- Open access
- Published: 02 October 2017

Awareness and current knowledge of breast cancer
- Muhammad Akram 1 ,
- Mehwish Iqbal 2 ,
- Muhammad Daniyal 2 &
- Asmat Ullah Khan 3 , 4
Biological Research volume 50 , Article number: 33 ( 2017 ) Cite this article
118k Accesses
736 Citations
20 Altmetric
Metrics details
Breast cancer remains a worldwide public health dilemma and is currently the most common tumour in the globe. Awareness of breast cancer, public attentiveness, and advancement in breast imaging has made a positive impact on recognition and screening of breast cancer. Breast cancer is life-threatening disease in females and the leading cause of mortality among women population. For the previous two decades, studies related to the breast cancer has guided to astonishing advancement in our understanding of the breast cancer, resulting in further proficient treatments. Amongst all the malignant diseases, breast cancer is considered as one of the leading cause of death in post menopausal women accounting for 23% of all cancer deaths. It is a global issue now, but still it is diagnosed in their advanced stages due to the negligence of women regarding the self inspection and clinical examination of the breast. This review addresses anatomy of the breast, risk factors, epidemiology of breast cancer, pathogenesis of breast cancer, stages of breast cancer, diagnostic investigations and treatment including chemotherapy, surgery, targeted therapies, hormone replacement therapy, radiation therapy, complementary therapies, gene therapy and stem-cell therapy etc for breast cancer.
Breast cancer is the most common cancer and also the primary cause of mortality due to cancer in female around the World. About 1.38 million new breast cancer cases were diagnosed in 2008 with almost 50% of all breast cancer patients and approximately 60% of deaths occurring in developing countries. There is a huge difference in breast cancer survival rates worldwide, with an estimated 5-year survival of 80% in developed countries to below 40% for developing countries [ 1 ]. Developing countries face resource and infrastructure constraints that challenge the objective of improving breast cancer outcomes by timely recognition, diagnosis and management [ 2 ]. In developed countries like the United States, about 232,340 female will be diagnosed and death of 39,620 female will occur due to breast cancer in 2013 [ 3 ]. The lifetime risk of developing breast cancer in an American female is 12.38% [ 3 ]. The significant decline in morality due to breast cancer in the United States from 1975 to 2000 is attributed to constant enhancement in both screening mammography and management [ 4 ]. According to the World Health Organization (WHO), enhancing breast cancer outcome and survival by early detection remains the foundation of breast cancer regulations. Different modern medicines are prescribed to treat breast cancer. Medical therapy of breast cancer with antiestrogens such as raloxifene or tamoxifen might avoid breast cancer in individuals who are at increased possibility of developing it [ 5 ]. Surgery of both breasts is an added preventative measure in some increased probability of developing cancer in female. In patients who have been identified with breast tumor, different strategies of management are used such as targeted therapy, hormonal therapy, radiation therapy, surgery and chemotherapy. In individuals with distant metastasis, managements are typically aimed at enhancing life quality and survival rate [ 6 ]. The unpleasant side effects of breast cancer treatment are one of the most motivating factors to find some alternative methods. The use of herbs for treating the patients having breast cancer is considered a natural alternative, because some plants may contain properties that naturally have the ability to treat breast cancer [ 7 , 8 , 9 , 10 , 11 ].
Epidemiology
Currently, one in twelve females in Britain between age of 1 and 85 years gets breast cancer. With one million new cases of cancers reported in the World, breast cancer is common in females and comprises 18% of all women cancer. Incidence of breast cancer is predicted to increase to 85 per 100,000 women by 2021 [ 12 ]. In 2012, 1.67 million new cases of breast cancer were diagnosed that is 25% of all cancers among women. Ferlay et al. [ 13 ] stated that 883,000 cases are in less developed countries and 794,000 in most developed countries. According to the data, 145.2 women in Belgium and 66.3 in Poland between 100,000 suffer from breast cancer [ 14 ]. Incidence of breast cancer in the United States is one out of eight women and In Asia one woman suffers from breast cancer out of 35. In Iran, there are 10 cases in 100,000 populations and 7000 new cases have been reported annually [ 15 ]. Prevalence of breast cancer is increasing in Pakistan [ 16 , 17 , 18 ]. Breast cancer is found mostly in highly populated areas of South Asian developing counties [ 19 , 20 ]. Breast cancers in males have been detected in Northern areas of Pakistan [ 21 ]. Yang et al. [ 22 ] stated that new cases of breast cancer in China were 168,013 in 2005 and 121,269 in 2000.
Anatomy of breast
Both males and females have breasts [ 23 ]. The breast is made up of fatty tissue called adipose tissue [ 24 ]. The female’s breasts usually contain more glandular tissue than that of the males [ 25 ]. Female breasts contain 12–20 lobes which are further divided into smaller lobules [ 26 ]. These lobes and lobules are connected via milk ducts. The adipose tissue of the breast is supplied by a network of nerves, blood vessels, lymph vessels, lymph nodes, and is also composed of fibrous connective tissue and ligaments [ 27 ]. The female breast is designed to provide optimal nourishment for babies and to provide sexual pleasure for the female herself. The breasts are glandular organs that are very sensitive to hormonal changes in the body [ 28 ]. They adopt cyclic changes in synchrony with the menstrual cycle. They are closely associated with the genital system of females. Nipple stimulation enhances secretion of prolactin from the pituitary gland. This hormone also affects the uterus and can cause contractions. Lymph node draining the breast tissues is also found in the armpits. After a female has had a baby and her milk comes in, mother may develop striking swelling under arms from engorgement of the breast tissue in that region. Breasts come in all sizes and shapes, as do nipples. Most female possess one breast that slightly smaller than the other [ 29 ]. The epidermis of the areola and nipple is very much pigmented and to some extent wrinkled, and the nipple skin contains several apocrine and sebaceous sweat glands and somewhat small hair. The 15–25 milk ducts go into the base of the nipple, wherever they expand to synthesize the milk sinuses. These milk ducts functions as the carriers of milk towards the nipples [ 30 ]. Slightly under the surface of nipple, these sinuses end in cone-shaped ampullae. The spherical areola is present around the nipple and is between 15 and 60 mm in diameter. Sebaceous glands, sweat glands and lanugo hairs are present on its skin, Montgomery’s glands, are big, modified sebaceous glands with tiny milk ducts that open into Morgagni’s tubercles in the areola epidermis. Deep in the nipple and areola, several smooth muscle fibers are set circularly and radially in the dense connective tissue and longitudinally alongside the lactiferous ducts that lengthen up into the nipple. These muscle fibers are cause emptying of milk sinuses, nipple erection and contraction of areola. The greater part of the breast parenchyma expand inferiorly from the point of the 2nd or 3rd rib to the inframammary fold, which is at about the point of the 6th or 7th rib, and crossways from the border of the sternum to the anterior axillary line. The mammary tissue also expands erratically into the axilla as the glandular tail of spence. The posterior surface of the breast rests on segment of the fasciae of the pectoralis major, rectus abdominis muscles, external abdominal oblique and serratus anterior.
A global prospective
Globalization, which thus greatly characterizes our period, was primarily linked with commercial-related actions, consequently with ecological concerns, and especially in recent times with the dark truth of terrorism. Up till now the “globalization” of numerous human being actions, together with health care, has been departing on for several decades, enhancing in step with improvement in information machinery. Correctly or incorrectly, and whether planned or not, numerous clinicians in developing countries keep an eye on what Americans are achieving, or are alleged to be achieving, as “state of the art” and recent most excellent performance that ought to be copied. The actions reviewed and our current narration with transplantation of bone marrow recommends that present “standard of care” United States described interventions are inappropriate to global utilization. Unluckily, extensive deficiency of community wellbeing strategies to breast cancer has made understanding of such rights for females not viable. Impractical, deadly, and extremely expensive treatments for breast cancer cannot assist the huge number of females in the earth at danger for or who develop breast cancer [ 31 ].
Types of breast cancer
According to site, it is divided into invasive and non-invasive breast cancers
Non-invasive breast cancer
It is a cancer that has not extended away from the lobule or ducts where it situated [ 32 ]. An example of a kind of non-invasive breast cancer is ductal carcinoma in situ. Ductal carcinoma in situ appears when atypical cells develop within the milk ducts, however have not extended to close proximity of tissue or outside. The word “in situ” describes “in place.” Even though the atypical cells have not extended to tissues outer the lobules or ducts, they can progress and grow into invasive breast cancer. The normal background of every scientific unit is demonstrated and a biological understanding of the accessible information is presented. Lobular carcinoma in-situ is understood merely a risky sign moderately than a predecessor for the successive growth of invasive cancer, so that one time the judgment is made, additional operative involvement is avoidable and sequential follow-up only is suggested. The management of ductal carcinoma in-situ should be kept in mind that breast-preserving treatment is at the present considered best therapy of breast cancer, the illness we are attempting to stop [ 33 ]. The pitfalls of suggested management based on retrospective statistics are have been taken into account and the requirement to conduct clinical studies intended to establish the best possible beneficial treatment of non-invasive breast cancer is affirmed [ 34 ].
Lobular carcinoma in situ (LCIS)
This type of breast cancer develops into breast lobules [ 35 ]. The breast cancer has not extended exterior to the lobules into the breast tissue [ 36 ]. Lobular carcinoma in situ is usually identified as non-invasive breast cancer [ 37 ].
Ductal carcinoma in situ
It is the most general kind of non-invasive breast cancer, is limited to the breast duct. Example of ductal carcinoma in situ is ductal comedocarcinoma [ 38 ].
Invasive breast cancer
It exists when abnormal cells from within the lobules or milk ducts split out into close proximity of breast tissue [ 39 ]. Cancer cells can pass through the breast to different parts of the body through immune system or the systemic circulation [ 40 ]. They may move early in the development when the tumor is a minute or afterward when the tumor is huge Invasive breast cancer is most occurring general carcinoma in females. The regions of elevated threat are the prosperous populations of Australia and Europe wherever 6% of females suffer from invasive breast cancer prior to 75 years of age. The prevalence of breast cancer enhances quickly with increasing age [ 41 ]. Invasive breast cancer that extends to different organs of the body is also recognized as metastatic breast cancer [ 42 ]. Most common organ to which these cells spread are brain, bones, lungs and liver. These cells once more segregate and expand irregularly and produce new cancers. The new forming cells are developing in different part of the body, it is still breast cancer [ 43 ].
Infiltrating lobular carcinoma (ILC)
Infiltrating lobular carcinoma is also recognized as invasive lobular carcinoma. ILC originates in the milk glands (lobules) of the breast, but frequently extends to other areas of the body [ 44 ].
Infiltrating ductal carcinoma
Infiltrating ductal carcinoma is also recognized as invasive ductal carcinoma. IDC originates in the milk ducts of the breast and extends to the duct wall, invading the breast fatty tissues and probably other parts of the body [ 45 ].
Medullary carcinoma
Medullary carcinoma is an invasive breast cancer that designs a discrete margin normal tissue and medullary tissue [ 46 ].
Mucinous carcinoma
It is recognized as colloid carcinoma , mutinous carcinoma is a uncommon breast cancer created by the mucus-forming cancer cells. Females with mutinous carcinoma usually have an improved prediction than females with additional general kinds of invasive carcinoma [ 47 ].
Tubular carcinoma
Tubular carcinomas are a particular kind of invasive breast carcinoma. Females with tubular carcinoma usually have an improved prospects than women with additional general kinds of invasive carcinoma [ 48 ].
Inflammatory breast cancer
Inflammatory breast cancer is the form of swollen breasts (red and warm) with dimples and/or broad ridges due to cancer cells blocking lymph vessels or channels in the skin over the breast. Though inflammatory breast cancer is uncommon and is tremendously fast-growing [ 49 ]. Treatment involves vigilant synchronization of all multidisciplinary strategies, including radiation therapy, surgery, chemotherapy and imaging. The administration of neoadjuvant chemotherapy has accorded considerably to enhancement in general survival from the time when the earliest report of this matter and has performed the function of locoregional treatment such as radiation and surgery significant to sustained improvements in this ailment [ 50 ].
Paget’s disease of the breast
It is the uncommon type of breast cancer that usually shows visible changes to the nipple of the breast [ 51 ]. Its symptoms include red itchy rashes involving the nipple and then it can sometime spread to the normal skin as well. However it resembles with the other skin conditions such as eczema and psoriasis but it can be differentiated as the other skin conditions usually affects both the breasts and can start from the areola rather than the nipple of the breast however Paget’s disease of the breast most often affects only one breast and starts with the nipple of the breast instead of areola (breastcancercare.org.uk) Nearly 1–3% of all the breast cancers are Paget’s disease and can affect both men as well as women. The actual theory behind the pathogenesis or development of Paget’s disease of the breast isn’t clear yet however there are few theories supporting it’s pathogenesis. Their warning signs include bleeding and oozing of discharge from the nipple, flattening or inversion of nipple, lump found in the breast etc. It can be diagnosed by using punch biopsy. It’s prognosis is good if it remains within the nipple or in ducts of the breast [ 52 ].
Phyllodes tumor
Phyllodes tumors are can be either benign or malignant [ 53 ]. Phyllodes tumors develop in the connective tissues of the breast and may be treated by surgical removal [ 54 ]. Phylloides tumors are extremely uncommon; fewer than 10 females die of this kind of breast cancer every year in the United States [ 55 ].
Triple-negative breast cancer
Breast cancer is at the present extensively documented that is a heterogeneous disorder with special sub-forms, distinguished by means of their dissimilar clinico-pathological characteristics, prevision and responses to management. Triple-negative breast cancer is described by the deficiency of progesterone receptor, human epidermal growth factor receptor 2 and estrogen receptor expression [ 56 ]. This type is mainly destructive, commonly observed in premenopausal females, and is responsible for 10–15% of cases in white females, with a elevated occurrence [ 57 ].
Pathogenesis of breast cancer
The breast is a complex tubulo-alveolar organ fixed within an asymmetrical connective tissue [ 58 ], that go through a chain of alteration from child bearing age to senility. The changes seen with every menstrual cycle and pregnancy guided us to assume the occurrence of precursor cells in the mature tissue that is able of synthesizing novel duct-lobular units [ 59 ]. The typical breast architecture contains a stratified epithelium bordered by a basement membrane and fixed in a template of blood vessels, lymphatic and stromal cells [ 60 ]. In the usual breast, the stratified epithelium comprised of two dissimilar cell populations, myoepithelial and epithelial, which can be distinguished by way of immunohistochemical staining with antibodies against myosin and CK, correspondingly. It has been postulated that the creation of cellular heterogeneity in breast disorders depends on the primary developmental series of the usual breast. This heterogenicity of the breast carcinoma might happen from the neoplastic change of either myoepithelial or epithelial cell, or yet from a stem cell that has the ability to develop into myoepithelial or epithelial cells [ 61 ]. According to the oncology of breast cancer, neoplastic cells differ from the normal body cells. Normal tissues of the body have limited growth promotion and regulation which helps to keep the structure and functions of tissues usual. However, cancerous cells have prolonged and chronic proliferation without any external stimuli [ 62 ]. Cancer cells overcome the growth suppressor genes [ 63 ]. Breast cancer is a malignant disease that initiates in the breast cells. Like other malignant tumors, there are numerous causes that can increase the possibility of developing breast cancer. Injure to the deoxyribonucleic acid (DNA) and hereditary alteration can guide to breast cancer have been associated with the exposure of estrogen. Some patients inherit fault in the deoxyribonucleic acid (DNA) and genes like the P53, BRCA1 and BRCA2 among others. The patients with a family history of breast or ovarian cancer have possibility of developing breast cancer [ 64 ]. Neoplastic cells require considerable potential to multiply and convert into a massive tumor [ 65 ]. The immune system usually tries to find out cancer cells and cells with injured deoxyribonucleic acid (DNA) and demolish them. Breast cancer might be outcome of malfunction of such an useful immune defence and surveillance. Breast cancer commonly occurs due to an association between genetic and environmental factors. RAS/MEK/ERK pathway and PI3K/AKT pathway defend normal cells from cell suicide. When mutation occurs in genes that are involved in encoding of these protective pathways, the cells become unable of committing suicide when they are no longer required which then leads to development of cancer. These mutations were confirmed to be experimentally associated with estrogen exposure [ 66 ]. It was recommended that deformity in the growth factors signaling can assist growth of malignant cells. Over expression of leptinin breast adipose tissue enhances proliferation of cell and cancer [ 67 ]. These are numerous growth factors signaling and other factors that interrelate between epithelial cells and stromal cells. Interruption in these might result in development of breast cancer. In cancer cells, enzyme telomerase turns away the chromosomal shortening and allows the extensive replication of cells [ 68 ]. Tumor cells get their nutrients and oxygen supply by angiogenesis [ 69 ]. Cancer cells break their boundaries and can enter into the blood, lymphatic tissues and other tissues of the body to produce a secondary tumor [ 70 ].
Causative factors and associated risks of breast carcinoma
Breast cancer is the leading cause of death among British females who are 40–55 years of age. Breast cancer is more common in single women than in married women [ 71 , 72 ]. The breast is an estrogen sensitive organ. Many females who have been on birth control pills or estrogen replacement have found that the medications result in enlarged and often tender breasts. The activity of this medication, combined with the standard western high fat, low fiber diet, which over-stimulates breast tissue, could be a trigger for breast cancer. Incidence of breast cancer is higher in women above 50 years of age and 2 cases per 1000 are reported in this age group. Epidemiological investigations have also suggested that those women who have many children possess lower risk of breast cancer than those women who have fewer children. Incidence of breast cancer is 10.04% among all cancers and, most commonly occurs in 40–50 aged women. Mean age of breast cancer in Iranian women is 48 years [ 73 ]. An association of clinic pathological characteristic and breast cancer subtypes has been determined in Iranian women [ 74 ]. Breast cancer mostly occurs in obese women [ 75 ]. Depression is most commonly found in women with breast cancer [ 76 ]. Andsoy et al. [ 77 ] conducted a study to investigate knowledge of colorectal, cervical and breast cancer. For this study 226 working nurses were screened. It is very interesting that certain epidemiological studies have claimed that women who give birth to their child before they attain the age of 20 years are known to have decreased risk of breast cancer than those women who have not given birth to any child or who have given birth to their first child after the age of 30 years. The risk increases with age rapidly during premenopausal and slowly during post-menopausal life. Breast feeding decreases the risk of breast cancer [ 78 ]. Menopause resulting from surgical removal of ovaries (oophorectomy) decreases the risk [ 79 ]. Presence of certain kinds of benign tumours in breast increases the risk of malignancy [ 80 ]. The ovaries stop producing the female hormones once the menopause sets in, but in obese women the fatty tissue can provide the estrogen as it is capable of producing it. This increase in hormone production seems to increase the risk of breast cancer in obese post menopausal women. Deficiency of vitamin D and lack of sun exposure is considered to be the important cause of breast cancer [ 81 ]. It is found to be more in women than men [ 82 ]. The risk of breast cancer increases with age however rarely found before the age of 20 years [ 83 ]. Carcinoma in one breast can increase the risk by four times in another breast. While the patients that have the history of ovarian, endometrial or colon cancer have 1–2 times increased risk to develop breast carcinoma [ 84 ]. A female who has had breast cancer has an enhanced danger of occurring breast cancer in the other breast [ 85 ]. The minimal role of the gene has been established in the development of breast cancer. BRCA-1 (breast cancer susceptibility gene) is considered to be the cause of 5–10% of breast cancer that is transferred from either father or mother to the next generation. The study indicates that right environmental conditions are required for cancer promoting gene for expression. Certain families have been recognized with a genetically higher incidence of early onset breast cancer. If some individuals of the female’s family have had a specific kind of cancer, female may have an enhanced danger risk of breast cancer [ 86 ]. The danger is maximum if the affected family member had breast cancer at a juvenile period, had cancer in both breasts, or if female is a close family member. First-degree family members such as daughter, sister and mother are mainly significant in estimating threat. Numerous second-degree relatives such as an aunt and grandmother with breast cancer might also enhance threat. Breast cancer in a male enhances the danger for the entire close female relatives. Women who have a positive family history of breast carcinoma are 2–4 times more likely to develop the cancer, especially the females who are the carriers of BRCA1 or BRCA2 genes have the significant chance to develop carcinoma of breast [ 87 ]. Breast cancer affects both male and females; though, the prevalence is more in female as compared to male. Generally, females are at 100-fold increased danger of breast cancer than male [ 88 ]. Early menarche, nulli parity, pregnancy after the age of 30, oral contraceptives or hormone replacement therapy all these factors can increase the risk of breast cancer [ 83 ]. Steroid hormones include androgens, progesterone and estrogen, which belong to a cluster of structurally connected hormones known as sex hormones that are released into the blood by the gonads and adrenal glands. They are synthesized from single general precursor, cholesterol through a reaction catalyzed by numerous enzymes to make a large diversity of hormones for diverse target organs and tissues [ 89 ]. This procedure is well regulated and the discharge of these hormones into the systemic circulation. These hormones cross the plasma membrane to reach the target cells and bind to specific receptors called steroid hormone receptors to exert their activity [ 90 ]. Oestrogens have important activities on differentiation, growth and performance of several tissues, including urogenital system of man and women, cardiovascular system, brain, uterus and breast [ 89 ]. In accordance with this, Kato et al. [ 91 ], reported that the progression of reproductive organ cancer like prostate and breast cancer frequently occurs because of the androgens, progesterone and estrogen, which exert numerous biological activities in normal as well as abnormal cells. The study indicates that the development of normal and abnormal epithelial cells of the breast can be modulated by stromal cells of the breast and can release growth factors after stimulation by the endogenous hormones. An aromatase enzyme is found in adipose tissues, which makes estradiol from the precursor molecule, cholesterol. Fat cells are found in excess amount in breast of aged females; therefore, the quantity of estradiol is higher in breast tissues of post menopausal female than their plasma level [ 92 ]. This most likely is responsible for the increasing occurrence of breast cancer in aged female and assists the action of steroid hormones in breast cancer pathogenesis. Benign tumors and proliferative lesions without or with atypia can increase the risk of breast cancer [ 85 ]. Breast cancer has been linked with high level of dietary fats and low level of certain nutrients for various years [ 93 ]. Animal fat stimulates colonal bacterial to form estrogen from cholesterol found in the diet, thus increasing level of estrogen in the body. The body fat is also involved in synthesis of oestrone, a type of estrogen. Obesity, increased fat consumption, radiation therapy [ 94 ]. Evidence is accumulating that certain environmental pollutants contribute to estrogenic activity and may contribute to the prevalence of breast problems in the industrialized world. Alcohol consumption is linked with breast cancer risk. This association was felt to be secondary to the fact that consumption of alcohol enhances level of hormones in the blood [ 95 ].
BRCA1 and BRCA2
These are two genes that have been recognized as possessing the firm relationship with breast cancer. Both emerge to contain comparable biological activities such as DNA damage repair and, in their variant kind, they enhance the danger of breast cancer and other ovarian cancers. The preeminent knowledge accessible to date is based on a joint investigation of 22 researches, 11 which established that the prevalence of breast cancer is 65% at 70 years of age in women who acquired a BRCA1 gene and 45% in those women who are carriers of BRCA2 genes. The prevalence of breast cancer in carrier of these genes is 10–30 times more than those females that have no inherited gene variants. In spite of the big boost in breast cancer danger linked with BRCA1 and BRCA2 genes, they are responsible approximately 5% of all breast cancers, as merely 1 in 1000 females have acquired one of them. There are several tribal Subgroups in which BRCA1 and BRCA2 genes are more possible to be innate (e.g. approximately 1% of females of Ashkenazi Jewish descent have acquired increased risk BRCA1 or BRCA2 genes; analogous variants are moreover familiar in women belong to Iceland and different Scandinavian countries). Individual risk indicator as an outcome of hereditary testing for BRCA1 and BRCA2 remains a demanding experience. Almost 2000 variants have been found in the two genes (BRCA1 and BRCA2) and, for numerous; it is yet not recognized whether or not they enhance prevalence of breast cancer. One possible sign is the site of the variant in the gene; it indicates that variants in few parts of the genes might cause bigger threat of breast cancer than others [ 96 , 97 ]. Even though all females who acquire a BRCA1 or BRCA2 variant do not essentially cause breast cancer, it is uncertain what other determinants such as genetic or environmental persuade the risk of breast. There is also promising data that determinants for breast cancer might perform in a different way for carriers of BRCA1 or BRCA2 variants than for females lacking hereditary vulnerability because of these genes [ 98 ]. Literature review also recommends that high-risk genes other than BRCA1 and BRCA2 possibly enhance the risk of developing breast cancer, mainly for younger females.
Fifth most common cause of cancer death is breast cancer. The mortality and age standardized prevalence of breast cancer is higher in the United States compared to world. In Poland, seventeen percent of disease cases occur due to cancer and 14% deaths occur due to cancerous changes. Worldwide death due to breast cancer calculated in 2004 was 519,000 [ 99 ]. In the United States alone, approximately 1,208,000 cancer cases are reported per year and that some 538,000 people die from the previous manifestation of this disease condition, representing about one fifth of the total annual deaths from all causes [ 74 ].
Stages of breast cancer
According to the report of breast cancer.org Stages of the breast cancer depends upon the size and type of tumor and how much the tumor cells have been penetrated in the breast tissues [ 100 ]. Whereas stage 0 describes the non invasive and stage 4 describes the invasive kind of tumor. Descriptions of those tumor stages are:
This is the non invasive stage of tumour which indicates that both cancerous and non cancerous cells are within the boundaries of that part of the breast in which the tumor begins to grow and no evidence found of their invasion in the surrounding tissues of that part, the example of this tumour stage is ductal cell carcinoma in situ (DCIS) [ 101 ].
This stage describes as the invasive breast carcinoma and microscopic invasion is possible in this stage. It has two categories that are 1A and 1B stage. The category 1A describes the tumor which measures up to 2 cm and none of the lymph nodes are involved in it while stage 1B describes that small group of cancer cells larger than 0.2 mm founds in lymph node [ 102 ].
Stage 2 also has two categories 2A and 2B. Stage 2A describes that the tumour is found in axillary lymph nodes or in sentinel lymph nodes but no tumor found in breast. The tumor can be smaller or larger than 2 cm but not more than 5 cm. However stage 2B describes that the tumor could be larger than 5 cm but can’t reach to the axillary lymph nodes [ 103 ].
It has been divided into three sub categories that are 3A, 3B and 3C. Amongst which stage 3A describes that no tumor is found in breast but it can be found in 4–9 axillary lymph nodes or in sentinel lymph nodes while stage 3B describes that the tumour can be of any size but have caused swelling or ulcer on the skin of the breast and can have spread up to 9 axillary lymph nodes or to sentinel lymph nodes stage 3B can be considered as inflammatory breast cancer which includes red, warm and swollen skin of the breast. However stage 3C describes the spread of tumor up to 10 or more than 10 axillary lymph nodes and it also have involved the lymph nodes above and below the clavicle [ 104 ].
This is the advanced and metastatic stage of cancer and this stage describes the spread to other organs of the body that is lungs, bones, liver brain etc [ 105 ].
History and physical examination
The clinical history of patients with breast cancer is aimed at investigating cancer threat and demonstrating the occurrence or lack of manifestations indicative of breast illness [ 106 ]. It must comprise age at menarche, menopausal condition, earlier pregnancies and utilization of hormone replacement therapy after menopause or utilization of oral contraceptives. Personal history as well as family history should be carried out in detail. Personal history includes age at diagnosis of breast cancer, previous breast biopsies and treatment of other cancer with use of radiations. Family history includes history of ovarian cancers and breast cancer in first degree relatives. Patents should be examined for particular manifestations such as breast pain, weight loss, pain in bone, tiredness and nipple discharge [ 107 ]. Physical examination includes inspection of breasts, area around neck and collarbone, and armpits (axillae) carried out by clinicians [ 108 ]. Breasts are observed for any deformities such as lumps or other manifestations of breast cancer. Lymph nodes are also examined that are usually enlarged in patients with breast cancer.
Self examination
Usefulness of the breast self-examination is contentious because the advantage in conditions of reduced deaths has not been established [ 109 ]. Most physicians educate females to carry out monthly BSE to become recognizable with their usual structure and authorize them with reference to their own healthcare [ 110 ]. Women are guided for self examination of the breast cancer. Women can find abnormalities in size and shape of breast on self examination [ 111 , 112 , 113 ]. Alipour et al. [ 114 ] conducted a study to investigate the the SMS based and paper based paper learner’s satisfaction and learning effect. Gynecologists gave printed materials and text messages regarding facts of breast cancer and breast cancer tests. Doctors found higher motivation and better effects in the SMS group than the printed material group. Sreedharan et al. conducted a study in United Arab States hospitals. Self administered structured questionnaire was used to investigate practices of self examination and knowledge. Satisfactory results were found from this study [ 115 ]. Ozkan et al. [ 116 ] investigated the level of knowledge regarding self examination of the breast cancer among 113 midwifery and nursing students. These researches have shown that continuous education program about breast cancer can raise the awareness among the population. Ceber et al. [ 117 ] conducted studies on breast self examination and health beliefs of Turkish women and stated that physical illnesses and early death can be prevented by early diagnosis of breast cancer. He further stated that one out of seven patients with breast cancer is diagnosed in time. Beydag and Karaoglan [ 118 ] investigated the awareness about breast self examination in 1st and 4th years students and concluded that 4th years students have more knowledge about breast examination than the 1st years students.
Ultrasound breast imaging
There are numerous researches behind the application of adjunctive screening ultrasound in elevated hazard women with thick breast tissue, which reveals a significant but established figure of false positives [ 119 , 120 ]. There is no randomized clinical study conducted for investigation of impact of screening ultrasonography on mortality rates of breast cancer. Entire breast ultrasound might permit the Physicians to display for breast tumors not measured by long-established mammography, particularly in thick breasts wherever mammography sensitivity is lesser [ 121 ]. Ultrasound breast imaging shows the size and position of tumour whether it is filled with fluid or is solid and needs to be biopsied to rule out cancer. This examination is quickly becoming a routine procedure for diagnosing lumps in young women [ 122 , 123 ].
Nuclear medicine
It is a type of molecular imaging wherever a radioactive substance (radiopharmaceutical) is introduced to an individual and the radiation from the radiopharmaceutical is displayed by perceptive emission detectors including gamma cameras and PET detectors and gamma Cameras located exterior to the body of patient. Combination of CT and gamma camera and the combination of CT and PET is a main progress in enhancing recognition and vicinity of disease.
Single photon emission computerised tomography (SPECT)
This procedure utilizes solitary photon radionuclides including gallium-67, iodine-131 and technicium-99 m that discharge gamma rays. It is a efficient scan and is precise for organ of curiosity. It can also be employed to the entire body, is comparatively secure in expressions of radiation quantity and is fine in recognition of primary and metastatic cancers. Iodine-131 is together indicative and remedial for cancer of thyroid [ 124 ].
Positron emission tomography (PET/CT)
In expressions of radiation quantity, PET/CT is also comparatively secure and utilizes positron emitting radionuclides including oxygen-15, flouoride-18 and carbon-11. The frequently utilized tracer in positron emission tomography is a radioactive type of glucose such as [18F]fluoro-2-deoxy- d -glucose. Tissues with enhanced metabolic requirements including developing cancer cells, demonstrate increased uptake of the tracer and displays on the scan. With combination of CT and PET, significant information regarding numerous situations affecting the different organs of the body is simply mapped. PET/CT is extremely perceptive and precise for predicating occult and different areas of loco-regional lymph nodal extent and/or far-away metastases not obvious by regular imaging, therefore altering staging in up to 25% of the patients. This procedure is employed for the management planning by describing spread of primary illness. It is also employed in re-staging after management ailment relapse and treatment follow up [ 125 ].
Tumor markers
Porika et al. [ 126 ] stated that tumour markers should be measured in all stages of the breast cancer including metastasis prediction, treatment, diagnosis and screening. Thirteen verities of tumor markers of breast cancer are measured, six out of 13 are novel for the guideline. The different varieties displayed proof of clinical use and are suggested for utilization in practice [ 127 ]. It is particularly significant that the comparative autonomy of the markers in reference to other accessible markers to demonstrated so as to evade the gratuitous price and expenditure of redundancy [ 128 ]. Furthermore, it is significant that the physician be attentive of the restrictions in together specificity and sensitivity of every marker so because not to specificity and sensitivity of every marker so since not to over- or under-interpret the prognostic worth of a few investigation. With these caveats in intelligence, trial submission of tissue, germ-line and soluble tumor markers can recover medical care of individuals at threat for and with breast cancer.
It can be employed for monitoring of patients with breast cancer. High blood levels are seen in <10% of patients in the beginning of breast cancer and in approximately 70% of patients with advanced stage of breast cancer. The levels of CA 15-3 typically fall after successful management. However CA 15-3 can also be high in other types of cancers and in few non-cancerous conditions including hepatitis and benign breast conditions.
It is another marker for monitoring of patients with breast cancer. This test does not seem to be any better to identify early or advanced stage of breast cancer. This tumor marker is seen in other types of cancers and in few non-cancerous disorders.
Estrogen and progesterone receptors
For the identification of breast cancer, breast cancer tissues are investigated for estrogen and progesterone receptors including HER2 antigen. These tests give information regarding the aggressiveness of cancer and response of certain drugs used for treatment of breast cancer.
Immunohistochemistry
Immunohistochemistry (IHC) has grown to be an essential component of pathology. Although eosin and hematoxylin stain is the primary foundation for diagnostic pathology of the breast, Immunohistochemistry stains give valuable and sometimes very important information. Furthermore, taking into consideration the part of hormonal treatment in hormone receptor–positive breast tumors, as well as the accessibility of targeted chemotherapeutic drugs for HER2-positive patients, Immunohistochemistry knowledge indicates a key element of workups. Careful use of Immunohistochemistry stains in combination with E & H test assists determine mainly diagnostic matters encountered by clinicians during their routine practice. Clinicians should be well-known to utilize the each immunostain and its restrictions to evade errors in interpretation. Immunohistochemistry stains assists in differential diagnosis of challenging epithelial disorders of the breast. They should be selectively and sensibly utilized and their results must be understood with the differential diagnoses in consideration and with an understanding of potential drawback [ 129 ].
MRI and breast cancer
Mammography has been considered as an appropriate screening method for breast cancer detection for many years [ 130 ] but it can’t distinguish between the solid and cystic masses and can miss up to 10–15% of the cases however MRI provides more accurate results and clear benefit to the women who are developing breast cancer due to the BRCA1 and BRAC2 genetic mutation and are present with the axillary lymph adenopathy [ 131 ].
Breast biopsy
Breast biopsy is the simply best technique for diagnosing breast cancer [ 132 ]. There are numerous different types of breast biopsies. To enhance diagnostic precision and get rid of as many false negative results as possible, breast imaging, clinical breast examination and biopsy are performed concurrently (triple test).
Fine needle aspiration
A thin prickle is employed to get cells from the abnormal area or a breast lump [ 133 ]. Ultrasound can be used to assist direct the prickle. A restricted anesthetic might be used to anesthetize the region where the prickle will be inserted [ 134 ].
Core biopsy
A wider prickle is to get a portion of tissue (a core) from the abnormal area or breast lump [ 135 ]. It is typically made under restricted anesthetic, thus breast is insensitive, while patient may experience little hurt or uneasiness at what time the anesthetic is given [ 136 ]. MRI, ultrasound and mammogram can be used to guide the prickle for the duration of core biopsy [ 137 ].
Vacuum-assisted stereotactic core biopsy
In this core biopsy, different tiny tissue samples are taken via single tiny incision in the skin with a prickle and a suction-type device [ 138 ]. It is carried out using local anaesthetic. MRI, ultrasound or a mammogram may be employed to direct the prickle into position. The patient may experience little uneasiness during the process [ 139 ].
Surgical biopsy
If the abnormal vicinity is too minute to be biopsied by another procedure or the biopsy outcome is not apparent, a surgical biopsy is carried out. Prior to the biopsy, a guide wire may be placed into the breast to assist the medical doctor locate the abnormal tissue. Local anesthetic can be used and the physician may use MRI, ultrasound and mammogram to direct the wire into position. The biopsy is after that carried out under a general anesthetic. Little area close to breast tissue and lump are detached, alongside the wire [ 140 , 141 ].
Digital mammography
It helps to find lumps in dense tissue. The image can also be easily stored and transmitted to another radiologist for a second opinion [ 142 , 143 , 144 ]. Tarhan et al. [ 12 ] stated mammography may give false negative and false positive results in patients with dense breast tissues. Kanaga et al. [ 145 ] stated that the practice of mammography is 19% in Malaysian women as compared to other study which was 10.5%. Lack of health insurance coverage, low income and embracement were the main barriers to mammography as mentioned in earlier studies. Mammography is considered as the gold standard test for early detection of breast cancer [ 146 ] but in case of scarce resources in some areas in breast health awareness program should be promoted for the early detection of breast cancers and the staff should also gets the training of clinical breast examination so that the patient get diagnosed at earlier stage especially in those areas where mammography is unavailable [ 147 ].
PEM and MRI in breast cancer patients
Hence both the positron emission mammography and magnetic resonance imaging have proven breast cancer detection sensitivity, however hormone replacement therapy, post menopausal status and breast tissue density has no influence on the sensitivity of PEM and MRI. Positron emission mammography can be used as an alternative of MRI in patients who don’t want to have an MRI due to multiple reasons such as time issues, limited budgets, lack of interest, claustrophobia (fear of being kept in as small space) [ 148 ]. However, both have the similar sensitivity to detect cancerous lesions comprehending invasive and ductal carcinoma in SITU [ 149 ].
In the management of breast cancer, aim is to preserve quality of life with prolonged life expectancy. The use of bioflavonoids may inhibit estrogen formation [ 150 ]. Effective communication between doctors and patients plays an important role to improve clinical outcome. Oshima et al. [ 151 ] reported that effective communication between doctors and patients is effective. A study conducted in Japan indicates that this communication helps the patients to cope with adverse effects. Doctor patient communication enhances the quality of life of breast cancer patients [ 152 ]. Previous studies have shown that less exposure from radiations, higher family monthly income, long years after diagnosis, higher education, initial stage cancer and younger age were considerably related with better quality of life (QOL) in patients with breast cancer [ 153 ]. Breast cancer is less common in breast feeding women, but the protective effect of this factor is not clearly investigated [ 154 ]. Cancer is a fatal disease affecting humankind in every country. Vinblastine and vincristine was introduced in 1961 as anti cancer drugs. CIPLA has improved the process of isolating vinblastine and vincristine in the World [ 155 ], and India is exporting these alkaloids to European countries and the demand is steadily increasing. The main forms of treatment for cancer in humans are surgery, radiation and chemotherapeutic agents. The drugs can often provide temporary relief of symptoms, lengthening of life and occasionally cures the disease. Many hundreds of chemical drugs of known classes of cancer chemotherapeutic agents have been synthesized [ 156 ]. The activity of these compounds is based on their capacity for biological alkylation. The effective dose of such alkylating agents was almost the same as the toxic dose. Multi-targeted therapy could be more effective, because the recurrence rate of cancer is high and death occurs due to metastasis. Deng et al. [ 157 ] reported that Pemetrexed and Lobaplatin is prescribed in metastatic breast cancer. Huang and Cao [ 158 ] reported that cantharidin sodium injection is effective in the management of breast cancer. Cantharidinate sodium injection is herbal origin and is prepared in China for treatment of breast cancer. Breast cancer management strategies differ depending on the step of the cancer—its mass, place, whether it has extended to other organs of the body and the physical condition of the individual. Present management for breast cancer includes targeted therapies, hormonal treatment, radiation therapy and surgery.
Psychological adjustment to breast cancer
Breast cancer is extremely common and very worrying experience for numerous females every year in developing and developed countries [ 159 ]. Psychological research has given an image of the emotional and community impact of breast cancer on females’ lives, and of factors linked with better versus worse amendment. Psychosocial mediations have been helpful in reducing patients’ grief and improving their life quality. Current study also recommends that psychological aspects might be associated with potentially significant biological ailment linked processes. Additionally, to giving an idea of the psychological aspects in breast cancer, investigation in this vicinity has given a foundation for further studies on adjustment to health-related nervous tension in common [ 160 ].
This is the foremost management strategy for individuals whose breast cancer has not extended to further areas of the body and is also a choice for further complex stages of the illness [ 161 , 162 , 163 ]. The kinds of breast cancer surgery vary in the quantity of tissue that is excised with the cancer; this depends on the cancer’s characteristics, whether it has extended, and the patient’s special feelings. A few of the most familiar kinds of surgery include:
Lumpectomy (breast conserving surgery)
Some patients diagnosed with breast cancer undergo some type of surgery [ 164 ]. According to American cancer society, lumpectomy or partial mastectomy is the procedure of removing the part of the breast that contains malignant tumor along with some healthy tissues and surrounding lymph nodes leaving the major part of the breast intact as possible [ 165 ]. This practice generally experienced in women that are in their initial phase of cancer, however the patient also requires another type of treatment such as radiation therapy, chemotherapy or hormone replacement therapy along with this procedure. Most surgeons and patients prefer lumpectomy initially rather than having the complete breast removal, especially if the patient is more concerned about losing her breast [ 166 ]. However, adverse effects of lumpectomy are tenderness, temporary inflammation, sclerosis and changed appearance of breast, etc [ 167 ].
Mastectomy is done to decrease the risk of development of breast cancer [ 168 ]. Bilateral prophylactic mastectomy decreases the chances of development of breast cancer but does not eliminate the risk of developing cancer completely [ 169 ]. Aromatase and tamoxifen decreases the risk of contra-lateral breast cancer and it is considered more effective than contra lateral prophylactic mastectomy [ 170 ]. Mastectomy is considered the most effective method of dealing with an already diffused case of breast cancer, for which a lumpectomy was not decisive enough. Nevertheless, the loss of breast leads to feeling of asexuality and loss of self-image and consequent depression in most women [ 171 ].
Reconstructive surgery
Females who have a mastectomy might as well have breast renovation, either immediate reconstruction or delayed reconstruction. It is performed to get better the look of the breast following tumor surgery. All females having a mastectomy must be presented the option to converse reconstructive surgical treatment [ 172 ]. Mastectomy is a comparatively simple surgical practice that typically results in stay in hospital for 1–2 days. Deficiency of the breast mass changes the patient’s special look and can create wearing a few forms of clothing difficult. The utilization of an exterior prosthesis to tackle these problems can be awkward and scratchy, particularly for females with huge breasts. Though, the most significant issue of mastectomy is the psychosocial effect of the physical and aesthetic distortion, which can comprise nervousness, sadness, and negative impacts on body figure and on sexual activity [ 173 ]. Breast reconstruction is commonly requested by females with breast cancer who are unable for breast-conserving treatment and females with an increased hereditary danger for breast cancer. Existing breast reconstruction procedures are miscellaneous and might engage the utilization of prosthetic implant or an autologous tissue flap, or both. Despite of the method employed, cancer might relapse in the reconstructed breast; additionally, in autologous tissue flaps reconstructed breasts, little complexity such as fat necrosis may take place. Researches recommend that breast reconstruction restores body representation, proves vigor, femaleness, and sexuality; and optimistically influences the patient’s feelings of comfort and life quality [ 174 ].
Ovarian ablation as adjuvant therapy for breast cancer
Ovarian ablation has been employed as management for breast cancer [ 175 ]. There are numerous techniques of ovarian ablation such as radiation induced ablation, surgical removal of ovaries and chronic utilization of luteinizing hormone-releasing hormone (LHRH) analogs. Additionally, there are few proposals that cytotoxic chemotherapy might perform by inducing ovarian ablation in premenopausal females with breast cancer. Of the abundant case series and clinical studies of ovarian ablation conducted in the earlier period, numerous have been laden with methodologic issues. Meta-analysis of randomized clinical studies demonstrates a momentous enhancement in overall survival and disease-free survival for females whose ovarian ablation were performed as adjuvant treatment compared to those females who did not. Literature review indicates that ovarian ablation may be employed an alternative therapy for breast cancer [ 176 ].
Role of estrogen and progesterone receptors in the management of breast cancer
The estrogen receptor assay has developed into a typical practice in the treatment of complex breast cancer [ 177 ]. Tumors missing estrogen receptor react occasionally to endocrine treatment, while improvement proportions of 50–60% are seen in estrogen receptor positive tumors. Current researches demonstrate that the estrogen receptor condition of the principal cancer is a superior interpreter of the endocrine reliance of metastatic cancers at the moment of clinical deterioration. Additionally, the deficiency of estrogen receptor in the primary cancer is an significant self-regulating predictive display of higher incidence of relapse and shorter survival. Quantitative investigation of estrogen receptor and an analysis for progesterone receptor are two procedures for enhancing the precision of selecting or rejecting individuals for hormonal treatment; cancers with a elevated quantitative estrogen receptor amount or those with a positive progesterone receptor show the maximum response. Initial investigation demonstrates that the existence of progesterone receptor might be a improved indicator of tumor hormone dependence than quantitative estrogen receptor [ 178 ].
Anti-estrogen therapy
