- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Overcoming Speech Impediment: Symptoms to Treatment
There are many causes and solutions for impaired speech
- Types and Symptoms
- Speech Therapy
- Building Confidence
Speech impediments are conditions that can cause a variety of symptoms, such as an inability to understand language or speak with a stable sense of tone, speed, or fluidity. There are many different types of speech impediments, and they can begin during childhood or develop during adulthood.
Common causes include physical trauma, neurological disorders, or anxiety. If you or your child is experiencing signs of a speech impediment, you need to know that these conditions can be diagnosed and treated with professional speech therapy.
This article will discuss what you can do if you are concerned about a speech impediment and what you can expect during your diagnostic process and therapy.
FG Trade / Getty Images
Types and Symptoms of Speech Impediment
People can have speech problems due to developmental conditions that begin to show symptoms during early childhood or as a result of conditions that may occur during adulthood.
The main classifications of speech impairment are aphasia (difficulty understanding or producing the correct words or phrases) or dysarthria (difficulty enunciating words).
Often, speech problems can be part of neurological or neurodevelopmental disorders that also cause other symptoms, such as multiple sclerosis (MS) or autism spectrum disorder .
There are several different symptoms of speech impediments, and you may experience one or more.
Can Symptoms Worsen?
Most speech disorders cause persistent symptoms and can temporarily get worse when you are tired, anxious, or sick.
Symptoms of dysarthria can include:
- Slurred speech
- Slow speech
- Choppy speech
- Hesitant speech
- Inability to control the volume of your speech
- Shaking or tremulous speech pattern
- Inability to pronounce certain sounds
Symptoms of aphasia may involve:
- Speech apraxia (difficulty coordinating speech)
- Difficulty understanding the meaning of what other people are saying
- Inability to use the correct words
- Inability to repeat words or phases
- Speech that has an irregular rhythm
You can have one or more of these speech patterns as part of your speech impediment, and their combination and frequency will help determine the type and cause of your speech problem.
Causes of Speech Impediment
The conditions that cause speech impediments can include developmental problems that are present from birth, neurological diseases such as Parkinson’s disease , or sudden neurological events, such as a stroke .
Some people can also experience temporary speech impairment due to anxiety, intoxication, medication side effects, postictal state (the time immediately after a seizure), or a change of consciousness.
Speech Impairment in Children
Children can have speech disorders associated with neurodevelopmental problems, which can interfere with speech development. Some childhood neurological or neurodevelopmental disorders may cause a regression (backsliding) of speech skills.
Common causes of childhood speech impediments include:
- Autism spectrum disorder : A neurodevelopmental disorder that affects social and interactive development
- Cerebral palsy : A congenital (from birth) disorder that affects learning and control of physical movement
- Hearing loss : Can affect the way children hear and imitate speech
- Rett syndrome : A genetic neurodevelopmental condition that causes regression of physical and social skills beginning during the early school-age years.
- Adrenoleukodystrophy : A genetic disorder that causes a decline in motor and cognitive skills beginning during early childhood
- Childhood metabolic disorders : A group of conditions that affects the way children break down nutrients, often resulting in toxic damage to organs
- Brain tumor : A growth that may damage areas of the brain, including those that control speech or language
- Encephalitis : Brain inflammation or infection that may affect the way regions in the brain function
- Hydrocephalus : Excess fluid within the skull, which may develop after brain surgery and can cause brain damage
Do Childhood Speech Disorders Persist?
Speech disorders during childhood can have persistent effects throughout life. Therapy can often help improve speech skills.
Speech Impairment in Adulthood
Adult speech disorders develop due to conditions that damage the speech areas of the brain.
Common causes of adult speech impairment include:
- Head trauma
- Nerve injury
- Throat tumor
- Stroke
- Parkinson’s disease
- Essential tremor
- Brain tumor
- Brain infection
Additionally, people may develop changes in speech with advancing age, even without a specific neurological cause. This can happen due to presbyphonia , which is a change in the volume and control of speech due to declining hormone levels and reduced elasticity and movement of the vocal cords.
Do Speech Disorders Resolve on Their Own?
Children and adults who have persistent speech disorders are unlikely to experience spontaneous improvement without therapy and should seek professional attention.
Steps to Treating Speech Impediment
If you or your child has a speech impediment, your healthcare providers will work to diagnose the type of speech impediment as well as the underlying condition that caused it. Defining the cause and type of speech impediment will help determine your prognosis and treatment plan.
Sometimes the cause is known before symptoms begin, as is the case with trauma or MS. Impaired speech may first be a symptom of a condition, such as a stroke that causes aphasia as the primary symptom.
The diagnosis will include a comprehensive medical history, physical examination, and a thorough evaluation of speech and language. Diagnostic testing is directed by the medical history and clinical evaluation.
Diagnostic testing may include:
- Brain imaging , such as brain computerized tomography (CT) or magnetic residence imaging (MRI), if there’s concern about a disease process in the brain
- Swallowing evaluation if there’s concern about dysfunction of the muscles in the throat
- Electromyography (EMG) and nerve conduction studies (aka nerve conduction velocity, or NCV) if there’s concern about nerve and muscle damage
- Blood tests, which can help in diagnosing inflammatory disorders or infections
Your diagnostic tests will help pinpoint the cause of your speech problem. Your treatment will include specific therapy to help improve your speech, as well as medication or other interventions to treat the underlying disorder.
