Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.

Harvard-led study IDs statin that may block pathway to some cancers
New Alzheimer’s study suggests genetic cause of specific form of disease

Had a bad experience meditating? You’re not alone.
“When my son was diagnosed [with Type 1], I knew nothing about diabetes. I changed my research focus, thinking, as any parent would, ‘What am I going to do about this?’” says Douglas Melton.
Kris Snibbe/Harvard Staff Photographer
Breakthrough within reach for diabetes scientist and patients nearest to his heart
Harvard Correspondent
100 years after discovery of insulin, replacement therapy represents ‘a new kind of medicine,’ says Stem Cell Institute co-director Douglas Melton, whose children inspired his research
When Vertex Pharmaceuticals announced last month that its investigational stem-cell-derived replacement therapy was, in conjunction with immunosuppressive therapy, helping the first patient in a Phase 1/2 clinical trial robustly reproduce his or her own fully differentiated pancreatic islet cells, the cells that produce insulin, the news was hailed as a potential breakthrough for the treatment of Type 1 diabetes. For Harvard Stem Cell Institute Co-Director and Xander University Professor Douglas Melton, whose lab pioneered the science behind the therapy, the trial marked the most recent turning point in a decades-long effort to understand and treat the disease. In a conversation with the Gazette, Melton discussed the science behind the advance, the challenges ahead, and the personal side of his research. The interview was edited for clarity and length.
Douglas Melton
GAZETTE: What is the significance of the Vertex trial?
MELTON: The first major change in the treatment of Type 1 diabetes was probably the discovery of insulin in 1920. Now it’s 100 years later and if this works, it’s going to change the medical treatment for people with diabetes. Instead of injecting insulin, patients will get cells that will be their own insulin factories. It’s a new kind of medicine.
GAZETTE: Would you walk us through the approach?
MELTON: Nearly two decades ago we had the idea that we could use embryonic stem cells to make functional pancreatic islets for diabetics. When we first started, we had to try to figure out how the islets in a person’s pancreas replenished. Blood, for example, is replenished routinely by a blood stem cell. So, if you go give blood at a blood drive, your body makes more blood. But we showed in mice that that is not true for the pancreatic islets. Once they’re removed or killed, the adult body has no capacity to make new ones.
So the first important “a-ha” moment was to demonstrate that there was no capacity in an adult to make new islets. That moved us to another source of new material: stem cells. The next important thing, after we overcame the political issues surrounding the use of embryonic stem cells, was to ask: Can we direct the differentiation of stem cells and make them become beta cells? That problem took much longer than I expected — I told my wife it would take five years, but it took closer to 15. The project benefited enormously from undergraduates, graduate students, and postdocs. None of them were here for 15 years of course, but they all worked on different steps.
GAZETTE: What role did the Harvard Stem Cell Institute play?
MELTON: This work absolutely could not have been done using conventional support from the National Institutes of Health. First of all, NIH grants came with severe restrictions and secondly, a long-term project like this doesn’t easily map to the initial grant support they give for a one- to three-year project. I am forever grateful and feel fortunate to have been at a private institution where philanthropy, through the HSCI, wasn’t just helpful, it made all the difference.
I am exceptionally grateful as well to former Harvard President Larry Summers and Steve Hyman, director of the Stanley Center for Psychiatric Research at the Broad Institute, who supported the creation of the HSCI, which was formed specifically with the idea to explore the potential of pluripotency stem cells for discovering questions about how development works, how cells are made in our body, and hopefully for finding new treatments or cures for disease. This may be one of the first examples where it’s come to fruition. At the time, the use of embryonic stem cells was quite controversial, and Steve and Larry said that this was precisely the kind of science they wanted to support.
GAZETTE: You were fundamental in starting the Department of Stem Cell and Regenerative Biology. Can you tell us about that?
MELTON: David Scadden and I helped start the department, which lives in two Schools: Harvard Medical School and the Faculty of Arts and Science. This speaks to the unusual formation and intention of the department. I’ve talked a lot about diabetes and islets, but think about all the other tissues and diseases that people suffer from. There are faculty and students in the department working on the heart, nerves, muscle, brain, and other tissues — on all aspects of how the development of a cell and a tissue affects who we are and the course of disease. The department is an exciting one because it’s exploring experimental questions such as: How do you regenerate a limb? The department was founded with the idea that not only should you ask and answer questions about nature, but that one can do so with the intention that the results lead to new treatments for disease. It is a kind of applied biology department.
GAZETTE: This pancreatic islet work was patented by Harvard and then licensed to your biotech company, Semma, which was acquired by Vertex. Can you explain how this reflects your personal connection to the research?
MELTON: Semma is named for my two children, Sam and Emma. Both are now adults, and both have Type 1 diabetes. My son was 6 months old when he was diagnosed. And that’s when I changed my research plan. And my daughter, who’s four years older than my son, became diabetic about 10 years later, when she was 14.
When my son was diagnosed, I knew nothing about diabetes and had been working on how frogs develop. I changed my research focus, thinking, as any parent would, “What am I going to do about this?” Again, I come back to the flexibility of Harvard. Nobody said, “Why are you changing your research plan?”
GAZETTE: What’s next?
MELTON: The stem-cell-derived replacement therapy cells that have been put into this first patient were provided with a class of drugs called immunosuppressants, which depress the patient’s immune system. They have to do this because these cells were not taken from that patient, and so they are not recognized as “self.” Without immunosuppressants, they would be rejected. We want to find a way to make cells by genetic engineering that are not recognized as foreign.
I think this is a solvable problem. Why? When a woman has a baby, that baby has two sets of genes. It has genes from the egg, from the mother, which would be recognized as “self,” but it also has genes from the father, which would be “non-self.” Why does the mother’s body not reject the fetus? If we can figure that out, it will help inform our thinking about what genes to change in our stem cell-derived islets so that they could go into any person. This would be relevant not just to diabetes, but to any cells you wanted to transplant for liver or even heart transplants. It could mean no longer having to worry about immunosuppression.
Share this article
You might like.
Cholesterol-lowering drug suppresses chronic inflammation that creates dangerous cascade
Findings eventually could pave way to earlier diagnosis, treatment, and affect search for new therapies

Altered states of consciousness through yoga, mindfulness more common than thought and mostly beneficial, study finds — though clinicians ill-equipped to help those who struggle
When should Harvard speak out?
Institutional Voice Working Group provides a roadmap in new report
Day to remember
One journey behind them, grads pause to reflect before starting the next
Had a bad experience meditating? You're not alone.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

