES is associated with increased risk for accidents (including motor vehicle accidents, burns, and poisoning) and interpersonal violence, including domestic violence (see review by Laflamme, Burrows, & Hasselberg, 2009 ).
In a predominately African American sample of 1,256 primary care patients with low SES who were living in an urban center, 46.2 percent met criteria for a PTSD diagnosis at some point during their lives ( Gillespie et al., 2009 ). The most common traumas for men in the study were serious accident or injury (experienced by 56.1 percent), being attacked with a weapon by someone other than an intimate partner (55.1 percent), being attacked without a weapon by someone other than an intimate partner (40.3 percent), and sudden life-threatening illness (30.7 percent). For women, the most common traumas were serious accident or injury (experienced by 42.2 percent), being attacked by an intimate partner without a weapon (33 percent), sexual abuse before age 14 (23.9 percent), and being attacked with a weapon by someone other than an intimate partner (21.8 percent).
Lower income has also been associated with significantly greater PTSD likelihood in other studies with different populations, including Cambodian refugees ( Marshall et al., 2005 ), African Americans in a large urban area ( Alim et al., 2006 ), and others. For some populations, however, lower SES may not be associated with increased trauma exposure and/or traumatic stress reactions. For example, in the AI-SUPERPFP study of two American Indian populations, both lower SES and less education were associated with significantly lower levels of trauma exposure ( Manson et al., 2005 ).
Data clearly show that lower SES is linked to greater risk for PTSD in one’s lifetime than is found in general population samples. For example, Wave 2 of NESARC found a significant association between lower income and a higher likelihood of having PTSD at some point during one’s life, with individuals in the $0 to $19,999 a year bracket having 2.3 times the risk and those in the $20,000 to $34,999 bracket having 1.8 times the risk compared with others in the survey ( Pietrzak et al., 2011a ). People with lower SES, again according to NESARC data, are also significantly more likely to report lower levels of perceived social support, a significant risk factor for both trauma exposure and PTSD ( Moak & Agrawal, 2010 ).
The association between lower income and higher rates of trauma/traumatic stress may partly reflect the fact that people with lower incomes can only afford to live in neighborhoods where community violence is high ( Gapen et al., 2011 ; Truman, 2011 ). Gapen and colleagues (2011) evaluated the relationship of perceived neighborhood disorder (measured with the Neighborhood Disorder Scale) and PTSD symptoms (assessed with the Modified PTSD Symptom Scale) among a group of largely (95 percent) African American users of an inner-city health clinic. They found a significant relationship between perceived neighborhood disorder and PTSD symptoms that was partially mediated by perceived community cohesion (assessed with the Community Cohesion Scale). The authors suggested that, in communities where high crime and other problems exist, residents develop a lack of trust that, in turn, can exacerbate PTSD symptoms.
Less education is also associated with significantly greater risk of having PTSD ( DiGrande et al., 2011 ; Galea et al., 2008 ; Pietrzak et al., 2011a ). People with lower incomes have fewer resources with which to address trauma, face more additional stressors that may increase the likelihood of developing PTSD, and may have learned fewer coping skills ( Kelly, Merrill, Shumway, Alvidrez, & Boccellari, 2010 ). The fact that losing economic resources as a result of a traumatic event can significantly increase PTSD risk (e.g., Hobfoll et al., 2008 ) may also support this explanation.
Lesbian, Gay, Bisexual, and Transgender People
Studies have documented greater exposure to trauma and higher PTSD rates among lesbian, gay, bisexual, and transgender people compared with people who are heterosexual ( Roberts, Austin, Corliss, Vandermorris, & Koenen, 2010 ). Elevated PTSD rates and trauma exposure in this population are perhaps best documented by Roberts and colleagues’ (2010) analysis of NESARC data, which included 145 individuals who self-identified as gay/lesbian, 161 who self-identified as bisexual, 314 who self-identified as heterosexual who reported same-sex partners, 953 who self-identified as heterosexual who reported attraction to members of the same gender but no partners, and 18,144 who self-identified as heterosexual who reported neither. According to these data, women who were lesbian, bisexual, or heterosexual with same-sex partners were significantly more likely, compared with heterosexual women (including those who had same-sex attraction but no same-sex partners), to have experienced childhood maltreatment, to have experienced most types of interpersonal violence, to have witnessed someone being injured/killed, and to have learned of trauma experienced by a close friend or relative. For men, being gay or self-identified as heterosexual with same-sex partners, but not being bisexual, was associated with significantly more likelihood of experiencing interpersonal violence and of having learned of trauma experienced by a close friend or relative.
For women who were exposed to traumatic events, being bisexual or heterosexual with same-sex partners was associated with a significantly higher likelihood of having PTSD, compared with being heterosexual with no same-sex partners. For men who were exposed to traumatic events, being gay or heterosexual with same-sex partners was associated with a significantly higher likelihood of having PTSD compared with being heterosexual with no same-sex partners. In a model that adjusted for gender, race/ethnicity, education, and age at the time of interview, being self-identified as gay/lesbian, bisexual, or heterosexual with same-sex partners was associated with more than twice the likelihood of developing PTSD when exposed to trauma. When the worst type of trauma experienced and the age of its occurrence were factored into the analysis, the odds ratios fell but remained high compared with heterosexual individuals with no same-sex partners. The greatest increase in the odds of having PTSD, 1.59 times, was found for self-identified heterosexuals who had same-sex partners.
Roberts and colleagues (2010) found elevated rates of childhood maltreatment only among women who were “sexual minorities,” but other studies have found high rates of childhood abuse among both men and women who are gay/lesbian or bisexual compared with those who are heterosexual. For example, Balsam, Rothblum, and Beauchaine (2005) found that lesbian, gay, or bisexual individuals were significantly more likely than were heterosexual siblings to report psychological and physical abuse by parents/caretakers during childhood and to report more childhood sexual abuse (not necessarily from caretakers). They also were significantly more likely to report abuse from partners in adulthood and sexual assaults in adulthood. The authors found larger differences in sexual victimization among men in the study than among women.
Little information is available about trauma and PTSD among transgender individuals. A German study involving 41 transgender individuals and 115 individuals receiving inpatient treatment for mental disorders found that the transgender individuals were significantly more likely to have experienced childhood emotional abuse/neglect but significantly less likely to have experienced childhood sexual abuse than were the inpatients ( Kersting et al., 2003 ). Balsam and colleagues (2010) evaluated the relationship of culture and childhood abuse for a group of lesbian, gay, or bisexual individuals ( N =669). They found that rates of childhood physical abuse were significantly higher for Latinos and Asian Americans than White Americans and that rates of childhood sexual abuse were significantly higher for Latinos and African Americans than White Americans.
Other research conducted with 528 lesbian, gay, or bisexual youth (ages 15 to 19) found that 80 percent had experienced verbal victimization, 11 percent physical victimization, and 8 percent sexual victimization outside the home because of their sexual orientation or atypical gender behavior. Physical victimization was significantly associated with PTSD ( D’Augelli, Grossman, & Starks, 2006 ). In an Internet survey of 662 gay, lesbian, or bisexual adults, approximately 20 percent reported being the victim of hate crimes involving physical violence or damage to property ( Herek, 2009 ).
People With Physical and/or Cognitive Disabilities
People with disabilities, compared with people without disabilities, are 4 to 10 times more likely to be victims of violence, abuse, and/or neglect ( Petersilia, 2001 ). For example, an analysis of school, foster care, and police records found that children with disabilities were 3.4 times more likely than other children to be abused/neglected and were over three times more likely to experience each specific type of abuse/neglect than children without disabilities ( Sullivan & Knutson, 2000 ). Govindshenoy and Spencer (2007) reviewed four studies that provide data on childhood abuse among people with disabilities. Three of the studies found a significant association between psychological/emotional disabilities and abuse, two between learning disabilities and abuse, and one between physical disabilities and abuse (see also Fisher, Hodapp, & Dykens, 2008 ).
Petersilia (2001) observed that studies from a number of Western countries have found that, compared with the general population, people with developmental disabilities have a significantly greater risk for being victims of violence and abuse (although data are limited). Other research indicates that women with significant physical disabilities are about four times more likely than other women to be sexually assaulted in adulthood ( Casteel, Martin, Smith, Gurka, & Kupper, 2008 ; Martin et al., 2006 ). Plummer and Findley (2012) reviewed these and other studies discussing the heightened risk for physical and sexual abuse of women with disabilities.
Research on resilience and traumatic stress reactions indicates that greater intelligence protects against PTSD (e.g., see Macklin, Litz, McNally, Lasko, Orr, & Pitman, 1998 ); therefore, cognitive disabilities may increase risk for developing PTSD following trauma exposure. Mevissen and de Jongh (2010) reviewed four studies that report PTSD rates in people with cognitive disabilities as ranging from 2.5 to 60 percent. Razza, Tomasulo, and Sobsey (2011) also reviewed research that supports the view that people with cognitive disabilities have an increased risk for developing PTSD following trauma exposure. They cited research indicating that developmental level affects how an individual processes traumatic experiences and that cognitive impairments may lead to increases in PTSD. Furthermore, they presented research indicating that trauma itself negatively affects intellectual abilities.
People Who Are Homeless
In the NCS-R, individuals who had been homeless for more than 1 week in their adult lives were significantly more likely than those who had remained domiciled to report being in a traumatic environment (e.g., a combat zone, a natural disaster), having a traumatic experience (e.g., being kidnapped, being in an automobile accident), experiencing personal violence directed toward themselves, and/or witnessing the trauma of others ( Greenberg & Rosenheck, 2010 ). In addition, those who reported at least 1 week of homelessness were significantly more likely to have had PTSD at some point during their lives, with 17.2 percent meeting those criteria compared with 6.3 percent of those who had not been homeless for 1 week or more.
Other research indicates that people who are homeless, compared with those who are domiciled, are significantly more likely to have experienced physical/sexual abuse in childhood ( Herman, Susser, Struening, & Link, 1997 ; Tam et al., 2003 ), to be victims of interpersonal violence as adults ( Wenzel et al. 2004 ), and to sustain unintentional injury ( Frencher et al., 2010 ). People who are homeless and have behavioral health disorders are significantly more likely than other people who are homeless to be victims of violence ( Lee & Schreck, 2005 ) and/or to have an unintentional injury ( Wan, Morabito, Khaw, Knudson, & Dicker, 2006 ).
Among people who are homeless, histories of childhood abuse are associated with significant increases in the likelihood of having mental health impairment ( Kim, Ford, Howard, & Bradford, 2010 ), and among individuals with mental disorders, histories of childhood abuse are associated with significant increases in the likelihood of being homeless ( Lu, Mueser, Rosenberg, & Jankowski, 2008 ; Rosenberg, Lu, Mueser, Jankowski, & Cournos, 2007 ). In their review of the research on trauma and homelessness, Hopper and colleagues (2010) concluded that “early developmental trauma—including child abuse, neglect, and disrupted attachment—provides a subtext for the narrative of many people’s pathways to homelessness” (p. 80). For more information on homelessness and traumatic stress reactions, refer to TIP 55, Behavioral Health Services for People Who Are Homeless ( SAMHSA, 2013b ).
People who have served in the armed forces, in addition to their exposure to combat-related trauma, also have high rates of exposure to other types of trauma before, during, and after their service. Veterans have high rates of motor vehicle accidents, especially while driving military vehicles ( Bell, Amoroso, Yore, Smith, & Jones, 2000 ; Rossen, Pollack, Canham-Chervak, Canada, & Baker, 2011 ) and of unintentional injuries related to activities such as exercising and training ( Jones & Knapik, 1999 ; Wilkinson et al., 2011 ).
Female veterans report high rates of sexual assault and rape, often occurring during their military service. Surveys of large groups of female veterans receiving U.S. Department of Veterans Affairs (VA) services include the following results:
- Hankin and colleagues (1999) found that 23 percent of female veterans reported military-related sexual assault (defined as unwanted sexual relations in which force or the threat of force was used).
- Skinner and colleagues (2000) found that 23 percent of their respondents reported being sexually assaulted (defined as being forced to have “sexual relations”).
- Sadler, Booth, Cook, and Doebbeling (2003) found that 28 percent of respondents reported being raped while in the military.
- Suris, Lind, Kashner, and Borman (2007) found that 33 percent of their sample reported a sexual assault while in the military.
- Kimerling and colleagues (2010) found that 15.1 percent of women and 0.7 percent of men reported experiencing sexual trauma while in the military.
- Booth, Mengeling, Torner, & Sadler (2011) found that 24.6 percent of their sample reported being raped while in the military. Among women who had served in a combat or war zone ( n =576), rape was most often cited (by 36 percent) as the worst trauma they had ever experienced.
Kang, Dalager, Mahan, and Ishii (2005) interviewed 1,381 Gulf War veterans with current PTSD and 10,060 without PTSD and found that sexual trauma (defined as sexual harassment and/or assault) was significantly more common among both male and female veterans who had PTSD than among male and female veterans who did not. Sexual assault during deployment was reported by 9.5 percent of women with PTSD and 2.2 percent of other women, and it was reported by 0.9 percent of men with PTSD and 0.1 percent of other men. The authors determined that, for women, sexual trauma (either harassment or assault) was associated with greater risk for PTSD than was combat exposure. Sexual trauma that occurs during a woman’s military service may also be more likely to result in PTSD than does such trauma experienced before entering or after leaving the military ( Himmelfarb, Yaeger, & Mintz, 2006 ). For more detailed information on the impact of trauma and deployment, see the planned TIP, Reintegration-Related Behavioral Health Issues in Veterans and Military Families (SAMHSA, planned f).
People in Specific Age Groups
Among adults, trauma exposure and traumatic stress reactions vary somewhat according to age. Norris and Slone (2007) reviewed research regarding differences in trauma exposure according to age group. They observed that overall trauma exposure is greatest among older adolescents and young adults (roughly ages 16 to 20), but that exposure to particular types of trauma varies more across age groups (e.g., sudden, unexpected death of a loved one is most common among individuals in their 40s). In the NCS, the lifetime risk of having PTSD among people who had been exposed to trauma peaked in those ages 25 to 35, whereas the lifetime risk of having been exposed to trauma peaked in those ages 35 to 44 ( Kessler et al., 1995 ).
Research regarding the incidence and prevalence of trauma exposure and current PTSD among older adults (typically defined as either ages 55 and older or ages 65 and older) in the United States is limited, but some studies are available. For example, national crime data indicate that older adults (age 50 and older) are much less likely than those who are younger to be the victims of violent crime ( Truman, 2011 ). Older adult women are also significantly less likely than other adult women to experience recent sexual or physical assault, according to a telephone survey of 3,209 women ( Acierno et al., 2002 ). This same study also found that older women who have sustained physical and/or sexual assault are less likely to develop PTSD and less likely to have certain types of PTSD symptoms than younger women who have been assaulted.
Overall, most research does indicate that current PTSD rates decline with age even for individuals in groups with high PTSD rates, such as former prisoners of war or Holocaust survivors. NCS-R data also indicate that PTSD is less common among older adults than in the general population ( Byers, Yaffe, Covinsky, Friedman, & Bruce, 2010 ). According to these data, 4.7 percent of older adults ages 55 to 64 had PTSD in the prior year, but only 0.6 percent of those ages 65 to 74, 0.1 percent of those ages 74 to 84, and 0.7 percent of persons ages 85 and older had PTSD in the prior year.
However, some studies from outside the United States have associated older age with increased PTSD risk. For example, among a group of survivors of the 2004 tsunami in Southern Asia, being age 40 or older was associated with being significantly more likely to develop PTSD ( Pyari, Kutty, & Sarma, 2012 ). In largely international research conducted with survivors of torture and civilian war trauma, older age was also associated with increased PTSD risk ( Johnson & Thompson, 2008 ). Böttche, Kuwert, & Knaevelsrud (2012) reviewed research on the course and severity of PTSD among older adults, much of it from European sources, observing that American and Swedish studies found lower lifetime PTSD prevalence for older adults compared with middle-aged and younger adults; however, they noted that two German studies found higher rates for older adults (this may reflect cultural differences, differences in exposure to war-related trauma, and/or differences in assessment methods). In addition, older adults in specific populations/groups may have even higher rates of trauma and traumatic stress reactions. One such group is older adults who are incarcerated (for review, see Maschi et al., 2011 ).
Older adults may also have somewhat different responses to traumatic stress than adults who are younger. Traumatic experiences (whether experienced in childhood or adulthood) may affect both depression and anxiety symptoms in older adults, according to a large ( N =1,216) study of older adults in New Zealand ( Dulin & Passmore, 2010 ). This study found that avoidance of prior traumatic memories and situations played a large role in late-life anxiety and depression, accounting for 49 percent of the variance between past trauma and depression and 46 percent of the variance between trauma and anxiety.
Cook and Niederehe (2007) reviewed research that generally indicates that PTSD for older adults is typically less severe and that their PTSD symptoms are less intense compared with other adults. Older adults also appear to experience more arousal symptoms and fewer intrusive symptoms, and they are less likely to experience depression and GAD in the wake of natural disasters than are other adults ( Cook & Niederhe, 2007 ). Grammer and Moran (2011) , in another review, observed that biological changes associated with PTSD differ between older adults and people who are younger (e.g., less variance in cortisol levels, higher levels of serum lipids).
Cultural factors appear to play a role in how age affects PTSD risk and traumatic stress reactions. Woodward and colleagues (2011) assessed a culturally diverse sample of adults age 55 and older ( N =3,046) using the DSM-IV Composite International Diagnostic Interview. Because they oversampled for members of certain cultural groups, they were able to report cultural, racial, and ethnic differences, but they only reported lifetime rates of disorders. These authors found that 4.6 percent of non-Hispanic White Americans, 4.5 percent of African Americans, 3.0 percent of Black Caribbean Americans, 2.1 percent of Latino Americans, and 2.0 percent of Asian Americans in this age group met criteria for PTSD at some point during their lives; differences between the groups did not reach the level of significance.
Norris and colleagues (2002) compared PTSD symptoms following exposure to natural disasters for individuals from different age groups and three different cultural groups (American, Mexican, and Polish). They found that among a mixed-race/ethnicity group of Americans who experienced Hurricane Andrew, middle-aged individuals had significantly more severe PTSD symptoms (assessed with the Revised Civilian Mississippi Scale [RCMS]) than older adults or younger adults; among Mexicans who experienced Hurricane Paulina, younger adults had significantly more severe PTSD symptoms, according to the RCMS, than older or middle-aged adults; and among Poles who experienced a flood, older adults had more severe PTSD symptoms than younger or middle-aged adults.
Among military service personnel and veterans, Brewin, Andrews, and Valentine (2000) observed that younger age was a PTSD risk factor in military (usually combat-exposed) but not civilian samples, which may mean that the role of age differed according to the different types of trauma commonly experienced by these groups. Other studies of either active-duty personnel or veterans also found that younger age (typically being age 25 and under) was associated with significantly higher risk of having PTSD ( Greiger et al., 2006 ; Seal et al., 2009 ; Tanielian et al., 2008 ). However, data from the NVVRS indicated that during the Vietnam War era, younger age was associated with significantly greater risk for PTSD for men but not women in the military ( King et al., 1996 ).
Data on OEF/OIF veterans indicate that older age (being 30 or older) is a PTSD risk factor for women but not for men ( Maguen, Ren, Bosch, Marmar, & Seal, 2010 ). Cook and Niederehe (2007) reviewed earlier research that found relatively low PTSD rates among World War II and Korean War veterans who were exposed to combat, suggesting that if PTSD had been present at levels similar to those seen in more recent conflicts, it likely resolved during older adulthood. Among older adult veterans in long-term care facilities, past PTSD symptoms were associated with a significantly greater likelihood of engaging in aggressive behavior, and observer-reported PTSD symptoms strongly correlated with patient anger ( Carlson, Lauderdale, Hawkins, & Sheikh, 2008 ).
Risk and protective factors for PTSD may also vary between age groups. Acierno, Kilpatrick, Resnick, Saunders, & Best (2006) compared risk factors for adults ages 60 and older ( n =1,130) and adults younger than 60 ( n =413) affected by the 2004 Florida hurricanes. They found that low income and a greater number of days displaced from one’s home significantly increased PTSD risk for older adults but not younger ones. Also, for older adults only, more days displaced also increased risk for depression and GAD, whereas greater out-of-pocket posthurricane expenses increased risk for GAD alone. Younger adults, however, did have significantly higher levels of PTSD symptoms than older adults. Another concern for older adults with trauma histories is the emergence of PTSD in older adulthood resulting from trauma experienced many years earlier. Little research is available on this subject, but Hiskey, Luckie, Davies, and Brewin (2008) reviewed 4 studies involving older adult male war veterans and 12 case studies that document this phenomenon.
- Responses to Trauma: Trauma and Behavioral Health
Not all traumas are equally likely to result in a traumatic stress reaction. Notably, PTSD risk is significantly higher for trauma involving interpersonal violence ( Breslau, 2002 ; Fetzner, McMillan, Sareen, & Asmundson, 2011 ; Kessler, 2000 ). Kessler (2000) observed that “the conditional risk of PTSD among trauma victims in U.S. samples varies enormously depending on the type of trauma to which they were exposed” (p. 6). As an example, he gave data from the NCS. For men in that survey, 65 percent of those who had experienced rape had PTSD, compared with 38.8 percent of those who had combat exposure, 12.2 percent of those who experienced another type of sexual assault, 6.4 percent of those who witnessed a traumatic event, 6.3 percent of those who had a life-threatening accident, 4.4 percent of those who had a loved one who sustained trauma, 3.7 percent of those who were in a natural disaster, and 1.9 percent of those who were threatened with a weapon. For women, the highest rate of PTSD (45.9 percent) was associated with rape. PTSD rates among women for other traumas were 32.6 percent for women who had been threatened with a weapon, 26.5 percent for sexual assault other than rape, 21.3 percent for physical attack, 10.4 percent for trauma occurring to a loved one, 8.8 percent for a life-threatening accident, 7.5 percent for witnessing a traumatic event, and 5.4 percent for experiencing a natural disaster.
Data from Wave 2 of NESARC indicate that people who have current PTSD, compared with people with histories of trauma exposure but no PTSD or partial PTSD, are more likely to have experienced certain types of trauma, including being mugged/held up (4.5 times more likely), childhood neglect (4.4 times), childhood physical abuse (4.4 times), military combat (4.3 times), witnessing family violence in childhood (4.2 times), sexual assault (4.1 times), being stalked (4.1 times), being kidnapped/held hostage (4.0 times), being assaulted by someone other than an intimate partner (4.0 times), and being assaulted by an intimate partner (3.2 times; Pietrzak et al., 2011a ). Trauma in which the individual fears for his or her life is also associated with increased PTSD risk. According to data from the Trauma Recovery Project, a large ( N =1,048) prospective study of trauma and its effects, perceived threat to life significantly predicted both early symptoms of acute stress and PTSD ( Holbrook, Hoyt, Stein, & Sieber, 2001 ). The odds of developing PTSD when there was a perceived threat to life were 1.6 times higher. Other significant factors associated with PTSD risk included perceiving a greater chance of the traumatic event occurring again, which increased the odds of developing PTSD 1.5 times; assaultive violence, which increased the odds 1.6 times; and sustaining a penetrative wound, which increased the odds 2.4 times. Research with military samples has also consistently found that greater perceived threat is associated with greater PTSD risk ( Maguen, Suvakm, & Litz, 2006 ).
Abuse in childhood often results in lasting and severe PTSD because it has physical and behavioral effects on the developing mind ( Cougle, Timpano et al., 2010 ). Wrenn and colleagues (2011) , using a largely African American, inner-city sample of people who had experienced trauma ( N =767), found that trauma in childhood was associated with significantly greater PTSD risk than trauma experienced in adulthood alone. Childhood abuse was associated with even greater risk than other childhood trauma. Sexual abuse, in adulthood or childhood, is also associated with high PTSD levels as well as other behavioral health disorders. In a meta-analytic review of 37 studies providing data on 3,162,318 individuals, Chen and colleagues (2010) found that a history of sexual abuse in childhood or adulthood was associated with more than three times the risk for an anxiety disorder compared with individuals who had no such history; more than twice the risk for depression, an eating disorder, or PTSD; and more than four times the risk for suicide attempts.
Brain Responses to Traumatic Stress
Neuroimaging studies demonstrate specific changes in the brains of people with PTSD, such as increased activity in the amygdala, decreased activity in the medial prefrontal cortex, and reduced hippocampal and anterior cingulate cortex volumes ( Garfinkel & Liverzon, 2009 ; Hughes & Shin, 2011 ). Neurochemical changes have also been found in people with PTSD, including increased dopamine levels, increased norepinephrine levels and/or activity, decreased concentrations of serotonin in parts of the brain, decreased gamma-aminobutyric acid activity, increased glutamate levels, decreased plasma levels of neuropeptide Y (NPY), and increased levels of beta-endorphin in the cerebrospinal fluid ( Sherin & Nemeroff, 2011 ). Brenner (2011) , Garfinkel and Liverzon (2009) , Hughes and Shin (2011) , and Sherin and Nemeroff (2011) reviewed research on changes in brain activity, chemistry, and volume related to PTSD. Brenner (2011) also attempted to distinguish these changes from those associated with traumatic brain injury (TBI).
Risk and Protective Factors
A number of risk and protective factors for trauma and for traumatic stress reactions (particularly PTSD) have been identified in the literature. Some of these factors are likely true risk/protective factors in that they increase or decrease risk in and of themselves, whereas others (e.g., elevated heart rate following trauma exposure) are likely indicative of other underlying risk factors, but both types of factors are discussed together in this literature review. As Layne, Warren, Watson, and Shalev (2007) observed in their review on PTSD-related risk and resilience, there is a lack of general agreement in the literature as to what defines protective or resilience factors, making it difficult to evaluate the relative importance of such factors. They noted that factors that promote resilience to traumatic stress reactions can range from genetic biological factors (e.g., greater levels of dehydroepiandrosterone, lower production of corticotrophin-releasing hormone), to personal attributes (e.g., greater intelligence, a stronger internal locus of control), to processes of adaptation to stressors/adversities, to social relationships.
Risk factors
Research has found a number of factors associated with increased risk for trauma exposure and traumatic stress reactions. Some of these factors are demographic in nature (e.g., SES, race/ethnicity, gender), whereas others involve individual and social characteristics (e.g., lower intelligence, less social support). Breslau, Lucia, and Alvarado (2006) found that youth with lower intelligence (as measured by intelligence quotient [IQ]) were significantly more likely to have been exposed in the 10 years following their assessment to traumatic events—specifically, nonassaultive trauma—and to have developed PTSD (conditioned upon not having anxiety disorders or high rates of externalizing problems at their initial assessment). In terms of social support, Moak and Agrawal (2010) , using data from Waves 1 and 2 of NESARC, found a modest but significant correlation between lower perceived social support and exposure to traumatic events.
A number of reviews and meta-analyses provide an overview of PTSD risk factors. Brewin and colleagues (2000) included 77 articles in their meta-analysis, which focused largely on demographic factors. They concluded that PTSD risk following trauma exposure increased with the following factors: female gender, lower SES, racial/ethnic minority status, less education, prior behavioral health disorders, a history of childhood abuse, a history of other prior trauma, other ACEs, a history of behavioral health disorders in one’s family, and a lack of social support. They cautioned, however, that only a prior history of behavioral health disorders, childhood abuse, and a family history of behavioral health disorders were uniformly found to increase risk in the studies that included them as variables. The authors also observed that risk factors differed somewhat between military and civilian samples, with female gender having no significant effect in military samples but younger age being associated with increased PTSD risk in military samples. Trauma severity also had a significantly greater effect on PTSD in military than in civilian samples (which may reflect differences in the nature of trauma typically experienced by these two groups). Brewin and colleagues (2000) found that risk factors vary somewhat by gender as well, so that, for example, childhood abuse has a significantly greater effect on women than on men, and younger age has an effect for men but not women (which may explain why it has an effect for largely male military samples but not civilian samples). These authors concluded that there was a great deal of heterogeneity across the studies and thus cautioned against trying to create a model in which pretrauma risk factors are considered universal rather than mediated by particular responses to trauma or factors associated with the trauma itself.
A meta-analysis by Ozer, Best, Lipsey, and Weiss (2003) included a larger group of studies (476) and focused on a different set of risk factors than did Brewin and colleagues’ (2000) review, namely factors associated with “psychological processing and functioning” and “aspects of the traumatic event or its sequelae” (p. 55). As such, they presented their review as complementary to that of Brewin and colleagues (2000) . Ozer and colleagues (2003) found seven significant risk factors for PTSD:
- A history of prior trauma
- Problems with behavioral health prior to the trauma (including preexisting mental disorders)
- A family history of behavioral health disorders
- A perceived threat to one’s life during the traumatic event
- Perceived social support following the trauma
- Intensely negative emotional responses immediately following the trauma (e.g., extreme fear, helplessness, horror, shame)
- Peritraumatic dissociation (i.e., dissociative experiences during or immediately following the trauma)
These authors found that stronger PTSD “predictors” were factors that were more proximal to the traumatic event, namely perceived threat to life, perceived social support, heightened peritraumatic emotional responses, and peritraumatic dissociation. In addition to differences in focus, Ozer and colleagues’ (2003) review differed from that of Brewin and colleagues (2000) in that it found social support to be a weaker predictor. The authors noted that this may reflect the fact that social support (or the lack thereof) had a larger effect in studies in which 3 or more years had elapsed since the trauma than in those that assessed individuals sooner after the traumatic event; their review included more of the latter. They noted that this may indicate that social support has a cumulative effect or is more important when individuals have more chronic PTSD (and less important in cases of ASD). Data from NESARC also indicate that lower perceived social support is associated with a number of other mental disorders (e.g., major depression, GAD) and behaviors such as suicidality (Moak & Agrawal, 2009).
Vogt, King, and King’s (2007) reviewed the literature on PTSD risk factors, paying special attention to the mechanisms through which such factors may affect PTSD. Their findings did not differ substantially from earlier reviews, but they observed some other factors associated with increased risk that were not included in the meta-analytic reviews cited previously, which had more strict inclusion criteria. They cited studies that found a dose–response relationship between severity of trauma and PTSD, as well as studies that found an increase in PTSD associated with trauma resulting in physical injury, trauma perceived as more malicious or horrifying, trauma in which one is actively involved (rather than a participant), and trauma that resulted in peritraumatic dissociation. The authors also observed that demographic factors (i.e., female gender, younger age, lower SES, lower education, lower intelligence, and certain racial/ethnic backgrounds) appeared to have a significant, but modest, relationship to PTSD risk. Prior trauma exposure, preexisting mental disorders, a history of childhood abuse, other exposure to ACEs, a family history of mental disorders, and lack of social support all appeared to have a somewhat large effect on increasing PTSD risk. They also noted that research, mostly conducted with veterans, indicated that the risk factors for onset and maintenance of PTSD appear to be different. Risk factors that existed prior to the traumatic experience did not have as strong an effect on the latter. However, other factors that came into play after the trauma may have affected the course of and recovery from PTSD. Examples of these include social supports available after the trauma (including community reactions), use of coping strategies, and cognitive appraisals of the nature of the trauma.
Recent studies (not included in the previously discussed reviews) that evaluate risk factors associated with PTSD symptoms not only generally confirm the prior findings; they also shed light on how different factors affect PTSD risk following different types of trauma exposure. For example, in a study that evaluated risk factors associated with PTSD symptoms (not PTSD diagnosis) for 2,001 New York residents following the 9/11 attack, risk factors included seeing the actual attack, living closer to the attack, experiencing a fear of injury/death at the time of the attack, being involved in the rescue effort, losing a job following the attack, having a friend or family member killed in the attack, experiencing greater media exposure to the attack, having more stressors in the year prior to the attack, and having less social support ( Lawyer et al., 2006 ). However, in a multivariate model that controlled for other historical, exposure, and demographic factors, the only risk factors that remained significant were heightened peritraumatic emotional responses and dissociation, peritraumatic panic/physiological arousal, greater life stressors in the year prior to the attacks, and being involved in the rescue effort.
In another study involving 527 adults admitted to a Level 1 trauma center with traumatic injuries, greater PTSD symptom severity was associated with younger age, being unmarried, being unemployed, having lower SES, being African American or Latino, and experiencing assaultive rather than nonassaultive trauma ( Chiu, deRoon-Cassini, & Brasel, 2011 ). A study of 1,386 patients at a trauma clinic found that patients were significantly more likely to screen positive for probably developing PTSD (in a screen that occurred a mean of 24 days after the traumatic event) if they were under 55 years old, were female, had sustained a blunt or penetrating wound (excluding self-inflicted or accidental wounds), and/or had been in a motor vehicle crash or had been the target of assaultive trauma (compared with all other traumas; Alarcon et al., 2012 ). Developmental risk factors (e.g., childhood abuse, preexisting mental disorders, mental disorders in one’s family), according to Koenen (2006) , affect an individual’s ability to self-regulate thoughts and feelings. The author noted that, although more research is needed, such risk factors may play a significant role in determining whether an individual is at risk for PTSD following trauma exposure.
Risk factors associated with material needs and losses are often ignored in research, but a number of studies have found that such factors do affect PTSD rates. For example, research from Israel indicates that the loss of economic resources following trauma exposure is associated with a significantly greater likelihood of PTSD ( Hobfoll et al., 2008 ). Loss of home and/or economic resources seems to affect PTSD onset and to affect specific populations differently. Research conducted with survivors of a large fireworks explosion in the Netherlands found that individuals whose homes were destroyed were significantly more likely than others affected by the disaster to have late-onset PTSD ( Smid et al., 2012 ) and were more sensitized to stressful events occurring after the disaster ( Smid et al., 2011 ). Material losses and lack of income appear to have a significantly greater effect on increasing PTSD risk for adults ages 60 and older compared with younger adults ( Acierno et al., 2006 )
In addition, a diagnosis of ASD following the traumatic event is a PTSD risk factor. Bryant (2011) reviewed 22 studies that evaluated the relationship of ASD to later PTSD development, concluding that an ASD diagnosis had a reasonable level of predictability (with at least half of individuals who had ASD later developing PTSD), but that it had poor sensitivity as a predictive measure (because the majority of individuals who developed PTSD did not have ASD). Cardeña and Carlson (2011) postulated that ASD is not a robust predictor of PTSD because ASD may be only one possible response to trauma and because protective factors that come into play after trauma exposure may help keep some individuals who have ASD from developing PTSD.
The importance of peritraumatic dissociation as a PTSD risk factor has been debated. Meta-analytic reviews by Breh and Seidler (2007) , Lensvelt-Mulders and colleagues (2008) , and Ozer, Best, and Lipsey, & Weiss (2003) all found evidence that peritraumatic dissociation represented a PTSD risk factor. Also, Cardeña and Carlson (2011) , following Lensvelt-Mulders and colleagues (2008) , concluded that peritraumatic dissociation has a stronger association with PTSD in studies with a prospective rather than a retrospective design, suggesting that the relationship between the two was not just a result of long-term recall being clouded by later PTSD.
However, another review by van der Velden and Wittmann (2008) , which included only prospective studies and controlled for persisting symptoms of dissociation, found that peritraumatic dissociation was a relatively weak PTSD predictor, whereas dissociation that persisted after the trauma was a much better predictor. Cardeña and Carlson (2011) also noted that other research confirms that dissociative symptoms that persist after trauma exposure are a relatively strong PTSD predictor, whereas peritraumatic dissociation is a relatively weak predictor. One reason that some studies have found a stronger relationship between peritraumatic dissociation and PTSD than have others is that the relationship appears to be significantly stronger among women than among men. Research conducted with 122 survivors of serious motor vehicle crashes found that the PTSD risk associated with peritraumatic dissociation was 7.55 times greater for women than for men ( Fullerton et al., 2001 ).
Some authors (e.g., Lawyer et al., 2006 ) have suggested that peritraumatic panic attacks are another possible PTSD predictor. However, Adams and Boscarino (2011) examined data on 1,681 survivors of 9/11 and found that, in a model that controlled for potentially confounding factors, a panic attack at the time of the incident predicted PTSD in the year after the event but not 2 years after the event. Insomnia and other sleep disturbances that begin following a traumatic event have also been associated with increased risk for developing PTSD ( Babson & Feldner, 2010 ). Some small studies have also found that individuals who develop PTSD following trauma exposure have elevated heart rates (e.g., 96 beats a minute and higher) soon after and up to a week after that exposure—significantly higher rates than for those who experience trauma but do not develop PTSD (e.g., Bryant, Creamer, O’Donnell, Silove, & McFarlane, 2011 ; Shalev et al., 1998 ). Research from France suggests that heart rate variability is a better predictor of PTSD than elevated heart rate alone. In this study, 35 survivors of automobile accidents had a positive predictive value of 75 percent and a negative predictive value of 90 percent in relation to the later development of PTSD ( Shaikh Al Arab et al., 2012 ).
Genetic factors appear to contribute to both trauma exposure and PTSD development in a number of ways. For example, research conducted with twins (which enables researchers to evaluate the relative contribution of common genetics) has found that a genetic predisposition is involved in assaultive trauma but not other kinds of trauma, which is likely related to behaviors that might make an individual more prone to becoming involved in situations where this type of trauma may occur ( Afifi, Asmundson, Taylor, & Jang, 2010 ). Other research included in this review indicated that genetics affect, to a moderate degree, whether an individual will develop PTSD symptoms as a result of trauma exposure; the degree to which genetic factors contribute may differ depending on the type of symptoms under consideration. Genetic factors may also differ according to the type of trauma and how many incidents of trauma are experienced (e.g., genetic factors may play a lesser role when a person experiences three or more types of trauma).
Other reviews reached similar conclusions regarding the contribution of genetic factors to the development of PTSD. For example, Cornelius, Nugent, Amstadter, and Koenen (2010) reviewed a wider range of research (not just twin studies), including information concerning the specific genes associated with PTSD. They also focused on some of the limitations of existing research (e.g., use of samples with relatively low PTSD rates, use of widely different methodologies). Sartor and colleagues (2011) looked specifically at genetic and environmental factors that play a role in both PTSD and substance use disorders for women, as fewer data are available on the role of genetics for women than for men. They found good evidence for a genetic link for both types of disorder among women.
Research conducted with veterans has found a common genetic influence on increased exposure to combat, increased alcohol use, and greater likelihood of having PTSD symptoms ( McLeod et al., 2001 ). Research reviewed by Afifi and colleagues (2010) confirmed that genetics may contribute to the co-occurrence of substance use disorders and PTSD as well as to exposure to assaultive trauma. Genetic factors may also play a role in maintaining PTSD and in an individual’s response to PTSD treatment. Bryant and colleagues (2011) found that, after controlling for pretreatment PTSD severity and number of treatment sessions attended, people with PTSD who had a given genotype had significantly more severe PTSD 6 months after receiving an 8-week exposure therapy (ET) intervention than others in the study.
Little information is available about specific risk and protective factors for ASD, although many of the factors relevant to PTSD would also likely apply ( Cardeña & Carlson, 2011 ). However, these authors did review literature indicating that the ability to be hypnotized (which has a genetic component), childhood abuse, disturbed attachment in childhood, and a tendency to view events as catastrophic have all been associated with increased risk for ASD.
Protective factors
Protective factors for trauma almost entirely reflect the risk factors discussed in the preceding “ Risk Factors ” section. For trauma, protective factors are typically contextual, including characteristics that make it less likely that a person will be in a situation where trauma might occur. A review by Ahmed (2007) listed internal characteristics that promote resilience to PTSD:
- Self-esteem
- Resourcefulness
- Self-efficacy
- Internal locus of control
- Secure attachments
- Sense of humor
- Self-sufficiency
- Sense of mastery
- Interpersonal abilities (e.g., social skills, problem-solving skills, impulse control)
Ahmed’s review (2007) also listed the following external resilience factors:
- Sense of safety
- Religious affiliation
- Strong role models
- Emotional sustenance (i.e., receiving from others understanding, companionship, a sense of belonging, positive regard)
A review by Agaibi and Wilson (2005) classified protective factors into five categories: personality factors (e.g., hardiness, internal locus of control, autonomy), affect regulation, coping skills (e.g., active problem-solving skills), ego defenses, and ability to mobilize and use resources (e.g., social support). These authors also presented a model for how these different factors relate to one another in affecting an individual’s response to traumatic stress and promoting adaptation and resilience. Guay, Billette, and Marchand (2006) reviewed research and theory on the protective aspects of social support, one of the protective factors most consistently found to have a significant role with regard to PTSD. Guay and colleagues (2006) reviewed research and theory regarding the protective aspects of social support as well as PTSD’s potential negative effects on social interactions. They observed that the most widely held belief is that social support positively affects PTSD symptoms because it influences individuals’ interpretations of traumatic events and their ability to process traumatic experiences.
In some studies, social support is the most significant factor, with such populations as survivors of childhood abuse ( Collishaw et al., 2007 ), women who were victims of sexual assault ( Kimerling & Calhoun, 1994 ), survivors of natural disasters ( Cook & Bickman, 1990 ), veterans exposed to combat trauma ( Pietrzak et al., 2010 ), law enforcement officers ( Martin, Marchand, Boyer, & Martin, 2009 ), women who experienced war trauma in Bosnia and Herzegovina ( Klarić et al., 2008 ), and survivors of torture ( Johnson & Thompson, 2008 ). However, the most important type of social support may vary according to the specific situation and the type of trauma; for example, for men exposed to combat trauma, military unit support and cohesion may be most important during deployment ( Office of the Surgeon Multinational Force-Iraq & Office of the Surgeon General, U.S. Army Medical Command, 2006 ), whereas for survivors of childhood abuse, support from caregivers and relationships with peers in childhood and with intimate partners in adulthood seem to be most significant ( Aspelmeier, Elliot, & Smith, 2007 ; Collishaw et al., 2007 ).
A good deal of research on protective factors has been conducted with military personnel and veterans. Some of the protective factors for this population are the same as for others, such as social support, positive/active coping skill use, greater self-esteem, greater mastery/self-sufficiency, more education, higher SES, and male gender ( Subcommittee on Posttraumatic Stress Disorder of the Committee on Gulf War and Health, 2006 ). In addition, better training and preparation for combat trauma (or at least, feeling more prepared), stronger unit cohesion, and responses from the civilian population upon returning from combat all have a protective function. In a study involving 207 combat veterans deployed to the Middle East, individuals’ sense of preparedness, as assessed prior to deployment, affected the relationship between perceived threat (greater perceived threat has been associated with increased risk for PTSD) and combat experiences. That is, those who had a better sense of preparedness perceived less threat from their combat experiences, which translated into lower levels of PTSD ( Renshaw, 2011 ).
Positive attitudes toward military service are related to significantly lower PTSD rates among military personnel deployed to Iraq ( N =2,583; Skopp et al., 2011 ). The same risk and resilience factors have also been found for veterans from other conflicts ( Vogt & Tanner, 2007 ), and for the National Guard as well as active-duty personnel ( Polusny et al., 2011 ). Protective factors assessed for other specific groups generally do not deviate much from those already mentioned. For example, Yuan and colleagues (2011) evaluated 233 police officers during their academy training and again after serving 2 years, finding that a stronger sense of self-worth, stronger beliefs in the benevolence of the world (assessed with the World Assumptions Scale), greater social support, and better social adjustment (assessed with the Social Adjustment Scale–Self Report) were all significant protective factors against later PTSD development. In another analysis of 132 Canadian police officers, the only significant protective factors identified were one dimension of the Short Hardiness Scale relating to an officer’s ability to perceive difficulties as challenges and social support from coworkers (but not from significant others; Martin et al., 2009 ).
In an evaluation of PTSD risk and protective factors for 600 women who were sexual assault victims, the only significant protective factor for PTSD symptoms identified was the victims’ perceptions that they had greater control over their recovery process ( Ullman, Filipas, Townesend, & Starzynski, 2007 ). For both risk and protective factors, the victims’ perceptions at the time of the assault and their postassault characteristics (e.g., negative social reactions, coping skills) had a stronger relationship to PTSD symptom severity than did preassault characteristics and the characteristics of the assault itself.
Religious belief/affiliation has been found to have a protective function in groups as diverse as Buddhist Cambodian refugees ( Cheung, 1994 ) and African American women who have been victims of intimate partner violence ( Bradley, Schwartz, & Kaslow, 2005 ). However, stronger religious beliefs may not always have a protective function, and much will depend on context. For example, in a study of Israeli settlers who were forced to move from their homes in the Gaza Strip ( N =104), a stronger secular identity (i.e., one that was not traditionally religious or orthodox) assessed prior to relocation was associated with significantly lower levels of PTSD symptoms assessed 9 months after relocation ( Ben-Zur, 2008 ). Other protective factors included greater perceived social support (from family, friends, community, and the government), higher levels of mastery/optimism, more education, and certain demographic factors (e.g., gender).
Many protective/resilience factors for PTSD (including social support) are essentially the same as protective factors for behavioral health disorders in general. Much of the research in this area has been conducted with youth and adolescents, but the protective factors thus identified do not vary much from those for adults. For example, Van Breda (2001) provided an indepth review of factors associated with resilience in general (i.e., better behavioral health and better resistance to stressors), which include hardiness, a sense of coherence, learned resourcefulness, self-efficacy, and a stronger internal locus of control, all of which may also be considered resilience/protective factors in relation to PTSD.
Certain coping styles and cognitive appraisals of traumatic events can reduce the occurrence and/or severity of PTSD. For example, Ginzburg, Solomon, and Bleich (2002) found that the use of repressive coping styles was linked to significantly lower levels of PTSD symptoms following trauma exposure. Earlier research conducted with 215 female victims of assault (either sexual or nonsexual) found that greater use of positive distancing (e.g., optimism, acceptance, cognitive distancing) was associated with significantly less severe PTSD, whereas reliance on wishful thinking was associated with worse PTSD ( Valentiner, Foa, Riggs, & Gershuny, 1996 ).
Research conducted with 102 women who reported histories of childhood sexual abuse found that those women who found their traumatic experience more central to their identity, who believed the trauma was a turning point in their lives, and/or who believed past trauma influenced their expectations for the future (all factors assessed using the Centrality of Events Scale) had significantly more severe PTSD (assessed with the PCL-Civilian Version) compared with other women in the study ( Robinaugh & McNally, 2011 ). Other research indicates that women with PTSD who have protective self-cognitions are less likely to lose resources (material, social, family, and work-related) than women with PTSD who do not have such protective cognitions. ( Walter, Horsey, Palmieri, & Hobfoll, 2010 ). Personality traits may also play a role in protecting individuals from PTSD. For instance, a British study involving a community sample of 364 individuals who were assessed in adolescence and again some 30 years later found that, among those with histories of childhood abuse, a more stable personality (assessed with the neuroticism scale of the Eyesnck Personality Questionnaire) was associated with being significantly more likely not to have an anxiety disorder (including PTSD) or depressive disorder in adulthood ( Collishaw et al., 2007 ).
Effects of Trauma and Traumatic Stress Reactions on Quality of Life, Health, and Functioning
Trauma, in and of itself, appears to have negative effects on quality of life and health, although trauma is not as well researched as the effects of PTSD on these outcomes. NCS-R data indicate that trauma itself often has a greater role in physical health problems than does PTSD, and it has often been ignored in the research evaluating the health consequences of PTSD (see Sledjeski, Speisman, & Dierker, 2008 ). Although trauma itself is associated with functional impairment and/or decrease in quality of life, a number of studies comparing individuals with PTSD and individuals who had trauma exposure without PTSD have found that those with PSTD have significantly lower quality of life and more impairments ( Breslau, Lucia, & Davis, 2004 ; Gellis, Mavandadi, & Oslin, 2010 ; Stein, Walker, Hazen, & Forde, 1997 ).
There is no doubt that traumatic experiences that result in physical injury negatively affect quality of life, health, and functioning ( Polinder et al., 2010 ; Polinder et al., 2012 ). Although it is difficult in many cases to tease out the relative effects of physical and psychological trauma (e.g., see discussion of burn victims by Corry, Pruzinsky, & Rumsey, 2009 ), research indicates that both quality of life and functioning are significantly more impaired among disaster survivors who sustain physical injury compared with those who do not (e.g., Sudaryo et al., 2012 ). In a study of Indonesian survivors of a large earthquake, physical injury and impairment had a more significant effect on quality of life ( Sudaryo et al., 2012 ).
In general, numerous studies conducted with a variety of different populations have found that people with PTSD have worse quality of life than do those who never had the disorder, even if they were exposed to trauma ( Olatunji, Cisler & Tolin, 2007 ; Schnurr, Lunney, Bovin & Marx, 2009 ). Partial PTSD has also been associated with significantly worse quality of life, although not to the extent of PTSD, compared with individuals who have had trauma exposure but not PTSD or partial PTSD ( Gellis et al., 2010 ). Although quality of life appears to be better for people who are in remission from PTSD, it remains worse compared with those who never had PTSD ( Westphal et al., 2011 ).
In a study conducted with 184 people with chronic PTSD (largely White American women), the strongest predictors of worse quality of life were arousal symptoms, depressive symptoms, and other anxiety symptoms ( Doctor, Zoellner, & Feeny, 2011 ). In another group of 156 Turkish men with alcohol dependence, dissociation symptoms and a lifetime diagnosis of PTSD were predictive of worse quality of life ( Evren et al., 2011 ). PTSD is also associated with significantly worse health ( Sala, Cox, & Sareen, 2008 ) and adjusted health status (a measure of quality of life and functional impairment as it relates to physical health; Mancino et al., 2006 ). Specifically, people with PTSD have an increased risk for myocardial infarction, coronary heart disease, psychogenic nonepileptic seizure, rheumatoid arthritis, thyroid disease, diabetes, psoriasis, and different types of cancer ( Sala, Cox, & Sareen, 2008 ). A review by Qureshi, Pyne, Magruder, Schulz, and Kunik (2009) found strong evidence for a link between PTSD and arthritis, but it also found conflicting evidence for links between PTSD and stroke, heart disease, and diabetes.
Using NCS-R data, Sledjeski and colleagues (2008) concluded that most types of physical ailments commonly associated with PTSD could be attributed to repeated trauma exposure. The exception was headache, which was significantly associated with PTSD even after controlling for trauma exposure. Most of the other chronic physical complaints included in the study were significantly associated with the number of traumas, except for high blood pressure and epilepsy. On the other hand, Del Gaizo, Elhai, and Weaver (2011) , using NCS-R data, found that PTSD mediated the relationship between a number of different traumatic experiences and gastrointestinal, musculoskeletal, and/or cardiovascular health problems, suggesting that trauma affected health indirectly through the effects of PTSD. This finding is in line with some earlier research (e.g., Taft, Vogt, Mechanic, & Resick, 2007 ). Interestingly, Del Gaizo and colleagues found that substance use/abuse did not mediate the relationship between PTSD and physical health problems, thus discounting another possible explanation for how trauma affects health.
It is unclear to what extent increased health problems linked with trauma reflect physiological differences (e.g., related to increased arousal) versus worse self-care ( Sala et al., 2008 ). Some research has found that people with PTSD are less likely to follow medication regimens, which can also contribute to worse health outcomes ( Shemesh et al., 2004 ). Services that address trauma have been found effective in improving physical health and promoting better health-related behaviors ( Weissbecker & Clark, 2007 ). Individuals with PTSD also frequently have chronic pain ( Asmundson, Abrams, & Collimore, 2008 ; Asmundson & Katz, 2009 ). According to NCS-R data, people with episodic migraines or chronic daily headaches are significantly more likely than others to have PTSD (according to both lifetime and past-year data; Peterlin et al., 2011 ). McWilliams, Cox, and Enns (2003) , using NCS data, found that PTSD was associated with 3.7 times the likelihood of also having a chronic pain complaint. Asmundson and Katz (2009) reviewed research and theory concerning the relationship of PTSD to chronic pain and suggested two theories to explain the relationship: a mutual maintenance model in which PTSD exacerbates pain and vice versa and a model in which individuals have a shared vulnerability (perhaps genetic) that predisposes them to develop PTSD and chronic pain conditions.
Both trauma and PTSD also affect family relationships and the behavioral health of family members who did not experience the trauma or do not have the disorder, and these effects can be lasting. For example, children of mothers who endured physical and/or emotional abuse in childhood have more pronounced physiological responses indicative of anxiety than children of mothers who were not abused as children ( Jovanovic et al., 2011 ), and increased maternal PTSD symptoms are associated with a number of other markers indicating worse behavioral health in children ( Bosquet et al., 2011 ). So too, adults whose parents had PTSD have a strong and significantly greater risk of having PTSD themselves, but the association between parental trauma exposure and PTSD in the absence of parental PTSD is rather weak ( Yehuda, Halligan, & Bierer, 2001 ). However, according to the same research, greater parental trauma exposure was associated with significantly higher rates of depressive disorder among offspring. In addition, children of adults with PTSD were more likely to report childhood trauma, which in turn was associated with increased risk for PTSD in adulthood ( Yehuda, Halligan, & Grossman, 2001 ).
A number of reviews have found evidence that, in families where one or more parents are veterans with PTSD, there are higher rates of marital problems, more parenting problems, a greater likelihood of family violence, worse perceived parenting behavior, more behavioral health problems among children and partners, and worse academic performance by children, even when controlling for such potentially confounding factors as substance abuse and the strength of the relationship prior to PTSD (e.g., Erbes, 2011 ; Galovski & Lyons, 2004 ; Karney et al., 2008 ; Monson, Taft, & Fredman, 2009 ). The relationship between PTSD symptoms and poor family functioning has been found to persist for as many as 14 years for some individuals ( Koenen, Stellman, Sommer, & Stellman, 2008 ). Avoidance/numbing PTSD symptoms have the strongest association with family dissatisfaction and problems with intimate relations ( Renshaw, Blais, & Caska, 2011 ), whereas hyperarousal PTSD symptoms have been associated with increased aggression and violent behavior for veterans ( Elbogen, Fuller et al., 2010 ).
Other research conducted with veterans indicates that the relationship between PTSD and family functioning is complex; a partner’s perceptions of the veteran’s PTSD symptom severity, what the partner attributes the PTSD to, and how great the partner perceives his or her own burden to be as a result of the PTSD all affect the degree to which the partner’s own behavioral health is influenced ( Renshaw, Blais, & Caska, 2011 ). For example, in research conducted with 49 male National Guard members returning from deployment, symptoms of PTSD and depression among their wives were not correlated with veterans’ actual PTSD symptom scores, but instead with the wives’ own ratings of perceived symptoms among their husbands ( Renshaw, Rodrigues, & Jones, 2008 ). The wives’ symptom severity was greatest when they perceived high symptom severity in their husbands, even when their husbands perceived their own symptom levels low.
PTSD also appears to impair the ability to use resources that could help individuals overcome that disorder and other negative trauma effects, thus perpetuating PTSD symptoms. Johnson, Palmieri, Jackson, and Hobfoll (2007) evaluated resource loss (using the Conservation of Resource–Evaluation) for 225 inner-city women who reported being victims of interpersonal violence during childhood or adulthood. PTSD assessed at an initial interview was significantly related to resources lost 6 months later, even after controlling for resources lost at the initial assessment and for depressive symptoms. In particular, the authors found that emotional numbing symptoms of PTSD accounted for the majority of the women’s resource loss.
In research conducted with veterans, PTSD is associated with a significantly higher likelihood of being unemployed ( Savoca & Rosenheck, 2000 ; Zivin et al., 2011 ), as is greater PTSD symptom severity ( Smith, Schnurr, & Rosenheck, 2005 ). Among veterans, PTSD is associated with decreased productivity ( Savoca & Rosenheck, 2000 ) and greater occupational impairment ( Schnurr & Lunney, 2011 ). Kessler (2000) observed that, according to NCS data, individuals with PTSD had significantly more lost work time compared with those who did not have the disorder and experienced an amount of work-related impairment comparable to that experienced by people with major depression. Research conducted with nonveterans seeking treatment for PTSD and/or alcohol use disorders also found that individuals who had both were significantly more likely than those who had only one of the two disorders to be unemployed, have low income, and not have a spouse or intimate partner ( Riggs, Rukstalis, Volpicelli, Kalmanson, & Foa, 2003 ).
Malta, Levitt, Martin, David, and Cloitre (2009) evaluated work-related functional impairment among a group of 95 individuals who had PTSD symptoms related to the 9/11 attack. They found that PTSD symptoms, particularly numbing symptoms, were significantly related to work-related impairment, as were having low expectancies about one’s ability to manage negative feelings, greater feelings of social discomfort, greater expectations of being disliked by others, and certain demographic factors (e.g., income level, relationship status). Thorp and Stein (2005) reviewed a number of studies indicating that people with PTSD, compared with people with trauma exposure but no PTSD and people in primary care settings with no current mental disorders, had significantly greater impairment in several areas, including employment. The authors also noted that many of the studies reviewed found a level of impairment comparable to major depression.
Other Disorders That May Be Related to Trauma
Other behavioral health disorders besides PTSD have been linked to both trauma exposure and traumatic stress reactions—at times, it is difficult to tease out which is the contributing factor, so both are discussed together in the following sections. The various disorders comprising SMI, which include psychotic disorders and bipolar disorder, are often grouped together in the literature and hence are discussed together. There is also evidence linking trauma exposure to other types of anxiety disorders, depression, certain personality disorders, eating disorders, substance use disorders, and psychotic disorders.
In addition, PTSD frequently co-occurs with other behavioral health disorders and has been associated in a number of studies with significantly higher rates of a number of different disorders. For example, in the NCS-R, Kessler and colleagues (2005) found the following co-occurring disorders:
- Mood disorders (e.g., major depression, dysthymia)
- Other anxiety disorders (e.g., GAD, OCD)
- Impulse control disorders including oppositional–defiant disorder and intermittent explosive disorder, but not conduct disorder
- Alcohol use/dependence (with no significant association with drug use/dependence disorders)
NCS data show that the norm for people with PTSD is to have at least one co-occurring behavioral health disorder; 88 percent of men and 79 percent of women with PTSD have at least one other diagnosis, and 59 percent of men with PTSD and 44 percent of women have three or more diagnoses ( Kessler et al., 1995 ). Kessler (2000) also presented NCS data indicating that a prior PTSD diagnosis significantly increased the risk of subsequently developing a substance use disorder, major depression, dysthymia, mania, GAD, panic disorder, social phobia, simple phobias, and/or agoraphobia.
Substance use disorders
Numerous studies have found that the use of alcohol and/or illicit drugs increases risk for a number of different types of trauma. For example, in a meta-analysis of studies evaluating the relationship between alcohol use and injury, Taylor and colleagues (2010) found a dose–response relationship between the amount of alcohol consumed and the odds of having vehicular crashes and nonvehicular accidents. Other research conducted with emergency room patients indicated a significant association between blood alcohol level and an increased likelihood of sustaining a violence-related injury ( Cherpitel, 1997 ). As expected, people with substance use disorders are at increased risk for a number of different types of trauma besides accidents, including violent victimization ( Farley, Golding, Young, Mulligan, & Minkoff, 2004 ). According to NESARC data, people with a past-year diagnosis of alcohol use disorder, cocaine use disorder, and/or opioid use disorder all had significantly elevated risk for having been victims of crime in the prior year, although not necessarily violent crime ( Vaughn et al., 2010 ).
A history of trauma exposure, whether or not the individual has a traumatic stress reaction, is associated with increased risk for substance use disorders ( Farley et al., 2004 ). In a sample of 959 clients receiving outpatient substance abuse treatment services, Farley and colleagues (2004) found that 88.6 percent reported at least one traumatic event. Among men, the most commonly reported traumas were serious accidents (reported by 39.9 percent), being robbed (38.2 percent), and seeing someone killed or injured (37.7 percent). Among women, the most common traumas were rape (47.4 percent), other sexual assault (44 percent), and serious accidents (40.4 percent). Histories of multiple traumas are also common among people in treatment for substance use disorders, with 82.7 percent of one inpatient sample from Great Britain reporting two or more trauma events ( Reynolds et al., 2005 ).
Certain types of trauma appear to be associated with increased substance use, regardless of whether that use results in a substance use disorder. Survey data from New York, NY, indicate that in the 6 months after the 9/11 attack, there was a 30.8 percent increase in the use of cigarettes, marijuana, and/or alcohol among the general population ( Vlahov, Galea, Ahern, Resnick, and Kilpatrick, 2004 ). Other studies similarly indicate a rise in alcohol consumption, binge drinking, illicit drug use, and/or smoking in communities after natural disasters ( Adams & Adams, 1984 ; Lutz, Kramer, Gonnerman, & Downs, 1995 ; Office of Applied Studies, 2008 ).
Data from the Multisite Adult Drug Court Evaluation study of 958 adult offenders who were not incarcerated and who used illicit drugs indicate that experiencing a physical or sexual assault is associated with a significant increase in illicit drug use in the year following the assault, even after controlling for other factors related to drug use ( Zweig, Yahner, & Rossman, 2012 ). These authors also found that the relationship between assaultive trauma and PTSD was mediated by depressive symptoms (assessed with a 10-item Likert scale). Similarly, in a large longitudinal study of violence and women ( N =3,006), experiences of physical and/or sexual assault were associated with a significant increase in the likelihood of using illicit drugs and of alcohol abuse in the following year ( Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997 ). The use of illicit drugs, but not the abuse of alcohol alone, was also associated with a significant increase in the likelihood of being assaulted in the following year.
Although there is evidence that PTSD is associated with a high rate of substance use disorders, not all studies have found a significant association. Some have found associations only between certain substance use disorders and PTSD or between substance use disorders and PTSD only for certain populations. For example, research from the Epidemiologic Catchment Area Study (ECA) regarding 2,985 participants in North Carolina found a significant association between drug use disorders and PTSD, but not between alcohol use disorders and PTSD ( Davidson, Hughes, Blazer, & George, 1991 ). More recently, in the NCS, men with a lifetime PTSD diagnosis were 2.06 times more likely to also have an alcohol use disorder at some point during their lives and 2.97 times more likely to have a drug use disorder, compared with men who never had PTSD ( Kessler et al., 1995 ). For women, PTSD increased the odds of having a substance use disorder to an even greater degree, with the odds of having an alcohol use disorder being 2.48 times higher compared with women who never had PTSD and the odds of having a drug use disorder 4.46 times higher.
Interestingly, according to these same data, men with alcohol abuse disorder were actually less likely (about half as likely) than men without the disorder to have PTSD at some point during their lives, but men with alcohol dependence disorder were significantly more likely than those without that disorder to also have PTSD at some point (3.2 times more likely; Kessler et al., 1997 ). Women with alcohol abuse disorder were about as likely as other women to have PTSD, whereas those with alcohol dependence were 3.6 times more likely to have PTSD.
Both trauma exposure and PTSD are related to smoking. Feldner, Babson, and Zvolensky (2007) reviewed epidemiological data on the relationship of smoking to both trauma exposure and PTSD. Research has consistently shown that trauma exposure, even without PTSD, is associated with increased smoking and nicotine dependence. Rates are much higher for individuals who have experienced rape or other sexual trauma, and for women, but not men, who have experienced a nonsexual physical assault. For example, in one study, women who had been physically assaulted during their lives were 1.82 times more likely to be smoking at the time of the assessment than were women who had never been assaulted ( Acierno, Kilpatrick, Resnick, Saunders, & Best, 1996 ). Feldner and colleagues (2007) also found that studies of smoking among people with PTSD report even higher rates than those found in people with trauma exposure alone. They concluded that, according to data drawn from multiple studies, approximately 45 percent of people with PTSD smoke—a rate more than twice as high as that in the general population.
However, other research indicates that certain types of trauma may increase an individual’s risk for substance abuse, even in the absence of PTSD. Different types of trauma may differently affect alcohol consumption and alcohol use disorder risk for individuals who do not develop PTSD. Using data from Wave 2 of NESARC, Fetzner and colleagues (2011) evaluated the relative risk of different types of trauma on the development of alcohol use disorders, with or without co-occurring PTSD. Using a model that adjusted for demographic factors and other co-occurring behavioral health disorders, they found that, for individuals who did not meet criteria for PTSD, experiences of childhood trauma (particularly sexual abuse), military combat, and assaultive violence were all associated with significantly higher rates of alcohol use disorders, as were having a serious/life-threatening accident, witnessing serious injury/death, having someone close to you die unexpectedly, and learning of trauma experienced by someone close to you. Being an unarmed civilian in a war zone and being a refugee were associated with significantly lower odds of having an alcohol use disorder for individuals without PTSD. For individuals with PTSD, experiences of childhood trauma (particularly sexual abuse), military combat, and assaultive violence were all associated with a significantly greater likelihood of having an alcohol use disorder.
Numerous smaller studies show that prevalence estimates for PTSD among people seeking treatment for substance use disorders are significantly higher than prevalence estimates obtained from general population studies. Prevalence estimates differ widely among these studies, however, depending on the study population and research methodology. Exhibit L-5 summarizes these figures.
Exhibit L-5
Prevalence of PTSD Among Individuals Who Received Substance Abuse Treatment.
Although less common, prospective studies of PTSD and substance use disorders support the idea that PTSD, but not necessarily trauma exposure, increases the likelihood that someone might develop a substance use disorder. For example, a 10-year study of 1,200 members of a Michigan HMO who were ages 21 to 30 at the initial assessment found that a PTSD diagnosis at an earlier assessment was associated with a significantly greater risk for subsequently developing an alcohol use disorder, drug use disorder, and/or nicotine dependence ( Breslau, Davis, & Schulz, 2003 ). Trauma exposure alone, without PTSD, was not associated with increased risk for developing these disorders—with one exception, which was that women, but not men, who were exposed to trauma but did not meet criteria for a PTSD diagnosis subsequently had a significantly greater risk than did other women for developing alcohol use disorders but not drug use disorders.
Individuals with PTSD who have a co-occurring substance use disorder, particularly a co-occurring alcohol use disorder (the most often studied type of disorder) have more severe PTSD symptoms, a greater chance that PTSD symptoms will return after remission, a greater chance of relapse to substance abuse, more severe symptoms of substance abuse, and more co-occurring health problems ( McCarthy & Petrakis, 2010 ). For example, a German study of 459 clients in substance abuse treatment programs found that those with co-occurring PTSD had significantly more severe substance abuse problems (as measured by ASI scores) than did those with partial PTSD, trauma exposure without PTSD, or no trauma exposure ( Driessen et al., 2008 ). Differences in ASI scores were largely accounted for by ASI subscores indicating more severe psychiatric, family, employment, and drug-related problems among individuals with PTSD. Individuals with PTSD were also significantly more likely to report frequent substance cravings and reported a significantly shorter longest period of abstinence from drug use. A study of 1,098 out-of-treatment African Americans who used illicit drugs also found that PTSD was associated with significantly earlier age of onset for many substance use disorders ( Johnson, Striley, & Cottler, 2006 ).
PTSD may also affect individuals’ choices regarding substances of abuse. For example, PTSD-related hyperarousal symptoms have been significantly associated with heroin use among individuals in substance abuse treatment ( Tull, Gratz, Aklin, & Lejuez, 2010 ) and (along with reexperiencing symptoms) with marijuana use among individuals in a methadone maintenance program ( Villagonzalo et al., 2011 ). However, an Australian study of individuals attending an inpatient detoxification program found no significant differences in the primary substance of concern between those who did and did not have current PTSD ( Dore et al., 2011 ).
Exposure to certain types of trauma may also affect treatment seeking. Among a group of 40 women with substance use disorders who were incarcerated, severity of childhood sexual abuse was negatively correlated with the number of prior episodes of substance abuse treatment ( Peltan & Cellucci, 2011 ). Simpson (2002) had a similar finding with a group of 72 women in public substance abuse treatment programs, although, unlike Peltan and Cellucci (2011) , she also found that greater use of mental health services correlated with severity of childhood sexual abuse.
Among individuals in treatment for PTSD, co-occurring substance use disorders are associated with clients being significantly more likely to drop out of treatment ( Difede et al., 2007 ) and having worse treatment outcomes in a number of areas ( Ouimette, Brown, & Najavits, 1998 ). A study of 428 clients who were being treated for cocaine dependence found that those who had co-occurring PTSD, compared with those without current PTSD, entered treatment with significantly greater impairments in a number of areas, so that even when they improved at a similar rate, their outcome measures were still worse at the end of treatment ( Najavits et al., 2007 ). Individuals with PTSD were also less likely to show significant improvements in a number of areas, including alcohol use, legal problems, family/social problems, and psychiatric problems (as measured by ASI subscales).
Reasons for co-occurrence of trauma-related disorders and substance use disorders
Chilcoat and Breslau (1998) suggested three major causal pathways to explain the relationship between PTSD and substance use disorders: people with PTSD use substances of abuse in an attempt to counteract or cope with PTSD symptoms (a “self-medicate” process); people who abuse substances have high trauma rates because of the effects of their substance abuse (i.e., they are at high risk for trauma and hence PTSD); and substance abuse, directly or indirectly, increases risk for developing PTSD in the wake of trauma exposure (i.e., these individuals have a high degree of susceptibility to PTSD).
The self-medication hypothesis ( Khantzian, 1997 ) holds that individuals with PTSD use substances as a way to manage or avoid distressing PTSD symptoms (e.g., intrusive memories and physical arousal). Substances such as alcohol, cocaine, barbiturates, opioids, amphetamines, or other drugs are frequently abused in attempts to relieve or numb emotional pain or forget the traumatic event. Whether or not substance abuse develops because the individual is using substances to self-medicate, PTSD does appear to increase risk for developing substance use disorders. For example, in the NCS, having PTSD increased the risk of subsequently meeting criteria for alcohol abuse disorder by 2 times for men and 2.1 times for women, of alcohol dependence disorder by 3 times for men and 3.2 times for women, of drug abuse disorder by 2.2 times for men and 3.7 times for women, and of drug dependence by 3.7 times for men and 4.2 times for women ( Kessler, 2000 ).
The high-risk hypothesis, proposed by Cottler, Compton, Mager, Spitznagel, & Janca (1992) , states that drug and alcohol use places people who use substances in high-risk situations increase their chances for being exposed to events that lead to PTSD. In a review of research on the co-occurrence of substance use disorders and PTSD, Johnson (2008) observed that a greater likelihood of engaging in violence (as either victim or perpetrator) among people with substance use disorders is likely involved in the high PTSD rates among that population. Among other research, she observed that some studies have found that the type and intensity of substances abused affect trauma exposure and hence PTSD.
The susceptibility hypothesis holds that people who use substances are more susceptible to developing PTSD after exposure to trauma than people who do not use substances. This increased vulnerability may be a result of the failure to develop effective stress management strategies. Changes in brain chemistry or damage to neurophysiological systems because of extensive substance use could also contribute to increased susceptibility ( Chilcoat and Breslau, 1998 ).
Kilpatrick and colleagues (1997) suggested a fourth possible explanation regarding the relationship between PTSD and substance use. They proposed a bidirectional relationship in which use is associated with a higher risk of victimization, and victimization tends to escalate substance use. Clients who have co-occurring PTSD and substance use disorders tend to perceive the two as linked, and many observe that when one disorder improves or worsens, so does the other ( Brown, Read, & Kahler, 1998 ).
It is possible that there is no direct causal pathway between PTSD and substance use disorders. Both disorders may be caused by a third factor, or both disorders may share common genetic causes ( Meyer, 1986 ). Twin studies have indicated that a genetic component common to both is likely, although environmental factors also play a role ( Xian et al., 2000 ).
Mood disorders
Laugharne, Lillee, & Janca (2010) found good evidence that a significant number of people will develop major depression in the wake of trauma exposure. In addition, trauma exposure may contribute to the development or return of depressive symptoms. The research they reviewed also indicated that preexisting symptoms of depression may increase risk for developing PTSD and have also been linked to having more severe PTSD. However, other researchers (e.g., Breslau, Davis, Peterson, & Schultz, 2000 ) have found that trauma exposure, in the absence of PTSD, does not increase risk for depression; thus, they suggest that PTSD is responsible for elevated rates of depression among those who have been exposed to trauma.
The effects of trauma on depression may also depend on the type of trauma experienced. Using data from an Australian twin study, McCutcheon and colleagues (2010) found that, among individuals who had experienced trauma, those who were the victims of assaultive violence had the greatest risk for major depression. In the context of trauma, it is important to note that symptoms of PTSD and depression often overlap (i.e., sleep problems, difficulty concentrating, avoidance/withdrawal, lack of interest/pleasure, and feelings of isolation may all be symptoms of either disorder; Brady, Killeen, Brewerton, & Lucerini, 2000 ). These reviewers also noted that there are physiological changes common to the two disorders involving the hypothalamic–pituitary–adrenal axis and the production of corticotrophin-releasing factor.
Larger studies, such as the NCS ( Kessler et al., 1995 ) and the NCS-R ( Kessler, Berglund et al., 2005 ), have found that PTSD is associated with significantly higher rates of all depressive disorders. In the NCS, lifetime rates of all affective disorders were significantly higher for individuals who had PTSD at some point during their lives compared with those who did not, with larger increases in the odds ratios found for affective disorders in men than in women ( Kessler et al., 1995 ). For example, PTSD was associated with 4.1 times greater odds of having major depression for women and 6.9 times greater odds for men. In the NCS-R, individuals who met criteria for PTSD in the prior year were significantly more likely than all others to also have major depression, dysthymia, or bipolar disorder ( Kessler, Berglund et al., 2005 ).
In Wave 2 of NESARC, people who had been diagnosed with PTSD at some point during their lives were also 2.6 times as likely to have had a mood disorder, 1.9 times as likely to have had major depression, 1.3 times as likely to have had dysthymic disorder, 2.1 times as likely to have had bipolar I disorder, and 1.4 times as likely to have had bipolar II disorder. Other studies have also found high rates of co-occurring PTSD among people with depression and vice versa. For example, data from the Sequenced Treatment Alternatives to Relieve Depression study for 1,376 adults being treated for major depression indicated that 18.8 percent had current co-occurring PTSD ( Rush et al., 2005 ).
Using both prospective and retrospective data from a large study of young adults ( N =1,007), Breslau and colleagues (2000) found that having had PTSD at some time prior to the initial assessment was associated with 2.8 times greater risk for developing major depression, whereas having a prior diagnosis of major depression was associated with 3.7 times greater risk for developing PTSD and 2.1 times greater risk for being exposed to trauma. However, prior trauma exposure was not associated with a significant increase in risk for major depression. They also found that trauma exposure occurring during the study further increased risk for developing depression among those who had prior PTSD, but not among those who did not have PTSD.
A number of explanations have been proposed to explain the relationships among trauma, PTSD, and depression. Breslau and colleagues (2000) reviewed literature proposing five different possibilities: preexisting depression increases risk for PTSD; PTSD increases risk for depression; depression increases risk for trauma (which then increases PTSD risk); there is a shared vulnerability to both PTSD and depression (e.g., a shared genetic factor that increases risk for both); or traumatic experiences increase risk for depression and potentially cause PTSD. Breslau and colleagues concluded, based on their own research, that trauma alone does not seem to contribute to the development of major depression, but PTSD does. Other researchers have argued that symptoms of both PTSD and depression represent the same, underlying construct (e.g., Elhai et al., 2011 ).
A study of 267 women with low incomes who were receiving treatment for depression found that those with co-occurring PTSD had more severe depression, more anxiety, and greater functional impairment ( Green et al., 2006 ). Another study that evaluated depression and trauma histories for 792 adults also found that prior trauma, especially childhood abuse, was associated with significantly greater severity of depression (measured with the Beck Depression Inventory), even after controlling for demographic factors and family mental disorder history ( Wingo et al., 2010 ). Earlier studies (e.g., Blanchard, Buckley, Hickling, & Taylor, 1998 ) also found that among individuals with PTSD, those who have co-occurring depression have greater role impairment, more subjective distress, and lower rates of remission from PTSD.
A study of 178 veterans in treatment for co-occurring depression and substance use disorders found that clients with PTSD had more severe depressive symptoms (assessed with the Hamilton Depression Rating Scale), but they experienced a decrease in depressive symptoms following treatment similar to that seen in clients without PTSD ( Norman, Tate, Wilkins, Cummins, & Brown, 2010 ). More information on the relationship of traumatic stress reactions to bipolar disorder can be found in the “ Serious Mental Illness ” section. The planned TIP, Managing Anxiety Symptoms in Behavioral Health Services (SAMHSA, planned d), discusses the relationship of mood and anxiety disorders (including PTSD) in more detail.
Anxiety disorders
A review by Laugharne and colleagues (2010) found some evidence that trauma exposure can contribute to the development of anxiety disorders, particularly GAD. They also found that preexisting anxiety symptoms and/or anxiety sensitivity may increase an individual’s risk for developing PTSD. Brady and colleagues (2000) reviewed research that indicates that PTSD frequently co-occurs with anxiety disorders, particularly panic disorder and SAD.
A number of studies confirm that PTSD frequently co-occurs with panic disorder. This co-occurrence may be even more common among individuals with certain cultural backgrounds, such as people from Southeast Asia ( Hinton et al., 2000 ; Hinton et al., 2001 ). Cougle, Feldner, Keough, Hawkins, and Fitch (2010) reviewed earlier studies that indicate that between 7.3 and 18.6 percent of men with PTSD and 12.6 and 17.5 percent of women with PTSD have co-occurring panic disorder. They noted that other research indicates that people with PTSD are about twice as likely as others to have had a panic attack (whether or not they have had panic disorder). Individuals who have been the victims of assaultive violence have greater risk for panic disorder than do those who have only experienced other kinds of trauma ( McCutcheon et al., 2010 ).
A study of 884 veterans found high rates of co-occurrence between PTSD and panic disorder, with more individuals ( n =40) having both PTSD and panic disorder than panic disorder alone ( n =33; Gros, Frueh, & Magruder, 2011 ). This study also found that individuals with PTSD who had co-occurring panic disorder had more severe PTSD, according to PCL scores, than did those who had PTSD alone. According to NCS-R data, 35 percent ( n =72) of individuals with a past-year diagnosis of PTSD reported having had one or more panic attacks ( Cougle et al., 2010 ). Individuals with PTSD who reported panic attacks also had greater PTSD-related disability, more traumatic experiences during their lives, and more time unemployed or absent from work, and they were more likely to have co-occurring depression and/or substance use disorders.
Some research indicates that individuals who have panic attacks have a greater risk than others for developing PTSD following trauma exposure ( Adams & Boscarino, 2011 ). Marshall-Berenz, Vujanovic, and Zvolensky (2011) also found, in a sample of 91 individuals who had experienced trauma, that a history of panic attacks in the absence of panic disorder was significantly related to PTSD-related reexperiencing and hyperarousal symptoms. Hinton, Hofmann, Pitman, Pollack, and Barlow (2008) proposed that panic attacks may be triggered by sensations associated with traumatic experiences, and in turn, panic attacks may worsen PTSD by increasing arousal and reactivating traumatic memories. This phenomenon may be affected by cultural beliefs. Hinton, Nickerson, and Bryant (2011) observed that, among Cambodian refugees, worry often precipitated panic attacks and increased trauma recall (including flashbacks) and hyperarousal, which in turn were associated with more severe PTSD.
SAD also frequently co-occurs with PTSD. Collimore, Carleton, Hofmann, and Asmundson (2010) reviewed research on this co-occurrence. Studies included in their review found that rates of past-year SAD among individuals with PTSD ranged from 4.3 percent to 72 percent in both clinical and nonclinical studies with different samples (e.g., veterans, disaster survivors). The authors considered a number of different factors that may contribute to this co-occurrence, including common genetic causes, heightened anxiety sensitivity, fears of negative evaluation, intolerance of uncertainty, increased guilt and/or shame, and co-occurring depression. For individuals with high levels of social anxiety, episodes of social embarrassment may be perceived as more traumatic than other events that are typically considered traumatic ( Carleton, Peluso, Collimore, & Asmundson, 2011 ). Other researchers have observed that there is an element of experiential avoidance that may be involved in the maintenance of both SAD and PTSD, which may also explain why the disorders frequently co-occur (e.g., Kashdan, Morina, & Priebe, 2009 ).
Personality disorders
Personality disorders frequently co-occur with other behavioral health disorders, and PTSD is not uncommon among individuals with many of these disorders. Because of its size and methodology, NESARC provides the most accurate epidemiological data on personality disorders in the United States. According to NESARC Wave 2 data regarding individuals who had been exposed to trauma, those who developed PTSD were significantly more likely to have borderline, narcissistic, and/or schizotypal personality disorders than were those who did not develop PTSD ( Pietrzak et al., 2011a ). For women, but not men, PTSD was also associated with significantly higher odds of having OCD. According to the initial NESARC data, 19.5 percent of respondents with a past-year diagnosis of narcissistic personality disorder had co-occurring PTSD, and 25.7 percent of those with a lifetime diagnosis of narcissistic personality disorder had co-occurring PTSD ( Stinson et al., 2008 ).
Rates of co-occurring PTSD are also high among people with borderline personality disorder (BPD). In NESARC, 31.2 percent of people with BPD in the past year also had PTSD in that year, whereas 39.2 percent of those with a lifetime diagnosis of BPD also had PTSD at some point ( Grant et al., 2008 ). However, because of the overlap in symptoms between the two disorders and the high rates of early trauma among those with BPD, there is also an ongoing debate as to whether BPD may in fact be a traumatic stress reaction ( Lewis & Grenyer, 2009 ).
In NESARC, individuals with schizotypal personality disorder had increased risk for co-occurring PTSD; 38.1 percent of women and 21.6 percent of men with schizotypal personality disorder also had co-occurring PTSD ( Pulay et al., 2009 ). Studies have also found high rates of co-occurring PTSD among individuals with ASPD. In reviewing prior research, Goldstein, Compton, and Grant (2010) observed that studies have found that between 8 and 21 percent of people with ASPD have PTSD. They also noted that, in NESARC, individuals with PTSD who had a co-occurring diagnosis of ASPD were significantly more likely to have a number of other co-occurring disorders, including substance use disorders, bipolar I disorder, and a number of other personality disorders.
In a large study of personality disorders, the majority ( n =102) of individuals with PTSD at the start of the 7-year study ( n =142) achieved remission during the study; 34 percent of those who did achieve remission had at least one relapse to PTSD (Ansell et al., 2010). Schizotypal personality disorder was the only disorder of the four included in the study that was associated with significantly lower remission (compared with individuals with no personality disorder, avoidant personality disorder, BPD, or OCD). Research has found that individuals who experience significant trauma (e.g., sexual abuse) as children are at increased risk for developing personality disorders ( Pratchett et al., 2010 ). There are gender differences in this pattern—women are more likely to develop BPD and men are more likely to develop ASPD—but individuals with both of those personality disorders are significantly more likely than those without either disorder to have experienced childhood abuse.
Eating disorders
Brewerton (2007) reviewed a number of studies that found high rates of trauma and PTSD among both men and women with eating disorders. Most eating disorder research does not include men. Brewerton (2007) found that although child sexual abuse is a particularly strong risk factor for later developing an eating disorder, other forms of trauma appear to increase the likelihood of developing eating disorders as well. He cited studies indicating that trauma is more common among women who have eating disorders with bulimic symptoms than among those who have eating disorders without such symptoms, and he noted that women with bulimic disorders are more likely than women without eating disorders or those with nonbulimic disorders to have had multiple episodes of trauma. Although trauma histories are not associated with any significant differences in severity of eating disorder symptoms, women with eating disorders who have trauma histories are more likely than other women with eating disorders to have major depression, substance use disorders, BPD, and anxiety disorders (including PTSD).
Swinbourne and Touyz (2007) reviewed research that provides epidemiological data on the co-occurrence of anxiety and eating disorders. They found PTSD rates ranging from 11 to 52 percent in samples of people (typically women) with eating disorders but also noted that studies that included individuals with both anorexia nervosa and bulimia nervosa found PTSD to be significantly more common among those with the latter disorder. Among women with histories of childhood sexual abuse ( N =50), eating disorders were associated with significantly lower self-esteem and significantly more symptoms of depression at the conclusion of treatment and at a 6-month follow-up assessment ( Harper, Richter, & Gorey, 2009 ).
Serious mental illness
SMI typically includes schizophrenia, schizoaffective disorder, and bipolar disorder. Individuals with these disorders have increased risk for a number of different types of trauma and for PTSD. According to NESARC data, people with psychotic disorders had a 78 percent greater chance of having been the victim of violence in the year prior to assessment, but the difference was not significant, given the relatively small numbers of people with such disorders included in the study (Vaughn et al., 2009). However, mood disorders, which include bipolar disorder, were found to be associated with a significantly greater likelihood of being a victim of violent crime (people with bipolar disorder had an increased risk of 32 percent in the adjusted model).
People with SMI also appear to have increased risk for trauma from accidents. In a study involving 1,709 admissions to a public hospital trauma unit, individuals with mental disorders (not limited to SMI, but involving psychosis/schizophrenia in 29 percent of cases) were more than twice as likely to have an unintentional injury ( Wan et al., 2006 ). Other research indicates that people with psychosis ( Kilcommons, Morrison, Knight, & Lobban, 2008 ; Read, van Os, Morrison, & Ross, 2005 ) and those with bipolar disorder ( Garno, Goldberg, Ramirez, & Ritzler, 2005 ; Goldberg & Garno, 2005 ) have high rates of childhood physical and/or sexual abuse. A large British study (N=8,580) found significant associations between a number of traumatic childhood experiences and increased likelihood of psychosis, with an especially strong association between childhood sexual abuse and psychosis ( Bebbington et al., 2004 ).
Goldberg and Garno (2005) evaluated trauma histories for 100 consecutive admissions to a bipolar disorders research clinic; 24 percent of participants had current PTSD. However, current PTSD was significantly more common (affecting 35 percent) for individuals with childhood traumatic experiences compared with those who did not report such experiences (13 percent of whom had PTSD). A greater number of childhood traumatic experiences correlated with a greater likelihood of PTSD in adulthood.
Whether trauma, particularly childhood trauma, contributes to the development of SMI is still a subject for debate; some evidence supports the fact that it does, and some does not. An Australian study of 1,612 individuals (1,327 female) who had been sexually abused in childhood (according to police records) and who had histories of receiving behavioral health services found no significant increase in psychotic disorders compared with a general population control group, but risk for psychotic disorders was elevated in both men and women who had histories of childhood sexual abuse (e.g., women who were sexually abused as children had 1.5 times greater risk for psychotic disorders as adults; Spataro, Mullen, Burgess, Wells, & Moss, 2004 ). Critics of the study, though, have pointed to methodological problems, including the fact that the study was limited to those whose abuse was recognized while they were children and who received services at the time; it excluded individuals whose abuse went unrecognized and who thus had more chronic and severe trauma histories ( Read & Hammersley, 2005 ).
A German study, which assessed 2,524 adolescents and young adults (ages 14 to 24) and then reassessed them an average of 42 months later, found that trauma reported at the initial assessment was significantly associated, in a dose–responsive manner, with the onset of psychotic symptoms at the follow-up assessment ( Spauwen, Krabbendam, Lieb, Wittchen, & van Os, 2006 ). All of the types of trauma evaluated were associated with significant increases in risk for psychotic symptoms, but the largest increase in relative risk for psychosis was associated with sexual trauma. Another German study conducted with 4,045 adults ages 18 to 64 also found that childhood abuse reported during an initial assessment was associated with 11.5 times greater risk for reporting psychotic symptoms at a follow-up 2 years later ( Janssen et al., 2004 ).
PTSD also appears to cause, for some individuals, some psychotic symptoms (see Braakman et al., 2009 ), and studies that examine the relationship between trauma and psychotic symptoms have found a significant association. Read and colleagues (2005) found evidence for a “strong relationship” between childhood abuse and both hallucinations and delusional ideations. Read, Agar, Argyle, and Aderhold (2003) found that sexual assault in adulthood was significantly associated with hallucinations, delusions, and thought disorder, whereas childhood physical and/or sexual abuse was significantly associated with hallucinations but not delusions or thought disorder.
Kilcommons and colleagues (2008) evaluated psychotic experiences among 40 survivors of sexual assault and 40 individuals who did not have sexual assault histories and interviewed a subset of 26 from the first group. They found that study participants who had been sexually assaulted were significantly more likely than those in the control group to have experienced psychotic symptoms (both delusional ideations and hallucinations). Sixty-six percent of survivors of sexual abuse met criteria for PTSD, but an even larger percentage reported psychotic symptoms (with 75 percent reporting the most common symptoms in the study). A study with a smaller sample ( n =32, 53 percent with current PTSD) of individuals with psychotic disorders ( Kilcommons & Morrison, 2005 ) also found that the severity of traumatic experiences was significantly associated with severity of PTSD and severity of psychotic symptoms.
Some evidence suggests that the experience of psychosis itself, and attendant issues such as forced hospitalization, may be traumatic and contribute to PTSD symptoms ( Beattie, Shannon, Kavanagh, & Mulholland, 2009 ). Sherrer (2011) , in an article discussing reasons for high PTSD rates among people with SMI, reviewed studies that found that between 24 and 43 percent of people with SMI have co-occurring PTSD. Some literature also indicates that PTSD rates are higher for individuals with bipolar disorder than for those with schizophrenia spectrum disorders ( O’Hare, Sherrer, & Shen, 2006 ).
Achim and colleagues (2011) conducted a meta-analytic review of studies giving prevalence data on co-occurring anxiety disorders among individuals diagnosed with schizophrenia. According to pooled prevalence data from 52 studies ( N =4,032), 12.4 percent had current PTSD. However, the authors noted a wide variation in rates among the studies they included.
In the NCS-R, 30.9 percent of respondents who had a lifetime diagnosis of bipolar I disorder and 34.3 percent of those with bipolar II also had PTSD at some point during their lives ( Merikangas et al., 2007 ). Some studies have found lower rates of co-occurring PTSD, however. One study of 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder found that 17.2 percent met criteria for a PTSD diagnosis at some point during their lives, and 5.1 percent had current PTSD at the time of assessment, with somewhat higher rates for participants with bipolar I disorder and somewhat lower rates for those with bipolar II ( Simon et al., 2004 ).
Provencher, Hawke, and Thienot (2011) reviewed research on the co-occurrence of bipolar and anxiety disorders (including PTSD). Some research has found that people with bipolar disorder who have co-occurring PTSD, compared with others with bipolar disorder, have longer affective episodes, are more likely to have a recurrence of affective episodes, are more likely to have rapid cycling, take longer to achieve remission, have greater risk for co-occurring substance use disorders, have worse health-related quality of life, and are more likely to attempt suicide ( Garno et al., 2005 ; Goldberg & Garno, 2005 ).
Other research indicates that individuals with schizophrenia or schizoaffective disorder who have PTSD also have more severe anxiety and dysphoria symptoms (according to the Positive and Negative Syndrome Scale [PANSS] and the Endler Multidimensional Anxiety Scale) compared with those who do not have co-occurring PTSD ( Newman, Turnbull, Berman, Rodrigues, & Serper, 2010 ). This study also found that a greater number of past traumatic experiences was associated with more severe psychosis, and a higher number of past experiences of victimization was associated with more severe cognitive/autistic symptoms (on the PANSS).
Several researchers have argued that PTSD with secondary psychotic features should be considered as a separate diagnostic category. Braakman, Kortmann, and van den Brink (2009) defined this diagnostic category as a syndrome in which an individual experiences PTSD symptoms followed in time by psychotic symptoms and found that certain facets of the syndrome distinguish it from PTSD and schizophrenia (e.g., elevated plasma dopamine β-hydroxylase and cerebrospinal concentrations of corticotrophin-releasing factor).
Possible explanations for high PTSD rates among people with SMI are that SMI predisposes people to trauma, that SMI directly or indirectly causes or contributes to developing PTSD (e.g., because psychotic episodes are themselves traumatic), and/or that traumatic experiences (e.g., childhood trauma) contribute to the development of SMI as well as PTSD. However, the most commonly held theory is that SMI affects how individuals interpret traumatic experiences and thus increases the likelihood of having PTSD as well as PTSD severity ( Sherrer, 2011 ).
Still, rates of crime victimization are high for people with SMI. Teplin and colleagues (2005) used data from a survey of 936 patients with SMI who attended mental health programs in the Chicago area from 1997 to 1999 and data from the National Crime Victimization Survey for residents of large cities during the same period and determined that, compared with others residing in large cities, people with SMI were over 10 times more likely to have been victims of violent crime in the prior year.
Sherrer (2011) theorized that high rates of co-occurring PTSD among people with SMI are attributable to problems in cognitive appraisal related to potentially traumatic events that may make people less objective in evaluating the nature of those events. She suggested that cognitive restructuring may be particularly useful for this population as a way to modify problematic cognitions related to trauma.
- Screening and Assessing Trauma and Trauma-Specific Disorders
Briere (2002) and others recommended that any behavioral health assessment inquire about trauma histories and assess traumatic stress reactions. Briere observed that assessments should elicit information about the client’s psychological functioning prior to the trauma; the exact nature of the traumatic event(s), including type, duration, frequency, and severity; social and family support available after the trauma; co-occurring behavioral health problems; and posttraumatic response, including PTSD symptoms.
Assessing Trauma Histories
Assessment of trauma histories is necessary not only as a first step in assessing traumatic stress reactions, but also for other forms of assessment and treatment planning. Such assessments need to take into account factors such as the client’s current level of safety (e.g., whether the client is at risk for further trauma), current psychological stability (e.g., whether the client is currently experiencing a level of acute psychological distress that might preclude indepth inquiries about traumatic experiences), and the client’s readiness for further assessment and treatment ( Briere & Scott, 2006 ). Briere and Scott (2006) gave some guidelines for assessing trauma exposure, such as establishing trust and a level of comfort before inquiring about traumatic experiences and being prepared for intense responses from clients. They also provided a detailed list of symptom responses to trauma that go beyond typical symptoms of traumatic stress reactions, including cognitive disturbances (e.g., low self-esteem, helplessness, shame), dysfunctional behaviors aimed at reducing trauma-related stress (e.g., self-mutilation, compulsive stealing), sexual disturbances, somatic complaints, symptoms of other behavioral health disorders, and culturally specific trauma responses. Hanson and Self-Brown (2010) provided some guidelines for assessing trauma resulting from criminal victimization.
Assessing traumatic experiences to see if a client meets Criterion A for a PTSD diagnosis is a first step in diagnosing PTSD ( Weathers, Keane, & Foa, 2009 ). O’Donnell, Creamer, and Cooper (2010) discussed some of the debate around Criterion A for PTSD and potential problems with using that criterion to guide trauma assessment. They observed that Criterion A may, for example, cause clinicians to ignore traumatic events that do not involve a clear memory of the incident. A number of assessment instruments are available to aid in assessing trauma histories or histories related to a particular type of trauma. These have almost always been developed for research purposes but may be useful in real-life settings as well. For example, researchers conducting the Women, Co-Occurring Disorders and Violence study selected the Life Stressor Checklist-Revised to assess exposure to lifetime and current traumatic experiences for women with co-occurring disorders and found it effective, reliable, and well tolerated in that context ( McHugo et al., 2005 ). Bailey, DeOliveira, Wolfe, Evans, and Hartwick (2012) used the Childhood Trauma Questionnaire to evaluate childhood traumatic experiences for mothers of preschool children and judged it a valid measure that helped them relate childhood traumatic experiences to parenting concerns and behaviors.
Corcoran, Green, Goodman, and Krinsley (2000) observed that trauma assessment instruments are not comprehensive and also reviewed potential complications in accurately assessing a client’s prior traumatic experiences. They focused on two trauma assessment instruments, the Stressful Life Events Screening Questionnaire (SLESQ) and the Evaluation of Lifetime Stressors instrument, with attention to how well these instruments capture experiences that meet Criterion A of a PTSD diagnosis. They noted that the SLESQ is a brief measure that does not collect as much information about objective and subjective aspects of trauma, and thus the two instruments may be useful in different contexts. Both instruments have good test–retest reliability and construct validity, and the SLESQ has good convergent validity as well.
The Traumatic Life Events Questionnaire (TLEQ) is a widely used self-report measure that evaluates 22 types of traumatic events and certain characteristics of those events (e.g., whether the event resulted in injury, how often it occurred; Kubany, Leisen, Kaplan, & Kelly, 2000 ). The instrument has good reliability and validity ( Orsillo, 2001 ). Compared with a single-item trauma assessment question from the SCID, the TLEQ elicited 900 percent more traumatic events in a group receiving treatment for opioid dependence ( Peirce, Burke, Stoller, Neufeld, & Brooner, 2009 ).
Cusack, Frueh, and Brady (2004) described a 13-item self-report version of the Trauma Assessment of Adults instrument (shortened to make it useful in clinical settings), which, unlike the aforementioned instruments, was developed for use in clinical settings. In their evaluation of the instrument with clients from a community mental health center, they found that a higher number of traumatic events reported on the instrument correlated with worse physical and behavioral health assessments using other measures. The authors concluded that the instrument is useful in behavioral health treatment settings and can help improve recognition of PTSD as well as guide other aspects of treatment. Some concern exists that trauma screening instruments may prime some respondents to report PTSD symptoms, but Reddy, Polusny, and Murdoch (2009) found this not to be the case in an evaluation of National Guard members. Fallot and Harris (2001) also suggested that behavioral health treatment programs check a client’s medical, social, and criminal histories for evidence of past trauma.
Screening and Assessing ASD
ASD may occur any time from the trauma exposure to 4 weeks after the exposure. The earliest time an assessment can be made is 2 days following trauma exposure, because symptoms must last at least 2 days for an ASD diagnosis ( APA, 2000 ). Bryant and Litz (2006) noted that assessments that occur too soon after trauma exposure are less likely to predict PTSD and that ASD assessed 4 weeks after trauma exposure is more than twice as accurate as a PTSD marker. Thus, they recommended that ASD assessment occur later in the window for ASD diagnosis to make the best use of resources. In Bryant and Litz’s review (2006) , they recommended three instruments for assessing ASD that are also useful for predicting PTSD: Stanford Acute Stress Reaction Questionnaire ( Cardeña, Koopman, Classen, Waelde, & Spiegel, 2000 ), Acute Stress Disorder Interview ( Brooks et al., 2008 ), and Acute Stress Disorder Scale ( Bryant, Moulds, & Guthrie, 2000 ).
Screening and Assessing PTSD
Clients who report trauma histories should generally be further assessed for traumatic stress symptoms and PTSD ( Australian Centre for Posttraumatic Mental Health [ACPMH], 2007 ). Screening instruments are available that can help clinicians decide which clients are more likely to have PTSD and thus require further assessment. For example, Boscarino and colleagues (2011) reported on a brief screening tool designed for use in clinical practice, the New York PTSD Risk Score, which inquires about PTSD symptoms including sleep problems, trauma exposure, suicidal thoughts, depression symptoms, and demographic factors that may mean an individual is at greater risk for PTSD. The instrument has been found effective for predicting PTSD up to 1 year after the initial assessment ( Boscarino et al., 2012b ) and has specific versions intended to assess men and women separately ( Boscarino et al., 2012a ). The National Center for PTSD (NCPTSD) Web site ( http://www.ptsd.va.gov ) provides descriptions and basic information on other commonly used PTSD screening instruments, including a table comparing them, reproduced below as Exhibit L-6 .
Exhibit L-6
Comparison of Screens for PTSD.
The ACPMH (2007) , as part of its review on the assessment and treatment of PTSD, recommended that individuals presenting in healthcare settings be asked about whether they have experienced trauma; when indicated, they should be given a comprehensive PTSD assessment. Such PTSD assessments should investigate not only PTSD symptoms, but also symptoms of other mental disorders, substance use/abuse behavior, marital and family functioning, vocational functioning, quality of life, psychological functioning, and physical health. Assessments should also establish strengths and sources of resilience. Symptoms should be assessed within the context of the time elapsed since trauma exposure, recognizing that symptoms experienced in the few weeks following trauma are likely to remit and also that, for some individuals, symptoms may not appear until a considerable amount of time after the trauma. Regular reassessment should also occur and needs to be culturally competent and to take into consideration the effects an individual’s trauma exposure may have on those close to him or her.
Steel, Dunlavey, Stillman, and Pape (2011) reviewed assessment of PTSD and depression for individuals who have experienced significant trauma. They addressed differential diagnosis with respect to TBI, the importance of cultural and sociodemographic factors, and potentially confounding effects of medications. They summarized reliability and validity data for a number of PTSD assessment instruments, including the PTSD interview, the CAPS, the Structured Interview for PTSD, the Posttraumatic Diagnostic Scale, the Impact of Events Scale-Revised, the Primary Care PTSD Screen, the PCL, the Harvard Trauma Questionnaire, the PENN Inventory, and the PTSD modules of the Composite International Diagnostic Interview and the Diagnostic Interview Schedule.
Orsillo (2001) also provided information on reliability and validity for these instruments as well as a number of others. Briere (2002) discussed specific screening and assessment instruments for both trauma and traumatic stress reactions and addressed how certain general measures of behavioral health may be used for assessing these. The NCPTSD Web site ( http://www.ptsd.va.gov ) also provides descriptions and basic information on clinician-delivered interview instruments and self-report measures for assessing PTSD. See Exhibits L-7 and L-8 , respectively.
Exhibit L-7
Clinician-Delivered Interview Instruments for Assessing PTSD.
Exhibit L-8
Self-Report Measures Instruments for Assessing PTSD.
A review by Johnson (2008) concerning the relationship of PTSD and substance use disorders discussed some of the issues involved in assessment and differential diagnosis for clients with both disorders. Najavits (2004) provided practical guidance on assessing trauma and traumatic stress reactions in individuals with substance use disorders.
Screening and Assessing Complex PTSD
The assessment of complex PTSD is likely to follow from a more general assessment of trauma and traumatic stress reactions, but it is a more complex process ( Briere & Spinazzola, 2009 ). Brown (2009) discussed assessment issues related to attachment styles for adults who have complex PTSD. Briere and Spinazzola (2009) discussed appropriate instruments for assessing trauma-related responses that may result from complex trauma (e.g., cognitive disturbance, dissociation, dysfunctional behaviors).
Cultural, Ethnic, and Gender Factors in Assessment
All behavioral health screening and assessment should be culturally competent and sensitive to gender, functional impairment, age, and religion/spiritual beliefs. Screening and assessment for trauma and traumatic stress reactions are no exception, particularly given that research suggests that culturally defined ways of interpreting traumatic experiences affect an individual’s reaction to trauma, including the type and degree of behavioral health problems that may result from the trauma exposure ( Wilson, 2007 ). The planned TIP, Improving Cultural Competence (SAMHSA, planned c), contains more detailed information on conducting culturally competent assessments in behavioral health settings.
In assessing the impact of trauma on clients with diverse cultural backgrounds, one must understand how their culture interprets the traumatic event, the historical and intergenerational context of the trauma, the types of responses to trauma that the culture considers appropriate, and what sources of strength/resilience people from that culture rely on in the wake of trauma ( Danieli, 2007 ; Hoshmand, 2007 ). Another important issue is how a client’s culture may shape his or her attitudes toward behavioral health services and behavioral health disorder diagnoses. For example, people from developing countries who have mood and/or anxiety disorders are about twice as likely as those from developed countries to perceive “stigma” associated with those disorders, which can affect their willingness to report symptoms ( Alonso et al., 2008 ).
Clients’ understanding and presentation of dissociative symptoms may also vary according to their cultural backgrounds. For example, a number of researchers and clinicians have observed that Asians and Asian Americans are more likely than members of many other cultural groups to present anxiety symptoms, including PTSD symptoms, as somatic complaints ( Hinton, Hofmann, Pollack & Otto, 2009 ). Others have observed that Asian Americans may be more reticent about discussing psychological complaints, because their cultures teach that stoic acceptance is the appropriate response to adversity ( Lee & Mock, 2005a , b ). Research from the Netherlands has found that people from non-Western cultures have more physical health-related anxieties following trauma exposure than do those from Western cultures exposed to the same traumatic event ( Verschuur et al., 2010 ).
Pole and colleagues (2008) observed that African American clients may be hesitant to discuss certain traumatic experiences with White American clinicians because they are concerned about being judged. Instead, they too may present themselves in a reserved or stoic manner that can be mistaken for the PTSD symptoms of avoidance or numbing. The authors noted that some Latinos may also somaticize PTSD symptoms or present complaints using terminology that may not fit easily into PTSD symptom categories (e.g., an attack of nerves).
Members of some cultural groups may also present dissociative symptoms in a manner that may not readily be assessed as dissociation (e.g., as possession by a spirit; Lewi-Fernández et al., 2007 ). Hinton, Pich, Marques, Nickerson, and Pollack (2010) found that severity of khyâl attacks, a panic-like symptom experienced by Cambodian people and attributed to disruption in personal energy, was strongly correlated with severity of PTSD symptoms. Certain traumas, given their importance to members of a culture, may also be more likely to cause traumatic stress reactions in members of a particular cultural group.
Some, but not all, assessment instruments have been evaluated with different cultural groups. Pole and colleagues’ (2008) review noted that the Mississippi Combat-Related PTSD Scale, the Keane PTSD Scale, the CAPS, and the PCL have been found to be effective with African American populations. It is worth noting that an assessment instrument may have been translated into another language, but this does not mean it is valid with every cultural group that speaks that language. For instance, Bourque and Shen (2005) found that the Spanish translation of the Civilian Mississippi Scale had significantly poorer correlations for Latinos than it did for White Americans compared with other PTSD measures. Fortuna, Porche, and Alegría (2009) recommended that clinicians use the Cultural Formulation from the DSM-5 (a model that takes into consideration cultural identity, the client’s cultural environment, the role of culture in the clinical relationship, and cultural factors related to behavioral health) when assessing PTSD. They explained its application but also observed that, in their own research involving community healthcare settings, the model is not widely used.
Special Issues in Assessment
Clinicians may have concerns that clients will not want to answer questions about certain types of trauma, such as childhood abuse. Research indicates that a considerable percentage of people who experience childhood sexual abuse do not report it when asked open-ended questions about childhood experiences. In earlier studies reviewed by Goodman and colleagues (2003) , 37 percent of women ( Williams, 1994 ) and 38 percent of women and men ( Widom & Morris, 1997 ) with child sexual abuse histories did not report it. Goodman and colleagues (2003) also reviewed research indicating that men are less likely than women to disclose childhood sexual abuse and that individuals are less likely to disclose instances of childhood sexual abuse when the perpetrator is a family member.
Goodman and colleagues’ (2003) own research involved 175 adults who had participated as children in a study regarding their sexual abuse and were reinterviewed by phone 13 years later, ostensibly for a study of their legal experiences and attitudes. They found that only 15.5 percent ( n =26) reported the abuse. They observed that their study, in contrast to the earlier studies they reviewed, had comprehensive records of the participants’ childhood sexual abuse, which enabled them to more accurately assess whether participants were disclosing information about the reported events. Factors associated with significantly lower likelihood of disclosing about childhood sexual abuse included abuse occurring at an early age (age 5 or earlier), less severe abuse, and less maternal support following the abuse. The authors did not find significant differences in disclosure between men and women. On the other hand, Edwards and colleagues (2003) found in the ACE study, as well as in some other research they reviewed, that most individuals who sustained childhood abuse are willing to discuss it and also believe that clinicians can help them cope with the effects of such abuse. The authors observed that differences in findings may reflect differences in how inquiries about childhood sexual abuse are made and how nonreporting of such abuse was evaluated, but also noted that the wrong assessment methods will fail to elicit reports about such trauma.
Clinicians may also have difficulties eliciting information about other types of interpersonal trauma, such as torture. Westermeyer, Hollifield, Spring, Johnson, and Jaranson (2011) assessed experiences of torture for 1,134 refugees from Eastern Africa, using a single direct question as to whether the individual had been tortured and a checklist of the 75 most common experiences of torture. They found a fair amount of disagreement between the two assessment methods; 14 percent of the sample reported 1 or more item of torture on the checklist but answered the single question negatively, and 9 percent of the sample answered that they had been tortured but indicated no experience that would be considered torture.
The authors suggested that those who reported an experience that qualifies as torture but did not indicate they had been tortured may have done so because they may have been so inundated with trauma in their environment that they did not perceive their experience as torture, they may have been afraid of being discriminated against because of their experiences, and/or they may have perceived their experiences to be punishment for political actions and not as victimization by torture. Those who indicated being tortured in answer to the general question but did not indicate any specific experiences differed from others in the study in that they were significantly more likely to be women; to be separated, divorced, or widowed; and to be significantly older (factors that may have played a role in shaping their response). The authors noted that this latter group was, like others in the study, highly traumatized and may have perceived their trauma as a form of torture, even if their specific experiences would not generally be categorized as torture. The results of this study suggest that multiple methods of screening/assessment may be needed to elicit information about certain types of trauma, such as torture.
Although childhood sexual abuse often goes unreported, another potential concern in assessment is whether recovered or discontinuous memories of childhood abuse (particularly childhood sexual abuse) are valid or accurate portrayals of an individual’s past trauma. Courtois (2000) discussed the reasons for the controversy surrounding recovered memories and the arguments given, both pro and con, concerning the validity of such memories. She also reviewed the conclusions of four expert panels that weighed in on the controversy. An APA panel cautioned that clinicians should not automatically disbelieve any reports of abuse, nor should they pressure clients to believe that abuse may have occurred. The APA similarly noted that all clinicians should take a neutral attitude toward reports of child abuse, and observed that despite it being possible to construct pseudomemories that may be mistaken for real events, there are no hard and fast rules as to when reports are inaccurate. She concluded that research has established that memories can be recovered, but also that false memories are possible.
Geraerts and colleagues (2007) reviewed, in greater detail, evidence that it is possible for individuals to regain previously forgotten memories of childhood abuse, but they observed that the cases where this has been established have not involved aggressive memory-recovery techniques (e.g., hypnosis). They also provided evidence from their own study of a self-selected sample of individuals with either continuous ( n =71) or discontinuous ( n =57) memories of childhood sexual abuse. They substantiated, using other sources, significantly more cases of discontinuous memory when the memory was recalled outside of therapy and, in fact, they could not substantiate any of the cases involving discontinuous memories that were recalled within the context of therapy. Similar percentages of continuous memories and discontinuous memories recalled outside of therapy were corroborated. Although this does not discount discontinuous memories first recalled within the context of therapy, it does suggest that it is more likely that some of them are not authentic.
In another study, Geraerts and colleagues (2009) evaluated the propensity to recall falsely and the tendency to forget prior instances of remembering among a Dutch sample of individuals who had memories of childhood sexual abuse recovered in therapy ( n =30) or recovered spontaneously ( n =30) or who had continuous memories of childhood sexual abuse ( n =30) or no such memories ( n =30). They found that individuals who recovered memories while in treatment appeared to be more susceptible to false memories; those who recovered memories outside treatment appeared more prone to forgetting past acts of remembering. Again, the tests used were not conclusive but do suggest underlying differences between those who may have false recall of childhood sexual abuse and those who may have forgotten and then recalled acts of childhood sexual abuse.
Certain aspects of traumatic stress reactions may also hinder effective assessment. Briere (2002) noted that avoidant PTSD symptoms, by their very nature, decrease clients’ responses to assessment questions and inhibit discussion of trauma. Such symptoms may even manifest as dissociative amnesia, which may make traumatic memories completely unavailable to clients.
- Prevention and Early Interventions for Traumatic Stress Reactions
This section covers a number of reviews and meta-analyses that evaluate different interventions for traumatic stress reactions (e.g., ACPMH, 2007 ; Bisson et al., 2007 ; Bisson & Andrew, 2009; Bradley, Greene, Russ, Dutra, & Western, 2005 ; Cloitre, 2009 ; Ehlers et al., 2010 ; Ponniah & Hollon, 2009 ; Seidler & Wagner, 2006 ). For more information on specific interventions and the seminal works that highlight them, refer to Part 1 of this TIP, “A Practical Guide for the Provision of Behavioral Health Services.” The following sections discuss the more commonly used or recommended interventions for preventing and treating traumatic stress reactions and provide information about selected research regarding the effectiveness of these interventions.
Prevention and Early Intervention
A number of interventions meant to reduce the effects of trauma and prevent the development of PTSD have been evaluated in the literature ( Resnick, Acierno, Kilpatrick, & Holmes, 2005 ; Zatzick et al., 2004 ). Such prevention activities may be presented as a form of psychological first aid delivered to everyone who has experienced a given type of trauma ( Everly, Phillips, Kane, & Feldman, 2006 ). Alternatively, indicated prevention may be provided for individuals who are considered at high risk for developing PTSD (e.g., people who have ASD) following trauma exposure.
Zohar, Sonnino, Juven-Wetzler, & Cohen (2009) explored whether PTSD can be prevented. They reviewed research indicating that individuals who have amnesia related to traumatic experiences are significantly less likely to develop PTSD. Animal research confirms this and also shows that stress related to trauma can be reduced/eliminated by chemically inducing amnesia. They noted that research with people who have had a myocardial infarction ( n =116) found that those who use a repressive coping style had significantly fewer symptoms of ASD and PTSD (the latter, up to 7 months after the event), suggesting that particular coping skills might aid in reducing traumatic stress reactions among those exposed to trauma (see Ginzburg et al., 2002 ).
Zohar and colleagues (2009) also reviewed research indicating that interventions that enhance a traumatic memory, such as some forms of psychological debriefing, are unlikely to be effective and may be harmful. Instead, the authors concluded that pharmacological interventions are likely to be the most effective means of preventing PTSD, although more research is needed to evaluate such interventions. Another review, conducted by Roberts, Kitchiner, Kenardy, and Bisson (2009a) , looked at 25 randomized controlled trials for multisession prevention interventions and concluded that trauma-focused cognitive–behavioral therapy (CBT) provided within 3 months of trauma exposure was effective at reducing PTSD symptoms, especially for those whose symptom levels met criteria for a PTSD diagnosis.
A review by Agorastos, Marmar, and Otte (2011) did not find sufficient evidence of any benefit from preventive interventions delivered within hours of trauma exposure, but they found some evidence that brief CBT delivered days or weeks after trauma reduced PTSD risk. These authors concluded that brief CBT interventions should be considered the best option for prevention. Prevention interventions that use CBT are difficult to distinguish from early treatment, but several other studies have also found them effective for reducing PTSD symptoms. For example, Israeli researchers compared four different early treatment options (prolonged ET, cognitive therapy, treatment with a selective serotonin reuptake inhibitor [SSRI], or placebo) with a waitlist control group ( Shalev et al., 2012 ). The researchers provided follow-up data for 182 participants. At the 5-month follow-up assessment, the PTSD prevalence rates were similar for the prolonged ET and cognitive therapy groups (21.4 percent and 18.2 percent of whom, respectively, had PTSD) and were significantly lower for participants who received those interventions compared with all others. Treatment compliance and completion rates were also similar across intervention groups.
A number of other reviews evaluating interventions to prevent traumatic stress reactions have been conducted. One that used stringent selection criteria was conducted for the Cochrane Collaboration ( DeSilva et al., 2009 ). This review evaluated prevention of physical and mental problems as well as impairments to social functioning that might result from trauma exposure. It did not, however, find convincing evidence for the effectiveness of interventions aimed at preventing behavioral health problems and, in fact, found three studies that provided good evidence that such interventions had a harmful effect on behavioral health.
Although less often recognized as prevention, material and social services provided to trauma victims appear to reduce PTSD risk. For example, among survivors of a tsunami in India, both satisfaction with services received and receiving three or more sessions of counseling were associated with significantly lower PTSD rates ( Pyari et al., 2012 ). Also, Ullman & Filipas (2001) found that having more services available was associated with a significant decrease in PTSD risk for women who had been raped or sexually abused. Kantor and Beckett (2011) reviewed more research that indicates that connecting trauma survivors with family, social support networks, and needed resources appears to be the most effective strategy for preventing traumatic stress reactions.
A number of models/interventions for providing social services to trauma victims have been developed, but most have not had high-quality evaluations. Walsh (2007) reviewed information on multisystemic, resilience-oriented interventions that have been used to help communities respond to large-scale traumatic events, drawing on examples from around the world. Agani, Landau, and Agani (2010) discussed the Linking Human Systems Community Resilience Model, which attempts to mobilize social resources to improve an entire community’s resilience in response to traumatic events. They also gave an example of the program’s use in Kosovo.
Principles of Effective PTSD Prevention
It is unclear whether a specific effective intervention is available for preventing PTSD, but some basic principles have been evaluated that many authors believe are helpful in the wake of trauma exposure. Hobfoll and colleagues (2007) delineated and reviewed research supporting the use of five basic principles to use when counseling someone who has recently been exposed to trauma:
- Promote a sense of safety . Research indicates that reestablishing a feeling of safety following trauma exposure can decrease PTSD risk, whereas individuals who exaggerate future risk following trauma have a higher rate of PTSD.
- Promote calmness . An initial reaction of anxiety and heightened emotional response is normal in the wake of trauma, yet studies indicate that when this type of response is prolonged, it is associated with a variety of behavioral health problems. Two interventions that work to calm individuals exposed to trauma or to teach skills for self-calming prior to trauma exposure have been evaluated and found effective at reducing PTSD: stress inoculation training ( Hembree & Foa, 2000 ) and ET ( Bryant, Harvey, Guthrie, & Moulds, 2003 ). Hobfoll and colleagues (2007) also recommend teaching problem-solving skills to improve clients’ abilities to appraise the nature of their problems realistically and provide psychoeducation about typical reactions to trauma to help them put feelings into context. Both techniques have strong theoretical support but lack research evaluating their effectiveness. Fostering positive emotions may also be helpful in this context, as such emotions have been found to have a protective relationship to behavioral health problems.
- Promote a sense of personal and collective efficacy. A belief in one’s own ability to recover from trauma (self-efficacy) and the ability of one’s community or group to do so (collective efficacy) has been shown to have a positive effect on one’s behavioral health. Skills can also be taught, for example, with CBT to improve self-efficacy. In the case of collective efficacy, providing social and economic resources is also important (as those individuals who lose more economically and socially have a harder time recovering from trauma).
- Promote connectedness. A number of studies have found that greater social support reduces the likelihood of developing PTSD following trauma exposure and improves recovery from it, and on the other hand, poor social support or a negative community response increases the odds that an individual will develop PTSD and hinders recovery. However, the quality of social support is important, not just the quantity. Studies have also demonstrated that negative social support, such as minimizing problems, invalidating feelings, or creating unrealistic expectations, is strongly associated with long-term distress following trauma (e.g., Andrews et al., 2003 ).
- Instilling hope. A greater sense of hope after trauma is associated with better outcomes in a number of areas. Research indicates that CBT can be used to address such factors as an exaggerated sense of personal responsibility or a tendency to classify experiences as catastrophic (e.g., turning every setback into a catastrophe), which can impede hope.
In a review that specifically addressed pharmacological interventions to prevent PTSD, Zohar and colleagues (2011) offered a different set of basic guidelines for preventing PTSD that should be followed when treating someone who has been recently exposed to trauma. These are: don’t pathologize (instead, explain that the individual’s response is normal given the abnormality of the situation), don’t psychologize (e.g., increase emotional reactions to the trauma or enhance traumatic memory through debriefing), and don’t pharmacologize (e.g., administer a benzodiazepine or sleeping pill in the first few hours). This last item has a caveat that medications are being researched (e.g., inderal, hydrocortisone) that may reduce PTSD if administered soon after trauma exposure.
Although most prevention activities for people who have been traumatized are aimed at preventing PTSD, it is possible to work to prevent other behavioral health problems in the wake of trauma. For example, Resnick, Acierno, Amstadter, Self-Brown, and Kilpatrick (2007) evaluated an intervention aimed at preventing substance abuse in the wake of sexual assault. According to data for 268 female adolescents and adults who received either a two-part psychoeducational intervention delivered via video or standard care alone and who were available for at least one of three follow-up assessments, viewing the video intervention was associated with significantly lower frequency of marijuana use at each of the follow-up times (less than 3 months, 3 to 6 months, or 6 months or longer post assault). However, women who did not have a prior rape history displayed higher PTSD and anxiety symptoms at 6 weeks. The results underscore the need to further explore other aspects of the findings.
Psychological First Aid
Some authors have adapted the basic principles suggested by Hobfoll and colleagues (2007 ; see “ Principles of Effective PTSD Prevention ”) as part of a program of psychological first aid (e.g., Kantor & Beckett, 2011 ; Ng & Kantor, 2010). Kantor and Beckett (2011) described the key features of psychological first aid as “contact and engagement, safety and comfort, stabilization, information gathering, practical assistance, connection with social supports, information on coping, and linkage with collaborative services” (p. 203). They also observed that psychological first aid is flexible and responsive to “the specific human needs and emotional style of an individual and his or her expressed needs at the moment of intervention” (p. 204).
Young (2006) observed that psychological first aid is indicated when an individual has an acute stress reaction in response to trauma (e.g., dissociative symptoms, extreme anxiety, a high level of cognitive impairment) or is at high risk for a traumatic stress reaction. The NCTSN and the NCPTSD (2006) created a manual, now in its second edition, that provides further guidelines for providing psychological first aid (available at http://www.nctsn.org/content/psychological-first-aid ). These guidelines have been widely accepted and adopted by organizations such as the American Red Cross ( Kantor & Beckett, 2011 ).
Military Prevention Programs
Prevention interventions have been developed specifically for members of the military who have been exposed to trauma (e.g., the Battlemind and the Master Resiliency Training Programs; see Reivich, Seligman, & McBride, 2011 ). Some of these programs are more immediate preventive measures delivered prior to deployment and/or after trauma exposure, and others are intended for the transition period when military personnel are returning from deployment. In a large study intended to evaluate these programs, Adler, Bliese, McGurk, Hoge, and Castro (2009) compared 4-month outcomes for 1,060 individuals who had returned from combat deployments in Iraq and had been randomly assigned to receive stress education delivered in large groups, a Battlemind debriefing session delivered in small groups, Battlemind training in small groups, or Battlemind training in large groups. At follow-up, participants in the Battlemind debriefing group with high levels of combat exposure had significantly fewer PTSD symptoms (according to PCL scores), fewer depression symptoms (according to scores on the Patient Health Questionnaire-Depression scale), and fewer sleep problems than did participants with high combat exposure who received stress education, but there were no significant differences for individuals with less combat exposure (and presumably less exposure to combat trauma). Individuals who participated in the large-group Battlemind training also had significantly fewer depression symptoms and fewer sleep problems than participants in the stress education group.
The VA and the U.S. Department of Defense ( VA/DoD; 2010 ) publication, Clinical Practice Guideline for Management of Post-Traumatic Stress , reviewed research on these programs and recommended four to five sessions of brief CBT as having the most benefit, although social support and psychoeducation/normalization also had some benefit. However, the guidelines did not address substance abuse or other comorbid conditions, and thus, their implementation requires careful evaluation depending on the complexity of the clientele.
Psychoeducation and Related Interventions for Prevention
Many interventions aimed at preventing traumatic stress reactions use psychoeducation to help people exposed to trauma understand psychological symptoms that may result from trauma, alter their perception of the traumatic event in a positive way, and be aware of behavioral health treatments available to alleviate posttraumatic psychological distress ( Wessely et al., 2008 ). There is evidence that psychoeducation can alleviate anxiety for some anxiety disorders (see discussion in the planned TIP, Managing Anxiety Symptoms in Behavioral Health Services [SAMHSA, planned d]). However, evidence concerning the use of psychoeducation for preventing PTSD is more complicated.
Wessely and colleagues (2008) reviewed research on psychoeducation interventions that have been evaluated for their ability to reduce posttraumatic psychological distress, some of which (e.g., stress inoculation approaches) have evidence supporting their use and others of which (e.g., single-session psychological debriefing) have been found ineffective or potentially harmful. The authors concluded that there is not yet sufficient evidence for psychoeducation in this context and that the quality of interventions for this purpose varies considerably. They noted that some evidence suggests that psychoeducation that “proactively encourages an expectation of resilience and, if necessary, help-seeking” may be beneficial (p. 296). The authors also warned that simply disseminating information about psychological symptoms and mental disorders that may result from trauma exposure is likely not to be useful and may be harmful. Other reviews (e.g., van Emmerik, Kamphuis, Hulsbosch, & Emmelkamp, 2002 ) and studies (e.g., Marchand et al., 2006 ) have found that a single session of incident stress debriefing is no better than no intervention for people exposed to various types of trauma. Educational debriefing and emotional ventilation debriefing were also found ineffective and actually associated with higher PTSD rates for individuals who had a high level of hyperarousal at the time of the intervention ( Sijbrandij, Olff, Reitsma, Carlier, & Gersons, 2006 ).
Medications To Prevent PTSD
Another possible way to prevent PTSD following trauma exposure is to administer a medication before or immediately following exposure. Fletcher, Creamer, and Forbes (2010) reviewed 15 studies that evaluated the use of medication for this purpose and concluded that, despite limited evidence, there are indications that hydrocortisone (which reduces the production of cortisol) and propranolol (which blocks norepinephrine reuptake) administered after trauma exposure may reduce PTSD rates. They noted that more extensive research is needed before medications such as these are used for trauma prevention (see also, Zohar et al., 2011 ).
Animal research appears to indicate that early administration of an SSRI following traumatic experiences may also significantly reduce PTSD-like behaviors, but more research is needed to confirm a positive effect for people ( Zohar, Sonnino et al., 2009 ). Notably, some medications that are used following trauma may actually make PTSD symptoms worse or increase the likelihood of developing PTSD. Zohar and colleagues (2011) reviewed two small human studies and one animal study that indicate that benzodiazepines administered following trauma exposure increase the likelihood of developing PTSD later on. Similarly, research from Germany indicates that ketamine administered to accident victims aggravates ASD symptoms and is associated with increased levels of PTSD symptoms 3 to 24 months after trauma exposure ( Schönenberg, Reichwald, Domes, Badke, & Hautzinger, 2005 , 2008 ).
Longer-Term Prevention Measures
Interventions 1 to 4 weeks after trauma exposure require different methods and are typically aimed at achieving different outcomes than are measures provided in the immediate aftermath of trauma ( Bryant & Litz, 2006 ). Interventions delivered 1 to 4 weeks after trauma exposure (such as interventions for people with ASD, discussed in the following section) more closely resemble treatment interventions and may even be labeled as assessment and early intervention rather than as prevention. Bryant and Litz (2006) reviewed some of the prevention tasks that might be used at this stage, including assessment of ASD and PTSD symptoms, trauma-focused CBT, ET, and eye movement desensitization and reprocessing (EMDR). They also observed that prevention activities at this stage will likely be targeted to individuals with ASD or those believed to be at high risk for PTSD.
Prevention for People With ASD
ASD following trauma exposure is associated with increased risk for developing PTSD later, so individuals with ASD are an appropriate target audience for indicated PTSD prevention. Ponniah and Hollon (2009) reviewed randomized clinical trials for both PTSD and ASD. Even though the research on ASD was limited to two studies, they concluded that, for preventing PTSD among people with ASD, trauma-focused CBT by itself or with an additional hypnosis component is more effective than supportive counseling and that imaginal and in vivo ET are more effective than either no treatment or cognitive restructuring.
Kornør and colleagues (2008) reviewed research on the delivery of trauma-focused CBT to people with ASD to prevent PTSD. All the studies included in their review compared trauma-focused CBT with supportive counseling. The authors concluded that trauma-focused CBT is superior to supportive therapy in terms of some PTSD outcomes (i.e., significantly lower PTSD rates at some, but not all, follow-up points; significantly lower levels of intrusion and avoidance symptoms up to 6 months later). However, the review included a limited number of studies (five trials, four of which were conducted by the same researchers), and further research is needed.
A review ( Roberts, Kitchiner, Kenardy, & Bisson, 2010b ) of interventions that treat ASD symptoms with the goal of preventing PTSD examined 15 studies that compared trauma-focused CBT, supportive counseling, cognitive restructuring (without exposure), behavioral activation, or stepped collaborative care with waitlist or treatment-as-usual controls; trauma-focused CBT was also compared with other active treatments (supportive counseling, structured writing therapy, or cognitive restructuring without exposure). Roberts and colleagues concluded that trauma-focused CBT is effective at reducing PTSD symptoms among those who meet criteria for ASD; weaker evidence suggests that it is effective with individuals who have symptoms of ASD without meeting all criteria for the diagnosis. Trauma-focused CBT compares favorably with waitlist and treatment-as-usual controls as well as supportive counseling, and some evidence indicates superior effectiveness 6 months after treatment compared with cognitive restructuring without exposure. They also found limited evidence that cognitive restructuring had a greater effect than waitlist controls. They found no evidence to support the use of other interventions.
It can be difficult to distinguish between interventions aimed at treating ASD and those intended to prevent the development of PTSD among people with ASD, as they largely focus on the same outcomes. For example, Bryant and colleagues (2008) evaluated imaginal/in vivo ET ( n =30), cognitive restructuring ( n =30), or assessment and a waitlist ( n =30) as treatment for ASD following either a vehicle crash or a nonsexual assault. Using an intent-to-treat analysis, they found that individuals who received ET were significantly less likely to have PTSD 6 months after treatment, had significantly fewer ASD/PTSD symptoms following treatment and at the 6-month posttreatment assessment, and had significantly better outcomes in terms of general distress, non-PTSD anxiety symptoms, and depressive symptoms. Individuals receiving cognitive restructuring also had significantly better outcomes than those in the waitlist control group, but effect sizes were about half as large as those found with the ET intervention.
- Trauma-Specific Treatments
Many different interventions and modalities are available for the treatment of trauma-related behavioral health problems. Although the focus of this TIP is on adults who have experienced trauma during their lifetimes, interventions have been designed and evaluated to address traumas across development that is, ET and EMDR are designed more for adult populations, whereas some CBTs have been tailored to reach a broader age range. Treatments need to be developmentally appropriate and specific. This section focuses on meta-analyses and reviews rather than seminal works to cover the prolific field of trauma research. For more detailed information on particular trauma-specific treatments, refer to Part 1 of this TIP, “A Practical Guide for the Provision of Behavioral Health Services.”
Most reviews and meta-analyses have found that the most effective trauma-related behavioral health treatments are trauma-focused CBTs, which are broadly defined to include ET and EMDR. These two approaches are usually found to be about equally effective. Some reviews (e.g., Bisson et al., 2007 ) have found that stress management and group CBT are effective, albeit somewhat less so than CBT and EMDR. Cloitre’s (2009) review provided mean effect sizes different treatments across multiple studies and found that trauma-focused CBT with cognitive restructuring had the largest mean effect size (8.83), followed by CBT with ET (8.04), ET alone (7.94), EMDR (5.89), and problem-centered therapy (5.67).
Mendes, Mello, Ventura, Passarela, and Mari (2008) reached somewhat different conclusions in their review of 23 clinical trials comparing CBT with other PTSD treatments. They found that CBT is associated with better remission rates than EMDR and with efficacy and compliance outcomes comparable to cognitive therapy and ET, suggesting that CBT is somewhat preferable to EMDR.
Clinical practice guidelines such as those from the ACMPH (2007) , the United Kingdom’s National Institute for Clinical Excellence ( NICE; 2005 ), and DoD and VA (2010) also generally endorse trauma-focused CBT and, in some cases, EMDR as the best initial approaches for treating PTSD. However, the National Institute of Medicine ( IOM, 2008 ), in its review and recommendations on PTSD treatment, found insufficient evidence supporting the use of EMDR, cognitive restructuring, coping skills therapy, and group therapy for PTSD, and endorsed only the use of ET, which they noted was a component of most CBT interventions. Benish, Imel, and Wampold (2008) —using a statistical approach that was conservative in design and analysis—concluded in their review that all interventions aimed at treating PTSD were basically equally effective. This review included trauma desensitization, EMDR, CBT, various forms of ET, stress inoculation, hypnotherapy, trauma-focused group therapy, psychodynamic therapy, and present-centered therapy. The authors also observed that about 25 percent of participants in the studies reviewed left treatment early, and thus concluded, “keeping patients in treatment would appear to be more important in achieving desired outcomes than would prescribing a particular type of psychotherapy” (p. 755).
Ehlers and colleagues (2010) raised two major objections in response to Benish and colleagues’ (2008) review. The review excluded some widely used treatments (notably, supportive therapy) because they did not meet their criteria of being a bona fide treatment but included others (e.g., present-centered therapy) that used many of the same components but were not as widely studied, and the review did not account for the need for treatments to show greater efficacy than natural recovery to establish their effectiveness. Ehlers and colleagues (2010) concluded that Benish and colleagues’ (2008) review findings are not sufficient to establish that all PTSD treatments (not just trauma-focused CBT and EMDR) are equally effective.
Large-scale reviews such as these present certain problems. As noted by IOM (2008) , interventions vary from one another in a number of different ways, such as “in their emphasis on re-exposure to trauma-related memories and stimuli, cognitive restructuring of the trauma experience, expression and management of emotion, training in stress management (including relaxation training), and general social and vocational support,” and few studies attempt to separate these components to evaluate their efficacy/effectiveness independently (p. 93). Thus, it is difficult to ascertain which parts of a given intervention produce positive change.
IOM (2008) also identified problems with PTSD research, such as study attrition, inadequate methods for addressing missing data, publication and investigator bias (e.g., pharmacological studies funded by drug companies), difficulties generalizing results found with one specific population or applying those results to another specific population, inadequate follow-up, and a dearth of high-quality randomized controlled studies. The report pointed out that even though a rigorous evidence base for a particular treatment or intervention may be lacking, this does not mean the particular treatment lacks clinical efficacy.
Cognitive–Behavioral Therapy
A number of specific PTSD interventions can be classified as CBT, and CBT for trauma and traumatic stress reactions typically includes multiple techniques/components. It is also usually trauma-focused (i.e., focused on helping clients address traumatic experiences). For example, in their review of CBT for trauma, Cahill, Rothbaum, Resick, and Follette (2009) evaluated seven different techniques/therapies, which they labeled as CBT: ET, stress inoculation training, cognitive processing therapy (CPT), cognitive therapy, relaxation training, dialectical behavior therapy (DBT), and acceptance and commitment therapy (ACT). CBT is a well-studied approach— Cahill and colleagues’ (2009) review included 64 randomized, controlled trials and many more nonrandomized trials. CBT is also generally recommended in the treatment of PTSD. Although much of the research has focused on CBT’s use in treating PTSD, a Cochrane review of treatments for ASD also found CBT to be more efficacious than waitlist controls or supportive counseling ( Roberts et al., 2010 ).
Reviews of CBT for the treatment of trauma and/or PTSD include those by Cahill and colleagues (2009) , Kar (2011) , and Mendes and colleagues (2008) . All concluded that evidence supports the effectiveness of CBT in the treatment of PTSD. Beck, Emery, and Greenberg’s (2005) book on a cognitive approach to treating anxiety disorders also has some discussion of how cognitive therapy may be applied to the treatment of PTSD.
Other reviews of CBT for anxiety disorders also found it to be an effective approach for treating PTSD and, in some cases, ASD ( Hofmann & Smits, 2008 ; Norton & Price, 2007 ; Otte, 2011 ; Stewart & Chambless, 2009 ). For example, Stewart and Chambless (2009) found that CBT performed significantly better in treating PTSD than nontreatment controls and had relatively large effect sizes in terms of reducing PTSD symptoms (with a combined standardized mean difference in effect size of 2.59, according to their meta-analysis). CBT has been successfully used for treating trauma and PTSD in a number of different populations, including child sexual abuse survivors with or without complex PTSD ( McDonagh et al., 2005 ; Resick, Nishith, & Griffin, 2003 ); women who have experienced domestic violence ( Johnson, Zlotnick, & Perez, 2011 ; Kubany et al., 2004 ); women who are victims of sexual assault ( Foa, Zoellner, & Feeny, 2006 ; Resick, Nishith, Weaver, Astin, & Feuer, 2002 ); people who survived motor vehicle crashes ( Beck, Coffey, Foy, Keane, & Blanchard, 2009 ; Maercker, Zöllner, Menning, Rabe, & Karl, 2006 ); victims of terrorism/civil conflict ( Duffy, Gillespie, & Clark, 2007 ; Hamblen, Gibson, Mueser, & Norris, 2006 ; Levitt, Malta, Martin, Davis, & Cloitre, 2007 ); refugees/asylum seekers ( Hinton et al., 2009 ; Paunovic & Öst, 2001 ); survivors of natural disasters ( Başoglu, Salcioglu, & Livanou, 2007 ; Hamblen et al., 2009 ); veterans/military personnel with combat trauma ( Kent, Davis, Stark, & Stewart, 2011 ; Khoo, Dent, & Oei, 2011 ; Schnurr, Friedman et al., 2003 ); and disaster aid workers ( Difede et al., 2007 ). Ruzek and colleagues (2008) specifically reviewed the use of CBT to treat trauma and traumatic stress responses in individuals who survived disasters or terrorist attacks, and Jaycox, Zoellner, and Foa (2002) reviewed its use with rape survivors.
CBT has also been effectively used to treat PTSD in clients with various co-occurring disorders, including panic disorder ( Falsetti, Resnick, & Davis, 2008 ; Hinton, Chhean, Pich et al., 2005 ), major depression ( Nixon & Nearmy, 2011 ), SMI (i.e., major depression, bipolar disorder, schizoaffective disorder, and/or schizophrenia; Mueser et al., 2008 ), substance use disorders (see the “ Integrated Approaches for Trauma and Substance Abuse ” section), BPD ( Dorrepaal et al., 2010 ), both depression and substance use disorders ( Norman et al., 2010 ), and chronic pain conditions ( Otis, Keane, Kerns, Monson, & Scioli, 2009 ). CBT has also been found to be an effective treatment for sleep problems associated with PTSD ( Carney & Edinger, 2010 ; DeViva, Zayfert, Pigeon, & Mellman, 2005 ; Nishith et al., 2003 ; Ulmer, Edinger, & Calhoun, 2011 ).
Trauma-focused CBT interventions have been culturally adapted for various client populations, including Latinas (Hinton, Hofmann et al., 2011), African refugees from two different nations ( Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004 ), Cambodians ( Hinton, Hofmann et al., 2009 ), and Vietnamese ( Hinton et al., 2004 ). Hinton, Kredlow, Bui, Pollack, & Hofmann (2012 ) discussed some of the ways in which CBT can be made more culturally relevant for refugees (and others) from non-Western cultures. For example, using emotional regulation techniques and imagery drawn from their cultural traditions, focusing on teaching psychological flexibility (an important skill for individuals trying to adapt to living in a multicultural environment), changing the focus of some CBT techniques (e.g., focusing on uncontrollable worry, a common expression of traumatic stress reactions in individuals from non-Western cultures), using culturally relevant rituals to mark transitions, and using CBT to address culturally specific syndromes (e.g., ataque de nervios among Latinos). CBT for trauma/traumatic stress reactions can be effectively delivered in groups as well as one on one (e.g., Beck et al., 2009 ; Kent et al., 2011 ). It has also been adapted for delivery by computer or over the Internet ( McLean, Steenkamp, Levy, & Litz, 2010 ).
Trauma-focused CBT can encompass a number of different techniques. Cahill and colleagues’ (2009) review listed various interventions/techniques that involve CBT principles and have been used for treating trauma/traumatic stress reactions These include ET (discussed separately in this section); stress inoculation training, a method of managing anxiety/stress; CPT, which teaches clients to address problematic cognitions such as self-blaming; cognitive therapy, another approach for modifying problematic/dysfunctional thinking; relaxation training, a behavioral approach for relaxing the body and mind to reduce stress/anxiety; DBT, a form of CBT developed to treat BPD; and ACT, an approach that fosters acceptance and awareness of internal states/feelings. Cahill and colleagues’ (2009) review summarized research supporting the use of each of these CBT interventions/techniques, noting that the strongest and most extensive research is for various exposure therapies; there are also multiple studies supporting the use of CPT, cognitive therapy, and stress inoculation training in this context.
Although the research on ACT for people with PTSD and trauma-related problems is limited, Walser and Westrup (2007) drew on theory and clinical experience to discuss why the approach may be effective with this population. They also provided a “how-to” guide for using ACT in this context. Researchers have found mixed results in comparing the effectiveness of different components of trauma-focused CBT; typically, this research has involved comparing ET and cognitive restructuring. Most studies have found that neither ET nor cognitive restructuring alone is more effective than the other, and although some studies have found that the combination of the two is more effective than either alone, others have not found that to be the case ( Resick et al., 2008 ).
Resick and colleagues (2008) took a somewhat different approach to evaluating the components of CPT, a CBT intervention that involves the use, separately and together, of cognitive therapy to address thinking patterns and narrative writing to enable clients to be exposed to traumatic memories in a relatively safe manner. Assessment 6 months after treatment showed no significant differences in symptoms of depression or PTSD between participants who received either component alone and those who received both components. However, when the participants who received cognitive therapy alone were compared with those who received the narrative therapy component alone, those in the former group had significantly lower levels of both PTSD and depression symptoms.
Not all CBT interventions used to treat PTSD are trauma-focused. For example, Monson, Rodriguez, and Warner (2005) compared CBT for PTSD that was trauma-focused (relying largely on ET to help clients reprocess traumatic experiences) with another CBT intervention that was skills-focused (helping clients learn and practice skills to manage PTSD symptoms). They did not find significant differences between the two in terms of outcomes for PTSD symptoms or alcohol abuse, but they did find that the perceived quality of clients’ intimate relationships prior to beginning treatment had a stronger negative relationship to violence perpetration (assessed using four questions from the NVRRS study) if the client received trauma-focused rather than skills-focused CBT, suggesting that clients with stronger intimate relationships may gain some added benefit from trauma-focused CBT.
Building strength and resilience can be the focus of a CBT intervention. In a pilot study, Kent and colleagues (2011) used a resilience-oriented CBT intervention with 39 veterans who had PTSD. The authors found large improvements in terms of affective symptoms and positive emotional health, a moderate improvement in memory, and a small-to-moderate improvement in executive functioning.
CBT has also been combined with other approaches/interventions to improve treatment of PTSD and other consequences of trauma. Positive outcomes have been found using CBT combined with behavioral activation, a more purely behaviorist approach to treatment ( Nixon & Nearmy, 2011 ), as well as with CBT combined with pharmacotherapy (see studies reviewed by Stein, Ipser, & McAnda, 2009 ). Although many CBT interventions are manualized, Levitt and colleagues (2007) , in a study that evaluated flexibility in the application of a manualized CBT treatment for 59 survivors of the 9/11 attack, found that effects sizes for the treatment using a more flexible approach were comparable to those observed in other studies that had more strict adherence to the manual.
Eye Movement Desensitization and Reprocessing
EMDR is a technique that helps desensitize clients to traumatic memories, replace distressing cognitions with positive ones, and learn to attend to bodily sensations, thoughts, and feelings in a manner similar to mindfulness meditation approaches ( Foa, Keane, Friedman, & Cohen, 2009 ; Spates, Koch, Cusack, Pagoto, & Waller, 2009 ). A number of literature reviews/meta-analyses have found EMDR to be an effective treatment for PTSD, with the caveat that the eye movements themselves do not appear to be necessary in order for the intervention to be effective ( Ehlers et al., 2010 ). Although IOM (2008) guidelines do not recommend EMDR, guidelines from Australia ( ACPMH, 2007 ) and Great Britain ( NICE, 2005 ) have included it as an effective approach. SAMHSA’s National Registry of Effective Evidence-Based Programs and Practices (NREPP; http://nrepp.samhsa.gov ) also recognizes EMDR as effective in reducing PTSD, anxiety, and depression symptoms.
Spates and colleagues (2009) reviewed research specifically on EMDR as a treatment for PTSD. Among the studies they reviewed are ones that found EMDR more effective than relaxation training, habituation training, fluoxetine, placebo pill, and standard care. They reported on two studies that found better outcomes for EMDR than for prolonged ET and other studies that found that ET produced better outcomes than EMDR. They concluded that the two treatments are about equally effective. One study they reviewed also indicated that EMDR produced significantly better outcomes for clients with adult-onset rather than childhood-onset trauma.
Ehlers and colleagues’ (2010) review concluded that, although EMDR is effective for PTSD, the eye movement component of the treatment is not necessary. Davidson and Parker (2001) reached a similar conclusion in an earlier meta-analysis of EMDR, finding that no additional effect could be found when EMDR was practiced with the eye movements compared with when it was practiced without them. Spates and colleagues (2009) also reviewed studies that evaluated the benefit of the eye movement component of EMDR. They observed that early research did not find any additional benefit, but that one small study found that bilateral eye movements (the type used in EMDR) produced somewhat quicker results than other types of eye movements. Other studies of this aspect of EMDR either have not used clinical samples or have other significant methodological problems.
Exposure Therapy
ET may be considered as a component of trauma-focused CBT (e.g., Cahill et al., 2009 ) or evaluated as an intervention in and of itself (e.g., IOM, 2008 ). It has been recommended for the treatment of PTSD in a number of guidelines (e.g., ACPMH, 2007 ; DoD/VA, 2010 ; IOM, 2008 ) and reviews (e.g., Bisson & Andrew, 2007 ; Bradley, Greene et al., 2005 ; Cloitre, 2009 ; Ehlers et al., 2010 ). Prolonged exposure (PE; Foa & Rothbaum, 1998 ; Foa, Hembree, & Rothbaum, 2007 ; see also NREPP ) is the specific model of ET for PTSD that has been the most widely researched and is recommended in a number of PTSD treatment guidelines and reviews (e.g., IOM, 2008 ).
In their review of PE, McLean and Foa (2011) described recommended practice, presented the theoretical underpinnings of the intervention, and briefly reviewed the research supporting its use. Reviewing 25 randomized, controlled trials, the authors concluded that studies have consistently found that PE is effective in reducing PTSD. A few studies also indicated that PE is effective for both acute and chronic PTSD, produces results that persist for 1 year or more, produces relatively quick results, and has relatively large effect sizes. PE is more effective than waitlist controls, relaxation training, supportive counseling, and treatment as usual; it is as effective as other recommended PTSD treatments.
