
Presentations made painless
- Get Premium

124 Healthcare Essay Topic Ideas & Examples
Inside This Article
Healthcare is a diverse and complex field that encompasses a wide range of topics, issues, and challenges. Whether you are studying healthcare as a student, working in the healthcare industry, or simply interested in learning more about this important area, there are countless essay topics that you can explore. To help you get started, here are 124 healthcare essay topic ideas and examples that you can use for inspiration:
- The impact of healthcare disparities on patient outcomes
- Strategies for improving access to healthcare in underserved communities
- The role of technology in transforming healthcare delivery
- The ethics of healthcare rationing
- The importance of diversity and inclusion in healthcare organizations
- The rise of telemedicine and its implications for patient care
- The impact of the opioid epidemic on healthcare systems
- The role of nurses in promoting patient safety
- The challenges of providing mental health care in a primary care setting
- The future of healthcare: personalized medicine and precision healthcare
- The role of healthcare providers in addressing social determinants of health
- The impact of climate change on public health
- The role of public health campaigns in promoting healthy behaviors
- The challenges of healthcare delivery in rural areas
- The impact of healthcare reform on the uninsured population
- The role of healthcare informatics in improving patient outcomes
- The importance of cultural competency in healthcare delivery
- The ethical implications of genetic testing and personalized medicine
- The impact of healthcare costs on patient access to care
- The role of healthcare administrators in shaping the future of healthcare delivery
- The challenges of implementing electronic health records in healthcare settings
- The impact of healthcare privatization on patient care
- The role of healthcare providers in promoting patient autonomy
- The challenges of providing end-of-life care in a healthcare setting
- The impact of healthcare disparities on maternal and child health outcomes
- The role of healthcare providers in addressing the opioid crisis
- The challenges of providing healthcare to undocumented immigrants
- The impact of the COVID-19 pandemic on healthcare systems
- The role of healthcare providers in promoting vaccination uptake
- The challenges of healthcare delivery in conflict zones
- The impact of healthcare disparities on LGBTQ+ populations
- The role of healthcare providers in promoting healthy aging
- The challenges of providing healthcare to homeless populations
- The impact of healthcare disparities on rural communities
- The role of healthcare providers in addressing food insecurity
- The challenges of providing healthcare to refugees and asylum seekers
- The impact of healthcare disparities on people with disabilities
- The role of healthcare providers in promoting mental health awareness
- The challenges of providing healthcare to incarcerated populations
- The impact of healthcare disparities on immigrant populations
- The role of healthcare providers in promoting sexual health education
- The challenges of providing healthcare to indigenous populations
- The impact of healthcare disparities on veterans' health outcomes
- The role of healthcare providers in promoting healthy lifestyles
- The challenges of providing healthcare to low-income populations
- The impact of healthcare disparities on minority populations
- The role of healthcare providers in promoting preventive care
- The challenges of providing healthcare to elderly populations
- The impact of healthcare disparities on women's health outcomes
- The role of healthcare providers in promoting maternal health
- The challenges of providing healthcare to children and adolescents
- The impact of healthcare disparities on mental health outcomes
- The role of healthcare providers in promoting substance abuse treatment
- The challenges of providing healthcare to homeless youth
- The impact of healthcare disparities on LGBTQ+ youth
- The role of healthcare providers in promoting healthy relationships
- The challenges of providing healthcare to LGBTQ+ youth
- The impact of healthcare disparities on transgender populations
- The role of healthcare providers in promoting gender-affirming care
- The challenges of providing healthcare to LGBTQ+ elders
- The impact of healthcare disparities on people of color
- The role of healthcare providers in promoting racial equity
- The challenges of providing healthcare to immigrant populations
- The impact of healthcare disparities on refugee populations
- The role of healthcare providers in promoting cultural competency
- The challenges of providing healthcare to non-English speaking populations
- The role of healthcare providers in promoting disability rights
- The challenges of providing healthcare to people with mental illnesses
- The impact of healthcare disparities on people experiencing homelessness
- The role of healthcare providers in promoting housing stability
- The challenges of providing healthcare to people living in poverty
- The impact of healthcare disparities on incarcerated populations
- The role of healthcare providers in promoting criminal justice reform
- The challenges of providing healthcare to veterans
- The impact of healthcare
Want to create a presentation now?
Instantly Create A Deck
Let PitchGrade do this for me
Hassle Free
We will create your text and designs for you. Sit back and relax while we do the work.
Explore More Content
- Privacy Policy
- Terms of Service
© 2023 Pitchgrade
ORDER YOUR PAPER
15% off today
from a verified trusted writer

Mastering the Art of Writing a Health Care Essay on a Good Topic
'A healthy nation is a wealthy nation' - this famous proverb inspires many young people to pursue a career in healthcare, becoming nurses, physicians, therapists, etc. However, some of them fail to realize the responsibility that comes with such occupations. This may bring about a situation whereby colleges and universities turn out unqualified healthcare and nursing experts. To prevent it from happening, professors who teach respective disciplines assign their students the task of writing a health care essay. Being either an essay or research paper, it presents the students with a choice: to examine the problem on their own using various tools and equipment or analyze all available sources on the given research question, offering some personal findings.
14 Amazing Health Care Essay Topics with Introduction Examples
In your essay about health care, you may either talk about various diseases, symptoms, diagnosis, treatment, or methods used by doctors to help their patients, as well as their roles in general. In most cases, students should criticize the modern healthcare system as it really is in need of improvement. It is necessary that they provide some vivid real-life examples if they wish to convince their audience of their point of view.
Approaches to healthcare in the US, UK, and Australia differ, so you may focus on discussing their pros and cons in the essays about health care.
To help you understand which issues to discuss, we have listed the best health care essay topics below. You can also find short answers to each question.
Why is Healthcare Important to Society?
"Healthcare and medicine is a broad term that refers to a system involving maintenance and enhancement of medical services to cater to the health demands of human beings and other living creatures. The quality of healthcare services is one of the most critical factors that predetermines a country's well-being. The system usually varies depending on the healthcare policies of the region. In highly industrialized countries (i.e.countries of the First World), the system is advanced, with almost every citizen having unrestricted access to healthcare services. The low economic level in underdeveloped countries exerts an adverse impact on the healthcare system of these nations."
Is Healthcare a Right or a Privilege
"In the countries of the Third World, healthcare and medicine are not developed enough to save the lives of all of their citizens. Most of them cannot afford quality services, and that is the main difference between developed and underdeveloped countries as far as healthcare is concerned. Unlike poor people, the rich should make health their priority. However, they often neglect to do so, wasting almost all their money on things that harm their body, such as tobacco, alcoholic beverages, drugs, etc. In other words, they tend to have more bad habits, and they value their health less."
Overweight is Putting Strain on the Health Care in the United States
"Childhood obesity in the United States has reached epidemic proportions. This type of disorder has adverse effects on both physical and mental health, as obese kids tend to fall victim to school bullies. The worst consequence of being overweight is Diabetes Type II, and, unfortunately, more and more US children are facing this problem. The pivotal role in the increase in fat intake is played by environmental factors, tastes and preferences, and culture. Highly stressful activities like homework assignments may cause the child to eat more sweets, while their parents do nothing to restrict their consumption of sugar-rich foods. And finally, the lack of physical exercises also takes its toll."
Is Healthcare a Human Right?
"According to NCBI, healthcare is not a human right. To understand why it is important to define both terms. 'Human right' refers to a moral right of great significance that each human being should be entitled to. Dictionaries define healthcare as 'the act of taking prevention or important procedures to make a person's well-being better.' Healthcare is even more complex and confusing to define. Its meaning is too broad to be considered a human right. So, is there a person ultimately responsible for providing healthcare to the entire world? Insisting that healthcare is a human right is, therefore, wrong and pointless."
Should the Government Provide Health Care Insurance?
"The US government is not the only one responsible for providing healthcare insurance to all its citizens. It is only typical of the representatives of the political left to believe that the government should do that. All parties agree that health care is a valuable service, but the government has other important things to take care of. Rather than take care of medicine and nursing, the government's main goal should be to monitor and control the political and economic situation in the country. In fact, each organization has its goals, and so does the government. The government may protect the customer's freedom to buy goods and services by putting in place the corresponding laws and regulations. That is the best thing the US government can do as far as healthcare is concerned."
Causes and Effects of Health Care Crisis in America
"While urban population is more or less OK with its healthcare system, the rural areas of the US keep on suffering from what they call an American healthcare crisis. Hospitals in these regions continue to close down, while those that remain operational provide services of increasingly poor quality. More than 80 rural hospitals have shuttered during the last eight years because their personnel lacked the qualifications to cure patients properly. More than 700 hospitals are at high risk of being closed down, as they lack qualified healthcare professionals. Therefore, emergency medical services are becoming very important, because this is the only way of providing help to patients suffering from strokes, heart attacks, and other heart-related conditions."
Professionalism in Healthcare
"Being a doctor is the most responsible job in the world. It is also the most in-demand one, even though not always properly remunerated. In the underdeveloped countries, the doctor's salaries are among the lowest. In the US, the situation is much better, but still needs improvement in many respects. Medical personnel in this country are granted a license to invest long hours in research and diligent evaluation. Licensure is the way to guarantee the doctor's excellent skills and rich experience in a specific field. It is their willingness to place personal needs after the needs of the patient."
What Has Been the Impact of Medicare on the Healthcare System?
"Quality medicare and teamwork are the essential prerequisites of professional attitude and behavior. The most essential qualities of any medical expert are integrity, accountability, motivation, altruism, and empathy. This way the crucial trust between the patient and professionals is developed. Advanced interpersonal and communication skills impact the quality of medicare as well. Over the past 20 years, we have been witnessing the resurgence of interest in professional training and fair evaluation in the US. It is, therefore, experienced doctors' job to support and guide young professionals on their way to success."
Why Do You Want to Pursue a Career in Healthcare?
"Several factors, the salary being probably the most important one, motivate a lot of young people to choose a career in healthcare. Everyone knows that good medical experts are valued extremely high in the United States. Jobs in healthcare guarantee great opportunities and full security. Quite a few students consider helping other people their priority because they lost their loved ones to fatal diseases. They want to contribute to the medical field by finding a cure to the most complicated disorders some day. And finally, a career in healthcare provides an excellent opportunity to live and work in different parts of the world."
Cultural Diversity in Healthcare
"The purpose of this research paper is to identify basic nuances and issues of cultural diversity in the context of medical treatment, as well as offer solutions aimed at preventing said issues. The main focus is on communication as a culture-based phenomenon, correlation between the patient's progress and expert's treatment, and possible communication characteristics that act as obstacles between healthcare staff and patients. Of the two theoretical approaches used in the study, the first one relates to the information processing, while the second one concerns changing behaviors and interpretation."
Healthcare in America
"Though considered one of the best in the world, the American health care system still has some catching up to do with other countries, including the US's closest neighbor Canada. The US lacks a uniform health system that could offer universal healthcare coverage. Its healthcare system can be referred to as hybrid as it is funded from different sources, such as private funds (48%), households funds (28%), and private businesses funds(20%). The majority of medical and nursing services in this country are privately-owned, even if they are financed by the government. What makes this system stand out from the rest of the world is its great professional staff."
Healthcare in Canada
"Canada has implemented one of the best healthcare reforms in the world. Over the past 4 decades, the country has introduced a number of improvements, making medical treatment affordable for almost every citizen. Urgent and essential health care services are provided based on the needs rather than financial opportunities. This fact alone shows how generous the Canadian government and its healthcare professionals are. When it comes to healthcare, they value fairness and equality more than other nations do. The local healthcare system keeps getting improved as the nation's population increases. It is also important to acknowledge that the very essence of healthcare is also undergoing change."
Public vs. Private Healthcare Sectors
"When comparing the public and private healthcare sectors, it is impossible to ignore the NHS or the National Health Service. The organization, whose staff is made up mostly of primary care nurses or emergency care nurses, provides free health care services to the UK population. That is the reason why the job of Registered Nurse is so prevalent in local healthcare institutions. Specialized caregivers account for another sizeable portion of the healthcare sector. Each young professional is provided with a lot of opportunities for professional development and further career growth.
Communication in Healthcare
"Communication is one of the most important factors in healthcare. Without knowing the details of the patient's conditions and their medical history, the doctor will not be able to make a proper diagnosis. The evidence obtained in the course of this study indicates that there's a direct correlation between the medical representative's communication skills and the patient's willingness to follow the doctor's advice. The doctor's duty is to help the patient control their chronic condition all by themselves, if needed, as well as acquire preventive behaviors. The doctor should not simply cure the patient, but rather teach them some significant lessons to help them remain healthy."
Hopefully, these samples of papers on medicine and nursing will help you choose the hottest topics and best introductions to your essays and research papers. Still having problems? We can offer affordably-priced assistance with any sort of academic writing, including an essay on health care! Try our services at any time, and you won't be disappointed!
- Stats & Feedback
Have your tasks done by our professionals to get the best possible results.
NO Billing information is kept with us. You pay through secure and verified payment systems.
All papers we provide are of the highest quality with a well-researched material, proper format and citation style.
Our 24/7 Support team is available to assist you at any time. You also can communicate with your writer during the whole process.
You are the single owner of the completed order. We DO NOT resell any papers written by our expert
All orders are done from scratch following your instructions. Also, papers are reviewed for plagiarism and grammar mistakes.
You can check the quality of our work by looking at various paper examples in the Samples section on our website.
Think we should be on a first-name basis at this point! The more papers I order here, the more satisfied I am with my performance! Proofreaders here can refine any writing easily, and now, I can prove it!
Don't like lab reports much because of all that preciseness, numbers, and details. So, it was a real relief to order my lab report here and forget about spending a night over this thing. Thanks for prompt and high-quality support!
- High School $11.23 page 14 days
- College $12.64 page 14 days
- Undergraduate $13.2 page 14 days
- Graduate $14.08 page 14 days
- PhD $14.59 page 14 days
Our service has received a swarm of positive reviews, around 596 testimonials proving our success rate to be 9.7 / 10 .
"If you need a refined assignment — trust no one but this writing service! I ordered an essay on politics and was provided with an A-grade paper in a moment's notice! Definitely will cooperate with you more :)"
"I've completely fallen out of reality! I got so caught up in the charity projects I've been doing that I forgot about my term paper. I'm forever grateful to your writers for saving my neck last-minute!"
"Didn’t expect to receive my research paper so fast, but you guys have impressed me. I didn’t even have to move a finger! The formatting wasn’t exactly what I asked for, but it was all revised and corrected on demand. Thank you!"
"Good! I hardly trust any online services and was kinda skeptic when ordered my coursework. Everything went ok though deadline extension was kinda unexpected. Quality was acceptable. "
"Not my first time and not the last, for sure) Good quality even for my urgent papers. I love my writer and will always ask for his help only. Add more services, I am sure you can do anything)"
"You are awesome! That is all I can tell you. I've used your service before, however this was the first time when I needed my paper be done in several hours. I was really surprised with your speed. A writer managed to complete my paper within the given time frames. Thank you, guys!"
- Essay Writing
- Term Paper Writing
- Research Paper Writing
- Coursework Writing
- Case Study Writing
- Article Writing
- Article Critique
- Annotated Bibliography Writing
- Research Proposal
- Thesis Proposal
- Dissertation Writing
- Admission / Application Essay
- Editing and Proofreading
- Multiple Choice Questions
- Group Project
- Lab Report Help
- Statistics Project Help
- Math Problems Help
- Buy Term Paper
- Term Paper Help
- Case Study Help
- Complete Coursework for Me
- Dissertation Editing Services
- Marketing Paper
- Bestcustomwriting.com Coupons
- Edit My Paper
- Hire Essay Writers
- Buy College Essay
- Custom Essay Writing
- Culture Essay
- Argumentative Essay
- Citation Styles
- Cause and Effect Essay
- 5 Paragraph Essay
- Paper Writing Service
- Help Me Write An Essay
- Write My Paper
- Research Paper Help
- Term Papers for Sale
- Write My Research Paper
- Homework Help
- College Papers For Sale
- Write My Thesis
- Coursework Assistance
- Custom Term Paper Writing
- Buy An Article Critique
- College Essay Help
- Paper Writers Online
- Write My Lab Report
- Mathematics Paper
- Write My Essay
- Do My Homework
- Buy a PowerPoint Presentation
- Buy a Thesis Paper
- Buy an Essay
- Comparison Essay
- Buy Discussion Post
- Buy Assignment
- Deductive Essay
- Exploratory Essay
- Literature Essay
- Narrative Essay
- Opinion Essay
- Take My Online Class
- Reflective Essay
- Response Essay
- Custom Papers
- Dissertation Help
- Buy Research Paper
- Criminal Law And Justice Essay
- Political Science Essay
- Pay for Papers
- College Paper Help
- How to Write a College Essay
- High School Writing
- Personal Statement Help
- Book Report
- Report Writing
- Cheap Coursework Help
- Literary Research Paper
- Essay Assistance
- Academic Writing Services
- Coursework Help
- Thesis Papers for Sale
- Coursework Writing Service UK
610 Healthcare Essay Topics & Research Questions to Write About
Are you looking for interesting healthcare essay topics? StudyCorgi has prepared an extensive list of health care topics to write about! Here, you’ll find title ideas for various healthcare fields, including healthcare management, ethics, administration, leadership, policy, finance, care quality, and issues faced by healthcare workers. Our topics are suitable for both high school students and college students. Check them out!
🏆 Best Health Care Topics to Write About
✍️ healthcare essay topics for college, 👍 good healthcare research topics & essay examples, 🌶️ hot medical essay topics to discuss, 🎓 most interesting health care essay examples, 💡 simple healthcare paper topics, 📌 easy healthcare essay topics, 👨⚕️ health titles for essays, 🏥 research topics about healthcare, 🚑 healthcare thesis topics, ❓ research questions about healthcare.
- Free Healthcare: Advantages and Disadvantages
- Application of Statistics in Healthcare
- Motivational Theories in Healthcare
- Artificial Intelligence in Healthcare
- The Effects of the Lack of Teamwork in Healthcare
- Healthcare Information Systems: Components, Benefits
- Paired and Independent T-Test in Healthcare Scenario
- Statistics Application in Healthcare and Nursing Statistical analyses are efficient mechanisms for obtaining accurate data based on calculations and affecting not only the quality of care.
- Hospital Revenue Sources and Models in Healthcare Industry Like any other business, healthcare organizations have to perform effective revenue management in order to maintain stable financial status and avoid critical losses.
- The Importance of Healthcare Management Healthcare organizations need healthcare management because healthcare nowadays requires high levels of coordination among multiple stakeholders.
- Organization Theory Improving Healthcare Operations Organizational theories explain the relationships between the business and its environment and how it affects its operation mode.
- The US and New Zealand: Healthcare Profiles Comparison This essay compares the healthcare profiles of the United States and New Zealand and discusses how the latter may have paved the way for the former’s much-needed improvement.
- The Value of PowerPoint Presentations for Healthcare Management In the fast-evolving spheres like healthcare, technologies play a crucial role in the achievement of health-promotional, educational, strategic, and developmental goals.
- The Healthcare Manager’s Role in Information Technology Management This article focuses on the role that a healthcare manager plays in ensuring the efficient execution of medical operations through the use of new technologies.
- Calgary Family Assessment Model in Healthcare Calgary Family Assessment Model is a tool utilized by health care specialists to evaluate the overall wellbeing of a family.
- Effects of Poor Communication in Healthcare Reviewing various categories of interactions within the healthcare system will enable an in-depth understanding of the effects of poor communication.
- The U.S Healthcare System and the Roemer Model Roemer’s model of a healthcare system demonstrates how a socialist healthcare system operates. This paper explores the entire U.S healthcare system in relation to Roemer’s model.
- Lack of Staffing and Training in Healthcare The essay discusses Lack of training affects the supply of trained nurses to health care organizations, thus, contributing to the nursing shortage in these organizations.
- Pros and Cons of the Gatekeeper Healthcare System The article describes the levels of the healthcare system, its advantages and disadvantages, while the author believes that the advantages outweigh.
- Expectancy Theory in the Healthcare Sector This paper explores the fundamentals of Expectancy Theory and applies it to the healthcare sector. Expectancy theory has found use in healthcare education contexts.
- Healthcare Information System and Its Application In modern society, the healthcare information system plays a critical role in defining the quality of healthcare offered in healthcare centers.
- Ethical Issues in Healthcare Essay: Ethical Dilemma This paper describes an ethical dilemma in healthcare, its specific characteristics, violated ethical principles, and existent barriers to ethical practice.
- Advantages of Computer Technology in Healthcare The emergence of computer technology within healthcare is the catalyst of changes that began to display the improvement of medical procedures and care quality.
- Risk Management in Healthcare Construction Projects A risk is any occurrence that has the potential to alter the progress of a project significantly. A risk may be positive or negative.
- Role of Family in Healthcare and How Culture Affects Health Beliefs The paper will discuss how family shapes the role of care and attitudes towards health and how culture affects health beliefs and community health.
- Comparing the American and Australian Healthcare Systems This paper will compare the American and Australian healthcare systems based on their costs, quality, and access and mention what the US can learn from the OCED member.
- Information Technology Applications in Healthcare Health IT applications as the most advanced tool that can potentially be used for enhancing patient education through patient-nurse communication.
- Quality Management in Healthcare Quality management in healthcare is essential to ensure patient safety. It is helpful by providing the opportunity to evaluate quality in healthcare organizations.
- Ethical and Legal Issues in Healthcare Services The article is an analysis of a number of situations that a patient may face and contains a detailed analysis of each of them from a legal and ethical point of view.
- Change Management in Healthcare Changes in the healthcare field are always associated with difficulties since they affect the ways care is delivered, as well as medical professionals’ and clients’ experiences.
- Regression Analysis for Healthcare Organization The paper studies the regression analysis that enables managers to evaluate the patterns within the health care organization and make predictions for decision-making.
- Virtual Reality in Healthcare and Education The beginnings of virtual reality can found throughout human history. This paper explores its emergence and development, and its influence in healthcare and education.
- Healthcare Problems in South Africa The state of health in South Africa differs from the most fundamental primary healthcare, provided for free by the government, to the highly professional and technologically advanced facilities.
- Supply and Demand of Healthcare and Automobiles This paper’s purpose is to examine the differences and peculiarities of the health care market, as well as analyze current trends in this field.
- Maternal Healthcare Overview Maternal health is a field that focuses on the well-being of women while pregnant, during childbirth, and throughout the postnatal period.
- Irish Healthcare System: HR Management and Financing The management of the healthcare sector requires using not only adequate leadership practices and approaches to monitoring employee performance.
- Steps in the Process of Risk Management in Healthcare Risk management is essential for any enterprise, but for healthcare organizations, it has even greater significance because, frequently, people’s lives are at stake.
- Nursing Informatics Policy and Its Influence on Healthcare Delivery The development of nursing information structures is an essential factor in improving the delivery of health services. It includes the development of regulations.
- Shared Decision-Making Principles in Healthcare The article argues that to provide effective care, healthcare workers need to understand the concepts of shared decision-making and follow the basic principles.
- Healthcare Manager’s Conceptual, Technical, and Interpersonal Skills A healthcare manager is a person who facilitates, administrates, and influences the healthcare system as a manager is an indispensable part of the medical system.
- Social Change: The Nurse’s Role in Global Healthcare To advocate for the global perspective on the issue of the opioid crisis and the need to change the current standards for opioid prescription.
- The Role of Cultural Relativism in Healthcare The Nacirema is a group of North Americans living in the territory between the “Canadian Cree, the Yaqui and Tarahumara of Mexico, and the Carib and Arawak of the Antilles”
- Artificial Intelligence in Healthcare: Pros & Cons Rapidly advancing artificial intelligence technologies are gradually changing health care practices and bring a paradigm shift to the medical system.
- Leadership Theories in the Healthcare Industry There has been extensive research on the effectiveness of leadership style and of theories in different areas of work such as business, nursing, education, military, and politics.
- American and Spanish Healthcare Systems The paper is aimed to contrast and compare the information and statistics related to health care systems in the United States (US) and Spain.
- High Taxes’ Benefits for Education and Healthcare High taxes have more benefits than drawbacks for the citizens as the payments are allocated to develop essential systems, such as healthcare and education.
- Healthcare Environment: Challenges to Teamwork and Collaboration Collaboration among staff members is one of the vital requirements for effective management of key tasks and responsibilities in the healthcare environment.
- Quality Improvement and Measurement Tools in Healthcare Quality tools are widely used to define and assess healthcare problems, especially in healthcare facilities that prioritize quality and safety problems.
- Healthcare in the United Kingdom The purpose of this paper is to examine the healthcare in the United Kingdom, providing recent data and covering the main issues in this area.
- Capstone Project Change Proposal in Healthcare Sector Nursing understaffing is caused primarily by the emotional exhaustion of medical workers due to the stressful workload in the sector.
- Healthcare Employee Recruitment and Selection Recruitment and selection are the starting points of staffing, which emphasizes their importance for providing the healthcare industry with employees.
- Importance of Education for Healthcare Professionals Education are important in promoting quality healthcare services by providing healthcare practitioners with knowledge and skills in handling different healthcare conditions.
- Performance Appraisals in Healthcare Settings The assessment of the achievements should be eliminated from the healthcare work setting because it focuses on the compensation rather than individual specifics.
- Quality Improvement in Healthcare Improving quality in health care is one of the essential tasks. The quality of hospital services depends on external factors, such as industrial manufacturing processes.
- Healthcare Problems of Modern Society The public health system, as an organizational construct of a social institution, affects the formation and effective use of human capital.
- Issues and Possible Solutions in the Healthcare Sector It is hard to disagree that healthcare is one of the most fundamental and intricate sectors playing a crucial role in people’s lives.
- Ethics, Morals, and Values in Healthcare In healthcare, ethics, morals, and values play a rather crucial role. It is important to be able to differentiate between the concepts and understand their influence on the field.
- US and Canada Healthcare Systems Comparison Although Canada is similar to the U.S., its health care system cannot be copied as the two countries do not share the same social ethos and history.
- Healthcare Organizations’ Mission, Vision and Values This project identifies four health organizations coupled with reviewing their vision, mission, and values and proposes changes to the organizations’ missions, visions, and values.
- Leadership and Change in Healthcare Management The paper outlines the essence of leadership and change in healthcare management focusing on the Patient safety, Understanding organizations, Health care management.
- Russian and American Healthcare Systems Comparison The comparison of the health care system of Russia and the health care system in America shows that neither system meets the health care needs of its populations.
- Cultural Barriers in Healthcare Management There are numerous barriers including language, cultural competence, and structural access to health care which prevent participation from cultural or ethnic minorities.
- Stages of Life and Influence of Age in Healthcare Age is a factor in the way patients interact with the healthcare system. This paper discusses the stages of life and the influence of age in healthcare from the patient’s perspective.
- Conflict Stages and Its Resolution in Healthcare The purpose of this paper is to describe the case related to the development of a conflict in a healthcare setting, identify its type and discuss four stages of a conflict.
- Healthcare Disparities in the LGBT Community Apart from the disparities representatives of the LGBT community face in everyday life, they also deal with some major challenges as to their access to appropriate health care services.
- Financial Management Role in Healthcare With the introduction of the Affordable Care Act, electronic health records, and the Medicare billing system, the financial aspect of healthcare requires extra attention.
- Project Management in Healthcare Project management in healthcare involves several skills and techniques that improve the efficiency of operations in medical facilities.
- Creating App in Healthcare: Business Plan In order to create the most effective app in healthcare, it is necessary to monitor trends in this area and implement them.
- Staffing Process in Healthcare The paper analyzes the essential functions, values, and components of effective health care organizational leadership and the challenges of leading modern healthcare organizations.
- Healthcare Services: Right or Privilege? It is believed that all people should have free access to healthcare. But today it is a privilege that only particular people can access even though it should be a human right.
- Practice in the Field of Healthcare: Literature Review The purpose of this study has been to determine how the evidence supports practice in the health care industry as well as the various problems health care.
- Management and Leadership in Healthcare The effectiveness of management of a medical organization can only be guaranteed by the figure of the chief physician as the main head of the clinic.
- Applying Ethical Principles in Healthcare Modern medical field requires new, high-quality ways of treating patients, considering the objective moral code.practice and help them in ethical decision-making process.
- Mintzberg’s Configuration in a Healthcare Organization The paper compares Mintzberg’s five basic organizational configurations, identifies the predominant design that works best for a health care organization.
- Evolution of Healthcare Information Systems Healthcare and hospital information systems have greatly changed in the past twenty years and this has been as a result of the improvement of information technology.
- Healthcare Management and Leadership The importance of healthcare management is being understood on the medicine front with various players and places.
- Evaluation in Nursing Education and Healthcare Organization Evaluation and assessment are key components of nursing education and healthcare practice since they are concerned with quality appraisal and revealing the need for improvement.
- Hospital Ownership Types and Impacts on Healthcare Finance The paper states that there is a significant difference in the level of the financial well-being of private, non-profit, and public hospitals.
- Benefits of Health Information Technology Information technology can assist patients in getting their medications, which can be prescribed on video and audio devices.
- Patient-Centered Healthcare Coordination Plan The paper states that the goal of the eventual care coordination plan is to ensure that all the many aspects of healthcare are addressed.
- Perfect Competition and the Cost of Healthcare The cost of healthcare in the US is extremely high, especially in contrast to other high-income countries; this high cost is attributed to labor, goods, and administrative costs.
- IT in Healthcare: Barcode Medication Administration System The integration of the information systems into the medical has improved a lot of issues, including reduction of errors relating to administration transcription.
- US and Singapore Healthcare Systems Comparison The Healthcare system is a major concern for many countries. Comparing and contrasting the quality of healthcare in the U.S. and Singapore might provide valuable insights.
- Demand and Supply of Healthcare Workforce in Oman There has been continued indication of the shortages of physicians and nurses in hospitals across Oman and this is often seen in the media on regular basis.
- Effects of Poor Workplace Culture on Healthcare Organizations The current paper provides a unique outlook on the fundamental value held by workplace culture in healthcare organizations.
- GBMC HealthCare System’s Competitive Advantage Strategic planning helps GBMC maintain steady value growth, decrease financial risks, and plan development for the services and employees.
- Healthcare in the Russian Federation There are a number of key factors that lead to major Russian healthcare issues, such as chronic diseases, poor lifestyle habits, and lack of health promotion.
- Interpersonal Communication Skills in Healthcare The problem of miscommunication in healthcare persists and tends to have negative impacts on patient outcomes, including those related to safety.
- Unionization and Magnet Accreditation in Healthcare This essay investigates the process of union organization in healthcare and provides a description of the steps needed to be undertaken.
- Non-traditional Healthcare Practices: Can It Replace the Actual Medicine? The three cultures that will be examined in this study will consist of the Filipino, Chinese and Finnish cultures. Their non traditional health practices significantly diverged from one another.
- Healthcare Regulatory Agencies in the US The purpose of this paper is to identify 5 major healthcare regulatory agencies in the US, describe the agency, level of regulatory authority, and role within the US healthcare system.
- Quality Improvement Team in Healthcare Institution The essay considers creation of an interdisciplinary quality improvement team, risks associated with working with such teams and the ways to address these issues.
- Intercultural Communication in Business, Education, and Healthcare The rules of communication vary depending on different contexts; that’s why this paper aims to discuss intercultural communication in business, education, and healthcare.
- Analysis of Limited Access to Healthcare The analysis will primarily focus on geographic and related factors in regards to the issue of healthcare access.
- The Ontological Basis for Participant Action Research in Healthcare The paper is interested in describing the ontological and epistemological basis for participant action research in healthcare with particular emphasis on non-medical prescribing.
- Financial Analysis in Healthcare Organizations There are four essential financial statements for a not-for-profit healthcare enterprise. They should be used for financial strategy formulation together.
- Leadership in Motivating Healthcare Staff to Increase Performance Transformation leadership is an approach that efficiently works to motivate healthcare staff to increase performance and teamwork and to improve patients’ outcomes.
- Ethical Professional Codes of Healthcare The current case study describes the basic principles of healthcare ethics. They include autonomy, beneficence, justice, and non-maleficence.
- Implementation of Healthcare Organizational Design In the case of a healthcare organization, the organization and management structure should support the design.
- Administrative and Financial System in Healthcare Administrative and financial system applications have advantages and disadvantages for healthcare; however, their benefits prevail over the challenges.
- GE Energy and GE Healthcare: Strategic Customer Relationships This article seeks to discuss the benefits of building strategic customer relationships for GE Energy and GE healthcare and their customers.
- NMC Healthcare Organization and Its Culture NMC Healthcare has several strengths that contribute towards its success. Having been operating for more than four decades, the firm has gained vast experience.
- The Consent Role and Aspects in Healthcare Consent represents a kind of agreement that is defined between two or more parties and highlights certain capacities and freedoms that are preserved by that agreement.
- Performance Appraisal Process in a Healthcare Organization The immediate goals of a nursing performance appraisal have to involve the improvement of care performance, which should lead to a positive healthcare organization outcome.
- Spain’s Current Healthcare System Governments across the globe implement powerful measures and allocate adequate resources to support their respective healthcare systems.
- Indian Healthcare Information System The technological aspects of Indian healthcare has undergone a profound transformation, especially when it comes to information systems.
- Healthcare Robotics Impact Today, robotics enters many spheres of life, including education, social life, and healthcare. The use of robots in healthcare allows advancing patient care and achieving better health outcomes.
- HCA Healthcare Corporation’s Strategic Analysis HCA is a corporation that offers a broad scope of healthcare services in areas that encompass surgery, oncology, orthopedics, and cardiology to mention a few.
- The Internet of Things (IoT) and Healthcare The Internet of Things (IoT) is a term that defines the way objects (things) can be connected to the Internet, which provides them with the capability to transmit information.
- Role of Ethics in Healthcare Leadership Healthcare administrators use the principle of nonmaleficence to resolve challenges associated with service delivery.
- Conflict Resolution in a Healthcare Setting The senior management of a healthcare setting must find a way to resolve a conflict in order not to undermine employees’ productivity and the quality of the provided care.
- The Importance of Interdisciplinary Collaboration in Healthcare Interdisciplinary cooperation has been on the rise in the last few years in the healthcare system and its impact has been substantial.
- The Healthcare System: Effects of Social Media Healthcare professionals are grasping social media as an instrument in careers advancement. Registered nurses and health practitioners must be registered for vocational reasons.
- Racial and Ethnic Disparities in Healthcare The government can improve health outcomes by ensuring equitable access to diagnosis, treatment, and management of chronic illnesses for marginalized populations.
- The US Healthcare Delivery System and Role of Nurses This paper aims to discuss changes implemented to reform the U.S. healthcare delivery system and the role of nurses in the altering environment.
- Theory, Risk, and Quality Management in Healthcare Facilities Risk management approaches were incorporated into the health sector following the increased malpractice crises. Hospitals were encountering increased compensation demands.
- Implementing Effective Management in Healthcare This study explores the importance of implementing effective management processes within the healthcare systems.
- The German Healthcare System: Key Aspects The German Healthcare System is among the most advanced healthcare systems that provide quality healthcare services, which are not only accessible but also affordable.
- Healthcare System in Republic of Panama The paper discusses the organization of the Panama health care system, patients’ bill of rights, medical ethical issues and complexities of advanced directives.
- Quality Healthcare and Its Aims Organizations and healthcare providers develop analytic frameworks for assessing quality to improve outcomes. Patient-centered care is an aim proposed by the Institute of Medicine.
- Comparison of Healthcare Systems: The United States and Switzerland According to AHRQ, there are cases when health disparities in the quality of care and access may be observed. It particularly relates to ethnic minorities and immigrants with low income.
- Healthcare for Hindus: Purnell Model for Cultural Competence This paper provides a detailed literature review on healthcare providers and Hinduism from the Purnell Model for Cultural Competence.
- Healthcare Database Design and Development The healthcare databases for patient data and human resources are likely to be different. Similarly, the database scope can define the specific needs and issues.
- South African and Namibian Healthcare The portfolio assesses the current state of South African health care compares it to Namibian health care system, and identifies future challenges and directions.
- The Right to Healthcare as a Basic Human Right This paper argues for the implementation of a universal healthcare system in the United States and emphasizes that healthcare is a basic human right.
- Healthcare Facility Expansion Funding The paper addresses the funding sources and other decision-making factors that the management will have to consider before expansion by 150 beds for the 253-bed healthcare facility.
- Healthcare: The Importance of Accessibility Healthcare plays a significant role in treating life-threatening illnesses, and the accessibility for everyone would save countless lives.
- Professional Relationships in Healthcare Successful professional relationships are essential to working effectively in healthcare settings and maintaining a positive climate within the organization.
- Healthcare Social Issue for Indigenous People in Canada It is worth pointing out that the social issue associated with the indigenous population of Canada and the health care system is relevant and open.
- Healthcare Professional Burnout and Its Effects Drained by work, the emotionally distressed healthcare professional can no longer confront the challenges of the job and may not engage successfully with others.
- Healthcare Delivery Systems in Different Countries The health care delivery system in Germany means accuracy, a high level of organization, and maximum efficiency.
- Artificial Intelligence: Integrated in Healthcare This paper aims to talk about AI as an innovative idea that can be integrated into healthcare. It will detail the strategies used in executing AI.
- Leadership in Healthcare Management & Administration Healthcare management needs administrators with a deep understanding of the medical practice and requires them to be influential leaders.
- The Effectiveness of the Internet in Healthcare Healthcare organizations that are making use of the internet to manage their information have received significant attention.
- Categorical Variables in a Healthcare Research Such categories as age, gender, height, weight can be applied in healthcare research. This paper describes categorical variables and analyzes categorical variables’ application.
- Partnering to Heal: Healthcare-Associated Infections Prevention The essay explains how healthcare providers and family members could have prevented the occurrence of healthcare-associated infections.
- Medicines and Healthcare Regulatory Agency (MHRA) The paper investigates the Medicines and Healthcare Regulatory Agency – its background, structure, the field of operation, impacts, and responsibilities.
- The Healthcare Information: Security and Privacy All employees should participate in a mandatory training program that is aimed at raising awareness of the importance of handling patient health records securely.
- Healthcare in Canada: Problems and Solutions The issue of the challenges that face Medicare in Canada is increasingly turning out to be a controversial subject; even as far as the politics of Canada are concerned.
- Major Third-party Payers to Healthcare Providers This paper includes a brief discussion of major reimbursement methods that are currently used in the country of the USA.
- Healthcare Professional Training and Development The articles that will be discovered in this paper mainly cover the topic of training and development of staff in healthcare establishments.
- Policies and Protocols in Healthcare Policies and protocols in a healthcare environment are essential, as they guide medical professionals in providing high-quality, evidence-based care to all patients.
- Effective Professional Teamwork in Healthcare Teamwork is an essential aspect embraced by many organizations not only in the healthcare sector but also in other industries.
- United Healthcare Group and Its Strategic Plan United Healthcare Group is a for-profit managed organization and one of the largest health care companies in the US, which provides a wide range of services to its clients.
- Medical Technologies Developing Healthcare In this case, the primary goal of this paper is to highlight a substantial role of technology in the advancement of medicine.
- Research Designs in Healthcare Research The paper introduces various research methods and types of designs, explaining how they can be applied within the healthcare industry.
- Scheduling Management in Healthcare In healthcare management, scheduling is an essential procedure that optimizes the workflow, leading to increased nurse satisfaction and balanced benefits expenses.
- Strategic Planning and Leadership in Healthcare Our paper today aims to refresh our knowledge of strategic planning and determine how applicable this concept is to healthcare.
- The Basic Level of Healthcare: H. Engelhardt’s and N. Daniels’ Perspectives H. Tristram Engelhardt Jr. and Norman Daniels are two prominent philosophers whose views on what constitutes a reasonable basic level of healthcare are opposed.
- Using of Virtual Reality in Healthcare The paper argues it is necessary to analyze several cases of application of VR developments in the field of healthcare.
- The Challenges Faced by Healthcare Workers The challenges faced by healthcare workers include transitioning from volume-based healthcare to value-based healthcare, increasing costs and expenses, and provider shortages.
- Clinical Career Ladders in Healthcare The main objective of the essay is to identify the relationship between successful Clinical Ladder Programs and nurses’ job satisfaction and the factors that contribute to it.
- Interprofessional Communication in the Healthcare Team Inadequate communication between professionals of the healthcare team often leads to errors and adverse events that adversely affect the patient and the healthcare team.
- Healthcare Delivery Models in Germany, the UK, and the US The goal of the research paper is to compare and contrast healthcare delivery models in three countries: Germany, the United Kingdom, and the U.S.
- The Analysis of Healthcare Organization The paper analyzes various organizational style, their advantages and disadvantages and importance of management for control.
- Healthcare: Interprofessional Collaboration The essay presents ethical and legal principles providing a positive shift from traditional views in the health care system and nursing in particular.
- Organizational Performance and Structure in Healthcare The structure and the leadership of a health organization influence the motivation, work environment and the general feeling of the patients and health care workers.
- Quality and Risk Management in Healthcare Management of risk in health care institutions seeks to reduce any potential negative occurrences to all stakeholders such as patients and staff.
- Teamwork and Collaboration in Healthcare Successful health outcomes are best attained when there are teamwork and collaboration among the individuals involved.
- Incivility Within the Healthcare Metaparadigm Incivility undermines the respect that underpins the relationship between the person who receives the care and the one who is in charge of the whole vital process.
- Behavioral Cues in Healthcare Behaviors Behavioral cues in healthcare behaviors can provide an indicator for providers as to what interventions should be implemented in order to improve behaviors.
- Developing a Feedback-Rich Environment in the Healthcare Timely and effective feedback is a critical part of a successful performance management program and should be applied in conjunction with setting performance goals.
- Impact of Technology on the Healthcare System Over the past ten year there has been a drastic change within the health care set up a factor that has greatly influenced the trend within the health care setup.
- Workplace Interpersonal Conflicts Among the Healthcare Workers The work in a healthcare setting is rather demanding and may sometimes require much more than a thorough preparation and the knowledge of one’s job.
- Ways to Improve the US Healthcare System The healthcare system in the United States is one of the main areas that need to be improved. This paper discusses the possible ways for the improvement of US health care.
- Restraint and Seclusion in Healthcare Restraint and seclusion have been used as measures of addressing patients’ behaviors that could cause harm to them and other people around.
- Healthcare Quality, Safety, and High-Reliability Healthcare quality is outcome-oriented. Healthcare safety encompasses the well-being of the patient. High reliability reduces errors and risks.
- Factors of Decision-Making by Healthcare Managers
- Career in Healthcare Administration
- Healthcare Informatics: Introduction to Theory
- Patient Identity Management Policy in Healthcare
- Strategic Planning in Healthcare
- The Action Research in Healthcare
- The Implementation of a Safety Improvement Initiative in Healthcare Institutions
- Women’s Healthcare: Eugenics and Sterilization
- Healthcare Professions: EMT and Occupational Therapist
- Healthcare Marketing and Its Evolution
- Electronic Resources in Healthcare
- Healthcare Accreditation and Licensing
- Cash vs. Accrual Accounting for Healthcare Organization
- Building Trust Within the Healthcare Setting
- Incomplete or Missing Documentation: Patient Safety in Healthcare
- The Importance of Moral Courage in the Healthcare
- Cash Versus Accrual Accounting Methods in Healthcare Organizations
- Absenteeism and Lateness in the Healthcare Field
- Evidence-Based Conflict Resolution Strategies in Healthcare
- Organizational Culture in Healthcare
- New Sustainable Development Goals in Healthcare
- Personality Type and Leadership in Healthcare
- Healthcare Quality Improvement Team Meeting Plan
- Patients Safety and Needs in Healthcare Environment
- Healthcare Governance and Its Common Features
- Data Breaches and Cyber Attacks on Healthcare Organizations
- Information Security Policies in Healthcare Organizations
- Risk and Quality Management in Healthcare
- Organizational Change in Healthcare
- Corruption in South Africa’s Healthcare Sector
- Strategic and Program Evaluation in Healthcare
- Healthcare Administrator: Profession Overview
- Ethical Dilemmas in Healthcare
- Cybersecurity and Protection in Healthcare
- Mental Healthcare Aspects of Latinos
- Overworked Healthcare Systems: The Case of the US and Canada
- Fraud Schemes in the Healthcare Industry
- The Pain Rating Scales in Healthcare
- Modern Healthcare Management: The Role of Information Technologies
- Medication Error Impact on Healthcare Quality
- Cuban Cultural Communication in Relation to Healthcare
- Roles of a Financial Manager in Healthcare
- The Forced-Air Prewarming Strategy in Healthcare
- Strategic Planning: Healthcare Organizations
- Organizational Mission, Vision, and Values in Healthcare
- Nurse’s Role in Healthcare Sentinel Events
- Quality Improvement and Transformation of Healthcare
- Healthcare Issues: The Cultural Assessment Framework
- Healthcare System in the Republic of Panama
- System Failures in Healthcare Facilities
- Cost Allocation in Healthcare Analysis
- Accountability in the Healthcare Industry
- Healthcare Root-Cause Analysis and Safety Improvement Plan
- Cloudlet Architecture in Healthcare Computing
- Afro-Latin Culture and Approach to Healthcare
- Ethical and Religious Directives for Catholic Healthcare Services
- AIDET Communication Process in the Healthcare
- Chinese Cultural Beliefs: Healthcare Assessment
- Teamworking Skills in Healthcare
- Healthcare Human Resources Management and Changes
- Trends in the Healthcare Sector
- Access of Healthcare: Factors Affecting the Access of Care and Barriers
- Emotional Intelligence and Feelings in Healthcare
- LGBT Healthcare Disparity: Theoretical Framework
- Code of Conduct in Healthcare Organizations
- Three-Step Change Theory and Its Phases in Healthcare
- Graphs, Statistical and Clinical Significance in Healthcare
- Emotional Intelligence in Healthcare Leaders and Nurses
- Healthcare Conflict Resolution Case
- Healthcare Technological Advancements: Pros & Cons
- Religion and Ethics in Healthcare Provision
- Diagnosis-Related Groups in Healthcare Research
- The Implication of Information Technology on Marketing Strategy of Healthcare Industry
- Future Trends in Healthcare
- Healthcare Quality Initiatives and Their Importance
- Using Smartphones in Healthcare: Ethical Issues
- Constructing Team Values in Healthcare
- Information Technology Projects in the Healthcare Sector
- Jehovah’s Witnesses’ Views on Healthcare
- Beliefs, Perceptions, and Behaviors Impacting Healthcare Utilization
- Marijuana and Its Use in Healthcare
- Analysis of Innovation in Healthcare
- Stakeholders’ Conflict of Interests in Healthcare Provision
- Telehealth and Its Impact on the Healthcare System
- Safety Culture in the Healthcare Workplace
- Aspects of Healthcare Costs
- Overcoming Personal Biases, Prejudice, and Stereotyping in Healthcare
- Informatics Technologies in Healthcare
- Compensation Structure in Healthcare
- United Healthcare Firm’s Readiness to Meeting Healthcare Needs
- Artificial Intelligence and Its Usage in Modern Warfare and Healthcare
- Operation Management and Value Chain in Healthcare
- Poverty and Poor Health: Access to Healthcare Services
- Ethics in the Healthcare Industry: Armando Dimas’ Case
- Healthcare Innovations and Improvements
- Peru’s Healthcare System Assessment
- Vanguard Healthcare Services, LLC: Health Organization Case Study
- Informatics in the Clinic Area Healthcare
- The Issue of Healthcare Compliance
- Technology and Future Trends in Healthcare
- Replication and Its Importance in Healthcare Research
- Mobile Apps Utilization in Modern Health Care
- Healthcare Management: Past, Present, and Future
- Patient Safety Culture in the Healthcare Workplace
- Healthcare: New Treatment Methods
- United Healthcare Organization and Citizens’ Needs
- Information Systems in Healthcare
- Science of Human Flourishing in Healthcare
- Healthcare Disparities and Potential Solutions
- Medical Devices Trade Agreements for Healthcare
- Healthcare Project Management Office’s Responsibilities
- Cross-Cultural Healthcare and Its Implications
- Healthcare Financing: Equipment Replace Proposal
- Muslim Faith and Healthcare Relationship
- Healthcare Policy, Leadership and Performance
- Healthcare Informatics: Infrastructure Evaluation
- Healthcare Regulatory Agencies
- Levine’s Conservation Theory in Healthcare Research
- Healthcare Change Management and Workforce Retention
- Team-Based Healthcare in Nursing Practice
- How Big Data Is Used in Health Care
- Conflict Management in Healthcare Facilities
- The PICOT Framework in Healthcare
- Leadership Models in Healthcare
- Time Management in the Healthcare Sector
- Big Data in the Healthcare Sector: Pros and Cons
- Billing and Coding Regulations in Healthcare
- Epidemiological Data and Its Role in Healthcare
- The Socio-Ecological Model of Access to Healthcare
- The Gibbs Reflection Cycle Method in Healthcare
- Advocacy and Communication in Healthcare
- Culture of the Nacirema in Modern Healthcare
- Strategic Planning Processes in Healthcare
- Risk Management in Healthcare Settings
- Healthcare Collection Policies and Procedures
- Effective Communication and Quality in Healthcare
- Agile-Scrum in Healthcare Project Management
- Trinity Healthcare’s Internal and External Barriers
- Aspects of Palliative Care in Healthcare
- Elder Abuse in the US Healthcare System
- Voluntary Accreditation in Healthcare: Requirements, Compliance, and Standards
- Occupational Stress Management in Healthcare
- Impact of IT on Healthcare During COVID-19
- Data Analytics and System Performance in Healthcare
- Competing Needs and Quadruple Aim in Healthcare
- Communication as a Barrier to Providing Healthcare
- Servant Leadership in Healthcare
- Integration of Health Information Management System (HIMS) into Healthcare
- Gender and Ethnic Diversity in Healthcare
- Ethical Theory in a Healthcare Scenario
- The Smartphone Technology in the Healthcare Sector
- “The HR Challenges Shaping the Healthcare Industry” Article Summary
- Racial Disparities in Healthcare Through the Lens of Systemic Racism
- Using of Statistics in Healthcare
- Abbreviated Quantitative Healthcare Research Plan
- Foundations in Professional Healthcare Practice
- Strategic Management Techniques and Tools in Healthcare
- Transformational Leadership in Healthcare
- Intentional Exaggeration: Healthcare Plans and Products
- Six Sigma’ Management Strategy in Healthcare
- Patient Rights When Interacting With Healthcare Providers
- Leadership in Healthcare Overview
- The Practice Reality of Quality Improvement in Healthcare
- Conflict in Nursing: Conflict Resolution in a Healthcare Setting
- Reducing the Number of Healthcare-Associated Infections
- Nursing Informatics in Healthcare
- Leadership and Communication in Healthcare Setting
- The Issue of Ethics in Healthcare
- Statistical Process Control in the Healthcare
- The Role of Chief Information Officers in Healthcare
- The Launch of Healthcare Projects
- Implementation Strategy in the Healthcare Sector: Implementation Stages Analysis
- Healthcare Marketing and Strategy in Prenatal Care Practice
- Key Employee Benefits in the Healthcare Sector
- Theory of Control in the Healthcare
- Financial Management of Healthcare Organizations
- Hospital-Acquired Pressure Ulcers in US Healthcare Organizations
- Financial Management in the Healthcare Industry
- Patient Safety in the Healthcare Workplace Culture
- Leadership Styles and Theories in Healthcare
- Cultural Pluralism and Sexism in Healthcare
- Improving Healthcare Quality With Bar-Coded Medication Administration
- Transgender People and Healthcare Barriers
- Interprofessional Collaboration in Healthcare
- Importance Skills in Healthcare Environment
- Change Management in Healthcare: Using the Principles of Transformational Leadership
- Healthcare Delivery Models and Nursing Trends
- Healthy Relationships in the Healthcare Workplace
- Tenet Healthcare Corporation’s Training and Development Plan
- ABC Healthcare Cyber and Computer Network Security
- Continuous Quality Improvement Strategies in Healthcare
- Healthcare Marketing Communication and Strategies
- Healthcare Workforce and Human Resource Management
- Using Technology in Healthcare Setting
- Use of Telehealth in Healthcare
- Political Activism in Nursing and Healthcare Provision
- Nursing Definition and Healthcare Actors
- Austrian vs. American Healthcare Systems
- Sickle Cell Disease and Healthcare Decisions
- Change and Conflict Theories in Healthcare Leadership
- Financial Viability in Healthcare
- Nursing Quality Models in Healthcare Institutions
- The Christian and Buddhist Perspectives in Healthcare
- Banner Healthcare Strategic Planning
- Evidence-Based Practice Role in Healthcare
- Healthcare Mission and Philosophy: Mercy Hospital Inc.
- Healthcare in the United States: Timeline and Reforms
- Healthcare Access: Financial Barriers
- Simulation in Healthcare Operational Decision-Making
- The United States Healthcare System Analysis
- The National Healthcare Quality and Disparities Report
- Factors Facilitating Quality Improvement in Healthcare
- Policies Addressing LGBT (Queer) Healthcare Disparities
- Quality Healthcare Improvement for Pregnant Women in New York City
- Negligence and Battery in Healthcare Units
- Risk Management, Quality and Safety in Healthcare
- Healthcare Affordability in the United States
- Healthcare Quality and Outcomes: Measurement and Management
- The Policy Standard in China’s Healthcare System
- Healthcare Financial Elements
- Patient-Centered Medical Home: Marketing in Healthcare
- How Analytics Can Help Improve Healthcare Decision-Making
- Evidence-Based Practice in Healthcare Organizations
- The Impact of Genomics on Policy and Practice in Healthcare
- Healthcare Costs Affected by the COVID-19 Pandemic
- Monitoring Compliance of IV Pump Integration in a Healthcare Setting
- Geography and Healthcare Equity in the U.S.
- Navigating Organizational Theories in Healthcare
- Challenges and Complexities in the U.S. Healthcare System
- The US vs. New Zealand Healthcare Systems
- Application of Blockchain in Healthcare
- Dental Healthcare Persons’ Infection Control
- Monitoring and Controlling Functions in Healthcare Organizations
- Abuses in a Healthcare Context
- The Canadian Healthcare System’s Key Challenges
- Healthcare as a Basic Human Right
- Data Analytics and Its Role in Healthcare
- Business Analytics in Healthcare
- Impacts of Organizational Culture and Structure on Healthcare Outcomes
- Healthcare Service Management Course
- Healthcare Organization Assessment
- Advanced Practice Nurse: Healthcare Policy
- Business Needs in the Healthcare Sector
- Information Technologies in Healthcare
- Management Tasks in Healthcare Organizations
- Risk Management in Healthcare
- Fraud and Abuse in Healthcare: Analysis
- Informed Decision-Making in Healthcare
- Diversity in Healthcare Organizations
- Managing Incremental Healthcare Costs in a Post Pandemic World
- Healthcare Change Implementation and Management Plan
- Healthcare Data Quality Elements
- Standardization as a Procedural Issue in Healthcare
- Cultural Diversity and Sensitivity in Healthcare
- Leading Interprofessional Collaboration in Healthcare
- Barriers to Healthcare in Refugee Communities
- Policy Analysis in Healthcare Industry
- Healthcare Research: Systematic Search Strategy
- Refugees’ Adjustment and Accessibility of Healthcare
- Professional Services Automation System in Healthcare
- VITAS Healthcare: Program Evaluation Proposal
- Healthcare Research Designs and Sampling Methods
- Healthcare Policy Evaluation in the US vs. Mexico
- Prevention in Healthcare and Social Science
- Interprofessional Team Management in Healthcare
- Implications of Healthcare Fraud and Abuse
- Impacts of Technology on the Healthcare System
- Healthcare Advocacy Plan for Nassau County
- Incorporating Telehealth Into the Healthcare System
- Healthcare Program: Informational Campaign on Dementia
- Initial Beliefs: Evidence-Based Management in Healthcare
- Q.I. Program for Vaccination Among Healthcare Workers
- How Healthcare Organizations Deal With COVID-19 Financial Issues
- Vocal Biomarkers in Healthcare
- Communication Problems in Healthcare Attendants
- Climate Change as a Healthcare Priority
- Rising Healthcare Costs as a Policy Issue
- Electronic Vulnerability in Healthcare
- Statistical Analysis in Healthcare
- Interprofessional Collaboration Examples in Nursing Case Study
- Access to Healthcare Services and Language Interpretation
- The Healthcare Labour Shortage: Practice, Theory, Evidence
- Healthcare Financing: USA vs. Switzerland
- Discussion: The Use of RFID in Healthcare
- Healthcare Insurance Organizations’ Risk of Fraud
- Mental Healthcare Provision & Barriers to Innovation
- The Healthcare Center for the Homeless
- Project Evaluation in Healthcare
- Healthcare Language Barrier for Afghani Refugees
- Advantages of Accreditation of Healthcare Organizations
- Technologies in Healthcare Delivery
- Antibiotics: The Use in Healthcare
- Challenges of Virtual Assistance Technology Implementation for Healthcare
- Universal Healthcare as a Basic Right of Humanity
- Evaluation of Virtual Reality in Healthcare
- Healthcare Interprofessional Team Members’ Perspectives on Caring
- Leadership Versus Management: Healthcare Leadership
- Third-Party Payers in Healthcare Reimbursement
- Organizational Change Regarding Language Barriers in Healthcare
- The Triple Aim Framework and Financial Issues in Healthcare
- How 911 Dispatcher Technology Has Reduced Healthcare Costs
- Applying Lean Principles in Healthcare
- Reducing Healthcare Expenses: Structural and Individual Measures
- Hansen vs. Baxter Healthcare Corporation
- The Role of Differential Diagnosis in Healthcare
- Issues in Healthcare and Effective Communication with Organization Stakeholders
- Issues of Healthcare in the US
- Healthcare Services for Vulnerable Populations in Georgia
- Report Specifications in Healthcare
- Importance of Healthcare Advocacy Plan
- The Healthcare Costs Regulation Strategies
- Malpractice, Abuse, and Neglect in Healthcare
- Healthcare Cost and Utilization Project
- The Healthcare Administrator: Leadership Abilities
- Queer People (LGBTQIA) in Healthcare System Context
- Informatics Systems in Healthcare
- Auburn Hospital’s Comprehensive Healthcare Strategies
- Healthcare during Tornados: Business Continuity
- Qualitative Research in Healthcare
- Interoperability in Healthcare
- Theories and Approaches in Healthcare
- The Significance of Healthcare Policy
- Legal and Ethical Issues in Healthcare System
- Consumer Involvement in the Healthcare System
- Significance of Accreditation in Healthcare
- Healthcare Trends and Innovations
- Pediatric and Adult Anatomy for Healthcare Providers
- Organizational Theory in Healthcare
- Licensed Professional Counseling in Mental Healthcare
- Healthcare Errors, Risks, and Project Management
- A Strategic Plan for a Healthcare Organization
- Technology in the Healthcare System
- Healthcare Insurance in the USA
- Population Aging and Healthcare Concerns
- Implementing and Evaluating a Healthcare Organization’s Strategic Plan
- Galen’s Experiential Philosophic Approach to Healthcare
- Economic Issues Confronting Healthcare System
- Doctor Michael R. Walker as Leader in Healthcare
- Role of Advance Directives in Healthcare
- Nursing Informatics: Healthcare Blockchain System
- “Top Challenges Facing the Healthcare Industry Today”: Three Challenges
- Healthcare Information Systems
- Technology in Healthcare and Care Coordination
- The Concept of Accountability in Healthcare
- Universal Healthcare in the United States
- Simulation Training for Healthcare Staff
- Mandatory COVID-19 Vaccination for Healthcare Employees
- Regulation of Patient Healthcare Records Release
- Telemedicine as a Healthcare Provision Technique
- Healthcare for Queer (LGBTQIA+) Patients
- The American College of Healthcare Executives: Leadership Reflection
- Strategic Planning Process in Healthcare
- The Assessment Process in Healthcare
- Competitive Forces in the Healthcare Market
- Impact of Obesity on Healthcare System
- Care Coordination Process in the Healthcare
- Social Welfare Policy and Healthcare Insurance
- Interprofessional Teamwork in Healthcare
- Quality Performance Is a Goal in Healthcare
- Revenue Cycle Processes and Pricing in Healthcare
- Billing Specialists in Healthcare
- Healthcare: Auditing Practices
- Community Healthcare Agency at Fairfax
- The Adoption of the EHR Framework in Healthcare Facilities
- Should Free Healthcare be a Right in America?
- Unlisted Procedures and Services in Healthcare
- Creating Value in Healthcare Settings
- Healthcare Disparity in the African American Community
- The Introduction of a Vaccine Against COVID-19 Among Healthcare Staff in Moldova
- The Healthcare Availability in the USA
- Improving a Healthcare Compliance Program
- The Healthcare Situation in the USA
- Human Resource Management: Healthcare
- Artificial Intelligence: Human Trust in Healthcare
- Researching of Fraud and Abuse in Healthcare
- Ethics of Care (EOC) and Healthcare
- Genetic Technologies in the Healthcare
- Racial Inequality, Immigration, and Healthcare in the US
- Cybersecurity in Healthcare Organizations
- Nurses’ Knowledge to Be Successful Healthcare Professionals
- The Risk of Using Abbreviations in Modern Healthcare
- The Use of Unmanned Aircraft Systems (UAS) in the Healthcare
- Women’s Healthcare and Social Darwinism
- Telepsychiatry as Innovative Healthcare Practice
- Language and Culture: Impact on Healthcare
- Health Costs and Insurance in Healthcare
- Healthcare Industry Challenges: Information and Service Integration
- Fraud in the Healthcare Industry
- Providing Quality Care in Healthcare Setting
- Occupational Therapy in Modern Healthcare Market
- Responsible Citizenship in Healthcare Administration
- Handwashing Compliance of Healthcare Workers
- Healthcare and Governmental Efforts
- Followership and Leadership in Healthcare
- Reducing Risks Facing a Healthcare Organization
- Public Education Initiatives in the Area of Healthcare
- Followership-Leadership Interaction in Healthcare
- The Importance of In-Team Communication in Primary and Emergency Healthcare
- Healthcare Leadership and Management Functions
- Mental Healthcare Services for Transgender Individuals
- Social Justice and Barriers in Healthcare
- Analysis of Implicit Bias in Healthcare
- Accreditation, Regulation, and Certification in the Healthcare Field
- Healthcare Settings: Financial Challenges
- Patient Consent in Healthcare Diagnostics
- Cultural Diversity in Healthcare
- Standard of Care in Healthcare System
- Joe Biden’s New Reform on Healthcare
- The Culture of an Open Attitude in Healthcare
- Global Issues in Healthcare: Cultural Competence and Patient Safety
- Language, Culture, and Healthcare
- International Classification of Functioning in Healthcare
- Analyzing Errors in Healthcare
- Healthcare Programs in Wyandotte County
- Affordable Healthcare Approach and Best Strategies
- Non- and Governmental Structures in Public Healthcare
- Statistics in Healthcare: Sun Rays Exposure
- Devices to Improve Healthcare Service Delivery
- What Are the Cross Cultural Healthcare Perspectives?
- How to Estimate the Optimal Size of Secondary Healthcare Providers in Slovenia?
- How Health Policy Shapes Healthcare Sector Productivity?
- How HRM Provides a Mandatory Organized Structure in the Healthcare System?
- How Medical Robotics Affect Healthcare Costs and Patient Care?
- How Medicare Has Impacted Healthcare Within the United States of America?
- How Reliable Are Surveys of Client Satisfaction With Healthcare Services?
- How Retractable Syringe Development Impacted Society and Healthcare?
- What Are the Applications of Simulation Within the Healthcare Context?
- What Are the Factors Influencing Healthcare Service Quality?
- What Is “Quality Improvement” and How Can It Transform Healthcare?
- What Is Interprofessional and Multiprofessional Collaboration in Healthcare?
- What Is Jamaica’s Ethnomedicine Potential in the Healthcare System?
- What Are the Characteristics of Healthcare Wastes?
- What Is a Canadian Model of Integrated Healthcare?
- What Are the Trends and Approaches in Lean Healthcare?
- Whar Are the Emerging Information Technologies for Enhanced Healthcare?
- What Are the Challenges for Design Researchers in Healthcare?
- How Well-organized Logistics Can Service Healthcare?
- What Are the Theories on Implementation of Change in Healthcare?
- How the Blockchain Technology Was Implemented in Healthcare?
- How To Improve Healthcare With Interactive Visualization?
- What Are the Essentials of Economic Evaluation in Healthcare?
- How Mobile Devices Are Transforming Healthcare?
- How to Develop Machine Learning Models for Healthcare?
Cite this post
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2021, December 21). 610 Healthcare Essay Topics & Research Questions to Write About. https://studycorgi.com/ideas/healthcare-essay-topics/
"610 Healthcare Essay Topics & Research Questions to Write About." StudyCorgi , 21 Dec. 2021, studycorgi.com/ideas/healthcare-essay-topics/.
StudyCorgi . (2021) '610 Healthcare Essay Topics & Research Questions to Write About'. 21 December.
1. StudyCorgi . "610 Healthcare Essay Topics & Research Questions to Write About." December 21, 2021. https://studycorgi.com/ideas/healthcare-essay-topics/.
Bibliography
StudyCorgi . "610 Healthcare Essay Topics & Research Questions to Write About." December 21, 2021. https://studycorgi.com/ideas/healthcare-essay-topics/.
StudyCorgi . 2021. "610 Healthcare Essay Topics & Research Questions to Write About." December 21, 2021. https://studycorgi.com/ideas/healthcare-essay-topics/.
These essay examples and topics on Healthcare were carefully selected by the StudyCorgi editorial team. They meet our highest standards in terms of grammar, punctuation, style, and fact accuracy. Please ensure you properly reference the materials if you’re using them to write your assignment.
This essay topic collection was updated on January 8, 2024 .
Home — Essay Samples — Nursing & Health — Health Care
Essays on Health Care
Five nursing pillars, optometrist: advantages and disadvantages, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Occupational Therapy Application
Aspects of nursing shortage, the importance of nursing philosophy, examples of icare values in healthcare, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Fresh Fruit, Broken Bodies: a Summary and Analysis
Analysis of "a walk to beautiful", universal health care: persuasive speech outline, the importance of hand washing in nursing, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
Sick Around America Documentary Analysis
Middle range theory of acute pain, patch adams reflection paper, nursing personal statement, self-assessment in nursing, vimax extender analysis, delegation in nursing case study, cleveland clinic mission statement, challenges of istj in nursing, topics in this category.
- Affordable Care Act
- Universal Health Care
- Nursing Care Plan
- Health Care Policy
- Healthcare Crisis
- Opioid Epidemic
- Nursing Theory
Popular Categories
- Public Health Issues
- Medical Practice & Treatment
- Nutrition & Dieting
- Neurology & Nervous System Diseases

Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
How to build a better health system: 8 expert essays

We need to focus on keeping people healthy, not just treating them when they're sick Image: REUTERS/Rupak De Chowdhuri
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Global Future Council on Health and Healthcare
Introduction
By Francesca Colombo , Head, Health Division, Organisation for Economic Co-operation and Development (OECD) and Helen E. Clark , Prime Minister of New Zealand (1999-2008), The Helen Clark Foundation
Our healthy future cannot be achieved without putting the health and wellbeing of populations at the centre of public policy.
Ill health worsens an individual’s economic prospects throughout the lifecycle. For young infants and children, ill health affects their capacity to acumulate human capital; for adults, ill health lowers quality of life and labour market outcomes, and disadvantage compounds over the course of a lifetime.
And, yet, with all the robust evidence available that good health is beneficial to economies and societies, it is striking to see how health systems across the globe struggled to maximise the health of populations even before the COVID-19 pandemic – a crisis that has further exposed the stresses and weaknesses of our health systems. These must be addressed to make populations healthier and more resilient to future shocks.
Each one of us, at least once in our lives, is likely to have been frustrated with care that was inflexible, impersonal and bureaucratic. At the system level, these individual experiences add up to poor safety, poor care coordination and inefficiencies – costing millions of lives and enormous expense to societies.
This state of affairs contributes to slowing down the progress towards achieving the sustainable development goals to which all societies, regardless of their level of economic development, have committed.
Many of the conditions that can make change possible are in place. For example, ample evidence exists that investing in public health and primary prevention delivers significant health and economic dividends. Likewise, digital technology has made many services and products across different sectors safe, fast and seamless. There is no reason why, with the right policies, this should not happen in health systems as well. Think, for example, of the opportunities to bring high quality and specialised care to previously underserved populations. COVID-19 has accelerated the development and use of digital health technologies. There are opportunities to further nurture their use to improve public health and disease surveillance, clinical care, research and innovation.
To encourage reform towards health systems that are more resilient, better centred around what people need and sustainable over time, the Global Future Council on Health and Health Care has developed a series of stories illustrating why change must happen, and why this is eminently possible today. While the COVID-19 crisis is severally challenging health systems today, our healthy future is – with the right investments – within reach.
1. Five changes for sustainable health systems that put people first
The COVID-19 crisis has affected more than 188 countries and regions worldwide, causing large-scale loss of life and severe human suffering. The crisis poses a major threat to the global economy, with drops in activity, employment, and consumption worse than those seen during the 2008 financial crisis . COVID-19 has also exposed weaknesses in our health systems that must be addressed. How?
For a start, greater investment in population health would make people, particularly vulnerable population groups, more resilient to health risks. The health and socio-economic consequences of the virus are felt more acutely among disadvantaged populations, stretching a social fabric already challenged by high levels of inequalities. The crisis demonstrates the consequences of poor investment in addressing wider social determinants of health, including poverty, low education and unhealthy lifestyles. Despite much talk of the importance of health promotion, even across the richer OECD countries barely 3% of total health spending is devoted to prevention . Building resilience for populations also requires a greater focus on solidarity and redistribution in social protection systems to address underlying structural inequalities and poverty.
Beyond creating greater resilience in populations, health systems must be strengthened.
High-quality universal health coverage (UHC) is paramount. High levels of household out-of-pocket payments for health goods and services deter people from seeking early diagnosis and treatment at the very moment they need it most. Facing the COVID-19 crisis, many countries have strengthened access to health care, including coverage for diagnostic testing. Yet others do not have strong UHC arrangements. The pandemic reinforced the importance of commitments made in international fora, such as the 2019 High-Level Meeting on Universal Health Coverage , that well-functioning health systems require a deliberate focus on high-quality UHC. Such systems protect people from health threats, impoverishing health spending, and unexpected surges in demand for care.
Second, primary and elder care must be reinforced. COVID-19 presents a double threat for people with chronic conditions. Not only are they at greater risk of severe complications and death due to COVID-19; but also the crisis creates unintended health harm if they forgo usual care, whether because of disruption in services, fear of infections, or worries about burdening the health system. Strong primary health care maintains care continuity for these groups. With some 94% of deaths caused by COVID-19 among people aged over 60 in high-income countries, the elder care sector is also particularly vulnerable, calling for efforts to enhance control of infections, support and protect care workers and better coordinate medical and social care for frail elderly.
Third, the crisis demonstrates the importance of equipping health systems with both reserve capacity and agility. There is an historic underinvestment in the health workforce, with estimated global shortages of 18 million health professionals worldwide , mostly in low- and middle-income countries. Beyond sheer numbers, rigid health labour markets make it difficult to respond rapidly to demand and supply shocks. One way to address this is by creating a “reserve army” of health professionals that can be quickly mobilised. Some countries have allowed medical students in their last year of training to start working immediately, fast-tracked licenses and provided exceptional training. Others have mobilised pharmacists and care assistants. Storing a reserve capacity of supplies such as personal protection equipment, and maintaining care beds that can be quickly transformed into critical care beds, is similarly important.
Fourth, stronger health data systems are needed. The crisis has accelerated innovative digital solutions and uses of digital data, smartphone applications to monitor quarantine, robotic devices, and artificial intelligence to track the virus and predict where it may appear next. Access to telemedicine has been made easier. Yet more can be done to leverage standardised national electronic health records to extract routine data for real-time disease surveillance, clinical trials, and health system management. Barriers to full deployment of telemedicine, the lack of real-time data, of interoperable clinical record data, of data linkage capability and sharing within health and with other sectors remain to be addressed.
Fifth, an effective vaccine and successful vaccination of populations around the globe will provide the only real exit strategy. Success is not guaranteed and there are many policy issues yet to be resolved. International cooperation is vital. Multilateral commitments to pay for successful candidates would give manufacturers certainty so that they can scale production and have vaccine doses ready as quickly as possible following marketing authorisation, but could also help ensure that vaccines go first to where they are most effective in ending the pandemic. Whilst leaders face political pressure to put the health of their citizens first, it is more effective to allocate vaccines based on need. More support is needed for multilateral access mechanisms that contain licensing commitments and ensure that intellectual property is no barrier to access, commitments to technology transfer for local production, and allocation of scarce doses based on need.