New and Emerging Technologies in Type 1 Diabetes
There has been a rapid advancement in the pace of development of new diabetes technologies and therapies for the management of type 1 diabetes over the past decade. The Diabetes Control and Complications Trial conclusively established that tight glycemic control with intensive insulin therapy decreases the rates of diabetes complications in proportion to glycemic control, and diabetes technologies have accordingly been developed to help patients reach these goals. In this review, the authors discuss new diabetes therapeutics and technologies, including new insulin analogues, insulin pumps, continuous glucose monitoring systems, and automated insulin delivery systems.”
- • Innovative and novel technologies for the management of type 1 diabetes hold promise for improving glycemia, decreasing burden of disease management, and improving long-term outcomes.
- • Improvements in the accuracy of real-time continuous glucose monitoring (CGM) have allowed for the development of automated insulin delivery systems that can adjust insulin delivery based on CGM glucose input.
- • The development of new drugs, such as ultrarapid-acting insulins that better mimic physiologic insulin secretion, may lead to improved postprandial glycemia. The advent of stable glucagon formulations may allow for development of dual-hormone closed-loop systems that could further improve glycemic regulation.
New technologies in type 1 diabetes
Intensive insulin therapy for the management of type 1 diabetes (T1D) was established as the standard of care based on the results of the Diabetes Control and Complication Trial (DCCT), which conclusively demonstrated the benefits of tight glycemic control. 1 However, those who received intensive insulin management were at increased risk for severe hypoglycemia, which can be acutely life threatening and can result in seizures, coma, or death. Based on DCCT and other data, the American Diabetes Association (ADA) recommends glycosylated hemoglobin (HbA1c) less than 7% in adults, and recently also in many children and adolescents, in order to decrease the risk of both macrovascular and microvascular complications. 2 To achieve these recommended glycemic targets, patients must monitor blood glucose multiple times a day, closely estimate carbohydrate intake to calculate appropriate meal coverage, and administer multiple doses of insulin, which can have varying effects based on several physiologic factors such as physical activity, illness, or stress. This program results in a significant burden of disease management. Recently published data from the T1D Exchange, which includes more than 22,000 children and adults in the United States, show that less than a quarter of patients with T1D are meeting HbA1c goals. 3 Diabetes technologies are being developed to help decrease disease burden and improve glycemic outcomes. In this article, the authors highlight diabetes technology and therapies including new insulin analogues, continuous glucose monitoring systems (CGM), continuous subcutaneous insulin infusion (insulin pump therapy), as well as automated insulin delivery (AID) systems that integrate CGM and insulin pump technology with mathematical algorithms that automatically adjust insulin delivery ( Box 1 ).
Box 1
Key definitions, glucose monitoring.
Self-monitoring of blood glucose (SMBG) with finger-stick glucose (FSG) concentrations has become a key component of diabetes care. The ability to obtain a blood glucose measurement and adjust therapy accordingly is a mainstay of treatment to reach glucose targets and prevent hypoglycemia. Glucometer accuracy has increased throughout the years, but not all meters available on the market today meet standards set forth by the Food and Drug Administration (FDA) and International Organization for Standardization. 4 Identifying glucose trends and patterns based on SMBG to make insulin adjustments had been the standard of care set forth by the DCCT, and increased frequency of SMBG is associated with improved glycemic control. 5 Some newer glucometers are Bluetooth enabled and can pair with smartphone applications for patients to better track and identify patterns. 6 However, FSG has limitations in that they provide only an instantaneous snapshot in time of current glucose and do not provide information on glucose trends or direction of change.
CGM and FGM devices measure interstitial glucose and estimate plasma glucose every 5 to 15 minutes, depending on the system. Real-time CGM systems (Dexcom G6, Senseonics Eversense, Medtronic Guardian) actively transmit glucose information to a dedicated receiver, insulin pump, smartphone/watch, and to a cloud network if desired and can provide real-time information to the user regarding (1) rate of glucose change, (2) hyperglycemia and hypoglycemia based on individualized thresholds, and (3) impending hypoglycemia alarms based on glucose trends. The glucose measurements can also be shared by patients with others, such as family members, in real-time for an added degree of security. In the only currently available FGM system (Abbott Freestyle Libre), data are stored within the sensor and can be obtained by scanning the device with dedicated receiver or smartphone. Of note, the next-generation Freestyle Libre 2 CGM recently approved by the FDA is capable of “pushing” optional real-time threshold alerts to a receiver or smartphone. Both CGM and FGM devices can be used in blinded mode to record glucose data on the device for later analysis of glycemic patterns to assist health care professionals in making therapeutic decisions.
Externally worn CGM (Dexcom G6, Medtronic Guardian) and FGM (Abbott Freestyle Libre) devices measure interstitial glucose via a transcutaneous sensor, a filament placed in the subcutaneous tissue connected to an overlying transmitter. More recently a CGM with an implantable sensor system with an externally worn transmitter, the Senseonics Eversense, has been approved for 3 or 6 months of use before replacement in the United States and Europe, respectively. Some devices require regular calibration, with FSG input required at least twice daily (Medtronic Guardian and Senseonics Eversense), or are factory calibrated with no additional measurements required (Dexcom G6 and Abbott Freestyle Libre).
Data from CGM and FGM devices can be downloaded by clinicians and provide a standardized ambulatory glucose profile with information regarding percentage of time spent in hypo- and hyperglycemic ranges, time in target range, and glucose variability. Mean glucose as determined by CGM can be used to calculate the glucose management indicator, which provides an estimate of HbA1c 7 to help determine if patients are achieving target glucose goals. 8 In fact, because the relationship between HbA1c and average glucose can be modified by the mean red blood cell lifespan, mean CGM glucose may be a better predictor of long-term complications than HbA1c when the measured HbA1c and GMI are not in agreement. 7 Recently the ADA has published consensus guidelines regarding the recommended percentage of time in target range as well as hyper- and hypoglycemic targets for patients with T1D. 9 Time in target range of 70 to 180 mg/dL (TIR) has been shown to correlate with mean glucose and HbA1c. TIR of 70% correlates to an HbA1c of approximately 7%. TIR has been suggested as a new treatment standard based on the argument that TIR is easier for people with diabetes to understand and is more actionable on a day-to-day basis. 2 , 10 Targets for time below range (TBR) and time above range (TAR) have also been established ( Table 1 ).
Table 1
Continuous glucose monitoring recommendations for patients with type 1 diabetes to achieve HbA1c 7% a
CGM accuracy has improved significantly since its inception, and many CGM devices have obtained approval for nonadjunctive use (Dexcom G6, Senseonics Eversense, Freestyle Libre), meaning that CGM data can be used as a replacement for FSG when making insulin-dosing decisions. 11 Studies have shown that CGM use is associated with improved HbA1c and a reduction in hypoglycemia. 12 , 13 More recently, the FDA has created an interoperable integrated continuous glucose monitoring system standard, which allows an approved CGM device to be used as part of an integrated system with other compatible medical devices and electronic interfaces, including insulin delivery systems. Approved systems (currently, the Dexcom G6 and the Freestyle Libre 2) meet accuracy and reliability standards set forth by the FDA, securely transmit glucose data to other devices, and may be used interchangeably with AID devices for the purpose of managing glycemia.
One of the major challenges to managing glycemia in patients with diabetes is the inability of currently available insulin formulations to mimic the kinetics and action of endogenous insulin secretion. 14 In individuals without diabetes, incretin-stimulated insulin release and a rapid hepatic exposure to insulin in response to a meal occur and lead to decreased hepatic glucose production. 15 This physiology is no longer intact in patients with T1D. Exogenous insulin administered in the subcutaneous tissue takes time to be absorbed in the systemic circulation. This delayed systemic delivery of exogenous insulin is a major physiologic difference with the immediate entry of endogenous insulin into the hepatic circulation for rapid effects. 16
Since the discovery of insulin in 1921, insulin therapy has greatly advanced from porcine and bovine insulin derivatives to the development of rapid-acting, and then ultrarapid-acting, insulin analogues. Older insulins such as Neutral Protamine Hagedorn and regular human insulin have a slow action of onset and long duration, which require patients to have rigid food consumption timing and routines to match the kinetics of insulin action. Rapid-acting insulin analogues (aspart, lispro, and glulisine) have a faster onset of action and quicker time to peak insulin action, which help better match postprandial glucose excursion. These rapid-acting insulins permit greater flexibility for patients: doses can be adjusted based on the timing and quantity of carbohydrates consumed rather. However, rapid-acting insulin analogues still require injection 10 to 15 minutes before meal intake for optimal action. 14
New ultrarapid-acting insulins have even faster on-off kinetics than rapid-acting insulin. 17 , 18 , 19 , 20 , 21 Faster aspart (also known as Fiasp) is currently FDA approved for adults and children with diabetes and uses nicotinamide as an excipient and l -arginine to increase stability. Ultrarapid lispro (URLi), which has recently completed a phase 3 trial, uses treprostinil to promote vasodilation and citrate as an excipient. 21 BioChaperone lispro, which uses BC222, an oligosaccharide modified with natural molecules and citrate as an excipient, is currently in development. Postprandial glucose were found to be lower with use of faster aspart in both pump and MDI delivery. 19 , 22 Overall rates of blood glucose–confirmed hypoglycemia and severe hypoglycemia have been reported to be similar between aspart and faster aspart. 19 Faster aspart is labeled for use to be administered up to 20 minutes after meal, which can provide further flexibility to patients. A trial of URLi in patients with T1D showed decreased postprandial glycemic excursions at 1 and 2 hours compared with lispro. 21 A short-term, cross-over trial comparing BioChaperone Lispro with insulin lispro has also shown decreases in early postprandial hyperglycemia. 20 In a head-to-head study, BioChaperone Lispro had slightly faster on-off kinetics than insulin lispro and may more closely mimic normal postprandial insulin secretion. 17 Inhaled insulin (Afrezza) is FDA approved and has much more rapid kinetics than injectable insulin delivered subcutaneously. Limitations in clinical use include lack of dose equivalency with injectable insulin and possible respiratory side effects including lung function decreases that are reversible on discontinuation. 23
Insulin delivery modalities
Multiple daily injection.
Insulin has been traditionally administered via MDI therapy via insulin syringe or insulin pen. Smart pen technology pairs the insulin pen with a smartphone to allow patients to more easily calculate and track insulin administration. The InPen (Companion Medical) is currently the only FDA-approved smart pen device, although others are in development. The InPen connects with a smartphone app via Bluetooth allowing patients to track insulin dosing history, calculate insulin doses, keep track of “insulin on board” (an estimate of rapid-acting insulin still in effect) and adjust calculated dosing accordingly, and set dosing reminders. 24 In addition, the phone application can also receive CGM data directly and in real time. Patients can export data collected from the application and share it with their health care team. Smart pen technology may have extra utility in certain patient populations or clinical scenarios, such as those who have difficulty remembering insulin dosing (eg, pediatric patients or those with cognitive or memory impairment) or those with limited health numeracy. 25 Accurate tracking of insulin dose administration is also of use to treatment teams to aid in insulin regimen adjustments. Further research is needed to determine clinical benefits of this technology, and other companies (including major insulin manufacturers) have announced plans to release smart pens in the future.
Insulin Pumps
Insulin pumps deliver a continuous infusion of insulin via a cannula placed in the subcutaneous tissue, sometimes referred to as continuous subcutaneous insulin infusion (CSII). Most of the pumps available use an infusion set with tubing to deliver insulin (in the United States, pumps from Tandem and Medtronic), but some systems known as patch pumps attach directly to the skin without the need for tubing (in the United States, the Insulet Omnipod system). Insulin pumps have programmable basal and bolus settings that can vary based on the time of the day. Insulin pumps track insulin usage and contain bolus calculators to assist in the calculation of meal-time insulin coverage and glucose correction. The pump also keeps track of “insulin on board” and adjusts calculated doses accordingly. The abilities to use different basal rates at different times of the day, to make temporary basal rate adjustments in response to glucose trend or activity level, and to deliver meal-time bolus insulin over extended periods of time based on user input are all unique to insulin pumps.