Another meta-analysis of PE, which included 13 studies and a total sample of 657, reached similar conclusions ( Powers, Helpern, Ferenschak, Gillihan, & Foa, 2010 ), finding it more effective than nontreatment control conditions and as effective as other active treatments (e.g., EMDR, CBT). According to Powers et al.’s analysis of combined data, the average client receiving PE had better posttreatment outcomes than 86 percent of participants in control groups. PE had high to medium effect sizes for primary and secondary outcomes at follow-up assessments. Rachamim, Nacasch, Shafran, Tzur, and Gilboa-Schechtman (2009) also reviewed research on the use of PE for PTSD, with particular attention to research conducted in Israel. Another meta-analytic review by Ougrin (2011) compared data on the effectiveness of cognitive therapy and ET and found no significant differences in effectiveness between the two.
A few studies of PE have been published since these reviews. One by Resick, Williams, Suvak, Monson, and Gradus (2012) followed up earlier research and provided long-term (i.e., 5 to 10 years after initial treatment) follow-up data for 126 women (out of an initial 171) who had been rape victims and had PTSD that was treated with either PE or CPT. Participants in both treatment groups had significant reductions in PTSD symptoms (according to both the PTSD Symptom Scale and the CAPS) that persisted over the long-term follow-up period, with no significant differences between the two treatment arms. At the long-term follow-up assessment, 93.4 percent of those who received CPT and 91.9 percent of those who received PE had 10-point reductions in CAPS scores from pretreatment levels, and 88.5 percent of those who received CPT and 88.7 percent of those who received PE had 20-point reductions. Also, at the long-term follow-up assessment, only 22.2 percent of those who received CPT and 17.5 percent of those who received PE met criteria for a current PTSD diagnosis (down from 100 percent at the start of treatment).
ET (typically PE) has been found to be effective with different populations, including female veterans ( Schnurr et al., 2007 ), male combat veterans ( Yoder et al., 2012 ), female victims of rape ( Resick et al., 2012 ), women who were victims of childhood sexual assault ( McDonagh et al., 2005 ), survivors of terrorist attacks ( Schneier et al., 2012 ), and refugees exposed to political violence/torture ( Paunovic & Öst, 2001 ). ET has been found to be effective when delivered in groups ( Ready et al., 2008 ) as well as individually.
Some research suggests that traditional ET models may not be suitable for members of all cultural groups and that individuals from non-Western cultures may find ET harder to tolerate or may have some degree of worsening of symptoms before they respond to treatment ( Hinton, Rivera, Hofmann, Barlow, & Otto, 2012 ). However, there is a lack of research evaluating this, and no significant data are available.
Hinton, Rivera, and colleagues (2012) recommended that, when using ET with refugees from non-Western cultures, clinicians should take a phased approach (e.g., teach emotional regulation skills such as meditation or muscle relaxation before using exposure techniques), use a trauma protocol (described in the article) that includes emotional regulation techniques and discussion to make ET more acceptable, and use interoceptive exposure techniques with positive reassociations (as this population has a high level of somatic complaints associated with their trauma, and those somatic sensations often perpetuate PTSD). They also recommended ways these techniques can be made more culturally relevant (e.g., understanding and using imagery and techniques drawn from clients’ cultural traditions when teaching emotional regulation). Their advice is also applicable to nonrefugee populations from diverse cultural backgrounds.
ET has also been adapted, as multiple channel exposure therapy, to treat co-occurring PTSD and panic disorder ( Falsetti et al., 2008 ), and it has been combined with DBT to treat co-occurring PTSD and BPD ( Harned, Korslund, Foa, & Linehan, 2012 ). Najavits, Schmitz, Gotthardt, and Weiss (2005) also reported on a small study ( N =5) combining ET and Seeking Safety for men with co-occurring PTSD and substance use disorders. Looking at whether ET may be made more effective and palatable if used in combination with other treatments, Foa, Rothbaum, and Furr (2003) reviewed five studies combining ET and other CBT interventions and found little significant improvement associated with the additional therapies (only one of the studies found some improvement in outcomes). A later study by Foa and colleagues (2005) also found no significant differences when cognitive restructuring was added to ET, but there was some evidence that individuals with severe trauma-related thoughts did better in ET alone than in the combined treatment.
More recent research suggests benefits to adding cognitive restructuring to ET. A study that randomly assigned 118 individuals with PTSD to receive imaginal exposure, in vivo exposure, both combined, or both with additional cognitive restructuring found that fewer participants in the combined group had PTSD at the 6-month follow-up; findings also showed significantly larger effect sizes for PTSD and depression outcomes in the combined treatment group compared with all others ( Bryant, Moulds et al., 2008 ). A randomized trial of ET with and without additional cognitive restructuring found that men who received ET alone ( n =32) had significantly higher levels of PTSD symptoms at a 6-month posttreatment follow-up assessment than did men who received ET plus cognitive therapy ( n =20) or women in either group ( n =56; Felmingham & Bryant, 2012 ). The authors concluded that these gendered differences in treatment responses suggest that the combined treatment is a better option for men with PTSD.
Beidel, Frueh, Uhde, Wong, and Mentrikoski (2011) compared ET alone with ET in combination with social–emotional rehabilitation for combat veterans ( N =35). They found no significant differences in PTSD outcomes, but they did find that people who received the additional treatment participated in social activities more frequently and spent a greater amount of time engaged in such activities. ET has also been effectively combined with pharmacotherapy. Schneier and colleagues (2012) found that PE combined with pharmacotherapy (Paroxetine) was associated with better outcomes than PE alone in a group of survivors of the 9/11 attack ( N =37).
One recent modification of ET is the use of virtual reality (VR) software to deliver exposure experiences in a more controlled and perhaps more realistic manner ( Alcañiz, Lozano, & Rey, 2004 ; Botella et al., 2004 ). Recent literature reviews by Gerardi, Cukor, Difede, Rizzo, and Rothbaum (2010) and Meyerbröker and Emmelkamp (2010) have found that VR shows promise as a way to enhance ET for people with PTSD. However, the studies included in these reviews are small, often do not use control groups or random assignment, and mostly involve veterans with combat-related PTSD. A study from Spain compared a VR intervention ( n =19) with standard CBT ( N =20) for individuals with a stress-related disorder (PTSD, pathological grief, or adjustment disorders) and found no significant differences in outcomes related to those disorders and significantly better outcomes in terms of depression, social interference, and relaxation for those who received the VR intervention ( Baños et al., 2011 ).
Another promising innovation in the delivery of ET is narrative ET, which was originally developed for use in countries with less economic development but has since been used in more developed nations ( Robjant & Fazel, 2010 ). This approach was designed to be delivered by individuals who are not mental health professionals and to require a relatively short treatment time; it was also intended to document atrocities as well as treat PTSD. It is a manualized approach and involves emotional exposure to memories of trauma that takes place in the context of creating a narrative about the traumatic event. Robjant and Fazel (2010) reviewed findings from six trials involving the treatment of both children and adults that were conducted in countries with low to medium economic development and four conducted in countries with high economic development (although typically with refugee populations). These studies found that participation in the intervention was associated with reductions in PTSD symptoms and, in some cases, with reductions in other mental disorder symptoms and improvements in overall psychological well-being. Studies found greater improvements in outcomes among those receiving the intervention compared with no treatment, treatment as usual, psychoeducation, interpersonal therapy, or supportive counseling.
Some authors have raised concerns that ET may worsen symptoms for some clients and that dropout rates are high because the treatment is unpalatable to some. Cahill, Foa, Hembree, Marshall, and Nacash (2006) reviewed research regarding dropout and worsening of symptoms in the context of a larger review on the dissemination of ET for PTSD. They observed that studies have found dropout rates for ET to be comparable to those of other active treatments but significantly higher than nontreatment controls; the amount of worsening of symptoms was no different from that found in other active treatments but significantly lower than found in nontreatment controls.
Psychodynamic Approaches
Most research reviews and meta-analyses have found psychodynamic therapies to be relatively ineffectual in the treatment of PTSD. However, in a review of research on psychodynamic treatments for PTSD, Schottenbauer, Glass, Arnkoff, & Gray (2008) argued that this is because such reviews consider only limited outcomes and claimed that psychodynamic approaches are helpful in ways that are typically not evaluated in the research, such as by improving self-esteem, relationships, problem-solving, and social functioning. They also noted that research indicates that such improvements often continue after treatment concludes. In addition, their review discussed how research and clinical observation indicate best uses for psychodynamic therapy with clients who have PTSD, particularly those with complex PTSD.
Kudler, Krupnick, Blank, Herman, & Horowitz (2009) reviewed research on psychodynamic therapy in the treatment of PTSD and derived similar conclusions. They observed that psychodynamic approaches place a priority on individualizing treatment but that such approaches are not indicated for every client. They also provided guidelines for which clients are best suited to this treatment modality.
Pharmacotherapy
A number of treatment guidelines also recommend pharmacotherapy as a possible treatment for PTSD, although typically not as the first line of treatment (e.g., ACPMH, 2007 ; Benedek, Friedman, Zatzick, & Ursano, 2009 ; DoD/VA, 2010 ; NICE, 2005 ). A variety of medications have been evaluated as PTSD treatments, but the most often recommended or suggested medications are, in order of preference, SSRIs, serotonin norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants, monoamine oxidase inhibitors (MAOs), and atypical antipsychotics (see reviews by Friedman & Davidson, 2007 ; Ravindran & Stein, 2009 ; Stein, Ipser, & Seedat, 2006 ). Paroxetine and sertraline (both SSRIs) have been approved by the Food and Drug Administration for the treatment of PTSD, the latter for long-term as well as short-term treatment (Ipser & Stein, 2011).
Various reviews and guidelines recommend SSRIs as the first medication to try when treating PTSD (see review by Stein et al., 2009 ). Ravindran and Stein (2009) agreed with other reviews in noting that SSRIs have the most research supporting their use in this context, and, of the SSRIs, fluoxetine is the most researched and has generally been found to be effective in alleviating PTSD symptoms, reducing the likelihood of relapse to PTSD once remission is achieved, and alleviating other mental disorder symptoms that might complicate treatment. Acute-phase trials of sertraline have had somewhat mixed results; at least one trial involving veterans with relatively severe PTSD found that symptom improvements associated with sertraline were not significantly better than those associated with placebo use. Stein et al. observed that current guidelines recommend that SSRIs be used for 6 to 12 months for acute PTSD and 12 to 24 months for chronic PTSD; in some cases, an even longer period of treatment may be required. Studies of longer-term use of sertraline have shown better results and have consistently found significantly better improvements than placebo use.
A Cochrane review by Stein and colleagues (2006) found that, in the 35 randomized controlled trials they evaluated, a significantly larger percentage of clients with PTSD responded to medications than to placebo; most of these studies indicate that SSRIs are effective for treating PTSD. Ravindran and Stein (2009) noted that paroxetine also has a number of studies supporting its use, albeit fewer than the other SSRIs; a few other SSRIs (i.e., citalopram, escitalopram, fluvoxamine) have also been found effective in more limited research. Research comparing different SSRIs/SNRIs has not generally found significant differences in PTSD outcomes ( Benedek et al., 2009 ).
A review by Ipser and Stein (2011) added to the knowledge base but also drew the same basic conclusions that SSRIs, the SNRI venlafaxine, and the atypical antipsychotic risperidone all are effective at reducing PTSD severity/symptoms. These authors also observed that sample characteristics do not appear to have a significant relationship to treatment response for these medications. Ravindran and Stein (2009) noted that the SNRI venlafaxine has been evaluated in a couple of research trials that found its use to be associated with significantly better outcomes than use of a placebo, although one trial did not find significant differences between venlafaxine and the SSRI sertraline. Other research has found no significant ethnic/racial or gender differences associated with response to venlafaxine, whereas differences in type of trauma were associated with significant differences in some outcomes (i.e., symptom-related disability, resilience) but not others (e.g., PTSD symptoms; Rothbaum et al., 2009).
Berger and colleagues (2009) specifically reviewed the use of medications other than SSRIs, which may be needed because many clients with PTSD do not respond to SSRIs. The authors found the strongest evidence for the use of atypical antipsychotics, especially risperidone, which has been found to be superior to placebo in reducing PTSD symptoms in three trials. Olazapine has also been found effective in this regard in some, but not all, studies. The authors observed, however, that these medications do not appear to have an effect on avoidance behavior or emotional numbness. In a meta-analytic review of atypical antipsychotics for PTSD, Pae and colleagues (2008) noted that, although these medications have been shown in a number of studies to reduce PTSD symptoms to a greater degree than placebos, most of the difference is a result of reduced intrusion symptoms. Ravindran and Stein (2009) noted that, as expected, these medications are particularly helpful for clients who have PTSD with psychotic symptoms, but the authors also cautioned about negative side effects, such as excessive weight gain.
Other medications evaluated for PTSD show less promise but may be indicated in cases where individuals do not respond to SSRIs. Ravindran and Stein (2009) noted that the tricyclic antidepressants amitriptyline and desipramine perform better than placebos in reducing some PTSD symptoms. Also, some, but not all, studies have found MAOs more effective than placebo in addressing PTSD symptoms. Both Berger and colleagues (2009) and Ravindran and Stein (2009) pointed to research indicating that the antiadrenergic agent prazosin is an effective medication for improving sleep quality and reducing nightmares among people with PTSD. More research on these medications is needed.
Not all reviews/guidelines recommend pharmacotherapy for PTSD, however. Notably, IOM (2008) found that for all the medications included in the review (including SSRIs and atypical antipsychotics), there was inadequate evidence to determine their efficacy in treating PTSD. One IOM panel member contributed a dissenting opinion in Appendix H of the report, stating that he believed this conclusion was incorrect and disagreed with the panel decision to group research conducted with civilian and veteran populations. He noted that if studies showing a lack of efficacy with veterans who had chronic PTSD were removed from the pool, remaining evidence would indicate that SSRIs and atypical antipsychotics could be effective treatments for PTSD.
Ravindran and Stein (2009) also observed, in response to the IOM report, that SSRI efficacy varies considerably among individuals, and hence, the modest effect sizes do not mean that these medications should be discounted. A review by Choi, Rothbaum, Gerardi, and Ressler (2010) of the use of pharmacological agents to improve the results of other therapies concluded that most studies have not found any additional improvement in outcomes associated with the addition of SSRIs. However, their review did not consider evidence for the use of SSRIs with individuals who have not been responsive to other therapies. They also suggested that there are new medications being evaluated (notably D-cycloserine) that may improve clients’ responses to PTSD therapy.
A Cochrane review by Hetrick, Purcell, Garner, and Parslow (2010) on combined pharmacotherapy and psychological therapies for PTSD looked at four that met more stringent inclusion criteria and concluded that there was insufficient data to determine whether combination therapy produced better results than pharmacotherapy or a psychological therapy alone. Little research evaluates the effects of culture on outcomes in pharmacotherapy for PTSD, but one study by Hinton, Kredlow, and colleagues (2012) found that CBT combined with paroxetine was effective in reducing not only PTSD symptoms, but also culturally salient somatic complaints and culturally specific disorders in a group of 56 Cambodian refugees with PTSD.
Group Therapy
Several of the therapies previously mentioned, and some discussed in the “ Other Interventions ” section, may be delivered in a group format. However, many of these interventions have not been evaluated as group treatments for clients who have PTSD and/or trauma histories. Group interventions may be particularly useful for clients with PTSD, because PTSD often causes isolation and disengagement from others ( Ford, Fallot, & Harris, 2009 ).
Therapeutic groups may consist of people who share a common type of trauma, such as combat trauma ( Schnurr et al., 2003 ) or torture/political violence ( Kira et al., 2012 ). Homogeneity in clients’ backgrounds may be advisable for reasons connected to trauma. For example, in an article on group therapy for refugees and torture survivors, Kira and colleagues (2012) recommended single-gender groups (to facilitate expression of taboo topics) and groups of a single ethnicity (to build self-esteem/group pride and avoid intergroup conflicts). Survivors of childhood sexual abuse ( Classen, Koopman, Nevill-Manning, & Spiegel, 2001 ) or other sexual trauma ( Lynch, 2011 ) are other populations for whom trauma-specific and/or gender-specific groups may be preferred.
Shea, McDevitt-Murphy, Ready, and Schnurr (2009) reviewed research on group therapy for PTSD. They noted that cognitive–behavioral group therapy, which has been evaluated with combat veterans and adult survivors of sexual abuse, is more effective than nontreatment controls and about as effective as present-centered group therapy at reducing PTSD symptoms. Another review of PTSD treatments by Bisson and Andrew (2009) similarly concluded that trauma-focused CBT groups are more effective than waitlist controls and not significantly different from group CBT not focused on trauma.
The major study evaluated by both these reviews found that both trauma-focused CBT and present-centered group interventions were associated with significant improvements in a number of PTSD symptom measures and significant reductions in the use of VA services during the year after the interventions ( Schnurr, Friedman et al., 2003 ). Although dropout rates were somewhat higher for clients who received the trauma-focused CBT group intervention, for those clients who completed 24 or more sessions (out of 35), participation in the trauma-focused CBT group was associated with more improvement in avoidance/numbing and hyperarousal PTSD symptoms than was participation in the other group. Shea and colleagues (2009) also noted that survivors of childhood sexual abuse who participated in interpersonal/process groups had better outcomes than nontreatment controls and outcomes that were not significantly different from those of survivors who participated in trauma-focused groups. However, this type of group intervention has been found to be ineffective in groups where one or more participants have BPD. Insight-oriented/supportive groups may be more effective than no-treatment controls.
Another study conducted with survivors of childhood sexual abuse ( N =166) found significantly greater reductions in PTSD symptoms among those who participated in either trauma-focused group or present-centered group therapy (both based on CBT principles) than among those assigned to a waitlist control group, but it found no significant differences in PTSD outcomes between the two treatment groups ( Classen et al., 2011 ). The only significant difference in outcomes between the two treatment groups was that participants in the trauma-focused group had a significantly greater reduction in anger. Additionally, Shea and colleagues (2009) observed that, although trauma-focused groups appeared to be as effective as other types of group therapy for treating PTSD, there was little evidence suggesting that they were any more effective. Likewise, there was no evidence that group therapy for PTSD was any more or less effective than one-on-one interventions (although they were only able to locate one study that made such a comparison).
Family and Couples Therapy
Although it is not recommended for everyone with PTSD, a number of reviews and guidelines indicate that family or couples therapy is a useful second-line approach to treating otherwise resistant PTSD and is a useful primary approach for clients who have significant family issues that need to be addressed as part of their treatment (e.g., Cukor, Spitalnick, Difede, Rizzo, & Rothbaum, 2009 ; DoD/VA, 2010 ; Sherman, Zanotti, & Jones, 2005 ). There is good reason to believe that family and couples interventions may be helpful for people with PTSD, and a family member’s PTSD will likely negatively affect family interactions and the entire family’s behavioral health ( Erbes, 2011 ; Guay et al., 2006 ). In their review of couples and family therapy for clients with PTSD, Riggs, Monson, Glynn, and Canterino (2009) observed that such interventions typically either focus on healing the disruptions to the family and/or relationship that results when one member has PTSD or involving the family/partner in treating one family member/partner’s PTSD, although some more recent interventions (e.g., Monson, Stevens, & Schnurr, 2005 ) attempt both. In some cases, for example in the wake of natural disasters, more than one family member may be exhibiting the effects of posttraumatic stress, and a somewhat different focus may be required.
Riggs and colleagues (2009) reviewed limited research regarding behavioral family therapy, behavioral marital therapy, cognitive–behavioral couples treatment, lifestyle management courses, emotionally focused couple therapy, spousal education and support programs, family systems-based therapy, and critical interaction therapy. They found relatively strong evidence supporting the use of behavioral family and behavioral marital therapies, somewhat weaker evidence supporting the use of cognitive–behavioral couples treatment and lifestyle management courses, and weak to no support for the other types of family interventions included in the review. Structured approach therapy (SAT) is yet another couples-based therapy for PTSD that has been evaluated with veterans and their spouses for reducing PTSD avoidance symptoms ( Sautter, Armelie, Glynn, & Wielt, 2011 ). Preliminary research indicates that participants (six Vietnam veterans and their partners) experienced significant reductions in avoidance symptoms (according to self-reports, clinician ratings, and partner ratings), emotional numbing, and overall PTSD severity according to both the CAPS and the PCL following participation in SAT ( Sautter, Glynn, Thompson, Franklin, & Han, 2009 ).
Fredman, Monson, and Adair (2011) recommended cognitive–behavioral conjoint therapy for PTSD specifically with veterans and their families and provided a case study in its use. Weine and colleagues (2008) recommended multiple-family groups for refugees with PTSD and their families to increase participation in behavioral health services. Some clients may express a preference for family/couples therapy, especially if it is offered as an option for treatment. For instance, a survey of 97 National Guard members with spouses and children (47 with PTSD) expressed a preference for family therapy ( Khaylis, Polusny, Erbes, Gewirtz, & Rath, 2011 ).
Other Interventions
Promising new approaches for treating PTSD are also being tried or evaluated but require further research before they can be recommended. Cukor and colleagues (2009) reviewed research on many of these, including couples/family therapy, behavioral activation, trauma management therapy, interoceptive exposure, mindfulness, imagery rescripting, imagery rehearsal therapy, DBT, ACT, thought-field therapy, trauma incident reduction, visual kinesthetic disassociation, and virtual reality ET. Their major conclusions in regard to these new approaches were:
- There is strong evidence supporting the use of new technology, including virtual reality, in the treatment of PTSD.
- D-cycloserine for use in enhancing ET is the most promising new medication being evaluated, and its use is likely to reduce the time needed for ET.
- There is good theoretical support and some evidence suggesting that family and couples therapy will be useful for some clients, but conclusive evidence is still lacking.
- ACT and DBT may be useful for increasing distress tolerance, and the latter has been found effective for women with histories of childhood abuse but not with other populations (whereas the former lacks research demonstrating its effectiveness for people with PTSD).
- Behavioral or cognitive–behavioral approaches (e.g., behavioral activation, mindfulness meditation therapy) have good evidence demonstrating their usefulness in ameliorating some PTSD symptoms.
- Trauma management therapy, used together with ET, shows promise as a treatment for negative PTSD symptoms.
- Imagery-based treatments (i.e., imagery rescripting and imagery rehearsal therapy) appear to be useful in some contexts, the former as a treatment for PTSD-related nightmares and the latter as a potential enhancement to imaginal ET.
For all of these interventions, further research is needed. The authors observed that some of the other approaches they considered (e.g., complementary approaches such as yoga and acupuncture) may also prove to be useful adjuncts to treatment. Hollifield (2011) also discussed the use of acupuncture to treat PTSD, noting that no research studies are available concerning its effectiveness, but some research and theory suggest that acupuncture may be effective given its action in other areas. People who are susceptible to hypnosis have an elevated risk for developing PTSD following trauma exposure, and for this and other reasons related to the nature of PTSD symptoms, several authors have recommended hypnosis as an adjunctive treatment for PTSD ( Cardeña, Maldonado, van der Hart, & Spiegel, 2009 ). This review also discussed methods for using hypnosis to help clients with PTSD. Creative therapies, such as art and music therapy, have been used with this population. Clinical reports indicate that they can be effective, but there is little research supporting their use with adults who have PTSD (more is available regarding children and adolescents; see review by Johnson, Lahad, & Gray, 2009 ).
Dropout and Treatment Response
Rates of dropout and nonresponse to treatment are high for most of the interventions discussed thus far, even those most often recommended for this population. Schottenbauer, Glass, Arnkoff, Tendick, and Gray (2008) reviewed data on dropout and nonresponse rates for the most commonly used PTSD treatments. They found dropout rates ranging from 0 to 50 percent for ET/PE, 5 to 32 percent for CBT, and 0 to 36 percent for EMDR. Nonresponse rates were 20 to 67 percent for ET/PE, 16 to 71 percent for CBT, and 7.3 to 92 percent for EMDR. Although the authors observed that these rates are high, they also cautioned against making comparisons of dropout/nonresponse between different types of interventions because of substantial differences in methodology. A meta-analysis that included 25 studies evaluating ET, CBT, or EMDR found that dropout rates for the three types of interventions did not differ significantly; control conditions had significantly lower dropout rates than either ET or CBT, but not EMDR ( Hembree et al., 2003 ).
Schottenbauer, Glass, Arnkoff, Tendick, and Gray (2008) also reviewed research associated with dropout and nonresponse to treatment. They found that dropout rates for a number of recommended treatments (ET, cognitive therapy, stress inoculation therapy, and EMDR) were higher than those found in control conditions, such as waitlists and relaxation training. Surveys of clients who had dropped out of treatment suggested that logistical issues (e.g., lack of transportation, inability to find child care) were often a problem, as were problems with social adjustment (the latter according to a study of ET conducted with clients who had PTSD and co-occurring alcohol dependence). Another study included in the review found that the credibility of the treatment for the client was a significant factor in dropout.
Zayfert and DeViva (2010) cited studies that found that the risk of treatment dropout is greater for clients with more severe PTSD symptoms (especially more severe avoidance symptoms), with greater anxiety, with more severe symptoms of depression, and with greater use of alcohol. Male clients are also more likely to drop out of treatment than female clients. These authors also observed that worsening of symptoms during treatment, which many clinicians believe is a cause of treatment dropout, has not been associated with increased dropout rates.
Zayfert and DeViva (2010) analyzed factors associated with treatment response, observing that studies have found that childhood trauma and/or complex trauma is associated with worse response, as is use of prescription sedatives, male gender, higher suicidality ratings, being single (rather than married or living with a partner), having more severe PTSD symptoms, having GAD, having greater anger, and having more physical pain. On the other hand, Schottenbauer, Glass, Arnkoff, Tendick, and Gray (2008) observed, based on their review, that demographic factors appear to have very little relationship to treatment response. Also, trauma severity (particularly severity of childhood abuse) may have a negative effect on outcomes, but not every study has found this to be the case. They also found mixed evidence on the effects of co-occurring depression, co-occurring personality disorders, anger related to trauma, and guilt/shame on PTSD treatment outcomes. They discussed some of the methods suggested in the literature to improve treatment response, including being flexible about the number of sessions and offering or using more than one treatment technique/intervention.
- Integrated Approaches for Trauma and Substance Abuse
Traumatic stress and PTSD frequently co-occur with substance use disorders. As a result, many clients seeking treatment for PTSD will require substance abuse treatment services and vice versa. Ouimette, Moos, and Brown (2003) reviewed early research on the treatment of co-occurring PTSD and substance use disorders and concluded, as did later reviews, that concurrent PTSD and substance abuse treatment is preferred.
Dass-Brailsford and Myrick (2010) reviewed research and clinical opinions on the importance of integrated treatment for clients with co-occurring PTSD and substance use disorders, discussing factors such as the potential benefits of integrated approaches, potential implementation barriers, and specific models of integrated substance abuse and trauma/PTSD treatment. Limited research suggests that some of the integrated treatment models they discussed are effective at reducing substance abuse, PTSD symptoms, and other mental disorder symptoms. They also observed that, because of the lack of research recommending one specific model over another, providers should consider other factors, such as training requirements, philosophical/theoretical orientations, and appropriate settings in selecting a specific intervention.
The specific interventions included in Dass-Brailsford and Myrick’s (2010) review were:
- Addictions and Trauma Recovery Integration , a 12-week program that uses psychoeducation, expressive therapy, mindfulness, and guided relaxation that can be provided in a group or individual format and is delivered by either peers or professionals ( Miller & Guidry, 2001 ).
- TRANSCEND , a 12-week CBT intervention intended for veterans in partial hospitalization settings ( Donovan, Padin-Rivera, & Kowaliw, 2001 ).
- Assisted Recovery Trauma and Substances , a 20-week, individual CBT intervention that addresses both PTSD and substance use disorders; it has been evaluated with clients in methadone maintenance and cocaine treatment programs ( Triffleman, 2002 ).
- Helping Women Recover , a 17-week, gender-responsive intervention that uses CBT, expressive arts, and relational theory ( Covington, 2008 ).
- Substance-Dependence Posttraumatic Stress Disorder Therapy (SDPT) , a 20-week intervention intended for outpatients that uses ET, psychoeducation, and coping skills training ( Triffleman, 2000 ).
- Concurrent Treatment of PTSD and Cocaine Dependence , which the developers believe can be used with any substance use disorders, and which uses coping skills training, cognitive restructuring, relapse prevention, and ET ( Coffey, Schumacher, Brimo, & Brady, 2005 ).
- Seeking Safety , a 25-session, present-focused therapy for co-occurring disorders, which is one of the more extensively evaluated of the integrated interventions included in the review ( Najavits, 2002 ).
- Trauma Affect Regulation: Guide for Education and Therapy (TARGET) , a nine-session, gender-specific intervention adapted from a trauma treatment intervention for clients with other mental disorders, which uses psychoeducation and present-centered therapy to help clients learn effective emotional regulation techniques ( Ford & Russo, 2006 ; Frisman, Ford, Lin, Mallon, & Chang, 2008 ).
- Trauma Recovery and Empowerment Model (TREM) , a 24- to 29-session group intervention originally developed for women who were survivors of physical/sexual abuse that since has been adapted for men (M-TREM); it has been implemented in a wide variety of treatment settings ( Fallot & Harris, 2002 ).
- The Triad Women’s Project , a 16-week group intervention for women that uses integrated case management services, a curriculum-based treatment group, and a peer support group ( Clark & Fearday, 2003 )
Torchalla, Nosen, Rostam, and Allen (2012) conducted a meta-analysis of 17 trials of integrated treatments for PTSD/trauma and substance use disorders. Their review included six of the interventions listed previously (i.e., Seeking Safety, TARGET, TREM, TRANSCEND, SDPT, and CTPCD) and an additional three, which were:
- Integrated CBT for PTSD in Addictions Treatment , an 8- to 12-session intervention that uses psychoeducation, skills training, and cognitive processing and restructuring ( McGovern et al., 2009 ; McGovern, Lambert–Harris, Alterman, Xie, & Meier, 2011 ).
- Dual Assessment and Recovery Track , a treatment for co-occurring substance use and other mental disorders (including PTSD) that involves 9 hours of treatment per week for a 12-week period and is designed to be implemented in a therapeutic community-oriented outpatient program ( Sacks, McKendrick, Sacks, Banks, & Harle, 2008 ).
- Integrated Tobacco Cessation Treatment , a six-session intervention involving behavioral counseling, stress management, and pharmacotherapy for smoking cessation ( McFall et al., 2006 ).
Torchalla and colleagues (2012) found that integrated treatments can reduce both PTSD symptoms and substance abuse, and across the reviewed studies, the data suggest that such treatments are associated with relatively large reductions in symptoms. However, most of the studies that compare integrated and nonintegrated treatments (the latter typically being substance abuse treatment interventions) did not report significant differences between the two in terms of either substance abuse or PTSD outcomes, nor did the authors’ meta-analysis find significant differences between these various integrated treatments (taken as an aggregate) and active controls. The authors explored reasons for their failure to find significant differences in outcomes between integrated and nonintegrated treatments, including low participation in many of the studies. They also pointed out that, even though some research suggests that integrated treatments do not have as great an effect on clients with low levels of PTSD symptoms, the majority of the studies did not limit participation to clients with diagnosable PTSD; integrated treatments may be effective in reducing PTSD symptoms because they either reduce substance abuse or affect general mental health. Comparison treatments in many of these studies accomplish the same ends.
One study included in Torchalla and colleagues’ (2012) review appears to contradict the idea that addressing substance abuse alone is usually sufficient to reduce PTSD symptoms’ severity. Hien, Campbell, Ruglass, Hu, and Killeen (2010) analyzed data from a National Institute on Drug Abuse clinical trial ( N =353). They found that participants who responded to treatment with improvements in PTSD symptoms (as measured with the CAPS) but not with reductions in the amount of substances used were significantly more likely to later be classified as “globally responsive” (indicating improvements in both PTSD and substance use) compared with those who showed improvements in substance abuse use outcomes but not PTSD. This suggests that if a sequential approach to treatment is used, it is probably more beneficial to address PTSD first.
In a recent study not included in the reviews previously discussed, the Integrated CBT for PTSD in Addictions Treatment intervention was found to be more effective than individual substance abuse treatment counseling for reducing PTSD reexperiencing symptoms and increasing remission from PTSD, whereas both options were comparable in terms of reducing substance abuse ( McGovern et al., 2011 ). In addition, participants in the study who received the integrated CBT intervention were more likely to initiate and engage in treatment than those who received individual substance abuse treatment counseling.
- Other Integrated Approaches
Although most of the integrated treatment interventions that address traumatic stress and PTSD are intended for people with substance use disorders, a few interventions have been developed for clients with PTSD and other mental disorders. A large percentage of people with BPD have significant trauma histories, and many have co-occurring PTSD. Harned and colleagues (2012) conducted a preliminary evaluation of a year-long integrated treatment that uses DBT for BPD and exposure therapy for PTSD. Of the 13 participants who completed at least one treatment session, 60 percent no longer met criteria for PTSD at the end of treatment (for treatment completers, 71.4 percent no longer had PTSD). Participants also showed significant improvements in terms of suicidal ideation, anxiety, shame, guilt, depression, and social adjustment, and they demonstrated no increase in self-injurious thoughts and behaviors.
A pilot study by Nixon and Nearmy (2011) of an integrated intervention for clients with PTSD and major depression that uses behavioral activation for depression and ET and cognitive restructuring for PTSD found the intervention to be promising. Twenty clients with those co-occurring disorders were included in the trial (14 of whom completed the intervention); 3 months after the intervention, participants had significant reductions in both PTSD and depression symptoms, with 60 percent no longer meeting criteria for a PTSD diagnosis and 70 percent no longer meeting criteria for major depression.
Integrated interventions have also been developed to treat co-occurring PTSD and panic disorder/attacks. Falsetti and colleagues (2008) evaluated one such integrated treatment, Multiple Channel Exposure Therapy, with 62 women who had PTSD and a history of panic attacks (89 percent of whom met criteria for a panic disorder diagnosis). They found that participants in the intervention had significantly greater improvements in terms of PTSD, panic attacks, and symptoms of depression than did participants assigned to a waitlist control group. Improvements in PTSD and panic symptoms had not diminished significantly at a 6-month follow-up. Another culturally relevant model of integrated CBT for PTSD and panic disorder was found to be effective in small trials with Cambodian ( Hinton et al., 2005 ) and Vietnamese ( Hinton et al., 2004 ) refugees.
- Treating Complex Trauma/PTSD
Although many existing guidelines for the treatment of PTSD may provide some guidance in treating the effects of complex trauma, there are no widely disseminated practice guidelines focused specifically on its treatment ( Courtois, Ford, & Cloitre, 2009 ). However, Cloitre and colleagues (2011) have provided guidance from an expert clinician survey of 50 clinical experts (25 of whom specialize in treatment for complex trauma). The survey respondents largely agreed that treatment for complex trauma should have a phased approach in which multiple interventions are available; if the client does not respond to the first option, others should be used. They also generally agreed that interventions should be tailored to the client’s specific needs, taking the client’s specific symptoms into account. There was almost universal agreement that treatment should be provided in an individual format, but that as a second-line approach, additional sessions of group treatment could be added. They generally agreed that treatment should be provided at least on a weekly basis in the initial phase.
Regarding specific treatment elements or interventions recommended by the expert panel, the only first-line approaches in terms of effectiveness, safety, and acceptability were ones that were emotion-focused or addressed emotion regulation ( Cloitre et al., 2011 ). Other approaches that were considered first-line in terms of effectiveness and with reasonably high ratings in safety and acceptability were anxiety/stress management, cognitive restructuring, and psychoeducation about the effects of trauma. Meditation and mindfulness approaches were frequently cited as appropriate second-line treatments useful for addressing emotional, attention-related, and behavioral problems. The survey respondents also recommended first- and second-line interventions for specific sets of symptoms. For example, psychoeducation, anxiety/stress management, and emotion regulation were recommended as the first approaches to use for hyperarousal, whereas narration of trauma memory and cognitive restructuring were recommended as second-line approaches for those symptoms.
In an earlier review, Courtois and colleagues (2009) provided specific recommendations for conducting therapy with clients who have complex PTSD. These recommendations included suggestions for assessment, defining treatment goals, specific tasks for treatment to meet those goals, and principles and tasks to guide clinicians through three phases of treatment (i.e., promoting safety and stabilization, processing traumatic memories, reintegration). Many of the approaches recommended for treating PTSD in other populations are also effective for clients with complex PTSD, including CBT (Jackson et al., 2009) and pharmacotherapy ( Opler, Grennan & Ford, 2009 ). Both family/couples interventions ( Ford & Saltzman, 2009 ; Johnson & Courtois, 2009 ; Schwartz, Schwartz, & Galperin, 2009 ) and group interventions ( Dorrepaal et al., 2010 ; Ford et al., 2009 ) may also be beneficial, and they may even be more important in cases of complex trauma, because complex trauma histories typically have a negative effect on an individual’s ability to form positive relationships with partners and friends ( Schwartz et al., 2009 ). Other clinicians have recommended the use of experiential and emotion-focused therapies ( Fosha, Paivio, Gleiser, & Ford, 2009 ) and sensorimotor techniques, such as mindfulness and sensorimotor memory processing ( Fisher & Ogden, 2009 ), with this population. Jackson and colleagues (2010) discussed basic steps involved in treating PTSD as well as commonly encountered problems, such as resistance to experiencing feelings, to change, and to improving interpersonal functioning.
Some of the studies discussed elsewhere in this TIP do include individuals who have experienced complex trauma. In particular, survivors of severe childhood abuse often have complex PTSD. The “ Survivors of Childhood Abuse ” section includes studies relevant in this context. Other populations with histories of repeated interpersonal violence, such as torture survivors ( Johnson & Thompson, 2008 ) and prisoners of war ( Solomon, Dekel, & Mikulincer, 2008 ), also often have complex trauma. However, few controlled trials are available that specifically focus on clients with complex PTSD, and more research in this area is needed ( Dorrepaal et al., 2010 ).
Some interventions have been developed specifically for clients with complex PTSD. Contextual behavior trauma therapy (CBTT) is another intervention designed specifically for clients with histories of complex trauma and the experiential avoidance and developmental deficits that result from such traumatic experiences ( Follette, Iverson, & Ford, 2009 ). CBTT uses techniques drawn from ACT, behavioral activation, DBT, and functional analytic psychotherapy. Contextual therapy was developed to treat adults who have sustained prolonged childhood abuse ( Gold, 2009 ). Contextual therapy looks at the context of a client’s trauma; it has an initial phase to help clients work on building a sense of safety/security prior to addressing trauma and a final phase to help clients integrate gains made in terms of interpersonal interactions, practical skills, and insight into experiences and behaviors.
A group intervention designed for people with complex trauma that was evaluated in the Netherlands is Stabilizing Group Treatment ( Dorrepaal et al., 2010 ). This 20-week intervention used psychoeducation and CBT skills training. In a pilot study, participants ( n =36) had significant reductions in PTSD and BPD symptoms from baseline to the end of the intervention. At a 6-month follow-up assessment, 78 percent no longer met criteria for complex PTSD. In a review concerning the use of psychodynamic approaches to treat trauma/PTSD, Schottenbauer, Glass, Arnkoff, & Gray (2008) suggested that psychodynamic approaches may be particularly relevant for clients with complex trauma/PTSD, because they may be well-suited for addressing problems with social/interpersonal relationships, general life functioning, and underlying personality problems that may have developed as the result of repeated trauma (particularly occurring in childhood).
- Treatment for Specific Populations
Any treatment for traumatic stress reactions should be tailored to the specific needs of each client, but general information pertaining to population characteristics may help guide that treatment.
People From Diverse Cultural Groups
As with any behavioral health treatment, it is extremely important that providers be culturally competent when treating clients with traumatic stress reactions and/or trauma histories. Cultural background influences how individuals respond to trauma and how they present traumatic stress reactions and other behavioral health problems related to traumatic experiences. The section entitled “ Cultural, Ethnic, and Gender Factors in Assessment ” provides more information on culture as a factor in assessing traumatic stress reactions.
Osterman and de Jong (2007) provided a good overview of some of the treatment issues involved in providing culturally responsive behavioral health services relating to trauma, including the adaptation of assessment instruments, theoretical ideas about how to respond to traumatic experiences and traumatic stress reactions with clients from culturally diverse backgrounds, and the somewhat limited research evaluating PTSD treatment with diverse cultural groups. The treatment sections refer to such literature when it is available (e.g., the CBT section includes references to studies evaluating trauma-focused CBT with members of diverse cultural groups). The section “ Refugees ” also discusses treatment options and adaptations that are useful with non-Western cultural groups.
Few studies are available that compare PTSD treatment outcomes for members of diverse cultural groups, and those that do often fail to account for potentially confounding factors, such as SES ( Lester, Resick, Young-Xu, & Artz, 2010 ). These authors compared outcomes and treatment retention rates for African American women ( n =94) and White American women ( n =214) who had been victims of interpersonal violence and had PTSD. They found that African American women were significantly more likely to drop out of treatment than were White American women, even after controlling for education and income. However, the authors observed that there were no significant differences in treatment outcomes between African Americans and White Americans, and this may indicate that a higher dropout rate reflected greater symptom improvement among African Americans who left treatment.
A volume edited by Marsella, Johnson, Watson, and Gryczynski (2008) discussed in greater detail how to address traumatic experiences with members of diverse cultural groups found in the United States. For individuals belonging to cultural groups that have sustained trauma for multiple generations, treatment should address issues of historical trauma and the relationship of the client’s traumatic experiences with those of his parents and other generations ( Danieli, 2007 ; Sotero, 2006 ). A few specific interventions have been developed for addressing historical trauma in Native Americans that might also guide similar interventions with other groups (e.g., Yellow Horse & Brave Heart, 2005 ). Culture can serve as a factor in building resilience and healing the effects of trauma; even so, individuals in certain trauma-related predicaments (e.g., internment during war) may have a strong desire to remove themselves from the persecuted culture, leading to accelerated deacculturation ( Danieli, 2007 ). In such cases, it may be even more important to integrate elements of the individual’s cultural background into treatment ( Danieli, 2007 ).
Although it is not just a cultural issue, the treatment of refugees from outside the United States also typically involves cross-cultural exchanges and requires cultural competence. Nickerson, Bryan, Silove, and Steel (2011) reviewed research on PTSD treatment that specifically involved refugee populations. They found two approaches that have been studied with this population: trauma-focused therapies (typically trauma-focused CBT) and multimodal treatments that attempt to address extensive behavioral and other health problems experienced by this population. The studies they reviewed indicate that trauma-focused therapies are associated with significant long-term reductions in PTSD symptoms, but the research involving multimodal approaches has generally not found significant long-term reductions (although shorter-term reductions have been observed). Although research is lacking, published clinical opinion generally agrees that ET is inappropriate for refugees. Hinton, Rivera, and colleagues (2012) discussed adapting CBT interventions for refugee populations with non-Western cultural backgrounds. Many of the suggestions they provided can also be used with other treatment interventions for this population.
The VA and DoD (2010) have published guidelines on treating PTSD for veterans and active-duty personnel entitled Clinical Practice Guideline for Management of Post-Traumatic Stress (described in the “ Military Prevention Programs ” section). Other guidance on appropriate treatments may be found in reviews on treating trauma/traumatic stress reactions in this population (e.g., Goodson et al., 2011 ; Hoge, 2011 ; Sharpless & Barber, 2011 ). However, these guidelines do not address co-occurring complexities, such as substance abuse, psychosis, individuals in danger of harming self or others, personality disorders, current homelessness or domestic violence, and other issues. Thus, for these populations, the clinician should use careful judgment in applying the guidelines.
Goodson and colleagues (2011) recommended treatments for veterans that are largely the same as those recommended for the general population. Their review found that treatments for PTSD in veterans, taken as a whole, have a medium effect size (i.e., d =0.43 across all the studies and d =0.48 for the controlled studies), with larger effect sizes for CPT and trauma-focused CBT. The review also observed that 66 percent of veterans included in the research reviewed had better outcomes than did those who were in control groups. More detailed information on PTSD treatment for veterans can be found in the planned TIP, Reintegration-Related Behavioral Health Issues in Veterans and Military Families (SAMHSA, planned f).
Survivors of Sexual Assault
Survivors of sexual assault have elevated risk for a number of behavioral health disorders and problems in addition to PTSD (e.g., eating disorders, depression, sleep disorders, other anxiety disorders, suicide attempts), and many will have complex trauma ( Chen et al., 2010 ), so behavioral health services for this population will often need to address multiple issues. Vickerman and Margolin (2009) reviewed research on behavioral health treatment for survivors of rape, including treatment for PTSD, depression, and/or other anxiety disorders. They concluded that CPT and PE have the most data supporting their effectiveness; EMDR has also been found effective, albeit in fewer studies. In research comparing interventions, CBT interventions have been found to be more effective than supportive counseling. Across all interventions, however, there is a high rate of dropout from treatment, with more than a third of clients leaving before completing treatment. Foa and Rothbaum (1998) also discussed behavioral health treatment for survivors of rape, with particular attention to CBT techniques. Women with sexual trauma may prefer working with female clinicians and/or all-female treatment groups ( Lee, Westrup, Ruzek, Keller, & Weitlauf, 2007 ; Nelson-Zlupko, Dore, Kauffman, & Kaltenbach, 1996 ), but perhaps more important than the gender of clinicians or group members is that services be responsive to gender issues and centered on the needs of women who have experienced such trauma.
Survivors of Childhood Abuse
As with other populations of people with PTSD, CBT has been found to be effective at reducing PTSD symptoms for adults with PTSD related to childhood abuse, which in most studies involved sexual abuse (e.g., Classen et al., 2011 ; McDonagh et al., 2005 ; Resick et al., 2003 ). Cloitre and colleagues (2010) noted that not all trauma-focused CBT interventions are designed to address the interpersonal, social adjustment, and/or emotional regulation problems that are common among people with histories of repeated childhood abuse, and thus caution must be used in selecting appropriate interventions. They also indicated that their own CBT intervention, Skills Training in Affective and Interpersonal Regulation (STAIR), was developed for this population.
Particular CBT interventions may be useful for addressing specific behavioral health symptoms/concerns. For example, a small ( n =9) pilot study found that two sessions of cognitive restructuring and imagery modification were effective at alleviating feelings of contamination experienced by survivors of childhood sexual abuse ( Steil, Jung, & Stangier, 2011 ). Only a few studies have evaluated optimum duration and intensity of treatment for adults with histories of childhood sexual abuse, but given that members of this population frequently drop out of treatment and often require long-term treatment ( Gilbert et al., 2009 ; Schumm et al., 2006 ), this issue may be even more important in their treatment. One study, which has some methodological problems, found that a 6-month group treatment for childhood sexual abuse was associated with somewhat better outcomes than a 12-month group treatment, leading the authors to conclude that a shorter, more intensive course of treatment may be preferred for this population ( Kreidler & Einsporn, 2012 ).
Treatment sequencing is another important issue with this population, as multiple interventions are often required to address complex trauma. Researchers randomly assigned 104 women with PTSD related to childhood sexual abuse to receive the STAIR intervention followed by narrative ET, supportive counseling followed by narrative ET, or STAIR followed by supportive counseling ( Cloitre et al., 2010 ). The authors found that participants in the first group were significantly more likely to achieve sustained remission from PTSD than were participants in the other two groups (whereas those in group 3 were more likely to do so than those in group 2). In terms of percentages, 27 percent of group 1 achieved sustained full remission, 13 percent of group 3 did, and none of the members in group 2 did. In a later analysis of study data, Cloitre, Petkova, Wang, and Lu (2012) found that the level of dissociative symptoms a client had at baseline did not significantly change these outcomes, except that participants with high levels of dissociative symptoms who were in group 1 continued to show improvements in PTSD symptoms during follow-up, but those assigned to the other two groups did not.
People with lower SES are likely to have multiple needs that should be addressed if treatment for PTSD is to succeed ( Kelly et al., 2010 ). Kelly and colleagues (2010) discussed case examples of medical and psychosocial needs relating to PTSD, methods of outreach and engagement, and suggestions for providing appropriate services for this population. Dropout rates are high for PTSD treatment, but a study of CBT treatment ( N =31) found significantly higher dropout rates for individuals with low income and lower levels of education ( Difede et al., 2007 ).
People With SMI
Only a few studies have addressed PTSD treatments specifically for people with SMI; these studies, along with some authors’ clinical opinions, suggest that CBT is likely the best option for this population. Most of the research on using trauma-focused CBT to treat PTSD in people with SMI found it to be an effective approach. In one study, 108 clients with SMI (85 percent of whom had a major mood disorder, 15 percent of whom had schizophrenia or schizoaffective disorder, and 25 percent of whom had co-occurring BPD) were randomly assigned to receive trauma-focused CBT or standard treatment ( Mueser et al., 2008 ). The authors found, using an intent-to-treat analysis to account for missing data, that CBT was associated at a 6-month follow-up with significantly better outcomes for PTSD symptoms, other mental disorder symptoms, and perceived health. CBT appeared to have the greatest effect on participants with more severe PTSD. The authors also found that homework completion was associated with greater reductions in PTSD symptoms, arguing for the importance of this CBT component. Sherrer (2011) argued that cognitive restructuring (another CBT intervention) is likely the most appropriate PTSD treatment for people with SMI, as this population has difficulties objectively evaluating traumatic experiences. Rakofsky and Dunlop (2010) also reviewed research on the treatment of PTSD and other anxiety disorders for clients with bipolar disorder. They covered little research specific to PTSD but presented some general considerations for treating anxiety and anxiety disorders in this population.
Hopper and colleagues (2010) reviewed literature regarding people who are homeless and gave recommendations for providing them with trauma-informed services. They concluded that providing trauma-informed services to this population can produce better behavioral health outcomes, improve housing stability, and decrease use of crisis-based services such as emergency room services. The authors also noted that these services are cost-effective for and well-received by this population.
People With Physical and Cognitive Disabilities
Few studies have looked at the treatment of trauma-related behavioral health problems in people with disabilities. Focht-New, Clements, Barol, Faulkner, and Service (2008) , however, provided guidelines on treating and assessing trauma and traumatic stress reactions in this population and reviewed some relevant research. Mevissen and de Jongh (2010) also reviewed research on assessment and treatment of PTSD in people with intellectual disabilities, discussing several adaptations to treatment, such as training caregivers and making changes to assessments.
Studies have been conducted concerning the treatment of PTSD in veterans with trauma-related disabilities (particularly TBI). Veterans from recent conflicts have high rates of both TBI and PTSD, and it is often difficult to distinguish resulting impairments, especially in cases of mild TBI ( Hill, Mobo, & Cullen, 2009 ). In their review of the literature on TBI and PTSD, Vasterling, Verfaellie, and Sullivan (2009) observed that there is good evidence that PTSD is even more common in cases of mild TBI than in more severe TBI, and mild TBI is even more common than PTSD among veterans of recent conflicts.
The VA and DoD have developed TBI screening tools that may aid in distinguishing TBI and PTSD ( Hill et al., 2009 ; Terrio, Nelson, Betthauser, Harwood, & Brenner, 2011 ). The combination of PTSD, mild TBI, and chronic pain complaints is common enough among veterans of OEF/OIF that it has been labeled “post-deployment multi-symptom disorder “ ( Walker, Clark, & Sanders, 2010 ). These authors suggested the use of an integrated treatment model to help improve coping and decrease functional disability, but more research is needed to evaluate the intervention.
- Trauma-Informed Intervention Considerations
Special considerations in the treatment of clients with traumatic stress reactions and/or trauma histories are not covered in the previous treatment sections but deserve special attention.
Self-Harm and Suicidality
Traumatic experiences may contribute to suicidal behaviors regardless of whether those events result in a traumatic stress reaction, and, in fact, some research suggests that PTSD does not increase suicidality after controlling for trauma exposure. In the largest study to date to evaluate suicidality and trauma exposure, 102,245 respondents in 21 countries were interviewed as part of the World Mental Health Survey ( Stein et al., 2010 ). A wide range of traumatic experiences were associated with increased odds of suicidal ideation and/or suicide attempts, but the greatest increase was associated with being the victim of sexual violence followed by interpersonal violence. Being exposed to war was associated with a significant increase in the odds of having a planned suicide attempt, whereas being the victim of sexual violence was associated with a significant increase in the odds of making an attempt without a plan (no other traumas were associated with significant increases in the rates of these two outcomes).
Trauma exposure also appears to have a cumulative effect on suicidality, with repeated experiences of trauma being associated with increased rates of suicidal ideation and attempts, but this effect appears to level off at a certain point (at seven traumatic events for ideation and six for attempts). When the authors evaluated trauma-related suicidality with respect to PTSD (according to DSM-IV diagnostic criteria), they did not find any further increase in suicidality associated with PTSD, suggesting that it was the traumatic experience and not the subsequent mental disorder that largely influenced suicidality. The association of trauma and suicidality was found to be valid for individuals from diverse cultural backgrounds and from both developing and developed nations.
Other research has found PTSD to be associated with increased suicidality, although not to the same degree as many other behavioral health disorders. For example, a study of veterans found that PTSD increased risk to a lesser degree than did substance use disorders, bipolar disorder, depression, schizophrenia, or other anxiety disorders, but this study did not control for trauma exposure ( Ilgen et al., 2010 ). Other research evaluating veterans with depression found that co-occurring PTSD did not increase suicide rates, although certain other co-occurring mental disorders did ( Pfeiffer, Ganoczy, Ilgen, Zivin, & Valenstein, 2009 ).
Other reviews on the subject have also concluded that PTSD does affect suicidality, independent of the effects of trauma exposure. Panagioti, Gooding, and Tarrier (2009) reviewed a wide range of research on PTSD and suicidality, including studies relating specifically to the effects of different types of trauma, the role of other co-occurring behavioral health disorders, and the relationship of the two in specific populations (i.e., people with HIV, refugees, and police officers). They concluded that PTSD does have an independent effect on increasing suicidality, and this is often further increased by the presence of co-occurring depression, which may mediate the relationship between PTSD and suicidality. This relationship exists regardless of the type of trauma involved. Research also indicates that the PTSD symptom of reexperiencing has the strongest relationship with suicidality.
Krysinska and Lester (2010) conducted a meta-analytic review of 50 studies that evaluated the relationship between PTSD and suicidality (defined as suicide attempts and/or suicidal ideation). They concluded that PTSD did have a significant relationship to suicidality, but that, when controlling for other behavioral health disorders, that relationship was substantially weaker. However, they did not find a significant relationship between PTSD and completed suicide. The evidence is somewhat stronger that PTSD is associated with increased self-harming behavior (self-harm is any type of intentionally self-inflicted harm, regardless of the severity of injury or whether suicide is intended). In research conducted with 2,854 soldiers returning from OIF, individuals with PTSD diagnoses were significantly more likely to report thoughts about self-harm than were those without PTSD, but they were not significantly more likely to report suicidal ideation ( Maguen et al., 2011 ).
Other research indicates that complex PTSD is associated with greater self-harming behavior than simple PTSD ( Dyer et al., 2009 ). Also, a study of deliberate self-harming behavior in substance abuse treatment clients found a significant association between symptoms of emotional dysregulation and self-harm behavior, suggesting that such symptoms may play a key role in promoting such behaviors among individuals with PTSD ( Gratz & Tull, 2010 ). Complex PTSD is also associated with more self-harming behavior than noncomplex PTSD ( Dyer et al., 2009 ). It is worth noting that the relative impact of PTSD on suicidality may vary by culture, as Joe, Baser, Breeden, Neighbors, and Jackson (2006) found that anxiety disorders appeared to have a significantly greater effect on suicide risk for African Americans than for members of other major racial/ethnic groups. More information on treating clients with suicidal thoughts and behaviors can be found in TIP 50, Addressing Suicidal Thoughts and Behaviors in Substance Abuse Treatment ( CSAT, 2009a ).
Sleep Disturbances
Although difficulties falling or staying asleep may be a symptom of PTSD and may respond to standard PTSD treatment, they often require specific interventions to be effectively treated ( Nappi, Drummond, & Hall, 2012 ). Carney and Edinger (2010) reviewed research indicating that the majority of people with PTSD will have some sleep disturbances and that sleep complaints following a traumatic event are associated with an increased risk for developing PTSD. Among returning OEF/OIF veterans with PTSD, sleep disturbances are the most commonly reported symptom and often predate the advent of other PTSD symptoms ( McLay, Klam, & Volkert, 2010 ). Other recent research also confirms that disordered/disrupted sleep is a core feature of PTSD ( Nappi et al., 2012 ). Sleep disturbances among people with PTSD are also associated with increased risk for suicidal ideation, neurocognitive deficits, impaired social functioning, and a variety of physical health complaints ( Nappi et al., 2012 ).
In another review, Babson and Feldner (2010) observed that traumatic events, whether or not the individual develops PTSD, can cause or exacerbate difficulties falling asleep, falling back to sleep after waking, and staying asleep through the night. Certain aspects of traumatic events also appear to affect sleep patterns, such that traumatic events of longer duration have a greater effect, and people experience more severe sleep disturbance when the event has occurred more recently. However, such problems, at least for those individuals who develop PTSD, also may persist for many years (as many as 45 years in one study). The authors also referenced literature indicating that sleep problems can interfere with recovery from PTSD.
Carney and Edinger (2010) and Nappi and colleagues (2012) also reviewed research on the treatment of sleep disturbances in people with PTSD. Nappi and colleagues (2012) concluded that some, but not all, research regarding the effects of standard PTSD treatments (e.g., trauma-focused CBT, EMDR) indicates that they can be effective at eliminating nightmares but not PTSD-related insomnia, which often continues after such treatment. Therefore, they recommended either psychological or pharmacological treatments specifically aimed at insomnia and reviewed available options.
Spirituality and Religious Beliefs
Religious beliefs have been found in a number of contexts to have a protective function relative to PTSD (e.g., Bradley, Schwartz, & Kaslow, 2005 ; Cheung, 1994 ), but not in every context ( Ben-Zur, 2008 ). It is also not clear whether changes in religiosity positively affect traumatic stress reactions among those who have been traumatized, as both posttrauma weakening and strengthening of religious beliefs have been associated with significant increases in PTSD symptoms compared with those individuals whose beliefs did not change ( Falsetti, Resick, & Davis, 2003 ; Hussain, Weisaeth, & Heir, 2011 ). Other research, however, indicates that certain types of trauma (e.g., combat trauma) may cause a spiritual crisis; for some clients, addressing that crisis may improve their behavioral health ( Baroody, 2011 ). Research conducted with veterans also indicates that loss of religious faith is a major factor in motivating individuals to seek treatment for PTSD ( Fontana & Rosenheck, 2004 ).
Religious belief/spirituality may also affect other factors, such as finding meaning in life or self-esteem. For example, according to NCS data, among survivors of childhood abuse, greater religiosity is associated with significantly higher self-esteem ( Reiland & Lauterbach, 2008 ). Owens, Steger, Whitesell, and Herrera (2009) conducted an Internet survey of 174 veterans and found that higher levels of PTSD symptom severity were significantly related to finding less meaning in life according to self-report. However, when depression was factored into the equation, a somewhat different picture emerged, so that for veterans with low to moderate levels of depression (measured with the Depression Anxiety Stress Scales-21), perceiving greater meaning in one’s life was associated with significantly less severe PTSD; the same was not true for veterans with severe depression. The authors concluded that improving an individual’s perception of meaning in his or her life may reduce PTSD symptom severity, except when the individual also has severe depression.
Although interventions targeting spirituality or religious beliefs are difficult to evaluate, small studies conducted with veterans have found that spiritual practices, such as mantra repetition (Bormann, Lui, Thorp, and & Lang, 2011) and transcendental meditation ( Rosenthal, Grosswald, Ross, & Rosenthal, 2011 ), typically presented in a nondenominational manner, are effective at reducing PTSD symptom severity. Lang and colleagues (2012) reviewed research and theoretical support for the use of meditation as an aid in PTSD treatment. Harris and colleagues (2011) evaluated an eight-session group treatment designed to help veterans who experienced combat trauma find religious/spiritual meaning in their experiences and found that participants who received the intervention had significantly less PTSD symptom severity than did those who were in a waitlist control group.
- Building a Trauma-Informed Workforce
There is general agreement that behavioral health programs where staff members need to address issues related to trauma and/or need to work with clients who have traumatic stress disorders should prepare their workforce to serve such clients and to be able to deal with the stress and problems they may experience as a result of that work. Failure to address these problems and related problems involving institutional practices may further traumatize clients and harm the staff members who work with them ( Bloom & Farragher, 2011 ).
Staff Development and Training
Weine and colleagues (2002) summarized findings from an international expert consensus panel on training behavioral health staff members to treat clients with trauma histories. Core components of trauma-informed training, according to this panel, involve teaching:
- Competence in listening.
- Ability to recognize psychosocial and mental problems to promote appropriate assessment.
- Familiarity with established interventions in the client population.
- The importance of understanding the local context, including help-seeking expectations, duration of treatment, attitudes toward intervention, cost-effectiveness of intervention, and family attitudes and involvement.
- Use of problem-solving strategies that can be used on individual, family, and community levels.
- Appropriate treatment approaches for medically unexplained somatic pain.
- Ability to collaborate with existing local resources and change agents (e.g., clergy, traditional healers, informal leaders).
- Counselor self-care skills.
Secondary Traumatization and Burnout
Both burnout and secondary traumatization (also known as vicarious trauma) can affect clinicians working with clients who have trauma issues. In a review concerning secondary traumatization and ways to prevent it, Trippany, Kress, and Wilcoxon (2004) distinguished vicarious trauma from burnout (the former is a reaction to specific information presented by clients and involves problems with trust, control, intrusive imagery, safety, and intimacy) and from general countertransference reactions (observing that even though vicarious trauma may involve countertransference, it is not inherent in or equated with countertransference). These authors also discuss the needs commonly experienced by clinicians with vicarious trauma (needs related to safety, trust, esteem, intimacy, and control) and some of the ways those needs may be met by programs. A similar review was conducted by Collins and Long (2003) .
Secondary trauma can lead to difficulty responding appropriately to clients’ feelings and/or cause clinical mistakes in judgment resulting from a failure to understand what the client is trying to express ( Figley, 2002 ). Figley (2002) presented a model for conceptualizing secondary trauma/compassion fatigue. Mathieu and colleagues (2007) provided self-care tips for behavioral health providers to help them reduce/overcome compassion fatigue. Elwood, Mott, Lohr, and Galovski (2011) also reviewed this issue, but focused more on the empirical literature that provides data on the prevalence of the problem. Research has found that the extent and severity of secondary traumatization varies widely across studies, which the authors accounted for both by differences in research methodology and difference in the client population involved (e.g., it does appear that clinicians working with clients who were sexually assaulted have a greater risk for secondary traumatization than do those who work with clients who experienced a variety of other types of trauma).
Elwood and colleagues (2011) also observed that a few studies have found a significant association between the percentage of clients with trauma issues whom a clinician serves and secondary trauma symptoms for that clinician, but that a greater number of studies have found no significant association. Some, but not all, studies have also found a significant association between weekly hours spent working with trauma clients and clinician burnout. Also, a few studies have found that having spent more time working with trauma clients is associated with greater secondary traumatization symptom severity, but again, other studies have found no such association. Additionally, some studies have found significantly higher risk for secondary traumatization among clinicians who have personal trauma histories, whereas other studies have not. The authors also observed that if prior trauma histories do play a significant role in what is labeled secondary traumatization, this may mean that what is really being evaluated is retraumatization brought on by discussions of similar traumatic experiences.
Whether factors such as counselors’ own trauma histories or hours spent with trauma clients affect secondary traumatization may also depend on the nature of the trauma involved. For example, a study of 114 women who specialized in treating sexual trauma did find a significant association between their own traumatic experiences and secondary traumatization ( Trippany, Wilcoxon, & Satcher, 2003 ). Similarly, a study by Schauben and Frazier (1995) found that having more clients who were victims of sexual violence was associated with increased PTSD symptoms among a group of female counselors.
Elwood and colleagues (2011) observed that, in one study, the clinicians described secondary traumatization symptoms that occurred after exposure to clients’ trauma stories, yet none of those clinicians mentioned symptoms occurring 6 weeks or more after the exposure, suggesting that long-term effects of secondary traumatization may be limited. Also, findings about the effects of secondary traumatization on employment or performance were not clear. One group of researchers found a significant association between secondary trauma symptoms and less expressed intent to remain in the behavioral health field, but clinicians interviewed in other research deny that secondary trauma symptoms affect their work performance. They concluded that research findings concerning secondary traumatization of providers “are neither clear nor consistent and warrant additional research” (p. 34).
Beck (2011) reviewed literature on secondary traumatization as it applies specifically to nurses, but some of the information provided, such as how to assess secondary traumatization, is applicable to other providers. Elwood and colleagues (2011) reviewed the instruments that have been used in research to assess secondary traumatization. Counselor burnout is not specific to providers working with trauma survivors, but it may affect them just as it does other counselors.
In a review of research regarding burnout among behavioral health counselors (with a focus on substance abuse treatment providers), Lacoursiere (2001) discussed instruments for assessing counselor burnout and noted some factors associated with an increased likelihood of burnout:
- Increased job stress/workplace pressure
- A lack of clarity about rules and policies
- A lack of organizational commitment to counselor goals
- Worse counselor coping skills
- Greater client/patient distress
- Worse management/supervision
- Lower professional status
- A lack of intellectual stimulation
- Unsatisfactory relationships with clients, client families, and other staff members
Preventing Burnout/Secondary Traumatization
Although burnout and secondary traumatization may increase counselor turnover, it is possible to implement program policies that ameliorate the problem—for example, by providing effective clinical supervision, because perceived quality of supervision has been associated with lower self-ratings of emotional exhaustion and desire to leave a counseling position ( Knudsen, Ducharme, & Roman, 2006 ). Trippany and colleagues (2004) also concluded that good peer supervision can help reduce the effects of secondary traumatization. Support from coworkers is also important for reducing burnout/emotional exhaustion; generally, a cohesive and supportive workplace will help reduce burnout ( Ducharme, Knudsen, & Roman, 2008 ; Lent, 2010 ).
Research with a group of behavioral health service providers who identified themselves as trauma specialists ( N =532) determined that the use of evidence-based practices in the workplace was associated with significantly less burnout and compassion fatigue and significantly greater satisfaction with doing an effective job ( Craig & Sprang, 2010 ). In addition, proper education regarding the provision of trauma services and how treating trauma clients may affect the clinician also appears to reduce symptoms of secondary traumatization, according to research reviewed by Trippany, Kress, and Wilcoxon (2004) . Counselors who have a stronger sense of personal efficacy, more job autonomy, more recognition of their ideas, a stronger sense that their programs are open to change, and a greater sense that work and rewards were fairly distributed across the organization (i.e., greater distributive justice) also have lower burnout rates ( Ducharme, Knudsen, & Roman, 2008 ; Garner, Knight, & Simpson, 2007 ; Knudsen et al., 2006 ; Shoptaw, Stein, & Rawson, 2000 ).
Adequate resources, including access to computers and sufficient staffing, have been associated with lower rates of burnout/emotional exhaustion in a group of 151 substance abuse counselors working with clients in the criminal justice system ( Garner et al., 2007 ). Awa, Plaumann, and Walter (2010) reviewed 25 program practices intended to reduce/prevent burnout that have been used in a variety of workplace settings. They grouped these as person-directed (i.e., focused on helping employees cope with workplace stress and burnout), organization-directed (i.e., focused on changing workplace organization/practices that may affect all staff), or combined (having features of both person-directed and organization-directed practices). They concluded that person-directed interventions have a greater effect in the short term (a period of 6 months or less after the practice is instituted) and that combined interventions have the longest-lasting effects (with positive effects lasting a year or more). In all cases, the positive effects of the interventions appear to diminish over time. In addition, practices that reduce stress may also help reduce burnout. Teaching counselors time management skills ( Hawkins & Klas, 1997 ), cognitive therapy techniques to address dysfunctional thought patterns ( Gardner, Rose, Mason, Tyler, & Cushway, 2005 ), and how to meditate ( Oman, Hedberg, & Thoresen, 2006 ) may all reduce stress.
- Achim AM, Maziade M, Raymond E, Olivier D, Merette C, Roy MA. How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophrenia Bulletin. 2011; 37 :811–821. [ PMC free article : PMC3122284 ] [ PubMed : 19959704 ]
- Acierno R, Brady K, Gray M, Kilpatrick DG, Resnick H, Best CL. Psychopathology following interpersonal violence: A comparison of risk factors in older and younger adults. Journal of Clinical Geropsychology. 2002; 8 :13–23.
- Acierno R, Kilpatrick DG, Resnick HS, Saunders BE, Best CL. Violent assault, posttraumatic stress disorder, and depression: Risk factors for cigarette use among adult women. Behavior Modification. 1996; 20 :363–384. [ PubMed : 8875812 ]
- Acierno R, Ruggiero KJ, Kilpatrick DG, Resnick HS, Galea S. Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. The American Journal of Geriatric Psychiatry. 2006; 14 :1051–1059. [ PubMed : 17035356 ]
- Adams PR, Adams GR. Mount Saint Helens’s ashfall: Evidence for a disaster stress reaction. American Psychologist. 1984; 39 :252–260. [ PubMed : 6711993 ]
- Adams RE, Boscarino JA. A structural equation model of perievent panic and posttraumatic stress disorder after a community disaster. Journal of Traumatic Stress. 2011; 24 :61–69. [ PMC free article : PMC3334528 ] [ PubMed : 21351165 ]
- Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: Randomization by platoon. Journal of Consulting and Clinical Psychology. 2009; 77 :928–940. [ PubMed : 19803572 ]
- Afifi TO, Asmundson GJG, Taylor S, Jang KL. The role of genes and environment on trauma exposure and posttraumatic stress disorder symptoms: A review of twin studies. Clinical Psychology Review. 2010; 30 :101–112. [ PubMed : 19892451 ]
- Agaibi CE, Wilson JP. Trauma, PTSD, and resilience: A review of the literature. Trauma, Violence, & Abuse. 2005; 6 :195–216. [ PubMed : 16237155 ]
- Agani F, Landau J, Agani N. Community–building before, during, and after times of trauma: the application of the LINC model of community resilience in Kosovo. American Journal of Orthopsychiatry. 2010; 80 :143–149. [ PubMed : 20397999 ]
- Agorastos A, Marmar CR, Otte C. Immediate and early behavioral interventions for the prevention of acute and posttraumatic stress disorder. Current Opinion in Psychiatry. 2011; 24 :526–532. [ PubMed : 21941180 ]
- Ahmed AS. Post-traumatic stress disorder, resilience and vulnerability. Advances in Psychiatric Treatment. 2007; 13 :369–375.
- Alarcon LH, Germain A, Clontz AS, Roach E, Nicholas DH, Zenati MS, et al. Predictors of acute posttraumatic stress disorder symptoms following civilian trauma: Highest incidence and severity of symptoms after assault. Journal of Trauma and Acute Care Surgery. 2012; 72 :629–635. [ PubMed : 22491546 ]
- Alcañiz M, Lozano JA, Rey B. Technological background about VR. In: Riva G, Botella C, Legeron P, Optale G, editors. Cybertherapy: Internet and virtual reality as assessment and rehabilitation tools for clinical psychology and neuroscience. Amsterdam: Ios Press; 2004. pp. 199–216.
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, et al. Prevalence of mental illness in immigrant and non–immigrant U.S. Latino groups. American Journal of Psychiatry. 2008; 165 :359–369. [ PMC free article : PMC2712949 ] [ PubMed : 18245178 ]
- Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, et al. Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. Journal of the National Medical Association. 2006; 98 :1630–1636. [ PMC free article : PMC2569763 ] [ PubMed : 17052054 ]
- Alonso J, Buron A, Bruffaerts R, He Y, Posada-Villa J, Lepine JP, et al. Association of perceived stigma and mood and anxiety disorders: Results from the World Mental Health Surveys. Acta Psychiatrica Scandinavica. 2008; 118 :305–314. [ PMC free article : PMC3040096 ] [ PubMed : 18754833 ]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: American Psychiatric Association; 1980.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd rev ed. Washington, DC: American Psychiatric Association; 1987.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th Text Revision ed. Washington, DC: American Psychiatric Association; 2000.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- Amstadter AB, Acierno R, Richardson LK, Kilpatrick DG, Gros DF, Gaboury MT, et al. Posttyphoon prevalence of posttraumatic stress disorder, major depressive disorder, panic disorder, and generalized anxiety disorder in a Vietnamese sample. Journal of Traumatic Stress. 2009; 22 :180–188. [ PMC free article : PMC2720525 ] [ PubMed : 19455707 ]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006; 256 :174–186. [ PMC free article : PMC3232061 ] [ PubMed : 16311898 ]
- Andrews B, Brewin CR, Rose S. Gender, social support, and PTSD in victims of violent crime. Journal of Traumatic Stress. 2003; 16 :421–427. [ PubMed : 12895025 ]
- Ansell EB, Pinto A, Edelen MO, Markowitz JC, Sanislow CA, Yen S, et al. The association of personality disorders with the prospective 7-year course of anxiety disorders. Psychological Medicine. 2011; 41 :1019–1028. [ PMC free article : PMC3606880 ] [ PubMed : 20836909 ]
- Antony MM, Orsillo SM, Roemer L. Practitioner’s guide to empirically based measures of anxiety. New York: Kluwer Academic/Plenum Publishers; 2001.
- Asmundson GJ, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depression and Anxiety. 2009; 26 :888–901. [ PubMed : 19691031 ]
- Asmundson GJG, Abrams MP, Collimore KC. Anxiety in health behaviors and physical illness. New York: Springer Science + Business Media; 2008. Pain and anxiety disorders; pp. 207–235.
- Asnaani A, Richey JA, Dimaite R, Hinton DE, Hofmann SG. A cross–ethnic comparison of lifetime prevalence rates of anxiety disorders. Journal of Nervous and Mental Disease. 2010; 198 :551–555. [ PMC free article : PMC2931265 ] [ PubMed : 20699719 ]
- Aspelmeier JE, Elliott AN, Smith CH. Childhood sexual abuse, attachment, and trauma symptoms in college women: The moderating role of attachment. Child Abuse & Neglect. 2007; 31 :549–566. [ PubMed : 17391758 ]
- Australian Centre for Posttraumatic Mental Health. Australian guidelines for the treatment of adults with acute stress disorder and posttraumatic stress disorder. 2007. Retrieved July 4, 2013, from: http://www .acpmh.unimelb .edu.au/resources /resources-guidelines.html . [ PubMed : 17620160 ]
- Awa WL, Plaumann M, Walter U. Burnout prevention: A review of intervention programs. Patient Education and Counseling. 2010; 78 :184–190. [ PubMed : 19467822 ]
- Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: A critical review of the empirical literature. Journal of Anxiety Disorders. 2010; 24 :1–15. [ PMC free article : PMC2795058 ] [ PubMed : 19716676 ]
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without Posttraumatic Stress Disorder: A comparison of substance use, trauma history and psychiatric comorbidity. American Journal on Addictions. 2000; 9 :51–62. [ PubMed : 10914293 ]
- Bailey HN, DeOliveira CA, Wolfe VV, Evans EM, Hartwick C. The impact of childhood maltreatment history on parenting: A comparison of maltreatment types and assessment methods. Child Abuse & Neglect. 2012; 36 :236–246. [ PubMed : 22444714 ]
- Balsam KF, Lehavot K, Beadnell B, Circo E. Childhood abuse and mental health indicators among ethnically diverse lesbian, gay, and bisexual adults. Journal of Consulting and Clinical Psychology. 2010; 78 :459–468. [ PMC free article : PMC2911995 ] [ PubMed : 20658803 ]
- Balsam KF, Rothblum ED, Beauchaine TP. Victimization over the life span: A comparison of lesbian, gay, bisexual, and heterosexual siblings. Journal of Consulting and Clinical Psychology. 2005; 73 :477–487. [ PubMed : 15982145 ]
- Baños RM, Guillen V, Quero S, Garcia-Palacios A, Alcañiz M, Botella C. A virtual reality system for the treatment of stress–related disorders: A preliminary analysis of efficacy compared to a standard cognitive behavioral program. International Journal of Human Computer Studies. 2011; 69 :602–613.
- Banyard VL, Williams LM, Siegel JA. Childhood sexual abuse: A gender perspective on context and consequences. Child Maltreatment. 2004; 9 :223–238. [ PubMed : 15245676 ]
- Baroody AN. Families under fire: Systemic therapy with military families. New York: Routledge/Taylor & Francis Group; 2011. Spirituality and trauma during a time of war: A systemic approach to pastoral care and counseling; pp. 165–190.
- Başoğlu M, Livanou M, Crnobaric C, Franciskovic T, Suljic E, Duric D, et al. Psychiatric and cognitive effects of war in former Yugoslavia: Association of lack of redress for trauma and posttraumatic stress reactions. JAMA. 2005; 294 :580–590. [ PubMed : 16077052 ]
- Başoğlu M, Salcioglu E, Livanou M. A randomized controlled study of single-session behavioural treatment of earthquake-related post-traumatic stress disorder using an earthquake simulator. Psychological Medicine. 2007; 37 :203–213. [ PubMed : 17254365 ]
- Beals J, Manson SM, Shore JH, Friedman MJ, Ashcraft M, Fairbank JA, et al. The prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: Disparities and context. Journal of Traumatic Stress. 2002; 15 :89–97. [ PubMed : 12013069 ]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Archives of General Psychiatry. 2005; 62 :99–108. [ PubMed : 15630077 ]
- Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, Manson SM. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: Mental health disparities in a national context. American Journal of Psychiatry. 2005; 162 :1723–1732. [ PubMed : 16135633 ]
- Beattie N, Shannon C, Kavanagh M, Mulholland C. Predictors of PTSD symptoms in response to psychosis and psychiatric admission. Journal of Nervous and Mental Disease. 2009; 197 :56–60. [ PubMed : 19155811 ]
- Bebbington PE, Bhugra D, Brugha T, Singleton N, Farrell M, Jenkins R, et al. Psychosis, victimisation and childhood disadvantage: Evidence from the second British National Survey of Psychiatric Morbidity. British Journal of Psychiatry. 2004; 185 :220–226. [ PubMed : 15339826 ]
- Beck AJ, Harrison PM, Berzofsky M, Caspar R, Krebs C. Sexual victimization in prisons and jails reported by inmates, 2008–09. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2010.
- Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books; 2005.
- Beck CT. Secondary traumatic stress in nurses: A systematic review. Archives of Psychiatric Nursing. 2011; 25 :1–10. [ PubMed : 21251596 ]
- Beck JG, Coffey SF, Foy DW, Keane TM, Blanchard EB. Group cognitive behavior therapy for chronic posttraumatic stress disorder: An initial randomized pilot study. Behav. Ther. 2009; 40 :82–92. [ PubMed : 19187819 ]
- Beidel DC, Frueh BC, Uhde TW, Wong N, Mentrikoski JM. Multicomponent behavioral treatment for chronic combat-related posttraumatic stress disorder: a randomized controlled trial. Journal of Anxiety Disorders. 2011; 25 :224–231. [ PMC free article : PMC3031665 ] [ PubMed : 20951543 ]
- Bell NS, Amoroso PJ, Yore MM, Smith GS, Jones BH. Self-reported risk-taking behaviors and hospitalization for motor vehicle injury among active duty army personnel. American Journal of Preventive Medicine. 2000; 18 :85–95. [ PubMed : 10736544 ]
- Benedek DM, Friedman MJ, Zatzick D, Ursano RJ. Guideline watch (March 2009: Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. FOCUS: The Journal of Lifelong Learning in Psychiatry. 2009; VII :204–213.
- Benish SG, Imel ZE, Wampold BE. The relative efficacy of bona fide psychotherapies for treating post-traumatic stress disorder: A meta-analysis of direct comparisons. Clinical Psychology Review. 2008; 28 :746–758. [ PubMed : 18055080 ]
- Ben-Zur H. Personal resources of mastery–optimism, and communal support beliefs, as predictors of posttraumatic stress in uprooted Israelis. Anxiety Stress Coping. 2008; 21 :295–307. [ PubMed : 18938288 ]
- Berger W, Mendlowicz MV, Marques-Portella C, Kinrys G, Fontenelle LF, Marmar CR, et al. Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: A systematic review. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2009; 33 :169–180. [ PMC free article : PMC2720612 ] [ PubMed : 19141307 ]
- Bisson J, Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews. 2007:CD003388. [ PubMed : 17636720 ]
- Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. British Journal of Psychiatry. 2007; 190 :97–104. [ PubMed : 17267924 ]
- Blanchard EB, Buckley TC, Hickling EJ, Taylor AE. Posttraumatic stress disorder and comorbid major depression: Is the correlation an illusion? Journal of Anxiety Disorders. 1998; 12 :21–37. [ PubMed : 9549607 ]
- Bloom SL, Farragher B. Destroying sanctuary: The crisis in human service delivery systems. New York: Oxford University Press; 2011.
- Bober T, Regehr C. Strategies for reducing secondary or vicarious trauma: Do they work? Brief Treatment and Crisis Intervention. 2006; 6 :1–9.
- Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting & Clinical Psychology. 2007; 75 :671–682. [ PubMed : 17907849 ]
- Booth BM, Mengeling M, Torner J, Sadler AG. Rape, sex partnership, and substance use consequences in women veterans. Journal of Traumatic Stress. 2011; 24 :287–294. [ PubMed : 21567476 ]
- Bormann JE, Liu L, Thorp SR, Lang AJ. Spiritual wellbeing mediates PTSD change in veterans with military-related PTSD. International Journal of Behavioral Medicine. 2012; 19 (4):496–502. [ PubMed : 21874605 ]
- Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE, Figley CR. A brief screening tool for assessing psychological trauma in clinical practice: development and validation of the New York PTSD Risk Score. General Hospital Psychiatry. 2011; 33 :489–500. [ PMC free article : PMC3557518 ] [ PubMed : 21777981 ]
- Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE, Figley CR. Predicting future PTSD using a modified New York Risk Score: Implications for patient screening and management. Minerva Psichiatrica. 2012; 53 :47–59. [ PMC free article : PMC3298362 ] [ PubMed : 22408285 ]
- Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE, Figley CR. The New York PTSD risk score for assessment of psychological trauma: Male and female versions. Psychiatry Research. 2012; 200 (2–3):827–834. [ PMC free article : PMC3434234 ] [ PubMed : 22648009 ]
- Bosquet EM, Kitts RL, Blood E, Bizarro A, Hofmeister M, Wright RJ. Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behav. Dev. 2011; 34 :487–503. [ PMC free article : PMC3180882 ] [ PubMed : 21862136 ]
- Botella C, Quero S, Baños RM, Perpina C, Garcia Palacios A, Riva G. Virtual reality and psychotherapy. In: Riva G, Botella C, Legeron P, Optale G, editors. Cybertherapy: Internet and virtual reality as assessment and rehabilitation tools for clinical psychology and neuroscience. Amsterdam: Ios Press; 2004. pp. 37–54.
- Böttche M, Kuwert P, Knaevelsrud C. Posttraumatic stress disorder in older adults: An overview of characteristics and treatment approaches. International Journal of Geriatric Psychiatry. 2012; 27 :230–239. [ PubMed : 21538540 ]
- Bourque LB, Shen H. Psychometric characteristics of Spanish and English versions of the Civilian Mississippi scale. Journal of Traumatic Stress. 2005; 18 :719–728. [ PubMed : 16382438 ]
- Braakman MH, Kortmann FA, van den Brink W. Validity of ‘post-traumatic stress disorder with secondary psychotic features’: A review of the evidence. Acta Psychiatrica Scandinavica. 2009; 119 :15–24. [ PubMed : 18764840 ]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005; 162 :214–227. [ PubMed : 15677582 ]
- Bradley R, Schwartz AC, Kaslow NJ. Posttraumatic stress disorder symptoms among low-income, African American women with a history of intimate partner violence and suicidal behaviors: Self-esteem, social support, and religious coping. Journal of Traumatic Stress. 2005; 18 :685–696. [ PubMed : 16382436 ]
- Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry. 2000; 61 :22–32. [ PubMed : 10795606 ]
- Brave Heart MYH. Gender differences in the historical trauma response among the Lakota. Journal of Health & Social Policy. 1999; 10 :1–20. [ PubMed : 10538183 ]
- Brave Heart MYH. The historical trauma response among natives and its relationship with substance abuse: A Lakota illustration. Journal of Psychoactive Drugs. 2003; 35 :7–13. [ PubMed : 12733753 ]
- Brave Heart MYH. The historical trauma response among natives and its relationship to substance abuse: A Lakota illustration. In: Nebelkopf E, Phillips M, editors. Healing and mental health for Native Americans: Speaking in red. Walnut Creek, CA: AltaMira Press; 2004. pp. 7–18.
- Breh DC, Seidler GH. Is peritraumatic dissociation a risk factor for PTSD? Journal of Trauma & Dissociation. 2007; 8 :53–69. [ PubMed : 17409054 ]
- Brenner LA. Neuropsychological and neuroimaging findings in traumatic brain injury and post-traumatic stress disorder. Dialogues in Clinical Neuroscience. 2011; 13 :311–323. [ PMC free article : PMC3182009 ] [ PubMed : 22034217 ]
- Breslau N. Gender differences in trauma and posttraumatic stress disorder. Journal of Gender Specific Medicine. 2002; 5 :34–40. [ PubMed : 11859685 ]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003; 60 :289–294. [ PubMed : 12622662 ]
- Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: A follow-up study at age 17 years. Archives of General Psychiatry. 2006; 63 :1238–1245. [ PubMed : 17088504 ]
- Breslau N, Lucia VC, Davis GC. Partial PTSD versus full PTSD: An empirical examination of associated impairment. Psychological Medicine. 2004; 34 :1205–1214. [ PubMed : 15697047 ]
- Breslau N, Davis C, Peterson EL, Schultz L. A second look at comorbidity in victims of trauma: The posttraumatic stress disorder–major depression connection. Biological Psychiatry. 2000; 48 :902–909. [ PubMed : 11074228 ]
- Brewerton TD. Eating disorders, trauma, and comorbidity: Focus on PTSD. Journal of Eating Disorders. 2007; 15 :285–304. [ PubMed : 17710567 ]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000; 68 :748–766. [ PubMed : 11068961 ]
- Briere J. Detailed assessment of posttraumatic stress: Professional manual. Odessa, FL: Psychological Assessment Resources; 2001.
- Briere J, Scott C. Principles of trauma therapy: A guide to symptoms, evaluation, and treatment. Thousand Oaks, CA: Sage Publications; 2006.
- Briere J, Scott C. Principles of trauma therapy: A guide to symptoms, evaluation, and treatment. 2nd ed. Thousand Oaks, CA: Sage; 2012.
- Briere J, Spinazzola J. Assessment of the sequelae of complex trauma: Evidence-based measures. In: Courtois CA, editor. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 104–123.
- Brooks R, Silove D, Bryant R, O’Donnell M, Creamer M, McFarlane A. A confirmatory factor analysis of the acute stress disorder interview. Journal of Traumatic Stress. 2008; 21 :352–355. [ PubMed : 18553413 ]
- Brown D. Assessment of attachment and abuse history, and adult attachment style. In: Courtois CA, editor. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 124–144.
- Brown PJ, Read JP, Kahler CW. Comorbid posttraumatic stress disorder and substance use disorders: Treatment outcomes and the role of coping. In: Ouimette P, Brown PJ, editors. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. Washington, DC: American Psychological Association; 2003. pp. 171–188.
- Brown PJ, Stout RL, Gannon-Rowley J. Substance use disorder–PTSD comorbidity: Patients’ perceptions of symptom interplay and treatment issues. Journal of Substance Abuse Treatment. 1998; 15 :445–448. [ PubMed : 9751003 ]
- Bryant RA. Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic review. Journal of Clinical Psychiatry. 2011; 72 :233–239. [ PubMed : 21208593 ]
- Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Heart rate after trauma and the specificity of fear circuitry disorders. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2011; 41 :2573–2580. [ PubMed : 21672298 ]
- Bryant RA, Harvey AG, Guthrie RM, Moulds ML. Acute psychophysiological arousal and posttraumatic stress disorder: a two-year prospective study. Journal of Traumatic Stress. 2003; 16 :439–443. [ PubMed : 14584627 ]
- Bryant RA, Litz BT. Intermediate Interventions. In: Ritchie EC, Watson PJ, Friedman MJ, editors. Interventions following mass violence and disasters: Strategies for mental health practice. New York: Guilford Press; 2006. pp. 155–173.
- Bryant RA, Mastrodomenico J, Felmingham KL, Hopwood S, Kenny L, Kandris E, et al. Treatment of acute stress disorder: A randomized controlled trial. Archives of General Psychiatry. 2008; 65 :659–667. [ PubMed : 18519824 ]
- Bryant RA, Moulds ML, Guthrie RM. Acute Stress Disorder Scale: A self-report measure of acute stress disorder. Psychological Assessment. 2000; 12 :61–68. [ PubMed : 10752364 ]
- Bryant RA, Moulds ML, Guthrie RM, Dang ST, Mastrodomenico J, Nixon RD, et al. A randomized controlled trial of exposure therapy and cognitive restructuring for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2008; 76 :695–703. [ PubMed : 18665697 ]
- Byers AL, Yaffe K, Covinsky KE, Friedman MB, Bruce ML. High occurrence of mood and anxiety disorders among older adults: The National Comorbidity Survey Replication. Archives of General Psychiatry. 2010; 67 :489–496. [ PMC free article : PMC2933177 ] [ PubMed : 20439830 ]
- Cahill SP, Foa EB, Hembree EA, Marshall RD, Nacash N. Dissemination of exposure therapy in the treatment of posttraumatic stress disorder. Journal of Traumatic Stress. 2006; 19 :597–610. [ PubMed : 17075914 ]
- Cahill SP, Rothbaum BO, Resick PA, Follette VM. Cognitive–behavioral therapy for adults. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 139–222.
- Cardeña E, Carlson E. Acute stress disorder revisited. Annual Review of Clinical Psychology. 2011; 7 :245–267. [ PubMed : 21275643 ]
- Cardeña E, Koopman C, Classen C, Waelde LC, Spiegel D. Psychometric properties of the Stanford Acute Stress Reaction Questionnaire (SASRQ): a valid and reliable measure of acute stress. Journal of Traumatic Stress. 2000; 13 :719–734. [ PubMed : 11109242 ]
- Cardeña E, Maldonado JR, van der Hart O, Spiegel D. Hypnosis. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 427–457.
- Carleton RN, Peluso DL, Collimore KC, Asmundson GJ. Social anxiety and posttraumatic stress symptoms: The impact of distressing social events. Journal of Anxiety Disorders. 2011; 25 :49–57. [ PubMed : 20800426 ]
- Carlson EB, Lauderdale S, Hawkins J, Sheikh JI. Posttraumatic stress and aggression among veterans in long-term care. Journal of Geriatric Psychiatry and Neurology. 2008; 21 :61–71. [ PubMed : 18287172 ]
- Carney CE, Edinger JD. Insomnia and anxiety. New York: Springer Science + Business Media; 2010.
- Carswell K, Blackburn P, Barker C. The relationship between trauma, post-migration problems and the psychological well-being of refugees and asylum seekers. International Journal of Social Psychiatry. 2011; 57 :107–119. [ PubMed : 21343209 ]
- Casteel C, Martin SL, Smith JB, Gurka KK, Kupper LL. National study of physical and sexual assault among women with disabilities. Injury Prevention. 2008; 14 :87–90. [ PubMed : 18388227 ]
- Catalano S. Intimate partner violence in the US. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2012.
- Center for Substance Abuse Treatment. Substance abuse treatment for persons with child abuse and neglect issues. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2000. HHS Publication No. (SMA) 00-3357.
- Center for Substance Abuse Treatment. Addressing suicidal thoughts and behaviors in substance abuse treatment. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2009. Treatment Improvement Protocol (TIP) Series 50. HHS Publication No. (SMA) 09-4381.
- Center for Substance Abuse Treatment. Substance abuse treatment: Addressing the specific needs of women. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2009. HHS Publication No. (SMA) 09-4426.
- Chen KW, Banducci AN, Guller L, Macatee RJ, Lavelle A, Daughters SB, et al. An examination of psychiatric comorbidities as a function of gender and substance type within an inpatient substance use treatment program. Drug and Alcohol Dependence. 2011; 118 :92–99. [ PMC free article : PMC3188332 ] [ PubMed : 21514751 ]
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, et al. Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clinic Proceedings. 2010; 85 :618–629. [ PMC free article : PMC2894717 ] [ PubMed : 20458101 ]
- Cherpitel CJ. Alcohol and violence-related injuries in the emergency room. Recent Developments in Alcoholism. 1997; 13 :105–118. [ PubMed : 9122492 ]
- Cheung P. Posttraumatic stress disorder among Cambodian refugees in New Zealand. International Journal of Social Psychiatry. 1994; 40 :17–26. [ PubMed : 8005775 ]
- Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addictive Behaviors. 1998; 23 :827–840. [ PubMed : 9801719 ]
- Chiu KB, deRoon–Cassini TA, Brasel KJ. Factors identifying risk for psychological distress in the civilian trauma population. Academic Emergency Medicine. 2011; 18 :1156–1160. [ PMC free article : PMC3220731 ] [ PubMed : 22044521 ]
- Choi DC, Rothbaum BO, Gerardi M, Ressler KJ. Pharmacological enhancement of behavioral therapy: Focus on posttraumatic stress disorder. Current Topics in Behavioral Neurosciences. 2010; 2 :279–299. [ PubMed : 21309114 ]
- Clark C, Fearday FE. Triad women’s project: Group facilitator’s manual. Tampa, FL: Louis de la Parte Florida Mental Health Institute, University of South Florida; 2003.
- Classen CC, Palesh OG, Aggarwal R. Sexual revictimization: A review of the empirical literature. Trauma, Violence, & Abuse. 2005; 6 :103–129. [ PubMed : 15753196 ]
- Classen CC, Palesh OG, Cavanaugh C, Koopman C, Kaupp JW, Kraemer HC, et al. A comparison of trauma-focused and present-focused group therapy for survivors of childhood sexual abuse: A randomized controlled trial. Psychological Trauma: Theory, Research, Practice, and Policy. 2011; 3 :84–93.
- Classen C, Koopman C, Nevill-Manning K, Spiegel D. A preliminary report comparing trauma-focused and present-focused group therapy against a wait-listed condition among childhood sexual abuse survivors with PTSD. Journal of Aggression, Maltreatment & Trauma. 2001; 4 :265–288.
- Cloitre M. Effective psychotherapies for posttraumatic stress disorder: A review and critique. CNS Spectrums. 2009; 14 :32–43. [ PubMed : 19169192 ]
- Cloitre M, Courtois CA, Charuvastra A, Carapezza R, Stolbach BC, Green BL. Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. Journal of Traumatic Stress. 2011; 24 (6):615–627. [ PubMed : 22147449 ]
- Cloitre M, Petkova E, Wang J, Lu LF. An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depression and Anxiety. 2012; 29 (8):709–717. [ PubMed : 22550033 ]
- Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, et al. Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry. 2010; 167 :915–924. [ PubMed : 20595411 ]
- Coffey SF, Schumacher JA, Brimo ML, Brady KT. Exposure therapy for substance abusers with PTSD: translating research to practice. Behavior Modification. 2005; 29 :10–38. [ PubMed : 15557477 ]
- Coker AL, Weston R, Creson DL, Justice B, Blakeney P. PTSD symptoms among men and women survivors of intimate partner violence: The role of risk and protective factors. Violence and Victims. 2005; 20 :625–643. [ PubMed : 16468442 ]
- Collimore KC, Carleton RN, Hofmann SG, Asmundson GJG. Posttraumatic stress and social anxiety: The interaction of traumatic events and interpersonal fears. Depression and Anxiety. 2010; 27 :1017–1026. [ PubMed : 20721907 ]
- Collins S, Long A. Too tired to care? The psychological effects of working with trauma. Journal of Psychiatric and Mental Health Nursing. 2003; 10 :17–27. [ PubMed : 12558918 ]
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse & Neglect. 2007; 31 :211–229. [ PubMed : 17399786 ]
- Cook A, Blaustein M, Spinazzola J, van der Kolk B. Complex trauma in children and adolescents. Durham, NC and Los Angeles: National Child Traumatic Stress Network; 2003. White Paper from the National Child Traumatic Stress Network, Complex Trauma Task Force.
- Cook JM, Niederehe G. Trauma in older adults. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York: Guilford Press; 2007. pp. 252–276.
- Cook JD, Bickman L. Social support and psychological symptomatology following a natural disaster. Journal of Traumatic Stress. 1990; 3 :541–556.
- Corcoran CB, Green BL, Goodman LA, Krinsley KE. Conceptual and methodological issues in trauma history assessment. In: Shalev AY, Yehuda R, McFarlane AC, editors. International handbook of human response to trauma. Dordrecht, Netherlands: Kluwer Academic Publishers; 2000. pp. 223–232.
- Cornelius MC, Nugent NR, Amstadter AB, Koenen KC. Genetics of post-traumatic stress disorder: Review and recommendations for genome-wide association studies. Current Psychiatry Reports. 2010; 12 :313–326. [ PMC free article : PMC3108177 ] [ PubMed : 20549395 ]
- Corry N, Pruzinsky T, Rumsey N. Quality of life and psychosocial adjustment to burn injury: Social functioning, body image, and health policy perspectives. International Review of Psychiatry. 2009; 21 :539–548. [ PubMed : 19919207 ]
- Cottler LB, Compton WM, Mager D, Spitznagel EL, Janca A. Posttraumatic stress disorder among substance users from the general population. American Journal of Psychiatry. 1992; 149 :664–670. [ PubMed : 1575258 ]
- Cougle JR, Feldner MT, Keough ME, Hawkins KA, Fitch KE. Comorbid panic attacks among individuals with posttraumatic stress disorder: associations with traumatic event exposure history, symptoms, and impairment. Journal of Anxiety Disorders. 2010; 24 :183–188. [ PubMed : 19914036 ]
- Cougle JR, Timpano KR, Sachs–Ericsson N, Keough ME, Riccardi CJ. Examining the unique relationships between anxiety disorders and childhood physical and sexual abuse in the National Comorbidity Survey–Replication. Psychiatry Research. 2010; 177 :150–155. [ PubMed : 20381878 ]
- Courtois CA. Implications of the memory controversy for clinical practice: An overview of treatment recommendations and guidelines. Journal of Child Sexual Abuse. 2000; 9 :183–210. [ PubMed : 17521996 ]
- Courtois CA, Ford JD, Cloitre M. Best practices in psychotherapy for adults. In: Courtois CA, editor. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 82–103.
- Covington SS. Helping women recover: A program for treating addiction. Revised (Loose Leaf) ed. San Francisco: Jossey-Bass; 2008.
- Craig CD, Sprang G. Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress & Coping: An International Journal. 2010; 23 :319–339. [ PubMed : 19590994 ]
- Cubbin C, Smith GS. Socioeconomic inequalities in injury: critical issues in design and analysis. Annual Review of Public Health. 2002; 23 :349–375. [ PubMed : 11910067 ]
- Cukor J, Spitalnick J, Difede J, Rizzo A, Rothbaum BO. Emerging treatments for PTSD. Clinical Psychology Review. 2009; 29 :715–726. [ PubMed : 19800725 ]
- Cusack KJ, Frueh BC, Brady KT. Trauma history screening in a community mental health center. Psychiatric Services. 2004; 55 :157–162. [ PubMed : 14762240 ]
- Danieli Y. Assessing trauma across cultures from a multigenerational perspective. In: Wilson JP, Tang CS, editors. Cross-cultural assessment of psychological trauma and PTSD. New York: Springer Science + Business Media; 2007. pp. 65–89.
- Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D, et al. Limbic scars: Long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biological Psychiatry. 2012; 71 :286–293. [ PubMed : 22112927 ]
- Dansky BS, Saladin ME, Brady KT, Kilpatrick DG, Resnick HS. Prevalence of victimization and posttraumatic stress disorder among women with substance use disorders: Comparison of telephone and in-person assessment samples. International Journal of the Addictions. 1995; 30 :1079–1099. [ PubMed : 7591350 ]
- Dass-Brailsford P, Myrick AC. Psychological trauma and substance abuse: The need for an integrated approach. Trauma, Violence, & Abuse. 2010; 11 :202–213. [ PubMed : 20823072 ]
- D’Augelli AR, Grossman AH, Starks MT. Childhood gender atypicality, victimization, and PTSD among lesbian, gay, and bisexual youth. Journal of Interpersonal Violence. 2006; 21 :1462–1482. [ PubMed : 17057162 ]
- Davidson JR, Hughes D, Blazer DG, George LK. Post-traumatic stress disorder in the community: An epidemiological study. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 1991; 21 :713–721. [ PubMed : 1946860 ]
- Davidson PR, Parker KC. Eye movement desensitization and reprocessing (EMDR): A meta-analysis. Journal of Consulting and Clinical Psychology. 2001; 69 :305–316. [ PubMed : 11393607 ]
- Del Gaizo AL, Elhai JD, Weaver TL. Posttraumatic stress disorder, poor physical health and substance use behaviors in a national trauma-exposed sample. Psychiatry Research. 2011; 188 :390–395. [ PubMed : 21481478 ]
- DeSilva M, Maclachlan M, Devane D, Desmond D, Gallagher P, Schnyder U, et al. Psychosocial interventions for the prevention of disability following traumatic physical injury. Cochrane Database of Systematic Reviews. 2009:CD006422. [ PMC free article : PMC3428876 ] [ PubMed : 19821365 ]
- DeViva JC, Zayfert C, Pigeon WR, Mellman TA. Treatment of residual insomnia after CBT for PTSD: Case studies. Journal of Traumatic Stress. 2005; 18 :155–159. [ PubMed : 16281208 ]
- Dietz PM, Spitz AM, Anda RF, Williamson DF, McMahon PM, Santelli JS, et al. Unintended pregnancy among adult women exposed to abuse or household dysfunction during their childhood. JAMA. 1999; 282 :1359–1364. [ PubMed : 10527183 ]
- Difede J, Malta LS, Best S, Henn–Haase C, Metzler T, Bryant R, et al. A randomized controlled clinical treatment trial for World Trade Center attack-related PTSD in disaster workers. Journal of Nervous and Mental Disease. 2007; 195 :861–865. [ PubMed : 18043528 ]
- DiGrande L, Neria Y, Brackbill RM, Pulliam P, Galea S. Long-term posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. American Journal of Epidemiology. 2011; 173 :271–281. [ PubMed : 21190987 ]
- Doctor JN, Zoellner LA, Feeny NC. Predictors of health-related quality-of-life utilities among persons with posttraumatic stress disorder. Psychiatric Services. 2011; 62 :272–277. [ PMC free article : PMC3238449 ] [ PubMed : 21363898 ]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science. 2006; 313 :979–982. [ PMC free article : PMC1584215 ] [ PubMed : 16917066 ]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. Continuing controversy over the psychological risks of Vietnam for U.S. veterans. Journal of Traumatic Stress. 2007; 20 :449–465. [ PubMed : 17721952 ]
- Donovan B, Padin-Rivera E, Kowaliw S. Transcend: Initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. Journal of Traumatic Stress. 2001; 14 :757–772. [ PubMed : 11776422 ]
- Dore G, Mills K, Murray R, Teesson M, Farrugia P. Post-traumatic stress disorder, depression and suicidality in inpatients with substance use disorders. Drug And Alcohol Review. 2011 [ PubMed : 21521385 ]
- Dorrepaal E, Thomaes K, Smit JH, van Balkom AJ, Van DR, Veltman DJ, et al. Stabilizing group treatment for Complex Posttraumatic Stress Disorder related to childhood abuse based on psycho-education and cognitive behavioral therapy: A pilot study. Child Abuse and Neglect. 2010; 34 :284–288. [ PubMed : 20303592 ]
- Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier M, et al. Trauma and PTSD in patients with alcohol, drug, or dual dependence: A multi-center study. Alcoholism: Clinical & Experimental Research. 2008; 32 :481–488. [ PubMed : 18215214 ]
- Drogendijk AN, van der Velden PG, Kleber RJ. Acculturation and post-disaster mental health problems among affected and non–affected immigrants: A comparative study. Journal of Affective Disorders. 2012; 138 :485–489. [ PubMed : 22377513 ]
- Drozdek B, Wilson JP. Wrestling with the ghosts from the past in exile: Assessing trauma in asylum seekers. In: Wilson JP, Tang CS, editors. Cross-cultural assessment of psychological trauma and PTSD. New York: Springer Science + Business Media; 2007. pp. 113–131.
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. JAMA: The Journal of the American Medical Association. 2001; 286 :3089–3096. [ PubMed : 11754674 ]
- Dube SR, Anda RF, Whitfield CL, Brown DW, Felitti VJ, Dong M, et al. Long-term consequences of childhood sexual abuse by gender of victim. American Journal of Preventive Medicine. 2005; 28 :430–438. [ PubMed : 15894146 ]
- Ducharme LJ, Knudsen HK, Roman PM. Emotional exhaustion and turnover intention in human service occupations: The protective role of coworker support. Sociological Spectrum. 2008; 28 :81–104.
- Duffy M, Gillespie K, Clark DM. Post-traumatic stress disorder in the context of terrorism and other civil conflict in Northern Ireland: Randomised controlled trial. BMJ: British Medical Journal. 2007; 334 :1147. [ PMC free article : PMC1885307 ] [ PubMed : 17495988 ]
- Dulin PL, Passmore T. Avoidance of potentially traumatic stimuli mediates the relationship between accumulated lifetime trauma and late-life depression and anxiety. Journal of Traumatic Stress. 2010; 23 :296–299. [ PubMed : 20419741 ]
- Dunlavy AC. The impact of acculturation, trauma, and post-migration stressors on the mental health of African immigrants and refugees in Sweden. Pittsburgh, PA: University of Pittsburgh; 2010.
- Dunn EC, Gilman SE, Willett JB, Slopen NB, Molnar BE. The impact of exposure to interpersonal violence on gender differences in adolescent-onset major depression: Results from the National Comorbidity Survey Replication (NCS–R). Depression and Anxiety. 2012 [ PMC free article : PMC4136968 ] [ PubMed : 22447513 ]
- Duran B, Duran E, Brave Heart MYH. Native Americans and trauma of history. In: Thornton R, editor. Studying Native America: Problems and prospects. Madison, WI: University of Wisconsin Press; 1998. pp. 60–76.
- Duran E, Duran B, Brave Heart MYH, Yellow Horse-Davis S. Healing the American Indian soul wound. In: Danieli Y, editor. International handbook of multigenerational legacies of trauma. New York: Plenum Press; 1998. pp. 341–354.
- Dyer KFW, Dorahy MJ, Hamilton G, Corry M, Shannon M, MacSherry A, et al. Anger, aggression, and self-harm in PTSD and complex PTSD. Journal of Clinical Psychology. 2009; 65 :1099–1114. [ PubMed : 19676110 ]
- Edwards VJ, Anda RF, Felitti VJ, Dube SR. Health consequences of abuse in the family: A clinical guide for evidence-based practice. Washington, DC: American Psychological Association; 2004. Adverse childhood experiences and health-related quality of life as an adult; pp. 81–94.
- Ehlers A, Bisson J, Clark DM, Creamer M, Pilling S, Richards D, et al. Do all psychological treatments really work the same in posttraumatic stress disorder? Clinical Psychology Review. 2010; 30 :269–276. [ PMC free article : PMC2852651 ] [ PubMed : 20051310 ]
- Elbogen EB, Fuller S, Johnson SC, Brooks S, Kinneer P, Calhoun PS, et al. Improving risk assessment of violence among military veterans: An evidence-based approach for clinical decision–making. Clinical Psychology Review. 2010; 30 :595–607. [ PMC free article : PMC2925261 ] [ PubMed : 20627387 ]
- Elbogen EB, Wagner HR, Fuller SR, Calhoun PS, Kinneer PM, Beckham JC. Correlates of anger and hostility in Iraq and Afghanistan war veterans. American Journal of Psychiatry. 2010; 167 :1051–1058. [ PMC free article : PMC3386845 ] [ PubMed : 20551162 ]
- El-Gabalawy R. Association between traumatic experiences and physical health conditions in a nationally representative sample. Silver Spring, MD: Anxiety and Depression Association of America; 2012.
- Elhai JD, de Francisco CL, Miguel FK, Palmieri PA, Primi R, Christopher FB. Testing whether posttraumatic stress disorder and major depressive disorder are similar or unique constructs. Journal of Anxiety Disorders. 2011; 25 :404–410. [ PubMed : 21129914 ]
- Elliott DE, Bjelajac P, Fallot RD, Markoff LS, Reed BG. Trauma-informed or trauma-denied: Principles and implementation of trauma-informed services for women. Journal of Community Psychology. 2005; 33 :461–477.
- Elwood LS, Mott J, Lohr JM, Galovski TE. Secondary trauma symptoms in clinicians: A critical review of the construct, specificity, and implications for trauma–focused treatment. Clinical Psychology Review. 2011; 31 :25–36. [ PubMed : 21130934 ]
- Engdahl B, Dikel TN, Eberly R, Blank A Jr. Posttraumatic stress disorder in a community group of former prisoners of war: A normative response to severe trauma. American Journal of Psychiatry. 1997; 154 :1576–1581. [ PubMed : 9356567 ]
- Erbes CR. Risk and resilience in US military families. New York: Springer Science + Business Media; 2011. Couple functioning and PTSD in returning OIF soldiers: Preliminary findings from the Readiness and Resilience in National Guard Soldiers Project; pp. 47–67.
- Evans DL, Foa EB, Gur RE, Herbert H, O’Brien CP, Seligman MEP, et al. Treating and preventing adolescent mental health disorders: What we know and what we don’t know: A research agenda for improving the mental health of our youth. New York: Oxford University Press; 2005.
- Evans-Campbell T. Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence. 2008; 23 :316–338. [ PubMed : 18245571 ]
- Everly GS Jr, Phillips SB, Kane D, Feldman D. Introduction to and overview of group psychological first aid. Brief Treatment and Crisis Intervention. 2006; 6 :130–136.
- Evren C, Dalbudak E, Cetin R, Durkaya M, Evren B. Relationship of alexithymia and temperament and character dimensions with lifetime post-traumatic stress disorder in male alcohol-dependent inpatients. Psychiatry and Clinical Neurosciences. 2010; 64 :111–119. [ PubMed : 20132531 ]
- Evren C, Sar V, Dalbudak E, Cetin R, Durkaya M, Evren B, et al. Lifetime PTSD and quality of life among alcohol-dependent men: Impact of childhood emotional abuse and dissociation. Psychiatry Research. 2011; 186 :85–90. [ PubMed : 20667600 ]
- Fallot RD, Harris M. A trauma-informed approach to screening and assessment. In: Harris M, Fallot RD, editors. Using trauma theory to design service systems. San Francisco: Jossey-Bass; 2001. pp. 23–31.
- Fallot RD, Harris M. The Trauma Recovery and Empowerment Model (TREM): Conceptual and practical issues in a group intervention for women. Community Mental Health Journal. 2002; 38 :475–485. [ PubMed : 12474935 ]
- Falsetti SA, Resick PA, Davis JL. Changes in religious beliefs following trauma. Journal of Traumatic Stress. 2003; 16 :391–398. [ PubMed : 12895022 ]
- Falsetti SA, Resnick HS, Davis JL. Multiple channel exposure therapy for women with PTSD and comorbid panic attacks. Cognitive Behaviour Therapy. 2008; 37 :117–130. [ PubMed : 18470742 ]
- Farley M, Golding JM, Young G, Mulligan M, Minkoff JR. Trauma history and relapse probability among patients seeking substance abuse treatment. Journal of Substance Abuse Treatment. 2004; 27 :161–167. [ PubMed : 15450649 ]
- Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clinical Psychology Review. 2007; 27 :14–45. [ PMC free article : PMC2575106 ] [ PubMed : 17034916 ]
- Felitti VJ. The relation between adverse childhood experiences and adult health: Turning gold into lead. The Permanente Journal. 2002; 6 :44–47. [ PMC free article : PMC6220625 ] [ PubMed : 30313011 ]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine. 1998; 14 :245–258. [ PubMed : 9635069 ]
- Felmingham KL, Bryant RA. Gender differences in the maintenance of response to cognitive behavior therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2012; 80 :196–200. [ PubMed : 22309472 ]
- Fetzner MG, McMillan KA, Sareen J, Asmundson GJ. What is the association between traumatic life events and alcohol abuse/dependence in people with and without PTSD? Findings from a nationally representative sample. Depression and Anxiety. 2011; 28 :632–638. [ PubMed : 21769995 ]
- Figley CR. Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical Psychology. 2002; 58 :1433–1441. [ PubMed : 12412153 ]
- Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: a comprehensive, national survey. Child Maltreatment. 2005; 10 :5–25. [ PubMed : 15611323 ]
- Fisher J, Ogden P. Sensorimotor psychotherapy. In: Courtois CA, editor. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 312–328.
- Fisher MH, Hodapp RM, Dykens EM. Child abuse among children with disabilities: What we know and what we need to know. In: Laraine MG, editor. International Review of Research in Mental Retardation. Volume 35 ed. Academic Press; 2008. pp. 251–289.
- Fletcher S, Creamer M, Forbes D. Preventing post traumatic stress disorder: Are drugs the answer? Australian and New Zealand Journal of Psychiatry. 2010; 44 :1064–1071. [ PubMed : 21070102 ]
- Foa EB.International Society For Traumatic Stress Studies. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009.
- Foa EB, Rothbaum BO. Treating the trauma of rape: Cognitive–behavioral therapy for PTSD. New York: Guilford Press; 1998.
- Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide. Oxford University Press; New York: 2007.
- Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005; 73 :953–964. [ PubMed : 16287395 ]
- Foa EB, Keane TM, Friedman MJ, Cohen JA. Introduction. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 1–20.
- Foa EB, Rothbaum BO, Furr JM. Augmenting exposure therapy with other CBT procedures. Psychiatric Annals. 2003; 33 :47–53.
- Foa EB, Zoellner LA, Feeny NC. An evaluation of three brief programs for facilitating recovery after assault. Journal of Traumatic Stress. 2006; 19 :29–43. [ PubMed : 16568461 ]
- Focht-New G, Barol B, Clements PT, Milliken TF. Persons with developmental disability exposed to interpersonal violence and crime: Approaches for intervention. Perspectives in Psychiatric Care. 2008; 44 :89–98. [ PubMed : 18366363 ]
- Follette VM, Iverson KM, Ford JD. Contextual behavior trauma therapy. In: Courtois CA, editor. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 264–285.
- Fontana A, Rosenheck R. Trauma, change in strength of religious faith, and mental health service use among veterans treated for PTSD. Journal of Nervous and Mental Disease. 2004; 192 :579–584. [ PubMed : 15348973 ]
- Fontana A, Rosenheck R. Treatment of female veterans with posttraumatic stress disorder: The role of comfort in a predominantly male environment. Psychiatric Quarterly. 2006; 77 :55–67. [ PubMed : 16397755 ]
- Ford JD. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. Neurobiological and developmental research: Clinical implications; pp. 31–58.
- Ford JD, Russo E. Trauma-focused, present-centered, emotional self-regulation approach to integrated treatment for posttraumatic stress and addiction: Trauma Adapative Recovery Group Education and Therapy (TARGET). American Journal of Psychotherapy. 2006; 60 :335–355. [ PubMed : 17340945 ]
- Ford JD, Saltzman W. Family systems therapy. In: Courtois CA, Ford JD, editors. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 391–414.
- Ford JD, Fallot RD, Harris M. Group therapy. In: Courtois CA, Ford JD, editors. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 415–440.
- Fortuna LR, Porche MV, Alegría M. Political violence, psychosocial trauma, and the context of mental health services use among immigrant Latinos in the United States. Ethnicity and Health. 2008; 13 :435–463. [ PMC free article : PMC2771411 ] [ PubMed : 18850369 ]
- Fortuna LR, Porche MV, Alegría M. A qualitative study of clinicians’ use of the cultural formulation model in assessing posttraumatic stress disorder. Transcult Psychiatry. 2009; 46 :429–450. [ PMC free article : PMC2879977 ] [ PubMed : 19837780 ]
- Fosha D, Paivio SC, Gleiser K, Ford JD. Experiential and emotion–focused therapy. In: Courtois CA, editor. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 286–311.
- Fredman SJ, Monson CM, Adair KC. Implementing cognitive–behavioral conjoint therapy for PTSD with the newest generation of veterans and their partners. Cognitive and Behavioral Practice. 2011; 18 :120–130.
- Frencher SK Jr, Benedicto CM, Kendig TD, Herman D, Barlow B, Pressley JC. A comparative analysis of serious injury and illness among homeless and housed low income residents of New York City. Journal of Trauma. 2010; 69 :S191–S199. [ PubMed : 20938307 ]
- Friedman MJ, Davidson JRT. Pharmacotherapy for PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York: Guilford Press; 2007. pp. 376–405.
- Friedman MJ, Marmar CR, Baker DG, Sikes CR, Farfel GM. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. Journal of Clinical Psychiatry. 2007; 68 :711–720. [ PubMed : 17503980 ]
- Frisman L, Ford J, Lin HJ, Mallon S, Chang R. Outcomes of trauma treatment using the TARGET model. Journal of Groups in Addiction and Recovery. 2008; 3 :285–303.
- Fullerton CS, Ursano RJ, Epstein RS, Crowley B, Vance K, Kao TC, et al. Gender differences in posttraumatic stress disorder after motor vehicle accidents. American Journal of Psychiatry. 2001; 158 :1486–1491. [ PubMed : 11532736 ]
- Galea S, Ahern J, Tracy M, Hubbard A, Cerda M, Goldmann E, et al. Longitudinal determinants of posttraumatic stress in a population-based cohort study. Epidemiology. 2008; 19 :47–54. [ PubMed : 18091003 ]
- Galea S, Vlahov D, Tracy M, Hoover DR, Resnick HS, Kilpatrick DG. Hispanic ethnicity and post-traumatic stress disorder after a disaster: evidence from a general population survey after September 11, 2001. Annals of Epidemiology. 2004; 14 :520–531. [ PubMed : 15350950 ]
- Galovski T, Lyons JA. Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran’s family and possible interventions. Aggression and Violent Behavior. 2004; 9 :477–501.
- Gapen M, Cross D, Ortigo K, Graham A, Johnson E, Evces M, et al. Perceived neighborhood disorder, community cohesion, and PTSD symptoms among low-income African Americans in an urban health setting. American Journal of Orthopsychiatry. 2011; 81 :31–37. [ PubMed : 21219273 ]
- Gardner B, Rose J, Mason O, Tyler P, Cushway D. Cognitive therapy and behavioural coping in the management of work–related stress: An intervention study. Work & Stress. 2005; 19 :137–152.
- Garfinkel SN, Liverzon I. Neurobiology of PTSD: A review of neuroimaging. Psychiatric Annals. 2009; 39 :370–381.
- Garner BR, Knight K, Simpson DD. Burnout among corrections-based drug treatment staff: Impact of individual and organizational factors. International Journal of Offender Therapy and Comparative Criminology. 2007; 51 :510–522. [ PubMed : 17615435 ]
- Garno JL, Goldberg JF, Ramirez PM, Ritzler BA. Impact of childhood abuse on the clinical course of bipolar disorder. British Journal of Psychiatry. 2005; 186 :121–125. [ PubMed : 15684234 ]
- Gellis LA, Mavandadi S, Oslin DW. Functional quality of life in full versus partial posttraumatic stress disorder among veterans returning from Iraq and Afghanistan. Primary Care Companion Journal of Clinical Psychiatry. 2010; 12 [ PMC free article : PMC2947536 ] [ PubMed : 20944775 ]
- Geraerts E, Lindsay DS, Merckelbach H, Jelicic M, Raymaekers L, Arnold MM, et al. Cognitive mechanisms underlying recovered-memory experiences of childhood sexual abuse. Psychological Science. 2009; 20 :92–98. [ PubMed : 19037903 ]
- Geraerts E, Schooler JW, Merckelbach H, Jelicic M, Hauer BJ, Ambadar Z. The reality of recovered memories: Corroborating continuous and discontinuous memories of childhood sexual abuse. Psychological Science. 2007; 18 :564–568. [ PubMed : 17614862 ]
- Gerardi M, Cukor J, Difede J, Rizzo A, Rothbaum BO. Virtual reality exposure therapy for post-traumatic stress disorder and other anxiety disorders. Current Psychiatry Reports. 2010; 12 :298–305. [ PubMed : 20535592 ]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, Erbes CR. Posttraumatic stress symptoms among National Guard Soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology. 2010; 78 :599–610. [ PMC free article : PMC3073229 ] [ PubMed : 20873896 ]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009; 373 :68–81. [ PubMed : 19056114 ]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, et al. Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry. 2009; 31 :505–514. [ PMC free article : PMC2785858 ] [ PubMed : 19892208 ]
- Ginzburg K, Solomon Z, Bleich A. Repressive coping style, acute stress disorder, and posttraumatic stress disorder after myocardial infarction. Psychosomatic Medicine. 2002; 64 :748–757. [ PubMed : 12271105 ]
- Gold SD, Marx BP, Soler-Baillo JM, Sloan DM. Is life stress more traumatic than traumatic stress? Journal of Anxiety Disorders. 2005; 19 :687–698. [ PubMed : 15927781 ]
- Gold SN. Contextual therapy. In: Courtois CA, Ford JD, editors. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 227–242.
- Goldberg JF, Garno JL. Development of posttraumatic stress disorder in adult bipolar patients with histories of severe childhood abuse. Journal of Psychiatric Research. 2005; 39 :595–601. [ PubMed : 16019032 ]
- Goldmann E, Aiello A, Uddin M, Delva J, Koenen K, Gant LM, et al. Pervasive exposure to violence and posttraumatic stress disorder in a predominantly African American Urban Community: The Detroit neighborhood health study. Journal of Traumatic Stress. 2011; 24 (6):747–751. [ PMC free article : PMC4433006 ] [ PubMed : 22144187 ]
- Goldstein RB, Compton WM, Grant BF. Antisocial behavioral syndromes and additional psychiatric comorbidity in posttraumatic stress disorder among U.S. adults: Results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of the American Psychiatric Nurses Association. 2010; 16 :145–165. [ PMC free article : PMC2909139 ] [ PubMed : 20661317 ]
- Gonzalez P, Gonzalez GM. Acculturation, optimism, and relatively fewer depression symptoms among Mexican immigrants and Mexican Americans. Psychological Reports. 2008; 103 :566–576. [ PubMed : 19102481 ]
- Goodman GS, Ghetti S, Quas JA, Edelstein RS, Alexander KW, Redlich AD, et al. A prospective study of memory for child sexual abuse: New findings relevant to the repressed-memory controversy. Psychological Science. 2003; 14 :113–118. [ PubMed : 12661671 ]
- Goodson J, Helstrom A, Halpern JM, Ferenschak MP, Gillihan SJ, Powers MB. The treatment of posttraumatic stress disorder in U.S. combat veterans: A meta-analytic review. Psychological Reports. 2011; 109 :573–599. [ PubMed : 22238857 ]
- Govindshenoy M, Spencer N. Abuse of the disabled child: A systematic review of population-based studies. Child: Care, Health and Development. 2007; 33 :552–558. [ PubMed : 17725777 ]
- Grammer GG, Moran SC. Geriatrics. In: Benedek DM, editor. Clinical manual for management of PTSD. Arlington, VA: American Psychiatric Publishing, Inc; 2011. pp. 371–381.
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008; 69 :533–545. [ PMC free article : PMC2676679 ] [ PubMed : 18426259 ]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV Psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004; 61 :1226–1233. [ PubMed : 15583114 ]
- Gratz KL, Tull MT. The relationship between emotion dysregulation and deliberate self-harm among inpatients with substance use disorders. Cognitive Therapy and Research. 2010; 34 :544–553. [ PMC free article : PMC2996045 ] [ PubMed : 21132101 ]
- Green BL, Krupnick JL, Chung J, Siddique J, Krause ED, Revicki D, et al. Impact of PTSD comorbidity on one-year outcomes in a depression trial. Journal of Clinical Psychology. 2006; 62 :815–835. [ PubMed : 16703602 ]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry. 2010; 67 :113–123. [ PMC free article : PMC2822662 ] [ PubMed : 20124111 ]
- Greenberg GA, Rosenheck RA. Mental health correlates of past homelessness in the National Comorbidity Study Replication. Journal of Health Care for the Poor and Underserved. 2010; 21 :1234–1249. [ PubMed : 21099075 ]
- Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE, Engel CC, et al. Posttraumatic stress disorder and depression in battle-injured soldiers. American Journal of Psychiatry. 2006; 163 :1777–1783. [ PubMed : 17012689 ]
- Gros DF, Frueh BC, Magruder KM. Prevalence and features of panic disorder and comparison to posttraumatic stress disorder in VA primary care. General Hospital Psychiatry. 2011; 33 :482–488. [ PubMed : 21816481 ]
- Guay S, Billette V, Marchand A. Exploring the links between posttraumatic stress disorder and social support: Processes and potential research avenues. Journal of Traumatic Stress. 2006; 19 :327–338. [ PubMed : 16788995 ]
- Hamblen JL, Gibson LE, Mueser KT, Norris FH. Cognitive behavioral therapy for prolonged postdisaster distress. Journal of Clinical Psychology. 2006; 62 :1043–1052. [ PubMed : 16700022 ]
- Hamblen JL, Norris FH, Pietruszkiewicz S, Gibson LE, Naturale A, Louis C. Cognitive behavioral therapy for postdisaster distress: A community based treatment program for survivors of Hurricane Katrina. Administration and Policy in Mental Health. 2009; 36 :206–214. [ PubMed : 19365725 ]
- Hankin CS, Skinner KM, Sullivan LM, Miller DR, Frayne S, Tripp TJ. Prevalence of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing sexual assault while in the military. Journal of Traumatic Stress. 1999; 12 :601–612. [ PubMed : 10646179 ]
- Hanson RF, Self-Brown S. Screening and assessment of crime victimization and its effects. Journal of Traumatic Stress. 2010; 23 :207–214. [ PubMed : 20336706 ]
- Harned MS, Korslund KE, Foa EB, Linehan MM. Treating PTSD in suicidal and self-injuring women with borderline personality disorder: Development and preliminary evaluation of a Dialectical Behavior Therapy Prolonged Exposure Protocol. Behaviour Research and Therapy. 2012; 50 :381–386. [ PMC free article : PMC3348973 ] [ PubMed : 22503959 ]
- Harper K, Richter NL, Gorey KM. Group work with female survivors of childhood sexual abuse: Evidence of poorer outcomes among those with eating disorders. Eating Behaviors. 2009; 10 :45–48. [ PubMed : 19171317 ]
- Harris JI, Erbes CR, Engdahl BE, Thuras P, Murray-Swank N, Grace D, et al. The effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma. Journal of Clinical Psychology. 2011; 67 :425–438. [ PubMed : 21294116 ]
- Harris M, Fallot RD. Trauma-informed inpatient services. In: Harris M, Fallot RD, editors. Using trauma theory to design service systems. San Francisco: Jossey-Bass; 2001. pp. 33–46.
- Harvard School of Medicine. NCS–R lifetime prevalence estimates: Table 1 Lifetime prevalence of DSM-IV/WMH-CIDI disorders by sex and cohort 1 (n=9282) National Comorbidity Survey (NCS) and National Comorbidity Survey Replication (NCS–R). Cambridge, MA: Harvard University Press; 2007.
- Harvard School of Medicine. NCS–R Twelve-month prevalence estimates: Table 2 12–month prevalence of DSM-IV/WMH-CIDI disorders by sex and cohort 1 (n=9282) National Comorbidity Survey (NCS) and National Comorbidity Survey Replication (NCS–R). Cambridge, MA: Harvard University Press; 2007.
- Haskell SG, Mattocks K, Goulet JL, Krebs EE, Skanderson M, Leslie D, et al. The burden of illness in the first year home: Do male and female VA users differ in health conditions and healthcare utilization. Women’s Health Issues. 2011; 21 :92–97. [ PMC free article : PMC3138124 ] [ PubMed : 21185994 ]
- Hawkins F, Klas L. Time management as a stressor for helping professionals: Implications for employment. Journal of Employment Counseling. 1997; 34 :2–6.
- Hembree EA, Foa EB. Posttraumatic stress disorder: Psychological factors and psychosocial interventions. Journal of Clinical Psychiatry. 2000; 61 :33–39. [ PubMed : 10795607 ]
- Hembree EA, Foa EB, Dorfan NM, Street GP, Kowalski J, Tu X. Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress. 2003; 16 :555–562. [ PubMed : 14690352 ]
- Herek GM. Hate crimes and stigma-related experiences among sexual minority adults in the United States: prevalence estimates from a national probability sample. Journal of Interpersonal Violence. 2009; 24 :54–74. [ PubMed : 18391058 ]
- Herman DB, Susser ES, Struening EL, Link BL. Adverse childhood experiences: Are they risk factors for adult homelessness? American Journal of Public Health. 1997; 87 :249–255. [ PMC free article : PMC1380802 ] [ PubMed : 9103105 ]
- Herman JL. Trauma and recovery. New York: Basic Books; 1992.
- Herman JL. Trauma and recovery. Rev ed. New York: Basic Books; 1997.
- Hetrick SE, Purcell R, Garner B, Parslow R. Combined pharmacotherapy and psychological therapies for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews. 2010:CD007316. [ PubMed : 20614457 ]
- Hien DA, Campbell ANC, Ruglass LM, Hu MC, Killeen T. The role of alcohol misuse in PTSD outcomes for women in community treatment: A secondary analysis of NIDA’s Women and Trauma Study. Drug and Alcohol Dependence. 2010; 111 :114–119. [ PMC free article : PMC2981092 ] [ PubMed : 20537811 ]
- Hill JJ III, Mobo BH Jr, Cullen MR. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: Preliminary findings from the Veterans Affairs traumatic brain injury screening program. American Journal of Physical Medicine and Rehabilitation. 2009; 88 :605–614. [ PubMed : 19620825 ]
- Hillis SD, Anda RF, Felitti VJ, Nordenberg D, Marchbanks PA. Adverse childhood experiences and sexually transmitted diseases in men and women: A retrospective study. Pediatrics. 2000; 106 :E11. [ PubMed : 10878180 ]
- Himmelfarb N, Yaeger D, Mintz J. Posttraumatic stress disorder in female veterans with military and civilian sexual trauma. Journal of Traumatic Stress. 2006; 19 :837–846. [ PubMed : 17195980 ]
- Hinton D, Ba P, Peou S, Um K. Panic disorder among Cambodian refugees attending a psychiatric clinic. Prevalence and subtypes. General Hospital Psychiatry. 2000; 22 :437–444. [ PMC free article : PMC2749726 ] [ PubMed : 11072060 ]
- Hinton D, Chau H, Nguyen L, Nguyen M, Pham T, Quinn S, et al. Panic disorder among Vietnamese refugees attending a psychiatric clinic: prevalence and subtypes. General Hospital Psychiatry. 2001; 23 :337–344. [ PMC free article : PMC2749719 ] [ PubMed : 11738465 ]
- Hinton DE, Chhean D, Pich V, Safren SA, Hofmann SG, Pollack MH. A randomized controlled trial of cognitive–behavior therapy for Cambodian refugees with treatment–resistant PTSD and panic attacks: A cross-over design. Journal of Traumatic Stress. 2005; 18 :617–629. [ PubMed : 16382423 ]
- Hinton DE, Hinton AL, Pich V, Loeum JR, Pollack MH. Nightmares among Cambodian refugees: The breaching of concentric ontological security. Culture, Medicine and Psychiatry. 2009; 33 :219–265. [ PubMed : 19333741 ]
- Hinton DE, Hofmann SG, Pollack MH, Otto MW. Mechanisms of efficacy of CBT for Cambodian refugees with PTSD: Improvement in emotion regulation and orthostatic blood pressure response. CNS Neuroscience & Therapeutics. 2009; 15 :255–263. [ PMC free article : PMC6494047 ] [ PubMed : 19691545 ]
- Hinton DE, Hofmann SG, Rivera E, Otto MW, Pollack MH. Culturally adapted CBT (CA–CBT) for Latino women with treatment–resistant PTSD: A pilot study comparing CA–CBT to applied muscle relaxation. Behaviour Research and Therapy. 2011; 49 :275–280. [ PubMed : 21333272 ]
- Hinton DE, Kredlow MA, Bui E, Pollack MH, Hofmann SG. Treatment change of somatic symptoms and cultural syndromes among Cambodian refugees with PTSD. Depression and Anxiety. 2012; 29 :148–155. [ PubMed : 22065554 ]
- Hinton DE, Nickerson A, Bryant RA. Worry, worry attacks, and PTSD among Cambodian refugees:A path analysis investigation. Social Science and Medicine. 2011; 72 :1817–1825. [ PMC free article : PMC3128797 ] [ PubMed : 21663803 ]
- Hinton DE, Park L, Hsia C, Hofmann S, Pollack MH. Anxiety disorder presentations in Asian populations: A review. CNS Neuroscience & Therapeutics. 2009; 15 :295–303. [ PMC free article : PMC6494053 ] [ PubMed : 19691549 ]
- Hinton DE, Pham T, Tran M, Safren SA, Otto MW, Pollack MH. CBT for Vietnamese refugees with treatment-resistant PTSD and panic attacks: A pilot study. Journal of Traumatic Stress. 2004; 17 :429–433. [ PMC free article : PMC2748790 ] [ PubMed : 15633922 ]
- Hinton DE, Pich V, Marques L, Nickerson A, Pollack MH. Khyal attacks: A key idiom of distress among traumatized Cambodia refugees. Culture, Medicine and Psychiatry. 2010; 34 :244–278. [ PubMed : 20407813 ]
- Hinton DE, Rivera EI, Hofmann SG, Barlow DH, Otto MW. Adapting CBT for traumatized refugees and ethnic minority patients: Examples from culturally adapted CBT (CA–CBT). Transcultural Psychiatry. 2012; 49 :340–365. [ PubMed : 22508639 ]
- Hiskey S, Luckie M, Davies S, Brewin CR. The emergence of posttraumatic distress in later life: a review. Journal of Geriatric Psychiatry and Neurology. 2008; 21 :232–241. [ PubMed : 19017780 ]
- Hobfoll SE, Canetti-Nisim D, Johnson RJ, Palmieri PA, Varley JD, Galea S. The association of exposure, risk, and resiliency factors with PTSD among Jews and Arabs exposed to repeated acts of terrorism in Israel. Journal of Traumatic Stress. 2008; 21 :9–21. [ PMC free article : PMC2802182 ] [ PubMed : 18302179 ]
- Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, et al. Five essential elements of immediate and mid–term mass trauma intervention: empirical evidence. Psychiatry. 2007; 70 :283–315. [ PubMed : 18181708 ]
- Hofmann SG, Smits JA. Cognitive–behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. Journal of Clinical Psychiatry. 2008; 69 :621–632. [ PMC free article : PMC2409267 ] [ PubMed : 18363421 ]
- Hoge CW. Public health strategies and treatment of service members and veterans with combat-related mental health problems. In: Adler AB, Bliese PD, Castro CA, editors. Deployment psychology: Evidence-based strategies to promote mental health in the military. Washington, DC, US: American Psychological Association; 2011. pp. 17–34.
- Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq War veterans. The American Journal of Psychiatry. 2007; 164 :150–153. [ PubMed : 17202557 ]
- Holbrook TL, Hoyt DB, Stein MB, Sieber WJ. Perceived threat to life predicts posttraumatic stress disorder after major trauma: Risk factors and functional outcome. Journal of Trauma. 2001; 51 :287–292. [ PubMed : 11493786 ]
- Holbrook TL, Hoyt DB, Stein MB, Sieber WJ. Gender differences in long-term posttraumatic stress disorder outcomes after major trauma: Women are at higher risk of adverse outcomes than men. Journal of Trauma. 2002; 53 :882–888. [ PubMed : 12435938 ]
- Hollifield M. Acupuncture for posttraumatic stress disorder: Conceptual, clinical, and biological data support further research. CNS Neuroscience & Therapeutics. 2011; 17 :769–779. [ PMC free article : PMC6493831 ] [ PubMed : 22070661 ]
- Hopper EK, Bassuk EL, Olivet J. Shelter from the storm: Trauma-informed care in homelessness services settings. The Open Health Services and Policy Journal. 2010; 3 :80–100.
- Horowitz MJ. American Psychiatric Association Task Force on Treatments of Psychiatric Disorders, editor. Treatments of psychiatric disorders: A task force report of the American Psychiatric Association. Washington, DC: American Psychiatric Association; 1989. Posttraumatic Stress Disorder; pp. 2065–2082.
- Hoshmand LT. Cross-cultural assessment of psychological trauma and PTSD. New York: Springer Science + Business Media; 2007. Cultural–ecological perspectives on the understanding and assessment of trauma; pp. 31–50.
- Huang MC, Schwandt ML, Ramchandani VA, George DT, Heilig M. Impact of multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic inpatients. Alcoholism, Clinical and Experimental Research. 2012; 36 (6):1099–1107. [ PMC free article : PMC3370064 ] [ PubMed : 22420670 ]
- Hughes KC, Shin LM. Functional neuroimaging studies of post-traumatic stress disorder. Expert Review of Neurotherapeutics. 2011; 11 :275–285. [ PMC free article : PMC3142267 ] [ PubMed : 21306214 ]
- Hussain A, Weisaeth L, Heir T. Changes in religious beliefs and the relation of religiosity to posttraumatic stress and life satisfaction after a natural disaster. Social Psychiatry and Psychiatric Epidemiology. 2011; 46 :1027–1032. [ PMC free article : PMC3173616 ] [ PubMed : 20676883 ]
- Ilgen MA, Bohnert AS, Ignacio RV, McCarthy JF, Valenstein MM, Kim HM, et al. Psychiatric diagnoses and risk of suicide in veterans. Archives of General Psychiatry. 2010; 67 :1152–1158. [ PubMed : 21041616 ]
- Institute of Medicine. Treatment of posttraumatic stress disorder: An assessment of the evidence. Washington, DC: Institute of Medicine; 2008.
- Ipser JC, Stein DJ. Evidence-based pharmacotherapy of post-traumatic stress disorder (PTSD). The International Journal of Neuropharmacology. 2012; 15 :825–840. [ PubMed : 21798109 ]
- Jackson C, Nissenson K, Cloitre M. Treatment for complex PTSD. In: Sookman D, editor. Treatment resistant anxiety disorders: Resolving impasses to symptom remission. New York: Routledge/Taylor & Francis Group; 2010. pp. 75–104.
- Jainchill N, Hawke J, Yagelka J. Gender, psychopathology, and patterns of homelessness among clients in shelter-based TCs. American Journal of Drug and Alcohol Abuse. 2000; 26 :553–567. [ PubMed : 11097192 ]
- Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, de GR, et al. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatrica Scandinavica. 2004; 109 :38–45. [ PubMed : 14674957 ]
- Jaycox LH, Zoellner L, Foa EB. Cognitive–behavior therapy for PTSD in rape survivors. Journal of Clinical Psychology. 2002; 58 :891–906. [ PubMed : 12115713 ]
- Joe S, Baser RE, Breeden GK, Neighbors HW, Jackson JS. Prevalence of and risk factors for lifetime suicide attempts among blacks in the United States. JAMA. 2006; 296 :2112–2123. [ PMC free article : PMC2718696 ] [ PubMed : 17077376 ]
- Johnson DM, Palmieri PA, Jackson AP, Hobfoll SE. Emotional numbing weakens abused inner-city women’s resiliency resources. Journal of Traumatic Stress. 2007; 20 :197–206. [ PubMed : 17427905 ]
- Johnson DM, Zlotnick C, Perez S. Cognitive behavioral treatment of PTSD in residents of battered women’s shelters: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2011; 79 :542–551. [ PMC free article : PMC3144508 ] [ PubMed : 21787052 ]
- Johnson DR, Lahad M, Gray A. Creative therapies for adults. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 479–490.
- Johnson H, Thompson A. The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clinical Psychology Review. 2008; 28 :36–47. [ PubMed : 17383783 ]
- Johnson H, Thompson A, Downs M. Non–Western interpreters’ experiences of trauma: The protective role of culture following exposure to oppression. Ethnicity and Health. 2009; 14 :407–418. [ PubMed : 19259848 ]
- Johnson SD. Substance use, post-traumatic stress disorder and violence. Current Opinion in Psychiatry. 2008; 21 :242–246. [ PubMed : 18382221 ]
- Johnson SD, Striley C, Cottler LB. The association of substance use disorders with trauma exposure and PTSD among African American drug users. Addictive Behaviors. 2006; 31 :2063–2073. [ PubMed : 16580784 ]
- Johnson SM, Courtois CA. Couple therapy. In: Courtois CA, Ford JD, editors. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 371–390.
- Jones BH, Knapik JJ. Physical training and exercise–related injuries. Surveillance, research and injury prevention in military populations. Sports Medicine. 1999; 27 :111–125. [ PubMed : 10091275 ]
- Jordan BK, Schlenger WE, Hough R, Kulka RA, Weiss D, Fairbank JA, et al. Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Archives of General Psychiatry. 1991; 48 :207–215. [ PubMed : 1996916 ]
- Jovanovic T, Smith A, Kamkwalala A, Poole J, Samples T, Norrholm SD, et al. Physiological markers of anxiety are increased in children of abused mothers. Journal of Child Psychology and Psychiatry. 2011; 52 :844–852. [ PMC free article : PMC3134615 ] [ PubMed : 21501167 ]
- Kang H, Dalager N, Mahan C, Ishii E. The role of sexual assault on the risk of PTSD among Gulf War veterans. Annals of Epidemiology. 2005; 15 :191–195. [ PubMed : 15723763 ]
- Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based survey of 30,000 veterans. American Journal of Epidemiology. 2003; 157 :141–148. [ PubMed : 12522021 ]
- Kantor EM, Beckett DR. Psychological first aid. In: Stoddard FJ Jr, Pandya A, Katz CL, editors. Disaster psychiatry: Readiness, evaluation, and treatment. Arlington, VA: American Psychiatric Publishing, Inc; 2011. pp. 203–212.
- Kar N. Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: A review. Neuropsychiatric Disease and Treatment. 2011; 7 :167–181. [ PMC free article : PMC3083990 ] [ PubMed : 21552319 ]
- Karney BR, Ramchand R, Osilla KC, Caldarone LB, Burns RM. Invisible wounds: Predicting the immediate and long term consequences of mental health problems in veterans of Operation Enduring Freedom and Operation Iraqi Freedom. Santa Monica, CA: RAND Corporation; 2008.
- Kashdan TB, Morina N, Priebe S. Post-traumatic stress disorder, social anxiety disorder, and depression in survivors of the Kosovo War: Experiential avoidance as a contributor to distress and quality of life. Journal of Anxiety Disorders. 2009; 23 :185–196. [ PMC free article : PMC2667796 ] [ PubMed : 18676121 ]
- Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: Three studies in reliability and validity. Journal of Consulting & Clinical Psychology. 1988; 56 :85–90. [ PubMed : 3346454 ]
- Kelly VG, Merrill GS, Shumway M, Alvidrez J, Boccellari A. Outreach, engagement, and practical assistance: Essential aspects of PTSD care for urban victims of violent crime. Trauma, Violence, and Abuse: A Review Journal. 2010; 11 :144–156. [ PubMed : 20554505 ]
- Kent M, Davis MC, Stark SL, Stewart LA. A resilience-oriented treatment for posttraumatic stress disorder: Results of a preliminary randomized clinical trial. Journal of Traumatic Stress. 2011; 24 :591–595. [ PubMed : 21898603 ]
- Kersting A, Reutemann M, Gast U, Ohrmann P, Suslow T, Michael N, et al. Dissociative disorders and traumatic childhood experiences in transsexuals. Journal of Nervous and Mental Disease. 2003; 191 :182–189. [ PubMed : 12637845 ]
- Kessler RC. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry, 61 Supplement. 2000; 5 :4–12. [ PubMed : 10761674 ]
- Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS–R): Background and aims. International Journal of Methods in Psychiatric Research. 2004; 13 :60–68. [ PMC free article : PMC6878416 ] [ PubMed : 15297904 ]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005; 62 :593–602. [ PubMed : 15939837 ]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005; 62 :617–627. [ PMC free article : PMC2847357 ] [ PubMed : 15939839 ]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997; 54 :313–321. [ PubMed : 9107147 ]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995; 52 :1048–1060. [ PubMed : 7492257 ]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Breslau NN. Epidemiological risk factors for trauma and PTSD. In: Yehuda R, editor. Risk factors for PTSD. Washington, DC: American Psychiatric Press; 1999. pp. 23–59.
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997; 4 :231–244. [ PubMed : 9385000 ]
- Khaylis A, Polusny MA, Erbes CR, Gewirtz A, Rath M. Posttraumatic stress, family adjustment, and treatment preferences among National Guard Soldiers deployed to OEF/OIF. Military Medicine. 2011; 176 :126–131. [ PubMed : 21366071 ]
- Khoo A, Dent MT, Oei TPS. Group cognitive behaviour therapy for military service–related post-traumatic stress disorder: Effectiveness, sustainability and repeatability. Australian and New Zealand Journal of Psychiatry. 2011; 45 :663–672. [ PubMed : 21870924 ]
- Kilcommons AM, Morrison AP. Relationships between trauma and psychosis: An exploration of cognitive and dissociative factors. Acta Psychiatrica Scandinavica. 2005; 112 :351–359. [ PubMed : 16223422 ]
- Kilcommons AM, Morrison AP, Knight A, Lobban F. Psychotic experiences in people who have been sexually assaulted. Social Psychiatry and Psychiatric Epidemiology. 2008; 43 :602–611. [ PubMed : 18560786 ]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997; 65 :834–847. [ PubMed : 9337502 ]
- Kim MM, Ford JD, Howard DL, Bradford DW. Assessing trauma, substance abuse, and mental health in a sample of homeless men. Health & Social Work. 2010; 35 :39–48. [ PubMed : 20218452 ]
- Kimerling R, Calhoun KS. Somatic symptoms, social support, and treatment seeking among sexual assault victims. Journal of Consulting and Clinical Psychology. 1994; 62 :333–340. [ PubMed : 8201071 ]
- Kimerling R, Ouimette P, Weitlauf JC. Gender issues in PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. Guilford Press; New York: 2007. pp. 207–228.
- Kimerling R, Street AE, Pavao J, Smith MW, Cronkite RC, Holmes TH, et al. Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. American Journal of Public Health. 2010; 100 :1409–1412. [ PMC free article : PMC2901286 ] [ PubMed : 20558808 ]
- King DW, King LA, Foy DW, Gudanowski DM. Prewar factors in combat-related posttraumatic stress disorder: structural equation modeling with a national sample of female and male Vietnam veterans. Journal of Consulting and Clinical Psychology. 1996; 64 :520–531. [ PubMed : 8698946 ]
- Kira IA, Ahmed A, Wasim F, Mahmoud V, Colrain J, Rai D. Group therapy for refugees and torture survivors: Treatment model innovations. International Journal of Group Psychotherapy. 2012; 62 :69–88. [ PubMed : 22229369 ]
- Kira IA, Lewandowski LA, Templin TN, Ramaswamy V, Ozkan B, Mohanesh J. The effects of post-retribution inter-group forgiveness: The case of Iraqi refugees. Peace and Conflict. 2009; 15 :385–413.
- Klariç M, Francciskovic T, Klariç B, Kresiç M, Grkoviç J, Lisica ID, et al. Social support and PTSD symptoms in war-traumatized women in Bosnia and Herzegovina. Psychiatria Danubina. 2008; 20 :466–473. [ PubMed : 19011587 ]
- Knoll J, Resnick PJ. The detection of malingered post-traumatic stress disorder. Psychiatric Clinics of North America. 2006; 29 :629–647. [ PubMed : 16904503 ]
- Knudsen HK, Ducharme LJ, Roman PM. Counselor emotional exhaustion and turnover intention in therapeutic communities. Journal of Substance Abuse Treatment. 2006; 31 :173–180. [ PubMed : 16919745 ]
- Koenen KC. Developmental epidemiology of PTSD: self-regulation as a central mechanism. Annals of the New York Academy of Sciences. 2006; 1071 :255–266. [ PubMed : 16891576 ]
- Koenen KC, Moffitt TE, Caspi A, Gregory A, Harrington H, Poulton R. The developmental mental–disorder histories of adults with posttraumatic stress disorder: A prospective longitudinal birth cohort study. Journal of Abnormal Psychology. 2008; 117 :460–466. [ PMC free article : PMC2666441 ] [ PubMed : 18489223 ]
- Koenen KC, Stellman SD, Sommer JF Jr, Stellman JM. Persisting posttraumatic stress disorder symptoms and their relationship to functioning in Vietnam veterans: A 14-year follow-up. Journal of Traumatic Stress. 2008; 21 :49–57. [ PMC free article : PMC2654776 ] [ PubMed : 18302174 ]
- Kornør H, Winje D, Ekeberg Ÿ, Weisaeth L, Kirkehei I, Johansen K, et al. Early trauma-focused cognitive–behavioural therapy to prevent chronic post-traumatic stress disorder and related symptoms: A systematic review and meta-analysis. BMC Psychiatry. 2008; 8 [ PMC free article : PMC2559832 ] [ PubMed : 18801204 ]
- Kreidler M, Einsporn R. A comparative study of therapy duration for survivors of childhood sexual abuse. Journal of Psychosocial Nursing and Mental Health Services. 2012; 50 :26–32. [ PubMed : 22421008 ]
- Krysinska K, Lester D. Post-traumatic stress disorder and suicide risk: A systematic review. Archives of Suicide Research. 2010; 14 :1–23. [ PubMed : 20112140 ]
- Kubany ES, Hill EE, Owens JA, Iannce–Spencer C, McCaig MA, Tremayne KJ, et al. Cognitive trauma therapy for battered women with PTSD (CTT–BW). Journal of Consulting and Clinical Psychology. 2004; 72 :3–18. [ PubMed : 14756610 ]
- Kubany ES, Leisen MB, Kaplan AS, Kelly MP. Validation of a brief measure of posttraumatic stress disorder: The distressing event questionnaire (DEQ). Psychological Assessment. 2000; 12 :197–209. [ PubMed : 10887766 ]
- Kudler HS, Krupnick JL, Blank AS Jr, Herman JL, Horowitz MJ. Psychodynamic therapy for adults. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 346–369.
- Kuhn JH, Nakashima J. Community Homelessness Assessment, Local Education and Networking Group (CHALENG) for veterans: The fifteenth annual progress report on public law 105–114 services for homeless veterans assessment and coordination March 11, 2009. Washington, DC: U.S. Department of Veterans Affairs; 2011.
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. The National Vietnam Veterans Readjustment Study: Tables of findings and technical appendices. Research Triangle Park, NC: Research Triangle Institute; 1990.
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. Trauma and the Vietnam war generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel; 1990.
- Kushner MG, Krueger R, Frye B, Peterson J. Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In: Stewart SH, Conrod PJ, editors. Anxiety and substance use disorders: The vicious cycle of comorbidity. New York: Springer Science + Business Media; 2008. pp. 3–17.
- Lacoursiere RB. “Burnout” and substance user treatment: The phenomenon and the administrator–clinician’s experience. Substance Use & Misuse. 2001; 36 :1839–1874. [ PubMed : 11795582 ]
- Laflamme L, Burrows S, Hasselberg M. Socioeconomic differences in injury risks: A review of findings and a discussion of potential countermeasures. Geneva: World Health Organization; 2009.
- Lalor K, McElvaney R. Child sexual abuse, links to later sexual exploitation/high-risk sexual behavior, and prevention/treatment programs. Trauma, Violence, & Abuse. 2010; 11 :159–177. [ PubMed : 20679329 ]
- Lang AJ, Strauss JL, Bomyea J, Bormann JE, Hickman SD, Good RC, et al. The theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification. 2012; 36 (6):759–786. [ PubMed : 22669968 ]
- Laugharne J, Lillee A, Janca A. Role of psychological trauma in the cause and treatment of anxiety and depressive disorders. Current Opinion in Psychiatry. 2010; 23 :25–29. [ PubMed : 19901834 ]
- Lawyer SR, Resnick HS, Galea S, Ahern J, Kilpatrick DG, Vlahov D. Predictors of peritraumatic reactions and PTSD following the September 11th terrorist attacks. Psychiatry. 2006; 69 :130–141. [ PubMed : 16822192 ]
- Layne CM, Warren JS, Watson PJ, Shalev AY. Risk, vulnerability, resistance, and resilience: Toward an integrative conceptualization of posttraumatic adaptation. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York: Guilford Press; 2007. pp. 497–520.
- Lee BA, Schreck CJ. Danger on the streets: Marginality and victimization among homeless people. American Behavioral Scientist. 2005; 48 :1055–1081.
- Lee CS, Chang JC, Liu CY, Chang CJ, Chen THH, Chen CH, et al. Acculturation, psychiatric comorbidity and posttraumatic stress disorder in a Taiwanese aboriginal population. Social Psychiatry and Psychiatric Epidemiology. 2009; 44 :55–62. [ PubMed : 18622537 ]
- Lee E, Mock MR. Asian families: An overview. In: McGoldrick M, Giordano J, Garcia-Preto N, editors. Ethnicity and family therapy. 3rd ed. Guilford Press; New York: 2005. pp. 269–289.
- Lee E, Mock MR. Chinese families. In: McGoldrick M, Giordano J, Garcia-Preto N, editors. Ethnicity and family therapy. 3rd ed. Guilford Press; New York: 2005. pp. 302–318.
- Lee TT, Westrup DA, Ruzek JI, Keller J, Weitlauf JC. Impact of clinician gender on examination anxiety among female veterans with sexual trauma: A pilot study. Journal of Women’s Health. 2007; 16 :1291–1299. [ PubMed : 18001185 ]
- Lensvelt-Mulders G, van der Hart O, van Ochten JM, van Son MJM, Steele K, Breeman L. Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis. Clinical Psychology Review. 2008; 28 :1138–1151. [ PubMed : 18502549 ]
- Lent J. Stressors and stress management of counselors: Findings from interviews of professional counselors. 2010. Retrieved July 4, 2013, from: http: //counselingoutfitters .com/vistas/vistas10/Article_73 .pdf .
- Lester K, Resick PA, Young–Xu Y, Artz C. Impact of race on early treatment termination and outcomes in posttraumatic stress disorder treatment. Journal of Consulting and Clinical Psychology. 2010; 78 :480–489. [ PubMed : 20658805 ]
- Levitt JT, Malta LS, Martin A, Davis L, Cloitre M. The flexible application of a manualized treatment for PTSD symptoms and functional impairment related to the 9/11 World Trade Center attack. Behaviour Research and Therapy. 2007; 45 :1419–1433. [ PubMed : 17350590 ]
- Lewis KL, Grenyer BF. Borderline personality or complex posttraumatic stress disorder? An update on the controversy. Harvard Review of Psychiatry. 2009; 17 :322–328. [ PubMed : 19832046 ]
- Lewis-Fernández R, Martínez-Taboas A, Sar V, Patel S, Boatin A. The cross-cultural assessment of dissociation. In: Wilson JP, Tang CS, editors. Cross-cultural assessment of psychological trauma and PTSD. New York: Springer Science + Business Media; 2007. pp. 279–317.
- Libby AM, Orton HD, Beals J, Buchwald D, Manson SM. Childhood abuse and later parenting outcomes in two American Indian tribes. Child Abuse & Neglect. 2008; 32 :195–211. [ PMC free article : PMC4530963 ] [ PubMed : 18304630 ]
- Lilly MM, Graham-Bermann SA. Ethnicity and risk for symptoms of posttraumatic stress following intimate partner violence. Journal of Interpersonal Violence. 2009; 24 :3–19. [ PubMed : 18299418 ]
- Lu W, Mueser KT, Rosenberg SD, Jankowski MK. Correlates of adverse childhood experiences among adults with severe mood disorders. Psychiatric Services. 2008; 59 :1018–1026. [ PubMed : 18757595 ]
- Luce H, Schrager S, Gilchrist V. Sexual assault of women. American Family Physician. 2010; 81 :489–495. [ PubMed : 20148503 ]
- Lutz GM, Kramer RE, Gonnerman ME, Lantz GL, Downs WR. Substance abuse and the Iowa flood disaster of 1993: Final report. Cedar Falls, IA: University of Northern Iowa; 1995.
- Lynch M, Cicchetti D. An ecological–transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, and children’s symptomatology. Development and Psychopathology. 1998; 10 :235–257. [ PubMed : 9635223 ]
- Lynch SM. Surviving sexual violence: A guide to recovery and empowerment. Lanham, MD: Rowman & Littlefield; 2011. Restoring relationships: Group interventions for survivors of sexual traumas; pp. 179–198.
- Macklin ML, Metzger LJ, Litz BT, McNally RJ, Lasko NB, Orr SP, et al. Lower precombat intelligence is a risk factor for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1998; 66 :323–326. [ PubMed : 9583335 ]
- Maercker A, Zöllner T, Menning H, Rabe S, Karl A. Dresden PTSD treatment study: Randomized controlled trial of motor vehicle accident survivors. BMC Psychiatry. 2006; 6 :29. [ PMC free article : PMC1543618 ] [ PubMed : 16824221 ]
- Maes M, Delmeire L, Mylle J, Atamura C. Risk and preventive factors of post-traumatic stress disorder (PTSD): Alcohol consumption and intoxication prior to a traumatic event diminishes the relative risk to develop PTSD in response to that trauma. Journal of Affective Disorders. 2001; 63 :113–121. [ PubMed : 11246087 ]
- Maguen S, Luxton DD, Skopp NA, Madden E. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. Journal of Psychiatric Research. 2011; 46 (3):311–316. [ PubMed : 22172997 ]
- Maguen S, Ren L, Bosch JO, Marmar CR, Seal KH. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. American Journal of Public Health. 2010; 100 :2450–2456. [ PMC free article : PMC2978175 ] [ PubMed : 20966380 ]
- Maguen S, Suvak M, Litz BT. Predictors and prevalence of posttraumatic stress disorder among military veterans. In: Adler AB, Castro CA, Britt TW, editors. Military life: The psychology of serving in peace and combat (2): Operational stress. Westport, CT: Praeger Security International; 2006. pp. 141–169.
- Malta LS, Levitt JT, Martin A, Davis L, Cloitre M. Correlates of functional impairment in treatment-seeking survivors of mass terrorism. Behavior Therapy. 2009; 40 :39–49. [ PubMed : 19187815 ]
- Mancino MJ, Pyne JM, Tripathi S, Constans J, Roca V, Freeman T. Quality-adjusted health status in veterans with posttraumatic stress disorder. Journal of Nervous and Mental Disease. 2006; 194 :877–879. [ PubMed : 17102715 ]
- Manson SM, Beals J, Klein SA, Croy CD. Social epidemiology of trauma among 2 American Indian reservation populations. American Journal of Public Health. 2005; 95 :851–859. [ PMC free article : PMC1449268 ] [ PubMed : 15855465 ]
- Marchand A, Guay S, Boyer R, Lucci S, Martin A, St-Hilaire MH. A Randomized controlled trial of an adapted form of individual critical incident stress debriefing for victims of an armed robbery. Brief Treatment and Crisis Intervention. 2006; 6 :122–129.
- Marques L, Robinaugh DJ, LeBlanc NJ, Hinton D. Cross-cultural variations in the prevalence and presentation of anxiety disorders. Expert Review of Neurotherapeutics. 2011; 11 :313–322. [ PubMed : 21306217 ]
- Marsella AJ. Ethnocultural aspects of PTSD: An overview of concepts, issues, and treatments. Traumatology. 2010; 16 :17–26.
- Marsella AJ, Christopher MA. Ethnocultural considerations in disasters: An overview of research, issues, and directions. Psychiatric Clinics of North America. 2004; 27 :521–539. [ PubMed : 15325491 ]
- Marsella AJ, Johnson JL, Watson P, Gryczynski J. Essential concepts and foundations. In: Marsella AJ, Johnson JL, Watson P, Gryczynski J, editors. Ethnocultural perspectives on disaster and trauma: Foundations, issues, and applications. New York: Springer Science + Business Media; 2008. pp. 3–13.
- Marshall GN, Schell TL, Miles JN. Ethnic differences in posttraumatic distress: Hispanics’ symptoms differ in kind and degree. Journal of Consulting & Clinical Psychology. 2009; 77 :1169–1178. [ PMC free article : PMC2821595 ] [ PubMed : 19968392 ]
- Marshall GN, Schell TL, Elliott MN, Berthold SM, Chun CA. Mental health of Cambodian refugees 2 decades after resettlement in the United States. JAMA. 2005; 294 :571–579. [ PubMed : 16077051 ]
- Marshall-Berenz EC, Vujanovic AA, Zvolensky MJ. Main and interactive effects of a nonclinical panic attack history and distress tolerance in relation to PTSD symptom severity. Journal of Anxiety Disorders. 2011; 25 :185–191. [ PMC free article : PMC3017224 ] [ PubMed : 20888732 ]
- Martin M, Marchand A, Boyer R, Martin N. Predictors of the development of posttraumatic stress disorder among police officers. Journal of Trauma & Dissociation. 2009; 10 :451–468. [ PubMed : 19821179 ]
- Martin SL, Ray N, Sotres-Alvarez D, Kupper LL, Moracco KE, Dickens PA, et al. Physical and sexual assault of women with disabilities. Violence Against Women. 2006; 12 :823–837. [ PubMed : 16905675 ]
- Maschi T, Dennis KS, Gibson S, MacMillan T, Sternberg S, Hom M. Trauma and stress among older adults in the criminal justice system: A review of the literature with implications for social work. Journal of Gerontological Social Work. 2011; 54 :390–424. [ PubMed : 21547829 ]
- Mathieu A, Mazza S, Petit D, Decary A, Massicotte-Marquez J, Malo J, et al. Does age worsen EEG slowing and attention deficits in obstructive sleep apnea syndrome? Clinical Neurophysiology. 2007; 118 :1538–1544. [ PubMed : 17507290 ]
- McCarthy E, Petrakis I. Epidemiology and management of alcohol dependence in individuals with post-traumatic stress disorder. CNS Drugs. 2010; 24 :997–1007. [ PubMed : 21090836 ]
- McCutcheon VV, Heath AC, Nelson EC, Bucholz KK, Madden PA, Martin NG. Clustering of trauma and associations with single and co-occurring depression and panic attack over twenty years. Twin Research and Human Genetics. 2010; 13 :57–65. [ PMC free article : PMC2850813 ] [ PubMed : 20158307 ]
- McDonagh A, Friedman M, McHugo G, Ford J, Sengupta A, Mueser K, et al. Randomized trial of cognitive–behavioral therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005; 73 :515–524. [ PubMed : 15982149 ]
- McFall M, Atkins DC, Yoshimoto D, Thompson CE, Kanter E, Malte CA, et al. Integrating tobacco cessation treatment into mental health care for patients with posttraumatic stress disorder. American Journal on Addictions. 2006; 15 :336–344. [ PubMed : 16966189 ]
- McGovern MP, Lambert-Harris C, Acquilano S, Xie H, Alterman AI, Weiss RD. A cognitive behavioral therapy for co-occurring substance use and posttraumatic stress disorders. Addictive Behaviors. 2009; 34 :892–897. [ PMC free article : PMC2720425 ] [ PubMed : 19395179 ]
- McGovern MP, Lambert–Harris C, Alterman AI, Xie H, Meier A. A randomized controlled trial comparing integrated cognitive behavioral therapy versus individual addiction counseling for co-occurring substance use and posttraumatic stress disorders. Journal of Dual Diagnosis. 2011; 7 :207–227. [ PMC free article : PMC3289146 ] [ PubMed : 22383864 ]
- McHugo GJ, Caspi Y, Kammerer N, Mazelis R, Jackson EW, Russell L, et al. The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. The Journal of Behavioral Health Services & Research. 2005; 32 :113–127. [ PubMed : 15834262 ]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: Associations with persistence of DSM-IV disorders. Archives of General Psychiatry. 2010; 67 :124–132. [ PMC free article : PMC2847359 ] [ PubMed : 20124112 ]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS–R) III: Associations with functional impairment related to DSM-IV disorders. Psychological Medicine. 2010; 40 :847–859. [ PMC free article : PMC2847368 ] [ PubMed : 19732483 ]
- McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Military Medicine. 2010; 175 :759–762. [ PubMed : 20968266 ]
- McLean CP, Anderson ER. Brave men and timid women? A review of the gender differences in fear and anxiety. Clinical Psychology Review. 2009; 29 :496–505. [ PubMed : 19541399 ]
- McLean CP, Foa EB. Prolonged exposure therapy for post-traumatic stress disorder: A review of evidence and dissemination. Expert Review of Neurotherapeutics. 2011; 11 :1151–1163. [ PubMed : 21797656 ]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research. 2011; 45 :1027–1035. [ PMC free article : PMC3135672 ] [ PubMed : 21439576 ]
- McLean CP, Steenkamp MM, Levy HC, Litz BT. Posttraumatic stress disorder. In: Cucciare MA, Weingardt KR, editors. Using technology to support evidence-based behavioral health practices: A clinician’s guide. New York: Routledge/Taylor & Francis Group; 2010. pp. 45–68.
- McLeod DS, Koenen KC, Meyer JM, Lyons MJ, Eisen S, True W, et al. Genetic and environmental influences on the relationship among combat exposure, posttraumatic stress disorder symptoms, and alcohol use. Journal of Traumatic Stress. 2001; 14 :259–275. [ PubMed : 11469155 ]
- McNamara C, Schumacher JE, Milby JB, Wallace D, Usdan S. Prevalence of nonpsychotic mental disorders does not affect treatment outcome in a homeless cocaine-dependent sample. American Journal of Drug and Alcohol Abuse. 2001; 27 :91–106. [ PubMed : 11373038 ]
- McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: An examination in a nationally representative sample. Pain. 2003; 106 :127–133. [ PubMed : 14581119 ]
- Mendes DD, Mello MF, Ventura P, Passarela CM, Mari JJ. A systematic review on the effectiveness of cognitive behavioral therapy for posttraumatic stress disorder. International Journal of Psychiatry in Medicine. 2008; 38 :241–259. [ PubMed : 19069570 ]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12–month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of General Psychiatry. 2007; 64 :543–552. [ PMC free article : PMC1931566 ] [ PubMed : 17485606 ]
- Mevissen L, de Jongh A. PTSD and its treatment in people with intellectual disabilities: A review of the literature. Clinical Psychology Review. 2010; 30 :308–316. [ PubMed : 20056303 ]
- Meyer RE. Psychobiology and the treatment of drug dependence: The biobehavioral interface. American Journal of Drug and Alcohol Abuse. 1986; 12 :223–233. [ PubMed : 3332558 ]
- Meyerbröker K, Emmelkamp PM. Virtual reality exposure therapy in anxiety disorders: a systematic review of process-and-outcome studies. Depression and Anxiety. 2010; 27 :933–944. [ PubMed : 20734361 ]
- Miller D, Guidry L. Addictions and trauma recovery: Healing the body, mind and spirit. New York: W W Norton & Co; 2001.
- Moak ZB, Agrawal A. The association between perceived interpersonal social support and physical and mental health: results from the National Epidemiological Survey on Alcohol and Related Conditions. Journal of Public Health: Oxford Journals. 2010; 32 :191–201. [ PMC free article : PMC2875984 ] [ PubMed : 19864495 ]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2010; 40 :899–909. [ PMC free article : PMC3572710 ] [ PubMed : 19719899 ]
- Mollica RF, McInnes K, Poole C, Tor S. Dose–effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. British Journal of Psychiatry. 1998; 173 :482–488. [ PubMed : 9926076 ]
- Monson CM, Rodriguez BF, Warner R. Cognitive–behavioral therapy for PTSD in the real world: Do interpersonal relationships make a real difference? Journal of Clinical Psychology. 2005; 61 :751–761. [ PubMed : 15546144 ]
- Monson CM, Stevens SP, Schnurr PP. Cognitive–behavioral couple’s treatment for posttraumatic stress disorder. In: Corales TA, editor. Focus on posttraumatic stress disorder research. Hauppauge, NY: Nova Science Publishers; 2005. pp. 245–274.
- Monson CM, Taft CT, Fredman SJ. Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clinical Psychology Review. 2009; 29 :707–714. [ PMC free article : PMC2783889 ] [ PubMed : 19781836 ]
- Mouton CP, Rodabough RJ, Rovi SL, Hunt JL, Talamantes MA, Brzyski RG, et al. Prevalence and 3-year incidence of abuse among postmenopausal women. American Journal of Public Health. 2004; 94 :605–612. [ PMC free article : PMC1448306 ] [ PubMed : 15054013 ]
- Mueser KT, Rosenberg SD, Xie H, Jankowski MK, Bolton EE, Lu W, et al. A randomized controlled trial of cognitive–behavioral treatment for posttraumatic stress disorder in severe mental illness. Journal of Consulting & Clinical Psychology. 2008; 76 :259–271. [ PMC free article : PMC3916092 ] [ PubMed : 18377122 ]
- Mylle J, Maes M. Partial posttraumatic stress disorder revisited. Journal of Affective Disorders. 2004; 78 :37–48. [ PubMed : 14672795 ]
- Najavits LM. Seeking safety: A treatment manual for PTSD and substance abuse. New York: Guilford Press; 2002.
- Najavits LM. Assessment of trauma, PTSD, and substance use disorder: A practical guide. In: Wilson JP, Keane T, editors. Assessing psychological trauma and PTSD. New York: Guilford; 2004. pp. 466–491.
- Najavits LM, Gastfriend DR, Barber JP, Reif S, Muenz LR, Blaine J, et al. Cocaine dependence with and without PTSD among subjects in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. American Journal of Psychiatry. 1998; 155 :214–219. [ PubMed : 9464200 ]
- Najavits LM, Harned MS, Gallop RJ, Butler SF, Barber JP, Thase ME, et al. Six-month treatment outcomes of cocaine-dependent patients with and without PTSD in a multisite national trial. Journal of Studies on Alcohol and Drugs. 2007; 68 :353–361. [ PubMed : 17446974 ]
- Najavits LM, Schmitz M, Gotthardt S, Weiss RD. Seeking safety plus exposure therapy: An outcome study on dual diagnosis men. Journal of Psychoactive Drugs. 2005; 37 :425–435. [ PubMed : 16480170 ]
- Nappi CM, Drummond SP, Hall JM. Treating nightmares and insomnia in posttraumatic stress disorder: A review of current evidence. Neuropharmacology. 2012; 62 :576–585. [ PMC free article : PMC5154613 ] [ PubMed : 21396945 ]
- Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence based estimates of mental disorders in the United States: Using a clinical significance criterion to reconcile 2 surveys’ estimates. Archives of General Psychiatry. 2002; 59 :115–123. [ PubMed : 11825131 ]
- National Child Traumatic Stress Network & National Center for PTSD. Psychological first aid: Field operations guide. White River Junction, VT: National Center for PTSD; 2006.
- National Institute for Health and Clinical Excellence. Post-traumatic stress disorder (PTSD). London: National Institute for Health and Clinical Excellence; 2005.
- Nelson-Zlupko L, Dore MM, Kauffman E, Kaltenbach K. Women in recovery: Their perceptions of treatment effectiveness. Journal of Substance Abuse Treatment. 1996; 13 :51–59. [ PubMed : 8699543 ]
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology. 2004; 72 :579–587. [ PubMed : 15301642 ]
- Newman JM, Turnbull A, Berman BA, Rodrigues S, Serper MR. Impact of traumatic and violent victimization experiences in individuals with schizophrenia and schizoaffective disorder. Journal of Nervous and Mental Disease. 2010; 198 :708–714. [ PubMed : 20921860 ]
- Nickerson A, Bryant RA, Silove D, Steel Z. A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clinical Psychology Review. 2011; 31 :399–417. [ PubMed : 21112681 ]
- Nishith P, Duntley SP, Domitrovich PP, Uhles ML, Cook BJ, Stein PK. Effect of cognitive behavioral therapy on heart rate variability during REM sleep in female rape victims with PTSD. Journal of Traumatic Stress. 2003; 16 :247–250. [ PubMed : 12816336 ]
- Nixon RDV, Nearmy DM. Treatment of comorbid posttraumatic stress disorder and major depressive disorder: A pilot study. Journal of Traumatic Stress. 2011; 24 :451–455. [ PubMed : 21755543 ]
- Noll JG, Horowitz LA, Bonanno GA, Trickett PK, Putnam FW. Revictimization and self-harm in women who experienced childhood sexual abuse: Results from a prospective study. Journal of Interpersonal Violence. 2003; 18 :1452–1471. [ PubMed : 14678616 ]
- Norman SB, Tate SR, Wilkins KC, Cummins K, Brown SA. Posttraumatic stress disorder’s role in integrated substance dependence and depression treatment outcomes. Journal of Substance Abuse Treatment. 2010; 38 :346–355. [ PubMed : 20363091 ]
- Norris FH, Slone LB. The epidemiology of trauma and PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. Guilford Press; New York: 2007. pp. 78–98.
- Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002; 65 :240–260. [ PubMed : 12405080 ]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002; 65 :207–239. [ PubMed : 12405079 ]
- Norris FH, Kaniasty KZ, Conrad ML, Inman GL, Murphy AD. Placing age differences in cultural context: A comparison of the effects of age on PTSD after disasters in the United States, Mexico, and Poland. Journal of Clinical Geropsychology. 2002; 8 :153–173.
- Norris FH, Perilla JL, Ibanez GE, Murphy AD. Sex differences in symptoms of posttraumatic stress: Does culture play a role? Journal of Traumatic Stress. 2001; 14 :7–28.
- Norton PJ, Price EC. A meta-analytic review of adult cognitive–behavioral treatment outcome across the anxiety disorders. Journal of Nervous and Mental Disease. 2007; 195 :521–531. [ PubMed : 17568301 ]
- O’Donnell ML, Creamer M, Cooper J. Criterion A: Controversies and clinical implications. In: Rosen GM, editor. Clinician’s guide to posttraumatic stress disorder. Hoboken, NJ, US: John Wiley & Sons Inc; 2010. pp. 51–75.
- Office of the Surgeon Multi-National Corps–Iraq & Office of The Surgeon General United States Army Medical Command. Mental Health Advisory Team (MHAT) IV Operation Iraqi Freedom 05–07. Final report 17 November 2006. Washington, DC: U. S. Army Medical Department; 2006.
- O’Hare T, Sherrer MV, Shen C. Subjective distress from stressful events and high-risk behaviors as predictors of PTSD symptom severity in clients with severe mental illness. Journal of Traumatic Stress. 2006; 19 :375–386. [ PubMed : 16788997 ]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review. 2007; 27 :572–581. [ PubMed : 17343963 ]
- Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychological Bulletin. 2007; 133 :183–204. [ PubMed : 17338596 ]
- Oman D, Hedberg J, Thoresen CE. Passage meditation reduces perceived stress in health professionals: A randomized, controlled trial. Journal of Consulting and Clinical Psychology. 2006; 74 :714–719. [ PubMed : 16881779 ]
- Opler LA, Grennan MS, Ford JD. Pharmacotherapy. In: Courtois CA, Ford JD, editors. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 329–349.
- Orsillo SM. Measures for social phobia. In: Antony MM, Orsillo SM, Roemer L, editors. Practitioner’s guide to empirically based measures of anxiety. Dordrecht, Netherlands: Kluwer Academic Publishers; 2001. pp. 165–187.
- Ortega AN, Rosenheck R. Mental and physical health and acculturation among Hispanic Vietnam Veterans. Military Medicine. 2001; 166 :894–897. [ PubMed : 11603242 ]
- Osterman JE, de Jong JTVM. Cultural issues and trauma. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. Guilford Press; New York: 2007. pp. 425–446.
- Otis JD, Keane TM, Kerns RD, Monson C, Scioli E. The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Med. 2009; 10 :1300–1311. [ PubMed : 19818040 ]
- Otte C. Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dialogues in Clinical Neuroscience. 2011; 13 :413–421. [ PMC free article : PMC3263389 ] [ PubMed : 22275847 ]
- Ougrin D. Efficacy of exposure versus cognitive therapy in anxiety disorders: Systematic review and meta-analysis. BMC Psychiatry. 2011; 11 :200. [ PMC free article : PMC3347982 ] [ PubMed : 22185596 ]
- Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addictive Behaviors. 1998; 23 :785–795. [ PubMed : 9801716 ]
- Ouimette P, Moos RH, Brown PJ. Substance use disorder–posttraumatic stress disorder comorbidity: A survey of treatments and proposed practice guidelines. In: Ouimette P, Brown PJ, editors. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. Washington, DC: American Psychological Association; 2003. pp. 91–110.
- Owens GP, Steger MF, Whitesell AA, Herrera CJ. Posttraumatic stress disorder, guilt, depression, and meaning in life among military veterans. Journal of Traumatic Stress. 2009; 22 :654–657. [ PubMed : 19924820 ]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003; 129 :52–73. [ PubMed : 12555794 ]
- Pae CU, Lim HK, Peindl K, Ajwani N, Serretti A, Patkar AA, et al. The atypical antipsychotics olanzapine and risperidone in the treatment of posttraumatic stress disorder: a meta-analysis of randomized, double-blind, placebo-controlled clinical trials. International Clinical Psychopharmacology. 2008; 23 :1–8. [ PubMed : 18090502 ]
- Palinkas L, Downs M, Patterson J, Russell J. Social, cultural, and psychological impacts of the Exxon Valdez oil spill. Human Organization. 1993; 52 :1–13.
- Panagioti M, Gooding P, Tarrier N. Post-traumatic stress disorder and suicidal behavior: A narrative review. Clinical Psychology Review. 2009; 29 :471–482. [ PubMed : 19539412 ]
- Paunovic N, Öst LG. Cognitive–behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behaviour Research and Therapy. 2001; 39 :1183–1197. [ PubMed : 11579988 ]
- Peirce JM, Burke CK, Stoller KB, Neufeld KJ, Brooner RK. Assessing traumatic event exposure: Comparing the Traumatic Life Events Questionnaire to the Structured Clinical Interview for DSM-IV. Psychological Assessment. 2009; 21 :210–218. [ PMC free article : PMC3037764 ] [ PubMed : 19485675 ]
- Peirce JM, Kindbom KA, Waesche MC, Yuscavage ASE, Brooner RK. Posttraumatic stress disorder, gender, and problem profiles in substance dependent patients. Substance Use & Misuse. 2008; 43 :596–611. [ PubMed : 18393079 ]
- Peller AJ, Najavits LM, Nelson SE, LaBrie RA, Shaffer HJ. PTSD among a treatment sample of repeat DUI offenders. Journal of Traumatic Stress. 2010; 23 :468–473. [ PubMed : 20690170 ]
- Peltan JR, Cellucci T. Childhood sexual abuse and substance abuse treatment utilization among substance-dependent incarcerated women. Journal of Substance Abuse Treatment. 2011; 41 :215–224. [ PubMed : 21550199 ]
- Perilla JL, Norris FH, Lavizzo EA. Ethnicity, culture, and disaster response: Identifying and explaining ethnic differences in PTSD six months after Hurricane Andrew. Journal of Social and Clinical Psychology. 2002; 21 :20–45.
- Peterlin BL, Rosso AL, Sheftell FD, Libon DJ, Mossey JM, Merikangas KR. Post-traumatic stress disorder, drug abuse and migraine: New findings from the National Comorbidity Survey Replication (NCS–R). Cephalalgia. 2011; 31 :235–244. [ PMC free article : PMC3105759 ] [ PubMed : 20813779 ]
- Petersilia JR. Crime victims with developmental disabilities: A review essay. Criminal Justice and Behavior. 2001; 28 :655–694.
- Pfeiffer PN, Ganoczy D, Ilgen M, Zivin K, Valenstein M. Comorbid anxiety as a suicide risk factor among depressed veterans. Depression and Anxiety. 2009; 26 :752–757. [ PMC free article : PMC2935592 ] [ PubMed : 19544314 ]
- Pico-Alfonso MA. Psychological intimate partner violence: The major predictor of posttraumatic stress disorder in abused women. Neuroscience and Biobehavioral Reviews. 2005; 29 :181–193. [ PubMed : 15652265 ]
- Pietrzak RH, Goldstein MB, Malley JC, Rivers AJ, Johnson DC, Southwick SM. Risk and protective factors associated with suicidal ideation in veterans of Operations Enduring Freedom and Iraqi Freedom. Journal of Affective Disorders. 2010; 123 :102–107. [ PubMed : 19819559 ]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Personality disorders associated with full and partial posttraumatic stress disorder in the U.S. population: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Psychiatric Research. 2011; 45 :678–686. [ PMC free article : PMC3388551 ] [ PubMed : 20950823 ]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders. 2011; 25 :456–465. [ PMC free article : PMC3051041 ] [ PubMed : 21168991 ]
- Plummer SB, Findley PA. Women with disabilities’ experience with physical and sexual abuse. Trauma, Violence, & Abuse. 2012; 13 :15–29. [ PubMed : 22070987 ]
- Pole N, Best SR, Metzler T, Marmar CR. Why are Hispanics at greater risk for PTSD? Cultural Diversity and Ethnic Minority Psychology. 2005; 11 :144–161. [ PubMed : 15884985 ]
- Pole N, Best SR, Weiss DS, Metzler T, Liberman AM, Fagan J, et al. Effects of gender and ethnicity on duty-related posttraumatic stress symptoms among urban police officers. Journal of Nervous & Mental Disease. 2001; 189 :442–448. [ PubMed : 11504321 ]
- Pole N, Gone JP, Kulkarni M. Posttraumatic stress disorder among ethnoracial minorities in the United States. Clinical Psychology: Science and Practice. 2008; 15 :35–61.
- Polinder S, Haagsma JA, Belt E, Lyons RA, Erasmus V, Lund J, et al. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health. 2010; 10 :783. [ PMC free article : PMC3019196 ] [ PubMed : 21182775 ]
- Polinder S, Haagsma JA, Lyons RA, Gabbe BJ, Ameratunga S, Cryer C, et al. Measuring the population burden of fatal and nonfatal injury. Epidemiologic Reviews. 2012; 34 :17–31. [ PubMed : 22113244 ]
- Polusny MA, Erbes CR, Murdoch M, Arbisi PA, Thuras P, Rath MB. Prospective risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq. Psychological Medicine. 2011; 41 :687–698. [ PubMed : 21144108 ]
- Ponniah K, Hollon SD. Empirically supported psychological treatments for adult acute stress disorder and posttraumatic stress disorder: A review. Depression and Anxiety. 2009; 26 :1086–1109. [ PubMed : 19957280 ]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010; 30 :635–641. [ PubMed : 20546985 ]
- Pratchett LC, Pelcovitz MR, Yehuda R. Trauma and violence: Are women the weaker sex? Psychiatric Clinics of North America. 2010; 33 :465–474. [ PubMed : 20385347 ]
- Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposure among US men. American Journal of Public Health. 2002; 92 :59–63. [ PMC free article : PMC1447389 ] [ PubMed : 11772762 ]
- Provencher MD, Hawke LD, Thienot E. Psychotherapies for comorbid anxiety in bipolar spectrum disorders. Journal of Affective Disorders. 2011; 133 :371–380. [ PubMed : 21093062 ]
- Pulay AJ, Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: Results From the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Primary Care Companion to the Journal of Clinical Psychiatry. 2009; 11 :53–67. [ PMC free article : PMC2707116 ] [ PubMed : 19617934 ]
- Pyari TT, Kutty RV, Sarma PS. Risk factors of post-traumatic stress disorder in tsunami survivors of Kanyakumari District, Tamil Nadu, India. Indian Journal of Psychiatry. 2012; 54 :48–53. [ PMC free article : PMC3339219 ] [ PubMed : 22556437 ]
- Qureshi SU, Pyne JM, Magruder KM, Schulz PE, Kunik ME. The link between post-traumatic stress disorder and physical comorbidities: A systematic review. Psychiatric Quarterly. 2009; 80 :87–97. [ PubMed : 19291401 ]
- Rachamim L, Nacasch N, Shafran N, Tzur D, Gilboa-Schechtman E. Exposure-based therapy for post-traumatic stress disorder in children and adults. Israel Journal of Psychiatry and Related Sciences. 2009; 46 :274–281. [ PubMed : 20635775 ]
- Rakofsky JJ, Dunlop BW. Treating nonspecific anxiety and anxiety disorders in patients with bipolar disorder: A review. Journal of Clinical Psychiatry. 2011; 72 :81–90. [ PubMed : 21208580 ]
- Rand MR, Robinson JF. Criminal victimization in the United States, 2008—Statistical tables. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2012.
- Ravindran LN, Stein MB. Pharmacotherapy of PTSD: Premises, principles, and priorities. Brain Research. 2009; 1293 :24–39. [ PMC free article : PMC2748176 ] [ PubMed : 19332035 ]
- Razza NJ, Tomasulo DJ, Sobsey D. Group psychotherapy for trauma-related disorders in people with intellectual disabilities. Advances in Mental Health and Intellectual Disabilities. 2011; 5 :40–45.
- Read J, Hammersley P. Child sexual abuse and schizophrenia. British Journal of Psychiatry. 2005; 186 :76. [ PubMed : 15690589 ]
- Read J, Agar K, Argyle N, Aderhold V. Sexual and physical abuse during childhood and adulthood as predictors of hallucinations, delusions and thought disorder. Psychology and Psychotherapy: Theory, Research and Practice. 2003; 76 :1–22. [ PubMed : 12689431 ]
- Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica. 2005; 112 :330–350. [ PubMed : 16223421 ]
- Ready DJ, Thomas KR, Worley V, Backscheider AG, Harvey LA, Baltzell D, et al. A field test of group based exposure therapy with 102 veterans with war–related posttraumatic stress disorder. Journal of Traumatic Stress. 2008; 21 :150–157. [ PubMed : 18404634 ]
- Reddy MK, Polusny MA, Murdoch M. On counterbalancing of symptom-reporting in trauma surveys. Psychological Reports. 2009; 105 :1154–1158. [ PubMed : 20229918 ]
- Reiland S, Lauterbach D. Effects of trauma and religiosity on self-esteem. Psychological Reports. 2008; 102 :779–790. [ PubMed : 18763449 ]
- Reivich KJ, Seligman ME, McBride S. Master resilience training in the U.S. Army. American Psychology. 2011; 66 :25–34. [ PubMed : 21219045 ]
- Renshaw KD. An integrated model of risk and protective factors for post-deployment PTSD symptoms in OEF/OIF era combat veterans. Journal of Affective Disorders. 2011; 128 :321–326. [ PubMed : 20692705 ]
- Renshaw KD, Blais RK, Caska CM. Distress in spouses of combat veterans with PTSD: The importance of interpersonally based cognitions and behaviors. In: Wadsworth SM, Riggs D, editors. Risk and resilience in US military families. New York: Springer Science + Business Media; 2011. pp. 69–84.
- Renshaw KD, Rodrigues CS, Jones DH. Psychological symptoms and marital satisfaction in spouses of Operation Iraqi Freedom veterans: Relationships with spouses’ perceptions of veterans’ experiences and symptoms. Journal of Family Psychology. 2008; 22 :586–594. [ PubMed : 18729672 ]
- Resick PA, Galovski TE, O’Brien UM, Scher CD, Clum GA, Young–Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008; 76 :243–258. [ PMC free article : PMC2967760 ] [ PubMed : 18377121 ]
- Resick PA, Nishith P, Griffin MG. How well does cognitive–behavioral therapy treat symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial. CNS Spectrums. 2003; 8 :340–355. [ PMC free article : PMC2970926 ] [ PubMed : 12766690 ]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive–processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting & Clinical Psychology. 2002; 70 :867–879. [ PMC free article : PMC2977927 ] [ PubMed : 12182270 ]
- Resick PA, Williams LF, Suvak MK, Monson CM, Gradus JL. Long-term outcomes of cognitive–behavioral treatments for posttraumatic stress disorder among female rape survivors. Journal of Consulting and Clinical Psychology. 2012; 80 :201–210. [ PMC free article : PMC3336190 ] [ PubMed : 22182261 ]
- Resnick HS, Acierno R, Amstadter AB, Self-Brown S, Kilpatrick DG. An acute post–sexual assault intervention to prevent drug abuse: Updated findings. Addictive Behaviors. 2007; 32 :2032–2045. [ PMC free article : PMC1986828 ] [ PubMed : 17275198 ]
- Resnick HS, Acierno R, Kilpatrick DG, Holmes M. Description of an early intervention to prevent substance abuse and psychopathology in recent rape victims. Behavior Modification. 2005; 29 :156–188. [ PubMed : 15557482 ]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol Dependence. 2005; 77 :251–258. [ PubMed : 15734225 ]
- Richardson JD, Elhai JD, Pedlar DJ. Association of PTSD and depression with medical and specialist care utilization in modern peacekeeping veterans in Canada with health-related disabilities. Journal of Clinical Psychiatry. 2006; 67 :1240–1245. [ PubMed : 16965202 ]
- Riggs DS, Monson CM, Glynn SM, Canterino J. Couple and family therapy for adults. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 458–478.
- Riggs DS, Rukstalis M, Volpicelli JR, Kalmanson D, Foa EB. Demographic and social adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol dependence: Potential pitfalls to PTSD treatment. Addictive Behaviors. 2003; 28 :1717–1730. [ PubMed : 14656555 ]
- Roberts AL, Austin SB, Corliss HL, Vandermorris AK, Koenen KC. Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. American Journal of Public Health. 2010; 100 :2433–2441. [ PMC free article : PMC2978167 ] [ PubMed : 20395586 ]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2011; 41 :71–83. [ PMC free article : PMC3097040 ] [ PubMed : 20346193 ]
- Roberts AL, McLaughlin KA, Conron KJ, Koenen KC. Adulthood stressors, history of childhood adversity, and risk of perpetration of intimate partner violence. American Journal of Preventive Medicine. 2011; 40 :128–138. [ PMC free article : PMC3023909 ] [ PubMed : 21238860 ]
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson J. Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic Reviews. 2009:CD006869. [ PubMed : 19588408 ]
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Systematic review and meta-analysis of multiple-session early interventions following traumatic events. American Journal of Psychiatry. 2009; 166 :293–301. [ PubMed : 19188285 ]
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews. 2010:CD007944. [ PubMed : 20238359 ]
- Robinaugh DJ, McNally RJ. Trauma centrality and PTSD symptom severity in adult survivors of childhood sexual abuse. Journal of Traumatic Stress. 2011; 24 :483–486. [ PubMed : 21793046 ]
- Robjant K, Fazel M. The emerging evidence for Narrative Exposure Therapy: A review. Clinical Psychology Review. 2010; 30 :1030–1039. [ PubMed : 20832922 ]
- Roht-Arriaza N. Punishment, redress, and pardon: Theoretical and psychological approaches. In: Roht-Arriaza N, editor. Impunity and human rights international law and practice. Oxford, England: Oxford University Press; 1995. pp. 13–23.
- Rosenberg SD, Lu W, Mueser KT, Jankowski MK, Cournos F. Correlates of adverse childhood events among adults with schizophrenia spectrum disorders. Psychiatric Services. 2007; 58 :245–253. [ PubMed : 17287383 ]
- Rosenthal JZ, Grosswald S, Ross R, Rosenthal N. Effects of transcendental meditation in veterans of Operation Enduring Freedom and Operation Iraqi Freedom with posttraumatic stress disorder: A pilot study. Military Medicine. 2011; 176 :626–630. [ PubMed : 21702378 ]
- Rossen LM, Pollack KM, Canham-Chervak M, Canada S, Baker SP. Motor vehicle crashes among active duty U.S. Army personnel, 1999 to 2006. Military Medicine. 2011; 176 :1019–1026. [ PubMed : 21987960 ]
- Rothbaum BO, Davidson JR, Stein DJ, Pedersen R, Musgnung J, Tian XW, et al. A pooled analysis of gender and trauma-type effects on responsiveness to treatment of PTSD with venlafaxine extended release or placebo. Journal of Clinical Psychiatry. 2008; 69 :1529–1539. [ PubMed : 19192435 ]
- Ruef AM, Litz BT, Schlenger WE. Hispanic ethnicity and risk for combat-related posttraumatic stress disorder. Cultural Diversity and Ethnic Minority Psychology. 2000; 6 :235–251. [ PubMed : 10938633 ]
- Rush AJ, Zimmerman M, Wisniewski SR, Fava M, Hollon SD, Warden D, et al. Comorbid psychiatric disorders in depressed outpatients: Demographic and clinical features. Journal of Affective Disorders. 2005; 87 :43–55. [ PubMed : 15894381 ]
- Ruzek J, Walser RD, Naugle AE, Litz B, Mennin DS, Polusny MA, et al. Cognitive–behavioral psychology: Implications for disaster and terrorism response. Prehospital and Disaster Medicine. 2008; 23 :397–410. [ PubMed : 19189609 ]
- Sacks JY, McKendrick K, Banks S. The impact of early trauma and abuse on residential substance abuse treatment outcomes for women. Journal of Substance Abuse Treatment. 2008; 34 :90–100. [ PubMed : 17574799 ]
- Sacks S, McKendrick K, Sacks JY, Banks S, Harle M. Enhanced outpatient treatment for co-occurring disorders: Main outcomes. Journal of Substance Abuse Treatment. 2008; 34 :48–60. [ PubMed : 17574795 ]
- Sadler AG, Booth BM, Cook BL, Doebbeling BN. Factors associated with women’s risk of rape in the military environment. American Journal of Industrial Medicine. 2003; 43 :262–273. [ PubMed : 12594773 ]
- Sala T, Cox BJ, Sareen J. Anxiety in health behaviors and physical illness. New York: Springer Science + Business Media; 2008. Anxiety disorders and physical illness comorbidity: An overview; pp. 131–154.
- Sartor CE, McCutcheon VV, Pommer NE, Nelson EC, Grant JD, Duncan AE, et al. Common genetic and environmental contributions to post-traumatic stress disorder and alcohol dependence in young women. Psychological Medicine. 2011; 41 :1497–1505. [ PMC free article : PMC3377473 ] [ PubMed : 21054919 ]
- Sautter FJ, Armelie AP, Glynn SM, Wielt DB. The development of a couple-based treatment for PTSD in returning veterans. Professional Psychology: Research and Practice. 2011; 42 :63–69.
- Sautter FJ, Glynn SM, Thompson KE, Franklin L, Han X. A couple–based approach to the reduction of PTSD avoidance symptoms: Preliminary findings. Journal of Marital and Family Therapy. 2009; 35 :343–349. [ PubMed : 19522786 ]
- Savoca E, Rosenheck R. The civilian labor market experiences of Vietnam-era veterans: The influence of psychiatric disorders. Journal of Mental Health Policy and Economics. 2000; 3 :199–207. [ PubMed : 11967456 ]
- Sayer NA, Carlson KF, Schnurr PP. Assessment of functioning and disability. In: Benedek DM, Wynn GH, editors. Clinical manual for management of PTSD. Arlington, VA: American Psychiatric Publishing, Inc; 2011. pp. 255–287.
- Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric Services. 2010; 61 :589–597. [ PubMed : 20513682 ]
- Schauben LJ, Frazier PA. Vicarious trauma: The effects on female counselors of working with sexual violence survivors. Psychology of Women Quarterly. 1995; 19 :49–64.
- Schneier FR, Neria Y, Pavlicova M, Hembree E, Suh EJ, Amsel L, et al. Combined prolonged exposure therapy and paroxetine for PTSD related to the World Trade Center attack: a randomized controlled trial. American Journal of Psychiatry. 2012; 169 :80–88. [ PMC free article : PMC3606709 ] [ PubMed : 21908494 ]
- Schnurr PP, Lunney CA. Work-related quality of life and posttraumatic stress disorder symptoms among female veterans. Women’s Health Issues. 2011; 21 :S169–S175. [ PubMed : 21724137 ]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. JAMA: The Journal of the American Medical Association. 2007; 297 :820–830. [ PubMed : 17327524 ]
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, et al. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a Department of Veterans Affairs Cooperative Study. Archives of General Psychiatry. 2003; 60 :481–489. [ PubMed : 12742869 ]
- Schnurr PP, Lunney CA, Bovin MJ, Marx BP. Posttraumatic stress disorder and quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical Psychology Review. 2009; 29 :727–735. [ PubMed : 19744758 ]
- Schnurr PP, Lunney CA, Sengupta A, Waelde LC. A descriptive analysis of PTSD chronicity in Vietnam veterans. Journal of Traumatic Stress. 2003; 16 :545–553. [ PubMed : 14690351 ]
- Schönenberg M, Reichwald U, Domes G, Badke A, Hautzinger M. Effects of peritraumatic ketamine medication on early and sustained posttraumatic stress symptoms in moderately injured accident victims. Psychopharmacology (Berlin). 2005; 182 :420–425. [ PubMed : 16012867 ]
- Schönenberg M, Reichwald U, Domes G, Badke A, Hautzinger M. Ketamine aggravates symptoms of acute stress disorder in a naturalistic sample of accident victims. Journal of Psychopharmacology. 2008; 22 :493–497. [ PubMed : 18208917 ]
- Schottenbauer MA, Glass CR, Arnkoff DB, Gray SH. Contributions of psychodynamic approaches to treatment of PTSD and trauma: A review of the empirical treatment and psychopathology literature. Psychiatry. 2008; 71 :13–34. [ PubMed : 18377203 ]
- Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008; 71 :134–168. [ PubMed : 18573035 ]
- Schubert CC, Punamäki RL. Mental health among torture survivors: Cultural background, refugee status and gender. Nordic Journal of Psychiatry. 2011; 65 :175–182. [ PubMed : 20854222 ]
- Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress. 2006; 19 :825–836. [ PubMed : 17195981 ]
- Schwartz RC, Schwartz MF, Galperin L. Internal family, editor. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. Internal family systems therapy; pp. 353–370.
- Schweitzer RD, Brough M, Vromans L, Asic-Kobe M. Mental health of newly arrived Burmese refugees in Australia: Contributions of pre-migration and post-migration experience. Australian and New Zealand Journal of Psychiatry. 2011; 45 :299–307. [ PubMed : 21303193 ]
- Schweitzer R, Melville F, Steel Z, Lacherez P. Trauma, post–migration living difficulties, and social support as predictors of psychological adjustment in resettled Sudanese refugees. Australian and New Zealand Journal of Psychiatry. 2006; 40 :179–187. [ PubMed : 16476137 ]
- Scott JC. Domination and the arts of resistance: Hidden transcripts. New Haven: Yale University Press; 1990.
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. American Journal of Public Health. 2009; 99 :1651–1658. [ PMC free article : PMC2724454 ] [ PubMed : 19608954 ]
- Seidler GH, Wagner FE. Comparing the efficacy of EMDR and trauma-focused cognitive–behavioral therapy in the treatment of PTSD: a meta-analytic study. Psychological Medicine. 2006; 36 :1515–1522. [ PubMed : 16740177 ]
- Shaikh Al, Arab A, Guedon-Moreau L, Ducrocq F, Molenda S, Duhem S, Salleron J, et al. Temporal analysis of heart rate variability as a predictor of post traumatic stress disorder in road traffic accidents survivors. Journal of Psychiatric Research. 2012 [ PubMed : 22425487 ]
- Shalev AY, Ankri Y, Israeli–Shalev Y, Peleg T, Adessky R, Freedman S. Prevention of posttraumatic stress disorder by early treatment: Results from the Jerusalem Trauma Outreach And Prevention study. Archives of General Psychiatry. 2012; 69 :166–176. [ PubMed : 21969418 ]
- Shalev AY, Sahar T, Freedman S, Peri T, Glick N, Brandes D, et al. A prospective study of heart rate response following trauma and the subsequent development of posttraumatic stress disorder. Archives of General Psychiatry. 1998; 55 :553–559. [ PubMed : 9633675 ]
- Sharpless BA, Barber JP. A clinician’s guide to PTSD treatments for returning veterans. Professional Psychology: Research and Practice. 2011; 42 :8–15. [ PMC free article : PMC3070301 ] [ PubMed : 21475611 ]
- Shea MT, McDevitt-Murphy M, Ready DJ, Schnurr PP. Group therapy. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 306–326.
- Shemesh E, Yehuda R, Milo O, Dinur I, Rudnick A, Vered Z, et al. Posttraumatic stress, nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosomatic Medicine. 2004; 66 :521–526. [ PubMed : 15272097 ]
- Sherin JE, Nemeroff CB. Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues in Clinical Neuroscience. 2011; 13 :263–278. [ PMC free article : PMC3182008 ] [ PubMed : 22034143 ]
- Sherman MD, Zanotti DK, Jones DE. Key elements in couples therapy with veterans with combat-related posttraumatic stress disorder. Professional Psychology–Research and Practice. 2005; 36 :626–633.
- Sherrer MV. The role of cognitive appraisal in adaptation to traumatic stress in adults with serious mental illness: A critical review. Trauma, Violence, & Abuse. 2011; 12 :151–167. [ PubMed : 21733943 ]
- Shoptaw S, Stein JA, Rawson RA. Burnout in substance abuse counselors: Impact of environment, attitudes, and clients with HIV. Journal of Substance Abuse Treatment. 2000; 19 :117–126. [ PubMed : 10963923 ]
- Sijbrandij M, Olff M, Reitsma JB, Carlier IV, Gersons BP. Emotional or educational debriefing after psychological trauma. Randomised controlled trial. British Journal of Psychiatry. 2006; 189 :150–155. [ PubMed : 16880485 ]
- Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide logitudinal study of psychological responses to September 11. Journal of the American Medical Association. 2002; 288 :1235–1244. [ PubMed : 12215130 ]
- Simon NM, Otto MW, Wisniewski SR, Fossey M, Sagduyu K, Frank E, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP–BD). American Journal of Psychiatry. 2004; 161 :2222–2229. [ PubMed : 15569893 ]
- Simpson TL. Women’s treatment utilization and its relationship to childhood sexual abuse history and lifetime PTSD. Substance Abuse. 2002; 23 :17–30. [ PubMed : 12444358 ]
- Skinner KM, Kressin N, Frayne S, Tripp TJ, Hankin CS, Miller DR, et al. The prevalence of military sexual assault among female Veterans’ Administration outpatients. Journal of Interpersonal Violence. 2000; 15 :291–310.
- Skopp NA, Reger MA, Reger GM, Mishkind MC, Raskind M, Gahm GA. The role of intimate relationships, appraisals of military service, and gender on the development of posttraumatic stress symptoms following Iraq deployment. Journal of Traumatic Stress. 2011; 24 :277–286. [ PubMed : 21547955 ]
- Sledjeski EM, Speisman B, Dierker LC. Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey–Replication (NCS–R). Journal of Behavioral Medicine. 2008; 31 :341–349. [ PMC free article : PMC2659854 ] [ PubMed : 18553129 ]
- Smid GE, Mooren TT, van der Mast RC, Gersons BP, Kleber RJ. Delayed posttraumatic stress disorder: Systematic review, meta-analysis, and meta-regression analysis of prospective studies. Journal of Clinical Psychiatry. 2009; 70 :1572–1582. [ PubMed : 19607763 ]
- Smid GE, van der Velden PG, Gersons BPR, Kleber RJ. Late-onset posttraumatic stress disorder following a disaster: A longitudinal study. Psychological Trauma: Theory, Research, Practice, and Policy. 2012; 4 :312–322.
- Smid GE, van der Velden PG, Lensvelt–Mulders GJ, Knipscheer JW, Gersons BP, Kleber RJ. Stress sensitization following a disaster: A prospective study. Psychological Medicine. 2011:1–12. [ PubMed : 22126800 ]
- Smith MW, Schnurr PP, Rosenheck RA. Employment outcomes and PTSD symptom severity. Mental Health Services Research. 2005; 7 :89–101. [ PubMed : 15974155 ]
- Solomon Z, Dekel R, Mikulincer M. Complex trauma of war captivity: A prospective study of attachment and post-traumatic stress disorder. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2008; 38 :1427–1434. [ PubMed : 18257940 ]
- Söndergaard HP, Theorell T. Language acquisition in relation to cumulative posttraumatic stress disorder symptom load over time in a sample of re-settled refugees. Psychotherapy and Psychosomatics. 2004; 73 :320–323. [ PubMed : 15292630 ]
- Sotero M. A conceptual model of historical trauma: Implications for public health practice and research. Journal of Health Disparities Research and Practice. 2006; 1 :93–108.
- Spataro J, Mullen PE, Burgess PM, Wells DL, Moss SA. Impact of child sexual abuse on mental health: Prospective study in men and women. British Journal of Psychiatry. 2004; 184 :416–421. [ PubMed : 15123505 ]
- Spates CR, Koch E, Cusack K, Pagoto S, Waller S. Eye movement desensitization and reprocessing. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 279–305.
- Spauwen J, Krabbendam L, Lieb R, Wittchen HU, van Os J. Impact of psychological trauma on the development of psychotic symptoms: Relationship with psychosis proneness. British Journal of Psychiatry. 2006; 188 :527–533. [ PubMed : 16738342 ]
- Spitzer RL, Williams JB, Gibbon M. Structured clinical interview for DSM-III-R—Patient version (SCID-P). New York: New York State Psychiatric Institute, Biometrics Research; 1987.
- Steel JL, Dunlavy AC, Stillman J, Pape HC. Measuring depression and PTSD after trauma: Common scales and checklists. Injury. 2011; 42 :288–300. [ PMC free article : PMC3295610 ] [ PubMed : 21216400 ]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van OM. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA. 2009; 302 :537–549. [ PubMed : 19654388 ]
- Steil R, Jung K, Stangier U. Efficacy of a two-session program of cognitive restructuring and imagery modification to reduce the feeling of being contaminated in adult survivors of childhood sexual abuse: a pilot study. Journal of Behavior Therapy and Experimental Psychiatry. 2011; 42 :325–329. [ PubMed : 21367358 ]
- Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, et al. Cross-national analysis of the associations between traumatic events and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLoS ONE. 2010; 5 [ PMC free article : PMC2869349 ] [ PubMed : 20485530 ]
- Stein DJ, Ipser JC, Seedat S. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews. 2006:CD002795. [ PMC free article : PMC6993948 ] [ PubMed : 16437445 ]
- Stein DJ, Ipser J, McAnda N. Pharmacotherapy of posttraumatic stress disorder: A review of meta-analyses and treatment guidelines. CNS Spectr. 2009; 14 :25–31. [ PubMed : 19169191 ]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: Findings from a community survey. American Journal of Psychiatry. 1997; 154 :1114–1119. [ PubMed : 9247398 ]
- Stewart RE, Chambless DL. Cognitive–behavioral therapy for adult anxiety disorders in clinical practice: a meta-analysis of effectiveness studies. Journal of Consulting and Clinical Psychology. 2009; 77 :595–606. [ PMC free article : PMC8022196 ] [ PubMed : 19634954 ]
- Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, Smith SM, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV narcissistic personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2008; 69 :1033–1045. [ PMC free article : PMC2669224 ] [ PubMed : 18557663 ]
- Subcommittee on Posttraumatic Stress Disorder of the Committee on Gulf War and Health: Physiologic, Psychologic, and Psychosocial Effects of Deployment-Related Stress. Posttraumatic stress disorder: Diagnosis and assessment. Washington, DC: The National Academies Press; 2006.
- Substance Abuse and Mental Health Services Administration. Behavioral health services for people who are homeless. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. Treatment Improvement Protocol (TIP) Series 55. (HHS Publication No SMA 13-4734)
- Substance Abuse and Mental Health Services Administration. Improving cultural competence. Rockville, MD: Substance Abuse and Mental Health Services Administration; (planned c) Treatment Improvement Protocol (TIP) Series.
- Substance Abuse and Mental Health Services Administration. Managing anxiety symptoms in behavioral health services. Rockville, MD: Substance Abuse and Mental Health Services Administration; (planned d) Treatment Improvement Protocol (TIP) Series.
- Substance Abuse and Mental Health Services Administration. Reintegration-related behavioral health issues in veterans and military families. Rockville, MD: Substance Abuse and Mental Health Services Administration; (planned f) Treatment Improvement Protocol (TIP) Series.
- Substance Abuse and Mental Health Services Administration & Office of Applied Studies. Impact of hurricanes Katrina and Rita on substance use and mental health. The NSDUH Report. Rockville, MD: Substance Abuse and Mental Health Services Administration and Office of Applied Studies; 2008.
- Substance Abuse and Mental Health Services Administration, Trauma and Justice Strategic Initiative. SAMHSA's working definition of trauma and guidance for trauma-informed approach. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012.
- Sudaryo MK, Besral Endarti AT, Rivany R, Phalkey R, Marx M, et al. Injury, disability and quality of life after the 2009 earthquake in Padang, Indonesia: A prospective cohort study of adult survivors. Global Health Action. 2012; 5 [ PMC free article : PMC3359784 ] [ PubMed : 22629236 ]
- Sullivan PM, Knutson JF. Maltreatment and disabilities: A population-based epidemiological study. Child Abuse & Neglect. 2000; 24 :1257–1273. [ PubMed : 11075694 ]
- Suris A, Lind L, Kashner TM, Borman PD. Mental health, quality of life, and health functioning in women veterans: Differential outcomes associated with military and civilian sexual assault. Journal of Interpersonal Violence. 2007; 22 :179–197. [ PubMed : 17202575 ]
- Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: A review. European Eating Disorders Review. 2007; 15 :253–274. [ PubMed : 17676696 ]
- Taft CT, Vogt DS, Mechanic MB, Resick PA. Posttraumatic stress disorder and physical health symptoms among women seeking help for relationship aggression. Journal of Family Psychology. 2007; 21 :354–362. [ PMC free article : PMC2971557 ] [ PubMed : 17874920 ]
- Tam TW, Zlotnick C, Robertson MJ. Longitudinal perspective: Adverse childhood events, substance use, and labor force participation among homeless adults. American Journal of Drug and Alcohol Abuse. 2003; 29 :829–846. [ PubMed : 14713142 ]
- Tanielian TL, Jaycox LH, Schell TL, Marshall GN, Burnam MA, Eibner C, et al. Invisible wounds of war: Summary and recommendations for addressing psychological and cognitive injuries. Santa Monica: RAND; 2008.
- Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C, et al. The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug and Alcohol Dependence. 2010; 110 :108–116. [ PMC free article : PMC2887748 ] [ PubMed : 20236774 ]
- Teplin LA, McClelland GM, Abram KM, Weiner DA. Crime victimization in adults with severe mental illness: Comparison with the national crime victimization survey. Archives of General Psychiatry. 2005; 62 :911–921. [ PMC free article : PMC1389236 ] [ PubMed : 16061769 ]
- Terrio HP, Nelson LA, Betthauser LM, Harwood JE, Brenner LA. Postdeployment traumatic brain injury screening questions: Sensitivity, specificity, and predictive values in returning soldiers. Rehabilitation Psychology. 2011; 56 :26–31. [ PubMed : 21401283 ]
- The APSAC handbook on child maltreatment. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc; 2002.
- Thompson MP, Kingree JB. The frequency and impact of violent trauma among pregnant substance abusers. Addictive Behaviors. 1998; 23 :257–262. [ PubMed : 9573429 ]
- Thorp SR, Stein MB. Posttraumatic stress disorder and functioning. PTSD Research Quarterly. 2005; 16 :1–7.
- Tjaden P, Thoennes N. Extent, nature, and consequences of intimate partner violence Findings from the National Violence Against Women Survey. Washington, DC: US Department of Justice, Office of Justice Programs; 2000.
- Torchalla I, Nosen L, Rostam H, Allen P. Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2012; 42 :65–77. [ PubMed : 22035700 ]
- Treating Compassion Fatigue. New York: Brunner-Routledge; 2002.
- Triffleman E. Gender differences in a controlled pilot study of psychosocial treatment in substance dependent patients with post-traumatic stress disorder: Design considerations and outcomes. Alcoholism Treatment Quarterly. 2000; 18 :113–126.
- Triffleman E. Implementing substance dependence posttraumatic stress disorder therapy in a community-based methadone clinic. In: Sorensen JL, Rawson RA, Guydish J, Zweben JE, editors. Research to practice, practice to research: Promoting scientific clinical interchange in drug abuse treatment. Washington, DC: American Psychological Association; 2002. pp. 227–248.
- Triffleman EG, Marmar CR, Delucchi KL, Ronfeldt H. Childhood trauma and posttraumatic stress disorder in substance abuse inpatients. Journal of Nervous & Mental Disease. 1995; 183 :172–176. [ PubMed : 7891064 ]
- Trippany RL, Kress VEW, Wilcoxon SA. Preventing vicarious trauma: What counselors should know when working with trauma survivors. Journal of Counseling & Development. 2004; 82 :31–37.
- Trippany RL, Wilcoxon SA, Satcher JF. Factors influencing vicarious traumatization for therapists of survivors of sexual victimization. Journal of Trauma Practice. 2003; 2 :47–60.
- Truman JL. Criminal victimization, 2010. Washington, DC: U.S. Department of Justice, Bureau of Justice Statistics; 2011.
- Tull MT, Gratz KL, Aklin WM, Lejuez CW. A preliminary examination of the relationships between posttraumatic stress symptoms and crack/cocaine, heroin, and alcohol dependence. Journal of Anxiety Disorders. 2010; 24 :55–62. [ PMC free article : PMC2808189 ] [ PubMed : 19767174 ]
- Turnbull GJ. A review of post-traumatic stress disorder; part I: Historical development and classification. Injury. 1998; 29 :87–91. [ PubMed : 10721399 ]
- Ullman SE, Filipas HH. Predictors of PTSD symptom severity and social reactions in sexual assault victims. Journal of Traumatic Stress. 2001; 14 :369–389. [ PMC free article : PMC3583013 ] [ PubMed : 11469163 ]
- Ullman SE, Filipas HH, Townsend SM, Starzynski LL. Psychosocial correlates of PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress. 2007; 20 :821–831. [ PubMed : 17955534 ]
- Ulmer CS, Edinger JD, Calhoun PS. A multi-component cognitive–behavioral intervention for sleep disturbance in veterans with PTSD: A pilot study. Journal of Clinical Sleep Medicine. 2011; 7 :57–68. [ PMC free article : PMC3041620 ] [ PubMed : 21344046 ]
- U.S. Department of Veterans Affairs & Department of Defense. VA/DoD clinical practice guideline for management of post-traumatic stress. Washington, DC: U. S. Department of Veterans Affairs; 2010.
- Valentiner DP, Foa EB, Riggs DS, Gershuny BS. Coping strategies and posttraumatic stress disorder in female victims of sexual and nonsexual assault. Journal of Abnormal Psychology. 1996; 105 :455–458. [ PubMed : 8772016 ]
- Van Breda AD. Resilience theory: A literature review. Gezina, South Africa: South African Military Health Service, Military Psychological Institute, Social Work Research & Development; 2001.
- van der Kolk BA, McFarlane AC, Van der Hart O. A general approach to treatment of posttraumatic stress disorder. In: van der Kolk BA, McFarlane AC, Weisaeth L, editors. Traumatic stress: The effects of overwhelming experience on mind, body, and society. New York: Guilford Press; 1996. pp. 417–440.
- van der Kolk BA, McFarlane AC, Weisaeth L. Traumatic stress: The effects of overwhelming experience on mind, body, and society. New York: Guilford Press; 1996.
- van der Velden PG, Wittmann L. The independent predictive value of peritraumatic dissociation for PTSD symptomatology after type I trauma: A systematic review of prospective studies. Clinical Psychology Review. 2008; 28 :1009–1020. [ PubMed : 18406027 ]
- Van Emmerik AAP, Kamphuis JH, Hulsbosch AM, Emmelkamp PMG. Single session debriefing after psychological trauma: a meta-analysis. Lancet. 2002; 360 :766–771. [ PubMed : 12241834 ]
- Vasterling JJ, Verfaellie M, Sullivan KD. Mild traumatic brain injury and posttraumatic stress disorder in returning veterans: Perspectives from cognitive neuroscience. Clinical Psychology Review. 2009; 29 :674–684. [ PubMed : 19744760 ]
- Vaughn MG, Fu Q, DeLisi M, Beaver KM, Perron BE, Howard MO. Criminal victimization and comorbid substance use and psychiatric disorders in the United States: Results from the NESARC. Annals of Epidemiology. 2010; 20 :281–288. [ PMC free article : PMC3266851 ] [ PubMed : 20097578 ]
- Verschuur MJ, Maric M, Spinhoven P. Differences in changes in health-related anxiety between Western and non-Western participants in a trauma-focused study. Journal of Traumatic Stress. 2010; 23 :300–303. [ PubMed : 20419742 ]
- Vest JR, Catlin TK, Chen JJ, Brownson RC. Multistate analysis of factors associated with intimate partner violence. American Journal of Preventive Medicine. 2002; 22 :156–164. [ PubMed : 11897459 ]
- Vickerman KA, Margolin G. Rape treatment outcome research: Empirical findings and state of the literature. Clinical Psychology Review. 2009; 29 :431–448. [ PMC free article : PMC2773678 ] [ PubMed : 19442425 ]
- Villagonzalo KA, Dodd S, Ng F, Mihaly S, Langbein A, Berk M. The relationship between substance use and posttraumatic stress disorder in a methadone maintenance treatment program. Comprehensive Psychiatry. 2011; 52 :562–566. [ PubMed : 21109242 ]
- Vlahov D, Galea S, Ahern J, Resnick H, Kilpatrick D. Sustained increased consumption of cigarettes, alcohol, and marijuana among Manhattan residents after September 11, 2001. American Journal of Public Health. 2004; 94 :253–254. [ PMC free article : PMC1448236 ] [ PubMed : 14759935 ]
- Vogt DS, Tanner LR. Risk and resilience factors for posttraumatic stress symptomatology in Gulf War I veterans. Journal of Traumatic Stress. 2007; 20 :27–38. [ PubMed : 17345645 ]
- Vogt DS, King DW, King LA. Risk pathways for PTSD: Making sense of the literature. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York: Guilford Press; 2007. pp. 99–115.
- Vogt DS, Pless AP, King LA, King DW. Deployment stressors, gender, and mental health outcomes among Gulf War I veterans. Journal of Traumatic Stress. 2005; 18 :272–284. [ PubMed : 16281224 ]
- Walker RL, Clark ME, Sanders SH. The postdeployment multi-symptom disorder: An emerging syndrome in need of a new treatment paradigm. Psychological Services. 2010; 7 :136–147.
- Walser RD, Westrup D. Acceptance & commitment therapy for the treatment of post-traumatic stress disorder & trauma-related problems: A practitioner’s guide to using mindfulness & acceptance strategies. Oakland, CA: New Harbinger Publications; 2007.
- Walsh F. Traumatic Loss and Major Disasters: Strengthening Family and Community Resilience. Family Process. 2007; 46 :207–227. [ PubMed : 17593886 ]
- Walter KH, Horsey KJ, Palmieri PA, Hobfoll SE. The role of protective self-cognitions in the relationship between childhood trauma and later resource loss. Journal of Traumatic Stress. 2010; 23 :264–273. [ PMC free article : PMC2860613 ] [ PubMed : 20419735 ]
- Wan JJ, Morabito DJ, Khaw L, Knudson MM, Dicker RA. Mental illness as an independent risk factor for unintentional injury and injury recidivism. Journal of Trauma. 2006; 61 :1299–1304. [ PubMed : 17159669 ]
- Weathers FW, Keane TM, Foa EB. Assessment and diagnosis of adults. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009. pp. 23–61.
- Weine S, Danieli Y, Silove D, Ommeren MV, Fairbank JA, Saul J. Guidelines for international training in mental health and psychosocial interventions for trauma exposed populations in clinical and community settings. Psychiatry. 2002; 65 :156–164. [ PubMed : 12108139 ]
- Weine S, Kulauzovic Y, Klebic A, Besic S, Mujagic A, Muzurovic J, et al. Evaluating a multiple-family group access intervention for refugees with PTSD. Journal of Marital and Family Therapy. 2008; 34 :149–164. [ PubMed : 18412823 ]
- Weissbecker I, Clark C. The impact of violence and abuse on womens physical health: Can trauma-informed treatment make a difference? Journal of Community Psychology. 2007; 35 :909–923.
- Wenzel SL, Tucker JS, Elliott MN, Hambarsoomians K, Perlman J, Becker K, et al. Prevalence and co-occurrence of violence, substance use and disorder, and HIV risk behavior: a comparison of sheltered and low-income housed women in Los Angeles County. Preventive Medicine. 2004; 39 :617–624. [ PubMed : 15313103 ]
- Wessely S, Bryant RA, Greenberg N, Earnshaw M, Sharpley J, Hughes JH. Does psychoeducation help prevent posttraumatic psychological distress? Psychiatry: Interpersonal and Biological Processes. 2008; 71 :287–302. [ PubMed : 19152276 ]
- Westermeyer J, Hollifield M, Spring M, Johnson D, Jaranson J. Comparison of two methods of inquiry for torture with East African refugees: Single query versus checklist. Torture. 2011; 21 :155–172. [ PubMed : 22057103 ]
- Westphal M, Olfson M, Gameroff MJ, Wickramaratne P, Pilowsky DJ, Neugebauer R, et al. Functional impairment in adults with past posttraumatic stress disorder: findings from primary care. Depression and Anxiety. 2011; 28 :686–695. [ PMC free article : PMC3647251 ] [ PubMed : 21681868 ]
- Whitbeck LB, Chen X, Hoyt DR, Adams GW. Discrimination, historical loss and enculturation: Culturally specific risk and resiliency factors for alcohol abuse among American Indians. Journal of Studies on Alcohol. 2004; 65 :409–418. [ PubMed : 15376814 ]
- Whitfield CL, Anda RF, Dube SR, Felitti VJ. Violent childhood experiences and the risk of intimate partner violence in adults: Assessment in a large health maintenance organization. Journal of Interpersonal Violence. 2003; 18 :166–185.
- Widom CS, Morris S. Accuracy of adult recollections of childhood victimization, Part 2: Childhood sexual abuse. Psychological Assessment. 1997; 9 :34–46.
- Wilcox J, Briones D, Suess L. Auditory hallucinations, posttraumatic stress disorder, and ethnicity. Comprehensive Psychiatry. 1991; 32 :320–323. [ PubMed : 1935021 ]
- Wilkinson DM, Blacker SD, Richmond VL, Horner FE, Rayson MP, Spiess A, et al. Injuries and injury risk factors among British army infantry soldiers during predeployment training. Injury Prevention. 2011; 17 :381–387. [ PubMed : 21507884 ]
- Williams LM. Recall of childhood trauma: A prospective study of women’s memories of child sexual abuse. Journal of Consulting and Clinical Psychology. 1994; 62 :1167–1176. [ PubMed : 7860814 ]
- Wilson JP. The lens of culture: Theoretical and conceptual perspectives in the assessment of psychological trauma and PTSD. In: Wilson JP, Tang CS, editors. Cross–cultural assessment of psychological trauma and PTSD. New York: Springer Science + Business Media; 2007. pp. 3–30.
- Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. Journal of Affective Disorders. 2010; 126 :411–414. [ PMC free article : PMC3606050 ] [ PubMed : 20488545 ]
- Woodward AT, Taylor RJ, Bullard KM, Aranda MP, Lincoln KD, Chatters LM. Prevalence of lifetime DSM-IV affective disorders among older African Americans, Black Caribbeans, Latinos, Asians and Non-Hispanic White people. International Journal of Geriatric Psychiatry. 2011 [ PMC free article : PMC3391316 ] [ PubMed : 21987438 ]
- World Health Organization. International statistical classification of diseases and related health problems. 9th revision ed. Geneva, Switzerland: World Health Organization; 1979.
- Wrenn GL, Wingo AP, Moore R, Pelletier T, Gutman AR, Bradley B, et al. The effect of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients. Journal of the National Medical Association. 2011; 103 :560–566. [ PMC free article : PMC3691279 ] [ PubMed : 21999030 ]
- Xian H, Chantarujikapong SI, Scherrer JF, Eisen SA, Lyons MJ, Goldberg J, et al. Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence in twin pairs. Drug and Alcohol Dependence. 2000; 61 :95–102. [ PubMed : 11064187 ]
- Xie Y, Greenman E. Research report: Segmented assimilation theory: A reformulation and empirical test. Ann Arbor, MI: University of Michigan; 2005.
- Yehuda R, Halligan SL, Bierer LM. Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research. 2001; 35 :261–270. [ PubMed : 11591428 ]
- Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Development and Psychopathology. 2001; 13 :733–753. [ PubMed : 11523857 ]
- Yellow Horse S, Brave Heart MYH. Chapter 3: Native American children. Colorado Springs, CO: White Bison, Inc.; 2005.
- Yoder M, Tuerk PW, Price M, Grubaugh AL, Strachan M, Myrick H, et al. Prolonged exposure therapy for combat-related posttraumatic stress disorder: Comparing outcomes for veterans of different wars. Psychol. Serv. 2012; 9 :16–25. [ PMC free article : PMC3427616 ] [ PubMed : 22449084 ]
- Young BH. The immediate response to disaster: Guidelines for adult psychological first aid. In: Ritchie EC, Watson PJ, Friedman MJ, editors. Interventions following mass violence and disasters: Strategies for mental health practice. New York: Guilford Press; 2006. pp. 134–154.
- Yuan C, Wang Z, Inslicht SS, McCaslin SE, Metzler TJ, Henn-Haase C, et al. Protective factors for posttraumatic stress disorder symptoms in a prospective study of police officers. Psychiatry Research. 2011; 188 :45–50. [ PMC free article : PMC3071439 ] [ PubMed : 21095622 ]
- Zatzick D, Roy-Byrne P, Russo J, Rivara F, Droesch R, Wagner A, Dunn C, Jurkovich G, Uehara E, Katon W. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Archives of General Psychiatry. 2004; 61 :498–506. [ PubMed : 15123495 ]
- Zayfert C, DeViva JC. Avoiding treatment failures in the anxiety disorders. New York: Springer Science + Business Media; 2010. Avoiding treatment failures in PTSD; pp. 147–168.
- Zivin K, Bohnert ASB, Mezuk B, Ilgen MA, Welsh D, Ratliff S, et al. Employment status of patients in the VA health system: Implications for mental health services. Psychiatric Services. 2011; 62 :35–38. [ PubMed : 21209297 ]
- Zohar J, Fostick L, Cohen A, Bleich A, Dolfin D, Weissman Z, et al. Risk factors for the development of posttraumatic stress disorder following combat trauma: A semiprospective study. Journal of Clinical Psychiatry. 2009; 70 :1629–1635. [ PubMed : 19852906 ]
- Zohar J, Juven-Wetzler A, Sonnino R, Cwikel-Hamzany S, Balaban E, Cohen H. New insights into secondary prevention in post-traumatic stress disorder. Dialogues in Clinical Neuroscience. 2011; 13 :301–309. [ PMC free article : PMC3182005 ] [ PubMed : 22033784 ]
- Zohar J, Sonnino R, Juven-Wetzler A, Cohen H. Can posttraumatic stress disorder be prevented? CNS Spectrums. 2009; 14 :44–51. [ PubMed : 19169193 ]
- Zweig JM, Yahner J, Rossman SB. Does recent physical and sexual victimization affect further substance use for adult drug-involved offenders? Journal of Interpersonal Violence. 2012 [ PubMed : 22328655 ]
Appendix. Methodology
Some of the sources cited in the Treatment Improvement Protocol (TIP) Trauma-Informed Care in Behavioral Health Services were suggested early on in the TIP’s development by consensus panel members, reviewers, and consultants working together with staff members of the Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) Knowledge Application Program (KAP) staff. More recently, broad searches were conducted to find research from the past 10 years involving trauma and behavioral health (including both mental health and substance abuse) as well as posttraumatic stress disorder (PTSD) and acute stress disorder.
At various times during the development of the TIP, searches on specific topics were conducted per the requests of SAMHSA staff and/or reviewers of the TIP. Early searches focused on trauma/PTSD and September 11, 2001, trauma/PTSD and Hurricane Katrina, trauma/PTSD and motivational interviewing, and historical trauma. Later in the TIP’s development, additional searches were conducted using the American Psychological Association’s PsychNet databases, the National Library of Medicine’s PubMed database, and, occasionally, Elsevier’s Scopus database as needed on topics such as:
- Trauma-informed care.
- Trauma teams.
- Stockholm syndrome/traumatic bonding.
- Vicarious trauma.
- Compassion fatigue and trauma.
- Environmental safety and trauma/PTSD.
- Sleep disorders and trauma.
- Ecological models and trauma.
- Psychological trauma/PTSD and quality of life.
- Psychological trauma/PTSD and culture.
- Trauma and health disparities.
- Trauma and rural health.
- Psychological trauma and torture.
- Recovered memories.
- Adverse childhood experiences/child abuse.
- Assessment and psychological trauma/PTSD.
- Trauma and mood disorders.
- Trauma and anxiety disorders (excluding PTSD).
- Trauma and personality disorders.
- Trauma and eating disorders.
- Trauma and substance use disorders.
- Trauma and schizophrenia.
- Self-harm/suicidality and trauma.
- Trauma and psychological first aid.
- Acute stress disorder/PTSD and prevention.
- Family therapy and trauma.
- Group therapy and trauma.
- Cognitive–behavioral therapy and PTSD.
- Eye movement desensitization and PTSD.
- Exposure therapy and PTSD.
- Pharmacotherapy/medication and PTSD.
Searches were generally conducted by the author of the literature review; abstracts were typically reviewed online by the TIP’s Expert Content Director, who then requested copies of promising citations. Relevant articles were reviewed by the writer in consultation with the KAP Senior Researcher and Applied Psychologist.
When available, review articles were acquired first and used to summarize older literature. Review articles as well as other articles that were retrieved suggested further promising or seminal literature, which was also obtained. In addition, Internet searches were conducted for relevant literature available from government and nongovernmental sources.
- Cite this Page Center for Substance Abuse Treatment (US). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. (Treatment Improvement Protocol (TIP) Series, No. 57.) Section 1, A Review of the Literature.
- PDF version of this title (5.2M)
In this Page
- Methodology
Other titles in these collections
- SAMHSA/CSAT Treatment Improvement Protocols
- Health Services/Technology Assessment Texts (HSTAT)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- A Review of the Literature - Trauma-Informed Care in Behavioral Health Services A Review of the Literature - Trauma-Informed Care in Behavioral Health Services
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Psychological Trauma: Theory, Research, Practice, and Policy
- Read this journal
- Read free articles
- Journal snapshot
- Advertising information
Journal scope statement
Psychological Trauma: Theory, Research, Practice, and Policy ® publishes empirical research on the psychological effects of trauma. The journal is intended to be a forum for an interdisciplinary discussion on trauma, blending science, theory, practice, and policy.
The journal publishes empirical research on a wide range of trauma-related topics, including:
- Psychological treatments and effects
- Promotion of education about effects of and treatment for trauma
- Assessment and diagnosis of trauma
- Pathophysiology of trauma reactions
- Health services (delivery of services to trauma populations)
- Epidemiological studies and risk factor studies
- Neuroimaging studies
- Trauma and cultural competence
The journal publishes articles that use experimental and correlational methods and qualitative analyses, if applicable.
All research reports should reflect methodologically rigorous designs that aim to significantly enhance the field's understanding of trauma. Such reports should be based on good theoretical foundations and integrate theory and data. Manuscripts should be of sufficient length to ensure theoretical and methodological competence.
Equity, diversity, and inclusion
Psychological Trauma: Theory, Research, Practice, and Policy supports equity, diversity, and inclusion (EDI) in its practices. More information on these initiatives is available under EDI Efforts .
Call for papers
- Call for abstracts: Special section on trauma-informed assessment: Process and measures
- Call for papers: The bidirectional relationship between PTSD and psychosis: Advancements in theory, research, practice, and policy
Author and editor spotlights
Explore journal highlights : free article summaries, editor interviews and editorials, journal awards, mentorship opportunities, and more.
Prior to submission, please carefully read and follow the submission guidelines detailed below. Manuscripts that do not conform to the submission guidelines may be returned without review.
To submit to the editorial office of Kathleen Kendall-Tackett, please submit manuscripts electronically through the Manuscript Submission Portal in Microsoft Word or Open Office format.
Prepare manuscripts according to the Publication Manual of the American Psychological Association using the 7 th edition. Manuscripts may be copyedited for bias-free language (see Chapter 5 of the Publication Manual ). APA Style and Grammar Guidelines for the 7 th edition are available.
Submit Manuscript
Kathleen Kendall-Tackett, PhD Praeclarus Press, LLC
General correspondence may be directed to the editor's office .
Authors must indicate in their cover letter whether they prefer masked or unmasked peer review. If anonymous review is requested, all author's names, their affiliations, and contact information should be removed from the manuscript. Note that the Open Science Framework provides instructions for creating anonymized links to data sets, codebooks, relevant scripts or materials, and preregistrations to protect the integrity of the masked review process.
In addition to addresses and phone numbers, please supply email addresses and fax numbers for use by the editorial office and later by the production office. Most correspondence between the editorial office and authors is handled by email, so a valid email address is important to the timely flow of communication during the editorial process.
Keep a copy of the manuscript to guard against loss.
Manuscripts for Psychological Trauma: Theory, Research, Practice, and Policy can vary in length, but may not exceed 28 double-spaced manuscript pages (including title page, abstract, manuscript body, references, and tables/figures.) Manuscripts that exceed this length may be returned without review. Authors do have the option of electronically archiving supplemental material, such as tables and figures, in order to assist them in keeping their articles to the required length (see below).
While Psychological Trauma primarily publishes original empirical studies, we are also open to reviewing high-quality literature reviews and clinical, qualitative, theoretical, and policy articles. Replication studies are welcome if they provide conclusive results.
Manuscript preparation
Prepare manuscripts according to the Publication Manual of the American Psychological Association using the 7th edition. Manuscripts may be copyedited for bias-free language (see Chapter 5 of the Publication Manual ).
Review APA's Journal Manuscript Preparation Guidelines before submitting your article.
Double-space all copy. Other formatting instructions, as well as instructions on preparing tables, figures, references, metrics, and abstracts, appear in the Manual . Additional guidance on APA Style is available on the APA Style website .
If your manuscript was mask reviewed, please ensure that the final version for production includes a byline and full author note for typesetting.
Below are additional instructions regarding the preparation of tables.
Use Word's insert table function when you create tables. Using spaces or tabs in your table will create problems when the table is typeset and may result in errors.
Author contributions statements using CRediT
The APA Publication Manual ( 7th ed. ) stipulates that “authorship encompasses…not only persons who do the writing but also those who have made substantial scientific contributions to a study.” In the spirit of transparency and openness, Psychological Trauma has adopted the Contributor Roles Taxonomy (CRediT) to describe each author’s individual contributions to the work. CRediT offers authors the opportunity to share an accurate and detailed description of their diverse contributions to a manuscript.
Submitting authors will be asked to identify the contributions of all authors at initial submission according to this taxonomy. If the manuscript is accepted for publication, the CRediT designations will be published as an author contributions statement in the author note of the final article. All authors should have reviewed and agreed to their individual contribution(s) before submission.
CRediT includes 14 contributor roles, as described below:
- Conceptualization —Ideas; formulation or evolution of overarching research goals and aims.
- Data curation —Management activities to annotate (produce metadata), scrub data and maintain research data (including software code, where it is necessary for interpreting the data itself) for initial use and later re-use.
- Formal analysis —Application of statistical, mathematical, computational, or other formal techniques to analyze or synthesize study data.
- Funding acquisition —Acquisition of the financial support for the project leading to this publication.
- Investigation —Conducting a research and investigation process, specifically performing the experiments, or data/evidence collection.
- Methodology —Development or design of methodology; creation of models.
- Project administration —Management and coordination responsibility for the research activity planning and execution.
- Resources —Provision of study materials, reagents, materials, patients, laboratory samples, animals, instrumentation, computing resources, or other analysis tools.
- Software —Programming, software development; designing computer programs; implementation of the computer code and supporting algorithms; testing of existing code components.
- Supervision —Oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
- Validation —Verification, whether as a part of the activity or separate, of the overall replication/reproducibility of results/experiments and other research outputs.
- Visualization —Preparation, creation and/or presentation of the published work, specifically visualization/data presentation.
- Writing —original draft—Preparation, creation and/or presentation of the published work, specifically writing the initial draft (including substantive translation).
- Writing —review & editing—Preparation, creation and/or presentation of the published work by those from the original research group, specifically critical review, commentary or revision—including pre- or post-publication stages.
Authors can claim credit for more than one contributor role, and the same role can be attributed to more than one author.
APA Style Journal Article Reporting Standards
Authors are expected to adhere to the updated APA Style Journal Article Reporting Standards (JARS) for quantitative , qualitative , and mixed methods research before submitting. These standards offer ways to improve transparency in reporting to ensure that readers have the information necessary to evaluate the quality of the research and to facilitate collaboration and replication. For further resources, including flowcharts, see the Journal Article Reporting Standards (JARS) website .
Brief reports
Brief reports are articles that do not exceed 12 pages including the cover page, abstract, tables, figures, and references. A brief report is appropriate when there are preliminary findings, or findings from a small sample size, that may not be appropriate for a full research report.
Academic writing and English language editing services
Authors who feel that their manuscript may benefit from additional academic writing or language editing support prior to submission are encouraged to seek out such services at their host institutions, engage with colleagues and subject matter experts, and/or consider several vendors that offer discounts to APA authors .
Please note that APA does not endorse or take responsibility for the service providers listed. It is strictly a referral service.
Use of such service is not mandatory for publication in an APA journal. Use of one or more of these services does not guarantee selection for peer review, manuscript acceptance, or preference for publication in any APA journal.
Submitting supplemental materials
APA can place supplemental materials online, available via the published article in the PsycArticles ® database. Please see Supplementing Your Article With Online Material for more details.
Abstract and keywords
All manuscripts must include a structured abstract divided into the following sections, with headings: objective, method, results, and conclusions. The objective should clearly communicate the novel contribution of the manuscript. In the conclusion, please identify at least one specific implication and avoid boilerplate language such as “Implications will be discussed.”
The abstract should be no longer than 250 words and should be followed by five keywords, or brief phrases.
Clinical impact statements
Authors are asked to include a short statement of no more than 100 words, written in conversational English, that summarizes the article's findings and why they are important to practice.
This new article feature allows authors greater control over how their work will be interpreted by a number of audiences (e.g., practitioners, policy makers, news media).
This text should appear in your manuscript, below the abstract, in a section titled "Clinical impact statement."
Please refer to the Guidance for Translational Abstracts and Public Significance Statements page to help you write this text.
Openness and transparency
Authors should state all sources of financial support for the conduct of the research (e.g., This research was supported by Award XX from the Eunice Kennedy Shriver Institute of Child Health and Human Development) in the author note. If the funding source was involved in any other aspects of the research (e.g., study design, analysis, interpretation, writing), then clearly state the role. If the funding source had no other involvement other than financial support, then simply state that the funding source had no other role other than financial support.
Authors should also provide a conflict of interest statement in the author note disclosing any real or potentially perceived conflict(s) of interest, including financial, personal, or other relationships with other organizations or companies that may inappropriately impact or influence the research and interpretation of the findings. If there are no conflicts of interest, this should be clearly stated.
Preregistration of studies and analysis plans can be useful for distinguishing confirmatory and exploratory analyses. We encourage investigators to preregister their studies and analysis plans prior to conducting the research (e.g., Open Science Framework, ClinicalTrials.gov). If any aspect of the study is preregistered, include the registry link in the author note.
Authors who have posted their manuscripts to preprint archives, such as PsyArXiv, prior to submission should include a link to the preprint in the author note.
Participant description and informed consent
The method section of each empirical report must contain a detailed description of the study participants, including (but not limited to) the following:
- nativity or immigration history
- socioeconomic status
- clinical diagnoses and comorbidities (as appropriate)
- any other relevant demographics (e.g., disability status; sexual orientation)
In both the abstract and in the discussion section of the manuscript, authors should discuss the diversity of their study samples and the generalizability of their findings.
The method section also must include a statement describing how informed consent was obtained from the participants (or their parents/guardians), including for secondary use of data if applicable, and indicate that the study was conducted in compliance with an appropriate Internal Review Board.
Registered reports, null results, and replications
In addition to full-length research papers reporting novel findings, the journal publishes registered reports, negative findings, and replications, regardless of result. Preregistration of replication studies is strongly recommended, but not required.
Registered reports require a two-step review process. The first step is the submission of the registration manuscript. This is a partial manuscript that includes hypotheses, rationale for the study, experimental design, and methods. The partial manuscript will be reviewed for rigor and methodological approach.
If the partial manuscript is accepted, this amounts to provisional acceptance of the full report regardless of the outcome of the study. The full manuscript will be reviewed for adherence to the preregistered design (deviations should be reported in the manuscript).
Data transparency
In order to reduce the likelihood of duplicate or piecemeal publication, authors are required to provide, in their cover letter, a list of published, in press, and under review studies that come from the same dataset as the one in the submitted manuscript, as well as a narrative description of how the submitted manuscript differs from the others.
This narrative description should include how the manuscript differs (or does not) in terms of research question and variables studied.
Authors also are required to submit a masked version of the narrative description that can be provided to reviewers. Please add this as an appendix table on the last page of the submitted manuscript.
Please base your description on the following examples, edited according to your specific data circumstances.
Do not provide the title of the manuscript, authors, or journal in which it was published. Do provide the names of the relevant variables (i.e., substitute the numbers in the examples for actual names, such as depressive symptoms, therapeutic alliance, etc.).
Narrative example: Multiple uses of data collected from the same sample
The data reported in this manuscript have been previously published and/or were collected as part of a larger data collection (at one or more points in time). Findings from the data collection have been reported in separate manuscripts. MS 1 (published) focuses on variables 1, 2, and 3; while MS 2 (in press) focuses on variables 4, 5, and 6. MS 3 (the current manuscript) focuses on variables 8, 9, and 15. MS 4 (soon to be submitted) will focus on variables 10, 12, and 14.
Narrative example: Publicly available dataset
The data reported in this manuscript were obtained from publicly available data, [name of project, along with website link to project description]. A bibliography of journal articles, working papers, conference presentations, and dissertations using the [name of project] is available at [website link to bibliography list]. The variables and relationships examined in the present article have not been examined in any previous or current articles, or to the best of our knowledge in any papers that will be under review soon. [Alternatively, clarify any overlap of variables, as done in the narrative example above].
Upon submission of the manuscript, authors will be required to attest to the provision of the required information described above.
Finally, upon acceptance of a manuscript, authors will be required to provide, as part of the author note, a list of related published papers that come from the same dataset, unless such papers are clearly described and referenced in the manuscript (specifically noting that findings come from the same dataset).
Open science badges
Articles are eligible for open science badges recognizing publicly available data, materials, and/or preregistration plans and analyses. These badges are awarded on a self-disclosure basis.
At submission, authors must confirm that criteria have been fulfilled in a signed badge disclosure form (PDF, 33KB) that must be submitted as supplemental material. If all criteria are met as confirmed by the editor, the form will then be published with the article as supplemental material.
Authors should also note their eligibility for the badge(s) in the cover letter.
For all badges, items must be made available on an open-access repository with a persistent identifier in a format that is time-stamped, immutable, and permanent. For the preregistered badge, this is an institutional registration system.
Data and materials must be made available under an open license allowing others to copy, share, and use the data, with attribution and copyright as applicable.
Available badges are:

Note that it may not be possible to preregister a study or to share data and materials. Applying for open science badges is optional.
List references in alphabetical order. Each listed reference should be cited in text, and each text citation should be listed in the references section.
Examples of basic reference formats:
Journal article
McCauley, S. M., & Christiansen, M. H. (2019). Language learning as language use: A cross-linguistic model of child language development. Psychological Review , 126 (1), 1–51. https://doi.org/10.1037/rev0000126
Authored book
Brown, L. S. (2018). Feminist therapy (2nd ed.). American Psychological Association. https://doi.org/10.1037/0000092-000
Chapter in an edited book
Balsam, K. F., Martell, C. R., Jones. K. P., & Safren, S. A. (2019). Affirmative cognitive behavior therapy with sexual and gender minority people. In G. Y. Iwamasa & P. A. Hays (Eds.), Culturally responsive cognitive behavior therapy: Practice and supervision (2nd ed., pp. 287–314). American Psychological Association. https://doi.org/10.1037/0000119-012
Preferred formats for graphics files are TIFF and JPG, and preferred format for vector-based files is EPS. Graphics downloaded or saved from web pages are not acceptable for publication. Multipanel figures (i.e., figures with parts labeled a, b, c, d, etc.) should be assembled into one file. When possible, please place symbol legends below the figure instead of to the side.
- All color line art and halftones: 300 DPI
- Black and white line tone and gray halftone images: 600 DPI
Line weights
- Color (RGB, CMYK) images: 2 pixels
- Grayscale images: 4 pixels
- Stroke weight: 0.5 points
APA offers authors the option to publish their figures online in color without the costs associated with print publication of color figures.
The same caption will appear on both the online (color) and print (black and white) versions. To ensure that the figure can be understood in both formats, authors should add alternative wording (e.g., “the red (dark gray) bars represent”) as needed.
For authors who prefer their figures to be published in color both in print and online, original color figures can be printed in color at the editor's and publisher's discretion provided the author agrees to pay:
- $900 for one figure
- An additional $600 for the second figure
- An additional $450 for each subsequent figure
Permissions
Authors of accepted papers must obtain and provide to the editor on final acceptance all necessary permissions to reproduce in print and electronic form any copyrighted work, including test materials (or portions thereof), photographs, and other graphic images (including those used as stimuli in experiments).
On advice of counsel, APA may decline to publish any image whose copyright status is unknown.
- Download Permissions Alert Form (PDF, 13KB)
Publication policies
For full details on publication policies, including use of Artificial Intelligence tools, please see APA Publishing Policies .
APA policy prohibits an author from submitting the same manuscript for concurrent consideration by two or more publications.
See also APA Journals ® Internet Posting Guidelines .
APA requires authors to reveal any possible conflict of interest in the conduct and reporting of research (e.g., financial interests in a test or procedure, funding by pharmaceutical companies for drug research).
- Download Full Disclosure of Interests Form (PDF, 41KB)
Ethical Principles
It is a violation of APA Ethical Principles to publish "as original data, data that have been previously published" (Standard 8.13).
In addition, APA Ethical Principles specify that "after research results are published, psychologists do not withhold the data on which their conclusions are based from other competent professionals who seek to verify the substantive claims through reanalysis and who intend to use such data only for that purpose, provided that the confidentiality of the participants can be protected and unless legal rights concerning proprietary data preclude their release" (Standard 8.14).
APA expects authors to adhere to these standards. Specifically, APA expects authors to have their data available throughout the editorial review process and for at least 5 years after the date of publication.
Authors are required to state in writing that they have complied with APA ethical standards in the treatment of their sample, human or animal, or to describe the details of treatment.
- Download Certification of Compliance With APA Ethical Principles Form (PDF, 26KB)
The APA Ethics Office provides the full Ethical Principles of Psychologists and Code of Conduct electronically on its website in HTML, PDF, and Word format. You may also request a copy by emailing or calling the APA Ethics Office (202-336-5930). You may also read "Ethical Principles," December 1992, American Psychologist , Vol. 47, pp. 1597–1611.
Other information
See APA’s Publishing Policies page for more information on publication policies, including information on author contributorship and responsibilities of authors, author name changes after publication, the use of generative artificial intelligence, funder information and conflict-of-interest disclosures, duplicate publication, data publication and reuse, and preprints.
Visit the Journals Publishing Resource Center for more resources for writing, reviewing, and editing articles for publishing in APA journals.
Editor-in-chief
Kathleen Kendall-Tackett, PhD Texas Tech University School of Medicine at Amarillo, United States
Associate editors
Tyson Bailey, PsyD Kenmore, Washington, United States
Diane Elmore Borbon, PhD, MPH Duke University School of Medicine, United States
Paul Frewen, PhD Western University, Ontario, Canada
Sylvia Marotta-Walters, PhD George Washington University, United States
Sandra Mattar, PsyD Boston University School of Medicine, Boston Medical Center & Center for Multicultural Training in Psychology, United States
Jack Tsai, PhD University of Texas at San Antonio, United States
Associate editor for statistics
Zhen Cong, PhD University of Texas at Arlington, United States
Editorial board
Shane Adams, PhD VA Palo Alto Health Care System, United States
Dean Ajdukovic, PhD University of Zagreb, Croatia
Carolyn Allard, PhD University of California at San Diego, United States
Siraj Alyami, MA Ashford University, United States
Hadis Amiri, PhD Kerman University of Medical Sciences, Iran
Catherine L. Anderson, PhD Bethesda, Maryland, United States
Gizem Arikan, PhD Ozyegin University, Turkey
Cherie Armour, PhD Ulster University, Ireland
Rebecca L. Babcock Fenerci, PhD Brown Medical School; Merrimack College, United States
Oyenike Balogun-Mwangi, PhD Salve Regina University, United States
Rose Barlow, PhD National Center for Posttraumatic Stress Disorder, United States
Erin R. Barnett, PhD Geisel School of Medicine at Dartmouth College, Dartmouth-Hitchcock Medical Center, United States
Alexandria G. Bauer, PhD Rutgers University New Brunswick, United States
Vera Békés, PhD Yeshiva University, United States
Charles A. Benincasa, MA Saint Mary’s University of Minnesota, United States
Nahaal Binazir, PsyD Louisiana State University, United States
Allyson Marie Blackburn University of Illinois at Urbana-Champaign, United States
Isabelle Blanchette, PhD Université du Québec à Trois-Rivières, Canada
Bethany L. Brand, PhD Towson University, United States
Douglas Bremner, MD Emory University School of Medicine, United States
Deborah J. Brief, PhD VA Boston Healthcare System, United States
Thema Bryant-Davis, PhD Pepperdine University, United States
Rodger K. Bufford, PhD George Fox University, United States
Brianna Byllesby, PhD University of South Dakota, United States
Clare E. B. Cannon, PhD University of California Davis, United States
Christy Capone, PhD Warren Alpert School of Medicine, Brown University, United States
Laura E. Captari, PhD Boston University, United States
Etzel Cardeña, PhD Lund University, Sweden
Eve B. Carlson, PhD National Center for Posttraumatic Stress Disorder, United States
Robert T. Carter, PhD Teachers College at Columbia University, United States
Sierra Elizabeth Carter, PhD Georgia State University, United States
Lorys Castelli, PhD University of Turin, Italy
Eduardo Cazabat, PsyD Argentine Society for Psychotrauma, Argentina
Christian S. Chan, PhD The University of Hong Kong, Hong Kong
Catherine C. Classen, PhD University of Toronto, Canada
Ashley N. Clausen, PhD Duke University Brain Imaging and Analysis Center, United States
Keren Cohen-Louck, PhD Ariel University, Israel
Ateka Contractor, PhD University of North Texas, United States
Joan M. Cook, PhD Yale School of Medicine, United States
Lisa Cromer, PhD University of Tulsa, United States
Constance J. Dalenberg, PhD Alliant International University, United States
Wendy D'Andrea, PhD The New School, United States
Andrea Danese, MD, PhD King's College London, United Kingdom
Priscilla Dass-Brailsford, EdD, MPH Georgetown University, United States
Christopher R. DeCou, PhD University of Washington, United States
Ian de Terte, PhD Massey University, New Zealand
Sharon Dekel, PhD Harvard Medical School, United States
John Delatorre, PsyD Private Practice, United States
Daniel Dogden, PhD US Department of Health & Human Services, United States
John Durkin, PhD Stage-28 International, Perth, Australia
Amy Ellis, PhD Nova Southeastern University, United States
Lisa Elwood, PhD Ponce Health Sciences University, United States
Brian Engdahl, PhD Veterans Affairs Healthcare System, United States
Alexander J. Erickson, PhD VA Greater Los Angeles Healthcare System, United States
Carolyn Fallahi, PhD Central Connecticut State University, United States
Michael Fitzgerald, PhD Oklahoma State University, United States
William F. Flack, PhD Bucknell University, United States
Edna Foa, PhD University of Pennsylvania, United States
Victoria Follette, PhD University of Nevada at Reno, United States
David Forbes, PhD Phoenix Australia Centre for Posttraumatic Mental Health, Australia
Julian Ford, PhD University of Connecticut Health Center, United States
Sheila B. Frankfurt, PhD VISN 17 Center of Excellence for Research on Returning War Veterans, United States
Molly R. Franz, PhD University of Maryland, Baltimore County (UMBC), United States
Mary Gail Frawley-O'Dea, PhD Presbyterian Samaritan Counseling Center, United States
Maria M. Galano, PhD University of Massachusetts Amherst, United States
Richard M. Ganley, PhD Veterans Administration Medical Center, United States
Dana Rose Garfin, PhD University of California Los Angeles, United States
Adrienne Gilmore-Thomas, PhD UTHealth Science Center Houston, United States
Steven N. Gold, PhD Nova Southeastern University, United States
David Graham, MBBS, MPsychMed, PhD University of Sydney, Australia
Jessica A. Graham, PsyD VA Salt Lake City Health Care System, United States
Sandra Graham-Bermann, PhD University of Michigan, United States
Michele Grassi, PhD Universita degli Studi di Trieste, Italy
Jonathan Green, PhD Veterans Affairs Boston Healthcare System, United States
Ricky Greenwald, PsyD Trauma Institute & Child Trauma Institute, United States
Sabina Gušić, PhD Lund University, Sweden
Muhammad M. Haj-Yahia, PhD The Hebrew University of Jerusalem, Israel
Brian James Hall, PhD University of Macau & Johns Hopkins Bloomberg School of Public Health, China
Erin P. Hambrick, PhD University of Missouri at Kansas City, United States
Hamka Hamka, PhD Universtas Muhammadiyah Kalimantan Timur, Indonesia
Catherine R. M. Hearne, PhD New Mexico Veterans Affairs Health Care System, United States
Philip Held, PhD Rush University Medical Center, United States
Melanie D. Hetzel-Riggin, PhD Penn State Behrend, United States
Stevan E. Hobfoll, PhD Rush University Medical Center, United States
Katherine Kelton, PhD, MSPH US Department of Veterans Affairs, United States
Mohsen Khosravi, MD Zahedan University of Medical Sciences, Iran (Islamic Republic of)
David Read Johnson, PhD c Post Traumatic Stress Center, United States
Russell Jones, PhD Virginia Polytechnic Institute and State University, United States
Terence M. Keane, PhD Veterans Affairs National Center for Posttraumatic Stress Disorder & Boston University School of Medicine, United States
Alicia M. Key, PhD Dartmouth College, United States
Ibrahim Aref Kira, PhD Center for Cumulative Trauma Studies, United States
Shaina A. Kumar, PhD Boston University Chobanian & Avedisian School of Medicine, United States
Sadie Larsen, PhD Milwaukee VA, Medical College of Wisconsin, United States
Daniel Lee, PhD National Center for PTSD, VA Boston Healthcare System, United States
Inna Levy, PhD Ariel University, Israel
Michelle Lilly, PhD Northern Illinois University, United States
Annett Lotzin, PhD University Medical Center Hamburg-Eppendorf, Germany
Shannon M. Lynch, PhD Idaho State University, United States
Kathryn S. Macia, PhD VA Palo Alto Healthcare System Menlo Park Division, United States
Grant Marshall, PhD RAND Corporation, United States
Brian Marx, PhD National Center for Posttraumatic Stress Disorder at Veterans Affairs Boston Healthcare System, United States
Laura E. Miller-Graff, PhD University of Notre Dame, United States
Ursula Myers, PhD Ralph H Johnson VAMC, United States
Viann N. Nguyen-Feng, PhD, MPH University of Minnesota–Duluth, United States
Barbara L. Niles, PhD National Center for PTSD, United States
Oluyinka Ojedokun, PhD Adekunle Ajasin University, Nigeria
Tapan A. Patel, MS Florida State University, United States
Nnamdi Pole, PhD Smith College, United States
Janne L. Punski-Hoogervorst, MD, MSc University of Haifa, Israel
Brenda Punsky, LCSW, LLM Terra Firma at Montefiore Bronx Health Collective, United States
Gilbert Reyes, PhD Tulalip Behavioral Health and Recovery, United States
George Rhoades, Jr., PhD Ola Hou Clinic, United States
Lisa Rocchio, PhD Johnston, Rhode Island, United States
Josef I. Ruzek, PhD National Center for Posttraumatic Stress Disorder at Veterans Affairs Palo Alto Health Care System, United States
Bareera Saeed, MPhil Psychology The University of Lahore, Pakistan
Kristin W. Samuelson, PhD University of Colorado at Colorado Springs, United States
Adriano Schimmenti, PhD Kore University of Enna, Italy
Lawrence J. Schneider, PhD University of North Texas, United States
Stefan E. Schulenberg, PhD University of Mississippi, United States
Jeremiah A. Schumm, PhD Trauma Recovery Center at Veterans Affairs Medical Center, United States
Julia Seng, PhD University of Michigan School of Nursing, United States
M. Tracie Shea, PhD Providence VA Medical Center, United States
Christina M. Sheerin, PhD Virginia Commonwealth University, United States
Allen Sherman, PhD Winthrop P. Rockefeller Cancer Institute at University of Arkansas for Medical Sciences, United States
Victoria A. Shivy, PhD Virginia Commonwealth University, United States
Amit Shrira, PhD Bar-Ilan University, Israel
Brian Smith National Center for PTSD at VA Boston Healthcare System and Boston University School of Medicine, United States
Ian H. Stanley, PhD University of Colorado, United States
Maureen Sullivan, PhD Oklahoma State University, United States
Casey Taft, PhD National Center for Posttraumatic Stress Disorder at Veterans Affairs Boston Healthcare System & Boston University School of Medicine, United States
Sarah E. Ullman, PhD University of Illinois at Chicago, United States
Emre Umucu, PhD University of Texas at El Paso, United States
Onno Van der Hart, PhD Utrecht University, Netherlands
Dawne Vogt, PhD Veterans Affairs Boston Healthcare System and Boston University, United States
Eleni Vousoura, PhD National and Kapodistrian University of Athens, Greece
Anka A. Vujanovic, PhD University of Houston, United States
Jennifer Schuster Wachen, PhD National Center for Posttraumatic Stress Disorder at Veterans Affairs Boston Healthcare System & Boston University School of Medicine, United States
Sharon Wagner, PhD University of Northern British Columbia, Canada
Rachel Wamser, PhD University of Missouri–St. Louis, United States
Frank W. Weathers, PhD Auburn University, United States
Charity B. Wilkinson-Truong, PsyD Stress & Anxiety Services of NJ and Rutgers University, United States
Jolin Yamin, PhD Beth Israel Deaconess Medical Center, United States
Yingying Ye, PhD Zhejiang University, China
Abstracting and indexing services providing coverage of Psychological Trauma: Theory, Research, Practice, and Policy ®
- Cabell's Directory of Publishing Opportunities in Psychology
- CINAHL Complete
- CINAHL Plus
- Current Contents: Social & Behavioral Sciences
- Journal Citations Report: Social Sciences Edition
- Mosby's Nursing Consult
- Social Sciences Citation Index
Special issue of APA's journal Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 16, No. S1, April 2024. In this special issue, there are new studies covering a wide range of topics including adverse childhood experiences, symptoms of childhood trauma, childhood trauma’s impact on maternal/parent–child interactions, and child and adult social integration. Child maltreatment rates increased during COVID, which affected whole families and communities, compounding the risk.
Special issue of APA's journal Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 15, No. 8, November 2023. The articles included in this special issue feature current research on trauma in the military.
Special issue of APA's journal Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 15, No. S2, September 2023. This special issue features current research on secondary trauma.
Special issue of the APA's Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 15, No. S1, May 2023. This special issue examines trauma symptoms and types of trauma exposure, resilience and posttraumatic growth, trauma treatment and barriers to care, and finally, measuring trauma in young people.
Special issue of APA's Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 14, No. S1, April 2022. The special issue was inspired by a desire to shine a light on new ways to think about stress and trauma through resilience, perseverance, and posttraumatic growth.
Special issue of the APA journal Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 12, No. 8, November 2020. The studies included evaluate several different approaches to trauma treatment that fall under the broad umbrella of complementary and integrative health interventions.
Special issue of the APA journal of Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 12, No. S1, August 2020. This special issue presents early finding from Wuhan, China and raise essential questions about the massive social experiment of mandated lockdown.
Special issue of the APA journal Psychological Trauma, Vol. 11, No. 4, May 2019. The articles represent four areas of emerging research on trauma in the military population: beliefs, cognitions, and moral injury; relationships and coping; symptoms and comorbidity; and recovery.
Special issue of the APA journal Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 9, Suppl. 1, 2017. Includes articles about integrating the military back into civilian life, factors that influence trauma symptoms, treatments, triggers and buffers, disasters, and intergenerational effects of mass trauma and political violence.
Special issue of the APA journal Psychological Trauma, Vol. 6, Supplement 1, 2014. The issue is divided into 4 sections: the National Child Traumatic Stress Network Core Data Set, Trauma Treatment Approaches and Outcomes, The Nature of Trauma and Traumatization, Trauma in College Students.
Special issue of the APA journal Psychological Trauma, Vol. 3, No. 3, September 2011. Articles discuss trauma education and training in undergraduate, graduate, and community contexts.
Special issue of the APA journal Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 2, No. 4, December 2010. Articles discuss cultural factors in intimate partner violence among African Americans, Asian Americans, Latinos, homeless women, HIV-positive women, and pregnant women.
Special issue of APA's journal Psychological Trauma: Theory, Research, Practice, and Policy, Vol. 2, No. 1, March 2010. Includes articles about ethic group comparisons and trauma-related factors among Latinos, African Americans, and Asian Americans.
Journal equity, diversity, and inclusion statement
Psychological Trauma: Theory, Research, Practice, and Policy ® is an interdisciplinary forum on the causes and effects of psychological trauma. While we recognize that trauma potentially affects all people, we also recognize that socio-historical and cultural factors mediate expressions of trauma response. Therefore, Psychological Trauma encourages submissions that include diverse populations, samples, and viewpoints. We especially encourage authors from underrepresented groups and those outside the U.S.
Possible trauma-related topics include:
- psychological effects of trauma
- trauma treatments
- health services
- delivery of trauma services to diverse populations
- assessment and diagnosis of trauma
- culturally sensitive measure of trauma
- pathophysiology of response to trauma
- neuroimaging studies
- epidemiological and risk factor studies
- trauma prevention, intervention, and treatment that is culturally and linguistically sensitive
The journal publishes quantitative and qualitative studies, systematic reviews, and meta-analyses. All reports should integrate theory and data and aim to significantly advance the understanding of trauma. Manuscripts must contain a detailed description of the sample and its generalizability. Sample characteristics should be considered throughout the manuscript.
Inclusive study designs
- Collaborative research models
- Diverse samples
- Registered Reports
Definitions and further details on inclusive study designs are available on the Journals EDI homepage .
Inclusive reporting standards
- Bias-free language and community-driven language guidelines (required)
- Author contribution roles using CRediT (required)
- Data sharing and data availability statements (required)
- Impact statements (required)
- Participant sample descriptions (required)
- Sample justifications (required)
More information on this journal’s reporting standards is listed under the submission guidelines tab .
Pathways to authorship and editorship
Editorial fellowships.
Editorial fellowships help early-career psychologists gain firsthand experience in scholarly publishing and editorial leadership roles. This journal offers an editorial fellowship program for early-career psychologists from historically excluded communities. Of the two available fellow positions, one editorial fellow position is specifically designated for a person of color.
The journal has a high percentage of international authors.
Reviewer mentorship program
This journal encourages reviewers to submit co-reviews with their students and trainees. The journal likewise offers a formal reviewer mentorship program where graduate students and postdoctoral fellows from historically excluded groups are matched with a senior reviewer to produce an integrated review.
Development editor assistance program
Development editor programs offer support to experts who have a promising idea for advancing the field of psychology but have little experience with academic writing and publishing. A development editor provides a structured process, feedback, and editorial guidance for creating a manuscript to be submitted to a given journal. This journal offers a formal development editor assistance program.
Education sessions
This journal offers education sessions for aspiring authors and offers assistance with English-language issues.
Other EDI offerings
Orcid reviewer recognition.
Open Research and Contributor ID (ORCID) Reviewer Recognition provides a visible and verifiable way for journals to publicly credit reviewers without compromising the confidentiality of the peer review process. This journal has implemented the ORCID Reviewer Recognition feature in Editorial Manager, meaning that reviewers can be recognized for their contributions to the peer review process.
Masked peer review
This journal offers masked peer review (where both the authors’ and reviewers’ identities are not known to the other). Research has shown that masked peer review can help reduce implicit bias against traditionally female names or early-career scientists with smaller publication records (Budden et al., 2008; Darling, 2015).
Psychological Trauma and COVID-19
- Differential impacts of COVID-19 on communities of color
- International perspectives on COVID-19
- COVID-19: Insights on the pandemic’s traumatic effects and global implications A special supplemental issue of Psychological Trauma (August 2020)
- Increasing early career participation in the scholarly publishing process
- The co-occurrence of PTSD and opioid use disorder in opioid agonist therapy
- Introducing the May 2016 issue of Psychological Trauma: Theory, Research, Practice, and Policy
- How adequate is coverage of child maltreatment in abnormal psychology textbooks?
- Introducing the March 2016 issue of Psychological Trauma: Theory, Research, Practice, and Policy
- Anger dimensions and PTSD treatment
From APA Journals Article Spotlight ®
- Childhood neglect and posttraumatic stress may negatively affect fertility
- Posttraumatic outcomes following a campus shooting
Journal Alert
Sign up to receive email alerts on the latest content published.
Welcome! Thank you for subscribing.
Subscriptions and access
- Pricing and individual access
- APA PsycArticles database
Calls for Papers
Access options
- APA publishing resources
- Educators and students
- Editor resource center
APA Publishing Insider
APA Publishing Insider is a free monthly newsletter with tips on APA Style, open science initiatives, active calls for papers, research summaries, and more.
Social media
Contact Journals
Trauma Through the Life Cycle: A Review of Current Literature
- Original Paper
- Published: 31 May 2014
- Volume 42 , pages 323–335, ( 2014 )
Cite this article

- Shulamith Lala Ashenberg Straussner 1 &
- Alexandrea Josephine Calnan 2
27k Accesses
41 Citations
16 Altmetric
Explore all metrics
The past is never dead. It’s not even past. William Faulkner
The conflict between the will to deny horrible events and the will to proclaim them aloud is the central dialectic of psychological trauma. Judith Lewis Herman
This paper provides an overview of common traumatic events and responses, with a specific focus on the life cycle. It identifies selected “large T” and “micro” traumas encountered during childhood, adulthood and late life, and the concept of resilience. It also identifies the differences in traumatic events and reactions experienced by men compared to women, those related to the experience of immigration, and cross generational transmission of trauma. Descriptions of empirically-supported treatment approaches of traumatized individuals at the different stages of the life cycle are offered.
Similar content being viewed by others

The Childhood Trauma Questionnaire—Short Form (CTQ-SF) used with adolescents – methodological report from clinical and community samples

Examining the short and long-term impacts of child sexual abuse: a review study
Intergenerational trauma and its relationship to mental health care: a qualitative inquiry.
Avoid common mistakes on your manuscript.
Introduction
As recognized by William Faulkner and Judith Herman, as well as by many other writers and mental health professionals, trauma can take a tremendous psychological toll that may not disappear even with the passage of time. The term “trauma” comes from the Greek language meaning a “wound” or “hurt” (Oxford Dictionaries, 2013 ). Psychologically, “trauma” refers to an experience that is emotionally painful, distressful, or shocking, and one that often has long-term negative mental and physical (including neurological) consequence. An event is thought to produce a traumatic response when the stress resulting from that event overwhelms the individual’s psychological ability to cope (McGinley and Varchevker 2013 ).
Although we often think of trauma as being synonymous with the identified objective cause of the trauma, such as a soldier losing his legs to a roadside bomb explosion, the effect of the trauma is always subjective and refers to the impact—the perceived “wound” or “hurt” as identified by the early Greeks—that it has on the individual (Miller 2004 ). Thus what might be a traumatizing, life-shattering event for one individual might have minimal effects on another. Such differential reaction is based on many factors, including the individual’s age, gender identity, pre-morbid ego strength, previous traumatic experiences, the chronicity of the trauma, family history of trauma, current life stressors, social supports, and one’s cultural, religious or spiritual attitude toward adversity (Amir and Lev-Wiesel, 2003 ; Brewin et al. 2000 ; Felitti et al. 1998 ; Foa et al. 2009 ; Stamm and Friedman 2000 ; Straussner and Phillips 2004a ).
Unfortunately, the experience of trauma is not uncommon. Although there is a lack of recent national epidemiological findings about trauma among adults [Centers for Disease Control and Prevention (CDC) 2006 ], studies during the 1990s found that over 60 % of men and 51 % of women in the United States report having experienced at least one traumatic event during their lifetime (Giaconia et al. 1995 ; Kessler et al. 1995 ). Traumatic stress can cause disorganization of thinking, awareness, impaired judgment, altered reaction time, hyper vigilance, and unhelpful attempts at coping. While most people will experience time limited reactions, such as acute stress disorder, a smaller percentage may continue to manifest more severe and often longer lasting trauma-related impacts. These may include panic disorders, depression, sleep disorders, substance use disorders, as well as post-traumatic stress disorder (PTSD) (Kessler et al. 1995 ; Leskin and Sheikh 2002 ; Ringel and Brandell 2012 ).
While trauma can impact an individual at any time in the life cycle, from pre-natal development through old age, the impact and the treatment approaches vary depending on the individual’s developmental needs and the psychosocial environment. The purpose of this article is to provide an overview of common traumatic events and responses with a specific focus on the life cycle—identifying selected traumas encountered during childhood and adolescences, adulthood and late life. The differential impact of trauma on men and women, on immigrants, transgenerational transmission of trauma, the concept of resilience, and the implications for the treatment of traumatized individuals at the different stages of the life cycle are identified.
Nature of Trauma: “Large T” and “Micro-Traumas”
There are many different kinds of traumas, ranging from what Francine Shapiro, the originator of Eye Movement Desensitization and Reprocessing (EMDR) treatment approach (Shapiro 1995 ) has termed “large - T” traumas to “ small - t” or, what Straussner ( 2012 ) refers to as “micro-traumas.” Large-T traumas can impact individuals, families, groups and communities and include natural disasters, such as hurricanes, floods, wildfires, or nuclear disasters, as well as human-caused disasters, such as deadly car accidents, individual and mass violence, and other one-time traumatic events. Large-T traumas can also include, what Judith Herman ( 1997 ) termed as “complex traumas,” and which others refer to as Complex Traumas and Disorders of Extreme Stress (DESNOS- disorders of extreme stress not otherwise specified )—traumas that involve events of prolonged duration or multiple traumatic events (van der Kolk, Roth, Pelcovitz, Sunday and Spinazzola, 2005 ). Examples of complex, large-T traumas [also referred to as Type II trauma by Terr (1991)], include on-going interpersonal violence, child physical or sexual abuse spanning several years, never-ending wars, or constant acts of terrorism.
Small-t or micro-traumas are the more common traumas encountered by many of us. While large-T traumas are easily identified, many micro-traumas, such as being bullied in school or in the workplace (Idsoe et al. 2012 ; Mishna 2012 ), being stalked by someone (Purcell et al. 2005 ), living in severe poverty (Kiser 2007 ), childbirth (Kendall-Tackett 2013 ), or being the recipient of on-going individual discrimination because of one’s race, religion, gender identity, or sexual orientation, often go unrecognized and unacknowledged. Yet these micro-traumas may still cause much psychic pain and life-long damage.
Exposure to and Impact of Trauma
In her classic book Shattered assumptions: Towards a new psychology of trauma , Janof-Bulman ( 1992 ) reflects on the psychological shattering of one’s worldview experienced by traumatized individuals, especially if the trauma is caused through deliberate human acts (Straussner and Phillips 2004a ). Whereas the world was previously viewed as being trustworthy and benevolent, this belief may become transformed into the sense that “people will hurt me, and I can’t trust anyone.” Additionally, trauma survivors might find that the world they used to perceive as being stable and predictable, now seems unpredictable and out of their control. Consequently, their previous sense of empowerment and of being in control of their environment and their lives gives way to one in which they feel disempowered, helpless, and unable to predict and plan for the future. They may even have a sense of being psychologically damaged and defective (Janof-Bulman 1992 ).
The idea that trauma could result in specific clusters of symptoms first became formalized by the inclusion of the diagnosis of PTSD in the third edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM; American Psychiatric Association (APA) 1980 ]. This new diagnostic category was precipitated by awareness of the psychological problems experienced by returning Vietnam War veterans in the late 1970s and the growing literature by European writers who survived their own traumatic experiences during the Second World War—such as Gunter Grass, Primo Levy, and Eli Wiesel among others—and who vividly described the profound impact of mass violence on individuals, families and communities (Straussner and Phillips 2004a ). Studies of survivors of the Nazi-caused Holocaust (Krystal and Niederland 1968 ) and of the Hiroshima atomic bombing by the United States (Lifton 1968 ), introduced the concept of “survivors’ guilt” into our vocabulary.
The more recent recognition that traumatic reactions can result from response to events other than war, such as sexual assault, exposure to child abuse, domestic violence, and accidents has made PTSD a widely recognized disorder throughout the world (Herman 1997 ; van der Kolk et al. 2005 ). The importance of PTSD as a diagnostic category is reflected in the newly revised DSM-5 (APA, 2013 ), where PTSD and related conditions are no longer listed under Anxiety Disorders or Adjustment Disorders as previously, but are located in a separate chapter titled “Trauma- and Stressors-Related Disorders.”
While the experience of trauma is common, PTSD diagnosis is relatively rare. The estimated lifetime prevalence rate of PTSD in the US is thought to range between 6 and 12 %, averaging around 9 % of the population (APA 2013 ; Breslau et al. 1991 ; Kessler et al. 1995 ; Resnick et al. 1993 ). However, the initial prevalence rates among active duty military exposed to war conditions and among survivors of mass trauma, such as the September 11, 2001 World Trade Centers in New York, can range as high as 30 % and more (Galea et al. 2005 ; Susser et al. 2002 ). According to the latest edition of the DSM, the “[h]ighest rates (ranging from one-third to more than one-half of those exposed) are found among survivors of rape, military combat and captivity, and ethnically or politically motivated internment and genocide” (APA 2013 , p. 276). Recent United States- based studies document higher rates of PTSD among African-Americans, Latinos and American Indians than among white or Asian populations (APA 2013 ). International annual prevalence rates are believed to be somewhat lower than those in the US (APA 2013 ; Landolt et al. 2013 ), although studies in areas with on-going conflict, such as in Israel and the Palestinian territories, point to rates that are similar to those in the US among individuals who have been or are still exposed to combat (Dimitry 2011 ; Gelkopf et al. 2008 ; Solomon et al. 1996 ).
As pointed out earlier, trauma has a differential impact depending on age, gender, and psychosocial factors, which are discussed below.
Trauma and Children
As is recognized in the new Diagnostic and Statistical Manual (DSM-5; APA 2013 ), while trauma has a profound impact on all individuals, its impact on young children is unique and particularly pernicious. Millions of children throughout the world are currently growing up amidst traumatic environments—they are being sexually and physically abused at home, bullied at school, and traumatized in their communities (Finkelhor et al. 2009 ). Many lack adequate food and shelter, and some live in unsafe communities and war zones witnessing violence occurring to friends and family, including rape, torture and murder. Numerous studies have shown evidence of long term repercussions of exposure to violence at an early age (Anda et al. 2006 ; Steele 2004 ). The implications of exposure to trauma are now believed to have an effect on the infant even before birth. A more detailed discussion of the impact of trauma on children follows, starting with prenatal impact.
Prenatal Impact
Preliminary research shows that children are impacted even before birth by trauma that is experienced by their mothers. Studies in New York City comparing pregnant women who were close to Twin Towers on September 11 and suffered “post traumatic stress syndrome” (PTSS) with pregnant women who were in different locations, found that newborns of mothers manifesting PTSS had significant smaller head circumference at birth (Engel et al. 2005 ). As we know, decrements in head circumference influence subsequent neurocognitive development. More recent studies, using modern technologies such as Functional MRI, reveal that fetal exposure to maternal stress is significantly associated with a variety of impacts on brain activity, endocrine function, and on autonomic nervous system function (Sandman and Davis 2012 ). While these studies have small sample sizes and need to be validated further, we are recognizing that it is not enough to assess, when appropriate, whether a child was born prematurely or not, or whether the mother was malnourished during pregnancy, but also whether she was being abused by her husband or partner, or lived in a violent community or a war zone during her pregnancy, and how this may be related to the some of the problems exhibited by her children (Lieberman and Van Horn 2008 ; Pine and Cohen 2002 ). It is also worth noting that the biophysiological impact of paternal trauma on the fetus and newborn child has yet to be considered as worth studying, even though there is growing evidence that spontaneous changes in genetic makeup in the sperms of fathers impacts on the mental health of their children (Kandel 2013 ). Whether paternal trauma impacts the sperm, and thus the child, needs to be researched in the future.
Impact on Young Children and Adolescents
The impact of trauma on the brain of traumatized children continues after birth and even during adolescence and young adulthood, as evidenced by recent studies suggesting that the brain continues its development until age 25 (Cicchetti and Curtis 2006 ; Giedd 2008 ). Trauma, particularly complex or ongoing trauma in early life, affects brain development, especially the development of right hemispheric brain functions, which include among other things, regulation of mood and social adjustment. Moreover, “[n]europsychological studies suggest an association between child abuse and deficits in IQ, memory, working memory, attention, response inhibition, and emotion discrimination. Structural neuroimaging studies provide evidence for deficits in brain volume, gray and white matter of several regions, most prominently the … prefrontal cortex but also hippocampus, amygdala, and corpus callosum (CC). Diffusion tensor imaging (DTI) studies show evidence for deficits in structural interregional connectivity between these areas, suggesting neural network abnormalities” (Hart and Rubia 2012 p. 52). While the authors acknowledge the limitations of such studies, particularly the lack of control for co-morbid psychiatric disorders, which make it difficult to disentangle which of the above effects are due to maltreatment, other researchers have found that even indirect exposure to trauma, such as witnessing family or community gang violence, plays an important role in altering brain mechanisms involved in the processing of emotions and may predispose children to problems managing strong emotions and difficulty with emotional regulation. Such children appear to experience changes in stress hormonal regulatory systems and neural patterns that are associated with heightened emotional reactivity as well as weakened emotional resiliency, increasing their vulnerability to problematic behaviors, future traumas, as well as their own potential for violence (Grasso et al. 2013 ; Heide and Soloman 2006 ).
Data from the well regarded Adverse Childhood Experiences (ACE) study (Felitti et al. 1998 ) suggests that ACEs are “related to a greater likelihood of developing a variety of behavioral, health, and mental health problems, including smoking, multiple sexual partners, heart disease, cancer, lung disease, liver disease, sexually transmitted diseases, substance abuse, depression, and suicide attempts” (Lu et al. 2008 p. 1018).
Various authors have identified other negative consequences resulting from exposure to trauma during early life:
Preschool children are likely to exhibit passive reactions and regressive symptoms, such as enuresis, decreased verbalizations and clinging behavior, indicative of anxious attachment (APA 2013 ; Lieberman and Van Horn 2008 ; Steele 2004 ).
School age children may display both more aggression and more inhibition. They also develop somatic complaints, depression, sleep disturbance, cognitive distortions and learning difficulties manifested by impaired concentration and memory problems (Steele 2004 ; Terr 1991 ).
Adolescents exposed to trauma tend to respond by acting-out and self–destructive behavior: substance abuse, promiscuity, delinquent behavior, and life-threatening reenactments of violent episodes (APA 2013 ; Bava and Tapert 2010 ; Brent and Silverstein 2013 ; Garbarino et al. 1992 ; Pat-Horenczyk et al. 2007 ).
Children and adolescents who witness the death of close friends or family members may experience survivor guilt (Herman 1997 ; Steele 2004 ).
Like many traumatized adults, children may exhibit classic symptoms of PTSD without any understanding of what is going on with them (Derluyn et al. 2004 ).
Some children exposed to severe trauma may not show many of the classical trauma symptoms until later in life, reflecting the new DSM-5 specifier of “delayed expression” (APA 2013 ).
Children may exhibit traumatic bonding reflecting maladaptive attachment as well as inappropriate modeling of the behaviors of their abusers (a behavior also seen in adults and known as “identification with the aggressor” or “the Stockholm syndrome”) (Cohen et al. 2006 ; Derluyn et al. 2004 ; Weierstall et al. 2012 ).
Studies show that almost 100 % of those witnessing the murder or the sexual assault of a parent, and 35 % of urban youth exposed to community violence develop PTSD, although some of these highly traumatized children are more resilient than others (Derluyn et al. 2004 ; Garbarino et al. 1992 ; Malmquist 1986 ).
These young people with a history of, or current trauma need to be identified and treated in order to prevent life-long physiological, cognitive, emotional, behavioral, and social sequelae of their traumas (Anda et al. 2006 ).
Impact of Trauma on Adults
Ever since the tragedy of September 11, 2001 much has been researched and written about the impact of trauma on adults, especially in the United States. A exploration of the literature finds a variety of specialized journals devoted to this topic (to wit: Journal of Trauma Practice , Journal of Loss and Trauma , Journal of Traumatic Stress , Traumatology , International Journal of Emergency Mental Health , Journal on Rehabilitation of Torture Victims and Prevention of Torture, among others), as well as various textbooks aimed at different health professions, including social work (e.g., Courtois and Ford 2009 ; Foa et al. 2009 ; Ringel and Brandell 2012 ; Straussner and Phillips 2004b , etc.). What we would like to emphasize in this article are some of the lesser known factors effecting millions of adults by focusing on gender differences Footnote 1 and the impact of trauma on immigrants and refugees.
Gender and Trauma: What Do We Know?
Studies have found that men and women experience trauma in very different ways with somewhat different consequences. For instance, while men are much more likely to experience trauma, women are more likely to develop PTSD (APA 2013 ): for every traumatized man, three women have a lifetime prevalence rate of PTSD (Foa et al. 2009 ). Moreover, men are two times as likely as women to experience trauma due to physical assault, yet women are fifteen times more likely to develop PTSD as a result [World Health Organization (WHO), 2011 a]. While there are a variety of hypothesized explanations for these findings, ranging from the fact that women are more likely to seek professional help than men to possible neurobiological and hormonal differences, to women’s greater exposure to intrusive interpersonal violence (Hien et al. 2009 ), there is a lack of conclusive studies explaining these findings. Moreover, it appears that for men the most common factors associated with a diagnosis of PTSD are: rape, combat exposure, childhood neglect, and childhood physical abuse, while women are most likely be diagnosed with PTSD that is associated with sexual molestation, physical attack, being threatened with a weapon, and childhood physical abuse (Janof-Bulman 1992 ). These differences are particularly noteworthy among young adults. Recent data on military veterans show that over 15 % of US women veterans returning from the wars in Afghanistan and Iraq report being sexually traumatized in the military compared to .7 % of the men (Kimerling et al. 2010 ; Risen 2012 ).
Violence against women seems to be a growing worldwide pandemic. According to Key Facts Regarding Intimate Partner and Sexual Violence Against Women in the World , published by the World Health Organization (WHO 2011 a):
Violence against women is a major public health problem and violation of women’s human rights. Approximately 20 % of women report being victims of sexual violence as children.
The WHO multi-country study found that between 15 and 70 % of women reported experiencing physical and/or sexual violence by an intimate partner at some point in their lives, ranging from the extremely high rate of 70 % of women in Ethiopia and Peru to a low rate of 15 % among women in Japan.
First sexual experience for many women is reported as forced, with 40 % of young women in South Africa having such an experience. Such violence results in physical, mental, sexual, and reproductive health problems, and may increase the vulnerability of women to HIV/AIDS.
Population-based studies of relationship violence among young people (i.e., “dating violence” or “date rape”) show that it affects a substantial proportion of youth throughout the world. Moreover, worldwide, 1 in 2 female murder victims are killed by their male partners, often during an ongoing, abusive relationship.
Finally, situations of political conflict, post conflict and displacement may exacerbate existing violence and present new forms of violence against women.
Trauma and Immigration/Migration
In 2010, some 214 million people—3 % of the world’s population—lived outside of their country of origin (Batalova and Lee 2012 ). While many people migrate for positive reasons, the so called pull factors –to seek better education or jobs, to reunite with family, and so on—more and more people today move for negative reasons, or push factors , i.e. they are being pushed from their home communities due to natural disasters, economic situations, or local conflicts and wars (Castex 2006 ). Worldwide, there are currently over 15 million refugees uprooted from their home countries, the highest number since the 1990s Rwandan genocide (McClelland 2014 ). For many of these individuals, trauma is compounded by grief over loss—loss of family members and friends, loss of homes, neighborhoods, language, and even familiar smells. Cultural anchors, such as local religious and educational institutions, familiar medicines, native healers and/or known medical and psychological treatment approaches are missing. For many, particular political refugees and those with undocumented status, migration itself becomes traumatic with numerous obstacles along the way and an uncertain future. For some, prejudice and discrimination, lack of recognition of previously achieved economic and personal status (the micro-traumas) compound the reactions. For those whose migration status is undocumented or illegal, seeking or obtaining help for their big T, much less their micro-traumas is often impossible; thus their trauma may remain unresolved and may carry over to the next generation.
The dynamics of intergenerational transmission of trauma was first identified in studies of adult children of Holocaust survivors (Danieli 1998 ; Yehuda et al. 2001 ). The growing attention in the US on what is being termed “historical trauma”, relating mainly to Native American populations (Heart 1999 ), and “Post Traumatic Slave Syndrome” (DeGruy Leary 2006 ), which focuses on the consequences of slavery on African Americans, point to the increasing recognition and need to address the psychological, social, political, and cultural impact of widespread trauma over time . A study by Mollica et al. ( 1998 ) found that in a group of Cambodian survivors the impact of trauma remains decades after the original experience and that mental health symptoms may increase when individuals experience additional traumas, findings that were confirmed by other researchers studying refugee populations from different parts of the world (Bogic et al. 2012 ; Steel et al. 2002 ). Thus, the frequency of traumatic events (multiple traumatic exposures) is an important predictor of long term mental health outcomes, especially for traumatized refugee populations.
Trauma and Older Adults
The finding that cumulative trauma is more likely to increase the risk of poor psychiatric outcomes is of particular relevance to aging populations. The global population of people aged 60 years and older is expected to reach about 1.2 billion in 2025, more than doubling in the last 30 years (WHO 2011 b). As the world’s population ages, the special issues of trauma among the elderly need to be recognized more widely. The concept of “cumulative life stressors” is well known in the psychosocial literature (Dohrenwend 1998 ), and “cumulative trauma” is seen as reflecting multiple traumas experienced by an individual in multiple situations (Landau and Litwin 2000 ; Mollica et al. 1998 ). Thus the older an individual, the more likely he or she is to have been exposed to a variety of traumatic situations, and the more frequent exposure to life-threatening events has been associated with a lower capability to handling stress and higher risks of PTSD (Brandler 2004 ; Ursano et al. 1995 ). Moreover, the elderly are at a greater risk for psychological distress post- disaster than middle aged adults due to a greater risk for bodily injury, loss of resources, and lack of social networks or supports (Marsella 2008 ; Ursano et al. 1995 ). These issues play an even greater role among disabled older adults who are dependent on others for both physical as well as emotional support.
While the elderly may suffer trauma from the same sources as younger people, like children they are particularly vulnerable to being maltreated or abuse at home and even more so in institutions aimed to protect them, such as nursing homes and hospitals. According to the WHO ( 2011 b), an estimated 4–6 % of elderly people in high-income countries have experienced some form of maltreatment at home. Many of the abusive acts against the elderly in homes or institutions consist of micro-traumas, such as: being physically restrained, deprived of dignity by being left in soiled clothes, being over- or under-medicated, and emotionally neglected and abused. One study found that more than half the residents of intermediate care facilities were receiving psychoactive drugs and 30 % received long-acting drugs not recommended for elderly persons (Beers et al. 1988 ). Some acts against older adults do rise up to the level of large-T traumas of physical abuse that can be life threatening or can result in serious, long-lasting, psychological consequences, including depression, anxiety and PTSD.
While accurate, generalizable data are scarce (Ben Natan and Lowenstein 2010 ), one survey of nursing-home staff in the US, found that (Pillemer and Moore 1989 ):
36 % witnessed at least one incident of physical abuse of an elderly patient in the previous year;
10 % committed at least one act of physical abuse towards an elderly patient;
40 % admitted to psychologically abusing patients.
For those cared for at home, studies indicate that the social isolation of both caregivers and the older adults, and the ensuing lack of social support, is a significant risk factor for elder maltreatment by caregivers. Thus help needs to be provided not only to the elderly, but also to their caregivers.
Moreover, when dealing with community trauma, whether natural, such as earthquakes, or man-made, such as a terrorist attack, or individual micro-traumas, such as having a spouse who has been diagnosed with Alzheimer’s, older adults are particularly vulnerable to what has been termed as “ambiguous loss” (Boss 2009 ) or “disenfranchised grief” (Doka 1989 ). For example, while the parents of an adult son killed in a terrorist attack may be acknowledged and supported by the community, the great-aunt of the murdered young man may be totally ignored, even though for many years he may have been her major source of emotional support. Finally, it is important to recognize that the nature of trauma among older adults varies among different ethnic and racial groups, even in the same community (Marsella 2008 ). For example, Higgins and Park ( 2012 ) in a comparison of African American and Caribbean Black older adults in New York found that African Americans experienced more spousal abuse, incarceration, and combat involvement, while Caribbean Black older adults experienced more natural disasters.
Trauma and Resilience: A Strength-Based Perspective
As George Bonanno ( 2004 ) reminds us, as professional helpers we tend to see people who have difficulties coping with trauma. We thus forget that many people are exposed to traumatic events at some point in their lives, and yet they continue to have positive emotional experiences and show only minor or transient disruptions in their ability to function. The concept of resilience reflects the individual’s ability to effectively use resources in the environment, notably relationships with others, as well as their own internal resources and potentialities (Bonanno et al. 2007 ; Bonanno et al. 2011 ). Hauser ( 1999 ; Hauser et al. 2006 ) point out that resilience is a process, not a state. Doing longitudinal studies of youth, most of whom were physically and sexually abused at home and then put into psychiatric hospitals, the authors found that those young men, who as adults were able to achieve a satisfying life despite horrendous childhoods, reflected three general characteristics:
A belief that one can influence one’s environment (self efficacy),
The ability to handle one’s thoughts and feelings (cognitive-behavioral skills), and
The capacity to form caring relationships.
What is important to note is that these traumatized yet resilient youth did not show a normative development. Their lives had not been easy; they made seemingly unwise choices and often got into social and legal troubles. What characterized them was, however, an ability to learn from experience . The authors point out is that “Resilience does not lie in either the competence or relationship; it lies in the development of competence or relationship where they did not exist before” (Hauser et al. 2006 , p. 261). It is this ability to learn from one’s traumatic experience and to achieve what we now refer to as Post - Traumatic Growth (PTG) (Tedeschi and Calhoun 2004 ; Zoeller and Maercker 2006 ) that is the ultimate goal of effective trauma treatment.
Treatment Approaches with Traumatized Individuals
The last few decades have brought extensive research and innovative treatment approaches to helping traumatized individuals. Since, as indicated previously, the experiencing and the consequences of trauma are highly subjective, there is no single treatment approach for helping all individuals who have experienced and suffered trauma, and particularly those suffering from chronic PTSD. Moreover, as trauma can occur at different ages, interventions must be age appropriate as well as gender and culturally relevant.
Interventions with Traumatized Children
As with traumatized adults, the main goal of treatment with traumatized children is to engage them in activities and experiences that allow them to safely express feelings, regulate their emotions and manage overwhelming sensations. The natural language of young children is play. Play therapy, and related expressive arts therapies (Harris 2007 ), provide a way for the child to reenact the traumatic event through symbolic play and movement, and is an empirically-based intervention for working with traumatized children from the age of 3–11 (Bratton et al. 2005 ; Malchiodi 2008 ; Ryan and Needan 2001 ; Webb 2011 ). Play therapy with a caring, empathic adult allows the traumatized child to develop a sense of trust and provides an opportunity to achieve a sense of control over their trauma (Steele 2004 ; Webb 2011 ). While play therapy is usually conducted with an individual child, other approaches focus on involving the parents, and include:
Child-Parent Psychotherapy (CPP) (Lieberman and Van Horn 2008 ). CPP is a psychodynamically based therapeutic approach has shown to be very effective in treating trauma in young children while working with parents to repair the impact of the trauma to the family system. CPP is a flexible, culturally sensitive intervention that can be utilized in unstructured weekly session over the course of a year. It focuses on helping the child to rebuild trust by creating a trauma narrative where the caregiver can act out the protective role through the use of play. CPP has been supported by a number of randomized trials showing efficacy in increasing attachment security and maternal empathy (Berlin et al. 2008 ).
Parent–Child Interaction Therapy (PCIT; Eyberg and Bussing, 2010 ). While not specific to traumatized children, it is an empirically-based behavioral short term intervention for children age 2–7 who are experiencing emotional and behavioral disorders. PCIT draws on both attachment and behavioral theories and is provided over the course of 12 1-h weekly sessions. PCIT involves the parent interacting with the child with the therapist observing through a one-way mirror and coaching through a hearing aid device. The coaching consists of helping the parents to utilize two sets of skills: a. Child Directed Interaction, which teaches parents to use traditional play therapy techniques, and b. Parent Directed Interaction, which teaches the parents skills to address disruptive behaviors while increasing compliance by the child. These skills include establishing rules, praising compliance, using time-out chair for non-compliance, and so on (Ware et al. 2008 ).
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT; Cohen and Mannarino 2008 ).
TF-CBT is a psychosocial intervention found to be effective in treating PTSD and other behavioral and emotional problems related to a variety of traumatic experiences in children and adolescents. It can be used with children and parents in individual and conjoined sessions, as well as in multi-family groups. TF-CBT usually lasts from 12 to 16 sessions. The treatment model focuses on applying the acronym PRACTICE, which summarizes the nine components of this model: Psychoeducation and parenting skills; Relaxation skills; Affect expression and regulation skills; Cognitive coping skills and processing; Trauma narrative; In-vivo exposure (when needed); Conjoint parent–child sessions; and Enhancing safety and future development (Cohen and Mannarino 2008 ; Cohen et al. 2006 ).
Intervention with Traumatized Adults
Many different treatment approaches have been shown to be effective for traumatized adults. They include: Psychoeducation, cognitive behavioral therapy, exposure therapy, desensitization and imaginal flooding, Eye Movement Desensitization and Reprocessing (EMDR), narrative therapy, group therapy and medications.
Psychoeducation
Psychoeducation is the “process of teaching clients with mental illness and their family members about the nature of the illness, including its etiology, progression, consequences, prognosis, treatment and alternatives” (Barker 2003 , p. 347). While there has been limited empirical evidence proving the importance of psychoeducation (Lukens and McFarlane 2004 ), clinical experience has shown that understanding the physiological responses to trauma can help individuals develop new coping strategies in dealing with others and learning to calm oneself physically (Creamer and Forbes 2004 ). It has also been shown to improve the quality of life for family members traumatized by others or to better understand the sometimes irrational behaviors of their traumatized loved one (Solomon et al. 2005 ).
Cognitive Behavioral Therapy [CBT]
CBT has been shown to be very effective at helping individuals who have experienced trauma by dealing with their thoughts and beliefs, as well as with their behavior patterns. Among the various empirically-based CB treatments are:
Exposure/Desensitization, which consists of direct confrontation with trauma by having individuals visualize the event, talk about it, and expose themselves gradually to stimuli which reminds them of the trauma. This is repeated several times until the person becomes accustomed or desensitized to these thoughts and images. Through these repeated exercises, the traumatic memory becomes just a regular memory, allowing the individual to have a sense of control rather than feeling helpless over the past traumatic event. One particular approach is known as “Prolonged Exposure” (PE; Foa et al. 2007 ), and is rooted in the tradition of exposure therapy for anxiety disorders and emotional processing for PTSD. PE uses both imaginal exposure (confront feared trauma memories and thoughts via imagining the feared object, event, or situation), and in vivo (experience/confront feared objects, places, events, and situations in real world settings). Individuals also are provided with psychoeducation on trauma reactions and on the use of PE to reduce symptoms, as well as breathing training to manage their anxiety. PE may not be appropriate for individual who have a history of multiple traumas (particularly in childhood), those with anger problems, and those who dissociate (Foa et al. 2007 , 2009 ).
Another empirically supported cognitive-behavioral treatment for PTSD is Dialectical Behavior Therapy (DBT) (Linehan 1993 ), which was developed for individuals diagnosed with borderline personality disorder (BPD). The emotional dysregulation that is the hallmark of BPD is also associated with symptoms of complex-PTSD (DESNOS). The treatment combines group skill training sessions, individual psychotherapy, and phone coaching. It is designed to help individuals label and regulate arousal, tolerate emotional distress, and trust their emotional reactions. Emotional regulation, interpersonal effectiveness, and self-management skills, including mindfulness and meditation skills are core skills in DBT. Validation and dialectical strategies are used to balance acceptance and change during treatment.
A different treatment model found to be effective in treating traumatized adults is Eye Movement Desensitization and Reprocessing (EMDR) (Shapiro 1995 ). For many traumatized individuals, remembering an event can feel as real as if it were happening again before their eyes. EMDR uses the person’s eye movements to help the natural processing and relaxation mechanisms available in the brain. During treatment, people are asked to think of a picture, emotion or thought relating to their trauma and at the same time to watch the therapist’s moving finger or listen to a repeating sound of a drum or a bell, leading to cognitive dissonance and a diminished power of the intrusive traumatic memory. EMDR can be delivered in a short series of sessions and does not involve detailed narrative of the traumatic event.
Narrative Therapy
This approach is based on the belief that trauma disrupts the normal narrative processing of everyday experiences by interfering with psychophysiological coordination, cognitive processes, and social connections, and such incomplete narrative leads to symptoms of posttraumatic distress (Wigren 1994 ). Narrative therapy thus allows for the completion and reframing of the traumatic event. While there is some evidence showing the effectiveness of this approach (Amir et al. 1998 ; Schaal et al. 2009 ), there seems to be no single narrative treatment model. Further research is needed in order to identify the best narrative approaches.
Group Therapy
While group therapy has been found to be effective at providing support for individuals in many circumstances, the use of certain group approaches, such as Critical Incidence Stress Debriefing (CISD) has been shown to have the potential for retraumatization. This is a particular danger for some individuals who are mandated to participate in such a group and listen to other people’s stories of their traumatic events before they had a chance to process their own trauma (Rose et al. 2002 ). Thus caution must be taken when utilizing any group approaches to trauma treatment.
One highly effective treatment model, used mainly in group settings, is Seeking Safety , developed by Lisa Najavitis ( 2006 ), The Seeking Safety Model is a present-focused therapy to help people attain safety from both trauma/PTSD and substance abuse. Treatment is flexible and utilizes 25 different topics that focus on both cognitive and behavioral areas. Seeking Safety is based on five central ideas: Safety as the priority of treatment; integrated treatment of trauma and substance use; a focus on ideals; content addressing cognitive, behavioral, interpersonal skills and case management; and attention to the clinician. Originally developed as an empowerment model for women, it is now recognized as being an effective and widely used approach for many others, including traumatized US veterans (Boden et al. 2012 ). The program focuses on teaching traumatized individuals to view themselves in more positive ways and helping clients build their self-esteem and self-confidence.
Medications
While there are no medications specific for trauma or PTSD, some medications have been shown to be effective at treating certain symptoms of PTSD, such as depression, anxiety or sleeping disorders. Currently the US Federal Drug Administration (FDA) has approved only two anti-depression medications for use with patients diagnosed with PTSD: sertraline (Zoloft) and paroxetine (Paxil), although other medications are being used off-label (Jeffreys 2013 ). It is worth noting that some medications have been found to be dangerous for those using or recovering from a substance use disorder, or those who are potentially suicidal (for a full review of medication use for those with PTSD, see Jeffreys 2013 ).
In general, when working with traumatized adults, the most important task is the establishment and maintenance of a physical and emotional sense of safety. It is critical to determine if the individual is at risk for imminent interpersonal violence or other maltreatment in their psychosocial environment, if they are suicidal or homicidal, and if they are psychologically stable and capable of caring for themselves (Briere and Scott 2012 ).
Interventions with Older Adults
While there is a growing acknowledgement of the need for psychosocial interventions with this population, the literature tends to focus more on programs and policies devoted to identification and reporting of elder abuse than actual clinical interventions (Brandler 2004 , Donovan and Regehr 2010 ). Literature on empirically supported interventions with traumatized older adults seems to be almost non-existent, although some believe that CBT may be effective (Foa et al. 2009 ). Obviously, more needs to be done to identify effective clinical approaches to this growing population.
Unfortunately, traumatized children and adults comprise a significant number of individuals in our communities and will continue to be with us in the foreseeable future. Many remain untreated. It is therefore critical for clinicians to be familiar with the various traumas encountered by individuals, families and communities, and to become knowledgeable about the most effective treatment approaches for a given population. Despite the growing research that is providing us with a base of scientific knowledge regarding promising interventions, there is much to be learned about effective interventions with traumatized children and adults—to make sure that we “do no harm.” Particularly important is research focusing on the resilience that many traumatized individuals’ exhibit and learning how best to encourage clients to access their strengths and abilities both in and out of the treatment process. Finally, because of the risk of experiencing secondary trauma, clinicians also need to be aware of the risk of working with high caseloads of traumatized individuals and to learn to take care of themselves so that they do not become part of the problem, but are an effective part of the solution.
While this article discusses the available research focusing on trauma among individuals with traditional gender identities, the authors recognize that transgender individuals experience disproportionate levels of trauma. Since a comprehensive discussion on this topic is beyond the scope of this paper, readers are referred to Mizock and Lewis ( 2008 ) for further information.
American Psychiatric Association (APA). (1980). Diagnostic and statistical manual of mental disorder , (3rd edn, DSM III ). Washington, DC: Author.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th edn, DSM-5). Washington, DC: Author.
Amir, M., & Lev-Wiesel, R. (2003). Time does not heal all wounds: Quality of life and psychological distress of people who survived the Holocaust as children 55 years later. Journal of Traumatic Stress, 16 , 295–299.
Article PubMed Google Scholar
Amir, N., Stafford, J., Freshman, M. S., & Foa, E. B. (1998). Relationship between trauma narratives and trauma pathology. Journal of Traumatic Stress, 11 (2), 385–392.
Anda, R. F., Felitti, V. J., Walker, J., Whitfield, C. L., Bremner, J. D., Perry, B. D., et al. (2006). The enduring effects of abuse and related experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256 , 174–186.
Article PubMed Central PubMed Google Scholar
Barker, R. L. (2003). Psychoeducation. Social Work Dictionary . Washington DC: NASW Press.
Google Scholar
Batalova, J and Lee, A. (2012). Frequently requested statistics on immigrants and immigration in the United States. Migration Information Source. Retrieved from http://www.migrationinformation.org/usfocus/display.cfm?ID=886#1 .
Bava, S., & Tapert, S. F. (2010). Adolescent brain development and the risk for alcohol and other drug problems. Neuropsychology Review, 20 (4), 398–413.
Beers, M., Avorn, J., Soumerai, S. B., Everitt, D. D., Sherman, D. S., & Salem, S. (1988). Psychoactive medication use in intermediate-care facility. Residents Journal of American Medical Association, 260 (20), 3016–3020.
Article Google Scholar
Ben Natan, M., & Lowenstein, A. (2010). Study of factors that affect abuse of older people in nursing homes. Nursing Management, 17 (8), 20–24.
Berlin, L., Zeanah, C. H., & Lieberman, A. F. (2008). Prevention and intervention programs for supporting early attachment security. In J. Cassidy & P. R. Shaver (Eds.), Handbook of attachment: Theory, research and clinical applications (2nd ed., pp. 745–761). New York: Guilford Press.
Boden, M. T., Kimerling, R., Jacobs-Lentz, J., Bowman, D., Weaver, C., Carney, D., et al. (2012). Seeking safety treatment for male veterans with a substance use disorder and PTSD symptomatology. Addiction, 107 , 578–586.
Bogic, M., Ajdukovic, D., Bremner, S., Franciskovic, T., Galeazzi, G. M., Kucukalic, A., et al. (2012). Factors associated with mental disorders in long-settled war refugees: Refugees from the former Yugoslavia in Germany, Italy and the UK. The British Journal of Psychiatry, 200 , 216–223.
Bonanno, G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59 , 20–28.
Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75 (5), 671–682.
Bonanno, G. A., Westphal, M., Anthony, D., & Mancini, A. D. (2011). Resilience to loss and potential trauma. The Annual Review of Clinical Psychology, 7 , 511–535.
Boss, P. (2009). Ambiguous loss: Learning to live with unresolved grief . New York: W.W. Norton and Co.
Brandler, S. (2004). Mass violence and the elderly. In S. L. A. Straussner & N. K. Phillips (Eds.), Understanding mass violence: A social work perspective (pp. 57–68). Boston: Allyn and Bacon.
Bratton, S., Ray, D., Rhine, T., & Jones, L. (2005). The efficacy of play therapy with children: A meta-analytic review of treatment outcomes. Professional Psychology: Research and Practice, 36 (4), 376–390.
Brent, D. A., & Silverstein, M. (2013). Shedding light on the long shadow of childhood adversity. Journal of American Medical Association, 309 (17), 1777–1778.
Breslau, N., Davis, G. C., Andreski, P., & Peterson, E. (1991). Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry, 48 (3), 216–222.
Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting Clinical Psychology, 68 (5), 748–766.
Briere, J. N., & Scott, C. (2012). Principles of trauma therapy: A guide to symptoms, evaluation, and treatment (2nd ed.). Thousand Oaks, CA: Sage.
Castex, G. (2006). Immigrant children in the United States. In N. K. Phillips & S. L. A. Straussner (Eds.), Children in the Urban Environment: Linking Social Policy and Clinical Practice (2nd ed., pp. 50–74). Springfield, IL: Charles C. Thomas.
Centers for Disease Control and Prevention [CDC], (2006). Adverse childhood experiences study: Major findings. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention. Retrieved from www.cdc.gov/nccdphp/ace/findings.htm .
Cicchetti, D., & Curtis, J. (2006). The developing brain and neural plasticity: Implications for normality, psychopathology, and resilience. In D. Cicchetti & D. J. Cohen (Eds.), Developmental psychopathology: Developmental neuroscience (Vol. 2, pp. 1–64). Hoboken: John Wiley and Sons Inc.
Cohen, J. A., & Mannarino, A. P. (2008). Trauma-focused cognitive behavioural therapy for children and parents. Child and Adolescent Mental Health, 13 (4), 158–162.
Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2006). Treating trauma and traumatic grief in children and adolescents . New York: Guilford Press.
Courtois, C. A., & Ford, J. D. (2009). Treating complex traumatic stress disorders (adults): Scientific foundations and therapeutic models . New York: Guilford Press.
Creamer, M., & Forbes, D. (2004). Treatment of posttraumatic stress disorder in military and veteran populations. Psychotherapy: Theory, Research, Practice Training, 41 (4), 388–398.
Danieli, Y. (Ed.). (1998). International handbook of multigenerational legacies of trauma . New York: Plenum Press.
DeGruy Leary, J. (2006). Post traumatic slave syndrome: America’s legacy of enduring injury and healing . Baltimore, MD: Upton Press.
Derluyn, I., Broekaert, E., Schuyten, G., & De Temmerman, E. (2004). Post-traumatic stress in former Ugandan child soldiers. Lancet, 363 (9412), 861–863.
Dimitry, L. (2011). A systematic review on the mental health of children and adolescents in areas of armed conflict in the Middle East. Child: Care, Health and Development, 38 (2), 153–166.
Dohrenwend, B. P. (Ed.). (1998). Adversity, stress and psychopathology . New York: Oxford University Press.
Doka, K. (1989). Disenfranchised grief: Recognizing hidden sorrow . New York: Lexington Books.
Donovan, K., & Regehr, C. (2010). Elder abuse: Clinical, ethical, and legal considerations in social work practice. Clinical Social Work Journal, 38 , 174–182.
Engel, S. M., Berkowitz, G. S., Wolff, M. S., & Yehuda, R. (2005). Psychological trauma associated with the World Trade Center attacks and its effect on pregnancy outcome. Paediatric and Perinatal Epidemiology, 19 (5), 334–341.
Eyberg, S.M. and Bussing, R. (2010). Parent-child interaction therapy. In M. Murrihy, A. Kidman and T. Ollendick (eds). A clinician’s handbook for the assessment and treatment of conduct problems in youth (pp. 139-162). New York: Springer. Faulkner, W. (1950). Requiem for a nun. NY: Random House.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14 (4), 245–258.
Finkelhor, D., Turner, H., Ormrod, R., & Hamby, S. L. (2009). Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics, 124 (5), 1411–1423.
Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide . New York: Oxford University Press.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (Eds.). (2009). Effective treatments for PTSD: Practice guidelines from the International Society of Traumatic Stress Studies (2nd ed.). New York: Guilford Press.
Galea, S., Nandi, A., Stuber, J., Gold, J., Acierno, R., Best, C. L., et al. (2005). Participant reactions to survey research in the general population after terrorist attacks. Journal of Traumatic Stress, 18 (5), 461–465.
Garbarino, J., Dubrow, N., Kostelny, K., & Pardo, C. (1992). Children in danger: Coping with the effects of community violence . San Francisco, CA: Jossey-Bass.
Gelkopf, M., Solomon, Z., Berger, R., & Bleich, A. (2008). The mental health impact of terrorism in Israel: A repeat cross-sectional study of Arabs and Jews. Acta Psychiatrica Scandinavica, 117 , 369–380.
Giaconia, R. M., Reinherz, H. Z., Silverman, A. B., Pakiz, B., Frost, A. K., & Cohen, E. (1995). Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal of American Academy of Child and Adolescent Psychiatry, 34 (10), 1369–1380.
Giedd, J. N. (2008). The teen brain: Insights from neuroimaging. Journal of Adolescent Health, 42 (4), 335–343.
Grasso, D. J., Ford, J. D., & Briggs-Gowan, M. J. (2013). Early life trauma exposure and stress sensitivity in young children. Journal of Pediatric Psychology, 38 (1), 94–103.
Harris, D. A. (2007). Dance/movement therapy approaches to fostering resilience and recovery among African adolescent torture survivors. Journal on Rehabilitation of Torture Victims and Prevention of Torture, 17 (2), 134–155.
Hart, H. and Rubia, K. (2012). Neuroimaging of child abuse: A critical review. Frontiers of Human Neuroscience. 5 , 52. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3307045/ .
Hauser, S. T. (1999). Understanding resilient outcomes: Adolescent lives across time and generations. Journal of Research on Adolescence, 9 , 1–24.
Hauser, S. T., Allen, J. P., & Golden, E. (2006). Out of the woods: Tales of resilient teens . Cambridge, MA: Harvard University Press.
Heart, M. B. Y. (1999). Gender differences in historical trauma response among the Lakota. Journal of Health and Social Policy, 10 (4), 1–21.
Heide, K. M., & Soloman, E. P. (2006). Biology, childhood trauma, and murder: Rethinking justice. International Journal of Law and Psychiatry, 29 (3), 220–233.
Herman, J. L. (1997). Trauma and recovery: The aftermath of violence from domestic abuse to political terror . New York: Basic Books.
Hien, D. A., Litt, L. C., Cohen, L. R., Miele, G. M., & Campbell, A. N. (2009). Trauma services for women in substance abuse treatment: An integrated approach . New York: American Psychological Association Press.
Book Google Scholar
Higgins, C. and Park, N. (2012). A community sample of older African Americans and Caribbean Blacks exposure to early life traumatic events and associated factors. Unpublished paper.
Idsoe, T., Dyregov, A., & Idsoe, E. C. (2012). Bullying and PTSD symptoms. Journal of Abnormal Child Psychology, 40 (6), 901–911.
Janof-Bulman, R. (1992). Shattered assumptions: Towards a new psychology of trauma . New York: The Free Press.
Jeffreys, M. (2013). Clinican’s guide to medications for PTSD. U.S. Department of Veterans Affairs. Retrieved from http://www.ptsd.va.gov/professional/pages/clinicians-guide-to - medications-for-ptsd.asp.
Kandel, R. R. (2013, Sept. 6). The New Science of Mind. New York Times . Retrieved from ww.nytimes.com/2013/09/08/opinion/Sunday/the-new-science-of-mind.html.
Kendall-Tackett, K. (2013, June). Childbirth-related psychological trauma: It’s finally on the radar and it affects breastfeeding. Science and Sensibility. Retrieved from http://www.scienceandsensibility.org/?p=682.1 .
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry, 52 , 1048–1060.
Kimerling, R., Street, A. E., Pavao, J., Smith, M. W., Cronkite, R. C., & Holmes, T. H. (2010). Military-related sexual trauma among veterans health administration patients returning from Afghanistan and Iraq. American Journal of Public Health, 100 (8), 1409–1412.
Kiser, L. J. (2007). Protecting children from the dangers of urban poverty. Clinical Psychology Review, 27 (2), 211–225.
Krystal, H., & Niederland, J. (1968). Massive psychic trauma . New York: International University Press.
Landau, R., & Litwin, H. (2000). The effects of extreme early stress in very old age. Journal of Traumatic Stress, 13 , 473–487.
Landolt, M. A., Schnyder, U., Maier, T., Schoenbucher, V., & Mohler-Kuo, M. (2013). Trauma exposure and posttraumatic stress disorder in adolescents: A national survey in Switzerland. Journal of Traumatic Stress, 26 , 209–216.
Leskin, G. A., & Sheikh, J. (2002). Lifetime trauma history and panic disorder: Findings from the national comorbidity survey. Journal of Anxiety Disorders, 16 (6), 599–603.
Lieberman, A. F., & Van Horn, P. (2008). Psychotherapy with infants and young children: Repairing the effects of stress and trauma in early attachment . New York: Guilford Press.
Lifton, R. J. (1968). Death in life: Survivors of Hiroshima . New York: Random House.
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder . New York: Guilford Press.
Lu, W., Mueser, K. T., Rosenberg, S. D., & Jankowski, M. K. (2008). Correlates of adverse childhood experiences among adults with severe mood disorders. Psychiatric Services, 59 , 1018–1026.
Lukens, E. P., & McFarlane, W. R. (2004). Psychoeducation as evidence-based practice: Considerations for practice, research, and policy. Brief Treatment and Crisis Intervention, 4 (3), 205–225.
Malchiodi, C. (2008). Creative interventions with traumatized children . New York: Guilford Press.
Malmquist, C. P. (1986). Children who witness parental murder: Posttraumatic aspects. Journal of American Academy of Child Psychiatry, 25 , 320–326.
Marsella, A. (2008). Ethnocultural aspects of PTSD: An overview of concepts, issues and treatment. Traumatology, 16 (4), 17–26.
McClelland, M. (2014, February 13). How to build a perfect refugee camp. New York Times Magazine. Retrieved from http://www.nytimes.com/2014/02/16/magazine/how-to-build-a-perfect-refugee-camp.html?emc=eta1&_r=0 .
McGinley, E., & Varchevker, A. (Eds.). (2013). Enduring trauma through the life cycle . London: Karnac Books.
Miller, M. (2004). Intervention with individuals and families affected by mass violence. In S. L. A. Straussner & N. K. Phillips (Eds.), Understanding mass violence: A social work perspective (pp. 23–40). Boston: Allyn and Bacon.
Mishna, F. (2012). Bullying: A guide to research, intervention, and prevention. Oxford Scholarship Line. Retrieved from http://www.oxfordscholarship.com/view/10.1093/acprof:oso/9780199795406.001.0001/a cprof- 9780199795406.
Mizock, L., & Lewis, T. K. (2008). Trauma in transgender populations: Risk, resilience, and clinical care. Journal of Emotional Abuse, 8 (3), 335–354. doi: 10.1080/10926790802262523 .
Mollica, R. F., Mclnnes, K., Poole, C., & Tor, S. (1998). Dose-effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. British Journal of Psychiatry, 173 , 482–488.
Najavits, L. M. (2006). Seeking safety: A new psychotherapy for posttraumatic stress disorder and substance use disorder: A randomized controlled trial. Journal of Behavioral Health Services and Research, 33 , 453–463.
Oxford Dictionaries (2013). Trauma. Retrieved from http://oxforddictionaries.com/definition/english/trauma .
Pat-Horenczyk, R., Peled, O., Miron, T., Villa, Y., Brom, D., & Chemtob, C. M. (2007). Risk- taking behaviors among Israeli adolescents exposed to recurrent terrorism. American Journal of Psychiatry, 164 (1), 66–72.
Pillemer, K., & Moore, D. (1989). Abuse of patients in nursing homes: Findings from a survey of staff. Gerontologist, 29 (3), 314–320.
Pine, D. S., & Cohen, J. A. (2002). Trauma in children and adolescents: Risk and treatment of psychiatric sequelae. Biological Psychiatry, 51 (7), 519–531.
Purcell, R., Pathé, M., & Mullen, P. E. (2005). Association between stalking victimisation and psychiatric morbidity in a random community sample. British Journal of Psychiatry, 187 , 416–420.
Resnick, H. S., Kilpatrick, D. G., Dansky, B. S., Saunders, B. E., & Best, C. L. (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61 (6), 984–991.
Ringel, S., & Brandell, J. (2012). Trauma: Contemporary directions in theory, practice, and research . New York: Sage Publications Inc.
Risen, J. (2012, Nov. 2). Military has not solved problem of sexual assault, women say. New York Times, p. A15.
Rose, S., Bisson, J., and Weseley, S. (2002). Psychological debriefing for preventing Posttraumatic Stress Disorder (PTSD). Cochrane Database Systematic Review, 2. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12076399 .
Ryan, V., & Needan, C. (2001). Non-directive play therapy with children experiencing psychic trauma. Clinical Child Psychology and Psychiatry, 6 (3), 437–453.
Sandman, C. A., & Davis, E. P. (2012). Neurobehavioral risk is associated with gestational exposure to stress hormones. Expert Review of Endocrinology and Metabolism, 7 (4), 445–459.
Schaal, S., Elbert, T., & Neuner, F. (2009). Narrative exposure therapy versus interpersonal psychotherapy. Psychotherapy and Psychosomatics, 78 , 298–306.
Shapiro, F. (1995). Eye movement desensitization and reprocessing: Basic principles, protocols and procedures . New York: Guilford Press.
Solomon, P. L., Cavanaugh, M. M., & Gelles, R. J. (2005). Family violence among adults with severe mental illness: A neglected area of research. Trauma, Violence, and Abuse, 6 (1), 40–54.
Solomon, Z., Laor, N., & McFArlane, A. C. (1996). Acute postramatic reactions in soldiers and civilians. In B. A. van der Kolk, A. C. McFarlane, & L. Weisaeth (Eds.), Traumatic stress: The effects of overwhelming experience on mind, body and society (pp. 102–113). New York: Guilford.
Stamm, B. H., & Friedman, M. J. (2000). Cultural diversity in the appraisal and expression of trauma. In A. Shalev, R. Yehuda, & A. Mcfarlane (Eds.), International handbook of human response to trauma (pp. 69–85). New York: Plenum.
Chapter Google Scholar
Steel, Z., Silove, D., Phan, T., & Bauman, A. (2002). Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. Lancet, 360 (9339), 1056–1062.
Steele, W. (2004). Helping traumatized children. In S. L. A. Straussner & N. K. Phillips (Eds.), Understanding mass violence: A social work perspective (pp. 41–68). Boston: Allyn and Bacon.
Straussner, S.L.A (2012, January 8). Micro-traumas. Presentation at the conference on Trauma Through The Life Cycle From a Strengths Perspective: An International Dialogue, Hebrew University: Jerusalem.
Straussner, S. L. A., & Phillips, N. K. (2004a). Social work interventions in the context of mass violence. In S. L. A. Straussner & N. K. Philips (Eds.), Understanding mass violence: A social work perspective (pp. 3–19). Boston: Allyn and Bacon.
Straussner, S. L. A., & Phillips, N. K. (Eds.). (2004b). Understanding mass violence: A social work perspective . Boston: Allyn and Bacon.
Susser, E. S., Herman, D. B., & Aron, B. (2002). Combating the terror of terrorism. Scientific American, 287 , 70–78.
Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15 , 1–18.
Terr, L. C. (1991). Childhood traumas: An outline and overview. American Journal of Psychiatry, 148 (1), 10–20.
PubMed Google Scholar
Ursano, R.J. Brian G. McCaughey, B. G. &, Fullerton, C. S. (Eds). (1995). Individual and community responses to trauma and disaster: The structure of human chaos . Cambridge, UK: Cambridge University Press.
van der Kolk, B. A., Roth, S., Pelcovitz, D., Sunday, S., & Spinazzola, J. (2005). Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress, 18 (5), 389–399.
Ware, L. M., McNeil, C. B., Masse, J. J., & Stevens, S. (2008). Efficacy of in-home parent-child interaction therapy. Child and Family Behavior Therapy, 30 (2), 99–126.
Webb, N. (2011). Play therapy for bereaved children: Adapting strategies to community, school and home settings. School Psychology International, 32 (2), 132–143.
Weierstall, R., Schalinski, I., Crombach, A., Hecker, T., & Elbert, T. (2012). When combat prevents PTSD symptoms–results from a survey with former child soldiers in Northern Uganda. BMC Psychiatry., 14 (12), 41.
Wigren, J. (1994). Narrative completion in the treatment of trauma. Psychotherapy: Theory, Research, Practice Training, 31 (3), 415–423.
World Health Organization [WHO]. (2011a). Key Facts Regarding Intimate Partner and Sexual Violence Against Women in the World . Geneva: Author.
World Health Organization, (2011b). Elder maltreatment. Fact sheet no.357. Geneva: Author. Retrieved from http://www.who.int/mediacentre/factsheets/fs357/en/ .
Yehuda, R., Halligan, S. L., & Grossman, R. (2001). Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD and cortisol excretion. Development and Psychopathology, 13 (3), 733–753.
Zoeller, T., & Maercker, A. (2006). Posttraumatic growth in clinical psychology: A critical review and introduction of a two component model. Clinical Psychology Review, 26 (5), 626–653.
Download references
Acknowledgments
This paper is based on a keynote presentation by the senior author at the international conference on Trauma Through The Life Cycle From a Strengths Perspective: An International Dialogue, Hebrew University, Jerusalem, January 8, 2012. The authors would like to thank Drs. April Naturale, Miriam Schiff and Shlomo Einstein for their helpful critiques of an earlier draft of this paper.
Author information
Authors and affiliations.
Silver School of Social Work, New York University, 1 Washington Sq. North, New York, NY, 10003, USA
Shulamith Lala Ashenberg Straussner
Howard Center, 1 So. Prospect Street, Burlington, VT, 05401, USA
Alexandrea Josephine Calnan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Shulamith Lala Ashenberg Straussner .
Rights and permissions
Reprints and permissions
About this article
Straussner, S.L.A., Calnan, A.J. Trauma Through the Life Cycle: A Review of Current Literature. Clin Soc Work J 42 , 323–335 (2014). https://doi.org/10.1007/s10615-014-0496-z
Download citation
Published : 31 May 2014
Issue Date : December 2014
DOI : https://doi.org/10.1007/s10615-014-0496-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Large-T and micro-traumas
- Neurobiology
- Gender differences
- Treatment approaches
- Find a journal
- Publish with us
- Track your research
Trauma, Resilience and Mental Health Disparities: A Literature Review
28 Pages Posted: 20 Oct 2023
Shima Oliaei Far
Independent.
Date Written: October 15, 2023
This literature review explores the intricate relationship between trauma, resilience, and mental health disparities. Trauma, whether experienced directly or indirectly, has profound and lasting effects on mental health. However, individuals and communities exhibit remarkable resilience in the face of adversity. This review synthesizes current research on the impact of trauma on mental health disparities and the role of resilience as a protective factor. It also examines the complex interplay of sociodemographic factors, systemic inequalities, and access to mental health care in shaping mental health disparities among diverse populations. The findings underscore the need for a comprehensive and equitable approach to mental health care that addresses trauma, fosters resilience, and reduces disparities.
Note: Funding Information: I, Shima Oliaei Far, would like to declare that I have not received any external funding or financial support for the research presented in the literature review titled "Trauma, Resilience and Mental Health Disparities." This review was conducted as part of my independent research efforts, and I did not have any financial assistance or grants from any organization, institution, or individual. Conflict of Interests: I, Shima Oliaei Far, declare that there are no competing interests associated with this literature review.
Keywords: Trauma, Recovery, Disorder, Resilience, Mental Health, LGBTQ+, Disparity, Race, Gender, Ethnicity, Culture, Minority, Socioeconomics, Inequality, Stigma
Suggested Citation: Suggested Citation
Shima Oliaei Far (Contact Author)
Do you have a job opening that you would like to promote on ssrn, paper statistics, related ejournals, race & social inequity ejournal.
Subscribe to this free journal for more curated articles on this topic
Psychological Anthropology eJournal
Subscribe to this fee journal for more curated articles on this topic
Legal Anthropology: Laws & Constitutions eJournal
Psychiatry ejournal, clinical & counseling psychology ejournal, medical & mental health sociology ejournal.
- Tools and Resources
- Customer Services
- African Literatures
- Asian Literatures
- British and Irish Literatures
- Latin American and Caribbean Literatures
- North American Literatures
- Oceanic Literatures
- Slavic and Eastern European Literatures
- West Asian Literatures, including Middle East
- Western European Literatures
- Ancient Literatures (before 500)
- Middle Ages and Renaissance (500-1600)
- Enlightenment and Early Modern (1600-1800)
- 19th Century (1800-1900)
- 20th and 21st Century (1900-present)
- Children’s Literature
- Cultural Studies
- Film, TV, and Media
- Literary Theory
- Non-Fiction and Life Writing
- Print Culture and Digital Humanities
- Theater and Drama
- Share This Facebook LinkedIn Twitter
Article contents
Trauma and memory studies.
- Karyn Ball Karyn Ball Department of English and Film Studies, University of Alberta
- https://doi.org/10.1093/acrefore/9780190201098.013.1129
- Published online: 23 February 2021
A focus on trauma’s institutional trajectory in literary and cultural theory serves to narrow the transnational and multidirectional scope of memory studies. While Sigmund Freud’s attempt in Beyond the Pleasure Principle to define trauma in order to account for World War I veterans’ symptoms might serve as a provisional departure point, the psychological afflictions that haunted American soldiers returning from the Vietnam War reinforced the explanatory value of what came to be called “posttraumatic stress disorder,” which the American Psychiatric Association added to the DSM-III (the Diagnostic and Statistical Manual of Mental Disorders) in 1980. Multiple dramatic films released in the 1980s about Vietnam conveyed images of the American soldier’s two-fold traumatization by the violence he not only witnessed but also perpetrated along with the ambivalent treatment he received upon his return to a protest-riven nation waking up to the demoralizing realization that US military prowess was neither absolute nor inherently just. Proliferating research and writing about trauma in the late 1980s reflected this juncture as well as the transformative impact of the new social movements whose consciousness-raising efforts inspired a generation of academics to revise secondary and post-secondary literary canons.
The publication in 1992 of both Judith Herman’s Trauma and Recovery as well as Shoshana Felman and Dori Laub’s Testimony: Crises of Witnessing; In Literature, Psychoanalysis, and History , along with Cathy Caruth’s editorial compilation entitled Trauma: Explorations in Memory (1995) and collected essays in Unclaimed Experience: Trauma, Narrative, and History (1996), crystallized a moment when trauma was manifestly coming into vogue as an object of inquiry. This trend was reinforced by simultaneous developments in Holocaust studies that included critical acclaim for Claude Lanzmann’s ten-hour documentary Shoah (released in 1985), the opening of the United States Holocaust Memorial Museum in Washington, DC in 1993, and, that same year, the international success of Stephen Spielberg’s Schindler’s List . Other key events that propelled the popularity of trauma studies in the 1990s included the fall of the Berlin wall, the dissolution of the Soviet Union and South African apartheid governments, and Toni Morrison receiving the 1993 Nobel Prize in Literature for Beloved . The latter additionally bolstered specialization in African American studies as a platform for investigating representations of slavery and its violent afterlives.
While some critics fault the 1990s confluence of Holocaust and trauma studies for its Eurocentrism, the research pursued by feminist, multiculturalist, and postcolonial scholars in the same period laid the foundation for increasingly diverse lines of inquiry. Postcolonial criticism in particular has inspired scholarship about the intergenerational aftereffects of civil war, partition, forced migration, and genocide as well as the damage that accrues as settler states continue to marginalize and constrain the indigenous groups they displaced. More recent trauma research has also moved beyond a focus on finite events to examine the compounding strain of the everyday denigrations and aggressions faced by subordinated groups in tandem with long-term persecution and systemically induced precarity. Ultimately, then, the scale of trauma and memory studies has become not only global but also planetary in response to intensifying public anxiety about extinction events and climate change.
- posttraumatic stress disorder (PTSD)
- Holocaust studies
- psychoanalysis
- constructivism
- identity politics
- postcolonial criticism
- figural and traumatic realism
- affect studies
- Afro-pessimism
Judith Herman opens the “Acknowledgments” section of her canonical monograph Trauma and Recovery: The Aftermath of Violence; From Domestic Abuse to Political Terror by foregrounding its debt to “the women’s liberation movement. Its intellectual mainspring,” as Herman articulates it, “is a collective feminist project of reinventing the basic concepts of normal development and abnormal psychology, in both men and women.” 1 Like first sentences in literary texts, this statement speaks volumes—beyond its immediate literal sense—about the moment when the book appears and its role in the emerging field of trauma studies. In 1992 , a convergence of recent intellectual trends and preoccupations was pushing literary and cultural critics in directions that promoted the currency of traumatic memory as an object of inquiry. While Herman spotlights women’s liberation, other new social movements—for civil rights and gay liberation—were also making themselves felt as the PhDs of the 1970s and ’80s gained a foothold in academia and began to diversify both the faculty and the curricula. This shift was most noticeable in the social sciences and humanities, but especially in literature departments where women were hired in rising numbers. In effect, the forces and events that inflected Herman’s psychiatric research were reshaping the university and, by extension, generations of students who read expanding canons while attending lectures on the structural dynamics of prejudice and marginalization.
In its attention to the cultural, social, and political valences of traumatic experience, Herman’s book has turned out to be prescient well beyond its initial intervention. At the same time that her standpoint on trauma reflected the institutional shifts that had given rise to recently formed women’s studies departments, Herman also helped to set an agenda for literary and cultural theory in the 1990s. Already in 1992 , Herman reinforced the intelligibility of “repeated traumas” such as incest and domestic abuse that left posttraumatic imprints on women’s experiences, as Laura Brown has also contended. 2 Herman’s distinction between Type I, or short-term, or finite traumas, and Type II, prolonged and recurrent trauma, pinpointed a pivotal distinction between male war veterans whose PTSD (posttraumatic stress disorder) originated with particular events, and women as well as girls subjected to recurrent humiliations and threats of violence under a law that, up until recently, denied them recourse to justice by reducing them to father’s or husband’s property.
It is also important that Herman’s now canonical Trauma and Recovery was published in the same period that Cathy Caruth’s highly influential contributions to trauma studies were also gaining traction in tandem with a theoretical and critical turn in Holocaust studies. This juncture turns out to have been pivotal to the ensuing popularity of trauma studies. Tracing the interrelations among various academic concerns in the late 1980s and early 1990s will disclose the coalescence of this subfield in literary and cultural theory as well as the issues that propelled its transformations over time. What follows, then, is an institutional history that will highlight shifts that have taken place since the 1980s and that continue to shape trauma and memory scholarship today. To the extent that the various disciplinary branches of memory research yield a potentially infinite array of directions, taking the emergence of trauma studies in the 1990s as a conspicuous object of inquiry will also serve to narrow the scope.
The Emergence of Trauma Studies in the 1990s: Key Events
Though the discussion spotlights the roles of Holocaust studies, critical theory, anti-foundationalist French thought, and identity politics in shaping literary discourses of trauma and memory in the 1990s, there were other signal events in the preceding decades that facilitated the literary-institutional evolution of the field. It has been frequently remarked that the term posttraumatic stress disorder (PTSD) gained currency in the 1970s in response to symptoms commonly manifested by Vietnam War veterans, and the American Psychiatric Association codified this diagnosis in 1980 in DSM-III (the Diagnostic and Statistical Manual of Mental Disorders). 3 It is also not incidental to trauma’s trajectory that this particular war fostered more medical recognition of PTSD and public compassion for veterans seeking to reintegrate with differing degrees of success into an American society still reeling from the cultural transformations that the new social movements sparked.
After a period of apparent latency, the Washington, DC Vietnam War memorial based on then twenty-one-year-old Maya Lin’s award-winning design was completed in 1982 , and, beginning in the late 1970s with Coming Home and The Deer Hunter followed by Apocalypse Now , a proliferation of films in the 1980s signaled that an American public was ready to grapple with the myriad meanings of the US military failure and atrocities committed by American troops. 4 The spring 1986 issue of Cultural Critique edited by Richard Berg and John Carlos Rowe on “American Representations of Vietnam” critically reflected the mood in assembling essays focused on literature as well as documentary, propaganda, and dramatic films about the war. The issue stimulated further academic interest in the Vietnam War as a belatedly recognized national trauma. 5
Another fulcrum event was the publication of Toni Morrison’s Beloved dedicated to the “Sixty Million/and more” who died in the Middle Passage. 6 The novel won both the Pulitzer Prize and the American Book Award in 1988 , sealing its canonical status as, arguably, the most quintessential of American ghost stories depicting the centuries-long trauma of slavery, a story so unbearable that it should not be passed on, yet will be. As Morrison went on to receive the Nobel Prize in Literature a few years later (in 1993 ), the novel’s spectacular success at a time when English departments were diversifying their curriculum ensured its author’s prominence in African American studies and American literature scholarship as a whole.
In his trenchant critique of the translation of PTSD into an increasingly conventional literary style, Alan Gibbs citing Roger Luckhurst’s The Trauma Question identifies the formal techniques that distinguish Beloved as a “paradigmatic” trauma text: First, “its disrupted narrative whereby the novel’s chronology is structured according to characters’ associative memories of trauma rather than adhering to a realist, linear chronology.” Second, Morrison’s pronounced pluralization of the novel’s “narrating voice” functions to simulate “psychic experience.” Third, she frequently employs repetition to convey her characters’ inability to confront their past directly. 7 Gibbs additionally illustrates less “conventional” aspects of the novel’s narrative structure—for example, its “shading from iterative to singulative narration” to stress memory’s “dangerous fluidity” as past elements suddenly and intrusively impinge upon everyday life. 8 In portraying the tragic consequences of an escaped slave’s response to a double bind that spurs her to murder a baby daughter to protect her from slavery, Beloved ’s brilliance not only spurred further interest in representations of trauma, it demonstrated literature’s power to conjure a historical record on behalf of those who have fallen through history’s cracks.
Another pivotal event that shaped trauma studies’ trajectory in the 1990s was Nelson Mandela’s 1990 release after twenty-seven years of imprisonment when F. W. de Klerk announced the repeal of the ban on the African National Congress. Apartheid’s dissolution led up to the establishment of the Truth and Reconciliation Committee, requiring perpetrators to confess their crimes (as forthrightly as possible) in exchange for amnesty. 9 These sessions were supposed to facilitate the process of coming to terms, or not, with the typically irreparable damages inflicted by centuries of state-authorized racism. Testimonies about territorial expropriation, ghettoization, persecution, abandonment, torture, and murder exposed the apartheid government’s merciless treatment of its majority black population. These accounts subsequently filtered into memoir and museum installations, as well as film, fiction, and other art forms as different communities of victims and perpetrators endeavored to work through memories of brutality, loss, guilt, and shame. The proliferation of “artifacts of barbarism” (as Walter Benjamin might have called such artworks) provided materials for studies of apartheid as a preeminent instance of longterm historical trauma.
Around the same time, the dissolution of the Soviet Union and the fall of the Berlin Wall meant not only the end of the Cold War but also a time of reckoning in the former East Germany where the Stasi had coerced ordinary people to spy on colleagues, friends, and family members. The tenuous relationships among the ethnic groups comprising the former Yugoslavia after World War II had already become strained following Tito’s death in 1980 , and the Soviet Union’s collapse precipitated genocidal conflict and mass rape. In the wake of this collapse, formerly closed archives gradually opened, thereby making available a trove of resources for historians to settle old questions about the Holodomor and collaboration in mass crimes against Jewish and Polish civilians while pursuing new queries that would have been unthinkable before. Those who witnessed the transformations of their government and society after the Soviet Union broke up also underwent extreme transitions that were often experienced as traumatic in varying degrees. 10
During a decade striated by the closing stages of the Cold War and apartheid, Silvester Stallone squaring off against Soviets in Rambo , and Morrison’s Pulitzer-winning Beloved , literary and cultural studies in the United States at the end of the 1980s and the beginning of the 1990s were awash in a multitude of explicitly political agendas and theoretical vocabularies including but not limited to feminism, multiculturalism, Marxism, critical theory, semiotics, hermeneutics, narratology, psychoanalysis, film theory, structuralism, poststructuralism, deconstruction, postcolonial criticism, and an incipient queer theory. Sometimes these perspectives melded fruitfully, but they were just as often in tension, except in immature writing where theoretical jargon salads prevailed. Literary scholarship devoted to the study of trauma thus emerged at the scene of a continental divide of sorts between a comparatist canon that privileged German and French philosophical lineages on one side, and, on the other, a politicized American agenda that mandated the study of inequality and subordination. For scholars committed to so-called high theory, what came to be known alternatively as “constructivism,” “postmodernism,” or “poststructuralism” initially signified a linguistically-turned engagement with major figures from the continental philosophical tradition including Immanuel Kant, G. W. F. Hegel, Karl Marx, Friedrich Nietzsche, Edmund Husserl, Martin Heidegger, Emmanuel Levinas, late 19th- and early 20th-century sociology, Ferdinand de Saussure’s semiotics, Freudian and Lacanian psychoanalysis, the Frankfurt School, and (for some) French feminism. The theoretical inclinations that shaped American trauma studies in the 1990s often reflected this Eurocentric canon in grappling with the moral and formal implications of a constructivist critique of empirical and historical referentiality.
At the height of deconstruction’s vogue, recently empowered feminist, multiculturalist, and postcolonial critics found that their ethical agendas came into tension with reading styles that foregrounded figural logics while calling the authority of personal and collective experience into question. The issue became how to affirm the reality of past and present suffering as formative to certain collective identifications and grievances. It may have even seemed all too convenient when, at the same time that women and minorities were finally achieving recognition on an institutional and curricular level, a philosophical stance arose simultaneously to “destroy” the foundational status of experience at the heart of testimony. 11
While acknowledging the past’s susceptibility to shifting concerns over time, psychoanalytic theory insisted that memory could still be treated as the unconsciously attenuated placeholder for something that took place. If, for both psychoanalysis and poststructuralism, subjects are never “fully present” in their experiences (a premise that Caruth’s understanding of trauma formalizes as an epistemological “missed encounter”), it is because fluctuating social affiliations and provisionally intense collective identifications continuously reshape memories and recalibrate their emotional force over time, as Maurice Halbwachs contends. 12 Freud’s theses on screen memory suggest that less affectively charged memories or elements in them sometimes displace anxiety-saturated or traumatic incidents from early childhood. 13 This lesson from Freud’s “psychopathology of everyday life” underscores the figurative operations of memory in selectively conveying (and distorting) contingently reanimated impressions of past phenomena. To the extent that Lacan reading Freud emphasized the figurative logics of unconscious processes while scorning the fetishism of the coherent ego, his linguistically-turned psychoanalysis facilitated a poststructuralist rejection of a unified subject. At this juncture, traumatic memory appeared as a perfect compromise between identity politics and poststructuralism, since it allowed literary critics to uphold the historical standing of memories of oppression while fulfilling the protocols of deconstructive rigor that called for a critical attitude toward the category of experience. 14 To a certain extent, then, the linguistic turn’s currency in the 1970s and ’80s propelled trauma’s appeal in the ’90s as a focus that allowed critics to carry on with the multiculturalist mandate to make space for “other” voices conveying memories suppressed by national glorifications of the white male-dominated “Western tradition,” which had heretofore serviced Empire’s false claim to universality.
The Symbiosis of Holocaust and Trauma Studies in and beyond Yale Deconstruction and the Rhetoric of Unrepresentability
Interest in the Holocaust burgeoned in the 1990s, though not only in academia. In 1978 , Jimmy Carter inaugurated the President’s Commission on the Holocaust under Elie Wiesel’s chair-ship; groundbreaking ceremonies for the United States Holocaust Memorial Museum took place on October 16, 1985 ; President Reagan presided over the cornerstone laying ceremony in October 1988 ; construction began in July 1989 ; and the museum opened in April 1993 . The 1985 release of Claude Lanzmann’s Shoah was another seminal event that took place in this period, which, as Richard Brody argues in his obituary for the director in the New Yorker , changed the history of filmmaking itself. 15 Inspired by Shoah , scholars’ considerations of the challenges of bearing witness to and representing mass murder subsequently shaped the passionate debates about the propriety of Steven Spielberg’s Schindler’s List and Roberto Begnini’s Life Is Beautiful that provoked further questions about the “limits of representation.”
With a shared commitment to honoring the victims alongside the emotional realities of the traumatized (the “survivors” of various human-led and natural catastrophes), Holocaust and trauma studies reciprocally drew upon each other in this period. Read together, pivotal contributions by Cathy Caruth, Shoshana Felman and Dori Laub, M. D., Saul Friedländer, Eric Santner, Dominick LaCapra, Geoffrey Hartman, Marianne Hirsch, Berel Lang, Lawrence Langer, Michael Rothberg, and James E. Young among many others helped to bring about the coextensive development of Holocaust studies and trauma studies, beginning in the late 1980s and continuing into the first few years of the postmillennial period. 16 This convergence inspired a surge of critical work focused on witnessing and testimony by Kelly Oliver, Michael Bernard-Donals and Richard Geljzer, Ana Douglass and Thomas A. Vogler, Gary Weissman, Jakob Lothe with Susan Rubin Suleiman and James Phelan, and Thomas Trezise. 17
In 1992 , the same year that Herman’s Trauma and Recovery appeared, Felman and Laub published Testimony: Crises of Witnessing in Literature, Psychoanalysis, and History , which, in its attempt to heed the different motivations for survivor and bystander silence, amalgamated the situational, aesthetic, and moral valences of unspeakability. 18 Felman and Laub’s Testimony was nevertheless pivotal in forging the 1990s symbiosis between Holocaust and trauma studies—in part because of the authors’ vicinity to the Fortunoff Video Archive at Yale University. Among Felman and Laub’s many illustrious colleagues, George Steiner, J. Hillis Miller, and Geoffrey Hartman shared the former’s preoccupation with the Holocaust in an intellectual arena at once elevated and haunted by the late Paul de Man. Unlike the others, de Man did not write about the Holocaust; however, as Pascale-Anne Brault and Michael Naas note, during his time at Yale, he had “transformed the field of literary theory, revitalizing all of the channels that irrigate it both inside and outside the university, in the United States and in Europe.” 19 Together with Hartman and Miller, de Man’s celebrity as the foremost literary critic of his era consolidated the Yale school of criticism’s prestige in and beyond academia. 20
In his New Yorker review of Evelyn Barish’s The Double Life of Paul de Man , Louis Menand notes that de Man was “generally admired as a thinker, esteemed as a colleague, and idolized as a teacher.” Many of his essays have been studied and several of his graduate students enjoyed “distinguished careers at Yale and elsewhere.” 21 Three and a half years after his death in 1983 , Belgian graduate student Ortwin de Graef discovery of de Man’s wartime writings for two Nazi-owned newspapers in occupied Belgium stunned his former colleagues and students. From the collection of his wartime journalism they published in 1987 , it became disturbingly evident that “the young de Man was a fascist. His eyes were open,” as Menand declares. De Man wrote most of his columns for Le Soir , the Nazi-co-opted, collaborationist-staffed newspaper; it was Belgium’s “biggest daily,” and it sometimes featured anti-Semitic articles on its front page. 22 In his columns, de Man adhered to a Nazi line as he “championed a Germanic aesthetic, denigrated French culture as effete, associated Jews with cultural degeneracy, praised pro-Nazi cowriters and intellectuals, and assured Le Soir ’s readers that the New Order had come to Europe. The war was over,” according to de Man, and it “was time to join the winners.” 23
The evidence of de Man’s collaboration with the Nazis cast a pall over his colleagues and admirers, and his former students in particular, whose own reputations drew strength from this institutional lineage; as a result, de Man’s status as one of the fathers of deconstruction, alongside his close friend Jacques Derrida, came under intense scrutiny. Deconstruction’s enemies touted the revelations about de Man’s past as proof of its treacherous amorality and as yet another reason to dismiss constructivist literary theory as a whole for so cavalierly positing the instability of reference in tandem with the historicity of values and fundamental categories including identity and truth. 24
The blow to Yale school criticism’s reputation was exacerbated as the de Man affair dovetailed with the publication of Victor Farías’s Heidegger and Nazism in French and English, which sparked an uproar in France and the United States in attesting to Heidegger’s early, vocal embrace of National Socialism and his participation as the Rector at the Universtät Freiburg in carrying out anti-Semitic policies. 25 To the extent that Heidegger along with Nietzsche played a fulcrum role in the writings of Jacques Derrida, Jean-François Lyotard, Michel Foucault, and Luce Irigaray among others, those suspicious of French poststructuralist thought were hereby provided with still more material with which to fan the flames against it.
Unfortunately, anti-intellectual and typically undifferentiated treatments of deconstruction as a movement fed into less motivated skepticism about its substance and rigor that extended to de Man’s fellow travelers and former students as well as his close association with Derrida and deconstruction. Felman joined Yale’s faculty in 1970 , the same year as de Man, and, as LaCapra has argued, her relationship with him colors her discussion of her late colleague’s historical and intellectual trajectory in the fifth chapter of the 1992 Testimony book; it would be reactionary, of course, to belittle Felman’s contributions to Holocaust and trauma studies solely on the basis of her fondness for deconstructive gestures and, certainly, her relationships with Dori Laub and Cathy Caruth are more manifestly vital to the 1990s interaction between these fields than her relationship with de Man. 26
A professor of Clinical Psychiatry, Dr. Laub deserves special mention. Born in Czernowitz, Romania in 1937 , he went on to complete an MD and MA in Israel, and, with Geoffrey H. Hartman, cofounded the Holocaust Survivors’ Film Project in 1979 , which later became the Fortunoff Video Archive for Holocaust Testimonies at Yale’s Sterling Memorial Library. He was also a cofounder along with Werner Bohleber, Jan Philipp Reemtsma, and Jörn Rüsen of the International Study Group for Trauma, Violence, and Genocide, a project inaugurated in 1996 and housed at the Hamburger Institut für Sozialforschung in Hamburg, Germany. As of 2020 , he was serving as Deputy Director for Trauma Research at Yale.
Felman and Caruth’s close intellectual relationship was also important to the co-evolution of Holocaust and trauma studies in the 1990s. Caruth completed a PhD in comparative literature at Yale in 1988 and remained affiliated with it as a teacher and researcher for a few years thereafter, before moving to Emory, where she helped to build the university’s comparative literature program and inaugurate its Trauma Network (she subsequently became the Frank H. T. Rhodes Professor of Humane Letters at Cornell University). Felman cites Caruth’s “Claims of Reference” article on de Man included in the fall 1990 issue of the Yale Journal of Criticism as well as “Unclaimed Experience: Trauma and the Possibility of History in Freud,” published by Yale French Studies in 1991 (both reappeared as chapters four and one respectively in Unclaimed Experience: Trauma, Narrative, and History ). 27 Reciprocally, in the “Acknowledgments” to Unclaimed Experience , Caruth expresses her gratitude for Felman’s “inspiring work on testimony” in the first sentence, followed by thanks to Hartman in the second sentence and Laub in the third. 28 Caruth had previously edited and introduced two issues of American Imago (1 and 4) under the title “Psychoanalysis, Culture and Trauma,” and the articles from both were republished under the title Trauma: Explorations in Memory , which, along with Herman’s Trauma and Recovery , became a requisite touchstone for trauma scholars in literary and cultural studies. 29
In the Testimony book, Felman poignantly stresses the Holocaust’s potentially dumbing impacts on survivors and bystanders through her recourse to the aporetic “crisis of witnessing” figure to designate either a shock-induced incapacity or a demoralized refusal to attempt to do justice to cruelty so horrific it might not be believed. Her fulcrum contention is that the scale and extremity of Nazi brutality along with the immeasurable anguish it caused constrained witnesses to attest only to the impossibility of witnessing. Yet even as unrepresentability and unspeakability overlap in Felman’s interpretation of survivor silence, these terms are not synonymous. In Herman’s introduction to Trauma and Recovery , she observes that, “[t]he ordinary response to atrocities is to banish them from consciousness,” adding that “[c]ertain violations of the social compact are too terrible to utter aloud. This,” as she suggests, “is the meaning of the word unspeakable .” 30 Taking distance from this figure, Naomi Mandel states that, “[t]he negation performed by the ‘un’ in ‘unspeakable’ can be more accurately described as a prohibition, a kind of taboo, itself untouchable, around which discourses and culture are structured but which also embodies the disturbing potential of violence and contamination.” 31 By extension, to describe an event or action as “unspeakable” implies that the transgression at stake carries over to the speech that would describe it, with the idea that some sort of ban has been dangerously or disrespectfully overturned. This is the meta-failure that the 1990s rhetoric of “unrepresentability” and “unspeakability” in Holocaust studies sacralized: it leaned on the logic of the Second Commandment, or “image prohibition,” to warn against any attempt to (melo)dramatize the Third Reich’s genocidal crimes. The ostensible impetus of such a sacralization was to avert trivializations of the severe dehumanization and loss of intergenerational life that mass murder begets.
The alternation between unspeakability and unrepresentability in Holocaust and trauma studies typically functioned to indicate a “sublime” failure of imagination in the face of the magnitude and pathos of mass murder. The aesthetic of the sublime increasingly assumed the force of an ethical protocol in debates about representing the Shoah, a phenomenon partly indebted to the influence of poststructuralism’s preference for negative, open-ended, and aporetic figures that were supposed to thwart totalizing and positivistic impulses. The Nietzschean, post-Hegelian, and posthumanist temperament of Michel Foucault, Jean-François Lyotard, Gilles Deleuze, and Jacques Derrida expressed itself in their shared wariness of mimetic, fixed, and finite definitions of truth and in their embrace of more fluid and open-ended metaphors that tended to trouble the prospect of a closure of interpretation. This sensibility aligned them implicitly with Theodor W. Adorno, whose own Nietzschean presentiments expressed themselves in an anti-identitarian aesthetics adapted from Immanuel Kant’s emplotment of the sublime.
A fulcrum inquiry for Kant’s project of aesthetics is, by definition, how the subject draws upon a differential play of “faculties” to sense or discern various phenomena. As Kant’s considerations of the beautiful suggest, questions about the limits of communicating taste also indicate a social dimension to aesthetic judgment: will the subject be able to convey their discernment, and will others agree? In this respect, Kant’s Critique of the Power of Judgment challenged generations of readers to contemplate the repercussions of aesthetic topoi standing in for moral ideas and vice versa. 32
In Kant’s canonical formulation, the sublime dervies from an initially negative experience that transpires when the faculty of imagination ( Einbildungskraft ) fails to produce a determinate internal image or “intuition” ( Anschauung ) of a mathematically or dynamically overwhelming phenomenon. “That is sublime,” Kant writes, “which even to be able to think demonstrates a faculty of the mind that surpasses every measure of the senses.” 33 In Kant’s conception, the subject finds compensation for this failure through the faculty of reason, which affirms its capacity to recognize limits, and thereby transcend them.
Adorno’s adaptation of the Kantian sublime sheds this compensatory resolution, thereby leaving the subject adrift in a failure of representation. Adorno develops this “negative” sublime in his discussions of modernist art and Ershütterung (shudder) in the unfinished Aesthetic Theory but also, notably, in his various comments about poetry, art, and culture “after Auschwitz.” In the sometimes polemical scholarship produced at the intersection of Holocaust and trauma studies, Adorno’s statements from “On Lyric Poetry and Society” and Negative Dialectics typically circulated out of context, though endeavors to amplify them in light of Adorno’s work as a whole yielded insight into his scorn for a refusal in and beyond Germany to recognize the modern subject’s defensive hardening against a proliferation of suffering. 34 Hence, if the mass murders are “unrepresentable,” it is because of a failure of moral imagination: complicity constitutes a hermeneutic horizon beyond which one cannot see.
As evinced in the opening line of the last chapter from the third section of Negative Dialectics entitled “Meditations on Metaphysics,” Adorno does not abide with the presumption of “immutable truth” privileged over and against an allegedly mobile, transitory appearance. To reinforce this point, he reproaches Hegel for redeeming the eternal from the destruction inherent in his temporality concept by converting that destruction into an abstraction. This criticism captures Adorno’s repugnance for redemptive and universalizing logics and his attendant embrace of what he refers to as the “micrological” standpoint focused on the unassimilability of the concrete particular.
The position of this criticism at the opening of the third section is additionally significant, because the first paragraph ends with one of Adorno’s most famous pronouncements: “After Auschwitz, our feelings resist any claim about the positivity of existence as sanctimonious, as wronging the victims.” Such feelings, Adorno says, “balk at squeezing any kind of sense out of the victims’ fate.” 35 This statement recodes his prior criticism of Hegel to the extent that Adorno once again repudiates the prospect of Sinnstiftung : the assertion of a universal moral lesson from mass murder that purports to redeem the victims’ anguish as a sacrifice while actually reaffirming the system that enjoins self-sovereignty and nurtures the disavowal of widespread suffering. This moment in Negative Dialectics resonates with the still more famous conclusion from “Cultural Criticism and Society,” where he proclaims that, “To write lyric poetry after Auschwitz is barbaric,” with the explanation that “absolute reification is preparing to absorb the mind entirely,” thus neutralizing presumptions about moral progress. 36 The challenge he poses here and elsewhere is that a genuine confrontation with others’ pain must not consolidate the ego’s sense of bounded coherence. It is a question of how to create art that conveys misery without fostering “self-satisfied contemplation.” 37 As is also well known, when Adorno subsequently refers back to this claim in his critique of politicized art entitled “Commitment,” he refuses to qualify it, insisting instead that, “it expresses, negatively, the impulse that animates committed literature.” 38
In keeping with Adorno’s rejection of identitarian and universalizing logics, Lyotard discovered fertile material in Kantian aesthetics and in the sublime in particular, which he adopts in The Differend to conceptualize the impact of transformative events such as “Auschwitz” and “May 1968” among others as negations of the Enlightenment narrative of progress and the “doctrine of parliamentary liberalism, respectively.” 39 Lyotard’s prominence in the 1980s American literary institution thus furthered an association between traumatic history, the sublime, and the motif of “unrepresentability” with respect to the Holocaust in particular.
In The Differend , Lyotard embraces an aporetic logic that, in dialogue with Kant, Hegel, Marx, Nietzsche, Wittgenstein, Adorno, and Levinas among many others, also embraces Derrida’s rejection of the metaphysics of presence. Lyotard introduces The Differend as a philosophical intervention in response to Robert Faurisson’s declaration that the existence of the gas chambers cannot be proven in the absence of living witnesses to attest to them. Knowing that there is more than sufficient evidence to satisfy any but the most ideological revisionists on the reality of the gas chambers, Lyotard treated Faurisson’s scandalous claim as a positivist ruse, to be countered philosophically through a commentary on the fragility of first-person testimony as an empirical form of evidence that fails to fulfill positivist criteria. This line of inquiry suited his critical Kantian preoccupation with the conditions and limits of moral judgment, particularly with respect to the perpetrators of mass murder whose crimes destroyed their witnesses along with other sources of evidence.
The titular differend is Lyotard’s term for situations in which those empowered to judge reject the validity of a plaintiff’s grievance, perhaps because they sympathize or align themselves with the perpetrators who would sidestep accountability. Countering Faurisson’s disingenuous call for proper evidence, Lyotard argues that if there is something like a “moment of truth,” it transpires when the audience feels the weight of justice left in abeyance from the plaintiff’s standpoint. Lyotard’s contention is that such a feeling is aesthetic and moral rather than cognitive or empirical; it therefore parries a positivist fetishism of facticity as well as a naive insistence upon the coherence and consistency of first-hand experience.
In The Differend , Lyotard employs Ludwig Wittgenstein’s conception of language games alongside a deconstruction of reference to translate Adorno’s “after Auschwitz” into a theory of the empirically, cognitively, morally, and aesthetically overwhelming event. With this critical aim, he foregrounds the witness’s anxiety about finding believable phrases that could do justice to the overwhelming magnitude and pathos of the cruelties that the Nazis and their collaborators perpetrated against Jews and other targets, the lost details of the lives blended into statistical approximations of how many were “exterminated.” The unrepresented becomes the unrepresentable, as respect for such profound suffering registers as a determinate negation of the longing for a complete image. Lyotard’s translation of Adorno’s negative sublime into Wittgenstein’s language games carried “unrepresentability” into discussions about the Holocaust as a trauma, including Felman’s; hence, the silence that Lyotard views as indicating a differend anticipates Felman’s “crisis of witnessing,” and, specifically, her understanding that firsthand witnesses of extreme dehumanization fear they will not be believed even if they could find the requisite words.
The question of the limits of depicting the mass murder of the Jews responsibly as a large-scale trauma also figured prominently at a 1990 conference organized by the historian Saul Friedlander at the University of California in Los Angeles. Selected presentations from the “Probing the Limits of Representation: Nazism and the ‘Final Solution’” conference subsequently appeared in a collection with the same title edited by Friedlander. As Wulf Kansteiner and Todd Presner observe, the conference and resulting volume “arguably defined the theoretical and historiographic contours of the field of Holocaust studies for two and a half decades” in staging a referendum on debates from the 1980s about “postmodernism and the alleged pitfalls of historical relativism.” 40
As both a survivor and an historian, Friedlander was concerned about the implications of the 1986–1987 Historians’ Debate, which mounted as conservatives in the Federal Republic argued that Germans were too obsessed with the Holocaust and that they needed (or perhaps deserved) a “positive” national history. The variants of revisionism showcased by the likes of Ernst Nolte challenged prevailing proprieties governing memory of the Third Reich’s atrocities as pivotal to the shaping of a Western-leaning “civilized” Bundesrepublik. 41 Yet if Nolte’s specious arguments against the Holocaust’s uniqueness goaded historians’ responses to revisionism and denial, then poststructuralist challenges to positivism, facticity, and referential stability presented them with another can of worms. Apart from critical and nuanced explorations of the term by Lyotard, Fredric Jameson, Harry Harootunian, Zygmunt Baumann, Jane Flax, and bell hooks among many others, the term postmodernism has typically been deployed like an expletive to homogenize and dismiss at once a range of diverse theoretical standpoints and heuristics that included post-Hegelian, post-positivist, and posthumanist responses to Nietzsche’s call for a transvaluation of values.
From the standpoint of both its proponents and critics, postmodernism understood as a philosophical framework derives predominantly from contributions by the generation of philosophers associated with the French “linguistic turn” who had been chastened by German occupation and French collaboration during World War II, France’s unraveling colonial heritage, and Stalin’s atrocities. This generation engaged critically with the intellectual currents of their day, including Marxism, structural anthropology, existentialism, phenomenology, semiotics, and psychoanalysis, through a Nietzschean and Heideggerian lens. The rejection of postmodernism has also targeted American theorists conversant with anti-positivist French theory whose work reflects a profound respect for the implications of language and perspectivalism with respect to identity, signification, and knowledge formation. Ultimately, then, those who repudiate postmodernism also tend to resent the identity politics propelled by the new social movements of the 1960s and ’70s (civil rights, women’s liberation, and Stonewall) seeking to make visible long-running inequities. The anti-intellectual conflation of these constituencies and their respective praxes reflected, on the one hand, a nostalgia for the “universal” foundations supposedly endemic to the white, patriarchal “Western civilization” curriculum in the humanities and, on the other, a reactionary paranoia about losing the ideal of scientific rigor defined as a dependably result-oriented methodological consistency.
Hayden White’s keynote, “Historical Emplotment and the Problem of Truth,” opens with his notorious proclamation to the effect that, “[t]here is an inexpungeable relativity in every representation of historical phenomena.” 42 This claim derives from his sense that the verisimilitude and authoritative force of a historical representation is contingent on “the language used to describe and thereby constitute events as possible objects of historical understanding.” The presuppositions he would hereby problematize are that narratives are neutral and natural “containers” for historical evidence, and that conventional plot types such as epic, comedy, tragedy, satire, and pastoral “inhere” in the facts. White not only contests these assumptions but also challenges the idea that the truth or falsity of a narrative can be evaluated, since stories “are linguistic entities that belong to the order of discourse.” 43
White raises other significant issues in response to the conference injunction to consider the limits of representation. Most significantly, he foregrounds the issue of propriety in the selection of certain plot types versus others to depict the Final Solution. The question then becomes whether or not the Holocaust belongs to a “special class of events” that are “emplottable in one way only,” or are they meaningful like other historical events that are “infinitely interpretable and ultimately undecidable”? 44 As is well known, White argues that judgments about the fidelity and appropriateness of a particular plot type mistakenly assume that narratives are literal to the extent that they are intrinsic to the most important facts, which evince “a ‘story’ kind of form and a ‘plot’ kind of meaning.” 45
White goes on to argue that literary modernism offers a more suitable mode of narration than the “literal” and “impersonal” yet nevertheless realist approach advocated by Berel Lang in Act and Idea because, according to the former’s articulation of the latter’s position, figuration allows the author’s personal perspective to “obtrude.” Drawing on Erich Auerbach and Lang’s own recourse to Roland Barthes’s conception of the middle voice, White contemplates the prospect that intransitive writing finesses the subject-object split in debates about the Jewish genocide. Ultimately, then, White’s lesson is that “our notion of what constitutes realistic representation must be revised to take account of experiences that are unique to our century and for which older modes of representation have proven inadequate.” 46
In “The Burden of History,” White echoes Nietzsche’s “The Uses and Disadvantages of History for Life,” his diatribe against the “malady” of excessive history that preempts creativity, discourages transformation, and stifles freedom. White’s magnum opus Metahistory which appeared in 1973 , which continued this line of argument, unleashed a storm of denunciations concerning his alleged conversion of “truth” into “rhetoric.” As of the spring 1990 , when the UCLA conference took place, he had published The Content of the Form , a collection of essays where he continued to explore the role of rhetoric, narrativity, and aesthetic ideas in historical discourse in order to highlight its poetic and imaginative potential at the expense of its scientific pretentions. Conference participants consequently made use of the days following his keynote to confront White’s “postmodernist” position on the “inexpungeably” interpretative work of constituting historical referents, which are then “emplotted” as evidence most typically in a conventionally realist third-person narrative form. 47
The impact of the “Probing the Limits” conference carried over to trauma studies, since, in the decade following the conference, many participants, including White himself along with Eric Santner, Dominick LaCapra, Berel Lang, and Geoffrey H. Hartman, published significant contributions exploring the ethics of representing the mass murder of Europe’s Jews. In the same year as the conference, Santner published Stranded Objects: Mourning, Memory, and Film in Postwar Germany , where he distinguished between a self-critically introspective and thus genuine form of working through and what he referred to as a “short-circuited” mode of compulsive narration, or “narrative fetishism” that avoids a substantive confrontation with historical complicity and the loss of shameful objects of desire: Hitler as father figure or national ego-ideal (as Alexander and Margarete Mitscherlich suggested) and the thousand-year Reich as a fantasy of unified community. 48 Lang’s participation in the conference was bridged by the edited collection Writing and the Holocaust and his monograph Act and Idea in the Nazi Genocide . 49
In 1996 , Hartman published a personal and scholarly reflection, The Longest Shadow: In the Aftermath of the Holocaust , which included his contribution to the Probing the Limits volume entitled “The Book of the Destruction.” It was preceded in 1994 by the edited collection Holocaust Remembrance: The Shapes of Memory , which featured Friedlander’s “Trauma, Memory, Transference” as well as a chapter by Felman on Lanzmann’s Shoah . 50 Taking up the conference injunction to reflect upon the limits of representing the Final Solution, Hartman expounds on the broader issue of how art poses this question more generally. The essay thus opens a window into the state of the theory and preoccupations informing Holocaust and trauma studies in the early 1990s, with references to the Fortunoff Video Archive that he cofounded with Laub and to Lyotard’s recourse to the sublime in his engagements with both art and “Auschwitz.”
Between 1994 and 2004 , LaCapra published no fewer than four collections of essays devoted to the Holocaust and trauma. 51 His prominence in the fields of intellectual history and interdisciplinary criticism in conjunction with his institutional prestige as a Cornell University professor shaped the trajectory of memory and trauma studies through the generations of students who worked with him or read him as well as the forums he participated in or organized himself. To a considerable extent, then, LaCapra’s interventions helped to consolidate the coextensive development of Holocaust and trauma studies.
Among the many valuable concepts that LaCapra has proposed is his adaptation of the psychoanalytic notion of transference to reflect on how historians’ and other scholars’ backgrounds might lead them unconsciously to identify with certain actors over others in historical events. Transpiring “at the intersection of the personal, political, and textual,” transference, in LaCapra’s words, indicates the manner “in which problems and processes active in the texts or artifacts we study are repeated in displaced and often disguised or distorted form in our very accounts of them.” 52 Hence, part of what motivates his criticisms of Felman along with other former colleagues and students of de Man’s is their apparent inability to reflect on their own transferential relationships with the one-time collaborator and his texts, which manifests as a failure to confront the nature of the trauma “caused (at least for some) by the discovery of the World War II journalism.” 53 As LaCapra observes, some commentators have “acted out” their trauma in tending “to exaggerate traces of self-contestation in the early writings, to rewrite the past in a manner that underwrites a more ‘positive’ identity in the present, and to overinterpret the role of self-criticism in the relation of the later to the earlier unacknowledged writings.” This response is “insufficiently attentive to an important public context for the controversy over de Man: revisionist interpretations of the Holocaust.” 54 Nothing less than “the pubic consequences of reading and interpretation” are at stake for LaCapra in his verdict that “private acts of friendship or love may be questionable as interventions in a politically fraught field of public discourse.” 55
In the concluding chapter of Representing the Holocaust , LaCapra also revises the opposition between “acting out” and “working through” in dialogue with Santner, who himself draws upon Freud, Adorno, and the Mitscherlichs’ The Inability to Mourn . 56 LaCapra aligns himself with both Adorno and Santner in privileging working through as a process of becoming conscious of the historically disavowed and repressed (particularly when perpetrator generations are concerned), reflecting critically on one’s own implication in the past, and stepping back from transferential projections that convert traumatic history into a vehicle for compulsively repeating (or “acting out”) one’s own defenses and anxieties. Without this distance, LaCapra insists, trauma cannot be integrated into an individual or collective past, since a fantasy-imbued emotional fixation renders it eternally present.
LaCapra’s 2001 collection of previously published articles entitled Writing History, Writing Trauma also provides a wealth of critical discernments and theoretical insights about the ethics of analyzing victim and perpetrator perspectives in representations of trauma. For example, LaCapra recommends the term historical trauma to distinguish actual events from the structural trauma that psychoanalytically inclined theorists such as Slavoj Zizek attribute to incursions of “the real.” 57 He criticizes Zizek’s figuration of the “traumatic real” because it converts trauma into a general disposition inseparable from any modern subject’s disavowal of responsibility for the social consequences of unconscious repetitions. In Zizek’s reading of Lacan, the symbiotic relationship between fantasy (the imaginary) and socialization (the symbolic) that constitutes identity is constructed to guard against the real, which is “traumatic” insofar as it can never be recognized the first time it irrupts, if at all. LaCapra would segregate such “structural” or ontological notions of trauma from “historical” trauma to preserve the moral import of events that lead to widespread and typically intergenerational forms of suffering. To the extent that structural trauma, by LaCapra’s account, revolves around absences that are misrecognized as losses rather than the types of violent bereavement and abjection that result from genocide and persecution, he insists that trauma researchers endeavor not to collapse them. 58 At stake is the moral necessity of respecting the dead and bereaved while holding perpetrators accountable.
On an experiential level, LaCapra’s distinction between historical and structural trauma is not sustainable, since coping with the emotional impact of massive violence may mobilize neurotic tendencies that preexisted the events. LaCapra’s analysis is nevertheless helpful as a corrective to melancholic idealizations of absences treated as losses, a tendency that, as he contends, resonated with a poststructuralist emphasis on referential instability (the “missing” referent that feels “lost”). In this respect, LaCapra’s polemic also betrays a certain prejudice against the supposed excesses of poststructuralist theory and deconstruction in particular as evinced in his criticisms of Caruth, a major trauma theorist whose claims about its imbrication with history LaCapra seems concertedly driven to debunk. 59
Throughout his work on the Holocaust and/as trauma, LaCapra reiterates a need to respect victims—both the murdered and bereaved—and to hold the intergenerational inheritors of perpetrator histories accountable, perhaps especially when they “act out” their self-interest in rationalizing, minimizing, or denying their crimes. One of the questions this understanding of the critic’s responsibility raises is how to adjudicate perpetrator accountability if unconscious narcissism protects one from becoming aware of the consequences of at least some of one’s actions.
Trauma beyond Deconstruction and Psychoanalysis: The Turn toward Affect
LaCapra was not the only critic with reservations about Caruth’s deconstructive style to find fault with her trauma theory. In Trauma: A Genealogy Ruth Leys carries out an exacting assessment of Caruth’s major claims about trauma: that, in the absence of anxiety about the precipitating incident, it names a wounding “experience” that was not actually experienced. According to Leys, Caruth depicts this “unclaimed” experience as a “literal engraving of the mind by an incomprehensible reality that ‘continually returns, in its exactness, at a later time.’” 60 Caruth’s assumption is that this “reality” will become belatedly intelligible through unconsciously motivated repetition and other symptoms. In Caruth’s words, “[t]he history that a flashback tells—as psychiatry, psychoanalysis, and neurobiology equally suggest—is, therefore, a history that literally has no place , neither in the past, in which it was not fully experienced, nor in the present, in which its precise images and enactments are not fully understood.” Insofar as the trauma insistently imposes itself on present consciousness “as both image and amnesia,” according to Caruth, it “seems to evoke the difficult truth of a history that is constituted by the very incomprehensibility of its occurrence.” The flashback is, thus, a belated “traumatic reenactment,” which conveys “both the truth of an event , and the truth of its incomprehensibility .” 61
The context of these contentions is important, because Caruth is paraphrasing Bessel A. van der Kolk and Onno van der Hart’s discussion of Pierre Janet, who, as Caruth states, “proposed that traumatic recall remains insistent and unchanged to the precise extent that it has never, from the beginning, been fully integrated into understanding.” 62 Because it was not “fully integrated as it occurred,” according to Caruth’s summary, it cannot be incorporated as a narrative “into a completed story of the past,” which, as she emphasizes, is required “both for the sake of testimony and for the sake of cure.” 63
Leys devotes an entire chapter to debunking van der Kolk and van der Hart and still another to excoriating Caruth in arguments that are sometimes too dismissive of the latter’s deconstructive style, especially in the chapters on Freud’s Moses and Monotheism . 64 The ethos of this style is to rebuff a regime of truth and the ideal of rigor that accompanies it while charting an ostensibly aleatory process of configuring meaning from coincidences as well as seemingly inadvertent and thus symptomatic repetitions signaling absent presences and latent transitions. This is not to say that deconstructive writing does not adhere to its own code of scholarly responsibility, but it often takes a loxodromic tack to open up interpretation through a build-up of evocations that allows readers to glimpse something gestural and provisional at a slant. 65 Among the points that Leys attacks most adamantly is Caruth’s proposition that the “unclaimed” traumatic experience lodges an intact yet repressed image that repetition among other symptoms symbolizes. In reproving Caruth’s reliance on van der Kolk and van der Hart to define trauma as a literal registration, Leys hereby exposes a decidedly less deconstructive Caruth who defines trauma as an actually missed origin.
Leys interrogates the “mimetic” assumptions in Caruth’s reading of Freud, and specifically the idea of an originary event that must be imitated or recreated as precisely as possible by the traumatized as they work through its belated affects. Yet unlike some contemporary work in trauma studies that treats Freudian psychoanalysis as a retrograde skin to be sloughed off, Leys’s Trauma offers a detailed reading of key contributors to psychoanalytic theory in the course of critiquing Caruth’s rewriting of Freud’s belatedness conception. According to Leys, Freud’s account of trauma is more balanced between mimetic and anti-mimetic standpoints. While understanding trauma “as a situation of unconscious imitation or identification with the traumatic scene . . . which occurs in a state akin to a trance,” he “sought to repudiate mimesis,” according to Leys, by “[positing] a subject capable of seeing and hence depicting to itself and others the objects of its fantasies and wishes.” It is in this respect that Freud “attempts to solve the problem of mimesis by redefining the relation between the subject and the other in antimimetic, spectatorial terms,” depicting the unconscious “as a stage,” in effect, “on which the subject in its traumatic dreams or fantasies observes himself or herself performing the scene.” 66
In Beyond the Pleasure Principle , Freud speculates on the systemic motivations for the compulsive repetitions that he observes in World War I veterans’ nightmares as well as children’s play. One major issue that troubles Freud is that veterans’ nightmares seemingly return them to painful scenes where they were injured or lost comrades, a symptom that, on the surface, contradicts his major premise from the Interpretation of Dreams to the effect that dreams indirectly enact unconscious wishes. 67 Observing his infant grandson’s “fort-da” game, as Freud designates it, spurs him to read the boy’s act of throwing a toy over the side of his crib as a dramatization of his mother’s disappearance when she leaves the room. Freud’s insight is that the game allows the child to convert a passive experience of loss into an active one and thereby master it.
The common ground Freud establishes for understanding the compulsive repetition that propels veterans’ nightmares and the grandson’s fort-da is “economic” in the sense of thermodynamic: the pleasure principle induces the neutralization of excessive stimuli that overburden the psychophysical apparatus. Yet Freud does not stop there, since the economic level itself seems to demonstrate a split between survival-oriented regulation and more “primal” destructive aims. Freud’s concept of the death drive enters the stage as a primal-masochistic urge to revert to an “inorganic” state by defusing all stressors, including the tension of life itself. Freud speculates that the repetition compulsion as a symptom of posttraumatic anxiety might also serve the death drive’s ends, which go beyond the pleasure principle in aiming for tension-free stasis.
Among the many reasons put forward for moving beyond Freudian psychoanalysis in trauma theory has been a rejection of his theorization of compulsive repetition as it emerged between the thermodynamic determinism of the pleasure principle and the phylogenetic masochism of the death drive. This distaste for Freud’s scientistic metaphysics was spurred on, in part, by Gilles Deleuze and Félix Guattari’s highly influential collaboration in Anti-Oedipus , where they propose a dynamically metonymic morphology that would free sexual energetics from archaeological and utilitarian models of interpretation, from the Oedipal matrix as well as a compartmentalizing functionally differentiated psychic and libidinal economy that operates as a closed system in subservience to the metaphor of scarcity. 68 As the work of Laura S. Brown and Lauren Berlant attests, there has also been an interest in thinking traumatic conditions beyond single catastrophic events, since many of the anxieties and other residues of everyday forms of aggression and humiliation—the kind that women and other subordinated groups continually face—cannot be reduced to finite episodes located in the past. 69
The interest in moving beyond the singular event in trauma studies coincided with intensifying frustration among the members of feminist and queer studies circles about the patriarchal and heteronormative blind spots of Freudian and Lacanian psychoanalysis. Their objections parallel Marxist-leaning postcolonial and globalization critics’ dismissals of an “ahistorical” psychoanalytic framework in their focus on the historical and hemispheric scopes of transnational exploitation. At the same time, posthumanists were grafting onto Deleuze and Guattari’s rejection of Freud-Lacan’s Oedipus fixation the outmoded naturalization of bounded subjects and surface-depth reading strategies.
Given the suspicion with which academic feminists and Marxists have regarded Freudian and Lacanian psychoanalysis, albeit for mostly different reasons, the desire to move beyond it was not altogether surprising. Because of the overwhelming frequency of his female patients’ accounts of incest and predation in their homes, Freud’s initial credence declined as he increasingly viewed such admissions as building blocks for his theory of fantasy. Certainly, for feminists, this shift was alienating, since it derealized the scandalous incidence of sexual abuse. 70 The notorious case of Dora also fanned feminist ire as Freud stubbornly clung to his own framework when confronted with a patient whose circumstances exposed its limits. 71
Marxists preoccupied with the historical development and social expression of economic exploitation found psychoanalysis ahistorical and, by extension, apolitical, since it seemed to convert the issues driving bourgeois neurotics into transhistorical principles. Though the work of the Frankfurt School, Louis Althusser, Fredric Jameson, and Slavoj Zizek offered a recourse for Marxists interested in the political-economic “unconscious” or ideology; for those preoccupied with “concrete particulars” and historical context as such, the fundamental insistence on ambivalence that a theory of the unconscious enjoins—that what could be “untrue” for an intentionally oriented consciousness could be “true” at the unconscious level—left them cold. Notably, this type of Marxist historicist was also alienated by the poetics of deconstruction, which embraced a psychoanalytic emphasis on symptomatic absences and repetitions while problematizing the latent-manifest heuristic as overly beholden to archaeological truth metaphors. Derridean deconstruction ironically enacted this manifest-latent oscillation at the level of form (through the incorporation of lengthy footnotes that subvert the main text, for example) and by attending to the historical and semantic layering of figures that undermines supposedly fundamental oppositions. Moreover, the multilingual erudition in continental philosophy and intellectual history that the best kind of deconstructive writing required tended to leave out monolingual academics with scientific aspirations, who favored decidability, and whose literal disposition inclined them to decontextualize theoretical concepts by applying them merely as “tools” for framing new lines of inquiry and categorizing results. A confluence between multiculturalism and postcolonial studies in the late nineties altered the critical mood, turning it against a Eurocentric trauma studies that derived its conceptual ground from Freud’s Beyond the Pleasure Principle while adopting the sacralizing tone of the negative sublime in the course of brandishing the Holocaust’s “uniqueness” and “unrepresentability.”
As a generation of PhDs inspired by Felman’s, Laub’s, and Caruth’s work on trauma initially drew upon an admixture of psychoanalytic figures and deconstructive motifs, the institutional rise of the multiculturalist agenda and postcolonial studies inculcated a mandate to consider minority and subaltern perspectives. The American curriculum wars of the 1980s and ’90s additionally sensitized this generation to find the repudiation of trauma studies’ Eurocentrism persuasive, and, without abandoning the lessons gained from studying the Shoah as a trauma, prominent contributors helped to push the field into new territories through their own work and by facilitating research and writing that dovetailed with ongoing scholarship on oppression and violence in women’s studies, postcolonial studies, racialized minority studies, and (in the nineties) a still emerging queer studies. A look through the tables of contents from edited collections on trauma, memory, and witnessing from this period reveals that editors often included one or two essays on the Holocaust but ultimately favored diversified topics illuminating various wounding pasts.
It is worth recalling these internal tensions among the different constituencies in cultural theory because they shed light on one of the many forms through which North American anti-intellectualism infected academia—as if some researchers had internalized a larger public antagonism toward “useless” (unprofitable or amoral) thinking (in other words, thinking, like art, for “its own sake”) while hypostasizing information. Of course, an image of the period should include a rapidly “corporatizing” or “neoliberalizing” university as reflected in the “metrics” for evaluating faculty performance. 72 To the extent that quantity and efficiency were easier metrics to judge by than quality, work that required a very time-intensive study of languages and intellectual lineages, that was less easily digestible, more difficult to create, and more challenging to teach has become decreasingly feasible for a streamlined PhD that is funded for four years, thus compelling students to read for their dissertation projects in order to finish as quickly as possible.
Such economic instrumentality had an impact on trauma and memory studies, since it expedited the intertwined fates of Lacanian psychoanalysis and Derridean deconstruction, which fell increasingly out of vogue in the post-millennial period. Lacan’s and Derrida’s notorious difficulty became yet another strike against the all-too-white male elitism of high theory, while Freud’s determinisms sufficed to throw out “his majesty the baby” (otherwise known as the subject of “On Narcissism: An Introduction”) with the humanist bathwater. 73 Without dismissing its limitations, psychoanalytic theory had, at the very least, provided some invaluable key terms without which it became difficult to speak about the relationship between memory and individual or collective identity. How might one understand national silences in the aftermath of major events such as the Jewish genocide and the Vietnam War without the concept of belatedness? How can the inability to acknowledge or even remember disturbing incidents be apprehended without the notions of repression or disavowal? Yet as trauma researchers stopped consciously relying on psychoanalytic theory, they gave up an explicitly common framework that nonetheless continued to undergird their work as a set of presuppositions, commonplaces, and dead metaphors. 74
Among the paradoxical offspring of an increasingly post-psychoanalytic trauma studies has been a turn toward affect , which is itself indebted to multiple developments and forces within cultural studies. 75 In the late 1990s and early millennial period, a few critics began to ask the question: why trauma and why now? To some extent the rise of trauma studies during the curriculum wars provided a mustering point for the work of giving voice to the marginalized, an agenda that increasingly shaped late 1980s and 1990s identity politics as previously ignored literature and cultural practices featuring formerly excluded histories assumed a new appeal for literature professors committed to diversifying the curriculum and the faculty. On a strategic level, the hope was that by giving women and minorities more cultural visibility in literary curricula, the marginalized might gradually achieve more sociopolitical agency because familiarity with their issues would encourage students to become more receptive to seeing their “others” represented in various professions and voting them into political leadership. Bringing formerly unheard voices into the classroom also allowed progressives to pursue an Enlightenment agenda: to prompt awareness and compassion among students from dominant groups while validating less advantaged students’ experiences and aspirations. Since the literature of persecuted communities often depicted scenes of suffering, cruelty, and injustice, it implicitly provided a trove of material for trauma studies beyond the Holocaust.
To a certain extent, poststructuralist theory facilitated this agenda by furthering an anti-foundationalist critique of essence and universality. Yet by the time that Joan Scott published her incisive intervention on “experience” in 1991 , which decried its fetishism as a stable repository of personal and collective “truth,” a sacred “property” of the victimized, scholars invested in honoring heretofore ignored histories of expropriation and subordination were faced with the perplexing task of saving their object of inquiry from a persuasive set of criticisms that seemed to sabotage its epistemological authority. 76 Considerations of memory, memorialization, and memory politics offered a means of thinking about the partial and contextually permeated representation of experiences of oppression without coveting an originary or coherent experiential referent. To the extent that finite experiences could not exist in the absence of memory as a representation in its own right, studies of memory lent themselves to potentially respectful responses to their figural disposition as an inevitable aspect of witnessing, if not also a symptom of an event’s overwhelming and wounding impact.
White and Rothberg addressed this aspect of trauma remembrance through their conceptualizations of “figural realism” and “traumatic realism,” respectively, based on the premise that representations of trauma will reflect an event’s emotional vicissitudes at the level of form—in other words, that the form itself bears a traumatic content, as if it were enacting (or mimicking) a symptomatology. 77 In amplifying this premise, White and Rothberg honor the ineluctability of shock and grief in responses to the Jewish genocide, thereby asserting their value over and against a pedantic defensiveness about the putative dangers of aestheticization and dramatization in the realms of historical fiction and docudrama.
While it would be inaccurate to assert that White’s and Rothberg’s interventions precipitated the turn toward affect, their work demonstrates how the anxiety, humiliation, and grief that traumatic history leaves behind assumes a structural externality that effectively collapses the boundary between the inside and outside of an event. White’s recourse to the term realism registers his insight from reading Virginia Woolf’s Between the Acts as a modernist mode of psychological mimesis, conveying the effect of intimacy with a subjective referent—the fragmentation and circuitousness precipitated by the interplay between perception and feeling, the affectively magnetized contiguities and encroachments that take place as the past slices through the present and vice versa. 78 For White as a reader of Woolf and Primo Levi, and for Rothberg as a reader of Ruth Klüger, Charlotte Delbo, and Art Spiegelman, the forms through which these authors depict their experiences configure painfully disruptive insinuations of the past into the present, and vice versa. From this standpoint, studies of writing about trauma would necessarily attend to the formalization of emotional dynamics through amalgamation, exaggeration, fixation, reduction and displacement as translated by emplotment, shifts in point of view, metaphor, metonymy, and synecdoche, among other vehicles. Emotion, feeling, and “affect” as such were the crux, then, as teaching trauma texts would likely entail guiding students to identify its causes and effects, and to grasp the moral significance of the catastrophes and atrocities through sympathy with the victims.
Yet there was another direction coming into focus. If trauma studies permitted identity politics to continue in the wake of the deconstruction of experience, then the question arises as to what aspects of the former framework needed to be “salvaged” in order to ensure that portrayals of the injustices generated by sexism, racism, homophobia, imperialism, and colonization were not only treated respectfully but could also retain a moral force that might direct public attention to historically accrued grievances. One answer seems to be affect generally understood as a psychophysical residue (taking the form of feelings, emotions, and moods) that arises in the aftermath of a transpired situation or succession of events. To be sure, pathos as an object of study has a long and rich lineage since Aristotle’s Poetics ; however, as trauma and memory studies became more self-reflexive, a preoccupation with “traumatic affect” fed into a renewed interest in conceptualizing affect more broadly.
Evidence for the “return” of feelings and emotions as a specific focus of inquiry in this period includes Teresa Brennan’s Transmission of Affect , which was posthumously published by Cornell University Press in 2004 , the same year that Sarah Ahmed put forward her invaluable concept of “affective economy” in The Cultural Politics of Emotion . 79 Noting that psychoanalysis offers a “theory of emotion as economy, as involving relationships of difference and displacement without positive value ,” she borrows from Marxist theory to add that emotions be viewed as a “form of capital,” which is to say that affect “does not reside positively in the sign or commodity, but is produced as an effect of its circulation.” In keeping with this premise, she contends that “[s]igns increase in affective value as an effect of the movement between signs: the more signs circulate, the more affective they become.” 80 Diverging from a liberal individualist view of the self as property, however, Ahmed asserts that “‘the subject’ is simply one nodal point in the [affective] economy, rather than its origin and destination.” 81
Lauren Berlant has also played a crucial role in facilitating the development of affect studies with her prescient considerations of sentimentality and intimacy. 82 More recently, Cruel Optimism consolidated a direction that had been building steadily since the late nineties. 83 In this landmark monograph, Berlant engages with affect beyond the models oriented by PTSD following a single, finite episode to consider instead how recurrent or continuous and thus “ordinary” experiences of humiliation, demoralization, and precarity foster fantasies of solace that are too often exorcised in self-destructive ways. Though well-versed in psychoanalytic theory (see Desire/Love ), Berlant moves beyond its characteristic gestures to provide a framework for elucidating everyday forms of alienation, futility, emotional support-seeking, and political longing. 84
From the standpoint of trauma and memory studies, such work furthered the aims of politicized research on trauma because it adhered to a commitment to bring attention to identity-formative differences that positioned some to flourish while others struggle merely to tread water or slowly die. In this respect, Berlant’s Cruel Optimism gained momentum in part because of the currency of Michel Foucault’s recently translated lectures on “biopower” and “biopolitics” as well as the traction of Giorgio Agamben’s revisions of these theses in a series where he reopened conceptions of sovereign power that Foucault’s genealogical emphasis on discursive effects and the “microphysics” of discipline tended to sideline. 85
Both Ahmed’s and Berlant’s interventions register a widespread disenchantment with Freud’s death-driven trauma theory and the psychoanalytic subject (not to mention Freud-Lacan’s heteronormative baseline). In moving beyond Freud’s thermodynamic understanding of belated affects tied to finite traumas, Ahmed and Berlant offer a vocabulary alongside concrete imagery for certain kinds of day-to-day anxieties and long-term pain. To the extent that Ahmed and Berlant consider affects such as self-destructive “optimism” and racial shame, their work nevertheless furthers the aims of the feminist, multicultural, Marxist, postcolonial, and queer studies agendas to create intelligibility for situations that are typically occulted by the biopolitical horizons of governments that position certain populations to thrive while leaving others to subsist or perish. 86 In effect, there are real dynamics and circumstances that are being disclosed as the basis for the “structures of feeling” these critics depict. 87 Their many innovations have provoked new questions for literary and cultural critics concerned about how neoliberal capitalism not only undermines physical health but also variegates socioeconomic damage at an affective level.
Elizabeth A. Povinelli’s Economies of Abandonment: Social Belonging and Endurance in Late Liberalism details the impact of long-term vulnerabilities that (neoliberal and imperial) state policies produce and exacerbate rather than alleviate. 88 “Abandonment” names the affective economy of learned helplessness—its gritty, demoralizing repercussions for individuals and their immediate communities struggling to survive seemingly insurmountable conditions. Povinelli’s anthropological lens forcefully conveys the concrete quotidian impasses that undermine survival without dismissing the creativity of the innovations people cobble together in order to navigate dire circumstances.
More “posthumanist” trends in affect theory have drifted away from the coalescence of interests that marked trauma studies in the United States as a seemingly natural outgrowth of the curriculum wars and the new canons showcasing the writing of marginalized groups. Trauma studies in the 1990s was very much consonant with the “giving voice” agenda in aiming to establish intelligibility for the experiences of heretofore silenced women and minorities, the “particulars” who were compelled to default to dominant groups’ “universal” ideas about normativity. This agenda translates to some extent into considerations of affect that remain individual and collective-subject centered, where anxiety, hopelessness, paranoia, ressentiment, and rage indicate the ongoing pressures of pasts that magnetize negative feelings and moods as though the events that provoked them were still present. In the meantime, however, another perspective in affect studies has seemingly dispensed with bounded notions of the subject in order to speculate on the virtual dimensions of sensory experience.
It is no coincidence that the “virtual turn” in affect studies coalesces with the intensifying popularity of Gilles Deleuze as well as his collaborations with Félix Guattari, a staunch critic of psychiatry. In his ingenious resurrections of Baruch Spinoza, David Hume, and Henri Bergson, and in the course of narrating cinema’s history as thought in the Cinema books, Deleuze postulates alternatives to the psychoanalytic view of affect, while his collaborations with Guattari in Anti-Oedipus and A Thousand Plateaus not only encouraged a growing repudiation of psychoanalytic theory’s archaeological and subject-centered hermeneutics but also enacted a plethora of surface reading strategies and posthumanist metaphors that dramatized the prospect of dispensing with bounded subjects altogether. 89
Deleuze and Guattari’s passionate excoriation of the psychoanalytic subject has inspired what might be called a virtual turn in affect theory. In place of Freudian topographies and thermodynamics, the virtual turn has promoted a definition of affect as the byproduct of a fluid relationship between the senses and stimuli that need not emanate from or inhere in an individual consciousness (or unconscious). 90 It is worth acknowledging that this desubjectifying turn away from Freudian and Lacanian understandings of affective investment manifestly extends the scope of posthumanist critique in motivating cultural critics to embrace fluidity, permeability, assemblage, and object-oriented ontology over and against what Wendy Brown criticized as liberalism’s “wounded attachments” to the traumas of historically oppressed groups. 91 More importantly, however, it also responds to a rising sense of dread about the lethal impacts of anthropocentrism that culminate in “extinction events” in the course of destroying the environment for humans among other species.
To counteract anthropocentrism in cultural theory, ecologically-minded posthumanists have sometimes lambasted constructivism for hypostasizing the agency of language and its categories in mediating perceptions and constituting knowledge. The endeavors of these critics to scale back constructivism’s alleged excesses have spurred the emergence of a “new materialist” perspective that grants silenced objects a “co-agential” status, allowing them, in effect, to be seen as well as “heard.” 92 To a certain extent, then, one moralism displaced another, as theory stripped of a cognizing, intentional subject lost still more of its Enlightenment steam. 93
New materialism registered in part as a backlash against the once institutionally powerful vocabularies and reading strategies that distinguished a Eurocentric high theory. One might wonder whether or not this backlash additionally reflected a kind of emotional exhaustion goaded by a multivalent demand for compassion that early multiculturalism and trauma studies seemed to mandate as each newly intelligible voice conveyed another world of suffering, another set of grievances to respond to or feel paralyzed by and guilty about, or all at once. 94 Perhaps, too, the location and scale of the stakes has metamorphosed since the 1990s: in the face of the devastating consequences of reckless greed, consumerism, and climate change denial, trauma has assumed the ubiquity of a present and imminent catastrophe that will overtake every one of the earth’s populations (and some sooner than others). 95 The time has long passed to begin to speculate on traumas to come—the future of trauma studies for a world without a human future.
Conclusion: The Global Scale of Trauma and Memory Studies
The task of sketching the parameters of memory and trauma studies is potentially infinite given the innumerable locations and situations that might serve as objects of inquiry. Possible foci multiply exponentially as memories migrate, circulate, articulate, and transform through different media among geographically dispersed communities. Indeed, insofar as the study of culture might encompass fictional along with real experiences, the prospects for research in memory and trauma studies are only as limited as the imagination. That said, there are, to be sure, various power structures and trends that have overdetermined and often narrowed the privileged academic gaze, which tends to favor writing over oral practices, thus instituting print culture and sites of industrialized reproduction as arbiters of uneven intelligibility. In this connection, the rise of English as a global language is a conspicuous force in focalizing interests in certain memories more than others, a hierarchy that reflects the economic and political dominance not just of the United States and England but also of the European Union’s member states whose elites have long embraced multilingual educations and whose mobile workers have compulsorily adapted to prevailing conditions. Indeed, even if a remembered past is “locally rooted,” it can, simultaneously, be “markedly globalized thanks to the appropriation of a globally circulating language of heritage.” 96 This is to emphasize, once again, that memories of catastrophe and violence are rarely finite and only provisionally collective, since they are subject to spatiotemporal and sociocultural shifts in meaning that can neither be completely neutralized nor permanently foreclosed.
Major events in the 1990s that corroded the insular American and Eurocentric cast of trauma theory at its inception included the dissolution of the South African apartheid government along with a widespread acknowledgment of its crimes and the Rwandan massacre, which resulted in the first International Criminal Court trials for “genocide” (since the UN adopted the Convention on the Prevention and Punishment of Genocide in 1948 , officially codifying Raphael Lemkin’s term). 97 At the same time, accounts detailing Japan’s exploitation of Korean “comfort women” and the “rape of Nanking” during World War II; the partition of India and Pakistan; the Palestinian Day of the Catastrophe (Nakba); Australia’s “Stolen Generations”; Canada’s “residential schools”; the Nigerian-Biafran War; los desaparecidos (“the disappeared”) of Argentina’s “dirty war”; and the Lebanese Civil War continue to claim a rightful place in the annals of world-historical trauma (among too many other “slaughterbench” events marked by mass murder and cultural genocide). 98 The long, entangled, and zigzagging legacies of colonization, forced migration, dire poverty, white supremacist terror, the subordination of and violence against women, sex trafficking, religious persecution, sectarian struggles, assaults on LGBTQ+ individuals, and child abuse by Catholic clergy among others have also frayed the edges of a critical meta-narrative that protests against the Holocaust’s hegemonic centrality in 1990s trauma studies and public culture. 99 It might even be argued that, in accentuating the vicious cross-fertilizations of imperialism and racism, Frantz Fanon and Hannah Arendt (among other proto-trauma theorists) already projected a need for a postcolonial criticism that would rewrite history as the legacy of trauma. 100
In 2009 , Rothberg published Multidirectional Memory: Remembering the Holocaust in the Age of Decolonization , an elegantly written and assiduously researched intervention against a competitive vision of memorial space as “real estate,” a scarce commodity registering a percentage of moral “capital” in the form of sociocultural recognition and an attendant entitlement to compassion. Rothberg notes the circulation of a cultural memory “deficit” figure in commentaries lambasting an “obsession” with the Holocaust as the presumed apex of transgressive cruelty. Critics mounting this attack derided “excessive” attention to the Jewish genocide “at the expense of” the West’s imperialist and colonial violences—traumas that took place outside of Europe. In a similar vein, Holocaust envy targets the Jews’ (“typical”) self-aggrandizement in appropriating more than their fair share of public attention as they secure “real estate” in historical museums and films (the so-called “Shoah business”). 101 In short, when deployed with reference to the Jewish genocide, the scarcity metaphor implies that other deserving communities are being deprived of an equitable allotment of moral capital and public recognition as such.
Moreover, as Israel’s occupation of Palestinian territory continues, a sense of indignation has mounted on the left that the Jews as a minority no longer deserve public sympathy and, indeed, that they deploy a centuries-long history that includes pogroms and mass murder to deflect responsibility for Israel’s crimes. The backlash is also bound up with anger at Israel and its supporters who too frequently invoke the Holocaust and anti-Semitism to intimidate Zionism’s critics. This silencing tactic has, predictably, backfired miserably among those who identify with the Palestinian struggle for a homeland, leaving these critics even less sympathetic both to the plight of Jewish refugees fleeing Europe during and after the World War II but also to the contemporary vulnerability of practicing Jews targeted by right-wing extremists. Putting reductive excoriations of Holocaust studies aside, the time is nevertheless ripe to give precedence to the Palestinians’ present and urgent grievances and to desist from deploying the Jewish genocide in the service of a self-congratulatory American narrative of progress that honors US soldiers and their allies as saviors. 102
Rothberg intervenes in this morass by pointing out that there is no actual “scarcity” where memory is concerned, since bringing up one historical trauma can foster sympathetic attention to another by heightening the latter’s intelligibility. To counter the perspective that figures “collective memory as competitive memory—as a zero-sum struggle over scarce resources,” Rothberg extends Alison Landsberg’s “prosthetic memory” concept to highlight the subject-formative agency of public culture, such as film, in spurring individuals to internalize and potentially act upon vicariously experienced historical pasts. Rothberg proposes to think along the lines of “multidirectional memory,” a more dynamic view of memory as “productive” rather than “privative” insofar as it is subject to ongoing negotiation, cross-referencing, and borrowing.” 103 To be sure, while the Nazis and their crimes have frequently been invoked to promote the cause of “never again,” the seemingly irresistible recourse to the 20th century ’s most frequently summoned specter of ultimate evil can just as likely elicit irritation or impatience. Rothberg is nevertheless right to depose the scarcity premise, especially as a source of resentment. After all, the millions annihilated by the Third Reich and its collaborators did not ask to become the paragon of maniacal cruelty; their memory should be guarded with deference, especially since the extremity of their fates fosters a prurient fascination that popular culture endlessly capitalizes on.
There is, of course, more than ample justification to reflect on how Eurocentrism has too often foreclosed public and academic attention to the southern hemisphere, as if history does not take place there. As Rebecca Saunders correctly observes, “while trauma theory has primarily been produced in Europe and the United States, trauma itself has, with equal if not greater regularity and urgency, been experienced elsewhere.” 104 On this score, postcolonial criticism has advanced knowledge of the circumstances and locations of historical violence as well as their aftereffects. 105 Insofar as memory and history have often been contested sites for various groups and nations at different points in time, both literary fiction and nonfiction as well as literary studies have, since the 1980s, increasingly reflected a range of expression aimed at pushing heretofore marginalized or unknown perspectives into the foreground.
While tracing the Holocaust’s transcultural and transhistorical interfaces, Rothberg has explicitly endeavored to model a “multidirectional” scholarship that acknowledges how more recent events draw upon the moral force and currency of past historical traumas. 106 In Postcolonial Witnessing: Trauma Out of Bounds , his special issue of Studies in the Novel co-edited with Gert Beulens as well as his collaboration with Lucy Bond and Pieter Vermeulen entitled Memory Unbound: Tracing the Dynamics of Memory Studies , Stef Craps has pursued a two-prong process of illuminating multidirectional currents in trauma literature by authors identified with or representing the global South while highlighting urgent new questions for memory studies as a whole. 107 In their introduction to Memory Unbound , Bond, Craps, and Vermeulen cite Marianne Hirsch’s delineation of “postmemory,” Alison Landsberg’s theory of “prosthetic memory,” Astrid Erll and Terri Tomsky on “traveling memory,” as well as Max Silverman’s concept of “palimpsestic memory,” thus productively expanding and updating memory studies’ repertoire of issues, dynamics, and frameworks. 108 The co-editors’s introduction also serves to re-map memory studies from “transcultural,” “transgenerational,” “transmedial,” and “transdisciplinary” perspectives as represented by well-known contributors to the broader field of memory studies such as Aleida Assmann, Marianne Hirsch in collaboration with her partner Leo Spitzer, alongside more recently established scholars such as Rick Crownshaw and Jessica K. Young. Crownshaw, in his turn, previously co-edited The Future of Memory with Jane Kilby and Antony Rowland featuring chapters by Caruth, Sara Guyer, Susan Rubin Suleiman, Dan Stone, Anne Whitehead, and James E. Young—all prominent contributors to trauma and memory studies. 109
In her capacity as a clinical psychologist and the Research Chair for Historical Trauma and Transformation at the University of Stellenbosch in South Africa, Pumla Gobodo-Madikizela has facilitated work on the intergenerational aftermaths of mass dehumanization and violent abuse in South Africa while convening international workshops and symposia that bring together trauma and memory specialists from different continents and arenas of engagement. Alongside her own research and reflections on trauma, cycles of repetition, shame, empathy, and forgiveness and its limits, Gobodo-Madikizela’s organizational work has shaped important dialogues about the backgrounds structuring ongoing situations in and beyond South Africa, bringing activists, social workers, therapists, and filmmakers into conversation with cultural theorists, literature scholars, sociologists, anthropologists, and historians. 110
Discussion of the Literature
Tacking along the interdisciplinary and international currents of literary studies over the last two decades, the following have mobilized new directions in trauma and memory studies that signal the field’s increasingly diverse present and future. Gert Beulens, Sam Durrant, and Robert Eaglestone have thoughtfully mapped emerging trajectories in the field in their edited volume entitled The Future of Trauma Theory: Contemporary Literary and Cultural Theory . 111 With a preface by Rothberg and contributions by the editors and other established scholars (including LaCapra, Roger Luckhurst, and Lyndsey Stonebridge), this volume provides a strong sense of contemporary dynamics in the field, which has been shifting from postcolonial criticism to globalization studies oriented by a Marxist emphasis on “capitalism as the crisis” while increasingly adopting a posthumanist, planetary standpoint that encourages work on climate and environmental trauma, as evinced in Ann Kaplan’s Climate Trauma: Foreseeing the Future in Dystopian Fiction and Film ; Lucy Bond, Ben de Bruyn, and Jessica Rapson’s co-edited Planetary Memory in Contemporary Fiction ; and an interview with Stef Craps headlined as “Memory Studies Goes Planetary” published in the interdisciplinary research journal Exchanges (see also his introduction co-written with Rick Crownshaw to a special issue of Studies in the Novel on climate change fiction). 112
There is not enough space to acknowledge every representative contribution, or to describe every recent direction in memory and trauma studies, but it is worth briefly mentioning a few subfields, critical preoccupations, and strains of inquiry that have dovetailed with these domains over the years. Under the rubric of memory politics, research across the disciplines into the aftermaths of conflict, imperial or colonial displacement, civil war, inter- and intra-racial violence, and genocide have been manifestly sharpened by the issues raised by memory and trauma studies. Psychoanalytic approaches consonant with Deborah P. Britzman’s theorization of “difficult knowledge” have furthered thinking about how to teach the histories and structural effects of human-inflicted catastrophe, especially when the students from dominant groups resist their implication in the traumatic pasts under discussion. 113 Perpetrator studies has assumed some currency in recent years, a counterpoint to a competing tendency to blame the state for various forms of “lateral violence” (such as domestic abuse) among members of historically aggrieved and biopolitically abandoned groups, or to the premise that everyone is implicated in historical processes of victimization. Research focused on “intersectionality” as proposed by Kimberlé Williams Crenshaw sheds light on how racialized oppression and violence are differentially over-determined by class, gender, and sexuality. The perspective referred to as “Afro-pessimism” broaches deeply disturbing arguments about the futility of a progressive narrative in the face of a pervasively entrenched racism that both presumes and ensures that black lives do not matter. 114
Arguing that the “history of capital is inextricable from the history of Atlantic chattel slavery,” Christina Sharpe borrows Maurice Blanchot’s phrasing to portray the writing of anti-Blackness as a disaster that is, paradoxically, never and always present. 115 To advance this claim, Sharpe cites Joy James and João Costa Vargas’s recognition that Black death is “a predictable and constitutive aspect of [American] democracy”—in other words, that the legal and extra-legal murder of unarmed Blacks is not only state-sanctioned but also normative. 116 Her question as to how African Americans are “to live in relation to this requirement for [their] death” is also a challenge to understand trauma beyond the finite or singular wounding event—to investigate it, instead, as the ontology, phenomenology, and epistemology of dwelling with the terrors of social death and imminent execution. 117
In her introduction to In the Wake: On Blackness and Being , Sharpe adopts the wake to convene a sense about the “precarities of the afterlives of slavery” that include “skewed life chances, limited access to health and education, premature death, incarceration, and impoverishment.” 118 Hence, wake refers, first, to “the track left on the water’s surface by a ship; the disturbance caused by a body swimming or moved, in water; it is the air currents behind a body in flight; a region of disturbed flow.” 119 Sharpe’s wake also stands in for a legacy of vulnerability and terror in the hands of police who shoot and kill unarmed Blacks with impunity, such that to be Black is to live “in the line of recoil (of a gun).” 120 As a figure for the ever imminent lethal violence that “precedes and exceeds Blacks” in Frank B. Wilderson III’s phrasing, the wake also signifies “a watch or vigil held beside the body of someone who has died” as well as the ritual through which the bereaved mourn a friend or relative, celebrate the dead person’s life, and watch over the body “from death to burial and the drinking, feasting, and other observances incidental to this.” 121 The interplay between vigil and vigilance is key to this figure, as Sharpe emphasizes, because of the ways Blacks have been repeatedly targeted for death, but also “because any- and everywhere [they] are, medical practitioners treat black people differently” (by not listening to them, and by rationing or denying them access to palliative medicine, for example). 122 Black survival depends on such vigilance, then, just as the cumulative pain of mourning vigils heightens its weathering impacts on physical and mental health. In charting the brutal legacies of the slave ships that brought Africans to American shores, Sharpe constitutes the “Afro-pessimist” standpoint as a parallel trauma studies archive comprising historical flash points, intellectual resources, and sociomoral problematics. This necessarily antidisciplinary archive bears the potential to disrupt white liberal academic longings for racial healing and emancipation through empathetic awareness. 123
A few of the innumerable contributions to trauma studies by researchers and practitioners from psychology, anthropology, and sociology deserve special mention. As Veena Das’s Life and Words: Violence and the Descent into the Ordinary and Avery Gordon’s Ghostly Matters: Haunting and the Sociological Imagination so powerfully illustrate, anthropological and sociological research in the area of violence studies attests to the infinite scope of memory studies, with results as varied as the places and populations that orient investigation. 124 In effect, then, while still abiding with the premise that the personal is the political, work in trauma and memory studies has come a long way since 1992 , when influential writing in the convergent domains of literary and cultural studies was propelled by the recent psychiatric recognition of PTSD, committed to a psychoanalytic framework, and sutured to debates about representing the emotional legacies of the Vietnam War, the Holocaust, slavery, apartheid, sexism, and ethno-racial prejudice. The emergence of this field in the 1990s additionally reflected a desire to reconcile memories of persecution and suffering with poststructuralist critiques of the categories of identity, experience, and reference; however, as such provocations faded over time, the early conceptual self-reflexivity and theoretical inventiveness that shaped the field gave way to the need to move beyond Eurocentric theory canons and to shed light on histories that had theretofore received little attention.
To be sure, as fields are emerging and, indeed, as Freud’s own shifting trajectory suggests, there is more impetus to call attention to their substantive uncertainties and the forms of their disciplinary self-constitution; however, once a field becomes institutionalized through successive iterations, there is less need to conceptualize or ground its authority. In addition, the Internet’s rise has fundamentally transformed not just research but also thinking and reading. Quick access to a vast array of resources has generated new information that invaluably supplements physical visits to sites and archives. Critical agendas that emerged in the 1980s and ’90s nonetheless continue to inform lines of inquiry as contemporary researchers sidestep the temptation to deliver purportedly generalizable insights, opting instead to reflect upon the circumstances and implications of particular cases. Trauma and memory studies has, for this reason, become more concrete yet also dynamic since Yale deconstruction’s heyday while engaging with a more geographically diverse range of voices and pasts.
Further Reading
- Alexander, Jeffrey C. , Ron Eyerman , Bernhard Giesen , Neil J. Smelser , and Piotr Sztompka . Cultural Trauma and Collective Identity . Berkeley and Los Angeles: University of California Press, 2004.
- Assmann, Aleida . Shadows of Trauma: Memory and the Politics of Postwar Identity. Translated by Sarah Clift . New York: Fordham University Press, 2015.
- Ball, Karyn , ed. Traumatizing Theory: The Cultural Politics of Affect in and beyond Psychoanalysis . New York: Other Press, 2007.
- Banki, Peter . The Forgiveness to Come: The Holocaust and the Hyper-Ethical . New York: Fordham University Press, 2018.
- Bennett, Jill . Empathic Vision: Affect, Trauma, and Contemporary Art . Stanford: Stanford University Press, 2005.
- Belau, Linda , and Petar Ramadanovic , eds. Topologies of Trauma: Essays on the Limits of Knowledge and Memory . New York: Other Press, 2002.
- Bond, Lucy , and Stef Craps . Trauma . Abingdon: Routledge, 2020.
- Casper, Monica J. , and Eric Wertheimer , eds. Critical Trauma Studies : Understanding Violence, Conflict, and Memory in Everyday Life . New York: New York University Press, 2016.
- Davis, Colin , and Hanna Meretoya , eds. The Routledge Companion to Literature and Trauma . London: Routledge, 2020.
- Fassin, Didier , and Richard Rechtman . Empire of Trauma: An Inquiry into the Condition of Victimhood . Princeton, NJ: Princeton University Press, 2009.
- Fletcher, John . Freud and the Scene of Trauma . New York: Fordham University Press, 2013.
- Ionesco, Arleen , and Maria Margaroni , eds. Arts of Healing: Cultural Narratives of Trauma . London: Rowman & Littlefield International Ltd, 2020.
- Kaplan, E. Ann . Trauma Culture : The Politics of Terror and Loss in Media and Literature . New Brunswick, NJ: Rutgers University Press, 2005.
- Kaplan, E. Ann , and Ben Wang , eds. Trauma and Cinema: Cross-Cultural Explorations. Hong Kong: Hong Kong University Press, 2009.
- Krämer, Sybille , and Sigrid Weigel , eds. Testimony/Bearing Witness: Epistemology, Ethics, History, and Culture . London: Rowman & Littlefield Publishers, 2019.
- Levy, Daniel , and Natan Sznaider . Human Rights and Memory . University Park: The Pennsylvania State University Press, 2011.
- Miller, Nancy K. , and Jason Tougau , eds. Extremities: Trauma , Testimony, and Community . Urbana and Chicago: University of Illinois Press, 2002.
- Rankine, Claudia . Citizen: An American Lyric . Minneapolis: Graywolf Press, 2014.
- Rothberg. Michael . The Implicated Subject: Beyond Victims and Perpetrators . Stanford: Stanford University Press, 2019.
- Whitlock, Gillian , and Kate Douglas , eds. Trauma Texts . Abingdon: Routledge, 2015.
1. Judith Herman, M. D., Trauma and Recovery: The Aftermath of Violence; From Domestic Abuse to Political Terror (New York: Basic Books, 1992), IX.
2. See Laura S. Brown, “Not Outside the Range: One Feminist Perspective on Psychic Trauma,” in Trauma: Explorations in Memory , ed. Cathy Caruth (Baltimore: Johns Hopkins University Press, 1995), 100–112. For an original treatment of incest from the standpoint of Holocaust and trauma studies, see Janet Walker, Trauma Cinema: Documenting Incest and the Holocaust (Berkeley and Los Angeles: University of California Press, 2005).
3. For a trenchant critique of the reification of PTSD, see Allan Young, The Harmony of Illusions: Inventing Post-Traumatic Stress Disorder (Princeton, NJ: Princeton University Press, 1995);as well as Alan Gibbs, Contemporary American Trauma Narratives (Edinburgh: Edinburgh University Press, 2014). Gibbs seems to accept Young’s standpoint wholeheartedly in characterizing the conversion of PTSD into a set of generic conventions that devolve into clichés in late postmodernist writing. For critical discussions of “trauma culture” and “post-traumatic culture,” see Mark Seltzer, Serial Killers: Death and Life in America’s Wound Culture (New York and London: Routledge, 1998); Kirby Farrell, Post-traumatic Culture: Injury and Interpretation in the Nineties (Baltimore: The Johns Hopkins University Press, 1998); John Mowitt, “Trauma Envy,” in a special issue on “Trauma and Its Cultural Aftereffects” edited by Karyn Ball. Cultural Critique 46 (fall 2000): 272–297; and Griselda Pollock, ed., Visual Politics of Psychoanalysis and the Image in Post-Traumatic Cultures (London and New York: I.B. Tauris, 2013).
4. The controversy over the memorial sometimes touched on its purportedly “emasculated” form. For a feminist analysis of the Vietnam War as an emasculating trauma, see Susan Jeffords, The Re-Masculinization of America: Gender and the Vietnam War (Bloomington: Indiana University Press, 1989). Martin Scorsese’s Palm d’Or–winning Taxi Driver from 1976 is widely viewed as an early cinematic representation of the dangerously traumatized Vietnam War veteran as portrayed by Robert De Niro; however, because the film focuses on a delusional veteran failing to adapt to life after discharge in New York City, it is also manifestly distinct from the films that followed in the 1980s, which tend to depict American soldiers becoming traumatized by the war they were fighting. The latter, significantly, also encouraged American audiences to sympathize with young soldiers scarred by the violence they not only witnessed but also perpetrated. An incomplete list of influential films released during this period includes Platoon (1986), Full Metal Jacket (1987), Good Morning, Vietnam (1987), Hamburger Hill (1987), Casualties of War (1989), and Born on the Fourth of July (1989).
5. Richard Berg and John Carlos Rowe, “American Representations of Vietnam,” special issue, Cultural Critique 3 (Spring 1986). The symptomatology associated with PTSD doubtlessly assumed greater cultural intelligibility for the generations born during and after the war as a result of films that represented American soldiers as “unwilling” perpetrators traumatized by their own violence. Jonathan Shay’s Achilles in Vietnam: Combat Trauma and the Undoing of Character (New York: Scribner, 2003), originally published in 1994, thus reflected and further intensified an investment in studying veterans’ PTSD.
6. Toni Morrison, Beloved: A Novel . New York: Vintage International, 1987).
7. Gibbs, Trauma Narratives , 72–73; and Roger Luckhurst, The Trauma Question (New York: Routledge, 2008).
8. Gibbs, Trauma Narratives , 73.
9. See Rebecca Saunders, “ Disgrace in the Time of a Truth Commission” in “Visceral Reason,” edited by Karyn Ball. Special issue, Parallax 36 (July-September 2005): 99–106
10. In this connection, see Piotr Sztompka’s insightful discussion in “The Trauma of Social Change: A Case of Postcommunist Societies,” in Cultural Trauma and Collective Identity , ed. Jeffrey Alexander, et al. (Berkeley: University of California Press, 2004), 155–195.
11. Barbara Christian, “The Race for Theory,” Feminist Studies 14, no. 1 (Spring 1988): 67–79.
12. See Maurice Halbwachs, On Collective Memory , ed., trans., and introduced by Lewis A. Coser (Chicago: University of Chicago Press, 1992). See also Jeffrey K. Olick, Vered Vinitzky-Seroussi, and Daniel Levy, eds., The Collective Memory Reader (New York: Oxford University Press, 2011). On the constitution of post-traumatic communities through disaster, see Kai Erikson, A New Species of Trouble: The Human Experience of Modern Disaster (New York: W.W. Norton and Company, 1995).
13. See Sigmund Freud, “Childhood Memories and Screen Memories,” The Standard Edition of the Complete Psychological Works of Sigmund Freud, vol. VI: The Psychopathology of Everyday Life (1901 ), translated and edited by. James Strachey in collaboration with Anna Freud (London: The Hogarth Press, 2001), 43–53.
14. Karyn Ball, “Introduction: Trauma and Its Institutional Destinies,” in “Trauma and Its Cultural Aftereffects,” ed. Karyn Ball, special issue, Cultural Critique 46 (2000): 1–44.
15. Richard Brody, “Claude Lanzmann Changed the History of Filmmaking with ‘Shoah’,” The New Yorker , July 6, 2018. Lanzmann’s nine-hour documentary along with Shoshana Felman’s and Dominick LaCapra’s respective chapters on it furthered the symbiosis between Holocaust and trauma studies, hinging on the question of how to represent the diversely fracturing impacts of genocide. See LaCapra, Chapter Four: Lanzmann’s Shoah : “Here There Is No Why,” History and Memory after Auschwitz (Ithaca, NY: Cornell University Press, 1998), 95–135; and Felman and Laub, “Chapter 7: The Return of the Voice: Claude Lanzmann’s Shoah,” Testimony: Crises of Witnessing in Literature, Psychoanalysis, and History (New York: Routledge, 1992), 204–283.
16. Cathy Caruth, ed., Trauma: Explorations in Memory (Baltimore: Johns Hopkins University Press, 1995); Cathy Caruth, Unclaimed Experience: Trauma, Narrative, and History (Baltimore: Johns Hopkins University Press, 1996); Shoshana Felman and Dori Laub, M. D., Testimony: Crises of Witnessing in Literature, Psychoanalysis, and History (New York: Routledge, 1992); Saul Friedländer, Reflections on Nazism: An Essay on Kitsch and Death , trans. Thomas Weyr (Bloomington and Indianapolis: Indiana University Press, 2000); Saul Friedlander, ed., Probing the Limits of Representation: Nazism and the “Final Solution” (Cambridge, MA: Harvard University Press, 1992); Eric L. Santner, Stranded Objects: Mourning, Memory, and Film in Postwar Germany (Ithaca, NY: Cornell University Press, 1990); Dominick LaCapra, Representing the Holocaust (Ithaca, NY: Cornell University Press, 1994); Dominick LaCapra, History and Memory after Auschwitz (Ithaca, NY: Cornell University Press, 1998); Dominick LaCapra, Writing History, Writing Trauma (Baltimore: Johns Hopkins University Press, 2001); Geoffrey H. Hartman, ed., The Longest Shadow: In the Aftermath of the Holocaust (Bloomington and Indianapolis: Indiana University Press, 1996); Marianne Hirsch, Family Frames: Photography, Narrative, and Postmemory (Cambridge, MA: Harvard University Press, 1997); Marianne Hirsch, The Generation of Postmemory: Writing and Visual Culture after the Holocaust (New York: Columbia University Press, 2012).
⤴ Berel Lang, ed., Writing and the Holocaust (Teaneck, NJ: Holmes & Meier Publishers, 1989); Berel Lang, Act and Idea in the Nazi Genocide (Chicago: University of Chicago Press, 1990); Berel Lang, Holocaust Representation: Art within the Limits of History and Ethics (Baltimore: Johns Hopkins University Press, 2000); Lawrence Langer, Holocaust Testimonies: The Ruins of Memory (New Haven, CT: Yale University Press, 1991); Michael Rothberg, Traumatic Realism: The Demands of Holocaust Representation (Minneapolis: University of Minnesota Press, 2000); James E. Young, Writing and Rewriting the Holocaust: Narrative and the Consequences of Interpretation (Bloomington: Indiana University Press, 1988); James E. Young, Texture of Memory: Holocaust Memorials and Meaning (New Haven, CT: Yale University Press, 1993); and James E. Young, At Memory’s Edge: After-Images of the Holocaust in Contemporary Art and Architecture (New Haven, CT: Yale University Press, 2000). Lang’s publications on the Holocaust are almost too numerous to list. The texts mentioned in this note were selected on the basis of their proximity to the “Probing the Limits of Representation” conference at UCLA in 1990.
17. Kelly Oliver, Witnessing beyond Recognition (Minneapolis: University of Minnesota Press, 2001); Michael Bernard-Donals and Richard Geljzer, Between Witness and Testimony: The Holocaust and the Limits of Representation (New York: State University of New York Press, 2001); Michael Bernard-Donals and Richard Geljzer, eds., Witnessing the Disaster: Essays on Representation and the Holocaust (Madison: University of Wisconsin Press, 2003); Ana Douglass and Thomas A. Vogler, eds., Witness and Memory: The Discourse of Trauma (New York: Routledge, 2003); Gary Weissman, Fantasies of Witnessing: Postwar Efforts to Experience the Holocaust (Ithaca, NY: Cornell University Press, 2004); Jakob Lothe with Susan Rubin Suleiman and James Phelan, After Testimony: The Ethics and Aesthetics of Holocaust Narrative for the Future (Columbus: Ohio State University Press, 2012); and Thomas Trezise, Witnessing Witnessing: On the Reception of Holocaust Survivor Testimony (New York: Fordham University Press, 2013).
18. Herman, Trauma and Recovery ; and Felman and Laub, Testimony .
19. Jacques Derrida, The Work of Mourning , ed. Pascale-Anne Brault and Michael Naas (Chicago: University of Chicago Press, 2003), 73.
20. Following a brief stint as a professor of humanities at Johns Hopkins, de Man joined the faculty at Yale University in 1970, where his membership in a cluster of exceptional scholars “brought fame and prestige to what was considered the center of deconstructive theory in the United States in the late 1970s and early 1980s”; Derrida, The Work of Mourning , 70. De Man’s colleagues, students, and imitators admired his innovations of rhetorical analysis and his sensitivity to the indeterminacies of meaning that arise as grammatical oddities and other material elements in a text belie its denotative register. One of de Man’s typical moves, as Kevin Newmark aptly characterizes it, is to show how historical terms, to name one example, “turn out not to be really historical after all, but rather are,” themselves, crude metaphors “for figural relationships”; Kevin Newmark, “Paul de Man’s History,” in Reading de Man Reading , eds. Lindsey Waters and Wlad Godzich (Minneapolis: University of Minnesota Press, 1989), 123. Newmark makes this observation in the course of examining de Man’s apparent dismissal of conventional literary-historical terms in Paul de Man, “Anthropomorphism and Trope in the Lyric,” in The Rhetoric of Romanticism (New York: Columbia University Press, 1986), 239–262. De Man is also well known for demonstrating how theoretical terminology and categories provide a means for critics to avoid actual reading.
21. Louis Menand, “The de Man Case: Does a Critic’s Past Explain His Criticism?” New Yorker , (March 17, 2014), 3.
22. Menand, “The de Man Case,” 4.
23. Menand, “The de Man Case,” 4.
24. On the de Man controversy, see Paul de Man, Wartime Journalism, 1939–1943 , ed. Werner Hamacher, Neil H. Hertz, and Thomas Keenan (Lincoln: University of Nebraska Press, 1988); Jacques Derrida, Memoires for Paul de Man , rev. ed., translations ed. Avital Ronell and Eduardo Cadava (New York: Columbia University Press, 1989); Jacques Derrida, “Paul de Man (1919–83): In Memorium; On the Soul,” in The Work of Mourning , ed. Pascalle-Anne Brault and Michael Naas (Chicago: University of Chicago Press, 2001), 69–75; Jacques Derrida, “Like the Sound of the Sea Deep Within a Shell: Paul de Man’s War,” trans. Peggy Kamuf in Werner Hamacher, Neil Hertz, and Thomas Keenan, eds., On Paul de Man’s Wartime Journalism (Lincoln: University of Nebraska Press, 1989), 127–164; David Lehman, Signs of the Times: Deconstruction and the Fall of Paul de Man (New York: Poseidon, 1991); Evelyn Barish, The Double Life of Paul de Man (New York: Liveright, 2014); Louis Menand, “ The de Man Case: Does a Critic’s Past Explain His Criticism?” ,” March 24, 2014, 1–12; and Marc Redfield, Theory at Yale: The Strange Case of Deconstruction in America (New York: Fordham University Press, 2015).
25. Victor Farías, Heidegger and Nazism (Philadelphia: Temple University Press, 1989).
26. Felman and Laub, Testimony . Felman accepted the Thomas E. Donnelly Professorship in French and Comparative Literature at Yale in 1986.
27. Cathy Caruth, “The Claims of Reference,” Yale Journal of Criticism 4.1 (1991): 193–205; Cathy Caruth, “Unclaimed Experience: Trauma and the Possibility of History in Freud,” Yale French Studies 79 “Literature and the Ethical Question” (winter 1991): 181–193. Both essays also appear in Caruth’s collection, Unclaimed Experience , chaps. 1 and 4. In disseminating the idea of the Holocaust’s “unrepresentability,” the translation and discussion of Lyotard and Adorno in venues such as Yale French Studies and New German Critique were vital. As the first American journal to focus on French and Francophone culture and writing, Yale French Studies in the 1980s and 1990s was instrumental in elevating the fortunes of linguistically turned post-war philosophers and theorists writing in French both before and after their translation into English. Another ascendant journal in this period was New German Critique , which was founded by David Bathrick, Andreas Huyssen, Anson Rabinbach, and Jack Zipes in the early 1970s. This cutting-edge journal played a crucial role in publishing and translating writings by and about the Frankfurt School, thereby introducing it to Anglophone readers, while making space for interdisciplinary scholarship devoted to problems connected with the Holocaust’s representations and their German receptions.
28. Caruth, Unclaimed Experience , ix.
29. Cathy Caruth, ed., “Psychoanalysis, Culture and Trauma,” special issue, American Imago 48.1 (Spring 1991) and Cathy Caruth, ed., “Psychoanalysis, Culture and Trauma,” special issue, American Imago 48.4 (winter 1991; Caruth, Trauma: Explorations in Memory ; and Herman, Trauma and Recovery .
30. Herman, Trauma and Recovery , 1.
31. Naomi Mandel, Against the Unspeakable: Complicity, the Holocaust, and Slavery in America (Charlottesville: University of Virginia Press, 2006), 7.
32. Immanual Kant, Critique of the Power of Judgment , ed. Paul Guyer, trans. Paul Guyer and Eric Matthews (Cambridge, UK: Cambridge University Press, 2000).
33. Kant, Critique , § 25, p. 134.
34. Theodor W. Adorno, “On Lyric Poetry and Society” in Notes to Literature , vol. 1, trans. Shierry Weber Nicholsen (New York: Columbia University Press 1991), 37–54; Theodor W. Adorno, Negative Dialectics , trans. E. B. Ashton (New York: Continuum, 1995); and Karyn Ball, Disciplining the Holocaust (New York: State University of New York Press, 2008).
35. Adorno, Negative Dialectics , 361.
36. Theodor W. Adorno, “On Cultural Criticism and Society,” in Prisms , trans. Samuel Weber and Shierry Weber (Cambridge, MA: MIT Press, 1997), 34.
37. Adorno, “On Cultural Criticism,” 34.
38. Theodor W. Adorno, “Commitment,” in Notes to Literature , vol. 2, trans. Shierry Weber Nicholsen (New York: Columbia University Press, 1992), 87.
39. For Lyotard’s conceptualization of “negative” signs of history, see the last chapter “The Sign of History,” in The Differend (Minneapolis: University of Minnesota Press, 1988), 151–181, 179.
40. Wulf Kansteiner and Todd Presner, “Introduction: The Field of Holocaust Studies and the Emergence of Global Holocaust Culture” in Probing the Ethics of Holocaust Culture (Cambridge, MA: Harvard University Press, 2016), 1–2.
41. See Ernst Nolte, “Zwischen Geschichtslegende und Revisionismus?,” in Historiker-“Streit”: Die Dokumentation der Kontroverse um die Einzigartigkeit der national-sozialistischen Judenvernichtung , ed. Ernst Reinhard Piper (Munich: Reinhard Piper Verlag, 1987), 13–35; and Ernst Nolte, “Vergangenheit, die nicht vergehen will,” in Historiker-“Streit”: Die Dokumentation der Kontroverse um die Einzigartigkeit der national-sozialistischen Judenvernichtung , ed. Ernst Reinhard Piper (Munich: Reinhard Piper Verlag, 1987), 39–47. For the translation of this debate, see James Knowlton and Truett Cates, trans., Forever in the Shadow of Hitler? Original Documents of the Historikerstreit, the Controversy Concerning the Singularity of the Holocaust (New Jersey: Humanities Press, 1993). See also Anson Rabinbach and John Torpey, eds., “Special Issue on the Historikerstreit,” special issue, New German Critique 44 (Spring–Summer 1988), a special issue devoted to the debate, which included, among other pivotal pieces, translations of Jurgen Habermas’s responses to Ernst Nolte.
42. Hayden White, “Historical Emplotment and the Problem of Truth,” in Probing the Limits of Representation: Nazism and the “Final Solution , ” ed. Saul Friedlander (Cambridge, MA: Harvard University Press, 1992), 37. It is worth observing that White’s essay, “The Modernist Event,” amplified this lesson in proclaiming modernism’s particular aptitude for simulating psychologically realist responses to events that derealized conventional oppositions between facts and meaning, truth and fantasy, as well as the “outside” and “inside” of an event; Hayden White, “The Modernist Event,” in Figural Realism: Studies in the Mimesis Effect (Baltimore and London: The Johns Hopkins University Press, 1999), 66–86. It was in this context that he notoriously positioned the “German genocide of six million European Jews” as “paradigmatic among such events” that “function in the consciousness of certain social groups exactly as infantile traumas are conceived to function in the psyche of neurotic individuals.” As he elaborates it, this comparison implies that, “they cannot be simply forgotten and put out of our of mind, or conversely, adequately remembered, which is to say, clearly and unambiguously identified as to their meaning and contextualized in the group memory in such a way as to reduce the shadow they cast over the group’s capacities to go into its present and envision a future free of their debilitating effects”; Hayden White, Figural Realism: Studies in the Mimesis Effect (Baltimore: Johns Hopkins University Press, 1999), 69. A careful reader of White’s work, Rothberg will subsequently identify this standpoint with the lessons he draws from reading Adorno’s and Maurice Blanchot’s respective “meditations on the ‘after Auschwitz’ epoch” to the effect that “post-Holocaust history has a traumatic structure – it is repetitive, discontinuous, and characterized by obsessive returns to the past and the troubling of simple chronology”; Rothberg, Traumatic Realism , 19; see also Maurice Blanchot, Writing the Disaster , trans. Ann Smock (Lincoln and London: University of Nebraska Press, 1995). Rothberg additionally suggests that this “traumatic version of modernism differs from realism in that it is primarily concerned not with the practice of representation, but rather with the metanarrative that the modern age tells about itself and its representational practices”; Rothberg, Traumatic Realism , 19. A passage in his introduction to Traumatic Realism where he disentangles the realist, modernist, and postmodernist strains that alternate in White’s “The Modernist Event” is worth quoting at length: “The realist aims at the mimesis of a certain spatial world, but in confronting the structural problem of the relationship between the extreme and the everyday finds herself caught in a traumatic temporality. The modernist, on the other hand, confronts a particular form of progressive time consciousness, but finds his attempt to establish a before and after frustrated as he is pulled back again and again toward the site of a genocidal crime. Finally, the postmodernist interrogates the reign of the pure image or simulacrum and attempts to negotiate between the demands of memory and the omnipresence of mediation and commodification.” He adds: “The constellation of the three categories corresponds to some of the emblematic figures of an era of extreme violence; the survivor, who attempts to document an undocumentable experience; the bystander, who feels impelled to bear an impossible witness to the extreme from a place of relative safety; and the latecomer or representative of the ‘postmemory’ generation, who, like Spiegelman, inherits the detritus of the twentieth century”; Rothberg, Traumatic Realism , 14.
43. White, “Historical Emplotment,” 37.
44. White, “Historical Emplotment,” 37–38.
45. White, “Historical Emplotment,” 39. His ensuing discussion of Art Spiegelman’s Maus demonstrates how the text “assimilates the events of the Holocaust to the conventions of comic book representation, and in this absurd mixture of a ‘low’ genre with the events of the most momentous significance,” succeeds in posing “all of the crucial issues regarding the ‘limits of representation’ in general” (White, “Historical Emplotment,” 42).
46. White, “Historical Emplotment,” 52; and Lang, Act and Idea .
47. White, “Historical Emplotment,” 37–53; see also the version reprinted in White, Figural Realism , 22–43; Hayden White, Metahistory: The Historical Imagination in Nineteenth Century Europe (Baltimore: The Johns Hopkins University Press, 1973); and Hayden White, The Content of the Form: Narrative Discourse and Historical Representation (Baltimore: Johns Hopkins University Press, 1987).
48. Santner, Stranded Objects .
49. Berel Lang, ed., Writing and the Holocaust (Teaneck, NJ: Holmes and Meier, 1988); and Lang, Act and Idea .
50. Geoffrey H. Hartman, The Longest Shadow ; Hartman, “The Book of the Destruction,” in Probing the Limits of Representation: Nazism and the “Final Solution , ” ed. Saul Friedlander (Cambridge, MA: Harvard University Press, 1992), 318–334; Hartman, ed., Holocaust Remembrance: The Shapes of Memory (Oxford: Basil Blackwell, 1994); Friedlander, “Trauma, Memory, Transference,” in Hartman, ed., Holocaust Remembrance: The Shapes of Memory (Cambridge, MA: Blackwell Publishers, 1994), 252–263; and Shoshana Felman, “Film as Witness: Claude Lanzmann’s Shoah ,” in Hartman, ed., Holocaust Remembrance: The Shapes of Memory (Cambridge, MA: Blackwell Publishers, 1994), 90–103.
51. LaCapra, Representing the Holocaust ; LaCapra, History and Memory ; LaCapra, Writing History ; and Dominick LaCapra, History in Transit: Experience, Identity, Critical Theory (Ithaca, NY: Cornell University Press, 2004).
52. LaCapra, Representing the Holocaust , 111.
53. LaCapra, Representing the Holocaust , 113. LaCapra has argued that Felman’s and Caruth’s discussions about de Man attest to a “transferential” relationship with him insofar as their deconstructive style deflects or attenuates the questions raised by his anti-Semitic war-time journalism and his silence about it afterward. This transference, for LaCapra at least, undermines the explanatory value of their poetically articulated reflections on trauma. LaCapra details this argument against not only Felman but also Derrida in “Paul de Man as Object of Transference,” chap. 4, in Representing the Holocaust: History, Theory, Trauma (Ithaca, NY and London: Cornell University Press, 1994), 111–136. A few years later, in the course of citing Caruth’s chapter on de Man from Unclaimed Experience , LaCapra wonders about “the extent to which [her] version of trauma theory, as an ambitious rewriting of de Manian deconstruction, is able to get beyond the repetition compulsion other than through allegories of excess, incomprehensibility, and empty utopian hope”; LaCapra, History and Memory , 208. What amounts to a guilt-by-association argument is, ultimately, not very persuasive, however, since it presumes that an author’s moral character is necessarily relevant to anything diverse readers might draw from her work. While it is worth contemplating what is at stake in reading a morally compromised author, or reflecting on how to read them (see, for example, Tom Rockmore, On Heidegger’s Nazism and Philosophy [Berkeley and Los Angeles: University of California Press, 1991]), de Man’s and Heidegger’s considerable faults (including but not limited to their anti-Semitism) do not preempt the import of their writing; neither should their disciples’ scholarship be condemned, unless they use it to engage in apologetics, or worse—embrace the master’s dehumanizing prejudices as their own.
54. LaCapra, Representing the Holocaust , 115–116.
55. LaCapra, Representing the Holocaust , 116.
56. Alexander Mitscherlich and Margarete Mitscherlich, The Inability to Mourn: Principles of Collective Behavior (New York: Grove Press, 1975).
57. In one of his most useful explanations of the Real (which he capitalizes), Zizek defines it as “that which resists symbolization: the traumatic point which is always missed but none the less always returns, although we try – through a set of different strategies – to neutralize it, to integrate it into the symbolic order.” Zizek situates this understanding in “the last stage of Lacanian teaching,” where it is figured as “precisely the symptom,” and “as such a real kernel of enjoyment, which persists as a surplus and returns through all attempts to domesticate it, to gentrify it . . . to dissolve it by means of explication, of putting-into-words its meaning”; Slavoj Zizek, The Sublime Object of Ideology (London: Verso, 1989), 69.