It can be used in such types of cancers that are affected by hormones and the tumor has hormone receptors such as estrogen receptors. Clarke et al. [ 179 ] stated that the most common category of drugs that are used in breast cancer is anti estrogen, which includes the agents that are (tamoxifen, raloxifene, toremifene etc). Tamoxifen inhibits the hormone oestrogen from entering into cells of the breast cancer. This mechanism inhibits the breast cancer cells from developing. Tamoxifen can be suggested to treat female of any age group. However tamoxifen is considered as the drug of choice in women that have positive estrogen receptor breast carcinoma. Tamoxifen is a selective estrogen receptor modulator (SERMS) and acts like estrogen on other parts of the body such as uterus. However, it demonstrates anti estrogen properties of breast tissues and competes with estrogen for binding to the estrogen receptors in the breast [ 180 ]. If we have to discuss about the toxic effects of anti estrogen therapy, comparatively there is very least toxicity found in it as compared to other cytotoxic drugs [ 181 ]. While some patients withdraw the treatment before completing the course of drug due to the side effects such as hot flushes, gastro intestinal problems and vaginitis etc. Though, the medical indications for discontinuing antiestrogen therapy include adeno carcinoma, sarcoma and thrombo embolic diseases etc. Any how the American society of clinical oncology recommends Tamoxifen as standard adjuvant therapy for patients with Estrogen positive breast carcinoma [ 182 ]. On the other hand Fulvestrant; Faslodex has entirely anti estrogenic action and is considered as estrogen antagonist it demonstrates anti neo plastic activities in breast tissues without having a positive effect on the uterus and bones, which may lead to certain side effects if taken for a long period of time such as osteoporosis [ 183 ]. Tamoxifen and raloxifene are selective estrogen receptor modulators (SERMs), a set of medicine that selectively prevents or motivates oestrogen-like activity in different tissues, affecting the estrogen receptors [ 184 ]. Tamoxifen exhibits its oestrogen antagonist action in numerous tissues such as uterus, liver, bone and breast [ 185 ]. It was used as adjuvant treatment in estrogen receptor positive patients and tamoxifen was accepted by the United States Food and Drug Administration (FDA) in 1998 for the impediment of breast cancer for females at elevated danger [ 186 ]. This verdict was based on the outcome of a experiment carried out by the United States National Cancer Institute that was interrupted premature as an intervening study indicated that tamoxifen decreased breast cancer prevalence by approximately one half [ 187 , 188 ]. Four big prospective studies have investigated the efficacy of tamoxifen versus placebo for breast cancer danger decline for females at elevated danger of breast cancer [ 189 ]. A summary of these studies demonstrated a 38% general decline in breast cancer occurrence for females at increased danger of breast cancer who administered tamoxifen for the period of 5 years and also indicated that tamoxifen inhibits only estrogen receptor positive breast cancers (RR ~ 50%) with no influence on estrogen receptor negative breast cancer [ 190 ]. A variety of adverse effects have been reported for females taking tamoxifen, such as venous thrombosis, cataract, endometrial cancer, menstrual disorders and hot flushes. A study indicated that the risk decreasing activity of tamoxifen expands beyond the vigorous management phase of 5 years, and remains for minimum 10 years, whereas the majority of adverse reactions do not carry on behind the 5 year management duration [ 191 ]. Raloxifene, has also been revealed to decrease danger of breast cancer, however seems to exert some adverse reactions [ 192 ]. During the precedent periods, clinical studies carried out to investigated the efficacy of raloxifen on fracture and osteoporosis, showed a 44–76% risk decline of breast cancer prevalence in the raloxifen treated patients as compared to the placebo group [ 193 ]. A randomized clinical study of Raloxifen and Tamoxifen was planned for comparing the efficacies of raloxifen and tamoxifen on postmenopausal females with an enhanced 5-year threat of breast cancer as expected by the Gail model [ 194 , 189 ]. The study demonstrated that raloxifen was comparable to the tamoxifen in decreasing the threat of invasive breast cancer and was linked with a minor danger of cataract and thromboembolism than tamoxifen. In 2007, approximately 10 years following the endorsement of tamoxifen, the FDA permitted raloxifen for the impediment of breast cancer for postmenopausal females with osteoporosis and for postmenopausal females at increased danger for breast cancer. In Australia, tamoxifen is prescribed for the treatment of breast cancer and osteoporosis.
Aromatase inhibitors
These are compound designed for decreasing oestrogen formation by targeting aromatase, the enzyme complex accountable for the last stair in the formation of estrogen [ 195 ]. The third-generation aromatase inhibitors including letrozole, exemastane and anastrozole are in present utilization [ 196 ]. Randomized clinical trial conducted for investigation of these agents in the treatment of breast cancer has indicated that these compounds contain an outstanding effectiveness in treating females with advanced disorder. Clinical study indicated that females managed with aromatase inhibitors had a superior contra lateral breast cancer threat decline than females managed with tamoxifen [ 131 ].
Radiation therapy
It is useful for reducing the necessity of mastectomies. A combination of a lumpectomy and radiation therapy is being increasingly used over a mastectomy in the early stages of breast cancer [ 197 ]. A study was conducted in India. For this study 135 women were selected, most of them had undergone mastectomy. At the time of analysis, there was no local recurrence after hypo fractioned radiation therapy and metastatic disease developed in only four patients [ 198 ]. Zhou et al. [ 199 ] reported that radiation therapy is effective in early breast cancer patients. This study was conducted on 143 women who underwent either routine or intra operative radiation therapy after breast conserving surgery. At 54 months of follow up, there was a significant local control of the tumour. High-energy rays from radiation therapy kill cancer cells. This therapy affects only the cells that are treated. Use of radiation therapy may be done after breast cancer surgery to destroy the remaining cells in the chest area.
Brachytherapy
It is a kind of radiotherapy [ 200 ]. It might be recognized as accelerated partial breast irradiation. It directs radiation merely to the area around the vicinity wherever the cancer was. This might replace the requirement to provide radiation to the whole breast. It also decreases the number of management sessions [ 201 ].
- Chemotherapy
The process of killing cancer cells by using certain medicines is termed as chemotherapy [ 202 , 203 ]. It can be given in both situations, before and after surgery, depending upon the condition of the patient. According to the American cancer society the medicines include in chemotherapy are Docetaxel, Paclitaxel, Platinum agents (cisplatin, carboplatin), Vinorelbine (Navelbine), Capecitabine (Xeloda), Liposomal doxorubicin (Doxil), Cyclophosphamide (Cytoxan), Carboplatin (Paraplatin) etc [ 204 ]. However it has various side effects [ 205 ]. Metastatic or secondary breast can is difficult to treat but it can be controlled and sometime for various years [ 206 ]. Chemotherapy can be prescribed to manage metastatic breast cancer to minimize or sluggish its development. It can also be administered to decrease some manifestations. Other treatment option can be initiated prior or alongside chemotherapy.
Taxol is used clinically in the treatment of ovarian cancers and is undergoing clinical trials against metastatic breast cancers [ 207 ]. It may also have potential value for lung, head and neck cancers. Taxotere is a side chain analogue of taxol, which has also been produced by semi synthesis from 10-deacetyl-baccatin III [ 208 ]. It has improved water solubility, and is being clinically tested against ovarian, and breast cancers. It can be used in those where resistance to cisplatin has been observed [ 209 ].
Anthracyclines
Anthracycline are commonly prescribed in the treatment of breast cancer [ 210 ]. They impede with enzymes associated the DNA copying, which is desired for cells to separate to create new cells. Epirubicin and doxorubicin are the most commonly used medicines in breast cancers. There is proof that anthracyclines functions better than various other chemotherapy medicines [ 211 ]. However these have adverse reactions such as damage to the heart and loss of hair [ 212 , 213 ]. Prior to start of medicines, patient should converse with clinician any probable adverse reactions of drugs used and how these medicines might influence life quality.
Thermochemotherapy
Medifocus heat management in combination with chemotherapy enhanced the shrinkage of median cancer in the thermochemotherapy arm to 88.4%, whereas for chemotherapy alone the shrinkage of median cancer was 58.8%. For the thermo-chemotherapy management arm, approximately 80% of breast cancers had a cancer size decrease of 80% or more, compared to merely 20% for the chemotherapy alone [ 214 ].
Complementary therapies
Women with breast cancer occasionally desire to use complementary therapies along with their medical therapy [ 215 ]. These therapies are usually not investigated in randomized clinical trials [ 216 ]. Some female believe that they have benefited from a number of these treatments [ 217 ]. Vitamins, nutritional supplements, yoga, meditation, visualization, traditional medicines and acupuncture are included in complementary therapies.
Medicinal plants
Screening of plant extracts for anticancer activity started in 1961 by National cancer institute in the USA, and up to 1981 (20 years) about 1,14,045 plants had been screened of which only 3.4% (representing about 3400 different species) have been observed to be active in one or more biological systems.
Ganoderma lucidum (Polyporaceae)
It contains ganoderic acid, ganoderic acid G, ergosta, ergosterol peroxide ganoderic acid G, ergosta, ergosterol peroxide, methyl ganoderate A, B, ganoderic acid C2. It is an anticancer [ 218 ]. Jiang et al. [ 219 ] reported that the Ganoderma lucidum suppresses growth of breast cancer cells through the inhibition of Akt/NF-kappa B signaling. It is used to treat cancer cells. It inhibits the transcription factor NF-kappa B and inhibits the invasive behavior of breast cancer cells. The exact mechanism for inhibition of cancer cells is not understood. The study showed that the proliferation of breast cancer MDA-MB-231 cells is inhibited and Akt/NF-kappa B signaling is suppressed. Phosphorylation of Akt at Ser473 is suppressed by this plant and expression of Akt is suppressed, as a result NF-kappa B activity in MDA-MB-231 cells is inhibited.
Momordica charantia (Cucurbitaceae)
The parts used are fruits, leaves and seeds. It contains glucoside, albuminoids, fatty acids, non polar lipid, linolinic acid, palmitic acid, myrtenol, hexenol, benzyl alcohol, acylglycosylsterols and glycoproteins [ 220 ]. It is hepatoprotective, tonic, stimulant, emetic, laxative, stomachic and cancer [ 221 ]. It is used to treat gout and rheumatism. Ray et al. [ 222 ] reported that Momordica charantia extract inhibits breast cancer by modulating cell cycle regulatory genes. This study was conducted in vitro models. An extract of this plant was investigated in human breast cancer cells, MCF-7 and MDA-MB-231, and primary human mammary epithelial cells. This extract was able to decrease cell proliferation and apoptotic cell death was induced. Survivin and claspin expression was inhibited by this extract.
Carthamus tinctorius (Asteraceae)
The parts used are flowers and seeds. It contains palmitic acid, hexadecanolenin, coumaric acid, daucosterol, apigenin, kaempferol, trans-3-tridecene-5, 7, 9, 11-tetrayne-1, 2-diol, trans-trans-3, 11-tridecadiene -5, 7, 9-triyne -1, 2-diol [ 223 ]. It is used in colds, flu, fevers, hysteria, anemia, and diabetes mellitus. It is an antioxidant [ 224 ] and alpha glucosidase inhibitor [ 225 ]. Loo et al. [ 226 ] reported the efficacy of this plant in breast cancer. MDA-MB-231 breast cancer cell and normal human mammary gland cell were treated with a compound that contains Carthamus tinctorius. This compound observed inhibition of cell proliferation. Inhibition of cell proliferation was dose dependent. Its cytotoxic activity was more than commonly used cytotoxic drugs.
Viscum album (Viscaceae)
Part used are leaves and stem. It contains sinapylflavanone, glucopyranoside, flavanone, hydroxy flavanone and viscin [ 227 ]. It is antioxidant, cardiac tonic, and anti-cancer [ 228 ]. It is used in palpitation, vascular spasms, asthma, dizziness, vertigo and headaches. Gunver et al. [ 229 ] reported the efficacy of this plant in breast cancer.
Calendula officinalis (Asteraceae)
The parts used are leaves. It contains triterpene, calendula glycoside, butyl ester, flavonol glycosides, and carotenoids [ 230 ]. It is anti-inflammatory and anti-cancer [ 231 ]. It is used in carcinoma of the vagina, and cervix. Pommier et al. [ 232 ] reported the efficacy of Calendula officinalis for the prevention of acute dermatitis during irradiation for breast cancer.
Citrullus colocynthis (Cucurbitaceae)
The parts used are seeds and fruit. It contains phytosterol, flavones C-glycosides, saponins, aspartic acid, arginine, colocynthin, colocynthitin and cucurbitacin glycosides [ 233 ]. It is used in constipation and carcinoma of the breast [ 234 ]. It is an emmenagogue, ecbolic, cathartic, hydragogue and antioxidant [ 235 ]. This plant has growth inhibitory activity. Cucurbitacin glucosides have been isolated from this plant. These glycosides prevent human breast cancer cells [ 234 ].
Indole-3-Carbinol (13C)
A compound known as indole-3-carbinol, which is a plant chemical derived from cruciferous vegetables such as Brussels sprouts and cabbage, changes the way estrogen is metabolized. This compound predictably alters the endogenous estrogen metabolism towards increased catechol estrogen production and may thereby provide a novel dietary means for decreasing risk of breast cancer [ 236 ].
Silibinin and Chrysin
Previous research indicates that chrysin and silibinin function synergistically and possess significant anti-cancer activities against T47D breast cells [ 187 , 188 ]. It shows potential that the synergistic efficacy is based, at least in part, by down-regulation of hTERT and cyclin D1. Their potential activities in the established synergism among Chrysin and Silibinin should be verified by additional in vitro or in vivo researches. Study demonstrates that Chrysin and Silibinin combined might come out as an eye-catching approach based on herbal medicine for the management of breast cancer [ 237 ].
Lactobacillus acidophilus
Breast cancer and hyperestrogenism may be decreased by the inclusion of lactobacillus acidophilus in the diet. This useful bacterium helps to metabolize estrogen properly in the bowel. Clinicians can prescribe lactobacillus acidophilus that is available in different forms, including capsules in patients with breast cancer [ 238 ].
Women with breast cancer have been shown to possess selenium levels that are lower than those of women without cancer. Selenium is a trace mineral that is often lacking in refined food diets. A contrary association exists among the prevalence of human breast cancer and concentration of dietary selenium. The adding of Selenium to the food has been revealed to reduce the occurrence of breast cancer [ 239 ].
Targeted therapies
These are drugs prescribed to manage some types of breast cancer. The mainly familiar targeted treatment is the drug Herceptin [ 240 ]. It is prescribed to manage HER2 positive breast cancer. It functions by preventing the cancer cells from developing and progressing [ 241 ].
Gene therapy for carcinoma of the breast
Gene therapy is a remedial strategy that is considered to correct particular molecular deformities associated with the progression or development of breast cancer [ 242 ]. Mutated BRCA1 and p53 genes recognized as cancer susceptibility gene are involved in progression of cancer [ 243 ]. Since mutational inactivation of gene activity is reserved to cancer cells in these contexts, cancer gene modification techniques may give an opening for selective targeting without major hazards of normal, non-cancer cells [ 244 , 245 ]. Both BRCA1 and p53 emerge to restrain tumor cells that lack mutations in these genes, indicating that the so-called gene modification techniques may contain broader efficacy than previously considered. Raising awareness of cancer genetics has recognized these and new genes as possible targets for gene substitute treatment [ 246 ]. Early patient study of BRCA1 and p53 gene therapy have given a number of indications of possible effectiveness, but have also recognized areas of clinical trials that are wanted prior to these therapeutic strategies may be broadly employed in patients with breast cancer [ 247 ].
Oncogenes inactivation
Numerous oncogenic proteins have been recognized and linked with a variety of cancers [ 248 ]. The frequently practical strategy in clinical studies is the employment of antisense options. Oncogenes transcription also can be prevented by means of adenoviral gene E1A, which hinder erbB-2 transcription, an option helpful in managing cancer that over express this oncogenic protein [ 249 ].
Augmentation of cancer suppressor genes
The mutations in tumor suppressor genes are linked with the development of numerous cancers. Some clinical studies are being conducted to deliver p53 via adenoviral vectors to different cancers. Likewise, viral vectors have been used to administer a breast cancer gene BRCA1 and retinoblastoma gene into ovarian cancer and bladder, correspondingly. In various circumstances, this strategy will fall short, as the mutant gene indicates dominant negative activity of the normal gene. To avoid this difficulty for p53 gene therapy, a genetic repair approach rather than a gene augmentation strategy might be more successful [ 250 ].
Cancer stem-cell therapy for breast cancer
Current investigation in biology of breast has provided the foundation for the cancer stem-cell hypothesis [ 251 ]. Two significant aspects of this theory are that cancer arises in progenitor cells or mammary stem cells as an outcome of dysregulation of the normally strongly regulated method of self-renewal. As a consequence, cancers posses and are obtained by a cellular subcomponent that keeps central stem-cell functions such as self-renewal, which directs differentiation and tumorigenesis that is responsible for cellular heterogeneity. Development in the stem-cell field have guided to the recognition of stem cells in normal and malignant tissue of the breast. The investigations of these stem cells have assisted to clarify the source of the molecular complexity of breast cancer in human. The cancer stem-cell theory has significant role for timely recognition, prevention, and management of human breast cancer. Dysregulation of stem cell renewal pathways are involved in the development of both sporadic and hereditary breast cancers. These abnormal stem cells may give targets for the improvement of cancer prevention options. In addition, since breast cancer stem cells may be extremely challenging to chemotherapy and radiation, the progress of additional efficient treatments for breast cancer may need the efficient targeting of this cell population [ 252 ].
Anti-oestrogens and prevention of breast cancer
With the accomplishment of anti-oestrogens in breast tumor management, numerous studies evaluated their use as an mediator to avert breast cancer in female at high risk [ 253 , 254 ]. Tamoxifen is the antiestrogen medicine employed most commonly in the treatment of breast cancer. Administration of tamoxifen as an adjuvant treatment following surgery, normally for 5 years, decreases the risk of hormone receptor breast cancer recurrence.
Metastatic breast cancer is also managed by tamoxifen. In numerous females, tamoxifen induce the manifestations of menopause such as mood swings, vaginal discharge and hot flushes. Toremifene is one more medicine strongly related to tamoxifen. It is used an alternate drug in postmenopausal female for the treatment of metastatic breast cancer. Fulvestrant is another drug that decreases the estrogen receptor numbers. It is usually useful in postmenopausal female, even in tamoxifen resistant breast cancer. In previous studies, tamoxifen was evaluated for its efficacy in 13, 388 females at higher risk of breast cancer for the period of 5 years. The study indicated a 49% decrease in risk of increasing invasive breast cancer and as well decreased risk of opposing side breast cancer, reappearance and extended existence in the female who had tamoxifen as accessory after operation [ 187 , 188 ]. Antioestrogens are currently suggested as chemoprevention for female with atypical hyperplasia, genetic tendency to develop cancer and important family history of breast tumor. They are also prescribed because component of practice post-operative concomitant management of those with estrogen receptor positive cancers for duration of 5 years following surgery [ 255 ].
Human monoclonal antibody
Monoclonal antibodies are prepared in the laboratory [ 256 ]. These are used alone or in combination with radiation therapy and chemotherapy to locate and target cancer cells. Usually, the body’s immune system attack to foreign antigens such as infectious agents. It will then create antibodies to assist fight it off. The body does not identify cancer cells as a kind of foreign attacker. So, antibodies are then not formed. A randomized clinical trial was conducted to investigate efficacy of denosumab, a completely human monoclonal antibody against receptor activator of nuclear factor κ B (RANK) ligand, in comparison with zoledronic acid in the prevention of skeletal-related events in breast cancers individuals with bone metastases. Denosumab was found better as compared to zoledronic acid in preventing or delaying the SREs in breast cancer patients with bone metastasis. It is demonstrated that denosumab is possible therapeutic alternative for individual with bone metastases [ 257 ].
Immunotherapy
It utilizes the immune system of the body to fight against the cancer cells [ 258 ]. Cancer vaccine is one of its examples. Parts of cancer cells or cancer cells are utilized for formation of vaccines. These cells excite the body’s immune system to assist assault and destroy cancer cells [ 259 ]. Immunotherapy has turn into a significant constituent in the management of breast cancer. HER2 targeted treatment are at the present an important part of HER2 over expressing breast tumor therapy. Trastuzumab, with the new current accompaniments of pertuzumab and TDM1, encompass considerably superior breast cancer prediction. With various Federal Drug and Administration recommended antibody treatments used in together the adjuvant and metastatic settings, development progresses to be done in the area of immunotherapies. Current achievements in targeted therapies, vigorous particular immunotherapy, grasp assure for continuous success in general endurance within the adjuvant setting. The extremely precise and targeted strategy of vaccine therapy not simply avoids the adverse effects of recent standard of care therapies, active and passive immunotherapies including ipilimumab; however presents remedial strategy beyond now the HER2-overexpressing individuals. Even though vaccines for breast cancers have been mainly ineffective in precedent clinical studies, the most of these studies conducted in the location of late-stage metastatic illness, adverse surroundings for agents intended to stop, as different to manage, disease. With present clinical studies conducted on the adjuvant settings, immunogenicity is at the present indicating association with medical response.
Anti–angiogenesis drugs
Angiogenesis and inflammation are host-dependent manifestations of tumors that can be targeted with impediment strategies long prior to cancer start and develop [ 260 ]. Numerous prescription and non-prescription medicines are now accessible for utilization in angioprevention. Angioprevention can be proposed at four levels; first for the healthy people, 2nd for population at enhanced risk of tumor, 3rd for preneoplastic disease and 4th for prevention of cancer relapse. There are numerous achievements in prevention of cancer that reveal medical possibility and levels of interference, from no to slight to strong clinician participation. To evade toxicity whereas maintaining effectiveness, angioprevention desires to attain a level of angiogenesis prevention that is not extremely oppressive, such that hale and hearty vascular activity is maintained. These drugs block angiogenesis. In the absence of blood supply to cancer cells, they cannot develop and die. Various drugs are under investigation for the management of metastatic breast cancer. In initial stage of breast cancer, they are also investigate in the neoadjuvant (before surgery) setting [ 261 ]. Antiangiogenic treatment in breast cancer presents important promise, and numerous continuing investigations are trying to better describe the best management settings and mediator assortment. For patients with estrogen receptor positive aliment, researches recommend a relationship among resistance of endocrine and cancer dependence on angiogenic networks, suggesting a possible curative advantage in mixing endocrine treatment with antiVEGF mediator. Findings from randomized clinical studies emphasize the multiplicity in reaction to antiVEGF treatment and recommend the requirement for better choice of patient subsets further to be expected to advantage from these therapies. The recognition of biomarkers for therapy response is solitary part of deep attention, though mainly study to date has become unsuccessful to discover a relationship linking cancer-associated markers including cancer mutations and EGF expression and scientific response.
Surveillance and follow up
A regular assessment of the important in print literature conducted by de Bock et al. [ 262 ], revealed that 40% of recurring cancers are identified in asymptomatic individuals during routine visits. This information intensifies the significance of surveillance and follow-up. Clinical investigation such as history and physical examination is suggested each 4–6 months for 5 years, after that each year with annual mammography. Female on tamoxifen should go through a yearly gynecologic evaluation if the uterus exists. Female who suffers from ovarian failure secondary to management or on an aromatase inhibitor should have checking of bone fitness with a bone mineral thickness determination at the start and sometimes subsequently. Women should also be advised to adopt variable risk factors, including lessening alcohol use, reducing BMI and enhancing physical activity.
The increase of information on the pathophysiologic mechanisms of breast cancer has brought extensive development in the figure of biomolecular markers. In addition, the development of targeted drug design has grown quickly and more complicated, providing numerous agents that target these markers for in vivo investigation in animal models as well as clinical studies. The enthusiasm among scientists and Physicians about the growing management strategies is tempered by apprehension that resources are insufficient to carry the mainstream of these agents to advanced clinical trials. The challenges, then, are to choose the most capable agents to be investigated and the proper clinical studies for such evaluations. We have adopted a justifying strategy to unfolding the most extensively documented molecular targets in breast cancer. Drugs that amend the NRF have not been evaluated comprehensively so far, and such studies can boost the chances for true ‘endocrine’ strategies for management of breast cancer. Furthermore, agents that amend angiogenesis and apoptosis demonstrate an thrilling area of research, mostly in vigilantly chosen combination regimens.
Coleman M, Quaresma M, Berrino F, Lutz JM, Angelis R, Capocaccia R, et al. Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Oncol. 2008;9:730–56.
Article PubMed Google Scholar
Anderson B, Yip C, Smith R, Shyyan R, Sener S, Eniu A, et al. Guideline implementation for breast healthcare in low-income and middle-income countries: overview of the breast health global initiative global summit 2007. Cancer. 2008;113:2221–43.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30.
Berry D, Cronin K, Plevritis S, Fryback D, Clarke L, Zelen M, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784–92.
Article CAS PubMed Google Scholar
Peng J, Sengupta S, Jordan VC. Potential of selective estrogen receptor modulators as treatments and preventives of breast cancer. Anti-Cancer Agents Med Chem. 2009;9:481–99.
Article CAS Google Scholar
Reeder J, Vogel V. Breast cancer prevention. Cancer Treat Res. 2008;141:149–64.
Abdull R, Noor N. Cruciferous vegetables: dietary phytochemicals for cancer prevention. Asian Pac J Cancer Prev. 2013;14:1565–70.
Article Google Scholar
Dwivedi V, Shrivastava R, Hussain S. Comparative anticancer potential of clove ( Syzygium aromaticum )—an Indian spice—against cancer cell lines of various anatomical origin. Asian Pac J Cancer Prev. 2011;12(8):1989–93.
PubMed Google Scholar
Mary J, Vinotha P, Pradeep A. Screening for in vitro cytotoxic activity of seaweed, Sargassum sp. against Hep-2 and MCF-7 cancer cell lines. Asian Pac J Cancer Prev. 2012;13:6073–6.
Mukherjee P, Wahile A. Integrated approaches towards drug development from Ayurveda and other Indian system of medicines. J Ethnopharmacol. 2006;103:25–35.
Zhu Y, Zhou L, Jiao S, Xu L. Relationship between soy food intake and breast cancer in China. Asian Pac J Cancer Prev. 2011;12:2837–40.
Han S, Guo Q, Wang T. Prognostic significance of interactions between ER alpha and ER beta and lymph node status in breast cancer cases. Asian Pac J Cancer Prev. 2013;14:6081–4.
Ferlay J, Soerjomataram I, Ervik M. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:359–86.
Agnieszka M, Magdalena K, Grazyna J, Iwanowicz P. Assessment of midwifery student preparation for erforming the role of breast cancer educator. Asian Pac J Cancer Prev. 2014;15:5633–8.
Haghighat S, Akbari M, Ghaffari S, Yavari P. Standardized breast cancer mortality rate compared to the general female population of Iran. Asian Pac J Cancer Prev. 2012;13:5525–8.
Bhurgri Y. Karachi cancer registry data implications for the national cancer control program of Pakistan. Asian Pac J Cancer Prev. 2004;5:77–82.
Hanif M, Zaidi P, Kamal S, Hameed A. Institution-based cancer incidence in a local population in Pakistan: 9 year data analysis. Asian Pac J Cancer Prev. 2009;10:227–30.
Khoker S, Muhammad U, Masooma R, Naseem A, Afaf S. Clinico-pathologic profile of breast cancer patients in Pakistan: 10 years data of a local cancer hospital. Asian Pac J Cancer Prev. 2012;13:693–8.
Badar F, Faruqui Z, Uddin N. Management of breast lesions by breast physicians in a heavily populated south Asian developing country. Asian Pac J Cancer Prev. 2011;12:827–32.
CAS PubMed Google Scholar
Moore M, Ariyaratne Y, Badar F. Cancer epidemiology in South Asia past, present and future. Asian Pac J Cancer Prev. 2009;10:49–67.
Google Scholar
Jamal S, Mamoon N, Mushtaq S, Luqman M. Carcinoma of the male breast: a study of 141 cases from Northern Pakistan. Asian Pac J Cancer Prev. 2006;7:119–21.
Yang L, Parkin D, Ferlay J. Estimates of cancer incidence in China for 2000 and projections for 2005. Cancer Epidemiol Biomarkers Prev. 2005;14:243–50.
Torre LA, Sauer AM, Chen MS, Kagawa-Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, native hawaiians, and pacific islanders, 2016: converging incidence in males and females. Cancer J Clin. 2016;66:182–202.
Aronson K, Miller A, Woolcott C, Sterns E, McCready D, Lickley L, et al. Breast adipose tissue concentrations of polychlorinated biphenyls and other organochlorines and breast cancer risk. Cancer Epidemiol Prev Biomarkers. 2000;9:55–63.
CAS Google Scholar
Stark G, Grandel S, Spilker G. Tissue suction of the male and female breast. Aesth Plast Surg. 1992;16:317–24.
Tanis P, Nieweg O, Olmos R, Kroon B. Anatomy and physiology of lymphatic drainage of the breast from the perspective of sentinel node biopsy1. J Amer Coll Surg. 2001;192:399–409.
Thomsen S, Tatman D. Physiological and pathological factors of human breast disease that can influence optical diagnosis. Ann N Y Acad Sci. 1998;838(1):171–93.
Jagannathan N, Sharma U. Breast tissue metabolism by magnetic resonance spectroscopy. Metabolites. 2017;7:25–30.
Article PubMed Central CAS Google Scholar
Brayboy L, Oulhen N, Long S, Voigt N, Raker C, Wessel G. Multidrug resistance transporter-1 and breast cancer resistance protein protect against ovarian toxicity, and are essential in ovarian physiology. Rep Toxicol. 2017;69:121–31.
Hassiotou F, Geddes D. Anatomy of the human mammary gland: current status of knowledge. Clin Anat. 2013;26:29–48.
Love RR, Love SM, Laudico AV. Breast cancer from a public health perspective. Breast J. 2004;10:136–40.
West A, Wullkopf L, Christensen A, Leijnse N, Tarp JM, Mathiesen J, et al. Division induced dynamics in non-Invasive and invasive breast cancer. Biophys J. 2017;112:123–5.
Posner MC, Wolmark N. Non-invasive breast carcinoma. Breast Cancer Res Treat. 1992;21(3):155–64.
Hang J, Sim L, Zakaria Z. Non-invasive breast cancer assessment using magnetic induction spectroscopy technique. Int J Integr Eng. 2017;9:15–20.
Inoue M, Nakagomi H, Nakada H, Furuya K, Ikegame K, Watanabe H. Specific sites of metastases in invasive lobular carcinoma: a retrospective cohort study of metastatic breast cancer. Breast Cancer. 2017;20:1–6.
Clauser P, Marino MA, Baltzer PA, Bazzocchi M, Zuiani C. Management of atypical lobular hyperplasia, atypical ductal hyperplasia, and lobular carcinoma in situ. Exp Rev Anticancer ther. 2016;16:335–6.
Chuba P, Hamre M, Yap J, Severson R, Lucas D, Shamsa F. Bilateral risk for subsequent breast cancer after lobular carcinoma-in-situ: analysis of surveillance, epidemiology, and end results data. J Clin Oncol. 2005;23:5534–41.
Nakhlis F, Morrow M. Ductal carcinoma in situ. Surg Clin. 2003;83:821–39.
Harris LN, Ismaila N, McShane LM, Andre F, Collyar DE, Gonzalez-Angulo AM, et al. Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer. J Clin Oncol. 2016;34:1134–50.
Article CAS PubMed PubMed Central Google Scholar
Ziperstein MJ, Guzman A, Kaufman LJ. Evaluating breast cancer cell morphology as a predictor of invasive capacity. Biophys J. 2016;110:621–5.
Prabhakaran S, Rizk V, Ma Z, Cheng C, Berglund A, Coppola D, et al. Evaluation of invasive breast cancer samples using a 12-chemokine gene expression score: correlation with clinical outcomes. Breast Cancer Res. 2017;19:71–4.
Article PubMed PubMed Central Google Scholar
Stevanovic A, Lee P, Wilcken N. Metastatic breast cancer. Aust Fam Phys. 2006;35:309–11.
Page K, Guttery D, Fernandez-Garcia D, Hills A, Hastings R, Luo J, et al. Next generation sequencing of circulating cell-free DNA for evaluating mutations and gene amplification in metastatic breast cancer. Clin Chem. 2017;63:532–41.
Arpino G, Bardou VJ, Clark GM, Elledge RM. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res. 2004;6:149–52.
Somiari R, Sullivan A, Russell S, Somiari S, Hu H, Jordan R, George A, Katenhusen R, Buchowiecka A, Arciero C, Brzeski H. High-throughput proteomic analysis of human infiltrating ductal carcinoma of the breast. Proteomics. 2003;3(10):1863–73.
Mateo A, Pezzi T, Sundermeyer M, Kelley C, Klimberg V, Pezzi C. Chemotherapy significantly improves survival for patients with T1c-T2N0M0 medullary Breast cancer. Ann Surg Oncol. 2017;24:1050–6.
Anuradha D, Lakshmi A. Mucinous carcinoma of breast with neuroendocrine differentiation: a rare case report with review of literature. Int J Res Med Sci. 2017;2:1751–4.
Priya V, Prasaad P. Tubulo-lobular carcinoma: a rare mixed invasive carcinoma of breast. Int J Res Med Sci. 2017;5:2818–20.
Joglekar-Javadekar M, Van Laere S, Bourne M, Moalwi M, Finetti P, Vermeulen PB, et al. Characterization and targeting of platelet-derived growth factor receptor alpha (PDGFRA) in inflammatory breast cancer (IBC). Neoplasia. 2017;19:564–73.
Cariati M, Bennett-Britton TM, Pinder SE, Purushotham AD. Inflammatory breast cancer. Surg Oncol. 2005;14:133–43.
Errichetti E, Avellini C, Pegolo E, De Francesco V. Dermoscopy as a supportive instrument in the early recognition of erosive adenomatosis of the nipple and mammary paget’s disease. Ann Dermatol. 2017;29:365–7.
Merrill A, White A, Howard-McNatt M. Paget’s disease of the breast: an institutional review and surgical management. Am Surg. 2017;83:96–8.
Strode M, Khoury T, Mangieri C, Takabe K. Update on the diagnosis and management of malignant phyllodes tumors of the breast. J Breast. 2017;33:91–6.
Sera T, Kashiwagi S, Takashima T, Asano Y, Goto W, Iimori N, et al. Multiple metastatic malignant phyllodes tumor of the breast with tonsillar metastasis: a case report. BMC Res Notes. 2017;10:55–60.
Nozad S, Sheehan C, Gay L, Elvin J, Vergilio J, Suh J, et al. Comprehensive genomic profiling of malignant phyllodes tumors of the breast. Breast Cancer Res Treat. 2017;162:597–602.
Liedtke C, Mazouni C, Hess KR, André F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–81.
Foulkes W, Smith I, Reis-Filho J. Triple-negative breast cancer. New Engl J Med. 2010;363:1938–48.
Stingl J, Raouf A, Emerman JT, Eaves CJ. Epithelial progenitors in the normal human mammary gland. J Mammary Gland Biol Neoplasia. 2005;10:49–59.
Villadsen R, Fridriksdottir AJ, Rønnov-Jessen L, et al. Evidence for a stem cell hierarchy in the adult human breast. J Cell Biol. 2007;177(1):87–101.
Stingl J, Raouf A, Eirew P, Eaves CJ. Deciphering the mammary epithelial cell hierarchy. Cell Cycle. 2006;5:1519–22.
Gusterson B, Warburton MJ, Mitchell D, Ellison M, Neville AM, Rudland PS. Distribution of myoepithelial cells and basement membrane proteins in the normal breast and in benign and malignant breast diseases. Cancer Res. 1982;42:4763–70.
Evan G, Vousden K. Proliferation, cell cycle and apoptosis in cancer. Nature. 2001;411:342–8.
Grana X, Reddy E. Cell cycle control in mammalian cells: role of cyclins, cyclin dependent kinases (CDKs), growth suppressor genes and cyclin-dependent kinase inhibitors (CKIs). Oncogene. 1995;11:211–20.
Hartwell L, Kastan M. Cell cycle control and cancer. Sci. 1994;266:1821–3.
Leighton J, Kalla R, Turner J, Fennell R. Pathogenesis of tumor invasion. Cancer Res. 1960;20:575–86.
Cavalieri E, Chakravarti D, Guttenplan J, Hart E, Ingle J, Jankowiak R, et al. Catechol estrogen quinones as initiators of breast and other human cancers: implications for biomarkers of susceptibility and cancer prevention. Biochim Biophys Acta. 2006;1766:63–8.
Jarde T, Perrier S, Vasson M, Caldefie-Chezet F. Molecular mechanisms of leptin and adiponectin in breast cancer. Eur J Cancer. 2011;47:33–43.
Hanahan D, Weinberg R. The hallmarks of cancer. Cell. 2000;100:57–70.
Jain R. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62.
Gupta G, Massagué J. Cancer metastasis: building a framework. Cell. 2006;127:679–95.
Shamsi U, Khan S, Usman S, Soomro S, Azam I. A multicenter matched case control study of breast cancer risk factors among women in Karachi, Pakistan. Asian Pac J Cancer Prev. 2013;14:183–8.
Donnelly T, Khater A, Al-Bader S. Arab women’s breast cancer screening practices: a literature review. Asian Pac J Cancer Prev. 2013;14(8):4519–28.
Harirchi I, Karbakhsh M, Kashefi A, Momtahen A. Breast cancer in Iran: results of a multi-center study. Asian Pac J Cancer Prev. 2004;5:24–7.
Kadivar M, Mafi N, Joulaee A. Breast cancer molecular subtypes and associations with clinicopathological characteristics in Iranian women, 2002–2011. Asian Pac J Cancer Prev. 2012;13:1881–6.
Alegre M, Knowles M, Robison R, O’Neill K. Mechanics behind breast cancer prevention-focus on obesity, exercise and dietary fat. Asian Pac J Cancer Prev. 2013;14:2207–12.
Zainal N, Nik-Jaafar N, Baharudin A, Sabki Z, Ng C. Prevalence of depression in breast cancer survivors: a systematic review of observational studies. Asian Pac J Cancer Prev. 2013;14:2649–56.
Andsoy I, Gul A. Breast, cervix and colorectal cancer knowledge among nurses in turkey. Asian Pac J Cancer Prev. 2014;15:2267–9.
Franca A, Ferreira M, Franca J, Franca E, Honorio-Franca A. Breastfeeding and its relationship with reduction of breast cancer: a review. Asian Pac J Cancer Prev. 2012;13:5327–32.
Kruk J. Association of lifestyle and other risk factors with breast cancer according to menopausal status: a case-control study in the region of Western Pomerania (Poland). Asian Pac J Cancer Prev. 2007;8:513–4.
Jacobs T, Byrne C, Colditz G, Connolly J, Schnitt S. Radial scars in benign breast-biopsy specimens and the risk of breast cancer. New Engl J Med. 1999;340:430–6.
Alco G, Igdem S, Dincer M. Vitamin D levels in patients with breast cancer: importance of dressing style. Asian Pac J Cancer Prev. 2014;15:1357–62.
Hasson-Ohayon I, Goldzweig G, Braun M, Galinsky D. Women with advanced breast cancer and their spouses: diversity of support and psychological distress. PsychoOncology. 2010;19:1195–204.
McPherson K, Steel C, Dixon J. Breast cancer-epidemiology, risk factors, and genetics. Brit Med J. 2000;321:624–8.
Kelsey J, Bernstein L. Epidemiology and prevention of breast cancer. Ann Rev Public Health. 1996;17:47–67.
Hartmann L, Sellers T, Frost M, Lingle W, Degnim A, Suman V. Benign breast disease and the risk of breast cancer. New Engl J Med. 2005;353:229–37.
Eberl M, Sunga A, Farrell C, Mahoney M. Patients with a family history of cancer: identification and management. JABFM. 2005;18:211–7.
Key T, Verkasalo P, Banks E. Epidemiology of breast cancer. The lancet Oncol. 2001;2:133–40.
Thomas DB. Breast cancer in men. Epidemiol Rev. 1993;15:220–31.
Weinberg O, Marquez-Garban D, Pietras R. New approaches to reverse resistance to hormonal therapy in human breast cancer. Drug Resist Updat. 2005;8:219–33.
Singh R, Kumar R. Steroid hormone receptor signalling in tumorigenesis. J Cell Biochem. 2005;96:490–505.
Kato S, Sato T, Watanabe T, Takemasa S, Masuhiro Y, Ohtake F. Function of nuclear sex hormone receptors in gene regulation. Cancer Chemother Pharmacol. 2005;56:4–9.
Article PubMed CAS Google Scholar
Malara N, Leotta A, Sidoti A, Lio S, D’Angelo R, Caparello B, et al. Ageing, hormonal behaviour and cyclin D1 in ductal breast carcinomas. Breast. 2006;15:81–9.
Lee H, Lee J, Gourley L, Duffy S, Day N, Estève J. Dietary effects on breast-cancer risk in Singapore. Lancet. 1991;8(337):1197–200.
Hulka B, Stark T. Breast cancer: cause and prevention. Lancet. 1995;346:883–7.
Zhao M, Howard E, Parris A, Guo Z, Zhao Q, Yang X. Alcohol promotes migration and invasion of triple-negative breast cancer cells through activation of p38 MAPK and JNK. Mol Carcinogen. 2017;56:849–62.
Antoniou A, Pharoah P, Narod S. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003;72:1117–30.
Scott C, Jenkins M, Southey M. Average age-specific cumulative risk of breast cancer according to type and site of germline mutations in BRCA1 and BRCA2 estimated from multiple-case breast cancer families attending Australian family cancer clinics. Hum Genet. 2003;112:542–51.
Nkondjock A, Ghadirian P. Epidemiology of breast cancer among BRCA mutation carriers: an overview. Cancer Lett. 2004;205:1–8.
Shaukat U, Ismail M, Mehmood N. Epidemiology, major risk factors and genetic predisposition for breast cancer in the Pakistani population. Asian Pac J Cancer Prev. 2013;14:5625–9.
Heim E, Valach L, Schaffner L. Coping and psychosocial adaptation: longitudinal effects over time and stages in breast cancer. Psychosom Med. 1997;59:408–18.
Bednarek A, Sahin A, Brenner A, Johnston D, Aldaz C. Analysis of telomerase activity levels in breast cancer: positive detection at the in situ breast carcinoma stage. Clin Cancer Res. 1997;3(1):11–6.
Segal R, Evans W, Johnson D, Smith J, Colletta S, Gayton J. Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol. 2001;19:657–65.
Moran M, Schnitt S, Giuliano A, Harris J, Khan S, Horton J. Society of surgical oncology–American society for radiation oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Int J Rad Oncol Biol Phys. 2014;88:553–64.
Jacquillat C, Weil M, Baillet F, Borel C, Auclerc G, Maublanc M. Results of neoadjuvant chemotherapy and radiation therapy in the breast-conserving treatment of 250 patients with all stages of infiltrative breast cancer. Cancer. 1990;66:119–29.
Neuman H, Morrogh M, Gonen M. Stage IV breast cancer in the Era of targeted therapy, Does surgery of the primary tumor matter. Cancer. 2015;116:1226–33.
Kerlikowske K, Grady D, Barclay J, Sickles EA, Eaton A, Ernster V. Positive predictive value of screening mammography by age and family history of breast cancer. JAMA. 1993;270(20):2444–50.
Shah R, Rosso K, Nathanson SD. Pathogenesis, prevention, diagnosis and treatment of breast cancer. World J Clin Oncol. 2014;5:283–8.
Kolb T, Lichy J, Newhouse J. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiology. 2002;225:165–75.
Kosters J, Gøtzsche P. Regular self-examination or clinical examination for early detection of breast cancer. Cochrane Database Syst Rev. 2003;2:3373–5.
McCready T, Littlewood D, Jenkinson J. Breast self-examination and breast awareness: a literature review. J Clin Nurs. 2005;14:570–8.
Gursoy A, Hindistan S, Nurall N. A comparison of three educational interventions on breast self examination knowledge and health belief. Asian Pac J Cancer Prev. 2009;10:765–72.
Redhwan A, Al-Naggar D, Bobryshev Y, Chen R, Assabri A. Practice and barriers toward breast self-examination among young Malaysian women. Asian Pac J Cancer Prev. 2011;12:1173–8.
Taha H, Halabi Y, Berggren V. Educational intervention to improve breast health knowledge among women in Jordan. Asian Pac J Cancer Prev. 2010;11:1167–73.
Alipour S, Moini A, Jafari-Adli S, Gharaie N, Mansouri K. Comparison of teaching about breast cancer via mobile or traditional learning methods in gynecology residents. Asian Pac J Cancer Prev. 2012;13:4593–5.
Sreedharan J, Muttappallymyalil J, Venkatramana M, Thomas M. Breast self-examination and practice among nurses in United Arab Emirates. Asian Pac J Cancer Prev. 2010;11:651–4.
Ozkan A, Malak A, Gürkan A, Turgay A. Do Turkish nursing and midwifery students teach breast self examination to their relatives. Asian Pac J Cancer Prev. 2010;11:1569–73.
Ceber E, Mermer G, Okcin F. Breast cancer risk and early diagnosis applications in Turkish women aged 50 and over. Asian Pac J Cancer Prev. 2013;14:5877–82.
Beydag K, Karaoğlan P. The effect of breast self examination (Bse) education given to midwifery students on their knowledge and attitudes. Asian Pac J Cancer Prev. 2010;11:1761–4.
Berg W, Blume J, Cormack J, Mendelson E, Lehrer D, Bohm-Velez M, et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA. 2008;299:2151–63.
Masood S, Rosa M. Borderline breast lesions: diagnostic challenges and clinical implications. Adv Anat Pathol. 2011;18:190–8.
Kelly K, Dean J, Comulada W, Lee S. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010;20:734–42.
Ahmed B. Awareness and practice of breast cancer and breast self examination among university students in Yemen. Asian Pac J Cancer Prev. 2010;11:101–6.
Cam O, Gvmvs A. Breast cancer screening behavior in Turkish women: relationships with health beliefs and self-esteem, body, perception and hopelessness. Asian Pac J Cancer Prev. 2009;10:49–56.
Husarik D, Steinert H. Single-photon emission computed tomography/computed tomography for sentinel node mapping in breast cancer. Semin Nuclear Med. 2007;37:29–33.
Antoch G, Saoudi N, Kuehl H, Dahmen G, Mueller SP, Beyer T, et al. Accuracy of whole-body dual-modality fluorine-18–2-fluoro-2-deoxy- d -glucose positron emission tomography and computed tomography (FDG-PET/CT) for tumor staging in solid tumors: comparison with CT and PET. J Clin Oncol. 2004;22:4357–68.
Porika M, Malotu N, Veldandi U-K. Evaluation of tumor markers in Southern Indian breast cancer patients. Asian Pac J Cancer Prev. 2010;2010(11):157–9.
Harris L, Fritsche H, Mennel R, Norton L, Ravdin P, Taube S, et al. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol. 2007;25:5287–312.
Hayes DF. Tumor markers for breast cancer. Ann Oncol. 1993;4:807–19.
Khazai L, Rosa M. Use of immunohistochemical stains in epithelial lesions of the breast. Cancer Control. 2015;22:220–5.
Nystrom L, Andersson I, Bjurstam N, Frisell J, Nordenskjöld B, Rutqvist L. Long-term effects of mammography screening: updated overview of the Swedish randomised trials. Lancet. 2002;359:909–19.
Richardson H, Johnston D, Pater J, Goss P. The national cancer institute of Canada clinical trials group MAP.3 trial: an international breast cancer prevention trial. Curr Oncol. 2007;14:89–96.
Boughey J, Nguyen T. Axillary staging after neoadjuvant chemotherapy for breast cancer: a pilot study combining sentinel lymph node biopsy with radioactive seed localization of pre-treatment positive axillary lymph bodes. Breast Dis YB Quart. 2016;27:282–4.
Sotiriou C, Powles TJ, Dowsett M, Jazaeri AA, Feldman AL, Assersohn L, Gadisetti C, Libutti SK, Liu ET. Gene expression profiles derived from fine needle aspiration correlate with response to systemic chemotherapy in breast cancer. Breast Cancer Res. 2002;4(3):3–7.
Kuenen-Boumeester V, Menke-Pluymers M, Kanter A, Obdeijn I, Urich D, Kwast T. Ultrasound-guided fine needle aspiration cytology of axillary lymph nodes in breast cancer patients. Eur J Cancer. 2003;39:170–4.
Elvecrog EL, Lechner MC, Nelson MT. Nonpalpable breast lesions: correlation of stereotaxic large-core needle biopsy and surgical biopsy results. Radiology. 1993;188(2):453–5.
Liberman L, Dershaw DD, Rosen PP, Abramson AF, Deutch BM, Hann LE. Stereotaxic 14-gauge breast biopsy: how many core biopsy specimens are needed. Radiology. 1994;192(3):793–5.
Damera A, Evans A, Cornford E, Wilson A, Burrell H, James J, et al. Diagnosis of axillary nodal metastases by ultrasound-guided core biopsy in primary operable breast cancer. Brit J Cancer. 2003;89:1310.
Jackman R, Burbank F, Parker S, Evans P, Lechner C, Richardson T, et al. Atypical ductal hyperplasia diagnosed at stereotactic breast biopsy: improved reliability with 14-gauge, directional, vacuum-assisted biopsy. Radiology. 1997;204:485–8.
Burak W, Owens K, Tighe M, Kemp L, Dinges S, Olsen J. Vacuum-assisted stereotactic breast biopsy: histologic underestimation of malignant lesions. Arch Surg. 2000;135:700–3.
Krag D, Weaver D, Alex J, Fairbank J. Surgical resection and radiolocalization of the sentinel lymph node in breast cancer using a gamma probe. Surg Oncol. 1993;2:335–40.
Lyman G, Temin S, Edge S, Newman L, Turner R, Weaver D, et al. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2014;32:1365–83.
Abdulkareem S. Breast magnetic resonance imaging indications in current practice. Asian Pac J Cancer Prev. 2014;2:569–75.
Ahmadian M, Samah A, Redzuan M, Emby Z. Predictors of mammography screening among Iranian women attending outpatient clinics in Tehran, Iran. Asian Pac J Cancer Prev. 2012;13:969–74.
Wang F, Chen F, Yin H. Effects of age, breast density and volume on breast cancer diagnosis: a retrospective comparison of sensitivity of mammography and ultrasonography in China’s rural areas. Asian Pac J Cancer Prev. 2013;4:2277–82.
Kanaga K, Nithiya J, Shatirah M. Awareness of breast cancer and screening procedures among Malaysian women. Asian Pac J Cancer Prev. 2011;12:1965–7.
Sardanelli F, Giuseppetti G, Panizza P, Bazzocchi M, Fausto A, Simonetti G, et al. Sensitivity of MRI versus mammography for detecting foci of multifocal, multicentric breast cancer in fatty and dense breasts using the whole-breast pathologic examination as a gold standard. Am J Roentgenol. 2004;183:1149–57.
Smith R, Caleffi M, Albert S, Tony H, Stephen W, Franceschi D. Breast cancer in limited resource countries: early detection and access to care. Breast J. 2006;12:16–26.
Berg W, Weinberg I, Narayanan D, Lobrano M, Ross E, Levine E. High-resolution fluorodeoxyglucose positron emission tomography with compression (“positron emission mammography”) is highly accurate in depicting primary breast cancer. Breast J. 2006;12(4):309–23.
Schilling K, Narayanan D, Judith E, Velasquez M, Kahn S, Saady M. Positron emission mammography in breast cancer presurgical planning: comparisons with magnetic resonance imaging. Eur J Nucl Med Mol Imaging. 2011;38:23–36.
Meng X, Sun H, Yang L, Yin R, Qi L. A hydroxylated flavonol, fisetin inhibits the formation of a carcinogenic estrogen metabolite. Steroids. 2017;31(119):53–6.
Oshima S, Kisa K, Terashita T. A qualitative study of Japanese patients’ perspectives on post-treatment care for gynecological cancer. Asian Pac J Cancer Prev. 2011;12:2255–61.
Sharifa E, Fuad I, Hayati Y. Observational Study on patient’s satisfactions and quality of life (QoL) among cancer patients receiving treatment with palliative care intent in a tertiary hospital in Malaysia. Asian Pac J Cancer Prev. 2014;15:695–701.
Shen F, Liu M, Zhang X. Health-related quality of life among breast cancer patients and its influencing factor in a Chinese population. Asian Pac J Cancer Prev. 2012;13:3747–50.
Lodha R, Nandeshwar S, Pal D. Risk factors for breast cancer among women in Bhopal urban agglomerate: a case-control study. Asian Pac J Cancer Prev. 2011;12:2111–5.
Debnath M, Malik C, Bisen P. Micropropagation: a tool for the production of high quality plant-based medicines. Curr Pharm Biotechnol. 2006;7(1):33–9.
Mehta R, Murillo G, Naithani R, Peng X. Cancer chemoprevention by natural products: how far have we come. Pharm Res. 2010;27:950–61.
Deng Q, Huang X, Ye L. Phase II trial of Loubo ® (Lobaplatin) and Pemetrexed for patients with metastatic breast cancer not responding to anthracycline or taxanes. Asian Pac J Cancer Prev. 2013;14:413–7.
Huang S, Cao K. Anti-invasive and anti-metastasis effect of norcantharidin on high-metastatic human breast cancer cell lines. J Trop Med. 2010;9:1034–45.
Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: sleep and psychological effects. J Clin Oncol. 2005;23:6083–96.
Compas BE, Luecken L. Psychological adjustment to breast cancer. Curr Direct Psychol Sci. 2002;11:111–4.
Ellis M, Suman V, Hoog J, Goncalves R, Sanati S, Creighton CJ, et al. Ki67 proliferation index as a tool for chemotherapy decisions during and after neoadjuvant aromatase inhibitor treatment of breast cancer: results from the American college of surgeons oncology group Z1031 trial (Alliance). J Clin Oncol. 2017;35:1061–9.
Houssami N, Turner R, Morrow M. Meta-analysis of pre-operative magnetic resonance imaging (MRI) and surgical treatment for breast cancer. Breast Cancer Res Treat. 2017;6:1–11.
Pearson R, Milligan R, Cain H. Radioactive iodine-125 seed localisation of breast carcinoma in advance of the day of surgery reduces pre-operative anxiety levels. Europ J Surg Oncol. 2017;43:7–10.
Vaz-Luis I, Hughes ME, Cronin A, Rugo HS, Edge SB, Moy B, Theriault RL, Hassett MJ, Winer EP, Lin NU. Trends in the use of mastectomy in women with small node-negative breast cancer treated at US academic centers. Breast Cancer Res Treat. 2016;155(3):569–78.
Fisher B, Anderson S, Redmond C, Cronin W. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. New Engl J Med. 1995;333:1456–61.
Dorval M, Maunsell E, Deschênes L, Brisson J. Type of mastectomy and quality of life for long term breast carcinoma survivors. Cancer. 1998;83:2130–8.
Yarnold J, Ashton A, Bliss J, Homewood J, Harper C, Hanson J. Fractionation sensitivity and dose response of late adverse effects in the breast after radiotherapy for early breast cancer: long-term results of a randomised trial. Radiother Oncol. 2005;75:9–17.
Voogd A, Nielsen M, Peterse JL, Blichert-Toft M, Bartelink H, Overgaard M, et al. Danish breast cancer cooperative group and the breast cancer cooperative group of the European organization for research and treatment of cancer. Differences in risk factors for local and distant recurrence after breast-conserving therapy or mastectomy for stage I and II breast cancer: pooled results of two large European randomized trials. J Clin Oncol. 2001;19:1688–97.
Rebbeck T, Friebel T, Lynch H, Neuhausen S, Veer L, Garber J, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol. 2004;22:1055–62.
Tuttle T, Habermann E, Grund E, Morris T, Virnig B. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–9.
Keskin G, Gumus A. Turkish hysterectomy and mastectomy patients-depression, body image, sexual problems and spouse relationships. Asian Pac J Cancer Prev. 2011;12:425–32.
Rowland JH, Desmond KA, Meyerowitz BE, Belin TR, Wyatt GE. Role of breast reconstructive surgery in physical and emotional outcomes among breast cancer survivors. J Nat Cancer Instit. 2000;92:1422–9.
Parker P, Youssef A, Walker S. Short-term and long-term psychosocial adjustment and quality of life in women undergoing different surgical procedures for breast cancer. Ann Surg Oncol. 2007;14:3078–89.
Elder EE, Brandberg Y, Björklund T. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast. 2005;14:201–8.
Thomson C, Twelves C, Mallon E, Leake R, Group S. Scottish cancer therapy network. adjuvant ovarian ablation vs CMF chemotherapy in premenopausal breast cancer patients: trial update and impact of immunohistochemical assessment of ER status. Breast. 2002;11:419–29.
Davidson N. Ovarian ablation as adjuvant therapy for breast cancer. Semin Oncol. 2001;30:67–71.
Hammond M, Hayes D, Dowsett M, Allred D, Hagerty K, Badve S, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Arch Pathol Lab Med. 2010;134:48–72.
Osborne C, Yochmowitz M, Knight W, McGuire W. The value of estrogen and progesterone receptors in the treatment of breast cancer. Cancer. 1980;46:2884–8.
Clarke R, Liu M, Bouker K, Gu Z, Lee R, Zhu Y. Antiestrogen resistance in breast cancer and the role of estrogen receptor signaling. Oncogene. 2003;22:7316–39.
Mehta S, Dhandapani K, De Sevilla L, Webb R, Mahesh V. Tamoxifen, a selective estrogen receptor modulator, reduces ischemic damage caused by middle cerebral artery occlusion in the ovariectomized female rat. Neuroendocrinology. 2003;77:44–50.