Patients can achieve target HbA1c goals with either MDI or insulin pump therapy, and extensive research has sought to determine if glycemic control with pump therapy is superior to that of MDI management. A systematic review and meta-analysis showed that both MDI and pump therapy resulted in comparable levels of glycemic control and incidence of severe hypoglycemia in children and adolescents with T1D and that pump therapy may have favorable effects on glycemic control in adults with T1D. 26 Insulin pump therapy is also associated with improved quality of life in both pediatric and adult populations. 27 , 28 By allowing varied basal rates, insulin pumps permit more flexible and physiologic insulin delivery that can be changed based on time of day and other factors such as exercise, as well as varied delivery of meal-time insulin bolus (eg, dual-wave or square-wave delivery set by the user) based on the type of food consumed. In addition, pump therapy eliminates the need for multiple daily injections of insulin, instead requiring only infusion set be changed every 2 to 3 days. Uptake of CSII has increased over the past decade, and currently nearly half of all patients with T1D in the United States manage their diabetes with pump therapy. 3
Automated Insulin Delivery
AID systems (also known as closed-loop, artificial pancreas, or bionic pancreas systems) use real-time glucose measurements fed into a control algorithm that automatically adjusts the rate of subcutaneous insulin delivery via an insulin pump ( Table 2 ). The earliest approved AID systems used threshold suspend, in which insulin delivery way automatically suspended when blood glucose level dropped less than a certain threshold. 29 Predictive glucose suspend improves on this feature by suspending insulin delivery when a hypoglycemic event is predicted in the future. Predictive low glucose suspend functionality decreases the percentage of time spent in hypoglycemic ranges in both the daytime and overnight. 30 By suspending insulin before a hypoglycemic event, this feature also reduces the duration of hypoglycemic events when they do occur.
Table 2
Current Food and Drug Administration–approved automated insulin delivery systems
Later generation AID systems entail more complex algorithms to not only suspend insulin delivery based on hypoglycemia but continuously adjust insulin delivery in response to glycemic trends. The most advanced AID systems that are commercially available today are referred to as hybrid closed-loop systems. Patient input is still required to count carbohydrates and administer correction boluses, but the system will additionally modulate insulin delivery in the background, and in some systems deliver partial correction boluses, based on glycemic trends. Other systems that have been studied but are not yet available use qualitative meal announcements to estimate carbohydrate content, describing meals as “typical,” “more than typical,” “less than typical,” or “a small bite,” rather than requiring quantitative carbohydrate counting. 31
Currently available FDA-approved hybrid closed-loop systems include the Medtronic 670G and Tandem t:slim X2 with Control IQ. The first hybrid closed-loop system available in United States, the Medtronic 670G, was approved in 2017 for adult and pediatric patients as young as age 7 years. The approval relied on a nonrandomized study without a control arm. 32 The system can be used as a traditional pump or in “auto mode,” in which the pump automatically adjusts basal insulin rates up to every 5 minutes by increasing, decreasing, or suspending delivery of insulin based on CGM trends. Patients are still required to count carbohydrates and enter them into the system, and meal boluses are calculated based on a programmed carbohydrate ratio. As a safety feature, the system may exit auto mode and revert to preprogrammed delivery if insulin delivery approaches maximum or minimum insulin delivery thresholds, if POC and CGM readings are discrepant, or if CGM signal is lost. In a real-world, prospective observational study of 92 youth who started this system, 30% discontinued use of the auto mode within the first 6 months. Another real-world cohort study of 79 pediatric and adult patients reported that 33% discontinued auto mode use within 12 months. 33 , 34 Reasons cited included the number of alarms, challenges with requiring calibrations, and dissatisfaction with glycemic control. 34
The second hybrid closed-loop device in the United States, the Tandem t:slim X2 with Control-IQ using the Dexcom G6 as the input CGM, was approved in 2019 for adults and pediatric patients older than or equal to 6 years. In the 6-month, randomized, controlled pivotal trial of this device, participants were randomized to closed-loop control or usual diabetes care with sensor-augmented pump therapy. 35 Patients randomized to closed-loop control had improvements in target range, mean CGM glucose, and HbA1c, as well as reduced rates of hypoglycemia. Unlike the Medtronic 670G, Control-IQ only reverts to preprogrammed insulin delivery when CGM signal is lost and does not require finger-stick calibration to continue AID. Trials are underway evaluating this device in younger children ( {"type":"clinical-trial","attrs":{"text":"NCT03844789","term_id":"NCT03844789"}} NCT03844789 ).
Experimental Automated Insulin Delivery Systems
Several AID systems that rely on different sets of mathematical algorithms, including proportional integral derivative, fuzzy logic, and model predictive control algorithms, are in development. These AID systems have been associated with increased time in target glucose range (typically 70–180 mg/dL) and in some cases with decreased mean glucose, lower HbA1c, and decreased time in the hypoglycemic range. Pivotal trials for several of these AID systems are currently ongoing, including the Omnipod Horizon hybrid closed-loop system ( {"type":"clinical-trial","attrs":{"text":"NCT04196140","term_id":"NCT04196140"}} NCT04196140 ) and the Beta Bionics iLet Bionic Pancreas ( {"type":"clinical-trial","attrs":{"text":"NCT04200313","term_id":"NCT04200313"}} NCT04200313 ).
One class of AID systems, called bihormonal or dual hormone systems, is capable of delivering a second hormone to further improve glycemic control. Given the kinetics of subcutaneous insulin delivery, the reduction and/or suspension of insulin may be insufficient to prevent hypoglycemia, especially in certain scenarios that may result in changes in insulin sensitivity such as exercise. Several bihormonal systems use microdosing of glucagon to prevent and treat hypoglycemia when suspension of insulin delivery is not sufficient. Glucagon has rapid on and off kinetics, and the addition of glucagon can allow for more aggressive glucose targets compared with insulin-only systems by reducing the potential for hypoglycemia. In short-term studies of bihormonal systems, subjects achieved increased time in target range, lower mean glucose, and decreased rates of hypoglycemia compared with sensor-augmented pump therapy. 31 , 36 Additional studies comparing bihormonal with insulin-only closed-loop systems suggest that bihormonal systems may further improve mean glucose, time in range, as well as reduce the time spent in hypoglycemic ranges. 37
Other classes of dual hormone systems that have been studied administer pramlintide (an amylin analogue) or glucagon-like peptide-1 (GLP-1) receptor agonist in combination with insulin. 38 , 39 Amylin is cosecreted with insulin from pancreatic beta cells and helps moderate postprandial glucose excursions by slowing gastric emptying, inhibiting glucagon secretion, and promoting satiety. A recent study examining an automated system delivering fixed dose ratio of insulin and pramlintide found increase in time in range compared with the insulin-only system. 38 Long-term studies of bihormonal systems are needed to establish their potential benefits.
A recent meta-analysis 37 reviewed published studies of artificial pancreas systems including insulin-only and dual hormone systems delivering glucagon in more than 500 adult and pediatric subjects with T1D. Most of these trials were small and for a short duration, but the analyses showed that AID systems achieved higher TIR compared with conventional pump therapy and that dual hormone systems resulted in greater improvements in TIR than insulin-only systems. Both classes of AID systems deliver improved glycemia overnight, which is a substantial benefit to patients, as fear of nocturnal hypoglycemia is a primary concern for patients and families. 37 , 40
Challenges to Fully Automated Insulin Delivery
One the main challenges to achieving fully automated closed-loop insulin delivery is overcoming the kinetics of nonphysiologic subcutaneous insulin administration related to postprandial glucose excursions. Given the kinetics of subcutaneous insulin delivery, increased insulin dosing that occurs only after the glucose excursion has begun may lead to prolonged hyperglycemia. Furthermore, because of variations in physiologic insulin needs and the kinetics of current insulin formulations, increased insulin delivery can result in late hypoglycemia. Exercise can compound these challenges by altering insulin sensitivity and increasing insulin-independent glucose uptake into muscles. Several approaches have been studied to ameliorate this issue. Adjunctive therapies including pramlintide (an amylin analogue), GLP-1 receptor agonists, dipeptidyl peptidase-4 inhibitors, and sodium–glucose cotransporter 2 inhibitors have all been studied in patients with T1D with the goal of decreasing postprandial glycemic excursions and reducing the need for aggressive insulin dosing. 41 Alternate approaches to insulin delivery, such as delivery of insulin directly to intraperitoneal space, enable faster pharmacokinetics/pharmacodynamics than subcutaneous insulin delivery. 42 Studies examining the utility of new ultrarapid-acting insulins in AID systems have suggested decreased glycemic variability with these newer insulin analogues. 43
Data management and telehealth
Technology including CGM, smartphones, smartwatches, and activity trackers generate large amounts of high-density data that can be difficult for clinicians to synthesize in the limited time available during visits. At present, SMBG, CGM, and pump data can be downloaded to review for patterns and make adjustments in treatment. Currently available software allows patients to download their pump and CGM at home and then share these data via cloud-based services with the patient’s clinical team to review, potentially allowing for more frequent patient contact between in-person visits. With advancement of artificial intelligence and machine learning, these data could be analyzed for automated generation of recommendations for therapy adjustment. Software systems have been developed to automatically generate insulin dose decision support recommendations. 44
The prevalence of technology at home and in clinics has led to great interest in telehealth—a broad term used to describe health care delivery with the aid of technology, which includes video visits, web-based portals, or text messaging. Telehealth has been applied across multiple specialties and conditions and can be used to conduct remote patient visits and patient education and behavioral management sessions. Telehealth strategies can help increase access to health care and reduce barriers to reaching providers, especially in resource limited settings or for those living far from treatment facilities. A recent meta-analysis found that telehealth intervention in patients with diabetes led to HbA1c improvements. 45 Concerns about spread of SARS-CoV-2 have dramatically increased use of telehealth visits for diabetic patients over a very short period of time in the first quarter of 2020 and will likely accelerate the movement of diabetes management visits to virtual formats.
Availability of data in the cloud has allowed companies to publish “real world” studies describing glycemic control in patients using their technologies. 46 The development of virtual diabetes clinics is likely on the horizon, as patient data are obtained from wearable devices including CGM and insulin pumps and then transmitted into the electronic health record for analysis with machine learning and decision support. 47
Diabetes technology holds promise for improving glycemic outcomes and decreasing burden of disease for patients and families with T1D. Rapid advancement of diabetes therapeutics and technologies have enhanced diabetes monitoring and insulin delivery capabilities. Devices that partially automate insulin delivery improve glycemic control, and more capable automated closed-loop systems will likely be available in the near future. Further research should determine the long-term benefits of these devices on glycemic control and quality of life in T1D.
J.S. Sherwood has nothing to disclose. S.J. Russell has patents and patents pending on aspects of the bionic pancreas that are assigned to Massachusetts General Hospital and are licensed to Beta Bionics, has received honoraria and/or travel expenses for lectures from Novo Nordisk, Roche, and Ascensia, serves on the scientific advisory boards of Unomedical and Companion Medical, has received consulting fees from Beta Bionics, Novo Nordisk, Senseonics, and Flexion Therapeutics, has received grant support from Zealand Pharma, Novo Nordisk, and Beta Bionics, and has received in-kind support in the form of technical support and/or donation of materials from Zealand Pharma, Ascencia, Senseonics, Adocia, and Tandem Diabetes. M.S. Putman has nothing to disclose.

Study provides preliminary evidence in favor of a new type 1 diabetes treatment

Type 1 diabetes is an autoimmune disease that causes the body's immune system to attack and destroy insulin-producing beta cells in the pancreas. Traditional management of type 1 diabetes has primarily involved replacing the missing insulin with injections which, though effective, can be expensive and burdensome. A new study led by researchers at the University of Chicago Medicine and Indiana University suggests that an existing drug could be repurposed to treat type 1 diabetes, potentially reducing dependence on insulin as the sole treatment.
The research centers on a medication known as α-difluoromethylornithine (DFMO), which inhibits an enzyme that plays a key role in cellular metabolism. The latest translational results are a culmination of years of research: In 2010, while corresponding author Raghu Mirmira, MD, PhD , was at Indiana University, he and his lab performed fundamental biochemistry experiments on beta cells in culture. They found that suppressing the metabolic pathway altered by DFMO helped protect the beta cells from environmental factors, hinting at the possibility of preserving and even restoring these vital cells in patients diagnosed with type 1 diabetes.
The researchers confirmed their observations preclinically in zebrafish and then in mice before senior author Linda DiMeglio, MD, MPH, Edwin Letzter Professor of Pediatrics at Indiana University School of Medicine and a pediatric endocrinologist at Riley Children's Health, launched a clinical trial to evaluate the safety and tolerability of the drug in type 1 diabetes patients. The results of the trial, which was funded by the Juvenile Diabetes Research Foundation (JDRF) and used DMFO provided by Panbela Therapeutics, indicated that the drug is safe for type 1 diabetes patients and can help keep insulin levels stable by protecting beta cells.
“As a physician-scientist, this is the kind of thing we’ve always strived for – to discover something at a very basic, fundamental level in cells and find a way to bring it into the clinic,” said Mirmira, who is now Professor of Medicine and an endocrinologist at UChicago Medicine. “It definitely underscores the importance of supporting basic science research.”
"It's been truly thrilling to witness the promising results in the pilot trial after this long journey, and we're excited to continue our meaningful collaboration," said DiMeglio.
Importantly, DFMO has already been FDA-approved as a high dose injection since 1990 for treating African Sleeping Sickness and received breakthrough therapy designation for neuroblastoma maintenance therapy after remission in 2020. Pre-existing regulatory approval could potentially facilitate its use in type 1 diabetes, saving effort and expense and getting the treatment to patients sooner.
“For a drug that’s already approved for other indications, the approval timeline can be a matter of years instead of decades once you have solid clinical evidence for safety and efficacy,” said Mirmira. “Using a new formulation of DFMO as a pill allows patients to take it by mouth instead of needing to undergo regular injections, and it has a very favorable side effect profile. It’s exciting to say we have a drug that works differently from every other treatment we have for this disease.”
To follow up on the recently published results, first and co-corresponding author Emily K. Sims, MD, Associate Professor of Pediatrics at IU School of Medicine and a pediatric endocrinologist at Riley Children's Health, launched a multi-center clinical trial, also funded by JDRF – with UChicago among the trial sites – to gather even stronger data regarding the efficacy of DFMO as a type 1 diabetes treatment.
"With our promising early findings, we hold hope that DFMO, possibly as part of a combination therapy, could offer potential benefits to preserve insulin secretion in individuals with recent-onset type 1 diabetes and ultimately also be tested in those who are at risk of developing the condition," said Sims.
“A new era is dawning where we’re thinking of novel ways to modify the disease using different types of drugs and targets that we didn’t classically think of in type 1 diabetes treatment,” said Mirmira.
The study, “Inhibition of Polyamine Biosynthesis Preserves β-Cell Function in Type 1 Diabetes,” was published in Cell Medicine Reports in November 2023. Co-authors include Emily K. Sims, Abhishek Kulkarni, Audrey Hull, Stephanie E. Woerner, Susanne Cabrera, Lucy D. Mastrandrea, Batoul Hammoud, Soumyadeep Sarkar, Ernesto S. Nakayasu, Teresa L. Mastracci, Susan M. Perkins, Fangqian Ouyang, Bobbie-Jo Webb-Robertson, Jacob R. Enriquez, Sarah A. Tersey, Carmella Evans-Molina, S. Alice Long, Lori Blanchfield, Eugene W. Gerner, Raghavendra Mirmira, and Linda A. DiMeglio.
- Utility Menu
GA4 tracking code

A new therapy for treating Type 1 diabetes
Promising early results show that longstanding harvard stem cell institute (hsci) research may have paved the way for a breakthrough treatment of type 1 diabetes. utilizing research from the melton lab, vertex pharmaceuticals has developed vx-880, an investigational stem cell-derived, fully differentiated pancreatic islet cell replacement therapy for people with type 1 diabetes (t1d). in conjunction with immunosuppressive therapy, vx-880 produced robust restoration of islet cell function on day 90 in the first patient in its phase 1/2 clinical trial..