58. See LaCapra, Writing History , 43–85.
59. See LaCapra, Representing the Holocaust , 14n; LaCapra, History and Memory , 208n; LaCapra, Writing History , 107–109n, 181–185; and LaCapra, History in Transit , 118–123. Despite the conspicuous evidence of LaCapra’s own highly invested repetition compulsion with respect to Caruth, he nevertheless remarks on Leys’s “extremely judgmental and affectively charged” treatment of the former’s recourses to Bessel van der Kolk; LaCapra, History in Transit , 87n.
60. Ruth Leys, Trauma: A Genealogy (Chicago: University of Chicago Press, 2000), 283; and Caruth, Trauma: Explorations in Memory , 153.
61. Caruth, Trauma: Explorations in Memory , 153. Emphasis in the original.
62. See Bessel A. Van der Kolk, and Onno van der Hart, “The Intrusive Past: The Flexibility of Memory and the Engraving of Trauma,” in Trauma: Explorations in Memory , ed., Cathy Caruth (Baltimore: The Johns Hopkins University Press, 1995), 158–182.
63. Caruth, Trauma: Explorations in Memory , 153.
64. See Caruth, Unclaimed Experience , 10–24, 57–72.
65. For an elegant example of this style, see Rebecca Comay, Mourning Sickness: Hegel and the French Revolution (Stanford, CA: Stanford University Press, 2011).
66. Leys, Trauma , 300. For a magisterial amplification of the staging metaphor throughout Freud’s work, but particularly in his trauma theory, see John Fletcher, Freud and the Scene of Trauma (New York: Fordham University Press, 2013) .
67. Sigmund Freud, Beyond the Pleasure Principle: The Standard Edition of the Complete Psychological Works of Sigmund Freud , vol. 18, trans. and ed. James Strachey in collaboration with Anna Freud (London: Hogarth Press, 2001), 7–64; and Sigmund Freud, Interpretation of Dreams The Standard Edition of the Complete Psychological Works of Sigmund Freud , vols. IV and V, trans. and ed. James Strachey in collaboration with Anna Freud (London: Hogarth Press, 2001).
68. Gilles Deleuze and Félix Guattari, Anti-Oedipus: Capitalism and Schizophrenia , trans. Robert Hurley, Mark Seem, and Helen Lane (Minneapolis: University of Minnesota Press, 1983).
69. Brown, “Not Outside the Range”; and Lauren Berlant, Cruel Optimism (Durham, NC: Duke University Press, 2011). Trauma scholars in literary and cultural fields may have come to know Laura S. Brown from her contribution to Caruth, Trauma: Explorations in Memory . It is worth pointing out that she is a founding member of the Division of Trauma Psychology of the American Psychological Association (APA).
70. See Jeffrey Moussaieff Masson, trans. and ed., The Complete Letters of Sigmund Freud to Wilhelm Fliess 1887–1904 (Cambridge, MA: Belknap Press, 1985); and Jeffrey Moussaieff Masson, The Assault on Truth: Freud’s Suppression of the Seduction Theory (New York: Pocket Books, 1998).
71. In this connection, see Hanna S. Decker, Freud, Dora, and Vienna 1900 (New York: Free Press, 1991); and Claire Kahane, “Chapter Two: Freud’s Passion/Dora’s Voice,” in Passions of the Voice: Hysteria, Narrative, and the Figure of the Speaking Woman, 1850–1915 , (Baltimore: Johns Hopkins University Press, 1995), 14–33.
72. Bill Readings, University in Ruins (Cambridge, MA: Harvard University Press, 1996).
73. Sigmund Freud, “On Narcissism: An Introduction,” in The Standard Edition of the Complete Psychological Works of Sigmund Freud , vol. 14: (1914–1916): On the History of the Psycho-Analytic Movement, Papers on Metapsychology and Other Works , trans. and ed. James Strachey in collaboration with Anna Freud (London: Hogarth Press, 2001), 73–102.
74. In 1997–1998, the Society for the Humanities at Cornell University invited scholars to participate in a year of conversations on “two sets of critical issues that often intersect” relating to the topic of “ 1997–98: Trauma and Psychoanalysis ”: “the widespread attention to trauma and the uses of psychoanalysis as an explanatory model.”
75. See Karyn Ball, “Introduction: Traumatizing Psychoanalysis,” Traumatizing Theory: The Cultural Politics of Affect in and beyond Psychoanalysis (New York: Other Press, 2007), xvii–li; and Maurice E. Stevens, “Trauma Is as Trauma Does: The Politics of Affect in Catastrophic Times,” in Critical Trauma Studies: Understanding Violence, Conflict, and Memory in Everyday Life (New York: New York University Press, 2016), 19–36.
76. Joan Scott, “The Evidence of Experience,” Critical Theory 17 (1991): 773–797.
77. White, Figural Realism ; and Rothberg, Traumatic Realism .
78. Virginia Woolf, Between the Acts (San Diego: Harcourt Brace, 1970).
79. Teresa Brennan, The Transmission of Affect (Ithaca, NY: Cornell University Press, 2004); and Sarah Ahmed, The Cultural Politics of Emotion (New York: Routledge, 2004). It might be recalled that Eve Sedwick co-edited a Silvan Tomkins reader devoted to shame with Adam Frank, which appeared in 1995; Eve Kosofsky Sedgwick and Adam Frank, eds., Shame and Its Sisters: A Silvan Tomkins Reader (Durham, NC: Duke University Press, 1995). This reader contributes more meaningfully to post-psychoanalytic affect theory than Sedgwick’s Touching Feeling: Affect, Pedagogy, Performativity (Durham, NC: Duke University Press, 2003), despite the latter collection’s title.
80. Ahmed, The Cultural Politics , 45. Emphasis in the original.
81. Ahmed, The Cultural Politics , 46.
82. Lauren Berlant, The Queen of America Goes to Washington City (Durham, NC: Duke University Press, 1997); and Lauren Berlant, ed., Intimacy (Chicago: University of Chicago Press, 2000).
83. Berlant, Cruel Optimism .
84. Lauren Berlant, Desire/Love (Brooklyn: Punctum Books, 2012).
85. Judith Butler’s attention to Agamben’s analysis of sovereignty in Judith Butler, Precarious Life: The Powers of Mourning and Violence (London: Verso, 2004) was also pivotal in spurring deeper considerations of biopolitics and precarity in the aftermath of 9/11 and the so-called “war on terror.” See also her chapter entitled “Survivability, Vulnerability, Affect,” in Frames of War: When Is Life Grievable , by Judith Butler (London: Verso, 2010), 33–62.
86. For insightful discussions of racial shame in Frantz Fanon’s Black Skin, White Masks and Toni Morrison’s The Bluest Eye respectively, see Kelly Oliver, “The Good Infection” in a special issue on “Visceral Reason” edited by Karyn Ball, Parallax 36 (2005): 87–98; and Kathleen Woodward’s “Traumatic Shame: Toni Morrison, Televisual Culture, and the Cultural Politics of the Emotions,” in a special issue on “Trauma and Its Cultural Aftereffects” edited by Karyn Ball. Cultural Critique 46 (fall 2000): 210–240.
87. See Raymond Williams, “Chapter 9: Structures of Feeling,” in Marxism and Literature , (Oxford: Oxford University Press, 1977), 129–135.
88. Elizabeth A. Povinelli, Economies of Abandonment: Social Belonging and Endurance in Late Liberalism (Durham, NC: Duke University Press, 2011).
89. Deleuze and Guattari, Anti-Oedipus ; and Gilles Deleuze and Félix Guattari, A Thousand Plateaus: Capitalism and Schizophrenia , trans. and foreword by Brian Massumi (Minneapolis: University of Minnesota Press, 1987).
90. Among the responses to this seemingly paradoxical juncture is Traumatic Affect , a volume of essays edited by Meera Atkinson and Michael Richardson, and featuring essays by Shoshana Felman, Anna Gibbs, and Magdaelna Zolkos among others, which encouraged contributors to rethink the emplotment, location, and intensity of trauma with respect to recent questions posed by affect studies. With a disciplinary home in political science, Zolkos’s work on forgiveness remains committed to subjects who endure, perpetrate, or confront it with varying degrees of cognition. Yet in her editing collaborations with Gerta Roelvink in special issues of Angelaki and Emotions, Space, and Society she has also invited scholars to consider the stakes of posthumanist and new materialist standpoints on affect. See Meera Atkinson and Michael Richardson, Traumatic Affect (Newcastle upon Tyne, UK: Cambridge Scholars, 2013). Magdalena Zolkos, Reconciling Community and Subjective Life: Trauma Testimony as Political Theorizing in the Work of Jean Améry and Imre Kertész (London: Continuum, 2010); Magdalena Zolkos, Restitution and the Politics of Repair: Tropes, Imaginaries, Theory (Edinburgh: Edinburgh University Press, 2020); Magdalena Zolkos and Gerta Roelvink, eds., “Posthumanist Perspectives on Affect,” special issue, Angelaki 20.3 (2015); and Magdalena Zolkos and Gerta Roelvink, eds., “Affective Ontologies: Posthumanist Perpsectives on the Self, Feeling and Intersubjectivity,” special issue, Emotion, Space, and Society 14 (2015).
91. See Wendy Brown, States of Injury: Power and Freedom in Late Modernity (Princeton, NJ: Princeton University Press, 1995).
92. See, for example, Karen Barad, “Posthumanist Performativity: Toward an Understanding of How Matter Comes to Matter,” Signs: A Journal of Women in Culture and Society 28, no. 3 (2003): 801–831.
93. Karyn Ball, “Losing Steam after Marx and Freud: On Entropy as the Horizon of the Community to Come,” Angelaki 3 (2015): 55–78.
94. For incisively argued critical analyses of the discourses of trauma and reparation as they pertain to the figure of the victim, see Didier Fassin and Richard Rechtman, Empire of Trauma: An Inquiry into the Condition of Victimhood (Princeton, NJ: Princeton University Press, 2009) ; and Carolyn Dean, Aversion and Erasure: The Fate of the Victim after the Holocaust (Ithaca, NY: Cornell University Press, 2010); though her previous book, The Fragility of Empathy after the Holocaust (Ithaca, NY: Cornell University Press, 2004), is also germane, albeit less directly.
95. Indeed, circulation and scale have become recent preoccupations in memory studies. See Chiara de Cesari and Ann Rigney, eds., Transnational Memory: Circulation, Articulation, Scale (Berlin, Germany: De Gruyter, 2014).
96. De Cesari and Rigney, Transnational Memory .
97. See Pumla Dineo Gqola, What Is Slavery to Me? Postcolonial/Slave Memory in Post-Apartheid South Africa (Witwatersrand: University of Witwatersrand, 2010); and Josias Semujanga, “Narratives of the Rwandan Genocide,” in The Routledge Companion to Literature , ed., Colin Davis and Hanna Meretoja (London and New York: Routledge, 2020), 395–406 .
98. Iris Chang, The Rape of Nanking: The Forgotten Holocaust of World War II (New York Penguin, 1998); Bashir, Bashir and Amos Goldberg, The Holocaust and the Nakba: A New Grammar of Trauma and History (New York: Columbia University Press, 2018); Rosanne Kennedy, “Moving Testimony: Human Rights, Palestinian Memory, and the Transnational Public Sphere” in Transnational Memory: Circulation, Articulation, Scales , ed., Chiara de Cesari and Ann Rigney (Berlin and Boston: Walter de Gruyter, 2014), 51–78; Rosanne Kennedy, “The Affective Work of Stolen Generations Testimony: From the Archive to the Classroom,” Biography 27, no. 1 (Winter 2004): 48–77. For a summary of research on intergenerational trauma connected with the residential schools in Canada, see Amy Bombay, Kimberly Matheson, and Hymie Anisman, “The Intergenerational Effects of Indian Residential Schools: Implications for the Concept of Historical Trauma,” Transcultural Psychiatry 51.3 (2014): 320–338; on the Nigerian Civil War, see Chinua Achebe, There Was a Country: A Memoir (New York: Penguin Books, 2012); and S. Elizabeth Bird and Fraser M. Ottanelli, The Asaba Massacre: Trauma, Memory, and the Nigerian Civil War (Cambridge, UK:Cambridge University Press, 2017); on los desaparecidos (the disappeared) of Argentina’s Dirty War, see Avery F. Gordon, “Chapter 3: “the other door, it’s floods [sic] of tears with consolation enclosed,” in Ghostly Matters: Haunting and the Sociological Imagination (Minneapolis: University of Minnesota Press, 2008), 63–136; and on cinematic responses to the Lebanese Civil War, see Nouri Gana, “Trauma Ties: Chiasmus and Community in Lebanese Civil War Literature” in Gert Beulens, Samuel Durrant, and Robert Eaglestone, eds., The Future of Trauma Theory: Contemporary Literary and Cultural Criticism (Abingdon, : Routledge, 2014), 77–90; and Zeina Tarraf, “Haunting and the Neoliberal Encounter in Terra Incognita and A Perfect Day ,” Cultural Dynamics 29, no. 1–2 (2017): 39–62.
99. Echoing Michael Rothberg, Chiari de Cesari and Ann Rigney observe that the Holocaust is itself global: “it is indeed the case that globally circulating memories and particularly the memory of the Holocaust – which has itself emerged as a paradigm and model for memory-making world-wide – have helped provide a language in which to articulate other narratives of suffering and loss.” De Cesari and Rigney, Transnational Memory , 10; and Michael Rothberg, Multidirectional Memory (Stanford, CA: Stanford University Press, 2009).
100. See Frantz Fanon, Black Skin, White Masks , trans. Richard Philcox (New York: Grove Press, 2008); and Hannah Arendt, The Origins of Totalitarianism (San Diego: Harcourt, 1994). Sam Durrant and Ryan Topper counter criticisms of Cathy Caruth’s Eurocentrism by foregrounding her conception of the implicated subject, arguing that it exemplifies how trauma theory has, simultaneously, always and never been postcolonial; see Sam Durrant and Ryan Topper, “Cosmological Trauma and Postcolonial Modernity,” in The Routledge Companion to Literature and Trauma , ed., Colin Davis and Hanna Meretoya (London: Routledge, 2020), 187–200 .
101. Rothberg, Multidirectional Memory ; and see Karyn Ball and Per Anders Rudling, “The Underbelly of Canadian Multiculturalism: Holocaust Obfuscation and Envy in the Debate about the Canadian Museum for Human Rights,” Holocaust Studies: A Journal of Culture and History 20, no. 3 (2014): 33–80.
102. Norman Finkelstein has gone so far as to accuse the field of Holocaust studies of rationalizing the ongoing occupation while providing sacred cover for the United States government’s failure to block Israel’s expansion and pursue justice for the Palestinians. See Norman Finkelstein, “Daniel Jonah Goldhagen’s ‘Crazy’ Thesis: A Critique of Hitler’s Willing Executioners ,” New Left Review 224 (July–August 1997): 39–87.
103. Rothberg, Multidirectional Memory , 3.
104. Stef Craps, Postcolonial Witnessing: Trauma out of Bounds (New York: Palgrave-MacMillan, 2013); and Rebecca Saunders, Lamentation and Modernity in Literature, Philosophy, and Culture (New York: Palgrave Macmillan, 2007), 15.
105. For a range of sociologically-oriented perspectives in postcolonial trauma studies, see Ron Eyerman and Giuseppe Sciortino, eds., The Cultural Trauma of Decolonization: Colonial Returnees (London and New York: Palgrave-MacMillan, 2019).
106. Rothberg, Multidirectional Memory .
107. Craps, Postcolonial Witnessing ; Crapsand GertBeulens, eds., “Postcolonial Trauma Novels,” special issue, Studies in the Novel 40, no. 1–2 (2008); and Lucy Bond, Stef Craps, and Pieter Vermeulen, Memory Unbound: Tracing the Dynamics of Memory Studies (New York: Berghahn, 2016).
108. Astrid Erll, “Traveling Memory,” Parallax 17.4 (2011): 4–18; and TerriTomsky, “From Sarajevo to 9/11: Traveling Memory and the Trauma Economy,” Parallax 17, no. 4 (2011): 49–60. Max Silverman’s study of what he calls “palimpsest memory” illuminates how the composite structure of the “buried” or repressed past overlays (and underlies) the present (and vice versa) as well as a “number of different moments, hence producing a chain of signification which draws together disparate spaces and times.” By virtue of this hybrid form, two disparate phenomena “are shown to be profoundly connected, so that what one might have thought of as distinct moments in time and space are recomposed to create a different spatio-temporal configuration.” In effect, what the palimpsest concept “captures most completely,” for Silverman, is “the superimposition and productive interaction of different inscriptions and the spatialization of time central to the work of memory.” Max Silverman, Palimpsestic Memory: The Holocaust and Colonialism in French and Francophone Fiction and Film (New York: Berghahn Books, 2013), 3–4.
109. Rick Crownshaw, Jane Kilby, and Antony Rowland, eds., The Future of Memory (New York: Berghahn Books, 2011).
110. See Pumla Gobodo-Madikizela, A Human Being Died That Night: A South African Woman Confronts the Legacy of Apartheid (New York: Mariner Books, 2004); and Pumla Gobodo-Madikizela, ed., Breaking Intergenerational Cycles of Repetition: A Global Dialogue on Historical Trauma and Memory (Cologne, Germany: Budrich Academic Press, 2016).
111. Beulens, Durrant, and Eaglestone, Future of Trauma Theory .
112. Kaplan, Climate Trauma ; Lucy Bond, Ben de Bruyn, and Jessica Rapson, Planetary Memory in Contemporary American Fiction (Abingdon: Routledge, 2018); Maria Roca Lizarazu and Rebekah Vince, “Memory Studies Goes Planetary: Interview with Stef Craps,” Exchanges: The Interdisciplinary Research Journal 5, no. 2 (2018): 1–15; and Stef Craps and Rick Crownshaw, “Introduction: The Rising Tide of Climate Change Fiction,” Studies in the Novel 50, no. 1 (Spring 2018): 1–8. Craps and Crownshaw’s various collaborations in the 2010s offer a lens on issues and subfields in trauma and memory and trauma studies. See, for example, their 2012 roundtable with Pieter Vermeulen, Ortwin de Graef, Andreas Huyssen, and Vivian Liska in Stef Craps, et al., “Dispersal and Redemption: The Future Dynamics of Memory Studies; A Roundtable,” Memory Studies 5, no. 2 (2012): 223–239; and their 2018 roundtable with Jennifer Wenzel, Rosanne Kennedy, and Claire Colebrook in Stef Craps, et al., “Memory Studies and the Anthropocene: A Roundtable,” Memory Studies 11, no. 4(2018): 498–515.
113. Deborah P. Britzman, Lost Subjects, Contested Objects: Toward a Psychoanalytic Inquiry of Learnin g (Albany: State University of New York Press, 1998).
114. Kimberle Williams Crenshaw, “Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color,” Stanford Law Review 43, no. 6 (July 1991): 1241–1299. For a thumbnail sketch and list of canonical works, see Patrice Douglass, Selamawit D. Terrefe, and Frank B. Wilderson III, “Afro-Pessimism,” Oxford Bibliographies , modified August 28, 2018. Among the more recent references, the entry lists Dionne Brand, A Map to the Door of No Return: Notes to Belonging (Toronto: Vintage, 2002); Matthieu Chapman, Anti-Black Racism in Early Modern English Drama: The Other “Other” (London: Routledge, 2017); Patrice Douglass and Frank B. Wilderson, “The Violence of Presence: Metaphysics in a Blackened World,” The Black Scholar 3, no. 4 (Winter 2013): 117–123; Lewis R. Gordon, Bad Faith and Antiblack Racism (Atlantic Highlands, NJ: Humanities Press, 1995); Saidiya Hartman, Lose Your Mother ; Jared Sexton, “Afro-Pessimism: The Unclear Word ,” Rhizomes 29 (2016); Sharpe, In the Wake ; Selamawit D. Terrefe, “Phantasmagoria: Or, The World Is a Haunted Plantation ,” The Feminist Wire , October 10, 2012; Sylvia Wynter, “No Humans Involved: An Open Letter to My Colleagues,” Forum N. H. I.: Knowledge for the 21st Century 1, no. 1 (Fall 1994): 1–11; Frank B. Wilderson, Incognegro: A Memoir of Exile and Apartheid (Durham, NC: Duke University Press, 2008); and Wilderson, Afropessimism . Names not mentioned in the bibliography but nevertheless pivotal to conversations about Afro-pessimism include Ta-Nehisi Coates, Between the World and Me (New York: Random House, 2015); David Marriott, On Black Men (New York: Columbia University Press, 2000); David Marriott, Haunted Life: Visual Culture and Black Modernity (New Brunswick, NJ: Rutgers University Press, 2007); Achille Mbembe, Necropolitics (Durham, NC: Duke University Press, 2019); Fred Moten, In the Break: The Aesthetics of the Black Radical Tradition (Minneapolis: University of Minnesota Press, 2003); Fred Moten and Stefano Harney, The Undercommons: Fugitive Planning & Black Study (Wivenhoe, NY: Minor Compositions, 2013); Tavia Nyong’o, “Black Survival in the Uchromatic Dark ,” Feminist Wire , December 18, 2012; Claudia Rankine, Citizen: An American Lyric (Minneapolis: Graywolf Press, 2014) ; and Claudia Rankine, “The Condition of Black Life Is One of Mourning ,” The New York Times , June 22, 2015.
115. Sharpe, In the Wake , 5.
116. Sharpe, In the Wake , 7; and Joy James and Costa Vargas, “Refusing Blackness-as-Victimization: Trayvon Martin and the Black Cyborgs,” in Pursuing Trayvon Martin: Historical Manifestations of Racial Dynamics , ed. George Yancy and Janine Jones (Lanham, MD: Lexington Books, 2014), 193.
117. Sharpe, In the Wake , 7.
118. Sharpe, In the Wake , 5; and Saidiya Hartman, Lose Your Mother: A Journey Along the Atlantic Slave Route (New York: Farrar, Strauss, and Giroux, 2007), 6. In this connection, see also Ron Eyerman, Cultural Trauma: Slavery and the Formation of African American Identity (Cambridge, UK: Cambridge University Press, 2001).
119. Sharpe, In the Wake , 3.
120. Sharpe, In the Wake , 8.
121. Sharpe 10–11 citing Frank B. Wilderson, Red, White, and Black: Cinema and the Structure of U.S. Antagonisms (Durham, NC: Duke University Press, 2010), 76.
122. Sharpe, In the Wake , 10.
123. Sharpe writes: “Despite knowing otherwise, we are often disciplined into thinking through and along lines that reinscribe our own annihilation, reinforcing and reproducing what Sylvia Wynter (1994, 70) has called our ‘narratively condemned status’”; Sharpe, In the Wake , 13.
124. Veena Das, Life and Words: Violence and the Descent into the Ordinary (Berkeley: University of California Press, 2007); and Avery Gordon, Ghostly Matters: Haunting and the Sociological Imagination (Minneapolis: University of Minnesota Press, 2007).
Related Articles
- Affect Studies
- Deconstruction
- History and Memory: Narrating the Japanese American Incarceration
- Ethics of Reading
- Mourning and Melancholia
Printed from Oxford Research Encyclopedias, Literature. Under the terms of the licence agreement, an individual user may print out a single article for personal use (for details see Privacy Policy and Legal Notice).
date: 11 June 2024
- Cookie Policy
- Privacy Policy
- Legal Notice
- Accessibility
- [109.248.223.228]
- 109.248.223.228
Character limit 500 /500
Literature review: connections between trauma and substance abuse
- January 2017
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Western University

- King's University College
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Burcu Kardaş B A

- James M. O'Neil

- Claire M. Renzetti
- J.L. Edleson
- Raquel Kennedy Bergen

- John P. Allen
- Marc A. Schuckit

- Claudia Garcia-Moreno
- Alcohol Health Res World
- J.S. Gavalier
- BIOL PSYCHIAT

- Robert L. Trestman

- Psychol Today
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Open access
- Published: 30 July 2022
Childhood trauma, posttraumatic stress disorder symptoms, early maladaptive schemas, and schema modes: a comparison of individuals with obesity and normal weight controls
- Dean Spirou 1 , 2 , 3 ,
- Jayanthi Raman 4 ,
- Ramy H. Bishay 2 , 3 ,
- Golo Ahlenstiel 3 , 5 , 6 &
- Evelyn Smith 7 , 8
BMC Psychiatry volume 22 , Article number: 517 ( 2022 ) Cite this article
3138 Accesses
4 Citations
Metrics details
Previous research on the psychological mechanisms of obesity has primarily focused on acute psychopathology. However, there is limited literature on the role of more complex and entrenched psychological processes in weight management. The current study aimed to expand previous research by examining more enduring psychological constructs, including early maladaptive schemas (EMS), schemas modes, and trauma.
Participants ( N = 125) comprised adults with normal weight ( n = 40) and obesity ( n = 85) from community and clinical settings in Australia. Eligible participants completed a series of self-report questionnaires via Research Electronic Data Capture (REDCap). Two, separate, one-way multivariate analysis of variance (MANOVA) were conducted to examine group differences on the outcome variables.
Findings indicated a significant effect of group on EMS and schema modes, V = .51, F (32, 92) = 2.97, p < .001, partial η 2 = .51. Follow-up univariate tests revealed that individuals with obesity endorsed significantly more maladaptive schemas and schema modes and significantly less healthy schema modes than individuals with normal weight. In addition, results demonstrated a significant effect of group on childhood trauma and posttraumatic stress disorder (PTSD) symptoms, V = .19, F (6, 118) = 4.70, p < .001, partial η 2 = .19. Subsequent univariate tests and chi-square analyses indicated that individuals with obesity reported significantly more childhood trauma as well as significantly more PTSD symptoms within the last month than normal weight individuals.
This was the first study to compare EMS and schema modes in treatment-seeking individuals with obesity and normal weight controls using the short form version 3 of the Young Schema Questionnaire and revised, 118-item, Schema Mode Inventory. Overall, findings revealed that individuals with obesity experience more complex and enduring psychological difficulties than normal weight individuals. Increased assessment and targeted treatment of these underlying mental health concerns may contribute to a more holistic conceptualisation of obesity and could improve the long-term success of weight management.
Peer Review reports
Introduction
Preventing weight regain after weight loss intervention remains the single greatest challenge for individuals with obesity [ 1 , 2 , 3 ]. Successful weight maintenance requires long-term modification of diet and physical activity as well ongoing support [ 1 , 2 , 3 , 4 ]. Psychological factors may impede adherence to diet and physical activity and may hinder long-term weight loss maintenance [ 1 , 4 , 5 , 6 ]. Research on the psychological mechanisms of obesity has predominantly focused on temporary or acute difficulties (e.g., depression, anxiety, binge eating), with limited attention on more complex and entrenched psychological processes. Recently, however, researchers have begun examining more enduring psychological constructs such as early maladaptive schemas (EMS), schemas modes, and trauma.
EMS are central to schema therapy, an integrated psychotherapy incorporating and extending elements of cognitive-behavioural therapy, Gestalt therapy, psychodynamic therapy, and attachment theory [ 7 ]. EMS refer to pervasive and enduring life patterns regarding oneself and one’s relationship with others, and consist of memories, cognitions, physiological sensations, and emotions [ 7 , 8 ]. EMS develop during childhood or adolescence and strengthen over time [ 7 ]. They are theorised to be a result of unmet core emotional needs in childhood (e.g., secure attachment to others, freedom to express valid needs and emotions), primarily due to the interplay between adverse childhood experiences (e.g., traumatisation or victimisation) and emotional temperament [ 7 ]. Young et al. [ 7 ] proposed 18 EMS that are categorised into five domains: Disconnection and Rejection, Impaired Autonomy and Performance, Impaired Limits, Other-Directedness, and Overvigilance and Inhibition (see Additional File 1 for a description of EMS) [ 7 ]. These schemas are initially adaptive coping responses to a child’s environment but become maladaptive over time and may elicit significant impairment [ 7 , 8 ].
Another key concept in schema therapy is the notion of schema modes. Schema modes are moment-to-moment coping responses and emotional states associated with one or several EMS (see Additional File 2 for a description of schema modes) [ 7 ]. Schema modes may be adaptive or maladaptive and are often triggered by contextual circumstances [ 7 ]. Arntz and Jacob [ 8 ] referred to EMS as being conceptually similar to traits, with schema modes depicting the states associated with those schemas. Four categories of modes have been proposed, including Child modes, Dysfunctional Parent modes, Dysfunctional Coping modes, and Healthy modes [ 7 , 8 ]. Child modes are considered universal and innate and resemble the notion of the “inner child” [ 7 , 8 ]. Dysfunctional Parent modes represent the individuals’ internalisation of dysfunctional parenting such as placing excessive pressure on oneself to meet high standards (e.g., critical or demanding voice) [ 7 , 8 ]. Dysfunctional Coping modes reflect an individual’s unhelpful coping strategies such as avoidance, overcompensation, or surrendering [ 7 , 8 ]. Finally, the Healthy modes represent one’s ability to realistically view themselves and life, and feel loved, connected, and joyful [ 7 , 8 ].
Furthermore, early childhood experiences are a critical component in schema therapy. Young et al. [ 7 ] asserted that adverse childhood experiences (e.g., toxic frustration of needs) are the primary origin for EMS. Supporting this notion, Pilkington et al. [ 9 ] found small to large associations between childhood adversity and EMS in adulthood, with the strongest link to a history of childhood emotional abuse. In addition, previous research has demonstrated a positive association between traumatic experiences (e.g., sexual abuse, physical abuse, peer bullying, interpersonal violence) and obesity [ 10 , 11 , 12 ] as well as posttraumatic stress disorder (PTSD) and obesity [ 12 ], with significantly greater impairment to self-esteem, psychosocial functioning, body image, physical health, and eating pathology among those with a lifetime history of PTSD [ 13 ]. Research has also demonstrated a link between traumatic experiences and eating disorders such as binge eating disorder (BED) [ 12 , 14 ]. Together, these findings emphasise the heightened risk of developing maladaptive schemas, eating disorders, and obesity for those with a history of trauma.
In recent years, the schema model has received increasing attention in the field of obesity. Thus far, three studies have utilised the Young Schema Questionnaire, Short Form, Version 2 (YSQ-S2) to compare EMS in individuals with overweight and obesity and normal weight controls [ 15 , 16 , 17 ]. First, Anderson et al. [ 15 ] found that individuals with obesity had significantly higher scores on the Defectiveness/Shame, Social Isolation/Alienation, and Failure schemas relative to normal weight controls. In addition, Basile et al. [ 16 ] reported that the Abandonment, Insufficient Self-Control, Subjugation, and Dependency schemas were significantly higher among the overweight and obesity group compared to the normal weight group. In contrast, however, da Luz et al. [ 17 ] found that individuals with obesity only had significantly higher scores on the Insufficient Self-Control schema compared to normal weight individuals, but this effect became non-significant after controlling for mental health. One explanation for this discrepancy is that da Luz et al. [ 17 ] employed stricter exclusion criteria regarding age, education, and cognitive ability, which limited the variability in their sample. In addition, more than half (54%) of their sample were receiving psychiatric medication at the time of the study, which may have attenuated the activation or presence of EMS, though further research is required to verify this claim. Moreover, one study has investigated differences in schema modes across weight classes using the 124-item Schema Mode Inventory [ 16 ]. Basile et al. [ 16 ] found that the Vulnerable Child, Impulsive Child, and Detached Protector modes were significantly higher among the overweight and obesity group, while the Happy Child and Healthy Adult modes were significantly higher among the normal weight group.
To date, no study has utilised the Young Schema Questionnaire, Short Form, Version 3 (YSQ-S3) to compare EMS in individuals with obesity and normal weight controls. In addition, previous studies using the YSQ-S2 have found inconsistent results regarding group differences. Further, the only study examining schema modes in obesity combined overweight and obesity participants from the community and utilised an earlier iteration of the Schema Mode Inventory, containing 124-items [ 16 ]. To our knowledge, no study has used the refined, 118-item, Short Schema Mode Inventory (SMI) to examine schema modes in treatment-seeking individuals with obesity and normal weight controls. Similarly, previous research on trauma and obesity has primarily focused on individuals in the community, with less emphasis on comparing differences in individuals with obesity attending tertiary services and normal weight controls. Investigating these relationships will contribute to the growing literature on trauma and schema modes in obesity and will contribute to clarifying inconsistent findings in the literature regarding EMS.
The goal of the current study was to examine whether there were significant differences in EMS and schema modes among treatment-seeking individuals with obesity and normal weight controls. This study extends previous research by comparing a normal weight control group to individuals with obesity attending a tertiary weight intervention service, and by utilising the latest iteration of the schema questionnaires, namely the YSQ-S3 and revised SMI. In addition, we aimed to investigate whether individuals with obesity and normal weight significantly differed on childhood trauma and PTSD symptoms. In light of previous research, we hypothesised that the obesity group would have significantly higher scores on the Abandonment, Defectiveness/Shame, Social Isolation/Alienation, Dependence/Incompetence, Failure, Insufficient Self-Control, and Subjugation schemas relative to normal weight controls. Given the existing literature on trauma and obesity, we also hypothesised that individuals with obesity would have significantly higher scores on the Mistrust/Abuse and Emotional Deprivation schemas compared to normal weight individuals. In addition, we predicted that individuals with obesity would have significantly higher scores on the Vulnerable Child, Impulsive Child, and Detached Protector schema modes, but significantly lower scores on the Happy Child and Healthy Adult modes compared to normal weight controls. Further, we hypothesised that the obesity group would have significantly higher scores on childhood trauma and PTSD symptoms compared to the normal weight group.
Participants
Participants ( N = 163) comprised adults with normal weight ( n = 58) and obesity ( n = 105) from Australia. This data overlaps with another study submitted for publication by the same authors, though focuses on distinct research questions and statistical analyses. Normal weight participants were recruited via community advertisements and social media. Participants with normal weight were eligible if aged 18 years or older and BMI was between 18.5 to 24.9 kg/m 2 . Participants with obesity were recruited from the Blacktown Metabolic and Weight Loss Program (BMWLP) at Blacktown Hospital, prior to commencing treatment. The BMWLP is a tertiary level service that provides multidisciplinary weight intervention for adults with obesity, including the option for bariatric surgery for eligible patients. To be eligible for enrolment in the BMWLP, participants required a BMI \(\ge\) 35 kg/m 2 with type 2 diabetes or a BMI \(\ge\) 40 kg/m 2 with at least two obesity-related complications (e.g., hypertension, hyperlipidaemia, sleep apnoea, fatty liver disease, cardiac disease, stroke disease, or joint disease). Recruitment occurred across a 12-month period. All participants were informed about the research aims. Participants in either group were excluded if they had a cognitive or speech impairment, neurological disorder, intellectual disability, head injury, or mental health condition which interfered with their ability to complete or understand the requirements of the study. Eligible participants completed a series of self-report questionnaires via Research Electronic Data Capture (REDCap), a secure web-based software platform [ 18 , 19 ]. The questionnaires took approximately 45–60 min to complete. Community participants were offered a $15 gift voucher as reimbursement. This study was approved by the Western Sydney Local Health District (5450 – 2019/ETH01915) and was ratified by the University of Technology Sydney (ETH20-5545; ETH20-6063).
Of the 163 participants, 37 were excluded because of missing data. One significant outlier was also excluded. The final sample ( N = 125) included males (32.8%) and females (67.2%) that ranged in age from 21 to 79 years ( M = 41.33, SD = 13.98) and ranged in BMI from 19.1 kg/m 2 to 75.4 kg/m 2 ( M = 42.04, SD = 15.77). Of these 125 participants, 40 (32%) were in the normal weight group and 85 (68%) were in the obesity group. Table 1 presents demographic characteristics of the final sample.
Demographics and Eligibility
Sociodemographic information (i.e., sex, age, employment status, education) was collected through a general self-report questionnaire. Mental and physical health information was also collected to determine participant eligibility.
Anthropometrics
Specialised wheelchair scales were used to measure participant height and weight for the obesity group. Self-reported height and weight was used for the normal weight group due to changes in recruitment procedures associated with COVID-19. BMI was computed by dividing weight in kilograms by height in metres squared (kg/m 2 ).
Young Schema Questionnaire – Short Form, Version 3 (YSQ-S3)
The YSQ-S3 is a 90-item self-report measure of EMS [ 20 ]. The YSQ-S3 comprises 18 scales (schemas) with 5 items in each scale. Participants rate a series of statements according to how accurately it reflects them over the past year. Items are rated on a 6-point Likert scale ranging from 1 ( completely untrue of me ) to 6 ( describes me perfectly ). A total score for each scale is derived by summing the scale items. Higher scores indicate greater endorsement of that schema. The YSQ-S3 has demonstrated good internal consistency in clinical and non-clinical samples across several languages (e.g., [ 21 , 22 , 23 , 24 ]).
Short Schema Mode Inventory (SMI)
The SMI is a 118-item self-report measure of moment-to-moment coping responses and cognitive and emotional states [ 25 ]. The SMI assesses 14 scales (schema modes) with 4 to 10 items in each scale. Items are rated on a 6-point Likert scale ranging from 1 ( never or almost never ) to 6 ( all of the time ). The score for each scale is derived by calculating the scale mean. Higher scores indicate greater endorsement of that schema mode. The SMI has demonstrated acceptable internal consistency and test–retest reliability [ 25 ].
Childhood Trauma Questionnaire – Short Form (CTQ-SF)
The CTQ-SF is a 28-item self-report screening measure of retrospective childhood abuse and neglect [ 26 ]. The CTQ-SF comprises five clinical scales: Emotional Abuse, Physical Abuse, Sexual Abuse, Emotional Neglect, and Physical Neglect. Each scale contains five items. Items are rated on a 5-point Likert scale ranging from 1 ( never true ) to 5 ( very often true ). The total score for each scale ranges from 5 to 25 with higher scores suggesting greater exposure to maltreatment. Two main approaches have been applied to interpreting the CTQ-SF. First, the total score for each scale can be classified according to four levels of maltreatment: None (or Minimal), Low (to Moderate), Moderate (to Severe), and Severe (to Extreme) [ 26 ]. Second, a dichotomous cut-off score can be used to differentiate the presence or absence of maltreatment [ 27 ]. Using the dichotomous approach, scores \(\ge\) 10 for Emotional Abuse, 8 for Physical Abuse, 8 for Sexual Abuse, 15 for Emotional Neglect, and 8 for Physical Neglect indicate the presence of maltreatment [ 27 ]. The CTQ-SF also contains a 3-item Minimisation/Denial scale assessing possible underreporting of maltreatment. On this scale, items rated 5 ( very often true ) were coded as 1 ( possible underreporting ), while items rated 1 ( never true ) through 4 ( often true ) were coded as 0 ( no underreporting ). The validity and reliability of the CTQ-SF has been well-supported across both clinical and non-referred samples [ 26 ].
PTSD Checklist for DSM-5 (PCL-5)
The PCL-5 is a 20-item self-report measure of PTSD symptoms within the past month [ 28 ]. Items are rated on a 5-point Likert scale ranging from 0 ( not at all ) to 4 ( extremely ). A total score ranging from 0 to 80 is calculated by summing the items. Higher scores indicate a greater frequency of PTSD symptoms. A provisional PTSD diagnosis is indicated using a cut-off score of 31 to 33. In the current study, participants scoring above 31 were coded as 1 ( provisional diagnosis ), while participants scoring below 31 were coded as 0 ( no diagnosis ). Each item also corresponds with a symptom of PTSD in the Diagnostic and Statistical Manual of Mental Disorders-fifth edition (DSM-5) [ 29 ]. Corresponding items scored 2 ( moderately ) or higher indicate a DSM-5 symptom has been endorsed. The PCL-5 has demonstrated high internal consistency, test–retest reliability, and convergent and discriminant validity [ 30 , 31 ].
Data Analyses
All analyses were carried out using SPSS Version 28.0. Initially, the data was inspected for outliers and missing values, and assumption testing was performed. Missing data was managed through listwise deletion. Two, separate, one-way multivariate analysis of variance (MANOVA) were conducted to examine group differences on the outcome variables. The choice to conduct two separate MANOVA was based on the theoretical and empirical relationship between these variables, and the research aims. It was also anticipated that two separate MANOVA would likely yield the most clinically meaningful interpretations given the paucity of research in this area. Further, fitting separate models has been recommended when there are reasonable theoretical grounds for separating outcome measures [ 32 ]. First, a one-way MANOVA was performed to explore group differences on EMS and schema modes. Second, a one-way MANOVA was conducted to examine group differences on childhood trauma and PTSD symptoms. In addition, chi-square (χ 2 ) analyses were performed to investigate whether groups differed on childhood trauma and provisional PTSD diagnosis using the dichotomous scoring method on the CTQ-SF and PCL-5, respectively. Pillai’s trace (V) was used to interpret the MANOVA results. Pillai’s trace has been recommended as the statistic of choice because of its robustness to model violations [ 33 , 34 , 35 ]. Following a significant MANOVA, separate univariate tests were conducted to examine group differences on the outcome variables. Partial eta-squared (η 2 ) was used as the effect size (.01 = small, .06 = medium, and .14 = large). Bonferroni correction was applied to circumvent inflation of the type 1 error rate due to multiple comparisons. The alpha level for the first and second MANOVA were adjusted to .002 and .008, respectively.
Data Screening
Data from the total sample ( N = 125) was utilised to examine group differences on the outcome variables. All observations were independent, measured on a ratio scale, and randomly sampled from the populations of interest. There were 33 (38.8%) participants in the obesity group and 10 (25%) participants in the normal weight group with scores on the CTQ-SF that suggested possible underreporting of maltreatment (i.e., false negatives). These participants were retained in the analyses. There were no concerns with multicollinearity and there was sufficient observed power (> .80) for all significant effects. Multivariate normality and homogeneity of covariance matrices were partially satisfactory. These model assumptions, however, are susceptible to deviations in large samples [ 32 ]. Nevertheless, the central limit theorem asserts that sampling distribution will be normally distributed in large samples [ 32 , 35 ].
Comparing EMS and Schema Modes Across Groups
Using Pillai’s trace, there was a significant effect of group on EMS and schema modes, V = .51, F (32, 92) = 2.97, p < .001, partial η 2 = .51. As hypothesised, separate univariate tests on the outcome variables revealed that individuals with obesity had significantly higher scores on the Abandonment ( p < .001), Mistrust/Abuse ( p < .001), Emotional Deprivation ( p < .001), Defectiveness/Shame ( p < .001), Social Isolation/Alienation ( p < .001), Dependence/Incompetence ( p < .001), Failure ( p < .001), Insufficient Self-Control ( p < .001), and Subjugation ( p < .001) schemas compared to normal weight controls. Unexpectedly, individuals with obesity also had significantly higher scores on the Vulnerability to Harm and Illness ( p < .001), Self-Sacrifice ( p = .002), Negativity/Pessimism ( p < .001), and Emotional Inhibition ( p < .001) schemas. Furthermore, as predicted, individuals with obesity demonstrated significantly higher scores on the Vulnerable Child ( p < .001), Impulsive Child ( p < .001), and Detached Protector ( p < .001) schema modes as well as significantly lower scores on the Happy Child ( p < .001) and Healthy Adult ( p < .001) modes compared to normal weight controls. Unexpectedly, individuals with obesity also exhibited significantly higher scores on the Angry Child ( p = .002), Undisciplined Child ( p < .001), Compliant Surrender ( p < .001), and Punitive Parent ( p < .001) modes. Table 2 presents the means, standard deviations, and univariate outcomes for EMS and schema modes.
Comparing Childhood Trauma and PTSD Symptoms Across Groups
Using Pillai’s trace, there was a significant effect of group on childhood trauma and PTSD symptoms, V = .19, F (6, 118) = 4.70, p < .001, partial η 2 = .19. As hypothesised, separate univariate tests on the outcome variables revealed that individuals with obesity had significantly higher scores on Emotional Abuse ( p < .001), Physical Abuse ( p < .001), Sexual Abuse ( p = .005), Emotional Neglect ( p = .004), Physical Neglect ( p < .001), and PTSD symptoms ( p < .001) compared to normal weight controls. Table 3 presents the means, standard deviations, and univariate outcomes for childhood trauma and PTSD symptoms.
Using the dichotomous scoring method on the CTQ-SF and PCL-5, chi-square analyses revealed that individuals with obesity reported a significantly higher proportion of Emotional Abuse, χ 2 (1, N = 125) = 6.18, p = .013, Physical Abuse, χ 2 (1, N = 125) = 8.16, p = .004, Sexual Abuse, χ 2 (1, N = 125) = 8.91, p = .003, Emotional Neglect, χ 2 (1, N = 125) = 8.78, p = .003, Physical Neglect χ 2 (1, N = 125) = 14.93, p < .001, and provisional PTSD diagnosis, χ 2 (1, N = 125) = 6.59, p = .010, compared to normal weight individuals. Table 4 presents frequency statistics for the presence of childhood trauma and provisional PTSD diagnosis using the dichotomous method on the CTQ-SF and PCL-5, respectively.
The current study was the first to compare early maladaptive schemas (EMS) and schema modes using the YSQ-S3 and revised SMI, respectively, in normal weight controls and individuals with obesity attending a tertiary weight intervention service. This study also investigated differences in childhood trauma and PTSD symptoms among treatment-seeking individuals with obesity and normal weight controls.
First, consistent with our hypotheses and previous research [ 15 , 16 ], individuals with obesity endorsed significantly higher scores on the Abandonment, Mistrust/Abuse, Emotional Deprivation, Defectiveness/Shame, Social Isolation/Alienation, Dependence/Incompetence, Failure, Insufficient Self-Control, and Subjugation schemas compared to normal weight controls. Unexpectedly, individuals with obesity also demonstrated significantly higher scores on the Vulnerability to Harm and Illness, Self-Sacrifice, Negativity/Pessimism, and Emotional Inhibition schemas. Notably, our findings revealed that all schemas in the Disconnection and Rejection domain were significantly higher in the obesity group, with medium to large effect sizes. The Disconnection and Rejection domain primarily reflects difficulties with developing secure attachments to others [ 7 , 8 ]. Previous research has demonstrated that elevations in this schema domain is related to eating disorders and predicts food addiction symptoms among women with overweight and obesity [ 36 , 37 ].
Specifically, these results suggested that compared to normal weight individuals, those with obesity may perceive their important relationships with others as more unstable (i.e., Abandonment) or may believe that others are more likely to abuse and treat them poorly (i.e., Mistrust/Abuse) and that their emotional needs will remain unsatisfied (i.e., Emotional Deprivation) [ 7 , 8 ]. They may also experience more shame or perceive themselves as more defective (i.e., Defectiveness/Shame) or have a stronger sense of not belonging to communities and social groups due to feeling dissimilar (i.e., Social Isolation/Alienation) [ 7 , 8 ]. In addition, they may believe they are less capable of independently managing daily responsibilities (i.e., Dependence/Incompetence), that catastrophic illness and injury (e.g., heart attack) is unpreventable and imminent (i.e., Vulnerability to Harm and Illness), and that they will inevitably fail and be less successful than peers (i.e., Failure) [ 7 , 8 ]. Furthermore, they may experience greater difficulties with self-control (i.e., Insufficient Self-Control), may be more likely to surrender control to others (i.e., Subjugation), or more likely to prioritise the needs of others at the expense of their own (i.e., Self-Sacrifice) [ 7 , 8 ]. Moreover, they may exhibit a greater preoccupation with negative aspects of life (i.e., Negativity/Pessimism) as well as a greater inhibition of emotion due to the belief that emotions are unnecessary or unpleasant to display (i.e., Emotional Inhibition) [ 7 , 8 ].
Second, consistent with our predictions and previous research [ 16 ], individuals with obesity demonstrated significantly higher scores on the Vulnerable Child, Impulsive Child, and Detached Protector modes as well as significantly lower scores on the Happy Child and Healthy Adult modes relative to normal weight individuals. Unexpectedly, individuals with obesity also displayed significantly higher scores on the Angry Child, Undisciplined Child, Compliant Surrender, and Punitive Parent modes. Specifically, these findings suggested that individuals with obesity experience a higher degree of sadness and desperation (i.e., Vulnerable Child) and may be more likely to act in anger and frustration due to unmet needs (i.e., Angry Child) or to behave in impulsive and uncontrolled ways to satisfy their needs (i.e., Undisciplined and Impulsive Child), but not in a more aggressive or violent manner than normal weight individuals (i.e., Enraged Child) [ 7 , 8 ]. In addition, individuals with obesity more frequently experience a harsh, unforgiving, and critical internalised parent/caregiver voice (i.e., Punitive Parent) but place a degree of pressure on themselves to meet high standards that is similar to normal weight individuals (i.e., Demanding Parent) [ 7 , 8 ]. Further, individuals with obesity adopt a more passive, submissive, and compliant coping method (i.e., Compliant Surrender) as well as a more avoidant, emotionally withdrawn, and detached coping style (i.e., Detached Protector). Moreover, normal weight individuals demonstrate less activated schemas, more satisfied core emotional needs, and more appropriate adult functioning than individuals with obesity (i.e., Happy Child, Healthy Adult) [ 7 , 8 ].
Third, as hypothesised, individuals with obesity demonstrated significantly higher scores on Emotional Abuse, Physical Abuse, Sexual Abuse, Emotional Neglect, Physical Neglect, and PTSD symptoms compared to normal weight individuals. Significant differences between groups were also observed on childhood trauma and provisional PTSD diagnosis using the dichotomous scoring methods on the CTQ-SF and PCL-5. Specifically, 58.8% of individuals with obesity reported the presence of Emotional Abuse, 49.4% reported the presence of Physical Abuse, 28.2% reported the presence of Sexual Abuse, 31.8% reported the presence of Emotional Neglect, 54.1% reported the presence of Physical Neglect, and 37.6% reported PTSD symptoms within the last month that were above the cut-off criteria to suggest a provisional diagnosis of PTSD. These results support previous studies that found an increased probability of developing obesity for those with childhood traumatic experiences and PTSD [ 10 , 11 , 12 , 38 ]. Similarly, these results are comparable with Walsh et al. [ 13 ], who found that one-third of their pre-bariatric surgery sample endorsed a history of physical or sexual abuse in childhood. Together, these findings reiterate that individuals with obesity experience considerably more traumatic experiences and current trauma symptoms than the general population, which may prove detrimental to their mental health and weight management.
Implications
Previous research on the psychological mechanisms of obesity has primarily concentrated on acute psychopathology. This study contributes to elucidating the relationship between obesity and more complex and entrenched psychological processes. Overall, our findings indicated that individuals with obesity endorsed significantly more maladaptive schemas and schema modes and significantly less healthy schema modes than individuals with normal weight. In addition, individuals with obesity reported significantly more childhood trauma as well as significantly more PTSD symptoms within the last month than normal weight individuals. These findings have several clinical implications for the management of obesity and mental health more broadly.
First, they highlight the importance of comprehensively assessing maladaptive schemas and schema modes in weight intervention programs. Identifying how patients view themselves, others, and the world, and their primary coping strategies, may provide valuable insight for targeted intervention. For instance, our findings revealed that individuals with obesity principally display a psychologically withdrawn and submissive or passive coping style. This suggests that patients have developed ways to emotionally detach from their experiences, but do not employ effective strategies to manage their emotional difficulties. These maladaptive coping mechanisms may be activated by underlying schemas and schema modes that are entrenched within the patient (e.g., Punitive Parent, Vulnerable Child). This formulation is conceptually consistent with the schema mode model of obesity proposed by Basile et al. [ 16 ], which theorises that the Compliant Surrender and Detached Protector/Detached Self-Soother modes arise from the patient’s attempt to cope with the Punitive Parent and Impulsive Child modes. Importantly, this pattern of functioning may interfere with weight management over time. Therefore, identifying entrenched schemas and schema modes, including their origins and triggers, could be a critical first step to improving long-term weight management for individuals with obesity.
Second, as part of weight intervention, maladaptive schemas and schema modes should be addressed through psychological treatments such as schema therapy. Schema therapy integrates cognitive, behavioural, and experiential techniques to modify maladaptive coping strategies, reduce the influence of the internalised parent modes, satisfy unmet core emotional needs, and foster healthy functioning [ 7 , 8 ]. Importantly, schema therapy focuses on establishing a safe therapeutic relationship that acknowledges the previously functional role of current maladaptive coping methods (e.g., in response to trauma) and substitutes them with more helpful coping strategies. If untreated, however, underlying schemas and schema modes may interfere with longer-term outcomes due to their pervasive and enduring nature. Therefore, intervention for obesity must inevitably replace maladaptive coping methods (e.g., binge eating) with more functional and adaptive responses. By developing more adaptive coping strategies and minimising maladaptive schema modes, individuals with obesity could remove barriers that potentially impede diet and physical activity and improve longer-term weight management.
Third, these findings emphasise the importance of comprehensively assessing trauma history in weight intervention programs. Research indicates that individuals with obesity with a history of childhood abuse and PTSD demonstrate significantly more eating psychopathology, physical health concerns, and psychological difficulties (e.g., substance misuse, body image) than those without a history of trauma or PTSD [ 13 ]. Further, childhood and adulthood trauma has been linked to eating disorders such as BED [ 12 , 14 ]. If untreated, BED may hinder weight loss outcomes and contribute to weight regain for those undertaking bariatric surgery [ 39 , 40 ]. Therefore, identifying individuals with a history of trauma may be critical to detecting those vulnerable to adverse medical and psychological outcomes. Importantly, however, individuals with obesity may underreport their clinical symptoms to appear more favourable during psychological assessments [ 41 ]. Similarly, they may require intensive intervention over time to accurately recall their traumatic experiences. As a result, it is essential for all health professionals within multidisciplinary teams to be cognisant of the markers of trauma to identify those at increased risk of less successful outcomes.
Finally, these findings reinforce the importance of treating mental health difficulties in weight intervention programs. Psychological difficulties (e.g., eating psychopathology, depression, anxiety, binge eating) have been linked to weight regain after bariatric surgery [ 5 , 42 ] and may interfere with longer-term weight management. As evidenced in our study, individuals with obesity also experience more complex and enduring psychological difficulties, including increased childhood trauma, PTSD symptoms, and maladaptive schemas and schema modes. Childhood trauma may also represent a transdiagnostic risk factor for other mental health concerns, including depression and psychosis [ 43 ]. Future obesity treatment models could consider routine screening for childhood trauma, PTSD, and maladaptive coping strategies, to identify those requiring more intensive intervention. This will contribute to a more holistic and individualised conceptualisation of weight management and could attenuate the influence of psychological mechanisms on long-term weight maintenance.
Limitations, Strengths, and Future Directions
Our results should be considered in the context of several limitations. First, we did not explicitly assess all types of childhood maltreatment (e.g., bullying, parental domestic violence, serious accident/death). As a result, some participants may have experienced childhood adversities that were not captured in this study. For example, MacDonald et al. [ 44 ] found that almost one-third of their participants experienced childhood adversities that were not identified by the CTQ-SF. In addition, childhood maltreatment is often assessed retrospectively, which may contribute to recall inaccuracies. These inaccuracies may be deliberate, due to fear of negative evaluation from others (e.g., stigma associated with the experience), or unintentional, because of an emotional avoidance of the traumatic experience. Future research could utilise longitudinal designs to minimise the potential effects of recall bias when assessing childhood trauma. Furthermore, as proposed by Pilkington et al. [ 9 ], future research could investigate the developmental period of maltreatment (e.g., first 12 months of life, adolescence) as well as the impact of different perpetrators (e.g., mother, father, grandparent, sibling, peer) on outcomes.
Second, responses on schema-related questionnaires may be influenced by active schemas or schema modes at the time of the assessment. For example, individuals in an avoidant coping mode (e.g., Detached Protector) may inadvertently minimise their clinical symptoms, whereas individuals in a Vulnerable Child mode may unintentionally inflate their concerns. Similarly, although EMS are considered relatively stable, it is unclear whether certain questions (e.g., trauma) prime responses or elicit emotional states that influence responding style. In addition, it is unclear whether certain psychiatric medication attenuates schema activation. The potential variability in schema activation at the time of the assessment may contribute to differences in outcomes across the literature, but future research is required to verify this claim. In addition, future research could examine these outcomes over multiple time points to circumvent potential response bias associated with active schemas and schemas modes.
Third, previous research has shown that treatment-seeking individuals with obesity may underreport their clinical symptoms due to fear of treatment ineligibility [ 41 ]. Supporting this claim, our findings indicated that 38.8% of participants in the obesity group provided scores that indicated possible underreporting of childhood maltreatment. This social desirability bias was also observed in the normal weight group, with 25% of participants possibly underreporting childhood maltreatment. Furthermore, we would expect that participants responded with a similar bias to the other questionnaires in our study; however, this was not formally assessed. Therefore, our results should be considered carefully, as they may underestimate the actual prevalence of childhood maltreatment in the current sample as well as the severity of EMS and schema modes. Future research could utilise a multi-method approach (e.g., self-report questionnaire, semi-structured interview) when assessing these constructs to mitigate potential social desirability bias.
Fourth, our sample predominantly consisted of female participants, with a large portion recruited from a clinical setting. Notably, this clinical setting resides in a lower socioeconomic area in Australia than the sample recruited by Anderson et al. [ 15 ] and is characterised by greater medical complexities than a community sample. Australian adults residing in lower socioeconomic regions have a greater likelihood of elevated psychological distress and adverse health complications such as obesity, relative to individuals from higher socioeconomic regions [ 45 , 46 ]. Importantly, community participants were recruited from the same socioeconomic area in Australia to minimise sociodemographic variance across groups. In addition, we excluded participants with severe mental and physical illness and cognitive/intellectual impairment to circumvent the influence of more severe presentations on outcomes. Nonetheless, future research could replicate these findings in a community sample with similar sex distribution and socioeconomic factors, which may improve the external validity of these results. Future studies could also examine whether trauma exposure and coping responses vary among men and women, especially in the context of potential biological differences and culturally acceptable forms of coping. For example, previous research has found that men are more susceptible to environmental stressors (e.g., abuse, neglect) due to differences in neural development [ 47 ], which may have implications for longer-term outcomes. Moreover, future research could investigate the relationship between the onset of obesity (i.e., childhood, adolescence, adulthood) and childhood trauma, EMS, and schema modes.
Finally, there are several notable strengths in the current study. First, we utilised the YSQ-S3 and refined, 118-item SMI, which are the latest iterations of the schema questionnaires. This extends previous literature that compared EMS and schema modes in individuals with obesity and normal weight controls using the YSQ-S2 and 124-item Schema Mode Inventory, respectively [ 15 , 16 , 17 ]. Importantly, though, the motivation and time taken to complete these questionnaires may have contributed to respondent boredom or fatigue, possibly impacting recruitment and the completion rate. Second, our clinical sample comprised treatment-seeking individuals with obesity attending a tertiary weight intervention service, with all participants containing a BMI in the obesity range. This extends the findings of previous studies that combined overweight and obesity participants into one group [ 16 ]. The use of a combined overweight and obesity group may contribute to differences in outcomes, but future research is required to investigate this further. In addition, the inclusion of a treatment-seeking sample elaborates previous research that compared schema modes in normal weight controls and individuals with obesity from the community [ 16 ].
This was the first study to utilise the YSQ-S3 and revised, 118-item, SMI to compare EMS and schema modes in normal weight controls and individuals with obesity attending a tertiary weight intervention service. This study also examined differences in childhood trauma and PTSD symptoms among treatment-seeking individuals with obesity and normal weight controls. Overall, results revealed that individuals with obesity endorsed significantly more maladaptive schemas and schema modes and significantly less healthy schema modes than individuals with normal weight. In addition, individuals with obesity reported significantly more childhood trauma as well as significantly more PTSD symptoms within the last month than normal weight individuals. Future obesity treatment models should incorporate routine assessment of these psychological difficulties, which may contribute to a more holistic conceptualisation of obesity. Moreover, addressing these underlying mental health concerns through evidence-based psychological interventions such as schema therapy, may attenuate the influence of psychological processes on weight management, and could improve the long-term success of patients with obesity.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005. https://doi.org/10.1111/j.1467-789X.2005.00170.x .
Article PubMed Google Scholar
Hall KD, Kahan S. Maintenance of lost weight and long-term management of obesity. Med Clin N Am. 2018. https://doi.org/10.1016/j.mcna.2017.08.012 .
Paixão C, Dias CM, Jorge R, Carraça EV, Yannakoulia M, de Zwaan M, Soini S, Hill JO, Teixeira PJ, Santos I. Successful weight loss maintenance: A systematic review of weight control registries. Obes Rev. 2020. https://doi.org/10.1111/obr.13003 .
Article PubMed PubMed Central Google Scholar
Varkevisser RDM, Van Stralen MM, Kroeze W, Ket JCF, Steenhuis IHM. Determinants of weight loss maintenance: A systematic review. Obes Rev. 2019. https://doi.org/10.1111/obr.12772 .
Mauro MFFP, Papelbaum M, Brasil MAA, Carneiro JRI, Coutinho ESF, Coutinho W, Appolinario JC. Is weight regain after bariatric surgery associated with psychiatric comorbidity? A systematic review and meta-analysis. Obes Rev. 2019. https://doi.org/10.1111/obr.12907 .
Raman J, Spirou D, Jahren L, Eik-Nes TT. The clinical obesity maintenance model: A theoretical framework for bariatric psychology. Front Endocrinol. 2020. https://doi.org/10.3389/fendo.2020.00563 .
Article Google Scholar
Young JE, Klosko JS, Weishaar ME. Schema therapy: A practitioner’s guide. New York: Guilford Press; 2003.
Google Scholar
Arntz A, Jacob G. Schema therapy in practice: An introductory guide to the schema mode approach. John Wiley & Sons; 2017.
Pilkington PD, Bishop A, Younan R. Adverse childhood experiences and early maladaptive schemas in adulthood: A systematic review and meta-analysis. Clin Psychol Psychother. 2021. https://doi.org/10.1002/cpp.2533 .
Gustafson TB, Sarwer DB. Childhood sexual abuse and obesity. Obes Rev. 2004. https://doi.org/10.1111/j.1467-789X.2004.00145.x .
Midei AJ, Matthews KA. Interpersonal violence in childhood as a risk factor for obesity: A systematic review of the literature and proposed pathways. Obes Rev. 2011. https://doi.org/10.1111/j.1467-789X.2010.00823.x .
Palmisano GL, Innamorat M, Vanderlinden J. Life adverse experiences in relation with obesity and binge eating disorder: A systematic review. J Behav Addict. 2016. https://doi.org/10.1556/2006.5.2016.018 .
Walsh E, Rosenstein L, Dalrymple K, Chelminski I, Zimmerman M. The importance of assessing for childhood abuse and lifetime PTSD in bariatric surgery candidates. J Clin Psych Med. 2017. https://doi.org/10.1007/s10880-017-9518-7 .
Trottier K, MacDonald DE. Update on psychological trauma, other severe adverse experiences and eating disorders: State of the research and future research directions. Curr Psychiatry Rep. 2017. https://doi.org/10.1007/s11920-017-0806-6 .
Anderson K, Rieger E, Caterson I. A comparison of maladaptive schemata in treatment-seeking obese adults and normal-weight control subjects. J Psychosom Res. 2006. https://doi.org/10.1016/j.jpsychores.2005.08.002 .
Basile B, Tenore K, Mancini F. Early maladaptive schemas in overweight and obesity: A schema mode model. Heliyon. 2019. https://doi.org/10.1016/j.heliyon.2019.e02361 .
da Luz FQ, Sainsbury A, Hay P, Roekenes JA, Swinbourne J, Da Silva DC, Oliveira DS. Early maladaptive schemas and cognitive distortions in adults with morbid obesity: Relationships with mental health status. Behav Sci. 2017. https://doi.org/10.3390/bs7010010 .
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. https://doi.org/10.1016/j.jbi.2008.08.010 .
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, Mcleod L, Delacqua G, Delacqua F, Kirby J, Duda SN, REDCap Consortium. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019; https://doi.org/10.1016/j.jbi.2019.103208 .
Young JE. Young Schema Questionnaire – Short Form 3 (YSQ-S3). Cognitive Therapy Center; 2005.
Bach B, Simonsen E, Christoffersen P, Kriston L. The Young Schema Questionnaire 3 Short Form (YSQ-S3). Euro J Psychol Assess. 2015. https://doi.org/10.1027/1015-5759/a000272 .
Hawke LD, Provencher MD. The Canadian French Young Schema Questionnaire: Confirmatory factor analysis and validation in clinical and nonclinical samples. Canadian J Behav Sci. 2012. https://doi.org/10.1037/a0026197 .
Kriston L, Schäfer J, Jacob GA, Härter M, Hölzel LP. Reliability and validity of the German version of the Young Schema Questionnaire – Short Form 3 (YSQ-S3). Eur J Psychol Assess. 2013. https://doi.org/10.1027/1015-5759/a000143 .
Phillips K, Brockman R, Bailey PE, Kneebone II. Young Schema Questionnaire-Short Form Version 3 (YSQ-S3): Preliminary validation in older adults. Aging Ment Health. 2019. https://doi.org/10.1080/13607863.2017.1396579 .
Lobbestael J, van Vreeswijk M, Spinhoven P, Schouten E, Arntz A. Reliability and validity of the short Schema Mode Inventory (SMI). Behav Cogn Psychother. 2010. https://doi.org/10.1017/S1352465810000226 .
Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003. https://doi.org/10.1016/s0145-2134(02)00541-0 .
Walker EA, Gelfand A, Katon WJ, Koss MP, Von Korff M, Bernstein D, Russo J. Adult health status of women with histories of childhood abuse and neglect. Am J Med. 1999. https://doi.org/10.1016/S0002-9343(99)00235-1 .
Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. PTSD: National Center for PTSD . 2013. http://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp . Accessed 16 Feb 2022.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). New York: American Psychiatric Pub; 2013.
Book Google Scholar
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J Trauma Stress. 2015. https://doi.org/10.1002/jts.22059 .
Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychol Assess. 2016. https://doi.org/10.1037/pas0000254 .
Field A. Discovering statistics using IBM SPSS statistics. 5th ed. Sage; 2017.
Olson CL. Comparative robustness of six tests in multivariate analysis of variance. J Am Statistical Assoc. 1974. https://doi.org/10.1080/01621459.1974.10480224 .
Olson CL. Practical considerations in choosing a MANOVA test statistic: A rejoinder to Stevens. Psychol Bull. 1979. https://doi.org/10.1037/0033-2909.86.6.1350 .
Tabachnick BG, Fidell LS. Using multivariate statistics. 7th ed. Pearson; 2019.
Imperatori C, Innamorati M, Lester D, Continisio M, Balsamo M, Saggino A, Fabbricatore M. The association between food addiction and early maladaptive schemas in overweight and obese women: A preliminary investigation. Nutrients. 2017. https://doi.org/10.3390/nu9111259 .
Pugh M. A narrative review of schemas and schema therapy outcomes in the eating disorders. Clin Psych Rev. 2015. https://doi.org/10.1016/j.cpr.2015.04.003 .
Danese A, Tan M. Childhood maltreatment and obesity: Systematic review and meta-analysis. Mol Psychiatry. 2014. https://doi.org/10.1038/mp.2013.54 .
Kofman MD, Lent MR, Swencionis C. Maladaptive eating patterns, quality of life, and weight outcomes following gastric bypass: Results of an Internet survey. Obesity. 2010. https://doi.org/10.1038/oby.2010.27 .
Luiz LB, de Souza Brito CL, Debon LM, Brandalise LN, de Azevedo JT, Monbach KD, Heberle LS, Mottin CC. Variation of binge eating one year after Roux-en-Y gastric bypass and its relationship with excess weight loss. PLoS ONE. 2016. https://doi.org/10.1371/journal.pone.0167577 .
Ambwani S, Boeka AG, Brown JD, Byrne TK, Budak AR, Sarwer DB, Fabricatore AN, Morey LC, O’Neil PM. Socially desirable responding by bariatric surgery candidates during psychological assessment. Surg Obes Relat Dis. 2013. https://doi.org/10.1016/j.soard.2011.06.019 .
Freire CC, Zanella MT, Segal A, Arasaki CH, Matos MIR, Carneiro G. Associations between binge eating, depressive symptoms and anxiety and weight regain after Roux-en-Y gastric bypass surgery. Eat Weight Disord. 2021. https://doi.org/10.1007/s40519-019-00839-w .
Haidl TK, Hedderich DM, Rosen M, Kaiser N, Seves M, Lichtenstein T, et al. The non-specific nature of mental health and structural brain outcomes following childhood trauma. Psychol Med. 2021. https://doi.org/10.1017/S0033291721002439 .
MacDonald K, Sciolla AF, Folsom D, Bazzo D, Searles C, Moutier C, Thomas ML, Borton K, Norcross B. Individual risk factors for physician boundary violations: The role of attachment style, childhood trauma and maladaptive beliefs. Gen Hosp Psychiatry. 2015. https://doi.org/10.1016/j.genhosppsych.2015.06.002 .
Australian Institute of Health and Welfare Overweight and obesity: An interactive insight. 2020. https://www.aihw.gov.au/reports/overweight-obesity/overweight-and-obesity-an-interactive-insight . Accessed 16 Feb 2022.
Isaacs AN, Enticott J, Meadows G, Inder B. Lower income levels in Australia are strongly associated with elevated psychological distress: Implications for healthcare and other policy areas. Front Psychiatry. 2018. https://doi.org/10.3389/fpsyt.2018.00536 .
Schore AN. All our sons: The developmental neurobiology and neuroendocrinology of boys at risk. Infant Ment Health J. 2017’ https://doi.org/10.1002/imhj.21616 .
Download references
Acknowledgements
The authors acknowledge the Blacktown Metabolic and Weight Loss Program at Blacktown Hospital (NSW, Australia) for their support with data recruitment.
This research was supported by an Australian Government Research Training Program Scholarship, the NSW Health Education and Training Institute Mental Health Research Award, and the Ainsworth donation.
Author information
Authors and affiliations.
Discipline of Clinical Psychology, Graduate School of Health, University of Technology Sydney, Sydney, NSW, Australia
Dean Spirou
Blacktown Metabolic and Weight Loss Program, Department of Endocrinology and Diabetes, Blacktown Hospital, Blacktown, Sydney, NSW, Australia
Dean Spirou & Ramy H. Bishay
School of Medicine, Western Sydney University, Sydney, NSW, Australia
Dean Spirou, Ramy H. Bishay & Golo Ahlenstiel
School of Psychological Sciences, University of Newcastle, Newcastle, NSW, Australia
Jayanthi Raman
Storr Liver Centre, Westmead Millennium Institute, Westmead Hospital, Sydney, NSW, Australia
Golo Ahlenstiel
Department of Gastroenterology and Hepatology, WSLHD, Blacktown and Mount Druitt Hospitals, Sydney, NSW, Australia
School of Psychology, Western Sydney University, Sydney, NSW, Australia
Evelyn Smith
Translational Health Research Institute, Western Sydney University, Sydney, NSW, Australia
You can also search for this author in PubMed Google Scholar
Contributions
DS and ES conceived the study. DS took the lead in collecting, screening, and analysing the data, as well as writing the manuscript. All authors provided critical feedback and read and approved the final manuscript.
Corresponding author
Correspondence to Evelyn Smith .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Western Sydney Local Health District Human Research Ethics Committee (5450 – 2019/ETH01915) and was ratified by the University of Technology Sydney Human Research Ethics Committee (ETH20-5545; ETH20-6063). All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
ES receives royalties from Taylor and Francis. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:, additional file 2:, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Spirou, D., Raman, J., Bishay, R.H. et al. Childhood trauma, posttraumatic stress disorder symptoms, early maladaptive schemas, and schema modes: a comparison of individuals with obesity and normal weight controls. BMC Psychiatry 22 , 517 (2022). https://doi.org/10.1186/s12888-022-04169-7
Download citation
Received : 16 February 2022
Accepted : 18 July 2022
Published : 30 July 2022
DOI : https://doi.org/10.1186/s12888-022-04169-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Early maladaptive schemas
- Schema modes
- Schema therapy
- Childhood trauma
- Posttraumatic stress disorder
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 13 July 2022
Goal setting with young people for anxiety and depression: What works for whom in therapeutic relationships? A literature review and insight analysis
- Jenna Jacob ORCID: orcid.org/0000-0003-1006-1547 1 ,
- Milos Stankovic 2 ,
- Inga Spuerck 2 &
- Farhad Shokraneh 3
BMC Psychology volume 10 , Article number: 171 ( 2022 ) Cite this article
15k Accesses
7 Citations
21 Altmetric
Metrics details
Goal setting and goal-focused work is widely used in young people’s mental health settings. However, little is known about how, why or for whom this is helpful. This study aims to explore the mechanisms of collaborative goal setting as part of therapeutic relationships: is it helpful for young people experiencing anxiety and/or depression, how and why/not, for whom, and under what circumstances?
Online database searches generated 10,907 records. Seven unique studies are included, combined with insight analysis from directed discussions with international advisors with lived experience of anxiety and/or depression and therapy (N = 8; mean age = 20.8), and mental health academics/clinicians (N = 6).
Findings are presented as a narrative synthesis and suggest that goal setting is helpful to young people experiencing anxiety and/or depression because it helps build good therapeutic relationships through open communication and building trust. Goal setting helps make things more manageable, enabling young people to feel supported and have ownership of their care. Individual preferences, or high levels of distress, trauma, low confidence, hopelessness, negative past experiences of goal setting, perfectionism, and rumination are considered limiting factors to goal setting. Additionally, contextual factors including country and long-term therapy are explored.
Whilst the resultant sample is small, emphasis on the voices of young people in the research is both prominent and of paramount importance. Several key literature gaps are identified, including evidenced links to the reduction in symptoms. Priority must be given to researching unhelpful mechanisms of goal setting for young people experiencing anxiety and/or depression, to avoid any potential iatrogenic effects.
Peer Review reports
Collaborative goal setting within therapeutic mental health settings refers to agreements made between young people and practitioners about specific therapy areas of focus: topics of personalised and meaningful outcome. Goals are concrete representations of intended endpoints, which fill the perceived gap between the current and desired end state [ 1 ]. Goals are usually formulated at the start of therapeutic interventions through a series of discussions. These differ from academic, physical rehabilitation, or general life goals, although there could be overlap. Progress towards these agreed goals may then be tracked over time, often through ratings on numerical scales, and there are tools available to support this. For example, the Goal Based Outcome tool (GBO; [ 2 ]) which comprises setting up to three goals and scoring progress between 0 and 10, is widely used to track progress against goal setting in youth mental health settings. Whilst goal tracking may lead to a shift in practitioners’ work to be goal focused [ 3 ], goals may also sit alongside usual clinical work, to track progress [ 4 ]. Goals set in therapy tend to be focused and specific, e.g., to deal with something in the immediacy, like a phobia [ 5 ], but it is important that these goals attain to more global goals [ 6 ], or are viewed as a “means to an end”.
Goals may take time to set, and can change and become more specific during the therapeutic process, for example, at the beginning of contact with a practitioner, a young person might have a general goal like “to feel less depressed”, but over time the young person, along with the practitioner, may learn more about the mechanisms behind the depression and may define more precise goals like “being able to stop negative thinking” or “being able to cope with flashbacks”. The types of phrases used by practitioners to help young people define goals may include: “what do you want to be different?”, “what will you get off your back?”, “where do you want to get to?”, and “how do you want things to change?” [ 4 , 6 ].
Goal setting and tracking in therapeutic settings is grounded in motivation theory [ 7 , 8 , 9 ] such that working towards goals is a continuous feedback loop which builds on self-efficacy, self-determination and motivation to continue to strive towards goals, acting as a self-regulation strategy [ 10 , 11 ]. Goal setting may be more feasible or acceptable to individuals with particular personality traits e.g., individuals who attribute successes and failures to external factors are less likely to find meaning in striving towards goals than those who attribute successes and failures to their own actions [ 12 ].
Further, young people have described recovery from depression as nested within relationships (e.g., [ 13 ]), portraying recovery as an intentional process, contingent on shared goals and joint action in relationships [ 14 ]. Good therapeutic relationships are considered a key element of effective therapy [ 15 , 16 , 17 , 18 ]. Also known as working relationships, or working/therapeutic alliance, this refers to the connection, bond or partnership between the young person and practitioner. Three key elements of therapeutic alliance have been identified in the literature: bond, tasks, and goals [ 19 ]. In a recent review of the effects of cognitive behavioural therapy (CBT) for young people experiencing anxiety and/or depression, three studies reported small-to-medium effect sizes for the correlational relationship between therapeutic alliance and symptom reduction [ 20 ]. This provides limited evidence linking goal collaboration to reduced anxiety/depression symptoms for young people, despite fair evidence supporting links between goal collaboration and positive adult anxiety and depression outcomes [ 21 ]. It is argued that goal agreement is a fundamental element missing from much work with young people, and it has been referred to as a “social contract” [ 22 ]. This emphasis on relationships is particularly important when working with young people with acute, or multifarious difficulties, where relationships are complex, difficult to develop and maintain (e.g., [ 23 ]).
Existing evidence suggests that there are certain elements of mental health support for young people that are effective, but there is a lack of identification and knowledge about mechanisms to refine and improve this support [ 24 ]. Specifically, there is a paucity of research exploring the mechanisms underpinning why goal setting may be helpful for some young people, and not others. There are likely to be confounding variables which interplay the effectiveness of goals, depression and/or anxiety, cognition, and motivation, yet there is little research that has explored this in clinical settings with young people.
The aim of this study is to summarise existing literature, supplemented by discussions with international advisors to contextualise and aid interpretation of the findings. The research question is:
“Is collaborative goal setting helpful or unhelpful to young people experiencing anxiety and/or depression, as an element of therapeutic relationships? a. Why/why not and how? b. For whom? c. Under what circumstances?”
A mixed methodological approach combined reviews of peer-reviewed, grey literature and additional sources (e.g., websites), with consultation with experts by experience. The risk of expert view biasing the findings was mitigated via the validating steps outlined below. The study was designed by the lead researcher, and other researchers in the team, in collaboration with the peer researchers.
Whilst it is acknowledged that there are important outcome areas such as quality of life and existential factors, aside from symptom reduction, the focus of this study was to specifically explore the research questions in relation to potential anxiety and depression symptom reduction. Anxiety and depression were focused on as the most common mental health difficulties worldwide. This focus on medicalised symptomology differs from quality of life, which is a multi-dimensional construct comprised of several domains, such as psychological, physical, and social wellbeing. Anxiety, depression, therapeutic relationships, and goal progress are routinely measured using self- and proxy-reported outcome measures, with numerical rating scales. It was anticipated that the research question would not be adequately explored through findings from outcome measures alone. Based on some initial scoping work, we determined that there would be more evidence on the effectiveness of goal setting and tracking via qualitative enquiry, including narratives. The exploration of the nuances identified in the research question was key to the study, and so it was important to give precedence to young people’s voices through existing research and youth advisors, combined with findings from any relevant supporting measures. Such explorations would not be possible through quantitative enquiry of outcome measure data.
Goal setting alongside usual clinical work and goals work (goal focused interventions) were differentiated from implicit goal-oriented practice, non-directive approaches and paternalistic approaches to support in this study. This meant that to be included in the literature synthesis, goals needed to be explicitly identified as an approach to progress tracking, and/or informing the work. This study also focused on individual settings, and whilst these relationships may include parents/carers in a triad, the primary focus was on the relationship built between the practitioner and the young person. This was due to the complexities and potential dilution of agreeing goals and developing therapeutic relationships in group work and with parents/carers in addition. Ethical approval was not required because this study did not involve collection nor analysis of primary data, and youth advisors were consulted on in the capacity of being part of the advisory group, rather than within the capacity of research participants [ 25 ].
Literature review
First, search terms and inclusion and exclusion criteria were agreed in collaboration with the academic/clinical and youth advisors (See Additional file 1 : Appendix 1 Inclusion and exclusion criteria and Search Strategies). The project was registered with PROSPERO (number: CRD42021259611).
Second, searches of ten online databases were conducted (PsycINFO (OVID), MEDLINE (OVID), EMBASE (OVID), Web of Science core collection, current contents connect, SciELOCitation Index, Cochrane Library of Systematic Reviews, CINAHL (EBSCO), ERIC (EBSCO), and child and adolescent studies (EBSCO)). The search strategy developed for each database comprised three concepts: anxiety and/or depression (condition), goals (intervention) and therapeutic alliance or general views on goal setting, e.g., perspective, view, narrative (intervention/outcome). Searches were restricted to the past 20 years (2000-present). Citation tracking of included papers was performed. Retrieved hits were exported to EndNote 20 [ 26 ], Rayyan [ 27 ] and Excel for title/abstract screening.
Third, two researchers (FS, JJ) independently screened titles and abstracts. Where one researcher (JJ) was an author in retrieved studies, screening was conducted by the other researcher (FS), to ensure unbiased screening. Fourth, two researchers (JJ, IS) explored resultant literature main texts, extracting and synthesising relevant information. Key literature identified by researchers and advisors was added. The quality of the studies was assessed using criteria for qualitative studies ([ 28 ]; See Additional file 1 : Appendix 2 Core Criteria for Quality Assessment of Qualitative Studies).
Grey literature search
Google and Google Scholar title search, Google Books, PsycEXTRA, PsyArXiv, and ProQuest Dissertations and Theses were used. Google's Site Search was used to search American Psychological Association, British Psychological Society, Australian Psychological Society, European Federation of Psychologists' Associations, International Association of Applied Psychology, Association for Psychological Science, International Union of Psychological Science, Canadian Psychological Association, and UN-affiliated websites (.int domains). To identify more relevant literature, ResearchRabbit.ai was used to track the citations to the included studies. As a result of Google title search, websites were identified and browsed. The searches were restricted to those: (1) written in English, (2) published from January 2000 to August 2021, (3) focused on goal setting with young people experiencing mental health difficulties. Two researchers (FS, JJ) independently screened titles and abstracts of the resultant sources for relevance.
Insight analysis
An advisory group was formed at the study’s outset, comprising: (1) young people with lived experience of anxiety and/or depression and therapy (N = 8; age range 15–26 years; mean age = 20.8; female (includes transgender) N = 5; and male (includes transgender) N = 3; located in Brazil, Pakistan, Spain, Turkey, and UK); and (2) academics and clinicians (N = 6; female N = 1, male N = 5; located in Norway and UK). Criteria for youth advisors to take part where that they were around the age of interest (14–24 years) and had lived experience of anxiety and/or depression and had previously -or currently-experienced receiving a mental health intervention. Youth advisors’ experience of anxiety and/or depression was balanced across advisors. Youth advisors were recruited via adverts circulated by a European network of peer advisors with international reach, and signed an agreement at the outset of the project, by way of consent to participate, which included specific duties and responsibilities of what would be expected of them, as well as hours and reimbursement details. For those under 18 years old, parent/carer consent and agreements were gained. One-to-one meetings between each youth advisor and the participation lead for the study were conducted before and after the study took place. A written agreement was made between the lead research organisation, and the participation organisation which facilitates the network of peer advisors.
Academic/clinical advisors were experienced and specialised in goals work and were recruited via existing networks. Criteria for academic/clinical advisors were that they had research and/or clinical experience in the field of mental health goal setting with young people (academic N = 6; clinical N = 4; categories not mutually exclusive). Written agreements were made between the lead research organisation, and each academic/clinical advisor.
Directed discussions were held at six advisory group meetings (two academic/clinical and four youth) facilitated by two researchers (JJ, MS) and conducted in English. All advisors spoke English, but time was given in the meetings to check understanding, as English was not a native language for many. The academic/clinical and youth advisors met separately, enabling the youth advisors to share openly with their peers. These discussions focused on the research question and drawing inferences about resultant findings, as well as appraising the evidence to identify key literature gaps. The summary of findings from the literature review was presented via PowerPoint to the advisors. The questions asked were broadly: is setting goals an important part of the relationship with the therapist and why/not; do these findings align with your experiences; is there anything you can think of that has not been considered; are there any elements of these findings that do not make sense in your experience; how do you interpret and understand these findings within the context of your own experience? Youth advisors were asked additional questions about the nature of language, for example, what do you think about the term “goal”? Is it the word you use, is it understandable, how does it translate to your national languages?. Field notes were taken, alongside notes in advisors’ own words on the JamBoard interactive workspace, allowing for anonymous contributions. Analysis comprised four stages. First, one researcher (MS) organised field notes and comments into a narrative summary. Second, one researcher (JJ) used the nuanced elements of the research question to organise the summary. Third, feedback was sought from advisors to evaluate and assess whether it was a true reflection of the discussions. Fourth, one researcher (JJ) refined and renamed the themes.
Online searches generated 10,907 records. Ten potentially eligible studies were identified. Upon screening full texts, seven unique studies met the selection criteria (See Fig. 1 and Table 1 ).
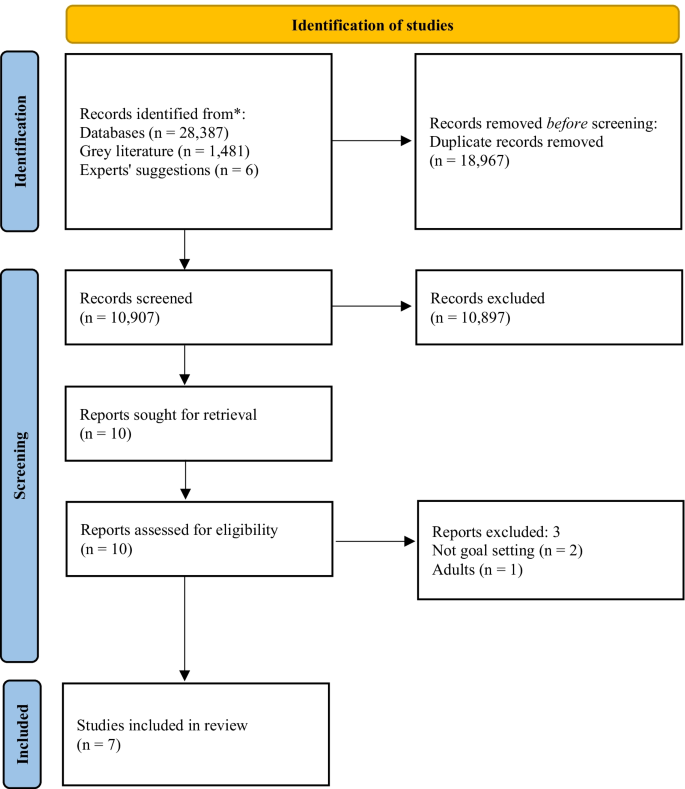
PRISMA flow chart of the study selection process. From: Page, M.J., McKenzie, J.E., Bossuyt, P.M., Boutron, I., Hoffmann, T.C., Mulrow, C.D. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(n71)
Included studies comprised three narrative case studies [ 29 , 30 , 31 ] a randomised control trial [ 32 ]; a narrative review [ 33 ] a practitioners’ guidance document [ 34 ]; and a naturalistic study [ 35 ]. Critical appraisal of the evidence (Table 1 ) demonstrates that caution must be exercised when considering the findings. The main strength of the included studies is the voice of young people through verbatim quotes, and for some, strong consideration of the researchers’ impact. However, less strength is attributed to the dependability or generalisability of the findings, mainly due to the high proportion of small-and-homogenous samples. The advisors’ discussion summaries were organised into themes within the nuances of the research question: Why/why not and how? For whom? Under what circumstances?”, and presented as a narrative synthesis.
Why/why not and how (mechanisms)
A conduit for open communication.
Six studies described collaborative goal setting as a conduit for communication [ 29 , 30 , 31 , 33 , 34 , 35 ]. Specifically, agreement on goals leads to open communication, a shared understanding of difficulties and ways forward [ 29 , 31 , 35 ]. Formulating goals was described as key to helping young people to feeling understood, valued and that practitioners are listening to them [ 33 , 34 , 35 ]. Collaborative goal setting enables young people and practitioners to make genuine disclosures, not necessarily otherwise possible [ 30 ] and facilitates mutual support [ 31 ].
Both academic/clinical and youth advisors said that open communication and trust were key, broadly agreeing that goal setting could be helpful to support building trusting relationships. It was agreed that collaboratively agreeing goals may take time and should not happen immediately. Rather, practitioners should work flexibly, aiming to understand what is comfortable for young people experiencing anxiety and/or depression. Some youth advisors said that relationships need to be built first, with trust established prior to goal setting, particularly when goal setting feels complicated. It was agreed by youth and academic/clinical advisors that goal setting should be led by young people and guided by practitioners, sharing responsibility. Youth advisors considered open communication the most crucial factor in therapy, with a sense that much therapeutic work cannot take place without it.
Feel supported and involved
Young people value receiving support to split actions into smaller manageable steps, with encouragement from practitioners stimulating validation that their goals are achievable ([ 35 ], and youth advisors). Being given choice about goal content and how this translates into the options for care was identified as an important part of the process in the literature [ 35 ]. Evidence suggests that this leads to a sense of autonomy and control over what happens to young people and enables them to feel involved in the process and increases engagement [ 30 , 33 , 35 ]. This was not directly addressed by the academic/clinical advisors in their discussions.
Nature of difficulties
All seven studies, and youth and academic/clinical advisors, suggested that goal setting was a helpful element of therapeutic relationships for young people experiencing anxiety and/or depression, and more broadly with other undefined presenting difficulties. Both academic/clinical and youth advisors agreed that there was no need to separate specific attributes of anxiety or depression, due in part, to high proportions of comorbidity.
Age, and previous experiences
Three studies described difficulties for young people engaging in goal setting [ 32 , 33 , 34 ]. These were: age-appropriate quests for independence interfering with establishing collaborative relationships with adults [ 32 ]; significant and repeated traumas impacting development, relationships and challenges ordering thoughts, particularly within the context of long-term therapy [ 34 ]; low confidence or feelings of hopelessness; and poor previous experiences of goal setting [ 33 ]. Youth advisors agreed that previous life experiences were important, e.g., views of goal setting in therapeutic settings were impacted by how successful they had been in achieving past goals, regardless of goal type. Academic/clinical advisors agreed that personal factors such as previous experiences and factors surrounding—or leading to—difficulties, may lead to challenges setting goals in the first instance.
Levels of distress, personality traits and preferences
Youth and academic/clinical advisors suggested that specific unhelpful elements may depend on the young person, and sometimes levels of distress, rather than the nature of difficulties. Some youth advisors expressed preferences for practitioner-directed work, particularly in times of high distress, e.g.,: “If I’m going through something very bad, I can be very frustrated/sad so I can’t think clear” (youth advisor) . It was also agreed that goals may exacerbate anxiety, particularly at times of overwhelm, whilst for others this could be a helpful anxiety reduction approach, e.g., in exposure therapy. Youth advisors said that ensuring goals are achievable is key to building good therapeutic relationships, and the impact on anxiety/depression; the individual’s capacity to set goals should be considered, e.g., someone struggling with day-to-day tasks may find even small goals too challenging. Youth advisors considered perfectionism to be important, where some people may feel pressure to achieve goals. A sense of hopelessness, or procrastination, and rumination also, where delaying tasks may result in delaying work on goals. For some youth advisors, goal setting felt especially important, whilst for others it was not, rather a supportive relationship was identified as most important, and they could not see how that would be developed through goal setting. Academic/clinical advisors said that young people’s preferences to work on goals, or not, was in itself of key importance to the therapeutic relationship. There was no evidence from the included literature to support/oppose these points.
Language and power dynamics
Linked to preferences, youth advisors said that young people tend not to like the term “goal” because they attribute it to work and formal settings, whereas “therapeutic goals” are personal with deeper meaning. Academic/clinical advisors discussed using alternative language for goal setting and goal directed work, and the importance of being led by the young person. Posing questions such as “What do you want to change?” is suggested as an alternative in the literature ([ 33 ]; p.47). Youth advisors said that whilst some young people may feel able to say they do not want to set goals, others may not, due to the young person-practitioner power imbalance, which has implications for relationships, and therapeutic work. There was no further evidence from the included literature to support/oppose these points.
Under what circumstances (contextual factors)
Broadly helpful.
All seven studies suggested that goal setting was a helpful element of therapeutic relationships for young people within the research contexts. This included year-long narrative therapy with interpersonal therapy and CBT techniques in alliance with the family [ 29 ]; multimodal family therapy [ 31 ]; Gestalt therapy [ 30 ]; either CBT, short-term psychoanalytic psychotherapy or brief psychosocial intervention [ 32 ]; UK child and adolescent mental health services [ 33 , 34 ] and UK inpatient settings [ 35 ]. All studies were based in Western high-income countries. Academic/clinical and youth advisors agreed with this assessment.
Review points and referral routes
Reviewing progress towards goals too frequently could give the impression that practitioners are more interested in gauging their own success, rather than in the young person as a whole person, and rating could end up being done by rote, making goals increasingly meaningless [ 34 ] . Academic/clinical and youth advisors agreed with this, discussing the need to work with goals in a flexible manner. Additionally, young people may not recognise the symptoms identified, particularly when referred for treatment by another party (e.g., parents/carers), which is crucial to enable collaborative goal setting [ 32 ]. Challenges associated with thinking of goals in this way was addressed by the academic/clinical and youth advisors in wider discussions elsewhere (see therapy contexts).
Culture and therapy contexts
Youth and academic/clinical advisors located in Western high-income countries agreed that it may depend on types of interventions offered and practitioner’s preferred working style, but young people largely have agency to set goals. However, it was recognised by the youth and academic/clinical advisors that some young people in some countries do not have agency to set goals. There, decisions are made by families, in collaboration with practitioners, and so less consideration is given to young people’s perspectives. It was suggested that, in some countries, there is no concept of setting goals (e.g., a youth advisor discussed their experience in Pakistan), and ongoing stigma associated with mental health difficulties, which may lead to distrust, scepticism in, and a disconnect with practitioners. Youth advisors said that this may also be true in other countries not represented. A youth advisor suggested that young people in Brazil were relaxed towards goal setting and would not mind if goals were not achieved; directed therapy was considered more helpful.
Youth and academic/clinical advisors discussed goals in long-term therapy as potentially feeling restrictive, with challenges associated with thinking of what goals might be. Both long-and short-term goal setting within this context may feel meaningless, which if then pressed by the practitioner, has a negative impact on relationships. Academic/clinical advisors said that the feasibility of goal setting in the first instance is likely to be attributable to the factors young people who might be offered long-term therapy might have, rather than the work itself leading to these challenges. Youth and academic/clinical advisors also said that where there are multiple needs and risks, goals need to be simpler to feel manageable. Youth advisors said that sometimes there were concerns about the achievement of goals equating to treatment ending, which felt unsettling. There was no evidence from the included literature to support/oppose these points.
This study aimed to provide a synthesis of existing literature, identifying knowledge gaps. Whilst much may be drawn from related research, caution must be exercised when translating findings into other contexts [ 11 ], and whilst promising, generalising adult findings to youth must be exercised with an abundance of caution. Evidence suggests that adults and children think differently; as children grow, their cognitive processes develop, and their contexts and perspectives change, impacting on understandings of the self and the world around them. Further, models of recovery from depression are notably different between adults and young people [ 14 ]. As such, we have focused on evidence from the youth field in our discussion, and further highlight the paucity of research with young people in this area.
The included evidence originates from Western high-income and largely specialist settings; further research in majority world countries is urgently required. Many studies identified in initial searches only partially met inclusion criteria. This evidence paucity may suggest goal setting is not embedded in service standards or practice in most countries, or other limiting factors such as the general underfunding of youth mental health research. Some examples were derived from the insight analysis, highlighting the advisors’ value, who helped contextualise and interpret evidence, grounded in lived experience. However, whilst the research question pertained to the effectiveness of goal setting as part of therapeutic relationships, the findings were related to the feasibility, or acceptability of goal setting itself. Links between effective goal setting, good therapeutic relationships and positive outcomes are inferred based on evidence that partially supports the research question, and the discussions with the advisory group, but no evidence relating to anxiety or depression outcomes was found in this study. Future research should consider in depth explorations of mechanisms of goal setting within therapeutic relationships, for young people experiencing anxiety and/or depression.
For many young people, goal setting is a helpful tool for building good therapeutic relationships via open communication. These findings support previous research which partially address the research question: young people find goal setting to be helpful to therapeutic relationships through the development of a shared language and understanding [ 3 ]. It has been suggested that goals are a mechanism of change via a means for “common ground” to be established [ 3 ]. Finding common ground and a shared understanding are particularly pertinent in youth mental health settings, where there are multiple stakeholders involved [ 36 , 37 , 38 ], which can be a balancing act [ 39 ]. Establishing this mutuality of situations is considered the key facilitator of engagement when referred for therapy by others [ 40 ]. Further, ownership of goals located with young people is important [ 41 ], which in turn gives young people ownership of their care, which can be motivational [ 42 , 43 ]. Young people experiencing anxiety may find goal setting an effective strategy due to links with avoidance motivation; such that they have reported pursuing approach goals to avoid negative emotional consequences of not doing so [ 44 ]. The ability of young people to maintain focus on the pursuit of personal goals has also been demonstrated as a moderator of depression and suicide [ 45 ].
One included study explicitly discussed parents/carers within collaborative goals and therapeutic relationships, as a foundation for mutual support [ 31 ]. Stronger relationships between both young people, parents/carers and practitioners and/or involving both young people and parents/carers in decision-making have been demonstrated to predict more positive outcomes [ 39 , 46 ]. Young people are often referred by their parents/carers, which must be considered, particularly where literature highlights challenges of setting goals when young people do not agree with the referral or recognise the difficulties [ 22 , 32 ]. Prior research has demonstrated that young people from minoritized ethnic groups are more likely to be referred for mental health support via social care and the youth justice system compared to their White British counterparts, who are commonly referred via primary care in the UK [ 47 ]. Further, evidence suggests that increases in emotional autonomy result in a shift from dependence on adults in adolescence, to reliance upon peers for support [ 48 ] particularly amongst girls [ 49 ], which may align with the developmental interference with building relationships outside of goal setting found by Cirasola and colleagues [ 32 ]. It has been argued that for young people who have difficulties building and maintaining relationships, the therapeutic relationship is particularly important (e.g., [ 23 ]). It is also noteworthy that young people in some countries may not have agency to set goals, a significant limiting factor. There are cultural and service level factors which were not explored. In some cultures, advice is sought from family and religious leaders over mental health professionals (e.g., [ 50 ]). Organisational level factors have also been found to hinder and influence therapeutic processes [ 40 ]. Further research is needed into referral routes, and intersections between systems, practice, and young people’s preferences.
Several elements of goal setting were identified as unhelpful for young people experiencing anxiety and/or depression, supporting previous literature. These discussions centred on the feasibility/acceptability of goals, rather than goal setting being detrimental to therapeutic relationships per se. Nevertheless, it is suggested that these factors were primarily related to the person, and that “personal” factors may be driven by underlying difficulties. For example, low confidence, hopelessness, levels of distress, perfectionism, and rumination (e.g., [ 51 , 52 , 53 , 54 , 55 ], may all be elements of anxiety and/or depression. Academic/clinical and youth advisors agreed that goals may become clearer over time, particularly for young people experiencing depression and purposeless, and through collaboration, goals could be formulated. The importance of considering specific challenges of goal setting during long-term therapy was highlighted. Academic/clinical and youth advisors discussed challenges associated with identifying priority areas for work, and that goals continue to flex and change, with the potential for goals work to feel too restrictive. This is in support of previous research suggesting that it is important that goals are worked on flexibly [ 3 ] with space for them to change; specifically in relation to depression. Compared to those with low levels of depression, young people with high levels of depression are more able to disengage with unhelpful goals over time and to set new goals, which in turn may predict lower levels of depressive symptoms over a year later [ 56 ]. This sense of goals flexing, feeling unique and changeable has been mirrored in descriptions of therapeutic relationships themselves [ 23 ]. There was a clear steer from youth advisors that the relationship independent of goal setting was key to good outcomes, and that this was a priority; that without the trusting relationship, there is no facilitator for goal setting. This is an important contradiction to the literature, warranting further exploration. One suggestion is that the initial goals for long-term therapy should be on relationship building, but reviewed, so the therapeutic relationship itself does not remain the primary goal [ 34 ]. Another key finding is that goals take time to establish, and pressure to set goals may render them meaningless, which also supports previous research [ 51 ]. Young people often do not know what their goals are [ 57 ], which impacts trust building, relationships and thus, therapeutic work. In support of prior research which defines recovery as contingent on shared goals and joint action in relationships [ 14 ], links found between goals, trust building and therapeutic relationships in the present study align with research on trauma informed care, and emotional and relational safety (see, [ 58 ]). Further consideration should be given to this area, particularly clinical implications, and interactions with levels of distress.
Whilst support approaches that incorporate structured goal setting are often characterised by a greater emphasis on client-centredness, the links between personally meaningful outcomes and the specific behaviour change techniques required to progress towards goals are not clear. Further, the person-centred focus is hypothesised as a conduit to positive ratings of self-efficacy, quality of life and service satisfaction, but evidence is lacking [ 11 ]. Whilst previous literature from within the youth mental health field suggests that working on goals is motivating and increases self-efficacy [ 34 , 42 ], evidence is still limited. Goal setting may be useful to young people because, whilst not necessarily synonymous, it has been demonstrated as a facilitative element of shared decision-making [ 59 , 60 ]. This collaborative way of working through shared understanding and the development of good therapeutic relationships [ 61 ] may be especially helpful to young people experiencing depression as it enables them to exercise control over their own feelings and behaviour [ 43 ] at a time when they may be experiencing feelings of hopelessness and purposeless. Whilst educated links are made to shared decision-making, further research should explore whether there is an embedded link to goals and therapeutic relationships.
Strengths and limitations
The mixed-methodological approach was a particular strength, with literature findings bolstered by lived experience. However, whilst advisors were from diverse demographic groups, not all groups were represented.
Whilst every attempt was made to include as many goal setting search terms as possible, the language is broad and fluid, meaning certain terms may have been missed. Still, the high number of results returned from literature searches suggests the strategy may need refinement. Nevertheless, we chose to ensure a large return given the subject’s broad nature. At the screening stage, the focus on explicitly identified goal setting and goal work made the identification of included studies less ambiguous, but meant that studies focused on implicit goals work would not have been included, reducing the number of studies included in the final synthesis.
Prior assumptions and knowledge of this topic will have influenced the researchers’ interpretation of the findings, even subconsciously. This includes the decision to use the nuanced elements of the research question to organise the findings. The researchers were located in Belgium, Germany, and the UK at the time of the study, which risks the perpetuation of the status quo of Western high-income-originating dominated research. Further, the findings were contextualised and linked to prior theory primarily by a researcher outside the age range of interest (JJ). The impact of both issues was mitigated via advisors, particularly those within majority world countries and the age range of interest, and the peer researchers entrenched in the research team (MS, IS), who provided contextual depth and understanding to the findings.
Literature focused on goal setting as helpful for young people with anxiety and/or depression is overwhelmingly supportive, but this leaves research gaps regarding in which ways, for whom and under what circumstances goal setting might be unhelpful. Priority must be given to researching unhelpful mechanisms of goal setting, to avoid potential iatrogenic effects. Accessibility could be improved through exploration of the intersections between systems/contexts (e.g., country), therapeutic practice (e.g., practitioner’s training/preferences) and young people’s preferences. Further research is also needed to explore mechanisms by which goal setting may help to reduce anxiety and/or depression symptoms, as well as other important areas of outcome, such as quality of life, using e.g., mediation analysis.
Scaling up in countries with well-developed systems could mean embedding goals in guidelines for anxiety and/or depression; in service specifications, including monitoring and reporting change mechanisms; staff training in consistency; and some interagency forums to align goal processes. For majority world countries with less developed systems, largely relying on non-specialist services e.g., NGOs, goals may be paradoxically more important for maximising limited resources. Despite nothing suggesting goal setting could not practically be scaled-up globally, cultural considerations may be a limiting factor in some places.
Preferences to not work on goals may be driven by the limiting factors identified, such as hopelessness or high distress. Practitioners should work through this first, reviewing the option to work on goals over time, respecting young people’s preferences. Flexibility is important, and ownership of goals located with young people is essential, particularly to those experiencing depression, enabling them to exercise control over their feelings and behaviour when they may be feeling hopeless and/or purposeless. Finally, there may be a unique opportunity for goals to facilitate work with young people experiencing high distress levels or who have experienced trauma, due to links to emotional and relational safety and building trusting relationships.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available to protect the confidentiality of the small number of advisors, but may be available from the corresponding author’s organisation, on reasonable request.
Abbreviations
Cognitive behavioural therapy
Goal based outcomes tool
United Kingdom
Austin JT, Vancouver JB. Goal constructs in psychology: structure, process, and content. Psychol Bull. 1996;122(3):338–75.
Article Google Scholar
Law D. Goals and goal based outcomes (GBOs): some useful information. London: Internal CORC Publication; 2011.
Google Scholar
Di Malta G, Oddli HW, Cooper M. From intention to action: a mixed methods study of clients’ experiences of goal-oriented practices. J Clin Psychol. 2019;75(20):1770–89.
Article PubMed Google Scholar
Law D, Jacob J. Goals and goal based outcomes: some useful information. 3rd ed. London: CAMHS Press; 2015.
Grosse M, Grawe HK. Bern inventory of treatment goals: part 1. Development and first application of a taxonomy of treatment goal themes. Psychother Res. 2002;12:79–99.
Law D. The goal-based outcome (GBO) tool. Guidance notes. [Internet]. Goals in Therapy. 2019. Available from: https://goalsintherapycom.files.wordpress.com/2019/02/gbo-version-2.0-guide-final-1st-feb-2019.pdf .
Bandura A. Self-regulation of motivation and action through goal systems. In: Bandura A, editor. Cognitive perspectives on emotion and motivation. Dordrecht: Springer; 1988. p. 37–61.
Chapter Google Scholar
Manderlink G, Harackiewicz JM. Proximal versus distal goal setting and intrinsic motivation. J Personal Soc Psychol. 1984;47:918–28.
Maslow AH. A theory of human motivation. Psychol Rev. 1943;50:370–96.
Harkin B, Webb TL, Chang BP, Prestwich A, Conner M, Kellar I, Benn Y, Sheeran P. Does monitoring goal progress promote goal attainment? A meta-analysis of the experimental evidence. Psychol Bull. 2016;142(2):198–229.
Levack WM, Weatherall M, Hay-Smith EC, Dean SG, McPherson K, Siegert RJ. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD009727.pub2 .
Article PubMed PubMed Central Google Scholar
Mellat N, Lavasani MG. The role of epistemological beliefs, motivational constructs and Information processing strategies in regulation of learning. Procedia Soc Behav Sci. 2011;30(1):1761–9.
Leavey JE. Youth experiences of living with mental health problems: emergence, loss, adaptation and recovery (ELAR). Can J Community Ment Health. 2009;24(2):109–26.
Simonds LM, Pons RA, Stone NJ, Warren F, John M. Adolescents with anxiety and depression: Is social recovery relevant? Clin Psychol Psychother. 2014;21(4):289–98.
Castonguay LG. Predicting the effect of cognitive therapy for depression: a study of unique and common factors. J Consult Clin Psychol. 1996;64:497–504.
Duncan BL. The heart and soul of change second edition: delivering what works in therapy. Washington: American Psychological Association; 2010.
Book Google Scholar
Messer SB. Let’s face facts: common factors are more potent than specific therapy ingredients. Clin Psychol Sci Pract. 2002;9:21–5.
Kazdin AE, Siegel TC, Bass D. Drawing on clinical practice to inform research on child and adolescent psychotherapy: survey of practitioners. Prof Psychol Res Pract. 1990;21(3):189–98.
Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theory Res Pract. 1979;16(3):252–60.
Luong HK, Drummond SPA, Norton PJ. Elements of the therapeutic relationship in CBT for anxiety disorders: a systematic review. J Anxiety Disord. 2020;76:102322. https://doi.org/10.1016/j.janxdis.2020.102322 .
Shick Tryon G, Birch SE, Verkuilen J. Meta-analyses of the relation of goal consensus and collaboration to psychotherapy outcome. Psychotherapy. 2018;55(4):372–83.
DiGiuseppe R, Linscott J, Jilton R. Developing the therapeutic alliance in child-adolescent psychotherapy. Appl Prev Psychol. 1996;5(2):85–100.
Hartley S, Redmond T, Berry K. Therapeutic relationships within child and adolescent mental health inpatient services: a qualitative exploration of the experiences of young people, family members and nursing staff Short. PsyArXiv. 2021. https://doi.org/10.31234/osf.io/w2nct .
Wolpert M, Pote I, Sebastian C. Identifying and integrating active ingredients for mental health. Lancet Psychiatry. 2021;8(9):741–3.
INVOLVE. Briefing note for researchers: Public involvement in NHS, public health and social care research [Internet]. 2012. Available from: https://www.invo.org.uk/wp-content/uploads/2012/04/INVOLVEBriefingNotesApr2012.pdf .
Gotschall T. EndNote 20 desktop version. J Med Libr Assoc JMLA. 2021;109(3):520.
PubMed Google Scholar
Ouzzani M, Hammady H, Fedorowicz ZEA. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10.
Hannes K. Chapter 4: Critical appraisal of qualitative research. In: Njbahkhahjlsl C, editor. Supplementary guidance for inclusion of qualitative research in cochrane systematic reviews of interventions version 1. London: Cochrane Collaboration Qualitative Methods Group; 2011. p. 4.
Bennett LR. Adolescent depression: meeting therapeutic challenges through an integrated narrative approach. J Child Adolesc Psychiatr Nurs. 2012;25(4):184–94.
Berdondini L, Elliott R, Shearer J. Collaboration in experiential therapy. J Clin Psychol. 2012;68(2):159–67.
Diamond GM, Diamond GS, Liddle HA. The therapist–parent alliance in family-based therapy for adolescents. J Clin Psychol. 2000;56(8):1037–50.
Cirasola A, Midgley N, Fonagy P, Martin P, MGoodyer I, Reynolds S, et al. The factor structure of the working alliance inventory short-form in youth psychotherapy: an empirical investigation. Psychother Res. 2021;31(4):535–47. https://doi.org/10.1080/10503307.2020.1765041 .
Feltham A, Martin K, Walker L. Using goals in therapy: the perspective of people with lived experience. In: Cooper M, Law D, editors. Working with goals in psychotherapy and counselling. Oxford: Oxford University Press; 2018. p. 73–85.
Law D, Wolpert M. Guide to using outcomes and feedback tools with children, young people and families. Formally known as the COOP document. London: CAMHS Press; 2014.
Martin K. A critical realist study of shared decision-making in young people’s mental health inpatient units. Bristol: Bristol University Press; 2019.
Hawks JM. Exploring the therapeutic alliance with adolescents and their caregivers: A qualitative approach. Diss Abstr Int Sect A Humanit Soc Sci. 2016;77(4-A(E)):No-Specified. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc13&NEWS=N&AN=2016-37856-098 .
Marks D. Fostering parental growth and enhancing the therapeutic alliance: key tasks for the child psychotherapist. J Child Psychother. 2020;46(1):20–34. https://doi.org/10.1080/0075417X.2020.1743736 .
Shpigel MS, Diamond GM. Good versus poor therapeutic alliances with non-accepting parents of same-sex oriented adolescents and young adults: a qualitative study. Psychother Res. 2014;24(3):376–91. https://doi.org/10.1080/10503307.2013.856043 .
Paul M. Decision-making about children’s health care. Adv Psychiatr Treat. 2004;10:301–11.
Stige SH, Eik I, Oddli HW, Moltu C. Negotiating system requirements to secure client engagement—therapist strategies in adolescent psychotherapy initiated by others. Front Psychol. 2021. https://doi.org/10.3389/fpsyg.2021.704136 .
Marshall SL, Oades LG, Crowe TP. Australian mental health consumers’ contributions to the evaluation and improvement of recovery oriented service provision. Isr J Psychiatry Relat Sci. 2010;47(3):198–205.
Cairns A, Kavanagh D, Dark F, McPhail SM. Setting measurable goals with young people: qualitative feedback from the goal attainment scale in youth mental health. Br J Occup Ther. 2015;78(4):253–9.
Grossoehme DH, Gerbetz L. Adolescent perceptions of meaningfulness of psychiatric hospitalization. Clin Child Psychol Psychiatry. 2004;9(4):589–96.
Dickson JM, Moberly NJ. Goal internalization and outcome expectancy in adolescent anxiety. J Abnorm Child Psychol. 2013;41(3):389–97.
Abrera AM. Depression and suicide risk among adolescents: exploring the moderating role of benevolence and goal-orientation. In: The 6 th ASEAN regional union psychological society (ARUPS) congress “driving mental revolution in the psychological century: enhancing psychological services for a better future. Bali; 2018. p. 56.
Edbrooke-Childs J, Jacob J, Argent R, Patalay P, Deighton JWM. The relationship between child-and parent-reported shared decision making and child-, parent-, and clinician-reported treatment outcome in routinely collected child mental health services data. Clin Child Psychol Psychiatry. 2016;21(2):324–38.
Edbrooke-Childs J, Patalay P. Ethnic differences in referral routes to youth mental health services. J Am Acad Child Adolesc Psychiatry. 2019;58(3):368–75.
Steinberg L, Silverberg SB. The vicissitudes of autonomy in early adolescence. Child Dev. 1986;57:841–51.
Slavin LA, Rainer KL. Gender differences in emotional support and depressive symptoms among adolescents: a prospective analysis. Am J Community Psychol. 1990;18(3):407–21.
Ciftci A, Jones N, Corrigan PW. Mental health stigma in the muslim community. J Muslim Ment Health. 2013;7(1):17–32.
Bromley C, Westwood S. Young people’s participation: views from young people on using goals. Child Fam Clin Psychol Rev. 2013;1:29–40.
Clarke SP, Oades LG, Crowe TP, Caputi P, Deane FP. The role of symptom distress and goal attainment in promoting aspects of psychological recovery for consumers with enduring mental illness. J Ment Health. 2009;18(5):389–97.
Trent ES, Viana AG, Raines EM, Woodward EC, Zvolensky MJCA. Exposure to parental threatening behaviors and internalizing psychopathology in a trauma-exposed inpatient adolescent sample: the role of difficulties with goal-directed behaviors. J Nerv Ment Dis. 2019;207(11):969–76.
Moberly NJ, Watkins ER. Negative affect and ruminative self-focus during everyday goal pursuit. Cogn Emot. 2010;24(4):729–39.
Steen A, Berghuis H, Braam AW. Lack of meaning, purpose and direction in life in personality disorder: a comparative quantitative approach using Livesley’s general assessment of personality disorder. Personal Ment Health. 2019;13(3):144–54.
Wrosch C, Miller GE. Depressive symptoms can be useful: self-regulatory and emotional benefits of dysphoric mood in adolescence. J Pers Soc Psychol. 2009;96(6):1181–90.
Troupp C. Distinguishing patient-generated outcome measures in CAMHS from a bespoke sandwich. Child Fam Clin Psychol Rev. 2013;1(1):19–28.
Taylor J, Shostak L, Rogers A, Mitchell P. Rethinking mental health provision in the secure estate for children and young people: a framework for integrated care (SECURE STAIRS). Safer Communities. 2018;17(4):193–201.
Cheng H, Hayes D, Edbrooke-Childs J, Martin K, Chapman L, Wolpert M. What approaches for promoting shared decision making are used in child mental health? A scoping review. Helen MIR mHealth uHealth. 2017;7(6):77.
Langer DA, Jensen-Doss A. Shared decision-making in youth mental health care: using the evidence to plan treatments collaboratively. J Clin Child Adolesc Psychol. 2018;47(5):821–31.
Coulter A, Edwards A, Elwyn G, Thomson R. Implementing shared decision making in the UK. Z Evid Fortbild Qual Gesundhwes. 2011;105(4):300–4.
Download references
Acknowledgements
The authors would like to thank the advisors, for their invaluable contribution from start to finish, including useful comments an early draft: Duncan Law, Elmas Aybike Yılmaz, Hanne Oddli, Isabella Valério, Jacob People, Josh D., Julian Edbrooke-Childs, Katya Proctor, Laura Calomarde Juárez, Mick Cooper, Nick Morgan, Panos Vostanis, Syeda Zeenat R., and Theo Jackson. Thank you to Bernice Appiah, Shade Davies and Shadia Robertson for helpful discussions about the findings, and assistance with evidence synthesis, and to Inês Pote from the Wellcome Active Ingredients team, and Jasmine Harju-Seppanen, for useful comments on a previous draft. The authors also wish to thank Zoe Thomas for incredibly useful advice and guidance regarding literature searches.
This work was funded by a Wellcome Trust Mental Health Priority Area “Active Ingredients” 2021 commission awarded to JJ at the Anna Freud Centre. It was a requirement of the funding team that the research design comprised a literature review, and that the involved and worked collaboratively with young people with lived experience of anxiety and/or depression throughout the course of the project. Members of the funding team provided feedback on an early draft of this manuscript.
Author information
Authors and affiliations.
Child Outcomes Research Consortium, Anna Freud Centre, 4-8 Rodney Street, London, N1 9JH, UK
Jenna Jacob
Euro Youth Mental Health, The Block, 35 Churchgate, Hitchin, SG5 1DN, UK
Milos Stankovic & Inga Spuerck
Systematic Review Consultants, 9 Sandfield Road, Nottingham, NG7 1QR, UK
Farhad Shokraneh
You can also search for this author in PubMed Google Scholar

Contributions
JJ conceptualised the study, prepared the first draft protocol and search strategy, refining this with the study authors and advisors. JJ undertook the library database searches for published literature, partially screened the titles and abstracts of literature, screened all full texts, led communication with study authors and advisors, led four advisory group meetings, maintained the databases which were used to extract and manage study data, prepared, and revised the manuscript. MS contributed to the first draft protocol and search strategy, led communication with youth advisors, led two advisory group meetings, created the narrative summaries, and contributed to the manuscript. IS contributed to the first draft protocol and search strategy, supported communication with youth advisors, screened full texts for further relevant literature, and contributed to the manuscript. FS conducted the grey literature searches, screened all potential title and abstracts from all searches (published and unpublished literature), maintained the databases which were used to extract and manage study data, and contributed to the manuscript. All study advisors were invited to comment on the protocol and initial search terms, and were invited to comment on earlier drafts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jenna Jacob .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this research was not required because it does not involve collection nor analysis of primary data, and youth advisors were consulted on in the capacity of being part of the advisory group, to discuss their interpretation of the findings, rather than within the capacity of research participants.
Consent for publication
Not applicable.
Competing interests
JJ works on the Child Outcomes Research Consortium (CORC) project at the Anna Freud National Centre for Children and Families, which encourages the use of outcome measures in youth mental health settings amongst its members. No other authors report any competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. appendix 1..
Inclusion and exclusion criteria and Search Strategies. Appendix 2 Core Criteria for Quality Assessment of Qualitative Studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jacob, J., Stankovic, M., Spuerck, I. et al. Goal setting with young people for anxiety and depression: What works for whom in therapeutic relationships? A literature review and insight analysis. BMC Psychol 10 , 171 (2022). https://doi.org/10.1186/s40359-022-00879-5
Download citation
Received : 16 March 2022
Accepted : 30 June 2022
Published : 13 July 2022
DOI : https://doi.org/10.1186/s40359-022-00879-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Youth mental health
- Goal setting
- Therapeutic alliance
- Outcome measurement
- Active ingredients
- Goal based outcomes
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Open access
- Published: 01 March 2022
Designing and conducting initial application of a performance assessment model for in-hospital trauma care
- Yalda Mousazadeh 1 , 2 ,
- Homayoun Sadeghi-Bazargani 3 ,
- Ali Janati 4 ,
- Mahboub Pouraghaei 5 ,
- Farzad Rahmani 3 &
- Mobin sokhanvar 6
BMC Health Services Research volume 22 , Article number: 273 ( 2022 ) Cite this article
1258 Accesses
2 Citations
Metrics details
Trauma is a major cause of death worldwide, especially in Low and Middle-Income Countries (LMIC). The increase in health care costs and the differences in the quality of provided services indicates the need for trauma care evaluation. This study was done to develop and use a performance assessment model for in-hospital trauma care focusing on traffic injures.
This multi-method study was conducted in three main phases of determining indicators, model development, and model application. Trauma care performance indicators were extracted through literature review and confirmed using a two-round Delphi survey and experts’ perspectives. Two focus group discussions and 16 semi-structured interviews were conducted to design the prototype. In the next step, components and the final form of the model were confirmed following pre-determined factors, including importance and necessity, simplicity, clarity, and relevance. Finally, the model was tested by applying it in a trauma center.
A total of 50 trauma care indicators were approved after reviewing the literature and obtaining the experts’ views. The final model consisted of six components of assessment level, teams, methods, scheduling, frequency, and data source. The model application revealed problems of a selected trauma center in terms of information recording, patient deposition, some clinical services, waiting time for deposit, recording medical errors and complications, patient follow-up, and patient satisfaction.
Performance assessment with an appropriate model can identify deficiencies and failures of services provided in trauma centers. Understanding the current situation is one of the main requirements for designing any quality improvement programs.
Peer Review reports
Trauma is one of the major causes of death worldwide, occurring mostly in the first four decades of life [ 1 ]. It is reported that nearly 5.8 million people die each year as a result of trauma [ 2 ]. Moreover, trauma occurs in all countries and is a common problem in modern societies [ 3 ]. On the other hand, a significant share of the burden of diseases is due to trauma [ 2 , 4 ]. Also, trauma annually leads to more than 50 million Disability-Adjusted Life Years (DALY) [ 5 ]. The other point is that traumatic injuries can cause higher mortality rates than Acquired Immune Deficiency Syndrome (AIDS), Malaria, and Tuberculosis [ 6 ]. Therefore, trauma is a critical and time-dependent health issue that requires an instant healthcare intervention to reduce the probability of mortality and disability [ 7 ].
Among the various types of trauma, trauma caused by a crash is a life-threatening condition for all age groups [ 8 ]. Traffic injuries are reported to have increased from 999,000 in 1990 to more than one million deaths in 2002, and were predicted to reach about two million deaths by 2020 [ 9 ]. Evidence shows that the trauma injuries from collisions leads to the death of 21 million people and the disability of 20-50 million people annually, most of whom are young [ 10 , 11 ]. Traffic injuries are the second leading cause of death in Iran, accounting for 40% of unusual deaths [ 12 , 13 ]. It is undeniable that the injuries caused by trauma are more severe in LMIC due to the lack of an organized trauma system and the extent of occasions leading to trauma, such as collisions [ 14 ].
In the case of trauma care, health organizations are responsible for providing cost-effective, patient-oriented, and safe health services to affected patients at the right time and place [ 3 ]. The key feature of good trauma care is rapid transfer to a medical center where appropriate trauma care is available and definitive treatment can be delivered within the first hour after injury [ 15 ]. Prevention activities, communication infrastructure, medical direction, trained workforce, pre-hospital care, transportation services, triage, in-hospital care, rehabilitation, public education, and trauma capacity assessment are key components of the trauma care system [ 15 ]. Reports indicate that people do not receive the same services for crash injuries even in the same environment. Also, evidence suggests that quality services are not always available to them [ 3 ]. Therefore, the quality of care provided to injured patients should be evaluated and improved [ 16 , 17 ]. Furthermore, the high and rising costs of health services confirm this need [ 18 ].
The Committee on Trauma of the American College of Surgeons was one of the first organizations to develop indicators for evaluating trauma care as part of a quality improvement program [ 19 ]. However, many LMIC do not have accreditation processes, standards, and specific assessment tools for trauma centers [ 20 ]. On the other hand, related indicators have been observed in developed countries for a long time. However, their use in low- and middle-income countries is limited due to resources shortage [ 21 ]. In addition, it is recommended to use context-related audit filters in the area of health services provision [ 5 ]. Nevertheless, the Iranian Ministry of Health and Medical Education (MOHME) defined only five general criteria as indicators of hospital emergency performance, which are not specifically related to trauma services. Hence, the present study was carried out to design and conduct the initial application of a model for assessing trauma care with a specific focus on traffic injuries.
This multi-method study was conducted between June 22, 2018 and October 22, 2019 in three main phases of determining the indicators, model development, and model application in the hospital.
Determining indicators
A comprehensive literature review was conducted by searching five electronic databases, including PubMed, Ovid Medline, Science Direct, ProQuest, Scopus, and Google Scholar search engine. In addition, Persian databases, including Scientific Information Database (SID) and Magiran, were searched. In the next step, the indicators regarding the assessment of in-hospital trauma services were extracted from related articles. Then, the the indicators extracted by a five-member panel were evaluated in terms of feasibility, importance, relationship with the health system, and compliance with context of the Iranian hospitals. Finally, the selected indicators were categorized by content and examined for content validity through a two-round Delphi survey. Accordingly, the Content Validity Index (CVI), Content Validity Ratio (CVR), and the modified kappa were calculated [ 22 , 23 ]. Participants ( n = 30) consisted of 17 physicians and specialists (general practitioner, emergency medicine, anesthesiologist, orthopedics, internists, and neurologist), four nurses, and nine faculty members on health policy, disaster and emergency health, and healthcare management. All the participants had work or research experience in trauma care.
The proposed indicators were rated using a self-administered questionnaire. In the first round of the Delphi survey, the questionnaires were distributed after providing sufficient explanations and a deadline of 2 weeks was set for their completion. In order to determine CVI, participants were asked to score each indicator, separately, in terms of their opinions and knowledge relating to three respects, “relevancy to the subject,” “simplicity” and “clarity” using a four-point Likert scale (completely relevant, relevant, relatively relevant, and not relevant). In order to determine CVR, participants were scored each indicator, in terms of “necessity” (necessary, useful but not necessary, and not necessary). They were also asked to comment on the proposed indicators. The formula to calculate CVI and CVR were as follows [ 23 ]:
In terms of CVI, each item with a score higher than 79% is appropriate. Items between 70 and 79% need to be corrected and less than 70% unacceptable. The acceptable CVR was 0.33 according to the number of participants (30 people).
To calculate the modified Kappa, the odds ratio of the agreement was first calculated. In this regard, a binomial random variable formula was used:
In this formula, N is the number of participants, and A is the number of people who agree (the number of raters giving a rating of 3 or 4). In the next step, the Kappa coefficient was calculated based on the following formula:
Based on the Polit and Beck view [ 23 ], the kappa coefficient in the range of 0.40-0.75 was at a good level, and above 0.75 was at a high level. The second round presented the indicators based on CVI scores, CVR, and the modified kappa. Finally, the approved indicators were listed and categorized in the second round.
Model development
Two Focus Group Discussions (FGD) were held (a total of 12 people in two sessions), and 16 semi-structured interviews were performed to identify how trauma care was assessed using the using extracted indicators. Each FGD and interview lasted 60 to 90 and 45 to 60 min, respectively. The participants were selected based on purposive sampling [ 24 ]. After obtaining informed consent, the participants’ statements were electronically recorded and then transcribed verbatim. The content analysis method [ 25 ] was used to analyze the text of interviews and FGDs. Eighty percent of the participants in this phase were related to the previous stage (Delphi and Panel). According to FGDs and interviews, the initial form of the model and its components were developed.
A three-part questionnaire was designed and provided to 10 selected experts in a separate session to conduct model approval. The majority of these people were faculty members and also worked in trauma centers. The first part consisted of socio-demographic variables of ten participants (Table 1 ). In the second part, the opinions of experts about the main and sub-components of the model were questioned according to the criteria of importance and necessity, simplicity, clarity, and relevance, based on the 9-point Likert scale. The components with scores between 7 and 9 were approvedand components with scores between 1 and 3 were removed. Agreement on components with a score of 4 to 6 was also discussed [ 26 ]. The third part of the questionnaire included questions for validation and agreement on the final form of the model. Accordingly, 12 areas were examined. These 12 areas included model feasibility, compatibility with upstream documents, acceptance of the proposed model by stakeholders, efficiency, flexibility, model sequence, model fit, the balance between model components, and a general question. According to these 12 items, a form was designed based on the 4-point Likert scale (1: very low, 2: low, 3: high, 4: very high), and experts expressed their opinions. Then, the Item-level Content Validity Index (I-CVI) and KAPPA were obtained [ 27 ].
Model application
The initial model application was conducted to assess in-hospital trauma care at the trauma center in the metropolitan city of Tabriz in the East Azerbaijan Province, Iran. Units involved in providing the data needed for general indicators included the medical record department, the emergency medicine department, the quality improvement office, the patient safety office, the nursing office, and the trauma ward. It should be noted that information on general indicators was collected for 1 year.
To collect data on specific indicators, 200 patients were selected who were to the referral trauma center in the emergency department for 3 months. A checklist consisting of 27 questions was designed based on the consensus of the research team and two emergency medicine specialists. Four other experts commented on the checklist, and thus, its validity was confirmed. Cronbach’s alpha coefficient for the four dimensions of the checklist was calculated to be 0.7, 0.65, 0.73, and 0.71, respectively. The checklist consisted of patient information, crash mechanism, patient triage level, vital signs, Glasgow Coma Scale (GCS), some procedures performed for the patient including (intubating, setting chest tube, fracture fixation, bleeding control, and blood and fluids transfusion), diagnostic procedures and related waiting time, patient satisfaction, and the final decision in the emergency department.
The data were collected using patient observation and measures taken to provide services, and interviewing patients and their accompanies, asking staff, and reviewing the patient's document. The gathered data were analyzed using Stata software (Stata 14 package statistical software). Then, the data were reported using descriptive statistics. One-Sample Kolmogorov-Smirnov Test was applied to test the normality of the distributions of the variables. Accordingly, Kruskal-Wallis, Chi-square, One Way ANOVA, and linear regression tests were also used to examine the relationship between variables. Figure 1 gives an overview of the study procedures.
Fig. 1 Flowchart of study procedure Full size image
In a comprehensive literature review, 140 indicators were associated with in-hospital trauma care after reviewing 51 articles, 3 guidelines, and 2 books. Then, some indicators were excluded or merged due to insignificance, differences in the management system of countries, lack of sufficient data (physical and electronic), time, human and physical resources shortage. Therefore, in the Delphi survey, 57 indicators were entered and investigated. In the first phase, CVR, CVI, and Modified Kappa were calculated to be 0.64, 0.85, 0.83, respectively. A total of 50 indicators were confirmed in the second phase of Delphi. Figure 2 provides an overview of this step of the study. Also, classification indicators for assessing in-hospital trauma care are shown in Fig. 3 .
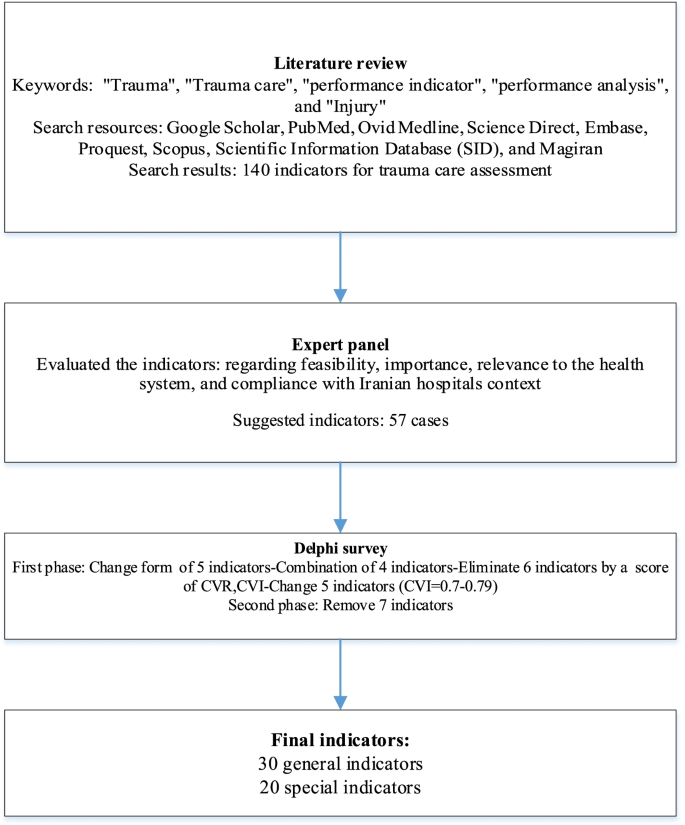
Flowchart of determining indicators
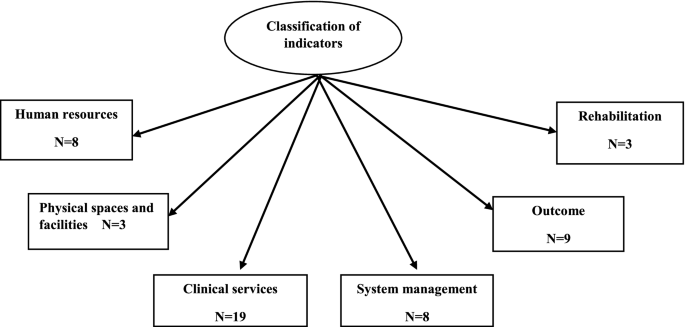
Classification of trauma care indicators for assessment
Prerequisites and assessment steps were determined based on expert opinions. Accordingly, assessment prerequisites included a component leader, support of service providers, determining the level of facilities and the nature of activities, and a person to collect data. The specialists insisted on constant review of indicators and updating if necessary. This was because the indicators had to be evidence-based and relevant to the results. Determining the assessment period (daily, weekly, monthly or annual) was another necessity. The experts believed that assessment should have broad dimensions and different aspects, including assessment of awareness, knowledge, attitude, service providers’ skill, and patient satisfaction. The experts asserted that both external assessments by auditing organizations and internal assessments by process owners should be considered. Finally, the experts suggested that the results of the evaluation be reviewed by hospital committees and relevant authorities. Then be made public. Figure 4 provides an overview of the FGDs and interviews findings.
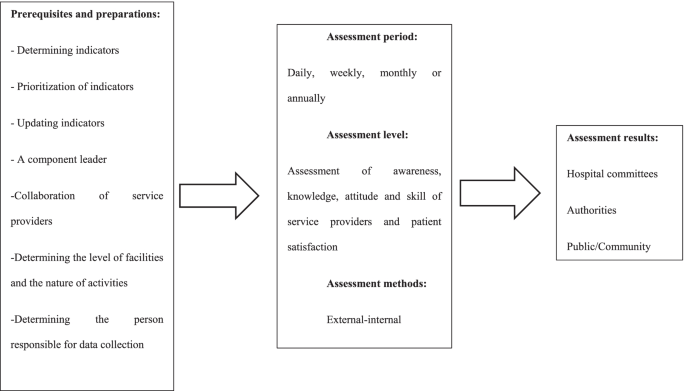
The FGDs and interviews finding
Based on the expert opinions, the initial form of the performance assessment model was designed in six components by the research team. These components were:
Selection of the assessment level (including hospital wards and patient/ staff views)
Assessment team (specialized and non-specialized)
Measurement method (assessment content based on the Donabedian framework Measuring tool)
Scheduling (based on plan or case)
Frequency of assessment (general and specific)
Data source (current reports, periodic reports, and case reports)
All components of the model scored an average of 7 to 9 in the Delphi survey and were therefore confirmed. The experts agreed on all the components as well as the general shape of the proposed model. The self-assessment team was added to the assessment teams based on their comments. Also, the k-score and I-ICV was obtained as 1 except for two areas of the model, including acceptability by stakeholders and the model’s simplicity in other areas under study. Figure 5 shows the final form of the model.
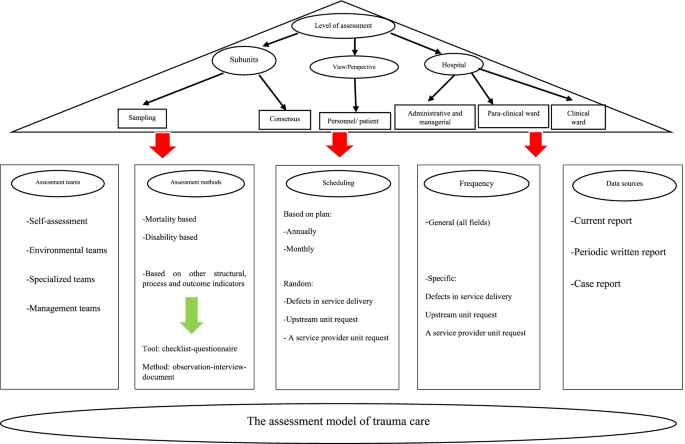
Assessment Model for in-Hospital Trauma Car
A total of 5163 crash patients were transported by ambulance in 1 year. The number of patients admitted to the emergency department was 330-340 patients per day. A total of 1951 patients were hospitalized, which was 0.04% of the total hospitalized patients. A trauma registry related to collisions was set up in the trauma center. The in-hospital trauma team consisted of emergency medicine specialists and senior residents in surgery, internal medicine, orthopedics, and neurologists. Eleven Root Cause Analyses (RCA) were performed over 1 year, none of which was for crash patients. Information related to Failure Modes and Effects Analysis (FMEA) was not recorded. The level of satisfaction of trauma patients referred to the emergency department was not assessed during a year. The patient’s functional status was not assessed after discharge, and there was no protocol for referral to rehabilitation centers. Table 2 shows the results of other general indicators.
In this study, 200 crash patients referred to the hospital emergency department were examined. The mean and Standard Deviation (SD) of patients’ age were 33.13 and 19.04, respectively. 42% of patients were sent to the hospital from different cities of East Azerbaijan province and 58% from Tabriz city. The mean (SD) of GCS in 170 patients was 14.41 (2.36). Out of 200 patients, imaging services were performed for 186 patients (93.47%). Table 3 shows some demographic characteristics and hospital information of the patients. Table 4 shows the waiting time for Para clinical procedures and patient outcomes in the emergency department.
The Chi-square test showed a statistically significant relationship between outcome and mechanism of injury, location of injury, and GCS group ( p < 0.05). Based on Kruskal–Wallis test, the relationship between the GCS score and the outcome was statistically significant ( p < 0.05). There was a statistically significant relationship between triage level and outcome ( p < 0.05). The waiting time to receive a CT scan increased the waiting time for discharge by 1.46 times ( p < 0.05). Also, the waiting time for receiving CXR increased the waiting time for discharge by 1.56 times ( p < 0.05).
Out of 200 patients, two patients were not triaged, or their triage was not recorded. In addition, five patients were re-triaged due to lower triage than the injury level of the patients. The neuromuscular status of 12 patients was not checked. There was no vacancy for treatment for eight patients in the operating room at the time of the medicines order. The decision was delayed in five patients due to a malfunction due to the failure of the Picture Archive and Communication System (PACS). There was a delay in depositing five patients due to receiving counseling. The hospitalization of five patients was delayed due to a lack of empty beds. Table 5 shows the quality of some of the procedures performed for patients.
This is a unique study from Iran in the field of trauma care. In this study, in-hospital trauma care indicators were extracted, and a model was developed to assess hospital performance in the management of trauma patients. Finally, a field study was firstconducted to apply the model in a trauma center, which contained positive findings and, of course, the shortcomings and weaknesses that were discussed.
A total of 50 indicators related to trauma care were identified and presented to be applicable in the Iranian hospital context. Indicators are used to compare the current situation with the standards, identify defects and shortcomings and fix them to improve performance [ 18 , 28 ]. Of course, the usefulness of using indicators is when they are compatible with the requirements of the context [ 28 ]. So, in this study, among the indicators extracted from the literature review, those were selected which fit the Iranian hospitals’ conditions based on the expert opinions. Evidence suggests that context-based filters will be useful. For example, the failure to use trauma care indicators in Asian countries has been due to a lack of standard data collection mechanisms and limited resources [ 5 ].
In this study, a six-dimensional model was also designed to assess the performance of in-hospital trauma care based on the expert opinions. The use of international indicators and models is essential in the event of localization, especially in developing countries that do not have an accreditation process for trauma centers [ 5 , 20 ]. Moeini et al. used the survival probability assessment system and concluded that despite the differences between the developed model of the countries as well as Iran; this model could be useful after localization and development of coefficients and variables derived from regional databases [ 29 ].
Experts in this study focused on important and applicable indicators due to the limitations of LMIC. Studies show that due to resource deficiencies, the use of low-cost interventions is more beneficial by increasing the efficiency and quality of care [ 30 , 31 ] . Studies in Iran and Pakistan have focused on improving trauma care processes to prevent death and disability even in low-resource centers [ 32 , 33 ]. In addition to the lack of resources, simpler indicators that can be collected based on current data allow for more comparisons. However, in hospitals with more resources, more advanced indicators can be used [ 5 ]. It is difficult to define the best performance in trauma, which is related to lack of financial resources and organizational problems such as the unclear definition of responsibilities within trauma teams and resistance to clinical guidelines. Therefore, in centers with the same level of resources, there is a difference in the quality of service [ 34 ]. These studies show that emphasizing the effectiveness of routine processes in evaluations is useful and allows comparisons that were also considered in designing the model of the present study.
Receiving the opinions of service recipients as an evaluation level was one of the strengths and innovations of the model presented in this study. Murray points out that the issue of quality has been raised from the service recipients in various health programs to continue to use care, ensure effectiveness, and participation of peopleand other stakeholders in health care [ 35 ]. Santana et al. also stated that a comprehensive, patient-centered assessment is achieved when patient perspectives are considered [ 36 ]. Simultaneous attention to structure, process, and outcomes is another strength of the model presented in this study, which is recommended by Donabedian [ 28 ].
Mortality was one of the leadings used indicators in this study which is a key indicator in assessing trauma care [ 19 ]. Findings showed that the mortality rate of crash patients was about 9% over a year. In Iran, the prevalence of collisions is twenty times higher than the global average [ 37 ]. Furthermore, the World Road Safety report revealed that the death rate due to crashs in Iran is estimated to be 32.1 per 100,000 people [ 38 ]. Disability was another indicator used in the current study. Unfortunately, the pilot assessment in a trauma center revealed that the functional status of the patients is not evaluated before discharge. This is while the findings of studies have shown that patients rarely have a definite and stable state of health at the time of discharge [ 39 , 40 ].
Assessment findings also showed that many quality improvements measures, including the death audit and comprehensive recording of errors and complications, RCA and FMEA at the study trauma center were in poor condition. While, in their review, authors concluded that most quality improvement measures could be useful in trauma care [ 41 ]. Suitable efforts to improve quality and support patient safety can improve patient-based outcomes and reduce costs [ 42 ].
Another important finding of the assessment was that most injured were pedestrians. In line with the present study, the classification of the patients injured in collisions in Iran showed that pedestrians with 39.8% had the most injuries [ 43 ]. Among different parts of the body, the head was the most frequently injured part in this study. In line with this finding, Taghipour et al. stated that head trauma had been the most frequent injury in driving accidents [ 44 ].
The length of stay in the emergency department was another investigated indicator which was very long in studied center. This is important because 75-85% of deaths occur in the first 20 min after an accident [ 45 ]. Also, in patient safety measures, results showed that only two cases of complications were studied, including postoperative infection and postoperative bleeding. This is while there were six cases of surgical site infection during the data collection period. Surgical site infections, with an incidence of 2 to 5%, account for 24% of nosocomial infections and increase morbidity and mortality [ 46 ].
Error reporting in the study center was not based on a precise mechanism, and most reports were provided by nurses. The most common errors reported were included registration errors and medication mistakes. As in the present study, findings reported by Bozorgzad and Hemmat showed that most of the reported errors were related to nurses [ 47 ]. Jolaee et al. reported medication mistakes as the most common error, consistent with findings of the present study [ 48 ].
Regarding the factors associated with patient satisfaction, the findings of this study showed that waiting time was an important factor in this regard. In line with this finding, in a study of physicians’ opinions working in the emergency department about the cause of patients’ dissatisfaction, 61% of them stated that waiting time is the main cause [ 49 ].
Finally, the initial application of the designed model revealed deficiencies in some of the equipment needed for trauma care. Lack of facilities to provide trauma services and shortage of related equipment in many developing countries is evident, as Mook et al. have concluded in the case of Mexico, Vietnam, Ghana, and India [ 50 ].
Limitations and strength
This study is the first to design an in-hospital trauma care assessment model by combining scientific evidence with expert opinions to be more in line with the conditions of Iranian hospitals. The development of this model is the first step in a series of research studies designed to improve our understanding and improve measurement and assessment of hospitals’ performance in terms of trauma care. However, this study also had some limitations. While every attempt was made to comprehensively search the literature. Indicators may have been excluded due to the impossibility of collecting data and as a result theindicators of in-hospital trauma care that may not have been examined. Initial application of the model in a trauma center is another potential limitation of the study. To validate the model, it is necessary to apply it in more centers.
The indicators and the steps required to assess the performance of in-hospital trauma care were designed based on a literature review and experts’ opinions and presented in the form of a model. The use of the model leads to a systematic assessment and comprehensive review of performance. Model application revealed some problems regarding information registration, complications recording, patient satisfaction, improper clinical services, follow-up and rehabilitation services, and waiting time. Identifying performance deficiencies may lead to appropriate planning and performing the necessary interventions. So, it can be expected to improve the outcomes of patients, hospitals, and the health system.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on request.
Abbreviations
Disability-Adjusted Life Years
Acquired Immune Deficiency Syndrome
Ministry of Health and Medical Education
Content Validity Index
Content Validity Ratio
Focus Group Discussion
Item-level Content Validity Index
Root Cause Analyses
Failure Modes and Effects Analysis
Standard Deviation
Picture Archive and Aommunication System
Doctor of Philosophy
Medical Doctor
the Advanced Trauma Life Support
the Advanced Trauma Care for Nurses
International Classification of Diseases
Cardiopulmonary Resuscitation
Incentive Care Unit
Temperature
Saturation of Oxygen
Prothrombin Ratio
Respiratory Rate
Blood Pressure
Glasgow Coma Scale
Diagnostic Peritoneal lavage
Computerized Tomography
Chest X-ray
Focused Assessment with Sonography for Trauma
Electrocardiogram
Scientific Information Database
World Health Organization
Moore L, Lavoie A, Sirois M-J, Swaine B, Murat V, Le Sage N, et al. Evaluating trauma center structural performance: the experience of a Canadian provincial trauma system. J Emerg Trauma Shock. 2013;6(1):3–10.
Article PubMed PubMed Central Google Scholar
Alharbi RJ, Lewis V, Mosley I, Miller C. Current trauma care system in Saudi Arabia: a scoping literature review. Accid Anal Prev. 2020;144:105653.
Article PubMed Google Scholar
Mousazadeh Y, Sadeghi-Bazargani H, Janati A, Pouraghaei M. Developing performance indicators for trauma care: A four-stage qualitative study. Trauma Mon. 2020;25(1):34–51.
Google Scholar
Glen J, Constanti M, Brohi K. Assessment and initial management of major trauma: summary of NICE guidance. Bmj. 2016;353:i3051.
Stewart BT, Gyedu A, Quansah R, Addo WL, Afoko A, Agbenorku P, et al. District-level hospital trauma care audit filters: Delphi technique for defining context-appropriate indicators for quality improvement initiative evaluation in developing countries. Injury. 2016;47(1):211–9.
Lashoher A, Schneider EB, Juillard C, Stevens K, Colantuoni E, Berry WR, et al. Implementation of the World Health Organization trauma care checklist program in 11 centers across multiple economic strata: effect on care process measures. World J Surg. 2017;41(4):954–62.
Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer’s effect on mortality. J Trauma. 2010;69:595–9.
Davtalab Esmaeili E, Sadeghi-Bazargani H, Shams Vahdati S, Shokouhi G, Safaiyan A, Salari LS. Assessment of survival and hospital care quality in patients with traffic injury in East Azerbaijan. Trauma Mon. 2017;22(5):e35303.
Nantulya VM, Reich MR. The neglected epidemic: road traffic injuries in developing countries. Bmj. 2002;324(7346):1139–41.
Ziyab AH, Akhtar S. Incidence and trend of road traffic injuries and related deaths in Kuwait: 2000–2009. Injury. 2012;43(12):2018–22.
Saladié Ò, Bustamante E, Gutiérrez A. COVID-19 lockdown and reduction of traffic accidents in Tarragona province. Spain TRIP. 2020;8:100218.
PubMed Google Scholar
Rasouli MR, Nouri M, Zarei M-R, Saadat S, Rahimi-Movaghar V. Comparison of road traffic fatalities and injuries in Iran with other countries. Chin J Traumatol (English Edition). 2008;11(3):131–4.
Article Google Scholar
Moafian G, Aghabeigi MR, Hoseinzadeh A, Lankarani KB, Sarikhani Y, Heydari ST. An epidemiologic survey of road traffic accidents in Iran: analysis of driver-related factors. Chin J Traumatol. 2013;16(3):140–4.
Mousazadeh Y, Sadeghi-Bazargani H, Janati A, Pouraghaei M, Rahmani F. Prediction of mortality risk in patients with traffic injury: A case study in Tabriz hospitals. Iran Arch Trauma Res. 2019;8(2):104–9.
Rasmussen TE. A national trauma care system: from call to action. JTrauma Acute Care Surg. 2016;81(5):813–5.
Stelfox HT, Straus SE, Nathens A, Bobranska-Artiuch B. Evidence for quality indicators to evaluate adult trauma care: a systematic review. Crit Care Med. 2011;39(4):846–59.
Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE. Quality indicators for evaluating trauma care: a scoping review. Arch Surg. 2010;145(3):286–95.
Moore L, Lavoie A, Sirois M-J, Amini R, Belcaïd A, Sampalis JS. Evaluating trauma center process performance in an integrated trauma system with registry data. J Emerg Trauma Shock. 2013;6(2):95–105.
Willis CD, Gabbe BJ, Cameron PA. Measuring quality in trauma care. Injury. 2007;38(5):527–37.
Latifi R, Ziemba M, Leppäniemi A, Dasho E, Dogjani A, Shatri Z, et al. Trauma system evaluation in developing countries: applicability of American College of Surgeons/committee on trauma (ACS/COT) basic criteria. World J Surg. 2014;38(8):1898–904.
Mousazadeh Y. Developing a hospital performance Assesment model for patients management with Trraffic injures: Tabriz University of Medical Sciences. School Manag Med. 2019:30–5.
Hajizadeh E, Asghari M. Statistical methods and analyses in health and biosciences a research methodological approach. 3rd ed. Tehran: Jahade Daneshgahi Publications; 2011.
Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recomm Res Nurs Health. 2007;30(4):459–67.
Tongco MDC. Purposive sampling as a tool for informant selection. Ethnobot ResAppl. 2007;5:147–58.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
De Villiers MR, De Villiers PJ, Kent AP. The Delphi technique in health sciences education research. Med Teach. 2005;27(7):639–43.
Hasanpoor E. Developing a model of evidence-based Management for Iranian Hospitals: Tabriz University of Medical Sciences. School Manage Med. 2018:53–54.
Santana MJ, Stelfox HT. Development and evaluation of evidence-informed quality indicators for adult injury care. Ann Surg. 2014;259(1):186–92.
Moini M, Rezaishiraz H, Zarineh A, Rasouli MR. Evaluation of quality of trauma care in a local hospital using a customization of ASCOT. Euro J trauma emerg surg. 2009;35(1):56–60.
Peabody JW, Taguiwalo MM, Robalino DA, Frenk J. Disease control priorities in developing countries. 2nd ed. Washington, DC: The International Bank for Reconstruction and Development/The World Bank Group; 2006.
Stewart B, Quansah R, Gyedu A, Ankomah J, Donkor P, Mock C. Strategic assessment of trauma care technology availability in Ghana. World J Surg. 2015;39:2428–40.
Zafarghandi MR, Modaghegh MH, Roudsari BS. Preventable trauma death in Tehran: an estimate of trauma care quality in teaching hospitals. J Trauma. 2003;55:459–65.
Jat AA, Khan MR, Zafar H, Raja AJ, Hoda Q, Rehmani R, et al. Peer review audit of trauma deaths in a developing country. Asian J Surg/Asian Surg Assoc. 2004;27:58–64.
Archambault PM, Turgeon AF, Witteman HO, Lauzier F, Moore L, Lamontagne F, Horsley T, Gagnon MP, Droit A, Weiss M, Tremblay S. Implementation and evaluation of a Wiki involving multiple stakeholders including patients in the promotion of best practices in trauma care: the WikiTrauma Interrupted Time Series Protocol. JMIR research protocols. 2015;4(1):e21.
Murray SA. Experiences with “rapid appraisal” in primary care: involving the public in assessing health needs, orientating staff, and educating medical students. Bmj. 1999;318(7181):440–4.
Article CAS PubMed PubMed Central Google Scholar
Santana MJ, Stelfox HT. Quality indicators used by trauma centers for performance measurement. J Trauma Acute Care Surg. 2012;72(5):1298–303.
Yadollahi M, Gholamzadeh S. Five-year forecasting deaths caused by traffic accidents in Fars province of Iran. BEAT. 2019;7(4):373.
World Health Organization (WHO). Global status report on road safety 2015. Geneva: World Health Organization; 2015.
Holbrook TL, Anderson JP, Sieber WJ, Browner D, Hoyt DB. Outcome after major trauma: discharge and 6-month follow-up results from the Trauma Recovery Project. J Trauma Acute Care Surg. 1998;45(2):315–24.
Article CAS Google Scholar
Holbrook TL, Anderson JP, Sieber WJ, Browner D, Hoyt DB. Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. J Trauma Acute Care Surg. 1999;46(5):765–73.
Juillard CJ, Mock C, Goosen J, Joshipura M, Civil I. Establishing the evidence base for trauma quality improvement: a collaborative WHO-IATSIC review. World JSurg. 2009;33(5):1075–86.
Bohnen JD, Anderson GA, Kaafarani HM. Quality and patient safety indicators in trauma and emergency surgery: National and global considerations. Curr Trauma Rep. 2018;4(1):9–24.
Ghafari Fam S, Sadeghi Bazargani H, Salarilak S. A survey on epidemiological and demographic aspects of pedestrian road accident victims in Shohada referral university hospital, East Azerbaijan province. J Urmia Uni Med Sci. 2014;25:549–60.
Taghipour H, Panahi F, Khoshmohabat H, Hojati Firoozabadi N, Moharamzad Y, Abbasi A. Causes and severity of fatal injuries in autopsies of victims of fatal traffic accidents. SSUJ. 2010;17(5):358–64.
Akbari M, editor. National strategies for quality improvement in emergency management 2002: Proceedingof national conference on qualityimprovmentin emergency medicine; 2002. 20-25.
Sorush AR, MakaremJ YM, Fazeli MS, Hajiabdolbaghi M, Noori M, et al. Surgical wound infection and factors affecting it in general surgery patients. JIMC. 2007;25(4):313–22.
Bozorgzad M, Hemati Z. Frequency of errors in nursing and associated factors in the cases referred to the mortality Committee in Shahrekord University of medical sciences during 2006-2012. J Clin Nurs Midwifery. 2015;4(2):52–8.
Jolaee S, Hajibabaee F, Peyravi H, Haghani H. Nursing medication errors and its relationship with work condition in Iran University of Medical Sciences. J Med Ethics Hist Med. 2009;3(1):65–76.
Mahabadi A, Ketabi S, Sajadi SM. Investigate the parameters which affect the patients waiting time in emergency department of orthopedic services in ayatollah Kashani hospital with the lean management approach. Health Inf Manag. 2015;11(7):1016–25.
Mock C, Nguyen S, Quansah R, Arreola-Risa C, Viradia R, Joshipura M. Evaluation of trauma care capabilities in four countries using the WHO-IATSIC guidelines for essential trauma care. World J Surg. 2006;30(6):946–56.
Download references
Acknowledgments
Authors thank the Research Deputy of Tabriz University of Medical Sciences for their financial support and the East Azerbaijan Medical Emergency and Accident Management Center, the Road Traffic Injury Prevention Research Center of Tabriz University of Medical Sciences, and Miss. Aysan Mohammad Namdar for technical cooperation. Special thanks are extended to all the experts to express their valuable views.
This research study was supported by Tabriz University of Medical Sciences ((grant number: 58043).
Author information
Authors and affiliations.
Department of Public Health, Khalkhal University of Medical Sciences, Khalkhal, Iran
Yalda Mousazadeh
Iranian Center of Excellence in Health Management, School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran
Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Homayoun Sadeghi-Bazargani & Farzad Rahmani
Department of Health Policy and Management, Iranian Center of Excellence in Health Management, School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran
Emergency Medicine Research Team, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Mahboub Pouraghaei
Department of Public Health, Khoy University of Medical Sciences, Khoy, Iran
Mobin sokhanvar
You can also search for this author in PubMed Google Scholar
Contributions
Study design: AJ, HS, YM, and MP; Data collection: YM, FR, MP, and MS; Data analyzing: HS, AJ, MS, and YM; Manuscript writing: all authors have read and approved the final manuscript.
Corresponding author
Correspondence to Ali Janati .
Ethics declarations
Ethics approval and consent to participate.
This study is part of a Ph.D. thesis in health services management. The main protocol of this study was reviewed and approved by the Ethics Committee of Tabriz University of Medical Sciences [IR.TBZMED.REC.1396.560]. All methods were carried out under relevant guidelines and regulations. Informed consent was obtained from all the participants before participating in the study.
Consent for publication
Not applicable.
Competing interests
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mousazadeh, Y., Sadeghi-Bazargani, H., Janati, A. et al. Designing and conducting initial application of a performance assessment model for in-hospital trauma care. BMC Health Serv Res 22 , 273 (2022). https://doi.org/10.1186/s12913-022-07578-2
Download citation
Received : 18 May 2021
Accepted : 01 February 2022
Published : 01 March 2022
DOI : https://doi.org/10.1186/s12913-022-07578-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Performance assessment
- Traffic injury
- Trauma care
- Trauma center
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Orthopaedic and trauma research in Tanzania: A scoping review
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation School of Medicine, University of Limerick, Limerick, Ireland
Roles Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing
Affiliation Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, United States of America
Roles Formal analysis, Project administration, Supervision, Validation, Writing – review & editing
Affiliation Department of Orthopaedic Surgery, Emory University School of Medicine, Atlanta, Georgia, United States of America
Roles Conceptualization, Methodology, Project administration, Supervision, Validation, Visualization, Writing – review & editing
Affiliations Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, United States of America, Department of Orthopaedic Surgery, Philadelphia, Pennsylvania, United States of America
- Benjamin Blackman,
- Sarah Barnett,
- Ajay Premkumar,
- Neil P. Sheth

- Published: June 5, 2024
- https://doi.org/10.1371/journal.pone.0304218
- Reader Comments
Tanzania is disproportionately burdened by musculoskeletal injuries as it faces unique challenges when dealing with trauma care. This scoping review aims to summarize and assess the current state of orthopaedic and trauma research in Tanzania. By identifying key themes, trends, and gaps in the literature, this review seeks to guide future research initiatives catered specifically to the needs of Tanzania’s healthcare system. Utilizing the PRISMA-ScR protocol, OVID Medline, PubMed, and CINAHL databases were searched from inception to June 17, 2023, using keywords such as “Orthopaedics” “Trauma” and “Tanzania”. One hundred and ninety-two eligible studies were included and the Arksey and O’Malley framework for scoping studies was followed. There was a notable growth of relevant publications from 2015 onward, with peaks in growth in the years 2019, 2021, and 2020. The studies employed diverse research methodologies, with cross-sectional (n = 41, 21%) and prospective studies (n = 39, 20%) being the most prevalent, and randomized-controlled trials being the least prevalent methodology, making up eight studies (4.2%). The most common study themes were trauma (n = 101, 52.6%), lower extremity (n = 31, 16%), and spine-related issues (n = 27, 14%). Only three studies looked at work-related injuries (1.6%). Road traffic injuries (RTIs) were the most common mechanism of trauma in 77.0% of the trauma focused studies. Fifty-three percent of the studies were conducted by a majority of Tanzanian authors. This scoping review highlights various trends in orthopaedic and trauma research in Tanzania, with a particular emphasis on road traffic-related injuries. Various gaps are explored, including a lack of research on work-related injuries and a paucity of experimental research. Our findings underline areas where future research is warranted. The future of orthopaedic and trauma care in Tanzania depends on the efforts and collaboration of both local and international stakeholders.
Citation: Blackman B, Barnett S, Premkumar A, Sheth NP (2024) Orthopaedic and trauma research in Tanzania: A scoping review. PLoS ONE 19(6): e0304218. https://doi.org/10.1371/journal.pone.0304218
Editor: Hans-Peter Simmen, University Hospital Zurich, SWITZERLAND
Received: January 11, 2024; Accepted: May 9, 2024; Published: June 5, 2024
Copyright: © 2024 Blackman et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Injuries make up 9% of global deaths, with 90% occurring in low and middle-income countries (LMIC) [ 1 ]. Alongside other developing countries, Tanzania faces unique challenges when dealing with orthopaedic and trauma care [ 2 ].
With a rapidly growing population and increased economic development, orthopaedic injuries continue to rise markedly, mainly due to road traffic injuries (RTI). In a one-day survey conducted in Tanzania, nearly half of all trauma cases were attributed to RTIs [ 3 ]. While the need for orthopaedic care is on the rise, there is a lack of available orthopaedic services and an insufficient number of adequately trained healthcare professionals in the field [ 4 ]. Limited access to surgical equipment and inadequate infrastructure for the volume of required care [ 5 ] renders orthopaedic and trauma management a significant strain on the country of Tanzania.
Multiple reports have highlighted the need for local healthcare research to improve health outcomes in developing countries [ 6 , 7 ]. Furthermore, local research in developing countries has been shown to be of utmost importance in contributing to infrastructural growth [ 8 – 10 ]. In Tanzania, the significance of generating robust local research becomes particularly pronounced due to persistent obstacles in the provision of adequate trauma care [ 11 , 12 ].
By employing a scoping review approach, this study aims to comprehensively survey and synthesize the existing orthopaedic and trauma literature within the context of Tanzania. This methodology facilitates the examination of a wide spectrum of literature by date of publication, research methodologies employed, and overarching themes addressed. This thorough assessment provides a comprehensive summary of the existing literature, as well as a foundational platform for future research endeavors. Moreover, this review seeks to align its findings with the unique requirements of Tanzania’s healthcare system, enhancing its capacity to contribute meaningfully to the advancement of orthopaedic and trauma care in the region.
A scoping review was chosen due to the breadth of the research topic and the expected variation in study design, and was conducted using the Arksey and O’Malley framework [ 13 ].
Identification of the research question
Our research question was, “What is the current state of orthopaedic and trauma literature in Tanzania, and where should future research be directed?”
The preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) protocol was used to present the study methodology and findings ( S1 Checklist ) [ 14 ].
Identification of the relevant studies
The authors executed a search using the following databases: OVID Medline, PubMed, and CINAHL using controlled vocabulary (e.g. MeSH) and keywords representing the topics “Orthopaedics”, “Trauma” and “Tanzania”.
Databases were searched from inception to June 17, 2023. With the goal of capturing the entirety of the relevant existing literature, no limits were applied. Results (n = 1573) were exported to Rayyan citation management system [ 15 ]. A detailed search strategy is available in S1 File .
Study selection
Two co-authors independently screened titles and abstracts of identified papers. After full-text screening by each reviewer, papers were categorized into retrospective cohort, prospective cohort, cross-sectional studies, case studies and reviews, randomized controlled trials, and other research (for e.g., cost analysis, discussion, mixed-method). Full-text extraction was then carried out using a data extraction sheet developed for the purpose of this study. Each author verified that the papers met the inclusion criteria and focused on the topic of interest. Discrepancies in reviewers’ decisions were resolved through discussion.
Inclusion and exclusion criteria
Studies met the inclusion criteria if they met the following criteria: (1) Study focused on orthopaedic conditions or injuries suffered from trauma, and (2) Study reported findings from a Tanzanian population.
Data charting
The same two co-authors independently reviewed each paper, discussed charted data, and updated a password protected Google Sheets [ 16 ] datasheet accordingly. Information extracted from the selected studies was organized and categorized as follows: authors and publication date, study type, study topic, and study context. Studies pertaining to trauma were further categorized by mechanism of injury from RTIs, falls, and violence, where the percentage of patients from each category was documented. Additionally, the country of origin pertaining to authorship was charted.
Collating and summarizing findings
A thematic data synthesis was performed to identify the state of orthopaedic literature in Tanzania. The synthesis includes useful information on past research focus, existing gaps, and suggested future initiatives.
Due to the heterogeneity of study designs and outcomes, a narrative summary of results is presented.
Search results
A preliminary search of scientific databases yielded a total of 1,573 studies. After removing the duplicates (n = 700), titles and abstracts of 873 studies were screened. This process excluded an additional 658 studies, leaving a sample of 215 studies. Screening of full texts yielded a total sample of 192 studies eligible for this review. A complete PRISMA study flow diagram is shown in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0304218.g001
Distribution of studies by year
There were no limits placed on the dates of studies included, as this scoping review aimed to capture all the relevant literature on orthopaedics and trauma in Tanzania. As a result, several decades of research were examined, dating back to 1966. Since then, the body of research grew sporadically, with the early 2000s showing a relatively steady increase. From 2015 onwards, there was a significant increase in published studies in this field. The years 2019, 2021, and 2020 marked the peaks in the literature, during which 23, 21, and 20 studies were published, respectively. In 2022, there were 16 studies, and in 2023, there have been 9 studies to date ( Fig 2 ).
https://doi.org/10.1371/journal.pone.0304218.g002
Research methodology
The scoping review examination of orthopaedic research and trauma care in Tanzania yielded diverse research methodologies that represented the multifaceted field of inquiry. The studies were primarily categorized as follows: retrospective cohort studies (14), cross-sectional studies (41), prospective studies (39), case studies (24), retrospective reviews (34), case series (9) and randomized controlled trials (8). Twenty-six studies fell in the category of other research: cost analysis (5), survey (4), qualitative (4), discussion (3), descriptive (3), mixed-method (3), modelling (1). A breakdown of study methodology is shown in Table 1 . This diversity in study methodologies presents opportunities and challenges when reviewing the data to guide future research in Tanzania.
https://doi.org/10.1371/journal.pone.0304218.t001
Thematic analysis
Various themes were identified which highlighted the existing breadth of research in the field and identified areas where research is lacking. There were 101 trauma-specific studies, which included a focus on RTIs, falls, violence, and other trauma. Fifty-six studies focused on fractures. Overall, 31 studies looked specifically at the lower extremity and seven focused on the upper extremity. Twenty-seven studies addressed spine-related issues, and 27 studies examined a pediatric population. Fifteen studies discussed infections, eight discussed genetic conditions, and four discussed cancer. Finally, seven studies addressed health economics, and seven addressed public health. These results are depicted in Table 2 .
https://doi.org/10.1371/journal.pone.0304218.t002
Trauma specific studies
Of the 101 trauma related studies, 61 (60.3%) further explored injury mechanisms in cohorts involving multiple admission causes (RTI, falls, violence, etc.). Of these studies, the most common cause of trauma were RTIs (77.0%), followed by falls (18.0%) and violence (4.92%). Almost 97% of trauma-focused studies included patients injured in RTI, 74.2% included patients injured from falls, and 50% included patients injured because of violence ( Table 3 ).
https://doi.org/10.1371/journal.pone.0304218.t003
Randomized controlled trials analysis
Of the eight studies classified in the category of RCT, there were four unique trials, one of which is in progress. There were five studies that reported results from RCTs [ 17 , 18 , 22 – 24 ], two RCT protocols [ 19 , 20 ], and one pilot study [ 21 ]. Four of the eight studies focused on infection prevention [ 17 – 20 ]. In 1989, Museru, Kumar, and Ickler compared isotonic saline, distilled water, and boiled water in irrigation of open fractures, and found no difference in outcomes [ 17 ]. In 2015, Marwa et al. examined the use of cefepime versus ceftriaxone prophylaxis in elective orthopaedic procedures and found no significant difference [ 18 ]. Two protocols were published with reference to the Go-Tibia trial, which aims to be completed by 2028 [ 19 , 20 ]. This trial is a masked randomized control trial assessing the rate of infection after gentamicin or saline administration in patients with open tibia fractures. The other four included RCTs related to a prospective trial comparing intramedullary nailing versus external fixation in the treatment of open tibial fractures [ 21 – 24 ]. The pilot study was published in 2018 [ 21 ], which was followed by a cost effectiveness analysis in 2019 [ 22 ], which revealed that intramedullary nailing was more cost effective and had better union rates at three months follow-up. The following publication at a one-year follow-up showed no difference in primary events, however found that intramedullary nailing yielded better coronal alignment [ 23 ]. A three to five year follow up of this cohort revealed that 25% of patients suffered chronic fracture-related infection and non-union, regardless of reintervention [ 24 ].
Work related injuries
There were three studies focusing specifically on work-related injuries. In 2010, Kishashu et al. surveyed 1385 patients with injuries from 2007 to 2008 and found that 638 (46%) were work related [ 25 ]. In 2013, Boniface et al. examined 248 miners suffering WRI from 2009 to 2012 and found that 98.7% of workers did not use protective gear and worked over 12 hours daily. Falling rocks were the leading cause of injury, and in total 41.3% of these patients died [ 26 ]. In 2021, Shewiyo et al. performed a retrospective review of 4578 claims to the Workers Compensatory Fund in Tanzania from 2016 to 2019. They concluded that motor accidents, machine faults, and falls were the most common causes of WRI. They also reported the odds of a work-related fatalities increased greater than 6-fold in injuries occurring during conveyance [ 27 ].
Country of origin
Of the 192 studies included, 91% had Tanzanian authors and 53% had a majority of Tanzanian authors. Of the studies with a majority of out-of-county authors, 55% of these studies had a majority of authors from the United States. Further, the USA was the most represented country after Tanzania, with 40% of all included studies including an American author. Africa was the most represented continent (54%), followed by North America (26%) and Europe (10.4%).
This scoping review outlines the evolution of orthopaedic trauma care in Tanzania, as reflected in the distribution of studies spanning several decades. The growth in orthopaedic and trauma research in Tanzania since 1966 is noteworthy as it represents shifts in scientific, societal, and health policy interests. The early years of research were marked by subtle and inconsistent growth, indicating the lower priority of trauma care in Tanzania. This is likely because infectious diseases such as HIV/AIDS, malaria, and tuberculosis had posed a more imminent threat to public health [ 28 ]. In particular, the last decade marked a significant period of growth for orthopaedic and trauma research. This may be attributed to increased awareness and international collaboration among world experts [ 29 , 30 ].
Road traffic injuries
The predominant focus on RTIs among trauma cases reveals the substantial burden created by these injuries. The increased incidence of RTIs is likely a result of the exponential proliferation of roads, which led to underdeveloped and unsafe driving conditions [ 31 , 32 ]. Roughly 10% of the roads in Tanzania are paved [ 33 ]. The increase in RTIs is multi-factorial and has increased due to more motorized vehicle use (e.g., cheaper foreign motorcycles from China and India) in conjunction with a lack of proper infrastructure (e.g., lack of sidewalks, lights on roads, road quality) and inadequate safety measures (e.g., seatbelt and helmet laws, traffic lights, stop signs) [ 34 – 36 ]. In 2011, the World Health Organization (WHO) and the World Bank launched a Decade of Action for Road Safety with the goal of cutting RTIs and deaths in half [ 37 ]. However, minimal progress has been made in LMICs [ 38 ], underscoring the need for further preventative initiatives.
Addressing road safety remains of utmost importance for the Tanzanian population. Ahmed et al. (2013) report that raising awareness of RTIs is integral in low-income countries [ 39 ]. They recommend increasing public awareness, road safety infrastructure, and traffic rules as the most effective means for reducing traffic accidents [ 39 ]. Thus, further research on the outcomes of these initiatives, and the formulation of health policy specific to the Tanzanian population, will be vital in minimizing the burden of RTIs.
In addition to raising awareness, future research should focus on rehabilitation and post-operative management of trauma patients, as this theme was seldom examined in the literature. By optimizing rehabilitation, patients will be better able to return to their livelihood, support their families, and contribute to the country’s economic growth, benefiting all shareholders [ 40 ].
Economic impact of injury
The financial implications of injuries remain a prevalent concern in Tanzania. On average, 52% of a citizen’s total health expenditure is out-of-pocket [ 41 ]. Over a one-month period, 75% of Tanzanians surveyed in the Kilimanjaro Christian Medical Center orthopaedic ward reported that their healthcare expenditure cost more than their monthly income, and roughly 40% of these patients reported losing their job due to their disability after their injury [ 42 ]. With nearly 26 million people in Tanzania living in extreme poverty (below 1.90 U.S. dollars a day) [ 43 ], the cost of health care augments the economic strain on trauma victims.
In addition to improving infrastructure and raising awareness, addressing work-related injuries (WRI) will help alleviate the overall trauma burden. When appropriate measures are put into place, WRIs are often preventable [ 44 ]. Such measures include safe working environments, appropriate protective equipment, appropriate training, and rehabilitation initiatives [ 45 ]. Poor workplace conditions place an economic and health burden on society [ 45 , 46 ]. The International Labour Organization (ILO) estimates that approximately 4% of the world’s gross domestic product is lost due to WRIs, and low-income countries are particularly affected [ 47 , 48 ]. In 2015, it was estimated that, in the Southern Africa region alone, 18,000 workers died from work-related accidents [ 49 ]. In Tanzania, WRI remains an unaddressed epidemic. This scoping review found a scarcity of research specifically related to WRI, with only three studies focusing on this topic. Although many of the trauma studies included patients who were injured at work, there is little research on interventions and initiatives focused on reducing injuries in the workplace.
Sustainability
Under conservative assumptions, over 90% of the Northern Tanzania population cannot access orthopaedic surgical services [ 50 ]. Tanzania has an estimated 118 orthopaedic surgeons for a population of over 60 million [ 51 ], which equates to one orthopaedic surgeon for every 508,000 citizens. In stark contrast, this ratio in America is one orthopaedic surgeon for every 10.8 thousand citizens [ 52 ].
In recent years, there has been increased enthusiasm for medical missions to developing countries as initiatives such as Doctors without Borders continue to expand [ 53 – 55 ]. As international orthopaedic surgeons volunteer in Africa on medical missions, addressing the long-term sequelae of their work is vital. These mission trips often involve completing many surgeries quickly, introducing new equipment and thus, potentially new complications, which further increase the burden on the local healthcare system [ 30 , 56 ]. For a more sustainable future of care, global collaboration is critical to develop adequate infrastructure for continuous orthopaedic management in Tanzania [ 30 , 57 , 58 ].
Future research
Given that developing countries constitute the majority of the global population [ 59 ], conducting research tailored to these populations is imperative. As delineated by the 10/90 phenomenon, only 10% of worldwide resources are devoted to the population which suffers 90% of the burden [ 60 ]. This scoping review found eight studies pertaining to randomized controlled trials, with four being unique trials. This scarcity highlights the need for further research into the population-specific determinants of health in Tanzania. In their systematic review of orthopaedic global outreach efforts, Nolte et al. concluded that orthopaedic outreach initiatives in LMICs are cost-effective and direct funding is needed to ameliorate global orthopaedic health [ 61 ]. Of the ten studies on surgical mission trips to Africa included in their review [ 61 ], none were in Tanzania, further highlighting the need for research in this specific population.
It is well-accepted that randomized clinical trials are the gold standard for assessing causal relationships in research [ 62 ]. However, this research methodology is often expensive and time-consuming [ 63 ]. In developing countries, various barriers exist to conducting high-quality research [ 64 ], such as lack of suitable research infrastructure, deficiency in policymakers understanding of the importance of research, and absence of research materials [ 65 – 67 ]. Historically, research in Tanzania has not been focused on the context-specific structural determinants of health and inequities, which warrants wider implementation of local investigator-initiated trials [ 64 , 67 ]. Further initiatives should focus on interdisciplinary collaboration in creating appropriate research infrastructure to better suit randomized controlled trials. As more experimental research is done in Tanzania, the management of orthopaedic conditions will be better understood to ultimately improve patient outcomes.
Most of the studies included were conducted by Tanzanian authors. Nevertheless, addressing orthopaedic and trauma care in other LMICs remains a global health priority. In LMICs, RTIs remains a significant health burden, due to similar factors discussed in this review [ 1 ]. Longitudinal partnerships and research that reflect the interests and goals of local populations in other LMICs are needed to further explore this topic, and ultimately improve global health outcomes [ 6 – 10 ].
Strengths and limitations
The major strength of this scoping review is its comprehensive overview of the literature. By including studies dating back to 1966, this review encapsulates the wide range of methodologies, focuses, and themes in orthopaedic and trauma research in Tanzania. This breadth of included studies allowed for a thorough review of trends and gaps in the literature, highlighting areas where future research is warranted. The main limitations are the lack of ability to perform a meta-analysis and lack of study quality (risk of bias) assessment.
The escalating orthopaedic and trauma crisis in Tanzania demands immediate attention and international intervention to mitigate the country’s massive health and economic burden. This scoping review offers a comprehensive analysis of orthopaedic and trauma research conducted in Tanzania from 1966 to 2023. Our findings highlight the prevalence of RTIs as a significant cause of injuries, emphasizing the pressing need for more effective interventions and health policies to reduce this burden. The notable scarcity of research on WRIs and randomized controlled trials indicates a significant gap in the existing literature, highlighting the need for high-quality research in these areas in Tanzania. A commitment to implementing sustainable orthopaedic and trauma care should be a local and global priority. This scoping review aims to catalyze further research endeavors and outreach initiatives in Tanzania’s orthopaedic and trauma sectors.
Supporting information
S1 checklist. prisma-scr checklist..
https://doi.org/10.1371/journal.pone.0304218.s001
S1 File. Search strategy.
https://doi.org/10.1371/journal.pone.0304218.s002
- 1. World Health Organization. Injuries and violence: the facts 2014 [Internet]. World Health Organization; 2014 [cited 2023 Aug 24]. 19 p. https://apps.who.int/iris/handle/10665/149798
- View Article
- PubMed/NCBI
- Google Scholar
- 8. World Health Organization. Local production and technology transfer to increase access to medical devices: addressing the barriers and challenges in low- and middle-income countries [Internet]. World Health Organization; 2012 [cited 2023 Aug 24]. iv, 144 p. https://apps.who.int/iris/handle/10665/336774
- 15. Rayyan—ai powered tool for systematic literature reviews [Internet]. 2021 [cited 2023 Aug 28]. https://www.rayyan.ai/
- 16. Google sheets: online spreadsheet editor | google workspace [Internet]. [cited 2023 Aug 28]. https://www.facebook.com/GoogleDocs/
- 29. Hardaker WM, Jusabani M, Massawe H, Pallangyo A, Temu R, Masenga G, et al. The burden of orthopaedic disease in sub-saharan africa: a focus on tanzania [Internet]. In Review; 2021 Apr [cited 2023 Aug 28]. https://www.researchsquare.com/article/rs-402380/v1
- 33. Clyde & Co LLP—Peter Kasanda. Lexology. 2014 [cited 2023 Sep 4]. An overview of the road infrastructure in Tanzania. https://www.lexology.com/library/detail.aspx?g=ba8c3064-6a64-4759-befc-2fecc5834b31
- 36. Kumar A. Understanding the emerging role of motorcycles in african cities: a political economy perspective. 2011 Apr [cited 2023 Sep 4]; http://hdl.handle.net/10986/17804
- 37. Second Decade of Action for road safety [Internet]. [cited 2023 Aug 28]. https://www.who.int/teams/social-determinants-of-health/safety-and-mobility/decade-of-action-for-road-safety-2021-2030
- 41. World health statistics 2013 [Internet]. [cited 2023 Aug 28]. https://www.who.int/publications-detail-redirect/9789241564588
- 43. Statista [Internet]. [cited 2023 Aug 28]. Tanzania: people in extreme poverty 2016–2025. https://www.statista.com/statistics/1230404/number-of-people-living-in-extreme-poverty-in-tanzania/
- 45. Abdalla S, Apramian SS, Cantley LF, Cullen MR. Occupation and risk for injuries. In: Mock CN, Nugent R, Kobusingye O, Smith KR, editors. Injury Prevention and Environmental Health [Internet]. 3rd ed. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017 [cited 2023 Aug 28]. http://www.ncbi.nlm.nih.gov/books/NBK525209/
- 47. ILO Estimates Over 1 Million Work-Related Fatalities Each Year [Internet]. 1999 [cited 2023 Aug 28]. http://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_007969/lang--en/index.htm
- 51. BOA. Women in surgery–tanzania [Internet]. [cited 2023 Aug 28]. https://www.boa.ac.uk/about-us/diversity-and-inclusion/international-women-s-day/women-in-surgery-tanzania.html
- 52. AAOS. ORTHOPAEDIC PRACTICE IN THE U.S. 2018 [Internet]. AAOS Department of Clinical Quality and Value; 2018. https://www.aaos.org/globalassets/quality-and-practice-resources/census/2018-census.pdf
- 55. Doctors Without Borders—USA [Internet]. [cited 2023 Aug 28]. Tanzania. https://www.doctorswithoutborders.org/what-we-do/where-we-work/tanzania
- 59. World Population Prospects The 2015 Revision. Key Findings and Advance Tables. Population Division: Department of Economic and Social Affairs; 2015.
- 66. Exploring the current state of health research in sub-saharan africa [Internet]. [cited 2023 Aug 29]. https://www.rand.org/randeurope/research/projects/health-research-sub-saharan-africa.html
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
2024 NABIS Conference on Brain Injury Abstracts
The North American Brain Injury Society is entirely responsible for the scientific content of these abstracts. These abstracts have undergone peer review by NABIS to determine suitability for their national conference. No additional peer review of these abstracts was performed by the editor or editorial board of Journal of Head Trauma Rehabilitation.

Letter from ABI2024:
Dear Colleagues,
It is with great pleasure that we present the accepted scientific abstracts from the North American Brain Injury Society’s 17th Annual Conference on Brain Injury in this issue of the Journal of Head Trauma Rehabilitation . The conference was held in Las Vegas, Nevada March 27-30th, 2024.
This year we were delighted to have received over 180 abstracts from investigators, clinicians, and researchers from around the world including some of the world’s leading clinical, academic, and research institutions. Moreover, we are proud of the high quality of research submitted and the broad range of relevant, interdisciplinary topics reflecting current advances being made across the continuum of care in the field of brain injury.
For those of you who were unable to attend the NABIS 2024 meeting, we are pleased to present accepted scientific abstracts in the Journal of Head Trauma Rehabilitation ( JHTR ). In addition to the scientific oral and poster abstracts, NABIS- ABI 2024 had over 50 invited speakers presenting on the latest advances in ABI neuroscience and rehabilitation research. With the theme of “Evidence Informed Best Practices and Guidelines in Brain Injury Medicine and Neurorehabilitation”, the conference planning committee developed a dynamic educational program aimed at achieving optimal outcomes through interdisciplinary collaborations. Clinicians, researchers, administrators, and other brain injury professionals gathered during this four-day multi-track event which covered a variety of adult and pediatric brain injury topics including medical best practices, rehabilitation, research, community integration, life-long living, with advocacy and a knowledge translation emphasis. The conference program is posted on the NABIS website, www.abi2024.org .
This past year, NABIS was also pleased to showcase six inspirational Pre-conference Courses. Pre-eminent leaders presented on Evidence Informed Management of Mild TBI’s, Assessment Tools for the Assessment and Management of Disorders of Consciousness: Novel Approaches for Motor Rehabilitation following ABI, and Pediatric Brain Injury: Best Practices to Enhance Clinical Care and Optimizing Outcomes. Finally, Brain Injury as a Chronic Health Condition and Training Emotional Recognition in Self and Others following ABI as half-day courses segued to the main conference. The main conference also featured leading experts presenting on essential ABI topics for every practicing clinician as well as researchers. Interactive sessions on Mild TBI, Disorders of Consciousness, Neuroplasticity, and Recovery Best Practices Rehabilitation were components of the broad-based program. Examples of practical education included but were not limited to headache evaluation management, pharmacologic rehabilitation, vision and vestibular current practices, neurologic music therapy and a context for applied complementary/alternative and integrative therapeutics. The educational offerings were rounded out with updated approaches to maximize community integration, lifelong living, and how best to manage ABI as a chronic condition to maximize one’s quality of life.
Thank you for all your contributions toward making ABI 2024 a most successful educational, informational and networking event. We look forward to seeing you at future NABIS/IBIA/IPBIS meetings. We also thank you for your support of this multi-disciplinary dynamic organization and are hopeful for new membership growth in the upcoming year. We welcome your feedback on how this society can improve and meeting your society membership needs. Whether it is in research or clinical care, NABIS and IBIA stand behind the premise that advances in scientific research and translational clinical care will ultimately provide the best outcomes for those individuals and families affected by brain injuries as well as the community.
Alan H. Weintraub, MD, FACRM, FAAPMR
ABI 2024 Conference Chair
Chair North American Brain Injury Society
10 Traumatic Brain Injury Induced Vision Impairment and Histone Methylation
Rajaneesh Gupta 1
1 Banaras Hindu University, Varanasi, India
Traumatic brain injury (TBI) is a major cause of mortality and morbidity in the world. TBI induces a chronic disease process causing visual loss which in turn affects day to day life of patients as well as their families. Understanding the underlying molecular mechanisms of TBI-induced vision impairment is a great challenge for neurobiologists, ophthalmologists, and other clinical practitioners. Our animal research study shows that TBI causes damage to the optic nerve and thinning of the retina culminating in compromised vision processing and perception. Axonal degeneration and demyelination in optic nerve and retinal ganglion cells (RGCs) loss in the retina is a crucial feature of vision impairment triggered by TBI. We have found that histone 3 dimethylation at lysine 9 residues (H3K9Me2) on antioxidants gene promoters like SOD can trigger oxidative stress in RGCs and oligodendrocyte precursor cells (OPCs) that was strongly correlated with retinal thinning, impairment of the retrograde transport of axons from visual cortex to neural retina, and demyelination of optic nerve following TBI. Our study suggests that epigenetic regulation of genes associated with oxidative stress could be a potential therapeutic target to restore visual deficits after TBI.
12 Strain-Rate Dependent Nature of Human Brain Tissue Under Shock Loading
Mariusz Ziejewski 1 ; Mohammed Hosseini Farid 1 ; Mehran Fereydoonpour 1 ; Ghodrat Karami 1
1 North Dakota State University, Fargo, United States
In the realm of biomechanical analysis of brain tissue, the precise understanding of the material properties of intracranial head organs holds utmost significance in the exploration of head injury biomechanics. Research has revealed the substantial rate-dependent nature of these biological tissues, thereby emphasizing the necessity to ascertain their material properties within the spectrum of deformation rates they encounter.
This paper employs a meticulously validated finite element model of the human head to delve into the biomechanics associated with impacts and blasts, both of which can result in traumatic brain injuries (TBIs). Our investigation encompasses simulations involving diverse impact directions and velocities. Additionally, we examine scenarios involving both helmeted and un-helmeted heads subjected to blast shock waves.
Our study illuminates that brain strain rates range from 36 to 241 s-1, which is approximately 1.9 and 0.86 times the head acceleration observed during impact and blast scenarios, respectively. The skull, on the other hand, experiences strain rates spanning from 14 to 182 s-1, translating to roughly 0.7 and 0.43 times the head acceleration associated with impact and blast situations.
Furthermore, the outcomes of our incident simulations unveil brainstem and dura mater strain rates within the ranges of 15 to 338 s-1 and 8 to 149 s-1, respectively. These findings not only contribute valuable insights into the characterization of brain tissue, cranial bone, brainstem, and dura mater, but also provide a foundational framework for the pre-selection of material properties in anticipation of computational dynamic studies concerning the human head and brain.
14 Is Virtual Service Delivery a Viable Way To Meet Clients’ Needs and Interests: A Needs Assessment of Virtual/Hybrid Day Programming for Clients With Acquired Brain Injury
Sydney Rossiter 1 ; Brooke Davis 1
1 University Of Ottawa, Ottawa, Canada
Vista Centre Brain Injury Services (VCBIS) offer clients with acquired brain injury a day program of social leisure activities with the objective of connecting them with other clients and promoting skill development to encourage self-efficacy in their community. During the COVID-19 pandemic, the VCBIS day program pivoted to virtual and hybrid programming to maintain service to clients. Program staff are now considering the future of these modes of service delivery. Evaluators conducted a needs assessment for the virtual and hybrid day program to determine whether this mode of program delivery would 1) meet clients’ needs and 2) be attractive to clients in a way that promotes participation in the program. Evaluators used a mixed methods approach, including a VCBIS record review, surveys of clients (n=28), VCBIS staff (n=3) and alternative service providers (n-6), and client focus groups (n=11). Findings from the evaluation indicated that clients have a similar experience of virtual and in-person programming (i.e., similar levels of enjoyment, interest in activities, social connection, skill development), even if clients generally had a preference for one mode of service delivery over the other due to personal interests and accessibility needs. Contrasting this finding, clients generally perceived hybrid programming less favorably on most measures. Clients rated their enjoyment of hybrid activities (M=2.10, SD=.89) significantly lower than the in-person (M=4.65, SD=.67) and virtual (M=4.19, SD=.87) activities; however, there was no significant difference in enjoyment ratings for in-person and virtual participation. During focus groups, clients frequently reported that they struggled to see or hear others clearly during hybrid programming. Staff and alternative service providers echoed these sentiments in their survey responses, indicating that hybrid programming was often challenging to facilitate due to client lack of interest in the programming and technological barriers. Clients did indicate, however, that participating in hybrid programming was much preferred over missing day programming sessions or having no access to programming at all (e.g., due to weather, COVID). Based on these findings, evaluators recommend that VCBIS: 1) continue to offer a virtual day program; 2) tailor program activities to the mode of service delivery; 3) adopt a flexible approach that allows clients to join virtually in cases where a session would otherwise be missed; and 4) implement ABI appropriate ongoing client feedback measures.
15 Improvement of Functional Mobility of Functional Neurologic Disorder (FND) Patients in the Inpatient Rehabilitation Facility Measured Using Wee FIM Scores
Evelyn David 1
1 Children Specialized Hospital, New Brunswick, United States
Functional Neurologic Disorder (FND), or conversion disorder, is a psychiatric disorder that has no organic basis with symptoms affecting sensory and motor function which are not consistent with known neurologic disorder or other medical diseases. Currently, the understanding of FND is largely limited and evolving. This retrospective study will increase the knowledge of how FND impacts the patient’s dysfunction in mobility and outcome of rehabilitation using Wee FIM scores.
There were total of 36 (26 females,10 males) patients who were admitted from 2016-2022. (n=1) in 2016, (n=4) in 2017, (n=2) in 2018, (n=4) in 2019, (n=12) in 2020, (n=9) in 2021, (n=4) in 2022. Patient admitted should have a formal diagnosis by a provider from the referring facility with caregiver’s acceptance of an FND diagnosis. Patients received Wee FIM scores on functional mobility on admission and discharge. Scores were compared from admission to discharge. Patients received therapies from a multidisciplinary team; medical, nursing, physical, occupational, child life, recreational, psychology, and psychiatry. Therapies were evaluated according to their individual needs and discussed weekly during the family meeting. Their length of stay was dependent on their daily progress and patient/family cooperation.
Wee FIM admission scores; Unable to walk; 1 is total assistance TA (44%). 2 is maximum assistance Max A (22.2%). 3 is moderate assistance Mod A (0%). 4 is minimal contact Min A (8.3%), 5 is supervision S (8.3%). 6 is modified independence Mod I (13.8%) and (2.7 %) was 7 for Total independence (TI). Unable to negotiate stairs; TA (75%), Max A (2.7%), Mod A (0%), Min A (2.7%), Needs supervision (5.5%), Mod I (13.8%), TI (0%). Transfers from bed to chair/chair to bed; TA (8.3%), Max A (5.5%), Mod A (8.3%), Min A (5.5%), supervision (22.2%), Mod I (41.6%), TI (8.3%). Discharge scores; (2.7%) was unable to walk, a decrease from 44%. Max A, Mod A, Min A were (0%), supervision (5.5%), Mod I (52.7%), patients who walked and TI (38.8%) an increase from (2.7%). Negotiating stairs; TA (2.7%), Max A, Mod A, Min A were (0%), supervision (5.5%), Mod I (55.5%) up from 41.6%, and 7 (36.1%) significantly improved from (8.3%). For transfer: none needed assistance or supervision, (50%) each for Mod I, increased from 13.8% and TI definitely up from (0%). Length of stay were from 1 day to 44 days.
FND can be very debilitating that needs a multidisciplinary team in a rehabilitation facility to improve the patient’s functional mobility. Treatment includes management of anxiety, depression, cognitive behavior, family, physical and occupational therapies.
16 Wernicke-Korsakoff Syndrome Following Sleeve Gastrectomy
Evelyn David 1, Wernicke-Korsakoff Syndrome Following Sleeve Gastrectomy Janay Parrish, Wernicke-Korsakoff Syndrome Following Sleeve Gastrectomy Lara Aunio, Wernicke-Korsakoff Syndrome Following Sleeve Gastrectomy Emily Lowry, Wernicke-Korsakoff Syndrome Following Sleeve Gastrectomy Erica Bissonnette
Case Diagnosis A 16-year old girl with a history of asthma, diagnosed with Wernicke-Korsakoff Syndrome following a sleeve gastrectomy.
Case Description or Program Description The patient presented to the emergency department with acute onset generalized weakness 3 months after a cosmetic sleeve gastrectomy in Mexico. She did not undergo pre-operative screening or education. Post-operatively, she reported vomiting and poor oral intake. She took Biotin, B12, and iron supplements but received no follow up. Neurologic exam revealed nystagmus, and labs showed thiamine deficiency. MRI demonstrated hyperintensities involving bilateral medial thalami, the periaqueductal grey, and bilateral mammillary bodies, consistent with Wernicke’s Encephalopathy. She completed a course of intravenous thiamine and was transferred to acute inpatient rehabilitation on oral supplementation.
Acute Inpatient Rehabilitation
Assessment/Results
The patient showed inattention, poor motivation, and short-term memory deficits during therapy. She was diagnosed with Wernicke-Korsakoff Syndrome on neuropsychological assessment. During her rehabilitation course, she made significant improvements in strength and activities of daily living. However, she had persistent cognitive deficits that limited her progress.
Discussion (relevance)
Wernicke’s encephalopathy is an uncommon complication of gastric sleeve procedures, developing within 6 months due to thiamine deficiency. Although B12 absorption in the small intestine is preserved, patients may develop thiamine deficiency through vomiting and poor oral intake. Typical symptoms include ataxia, nystagmus, and diplopia. Many patients make a full recovery following thiamine supplementation. Here, we describe a progression from Wernicke’s Encephalopathy to Wernicke Korsakoff syndrome in the setting of poor follow up. Therapy interventions were beneficial for the patient. However, she suffered long term impairment.
Conclusions
Wernicke Korsakoff Syndrome is a permanent neurological condition that can significantly impair quality of life and functional status. With new guidelines recommending bariatric surgeries at an earlier age, it is important to ensure adequate follow up and education on nutritional supplementation and to recognize the symptoms of thiamine deficiency post-operatively.
17 Immersive, Interactive Virtual Reality Scenarios for Traumatic Brain Injury Memory and Eye Recovery: A Pilot Study
Kristen Linton 1 ; Bahareh Abbasi 1 ; Melissa Gutierrez Jimenez 1 ; Jaylyn Aragon 1 ; Savanna Monson 1
1 California State University Channel Islands, Camarillo, United States
Early rehabilitation is necessary for people with traumatic brain injuries (TBI) to recover, yet 77-88% of people with TBI ever receive rehabilitation. People with TBI who are Hispanic, those without insurance, public insurance, or transportation challenges are even less likely than others to receive rehabilitation. Due to its potential to be mobile and low cost, Virtual reality (VR) is recommended as a rehabilitation option that addresses these challenges. Immersive, interactive VR has improved outcomes for people with TBI including memory and eye tracking.
This community-based participatory research project included focus groups with people with TBI (N = 12) to design virtual reality scenarios to address common rehabilitative needs. Prospective memory and eye tracking were described as the most common challenges. The authors then developed and assessed the rehabilitative effects of two new virtual reality scenarios using a HTC Vive headset on prospective memory and eye tracking among people with brain injuries (N = 11) randomized to intervention and control groups. The intervention group (n = 6) participated in the 12-minute memory scenario twice a week for 6 weeks. The control group (n = 5) participated in a memory card game for 20 minutes twice a week for 6 weeks and then participated in the memory VR scenario twice a week for 6 weeks. Four participants received 12 sessions of the 6-minute eye tracking scenario.
On an objective memory test, participants in the VR intervention group (66%) improved their memory more often than the memory card control group (0%) after about 12 sessions each. On a PMRQ memory scale, the intervention and control group did not have statistically significant different mean scores after six weeks. Three out of four (75%) of participants improved their eye tracking ability after they completed the eye tracking VR scenario.
Implications
An efficacy study of the two new VR scenarios will be conducted next. Future research should assess the appropriateness of VR for different types of brain injury and co-occurring conditions.
18 VA Tele-Traumatic Brain Injury (TBI) Program: Increasing Veterans’ Access to TBI Care
Mi-Hyon Cho 1
1 VA Hudson Valley Health Care System, Wappingers Falls, United States
Traumatic Brain Injuries (TBI) have been described as the “signature injury” from the Iraq and Afghanistan wars due to the high prevalence of blast exposure. In 2007, the Veterans Health Administration (VHA) implemented a national clinical guideline that required that providers screen all Veterans who served in combat operations for TBI. Then if a Veteran has a positive TBI screen, a TBI specialist should perform a comprehensive TBI evaluation (CTBIE) to determine a diagnosis and develop an individualized treatment plan. However, due to shortages in TBI specialists, some VA facilities were not able to complete CTBIEs for Veterans who screened positive.
To fill this gap, in 2016, VA Hudson Valley (HV) TBI care provider Dr. Cho reached out to a VA facility in Hawaii that needed assistance. To allow VA HV to provide virtual care for their Veterans, they developed a Telehealth Service Agreement (TSA). Using a modality called Clinical Video Telehealth (CVT), Veterans could go to the closest VA facility in Hawaii and connect virtually with a provider in HV, New York to complete a CTBIE. After providing successful gap coverage and a warm handoff to a newly hired TBI provider at the site in Hawaii, Dr. Cho used the framework to partner with other VA facilities who needed support providing TBI specialty care for their Veterans.
In 2021, VA HV was awarded funding from the VA Office of Rural Health which allowed them to form a more comprehensive Tele TBI Program - consisting of three TBI providers, two speech therapists, one psychologist and a TBI coordinator. To reduce patient drive times, reduce COVID-19 exposure, and improve access to care, the team also rolled out a new virtual care modality that allowed Veterans to connect with providers in HV from their personal devices.
To date, the program has provided TBI virtual care consults to over 1,400 Veterans at 20 VA facilities across the US and is working on expanding care to Active Duty Service Members (ADSM) at a Department of Defense site.
Since November 2022, 12% of HV Tele-TBI patients (169) were surveyed using a ten-question patient satisfaction survey. On average, patient satisfaction total scores were 4.7 out of 5.0. Of the 169 patients surveyed, 98% reported that they “felt comfortable discussing medical issues with their provider during the Telehealth visit,” 95% “would recommend tele-health to others,” and 98% said “overall, they were satisfied with the telehealth visit.”
22 Symptoms and Biological Markers in Traumatic Brain Injury Patients 3-12-Months Post-Injury
Kathryn Gerber 1 ; Gemayaret Alvarez 1 ; Victoria Behar-Zusman 1 ; Arsham Alamian 1 ; Charles Downs 1
1 University Of Miami School Of Nursing And Health Studies, Miami, United States
Neuroinflammation is an important feature of traumatic brain injury (TBI). However, the biological markers of TBI and their connections with cognitive, affective, and physical symptoms remain poorly understood, particularly in the 3-12-month time-period post-injury. Thus, the objective of our study was to examine the relationships between symptoms, biomarkers of neuroinflammation, and functional outcomes in TBI patients 3-12 months post-injury.
A cross-sectional study of 39 TBI patients was performed at a South Florida TBI clinic between May 2022 and June 2023. All patients were between 3-12 months post-injury during study participation. Clinical data, including initial Glasgow Coma Scale (GCS) score, pharmacological information, and patient co-morbidities, was obtained from the Electronic Health Record. Participants also completed a Sorting-Working Memory Test, Neuro-QOL Cognitive Function, Anxiety, Depression, and Sleep Disturbance inventories, a modified symptom checklist from the Brain Injury Association of Virginia, and the Disability Rating Scale (DRS) and Satisfaction with Life Scale (SWLS) as measures of physical function and quality of life, respectively. Multiple plasma biomarkers were assayed. The sample was characterized and associations between symptoms, biomarkers, and functional outcomes were examined using linear regression. Group means were calculated for outcomes and biological data, and analysis of variance (ANOVA) was used to compare between-group means.
The sample consisted of 69.23% male participants, with the most common cause of TBI being motor vehicle accident (71.79%). The top 5 symptoms reported by participants included (1) memory problems, (2) difficulty concentrating, (3) easily agitated, (4) trouble focusing with background noise, and (5) having to check and recheck. Of the top 25 symptoms reported by TBI patients, nearly half (12 out of 25) were cognitive symptoms. Changes in concentrations of the biomarkers over time was assessed, and BDNF levels were found to increase (4191.38 ±275.87 pg/ml 3-6 months post-TBI, 5121.33 ±251.70 pg/ml 6-9 months post-TBI, and 5872.92 ±195.54 pg/ml 9-12 months post-TBI, p = .045), while injury severity was not associated with difference in mean concentrations. GCS category and Satisfaction with Life (SWLS) were also significant [F(1, 34) = 5.17, p = .029]. BDNF was inversely associated with cognitive battery outcomes and positively associated with time since injury. S-100β was positively associated with anxiety score, depression score and hospital length of stay; GFAP was also positively associated with anxiety score and hospital length of stay. IL-6 was inversely associated with time since injury and cognitive function.
Several biological markers were associated with functional outcomes during the 3-12-month post-injury period. We found S-100β, GFAP, IL-6 and BDNF to play a larger role in the TBI recovery period than other biomarkers examined. Additionally, focus on cognitive symptoms should be clinically integrated into patient care to improve TBI patient outcomes.
23 Summary of the Centers for Disease Control and Prevention’s Self-reported Traumatic Brain Injury Survey Efforts
Jill Daugherty 1 ; Alexis Peterson 1 ; Lindsey Black 2 ; Dana Waltzman 1
1 Centers for Disease Control and Prevention, Atlanta, United States; 2 Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Division of Health Interview Statistics, Atlanta, United States
Introduction
Caused by a bump, blow, or jolt to the head, a traumatic brain injury (TBI) affects how the brain works. Determining the prevalence of TBI, including concussion, in the United States is difficult. Surveillance of TBI in the United States has historically relied on healthcare administrative datasets. The most recent numbers find that about 214,000 Americans are hospitalized and 69,000 Americans die from a TBI every year. However, these numbers likely undercount the true burden of TBI as they do not include people who seek care for their injuries outside of hospital settings or people who do not seek care. An alternative approach to TBI surveillance is to make use of national self-report surveys that ask respondents to report their experience with head injuries. The Centers for Disease Control and Prevention (CDC) has recently added TBI prevalence questions to several national surveys. The objective of this presentation is to summarize CDC’s recent efforts in TBI self-reporting.
CDC added various 12-month and lifetime TBI prevalence questions to a series of nationally representative surveys (e.g., Porter Novelli’s ConsumerStyles survey, National Health Interview Survey, Youth Risk Behavior Survey). Each survey’s questions were slightly different, and they varied by time period assessed and whether they focused on adult or youth respondents.
Depending on the survey methodology and question wording used, 12-month prevalence of concussion/TBI among adults ranged from 3-12% while lifetime prevalence ranged from about 21-28%. Twelve-month prevalence of concussion/TBI among children and adolescents was about 10% while lifetime prevalence ranged from 7-14%.
These results demonstrate that TBI is a common health condition in the United States, and one that is likely consistently underestimated by traditional surveillance methods, which rely on hospital-based datasets. Allowing respondents to self-report their suspected concussions and TBIs resulted in larger prevalence estimates than those captured via traditional surveillance methods. Analysis of the various surveys shows that how the questions are asked, and what terminology is used (e.g., concussion vs. mild traumatic brain injury), affects the estimate. CDC has used the data collected to better refine the questions added to the surveys to ensure the most accurate prevalence estimates are being obtained. These data can be used to optimize and standardize data collection approaches across the field of TBI surveillance.
25 Factors Related to the Quality and Stability of Partner Relationships After Stroke: A Systematic Literature Review
Boudewijn Bus 1,2 ; Brenda van den Broek 1,2,3 ; Laura Verrijt 1 ; Sophie Rijnen 1,2 ; Caroline van Heugten 2,3,4
1 Multidisciplinary Specialist Centre for Brain Injury and Neuropsychiatry, GGZ Oost-Brabant, Huize Padua, the Netherlands; 2 Limburg Brain Injury Centre, Maastricht University, Maastricht, the Netherlands; 3 School for Mental Health and Neuroscience, Maastricht University, Maastricht, the Netherlands; 4 Department of Neuropsychology and Psychopharmacology, Maastricht University, Maastricht, the Netherlands
Provide an overview of the current state of knowledge on factors related to relationship quality and stability following stroke.
Data Sources
Cumulative Index to Nursing and Allied Health, Embase, MEDLINE, Psychology and Behavioral Sciences Collection, APA PsycINFO, and PubMed were searched on November 15, 2022, for literature on factors associated with (1) relationship quality and (2) relationship stability after stroke.
Study Selection
English quantitative and qualitative studies investigating factors associated with relationship quality and/or stability after stroke were included. Three reviewers independently assessed eligibility. Consensus meetings were held in case of divergent opinions. Forty-four studies were included
Data Extraction
Information regarding study objectives and characteristics, participant demographics, independent and dependent variables, and main findings was extracted. Study quality was rated using the JBI Checklist for Analytical Cross-Sectional Studies and/or the CASP Checklist for Qualitative Research. Both were performed by the lead reviewer and checked by the second reviewer. Identified factors are described and presented according to the domains of the International Classification of Functioning, Disability, and Health model.
Data Synthesis
Thirty-seven factors related to relationship quality after stroke were identified, covering the domains of body functions and structures (e.g., cognitive problems), activities (e.g., decrease of physical intimacy), participation (e.g., being socially active), environment (e.g., medication side effects), and personal factors (e.g., hyper-vigilance). Eight factors related to relationship stability were identified, covering the domains of participation (agreement on reciprocal roles) and personal factors (e.g., quality of pre-stroke relationship).
Relationship quality and stability after stroke are related to a multitude of factors. Future research should confirm the relevance of factors found in few studies of suboptimal quality, explore possible associations between relationship stability and factors falling in the domains of body functions & structure, activity, and environmental factors, and explicitly explore potential positive effects of stroke on relationships.
26 The Role of Whiplash Associated Disorders on Concussion Recovery: A Retrospective Study.
Stéphanie Flageol 1,2 ; Evan Foster 2 ; Paul Comper 2 ; Mark Bayley 2,3 ; Tharshini Chandra 2 ; Alan Tam 2,3
1 IRDPQ, Quebec, Canada; 2 Toronto Rehabilitation Institute, University Health Network, Toronto, Canada; 3 Division of Physical Medicine and Rehabilitation, Department of Medicine, University of Toronto, Toronto, Canada
Examine the effect of whiplash associated disorders (WAD) on concussion outcomes among adults evaluated within 7 days of injury.
The study was carried out at the Hull-Ellis Concussion and Research Clinic (Toronto Rehabilitation Institute, Canada).
The authors analyzed patient’s clinical charts and routinely collected data from individuals that were admitted to the clinic between July 2019 and March 2020 from one-week to eight-weeks post-injury. The presence of WAD was determined by the presence of neck pain and cervical spine tenderness or restricted range of motion on physical examination by a clinic physician. Patients’ characteristics and outcomes were described according to the presence or absence of concomitant whiplash associated disorders (WAD).
82 medical files were reviewed retrospectively. 19 cases were excluded due to missing data and 63 cases were included in the study. 25 (40%) patients included were deemed to have a concurrent WAD. The WAD group presented with higher symptom severity (mean of 59/132 (SD 32) versus 39/132 (SD 26) for the no WAD group) and number of symptoms (mean of 18/22 (SD 5) versus 15/22 (SD 6) for the no WAD group) on the SCAT5 on initial assessment. By the end of the follow-up (eight weeks post-injury), fewer individuals with WAD had recovered from their concussion than those without WAD (44% with WAD versus 66% without WAD).
Our findings show that the combination of both concussion and neck symptoms can result in an overall greater frequency and intensity of initial symptoms, and a longer duration is required for recovery of all injury-related symptoms. Recognition of cervical injury in tandem with a diagnosed concussion soon after injury may facilitate earlier referral to appropriate rehabilitation.
27 American Congress of Rehabilitation Medicine Disorders of Consciousness Family Education Project: Implementation and Dissemination of New Web-Based Resource for Caregivers
Brooke Murtaugh 1 ; Kathryn Farris 2 ; Shanti Pinto 3 ; Amy Shapiro-Rosenbaum 4 ; Susan Johnson 5
1 Madonna Rehabilitation Hospitals, Lincoln, United States; 2 Shepherd Center, Atlanta, United States; 3 UT Southwestern, Dallas, United States; 4 Park Terrace Care Center, Queens, United States; 5 Georgia RSVP Clinic, Atlanta, United States
There is an array of educational material available to families and caregivers of severe brain injury experiencing Disorders of Consciousness (DoC). However, it is difficult to find information that is accurate and easy to navigate. Families and caregivers experience trauma along a continuum from hospital to community (Cameron and Gignac 2008). The need for caregivers to prepare for changes in role and caring for their loved one evolves over the course of recovery, but often not fully addressed by their clinical care team. This can lead to added stress, ambiguity and compound trauma for family and caregivers. The American Congress of Rehabilitation Medicine (ACRM) Brain Injury Interdisciplinary Special Interest Group: DoC Task Force, Family Education Subcommittee has developed a compendium of shared educational resources. During the last seven years, the committee engaged in an environmental scan of existing family education content from providers and websites that had information specific to DoC. We then developed a structure for delivering information that is simple, easy to read and organized in a way that that families/caregivers can find specific information across the course of recovery all located in a central, accessible location. The organization of content is separated into three sections: Body/Mind, Taking Care of Self and Resources. Focus groups and surveys were completed with 22 families and 16 professionals to validate the overall structure and included content for accuracy and health literacy. Consumer and professional survey responses were analyzed. Results of the family surveys 67-100% of respondents found content was easy to understand, descriptive and prompted end users to further engage with the additional website links embedded into the content. Professional surveys resulted in 100% of respondents approving the overall content included. The final product of family-focused DoC education will be accessible within a Treatment Hub on www.BrainLine.org . This poster will highlight the overall evolution of the project, content, the review process, partnership with BrainLine.org and the funding efforts to build the Treatment Hub and BrainLine. Our objective is to facilitate knowledge translation of this web-based resource to support further dissemination to the family end user experiencing acute and chronic DoC. Implementation to support utilization of this educational resource, by families, will be dependent on expanding knowledge and collaboration with brain injury medicine professionals across the care continuum for persons experiencing DoC.
28 A Case Report of Arachnoiditis in a Stroke Patient
Shubhangi Kumar, Physical Medicine and Rehabilitation PGY3 1 Kaitlyn Brunworth, M.D. 1 ; Assistant Professor Gemayaret Alvarez 1
1 Nova Southeastern University, Davie, United States; 2 University of Miami/Jackson Memorial Hospital, Miami, United States
This is the case of a 48-year-old female with a past medical history of hypertension who presented to the emergency room with “the worst headache” of her life. She was found to have diffuse subarachnoid hemorrhage and left frontal intraparenchymal hemorrhage, requiring ventriculoperitoneal shunt placement. After the procedure, the patient complained of new-onset bilateral lower extremity paresthesias and weakness. Lab results ruled out cobalamin and folate deficiencies. Electrodiagnostic studies showed bilateral lumbosacral root dysfunction primarily affecting L5-S2. Lumbar MRI showed clumping and diffuse enhancement of cauda equina nerve roots. These findings raised concern for possible arachnoiditis. Arachnoiditis is defined as a persistent inflammation of arachnoid mater that involves membrane thickening, dural adhesions, and clumping of nerve roots. It has no well-defined epidemiology and is considered quite rare and difficult to diagnose. Potential causes for arachnoiditis range from physical or chemical irritants such as injections, surgery, infectious causes such as HIV or TB, or mechanical irritants such as subarachnoid hemorrhage. It has variable timing from the onset of injury until clinical manifestations appear and presents with varying imaging results. Clinically, patients present with an insidious onset of chronic and debilitating pain, most commonly back pain, progressing to radicular pain and sensory defects. Arachnoiditis is managed with supportive care such as physical therapy, pain medication, muscle relaxants, and neurostimulation. It often goes unrecognized and untreated because it is exceedingly rare and difficult to diagnose. Understanding the causes of arachnoiditis and detecting the signs on imaging and physical examination is important to cultivate treatment regimens for future patients. With supportive management through medication and physical therapy, our patient has shown improvement in symptoms and functionality.
29 Characterizing Genetic Risk Factors for Post Traumatic Epilepsy Following Combat Brain Injury
Justin Weppner 1,2,3 ; Jerry Zhang 4 ; Erica Fan 5 ; Nabil Awan 6 ; Mark Linsenmeyer 7 ; Yvette Conley 8 ; Jordan Grafman 9 ; Amy Wagner 4,10,11,12
1 Carilion Clinic Brain Injury Center, Roanoke, United States; 2 Virginia Tech Carilion School of Medicine, Roanoke, United States; 3 Edward Via College of Osteopathic Medicine, Blacksburg, United States; 4 Department of Physical Medicine and Rehabilitation, University of Pittsburgh, Pittsburgh, United States; 5 Department of Epidemiology, University of Pittsburgh, Pittsburgh, United States; 6 Department of Biostatistics, University of Pittsburgh, Pittsburgh, United States; 7 Sunnyview Rehabilitation Hospital, Schenectady, United States; 8 Department of Health Promotion, University of Pittsburgh, Pittsburgh, United States; 9 Shirley Ryan Ability Laboratory, Northwestern University, Chicago, United States; 10 Safar Center for Resuscitation Research, University of Pittsburgh, Pittsburgh, United States; 11 Department of Neuroscience, University of Pittsburgh, Pittsburgh, United States; 12 Clinical and Translational Science Institute, University of Pittsburgh, Pittsburgh, United States
Posttraumatic epilepsy (PTE) is a significant concern after traumatic brain injury (TBI), particularly in military contexts. This study investigated genetic risk factors associated with PTE following combat brain injury using a Gene Risk Score (GRS) approach, utilizing data from the Vietnam Veterans Head Injury Study (VHIS) cohort.
We included 120 genotyped subjects with penetrating TBI (pTBI) and known PTE status monitored over a 35-year period. DNA samples were genotyped for 20 single nucleotide polymorphisms (SNPs) across nine genes linked to PTE in civilians with moderate-to-severe TBI (msTBI). SNPs were assessed using iPLEX Gold or TaqMan Assay, with double-masked genotype assignments. Covariate adjusted logistic regression was used to identify SNP associations with PTE. Covariates included education, post-traumatic stress disorder (PTSD), race, pre-injury intelligence (AFQI), pTBI-related surgery, loss of consciousness (LOC), and pTBI-related amnesia. A weighted gene risk score (wGRS) was then calculated for each individual based on beta-weights derived from univariate logistic regressions generated for each SNP located within individual genes, reaching a p=0.10 threshold in its association with PTE. Ridge regression was used to generate beta-weights for threshold associated SNPs located in the same gene (e.g. IL-1β). This wGRS was used in multivariate logistic regression to assess its added value, above covariates alone, in characterizing PTE risk.
Among this cohort, 44.1% experienced PTE over the 35-year follow-up period. Covariate adjusted logistic regression showed threshold associations between four SNPs (rs16944, rs1801131, rs1143634, and rs769391) and PTE status. For the IL-1β SNP rs16944, AA homozygotes had an 80% PTE rate compared to 30-40% in G-carriers. TT homozygotes for the MTHFR SNP rs1801131 had a 50% PTE rate. Heterozygotes had lower PTE incidence for the IL-1β SNP rs1143634 and for the GAD1 SNP rs769391. A higher number of risk genotypes was positively associated with greater seizure incidence; those with four risk genotypes had a >80% 35-year incidence of PTE while individuals with only one risk allele had ~30% PTE incidence. The wGRS was significantly associated with increased risk for PTE at 35 years, with an odds ratio of 3.64 (1.77-7.52); P<0.001) and enhanced the area under the receiver operating curve (AUROC) by 11% compared to covariates alone.
Key SNP associations—IL-1β rs16944, rs1143634, MTHFR rs1801131, GAD1 rs769391—and the GRS enhanced PTE risk assessment beyond covariate factors alone. This wGRS-based approach showcases the cumulative genetic influence on PTE susceptibility among individuals with combat pTBI.
The study highlights genetic contributions to PTE risk after combat TBI. wGRS inclusion significantly improved multivariable model performance over covariates alone. Future work should consider GRS incorporation when assessing PTE risk among contemporary combat TBI populations to support early screening, prevention, and management strategies.
30 The Effectiveness of Trazodone for Management of Acute Agitation in Patients With Traumatic Brain Injury: A Retrospective Chart Review
Kian Nassiri 1,2 ; Sangeeta Driver 1,2
1 Shirley Ryan AbilityLab, Chicago, United States; 2 McGaw Medical Center of Northwestern University, Chicago, United States
Acute agitation is a common complication in patients who have sustained traumatic brain injury (TBI) and can be measured using the Agitated Behavior Scale (ABS), a validated tool that drives clinical management. There is no consensus regarding use of as needed agents for pharmacologic management of acute agitation in people with TBI.
The primary objective of this study is to assess the effectiveness of as needed trazodone on reduction of agitation as reflected by lower ABS scores in patients with TBI and to demonstrate consistency in reduction of score across various demographic factors of patients with TBI.
A retrospective chart review was performed of patients admitted to acute inpatient rehabilitation over a 2-year period, who had age > 18 years old and were diagnosed with TBI. Data collected included: demographic information, length of stay, number of trazodone administrations, and pre-/post-trazodone administration ABS scores. Patients were organized into subgroups based on demographic characteristics.
The mean change [CI] in ABS score and total percent change in ABS score for all 128 patients were 8.2 [7.6, 8.8] and 14.6% [13.6%, 15.7%], respectively. For gender, males represented 84.4% (N=108) and females 15.6% (N=20). Mean change and percent change of total ABS based on gender were as follows: males 8.1 [7.4, 8.7] and 14.4% [13.3%, 15.6%], and female 8.7 [7.0, 10.3] and 15.5% [12.5%, 18.4%]. ANOVA showed no significant variance in mean change of ABS based on gender (p=0.51). For race, white represented 52.2% (N=67), black 19.5% (N=25), other 8.6% (N=11), and patients who declined to answer 19.5% (N=25). Mean change and percent change of total ABS based on race were as follows: white 8.3 [7.6, 9.1] and 14.9% [13.5%, 16.3%], black 7.9 [6.3, 9.4] and 14.0% [11.3%, 16.8%], other 8.5 [6.7, 10.2] and 15.1% [12.0%, 18.2%], and declined to answer 8.4 [6.3, 9.6] and 14.2% [11.2%, 17.0%]. ANOVA showed no significant variance based on race (p=0.91). For mechanism of injury, falls represented 46.9% (N=60), motor vehicle collision (MVC) 32.8% (N=42), gunshot wound (GSW) 6.3% (N=8), blunt force trauma (BFT) 9.4% (N=12), and other 4.7% (N=6). Mean change and percent change of total ABS based on mechanism of injury were as follows: falls 8.4 [7.5, 9.3] and 15.0% [13.3%, 16.6%], MVC 7.5 [6.5, 8.4] and 13.4% [11.7%, 15.6%], GSW 7.2 [4.9, 9.4] and 12.8% [8.9%, 16.8%], BFT 10.0 [7.9, 12.2] and 17.9% [14.1%, 21.8%], and other 8.7 [4.8, 12.6] and 15.6% [8.6%, 22.5%]. ANOVA showed no significant variance in mean change of ABS based on mechanism of injury subgroup (p=0.20).
Use of as needed trazodone was associated with consistent reduction in ABS scores of people with TBI, independent of subgroup characteristics based on age, gender, race, and mechanism of injury.
31 Enhancing Interdisciplinary TBI Treatment for Military Veterans and Service Members With Co-Occurring Substance Use: Program Development, Access to Care, and Early Treatment Outcomes
Katherine McCauley 1 ; Tracey Wallace 1 ; Dina Forehand 1 ; Javier Palacios 1 ; Jackie Breitenstein 1 ; Russell Gore 1
1 Shepherd Center, Atlanta, United States
Traumatic brain injury (TBI) and problems related to substance use (SU) commonly co-occur in the military and veteran population. Individuals with co-occurring TBI and SU (TBI + SU) are at greater risk for multiple negative outcomes, including death by suicide. Intensive interdisciplinary treatment for TBI can support improvement in symptoms and quality of life, but individuals using substances are often denied access to TBI treatment until they maintain lengthy periods of abstinence.
Our interdisciplinary treatment program for military TBI has undertaken efforts to: 1) characterize substance use among those seeking treatment, 2) develop and implement an approach to assessment, integrated treatment, and follow-up support for TBI + SU, and 3) evaluate access and treatment outcomes. We categorized all individuals who inquired about or applied for care within a 26-month period according to level of care accessed or reason for no access. Among 160 participants consented, 101 started intensive outpatient treatment (IOP) for TBI and completed measures related to substance use in addition to assessments for clinical care. This group was divided based on scores on SU-related measures into TBI (n = 59) and TBI + SU (n = 42) groups. Mixed ANOVAs were conducted to determine effects of treatment and group membership on TBI symptoms and consequences related to SU, captured by scores on the Neurobehavioral Symptom Inventory (NSI) and the Short Inventory of Problems - Revised (SIP-R).
An integrated care model of TBI treatment for clients with co-occurring SU was developed by modifying programing and adding resources to help those with TBI + SU safely and effectively participate in interdisciplinary TBI care. There was a significant main effect of treatment (F(1, 100) = 64.37, p < 0.001) on NSI scores, with decreased symptoms at discharge across both groups. Between-group differences were not significant, indicating that groups had similar NSI score reductions with treatment. There was a significant main effect of treatment F(1, 100) = 18.45, p < 0.001 and group membership F(1, 100) = 21.41, p < 0.001 and a group x time interaction F(1, 100) = 9.34, p = 0.003 on SIP-R scores, showing higher SIP-R scores among the TBI + SU group prior to treatment and greater reductions in SIP-R scores for the TBI + SU group with treatment. Among research participants who engaged in IOP treatment during this timeframe (n = 101), four were early discharges, and one of these instances was related to substance use.
This programming has enabled entry and retention in treatment for many clients with TBI + SU. Initial results related to treatment outcomes are promising, with follow-up data collection ongoing. Lessons from these efforts may inform programming in other interdisciplinary programs treating individuals with TBI + SU.
32 OculoMotor and Vestibular Endurance Screening (MoVES) Protocol Adult Concussion Data
Chang Yaramothu 1 ; Jacqueline Theis 2 ; Stuti Mohan 1
1 New Jersey Institute Of Technology, Newark, United States; 2 Virginia Neuro-Optometry, Richmond, United States
To evaluate the effectiveness of the OculoMotor and Vestibular Endurance Screening (MoVES) protocol in identifying concussed adults.
Participants between the ages of 18 to 65 years old were recruited from the Virginia Neuro-Optometry and were referred to the clinic after a concussion diagnosis. Data were collected in the first visit following the MoVES protocol with the following seven assessments: 1) near point of convergence (NPC), 2) amplitude of accommodation for both eyes (AA),3) horizontal saccades, 4) vertical saccades, 5) vergence jumps, 6) horizontal vestibular oculomotor reflex (VOR), and 7) vertical VOR. The OculoMotor Assessment Tool (OMAT, Gulden Ophthalmics, Elkins Park, PA, USA, product number 18009) was utilized to provide eye movement targets for all assessments. Saccadic and vergence jump assessments were performed using methods described in the OMAT Normative study, and NPC/AA were performed utilizing methods described in CITT studies. VOR assessments were performed with the participant holding the larger slider of the OMAT tool at arm’s length and rotating the head horizontally or vertically while fixating on the target letters on the slider. The saccadic, vergence, and VOR movements were performed for one minute each, and the number of repetitions was counted by an operator utilizing the OMAT companion smartphone application. The OMAT smartphone app displayed the number of eye movements or head turns performed in one-minute in 15-second intervals.
Presented data was collected on 33 participants (6 males) with an average age of 39.1 ± 12.3 years and an average of 22.1 ± 34.0 months since injury (3 participants were seen 109, 123, and 126 months after injury). On average, the participants made 24.8, 22.5, 19.0, and 17.2 horizontal saccadic eye movements in each of the 15-second intervals. A similar trend of decreasing number of eye movements or head rotations was observed in all the movements: vertical saccades (24.0, 18.1, 15.2, 12.6), vergence jumps (15.2, 13.1, 11.4, 10.5), HVOR (25.0, 21.6, 19.3, 13.6), VVOR (24.6, 20.4, 19.2, 14.6). The average NPC break was 10.5 ± 7.9 cm with a recovery of 14.9 ± 10.6 cm. The number of eye or head movements presented by this cohort was significantly lower than that observed in normative non-concussed cohorts in previous studies.
These data indicate that the MoVES protocol can potentially be utilized to identify a concussive event in the adult population. Additionally, the MoVES protocol has the potential to be used as an objective quantitative tracking tool for recovery. Healthy controls show no statistical significance in the number of eye or head movements; however, concussed individuals show a consistent decrease in the number of eye or head movements in the first to last interval.
33 Vision Quality of Life With Time (VisQuaL-T) Survey Adult Concussion Data
To evaluate the effectiveness of the Vision Quality of Life with Time (VisQuaL-T) survey in assessing the visual quality of life in concussed adults.
Participants between the ages of 18 to 65 years old were recruited from the Virginia Neuro-Optometry and were referred to the clinic after a concussion diagnosis. Data was collected on the first visit, where the participants responded to the 10 questions in the survey. The survey consisted of a list of the following activities: 1) reading for pleasure, 2) studying for a test/exam, 3) completing homework, 4) completing work in an office setting, 5) being in a crowded location, 6) tolerating habitual lighting, 7) using a smartphone/tablet, 8) playing a computer/console video game, 9) using a computer for general purposes, 10) watching a show on a large screen. Participants were asked to indicate how long it took them to experience any of the following symptoms: headache, dizziness, eye strain, double vision, floating words, blurry vision, inability to pay attention, easily distracted, or sleepy/drowsy. The possible time ratings, a novel feature of VisQuaL-T, were 0-15 min, 15-30 min, 30-45min, 60+ min, and N/A (for activities a participant does not participate in). A composite score between 0 and 3 was derived utilizing the methods in the VisQuaL-T normative manuscript by Dungan Et al. 2023.
Presented data was collected on 40 participants (6 males) with an average age of 39.2 ± 12.4 years and an average of 21.8 ± 33.3 months since injury (4 participants were seen 98, 109, 123, and 126 months after injury). Participants had an average composite score of 1.56 ± 0.57.
An average composite score of 1.56 is equivalent to approximately 20 minutes. Prior studies have shown that the general population scores an average composite score of 2.4. The utilization of time as a measurement factor has the potential to illicit more concise and quantitative data from a concussed individual. The presented instrument can potentially be more clinically relevant as questions examine how long a patient can perform a task before the onset of symptoms rather than simply reporting whether symptoms are present. This non-generalized symptom scale may potentially be a better indication of their quality of life. The VisQuaL-T can potentially indicate quality of life problems in patients after a concussive event and potentially guide clinical intervention. The survey also has the potential to be used as a recovery tracking tool.
34 Are We Providing Older Persons After Brain Injury the Same Care as Younger Persons? A Retrospective Population-Based Study
Narhari Timilshina 1 ; Arman Ali 1 ; Laura Langer 1 ; Judith Gargaro 1 ; Mark Bayley 1
1 University Health Network, Toronto, Canada
Traumatic brain injury (TBI) is a major public health problem resulting in hospitalizations, morbidity, and mortality globally. Despite the large proportion of elderly persons experiencing TBI, limited data exist at the population level.
To apply quality indicators (QI) to examine TBI care quality for older persons (65 years and older).
Provincial administrative health services data from publicly funded healthcare were used. We co-developed 12 QIs with healthcare partners and persons with lived experience, and measured care quality for patients 65+ years with TBI between 2016 and 2021. Age and gender adjusted incidence and QIs with 95% confidence limits were calculated. Variations in QI performance was explored according to age group, sex, geographic region, and income quintile.
A total of n=15,194 complex-mild and n=19,237 moderate/severe brain injury cases were identified between 2016-2021. The age and gender adjusted incidence rate for all severities of TBI increased with age. Older persons were more likely to get admitted to general rehab than specialized TBI rehab after discharged from acute care (8.35% vs 3.04% for persons with moderate to severe TBI). Higher ED visits rates in years 1 and 2 increased with age (156.8 per 100 PY in 80+ age group vs. 114.9 per 100 PY in 65-79 years age) group). The rate of falls in the first two years after moderate-severe TBI was higher among elderly patients (43.7 per 100 PY in 80+ age group vs. 30.6 per 100 PY in 65-79 year group).
This study establishes a foundation for quality-of-care assessments and monitoring disparity in care for older adults with TBI at a population level. Gaps were identified in receiving rehabilitation services after discharge from acute care, and follow-up with health professionals. Ensuring that older persons receive appropriate rehabilitation and community support to reduce falls is necessary to maintain independence in the community.
35 Short-Term Changes in Primary Motor Cortex Intracortical Inhibition Following Head Impact Exposure in Varsity Canadian Football
Géraldine Martens 1,2 ; Sophie-Andrée Vinet 2 ; Samuel Guay 1,2 ; Amélie Apinis-Deshaies 2 ; Johan Merbah 2 ; Betrand Caré 2 ; Laurie-Ann Corbin-Berrigan 3 ; Eric Wagnac 4 ; Louis De Beaumont 1,2
1 University Of Montréal, Montréal, Canada; 2 Montreal Sacred Heart Hospital Research Center, Montréal, Canada; 3 Université du Québec à Trois-Rivières, Trois-Rivières, Canada; 4 École de technologie supérieure, Montréal, Canada
Repetitive head impacts and sport-related concussions are significant concerns in contact sports due to their potential adverse effects on brain health. This study investigated the association between head impact exposure (HIE) during varsity football games and short-term changes in cortical excitability of the primary motor cortex (M1) using transcranial magnetic stimulation (TMS). A convenience sample of forty-nine university-level male athletes (median [IQR] age: 23.0 [2.0] years] were recruited. Twenty-nine athletes wore instrumented mouthguards during a football game to measure HIE (head impact group). TMS measurements were conducted 24 hours before and 1-2 hours after the game. Another twenty control football athletes underwent a non-contact training session and underwent identical TMS assessments (control group). For the head impact group, the median [IQR] number of impacts (> 10g) per player during a game was 11.6 [15.0]; the magnitude of each head impact was 18.9 [7.1] g and the cumulative force sustained per player was 234 [312.9] g. TMS results showed that whereas short-interval intracortical inhibition (SICI) ratios increased by 0.054 (± 0.0614) in the head impact group in the hours following the game, it decreased by 0.0704 (±0.0352) in the control group within the same time interval following the non-contact training session. A 2X2 mixed ANOVA on SICI ratios showed a significant Time * Group interaction (F(1, 44) = 5.192, p = .028, η2 = 0.106). Neither the main effect of groups (head impact versus control; p = .058) nor the main effect of time (24 hours before sport vs 1-2 hours after sport; p = 0.756) on SICI measures reached statistical significance. The relationship between HIE (i.e., number, magnitude and cumulative forces of impacts) and SICI was also investigated using two-tailed Pearson’s correlations. SICI modulation following the game was found to be unrelated to the mean number of impacts (p˂ .05) as well as to the cumulative forces of impacts across low-magnitude impact ranges (p˂ .05). However, the observed SICI disinhibition following the game was significantly related to the number of high-magnitude head impacts beyond 40g (r(29)=-0.397, p = 0.041) and the cumulative forces beyond 40g (r(29)=-0.468, p = 0.014) after False Discovery Rate corrections for multiple comparisons were applied. Likewise, this SICI disinhibition strongly correlated with the number of head impacts over 60g (r(29)=-0.629, p < 0.001) and cumulative forces over 60g (r(29)=-0.648, p = 0.014). Athletes exposed to subconcussive hits associated to a football game exhibit abnormal M1 corticomotor inhibition function, particularly when recorded impact magnitude ranges above 40g. Given the deleterious effects of decreased inhibition on motor control and balance, systematically tracking head impact forces at each game and practice with contacts could reveal useful for injury prevention in contact sports.
36 Updating the Concussion Awareness Training Tool (CATT): Translating the Expanding Concussion Evidence Into Accessible Resources
Shelina Babul 1,2 ; Kate Turcotte 1 ; Shazya Karmali 1 ; Vanessa Linton 1
1 BC Injury Research & Prevention Unit, BC Children’s Hospital, Vancouver, Canada; 2 University of British Columbia, Vancouver, Canada
Concussions occur inside and outside of the sports realm – including those resulting from falls, motor vehicle crashes, and violence – yet the emerging concussion response and management evidence is predominantly from the sports perspective. The 6th International Conference on Concussion in Sport, held in October 2022, prompted widespread updating of concussion training and resources. Notably, assessments for concussion, and the roles of rest and aerobic physical activity supporting recovery, have been considerably refined.
The Concussion Awareness Training Tool (CATT) provides free evidence-based concussion training tailored to diverse audiences, extending beyond medical professionals, coaches, youth, athletes, and their caregivers, to include educators, workers, and their employers, and those supporting survivors of intimate partner violence. Recently launched on its new online platform, the CATT offers up-to-date educational eLearning modules and downloadable resources, each created using an integrated knowledge translation approach. CATT resources include the Concussion Pathway (also adapted for the Motion Picture, Film, and Live Performance industry, and for neurodiverse students); questions to ask your doctor; strategies for return to activity, school, school, and work; accommodations during concussion recovery; and considerations for managing mental health symptoms.
To date, over 175,000 people worldwide have completed CATT training. The cattonline.com website receives over 17,000 visits per month from over 50 countries: primarily Canada and the United States, as well as the United Kingdom, Australia, China, New Zealand, Ireland, India, South Africa, France and elsewhere. This wide-reaching approach to online concussion education, originally launched in 2013, provides information in both English and French. ELearning modules for medical professionals, coaches, and school professionals are also available Arabic. CATT training has been mandated by over 100 sporting associations, universities, schools, and other organizations in Canada and the United States. This includes 32 universities/colleges across Canada, and BC School Sports representing 450 schools in British Columbia. Furthermore, the University of British Columbia is the first medical school in Canada to incorporate concussion education into its curriculum, using the CATT resources.
Global education efforts using CATT have focused on East Africa (Uganda, Kenya, Tanzania), Pakistan, Japan, Lebanon, and South Africa. CATT is currently seeking engagement with Indigenous partners within Canada to create culturally appropriate concussion resources.
37 Harnessing Chat-Bot Artificial Intelligence: Assessing the Accuracy and Comprehensiveness of ChatGPT-3.5 and 4.0 in Traumatic Brain Injury Information Dissemination
Matthew Lee 1 ; Angelo Cadiente 1 ; Jamie Chen 1 ; Yi Zhou 1,2 ; Brian Greenwald 1,2
1 Hackensack Meridian School Of Medicine, Nutley, United States; 2 JFK Johnson Rehabilitation Institute, Edison, USA
Accessibility to accurate and comprehensive information is crucial for patients and caregivers after a traumatic brain injury (TBI). While fact sheets offer standardized information, the rise of chat-bot artificial intelligence (AI) presents an alternative source of information. This study evaluates and compares the accuracy and comprehensiveness of responses from ChatGPT-3.5 and ChatGPT-4.0, utilizing the most-viewed TBI fact sheets from the Model Systems Knowledge Translation Center (MSKTC) as the gold standard.
Five TBI fact sheets were chosen from the MSKTC based on total views from 12/1/22-5/31/2023. Subheadings from the fact sheets were formatted into questions to simulate real-world queries. These questions were posed to both ChatGPT-3.5 and ChatGPT-4.0. Its output was compared to corresponding MSKTC fact sheet content and was scored by 3 blinded, independent graders using a 1-5 Likert scale based on accuracy, comprehensiveness, and additional factual and useful information. The mode score among graders was used as the consensus score.
Analysis of 38 prompts demonstrated a significant difference in accuracy and comprehensiveness scores between ChatGPT-3.5 and ChatGPT-4.0 (p = 0.04). The mean ChatGPT-4 score was 3.63 (SD = 0.94), indicating its responses were generally accurate but occasionally lacked comprehensiveness. In comparison, ChatGPT-3.5 had a mean score of 3.21 (SD = 0.84), indicating its responses were mostly accurate but often missing key details present in MSKTC fact sheets. The standardized mean difference (SMD) was -0.47 (95% CI: -0.92, -0.01). Further analysis of individual spreadsheets showed that ChatGPT-4.0 outperformed ChatGPT-3.5 in regards to discussing details about the vegetative state, the relationship between memory and TBI and the relationship between headaches and TBI.
This study demonstrates the advancements in AI from ChatGPT-3.5 to ChatGPT-4.0, with the latter showing a statistically significant improvement in accuracy and comprehensiveness when providing information on traumatic brain injuries. While both versions of ChatGPT can serve as valuable tools for disseminating TBI information, ChatGPT-4.0 appears to be a more reliable source, particularly in discussing complex topics like vegetative state and memory-related issues post-TBI. However, caution is advised as occasional gaps in comprehensiveness were observed in both versions. Continued advancements in AI and regular updates based on reliable sources such as MSKTC are essential for optimal patient and caregiver support.
38 Falling Out of Place: An Equity-Focused Characterization of mTBI/Concussion Healthcare
Arman Ali 1 ; Judith Gargaro 1 ; Lesley Plumptre 2 ; Jiming Fang 2 ; Mark Bayley 1
1 University Health Network (KITE-Toronto Rehab), Toronto, Canada; 2 Institute for Clinical Evaluative Sciences (ICES), Toronto, Canada
Although often classified as ‘mild’ traumatic brain injuries (mTBI), concussions can have serious public health consequences, with approximately 32,000 people experiencing persisting symptoms in Ontario each year. Due to the lack of a standardized care pathway, care quality and receipt depend on social, geographic, and demographic factors. Concussion treatment in Ontario is provided through a combination of public and third party funded care, the nature of which is determined by the cause of injury. Third party funded care is accessible if injured in an insured motor vehicle collision or at the workplace, while those injured by falls typically only receive publicly or self-funded care. As a result, equity deserving groups are disproportionately affected, impacting the level of care received and recovery. There is little health equity-focused research characterizing the concussion population and their healthcare utilization.
To 1) characterize mTBI/concussion and identify inequities related to healthcare utilization, and 2) highlight implications for subpopulations that may be disproportionately impacted.
Individuals a formal mTBI/concussion diagnosis between 2016 to 2022 were identified using administrative databases (e.g., Discharge Abstract Database, National Ambulatory Care Reporting System, Ontario Health Insurance Plan, and National Rehabilitation Reporting System). Incidence and healthcare utilization rates (e.g., emergency department (ED) visits) were calculated.
A total of 1,075,791 cases of mTBI/concussion were identified in Ontario. Of this cohort, nearly 30% of people sustained their injury through a fall, while sport-related injuries and motor vehicle collision comprised just 5% and 3% of all mTBI/concussions respectively. The incidence rate of concussion was 1.5 times higher among those with mental health comorbidities (14.07 vs 9.61 per 1000) and nearly 3 times higher among those with cognitive comorbidities (22.44 vs 7.87 per 1000). The ED visit rate during the two years post-concussion was considerably higher in people aged 65-79 (101 visits per 100 patient years (PY))) and 80+ (139.8 visits per 100 PY) compared to the overall provincial rate (79.3 visits per 100 PY). Those in rural or Northern areas, in the lowest income quintile, with pre-existing cognitive comorbidities, and who sustained their injury by falling also had considerably higher ED visit rates compared to the overall rate. The most utilized healthcare resource among people with concussion in the years following their injury was mental health-related care (95.8 per 100 PY).
Concussions occur frequently among older adults and people with mental health or cognitive comorbidities, who are all at greater risk of becoming high users of the healthcare system. Administrative data show that most concussions are caused by falls, which carries important implications, as fall-related injuries are unlikely to be covered by insurance-funded healthcare. Fall prevention efforts should be targeted toward these subgroups to decrease the burden on healthcare systems.
39 How Far are We From Achieving Ideal TBI Care? Evaluating TBI Care Quality and Equity Through Evidence-Based Quality Indicators
Traumatic brain injuries (TBI) are chronic conditions requiring ongoing care. However, the long-term supports needed by people with moderate-severe TBIs are often not in place after inpatient care, despite community living constituting most of their lifetime. This is complicated by the fact that care quality varies tremendously depending on socio-economic and regional factors, often disproportionately affecting equity-deserving groups. Despite these challenges, few jurisdictions have developed care quality evaluation strategies grounded in evidence-based, standardized, and equity-focused care pathways that span the care continuum.
To 1) evaluate TBI care quality and equity within the context of the care pathways approach and 2) use Quality Indicator data to identify system-level gaps and target improvement initiatives.
Residents admitted to acute care with a formal TBI diagnosis between 2016 to 2022 were identified using administrative databases (e.g., Discharge Abstract Database, National Ambulatory Care Reporting System, Ontario Health Insurance Plan, and National Rehabilitation Reporting System). From this cohort, data for 13 Quality Indicators were collected to reflect the stages of the TBI care pathway: pre-acute (n=2 indicators), acute (n=1), rehabilitation (n=3), community (n=7).
A total of 34,431 incident cases of TBI with hospital stay were identified. Over half of the people with TBI in this cohort were older adults (65+), and nearly 70% sustained their injury by falling. Older adults had a substantially higher incidence rate of moderate-severe TBI (39 per 100,000 for 65–79-year-olds and 173 per 100,000 for those aged 80+) than the overall rate (19 per 100,000). People with pre-existing cognitive comorbidities had an incidence rate six times higher than that for people without such comorbidities (161 per 100,000 vs 26 per 100,000). Admission to inpatient rehab was low across the province, with 22% of moderate-severe TBI patients admitted to any inpatient rehab and only 9% admitted to a specialized facility. For older adults, people with cognitive comorbidities, and people in Northern Ontario, specialized inpatient rehab admission was further limited. Of those who did not receive inpatient rehab, 55% were not followed-up by any medical professional in the community within 30 days of acute discharge. Within one year of acute discharge, just 10% were followed-up by a relevant specialist (e.g., physiatrist).
Care quality and equity gaps were identified in the rehabilitation and community stages of care. Admission to specialized inpatient rehabilitation was extremely limited, particularly in Northern regions, and for older adults and people with cognitive comorbidities, despite the latter groups being at higher risk of sustaining these injuries. Few people with TBI received timely primary care follow-up in the community. It is imperative to target injury prevention and quality improvement efforts toward these inequities and gaps to enhance TBI care quality, improve long-term outcomes, and optimize recovery.
40 How Can We Provide Better Care for Persons Who Have Sustained a Traumatic Brain Injury (TBI)? Living Clinical Practice Guidelines and Clinical Tools Are at Your Fingertips to Ensure Best Care Practice
Aishwarya Nair 1 ; Parwana Akbari 1 ; Judith Gargaro 1 ; Mark Bayley 1
The Canadian Clinical Practice Guideline (CPG) for the Rehabilitation of Adults with Moderate to Severe Traumatic Brain Injury (TBI) helps inform TBI care across jurisdictions through its ongoing and comprehensive review of research and clinical evidence. This review helps the CPG produce best-practice recommendations to improve the quality and consistency of care provided by healthcare professionals, as well as patient health outcomes. The CPG’s beneficial effects, however, are contingent on not only a methodologically rigorous guideline development process, but also on the successful knowledge translation (KT) and implementation of the resulting recommendations and associated tools.
Orient healthcare professionals to the CPG and help 1) increase understanding of the clinical value and utility of the living CPG and Ideal Care Pathways, which promote quality care and equity of access across the care continuum, and 2) guide implementation of the up-to-date best-practice recommendations, resources, and clinical tools.
Regulated Health Professional Associations in Ontario, Canada were approached to partner in and co-develop targeted KT activities rooted in the principles of adult learning: 1) self-concept; evidenced in CPG KT’s self-directed, asynchronous learning model, 2) adult learner experience, readiness to learn, orientation to learning, and motivation to learn; evidenced in CPG KT’s target audience and voluntary attendance, and 3) active learning; evidenced in CPG KT’s real-life case examples presented by healthcare professionals and interactive discussion. The KT activities promoted the relevance of the CPG by using clinical data, partnering with relevant practicing clinicians, and addressing current clinical issues in TBI care. The primary target audience was healthcare professionals who may not routinely encounter individuals who have sustained a TBI, and/or who may not be up to date on TBI best care practices.
The most popular KT method was interactive webinars, but in many cases, multiple methods, including newsletter articles, blog posts, website links and all-member emails, were used. All webinars were recorded, and their slide decks were made available for asynchronous learning. The KT activities have been ongoing since June 2023, and have shown excellent engagement as evidenced in the increasing number of visits to the CPG website, with 7700 visits in July 2023 to 9205 visits in September 2023. Invitations have been forth coming to return for further interactive sessions and to present at relevant RHP conferences. Further data on the CPG KT engagement, follow-up activities, and Google Analytics for the online resources will be presented.
Our multi-faceted and collaborative KT strategy for the CPG and Ideal Care Pathways is key in helping healthcare professionals make informed TBI clinical care decisions based on the most up-to-date scientific evidence for quality care, supporting the overall vision to provide ideal and equitable lifelong care for ALL after a brain injury.
41 “I Am Seen, I Am Heard, I Matter:” A Case Study of a Somatic, Contemplative Approach to Embodied Recovery From Functional Neurological Disorder, Traumatic Brain Injury, and Post Traumatic Stress Disorder Among Special Operations Forces
Esther Estey 1,2,3 ; Carey Pawlowski 1 ; Wendy Guyker 3
1 Veterans Affairs Palo Alto Healthcare System, Palo Alto, United States; 2 Harvard Medical School, Center For Mindfulness, Malden, United States; 3 University at Buffalo, The State University of New York, Buffalo, United States
Functional neurological disorder (FND) denotes neurological disorders of unknown origin that are not explained by other mental or medical disorders or structural injury to the brain. Symptoms can include motor/sensory loss, seizures, tremors, and other disturbances that affect critical areas of functioning. Traumatic brain injury (TBI) can be a precipitant, along with trauma and Post Traumatic Stress Disorder (PTSD) – both of which may serve as either predisposing or precipitating factors for FND. The prevalence rate of FND is higher among active-duty service members than the U.S. civilian population, with those presenting with a history of mood or PTSD symptoms at greater risk. Emergent findings on clinical treatment integrating cognitive, mindfulness, and compassion-based approaches for FND are promising but limited. There is no current evidence on body-oriented, somatic therapies which may holistically address the range of symptoms causing distress and/or dysfunction for adults with FND.
A 3-week course of integrative treatment was delivered to a 33-yr old Special Operations Forces, male service member presenting with FND, TBI, PTSD, Generalized Anxiety Disorder, Adjustment Disorder with Depressed Mood, insomnia (clinically significant, in severe range), and chronic pain. The service member received 1-hour psychotherapy sessions, 3 to 4 times per week during an intensive post-acute inpatient brain injury rehabilitation program. Treatment consisted of a somatic and embodiment-based approach integrating cognitive behavioral psychotherapy for PTSD and chronic pain, psychoeducation, body-oriented interventions, mindful movement, meditation, self-compassion exercises, and homework. Repeated measures analyses examined change in pre-post outcomes on the General Anxiety Disorder-7, Patient Health Questionnaire-9, PTSD Checklist for DSM-5, Insomnia Severity Index, Neurobehavioral Symptom Inventory, and Self-Efficacy for Symptom Management Scale.
At post-intervention, there were significant decreases in neurobehavioral symptoms (31 points), PTSD (10 points), anxiety (5 points), and depression (11 points). A significant increase in self-efficacy was also found (30 points). There was a non-significant downward trend in insomnia severity (3 points). Feasibility and acceptability were established.
To our knowledge, this is the first evidence of efficacy, feasibility, and acceptability of third-wave cognitive behavioral treatment with a military service-member, as well as the first evidence for any integrated psychotherapy approach for adults addressing FND, TBI, and PTSD concurrently. Further adding to the literature, this is also the first investigation to demonstrate support for the effectiveness of an embodiment-focused, somatic approach to FND recovery. Further investigations based on experimental designs are needed to expand upon these preliminary findings. Recommendations for future studies and trauma-sensitive, somatic, and compassion-based approaches in intensive rehabilitation of FND and comorbid TBI and PTSD are provided.
42 Spectrophotometric Evaluation of Light Sources that Trigger Photophobia in Patients with Brain Injury and the Corresponding Reduction with Tinted Lenses and/or Environmental Adaptations for Indoors, Outdoors, and Electronic Devices
Jacqueline Theis 1,2,3 ; Joyce Stern 4
1 Virginia Neuro-optometry, Richmond, United States; 2 Concussion Care Centre of Virginia, Richmond, United States; 3 Department of PMR, Uniformed Services University, Bethesda, United States; 4 University of Richmond, Richmond, United States
Photophobia is a common symptom in traumatic brain injury that can persist months and even years post injury. Currently, there is a lack of scientific guidance as to the best method to treat these patients.
We did a retrospective review of patients presenting post-TBI to a neuro-optometric clinic complaining of photophobia and evaluated what types of light sources they found to be most triggering, as well as which treatment option they found to be most alleviating of their symptoms. We then used a spectrophotometer to measure the spectral irradiance and light intensity of the most common triggers (computer, phone, fluorescent lights, indoor incandescent bulbs, and outdoor sunlight), and the change in irradiance and light intensity when using different tinted lenses, reducing screen brightness, and using an anti-glare computer screen.
Direct sunlight has the highest spectral irradiance over 5x that of indoor lighting and electronics. Unlike sunlight, which had a widespread spectral irradiance over all wavelengths, Indoor fluorescent lights and electronics had small, specific peaks of irradiance. Indoor fluorescent light had peaks of irradiance at 435nm, 490nm, 545nm 585nm, 615nm and 710nm, and electronics on full brightness had peaks at 430nm, 450nm, 485nm, 540nm, 585nm, 615nm, 630nm and 650nm and 710nm which were very similar in wavelength but less intense than fluorescent lights. The intensity of the light outside was 60x more intense than fluorescent lights, and 600x more intense than electronics. Patients were variable in their photophobia triggers, with some noting all light sources as triggers, but the majority of patients only reported a profile of specific triggers (ex: fluorescent lights and electronics). Spectrophotometry of 10 different brands of “FL41” tinted lenses revealed that each tint had different spectral profile in reducing light emitted from the computer even though all are marketed as being effective in “blocking blue light.” Online purchased “blue blockers” that were clear with a slight yellow tint and prescription reading glasses with an anti-reflective coating had slight reduction in light transmission at 444-476nm, and 504-536nm, 556-576nm, 628 and 648nm, but the reduction was not as effective as using an anti-glare computer screen or adjusting the brightness of the computer. The most effective tints in reducing spectral irradiance peaks from fluorescent lights included certain but not all FL41 tints, 50% blue and 81% NOIR but that was not what the patient always said was subjectively their preferred tint for comfort.
Not all patients post-TBI are photophobic to the same light sources. The most cost effective solution is to turn the brightness down on devices and overhead lighting, and if that is not effective try an FL41, blue or NOIR tint if the patient requires it to return to ADLs.
43 Immunologically Mediated Biochemical Injury to the Trigeminal Ganglion by COVID-19 Vaccine Administration: An Understanding for the Pathophysiology of Trigeminal Neuralgia
Christopher Ogunsalu 1 ; Lissa Pinkney-Gayle 1 ; Arif Saqui 1
1 International Post Graduate College, Montego Bay, Jamaica
The trigeminal neuralgia is a relatively uncommon condition which affects less than 0.5% of the general population. This condition is characterized by episodic attacks of sharp pains which is almost always unilateral in the region of the face with the fifth cranial nerve (CN V) distribution. This attack is triggered by movements of the facial muscles, cold temperature, touch and are spontaneous in nature and has ill-defined etiology.
The purpose of this current work is to positively implicate the administration of the COVID-19 vaccine in the pathophysiology of this facial neuralgia which is not unlike Trigeminal neuralgia. It will as such be reasonable to implicate an immunologically mediated biochemical injury to the trigeminal ganglion as the pathway for the expressed pain.
Since Trigeminal neuralgia has existed in the past long before the introduction of COVID-19 vaccination, it may be reasonable that this condition is called a post-traumatic trigeminal neuropathic pain due to biochemical injury to the trigeminal ganglion sequel to an immunological pathway initiated by COVID-19 vaccine. It must as such be a distinct clinic-pathologic entity from trigeminal neuralgia.
44 Defining Concussion Symptom Trajectories and Rates of Persisting Post-Concussive Symptoms Among Youths
Steve Hicks 1 ; Keith Yeates 2 ; Christina Master 3 ; Rebekah Mannix 4 ; Frank Middleton 5 ; John Leddy 6 ; Deborah Levine 7
1 Penn State University, Department of Pediatrics, Hershey, USA; 2 University of Calgary, Department of Psychology, Calgary, Canada; 3 Children’s Hospital of Philadelphia, Department of Pediatrics, Philadelphia, USA; 4 Boston Children’s Hospital, Department of Emergency Medicine, Boston, USA; 5 SUNY Upstate Medical University, Department of Neuroscience, Syracuse, USA; 6 SUNY Buffalo, Department of Clinical Orthopedics and Rehabilitation Medicine, Buffalo, USA; 7 Weill Cornell College of Medical Sciences, Department of Emergency Medicine, New York, USA
Concussions involve symptoms that arise following mild traumatic brain injury (mTBI). There is limited understanding about the evolution of concussion symptoms, particularly among children. This limits clinicians’ ability to predict concussion duration, or even define persisting post-concussive symptoms (PPCS). The objective of this study was to characterize the trajectory of concussion symptoms among youths and define the prevalence of PPCS.
This cohort study included 1132 youths, 12-21 years. There were 399 youths with mTBI (enrolled 2.9 ± 2 days after mTBI) and 733 without mTBI. Both groups were recruited at emergency departments and outpatient clinics. The Post-Concussion Symptom Inventory (PCSI) was used to assess 22 concussion symptoms. In total, 2074 PCSI were completed: 1076 uninjured ratings (865 from youths without mTBI, and 211 retrospective estimates from youths with mTBI); 998 longitudinal ratings from youths with mTBI: 390 at enrollment, 351 at 1-2 weeks, and 257 at 1 month. Uninjured ratings were used to determine mean symptom burden in the absence of mTBI. Longitudinal ratings were used to characterize symptoms after mTBI. Incidence of PPCS 1 month after mTBI was assessed with 3 approaches: 1) compared to individual uninjured symptoms; 2) compared to the mean symptom severity of uninjured youths; 3) using one question, “What percentage of normal do you feel?” (>95% at 1 month = recovered).
Participants were 49% male, 77% white, and 9% Hispanic. The majority were in in high school (44%) or middle school (32%), and 69% were athletes. History of headaches (29%), attention problems (30%), and depression (25%) were common. Many (22%) had a prior mTBI. Uninjured youths endorsed 6.7 of 22 symptoms, with a mean symptom severity of 16 out of 132. Following mTBI (n=399), mean symptom severity was 36 at enrollment, 19 at 1 week, and 9 at 1 month. Headache was the most common symptom at enrollment (88%), 1 week (66%), and 1 month (38%). Difficulty concentrating (33%) was also common at 1 month. One month after mTBI, 35% met PPCS criteria compared to personal uninjured ratings, 25% met PPCS criteria compared to the mean symptom severity of uninjured youths, and 30% met PPCS criteria based on estimated “percent normal.” There was significant agreement between measures (ĸ = 0.62, p < 0.001).
Many youths endorse concussion-like symptoms, even without mTBI. Headache is the predominant symptom in the first month after mTBI. Rates of PPCS in youths are 25-35%, and may be captured with a single self-report question, “What percentage of normal do you feel”
45 Success Is a Journey: Pilot Implementation of the Ideal Care Pathway for Traumatic Brain Injury
Judith Gargaro 1 ; Matheus Joner Wiest 1
1 UHN-Kite Research Institute, Toronto, Canada
There are no evidence-based standardized care pathways implemented at the healthcare system level that provide expert-informed guidance related to care and service provision from time of injury to life in the community, while considering the social determinants of health. Engaging diverse key partners, the Neurotrauma Care Pathways developed Ideal Care Pathways for mild traumatic brain injuries (TBI - concussions) and for moderate to severe TBIs. The TBI Care Pathways address known gaps in care related to, for example, unclear expectations during patient journeys, non-standardized concussion identification, and the much-needed lifelong community supports, especially related to mental health. With the Pathways at hand, it is time to start the journey to address these gaps.
to describe the process and outcomes of implementation projects addressing key elements of the TBI Care Pathways.
Provincial Working Groups composed of over 200 people with lived experience (PWLE) and their families, clinicians, healthcare administrators, community service providers, policymakers and researchers met to identify crucial components that constitute ideal care, highlighted system-level gaps, and developed and prioritized companion quality indicators by ranking them on significance and feasibility. Groups set regional and provincial implementation priorities. We identified regional teams to champion the implementation of three projects. Each team received a grant to co-design with persons with lived experience and their families a care map and implementation manual related to the implementation priorities. The projects had to implement an ongoing sustainability plan and evaluation strategies and ground their work in the principles of implementation science.
A set of implementation priorities was established which included two common priorities across the province: education for persons with lived experience and their families, and care coordination and navigation. Out of 6 pilot implementation projects, three involve TBI Care Pathways; these include: 1) a large urban concussion care clinic partnering with the TBI system navigator to optimize referral services; 2) a justice-involved support organization and a TBI system navigator creating a resource list for those living with complex needs, and 3) a community base provider facilitating post-traumatic stress disorder training after TBI. Each group developed the requisite care map, implementation manual, sustainability plan and collected evaluation data specific to their project. The teams presented their work at a provincial summit attended by PWLE and their families, clinical managers, system planners, injury-specific navigators, and funded and government officials to discuss opportunities for scale and spread.
These evidence-based Ideal Care Pathways represent a road map for quality improvement with a strong emphasis on community care and transitions. The implementation projects are initial steps of the journey towards ensuring that all persons living with TBI and their families receive equitable care and supports to address their chronic needs over the lifespan.
46 The Abbreviated Spokane mTBI Exam (aSME): A Potent Tool in Detecting Neurologic Dysfunction From Subconcussive Blows
Grace Wandler 3 ; Reese Beisser 1,2 ; Greg Carter 1,2 ; Valerie Moody 1 ; Reese Beisser 2
1 University Of Montana, Neural Injury Center, Missoula, United States; 2 Providence St. Luke’s Rehabilitation Institute, Spokane, USA; 3 Hellgate High School, Missoula, USA
A subconcussive impact is defined as a bump, blow, or jolt to the head that does not manifest any overt clinical symptoms. Such events carry a latent potential for neurological impairment, and thus should be of particular concern in contact sports. Existing assessments for sports-related concussions (SRC) predominantly focus on explicit, self-reported symptoms and more obvious neurological impairments, leaving subtle neurological signs in athletes largely undetected and inadequately assessed. These subtle neurological findings are termed soft signs and represent non-localizing abnormalities within the central nervous system. Growing research illustrates that repetitive subconcussive impacts can lead to consequential neurological outcomes and may ultimately culminate in chronic traumatic encephalopathy (CTE). One study demonstrated acute vestibular dysfunction in female soccer players following a single heading practice. Another study demonstrated white matter changes on diffusion tensor imaging in the brains of high school football players post-season, despite no formal concussion diagnoses. Moreover, multiple studies have shown that athletes deemed clinically recovered from SRC are at increased risk for further injuries; our prior research revealed soft signs of residual neurologic damage in such post-concussed athletes. These findings indicate that the existing SRC evaluations lack sensitivity in identifying residual neurological impairments. The Spokane mTBI Exam (SME) was previously developed by our group as a tool to identify soft signs following mTBI/concussion. In the present study, we used an abbreviated version of the SME (aSME) to screen 19 male amateur boxers, compared to 9 non-contact male athletes, swimmers. Participants ages 9 to 22 were evaluated pre- and post-activity using the following metrics: near point convergence (NPC), saccades, ocular smooth pursuits, vestibular-ocular reflex, finger-to-nose testing (dysmetria), and hip flexor strength. Findings revealed that 14 of 19 assessed boxers exhibited post-activity deterioration in their aSME evaluations, and 10 of these 14 exhibited worsening in multiple metrics. Loss of hip flexor strength, deterioration of NPC, and dysmetria, in that order, were the most common changes noted in the boxers. Two out of 9 swimmers revealed a post-activity deficit in 2 of these metrics, which normalized on repeat testing. In contrast, boxers who exhibited a post-activity deficit in NPC either stayed the same or worsened on repeat testing. The post-activity decreases in hip flexor strength observed in boxers cannot be attributed solely to fatigue because swimmers, following a comparable duration and intensity of exercise, showed either stable or improved hip flexor strength. Our findings substantiate the aSME as a pivotal tool for bolstering diagnostic sensitivity in detecting and tracking subconcussive trauma. By objectively monitoring neurological soft signs, the aSME fosters a refined and targeted approach to post-traumatic assessments, which may be used to guide informed return-to-play decisions in contactsports and potentially pave the way for tailored rehabilitation strategies.
47 The Spokane mTBI Exam (SME): A Neurologic Soft Sign Assessment Tool for Mild Traumatic Brain Injury (mTBI)
Reese Beisser 2 ; Greg Carter 1,2 ; Grace Wandler 3 ; Valerie Moody 1 ; Reese Beisser 1,2
1 University of Montana, Neural Injury Center, Missoula, United States; 2 Providence St. Luke’s Rehabilitation Institute, Spokane, United States; 3 Hellgate High School, Missoula, United States
To date, no definitive physical exam has emerged for identifying objective residual dysfunction following mTBI. Because the TBI spectrum involves subtle damage to a diffuse network of neuronal connectivity within the cortex, brainstem, cervical cord, and/or autonomic nervous system, abnormalities cannot always be localized to a focal lesion. Such findings are termed “soft signs,” and may be the only neurologic sequelae from an mTBI. These signs may persist chronically following an injury, latently impacting neurologic function and resilience. However, because the traditional neurologic exam is designed to detect focal lesions, it is often normal in patients affected by mTBI and therefore of limited utility in their diagnosis and management. In the absence of an objective, sensitive examination that assesses soft signs, many clinicians still commonly rely on subjective impressions to identify or exclude mTBI. This leads to diagnostic errors, false expectations about recovery, and limits the effective analysis of treatment interventions. A helpful contribution to this gap in validated assessment methods is the physical and neurologic examination of soft signs (PANESS), which was developed in 1984 as a tool for assessing developmental neurologic conditions in children. The PANESS has been shown to be more accurate at identifying subtle dysfunction after a concussion than the sports concussion assessment tool (SCAT). However, the PANESS does not incorporate newer research on mTBI (e.g., the VOMS), and is not standardized for adults. Considering this, we propose the SME, a soft sign assessment tool that complements the traditional neurologic bedside examination and is specific for concussion/mTBI. It integrates information from medical literature, academic conference presentations, and our research team’s more than 90 years of combined experience evaluating and studying mTBI patients. The SME focuses on identifying visual, motor, balance, and autonomic nervous system soft signs following an mTBI. These selected domains appear to be most vulnerable to damage following craniocervical neurotrauma. This premise is supported by studies on concussed athletes examined with the PANESS, by the work of other authors, and by our own prior and ongoing research evaluating processing speed, reaction time, vision, and hip flexor strength in mTBI patients. An abbreviated subset of the SME (the aSME) has recently shown effectiveness in capturing neurologic changes in subconcussed boxers compared to age-matched swimmers, post-activity. Our clinical experience and ongoing quantitative studies support the validity of the SME as a soft sign exam with the promise of being an effective tool for assessing and monitoring impairments acquired after neurotrauma. Our goal is to continue refining the SME to make it a standardized tool, available to all clinicians who evaluate and treat this complex patient population. Such an exam is necessary to improve diagnostic accuracy, guide treatment interventions, evaluate their efficacy, and assist in outcome prediction.
48 A Scoping Review of Long-Term Prognosis of Cognitive Function in Traumatic Brain Injury (TBI)
Tamami Aida, Shuhei Tateoka, Riho Hirose
1 Mejiro University Graduate School of Rehabilitation, Tokyo/Shinjuku/Nakaochiai, Japan
Traumatic brain injury (TBI) has been noted to be a chronic disease state. Uncertainty over predictors of long-term outcomes causes great distress for individuals with disabilities and their families.
The purpose of this study was to determine the factors involved in the long-term prognosis of cognitive impairments and the long-term prognosis of each cognitive impairment.
Long-term prognosis was defined as a state of 5 years or more from injury, and on May 23rd, 2023, we looked through articles from 1990 to May 23rd, 2023. A scoping review of the literature was conducted following the 2018 PRISMA-ScR Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews. Exclusion criteria were involving participants under 25 years old, not addressing Cerebrovascular Disease (CVD) and TBI, and no mention of cognitive impairments.
A total of 9 peer-reviewed articles were included for review. Factors involved in the long-term prognosis of cognitive impairment were that the severity of cognitive impairment was related with Glasgow Outcome Scale (GOS) and post-traumatic amnesia (PTA) (n= 2), not related with the pre-injury social environment, but with pre-injury intelligence and educational level (n= 2), that there was significant improvement between 1 and 3 years after injury (n= 7), that there was no difference in cognitive ability after 5 and 10 years, and that some subjects have reduced memory and working memory after 10 to 15 years (n= 2). The 10-year group scored worse on NSI total score and Traumatic Brain Injury Quality Of Life (TBI-QOL) Cognitive Concerns-General, the TBI group had more physical and neurological complaints than the non-TBI group, and the neurocognitive characteristics of participants with fewer symptoms of psychological distress were better. They also stated that the prevalence of impairment of simple attention was low, with the majority of patients not impaired by 5 years post-injury, and that working memory impairment was still present at 5 years but improved between 6 months and 1 year post-injury. Visual perceptual impairment was shown to improve mostly between 1 and 5 years, and the majority of patients were free of impairment at 5 years. The prevalence of executive dysfunction was low, with the majority of participants showing no impairment by 5 years after injury, with significant improvement between 6 months and 5 years.
Discussions
Predictors of cognitive impairment due to TBI were prior education level and severity of TBI, with visual perceptual function, attention recovered earlier from onset, and executive function and working memory recovery taking longer. However, the association between symptoms of emotional distress and cognitive function and the fact that TBI patients often have complaints suggest that the possibility that some subjects may experience memory and working memory deficits should be addressed.
51 Using Machine Learning to Discover Traumatic Brain Injury Patient Phenotypes: National Concussion Surveillance System Pilot
Dana Waltzman 1 ; Jill Daugherty 1 ; Alexis Peterson 1 ; Angela Lumba-Brown 2
1 Centers For Disease Control And Prevention, Atlanta, United States; 2 Stanford University School of Medicine, Stanford, United States
Current systems of classifying traumatic brain injury (TBI) frequently result in limitations to care. Clinical trials that use traditional classification schemes for TBI (e.g., mild, moderate, and severe) have failed to optimally translate to effective treatment and recovery in the real world, which may inhibit the discovery of effective therapies that improve outcomes based on more granular clinical profiles. Data-driven, alternative methods of classification may stratify TBI patient subpopulations more accurately for optimal identification and treatment. Data from the Centers for Disease Control and Prevention’s pilot National Concussion Surveillance System (n = 10,130 adults) were analyzed. Respondents who self-reported a head injury in the past 12 months were retained in the analysis (n = 1,364) and were queried for injury, outcome, and clinical characteristics. To identify potential TBI phenotypes among those reporting a head injury, respondents were grouped into clusters based upon 12 TBI signs and symptoms. Gower’s dissimilarity matrix was computed due to the nature of the binary input data (i.e., presence or absence of each sign or symptom). The partitioning around medoids (PAM) algorithm was used to cluster observations. To determine the association between outcomes and phenotypes, separate logistic regressions were run using the phenotype characterized by the least severity (e.g., Phenotype A [“cluster 1”]) as the reference group. The algorithm grouped the respondents into five clusters (TBI phenotypes A-E). Each TBI phenotype demonstrated unique clinical characteristics that corresponded to specific differences in outcomes and unique demographic profiles. Phenotype C represented more clinically severe TBIs with the highest prevalence of symptoms (i.e., >50% of respondents in this cluster self-reported 11 out of the 12 signs/symptoms) and a higher association with worse outcomes when compared to individuals in Phenotype A, a group with few TBI-related signs and symptoms: medical evaluation (odds ratio [OR] = 9.4, 95% confidence interval [CI] = 5.8-15.3), symptoms that were not currently resolved or resolved in 8+ days (OR = 10.6, 95% CI = 6.2-18.1), and more likely to report at least moderate, as compared to no or slight, impacts on social (OR = 54.7, 95% CI = 22.4-133.4) and work (OR = 25.4, 95% CI = 11.2-57.2) functioning. These results demonstrate that machine learning can be used to classify patients into unique TBI phenotypes. Further research might examine the utility of such classifications in supporting clinical diagnosis and patient recovery for this complex health condition.
52 Steps Toward Titrating Educational and Related Service Sessions to Minimize the Occurrence of Seizure-Like Events in a School Setting
Diane Bienek 1 ; Arletis Bueno Martinez 1 ; Ashley Hannon 1 ; Connor Wilson 1 ; Samantha Cotugno 1 ; Rutika Naik 1 ; Caleb Asomugha 1 ; Victor Pedro 1
1 International Institute for the Brain, New York, United States
This case study describes the history of seizure-like events of a 17-year-old Caucasian female diagnosed with spastic quadriplegic cerebral palsy and Lennox-Gastaut syndrome, intractable, with status epilepticus. This individual was enrolled at the International Institute for the Brain (iBRAIN), which establishes and implements an individualized education program (IEP) for each student annually. The student’s 2022 educational plan included mandates of weekly physical (5 h), occupational (5 h), music (2 h individual; 1 h group), and speech-language therapy (5 h). Hearing (0.5 h), vision (3 h), and assistive technology services (1 h) are also included in the student’s plan. For academic sessions, the student participated in a 6:1:1 special education classroom.
As an academy, iBRAIN does not diagnose seizures. Rather, suspected occurrences were reported as seizure-like events. Information captured from a seizure-like event include, but not limited to, time of day, sensory stimulation and service rendered at time of the event, prior state of arousal, and vital signs during the postictal phase. Pulse rate, respiration rate, and saturated oxygen levels were taken, using an over-the-counter pulse oximeter with respiratory rate device (Item # 793251, Walgreens Boots Alliance, Inc., Deerfield, IL). Herein, we conduct statistical analyses of the reported seizure-like events, considering time of day, sensory stimulation, arousal level, and vital signs.
Within a 16-week period, 38 seizure-like events were reported during this student’s school attendance. The observed frequency distribution of seizure-like events throughout the day was different (P < 0.05) from its expected distribution (i.e., equivalent number of occurrences throughout the day). The occurrence of seizure-like events was influenced (P < 0.05) by the type of sensory stimulation. Altogether, the highest seizure-like event occurrence was (in descending order) during a combination of sensory stimuli, feeding, visual, auditory, and movement. Notably, no seizure-like events were reported when the service sessions were primarily stretching exercises. In sessions where seizure-like events were reported, the mean pulse rate was 22 beats per minute higher (P < 0.05) than when no event was reported. Likewise, the mean number of respirations per minute was higher (P < 0.05) when seizure-like events were reported. Saturated oxygen levels did not differ statistically, when comparing sessions with the presence or absence of seizure-like events.
Understanding patterns of seizure-like events in a school setting could be used to dose or titrate educational and related service sessions. In this case, accommodation for arousal level and increased integration of muscular stretching may be indicated.
53 Factors Influencing Adherence to Insomnia and Obstructive Sleep Apnea Treatments Among Veterans With Mild Traumatic Brain Injury
Adam Kinney 1 ; Lisa Brenner 1 ; Morgan Nance 1 ; Joseph Mignogna 1 ; Audrey Cobb 1 ; Jeri Forster 1 ; Christi Ulmer 1 ; Risa Nakase-Richardson 1 ; Nazanin Bahraini 1
1 VA Rocky Mountain MIRECC, Aurora, United States
Insomnia disorder and obstructive sleep apnea (OSA) are common co-morbidities among Veterans with mild traumatic brain injury (mTBI). Clinical practice guidelines include recommendations for evidence-based interventions that effectively treat insomnia (e.g., cognitive behavioral therapy for insomnia) and OSA (e.g., positive airway pressure), but clinical benefit depends on Veterans’ consistent adherence to treatment. While adherence to interventions for insomnia disorder and OSA are challenging for many patients, Veterans with mTBI may experience unique barriers worthy of consideration. However, such barriers to adherence are poorly understood in this population. The purpose of this study was to understand factors influencing adherence to recommended treatment for insomnia and OSA among Veterans with mTBI.
Semi-structured interviews (n=49) with 29 clinical stakeholders and 20 Veterans were conducted. Clinical stakeholders included Veterans Health Administration providers and policymakers involved in the management of mTBI and/or sleep disorders. Veterans included those with a clinician-confirmed mTBI with a recent history of insomnia disorder and/or OSA treatment. Themes were identified using a Descriptive and Interpretive approach.
Barriers to sleep disorder treatment adherence included factors associated with the patient (e.g., negative appraisal of treatment benefit), intervention (e.g., side effects), health conditions (e.g., mTBI sequalae), health care system (e.g., limited availability of care), and socioeconomic status (e.g., economic instability). Similarly, facilitators of adherence included patient- (e.g., positive appraisal of treatment benefit), intervention- (e.g., flexible delivery format), condition- (e.g., accommodating cognitive impairments), health care system- (e.g., access to adherence support), and socioeconomic-related factors (e.g., social support).
Interviews revealed the multi-faceted nature of factors influencing adherence to sleep disorder treatment among Veterans with mTBI. Findings can inform the development of novel interventions and care delivery models that meet the complex needs of this population, ensuring they sustain treatment engagement and reap the desired clinical benefits.
54 Iberian Observatory for Disorders of Consciousness
Prof. Liliana Teixeira 1,2 ; Dr. Caroline Schnakers 3 ; Enrique Noe 4
1 Center for Translational Health and Medical Biotechnology Research, Portugal; 2 Center for Innovative Care and Health Technology, Portugal; 3 Casa Colina Hospital and Centers for Healthcare, United States; 4 IRENEA-Instituto de Rehabilitación Neurológica, Fundación Hospitales Vithas, España
This poster presents the main goals of the Iberian Observatory for Disorders of Consciousness and what the developers intend to do to ensure the success of this international project.
The high rate of misdiagnosis for people with disorders of consciousness (DoC) is well known and widely reported in the literature. Most of these studies have been carried out in countries where there are validated tools for the assessment of DoC (Childs & Mercer, 1996; Andrews et al., 1996; Gill-Thwaites & Munday, 2004; Schnakers et al., 2009; Wang et al., 2020). The JFK Coma Recovery Scale-revised is the gold standard assessment for DoC and has already been translated and validated in many countries. However, there are still countries where there are no translated or validated assessment tools and/or where there is little knowledge among health professionals about this population. Portugal and Spain are among those countries. Thus, it became imperative to create an observatory that would help to organize research in this field and to shed a light on this spectrum of often forgotten population.
The main aim of this Observatory is to contribute to understanding the reality of DoC in Portugal and Spain, to understand the trajectory of patients’ general state of health, and above all to give visibility to a spectrum of disorders that are little talked about in both countries. By creating partnerships with health institutions, medical and other health professionals’ societies, research centers, and other stakeholders it is hoped to open a path for high quality standard research.
It is also the Observatory’s responsibility to promote international scientific research activities in the area, contribute to the validation of diagnostic tools in Spanish and Portuguese and share knowledge to the community through the organization of short courses as well as by providing support for undergraduate and postgraduate training in this area.
56 Adolescents with a High Burden of New Onset Mood Symptoms after Sport-Related Concussion Benefit from Prescribed Aerobic Exercise
Matthew Castellana 1 ; George Burnett 1,2 ; Andrew Gasper 3 ; Muhammad Nazir 4 ; John Leddy 4,5 ; Christina Master 6 ; Rebekah Mannix 7 ; William Meehan 8 ; Haley Chizuk 4,5 ; Barry Willer 1,4 ; Mohammad Haider 4,5
1 Department of Psychiatry, Jacobs School of Medicine and Biomedical Sciences, State University of New York at Buffalo, Buffalo, United States, 2Buffalo Psychiatric Center, Buffalo, United States; 3 Jacobs School of Medicine and Biomedical Sciences, State University of New York at Buffalo, Buffalo, United States; 4 University Concussion Management Clinic and Research Center, UBMD Orthopaedics and Sports Medicine, Buffalo, United States; 5 Department of Orthopedics, Jacobs School of Medicine and Biomedical Sciences, State University of New York at Buffalo, Buffalo, United States; 6 Department of Pediatrics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, United States; 7 Department of Pediatrics and Emergency Medicine, Harvard Medical School, Boston, United States; 8 Department of Pediatrics and Orthopedics, Harvard Medical School, Boston, United States
Sport-related concussion (SRC), a subtype of mild traumatic brain injury (mTBI), is common in adolescents. A common clinical outcome of SRC is the development of new anxiety and depressive mood symptoms, which can impair SRC recovery. This study assesses the effect of early, targeted aerobic exercise treatment versus a placebo-like stretching program on recovery in adolescent athletes who report high and low initial mood symptom burden after SRC.
Exploratory secondary analysis using data from two randomized trials collected in four outpatient clinic settings. Male and female adolescents (13-18 years) diagnosed with SRC within ten days of injury were divided into low (< 6/24 points) or high (≥ 6/24 points) burden based on self-reported symptoms of irritability, sadness, nervousness and feeling more emotional on a 0-6 Likert scale. The main outcome measure was recovering during the intervention period and incidence of Persisting Post-Concussive Symptoms (PPCS).
Out of 198 adolescents with SRC, 156 (79%) reported a low burden of mood symptoms (mean = 1.2 ± 1.65) and 42 (21%) reported a high burden (mean = 9.74 ± 3.70) before randomization. The effect of intervention (exercise versus stretching) was not significant in the low mood symptom burden group (hazard ratio = 0.767, p = 0.128) and was significant in the high burden group (hazard ratio = 0.290, p = 0.005). This corresponds to a 71% reduction in risk for PPCS in the high burden group. High burden of mood symptoms had a positive correlation with high physical, cognitive and sleep symptoms, and a higher number of abnormalities on physical exam, but did not correlate with participant sex or level of exercise tolerance.
Early prescribed aerobic exercise treatment facilitates recovery and significantly reduces the incidence of PPCS in adolescents reporting a high burden of new onset mood symptoms after SRC and should be considered as part of a comprehensive treatment plan for these patients.
57 Inflammasome Activation in Alzheimer’s Disease Pathology in the Chronic Stages of Traumatic Brain Injury
Erika Cabrera Ranaldi 1 ; Nathan H Johnson 1 ; Nadine A Kerr 1 ; Helen M Bramlett 1 ; Robert W Keane 1 ; Dr. W Dalton Dietrich 1 ; Juan Pablo de Rivero Vaccari 1
1 University Of Miami, Miami, United States
Traumatic brain injury (TBI) affects millions of individuals annually, resulting in reduced quality of life in patients and substantial financial costs. TBI impacts learning and memory functionality and is a recognized risk factor for the development of Alzheimer’s disease (AD). A key component of the immune response in TBI and AD is activation of the inflammasome. The inflammasome is a multi-protein complex that activates pro-inflammatory cytokines interleukin (IL)-1β and IL-18, through the recruitment of caspase-1 and apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC). Activation results in pyroptotic cell death through cleavage and formation of the GSDM-D pore. We have previously demonstrated that genetic predisposition to AD, utilizing the 3XTg mouse model, significantly exacerbates inflammasome activation in the acute injury phase of TBI and leads to greater cognitive impairment. Furthermore, we showed that inhibition of the inflammasome through use of an anti-ASC therapeutic monoclonal antibody (IC100), was effective in reducing inflammasome activated IL-1β in 3xTg mice after TBI. Our current work investigates the chronic inflammatory response of TBI pathology in familial AD. 5-month-old wild-type (WT) and 3xTg (AD) mice underwent either sham surgery or moderate controlled cortical impact (CCI). At 3-months after surgery, animals were sacrificed and the ipsilateral cortex was dissected, homogenized, and immunoblotted for inflammasome proteins and IL-1β. A Simple Plex assay was completed using cortical lysates to assess neurodegeneration and astroglia reactivity by probing for neurofilament-light (NfL) and glial fibrillary acidic protein (GFAP), respectively. Histology and immunohistochemistry was also conducted on whole brain sections blotted for ASC, NfL, and GFAP. Sections were used to assess cortical and hippocampal tissue loss after injury using volumetric analysis. Our results demonstrate that IL-1β protein remains significantly elevated in the chronic stages after injury in AD animals compared to WT. We also observed a persistent elevation of the inflammasome proteins NLRP3, caspase-8, and ASC in injured AD mice which was not present in injured WT animals. Moreover, there is a chronic increase in NfL expression after TBI, with evidence of ASC co-localization after injury. Interestingly, only injured AD mice demonstrated continued elevation of GFAP. GFAP+ cells additionally demonstrated ASC co-localization in the injured AD mice. Finally, there was a significant loss in total cortical volume and total hippocampal volume in injured AD mice compared to the injured WT mice. In conclusion, we provide evidence that genetic predisposition to AD leads to chronic inflammasome activation and pro-inflammatory cytokine release after TBI leading to even greater neurodegeneration. Importantly, our results indicate that the inflammasome could be a promising therapeutic target for TBI with AD.
58 Salivary Brain-Derived Neurotrophic Factor in Athletes With Acute Sport-Related Concussion Throughout Exercise Intervention
Haley Chizuk 1,2 ; Alexander Rawlings 1 ; Jaffer Sayeed 1 ; Dr. Mohammad Haider 1,2 ; Barry Willer 1,3 ; John Leddy 1,2 ; Praveen Arany
1 University Concussion Management Clinic and Research Center, UBMD Orthopaedics and Sports Medicine, Buffalo, United States; 2 Department of Orthopedics, Jacobs School of edicine and Biomedical Sciences, State University of New York at Buffalo, Buffalo, United States; 3 Department of Psychiatry, Jacobs School of Medicine and Biomedical Sciences, Buffalo, United States, 4Department of Oral Biology, School of Dental Medicine, State University of New York at Buffalo, Buffalo, United States
Brain-Derived Neurotrophic Factor (BDNF) mediates the neuronal response to injury. It has been hypothesized that BDNF is a potential biomarker of sport-related concussion (SRC). BDNF expression is exercise-dependent, and aerobic exercise is a standard treatment for SRC. This study assessed salivary BDNF expression in athletes with acute SRC and throughout a 2-week aerobic exercise intervention.
Athletes with acute SRC (n= 32, 66% male, 15.6 ± 1.4 years) and healthy controls (n= 28, 66% male, 16.0 ± 1.6 years) provided saliva samples weekly (Day 0, 7 and 14). Concussed and control participants were randomly prescribed individualized aerobic exercise at high (5 days/week for 30 minutes) or low volumes (3 days/week for 20 minutes). Prescribed exercise intensity was based on the results from each participant’s graded exercise test. Participants completed standard clinical examinations and symptom reports during each visit. An optimized Enzyme-Linked Immunosorbent Assay (ELISA) for BDNF (R&D systems) was used to assess samples in triplicate.
ELISA standard curves were high quality (healthy r2= 1.00, concussed r2= 0.98). At the initial visit, concussed females had higher salivary BDNF than healthy participants (p=0.002). There was no difference between concussed and healthy males’ BDNF at the initial visit (p=0.627). Over time, concussed females consistently showed higher salivary BDNF expression than healthy females, whereas males were not different. BDNF level was not affected by the volume of exercise participants completed (p=0.767) or by history of prior concussions (p=0.85).
The data suggest that salivary BDNF may be assessed for post-concussion monitoring in adolescent athletes but may be more informative for females. Unexpectedly, exercise volume did not affect BDNF, suggesting that a longer exercise intervention would be required to impact BDNF expression. BDNF levels were not affected by time, regardless of recovery, consistent with reports that physiological dysfunction persists beyond clinical recovery from SRC. In conclusion, salivary BDNF offers a non-invasive and convenient analyte that may aid in concussion diagnosis and for monitoring post-concussion treatment response. However, further research is needed to understand the effects of sex, exercise, and recovery on salivary BDNF after SRC.
Acknowledgment
Support for this project by the Clinical Translational Science Institute at the University at Buffalo (UL1TR001412).
59 Disparities in Trauma-Informed Care: Understanding Mental Health Providers’ Ability to Identify Clients With Traumatic Brain Injury Resulting From Physical Violence
Jack Poon 1 ; Mandisa Keswa 2 ; Julia Stork 3 ; Wendy Wood-Kjelvik, Helene Smith, Nicole Infantino 4 ; Edie Zusman 5
1 University of Chicago, Chicago, United States of America, 2Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, United States of America; 3 Northwestern University, Evanston, United States of America; 4 Touro University Nevada, Henderson, United States of America; 5 Neuroscience Partners, Palo Alto, United States
Traumatic brain injury (TBI) is a serious medical condition well recognized among veterans and athletes, but less is known about TBI as a consequence of physical violence, particularly domestic violence and intimate partner violence (DV/IPV). An estimated 25% of women and 10% of men in the United States experience DV/IPV during their lifetime, with 74% of individual violent events involving injury to the head, neck or face. Half of these events include strangulation causing hypoxic brain injury. Despite a recent study which found that 58% of women entering DV shelters had sustained one or more concussions from DV/IPV, survivors more often engage with mental health professionals (MHPs) for TBI symptoms such as anxiety, depression, and PTSD than with concussion experts. MHPs have an unique opportunity to recognize TBI in clients who have experienced physical violence or abuse, incorporate an understanding of brain injury into their care programs, and refer to TBI experts as appropriate.
The primary objective is to estimate the percentage of MHPs who care for survivors of physical violence in their practice. The secondary objective is to assess among MHPs who care for survivors of physical violence their self-reported comfort and training to recognize signs and symptoms of TBI among their clients.
A ten question anonymous online survey tool was vetted, validated, and sent to a cohort of U.S. health care professionals inclusive of MHPs affiliated with DV/IPV organizations. The 5-10 minute survey includes respondent demographics and utilizes standard Likert scales to assess self-reported experience, training and comfort in assessing TBI.
Of an estimated 350 surveys sent out, 102 responses were returned with 74 responses sufficiently completed for inclusion in the analysis. While 89.2% of MHPs reported that their clientele includes individuals who have experienced physical violence, only 16.2% of MHPs responded that they felt very comfortable or extremely comfortable in evaluating clients for TBI. 45.9% of MHPs reported receiving no training in TBI assessment; however, 70.2% reported that they are very interested or extremely interested in further TBI training.
While the majority of MHPs reported seeing clients who have experienced physical violence, a population with a high rate of TBI, the results of this study highlight the potential knowledge gap about TBI among MHPs. Given the disparity, it is encouraging that the majority of MHPs reported high interest in further training to recognize the signs and symptoms of brain injury among their clients, suggesting an opportunity to improve trauma-informed mental health services for survivors of DV/IPV.
60 Identifying the Influence of Lung-Related Injuries on Delirium in Traumatic Brain Injury Patients: A National Analysis
Jordan Shin 1 ; Jeffry Nahmias 1 ; Patrick Chen 1 ; Jefferson Chen 1 ; Michael Lekawa 1 ; Lily Nguyen 1 ; Areg Grigorian 1
1 University of California, Irvine, Department of Trauma Surgery and Surgical Critical Care, Orange,
Traumatic brain injury (TBI) is a known risk factor for delirium, a condition associated with prolonged hospitalization and cognitive deterioration. Although the relationship between TBI and delirium is established, a detailed understanding of specific predictors remains limited. Respiratory disorders can significantly influence the central nervous system, with sequelae such as hypoxia, hypercapnia, and respiratory acidosis causing neurologic dysfunction. Therefore, we hypothesize that lung-associated conditions, stemming either from direct injuries or subsequent surgeries will increase the risk of developing delirium in TBI patients.
The 2017-2021 Trauma Quality Improvement Program database was queried for patients with TBI, excluding for those with pre-existing dementia. TBI patients developing delirium were compared to those without delirium. A multivariable logistic regression analysis was performed to determine predictors of delirium.
Among 155,252 TBI patients, 3,244 (2.1%) developed delirium. Delirium-afflicted patients showed elevated rates of lung injury (25.0% vs 13.3%, p<0.001), severe head trauma (Abbreviated Injury Score ≥ 3) (51.4% vs 37.8%, p<0.001), sepsis complications (3.1% vs. 0.5%, p<0.001) and more commonly underwent pulmonary operations (21.8% vs. 6.6%, p<0.001). The strongest associated risk factors for delirium included functional dependence (OR 2.70, CI 2.43-3.00, p<0.001), intubation (OR 2.33, CI 2.13-2.56, p<0.001), concurrent lung injury (OR 1.21, CI 1.20-1.33, p<0.001) and pulmonary surgery (OR 1.64, CI 1.48-1.82, p<0.001).
Delirium affected approximately 2% of the national TBI population. Our analysis not only reaffirms known predictors but also emphasizes the critical influence of lung-related conditions on delirium onset. Systemic inflammatory response, frequently instigated by lung injuries, might intensify neurological issues, escalating risk of delirium. Recognizing these risk factors is crucial in refining delirium prediction, prevention, and treatment in the setting of TBI.