Man S, Bocci G, Francia G, Green S, Jothy S, Hanahan D. Antitumor effects in mice of low-dose (metronomic) cyclophosphamide administered continuously through the drinking water. Cancer Res. 2002;62:2731–5.
Visvanathan K, Chlebowski R, Hurley P, Col F, Ropka M, Collyar D. American society of clinical oncology clinical practice guideline update on the use of pharmacologic interventions including tamoxifen, raloxifene, and aromatase inhibition for breast cancer risk reduction. J Clin Oncol. 2009;27:3235–58.
Journe F, Body J, Leclercq G, Laurent G. Hormone therapy for breast cancer, with an emphasis on the pure antiestrogen fulvestrant: mode of action, antitumor efficacy and effects on bone health. Exp Opin Drug Safe. 2008;7:241–58.
Riggs B, Hartmann L. Selective estrogen-receptor modulators—mechanisms of action and application to clinical practice. New Engl J Med. 2003;348:618–29.
Nayfield S, Karp J, Ford L, Dorr F, Kramer B. Potential role of tamoxifen in prevention of breast cancer. J Nat Cancer Inst. 1991;83:1450–9.
Jordan V. New insights into the metabolism of tamoxifen and its role in the treatment and prevention of breast cancer. Steroids. 2007;72:829–42.
Fisher B, Costantino J, Wickerham D, Redmond C, Kavanah M, Cronin W, et al. Tamoxifen for prevention of breast cancer: report of the national surgical adjuvant breast and bowel project P-1 Study. J Nat Cancer Inst. 1998;90:1371–88.
Fisher B, Costantino J, Wickerham D. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371–88.
Vogel V, Costantino J, Wickerham D. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP study of tamoxifen and raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727–41.
Cuzick J, Powles T, Veronesi U. Overview of the main outcomes in breast-cancer prevention trials. Lancet. 2003;361:296–300.
Cuzick J, Forbes J, Sestak I. Long-term results of tamoxifen prophylaxis for breast cancer—96-month follow-up of the randomized IBIS-I trial. J Natl Cancer Inst. 2007;99:272–82.
Mortimer J, Urban J. Long-term toxicities of selective estrogen-receptor modulators and antiaromatase agents. J Oncol. 2003;17:652–9.
Vogel V. Chemoprevention strategies 2006. Curr Treat Options Oncol. 2007;8:74–88.
Land S, Wickerham D, Costantino J. Patient-reported symptoms and quality of life during treatment with tamoxifen or raloxifene for breast cancer prevention: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2742–51.
Goss P, Strasser K. Aromatase inhibitors in the treatment and prevention of breast cancer. J Clin Oncol. 2001;19:881–94.
Winer E, Hudis C, Burstein H, Wolff A, Pritchard K, Ingle J, et al. American Society of Clinical Oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor–positive breast cancer: status report 2004. J Clin Oncol. 2005;23:619–29.
Hall E, Brenner D. Cancer risks from diagnostic radiology. Br J Radiol. 2008;81:362–78.
Nandi M, Mahata A, Mallick I. Hypofractionated radiotherapy for breast cancers–preliminary results from a tertiary care center in eastern India. Asian Pac J Cancer Prev. 2014;15:2505–10.
Zhou S, Shi W, Meng D. Interoperative radiotherapy of seventy-two cases of early breast cancer patients during breast-conserving surgery. Asian Pac J Cancer Prev. 2012;13:1131–5.
Keisch M, Vicini F, Kuske R, Hebert M, White J, Quiet C, et al. Initial clinical experience with the MammoSite breast brachytherapy applicator in women with early-stage breast cancer treated with breast-conserving therapy. Int J Radiat Oncol Biol Phys. 2003;55:289–93.
King A, Bolton J, Kuske R, Fuhrman G, Scroggins T, Jiang X. Long-term results of wide-field brachytherapy as the sole method of radiation therapy after segmental mastectomy for T is, 1, 2 breast cancer. Am J Surg. 2000;180:299–304.
Johnstone R, Ruefli A, Lowe S. Apoptosis: a link between cancer genetics and chemotherapy. Cell. 2002;108:153–64.
Masood S. Neoadjuvant chemotherapy in breast cancers. Womens Health (Lond). 2016;12:480–91.
Benson I, Schrag D, Somerfield M, Cohen A, Figueredo A, Flynn P. American society of clinical oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol. 2004;22(16):3408–19.
Shapiro C, Recht A. Side effects of adjuvant treatment of breast cancer. New Engl J Med. 2001;344:1997–2008.
Muller A, Homey B, Soto H, Ge N. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–5.
Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez E. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. New Engl J Med. 2007;357:2666–76.
Ringel I, Horwitz S. Studies with RP 56976 (taxotere): a semisynthetic analogue of taxol. J Nat Cancer Inst. 1991;83:288–91.
Wist E, Sommer H, Ostenstad B, Risberg T, Fjaestad K. Weekly 1-hour paclitaxel as first-line chemotherapy for metastatic breast cancer. Acta Oncol. 2004;43:11–4.
Tan D, Marchió C, Jones R, Savage K, Smith I, Dowsett M, et al. Triple negative breast cancer: molecular profiling and prognostic impact in adjuvant anthracycline-treated patients. Breast Cancer Res Treat. 2008;111:27–44.
Oshaughnessy J, Miles D, Vukelja S, Moiseyenko V, Ayoub JP, Cervantes G, et al. Superior survival with capecitabine plus docetaxel combination therapy in anthracycline-pretreated patients with advanced breast cancer: phase III trial results. J Clin Oncol. 2002;20:2812–23.
Grevelman E, Breed W. Prevention of chemotherapy-induced hair loss by scalp cooling. Ann Oncol. 2005;16:352–8.
Monsuez J, Charniot JC, Vignat N, Artigou JY. Cardiac side-effects of cancer chemotherapy. Int J Cardiol. 2010;144:3–15.
Digianni L, Garber J, Winer E. Complementary and alternative medicine use among women with breast cancer. J Clin Oncol. 2002;2002(20):34–8.
Yates J, Mustian K, Morrow G, Gillies L, Padmanaban D, Atkins J. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Support Care Cancer. 2005;13:806–11.
Linde K, Jonas W, Melchart D, Willich S. The methodological quality of randomized controlled trials of homeopathy, herbal medicines and acupuncture. Int J Epidemiol. 2001;30:526–31.
Thorne S, Paterson B, Russell C, Schultz A. Complementary/alternative medicine in chronic illness as informed self-care decision making. Int J Nurs Stud. 2002;39:671–83.
Wang S, Hsu L, Hsu H, Lee S, Shiao M, Ho C. The anti-tumor effect of Ganoderma lucidum is mediated by cytokines released from activated macrophages and T lymphocytes. Int J Cancer. 1997;70:699–705.
Jiang J, Slivova V, Harvey K. Ganoderma lucidum suppresses growth of breast cancer cells through the inhibition of Akt/NF-kappaB signaling. Nutr Cancer. 2004;49:209–16.
Harinantenaina L, Tanaka M, Takaoka S, Oda M, Mogami O, Uchida M. Momordica charantia constituents and antidiabetic screening of the isolated major compounds. Chem Pharm Bull. 2006;54:1017–21.
Basch E, Gabardi S, Ulbricht C. Bitter melon ( Momordica charantia ): a review of efficacy and safety. Amer J HealthSyst Pharm. 2003;60:356–9.
Ray B, Raychoudhuri A, Steele R. Bitter melon ( Momordica charantia ) extract inhibits breast cancer cell proliferation by modulating cell cycle regulatory genes and promotes apoptosis. Cancer Res. 2010;70:1925–31.
Roh J, Han J, Kim J, Hwang J. Inhibitory effects of active compounds isolated from safflower ( Carthamus tinctorius L.) seeds for melanogenesis. Biol Pharm Bull. 2004;27:1976–8.
Zhang H, Nagatsu A, Watanabe T. Antioxidative compounds isolated from safflower ( Carthamus tinctorius L.) oil cake. Chem Pharm Bull. 1997;45:1910–4.
Takahashi T, Miyazawa M. Potent α-glucosidase inhibitors from safflower ( Carthamus tinctorius L.) seed. Phytother Res. 2012;26:722–6.
Loo T, Cheung N, Chow W. The inhibitory effect of herbal formula comprising ginseng and Carthamus tinctorius on breast cancer. Life Sci. 2004;76:191–200.
Urech K, Scher J, Hostanska K, Becker H. Apoptosis inducing activity of viscin, a lipophilic extract from Viscum album L. J Pharm Pharmacol. 2005;57:101–9.
Grossarth-Maticek R, Kiene H, Baumgartner S, Ziegler R. Use of Iscador, an extract of European mistletoe ( Viscum album ), in cancer treatment: prospective nonrandomized and randomized matched-pair studies nested within a cohort study. Altern Ther Health Med. 2001;7:57.
Gunver S, Anja G, Michael S. Viscom album extracts in breast and gynaecological cancers: a systematic review of clinical and preclinical research. J Exp Clin Cancer Res. 2009;28:79.
Pintea A, Bele C, Andrei S, Socaciu C. HPLC analysis of carotenoids in four varieties of Calendula officinalis L. flowers. Acta Biol. 2003;47:37–40.
Ukiya M, Akihisa T, Yasukawa K, Tokuda H, Suzuki T. Anti-inflammatory, anti-tumor-promoting, and cytotoxic activities of constituents of marigold ( Calendula officinalis ) flowers. J Nat Products. 2006;69:1692–6.
Pommier P, Gomez F, Sunyach P. Phase III randomized trial of Calendula officinalis compared with trolamine for the prevention of acute dermatitis during irradiation for breast cancer. J Clin Oncol. 2004;22:1447–53.
Delazar A, Gibbons S, Kosari A, Nazemiyeh H, Modarresi M, Nahar L. Flavone C-glycosides and cucurbitacin glycosides from Citrullus colocynthis . DARU J Pharm Sci. 2006;14:109–14.
Tannin-Spitz T, Grossman S, Dovrat S, Gottlieb H, Bergman M. Growth inhibitory activity of cucurbitacin glucosides isolated from Citrullus colocynthis on human breast cancer cells. Biochem Pharmacol. 2007;73:56–67.
Kumar S, Kumar D, Jusha M, Saroha K, Singh N, Vashishta B. Antioxidant and free radical scavenging potential of Citrullus colocynthis (L.) Schrad. methanolic fruit extract. Acta Pharm. 2008;58:215–20.
Weng J, Tsai C, Kulp S, Chen C. Indole-3-carbinol as a chemopreventive and anti-cancer agent. Cancer Lett. 2008;262:153–63.
Maasomi Z, Soltanahmadi Y, Dadashpour M, Alipour S, Abolhasani S, Zarghami N. Synergistic anticancer effects of silibinin and chrysin in T47D breast cancer cells. Asian Pac J Cancer Prev. 2017;18:1283–7.
PubMed Central Google Scholar
Maroof H, Hassan Z, Mobarez A, Mohamadabadi M. Lactobacillus acidophilus could modulate the immune response against breast cancer in murine model. J Clin Immunol. 2012;1:1–7.
McConnell K, Jager R, Bland K, Blotcky A. The relationship of dietary selenium and breast cancer. J Surg Oncol. 1980;15:67–70.
Smith I, Procter M, Gelber RD, Guillaume S, Feyereislova A, Dowsett M, et al. 2-year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet. 2007;369:29–36.
Vogel C, Cobleigh M, Tripathy D, Gutheil J, Harris L, Fehrenbacher L, et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002;20:719–26.
Liang Q, Li W, Zhao Z, Fu Q. Advancement of Wnt signal pathway and the target of breast cancer. Open Life Sci. 2016;11:98–104.
Churpek JE, Marquez R, Neistadt B, Claussen K, Lee MK, Churpek MM, Huo D, Weiner H, Bannerjee M, Godley LA, Le Beau MM. Inherited mutations in cancer susceptibility genes are common among survivors of breast cancer who develop therapy-related leukemia. Cancer. 2016;122(2):304–11.
Bon E, Driffort V, Gradek F, Martinez-Caceres C, Anchelin M, Pelegrin P, et al. SCN4B acts as a metastasis-suppressor gene preventing hyperactivation of cell migration in breast cancer. Nat Commun. 2016;7:136–8.
Nik-Zainal S, Davies H, Staaf J, Ramakrishna M, Glodzik D, Zou X, et al. Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature. 2016;534:47–54.
Manchanda R, Jacobs I. Genetic screening for gynecological cancer: where are we heading? Future Oncol. 2016;12(2):207–20.
Obermiller P, Tait D, Holt J. Gene therapy for carcinoma of the breast: therapeutic genetic correction strategies. Breast Cancer Res. 1999;2:28–30.
Karin M, Greten FR. NF-[kappa] B: linking inflammation and immunity to cancer development and progression. Nature Rev Immunol. 2005;5:749–52.
Osborne C, Wilson P, Tripathy D. Oncogenes and tumor suppressor genes in breast cancer. Potential diagnostic and therapeutic applications. Oncologist. 2004;4:361–77.
Sharma G, Dave R, Sanadya J, Sharma P, Sharma K. Various types and management of breast cancer: an overview. J Adv Pharm Technol Res. 2010;1:109–11.
PubMed PubMed Central Google Scholar
Ricardo S, Vieira AF, Gerhard R, Leitão D, Pinto R, Cameselle-Teijeiro JF, Milanezi F, Schmitt F, Paredes J. Breast cancer stem cell markers CD44, CD24 and ALDH1: expression distribution within intrinsic molecular subtype. J Clin Pathol. 2011;64(11):937–46.
Kakarala M, Wicha M. Implications of the cancer stem-cell hypothesis for breast cancer prevention and therapy. J Clin Oncol. 2008;26:2813–20.
Noyce P. Improving long-term adjuvant anti-oestrogenic therapy for breast cancer. New Commun. 2017;13:43–7.
Shibata T, Watari K, Izumi H, Kawahara A, Hattori S, Fukumitsu C, et al. Breast cancer resistance to antiestrogens is enhanced by increased ER degradation and ERBB2 expression. Cancer Res. 2017;77:545–56.
Awolaran T. Cellular mechanisms of estrogen in breast cancer development. J Sci Technol. 2015;3:1–7.
Slamon D, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. New Engl J Med. 2001;344(11):783–92.
Stopeck A, Lipton A, Body J, Steger G, Tonkin K, De Boer R, et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol. 2010;28:5132–9.
Hadden J. Review Article The immunology and immunotherapy of breast cancer: an update. Int J Immunopharmacol. 1999;21:79–101.
Wright S. Immunotherapy of breast cancer. Expert Opin Biol Ther. 2012;12:479–90.
Ono M. Molecular links between tumor angiogenesis and inflammation: inflammatory stimuli of macrophages and cancer cells as targets for therapeutic strategy. Cancer Sci. 2008;99:1501–6.
Mu J, Zhu D, Shen Z, Ning S, Liu Y, Chen J. The repressive effect of miR-148a on Wnt/β-catenin signaling involved in Glabridin-induced anti-angiogenesis in human breast cancer cells. BMC Cancer. 2017;17:307–9.
de Bock G, Bonnema J, van der Hage J, Kievit J, van de Velde C. Effectiveness of routine visits and routine tests in detecting isolated locoregional recurrences after treatment for early-stage invasive breast cancer: a meta-analysis and systematic review. J Clin Oncol. 2004;22:4010–8.
Download references
Authors’ contributions
MA provided concept and design of the manuscript. MI wrote the draft of Manuscript. MD and AUK revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Consent for publication, ethics approval and consent to participate.
No funding received from any source.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Department of Eastern Medicine and Surgery, Directorate of Medical Sciences, GC University Faisalabad, Old Campus, Allam Iqbal Road, Faisalabad, 38000, Pakistan
Muhammad Akram
Faculty of Eastern Medicine, Hamdard University Karachi, Main Campus, Sharea Madinat al-Hikmah, Mohammad Bin Qasim Avenue, Karachi, 74600, Sindh, Pakistan
Mehwish Iqbal & Muhammad Daniyal
Laboratory of Neuroanatomy & Neuropsychobiology, Department of Pharmacology, RibeirãoPreto Medical School of the University of São Paulo, AV. Bandeirantes, 3900, RibeirãoPreto, 14049-900, São Paulo, Brazil
Asmat Ullah Khan
Department of Eastern Medicine and Surgery, School of Medical and Health Sciences, University of Poonch Rawalakot, Hajira Road, Shamsabad, Rawalakot, 12350, Azad Jammu and Kashmir, Pakistan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Muhammad Akram .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Akram, M., Iqbal, M., Daniyal, M. et al. Awareness and current knowledge of breast cancer. Biol Res 50 , 33 (2017). https://doi.org/10.1186/s40659-017-0140-9
Download citation
Received : 15 July 2017
Accepted : 22 September 2017
Published : 02 October 2017
DOI : https://doi.org/10.1186/s40659-017-0140-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Gene therapy
- Stem cell therapy
Biological Research
ISSN: 0717-6287
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 16 September 2024
Breast cancer screening motivation among women: an application of self-determination theory
- Chau Thi Dang 1 , 3 ,
- Tu Thi Ngoc Nguyen 1 , 3 ,
- Trang Thi Thuy Ho 1 &
- Sunjoo Kang 2
BMC Primary Care volume 25 , Article number: 339 ( 2024 ) Cite this article
Metrics details
Breast cancer is a major health concern worldwide, especially in Vietnam. This study aimed to explore women’s motivation for and factors related to breast cancer screening.
A mixed-methods study was conducted in Danang, Vietnam, using a convergent parallel approach. This study utilized both quantitative and qualitative methods to gather the data. The quantitative approach involved surveys to assess motivation levels and related factors, including demographic information and experience with breast cancer screening. In-depth qualitative interviews were used to gain deeper insights into participants' perspectives and experiences related to breast cancer screening.
The average motivation score for breast cancer screening was moderate (3.55 ± 0.55). Ethnicity, regular health check-ups, family history of breast cancer, receiving information about breast cancer, and women’s health issues have direct relationships with breast cancer screening motivation. According to the qualitative data, three categories emerged: intrinsic motivation, external motivation/internalization, and amotivation. The individual, and sociocultural environmental factors impacted screening motivation.
Conclusions
This study highlights the motivations behind breast cancer screening among women. Healthcare providers could use these findings to improve screening policies and guidelines and encourage more women to undergo regular screening, ultimately reducing the incidence of breast cancer in the community.
Peer Review reports
Introduction
Motivation plays a crucial role in influencing people's behavior and autonomous decision-making. It assists individuals in overcoming obstacles and challenges that might arise while pursuing their goals over time. Furthermore, the motivation for breast cancer screening lies in the numerous benefits it offers for individuals' health and well-being [ 1 , 2 , 3 , 4 ]. Early detection, improved treatment options, enhanced quality of life, and reduced healthcare costs were among the positive outcomes motivating screening for individuals and the broader community [ 4 , 5 ].
In Vietnam, breast cancer was the most common cancer, accounting for 11.8% of all new cancer cases and 124.65 per 100,000 of 5-year incidence among survivors in 2020 [ 6 ]. Although the Ministry of Health proposed the National Cancer Control Programme, the implementation of breast cancer screening was uncommon and highlighted some of the obstacles faced in healthcare systems [ 7 ]. Continued efforts to increase awareness, promote early detection, and provide effective treatment and support for individuals affected by breast cancer are vital for improving outcomes and reducing the impact of this disease. However, previous studies highlighted that there was no awareness of the importance of early detection or the availability of breast cancer screening programs [ 8 , 9 ]. Thus, motivation for screening is essential for raising awareness about the benefits of screening, encouraging individuals to initiate the screening process, and helping individuals make a broader commitment to a healthy lifestyle.
Moreover, motivation for breast cancer screening was not only an observable phenomenon but also focused on effective factors and outcomes [ 10 ]. Several reasons for low screening motivation have been identified, such as age, educational background, absence of family history, poor access to screening, fear, belief about cancer, maintaining health, and illness monitoring [ 1 , 11 , 12 ]. Thus, understanding the reasons behind the lack of motivation for screening and implementing strategies to address these factors could lead to increased participation in crucial healthcare screening programs.
To explore the motivations behind breast cancer screening, self-determination theory was utilized as an explanatory model. This theory focuses on understanding human motivation and the factors that influence individuals' behaviors and decisions. There are three types of motivation: intrinsic motivation, external motivation, and amotivation [ 13 ]. This theory has been widely applied and provides insights into how to create environments to support individuals' natural tendencies, ultimately enhancing overall motivation and well-being.
To tailor affordable and sustainable lifestyle interventions to individuals, it is crucial to fully understand the motivation for breast cancer screening. Consequently, the purpose of this study was to investigate the levels of motivation and related factors among Vietnamese women in relation to breast cancer screening. The findings from this study may provide some information that enhances healthcare providers’ understanding of women's motivations for breast cancer screening and encourages and exacerbates screening practices.
Study design
A convergent parallel design was used to determine the motivations behind breast cancer screening among Vietnamese women. This approach allowed for a thorough exploration of women's perceptions. The research methodology involved a two-stage data collection and analysis process initiated by the quantitative data and followed by the qualitative data. Qualitative data were then combined with quantitative data to provide a holistic view of the drivers behind breast cancer screening participation in Vietnamese women.
Population and sample
Participants were selected from a quantitative study using the convenience sampling method. To be included in the study, participants had to be 18 years or older; able to read, write and speak Vietnamese; and have access to a smartphone or a computer with internet connectivity. Women with a history of breast cancer were excluded from the study. Participants were recruited from February to September 2022 from women living in Danang city, Vietnam, through a Google form.
The present research study employed purposive sampling to select participants for in-depth interviews. The interviews were conducted at convenient locations such as the office of the Vietnam Women's Union or the People's Committee of the District. These settings were chosen to ensure participants felt comfortable and safe during the interview process. This approach also facilitated access to participants who were already familiar with these venues, contributing to a more relaxed and open interview environment. Inclusion criteria required participants to be 18 years of age or older and willing to report their personal experiences, regardless of their place of residence or marital and educational statuses.To meet the principle of sample saturation, a total of 15 women were selected for participation.
A sample size calculation was used to determine the sample size [ 14 ]. We chose an acceptable error level of 0.6%, and the estimated standard deviation of the scale from our pilot study was 0.75. At the 5% Type I error rate, the sample size is 601. In the case that some samples are inadequate or unfinish the survey, we add 20% of the initial sample; therefore, the final needed sample is 721. After nine months of study completion, 1041 women met the inclusion criteria and completed the Google Form. After removing duplicate and unfit cases, 649 official responses remained.
Quantitative measures
Participants provided demographic information, including age, ethnicity, educational level, marital status, monthly income, family history related to breast cancer, and experience with breast cancer screening. The Treatment Self-Regulation Questionnaire [ 15 ], which originally assesses motivation for health behaviors such as tobacco use, diet, and exercise, was adapted by researchers to focus on breast cancer screening. The questionnaire was translated from English to Vietnamese using a rigorous back-translation process [ 16 ]. Each item was carefully revised to ensure its relevance to breast cancer screening, and the modified questionnaire was validated through consultations with four experts to accurately assess women's motivation for undergoing breast cancer screening.
We conducted cognitive interviews with participants from the target population, asking them to verbalize their thoughts as they responded to each item. This process allowed to observe how respondents interpreted and understood the questions, supporting to identify any confusion or misinterpretation. We focused on ensuring that the language was clear, culturally relevant, and that the response categories were interpreted consistently. Based on the insights gained from these interviews, the revisions was improved the clarity and appropriateness of the items. Additionally, we incorporated feedback from linguistic and subject matter experts, who reviewed the translated questionnaire for both linguistic accuracy and cultural relevance. Their input was instrumental in refining technical terminology and addressing potential cultural sensitivities. After incorporating this expert feedback, we conducted further cognitive interviews to confirm that the revisions successfully addressed the identified issues. This iterative process ensured that the final version of the questionnaire was clear, culturally appropriate, and aligned with the intended meaning of the original instrument. Finally, the instrument is composed of 15 items related to continuous motivation, including amotivation, external motivation, introjection, and autonomous motivation. These items were responded to on a five-point Likert-type scale ranging from 1 (not at all true) to 5 (very true). The Content Validity Index of the items ranged from 0.67–1.00, and a total content validity index of 0.93 indicated a high level of content validity for this scale. In the pilot study, we administered the questionnaire to 65 women in a community setting. The participants had an average age of 46.8 years, and all were part of the King group. The primary goal of the pilot test was to assess the initial reliability of the questionnaire and gather input on its clarity and relevance. The findings revealed a strong internal consistency among the questionnaire items, with a Cronbach's alpha coefficient of 0.91. Taking into account the feedback and the reliability outcomes, we made several adjustments to improve the questionnaire. This pilot testing process was instrumental in ensuring that the final version of the questionnaire was not only reliable but also tailored to effectively measure motivation for breast cancer screening.
Qualitative measures
The data were collected either face-to-face or via video calling interviews during follow-up. The interviews were conducted using a semi-structured interview guide developed by the research team. During the interviews, patients' tone, appearance, facial expressions and other nonverbal messages were recorded and analysed.
The open-closed questions included the following: Please tell me your experience examining breast cancer screening? Which motivation for breast cancer screening? Do you have any other comments about your experience promoting breast cancer screening? Which factors impact the motivations behind breast cancer screening? All interviews were audio recorded and professionally transcribed.
Data collection
During the data collection process, we worked closely with the Vietnam Women's Union to connect with women in the community who were willing to participate in the study. The Vietnam Women's Union holds frequent meetings in the community, and their staff helped with collecting data. We obtained consent forms either during the meetings or by visiting participants at their homes. Afterwards, we provided the consenting participants with a personalized, secure link to the study questionnaire via email or social media. We also sent three periodic reminders to encourage completion of the questionnaires and/or scheduling of a phone interview. Before collecting any data, we made sure to obtain explicit written consent from all participants. Additionally, both the research personnel and the staff of the Vietnam Women's Union carefully checked the participant roster and consent documentation.
A subset of participants was chosen to be interviewed over the phone to schedule an appointment for a face-to-face interview. The interviews took place at community locations and lasted approximately 60 min. Each interview was audio-recorded and transcribed verbatim, and the transcripts were cross-checked against the audio recordings to ensure accuracy. At the end of the interview, we provided a gift to each participant as compensation for their transportation.
Statistical analysis
We analysed both the quantitative and qualitative data for each outcome. Quantitative analyses were conducted with SPSS 26.0 software (SPSS, Inc., Chicago, USA). Descriptive statistics and multivariable linear regression were employed to analyze the data and describe the characteristics of the participants.
Responses from open-ended questions assessing women’s reports of motivation for breast cancer screening were entered into ATLAS.ti version 9.0. All the recorded visits were transcribed verbatim for analysis. A content analysis approach was used to analyse the qualitative data of Elo and Kyngäs [ 17 ]. To ensure the accuracy and consistency of the analysis, we followed the guidelines of Graneheim and Lundman (2004) and Elo et al. [ 18 ]. These included having two independent authors read and code the response data and utilizing trustworthiness methods such as interviews, observations, and field notes. The qualitative coding process followed a structured and systematic approach, beginning with the development of preliminary codes based on research questions and emerging data themes. These codes were then formalized into a comprehensive codebook containing detailed definitions, inclusion criteria, and illustrative examples for clarity and consistency. To prevent overlaps, a code dictionary was established to provide specific definitions and guidelines for each code's application. The researchers independently applied the codes to data subsets, with regular meetings held to compare results, discuss any discrepancies, and reach consensus on coding decisions. Inter-coder reliability was assessed to ensure consistency, and any coding differences were resolved through discussion and adjustments to the codebook. This iterative and collaborative approach ensured a rigorous and reliable coding process, leading to a nuanced and accurate analysis of the qualitative data.
Quantitative results
Overall, 649 patients completed the questionnaire. According to the study findings, the research subjects were mainly middle-aged individuals who were identified as Kinh and did not follow any religion. Notably, women with a high school education constituted a significant portion of the study population, with more than half of the participants falling under this category and earning an average income of more than 5 million VND. Of the patients, half had previously undergone breast cancer screening. Most of them did not have relatives who had breast cancer (84.9%) (Table 1 ).
Breast cancer screening motivation
Table 2 showed that the mean breast cancer screening motivation score observed among participants was 3.55 ± 0.55. In particular, the average scores for external regulation, autonomous regulation, and introjected regulation were 3.71 ± 0.56, 3.56 ± 0.59, and 3.52 ± 0.73, respectively. Women had a lower average score for introjected regulation (3.2 ± 0.69).
Multiple linear regression
Table 3 presents the results of a multivariate linear regression model that was performed to identify factors associated with breast cancer screening motivation and subscale scores. According to the parameters of the multiple linear regression model, breast cancer screening motivation was explained significantly by ethnicity, having regular health check-ups, a family history of breast cancer, regularly receiving information about breast cancer, and having a woman’s health issues in the past, with a direct relationship between these variables. Ethnicity, religion, regular health check-ups, and having a woman’s health issues were positively associated with autonomy. Having relatives who had breast cancer and having a history of women’s health issues were positively associated with introjected regulation ( p < 0.05). Ethnicity, having regular health check-ups, a family history of breast cancer, and regularly providing information about breast cancer were strongly associated with external regulation ( p < 0.05). Amotivation was related to having relatives who had breast cancer and having a history of women’s health issues.
Qualitative results
This study highlights the importance of breast cancer screening for women in Vietnam. Table 4 highlighted that participants were between 25 and 75 years old, and the mean age was 45 years. Over 60% of the participants held high-level degrees, while the rest either finished high school or had not yet graduated. Most of the women were married and employed as homemaker.
After conducting a thorough analysis, authors identified three categories of motivation based on self-determination theory: amotivation, intrinsic motivation, and extrinsic motivation. Factors that impact an individual's motivation for screening were categorized into two groups: individual and sociocultural factors. In addition, the following factors influenced the motivation for breast cancer screening, as shown in Fig. 1 .
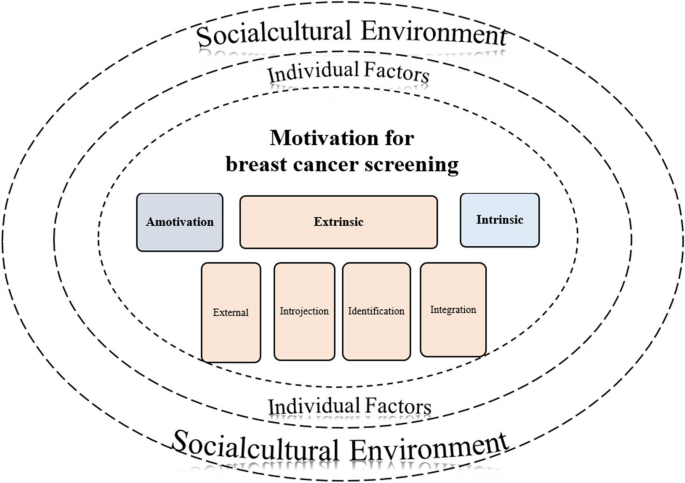
Motivation for breast cancer screening and its factors
Motivation for breast cancer screening
Intrinsic motivation.
Participants exhibited their innate motivation to maintain their well-being by regularly undergoing breast cancer screening, which reflected their intrinsic motivation. This practice was not contingent on external demands, as women may even unconsciously engage in it. According to the participants' experiences, this screening was often conducted individually or integrated with other self-care activities, such as bathing or massaging. This intrinsic motivation was typically more evident in the case of breast self-examination than in the case of other screening methods.
Participants shared that “I do it every day, I check it when taking showe r” (ID10, 52 years old, Bachelor's degree) and “I have been doing it for a long time, it is like it is my lifestyle, well… and it is also regular” (ID08, 36 years old, Bachelor's degree).
Extrinsic motivation
A variety of extrinsic motivations for breast cancer screening, including external, introjection, identification, and integration, emerged from the data. The extent of volition increased from external to integration regulation and became closer to intrinsic motivation. The present discourse expounds on the phenomenon whereby volition transitions from external regulation to integration regulation and attains proximity to intrinsic motivation. The detailed information is described below.
Providing favorable screening conditions such as insurance or agency and organizational support has proven to be essential in facilitating women's access to screening services. Furthermore, government-supported screening programmes play a crucial role in encouraging women to undergo screening by giving them opportunities to do so. Women who might not have considered screening earlier, who participate in the program when they receive support and who are free. Although there could be other factors that influence their decision, in general, they did not feel the intention to undergo screening until they were offered support. Alternatively, they might undergo screening under pressure from those around them. Participants highlighted, “My insurance covered 100 percent, so why do not I go see a doctor? It will not cost you money ” (D12, 41 years old, High school diploma) ; "If the doctor tells me to stay at home, I need to check it from time to time, so I will just do it” (D11, 48 years old, Bachelor's degree ); My mother, she often worries, also often tells her children, as women, to check this and that. Sometimes, she asks, "I told you so, have you gone to check yet?" (D13, 38 years old, High school diploma).
Introjection
Introjection occurred when the participant feft a danger or problem that was personally relevant and began to change from within. Breast cancer is increasingly common, and the risk of cancer is very high. In addition, some participants shared that they had experience with breast cancer and its consequences. Therefore, they started doing screening consciously and intentionally. Some women shared, “I feel cancer is getting more common among younger adults, not like in the past, only a few people got it” (D03, 35 years old, High school diploma).
Identification
Women were motivated to undergo breast cancer screening not only for their health but also for the sake of their behavior and well-being. The emphasis was on their own values, awareness of the effectiveness of screening, and a desire to take proactive steps in ensuring a healthy and worry-free future. This type of motivation reflects a self-driven commitment to maintaining good health and enjoying life without the burden of potential diseases such as breast cancer. One woman mentioned , "Then, I think about my health. Now health is gold. If I live for myself, I have motivation." (D13, 38 years old, High school diploma): “In the past, breast cancer was an incurable disease, but now, if detected early, it can be cured, so we have to regularly screen for it” (ID08, 36 years old, Bachelor's degree).
Integration
Participants might initially be motivated by external factors; however, through a process of internalization, they begin to adopt these motivations on their own. This could result in a motivation that was unified with intrinsic motivation, meaning that the individual now engages in the behavior because they truly value and identify with it. Therefore, this approach leads to a sense of autonomy and self-awareness in individuals’ pursuit of behavior. Those women believed that they were screened because of their role as mothers or wives in the family; because of their support for their children; because of setting examples for other women; or because they want/have to be proactive and independent in life as well as because they comply with personal principles. In addition, they are people with a special interest in health care, not only for themselves but also for those around them. In particular, when they strongly believe in the effectiveness of screening and screening because of the spiritual value it brings. Women who engaged in behavior for reasons that went beyond the actual benefits of the behavior and related to what is most about themselves or their lives. Some women shared their story: “ It (screening) brings two different spiritual values. When I have done my best, but it does not work, I'm satisfied. If I do not do anything, I feel regretful. because I have not done it yet”” (D09, 60 years old, Bachelor's degree); “ I am the main breadwinner for the family… but… (now) I only have 3 children left, and if something happens to me, my children will suffer.” (D12, 41 years old, High school diploma).
Amotivation
Amotivation is a phenomenon characterized by a lack of motivation among women to undergo cancer screening or even express an intention to do so. This lack of motivation could be due to their strong belief in their own good health, which led them to ignore the importance of screening. Additionally, being overly subjective about the potential results or consequences of a breast cancer diagnosis could also contribute to amotivation. A 35-year-old woman said, “I am still young, I don’t care (breast cancer screening) because sometimes I am also confident about my health” (D03, 35 years old, High school diploma).
Factors influencing breast cancer screening motivation
The importance of women's motivation for their ability to undergo the screening process and maintain it over time. The factors impacting motivation included individual, and sociocultural factors.
Individual factors , including emotions, and personal experiences could influence women's motivations and decisions regarding breast cancer screening. Emotional states could play a significant role in shaping attitudes and behaviors, including a range of emotions such as anxiety, shyness, curiosity, optimism, and even phobias related to breast cancer and a willingness to undergo screening. Personal experiences related to breast cancer and diseases, such as age, menopause status, previous experiences with screening, in general, could impact screening decisions. Discomfort or pain during mammography may discourage women from screening, leading to avoidance of early detection benefits. The inconvenience and potential delays associated with crowded public hospitals could contribute to a decline in motivation to prioritize screening. Furthermore, previous health experiences could shape an individual's perspective and attitude toward healthcare practices. These challenges create barriers that discourage women from accessing essential screening services, impacting overall screening rates and potentially resulting in delayed diagnosis and treatment.
Some stated “I am old and need to pay more attention to my health as it can impact my children and grandchildren if I get sick.” (D14, 63 years old, High school diploma) ; and “when I go for a genital or breast exam, I don't want to go to the doctor because I'm shy, really embarrassed”.” (D02, 32 years old, High school diploma).
The sociocultural environment encompasses a range of beliefs, attitudes, and societal pressures that could shape women's motivations for breast cancer screening. Societal perceptions and beliefs regarding diseases are specific to women and girls; folk beliefs, such as those related to "trái chàm”; beliefs about abnormalities and visiting the doctor; acceptance of fate and perception that having cancer means inevitable death; and modern life with myriad pressure that contributes to hesitation or avoidance of screening. In contrast, the widespread availability of online information could empower women to make informed decisions about their health and remind them about breast cancer and screening. Some mentioned: “I believe that when Heaven appoints, man must obey” (D12, 41 years old, High school diploma) ; “The old ladies said that if you have "trái chàm”, you will easily get cancer” (D09, 60 years old, Bachelor's degree).
The present study used a mixed methods approach to explore the motivations for breast cancer screening and the underlying factors in Vietnamese women. The results of the present study showed that overall, women’s cancer screening motivation was moderate. They described their incentives for cancer screening through amotivation and extrinsic and intrinsic motivation. Breast cancer screening should be a priority for women seeking effective early detection and prevention. Although there might be some degree of motivation to undergo screening, it is imperative to ensure that the level of motivation is sufficient to have a meaningful impact. Our findings are consistent with research conducted by Talley et al. that investigated the associations between motivation, clinical breast exam results, and clinical breast exam screening results [ 3 ]. Observing the varying levels of motivation for breast cancer screening among individuals with diverse ethnic backgrounds underscores the significance of factoring one's ethnicity when evaluating one’s breast cancer risk and promoting screening. Access to essential resources and knowledge is crucial to guarantee that everyone can make informed decisions regarding their health. Women's health issues, regular health examinations, and family history of breast cancer encompass a wide range of conditions. Individuals experiencing such health issues may be more motivated to undergo cancer screening as part of their overall health management.
This study also showed that autonomous forms of motivation had moderate effects on self-esteem and the role of other factors in autonomy. The results of our study showed that cultural and personal factors influenced autonomous motivation. In addition, our research showed that women are primarily self-motivated to undergo breast cancer screening. Research conducted by Haley and his colleagues has shed light on the motivations behind rural women's prioritization of their health and participation in breast cancer screenings [ 19 ]. Their findings indicate that women who recognize and embrace their independence are more inclined to undergo screening and take proactive measures to safeguard their health. Our own observations support this, underscoring the importance of self-reliance as a motivating factor. Notably, this sense of independence also leads to heightened self-confidence in breast cancer screening [ 20 ].
Motivation is not necessarily based on women's own intentions or desires to undergo screening. The screening of women for breast cancer is often a result of external regulation, such as demands from family members, directives from healthcare professionals, or opportunities provided by government agencies, unions, or other entities. The research findings show that women are acutely aware of their vital role in their families and are thus more attuned to healthcare practices that promote the health and safety of their loved ones, particularly their children. Notably, a significant number of women reported apprehension about their children's well-being and worried that a breast cancer diagnosis would limit their time together. Even though they accept illness as inevitable, their primary concern is the welfare of their loved ones rather than their own challenges.
Hassan et al. reported that the guidance of physicians could be a significant motivating factor for women in this regard [ 21 ]. Similarly, the support and encouragement of family members, particularly husbands, also play a role in motivating women to undergo breast cancer screening. These findings are consistent with the findings of the study conducted by Safizadeh et al., who also suggested that healthcare professionals provide guidance to women regarding the significance of various breast cancer screening methods for the early detection of breast cancer [ 22 ].
Intrinsic motivation in research is the result of the internalization process that turns screening into a habit and daily lifestyle. In comparison to the findings of Nur et al. [ 23 ], our study has shown a lower proportion of women who possess intrinsic motivation [ 23 ]. Compared with the findings of previous studies on the types of motivation to change lifestyles in individuals with newly diagnosed diabetes, the intrinsic motivation reported for this behavior is similar to the results of our study [ 24 ]. Low levels of intrinsic motivation can cause women to exhibit indifference toward screening, as they lack the willingness and readiness to undergo the process. In addition, breast cancer screening behavior does not involve intrinsic motivation. Nevertheless, women who engage in breast cancer screening out of a sense of secondary intrinsic motivation still achieve positive outcomes and exhibit advanced screening techniques, indicating a sense of efficacy and knowledge of best practices.
A recent study revealed that individuals who possess self-confidence in their health and exhibit a subjective perception of illness are more prone to experiencing amotivation. A lack of motivation has been identified as a contributing factor to women's reluctance to undergo breast cancer screening [ 25 ]. According to self-determination theory, a deficiency in motivation is a powerful negative predictor of health-related behaviors [ 26 ]. The results of our study are similar to those of Umami's study, in which individuals who perceived themselves to be in good health and displayed no symptoms of illness were less inclined to undergo cancer screenings [ 27 ]. Furthermore, our findings showed that amotivation was related to a family history of breast cancer and was not associated with women’s health issues. This finding underscores the importance of understanding and addressing various psychological and emotional barriers that can impede individuals from seeking necessary medical care. Efforts to promote awareness and education related to breast cancer screening are crucial. Addressing the root causes of low motivation ensures that individuals have access to the care they need to maintain optimal health and well-being.
The quantitative findings revealed that culture, regular health check-ups, a family history of breast cancer, regularly provided information about breast cancer, and having a woman’s health issues were related to breast cancer screening motivation. In addition, participants highlighted that individual factors, and sociocultural environment were factors that impacted their motivation for having breast cancer. Previous studies have indicated that lack of familiarity with breast examination techniques, insufficient access to screening services, and financial constraints serve as barriers preventing women from engaging in breast self-examination [ 28 , 29 , 30 ]. In our study, women who regularly received information related to breast cancer also had greater motivation for breast cancer screening than did those who were not regularly exposed. It has been found that providing more information about breast cancer screening can increase confidence in screening, as highlighted by participants in a study conducted in Iran [ 22 ]. As identified by Umami et al., women who have a history of breast disease are also motivated to undergo breast cancer screening, in addition to their knowledge of disease and the availability of related services [ 27 ]. In line with the Health Belief Model and Protection Motivation Theory, threat perception plays a crucial role in motivating behavior.
This study has several limitations. First, because of its cross-sectional design, no longitudinal studies could be inferred to be needed to further confirm our findings. Second, this study included only respondents from Danang, so the results cannot be generalized to other regions in Vietnam, a country with diverse socioeconomic and cultural backgrounds. Future research should include larger samples and replicate and expand this work in urban settings.
The motivation for breast cancer screening varies and continues to increase from amotivation to intrinsic motivation. In our quantitative study, the extent of motivation for breast cancer screening was average, while the qualitative study exhaustively evaluated kinds of motivation. The internalization process and factors influencing motivation are categorized into individual, and sociocultural environment factors. Understanding the various motivations for breast cancer screening is essential for effective healthcare strategies and interventions.
Availability of data and materials
The datasets utilized and/or analyzed during the present study are accessible from the corresponding authors upon a reasonable request.
Bhandari D, Shibanuma A, Kiriya J, Hirachan S, Ong KIC, Jimba M. Factors associated with breast cancer screening intention in Kathmandu Valley. Nepal PLoS One. 2021;16(1):e0245856.
Article PubMed CAS Google Scholar
Estebsari F, Rahimi Khalifehkandi Z, Latifi M, Farhadinasab A, Vasli P, Mostafaie D. Protection Motivation Theory and Prevention of Breast Cancer: A Systematic Review. Clin Breast Cancer. 2023;23(4):e239–46.
Article PubMed Google Scholar
Talley CH, Yang L, Williams KP. Breast Cancer Screening Paved with Good Intentions: Application of the Information–Motivation–Behavioral Skills Model to Racial/Ethnic Minority Women. J Immigrant Minority Health. 2017;19(6):1362–71.
Article Google Scholar
Zhang M, Wei W, Li Q, Chen X, Zhang M, Zuo D, et al. Determinants of Intention to Participate in Breast Cancer Screening among Urban Chinese Women: An Application of the Protection Motivation Theory. Int J Environ Res Public Health. 2021;18(21):11093.
Article PubMed PubMed Central Google Scholar
Newman LA. Breast cancer screening in low and middle-income countries. Best Pract Res Clin Obstet Gynaecol. 2022;83:15–23.
Global Cancer Observatory. International Agency for Research on Cancer. 2021 . Cancer today. Available from: http://gco.iarc.fr/today/home . [Cited 2023 Aug 19].
Huong TTT et al. Cancer control in vietnam: where are we now? Cancer control. 2016;99–106. Available from: https://www.cancercontrol.info/cc2016/cancer-control-in-vietnam-where-we-are/ .
Kaur K, Jajoo R, Naman S, Kandwal T, Brar GS, Garg P, et al. Identifying barriers to early diagnosis of breast cancer and perception of women in Malwa region of Punjab. India Global Health J. 2023;7(1):34–42.
Mohan R, Thulaseedharan JV. Awareness of risk factors, symptoms and screening of breast cancer: A cross-sectional survey among 35–65-year-old women in Alappuzha district, Kerala. India J Family Med Prim Care. 2023;12(10):2401–7.
Asadi N, Memarian R, Vânki Z. Motivation to Care: A Qualitative Study on Iranian Nurses. J Nurs Res. 2019;27(4):e34.
Labrie NHM, Ludolph R, Schulz PJ. Investigating young women’s motivations to engage in early mammography screening in Switzerland: results of a cross-sectional study. BMC Cancer. 2017;17(1):209.
Yang RJ, Huang LH, Hsieh YS, Chung UL, Huang CS, Bih HD. Motivations and reasons for women attending a breast self-examination training program: a qualitative study. BMC Womens Health. 2010;10(10):23.
Huang H, Wang HHX, Donaghy E, Henderson D, Mercer SW. Using self-determination theory in research and evaluation in primary care. Health Expect. 2022;25(6):2700–8.
Riley RD, Ensor J, Snell KIE, Harrell FE, Martin GP, Reitsma JB, et al. Calculating the sample size required for developing a clinical prediction model. BMJ. 2020;18:m441.
Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Educ Res. 2007;22(5):691–702.
Ozolins U, Hale S, Cheng X, Hyatt A, Schofield P. Translation and back-translation methodology in health research - a critique. Expert Rev Pharmacoecon Outcomes Res. 2020;20(1):69–77.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative Content Analysis: A Focus on Trustworthiness. SAGE Open. 2014. Available from: https://journals.sagepub.com/doi/10.1177/2158244014522633 . [Cited 2020 Apr 26].
Haley E, Avery EJ, McMILLAN SJ. Developing Breast Health Messages for Women in Rural Populations. J Consum Aff. 2011;45(1):33–51.
Oo Lwin M. Examining Asian Women’s Motivations to Undergo Breast Cancer Screening. J Women’s Health Care [Internet]. 2014 [cited 2023 Sep 26];03(03). Available from: http://www.omicsgroup.org/journals/examining-asian-womens-motivations-to-undergo-breast-cancer-screening-2167-0420.1000158.php?aid=25740 .
Hassan N, Ho WK, Mariapun S, Teo SH. A cross sectional study on the motivators for Asian women to attend opportunistic mammography screening in a private hospital in Malaysia: the MyMammo study. BMC Public Health. 2015;12(15):548.
Safizadeh H, Amirzadeh N, Mangolian SP. Motivational Factors for Breast Cancer Screening Behaviors in Iranian Women: A Qualitative Study. Asian Pac J Cancer Prev. 2020;21(10):3109–14.
Article PubMed Central Google Scholar
Nur NR, Ermiati E, Praptiwi A. Women’s Intrinsic Motivation in Conducting Breast Self-Examination. J Nurs Care. 2018 ;1(2). Available from: http://jurnal.unpad.ac.id/jnc/article/view/16326 . [Cited 2023 Oct 5].
Sebire SJ, Toumpakari Z, Turner KM, Cooper AR, Page AS, Malpass A, et al. “I’ve made this my lifestyle now”: a prospective qualitative study of motivation for lifestyle change among people with newly diagnosed type two diabetes mellitus. BMC Public Health. 2018;18(1):204.
Özkan İ, Taylan S. Barriers to women’s breast cancer screening behaviors in several countries: A meta-synthesis study. Health Care Women Int. 2021S;42(7–9):1013–43.
Ryan RM, Deci EL. Intrinsic and extrinsic motivation from a self-determination theory perspective: Definitions, theory, practices, and future directions. Contemp Educ Psychol. 2020;1(61):101860.
Umami A, Sudalhar S, Pratama TWY, Fitri I, Firmansyah A. Knowledge, Barriers, and Motivation Related to Breast and Cervical Cancer Screening Among Women in Bojonegoro, East Java: A Qualitative Study. J Health Promot Behav. 2020;5(1):1–10.
Akhtari-Zavare M, Juni MH, Ismail IZ, Said SM, Latiff LA. Barriers to breast self examination practice among Malaysian female students: a cross sectional study. Springerplus. 2015;11(4):692.
Camillus B, Nyinaku P, Mingle D, Adiasani C. ‘I want to live for them’; Determinants of Uptake of Clinical Breast Examination: A Qualitative Inquiry. Rwanda J Med Health Sci. 2022;5(1):85–98.
Malhotra C, Bilger M, Liu J, Finkelstein E. Barriers to Breast and Cervical Cancer Screening in Singapore: a Mixed Methods Analysis. Asian Pac J Cancer Prev. 2016;17(8):3887–95.
PubMed Google Scholar
Download references
This research did not receive any specific grant from any funding agency.
Author information
Authors and affiliations.
Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam
Chau Thi Dang, Tu Thi Ngoc Nguyen & Trang Thi Thuy Ho
Graduate School of Public Health Yonsei University, Seoul, Republic of Korea
Sunjoo Kang
Da Nang University of Medical Technology & Pharmacy, Danang, Vietnam
Chau Thi Dang & Tu Thi Ngoc Nguyen
You can also search for this author in PubMed Google Scholar