The patient was treated with a single infusion of VX-880 at half the target dose in conjunction with immunosuppressive therapy. The patient, who was diagnosed with T1D 40 years ago and has been dependent on exogenous (injected) insulin, achieved successful engraftment and demonstrated rapid and robust improvements in multiple measures. These included increases in fasting and stimulated C-peptide, improvements in glycemic control, including HbA1c, and decreases in exogenous insulin requirement, signifying the restoration of insulin-producing islet cells.
VX-880 is not only a potential breakthrough in the treatment of T1D, it is also one of the very first demonstrations of the practical application of embryonic stem cells, using stem cells that have been differentiated into functional islets to treat a patient, explained Doug Melton, Ph.D., co-director of HSCI, is the Xander University Professor at Harvard and an Investigator of the Howard Hughes Medical Institute. Unlike prior treatments, this innovative therapy gives the patient functional hormone producing cells that control glucose metabolism. This potentially obviates the lifelong need for patients with diabetes to self-inject insulin as the replacement cells “provide the patient with the natural factory to make their own insulin,” explained Melton.
These results from the first patient treated with VX-880 are unprecedented. What makes these results truly remarkable is that they were achieved with only half the target dose,” said Bastiano Sanna, Ph.D., Executive Vice President and Chief of Cell and Genetic Therapies at Vertex. “While still early, these results support the continued progression of our VX-880 clinical studies, as well as future studies using our encapsulated islet cells, which hold the potential to be used without the need for immunosuppression.”
“As a surgeon who has worked in the field of islet cell transplantation for decades, this approach, which obviates the need for an organ donor, could be a game changer,” said James Markmann, M.D., Ph.D., Professor of Surgery and Chief of the Division of Transplant Surgery at Massachusetts General Hospital. “We are excited to progress this unique and potentially transformative medicine through clinical trials and to patients.”
“More than a decade ago our lab had a vision for developing an islet cell replacement therapy to provide a functional cure to people suffering from T1D,” said Melton, a founder and one of the first co-chairs of the Harvard Stem Cell and Regenerative Biology Department. “These promising results bring great hope that stem cell-derived, fully differentiated islet cells could deliver a life-changing therapy for people who suffer from the relentless life-long burden of T1D. I'm so grateful that Harvard and the Harvard Stem Cell Institute have supported this work.”
Latest News
How a small fish could lead to better strategies to repair tendon tears, jason buenrostro lands macarthur ‘genius grant’, new model for in vitro production of human brown fat cells lays groundwork for obesity, diabetes cell therapy, share this story, news by topic.
- Alzheimer's Disease (8)
- Bioengineering (31)
- Blood Diseases (52)
- Cancer (55)
- Cardiovascular Disease (25)
- Diabetes (30)
- Endocrine Disease (1)
- Eye Diseases (10)
- Fibrosis (6)
- Gastrointestinal Disease (8)
- Genetics/Epigenetics (24)
- Graft-Versus-Host Disease (1)
- Hearing Loss (5)
- Immunology (15)
- Kidney Disease (12)
- Liver Disease (6)
- Lung Disease (9)
- Multiple Sclerosis (1)

Apr. 27, 2023
Study unlocks potential breakthrough in type 1 diabetes treatment, rice u. scientists optimize biomaterials screening, identify ‘winning’ formulations.
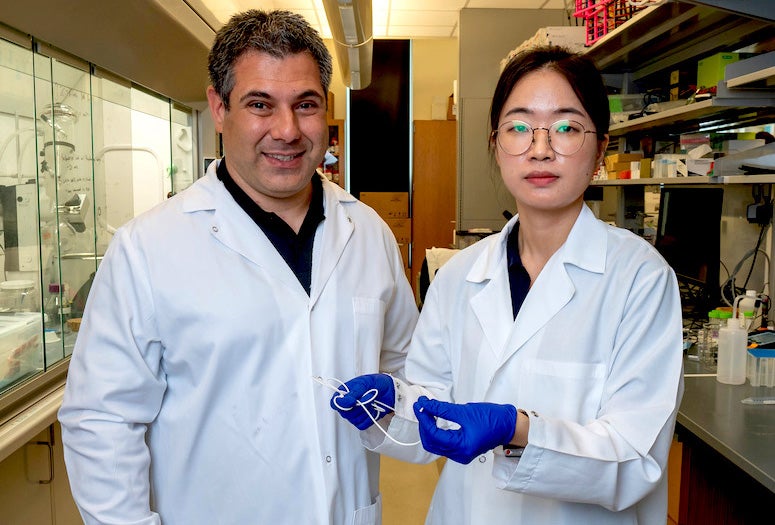
For the over 8 million people around the globe living with Type 1 diabetes , getting a host immune system to tolerate the presence of implanted insulin-secreting cells could be life-changing.
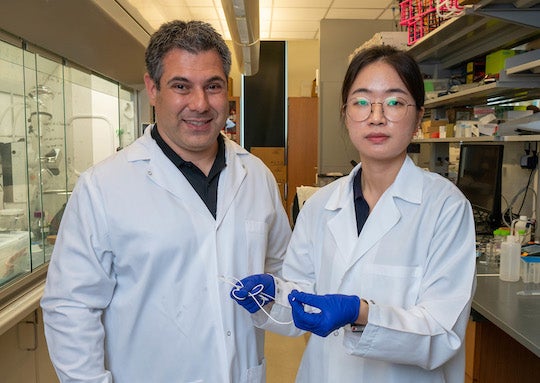
Rice University bioengineer Omid Veiseh and collaborators identified new biomaterial formulations that could help turn the page on Type 1 diabetes treatment, opening the door to a more sustainable, long-term, self-regulating way to handle the disease.
To do so, they developed a new screening technique that involves tagging each biomaterial formulation in a library of hundreds with a unique “barcode” before implanting them in live subjects.
According to the study in Nature Biomedical Engineering , using one of the alginate formulations to encapsulate human insulin-secreting islet cells provided long-term blood sugar level control in diabetic mice. Catheters coated with two other high-performing materials did not clog up. “This work was motivated by a major unmet need,” said Veiseh, a Rice assistant professor of bioengineering and Cancer Prevention and Research Institute of Texas scholar. “In Type 1 diabetes patients, the body’s immune system attacks the insulin-producing cells of the pancreas. As those cells are killed off, the patient loses the ability to regulate their blood glucose.”

For decades, scientists labored toward what Veiseh called a “‘holy grail’ goal of housing islet cells inside a porous matrix made out of a protective material that would allow the cells to access oxygen and nutrients without getting clobbered by the host’s immune system.”
However, materials with optimal biocompatibility proved very hard to find, due in part to screening constraints. On one hand, immune system response to a given implanted biomaterial can only be assessed in a live host.
“The problem is the immune response needs to be investigated inside the body of these diabetic mice, not in a test tube,” said Boram Kim, a graduate student in the Veiseh lab and co-lead author on the study. “That means that if you want to screen these hundreds of alginate molecules, then you need to have hundreds of animal test subjects. Our idea was to screen for hundreds of biomaterials at the same time, in the same test subject.”

On the other hand, different biomaterial formulations look the same, making it impossible to identify high-performing ones in the absence of some telltale trait. This made testing more than one biomaterial per host unfeasible.
“They are different materials but they look the same,” Veiseh said. “And once they are implanted in the body of a test subject and then taken out again, we cannot distinguish between the materials and we would be unable to identify which material formulation worked best.”
To overcome these constraints, Veiseh and collaborators came up with a way to tag each alginate formulation with a unique ‘barcode’ that allowed them to identify the ones that performed best.

“We paired each modified biomaterial with human umbilical vein endothelial cells (HUVEC) from a different donor,” Kim said.
“The HUVEC cells, because they come from unique donors, act as a barcode that allows us to tell what material was used initially,” Veiseh added. “The winners are the ones that have live cells in them. Once we found them, we sequenced the genome of those cells and figured out which material was paired with it. That’s how we uncovered the greatest hits.”
Trials are underway for stem cell-derived islet cell use in diabetic patients. However, current islet treatments require immunosuppression, making it a taxing way to treat Type 1 diabetes. “Currently, in order to use implanted islet cells in diabetic patients, you have to suppress the entire immune system, just as if you were trying to do an organ transplant,” Veiseh said. “That comes with a lot of complications for the patient.

“They can develop cancer, they can’t fight infections, so, for the vast majority of patients, it’s better to actually do the insulin therapy where they inject themselves. With this biomaterial-encapsulation strategy, no immunosuppression is needed.”
Placing actual HUVEC cells inside the biomaterial capsules increased the likelihood that the host immune system would detect a foreign presence. This makes the experiment more robust than simply testing for immune response to the biomaterials alone.
“We wanted to test a library of these materials, with the selection pressure of having cells inside the beads that makes it harder for the material to not get noticed by the immune system,” Veiseh said. “There’s a lot of interest from all the islet cell manufacturers to be able to get rid of immunosuppression and instead use these alginate hydrogel matrices to protect the implanted cells.” The new high-throughput “barcoding” approach can be deployed to screen for other medical applications using fewer live test subjects.

“That actually feeds into a lot of other projects in my lab where we’re doing biologic production from cells for other disease indications,” Veiseh said. “The same modifications can be applied to all types of materials that go into the body. This is not limited only to cell transplantation. The technology we developed can be paired with a lot of different device concepts.
“For instance, some diabetic patients use automated pump systems to self-administer insulin. The catheters on those pump systems have to be replaced every few days because they get clogged. We were able to show that coating the catheters with these new materials prevented clogging.”
“With this new cell-based barcoding technology, biomaterials research just got an unprecedented boost that will accelerate the translation to clinically applicable products, and make it more affordable,” said Dr. José Oberholzer, a transplant surgeon and bioengineer at the University of Virginia.
“This is a real paradigm shift. With this method, we can now screen hundreds of biomaterials at once and select those that the human body does not reject. We can protect cellular grafts from the assaults of the immune system, without the need for immunosuppressive medications,” Oberholzer added.

Former Rice bioengineering professor and current NuProbe U.S. CEO David Zhang noted that “high-throughput DNA sequencing has revolutionized many biomedical fields.”
“I am pleased to work with Omid to enable the development of improved biomaterials using my team's expertise in DNA sequencing,” added Zhang, who was a co-investigator on the grant. “These improved biomaterials can enable durable implanted cell therapies to function as living drug factories, and can have a positively disruptive impact on patients with a variety of chronic diseases.” The National Institutes of Health (R01 DK120459), JDRF (3-SRA-2021-1023-S-B), the National Science Foundation (CBET1626418), the Rice University Academy Fellowship and Rice’s Shared Equipment Authority supported the research.
Screening hydrogels for antifibrotic properties by implanting cellularly barcoded alginates in mice and a non-human primate | Nature Biomedical Engineering | DOI: 10.1038/s41551-023-01016-2 Authors: Sudip Mukherjee, Boram Kim, Lauren Cheng, Michael David Doerfert, Jiaming Li, Andrea Hernandez, Lily Liang, Maria Ruocco, Peter Rios, Sofia Ghani, Irax Joshi, Douglas Isa, Trisha Ray, Tanguy Terlier, Cody Fell, Ping Song, Roberto Miranda, Jose Oberholzer, David Yu Zhang and Omid Veiseh https://www.nature.com/articles/s41551-023-01016-2
https://news-network.rice.edu/news/files/2023/03/230310_Veiseh-Lab_LG.jpg CAPTION: Omid Veiseh is a Rice assistant professor of bioengineering and Cancer Prevention and Research Institute of Texas scholar. (Photo by Gustavo Raskoksy/Rice University) https://news-network.rice.edu/news/files/2023/03/230310_Boram_Kim_LG.jpg CAPTION: Boram Kim is a Rice graduate student and co-lead author on the study. (Photo by Gustavo Raskosky/Rice University) https://news-network.rice.edu/news/files/2023/03/230310_Veiseh_Kim_LG.jpg CAPTION: Omid Veiseh and Boram Kim. Kim is holding a medical-grade catheter similar to ones used in the study experiments. (Photo by Gustavo Raskosky/Rice University) https://news-network.rice.edu/news/files/2023/03/230310_Veiseh-Lab_capsules1.jpg CAPTION: Different biomaterial formulations look the same, making it impossible to identify high-performing ones in the absence of some telltale trait. To overcome these constraints, Rice researchers tagged each alginate formulation with a unique “barcode” that allowed them to identify the ones that performed best. The multicolored beads illustrate the barcoded biomaterial capsules. (Photo by Gustavo Raskosky/Rice University) https://news-network.rice.edu/news/files/2023/03/230310_Veiseh-Lab_capsules2.jpg CAPTION: The new high-throughput “barcoding” approach can be deployed to screen for other medical applications using fewer live test subjects. (Photo by Gustavo Raskosky/Rice University) https://news-network.rice.edu/news/files/2023/03/José_Oberholzer_LG.jpeg CAPTION: Dr. José Oberholzer is a researcher and transplant surgeon at the University of Virginia. (Photo courtesy of José Oberholzer) https://news-network.rice.edu/news/files/2023/03/Lauren_Cheng_LG.jpg CAPTION: Lauren Cheng is a Rice alum and co-lead author on the study. (Photo courtesy of Lauren Cheng) https://news-network.rice.edu/news/files/2023/03/Sudip_Mukherjee_LG.jpg CAPTION: Sudip Mukherjee, a former Rice postdoctoral associate, is an assistant professor in the School of Biomedical Engineering at the Indian Institute of Technology Varanasi and co-lead author on the study. (Photo courtesy of Sudip Mukherjee)
Fats help tag medical implants as friend or foe: https://news.rice.edu/news/2023/fats-help-tag-medical-implants-friend-or-foe Upgraded tumor model optimizes search for cancer therapies: https://news.rice.edu/news/2023/upgraded-tumor-model-optimizes-search-cancer-therapies HIV ‘drug factory’ implant promises once-a-year therapy: https://news.rice.edu/news/2022/hiv-drug-factory-implant-promises-once-year-therapy Rice lab’s ‘drug factory’ implants cleared for human trials: https://news.rice.edu/news/2022/rice-labs-drug-factory-implants-cleared-human-trials
Department of Bioengineering: https://bioengineering.rice.edu/ Veiseh lab: https://veisehlab.rice.edu/team Cancer Prevention and Research Institute of Texas (CPRIT): https://www.cprit.state.tx.us/
Located on a 300-acre forested campus in Houston, Rice University is consistently ranked among the nation’s top 20 universities by U.S. News & World Report. Rice has highly respected schools of Architecture, Business, Continuing Studies, Engineering, Humanities, Music, Natural Sciences and Social Sciences and is home to the Baker Institute for Public Policy. With 4,552 undergraduates and 3,998 graduate students, Rice’s undergraduate student-to-faculty ratio is just under 6-to-1. Its residential college system builds close-knit communities and lifelong friendships, just one reason why Rice is ranked No. 1 for lots of race/class interaction and No. 1 for quality of life by the Princeton Review. Rice is also rated as a best value among private universities by Kiplinger’s Personal Finance.
Type 1 Research Highlights
While the Association’s priority is to improve the lives of all people affected by diabetes, type 1 diabetes is a critical focus of the organization. In fact, in 2016, 37 percent of our research budget was dedicated to projects relevant to type 1 diabetes. Read more about the critical research made possible by the American Diabetes Association.

Smart Insulin Patch
American Diabetes Association Pathway to Stop Diabetes Scientist Zhen Gu, PhD, recently published a paper describing the development of an innovative "smart insulin" patch that imitates the body's beta cells by both sensing blood glucose levels and releasing insulin.
A Possible Trigger for Type 1 Diabetes
In order to prevent or reverse the development of type 1 diabetes, it is essential to understand why and how the immune system attacks the body’s own cells. Association-funded Researcher Thomas Delong, PhD, found a possible answer to these questions.
Enhancing Survival of Beta Cells for Successful Transplantation
Islet transplantation has long offered hope as a curative measure for type 1 diabetes. However, more than 80% of transplanted islets die within one week after transplantation. Research efforts are working to improve their survival and the promise of stem cells to reverse diabetes.
Explore: Type 1 Research Highlights
Investments in type 1 diabetes research
The CDC estimates that nearly 1.6 million Americans have it, including about 187,000 children and adolescents. The American Diabetes Association funds a productive research portfolio that offers significant progress and hope for improved outcomes for people with type 1 diabetes.
Identifying type 1 diabetes before beta cell loss
Dr. Hessner is investigating so-called “biomarkers,” which are components in blood or tissue samples that can be measured to predict which individuals are most likely to develop type 1 diabetes.
Beta cell replacement
Both type 1 and type 2 diabetes result from a complete or partial loss of beta cell number and function. Finding a way to successfully replace functional beta cell is key to efforts to one day cure diabetes.
Enhancing survival of beta cells for successful transplantation
Islet transplantation has long offered hope as a curative measure for type 1 diabetes. However, more than 80% of transplanted islets die within one week after transplantation. Research efforts are working to improve their survival and the promise of stem cells to reverse diabetes.
New insight into how diabetes leads to blindness
New research is uncovering how diabetes changes the kinds of proteins that are made in the eye. These changes may lead to diabetic retinopathy, a leading cause of blindness. This information is allowing researchers to identify new targets for therapies that could delay or prevent the development of diabetic retinopathy.

Give Today and Change Lives!

Type 1 Diabetes Research
Through the JDRF – Beyond Type 1 Alliance , Beyond Type 1 has partnered with JDRF—the world’s biggest nonprofit funder of type 1 diabetes research —to educate our community on the important role research plays in the lives of everyone affected by type 1 diabetes (T1D). It was diabetes research that led to the discovery of insulin in 1921. It was research that led to the creation of the first insulin pump in 1963, and research that led to the modern analog insulins used by many living with T1D today. Without research, we wouldn’t have continuous glucose monitors (CGMs), hybrid closed loop systems, or treatment for the complications that arise from living with diabetes. And it is research that will some day lead to the cure for type 1 diabetes.
Cure Research: The most promising cures for Type 1 diabetes will need to address two challenges: the loss of insulin-producing beta cells, and the immune system’s attack on those beta cells.

Vertex VX-880 Clinical Results Lead To Insulin-Independence

Explaining the Research: What Will It Take to Cure Diabetes?

Vertex Acquires ViaCyte, Combining Resources Toward a T1D Cure
Beta Cell Replacement Therapy: A Pathway to a Cure for Type 1 Diabetes?

New Documentary: ‘The Human Trial’ is a Quest to Cure Type 1 Diabetes
Beta Cell Therapies

Immunotherapies
Improving lives: a future cure is not enough for people living with t1d today. research also focuses on improving lives through glucose control and treating complications..

Glucose Control Therapies

Complications Treatment Research
Learn more about t1d research and the importance of trial participation.

