The evolving profile of eating disorders and their treatment in a changing and globalised world
Affiliations.
- 1 Centre for Research in Eating and Weight Disorders, Department of Psychological Medicine, Institute of Psychiatry, Psychology, and Neuroscience, King's College London, London SE5 8AF, UK; South London and Maudsley NHS Foundation Trust, London, UK. Electronic address: [email protected].
- 2 Centre for Research in Eating and Weight Disorders, Department of Psychological Medicine, Institute of Psychiatry, Psychology, and Neuroscience, King's College London, London SE5 8AF, UK.
- 3 Center for Eating and Feeding Disorders Research, Mental Health Center Ballerup, Copenhagen University Hospital-Mental Health Services CPH, Copenhagen, Denmark; Institute of Biological Psychiatry, Mental Health Center Sct. Hans, Mental Health Services Copenhagen, Roskilde, Denmark.
- 4 Psychiatry Department, St Paul Hospital Millennium Medical College, Addis Ababa, Ethiopia.
- 5 Centre for Research in Eating and Weight Disorders, Department of Psychological Medicine, Institute of Psychiatry, Psychology, and Neuroscience, King's College London, London SE5 8AF, UK; South London and Maudsley NHS Foundation Trust, London, UK.
- PMID: 38705161
- DOI: 10.1016/S0140-6736(24)00874-2
- Publications
- Published Papers, 2021

Published Papers by year
Walter Kaye and the UCSD Eating Disorders Research team have published over 250 papers on the neurobiology of eating disorders. These publications include behavioral, treatment, and cognitive neuroscience studies that have improved understanding of the clinical presentation, genetics, neurotransmitter systems, and neural substrates involved in appetite dysregulation and disordered eating. These studies are guiding the development of more effective, neurobiologically informed interventions.
- Treatment of Patients With Anorexia Nervosa in the US – A Crisis in care
- Walter H. Kaye, MD; Cynthia M. Bulik, PhD
- Association of Brain Reward Response With Body Mass Index and Ventral Striatal-Hypothalamic Circuitry Among Young Women With Eating Disorders
- Guido K. W. Frank, MD; Megan E. Shott, BS; Joel Stoddard, MD; Skylar Swindle, BS; Tamara L. Pryor, PhD
- The acceptability, feasibility, and possible benefits of a neurobiologically-informed 5-day multifamily treatment for adults with anorexia nervosa.
- Wierenga CE, Hill L, Knatz Peck S, McCray J, Greathouse L, Peterson D, Scott A, Eisler I, Kaye WH.
- Int J Eat Disord. 2018 May 2. doi: 10.1002/eat.22876. [Epub ahead of print]
- PMID: 29722047
- Free PMC Article
- Research Program
- Current Research Studies
- Genetic Studies
- Participate in Our Studies
Multi-family Therapy for Eating Disorders Across the Lifespan
- Open access
- Published: 06 May 2024
Cite this article
You have full access to this open access article

- Julian Baudinet ORCID: orcid.org/0000-0002-7840-4158 1 , 2 &
- Ivan Eisler ORCID: orcid.org/0000-0002-8211-7514 1 , 2
278 Accesses
Explore all metrics
Purpose of Review
This review aims to report on recent evidence for multi-family therapy for eating disorders (MFT) across the lifespan. It is a narrative update of recent systematic, scoping and meta-analytic reviews.
Recent Findings
There has been a recent increase in published theoretical, quantitative and qualitative reports on MFT in the past few years. Recent and emerging data continues to confirm MFT can support eating disorder symptom improvement and weight gain, for those who may need to, for people across the lifespan. It has also been associated with improved comorbid psychiatric symptoms, self-esteem and quality of life. Data are also emerging regarding possible predictors, moderators and mediators of MFT outcomes, as well as qualitative data on perceived change processes. These data suggest families with fewer positive caregiving experiences at the start of treatment may particularly benefit from the MFT context. Additionally, early change in family functioning within MFT may lead to improved outcomes at end of treatment.
MFT is a useful adjunctive treatment across the lifespan for people with eating disorders. It helps to promote change in eating disorder and related difficulties. It has also been shown to support and promote broader family and caregiver functioning.
Similar content being viewed by others

Toward the Integration of Family Therapy and Family-Based Treatment for Eating Disorders

Life is different now – impacts of eating disorders on Carers in New Zealand: a qualitative study

A systematic review of the impact of carer interventions on outcomes for patients with eating disorders
Avoid common mistakes on your manuscript.
Introduction
Multi-family therapy (MFT) is increasingly being implemented in eating disorder services internationally [ 1 •]. MFT models differ significantly depending on the country and service context. What they all have in common is that they are (a) group-based, (b) involve several families working together as part of treatment with the support of a clinical team and, (c) in the context of eating disorders, are most commonly delivered in blocks of several hours or full days of treatment [ 2 , 3 ]. MFT has been described in the mental health literature since the 1960s. The earliest groups described were for people struggling with schizophrenia [ 4 , 5 ], substance misuse [ 6 ] and depression [ 7 , 8 ]. Nowadays, MFT is used internationally to support people with a range of presentations across the lifespan including eating disorders, mood disorders, schizophrenia, addiction and medical illnesses [ 9 ].
MFT for eating disorders was first described for young adults with bulimia nervosa [ 10 ] and anorexia nervosa [ 11 ] in the 1980s. Adolescent-specific MFT models emerged in the 1990s, initially from teams in Germany [ 12 , 13 ] and the UK [ 14 ]. These MFT models integrated the theoretical concepts of eating disorder focused family therapy [ 15 , 16 , 17 , 18 ] with more general concepts of MFT [ 14 , 19 , 20 ].
The overarching aim of current MFT models are to speed up the recovery process by offering brief, intensive support in the early stages of treatment when families are feeling most in need of urgent support. MFT differs from other intensive outpatient treatment options (e.g., day programmes, partial hospitalisation programmes, intensive outpatient treatment, etc.) by being entirely group-based and typically adjunctive to other therapeutic interventions [ 21 ]. By bringing multiple families together, MFT provides an opportunity for them to learn from each other and share experiences with a wider range of people, including others with lived experience [ 13 , 22 ]. This is described as helping to reduce stigma and a sense of isolation [ 23 , 24 ]. The MFT milieu has also been described as a “hot house” learning environment in which it is safe to try out new behaviours and express emotions with increased support [ 19 ]. The collaborative environment of MFT may also help to highlight and address any deleterious staff-patient dynamics that can otherwise hamper treatment engagement and progress [ 13 ].
Several systematic, scoping and meta-analytic reviews have been published on MFT across the lifespan in recent years [ 1 , 25 , 26 ]. MFT Manuals have been produced in English [ 27 , 28 , 29 •, 30 ], French [ 31 ], Swedish [ 32 , 33 ], and German [ 34 ].
Typically, MFT is offered in an outpatient context, although day- and inpatient models have also been described. The briefest MFT models provide three [ 35 ] or five [ 28 , 36 , 37 , 38 , 39 ] consecutive days of MFT offered as a stand-alone intervention. The latter five-day model has been manualised by a team at the University of California, San Diego, and named Temperament-Based Therapy with Support (TBT-S [ 28 ]). Other models, such as the Maudsley model, offer six to ten days of MFT spread across 6–12 months [ 29 •, 40 ]. Others offer up to 20 days or more of MFT [ 41 , 42 , 43 •] spread across a period of 12 months or more. Inpatient MFT models tend to be more heterogeneous. Those described in the literature range from the aforementioned three and five day models to eight-week [ 44 ], 26-week [ 45 ] and 12-month models [ 46 ].
The majority of programmes described in this paper are outpatient child and adolescent MFT models for anorexia nervosa (MFT-AN), although the number of adult studies is growing. Only recently have MFT models specifically for bulimia nervosa (MFT-BN) been developed [ 47 , 48 ]. Several services offer MFT for mixed eating disorder groups [ 36 , 46 , 49 •]. During child and adolescent MFT, parents and siblings are typically invited to attend, whereas adult models may also include partners, other significant people in the participant’s life, and/or parents/caregivers.
This review aims to narratively synthesise key MFT findings and provide an update on new quantitative and qualitative data published since our most recent systematic scoping review [ 1 ]. While the full systematic scoping review process was not repeated, the same search terms and strategy were implemented using the same databases (PsycInfo, Medline, Embase, CENTRAL) with the date range set for April 2021 to the present.
Outpatient Multi-family Therapy Outcomes
Regardless of age or MFT model, the pattern of findings is relatively similar across studies. One outpatient MFT-AN randomized controlled trial (RCT) has been published to date ( N = 169, age range 12–20 years) [ 50 •], although two other RCT protocols have been reported [ 51 , 52 ], suggesting more is to follow. Eisler et al. [ 50 •] randomised participants to 12 months of single-family therapy alone or single-family therapy with the addition of 10 days of adjunctive MFT-AN spread across treatment. Both groups reported significant improvements in weight, eating disorder psychopathology and mood, as well as parent-rated negative aspects of caregiving. Participants who received MFT-AN were significantly more likely to have a better global outcome, using the Morgan Russel outcome criteria [ 53 ], compared to those who received single-family therapy alone. At six-month follow-up (18 months post-randomisation) this difference was no longer significant, however, weight was significantly higher for those who received MFT-AN compared to single-family therapy [ 50 •].
Findings from uncontrolled comparison studies and case series’ confirm MFT is associated with weight gain for those who are underweight [ 43 •, 49 •, 50 •, 54 , 55 , 56 , 57 ] and a reduction in eating disorder symptoms [ 3 , 43 •, 49 •, 50 •, 56 , 57 ].
Meta-analytic review findings suggest a large effect size for weight ( n = 8 studies) and medium effect size for self-reported eating disorder symptoms ( n = 4 studies) from baseline to post-MFT intervention, although no differences were reported between MFT and comparison interventions [ 26 ]. When subgroup analyses of weight outcomes were assessed by age, adolescent MFT was associated with significant weight gain with a large effect (standard mean difference = 1.15, 95% CI = 0.94, 1.36), but adult MFT was not (standard mean difference = 0.18, 95% CI = − 0.09, 0.45). It is worth noting that only three adult studies [ 39 , 45 , 46 ] were included in this analysis, all of which had very different treatment lengths and intensity (range 5 days – 12 months). Two included participants with mixed eating disorder diagnoses [ 39 , 46 ] and one included restrictive eating disorder presentations only [ 45 ]. Only one MFT study across the lifespan in this review did not find a significant improvement in weight during MFT, however, participants ( N = 10) in this study reported significant improvements in eating disorder symptoms and mean BMI at the start of treatment was 20.7 (sd = 3.3, range = 16.0–26.1), which was maintained during treatment [ 45 ].
Regarding broader psycho-social functioning, there is evidence that MFT is associated with improved quality of life [ 56 , 58 ], self-perception and self-image [ 57 ], self-esteem [ 58 , 59 ], reduced caregiver burden [ 54 ], changes in expressed emotion [ 60 ], as well as improved general family functioning [ 39 , 43 •, 61 , 62 ] and communication [ 63 ]. Notably, change in family functioning and expressed emotion are more varied and not consistently reported between studies.
Within the last few years, data are also beginning to emerge regarding possible moderators, mediators and predictors (baseline individual and family factors) of MFT outcomes. Terache et al. [ 43 •] found that MFT was associated with improvements in all aspects of family functioning on the Family Assessment Device [ 64 ], and that two subscales (roles, communication) and the general family functioning score each mediated improvements in some aspects of eating disorder symptomatology measures using the Eating Disorder Inventory, second edition (EDI-II) [ 65 ]. Most notably, an improvement in the clarity of family roles mediated changes in drive for thinness [ 43 •]. However, in the same study, family functioning did not mediate improvements in weight [ 43 •]. In another study, decreases in parental perceived isolation was associated with improved young person physical health and general functioning at the end of treatment [ 54 ].
Regarding baseline predictors of outcome, Funderud et al. [ 49 •] reported that lower baseline weight was not significantly associated with change in eating disorder symptoms or distress. Dennhag et al. [ 54 ] found that baseline maternal level of guilt was associated with poorer end-of-treatment eating disorder symptom outcomes in their case series. Additionally, greater paternal social isolation and perceived burden of dysregulated behaviours was associated with poorer physical health outcomes for the young person at end of treatment [ 54 ].
In a secondary analysis of the Eisler et al. [ 50 •] RCT, six hypothesised moderators of treatment effect were recently explored; (1) age, (2) eating disorder symptom severity, (3) perceived conflict from the 3) young person and (4) parent/caregiver perspective, parent-rated (5) positive and (6) negative experiences of caregiving [ 66 ]. Positive experiences of caregiving significantly moderated treatment effect. Families presenting with fewer parent-rated positive caregiving experiences at baseline had higher weight at follow-up if they had MFT-AN alongside single-family therapy compared to single-family therapy alone. This is striking given consistent findings from three studies that positive caregiving experiences do not change during MFT [ 35 , 50 •, 61 ]. Taken together, these data suggest that MFT-AN may help protect against this impacting outcome for the adolescent, however, it does not seem help improve parental sense of caregiving itself. The findings from this moderator study extend previous findings that weight at commencement of treatment does not seem to impact on outcome [ 49 •] by demonstrating that it also does not seem to moderate treatment effect [ 66 ].
Outcome data for MFT-BN is still very limited, and all data are generated from one outpatient specialist child and adolescent eating disorder clinic, the Maudsley Centre for Child and Adolescent Eating Disorders. Quantitative outcomes ( N = 50) from this 14-week programme consisting of weekly 90 min sessions indicate it is associated with a reduction in binge-purge behaviours, as well as improvements in eating disorder symptoms, anxiety, depression and emotion dysregulation [ 48 ]. Caregiver burden and parental mood also significantly improved in the same study, although level of anxiety in the young person did not [ 48 ]. While promising, more data are needed to confirm MFT-BN’s effectiveness and replicability in different contexts.
Multi-family Therapy Outcomes in Day- and Inpatient Settings
A much smaller amount of data have been reported on for inpatient/day-patient MFT models. Regarding quantitative data, three inpatient (two young person [ 61 , 67 ] and one adult [ 35 ] studies) and one adult day programme MFT study [ 44 ] have been published. All studies compared MFT to another type of treatment, namely, single family therapy [ 35 , 44 , 67 ] or a parent-only group intervention [ 61 ]. Two were small RCTs ( N = 25 [ 67 ], N = 48 [ 35 ]) and the other two used a non-randomised, uncontrolled comparison design.
Regarding outcomes, MFT within intensive treatment settings has been associated with weight gain and eating disorder symptom improvement [ 35 , 44 , 61 ], as well as broader factors such as expressed emotion [ 35 , 44 ], perceived caregiver burden [ 61 ], family member depressive symptoms [ 44 ], carer distress [ 35 ] and family functioning [ 61 ].
Notably, findings are more mixed than in the outpatient context. One study found no change in eating disorder symptoms and a worsening in perceived family functioning, which the authors attributed to increased family insight into their difficulties [ 67 ]. This may reflect the more heterogeneous treatment models tested and the fact that much more intervention is offered alongside MFT in inpatient and day-patient settings, such as other therapeutic group work, meal support, individual and family therapy sessions, etc.
Qualitative Findings and Perceived Change Processes During MFT
Due to the multiple co-occurring family needs and dynamics within MFT, increasingly qualitative studies are being produced to better understand participant, caregiver and clinician experiences of treatment. Based on data generated using observational, individual interviews and focus groups, MFT has been described as challenging and helpful, regardless of model, setting or age [ 1 ]. Specifically, people describe it as promoting understanding, identity development, mentalising and holistic recovery-oriented change [ 47 , 63 , 68 , 69 , 70 , 71 ]. Benefits include participants (particularly caregivers) feeling empowered, more confident and more able to share experiences [ 45 , 72 , 73 , 74 ]. Many also speak of the intensity and comparisons that arise out of the group process, and how this can generate and lead to the expression of strong emotion – described as both a challenge and a benefit [ 62 , 68 ]. Being able to learn and experiment through non-verbal and activity-based tasks has also been described as helpful and unique to MFT [ 68 ].
In the only study exploring the experience of MFT delivered online vs. face-to-face, data were mixed with participants describing both the convenience of online MFT as well as the potential loss of non-verbal communication during online working [ 62 ].
Most recently, qualitative studies have explored how participants and clinicians perceived change to occur within MFT [ 68 , 75 ]. Considering data from these three different perspectives suggests four inter-related elements (1. Intensity and immediacy, 2. Flexibility, 3. Peer connection and comparisons, 4. New ideas and channels of learning) may combine to contain the family system by building trust, engagement, hope and confidence. It seems that from this (re)established secure base, recovery-oriented behaviour change may (re)commence. See Fig. 1 for a proposed model of change in MFT-AN that incorporates data from clinician [ 75 ], young person and parent/caregiver [ 68 ] data. To date, no data have been collected regarding potential change processes in MFT-BN.

Proposed model of change in MFT-AN that incorporates young person, parent/caregiver and clinician perspectives from two recent qualitative studies [ 68 , 75 ]
Within this model (Fig. 1 ), the step of ‘containment’ may reflect the quantitative findings that improved family functioning mediates MFT outcomes [ 43 •]. Qualitative data suggests families need to move from a place of uncertainty and distress to connection to be able to take positive steps forward. This fits closely theoretically with the aspects of family functioning (roles, communication, general family functioning) that mediated outcomes in the Terache et al. [ 43 •] quantitative study. It also supports the idea that MFT (and possibly other intensive treatments) may (re)activate several change processes recently reported for single-family therapy [ 76 ].
These data also fit theoretically with qualitative data on young person and parent experiences of intensive day programme treatment [ 77 , 78 ]. While, day programme treatments are somewhat different from MFT, some do include multi-family elements. Other similarities include the intensity, increased level of support and additional hours of intervention per week. In both settings, the importance of immediacy, intensity and connecting with others are all described by young people and parents/caregivers as key factors in supporting people to (re)engage in less intensive outpatient treatment.
Conclusions
Available data are encouraging and suggest MFT is an effective adjunctive treatment for people with eating disorders across the lifespan. The available data are predominantly focused on adolescent MFT-AN models, specifically. Conclusions are more mixed regarding adult MFT models and MFT-BN. Findings for this review indicate that more is needed to confirm these effects in more diverse and larger groups, and settings. It will be important for future research to begin empirically investigating which components or aspects of MFT are most effective and whether this differs according to individual, family, cultural and service contexts.
Data Availability
No datasets were generated or analysed during the current study.
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Baudinet J, Eisler I, Dawson L, Simic M, Schmidt U. Multi-family therapy for eating disorders: a systematic scoping review of the quantitative and qualitative findings. Int J Eat Disord. 2021;54:2095–120. This article is a recent comprehensive scoping review of quantitative and qualitative findings for MFT-ED across the lifespan.
Article PubMed PubMed Central Google Scholar
Cook-Darzens S, Gelin Z, Hendrick S. Evidence base for multiple family therapy (MFT) in non-psychiatric conditions and problems: a review (part 2): evidence base for non-psychiatric MFT. J Fam Ther. 2018;40:326–43.
Article Google Scholar
Gelin Z, Cook-Darzens S, Simon Y, Hendrick S. Two models of multiple family therapy in the treatment of adolescent anorexia nervosa: a systematic review. Eat Weight Disord. 2016;21:19–30.
Article PubMed Google Scholar
Laqueur HP, Laburt HA, Morong E. Multiple family therapy. Curr Psychiatr Ther. 1964;4:150–4.
CAS PubMed Google Scholar
McFarlane WR. Multifamily groups in the treatment of severe Psychiatric disorders. New York & London: Guilford Press; 2002.
Google Scholar
Kaufman E, Kaufmann P. Multiple family therapy: a new direction in the treatment of drug abusers. Am J Drug Alcohol Abus. 1977;4:467–78.
Article CAS Google Scholar
Anderson CM, Griffin S, Rossi A, Pagonis I, Holder DP, Treiber R. A comparative study of the Impact of Education vs. process groups for families of patients with affective disorders. Fam Process. 1986;25:185–205.
Article CAS PubMed Google Scholar
Lemmens GMD, Eisler I, Buysse A, Heene E, Demyttenaere K. The effects on mood of adjunctive single-family and multi-family group therapy in the treatment of hospitalized patients with major depression a 15-month follow-up study. Psychother Psychosom. 2009;78:98–105.
Van Es CM, El Khoury B, Van Dis EAM, Te Brake H, Van Ee E, Boelen PA, et al. The effect of multiple family therapy on mental health problems and family functioning: a systematic review and meta-analysis. Fam Process. 2023;62:499–514.
Wooley OW, Wooley SC, Deddens JA. Outcome evaluation of an intensive residential treatment program for bulimia. J Psychother Pract Res. 1993;2(3):242–56. PMID: 22700149; PMCID: PMC3330336.
Slagerman M, Yager J. Multiple family group treatment for eating disorders: a short term program. Psychiatr Med. 1989;7:269–83.
Asen E. Multiple family therapy: an overview. J Family Therapy. 2002;24:3–16.
Scholz M, Asen E. Multiple family therapy with eating disordered adolescents: concepts and preliminary results. Eur Eat Disorders Rev. 2001;9:33–42.
Dare C, Eisler I. A multi-family group day treatment programme for adolescent eating disorder. Eur Eat Disorders Rev. 2000;8:4–18.
Baudinet J, Simic M, Eisler I. From treatment models to manuals: Maudsley single- and multi-family therapy for adolescent eating disorders. In: Mariotti M, Saba G, Stratton P, editors. Systemic approaches to manuals. Switzerland: Springer, Cham; 2021. p. 349–72.
Dare C, Eisler I, Russell GFM, Szmukler GI. The clinical and theoretical impact of a controlled trial of family therapy in anorexia nervosa. J Marital Fam Ther. 1990;16:39–57.
Eisler I. The empirical and theoretical base of family therapy and multiple family day therapy for adolescent anorexia nervosa. J Family Therapy. 2005;27:104–31.
Eisler I, Simic M, Blessitt E, Dodge L, MCCAED Team. Maudsley Service Manual for Child and Adolescent Eating Disorders. 2016. https://mccaed.slam.nhs.uk/wp-content/uploads/2019/11/Maudsley-Service-Manual-for-Child-and-Adolescent-Eating-Disorders-July-2016.pdf .
Asen E, Scholz M. Multi-family therapy: concepts and techniques. London/New York: Routledge; 2010.
Book Google Scholar
Simic M, Eisler I. Family and multifamily therapy. In: Eating and its Disorders. 2012. p. 260–79.
Chapter Google Scholar
Baudinet J, Simic M. Adolescent eating Disorder Day Programme Treatment models and outcomes: a systematic scoping review. Front Psychiatry. 2021;12:539.
Blessitt E, Baudinet J, Simic M, Eisler I. Eating disorders in children, adolescents, and young adults. The handbook of systemic family therapy. John Wiley & Sons, Ltd; 2020. pp. 397–427.
Dawson L, Baudinet J, Tay E, Wallis A. Creating community - the introduction of multi-family therapy for eating disorders in Australia. Australian New Z J Family Therapy. 2018;39:283–93.
Simic M, Eisler I. Multi-family therapy. In: Loeb KL, Le Grange D, Lock J, editors. Family Therapy for Adolescent Eating and Weight disorders. New York: Imprint Routledge; 2015. pp. 110–38.
Gelin Z, Cook-Darzens S, Hendrick S. The evidence base for multiple family therapy in psychiatric disorders: a review (part 1). J Family Therapy. 2018;40:302–25.
Zinser J, O’Donnell N, Hale L, Jones CJ. Multi-family therapy for eating disorders across the lifespan: a systematic review and meta‐analysis. Euro Eat Disorders Rev 2022;30(6):723–45. https://doi.org/10.1002/erv.2919
Balmbra S, Valvik M, Lyngmo S. Coming together, letting go. Bodo, Norway, 2019. Retrieved from: https://www.nordlandssykehuset.no/siteassets/documents/Ressp/Coming-together-2019-10d-B5.pdf .
Hill LL, Knatz Peck S, Wierenga CE. Temperament based therapy with support for Anorexia Nervosa: a Novel treatment. Cambridge: Cambridge University Press; 2022. https://doi.org/10.1017/9781009032063 .
• Simic M, Baudinet J, Blessitt E, Wallis A, Eisler I. Multi-family therapy for anorexia nervosa: a treatment manual. 1st edition. London, UK: Routledge; 2021. https://doi.org/10.4324/9781003038764 . This is a treatment manual covering theory and practice of MFT-AN for young people. This is the model used in the only outpatient MFT-ED RCT.
Tantillo M, McGraw JS, Le Grange D. Multifamily therapy group for young adults with anorexia nervosa: reconnecting for recovery. 1st ed. London, UK: Routledge; 2020.
Duclos J, Carrot B, Minier L, Cook-Darzens S, Barton-Clegg V, Godart N, Criquillion-Doublet S. Manuel de Thérapie Multi-Familiale. 2021. https://www.researchgate.net/publication/350906742_Manuel_de_Therapie_Multi-Familiale_approche_integrative_pour_la_prise_en_charge_d%27adolescents_souffrant_d%27Anorexie_Mentale_et_de_leurs_familles .
Wallin U. Multi-family therapy with anorexia nervosa. A treatment manual. Lund: Lund University; 2007.
Wallin U. Multifamiljeterapi vid anorexia nervosa [Multifamily therapy of anorexia nervosa]. Lund, Sweden: Behandlingsmanual; 2011.
Scholz M, Rix M, Hegewald K. Tagesklinische multifamilientherapie bei anorexia nervosa – manual Des Dresdner modells [Outpatient multifamiliy therapy for anorexia nevrosa – manual of the Dresdner model]. In: Steinbrenner B, Schönauer CS, editors. Essst ̈ orungen – anorexie – bulemie-adipositas – therapie in theorie und praxis [Eating disorders. Anorexia – bulimia-obesity – therapy in theory and practice]. Vienna: Maudrich; 2003. pp. 66–75.
Whitney J, Murphy T, Landau S, Gavan K, Todd G, Whitaker W, et al. A practical comparison of two types of family intervention: an exploratory RCT of Family Day Workshops and Individual Family Work as a supplement to Inpatient Care for adults with Anorexia Nervosa. Eur Eat Disorders Rev. 2012;20:142–50.
Knatz Peck S, Towne T, Wierenga CE, Hill L, Eisler I, Brown T, et al. Temperament-based treatment for young adults with eating disorders: acceptability and initial efficacy of an intensive, multi-family, parent-involved treatment. J Eat Disord. 2021;9:110.
Marzola E, Knatz S, Murray SB, Rockwell R, Boutelle K, Eisler I, et al. Short-term intensive family therapy for adolescent eating disorders: 30-month outcome. Eur Eat Disord Rev. 2015;23:210–8.
Stedal K, Funderud I, Wierenga CE, Knatz-Peck S, Hill L. Acceptability, feasibility and short-term outcomes of temperament based therapy with support (TBT-S): a novel 5-day treatment for eating disorders. J Eat Disord. 2023;11:156.
Wierenga CE, Hill L, Knatz Peck S, McCray J, Greathouse L, Peterson D, et al. The acceptability, feasibility, and possible benefits of a neurobiologically-informed 5-day multifamily treatment for adults with anorexia nervosa. Int J Eat Disord. 2018;51:863–9.
Baudinet J, Eisler I, Simic M. Thérapie multifamiliale intensive pour adolescents avec troubles des conduits alimentaires (TMF-AM) [Intensive multi-family therapy for adolescents with eating disorders]. In: Cook-Darzens S, Criquillion-Doublet S, editors. Les Thérapies multifamiliales appliquées aux troubles des conduites alimentaires [Multi-family therapies: applications to eating disorders]. Elsevier Masson: France,; 2023. pp. 13–35.
Minier L, Carrot B, Cook-Darzens S, Criquillion‐Doublet S, Boyer F, Barton‐Clegg V, Simic M, Voulgari S, Godart N, Duclos J, the THERAFAMBEST group. Conceptualising, designing and drafting a monthly multi‐family therapy programme and manual for adolescents with anorexia nervosa. J Fam Ther 2022;1467–6427.12403. https://doi.org/10.1111/1467-6427.12403 .
Scholz M, Rix M, Scholz K, Gantchev K, Thomke V. Multiple family therapy for anorexia nervosa: concepts, experiences and results. J Family Therapy. 2005;27:132–41.
• Terache J, Wollast R, Simon Y, Marot M, Van der Linden N, Franzen A, et al. Promising effect of multi-family therapy on BMI, eating disorders and perceived family functioning in adolescent anorexia nervosa: an uncontrolled longitudinal study. Eat Disord. 2023;31:64–84. This recent naturalistic study includes a relatively large sample and includes mediator analyses.
Dimitropoulos G, Farquhar JC, Freeman VE, Colton PA, Olmsted MP. Pilot study comparing multi-family therapy to single family therapy for adults with anorexia nervosa in an intensive eating disorder program. Eur Eat Disord Rev. 2015;23:294–303.
Tantillo M, McGraw JS, Lavigne HM, Brasch J, Le Grange D. A pilot study of multifamily therapy group for young adults with anorexia nervosa: reconnecting for recovery. Int J Eat Disord. 2019;52:950–5.
Skarbø T, Balmbra SM. Establishment of a multifamily therapy (MFT) service for young adults with a severe eating disorder – experience from 11 MFT groups, and from designing and implementing the model. J Eat Disord. 2020;8:9.
Escoffié A, Pretorius N, Baudinet J. Multi-family therapy for bulimia nervosa: a qualitative pilot study of adolescent and family members’ experiences. J Eat Disord. 2022;10:91.
Stewart CS, Baudinet J, Hall R, Fiskå M, Pretorius N, Voulgari S, et al. Multi-family therapy for bulimia nervosa in adolescence: a pilot study in a community eating disorder service. Eat Disord. 2021;29:351–67.
• Funderud I, Halvorsen I, Kvakland A-L, Nilsen J-V, Skjonhaug J, Stedal K, et al. Multifamily therapy for adolescent eating disorders: a study of the change in eating disorder symptoms from start of treatment to follow-up. J Eat Disord. 2023;11:92. This larger naturalistic study conducted in Norway includes investigation of whether some baseline factors predict treatment response.
• Eisler I, Simic M, Hodsoll J, Asen E, Berelowitz M, Connan F, et al. A pragmatic randomised multi-centre trial of multifamily and single family therapy for adolescent anorexia nervosa. BMC Psychiatry . 2016;16:422. This is the only outpatient RCT for MFT-ED with a relatively large sample size compared to may MFT-ED studies.
Baudinet J, Eisler I, Simic M, Schmidt U. Brief early adolescent multi-family therapy (BEAM) trial for anorexia nervosa: a feasibility randomized controlled trial protocol. J Eat Disord. 2021;9:71.
Carrot B, Duclos J, Barry C, Radon L, Maria A-S, Kaganski I, et al. Multicenter randomized controlled trial on the comparison of multi-family therapy (MFT) and systemic single-family therapy (SFT) in young patients with anorexia nervosa: study protocol of the THERAFAMBEST study. Trials. 2019;20:249.
Russell GFM, Szmukler GI, Dare C, Eisler I. An evaluation of Family Therapy in Anorexia Nervosa and Bulimia Nervosa. Arch Gen Psychiatry. 1987;44:1047.
Dennhag I, Henje E, Nilsson K. Parental caregiver burden and recovery of adolescent anorexia nervosa after multi-family therapy. Eat Disorders: J Treat Prev. 2019. https://doi.org/10.1080/10640266.2019.1678980 .
Gabel K, Pinhas L, Eisler I, Katzman D, Heinmaa M. The effect of multiple family therapy on Weight Gain in adolescents with Anorexia Nervosa: Pilot Data. J Can Acad Child Adolesc Psychiatry. 2014;23:4.
Gelin Z, Fuso S, Hendrick S, Cook-Darzens S, Simon Y. The effects of a multiple family therapy on adolescents with eating disorders: an outcome study. Fam Process. 2015;54:160–72.
Hollesen A, Clausen L, Rokkedal K. Multiple family therapy for adolescents with anorexia nervosa: a pilot study of eating disorder symptoms and interpersonal functioning: outcome of multiple family therapy. J Fam Ther. 2013;35:53–67.
Mehl A, Tomanova J, Kubena A, Papezova H. Adapting multi-family therapy to families who care for a loved one with an eating disorder in the Czech Republic combined with a follow-up pilot study of efficacy. J Fam Ther. 2013;35:82–101.
Salaminiou E, Campbell M, Simic M, Kuipers E, Eisler I. Intensive multi-family therapy for adolescent anorexia nervosa: an open study of 30 families: multi-family therapy for adolescent anorexia nervosa. J Family Therapy. 2017;39:498–513.
Uehara T, Kawashima Y, Goto M, Tasaki S, Someya T. Psychoeducation for the families of patients with eating disorders and changes in expressed emotion: a preliminary study. Compr Psychiatry. 2001;42:132–8.
Depestele L, Claes L, Dierckx E, Colman R, Schoevaerts K, Lemmens GMD. An adjunctive multi-family group intervention with or without patient participation during an inpatient treatment for adolescents with an eating disorder: a pilot study. Eur Eat Disorders Rev. 2017;25:570–8.
Yim SH, White S. Service evaluation of multi-family therapy for anorexia groups between 2013–2021 in a specialist child and adolescent eating disorders service. Clin Child Psychol Psychiatry. 2023. https://doi.org/10.1177/13591045231193249 .
Voriadaki T, Simic M, Espie J, Eisler I. Intensive multi-family therapy for adolescent anorexia nervosa: adolescents’ and parents’ day-to-day experiences. J Fam Ther. 2015;37:5–23.
Epstein NB, Baldwin LM, Bishop DS. The McMasters Family Assessment device. J Marital Fam Ther. 1983;9:171–80.
Garner DM. Eating disorder inventory-2: professional manual. Psychological Assessment Resources, Odessa. 1991.
Baudinet J, Eisler I, Konstantellou A, Hunt T, Kassamali F, McLaughlin N, Simic M, Schmidt U. Perceived change mechanisms in multi-family therapy for anorexia nervosa: a qualitative follow-up study of adolescent and parent experiences. Eur Eat Disord Rev. 2023;31(6):822–36. https://doi.org/10.1002/erv.3006 .
Geist R, Heinmaa M, Stephens D, Davis R, Katzman DK. Comparison of family therapy and family group psychoeducation in adolescents with anorexia nervosa. Can J Psychiatry. 2000;45:173–8.
Baudinet J, Eisler I, Konstantellou A, Hunt T, Kassamali F, McLaughlin N, et al. Perceived change mechanisms in multi-family therapy for anorexia nervosa: a qualitative follow-up study of adolescent and parent experiences. Eur Eat Disord Rev. 2023;31:822–36.
Baumas V, Zebdi R, Julien-Sweerts S, Carrot B, Godart N, Minier L, et al. Patients and parents’ experience of multi-family therapy for Anorexia Nervosa: a pilot study. Front Psychol. 2021;12:584565.
Coopey E, Johnson G. Exploring the experience of young people receiving treatment for an eating disorder: family therapy for anorexia nervosa and multi-family therapy in an inpatient setting. J Eat Disord. 2022;10:101.
Escoffié A, Pretorius N, Baudinet J. Multi-family therapy for bulimia nervosa: a qualitative pilot study of adolescent and family members’ experiences. J Eat Disord. 2022;10(1):91. https://doi.org/10.1186/s40337-022-00606-w .
Brinchmann BS, Krvavac S. Breaking down the wall’ patients’ and families’ experience of multifamily therapy for young adult women with severe eating disorders. J Eat Disord. 2021;9:56.
Whitney J, Currin L, Murray J, Treasure J. Family Work in Anorexia Nervosa: a qualitative study of Carers’ experiences of two methods of family intervention. Eur Eat Disorders Rev. 2012;20:132–41.
Wiseman H, Ensoll S, Russouw L, Butler C. Multi-family therapy for Young People with Anorexia Nervosa: clinicians’ and Carers’ perspectives on systemic changes. J Systemic Ther. 2019;38:67–83.
Baudinet J, Eisler I, Roddy M, Turner J, Simic M, Schmidt U. Clinician perspectives on the change mechanisms in multi-family therapy for anorexia nervosa: a qualitative study. J Eat Disord. under review.
Baudinet J, Eisler I, Konstantellou A, Simic M, Schmidt U. How young people perceive change to occur in family therapy for anorexia nervosa: a qualitative study. J Eat Disord. 2024;12:11.
Colla A, Baudinet J, Cavenagh P, Senra H, Goddard E. Change processes during intensive day programme treatment for adolescent anorexia nervosa: a dyadic interview analysis of adolescent and parent views. Front Psychol. 2023;14. https://doi.org/10.3389/fpsyg.2023.1226605 .
Gledhill LJ, MacInnes D, Chan SC, Drewery C, Watson C, Baudinet J. What is day hospital treatment for anorexia nervosa really like? A reflexive thematic analysis of feedback from young people. J Eat Disord. 2023;11:223.
Download references
Author information
Authors and affiliations.
Maudsley Centre for Child and Adolescent Eating Disorders (MCCAED), Maudsley Hospital, De Crespigny Park, Denmark Hill, London, SE5 8AZ, UK
Julian Baudinet & Ivan Eisler
Centre for Research in Eating and Weight Disorders (CREW), Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King’s College London, De Crespigny Park, Denmark Hill, London, SE5 8AF, UK
You can also search for this author in PubMed Google Scholar
Contributions
JB and IE were involved in study design. JB drafted the initial manuscript. JB and IE reviewed the final version.
Corresponding author
Correspondence to Julian Baudinet .
Ethics declarations
Competing interests.
Both authors receive royalties from Routledge for a published manual on multi-family therapy for adolescent anorexia nervosa [ 29 •].
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Baudinet, J., Eisler, I. Multi-family Therapy for Eating Disorders Across the Lifespan. Curr Psychiatry Rep (2024). https://doi.org/10.1007/s11920-024-01504-5
Download citation
Accepted : 14 April 2024
Published : 06 May 2024
DOI : https://doi.org/10.1007/s11920-024-01504-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Maudsley family therapy
- Multi-family therapy
- Family based treatment
- Anorexia nervosa
- Bulimia nervosa
- Group therapy
Advertisement
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 30 May 2023
Eating disorder outcomes: findings from a rapid review of over a decade of research
- Jane Miskovic-Wheatley 1 , 2 ,
- Emma Bryant 1 , 2 ,
- Shu Hwa Ong 1 , 2 ,
- Sabina Vatter 1 , 2 ,
- Anvi Le 3 ,
- National Eating Disorder Research Consortium ,
- Stephen Touyz 1 , 2 &
- Sarah Maguire 1 , 2
Journal of Eating Disorders volume 11 , Article number: 85 ( 2023 ) Cite this article
14k Accesses
14 Citations
277 Altmetric
Metrics details
Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and interventions that may reduce the detrimental impact of illness and to optimise recovery. This paper aims to synthesise the literature on outcomes for people with ED, including rates of remission, recovery and relapse, diagnostic crossover, and mortality.
This paper forms part of a Rapid Review series scoping the evidence for the field of ED, conducted to inform the Australian National Eating Disorders Research and Translation Strategy 2021–2031, funded and released by the Australian Government. ScienceDirect, PubMed and Ovid/MEDLINE were searched for studies published between 2009 and 2022 in English. High-level evidence such as meta-analyses, large population studies and Randomised Controlled Trials were prioritised through purposive sampling. Data from selected studies relating to outcomes for people with ED were synthesised and are disseminated in the current review.
Of the over 1320 studies included in the Rapid Review, the proportion of articles focused on outcomes in ED was relatively small, under 9%. Most evidence was focused on the diagnostic categories of AN, Bulimia Nervosa and Binge Eating Disorder, with limited outcome studies in other ED diagnostic groups. Factors such as age at presentation, gender, quality of life, the presence of co-occurring psychiatric and/or medical conditions, engagement in treatment and access to relapse prevention programs were associated with outcomes across diagnoses, including mortality rates.
Results are difficult to interpret due to inconsistent study definitions of remission, recovery and relapse, lack of longer-term follow-up and the potential for diagnostic crossover. Overall, there is evidence of low rates of remission and high risk of mortality, despite evidence-based treatments, especially for AN. It is strongly recommended that research in long-term outcomes, and the factors that influence better outcomes, using more consistent variables and methodologies, is prioritised for people with ED.
Plain English summary
Eating disorders are complex psychiatric conditions that can seriously impact a person’s physical health. Whilst they are consistently associated with high mortality rates and significant psychosocial difficulties, lack of agreement on definitions of recovery, remission and relapse, as well as variations in methodology used to assess for standardised mortality and disability burden, means clear outcomes can be difficult to report. The current review is part of a larger Rapid Review series conducted to inform the development of Australia’s National Eating Disorders Research and Translation Strategy 2021–2031. A Rapid Review is designed to comprehensively summarise a body of literature in a short timeframe to guide policymaking and address urgent health concerns. This Rapid Review synthesises the current evidence-base for outcomes for people with eating disorders and identifies gaps in research and treatment to guide decision making and future clinical research. A critical overview of the scientific literature relating to outcomes in Western healthcare systems that may inform health policy and research in an Australian context is provided in this paper. This includes remission, recovery and relapse rates, diagnostic cross-over, the impact of relapse prevention programs, factors associated with outcomes, and findings related to mortality.
Introduction
Eating disorders (ED), especially Anorexia Nervosa (AN), have amongst the highest mortality and suicide rates in mental health. While there has been significant research into causal and maintaining factors, early identification efforts and evidence-based treatment approaches, global incidence rates have increased from 3.4% calculated between 2000 and 2006 to 7.8% between 2013 and 2018 [ 1 ]. While historically seen as a female illness, poorer outcomes are increasingly seen in other genders, including males [ 2 ].
Over 3.3 million healthy life years are lost worldwide due to ED each year, and many more lost to disability due to medical and psychiatric complications [ 3 ]. Suicide accounts for approximately 20% of non-natural deaths among people with ED [ 4 ]. As this loss of healthy life is preventable, there is a grave responsibility to better understand outcomes for people with ED, including factors which may minimise the detrimental impact they have on individuals, carers, and communities, as well as to optimise recovery.
There has been considerable debate within the clinical, scientific and lived experience (i.e., patient, consumer, carer) communities about the definition and measurement of key outcomes in ED, including ‘remission’ from illness (a period of relief from symptoms), ‘relapse’ (a resumption of symptoms) and ‘recovery’ (cessation of illness) [ 5 , 6 ], which can compromise outcome comparisons. Disparities include outcome variables relating to eating behaviours as well as medical, psychological, social and quality of life factors. There is increasing awareness in the literature of the elevated likelihood of diagnostic crossover [ 7 ]; research examining specific diagnostic profiles potentially misses outcomes where symptom experience transforms rather than alleviates. Methodological approaches in outcomes research are varied, the most significant being length of time to follow up, compromising direct study comparisons.
The aim of this Rapid Review (RR) is to synthesise the literature on outcomes for people with ED, including rates of remission, recovery and relapse, diagnostic crossover, and mortality. Factors influencing outcomes were summarised including demographic, illness, treatment, co-morbidities, co-occurring health conditions, societal factors, and impact of relapse prevention programs. This RR forms one of a series of reviews scoping the field of ED commissioned to inform the Australian National Eating Disorders Research and Translation Strategy 2021–2031 [ 8 ]. The objective is to evaluate the current literature in ED outcomes to identify areas of consensus, knowledge gaps and suggestions for future research.
The Australian Government Commonwealth Department of Health funded the InsideOut Institute for Eating Disorders (IOI) to develop the Australian Eating Disorders Research and Translation Strategy 2021–2031 [ 8 ] under the Psych Services for Hard to Reach Groups initiative (ID 4-8MSSLE). The strategy was developed in partnership with state and national stakeholders including clinicians, service providers, researchers, and experts by lived experience (including consumers and families/carers). Developed through a 2 year national consultation and collaboration process, the strategy provides the roadmap to establishing ED as a national research priority and is the first disorder-specific strategy to be developed in consultation with the National Mental Health Commission. To inform the strategy, IOI commissioned Healthcare Management Advisors (HMA) to conduct a series of RRs to broadly assess all available peer-reviewed literature on the six DSM-V [ 9 ] listed ED. RR’s were conducted in the following domains: (1) population, prevalence, disease burden, Quality of Life in Western developed countries; (2) risk factors; (3) co-occurring conditions and medical complications; (4) screening and diagnosis; (5) prevention and early intervention; (6) psychotherapies and relapse prevention; (7) models of care; (8) pharmacotherapies, alternative and adjunctive therapies; and (9) outcomes (including mortality) (current RR), with every identified paper allocated to only one of the above domains from abstract analysis by two investigators. Each RR was submitted for independent peer review to the Journal of Eating Disorders special edition, “Improving the future by understanding the present: evidence reviews for the field of eating disorders”.
A RR Protocol [ 10 ] was utilised to swiftly synthesise evidence to guide public policy and decision-making [ 11 ]. This approach has been adopted by several leading health organisations, including the World Health Organization [ 12 ] and the Canadian Agency for Drugs and Technologies in Health Rapid Response Service [ 13 ], to build a strong evidence base in a timely and accelerated manner, without compromising quality. RR was chosen as the most suitable design as it is conducted with broader search terms and inclusion criteria allowing to gain a better understanding of a specific field, returning a larger number of search results and providing a snapshot of key findings detailing the current state of a field at study [ 10 ]. A RR is not designed to be as comprehensive as a systematic review—it is purposive rather than exhaustive and provides actionable evidence to guide health policy [ 14 ].
The RR is a narrative synthesis adhering to the PRISMA guidelines [ 15 ]. It is divided by topic area and presented as a series of papers. Three research databases were searched: ScienceDirect, PubMed and Ovid/MEDLINE. To establish a broad understanding of the progress made in the field of eating disorders, and to capture the largest evidence base on the past 13 years (originally 2009–2019, but expanded to include the preceding two years), the eligibility criteria for included studies into the RR were kept broad. Therefore, included studies were published between 2009 and 2022, in English, and conducted within Western healthcare systems or health systems comparable to Australia in terms of structure and resourcing. The initial search and review process was conducted by three reviewers between 5 December 2019 and 16 January 2020. The re-run for the years 2020–2021 was conducted by two reviewers at the end of May 2021 and a final run for 2022 conducted in January 2023 to ensure the most up to date publications were included prior to publication.
The RR had a translational research focus with the objective of identifying evidence relevant to developing optimal care pathways. Searches, therefore, used a Population, Intervention, Comparison, Outcome (PICO) approach to identify literature relating to population impact, prevention and early intervention, treatment, and long-term outcomes. Purposive sampling focused on high-level evidence studies such as: meta-analyses; systematic reviews; moderately sized randomised controlled trials (RCTs) ( n > 50); moderately sized controlled-cohort studies ( n > 50), or population studies ( n > 500). However, the diagnoses Avoidant Restrictive Food Intake Disorder (ARFID), Eating Disorder Not Otherwise Specified (EDNOS), Other Specified Feeding or Eating Disorder (OSFED) and Unspecified Feeding or Eating Disorder (UFED) necessitated a less stringent eligibility criterion due to a paucity of published articles. As these diagnoses are newly captured in the DSM-V [ 9 ] (released in 2013, within the allocated search timeframe), the evidence base is emerging, and fewer studies have been conducted. Thus, smaller studies ( n ≤ 20) and narrative reviews were also considered and included. Grey literature, such as clinical or practice guidelines, protocol papers (without results) and Masters’ theses or dissertations, was excluded.
Full methodological details including eligibility criteria, search strategy and terms and data analysis are published in a separate protocol paper [ 10 ]. The full RR included a total of over 1320 studies (see Additional file 1 : Fig. S1). Data from included studies relating to outcomes for eating disorders were synthesised and are presented in the current review.
Of the 1320 articles included in the RR, the proportion of articles focused on outcomes in ED was relatively small, just less than 9% ( n = 116) (see Additional file 2 : Table S1). Studies typically examined outcomes in AN, Bulimia Nervosa (BN) and Binge Eating Disorder (BED), with limited research in other diagnostic groups. Whereas most outcome studies reported recovery, remission and relapse rates, others explored factors impacting outcomes, such as quality of life, co-occurring conditions, and outcomes from relapse prevention programs.
ED, particularly AN, have long been associated with an increased risk of mortality. The current review summarises best available evidence exploring this association. Several factors complicate these findings including a lack of consensus on definitions of remission, recovery and relapse, widely varying treatment protocols and research methodologies, and limited transdiagnostic outcome studies or syntheses such as meta-analyses. Table 1 provides a summary of outcomes reported by studies identified in this review. There is considerable heterogeneity in the reported measures.
Overall outcomes
A good outcome for a person experiencing ED symptomatology is commonly defined as either remission or no longer meeting diagnostic criteria, as well as improved levels of psychosocial functioning and quality of life [ 28 , 29 ]. However, such a comprehensive approach is rarely considered, and there is no consensus on a definition for recovery, remission, or relapse for any of the ED diagnoses [ 30 , 31 ]. To contextualise this variation, definitions and determinants for these terms are presented in Table 2 .
The terms ‘remission’ and ‘recovery’ appear to be used interchangeably in the literature. Whilst ‘remission’ is usually defined by an absence of diagnostic symptomatology, and ‘recovery’ an improvement in overall functioning, the period in which an individual must be symptom-free to be considered ‘remitted’ or ‘recovered’ varies greatly between studies, follow-up (FU) time periods are inconsistent, and very few studies examine return to psychosocial function and quality of life (QoL) after alleviation of symptoms. The current review uses the terms adopted by the original studies. ‘Relapse’ is typically defined by a return of symptoms after a period of symptom relief. The reviewed studies report a variety of symptom determinants including scores on standardised psychological and behavioural interviews or questionnaires, weight criteria [including Body Mass Index (BMI) or %Expected Body Weight (%EBW)], clinical assessment by a multidisciplinary team, self-reported ED behaviours, meeting diagnostic criteria, or a combination of the above.
Remission, recovery, and relapse
In a global overview of all studies reviewed, remission or recovery rates were reported for around half of the cohort, regardless of diagnostic group. For example, a 30 month FU study of a transdiagnostic cohort of patients found 42% obtained full and 72% partial remission, with no difference between diagnostic groups for younger people; however, bulimic symptoms emerged frequently during FU, regardless of initial diagnosis [ 44 ]. A 6 year study following the course of a large clinical sample ( n = 793) reported overall recovery rates of 52% for AN, 50–52% for BN, 57% for EDNOS-Anorectic type (EDNOS-A), 60–64% for BED and 64–80% for EDNOS-Bulimic type (EDNOS-B) [ 7 ]. Of those who recorded full remission at end of treatment (EOT), relapse was highest for AN (26%), followed by BN (18%), and EDNOS-B (16%). Relapse was less common for individuals with BED (11–12%), and EDNOS-A (4%). Change in diagnosis (e.g., from AN to BN) was also seen within the relapse group [ 7 ].
Longer-term FU studies may more accurately reflect the high rates of relapse and diagnostic crossover associated with ED. A 17 year outcome study of ED in adult patients found only 29% remained fully recovered, with 21% partially recovered and half (50%) remaining ill [ 52 ], noting the protracted nature of illness for adults with longstanding ED. Relapse is observed at high rates (over 30%) among people with AN and BN at 22 year FU [ 61 ]. In a large clinical study using predictive statistical modelling, full remission was more likely for people with BED (47.4%) and AN (43.9%) compared to BN (25.2%) and OSFED (23.2%) [ 41 ]. This result is distinct from other studies citing AN to have the worst clinical outcomes within the diagnostic profiles [ 52 ]. The cut‐off points for the duration of illness associated with decreased likelihood of remission were 6–8 years for OSFED, 12–14 years for AN/BN and 20–21 years for BED [ 41 ]. As with recovery rates, reported rates of relapse are highly variable due to differing definitions and study methodologies used by researchers in FU studies [ 35 , 61 ].
Evidence from a meta-analysis of 16 studies found four factor clusters that significantly contributed to relapse; however, also noted a substantial variability in procedures and measures compromising study comparison [ 62 ]. Factors contributing to heightened risk of relapse included severity of ED symptoms at pre- and post-treatment, presence and persistence of co-occurring conditions, higher age at onset and presentation to assessment, and longer duration of illness. Process treatment variables contributing to higher risk included longer duration of treatment, previous engagement in psychiatric and medical treatment (including specialist ED treatment) and having received inpatient treatment. These variables may indicate more significant illness factors necessitating a higher intensity of treatment.
Importantly, full recovery is possible, with research showing fully recovered people may be indistinguishable from healthy controls (HCs) on all physical, behavioural, and psychological domains (as evaluated by a battery of standardised assessment measures), except for anxiety (those who have fully recovered may have higher general anxiety levels than HCs) [ 29 ].
Diagnostic crossover
Most studies reported outcomes associated with specific ED diagnoses; however, given a significant proportion of individuals will move between ED diagnoses over time, it can be challenging to determine diagnosis-specific outcomes. Results from a 6 year FU study indicated that overall individuals with ED crossed over to other ED diagnoses during the FU observational period, most commonly AN to BN (23–27%), then BN to BED (8–11%), BN to AN (8–9%) and BED to BN (7–8%) [ 7 ]. Even higher crossover trends were observed in the subgroup reporting relapse during the FU period, with 61.5% of individuals originally diagnosed with AN developing BN, 27.2% and 18.1% of individuals originally diagnosed with BN developing AN and BED respectively, and 18.7% of people with a previous diagnosis of BED developing BN [ 7 ].
A review of 79 studies also showed a significant number of individuals with BN (22.5%) crossed over to other diagnostic groups (mostly OSFED) at FU [ 63 ]. A large prospective study of female adolescents and young adults in the United States ( n = 9031) indicated that 12.9% of patients with BN later developed purging disorder and between 20 and 40% of individuals with subthreshold disorders progressed to full threshold disorders [ 64 ]. Progression from subthreshold to threshold eating disorders was higher for BN and BED (32% and 28%) than for AN (0%), with researchers suggesting higher risk for binge eating [ 66 ]. Progression from subthreshold to full threshold BN and BED was also common in adolescent females over the course of an 8 year observational study [ 33 ]. Some researchers contend that such diagnostic ‘instability’ demonstrates a need for ‘dimensional’ approaches to research and treatment which have greater focus on the severity rather than type of symptoms [ 7 ]. Diagnostic crossover is common and should be considered in the long-term management and monitoring of people with an ED.
Anorexia nervosa (AN)
People with restrictive-type ED have the poorest prognosis compared to the other diagnostic groups, particularly individuals displaying severe AN symptomatology (including lower weights and higher body image concerns) [ 44 ]. There is a paucity of effective pharmacological and/or psychological treatments for AN [ 65 ]. Reported rates of recovery vary and include 18% [ 56 ] to 52% at 6 year FU [ 7 ] to 60.3% at 13 year FU [ 20 ] and 62.8% at 22 year-FU [ 61 ]. Reported relapse rates in AN also vary, for example, 41.0% at 1 year post inpatient/day program treatment [ 35 ] to 30% at 22 year FU [ 61 ]. Average length of illness across the reviewed studies also varies from 6.5 years [ 56 ] to 14 years [ 41 ].
A variety of reported outcomes from treatment studies is likely due to the breadth of treatments under investigation, diverse study protocols and cohorts. For example, in a mixed cohort of female adult patients with AN and Atypical AN (A-AN), 33% were found to have made a full recovery at 3 year FU after treatment with cognitive behavioural therapy (CBT) [ 57 ], while 6.4% had a bad outcome and 6.4% a severe outcome. However, in a 5–10 year FU study of paediatric inpatients (mean age 12.5 years) approximately 41% had a good outcome, while 35% had intermediate and 24% poor outcome [ 66 ]. Multimodal treatment approaches including psychiatric, nutritional, and psychological rehabilitation have been found to be most efficacious for moderate to severe and enduring AN but noting a discrete rate of improvement [ 67 ].
Very few factors were able to predict outcomes in AN. Higher baseline BMI was consistently found to be the strongest predictor of recovery, and better outcomes were associated with shorter duration of illness [ 7 , 55 , 61 , 66 ]. Earlier age of illness onset [ 59 , 68 , 69 ] and older age at presentation to treatment [ 30 ] were related to chronicity of illness and associated with poorer outcome.
There was a consensus across a variety of studies that engagement in binge/purge behaviours (Anorexia Nervosa Binge/Purge subtype; AN-BP) was associated with a poorer prognosis [ 20 , 56 , 70 ]. Similarly, individuals with severe and enduring AN restrictive sub-type (AN-R) are likely to have a better outcome than individuals with AN-BP. AN-BP was associated with a two-fold greater risk of relapse compared to AN-R [ 30 , 35 ]. Some studies, however, were unable to find an association between AN subtype and outcome [ 55 ]. Other factors leading to poorer outcome and higher probability of relapse were combined ED presentations, such as combined AN/BN [ 35 ], higher shape concern [ 57 ], lower desired weight/BMI [ 44 ], more ED psychopathology at EOT, low or decreasing motivation to recover, and comorbid depression [ 35 , 61 ].
Preliminary genetic work has found associations between a single nucleotide polymorphism (SNP) in a ghrelin production gene (TT genotype at 3056 T-C) and recovery from AN-R [ 71 ], and the S-allele of the 5-HTTLPR genotype increasing the risk susceptibility for both depressive comorbidity and diagnostic crossover at FU of AN patients [ 72 ]. These studies, however, need to be interpreted with caution as they were conducted over a decade ago and have not since been replicated. Research in eating disorder genetics is a rapidly emerging area with potential clinical implications for assessment and treatment.
Bulimia nervosa (BN)
Overall, studies pertaining to a diagnostic profile of BN report remission recovery rates of around 40–60%, depending on criteria and FU period, as detailed below. Less than 40% of people achieved full symptom abstinence [ 73 ] and relapse occurred in around 30% of individuals [ 61 ]. A meta-analysis of 79 case series studies reported rates of recovery for BN at 45.0% for full recovery and 27.0% for partial remission, with 23.0% experiencing a chronic course and high rates of treatment dropout [ 63 ]. At 11 year FU, 38.0% reported remission in BN patients, increasing to 42.0% at 21 year [ 45 ]. At 22 year FU, 68.2% with BN were reported to have recovered [ 41 ]. Higher frequency of both objective binge episodes and self-induced vomiting factors influencing poorer outcomes [ 44 ].
Considering impact of treatment, analysis of engagement in self-induced vomiting as a predictor for outcome indicated there were no differences between groups in treatment dropout or response to CBT among a sample of 152 patients with various types of EDs (AN-BP, BN, EDNOS) at EOT [ 74 ]. Meta-analysis of results from 45 RCTs on psychotherapies for BN found 35.4% of treatment completers achieved symptom abstinence [ 73 ] with other studies indicating similar rates of recovery (around 52–59% depending on DSM criteria) [ 7 ].
Studies delivering CBT or other behavioural therapies reported the best outcomes for BN [ 73 ]. Specifically, early treatment progression, elimination of dietary restraint and normalisation of eating behaviour resulted in more positive outcomes [ 22 ]. These findings are supported by results from a study comparing outcomes of CBT and integrative cognitive-affective therapy (ICAT) [ 75 ]. Additional moderating effects were shown at FU (but not EOT), with greater improvements for those with less baseline depression, higher stimulus seeking (the need for excitement and stimulation) and affective lability (the experience of overly intense and unstable emotions) in the ICAT-BN group and lower stimulus seeking in the Enhanced Cognitive Behavioural Therapy (CBT-E) group. Lower affective lability showed improvements in both treatment groups [ 75 ]. Such findings indicate personality factors may deem one treatment approach more suitable to an individual than another.
A review of 4 RCTs of psychotherapy treatments for BN in adolescents (including FBT and CBT) reported overall psychological symptom improvement by EOT predicting better outcomes at 12 months, which underscored the need for not only behavioural but psychological improvement during 6 month treatment [ 31 ]. Other factors leading to poorer outcomes included less engagement in treatment, higher drive for thinness, less global functioning, and older age at presentation [ 45 ]. More research is needed into consistent predictors, mediators and moderators focused on treatment engagement and outcomes [ 22 ].
While many studies combine findings for BN and BED, one study specifically considered different emotions associated with binge eating within the two diagnostic profiles [ 60 ]. At baseline, binge eating was associated with anger/frustration for BN and depression for BED. At FU, objective binge eating (OBE) reduction in frequency (a measure of recovery) was associated with lower impulsivity and shape concern for BN but lower emotional eating and depressive symptoms for BED. These differences may provide approaches for effective intervention targets for differing presentations; however, how these may play out within a transdiagnostic approach requires further enquiry.
Binge eating disorder (BED)
BED is estimated to affect 1.5% of women and 0.3% of men worldwide, with higher prevalence (but more transient) in adolescents. Most adults report longstanding symptoms, 94% lifetime mental health conditions and 23% had attempted suicide, yet only half were in recognised healthcare or treatment [ 76 ].
Compared with AN and BN, long-term outcomes, and treatment success for individuals with BED were more favourable. Meta-analysis of BED abstinence rates suggests available psychotherapy and behavioural interventions are more effective for this population [ 77 ]. Additionally, stimulant medication (i.e., Vyvanse) has been found to be particularly effective to reduce binge eating [see [ 78 ] for full review]. Results from a study of people who received 12 months of CBT for BED indicated high rates of treatment response and favourable outcomes, maintained to 4 year FU. Significant improvements were observed with binge abstinence increasing from 30.0% at post-treatment to 67.0% at FU [ 79 ]. A meta-analysis reviewing psychological or behavioural treatments found Interpersonal Therapy (IPT) to be the treatment producing the greatest abstinence rates [ 73 ]. In a comparative study of IPT and CBT, people receiving CBT experienced increased ED symptoms between treatment and 4 year FU, while those who received IPT improved during the same period. Rates of remission at 4 year FU were also higher for IPT (76.7%) versus CBT (52.0%) [ 80 ].
One study specifically explored clinical differences between ED subtypes with and without lifetime obesity over 10 years. Prevalence of lifetime obesity in ED was 28.8% (ranging from 5% in AN to 87% in BED), with a threefold increase in lifetime obesity observed over the previous decade. Observed with temporal changes, people with ED and obesity had higher levels of childhood and family obesity, older-age onset, longer ED duration, higher levels of ED (particularly BED and BN) and poorer general psychopathology than those who were not in the obese weight range [ 81 ], suggesting greater clinical severity and poorer outcomes for people of higher weight.
Comparison of 6 year treatment outcomes between CBT and Behavioural Weight Loss Treatment (BWLT) found CBT more effective at post-treatment but fading effectiveness over time, with remission rates for both interventions lower than other reported studies (37%) [ 82 ]. A meta-analytic evaluation of 114 published and unpublished psychological and medical treatments found psychological treatments, structured self-help, and a combination of the two were all effective at EOT and 12 month FU but noted a wide variation in study design and quality, and the need for longer term FU. Efficacy and FU data for pharmacological and surgical weight loss treatments were lacking [ 77 ].
Whilst high weight and associated interventions (such as bariatric surgery) can be associated with any ED, they are frequently studied in relation to BED. A significant proportion of individuals seeking bariatric surgery (up to 42%) displayed binge eating symptomatology [ 83 ], yet little is known about the effect of these interventions on ED psychopathology and whether this differs by type of intervention. A systematic review of 23 studies of changes in ED behaviour following three different bariatric procedures found no specific procedure led to long term changes in ED profiles or behaviours [ 84 ]; however, another study investigating the placement of an intragastric balloon in obese patients found post-surgical reductions in grazing behaviours, emotional eating and EDNOS scores [ 85 ]. Bariatric surgery in general is associated with a reduction in ED, binge eating and depressive symptoms [ 86 ].
Outcomes among patients receiving bariatric surgery with and without BED were assessed where weight loss was comparable between the groups at 1 year FU. However, compared with participants receiving a BWLT-based lifestyle modification intervention instead of surgery, bariatric surgery patients lost significantly less weight at a 10.3% difference between groups. There was no significant difference between lifestyle modification and surgery groups in BED remission rates [ 87 ]. These results indicate that BLWT-type interventions are more effective than surgery at promoting weight loss in individuals with BED over a 1 year FU period, and people with BED and higher BMI were able to maintain weight loss in response to psychotherapy (CBT) at up to 5 year FU [ 88 ]. In analysis of health-related quality of life (HRQoL) in people with BED who received various levels of CBT (therapist-led, therapist-assisted and self-help), evaluation indicated that all modalities resulted in improvements to HRQoL. Poorer outcomes were associated with obesity and ED symptom severity at presentation, stressing the importance of early detection and intervention measures [ 89 ]. Research into the role of CBT in strengthening the effect of bariatric surgery for obesity is ongoing but promising [ 90 ].
EDNOS, OSFED and UFED
Similarly to BED, a diagnosis of DSM-IV EDNOS (now OSFED) was associated with a more favourable outcome than AN or BN, including shorter time to remission. One study reported remission rates for both EDNOS and BED at 4 year FU of approximately 80% [ 21 ]. The researchers suggested that an ‘otherwise specified’ diagnostic group might be comprised of individuals transitioning into or out of an ED rather than between diagnostic categories; however, more work is needed in this area to fully understand this diagnostic profile. The reported recovery rate from EDNOS-A has been found to be much lower at 57% than for EDNOS-B at 80% (DSM-V). One factor suggested leading to poorer outcomes for EDNOS-A was a higher association with a co-occurring condition of major depression and/or dysthymia not found in other EDNOS subtypes [ 7 ]. Another study found purging occurred in 6.7% from total (cross-diagnostic) ED referrals, but this subtype did not have different post-treatment remission rates or completion rates compared to non-purging profiles [ 91 ], so results are mixed.
Acknowledging the scarcity of research within these diagnostic groups, remission rates for adolescents including those with a diagnosis of Other Specified Feeding or Eating Disorder (OSFED) and Unspecified Feeding or Eating Disorder (UFED) was reported to be 23% at 12 month FU in the one study reviewed, but no detail was provided on recovery rates by diagnosis [ 26 ]. No available evidence was identified specifically for the DSM-V disorders OSFED or UFED for adults.
Avoidant/Restrictive Food Intake Disorder (ARFID)
Research into outcomes for people with ARFID is lacking, with only three studies meeting criteria for the review [ 23 , 24 , 25 ]. While, like AN, recovery for people with ARFID is usually measured by weight gain targets, one of the three studies [ 63 ] identified by this review instead reported on outcomes in terms of meeting a psychiatric diagnosis, making comparison between the studies difficult.
In a cross-diagnostic inpatient study, individuals presenting with ARFID were younger, had fewer reported ED behaviours and co-occurring conditions, less weight loss and were less likely to be bradycardic than individuals presenting with AN [ 25 ]. Although both groups received similar caloric intakes, ARFID patients relied on more enteral nutrition and required longer hospitalisations but had higher rates of remission and fewer readmissions than AN patients at 12 months. This study highlights the need for further investigation into inpatient treatment optimisation for different diagnostic profiles.
People with ARFID who had achieved remission post-treatment were able to maintain remission until 2.5 year FU, with most continuing to use outpatient treatment services [ 23 ]. In a 1 year FU study assessing ARFID, 62.0% of patients had achieved remission as defined by weight recovery and no longer meeting DSM-V criteria [ 25 ]. In a study following children treated for ARFID to a mean FU of 16 years post-treatment (age at FU 16.5–29.9 years), 26.3% continued to meet diagnostic criteria for ARFID with no diagnostic crossover, suggesting symptom stability [ 24 ]. Rates of recovery for ARFID patients in this study were not significantly different to the comparison group who had childhood onset AN, indicating similar prognoses for these disorders. No predictors of outcome for patients with ARFID were identified by the articles reviewed [ 63 ].
Community outcomes
While most outcome studies derive from health care settings, two studies were identified exploring outcomes of ED within the community. The first reported the 8 year prevalence, incidence, impairment, duration, and trajectory of ED via annual diagnostic interview of 496 adolescent females. Controlling for age, lifetime prevalence was 7.0% for BN/subthreshold BN, 6.6% for BED/subthreshold BED, 3.4% for purging disorder, 3.6% for AN/atypical AN, and 11.5% for feeding and eating disorders not otherwise classified. Peak onset age across the ED diagnostic profiles was 16–20 years with an average episode duration ranging from 3 months for BN to a year for AN; researchers noted that these episodes were shorter than the average duration estimates reported in similar research and may be representative of the transient nature of illness rather than longer term prognosis. ED were associated with greater functional impairment, distress, suicidality, and increased use of mental health treatment [ 27 ].
A second study followed 70 young people (mean age of 14 years at study commencement) meeting DSM-IV criteria for a binge eating or purging ED and found 44% no longer met criteria at ages 17 or 20, while 25% still met criteria at age 20 (the latter individuals were more likely to have externalising behaviour problems and purging behaviour at age 17). Those who experienced a persistent ED were less likely to complete secondary education and report higher depressive and anxiety symptoms at age 20, indicating the ongoing impacts of ED on education and quality of life [ 92 ]. These studies provide information about the course and outcome of early onset ED at the population level with indicators of predictive and maintaining factors.
Factors relating to outcomes
Several factors relating to outcomes have been studied across ED presentations and in specific diagnostic profiles. These include predictors of outcome, moderators or mediators of outcome, and illness reinforcers, considering age of presentation and duration of illness, ED symptomatology, presence of co-occurring medical and psychiatric conditions, and treatment characteristics.
Age of presentation
Age of presentation to treatment has been shown to have a significant impact on outcome in all diagnoses. One study considering ED in general (including AN, BN and EDNOS) showed presentation at mid-life drastically decreased chances of achieving a good outcome in response to treatment (“good” outcome defined as BMI ≥ 18.5, 3 month remission of symptoms and Eating Disorder Examination Questionnaire (EDE-Q) scores within or better than normal range). Six percent of mid-life (≥ 40 years) presentations achieved a good outcome post-treatment compared to 14% of young adults (18–39 years) and 28% of younger people (< 18 years) [ 28 ]. This finding has also been seen in research comparing 22 year outcomes of AN and BN [ 61 ].
People presenting in mid-life often have more complex medical and psychiatric profiles as well as life circumstances. They are also far more likely to have a sustained length of illness by the time of initial presentation: 27.8 years compared with 1.2 years for youths [ 28 ]. Longer duration of illness is associated with greater increase in self-reported clinical impairment [ 93 ]; however, illness duration does not necessarily influence treatment outcome, though wide variation in study protocol and quality limit the interpretability of these findings [ 37 , 94 ]. The disparity in rates of favourable outcome between age groups highlights the importance of prevention, screening, awareness of ED in primary care settings and early intervention programs, as well as targeted programs for those presenting with more complex psychosocial and life challenges.
Clinical features and co-occurring conditions
A systematic review assessed the average duration of untreated illness duration in help-seeking populations at first contact to treatment services at 29.9 months for AN, 53.0 months for BN and 67.4 months for BED [ 69 ]. ED clinical factors significantly influence outcomes, with poorer prognosis in those with time of untreated illness, primary diagnosis of AN [ 95 ], lower BMI at presentation [ 93 ], and presence of binge/purge symptomatology [ 20 , 56 ]. Certain ED behaviours and cognitions at intake predict better outcome such as lower rates of purging behaviour, higher rates of body image flexibility [ 96 ], and lower EDE-Q scores at baseline [ 97 ].
There is strong evidence for the presence of co-occurring medical and psychiatric conditions as a predictor of outcome in ED. At 22 year FU, the presence of co-occurring psychiatric conditions including Major Depressive Disorder (MDD) and Substance Use Disorder (SUD) were negatively correlated with recovery, with those who had recovered from an ED being 2.17 times less likely to have MDD and 5.33 times less likely to have SUD [ 98 ]. Co-occurring mood disorders consistently lead to poorer outcomes [ 47 , 51 , 55 , 99 ] and greater chance of moving between ED diagnoses [ 7 ]. In one study, presence of a mood disorder was the strongest predictor of classification of AN-R (but not AN-BP) [ 61 ]. Comorbid personality disorder was found in several studies to be the most common predictor of poorer outcome in ED [ 20 , 41 , 44 , 67 ].
In an adolescent sample, 39% of individuals with AN met criteria for at least one other psychiatric disorder and poorer prognosis was associated with co-occurring diagnoses of Obsessive Compulsive Disorder (OCD) and autistic traits [ 59 ]. In a large community childhood health longitudinal study, presence of any ED profile was predictive of later anxiety and mood disorders. AN was prospectively associated with long term low weight, while BN and BED with obesity, drug use and deliberate self-harm compared to age-matched children who did not have an ED profile [ 100 ].
Personality traits have also been found to be associated with poorer outcomes such as low persistence and harm avoidance in AN, lower self-directedness (BN) and reward dependence (BED) [ 41 ]. Higher perfectionism at intake predicted a lower likelihood of remission at 12 months in an adolescent sample [ 26 ], a finding consistent with previous research in adult cohorts [ 41 ].
Medical comorbidities such as malnutrition [ 72 ], concurrent type 1 diabetes [ 39 , 42 ], bodily pain [ 55 ] and viral infections [ 72 ] have been identified as risk factors for poorer outcomes and increased rates of relapse. Other co-occurring factors associated with poorer outcomes for people with ED include anxiety [ 47 , 56 , 93 ], dissociative experiences [ 101 ], impulsivity [ 56 ], adjustment disorder [ 95 ], use of psychotropic medications [ 30 ], and autistic traits have been associated with greater use of ED treatment [ 102 ].
Psychosocial, environmental and health factors
A large United States community study found positive correlation between higher rates of smoking behaviour and ED in women [ 99 ]. The same study also reported birth-related outcomes in women with ED including having a later first birth, pregnancy health concerns, experience of miscarriage or abortion [ 99 ], and women with ED may have increased experience of adverse pregnancy and neonatal outcomes, and lower numbers of children [ 3 ]. For women with a history of ED, ED symptoms tend to alleviate during pregnancy; however, they commonly resurface during the postnatal period, and up to a third of women with ED report postnatal depression [ 103 , 104 ].
Demographic factors leading to poorer prognosis include being male [ 72 ], of the LGBTQIA + community [ 105 ], being from a non-white ethnic background, low family education levels [ 99 ], lower socioeconomic status, living in a remote or rural area [ 72 ], poor employment and social adjustment [ 30 ], functional impairment [ 47 ], and having a family member with an ED [ 99 ]. Complicating prognosis are additional factors such as financial stress (individuals with ED face yearly health care costs 48% higher than the general population, while the presence of co-occurring psychiatric conditions is associated with 48% lower yearly earnings [ 3 ]. These financial challenges limit ability to access evidence-based treatments (especially in countries lacking in publicly funded health care) which may prolong illness.
There is strong evidence to suggest QoL is reduced in people with an ED [ 3 , 106 ]. It is important to consider associations between QoL, ED symptomatology and treatment outcome. Evidence-based treatments have demonstrated positive effects on QoL in addition to reduction in ED symptomatology, for example, improvements in QoL and psychological functioning and well-being were seen in response to CBT in a cross-diagnostic sample [ 43 ]. However, a meta-analysis of ED outcome studies found that the QoL of recovered ED patients remained lower than in healthy populations, highlighting the importance of prevention efforts [ 107 ] and restoration of QoL in relapse prevention. These studies highlight the high public health and clinical burden of eating disorders and the need to consider co-occurring medical and psychiatric conditions during comprehensive assessment history-taking, treatment planning and provision.
Treatment factors
Early progression in treatment can provide indication of treatment outcomes. In an RCT comparing Family Based Treatment (FBT) and Adolescent Focused Therapy (AFT) for adolescents with AN, most people who achieved remission at 1 year FU maintained recovery to 4 years FU regardless of treatment arm with remission rates tended to remain stable after 1 year [ 108 ]. The First Episode Rapid Early Intervention for Eating Disorders (FREED) service model for young adults with AN reported significant and rapid clinical improvements in over 53.2% of people compared to 17.9% TAU and also reported more cost-effective treatment [ 109 ]. In a transdiagnostic study comparing inpatient vs outpatient settings, rapid response to treatment (defined here as a clinically meaningful reduction in disorder-specific symptoms within the first ten sessions) was the only outcome predictor accounting for 45.6% of variance in ED symptoms, suggesting future work should evaluate mediators and moderators of rapid response [ 37 ]. A systematic review of outcome predictors and mediators in response to CBT indicated that early behavioural and cognitive change was associated with positive outcomes across ED diagnoses [ 22 ]. Similarly, a recent systematic review and meta-analysis of 20 years of accumulated evidence concluded early response to treatment the most robust predictor of better treatment outcomes, however, only half of people investigated across numerous studies showed early change, and more research was needed to determine outcome predictors [ 110 ]. Ongoing assessment to identify individuals who do not show early response to treatment (defined by healthy weight and absence of ED behaviours at 12 month FU), as well as provision of targeted engagement approaches, may improve outcomes [ 47 ].
Due to the frequent need for medical stabilisation in the early and acute stages of AN, the role of hospitalisation needs to be considered in the evaluation of treatment outcomes. In a large patient cohort study ( n = 7505) with 5 year FU, a clear trend was observed with the per-patient 5 year cumulated number of inpatient days decreasing by 6% per annum after adjustment for age at diagnosis, parental mental health, and household income. The number of hospital admissions decreased by 2% per year, although there was no change in outpatient visits [ 111 ]. Factors contributing to better outcomes were not identified in this study, but in other research, early change in %EBW and ED psychopathology in adolescent inpatients predicted later change in the same ED variables [ 18 ]. Another study showed longer first admission predicted increased use of the health system in young adults [ 112 ].
In a multicentre RCT there was no difference between higher or lower calorie refeeding on clinical remission or medical hospitalisation to 12 month FU [ 113 ]. A systematic scoping review of 49 studies found adolescent day programs (intensive treatment programmes that do not involve an overnight stay at the treatment facility) can be an effective alternative to inpatient hospitalisation or step up/down in treatment intensity and are generally associated with weight gain and improvements in ED and comorbid psychopathology [ 114 ]. Outcomes in the review were sustained from 3 months to 2 years from EOT; however, due to large variability in the content, structure and theoretical underpinnings of reviewed programs, findings should be interpreted with caution.
Difficulties with emotion regulation are also associated with poor outcome across diagnostic profiles. There is evidence to suggest emotion-focused treatment is beneficial both to emotional functioning and mood as well as ED severity for people with elevated emotion regulation issues at baseline with positive effects lasting up to 5 years FU [ 115 ].
Self-esteem, self-compassion, and motivation
There is little conclusive evidence regarding predictors of poor response to evidence-based treatments [ 22 , 58 ]; however, low self-esteem has been implicated across all ED diagnoses [ 98 , 101 ], particularly AN [ 55 ]. A meta-analysis exploring the role of self-esteem on treatment outcomes indicated that while self-esteem did not predict remission or long-term weight related outcomes, it did mediate progression during inpatient treatment (greater increase in self-esteem during inpatient treatment was associated with higher remission and lower relapse rates at FU) [ 116 ]. Relatedly, high fear of self-compassion was associated with greater severity of ED symptoms in individuals with an active ED, suggesting that a fearful unwillingness to become more self-compassionate, rather than the absence of self-compassion, may lead to more detrimental outcomes [ 117 ].
Greater pre-treatment motivation has also been associated with ED symptom improvement and management of co-occurring anxiety and depression, in a systematic review and meta-analysis of 42 longitudinal studies [ 118 ]. Therapeutic interventions that include enhancement of motivation, self-esteem and self-compassion have been shown across studies to improve treatment outcomes across diagnostic profiles [ 117 ].
Relapse prevention programs
Whilst the role of treatment is crucial in the alleviation of symptoms and restoration of wellbeing, active provision of evidence-based post-treatment recovery care may be an important determining factor in relapse prevention. Research suggests the period in which individuals are at greatest risk of relapse is between four and nine-months following discharge [ 35 ], with between 31 and 41% relapsing at one to two years post-discharge [ 62 ].
To reduce readmission among a group of females receiving inpatient treatment for AN at an Australian specialist child and adolescent ED service, a 10 week transition ‘day’ program was developed and evaluated. The delivered program allowed for a ‘step down’ option and was found to have significant benefit for participants, who achieved an average weight gain of over 1 BMI point and decreased ED symptomatology at six-month FU [ 65 ]. Promising findings were also seen in a 6-session post-(inpatient and/or outpatient) treatment relapse prevention program designed by clinicians, parents, and patients in the Netherlands, which included a take-home workbook and appointments up to 18 months (frequency dependent on patient progress). Evaluated with young people with AN-R and AN-BP, 70% maintained post-discharge recovery to the end of the study period [ 36 ]. Such programs were evaluated in the context of a comprehensive specialist service with no control group comparison to measure the impact of the specific intervention, and there was no FU assessment following conclusion of the intervention to assess maintenance. Although more work is needed, these studies indicate the value of targeted relapse prevention programs.
Online relapse prevention programs
There is emerging evidence to support the safety and efficacy of internet-based relapse prevention programs aimed at preventing readmission to intensive ED treatment following discharge. These programs have the potential to be widely disseminated to individuals who may otherwise disengage from ongoing support due to access issues (e.g., living in an underserviced area, financial burden) or personal reasons such as stigma or shame [ 119 , 120 ].
A 9-session (1/month) CBT-based online relapse prevention program for women with AN discharged from inpatient treatment (baseline BMI x̄ = 17.7) found participants who completed the program had significant gains in BMI at end of program ( x̄ = 19.1) while the treatment as usual (TAU) control group did not ( x̄ = 17.7). Of note, participants who were 1–2 sessions short of completing the program maintained a higher BMI ( x̄ = 18.0) than the TAU group, whereas participants with less than 50% completion had a significantly lower BMI than any group including TAU ( x̄ = 17.0) [ 121 ]. A similar CBT-based online program targeted toward women discharged from inpatient treatment for BN found that the intervention group reported 46.0% fewer vomiting episodes compared to TAU, with some improvement in symptom abstinence (intervention group: 21.4%, TAU control = 18.9%), although this finding was not statistically significant [ 122 ].
In Hungary, an internet-based aftercare support program for individuals who had received inpatient or outpatient treatment for BN or related EDNOS in the 12 months prior to the study included information and support offered via 30 min chat sessions with peers and clinicians. Results showed 40.6% of the intervention group reported improvement compared to TAU waitlist controls (24.4%), although this difference was not statistically significant. The study noted that, although on the waitlist for the internet-based aftercare support program, the TAU group could still access additional treatment if so required. Evaluation findings report the program was feasible and well accepted [ 123 ].
Text messaging-based interventions have also been trialled to maintain engagement post-treatment, whereby participants send regular symptom reports to the clinical team with feedback provided. A 12 week ‘mobile therapy’ study with a group of women exiting CBT treatment for BN resulted in significant improvement in binge/purge frequency, ED and depressive symptoms from baseline to FU, with high rates of protocol adherence (87.0%), although there was no control group comparison [ 124 ]. Further evidence was provided in a 16 week weekly symptom report study of women with BN following inpatient discharge, with a significantly larger proportion of the intervention group achieving remission (51%) compared with TAU (36%) at 8 months FU. There was no significant difference between groups in terms of outpatient service use [ 125 ]. Results from these studies conflict with evidence from a systematic review of 15 studies, which was unable to support the effectiveness of text messaging-based programs for people with ED as either a sole or adjunctive component of the intervention [ 126 ]; however, this review noted the lack of a common evaluation framework making comparison difficult.
Despite advances in awareness and treatment, ED, particularly AN, continue to be associated with increased risk of mortality [ 4 ]. Studies identified that focus on the assessment of ED mortality, as well as data from the Global Burden of Disease Study 2016 are discussed in this section. Importantly, there are several different metrics used to report mortality. These include the Standardised Mortality Ratio (SMR), or the number of observed deaths in a cohort versus the number of expected deaths in a reference population (where a rate greater than one is interpreted as excess mortality); Weighted Mortality Ratio (WMR), or the weighted average of age-specific mortality rates per 100,000 persons; Crude Mortality Rate (CMR) , or the number of deaths in a given period divided by the population exposed to risk of death in that period; and Years of Life Lost (YLL), a summary measure of premature mortality calculated by subtracting the age at death from the standard life expectancy in a reference population.
Standardised, weighted, and crude mortality
AN is consistently described as having the highest mortality rate of the ED, but actual rate difference varies between studies. A summary of Standardised Mortality Ratios across studies is presented in Table 3 . SMRs from a meta-analysis suggest that measured mortality of AN is approximately three times as high as for other ED diagnoses, and in a UK study of ED patients ( n = 1892) accessing services between 1992 and 2004, the SMR for AN was almost five times higher than other ED [ 127 ]. This is consistent with other research (a meta-analysis summarising 41 studies) reporting people with AN were 5.2 [3.7–7.5] times more likely to die prematurely from any cause [ 128 ]. A longitudinal study ( n = 246) found SMR of AN to be only twice as high compared to BN, but still 6.5 times the rate expected in the general population [ 49 ].
Some studies did not report higher SMR for AN compared to other ED, however, methodological differences need to be considered. For example, some studies reported comparable SMR for AN to other ED, but subthreshold AN cases were included (previously catagorised as EDNOS) which may have reduced the calculated AN SMR [ 104 , 108 ]. In a British study using English National Hospital Episodes Statistics (2001–2009) comparing AN and BN, little difference in SMRs was reported [ 132 ]. The diagnosis of BN was less likely than other diagnosis to be recorded as the primary diagnosis and may not have been representative.
In a 22 year trial FU of a large sample of inpatients treated for BN, 2.4% had died [ 45 ]; the CMR for BN was 0.32% [ 63 ] and in severely malnourished patients, the crude mortality rate rose to 11.5% with SMR 15.9 [CI 95% (11.6–21.4)], just over 5 years post-treatment [ 137 ]. WMR has been found to be 5.1 for AN, 1.7 for BN, and 3.3 for EDNOS. SMRs were 5.86 for AN, 1.93 for BN, 1.92 for EDNOS [ 4 ] and 1.5–1.8 for BED [ 76 ].
Mortality rates in AN were highest during the first year after admission to treatment, while in BN it is in the first two years [ 134 ], with a higher risk in adolescence [ 140 ]. In AN, peak age of risk of death has been reported to be 15 years of age, BN 22 years and EDNOS 18–22 years [ 141 ]. Substance use disorders (including alcohol and/or cannabis) increased mortality in people with eating disorders across the diagnostic profiles [ 142 ].
In ED, peak age of risk for males may be earlier than females [ 141 ]. SMRs are higher for males (SMR = 7.24; 95% CI 6.58–7.96) relative to females (SMR = 4.59; 95% CI 4.34–4.85) overall, and in all age groups [ 131 ]. This may be due to the lower likelihood of males to self-identify or be identified with ED resulting in treatment delays and higher severity of illness when finally seeking help [ 131 ]. In mortality research conducted with a male-only sample, similarly high SMRs for males with BN and particularly AN as in majority female samples [ 2 ] were reported; however, mortality rates of EDNOS in males were considerably higher than those reported in female-dominant or female-only samples. Moreover, a case-controlled study found there was a sex difference across all diagnostic categories in CMR, with male to female being 15–5% in AN, 8–3% in BN, and 4–3% in EDNOS, but there were no significant sex differences in SMR for any diagnostic group, with males showing a shorter survival time after onset [ 2 ]. Researchers have suggested that increased mortality in males could be due to several factors, including reluctance to seek treatment and current treatment approaches being less effective in males [ 138 ]. Further research in males with ED is required to better understand the impact and response in male patients. Regardless of the mortality metric used, these studies indicate the vital importance of considering elevated mortality risk across the range of ED diagnoses.
Years of life lost/years lived with disability
The Global Burden of Disease Study 2016 reported that YLL due to premature death attributable to AN was 0.4 per 100,000. No YLL were attributed to BN; however, cause-specific mortality (CSM)—where each death is attributed to a single underlying cause—was, per thousand, 0.5 for AN (with a 2.9% increase from 1980 to 2016) and 0.1 for BN (21.8% increase from 1980 to 2016) [ 143 ]. The 2019 extension advocated for the inclusion of BED and OSFED in the Global Burden of Disease Study, previously excluded, as both diagnostic groups accounted for the majority of global ED cases and accounted for an unrepresented 41.9 million people living with ED [ 144 ].
Estimates are that over 3.3 million healthy life years are lost per year worldwide due to eating disorders. Years lived with a disability (YLDs) have increased from 2007 to 2017 for both AN (6.2% increase) and BN (10.3%), a higher rate than other mental disorders (− 0.1%). ED outcomes include reduced self-reported quality of life and estimated health care costs at 48% higher than for the general population [ 3 ].
Risk factors
Little is known about specific risk factors for mortality, although some variables have been reported in the literature. People who receive inpatient treatment for AN have more than five to seven times mortality risk when matched to age and gender and compared to other ED diagnoses [ 3 , 131 , 133 ]. For individuals receiving AN or BN treatment in outpatient settings, the risk is still twice that of controls [ 3 ]. Older age of presentation is a significant risk; adult presentations are associated with much higher mortality rates than adolescent presentations likely due to longer duration of illness at presentation, higher rates of medical and psychiatric complications and less engagement in treatment [ 4 , 28 , 68 , 137 , 139 ]. Higher mortality rates (especially in AN) are associated with lower BMI, longer duration of illness at service presentation [ 4 , 49 , 68 , 137 , 139 ], diuretic use [ 68 ], and occurrence of an in-hospital suicide attempt [ 68 , 137 ]. Certain treatment factors may be associated with higher risk of mortality, including transfer to medical intensive care unit, discharge against medical advice, and shorter hospital stays [ 137 ]. Other factors associated with increased risk of mortality include poor psychosocial functioning, substance use [ 28 , 49 ] and absence of family ED history [ 28 ].
Cause of death
Results from a large prospective 20 year (1985–2005) longitudinal study of individuals admitted to inpatient services in Germany ( n = 5839) showed people with AN were likely to die from health issues caused by their disorder, most commonly circulatory failure, cachexia, and multiple organ failure [ 133 ]. Other studies have identified somatic risk factors including anaemia, dysnatremia, infection, cardiac complications and haematological comorbidities [ 137 ]. A 2021 study reported rates of medical complications for severe AN, which included anaemia (79%), neutropenia (53.9%), hypertransaminasemia (53.7%), osteoporosis (46.3%), hypokalemia (39.5%), hypophosphatemia (26%), hypoglycaemia (13.8%), infectious complications (24.3%), cardiac dysfunction (7.1%), and proven gelatinous bone marrow transformation (6.5%). Five (1.4%) of the patients in this study died of the following causes: septic shock of pulmonary origin ( n = 1), septic shock of urinary origin ( n = 1) and suicide ( n = 3) [ 145 ].
Suicide is the most common non-natural cause of death in people with AN, BN, BED and EDNOS [ 133 ]. High rates of suicidality were reported in a meta-analysis of 36 studies published between 1966 and 2010 with data showing one in five individuals who died from an ED did so by suicide [ 4 ]. Risk of suicide may be particularly elevated in AN [Hazard Ratio (HR) 5.07; 95% CI 1.37–18.84] and BN (HR 6.07; 95% CI 2.47–14.89) even when specialised treatments are available [ 134 ]: people with AN are 18.1 [11.5–28.7] times more likely to die by suicide than 15–34 year old females in the general population [ 128 ]. This is supported by results from a meta-review exploring risk of all-cause and suicide across major mental disorders. 1.7 million patients and over a quarter of a million deaths were examined, finding all mental health disorders had an increased mortality rate to the general population; however, substance use and AN were the highest, translating into 10–20 year reductions in life expectancy, with borderline personality disorder, AN, depression and bipolar disorder having the highest suicide risk [ 146 ].
This rapid review, which synthesised the available literature on ED remission, relapse and recovery rates including associated moderating and mediating variables such as psychosocial and treatment characteristics, highlighted significant challenges of synthesising outcome literature. This includes a wide variety of ways in which key outcomes ‘remission’, ‘relapse’ and ‘recovery’ are not only defined but also how they are measured and analysed. There is no consensus among clinical or research communities on these definitions for any of the ED diagnoses [ 30 , 31 , 94 ]; thus, comparison between studies is challenging.
As EDs have amongst the highest rates of mortality of the mental health disorders, including one in five deaths caused by suicide, research into preventable causes of death, mitigatable risk, prevention and treatment efficacy is of paramount importance. It is noteworthy that current reported YLL and YLD for ED are likely an underestimate due to lack of robust epidemiological data, methodological limitations of burden of disease studies, absence of the illness group from national surveys and underreporting of mortality [ 147 ].
‘Relapse’ is typically defined by a return of symptoms after a period of reduced symptomatology; however, reviewed studies report a variety of methods to measure this, including multidisciplinary healthcare team assessment, scores on standardised psychological and behavioural interviews or questionnaires, weight criteria (including BMI or %EBW), reported eating disorder behaviours, meeting DSM (IV or V) diagnostic criteria, or a combination of the above. More difficult is determining if there is a difference between ‘remission’ and ‘recovery’, with remission usually determined by an absence of diagnostic symptomatology (again, characterised by a variety of methods), and recovery an improvement in overall functioning. Many studies report remission and recovery interchangeably, and very few incorporate returns to psychosocial functioning and QoL post alleviation of symptoms [ 29 ]. More standardised definitions may progress research [ 148 ] by allowing direct comparison between outcome studies, improving the ability of future investigations to predict and report relapse versus recovery rates and to comprehensively evaluate intervention and relapse prevention approaches.
An additional challenge across studies is a highly variable period between initial assessment or baseline and the time at which ‘outcome’ is assessed—ranging from as little as one week up to 25 years. As rates of relapse increase with illness progression, relatively short FU periods may compromise the understanding of true long-term outcomes. Longer-term FU studies are crucial to understand optimised models of care for sustained recovery and wellbeing.
Along with illness progression over time in individuals, the shift of diagnostic profiles among the individual may differ the definition of relapse or remission and thus impacts on outcome measures. Most research protocols adopt a firm inclusion/exclusion criterion, focusing on specific diagnostic profiles; however, findings from this review suggest considering a transdiagnostic approach in outcomes research which may better reflect the potentially transient nature of ED symptomatology [ 44 ]. This may have implications for diagnoses such as OSFED, potentially a transient category [ 21 ], rather than categorisation in or out of full ED diagnostic syndromes. Identification and consideration of transdiagnostic profiles, combined ED presentations and co-occurring mental health conditions should be considered in the long-term management and monitoring of individuals.
Studies within this review reported on cohorts of individuals with a formal diagnosis and research conducted within treatment settings. However, previous research has suggested that incidence rates within the community are considerable, and yet help-seeking of any type for a problem related to ED symptoms is uncommon, ranging between 22 and 40% [ 106 ] and there can be a significant time delay from first symptom experience [ 69 ]. A recent large community survey of the impact of COVID-19 on people with ED reported up to 70% of people who experienced ED symptoms were not in treatment [ 149 ] suggesting a significant proportion of people with an ED are not captured within this outcome review. Outcomes for this population are largely unknown [ 150 ] but preliminary research suggests they may be less favourable [ 151 , 152 ].
Improved QoL has been shown to be a significant predictor of positive outcome and is an opportunity for broader scope interventions for people with ED [ 107 ], and yet consistent and more wholistic markers of life quality are rarely integrated into research or clinical decision making [ 153 , 154 ]. It is also noted that outcome determinants in the reviewed studies are predominantly biometric (e.g., weight) and ED symptom related, whereas qualitative lived experience evidence suggests a broader range of person-centred metrics should be used to measure outcome. These include supportive relationships (e.g., receiving support, advice and encouragement from others, including family, friends, and/or professional carers), sense of hope, identity, meaning and purpose, feelings of empowerment and self-compassion [ 155 ]. Involvement of those to whom the work pertains (i.e., individuals with lived experience) is essential in future outcomes research to add richness and utility to theoretical frameworks, methodological approaches and conclusions [ 156 ].

Key findings
ED frequently take a chronic course, with less than half of individuals achieving recovery at long-term FU [ 41 , 44 , 52 ]. Between 30 and 41% of people will relapse within two years of receiving treatment [ 35 , 61 ], and between 20 and 61% will experience more than one type of eating disorder [ 7 , 63 , 64 ]. As with much of the extant ED literature, most outcome research has been conducted in AN. Restrictive ED are consistently associated with the poorest prognosis. This review identified recovery rates in the range of 18–60% for AN and an average length of illness of between 6.5 and 14 years [ 41 , 56 ]. Binge/purge symptomatology within AN is associated with worse outcome [ 20 , 56 ]. Recovery rates for BN are slightly more optimistic at 35–59% [ 7 , 45 , 63 , 157 ], and similarly for BED at 37–77% [ 79 , 80 , 82 ]. There is limited data available on outcomes in ARFID, OSFED, and UFED.
Factors associated with a more positive long-term outcome include lower age of presentation [ 28 , 61 ], shorter duration of illness at first presentation [ 69 , 93 , 94 ], higher pre-treatment motivation to recover [ 116 ], and demonstrated early response to treatment [ 18 , 75 , 110 , 112 ]. Factors associated with poorer outcome are lower BMI at presentation [ 93 ], presence of binge/purge symptomatology [ 20 , 30 , 44 , 56 ], and presence of comorbid psychiatric condition/s such as depression, anxiety, or personality disorder [ 44 , 47 , 51 , 55 , 67 , 98 , 99 ]. Males, LGBTQIA + community [ 104 , 105 ], neurodiversity [ 102 ], individuals from non-white/ethnic backgrounds, and those from lower socioeconomic brackets or rural/remote communities are also more likely to experience a poor outcome [ 18 , 72 , 76 , 77 ].
Relapse following ED treatment is common [ 11 , 35 , 36 , 62 , 148 ] and is most likely to occur 4–9 months post discharge [ 35 ]. Up to 41% of individuals will relapse by the second-year post-discharge [ 62 ]. Aftercare relapse prevention programs, including online and face-to-face initiatives such as text-message based interventions, daily feedback to clinicians and intensive day programs have been shown to increase chance of maintaining recovery [ 121 , 123 – 125 ]. The implementation of such programs may be key to improving long-term recovery rates particularly for those individuals who may otherwise disengage from treatment for access reasons (such as living in an underserviced area) or because of the stigma of engaging with mental health care [ 119 , 120 ]. There is emerging evidence in the effectiveness of online intervention for preventing relapse and promoting treatment gains when individuals are motivated to change; however, evidence is not conclusive potentially due to the high variability of the interventions and evaluations of such programs.
ED are associated with unacceptably high mortality rates, and particularly high risk of suicide [ 128 , 133 ]. Of the ED, AN carries the highest mortality risk [ 49 , 127 , 128 ]. Standardised mortality ratios (SMRs) identified by this review ranged between 1.2 and 15.9 for AN; 1.4 and 4.8 for BN; 1.01 and 3.3 for BED; and 1.3 to 4.7 for EDNOS/OSFED [ 2 , 4 , 20 , 121 , 127 , 128 , 132 , 134 , 135 , 137 , 139 ]. Factors associated with increased risk of mortality include having received inpatient treatment [ 3 , 131 , 133 ], longer duration of untreated illness [ 4 , 28 , 68 , 68 , 137 , 139 ] and lower BMI at presentation [ 4 , 49 , 68 , 137 , 139 ]. Males are at higher risk of death than females [ 2 ].
Strengths and limitations
This rapid review has several strengths inherent to the methodological approach of the series, conducted to inform the Australian Eating Disorders Research and Translation Strategy 2021–2031 [ 1 ]. The RR process broadly assessed all available high-level evidence peer-reviewed literature swiftly [ 24 ], included all diagnostic categories covering transdiagnostic continuums, considered the full demographic range available and reported a variety of methodological designs including clinical trials (across a variety of settings), systematic reviews, meta-analyses, and population-level research. It aimed to provide the most comprehensive and current review possible with coordination of complex findings into a more cohesive structure. It was noted where applicable the limitations of conclusions drawn from this review, such as the widely disparate definitions and measurements for key outcome data (i.e., remission, relapse, and recovery rates), crossover from DSM-IV to DSM-V criteria (due to timeframe of search), vastly different periods of follow up impacting findings, and conflicting evidence. As with the series of rapid reviews, the inclusion criteria of evidence may have potentially excluded relevant evidence, and it is noted that evidence is always emerging.
This RR of outcomes in ED identified several gaps in current knowledge and provides direction for future strategic research directives, specifically, defining the key outcomes of remission, recovery, and relapse, with consensus of determinants and inclusion of broader QoL measures and lived experience. Identifying and refining risk factors, mediating and moderating factors that may influence outcomes is ongoing, with longer-term FU research needed to track remission versus relapse, diagnostic crossover and optimisation of treatment engagement and recovery. Regarding mortality literature, this review noted considerable gaps [ 146 ], with variety reporting methods, a paucity of research between population level reporting and small hospital outcome studies, and minimal investigation into life circumstances relating to death, especially as many of these deaths may be preventable. With low rates of remission despite evidence-based care and high risk of mortality, especially for AN, it is strongly recommended that focused, long-term follow-up research is prioritised for people with ED.
Availability of data and materials
Not applicable—all citations provided.
Abbreviations
Atypical anorexia nervosa
Adolescent focused therapy
- Anorexia nervosa
Anorexia nervosa binge/purge subtype
Anorexia nervosa restricting subtype
Avoidant restrictive food intake disorder
- Binge eating disorder
Body mass index
- Bulimia nervosa
Behavioural weight loss therapy
Cognitive behaviour therapy
Enhanced cognitive behavioural therapy
Crude mortality rate
Diagnostic and statistical manual of mental disorders
Expected body weight
- Eating disorders
Eating disorder examination questionnaire
Eating disorder not otherwise specified
Eating disorder not otherwise specified-anorectic type
Eating disorder not otherwise specified-bulimic type
End of treatment
Family-based therapy
Healthcare management advisors
Health related quality of life
Integrative cognitive-affective therapy
InsideOut Institute
Interpersonal therapy
Major depressive disorder
Objective binge eating
Obsessive compulsive disorder
Other specified feeding or eating disorder
Quality of life
Randomised controlled trial
National eating disorder research & translation strategy rapid review
Standardised mortality ratio
Substance use disorder
Treatment as usual
Unspecified feeding or eating disorder
Weighted mortality ratio
Years of life lost
Years lived with a disability
Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402–13.
Article PubMed Google Scholar
Fichter MM, Naab S, Voderholzer U, Quadflieg N. Mortality in males as compared to females treated for an eating disorder: a large prospective controlled study. Eat Weight Disord. 2021;26(5):1627–37.
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatr. 2020;33(6):521–7.
Article Google Scholar
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatr. 2011;68(7):724.
Bardone-Cone AM, Hunt RA, Watson HJ. An overview of conceptualizations of eating disorder recovery, recent findings, and future directions. Curr Psychiatr Rep. 2018;20(9):79.
Noordenbos G, Seubring A. Criteria for recovery from eating disorders according to patients and therapists. Eat Disord. 2006;14(1):41–54.
Castellini G, Lo Sauro C, Mannucci E, Ravaldi C, Rotella CM, Faravelli C, et al. Diagnostic crossover and outcome predictors in eating disorders according to DSM-IV and DSM-V proposed criteria: a 6-year follow-up study. Psychosom Med. 2011;73(3):270–9.
InsideOut Institute for Eating Disorders. Australian Eating Disorders Research and Translation Strategy 2021–2031. 2021.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders [Internet]. Fifth Edition. American Psychiatric Association; 2013 [cited 2022 Mar 15]. Available from: https://psychiatryonline.org/doi/book/ https://doi.org/10.1176/appi.books.9780890425596 .
Aouad P, Bryant E, Maloney D, Marks P, Le A, Russell H, et al. Informing the development of Australia’s national eating disorders research and translation strategy: a rapid review methodology. J Eat Disord. 2022;10(1):31.
Article PubMed PubMed Central Google Scholar
Grilo CM, Pagano ME, Stout RL, Markowitz JC, Ansell EB, Pinto A, et al. Stressful life events predict eating disorder relapse following remission: six-year prospective outcomes. Int J Eat Disord. 2012;45(2):185–92.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20.
Canadian Agency for Drugs and Technologies in Health. About the Rapid Response Service [Internet]. [Cited 2021 Jun 19]. Available from: https://www.cadth.ca/about-cadth/what-we-do/products-services/rapid-response-service .
Hamel C, Michaud A, Thuku M, Skidmore B, Stevens A, Nussbaumer-Streit B, et al. Defining rapid reviews: a systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. J Clin Epidemiol. 2021;129:74–85.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372: n160.
Le Grange D, Hughes EK, Court A, Yeo M, Crosby RD, Sawyer SM. Randomized clinical trial of parent-focused treatment and family-based treatment for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatr. 2016;55(8):683–92.
Guarda AS, Cooper M, Pletch A, Laddaran L, Redgrave GW, Schreyer CC. Acceptability and tolerability of a meal-based, rapid refeeding, behavioral weight restoration protocol for anorexia nervosa. Int J Eat Disord. 2020;53(12):2032–7.
Brown TA, Murray SB, Anderson LK, Kaye WH. Early predictors of treatment outcome in a partial hospital program for adolescent anorexia nervosa. Int J Eat Disord. 2020;53(9):1550–5.
Fichter MM, Quadflieg N, Lindner S. Internet-based relapse prevention for anorexia nervosa: nine-month follow-up. J Eat Disord. 2013;1(1):23.
Rigaud D, Pennacchio H, Bizeul C, Reveillard V, Vergès B. Outcome in AN adult patients: a 13-year follow-up in 484 patients. Diabetes Metab. 2011;37(4):305–11.
Agras WS, Crow S, Mitchell JE, Halmi KA, Bryson S. A 4-year prospective study of eating disorder NOS compared with full eating disorder syndromes. Int J Eat Disord. 2009;42(6):565–70.
Linardon J, de la Piedad GX, Brennan L. Predictors, moderators, and mediators of treatment outcome following manualised cognitive-behavioural therapy for eating disorders: a systematic review: predictors, moderators, and mediators of outcome for eating disorders. Eur Eat Disorders Rev. 2017;25(1):3–12.
Bryson AE, Scipioni AM, Essayli JH, Mahoney JR, Ornstein RM. Outcomes of low-weight patients with avoidant/restrictive food intake disorder and anorexia nervosa at long-term follow-up after treatment in a partial hospitalization program for eating disorders. Int J Eat Disord. 2018;51(5):470–4.
Lange CRA, Ekedahl Fjertorp H, Holmer R, Wijk E, Wallin U. Long-term follow-up study of low-weight avoidant restrictive food intake disorder compared with childhood-onset anorexia nervosa: psychiatric and occupational outcome in 56 patients. Int J Eat Disord. 2019;52(4):435–8.
Strandjord SE, Sieke EH, Richmond M, Rome ES. Avoidant/restrictive food intake disorder: Illness and hospital course in patients hospitalized for nutritional insufficiency. J Adolesc Health. 2015;57(6):673–8.
Johnston J, Shu CY, Hoiles KJ, Clarke PJF, Watson HJ, Dunlop PD, et al. Perfectionism is associated with higher eating disorder symptoms and lower remission in children and adolescents diagnosed with eating disorders. Eat Behav. 2018;30:55–60.
Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Psychol. 2013;122(2):445–57.
Ackard DM, Richter S, Egan A, Cronemeyer C. Poor outcome and death among youth, young adults, and midlife adults with eating disorders: an investigation of risk factors by age at assessment: poor outcome and death. Int J Eat Disord. 2014;47(7):825–35.
Bardone-Cone AM, Harney MB, Maldonado CR, Lawson MA, Robinson DP, Smith R, et al. Defining recovery from an eating disorder: conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behav Res Ther. 2010;48(3):194–202.
Le Grange D, Fitzsimmons-Craft EE, Crosby RD, Hay P, Lacey H, Bamford B, et al. Predictors and moderators of outcome for severe and enduring anorexia nervosa. Behav Res Ther. 2014;56:91–8.
Gorrell S, Matheson BE, Lock J, Le Grange D. Remission in adolescents with bulimia nervosa: empirical evaluation of current conceptual models. Eur Eat Disorders Rev. 2020;28(4):445–53.
Keel PK, Dorer DJ, Franko DL, Jackson SC, Herzog DB. Postremission predictors of relapse in women with eating disorders. AJP. 2005;162(12):2263–8.
Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J Abnorm Psychol. 2009;118(3):587–97.
Agras WS, Walsh BT, Fairburn CG, Wilson GT, Kraemer HC. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Arch Gen Psychiatr. 2000;57(5):459.
Carter JC, Mercer-Lynn KB, Norwood SJ, Bewell-Weiss CV, Crosby RD, Woodside DB, et al. A prospective study of predictors of relapse in anorexia nervosa: implications for relapse prevention. Psychiatr Res. 2012;200(2–3):518–23.
Berends T, van Meijel B, Nugteren W, Deen M, Danner UN, Hoek HW, et al. Rate, timing and predictors of relapse in patients with anorexia nervosa following a relapse prevention program: a cohort study. BMC Psychiatr. 2016;16(1):316.
Walker DC, Donahue JM, Heiss S, Gorrell S, Anderson LM, Brooks JM, et al. Rapid response is predictive of treatment outcomes in a transdiagnostic intensive outpatient eating disorder sample: a replication of prior research in a real-world setting. Eat Weight Disord. 2021;26(5):1345–56.
Taylor MB, Daiss S, Krietsch K. Associations among self-compassion, mindful eating, eating disorder symptomatology, and body mass index in college students. Transl Issues Psychol Sci. 2015;1(3):229–38.
Custal N, Arcelus J, Agüera Z, Bove FI, Wales J, Granero R, et al. Treatment outcome of patients with comorbid type 1 diabetes and eating disorders. BMC Psychiatr. 2014;14(1):140.
Agüera Z, Riesco N, Jiménez-Murcia S, Islam MA, Granero R, Vicente E, et al. Cognitive behaviour therapy response and dropout rate across purging and nonpurging bulimia nervosa and binge eating disorder: DSM-5 implications. BMC Psychiatr. 2013;13(1):285.
Fernández-Aranda F, Treasure J, Paslakis G, Agüera Z, Giménez M, Granero R, et al. The impact of duration of illness on treatment nonresponse and drop-out: exploring the relevance of enduring eating disorder concept. Eur Eat Disorders Rev. 2021;29(3):499–513.
Colton PA, Olmsted MP, Daneman D, Farquhar JC, Wong H, Muskat S, et al. Eating disorders in girls and women with type 1 diabetes: a longitudinal study of prevalence, onset, remission, and recurrence. Diabetes Care. 2015;38(7):1212–7.
Tomba E, Tecuta L, Schumann R, Ballardini D. Does psychological well-being change following treatment? An exploratory study on outpatients with eating disorders. Compr Psychiatr. 2017;74:61–9.
Helverskov JL, Clausen L, Mors O, Frydenberg M, Thomsen PH, Rokkedal K. Trans-diagnostic outcome of eating disorders: a 30-month follow-up study of 629 patients. Eur Eat Disorders Rev. 2010;18(6):453–63.
Quadflieg N, Fichter MM. Long-term outcome of inpatients with bulimia nervosa—results from the Christina Barz study. Int J Eat Disord. 2019;52(7):834–45.
Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: norms for young adolescent girls. Behav Res Ther. 2001;39(5):625–32.
Wade T, Ambwani S, Cardi V, Albano G, Treasure J. Outcomes for adults with anorexia nervosa who do not respond early to outpatient treatment. Int J Eat Disord. 2021;54(7):1278–82.
Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJV. Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther. 2004;42(5):551–67.
Franko DL, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, et al. A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. AJP. 2013;170(8):917–25.
Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J Clin Psychiatr. 2017;78(02):184–9.
Lydecker JA, Grilo CM. Psychiatric comorbidity as predictor and moderator of binge-eating disorder treatment outcomes: an analysis of aggregated randomized controlled trials. Psychol Med. 2021;52(16):4085–93.
Eielsen HP, Vrabel K, Hoffart A, Rø Ø, Rosenvinge JH. The 17-year outcome of 62 adult patients with longstanding eating disorders—a prospective study. Int J Eat Disord. 2021;54(5):841–50.
Dare C, Eisler I, Russell G, Treasure J, Dodge L. Psychological therapies for adults with anorexia nervosa: randomised controlled trial of out-patient treatments. Br J Psychiatr. 2001;178(3):216–21.
Kordy H, Krämer B, Palmer RL, Papezova H, Pellet J, Richard M, et al. Remission, recovery, relapse, and recurrence in eating disorders: conceptualization and illustration of a validation strategy. J Clin Psychol. 2002;58(7):833–46.
Wild B, Friederich HC, Zipfel S, Resmark G, Giel K, Teufel M, et al. Predictors of outcomes in outpatients with anorexia nervosa—results from the ANTOP study. Psychiatr Res. 2016;244:45–50.
Zerwas S, Lund BC, Von Holle A, Thornton LM, Berrettini WH, Brandt H, et al. Factors associated with recovery from anorexia nervosa. J Psychiatr Res. 2013;47(7):972–9.
Ricca V, Castellini G, Lo Sauro C, Mannucci E, Ravaldi C, Rotella F, et al. Cognitive-behavioral therapy for threshold and subthreshold anorexia nervosa: a three-year follow-up study. Psychother Psychosom. 2010;79(4):238–48.
Winkler LAD, Bilenberg N, Hørder K, Støving RK. Does specialization of treatment influence mortality in eating disorders?—A comparison of two retrospective cohorts. Psychiatr Res. 2015;230(2):165–71.
Wentz E, Gillberg IC, Anckarsäter H, Gillberg C, Råstam M. Adolescent-onset anorexia nervosa: 18-year outcome. Br J Psychiatr. 2009;194(2):168–74.
Castellini G, Mannucci E, Lo Sauro C, Benni L, Lazzeretti L, Ravaldi C, et al. Different moderators of cognitive-behavioral therapy on subjective and objective binge eating in bulimia nervosa and binge eating disorder: a three-year follow-up study. Psychother Psychosom. 2012;81(1):11–20.
Franko DL, Tabri N, Keshaviah A, Murray HB, Herzog DB, Thomas JJ, et al. Predictors of long-term recovery in anorexia nervosa and bulimia nervosa: data from a 22-year longitudinal study. J Psychiatr Res. 2018;96:183–8.
Berends T, Boonstra N, van Elburg A. Relapse in anorexia nervosa: a systematic review and meta-analysis. Curr Opin Psychiatr. 2018;31(6):445–55.
Steinhausen HC, Weber S. The outcome of bulimia nervosa: findings from one-quarter century of research. AJP. 2009;166(12):1331–41.
Glazer KB, Sonneville KR, Micali N, Swanson SA, Crosby R, Horton NJ, et al. The course of eating disorders involving bingeing and purging among adolescent girls: prevalence, stability, and transitions. J Adolesc Health. 2019;64(2):165–71.
Goldstein M, Peters L, Baillie A, McVeagh P, Minshall G, Fitzjames D. The effectiveness of a day program for the treatment of adolescent anorexia nervosa. Int J Eat Disord. 2011;44(1):29–38.
Herpertz-Dahlmann B, Dempfle A, Egberts KM, Kappel V, Konrad K, Vloet JA, et al. Outcome of childhood anorexia nervosa-the results of a five- to ten-year follow-up study. Int J Eat Disord. 2018;51(4):295–304.
Amianto F, Spalatro A, Ottone L, Abbate Daga G, Fassino S. Naturalistic follow-up of subjects affected with anorexia nervosa 8 years after multimodal treatment: personality and psychopathology changes and predictors of outcome. Eur psychiatr. 2017;45:198–206.
Huas C, Caille A, Godart N, Foulon C, Pham-Scottez A, Divac S, et al. Factors predictive of ten-year mortality in severe anorexia nervosa patients: mortality in severe anorexia nervosa patients. Acta Psychiatr Scand. 2011;123(1):62–70.
Austin A, Flynn M, Richards K, Hodsoll J, Duarte TA, Robinson P, et al. Duration of untreated eating disorder and relationship to outcomes: a systematic review of the literature. Eur Eat Disorders Rev. 2021;29(3):329–45.
Dechartres A, Huas C, Godart N, Pousset M, Pham A, Divac SM, Rouillon F, Falissard B. Outcomes of empirical eating disorder phenotypes in a clinical female sample: results from a latent class analysis. Psychopathology. 2011;44:12–20.
Ando T, Komaki G, Nishimura H, Naruo T, Okabe K, Kawai K, et al. A ghrelin gene variant may predict crossover rate from restricting-type anorexia nervosa to other phenotypes of eating disorders: a retrospective survival analysis. Psychiatr Genet. 2010;20(4):153–9.
Castellini G, Ricca V, Lelli L, Bagnoli S, Lucenteforte E, Faravelli C, et al. Association between serotonin transporter gene polymorphism and eating disorders outcome: a 6-year follow-up study. Am J Med Genet. 2012;159B(5):491–500.
Linardon J. Rates of abstinence following psychological or behavioral treatments for binge-eating disorder: meta-analysis. Int J Eat Disord. 2018;51(8):785–97.
Dalle Grave R, Calugi S, Marchesini G. Self-induced vomiting in eating disorders: associated features and treatment outcome. Behav Res Ther. 2009;47(8):680–4.
Accurso EC, Wonderlich SA, Crosby RD, Smith TL, Klein MH, Mitchell JE, et al. Predictors and moderators of treatment outcome in a randomized clinical trial for adults with symptoms of bulimia nervosa. J Consult Clin Psychol. 2016;84(2):178–84.
Keski-Rahkonen A. Epidemiology of binge eating disorder: prevalence, course, comorbidity, and risk factors. Curr Opin Psychiatr. 2021;34(6):525–31.
Hilbert A, Petroff D, Herpertz S, Pietrowsky R, Tuschen-Caffier B, Vocks S, et al. Meta-analysis on the long-term effectiveness of psychological and medical treatments for binge-eating disorder. Int J Eat Disord. 2020;53(9):1353–76.
Rodan S, Bryant E, Le A, Maloney D, National Eating Disorders Collaboration, Touyz S, et al. Pharmacotherapy, adjunctive and alternative therapies: findings from a rapid review. J Eat Disord. (Under Review).
Fischer S, Meyer AH, Dremmel D, Schlup B, Munsch S. Short-term cognitive-behavioral therapy for binge eating disorder: long-term efficacy and predictors of long-term treatment success. Behav Res Ther. 2014;58:36–42.
Hilbert A, Bishop ME, Stein RI, Tanofsky-Kraff M, Swenson AK, Welch RR, et al. Long-term efficacy of psychological treatments for binge eating disorder. Br J Psychiatr. 2012;200(3):232–7.
Villarejo C, Fernández-Aranda F, Jiménez-Murcia S, Peñas-Lledó E, Granero R, Penelo E, et al. Lifetime obesity in patients with eating disorders: increasing prevalence, clinical and personality correlates. Eur Eat Disorders Rev. 2012;20(3):250–4.
Munsch S, Meyer AH, Biedert E. Efficacy and predictors of long-term treatment success for cognitive-behavioral treatment and behavioral weight-loss-treatment in overweight individuals with binge eating disorder. Behav Res Ther. 2012;50(12):775–85.
Opolski M, Chur-Hansen A, Wittert G. The eating-related behaviours, disorders and expectations of candidates for bariatric surgery: eating in bariatric surgery candidates. Clin Obes. 2015;5(4):165–97.
Opozda M, Chur-Hansen A, Wittert G. Changes in problematic and disordered eating after gastric bypass, adjustable gastric banding and vertical sleeve gastrectomy: a systematic review of pre-post studies: problematic/disordered eating in bariatric surgeries. Obes Rev. 2016;17(8):770–92.
Genco A, Maselli R, Frangella F, Cipriano M, Paone E, Meuti V, et al. Effect of consecutive intragastric balloon (BIB®) plus diet versus single BIB® plus diet on eating disorders not otherwise specified (EDNOS) in obese patients. Obes Surg. 2013;23(12):2075–9.
Ferreira Pinto T, Carvalhedo de Bruin PF, Sales de Bruin VM, Ney Lemos F, Azevedo Lopes FH, Marcos Lopes P. Effects of bariatric surgery on night eating and depressive symptoms: a prospective study. Surg Obes Relat Dis. 2017;13(6):1057–62.
Wadden TA, Faulconbridge LF, Jones-Corneille LR, Sarwer DB, Fabricatore AN, Thomas JG, et al. Binge eating disorder and the outcome of bariatric surgery at one year: a prospective, observational study. Obesity. 2011;19(6):1220–8.
Calugi S, Ruocco A, El Ghoch M, Andrea C, Geccherle E, Sartori F, et al. Residential cognitive-behavioral weight-loss intervention for obesity with and without binge-eating disorder: a prospective case-control study with five-year follow-up: treatment for obesity with binge-eating disorder. Int J Eat Disord. 2016;49(7):723–30.
Mason TB, Crosby RD, Kolotkin RL, Grilo CM, Mitchell JE, Wonderlich SA, et al. Correlates of weight-related quality of life among individuals with binge eating disorder before and after cognitive behavioral therapy. Eat Behav. 2017;27:1–6.
Paul L, van Rongen S, van Hoeken D, Deen M, Klaassen R, Biter LU, et al. Does cognitive behavioral therapy strengthen the effect of bariatric surgery for obesity? Design and methods of a randomized and controlled study. Contemp Clin Trials. 2015;42:252–6.
Tasca GA, Maxwell H, Bone M, Trinneer A, Balfour L, Bissada H. Purging disorder: psychopathology and treatment outcomes. Int J Eat Disord. 2012;45(1):36–42.
Allen KL, Byrne SM, Oddy WH, Crosby RD. Early onset binge eating and purging eating disorders: course and outcome in a population-based study of adolescents. J Abnorm Child Psychol. 2013;41(7):1083–96.
Glasofer DR, Muratore AF, Attia E, Wu P, Wang Y, Minkoff H, et al. Predictors of illness course and health maintenance following inpatient treatment among patients with anorexia nervosa. J Eat Disord. 2020;8(1):69.
Radunz M, Keegan E, Osenk I, Wade TD. Relationship between eating disorder duration and treatment outcome: systematic review and meta-analysis. Int J Eat Disord. 2020;53(11):1761–73.
Li A, Cunich M, Miskovic-Wheatley J, Maloney D, Madden S, Wallis A, et al. Factors related to length of stay, referral on discharge and hospital readmission for children and adolescents with anorexia nervosa. Int J Eat Disord. 2021;54(3):409–21.
Bluett EJ, Lee EB, Simone M, Lockhart G, Twohig MP, Lensegrav-Benson T, et al. The role of body image psychological flexibility on the treatment of eating disorders in a residential facility. Eat Behav. 2016;23:150–5.
Wade TD, Hart LM, Mitchison D, Hay P. Driving better intervention outcomes in eating disorders: a systematic synthesis of research priority setting and the involvement of consumer input. Eur Eat Disorders Rev. 2021;29(3):346–54.
Keshishian AC, Tabri N, Becker KR, Franko DL, Herzog DB, Thomas JJ, et al. Eating disorder recovery is associated with absence of major depressive disorder and substance use disorders at 22-year longitudinal follow-up. Compr Psychiatr. 2019;90:49–51.
O’Brien KM, Whelan DR, Sandler DP, Hall JE, Weinberg CR. Predictors and long-term health outcomes of eating disorders. PLoS ONE. 2017;12(7):e0181104.
Micali N, Solmi F, Horton NJ, Crosby RD, Eddy KT, Calzo JP, et al. Adolescent eating disorders predict psychiatric, high-risk behaviors and weight outcomes in young adulthood. J Am Acad Child Adolesc Psychiatry. 2015;54(8):652-659.e1.
La Mela C, Maglietta M, Lucarelli S, Mori S, Sassaroli S. Pretreatment outcome indicators in an eating disorder outpatient group: the effects of self-esteem, personality disorders and dissociation. Compr Psychiatr. 2013;54(7):933–42.
Li Z, Halls D, Byford S, Tchanturia K. Autistic characteristics in eating disorders: treatment adaptations and impact on clinical outcomes. Euro Eat Disord Rev. 2022;30(5):671–90.
Bye A, Martini MG, Micali N. Eating disorders, pregnancy and the postnatal period: a review of the recent literature. Curr Opin Psychiatr. 2021;34(6):563–8.
Sollid C, Clausen L, Maimburg RD. The first 20 weeks of pregnancy is a high-risk period for eating disorder relapse. Intl J Eat Disord. 2021;54(12):2132–42.
Grammer AC, Vázquez MM, Fitzsimmons-Craft EE, Fowler LA, Rackoff GN, Schvey NA, et al. Characterizing eating disorder diagnosis and related outcomes by sexual orientation and gender identity in a national sample of college students. Eat Behav. 2021;42: 101528.
Hay PJ, Buettner P, Mond J, Paxton SJ, Quirk F, Rodgers B. A community-based study of enduring eating features in young women. Nutrients. 2012;4(5):413–24.
Winkler LA. Funen anorexia nervosa study—a follow-up study on outcome, mortality, quality of life and body composition. Danish Med J. 2017;64(6):B5380.
Google Scholar
Le Grange D, Lock J, Accurso EC, Agras WS, Darcy A, Forsberg S, et al. Relapse from remission at two- to four-year follow-up in two treatments for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatr. 2014;53(11):1162–7.
Austin A, Flynn M, Shearer J, Long M, Allen K, Mountford VA, et al. The first episode rapid early intervention for eating disorders-upscaled study: clinical outcomes. Early Interv Psychiatr. 2022;16(1):97–105.
Chang PGRY, Delgadillo J, Waller G. Early response to psychological treatment for eating disorders: a systematic review and meta-analysis. Clin Psychol Rev. 2021;86: 102032.
Støving RK, Larsen PV, Winkler LA, Bilenberg N, Røder ME, Steinhausen H. Time trends in treatment modes of anorexia nervosa in a nationwide cohort with free and equal access to treatment. Int J Eat Disord. 2020;53(12):1952–9.
McClelland J, Simic M, Schmidt U, Koskina A, Stewart C. Defining and predicting service utilisation in young adulthood following childhood treatment of an eating disorder. BJPsych open. 2020;6(3): e37.
Golden NH, Cheng J, Kapphahn CJ, Buckelew SM, Machen VI, Kreiter A, et al. Higher-calorie refeeding in anorexia nervosa: 1-year outcomes from a randomized controlled trial. Pediatrics. 2021;147(4): e2020037135.
Baudinet J, Simic M. Adolescent eating disorder day programme treatment models and outcomes: a systematic scoping review. Front Psychiatr. 2021;12: 652604.
Thompson-Brenner H, Singh S, Gardner T, Brooks GE, Smith M, Lowe M, et al. The Renfrew unified treatment for eating disorders and comorbidity: long-term effects of an evidence-based practice implementation in residential treatment. Front Psychiatr. 2021;12:641601.
Kästner D, Löwe B, Gumz A. The role of self-esteem in the treatment of patients with anorexia nervosa—a systematic review and meta-analysis. Int J Eat Disord. 2019;52(2):101–16.
Kelly AC, Vimalakanthan K, Carter JC. Understanding the roles of self-esteem, self-compassion, and fear of self-compassion in eating disorder pathology: an examination of female students and eating disorder patients. Eat Behav. 2014;15(3):388–91.
Sansfaçon J, Booij L, Gauvin L, Fletcher É, Islam F, Israël M, et al. Pretreatment motivation and therapy outcomes in eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2020;53(12):1879–900.
Griffiths S, Mond JM, Li Z, Gunatilake S, Murray SB, Sheffield J, et al. Self-stigma of seeking treatment and being male predict an increased likelihood of having an undiagnosed eating disorder: predicting undiagnosed eating disorders. Int J Eat Disord. 2015;48(6):775–8.
Foran A, O’Donnell AT, Muldoon OT. Stigma of eating disorders and recovery-related outcomes: a systematic review. Eur Eat Disord Rev. 2020;28(4):385–97.
Fichter MM, Quadflieg N, Nisslmüller K, Lindner S, Osen B, Huber T, et al. Does internet-based prevention reduce the risk of relapse for anorexia nervosa? Behav Res Ther. 2012;50(3):180–90.
Jacobi C, Beintner I, Fittig E, Trockel M, Braks K, Schade-Brittinger C, et al. Web-based aftercare for women with bulimia nervosa following inpatient treatment: randomized controlled efficacy trial. J Med Internet Res. 2017;19(9): e321.
Gulec H, Moessner M, Túry F, Fiedler P, Mezei A, Bauer S. A randomized controlled trial of an internet-based posttreatment care for patients with eating disorders. Telemed e-Health. 2014;20(10):916–22.
Shapiro J, Bauer S, Andrews E, Pisetsky E, Bulik-Sullivan B, Hamer R, et al. Mobile therapy: use of text-messaging in the treatment of bulimia nervosa. Int J Eat Disord. 2010;43(6):513–9.
Bauer S, Okon E, Meermann R, Kordy H. Technology-enhanced maintenance of treatment gains in eating disorders: efficacy of an intervention delivered via text messaging. J Consult Clin Psychol. 2012;80(4):700–6.
Anastasiadou D, Folkvord F, Lupiañez-Villanueva F. A systematic review of mHealth interventions for the support of eating disorders. Eur Eat Disord Rev. 2018;26(5):394–416.
Button EJ, Chadalavada B, Palmer RL. Mortality and predictors of death in a cohort of patients presenting to an eating disorders service. Int J Eat Disord. 2010;43(5):387–92.
PubMed Google Scholar
Keshaviah A, Edkins K, Hastings ER, Krishna M, Franko DL, Herzog DB, et al. Re-examining premature mortality in anorexia nervosa: a meta-analysis redux. Compr Psychiatr. 2014;55(8):1773–84.
Ward ZJ, Rodriguez P, Wright DR, Austin SB, Long MW. Estimation of eating disorders prevalence by age and associations with mortality in a simulated nationally representative US cohort. JAMA Netw Open. 2019;2(10): e1912925.
Nielsen S, Vilmar JW. What can we learn about eating disorder mortality from eating disorder diagnoses at initial assessment? A Danish nationwide register follow-up study using record linkage, encompassing 45 years (1970–2014). Psychiatr Res. 2021;303: 114091.
Iwajomo T, Bondy SJ, de Oliveira C, Colton P, Trottier K, Kurdyak P. Excess mortality associated with eating disorders: population-based cohort study. Br J Psychiatr. 2021;219(3):487–93.
Hoang U, Goldacre M, James A. Mortality following hospital discharge with a diagnosis of eating disorder: national record linkage study, England, 2001–2009: mortality following a diagnosis of eating disorder. Int J Eat Disord. 2014;47(5):507–15.
Fichter MM, Quadflieg N. Mortality in eating disorders—results of a large prospective clinical longitudinal study: mortality in eating disorders. Int J Eat Disord. 2016;49(4):391–401.
Suokas JT, Suvisaari JM, Gissler M, Löfman R, Linna MS, Raevuori A, et al. Mortality in eating disorders: a follow-up study of adult eating disorder patients treated in tertiary care, 1995–2010. Psychiatr Res. 2013;210(3):1101–6.
Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, et al. Increased mortality in bulimia nervosa and other eating disorders. AJP. 2009;166(12):1342–6.
Castellini G, Caini S, Cassioli E, Rossi E, Marchesoni G, Rotella F, et al. Mortality and care of eating disorders. Acta Psychiatr Scand. 2023;147(2):122–33.
Guinhut M, Godart N, Benadjaoud M, Melchior J, Hanachi M. Five-year mortality of severely malnourished patients with chronic anorexia nervosa admitted to a medical unit. Acta Psychiatr Scand. 2021;143(2):130–40.
Quadflieg N, Strobel C, Naab S, Voderholzer U, Fichter MM. Mortality in males treated for an eating disorder—a large prospective study. Int J Eat Disord. 2019;52(12):1365–9.
Rosling AM, Sparén P, Norring C, von Knorring AL. Mortality of eating disorders: a follow-up study of treatment in a specialist unit 1974–2000. Int J Eat Disord. 2011;44(4):304–10.
Crow SJ, Swanson SA, le Grange D, Feig EH, Merikangas KR. Suicidal behavior in adolescents and adults with bulimia nervosa. Compr Psychiatr. 2014;55(7):1534–9.
Zerwas S, Larsen JT, Petersen L, Thornton LM, Mortensen PB, Bulik CM. The incidence of eating disorders in a Danish register study: associations with suicide risk and mortality. J Psychiatr Res. 2015;65:16–22.
Mellentin AI, Mejldal A, Guala MM, Støving RK, Eriksen LS, Stenager E, et al. The impact of alcohol and other substance use disorders on mortality in patients with eating disorders: a nationwide register-based retrospective cohort study. AJP. 2021;179(1):46–57.
Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210.
Santomauro DF, Melen S, Mitchison D, Vos T, Whiteford H, Ferrari AJ. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. Lancet Psychiatr. 2021;8(4):320–8.
Guinhut M, Melchior JC, Godart N, Hanachi M. Extremely severe anorexia nervosa: hospital course of 354 adult patients in a clinical nutrition-eating disorders-unit. Clin Nutr. 2021;40(4):1954–65.
Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatr. 2014;13(2):153–60.
Bryant E, Koemel N, Martenstyn J, Marks P, Hickie I, Maguire S. Mortality and mental health funding—when the dollars don’t add up: a portfolio analysis of eating disorder research funding in Australia 2009–2021. Lancet Regional Health (Western Pacific).
Khalsa SS, Portnoff LC, McCurdy-McKinnon D, Feusner JD. What happens after treatment? A systematic review of relapse, remission, and recovery in anorexia nervosa. J Eat Disord. 2017;5(1):20.
Miskovic-Wheatley J, Koreshe E, Kim M, Simeone R, Maguire S. The impact of the COVID-19 pandemic and associated public health response on people with eating disorder symptomatology: an Australian study. J Eat Disord. 2022;10(1):9.
Smink FRE, van Hoeken D, Hoek HW. Epidemiology, course, and outcome of eating disorders. Curr Opin Psychiatr. 2013;26(6):543–8.
Vinchenzo C, McCombie C, Lawrence V. The experience of patient dropout from eating disorders treatment: a systematic review and qualitative synthesis. BJPsych open. 2021;7(S1):S299–S299.
Article PubMed Central Google Scholar
Björk T, Björck C, Clinton D, Sohlberg S, Norring C. What happened to the ones who dropped out? Outcome in eating disorder patients who complete or prematurely terminate treatment. Eur Eat Disorders Rev. 2009;17(2):109–19.
Jenkins PE, Hoste RR, Meyer C, Blissett JM. Eating disorders and quality of life: a review of the literature. Clin Psychol Rev. 2011;31(1):113–21.
Calvete E, Las Hayas C, Gómezdel Barrio A. Longitudinal associations between resilience and quality of life in eating disorders. Psychiatr Res. 2018;259:470–5.
Wetzler S, Hackmann C, Peryer G, Clayman K, Friedman D, Saffran K, et al. A framework to conceptualize personal recovery from eating disorders: a systematic review and qualitative meta-synthesis of perspectives from individuals with lived experience. Int J Eat Disord. 2020;53(8):1188–203.
Musić S, Elwyn R, Fountas G, Gnatt I, Jenkins ZM, Malcolm A, et al. Valuing the voice of lived experience of eating disorders in the research process: benefits and considerations. Aust N Z J Psychiatr. 2022;56(3):216–8.
Linardon J, Wade TD. How many individuals achieve symptom abstinence following psychological treatments for bulimia nervosa? A meta-analytic review. Int J Eat Disord. 2018;51(4):287–94.
Download references
Acknowledgements
The InsideOut Institute is a collaboration between the University of Sydney and Sydney Local Health District. We thank all the staff from the Institution for their support of this significant project. The authors would like to thank and acknowledge the hard work of Healthcare Management Advisors (HMA) who were commissioned to undertake the Rapid Review. Additionally, the authors would like to thank all members of the consortium and consultation committees for their advice, input, and considerations during the development process. Further, a special thank you to the carers, consumers and lived experience consultants that provided input to the development of the Rapid Review and wider national Eating Disorders Research & Translation Strategy. Finally, thank you to the Australian Government—Department of Health for their support of the current project. National Eating Disorder Research Consortium Members (alphabetical order of surname): *indicates named authors. Phillip Aouad InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Sarah Barakat InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Robert Boakes School of Psychology, Faculty of Science, University of Sydney, NSW Australia. Leah Brennan School of Psychology and Public Health, La Trobe University, Victoria, Australia. Emma Bryant* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Susan Byrne School of Psychology, Western Australia, Perth, Australia. Belinda Caldwell Eating Disorders Victoria, Victoria, Australia. Shannon Calvert Perth, Western Australia, Australia. Bronny Carroll InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. David Castle Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia. Ian Caterson School of Life and Environmental Sciences, University of Sydney, Sydney, New South Wales, Australia. Belinda Chelius Eating Disorders Queensland, Brisbane, Queensland, Australia. Lyn Chiem Sydney Local Health District, New South Wales Health, Sydney, Australia. Simon Clarke Westmead Hospital, Sydney, New South Wales, Australia. Janet Conti Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Lexi Crouch Brisbane, Queensland, Australia. Genevieve Dammery InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Natasha Dzajkovski InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Jasmine Fardouly School of Psychology, University of New South Wales, Sydney, New South Wales, Australia. John Feneley New South Wales Health, New South Wales, Australia. Amber-Marie Firriolo University of Sydney, NSW Australia. Nasim Foroughi Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Mathew Fuller-Tyszkiewicz School of Psychology, Faculty of Health, Deakin University, Victoria, Australia. Anthea Fursland School of Population Health, Faculty of Health Sciences, Curtain University, Perth, Australia. Veronica Gonzalez-Arce InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Bethanie Gouldthorp Hollywood Clinic, Ramsay Health Care, Perth, Australia. Kelly Griffin InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Scott Griffiths Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia. Ashlea Hambleton InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Amy Hannigan Queensland Eating Disorder Service, Brisbane, Queensland, Australia. Mel Hart Hunter New England Local Health District, New South Wales, Australia. Susan Hart St Vincent’s Hospital Network Local Health District, Sydney, New South Wales, Australia. Phillipa Hay Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Ian Hickie Brain and Mind Centre, University of Sydney, Sydney, Australia. Francis Kay-Lambkin School of Medicine and Public Health, University of Newcastle, New South Wales, Australia. Ross King School of Psychology, Faculty of Health, Deakin University, Victoria, Australia. Michael Kohn Paediatrics & Child Health, Children's Hospital, Westmead, Sydney, Australia. Eyza Koreshe InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Isabel Krug Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia. Jake Linardon School of Psychology, Faculty of Health, Deakin University, Victoria, Australia. Randall Long College of Medicine and Public Health, Flinders University, South Australia, Australia. Amanda Long Exchange Consultancy, Redlynch, New South Wales, Australia. Sloane Madden Eating Disorders Service, Children’s Hospital at Westmead, Sydney, New South Wales, Australia. Sarah Maguire* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Danielle Maloney InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Peta Marks InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Sian McLean The Bouverie Centre, School of Psychology and Public Health, La Trobe University, Victoria, Australia. Thy Meddick Clinical Excellence Queensland, Mental Health Alcohol and Other Drugs Branch, Brisbane, Queensland, Australia. Jane Miskovic-Wheatley* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Deborah Mitchison Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Richard O’Kearney College of Health & Medicine, Australian National University, Australian Capital Territory, Australia. Shu Hwa Ong* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Roger Paterson ADHD and BED Integrated Clinic, Melbourne, Victoria, Australia. Susan Paxton La Trobe University, Department of Psychology and Counselling, Victoria, Australia. Melissa Pehlivan InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Genevieve Pepin School of Health & Social Development, Faculty of Health, Deakin University, Geelong, Victoria, Australia. Andrea Phillipou Swinburne Anorexia Nervosa (SWAN) Research Group, Centre for Mental Health, School of Health Sciences, Swinburne University, Victoria, Australia. Judith Piccone Children's Health Queensland Hospital and Health Service, Brisbane, Queensland, Australia. Rebecca Pinkus School of Psychology, Faculty of Science, University of Sydney, NSW Australia. Bronwyn Raykos Centre for Clinical Interventions, Western Australia Health, Perth, Western Australia, Australia. Paul Rhodes School of Psychology, Faculty of Science, University of Sydney, NSW Australia. Elizabeth Rieger College of Health & Medicine, Australian National University, Australian Capital Territory, Australia. Karen Rockett New South Wales Health, New South Wales, Australia. Sarah-Catherine Rodan InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Janice Russell Central Clinical School Brain & Mind Research Institute, University of Sydney, New South Wales, Sydney. Haley Russell InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Fiona Salter Ramsay Health Care, Perth, Australia. Susan Sawyer Department of Paediatrics, The University of Melbourne, Australia. Beth Shelton National Eating Disorders Collaboration, Victoria, Australia. Urvashnee Singh The Hollywood Clinic Hollywood Private Hospital, Ramsey Health, Perth, Australia. Sophie Smith Sydney, New South Wales, Australia. Evelyn Smith Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Karen Spielman InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Sarah Squire The Butterfly Foundation, Sydney, Australia. Juliette Thomson The Butterfly Foundation, Sydney, Australia. Stephen Touyz* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Ranjani Utpala The Butterfly Foundation, Sydney, Australia. Lenny Vartanian School of Psychology, University of New South Wales, Sydney, New South Wales, Australia. Sabina Vatter* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Andrew Wallis Eating Disorder Service, The Sydney Children’s Hospital Network, Westmead Campus, Sydney, Australia. Warren Ward Department of Psychiatry, University of Queensland, Brisbane, Australia. Sarah Wells University of Tasmania, Tasmania, Australia. Eleanor Wertheim School of Psychology and Public Health, La Trobe University, Victoria, Australia. Simon Wilksch College of Education, Psychology and Social Work, Flinders University, South Australia, Australia. Michelle Williams Royal Hobart, Tasmanian Health Service, Tasmania, Australia.
The RR was in-part funded by the Australian Government Department of Health in partnership with other national and jurisdictional stakeholders. As the organisation responsible for overseeing the National Eating Disorder Research & Translation Strategy, InsideOut Institute commissioned Healthcare Management Advisors to undertake the RR as part of a larger, ongoing, project. Role of Funder: The funder was not directly involved in informing the development of the current review.
Author information
Authors and affiliations.
Faculty of Medicine and Health, InsideOut Institute for Eating Disorders, University of Sydney, Level 2, Charles Perkins Centre (D17), Sydney, NSW, 2006, Australia
Jane Miskovic-Wheatley, Emma Bryant, Shu Hwa Ong, Sabina Vatter, Phillip Aouad, Sarah Barakat, Emma Bryant, Bronny Carroll, Genevieve Dammery, Natasha Dzajkovski, Veronica Gonzalez-Arce, Kelly Griffin, Ashlea Hambleton, Eyza Koreshe, Sarah Maguire, Danielle Maloney, Peta Marks, Jane Miskovic-Wheatley, Shu Hwa Ong, Melissa Pehlivan, Sarah-Catherine Rodan, Haley Russell, Karen Spielman, Stephen Touyz, Sabina Vatter, Stephen Touyz & Sarah Maguire
Sydney Local Health District, Sydney, Australia
Healthcare Management Advisors, Melbourne, Australia
School of Psychology, Faculty of Science, University of Sydney, Sydney, NSW, Australia
Robert Boakes, Rebecca Pinkus & Paul Rhodes
School of Psychology and Public Health, La Trobe University, Victoria, Australia
Leah Brennan & Eleanor Wertheim
School of Psychology, Perth, Western Australia, Australia
Susan Byrne
Eating Disorders Victoria, Victoria, Australia
Belinda Caldwell
Perth, Australia
Shannon Calvert
Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia
David Castle
School of Life and Environmental Sciences, University of Sydney, Sydney, NSW, Australia
Ian Caterson
Eating Disorders Queensland, Brisbane, QLD, Australia
Belinda Chelius
Sydney Local Health District, New South Wales Health, Sydney, Australia
Westmead Hospital, Sydney, NSW, Australia
Simon Clarke
Translational Health Research Institute, Western Sydney University, Sydney, NSW, Australia
Janet Conti, Nasim Foroughi, Phillipa Hay, Deborah Mitchison & Evelyn Smith
Brisbane, Australia
Lexi Crouch
School of Psychology, University of New South Wales, Sydney, NSW, Australia
Jasmine Fardouly & Lenny Vartanian
University of Sydney, Sydney, NSW, Australia
Carmen Felicia & Amber-Marie Firriolo
New South Wales Health, Sydney, NSW, Australia
John Feneley & Karen Rockett
School of Psychology, Faculty of Health, Deakin University, Victoria, Australia
Mathew Fuller-Tyszkiewicz & Ross King
School of Population Health, Faculty of Health Sciences, Curtain University, Perth, Australia
Anthea Fursland
Hollywood Clinic, Ramsay Health Care, Perth, Australia
Bethanie Gouldthorp & Jake Linardon
Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia
Scott Griffiths & Isabel Krug
Queensland Eating Disorder Service, Brisbane, QLD, Australia
Amy Hannigan
Hunter New England Local Health District, New Lambton, NSW, Australia
St Vincent’s Hospital Network Local Health District, Sydney, NSW, Australia
Brain and Mind Centre, University of Sydney, Sydney, Australia
School of Medicine and Public Health, University of Newcastle, Newcastle, NSW, Australia
Francis Kay-Lambkin
Westmead Hospital, Sydney, Australia
Michael Kohn
College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia
Randall Long
Exchange Consultancy, Redlynch, NSW, Australia
Amanda Long
Eating Disorders Service, Children’s Hospital at Westmead, Sydney, NSW, Australia
Sloane Madden
The Bouverie Centre, School of Psychology and Public Health, La Trobe University, Victoria, Australia
Sian McLean
Clinical Excellence Queensland, Mental Health Alcohol and Other Drugs Branch, Brisbane, QLD, Australia
Thy Meddick
College of Health and Medicine, Australian National University, Canberra, ACT, Australia
Richard O’Kearney & Elizabeth Rieger
ADHD and BED Integrated Clinic, Melbourne, VIC, Australia
Roger Paterson
Department of Psychology and Counselling, La Trobe University, Victoria, Australia
Susan Paxton
School of Health and Social Development, Faculty of Health, Deakin University, Geelong, VIC, Australia
Genevieve Pepin
Swinburne Anorexia Nervosa (SWAN) Research Group, Centre for Mental Health, School of Health Sciences, Swinburne University, Victoria, Australia
Andrea Phillipou
Children’s Health Queensland Hospital and Health Service, Brisbane, QLD, Australia
Judith Piccone
Centre for Clinical Interventions, Western Australia Health, Perth, WA, Australia
Bronwyn Raykos
Central Clinical School Brain & Mind Research Institute, University of Sydney, Sydney, NSW, Australia
Janice Russell
Ramsay Health Care, Perth, Australia
Fiona Salter
Department of Paediatrics, The University of Melbourne, Parkville, Australia
Susan Sawyer
National Eating Disorders Collaboration, Victoria, Australia
Beth Shelton
The Hollywood Clinic Hollywood Private Hospital, Ramsey Health, Perth, Australia
Urvashnee Singh
Sydney, Australia
Sophie Smith
The Butterfly Foundation, Sydney, Australia
Sarah Squire, Juliette Thomson & Ranjani Utpala
Eating Disorder Service, The Sydney Children’s Hospital Network, Westmead Campus, Sydney, Australia
Andrew Wallis
Department of Psychiatry, University of Queensland, Brisbane, Australia
Warren Ward
University of Tasmania, Hobart, TAS, Australia
Sarah Wells
College of Education, Psychology and Social Work, Flinders University, Adelaide, SA, Australia
Simon Wilksch
Royal Hobart, Tasmanian Health Service, Hobart, TAS, Australia
Michelle Williams
You can also search for this author in PubMed Google Scholar
National Eating Disorder Research Consortium
- Phillip Aouad
- , Sarah Barakat
- , Robert Boakes
- , Leah Brennan
- , Emma Bryant
- , Susan Byrne
- , Belinda Caldwell
- , Shannon Calvert
- , Bronny Carroll
- , David Castle
- , Ian Caterson
- , Belinda Chelius
- , Lyn Chiem
- , Simon Clarke
- , Janet Conti
- , Lexi Crouch
- , Genevieve Dammery
- , Natasha Dzajkovski
- , Jasmine Fardouly
- , Carmen Felicia
- , John Feneley
- , Amber-Marie Firriolo
- , Nasim Foroughi
- , Mathew Fuller-Tyszkiewicz
- , Anthea Fursland
- , Veronica Gonzalez-Arce
- , Bethanie Gouldthorp
- , Kelly Griffin
- , Scott Griffiths
- , Ashlea Hambleton
- , Amy Hannigan
- , Susan Hart
- , Phillipa Hay
- , Ian Hickie
- , Francis Kay-Lambkin
- , Ross King
- , Michael Kohn
- , Eyza Koreshe
- , Isabel Krug
- , Jake Linardon
- , Randall Long
- , Amanda Long
- , Sloane Madden
- , Sarah Maguire
- , Danielle Maloney
- , Peta Marks
- , Sian McLean
- , Thy Meddick
- , Jane Miskovic-Wheatley
- , Deborah Mitchison
- , Richard O’Kearney
- , Shu Hwa Ong
- , Roger Paterson
- , Susan Paxton
- , Melissa Pehlivan
- , Genevieve Pepin
- , Andrea Phillipou
- , Judith Piccone
- , Rebecca Pinkus
- , Bronwyn Raykos
- , Paul Rhodes
- , Elizabeth Rieger
- , Sarah-Catherine Rodan
- , Karen Rockett
- , Janice Russell
- , Haley Russell
- , Fiona Salter
- , Susan Sawyer
- , Beth Shelton
- , Urvashnee Singh
- , Sophie Smith
- , Evelyn Smith
- , Karen Spielman
- , Sarah Squire
- , Juliette Thomson
- , Stephen Touyz
- , Ranjani Utpala
- , Lenny Vartanian
- , Sabina Vatter
- , Andrew Wallis
- , Warren Ward
- , Sarah Wells
- , Eleanor Wertheim
- , Simon Wilksch
- & Michelle Williams
Contributions
AL carried out and wrote the initial review from the first search; JMW conducted subsequent reviews, analysed results, wrote the first manuscript and the final edit; EB, SHO and SV contributed to specific sections, detailed tables and figures, responded to review comments and contributed to ongoing drafts to manuscript completion; the National Eating Disorder Research Consortium reviewed and provided expert feedback; ST and SM provided project direction, methodological design, comprehensively reviewed the manuscript and provided overall supervision and leadership. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jane Miskovic-Wheatley .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
ST receives royalties from Hogrefe and Huber, McGraw Hill and Taylor and Francis for published books/book chapters. He has received honoraria from the Takeda Group of Companies for consultative work, public speaking engagements and commissioned reports. He has chaired their Clinical Advisory Committee for Binge Eating Disorder. He is the Editor in Chief of the Journal of Eating Disorders. He is a committee member of the National Eating Disorders Collaboration as well as the Technical Advisory Group for Eating Disorders. AL undertook work on this RR while employed by HMA. JMW and SM are guest editors of the special issue “Improving the future by understanding the present: evidence reviews for the field of eating disorders.”
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: fig. s1..
PRISMA flow diagram.
Additional file 2: Table S1.
Studies included in the Rapid Review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Miskovic-Wheatley, J., Bryant, E., Ong, S.H. et al. Eating disorder outcomes: findings from a rapid review of over a decade of research. J Eat Disord 11 , 85 (2023). https://doi.org/10.1186/s40337-023-00801-3
Download citation
Received : 28 February 2023
Accepted : 05 May 2023
Published : 30 May 2023
DOI : https://doi.org/10.1186/s40337-023-00801-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Transdiagnostic
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]
- Methodology
- Open access
- Published: 20 September 2023
Co-producing principles to guide health research: an illustrative case study from an eating disorder research clinic
- Cat Papastavrou Brooks ORCID: orcid.org/0000-0002-3055-5301 1 , 2 ,
- Eshika Kafle 2 ,
- Natali Butt 2 ,
- Dave Chawner 2 , 3 ,
- Anna Day 2 ,
- Chloë Elsby-Pearson ORCID: orcid.org/0000-0002-2235-2379 2 ,
- Emily Elson 2 ,
- John Hammond 2 ,
- Penny Herbert 2 ,
- Catherine L. Jenkins 2 ,
- Zach Johnson 2 ,
- Sarah Helen Keith-Roach 2 ,
- Eirini Papasileka 2 , 4 ,
- Stella Reeves 2 , 5 ,
- Natasha Stewart 2 ,
- Nicola Gilbert 2 , 6 &
- Helen Startup 2
Research Involvement and Engagement volume 9 , Article number: 84 ( 2023 ) Cite this article
1710 Accesses
2 Citations
10 Altmetric
Metrics details
There is significant value in co-produced health research, however power-imbalances within research teams can pose a barrier to people with lived experience of an illness determining the direction of research in that area. This is especially true in eating disorder research, where the inclusion of co-production approaches lags other research areas. Appealing to principles or values can serve to ground collaborative working. Despite this, there has not been any prior attempt to co-produce principles to guide the work of a research group and serve as a basis for developing future projects.
The aim of this piece of work was to co-produce a set of principles to guide the conduct of research within our lived experience led research clinic, and to offer an illustrative case for the value of this as a novel co-production methodology. A lived experience panel were recruited to our eating disorder research group. Through an iterative series of workshops with the members of our research clinic (composed of a lived experience panel, clinicians, and researchers) we developed a set of principles which we agreed were important in ensuring both the direction of our research, and the way in which we wanted to work together.
Six key principles were developed using this process. They were that research should aim to be: 1) real world—offering a clear and concrete benefit to people with eating disorders, 2) tailored—suitable for marginalised groups and people with atypical diagnoses, 3) hopeful—ensuring that hope for recovery was centred in treatment, 4) experiential—privileging the ‘voice’ of people with eating disorders, 5) broad—encompassing non-standard therapeutic treatments and 6) democratic—co-produced by people with lived experience of eating disorders.
Conclusions
We reflect on some of the positives as well as limitations of the process, highlighting the importance of adequate funding for longer-term co-production approaches to be taken, and issues around ensuring representation of minority groups. We hope that other health research groups will see the value in co-producing principles to guide research in their own fields, and will adapt, develop, and refine this novel methodology.
Plain English summary
It important that when researchers are trying to understand illnesses they do this together with people who have experienced them. This can be difficult, because researchers often take over—even if everyone is meant to be working as a team. We are a group of people trying to understand eating disorders and help people who have them get better. In our group there are some people that have experienced an eating disorder, health workers and researchers.
We thought it might be helpful if we could start by working out what things were most important to us as a group, and then try to stick by them. We talked a lot together to come up with a list of principles.
The six principles we thought were the most important were that research should make a difference to people’s lives, see people as individuals, be hopeful, make sure that people have a voice, look at things that aren’t traditional therapies, and always work together as equals.
There are some issues with what we did; we found it hard to get a good mix of people in our group, and we were lucky in having enough money to pay people to do what we wanted to do, which is not always true. Despite this, we still hope that other teams might look at what we have done, and see if they could build on it, or change it, so it would work for them.
Peer Review reports
Co-production approaches
Co-production has been defined as the delivery of “public services in an equal and reciprocal relationship between professionals, people using services, their families and their neighbours” [ 21 ], placing a strong emphasis on the importance of citizens’ power and worth [ 26 ]. The initial emergence of co-production within health services stemmed from a critique of the limited power patients had to shape the service they received, and the failure of services to acknowledge and respond to patients’ often negative experiences [ 32 ]. Despite the argued importance of co-production in terms of its substantive, instrumental, normative and political value [ 94 ] there have been significant criticisms of what is typically described as ‘co-production’ in health services. This includes the claim that co-production rarely involves a transfer of power to patients [ 136 ], instead involving a co-option of people’s lived experience to be used for agendas which are foreign to them and their interests [ 102 ]. Genuine co-production is often impossible due to the reality of the power imbalances present in the psychiatric system [ 97 ], and—by masking and de-politicising these imbalances—it can serve to exacerbate them [ 124 ].
Within health research, co-production approaches come with their own associated set of difficulties [ 79 ]. Relationships within research often mirror those between patient and clinician and there can be a division between researchers who are seen as active, knowing and rational in contrast to the passive, known and irrational objects of health research—patients [ 66 ]. Although evidence-based practice is often reified as a values-neutral methodology [ 14 ], it involves the privileging a specific scientific or rationalistic voice, excluding ways of knowing which do not conform to this and often constituting a form of injustice against epistemically marginalized groups [ 30 , 37 ]. This critique is foundational to the emerging field of mad studies, which seeks not to just include mad people within mental health research by forcing them to assimilate within traditional methodological frameworks but demands instead substantial changes to the way we conceive of and conduct research [ 44 , 63 ]. Thus the aims of mad studies include both “showing that there is method in our madness; and on the other side, preserving madness in our method” [ 63 ].
In addition to these theoretical issues, co-producing research with patients can often have significant psychological and emotional costs for them, partially as a result of increased interpersonal conflict which often occurs [ 94 ]. Collaborating with patients on mental health research has been conceptualised as occurring on one of three distinct levels: consultation, collaboration, and user-controlled,Rose and Kalathil [ 105 ] argue that consultation is superficial and lacks value, and that collaboration only requires power imbalances to be hidden as opposed to abolished, meaning it inevitably collapses into consultation. On this model, methodologies like participatory action research—which centre around collaboration between researchers and participants [ 54 ] though do not challenge either the conceptual distinction or the power-relations between them typically fall under the category of collaboration. Only user-controlled research can preserve patients’ autonomy and ability to affect the research process without the risk of co-option [ 105 ].
Co-producing eating disorder research
Eating disorders (EDs) are a classification of disorders which involve feeding and eating disturbances which cause significant clinical distress [ 76 ]. An estimated 725,000 people in the UK are affected by EDs, at an estimated cost of 3.9–4.6 billion pounds annually to the NHS [ 15 ]. Anorexia Nervosa (AN) and Bulimia Nervosa (BN) are two eating disorders with high mortality rates, compared to the general population [ 11 , 128 ] with AN leading to the highest mortality rates compared to all other psychiatric illnesses [ 11 ].
Despite this, the strength of evidence for eating disorder treatments is modest [ 23 , 58 ] with no gold standard psychological interventions available for adult presentations of AN [ 83 ] or BN [ 96 ]. Systematic reviews of randomised control trials (RCTs) in eating disorders have found the evidence for psychological therapies for eating disorders inconclusive [ 24 , 58 ]. Therapies for eating disorders have a minimal evidence base, consisting of a very small number of studies [ 113 ], with and high impact factor journals publish significantly fewer papers on eating disorders than other psychiatric conditions [ 113 ]. This may be due, in part, to a deficit in funding for eating disorder research in comparison to the burden of illness [ 38 , 83 ], mirroring a lack of funding for clinical services [ 6 ].
However, another reason for the lack of effective evidence-based treatments for people with eating disorders could be comparative failings of integrating lived-experience perspectives into research in this area. Aspects of co-production have been incorporated into case-studies [ 4 , 5 , 19 ], the development of novel pathways such as FREED [ 7 ], within service delivery [ 75 ] and in research priority setting [ 9 , 92 ]. Feminist approaches within an eating disorder context have also been significant in challenging the politics and validity of diagnoses and power-imbalances within treatment, through drawing on women’s embodied and socially situated lived experience of having an eating disorder [ 72 ]. However, co-production within eating disorder research is not as established as service-user /survivor led research in other areas [ 44 , 104 ], where research teams and projects are either headed by or predominantly composed of lived-experience researchers.
Principles for co-production
A barrier to co-production in health research more generally, and eating disorder research specifically, might be that people with lived experience of an illness are often brought in to work on a specific research project, the parameters, aims and methodology of which have been set prior to their involvement. This contrasts with longer term work conducted by research teams including people with lived experience as key members—who might have the capacity to work together over a longer time-period to decide the direction they want their research to go in, and co-produce projects from the ground-up. Developing projects according to research principles has been found to be helpful in enabling this kind of longer-term collaboration, particularly around ideas of sharing power and building trust [ 31 ]. Many historically significant groups of mental patients advocating for their rights and to change mental health services have manifestos structured around shared values they collectively organize on the basis of CAPO [ 28 ], Mental Patients Union [ 81 ], MPU [ 82 ]. Within mental health services, there has been work carried on co-producing principles to guide the development and evaluation of peer worker roles [ 50 ], for best practice in school mental health [ 133 ] and within health research to develop principles for community-based research [ 107 ]. However, to our knowledge, there has not been an attempt to develop principles to form the basis for co-producing research between people with lived experience of a particular mental health issue and researchers, who though they might happen to have lived experience of what they are researching, are not employed in that capacity. Principles may help to guide the research process, facilitate collaborative working, and form the shared basis from which to derive research priorities. We believe that doing so could be an important way of preventing the collapse of collaboration into consultation [ 105 ].
The SPIRED research clinic
SPIRED (Sussex Partnership Innovation and Research in Eating Disorders) research clinic was founded in January 2021 and is composed of people with lived experience of eating disorders, researchers and clinicians working in the Sussex Eating Disorders Services within Sussex Partnership NHS Foundation Trust (SPFT). These identities are not mutually exclusive; many SPIRED clinic members will fall under two or more of these categories, and we aspire to be a team where clinicians and researchers are able to share their own experiences of mental health issues, regardless of their formal role [ 70 ].
To ensure those with lived experience had oversight in the research activities of the clinic, a lived experience panel was recruited in collaboration with SPFT’s Patient and Public Involvement (PPI) team [ 115 ]. The PPI team oversees the development of lived experience advisory panels (LEAPs) to ensure that those with lived experience can provide insight into the research conducted within SPFT. An advert was circulated on social media, within SPFT and with partner organisations to recruit individuals with diverse experiences of eating disorders and eating disorder treatment and was also circulated to patients within the trust eating disorder service who were at point of discharge. Sixteen individuals were recruited to the lived experience panel, and consequently SPIRED. The criteria for recruitment were that they had to identify as having experienced an eating disorder, regardless of whether that had been formally diagnosed. They were not required to reveal any information about their eating disorder. Since the eating disorder service SPIRED is connected to is for adults, all SPIRED lived experience panel members are over eighteen. Although these individuals were specifically recruited for a lived experience role, some of them also had clinical experience within the NHS, as well as research expertise. A co-production approach is followed in research conducted by SPIRED [ 32 ], echoing the rhetoric 'no decision about me without me' [ 41 ]. Within SPIRED, those with lived experience of EDs contribute to developing ideas, overseeing projects and conducting research.
To co-produce a set of principles to guide research, within an eating disorder research clinic composed of people with lived experience of an eating disorder, clinicians, and other researchers.
To provide an illustrative case for our approach as a novel co-production methodology, by demonstrating how co-producing developing principles can lead to a clear and defined research agenda.
Development of principles
Prior to the first SPIRED team meeting, the lived experience panel and SPIRED team members were invited to complete a questionnaire. The questionnaire was developed by the SPIRED clinic research assistant, a Service User and Carer Involvement Coordinator from the SPFT PPI team, and a member of the lived experience panel.
The questionnaire consisted of four open ended questions, and asked members to share whatever they felt comfortable sharing: their experience of eating disorders and eating disorder services, their view of what lived experience involvement in research meant, what they wanted to contribute to SPIRED aside from their lived experience of an eating disorder, and what they felt should be the key priorities for eating disorder research.
Responses were loosely summarised by theme and presented at the first SPIRED clinic meeting (facilitated over an online platform), where seventeen members were present, including eleven members of the lived experience panel. Small group discussions were held in break-out rooms to develop key principles, followed by feedback and a discussion with the whole group. Extensive notes were taken of all these discussions.
These notes formed the starting point of a smaller working group, with three lived experience panel members and two other SPIRED clinic members. A consensus-based decision making methodology [ 56 ] was used to derive core principles from the discussions of the wider SPIRED group. All the key principles derived from the initial meeting were discussed individually, with each working group member holding veto-power for any decision around a particular principle (whether that was to include or to exclude it). This then halted the decision, and the principle was then re-discussed and modified until consensus could be reached [ 56 ]. Following agreement about which principles to include, this consensus-based process was used for decision-making around which of the principles could be synthesized.
A group facilitator chaired the meeting and made notes on ongoing discussions to enable further reflection. The lead author then wrote up the main sections of this paper, which were then circulated to all SPIRED clinic members for comments and feedback, following which extensive changes were made to this paper.
Reflexivity
Everyone who has contributed to this paper at any stage has been invited to co-author (including the lived experience panel). Although we felt it was vital to highlight the extent of the contribution of the lived experience panel in the co-production of these principles, we did not want to force any individual to identify themselves as someone with lived experience of an eating disorder. Therefore, all authors are listed solely as SPIRED clinic members.
The SPIRED clinic consists of individuals with a range of experiences of different eating disorders, eating disorder services, clinicians, and researchers. We aimed to ensure representation from neurodivergent people, LGBTIA people, men, and people of colour (POC), all of which are often marginalised within eating disorder treatment. However, we recognise that POC are particularly underrepresented on our lived experience panel, which may have impacted on the principles that our research team chose to prioritise.
The SPFT Research Governance department confirmed that ethical approval was not necessary for this project, as there were no participants.
Because of the increased sensitivity of sharing personal information about mental health, co-authors who were lived experience panel members also signed a consent form to be anonymously quoted in this paper.
As a result of the process outlined above, the following six principles were determined to be fundamental in guiding our research. We believe in eating disorder research which is: real world, tailored, hopeful, experiential, broad and democratic (see Fig. 1 ).
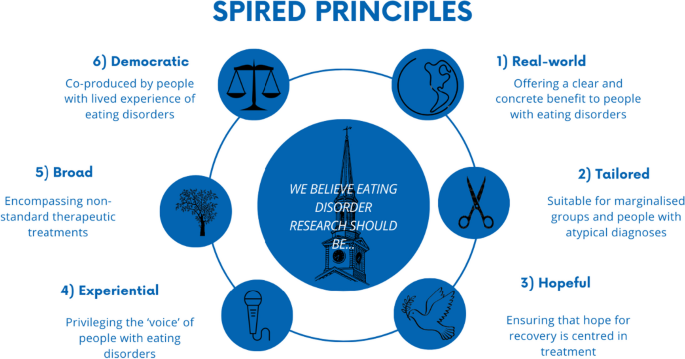
Overview of SPIRED principles
We have chosen in this section to integrate the ‘results’ of our decision-making with existing literature, as this best reflects both our aims in doing this work and the process through which the principles came about. Traditional qualitative research results focus solely on ‘participant data’, viewing people experiences, viewpoints, and theorizing as data-points to be analysed by a researcher, and then contextualized within the discussion section of a paper. However, our lived experience panel (along with other clinic members) are not participants, but researchers, and drew on both their own individual experiences but also their understanding and critical assessment of the research literature during this process. This demonstrates the capacity of lived-experience led research to create new forms of knowing outside traditional research binaries, such as those between researcher and researched [ 63 ]. Because our discussions as a group, both in the meetings, and over email, involved sharing and reflecting on research findings, this structure has been mirrored in our write-up. The point of this work was to create a set of principles that would be foundational for our work together and could be shared with others. Although this paper describes the process by which we developed these principles, we consider the below results section not the output of a novel co-production process, but also an argument for change [ 16 ].
Given the paucity of research on efficacy and acceptability of ED treatments, there is an urgent need for research which is ‘real world’ and makes an immediate, practical impact on the lives of people with eating disorders. Within SPIRED, this could include developing and evaluating novel interventions for eating disorders [ 93 ], evaluating, improving and developing ED service provision [ 109 ] or engaging with policymaking to ensure it is evidence-based.
Current research does not seem to consistently meet the needs of those with EDs. Although recent research has established connections between the presence of an ED and brain structure and functioning [ 42 , 117 ], translating findings on neurofeedback and biofeedback into effective treatment has proven difficult, with current therapeutic options proving too invasive and costly [ 126 ].
Due to the high mortality rate of EDs and current lack of evidence-based treatment, we call for urgent prioritisation of funding for well-targeted research that can be translated into concrete and immediate changes in service provision [ 55 ].
Where evidence-based treatments do exist, researchers have often been slow to adapt them effectively for marginalised groups [ 2 ]. We believe that eating disorder treatments and services should adopt an intersectional approach [ 25 ], recognising that people have differing identities, such as race, class, gender and sexuality, which interact and result in differing experiences of oppression [ 36 ]. Consequently, ED research should offer evidence-based ways of tailoring existing interventions to include minority groups and acknowledge the systemic factors which may create inequalities in accessing ED treatment [ 17 ].
Within ED research, particular groups have been excluded from treatment development, and treatment and service provision, so are often missing in the dialogue within eating disorder research. These include: people with other comorbid mental health issues [ 10 , 17 , 69 , 137 ], autistic spectrum conditions [ 3 , 22 , 40 , 62 , 118 , 121 ], people with binge-eating disorder, EDNOS/OSFED or ARFID [ 11 , 13 , 106 ], men [ 103 , 112 , 120 , 134 , 138 , 140 ], racially minoritized groups [ 1 , 20 , 52 , 53 , 77 , 114 , 119 , 139 ] and LGBTIA people [ 8 , 27 , 51 , 80 , 85 , 95 , 98 ].
Whilst acknowledging the issues within current ED research is important, it is vital to hold an optimistic and forward-thinking stance on treatment for EDs. Individuals with eating disorders often experience high levels of hopelessness [ 116 ], and as a result interventions which target “hope” and forward looking thinking have been found to be effective in facilitating recovery [ 64 , 116 ]. Empathy and the provision of hope have been repeatedly found to be the most important features in health professionals working with patients with eating disorders [ 43 , 46 , 65 , 135 ].
Evidence suggests that peer support can provide the support and connection necessary to increase people’s sense of hope for recovery, as a key mechanism of change [ 29 , 48 , 86 , 101 , 110 ].
Interventions which harness peer support have included online discussion forums [ 67 , 86 ], formal mentoring programmes [ 57 , 99 , 100 ] and clinicians use of their own personal recovery in the treatment of eating disorders [ 34 , 131 ].
Experiential
Eating disorder research often focuses on quantitative outcomes such as BMI to evaluate interventions [ 12 , 24 ]. However solely focusing on BMI as an indicator of recovery is not recommended by NICE guidelines [ 90 ]. This narrow focus on BMI can cause iatrogenic harm to patients [ 88 ], and marginalise patients with diagnoses aside from AN [ 130 ].
The importance placed on measuring people with eating disorders bodies, over listening to their experience, can be understood utilizing the philosophical concept of epistemic injustice; whereby patients’ knowledge about their own condition is disregarded, and they are reduced to passive ‘objects’ to be measured, instead of active and knowing subjects [ 37 ].
A significant part of recovery from eating disorders can involve developing a “recovery” voice separate from the illness [ 18 ], with effective therapeutic interventions utilising creative ways of developing this [ 59 , 60 ]. The current focus on BMI as an indicator of recovery does not take patients own knowledge and understanding of their illness into account and overlooks the subjective experiences of those with EDs receiving treatment.
We feel there is a need for an increase in qualitative research which explores the perspectives of ED sufferers and aims to understand their experiences. This may be key for developing more effective interventions in this area [ 35 ].
Although traditional therapies for EDs can form an important part of ED recovery, they do not address all the factors which have the capacity to have a positive impact of the lives of those with EDs. It is well established in the literature that carers play an important role in recovery [ 108 , 123 ], as well as peers [ 57 ]. Despite acknowledgment that carers might struggle in these roles [ 33 ], research exploring which factors impact carer wellbeing, and what support they might benefit from, is still a comparatively new field [ 122 ].
There is an emerging evidence base on the impact of holistic therapies on EDs, including art therapy [ 47 , 61 ], dance [ 71 ] and comedy [ 78 ]. This is consistent with an understanding that ED recovery involves rebuilding a life outside the ED [ 135 ] beyond simply managing the illness [ 39 , 74 , 111 ].
We believe that it is important to broaden out the research focus from the development and evaluation of therapies, to consider provision of support to all parts of the ‘system’ (family members, carers, peers, clinicians) as well as focusing on the development of novel and creative interventions.
Despite the importance of involving patients and carers in eating disorder research and service provision there is often limited ‘co-production in this area’ [ 87 ], with inclusion of lived-experience perspectives “scarce to date” [ 84 ].
It is our belief that many of the current issues we have highlighted in eating disorder research are the result of not including the perspectives and expertise of people who have experience of eating disorders. Co-production in eating disorder research is particularly important in determining how to define and evaluate recovery in eating disorders (moving away from narrow outcomes like BMI) [ 68 , 125 ] and towards a richer understanding of the recovery process [ 135 ].
We advocate an approach to research that involves service-users/survivors and clinicians working in partnership with other researchers, in all aspects of eating disorder research. This could include setting research priorities, designing research projects, conducting all aspects of research, and disseminating research and engaging the public.
We wanted to trial a ‘principles-first’ approach in developing research projects within our eating disorder research clinic (SPIRED), as we hoped that it would give us a direction and mandate for our work stemming from all members of the clinic. Through a series of workshops, we co-produced a set of principles to guide the direction and process of our work together, agreeing that the eating disorder research we conducted would be real world, tailored, hopeful, experiential, broad, and democratic.
In this section we first offer some reflections on the process from clinic members, highlighting strengths and weaknesses of the approach we took, before setting these in the context of the broader literature.
Reflections
Members of the SPIRED research clinic wrote reflections on their experience of co-producing principles to guide our research and collaborating on this paper. We present these in their individuality and diversity, instead of coming to a single reflexive position (as authors) on the strengths and limitations of the process we took.
There was consensus that any division between members of the lived experience panel and other researchers and clinicians was not only artificial (as members had a multiplicity of roles and identities in their lives), but also undermined the democratic way we aimed to work together. People are identified here by whether they are a professional member or a lived experience panel member within the SPIRED clinic, however we wanted to emphasize that they will have other identities and areas of expertise. We identified people in this way as we thought it was important to acknowledge the power imbalances that exist between lived experience panel members, and those employed by the trust in a more permanent capacity.
“[Contrasting lived experience perspectives with clinicians and researchers] creates an artificial binary where our ED defines us—instead of recognising multiple identities. I fit into each of these 'categories’, but the research process runs the risk of reinforcing power differentials and that we ARE the ED. An ED can silence our sense of self and other aspects of identity—the research process shouldn't replay this.” -Lived Experience Panel Member
"I was looking forward to contributing as someone with Lived Experience, because I work as a research student in my day job, so I wear two hats and have seen first-hand the value in incorporating Lived Experience perspectives.” -Lived Experience Panel Member
“As a clinician and researcher who has also had experiences of being on the other side of service provision, I was acutely aware of the ‘us and them’ divisions that play out in both clinical and research settings, and how these divisions can make it harder for people to open up and express fully their views about any care they might or might not have received. We are then missing important information around how to develop interventions and improve care delivery.” -Professional Member
One of the most significant things about the process for many SPIRED members was that the initial meeting was one of the first times they were able to be open about, integrate and use their multiple identities. This meeting was felt by many as cathartic, hopeful and powerful, as well as providing a solid foundation for collaboration.
“As a mental health professional, who was sharing my experiences of being a service user for the first time in front of other professionals, I felt scared and shy at first. Everyone was supportive and reassuring, and I never felt “less than” for sharing my lived experience.” -Lived Experience Panel Member
“I was keen that the LEAP was a place that welcomed all perspectives and we put a lot of thought into the initial meetings to create a psychologically safe arena for people to know they could be open and honest. An example of this was me sharing that I had not had good experiences of service use, to help others feel that all perspectives were welcome and to counter the us and them divide.” -Professional Member
“There was such a really open atmosphere in that first meeting—I shared things about my mental illness for the first time in a work context. I think this was such a respectful and trusting basis for the later consensus-based decision-making work we did together in developing the principles.” -Professional Member
Part of why the process of co-producing principles was felt to be successful, was because everyone shared similar motivations for wanting to be part of the SPIRED research clinic. These included a motivation to improve eating disorder treatment, alongside a commitment to genuine co-production, as opposed to lived experience involvement just having a ‘rubber-stamping’ function.
“Having been denied help because of a “normal BMI”, deteriorating and then being on a waiting list for months I felt the need to do something- just anything to take this disappointment and anger towards services and turn it into something a bit positive.” -Lived Experience Panel Member
“I think my main motivations for helping out are guilt, being bluntly honest. I had amazing treatment—the best. Not everyone is so lucky. So, I want to pay that forward and try in any meagre way to give back.” -Lived Experience Panel Member
“I really wanted to work at SPIRED because the people who set it up were so clear about how much they valued co-production as core to the way they worked.” -Professional Member
“I was happy that everyone seemed to be on the same page and have a shared passion for improving lives for people with eating disorders.” -Lived Experience Panel Member
All the co-authors of this paper except two, were present for the initial meeting and subsequent discussions. However even those who joined the process later, felt aligned with what had already been done.
“I have been struck by the paucity of research focused on ED interventions, particularly the lack of research which is co-produced with those with lived experience. Despite not being involved in the discussions in which SPIRED principles emerged, I believe the research priorities outlined by SPIRED are incredibly important and reflective of my own values.” -Professional Member
“As I was reading through, I couldn’t believe how aligned they were with my own personal views on co-production and the importance of lived experience perspectives in research […]. This is such a hopeful piece of work.” -Professional Member
Those responsible for facilitating the initial meeting, and supporting the lived experience panel going forward, were keen to reduce the burden on them from engaging in this work.
“I was also aware that speaking about your own difficult experiences can be exhausting, triggering and recovery is not neat; people can relapse and struggle. I didn’t want there to be only a couple of people who were relied on excessively for contributions, so there was an idea that people could dip in and out depending on capacity and interest.” -Professional Member
However, despite the shared wish to make lived experience work core to the SPIRED clinic, structural inequalities between the clinic members were a significant barrier to democratic working. Clinicians and researchers were employed on a substantive basis, whereas the lived experience panel were employed on a casualized basis, occasionally doing work—but with limited funding. This meant that often they were not able to lead on aspects of the research.
“Although I do have lived experience of mental illness (including disordered eating) I’m not one of the Lived Experience Panel members for SPIRED, and it should have been one or many of them that wrote up this paper—which they would have been much better placed to do than me. However sadly we didn’t have a permanently employed lived experience researcher, or enough in our PPI budget to pay for this work to be done on a casualised basis.” -Professional Member
Some people felt that this led to differences between how lived experience panel members and other SPIRED clinic members were treated, though others didn’t share this view.
“[There was a] 'distance' between the researchers and those assigned a 'lived experience' identity in having limited communications from the project.” -Lived Experience Panel Member
"Every communication I had from the PPI team felt like they were talking to an equal member of the team. Same for the paper- I didn’t feel like my thoughts and comments counted less because I was a LEAP member and not a researcher." -Lived Experience Panel Member
In general, people felt pride in what we’d achieved together and positive about the personal benefits of creating this paper.
“I remember feeling very proud of having contributed on that piece of collective work.” -Lived Experience Panel Member
“Lived Experience contributors don't often have a "career pathway" or professional development opportunities, so helping to shape an academic paper—and this was before I had published anything in my own field, as a student—was a really valuable experience.” -Lived Experience Panel Member
Our work in context
We set-up our lived experience led research clinic due to a belief that ED research was not currently adequately meeting the needs of the population it aimed to serve.
It is our view current issues in ED research are partially due to the distinct absence of the voices of those with lived experience of EDs and a lack of co-production in ED research.
We wanted to address the absence or superficiality of co-production in ED research by co-producing a set of principles which would be a mandate for our work together and ensure that it was grounded in what we cared about as a team. Although it initially seemed unlikely that a consensus-based decision-making methodology [ 56 ] would be successful, given the range of people with different backgrounds and experiences and priorities in our initial clinical meeting, this has not been our experience. Even the initial questionnaires that were completed by all clinic members — prior to meeting —s howed significant overlap in which principles people wanted to prioritize, and discussions further solidified these shared understandings and commitment. There was debate at all stages of the process of developing the principles, from initial workshops through to comments on drafts of the paper. These issues were resolved through discussion (during meetings as well as via email),this resolution tended to occur by describing the principles in a nuanced way that incorporated critical feedback from clinic members. All members enthusiastically agreed with the way the principles were framed in the final draft of this paper.
We were fortunate as a research clinic in having funding allocated to us for about 60 h of PPI time annually, as well as a dedicated PPI co-ordinator for our clinic, and a broader PPI team within our NHS trust who were able to advise on issues. This enabled us to take a longer-term strategy for PPI, as opposed to only having funding tied to specific research projects — where the aims and the method of the project had already been determined. Even though UK funders often include a requirement for PPI to have occurred at the project development stage [ 91 ], meaning that research institutions often have funding available for this specific purpose, it is rarer that PPI funding is allocated to a research team to spend in any way they think appropriate. However, this was essential to the kind of approach we were able to take. Additional funding would have allowed us time and research capacity to use a wider variety of methodological approaches to co-produce principles,we would love to see the work outlined in this paper built on and added to by other researchers trialling different and more systematic approaches for doing so. We believe that it is important to have more substantive lived-experience positions in research, something that we would like to see in our research clinic.
We recruited our PPI panel from social media, as well as patients who were at the point of discharge. As outlined above, POC are not adequately represented on our lived experience advisory panel, something that is a significant issue with many cases of co-production and PPI within research [ 49 ]. Developing ongoing collaborations with organisations focused on health research specific to POC, as well as putting systems in place to enhance recruitment of POC to senior positions within research teams [ 45 ] are both strategies that could improve these issues. However, neither of these constitutes a ‘quick fix’, and we were keen to work to address the underlying issue causing under-presentation of POC on our LEAP, as opposed to just advertising specifically for more POC which we felt was tokenistic.
We wanted to ensure that the research funding that we applied for corresponded to our research agenda — which was derived directly from our principles. However, in trying to develop competitive funding applications which fell under the ‘broad’ principle (i.e., developing and evaluating non-standard therapeutic treatments, including peer-support) it became clear that fewer health research funding sources would consider these kinds of treatments, as opposed to more traditional therapies. It appears that currently, ED research priorities can be guided by funders [ 38 ], rather than those with lived experience of EDs, who can provide valuable insight into where research efforts need to be urgently directed.
Priorities and principles and developed as a result of co-production approaches such as that one taken in this paper are often critical in approach and conflict with existing recommendations for eating disorder treatments [ 89 ], as approaches which seek to elevate the voices of service users have found in other areas [ 129 ]. However, we feel that this conflict has arisen because of the historic marginalization of lived experience voices within mental health research, and the lack of power people with lived experience still have in collaborating on research projects [ 73 ]. Given the evidence that research priorities determined by ED service-users produce better interventions and outcomes [ 132 ], and the ineffectiveness of current ED treatments [ 58 ], we believe it time for a new approach—led by those with lived-experience of eating disorders.
To our knowledge, we are the first health research group to have co-produced principles as the basis for our work together—putting us more in line with grassroots campaigning organisations [ 81 , 82 ]. However, these historic organizations rarely outline the process by which they produce their manifestos, which makes it hard to replicated and develop their methodology. There are several limitations to this piece of work, however we hope that other researchers will both build upon and refine the approach outlined in this paper and develop new methodologies for enhancing co-production within health research through the creation of principles to guide their collaborative work. More broadly, we wanted to provide an illustrative case for the value and generative potential of co-producing principles to guide health research and enable long-term collaboration between people with lived experience of an illness, and other researchers [ 127 ].
Following the development of SPIRED principles they were included in an All-Party parliamentary group report on eating disorders led by BEAT [ 16 ], as an example of how "a relatively small investment can make a big impact in building local research capacity and supporting the application of research findings into clinical practice."
Availability of data and materials
Not applicable.
Abbreviations
- Anorexia nervosa
- Bulimia nervosa
Eating disorder
Patient and public involvement (in research)
Sussex Partnership NHS Foundation Trust
Abood DA, Chandler SB. Race and the role of weight, weight change, and body dissatisfaction in eating disorders. Am J Health Behav. 1997;21(1):21–5.
Google Scholar
Acle A, Cook BJ, Siegfried N, Beasley T. Cultural considerations in the treatment of eating disorders among racial/ethnic minorities: a systematic review. J Cross Cult Psychol. 2021;52(5):468–88.
Article Google Scholar
Adamson J, Kinnaird E, Glennon D, Oakley M, Tchanturia K. Carers’ views on autism and eating disorders comorbidity: qualitative study. BJPsych Open. 2020. https://doi.org/10.1192/bjo.2020.36 .
Article PubMed PubMed Central Google Scholar
Adlam J. Shared work and existential engagement in the therapeutic milieu. (2016)
Adlam J. ‘Project Antigone’: a psychosocial exploration of the dynamics of food refusal and force feeding (2014). Doi: https://doi.org/10.13140/2.1.4963.2328
Allen KL, Mountford VA, Elwyn R, Flynn M, Fursland A, Obeid N, Partida G, Richards K, Schmidt U, Serpell L, Silverstein S, Wade T. A framework for conceptualising early intervention for eating disorders. Eur Eat Disord Rev. 2023;31(2):320–34. https://doi.org/10.1002/erv.2959 .
Article PubMed Google Scholar
Allen KL, Mountford V, Brown A, Richards K, Grant N, Austin A, Glennon D, Schmidt U. First episode rapid early intervention for eating disorders (FREED): from research to routine clinical practice. Early Interv Psychiatry. 2020;14(5):625–30. https://doi.org/10.1111/eip.12941 .
Amianto F. Homosexuality and anorexia nervosa: an explorative study on personality traits. Acta Psychopathol. 2016. https://doi.org/10.4172/2469-6676.100068 .
Aouad P, Hambleton A, Marks P, Maloney D, Calvert S, Caldwell B, McLean SA, Shelton B, Cowan K, Feneley J, Pepin G, Paxton S, Williams M, Meddick T, Squire S, Hickie I, Kay Lambkin F, Touyz S, Maguire S. Setting the top 10 eating disorder research and translation priorities for Australia. Aust N Z J Psychiatry. 2022. https://doi.org/10.1177/00048674221128754 .
Araujo DMR, da Santos GF, Nardi AE. Binge eating disorder and depression: a systematic review. World J Biol Psychiatry. 2010;11(2–2):199–207. https://doi.org/10.3109/15622970802563171 .
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–31. https://doi.org/10.1001/archgenpsychiatry.2011.74 .
Atwood ME, Friedman A. A systematic review of enhanced cognitive behavioral therapy (CBT-E) for eating disorders. Int J Eat Disord. 2020;53(3):311–30. https://doi.org/10.1002/eat.23206 .
Bailey AP, Parker AG, Colautti LA, Hart LM, Liu P, Hetrick SE. Mapping the evidence for the prevention and treatment of eating disorders in young people. J Eat Disord. 2014;2(1):5. https://doi.org/10.1186/2050-2974-2-5 .
Beale J. Scientism and scientific imperialism. Int J Philos Stud. 2019;27(1):73–102. https://doi.org/10.1080/09672559.2019.1565316 .
BEAT. Types of Eating Disorder—Beat (2020). https://www.beateatingdisorders.org.uk/types
BEAT. All-Party Parliamentary Group (APPG) on Eating Disorders (2021). Beat. https://www.beateatingdisorders.org.uk/about-beat/policy-work/all-party-parliamentary-group-appg-on-eating-disorders/
Becker AE, Eddy KT, Perloe A. Clarifying criteria for cognitive signs and symptoms for eating disorders in DSM-V. Int J Eat Disord. 2009;42(7):611–9. https://doi.org/10.1002/eat.20723 .
Bell NJ. Rhythm and semiotic structures of long-term ambivalence in the dialogical self: eating disorder and recovery voices. J Constr Psychol. 2013;26(4):280–92. https://doi.org/10.1080/10720537.2013.812857 .
Blackburn J, Minogue V. Developing an eating disorder pathway: a case study. J Ment Health Train Educ Pract. 2014;9(4):244–60. https://doi.org/10.1108/JMHTEP-06-2014-0016 .
Bodell LP, Wildes JE, Cheng Y, Goldschmidt AB, Keenan K, Hipwell AE, Stepp SD. Associations between race and eating disorder symptom trajectories in black and white girls. J Abnorm Child Psychol. 2018;46(3):625–38. https://doi.org/10.1007/s10802-017-0322-5 .
Boyle D, Harris M. The challenge of co-production. Lond New Econ Found. 2009;56:18.
Brede J, Babb C, Jones C, Elliott M, Zanker C, Tchanturia K, Serpell L, Fox J, Mandy W. “For me, the anorexia is Just a symptom, and the cause is the autism”: investigating restrictive eating disorders in autistic women. J Autism Dev Disord. 2020;50(12):4280–96. https://doi.org/10.1007/s10803-020-04479-3 .
Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):337–48. https://doi.org/10.1002/eat.20370 .
Bulik CM, Berkman ND, Brownley KA, Sedway JA, Lohr KN. Anorexia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):310–20. https://doi.org/10.1002/eat.20367 .
Burke NL, Schaefer LM, Hazzard VM, Rodgers RF. Where identities converge: the importance of intersectionality in eating disorders research. Int J Eat Disord. 2020;53(10):1605–9.
Cahn ES. No more throw-away people: the co-production imperative. Edgar Cahn (2000)
Calzo JP, Austin SB, Micali N. Sexual orientation disparities in eating disorder symptoms among adolescent boys and girls in the UK. Eur Child Adolesc Psychiatry. 2018;27(11):1483–90. https://doi.org/10.1007/s00787-018-1145-9 .
CAPO. Introduction, manifesto, demands (n.d.). https://tonybaldwinson.files.wordpress.com/2018/07/undated-campaign-against-psychiatric-oppression-capo.pdf
Cardi V, Ambwani S, Crosby R, Macdonald P, Todd G, Park J, Moss S, Schmidt U, Treasure J. Self-help and recovery guide for eating disorders (SHARED): study protocol for a randomized controlled trial. Trials. 2015;16(1):165. https://doi.org/10.1186/s13063-015-0701-6 .
Carel H, Kidd IJ. Epistemic injustice in medicine and healthcare. In: Kidd IJ, Medina J, Pohlhaus G Jr, editors. The Routledge handbook of epistemic injustice. Routledge; 2017. p. 336–46.
Christopher S, Saha R, Lachapelle P, Jennings D, Colclough Y, Cooper C, Cummins C, Eggers MJ, FourStar K, Harris K, Kuntz SW, LaFromboise V, LaVeaux D, McDonald T, Bird JR, Rink E, Webster L. Applying indigenous community-based participatory research principles to partnership development in health disparities research. Fam Commun Health. 2011;34(3):246–55. https://doi.org/10.1097/FCH.0b013e318219606f .
Clark M. Co-production in mental health care. Ment Health Rev J. 2015;20(4):213–9. https://doi.org/10.1108/MHRJ-10-2015-0030 .
Coomber K, King RM. Coping strategies and social support as predictors and mediators of eating disorder carer burden and psychological distress. Soc Psychiatry Psychiatr Epidemiol. 2012;47(5):789–96. https://doi.org/10.1007/s00127-011-0384-6 .
Costin C. Been there, done that: clinicians’ use of personal recovery in the treatment of eating disorders. Eat Disord. 2002;10(4):293–303.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: The new medical research council guidance. Int J Nurs Stud. 2013;50(5):587–92.
Crenshaw K. Demarginalizing the intersection of race and sex: a Black feminist critique of antidiscrimination doctrine, feminist theory, and antiracist politics [1989]. In: Bartlett K, editor. Feminist legal theory. Routledge; 2018. p. 57–80.
Crichton P, Carel H, Kidd IJ. Epistemic injustice in psychiatry. BJPsych Bull. 2017;41(2):65–70.
Davies H. Eating disorders bear the brunt of the paucity in mental health research funding. The Psych PhD Pathway. 2020. https://thepsychphdpathway.com/2020/09/15/eating-disorders-research-funding/ .
Dawson L, Rhodes P, Touyz S. “Doing the impossible”: the process of recovery from chronic anorexia nervosa. Qual Health Res. 2014;24(4):494–505. https://doi.org/10.1177/1049732314524029 .
Dell’Osso L, Carpita B, Gesi C, Cremone IM, Corsi M, Massimetti E, Muti D, Calderani E, Castellini G, Luciano M, Ricca V, Carmassi C, Maj M. Subthreshold autism spectrum disorder in patients with eating disorders. Compr Psychiatry. 2018;81:66–72. https://doi.org/10.1016/j.comppsych.2017.11.007 .
Department of Health. Liberating the NHS: No decision about me, without me. 2012.
Donnelly B, Touyz S, Hay P, Burton A, Russell J, Caterson I. Neuroimaging in bulimia nervosa and binge eating disorder: a systematic review. J Eat Disord. 2018;6(1):3. https://doi.org/10.1186/s40337-018-0187-1 .
Evans EJ, Hay PJ, Mond J, Paxton SJ, Quirk F, Rodgers B, Jhajj AK, Sawoniewska MA. Barriers to help-seeking in young women with eating disorders: a qualitative exploration in a longitudinal community survey. Eat Disord. 2011;19(3):270–85. https://doi.org/10.1080/10640266.2011.566152 .
Faulkner A. Survivor research and mad studies: the role and value of experiential knowledge in mental health research. Disabil Soc. 2017;32(4):500–20. https://doi.org/10.1080/09687599.2017.1302320 .
Faulkner A, Thompson R. Uncovering the emotional labour of involvement and co-production in mental health research. Disabil Soc. 2021. https://doi.org/10.1080/09687599.2021.1930519 .
Fogarty S, Ramjan LM. Factors impacting treatment and recovery in anorexia nervosa: qualitative findings from an online questionnaire. J Eat Disord. 2016;4(1):18. https://doi.org/10.1186/s40337-016-0107-1 .
Frisch MJ, Franko DL, Herzog DB. Arts-based therapies in the treatment of eating disorders. Eat Disord. 2006;14(2):131–42.
Gallagher MW, Long LJ, Richardson A, D’Souza J, Boswell JF, Farchione TJ, Barlow DH. Examining hope as a transdiagnostic mechanism of change across anxiety disorders and CBT treatment protocols. Behav Ther. 2020;51(1):190–202.
Gibbins KJ, Lo JO. What matters to whom: patient and public involvement in research. Clin Obstet Gynecol. 2022;65(2):268–76.
Gillard S, Foster R, Gibson S, Goldsmith L, Marks J, White S. Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Ment Health Soc Incl. 2017;21(3):133–43. https://doi.org/10.1108/MHSI-03-2017-0016 .
Goldhammer HB, Maston ED, Keuroghlian AS. Addressing eating disorders and body dissatisfaction in sexual and gender minority youth. Am J Prev Med. 2019;56(2):318–22. https://doi.org/10.1016/j.amepre.2018.09.011 .
Gordon KH, Brattole MM, Wingate LR, Joiner TE. The impact of client race on clinician detection of eating disorders. Behav Ther. 2006;37(4):319–25. https://doi.org/10.1016/j.beth.2005.12.002 .
Gordon KH, Perez M, Joiner TE. The impact of racial stereotypes on eating disorder recognition. Int J Eat Disord. 2002;32(2):219–24. https://doi.org/10.1002/eat.10070 .
Grattidge L, Purton T, Auckland S, Lees D, Mond J. Participatory action research in suicide prevention program evaluation: opportunities and challenges from the National Suicide Prevention Trial, Tasmania. Aust N Z J Public Health. 2021;45(4):311–4. https://doi.org/10.1111/1753-6405.13116 .
Great Britain & Parliamentary and Health Service Ombudsman. Ignoring the alarms: how NHS eating disorder services are failing patients. 2017.
Guinaudie C, Mireault C, Tan J, Pelling Y, Jalali S, Malla A, Iyer SN. Shared decision making in a youth mental health service design and research project: insights from the pan-canadian access open minds network. Patient Patient-Center Outcomes Res. 2020;13(6):653–66. https://doi.org/10.1007/s40271-020-00444-5 .
Hanly F, Torrens-Witherow B, Warren N, Castle D, Phillipou A, Beveridge J, Jenkins Z, Newton R, Brennan L. Peer mentoring for individuals with an eating disorder: a qualitative evaluation of a pilot program. J Eat Disord. 2020;8(1):29. https://doi.org/10.1186/s40337-020-00301-8 .
Hay P. A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. Int J Eat Disord. 2013;46(5):462–9. https://doi.org/10.1002/eat.22103 .
Hilliard RE. The use of cognitive-behavioral music therapy in the treatment of women with eating disorders. Music Ther Perspect. 2001;19(2):109–13. https://doi.org/10.1093/mtp/19.2.109 .
Hodge L, Simpson S. Speaking the unspeakable: artistic expression in eating disorder research and schema therapy. Arts Psychother. 2016;50:1–8. https://doi.org/10.1016/j.aip.2016.05.005 .
Holmqvist G, Persson CL. Is there evidence for the use of art therapy in treatment of psychosomatic disorders, eating disorders and crisis? A comparative study of two different systems for evaluation. Scand J Psychol. 2012;53(1):47–53.
Huke V, Turk J, Saeidi S, Kent A, Morgan JF. Autism spectrum disorders in eating disorder populations: a systematic review. Eur Eat Disord Rev. 2013;21(5):345–51. https://doi.org/10.1002/erv.2244 .
Ingram RA. Doing mad studies: making (non)sense together. Intersect Glob J Soc Work Anal Res Polity Pract. 2016;5(3):11–7.
Irving LM, Cannon R. Chapter 14 - starving for hope: goals, agency, and pathways in the development and treatment of eating disorders. In: Snyder CR, editor. Handbook of hope. Cambridge: Academic Press; 2000. p. 261–283. https://doi.org/10.1016/B978-012654050-5/50016-6 .
Chapter Google Scholar
Jewell T, Blessitt E, Stewart C, Simic M, Eisler I. Family therapy for child and adolescent eating disorders: a critical review. Fam Process. 2016;55(3):577–94. https://doi.org/10.1111/famp.12242 .
Karnieli-Miller O, Strier R, Pessach L. Power relations in qualitative research. Qual Health Res. 2009;19(2):279–89.
Kendal S, Kirk S, Elvey R, Catchpole R, Pryjmachuk S. How a moderated online discussion forum facilitates support for young people with eating disorders. Health Expect. 2017;20(1):98–111. https://doi.org/10.1111/hex.12439 .
Kenny TE, Lewis SP. reconceptualizing recovery: integrating lived experience perspectives into traditional eating disorder recovery frameworks. Psychiatr Serv. 2021. https://doi.org/10.1176/appi.ps.202000447 .
Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry. 2016;29(6):340–5. https://doi.org/10.1097/YCO.0000000000000278 .
King AJ, Brophy LM, Fortune TL, Byrne L. factors affecting mental health professionals’ sharing of their lived experience in the workplace: a scoping review. Psychiatr Serv. 2020;71(10):1047–64. https://doi.org/10.1176/appi.ps.201900606 .
Krantz AM. Growing into her body: dance/movement therapy for women with eating disorders. Am J Dance Ther. 1999;21(2):81–103.
LaMarre A, Levine MP, Holmes S, Malson H. An open invitation to productive conversations about feminism and the spectrum of eating disorders (part 1): basic principles of feminist approaches. J Eat Disord. 2022. https://doi.org/10.1186/s40337-022-00532-x .
Lambert N, Carr S. ‘Outside the original remit’: co-production in UK mental health research, lessons from the field. Int J Ment Health Nurs. 2018;27(4):1273–81.
Lamoureux M, Bottorff J. “Becoming the real me”: recovering from anorexia nervosa. Health Care Women Int. 2005;26(2):170–88. https://doi.org/10.1080/07399330590905602 .
Lewis HK, Foye U. From prevention to peer support: a systematic review exploring the involvement of lived-experience in eating disorder interventions. Ment Health Rev J. 2021.
Lindvall Dahlgren C, Wisting L, Rø Ø. Feeding and eating disorders in the DSM-5 era: a systematic review of prevalence rates in non-clinical male and female samples. J Eat Disord. 2017;5(1):56. https://doi.org/10.1186/s40337-017-0186-7 .
Lynch SL. Eating disorders in African American women: Incorporating race into considerations of etiology and treatment [Psy.D., Widener University, Institute for Graduate Clinical Psychology]. 2003. https://search.proquest.com/docview/305257106/abstract/3009282B20AE4BC6PQ/1 .
MacRury I. Humour as ‘social dreaming’: stand-up comedy as therapeutic performance. Psychoanal Cult Soc. 2012;17(2):185–203. https://doi.org/10.1057/pcs.2012.20 .
Madden M, Speed E. Beware zombies and unicorns: toward critical patient and public involvement in health research in a neoliberal context. Front Sociol. 2017. https://doi.org/10.3389/fsoc.2017.00007 .
McClain Z, Peebles R. Body image and eating disorders among lesbian, gay, bisexual, and transgender youth. Pediatr Clin. 2016;63(6):1079–90.
Mental Patients Union. Declaration of Intent. 1973. https://libcom.org/article/mental-patients-union-1973 .
MPU. The Need for a Mental Patients’ Union. Some Proposals. 1976.
Murray SB, Pila E, Griffiths S, Le Grange D. When illness severity and research dollars do not align: are we overlooking eating disorders? World Psychiatry. 2017;16(3):321. https://doi.org/10.1002/wps.20465 .
Musić S, Elwyn R, Fountas G, Gnatt I, Jenkins ZM, Malcolm A, Miles S, Neill E, Simpson T, Yolland CO, Phillipou A. Valuing the voice of lived experience of eating disorders in the research process: benefits and considerations. Aust N Z J Psychiatry. 2021. https://doi.org/10.1177/0004867421998794 .
Nagata JM, Ganson KT, Austin SB. Emerging trends in eating disorders among sexual and gender minorities. Curr Opin Psychiatry. 2020;33(6):562–7. https://doi.org/10.1097/YCO.0000000000000645 .
Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatr Sci. 2016;25(2):113–22. https://doi.org/10.1017/S2045796015001067 .
Article CAS PubMed PubMed Central Google Scholar
Newton T. Consumer involvement in the appraisal of treatments for people with eating disorders: a neglected area of research? Eur Eat Disord Rev. 2001;9(5):301–8. https://doi.org/10.1002/erv.435 .
NHS England. Adult eating disorders: community, inpatient and intensive day patient care: guidance for commissioners and providers, 28 (2019).
NICE. Eating disorders: Recognition and treatment (2017a).
NICE. Overview | Eating disorders: recognition and treatment | Guidance | NICE. (2017b). NICE. https://www.nice.org.uk/guidance/ng69 .
NIHR. A brief guide to public involvement in funding applications. 2020. https://www.nihr.ac.uk/documents/a-brief-guide-to-public-involvement-in-funding-applications/24162 .
Obeid N, McVey G, Seale E, Preskow W, Norris ML. Cocreating research priorities for anorexia nervosa: the Canadian eating disorder priority setting partnership. Int J Eat Disord. 2020;53(5):662–72. https://doi.org/10.1002/eat.23234 .
Oldershaw A, Lavender T, Basra R, Startup H. SPEAKS study: study protocol of a multisite feasibility trial of the Specialist Psychotherapy with Emotion for Anorexia in Kent and Sussex (SPEAKS) intervention for outpatients with anorexia nervosa or otherwise specified feeding and eating disorders, anorexia nervosa type. BMJ Open. 2022;12(2):e050350.
Oliver K, Kothari A, Mays N. The dark side of coproduction: do the costs outweigh the benefits for health research? Health Res Policy Syst. 2019;17(1):1–10.
Parker LL, Harriger JA. Eating disorders and disordered eating behaviors in the LGBT population: a review of the literature. J Eat Disord. 2020;8(1):51. https://doi.org/10.1186/s40337-020-00327-y .
Peat CM, Berkman ND, Lohr KN, Brownley KA, Bann CM, Cullen K, Quattlebaum MJ, Bulik CM. Comparative effectiveness of treatments for binge-eating disorder: systematic review and network meta-analysis. Eur Eat Disord Rev. 2017;25(5):317–28. https://doi.org/10.1002/erv.2517 .
Pilgrim D. Co-production and involuntary psychiatric settings. Ment Health Rev J. 2018;23(4):269–79. https://doi.org/10.1108/MHRJ-05-2018-0012 .
Protos K. Restricting the gendered body: understanding the trans-masculine adolescent with anorexia. Clin Soc Work J. 2020. https://doi.org/10.1007/s10615-020-00758-9 .
Purcell J, Lister S, McCormack J, Caswell J, Logie K, Wade S, Stringer M. Reaching out for hope—a peer support program. J Eat Disord. 2014;2(1):O63. https://doi.org/10.1186/2050-2974-2-S1-O63 .
Article PubMed Central Google Scholar
Ramjan LM, Fogarty S, Nicholls D, Hay P. Instilling hope for a brighter future: a mixed-method mentoring support programme for individuals with and recovered from anorexia nervosa. J Clin Nurs. 2018;27(5–6):e845–57. https://doi.org/10.1111/jocn.14200 .
Ranzenhofer LM, Wilhelmy M, Hochschild A, Sanzone K, Walsh BT, Attia E. Peer mentorship as an adjunct intervention for the treatment of eating disorders: a pilot randomized trial. Int J Eat Disord. 2020;53(5):767–79. https://doi.org/10.1002/eat.23258 .
recoveryinthebin, A. A simple guide to co-production. Recovery in the Bin. 2018. https://recoveryinthebin.org/2018/07/03/a-simple-guide-to-co-production/ .
Robinson KJ, Mountford VA, Sperlinger DJ. Being men with eating disorders: perspectives of male eating disorder service-users. J Health Psychol. 2013;18(2):176–86. https://doi.org/10.1177/1359105312440298 .
Rose D. Service user/survivor-led research in mental health: epistemological possibilities. Disabil Soc. 2017;32(6):773–89. https://doi.org/10.1080/09687599.2017.1320270 .
Rose D, Kalathil J. Power, privilege and knowledge: the untenable promise of co-production in mental “health.” Front Sociol. 2019;4:57.
Santomauro DF, Melen S, Mitchison D, Vos T, Whiteford H, Ferrari AJ. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. Lancet Psychiatry. 2021;8(4):320–8. https://doi.org/10.1016/S2215-0366(21)00040-7 .
Schulz AJ, Israel BA, Selig SM, Bayer IS. Development and implementation of principles for community-based research in public health. In:Research strategies for community practice. Routledge; 1998.
Sepulveda AR, Lopez C, Todd G, Whitaker W, Treasure J. An examination of the impact of “the Maudsley eating disorder collaborative care skills workshops” on the well being of carers: a pilot study. Soc Psychiatry Psychiatr Epidemiol. 2008;43(7):584–91. https://doi.org/10.1007/s00127-008-0336-y .
Shaw H, Robertson S, Ranceva N. What was the impact of a global pandemic (COVID-19) lockdown period on experiences within an eating disorder service? A service evaluation of the views of patients, parents/carers and staff. J Eat Disord. 2021;9(1):14. https://doi.org/10.1186/s40337-021-00368-x .
Smale K, Pitt J. Eating disorder mentor program. J Eat Disord. 2013;1(1):O11. https://doi.org/10.1186/2050-2974-1-S1-O11 .
Smethurst L, Kuss D. ‘Learning to live your life again’: an interpretative phenomenological analysis of weblogs documenting the inside experience of recovering from anorexia nervosa. J Health Psychol. 2018;23(10):1287–98. https://doi.org/10.1177/1359105316651710 .
Soban C. What about the boys?: addressing issues of masculinity within male anorexia nervosa in a feminist therapeutic environment. Int J Men’s Health. 2006;5(3):251–67.
Solmi F, Bould H, Lloyd EC, Lewis G. The shrouded visibility of eating disorders research. Lancet Psychiatry. 2021;8(2):91–2. https://doi.org/10.1016/S2215-0366(20)30423-5 .
Sonneville KR, Lipson SK. Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. Int J Eat Disord. 2018;51(6):518–26. https://doi.org/10.1002/eat.22846 .
Article CAS PubMed Google Scholar
SPFT. Get Involved in Research. Sussex Partnership NHS Foundation Trust. 2023c. https://www.sussexpartnership.nhs.uk/our-research/get-involved-our-research
Stavarski DH, Alexander RK, Ortiz SN, Wasser T. Exploring nurses’ and patients’ perceptions of hope and hope-engendering nurse interventions in an eating disorder facility: a descriptive cross-sectional study. J Psychiatr Ment Health Nurs. 2019;26(1–2):29–38. https://doi.org/10.1111/jpm.12507 .
Steward T, Menchon JM, Jiménez-Murcia S, Soriano-Mas C, Fernandez-Aranda F. Neural network alterations across eating disorders: a narrative review of fMRI studies. Curr Neuropharmacol. 2018;16(8):1150–63. https://doi.org/10.2174/1570159X15666171017111532 .
Stewart CS, McEwen FS, Konstantellou A, Eisler I, Simic M. Impact of ASD traits on treatment outcomes of eating disorders in girls. Eur Eat Disord Rev. 2017;25(2):123–8. https://doi.org/10.1002/erv.2497 .
Striegel-Moore RH, Wilfley DE, Pike KM, Dohm F-A, Fairburn CG. Recurrent binge eating in black American women. Arch Fam Med. 2000;9(1):83.
Thapliyal P, Mitchison D, Hay P. Insights into the experiences of treatment for an eating disorder in men: a qualitative study of autobiographies. Behav Sci. 2017. https://doi.org/10.3390/bs7020038 .
Treasure J. Coherence and other autistic spectrum traits and eating disorders: building from mechanism to treatment. The Birgit Olsson lecture. Nord J Psychiatry. 2013;67(1):38–42. https://doi.org/10.3109/08039488.2012.674554 .
Treasure J, Nazar BP. Interventions for the carers of patients with eating disorders. Curr Psychiatry Rep. 2016;18(2):16. https://doi.org/10.1007/s11920-015-0652-3 .
Treasure J, Todd G. Interpersonal maintaining factors in eating disorder: skill sharing interventions for carers. In: Latzer Y, Stein D, editors. Bio-psycho-social contributions to understanding eating disorders. Berlin: Springer International Publishing; 2016. p. 125–37. https://doi.org/10.1007/978-3-319-32742-6_9 .
Turnhout E, Metze T, Wyborn C, Klenk N, Louder E. The politics of co-production: participation, power, and transformation. Curr Opin Environ Sustainabil. 2020;42:15–21. https://doi.org/10.1016/j.cosust.2019.11.009 .
Turton P, Demetriou A, Boland W, Gillard S, Kavuma M, Mezey G, Mountford V, Turner K, White S, Zadeh E, Wright C. One size fits all: or horses for courses? recovery-based care in specialist mental health services. Soc Psychiatry Psychiatr Epidemiol. 2011;46(2):127–36. https://doi.org/10.1007/s00127-009-0174-6 .
Val Laillet D, Aarts E, Weber B, Ferrari M, QuaresimaStoeckel VLE, Alonso-Alonso M, Audette M, Malbert CH, Stice E. Neuroimaging and neuromodulation approaches to study eating behavior and prevent and treat eating disorders and obesity. NeuroImage Clin. 2015;8:1–31. https://doi.org/10.1016/j.nicl.2015.03.016 .
van Furth EF, van der Meer A, Cowan K. Top 10 research priorities for eating disorders. Lancet Psychiatry. 2016;3(8):706–7. https://doi.org/10.1016/S2215-0366(16)30147-X .
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33(6):521–7. https://doi.org/10.1097/YCO.0000000000000641 .
Verschuere B, Brandsen T, Pestoff V. Co-production: the state of the art in research and the future agenda. VOLUNTAS Int J Volunt Nonprofit Organ. 2012;23(4):1083–101. https://doi.org/10.1007/s11266-012-9307-8 .
Virgo H, NCMH, Stewart C. Dump The Scales Campaign. NCMH. 2019. https://www.ncmh.info/2019/02/25/dump-the-scales/ .
de Vos JA, Netten C, Noordenbos G. Recovered eating disorder therapists using their experiential knowledge in therapy: a qualitative examination of the therapists’ and the patients’ view. Eat Disord. 2016;24(3):207–23. https://doi.org/10.1080/10640266.2015.1090869 .
Wade TD, Hart LM, Mitchison D, Hay P. Driving better intervention outcomes in eating disorders: a systematic synthesis of research priority setting and the involvement of consumer input. Eur Eat Disord Rev. 2021;29(3):346–54.
Weist MD, Sander MA, Walrath C, Link B, Nabors L, Adelsheim S, Moore E, Jennings J, Carrillo K. Developing principles for best practice in expanded school mental health. J Youth Adolesc. 2005;34(1):7–13. https://doi.org/10.1007/s10964-005-1331-1 .
Weltzin TE, Weisensel N, Franczyk D, Burnett K, Klitz C, Bean P. Eating disorders in men: update. J Men’s Health Gend. 2005;2(2):186–93. https://doi.org/10.1016/j.jmhg.2005.04.008 .
Wetzler S, Hackmann C, Peryer G, Clayman K, Friedman D, Saffran K, Silver J, Swarbrick M, Magill E, van Furth EF, Pike KM. A framework to conceptualize personal recovery from eating disorders: a systematic review and qualitative meta-synthesis of perspectives from individuals with lived experience. Int J Eat Disord. 2020;53(8):1188–203. https://doi.org/10.1002/eat.23260 .
Williams O, Robert G, Martin G, Hanna E, O’Hara J. Is Co-production just really good PPI? Making sense of patient and public involvement and co-production networks. Decent Health Care Netw Reshap Org Deliv Healthc. 2020;2:13–237. https://doi.org/10.1007/978-3-030-40889-3_10 .
Woodside BD, Staab R. Management of psychiatric comorbidity in anorexia nervosa and bulimia nervosa. CNS Drugs. 2006;20(8):655–63. https://doi.org/10.2165/00023210-200620080-00004 .
Wooldridge T, Lytle PP. An overview of anorexia nervosa in males. Eat Disord. 2012;20(5):368–78. https://doi.org/10.1080/10640266.2012.715515 .
Yanovski SZ. Eating disorders, race, and mythology. Arch Fam Med. 2000;9(1):88. https://doi.org/10.1001/archfami.9.1.88 .
Zhang C. What can we learn from the history of male anorexia nervosa? J Eat Disord. 2014;2(1):138. https://doi.org/10.1186/s40337-014-0036-9 .
Download references
Acknowledgements
Verity Millar-Sarahs edited a final draft of this paper, improving the clarity and quality of expression significantly. We are also grateful to the four anonymous reviewers for their thoughtful, comprehensive, and generous comments on this paper which have strengthened and shaped it substantially.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Population Health Sciences, Bristol Medical School, University of Bristol, Canynge Hall, 39 Whatley Road, Bristol, BS8 2PS, UK
Cat Papastavrou Brooks
SPIRED Clinic, Research and Development Department, Sussex Partnership NHS Foundation Trust, Sussex Education Centre, Nevill Avenue, Hove, BN3 7HZ, UK
Cat Papastavrou Brooks, Eshika Kafle, Natali Butt, Dave Chawner, Anna Day, Chloë Elsby-Pearson, Emily Elson, John Hammond, Penny Herbert, Catherine L. Jenkins, Zach Johnson, Sarah Helen Keith-Roach, Eirini Papasileka, Stella Reeves, Natasha Stewart, Nicola Gilbert & Helen Startup
Comedy for Coping, Aesthetics Research Centre, University of Kent, Room 2.16, Jarman Building, Canterbury, Kent, CT2 7UG, UK
Dave Chawner
Department of Psychology, City, University of London, Northampton Square, London, EC1V 0HB, UK
Eirini Papasileka
School of Human and Behavioural Sciences, Bangor University, Bangor, LL57 2DG, UK
Stella Reeves
Maudsley Learning, ORTUS Conferencing and Events Venue, 82-96 Grove Lane, London, SE5 8SN, UK
Nicola Gilbert
You can also search for this author in PubMed Google Scholar
Contributions
CPB led on writing up this paper, with significant contributions to write-up by EK. CPB, NG, HS and JH designed the methodology of the paper. All authors significantly contributed to the development of the ideas in this paper (as outlined in the ‘process’ section), gave substantive comments on drafts of this paper, and agreed a final draft of this paper.
Corresponding author
Correspondence to Cat Papastavrou Brooks .
Ethics declarations
Ethical approval and consent to participate.
The SPFT Research Governance department confirmed that ethical approval was not necessary for this project, as there were no participants. Because of the increased sensitivity of sharing personal information about mental health, co-authors who were lived experience panel members also signed a consent form to be anonymously quoted in this paper.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Papastavrou Brooks, C., Kafle, E., Butt, N. et al. Co-producing principles to guide health research: an illustrative case study from an eating disorder research clinic. Res Involv Engagem 9 , 84 (2023). https://doi.org/10.1186/s40900-023-00460-3
Download citation
Received : 21 February 2023
Accepted : 26 June 2023
Published : 20 September 2023
DOI : https://doi.org/10.1186/s40900-023-00460-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Co-production
- Lived experience
- Eating disorders
- Research priority setting
- Service-user led research
Research Involvement and Engagement
ISSN: 2056-7529
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychol Med
- v.41(4); Jul-Aug 2019
Eating Disorders: An Overview of Indian Research
Sivapriya vaidyanathan.
Department of Psychiatry, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Pooja Patnaik Kuppili
1 Department of Psychiatry, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
Vikas Menon
There has been sporadic research on eating disorders in India, with no published attempt to collate and summarize the literature landscape. Hence, the present narrative review aims to summarize Indian work related to eating disorders, discern current trends, and highlight gaps in research that will provide directions for future work in the area. Electronic search using the MEDLINE, Google Scholar, and PsycINFO databases was done to identify relevant peer-reviewed English language articles, in October 2018, using combinations of the following medical subject headings or free text terms: “eating disorders,” “anorexia nervosa,” “bulimia,” “treatment,” “epidemiology,” “co-morbidity,” “management,” “medications,” “behavioral intervention,” and “psychosocial intervention.” The data extracted from studies included details such as author names, year, from which of the states in India the work originated, type of intervention (for interventional studies), comparator (if any), and major outcomes. There is increasing research focused on eating disorders from India over the last decade, but it continues to be an under-researched area as evidenced by the relative paucity of original research. The cultural differences between east and west have contributed to variations in the presentation as well as challenges in the diagnosis. Hence, there is a need for the development of culturally sensitive instruments for diagnosis, as well as generating locally relevant epidemiological data about eating disorders from community and hospital settings.
The earliest description of an eating disorder (ED)-like syndrome appears in a treatise by Morton (1694), under the section “Nervous Consumption,” where the author talks about two adolescents who presented with loss of appetite, extreme fasting, weight loss, and their treatment and outcome.[ 1 ] Historical reports point to the existence of ED even in the 17 th century, referred to as “holy anorexia.” However, one of the first scientific reports of this condition, in the late 19 th century, was by William Gull who is credited with coining the term anorexia nervosa (AN).[ 2 ] In India, the occurrence of ED was not reported until the late 20 th century.[ 3 ] Perhaps, media-related glorification of “size zero” body type and culturally sanctioned drive for thinness, body shaming, and dissatisfaction have contributed to the recent upsurge of ED cases.[ 4 , 5 , 6 ] Traditionally, these parameters have been less of a concern in India than other countries.[ 4 ] Yet, another reason for the recent increase in the incidence of ED such as bulimia nervosa (BN) and binge eating disorder (BED) is more easy access to media outlets promoting unhealthy body types and higher socioeconomic status of people.[ 7 , 8 ]
Notwithstanding its increasing prevalence rates, ED continues to be an area that is under-reported and under-researched. There are several reasons why ED must be given increasing focus in health care research and policy planning in today's scenario. AN, a prototype ED, has the highest mortality rate among mental health disorders.[ 9 , 10 ] The economic and social impact of ED was estimated to be upwards of $15 billion (INR 1057.8 billion) in 2012, which is comparable to the productivity impact of anxiety and depression, estimated at $17.9 billion (INR 1262.3 billion) in 2010.[ 9 ] Though, relatively rare in the general population, the individual impact of ED can be quite debilitating and long-term treatments are often expensive. ED have high rates of psychiatric and medical co-morbidity.[ 9 , 10 , 11 , 12 ]
Though there has been sporadic research on ED in India, there has been no attempt to collate and summarize the literature landscape. We undertook the present narrative review with the objectives of summarizing Indian work related to ED, discern current trends, and highlight gaps in research that will provide directions for future work in the area. These would potentially answer key questions on the clinical presentation and trajectories of ED in our setting.
METHODOLOGY
Search strategy and study selection.
Electronic search using the MEDLINE, Google Scholar, and PsycINFO to identify relevant peer-reviewed English language articles was carried out to include articles between April 1967 to October 2018. We used random combinations of the following medical subject headings or free text terms: “eating disorders,” “anorexia nervosa,” “bulimia,” “treatment,” “epidemiology,” “co-morbidity,” “management,” “medications,” “behavioral intervention,” and “psychosocial intervention.”
This being a narrative review and because research on ED in India is relatively sparse, we included all types of research reports, including case reports, to gain a true picture of the research landscape. The initial search yielded 84 articles. From the initial search, 39 articles were relevant and therefore selected for inclusion in the review. The full text of these articles was retrieved electronically. Additionally, the reference section of all articles was manually screened to identify potentially relevant articles. We only selected articles describing research from India. There was no restriction on the date of publication. Citation indexing services and gray literature such as conference proceedings were not included in the present review.
Data extraction
The data extracted from studies included details such as author names, year, from which of the states in India the work originated, type of intervention (for interventional studies), comparator (if any), and major outcomes.
A major part of the literature on ED from India is derived from case reports and case series ( n = 24). In comparison, there are 15 original studies summarized in Table 1 .
Summary of original studies on eating disorders in India
AN – Anorexia nervosa; BDI – Beck’s Depression Inventory; BED – Binge eating disorder; BITE – Bulimia investigatory test; BSQ – Body shape questionnaire; BN – Bulimia nervosa; DSM-IV – Diagnostic and Statistical Manual of Mental Disorders Version IV; DSM-III – Diagnostic and Statistical Manual of Mental Disorders Version III; EAT – Eating attitudes test; EDS – Eating distress syndrome; ICD-10 – International Classification of Diseases; QOL EDs – Quality-of-life for eating disorders questionnaire; SCOFF – Sick, Control, One-stone (14 lbs/6.5 kg), Fat, Food; SRQ – Self-report questionnaire; SQ-EDS – Screening questionnaire for eating distress syndrome
The earliest reports of ED date back to 1966. The case was of AN in a 42-year-old female with episodes of compulsive fasting for 2 years. The patient was treated with 100 mg chlorpromazine, 100 ml of 25% glucose with vitamin C 500 mg intravenously, 10 injections of liver extract 2 ml intramuscularly biweekly, and 9 sessions of electroconvulsive treatment. After 46 days of intensive pharmacotherapy and supportive psychotherapy, she showed improvement and was kept in close follow up.[ 3 ] Following this, there has been increasing reports of ED cases in the last two decades. Majority of the cases were of AN, especially restrictive subtype. The typical profile of cases described from India is of adolescent females,[ 26 , 27 , 28 , 29 , 30 , 31 ] belonging to Hindu religion,[ 29 , 31 , 32 ] and coming from an upper- or middle-socioeconomic background[ 26 , 27 , 28 , 29 , 31 , 33 ] In contrast, there are only four cases of male AN reported.[ 27 , 34 ] There is a single case report of AN described in a pair of monozygotic twins too.[ 35 ]
Cases of AN have been described in Indian adolescents belonging to Sikh religions, living in the United Kingdom.[ 34 ] The symptoms of AN were found to flare up after being teased by peers about weight which was followed by concerns about weight gain, in the majority of cases.[ 27 , 29 ] There is also a case of AN which had atypical features such as denial of fears of weight gain.[ 36 ] One report of disordered eating described a young female, in whom “not eating” was conceptualized as a resistance to the patriarchal system and this highlights the role of Indian sociocultural factors for developing an ED.[ 37 ]
Bradycardia, hypotension, anemia, and dyselectrolytemia have been reported at the time of presentation to a psychiatrist.[ 27 , 28 , 38 ] Wernicke–Korsakoff syndrome was the presenting symptom for a 39-year-old female who had AN from adolescence.[ 39 ] Surreptitious use of metformin, with episodes of hypoglycemia, was the presenting symptom in another case of AN in a 21-year-old female.[ 33 ] Though the nature of psychiatric co-morbidity has not been described, psychiatric co-morbidity was noted in all the cases of a case series.[ 27 ] Obsessive traits of symmetry and order,[ 32 ] obsessive compulsive disorder (OCD),[ 40 ] and major depressive disorder have been reported as co-morbidities.[ 33 ] Menstrual abnormalities and poorly developed secondary sexual characteristics have been noted in the majority of cases.[ 26 , 27 , 28 , 32 , 41 ]
There have been only five cases of BN reported till date.[ 42 , 43 , 44 , 45 , 46 ] Two of the cases were females: one was a 22-year-old medical student, with the onset of symptoms around 13 years of age, with binging and purging with isabgol husk and consumption of orlistat.[ 44 , 45 ] The other three cases were atypical, with an absence of concerns for body weight or body image, along with an absence of concurrent use of diuretics or laxatives in a 37-year-old male,[ 46 ] 15-year-old female,[ 43 ] and a 24-year-old female.[ 42 ]
Cases of ED have been described occurring co-morbid to physical illnesses such as systemic lupus erythematosus[ 26 ] and secondary to traumatic brain injury[ 31 ] or due to an adverse drug reaction to zolpidem consumption termed as a nocturnal sleep-related ED.[ 47 ] Further, AN has been found to mask physical illnesses such as carcinoma.[ 48 ] Treatment described in these cases included comprehensive treatment involving mental health professionals and dieticians.[ 26 , 27 ]
Majority of cases were managed in the in-patient setting.[ 3 , 26 , 27 ] In AN, high-calorie high-protein diet has been advised, with careful monitoring for re-feeding syndrome.[ 26 , 27 ] In the 1960s, chlorpromazine and modified insulin therapy were the treatment options used.[ 3 ] Cyproheptadine in combination with chlorpromazine,[ 26 ] combination of cyproheptadine and olanzapine,[ 41 ] mirtazapine,[ 27 ] risperidone,[ 27 ] trazodone,[ 27 ] citalopram,[ 27 ] and fluoxetine at 20 mg/day[ 28 ] have been used for treatment of AN. Combinations of olanzapine and fluvoxamine or olanzapine and fluoxetine have been used in cases of AN with obsessive traits and OCD, respectively.[ 32 , 40 ] Sertraline[ 42 ] and fluoxetine at low dose of 20 mg/day[ 44 ] as well as at 80 mg/day[ 42 ] has been described in the management of BN, with good response.
The non-pharmacological therapy of ED included family therapy, cognitive behavioral therapy (CBT), supportive psychotherapy, contingency management, hypnotherapy, and play therapy.[ 26 , 27 , 29 , 31 , 42 , 43 , 44 , 49 ] High-frequency repetitive transcranial magnetic stimulation (rTMS) over the left dorsolateral prefrontal cortex was given as augmentation strategy in a 23-year-old female who earlier had only a partial response to antidepressants as well as atypical antipsychotics and CBT. rTMS was found to improve attitude toward body weight and body shape, with an improvement of weight.[ 38 ]
This review attempted to summarize the Indian research on ED. The literature is largely comprised of case reports, as noted in the previous reviews.[ 50 , 51 ] However, there has been an increase in the number of published original research articles over the last 5–6 years. There are no studies available which determined the prevalence of ED from the community setting. There is a single hospital-based retrospective review, which reported a prevalence of 1.25% for ED.[ 16 ] Of them, almost 85% had psychogenic vomiting and about 15% had AN. This is in contrast to the international literature, wherein the frequency of occurrence of BN and BED is more common than that of AN. A meta-analysis of 15 studies from various settings reported that the estimated lifetime prevalence of any ED was 1.01%, and those of AN, BN, and BED were 0.21%, 0.81%, and 2.22%, respectively.[ 52 ] BED had the highest point prevalence of ED, followed by BN and AN, among young females across China, Japan, Africa, and Latin America.[ 53 ] In comparison, in the Indian setting, there are no cases reported of BED, and only five cases have been reported of BN.[ 42 , 43 , 44 , 45 , 46 ] Further, the two-step assessment (initial screening by self-rated questionnaire, followed by assessment by semi-structured or diagnostic interview) is the standard procedure followed globally. However, there is a single study using the two-step procedure and found no cases.[ 14 ] Majority of the Indian studies used only the screening, self-rated assessment. The frequency of disordered eating/probable ED ranged from 4 to 45.4%.[ 18 , 25 ]
It is possible that subsyndromal ED cases may not be captured by a self-rated assessment. Two studies reported the prevalence of eating distress syndrome (EDS) to be 11% and 14.8%.[ 14 , 15 ] EDS refers to subsyndromal forms of AN or BN, with patients having distressing and conflicting thoughts about body shape and eating habits. EDS is characterized by strict dieting, and bingeing in a few cases, with no significant weight loss or behaviors such as resorting to severe measures of weight loss such as diet pills, starvation, purging, or vomiting.[ 14 ] However, there has been practically no Indian research on EDS in the last 20 years.
There are several methodological issues in Indian studies which need to be addressed. Firstly, many of the studies have employed convenient sampling on medical and nursing students.[ 14 , 15 , 18 , 22 , 24 , 25 ] This may lead to selection bias and such samples may not be truly representative of the population at large. However, this practice of studying medical students is popular worldwide. The rationale given to support this being the “stressful” nature of medical training, which could be a risk factor for ED.[ 54 , 55 , 56 ] But this may also imply that the prevalence rates obtained in these studies may be an inflated figure.
Secondly, in the measurement of the frequency of disordered eating, it was found to be higher as per the Sick, Control, One-stone, Fat, Food questionnaire (SCOFF) compared to the Eating Attitudes Test-26 item (EAT-26) questionnaire.[ 23 , 25 ] The frequency with SCOFF ranged from 17.2% in women to 45.4% in men, and the frequency with EAT-26 ranged from 4% to 31%.[ 6 , 18 , 24 , 25 ] Thirdly, there are limitations in the translation and implementation of the questionnaires in a setting like India that has such linguistic diversity. Though the EAT-26 questionnaire has been translated into Hindi, the cut-off score for the Hindi version has not been defined.[ 24 ] Also, the rationale for using the same cut-off of the English version in the Kannada version is not clear.[ 6 ] Hence, due to cultural differences between the western and Indian settings, there is a definite need for the development of culturally sensitive scales for screening ED.
Culture bears a strong influence on the presentation of ED in India. One unique point noted in the Indian presentations of ED is relative lack of concern for body fat/shape. This has been termed as “Non-fat phobic” variant of AN.[ 50 ] This has been described in Hong Kong as well. In this form, food restriction is attributed to somatic complaints such as abdominal bloating, pain, and lack of appetite, rather than concern for body fat. Similar atypical features have been noted in cases of BN too from India. Also, the concept of EDS is in accordance with this concept.[ 50 , 57 ] Further, food restriction is culturally sanctioned in Indian culture when one is unwell, for “cleansing the bowel.”[ 36 ] However, several recent studies show an association between perception of body shape and higher scores on EAT-26.[ 18 , 22 , 24 ] This could be explained by the ongoing rapid societal transitions in India and the increasing influence of western ideals.
At least 50% of patients with an ED are known to have a psychiatric co-morbidity, with depression being the most common.[ 58 , 59 ] In contrast, a few cases had syndromal co-morbidity.[ 27 , 40 ] The principles of management of ED adopted in India is similar to the west. Most reports of AN and BN describe using a combination of pharmacotherapy and psychotherapy. Selective serotonin reuptake inhibitors (SSRIs), second-generation antipsychotics, and cyproheptadine have been found to be effective for AN.[ 60 ] Patients with BN were treated with 20–80 mg/day of fluoxetine in the case reports.[ 42 , 44 ] In contrast, globally, a higher dose of SSRIs, especially fluoxetine, has been found to be effective in cases of BN.[ 61 ] Psychotherapeutic approaches used in the Indian setting, such as family-based therapy and CBT, therapy match global practices.[ 62 ]
To conclude, there is increasing research focus on ED from India over the last two decades. Lower prevalence of ED could be the reason for the relative paucity of studies. But, with the increasing impact of westernization of society, ED merit renewed focus. The cultural differences between east and west have contributed to variations in presentation as well as challenges in diagnosis. Hence, there is a need for the development of culturally sensitive instruments for diagnosis as well as generating locally relevant epidemiological data about ED from the community and hospital settings.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.

IMAGES
VIDEO
COMMENTS
The nine item avoidant/restrictive food intake disorder screen (NIAS) is a short and practical assessment tool specific to ARFID with three ARFID phenotypes such as "Picky eating," "Fear," and "Appetite". This... Hakan Öğütlü, Meryem Kaşak, Uğur Doğan, Hana F. Zickgraf and Mehmet Hakan Türkçapar. Journal of Eating Disorders ...
Aims and scope. Journal of Eating Disorders is the first open access, peer-reviewed journal publishing leading research in the science and clinical practice of eating disorders. It disseminates research that provides answers to the important issues and key challenges in the field of eating disorders and to facilitate translation of evidence ...
Advances and the current status of evidence‐based treatment and outcomes for the main eating disorders, anorexia nervosa, bulimia nervosa and BED are discussed with focus on first‐line psychological therapies. Deficits in knowledge and directions for further research are highlighted, particularly with regard to treatments for BED and ARFID ...
Methods. This paper forms part of a Rapid Review series scoping the evidence for the field of ED, conducted to inform the Australian National Eating Disorders Research and Translation Strategy 2021-2031, funded and released by the Australian Government.
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes ...
Epidemiology. Although eating disorders contribute significantly to the global burden of disease, they remain relatively uncommon. A study published in September 2018 by Tomoko Udo, Ph.D., and Carlos M. Grilo, Ph.D., in Biological Psychiatry examined data from a large, nationally representative sample of over 36,000 U.S. adults 18 years of age and older surveyed using a lay-administered ...
The current Rapid Review paper forms part of a series of reviews commissioned by the Australian Federal Government to inform the Australian National Eating Disorders Research and Translation Strategy 2021-2031. This paper aims to identify and explore the risk factors associated with EDs by summarising the existing evidence related to ...
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes in the food environment have been implicated.
Meet the Editor. Ruth Weissman is a Walter Crowell University Professor of Social Sciences, Emerita, at Wesleyan University, USA. She is a clinical psychologist with research expertise in eating and weight disorders. Her scholarship focuses on reducing the burden of suffering associated with eating and weight problems, and past projects have included work on defining and classifying eating ...
Affiliations 1 Centre for Research in Eating and Weight Disorders, Department of Psychological Medicine, Institute of Psychiatry, Psychology, and Neuroscience, King's College London, London SE5 8AF, UK; South London and Maudsley NHS Foundation Trust, London, UK. Electronic address: [email protected]. 2 Centre for Research in Eating and Weight Disorders, Department of Psychological ...
W ellington, 6012, New Zealand. EXPLANA TION OF EA TING DISORDERS 1. Abstract. Eating disorders (EDs) are one of the most severe and complex mental health problems. facing researchers and ...
Walter Kaye and the UCSD Eating Disorders Research team have published over 250 papers on the neurobiology of eating disorders. These publications include behavioral, treatment, and cognitive neuroscience studies that have improved understanding of the clinical presentation, genetics, neurotransmitter systems, and neural substrates involved in appetite dysregulation and disordered eating.
Using electronic health records of 5·2 million young people, Taquet and colleagues demonstrated that the overall incidence of eating disorders increased during the COVID-19 pandemic by 15·3% in 2020, compared with previous years. The relative risk of eating disorders increased steadily from March, 2020, onwards, exceeding 1·5 by the end of ...
Walter Kaye and the UCSD Eating Disorders Research team have published over 250 papers on the neurobiology of eating disorders. These publications include behavioral, treatment, and cognitive neuroscience studies that have improved understanding of the clinical presentation, genetics, neurotransmitter systems, and neural substrates involved in appetite dysregulation and disordered eating.
How we research eating disorder (ED) recovery impacts what we know (perceive as fact) about it. In this paper we aim to provide an overview of the ED field's current perspectives on recovery, discuss how our methodologies shape what is known about recovery, and suggest a broadening of our methodological "toolkits" in order to form a more complete picture of recovery.
Published Papers, 2021. Published Papers by year. Walter Kaye and the UCSD Eating Disorders Research team have published over 250 papers on the neurobiology of eating disorders. These publications include behavioral, treatment, and cognitive neuroscience studies that have improved understanding of the clinical presentation, genetics ...
Abstract. Public health concerns largely have disregarded the important overlap between eating disorders and obesity. This Special Issue addresses this neglect and points to how progress can be made in preventing and treating both. Thirteen primary research papers, three reviews, and two commentaries comprise this Special Issue.
Eating disorders are actually serious and often fatal illnesses,... | Find, read and cite all the research you need on ResearchGate ... All the papers from 2000-2022 were reviewed from Google ...
To quantify the magnitude of the disparity between research on eating disorders and other mental illnesses, we searched Web of Science for papers mentioning eating disorders in their title ("anorexia nervosa" OR "bulimia nervosa" OR "binge eating disorder" OR "binge eating" OR "eating disorders" OR "disordered eating") and found that, in 2018, only 1390 studies were ...
Purpose of Review This review aims to report on recent evidence for multi-family therapy for eating disorders (MFT) across the lifespan. It is a narrative update of recent systematic, scoping and meta-analytic reviews. Recent Findings There has been a recent increase in published theoretical, quantitative and qualitative reports on MFT in the past few years. Recent and emerging data continues ...
Eating disorders have increasingly become the focus of research studies due to their prevalence, especially in Western cultures. Of the adolescent and young adult populations in the United States, for example, between .3 and .9 % are diagnosed with anorexia nervosa (AN), between .5 and 5 % with bulimia nervosa (BN), between 1.6 and 3.5 % with binge eating disorder (BED), and about 4.8 % with ...
This article reviews 16 prevention-related publications in Eating Disorders during 2023. Using phases of the prevention cycle shown in Figure 1, these articles are categorized in Table 1, and in the References section they are preceded by an *.For each phase, Table 1 also recommends two or three reviews or research articles published in other journals in 2023.
Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and interventions ...
Since the main foci of the aforementioned ED-specialized journals can vary, we chose one journal to control the influence of journal features on bibliometric results. Papers published in Eating Disorders, for example, have been available in the WoS since 2012, and papers published in Journal of Eating Disorders have been available since 2017 ...
Co-producing eating disorder research. Eating disorders (EDs) are a classification of disorders which involve feeding and eating disturbances which cause significant clinical distress . An estimated 725,000 people in the UK are affected by EDs, at an estimated cost of 3.9-4.6 billion pounds annually to the NHS .
Introduction. In 2009, when it appeared likely that binge eating disorder (BED) would be recommended for inclusion as an official diagnosis in the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a number of researchers believed that it was important to initiate planning for the next generation of research.
Two step procedure Step 1: Screening of probable cases. They were defined as : Scoring >30 on 40-item EAT. Scoring >10 on 33-item BITE. Step 2: Clinical assessment and diagnosis of eating disorder as per DSM-III in all probable subjects as well as 1/3 of screen negative subjects selected by random sampling.