Contributions
TTTH, SK, and CTD were responsible for conceptualization and methodology. CTD and TTNN collected the data. TTTH, TTNN, and CTD, validated the data. CTD and TTNN performed the formal analysis with contributions of TTTH. TTTH, SK, TTNN, and CTD wrote the original draft and edited the original draft. TTTH and SK was responsible for the research activity planning and execution, including mentorship external to the core team. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Trang Thi Thuy Ho or Sunjoo Kang .
Ethics declarations
Ethics approval and consent to participate.
This research followed the Declaration of Helsinki, and the Ethics Committee of Hue University of Medicine and Pharmacy approved the protocol (No. H2021/258). The researcher disseminated pertinent information to participants, including the objectives and goals of the study. Written consent was obtained from all participants prior to the collection of data. Confidentiality and anonymity were upheld throughout the study, and participants were given the freedom to withdraw from the study at any juncture.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Dang, C.T., Nguyen, T.T.N., Ho, T.T.T. et al. Breast cancer screening motivation among women: an application of self-determination theory. BMC Prim. Care 25 , 339 (2024). https://doi.org/10.1186/s12875-024-02594-z
Download citation
Received : 14 February 2024
Accepted : 06 September 2024
Published : 16 September 2024
DOI : https://doi.org/10.1186/s12875-024-02594-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer screening
- Mixed methods
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Journal Proposal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Categorising subjective perceptions of middle-aged breast cancer patients using q methodology.