The pandemic offers huge opportunities to learn lessons for health system preparedness and resilience. Greater focus on anticipating responses, solidarity within and across countries, agility in managing responses, and renewed efforts for collaborative actions will be a better normal for the future.
OECD Economic Outlook 2020 , Volume 2020 Issue 1, No. 107, OECD Publishing, Paris
OECD Employment Outlook 2020 : Worker Security and the COVID-19 Crisis, OECD Publishing, Paris
OECD Health at a Glance 2019, OECD Publishing, Paris
https://www.un.org/pga/73/wp-content/uploads/sites/53/2019/07/FINAL-draft-UHC-Political-Declaration.pdf
OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies, OECD Publishing, Paris
Working for Health and Growth: investing in the health workforce . Report of the High-Level Commission on Health Employment and Economic Growth, Geneva.
Colombo F., Oderkirk J., Slawomirski L. (2020) Health Information Systems, Electronic Medical Records, and Big Data in Global Healthcare: Progress and Challenges in OECD Countries . In: Haring R., Kickbusch I., Ganten D., Moeti M. (eds) Handbook of Global Health. Springer, Cham.
2. Improving population health and building healthy societies in times of COVID-19
By Helena Legido-Quigley , Associate Professor, London School of Hygiene and Tropical Medicine
The COVID-19 pandemic has been a stark reminder of the fragility of population health worldwide; at time of writing, more than 1 million people have died from the disease. The pandemic has already made evident that those suffering most from COVID-19 belong to disadvantaged populations and marginalised communities. Deep-rooted inequalities have contributed adversely to the health status of different populations within and between countries. Besides the direct and indirect health impacts of COVID-19 and the decimation of health systems, restrictions on population movement and lockdowns introduced to combat the pandemic are expected to have economic and social consequences on an unprecedented scale .
Population health – and addressing the consequences of COVID-19 – is about improving the physical and mental health outcomes and wellbeing of populations locally, regionally and nationally, while reducing health inequalities.¹ Moreover, there is an increasing recognition that societal and environmental factors, such as climate change and food insecurity, can also influence population health outcomes.
The experiences of Maria, David, and Ruben – as told by Spanish public broadcaster RTVE – exemplify the real challenges that people living in densely populated urban areas have faced when being exposed to COVID-19.¹
Maria is a Mexican migrant who has just returned from Connecticut to the Bronx. Her partner Jorge died in Connecticut from COVID-19. She now has no income and is looking for an apartment for herself and her three children. When Jorge became ill, she took him to the hospital, but they would not admit him and he was sent away to be cared for by Maria at home with their children. When an ambulance eventually took him to hospital, it was too late. He died that same night, alone in hospital. She thinks he had diabetes, but he was never diagnosed. They only had enough income to pay the basic bills. Maria is depressed, she is alone, but she knows she must carry on for her children. Her 10-year old child says that if he could help her, he would work. After three months, she finds an apartment.
David works as a hairdresser and takes an overcrowded train every day from Leganés to Chamberi in the centre of Madrid. He lives in a small flat in San Nicasio, one of the poorest working-class areas of Madrid with one of the largest ageing populations in Spain. The apartments are very small, making it difficult to be in confinement, and all of David’s neighbours know somebody who has been a victim of COVID-19. His father was also a hairdresser. David's father was not feeling well; he was taken to hospital by ambulance, and he died three days later. David was not able to say goodbye to his father. Unemployment has increased in that area; small local shops are losing their customers, and many more people are expecting to lose their jobs.
Ruben lives in Iztapalapa in Mexico City with three children, a daughter-in-law and five grandchildren. Their small apartment has few amenities, and no running water during the evening. At three o’clock every morning, he walks 45 minutes with his mobile stall to sell fruit juices near the hospital. His daily earnings keep the family. He goes to the central market to buy fruit, taking a packed dirty bus. He thinks the city's central market was contaminated at the beginning of the pandemic, but it could not be closed as it is the main source of food in the country. He has no health insurance, and he knows that as a diabetic he is at risk, but medication for his condition is too expensive. He has no alternative but to go to work every day: "We die of hunger or we die of COVID."
These real stories highlight the issues that must be addressed to reduce persistent health inequalities and achieve health outcomes focusing on population health. The examples of Maria, David and Ruben show the terrible outcomes COVID-19 has had for people living in poverty and social deprivation, older people, and those with co-morbidities and/or pre-existing health conditions. All three live in densely populated urban areas with poor housing, and have to travel long distances in overcrowded transport. Maria’s loss of income has had consequences for her housing security and access to healthcare and health insurance, which will most likely lead to worse health conditions for her and her children. Furthermore, all three experienced high levels of stress, which is magnified in the cases of Maria and David who were unable to be present when their loved ones died.
The COVID-19 pandemic has made it evident that to improve the health of the population and build healthy societies, there is a need to shift the focus from illness to health and wellness in order to address the social, political and commercial determinants of health; to promote healthy behaviours and lifestyles; and to foster universal health coverage.² Citizens all over the world are demanding that health systems be strengthened and for governments to protect the most vulnerable. A better future could be possible with leadership that is able to carefully consider the long-term health, economic and social policies that are needed.
In order to design and implement population health-friendly policies, there are three prerequisites. First, there is a need to improve understanding of the factors that influence health inequalities and the interconnections between the economic, social and health impacts. Second, broader policies should be considered not only within the health sector, but also in other sectors such as education, employment, transport and infrastructure, agriculture, water and sanitation. Third, the proposed policies need to be designed through involving the community, addressing the health of vulnerable groups, and fostering inter-sectoral action and partnerships.
Finally, within the UN's Agenda 2030 , Sustainable Development Goal (SDG) 3 sets out a forward-looking strategy for health whose main goal is to attain healthier lives and wellbeing. The 17 interdependent SDGs offer an opportunity to contribute to healthier, fairer and more equitable societies from which both communities and the environment can benefit.
The stories of Maria, David and Ruben are real stories featured in the Documentary: The impact of COVID19 in urban outskirts, Directed by Jose A Guardiola. Available here. Permission has been granted to narrate these stories.
Buck, D., Baylis, A., Dougall, D. and Robertson, R. (2018). A vision for population health: Towards a healthier future . [online] London: The King's Fund. [Accessed 20 Sept. 2020]
Wilton Park. (2020). Healthy societies, healthy populations (WP1734). Wiston House, Steyning. Retrieved from https://www.wiltonpark.org.uk/event/wp1734/ Cohen B. E. (2006). Population health as a framework for public health practice: a Canadian perspective. American journal of public health , 96 (9), 1574–1576.
3. Imagine a 'well-care' system that invests in keeping people healthy
By Maliha Hashmi , Executive Director, Health and Well-Being and Biotech, NEOM, and Jan Kimpen , Global Chief Medical Officer, Philips
Imagine a patient named Emily. Emily is aged 32 and I’m her doctor.
Emily was 65lb (29kg) above her ideal body weight, pre-diabetic and had high cholesterol. My initial visit with Emily was taken up with counselling on lifestyle changes, mainly diet and exercise; typical advice from one’s doctor in a time-pressured 15-minute visit. I had no other additional resources, incentives or systems to support me or Emily to help her turn her lifestyle around.
I saw Emily eight months later, not in my office, but in the hospital emergency room. Her husband accompanied her – she was vomiting, very weak and confused. She was admitted to the intensive care unit, connected to an insulin drip to lower her blood sugar, and diagnosed with type 2 diabetes. I talked to Emily then, emphasizing that the new medications for diabetes would only control the sugars, but she still had time to reverse things if she changed her lifestyle. She received further counselling from a nutritionist.
Over the years, Emily continued to gain weight, necessitating higher doses of her diabetes medication. More emergency room visits for high blood sugars ensued, she developed infections of her skin and feet, and ultimately, she developed kidney disease because of the uncontrolled diabetes. Ten years after I met Emily, she is 78lb (35kg) above her ideal body weight; she is blind and cannot feel her feet due to nerve damage from the high blood sugars; and she will soon need dialysis for her failing kidneys. Emily’s deteriorating health has carried a high financial cost both for herself and the healthcare system. We have prevented her from dying and extended her life with our interventions, but each interaction with the medical system has come at significant cost – and those costs will only rise. But we have also failed Emily by allowing her diabetes to progress. We know how to prevent this, but neither the right investments nor incentives are in place.
Emily could have been a real patient of mine. Her sad story will be familiar to all doctors caring for chronically ill patients. Unfortunately, patients like Emily are neglected by health systems across the world today. The burden of chronic disease is increasing at alarming rates. Across the OECD nearly 33% of those over 15 years live with one or more chronic condition, rising to 60% for over-65s. Approximately 50% of chronic disease deaths are attributed to cardiovascular disease (CVD). In the coming decades, obesity, will claim 92 million lives in the OECD while obesity-related diseases will cut life expectancy by three years by 2050.
These diseases can be largely prevented by primary prevention, an approach that emphasizes vaccinations, lifestyle behaviour modification and the regulation of unhealthy substances. Preventative interventions have been efficacious. For obesity, countries have effectively employed public awareness campaigns, health professionals training, and encouragement of dietary change (for example, limits on unhealthy foods, taxes and nutrition labelling).⁴,⁵ Other interventions, such as workplace health-promotion programmes, while showing some promise, still need to demonstrate their efficacy.

The COVID-19 crisis provides the ultimate incentive to double down on the prevention of chronic disease. Most people dying from COVID-19 have one or more chronic disease, including obesity, CVD, diabetes or respiratory problems – diseases that are preventable with a healthy lifestyle. COVID-19 has highlighted structural weaknesses in our health systems such as the neglect of prevention and primary care.
While the utility of primary prevention is understood and supported by a growing evidence base, its implementation has been thwarted by chronic underinvestment, indicating a lack of societal and governmental prioritization. On average, OECD countries only invest 2.8% of health spending on public health and prevention. The underlying drivers include decreased allocation to prevention research, lack of awareness in populations, the belief that long-run prevention may be more costly than treatment, and a lack of commitment by and incentives for healthcare professionals. Furthermore, public health is often viewed in a silo separate from the overall health system rather than a foundational component.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Fee-for-service models that remunerate physicians based on the number of sick patients they see, regardless the quality and outcome, dominate healthcare systems worldwide. Primary prevention mandates a payment system that reimburses healthcare professionals and patients for preventive actions. Ministries of health and governmental leaders need to challenge skepticism around preventive interventions, realign incentives towards preventive actions and those that promote healthy choices by people. Primary prevention will eventually reduce the burden of chronic diseases on the healthcare system.
As I reflect back on Emily and her life, I wonder what our healthcare system could have done differently. What if our healthcare system was a well-care system instead of a sick-care system? Imagine a different scenario: Emily, a 32 year old pre-diabetic, had access to a nutritionist, an exercise coach or health coach and nurse who followed her closely at the time of her first visit with me. Imagine if Emily joined group exercise classes, learned where to find healthy foods and how to cook them, and had access to spaces in which to exercise and be active. Imagine Emily being better educated about her diabetes and empowered in her healthcare and staying healthy. In reality, it is much more complicated than this, but if our healthcare systems began to incentivize and invest in prevention and even rewarded Emily for weight loss and healthy behavioural changes, the outcome might have been different. Imagine Emily losing weight and continuing to be an active and contributing member of society. Imagine if we invested in keeping people healthy rather than waiting for people to get sick, and then treating them. Imagine a well-care system.
Anderson, G. (2011). Responding to the growing cost and prevalence of people with multiple chronic conditions . Retrieved from OECD.
Institute for Health Metrics and Evaluation. GBD Data Visualizations. Retrieved here.
OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris.
OECD. (2017). Obesity Update . Retrieved here.
Malik, V. S., Willett, W. C., & Hu, F. B. (2013). Global obesity: trends, risk factors and policy implications. Nature Reviews Endocrinology , 9 (1), 13-27.
Lang, J., Cluff, L., Payne, J., Matson-Koffman, D., & Hampton, J. (2017). The centers for disease control and prevention: findings from the national healthy worksite program. Journal of occupational and environmental medicine , 59 (7), 631.
Gmeinder, M., Morgan, D., & Mueller, M. (2017). How much do OECD countries spend on prevention? Retrieved from OECD.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198.
Richardson, A. K. (2012). Investing in public health: barriers and possible solutions. Journal of Public Health , 34 (3), 322-327.
Yong, P. L., Saunders, R. S., & Olsen, L. (2010). Missed Prevention Opportunities The healthcare imperative: lowering costs and improving outcomes: workshop series summary (Vol. 852): National Academies Press Washington, DC.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved here .
McDaid, D., F. Sassi and S. Merkur (Eds.) (2015a), “Promoting Health, Preventing Disease: The Economic Case ”, Open University Press, New York.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved from OECD.
4. Why e arly detection and diagnosis is critical
By Paul Murray , Head of Life and Health Products, Swiss Re, and André Goy , Chairman and Executive Director & Chief of Lymphoma, John Theurer Cancer Center, Hackensack University Medical Center
Although healthcare systems around the world follow a common and simple principle and goal – that is, access to affordable high-quality healthcare – they vary significantly, and it is becoming increasingly costly to provide this access, due to ageing populations, the increasing burden of chronic diseases and the price of new innovations.
Governments are challenged by how best to provide care to their populations and make their systems sustainable. Neither universal health, single payer systems, hybrid systems, nor the variety of systems used throughout the US have yet provided a solution. However, systems that are ranked higher in numerous studies, such as a 2017 report by the Commonwealth Fund , typically include strong prevention care and early-detection programmes. This alone does not guarantee a good outcome as measured by either high or healthy life expectancy. But there should be no doubt that prevention and early detection can contribute to a more sustainable system by reducing the risk of serious diseases or disorders, and that investing in and operationalizing earlier detection and diagnosis of key conditions can lead to better patient outcomes and lower long-term costs.
To discuss early detection in a constructive manner it makes sense to describe its activities and scope. Early detection includes pre-symptomatic screening and treatment immediately or shortly after first symptoms are diagnosed. Programmes may include searching for a specific disease (for example, HIV/AIDS or breast cancer), or be more ubiquitous. Prevention, which is not the focus of this blog, can be interpreted as any activities undertaken to avoid diseases, such as information programmes, education, immunization or health monitoring.