61 Behavior Analytic Services in Acquired Brain Injury Rehabilitation: Identifying Barriers and Promoting Progress
Megan Heinicke 1 ; Shelby Bryeans 1
1 California State University - Sacramento, Sacramento, US
Acquired brain injury (ABI) is a major public health concern in the United States (Schiller et al., 2012) and can result in behavioral consequences, such as physical aggression, sexually inappropriate behavior, and refusals, that impede rehabilitation goals and limit independent living options (Heinicke & Carr, 2014). One way to help rehabilitation professionals manage behavioral concerns and in turn increase the efficacy of their services is to include behavior analysts on their treatment teams. Historically, the most prolific practice area for behavior analysts has been autism spectrum disorder and other developmental disabilities (Normand & Kohn, 2013), but behavior analysts are also well equipped to serve ABI survivors (e.g., robust literature base to support their practice, ethical responsibility to individualize treatment, training in single-case experimental designs and repeated measurement; LeBlanc et al., 2013; Mozzoni, 2008). However, only 0.08% of board certified behavior analysts (BCBAs) report ABI rehabilitation as their primary practice area (BACB, n.d.). Therefore, the purpose of this study was to evaluate why limited visibility and recognition of applied behavior analysis remains a critical barrier to workforce development in ABI settings for BCBAs. We asked 12 subject matter experts (i.e., BCBAs currently serving ABI survivors with a history of doing so for at least five years) to describe their experiences regarding their company’s history with behavioral programming, perceived value of including BCBAs on rehabilitation teams, and barriers while working in ABI rehabilitation via semi-structured interviews. Our interviews included 23 questions, and we conducted a thematic analysis using a semantic approach as well as descriptive statistics to analyze the subject matter experts’ responses (Braun & Clark, 2006; 2013). We organized our results into the following domains: employment demographics (e.g., teaming models, other rehabilitation disciplines included on their teams, common behavioral excesses and deficits addressed), company history with behavior analysis (e.g., who advocated for the addition of BCBAs), value (e.g., the value they felt they contributed to their team vs. the perceived value of BCBAs from their team), workplace barriers (e.g., which barriers exist, why those barriers exist, potential solutions), and final thoughts (e.g., advice for behavior analysts). We will discuss how a better understanding of the identified barriers can aid in informing more specific and effective strategies to increase collaboration across rehabilitation disciplines and ABI survivors’ access to behavior analytic services.
62 Be Pain Smart - A New Way to Manage Pain after Traumatic Brain Injury
Regina Schultz 1,2 ; Jennifer Johnson 2 ; Jane Bradshaw 1 ; Raj Anand 1 ; Tejas Kanhere 1 ; Nicole Kennedy 1
1 Royal Rehab, Ryde, Australia; 2 Agency for Clinical Innovation, St Leonards Australia
Chronic pain is a multifaceted health problem which is a recognized concomitant of traumatic brain injury (TBI) that can significantly impact on the achievement of individual goals, social participation, activities of daily living and functional capacity. While the estimated prevalence rate is approximately 50% following moderate to severe TBI, there remains limited research and access to appropriate resources and specialized pain services for this population. The Be Pain Smart (BPS) clinic pilot project was developed to provide specialized pain management consultancy for people with a TBI and/or spinal cord injury (SCI). The BPS clinic provided an interdisciplinary comprehensive pain assessment, pain management plan and support to local clinicians to assist the participants to manage their pain. This state-wide service allowed increased access to pain management healthcare for metropolitan, rural, and regional participants. A sample of 40 BPS participants scores on the Patient Reported Outcome Measurement Information System – 29 (PROMIS-29+) and Brief Pain Inventory (BPI) were compared at baseline and follow-up. High rates of referrals were noted throughout the BPS clinic project period. The 40 participants were predominately male (70%), with a mean age of 48.48 years and on average 6.39 years post-injury. On the BPI from baseline to follow-up, on average the participants reported decreased pain scores (worst pain, and average pain) and on pain interference measures including overall pain interference, and more specific areas of pain interference: general activity, mood, walking ability, normal work, relationships with other people, sleep, and enjoyment of life. 75% of participants reported a clinically significant improvement on their overall BPI pain interference scores. Participants also reported improved scores on the PROMIS – 29+ including a decrease in pain interference and pain intensity, and a decrease in anxiety, depression, fatigue, and sleep disturbance symptoms. Participants also reported improvement on the participation in social roles and activities domain. Overall, 70% of participants reported a clinically significant improvement on their overall pain interference scores. Consequently, these preliminary results from this pilot study provides burgeoning evidence for the effectiveness of the BPS clinics in reducing pain interference for these two complex cohorts. Access to the BPS clinic reduced the level of interference of pain in the lives of TBI participants which lead to additional improvements in other domains, this emphasizes the critical role of an interdisciplinary, patient-centered approach to pain management in this highly complex cohort. The ongoing high referral rate highlights the importance of embedding specialized models of care into existing clinical services to optimize referrals and overall increasing the capacity of the system to manage pain in these populations. In conclusion, a specialized patient-centered, interdisciplinary pain clinic for people with TBI reduced overall pain interference and led to improvements in other key functional domains.
63 Be Pain Smart – Evaluation of Online Clinician Pain Management Education Modules
Regina Schultz 1 ; Tania Gardner 2 ; Jennifer Johnson 1
1 Agency for Clinical Innovation, Ryde, Australia; 2 University of Sydney, Sydney, Australia
There is a growing body of literature aimed at understanding the assessment and management of chronic pain after moderate to severe traumatic brain injury (M/S-TBI). Multidisciplinary (MDT) pain management is accepted as gold standard for chronic pain, but there is limited evidence to guide clinicians on how to modify general pain management strategies for people with a M/S-TBI. The Be Pain Smart – Online Education Modules (BPS-OEM) are a suite of online modules, providing evidence-based training for clinicians on pain management strategies for people with a M/S-TBI. The modules have utilized optimal adult learning principles within the design to support the learning of pain management strategies and clinical decision making aligned with the BPS clinical reasoning framework. The online delivery allows for maximum accessibility to facilitate the training of clinicians across metropolitan and rural/remote regions. The aim of this study is to evaluate the feasibility and acceptability of the BPS-OEM, particularly examining clinicians’ pain beliefs, confidence and clinical practice when managing pain with people who have a M/S-TBI. A sample of allied health clinicians were recruited via advertisements through the relevant New South Wales (NSW) networks. Data was collected via an online survey with outcome measures targeting clinical practice, knowledge, confidence, pain beliefs and clinical value of the BPS-OEM. Results demonstrated improvement in clinician confidence and pain knowledge, and changes in pain beliefs to be more aligned with MDT pain management approaches. The BPS clinical reasoning framework with an online interactive clinical reasoning tool will be presented with accessibility and usability results presented. The authors will discuss how improvements in clinician confidence and pain knowledge will lead to increased capacity within existing services to assess and manage chronic pain in the TBI population. The added value of additional 6 group mentoring sessions to compliment the BPS-OEM will be reviewed. The BPS-OEM provides training and a clinical reasoning framework to assist clinicians to improve access to and the delivery of appropriate pain management services for people with a M/S-TBI.
64 “An Individualized Wallet-Card Addresses Financial Capability Challenges for Adults Living With Acquired Brain Injury: A Longitudinal Qualitative Intervention Pilot Study.”
Lisa Engel 1 ; Roheema Ewesesan 1 ; Kafayat Adedotun 1 ; Celine Latulipe 1 ; Mohammad N. Khan 1 ; Anne Hunt 2 ; Ibiyemi Arowolo 1 ; Frederique Poncet 3 ; Jane Karpa 4
1 The University of Manitoba, Winnipeg, Canada; 2 University of Toronto, Toronto, Canada; 3 Chercheure au Centre de réadaptation Lethbridge-Layton-Mackay, Canada; 4 Brandon University, Winnipeg Campus, Canada
Acquired brain injury (ABI) is associated with financial capability challenges. This includes challenges with financial-related social interactions and remembering financial cues or behavioral strategies. In a previous focus-group study, people living with ABI discussed an individualized financial wallet-card as a novel intervention idea.
To develop and explore the feasibility, acceptability, uses, and outcomes related to the use of an individualized financial wallet-card for adults living with ABI.
We used a longitudinal qualitative intervention design. We recruited 10 adult participants who live with ABI (70% female; 1 to 59 years post-ABI). We co-designed a two-sided wallet card with each participant: one side addressed how others can better help the participant in social financial-related situations, and the other side addressed personal financial reminders or strategies. After co-designing their card, we interviewed participants and sent them copies of their cards in printed/laminated and electronic versions. Participants then completed up to five more interviews about their cards over 15 weeks. Participants had the opportunity to update their cards at the final interview. We analyzed longitudinal interviews and wallet-card content using content analysis.
Participants reported using the printed/laminated card more than the electronic version. There were many similarities across participants’ cards, with almost all participants including information related to living with invisible disabilities. Multiple participants reported the importance of card individualization. Common social cues included were to ask others to provide them time, speak slower, or provide written information. Common personal financial reminders were to focus on their needs before their wants, take time or talk with a trusted other person before making financial decisions, or make and check a monthly spending plan. Most participants reported the card very helpful to addressing some of their financial capability challenges. More reported the social situations side to be more helpful, especially to get the help they needed, with many reporting using the card beyond finance-related social situations. Multiple participants noted the personal financial reminders helped to keep them accountable and make better financial decisions. Two participants noted other people expressing negative attitudes about the card, although this was from family members and not from general community members. Some participants reported not using the card much or forgetting to use the card; for two participants, this tended to be in familiar environments where people knew them well.
The co-designed financial wallet-card is a potential low-cost technology to address some of the financial capability challenges experienced by some adults living with ABI. It was beneficial and helpful to many participants. Individualization of cards was important, as some people had unique contexts. Future improvements to the card would be to improve the official look of the card and increase the efficiency in card production.
65 Chronic Pain and Endogenous Pain Control Mechanisms After Brain Injury
David Clark 1,2 ; Karen-Amanda Irvine 2,3 ; Peyman Sahbaie 2,3 ; Xiaoyou Shi 1,2 ; QiLiang Chen 1
1 Stanford University, Palo Alto, United States; 2 VA Palo Alto Healthcare System, Palo Alto, United States; 3 Palo Alto Veterans Institute for Research, Palo Alto, USA
Chronic pain is a remarkably frequent outcome of mild TBI (mTBI). Common syndromes include headache, backache, limb pain and prolonged pain in the context of other injuries. Chronic pain after TBI leads to personal suffering, suboptimal functional recovery and increases exposure to opioids. Recent human and laboratory data suggest that dysfunctional endogenous pain control circuits, particularly those centered in the brainstem, may contribute to these pain problems. We hypothesized that descending pain modulatory circuits and aberrant serotonergic signaling are involved.
To address the effects of mTBI on descending pain modulation, both rat lateral fluid percussion and mouse closed head models were employed. Pain-related changes were measured using tests of mechanical allodynia in the facial region and hindlimbs. The bright light stress model of headache was used as were injury models including hindpaw incision and tibial fracture. Pharmacologic tools involved systemic, intrathecal and stereotactically targeted injections of selective adrenergic and serotonergic agents as well as neurotoxins such as dermorphin-saporin to eliminate cells expressing mu-opioid receptor. To control the activity of the locus coeruleus and periaqueductal gray matter, virally encoded Designer Receptors Exclusively Activated by Designer Drugs (DREADDs) were administered. Finally, running wheel equipped enclosures were used to study the effects of exercise on endogenous pain control systems after TBI.
We observed that TBI leads to an acute but transient period of pain sensitization characterized by facial and hindlimb allodynia supported by descending signaling through spinal 5-HT3 receptors. After recovery from this sensitization, however, the mice and rats showed profound disruption and plasticity of descending noradrenergic and serotonergic circuits. Maintenance of normal pain thresholds after TBI required the activity of endogenous opioid signaling. In this chronic setting, treatment of the mice or rats with serotonin selective reuptake inhibitors (SSRIs) was effective in restoring endogenous pain control systems and in reducing sensitization after limb injuries. Augmenting descending pain modulation through DREADD stimulation in the locus coeruleus or periaqueductal gray matter provided analgesia in the TBI animals. Finally, exercise beginning days after TBI could restore normal endogenous pain control systems.
Even mild TBI leads to a state of profound and long-lasting disruption of endogenous pain control systems. Pain control centers in the brainstem are central to this phenomenon. The augmentation of serotonergic signaling using clinically available SSRI drugs or exercise seem to be viable options for the restoration of normal endogenous pain control, and translational studies are indicated.
66 Assessment of Stimulated Blink Reflex and Symptoms Over Time in Collegiate Athletes With Sport-Related Concussion
Haley Chizuk 1 ; Mohammad Haider 1 ; John Leddy 1 ; Dena Garner 2
1 UBMD Orthopedics and Sports Medicine, Buffalo, United States; 2 Department of Health and Human Performance, The Citadel Charleston, United States
Recovery times for collegiate athletes with sport-related concussion (SRC) range from 2 to 4 weeks. The stimulated blink reflex is abnormal after SRC. This study assessed the blink reflex daily from initial assessment (within 2 days of injury) to recovery and compared it with symptom recovery.
Prospective cohort. Blink reflex (EyeStat) and Post-Concussion Symptom Scale (max=126) were assessed daily from injury to recovery. Blink reflex parameters: time to ipsilateral blink (latency), contralateral blink (differential latency), initial velocity, time to open, time to close, number of oscillations, and distance traveled (excursion). Associations over time were assessed using regression.
41 SRC (from 36 unique athletes, 20.46±1.50 y/o, 79.5% male, 0.95±1.2 days since injury) are included in analysis. Mean symptom severity at initial assessment was 25.00±17.3 and mean time to symptom resolution was 10.87±7.3 days. No significant correlation over time (i.e. p-value of interaction term of blink reflex parameter with days since injury) was observed between daily symptom severity and differential latency (p=0.097), initial velocity (p=0.150), time to open (p=0.506) and number of oscillations (p=0.228). However, a significant association was found for latency (p=0.016), time to close (p=0.017) and excursion (p=0.012). In all three of these regression models, symptom severity significantly decreased over time (p=0.013, 0.017 and 0.013, respectively) and correlated with individual blink reflex parameters throughout the recovery period (p=0.002, <0.001 and <0.001, respectively).
Certain stimulated blink reflex parameters (latency, time to close and excursions) have a significant association with daily symptom reporting over time, meaning that they are abnormal when athletes report a high number of symptoms and return to baseline when athletes are asymptomatic.
Significance
Identifying patterns on how the blink reflex changes throughout recovery and identifying those that are associated with symptom recovery can help develop algorithms that can use change in blink reflex parameters to predict symptom recovery.
67 Stimulated Blink Reflex Abnormalities Before and After Sport-Related Concussion and Association With Self-Reported Symptoms
Haley Chizuk 1 ; Nadir Haider 1 ; John Leddy 1 ; Dena Garner 2
1 UBMD Orthopedics and Sports Medicine, University at Buffalo, Buffalo, United States; 2 Department of Health and Human Performance, The Citadel Charleston, United States
Athletes with sport-related concussion (SRC) have blink reflex abnormalities, and can report combinations of physical, cognitive, fatigue or mood-related symptoms after injury. This study compares blink reflex before and after injury and identifies associations with self-reported symptoms.
Blink reflex (EyeStat, BlinkCNS) and Post-Concussion Symptom Scale (max=126) were assessed preseason and within 2 days of SRC. Clustering identified High (HS) and Low (LS) symptom groups. Blink reflex parameters: time to ipsilateral blink (latency), contralateral blink (differential latency), initial velocity, time to open, time to close, number of oscillations, and distance traveled (excursion).
Differential latency increased (baseline: 4.28±1.8 vs post-injury: 5.33±3.0 ms, p=0.047) and time to close decreased (34.30±5.6 vs 32.38±4.3 ms, p=0.022) after injury on paired t-test, and there was a trend for significance for latency (p=0.094) and oscillations (p=0.074). HS (n=15, 87% male, 20.8±1.5 years, symptoms=43.3±11.4) had slower initial velocity (4.23±0.7 vs 5.16±1.0 pixel/s, p=0.002) than LS (n=23, 74% male, 20.1±1.4 years, symptoms=13.0±6.3), and there was a trend for significance for excursions (p=0.081). Physical symptoms correlated with latency (rho=-0.28, p=0.026) and oscillations (rho=0.37,p=0.003); cognitive correlated with initial velocity (rho=-0.36, p=0.003) and exclusions (rho=-0.38,p=0.002); fatigue correlated with initial velocity (rho=-0.48, p<0.001), time to close (rho=-0.26, p=0.034) and excursion (rho=-0.49, p<0.001). Mood correlated with differential latency (rho=0.49, p<0.001) and initial velocity (rho=-0.30, p=0.014).
The stimulated blink reflex is abnormal acutely after SRC. Increase in differential latency is suggestive that the contralateral blink reflex arch is less efficient. Decreased time to close with a trend that latency is also faster is suggestive that the blink reflex is excited. The strongest correlations were between increasing differential latency and increasing mood symptoms and decreasing excursions and increasing fatigue.
The corneal blink reflex is a primitive brainstem response initiated by light, touch, or sound. Technology-assisted objective assessment using a portable blink reflexometer has the potential to aid in SRC diagnosis and validate self-reported symptoms.
68 Iterative User-Centered Design of the SwapMyMood Mobile App: Real-World Clinical Insights
Tracey Wallace 1 ; John Morris 1 ; Rebecca Gartell 1 ; Katherine McCauley 1 ; Russell Gore 1
SwapMyMood is an innovative mobile app designed to assist individuals with traumatic brain injury (TBI) in implementing problem-solving and emotion regulation strategies based on the clinically validated Short-Term Executive Plus (STEP) cognitive rehabilitation interventions. SwapMyMood’s genesis stems from experiences of patients undergoing TBI rehabilitation who reported challenges recalling and initiating the STEP program process and strategies, particularly in stressful situations. The app was designed to provide a portable solution that electronically guides users through problem-solving and emotion regulation strategies based on the content of the STEP intervention paper manual. App development followed an iterative user-centered design process involving interviews, surveys, sit-by demonstrations, and take-home testing with participants with TBI and clinical experts, incorporating end-user feedback at every stage of design. Three previous design cycles were completed with input by twelve subject matter experts (SMEs) and 24 people with the lived experience of TBI leading up to the current iteration of the app.
To describe usability results of the most recent of user-centered design testing of the recently launched 2023 version (v.1.0.10) of SwapMyMood. Usability testing ensures that the new version is functioning correctly and meets the needs of target users. It also helps identify opportunities for future improvement.
The study included six military service members/veterans with persistent mild TBI (mTBI) symptoms who were participating in an intensive outpatient TBI rehabilitation program, along with four SME clinicians providing care to one or more of the participants. Two additional SMEs outside the clinical setting also provided feedback. Participants used the app in the clinic, home and community for up to two weeks and completed interviews and surveys regarding their experience with the app. Participants with TBI completed the System Usability Scale (SUS). All participants answered questions on app usefulness and desired features.
All testers rated the app’s design and usability positively. SUS scores indicated high acceptability and usability (M=92.08). Users with mTBI reported an increase in knowledge of the app’s supported strategies following take-home use. All SMEs believed the app could benefit people with TBI and that it could be useful in their own professional practice. Valuable feedback from participants suggested the need to further refine some features to enhance support for users with TBI-associated memory challenges in accessing the app’s interventions.
The iterative user-centered design process for the SwapMyMood mobile app, conducted in a real-world clinical setting, has shown promising results. Users and SMEs are enthusiastic about its potential to support TBI patients in managing their symptoms and enhancing their quality of life. The valuable feedback collected from participants will guide ongoing app refinement, making it a more effective tool for both patients and professionals in the field of TBI rehabilitation.
69 Applying Behavior Analysis to the Interdisciplinary Inpatient Brain Injury Team
Arielle Reindeau 1
1 Craig Hospital, Englewood, United States
Behavioral disturbances are some of the most pervasive and persistent phenomena that follow an acquired brain injury (Corrigan, 1985). Rehabilitation sites across the United States struggle to provide services for individuals who consistently engage in challenging behaviors (Ketzmer et. al, 2022). At Craig Hospital, in Englewood, Colorado, Physicians and Board Certified Behavior Analysts (BCBA) are integrating the science of Applied Behavior Analysis (ABA) into the acute inpatient setting. This science, based on human behavior, is reshaping and redefining how clinical staff in this early phase of recovery gain information about patient behaviors, communicate about behavioral needs, and utilize their environments to shape socially appropriate behaviors.
The interdisciplinary teams, in conjunction with the newly added BCBA positions, have created novel systems to collect individualized data around behaviors that most impact the current rehab process. Day-to-day data is facilitated by nursing staff and used by the entire interdisciplinary team to help inform decisions. Data is operationally defined using tools validated through the ABA community. Rehab teams focus on the ability to define behavior prior to trying to measure it for best results. The current site utilizes a 15-minute partial-interval time-sampling template with up to 4 operationally defined behaviors. These individualized systems are used in tandem with reliable and validated assessments such as the Agitated Behavior Scale (ABS) (Corrigan, 1985).
Communication for behavioral needs and escalated events have been a primary focus of this program. Staff have received education, feedback and debriefs for all information provided through our quality improvement system. Most importantly, physicians and BCBAs have focused heavily on creating a language around behavior that allows staff to communicate in a way that is intentional and functional. Staff have been encouraged and engaged with the opportunities to improve the way behavior management flows.
Globally, the focus has been on indicating how the environment shapes patient behavior. Utilizing the building blocks we all know - consistency and structure - ABA fills a crucial gap in rehabilitation implementation that exists within the current structure. Although many team members with insight into behavior do exist, behavior analysts uniquely carry skills that allow them to both intervene and educate on behavioral principles across activities of the day. Our talk will include the process used to determine the effectiveness of medications utilized for behavior management. We will describe how staff are able to also use daily information to determine location, interaction structure and reinforcement for patients. The purpose of the current oral presentation will be to provide clinicians with an overview of the science that they can use in any setting to better manage behavior.
70 NASHIA’s Collaborative on Children’s Brain Injury: Working to Improve National Educational Support for Children With Brain Injury
Jennifer Lundine 1 ; Brenda Eagan-Johnson 2 ; Melissa McCart 3
1 The Ohio State University, Columbus, United States, 2BrainSTEPS Brain Injury Consulting Program, Pittsburgh, USA, 3Center on Brain Injury Research and Training, University of Oregon, Eugene, USA
In 2022, the National Association of State Head Injury Administrators (NASHIA) launched its first special interest group, NASHIA’s Collaborative on Children’s Brain Injury (NCCBI). NCCBI’s mission is to improve services and support for children with acquired brain injury. In 2014, NCCBI was formed outside of NASHIA, and in 2023, partnered with NASHIA to expand the group’s impact. NCCBI’s goals include 1) Identifying and addressing critical gaps in the continuum of services and supports, 2) Collaborating with national key partner groups to establish common language, practices, and to make policy/research recommendations, and 3) Educating, sharing information, developing tools, and resources on supports and services. NCCBI has two active working groups. The Standards of Practice workgroup is reviewing documents used across the United States to assess student history of brain injury. The Educational Policy workgroup focuses on early childhood brain injury and examining the processes to qualify for early intervention by state. The NCCBI workgroup’s findings will inform future projects to address the under-identification of children and adolescents who experience brain injury.
The three co-chairs of NCCBI, and colleagues representing school counseling and school psychology, recently submitted a commentary on eligibility determination for school-age children with traumatic brain injury (TBI). This paper explains the public-school evaluation process, including assessment considerations specific to students with TBI. A significant obstacle contributing to the under-identification of students with TBI is that many school districts require a medical statement for a TBI special education eligibility. To remedy this barrier, the authors propose using a guided credible history interview (GCHI) as an alternative to a medical statement. A GCHI is conducted by a school professional who is familiar with a TBI’s physical, cognitive, emotional, and behavioral effects and symptoms can emerge over time. The person interviewed is someone with knowledge of the TBI event, such as a parent or guardian. The information provided in the GCHI can then be used by schools instead of a medical statement, increasing the likelihood of identification of students with TBI. In 2020, the state legislature in Oregon adopted the GCHI process. First-year implementation data indicates that the number of students identified under Oregon’s TBI special education category increased 21%.
Future research is needed to evaluate the effectiveness of the GCHI to expand the identification of students with TBI so that they receive appropriate learning and behavior support. Students with TBI have nuanced needs that cannot be identified through clinical testing alone. NCCBI will identify and support educational policies that promote expanded use and interpretation of curriculum-based assessments and school-day observation to ensure that investigation of a student’s functional skills occurs where they are likely to show actual deficits.
72 School Transition After Traumatic Brain Injury (STATBI) – Caregiver Perspectives on Services for Students
Jennifer Lundine 1 ; Angela Ciccia 2 ; Erika Hagen 1 ; Nicole Viola 1
1 The Ohio State University, Columbus, United States; 2 Case Western Reserve University, Cleveland, USA
Traumatic brain injury (TBI) is considered a leading cause of acquired disability for children in the US. Despite the high incidence of negative long-term academic, social, and health outcomes for children with TBI, few receive appropriate educational supports. Return to school (RTS) programs have been developed to better assist children with TBI as they return to the classroom. These programs vary widely by state, and no existing RTS program has been systematically evaluated to determine its impact on outcomes for students with TBI. The objective of the School Transition After Traumatic Brain Injury (STATBI) project is to rigorously evaluate the impact of BrainSTEPS, a formal return-to-school (RTS) program, on academic, social, and health outcomes for students in grades K-12 who have experienced TBI of any severity, compared to students who have no formal RTS programming (control arm). STATBI uses a mixed method, cohort-controlled research design. The protocol includes electronic survey administration and virtual interviews with parents and children. This presentation will include data from nine focus groups completed with caregivers from the experimental and control groups during summer and fall 2023. Twenty-five caregivers (100% female) participated in focus groups, with four groups from the control arm and five groups from the experimental arm. The sample included students with mild, moderate, and severe TBI. Questions and discussion focused on how caregivers accessed services, facilitators and barriers to finding care, and their satisfaction with services their child received following TBI. Preliminary analysis of focus group transcripts reveals persistent challenges that caregivers face attempting to find and access necessary supports for mental health and school services for their children with TBI. Caregivers receiving formal RTS support through BrainSTEPS discussed the relief and support provided to them by school-related programming. Caregivers in the control arm discussed persistent difficulties in identifying providers and accessing supports for their children. When supports were identified and provided, unsurprisingly, caregivers were more satisfied with overall service provision. Focus group data is being analyzed further for themes associated with injury severity and time post injury. The STATBI project is unique in its focus on RTS for youth with TBI, and this presentation will describe caregiver perspectives of access to and satisfaction with services for school-age youth with TBI who participate in either formal or non-formal RTS program. Additionally, the sample includes many students who reported having mild injuries but who continued to have academic needs past the typical recovery period that warranted ongoing support services. These findings have important implications for assessing students with TBI as they progress through school. This talk will highlight ongoing study progress and implications for those studying RTS programs for students with TBI.
73 Multidisciplinary Rehabilitation for ABI Patients With Movement Disorders
Fernanda Lapietra de Carvalho 2 ; Karen Madden 2 ; Fran Richardson 2 ; Gemma Bailley 2 ; Esther McEvoy 2 ; Ivana Jankovic 2 ; Sarah Luxon 2 ; Sandra Sanmartin 2 ; Jesse Tulipano 2 ; Tara Dingman 2 ; Zhihui(Joy) Deng 1,2
1 Mcmaster University, Department of Medicine, Hamilton, Canada; 2 Regional Rehab Centre, Hamilton Health Sciences, Hamilton, Canada
Movement disorders are commonly seen clinical phenomena in patients who have suffered a moderate to severe acquired brain injury (ABI). While spasticity and ataxia are well known neurological deficits, less common types of movement disorders are encountered in our inpatient rehab program, which is the focus of this study. Early diagnosis and identification of contributing factors is key to reaching favorable functional outcomes for those patients. Here we present 6 types of clinical conditions including: (1) Parkinsonism with the etiology of ABI versus medication adverse effects. Dopamine agonists and anticholinergic agents may be beneficial for the former while discontinuation of culprit medications is important for the latter; (2) Dystonia with a similar etiology and pharmacological management as parkinsonism; (3) Tardive dyskinesia commonly seen as an adverse effect of dopamine antagonists, for which management is more challenging; (4) Tremor mimicking the symptoms of essential tremor (ET) seen after an injury to the cerebellum or brain stem, for which primidone is usually effective while some other antiepileptic drugs may worsen symptoms; (5) Palatal myoclonus seen after an injury involving the dentato-rubro-olivary pathway, for which antiepileptic medications can be trialed to alleviate symptoms; (6) Chronic post-hypoxic myoclonus which may be well managed with antiepileptic agents such as valproic acid, clonazepam and levetiracetam. We are a multidisciplinary team that specializes in adult ABI rehabilitation. Our team is comprised of physician specialists and allied health professionals including but not limited to pharmacists, physiotherapists, occupational therapists, speech-language pathologists and rehab therapists. We also have ready access to consulting specialists to assist in differential diagnosis and management planning if needed. In addition to medications, non-pharmacological interventions are essential to successfully enhance the function of ABI patients with movement disorders. Allied health teams can assist with positioning, developing strategies and utilizing assistive devices for more controlled movement, and thus creating opportunities to practice. The impact of the above-mentioned neurological conditions on functional movement patterns is assessed throughout the medication trials as the side effects of various medications can take time to develop. Multidisciplinary rehabilitation requires close collaboration among all team members to determine appropriate and effective strategies that, when implemented together, will optimize physical, communication, swallowing, and cognitive function. Continuous collaboration between allied health team members and the medical team is imperative to determine appropriate and effective pharmacological interventions (i.e. to address/manage tremor, hypertonia, movement initiation, etc.) that, in combination with evidence based therapeutic interventions, will enhance and maximize recovery for each patient experiencing movement disorders secondary to ABI.
74 The Back2Play App: A Concussion Management Platform for Children and Youth to Bridge the Gap Between Research and Practice
Joe Steinman 1,2 ; Kristele Pan 1,2 ; Kathy Stazyk 1,3 ; Samantha Perrotta 1,3 ; Maliah Leblanc 1 ; Richard Zhang 1 ; Vereena Andrawes 1 ; Carol DeMatteo 1,3
1 CanChild Centre for Childhood Disability Research, McMaster University, Hamilton, Canada; 2 Michael G. DeGroote School of Medicine, Faculty of Health Sciences, McMaster University, Hamilton, Canada; 3 School of Rehabilitation Science, Faculty of Health Sciences, McMaster University, Hamilton, Canada
Traumatic brain injury (TBI) is the leading cause of death and disability for the pediatric population worldwide. With concussions comprising the majority of these TBIs, concussions among children and youth are an established public health concern. However, the management of pediatric concussions, particularly the decision to return to school and activity following concussion, is often inconsistent and a one-size-fits-all approach. To (1) individualize concussion management to each patient’s unique recovery, (2) provide guidance and monitoring for optimal rehabilitation, and (3) revolutionize concussion management in the digital age, the Back2Play App was developed based on CanChild’s evidence-based management strategies and the expertise of pediatric, psychology, and rehabilitation clinicians, machine learning engineers, and exercise science specialists. The purpose of this randomized controlled trial was to evaluate whether the App supports safe and symptom-free return to school and activity.
Eligible children and youth aged 10-18 were randomized into an App Group and Usual Care Group. Usual Care Group participants completed a symptom survey once daily, and received typical care which usually includes generic guidelines provided by their physicians. App Group participants received an Apple watch with the Back2Play App that provided interactive feedback and monitored real-time biological variables including heart rate and movement; completed a symptom survey thrice daily; and followed CanChild’s evidence-based management strategies. All participants completed two follow-up interviews to assess recovery progress and ascertain if re-injury occurred.
Preliminary results indicate that at follow-up, 78.7% (37/47) of App Group participants had returned to sports, compared to 59.6% (28/47) of Usual Care Group participants (p = 0.074). At the early stages of the Return to School protocol (RTS Stage 1), the mean self-assessed cognitive scale score that measures cognitive activity was greater in the App Group than in the Usual Care Group (2.70 +/- 0.27 [N=53] vs. 2.01 +/- 0.21 [N=45], p < 0.01; error = 95% CI).
Recruitment for Phase 3 of this study is nearing completion, with 130 participants of the 160 targeted already recruited. Although not statistically significant, the number of participants having returned to sports at follow-up was greater in the App Group than in the Usual Care Group, potentially indicating a higher likelihood of returning to normal activities. The mean cognitive scale score was also higher in the App Group compared to the Usual Care Group at the earliest RTS stage, suggesting higher cognitive activity at the early stages of recovery in line with CanChild’s management strategies.
Results from this study can inform clinicians of the efficacy of app-based interventions within this population and address the dearth of consistency and personalization in concussion management, ultimately enabling children and youth who have experienced a concussion to return to school and activity safer and sooner.
75 Exploring Hypoxic and Ischemic Brain Injury: Observational Insights and Treatment Approaches in Indian Children With Cerebral Palsy
Priya Kapoor 1 ; Sakshi Pal
1 Bharati Vidyapeeth(Deemed To Be University) School Of Audiology And Speech Language Pathology, Pune, India
This study examines hypoxic ischemic brain injuries in the context of cerebral palsy (CP) in India. Children with CP commonly experience issues like epilepsy, hearing loss, and feeding difficulties. These feeding problems result from communication barriers, oral-motor dysfunction, and aspiration. Despite various assessment tools for feeding issues, there’s a lack of options in Indian languages. This study focuses on the complexities of hypoxic ischemic brain injuries, particularly within the context of CP. The objectives of the study are to evaluate the impact of hypoxic and ischemic brain injuries on individuals’ neurological and cognitive functions and provide observational insights to enhance the scientific understanding of these injuries.
The research took place in Pune, Maharashtra, employing a cross-sectional design and convenient sampling. Marathi-translated version of the Behavioral Pediatrics Feeding Assessment Scale (BPFAS) was utilized, comprising 35 items. These items allowed parents to assess both their child’s eating behaviors and their own feelings or strategies concerning feeding issues. The translated BPFAS was administered to parents of children diagnosed with CP. Using the Marathi-translated BPFAS, the questionnaire was structured into five categories: ‘Picky Eaters,’ ‘General Toddler Refusal,’ ‘Toddler Refusal—Textured Foods,’ ‘General Older Children Refusal,’ and ‘Stallers.’
A sample was gathered from the School of Audiology and Speech Language Pathology at Bharati Vidyapeeth (deemed to be a university). Out of the initial group of 50 participants, aged between 9 months and 7 years and diagnosed with cerebral palsy (CP), two participants declined to provide consent for the study, and 21 participants were excluded due to not meeting the inclusion criteria. The inclusion criteria required parents to be native Marathi speakers and their children to be aged 9 months to 7 years with CP attributed to hypoxic ischemic encephalopathy; the rest were excluded.
A descriptive analysis calculated standard deviations and means, revealing no significant gender impact on BPFAS scores. Notably, the study identified distinct feeding challenges among children with CP who displayed milder picky eating tendencies, while younger children in the ‘General Toddler Refusal’ category exhibited common issues like whining and food refusal. The ‘Toddler Refusal—Textured Foods’ category emphasized difficulties with specific food textures, underscoring the need for tailored interventions. Additionally, the ‘General Older Children Refusal’ and ‘Stallers’ categories highlighted CP-related behaviors in food choice negotiation and eating habits. This study offers valuable insights into mealtime behavior patterns in children with CP, underscoring the significance of tailored feeding interventions.
In conclusion, this study sheds light on the multifaceted challenges faced by children with CP in India. The prevalence of CP, its associated comorbidities, and the impact on feeding and communication are important considerations. The findings highlight the pressing need for high-quality prevalence studies in India to better understand the CP landscape and its associated issues.
76 Interdisciplinary Management of Mild Traumatic Brain Injury (mTBI): A Model of Care for Persistent Symptoms in a Pediatric Setting
Lindsay Cirincione 1,2 ; Carolyn Caldwell 1 ; Gray Vargas 1 ; Sherri Clark 1 ; William Ide 1,2 ; J. Alfredo Caceres 1,2
1 Kennedy Krieger Institute/Johns Hopkins School of Medicine, Baltimore, United States; 2 Johns Hopkins School of Medicine, Baltimore, 21205
Existing literature is clear that multidisciplinary treatment of persistent mTBI (concussion) symptoms is critical in improving patient outcomes. Institutions are often left to their own devices to determine how to provide this type of care in a way that is viable for providers, maximizes interdisciplinary potential, and is most helpful to patients and families. This study illustrates one model of achieving interdisciplinary care for a patient population with complex, varied, and persistent symptoms following remote mTBI. An interdisciplinary care model involving Medicine, Nursing, Neuropsychology, and Pediatric Psychology is presented using a case series to illustrate common symptom presentation, in-clinic assessment methods, and treatment recommendations. Twelve months of preliminary descriptive data is presented in this abstract, with five years of analysis available by date of presentation. Considerations related to equity, diversity, and inclusion within this population will be discussed.
Retrospective chart review was conducted of patients experiencing persistent symptoms > six months following an mTBI who were evaluated in a pediatric mTBI multidisciplinary clinic. Patients with findings on neuroimaging were excluded. Three cases with persistent symptoms are illustrated. The interdisciplinary care model is presented with an emphasis on each discipline’s role, assessment methods, and treatment recommendations.
Preliminary data extraction of cases over the course of 12 months was reviewed (n = 23). The mean age of patients was 15.8 years (range: 10-21 years). Patients were primarily female (65.2%; sex assigned at birth), White (73.9%), and not Hispanic (65.2%). Mean time since injury was 22.3 months (range 6-72 months). Most common presenting symptoms included mood-related concerns (83%), headaches (78%), and cognitive complaints (65%). The majority of patients (91%) were fully cleared from a mTBI perspective following the interdisciplinary team evaluation. Mental health support was recommended for 96% of patients and 35% were referred to physical therapy. Analysis including a total of five years of data will be reviewed.
An interdisciplinary care model provides specialty evaluation and treatment across physical, cognitive, and emotional domains of functioning while decreasing overall medical utilization rates, reducing the potential for conflicting recommendations among providers, and lessening time away from school and work for patients and their families. Most importantly, interdisciplinary management provides a comprehensive treatment plan, making the path to recovery clear and achievable. It also allows for a broader focus on factors predictive of recovery, which may fall outside the scope of a single-discipline visit.
77 Untangling the Everyday-Using the Rehabilitation Treatment Specification System (RTSS) to Uncloak the Rehabilitation Opportunities Inherent Within CONNECT’s Life Redesign Model to See the Possibilities of the Everyday.
Adam Van Sickle 1 ; Deidre Sperry
1 Connect Communities, Hamilton, Canada
This presentation or poster will make use of case examples to demonstrate how the Rehabilitation Treatment Specification System (RTSS) provides the means of moving knowledge from rehabilitation literature to the front lines all in an effort to enhance the work being done at CONNECT. We will explore how the RTSS framework has helped build a greater understanding of the many opportunities for rehabilitation that are present at CONNECT.
For 30 years, CONNECT Communities has supported people in redesigning their lives after brain injury and stroke. CONNECT’s Leading Practice Life Redesign Model includes meaningful community participation with an emphasis on social capital within a context of supported risk-taking. CONNECT originated in British Columbia and is now also located in Hamilton Ontario. In partnership with the local hospital system, Hamilton Health Sciences, people living with Acquired Brain Injury (ABI) are supported to engage in everyday activities to support their Life Redesign Plan. This requires close collaboration with professional team members, those who provide direct daily support (Life Redesign Coaches), and most importantly, the individual and their family. Being able to untangle complex everyday activities to allow for outcome measurement and maximized consistency of approach across the organization is a challenge. In 2016, The RTSS was introduced to rehabilitation Science. The RTSS provides a means of better analyzing, documenting, researching, and discussing the many components of any rehabilitation program. At CONNECT, the RTSS is providing the means of untangling the everyday to describe rehabilitation opportunities for individuals with ABI within CONNECT’s Life Redesign Model.
Utilizing the RTSS, the regulated health professional coaches reviewed the existing Life Redesign Goals and Plans that guide the rehabilitation of 10 residents at CONNECT. The process revealed a new way of seeing rehabilitation. When viewed through a different lens, it was possible to better describe Life Redesign at CONNECT, in terms of the aims, targets, and ingredients of the RTSS. In turn, this created opportunities to disseminate knowledge to all involved. Ultimately, the collaboration among professionals, frontline coaches, family, and the individuals we support, has allowed for greater unity and a better understanding of the rehabilitation layered into the everyday.
79 Minding the Early Brain: Perinatal Events and Intrapartum Exposures as Influences on Child Neurodevelopment
Lisa Kurth 1
1 University of Colorado School of Medicine, Developmental Pediatrics, Fort Collins, United States
Pediatric traumatic brain injury may consider expanding to include perinatal events and exposures involved in complicated childbirth, since research reveals adverse influences for child neurodevelopmental trajectory. Epidemiological studies link specific intrapartum complexities presenting during labor and delivery with rising child neuropsychiatric outcomes, justifying the novel concept of perinatal neurotrauma. These overlapping, interacting factors combined with elevated maternal gestational BMI, confer a disruptive cascade of neural events which may risk lifelong impairments for children. Rising neuropsychiatric conditions including ADHD and Autism have unconfirmed etiologies, yet complicated childbirth associations. Concomitant cognitive dysexecutive symptoms, emotional dysregulation, social and academic issues often persist into adulthood. While research has considered genetic etiology, it is unlikely genetics alone trigger these outcomes. Plausibly, events introduced during most sensitive developmental periods may affect the malleable fetal brain with risky downstream effects, altering child neurodevelopment. Birth complications typically involve well-respected measures aimed at expediting childbirth. One first-line, synthetic uterine simulant effectively assists > 50% of all U.S. childbirths, despite its poorly understood fetal impact. Exponential increases in exogenous uterine stimulation and dosage inconsistencies raise concerns of consequential maternal-fetal transmission. Labor duration and pharmacological dosages are important algorithms to disentangle since these are all modifiable factors. Established repercussions of this early environmental exposure include fetal distress, low Apgar scores, uterine hyperactivity, FHR abnormalities, NICU admissions and ischemia/asphyxia/hypoxia. Putative neuropathophysiological models include fetal intolerance to prolonged dosages, labor impact; epigenetic triggering, oxytocin receptor hyperstimulation and/or receptor oversaturation. Other considerations include neuroinflammation; hypertonic uterine contraction pressure imposing neuropathogenic alterations and diffuse axonal injury. Plausibly, disharmonious compounds, GABA downregulation; blood-brain barrier breach and/or placental permeability may interactively compromise fetal neuroprotective integrity. Additionally, the underexplored neuropathophysiological interpretation of pharmacokinetics involving synthetic properties may play a key role in fetal brain impact. Interestingly, maternal BMI/adiposity, a modifiable gestational health factor, increases odds for medically assisted childbirth owing to diminished uterine contractility in obese mothers. The shared effects of maternal BMI with chemically expedited labor, and its two-fold impact on offspring brain development is under-investigated, begging further exploration since its potential future contribution to the study of pediatric traumatic brain injury is imperative. While a signature, underlying, neuropathophysiological mechanism(s) linking childbirth complications and maternal gestational BMI to pediatric brain injury lacks confirmation, mixed evidence associates these factors directly with child neuropsychiatric phenotypes. Logically, the vulnerable fetal brain’s reaction to early, overlapping events and exposures is important to better understand. It is crucial to appreciate that a constellation of perinatal factors may risk future functional and behavioral impairments for children. Early vulnerabilities, potentially linked to in-utero exposures and obstetric dynamics, may destabilize and/or disrupt fetal brain development, warranting aggressive research and inclusion in the burgeoning field of pediatric brain injury as a critical child public health issue.
80 “You Should Be Better By Now!” Clinical Guidelines for Managing Prolonged Symptom Sequelae in TBI
The landscape of prolonged symptomatology and functional impairments following traumatic brain injury (TBI) can become perplexing and enigmatic to unravel etiologically. This constellation of TBI-induced symptoms can present curious, latent emerging symptoms which are difficult to distinguish across clinical settings. Since the specific biomechanics and aerodynamics involved in each injury scenario can vary widely, the combination of variability across individual coping styles, as coupled with personalized immune system responses, can interactively determine lingering and evolutionary injury-induced symptom sequelae. A sizeable amount of these persistent, post-morbid TBI symptom profiles may functionally overlap, and can feature multi-organ-system involvement. As an additional complication, impaired symptom awareness can amplify TBI-induced trauma and PTSD symptomatology for the injured individual, since an association to actual injury dynamics often goes underrecognized, and/or misdiagnosed, subsequently postponing essential treatment(s). When an injured individual discloses or displays curious, continuous and/or newly emerged TBI-related symptoms which are not taken seriously by others, these courageous communications may become misunderstood, dismissed, disbelieved, and underappreciated. Misinterpretation of symptom self-disclosures as being insincere, confabulated, or malingering can be difficult to cope with, especially when originating from family, friends and across other meaningful relationships. These discrediting impressions add baffling layers of burden to an individual suffering with a TBI, complicating the already challenging task of healing and recapturing pre-injury functioning. When the response of others involves questioning the authenticity of prolonged symptoms, this feedback translates atmospheric doubt, conveying non-supportive recovery expectations. This stress provocative dynamic can dilute relationship integrity, induce trauma triggers, reactivate, and amplify residual PTSD, and compound unresolved, post-morbid symptoms for the injured individual. A self-protective avoidance response of social disengagement is common, as the individual withdraws or self-isolates to minimize negative exposure impact. Essential treatment targets should encompass a thorough exploration of pre-morbid vs. post-morbid profiles, based on patient self-report, collateral input, and findings from standardized testing aimed at assessing and quantifying post-morbid functional impairment(s) and pre- vs. post-morbid discrepancies. Referral to well-informed, multidisciplinary providers who rely on evidence-based, specialized ancillary services can assist in discerning symptom persistence and its link to TBI-related events, while expediting multimodal interventions as may be warranted. A two-pronged psychotherapeutic approach should prioritize providing guidance and support in identifying and recognizing unrelenting post-morbid symptom comorbidities featuring neuropathophysiological, multi-system involvement. Secondly, evidence-informed psychoeducation should include didactic, portable coping skills which focus on tracking routine functioning across atmospheres, monitoring sleep architecture, nutrition, integrating modest exercise, budgeting energy output, mood regulation, promoting a self-healing mentality, and bolstering confidence in healing, health resilience and recovery. Restoring a sense of dignity for the TBI-injured individual by validating symptom legitimacy and launching endeavors to clinically investigate symptom etiology via referral(s) and clinical collaboration with multidisciplinary providers are essential approaches in addressing prolonged TBI-induced symptomatology.
82 Neuroprotective Effects After TBI of Enteric Hydrogen Generation From Si-Based Agent in Mice Model
Sanae Hosomi 1 ; Hiroshi Ito 1 ; Yoshihisa Koyama 2,3 ; Yuki Kobayashi 4 ; Hiroshi Ogura 1 ; Hikaru Kobayashi 4 ; Shoichi Shimada 2,3 ; Jun Oda 1
1 Department of Traumatology and Acute Critical Medicine, Osaka University Graduate School of Medicine, Suita, Japan; 2 Department of Neuroscience and Cell Biology, Osaka University Graduate School of Medicine, Suita, Japan; 3 Addiction Research Unit, Osaka Psychiatric Research Center, Osaka Psychiatric Medical Center, Suita, Japan; 4 Institute of Scientific and Industrial Research, Suita, Japan
Traumatic brain injury (TBI) is a condition that can cause oxidative stress, inflammation, and cell death in the brain. Antioxidant therapies have been studied as a potential treatment for TBI, including hydrogen treatment. Si-based agent continues generating hydrogen for more than 24 hours by the reaction with water and generates approximately 400 mL of hydrogen. However, there is no specific information available on the effectiveness of Si-based agents for TBI. This study aimed to investigate the beneficial effects of the Si-based agent for TBI in a mice model. We used the controlled cortical impact model (CCI) mice. The mice were fed a control diet or a diet containing the Si-based agent for one week before CCI. One week after CCI, the Y-maze and open-field tests were performed as behavioral tests. As a result, mice treated with Si-based agents (n=19) showed a notable increase in the spontaneous alternation values compared to the control group (n=19) (control group vs treatment group = 61.7% (51.9-69.2%) vs 74.2% (60.3-85.7%): p=0.03). However, there were no significant differences between the control group and treatment group in the open-field test (time in the inside zone; control group vs treatment group = 27.2 seconds (22.6-34.5 seconds) vs 30.1 seconds (16.8-34.2 seconds): p=0.99, total distance; control group vs treatment group = 29.1 meters (22.5-34.3 meters) vs 28.8 meters (23.1-35.8 meters)). These findings indicate that the Si-based agent is found to prevent impairment of spatial learning and memory after CCI, which should be considered as a novel hydrogen administration method for TBI.
83 Correlation of Computerized Posturography and Saccadic Latency in the Rehabilitation of Postural Abnormalities
Victor Pedro 1 ; Richard Lyon 1 ; Diane Bienek 1
Research into the dysfunction of the postural control system in humans has been inconclusive as to the rehabilitative role of the oculomotor subsystem. Studies on the relationship between pursuit and saccadic activities in the rehabilitation of postural abnormalities have had conflicting findings regarding the predictable role of oculomotor activities in rehabilitation. Most studies are performed on healthy athletes rather than challenging compromised patients in a clinical setting. The aim of this study was to measure computerized posturography and saccadic latency of a subject population with loss of postural control to include migraine headaches (39.3%), post-concussion syndrome/traumatic brain injury (35.7%), vertigo (17.9%), and other brain disorders (7.1%) as primary diagnoses.
A matched pairs design (pre- and post-treatment assessments) was used to assess the efficacy of a course of personalized Cortical Integrative Therapy, as the rehabilitative strategy. Postural control of 28 refractory adult patients, aged 18 to 64, was measured by computerized posturography and saccadic latency by videonystagmography. As head movements challenge the subject by generating a vestibular stimulus in addition to that generated by the subject’s sway, computerized posturography was conducted with the head in neutral position, right and left. Posturography scores in the three testing positions were compared to right and left horizontally directed saccades latency. These measurements were taken over the intervention course (mean = 7.66 weeks, range 0.57 to 20.29 weeks).
Efficacy of the personalized Cortical Integrative Therapy was indicated by a near 25% (P < 0.05) improvement in the posturography value. Post-intervention, the average latency values with the head in the neutral position and the head in left rotation demonstrated a negative linear correlation (P ≤ 0.05) in both directions of saccadic activity. In contrast, right head rotation testing yielded no statistically significant correlation between latency and posturography values. As expected, no correlation was observed between the postural stability and oculomotor function at baseline pretreatment testing.
The relationship between saccadic activities in the rehabilitation of postural abnormalities was demonstrated in a heterogeneous subject population with varied brain injuries and brain-based disorders. Moreover, computerized posturography data suggests that head rotation can help direct therapeutic strategy. Altogether these data suggest a rehabilitative role of vestibular postural systems in conjunction with oculomotor systems, which beckons development and implementation of new intervention approaches for broad-based clinical practice.
84 Advancing Traumatic Brain Injury Treatment: The Potential of Photobiomodulation, Its Mechanisms and Clinical Evidence
1 Vielight, Inc., Toronto, Canada
This abstract investigates the utility of Photobiomodulation (PBM) for Traumatic Brain Injury (TBI) treatment, aiming to expand therapeutic options beyond symptom management. It presents a synthesis of PBM’s biological mechanisms, a compilation of clinical evidence, and an overview of its regulatory considerations.
Methods and Mechanisms
PBM introduces red and near-infrared (NIR) light to targeted tissues, instigating a cascade of mitochondrial and cellular responses conducive to brain healing. This review elucidates PBM’s action in modulating the mitochondrial electron transport chain, fostering gene transcription, and stimulating growth factor production. The activity also attenuates the excitotoxicity and inflammation which are characteristic of TBI.
Clinical Evidence
Emphasizing clinical outcomes, substantial evidence from recent studies is presented, demonstrating PBM’s effectiveness in improving cognitive and behavioral symptoms associated with TBI. Specific improvements in depression, sleep quality, cognitive function, and PTSD symptoms have been consistently reported. Notably, reaction time and grip strength enhancements serve as additional objective metrics of PBM’s impact on neural recovery. Additionally, case reports involving former athletes with suspected chronic traumatic encephalopathy (CTE) reveal symptom alleviation in similar domains, reinforcing PBM’s therapeutic potential even in a worrying spectrum of brain injuries. The parallels drawn between PBM’s effects on CTE and clinical evidence for Alzheimer’s disease underlines a broader application for neurodegenerative disorders.
Personalization Through Technology
Recognizing the heterogeneity of TBI, this presentation advocates for the use of artificial intelligence (AI) to personalize PBM treatment. By analyzing individual brain activity through EEG and fMRI, AI algorithms can optimize PBM settings, tailoring the therapeutic regimen to patient-specific neurophysiological profiles.
Pivotal Trial and Regulatory Progress
Looking forward, the presentation details the design of an upcoming multi-site randomized controlled trial (RCT) encompassing 280 subjects to substantiate PBM’s efficacy for chronic TBI symptoms. This RCT is a critical step toward obtaining FDA clearance, a milestone that would validate PBM as a sanctioned therapy for TBI.
PBM is posited as an innovative, non-invasive treatment modality for TBI, distinguished by its ease of use and potential for integration into home settings. The convergence of promising clinical evidence and ongoing research underscores the need for continued exploration into PBM’s capabilities. With AI’s advent, the personalization of treatment parameters is anticipated to further enhance PBM’s clinical applicability and outcomes in TBI recovery.
87 De Novo Rehabilitation Recommendations for American College of Surgeons Traumatic Brain Injury Best Practice Guidelines 2024
Brooke Murtaugh 1 ; Joseph Giacino 2 ; Alan Weintraub 3 ; Flora Hammond 4 ; Geoffrey Manley 5
1 Madonna Rehabilitation Hospitals, Lincoln, United States; 2 Harvard University, Boston, United States; 3 Paradigm Corporation, Littleton, United States; 4 Indiana University School of Medicine, Indianapolis, United States; 5 University of California San Francisco, San Francisco, United States
In 2015, the American College of Surgeons (ACS) Trauma Quality Improvement Program (TQIP) published Best Practices in the Management of Traumatic Brain Injury which provided practice and care recommendations for patients with Traumatic Brain Injury (TBI) served by trauma centers. The purpose of the TBI Best Practice Guidelines (BPG) is to provide ACS verified trauma centers evidence and expert-based recommendations to determine best practices and quality care for TBI to support optimal long-term outcomes and recovery. These 2015 BPGs were developed by a committee consisting of neurotrauma, neurosurgery, neurocritical care and nursing experts and were endorsed by ACS and TQIP.
Since 2015, TBI research, published evidence and clinical care has evolved in multiple domains warranting a re-evaluation of the current TBI BPGs. ACS and TQIP supported an update to the 2015 publication to be congruent with current evidence and recommendations. The revised TBI Best Practice Guidelines builds on the work of the first edition from 2015. The updated 2024 TBI Best Practice Guidelines includes De Novo sections of TBI trauma care that were not included in the previous edition. Recently, ACS has been deliberate in pursuing collaboration with rehabilitation experts as the benefit of early rehabilitation improves outcomes from trauma and TBI patients and lead to the genesis of a focused rehabilitation best practice recommendation section within the new 2024 TBI BPGs as a de Novo section.
A cadre of TBI and rehabilitation experts were assembled to participate in the ACS TBI BPG committee to develop novel rehabilitation recommendations for trauma centers. Rehabilitation experts conducted in-depth review of rehabilitation literature to guide development of robust rehabilitation recommendations that would promote early initiation of rehabilitation within the ICU setting, emphasize the benefits of early rehabilitation for all severities of TBI and support the integration of rehabilitation experts into the core trauma team.
This poster will disseminate the final “key points” that summarize the evidence and expert consensus for rehabilitation best practice after TBI for trauma centers. These key points will be included in the final publication and will be available as open access in January 2024. The six finalized recommendations address rehabilitation for the spectrum of TBI severity and emphasize the importance of rehabilitation specialists as core members of the trauma team.
88 Investigating Longitudinal Cognitive Outcomes and Mental Health in Moderate-Severe TBI
Marina Everest 1 ; Jeremy Brand 1 ; Loretta Norton 1
1 Kings University College at Western University, London, Canada
Brain injury is the leading cause of death and disability for Canadians under the age of 40 and approximately 1.5 million Canadians live with the effects of an acquired brain injury. Cognitive impairment is a common sequelae of a traumatic brain injury (TBI). One limitation of current research in understanding cognitive deficits is that the focus has been predominantly on cross-sectional data, which does not detect the natural progression of cognitive recovery. Thus, the objective of the current study is to use a longitudinal approach using a web-based neurocognitive assessment tool to document the natural course of cognitive recovery in adults with moderate-to-severe TBI. Additionally, one factor to consider in predicting long-term outcomes after TBI is the presentation of mood disturbances. As such, this study also aims to longitudinally examine the relationship between cognitive impairment after TBI and the possible mediating effect of mood difficulties during recovery.
We recruited 34 patient participants (12 TBI, 22 traumatic body-only injury) through the London Health Sciences Trauma Program’s Outpatient Clinic in London, Ontario and 34 age and sex-matched healthy control participants. Participants were English-speaking, between 18-65 years old (M=41.10, SD=14.62), with no prior history of neurological or cognitive impairments. Brain injury participants were considered to have severe-moderate traumatic brain injury as defined by the Mayo TBI Severity Classification System and traumatic body-only injury patients required admission to hospital for traumatic injury that did not involve a brain injury. Both groups were assessed at three time points: 2 weeks post-hospital discharge, three months, and six months. At each time point, participants completed seven online neurocognitive tests and reported their levels of anxiety, depression, and quality of life.
Both TBI and traumatic injury to body groups had significant impairment in their verbal ability compared to healthy controls and no improvements were observed over the 6-month period. TBI patients performed worse than the traumatic body-injured group on cognitive measures of reasoning but not short-term memory. TBI and traumatic body-injured patients did not differ significantly with respect to anxiety or depression. However, TBI patients reported a significantly lower quality of life than the non-brain-injured group.
Significant domain-specific cognitive impairments were found in TBI patients even when compared to those with traumatic body injuries. The findings highlight the value of a longitudinal assessment that can be self-administered remotely by patients to allow for a clearer understanding of the natural course of cognitive recovery.
90 Screening for Cognitive Impairment Post-Concussion in a Non-Athlete Population – Findings From the Toronto Concussion Study
Evan Foster 1 ; Paul Comper 1,2 ; Tharshini Chandra 1 ; Lesley Ruttan 1 ; Laura Langer 1 ; Aaryan Adnan 1 ; Elizabeth L Inness 1,2,3 ; George Mochizuki 1,2,4 ; Catherine Wiseman-Hakes 1 ; Mark Bayley 1,2
1 Toronto Rehab Institute - UHN, Toronto, Canada; 2 Rehabilitation Sciences Institute, University of Toronto, Toronto, Canada; 3 Department of Physical Therapy, University of Toronto, Toronto, Canada; 4 School of Kinesiology and Health Science, York University, Toronto, Canada
Measuring cognitive difficulties post-concussion is challenging. ‘Baseline’ testing paradigms have individuals complete neurocognitive tests before a concussion occurs (e.g., pre-season for an athlete), followed by post-injury testing for comparative purposes. Evidence suggests that this is effective but is not always feasible. The second, ostensibly more common method, is to compare an individual’s post-concussion neurocognitive test scores to published norms. The purpose of this project was to examine the utility of neurocognitive testing to screen for cognitive impairment following concussion in a general adult population, using two study designs. Study 1 involved 343 adults (17-85 years of age) seen within seven days of concussion. Subjective cognitive difficulties were characterized by the Sport Concussion Assessment Tool (SCAT) scores for the four cognitive items. Objective neurocognitive measures included Trails A & B and Symbol Search & Coding (administered at Weeks 1, 2, and 12 post-injury), and a measure of verbal learning and recall and Digit Span (Weeks 2 and 12). Scores placing at or below the 3rd percentile on any measure were classified as ‘impaired’. 174 (50.7%) participants reported ‘mild’ cognitive SCAT symptoms; 124 (36.2%) as ‘moderate’; 45 (13.1%) as ‘severe’. Between 1-26 participants (0.3-7.6%) were classified as ‘impaired’, depending on the neurocognitive measure used. Those with severe subjective cognitive difficulties had lower neurocognitive test scores compared to the other groups, however they were still within the ‘average’ range using normative data. Determining an objective indicator of cognitive impairment related to subjective difficulties using a norms-based approach was not established. Study 2 employed a case-control design using 30 adults with acute concussion and 30, non-concussed control participants. A preliminary analysis of 29 non-concussed controls (median age: 24 [IQR 23-28] years, 20 females (67%), average years of education: 16.4 [SD: 1.4]) and 12 age, sex, and education-matched individuals with concussion (median age: 26 [IQR 24-30] years, 11 (92%) females, average years of education: 16.0 [SD: 2.8]), completed the same neurocognitive measures at Weeks 1, 2, and 8 post-injury. Preliminary analyses showed there were few measures with significant differences between cohorts at any single assessment (Coding Week 1, p=0.047; Delayed Recall Week 8, p=0.028). However, the non-concussed cohort improved significantly on several tests over time where the concussed cohort did not (i.e., Learning Week 1 to 8, non-concussed p=0.002, concussed p=0.134), suggesting an absence of learning effect in the concussed cohort. Full dataset to be presented at the conference. Without a baseline approach, using test norms to qualify and quantify a person’s subjective cognitive symptoms may yield false negative results. Therefore, more specific normative data (i.e., adjusting for learning effects) is needed to accurately evaluate cognitive performance post-concussion. Without this, the clinical focus shouldbe to provide treatment and education for any specific self-reported symptoms.
91 Social Determinants of Health and Lifetime History of Concussion in School-Aged Children and Adolescents in the United States
Grant Iverson 1,2,3,4 ; Julia Maietta 1,2,3 ; Nathan Cook 1,2,3
1 Massachusetts General Hospital, Cambridge, United States; 2 Harvard Medical School, Boston, USA; 3 Spaulding Rehabilitation Hospital, Charlestown, USA; 4 Schoen Adams Research Institute at Spaulding Rehabilitation, Charlestown, USA
Social determinants of health (SDoH) include socioeconomic and environmental factors that can influence health outcomes. SDoH are understudied in the concussion literature. Previous research suggests racial/ethnic and socioeconomic disparities in concussion care access. However, whether SDoH are associated with increased likelihood of sustaining a concussion remains unknown. The current study investigated whether SDoH are associated with parent-reported lifetime history of concussion in children and adolescents in a national sample.
The 2021 National Survey of Children’s Health is a national survey that collects parents’ self-reported health data on their children. Data from 34,077 youth (ages 5-17) were selected with complete data on the lifetime concussion history survey question. SDoH variables of interest included: primary language spoken at home, family income, parental level of education, and current health insurance. Separate binary logistic regressions were conducted with parent-reported lifetime concussion history as the dependent variable and demographics/SDoH variables as the predictor variables. A multivariable logistic regression was conducted including all predictors in the same model to examine the independence and magnitude of their associations.
In the univariable logistic regressions male sex (OR = 1.4, p < .001), adolescent age (OR = 3.1, p < .001), playing a sport in the past 12 months (OR = 1.9, p < .001), and having current healthcare coverage (OR = 1.5, p < .01) were associated with significantly higher lifetime history of concussion. Hispanic/Latino ethnicity (OR = 0.69, p < .001), non-English primary language (OR = 0.23, p < .001), lower level of parental education (OR = 0.82, p < .001), living in poverty (OR = 0.63, p < .001), and identifying as Black or Asian (OR = 0.55 and 0.31, respectively, p < .001) were associated with significantly lower lifetime history of concussion. In the multivariable model, after accounting for the combined effects of all predictors, significant independent predictors of lower lifetime history of concussion were lower level of parental education (OR = 0.92, p < .05), non-English primary language (OR = 0.36, p < .001), and identifying as Black or Asian (OR = 0.54 and 0.36 respectively, p < .001).
Several demographic and SDoH variables were associated with lower parent-reported lifetime history of concussion in school-aged children and adolescents including younger age, female sex, Black or Asian race, and Hispanic ethnicity. Adjusting for all variables, lower parental education, not speaking English as the primary language at home, and Black or Asian race were independently associated with lower lifetime history of concussion. Lower health literacy or access to care may contribute to families being less likely to recognize symptoms of concussion or seek out medical care for such an injury.
92 Lifetime History of Concussion Among Children and Adolescents With ADHD: Examining Differences Based on Age, Medication Status, and Parent-Reported ADHD Severity
Julia Maietta 1,2,3 ; Grant Iverson 1,2,3,4 ; Nathan Cook 1,2,3
Previous research has suggested greater lifetime concussion history among children/adolescents with attention-deficit/hyperactivity disorder (ADHD) compared to peers without ADHD. This research has focused on youth athlete’s self-reported ADHD history, as opposed to parent-reported diagnoses, and those studies have not examined differences across broad age spans. It is unclear if ADHD severity or medication status are associated with greater lifetime history of concussion. The current study investigated the association between parent-reported ADHD, ADHD severity, and medication status with lifetime concussion history in a national sample. We hypothesized that parent-reported ADHD severity would be associated with greater parent-reported lifetime concussion history, and that this would not differ across age ranges. We also hypothesized that, among youth with ADHD, those who were taking ADHD medication and those with mild (vs. moderate/severe) ADHD would have lower lifetime concussion history.
A sample of 33,914 children/adolescents (ages 5-17, mean = 11 years, SD = 4; 47.9% female) were selected from the 2021 National Survey of Children’s Health (those with complete data on the variables of interest). Overall, 6.2% of youth had parent-reported history of concussion (n = 2,103) and 13.4% had a history of parent-reported ADHD (n = 4,560). ADHD severity (mild or moderate/severe) and medication status (yes/no) were parent-reported for those children/adolescents who had current ADHD. A Mantel-Haenszel analysis was used to assess the associations between ADHD and lifetime concussion history across 5 age groups (5-7, 8-10, 11-13, 14-15, and 16–17-year-olds). Additional Mantel-Haenszel analyses were used to assess the associations between lifetime history of concussion and ADHD severity as well as medication status across the different age groups.
Youth with ADHD were more likely to have greater parent-reported history of concussion across all 5 age bands (χ 2 Mantel-Haenszel = 80.97, p < .001). However, odds ratios (OR) differed across age-groups (χ 2 Breslow-Day = 18.48, p = .001). The greatest difference was found in the 5-7-year-old age band (OR = 3.05) and ORs for older ages were smaller (8-10 OR = 1.68; 11-13 OR = 2.04; 14-15 OR = 1.62; 16-17 OR = 1.30). There were no differences in lifetime concussion history for those with mild ADHD versus moderate/severe ADHD (χ 2 Mantel-Haenszel = 0.02, p = .90). Similarly, there were no differences in lifetime concussion history for those taking ADHD medication versus those who were not taking medication (χ 2 Mantel-Haenszel = 0.78, p = .38).
Consistent with previous literature, youth with ADHD had greater lifetime concussion history. Contrary to our hypotheses, this difference was not consistent across ages, as differences between those with and without ADHD were larger for younger children compared to older children and adolescents. Also, among youth with ADHD, parent-reported ADHD severity and medication status were not associated with lifetime concussion history.
93 Patient, Caregiver, and Physician Perspectives of Acute Concussion Care and Management
Evan Foster 1 ; Monica Szczypinski 1 ; Tharshini Chandra 1 ; Paul Comper 1,2 ; Mark Bayley 1,2,3
1 Toronto Rehab Institute, University Health Network, Toronto, Canada; 2 Rehabilitation Sciences Institute, University of Toronto, Toronto, Canada; 3 Division of Physical Medicine and Rehabilitation, Department of Medicine, University of Toronto, Toronto, Canada
Concussion is a significant public health concern due to the underestimated frequency of the injury and in some cases, the potential for prolonged disability. In recent years, there has been a shift to participatory-action research models in health research whereby individuals with the disease or injury of interest are directly involved in the research itself. Employing a participatory-action research model on a local level can provide important feedback and guidance to research teams to help shape future research and care. This project employs a participatory-action research model to understand patient, caregiver, and physician experiences, and to determine stakeholder-informed research objectives that can be investigated in an acute concussion clinic. This study uses a modified Delphi approach. Semi-structured interviews have been conducted with individuals with concussion (or who have recently recovered from their concussion), their caregivers/family, and clinic physicians. All participants were 18 years of age or older and recruited from an acute concussion clinic in Toronto, Canada. Interviews were audio-recorded and transcribed, and transcripts were analyzed qualitatively and sorted into themes. To ensure that the patient perspective is continuously kept at the forefront of this work, an advisory committee of past patients has been recruited to help inform the: 1) research study design; 2) interview questions; 3) interpretation of the results; and 4) ways in which results should be disseminated. 11 participants have completed a semi-structured interview to date (n=5 individuals with concussion, n=3 caregivers, n=3 clinic physicians). An additional 9 participants will be recruited, and full results will be shared at the conference. After an interim qualitative analysis of the interview transcripts, the following themes were defined (in consultation with the advisory committee): concussion symptoms (i.e., direct experience with headache, cognitive difficulties), subjective experience with symptoms (i.e., being overwhelmed by concussion symptoms, frustration with fluctuating symptoms), caregiver experience (i.e., feelings of helplessness, providing household support), facilitators of recovery (i.e., normalizing recovery experience, value of early intervention), return to activities (i.e., modified work duties, supportive work environment), and challenges with providing/receiving care (i.e., financial burden of treatment, compliance with recommendations). These interviews have provided unique perspectives on the barriers, facilitators, and experiences of individuals with concussion, their caregivers/families, and clinic physicians in the context of an acute concussion clinic. The next steps consist of collaborating with the advisory committee to interpret interview themes into research objectives which will be ranked by a second group of participants to create stakeholder-informed research priorities that can be investigated in the future.
94 Aerobic Exercise Post-concussion: Can Findings Be Translated Into a Non-Athlete, Adult Population? Results From a Pilot Study
Evan Foster 1 ; Laura Langer 1 ; Mark Bayley 1,2,3 ; Paul Comper 1,3 ; Tharshini Chandra 1 ; Aidan Snaiderman 1,4 ; Ainsley Kempenaar 1,2 ; Elizabeth L Inness 1,3 ; Cynthia Danells 1 ; David Lawrence 1
1 Toronto Rehabilitation Institute, University Health Network, Toronto, Canada; 2 Division of Physical Medicine and Rehabilitation, Department of Medicine, University of Toronto, Toronto, Canada; 3 Rehabilitation Sciences Institute, University of Toronto, Toronto, Canada; 4 University of Guelph, Guelph, Canada
A growing body of literature has demonstrated that aerobic exercise (AE) can be beneficial in improving outcomes from concussion. This evidence resulted in an update to recent consensus guidelines for the treatment of sport-related concussion, which recommend initiating light AE within two days of injury. Most research has focused on athletes recovering from sport-related concussion. Less is known about the principles of AE following non-sport-related concussion. The goal of this pilot study was to examine the efficacy of various methods to inform AE recommendations post-concussion in a general adult population.
This pilot study represents a subset of the Toronto Concussion Study population. Participants were eligible for pilot study inclusion if they were 18-45 years of age and at low risk for underlying cardiac disease (determined by the treating physician). Participants who were either uninterested or ineligible were followed regularly by the clinic physician (“Usual Care” cohort). Eligible participants were randomly assigned to either the “Exercise Testing (ET) plus Usual Care” cohort, or the “Exercise Testing (ET) plus Individualized Prescription” cohort. All randomized participants completed a Buffalo Concussion Treadmill Test (BCTT) within seven days of injury. The “ET plus Usual Care” cohort received usual care AE recommendations, while the “ET plus Individualized Prescription” cohort received an individualized prescription based on their BCTT performance. Participants enrolled in both “ET” cohorts were provided with a heart rate (HR) monitor to wear during all waking hours, until they were deemed to be recovered from their concussion by a clinic physician. Kaplan-Meier survival analyses were conducted to evaluate for differences in time to recovery between each of the study cohorts. Log rank tests were used to compare the survival curves for all analyses.
75 participants were included in this analysis (average age: 31.2 years [SD 11.4], 65.7% female). 20 participants were eligible and randomized to either the “ET plus Usual Care” cohort, or the “ET plus Individualized Prescription” cohort (10 per arm). There was an observed longer time (restricted mean survival time [RMST]) to recovery of the “Usual Care” cohort (n=55, 7.2 weeks) compared to the combined “ET” cohorts (n=20, 5.7 weeks, p=0.046). However, there was no significant difference in time to recovery between the “ET plus Usual Care” cohort (n=10, 6.2 weeks) and the “ET plus Individualized Prescription” cohort (n=10, 5.0 weeks, p=0.350). There was no significant difference in minutes spent above certain HR thresholds (50-90% of age-predicted max HR) between the two “ET” cohorts (p=0.295-0.968).
Normalization of AE early post-concussion, under supervision, appears to improve recovery time post-concussion. Individualized AE prescription did not improve outcomes, nor did it alter activity levels in our sample. Future rigorous studies should further examine the role of supervised AE in the acute phase post-concussion.
95 What Do You Do When There Are Gaps in Peer-Reviewed Evidence? Insights From the Canadian Guideline for Rehabilitation of Adults With Moderate to Severe Traumatic Brain Injury
Eleni Patsakos 1 ; Judith Gargaro 1 ; Olga Yaroslavtseva 1 ; Aishwarya Nair 1,2 ; Mark Bayley 1,2
1 University Health Network, Toronto, Canada; 2 University of Toronto, Toronto, Canada
The quality and quantity of evidence varies widely across different aspects of Moderate to Severe Traumatic Brain Injury (MSTBI) Rehabilitation research. There is a notable lack of published research evidence to inform evidence-based recommendations. This is especially prominent in the new and emerging areas of rehabilitation, such as Telehealth and Intimacy and Sexuality. The Canadian Clinical Practice Guideline for the Rehabilitation of Adults with Moderate to Severe Traumatic Brain Injury addresses this gap following a robust living update process that consists of ongoing identification of research literature, expert panel review, rigorous evaluation of evidence quality and achieving clinical consensus in consultation with persons with lived experience (PWLE) to develop and modify current evidence-based recommendations in the areas that lack published research.
A rigorous multi-component guideline review process was developed and refined to ensure that recommendations reflect the rapidly emerging evidence and address the priorities identified by end users and people with lived experience.
1) Systematic review of published MSTBI evidence
2) Priorities identified by PWLE of MSTBI and guideline end users through surveys and focus groups
3) Diverse interdisciplinary expert panels that include PWLE
4) Online and offline review of the current published evidence, clinical and lived experience
5) Rigorous grading of available evidence
6) Expert panel voting to achieve a minimum of 75% by 80% of the expert panel
Since 2015, this review process has yielded 351 recommendations divided into 21 chapters focusing on different domains of MSTBI rehabilitation. Currently, the Guideline includes 239 Consensus-based recommendations which comprise 68% of the Guideline. Two new sections were added in 2022/23: Telerehabilitation - 14 recommendations including 11 (79%) consensus-based and Intimacy and Sexuality - 10 recommendations including 9 (90%) consensus-based. Recommendations were added that responded to PWLE comments that the guideline did not stress the importance of continuing rehabilitation into the community through participation in daily activities and promoting hope for ongoing improvements. Focus has also been on developing algorithms and tools to facilitate implementation.
This comprehensive TBI rehabilitation guideline uses a transparent and methodologically robust review process that integrates knowledge and experience of diverse interdisciplinary expert panels including the people with lived experience of MSTBI. This process allows the development of high-quality recommendations in the priority areas where published evidence is currently lacking. Including consensus-based recommendations and tools helps ensure that the guideline contains all relevant, current and critically evaluated recommendations that integrate the new areas of rehabilitation and incorporate the needs, values and preferences of PWLE.
96 Relationship Between Extreme Pain Phenotypes and Psychosocial Outcomes in Persons With Chronic Pain Following Traumatic Brain Injury
Jessica Ketchum 1 ; Jeanne Hoffman 2 ; Stephanie Agtarap 1 ; Flora Hammond 3 ; Aaron Martin 4,5 ; William Walker 6 ; Ross Zafonte 7 ; Cynthia Harrison-Felix 1 ; Risa Nakase-Richardson 8,9,10
1 Craig Hospital, Englewood, United States; 2 Department of Rehabilitation Medicine, University of Washington School of Medicine, Seattle, USA; 3 Department of Physical Medicine and Rehabilitation, Indiana University School of Medicine & Rehabilitation Hospital of Indiana, Indianapolis, USA; 4 Mental Health and Behavioral Science Service, James A. Haley Veterans Hospital, Tampa, USA; 5 Department of Psychiatry and Behavioral Neurosciences, University of South Florida, Tampa, USA; 6 Department of Physical Medicine and Rehabilitation, School of Medicine, Virginia Commonwealth University, Richmond, USA; 7 Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, and Harvard Medical School, Boston, USA; 8 MHBS/Polytrauma, James A. Haley Veterans Hospital, Tampa, USA; 9 Sleep and Pulmonary Division, Department of Internal Medicine, University of South Florida, Tampa, USA; 10 Defense Health Agency Traumatic Brain Injury Center of Excellence, Tampa, USA
The objective of this secondary analysis was to examine the relationship between extreme pain phenotypes (based on pain interference and perceived improvement) and psychosocial outcomes among persons with chronic pain after moderate-to-severe traumatic brain injury (TBI). In total, 1762 TBI Model Systems (TBIMS) participants 1 to 30 years postinjury reporting chronic pain were recruited as part of a multisite, cross-sectional, observational cohort TBIMS addendum study on Chronic Pain. Extremely low and high pain phenotypes were identified by the Brief Pain Inventory (BPI) interference scale, and the Patient’s Global Impression of Change (PGIC). Clinical outcomes of interest included life satisfaction, posttraumatic stress, depression and anxiety symptoms, sleep and participation. Generally, extreme phenotypes based on interference had greater association with psychosocial outcomes compared to improvement-based phenotypes. Those identified as extremely high pain interference phenotype had poorer psychosocial outcomes compared to the extremely low phenotype group. After controlling for covariates, large effect sizes (ES) related to pain interference were observed for posttraumatic stress symptomatology (ES = -1.14), sleep quality (ES = -1.10), depression (ES = -1.08), anxiety (ES = -0.82), and life satisfaction (ES = 0.76); effect sizes for participation outcomes, although significant, were relatively small (ES = 0.21-0.36). Effect sizes related to perceived improvement were small for life satisfaction (ES = 0.20) and participation (ES = 0.16-0.21) outcomes. Pain intensity was identified as a meaningful confounding factor of the relationships between extreme phenotypes and posttraumatic stress, depression, anxiety, and sleep quality. Results suggest that the relationships among a variety of characteristics of the person, their experience with pain, and treatment of pain are complex. However, examination of subgroups defined by extreme phenotypes of interference (and to an extent, perceived improvement) were able to identify pronounced differences in the psychosocial experience of individuals living with chronic pain and TBI. Further research is needed to better understand these complex relationships and how differences in pain interference and perceived improvement from treatment can assist in assessment and treatment of chronic pain after TBI.
97 Anterior Prefrontal Cortex Resting-State Functional Connectivity Associated With Depressive Symptoms in Chronic Moderate-to-Severe Traumatic Brain Injury: A Preliminary Study
Layan Elfaki 1,2 ; Bhanu Sharma 3 ; Liesel-Anne Meusel 2 ; Isis So 4 ; Brenda Colella 2 ; Robin Green 1,2,5
1 Temerty Faculty Of Medicine, University Of Toronto, Toronto, Canada; 2 KITE-Toronto Rehabilitation Institute, University Health Network, Toronto, Canada; 3 Department of Medical Sciences, McMaster University, Hamilton, Canada; 4 Schulich School of Medicine and Dentistry, University of Western Ontario, London, Canada; 5 Rehabilitation Sciences Institute, University of Toronto, Toronto, Canada
Background & aims
Depression in the context of moderate-to-severe TBI (msTBI) is highly prevalent, but its neural underpinnings are little understood. This pilot study focused on this gap through exploring voxel-wise associations between depressive symptoms and anterior prefrontal cortex (aPFC) resting-state functional connectivity (rsFC).
In a secondary analysis, BOLD fMRI resting-state scans and Personality Assessment Inventory Depression scale (PAI-DEP) scores were acquired from the Toronto Rehab TBI Recovery Study database. We examined n=32 patients with chronic msTBI and n=17 age and education-matched healthy controls. Patients with TBI were operationally grouped as Depressed (n = 13) with PAI-DEP scores ≥ 60 or as Nondepressed (n = 19) with T-scores < 60. To compare bilateral aPFC rsFC across our three study groups, we performed F-tests through seed-based connectivity analyses, while controlling for age and education. Nonparametric permutation testing was performed with threshold-free cluster enhancement (TFCE) and family-wise error (FWE) correction to identify significant group differences.
Although there were no significant differences in the rsFC of the right aPFC, the left aPFC demonstrated significantly increased rsFC with the bilateral fusiform gyri, right superior temporal lobe, and right precentral gyrus (TFCE-corrected pFWE < 0.05) in the group with comorbid TBI and depression as compared to the healthy control group.
This preliminary study adds to limited literature that implicates the aPFC in the pathophysiology of depressive symptoms occurring in chronic msTBI. Increased rsFC between the aPFC and these four sensory and motor regions could be a clue signifying vulnerability to depression post-TBI, offering testable hypotheses for future research.
99 Packed Red Blood Cell Transfusion: A Catalyst for Thrombosis in Patients With Traumatic Brain Injury?
Lily Nguyen 1 ; Jeffry Nahmias 1 ; Patrick Chen 1 ; Jefferson Chen 1 ; Michael Lekawa 1 ; Jordan Shin 1 ; Areg Grigorian 1
1 University Of California - Irvine, Orange, United States
While blood transfusions can be lifesaving, they also carry risks including thromboembolic events. This is due to multiple factors including increased blood viscosity, inflammatory response to transfused blood, and changes in the coagulation cascade. Traumatic brain injury (TBI) exhibits a unique coagulopathy, which may predispose patients to both bleeding and clotting complications. Transfusing TBI patients may add an additional layer of complexity to their coagulation profile. Therefore, this study aimed to investigate the relationship between trauma patients with TBI who receive packed red blood cell (pRBC) transfusions and the incidence of venous thromboembolism (VTE) hypothesizing that transfusion of pRBC during the initial resuscitation increases the risk of VTE.
The Trauma Quality Improvement Program (TQIP) was queried from 2017-2021 to identify adult (>18 years-old) patients with TBI. Patients receiving pRBC transfusions were compared to those who did not receive pRBC transfusions within 4 hours of presentation. Patients that died or were discharged within 48-hours, and all transferred patients were excluded. Outcomes were compared using bivariate analyses and a multivariable logistic regression analysis to identify predictors of VTE while controlling for age, sex, obesity, vitals on arrival, surgical intervention and fractures to the pelvis, spine, and lower extremities.
Of 422,831 TBI patients, 28,230 (6.7%) received pRBC transfusion. Patients who were transfused were younger (median: 45 vs 61 years old, p< 0.001), but had increased injury severity score ≥ 25 (72.5% vs 20.6%, p< 0.001) and a higher rate of emergent operations (39.4% vs 6.7%, p< 0.001). Transfused patients had higher rates of pelvic fractures (29% vs 4.4%, p< 0.001), spine fractures (50.8% vs 15.7%, p< 0.001), and lower extremity fractures (37% vs 8.6%, p< 0.001). Thrombotic events were more frequently observed in pRBC transfused patients, including cerebrovascular accident (2.7% vs 0.6%, p< 0.001), and VTE (8.1% vs 1.5%, p< 0.001) comprised of deep vein thrombosis (6.4% vs 1.2%, p< 0.001), and pulmonary embolism (2.4% vs 0.4%, p< 0.001). Multivariable regression analysis found undergoing any surgery (OR = 4.78, p<0.001) followed by transfusion of pRBC within 4 hours of presentation (OR = 1.438, p < 0.001) as the strongest predictors of VTE. Additional associated risk factors were ISS ≥ 25 (OR = 1.797, p< 0.001) and male sex (OR = 1.46, p< 0.001).
Trauma patients with TBI undergoing pRBC transfusion within 4 hours of arrival had an over 40% increased associated risk of VTE, compared to patients not undergoing transfusion. Providers should be vigilant in assessing the need for transfusions in TBI patients, balancing acute TBI management with thrombotic risks. Increased provider awareness of these findings may foster better patient outcomes by avoiding unnecessary transfusions in this high-risk population.
100 Prevalence of Concussion and Traumatic Brain Injury Secondary to Domestic and Intimate Partner Violence: A Systematic Review and Meta Analysis
Rachel Plouse 1,2 ; Diego Martell 2,3 ; Nicolette McNair 1,2 ; Suzannah Henderson 2,4 ; Edie Zusman 2,5
1 Touro University Nevada, Henderson, United States; 2 Safe Living Space, San Francisco, United States; 3 Yale University, New Haven, United States; 4 University of California,San Francisco, San Francisco, United States; 5 Neuroscience Partners, Moraga, United States
Domestic violence (DV/IPV) is a pressing global issue, affecting 25% of women and 10% of men. In the US alone, 58 million men and women experience DV/IPV within their lifetime. The most common physical assault in DV/IPV events is injury to the head and neck, occurring in 50-80% of altercations. However, there is currently no standardized or routine evaluation of TBI in DV/IPV situations. Debilitating physical, behavioral, and cognitive symptoms can result from such injuries, interfering with the ability to perform daily tasks and increasing the long-term risk of Parkinson’s, Dementia and Chronic Traumatic Encephalopathy (CTE). The purpose of this meta-analysis is to evaluate the prevalence of TBI secondary to DV/IPV.
A PubMed search from September 2014, the publication date of neurosurgical concussion guidelines used for sports, to September 2022 was conducted using keywords domestic violence and/or intimate partner violence in conjunction with concussion, traumatic brain injury, and/or head injury. The resulting primary research articles were then selected based on the following inclusion criteria: participants were ≥ 18 years old, participants had experienced violence by an intimate partner, the screening tool included questions about signs and symptoms of TBI as well as an experience that could cause a TBI, and a TBI diagnosis was not required for inclusion in the study. Data collection was then performed. Inter-reviewer validation and risk of bias assessment were conducted to ensure validity of data collection.
Of the 8,218 publications on domestic and/or intimate partner violence, only 46 (0.6%) included keywords concussion, traumatic brain injury, or head injury. Of those 46, 11 papers were included in this meta-analysis. From these 11 papers, the meta-analysis had a total sample size of 1,498. The prevalence of IPV-related TBI within this aggregated sample was 56.1% (n=841). Two studies with a total of 119 subjects included questions to evaluate the prevalence of multiple TBIs. In this subset, the prevalence of multiple TBIs was 50.4% (n=60). To assess for TBI prevalence, three papers utilized the Brain Injury Severity assessment (BISA), two studies used the HELPS tool, three performed a semi-structured interview, two utilized a modified VA TBI screening tool, and one used a modified Miller Abuse Physical Symptoms and Injury Scale (MAPSAIS).
There is a paucity of research into TBI within the DV/IPV population as well as a lack of standardized screening and evaluation. This meta-analysis suggests that more than half of people experiencing DV/IPV have sustained one or more brain injuries. Based on concussion research in sports, prospective studies are needed to optimize the screening, evaluation, and care of concussion and TBI within the DV/IPV population.
101 Multi-Session Transcranial Alternating Current Stimulation in Subacute Severe Brain-Injured Patients
Beatrice P. De Koninck 1,2,3 ; Daphnee Brazeau 1,2 ; Amelie Apinis-Deshaies 2 ; Marie-Michèle Briand 1,2,4 ; Charlotte Maschke 3,5 ; Virginie Williams 2 ; Caroline Arbour 1,2 ; David Williamson 1,2 ; Catherine Duclos 1,2 ; Francis Bernard 1,2 ; Stefanie Blain-Moraes 3,5 ; Louis De Beaumont 1,2
1 University Of Montreal, Montreal, Canada; 2 CIUSSS du Nord-de-l’Île-de-Montréal Research Center, Montreal, Canada; 3 Montreal General Hospital, McGill University Health Centre, Montreal, Canada; 4 Institut de réadaptation en déficience physique de Québec, Physical Medicine and Rehabilitation Department, Quebec, Canada; 5 McGill University, Montreal, Canada
Therapeutic interventions for disorders of consciousness (DoC) lack consistency; evidence supports non-invasive brain stimulation, but few studies assess neuromodulation in acute-to-subacute brain-injured patients. Interventions targeting the latter phase of DoC following a severe brain injury (i.e., severe traumatic brain injury (sTBI) or global hypoxic-ischemic encephalopathy (HIE)) may be critical to promote consciousness and long-term functional recovery. This study aims to validate the feasibility and assesses the effect of a multi-sessions transcranial Alternating Current Stimulation (tACS) intervention in brain-injured patients on recovery of consciousness, related brain oscillations and brain network dynamics.
This study was conducted in twelve medically stable brain-injured adult patients (sTBI and HIE), with a Glasgow Coma Scale score ≤ 12 after continuous sedation withdrawal. Recruitment took place at the intensive care unit (ICU) of a Level 1 Trauma Center in Montreal, Quebec, Canada. The intervention included a 20-minute 10-Hz tACS at 1 mA intensity or a sham session over parieto-occipital cortical sites, repeated over 5 consecutive days. The stimulation frequency targeted alpha brain oscillations (8-13 Hz), known to be associated with consciousness. Resting-state electroencephalogram (EEG) was recorded according to the intervention’s administration: pre- and post-intervention, at 60 and 120 minutes post-intervention. Two additional recordings were included: 24 hours and one week post protocol. Multimodal measures [blood samples, pupillometry, behavioral consciousness assessments (Coma Recovery Scale-revised), actigraphy measures] were acquired from baseline up to one week after the stimulation. EEG signal analyses focused on the alpha bandwidth (8-13 Hz) using spectral and functional network analyses. Phone assessments were conducted at 3, 6 and 12 months post-tACS to measure long-term functional recovery, quality of life, and caregivers’ burden.
Results demonstrate the feasibility of a 5-day tACS protocol on subacute brain-injured patients in the ICU, as well as multimodal and long-term measurements without interfering with the care team and while preserving constant relatives’/caregivers’ adherence to longitudinal follow-up sessions up to 12 months post-injury. Functional connectivity measures, such as the weighted phase lag index and the directed phase lag index, along with network hubs and power topography (i.e., topographic network properties) in the alpha bandwidth, were shown effective in detecting changes throughout the repeated protocol. Brain activity changes are also reflected by behavioral improvements according to CRS-R assessments.
These initial results support the expansion of this study to a clinical trial including a sham stimulation to assess the efficacy of a repetitive tACS protocol on the modulation of alpha band activity, as well as recovery of signs of consciousness. This experimental design includes repeated, rigorous multimodal assessments to allow the optimal capture of subtle changes in consciousness recovery status. Finally, such a protocol may allow the identification of conditional endotypes of responders to develop a targeted intervention.
102 Rapid Blood- Based Dipstick Test for Mitochondrial Electron Transport Chain Damage and Severity of Blast TBI in Rats
Pushpa Sharma 1 ; Geetaram Sahu 2 ; Biswajit Saha 3
1 Uniformed Services University, Bethesda, USA; 2 Uniformed Services University, Bethesda, USA; 3 Uniformed Services University, Bethesda, USA
Blast trauma is unique because of its complex mechanism of injury to the brain and other vital organs due to over pressure air and bleeding from internal organs. Severe loss of blood leading to hemorrhagic shock (HS) results in inadequate supply of oxygen and fuel to the cells for the generation of ATP from the mitochondria for the cell survival. Mitochondria generate ATP for cell survival through the orchestrated action of its electron transport chain enzyme’s activities, mainly through complex I-IV and mitochondrial gatekeeper enzyme” pyruvate dehydrogenase complex. Any damage to these enzymes results in increased oxidative damage to the cells, organ’s dysfunctions and neurological disorders. Although clinical symptoms of metabolic disruption are evident soon after the injury, but actual damage mechanisms at the molecular, cellular and organ system level persists for days to years post injury.
1) utilize our rapid blood -based dipstick test to monitor the severity of mitochondrial electron transport chain damage in response to blast exposure and HS, and 2) develop mitochondrial targeted therapeutic strategies.
Pre-clinical and military relevant rat model with blast exposure accompanied with or without HS and resuscitation was used. The animals underwent three repeated blast injuries of 20PSI at 15 minutes interval. After circulatory variables (MAP and pulse rate) were determined, controlled hemorrhage was induced. Rats were then bled over a 15-minute period to a MAP of 40 mmHg. Blood was collected in pre-heparinized tubes. MAP was sustained at 40 mmHg for 40 minutes by withdrawal or infusion of shed blood. Resuscitation (T60-120) followed by Blood Transfusion (T120-150). After the HS, animals were infused with either hypertonic sodium pyruvate (2M) or osmolality and volume matched control hypertonic saline. Blood collected at T0 (baseline), T60 (after injury), and T180 (end) was analyzed for plasma mitochondrial electron transport enzymes complex I, IV and pyruvate dehydrogenase by our published dipstick test.
Compared with baseline values, a significant decreased activity of complex I, IV and Pyruvate Dehydrogenase Complex (PDH) was noted after blast and HS in all of the animal groups. The animals also had a significantly elevated plasma lactate concentration. Although pyruvate treatment was effective in preventing the loss of these mitochondrial ETC enzyme activities, and also corrected the hyperlactatemia at the end, but it was unable to restore them to the baseline levels, suggesting the need for a combined therapeutic strategy targeted at preventing the mitochondrial damage, inflammatory cascade, antioxidant, and cell death mechanisms.
Serial monitoring and optimization of blood complex I, IV and PDH activity could aid in prognostication and potentially guide in using mitochondrial targeted therapies to reduce the mortality from the severity of combined traumatic injuries associated with hemorrhagic shock.
103 Safety and Feasibility of Paired Robotic Tilt Table and Transcutaneous Auricular Vagus Nerve Stimulation in a Patient With Chronic Disorders of Consciousness: A Case Study
Jessica Polizzi 1 ; Wilber Parada-Iraheta 1 ; Gabriela Rozanski 1 ; Christopher P. Kellner 2 ; Neha Dangayach 2 ; David Putrino 1 ; Jenna Tosto-Mancuso 1
1 Department of Rehabilitation and Human Performance Icahn School of Medicine at Mount Sinai, New York, United States; 2 Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, United States
Rehabilitation for patients after severe acute brain injury (SABI) and subsequent disorders of consciousness (DOC) is a complex balance of restorative strategies and medical management. There is an emerging body of evidence supporting early mobilization and rehabilitation in the acute and subacute phases of rehabilitation after SABI, including the implementation of progressive upright mobilization to support arousal, attention, and hemodynamic stability. 1, 2 Further, new evidence suggests transcutaneous auricular vagus nerve stimulation (taVNS) as a potentially effective, non-invasive neuromodulatory therapy for patients with (DOC) in both acute and chronic stages. 3, 4, 5 Little is known, however, about the safety and feasibility of paired upright mobilization and taVNS interventions in the rehabilitation of patients with chronic DOC. This work reports on the safety and feasibility of robotic enabled upright mobilization with paired taVNS for a patient with chronic DOC following SABI.
Patient is a 50 year old male with no significant past medical history prior to diagnosis of SARS- CoV2 infection in June of 2022. Following recovery from acute respiratory symptoms, the patient began to experience new onset fatigue and shortness of breath. Medical examination identified pulmonary emboli. The patient was treated with surgical thrombectomy where he suffered an intraoperative myocardial infarct. He was subsequently diagnosed with a SABI and remains in a minimally conscious state to date. He was seen at the Abilities Research Center Advanced Technology Rehabilitation Program where he underwent 6 weeks of advanced technology physical therapy. Interventions included 2 sessions per week of progressive upright mobilization with robotic assisted-stepping using Erigo (HOCOMA) and paired taVNS (PARASYM). The first 5 weeks consisted of mobilization with Erigo alone, with the addition of paired taVNS during the 6th week. Safety and feasibility were assessed using adverse event reporting. Clinical outcomes were assessed using the Coma Recovery Scale-Revised (CRS-R) and Glasgow Coma Scale (GCS) at baseline and 4 weeks.
The patient participated in 6 weeks of progressive verticalization with the addition of taVNS during the 6th week. No adverse events were reported. The patient tolerated an average of 32.36 (+/-12.14) minutes time on task. The patient tolerated an average tilt angle of 42.75 (+/- 26.66) degrees with a maximum tilt of 74 degrees. At baseline the patient scored 7/15 on GCS and 8/23 on CRS-R. At 4 week reassessment, GCS increased to 9/15. Overall CRS-R score remained 8/23 however motor function subscale score increased and arousal subscale decreased, each by 1 point respectively.
These findings suggest that robotic enabled mobilization with paired taVNS, is a feasible and safe intervention for persons with chronic DOC. Future work will continue to investigate short and long term feasibility, safety, and efficacy of the intervention in patients with chronic DOC.
104 Traumatic Brain Injury Among Veterans Accessing VA Justice-Related Services
Ryan Holliday 1,2 ; Alexandra Smith 1,2 ; Adam Kinney 1,2 ; Jeri Forster 1,2 ; Nazanin Bahraini 1,2 ; Lindsey Monteith 1,2 ; Lisa Brenner 1,2
1 Rocky Mountain Mental Illness Research, Education And Clinical Center for Suicide Prevention, Aurora, United States; 2 University of Colorado Anschutz Medical Campus, Aurora, United States
Risk for traumatic brain injury (TBI) within both the Veteran population and among individuals with a history of criminal justice involvement is notably high. Despite this, research examining TBI among Veterans with a history of criminal justice involvement (i.e., justice-involved Veterans) remains limited. Such a gap is disconcerting as the sequelae of TBI can impact justice-involved Veterans’ engagement in Department of Veterans Affairs (VA) justice-related services (i.e., Veterans Justice Outreach and Health Care for Re-entry Veterans), thus potentially increasing risk for recidivism and impacting post-release rehabilitation and psychosocial functioning. As such, further understanding of TBI risk among justice-involved Veterans is an integral first step to informing the potential need for tailored screening and interventional efforts within VA justice-related service settings. Given this, the current project sought to better understand relative risk for TBI diagnosis among male and female Veteran recipients and non-recipients of VA justice-related services.
Data Source
Data were gathered from electronic medical record data for Veterans accessing VA services from 2005 to 2018.
1,517,447 (12.48% justice-involved) male and 126 237 (8.89% justice-involved) female Veterans were included in the current cohort.
Study Design
The current project was a cross-sectional examination of national VA electronic medical record data. Sex-stratified analyses were conducted to examine relative risk of TBI diagnosis based on use of VA justice-related services.
Documented TBI diagnosis was the outcome of interest (as determined by ICD-9 and ICD-10 codes). Covariates included for adjusted models included: VA service use, age, race, and ethnicity.
Both male and female Veterans accessing VA justice-related services were more likely to have a documented TBI diagnosis in their electronic VA medical record. Associations were attenuated, yet maintained significance, in all adjusted models.
Given relative risk for TBI, enhancing and tailoring care for justice-involved Veterans may be critical to facilitating rehabilitation and reducing recidivism. It is likely that military (e.g., combat exposure) and non-military (e.g., physical assault in prison; childhood abuse) likely contributed to notably high rates of TBI among this population. Examination of existing services within justice-related settings and methods of augmenting care is an important next step. More specifically, determining methods of further implementing TBI screening as well as addressing TBI-related sequelae in these Veterans may be a pragmatic and necessary approach.
106 Home Safety Concerns for Adolescents With Acquired Brain Injuries: A Mixed-Methods Study Among Key Stakeholders
Sarah Anderson 1 ; Sarah Pierce 1 ; Taylor Stamper 1 ; Jennifer Lundine 1,2 ; Carmen DiGiovine 1 ; Emily Patterson 1 ; Scott Swearingen 1 ; Lauren Wengerd 1 ; Amy Darragh 1
1 The Ohio State University, Columbus, United States; 2 Nationwide Children’s Hospital, Columbus, United States
Acquired brain injury (ABI) is a leading cause of death and disability among children and adolescents, who experience a variety of cognitive, motor, and functional impairments. These youth are at an increased risk for additional injury in the home and community environments.
We aim to identify the home safety concerns adolescents with ABI, caregivers, and healthcare providers have for these adolescents with ABI.
We recruited healthcare providers, adolescents with ABI, and caregivers of adolescents with ABI for this mixed-methods study. Participants completed questionnaires on demographics (including injury severity) and pre-identified home safety hazards. They also engaged in individual or group interviews to examine their clinical/rehabilitation experiences and home safety hazards and concerns. Finally, they participated in a self-identified hazard prioritization matrix activity. Questionnaire data were analyzed with descriptive statistics (mean, standard deviation, frequency, etc.), and interview recordings were transcribed and analyzed via qualitative thematic analysis. Matrix data were analyzed with both descriptive statistics (hazard frequencies) and qualitative analyses (coding and thematic analysis of hazard descriptions).
Participants included thirteen healthcare providers (30.8% OT, 30.8% PT, 23.1% SLP, mean age 37.5 years), five adolescent patients with TBI (mean age 15.2 years), and five caregivers of adolescents with TBI (mean age 46.2 years). A percentage of the 67 pre-identified hazards were rated as concerning by at least one participant (100% providers, 26.9% caregivers, 31.3% patients). Self-identified safety hazards were 59 for providers, 21 for caregivers, and 10 for patients. In addition, 60% of patients identified no hazards, as compared to every provider and caregiver participant self-identifying at least one hazard. We found seven themes in hazards: hazardous activities, hazardous situations, hazardous objects, hazardous others, hazardous spaces, harms, and patient-specific factors (e.g., impulsivity).
This research study elucidates the safety hazards that pose risks to adolescents with ABI after hospital discharge to their homes. While all stakeholders expressed concerns for this population, providers identified more hazards and higher levels of concern than patients and caregivers. These findings provide insights to improve home safety interventions delivered to adolescents with ABI and their families.
107 Stakeholder Perceptions of a Home Safety Virtual Simulation Training System for Adolescents With ABI
Acquired brain injury (ABI) is a leading cause of death and disability among children and adolescents, who experience cognitive, motor, and functional impairments. These youth are at an increased risk for injury in the home and community environments. However, few tools exist to reduce the risk of injury.
We aim to assess the usability, usefulness, and desirability characteristics of a previously developed home safety program, the Home Healthcare Virtual Simulation Training System (HH-VSTS), and then identify modifications to tailor the program to adolescents with ABI.
Individual or multiple participants viewed a real-time demonstration of the HH-VSTS or test-played it themselves. They simultaneously participated in semi-structured, recorded interviews that elicited suggestions for program improvements. Healthcare providers, adolescents with ABI, and caregivers of adolescents with ABI were recruited to participate in this mixed-methods study. Participants completed demographics (including injury severity) and HH-VSTS usability (examining usability, usefulness, and desirability) questionnaires. Transcriptions from the interviews were analyzed via qualitative thematic analysis, and questionnaire data were analyzed with descriptive statistics.
Participants included thirteen healthcare providers (30.8% OT, 30.8% PT, 23.1% SLP, mean age 37.5 years), five adolescent patients with TBI (mean age 15.2 years), and five caregivers of adolescents with TBI (mean age 46.2 years). On a 1-7 numeric rating scale with 1 as not demonstrating that quality and 7 as very demonstrative of that quality, all participants rated the HH-VSTS as having good usability (mean 5.48/7), usefulness (mean 6.09/7), and desirability (mean 5.52/7). Patients consistently rated these qualities high, while clinicians and caregivers rated them lower. Themes were modifications to enhance HH-VSTS characteristics: learning, enjoyment, graphics, content, usability, and utility.
We confirmed that participants, and particularly the intended user group, rated overall usability as moderate. We identified necessary modifications to improve the relevance, accessibility, and enjoyment of the HH-VSTS for adolescents with ABI. These findings provide insights to tailor the HH-VSTS for adolescents with ABI, while supported by their families and providers. Future research is anticipated to re-design, re-develop, and assess a revised HH-VSTS for this population. There are no conflicts of interest.
108 A Case Report: Anti-Inflammatory Supplementation Dramatically Improves Post-Neurosurgical Recovery in a Pediatric Patient Requiring Functional Hemispherotomy
Melissa Kopolow 2 ; Michael Lewis 1 ; Chima Oluigbo 3
1 Brain Health Education and Research Institute, Potomac, United States; 2 Hydrocephalus Association, Bethesda, United States; 3 Department of Neurosurgery, Children’s National Medical Center, Washington, United States
AM was a complicated 8-year old female with a three year history of intractable seizures unresponsive to numerous medications. Born a 25-week micropreemie, twin B, she suffered a bilateral intraventricular hemorrhage grade III/IV on day 2 of life resulting in hydrocephalus. By age 5, she had twelve brain surgeries, all related to hydrocephalus, before she developed new onset left hemisphere focal seizures. Following two unsuccessful thermal ablations of her left amygdala and hippocampus, the decision was made to undertake a functional hemisphereotomy, isolating her left hemisphere. Starting one month prior to surgery and continuing without interruption, the patient’s mother instituted a regimen of twice daily supplementation using an omega-3 fish oil product that also contained Curcumin Extract, N-Acetyl-Cysteine, and Reduced L-Glutathione. The eight-hour surgical procedure went without complication.
Normal protocol dictates three days in the PICU, one week on the neuro-ward monitoring CSF output, fever, and edema, all very common following this procedure. Following removal of the externalized drain, patients typically spend an additional two to six weeks in inpatient rehabilitation. This patient, however, asked for, and ate, a full meal immediately upon waking, spent only one night in PICU, and as she was ambulatory the next day, she was transferred to the neuro-ward. Instead of three to five days of edema and fever as is typical, the patient had less than 24 hours of edema, no fever, and drain was removed on day three making her eligible for discharge to home for outpatient rehabilitation. However, due to COVID, outpatient rehabilitation was unavailable, so the patient was kept for one-week inpatient rehab. No further seizure activity has been noted since, now over three years later, and has been off all medications for over two years.
Here we present a case of arguably the most radical neurosurgical intervention that typically requires minimum of three weeks hospitalization. In this particular instance, the outcome was dramatically altered where the patient was proactively placed on an anti-inflammatory supplement regimen before, during, and after hospitalization resulting in her eligibility for discharge to home in three days instead of three to eight weeks.
109 Targeting the Neuro-Inflammasome With Nutritional Therapy for TBI Management and Prevention
Michael Lewis 1
1 Brain Health Education and Research Institute, Potomac, United States
Managing concussions and TBI remains a complex challenge in sports medicine and healthcare. A one-size-fits-all approach isn’t going to work. While current standard of care primarily involves rest and symptomatic management, emerging research suggests that active recovery and specific nutritional strategies may expedite concussion recovery. Therapies targeting the inflammasome are essential to maintain or regain brain health after injury. Presented here is a comprehensive overview of the potential efficacy of targeted nutritional interventions in ameliorating the effects of concussions and diminishing the risk of recurring injuries.
There exists a complex interplay between omega-3s and omega-6s and the endocannabinoid system. The endocannabinoid system has well-established roles in neuroinflammation, synaptic plasticity and neurogenesis. The endocannabinoid system comprises cannabinoid receptors, their endogenous ligands, the endocannabinoids, and their biosynthetic and degradation enzymes. Arachidonic acid (ARA) and docosahexaenoic acid (DHA) are essential for optimal brain development and function with and through the cannabinoid system. Omega long-chain polyunsaturated fatty acids (LCPUFA), including ARA, DHA, and EPA (eicosapentaenoic acid), are essential components of membrane phospholipids and precursors to a number of bioactive lipid mediators. Anandamide (AEA) and 2-arachidonoylglycerol (2-AG) are the most widely studied endocannabinoids and are both derived from phospholipid-bound ARA. Yet, DHA and EPA supplementation reduce AEA and 2-AG levels, with reciprocal increases in levels of the analogous endocannabinoid-like DHA and EPA-derived molecules, docosahexaenoyl ethanolamide (DHEA) and eicosapentaenoyl ethanolamide (EPEA). Dietary enrichment with DHA and EPA have shown beneficial effects on learning and memory, neuroinflammatory processes, synaptic plasticity, and neurogenesis.
This review contributes to the evolving landscape of concussion management by highlighting the pivotal role of targeted nutritional therapy as a therapeutic approach. These interventions can modulate neuroinflammation, enhance neuroprotection, and facilitate neurorepair following a concussion. Furthermore, practical considerations for implementing targeted nutritional interventions across diverse populations, from athletes to military personnel and individuals at risk of recurrent head injuries, are to be addressed. This underscores the importance of acknowledging nutrition as a complementary strategy in the multifaceted domain of concussion management and prevention. As we persist in our endeavors to augment patient outcomes and alleviate the societal burden of concussions and TBI, the application of targeted nutritional interventions warrants further exploration and clinical integration within the field of traumatic brain injury.
110 The Use of Motion Capture Technology and the eTherapy App With Patients With Post-concussion Visual Gaze Deficits: A Case Study Design
Daniel Panchik 1 ; Elizabeth Hice 1 ; Conlin Shellenberger 1 ; Shannon Young 1 ; Angelo Botticelli 1
1 Elizabethtown College, Elizabethtown, United States
The eTherapy app was created through a collaboration of computer engineering and occupational therapy and developed for patients with orthopedic injuries working on motor re-education. The app uses motion capture technology and a brand of inertia measurement units called Notches to measure a range of motion (ROM) and response time. The Notches are attached to the patient on both sides of a targeted joint and connected through Bluetooth to the mobile device with the app. This study finds novel uses for this app in patients with traumatic brain injuries. Concussion clients can experience long-term symptoms, including visual gaze deficits and changes in reaction time. They can also experience behavior or personality changes, including increased susceptibility to frustration 1 .
Researchers utilized a case study methodology with an expert opinion process 2 . The eTherapy app was introduced to an occupational therapist (OT) specializing in concussion rehabilitation and demonstrated its current capabilities. Then, researchers conducted a semi-structured interview with the OT about using the app for clients with vision deficits.
In the interview, the therapist reported that the current functioning of the app and its crashes would increase frustration in concussion clients and slow down their progress. Through collaboration with the researchers, a method was developed to assess visual tracking by placing one sensor on the forehead and one on the back of the hand. The therapist also reported that the app’s margin of error when measuring ROM should be decreased. With the changes made, the OT believes that the app could be a useful tool for this population 3 . The app is portable and inexpensive, making it appropriate to use both in-clinic and as part of a home program.
Through expert opinion, we determined that if this app is to be utilized in a population with post-concussion visual gaze deficits, it should be further developed. It is viable to continue the development of the app in-clinic or in a home program with a client in this population. The app can calculate data for visual tracking and reaction time to gather objective information in real-time. The app’s final development must be consistent in its utility and function without the application crashing.
111 Longitudinal Evaluation of Gut Microbiome and Inflammation Among Those Seeking Care in the Emergency Department for Acute Mild Traumatic Brain Injury
Andrew Hoisington, Molly Pezenik, Kelly Stearns-Yoder, Christoper Lowry, Teodor Postolache, Claire A. Hoffmire, Marian Betz, Christopher Stamper, Jeri Forster, Lisa Brenner
1 Department Of Veteran Affairs, Aurora, United States
Acute traumatic brain injury (TBI) exerts damage to the brain through an external force that activates a cerebral inflammatory response. In some cases, maladaptive inflammation may result in chronic inflammatory conditions and/or changes to the gut microbiome. Inflammation and the gut microbiome have a complex bidirectional relationship that plays a part in neurogenerative processes, behavior, and cognition. Currently few treatment options exist for TBI patients, therefore a better understanding of biological responses that are connected to physical and mental health outcomes is needed in human studies. In this study, longitudinal sampling was conducted from emergency department patients with post-acute mild TBI (mTBI). Samples included the fecal microbiome within 48 hours of admission (baseline) and at monthly intervals for up to 12 months in 23 participants for 167 total fecal samples (mean >7 samples per participant). Plasma was collected at baseline for all participants and at 12 months for a subset of 11 participants and analyzed for changes in inflammatory markers (i.e., C-reactive protein, interleukin (IL)-1β, IL-6, IL-8, tumor necrosis factor). Data regarding psychological histories/symptoms were obtained at baseline and each month of participation. Preliminary analysis was conducted to explore the microbiome and inflammatory changes post-acute mTBI. In a linear mixed model to account for related samples from the same participants, the overall microbial community was significantly divergent across the sampling time when compared to baseline. A rapid reduction in abundance, with no long-term recovery, of the potentially anti-inflammatory genus Akkermansia partially explained the trend. Akkermansia muciniphila promotes intestinal barrier function, in part by enhancing mucus production. A similar trend was not observed in other genera commonly associated with anti-inflammatory effects (e.g. Bacteroides, Faecalibacterium, Lactobacillus). Plasma concentrations of IL-6 were significantly reduced from baseline to 12 months, consistent with previous studies documenting elevated plasma concentrations of IL-6 immediately after a TBI. Findings support previous work highlighting relationships between TBI, inflammatory response, and the gut microbiome. Analysis of the factors associated with changes in the gut microbiome and/or biomarkers of inflammation is ongoing, including analysis of associations of physiologic responses with mental health outcomes subsequent to post-acute mTBI.
113 Disparities in Transitions of Care for Individuals with Traumatic Brain Injury
Amol Karmarkar 1 ; Alexandra Ulbing, Charmi Kanani, Amber Walter
1 Virginia Commonwealth University/sheltering Arms Institute, Richmond, United States
Navigating care following the initial hospital discharge can be a complex and vulnerable time for individuals with Traumatic Brain Injury (TB). After acute hospitalization, individuals with TBI may be discharged to different postacute settings, not limited to: inpatient rehabilitation facilities (IRF), skilled nursing facilities (SNF), long-term acute care hospitals (LTCH), and home health (HH). When the right transitions are not made at the right times, individuals with TBI face poor outcomes such as hospital readmissions. Also, there exists disparity in these care transitions by gender, race/ethnicity, and living situation (rural versus urban settings). Our study objectives were, to examine care transitions patterns and differences for individuals with TBI in a 90-day post-hospitalization period, and to examine 30- and 90-day hospital readmission risk. This was a retrospective cohort study. We conducted secondary analysis of data from Virginia All-Payer Claims Database (APCD) for the years 2027-2021. Virginia APCD comprised of commercial, Medicare, Medicaid, etc. claims from about 5 million Virginia residents associated with health services (acute, postacute, and community-based) utilization. We selected records of individuals with TBI admitted to acute hospitals and followed their care transitions through postacute and community-based health services in 30- and 90-day follow-up period. We also calculated risk adjusted 30- and 90-day hospital readmission and examined if the hospital readmission risk is different by gender, race/ethnicity, locations, and type of postacute services they received, controlling for all the other covariates. Our analytical cohort comprised of 18,215 individuals with TBI with index acute hospitalization in the years of 2017-2021. The mean age of our cohort was 70.8 (18.7) years, 51% male, 33% non-white, and 5% living in rural locations. Only 61% (11,106) of our study cohort received any postacute care, with 30% going to SNFs, 18% to HHs, and 12% to IRFs. The unadjusted 30-day readmission rate was 3.6%, and 5% for 90-day hospital readmission. In the fully adjusted models, controlling for other covariates, we found higher likelihood of 30-day hospital readmission for those going to SNFs (OR=1.9, 95%CI=1.5-2.4), and IRFs (OR=2.9, 95%CI=2.3-3.8) relative to those without any postacute follow-up. Also, we found lower likelihood of 30-day hospital readmission for Blacks compared to non-Hispanic Whites (OR=0.68, 95%CI=0.50-0.93). For 90-day hospital readmission, we found higher likelihood with SNFs and IRFs discharges and lower likelihood for Blacks as compared to non-Hispanic Whites. Our study findings highlight need for equitable access to postacute care is an important consideration for individuals with TBI to maintain care continuity, and achieve desirable health outcomes, and more importantly avoidance of undesirable outcomes, such as hospital readmissions.
114 Heads Together - Understanding Acquired Brain Injury: An Interdisciplinary Collaboration Addressing the Knowledge and Skills Gap in Social Work Education to Improve Practice and Outcomes
Akudo Amadiegwu 2 ; Caroline Bald 2 ; Andrew Bateman 2
1 Canterbury Christ Church University, Canterbury, United Kingdom; 2 University Of Essex, Colchester, United Kingdom
Brain Injury is the leading cause of death and disability in the UK for people aged 0-40 (Centre for Mental Health “CMH” 2018) and diagnosed in 70% of all cases of head injury (Ponsford, Sloan and Snow 2013). However, there is limited knowledge and understanding about this topic (Norman 2020, Mantell 2017) with very little known about social care and social work with people with brain injury (Holloway 2020) even though, social work plays an important role in the assessment and treatment of people with this condition (Linden et al 2023). The complexity and hidden nature of the condition can lead to misdiagnosis and inappropriate care and support. Safeguarding Adult Reviews repeatedly identify social workers’ poor understanding of ABI as a contributing factor to the premature deaths of people who struggle post-injury. Heads Together is an interdisciplinary effort led by Prof. Andrew Bateman and other brain injury experts and researchers including psychologists, social workers, academics from 5 universities in the UK and experts by experience funded by the NIHR with the aim of addressing this knowledge and skills gap. This unique project has five work packages including a systematic review of existing brain injury social work literature recently accepted for publication. Topic: Social workers’ understanding of acquired brain injury: A systematic review of the current evidence-base. We have surveyed 152 students, 65 social work educators and interviewed newly qualified and experienced social workers and commissioners in the UK to inform outputs. A recent addition to our project is Making Headway, a play in collaboration with local specialist brain injury charities brings the brain injury experience to life and serves as a trans-disciplinary teaching tool for health and social care students and other disciplines.
The play is supported by actor-led, interdisciplinary student workshops shown to over 150 University of Essex students in March, phase two is to tour four universities reaching 600 students by April 2024. Making Headway was presented at a Think Tank at the IBIA World Congress on Brain Injury in Dublin, with members of the team making presentations at this and other conferences including the Joint Universities Social Work Education Conference in Glasgow and has been nominated for a global interprofessional award. The team has influenced policy by contributing to two UK Parliament Post Notes and NICE Guidelines reviews and training social workers in a local authority where a safeguarding adult review into the death of a person with ABI was conducted. Heads Together is developing practice improvement resources including a website and interactive modules which present brain injury in a clear and concise manner and ultimately, improves outcomes for people affected by ABI. The brain injury social work toolkit will be launched during World Social Work Week 2024.
115 Social Work Educator Views of Student Training Needs in Preparation for Supporting People With ABI
Akudo Amadiegwu 2 ; Caroline Bald 2
Social work education in the United Kingdom is governed by four regulatory bodies with no common curricula, with Social Workers in England alone undertaking multiple education routes in 82 higher education institutions (HEI). A growing body of evidence has demonstrated a potentially significant gap in Acquired Brain Injury (ABI) curricula inclusion in initial social work education. Little is known about the gap at a micro curriculum level or Social Work Educators’ views of ABI relevance in initial education. An intra-disciplinary, UK-wide NIHR funded project, Heads Together, is researching social work education curricula to evidence the preparedness of graduating social workers for ABI practice and to develop resource database for curricula development. As part of the research project, a 12-point online survey was deployed to UK-based Social Work Educators with the support of the Joint Universities Social Work Committee (JUSWEC) and the British Association of Social Workers (BASW). Thematic analysis of 28 responses found four key themes: 1) an acknowledged gap in ABI curricula inclusion in initial social work education including that of respondents; 2) a significant numbers of respondents had personal experience of ABI (self, family, or close friends); 3) a majority viewed that ABI should be mandatory part of initial social work education; and finally, 4) there are pockets of good practice often prompted by local practice. The survey findings will, in combination with interviewing newly qualified, specialist and commissioning social workers, inform curricula inclusion of ABI in social work education in the UK. Underpinning and guiding the project is a governance board of experts by experience including people with brain injury, family, and brain injured social workers.
117 Opioid Weaning in a Patient With Anoxic Brain Injury After a 273-Day Inpatient Hospitalization: A Case Report
Harry Liu 1 ; David Ibrahim 2 ; Alexander Turfe 1 ; David Rustom 1
1 Wayne State University/Rehab Institute of Michigan, Royal Oak, United States; 2 MSU College of Osteopathic Medicine, East Lansing, United States
Case Diagnosis
Opioid weaning in a patient with anoxic brain injury and an extensive hospital stay.
Case Description
A 33-year-old male with an anoxic brain injury, related to complications after a gunshot wound (entry through ear into posterior cervical spine) was admitted to our hospital after discharge from a long-term care facility. He had tracheostomy, gastric feeding tube placed and was ultimately ventilator dependent. Upon nearing his discharge from prolonged hospital stay, our PMR/Pain management team was consulted. His pain regimen included Hydromorphone 0.5 mg Q4H prn, Acetaminophen 650 mg Q6H, Methocarbamol 1000 mg Q8H prn, Gabapentin 300 mg TID, and a Fentanyl patch 75 mcg/hr Q72H. Hypotension was an issue and made pain control even more challenging. Our goal on hospital discharge after nearly 273 days of admission was to be off intravenous medications and to reduce his overall morphine equivalent dose. We evaluated pain primarily via facial grimacing, as communication was limited due to his orientation, and his tetraplegic status. His total pre weaning morphine equivalent dose was 279. Over the course of 5 days, we were able to reduce morphine requirements to 150, while eliminating his intravenous medications.
Opioids should be used sparingly and every attempt for weaning should be made possible. They have been shown to further complicate treatment, worsen respiratory/cognitive status and have known to become an issue when attempting to wean if they have been administered over long periods of time. Additionally, higher morphine equivalent doses can lead to suppressed respiratory drive, dysautonomia, and decreased arousal, all issues we try to avoid potentiating in traumatic brain injury. Painful syndromes are characterized in traumatic brain injury and are challenging to diagnose, treat, and witness responses to treatment. Although localization may be difficult with nonverbal patients, we can use family, nursing staff, and physical examination maneuvers while monitoring for grimacing, blood pressure fluctuations, and mentation changes. Conservative pain-relieving options include pressure relief, correction of posture deficits, bracing, manual therapies, and non-opioid medications. If these fail, we do resort to the use of opioids and suggest beginning with the least restrictive dose, limiting progression or increases to tolerance.
Opioid weaning strategies should be employed early on in the treatment plan and attempted several times over. It can be discouraging and so we suggest slow weaning protocols varying from 10-20% reductions over the course of several days in a supervised setting.
118 Communication Partner Training for Health Care Workers, Families, Friends and Community Agencies Who Interact With People With Acquired Brain Injury: Pilot Data for a Free Online Resource Called Interact-ABI-lity
Leanne Togher 1 ; Petra Avramovic 1 ; Melissa Brunner 1 ; Emma Power 2 ; Sophie Brassel 1 ; Rachael Rietdijk 1
1 The University of Sydney, Sydney, Australia; 2 The University of Technology, Sydney, Australia
Communicating with people with acquired brain injury (ABI) can be challenging given that 75% of people experience social communication impairments (Macdonald, 2017). These difficulties can lead to less successful and less enjoyable interactions with others, including family and health professionals. To address these difficulties, it is internationally recognized best practice that the communication partners of people with a brain injury should receive education about how best to support communication (Togher et al., 2023). This paper presents pilot data for a free communication partner training (CPT) program called interact-ABI-lity.
Interact-ABI-lity is a self-guided resource which provides education to family members, friends, and health professionals who interact with a person with an ABI. It was developed via collaborative design and pilot testing (Miao et al., 2022). interact-ABI-lity is a two-hour, web-based CPT program for partners of adults with cognitive-communication disorders, aphasia or dysarthria after ABI. The free, seven-module program is available on desktop, tablet and phone devices as part of the ‘Social Brain Toolkit’. The pilot study entailed the recruitment of two groups: 1. Eleven participants (six support workers, three clinicians, two student health professionals) who were interested in improving their skills, and 2. Five clinicians (two speech pathologists, one occupational therapist, one physiotherapist, one psychologist) with at least four years’ experience working with an ABI caseload. Data collection for group 1 included the number of people who completed the course, their ratings of the likelihood to recommend the course to others and their ratings of their confidence in interacting with people with TBI, and for the clinicians, feedback interviews were also conducted at course completion.
Of the 11 learners in group 1, five fully completed the training, while all participants in group 2 fully completed all modules. Of the five completers, four learners rated their likelihood as 10/10 to recommend the course to others and three reported increased confidence in interacting with people with ABI at the end of the program. Feedback included the need for additional demonstration videos and provision of definitions of the technical language used.
interact-ABI-lity may address the need for a short, accessible educational resource about how to communicate with a person with an ABI. The pilot testing process was informative to identify ways to improve interact-ABI-lity. These included building in motivators (e.g., certificate of completion), prioritizing development of videos of people with ABI and their family members, and specific additions to the course content (e.g., glossaries of technical terms). Since this pilot study, the program has been updated and the final version will be presented at NABIS. Since launch in Feb 2022, there have been 2280 registrations for interact-ABI-lity, and it is now incorporated into training for assistants, clinicians, and students internationally.
120 Developing an Animal Model of Coal Mine Gas Explosion and Understanding the Injury Mechanism
Linqiang Tian 1,3 ; Zihui Zhao 1,3 ; Tingting Lei 1,3 ; Zhaodong Wang 1,3 ; Zhenzhou Sun 1,3 ; Hongxia Xing 1 ; Jianan Chen 2 ; Jie Liu 1,3 ; Wenjie Ren 3
1 The 3rd Affiliated Hospital of Xinxiang Medical University, Xinxiang, China; 2 School of Biological Science and Medical Engineering, Beihang University, Beijing, China; 3 Clinical Medical Center of Tissue Engineering and Regeneration, Xinxiang Medical University, Xinxiang, China
Although safety of coal mine production facilities and regulations continue to improve around the world, gas explosion accidents still exist. Brain damage caused by coal mine gas explosions is a unique type of injury that is different from those that are generally seen by the explosions in wars and open spaces. Specifically, it is caused by the gas explosions from the superposition of repeated shock waves in a closed space and subsequent poisonous gases such as carbon monoxide (CO), which is a particular combination of physical and chemical injuries. Currently, there are many models of simple explosion shock wave or CO poisoning separately, and it was also reported both experimentally and clinically that these injuries do not only cause neurological dysfunction in acute phase but is also more susceptible to develop neurodegenerative diseases in later stage. However, animal model of coal mine gas explosions with combined injuries does not exist currently, which prevent us from better understanding the difference between the single and combined injuries. We speculate that the combined injuries in coal mine gas explosions are more complex and severe than single injuries. This study will develop an animal model of gas explosion with combined injury by simulating gas explosion condition in coal mine tunnel and use the model to understand the injury mechanism. We believe that the results will be useful for finding effective intervention methods and early treatments for patients in coal mine gas explosion accidents in the future.
20 adult Kunming white mice were divided into four groups: (1) Single gas explosion (SGE), received one explosion in a customized device; (2) Continuous CO poisoning (CCP), received four CO intraperitoneal injections within 24 hours; (3) SGE+CCP, received single explosion immediately followed by four CO injections within 24 hours; (4) Normal control (NC), received no injury. Behavior tests were performed three and seven days after injuries, then the animals were terminated for molecular biology tests.
The elevated plus maze test shows that in both 3 days and 7 days after injury,all injured groups presented significantly lower entering number when compared to NC group (P < 0.05); while SGE+CCP group also presented significantly lower entering number when compared to SGE and CCP groups (P < 0.05). RT-qPCR test shows that the brain tissues from SGE+CCP group presented significantly higher expression of IL-1β and TNF-α in 3 days after injury as well as higher expression of IL-6 and TNF-α in 7 days after injury when compared to other groups (P < 0.05).
A mouse model of coal mine gas explosion was developed. The combined injury was found to be more severe than the single injuries behaviorally, which may be related to the more severe inflammation.
122 Rethinking the Outcomes and Burden of Diffuse Axonal Injury: A Nationwide Analysis
Amelia Maiga 1 ; Shayan Rakhit 1 ; Kun Bai 1 ; Fei Ye 1 ; Areg Grigorian 2 ; Bellal Joseph 3 ; Susanne Muehlschlegel 4 ; Mayur Patel 1
1 Vanderbilt University Medical Center, Nashville, United States; 2 University of California, Irvine, Irvine, United States; 3 University of Arizona, Tucson, United States; 4 Johns Hopkins, Baltimore, United States
Diffuse axonal injury (DAI) is a subtype of traumatic brain injury (TBI) thought to portend poor outcomes, perhaps prompting early withdrawal of life-sustaining therapies. However, large-scale studies are limited. Because DAI can be subtle or invisible on initial head CT imaging, diagnostic delay is common until other causes of encephalopathy are ruled out and MRI can be performed safely. We hypothesized that TBI with DAI would have increased in-hospital mortality compared to comparable TBI without DAI in a large nationwide database.
This retrospective cohort study included adults from the 2017-2020 American College of Surgeons Trauma Quality Improvement Program admitted with blunt, moderate-severe TBI. Exclusion criteria were bilateral nonreactive pupils. We compared patients with and without DAI and adjusted for age, injury severity score (ISS), presenting hemodynamics, TBI severity, and hospital characteristics. Logistic regression was used for the binary outcomes of inpatient mortality and hospital discharge disposition (proxy for short-term functional status). Linear regression was used for the continuous outcomes of time to intracranial pressure monitor (ICPm) placement and hospital length of stay (LOS).
Of 65,448 patients with moderate-severe TBI (median GCS 8 [interquartile range, IQR 6,10]), 7765 patients (12%) had DAI. DAI patients were significantly younger (median 36 years [25,55] vs. 55 years [32,71]) with higher ISS (33 [26,38] vs. 25 [17,29]), less midline shift (16% vs. 30%), and higher ICPm usage (43% vs. 24%, p<0.01). In multivariable analyses, DAI was associated with lower inpatient mortality (odds ratio [OR] 0.967, 95%CI 0.956-0.978), a 3.2-hour delay in ICPm placement (95%CI 0.1-6.3h), more than 3 days longer LOS (95% CI: 3.33-4.18), and worse short-term functional status (OR 1.06, 1.05-1.07) as measured by hospital discharge disposition.
Previous beliefs about early mortality and withdrawal of life-sustaining care for DAI are challenged by our findings. Further research is needed to clarify reasons for delays in ICPm placement (e.g., diagnostic delay, fatalism, etc.), and to determine if ICPm placement even improves outcomes in DAI. Although DAI prolongs hospitalization and is associated with worse functional status at discharge, the long-term trajectories of recovery remain unknown.
123 Gender Differences in Patients With Traumatic Brain Injury – A Retrospective Pilot Analysis
Jeffrey Lam Shin Cheung 1 ; Hajer Nakua 2 ; Anil Dosaj 3 ; Shweta Aswani 3 ; Ananya Pathak 4 ; Fallon Ponnambalam 3 ; Jeffrey Smallbone 1 ; Myriam Vigny-Pau 1 ; Shree Bhalerao 3
1 Faculty of Medicine,University of Toronto, Toronto, Canada; 2 Institute of Medical Science, University of Toronto, Toronto, Canada; 3 St. Michael’s Hospital, Toronto, Canada; 4 University of Guelph-Humber, Etobicoke, Canada
In recent years, the incidence of traumatic brain injury (TBI) in Canada has doubled, with females having a higher prevalence. Current literature shows no consensus regarding how gender may influence post-TBI outcomes, thus prompting further investigations. Here, we sought to study whether gender impacts post-TBI outcomes specific to psychiatric well-being.
A retrospective cohort study of patients admitted to St. Michael’s Hospital for TBI was analyzed. Using health consultation reports, we collected patient demographic characteristics, cause of TBI, past medical history, diagnoses following TBI and treatments. All measures analyzed were qualitative and coded as no or yes (e.g. suffered from depression: no or yes). Chi-square tests were used to assess whether males or females had differing TBI. Multiple comparisons were corrected for using the Bonferroni Correction.
Data was collected and analyzed for 39 patients (n=16 males, n=23 females, mean age = 38.5 ± 12.7 years). The causes of TBI included 16 (41.0%) motor vehicle accidents, 8 (20.5%) pedestrian accidents, 3 (7.7%) bicycle accidents, 10 (25.6%) cases of falls, 5 (12.8%) cases of physical assaults, and 3 (7.7%) sports-related injuries. Long-term disabilities resulting from TBI occurred in 14 patients (35.9%). Females were significantly more likely to experience orthopedic issues resulting from TBI compared to males (X2 = 5.35, p = 0.021), but this significance did not make it past multiple comparison corrections. No other significant differences were noted.
We did not find better post-TBI outcomes specific to psychiatric well-being in either gender in this pilot retrospective analysis. A larger sample and quantitative data are necessary to substantiate the findings.
124 The Boston Assessment of Traumatic Brain Injury Lifetime, Second Edition (BATL-2): Development and Initial Psychometric Evaluation in Post-9/11 Military Veterans
Catherine Fortier 1,2,3 ; Alexandra Kenna 1 ; Tristan Colaizzi 1 ; Alyssa Currao 1 ; Christine Clermont 1 ; William Milberg 1,2,3
1 Translational Research Center for TBI and Stress Disorders (TRACTS), VA Boston Healthcare System, Boston, United States; 2 Department of Psychiatry, Harvard Medical School, Boston, United States; 3 New England GRECC, Boston, United States
The BATL is an extensively validated and widely used semi-structured clinical interview designed to diagnose traumatic brain injury (TBI) across the lifespan in post-9/11 military veterans with particular attention to blast-related injury. The BATL uses a forensic approach designed to differentiate clinical symptoms of TBI (e.g., altered mental status, posttraumatic amnesia, loss of consciousness) from other common physiological and psychological reactions to head injury and trauma. The BATL has been updated to: (1) incorporate the most up-to-date TBI diagnostic criteria (American Congress of Rehabilitation Medicine [ACRM] 2023; Veterans Affairs [VA]/Department of Defense [DoD] Clinical Practice Guidelines); (2) assess for subconcussive repetitive head injury risk from blast and blunt force trauma; and (3) offer a flexible battery approach to allow clinicians and researchers to select modules specifically tailored to high-risk TBI contexts (e.g., military, civilian, intimate partner violence, and sports). These changes will expand the breadth of context in which the BATL can be utilized and reduce time burden for administering the BATL interview based on research and clinical goals. Prevalence of injury using the BATL-2 will be presented for a large cohort of U.S. Veterans from the Translational Research Center for TBI and Stress Disorders (TRACTS), a 15-year, 2-site VA Rehabilitation Research and Development National Center for TBI Research. The sample consists of 878 combat exposed post-9/11 Veterans, 90% male, 71% Non-Hispanic White, with mean age of 35 (SD = 9.2) and mean education level of 14 years (SD = 2.2). On average, they served in 1.68 tours (SD = 1.1) for 16 months (SD = 11.2) and completed the BATL interview 70 months (SD = 52.0) after returning from their last deployment. TBI was highly prevalent, as 74% (n = 645) sustained a TBI in their lifetime and 54% (n = 474) sustained a TBI during military service. Additionally, 32% (n = 284) of Veterans sustained a blast force military TBI, while 33% (n = 290) sustained a blunt force military TBI. Data on subconcussive blast and blunt exposure were collected in a subset of 228 of these veterans, revealing that 60% (n = 137) reported exposure to subconcussive blast events and 43% (n = 99) reported exposure to subconcussive blunt force trauma. Results of an initial psychometric evaluation of BATL-2 scores in 2 samples of military veterans will be presented. Overall, results indicate that the BATL-2 is a psychometrically sound measure of both ACRM 2023 and VA/DoD TBI diagnosis and symptom severity. Importantly, the BATL-2 strongly corresponds with the BATL-1, suggesting the BATL-2 provides continuity in evidence-based assessment of TBI with the transition to ACRM 2023 criteria.
125 Recidivism Risk in Incarcerated Individuals With Traumatic Brain Injury in Relation to Aggression and Executive Functioning
Devan Parrott 1 ; Dawn Neumann 1 ; Anthony Laffooon 1
1 Indiana University School of Medicine, Greenwood, United States
To examine aggression, executive functioning, and recidivism risk in a sample of incarcerated males with traumatic brain injury (TBI).
Cross-sectional study including 89 males with TBI. Data was collected as a baseline assessment for a clinical trial. Participants were recruited within 12 months of anticipated release date.
The Aggression Questionnaire (AQ) total score was used to assess aggression in addition to the verbal and physical aggression subscales. The Behavioral Rating Inventory of Executive Function-Adult Version (BRIEF-A) was used to measure self-regulation. The Level of Service Inventory–Revised (LSI-R) is a structured interview for correctional populations used to predict recidivism risk, adjustment, and institutional misconduct using criminal history, education, employment, finances, relationships, alcohol and drug problems, emotional/personal factors, and attitudes.
The majority of the sample (59%) reported high-very high aggression (T-scores = 60) on the total AQ (mean T-score = 59.93, 95% CI [57.95, 61.91]). 54% of the sample reported high-very high verbal aggression (mean T-score = 56.55, 95% CI [54.58, 58.53]) and 51% reported high-very high physical aggression (mean T-score = 58.89, 95% CI [56.40, 61.39]). Scores on the BRIEF-A were also clinically significant with a mean Global Executive Composite (GEC) T-score of 68.80 (95% CI: [65.95, 71.66]) indicating significant difficulty with executive functioning. The Behavioral Regulation Index (BRI) was also elevated (mean T-score = 69.70, 95% CI [67.07, 72.33]) suggesting increased deficits related to inhibiting impulsive responses and controlling emotions and behavior. The Metacognition Index (MI) was also above average (mean T-score = 66.03, 95% CI [62.90, 69.16]) suggesting impairments related to self-management of tasks and self-monitoring. The sample also showed an increased recidivism risk with a mean LSI-R score of 29.77 (moderate risk), 95% CI [28.26, 31.27] and the majority of the sample (86%) scoring in the moderate or higher risk categories. LSI-R risk scores were significantly correlated with AQ total aggression (r =.404; p<.001) and physical aggression (r=.393; p<.001), but not verbal aggression (r = .081; p=.498). LSI-R scores were also significantly correlated with executive function impairment: GEC (r =.489; p<.0001), BRI (r =.494; p<.0001), and MI (r =.446; p<.0001).
Aggression and executive dysfunction are common consequences of TBI that are believed to contribute to high incarceration and recidivism rates. The results from this sample suggest that incarcerated individuals with TBI are more likely to display elevated levels of aggression as well as suffer from executive dysfunction. Furthermore, the significant linear relationships between aggression (especially physical) and executive functioning with recidivism risk highlight the need for interventions designed to address and mitigate these deficits in individuals with TBI within the corrections environment as a strategy to potentially reduce recidivism and reincarceration.
126 The STEP-Home Skills-Based Group Reintegration Workshop Improves Anger, Inhibitory Control, and Neurobehavioral and Mental Health Symptoms in Veterans With TBI and Other Common Comorbidities
Alexandra Kenna 1 ; Dylan Katz 1 ; Caroline Sablone 1 ; Alyssa Currao 1 ; Adam Lebas 1 ; Catherine Fortier 1,2
1 Translational Research Center for TBI and Stress Disorders (TRACTS),VA Boston Healthcare System, Boston, United States; 2 Department of Psychiatry, Harvard Medical School, Boston, United States
Post-9/11 U.S. Veterans are clinically complex with multiple co-occurring health conditions contributing to morbidity/mortality and decreased quality of life. Traumatic Brain Injury (TBI) diagnosis can worsen these outcomes. STEP-Home is a cognitive-behavioral transdiagnostic intervention for TBI and common comorbidities.
Determine if STEP-Home improves anger and impulse control, frontal system function, civilian readjustment, neurobehavioral symptoms, and work/life functioning in post-9/11 Veterans. TBI may influence Veterans’ ability to learn core skills and, thus, impact response to treatment. Treatment outcomes for Veterans with and without TBI will be explored.
A total of 56 (39M/17F; mean age = 40) post-9/11 Veterans with high rates of psychiatric comorbidity, with and without TBI received 12 weeks of the STEP-Home transdiagnostic group intervention. STEP-Home sessions teach cognitive behavioral skills relevant across diagnostic category, including Problem Solving (PS) and Emotional Regulation (ER). These skills are integrated and applied across Veteran-specific content areas to assist in community reintegration and functioning. Assessments at baseline, posttreatment (12 weeks), and follow-up (24 weeks) included: State-Trait Anger Expression Inventory 2 (STAXI-2); Military to Civilian Questionnaire (M2CQ); Post-Deployment Readjustment Inventory (PDRI); Frontal Systems Behavioral Scale (FrSBe); Neurobehavioral Symptom Inventory (NSI); World Health Disability Scale (WHODAS); PTSD Checklist (PCL-5); Depression Anxiety and Stress Scale (DASS-21).
STEP-Home significantly improved anger expression (STAXI-2 p = .0320), inhibitory control (FrSBe p =.0001), and reintegration status (MC2Q p=.0001; PDRI p =.0097) posttreatment. Similar improvements were seen in neurobehavioral symptoms, work/life functioning, PTSD, depression, and stress (p’s < .01). Treatment gains were maintained at follow-up (p < .001). Treatment response did not differ by TBI status.
STEP-Home teaches Veterans cognitive-behavioral skills to improve anger, impulse control, executive functioning, reintegration, and work/life functioning. STEP-Home is equally as effective for participants with and without TBI. There was no effect of TBI status on treatment maintenance over time. This is critical given TBI prevalence among post-9/11 Veterans and the need for additional palatable treatment options.
128 Advancing a Precision Medicine Approach to Traumatic Brain Injury Longitudinal Outcomes Research
David Cifu 1 ; Lisa Brenner 2 ; Maya O’Neil 3 ; Elisabeth Wilde 4 ; Catherine Fortier 5 ; William Milberg 6
1 Virginia Commonwealth University; Central Virginia VA Healthcare System, Richmond, United States; 2 University of Colorado; VA Rocky Mountain Mental Illness Research Education and Clinical Center, Aurora, United States; 3 VA Portland Health Care System; Oregon Health and Science University, Portland, United States; 4 VA Salt Lake City HealthCare System; University of Utah, Salt Lake City, United States; 5 VA Boston Healthcare System; Harvard Medical School, Boston, United States; 6 VA Boston Healthcare System; Harvard Medical School, Boston, Unites States
Traumatic brain injury (TBI) exposures and poor health and functional outcomes are well established, particularly in the context of traumatic stressors common among those with histories of military deployments. Our team is advancing precision medicine approaches to predicting longitudinal outcomes through largescale, multi-study data harmonization and machine learning analytics. We combined data from the two largest mild TBI (mTBI) longitudinal cohort studies: The Long-Term Impact of Military-Relevant Brain Injury Consortium Chronic Effects of Neurotrauma Consortium (LIMBIC) Prospective Longitudinal Study (PLS) is a 10-year, 17-site cohort of more than 2,800 combat exposed service members and veterans. The Translational Research Center for TBI and Stress Disorders (TRACTS) is a VA RR&D National Center for TBI research including a 15-year, 2-site longitudinal cohort study of more than 950 combat exposed veterans. This proof-of-concept, precision medicine approach to mTBI longitudinal outcome research includes: 1) defining standardization methods and creating a crosswalk for the modalities and domains of LIMBIC and TRACTS longitudinal cohorts to create a unified assessment profile; 2) identifying a rigorous harmonization approach to allow for overall data analyses using the unified data set; 3) developing a multi-modal, analytic approach for the harmonized data sets; 4) pilot testing the use of a VA-supported machine-learning approach to identify multimodal patterns relevant to predicting long-term posttraumatic brain health; 5) establishing a program of research to analyze the prospective, longitudinal dataset and enable identification of risk factors associated with brain disorders and recovery; and, 6) developing, pilot testing, and proposing follow-up “FAIR” (Findable, Accessible, Interoperable, Reusable) data methods to apply the systems developed in this proposal to incorporate additional relevant, largescale, longitudinal veteran/military data (e.g., Million Veteran Project, VA Electronic Health Record Corporate Data Warehouse) to this robust data resource. We will present harmonized biomarker, imaging, functional, and mental health meta-data, outcomes, and methods designed to be scalable and publicly accessible to further advance precision medicine analytics for TBI.
129 Establishing Therapist Training and Fostering Interdisciplinary Care for Evaluation and Treatment of Patients With Disorders of Consciousness
Emily Axelson 1 ; Allison Bauer 1 ; Kayla Johnson 1
1 Mayo Clinic, Rochester, United States
Patients with disorders of consciousness (DOC) are a population within the rehabilitation team’s scope of practice, but about whom limited education may be available to the therapy staff designated to support them. This was recognized as an area for development and efforts were undertaken to support more systematic, effective, and evidence-based approach to evaluation and treatment. This presentation will describe the development and implementation of procedures for allied health staff’s involvement in evaluating and treating patients with DOC. A survey with eight questions was distributed to 18 therapy staff at Mayo Clinic in Rochester, asking them to rate their confidence level in evaluating, treating, and reporting results to medical staff or patient’s family. Staff rated their confidence level on a scale of one-five where one was “not confident requires full supervision” and five was “confident, provides training to others.” We asked each participant to rate their familiarity with terms associated with this patient population, where one was “this term is unfamiliar” and five was “I could provide education on this term.” Of 18 therapy staff, 15 responded and their data is included here. Initial data gathered indicates 66.7 percent of occupational therapists (OT), physical therapists (PT), and speech-language pathologists (SLP), who are currently evaluating/treating these patients feel they require some level of supervision and are not independent. 86.7 percent reported that they were not confident in reporting the results of their evaluation to other medical professional or patient’s family. Lastly, 26.6 percent of participants reported no training outside of what was provided in their curriculum or did not have education specific to DOC in their program, and 40 percent reported no additional training outside of on-site orientation/mentorship. Despite limited experience and education, the expectation is to provide quality care to patients with these complex diagnoses. This gap in knowledge and comfort revealed therapeutic approaches that were inconsistent across the therapy team and did not align with the recommended best practice guidelines published in 2018. To optimize knowledge and therapeutic skillset within the interdisciplinary team, this cohort of 18 rehab professionals (OTs, PTs, and SLPs), were identified and education and training was provided on evaluation measures (JFK Coma Recovery Scale Revised) and therapeutic interventions. As this is an ongoing project, post implementation data will be collected and used to develop an objective and defined evidence-based training protocol for all subsequent treating clinicians that aligns with published best practice guidelines.