1. Introduction
2. research method, 2.1. q population construction and q sample selection, 2.2. p sample, 2.3. q sorting, 2.4. data analysis, 3. research results, 3.1. analysis of results, 3.2. characteristics of perception types, 3.2.1. type 1: embracing a new life.
I lived too hard. When I got cancer, it felt like it was bound to happen, so accepting the fact was easier for me. The initial shock of the diagnosis was natural. After overcoming the initial fear, I’ve come to appreciate each day just for being alive. Additionally, I find myself grateful for life and even volunteering. (P24)
Rather than desires about death or wanting to live, I realised I’m still alive, and there are still things for me to do. I decided to live gratefully and joyfully. Changing my mindset like that, I’m not afraid of death anymore, and I dare to speak up. In doing so, I avoid harbouring resentment or greed and always try to shift my thoughts positively. (P29)
I realised that life and death are not areas I can control. So I thought it would be better to do what I can. When people ask me questions, I sincerely answer with all the knowledge I have. I hope I can be of some help, even if it’s small. (P11)
3.2.2. Type 2: Finally Focusing on Myself
When I’m sick, it only upsets me. I thought it would be less of a burden on my family if I were healthy. Instead of asking my son and husband to take care of me, I think it’s better for me to manage myself and live healthily. (P15)
I used to think the company and home couldn’t run without me, but I learned they can manage fine. Since then, I’ve let go of everything and decided to take care of myself first. If I’m sick, nothing else matters. (P17)
3.2.3. Type 3: Struggling Amidst Confusion
No matter the type of cancer, once you become a cancer patient, living with the fear of recurrence and metastasis is a common sentiment. I try to stay positive and forget, but being a cancer patient, I often feel trapped in this anxiety, and it makes me feel unhappy. (P34)
As I get older, I just need to live as a human being. I hate it when people dismiss my concerns about being a woman. But there’s truth to it. So, since this is how things are, I just aim to live as a good human being. (P4)
3.2.4. Type 4: Sorrowfully Withdrawing from the World
Even though I’m older, I’m still a woman. Because of the treatment, they removed my nipples. I took tamoxifen, which thickened my endometrial lining, so they removed my uterus too. I’ve lost everything that made me a woman—my uterus, ovaries, and breasts. There are times when I feel submerged in thoughts of whether I am still a woman. Every time I shower and see my body, it doesn’t feel good. My self-esteem has plummeted. (P14)
I underwent another surgery. I don’t like my body; how could others? On top of that, I’ve gained so much weight due to the side effects of tamoxifen. Because of the treatment, I quit my job, and I’m increasingly disliking meeting people and going out. (P20)
3.2.5. Type 5: Pushed to the Edge of Fear
Without realizing it, I become concerned over minor changes or pain in my body, worrying if they might indicate a recurrence or metastasis, becoming hypersensitive. The anxiety overwhelms me, especially when I hear about other patients experiencing recurrence or metastasis.
4. Discussion
5. limitations, 6. conclusions and recommendations, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
- Statistics Korea. Available online: https://kostat.go.kr (accessed on 5 March 2023).
- National Cancer Information Centre. Available online: https://www.cancer.go.kr (accessed on 7 April 2023).
- Park, G.E.; Kang, B.J. Trends in Korean breast cancer patients based on survival rate data from a single institution. J. Korean Soc. Breast Screen. 2021 , 18 , 102–107. [ Google Scholar ]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021 , 71 , 209–249. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lim, S.J.; Yi, M.S. Study on cancer patients who visited an emergency department with the side effects of chemotherapy. J. Korean Clin. Nurs. Res. 2014 , 20 , 75–89. [ Google Scholar ]
- Harris, P.F.; Remington, P.L.; Trentham-Dietz, A.; Allen, C.I.; Newcomb, P.A. Prevalence and treatment of menopausal symptoms among breast cancer survivors. J. Pain Symptom Manag. 2002 , 23 , 501–509. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Alagizy, H.A.; Soltan, M.R.; Soliman, S.S.; Hegazy, N.N.; Gohar, S.F. Anxiety, depression and perceived stress among breast cancer patients: Single institute experience. Middle East Curr. Psychiatry 2020 , 27 , 29. [ Google Scholar ] [ CrossRef ]
- Lee, R.; Kim, S.H.; Lee, K.S.; Seo, M.K. Development and validation of Self–Efficacy Scale for Self–Management of Breast Cancer (SESSM–B). J. Korean Acad. Nurs. 2012 , 42 , 385–395. [ Google Scholar ] [ CrossRef ]
- Dinapoli, L.; Colloca, G.; Di Capua, B.; Valentini, V. Psychological aspects to consider in breast cancer diagnosis and treatment. Curr. Oncol. Rep. 2021 , 23 , 38. [ Google Scholar ] [ CrossRef ]
- Gallagher, J.; Parle, M.; Cairns, D. Appraisal and psychological distress six months after diagnosis of breast cancer. Br. J. Health Psychol. 2002 , 7 , 365–376. [ Google Scholar ] [ CrossRef ]
- Sharpe, L.; Curran, L.; Butow, P.; Thewes, B. Fear of cancer recurrence and death anxiety. Psycho-Oncology 2018 , 27 , 2559–2565. [ Google Scholar ] [ CrossRef ]
- Stark, D.P.H.; House, A. Anxiety in cancer patients. Br. J. Cancer 2000 , 83 , 1261–1267. [ Google Scholar ] [ CrossRef ]
- Boquiren, V.M.; Esplen, M.J.; Wong, J.; Toner, B.; Warner, E.; Malik, N. Sexual functioning in breast cancer survivors experiencing body image disturbance. Psycho-Oncology 2016 , 25 , 66–76. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Koçan, S.; Gürsoy, A. Body image of women with breast cancer after mastectomy: A qualitative research. J. Breast Health 2016 , 12 , 145–150. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kwan, A.N.; Kim, T.H.; Lee, Y.M. The influence of post-operative discomfort, sense of loss, and family support on resilience in patients after breast cancer surgery. J. Korean Crit. Care Nurs. 2017 , 10 , 34–44. [ Google Scholar ]
- Park, S.Y.; Park, H.K.; Baek, H.N.; Koo, H.N. Living after diagnosis of middle-aged and elderly breast cancer survivors at early stages. Health Soc. Welf. Rev. 2020 , 40 , 90–123. [ Google Scholar ]
- Brunet, J.; Sabiston, C.M.; Burke, S. Surviving breast cancer: Women’s experiences with their changed bodies. Body Image 2013 , 10 , 344–351. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Keesing, S.; Rosenwax, L.; McNamara, B. A dyadic approach to understanding the impact of breast cancer on relationships between partners during early survivorship. BMC Women’s Health 2016 , 16 , 57. [ Google Scholar ] [ CrossRef ]
- Park, S.K.; Yoo, K.Y.; Kang, D.H.; Ahn, S.H.; Noh, D.Y.; Choe, K.J. The estimation of breast cancer disease–probability by difference of individual susceptibility. Res. Treat. 2003 , 35 , 35–51. [ Google Scholar ] [ CrossRef ]
- Oh, J.E. An integrated perspective of mid-life crisis: Focused on the most important three dimensions in human development. Korean J. Humanit. Soc. Sci. 2013 , 37 , 141–166. [ Google Scholar ]
- Lachman, M.E. Mind the gap in the middle: A call to study midlife. Res. Hum. Dev. 2015 , 12 , 327–334. [ Google Scholar ] [ CrossRef ]
- Kim, J.Y. Menopausal symptoms in breast cancer patients. Women’s Health 2017 , 18 , 19–35. [ Google Scholar ]
- Hwang, S.Y. Risk factors for depression and anxiety among breast cancer survivors in their 40s. J. Korea Contents Assoc. 2015 , 15 , 313–323. [ Google Scholar ] [ CrossRef ]
- Waldrop, D.P.; O’Connor, T.L.; Trabold, N. Waiting for the other shoe to drop: Distress and coping during and after treatment for breast cancer. J. Psychosoc. Oncol. 2011 , 29 , 450–473. [ Google Scholar ] [ PubMed ]
- Mehnert, A.; Koch, U. Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: A prospective study. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2007 , 16 , 181–188. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kazlauskiene, J.; Bulotiene, G. Prevalence of post-traumatic stress disorder among Lithuanian breast cancer patients and its risk factors. J. Psychosom. Res. 2020 , 131 , 109939. [ Google Scholar ] [ CrossRef ]
- Groleau, J.M.; Calhoun, L.G.; Cann, A.; Tedeschi, R.G. The role of centrality of events in post-traumatic distress and post-traumatic growth. Psychol. Trauma: Theory Res. Pract. Policy 2013 , 5 , 477–483. [ Google Scholar ] [ CrossRef ]
- Menger, F.; Mohammed Halim, N.A.; Rimmer, B.; Sharp, L. Post-traumatic growth after cancer: A scoping review of qualitative research. Support. Care Cancer 2021 , 29 , 7013–7027. [ Google Scholar ] [ CrossRef ]
- Tedeschi, R.G.; Calhoun, L.G. Post-traumatic growth: Conceptual foundations and empirical evidence. Psychol. Inq. 2004 , 15 , 1–18. [ Google Scholar ] [ CrossRef ]
- Cordova, M.J.; Cunningham, L.L.; Carlson, C.R.; Andrykowski, M.A. Post-traumatic growth following breast cancer: A controlled comparison study. Health Psychol. 2001 , 20 , 176–185. [ Google Scholar ] [ CrossRef ]
- Park, H.Y.; Choi, J.Y. Factors associated with post-traumatic growth in patients with breast cancer based on a model of post-traumatic growth. Asian Oncol. Nurs. 2022 , 22 , 65–73. [ Google Scholar ] [ CrossRef ]
- Chang, O.; Choi, E.K.; Kim, I.R.; Nam, S.J.; Lee, J.E.; Lee, S.K.; Im, Y.H.; Park, Y.H.; Cho, J.H. Association between socioeconomic status and altered appearance distress, body image, and quality of life among breast cancer patients. Asian Pac. J. Cancer Prev. 2014 , 15 , 8607–8612. [ Google Scholar ] [ CrossRef ]
- Chaoul, A.; Milbury, K.; Spelman, A.; Basen-Engquist, K.; Hall, M.H.; Wei, Q.; Shih, Y.C.T.; Arun, B.; Valero, V.; Perkins, G.H.; et al. Randomized trial of Tibetan yoga in patients with breast cancer undergoing chemotherapy. Cancer 2018 , 124 , 36–45. [ Google Scholar ] [ CrossRef ]
- Maass, S.W.M.C.; Boerman, L.M.; Verhaak, P.F.M.; Du, J.; de Bock, G.H.; Berendsen, A.J. Long-term psychological distress in breast cancer survivors and their matched controls: A cross-sectional study. Maturitas 2019 , 130 , 6–12. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ahn, J.H.; Suh, E.Y. The lived experience of body alteration and body image with regard to immediate breast reconstruction among women with breast cancer. J. Korean Acad. Nurs. 2021 , 51 , 245–259. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hur, S.S. The Lived Experience of Being Healed in Breast Cancer Patients. Ph.D. Thesis, Hanyang University, Seoul, Republic of Korea, 2016. [ Google Scholar ]
- Hong, E.Y. A Narrative Inquiry into the Life Experiences of Middle-Aged Women with Terminal Breast Cancer. Ph.D. Thesis, Dankook University, Seoul, Republic of Korea, 2021. [ Google Scholar ]
- Amin, Z. Q methodology: A journey into the subjectivity of human mind. Singap. Med. J. 2000 , 41 , 410–414. [ Google Scholar ]
- McKeown, B.; Thomas, D.B. Q Methodology ; Sage Publications: Thousand Oaks, CA, USA, 2013; Volume 66. [ Google Scholar ]
- Ramlo, S. Mixed method lessons learned from 80 years of Q methodology. J. Mix. Methods Res. 2016 , 10 , 28–45. [ Google Scholar ] [ CrossRef ]
- Watts, S.; Stenner, P. Doing Q Methodological Research ; Sage Publications: Thousand Oaks, CA, USA, 2012. [ Google Scholar ]
- Kim, H.K. Q Methodology: Philosophy, Theories, Analysis, and Application ; Communication Books: Seoul, Republic of Korea, 2008. [ Google Scholar ]
- Fallbjörk, U.; Rasmussen, B.H.; Karlsson, S.; Salander, P. Aspects of body image after mastectomy due to breast cancer—A two-year follow-up study. Eur. J. Oncol. Nurs. 2013 , 17 , 340–345. [ Google Scholar ] [ CrossRef ]
- Jeon, J.M. A study on the face validity of Cloze test and its effective method of use in the classroom. J. Mil. Sci. Res. 2020 , 71 , 7–28. [ Google Scholar ]
- Kwon, D.H. Educational Evaluation ; HAKJISA: Seoul, Republic of Korea, 2005. [ Google Scholar ]
- Brown, S.R. Political Subjectivity ; Yale University Press: New Haven, CT, USA, 1980. [ Google Scholar ]
- Kim, S.E. Theory and philosophy of Q methodology. Korean Soc. Public Adm. 2010 , 20 , 1–25. [ Google Scholar ]
- Park, J.S. A qualitative case study on the coping experiences of cancer survivors in their middle years. Health Soc. Welf. Rev. 2017 , 40 , 90–123. [ Google Scholar ]
- Karlsson, M.; Friberg, F.; Wallengren, C.; Öhlén, J. Meanings of existential uncertainty and certainty for people diagnosed with cancer and receiving palliative treatment: A life-world phenomenological study. BMC Palliat. Care 2014 , 13 , 28. [ Google Scholar ] [ CrossRef ]
- Seligman, M.E.P. Flourish: A Visionary New Understanding of Happiness and Well-Being ; Simon & Schuster: New York, NY, USA, 2014. [ Google Scholar ]
- Kang, M.Y. A Subjectivity Study on the Meaning of the Life of Breast Cancer Survivors: Focused on the Participation of the Support Groups. Master’s Thesis, Hanyang University, Seoul, Republic of Korea, 2009. [ Google Scholar ]
- Lim, I.S. Breast cancer, damaged body and a sense of femininity in crisis. J. Korean Women’s Stud. 2006 , 22 , 5–46. [ Google Scholar ]
- Pinto-Gouveia, J.; Duarte, C.; Matos, M.; Fráguas, S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clin. Psychol. Psychother. 2014 , 21 , 311–323. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yousefi, A.M.; Masoumi, S. Psychological well-being and death anxiety among breast cancer survivors during the COVID-19 pandemic: The mediating role of self-compassion. BMC Women’s Health 2021 , 21 , 387. [ Google Scholar ]
- Yun, M.R.; Song, M.S. A qualitative study on breast cancer survivors’ experiences. Perspect. Nurs. Sci. 2013 , 10 , 41–51. [ Google Scholar ]
- Joo, E.K.; Kim, H.Y. A narrative exploration of the life experiences of young breast cancer survivors. J. Humanit. Soc. Sci. 2022 , 13 , 489–504. [ Google Scholar ]
- Lindwall, L.; Bergbom, I. The altered body after breast cancer surgery. Int. J. Qual. Stud. Health Well-Being 2009 , 4 , 280–287. [ Google Scholar ] [ CrossRef ]
- Maheu, C.; Singh, M.; Tock, W.L.; Eyrenci, A.; Galica, J.; Hébert, M.; Frati, F.; Estapé, T. Fear of cancer recurrence, health anxiety, worry, and uncertainty: A scoping review about their conceptualization and measurement within breast cancer survivorship research. Front. Psychol. 2021 , 12 , 644932. [ Google Scholar ] [ CrossRef ]
- Vickberg, S.J. Fears about breast cancer recurrence: Interviews with a diverse sample. Cancer Pract. 2001 , 9 , 237–243. [ Google Scholar ] [ CrossRef ]
- Wu, X.; Wang, J.; Cofie, R.; Kaminga, A.C.; Liu, A. Prevalence of post-traumatic stress disorder among breast cancer patients: A meta-analysis. Iran. J. Public Health 2016 , 45 , 1533–1544. [ Google Scholar ]
- Moon, U.M. The third wave of cognitive-behavioral therapy. Korean J. Couns. Psychother. 2005 , 17 , 15–33. [ Google Scholar ]
- Lee, S.Y. Mental health and acceptance-commitment therapy. Couns. Guid. 2018 , 53 , 113–135. [ Google Scholar ]
- Lee, E.; Faber, J.; Bowles, K. A review of trauma-specific treatments (TSTS) for post-traumatic stress disorder (PTSD). Clin. Soc. Work. J. 2022 , 50 , 147–159. [ Google Scholar ] [ CrossRef ]
- Lim, S. Perception of the Meaning in Life in Early Breast Cancer Survivors: Using the Q methodology. Master’s Thesis, Ewha Womans University, Seoul, Republic of Korea, 2021. [ Google Scholar ]
Click here to enlarge figure
| Perceptions and Attitudes Towards Oneself | Perception and Attitude Towards Relationships and Environment | |
|---|---|---|
| Positive | ||
| Negative | ||
| Neutral |
| N | Q Statements |
|---|---|
| Q1 | I am grateful just to be alive right now. |
| Q2 | I feel fortunate that breast cancer, with its higher survival rates compared to other cancers, happened to me. |
| Q3 | I have come to appreciate the small joys of daily life that I didn’t notice before. |
| Q4 | The treatment process for breast cancer is too painful. |
| Q5 | I feel sad because my physical strength has declined so much that my daily life feels shattered. |
| Q6 | I often feel fearful about not knowing when I might die. |
| Q7 | I try to calm myself by thinking, “This too shall pass”. |
| Q8 | When I look back on my life, I try to accept that cancer was something I was meant to have. |
| Q9 | Breast cancer has been a turning point that allowed me to live a new life. |
| Q10 | I am more proactive in expressing my thoughts and emotions than before. |
| Q11 | I have developed a stronger attachment to life than before I got sick. |
| Q12 | To distract myself from forgetting the reality of being a breast cancer patient, I find things on which to focus. |
| Q13 | When I think about metastasis or recurrence, I feel overwhelmed with fear. |
| Q14 | Even minor pain or physical changes make me worry excessively about my health. |
| Q15 | Due to an uncertain future, I have abandoned my life goals. |
| Q16 | If breast cancer is my fate, I think I should accept it. |
| Q17 | I strive to let go of things and desires to which I used to cling. |
| Q18 | I have started reflecting on my life instead of just charging forward. |
| Q19 | Breast cancer has allowed me to find relaxation in my otherwise busy life. |
| Q20 | Thinking I may not have much time left, I do my best in my tasks. |
| Q21 | I encourage and support myself more than before. |
| Q22 | I want to focus more on the present moment rather than the future. |
| Q23 | Feeling that I have to handle and overcome cancer alone makes me feel lonely. |
| Q24 | I pity myself for being sick and anxious about breast cancer. |
| Q25 | Despite feeling relieved to have gotten this far, I cannot help feeling anxious. |
| Q26 | Now, my life’s priority is “myself”. |
| Q27 | Believing that health is most important, I am trying to change my diet and exercise habits. |
| Q28 | I am grateful to my family (husband, children, parents, siblings, etc.) who support me. |
| Q29 | Since being diagnosed with breast cancer, I have grown closer to my family. |
| Q30 | I worry about how my family will live without me. |
| Q31 | I want to witness my family grow and grow old together. |
| Q32 | Even my family doesn’t fully understand my suffering. |
| Q33 | I have been hurt by acquaintances who tried to comfort me. |
| Q34 | I no longer maintain relationships with friends I feel do not understand me. |
| Q35 | I feel discouraged by people around me who treat me as a patient. |
| Q36 | Now, the most important people who provide me with psychological support, stability, information, etc., are fellow breast cancer patients. |
| Q37 | It is difficult for me to go to public places like saunas or swimming pools where I must undress. |
| Q38 | I find listening to people telling me to think positively is much harder. |
| Q39 | Changes in my chest and body shape undermine my self-esteem. |
| Q40 | I dislike the idea of people around me knowing that I am a breast cancer patient. |
| Content/Type | Type 1 | Type 2 | Type 3 | Type 4 | Type 5 |
|---|---|---|---|---|---|
| Eigenvalues | 11.86 | 3.54 | 3.20 | 2.69 | 1.88 |
| Variance (%) | 30.42% | 9.08% | 8.19% | 6.90% | 4.83% |
| Cumulative (%) | 30.42% | 39.50% | 47.70% | 54.59% | 59.43% |
| Type | P # | Age | Stage | Duration of Treatment | Cancer Metastasis | Factor Weight |
|---|---|---|---|---|---|---|
| Type 1 (N = 13) | 1 | 48 | 2 | 7 years | O | 0.7127 |
| 2 | 52 | 3 | 1 year 1 month | O | 1.1638 | |
| 5 | 42 | 3 | 3 years 1 month | O | 1.6369 | |
| 6 | 43 | 3 | 9 months | O | 0.7766 | |
| 7 | 55 | 4 | 3 years 10 month | O | 1.2371 | |
| 9 | 54 | 1 | 2 years 6 months | X | 0.7345 | |
| 11 | 50 | 3 | 6 years | X | 0.8619 | |
| 13 | 54 | 2 | 1 year 6 months | X | 0.4932 | |
| 22 | 48 | 1 | 1 year 5 months | X | 1.1143 | |
| 24 | 54 | 3 | 9 months | X | 1.9371 | |
| 27 | 52 | 3 | 6 months | X | 0.6091 | |
| 29 | 53 | 1 | 3 years | X | 1.6828 | |
| 35 | 61 | 2 | 2 years 10 months | X | 1.1930 | |
| Type 2 (N = 6) | 3 | 43 | 1 | 3 years 6 months | X | 0.7648 |
| 15 | 55 | 2 | 4 years 8 months | O | 1.4540 | |
| 17 | 40 | 3 | 1 year 5 months | O | 0.6942 | |
| 23 | 52 | 3 | 1 year | O | 1.1938 | |
| 31 | 51 | 1 | 7 months | X | 0.7761 | |
| 37 | 45 | 1 | 2 months | X | 0.7311 | |
| Type 3 (N = 10) | 4 | 56 | 1 | 6 months | X | 0.2439 |
| 16 | 47 | 2 | 6 months | O | 1.2001 | |
| 18 | 59 | 3 | 7 years 1 month | O | 0.5215 | |
| 21 | 49 | 2 | 1 year 2 months | O | 0.9271 | |
| 26 | 47 | 3 | 9 months | X | 1.3674 | |
| 30 | 60 | 1 | 2 years 8 months | X | 0.9474 | |
| 32 | 52 | 1 | 5 years 10 months | X | 0.9709 | |
| 33 | 54 | 2 | 1 year 6 months | X | 1.0602 | |
| 34 | 43 | 2 | 1 year 2 months | O | 1.5733 | |
| 38 | 46 | 2 | 4 months | O | 1.1003 | |
| Type 4 (N = 5) | 10 | 49 | 2 | 2 years | X | 0.5661 |
| 14 | 64 | 1 | 2 years 9 months | X | 2.5126 | |
| 19 | 64 | 1 | 4 months | X | 0.9028 | |
| 20 | 41 | 2 | 1 year 1 month | X | 1.0662 | |
| 39 | 46 | 3 | 3 years 9 months | O | 0.9047 | |
| Type 5 (N = 5) | 8 | 47 | 2 | 2 years 6 months | X | 0.6623 |
| 12 | 52 | 1 | 3 years 6 months | X | 2.4584 | |
| 25 | 51 | 2 | 1 year 9 months | X | 1.1328 | |
| 28 | 53 | 3 | 8 months | O | 0.5852 | |
| 36 | 48 | 2 | 2 years 8 months | O | 0.9701 |
| No. | Statement | Z Score |
|---|---|---|
| 1 | I am grateful just to be alive right now. | 1.89 |
| 9 | Breast cancer has been a turning point that allowed me to live a new life. | 1.72 |
| 19 | Breast cancer has allowed me to find relaxation in my otherwise busy life. | 1.45 |
| 3 | I have come to appreciate the small joys of daily life that I didn’t notice before. | 1.38 |
| 22 | I want to focus more on the present moment rather than the future. | 1.25 |
| 35 | I feel discouraged by people around me who treat me as a patient. | −1.02 |
| 23 | Feeling that I have to handle and overcome cancer alone makes me feel lonely. | −1.13 |
| 6 | I often feel fearful about not knowing when I might die. | −1.44 |
| 24 | I pity myself for being sick and anxious about breast cancer. | −1.72 |
| 15 | Due to an uncertain future, I have abandoned my life goals. | −1.76 |
| No. | Statement | Z Score |
|---|---|---|
| 22 | I want to focus more on the present moment rather than the future. | 1.63 |
| 26 | Now, my life’s priority is “myself”. | 1.36 |
| 13 | When I think about metastasis or recurrence, I feel overwhelmed with fear. | 1.33 |
| 21 | I encourage and support myself more than before. | 1.28 |
| 9 | Breast cancer has been a turning point that allowed me to live a new life. | 1.12 |
| 35 | I feel discouraged by people around me who treat me as a patient. | −1.03 |
| 24 | I pity myself for being sick and anxious about breast cancer. | −1.42 |
| 39 | Changes in my chest and body shape undermine my self-esteem. | −1.62 |
| 15 | Due to an uncertain future, I have abandoned my life goals. | −1.73 |
| 8 | When I look back on my life, I try to accept that cancer was something I was meant to have. | −2.09 |
| No. | Statement | Z Score |
|---|---|---|
| 1 | I am grateful just to be alive right now. | 2.23 |
| 13 | When I think about metastasis or recurrence, I feel overwhelmed with fear. | 1.38 |
| 31 | I want to witness my family grow and grow old together. | 1.35 |
| 7 | I try to calm myself by thinking, “This too shall pass”. | 1.32 |
| 14 | Even minor pain or physical changes make me worry excessively about my health. | 1.20 |
| 33 | I have been hurt by acquaintances who tried to comfort me. | −1.06 |
| 40 | I dislike the idea of people around me knowing that I am a breast cancer patient | −1.38 |
| 15 | Due to an uncertain future, I have abandoned my life goals. | −1.49 |
| 35 | I feel discouraged by people around me who treat me as a patient. | −1.68 |
| 39 | Changes in my chest and body shape undermine my self-esteem. | −1.76 |
| No. | Statement | Z Score |
|---|---|---|
| 37 | It is difficult for me to go to public places like saunas or swimming pools where I must undress. | 2.02 |
| 25 | Despite feeling relieved to have gotten this far, I cannot help feeling anxious. | 1.90 |
| 13 | When I think about metastasis or recurrence, I feel overwhelmed with fear. | 1.49 |
| 39 | Changes in my chest and body shape undermine my self-esteem. | 1.29 |
| 33 | I have been hurt by acquaintances who tried to comfort me. | 1.02 |
| 21 | I encourage and support myself more than before. | −1.02 |
| 11 | I have developed a stronger attachment to life than before I got sick. | −1.26 |
| 15 | Due to an uncertain future, I have abandoned my life goals. | −1.77 |
| 20 | Thinking I may not have much time left, I do my best in my tasks. | −1.96 |
| 6 | I often feel fearful about not knowing when I might die. | −2.13 |
| No. | Statement | Z Score |
|---|---|---|
| 13 | When I think about metastasis or recurrence, I feel overwhelmed with fear. | 1.87 |
| 32 | Even my family doesn’t fully understand my suffering. | 1.34 |
| 6 | I often feel fearful about not knowing when I might die. | 1.20 |
| 27 | Believing that health is most important, I am trying to change my diet and exercise habits. | 1.11 |
| 14 | Even minor pain or physical changes make me worry excessively about my health. | 1.11 |
| 39 | Changes in my chest and body shape undermine my self-esteem. | −1.14 |
| 28 | I am grateful to my family (husband, children, parents, siblings, etc.) who support me. | −1.19 |
| 29 | Since being diagnosed with breast cancer, I have grown closer to my family. | −1.34 |
| 30 | I worry about how my family will live without me. | −1.60 |
| 5 | I feel sad because my physical strength has declined so much that my daily life feels shattered. | −2.10 |
| No. | Statement | Z Score |
|---|---|---|
| 22 | I want to focus more on the present moment rather than the future. | 1.074 |
| 15 | Due to an uncertain future, I have abandoned my life goals. | −1.610 |
| 20 | Thinking I may not have much time left, I do my best in my tasks. | −1.176 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Shim, M.-J.; Lee, S.-Y.; Ha, O.-S. Categorising Subjective Perceptions of Middle-Aged Breast Cancer Patients Using Q Methodology. Healthcare 2024 , 12 , 1873. https://doi.org/10.3390/healthcare12181873
Shim M-J, Lee S-Y, Ha O-S. Categorising Subjective Perceptions of Middle-Aged Breast Cancer Patients Using Q Methodology. Healthcare . 2024; 12(18):1873. https://doi.org/10.3390/healthcare12181873
Shim, Min-Jeung, Song-Yi Lee, and Oh-Sun Ha. 2024. "Categorising Subjective Perceptions of Middle-Aged Breast Cancer Patients Using Q Methodology" Healthcare 12, no. 18: 1873. https://doi.org/10.3390/healthcare12181873
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Skip to main content
- Accessibility information

- Enlighten Enlighten
Enlighten Theses
- Latest Additions
- Browse by Year
- Browse by Subject
- Browse by College/School
- Browse by Author
- Browse by Funder
- Login (Library staff only)
In this section
Breast cancer awareness among female residents of Kuwait
Almajed, Hanan (2023) Breast cancer awareness among female residents of Kuwait. PhD thesis, University of Glasgow.
| |
Background and aim Breast cancer is the most common cancer among females and the second leading cause of death worldwide. Incidence in developed countries is slightly higher than developing countries; yet mortality rate in developing countries is higher than developed ones. A main reason for this is late presentation of the disease, which is common in Gulf Coorporation Council countries (GCC), and in Kuwait especially. Evidence regarding the reasons behind late presentation is insufficient. This thesis aimed to provide a comprehensive insight into breast cancer awareness and its screening methods among females in Kuwait.
Method A multi-method approach was adopted to address the research objectives and gain a deeper understanding in a robust way. Three interlinked studies were carried out. A systematic review of literature attempted to understand the awareness, beliefs and attitudes towards breast cancer and breast cancer screening behavior in GCC countries region. The second epidemiological study was conducted to evaluate the level of knowledge and awareness about breast cancer non-lump symptoms, risks, and screening programs in the general population of females in Kuwait. The research was done using an internationally validated tool, the Breast Cancer Awareness Measure (BCAM). Participants were women who attended primary healthcare centres in the five districts of Kuwait and selected by systematic random sampling. Analysis included multivariable logistic regression analysis to quantify the relationship between the domains of the BCAM and breast cancer awareness. The qualitative study sought to explore and identify the best approaches to improve breast cancer awareness in Kuwait. Key stakeholders involved in breast cancer and breast screening awareness were selected because of their role. Individual in-depth interviews were built around video elicitation, where key stakeholders viewed a series of international breast cancer campaign videos. Reaction to the videos and a topic guide that included ten open-ended questions allowed the exploration of their views of breast cancer awareness in Kuwait. An Inductive thematic analysis was applied to the interview data.
Results A total of 53 studies were eligible for inclusion in the systematic review. A narrative synthesis approach resulted in five main themes, each with sub-themes. The synthesis of included studies concluded that awareness about breast cancer and its screening method was low compared to developed countries. Similarly, findings from the cross-sectional BCAM survey shown a lack of knowledge about breast cancer and breast screening methods. In the qualitative study, 14 participants were interviewed. The analysis identified eight themes and sub-themes. Participants discussed the reasons responsible for the low awareness of breast cancer and low uptake of mammography. Fear was a major resisting factor to screening, others mentioned social stigma and taboo and feeling shy, reflecting the cultural norm. Participants also explored different approaches to improve breast cancer awareness among the population of Kuwait.
Conclusion Findings from all three studies confirmed the low awareness about breast cancer and its screening methods among female residents of Kuwait. Areas of improvement were discussed and shared by interviewees. A number of recommendations for future awareness raising campaigns have been made. Improvement lies in the form of targeting campaigns for both healthcare professionals and females. Introducing factual females’ health programmes in early school was recommended by most stakeholders.
| Item Type: | Thesis (PhD) | |||
|---|---|---|---|---|
| Qualification Level: | Doctoral | |||
| Subjects: | > > | |||
| Colleges/Schools: | > > | |||
| Supervisor's Name: | Macdonald, Professor Sara, Nicholl, Dr. Barbara and Robb, Professor Katie | |||
| Date of Award: | 2023 | |||
| Depositing User: | ||||
| Unique ID: | glathesis:2023-83539 | |||
| Copyright: | Copyright of this thesis is held by the author. | |||
| Date Deposited: | 19 Apr 2023 08:09 | |||
| Last Modified: | 19 Apr 2023 08:12 | |||
| Thesis DOI: | ||||
| URI: |
| View Item |
Downloads per month over past year
View more statistics

The University of Glasgow is a registered Scottish charity: Registration Number SC004401
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Impact of Health Education Intervention on Breast Cancer Awareness among Rural Women of Tamil Nadu
Affiliations.
- 1 Department of Community Medicine, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
- 2 Department of Community Medicine, Chettinad Academy of Research and Education, Chennai, Tamil Nadu, India.
- PMID: 32905196
- PMCID: PMC7467190
- DOI: 10.4103/ijcm.IJCM_173_19
Background: The most common cancer among Indian females is breast cancer. Limited access to early detection and treatment is responsible for more than half of the deaths, primarily in rural areas, where organized mammography screening is neither affordable nor feasible. Therefore, imparting awareness on breast health and breast self-examination (BSE) is highly recommended. This study aimed to assess the impact of a health education interventional program on breast health awareness and BSE among rural women of Tamil Nadu.
Methodology: A quasi-experimental study was conducted among 266 women. A preinterventional survey was done using a pretested validated questionnaire. A multipronged breast health education intervention was administered and its effectiveness was measured after 3 months using the same tool.
Results: There was a statistically significant ( P = 0.0001) improvement in the knowledge of breast health, perceived susceptibility, and reasons for practice and proficiency of BSE practice of the interventional group from pre- to post-test. After the interventional program, 71.8% of increase in knowledge about breast health and BSE was observed. In addition, 64.7% of the women practiced BSE compared to 7.14% pretest.
Conclusion: This study highlights the awareness needs by the women and application of extensive strategies to increase the acceptance of cancer screening programs.
Keywords: Breast cancer awareness; breast self-examination; health education; impact; quasi-experimental; rural women.
Copyright: © 2020 Indian Journal of Community Medicine.
PubMed Disclaimer
Conflict of interest statement
There are no conflicts of interest.
Impact of health educational intervention
Similar articles
- Determinants of Awareness and Practice of Breast Self Examination Among Rural Women in Trichy, Tamil Nadu. Kumarasamy H, Veerakumar AM, Subhathra S, Suga Y, Murugaraj R. Kumarasamy H, et al. J Midlife Health. 2017 Apr-Jun;8(2):84-88. doi: 10.4103/jmh.JMH_79_16. J Midlife Health. 2017. PMID: 28706409 Free PMC article.
- Impact of a health education intervention program regarding breast self examination by women in a semi-urban area of Madhya Pradesh, India. Gupta SK. Gupta SK. Asian Pac J Cancer Prev. 2009;10(6):1113-7. Asian Pac J Cancer Prev. 2009. PMID: 20192594
- Effectiveness of educational intervention on breast cancer knowledge and breast self-examination among female university students in Bangladesh: a pre-post quasi-experimental study. Sarker R, Islam MS, Moonajilin MS, Rahman M, Gesesew HA, Ward PR. Sarker R, et al. BMC Cancer. 2022 Feb 22;22(1):199. doi: 10.1186/s12885-022-09311-y. BMC Cancer. 2022. PMID: 35193526 Free PMC article. Clinical Trial.
- Interventions Promoting Breast Cancer Screening Among Turkish Women With Global Implications: A Systematic Review. Secginli S, Nahcivan NO, Gunes G, Fernandez R. Secginli S, et al. Worldviews Evid Based Nurs. 2017 Aug;14(4):316-323. doi: 10.1111/wvn.12245. Epub 2017 Jun 12. Worldviews Evid Based Nurs. 2017. PMID: 28605115 Review.
- Awareness and Practice of Breast Self Examination among Women in Different African Countries: A 10-Year Review of Literature. Johnson OE. Johnson OE. Niger Med J. 2019 Sep-Oct;60(5):219-225. doi: 10.4103/nmj.NMJ_84_19. Epub 2019 Nov 26. Niger Med J. 2019. PMID: 31844349 Free PMC article. Review.
- Effectiveness of a Health Educational Program in Enhancing Breast Cancer Knowledge Among Women in Rural Karnataka, South India. Mainaz M, Guthigar M, Naik P. Mainaz M, et al. Cureus. 2024 Mar 14;16(3):e56157. doi: 10.7759/cureus.56157. eCollection 2024 Mar. Cureus. 2024. PMID: 38618335 Free PMC article.
- Awareness of risk factors, symptoms and screening of breast cancer: A cross-sectional survey among 35-65-year-old women in Alappuzha district, Kerala, India. Mohan R, Thulaseedharan JV. Mohan R, et al. J Family Med Prim Care. 2023 Oct;12(10):2401-2407. doi: 10.4103/jfmpc.jfmpc_700_23. Epub 2023 Oct 11. J Family Med Prim Care. 2023. PMID: 38074240 Free PMC article.
- An educational intervention study to enhance breast cancer awareness among women and primary healthcare providers of an urban health center area, Visakhapatnam. Potluri TS, Vadlamani S, Gujjarlapudi C, Nerusu NG, Rongala MV. Potluri TS, et al. J Family Med Prim Care. 2023 Aug;12(8):1697-1703. doi: 10.4103/jfmpc.jfmpc_932_23. Epub 2023 Aug 29. J Family Med Prim Care. 2023. PMID: 37767416 Free PMC article.
- Evaluation of an Interventional Health Education Project: Screening of Breast Cancer and Health Education (SHE). Khapre M, Ravi B, Sharda P, Mehta A, Kumari R. Khapre M, et al. Asian Pac J Cancer Prev. 2022 Jul 1;23(7):2361-2366. doi: 10.31557/APJCP.2022.23.7.2361. Asian Pac J Cancer Prev. 2022. PMID: 35901342 Free PMC article.
- Understanding Social Media Usage and Engagement among Women to inform Breast Cancer Knowledge and Prevention Practices: Cross - sectional study in Delhi -National Capital Region of India. Sinha N, Sharma A. Sinha N, et al. Indian J Community Med. 2021 Jul-Sep;46(3):411-415. doi: 10.4103/ijcm.IJCM_429_20. Epub 2021 Oct 13. Indian J Community Med. 2021. PMID: 34759477 Free PMC article.
- GLOBACON 2018 Cancer Fact Sheets: Breast Cancer. 2019. [Last accessed on 2019 Mar 23]. Available from: http://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-shee... .
- Gadgil A, Roy N, Sankaranarayanan R, Muwonge R, Sauvaget C. Effect of comprehensive breast care on breast cancer outcomes: A community hospital based study from Mumbai, India. Asian Pac J Cancer Prev. 2012;13:1105–9. - PubMed
- American Cancer Society Guidelines for the Early Detection of Cancer. [Last accessed on 2016 Sep 21]. Available from: http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/... .
- Petro-Nustas W, Tsangari H, Phellas C, Constantinou C. Health beliefs and practice of breast self-examination among young Cypriot women. J Transcult Nurs. 2013;24:180–8. - PubMed
- Census of India Website: Office of the Registrar General and Census Commissioner, India. [Last accessed on 2016 Aug 26]. Available from: http://censusindia.gov.in/
Related information
Linkout - more resources, full text sources.
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
ORIGINAL RESEARCH article
Evaluation of knowledge, perception, and risk awareness about breast cancer and its treatment outcome among university of gondar students, northwest ethiopia.