Expenditures for prevention and early detection vary by country and typically range between 1-5% of total health expenditures.¹ During the 2008 global financial crisis, many countries reduced preventive spending. In the past few years, however, a number of countries have introduced reforms to strengthen and promote prevention and early detection. Possibly the most prominent example in recent years was the introduction of the Affordable Care Act in the US, which placed a special focus on providing a wide range of preventive and screening services. It lists 63 distinct services that must be covered without any copayment, co-insurance or having to pay a deductible.

Whilst logic dictates that investment in early detection should be encouraged, there are a few hurdles and challenges that need to be overcome and considered. We set out a few key criteria and requirements for an efficient early detection program:
1. Accessibility The healthcare system needs to provide access to a balanced distribution of physicians, both geographically (such as accessibility in rural areas), and by specialty. Patients should be able to access the system promptly without excessive waiting times for diagnoses or elective treatments. This helps mitigate conditions or diseases that are already quite advanced or have been incubating for months or even years before a clinical diagnosis. Access to physicians varies significantly across the globe from below one to more than 60 physicians per 10,000 people.² One important innovation for mitigating access deficiencies is telehealth. This should give individuals easier access to health-related services, not only in cases of sickness but also to supplement primary care.
2. Early symptoms and initial diagnosis Inaccurate or delayed initial diagnoses present a risk to the health of patients, can lead to inappropriate or unnecessary testing and treatment, and represents a significant share of total health expenditures. A medical second opinion service, especially for serious medical diagnoses, which can occur remotely, can help improve healthcare outcomes. Moreover, studies show that early and correct diagnosis opens up a greater range of curative treatment options and can reduce costs (e.g. for colon cancer, stage-four treatment costs are a multiple of stage-one treatment costs).³
3. New technology New early detection technologies can improve the ability to identify symptoms and diseases early: i. Advances in medical monitoring devices and wearable health technology, such as ECG and blood pressure monitors and biosensors, enable patients to take control of their own health and physical condition. This is an important trend that is expected to positively contribute to early detection, for example in atrial fibrillation and Alzheimers’ disease. ii. Diagnostic tools, using new biomarkers such as liquid biopsies or volatile organic compounds, together with the implementation of machine learning, can play an increasing role in areas such as oncology or infectious diseases.⁴
4. Regulation and Intervention Government regulation and intervention will be necessary to set ranges of normality, to prohibit or discourage overdiagnosis and to reduce incentives for providers to overtreat patients or to follow patients' inappropriate requests. In some countries, such as the US, there has been some success through capitation models and value-based care. Governments might also need to intervene to de-risk the innovation paradigm, such that private providers of capital feel able to invest more in the development of new detection technologies, in addition to proven business models in novel therapeutics.
OECD Health Working Papers No. 101 "How much do OECD countries spend on prevention" , 2017
World Health Organization; Global Health Observatory (GHO) data; https://www.who.int/gho/health_workforce/physicians_density/en/
Saving lives, averting costs; A report for Cancer Research UK, by Incisive Health, September 2014
Liquid Biopsy: Market Drivers And Obstacles; by Divyaa Ravishankar, Frost & Sullivan, January 21, 2019
Liquid Biopsies Become Cheap and Easy with New Microfluidic Device; February 26, 2019
How America’s 5 Top Hospitals are Using Machine Learning Today; by Kumba Sennaar, February 19, 2019
5. The business case for private investment in healthcare for all
Pascal Fröhlicher, Primary Care Innovation Scholar, Harvard Medical School, and Ian Wijaya, Managing Director in Lazard’s Global Healthcare Group
Faith, a mother of two, has just lost another customer. Some households where she is employed to clean, in a small town in South Africa, have little understanding of her medical needs. As a type 2 diabetes patient, this Zimbabwean woman visits the public clinic regularly, sometimes on short notice. At her last visit, after spending hours in a queue, she was finally told that the doctor could not see her. To avoid losing another day of work, she went to the local general practitioner to get her script, paying more than three daily wages for consultation and medication. Sadly, this fictional person reflects a reality for many people in middle-income countries.
Achieving universal health coverage by 2030, a key UN Sustainable Development Goal (SDG), is at risk. The World Bank has identified a $176 billion funding gap , increasing every year due to the growing needs of an ageing population, with the health burden shifting towards non-communicable diseases (NCDs), now the major cause of death in emerging markets . Traditional sources of healthcare funding struggle to increase budgets sufficiently to cover this gap and only about 4% of private health care investments focus on diseases that primarily affect low- and middle-income countries.
In middle-income countries, private investors often focus on extending established businesses, including developing private hospital capacity, targeting consumers already benefiting from quality healthcare. As a result, an insufficient amount of private capital is invested in strengthening healthcare systems for everyone.

Why is this the case? We discussed with senior health executives investing in Lower and Middle Income Countries (LMIC) and the following reasons emerged:
- Small market size . Scaling innovations in healthcare requires dealing with country-specific regulatory frameworks and competing interest groups, resulting in high market entry cost.
- Talent . Several LMICs are losing nurses and doctors but also business and finance professionals to European and North American markets due to the lack of local opportunities and a significant difference in salaries.
- Untested business models with relatively low gross margins. Providing healthcare requires innovative business models where consumers’ willingness to pay often needs to be demonstrated over a significant period of time. Additionally, relatively low gross margins drive the need for scale to leverage administrative costs, which increases risk.
- Government Relations. The main buyer of health-related products and services is government; yet the relationship between public and private sectors often lacks trust, creating barriers to successful collaboration. Add to that significant political risk, as contracts can be cancelled by incoming administrations after elections. Many countries also lack comprehensive technology strategies to successfully manage technological innovation.
- Complexity of donor funding. A significant portion of healthcare is funded by private donors, whose priorities might not always be congruent with the health priorities of the government.
Notwithstanding these barriers, healthcare, specifically in middle-income settings, could present an attractive value proposition for private investors:
- Economic growth rates . A growing middle class is expanding the potential market for healthcare products and services.
- Alignment of incentives . A high ratio of out-of-pocket payments for healthcare services is often associated with low quality. However, innovative business models can turn out of pocket payments into the basis for a customer-centric value proposition, as the provider is required to compete for a share of disposable income.
- Emergence of National Health Insurance Schemes . South Africa, Ghana, Nigeria and others are building national health insurance schemes, increasing a population’s ability to fund healthcare services and products .
- Increased prevalence of NCDs. Given the increasing incidence of chronic diseases and the potential of using technology to address these diseases, new business opportunities for private investment exist.
Based on the context above, several areas in healthcare delivery can present compelling opportunities for private companies.
- Aggregation of existing players.
- Leveraging primary care infrastructure. Retail companies can leverage their real estate, infrastructure and supply chains to deploy primary care services at greater scale than is currently the case.
- Telemedicine . Telecommunications providers can leverage their existing infrastructure and customer base to provide payment mechanisms and telehealth services at scale. As seen during the COVID-19 pandemic, investment in telemedicine can ensure that patients receive timely and continuous care in spite of restrictions and lockdowns.
- Cost effective diagnostics . Diagnostic tools operated by frontline workers and combined with the expertise of specialists can provide timely and efficient care.
To fully realize these opportunities, government must incentivise innovation, provide clear regulatory frameworks and, most importantly, ensure that health priorities are adequately addressed.
Venture capital and private equity firms as well as large international corporations can identify the most commercially viable solutions and scale them into new markets. The ubiquity of NCDs and the requirement to reduce costs globally provides innovators with the opportunity to scale their tested solutions from LMICs to higher income environments.
Successful investment exits in LMICs and other private sector success stories will attract more private capital. Governments that enable and support private investment in their healthcare systems would, with appropriate governance and guidance, generate benefits to their populations and economies. The economic value of healthy populations has been proven repeatedly , and in the face of COVID-19, private sector investment can promote innovation and the development of responsible, sustainable solutions.
Faith – the diabetic mother we introduced at the beginning of this article - could keep her client. As a stable patient, she could measure her glucose level at home and enter the results in an app on her phone, part of her monthly diabetes programme with the company that runs the health centre. She visits the nurse-led facility at the local taxi stand on her way to work when her app suggests it. The nurse in charge of the centre treats Faith efficiently, and, if necessary, communicates with a primary care physician or even a specialist through the telemedicine functionality of her electronic health system.
Improving LMIC health systems is not only a business opportunity, but a moral imperative for public and private leaders. With the appropriate technology and political will, this can become a reality.
6. How could COVID-19 change the way we pay for health services?
John E. Ataguba, Associate Professor and Director, University of Cape Town and Matthew Guilford, Co-Founder and Chief Executive Officer, Common Health
The emergence of the new severe acute respiratory syndrome coronavirus (SARS-Cov-2), causing the coronavirus disease 2019 (COVID-19), has challenged both developing and developed countries.
Countries have approached the management of infections differently. Many people are curious to understand their health system’s performance on COVID-19, both at the national level and compared to international peers. Alongside limited resources for health, many developing countries may have weak health systems that can make it challenging to respond adequately to the pandemic.
Even before COVID-19, high rates of out-of-pocket spending on health meant that every year, 800 million people faced catastrophic healthcare costs ,100 million families were pushed into poverty, and millions more simply avoided care for critical conditions because they could not afford to pay for it.
The pandemic and its economic fallout have caused household incomes to decline at the same time as healthcare risks are rising. In some countries with insurance schemes, and especially for private health insurance, the following questions have arisen: How large is the co-payment for a COVID-19 test? If my doctor’s office is closed, will the telemedicine consultation be covered by my insurance? Will my coronavirus care be paid for regardless of how I contracted the virus? These and other doubts can prevent people from seeking medical care in some countries.
In Nigeria, like many other countries in Africa, the government bears the costs associated with testing and treating COVID-19 irrespective of the individual’s insurance status. In the public health sector, where COVID-19 cases are treated, health workers are paid monthly salaries while budgets are allocated to health facilities for other services. Hospitals continue to receive budget allocations to finance all health services including the management and treatment of COVID-19. That implies that funds allocated to address other health needs are reduced and that in turn could affect the availability and quality of health services.
Although health workers providing care for COVID-19 patients in isolation and treatment centres in Nigeria are paid salaries that are augmented with a special incentive package, the degree of impact on the quality improvement of services remains unclear. The traditional and historical allocation of budgets does not always address the needs of the whole population and could result in poor health services and under-provision of health services for COVID-19 patients.
In some countries, the reliance on out-of-pocket funding is hardly better for private providers, who encounter brand risks, operational difficulties, and – in extreme cases – the risk of creating “debtor prisons” as they seek to collect payment from patients. Ironically, despite the huge demand for medical services to diagnose and treat COVID-19, large healthcare institutions and individual healthcare practitioners alike are facing financial distress.
Dependence on a steady stream of fee-for-service payments for outpatient consultations and elective procedures is leading to pay cuts for doctors in India , forfeited Eid bonuses for nurses in Indonesia , and hospital bankruptcies in the United States . In a recent McKinsey & Company survey, 77% of physicians reported that their business would suffer in 2020 , and 46% were concerned about their practice surviving the coronavirus pandemic.
COVID-19 is exposing how fee-for-service, historical budget allocation and out-of-pocket financing methods can hinder the performance of the health system. Some providers and health systems that deployed “value-based” models prior to the pandemic have reported that these approaches have improved financial resilience during COVID-19 and may support better results for patients. Nevertheless, these types of innovations do not represent the dominant payment model in any country.
How health service providers are paid has implications for whether service users can get needed health services in a timely fashion, and at an appropriate quality and an affordable cost. By shifting from fee-for-service reimbursements to fixed "capitation" and performance-based payments, these models incentivize providers to improve quality and coordination while also guaranteeing a baseline income level, even during times of disruption.
Health service providers could be paid either in the form of salaries, a fee for services they provide, by capitation (whether adjusted or straightforward), through global budgets, or by using a case-based payment system (for example, the diagnostics-related groups), among others. Because there are different incentives to consider when adopting any of the methods, they could be combined to achieve a specific goal. For example, in some countries, health workers are paid salaries , and some specific services are paid on a fee-for-service basis.
Ideally, health services could be purchased strategically , incorporating aspects of provider performance in transferring funds to providers and accounting for the health needs of the population they serve.
In this regard, strategic purchasing for health has been advocated and should be highlighted as crucial with the emergence of the COVID-19 pandemic. There is a need to ensure value in the way health providers are paid, inter alia to increase efficiency, ensure equity, and improve access to needed health services. Value-based payment methods, although not new in many countries, provide an avenue to encourage long-term value for money, better quality, and strategic purchasing for health, helping to build a healthier, more resilient world.
7. L essons in integrated care from the COVID-19 pandemic
Sarah Ziegler, Postdoctoral Researcher, Department of Epidemiology and Biostatistics, University of Zurich, and Ninie Wang, Founder & CEO, Pinetree Care Group.
Since the start of the COVID-19 pandemic, people suffering non-communicable diseases (NCDs) have been at higher risk of becoming severely ill or dying. In Italy, 96.2% of people who died of COVID-19 lived with two or more chronic conditions.
Beyond the pandemic, cardiovascular disease, cancer, respiratory disease and diabetes are the leading burden of disease, with 41 million annual deaths. People with multimorbidity - a number of different conditions - often experience difficulties in accessing timely and coordinated healthcare, made worse when health systems are busy fighting against the pandemic.
Here is what happened in China with Lee, aged 62, who has been living with Chronic Obstructive Pulmonary Disease (COPD) for the past five years.
Before the pandemic, Lee’s care manager coordinated a multi-disciplinary team of physicians, nurses, pulmonary rehabilitation therapists, psychologists and social workers to put together a personalized care plan for her. Following the care plan, Lee stopped smoking and paid special attention to her diet, sleep and physical exercises, as well as sticking to her medication and follow-up visits. She participated in a weekly community-based physical activity program to meet other COPD patients, including short walks and exchange experiences. A mobile care team supported her with weekly cleaning and grocery shopping.
Together with her family, Lee had follow-up visits to ensure her care plan reflected her recovery and to modify the plan if needed. These integrated care services brought pieces of care together, centered around Lee’s needs, and provided a continuum of care that helped keep Lee in the community with a good quality of life for as long as possible.
Since the COVID-19 outbreak, such NCD services have been disrupted by lockdowns, the cancellation of elective care and the fear of visiting care service . These factors particularly affected people living with NCDs like Lee. As such, Lee was not able to follow her care plan anymore. The mobile care team was unable to visit her weekly as they were deployed to provide COVID-19 relief. Lee couldn’t participate in her community-based program, follow up on her daily activities, or see her family or psychologists. This negatively affected Lee’s COPD management and led to poor management of her physical activity and healthy diet.
The pandemic highlights the need for a flexible and reliable integrated care system to enable healthcare delivery to all people no matter where they live, uzilizing approaches such as telemedicine and effective triaging to overcome care disruptions.