Research Trials

Research News

Research Funding
To learn more about all the great T1D research being funded by JDRF, visit their research and impact page here.
WRITTEN BY BT1 Editorial Team, POSTED 02/13/21, UPDATED 01/03/23
A mother’s cautionary tale -, diabetes management -, diabetes news -, type 1 pregnancy risks and how to minimize them -, 9 bad diabetes photos -.

- TERMS OF USE
- 400 CONCAR DR.
- SAN MATEO, CA 94402

- BEYOND TYPE 1 BEYOND TYPE 1 EN ESPAÑOL
- IN ENGLISH EN ESPANOL BEYOND TYPE 1 AUF DEUTSCH BEYOND TYPE 1 IN ITALIANO BEYOND TYPE 1 EN FRANÇAIS BEYOND TYPE 1 IN HET NEDERLANDS BEYOND TYPE 1 PÅ SVENSKA BEYOND TYPE 1 EM PORTUGUÊS BEYOND TYPE 1 بالعربية

- BEYOND TYPE 2 BEYOND TYPE 2 EN ESPAÑOL IN ENGLISH EN ESPANOL BEYOND TYPE 2 AUF DEUTSCH BEYOND TYPE 2 en Français BEYOND TYPE 2 in Italiano BEYOND TYPE 2 Canada (French) BEYOND TYPE 2 Canada (English)
- KSAT Insider
- KSAT Connect
- Entertainment
WEATHER ALERT
2 severe thunderstorm watches in effect for 4 counties in the area
Could a person with type 1 diabetes re-grow their own pancreas a san antonio study is about to find out, local patients being asked to participate in a never-before-seen clinical trial.
Courtney Friedman , Anchor/Reporter
Luis Cienfuegos , Photojournalist
SAN ANTONIO – A person being able to re-grow their own damaged pancreas inside their body might sound like science fiction, but a new local research study wants to know if it could be real.
“Is there anything on the market like this? No. Is there anything much like this in research? Not that I know of,” Dr. Sherwyn Schwartz said.
Schwartz is the senior medical consultant of the Evolution Research Group and a longtime local doctor who has spent his career bringing important research studies to San Antonio.
That one-of-a-kind research happening right here in San Antonio could change everything for Type 1 diabetes patients.
To fully understand the study, Schwartz said it’s important to understand Type 1 diabetes is an autoimmune disease and very different than Type 2 diabetes.
The process starts with sugar, which our bodies use for fuel. For sugar to travel through the body and be used as energy, the human body needs insulin, a hormone located inside the pancreas.
For Type 1 diabetes patients, the pancreas makes very little or no insulin. As a result, sugar builds up in the bloodstream. Patients may have to be dependent on insulin shots or pumps for life.
“If someone’s got Type 1 diabetes right now, there’s really no treatment except insulin, so we can’t reverse anything,” Schwartz said.
Schwartz is hoping he and his team can change that.
“It’s a national study at several sites, including San Antonio — thank God — where they have a compound they’re working on that will make the pancreas potentially grow its insulin cells back,” Schwartz said. “And it’s never been done before.”
Schwartz and his team are investigating if an injection of the compound could allow patients’ own bodies to repair their damaged pancreas.
If it works, the study could be a major step in finding a cure for Type 1 diabetes.
“To try to make the pancreas grow back and protect them, so they just don’t have to take insulin the rest of their life,” Schwartz said.
Schwartz wants residents in and around San Antonio to be a part of history, and sign up to participate in the study.
The study is looking for participants right now.
You qualify if you’re:
- a Type 1 diabetes patient between 18 and 60 years old
- your disease is early on
- you have no other serious medical problems.
Schwartz said participants will be compensated for their time.
For more information, call 210-934-0500.
Copyright 2024 by KSAT - All rights reserved.
About the Authors
Courtney friedman.
Courtney Friedman anchors KSAT’s weekend evening shows and reports during the week. Her ongoing Loving in Fear series confronts Bexar County’s domestic violence epidemic. She joined KSAT in 2014 and is proud to call the SA and South Texas community home. She came to San Antonio from KYTX CBS 19 in Tyler, where she also anchored & reported.
Luis Cienfuegos
Luis Cienfuegos is a photographer at KSAT 12.
Recommended Videos
Chinese scientists cure diabetes using stem cells in world first

- The 59-year-old patient of 25 years received a transplant of pancreatic cells derived from his own stem cells in 2021. He is now insulin independent.
- This marks the world’s first successful use of stem cell-derived islet transplantation to cure diabetes .
- The achievement, published on Cell Discovery on April 30, comes after over a decade of research at Shanghai Changzheng Hospital.
- Diabetes is a major health threat, affecting 422 million people worldwide. While there is still no known cure for diabetes, methods of management include insulin injections and other medications.
- The patient reportedly suffered a significant decline in pancreatic islet function, which regulates blood sugar, after undergoing a kidney transplant in 2017. Since then, he had been dependent on daily multiple insulin injections.
- In July 2021, a team at the hospital led by researcher Yin Hao used the patient’s own blood cells to create stem cells, which were then converted into pancreatic islet cells.
- The transplant successfully eliminated the patient’s need for external insulin within 11 weeks. Oral medication was also gradually reduced and ultimately discontinued a year later.
- Follow-up exams showed restored pancreatic function and normal kidney function, suggesting that the patient has been cured .
- In 2023, the FDA approved a similar cell therapy treatment by a Chicago-based startup for type 1 diabetes.
- The Chinese researchers say more research is needed to confirm the long-term efficacy and broaden applicability of this treatment.

Asian Americans Have Higher Risk for Undiagnosed Heart Diseases Than White Americans

Incredible Dog in Singapore Has a Special Power That Helps Diabetic Patients

16-Year-Old Nearly Dies After Drinking Boba Tea EVERY DAY
- Happening Now
- San Francisco
- Los Angeles
- Orange County
- About NextShark
- AAPI Resources
Subscribe to NextShark's Newsletter

Ozempic reduces risk of serious illness and death in people with diabetes and kidney disease, study finds
W eekly injections of semaglutide medications like Ozempic significantly reduce the risk of serious kidney outcomes, major cardiovascular events and death among people who have type 2 diabetes and chronic kidney disease, according to a new study.
Diabetes is a key risk factor for kidney disease, which is one of the leading causes of death in the United States and worldwide; about 1 in 3 people with diabetes also has chronic kidney disease, according to the US Centers for Disease Control and Prevention.
But new research shows that weekly injections of semaglutide cut the risk of severe outcomes from diabetic kidney disease by about 24%.
These severe outcomes – including significant loss of kidney function, kidney failure and death from kidney or cardiovascular causes – occurred 331 times among trial participants who were treated with semaglutide, compared with 410 events among those who received the placebo. When scaled by the number of years each person was in the trial, there were 5.8 events for every 100 years of follow-up among those taking semaglutide, compared with 7.5 events for every 100 years of follow-up among those who received the placebo.
High sugar levels in the blood of people with diabetes can damage the blood vessels of the kidneys, and this can also cause strain on the heart. The new study found even broader related benefits of semaglutide treatment among people with diabetic kidney disease.
Kidney function declined more slowly overall, the risk of major cardiovascular events such as heart attack was 18% lower and the risk of death from any cause was 20% lower among people who were treated with semaglutide compared with those who received the placebo, the research found.
The study, published Friday in the New England Journal of Medicine and presented at the European Renal Association Congress, is based on the results of a drug trial conducted among about 3,500 people across 28 countries who were living with both type 2 diabetes and kidney disease. About half of the participants received weekly 1-milligram injections of semaglutide – the dose approved to treat type 2 diabetes under the brand name Ozempic in the US – and the others got a placebo treatment.
Overall, the study participants were followed for an average of about 3½ years. The trial was initially expected to last about four or five years, but findings at the midpoint check-in were so promising that an independent monitoring committee recommended that it end early.
“In this trial, we’re able to show benefits that highlight how transforming semaglutide can be for people with diabetes and kidney disease,” said Dr. Vlado Perkovic, a nephrologist and provost at the the University of New South Wales Sydney. He chairs the trial’s steering committee and was lead author of the new study.
“The effect size was a bit larger than we had expected, and therefore, the results were highly statistically significant. So the likelihood of this being a chance finding is infinitesimally small, and I think we can be highly confident that the results are robust and real.”
Three other drug treatments have been shown to provide benefits for people with diabetic kidney disease, and the researchers note in the new study that “clinicians and patients will need to consider the order and priority of use for semaglutide.”
A combination of therapies could be important, and many of the trial participants were also receiving some other type of treatment for their diabetes.
“Semaglutide showed some benefits on top of what is currently considered standard of care,” said Martin Holst Lange, executive vice president of development for Novo Nordisk. The Danish company is the only drug manufacturer with semaglutide products that are approved for use in the US – Ozempic for treatment of diabetes and Wegovy for treatment of obesity – and it funded the new study.
Similar benefits were found across all levels of starting kidney function, but there was a particular focus on those at highest risk. More than two-thirds of trial participants were considered to be at very high risk of severe outcomes including kidney failure, cardiovascular events or death, according to risk calculators outlined in global clinical practice guidelines .
In part, focusing on this high-risk group offers clearer insight into the benefits of treatment. But, experts say, many people also don’t realize they have kidney disease until it has reached later stages – and many don’t realize just how dangerous it can be. During each year of this trial, about 8% of the participants had a major kidney event, and almost 5% of people died.
“Kidney disease attributed to diabetes, or diabetic kidney disease, is one of the most common and deadly complications of diabetes. Yet, unfortunately, there’s very low awareness around it,” said Dr. Katherine Tuttle, chair of the Diabetic Kidney Disease Collaborative for the American Society of Nephrology. She is also the executive director for research at Providence Inland Northwest Health, an investigator with the Institute of Translational Health Sciences and professor of medicine at the University of Washington.
“Part of the problem is that the condition is asymptomatic until late stages, so physicians and patients have to be very intentional about identifying kidney disease.”
It’s recommended that people with diabetes get tested for kidney disease every six months with blood or urine tests. But this doesn’t always happen, and some people wait until they have symptoms such as fatigue, swelling or changes in urination frequency.
Diabetes treatments are in high demand because it’s such a common disease, said Tuttle, who was also part of the new research. But semaglutide is so promising because it seems to have benefits that apply to multiple complications that can arise because of it. In addition to lowering blood sugar, semaglutide products have been shown to help with weight loss, heart failure and potentially curbing addictive behaviors .
“I think these drugs that affect multiple final common pathways are really highly effective because when we try to just treat one risk factor, it’s almost like putting your finger in the dike. You can’t plug all the holes. To me, what semaglutide really does is, it addresses a broad spectrum of risk,” she said. “It does reduce weight, it does lower glucose in does lower blood pressure a little bit, and then we think on top of that, it has the direct effects on the kidney. It’s really the whole package.”
There are significant disparities in diabetes prevalence and kidney disease in the US. Black, Hispanic and American Indian adults are nearly twice as likely to have diabetes than White adults, according to CDC data . And Black people in the US are about three times more likely to have kidney failure than White adults.
However, most of the participants in the semaglutide trial were White, and the findings could not be assessed among important subgroups.
“When we have something that’s effective, we also have to turn our sights to getting treatments to patients,” Tuttle said. But many of the highest-risk people who could benefit most from treatment don’t have access to it.
“Now, we have a highly effective therapy that reduces things that really matter to patients, families and communities: keeping their kidney function, preserving life and reducing the rates of cardiovascular events. But that’s all great only if people get the treatment,” she said. “So now, really, the challenge before all of us is to move much more expeditiously from evidence generation to implementation.”
For more CNN news and newsletters create an account at CNN.com


IMAGES
VIDEO
COMMENTS
Type 1 diabetes (also known as diabetes mellitus) is an autoimmune disease in which immune cells attack and destroy the insulin-producing cells of the pancreas. ... Latest Research and Reviews ...
Type 1 diabetes is an autoimmune condition resulting in insulin deficiency and eventual loss of pancreatic β cell function requiring lifelong insulin therapy. Since the discovery of insulin more than 100 years ago, vast advances in treatments have improved care for many people with type 1 diabetes. Ongoing research on the genetics and immunology of type 1 diabetes and on interventions to ...
Study unlocks potential breakthrough in type 1 diabetes treatment. Cell barcoding strategy enables high-throughput materials screening. Credit: Nature Biomedical Engineering (2023). DOI: 10.1038 ...
Both are now adults, and both have Type 1 diabetes. My son was 6 months old when he was diagnosed. And that's when I changed my research plan. And my daughter, who's four years older than my son, became diabetic about 10 years later, when she was 14. When my son was diagnosed, I knew nothing about diabetes and had been working on how frogs ...
In its early stage (Stage 1), type 1 diabetes is usually asymptomatic; however, the development of autoimmunity is often detectable in early life, with circulating autoantibodies targeting insulin or other proteins, such as GAD65, insulinoma-associated protein 2 (IA2) or zinc transporter 8 (ZNT8) [].When a large portion of the beta cell mass has become dysfunctional or lost, asymptomatic ...
To the Editor: Most patients with new-onset type 1 diabetes have substantial intact beta-cell reserve. 1 Thus, we analyzed the efficacy of semaglutide, an agonist of glucagon-like peptide 1 (GLP-1 ...
New technologies in type 1 diabetes. Intensive insulin therapy for the management of type 1 diabetes (T1D) was established as the standard of care based on the results of the Diabetes Control and Complication Trial (DCCT), which conclusively demonstrated the benefits of tight glycemic control. 1 However, those who received intensive insulin ...
A new study led by researchers at the University of Chicago Medicine and Indiana University suggests that an existing drug could be repurposed to treat type 1 diabetes, potentially reducing dependence on insulin as the sole treatment. The research centers on a medication known as α-difluoromethylornithine (DFMO), which inhibits an enzyme that ...
As of 2021, about 8.4 million people around the world live with type 1 diabetes — a chronic disease where the pancreas is not able to produce enough insulin for the body to function correctly ...
Vertex Pharmaceuticals has developed VX-880, a stem cell-derived islet cell replacement therapy for T1D, based on research from the Melton Lab. The first patient treated with VX-880 achieved robust improvements in glycemic control and insulin independence.
For the over 8 million people around the globe living with Type 1 diabetes, getting a host immune system to tolerate the presence of implanted insulin-secreting cells could be life-changing.. Omid Veiseh and Boram Kim. Kim is holding a medical-grade catheter similar to ones used in the study experiments. (Photo by Gustavo Raskosky/Rice University)
Study provides preliminary evidence in favor of a new type 1 diabetes treatment. by University of Chicago Medical Center. Credit: Cell Reports Medicine (2023). DOI: 10.1016/j.xcrm.2023.101261 ...
Identification of a new player in type 1 diabetes risk. Type 1 diabetes is caused by an autoimmune attack of insulin-producing beta-cells. While genetics and the environment are known to play important roles, the underlying factors explaining why the immune system mistakenly recognize beta-cells as foreign is not known.
The burden of type 1 diabetes remains substantial, and more research is needed to improve the lives of people with type 1 diabetes and to find a cure. To this end, ADA-funded research continues to drive progress by funding research projects topics spanning technology, islet transplantation, immunology, improving transition to self-management ...
Improving lives, today and tomorrow. While our focus is on curing type 1 diabetes (T1D), we also pursue new treatments to keep people with T1D healthy until that day comes. Outside of the lab, we push for increased government funding for research, and work with academia, clinicians, insurers and regulators to get new therapies and devices to ...
Researchers conducted a Phase III trial to test the 100-year-old Bacillus Calmette-Gu rin (BCG) vaccine in people with type 1 diabetes during the COVID-19 pandemic. In new research, investigators ...
Type 1 Research Highlights. While the Association's priority is to improve the lives of all people affected by diabetes, type 1 diabetes is a critical focus of the organization. In fact, in 2016, 37 percent of our research budget was dedicated to projects relevant to type 1 diabetes. Read more about the critical research made possible by the ...
The Diabetes Research Institute houses teams of scientists, engineers, and clinicians with the expertise required to tackle diabetes from many angles. This integration of medicine and technology drives the vision behind the DRI strategy, a comprehensive, multidisciplinary approach to cure diabetes. The strategy builds upon decades of cure ...
Writing Team for the Diabetes C, I. Complications Trial/Epidemiology of Diabetes, and G. Complications Research (200) Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the Epidemiology of Diabetes Interventions and Complications (EDIC) study. JAMA 290(16): 2159-67
Through the JDRF - Beyond Type 1 Alliance, Beyond Type 1 has partnered with JDRF—the world's biggest nonprofit funder of type 1 diabetes research —to educate our community on the important role research plays in the lives of everyone affected by type 1 diabetes (T1D).It was diabetes research that led to the discovery of insulin in 1921. It was research that led to the creation of the ...
There has been a redistribution in the risk of arterial disease in type 1 and 2 diabetes. The risks of heart attack and stroke have decreased significantly, while complications in more peripheral ...
For Type 1 diabetes patients, the pancreas makes very little or no insulin. As a result, sugar builds up in the bloodstream. Patients may have to be dependent on insulin shots or pumps for life.
In 2023, the FDA approved a similar cell therapy treatment by a Chicago-based startup for type 1 diabetes. The Chinese researchers say more research is needed to confirm the long-term efficacy and ...
We randomly assigned patients with type 2 diabetes and chronic kidney disease (defined by an estimated glomerular filtration rate [eGFR] of 50 to 75 ml per minute per 1.73 m 2 of body-surface area ...
Three-quarters had type 2 diabetes, and 58% had public insurance. "We found insurance denied the GLP1Ra prescriptions in 64% of patients with obesity and 32% of patients with type 2 diabetes ...
But new research shows that weekly injections of semaglutide cut the risk of severe outcomes from diabetic kidney disease by about 24%. ... the dose approved to treat type 2 diabetes under the ...