- School of Pharmacy, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
Background: Breast cancer is among the most common life-threatening public health problems of global concern including Ethiopia. Knowledge and awareness about the disease will help to reduce the number of cases who present at late stages of the disease. The objective of this survey was to assess the knowledge, perception and risk awareness about breast cancer among female medical and health science students of University of Gondar, Ethiopia.
Methods: A cross sectional survey was conducted from May 03 to June 01, 2017 at University of Gondar, Ethiopia. Three hundred students were proportionally selected from nine departments using simple random sampling method. Using a structured questionnaire data on risk factors, symptoms and perception about breast cancer and its management approach was collected. Data were entered to and analyzed using SPSS version 21.
Results: A total of 300 students had fully completed the survey making the response rate 95.24. The participants' mean age was 21.4 years with the standard deviation (SD) of 2.13 years. The overall level of knowledge on breast cancer was low. Majority of the participants were unaware for complex risk factors such as first child after the age of 30 years (51%), early onset of menses (55.3%), and menopause after the age of 55 years (47.7%) are liked with breast cancer even though they acknowledged old age, family history, and smoking as possible risk factors for breast cancer. Pain in the breast region, change in the shape of the breast, and nipple discharge were the most frequently correctly identified symptoms of breast cancer. Majority of the study participants had also correct beliefs about breast cancer management and its outcomes. however, they had negative perception of breast cancer treatment by considering it to be a long-term and painful process. In binary logistic regression analysis department ( p = 0.000) and year of study ( p = 0.008) were found to be an independent predicting factors for knowledge among the study participants.
Conclusions: The overall level of knowledge on breast cancer and clinical breast examination guidelines was found to be low even though majority had positive perception toward the treatment and its outcomes. Hence, intensive breast health awareness campaign, which should also stress on the importance of early detection and reporting, is necessary to improve the knowledge about breast cancer.
Introduction
Breast cancer is one of the top most public health concern jeopardizing the lives of many peoples worldwide ( 1 , 2 ). This kind of cancer is malignant by nature endangers breast tissue, and may involve either the tubules carrying milk or ducts which produce the milk. This type of disease can metastasize to distant areas or invade surrounding tissues. Commonly, the disease happens in women population although males may also suffer from it ( 3 ).
Globally, the incidence of breast cancer has increased from 641 000 in 1980 to 1 643 000 in 2010 with an annual increment of 3.1% ( 4 ). Different reports revealed that in sub-Saharan African and other resource limited countries the rate of occurrence of breast carcinoma is significantly increasing ( 5 , 6 ). The overall incidence in Ethiopia is also increasing, it is estimated around 10,000 women and men taking in consideration that more number of cases were unreported since women from country side usually prefer to go to cultural treatment providers than looking for health care institution ( 7 ). Some of contributing factors implicated in steady rise in breast cancer incidence in developing countries are widespread urbanization, changing patterns of reproductive and environmental risks factors, obesity, decreased physical activity, and increasing life expectancy ( 8 , 9 ). Since 1980, the mortality of breast cancer has also increased from 250,000 to 425,000 in 2010. About 60% of deaths from breast cancer are occurring in low income countries ( 4 ).The high mortality associated with breast cancer in countries like Ethiopia is most importantly due to knowledge shortage about the disease that may leads to late diagnosis ( 10 ).
The exact reasons for the occurrence of breast cancer have not been fully understood. However, numerous researchers have identified a number of predictors that can increase one's likelihood of getting breast cancer. They called them risk factors and includes family and individual backgrounds of breast cancer; delayed menopause (>55 years); early menarche (<12 years); late age at first full-term pregnancy (>30 years); alcohol use; aging; never breastfeeding a child; exposure to contraceptives; tobacco smoking; high fat diet; obesity (postmenopausal); recent and long-term consumption of hormonal replacements; physical inactivity; high-dose x-ray to chest ( 11 , 12 ).
Although in developed countries, screening of such malignant tumor is usually performed using mammograms, the access to most women in sub Saharan countries are limited. From the existing situation it is uncertain to have amendments in the upcoming days ( 13 ). Breast self-examination (BSE) is the mere, reasonable and practical option of screening for women living in Africa in case of non-appearance of mammography ( 13 , 14 ). With applicable training of BSE along with clinical breast examination and comprehensive health education of the disease, it is likely to early detect the disease. Women who repeatedly do BSE tend to accustom both the feeling and appearance of their breasts this in turn will help them to early identify any changes. However, if it is done improperly, there might be untrue positive or negative findings associated with poor BSE and this may raise a great disappointment to undergo mammographic screening even in the set up where it is available and easily accessible ( 15 ).
In Ethiopia poor awareness is the core concern and there is also stigma and misconceptions/understanding about cancer, that all cancer cases are incurable. Associated with this little work was done so far to promote the awareness that most cancer cases can be prevented, even cured if detected early, and quality of life can also be improved ( 16 ).
As the principal focus of the present study was students, it strengthens cancer detection and prevention strategies at an early age, creates education opportunities for shaping health behaviors into adulthood and also encourage discussions between students and their guardians as well as relatives. Therefore, the purpose of the present survey was to explore the knowledge, perception and risk awareness toward breast cancer among female medical and health science students of University of Gondar, Ethiopia.
Study Design and Setting
An institutional based cross sectional study was employed among female medical and health science students of University of Gondar (UOG). UOG is among the first born universities in Ethiopia and located 737 km from the capital of Ethiopia, in northwest direction. It has 5 campuses such as Atse Tewodros, Maraki, College of Medicine and Health Sciences (CMHS), Atse Fasil, and Meles Zenawi. At present, with the nine academic offices it offers about 56 undergraduate and 64 postgraduate programs in regular, distance, extension and summer programs.
Study Samples
Female students who had interest to complete the self-administered questionnaire were included. However, students with already existing disease and unable to understand the questionnaire were excluded.
Sample Size Determination and Sampling Technique
Appropriate sample size was estimated using a single proportion formula ( 17 )
Where n is the need sample size; d , marginal error ( d = 0.05); Z , the required degree of accuracy at 95% confidence level, which is 1.96; P = 0.5 (50%) level of knowledge, as there was no study conducted in the study area to the best of literature search made. Using the above formula, the sample size was calculated as follows:
Since the sample was drawn from the gross population of 1463, which is <10,000, the required final sample size was determined after applying the correction factor;
Considering 5% for probable non-respondent, the required final sample size was 315.
Sampling Technique/Procedure
The final sample was distributed proportionally across different departments. Using simple random sampling technique the required samples from each department were recruited in the study (Figure 1 ).
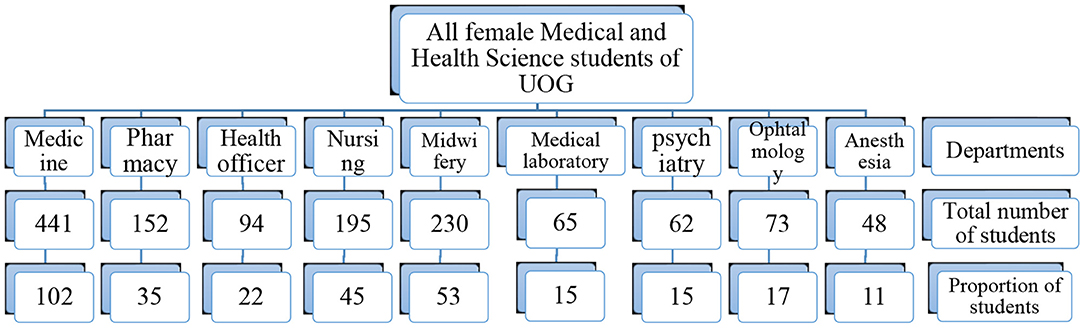
Figure 1 . A flow chart describing the sampling technique, UOG, 2017.
Data Collection Technique and Management
Three principal investigators were responsible for conducting the data collection. The data were obtained through self-administered questionnaire. The tool used was adopted from prior studies conducted in this area and prepared in English ( 18 – 23 ). The data collection tool has three sections: The first part includes socio-demographic variables while the second one comprises knowledge of breast cancer risk factors, symptoms and screening tests and the third part focuses on perception of management and outcomes. Participants' response was given 1 point for correct and zero for incorrect answer or do not know. The knowledge status was considered as “low,” “moderate,” and “high” if the scores fall in the range of 0–49, 50–79, and 80–100%, respectively ( 24 ). Likert scale of 1–5 was also employed to rate the responses of participants regarding perception related questions. It was also pretested on 25 participants who were not included in the final analysis before the commencement of actual data collection. Moreover, training on the familiarization of the instrument and strategies to approach the students were provided for the investigators.
Data Entry and Analysis
The collected data using quantitative method was entered to and analyzed using Statistical packages for social sciences (SPSS) version 21 statistical software. Frequencies, percentages, tables, flow chart were used to describe study variables. Binary logistic regression analysis was done to examine the association among different variables. For determining statistically significant associations, P < 0.05 and confidence interval (CI) of 95% were used as cut points.
Ethical Considerations
The study was ethically approved by the ethical review committee of School of Pharmacy (SoP), University of Gondar (UoG) with an approval number of UoG-SoP-140/2017. Informed consent was gained from each participant before the start of the study. They were also informed that involvement in the study was fully voluntarily and withdrawal at any stage if they refused to participate was assured. Information obtained from the survey was kept confidential. In addition, patient identifiers were not used.
Socio-Demographic Characteristics of the Participants
In the current study, out of the total interview guides/questionnaires of sample of 315 students who were interviewed 300 were included in the analysis, and 15 encounters were excluded due to incompleteness making the response rate 95.24%. The average age of the study respondents were 21.4 years with the standard deviation (SD) of 2.13 years.
More than two third 188 (62.7%) of the participants had no previous participation in breast care awareness. However, they had interest to participate in activities that encourages breast cancer awareness 234 (78.0%) (Table 1 ).
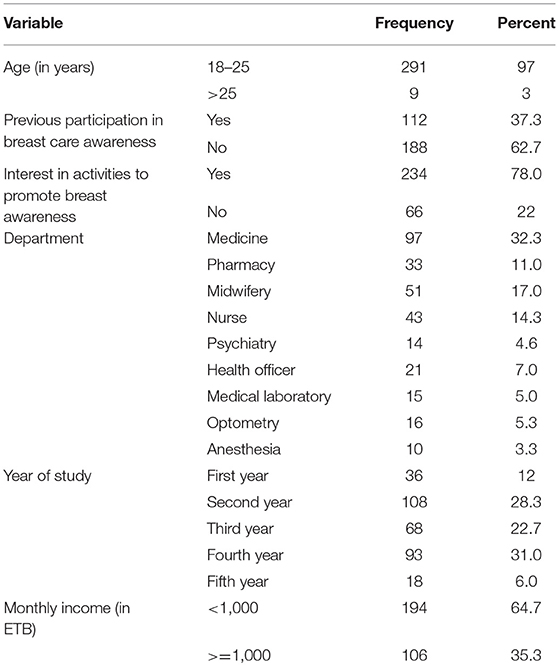
Table 1 . Distribution of participants by socio-demographic characteristics, UOG, 2017.
Knowledge of Breast Cancer Symptoms, Risk Factors, and Screening Test
More than two third of the participants acknowledged old age, family history, and smoking as possible risk factors for breast cancer. Majority of the participants were unaware for complex risk factors such as first child after the age of 30 years (51%), early onset of menses (55.3%), and menopause after the age of 55 years (47.7%) are liked with breast cancer. Pain in the breast region, Change in the morphology/shape of the breast and nipple discharge were the most frequently correctly identified symptoms of breast cancer. Moreover, 168 (56.0%) of the participants were aware about once a month recommendations for practicing breast self-examination (BSE) and 108 (36%) for once a year clinical breast examination (CBE) (Table 2 ).
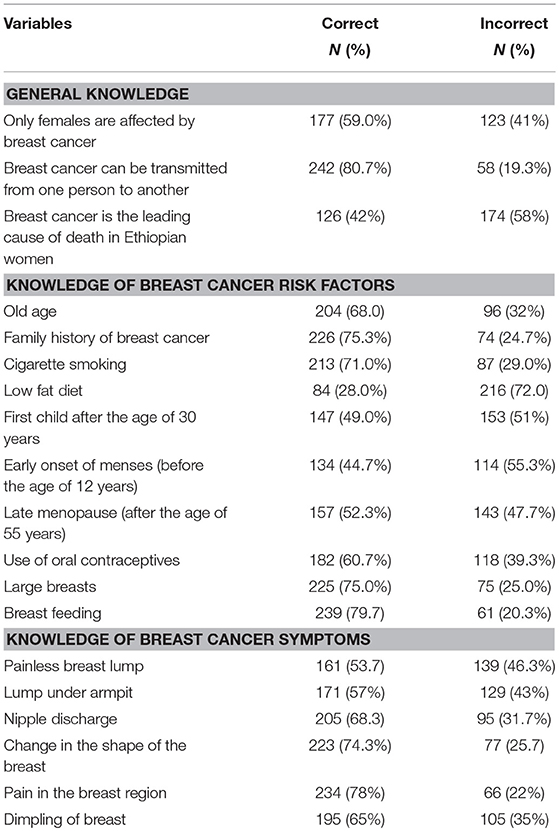
Table 2 . Participants' response to important knowledge related questions, UOG, 2017.
The overall level of knowledge was described by nineteen questions on breast cancer for general knowledge, risk factors and symptoms of breast cancer. Although the overall level of knowledge on breast cancer was low, high level of knowledge was observed in questions related to general knowledge about breast cancer 70 (23.3%) (Table 3 ).
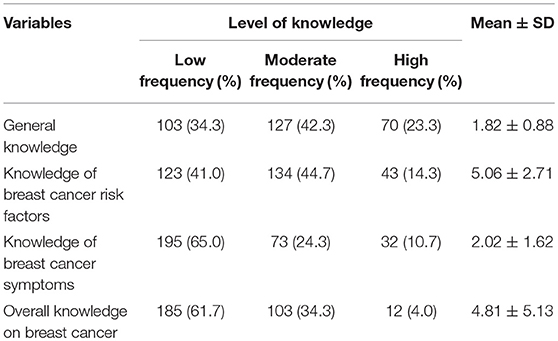
Table 3 . Knowledge about breast cancer, UOG, 2017.
Perception Toward Breast Cancer Treatment and Its Outcomes
Majority of study participants had correct beliefs about breast cancer management and its outcomes. however, they had negative perception of breast cancer treatment by considering it to be a long-term and painful process (Table 4 ).
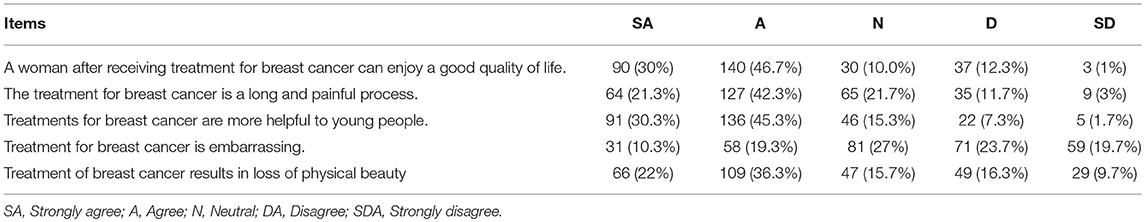
Table 4 . Perception toward breast cancer treatment and its outcomes, UOG, 2017.
Predictors of Knowledge of Breast Cancer Among the Participants
In binary logistic regression analysis department and year of study were found to be an independent predicting factors for knowledge among the participants. Students in pharmacy department (AOR = 0.839, CI = 0.312–2.255) were found to have 16.1% less likely to have good knowledge of breast cancer compared to public health officer students. On the other hand, students under first year of study (AOR = 2.661, CI = 0.407–17.389) were found to have 1.661 times more likely to have poor knowledge of breast cancer compared to fifth year students (Table 5 ).
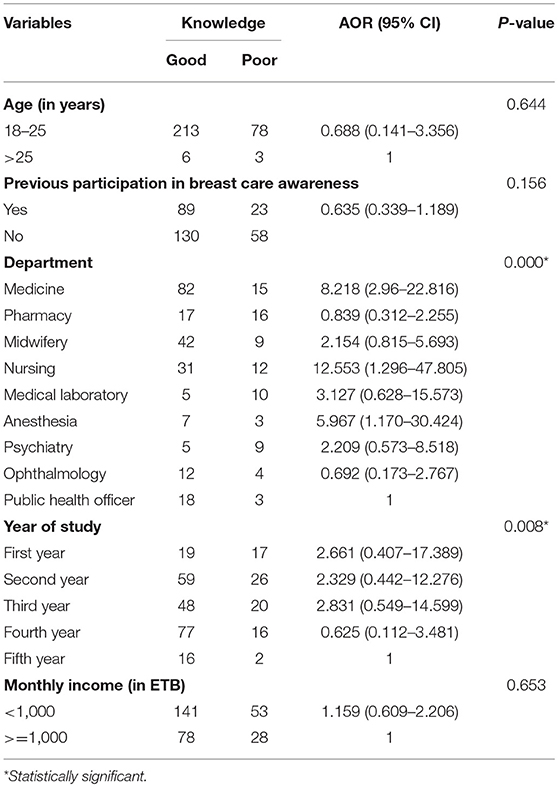
Table 5 . Predictors of knowledge of breast cancer among the participants, UOG, 2017.
It is an unconcealed evidence that breast cancer turn out to be one of the frequently occurring cancers among female population of Ethiopia and barriers associated with detection and management of the case decreases survival rates ( 1 , 25 ). The present study indicates that huge number of the study respondents had no previous involvement in breast care awareness. However, they had interest to involve in activities to encourage breast cancer awareness. This finding concurs with the report from United Arab Emirates ( 19 ).
This study stated that, beyond two third of the study subjects revealed to have low overall knowledge toward risk factors, general knowledge, and clinical manifestations of the malignant tumor, which was similar with the reports from Malaysia, Saudi, Egypt, and Nigeria ( 21 , 26 – 28 ). Many female students in such higher institutions are unacquainted of clinical breast examination (CBE), the predictors, and early presentation of the tumor. This might be the cause for the delayed presentation of the disease in developing countries. Therefore, it is crucial to provide comprehensive breast cancer and health awareness programs for female youngsters.
Bulk of the respondents acknowledged old age, family history, and tobacco use as potential predisposing factors for the tumor. Most of the participants were also unaware of complex risk factors such as first child after the age of 30 years (51%), early onset of menses (55.3%), and menopause after the age of 55 years (47.7%) are liked with breast cancer. This finding was comparable with studies done in Malaysia, Egypt, Oman and Britain ( 18 , 22 , 23 , 29 ).
Most of the study participants identified pain in the breast region as a symptom for breast cancer followed by swing in the morphology/shape of the breast and nipple discharge. However, more than one third of the respondents had less knowledge about under armpit lump and painless breast lump as cautioning signs of the disease. This finding concurs with the reports from Malaysia, Egypt, Nigeria, and Oman ( 18 , 22 , 23 , 28 ). However, it was higher when matched to the findings from Madawolabo ( 30 ). This could be justified as the respondents were merely from medical and health science streams, it was expected that awareness about manifestations of the disease to be good when matched to other technology campuses in the university.
Numerous respondents had the factual perception about breast cancer management and its outcomes. however, they had negative view of the tumor treatment by seeing the length of treatment and painful process, which was similar with the report from Malaysia and Nigeria ( 18 , 28 ). This finding suggest the need for customized educational interventions using different lines such as social media, distribution of leaflets, television/ radio broadcasts and proper counseling as tools for improving the knowledge and perception about the tumor and the treatment outcomes.
Binary logistic regression analysis was performed and factors such as department and study year were recognized as independent predictors for disease related knowledge among the study participants. Pharmacy students (AOR = 0.839 CI = 0.312–2.255) were 16.1% less likely to own good knowledge of breast cancer when equated to public health officer students. The study also mentioned that the odds of having poor knowledge toward the disease were 1.661 times higher among students enrolled under first year of study (AOR = 2.661, CI = 0.407–17.389) compared to fifth year students. This might be due more exposure and familiarization about breast cancer and related health issues in different courses, trainings and seminars will be embraced as academic year goes up.
As a drawback, although this research is the first in its kind in the study setting that can be used as an input for implementing basic projects, it is conducted only in one institution that the generalization to all over university students will be in question. With this, we highly recommended a large scale and multi centered survey that comprises diverse participants to validate our output and provide more representative findings.
Conclusions
In this study, the overall level of knowledge on breast cancer was low. Majority of the participants were unaware for complex risk factors such as first child after the age of 30 years, early onset of menses, and menopause after the age of 55 years are liked with breast cancer. However, small proportion of the participants were aware about clinical breast examination guidelines. Pain in the breast region, change in the shape of breast and nipple discharge were the most frequently correctly identified symptoms of breast cancer. On the other hand, majority of the participants acknowledged old age, family history, and smoking as possible risk factors for breast cancer and they had also positive perception toward breast cancer treatment and its outcomes. Department and year of study were found to be an independent predicting factors for knowledge among the participants.
Implications
Bearing in mind the greatest prominence of knowledge, perception and risk awareness about such tumor, institutions and different stakeholders working on cancer should offer a tailored health promotion and awareness creation to university youngsters, in line with cultivating facilities that let them do the screening examination regularly. In addition, the country ministry of education and health has to work on incorporating capacity building regular trainings regarding such disease avoidance and early detection in such organizations.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Ersumo T. Breast cancer in an Ethiopian population, Addis Ababa. East Central Afr J Surg. (2006) 11:81–6. Available online at: https://www.ajol.info/index.php/ecajs/article/view/136575
Google Scholar
2. American Cancer Society. Breast Cancer Facts & Figures 2013 – 2014 . Atlanta USA, Inc. (2013). Available online at: http://www.cancer.org/research/cancerfactsstatistics/breast-cancer-facts-figures
3. American Cancer Society. Breast Cancer Facts and Figures . Atlanta, GA: American Cancer Society (2011).
4. Maznah D, Daniel EHG, Nur AT, Ranjit P, Jennifer L. Predictors of breast cancer screening uptake: a pre intervention community survey in Malaysia. Asian Pac J Cancer Prev. (2012) 13:3443–9. doi: 10.7314/apjcp.2012.13.7.3443
CrossRef Full Text | Google Scholar
5. Fregene A, Newman A. Breast cancer in Sub-Saharan Africa: how does it relate to breast cancer in African-American women? Cancer (2005) 103:1540–50. doi: 10.1002/cncr.20978
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Ly M, Antoine M, Andre F, Callard P, Bernaudin JF, Diallo DA. Breast cancer in Sub-Saharan African women: review. Bull Cancer (2011) 98:797–806. doi: 10.1684/bdc.2011.1392
7. Dye TD, Bogale S, Hobden C, Tilahun Y, Deressa T, Reeler A. Experience of Initial symptoms of breast cancer and triggers for action in Ethiopia. Intrational J Breast Cancer (2011) 2012:1–5. doi: 10.1155/2012/908547
8. Lingwood RJ, Boyle P, Milburn A, Ngoma T, Arbuthnott J, McCaffrey R, et al. The challenge of cancer control in Africa. Nat Rev Cancer (2008) 8:398–403. doi: 10.1038/nrc2372
9. Akarolo-Anthony SN, Ogundiran TO, Adebamowo CA. Emerging breast cancer epidemic: evidence from Africa Breast Cancer Res. (2010) 12:8. doi: 10.1186/bcr2737
10. Martha NS, Benford M. Breast cancer knowledge and awareness among university students in Angola. Pan Afr Med J (2012) 11:70.
11. Parkin DM, Whelan SI, Ferlay J, Storm H. Cancer Incidence in Five Continents . Vol. 1–8. Lyon: IARC Press; IARC Cancer Base no 6 (2005).
PubMed Abstract
12. Ricci Susan Scott. Women's Health Throughout the Lifespan: Maternity and Pediatric Nursing . Philadelphia, PA: Wolters Kluwer Health, Lippincott Williams & Wilkins (2009). p. 180–96.
13. Panieri E. Breast cancer screening in developing countries. Best Pract Res Clin Obstet Gynaecol . (2012) 26:283–90. doi: 10.1016/j.bpobgyn.2011.11.007
14. Anderson BO, Braun S, Lim S, Smith RA, Taplin S, Thomas DB. Early detection of breast cancer in countries with limited resources. Breast J . (2003) 9 (Suppl. 2):S51–9. doi: 10.1046/j.1524-4741.9.s2.4.x
15. McCready T, Littlewood D, Jenkinson J. Breast self-examination and breast awareness: a literature review. J Clin Nurs . (2005) 14:570–8. doi: 10.1111/j.1365-2702.2004.01108.x
16. Mathiwos Wondu Ethiopian Cancer Society (MWECS). World Cancer Day Press Release (2011).
17. Lwanga SK, Lemeshow S. Sample Size Determination for Health Studies: A Practical Manual . Geneva: World Health Organization (1991).
18. Hadi MA, Hassali MA, Shafie AA, Awaisu A. Evaluation of breast cancer awareness among female university students in Malaysia. Pharm Prac. (2010) 8:29–34. doi: 10.4321/S1886-36552010000100003
19. Abduelmula RA, Fatima KS, Salma S, Talal AA. Evaluation of breast cancer awareness among female university students in university of Sharjah, UAE. Adv Breast Cancer Res . (2015) 4:9–21. doi: 10.4236/abcr.2015.41002
20. Kalandar A, Salah MA, Sanjoy KP, Khalid A, Gebrehiwot GK. Breast cancer awareness and practice of breast self-examination among female medical students in Haramaya University, Harar, Ethiopia. IJIMS (2014) 2:109–19. Available online at: https://pdfs.semanticscholar.org/d1c2/5a1e63799f40bc5a3fc4fc07eb19fd63707e.pdf
21. Mehrnoosh AZ, Latiffah AL, Muhamad HJ, Salmiah MS, Irmi ZI. Knowledge of female undergraduate students on breast cancer and breast self-examination in klang valley, Malaysia. Asian Pac J Cancer Prev . (2015) 16:6231–5. doi: 10.7314/APJCP.2015.16.15.6231
22. Boulos DN, Ghali RR. Awareness of breast cancer among female students at ain shams university, Egypt. Glob J Health Sci . (2014) 6:154–61. doi: 10.5539/gjhs.v6n1p154
23. Reem MAJ, Shah AK. Knowledge and awareness of breast cancer among university female students in Muscat, Sultanate of Oman- A pilot study. J Appl Pharm Sci . (2011) 1:146–9. Available online at: http://japsonline.com/admin/php/uploads/316_pdf.pdf
24. Lamport L, Andre T. AIDS knowledge and responsibility. Youth Soc. (1993) 25:38–62. doi: 10.1177/0044118X93025001003
25. Yip C, Mohd TN, Ibraham M. Epidemiology of breast cancer in Malaysia. Asian Pac J Cancer Prev . (2006) 7:369–74.
PubMed Abstract | Google Scholar
26. Elsadig YM, Waqas S, Abdullah AA, Abdulrahman MA, Ahmad KA, Khalid MA. Breast cancer awareness and breast self-examination among future female university graduates: comparison between medical and non-medical students. Int J Res Med Sci . (2016) 4:685–9. doi: 10.18203/2320-6012.ijrms20160505
27. Doaa GM, Eman SAA, Nadia MT. Effect of a Breast-Self Examination (BSE) educational intervention among female university students. Am J Nurs Sci. (2015) 4:159–65. doi: 10.11648/j.ajns.20150404.13
28. Deborah OO, Mildred UE, John EA, Amaka AM. Knowledge and awareness of breast cancer among university students in South-South Nigeria. Sch. Acad. J. Pharm . (2017) 6:4–15.
29. Grunfeld EA, Ramirez AJ, Hunter MS, Richards MA. Women's knowledge and beliefs regarding breast cancer. Br J Cancer (2002) 86:1373–8. doi: 10.1038/sj.bjc.6600260
30. Fetene KA. Assessment of Breast Cancer Knowledge and Practice of Breast Self - Examination Among Female Students in Madawalabu University . Masters' thesis, Addis Ababa University, Bale (2014).
Keywords: breast cancer, awareness, self-examination of breast, treatment-outcome, Ethiopia
Citation: Gebresillassie BM, Gebreyohannes EA, Belachew SA and Emiru YK (2018) Evaluation of Knowledge, Perception, and Risk Awareness About Breast Cancer and Its Treatment Outcome Among University of Gondar Students, Northwest Ethiopia. Front. Oncol . 8:501. doi: 10.3389/fonc.2018.00501
Received: 09 August 2018; Accepted: 15 October 2018; Published: 02 November 2018.
Reviewed by:
Copyright © 2018 Gebresillassie, Gebreyohannes, Belachew and Emiru. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yohannes Kelifa Emiru, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Breast cancer awareness, risk factors and screening practices among future health professionals in Ghana: A cross-sectional study
Roles Data curation, Investigation, Methodology, Project administration, Writing – review & editing
Affiliation Department of Physician Assistantship, School of Medicine, University of Health and Allied Sciences, Ho, Ghana
Roles Supervision, Writing – review & editing
Affiliation Department of Psychological Medicine and Mental Health, School of Medicine, University of Health and Allied Sciences, Ho, Ghana
Roles Formal analysis, Software, Validation, Writing – review & editing
Affiliation Department of Epidemiology and Biostatistics, School of Public Health, University of Health and Allied Sciences, Ho, Ghana
Roles Writing – review & editing
Affiliation Department of Population and Behavioural Sciences, School of Public Health, University of Health and Allied Sciences, Ho, Ghana
Roles Resources, Supervision, Writing – review & editing
Affiliation Directorate of Human Resource, University of Cape Coast, Cape Coast, Ghana
Roles Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Population and Behavioural Sciences, School of Public Health, University of Health and Allied Sciences, Ho, Ghana, Department of Public Health Graduate School, Yonsei University, Seoul, Republic of Korea
- Sandra Osei-Afriyie,
- Albert Kwesi Addae,
- Samuel Oppong,
- Hubert Amu,
- Emmanuel Ampofo,

- Published: June 24, 2021
- https://doi.org/10.1371/journal.pone.0253373
- Reader Comments
Like many other women in the developing world, the practice of breast cancer screening among Ghanaian women is unsatisfactory. As a result, many cases are diagnosed at advanced stages leading to poor outcomes including mortalities. An understanding of the awareness and predictors of breast examination is an important first step that may guide the design of interventions aimed at raising awareness across the general population. This study aimed to explore the awareness, risk factors, and self-reported screening practices of breast cancer among female undergraduate students at the University of Health and Allied Sciences.
This cross-sectional study was conducted among 385 female undergraduate students using a pre-tested questionnaire. Data were analysed using Stata Version 13.1 and presented using descriptive and inferential statistics comprising frequency, percentage, chi-square, and binary logistic regression. Odds ratios and 95% confidence intervals were computed to quantify the association between regular Breast-Self Examination (BSE) and socio-demographic characteristics of respondents.
Seventy-three per cent of the students were aware of breast cancer, with social media being the most important source of information (64.4%). The prevalence of breast cancer risk factors varied from 1% of having a personal history of breast cancer to 14.3% for positive family history of breast cancer. Current use of oral pills/injectable contraceptives was confirmed by 13.2% of participants; 20% were current alcohol users and10.1% were physically inactive. Regarding breast examination, 42.6% performed BSE; 10.1% had Clinical Breast Examination (CBE), while 2.3% had undergone mammography in the three years preceding the study. Women who did not believe to be susceptible to breast cancer (AOR: 0.04; 95%CI: 0.02–0.09) and those who did not know their risk status (AOR: 0.02; 95%CI: 0.005–0.57) were less likely to perform regular BSE compared to those who displayed pessimism. Further, women with no religious affiliation had 0.11 (95%CI: 0.02–0.55) odds of examining their breast regularly compared to Christians.
This study demonstrated moderate awareness of the modalities of breast cancer screening and the risk factors of breast cancer among the students. However, there exists a gap between awareness and practice of breast cancer screening, which was influenced by optimism in breast cancer risk perception and religion. Awareness campaigns and education should be intensified in the University to bridge this gap.
Citation: Osei-Afriyie S, Addae AK, Oppong S, Amu H, Ampofo E, Osei E (2021) Breast cancer awareness, risk factors and screening practices among future health professionals in Ghana: A cross-sectional study. PLoS ONE 16(6): e0253373. https://doi.org/10.1371/journal.pone.0253373
Editor: Antonio Simone Laganà, University of Insubria, ITALY
Received: July 4, 2020; Accepted: June 4, 2021; Published: June 24, 2021
Copyright: © 2021 Osei-Afriyie et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its S1 Data , S1 Questionnaire files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Breast cancer is the most prevalent cancer in women and generally the second most common cancer globally, with approximately 1.4 million cases diagnosed annually [ 1 ]. In 2018, 2.1 million incident cases of breast cancer were diagnosed worldwide (second most common cancer overall after lung cancer) representing nearly 12% of all incident cancer cases and an estimated 627,000 deaths were expected to occur globally [ 2 , 3 ]. Generally, the breast cancer rate is higher in the developed world than the developing countries, which may be as a result of certain lifestyles and reproductive factors that are more common in the developed world. The difference may be exaggerated due to relatively low awareness, screening practices, and diagnoses in the developing countries, though the rates are increasing rapidly in many developing countries [ 4 ].
In Ghana, breast cancer is becoming a great public health challenge among women. With about 2,900 incident cases occurring annually, and one-eighth of them dying from it, the disease has become the most common cancer-related death among Ghanaian women [ 5 , 6 ]. Previous studies have revealed an increased breast cancer burden in Ghana over the past decade. Clegg-Lamptey et al. [ 7 ] reported in 2009 that breast cancer now accounts for about 16% of all cancers and the most common cancer female cancer in Ghana. Naku et al. [ 8 ] estimated the incidence of breast cancer to be 76 per 100 000 Ghanaian women.
It is anticipated that the incidence of breast cancer will increase as Ghana’s population ages and women adopt western lifestyles [ 9 ]. Studies have shown that breast cancer is increasingly becoming common among younger Ghanaian women, and they present at a more advanced stage of the disease [ 5 , 7 , 10 ]. The advance stage at diagnosis is due to patients’ delay in seeking healthcare, which can be up to 10 months after the onset of symptoms, as a result of lack of awareness of the disease at its early stage and stigma associated with the disease [ 8 , 11 , 12 ].
Like most cancers, the primary risk factor for breast cancer in women is older age. Many other risk factors alter the exposure of breast tissues to reproductive hormones [ 4 ]. Some of these are modifiable, and include weight gain or being overweight/obese, long term use of the postmenopausal hormone, alcohol consumption, and physical inactivity [ 4 , 13 ]. Long menstrual history (younger age at menstruation and/or end later age at onset of menopause), never given birth, having one’s first child after age 30, and current use of hormonal contraceptives are other reproductive factors that influence the risk of breast cancer [ 11 , 12 ]. Personal medical or family history of breast cancer are also known to increase one’s risk for breast cancer [ 4 ].
Early diagnosis of breast cancer can increase the chance of early case detection and favourable outcomes, resulting in improved survival rates and quality of life of women and is therefore important public health strategy at all settings [ 2 ]. However, studies have demonstrated that factors related to women´s awareness, knowledge and perceptions about the disease may contribute significantly to health-seeking behaviours [ 14 , 15 ].
Notwithstanding that mammography is known to be the most effective screening tool for early detection of breast cancer [ 16 ], Breast-Self Examination (BSE) may be useful in resource-limited countries to detect any abnormalities in the breast as it provides an opportunity for women to be familiar with their breasts and promptly report any changes [ 17 ]. Additionally, clinical encounters by women provide the opportunity for women to have a number of important clinical activities such as breast cancer risk assessment, education about lifestyle, counselling, and clinical breast examination (CBE) that may not otherwise be done [ 17 ]. There are no current national breast cancer screening protocols in Ghana or countrywide literacy initiatives, and there is limited availability of mammography or ultrasound machines [ 5 ]. Although the effectiveness of BSE and CBE in detecting breast cancer is debatable [ 16 ], they have been campaigned as major screening tools given their availability at little to no cost among limited-resource settings in most developing countries.
Women who practice regular breast screening have been known to have a lower risk of developing an advanced form of breast cancer than those who do not. Reports have shown low uptake of breast cancer screening among women in many sub-Saharan African countries and this results in late detection and increased mortality in affected women [ 18 ].
Even though the incidence and mortality of breast cancer have been on the increase, there is a paucity of the empirical literature on student’s awareness, risk factors and screening practices in Ghana. This population is especially important because they have abundant access to health information as health students and they are potential sources of information for non-health students and the general population. College students have a significant influence on colleague students and also, findings regarding this target group have implications for their capacity in the role of promoting screening for breast cancer as potential health professionals. This study, therefore, explored breast cancer awareness, selected risk factors, and screening practices among female undergraduate students, to provide information for the control, prevention, and early treatment of the disease.
Materials and methods
Study site and design.
We conducted a cross-sectional study among female undergraduate students at the University of Health and Allied Sciences (UHAS), Ghana in February 2019. Ghana has a projected population of 30,280,482 in 275 districts distributed among 16 administrative regions as of June 2019 and is divided into some 75 ethnic groups with the Akans forming the majority. UHAS is among the newest public Universities in Ghana which was established in 2011 and is located at Ho in the Volta Region. UHAS is so far the only public University solely dedicated to the training of varied health professionals such as medical doctors, nurses, midwives, pharmacists, public health professionals etc. in Ghana. The University has two main campuses; the main campus, which is located at Ho (where this study was carried out), and the Hohoe campus, which has the School of Public Health. There are currently six schools/colleges in the University, with a current student population of about 3,752. Among the programmes offered by the University are Medicine, Physician Assistantship, Nursing, Midwifery, Physiotherapy, Pharmacy, Dietetics, Speech and Language Therapy, and Public Health [ 19 ].
Sample size determination
We obtained the required sample size for this study using Cochran’s single proportion formula; n = z 2 pq/d 2 , where n = sample size, z = z-score at 95% confidence level, p = estimated proportion of an attribute that is present in the population, q = 1-p, d = margin of error. This study assumed a margin of error(d) of 0.05 at 95% confidence level and an estimated proportion of 60.9% women with regular breast screening practice [ 20 ]. Adjusting for a non-response rate of 5%, 385 students were sampled and participated in the study. Thus, we sampled 385 students of which all participated.
Sampling procedure
We used two levels of stratified sampling method to select the study participants from to ensure representativeness. First, students were stratified according to faculty (school), defined as one of the 5 constituent schools in the University, namely, School of Allied Health Sciences; School of Basic and Biomedical Sciences; School of Medicine; School of Nursing and Midwifery; and School of Pharmacy. For each faculty, students were stratified according to their level (year) of study, where simple random sampling was used to select the required number of students separately from each faculty and academic year. This was done by obtaining names of all female students according to their faculty and level of study from the University’s administration. The names of eligible students were arranged and numbered alphabetically separately for each faculty and level in a Microsoft excel sheet, where random numbers were generated, and the corresponding students selected to take part of the study. The number of students selected from each academic year and faculty was proportional to the students’ population. Selected students were approached by the lead author who was also a student in the University in January 2019 and after explaining the study’s objectives and procedures to them, all (100%) agreed to participate in the study. Students who were under 18 years of age were excluded from this study.
Data collection tools and procedure
A structured pre-tested questionnaire was used to collect data from participants. The questionnaire contained closed-ended questions adapted from previously published studies that adapted validated questions and had the following sections: demographic information, breast screening practices, risk factors of breast cancer (Behavioural, reproductive, and hormonal factors), and awareness of breast cancer.
Consenting participants were handed printed copies of the questionnaire and were given 24 hours to fill their responses and return them anonymously to the researchers. The objectives of the study were explained to all participants before the questionnaires were given out. Filled questionnaires were checked daily by the researchers for consistency and omissions before collection. Where there were inconsistencies, participants were made to correct them in the presence of the researchers before they were taken.
Definition of variables.
Table 1 presents the definitions of some of the study variables measured in this study.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0253373.t001
Data analysis
All analyses were carried out using STATA (Stata Corp, College Station) statistical package Version 13. Descriptive statistics were used to describe the study population in relation to relevant variables. Bivariable and multivariable logistic regression models were used to identify significant predictors of regular BSE defined as having examined the breast at least once every month. First, the association of regular BSE with each variable of interest (Participant’s age, religion, ethnicity, faculty of study, academic year, family history of breast cancer, having known or seen a breast cancer patient, perceived risk for breast cancer, physical activity, current Alcohol use and current use of contraception) was examined. Second, variables with p-value <0.20 in the first model were considered for inclusion to construct a model with risk factors independently associated with the outcome variable. The degree of association between dependent and independent variables was assessed using odds ratios (OR) with 95% confidence intervals (CI).
Ethical issues
The study approval by the University of Health and Allied Sciences’ Ethics Review Committee with reference UHAS-REC A.8 [ 56 ] 18–19. Written informed consent was obtained from each respondent after explaining the study’s procedure and potential risk and benefits to them. Participants’ identifiers such as name and address were not collected.
General characteristics of respondents
All 385 participants returned their completed questionnaire. The mean age of the study population was 22 ± 2.78. The majority (55.8%) were between 20 and 24 years old, while 1.3% were 30 years and above; 16.4% were currently married and 83.1% were single; 74.0% were Christians and 18.9% were Muslims. Regarding ethnicity, Akans were the majority (38.4%), followed by Ewes (30.9%), while 14.3% belonged to the Ga-Dangbe ethnic group. Respondents constituting 26.2% (n = 101) were in their first year of study, 21.8% were in the second year, 30.2% in the third year and 21.8% were fourth-year students. The comparative majority (52.5%) were studying Nursing and midwifery, 22.3% were Medical students, and 19.7% were Allied Health Sciences students ( Table 2 ).
https://doi.org/10.1371/journal.pone.0253373.t002
Breast cancer awareness and risk perception
Regarding breast cancer awareness, 281 (73.0%) of the respondents reported having ever heard of breast cancer. The remaining items in Table 2 were asked of the 281 women who had heard of breast cancer. The social media remained the most important source of information on breast cancer (181;64.4%), followed by teachers (173; 62%) and the electronic media (172; 61%). As presented in Table 2 , the majority (200; 71.1%) of respondents were aware of mammography as a screening method for breast cancer; 196 (69.8%) were aware of BSE; while 28 (10.0%) of them did not know of any the screening methods. Family history of breast cancer (n = 236, 83.9%), genetics (n = 229, 81.7%) female sex (n = 173, 71.9%) and individual lifestyle (n = 176, 62.6%) were the most frequently indexed risk factors for breast cancer. Meanwhile, nulliparity (n = 100, 35.6%), early menses/menopause (n = 116,41.3%), and Obesity (n = 159, 56.6%) were the least known risk factors. Putting money in the brassiere was implicated as a potential risk factor for breast cancer by more than a third (n = 106, 37.7%) of study participants. The most common presentation of breast cancer aware of was a lump in the breast (n = 259, 92.2%), followed by nipple discharge (n = 219, 77.9%), and lymph node in the armpit (n = 191, 68%) while pulling off a nipple (n = 47, 16.7%), nipple itch (n = 55, 19.6), and swollen nipple (n = 97, 34.5) were the least known sign/symptom of breast cancer.
Among students who were aware of breast cancer, 129 (45.9%) thought that they do not have the chance of getting breast cancer, while 46 (16.4%) did not know whether they were at risk or not ( Table 3 ).
https://doi.org/10.1371/journal.pone.0253373.t003
Breast cancer risk factors
Among the 385 study participants, menarche occurred below age 12 in 48 (12.5%) of them, while 72 (18.7%) were more than 14 years at menarche. The prevalence of current oral pill/injectable contraceptive use was 13.2% (n = 51). The occurrence of breast cancer in the family was confirmed in 55 (14.3%) of the respondents; 14 (4%) had their first-degree relatives (Mother, Sister) affected with the disease, while 41 (11%) were second-degree relatives. Four (1%) of the students had a personal history of breast cancer. Regarding behavioural factors, 39 (10.1%) did not engage in physical activity and 77 (20%) currently use at least one standard of alcohol per day ( Table 4 ).
https://doi.org/10.1371/journal.pone.0253373.t004
Breast cancer screening practices
Of the 385 participants, 212 (55.1%) ever applied at least one breast cancer screening method. Of these, 164 (42.6%) practised BSE, 39(10.2%) had undergone CBE, and 9 (2.3%) were screened for breast cancer via mammography. Of those who performed BSE, 136 (82.9%) did it at least once in every month; 6 (3.7%) examine their breast yearly, and 22 (13.4%) did it at random; 115 (70.1%) of them learned BSE skills from their school-teachers, 112 (68.3%) from the media, 37 (22.6%) were taught by their friends, and 26 (15.9%) learned it from their mothers. The most common (28.1%) reason for not practising BSE was “1 do not know how to perform it” followed by “I have no family history of breast cancer” (23.1%) and “I am not at risk of breast cancer” (17.2%), while 63 (28.5%) had no reason for not doing BSE ( Table 5 ).
https://doi.org/10.1371/journal.pone.0253373.t005
Predictors of breast self-examination
Table 6 shows the results of bivariable and multivariable logistic regression analyses aimed at identifying variables associated with the odds of performing regular BSE. After adjusting for confounding effect of the variables, women who were between 25 and 29 years old were 5.13 (95%CI: 1.18–22.26; P = 0.03) times more likely to perform regular BSE compared to those less than 20 years. Further, women with no religious affiliation had 60% less odds of performing regular BSE compared to Christians. Women who expressed optimism regarding breast cancer risk (AOR: 0.04; 95%CI: 0.02–0.09; p<0.001) and those who did not know their risk level (AOR: 0.02; 95%CI: 0.005–0.57; p<0.001) were less likely to perform regular BSE compared to those who were pessimistic about breast cancer risk.
https://doi.org/10.1371/journal.pone.0253373.t006
This study though has demonstrated considerable awareness about the existence of breast cancer, insufficient knowledge, and misconceptions regarding its risk factors and causes and disease presentation also existed among participants. Less than three-quarters of our study participants had heard about breast cancer. This is unexpectedly far lower than the 100% observed in medical students in Harar, Ethiopia [ 23 ], 98.7% among University of Ibadan female students [ 24 ], 95% previously reported among female students of Faculty of Health and Medical Sciences in Ghana [ 25 ], and 88.1% among Teacher Training college students in Cameroon [ 26 ]. The difference in the awareness rate found in this study and that of the aforementioned studies cannot directly be explained. However, breast cancer has been adopted in the curriculum of the first two aforementioned studies in an attempt to create awareness among students and might have had a positive impact on the students’ awareness about the disease. Ours finding further show unsatisfactory levels of awareness and understanding of breast cancer risk factors and disease presentation. More than one-third of participants were not recognised increasing age, nulliparity, obesity, and early menstruation and late menopause as potential risk factors for breast cancer, while 5% did not know any risk factor for breast cancer. This finding confirms reports from previous studies in Ethiopia [ 27 ], Nigeria [ 28 ], Egypt [ 29 ], and Angola [ 30 ] where general knowledge and risk factors of breast cancer were found to be low among female college students. Knowledge gaps have also been identified among the general population elsewhere [ 31 , 32 ]. About one-third of our respondents held the belief that putting money in the brassiere can result in breast cancer. This is in line with other studies among women in the general population [ 33 , 34 ] as well as university students [ 24 ] that suggest that women still have misperceptions about the cause of breast cancer with some attributing it to the spiritual origins. Additionally, as reported by previous studies elsewhere, [ 23 , 26 ] awareness of other clinical manifestations of breast cancer other than breast lump was worryingly low. These existing knowledge gaps and misconceptions may impact health-seeking behaviours and uptake of breast screening resulting in late diagnosis which in turn may lead to complications and death. Thus, the need for health education programmes aiming to increase awareness about the causes, risk factors and clinical presentation of breast cancer is warranted.
Predictors of breast cancer risk are varied, including individual lifestyle, reproductive status, and genetics. This study attempted to identify some of these risk factors among the students. First menstruation at an early age (early menarche) is known to be associated with increased levels of endogenous hormones (estrogen and progesterone) in a woman’s lifetime which increases the risk of breast cancer [ 17 ]. In this study, about 13% of participants had their menarche at an age younger than 12 years. In the Lublin region of Poland, menarche occurred at 11 years in only about 3% of women attending screening a programme [ 35 ].
Among the most extensively researched risk factors of breast cancer is the use of exogenous hormones in the form of oral contraceptives and hormone replacement therapy (HRT) [ 36 ]. Lina et al. [ 37 ] in their study to assess the association between the use of hormonal contraception and the risk of invasive breast cancer among 1.8 million Danish women demonstrated that current and recent users of hormonal contraception had 20% increased risk of breast cancer compared with those who had never used hormonal contraception. We found in this study that, about 13% of women were current users of oral pills/injectables. None of them was however on HRT.
A positive family history of breast cancer in a first-degree relative is the most commonly known risk factor for the disease [ 38 ]. Women with a family history of breast cancer in a mother or sister have up to a 3-fold increase in the risk of developing breast cancer [ 38 ]. In this present study, about 14% of the participants had a positive family history of breast cancer, among whom 4% occurred in first degree relatives (mother and sister), and hence have increased risk of the disease. Our result is higher than that reported in the previous study in Ghana, where 1.4% of women had a first-degree family history of breast cancer [ 8 ]. and another study among university students in Ajman, UAE, where a positive family history of breast cancer was found in 9% of students and about 1% with the first-degree relative affected with breast cancer [ 39 ]. Researchers have devoted much attention to understanding the role that genes play in the development of breast cancer. This has helped in recognizing that some women could be at increased risk as a result of inherited predisposition. It must be acknowledged however that other than genes, families also share other factors such as cultural background and environmental exposures, which are themselves potential predictors of breast cancer [ 39 ].
The relationship between alcohol consumption and an increased risk of developing breast cancer has been the subject of many studies. Compared with non-alcohol drinkers, women who drink even in small amounts, have increased risk of breast cancer. The risk increases with an increased amount of alcohol consumed per day [ 40 ]. In many traditional African societies including Ghana, alcohol consumption is not common among females and the youth and people usually frown on alcohol intoxication [ 41 ]. The prevalence of alcohol consumption in African women varies from 1% in Malawi to 30% in Burkina Faso with about 81% of women in Africa reporting lifetime abstinence [ 42 ]. The prevalence of current alcohol consumption (20%) among female undergraduates found in this study is similar to levels (19.6%) reported among women in the WHO African regions in 2012 [ 43 ]. Martinize et al. [ 42 ] reported that about two-thirds of Ghanaian women abstain from alcohol in their lifetime. Kofi Adesi Kyei and colleagues found in their previous 5-year retrospective review to identify predominant lifestyle risk factors of breast cancer among Ghanaian women that alcohol contributed to about 19% to the disease with respect to preventable risk factors [ 44 ] and concluded that alcohol is not the most important preventable risk factor for breast cancer in Ghana. However, having 2 in 10 future female health professionals drinking alcohol is significant enough to warrant public health action due to the health consequences of alcohol on women.
Many studies have reported an inverse relationship between regular physical activity and breast cancer risk. Several biologic mechanisms have supported the protective effect of physical activity on breast cancer which includes effect on immune, endogenous sex steroid hormone production, and antioxidant system [ 44 – 46 ]. In this present study, 1 in 10 women was not physically active. Of those who were, the majority engaged in brisk walking. Comparing the most active and least active women, most studies estimate the risk reduction of breast cancer to be between 20 and 40% and recognise the dose-response relationship with risk increase levels of risk reduction [ 47 – 49 ]. Several mechanisms might be the cause of this inverse association with physical activity. Increased levels of activity are known to reduce body weight, thus reducing the risk of breast cancer. Physical activity may also influence the production, metabolism, and excretion of endogenous hormones that can result in lower levels of bioactive oestrogen, insulin, and other growth factors [ 50 ].
Accurate and early diagnosis of breast cancer depends mainly on the "opportunist approach". Given the challenges faced by resource-limited countries, improving breast cancer awareness and the application of screening methods remains a practical option for early detection and treatment of breast cancer. Similar to reports from previous studies done in different parts of the world including Ghana at different times, the performance of breast cancer examination is generally low [ 51 – 56 ]. Notably in this study, less than half of the participants performed BSE, 10% had CBE, and an even lower percentage (2.3%) had Mammography. This is a worrying phenomenon owing to the fact that breast cancer is increasingly becoming common in this part of the world, hence women and young ladies need to frequently subject themselves to screening for early detection and treatment to avoid complications and death. The low coverage of breast cancer screening among our study population could perhaps be explained by their young age as breast cancer has been known to be common among older women.
While the effectiveness of BSE to detect breast malignant tumour remains debatable, its importance in breast self-awareness creation in resource-limited countries with non-existent population screening programmes cannot be overemphasis, thus deserves consideration. The level of BSE practice in this study is, however, higher than that reported among over 10,000 undergraduate students from 24 countries across Africa, Asia and America. (9.1%) [ 57 ], and that of other studies among students in Ethiopia (39.4%), Cameroon (3%), Libya (23.5%) [ 53 , 58 , 59 ]. The rising trends in the incidence of breast cancer in Africa may be explained by the lack of health consciousness of young women to examine themselves for the timely identification of any breast abnormality. In this study, lack of skills, no family history of breast cancer and pessimism about the risk of the disease were the most important reasons for not performing BSE. This is a worrying finding since these are future healthcare professionals who are required to educate others in the community about the disease and the need for primary prevention. University students are among the well-informed group of women in Ghana. Their lack of skills in performing breast screening and the need for periodic screening, therefore, is indicative of a greater lack of skills and awareness among the general population of less-educated women. Similar, in Ethiopia, being healthy and lack of knowledge were the overriding factors given [ 53 ]. In a previous study among Presbyterian university college students in Ghana, varied reasons including, lack of time, forgetfulness, procrastination, and fear were the reasons for not performing BSE [ 25 ]. The social media could be an important tool that can be harnessed to educate women on the need for regular and correct practice of BSE since it remained the most important source of education for women who performed BSE in this study.
Expectedly, this study demonstrates that risk perception, an important component of behavioural change paradigm, is a sufficient enough variable that is capable of affecting women’s breast cancer screening behaviour. Women who did not believe to be vulnerable to breast cancer and those who did not know their risk status were less likely to practice BSE regularly compared to those who were pessimistic about their risk of the disease. Our result confirms the assertion of the Health Belief model that women who with a higher risk for breast cancer, perceive breast cancer as a serious threat, have a lower perception barrier, and who hold a higher perception of the benefits are more likely to perform regular BSE [ 60 ]. Erbil and Bolukbas also suggest that women’s health beliefs and attitudes remain the predominant factors that influence whether or not they will get themselves screened for breast cancer [ 61 ]. Among Korean women, those with lower perceived comparative risk were more likely to have no intention of getting a mammogram [ 62 ]. Further, this study demonstrated that who were not affiliated to any religion were less likely to examine their breast regularly compared to their counterparts who belonged to the Christianity religion perhaps due to exposure to breast cancer information in churches.
It is interesting to note that other risk variables such as physical activity, Alcohol consumption, and contraception use, and positive family history did not influence breast BSE in this present study. This is a worrying finding because women with risk factors are expected to perform regular breast examinations to detect the disease at its early stage to prevent complications and death. It can be suggested that university women do not practice BSE even though they have some risk factors of breast cancer.
There are three limitations of our study worth mentioning. First, the findings cannot be generalised beyond the study population since they are young and well-educated women. University students are not representative of young adults in general, and the risk perception, risk factors, and breast cancer screening practice may differ from that of the general population. Secondary, all data were self-reported with no objective measures to assess the accuracy of these reports. Lastly, the instrument used was not tested for its validity, however, questions used were taken from validated tools from previous studies at other settings. Nevertheless, the results of this study provide some understanding regarding perceived risk and the practice of breast screening among future health professionals, which can be useful for directed health promotion and education.
The research concludes that the awareness of breast cancer and its causes, risk factors, and disease manifestation was generally unsatisfactorily low. Additionally, even though some students possess some important risk factors of the disease, the practice of BSE coverage which was influenced by risk perception and religion was low. Improved methods of risk communication are recommended to ensure that women have appropriate risk information to make informed choices about risk management options and preventative interventions. Social media can also be a reliable tool for health education on breast cancer.
Supporting information
S1 data. anonymised data set used for this study..
https://doi.org/10.1371/journal.pone.0253373.s001
S1 Questionnaire. Assessment of breast cancer risk factors and screening practices among university female students, Ghana.
https://doi.org/10.1371/journal.pone.0253373.s002
Acknowledgments
SOA acknowledge the support provided to her by all faculty in the department of Physician Assistantship, University of Health and Allied Sciences, Ho, Ghana. Sincere thanks go to all study participants.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. World Health Organization, “Cancer,” retrieved from http://www.who.int/topics/cancer/en/ on February 10, 2019.
- 16. American Cancer Society, “American Cancer Society recommendations for the early detection of breast cancer”. https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html . On February 12 2020.
- 17. Bevers T, El-Serag H, Hanash S, Thrift AP, Tsai K, Maresso KC, et al. Screening and early detection. In Abellof’s Clinical Oncology, sixth edition; 2020. Elsevier. ISBN 978-0-323-47674-4.
- 19. The University of Health and Allied Sciences, Ghana. http://www.uhas.du.gh .
- 21. World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm. Geneva: WHO; 2000.
- 22. Global Physical Activity Questionnaire (GPAQ) Analysis Guide. https://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf (accessed April 20, 2020).
- 38. National Breast and Ovarian Cancer Centre. Breast cancer risk factors: a review of the evidence. National Breast and Ovarian Cancer Centre, Surry Hills, NSW, 2009.
- 41. Oshodin OG. Nigeria. In Heath B. D. (Ed.), International handbook on alcohol and culture (First ed., pp. 213–223). Westport: Greenwood Press. 1995.
- 49. Vainio H, Bianchini F. IARC Working group on the evaluation of cancer-preventive agents. Weight control and physical activity. Lyon, France: International Agency for Research on Cancer (IARC), 2002.
- Open access
- Published: 31 August 2022
Factors that influence breast cancer screening among women of reproductive age in the Nandom Municipality, Ghana
- Margaret Mary Wuur 1 ,
- Dillys Adomakoa Duodu 4 &
- Elvis Enowbeyang Tarkang 1 , 2 , 3
BMC Women's Health volume 22 , Article number: 359 ( 2022 ) Cite this article
3192 Accesses
3 Citations
1 Altmetric
Metrics details
In Ghana, breast cancer is a major public health concern and the most common type of cancer among women in terms of mortality and incidence. This study determined the factors influencing breast cancer screening among women of reproductive age in Nandom Municipality, Ghana using the Health Belief Model as the conceptual model.
The study was cross-sectional in design. A pretested structured questionnaire was administered to 243 womens of reproductive age in the Nandom Municipality. Descriptive and inferential statistics were performed using STATA version 16 at a 0.05 level of significance.
The uptake of breast cancer screening was 51.9%. Respondents who had a tertiary level of education were less likely to be screened for breast cancer [AOR = 0.10 (95% CI = 0.02–0.54); p = 0.008]. Respondents who perceived high susceptibility to breast cancer were more likely to get screened [AOR = 1.97 (95% CI = 1.12–3.47), p = 0.019]. Respondents who perceived the high severity of breast cancer were more likely to be screened for breast cancer [AOR = 4.55 (95% CI = 1.32–15.76), p = 0.017]. Also, respondents who perceived high barriers to breast cancer screening were more likely to be screened for breast cancer [AOR = 0.15(95% CI = 1.42–4.22), p < 0.001].
The uptake of screening among women of reproductive age in the Nandom Municipality is low. Health promotion interventions to improve breast cancer screening should target women with a tertiary level of education and should focus on heightening the perceived threat of breast cancer and minimizing barriers to breast cancer screening.
Peer Review reports
Breast cancer kills approximately 425,000 women and is the leading cause of cancer deaths amongst women globally [ 1 ]. There were over two million breast cancer cases in 2018 worldwide representing 15.3% of all cancer cases and 627,000 women died from the disease [ 1 , 2 ]. The annual incident rate is 5.8% [ 3 ].
In Ghana, breast cancer remains a public health concern and the most common type of cancer among women in terms of incidence and mortality. Current epidemiological data on breast cancer are inadequate as most studies are based on clinic pathological characteristics [ 4 , 5 , 6 ]. However, interestingly, 30% of breast cancer cases in Ghana are below 35 years, which may indicate a relative possible shift of cancer burden to women in their early thirties compared to western countries [ 7 ].
Breast cancer screening is the cornerstone of early detection [ 8 ]. Four main screening modalities can be used to help detect breast cancer. The screening methods include breast self-examination (BSE), Clinical breast examination (CBE) (by a doctor or a nurse), Ultrasound of the breast and mammography. Breast cancer requires advanced facilities to diagnose and treat, which are mainly by surgery, chemotherapy, and radiotherapy which are done in few hospitals in the urban areas of Ghana. This creates a geographical barrier to accessibility for most Ghanaian women [ 9 ]. With the National Health Insurance Scheme not at its best, financial barriers to breast cancer screening thus exist, amongst other factors. Since breast cancer is a complex and heterogeneous disease with ethnic and social variations [ 10 ], each District or population in Ghana must have accurate knowledge that defines the characteristics of the disease amongst its people to determine ways of controlling its mortality. Many factors however are bound to influence breast cancer screening amongst women of reproductive age.
The Nandom Municipality has had its fair share of this galloping cancer as it is estimated according to end of year review that, out of every ten women who report to the various Maternal and Child Health Clinics in the various sub-Municipalities, at least one has a complaint of breast swelling, lumps or sore nipples, which are signs of breast cancer [ 11 ]. Unfortunately, because mammography is not done in the municipality women have to be referred to as far as to Tamale Teaching Hospital for the screening. Due to this breast cancer screening is a challenge in the municipality.
It is imperative therefore to unearth the factors that influence breast cancer screening in the Nandom Municipality to find ways of detecting and diagnosing the disease early to be able to stand a chance of curbing its menace. This can be achieved through systematic and thorough research. Nandom Municipality has no detailed literature on breast cancer screening so this study came out with some literature. Guided by the Health Belief Model (HBM), this study determined the factors influencing breast cancer screening among women in the Nandom Municipality of Ghana.
The current study was grounded on the HBM [ 12 ]. The HBM is a psychosocial model, which is widely used in health education and promotion. The idea of the HBM is that an individual’s health behavior is determined by his/her beliefs or perceptions about the disease and available plans to reduce the incidence of the disease [ 12 ].
The model focuses on six main constructs; perceived susceptibility, perceived seriousness, perceived barriers, perceived benefits, self-efficacy, and cues to action [ 12 ]. These constructs together determine a person’s likelihood of partaking in screening practices.
Nandom Municipality is one of the five Municipalities in the Upper West Region. The Municipality is located in the North-Western corner of the Upper West Region of Ghana between latitude 5° 18 W to 50° 10 W longitude of 1° 20 N to 2° 25 N. It shares boundaries with the Lambussie-Karni District to the East and Lawra District to the South and Burkina Faso to the North. The population of the Municipality in the 2010 population census stood at about 56,089 people with about 53.7% being females [ 13 ]. This showed the need to assess the factors that influenced the screening of breast cancer among women of reproductive age.
Study population
The study included women of reproductive age (18–49) in the Nandom Municipality.
Inclusion and exclusion criteria
All women of reproductive age and from Nandom Municipality who were available and consented to be part of the study. Those who fell within the inclusion criteria but who were seriously sick and admitted to a health facility were excluded.
Study design
A quantitative study approach using a descriptive cross-sectional design was employed in this study using a survey-type questionnaire.
Sample size determination and sampling method
The sample size was calculated using the formula by Degu and Tessema (2005) [ 14 ]. It was calculated based on 21.1% CBE among nurses in Ghana [ 15 ]. Assuming a Z score of 1.96 for a 95% level of confidence and a 5% margin of error, the sample size was 243.
\(n=\frac{{Z(\alpha /2)}^{2}p(1-p)}{{e}^{2}},\) where n = sample size.
Zα/2 = Z score of 1.96 at 95% confidence interval (CI).
P = proportion of women of higher risk of breast cancer in Ghana, 21.2%
e = margin of error, 5%
n = \(\frac{{\left( {1.96^{2} } \right)*0.2*\left( {1 - 0.212} \right)}}{{0.05^{2} }}\)
The study respondents were selected using a multistage sampling technique. The Nandom Municipality has five (5) sub-Municipalities, which are Ketuo, Ko, Baseble, Gengenkpe, and Nandom. To get a true representation of the Municipality, participants were selected evenly from each of the five sub-Municipality to participate based on consent. In each sub-Municipality, the names of all the communities were written on pieces of paper. These were mixed up and one community was picked randomly. A convenience sampling technique was then used to select participants. The researcher visited the child welfare clinic (CWC) of the selected communities from each sub-Municipality to administer the questionnaire to 49 women in each of the communities. The purpose of the study was explained to the nurses at the CWC by the research team. The nurses explained the purpose of the study to the women who brought their children for CWC services and directed them to the study team. The purpose of the study was further explained to the mothers by the research team. Participant information and consent forms (PICFs) were given to the participants and the study team members were available to answer questions raised by the participants. Those who consented to participate were selected for the study.
Data collection procedure
The data were collected by the use of a standardized questionnaire in October 2021. The completion of the questionnaires was done in the participants’ homes and the CWCs. Data were collected from participants who consented to participate in the study. Two persons at the various sub-Municipalities were trained to assist the researcher in the data collection. A pretested structured questionnaire adapted from Aba (2019) [ 16 ] was used to collect data on socio-demographic characteristics, uptake of breast cancer screening and factors that influence breast cancer screening based on the constructs of the HBM. At the end of every data collection session, the research assistants and the principal researcher reviewed all the questionnaires for accuracy and completeness before they were placed in files. This process continued till the sample size for the study was attained.
The uptake of breast cancer screening (dependent variable) was measured by using the number of people who have ever screened for breast cancer and those who have never screened. Additionally, composite scores were generated for the constructs of the HBM (independent variables). For all the constructs of the HBM, the responses ‘Strongly agree’ and ‘Agree’ were combined into ‘Agree’. Also, the responses ‘Strongly disagree’ and ‘Disagree’ were combined into ‘Disagree’. On the construct perceived susceptibility, 3 items were used: ‘I am likely to get breast cancer’, ‘The chances of getting breast cancer in the next few months are high’ and ‘I feel I will get breast cancer at a point in life’. Furthermore, the number of items used to measure perceived severity and perceived benefits were 3 (breast cancer can lead to death, breast cancer can lead to cutting of the beast & breast cancer is very dangerous to all women) and 6 (my family will benefit if I screen for breast cancer, I am not worried if nothing is found, screening can detect lumps early, treatment could be easier if a lump is detected early, screening is the best way to find a very small lump & screening can reduce my chances of dying from breast cancer) respectively. Twelve items were used to measure perceived barriers (I do not understand the screening procedure, I am afraid of a positive result, I do not know how to go about getting screened for breast cancer, It is too embarrassing to be screened, screening procedure takes too much time, health workers doing the screening are rude to patients, screening will expose me to unnecessary radiation, it is difficult to schedule a breast cancer screening, breast cancer screening is not a priority to me, I am too old to need a routine breast cancer screening, breast cancer screening is too painful & breast cancer screening is expensive) while 9 items measured self-efficacy (I can arranged for transportation to get screened for breast cancer, I can create time to have a breast cancer screening, I am confident to talk to staff at the screening center about my concerns, I have the confidence to go for breast cancer screening, I can afford the cost for breast cancer screening, I can schedule an appointment for breast cancer screening, I can always go for screening if I want to, I know how to go about getting screening for breast cancer, & I can locate a breast cancer screening center). Composite scores were generated from the responses using the 50th percentile (median). This was done to generate a binary composite score for each construct. The median was therefore used as the point to categorise the respondents into those with low and high perceived susceptibility, severity, benefits, barriers and self-efficacy.
Statistical analysis
The collected data were entered into EPI Data version 4.0.2.101 and exported into the STATA version 16 for analysis. Descriptive statistics such as frequencies and percentages were used to summarise the data. Binary logistic regression analysis was used to determine the association between breast cancer screening uptake and the independent variables (demographic variables and the constructs of the HBM) at the 0.05 level of significance and at a 95% confidence interval.
Demographic characteristics of respondents
From Table 1 , the majority 138(56.8%) of the respondents were aged less than 30 years; 69(28.4%) had a Junior High School (JHS) level of education and the majority 211(86.8%) were Christians. The majority 189(77.8%) were married and 138(56.8%) were housewives.
Uptake of breast cancer screening
The majority of the respondents 126(51.9%) had ever screened for breast cancer. Also, only 35(14.4%) had ever had their breast examined by a healthcare provider (CBE). To add, 56(23.0%) of the respondents had been screened more than a year ago and 29(11.9%) had their screening between 3 and 6 months ago (Table 2 ).
Association between demographic characteristics and breast cancer screening
The associations between the demographic characteristics of respondents and breast cancer screening uptake are presented in Table 3 . Respondents who had a tertiary level of education were less likely to be screened for breast cancer [AOR = 0.10 (95% CI = 0.02–0.54); p = 0.008].
Constructs of the health belief model
Overall, the majority of the respondents 159(65.4%) perceived that they were susceptible to breast cancer; most 225(92.6%) believed that breast cancer is a serious condition; the majority (96.3%) believed that breast cancer screening is beneficial; most 138 (56.8%) perceived some barriers prevented them from getting screened for breast cancer and the majority 227 (93.4%) had a high self-efficacy for breast cancer screening (Table 4 ).
Logistic regression of factors influencing breast cancer screening based on the HBM
The associations between the uptake of breast cancer screening and the constructs of the HBM are shown in Table 5 . Respondents who perceived high susceptibility to breast cancer were more likely to be screened for it [AOR = 1.97 (95% CI = 1.12–3.47), p = 0.019]. Respondents who perceived the high severity of breast cancer were more likely to be screened for it [AOR = 4.55 (95% CI = 1.32–15.76), p = 0.017]. Also, respondents who perceived high barriers to breast cancer screening were less likely to be screened for it [AOR = 0.15(95% CI = 1.42–4.22), p < 0.001].
This current study revealed that a majority (51.9%) of the respondents had ever screened for breast cancer. The study also reported that only 2.5% of the women had ever examined their breasts using a mammogram. Low rates of using mammography for breast cancer screening have been reported in similar studies conducted in Ghana [ 17 , 18 , 19 , 20 ]. Mammography is often used as a diagnostic examination rather than for screening because of the lack of routine screening mammography services and the high cost involved in Ghana [ 17 ]. The addition of mammography services to the Ghana National Health Insurance Scheme (NHIS) would be beneficial and would catalyze breast cancer screening.
Also, the current study revealed that only 14.4% of the respondents had undergone CBE. This result is very low as CBE is less expensive and effective in the detection of lumps and other abnormalities in the breast. Similarly, other studies conducted in Ghana reported low usage of CBE [ 17 , 20 , 21 ]. Further, an interventional study conducted in Kenya reported that the rate of CBE uptake among women increased by 38.0% as the intervention group received community-based health education from community health workers [ 22 ]. This indicates the need to create CBE awareness in the communities to improve upon the low uptake rate for early detection and treatment of cancer. The low uptake of CBE in Ghana is worrying as the survival rate of breast cancer is 39% [ 23 ]. The absence of a national cancer registry could also mean that the cases are under-reported. Furthermore, 33.7% of the respondents in the current study practised BSE. A slightly higher percentage (42.6%) of trainee health professionals in Ghana undergoing BSE has also been reported by Osei-Afriyie et al. (2021) [ 20 ]. Another study conducted among breast cancer patients in Ghana revealed that respondents rarely performed BSE before their diagnosis [ 24 ].
The current study revealed that respondents who had a tertiary level of education were less likely to be screened for breast cancer. However, a similar study conducted in Accra and Sunyani, Ghana, showed that a higher educational level was significantly associated with the uptake of breast cancer screening [ 17 ]. The finding from the current study could mean that women who have attained tertiary education might be overwhelmed with work schedules and not able to attend or book an appointment for breast cancer screening. Also, a study conducted in Ghana showed that respondents who had ever attended school were more likely to take up breast cancer screening [ 19 ]. Also, a study conducted among women in Iran showed that educational status was significantly associated with BSE [ 25 ].
The factors that may influence the uptake of breast cancer screening investigated in the current study include the constructs of the HBM (perceived susceptibility, perceived severity, perceived benefits, perceived barriers and self-efficacy). Concerning perceived susceptibility, the current study revealed that the majority (65.4%) of the respondents believed they were susceptible to breast cancer. In contrast, a study conducted in Ghana among female clinicians in Ga West and South revealed that 55.0% of the respondents had low perceived susceptibility to breast cancer [ 26 ].
Regarding the perceived severity of breast cancer, the current study revealed that the majority of the respondents (92.6%) believed that getting breast cancer would be dangerous. This is similar to a cross-sectional study conducted among students in Iran, which reported a high perceived severity of breast cancer [ 27 ]. From the current study, the belief that breast cancer could lead to death, cutting off the breast, and the danger of breast cancer accounted for the high perceived severity recorded. This implies that respondents would be more likely to take up breast cancer screening to prevent the seriousness of breast cancer. Health interventions should, therefore, heigthen the severity of breast cancer in health promotion interventions so that people can get screened for early detection and treatment.
Additionally, 96.3% of the respondents in the current study believed that breast cancer screening is beneficial. A comparable study conducted in Ghana reported similar findings [ 26 ]. In divergence, a study conducted Ghana in the Accra Metropolitan area among nurses and midwives revealed that 67.0% perceived breast cancer screening not to be beneficial [ 21 ].
About 56.8% of the respondents in the current study believed that there are barriers that prevent them from undertaking breast cancer screening. A similar study conducted in Ghana among female clinicians revealed that 51.0% of them perceived high barriers to breast cancer screening [ 26 ]. Some of the barriers stated by respondents in this current study include: fear to find out something is wrong (49.8%), and did not know where to get screened (40.9%). Also, 43.2% and 35.0% believed that the screening was painful and expensive respectively. These barriers need to be minimised or removed to encourage women to take up breast cancer screening. For instance, breast cancer screening could be covered by the NHIS so that women would not have to pay additional money to get screened if they visit the health facility.
On perceived self-efficacy, 93.4% of the respondents in the current study were confident that they could take up breast cancer screening. This implies that they believed they could overcome the existing barriers that exist and get screened for breast cancer. Similar results were found from a cross-sectional study conducted among students in Iran, which showed that perceived self-efficacy was high among the respondents [ 27 ]. This indicates that increasing the confidence of women toward breast cancer screening is, therefore recommended to improve the uptake of the services. Also, a study among clinicians in Ga West and South Districts of Ghana showed that about 54% of the respondents had low self-efficacy regarding breast cancer screening [ 26 ]. This further iterates the need to increase the confidence of women so that they can easily take up breast cancer screening.
The association between the constructs of the HBM and breast cancer screening uptake showed that respondents who perceived high susceptibility to breast cancer were more likely to be screened for breast cancer. Similarly, a study conducted in Turkey among women who were 40 years and above showed that perceived susceptibility was a strong predictor of breast cancer screening [ 28 ]. Also, a study among undergraduate students in the Volta Region in Ghana showed that those who did not believe to be susceptible to breast cancer were less likely to get screened [ 20 ]. It can be inferred from the current finding that designing interventions to target the perceived susceptibility of respondents is essential as it would make clear the risk factors of breast cancer.
Also, the current study revealed that respondents who perceived a high severity of breast cancer were more likely to be screened for the disease. The perceived seriousness of breast cancer was also found to be a strong predictor of breast cancer screening among older women in Turkey [ 28 ]. A similar study conducted among students in Northwest Iran showed that high perceived severity was a predictor of breast cancer screening behaviour [ 27 ]. The severity of breast cancer to the individual, the family and the society at large should be made a central point in health promotion interventions so that women would be compelled to get screened.
Furthermore, respondents who perceived high barriers to breast cancer screening were less likely to be screened for breast cancer. In consonance, a similar study conducted in Iran showed that perceived barriers were significantly associated with breast cancer screening [ 25 ]. A study conducted in Turkey reported that perceived barriers had a strong association with breast cancer screening [ 28 ]. Also, a similar study conducted among clinicians in Ghana showed that perceived barriers were significantly associated with the uptake of breast cancer screening [ 26 ]. In this current study, it can be said that respondents who perceive barriers could find it difficult to get screened for breast cancer. Health promotion interventions to improve breast cancer screening should focus on reducing barriers to screening.
The current results should, however, be interpreted in line with some limitations. The convenience sampling used at the last stage of the multistage sampling is a non-probability sampling method and may limit the generalizability of the findings of this research. The cross-sectional nature of the study design limits the ability to attribute a causal relationship between the factors associated with breast cancer screening and screening uptake among the participants. Also, the study used a questionnaire to elicit responses on a sensitive topic (breast cancer screening) that has the potential of introducing social desirability bias and there was no way to validate what the respondents reported. However, the assurance of anonymity and confidentiality of the responses should have minimized possible limitations. Cultural factors could also shape breast screening behaviour in the Ghanaian context, but these factors are not accounted for in the HBM. Despite these limitations, this study provides insight into the factors influencing breast cancer screening among women of reproductive age in the Nandom Municipality, Ghana using the HBM.
The uptake of breast cancer screening among women of reproductive age in the Nandom Municipality was considerably low (51.9%). Health promotion interventions to improve breast cancer screening should target women with a tertiary level of education and should focus on heightening the perceived threat of breast cancer and minimizing barriers to breast cancer screening.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
World Health Organization [WHO]. Factors influencing breast cancer screening. Geneva: WHO; 2018.
Google Scholar
National Cancer Institute [NCI]. Cases of breast cancers. Maryland: NCI; 2018.
World Cancer Research Fund. Annual incidence of cancer cases. London: WCRF International; 2018.
Ohene-Yeboah M, Adjei E. Breast cancer in Kumasi, Ghana. Ghana Med J. 2012;46:8–13.
CAS PubMed PubMed Central Google Scholar
Clegg-Lamptey J, Hodasi W. A study of breast cancer in Korle Bu teaching hospital. Assessing the impact of health education. Ghana Med J. 2007;41:72–7.
PubMed PubMed Central Google Scholar
Edmund DM, Naaeder SB, Tettey Y, Gyasi RK. Breast cancer in Ghanaian women: What has changed? Am J Clin Pathol. 2013;140(1):97–102.
Article Google Scholar
Ghartey Jnr FN, Anyanful A, Eliason S, Adamu SM, Debrah S. Pattern of breast cancer distribution in Ghana: a survey to enhance early detection, diagnosis, and treatment. Int J Breast Cancer. 2016;2016:1–9. https://doi.org/10.1155/2016/3645308 .
Nazzal Z, Sholi H, Sholi S, Sholi M, Lahaseh R. Mammography screening uptake among female health care workers in primary health care centers in Palestine- motivators and barriers. Asian Pac J Cancer Prev. 2016;17(5):2549–54.
PubMed Google Scholar
Zelle SG, Nyarko KM, Bosuetal WK. Cost, effects and cost-effectiveness of breast cancer control in Ghana. Trop Med Int Health. 2012;17(8):1031–43.
Carey LA, Perou CM, Livasyetal CA. Race, breast cancer subtypes, and survival in the Carolina Breast cancer study. J Am Med Assoc. 2006;295(21):2492–502.
Article CAS Google Scholar
District Health Management Information System (DHMIS) 2. Nandom Municipality. From: https://dhims.chimgh.org
Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2:328–35.
Ghana Statistical Service. 2010 Population and Housing Census. District Analytical report. Nandom District. Ghana Statistical Service, Accra, Ghana. 2014.
Degu G, Tessema F. Biostatistics for health sciences students: lecture note series. Addis Ababa: The Carter Centre 9EPHTI; 2005.
Ohene-Yeboah M, Adofo K, Akpaloo M. Breast cancer awareness among Nurses In Kumasi Ghana: Knowledge, Attitudes And Practice. Postgraduate Medical Journal of Ghana (Vol.2). 2013; Retrieved from http://www.gcps.edu.gh/gcps_repository/files/original/c6b0f0c2b31b1b7dc9f8c7254f14e763.pdf
Aba AG. Factors influencing breast cancer screening among female clinicians at the Ga West and Ga South Municipal Hospital in Accra. 2019. http://ugspace.ug.edu.gh .
Opoku SY, Benwell M, Yarney J. Knowledge, attitudes, beliefs, behaviour and breast cancer screening practices in Ghana, West Africa. Pan African Med J. 2012; 11(1)
Amenuke-Edusei M, Birore CM. The influence of sociodemographic factors on women’s breast cancer screening in Accra, Ghana. Adv Soc Work. 2020;20(3):756–77.
Ayanore MA, Adjuik M, Ameko A, Kugbey N, Asampong R, Mensah D, Zotor F. Self-reported breast and cervical cancer screening practices among women in Ghana: predictive factors and reproductive health policy implications from the WHO study on global AGEing and adult health. BMC Womens Health. 2020;20(1):1–10.
Osei-Afriyie S, Addae AK, Oppong S, Amu H, Ampofo E, Osei E. Breast cancer awareness, risk factors and screening practices among future health professionals in Ghana: a cross-sectional study. PLoS ONE. 2021;16(6): e0253373.
Okoh AA. Breast cancer screening among nurses and midwives in maamobi general hospital and Achimota Hospital. Doctoral dissertation, University of Ghana. 2018.
Muinde FN, Nzioki JM, Mahmoud MK. Effect of a community health worker intervention on uptake of breast cancer screening services among women of reproductive age in Kitui County. Kenya African J Health Sciences. 2020;33(2):35–43.
Thomas AS, Kidwell KM, Oppong JK, Adjei EK, Osei-Bonsu E, Boahene A, Merajver SD. Breast cancer in Ghana: demonstrating the need for population-based cancer registries in low-and middle-income countries. J Global Oncol. 2017;3(6):765–72.
Agbokey F, Kudzawu E, Dzodzomenyo M, Ae-Ngibise KA, Owusu-Agyei S, Asante KP. Knowledge and health seeking behaviour of breast cancer patients in Ghana. Int J Breast Cancer. 2019. https://doi.org/10.1155/2019/5239840 .
Article PubMed PubMed Central Google Scholar
Mousavi F, Shojaei P, Homasan S. Health beliefs as predictors of breast self-examination behavior. Int J Women Health Wellness. 2018;4:1–10.
Ghansah AA. Factors influencing breast cancer screening among female clinicians at the Ga West and Ga South Municipal Hospitals in Accra. Doctoral dissertation, University of Ghana. 2019.
Didarloo A, Nabilou B, Khalkhali HR. Psychosocial predictors of breast self-examination behavior among female students: an application of the health belief model using logistic regression. BMC Public Health. 2017;17(1):1–8.
Tarı Selçuk K, Avcı D, Yılmaz Dündar G, Mercan Y. Breast cancer screening behaviors in women aged 40 years and over in a semi-urban region in Turkey: relationships with health beliefs. Healthcare. 2020;8(2):171.
Download references
Acknowledgements
The authors are thankful to all respondents and the Nandom Municipal Health Directorate for the permission given to conduct the study.
The authors did not receive any funding to conduct the current study.
Author information
Authors and affiliations.
Department of Population and Behavioural Sciences, School of Public Health, University of Health and Allied Sciences, Ho, Ghana
Margaret Mary Wuur & Elvis Enowbeyang Tarkang
HIV/AIDS Prevention Research Network Cameroon, Kumba, Cameroon
Elvis Enowbeyang Tarkang
Department of Public Health Medicine, School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
Department of Epidemiology and Biostatistics, School of Public Health, University of Health and Allied Sciences, Ho, Ghana
Dillys Adomakoa Duodu
You can also search for this author in PubMed Google Scholar
Contributions
EET and MMW conceptualised and designed the study and analysed the data; MMW collected the data; EET and DAD supervised the data collection; EET, MMW and DAD led the writing of the manuscript; EET, MMW and DAD critically reviewed the manuscript; All the authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Elvis Enowbeyang Tarkang .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was obtained from the University of Health and Allied Sciences Research Ethics Committee (UHAS-REC A.9[182] 20–21). This study was conducted following all accepted principles on the ethics of this REC. Written informed consent was obtained from all participants before enrolment into the study. Permission was also obtained from the Nandom Municipal Health Directorate and local authorities before the conduct of the study.
Consent for publication
The authors give consent to the Publisher to publish this article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wuur, M.M., Duodu, D.A. & Tarkang, E.E. Factors that influence breast cancer screening among women of reproductive age in the Nandom Municipality, Ghana. BMC Women's Health 22 , 359 (2022). https://doi.org/10.1186/s12905-022-01946-0
Download citation
Received : 11 June 2022
Accepted : 17 August 2022
Published : 31 August 2022
DOI : https://doi.org/10.1186/s12905-022-01946-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer screening
- Women of reproductive age
- Health belief model
- Nandom municipality
BMC Women's Health
ISSN: 1472-6874
- General enquiries: [email protected]
- Neoplasms by Site
- breast neoplasms
- Breast Cancer
Breast cancer
- December 2019
- Nature Reviews Disease Primers 5(1)
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Centre Jean Perrin

- Vall d’Hebron Institute of Oncology

- Medical University of Vienna
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Sufiyan Bashir Mukadam
- Hemprasad Yashwant Patil
- BIOL DIRECT
- MOL CELL BIOCHEM
- PROSTAG OTH LIPID M
- YangZi Cheng
- COMPUT BIOL CHEM

- Dilipkumar Preetha
- Sasi Nivruthi

- Jiahang Tian

- Qingfeng Du
- CRIT REV FOOD SCI

- Qingshuang Wang
- LANCET ONCOL

- Anne-Laure Vallier
- Fatima Cardoso

- Sacha Howell

- Gail S. Wright
- William J Gradishar

- Yin-Hsun Feng

- E.M. Ciruelos

- Paul McGale

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- DSpace Home
- Graduate School
- Public Health
Show simple item record
The Lived experiences of Filipino women with breast cancer
| dc.contributor.author | Almocera, Dianne Pearl | |
| dc.date.accessioned | 2021-06-10T02:42:28Z | |
| dc.date.available | 2021-06-10T02:42:28Z | |
| dc.date.issued | 2020-03 | |
| dc.identifier.uri | https://dspace.aiias.edu/xmlui/handle/20.500.12977/405 | |
| dc.description | Unpublished Thesis (MPH) Shelf Location: RC280.B8 .A56 2020 ATDC | en_US |
| dc.description.abstract | In 2015, breast cancer ranked third among the leading new cancer deaths and had the highest incidence among cancer cases in the Philippines (International Agency for Research in Cancer [IARC], 2017; Laudico et al., 2015). However, after a thorough review of literature, there is no study found that explored the lived experiences of Filipino women with breast cancer. Thus, the purpose of this paper aims to describe the lifeworld of Filipino women diagnosed with breast cancer. For my methodology, I used transcendental phenomenology. I chose my participants, seven of them, through snowball and purposive sampling techniques. I gathered data through in-depth interviews, observation, and analytical memos. I analyzed using Moustakas’ transcendental phenomenological analysis. The findings showed that the participants engaged in an unhealthy lifestyle before the onset of breast cancer, specifically (a) eating unhealthy food, (b) being overworked, and (c) having psychological stress responses such as anger and worry. The participants’ lifeworld could be described as (a) living a life of distress, (b) facing punishment, (c) passing through the shadow of death, (d) being haunted by the unknown, (e) pleading with the ultimate healer, (f) coping with the uncertainties, and (g) turning curse into a blessing. The participants yearned for a bright future, such as engaging in a productive job and preparing themselves for a life in Heaven. I would like to recommend that healthcare providers and family members provide loving support to women with breast cancer as they go through this challenging phase of their lives. Moreover, this paper found that most of the women with breast cancer long to be a part of finishing the gospel commission. Thus, church leaders should consider giving women with breast cancer responsibilities in their respective churches and providing them the opportunity to participate in evangelism endeavors. | en_US |
| dc.language.iso | en_US | en_US |
| dc.publisher | Adventist International Institute of Advanced Studies | en_US |
| dc.subject | Breast -- Cancer -- Psychological aspects. | en_US |
| dc.subject | Breast cancer patients' writings. | en_US |
| dc.subject | Breast -- Cancer -- Research. | en_US |
| dc.title | The Lived experiences of Filipino women with breast cancer | en_US |
| dc.type | Thesis | en_US |
Files in this item

This item appears in the following Collection(s)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Basic Clin Pharm
- v.5(3); June 2014-August 2014
Awareness and attitudes regarding breast cancer and breast self-examination among female Jordanian students
Amal k. suleiman.
Department of Clinical Pharmacy, Pharmacy School, Princess Nora University, Riyadh, Kingdom of Saudi Arabia
Background:
Despite huge efforts to increase the level of breast cancer awareness, breast self-examination (BSE) is still poorly practiced across Jordan. This baseline study aimed to assess the awareness of female Jordanian students about breast cancer and their practice of BSE.
Materials and Methods:
Using a cross-sectional research design, a self-administered survey was used, via a pre-validated pre-piloted questionnaire was distributed to 900 female students aged between 18 and 37 years recruited from the University of Jordan in Amman. The questionnaire was divided into four domains: Socio-demographic characteristics; the respondent's knowledge of breast cancer and BSE; their attitude towards risk factors for breast cancer; their experience of breast cancer screening and BSE. Statistical analysis was performed using Epi-Info version 6.4 statistical Software.
The overall response rate was 93.3%. Approximately half of the respondents 435 (51.8%) were aware of breast cancer. Of these, 99 (22.7%) believed that it was caused by a medical condition, followed by old age (71; 16.4%), lack of breastfeeding (58; 13.3%), heredity (56; 12.8%), late marriage (44; 10.3%), pregnancies in older women (33; 7.5%), the use of brassieres (18; 4.1%), excessive breastfeeding (17; 3.9%), being unmarried (14; 3.2%), and spirituality (11; 2.6%). Overall, 152 participants (34.9%) were aware of BSE, but only 93 (11%) had performed it.
Conclusions:
The current status of awareness of breast cancer in Jordanian students and their use of BSE are insufficient. Women need to be encouraged to self-monitor in order to detect abnormalities in their breasts. Appropriate educational interventions are urgently required to encourage women to engage in regular BSE.
Introduction
Breast cancer is the most common cancer among females, and represents a major global health problem.[ 1 ] Almost 70% of women with breast cancer are aged over 50 years, and only 5% are younger than 40 years old.[ 1 ] Approximately 700,000 cases are reported annually worldwide, of which 57% of these cases present in developing countries.[ 1 , 2 , 3 ] The global incidence of breast cancer is rising, particularly in developing countries that formerly had a low incidence.[ 2 , 4 ] Omotara et al . proposed that the incidence of breast cancer is increasing in the developing world due to increased life expectancy, increased levels of urbanization and the adoption of western lifestyles.[ 5 ] According to a recent report by the World Health Organization, the largest increase in cancer incidence over the next 15 years will be in Middle Eastern countries.[ 2 ] The mortality rate from all types of cancer in the Middle East is currently 70%, compared to 40-55% in western countries. Furthermore, by the year 2020, the number of new cancer cases diagnosed each year is estimated to increase by 40%.[ 2 ] Urgent interventions are, therefore, needed to raise awareness of all cancers in this region in order to improve the rates of early detection and increase the chance of curative treatment.
In Jordan, cancer is the second most common cause of death after cardiovascular disease,[ 6 ] and breast cancer was the most common of all cancers in women over the last decade.[ 7 ] In 2008, the latest year for which the Jordan National Cancer Registry has available data, 4606 new cases in Jordanian citizens and 1608 additional non-Jordanian cases were recorded. The early detection of breast cancer can be achieved through a combination of monthly breast self-examination (BSE), regular clinical breast examinations and annual mammography beginning at the age of 40 years, are the best ways to limit morbidity and mortality associated with breast cancer.[ 8 , 9 , 10 ] It is essential for the target population to have comprehensive knowledge, appropriate attitudes and practice of the screening methods. This is supported by evidence that earliest breast tumors are self-discovered and that the majority of early discoveries are made by BSE performers.[ 9 ] Some studies have reported that improved knowledge and attitudes have a positive effect on the screening attendance of women.[ 10 , 11 ]
Breast cancer awareness in developing countries is not well documented, and what is known is far from encouraging,[ 11 , 12 , 13 , 14 , 15 , 16 , 17 ] as comparatively few women in these areas have adequate knowledge of the risk factors and preventive measures or screening techniques for early detection. The lack of knowledge and incorrectly held beliefs about breast cancer prevention among females are responsible for the negative perception of the curability of cancer detected early and of the efficacy of the screening tests.[ 18 ] It is, therefore, important to assess the level of awareness of risk factors in our communities. This study aimed to assess awareness of breast cancer, and practice of breast cancer screening among female students in Jordan.
Materials and Methods
Using a cross-sectional research design, this study examined the knowledge of Jordanian female students with regards to breast cancer, in addition to their awareness and practice of breast cancer screening techniques, including BSE.
The target population of the study was all the Jordanian female students registered at Jordan University without inclusion or exclusion criteria of the target population. The total number of female students was around 18,900 students registered in the university during the time of this study. Based on the rule-of-thumb, sample size was determined with 643 students having 99% confidence intervals, and a margin of error of ± 5%. This study location was selected because the governorate estimated that the number of female breast cancer cases was highest in Amman, affecting 52.3 out of 100,000 females.
A quantitative research approach was conducted using a self-administered survey. Researcher used a prevalidated prepiloted questionnaire was adapted from a previous study conducted in Northeast Nigeria.[ 5 ] After attaining permission to use the questionnaire, the questionnaire was translated into Arabic language, modified to be applicable in Jordan, and then translated back to English to assure the translation equivalency and appropriateness. The final Arabic version was approved by a bilingual Arabic professor of pharmacy. The questionnaire was piloted on a convenience sample of fifteen out of the main target sample so that final modifications could be made to the questionnaire. Cultural differences were discussed by the author, and the data from the pilot sample were excluded from the final analysis. The study protocol was approved by the departmental Ethics Committee at our institution.
The questionnaire included four sections: (i) The demographic background of the respondent; (ii) the respondent's knowledge of breast cancer and BSE; (iii) their attitude towards risk factors for breast cancer; and (iv) their current practice for breast cancer screening and BSE.
Data collection took place between 2 nd June 2012 and 10 th September 2012. Based on a convenience sampling method 900 questioners were distrusted to ensure the highest response, participating was invited by a formal covering letter to complete the prepiloted questionnaire. The covering letter explained the main objectives of the study and assured participants of the confidentiality and anonymity of data. The questionnaire was hand-delivered by researcher to the students with appropriate instructions regarding its completion, and picked up at a later time after completion, with no reminders. Subjects were informed about the increased incidence of breast cancer in Jordan, especially among younger women. Respondents were informed that participation in the study was voluntary where, a small box was created fixed at the main entrance of the pharmacy school allows participants to drop the completed questionnaires. Thus, their responses would be confidential and analyzed only as part of a cohort.
The questionnaire data were anonymized, numbered and assessed manually for errors, before being entered into a computer database for analysis and data were assessed in an observational manner using Epi-Info version 6.4 Statistical Software.
Of 900 questionnaires distributed to all colleges of the University of Jordan, 840 were completed and returned, yielding a response rate of 93.3%. Table 1 reveals the demographic characteristics of the female students who participated. The study group was aged from 18 to 37 years (median, 5.0). Of the 840 female students that responded, only 435 (51.8%) had any awareness of breast cancer as shown in Table 2 . The majority of these respondents had obtained their knowledge from either friends or health workers [ Figure 1 ].
Demographic characteristics of participating female students at Jordan University, Amman

Breast cancer awareness among participating female students at Jordan University, Amman

Source of breast cancer information among participating female students at Jordan University, Amman
Table 3 indicates that, of the 435 respondents who were aware of breast cancer, 99 (22.7%) perceived the cause to be brought about by a medical condition. This was followed, in descending order, by 58 (13.3%) who felt that the lack of breastfeeding caused breast cancer, 56 respondents (12.8%) who attributed the cause to heredity, 71 (16.3) to old age, 44 (10.3) to individuals marrying at a later age, 33 (7.5) to pregnancy at a later age, 18 (4.1%) to the use of brassieres, 17 (3.9%) to excessive breastfeeding and 11 (2.6%) to spirituality.
Perceived risk factors for breast cancer among participating female students at Jordan University, Amman

A total of 340 (78.2%) out of the 435 did not agree that breast cancer patients should be isolated or stigmatized and 308 (70.8%) did not believe that the disease was a punishment from God. The majority agreed that breast cancer patients should live in the community (95.6%) and be supported (97.9%). Nevertheless, 292 (67.1%) of the respondents were afraid of patients with the disease [ Table 4 ].
Assessment of attitudes towards breast cancer among female students who were aware of breast cancer at Jordan University, Amman ( n =435)

With regards to BSE, only 152 (34.9%) of those aware of breast cancer knew of BSE as a method for the early detection of breast cancer, and only 93 (61.1%) had ever undergone screening or performed BSE themselves [ Table 5 ]. Of those 93, 23 (24.7%) did so on the advice of health workers, and 28 (30.2%) did so as part of a routine medical examination. As for those respondents who were aware of breast cancer, 198 (45.5%) would undergo screening or perform BSE if it was of benefit to them, 111 (25.5%) if their family agreed, and 84 (19.3%) only if there was a known cure for breast cancer.
Awareness and practice of BSE among participating female students at Jordan University, Amman

The evaluation of public awareness, attitudes and practice of BSE is of fundamental importance for the successful implementation of breast cancer control activities.[ 19 ] There are no known proven means to prevent breast cancer, which increases our reliance on the methods for early detection in order to improve patient outcomes. The primary goal of breast cancer awareness programs in developing countries is to promote and develop awareness about the importance of its early detection.[ 5 ]
Projections show that the population in Jordan will have increased from the current figure of 6.3-7.1 million by 2020, with the number of breast cancer cases in Jordanians increasing from 5110/year into 7281/year.[ 3 ] Cancer is increasing at a faster rate than population growth, for unknown reasons, but these projections should be used to properly plan for future cancer care requirements and to pinpoint resources to improve survival rates.
The current study revealed that Jordanian women had worryingly poor levels of knowledge of breast cancer. This finding is supported by the study of Jaradeen,[ 20 ] which revealed a low mean level of knowledge about breast cancer (49%) in 150 female hospital workers in Jordan. In addition, Ahmed et al .[ 21 ] found that knowledge of breast cancer was low among 411 Jordanian woman aged 18-70 years in Amman, the capital of Jordan. As the current study involved highly educated university students, it was expected that they would have greater awareness and knowledge of breast cancer than the general population. However, the findings were disappointing.
In the current study, of the 435 respondents who were aware of breast cancer, 51.8% obtained their information on breast cancer from friends and health workers. This was in contrast to the results of a study conducted in South Eastern Nigeria by Ibrahim and Odusanya,[ 19 ] which showed that health workers were the main source of information about breast cancer. Friends and family also seem to play a major role in terms of breast cancer awareness in Middle Eastern communities, as exemplified by the finding that 25.5% of the respondents who were aware of breast cancer would only undergo breast cancer screening if their family agreed. In the Middle East, breast cancer comes with a heavy cultural stigma, as exemplified by the study in which Laura Bush stated that, “Women in [the] Middle East are sometimes abandoned by their family when the disease is diagnosed, [and] such stories are discouraging”.[ 22 ]
In this study, the majority of women who were aware of breast cancer (308, 70.8%) did not believe that breast cancer was a punishment from God, which was in contrast to the findings of previous studies from developing countries.[ 5 , 12 ] The majority of respondents in the current study (78.2%) disagreed that breast cancer patients should be isolated and nearly all agreed that these patients should be allowed to live freely in their community (95.6%). This may be due to the Islamic religious beliefs of the majority of respondents, which encourages communities to support those suffering from any kind of disease.[ 20 ]
The current study shows that the practice of BSE was low amongst the sample tested. Only 152 (34.9%) of those aware of breast cancer knew of BSE as a method for detecting breast cancer, and only 93 of those respondents (61.1%) had ever performed it. This is in line with the findings of Abdel Hadi,[ 23 ] who found that 37.3% of his study population practiced BSE. In studies of other populations, the percentage of BSE awareness was 52% among Jordanian nurses,[ 24 ] 37% among Australian students,[ 25 ] and 31% among Pennsylvanian women.[ 26 ] Other studies that showed low rates of BSE practice suggested that the practice is globally low among women, regardless of their age and occupation.[ 21 , 23 ] However, the rates reported in this current study were higher than those described by previous Egyptian and Iranian studies, in which only 6% and 2.65% of the general study populations practiced BSE monthly, respectively.[ 21 , 27 ]
The current study suggested several reasons why Jordanian female students did not partake in breast cancer screening practices. More than a third of students who were aware of breast cancer did not feel that screening was necessary, and 28.8% of women reported being too busy. The provision of systematic health education (e.g. at college) may help to encourage breast cancer screening and change perceptions regarding screening. It is important to raise women's awareness regarding the potentially life-saving benefits of BSE practice. In addition, the accessibility of screening practices should be expanded with government support.
Limitations of the study
One of the limitations of the study is that the participants in the questionnaire enrolled in the study voluntarily. The results might therefore be biased as the sample was not selected at random. The students who chose to participate may have had different attitudes or knowledge than those who did not volunteer.
Conclusions
In contrast to western nations, most patients in developing countries, including Jordan, present with an advanced stage of cancer, when little or no benefit can be derived from therapy. The findings of this study are in keeping with previous research in which breast cancer awareness has been found to be low among women in developing countries. Breast cancer awareness among Jordanian students was less than 50% and knowledge was limited in its range and accuracy. The findings of this study suggest a number of avenues for future research and could be used to contribute to the development of preventative and screening programs for breast cancer across the population. This study emphasizes the need to raise breast cancer awareness and to teach individuals about the importance of practices for early detection techniques, such as BSE, which will enable breast cancer to be detected at an earlier stage. Interventions should be developed with the aim of providing information and services for all age groups, educational levels, cultures and social strata. In order to improve women's awareness and knowledge of breast cancer, it is important to initiate interventions that seek to provide health education, and to encourage preventive healthcare behaviors. The data presented here indicate an important myths factors about breast cancer among female Jordanian students that can provide insight and background, into exploring the strategies for promoting awareness among women according to the students.
Acknowledgment
Thanks to Dr. Natalie Morris of Oxford Science Editing for her assistance in manuscript English editing, and Dr. Abbas Al barq for his unconditional support.
Source of Support: Nil
Conflict of Interest: No
Downloadable Content
Reproducing neoliberal breast cancer awareness: a discourse analysis of pinkwashing campaigns
- Masters Thesis
- Robinson, Rebecca Elizabeth
- Baker, J. Mark
- California State Polytechnic University, Humboldt
- Environmental Health Justice
- Heteronormative femininity
- Political economy of breast cancer
- Pinkwashing
- Political Economy of breast cancer
- Environmental pollution
- Neoliberalism
- Critical Discourse Analysis
- Critical discourse analysis
- Survivorship/Optimism
- Commodification
- Toxic chemicals
- Sexualization of women
- Environmental Pollution/Toxic Chemicals
- Environmental health justice
- Breast cancer awareness
- Pink Ribbon
- Individual Responsibility
- Objectification of breasts
- Cause-related marketing
- Humboldt State University -- Theses -- Environment and Community
- Heteronormative Femininity
- Breast Cancer Awareness
- Pink ribbon
- 2016-08-29T15:32:33Z
- http://hdl.handle.net/10211.3/176165
- Thesis (M.A.)--Humboldt State University, Social Sciences: Environment and Community, 2016

| Thumbnail | Title | Date Uploaded | Visibility | Actions |
|---|---|---|---|---|
| 2020-08-06 | Public | |||
| 2020-08-06 | Public | |||
| 2020-08-06 | Public | |||
| 2020-08-06 | Public | |||
| 2020-08-06 | Public | |||
| 2020-08-06 | Public | |||
| 2020-08-06 | Public |
Items in ScholarWorks are protected by copyright, with all rights reserved, unless otherwise indicated.

IMAGES
VIDEO
COMMENTS
Breast cancer awareness and risk perception. Regarding breast cancer awareness, 281 (73.0%) of the respondents reported having ever heard of breast cancer. The remaining items in Table 2 were asked of the 281 women who had heard of breast cancer. The social media remained the most important source of information on breast cancer (181;64.4% ...
Breast cancer remains a worldwide public health dilemma and is currently the most common tumour in the globe. Awareness of breast cancer, public attentiveness, and advancement in breast imaging has made a positive impact on recognition and screening of breast cancer. Breast cancer is life-threatening disease in females and the leading cause of mortality among women population. For the previous ...
Introduction. Breast cancer (BC) was allocated 11.7% of all kinds of cancers in 2020.[] To date, the new cases of the disease were beyond two million, forecasted to reach more than 3 million cases with more than one million deaths by 2040.[2,3]BC was imposed a considerable economic burden on countries as well as public health problems[4,5] while it can be prevented by early detection ...
The early detection of breast cancer can be accomplished by establishing proactive screenings for women at risk, encouraging yearly mammograms and raising awareness . Women in Saudi Arabia are being educated about breast cancer through a national awareness campaign . Saudi Arabian Ministry of Health recommends that all women aged 40-50 ...
Background: "Breast awareness" is a recommendation that women understand the symptoms of breast cancer and become familiar with the usual look and feel of their breasts. It is recommended for women of all ages in breast cancer screening guidelines around the world. The objective of this study was to assess the evidence for breast awareness by investigating its effect on breast cancer outcomes ...
1. Introduction. Breast cancer is a disease in which cells in the breast grow out of control [], and it is the most prevalent cancer among women worldwide, affecting both developed and developing countries [].In 2017, there were approximately 2 million cases of breast cancer globally, with a mortality rate exceeding 50% [].It is estimated that up to 13% of women worldwide will experience ...
Introduction Awareness of screening procedures and illness warning signals is critical for expanding and implementing screening programs in society, which would improve the odds of early identification of breast cancer. Objectives This study aimed to evaluate the knowledge, awareness, attitudes, and practices related to breast cancer risk factors, signs, symptoms and methods of screening among ...
Background Breast cancer is a major health concern worldwide, especially in Vietnam. This study aimed to explore women's motivation for and factors related to breast cancer screening. Methods A mixed-methods study was conducted in Danang, Vietnam, using a convergent parallel approach. This study utilized both quantitative and qualitative methods to gather the data. The quantitative approach ...
3.3 Breast Cancer worldwide. Breast cancer is the most common type of cancer in women around the globe. It affects women from low, middle and high-income countries (Rohani, Abedi, Omranipour, & Langius-Eklöf, 2015, 2). Breast cancer prevalence has increased within the last few years in middle- and low-income countries.
Breast cancer awareness interventions were found to increase the uptake of breast self-examination behaviours and increase the likelihood of breast cancer screening attendance. Predicting the impact of these interventions on survivability and general morbidity/mortality outcomes remains a challenge due to a shortage of suitably evaluated campaigns.
2014). Awareness in breast cancer is very important because detecting cancer in early phase can save life. Awareness regarding breast cancer helps people to acknowledge about the disease which not only benefits reducing breast cancer stigmas but also im-proving health literacy. Awareness in the context of this thesis can be defined as the
The prevalence of breast cancer risk factors varied from 1% of having a personal history of breast cancer to 14.3% for positive family history of breast cancer.
Background/Objectives: This study explores the characteristics of different perception types in middle-aged female breast cancer patients and proposes psychological counselling interventions tailored to each type. Methods: The study used the Q methodology, starting with the construction of 40 Q samples and 39 P samples. Results: We categorised middle-aged female patients' subjective ...
Methods: Breast cancer awareness advertisements from October 2015 and October 2016 on internet platforms belonging to men and women's wear brand categories were selected. Out of the sixty (60) advertisements collected, a content analysis was conducted on thirty-five (35) of the advertisements.
This thesis aimed to provide a comprehensive insight into breast cancer awareness and its screening methods among females in Kuwait. Method. A multi-method approach was adopted to address the research objectives and gain a deeper understanding in a robust way. Three interlinked studies were carried out.
Participants also advocated for breast and other cancer awareness to be broadly publicized as was Covid-19 on television, radio, and social media e.g., Instagram, Twitter, Facebook as well as a specialized mobile cancer service. In addition, participants also called for regular cancer screening announcements made from the department of health ...
After the interventional program, 71.8% of increase in knowledge about breast health and BSE was observed. In addition, 64.7% of the women practiced BSE compared to 7.14% pretest. Conclusion: This study highlights the awareness needs by the women and application of extensive strategies to increase the acceptance of cancer screening programs ...
Presence in one or both breasts of one or more "hard masses" lumps of any size, shape, texture, with smooth or non-smooth edges. Inflammation (redness, swelling, increase of temperature) of the entire breast, or some part of it. Change of the skin of breast: noticeable depressions, redness, or thickening.
However, they had interest to participate in activities that encourages breast cancer awareness 234 (78.0%) (Table 1). TABLE 1. ... Masters' thesis, Addis Ababa University, Bale (2014). Keywords: breast cancer, awareness, self-examination of breast, treatment-outcome, Ethiopia.
Breast cancer awareness and risk perception. Regarding breast cancer awareness, 281 (73.0%) of the respondents reported having ever heard of breast cancer. The remaining items in Table 2 were asked of the 281 women who had heard of breast cancer. The social media remained the most important source of information on breast cancer (181;64.4% ...
Background In Ghana, breast cancer is a major public health concern and the most common type of cancer among women in terms of mortality and incidence. This study determined the factors influencing breast cancer screening among women of reproductive age in Nandom Municipality, Ghana using the Health Belief Model as the conceptual model. Methods The study was cross-sectional in design. A ...
Breast cancer is the most frequent malignancy in women worldwide and is curable in ~70-80% of patients with early-stage, non-metastatic disease. ... and an increase in awareness a nd mammography ...
Unpublished Thesis (MPH) Shelf Location: RC280.B8 .A56 2020 ATDC: en_US: dc.description.abstract: In 2015, breast cancer ranked third among the leading new cancer deaths and had the highest incidence among cancer cases in the Philippines (International Agency for Research in Cancer [IARC], 2017; Laudico et al., 2015).
Introduction. Breast cancer is the most common cancer among females, and represents a major global health problem.[] Almost 70% of women with breast cancer are aged over 50 years, and only 5% are younger than 40 years old.[] Approximately 700,000 cases are reported annually worldwide, of which 57% of these cases present in developing countries.[1,2,3] The global incidence of breast cancer is ...
This thesis examines conventional approaches to addressing breast cancer within the United States, as they are reinforced by breast cancer awareness campaigns. Through these campaigns, companies and organizations emphasize the importance of making people aware of the disease and raising money for research by hosting fundraising events and ...