Lee’s care manager created short videos to assist her family through each step of her care and called daily to check in on the implementation of the plan and answer questions. Lee received tele-consultations, and was invited to the weekly webcast series that supported COPD patient communities. When her uncle passed away because of pneumonia complications from COVID-19 in early April, Lee’s care manager arranged a palliative care provider to support the family through the difficult time of bereavement and provided food and supplies during quarantine. Lee could even continue with her physical activity program with an online training coach. There were a total of 38 exercise videos for strengthening and stretching arms, legs and trunk, which she could complete at different levels of difficulty and with different numbers of repetitions.
Lee’s case demonstrates that early detection, prevention, and management of NCDs play a crucial role in a global pandemic response. It shows how we need to shift away from health systems designed around single diseases towards health systems designed for the multidimensional needs of individuals. As part of the pandemic responses, addressing and managing risks related to NCDs and prevention of their complications are critical to improve outcomes for vulnerable people like Lee.
How to design and deliver successful integrated care
The challenge for the successful transformation of healthcare is to tailor care system-wide to population needs. A 2016 WHO Framework on integrated people-centered health services developed a set of five general strategies for countries to progress towards people-centered and sustainable health systems, calling for a fundamental transformation not only in the way health services are delivered, but also in the way they are financed and managed . These strategies call for countries to:
- Engage and empower people / communities: an integrated care system must mobilize everyone to work together using all available resources, especially when continuity of essential health and community services for NCDs are at risk of being undermined.
- Strengthen governance and accountability, so that integration emphasizes rather than weakens leadership in every part of the system, and ensure that NCDs are included in national COVID-19 plans and future essential health services.
- Reorient the model of care to put the needs and perspectives of each person / family at the center of care planning and outcome measurement, rather than institutions.
- Coordinate services within and across sectors, for example, integrate inter-disciplinary medical care with social care, addressing wider socio-economic, environmental and behavioral determinants of health.
- Create an enabling environment, with clear objectives, supportive financing, regulations and insurance coverage for integrated care, including the development and use of systemic digital health care solutions.
Whether due to an unexpected pandemic or a gradual increase in the burden of NCDs, each person could face many health threats across the life-course.
Only systems that dynamically assess each person’s complex health needs and address them through a timely, well-coordinated and tailored mix of health and social care services will be able to deliver desired health outcomes over the longer term, ensuring an uninterrupted good quality of life for Lee and many others like her.
- Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020;12: 6049–57.
- WHO. Noncommunicable diseases in emergencies. Geneva: World Health Organization, 2016.
- WHO. COVID-19 significantly impacts health services for noncommunicable diseases. June 2020.
- Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicalbe diseases in the COVID-19 response. The Lancet. 2020. 395:1678-1680
- WHO. Framework on integrated people-centred health services. Geneva: World Health Organization, 2016.
8 . Why access to healthcare alone will not save lives
Donald Berwick, President Emeritus and Senior Fellow, Institute for Healthcare Improvement; Nicola Bedlington, Special Adviser, European Patient Forum; and David Duong, Director, Program in Global Primary Care and Social Change, Harvard Medical School.
Joyce lies next to 10 other women in bare single beds in the post-partum recovery room at a rural hospital in Uganda. Just an hour ago, Joyce gave birth to a healthy baby boy. She is now struggling with abdominal pain. A nurse walks by, and Joyce tries to call out, but the nurse was too busy to attend to her; she was the only nurse looking after 20 patients.
Another hour passes, and Joyce is shaking and sweating profusely. Joyce’s husband runs into the corridor to find a nurse to come and evaluate her. The nurse notices Joyce’s critical condition - a high fever and a low blood pressure - and she quickly calls the doctor. The medical team rushes Joyce to the intensive care unit. Joyce has a very severe blood stream infection. It takes another hour before antibiotics are started - too late. Joyce dies, leaving behind a newborn son and a husband. Joyce, like many before her, falls victim to a pervasive global threat: poor quality of care.
Adopted by United Nations (UN) in 2015, the Sustainable Development Goals (SDG) are a universal call to action to end poverty, protect the planet and ensure that all enjoy peace and prosperity by 2030. SDG 3 aims to ensure healthy lives and promote wellbeing for all. The 2019 UN General Assembly High Level Meeting on Universal Health Coverage (UHC) reaffirmed the need for the highest level of political commitment to health care for all.
However, progress towards UHC, often measured in terms of access, not outcomes, does not guarantee better health, as we can see from Joyce’s tragedy. This is also evident with the COVID-19 response. The rapidly evolving nature of the COVID-19 pandemic has highlighted long-term structural inefficiencies and inequities in health systems and societies trying to mitigate the contagion and loss of life.
Systems are straining under significant pressure to ensure standards of care for both COVID-19 patients and other patients that run the risk of not receiving timely and appropriate care. Although poor quality of care has been a long-standing issue, it is imperative now more than ever that systems implement high-quality services as part of their efforts toward UHC.
Poor quality healthcare remains a challenge for countries at all levels of economic development: 10% of hospitalized patients acquire an infection during their hospitalization in low-and-middle income countries (LMIC), whereas 7% do in high-income countries. Poor quality healthcare disproportionally affects the poor and those in LMICs. Of the approximately 8.6 million deaths per year in 137 LMICs, 3.6 million are people who did not access the health system, whereas 5 million are people who sought and had access to services but received poor-quality care.
Joyce’s story is all too familiar; poor quality of care results in deaths from treatable diseases and conditions. Although the causes of death are often multifactorial, deaths and increased morbidity from treatable conditions are often a reflection of defects in the quality of care.
The large number of deaths and avoidable complications are also accompanied by substantial economic costs. In 2015 alone, 130 LMICs faced US $6 trillion in economic losses. Although there is concern that implementing quality measures may be a costly endeavor, it is clear that the economic toll associated with a lack of quality of care is far more troublesome and further stunts the socio-economic development of LMICs, made apparent with the COVID-19 pandemic.
Poor-quality care not only leads to adverse outcomes in terms of high morbidity and mortality, but it also impacts patient experience and patient confidence in health systems. Less than one-quarter of people in LMICs and approximately half of people in high-income countries believe that their health systems work well.
A lack of application and availability of evidenced-based guidelines is one key driver of poor-quality care. The rapidly changing landscape of medical knowledge and guidelines requires healthcare workers to have immediate access to current clinical resources. Despite our "information age", health providers are not accessing clinical guidelines or do not have access to the latest practical, lifesaving information.
Getting information to health workers in the places where it is most needed is a delivery challenge. Indeed, adherence to clinical practice guidelines in eight LMICs was below 50%, and in OECD countries, despite being a part of national guidelines, 19-53% of women aged 50-69 years did not receive mammography screening.4 The evidence in LMICs and HICs suggest that application of evidence-based guidelines lead to reduction in mortality and improved health outcomes.
Equally, the failure to change and continually improve the processes in health systems that support the workforce takes a high toll on quality of care. During the initial wave of the COVID-19 pandemic, countries such as Taiwan, Hong Kong, Singapore and Vietnam, which adapted and improved their health systems after the SARS and H1N1 outbreaks, were able to rapidly mobilize a large-scale quarantine and contact tracing strategy, supported with effective and coordinated mass communication.
These countries not only mitigated the economic and mortality damage, but also prevented their health systems and workforce from enduring extreme burden and inability to maintain critical medical supplies. In all nations, investing in healthcare organizations to enable them to become true “learning health care systems,” aiming at continual quality improvement, would yield major population health and health system gains.
The COVID-19 pandemic underscores the importance for health systems to be learning systems. Once the dust settles, we need to focus, collectively, on learning from this experience and adapting our health systems to be more resilient for the next one. This implies a need for commitment to and investment in global health cooperation, improvement in health care leadership, and change management.
With strong political and financial commitment to UHC, and its demonstrable effect in addressing crises such as COVID-19, for the first time, the world has a viable chance of UHC becoming a reality. However, without an equally strong political, managerial, and financial commitment to continually improving, high-quality health services, UHC will remain an empty promise.
1. United Nations General Assembly. Political declaration of the high-level meeting on universal health coverage. New York, NY2019.
2. Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the Marmot review 10 years on. Institute of Health Equity;2020.
3. National Academies of Sciences, Engineering, and Medicine: Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: Improving health care worldwide. Washington, DC: National Academies Press;2018.
4. World Health Organization, Organization for Economic Co-operation and Development, World Bank Group. Delivering quality health services: a global imperative for universal health coverage. World Health Organization; 2018.
5. Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. 2018;6(11):e1196-e1252.
6. Ricci-Cabello I, Violán C, Foguet-Boreu Q, Mounce LT, Valderas JM. Impact of multi-morbidity on quality of healthcare and its implications for health policy, research and clinical practice. A scoping review. European Journal of General Practice. 2015;21(3):192-202.
7. Valtis YK, Rosenberg J, Bhandari S, et al. Evidence-based medicine for all: what we can learn from a programme providing free access to an online clinical resource to health workers in resource-limited settings. BMJ global health. 2016;1(1).
8. Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America . Washington, DC: National Academies Press 2012.
Career mentorship, clinical and technology skills
- See us on facebook
- See us on youtube
- See us on instagram
APPLICATION GUIDE Clinical Science, Technology and Medicine Summer Internship
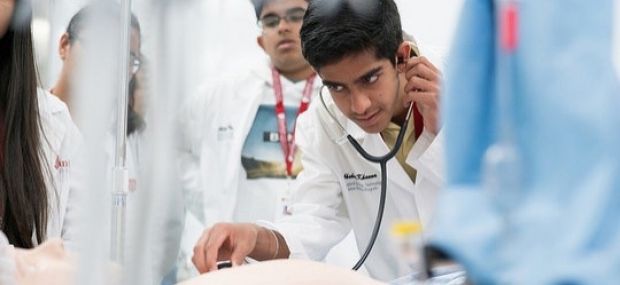
Applications Now Open
Applications open for the 2020 Clinical Science, Technology and Medicine Summer Internship program. Program application deadline is February 14, 2020.
How to write "the change you want to see in health care" essay

By SeventyFourImages via EnvatoElements
By Urvi Gupta
There are many ways of approaching an essay such as this one. Here are some methods that we find useful, and we hope they will be helpful to you as well.
The most powerful essays are those which could not be written by anyone other than yourself. Keep this in mind as you begin your brainstorm. Finding stories which are personal and teach the reader something about you is crucial.
Pull out some pen and paper. Set a 5-minute timer on your phone. Use this time to jot down every thought that comes into mind about the ways you wish our health care system was better. Try to keep your pen to the paper and keep writing throughout the 5 minutes.
Look over your list. Which ones stick out to you as the most compelling? Through your interactions with healthcare, have any of the challenges you brainstormed impacted you personally? Have you had any experiences where you worked towards any of these goals? Use these questions to pick 1-3 topics from your list.
Begin outlining your essay. For each of your topics, try to include answers to the following questions:
Briefly describe the topic/issue.
Why is this topic important to you specifically? How has it affected you/the people around you/the world? Give concrete examples.
How do you propose you can make it better? Again, be specific and try to draw inspiration from your own life.
Begin writing!
Read your draft out loud to yourself or a friend/family member to look for areas that are unclear or that could be improved.
Remember that it is less important as to what you pick for the change you want to see in health care and more important that you have something compelling and personal to say about it. We want to learn about you!
The views expressed here are the authors and they do not necessarily reflect the views and opinions of Stanford University School of Medicine. External websites are shared as a courtesy. They are not endorsed by the Stanford University School of Medicine.
The most powerful essays are those which could not be written by anyone other than yourself.
Urvi Gupta, BS SASI Teaching Assistant
Home / Essay Samples / Health / Health Care
Essays on Health Care
Importance of cleanliness: a path to health and well-being.
Cleanliness is not just a habit; it's a way of life that has far-reaching implications for both individuals and communities. From maintaining physical health to fostering a sense of discipline, the importance of cleanliness cannot be overstated. It encompasses personal hygiene, environmental cleanliness, and the...

Japan Vs Us Healthcare System
The healthcare systems of different countries reflect unique approaches to providing medical services, managing costs, and ensuring access to care. Two notable examples are Japan and the United States, each representing distinct models. This essay delves into a comparative analysis of the healthcare systems in...
The Benefits of Exercise for Mental and Physical Health
When it comes to leading a healthy and fulfilling life, there is one undeniable truth - regular exercise is a cornerstone. This essay explores the myriad benefits of exercise for health. In an era where sedentary lifestyles and desk-bound jobs are increasingly prevalent, understanding and...
Universal Healthcare: Examinin the Complexities
Universal healthcare is a topic of significant debate and discussion in countries around the world. It represents a system where every citizen has access to essential medical services regardless of their financial situation. The concept of universal healthcare has both fervent supporters and vehement critics....
Arguments for Euthanasia: a Comprehensive Examination
Euthanasia, the act of intentionally ending a person's life to relieve suffering, is a deeply divisive and ethically complex issue. Proponents argue that euthanasia is a compassionate and dignified option for individuals facing unbearable pain and terminal illnesses. In this essay, we will explore the...
Why Euthanasia Should not Be Legal: a Critical Examination
Euthanasia, often described as "mercy killing" or "assisted suicide," is a highly controversial and morally complex issue. It involves the deliberate ending of a person's life, usually in cases of terminal illness or unbearable suffering, with the assistance of a physician or another individual. While...
My Trip to the Dentist: a Tale of Dental Care
A trip to the dentist is often met with mixed feelings, ranging from a sense of responsibility to a hint of anxiety. However, this routine visit is an essential part of maintaining oral health and preventing potential issues. In this essay, I will recount my...
Medical Care Should Be Free for Everybody
The provision of free medical care for all individuals is a topic that has sparked intense debates globally. This essay explores the arguments in favor of providing medical care free of charge, highlighting the potential benefits to society in terms of public health, economic well-being,...
Wealth is More Important than Health
The age-old debate about whether wealth is more important than health continues to stir discussions across societies. Both wealth and health are essential aspects of a fulfilling life, yet they are often viewed as mutually exclusive. In this essay, we will explore the nuanced relationship...
Exercise and Fitness: a Path to Health and Well-being
Exercise and fitness play a pivotal role in maintaining a healthy lifestyle and promoting overall well-being. In a world marked by sedentary routines and modern conveniences, the importance of physical activity cannot be overstated. This essay delves into the significance of exercise, its benefits for...
Trying to find an excellent essay sample but no results?
Don’t waste your time and get a professional writer to help!
- Assisted Suicide
- Physical Exercise
- Nursing Home
- Universal Health Care
- Health Care Policy
- Dental Care
- Public Health
- Palliative Care
- Nursing Care Plan
- Health Promotion
- Healthcare Crisis
- Mental Health
- Reproductive Health
samplius.com uses cookies to offer you the best service possible.By continuing we’ll assume you board with our cookie policy .--> -->