For example, if you are diagnosed with MS, you would likely receive disease-modifying therapy to help prevent MS progression. And if you are diagnosed with a brain tumor, you may need surgery, chemotherapy, or radiation to treat the tumor.
Therapy to Address Speech Impediment
Therapy for speech impairment is interactive and directed by a specialist who is experienced in treating speech problems . Sometimes, children receive speech therapy as part of a specialized learning program at school.
The duration and frequency of your speech therapy program depend on the underlying cause of your impediment, your improvement, and approval from your health insurance.
If you or your child has a serious speech problem, you may qualify for speech therapy. Working with your therapist can help you build confidence, particularly as you begin to see improvement.
Exercises during speech therapy may include:
- Pronouncing individual sounds, such as la la la or da da da
- Practicing pronunciation of words that you have trouble pronouncing
- Adjusting the rate or volume of your speech
- Mouth exercises
- Practicing language skills by naming objects or repeating what the therapist is saying
These therapies are meant to help achieve more fluent and understandable speech as well as an increased comfort level with speech and language.
Building Confidence With Speech Problems
Some types of speech impairment might not qualify for therapy. If you have speech difficulties due to anxiety or a social phobia or if you don’t have access to therapy, you might benefit from activities that can help you practice your speech.
You might consider one or more of the following for you or your child:
- Joining a local theater group
- Volunteering in a school or community activity that involves interaction with the public
- Signing up for a class that requires a significant amount of class participation
- Joining a support group for people who have problems with speech
Activities that you do on your own to improve your confidence with speaking can be most beneficial when you are in a non-judgmental and safe space.
Many different types of speech problems can affect children and adults. Some of these are congenital (present from birth), while others are acquired due to health conditions, medication side effects, substances, or mood and anxiety disorders. Because there are so many different types of speech problems, seeking a medical diagnosis so you can get the right therapy for your specific disorder is crucial.
Centers for Disease Control and Prevention. Language and speech disorders in children .
Han C, Tang J, Tang B, et al. The effectiveness and safety of noninvasive brain stimulation technology combined with speech training on aphasia after stroke: a systematic review and meta-analysis . Medicine (Baltimore). 2024;103(2):e36880. doi:10.1097/MD.0000000000036880
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, language .
Mackey J, McCulloch H, Scheiner G, et al. Speech pathologists' perspectives on the use of augmentative and alternative communication devices with people with acquired brain injury and reflections from lived experience . Brain Impair. 2023;24(2):168-184. doi:10.1017/BrImp.2023.9
Allison KM, Doherty KM. Relation of speech-language profile and communication modality to participation of children with cerebral palsy . Am J Speech Lang Pathol . 2024:1-11. doi:10.1044/2023_AJSLP-23-00267
Saccente-Kennedy B, Gillies F, Desjardins M, et al. A systematic review of speech-language pathology interventions for presbyphonia using the rehabilitation treatment specification system . J Voice. 2024:S0892-1997(23)00396-X. doi:10.1016/j.jvoice.2023.12.010
By Heidi Moawad, MD Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Speech and Communication Disorders
Living with, related issues, see, play and learn.
- No links available
Statistics and Research
Clinical trials.
- Journal Articles
Reference Desk
Find an expert, patient handouts.
Many disorders can affect our ability to speak and communicate. They range from saying sounds incorrectly to being completely unable to speak or understand speech. Causes include:
- Hearing disorders and deafness
- Voice problems , such as dysphonia or those caused by cleft lip or palate
- Speech problems like stuttering
- Developmental disabilities
- Learning disabilities
- Autism spectrum disorder
- Brain injury
Some speech and communication problems may be genetic. Often, no one knows the causes. By first grade, about 5% of children have noticeable speech disorders. Speech and language therapy can help.
NIH: National Institute on Deafness and Other Communication Disorders
- Speech and Language Impairments (Center for Parent Information and Resources) Also in Spanish
- Speech to Speech Relay Service (Federal Communications Commission)
- Telecommunications Relay Service (TRS) (Federal Communications Commission)
- Aphasia vs. Apraxia (American Stroke Association)
Journal Articles References and abstracts from MEDLINE/PubMed (National Library of Medicine)
- Article: Development and validation of a predictive model for poor prognosis of...
- Article: Communication strategies for adults in palliative care: the speech-language therapists' perspective.
- Article: Pain assessment tools in adults with communication disorders: systematic review and...
- Speech and Communication Disorders -- see more articles
- Speech Problems (Nemours Foundation)
- Apraxia (Medical Encyclopedia) Also in Spanish
- Dysarthria (Medical Encyclopedia) Also in Spanish
- Phonological disorder (Medical Encyclopedia) Also in Spanish
- Selective mutism (Medical Encyclopedia) Also in Spanish
- Speech impairment in adults (Medical Encyclopedia) Also in Spanish
The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.

- Bachelor’s Degrees
- Master’s Degrees
- Doctorate Degrees
- Certificate Programs
- Nursing Degrees
- Cybersecurity
- Human Services
- Science & Mathematics
- Communication
- