
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
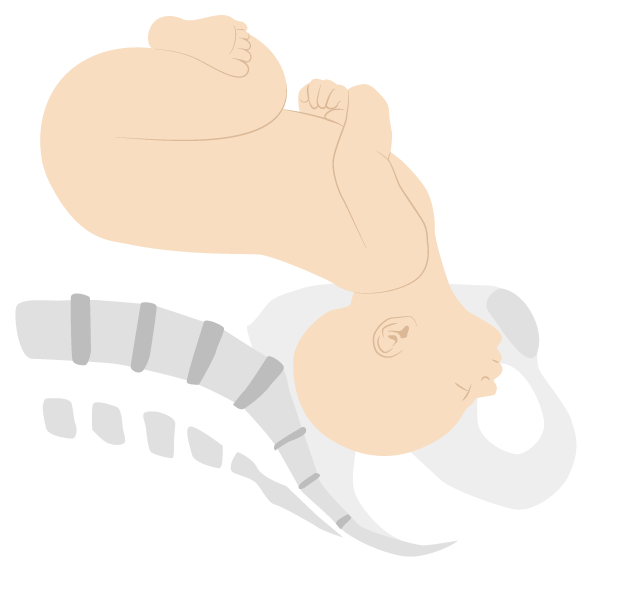
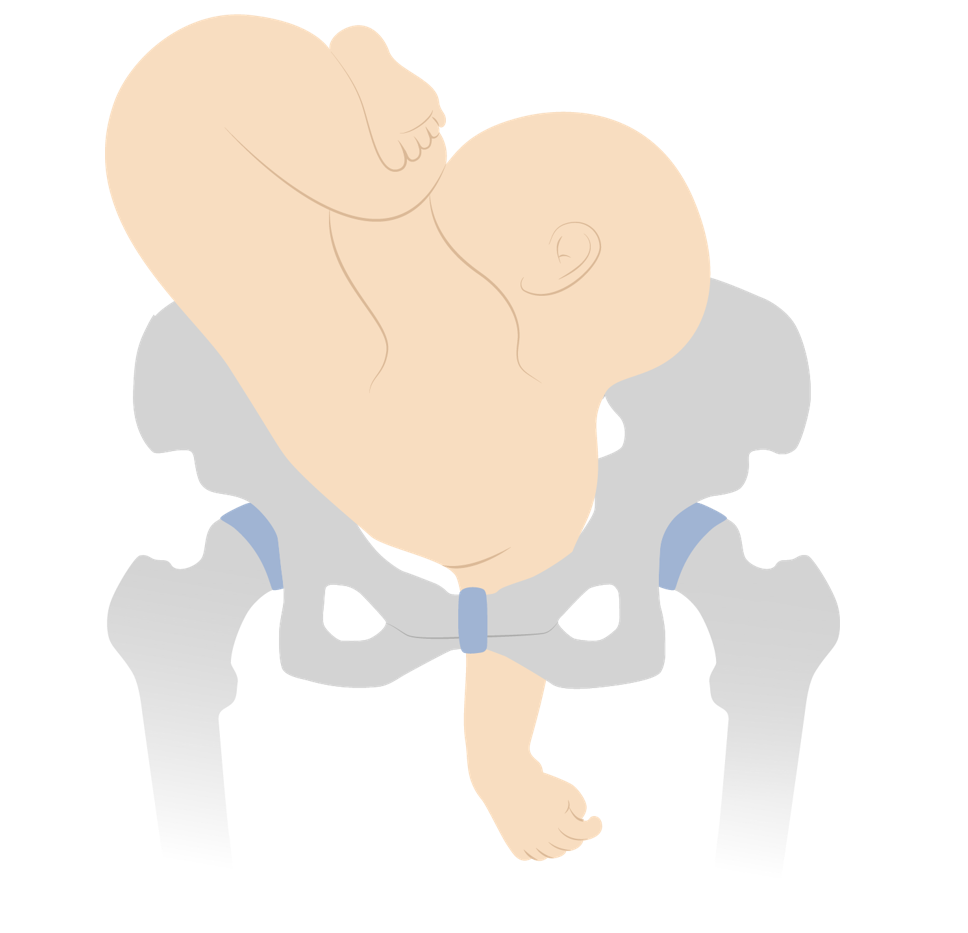
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
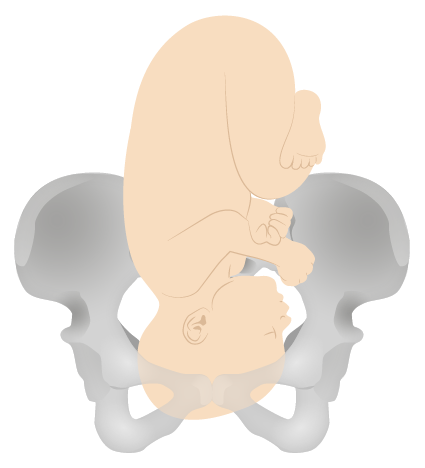
Breech presentation
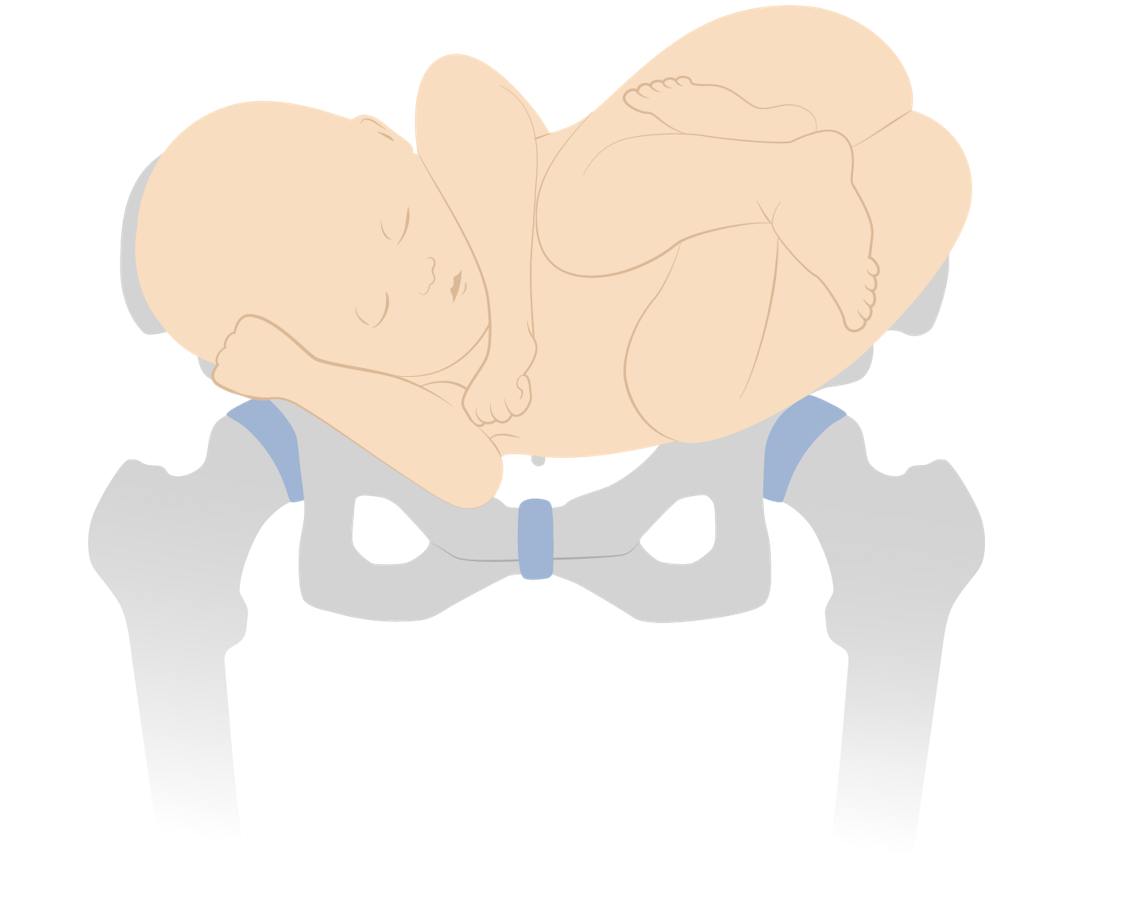
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
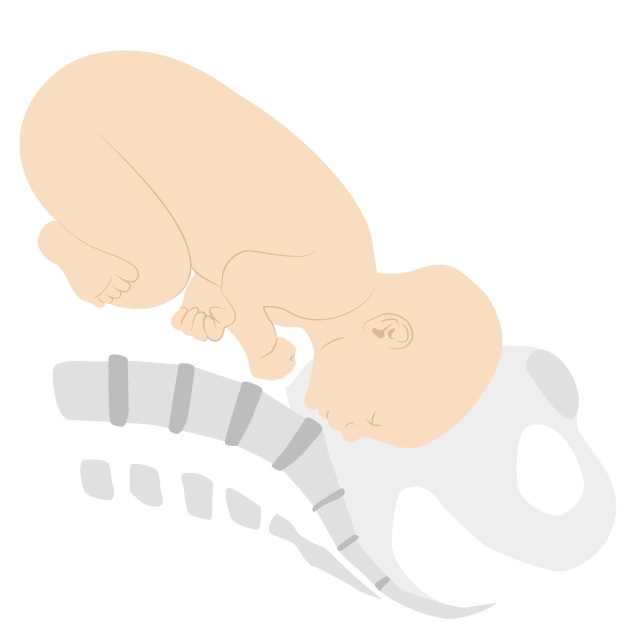
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).
Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
● The curvature of the fetal spine is oriented downward (also called "back down" or dorsoinferior), and the fetal shoulder presents at the cervix ( figure 1 ).
● The curvature of the fetal spine is oriented upward (also called "back up" or dorsosuperior), and the fetal small parts and umbilical cord present at the cervix.
(Note: Lie refers to the long axis of the fetus relative to the longitudinal axis of the uterus; the long axis of the fetus can be transverse to, oblique to, or parallel to [longitudinal lie] the longitudinal axis of the uterus. Presentation refers to the fetal part that directly overlies the pelvic inlet; it is usually cephalic [head] or breech [buttocks] but can be a shoulder, compound [eg, head and hand], or funic [umbilical cord]. Position is the relationship of a nominated site of the presenting part to a denominating location on the maternal pelvis [eg, right occiput anterior].)
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
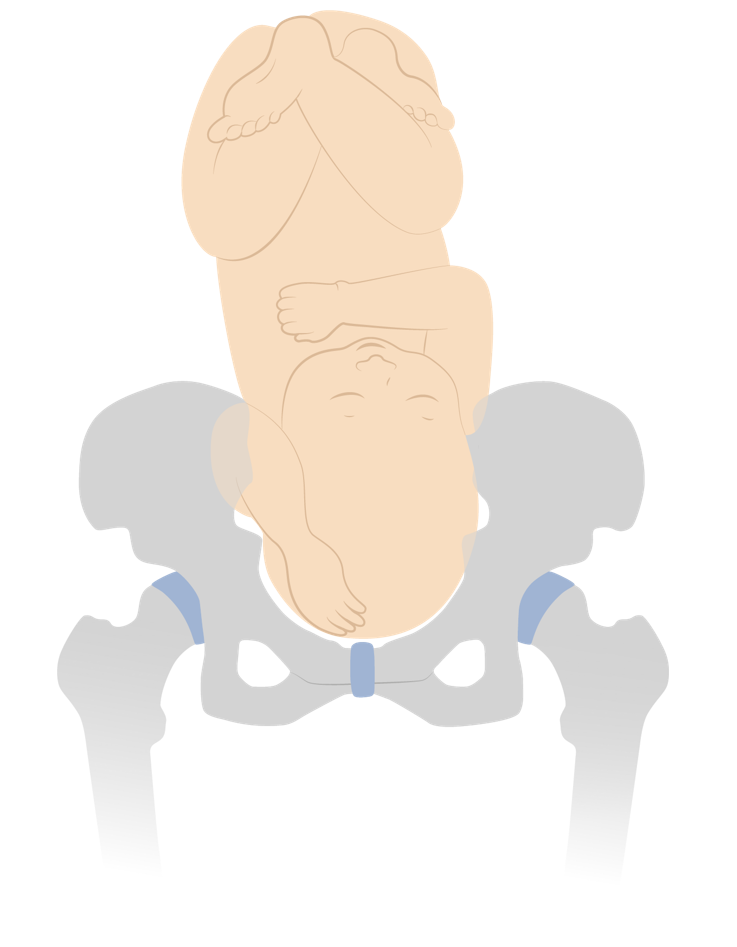
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.
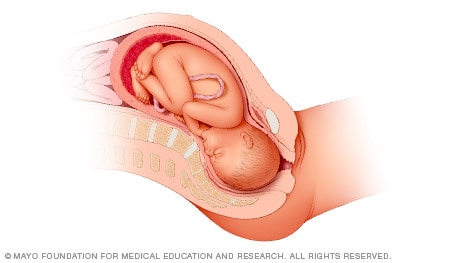
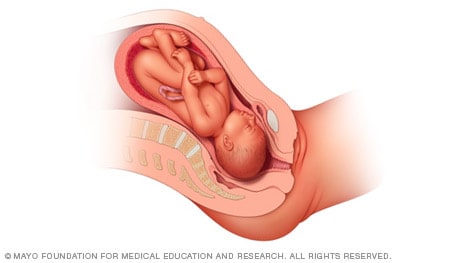
Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.
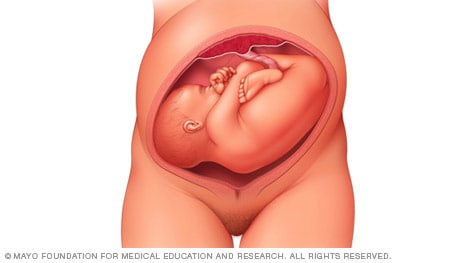
Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

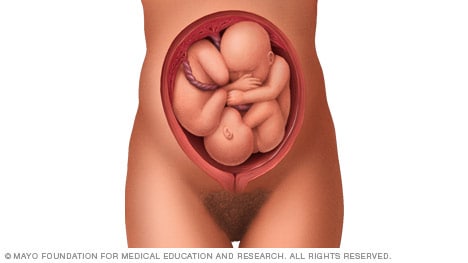
Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.
If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.
- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Your baby in the birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between their head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Alternative Names
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal

Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Review Date 11/10/2022
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
Fastest Obstetric, Gynecology and Pediatric Insight Engine
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Normal Labor
Fetal Lie The relation of the fetal long axis to that of the mother is termed fetal lie and is either longitudinal or transverse . Occasionally, the fetal and the maternal axes may cross at a 45-degree angle, forming an oblique lie . This lie is unstable and becomes longitudinal or transverse during labor. A longitudinal lie is present in more than 99 percent of labors at term. Predisposing factors for transverse fetal position include multiparity, placenta previa, hydramnios, and uterine anomalies ( Chap. 23 , p. 468 ). Fetal Presentation The presenting part is that portion of the fetal body that is either foremost within the birth canal or in closest proximity to it. It typically can be felt through the cervix on vaginal examination. Accordingly, in longitudinal lies, the presenting part is either the fetal head or breech, creating cephalic and breech presentations , respectively. When the fetus lies with the long axis transversely, the shoulder is the presenting part. Table 22-1 describes the incidences of the various fetal presentations. TABLE 22-1. Fetal Presentation in 68,097 Singleton Pregnancies at Parkland Hospital Cephalic Presentation Such presentations are classified according to the relationship between the head and body of the fetus ( Fig. 22-1 ). Ordinarily, the head is flexed sharply so that the chin is in contact with the thorax. The occipital fontanel is the presenting part, and this presentation is referred to as a vertex or occiput presentation . Much less commonly, the fetal neck may be sharply extended so that the occiput and back come in contact, and the face is foremost in the birth canal— face presentation ( Fig. 23-6 , p. 466 ). The fetal head may assume a position between these extremes, partially flexed in some cases, with the anterior (large) fontanel, or bregma, presenting— sinciput presentation —or partially extended in other cases, to have a brow presentation ( Fig. 23-8 , p. 468 ). These latter two presentations are usually transient. As labor progresses, sinciput and brow presentations almost always convert into vertex or face presentations by neck flexion or extension, respectively. Failure to do so can lead to dystocia, as discussed in Chapter 23 ( p. 455 ). Figure 22-1 Longitudinal lie. Cephalic presentation. Differences in attitude of the fetal body in (A) vertex, (B) sinciput, (C) brow, and (D) face presentations. Note changes in fetal attitude in relation to fetal vertex as the fetal head becomes less flexed. The term fetus usually presents with the vertex, most logically because the uterus is piriform or pear shaped. Although the fetal head at term is slightly larger than the breech, the entire podalic pole of the fetus—that is, the breech and its flexed extremities—is bulkier and more mobile than the cephalic pole. The cephalic pole is composed of the fetal head only. Until approximately 32 weeks, the amnionic cavity is large compared with the fetal mass, and the fetus is not crowded by the uterine walls. Subsequently, however, the ratio of amnionic fluid volume decreases relative to the increasing fetal mass. As a result, the uterine walls are apposed more closely to the fetal parts. If presenting by the breech, the fetus often changes polarity to make use of the roomier fundus for its bulkier and more mobile podalic pole. As discussed in Chapter 28 ( p. 559 ), the incidence of breech presentation decreases with gestational age. It approximates 25 percent at 28 weeks, 17 percent at 30 weeks, 11 percent at 32 weeks, and then decreases to approximately 3 percent at term. The high incidence of breech presentation in hydrocephalic fetuses is in accord with this theory, as the larger fetal cephalic pole requires more room than its podalic pole. Breech Presentation When the fetus presents as a breech, the three general configurations are frank, complete , and footling presentations and are described in Chapter 28 ( p. 559 ). Breech presentation may result from circumstances that prevent normal version from taking place. One example is a septum that protrudes into the uterine cavity ( Chap. 3 , p. 42 ). A peculiarity of fetal attitude, particularly extension of the vertebral column as seen in frank breeches, also may prevent the fetus from turning. If the placenta is implanted in the lower uterine segment, it may distort normal intrauterine anatomy and result in a breech presentation. Fetal Attitude or Posture In the later months of pregnancy, the fetus assumes a characteristic posture described as attitude or habitus as shown in Figure 22-1 . As a rule, the fetus forms an ovoid mass that corresponds roughly to the shape of the uterine cavity. The fetus becomes folded or bent upon itself in such a manner that the back becomes markedly convex; the head is sharply flexed so that the chin is almost in contact with the chest; the thighs are flexed over the abdomen; and the legs are bent at the knees. In all cephalic presentations, the arms are usually crossed over the thorax or become parallel to the sides. The umbilical cord lies in the space between them and the lower extremities. This characteristic posture results from the mode of fetal growth and its accommodation to the uterine cavity. Abnormal exceptions to this attitude occur as the fetal head becomes progressively more extended from the vertex to the face presentation (see Fig. 22-1 ). This results in a progressive change in fetal attitude from a convex (flexed) to a concave (extended) contour of the vertebral column. Fetal Position Position refers to the relationship of an arbitrarily chosen portion of the fetal presenting part to the right or left side of the birth canal. Accordingly, with each presentation there may be two positions—right or left. The fetal occiput, chin (mentum), and sacrum are the determining points in vertex, face, and breech presentations, respectively ( Figs. 22-2 to 22-6 ). Because the presenting part may be in either the left or right position, there are left and right occipital, left and right mental, and left and right sacral presentations. These are abbreviated as LO and RO, LM and RM, and LS and RS, respectively. FIGURE 22-2 Longitudinal lie. Vertex presentation. A. Left occiput anterior (LOA). B. Left occiput posterior (LOP). FIGURE 22-3 Longitudinal lie. Vertex presentation. A . Right occiput posterior (ROP). B . Right occiput transverse (ROT). FIGURE 22-4 Longitudinal lie. Vertex presentation. Right occiput anterior (ROA). FIGURE 22-5 Longitudinal lie. Face presentation. Left and right mentum anterior and right mentum posterior positions. FIGURE 22-6 Longitudinal lie. Breech presentation. Left sacrum posterior (LSP). Varieties of Presentations and Positions For still more accurate orientation, the relationship of a given portion of the presenting part to the anterior, transverse, or posterior portion of the maternal pelvis is considered. Because the presenting part in right or left positions may be directed anteriorly (A), transversely (T), or posteriorly (P), there are six varieties of each of the three presentations as shown in Figures 22-2 to 22-6 . Thus, in an occiput presentation, the presentation, position, and variety may be abbreviated in clockwise fashion as: Approximately two thirds of all vertex presentations are in the left occiput position, and one third in the right. In shoulder presentations, the acromion (scapula) is the portion of the fetus arbitrarily chosen for orientation with the maternal pelvis. One example of the terminology sometimes employed for this purpose is illustrated in Figure 22-7 . The acromion or back of the fetus may be directed either posteriorly or anteriorly and superiorly or inferiorly. Because it is impossible to differentiate exactly the several varieties of shoulder presentation by clinical examination and because such specific differentiation serves no practical purpose, it is customary to refer to all transverse lies simply as shoulder presentations . Another term used is transverse lie , with back up or back down , which is clinically important when deciding incision type for cesarean delivery ( Chap. 23 , p. 468 ). FIGURE 22-7 Transverse lie. Right acromiodorsoposterior (RADP). The shoulder of the fetus is to the mother’s right, and the back is posterior. Diagnosis of Fetal Presentation and Position Several methods can be used to diagnose fetal presentation and position. These include abdominal palpation, vaginal examination, auscultation, and, in certain doubtful cases, sonography. Rarely, plain radiographs, computed tomography, or magnetic resonance imaging may be used. Abdominal Palpation—Leopold Maneuvers Abdominal examination can be conducted systematically employing the four maneuvers described by Leopold in 1894 and shown in Figure 22-8 . The mother lies supine and comfortably positioned with her abdomen bared. These maneuvers may be difficult if not impossible to perform and interpret if the patient is obese, if there is excessive amnionic fluid, or if the placenta is anteriorly implanted. FIGURE 22-8 Leopold maneuvers (A–D) performed in a fetus with a longitudinal lie in the left occiput anterior position (LOA). The first maneuver permits identification of which fetal pole—that is, cephalic or podalic—occupies the uterine fundus. The breech gives the sensation of a large, nodular mass, whereas the head feels hard and round and is more mobile and ballottable. Performed after determination of fetal lie, the second maneuver is accomplished as the palms are placed on either side of the maternal abdomen, and gentle but deep pressure is exerted. On one side, a hard, resistant structure is felt—the back. On the other, numerous small, irregular, mobile parts are felt—the fetal extremities. By noting whether the back is directed anteriorly, transversely, or posteriorly, fetal orientation can be determined. The third maneuver is performed by grasping with the thumb and fingers of one hand the lower portion of the maternal abdomen just above the symphysis pubis. If the presenting part is not engaged, a movable mass will be felt, usually the head. The differentiation between head and breech is made as in the first maneuver. If the presenting part is deeply engaged, however, the findings from this maneuver are simply indicative that the lower fetal pole is in the pelvis, and details are then defined by the fourth maneuver. To perform the fourth maneuver, the examiner faces the mother’s feet and, with the tips of the first three fingers of each hand, exerts deep pressure in the direction of the axis of the pelvic inlet. In many instances, when the head has descended into the pelvis, the anterior shoulder may be differentiated readily by the third maneuver. Abdominal palpation can be performed throughout the latter months of pregnancy and during and between the contractions of labor. With experience, it is possible to estimate the size of the fetus. According to Lydon-Rochelle and colleagues (1993), experienced clinicians accurately identify fetal malpresentation using Leopold maneuvers with a high sensitivity—88 percent, specificity—94 percent, positive-predictive value—74 percent, and negative-predictive value—97 percent. Vaginal Examination Before labor, the diagnosis of fetal presentation and position by vaginal examination is often inconclusive because the presenting part must be palpated through a closed cervix and lower uterine segment. With the onset of labor and after cervical dilatation, vertex presentations and their positions are recognized by palpation of the various fetal sutures and fontanels. Face and breech presentations are identified by palpation of facial features and fetal sacrum, respectively. In attempting to determine presentation and position by vaginal examination, it is advisable to pursue a definite routine, comprising four movements. First, the examiner inserts two fingers into the vagina and the presenting part is found. Differentiation of vertex, face, and breech is then accomplished readily. Second, if the vertex is presenting, the fingers are directed posteriorly and then swept forward over the fetal head toward the maternal symphysis ( Fig. 22-9 ). During this movement, the fingers necessarily cross the sagittal suture and its linear course is delineated. Next, the positions of the two fontanels are ascertained. For this, fingers are passed to the most anterior extension of the sagittal suture, and the fontanel encountered there is examined and identified. Then, with a sweeping motion, the fingers pass along the suture to the other end of the head until the other fontanel is felt and differentiated ( Fig. 22-10 ). Last, the station, or extent to which the presenting part has descended into the pelvis, can also be established at this time ( p. 449 ). Using these maneuvers, the various sutures and fontanels are located readily ( Fig. 7-11 , p. 139 ). FIGURE 22-9 Locating the sagittal suture by vaginal examination. FIGURE 22-10 Differentiating the fontanels by vaginal examination. Sonography and Radiography Sonographic techniques can aid fetal position identification, especially in obese women or in women with rigid abdominal walls. Zahalka and associates (2005) compared digital examinations with transvaginal and transabdominal sonography for fetal head position determination during second-stage labor and reported that transvaginal sonography was superior. Occiput Anterior Presentation In most cases, the vertex enters the pelvis with the sagittal suture lying in the transverse pelvic diameter. The fetus enters the pelvis in the left occiput transverse (LOT) position in 40 percent of labors and in the right occiput transverse (ROT) position in 20 percent (Caldwell, 1934). In occiput anterior positions—LOA or ROA— the head either enters the pelvis with the occiput rotated 45 degrees anteriorly from the transverse position, or this rotation occurs subsequently. The mechanism of labor in all these presentations is usually similar. The positional changes of the presenting part required to navigate the pelvic canal constitute the mechanisms of labor . The cardinal movements of labor are engagement, descent, flexion, internal rotation, extension, external rotation, and expulsion ( Fig. 22-11 ). During labor, these movements not only are sequential but also show great temporal overlap. For example, as part of engagement, there is both flexion and descent of the head. It is impossible for the movements to be completed unless the presenting part descends simultaneously. Concomitantly, uterine contractions effect important modifications in fetal attitude, or habitus, especially after the head has descended into the pelvis. These changes consist principally of fetal straightening, with loss of dorsal convexity and closer application of the extremities to the body. As a result, the fetal ovoid is transformed into a cylinder, with the smallest possible cross section typically passing through the birth canal. Figure 22-11 Cardinal movements of labor and delivery from a left occiput anterior position. Engagement The mechanism by which the biparietal diameter—the greatest transverse diameter in an occiput presentation—passes through the pelvic inlet is designated engagement . The fetal head may engage during the last few weeks of pregnancy or not until after labor commencement. In many multiparous and some nulliparous women, the fetal head is freely movable above the pelvic inlet at labor onset. In this circumstance, the head is sometimes referred to as “floating.” A normal-sized head usually does not engage with its sagittal suture directed anteroposteriorly. Instead, the fetal head usually enters the pelvic inlet either transversely or obliquely. Segel and coworkers (2012) analyzed labor in 5341 nulliparous women and found that fetal head engagement before labor onset did not affect vaginal delivery rates in either spontaneous or induced labor. Asynclitism. The fetal head tends to accommodate to the transverse axis of the pelvic inlet, whereas the sagittal suture, while remaining parallel to that axis, may not lie exactly midway between the symphysis and the sacral promontory. The sagittal suture frequently is deflected either posteriorly toward the promontory or anteriorly toward the symphysis ( Fig. 22-12 ). Such lateral deflection to a more anterior or posterior position in the pelvis is called asynclitism . If the sagittal suture approaches the sacral promontory, more of the anterior parietal bone presents itself to the examining fingers, and the condition is called anterior asynclitism . If, however, the sagittal suture lies close to the symphysis, more of the posterior parietal bone will present, and the condition is called posterior asynclitism . With extreme posterior asynclitism, the posterior ear may be easily palpated. FIGURE 22-12 Synclitism and asynclitism. Moderate degrees of asynclitism are the rule in normal labor. However, if severe, the condition is a common reason for cephalopelvic disproportion even with an otherwise normal-sized pelvis. Successive shifting from posterior to anterior asynclitism aids descent. Descent This movement is the first requisite for birth of the newborn. In nulliparas, engagement may take place before the onset of labor, and further descent may not follow until the onset of the second stage. In multiparas, descent usually begins with engagement. Descent is brought about by one or more of four forces: (1) pressure of the amnionic fluid, (2) direct pressure of the fundus upon the breech with contractions, (3) bearing-down efforts of maternal abdominal muscles, and (4) extension and straightening of the fetal body. Flexion As soon as the descending head meets resistance, whether from the cervix, pelvic walls, or pelvic floor, it normally flexes. With this movement, the chin is brought into more intimate contact with the fetal thorax, and the appreciably shorter suboccipitobregmatic diameter is substituted for the longer occipitofrontal diameter ( Figs. 22-13 and 22-14 ). FIGURE 22-13 Lever action produces flexion of the head. Conversion from occipitofrontal to suboccipitobregmatic diameter typically reduces the anteroposterior diameter from nearly 12 to 9.5 cm. FIGURE 22-14 Four degrees of head flexion. The solid line represents the occipitomental diameter, whereas the broken line connects the center of the anterior fontanel with the posterior fontanel. A. Flexion poor. B. Flexion moderate. C. Flexion advanced. D. Flexion complete. Note that with complete flexion, the chin is on the chest. The suboccipitobregmatic diameter, the shortest anteroposterior diameter of the fetal head, is passing through the pelvic inlet. Internal Rotation This movement consists of a turning of the head in such a manner that the occiput gradually moves toward the symphysis pubis anteriorly from its original position or, less commonly, posteriorly toward the hollow of the sacrum ( Figs. 22-15 to 22-17 ). Internal rotation is essential for completion of labor, except when the fetus is unusually small. FIGURE 22-15 Mechanism of labor for the left occiput transverse position, lateral view. A. Engagement. B. After engagement, further descent. C. Descent and initial internal rotation. D. Rotation and extension. FIGURE 22-16 Mechanism of labor for left occiput anterior position. FIGURE 22-17 Mechanism of labor for right occiput posterior position showing anterior rotation. Calkins (1939) studied more than 5000 women in labor to ascertain the time of internal rotation. He concluded that in approximately two thirds, internal rotation is completed by the time the head reaches the pelvic floor; in about another fourth, internal rotation is completed shortly after the head reaches the pelvic floor; and in the remaining 5 percent, rotation does not take place. When the head fails to turn until reaching the pelvic floor, it typically rotates during the next one or two contractions in multiparas. In nulliparas, rotation usually occurs during the next three to five contractions. Extension After internal rotation, the sharply flexed head reaches the vulva and undergoes extension. If the sharply flexed head, on reaching the pelvic floor, did not extend but was driven farther downward, it would impinge on the posterior portion of the perineum and would eventually be forced through the perineal tissues. When the head presses on the pelvic floor, however, two forces come into play. The first force, exerted by the uterus, acts more posteriorly, and the second, supplied by the resistant pelvic floor and the symphysis, acts more anteriorly. The resultant vector is in the direction of the vulvar opening, thereby causing head extension. This brings the base of the occiput into direct contact with the inferior margin of the symphysis pubis (see Fig. 22-16 ). With progressive distention of the perineum and vaginal opening, an increasingly larger portion of the occiput gradually appears. The head is born as the occiput, bregma, forehead, nose, mouth, and finally the chin pass successively over the anterior margin of the perineum (see Fig. 22-17 ). Immediately after its delivery, the head drops downward so that the chin lies over the maternal anus. External Rotation The delivered head next undergoes restitution (see Fig. 22-11 ). If the occiput was originally directed toward the left, it rotates toward the left ischial tuberosity. If it was originally directed toward the right, the occiput rotates to the right. Restitution of the head to the oblique position is followed by external rotation completion to the transverse position. This movement corresponds to rotation of the fetal body and serves to bring its bisacromial diameter into relation with the anteroposterior diameter of the pelvic outlet. Thus, one shoulder is anterior behind the symphysis and the other is posterior. This movement apparently is brought about by the same pelvic factors that produced internal rotation of the head. Expulsion Almost immediately after external rotation, the anterior shoulder appears under the symphysis pubis, and the perineum soon becomes distended by the posterior shoulder. After delivery of the shoulders, the rest of the body quickly passes. Occiput Posterior Presentation In approximately 20 percent of labors, the fetus enters the pelvis in an occiput posterior (OP) position (Caldwell, 1934). The right occiput posterior (ROP) is slightly more common than the left (LOP). It appears likely from radiographic evidence that posterior positions are more often associated with a narrow forepelvis. They also are more commonly seen in association with anterior placentation (Gardberg, 1994a). In most occiput posterior presentations, the mechanism of labor is identical to that observed in the transverse and anterior varieties, except that the occiput has to internally rotate to the symphysis pubis through 135 degrees, instead of 90 and 45 degrees, respectively (see Fig. 22-17 ). Effective contractions, adequate head flexion, and average fetal size together permit most posteriorly positioned occiputs to rotate promptly as soon as they reach the pelvic floor, and labor is not lengthened appreciably. In perhaps 5 to 10 percent of cases, however, rotation may be incomplete or may not take place at all, especially if the fetus is large (Gardberg, 1994b). Poor contractions, faulty head flexion, or epidural analgesia, which diminishes abdominal muscular pushing and relaxes pelvic floor muscles, may predispose to incomplete rotation. If rotation is incomplete, transverse arrest may result. If no rotation toward the symphysis takes place, the occiput may remain in the direct occiput posterior position, a condition known as persistent occiput posterior . Both persistent occiput posterior and transverse arrest represent deviations from the normal mechanisms of labor and are considered further in Chapter 23 . Fetal Head Shape Changes Caput Succedaneum In vertex presentations, labor forces alter fetal head shape. In prolonged labors before complete cervical dilatation, the portion of the fetal scalp immediately over the cervical os becomes edematous ( Fig. 33-1 , p. 647 ). This swelling, known as the caput succedaneum , is shown in Figures 22-18 and 22-19 . It usually attains a thickness of only a few millimeters, but in prolonged labors it may be sufficiently extensive to prevent differentiation of the various sutures and fontanels. More commonly, the caput is formed when the head is in the lower portion of the birth canal and frequently only after the resistance of a rigid vaginal outlet is encountered. Because it develops over the most dependent area of the head, one may deduce the original fetal head position by noting the location of the caput succedaneum. FIGURE 22-18 Formation of caput succedaneum and head molding.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Fetal Disorders
- Neurological Disorders
- Fetal-Growth Disorders
- Cardiovascular Disorders
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

Achieve Mastery of Medical Concepts
Study for medical school and boards with lecturio.
USMLE Step 1 | USMLE Step 2 | COMLEX Level 1 | COMLEX Level 2 | ENARM | NEET
Fetal Malpresentation and Malposition
Fetal presentation describes which part of the fetus will enter through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first, while position is the orientation Orientation Awareness of oneself in relation to time, place and person. Psychiatric Assessment of the fetus compared to the maternal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 "hip" bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy . Presentations include vertex (the fetal occiput will present through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first), face, brow, shoulder, and breech. If a fetal limb is presenting next to the presenting part (e.g., the hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy is next to the head), this is known as a compound presentation. Malpresentation refers to any presentation other than vertex, with the most common being breech presentations. Vaginal delivery of a breech infant increases the risk for head entrapment and hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage , so, especially in the United States, mothers are generally offered a procedure to help manually rotate the baby to a head-down position instead (known as an external cephalic version) or a planned cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery .
Last updated: Feb 14, 2023
Fetal Lie and Presentation
Presenting diameter, management of cephalic and compound presentations, risks and management of breech and transverse presentations.
Share this concept:
- The “presenting part” refers to the part of the baby that will come through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first.
- The position refers to how that body part (and thus the baby) is oriented within the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
- The uterine fundus Fundus The superior portion of the body of the stomach above the level of the cardiac notch. Stomach: Anatomy is typically roomier, so babies tend to orient themselves head down so that their body and limbs occupy the larger portion of the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy .
Clinical relevance
- The maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy has a diameter of about 10 cm, through which the fetus must pass.
- The presentation and position of the fetus will determine how wide the fetus is (known as the “presenting fetal diameter”) as it attempts to pass through the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
- Certain presentation/positions are more difficult (or even impossible) to pass through the pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy because of their large presenting diameter.
- Knowledge of the presentation and position are required to safely manage labor and delivery.
Risk factors for fetal malpresentation
- Multiparity (which can result in lax abdominal walls)
- Multiple gestations (e.g., twins)
- Prematurity Prematurity Neonatal Respiratory Distress Syndrome
- Uterine abnormalities (e.g., leiomyomas, uterine septa)
- Narrow pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy shapes
- Fetal anomalies (e.g., hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage )
- Placental anomalies (e.g., placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities , in which the placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity covers the internal cervical os)
- Polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios (too much fluid)
- Oligohydramnios Oligohydramnios Oligohydramnios refers to amniotic fluid volume less than expected for the current gestational age. Oligohydramnios is diagnosed by ultrasound and defined as an amniotic fluid index (AFI) of ‰¤ 5 cm or a single deep pocket (SDP) of Oligohydramnios (not enough fluid)
- Malpresentation in a previous pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
Epidemiology
Prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency rates for different malpresentations at term:
- Vertex presentation, occiput posterior position: 1 in 19 deliveries
- Breech presentation: 1 in 33 deliveries
- Face presentation: 1 in 600–800 deliveries
- Transverse lie: 1 in 833 deliveries
- Compound presentation: 1 in 1500 deliveries
Related videos
Fetal lie is how the long axis of the fetus is oriented in relation to the mother. Possible lies include:
- Longitudinal: fetus and mother have the same vertical axis (their spines are parallel).
- Transverse: fetal vertical axis is at a 90-degree angle to mother’s vertical axis (their spines are perpendicular).
- Oblique: fetal vertical axis is at a 45-degree angle to mother’s vertical axis (unstable, and will resolve to longitudinal or transverse during labor).
Presentation
Presentation describes which body part of the fetus will pass through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first. Presentations include:
- Cephalic: head down
- Breech: bottom/feet down
- Transverse presentation: shoulder
- Compound presentation: an extremity presents alongside the primary presenting part
Cephalic presentations
Cephalic presentations can be categorized as:
- Vertex presentation: chin Chin The anatomical frontal portion of the mandible, also known as the mentum, that contains the line of fusion of the two separate halves of the mandible (symphysis menti). This line of fusion divides inferiorly to enclose a triangular area called the mental protuberance. On each side, inferior to the second premolar tooth, is the mental foramen for the passage of blood vessels and a nerve. Melasma flexed, with the occipital Occipital Part of the back and base of the cranium that encloses the foramen magnum. Skull: Anatomy fontanel as the presenting part
- Face presentation
- Brow presentation: forehead Forehead The part of the face above the eyes. Melasma is the presenting part
Vertex presentation
Face presentation (mentum anterior position)
Brow presentation (mentum posterior position)
Breech presentations
Breech presentations can be categorized as:
- Frank breech: bottom down, legs extended (50%–70%)
- Complete breech: bottom down, hips and knees both flexed
- Incomplete breech: 1 or both hips not completely flexed
- Footling breech: feet down
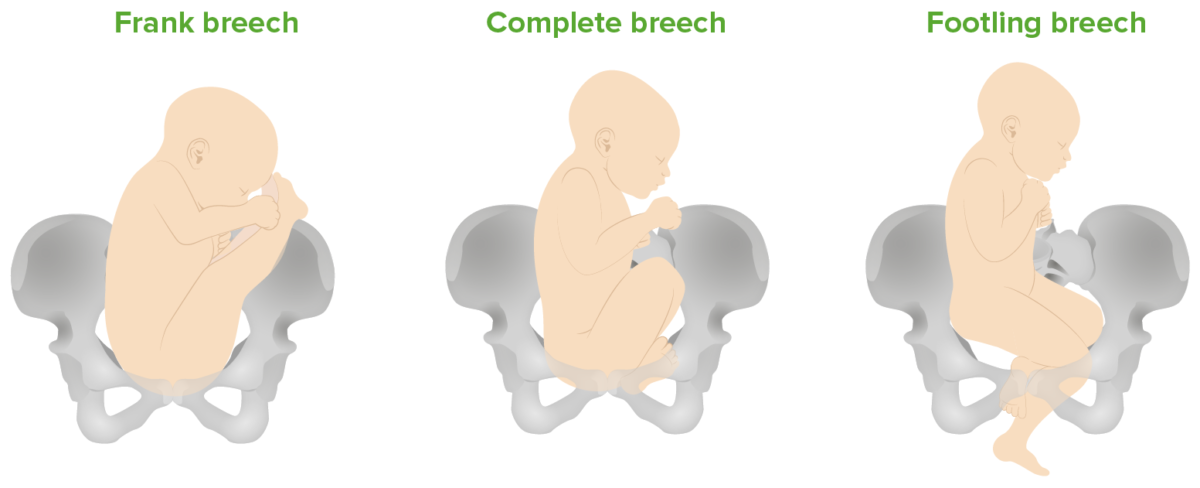
Breech presentations: Frank (bottom down, legs extended), complete (bottom down, hips and knees both flexed), and footling (feet down) breech presentations
Transverse and compound presentations
- Uncommon, but when they occur, the presenting fetal part is the shoulder.
- If the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy begins dilating, the arm Arm The arm, or “upper arm” in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy may prolapse through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy .
- In compound presentations, the most common situation is a hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy or arm Arm The arm, or “upper arm” in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy presenting with the head.
Shoulder presentation (transverse lie)
Neglected shoulder presentation resulting in arm prolapse during labor
Vertex presentation with a compound hand
Fetal malpresentation
- Any presentation other than vertex
- Clinically, this means breech, face, brow, and shoulder presentations.
Position describes the relation of the fetal presenting part to the maternal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
Vertex positions
Positions for vertex presentations describe the position of the fetal occiput .
- Identified on cervical exam as the area in the midline between the anterior and posterior fontanelles Fontanelles Physical Examination of the Newborn
- Anterior, posterior, or transverse in relation to the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy
- Being on the maternal right or left
- Right or left occiput anterior
- Right or left occiput posterior
- Right or left occiput transverse
- Direct occiput anterior or posterior
- The most common positions (and easiest for vaginal delivery) are occiput anterior.
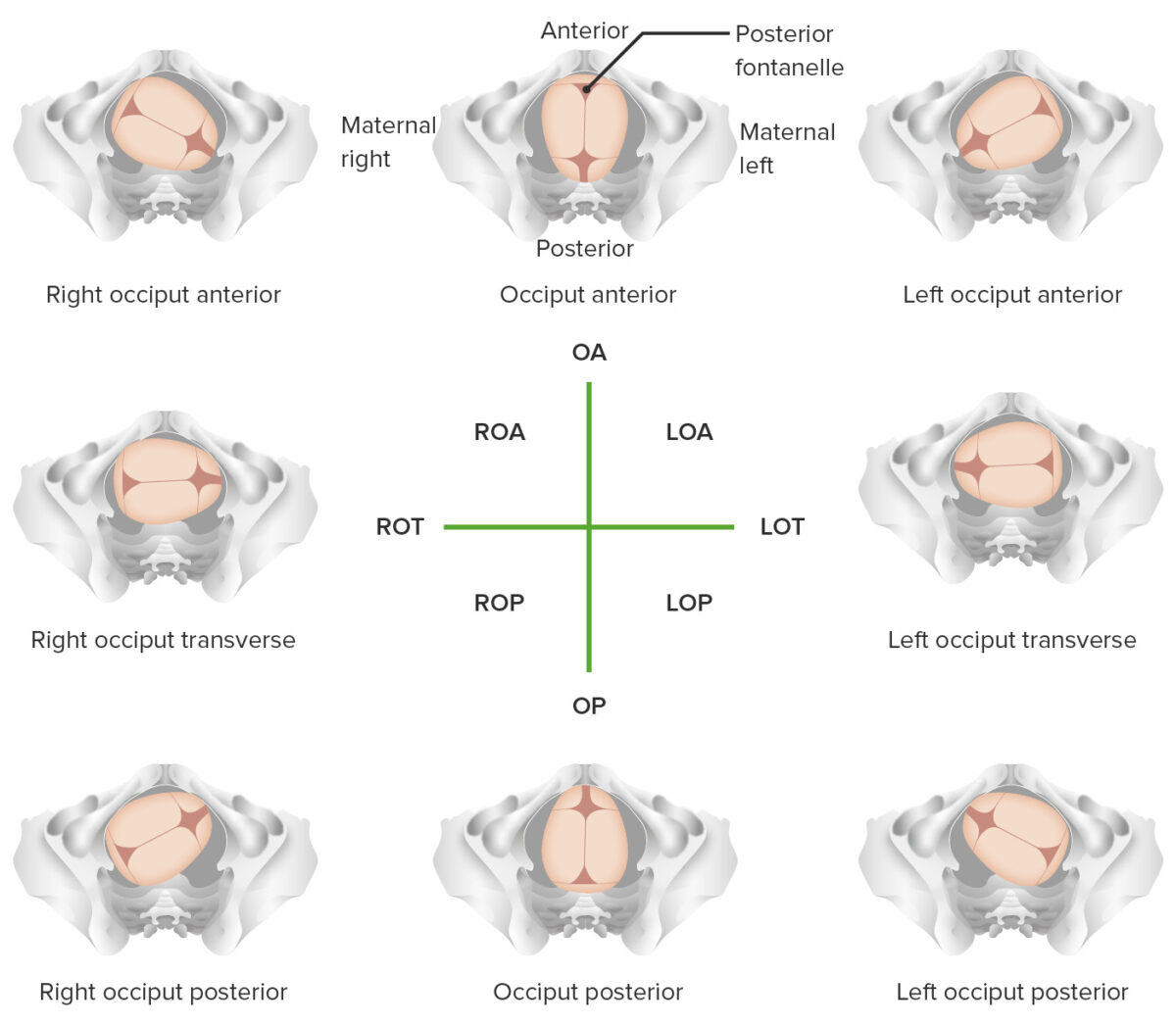
Overview of different vertex positions LOA: left occiput anterior LOP: left occiput posterior LOT: left occiput transverse OA occiput anterior OP: occiput posterior ROA: right occiput anterior ROP: right occiput posterior ROT: right occiput transverse
Face and brow positions
Positions for face and brow presentations describe the position of the chin Chin The anatomical frontal portion of the mandible, also known as the mentum, that contains the line of fusion of the two separate halves of the mandible (symphysis menti). This line of fusion divides inferiorly to enclose a triangular area called the mental protuberance. On each side, inferior to the second premolar tooth, is the mental foramen for the passage of blood vessels and a nerve. Melasma .
- The chin Chin The anatomical frontal portion of the mandible, also known as the mentum, that contains the line of fusion of the two separate halves of the mandible (symphysis menti). This line of fusion divides inferiorly to enclose a triangular area called the mental protuberance. On each side, inferior to the second premolar tooth, is the mental foramen for the passage of blood vessels and a nerve. Melasma is referred to as the mentum.
- Right or left mentum anterior
- Right or left mentum posterior
- Right or left mentum transverse
- Direct mentum anterior or posterior
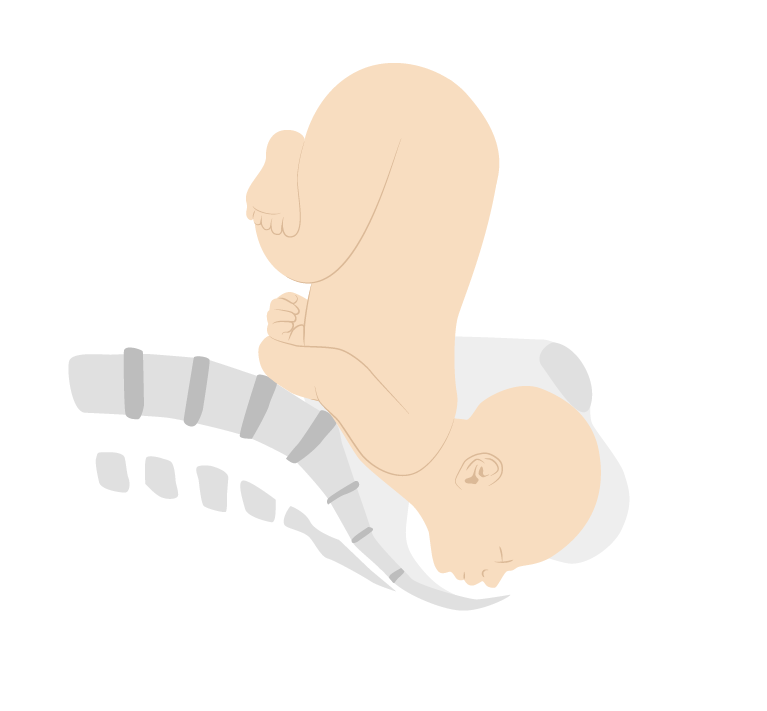
Face presentation (mentum posterior position)
Breech and shoulder positions
- Positions for breech presentations describe the position of the sacrum Sacrum Five fused vertebrae forming a triangle-shaped structure at the back of the pelvis. It articulates superiorly with the lumbar vertebrae, inferiorly with the coccyx, and anteriorly with the ilium of the pelvis. The sacrum strengthens and stabilizes the pelvis. Vertebral Column: Anatomy . Similar to other presentations, they include anterior, posterior, and transverse and right, left, and direct.
- Dorso-superior (back up)
- Dorso-inferior (back down)
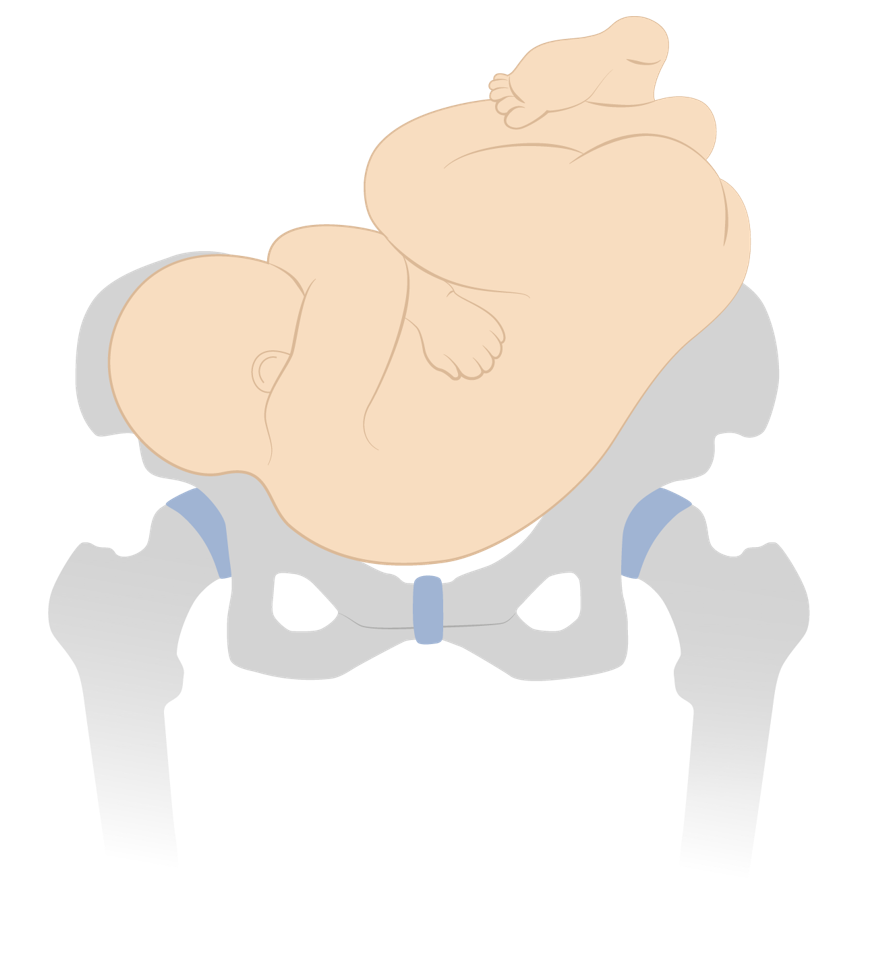
Dorso-inferior shoulder presentation
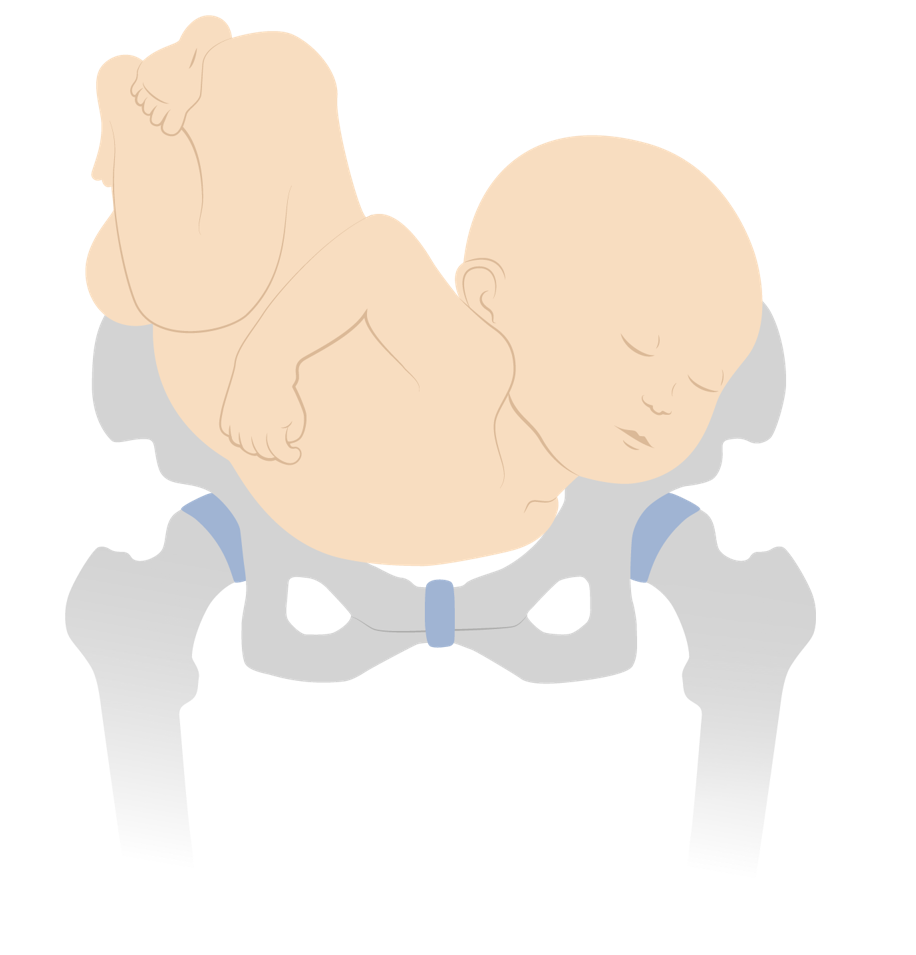
Dorso-superior shoulder presentation
Attitude and asynclitism
- Attitude: amount of flexion Flexion Examination of the Upper Limbs or extension Extension Examination of the Upper Limbs of the fetal head
- Lateral deflection of the sagittal Sagittal Computed Tomography (CT) suture to 1 side or the other
- Mild degrees of asynclitism are normal.
- More severe asynclitism increases the presenting fetal diameter and makes it more difficult for the fetal head to pass through the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
Fetal malposition
- Commonly refers to any position other than right occiput anterior, left occiput anterior, or direct occiput anterior
- All nonvertex presentations are also malpositioned.
- The terms fetal malpresentation and fetal malposition are often used interchangeably.
- The presenting diameter refers to the width of the presenting part.
- The maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy is about 10 cm at its narrowest point; the infant must orient itself so that it can fit through.
- Most commonly, the infant will move into a cephalic, vertex presentation, in 1 of the occiput anterior positions → presents the narrowest diameter
- Vertex presentation: suboccipitobregmatic diameter, approximately 9.5 cm
- Vertex presentation with deflexed head: occipitofrontal diameter, approximately 11.5 cm
- Brow presentation: occipitomental diameter, approximately 13 cm
- Face presentation: submentobregmatic diameter, approximately 9.5 cm
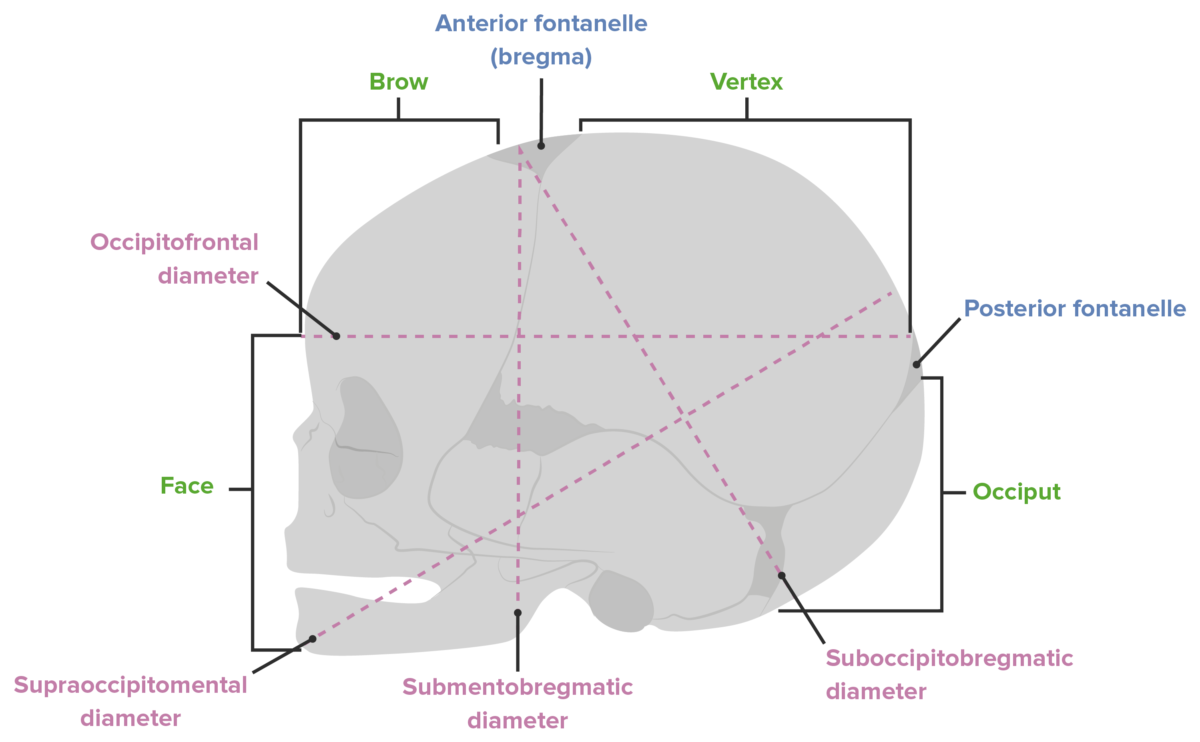
Diameters of the fetal head
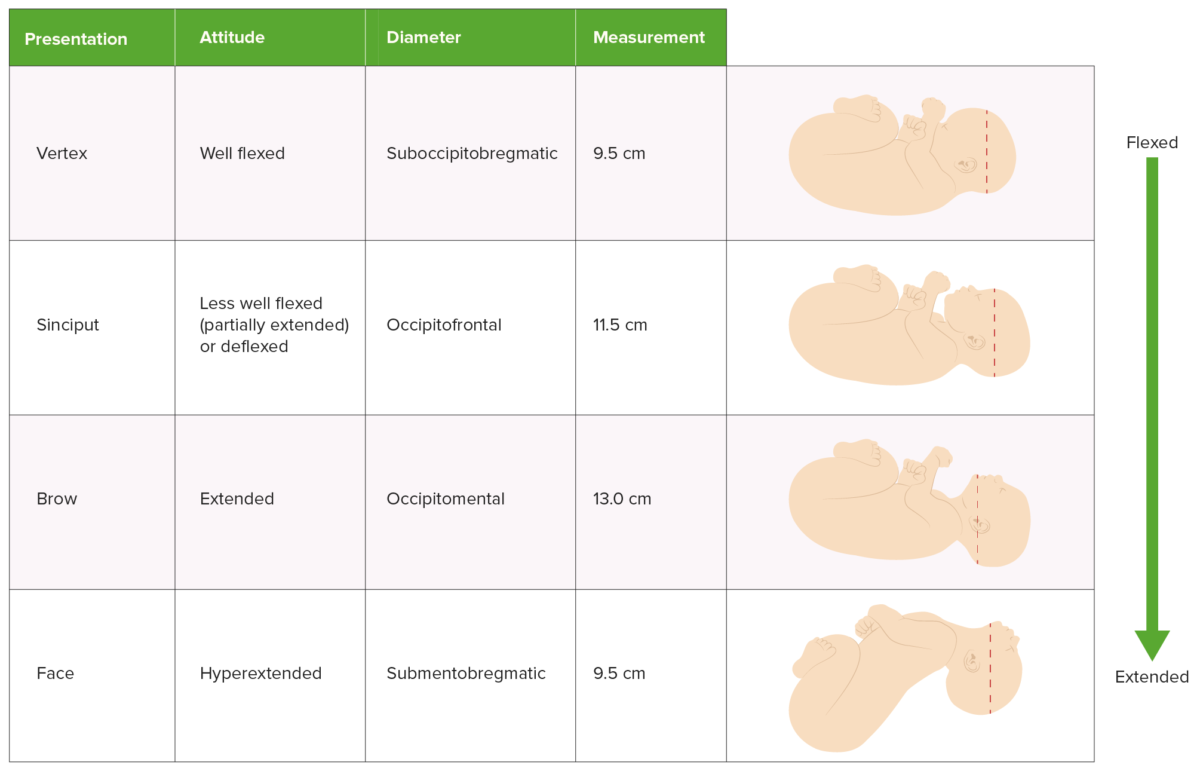
Comparison of presentation, attitude, and presenting diameter

How to establish lie, presentation, and position
Delivery is managed differently depending on the presentation and position of the infant. This information can be established in several different ways:
Leopold’s maneuvers
Ultrasonography.
- Cervical examination
- Techniques using abdominal palpation Abdominal Palpation Abdominal Examination to determine the presentation of the fetus
- The fetal head will be hard and round.
- The lower body will be bulkier, nodular, and mobile.
- The back will be hard and smooth.
- The other side (anterior surface of the fetus) will be filled with irregular, mobile fetal parts.
- Experienced providers can also estimate the fetal weight using these maneuvers.
- Bedside abdominal ultrasonography can easily identify the fetal head and its orientation Orientation Awareness of oneself in relation to time, place and person. Psychiatric Assessment .
- Quick bedside ultrasonography Bedside Ultrasonography ACES and RUSH: Resuscitation Ultrasound Protocols on admission to labor and delivery to assess fetal presentation is considered standard of care Standard of care The minimum acceptable patient care, based on statutes, court decisions, policies, or professional guidelines. Malpractice .
- The fetal head will typically encompass the entire window and appear like a large white circle (the fetal skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy ).
- Identification Identification Defense Mechanisms of the eyes can help determine position.
- It is quick and easy to perform and presents minimal risk to mother and infant.
- Allowing mothers to labor with infants in a noncephalic presentation significantly increases the risks to both of them.
Suprapubic bedside ultrasound showing the large white circle of the fetal skull, confirming a cephalic presentation F: fetal falx
Vaginal and cervical examination
- As the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy dilates, the fetal fontanelles Fontanelles Physical Examination of the Newborn can be directly palpated.
- Identifying the location of the fetal fontanelles Fontanelles Physical Examination of the Newborn allows the practitioner to establish the position.
- Insert 1–2 fingers through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy posteriorly.
- Sweep fingers along the fetal head moving anteriorly.
- This maneuver allows for identification Identification Defense Mechanisms of the sagittal Sagittal Computed Tomography (CT) suture.
- The fontanelles Fontanelles Physical Examination of the Newborn are then identified by moving along the sagittal Sagittal Computed Tomography (CT) suture.
Vertex presentations
- Expectant management
- All have high chances of successful vaginal delivery.
Compound presentations
- Observation when labor is progressing normally (many compound presentations will resolve spontaneously intrapartum).
- Can attempt to gently pinch the compound extremity trying to provoke the fetus into withdrawing the part (no good quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement evidence, but unlikely to be harmful)
- Can attempt to manually replace the compound extremity
- If labor is prolonged and the compound part remains, cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery (CD) should be performed.
- Prolonged labor
- Umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity prolapse
- Increased maternal morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status from lacerations
- Ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage of the compound part
Brow presentations
- The majority spontaneously convert to a vertex presentation.
- Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery may be required if labor is prolonged.
Face presentations
- Management depends on the position.
- Can be delivered vaginally by an experienced provider
- Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery may be required.
- Head is fully extended and unable to pass through the birth canal Birth canal Pelvis: Anatomy .
- Normally, the fetal head flexes as it passes under the pubic bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types ; however, this is impossible in an MP position.
- Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery is always required (unless the infant spontaneously rotates to a mentum anterior (MA) position).
There are 3 primary options for managing breech presentations: performing CD, attempting an external cephalic version to manually rotate the baby into a vertex presentation for attempted vaginal delivery, or a planned vaginal breech delivery (which is generally not done in the United States).
Natural history of breech presentations
Most infants will spontaneously rotate to a vertex presentation as the pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care progresses. At different gestational ages, the prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of breech presentations is:
- < 28 weeks: 20%–25%
- 32 weeks: 10%–15%
- Term (> 37 weeks): 3%
- Spontaneous version is possible even at > 40 weeks.
- Flexed fetal legs
- Polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios
- Longer umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity
- Lack of fetal/uterine anomalies
- Multiparity
Fetal risks associated with breech presentations
The following risks are associated with breech presentations in utero, regardless of mode of delivery:
- ↑ Association with congenital Congenital Chorioretinitis malformations
- Torticollis Torticollis A symptom, not a disease, of a twisted neck. In most instances, the head is tipped toward one side and the chin rotated toward the other. The involuntary muscle contractions in the neck region of patients with torticollis can be due to congenital defects, trauma, inflammation, tumors, and neurological or other factors. Cranial Nerve Palsies
- Developmental hip dysplasia
Fetal risks associated with vaginal breech delivery
The primary risk of a vaginal breech delivery is fetal head entrapment:
- The fetal body delivers, but the head remains trapped in the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy .
- Causes compression Compression Blunt Chest Trauma of the umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity running past the head (between the delivered umbilicus and the undelivered placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity )
- Leads to hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage until head is delivered → ↑ risk of fetal death
- The cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy may not be fully dilated enough to accommodate the head.
- The fetal head may not fit through the bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
- The mother’s expulsive efforts are unable to quickly deliver the head.
- Umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity prolapse during labor → requires emergent CD
- Birth injuries to the fetus (e.g., brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region injury)
Vaginal breech delivery
Vaginal breech deliveries for singleton gestations may be considered for certain low-risk women if vaginal delivery is strongly desired by the mother. In contrast, vaginal breech deliveries are done frequently for breech 2nd twins; the procedure is known as a breech extraction.
- Mothers must be fully counseled on risks.
- Mothers and infants should be monitored throughout labor with continuous electronic fetal heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology (FHR) and tocometry monitors.
- Mothers should understand that a CD will be recommended if there are signs of fetal distress or prolonged labor.
- Avoid artificial rupture of membranes to ↓ risk of cord prolapse.
- Frank or complete breech presentation with no hyperextension of the fetal head on ultrasonography
- No contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation to a vaginal birth
- No prior CDs
- Prior successful vaginal deliveries (i.e., multiparity)
- Gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care ≥ 36 weeks
- Spontaneous labor
- Normal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy shown on X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests
- Estimated fetal weight Estimated Fetal Weight Obstetric Imaging between approximately 2500 and 3500 grams (exact range varies based on clinician Clinician A physician, nurse practitioner, physician assistant, or another health professional who is directly involved in patient care and has a professional relationship with patients. Clinician–Patient Relationship )
- Immediately after delivery of the 1st twin in the cephalic presentation, the physician reaches up into the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy , manually grabs the infant’s legs, and gently guides them down through the birth canal Birth canal Pelvis: Anatomy while the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy is still fully dilated.
- ↓ Risk of head entrapment compared to singleton vaginal breech deliveries
External cephalic version
An external cephalic version (ECV) is a procedure in which the physician attempts to manually rotate the fetus from a breech to a cephalic presentation by pushing on the maternal abdomen.
- Approximately 50%–60% (higher in multiparous Multiparous A woman with prior deliveries Normal and Abnormal Labor than in nulliparous women)
- 97% of infants remained cephalic at birth.
- 86% delivered vaginally.
- Women who are candidates for ECV should be counseled on their options to attempt an ECV, or they may simply elect to schedule a CD.
- Infant is full term in case emergent CD is required because of complications from the procedure (e.g., placental abruption Placental Abruption Premature separation of the normally implanted placenta from the uterus. Signs of varying degree of severity include uterine bleeding, uterine muscle hypertonia, and fetal distress or fetal death. Antepartum Hemorrhage ).
- Better ratio of infant size to fluid level than later in pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
- Allows infant more time for spontaneous version than if the procedure was done earlier
- After a successful version, the mother can await spontaneous labor or be induced immediately, depending on the situation.
- There is still a chance that the infant may spontaneously rotate between the failed ECV and the planned CD date; therefore, presentation should always be checked immediately prior to CD.
- Another contraindication for a vaginal delivery (e.g., placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities )
- Severe oligohydramnios Oligohydramnios Oligohydramnios refers to amniotic fluid volume less than expected for the current gestational age. Oligohydramnios is diagnosed by ultrasound and defined as an amniotic fluid index (AFI) of ‰¤ 5 cm or a single deep pocket (SDP) of Oligohydramnios
- Nonreassuring fetal monitoring Fetal monitoring The primary goals of antepartum testing and monitoring are to assess fetal well-being, identify treatable situations that may cause complications, and evaluate for chromosomal abnormalities. These tests are divided into screening tests (which include cell-free DNA testing, serum analyte testing, and nuchal translucency measurements), and diagnostic tests, which provide a definitive diagnosis of aneuploidy and include chorionic villus sampling (CVS) and amniocentesis. Antepartum Testing and Monitoring prior to the procedure
- A hyperextended fetal head
- Significant fetal or uterine anomalies
- Leads to fetal and maternal hemorrhage
- An immediate CD is required.
- If the version was successful, labor should be induced immediately.
- If the version was unsuccessful, the mother should undergo immediate CD.
- Cord prolapse: can occur with PROM PROM Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, refers to the rupture of the amniotic sac before the onset of labor. Prelabor rupture of membranes may occur in term or preterm pregnancies. Prelabor Rupture of Membranes and requires immediate/emergent CD.
- Common during the procedure, but typically resolves shortly after pressure on the abdomen is released.
- If distress persists, the mother should undergo an immediate CD.
Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery
- Scheduled at 39 weeks’ gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care (WGA) if the infant is known to be in the breech presentation.
- Alternative option to attempting ECV
- Postpartum hemorrhage Postpartum hemorrhage Postpartum hemorrhage is one of the most common and deadly obstetric complications. Since 2017, postpartum hemorrhage has been defined as blood loss greater than 1,000 mL for both cesarean and vaginal deliveries, or excessive blood loss with signs of hemodynamic instability. Postpartum Hemorrhage
- Postpartum endomyometritis
- Maternal injury
- Longer recovery time postpartum
- Complications in future pregnancies (e.g., placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities , placenta accreta Placenta Accreta Abnormal placentation in which all or parts of the placenta are attached directly to the myometrium due to a complete or partial absence of decidua. It is associated with postpartum hemorrhage because of the failure of placental separation. Placental Abnormalities , uterine rupture Uterine Rupture A complete separation or tear in the wall of the uterus with or without expulsion of the fetus. It may be due to injuries, multiple pregnancies, large fetus, previous scarring, or obstruction. Antepartum Hemorrhage )
- Maternal request (mother declines ECV attempt)
- ECV contraindicated
- ECV unsuccessful
- Fetal distress during labor
Management of transverse presentations
- As with breech presentations, mothers may be offered an attempt at ECV or a CD.
- Unlike breech presentations, vaginal transverse delivery is always contraindicated.
- Hofmeyr, G.J. (2021). Overview of breech presentation. In Barss, V.A. (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/overview-of-breech-presentation
- Hofmeyr, G.J. (2021). Delivery of the singleton fetus in breech presentation. In Barss, V.A. (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/delivery-of-the-singleton-fetus-in-breech-presentation
- Hofmeyr, G.J. (2021). External cephalic version. In Barss, V.A. (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/external-cephalic-version
- Julien, S., and Galerneau, F. (2021). Face and brow presentations in labor. In Barss, V.A., (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/face-and-brow-presentations-in-labor
- Strauss, R.A., Herrera, C.A. (2021). Transverse fetal lie. In Barss, V.A., (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/transverse-fetal-lie
- Barth, W.H. (2021). Compound fetal presentation. In Barss, V.A., (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/compound-fetal-presentation
- Cunningham, F. G., Leveno, K. J., et al. (2010). Williams Obstetrics, 23rd ed., pp. 374‒382.
Study with Lecturio for
Medical School
Nursing School
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Create your free account or log in to continue reading!
Sign up now and get free access to Lecturio with concept pages, medical videos, and questions for your medical education.
Log in to your account
User Reviews
Get Premium to test your knowledge
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
Labour and Delivery Care Module: 8. Abnormal Presentations and Multiple Pregnancies
Study session 8 abnormal presentations and multiple pregnancies, introduction.
In previous study sessions of this module, you have been introduced to the definitions, signs, symptoms and stages of normal labour, and about the ‘normal’ vertex presentation of the fetus during delivery. In this study session, you will learn about the most common abnormal presentations (breech, shoulder, face or brow), their diagnostic criteria and the required actions you need to take to prevent complications developing during labour. Taking prompt action may save the life of the mother and her baby if the delivery becomes obstructed because the baby is in an abnormal presentation. We will also tell you about twin births and the complications that may result if the two babies become ‘locked’ together, preventing either of them from being born.
Learning Outcomes for Study Session 8
After studying this session, you should be able to:
8.1 Define and use correctly all of the key words printed in bold . (SAQs 8.1 and 8.2)
8.2 Describe how you would identify a fetus in the vertex presentation and distinguish this from common malpresentations and malpositions. (SAQs 8.1 and 8.2)
8.3 Describe the causes and complications for the fetus and the mother of fetal malpresentation during full term labour. (SAQ 8.3)
8.4 Describe how you would identify a multiple pregnancy and the complications that may arise. (SAQ 8.4)
8.5 Explain when and how you would refer a woman in labour due to abnormal fetal presentation or multiple pregnancy. (SAQ 8.4)
8.1 Normal and abnormal presentations
8.1.1 vertex presentation.
In about 95% of deliveries, the part of the fetus which arrives first at the mother’s pelvic brim is the highest part of the fetal head, which is called the vertex (Figure 8.1). This presentation is called the vertex presentation . Notice that the baby’s chin is tucked down towards its chest, so that the vertex is the leading part entering the mother’s pelvis. The baby’s head is said to be ‘well-flexed’ in this position.
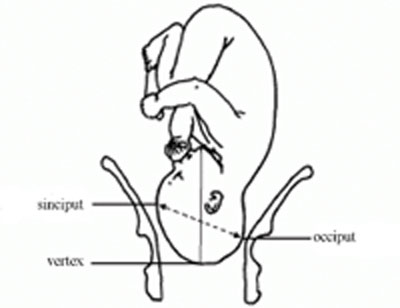
During early pregnancy, the baby is the other way up — with its bottom pointing down towards the mother’s cervix — which is called the breech presentation . This is because during its early development, the head of the fetus is bigger than its buttocks; so in the majority of cases, the head occupies the widest cavity, i.e. the fundus (rounded top) of the uterus. As the fetus grows larger, the buttocks become bigger than the head and the baby spontaneously reverses its position, so its buttocks occupy the fundus. In short, in early pregnancy, the majority of fetuses are in the breech presentation and later in pregnancy most of them make a spontaneous transition to the vertex presentation.
8.1.2 Malpresentations
You will learn about obstructed labour in Study Session 9.
When the baby presents itself in the mother’s pelvis in any position other than the vertex presentation, this is termed an abnormal presentation, or m alpresentation . The reason for referring to this as ‘abnormal’ is because it is associated with a much higher risk of obstruction and other birth complications than the vertex presentation. The most common types of malpresentation are termed breech, shoulder, face or brow. We will discuss each of these in turn later. Notice that the baby can be ‘head-down’ but in an abnormal presentation, as in face or brow presentations, when the baby’s face or forehead (brow) is the presenting part.
8.1.3 Malposition
Although it may not be so easy for you to identify this, the baby can also be in an abnormal position even when it is in the vertex presentation. In a normal delivery, when the baby’s head has engaged in the mother’s pelvis, the back of the baby’s skull (the occiput ) points towards the front of the mother’s pelvis (the pubic symphysis ), where the two pubic bones are fused together. This orientation of the fetal skull is called the occipito-anterior position (Figure 8.2a). If the occiput (back) of the fetal skull is towards the mother’s back, this occipito-posterior position (Figure 8.2b) is a vertex malposition , because it is more difficult for the baby to be born in this orientation. The good thing is that more than 90% of babies in vertex malpositions undergo rotation to the occipito-anterior position and are delivered normally.
You learned the directional positions: anterior/in front of and posterior/behind or in the back of, in the Antenatal Care Module, Part 1, Study Session 3.
Note that the fetal skull can also be tilted to the left or to the right in either the occipito-anterior or occipito-posterior positions.

8.2 Causes and consequences of malpresentations and malpositions
In the majority of individual cases it may not be possible to identify what caused the baby to be in an abnormal presentation or position during delivery. However, the general conditions that are thought to increase the risk of malpresentation or malposition are listed below:
Multiple pregnancy is the subject of Section 8.7 of this study session. You learned about placenta previa in the Antenatal Care Module, Study Session 21.
- Abnormally increased or decreased amount of amniotic fluid
- A tumour (abnormal tissue growth) in the uterus preventing the spontaneous inversion of the fetus from breech to vertex presentation during late pregnancy
- Abnormal shape of the pelvis
- Laxity (slackness) of muscular layer in the walls of the uterus
- Multiple pregnancy (more than one baby in the uterus)
- Placenta previa (placenta partly or completely covering the cervical opening).
If the baby presents at the dilating cervix in an abnormal presentation or malposition, it will more difficult (and may be impossible) for it to complete the seven cardinal movements that you learned about in Study Sessions 3 and 5. As a result, birth is more difficult and there is an increased risk of complications, including:
You learned about PROM in Study Session 17 of the Antenatal Care Module, Part 2.
- Premature rupture of the fetal membranes (PROM)
- Premature labour
- Slow, erratic, short-lived contractions
- Uncoordinated and extremely painful contractions, with slow or no progress of labour
- Prolonged and obstructed labour, leading to a ruptured uterus (see Study Sessions 9 and 10 of this Module)
- Postpartum haemorrhage (see Study Session 11)
- Fetal and maternal distress, which may lead to the death of the baby and/or the mother.
With these complications in mind, we now turn your attention to the commonest types of malpresentation and how to recognise them.
8.3 Breech presentation
In a b reech presentation , the fetus lies with its buttocks in the lower part of the uterus, and its buttocks and/or the feet are the presenting parts during delivery. Breech presentation occurs on average in 3–4% of deliveries after 34 weeks of pregnancy.
When is the breech position the normal position for the fetus?
During early pregnancy the baby’s bottom points down towards the mother’s cervix, and its head (the largest part of the fetus at this stage of development) occupies the fundus (rounded top) of the uterus, which is the widest part of the uterine cavity.
8.3.1 Causes of breech presentation
You can see a transverse lie in Figure 8.7 later in this study session.
In the majority of cases there is no obvious reason why the fetus should present by the breech at full term. In practice, what is commonly observed is the association of breech presentation at delivery with a transverse lie earlier in the pregnancy, i.e. the fetus lies sideways across the mother’s abdomen, facing a sideways implanted placenta. It is thought that when the placenta is in front of the baby’s face, it may obstruct the normal process of inversion, when the baby turns head-down as it gets bigger during the pregnancy. As a result, the fetus turns in the other direction and ends in the breech presentation. Some other circumstances that are thought to favour a breech presentation during labour include:
- Premature labour, beginning before the baby undergoes spontanous inversion from breech to vertex presentation
- Multiple pregnancy, preventing the normal inversion of one or both babies
- Polyhydramnios: excessive amount of amniotic fluid, which makes it more difficult for the fetal head to ‘engage’ with the mother’s cervix (polyhydramnios is pronounced ‘poll-ee-hy-dram-nee-oss’. Hydrocephaly is pronounced ‘hy-droh-keff-all-ee’)
- Hydrocephaly (‘water on the brain’) i.e. an abnormally large fetal head due to excessive accumulation of fluid around the brain
- Placenta praevia
- Breech delivery in the previous pregnancy
- Abnormal formation of the uterus.
8.3.2 Diagnosis of breech presentation
On abdominal palpation the fetal head is found above the mother’s umbilicus as a hard, smooth, rounded mass, which gently ‘ballots’ (can be rocked) between your hands.
Why do you think a mass that ‘ballots’ high up in the abdomen is a sign of breech presentation? (You learned about this in Study Session 11 of the Antenatal Care Module.)
The baby’s head can ‘rock’ a little bit because of the flexibility of the baby’s neck, so if there is a rounded, ballotable mass above the mother’s umbilicus it is very likely to be the baby’s head. If the baby was ‘bottom-up’ (vertex presentation) the whole of its back will move of you try to rock the fetal parts at the fundus (Figure 8.3).
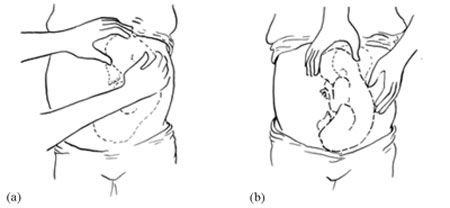
Once the fetus has engaged and labour has begun, the breech baby’s buttocks can be felt as soft and irregular on vaginal examination. They feel very different to the relatively hard rounded mass of the fetal skull in a vertex presentation. When the fetal membranes rupture, the buttocks and/or feet can be felt more clearly. The baby’s anus may be felt and fresh thick, dark meconium may be seen on your examining finger. If the baby’s legs are extended, you may be able to feel the external genitalia and even tell the sex of the baby before it is born.
8.3.3 Types of breech presentation
There are three types of breech presentation, as illustrated in Figure 8.4. They are:
- Complete breech is characterised by flexion of the legs at both hips and knee joints, so the legs are bent underneath the baby.
- Frank breech is the commonest type of breech presentation, and is characterised by flexion at the hip joints and extension at the knee joints, so both the baby’s legs point straight upwards.
- Footling breech is when one or both legs are extended at the hip and knee joint and the baby presents ‘foot first’.
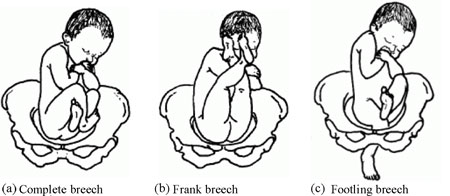
8.3.4 Risks of breech presentation
Regardless of the type of breech presentation, there are significant associated risks to the baby. They include:
- The fetal head gets stuck (arrested) before delivery
- Labour becomes obstructed when the fetus is disproportionately large for the size of the maternal pelvis
- Cord prolapse may occur, i.e. the umbilical cord is pushed out ahead of the baby and may get compressed against the wall of the cervix or vagina
- Premature separation of the placenta (placental abruption)
- Birth injury to the baby, e.g. fracture of the arms or legs, nerve damage, trauma to the internal organs, spinal cord damage, etc.
A breech birth may also result in trauma to the mother’s birth canal or external genitalia through being overstretched by the poorly fitting fetal parts.
Cord prolapse in a normal (vertex) presentation was illustrated in Study Session 17 of the Antenatal Care Module, and placental abruption was covered in Study Session 21.
What will be the effect on the baby if it gets stuck, the labour is obstructed, the cord prolapses, or placental abruption occurs?
The result will be hypoxia , i.e. it will be deprived of oxygen, and may suffer permanent brain damage or die.
You learned about the causes and consequences of hypoxia in the Antenatal Care Module.
8.4 Face presentation
Face presentation occurs when the baby’s neck is so completely extended (bent backwards) that the occiput at the back of the fetal skull touches the baby’s own spine (see Figure 8.5). In this position, the baby’s face will present to you during delivery.
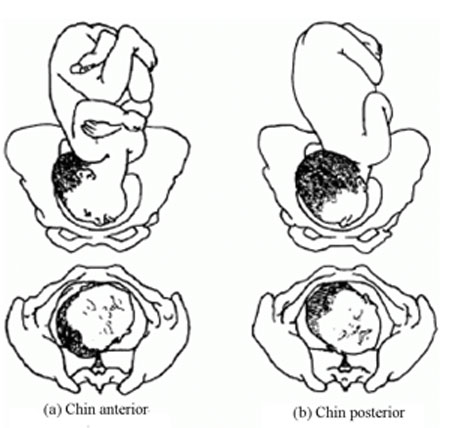
Refer the mother if a baby in the chin posterior face presentation does not rotate and the labour is prolonged.
The incidence of face presentation is about 1 in 500 pregnancies in full term labours. In Figure 8.5, you can see how flexed the head is at the neck. Babies who present in the ‘chin posterior’ position (on the right in Figure 8.5) usually rotate spontaneously during labour, and assume the ‘chin anterior’ position, which makes it easier for them to be born. However, they are unlikely to be delivered vaginally if they fail to undergo spontaneous rotation to the chin anterior position, because the baby’s chin usually gets stuck against the mother’s sacrum (the bony prominence at the back of her pelvis). A baby in this position will have to be delivered by caesarean surgery.
8.4.1 Causes of face presentation
The causes of face presentation are similar to those already described for breech births:
- Laxity (slackness) of the uterus after many previous full-term pregnancies
- Multiple pregnancy
- Polyhydramnios (excessive amniotic fluid)
- Congenital abnormality of the fetus (e.g. anencephaly, which means no or incomplete skull bones)
- Abnormal shape of the mother’s pelvis.
8.4.2 Diagnosis of face presentation
Face presentation may not be easily detected by abdominal palpation, especially if the chin is in the posterior position. On abdominal examination, you may feel irregular shapes, formed because the fetal spine is curved in an ‘S’ shape. However, on vaginal examination, you can detect face presentation because:
- The presenting part will be high, soft and irregular.
- When the cervix is sufficiently dilated, you may be able to feel parts of the face, such as the orbital ridges above the eyes, the nose or mouth, gums, or bony chin.
- If the membranes are ruptured, the baby may suck your examining finger!
But as labour progresses, the baby’s face becomes o edematous (swollen with fluid), making it more difficult to distinguish from the soft shape you will feel in a breech presentation.
8.4.3 Complications of face presentation
Complications for the fetus include:
- Obstructed labour and ruptured uterus
- Cord prolapse
- Facial bruising
- Cerebral haemorrhage (bleeding inside the fetal skull).
8.5 Brow presentation

In brow presentation , the baby’s head is only partially extended at the neck (compare this with face presentation), so its brow (forehead) is the presenting part (Figure 8.6). This presentation is rare, with an incidence of 1 in 1000 deliveries at full term.
8.5.1 Possible causes of brow presentation
You have seen all of these factors before, as causes of other malpresentations:
- Lax uterus due to repeated full term pregnancy
- Polyhydramnios
8.5.2 Diagnosis of brow presentation
Brow presentation is not usually detected before the onset of labour, except by very experienced birth attendants. On abdominal examination, the head is high in the mother’s abdomen, appears unduly large and does not descend into the pelvis, despite good uterine contractions. On vaginal examination, the presenting part is high and may be difficult to reach. You may be able to feel the root of the nose, eyes, but not the mouth, tip of the nose or chin. You may also feel the anterior fontanel, but a large caput (swelling) towards the front of the fetal skull may mask this landmark if the woman has been in labour for some hours.
Recall the appearance of a normal caput over the posterior fontanel shown in Figure 4.4 earlier in this Module.
8.5.3 Complications of brow presentation
The complications of brow presentation are much the same as for other malpresentations:
- Cerebral haemorrhage.
Which are you more likely to encounter — face or brow presentations?
Face presentation, which occurs in 1 in 500 full term labours. Brow presentation is more rare, at 1 in 1,000 full term labours.
8.6 Shoulder presentation
Shoulder presentation is rare at full term, but may occur when the fetus lies transversely across the uterus (Figure 8.7), if it stopped part-way through spontaneous inversion from breech to vertex, or it may lie transversely from early pregnancy. If the baby lies facing upwards, its back may be the presenting part; if facing downwards its hand may emerge through the cervix. A baby in the transverse position cannot be born through the vagina and the labour will be obstructed. Refer babies in shoulder presentation urgently.

8.6.1 Causes of shoulder presentation
Causes of shoulder presentation could be maternal or fetal factors.
Maternal factors include:
- Lax abdominal and uterine muscles: most often after several previous pregnancies
- Uterine abnormality
- Contracted (abnormally narrow) pelvis.
Fetal factors include:
- Preterm labour
- Placenta previa.
What do ‘placenta previa’ and ‘polyhydramnios’ indicate?
Placenta previa is when the placenta is partly or completely covering the cervical opening. Polyhydramnios is an excess of amniotic fluid. They are both potential causes of malpresentation.
8.6.2 Diagnosis of shoulder presentation
On abdominal palpation, the uterus appears broader and the height of the fundus is less than expected for the period of gestation, because the fundus is not occupied by either the baby’s head or buttocks. You can usually feel the head on one side of the mother’s abdomen. On vaginal examination, in early labour, the presenting part may not be felt, but when the labour is well progressed, you may feel the baby’s ribs. When the shoulder enters the pelvic brim, the baby’s arm may prolapse and become visible outside the vagina.
8.6.3 Complications of shoulder presentation
Complications include:
- Trauma to a prolapsed arm
- Fetal hypoxia and death.
Remember that a shoulder presentation means the baby cannot be born through the vagina; if you detect it in a woman who is already in labour, refer her urgently to a higher health facility.
8.7 Multiple pregnancy
In this section, we turn to the subject of multiple pregnancy , when there is more than one fetus in the uterus. More than 95% of multiple pregnancies are twins (two fetuses), but there can also be triplets (three fetuses), quadruplets (four fetuses), quintuplets (five fetuses), and other higher order multiples with a declining chance of occurrence. The spontaneous occurrence of twins varies by country : it is lowest in East Asia n countries like Japan and China (1 out of 1000 pregnancies are fraternal or non-identical twins), and highest in black Africans , particularly in Nigeria , where 1 in 20 pr egnancies are fraternal twins. In general, compared to single babies, multiple pregnancies are highly associated with early pregnancy loss and high perinatal mortality, mainly due to prematurity.
8.7.1 Types of twin pregnancy
Twins may be identical (monozygotic) or non-identical and fraternal (dizigotic). Monozygotic twins develop from a single fertilised ovum (the zygote), so they are always the same sex and they share the same placenta . By contrast, dizygotic twins develop from two different zygotes, so they can have the same or different sex, and they have separate placenta s . Figure 8.8 shows the types of twin pregnancy and the processes by which they are formed.

8.7.2 Diagnosis of twin pregnancy
On abdominal examination you may notice that:
- The size of the uterus is larger than the expected for the period for gestation.
- The uterus looks round and broad, and fetal movement may be seen over a large area. (The shape of the uterus at term in a singleton pregnancy in the vertex presentation appears heart-shaped rounder at the top and narrower at the bottom.)
- Two heads can be felt.
- Two fetal heart beats may be heard if two people listen at the same time, and they can detect at least 10 beats different (Figure 8.6).
- Ultrasound examination can make an absolute diagnosis of twin pregnancy.

8.7.3 Consequences of twin pregnancy
Women who are pregnant with twins are more prone to suffer with the minor disorders of pregnancy, like morning sickness, nausea and heartburn. Twin pregnancy is one cause of hyperemesis gravidarum (persistent, severe nausea and vomiting). Mothers of twins are also more at risk of developing iron and folate-deficiency anaemia during pregnancy.
Can you suggest why anaemia is a greater risk in multiple pregnancies?
The mother has to supply the nutrients to feed two (or more) babies; if she is not getting enough iron and folate in her diet, or through supplements, she will become anaemic.
Other complications include the following:
- Pregnancy-related hypertensive disorders like pre-eclampsia and eclampsia are more common in twin pregnancies.
- Pressure symptoms may occur in late pregnancy due to the increased weight and size of the uterus.
- Labour often occurs spontaneously before term, with p remature delivery or premature rupture of membranes (PROM) .
- Respiratory deficit ( shortness of breath, because of fast growing uterus) is another common problem.
Twin babies may be small in comparison to their gestational age and more prone to the complications associated with low birth weight (increased vulnerability to infection, losing heat, difficulty breastfeeding).
You will learn about low birth weight babies in detail in the Postnatal Care Module.
- Malpresentation is more common in twin pregnancies, and they may also be ‘locked’ at the neck with one twin in the vertex presentation and the other in breech. The risks associated with malpresentations already described also apply: prolapsed cord, poor uterine contraction, prolonged or obstructed labour, postpartum haemorrhage, and fetal hypoxia and death.
- Conjoined twins (fused twins, joined at the head, chest, or abdomen, or through the back) may also rarely occur.
8.8 Management of women with malpresentation or multiple pregnancy
As you have seen in this study session, any presentation other than vertex has its own dangers for the mother and baby. For this reason, all women who develop abnormal presentation or multiple pregnancy should ideally have skilled care by senior health professionals in a health facility where there is a comprehensive emergency obstetric service. Early detection and referral of a woman in any of these situations can save her life and that of her baby.
What can you do to reduce the risks arising from malpresentation or multiple pregnancy in women in your care?
During focused antenatal care of the pregnant women in your community, at every visit after 36 weeks of gestation you should check for the presence of abnormal fetal presentation. If you detect abnormal presentation or multiple pregnancy, you should refer the woman before the onset of labour.
Summary of Study Session 8
In Study Session 8, you learned that:
- During early pregnancy, babies are naturally in the breech position, but in 95% of cases they spontaneously reverse into the vertex presentation before labour begins.
- Malpresentation or malposition of the fetus at full term increases the risk of obstructed labour and other birth complications.
- Common causes of malpresentations/malpositions include: excess amniotic fluid, abnormal shape and size of the pelvis; uterine tumour; placenta praevia; slackness of uterine muscles (after many previous pregnancies); or multiple pregnancy.
- Common complications include: premature rupture of membranes, premature labour, prolonged/obstructed labour; ruptured uterus; postpartum haemorrhage; fetal and maternal distress which may lead to death.
- Vertex malposition is when the fetal head is in the occipito-posterior position — i.e. the back of the fetal skull is towards the mother’s back instead of pointing towards the front of the mother’s pelvis. 90% of vertex malpositions rotate and deliver normally.
- Breech presentation (complete, frank or footling) is when the baby’s buttocks present during labour. It occurs in 3–4% of labours after 34 weeks of pregnancy and may lead to obstructed labour, cord prolapse, hypoxia, premature separation of the placenta, birth injury to the baby or to the birth canal.
- Face presentation is when the fetal head is bent so far backwards that the face presents during labour. It occurs in about 1 in 500 full term labours. ‘Chin posterior’ face presentations usually rotate spontaneously to the ‘chin anterior’ position and deliver normally. If rotation does not occur, a caesarean delivery is likely to be necessary.
- Brow presentation is when the baby’s forehead is the presenting part. It occurs in about 1 in 1000 full term labours and is difficult to detect before the onset of labour. Caesarean delivery is likely to be necessary.
- Shoulder presentation occurs when the fetal lie during labour is transverse. Once labour is well progressed, vaginal examination may feel the baby’s ribs, and an arm may sometimes prolapse. Caesarean delivery is always required unless a doctor or midwife can turn the baby head-down.
- Multiple pregnancies are always at high risk of malpresentation. Mothers need greater antenatal care, and twins are more prone to complications associated with low birth weight and prematurity.
- Any presentation other than vertex after 34 weeks of gestation is considered as high risk to the mother and to her baby. Do not attempt to turn a malpresenting or malpositioned baby! Refer the mother for emergency obstetric care.
Self-Assessment Questions (SAQs) for Study Session 8
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 8.1 (tests Learning Outcomes 8.1, 8.2 and 8.4)
Which of the following definitions are true and which are false? Write down the correct definition for any which you think are false.
A Fundus — the ‘rounded top’ and widest cavity of the uterus.
B Complete breech — where the legs are bent at both hips and knee joints and are folded underneath the baby.
C Frank breech — where the breech is so difficult to treat that you have to be very frank and open with the mother about the difficulties she will face in the birth.
D Footling breech — when one or both legs are extended so that the baby presents ‘foot first’.
E Hypoxia — the baby gets too much oxygen.
F Multiple pregnancy — when a mother has had many babies previously.
G Monozygotic twins — develop from a single fertilised ovum (the zygote). They can be different sexes but they share the same placenta.
H Dizygotic twins — develop from two zygotes. They have separate placentas, and can be of the same sex or different sexes.
A is true. The fundus is the ‘rounded top’ and widest cavity of the uterus.
B is true. Complete breech is where the legs are bent at both hips and knee joints and are folded underneath the baby.
C is false . A frank breech is the most common type of breech presentation and is when the baby’s legs point straight upwards (see Figure 8.4).
D is true. A footling breech is when one or both legs are extended so that the baby presents ‘foot first’.
E is false . Hypoxia is when the baby is deprived of oxygen and risks permanent brain damage or death.
F is false. Multiple pregnancy is when there is more than one fetus in the uterus.
G is false. Monozygotic twins develop from a single fertilised ovum (the zygote), and they are always the same sex , as well as sharing the same placenta.
H is true. Dizygotic twins develop from two zygotes, have separate placentas, and can be of the same or different sexes.
SAQ 8.2 (tests Learning Outcomes 8.1 and 8.2)
What are the main differences between normal and abnormal fetal presentations? Use the correct medical terms in bold in your explanation.
In a normal presentation, the vertex (the highest part of the fetal head) arrives first at the mother’s pelvic brim, with the occiput (the back of the baby’s skull) pointing towards the front of the mother’s pelvis (the pubic symphysis ).
Abnormal presentations are when there is either a vertex malposition (the occiput of the fetal skull points towards the mother’s back instead towards of the pubic symphysis), or a malpresentation (when anything other than the vertex is presenting): e.g. breech presentation (buttocks first); face presentation (face first); brow presentation (forehead first); and shoulder presentation (transverse fetal).
SAQ 8.3 (tests Learning Outcomes 8.3 and 8.5)
- a. List the common complications of malpresentations or malposition of the fetus at full term.
- b. What action should you take if you identify that the fetus is presenting abnormally and labour has not yet begun?
- c. What should you not attempt to do?
- a. The common complications of malpresentation or malposition of the fetus at full term include: premature rupture of membranes, premature labour, prolonged/obstructed labour; ruptured uterus; postpartum haemorrhage; fetal and maternal distress which may lead to death.
- b. You should refer the mother to a higher health facility – she may need emergency obstetric care.
- c. You should not attempt to turn the baby by hand. This should only be attempted by a specially trained doctor or midwife and should only be done at a health facility.
SAQ 8.4 (tests Learning Outcomes 8.4 and 8.5)
A pregnant woman moves into your village who is already at 37 weeks gestation. You haven’t seen her before. She tells you that she gave birth to twins three years ago and wants to know if she is having twins again this time.
- a. How would you check this?
- b. If you diagnose twins, what would you do to reduce the risks during labour and delivery?
- Is the uterus larger than expected for the period of gestation?
- What is its shape – is it round (indicative of twins) or heart-shaped (as in a singleton pregnancy)?
- Can you feel more than one head?
- Can you hear two fetal heartbeats (two people listening at the same time) with at least 10 beats difference?
- If there is access to a higher health facility, and you are still not sure, try and get the woman to it for an ultrasound scan.
- Be extra careful to check that the mother is not anaemic.
- Encourage her to rest and put her feet up to reduce the risk of increased blood pressure or swelling in her legs and feet.
- Be alert to the increased risk of pre-eclampsia.
- Expect her to go into labour before term, and be ready to get her to the health facility before she goes into labour, going with her if at all possible.
- Get in early touch with that health facility to warn them to expect a referral from you.
- Make sure that transport is ready to take her to a health facility when needed.
Except for third party materials and/or otherwise stated (see terms and conditions ) the content in OpenLearn is released for use under the terms of the Creative Commons Attribution-NonCommercial-Sharealike 2.0 licence . In short this allows you to use the content throughout the world without payment for non-commercial purposes in accordance with the Creative Commons non commercial sharealike licence. Please read this licence in full along with OpenLearn terms and conditions before making use of the content.
When using the content you must attribute us (The Open University) (the OU) and any identified author in accordance with the terms of the Creative Commons Licence.
The Acknowledgements section is used to list, amongst other things, third party (Proprietary), licensed content which is not subject to Creative Commons licensing. Proprietary content must be used (retained) intact and in context to the content at all times. The Acknowledgements section is also used to bring to your attention any other Special Restrictions which may apply to the content. For example there may be times when the Creative Commons Non-Commercial Sharealike licence does not apply to any of the content even if owned by us (the OU). In these stances, unless stated otherwise, the content may be used for personal and non-commercial use. We have also identified as Proprietary other material included in the content which is not subject to Creative Commons Licence. These are: OU logos, trading names and may extend to certain photographic and video images and sound recordings and any other material as may be brought to your attention.
Unauthorised use of any of the content may constitute a breach of the terms and conditions and/or intellectual property laws.
We reserve the right to alter, amend or bring to an end any terms and conditions provided here without notice.
All rights falling outside the terms of the Creative Commons licence are retained or controlled by The Open University.
Head of Intellectual Property, The Open University
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
External cephalic version.
Meaghan M. Shanahan ; Daniel J. Martingano ; Caron J. Gray .
Affiliations
Last Update: December 13, 2023 .
- Continuing Education Activity
In carefully selected patients, an external cephalic version (ECV) may be an alternative to cesarean delivery for fetal malpresentation at term. ECV is a noninvasive procedure that manipulates fetal position through the abdominal wall of the gravida. With the global cesarean section rate reaching 34%, fetal malpresentation ranks as the third most common indication for cesarean delivery, accounting for nearly 17% of cases. Studies suggest a 60% mean success rate for ECV, emphasizing its cost-effectiveness and potential to decrease cesarean delivery rates significantly. While particularly crucial in resource-limited settings where access to medical services during labor is constrained or cesarean delivery is unavailable or unsafe, ECV presents a viable option to improve rates of vaginal delivery in singleton gestations in all settings.
This activity reviews the indications, contraindications, necessary equipment, preferred personnel, procedural technique, risks, and benefits of ECV and highlights the role of the interprofessional team in caring for patients who may benefit from this procedure.
- Select suitable candidates for an external cephalic version based on their clinical history and presentation.
- Screen patients effectively regarding the risks and benefits of an external cephalic version.
- Apply best practices when performing an external cephalic version.
- Develop and implement effective interpersonal team strategies to improve outcomes for patients undergoing external cephalic version.
- Introduction
The global cesarean section rate has increased from approximately 23% to 34% in the past decade. Fetal malpresentation is now the third-most common indication for cesarean delivery, encompassing nearly 17% of cases. Almost one-fourth of all fetuses are in a breech presentation at 28 weeks gestational age; this number decreases to between 3% and 4% at term. In current clinical practice, most pregnancies with a breech fetus are delivered by cesarean section.
Individual and institutional efforts are increasing to reduce the overall cesarean delivery rate, particularly for nulliparous patients with term, singleton, and vertex gestations. [1] [2] An alternative to cesarean delivery for fetal malpresentation at term is an external cephalic version (ECV), a procedure to correct fetal malpresentation. ECV may be indicated when the fetus is breech or in an oblique or transverse lie after 37 0/7 weeks gestation. [3] The overall success rate for ECV approaches 60%, is cost-effective, and can lead to decreased cesarean delivery rates. [4] ECV is of particular importance in resource-poor environments, where patients may have limited access to medical services during labor and delivery or where cesarean delivery is unavailable or unsafe.
- Anatomy and Physiology
ECV can be attempted when managing breech presentations or fetuses with a transverse or oblique lie. Three types of breech presentation are established concerning fetal attitude: complete, frank, and incomplete, which is sometimes referred to as footling breech. In complete breech, the fetal pelvis engages with the maternal pelvic inlet, and the fetal hips and knees are flexed. In frank breech, the fetal pelvis engages with the maternal pelvic inlet, the fetal hips are flexed, the knees are extended, and the feet are near the head. In incomplete or footling breech, one (single footling) or both (double footling) feet are extended below the level of the fetal pelvis.
A fetus with a transverse lie is positioned with their long axis, defined as the spine, at a right angle to the long axis of the gravida. The fetal head may be to the right or left side of the maternal spine. The fetus may be facing up or down. The long axis of the fetus characterizes an oblique lie at any angle to the maternal long axis that is not 90°. An oblique fetus is usually positioned with their head in the right or left lower quadrants, although this is not universal.
- Indications
ECV may be indicated in carefully selected patients. The fetus must be at or beyond 36 0/7 weeks of gestation with malpresentation, and there must be no absolute contraindications to vaginal delivery, such as placenta previa, vasa previa, or a history of classical cesarean delivery. Fetal status must be reassuring, and preprocedural nonstress testing is recommended. While ECV may be performed as early as 36 0/7 weeks gestation, many practitioners will delay ECV until 37 0/7 weeks gestation to ensure delivery of a term fetus.
ECV is more successful in multigravidas, those with a complete breech or transverse or oblique presentation, an unengaged presenting part, adequate amniotic fluid, and a posterior placenta. Nulliparous patients and those with an anterior, lateral, or cornual placenta have lower success rates. Patients with advanced cervical dilatation, obesity, oligohydramnios, or ruptured membranes also have lower success rates. Additionally, if the fetus weighs less than 2500 g, is at a low station with an engaged presenting part, is frank breech, or the spine is posterior, the success of ECV is decreased. [5]
Evidence supports the use of parenteral tocolysis, most often with the beta-2-agonist medication terbutaline, to improve the success of ECV; most studies evaluating the various aspects of ECV aspects include using a tocolytic agent. [6] [7] [8] [9] Data regarding the improved success of ECV incorporating regional anesthesia is inconsistent.
- Contraindications
Any contraindication to vaginal delivery would also be a contraindication to ECV. These contraindications include but are not limited to placenta previa, vasa previa, active genital herpes outbreak, or a history of classical cesarean delivery. A history of low transverse cesarean delivery is not an absolute contraindication to ECV. [10] The overall success rate of ECV in patients with a previous cesarean birth ranges from 50% to 84%; no cases of uterine rupture during ECV were reported in the four trials evaluating this outcome in patients with a prior cesarean delivery. [11] [12] [13] [14]
Antepartum ECV is contraindicated in multiple gestations, although it can be utilized for twin gestations that would otherwise be suitable candidates for breech extraction. [15] [16]
Patients with severe oligohydramnios, nonreassuring fetal monitoring, a hyperextended fetal head, significant fetal or uterine anomaly, fetal growth restriction, and maternal hypertension carry a low likelihood of successful ECV and a significantly increased risk of poor fetal outcomes; ECV in such situations requires careful consideration.
If a gravida who is otherwise a suitable candidate for ECV presents in early labor with fetal malpresentation, ECV may be a reasonable option if the presenting part is unengaged, the amniotic fluid index is within the normal range, and there are no contraindications to ECV or vaginal delivery. Data from the Nationwide Inpatient Sample from 1998 to 2011 noted a success rate of 65% for ECV performed in carefully selected patients during the admission for delivery. [17] ECV performed in this circumstance resulted in a significantly lower cesarean birth rate and hospital stay of greater than 7 days compared to patients with a persistent breech presentation at the time of delivery. [17]
External cephalic versions should be attempted only in settings where cesarean delivery services are readily available. Therefore, the required equipment for ECV includes all such requirements for cesarean delivery, including anesthesia services. Access to tocolytic agents, bedside ultrasonography, and external fetal heart rate monitoring equipment is also required. Following ECV, fetal status must be assessed; nonstress testing is preferred. If nonstress testing is unavailable, Doppler indices of the umbilical artery, middle cerebral artery, and ductus venosus may be performed. [18]
The personnel typically required to perform an ECV include:
- Obstetrician
- Labor and delivery nurse.
ECV may only be performed in a setting where cesarean delivery services are readily available. Personnel typically required for cesarean delivery include:
- Surgical first assistant
- Anesthesia personnel
- Surgical technician or operating room nurse
- Circulating or operating room nurse
- Pediatric personnel
- Note: for cesarean delivery, labor and delivery nurses may serve as surgical technicians, circulating, or operating room roles.
- Preparation
Before attempting ECV, informed consent must be obtained; this should include tocolysis and neuraxial analgesia if those procedures will be performed. Some clinicians will obtain consent from the patient for potential emergency cesarean delivery at this time, although this practice is not universal. Additionally, an ultrasound examination should be performed to verify fetal presentation, exclude fetal and uterine anomalies, locate the placental position, and evaluate the amniotic fluid index. Many clinicians will evaluate preprocedural fetal status with a nonstress test.
The current evidence supports the administration of terbutaline 0.25mg subcutaneously 15 to 30 minutes before the ECV but does not support using calcium channel blockers or nitroglycerin for preprocedural tocolysis. [19] While multiple studies report the increased success of ECV in patients who are administered epidural or spinal neuraxial anesthesia, overall data is insufficient to warrant a universal recommendation; neuraxial anesthesia may improve success rates for ECV in situations where tocolysis alone was unsuccessful. [20]
- Technique or Treatment
The gravida should be supine with a leftward tilt using a wedge support to relieve pressure on the great vessels. ECV is best performed using a 2-handed approach.
If the fetal presentation is breech, lift the breech out of the pelvis with one hand and apply downward pressure to the posterior fetal head to attempt a forward roll. If a forward roll is unsuccessful, a backward roll can be attempted. If the fetus is in either a transverse or oblique presentation, similar manipulation of the fetus is used to try to move the fetal head to the pelvis. [21]
Fetal well-being should be evaluated intermittently with Doppler or real-time ultrasonography during ECV. ECV should be abandoned if there is significant fetal bradycardia, patient discomfort, or if a version is not achieved easily. After a successful or unsuccessful ECV, external fetal heart rate monitoring should be performed for 30 to 60 minutes. If the gravida is Rh negative, anti-D immune globulin should be administered.
Immediate induction of labor to minimize reversion is not recommended. If the initial attempt at ECV is unsuccessful, additional attempts can be made during the same admission or at a later date.
- Complications
Complications of ECV are rare and occur in only 1% to 2% of attempts. The most common complication associated with ECV is fetal heart rate abnormalities, particularly bradycardia, occurring at a rate of 4.7% to 20%; these abnormalities usually are transient and improve upon completion or abandonment of the procedure.
More severe complications of ECV occur at a rate of less than 1% and include premature rupture of membranes, cord prolapse, vaginal bleeding, placental abruption, fetomaternal hemorrhage, emergent cesarean delivery, and stillbirth. Many of these rare complications require emergent cesarean delivery; some clinicians choose to perform ECV in the operating room, although this is neither necessary nor universal. [22]
ECV is associated with changes in Doppler indices that may reflect decreased placental perfusion. It appears these changes are short-lived and have no detrimental effects on the outcomes of uncomplicated pregnancies. A recent prospective study investigating the effects of ECV on fetal circulation in the antepartum period noted no differences in the Doppler evaluation of the middle cerebral artery or ductus venosus; all studied patients remained stable and were discharged home after the procedure. [18]
- Clinical Significance
Some data indicate that only 20% to 30% of eligible candidates are offered ECV. [23] Patients who undergo a successful ECV procedure have a lower cesarean delivery rate than patients who do not but are still at a higher risk of cesarean delivery than patients with cephalic fetuses who do not require ECV. ECV is cost-effective if the probability of a successful ECV exceeds 32%. Overall, ECV is successful in 58% of attempts, reduces the risk for CS by two-thirds, and enables 80% of these patients to deliver vaginally. [24]
- Enhancing Healthcare Team Outcomes
ECV is not a benign procedure and is most successful when performed under the care of an interprofessional team. Labor and delivery nurses play an integral role in the success of ECV as they frequently assist in the procedure, prepare the patient for ECV, and implement external fetal monitoring before, during, and after the procedure. Additionally, the support of emergent operating room staff promotes the safe delivery of a healthy fetus should complications arise during the ECV procedure. Clear and concise anticipatory interprofessional communication improves safety and outcomes for the gravida and the fetus should complications occur.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Meaghan Shanahan declares no relevant financial relationships with ineligible companies.
Disclosure: Daniel Martingano declares no relevant financial relationships with ineligible companies.
Disclosure: Caron Gray declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Shanahan MM, Martingano DJ, Gray CJ. External Cephalic Version. [Updated 2023 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Value of routine ultrasound examination at 35-37 weeks' gestation in diagnosis of non-cephalic presentation. [Ultrasound Obstet Gynecol. 2020] Value of routine ultrasound examination at 35-37 weeks' gestation in diagnosis of non-cephalic presentation. De Castro H, Ciobanu A, Formuso C, Akolekar R, Nicolaides KH. Ultrasound Obstet Gynecol. 2020 Feb; 55(2):248-256.
- External cephalic version at 38 weeks' gestation at a specialized German single center. [PLoS One. 2021] External cephalic version at 38 weeks' gestation at a specialized German single center. Zielbauer AS, Louwen F, Jennewein L. PLoS One. 2021; 16(8):e0252702. Epub 2021 Aug 30.
- External cephalic version in singleton pregnancies at term: a retrospective analysis. [Gynecol Obstet Invest. 2008] External cephalic version in singleton pregnancies at term: a retrospective analysis. Zeck W, Walcher W, Lang U. Gynecol Obstet Invest. 2008; 66(1):18-21. Epub 2008 Jan 30.
- Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - External Cephalic Version and other Interventions to turn Breech Babies to Cephalic Presentation]. [Gynecol Obstet Fertil Senol. 2...] Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - External Cephalic Version and other Interventions to turn Breech Babies to Cephalic Presentation]. Ducarme G. Gynecol Obstet Fertil Senol. 2020 Jan; 48(1):81-94. Epub 2019 Oct 31.
- Review Association between hospitals' cesarean delivery rates for breech presentation and their success rates for external cephalic version. [Eur J Obstet Gynecol Reprod Bi...] Review Association between hospitals' cesarean delivery rates for breech presentation and their success rates for external cephalic version. Athiel Y, Girault A, Le Ray C, Goffinet F. Eur J Obstet Gynecol Reprod Biol. 2022 Mar; 270:156-163. Epub 2022 Jan 13.
Recent Activity
- External Cephalic Version - StatPearls External Cephalic Version - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Breaking Down Upfronts: How Networks and Streamers Used A-Listers, Athletes and ‘Texas Hold ‘Em’ to Entice Ad Buys

Network executives once came to the upfronts on a mission to get advertisers excited about a handful of new series coming in the fall. This year, TV’s big players took a T-shirt cannon approach.
Every one of the major presentations during the May 13-15 sprint in midtown Manhattan — NBCUniversal, Fox, Disney, Amazon, Warner Bros. Discovery and Netflix — emphasized the breadth of the company’s content offerings. Call it the everything-everywhere-all-at-once strategy for the streaming age.
Popular on Variety
1) Star-Power Surge
Last year, the writers strike kept boldface names from appearing at the upfronts. This year, everybody turned up the star power to 11. NBCUniversal stuffed its presentation with performances from Little Big Town, Michael Bublé and Kelly Clarkson. Amazon went overboard with a nonstop parade of A-listers, including Reese Witherspoon, Will Ferrell, Jake Gyllenhaal and tennis great Roger Federer, with none other than Alicia Keys as the opening act (and yes, she promoted her Amazon line of skin care products). Disney also hauled out the heavy hitters: Ryan Reynolds, Michelle Williams, Sterling K. Brown, Steve Martin, Martin Short and Selena Gomez, just to name a few. Opening Disney’s upfront was Emma Stone, introducing CEO Bob Iger while getting in one more plug for her Oscar-winning film “Poor Things.” The sheer number of movie mentions (NBCU took time to debut the trailer to “Wicked”) felt unusual at an event traditionally tailored to ad-supported television. But in the streaming age, everything’s for sale — and there’s nothing advertisers like more than cozying their messages up to the biggest names in showbiz.
2) The Sporting Life
3) Franchise Fever
If you thought the big push into IP-based content of the past few years was a lot, buckle up. The power of IP was on full display as media companies tried to wow advertisers with plans to reinvent, reboot and reimagine programs and movies rooted in established properties. Disney and Amazon in particular dug deep into their vaults for new projects. WB Discovery hyped shows like its “Dune” prequel; “House of the Dragon” Season 2 and fellow “Game of Thrones” universe show “A Knight of the Seven Kingdoms: The Hedge Knight”; and a “Harry Potter”-themed baking series. Amazon burrowed into the MGM archive to conjure a “Tomb Raider” show from Phoebe Waller-Bridge, a “Legally Blonde” prequel and a Spider-Man Noir series starring Nicolas Cage.
4) Upfront MVPs
Applause, please. It’s not an EGOT-level honor, but appearing at more than one upfront event is never a bad sign for a person’s career. This time around, Jamie Foxx enlivened the Fox and Netflix presentations. NASCAR hero Dale Earnhardt Jr. revved up Amazon and WB Discovery. Mindy Kaling made like a multi-hyphenate by presenting shows that she produces for WBD’s Max (“The Sex Lives of College Girls”) and Netflix (“Running Point”).
More From Our Brands
Who’s afraid of ‘white boy summer’, the macallan and balmoral hotel have teamed up for an ultra-luxe whisky experience, the case to end college football, the best loofahs and body scrubbers, according to dermatologists, the way home premiere: chyler leigh, evan williams talk kat and elliot’s tense reunion, the search for jacob, verify it's you, please log in.
- Search Menu
- Sign in through your institution
- Volume 2024, Issue 5, May 2024 (In Progress)
- Volume 2024, Issue 4, April 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case report, conclusions, conflict of interest statement, inflammatory myofibroblastic tumor of the cecum presenting as acute abdomen, a rare pathology with a rarer presentation.
- Article contents
- Figures & tables
- Supplementary Data
Gabriel A Molina, Carolina Ludeña, Paul Alexander Carrera, Andrea E Heredia, Galo E Jimenez, Diana E Parrales, Carolina Alexandra Portilla, Sebastian Nicolay Martinez, Miguel Jacob Ochoa-Andrade, Inflammatory myofibroblastic tumor of the cecum presenting as acute abdomen, a rare pathology with a rarer presentation, Journal of Surgical Case Reports , Volume 2024, Issue 5, May 2024, rjae330, https://doi.org/10.1093/jscr/rjae330
- Permissions Icon Permissions
Inflammatory myofibroblastic tumor is an extremely rare neoplastic lesion with a predilection for aggressive local and recurrent behavior. The tumor tends to occur in the lungs of children and young adults, and although it can develop in older patients and other organs, this is extremely rare. Symptoms are nonspecific and depend on the location and size of the tumor. The gastrointestinal tract is rarely this mass’s primary site of origin, and the cecum is an even rarer location. We present the case of an otherwise healthy 55-year-old female who presented with an acute abdomen and a mass in her abdomen; after successful surgery, she fully recovered. Inflammatory myofibroblastic tumor causing acute abdomen was the final diagnosis.
Inflammatory myofibroblastic tumors are rare lesions formed by the proliferation of fibroblastic–myofibroblastic cells [ 1 ]. They usually appear during infancy and youth with non-specific symptoms, and although they may show a benign appearance, they have an intermediate malignant potential [ 1 , 2 ]. Therefore, surgery is the treatment of choice. These tumors are extremely rare in the colorectal segment, with fewer than 30 cases ever described in the literature [ 3 ].
We present the case of a 55-year-old female who presented with an acute abdomen and a mass in her abdomen; after successful surgery, she fully recovered. Inflammatory myofibroblastic tumor causing acute abdomen was the final diagnosis.
Patient is a 55-year-old female without any medical history; she suffered from sudden severe lower abdominal pain without nausea or vomits. As the pain persisted and did not improve, even with over-the-counter analgesics, she presented to the emergency room. We encountered a tachycardic, febrile (38 C) patient with lower abdominal pain with tenderness. A hard, palpable mass was detected in her lower abdomen, but no lymph nodes were found.
Complementary exams revealed normal leukocytes (9.86 × 10 9 /l) without neutrophilia and an elevated C-reactive protein. Due to the pain and the palpable mass, a contrast-enhanced computed tomography (CT) was needed. It revealed a 15 × 15 cm heterogeneous mass that compromised the cecum and ileocecal valve; it also had mesentery involvement, with focal strands radiating into the mesenteric fat ( Fig. 1 ).

Abdominal CT, the mass is seen in the cecum and ileocecal valve.
Surgical consultation was needed with these findings, and after explaining it to our patient, surgery was planned.
At laparoscopy, multiple adhesions were discovered between the abdominal wall and omentum, which were released using an ultrasound energy device (Harmonic, Ethicon NJ). Then, the mass was unveiled; it measured 15 × 10 cm and compromised the mesentery, the cecum wall, and the ileocecal valve. The mesentery seemed hardened and had many lymph nodes. Due to this, a right hemicolectomy was performed; the ileum was stapled 10 cm away from the ileocecal valve using mechanical staplers (Echelon Flex, Ethicon NJ), and the colon was exposed and released. The ileocolic and right colic arteries were clamped as they branched from the superior mesenteric artery. Afterward, the hepatic flexure of the colon was released and stapled, and the mass was removed entirely through the umbilicus. After that, a side-to-side ileo-transverse anastomosis with staples was completed, and the enterotomy was closed with a 2-0 Polyglactin 910 Suture (Ethicon Coated Vicryl, Ethicon NJ). A drain was placed, and the procedure was completed without complications.
Pathology reported a 10 × 6 cm tumor. It expanded from the cecum into the ileocecal valve and had a soft exterior. Microscopically, it was formed by multiple myofibroblastic spindle cells with borderline malignancy. Numerous plasma cells and lymphocytes were also seen ( Fig. 2 ). Immunohistochemistry was positive for actin and ALK ( Fig. 3 ). Margins were free of tumors, and all lymph nodes were negative for invasion. Inflammatory myofibroblastic tumor was the final diagnosis.

The mass is completely removed from the patient; it involves the cecum and ileocecal valve.

Immunohistochemistry: positive for actin and ALK.
The patient’s postoperative course was uneventful; she was on a liquid diet on postoperative Day 2, and after she passed gas and stool, she was discharged without complications. On follow-ups, she is doing well.
Inflammatory myofibroblastic tumors are a rare subset of tumors first described by Harold Brunn et al. in 1939 [ 1 ]. They are formed by a combination of myofibroblasts or fibroblasts and a variable number of inflammatory cells (eosinophils, plasma cells, and lymphocytes) [ 1 , 2 ]. They were once considered inflammatory benign tumors; however, they can show aggressive behavior with recurrences [ 2 , 3 ]. Therefore, they are now classified as intermediate-grade neoplasms, which have a high recurrence rate after excision and exhibit low metastatic potential [ 2 ].
The etiology of this disease is still under study; however, they are believed to arise from chronic infections, autoimmune diseases (IgG4 disease), and trauma [ 1–3 ]. They typically affect children and young adults and have an indolent course [ 2 ]. They predominantly affect the lungs and abdomen (75%) [ 2 , 3 ]. However, any body part, including the head, neck, chest, and central nervous sensations, can be affected [ 1 , 3 ].
Symptoms are nonspecific and frequently associated with general inflammatory symptoms such as fever or malaise; nonetheless, they will depend on where the tumor develops and are associated with the tumor mass effect, swelling, and subsequent inflammation [ 2 , 3 ]. In our case, the patient experienced acute abdomen and not obstruction due to the tumor, a rare event that has not been well described in the literature. For instance, tumors in the airways will cause dyspnea and epistaxis. In contrast, tumors in the intestine will cause obstruction [ 4 ].
Laboratory exams will be nonspecific as these lesions usually lead to an elevation of inflammatory parameters such as C-reactive protein and erythrocyte sedimentation rate, similar to other nonspecific surgical conditions [ 1 , 5 ]. Nonetheless, imaging will help in the diagnosis and preoperative planning [ 1 ]. In our case, the patient suddenly presented with an acute abdomen and a palpable mass. After evaluation, C-reactive protein was elevated, and the CT revealed the tumor in the intestine.
CT or magnetic resonance imaging (will show the tumor as a heterogeneous or homogeneous mass depending on the organ in which it is found [ 1 ]. Therefore, they are often misdiagnosed as malignant neoplasms [ 1 , 6 ]. Pathology is the only way to achieve a final diagnosis [ 1 , 2 ].
The differential includes benign and malignant tumors such as gastrointestinal stromal tumor (GIST) (1 out of 100 000 adults per year), inflammatory fibroid polyp (0.1%–3.0% of all polyps in this body), lymphoma (0.2%–1% of all colonic malignancies), and adenocarcinomas (3.2 to 4.2 per 100 000 persons), among others [ 2 , 4 ].
Pathology reveals a proliferation of fibroblasts and myofibroblasts, accompanied by mixed inflammatory infiltration by plasma cells, lymphocytes, eosinophils, and histiocytes [ 7 ]. Myxoid intercellular content, ganglion-like cells, necrosis, lymphovascular invasion, and high mitotic activity are considered adverse factors that worsen the prognosis [ 1 , 7 ]. These tumors show positivity for smooth muscle actin and can be positive or negative for other myoids (desmin, transgelin, etc.) [ 1 , 2 , 8 ], as it was found in our patient.
Recurrence appears in up to 5% of all cases and is associated with abdominopelvic location, tumor size beyond 8 cm, and older patients [ 1 , 2 , 8 ]. Surgical resection with negative margins is the only treatment that can offer a complete cure; in cases where the tumor cannot be resected because of its location or because of the invasion of vital organs, antihumoral drug therapy such as tyrosine kinase inhibitors (crizotinib, etc.) can be used [ 1–3 ].
Inflammatory myofibroblastic tumors are rare mesenchymal tumors, and due to their rarity, their clinical features are still being studied. Rare presentations like our patient in which there is an acute abdomen with a mass should raise our awareness of this rare pathology and remind us that these infrequent pathologies should always be kept in the differential.
None declared.
Siemion K , Reszec-Gielazyn J , Kisluk J , et al. What do we know about inflammatory myofibroblastic tumors? A systematic review . Adv Med Sci 2022 ; 67 : 129 – 38 . https://doi.org/10.1016/j.advms.2022.02.002 .
Google Scholar
Cantera JE , Alfaro MP , Rafart DC , et al. Inflammatory myofibroblastic tumours: a pictorial review . Insights Imaging 2014 ; 6 : 85 – 96 . https://doi.org/10.1007/s13244-014-0370-0 .
Coffin CM , Hornick JL , Fletcher CDM . Inflammatory myofibroblastic tumor . Am J Surg Pathol 2007 ; 31 : 509 – 20 . https://doi.org/10.1097/01.pas.0000213393.57322.c7 .
Palaskar S , Koshti S , Maralingannavar M , Bartake A . Inflammatory myofibroblastic tumor . Contemp Clin Dentist 2011 ; 2 : 274 – 4 . https://doi.org/10.4103/0976-237x.91787 .
Khalil S , Ghafoor T , Raja F . Inflammatory myofibroblastic tumor: a rare presentation and an effective treatment with crizotinib . Case Rep Oncol Med 2020 ; 2020 : 1 – 6 . https://doi.org/10.1155/2020/6923103 .
Appak YÇ , Sahin GE , Ayhan S , et al. Inflammatory myofibroblastic tumor of the colon with an unusual presentation of intestinal intussusception . Eur J Pediatr Surg Rep 2014 ; 02 : 054 – 7 . https://doi.org/10.1055/s-0034-1370774 .
Surabhi VR , Chua S , Patel RP , et al. Inflammatory myofibroblastic tumors . Radiol Clin North Am 2016 ; 54 : 553 – 63 . https://doi.org/10.1016/j.rcl.2015.12.005 .
Bettach H , El Bouardi N , Haloua M , et al. A case report of inflammatory myofibroblastic tumor of cecum mimicking malignant wall thickening . Int J Surg Case Rep 2022 ; 94 : 107166 – 6 . https://doi.org/10.1016/j.ijscr.2022.107166 .
Email alerts
Citing articles via, affiliations.
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- iSchool Connect
Introductory course teaches information science concepts through game design
As part of Teaching Associate Professor Judith Pintar's Introduction to Information Sciences (IS 101) course, students are tasked with creating board games that teach various aspects of information science targeted to particular audiences. The students presented their creations on April 19 at the Game Studies and Design Spring 2024 Showcase. In addition to the game demonstrations, the event featured posters and presentations by students and faculty.
The IS 101 students' games covered a range of information science topics–from internet safety to misinformation. Team members Sam Kitzke, Christina Jordan, Brendan McCarthy, and Antonio Iglesias created "Information Domination," a chance-heavy, trivia-based game with a runtime of twenty minutes that highlights the digital divide. The purpose of this game is to teach players about the gap between those who have access to modern information and technology resources, such as smartphones and computers, and those who have limited to no access.
According to Pintar, integrating game design into her curriculum is beneficial to elevating a student’s learning experience. "Games are cognitively engaging and board games are kinesthetically engaging as well," she said.
"It’s easy to access information and it’s easy to lose information, just like in real life," shared Kitzke. "One of the reasons why I took this course is because I wanted to learn more about how information travels and how to keep data secure."
In the course, students delve into the historical and contemporary context for understanding the role of information in society. Students learn to apply concepts and understand how skills are relevant to addressing significant information challenges of our day, including censorship, misinformation, algorithmic bias, ethical AI, and other important topics.
"As students take on the responsibilities of the information professions, they need to understand the context within which information–at every point in the information life cycle–is understood, managed, and communicated," said Pintar. "They need to understand that their actions create, shape, and design information–there are responsibilities associated with that, and their designs are also iterative and can be improved. All of these things game design teaches."
Pintar serves as the director of the Game Studies and Design Program. Her research and teaching interests include narrative design, game studies, and gameful pedagogies which she pursues through the Extended Literatures & Literacies Lab (EL3).
- Education of Information Professionals
- school news
- student news
- undergraduate

IMAGES
VIDEO
COMMENTS
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse. ... In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord. ...
Presentation refers to the part of the fetus's body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way. ... In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder ...
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). ... If your baby stays in a transverse lie until the end of your pregnancy, it can ...
Transverse lie refers to a fetal presentation in which the fetal longitudinal axis lies perpendicular to the long axis of the uterus. It can occur in either of two configurations: ... compound [eg, head and hand], or funic [umbilical cord]. Position is the relationship of a nominated site of the presenting part to a denominating location on the ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
If the fetus remains in a transverse lie, it cannot deliver deliver vaginally as the diameter of the fetal presenting part (the whole body, in this case) cannot descend through the birth canal. If labor is allowed to continue for enough time with the fetus in transverse lie, the uterus will rupture.
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
In the transverse lie, the presentation is usually the back or shoulder; in the oblique lie, it is usually the shoulder or the arm. ... If the presenting part is nonpalpable, it is in a floating station; if it is well applied against the cervix, but above the spines, it can range from -1 to -3. There is a significant subjective variation among ...
Relationship of presenting part to maternal pelvis based on presentation. The fetus enters the pelvis in the occipito-transverse plane (left or right), descent, and flexion and then rotates 90 degrees to the occipitoanterior (most commonly). Cephalic presentation. Vertex presentation with longitudinal lie:
Diagnosis of Transverse Presentation. Abdominal examination— In transverse position, the presenting part of the fetus is typically the shoulder. During abdominal examination, the head or the ...
Face presentation - an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. ... Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow ...
Fetal position reflects the orientation of the fetal head or butt within the birth canal. Anterior Fontanel. The bones of the fetal scalp are soft and meet at "suture lines." Over the forehead, where the bones meet, is a gap, called the "anterior fontanel," or "soft spot." This will close as the baby grows during the 1st year of life, but at ...
The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet. ... The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time ...
Oblique and transverse lie most often result in the fetal shoulder as the deepest presenting part and affects approximately 0.03% of deliveries.29 Diagnosis is made by Leopold maneuver and by ultrasound examination. These presentations are most often seen in conditions whereby the fetus is small, from growth restric-
The occipital fontanel is the presenting part, and this presentation is referred to as a vertex or occiput presentation. Much less commonly, ... For still more accurate orientation, the relationship of a given portion of the presenting part to the anterior, transverse, or posterior portion of the maternal pelvis is considered. ...
Transverse and compound presentations. Transverse presentations: Uncommon, but when they occur, the presenting fetal part is the shoulder. If the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to ...
Malpresentations are all presentations of the fetus other than vertex, which includes the breech presentation, transverse and oblique lie. Spontaneous vaginal delivery is most common when a cephalic-presenting fetus is in the occiput anterior position. ... This maneuver identifies which presenting part is in the lower uterine pole. To perceive ...
Cesarean section in breech or transverse presentation involves more complicated procedures than cesarean section in cephalic presentation because the former requires additional manipulations for guiding the presenting part of the fetus, liberation of the arms, and the after-coming head delivery; therefore, those cesarean sections are likely to be more invasive.
8.1 Normal and abnormal presentations 8.1.1 Vertex presentation. In about 95% of deliveries, the part of the fetus which arrives first at the mother's pelvic brim is the highest part of the fetal head, which is called the vertex (Figure 8.1).This presentation is called the vertex presentation.Notice that the baby's chin is tucked down towards its chest, so that the vertex is the leading ...
Ultrasound characteristics of face presentations have been published previously, but 3D ultrasound was not used in the transperineal acquisitions 3, 4. Deep transverse occiput position (TOP) may lead to arrest of labor, and persistent TOP in the second stage of labor is defined as TOP that continues for an hour or more 5.
presentation, in childbirth, the position of the fetus at the time of delivery. The presenting part is the part of the fetus that can be touched by the obstetrician when he probes with his finger through the opening in the cervix, the outermost portion of the uterus, which projects into the vagina. In nearly all deliveries the presenting part ...
Additionally, if the fetus weighs less than 2500 g, is at a low station with an engaged presenting part, is frank breech, or the spine is posterior, the success of ECV is decreased. ... If the fetus is in either a transverse or oblique presentation, similar manipulation of the fetus is used to try to move the fetal head to the pelvis.
Shaquille O'Neal, a host of TNT's "Inside the NBA," and Conan O'Brien wrapped up WBD's presentation with a bit of awkward banter. "He thought I was Larry Bird's sister," O ...
Inflammatory myofibroblastic tumor of the cecum presenting as acute abdomen, a rare pathology with a rarer presentation ... a side-to-side ileo-transverse anastomosis with staples was completed, and the enterotomy was closed with a 2-0 Polyglactin 910 Suture (Ethicon Coated Vicryl, Ethicon NJ). ... any body part, including the head, neck, chest ...
As part of Teaching Associate Professor Judith Pintar's Introduction to Information Sciences (IS 101) course, students are tasked with creating board games that teach various aspects of information science targeted to particular audiences. The students presented their creations on April 19 at the Game Studies and Design Spring 2024 Showcase. In addition to the game demonstrations, the event ...