132 Evaluating Neuropsychological Outcomes and Balance in Retired Contact Sports Players With Post-Concussion Syndrome: An Initial Investigation
Camille Charlebois-Plante 1,2 ; Samuel Guay 1,2 ; Marie-Ève Bourassa 1 ; Catherine Provost 1 ; Marie-Louise Charette 1 ; Raphaëlle Créniault 1 ; François Prince 1,3 ; Louis De Beaumont 1,3
1 Département de psychologie, Université De Montréal, Montréal, Canada; 2 Centre de recherche du CIUSSS du Nord-de-l’Île de Montréal (Hôpital du Sacré-Coeur), Montréal, Canada; 3 Département de Chirurgie, faculté de médecine, Université de Montréal, Montréal, Canada
The impact of post-concussion syndrome (PCS) on cognitive and motor abilities in ex-contact sports players is increasingly recognized. Research has predominantly focused on elite athletes, leaving a gap in understanding PCS’s functional effects in the general population.
Our research aimed to thoroughly examine neuropsychological outcomes and balance control in ex-athletes from non-professional backgrounds, with a focus on the enduring consequences of PCS symptoms.
We conducted an extensive neuropsychological assessment to evaluate cognitive functions and utilized a dual force plate system to measure center-of-pressure (COP) displacement and velocity, considering age and education as covariates.
Participants with PCS showed notable impairments in visual-spatial skills, immediate memory, and episodic memory. Regarding balance, no significant differences were observed in basic stances between the groups. However, under more challenging conditions, such as on uneven surfaces or during cognitive multitasking, the PCS group exhibited significant instability. This was particularly evident in medio-lateral balance during proprioceptive tests and in conditions of sensory limitation.
This study sheds light on the complex challenges former athletes with PCS encounter. The interaction between cognitive function and balance control, especially in demanding scenarios, highlights the necessity for individualized intervention strategies. These insights lay the groundwork for further investigations into the underlying mechanisms and potential treatment options for PCS in former athletes.
Post-concussion syndrome, neuropsychological outcomes, cognition, postural control, center-of-pressure, former contact sports athletes
133 Social Determinants of Health (SDOH) and Context in Initial Access, Symptom Report and Recovery Within Pediatric Mild Traumatic Brain Injury (mTBI) Care
Sydney Wing 1 ; Phillip Rosenbaum 1 ; Neil Bhathela 2 ; Daniel Ignacio 1 ; Joshua Caiquo 1 ; Natalie Gavi 1 ; Brad Barney 3 ; Faustina France-Nkansah 3 ; Christopher Giza 1 ; Talin Babikian 1
1 UCLA Steve Tisch BrainSPORT Program, Los Angeles, United States; 2 Atrium Health, Charlotte, United States; 3 University of Utah, Salt Lake City, United States
There is growing awareness of the degree to which Social Determinants of Health (SDOH) – encapsulated by social identities and demographic variables – impact many aspects of healthcare outcomes, including concussion care and recovery, making it imperative to consider the impact on patients with historically marginalized gender, racial, linguistic, and ethnic identities. Using retrospective data collected from the Four Corners Youth Consortium, we examined the impact of SDOH variables (e.g., race, ethnicity, insurance type, gender, age, and special educational services) on time to presentation (initial clinic contact), reported time to recovery, and symptom report (parent and child Post-Concussion Symptom Inventory [PCSI]) using multiple logistic regression and Cox proportional hazard regression statistical models. Included participants (n = 702) represented a primarily White (68.3%), Non-Hispanic/Latinx (79.1%) sample that has access to insurance (82.3%) and does not receive special education (82.5%). Gender, neurodiversity (whether child receives special education services), race and insurance were significant predictors of symptom report and recovery. Female adolescents (b = 8.33, p < .001) and their parents (b = 6.57, p < .001) reported higher increases in overall post-injury symptoms, including greater changes in physical, cognitive, emotional and fatigue symptoms. Neurodiverse (b = 1.07), p < .02), and Non-White (bBIPOC = 0.75, bOther = 1.32; p < .05) children self-reported heightened symptoms of fatigue. Insured patients (HR = 1.5, p = .03) experienced faster recovery, while female participants (HR = 0.77, p = .025) experienced slower time to recovery. Findings demonstrate that varying marginalized identities carry a higher symptom burden following a concussion, potentially facing more challenges for recovery. These findings reflect how social experiences related to privilege and marginalized status can ameliorate or compound the course of concussion symptomatology and recovery.
134 Detecting Covert Consciousness in the Intensive Care Unit Using Functional Near-Infrared Spectroscopy
Karnig Kazazian 1 ; Sergio Novi 1 ; Androu Abdalmalak 1 ; Loretta Norton 2 ; Derek Debicki 3 ; Adrian Owen 4
1 Western Institute Of Neuroscience, Western University, London, Canada; 2 Department of Psychology, King’s University College at Western University, London, Canada; 3 Department of Clinical Neurological Sciences, Western University, London, Canada; 4 Depart of Physiology and Pharmacology, Western University, London, Canada
The assessment of consciousness in patients who have sustained a severe brain injury in the intensive care unit (ICU) poses a significant challenge. Covert consciousness refers to a state where patients exhibit no overt signs of behavioral responsiveness, yet their brain activity – as indexed through functional neuroimaging - demonstrates preserved awareness and cognitive function. In the ICU setting, accurately identifying such cases is crucial for appropriate patient care and medical decision-making. Functional near-infrared spectroscopy (fNIRS) is a promising modality for measuring and mapping brain function, as it is portable and can be safely used at the bedside This study explores the feasibility of using fNIRS to detect covert consciousness in patients with acute brain injury in the ICU.
16 behaviorally unresponsive ICU patients with varying brain injury etiology were enrolled. Patients were asked to imagine playing a game of tennis while undergoing fNIRS monitoring. The fNIRS technique enables the measurement of cerebral hemodynamic changes associated with cognitive processes, providing a window into the neural activity underlying motor imagery. 24 age and sex-matched healthy controls were also enrolled. The fNIRS setup consisted of a 129-channel NIRScoutXP system. A channel was considered activated if there was a significant increase in oxyhemoglobin and a concurrent decrease in deoxyhemoglobin (p<0.05).
Of the 16 patients tested, two demonstrated the ability to follow commands during the motor imagery task despite the absence of observable signs of behavioral consciousness. Analysis of the fNIRS data revealed distinct patterns of neural activation during the motor imagery task in both patients and healthy controls. These findings were supported by positive responses to a language comprehension task.
Discussion: This study highlights the capability and feasibility of fNIRS to detect convert consciousness in patients who appear behaviorally non-responsive in the ICU. The results underscore the need for more nuanced and sensitive approaches to consciousness assessment in critical care settings. Further research and validation of fNIRS as a tool for detecting covert consciousness could revolutionize our understanding of patient awareness in the ICU, impacting treatment decisions and enhancing patient care strategies.
135 The Role of Bilingualism in Story-Telling Performance in Adults With Mild Traumatic Brain Injury
Monserrath Diaz 1 ; Lillian Thornock 1 ; Alexa Ybarra 1 ; Megan Morton 1 ; Rocio Norman 1
1 University of Texas Health San Antonio, San Antonio, United States
Communication skills, while often overlooked in the rehabilitation of adults with mild traumatic brain injury (mTBI) are critical to successful community reintegration and re-entry into society. Assessment of language is often challenging in mTBI due to the lack of available sensitive and specific published tools (Duff et al). Recently, the use of story-telling discourse assessment has been explored in mTBI (Norman et al, 2020) but there is limited research on the expected performance of adults who speak a second language. In the US in particular, it is critical for clinical providers to understand the role of second language proficiency in order to accurately assess patients and plan treatment.
A main concept analysis (MCA) was implemented on “Cinderella” story re-tell samples of thirty-six participants with mTBI to quantify the accuracy and completeness of the story-telling using a well-validated task. The participants were divided into three groups (individuals who learned Spanish before the critical age of seven; individuals who learned Spanish after seven years; individuals who consider themselves monolingual). Relevant concepts based on the story were identified and scaled according to a coding system. Participants were assigned codes based on if key concepts of the story were included in their story-telling discourse and the level of accuracy in their performance.
The final sample included 20 individuals who identified as bilingual before age age seven, seven bilingual individuals who identified as bilingual after age seven and eight monolingual individuals. Preliminary analyses indicated that mean MCA scores for the individuals who identified as bilingual before age seven outperformed the sequential and monolingual individuals, however, statistical significance was not reached. Further linguistic and grammatical analyses are underway to determine if differences at the microlinguistic level exist.
The precise measurement of language performance after mTBI is currently elusive, as traditional language tests fail to sufficiently capture linguistic changes specific to mTBI. For individuals who speak one or more languages, assessment is further complicated however, this study is a first step in understanding these differences which in turn can help refine and optimize rehabilitation approaches for individuals from a variety of cultural and language backgrounds.
136 TET3 Activator Ascorbate Mitigates Motor and Cognitive Deficits Following Controlled Cortical Impact Brain Injury in Mice
Raghu Vemuganti 1
1 University of Wisconsin-Madison, Madison, United States
Ten eleven translocases (TETs) mediate the conversion of 5-hydroxymethyl cytosine (5-mC) to 5-hydroxymethyl cytosine (5-hmC). The TET3 isoform and 5hmC are known to be enriched in the neurons in brain. TET3 is known to promote cell survival by inducing the expression of anti-inflammatory genes. Vitamin C (ascorbate) is a potent activator of TET3. Hence, we tested the efficacy of ascorbate in curtailing secondary brain damage and promoting motor and cognitive functional recovery after traumatic brain injury (TBI) induced in adult C57BL/6 mice by controlled cortical impact (CCI). Mice were given 3 doses of 500 mg/Kg ascorbate i.p. at 5 min, 1 day and 2 days after CCI injury (n =7/cohort). Seven saline treated mice were used as control. Both cohorts of mice were subjected to motor function analysis by rotarod test (between days 5 and 28) and cognitive function analysis (between days 21 and 23) after the injury. Mice were pretrained for 3 days before each test. Mice were euthanized on day 21 and the cortical injury (lesion) volume was estimated using cresyl violet stained serial brain sections. Post-TBI motor dysfunction was significantly reduced in the ascorbate-treated cohort compared to vehicle control (p < 0.05 by 2-way repeated measures ANOVA with Sidak’s post hoc test). Ascorbate treated cohort stayed in the platform quadrant significantly longer than the vehicle control mice in the Morris water maze test (probe trial on day 24; p < 0.05 by Mann-Whitney U test). In addition, the cortical lesion volume was also significantly smaller in the ascorbate treated mice compared with the vehicle treated mice (p < 0.05 by Mann-Whitney U test). These results indicate that epigenetic modulation by ascorbate is promoter of better functional outcomes after TBI.
137 Acute Post-Concussion Changes in Oculomotor Function From Baseline: A Case Series
Jacqueline Theis 1,2,3 ; Casey Batten 4 ; Michael Silver 2
1 Virginia Neuro-optometry, Richmond, United States; 2 University of California at Berkeley, Berkeley, United States; 3 Uniformed Services University, School of Medicine, Bethesda, United States; 4 Cedars-Sinai, Kerlan Jobe Institute, Los Angeles, United States
Recent studies have shown that concussion may lead to clinical impairment of the oculomotor pathways, and this has led to increasing research in the clinical assessment of post-concussion oculomotor dysfunction and its roles in diagnosis and treatment of concussion.
All experimental procedures were approved by the Committee for the Protection of Human Subjects (CPHS), the defined Institutional Review Board (IRB) of University of California, Berkeley, and followed the tenets of the Declaration of Helsinki. Intercollegiate athletes at the University of California, Berkeley were asked to participate in an oculomotor assessment at baseline and after a concussion. All recruited athletes were clinically determined to be free from acute or subacute concussion at the time of the baseline examination by the team physician and diagnosed with a concussion by the same team physician. All post-concussion oculomotor assessments were evaluated 0-5 days post-injury (average of 2.55 days). All baseline and post-concussion eye examinations were conducted by the same optometrist and included a comprehensive clinical test battery to assess fixation, accommodation, vergence, saccades, smooth pursuits, versions, and vestibular-ocular reflex.
A total of nine subjects (age 18-22 years; two female; seven male) were evaluated for this case series. Five of these subjects had a history of a previous concussion, with the number of previous concussions per subject ranging from 1-5, with an average of 2.0. Paired statistical comparisons of baseline versus post-concussion binary measures (fixation, saccades, pursuits, and versions) as well as nineteen continuous function variables (fusional vergence, near point of convergence, near point of accommodation, accommodative facility, and DEM subtest values) did not reveal statistically significant differences among the individual oculomotor metrics, possibly because of limited sensitivity due to the small sample size. When comparing the baseline data to clinical norms, seven of the nine subjects (77.8%) exhibited a pre-existing oculomotor abnormality. Of those seven, all had additional oculomotor abnormalities post-concussion when compared both to clinical norms as well as to their individual baseline assessments.
Changes in oculomotor function from baseline data following concussion in this case series provide clinical evidence in support of the hypothesis that concussive injury itself causes oculomotor dysfunction beyond possible pre-existing abnormalities. Without the baseline data in this case series, a number of these subjects would have been misdiagnosed post-concussion with symptoms that were based on pre-existing oculomotor abnormalities, and this could have delayed their return-to-play. Given increased use of oculomotor assessments in concussion diagnosis and management, this case series demonstrates the value of baseline assessments for increasing the accuracy and utility of oculomotor metrics in concussion management decisions.
138 Utilization of Computerized Dynamic Posturography Scores to Inform Rehabilitation Strategies in Dysfunctions of Postural Control
Refractory postural instability is among the most challenging conditions, given the complex subsystems integrating into postural control. The rehabilitation of postural dysfunction relies on various assessments and treatment modalities, both low and high-tech, to address deficits in variably weighted sensory or motor subsystem inputs. Dynamic computerized posturography is a reliable, objective metric to assess postural stability in varying testing conditions. These scores are expressed as a percentage of the theoretical limit of stability. There needs to be more information regarding the use of computerized posturography to help direct interventions. This retrospective study aims to determine the efficacy of computerized posturography in informing therapeutic strategies. Specifically, in this cohort, the percentage stability score was used to help guide the rehabilitation mechanism (feedback, feedforward, or efferent copy), as well as the laterality of the treatment application to optimally engage the activity map of the cortico-cerebellar loops underlying motor planning.
The subject population with loss of postural control included migraine headaches (23.1%), post-concussion syndrome/traumatic brain injury (37.5%), dizziness/vertigo (21.2%), dysautonomia (2.9%), post-traumatic orthostatic tachycardic syndrome (2.9%), and other brain disorders (12.5%) as the primary diagnoses. The pre-treatment posturography stability scores were compared and the direction of head rotation with the greater stability score dictated the side of individualized Cortical Integrative Therapy (CIT) treatment. Post-treatment posturography stability scores were taken over the intervention course (mean = 3.77 weeks, range 1 day to 20.29 weeks). Analyses considered the laterality of treatment, pre- and post-treatment stability scores, and the primary diagnosis.
The efficacy of the CIT treatment was indicated by over a 10% improvement (P < 0.001) in the mean post-treatment posturography stability score. Treatment ipsilateral to head rotation with the greater stability score produced near-equal results in all head positions. For example, the mean post-CIT treatment stability scores were comparable to the manufacturer’s normative data (CDP range of 69.8 to 74.9) for perturbed stability, eyes closed testing conditions. While improvement was observed with all primary diagnoses, the percent of control calculations (post-treatment score ÷ pre-treatment score X 100) indicated that patients with a primary diagnosis of dizziness/vertigo had the greatest improvement in stability scores (nearing 150% of control).
The stability score-informed intervention strategy, predicated on posturography results, optimized the efficiency of the motor planning loop. Based upon the level of compromise, the posturography stability scores can direct the laterality of treatment application in real-time. Further study of the use of dynamic posturography can identify its potential role in informing treatment strategies to improve the dysfunctional loop mechanisms.
139 Where Does Behavior Analysis Fit? Applying the Science of Behavior to All Aspects and Phases of Post-Acute Brain Injury Rehabilitation
Chris Schaub 1 ; Marla Baltazar-Mars 2 ; Paige Salinas 1
1 Collage Rehabilitation Partners, Paoli, United States; 2 Collage Rehabilitation Partners-Learning Services, Lakewood, USA
Acquired brain injuries (ABI) can result in sequelae across multiple systems and domains that disrupt and impact the individual’s interactions with the environment, thus affecting behavioral relations. The term “neurobehavioral” is used to classify a wide array of challenging excesses and/or deficits of behavior resulting from ABI, that impact or impede an individual’s progress in rehabilitation and recovery and can ultimately pose safety concerns for the individual and caregivers. This presentation will include a discussion of how evidence-based, behavior analytic principles and practices can be applied at multiple levels of treatment, e.g. to address individual behaviors, in support of interdisciplinary collaboration, and to underpin case conceptualization. Two case studies will be presented to illustrate these areas of application and involvement, including data to highlight and support efficacy.
The first case study calls attention to the significance of the behavioral history of adults with ABI, which may include challenging behaviors pre-injury that can be exacerbated post-injury and complicate treatment planning and programming. The subject of this case study had a pre-injury history of physical and emotional trauma, as well as a diagnosis of borderline personality disorder, that required both inpatient and outpatient treatment. Following an ABI in their late twenties, resulting from a rollover car accident at high speed, pre-injury repertoires and sensitivities were profoundly disrupted, and at-risk behavior occurred at high levels across all dimensions and settings during rehabilitation. The principles and practices of behavior analysis helped to inform medication adjustments that proved instrumental in stabilization efforts and guided the acquisition and generalization of replacement behaviors that established readiness for access to the community and an eventual discharge to home.
The second case study will demonstrate how behavior analysis can play a less direct, but no less valuable role, in the rehabilitation process. A married, middle-aged individual with adult children, working in a management capacity at the time of injury, sustained an ABI in a pedestrian vs. motor vehicle accident. Efforts in acute and post-acute rehabilitation were significantly impacted by sequelae such as confusion, suspiciousness, paranoia and delusionality. This required management of non-reality-based behaviors and close monitoring of medical and behavioral stability, which in the post-acute phase included disrupted sleep, disorientation, irritability, at-risk wandering/mobility, etc. Throughout the rehab process, data collection and analysis supported medication considerations and adjustments. Eventually, following stabilization, behavior analytic input helped to guide systematic efforts to generalize behavior to the community and to establish readiness for a successful return home.
These case presentations represent programming and treatment efforts to address complex neurobehavioral sequelae in an intensive, residential, post-acute rehabilitation setting. Overall, key points of discussion will include data collection, challenging behaviors, specific treatment interventions to promote stabilization and readiness, interdisciplinary collaboration, and medication-related decisions.
140 Apply Knowledge Translation to Promote Rehabilitation Outcomes for People With Traumatic Brain Injury
Xinsheng Cindy Cai 1
1 Model System Knowledge Translation Center (MSKTC), Arlington, United States
This presentation describes the knowledge translation approach that the Model Systems Knowledge Translation Center (MSKTC) and Traumatic Brain Injury Model System (TBIMS) researchers take to develop and disseminate user-friendly print and video resources to promote rehabilitation outcomes for people living traumatic brain injury (TBI). TBIMS centers provide clinical care and conduct research to improve the lives of people with TBI. The MSKTC supports TBIMS centers to conduct knowledge translation activities, identifies health information needs, and develops and disseminates information resources based on Model Systems research and available evidence. The MSKTC also collaborates with the Spinal Cord Injury Model System and Burn Injury Model System Programs to conduct similar knowledge translation activities. Both the MSKTC and the TBIMS are funded by the National Institute on Disability, Independent Living, and Rehabilitation Research, U.S. Department of Health and Human Services.
Knowledge translation is “the exchange, synthesis and ethically-sound application of knowledge—within a complex system of interactions among researchers and users—to accelerate the capture of the benefits of research” (Canadian Institutes of Health Research, n.d.). To maximize the impact of research and development activities to improve the lives of patients and families, it is important to engage stakeholders throughout the entire process (Barwick, Dubrowski, & Petrecca, 2020; Bowen, Botting, Graham, & Huebner, 2016; Nguyen et al., 2020; Parry, Salsberg & Macauley, 2015). The MSKTC collaborates with the TBIMS researchers to apply knowledge translation strategies and engage TBI survivors and their family members to develop, test, and disseminate free research-based resources.
The MSKTC has worked with the TBI model system researchers to develop resources on over 30 rehabilitation topics in multiple user-friendly formats such as factsheets, infocomics, videos, narrated slides, and podcasts. A MSKTC user feedback survey showed that 90.8% of the participants strongly agreed or agreed that MSKTC factsheets directly “apply to me or someone I know;” and 87.3% rated MSKTC factsheet quality as good or excellent. Between January 1, 2012 to October 31, 2023, over 5 million people from over 203 countries consumed the TBI contents on the MSKTC.org website. The MSKTC.org has been the go-to place for high quality rehabilitation resources for people living with TBI in the US and across the globe.
Knowledge translation can be an effective framework to help researchers better understand the needs of patients with TBI and families and develop strategies to meet their needs and improve their rehabilitation outcomes.
141 Escape Room: A TBI Case Based Interprofessional Study for OTD, DPT, and SLP Graduate Students
Rita Lenhardt 1 ; Melissa Goodman 1 ; Dianna Lunsford 1 ; Andrew T. Caswell 2
1 Gannon University, Ruskin, United States; 2 Gannon University, Erie, United States
We employed a mixed-method design (n=18) to investigate an innovative educational approach for allied healthcare professionals. The study centers around an escape room experience, where occupational therapy doctorate, doctor of physical therapy, and speech-language pathology graduate students collaboratively tackle a traumatic brain injury (TBI) case through puzzle-solving. The case was meticulously designed to address the knowledge required for interprofessional treatment of TBI. Puzzle scenarios encompassed assessments, impairments, and functional outcomes post-TBI, incorporating tools such as Rancho Los Amigos Levels of Cognitive Functioning Scale, Brunnstrom Stages of Stroke Recovery, Berg Balance Scale, aphasia symptoms, and patient management. Pre- and post-measures utilized the SPICE-R2 questionnaire, followed by structured focus group discussions. We averaged scores on the SPICE-R2 to create a full-scale composite, as well as composites for each of the three subscales for both the pre- and post-escape room surveys. We submitted the scores to a repeated measures t-test for each of the four pairs of composites and found significant increases in scores on four measures from pre-test to post-test, all ts < 3.20, all ps < .005. Qualitative analysis of narrative data obtained from focus group sessions unveiled two strong themes. Theme one: enjoyable educational approach. Participants expressed their enjoyment of the experimental learning format and this edutainment approach. Theme two: improved understanding of interdisciplinary contributions. This theme highlights the effectiveness of teamwork and the acquisition of insights into perspectives by other professions. The incorporation of case-based escape rooms as a pedagogical tool holds promise in enhancing the education of allied healthcare professionals, facilitating holistic comprehension of TBI management, and encouraging collaboration. Engaging in case-based activities during their training can potentially foster future interprofessional collaboration among healthcare practitioners. The long-term benefits to interprofessional cooperation are well documented and include favorable effects on patient outcome metrics, contentment with delivered healthcare services, and substantial cost reductions within the healthcare system. For a comprehensive evaluation of the long-term impact on knowledge acquisition related to TBI and interprofessional collaboration in clinical settings, further research in the form of a longitudinal study is warranted. This study holds potential in shaping future educational strategies in allied health professions, with applications in neurogenic disorders and beyond.
143 Treatment of Emotional Changes in an Infant With Traumatic Brain Injury: A Case Study
Theophilus Lazarus 1 ; Gershom Lazarus 1
1 Emory University, Atlanta, United States
Following the motor vehicle accident, this two-and-a-half-year-old patient was rendered comatose, with a hospital admission GCS score of 8/15 and left frontal subdural hematoma associated with mild midline shift found on CT Brain Scan. Following conservative management and recovery from coma after 4 to 6 days, patient recovered from right-sided weakness but two years later displayed residual emotional and behavioral changes such as anger, regressed emotional attachment to his mother, indiscriminate aggression to familiar family members and social-emotional interaction problems. Patient underwent weekly sessions of family integration therapy with involvement of his mother initially, and with gradual introduction of his grandmother and thereafter his siblings into the therapeutic setting for a period of 12 months, using the Infant-Toddler Social and Emotional Assessment (ITSEA) as per-and post-treatment tool to assess changes. Patient’s emotional balance and behavioral control showed improvement within the family setting the stage on the ITSEA, This paper outlines the remediation of emotional and behavioral changes in a young TBI patient in a family setting.
144 Multidimensional Health Perceptions: Preliminary Reliabilities of a Measure and Initial Characterization Among Persons in the Traumatic Brain Injury Model Systems
Shannon Juengst 1,2 ; Angelle Sander 1,3 ; Monique Pappadis 4 ; Dawn Neumann 5 ; Amanda Rabinowitz 6 ; Therese O’Neil-Pirozzi 7 ; Librada Callender 8
1 TIRR Memorial Hermann, Houston, United States; 2 UT Houston Health Sciences Center, Houston, United States; 3 Baylor College of Medicine, Houston, United States; 4 University of Texas Medical Branch, Galveston, United States; 5 Indiana University, Indianapolis, United States; 6 Moss Rehabilitation Research Institute, Elkins Park, United States; 7 Spaulding Hospital, Boston, United States; 8 Baylor Scott and White, Dallas, United States
Beliefs and perceptions about health can affect healthcare engagement, treatment adherence, and health outcomes. The Multidimensional Health Perceptions Questionnaire (MHPQ) was designed to assess: 1) health perceptions about the causes and consequences of health conditions; 2) the benefits and barriers to maintaining and improving health; 3) how to best accomplish health-related goals and control health circumstances; 4) the role of religion and/or spirituality in healthcare, perceived discrimination and its effects on care; 5) and trust in healthcare providers. Prior research in a mixed clinical and general population sample showed the MHPQ had a high content validity index of 98.1% and factor structure with seven domains. Items in seven health perceptions domains, or subscales, are averaged to produce a score ranging from 1 (low agreement) to 5 (high agreement). These subscales are: Anticipated Discrimination and Judgement, Spiritual Health Beliefs, Social and Emotional Well-being Beliefs, Confidence and Trust in Healthcare providers and Medicine, Health Self-Efficacy, Trust in Social Health Advice, and Health Literacy. The objectives of the current study are to validate the MHPQ among persons with traumatic brain injury (TBI) and characterize their health perceptions profiles to healthcare communication via a multisite study in five TBI Model Systems centers in the United States. Herein we present preliminary data from that study on the internal consistency of the MHPQ (English version) subscales, as well as descriptive characterization of these health perceptions domains among persons with chronic TBI. Forty-eight participants, at least one year after moderate-to-severe TBI, completed the MHPQ once (85.4% via electronic survey, 14.6% via telephone interview, with an average completion time of 9.2 minutes). Participants in the sample were 19-79 years old (mean=46.0) and were mostly men (64.6%), Non-Hispanic/Latino (85.4%), and White (64.6%). Internal consistent reliabilities (Cronbach’s α; >.70 considered “good”) and descriptive characterization of the domains [mean (M), standard deviation (SD), range (R)] were as follows: Anticipated Discrimination and Judgement (α=.90, M=2.1, SD=0.6, R=1.0-3.5); Spiritual Health Beliefs (α=.89, M=3.1, SD=0.8, R=1.2-4.6); Social and Emotional Well-being Beliefs (α=.79, M=3.5, SD=0.7, R=1.4-4.6); Confidence and Trust in Healthcare Providers and Medicine (α=.72, M=3.7, SD=0.4, R=3.1-5.0); Health Self-Efficacy (α=.75, M=3.9, SD=0.5, R=2.5-4.9); Trust in Social Health Advice (α=.83, M=2.8, SD=0.8, R=1.3-5.0); and Health Literacy (α=.86, M=4.1, SD=0.5, R=2.2-5.0). Findings support that the MHPQ has good to excellent internal consistency reliability across its subscales and that it captures a range of health perceptions in a relatively short amount of time. Understanding health perceptions of those with TBI is a critical first step towards personalizing communication and intervention approaches to be responsive to diverse individuals across cultures and populations. These findings can be used to provide healthcare professionals with information that can guide communications with people with TBI to be more personalized and culturally humble.
145 Red Eye: Concurrent Etiologies in a Patient With Moderately Severe Traumatic Brain Injury
Alex Rose 1 ; Michelle Andary 1 ; Stuart Yablon 1
1 Mary Free Bed Rehabilitation Hospital, Grand Rapids, United States
A 47-year-old male presented to acute inpatient rehabilitation with a moderately severe traumatic brain injury (TBI) 12 days after falling off a retaining wall. Initial neuroimaging demonstrated extensive orbitofrontal and bitemporal hemorrhagic contusions, and intraventricular hemorrhage. Other injuries included skull fracture and T12 compression fracture with resulting severe headache, back pain, right sided hearing loss, and vision problems. Physical examination was remarkable for bilateral chemosis and injected sclera. Pupils were equal, round, and reactive to light with accommodation. Extraocular movements displayed impaired lateral and dysconjugate gaze bilaterally. There was right facial weakness with injection of the right eye. Accordingly, neuro-ophthalmology was consulted. On ocular examination, a corneal ulcer was demonstrated in the right eye. After pupillary dilation, photo-retinography demonstrated impressive papilledema. RI/MRV of the brain revealed impressive bilateral temporal and frontal hemorrhagic contusions with no evidence of sinus thrombosis. The patient eventually recovered after symptomatic treatment.
146 Dimensions of Participation as Predictors of Satisfaction with Roles and Abilities after Traumatic Brain Injury: A TBI Model Systems Study
Amanda Wisinger 1 ; Robiann Broomfield 1,2 ; Shannon Juengst 1 ; Angelle Sander 1,2 ; Mark Sherer 1,2
1 TIRR Memorial Hermann, Houston, United States; 2 Baylor College of Medicine, Houston, United States
Background/Rationale
Participation refers to involvement in meaningful social roles, such as work or school, relationships, and leisure activities. Moderate to severe traumatic brain injury (TBI) is known to affect frequency of participation in these activities. However, participation frequency is not always equivalent to participation satisfaction. A better understanding of meaningful participation that reflects a person’s abilities and values may aid in identifying better targets for rehabilitation after TBI.
Main Objective
To determine the contribution of various dimensions of participation to satisfaction with social roles and abilities in a sample of individuals with complicated mild to severe TBI.
(including design, setting, sample/patient characteristics, and measures): Secondary analysis of baseline data from participants enrolled in a longitudinal intervention trial. We used data from 127 participants [mean age=35.24; 64.6%; predominately female (64.6%) and non-Hispanic White (70.1%)] who had completed a demographic questionnaire, portions of the TBI Quality of Life Scale (TBI-QOL), and the Participation Assessment with Recombined Tools-Objective (PART-O). Results: We performed a hierarchical regression to predict satisfaction with social roles and abilities using different dimensions of participation including objective (PART-O Out-and-About, Social Relations, and Productivity scores) and subjective (TBI-QOL Ability to participate in social roles and activities, Independence, and Stigma) dimensions. PART-O scores explained 17% of the variance [R2change=.17, p<.001] in satisfaction with social roles and abilities. Ability to participate in social roles and activities and Independence explained 40% of additional variance [R2change =.40, p<.001] in satisfaction with roles and abilities. Stigma explained an additional 2.3% of the variance [R2change =.023, p=.01].
Conclusions/Future Implications
How one perceives their abilities to participate and be independent, rather than the objective frequency of participation, accounted for a larger portion of the variance in how satisfied one was with their ability to participate in social roles and activities. Investigating different dimensions of participation in this population, rather than simply frequency, may result in more meaningful participation in this population.
147 Return to Driving following Moderate-to-Severe Traumatic Brain Injury: A Longitudinal Multi-Center Investigation
Thomas Novack 1 ; Yue Zhang 1 ; Jennifer Marwitz 1 ; Thomas Bergquist 2 ; Charles Bombardier 3 ; Richard Kennedy 1 ; Lisa Rapport 4 ; Candice Tefertiller 5 ; Thomas Watanabe 6 ; William Walker 7 ; Robert Brunner 1
1 University of Alabama at Birmingham, Birmingham, United States; 2 Mayo Clinic, Rochester, United States; 3 University of Washington, Seattle, United States; 4 Wayne State University, Detroit, United States; 5 Craig Hospital, Englewood, United States; 6 Moss Rehabilitation Research Institute, Elkins Park, United States; 7 Virginia Commonwealth University, Richmond, United States
To determine rates of return to driving following traumatic brain injury (TBI) and explore driving patterns and crash rates pre- and post-injury.
Adults (N = 334) with moderate-to-severe TBI enrolled by eight TBI Model System sites. A driving survey was completed during inpatient rehabilitation (for pre-injury information) and at one- and two-years post-injury.
Rates of return to driving were 65% at one-year follow-up and 70% at two-year follow-up. Return to driving was associated with higher levels of family income. Frequency of driving and distance driven were diminished compared to pre-injury as was frequency of driving in risky conditions (heavy traffic, bad weather, at night). Crash rates were 14.9% in the year prior to injury (excluding the crash that resulted in TBI), 9.9% in the first year post-injury, and 6% during the second year post-injury. Post-injury, the odds of a participant having at least one crash was decreased by 40% (95% CI: 15% - 59%) per year (p=0.005). Amongst participants who endorsed crashes in the year prior to their injury, the average number of crashes reported was 1.57 (77 crashes reported by 49 participants). At follow-up, these averages were 1.50 for the 1-year follow-up (i.e., 18 crashes for 12 participants) and 1.33 for the 2-year follow-up (i.e., 12 crashes by 9 participants). Logistic regression examining those who did or did not experience a crash did not reveal any significant findings for Year One. At Year Two the only significant finding was for participants’ time to follow commands. Those with milder injuries were more likely to experience a crash.
Consistent with prior reports, this investigation has shown that return to driving is a common occurrence following TBI, although individuals may limit their driving in terms of frequency of driving or total distances driven compared to pre-injury. Also, restriction of driving in particular situations is common. Incidence of crashes in this population is shown to be higher than population-based statistics, but this investigation highlights the critical importance of considering the possibility that, as a group, individuals who sustain a TBI are at higher risk of crash even prior to their injury. Discussion of crash risk needs to be tempered by the finding that 85% of those who returned to driving after injury did not report experiencing any crashes during follow-up interviews. Future work is needed to identify both premorbid and post-injury characteristics that may influence likelihood for adverse events while driving. Such studies will assist in development of screening tools and appropriate regulations to promote appropriate return to driving following TBI.
148 Postural Orthostatic Tachycardia Syndrome (POTS): Transcranial Magnetic Stimulation (TMS) as a Therapeutic Option.
Ananth Karanam 1 ; Rueshil Fadia 1 ; Ingrid Contreras 1 ; Ameer Chaudry 1 ; Ahmed Marabeh 1 ; Mohammed Ahmed 1
1 Kaizen Brain Center, La Jolla, United States
Postural orthostatic tachycardia syndrome (POTS) is a disorder of the autonomic nervous system which results in lightheadedness following a postural change from supine to standing upright and an associated rapid rise in heart rate. Other symptoms include physical and mental fatigue, exercise intolerance, anxiety, blurry vision, and headaches. POTS symptoms are often difficult to manage, as limited treatment options exist. Transcranial magnetic stimulation (TMS) is an FDA-approved treatment for depression and anxiety. We hypothesize that by addressing the anxiety symptoms of the POTS spectrum with TMS, other POTS symptoms may improve.
Two patients with POTS underwent TMS treatment at Kaizen Brain Center. One received Kaizen’s Accelerated TMS (KATMS) protocol (ten, 1800-pulse iTBS sessions daily; 45-minute interval between sessions) for five consecutive days and the other received the regular POTS TMS protocol (one, 1800-pulse iTBS session daily) for thirty-five consecutive weekdays. Resting state fMRI (RS-fMRI) was used to individually target the region of the amygdala most associated with anxiety in each patient. Treatment was administered at each patient’s unique resting motor threshold. HRV, heart rate, cognitive fatigue, depression, and anxiety were measured and monitored using questionnaires and electronic devices at baseline, throughout treatment, and post-treatment.
Two weeks post-treatment, the patient that received KATMS experienced a 20% decrease in anxiety (measured during a follow-up visit), a 10-point increase in HRV (measured using the Elite HRV App), and a 7.5% improvement in orthostatic intolerance (measured by the NASA-10 Lean Test). This patient will continue to be monitored. The patient receiving the regular POTS TMS protocol is four weeks into treatment and has already experienced a 13% improvement in orthostatic intolerance (measured by the NASA-10 Lean Test), as well as increased physical stamina and a rejuvenated appetite. Additional data will become available throughout this patient’s treatment and follow-ups.
TMS has shown some promise in addressing POTS symptoms.
149 Pattern of Functional and Somatic Symptoms and Symptoms of Illness Anxiety After Recent and Remote Mild Head Injuries
Mohamed Gheis 1
1 University Of British Columbia, Victoria, Canada
Functional Neurological Disorder (FND), Somatic Symptom Disorder (SSD) and Illness Anxiety Disorder are the main categories of Somatic Symptom and related conditions of the DSM 5. These conditions are recognized to occur following head trauma. Psychological factors associated with these conditions are thought to play a role in perpetuating some complications of mild head injury. The role of sensitizing physical events, such as trauma, is also thought to affect emerging psychopathologies of functional and somatic symptoms.
To evaluate potential differences in the pattern of functional and somatic symptoms and symptoms of illness anxiety in patients with mild head trauma in comparison to patients with the primary diagnosis of FND, SSD and illness anxiety disorder.
To explore whether any potential differences are related to the duration of the diagnosis.
This is a retrospective data analysis of thirty-four patients with FND-SSD and illness anxiety disorder consecutively referred to a specialist neuropsychiatric service. The patients’ somatic scales and subscales of the Personality Assessment Inventory (PAI) were analyzed and compared against a control sample of patients with FND-SSD without head trauma. These scale-subscales include overall somatic symptoms, somatization, conversion, and health concerns. The results were subsequently stratified based on the duration of the illness.
There was a statistically significant difference specifically in the conversion subscale between the groups with and without head trauma, with a mean Conversion T Score of 66 in the former and 84 in the latter (p=0.012), denoting less severe conversion processes post-head trauma but equally severe somatization and illness anxiety pathologies in patients with and without head injuries. Patients with post-trauma diagnosis tended to have a mean duration of illness approximately four years shorter than patients with FND-SSD-illness anxiety without head trauma. We were not able to establish a statistically significant association between the duration of illness and the pattern of symptoms in patients with or without head trauma. The difference between the two groups may be related to the nature of psychopathological processes rather than duration.
Conclusions: Patients with post-head injury FND-SSD may have some unique psychopathological and symptomatologic presentations of their SSD and related conditions.
151 Prevalence & Psychosocial Dysfunction in Community-Based Survivors of Traumatic Brain Injury Over Three Decades: A Randomized and Representative California Sample
Daniel Ignacio 1,2,3 ; Talin Babikian 2 ; Charles Degeneffe 1,4 ; Todd Higgins 1,5
1 Department of Rehabilitation TBI Advisory Board: Data Analytics Committee, Sacramento, United States; 2 Steve Tisch UCLA BrainSPORT Program, Los Angeles, United States; 3 St. Jude’s Brain Injury Network: HI-CARES, Fullerton, United States; 4 San Diego State University, San Diego, United States; 5 Disability Rights California, Sacramento, United States
Rates of traumatic brain injury (TBI) have traditionally relied on medical incidences to estimate prevalence. However, issues related to reporting and accessing medical care (e.g., unaware, uninsured, undocumented; Rao et al., 2020), charting medical encounters (e.g., unspecified head injury S09; Peterson et al., 2020), and diagnosis/definition (Patricios et al., 2023; Silverberg et al., 2023), have raised questions regarding the true prevalence of TBI in the community. Moreover, there have been organized efforts to move away from simple tripartite classification of TBI as mild, moderate, or severe to incorporating other severity indicators and risk stratification by outcome.
The present retrospective cohort study is an community-based surveillance methods that utilized three probability-based sampling methods for recruitment using a combination of mixed-mode random probability selection method using the United States Postal Service Delivery Sequence File (geographically stratified by population density; n = 25,000), Computer Assisted Telephone Interviewing technology (65% mobile/cellular; n = 15,000), random digit-dialing telephone recruitment of Californian participants (n = 10,000) of the National Behavioral Risk Factor Surveillance Survey, and quota-based recruitment method using registered California voter demographics.
In the total sample of California residents (N = 1,052), 42% self-endorsed a history of at least one event of any head/neck injury (M = 3.89, SD = 10.07), with 25% endorsing an associated period of lost consciousness (15% of sample). An average of three decades (M = 30.4, SD = 16.2) had elapsed since initial head trauma for the present sample, which were then compared on self-endorsements of cognitive, physical, and social dysfunction to the general California subgroup without head injury.
Ordinary least squared models were used to regress endorsements of employment difficulties, justice system involvements, and experiences with marginalized housing on endorsements of persistent depressive symptoms, generalized anxiety symptoms, neurocognitive disturbances, frequency of intoxication, presence of psychosis, and physical difficulties (e.g., ADLs) after controlling for age, gender, years of education, and income. All models significantly predicted the psychosocial outcome of interest with the head trauma estimates consistently ranking as a top predictor right next to frequency of intoxication for experiences with marginalized housing, presence of psychosis for justice system involvements, and difficulties with independently completing ADLs for employment difficulties. These findings provide initial evidence that suggests that complications associated with TBI manifest, over decades, as psychosocial dysfunction in a disease-like fashion. This may have a number of direct and indirect explanations, which in addition to a biological TBI signature, include lack of needed environmental supports (e.g., HCBS Medicaid) to manage cognitive and affective symptoms that may be ancillary to a brain injury, unfortunate community messaging (e.g., media, poor acute/post-acute medical management of symptoms and attributions), or inaccurate education about appropriate expectations and health-risk behaviors to enhance successful community reintegration following TBI.
152 Are the Symptoms of Peripartum Depression a Consequence of Undiagnosed Brain Injury From Intimate Partner Violence?
Rachel Plouse 1,5 ; Jessica Almgren-Bell 2,5 ; Nicolette McNair 1,5 ; Elsa Nico 3,5 ; Grayson Elliott 4,5 ; Brooklyn Copeland 5 ; Zofia Lowy 5 ; Edie Zusman 5,6 ; Erica Montes 5,7
1 Touro University Nevada College of Osteopathic Medicine, Henderson, United States; 2 Northwestern University, Chicago, United States; 3 University of Illinois College of Medicine at Chicago, Chicago, United States; 4 Watauga High School, Boone, United States; 5 Safe Living Space, Moraga, United States; 6 Neuroscience Partners, Moraga, United States; 7 Deborah Wilson MD and Associates Gynecology, Scottsdale, United States
Homicide is one of the leading causes of maternal mortality in the U.S. and approximately half of these deaths are associated with domestic and intimate partner violence (DV/IPV). With medical advances, maternal obstetric complications have declined in recent years, however maternal mortality continues to increase in part due to violence. Research has shown that DV/IPV increases in both incidence and severity during pregnancy. Understanding that 74% of individual DV/IPV events include injury to the head and neck, including strangulation, it is likely that many women sustain peripartum concussions and abuse induced brain injuries (AIBI). Abuse induced brain Injury often presents with a depressed mood, difficulty concentrating, sleep problems, emotional lability, and/or fatigue, similar to the presentation of peripartum depression (PPD). Given the similarity of clinical symptomatology, are a subset of women with PPD actually suffering from an AIBI? In this review, we explore the association between peripartum depression, domestic violence, and brain injury.
A PubMed search was performed from January 2016, the publication date of the U.S. Preventive Services Task Force Recommendation for postpartum depression screening, to July 2022 for keywords prenatal, peripartum, or postpartum depression combined with domestic and/or intimate partner violence. 120 articles met criteria for review to assess available prevalence data and associations between PPD and DV.
The mean prevalence of prenatal, peripartum, and postpartum depression was 25.0%, 17.7%, and 21.1% respectively, with an overall average of 23.5% and range of 5.8-50.5% across all groups. An average of 19.6% women experienced DV/IPV during pregnancy. Of the 98 papers that commented on DV/IPV, 73 (74.5%) found that DV/IPV was strongly associated with PPD. No papers commented on head injury, brain injury, or concussion surrounding pregnancy.
Our results show that approximately one in five women experience DV/IPV during pregnancy. While 74% of DV/IPV victims report head injury, to date, no studies have investigated DV/IPV-associated brain injury during the peri- or post-partum period. Given the significant similarities between AIBI and PPD symptoms, there is a critical need for research on the prevalence of peripartum abuse induced brain injury potentially including screening for peripartum brain injury with the current practice of peripartum depression assessment.
153 Corpus Callosum (CC) Integrity and Associated Neurocognitive Functions After Pediatric Brain Injury
Daniel Ignacio 1,2 ; K. C. Bickart 1,5 ; E. L. Dennis 3 ; Aliyah Snyder 4 ; Robert Asarnow 5 ; Christopher Giza 1,5 ; Anne Brown 1 ; Talin Babikian 1,5
1 Steve Tisch UCLA BrainSPORT Program, Fullerton, United States; 2 St. Jude Brain Injury Network: HI-CARES, Fullerton, United States; 3 University of Utah, Salt Lake City, United States; 4 University of Florida, Gainesville, United States; 5 UCLA Health, Los Angeles, United States
Moderate/Severe Traumatic brain injury (msTBI) often results in diffuse injury to white matter (WM), particularly to the corpus callosum (CC) (Dennis et al., 2015). Linking this CC vulnerability to cognitive outcomes has been more difficult given that CC function has been understudied and cognitive outcomes following msTBI are heterogeneous. This is an especially important problem for younger patients whose brains are in a period of ongoing rapid development. One indicator of CC function, which may mediate a link between CC structural integrity and cognitive outcomes, is interhemispheric transfer time (IHTT) (Ellis et al., 2016). Within pediatric msTBI samples, a bimodal distribution in IHTT exists, revealing a subgroup of children with either IHTT times comparable to healthy controls or significantly slower (Dennis et al., 2017). The IHTT subgroups demonstrate divergent trajectories of CC structural recovery as measured by Mean Diffusivity (MD) in the CC, an index of structural integrity measured by Diffusion Tensor Imaging (DTI). Both slow and normal IHTT subgroups showed worse MD in the CC in the post-acute timeframe after msTBI, but only the normal IHTT subgroup normalized MD in the CC at the chronic timeframe. Although in that study, IHTT subgroups did not differ on a broad index of cognitive functioning, another study showed that slow IHTT predicted worse cognitive outcomes post-acutely in pediatric msTBI (Moran et al., 2016). In this study, we aimed to reconcile these findings by testing whether IHTT could predict not only divergent MD recovery trajectories after pediatric msTBI but also more discrete cognitive outcomes.
In this study, 34 survivors of pediatric msTBI were compared to 45 well-matched controls (e.g., community members, uninjured siblings) on measures of IHTT, DTI, and standardized neurocognitive tasks of working memory. The sample was evaluated as early as one month (M = 4.18, SD = 2.24) following msTBI (baseline) and re-evaluated as far out as 24 months (M = 17.16, SD = 2.34). ANCOVA models with years of parental education, age, and gender as covariates revealed that trajectories (interaction) of structural WM improvement versus disorganization in CC projections (i.e., frontal, temporal, parietal), as measured by MD, matched the working memory scaled scores (age-adjusted) of the subgroups, F (2, 70) = 3.22, p = .046, ηp2 = .084. Neurocognitive and brain imaging biomarkers as stratified by an IHTT biomarker collected at an early stage of recovery post-msTBI resemble one another at baseline and one-year follow-up, suggesting that significantly higher MD is consistently associated with significantly poorer letter number sequencing at both time points for Slow IHTT, but not Normal IHTT. Future research will assess associations with adaptive behaviors, family factors, and functional outcomes to potentially identify which children may need more environmental/community support following msTBI in service toward successful reintegration.
154 Improving Post-TBI Participation: The Community-Based Neuropsychological Rehabilitation Approach
Yingying Liu 1 ; Daniel Ignacio 1 ; Elvina Chow 1 ; Ren Mizuhara 1 ; Samandeep Mankatala 1 ; Phu Uong 1
1 St Jude Brain Injury Network HI-CARES, Fullerton, United States
Reduction in participation in various activities (e.g., social, household) is a common functional outcome of traumatic brain injury (TBI) and is associated with lower quality of life (Goverover et al., 2017). The Community-Based Neuropsychological Rehabilitation (CBNPR) Model (Judd & DeBoard, 2009) emphasizes the importance of not only addressing individual deficits but also facilitating socio-environmental changes to improve the participation of individuals with neurological conditions during neuropsychological rehabilitation (NPR). Existing studies examined the effects of individual factors (e.g., mental health, pain, cognition) and socio-environmental factors on post-TBI participation separately (Kersey et al., 2020); research that investigates the interaction between the two is needed.
the present study aims to 1) determine the effect of Insurance Provider on post-TBI Participation; and 2) examine the interaction effect between Insurance Provider, Depression, Anxiety, Physical Difficulties, and Neurocognitive Symptoms on Participation.
CATBI registration packets that include relevant symptoms checklists, Mayo-Portland Adaptability Inventory Participation Index (M2PI), and Community Integration Questionnaire (CIQ) were collected from 229 survivors with TBI between 20 to 89 years old (M = 50.87, SD = 15.46). The participation of participants with Medicaid, Medicare, Medi/Medi, Commercial/Employer-provided/Private insurance was examined by a one-way MANOVA. A one-way MANCOVA was conducted to test the interaction effect of Insurance Provider, Depression, Anxiety, Physical Difficulties, and Neurocognitive Symptoms on Participation.
The combined Participations (i.e., M2PI and CIQ) of survivors with different Insurance Providers were significantly different (p < .05). Participants with Commercial/Employer-provided/Private insurance scored significantly lower on M2PI than participants with Medicare and Medi/Medi. There was a statistically significant five-term interaction between Insurance Provider, Depression, Anxiety, Physical Difficulties, Neurocognitive Symptoms (p < .001). However, after controlling for the covariates, the only significant difference lies between the CIQ scores of individuals with Medi/Medi and Commercial/Employer-Provided/Private insurance.
The significant five-term interaction between Insurance Provider, Depression, Anxiety, Physical Difficulties, and Neurocognitive symptoms supports the CBNPR model in terms of incorporating both individual-health and environmental factors to promote participation post TBI. The present study underscores the pivotal role of insurance providers in shaping post-TBI participation outcomes. Notably, participants covered by Commercial/Employer-provided/Private insurance experienced less perceived obstacles for participation. Insurance transformation, such as Enhanced Care Management, that extends beyond traditional healthcare to include community-based resources could facilitate the reintegration process following TBI. Future research should also investigate other socio-environmental factors to better understand their interaction with individual-health factors. The findings also highlight the need to incorporate physical, mental, and cognitive health support (e.g., by resource facilitation) in NPR to promote participation of individuals with disadvantaged socioeconomic status and disabling conditions.
155 Framing Racial Disparities within Mild Traumatic Brain Injury from an Ecological Systems Perspective: A Systematic Literature Review of Risk Factors for Black Athletes
Sydney Wing 1 ; Joshua Caiquo 1 ; Chanté Butler 2 ; Talin Babikian 1
1 UCLA Steve Tisch BrainSPORT Program, Los Angeles, United States; 2 Medical College of Wisconsin, Milwaukee, United States
There is an apparent phenomenon where Black adult and pediatric athletes face disparities within their care, treatment, and recovery from mild traumatic brain injury (mTBI), or concussion while playing their sport. Previous literature has demonstrated that Black athletes who have experienced sports-related concussions (SRC) are less likely to receive formal concussion diagnoses, and subsequent referrals to tertiary concussion care. Additionally, Black athletes have demonstrated lowered access to clinical care, concussion knowledge and symptom identification, as well as intention to report injury and overall poorer psychosocial outcomes following injury. Overall, the current body of literature has identified that race is a salient social determinant of health for general mTBI and SRC – the axis of privilege and marginalization associated with race, can impact presentation for care, receiving diagnoses, symptom reporting and tracking, and the process of recovery or return to baseline functioning. However, these empirical findings do not elucidate why nor how these various factors compound. Thus, there is a need for a framework to conceptualize and create a clear theory for how these factors compound. Particularly, there is a need to encapsulate how sociocultural experiences of power, access, and biases can impact Black athletes experiencing mTBI. The authors use Ecological Systems Theory (EST; Bronfenbrenner, 1979) to create a novel organization-systems model of identified findings and theory that demonstrate and support racial disparities within general mTBI and SRC. A comprehensive literature search was employed to identify recent (published ≤10 years) empirical studies and theoretical perspectives on racial disparities in mTBI for Black patients and athletes. Using EST as a framework, the literature review examines and organizes these findings within the context of (1) historical and sociopolitical events and systems, (2) sociocultural ideologies and policy, (3) indirect and (4) direct community and cultural factors, as well as (5) person-centered social experiences and identities (social determinants of health). Ultimately, the organizational structure provides a clear thread on how macro-level policy and perceptions, can impact micro-level clinical care and decision-making for Black athletes and their experiences with mTBI.
156 Restoring Efficient Sleep After TBI: A Randomized Controlled Trial of a Guided Computerized CBT-I Intervention
Molly Sullan 2 ; Lisa Brenner 1 ; Adam Kinney 1,2 ; Kelly Stearns-Yoder 2 ; Daniel Reis 2 ; Emerald Saldyt 2 ; Jeri Forster 2 ; Nazanin Bahraini 2
1 University of Colorado, Aurora, United States; 2 Department of Veterans Affairs, Rocky Mountain MIRECC, Aurora, United States
Individuals with a history of moderate-severe traumatic brain injury (TBI) experience a significantly higher prevalence of sleep-related problems including insomnia compared to members of the general population. While individuals living with TBI have been shown to benefit from traditional insomnia interventions (e.g., face-to-face [F2F]), such as Cognitive Behavioral Therapy for Insomnia (CBT-I), multiple barriers exist (e.g., cost, insufficient numbers of adequately trained healthcare providers, limited transportation, patient perceptions) that limit access to such F2F evidence-based treatments. Although computerized CBT-I (CCBT-I) has been shown to be efficacious in terms of reducing insomnia symptoms, individuals with moderate-severe TBI may require support to engage in such treatment.
This is an RCT of a guided CCBT-I intervention for individuals with a history of moderate-severe TBI and insomnia. The primary outcome is self-reported insomnia severity, pre- to post-intervention. Exploratory outcomes include changes in sleep misperception following CCBT-I and describing the nature of guidance needed by the Study Clinician during the intervention.
Data collection is underway, with a notable number of individuals already having completed the trial. With the grant ending (Spring 2024) it is expected that sufficient data will be collected to present feasibility/acceptability data, as well as initial outcome findings.
This study represents an innovative approach to facilitating broader engagement with an accessible and readily available no-cost evidence-based online treatment for insomnia among those with a history of moderate-severe TBI. Findings will provide evidence for the level and nature of support needed to implement guided CCBT-I. Moreover, should results suggest efficacy, this study would provide support for a strategy by which to deliver guided CCBT-I (with support) to individuals with a history of moderate-severe TBI.
157 Investigating Seasonal Affective Disorder in a Population With Traumatic Brain Injury From the Ottawa Vista Centre for Brain Injury Services Using the SPAQ
Justine Tubin 1
1 Ottawa Vista Centre Brain Injury Services/University of Ottawa, Ottawa, Canada
Up to 40% of patients will suffer from 2 or more psychiatric disorders following traumatic brain injury (TBI)6. A positive correlation between Axis-1 affective disorders, such as major depressive disorder (MDD) and TBI has been identified by a growing amount of literature1. Seasonal affective disorder (SAD) is characterized in the DSM-V as a subtype of MDD, including at least 2 episodes of MDD in the last 2 years demonstrating evident seasonal variability and is marked by full remission at the end of the season (mostly associated with winter)2. However, there’s limited data investigating the relationship between TBI and SAD. Interestingly, proposed mechanisms for the pathophysiology of both SAD and TBI involve dysregulation of serotonergic pathways in the CNS3. Studies have shown that patients with SAD have an upregulation of SERT in the winter compared to healthy controls, causing less available 5-HT in the synaptic cleft and TBI has been associated with as much as a 17% loss of serotonergic neurons4,8,9. Using the Seasonal Pattern Assessment Questionnaire (SPAQ), a widely used screening tool for SAD, this study aims to determine if there is a significant difference in the results of the questionnaire in a population with TBI from the Ottawa Vista Centre for Brain Injury Services compared to a control group5. More specifically, we will be comparing the mean Global Seasonality Score (GSS) between the groups using ANOVA as well as the number of positive screens for SAD in each group. A positive screen for SAD is a GSS of 11 or greater with a score of “moderate” or higher on question 17 of the SPAQ7. Exclusion criteria include actively taking anti-depressants as well as ETOH abuse3. The control group consists of students at the University of Ottawa who volunteered to fill out the SPAQ. We hope the results of this study will help direct best practice guidelines in caring for people post-TBI by helping to understand what cognitive and psychiatric illnesses can impact their independent functioning by acting as a barrier to reintegration into the community.
158 Evolving Practices: 2023 Updates to Pediatric Concussion Care
Jennifer Dawson 1 ; Nick Reed 2 ; Andree-Anne Ledoux 1,3 ; Roger Zemek 1,3
1 Children’s Hospital of Eastern Ontario Research Institute, Ottawa, Canada; 2 University of Toronto, Toronto, Canada; 3 University of Ottawa, Ottawa, Canada
Clinical guideline recommendations for pediatric post-concussion care and management have undergone major updates in 2023. The Living Guideline team includes 48 concussion clinical experts, researchers, and individuals with lived experience from across the US and Canada. This team collaborates on the Living Guideline for Pediatric Concussion Care (PedsConcussion) project to review new evidence and update the 80+ clinical recommendations, clinical algorithms, return-to-sport/activity, and return-to-learn/school concussion protocols as the evidence evolves. The best evidence from 2023 was collated and assessed, and new critical papers were shared in a living evidence map (EPPIreviewer). A quorum of 88% or more of the 48 experts voted on each update and consensus at 97-100% agreement was attained for all updates that were implemented. Significant updates to guideline recommendations involve revisions to the steps of the return-to-sport and activity protocol, highlighting the benefits of aerobic exercise in concussion treatment. Activities that pose no risk of sustaining a second concussion should be gradually resumed after 1-2 days even if mild symptoms are present. These symptoms may worsen mildly during activity as tolerated. Definitions of relative rest, mild to moderate intensity aerobic exercise, and mild symptom exacerbation have been harmonized with the Amsterdam International Consensus Statement on Concussion in Sport. Additionally, updates have been made to the timing of medical clearance and the definitions associated with it. The new return-to-school protocol reinforces the importance of promptly resuming school activities that do not have a risk of falling or being hit on the head, as tolerated, with the provision for academic accommodations if needed. It also emphasizes that the return to non-contact and low-risk school activities should not be restricted if the individual is effectively tolerating cognitive activities. The importance of restricting screen time in the early stage of recovery is now supported by strengthened evidence. Any activity with a risk of head impact or falling must still be entirely avoided until reassessment and medical clearance are obtained. All patients with a diagnosed concussion are recommended to return for a repeat medical assessment 7-10 days after the initial diagnosis and patients should be referred to specialized care with an interdisciplinary concussion team if post-concussion symptoms do not resolve by 2-4 weeks. Youth at increased risk of prolonged recovery require immediate referral. For more detailed information, including consensus voting details and complete recommendations, the pedsconcussion.com website serves as a valuable resource. Dissemination and implementation of these updates is essential to continue to improve outcomes for all pediatric patients with concussion. The collective efforts of the Living Guideline team highlight a commitment to continually advancing and improving pediatric post-concussion care practices.
159 Are We Putting the Best Interests of Patients First When Planning and Delivering Community-Based Care After Brain Injury?
Judith Gargaro 1 ; Matthew Galati 2 ; Nora Cullen 3
1 UHN-Kite Research Institute, Toronto, Canada; 2 Scarborough Family Health Team, Toronto, Canada; 3 Hamilton Health Sciences, Hamilton, Canada
Traumatic Brain Injury is the leading global cause of disability. In Canada alone, 2% of the population lives with a TBI and many survivors require significant ongoing support and rehabilitation post injury in order to return to functional independence and achieve meaningful goals. In recent years, holistic treatment for TBI has become an increasingly popular approach to provide the brain with the best possible environment to heal. Some key lifestyle modalities, which may support a recovering brain, include nutrition, exercise, mindfulness, cognitive activity, good sleep and limiting harmful exposure. Although some of these interventions have evidence for supporting rehabilitation post TBI, the effects of combining these modalities into a larger program have not yet been studied. Furthermore, vital allied health care services needed to provide well-rounded care are costly for most individuals and persons who are members of traditionally marginalized groups are overrepresented in the population who do not have access to this type of care. Consequently, many patients are left untreated and lost to follow-up after their acute injury has been addressed and stabilized. This in turn leads to a tremendous burden on our healthcare system, as we know earlier and intensive treatment post TBI is important to mitigate long term disability.
To pilot a novel primary care clinical model designed to address gaps in TBI care and provide effective, equitable access to care,
The novel primary care model was developed through review of published evidence for key lifestyle modalities, which are the cornerstones of holistic care: nutrition, exercise, mindfulness, cognitive activity, good sleep and limiting harmful exposure. The model was refined through consultation persons with lived experience and clinicians to ensure feasibility and relevance to address current gaps in care. The model was piloted utilizing government funded regulated health professionals using a Family Health Team framework to promote continuity of care following discharge from acute care facilities.
A structured model of care was developed that included quality indicators to assess process, outcome, and acceptability of care. This care model is consistent with the Ideal Care Pathways that is currently being implemented In Ontario. All patients referred to the care team were included in the pilot, regardless of severity of injury and personal circumstances. All had access to community based rehabilitative care with medical oversight that otherwise would not have been available to them. Patients reported high satisfaction with the model of care and the progress towards their identified goals.
This pilot represents an example of how holistic Family Health Team care can be effectively and efficiently provided in the community to support patients’ goals of living meaningful lives after brain injury.
160 Chronic Brain Injury: A Holistic Intake Assessment Tool for Clinical Practice
Thomas Watanabe 1 ; Alan Weintraub 2 ; Jacob Koffer 3 ; Morgan Pyne 4 ; Flora Hammond 5
1 Drucker Brain Injury Center MossRehab, Elkins Park, United States; 2 University of Colorado School of Medicine, Aurora, United States; 3 MossRehab, Elkins Park, United States; 4 James A Haley Veterans Hospital, Tampa, United States; 5 Indiana University School of Medicine, Indianapolis, United States
Chronic brain injury is associated with specific neurological, medical and psychological conditions that may decrease an individual’s functional capacities, their ability to live successfully, return to school or vocational endeavors, affect their relationships with others, and alter an individual’s quality of life. Over the last decade, numerous clinicians and researchers have emphasized the importance toward implementing a Chronic Care Model to manage the long term and often lifelong sequelae of Brain Injury. 1 A model for service delivery was originally introduced by Masel and DeWitt 2 who stressed the importance of systematic Brain Injury care that extends beyond the acute and inpatient rehabilitation phase of management. This would include proactive expectant management of the lifelong needs for patients, families, and caregivers. timely and appropriate rehabilitation services, and addressing concomitant psychosocial issues such that individuals can maximize their capacities for community integration and societal participation. A formal and agreed upon standard of practice to evaluate and/or manage the complex needs of brain injury individuals and how those needs may dynamically change over time does not exist.
Aims: As part of the BeHEALTHY 3 initiative, this feasibility project aligns with the goals of advancing a chronic disease management model for individuals with brain injury, their caregivers and health care providers. Following a systematic literature review, a BeHEALTHY working task force developed an easy to administer holistic and comprehensive intake tool for clinicians to utilize regardless of their specialty when managing the sequelae of chronic brain injury. Key concepts incorporated into the tool include:
1. A shared responsibility among the patient/family/caregivers and health care professionals emphasizing self-advocacy.
2. Promoting proactive and goal-oriented management plans aimed at meeting the dynamic and individualized needs of patients, families, and caregivers.
3. Emphasize collecting relevant preinjury and post injury medical and psychosocial history including mental health.
4. Emphasize the importance of evaluating an individual’s sensory-motor, neurocognitive, behavioral, social, community integration and societal participation status.
Components of the intake tool entails a Pre-visit assessment obtaining salient demographic information, relevant injury history, past medical and surgical history, medications, allergies, past hospitalization’s, current health care providers, family, educational and social history and a functional review of systems. This pre-visit tool will prepare the clinical providers for an in-person, holistic, targeted and time efficient initial intake that can be followed by personalized components of a general medical exam, neurological exam and “problem-specific and/or targeted functional exam.” Utilizing qualitative research methods for tool validation, reproducibility, comprehensiveness and ease of use, this can equip clinicians with a systematic tool useful in developing both a short- and long-term integrated management plan that can serve as a foundation for lifelong management.
161 Pharmacologic Use of PRN Medications for Agitation: “Examining the Weekend Effect”
Erin Miller 1 ; Mitch Sevigny 2 ; Stephanie Agtarap 3 ; Alan Weintraub 4 ; Robin Wackernah 5
1 HCA Florida Memorial Hospital, Jacksonville, United States; 2 Craig Hospital, Englewood, United States; 3 Craig Hospital, Englewood, United States; 4 University of Colorado School of Medicine, Englewood, United States; 5 Craig Hospital, Englewood, United States
To determine if PRN antipsychotic or benzodiazepine medication administration is increased over the weekends as compared to weekdays.
Retrospective chart review
Acute inpatient neurorehabilitation hospital
Patients admitted for moderate-severe traumatic brain injury and prescribed antipsychotics or benzodiazepines for agitation and/or aggression on an as-needed basis between 1900 Friday evenings and 0700 Monday mornings.
Main Measures
Primary outcome was the comparison of average daily number of administrations and daily medication dose between weekly and weekend PRN antipsychotic or benzodiazepine administration for agitation or aggression.
Fifty-Seven patients with a total of 4,485 PRN administrations were included in the chart review. On the weekdays, benzodiazepine had an average prn dose of 4.3 mg and antipsychotics had an average prn dose of 78.7 mg. The weekend days showed an average prn dose of 3.5 mg and 82.6 mg for benzodiazepine and antipsychotics respectively. Statistically significant differences were found with benzodiazepines where there were larger doses administered on the weekdays when compared to the weekend days on average. No statistical differences were found with the antipsychotic doses.
There was no significant difference found between weekday and weekend administration with prn medications indicated for aggression/agitation to support higher antipsychotic or benzodiazepine use on the weekends. Further research to explore the consequences of and the key components of a deleterious negative “weekend effect” whereby no formal rehabilitative therapies occur on the weekends is warranted for programs treating persons with traumatic brain injury.
162 DTI Imaging of Decreased Fractional Anisotropy Demonstrating a Correlation With the Dysregulation of Emotions
Nickalus Yasunaga 1 ; Mohammed Ahmed 1
TBI leads to emotional dysregulation which is the inability to control one’s emotions (Weis et al., 2022). Diffuse Axonal Injury (DAI) is a hallmark of TBI which can be screened using Diffusion Tensor Imaging (DTI) sequencing in MRI. The exact neural correlate is unclear. Some earlier studies suggested axonal injury in the anterior limb of the internal capsule involving the white matter tracts. (Floeter et al., 2014)
Does DAI in the genu of the corpus callosum based on MRI with DTI sequence lead to emotional dysregulation in patients with TBI?
This paper aims to support the claim that there is a pathological problem associated with emotional dysregulation rather than it being due to an underlying mood or personality disorder (Parvizi et al., 2009).
We analyzed clinical records of patients between 2017-2023 at Kaizen Brain Center who were diagnosed with TBI related emotional dysregulation by a TBI specialist. We found 18 patients who had abnormal DTI on their MRI and then probed their clinical notes for emotional dysregulation based on the physician’s impression.
Of the 92 TBI patients, 18 were found to have DAI in corpus callosum and diagnosed with emotional dysregulation. However, we did find that abnormalities in the genu were not exclusive to this correlation. Decreased FA in the splenium and other areas of the body also correlated with emotional dysregulation.
Abnormal DTI results due to DAI in corpus callosum may be a neural correlate of emotional dysregulation found in TBI Affective Disorder.
163 High School Football Players’ Knowledge and Attitude Regarding Concussions Contribute to a Staggering Occurrence of Unreported and Unrecognized Brain Injury
Grayson Elliott 1,2 ; Diego Martell 2,3 ; Edie Zusman 2,4
1 Watauga High School,Boone, United States; 2 Safe Living Space, Oakland, United States; 3 Yale University, New Haven, United States; 4 Neuroscience Partners, Oakland, United States
Concussions are a prevalent medical condition well recognized within professional and collegiate American football athletes, but less is known about the implications of concussions within adolescent populations. Recent studies indicate that approximately 67,000 high school football athletes are diagnosed with a concussion every year. Even with the high numbers of concussions diagnosed, high school football players may not adequately recognize or report the signs and symptoms of a concussion. Unrecognized and unreported brain injury should be of concern to health care providers given that adolescents experience longer and more diffuse cerebral swelling following neurological trauma compared to an adult population. Understanding the occurrence of concussions in high school American football athletes enables health care providers and coaches to properly assess adolescent athletes, while cultivating safer playing environments.
The primary objective is to determine the occurrence of undiagnosed head trauma resulting from participation in high school football. The secondary objective is to understand why high school football athletes fail to recognize and report experiencing concussion-like symptoms.
A five question anonymous online survey tool was shared with a cohort of high school varsity football players at a single institution. The survey includes questions regarding the participant’s concussion history, presence of unreported concussion symptoms, and questions allowing respondents to further elaborate on their attitude and knowledge of concussion symptoms.
Of 38 surveys shared, 81.6% (31 responses) were returned. While 90.1% of survey respondents reported having experienced concussion-like symptoms following a hit to the head during a game or practice within the most recent season, only 18.2% responded that they immediately left the field of play or sought medical attention. 12.9% of survey respondents were evaluated and diagnosed with concussion within the most recent football season. While 57% of survey respondents felt unable to determine if they may have had concussion symptoms, 35% of respondents who felt comfortable identifying their own concussions symptoms did not report them to a coach or trainer. The primary reason provided for not reporting recognized concussions symptoms was “fear of not immediately returning to the field of play.” Twenty-eight percent of study respondents reported that they experience prolonged concussion symptoms, lasting several weeks or even months.
While the majority of high school football players surveyed reported experiencing concussion-like symptoms, for many players the symptoms were not recognized and if recognized were not reported resulting in few players receiving standard medical treatment such as placement into a stepwise concussion protocol. Understanding why knowledge and attitudes about a concussion affects an individual’s willingness to seek medical attention immediately following head trauma is crucial to developing new narratives of concussion diagnostics, establishing general concussion awareness, and preventing long term health consequences.
164 Temporal Assessment of Hippocampal Susceptibility to Traumatic Brain Injury
Diana Gonzalez-Duque 1 ; Efrain Buriticá 1 ; Martha Escobar 1 ; Gabriel Arteaga 1 ; Melany Ayala 1 ; DVictor Moreno 1
1 Universidad Del Valle, Cali, Colombia
Traumatic Brain Injury (TBI) constitutes a public health problem around the world that annually claims thousands of lives and is associated with extensive disability and great economic impact; it is defined as the sudden alteration of the brain tissue or its physiological functions as a result of the influence of external forces that exceed the resistance of the tissue. The objectives of this work were to temporally characterize the tissue, behavioral and molecular changes of the hippocampus after moderate TBI in Wistar rats as well as to determine if early management with minocycline can reverse and/or improve the consequences of the injury. It was found that diffuse TBI is associated with neuronal loss in the hippocampus, alterations in the axons and myelin sheaths, as well as reactive gliosis in all subregions, with increased activity of the matrix protease MMP9. Early intervention with minocycline achieved a positive effect on the reduction of neuronal dead, axonal degeneration, and neurofilament compaction with a very slight effect on MMP9 activity. This work is expected to contribute to the knowledge of the phenomena associated with the temporal pathophysiology of diffuse TBI in the hippocampus and further open up the possibilities of pharmacological intervention.
167 The BEST Approach for Cognitive Retraining After Medical Neurorehabilitation: An Educational Model for Building Skills, Independence, and Community
Michelle Wild 1
1 Brain Education Strategies & Technology, Laguna Hills, United States
Brain Education Strategies and Technology, Inc. (BEST) is a nonprofit organization started by Michelle Ranae Wild to share the theories she has developed over more than 30 years as a professor in Coastline Community College’s Acquired Brain Injury program to help people with acquired brain injury (ABI) retrain their brains, learn compensatory skills, and rebuild their lives. Through its unique, educational model, BEST provides people with ABI a curriculum and a community to help them continue to make progress after completing medical neurorehabilitation. BEST recognizes that ABI recovery is life-long and thus meets people at any stage of their journey.
BEST offers free webinars, multi-week workshops, facilitated discussions, and asynchronous online courses that are designed to teach people with ABI, their family members, and clinicians (1) how ABI can create physical, cognitive, behavioral, and emotional challenges and (2) practical strategies they can personalize to help them navigate those challenges. In the process, BEST provides participants with a supportive community where they can feel less isolated and learn from the experiences of others.
BEST introduces cognitive and technology topics through interactive webinars that include instruction, polls, monitored live chats, and Q&A sessions. The webinars are followed by facilitated “after hours” discussions on Zoom. These peer collaboration sessions are much-loved by BEST regulars and newcomers alike, because they reduce isolation and allow participants to feel like members of a safe, supportive community where they can share how the concepts taught in the webinar relate to their lives.
BEST workshop series address webinar topics in a more comprehensive, hands-on manner. They include a multi-week curriculum delivered through interactive, weekly Zoom sessions that feature breakout groups, whole class discussions, Q&A sessions, live chats, and the integration of technology tools as appropriate. Each session begins with an iterative review, designed to reactivate and consolidate learning from prior sessions. As with webinars, participants receive presentation slides, supplemental worksheets, and session recordings so they can engage and re-engage with the content at their own pace.
Program topics include cognitive rehabilitation, neurofatigue, executive function, self-regulation, problem solving, learning styles, communication, self-efficacy, initiation, and many more. BEST also teaches people with ABI how to use technology to compensate for ABI deficits. The BEST Suite of apps helps people organize their lives and apply the strategies they learn in BEST programs.
Data from participant evaluations indicates that BEST’s programs are indeed meeting participants’ needs. More than half have attended 6 or more BEST programs. A staggering 96% rate information they learned in the webinar as “very useful,” with 97% saying they learned something they can use in daily life.
This session will share the BEST approach to cognitive/neurorehabilitation and the feedback from participants.
168 Could Abuse-Induced Brain Injury and Strangulation Be a Physiological Risk Factor for Developing Multiple Sclerosis?
Larkin Stephenson 1,4 ; Rachel Plouse 1,2 ; Edie E. Zusman 1,3
1 Safe Living Space, San Francisco, United States; 2 Touro Medical School Nevada, Henderson, United States; 3 Neuroscience Partners, Moraga, United States; 4 Northeastern University, Boston, United States
Traumatic Brain Injury (TBI) is a commonly identified condition in athletes, veterans, and car accidents, however, TBI in the domestic violence and intimate partner violence (DV/IPV) population is critically underrecognized. Current literature estimates 74% of these violent events result in mechanical trauma to the head, neck, and face. Additionally, half of these injuries further result in an ischemic brain injury caused by strangulation. Repeated head trauma has been linked to an increased risk of developing multiple sclerosis (MS), predominantly in cohorts of women and children. Approximately 38%-63% of women with MS report prior experiences of abuse, and abuse may lead to earlier onset of illness and higher relapse rates. There are no identified interventional studies that address DV/IPV-induced TBI in the MS population.
The primary objective is to propose abuse-induced brain injury and strangulation as a physiologic risk factor for developing MS.
A PubMed search of articles September 2014 to November 2023 using key words multiple sclerosis in conjunction with traumatic brain injury, head injury, concussion, and/or strangulation as well as domestic violence and/or intimate partner violence retrieved ten papers. Articles were reviewed for proposed mechanisms and connections between TBI, MS, and DV/IPV.
While no papers met all inclusion criteria, there is a significant epidemiological overlap between populations at risk of DV/IPV-induced TBI and those who develop MS. There is support in the literature for physiological mechanisms of increased intracranial pressure from venous outflow occlusion with strangulation, paired with the activation of astrocytes, degradation of tight junctions and a loss of blood-brain barrier (BBB) integrity seen with TBI. Disruptions of the BBB from central nervous system (CNS) injury proteins, including S100B, MBP, NSE, GFAP, UCHL-1, and NfL, enter the bloodstream and trigger an immune antibody response. Accumulation of TBI-induced proteins is linked to an increased risk of developing neurological diseases. Serum antibody IgG is released as a secondary immune response following IgM, which the injured CNS is unequipped to defend against following TBI-induced BBB degradation. Similar to ischemic brain injury, 24.8% of ischemic stroke patients have shown elevated oligoclonal IgG bands. Elevated levels of IgG have been established as a risk factor for MS. In TBI, the level of IgG has been associated with the severity and frequency of ischemia and TBI.
The literature suggests that TBI and venous outflow obstruction from strangulation may lead to inflammation thus activating the immune system and increasing the likelihood of developing the clinical syndrome of multiple sclerosis. This evidence-based theory highlights the probable link between abuse-induced brain injury and the risk of developing MS. Further research is necessary to establish this relationship and begin education, prevention, and care programs.
169 Lack of Accessible Health and Rehabilitation Services in Rural Counties Impacts Community Integration Following Traumatic Brain Injury
Elly O’Bryant 1,2 ; Ren Mizuhara 1 ; Daniel Ignacio 1
1 Saint Judes Brain Injury Network: HI-CARES, Fullerton, United States; 2 California State University, Chico, Chico, United States
Incidences of traumatic brain injury (TBI) are responsible for over one million emergency department visits a year, and rehabilitation costs in the United States may well exceed $100,000, depending on the observed population and injury severity (Dismuke et al., 2015). A national inpatient survey found that the majority of TBI-related hospitalizations for urban (99.6%) and rural (80.3%) residents were located at an urban hospital (Daugherty et al., 2022). When comparing health care costs, individuals living in rural areas experience higher costs yet receive fewer services than urban residents (Graves et al., 2018). Additionally, individuals living in rural areas are at risk for poorer outcomes following TBI due to a lack of accessible resources (e.g., hospital care, neurosurgical interventions, and post discharge rehabilitative services) and must often utilize transportation services to travel to their providers (Brown et al., 2019). The disparities between rural and urban post-TBI care and rehabilitative services are a public health issue, and the overall stress due to lack of accessibility and decreased support can lead to further psychological, cognitive, and physical post-concussive symptoms. For the present study, data was collected from a representative and randomized sample of California residents in collaboration with California Department of Rehabilitation’s TBI Advisory Board and The California State Survey Panel, and from individual assessment packets from 2 out of 12 California Association for Traumatic Brain Injury (CATBI) sites in Northern and Southern California who provide services to improve the independent living and community reintegration for survivors of brain injury. The findings indicate that individuals living in rural counties engage in less community participation than those residing in urban counties. These differences can be explained by how accessible outpatient and rehabilitative services are in an individual’s residence. People with TBIs living in rural areas face many barriers as they reintegrate into their community, especially a lack of knowledge about programs and resources. The disparities between rural and urban post-TBI services and community integration can be diminished by increasing access to transportation and information about resources that are available.
171 Intersection of Traumatic Brain Injury and POTS (Postural Orthostatic Tachycardia Syndrome): Single Center Case Series
Sydney Myers 1,2,3 ; Jaewon Choi 1,4 ; Edie Zusman 1,5
1 Safe Living Space, San Francisco, US; 2 University of California, Los Angeles, Los Angeles, USA; 3 Lawrence Livermore National Laboratory, Livermore, USA; 4 University of California, Berkeley, Berkeley, USA; 5 Neuroscience Partners, Sacramento, USA
While traumatic brain injury (TBI) is a recognized cause of postural orthostatic tachycardia syndrome (POTS), the prevalence of POTS among TBI patients is unknown, and the etiology of POTS following TBI is not well understood. POTS is characterized by orthostatic symptoms including dizziness, lightheadedness, fainting, and near syncope, but is also associated with cognitive dysfunction/attention deficits, sleep issues, headache, and anxiety. This collection of symptoms is attributed to dysfunction of the autonomic nervous system and can be seen in a subset of patients following TBI. Without a Tilt Table Test (TTT), POTS symptoms are often considered post-concussive and/or psychological leaving the underlying medical condition undiagnosed, with potential for increased concussion recovery time and decreased quality of life for TBI patients.
The goal of this retrospective case review is to determine the prevalence of POTS in a series of refractory post-concussion symptom patients, 6 months or more post injury, who were evaluated at a single interdisciplinary TBI and Concussion Clinic.
A retrospective chart review of 55 consecutive TBI patients evaluated between October 2022 and November 2023 was conducted. The patient’s gender, mechanism of injury, and symptoms associated with POTS were assessed.
Sixty-five percent (36) had orthostatic issues characteristic of POTS including dizziness, lightheadedness, orthostasis, or near syncope. Additional symptoms often associated with POTS were also observed. Eighty nine percent (49) of patients had cognitive dysfunction/attention selectivity issues, 73% (40) had headaches, 67% (37) had anxiety, 56% (31) had sleep issues, 45% (25) had balance issues. Sixty-one percent of the patients with orthostatic symptoms were female.
Symptoms associated with POTS were seen in the majority of patients with refractory post concussive symptoms. These findings suggest that patients with refractory post concussive symptoms should be routinely evaluated for POTS. Conversely, given the correlation between TBI and POTS, patients with POTS should be assessed for signs and symptoms of TBI as many in this demographic may have unrecognized brain injury including sports injuries and abuse induced brain injury/strangulation. Further research is warranted on the intersection of TBI and POTS.
172 Optimal Positioning of Mandibular Occlusion: A Possible Important Factor to Reduce Head Concussive Injuries.
Denise Gobert 1 ; Gregg Ueckert 2 ; Mark Strickland 3 ; Eric Linberg 1 ; Leeda Rasoulian 1 ; Bevyn Bryson 1 ; Andrew Long 1 ; Olivia Siciliano 1 ; Ashley Aurit 1 ; Clint Kennedy 1 ; Dilyn Lyle 1 ; Conlin Penland 1 ; Meredith Moreland 1
1 Texas State University, Round Rock, United States; 2 Ueckert Dentistry, Austin, USA; 3 Strickland Physical Therapy Associates, Austin, United States
Risk management of concussive blows to the head continues to be a challenge during several occupational and sports activities. Recent evidence suggests that there may be a significant negative relationship between neck strength/endurance and risk levels for concussion. (Collins 2014, Chavarro-Nieto 2021)
To evaluate immediate differences in neck strength and endurance with and without customized, optimal mandibular interocclusal appliance positioning.
Cohort Study Design with repeated testing.
University Outpatient Physical Therapy Clinic
12 healthy participants (6 females/6 males) ages >18 yrs. were sampled by convenience. Inclusion criteria: normal cervical spine AROM, no recent head or neck trauma or surgery. Exclusion criteria: active cervical pain and any cervical spine postural abnormalities. Participants were fitted with a customized, mouth guard to properly align occlusal “bite” by a dentist while an orthopedic specialist, physical therapist assessed neck extension/flexion/rotation strength using the MicroFit® pressure gauge (Newtons) and grip strength using the Jamar hand dynamometer (kg/ psi). Last of all, timed isometric, cervical muscle contraction for neck flex/extension endurance was measured in seconds. Participants were tested in each activity without and then with the interocclusal appliance in place. Quality of life outcomes including the Neck Disability Index (NDI) and Disability Assessment of Shoulder & Hand (DASH) were used as psychosocial factors or covariates in all analyses.
Statistical Analysis
SPSS (vs.26.0, IBM Inc.) was used for descriptive statistics, paired T-Tests and 2-way repeated measures ANOVA to explore differences at p = 0.05 with a Greenhouse-Geisser correction factor. Multivariate mixed effects models were constructed to assess separate and combined influences of gender and condition on strength and endurance outcomes.
There were significant differences found in strength based on Condition (F (1) 8.834, p =.018) and Position (F (1,8) = 134.226, p < 0.001). Significant differences were also observed in grip strength without vs with the MG (t (8) = -6.378, p < 0.001). There were also significant differences in endurance in both directions: Neck Flex Endurance Test-Supine, (t (8)= -2.334, p= 0.048), Neck Ext Endurance Test-Prone, (t (8)= -4.078, p = 0.002).
Preliminary results indicate a significantly increased neck strength and endurance with a jaw interocclusal appliance for optimized positioning compared to no appliance use.
Clinical Relevance
Suggested gains in cervical spine strength and endurance may assist concussion risk management for contact sports at all levels. Preliminary results also suggest the need for further research about how proper jaw alignment might optimize neck muscle strength over a broad spectrum of subjects regardless of sex, ages or athletic ability.
173 Prevalence of Accommodative and Vergence Dysfunction in Collegiate Varsity Athletes With and Without History of Concussion
Jacqueline Theis 1 ; Casey Batten 4 ; Michael Silver 2
1 Virginia Neuro-optometry, Richmond, United States; 2 University of California at Berkeley, Berkeley, United States; 3 Uniformed Services University, Bethesda, United states; 4 Cedars Sinai - Kerlan Jobe, Los Angeles, United States
Oculomotor dysfunctions, including convergence and accommodative disorders, are common in up to 80% of patients with acute concussion and 30-40% with chronic concussion. However, convergence and accommodative disorders are not specific to concussion, and they can also be present from development/non-traumatic origin. While there is a high (20-30%) prevalence of oculomotor dysfunctions in the non-concussed clinical pediatric population, prevalence of oculomotor dysfunctions in collegiate athletes is currently unknown, and this imposes strong limits on conclusions that can be drawn from studies of visual and vestibular-oculomotor dysfunction following suspected concussion. This study collected baseline oculomotor data to assess the presence of vergence and accommodative dysfunctions in collegiate varsity athletes with and without a history of concussion.
All experimental procedures were IRB approved. Intercollegiate varsity athletes at the University of California, Berkeley were asked to participate in a comprehensive oculomotor assessment. Athletes were asked about their concussion history and were cleared from prior concussions by the team physician prior to baseline testing. All baseline oculomotor examinations were conducted by the same optometrist.
Baseline data were collected on a total of 179 athletes. Athletes were assigned to groups either with (n=63, 17 females, 45 males) or without (n=116, 32 females, 85 males; control group) a history of a diagnosed concussion. Refractive correction of either glasses or contact lenses were worn by 22.9% (n=41) of the sample. Participants reported whether they had received at least one eye examination with an eyecare provider in their lifetime (52.5%; n=94) and whether they had received an eye examination within the last year (35.75%; n=64).
Baseline binary variables (proportions) were compared using Fisher’s exact test, and continuous variables were compared using the non-parametric Wilcoxon rank sum test. There were no statistically significant differences between groups for any of the oculometric measures. Notably, when compared to clinical norms, there were multiple clinically relevant oculomotor dysfunctions at baseline, including abnormal near cover test (11.2%), reduced fusional divergence at near (15.1%), reduced fusional convergence at near (29.1%), reduced near point of convergence (6.2%), reduced near point of accommodation (13.4%), and reduced accommodative facility (20.1%).
There were no statistically significant differences between athletes with or without a history of concussion for convergence or accommodative (dys)functions. Athletes exhibited clinically relevant levels of accommodative and vergence dysfunction at baseline, and 47.5% of the sample had never had a comprehensive eye exam in their lifetime. This lack of information regarding baseline oculomotor function in athletes confounds possible baseline abnormalities with those resulting from suspected concussions. This, in turn, can impact their education, sports performance and pull-from-play and return-to-play decisions.
174 Differentiation of Cervical, Oculomotor, and/or Vestibular Dysfunction: Using Clinical Testing to Optimize Evaluations and Rehabilitation Triage Post-Concussion COVA Study Group
Jacqueline Theis 1,2,3 ; Sara Etheredge 3 ; Edie Zusman 4 ; Cristen Kaae 5 ; Kristen Cadigan 5 ; Vera Pertsovskaya
1 Virginia Neuro-optometry, Richmond, United States; 2 Uniformed Services University, School of Medicine, Bethesda, United States; 3 Concussion Care Centre of Virginia, Richmond, United States; 4 Neuroscience Partners, Moraga, United States; 5 Kaiser Permanente Medical Center, Vallejo, United States
Patients who suffer from traumatic head injury are at risk of developing traumatic brain injury, traumatic whiplash injury, or both. The majority of these patients present to multiple disciplines of providers including pediatricians, internal medicine, sports medicine, and emergency medicine with nonspecific complaints including headache, dizziness, nausea, brain fog, and anxiety. The majority of these patients self-resolve within 4-6 weeks however approximately 10% will have persistent symptoms for months, years, or indefinitely. Tools like the VOMS (Vestibular Oculomotor Screening Assessment) have been instrumental in screening for visual-vestibular disorders to allow for referral to vestibular physical therapy. However, not all patients fully resolve with standard vestibular physical therapy and may worsen if the etiology is cervical or oculomotor.
We present a case series of 15 patients who presented to a transdisciplinary brain injury clinic to be evaluated by neuro-optometry and orthopedic physical therapy after failing vestibular physical therapy post-concussion. The cases have been reviewed with a distinguished national cohort of concussion experts including neuro-optometry, neurosurgery, orthopedic and vestibular physical therapy to propose a novel clinical assessment. Cervical-Oculomotor-Vestibular Assessment (COVA) that could help all providers differentiate cervical, vestibular, and oculomotor dysfunctions to provide more appropriate referrals to rehabilitation specialists and specialty providers.
The subset of patients with refractory or worsening post concussive symptoms following vestibular physical therapy benefit from a clinical assessment based on simple, subjective and objective testing which can be done chairside or bedside based on the nuances of neuro-anatomy and pathophysiology of whiplash vs traumatic brain injury vs traumatic brainstem injury.
The cervical, oculomotor, and vestibular systems are intimately connected neuro-anatomically and are often underlying causes of common post-traumatic symptoms like headaches, nausea, dizziness, and brain fog. By varying the methodology of oculomotor testing from current clinical screening assessments, clinicians may be better able to identify the underlying trigger for symptoms, and triage to the appropriate provider and rehabilitation type.
175 Primary Care Provider Follow-up and 90-Day Outcomes Following Community Discharge Among Older Medicare Beneficiaries With Traumatic Brain Injury (TBI) in Texas
Monique Pappadis 1,2 ; Ioannis Malagaris 1 ; Yong-Fang Kuo 1 ; Natalie Leland 3 ; Janet Freburger 3 ; James Goodwin 1
1 University of Texas Medical Branch, Galveston, United States; 2 Brain Injury Research Center at TIRR Memorial Hermann Hospital, Houston, United States; 3 University of Pittsburgh, Pittsburgh, United States
Primary care providers (PCP) are essential during the transition from hospital to community, but little is known about whether having a primary care visit will improve post-hospital outcomes among older adults with TBI. Therefore, we examined the predictors of PCP follow-up with an established PCP or any PCP, and its association with 90-day emergency department (ED) use and all-cause hospital readmission, using Cox regression models based on competing risks (death and hospice admission) and censoring (until loss of Medicare coverage, by 90th follow-up day, or by December 31, 2019). The interaction effect of visiting any PCP or established PCP with discharge destination (i.e., home, home health, skilled nursing facility (SNF), inpatient rehabilitation facility (IRF), nursing home, other facility) was also examined. Using 100% Texas Medicare data, we identified 27,480 older patients aged 66 and older hospitalized for TBI from January 1, 2014 and discharged by September 30, 2019, and returned home within 90 days following hospital discharge. Prior to the TBI, about 70% of older patients had an established PCP. By 90 days following discharge home, 79.5% of patients with an established PCP saw their provider, whereas 37% of patients without an established PCP saw any PCP. Patients who were more likely to see any PCP within 90 days after discharge home were female, of Hispanic ethnicity, discharged home from an IRF, or had an established PCP. Patients aged 70-84, of Black race, Medicare/Medicaid dual eligible, with primary TBI diagnosis, and discharged from an IRF were more likely to see their established PCP within 90 days from discharge home. Patients who saw any PCP and were discharged home were less likely to have an ED visit (HR=0.81; CI: 0.76-0.87) and hospital readmission (HR=0.87; CI: 0.81-0.95). Increased likelihood of ED service utilization was found among patients who visited any PCP and were discharged from either a SNF (HR=1.12; CI: 1.02-1.22) or IRF (HR=1.17; CI: 1.06-1.28). Those who visited any PCP and discharged home from an IRF were also more likely to be readmitted (HR=1.16; CI: 1.04-1.30). Patients with a previously established PCP who saw the same PCP and were discharged home following hospitalization were less likely to have an ED visit (HR=0.82; CI: 0.75-0.89) and be readmitted (HR=0.84; CI: 0.77-0.92). Older patients who visited their established PCP and were discharged from an IRF were more likely to have an ED visit (HR=1.16; CI: 1.04-1.29) and be readmitted (HR=1.14; CI: 1.00-1.29, p=0.046). In summary, for older patients with TBI who did not receive post-acute care, having a PCP was associated with better post-hospital outcomes, while those who received post-acute care may need care transition support. The role of continuity of primary care plays in TBI outcomes needs to be further explored.
176 The Impact of REM Sleep in Memory After a Traumatic Brain Injury and the Importance of Considering Sex a Biological Variable
Stefanie Howell, Grace Griesbach
1 Centre for Neuro Skills, Tarzana, United States; 2 David Geffen School of Medicine, UCLA, Los Angeles, United States
Sleep-wake disturbances (SWD) are common following TBI, and often extend into the chronic phase of recovery. Such disturbances in sleep can lead to deficits in executive functioning, attention, and memory consolidation, which may ultimately impact the recovery process. We examined if SWDs following TBI were associated with morbidity during the post-acute period. Particular attention was placed on the impact of sleep architecture on learning and memory. Because women are more likely to report SWDs, we examined sex as a biological variable. We also examined subjective quality of life, depression, and disability levels. Data was retrospectively analyzed for fifty-seven TBI patients that underwent an overnight polysomnography. Medical records were reviewed to determine cognitive and functional status during the period of the sleep evaluation. Consideration was given to medications, as a high number of these are likely to have secondary influences on sleep characteristics. Women showed significantly higher levels of disability and reported more depression and lower quality of life. A sex dependent disruption in sleep architecture was observed, with women having lower percent time in REM sleep. An association between percent of time in REM and better episodic memory scores was found. Melatonin utilization had a positive impact on REM duration. Improvements in understanding the impact of sleep-wake disturbances on post-TBI outcome will aid in defining targeted interventions for this population. Findings from this study support the hypothesis that decreases in REM sleep may contribute to chronic disability and underlie the importance of considering sex differences when addressing sleep.
177 Coma Recovery Scale–Revised is Better to Be Performed in an Upright Position Rather Than a Lying Position in Patients With Disorders of Consciousness
Bei Zhang, Andrew DaCosta 2,3 ; Aya Bou Fakhreddine 4 ; Stephanie Stroever 4 ; Katherine O’Brien 2,3,5
1 Division of Physical Medicine and Rehabilitation, Department of Neurology, Texas Tech University Health Sciences Center, Lubbock, USA; 2 TIRR Disorders of Consciousness Program, TIRR Memorial Hermann, Houston, United States; 3 Department of Physical Medicine and Rehabilitation, McGovern Medical School, University of Texas Health Science Center at Houston, Houston, United States; 4 Division of Biostatistics, Clinical Research Institute, Texas Tech University Health Science Center at Houston, Lubbock, United States; 5 H. Ben Taub Department of Physical Medicine and Rehabilitation, Baylor College of Medicine, Houston, United States
It is unclear whether the assessment position of patients with Disorders of Consciousness (DoC) affects the result of Coma Recovery Scale–Revised (CRS–R). Currently, only the arousal protocol is required to facilitate patients’ engagement and accurate scoring. The study aims to investigate the impact of positioning on the CRS-R total score. This is a retrospective study analyzing a total of 1470 CRS-Rs performed on 232 patients in four different positions, i.e., lying in bed (Bed), sitting at the edge of a mat (Mat), sitting in a wheelchair (Wheelchair), and up in a standing position (Standing), in an acute inpatient rehabilitation setting. A conditional random coefficients multi-level model was used to examine the changes of CRS–R based on the position, accounting for repeated measurements within subjects and the variability introduced by different raters. The cohort contains 65.1% male, age 37.4±16.2, and includes primarily traumatic brain injury (47.0%) and hypoxic-ischemic brain injury (26.7%). Each patient underwent an average of 10.3±6.8 CRS–Rs. The mean CRS–R total score was 7.4±4.1. The average arousal protocol used was 3.0±2.1 per session. We found that the CRS–R total score was significantly associated with the assessment position. Using the Bed as reference (controlling age, gender, etiology, number of arousal protocol used, and days post-injury), patients assessed in the Mat, Wheelchair, and Standing had estimated 1.3-, 1.1-, and 1.5-point increases in the CRS–R total score, respectively (P = 0.002, 0.008, and 0.050; overall, upright vs. lying, 1.2-point increase, P = 0.003). The CRS–R total score was found significantly associated with the number of arousal protocols used. However, it was estimated that with every additional administration of the arousal protocol, the CRS–R total score decreased by 0.8-point (P < 0.001). We further identified that, using the Bed as reference, the number of arousal protocol used was not associated with the assessment position, with and without controlling the abovementioned factors. Our results demonstrated that the increased use of arousal protocols indicated lower arousal level at baseline, thus, poorer CRS–R performance. The increased use of arousal protocols did not serve to improve CRS–R performance. The assessment position appears to be more important. Patients scored significantly higher in an upright position. One point change could potentially make a diagnostic difference in the CRS–R. The finding may be related to generally improved physical and cognitive functionality in an upright body position, rather than to arousal only. The arousal protocol needs to be applied as indicated regardless of the assessment position. In conclusion, CRS–R is better to be performed in an upright position rather than a lying position in patients with DoC.
178 Value of Group Holidays for Clients With Catastrophic Injury
Maggie Sargent
I arrange ski trips for adults and children, safaris in Africa, surfing in the UK, and camping in Europe. We have captured in pictures on our poster our clients in different environments and facing new challenges, and we have feedback from our clients confirming the benefit they and their families obtain from these experiences. The group holidays increase their confidence and self-esteem, and clients have discussed with me that they gained an insight into their own conditions from the experience and how ‘It was the first time I felt normal’ and, ‘I realized that I could function in a group and enjoy myself’ and are part of the story of how they progressed.
We saw physiotherapy benefits from surfing in the UK and in Africa. We took a brain-damaged, ventilated client skiing in France, showing there are no physical boundaries. We facilitate children’s trips that show us the value of activities with siblings e.g. a child going down an advanced run in contrast to the rest of the family, who are on basic runs! These trips demonstrate that such activities benefit both family and carers.
It is not necessary to go overseas for some clients: similar benefits can be obtained from a surfing holiday in Devon, UK. The safari was a very positive experience, ranging from snorkeling and shark cage diving, to surfing. We saw animals from an accessible open-top vehicle and hippos from a boat and took a group to a special-needs orphanage, and they raised money for the children and we then took the children to the beach for what was their first outing. It became difficult to tell who were clients, guides, support workers, or family.
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Abstracts of the 3rd annual meeting of the canadian concussion network/réseau..., genetic variants and persistent impairment following mild traumatic brain..., abstracts of the 4th annual canadian concussion network/réseau canadien des..., the prevalence of traumatic brain injury among young offenders in custody: a..., screening for traumatic brain injury: findings and public health implications.
- Open access
- Published: 11 June 2024
Video livestreaming from medical emergency callers’ smartphones to emergency medical dispatch centres: a scoping review of current uses, opportunities, and challenges
- Carin Magnusson 1 ,
- Lucie Ollis 1 ,
- Scott Munro 1 ,
- Jill Maben 1 ,
- Anthony Coe 2 ,
- Oliver Fitzgerald 2 &
- Cath Taylor 1
BMC Emergency Medicine volume 24 , Article number: 99 ( 2024 ) Cite this article
Metrics details
Timely dispatch of appropriate emergency medical services (EMS) resources to the scene of medical incidents, and/or provision of treatment at the scene by bystanders and medical emergency lay callers (referred to as ‘callers’ in this review) can improve patient outcomes. Currently, in dispatch systems worldwide, prioritisation of dispatch relies mostly on verbal telephone information from callers, but advances in mobile phone technology provide means for sharing video footage. This scoping review aimed to map and identify current uses, opportunities, and challenges for using video livestreaming from callers’ smartphones to emergency medical dispatch centres.
A scoping review of relevant published literature between 2007 and 2023 in the English language, searched within MEDLINE; CINAHL and PsycINFO, was descriptively synthesised, adhering to the PRISMA extension for scoping reviews.
Twenty-four articles remained from the initial search of 1,565 articles. Most studies were simulation-based and focused on emergency medical dispatchers’ (referred to as ‘dispatcher/s’ in this review) assisted video cardiopulmonary resuscitation (CPR), predominantly concerned with measuring how video impacts CPR performance. Nine studies were based on real-life practice. Few studies specifically explored experiences of dispatchers or callers. Only three articles explored the impact that using video had on the dispatch of resources. Opportunities offered by video livestreaming included it being: perceived to be useful; easy to use; reassuring for both dispatchers and callers; and informing dispatcher decision-making. Challenges included the potential emotional impact for dispatchers and callers. There were also concerns about potential misuse of video, although there was no evidence that this was occurring. Evidence suggests a need for appropriate training of dispatchers and video-specific dispatch protocols.
Research is sparse in the context of video livestreaming. Few studies have focussed on the use of video livestreaming outside CPR provision, such as for trauma incidents, which are by their nature time-critical where visual information may offer significant benefit. Further investigation into acceptability and experience of the use of video livestreaming is warranted, to understand the potential psychological impact on dispatchers and callers.
Peer Review reports
In recent years, the rapid uptake in ownership of smartphones (with integral video technology) has influenced communication in healthcare. Many healthcare providers worldwide now offer remote patient consultations via video, in particular following the COVID-19 pandemic [ 1 ].
In the emergency medical dispatch context, timely and effective dispatch of appropriate emergency medical services (EMS) resources is critical, in order to save lives [ 2 ]. However, emergency medical dispatch response has been described as the weakest link in the EMS response chain [ 3 ]. There are several different dispatch systems around the world, commonly categorised into two different systems; the criteria-based dispatch (CBD) system, and the Medical Priority Dispatch system (MPDS) [ 4 ]. Both systems rely almost exclusively on audio and verbal information from the incidents, to determine the severity of the incident and inform dispatch decision making. Evidence suggests that dispatch and resource allocation is often inappropriate (either under or over resourced) resulting in additional costs and unfavourable clinical outcomes [ 5 ]. Similarly, support and instructions to bystanders and medical emergency callers (referred to as ‘callers’ in this review) to provide help at the scene also relies predominantly on verbal (usually telephone) communication. In recent years, the uptake of smartphone ownership means that visual as well as verbal information could be used at the scene. Video livestreaming (also referred to as ‘video’ in this review) from callers’ smartphones has the potential to facilitate the timely dispatch of appropriate EMS resources and improve treatment/care delivered by bystanders and callers, and to potentially assist callers, for example when carrying out CPR [ 6 ].
Previous reviews of use of video livestreaming have focussed exclusively on its use for out-of-hospital cardiac arrest (OHCA), in particular the use of video-instructed dispatcher-assisted bystander cardiopulmonary resuscitation (CPR) (V-DACPR). These reviews have reported that dispatcher video-instructed CPR significantly improved the chest compression rate compared to the audio-instructed method [ 7 ] and that V-DACPR significantly increased the return of spontaneous circulation (ROSC) and survival to hospital discharge [ 8 ]. A further review [ 9 ] examined the scope and nature of research publications on the topic of video emergency calls but did not synthesise or thematically analyse the findings in a way that could inform practice. None of the aforementioned reviews have examined the experiences of patients, healthcare staff or callers use of video livestreaming from medical incidents. This review therefore aimed to address these deficiencies by focusing on the current uses, opportunities, and challenges for using video livestreaming from callers’ smartphones to emergency medical dispatch centres (EMDCs).
Review question
The aim of this review was to map and synthesise the published international literature regarding video livestreaming (streaming of video in real time) between callers’ smartphones and EMDCs. The review questions were:
What are the current uses for video livestreaming from callers’ smartphones to emergency medical dispatch centres?
What are the challenges and opportunities when using video livestreaming between emergency medical dispatch centres and callers’ smartphones?
Arksey and O’Malley’s [ 10 ] five-stage scoping review method was used to guide the review. A scoping review synthesises and maps the literature in a particular area of practice, highlights the different types of evidence and identifies knowledge gaps in an emerging field. We chose to do a scoping review, as there had been limited research concerning video livestreaming in the dispatch context. There was a need to get an initial understanding of the topic area to understand the scope and nature of current evidence. We adhered to the PRISMA extension for scoping reviews [ 11 ]. The PRISMA-ScR checklist can be found in Supplementary File 1 . The review protocol has not been published.
Stage 1: identifying the research question
We started by identifying the research question following initial scoping of the evidence. Due to limited number of relevant articles, it was agreed to include all types of clinical focus (such as trauma or CPR), as well as both real-life and simulation-based studies. We also agreed to focus on medical emergency lay callers only as this was our primary interest.
Study types and characteristics
This review included quantitative, qualitative, and mixed methods primary research studies, published in peer-review journals in any country in the English language between 2007 (introduction of smartphone video technology) and 2023. Reviews were excluded. Both ‘real-life’ and simulation studies were included due to the limited evidence base available for real-life studies only, and also due to the opportunity for learning from simulation settings, but papers were synthesised, and results are presented separately.
Stage 2: identifying relevant studies
MEDLINE; CINAHL and PsycINFO databases were searched in February 2023. Key words in context to the title/abstract were identified. Key terms included emergency medical dispatch, emergency medical services, air ambulance, cell phone, smartphone, telemedicine, video, livestreaming, and relevant Medical Subject Headings (MESH) using Boolean operators. An example Medline string can be found in Supplementary file 2 .
Stage 3: study selection/screening
Once the search was completed, citations were uploaded to Zotero, the reference management software and duplicates were removed resulting in 1565 papers. Title and abstracts were screened, and articles removed if they were not directly relevant to video livestreaming or dispatch. This resulted in 58 remaining articles. There was much literature covering specific video-diagnostic equipment such as laryngoscopy and other video devices used in the pre-hospital and emergency care environment, that was not relevant to this study. These were removed. Full-text review of the remaining articles ( n = 58) were independently assessed (CM & LO) for eligibility using the inclusion/exclusion criteria. There was 100% agreement regarding inclusion/exclusion of these articles. In total, 24 studies were included (see Fig. 1 Prisma flowchart).
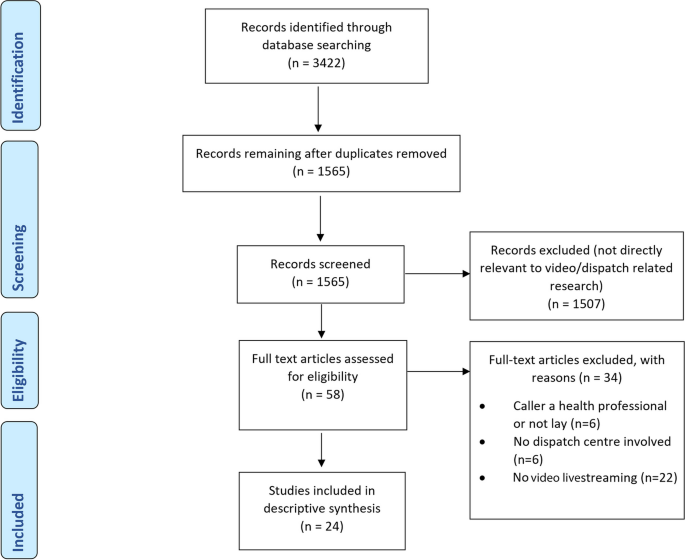
PRISMA flow diagram 19
Review inclusion & exclusion criteria
Inclusion criteria included:
Studies concerning use of video livestreaming between a lay caller and an emergency medical dispatch centre (or participant acting in the role of emergency medical dispatcher/call taker in simulation studies) AND
Studies where the caller was a lay person (or acting in the role of a lay person in simulation studies) AND
Studies set in an emergency medical dispatch centre or simulating that setting.
Exclusion criteria included: caller being a health professional or not a lay caller (such as the police); research not involving emergency dispatch or an emergency medical dispatch centre; or did not involve video livestreaming.
Stage 4: charting the data/data extraction
Data were extracted independently by the first author (CM all articles) and repeated by one of two research paramedic co-authors (AC and OF, each randomly allocated 50% of articles) using a bespoke data extraction tables in Word (see Tables 1 and 2 ). These were designed to comprehensively capture generic study information (i.e., aims, objectives, study settings/country etc.), as well as key study characteristics such as design/methodology, and information about the study population. We also extracted information about whether the study was real-life or simulation, whether the video communication was one- or two-way, study clinical focus, and reported key challenges and opportunities to using video livestreaming. Data extraction was compared between the three reviewers and any differences were discussed and agreed between reviewers. We did not appraise the methodological quality of the articles, consistent with scoping review guidance [ 10 ].
Stage 5: collating, summarising and reporting the results
The findings were synthesised descriptively (real-life and simulation separately) according to Arksey and O’Malley’s [ 10 ] framework using thematic analysis to answer the review questions. Key themes were identified (and sub-themes). Results were organised and mapped according to the review questions (opportunities and challenges) for each theme. This process was iterative and involved updating data extraction tables and additional re-reading of the papers to make sure that all relevant data relating to the themes or main themes had been included in the analysis.
In total, 24 studies were included (see Fig. 1 , PRISMA Diagram). Nine of the studies were based on real-life clinical practice (see Table 1 ) and fifteen were simulation studies (see Table 2 ). Ten of the fifteen simulation studies used comparison groups (nine used audio/voice calls and one study suboptimal light and sound conditions) as part of the research design. Only two of the real-life studies [ 14 , 15 ] used comparison groups, both focussing on dispatcher-assisted CPR clinical outcomes. In total, half of the included 24 studies used comparison groups and the other half relied on less robust study designs and used self-report data only. Most studies were conducted in Norway ( n = 6) and South Korea ( n = 6), followed by Belgium ( n = 2), Denmark ( n = 2), England ( n = 2), Germany ( n = 2). One study was conducted in each of the following countries: Canada [ 17 ], Israel [ 30 ], Japan [ 25 ] and Taiwan [ 33 ]. Nine of the studies reported using one-way video (caller not able to see the dispatcher), seven studies used two-way video communication (caller and dispatcher could see each other) and the remainder did not report mode of use (see Tables 1 and 2 ). Most included studies were quantitative ( n = 17), four were qualitative, and three were mixed methods. The design, source characteristics and results are summarised in Table 1 (real-life studies) and Table 2 (simulation studies). The results of the thematic synthesis of findings are organised under four main heading, and key findings are presented in Fig. 2 (below).
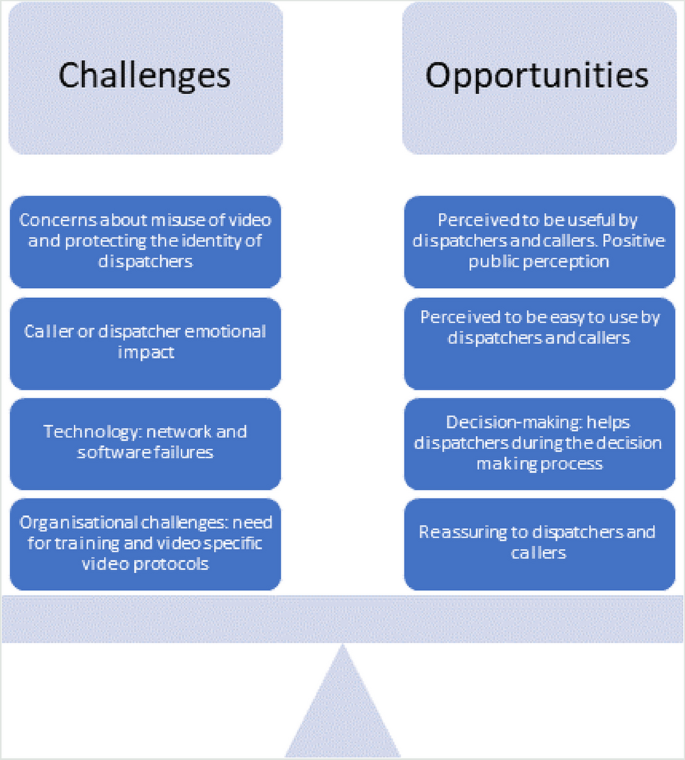
Challenges and opportunities to using video livestreaming
Current uses of video livestreaming between callers and emergency medical dispatch centres
In the nine real-life studies, three focussed on CPR only [ 14 , 15 , 16 ] and six had a broad clinical focus (with limited further detail included in the papers) ranging from trauma incidents to lower priority calls (see Table 1 ). These studies were undertaken in various countries including Norway, where a study had piloted video in four medical emergency medical communication centres [ 13 ]; Denmark [ 6 ], where dispatchers were able to decide when to use video streaming, and reported that video was used more frequently in cases with sick children or unconscious patients; and Seoul, South Korea, video was added to their dispatcher-assisted CPR programme in 2017 [ 15 ].
In the 14 simulation studies, ten focused on dispatcher-assisted CPR (see Table 2 ), two on incidents simulating foreign bodies in mouth (used as simulation scenario) [ 25 , 29 ], and two investigated the feasibility of using video call to guide lay people using automated external defibrillators (AEDs) following simulated cardiac arrests [ 20 , 34 ]. The majority of simulation studies focussed on adult casualties, but two used paediatric cases [ 25 , 31 ].
Emergency medical dispatchers’ perspectives: opportunities and challenges
Over half of the papers ( n = 14/24) included some information (though few had this as the study focus) on the views of the dispatchers (or those acting as dispatchers in simulation studies) about video livestreaming. Perspectives reported in these papers were overwhelmingly positive, with dispatchers reporting video livestreaming to be acceptable and easy to use, reporting various benefits of video livestreaming including its use as an aid for emergency medical dispatch decision-making, video dispatcher-assisted CPR improving caller technique when performing CPR, more accurate patient assessment and/or supporting better/more effective decision-making. Challenges included the potential emotional impact of seeing traumatic incidents that dispatchers would normally only ‘hear’, the potential for additional fatigue and workload, and concerns about the potential misuse of video were also reported. There was no evidence provided in any of the papers to support these concerns other than perceived potential impact. However in one real-life Norwegian study [ 18 ] dispatchers referred to colleagues having visual impressions that they were not prepared for.
Real-life studies
Clinicians reported that video ‘consultations’ (following medical emergency calls) were superior to audio only [ 12 ], easy to use [ 26 ], and that they wanted to use video in the future, especially for dispatcher-assisted CPR [ 23 ]. Dispatchers reported finding video livestreaming extremely useful [ 6 ], that it improved communication with callers [ 13 ], and also provided dispatchers with general reassurance in their decision-making [ 13 ]. Additional benefits included the ability to make a more thorough assessment of patients’ needs compared to telephone alone [ 12 , 13 ]. Dispatchers also reported that video streaming helped them assess the quality of CPR, obstructed airways, or position of the patient [ 16 ], and more easily evaluate different situational elements (such as bleeding or context of incidents) [ 18 ]. There was some preliminary evidence that video livestreaming impacted positively on dispatch decisions, prioritisation, and/or resource allocation. For example, in one study the medical dispatchers changed the dispatch response in approximately one quarter of calls after viewing the video [ 18 ]. In another study, dispatchers reported that video supported more precise resource allocation [ 13 ]. Challenges reported in real-life studies (self-report) included the potential emotional impact of viewing video footage [ 18 ], in particular when the call involved children [ 13 ]. In this Norwegian study, dispatchers could choose to use live video as an additional tool for communication, and a few of the dispatchers interviewed described that they felt uncomfortable activating video when children were involved [ 13 ]. Additionally, some dispatchers reported in interviews that using video livestreaming was more time-consuming and might divert their attention, potentially leading them to forget other tasks [ 13 ], increased their workload [ 6 ] and created potential information overload, although the dispatchers in the study [ 17 ] had never used video streaming.
Simulation studies
In simulation studies, video was reported to be superior to audio alone, helped to clarify misunderstandings with callers and motivated callers to continue with CPR [ 22 , 23 , 24 ]. Dispatchers reported that video helped them to save time gathering information from the callers, as they did not need to ask all of the standard questions [ 26 ]. Half of the dispatchers in a German simulation study (51%) agreed that video “supported them in making a diagnosis” [ 24 ]. Only two of the simulation studies covered challenges with video streaming from the dispatchers’ perspective [ 23 , 26 ]. Ecker et al. [ 23 ] surveyed dispatchers following simulated cardiac arrests and 30% agreed that they found using live video more stressful or exhausting compared to normal telephone (audio) protocol (simulation used video only, we make the assumption that the dispatchers compared this to their normal audio practice). Similarly, in Johnsen and Bolle’s [ 26 ] study, some of the dispatchers interviewed felt that video had the potential to cause extra strain and stress, for example, when witnessing deaths. The dispatchers in this simulation study were also worried about the videos potentially being misused and distributed by callers to mass media, as well as the loss of identity protection, as in this study dispatchers were visible to callers [ 26 ].
Caller perspectives: opportunities and challenges
Ten studies included perspectives from or regarding the callers (or those acting as callers in simulation studies). Most of these studies ( n = 6) reported proxy views of the callers’ perspectives from dispatchers, for example describing their experience of dealing with the caller, and sometimes speculating what callers may do if they added video to a call. The evidence in these papers suggested that callers in both real-life and simulation studies had positive attitudes and experiences of video livestreaming. On the basis of these studies, video streaming technology appears largely acceptable to callers, and few challenges were reported. Callers were generally positive, reported feeling reassured by the video, comforted by not being alone, and satisfied with the help they received. Very few challenges from the caller perspective were reported in the included articles, but some contained instances when video was reported to potentially increase callers’ stress, was disruptive or divided/diverted attention from the scene.
Four of the real-life studies included assessment of acceptability to callers or satisfaction with the use of video livestreaming (all these studies used self-report, see further below). Callers found video reassuring, comforting and not feeling “alone” [ 13 ], and enabled them to express their needs in a better way [ 12 ]. Linderoth et al. [ 6 ], surveyed callers in Denmark following real-life emergencies using live video, and nearly all (97.3%) reported that live video should be implemented. Although Ter Avest et al. [ 19 ] did not specifically ask callers about their experience, all of the callers in the study ( n = 21) were willing to attempt video livestreaming and the dispatchers reported that all callers were able to follow their instructions. Dispatchers rated their perception of callers’ acceptability of using video as “excellent” in all calls [ 19 ]. An interesting observation was made in a real-life study [ 14 ] in Seoul, South Korea, where video-instructed dispatcher-assisted CPR has been well established in practice for some time. It was noted anecdotally that increasing public awareness of its use through national news items reduced the tendency of callers to reject the change from audio to video instructions, hence improving acceptability. Challenges reported in real-life studies included dispatchers perceiving that, at times, the use of video increased callers’ stress [ 13 ] and some callers reporting technical difficulties such as video freezing [ 12 ].
As per the real-life studies above, callers in simulation studies have reported that sharing the scene with the dispatchers through video gave them comfort that they were not alone [ 27 ] and feeling reassured that dispatchers “could see whether I did the right thing” [ 12 ]. Most of the callers in Bolle’s et al.’s [ 21 ] Norwegian study reported that using video was better than standard telephones during medical simulated emergencies and improved their confidence when performing CPR. Challenges reported in simulation studies were very rare, although one survey participant (caller) in a Norwegian simulation study reported that they were concentrating more on recording the video than the situation [ 21 ]. In a Korean study [ 27 ], callers reported being concerned about how they would manage the situation if connection was lost during a video call, though none of them reported that this had happened.
Organisational perspectives: opportunities and challenges
Although none of the studies specifically focused on organisational issues, or systematically collected such data, ten studies offered important insights into the challenges and opportunities of using video livestreaming from an organisational perspective. The reported evidence in these papers suggest a need for training, video-specific protocols and a need to consider how best to implement video livestreaming into existing organisational structures. No specific organisational benefits were reported in the studies, although the benefits reported by callers and dispatchers earlier is suggestive of benefits to the organisation, for example by improving resource allocation.
Linderoth et al. [ 6 ] reported that video livestreaming could potentially interfere with existing symptom-based dispatch protocols; it was observed by the researchers that some of the dispatchers appeared to avoid using video livestreaming during particularly busy times. Other studies have supported the need to implement dispatch protocols and guidelines for the specific purpose of video livestreaming, as well as highlighting the need to fully integrate video features into existing IT-systems and processes [ 18 ]. Dispatchers have highlighted the need for experience in using the new technology [ 13 ] and the authors in another study suggested that the helicopter emergency medical service (HEMS) dispatchers in their pilot study needed to be provided with adequate support when potentially witnessing images that were unusual in their role [ 19 ]. Although not specifically measured, the authors in one of the real-life studies noted that there had been positive effects between the dispatcher and caller via video-instructed CPR, such as providing real-time feedback [ 14 ].
Similar findings about the importance of protocols and training were reported in the simulation studies. Ecker et al. [ 24 ] argued that training and additional support is needed to help dispatchers to develop new skills in using video. In another study, it was argued that training was also needed to help dispatchers integrate video CPR into existing workflows [ 23 ]. Stipulante et al. [ 32 ] developed and validated a protocol for video-assisted CPR and the new protocol supported improvement in some of the CPR performance indicators. Similarly, Perry et al. [ 30 ] used a ‘filming protocol’ for dispatcher video-assisted CPR and findings showed that the bespoke protocol improved CPR effectiveness. Perry et al. [ 30 ] also stressed that to maximise the use of the new technology, special attention is needed to implement video streaming in practice.
Technological factors: opportunities and challenges
Ten studies (five real-life and five simulation studies) included findings regarding the streaming technology, such as impact of lighting conditions, visibility, and sound quality. The few technical challenges that were identified in this review included problems with SMS/links, the positioning of the video camera, and lack of network coverage, although this was rare. Despite some difficulties in relation to these issues, in the majority of uses within all studies (both real-life and simulation studies), few technical barriers were reported. Both real-life and simulation studies reported high video call success connection rates.
Two studies reported video call success rates; nineteen out of 21 calls were successful in obtaining video from the scene in a small feasibility study [ 19 ] and live video succeeded in over 80% of calls ( N = 838) in a study in Denmark [ 6 ]. The small number of unsuccessful calls in these two studies were reported to be due to technical issues, lack of caller skills or callers not receiving the SMS with the link to activate the video. Some dispatchers in a Canadian study were worried about potential technical challenges with the CAD (computer aided dispatch) system and transferring calls, although they had never personally used video for dispatch purposes [ 17 ].
One study [ 29 ] specifically investigated using video livestreaming under different sound and light conditions. The authors concluded that video calls can be used successfully in suboptimal conditions, such as during night-time, poor lighting, and noisy conditions. Dispatchers in a simulation study carried out in Germany judged both the video audio quality and the video quality as excellent in nearly all calls. Several of the simulation studies explored video call success connection rates. Video calls succeeded in 76% of calls in a Japanese study [ 25 ] and in 85% of calls in a German study [ 24 ]. The technical reasons for unsuccessful calls were due to network failure, application software failures, and IT server problems. Dispatchers interviewed in a Norwegian study [ 26 ] reported some technical challenges, such as the image quality depending on how steadily the camera was held. Others reflected that if the call had been outside, the wind and noise from people and cars may be disruptive [ 26 ].
Our review has shown that despite the increased uptake of video livestreaming in emergency services, the evidence base remains sparse. Much of the previous research focuses on one aspect of emergency care, the use of CPR, and many of the studies are simulation-based rather than real-life clinical settings. Furthermore, methodological limitations have made attribution of findings to the use of video challenging, such as the lack of control groups or use of randomised designs, and there is a reliance on self-reported data.
Nevertheless, with these caveats, evidence from this synthesis suggests that video streaming is acceptable and easy to use to both callers and dispatchers and could be beneficial in relation to supporting video dispatcher-assisted CPR, and reassuring dispatchers and callers. There is limited research regarding callers overall experiences of calling EMDCs, but a literature review [ 35 ] found that bystanders at motor vehicle accidents often experienced fear of liability or fear of further harming the victim/patient. Video livestreaming offering reassurance to callers may provide additional benefits in these situations. Our results highlighted that callers were generally positive to video livestreaming, but most of the evidence relied on proxy views of the callers’ perspectives from dispatchers. Only two of the real-life studies surveyed callers [ 6 , 12 ] regarding their experience, and response rates were relatively low (below 22% in both studies), making it challenging to conclude what impact that video livestreaming may have on callers. Evidence from our review also suggests that video livestreaming could improve dispatchers’ clinical assessment and decision-making. Currently, dispatchers’ situational awareness and decision-making skills rely on the ability to obtain information about the incident and on their verbal communication skills [ 36 ]. Our review did not find any evidence of how or why video livestreaming impacts on decision-making processes, highlighting a gap in evidence.
Challenges included potential for additional dispatcher workload, stress, and the emotional impact of viewing video footage. In the simulation studies it was not possible to decipher whether the stress was partly induced by the simulated scenarios. Research has shown that simulation often creates anxiety and stress in participants [ 37 ]. Nevertheless, dispatchers are known to be at increased risk of stress, anxiety and depression [ 38 ]. New working practises, such a video livestreaming, need to consider approaches to minimise potential additional stress to dispatchers.
Our review raised important questions whether video livestreaming should be used selectively for specific conditions, high/low acuity, or for every call. As outlined in our results, most of the included studies investigated the use of video livestreaming for CPR only, reporting a range of positive outcomes [ 14 , 15 , 16 , 23 , 26 ], indicating usefulness in this area. In one of the real-life studies [ 6 ] the dispatchers chose when to initiate video livestreaming. Video was used more frequently with children and unconscious patients, described as “unable to talk for themselves”. Another study [ 12 ] investigated the use of video triage for low-acuity calls (such as diarrhoea, vomiting, and urine infection) during covid-19. Over half of the category 5 (low acuity) calls were upgraded after the video consultation, representing a potential important use for low-acuity calls. Further research is needed to understand for what type of calls video livestreaming is most beneficial.
The results of our review highlighted several additional significant topics that need to be considered when conducting research and implementing video livestreaming into practice. First, improving public awareness about the use of livestreaming by emergency services may help to increase caller acceptance and compliance rates, as highlighted in a study in South Korea, where dispatcher-assisted video CPR has been in use for some time [ 14 ]. Second, a number of the studies [ 13 , 19 ] also emphasised the importance of training dispatchers in using video technology. Our results indicate that dispatchers may need training in developing new skills in using video livestreaming and to help them integrate video into existing workflows. Internationally, there are several types of emergency medical dispatch systems and the professional background of call takers and dispatchers varies from no healthcare training to being trained health professionals with extensive experience [ 4 ]. The impact of professional/clinical backgrounds on using livestreaming is currently unknown. Future implementation of video livestreaming in this context is likely to require bespoke training programmes that consider local and national medical emergency systems and processes. Indeed, Linderoth et al. [ 6 ] argued that dispatcher training to use video livestreaming needs a comprehensive approach as the additional visual information may add further complexity to the decision-making process. Third, our review also drew attention to the need to carefully review dispatch protocols and organisational systems to ensure that they are compatible with video livestreaming technology. Fourth, dispatchers in one Norwegian study [ 26 ] voiced concern about the potential misuse of the videos and the loss of identity protection. Two-way video communication (where caller and dispatcher could see each other) was used in seven of the studies, raising potential concerns regarding privacy and identity for dispatchers. Overall, our review found limited information regarding the ethical aspects of video livestreaming from medical emergency callers’ smartphones. Many of the studies had local research ethical review only, or ethical review approval ‘waived’ and provided limited information regarding the caller and/or patient consent processes. Two of the studies [ 13 , 18 ] mentioned that dispatchers told callers during the consent process that the video was not being stored and callers’ smartphones could not be accessed. Future research needs to explore key ethical issues, such as privacy, dignity, information-governance and provide recommendations regarding how to best approach caller and patient consent.
Key gaps identified by our review were that few studies included data collected specifically from the callers and none of the studies included any health economic analysis. Only three of the studies included analysis of change in dispatch decisions regarding resources sent to scenes of incidents. There was also a lack of qualitative studies exploring the experiences of callers, dispatchers, and patients. Future research would benefit from including ethnographic observations ‘in the field’, taking account of important organisational factors and prevailing cultures, as these are known to have an impact on the implementation of new technologies [ 39 ], such as video livestreaming.
Strengths and limitations
The review used a comprehensive search strategy that enabled capture and synthesis of international evidence related to the use of video livestreaming in this context. It uniquely synthesises the potential benefits, challenges and opportunities to inform future research and practice. The review included both real-life and simulation studies and presented the results separately which allowed a systematic overview of evidence base. The review was limited to papers written in the English Language and it is possible that it therefore omits some key international literature. The chosen search terms may have limited inclusion, although a broader search strategy was initially used, in order to determine how best to use limiters to only focus on relevant literature.
The evidence base into the use of video livestreaming in this context is sparse. There are few studies of real-life practice, studies generally employ weak study designs, and caller perspectives are lacking. Over half of the studies focussed on dispatcher-assisted CPR. Nevertheless, there is growing evidence of potential opportunities to using this technology, including for improved clinical assessment and decision-making. These need to be balanced with consideration of the challenges uncovered in this review. Further well-designed robust research is needed, in particular into the experiences, acceptability and attitudes of both callers and dispatchers in real-life studies, and robust evidence of the effectiveness and cost effectiveness of implementing such technologies.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
Automated External Defibrillators
Computer Aided Dispatch
Criteria-based dispatch
Cardiopulmonary resuscitation
Emergency Medical Dispatch Centre
Emergency Medical Services
Medical Subject Headings
Medical Priority Dispatch System
Out-of-hospital cardiac arrest
Return of Spontaneous Circulation
Video-instructed dispatcher-assisted bystander cardiopulmonary resuscitation
Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19. BMJ. 2020;368:m998.
Article PubMed Google Scholar
Duke M, Tatum D, Sexton K, Stuke L, Robertson R, Sutherland M, et al. When minutes fly by: what is the true “golden hour” for air care? Am Surg. 2018;84:862–7.
Schellhaaß A, Popp E. [Air rescue: current significance and practical issues]. Anaesthesist. 2014;63:971–80; quiz 981–2.
Bohm K, Kurland L. The accuracy of medical dispatch - a systematic review. Scand J Trauma Resusc Emerg Med. 2018;26:94.
Article CAS PubMed PubMed Central Google Scholar
Eaton G, Brown S, Raitt J. HEMS dispatch: a systematic review. Trauma. 2018;20:3–10.
Article Google Scholar
Linderoth G, Lippert F, Østergaard D, Ersbøll AK, Meyhoff CS, Folke F, et al. Live video from bystanders’ smartphones to medical dispatchers in real emergencies. BMC Emerg Med. 2021;21:101.
Article PubMed PubMed Central Google Scholar
Lin YY, Chiang WC, Hsieh MJ, Sun JT, Chang YC, Ma MHM. Quality of audio-assisted versus video-assisted dispatcher-instructed bystander cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation. 2018;123:77–85.
Bielski K, Böttiger BW, Pruc M, Gasecka A, Sieminski M, Jaguszewski MJ, et al. Outcomes of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation: a systematic review and meta-analysis. Ann Med. 2022;54:464–71.
Sýkora R, Peřan D, Renza M, Bradna J, Smetana J, Duška F. Video emergency calls in medical dispatching: a scoping review. Prehosp Disaster Med. 2022;37:819–26.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Bell F, Pilbery R, Connell R, Fletcher D, Leatherland T, Cottrell L, et al. The acceptability and safety of video triage for ambulance service patients and clinicians during the COVID-19 pandemic. Br Paramedic J. 2021;6:49–58.
Idland S, Iversen E, Brattebø G, Kramer-Johansen J, Hjortdahl M. From hearing to seeing: medical dispatchers’ experience with use of video streaming in medical emergency calls – a qualitative study. BMJ Open. 2022;12:e063395.
Lee HS, You K, Jeon JP, Kim C, Kim S. The effect of video-instructed versus audio-instructed dispatcher-assisted cardiopulmonary resuscitation on patient outcomes following out of hospital cardiac arrest in Seoul. Sci Rep. 2021;11:15555.
Lee SY, Song KJ, Shin SD, Hong KJ, Kim TH. Comparison of the effects of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation on resuscitation outcomes after out-of-hospital cardiac arrest. Resuscitation. 2020;147:12–20.
Linderoth G, Rosenkrantz O, Lippert F, Østergaard D, Ersbøll AK, Meyhoff CS, et al. Live video from bystanders’ smartphones to improve cardiopulmonary resuscitation. Resuscitation. 2021;168:35–43.
Neustaedter C, Jones B, O’Hara K, Sellen A. The benefits and challenges of video calling for emergency situations. In: Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. New York: Association for Computing Machinery; 2018. p. 1–13.
Google Scholar
Steen-Tveit K, Munkvold BE, Radianti J. Using live video for communication between lay bystanders and emergency dispatchers in command and control centres. Int J Emerg Manag. 2021;17:154–76.
Ter Avest E, Lambert E, de Coverly R, Tucker H, Griggs J, Wilson MH, et al. Live video footage from scene to aid helicopter emergency medical service dispatch: a feasibility study. Scand J Trauma Resusc Emerg Med. 2019;27:55.
Bang JY, Cho Y, Cho GC, Lee J, Kim IY. Can mobile videocall assist laypersons’ use of automated external defibrillators? A randomized simulation study and qualitative analysis. Biomed Res Int. 2020;2020:1–7.
Bolle SR, Johnsen E, Gilbert M. Video calls for dispatcher-assisted cardiopulmonary resuscitation can improve the confidence of lay rescuers–surveys after simulated cardiac arrest. J Telemed Telecare. 2011;17:88–92.
Bolle SR, Scholl J, Gilbert M. Can video mobile phones improve CPR quality when used for dispatcher assistance during simulated cardiac arrest? Acta Anaesthesiol Scand. 2009;53:116–20.
Ecker H, Wingen S, Hagemeier A, Plata C, Bottiger B, Wetsch W. Dispatcher self-assessment and attitude toward video assistance as a new tool in simulated cardiopulmonary resuscitation. WestJEM. 2022;23:229–34.
Ecker H, Wingen S, Hamacher S, Lindacher F, Böttiger BW, Wetsch WA. Evaluation of CPR quality via smartphone with a video livestream - a study in a metropolitan area. Prehosp Emerg Care. 2021;25:76–81.
Igarashi Y, Suzuki K, Norii T, Motomura T, Yoshino Y, Kitagoya Y, et al. Do video calls improve dispatcher-assisted first aid for infants with foreign body airway obstruction? A randomized controlled trial/simulation study. J Nippon Med Sch. 2022;89:526–32.
Johnsen E, Bolle SR. To see or not to see—better dispatcher-assisted CPR with video-calls? A qualitative study based on simulated trials. Resuscitation. 2008;78:320–6.
Kim HJ, Kim JH, Park D. Comparing audio- and video-delivered instructions in dispatcher-assisted cardiopulmonary resuscitation with drone-delivered automatic external defibrillator: a mixed methods simulation study. PeerJ. 2021;9: e11761.
Lee SGW, Kim TH, Lee HS, Shin SD, Song KJ, Hong KJ, et al. Efficacy of a new dispatcher-assisted cardiopulmonary resuscitation protocol with audio call-to-video call transition. Am J Emerg Med. 2021;44:26–32.
Article CAS PubMed Google Scholar
Melbye S, Hotvedt M, Bolle SR. Mobile videoconferencing for enhanced emergency medical communication - a shot in the dark or a walk in the park? –– A simulation study. Scand J Trauma Resusc Emerg Med. 2014;22:35.
Perry O, Wacht O, Jaffe E, Sinuany-Stern Z, Bitan Y. Using a filming protocol to improve video-instructed cardiopulmonary resuscitation. Technol Health Care. 2020;28:213–20.
Peters M, Stipulante S, Cloes V, Mulder A, Lebrun F, Donneau AF, et al. Can video assistance improve the quality of pediatric dispatcher-assisted cardiopulmonary resuscitation? Pediatr Emerg Care. 2022;38:e451-457.
Stipulante S, Delfosse AS, Donneau AF, Hartsein G, Haus S, D’Orio V, et al. Interactive videoconferencing versus audio telephone calls for dispatcher-assisted cardiopulmonary resuscitation using the ALERT algorithm: a randomized trial. Eur J Emerg Med. 2016;23:418–24.
Yang C-W, Wang H-C, Chiang W-C, Chang W-T, Yen Z-S, Chen S-Y, et al. Impact of adding video communication to dispatch instructions on the quality of rescue breathing in simulated cardiac arrests–a randomized controlled study. Resuscitation. 2008;78:327–32.
You JS, Park S, Chung SP, Park JW. Performance of cellular phones with video telephony in the use of automated external defibrillators by untrained laypersons. Emerg Med J. 2008;25:597–600.
Hall A, Wooton K, Hutton A. Bystander Experiences at and after a Motor Vehicle Accident: A review of the literature. Australas J Paramed. 2013;10:1–10.
Møller TP, Jensen HG, Viereck S, Lippert F, Østergaaard D. Medical dispatchers’ perception of the interaction with the caller during emergency calls - a qualitative study. Scand J Trauma Resusc Emerg Med. 2021;29:45.
Paskins Z, Peile E. Final year medical students’ views on simulation-based teaching: a comparison with the best evidence medical education systematic review. Med Teach. 2010;32:569–77.
Smith EC, Holmes L, Burkle FM. Exploring the physical and mental health challenges associated with emergency service call-taking and dispatching: a review of the literature. Prehosp Disaster Med. 2019;34:619–24.
Jennett P, Yeo M, Pauls M, Graham J. Organizational readiness for telemedicine: implications for success and failure. J Telemed Telecare. 2003;9(2 suppl):27–30.
Download references
Acknowledgements
Extended thank you to Freda Mold for assistance with search strategy and search strings. This review was completed as part of the SEE-IT trial ( https://fundingawards.nihr.ac.uk/award/NIHR130811 ). The SEE-IT trial group also include: Kate Bennett-Eastley, Mark Cropley, Heather Gage, Matthew Glover, Janet Holah, Richard Lyon, Craig Mortimer, Simon S Skene and Julia Williams.
This project was funded by the National Institute for Health and Care Research (NIHR130811) Health and Social Care Delivery Research programme and will be published in Health and Social Care Delivery Research. See the NIHR Journals Library website for further project information.
Author information
Authors and affiliations.
School of Health Sciences, University of Surrey, Guildford, Surrey, UK
Carin Magnusson, Lucie Ollis, Scott Munro, Jill Maben & Cath Taylor
South East Coast Ambulance Service NHS Foundation Trust, Crawley, West Sussex, UK
Anthony Coe & Oliver Fitzgerald
You can also search for this author in PubMed Google Scholar
Contributions
CM, JM, LO and CT made substantial contributions to the conception of the review and the development of the review focus. CM carried out all database searches. CM and LO independently assessed articles for eligibility using the inclusion and exclusion criteria. CM, AC, OF and SM extracted the data from the final included full text articles. The first draft of the manuscript was drafted by CM and CT, and critically reviewed by all other authors named. All authors agree with manuscript results and conclusion. All authors approved the final version of the manuscript.
Corresponding author
Correspondence to Cath Taylor .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval not required for this review and the information included is publicly available.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Magnusson, C., Ollis, L., Munro, S. et al. Video livestreaming from medical emergency callers’ smartphones to emergency medical dispatch centres: a scoping review of current uses, opportunities, and challenges. BMC Emerg Med 24 , 99 (2024). https://doi.org/10.1186/s12873-024-01015-9
Download citation
Received : 03 November 2023
Accepted : 27 May 2024
Published : 11 June 2024
DOI : https://doi.org/10.1186/s12873-024-01015-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency medical dispatch
- Emergency medical services
- Video livestreaming
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Providing a comprehensive literature review on trauma, traumatic stress, trauma-informed care (TIC), and trauma-related interventions is a daunting task when considering the quantity and prolific production of research in this area in the past 20 years. To manage the volume of information, this literature review mainly focuses on reviews and meta-analyses rather than seminal work to address ...
Journal scope statement. Psychological Trauma: Theory, Research, Practice, and Policy® publishes empirical research on the psychological effects of trauma. The journal is intended to be a forum for an interdisciplinary discussion on trauma, blending science, theory, practice, and policy. The journal publishes empirical research on a wide range ...
A exploration of the literature finds a variety of specialized journals devoted to this topic (to wit: Journal of Trauma Practice, Journal of Loss and Trauma, Journal of Traumatic Stress, Traumatology, International Journal of Emergency Mental Health, Journal on Rehabilitation of Torture Victims and Prevention of Torture, among others), as well ...
None of the studies considered in the present literature review assessed the effect of compassion fatigue, burnout, secondary traumatic stress, or vicarious trauma on TIC practices. Given the centrality of the MHN therapeutic relationship to achieving TIC, service-based responses around funding clinical supervision and more frequent rotation of ...
A related review of vicarious trauma measures yielded two that are predominant in this literature. Among the 13 measures identified, there was significant diversity in what aspects of T(V)IC are assessed, with a clear emphasis on "knowledge" and "safety", and less on "collaboration/choice" and "strengths-based" concepts.
Based on the available literature, this review article investigates the issue of resilience in relation to trauma and posttraumatic stress disorder. Resilient coping to extreme stress and trauma is a multifaceted phenomena characterized as a complex repertoire of behavioral tendencies. An integrative Person × Situation model is developed based ...
Literature around trauma-informed systems of care include schools, with the teachers and staff who work in them, as components of multitiered systems of supports (Chafouleas, Johnson, Overstreet, & Santos, 2016).However, the empirical work informing trauma-informed teaching and teacher education that is reflected back to education audiences is less established, "specifically studies that ...
Abstract. This literature review explores the intricate relationship between trauma, resilience, and mental health disparities. Trauma, whether experienced directly or indirectly, has profound and lasting effects on mental health. However, individuals and communities exhibit remarkable resilience in the face of adversity.
Remembering Trauma, a review of new research that has been widely viewed as a shot over the bow of the trauma studies establishment—and that is now essential reading for specialists.2 In it, McNally summarizes dozens of new studies—both his own and others'—that challenge some of the field's sacred truths. Though his research is ex
Chapter 2 consists of the methodology for the project™s literature review and databases and key terms used to locate relevant research are listed. Chapters 3, 4, and 5 consist of the literature review on childhood trauma, brain development and the brain™s response to trauma, respectively. These three chapters detail an introduction to brain
PDF | On Nov 30, 2016, Shannon Eaton Allen published Childhood Trauma: A Comprehensive Review of Effects, Assessments, and Treatments | Find, read and cite all the research you need on ResearchGate
A literature review [12] identified that the most common definition for major trauma is a retrospective ISS of > 15. The injury severity score is an aggregation of the main injuries from each body ...
Section 1—A Review of the Literature Introduction to Trauma and Traumatic Stress Reactions Providing a comprehensive literature review on trauma, traumatic stress, trauma-informed care (TIC), and trauma-related interventions is a daunting task when considering the quantity and prolific production of research in this area in the past 20 years.
The Emergence of Trauma Studies in the 1990s: Key Events. Though the discussion spotlights the roles of Holocaust studies, critical theory, anti-foundationalist French thought, and identity politics in shaping literary discourses of trauma and memory in the 1990s, there were other signal events in the preceding decades that facilitated the literary-institutional evolution of the field.
Mulvihill DLRN (2017) Literature review: connections between trauma and substance abuse Ment Health Addict Res, 2017 doi: 10.15761/MHAR.1000147 V olume 2(4): 11-15 reduction is the best treatment ...
deep breathing exercises. meditation. progressive relaxation techniques. tai chi. yoga. Aerobic exercise is also an accessible option. Research shows that it can relax the nervous system and ...
Given the existing literature on trauma and obesity, we also hypothesised that individuals with obesity would have significantly higher scores on the Mistrust/Abuse and Emotional Deprivation schemas compared to normal weight individuals. ... Interpersonal violence in childhood as a risk factor for obesity: A systematic review of the literature ...
Some therapists use somatic or body-based techniques to help the mind and the body process trauma. A review of the literature in the Psychotherapy and Counselling Journal of Australia found that ...
Included studies comprised three narrative case studies [29,30,31] a randomised control trial []; a narrative review [] a practitioners' guidance document []; and a naturalistic study [].Critical appraisal of the evidence (Table 1) demonstrates that caution must be exercised when considering the findings.The main strength of the included studies is the voice of young people through verbatim ...
In a comprehensive literature review, 140 indicators were associated with in-hospital trauma care after reviewing 51 articles, 3 guidelines, and 2 books. Then, some indicators were excluded or merged due to insignificance, differences in the management system of countries, lack of sufficient data (physical and electronic), time, human and ...
Tanzania is disproportionately burdened by musculoskeletal injuries as it faces unique challenges when dealing with trauma care. This scoping review aims to summarize and assess the current state of orthopaedic and trauma research in Tanzania. By identifying key themes, trends, and gaps in the literature, this review seeks to guide future research initiatives catered specifically to the needs ...
Long-term prognosis was defined as a state of 5 years or more from injury, and on May 23rd, 2023, we looked through articles from 1990 to May 23rd, 2023. A scoping review of the literature was conducted following the 2018 PRISMA-ScR Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews.
A scoping review of relevant published literature between 2007 and 2023 in the English language, searched within MEDLINE; CINAHL and PsycINFO, was descriptively synthesised, adhering to the PRISMA extension for scoping reviews. ... Eaton G, Brown S, Raitt J. HEMS dispatch: a systematic review. Trauma. 2018;20:3-10. Article Google Scholar ...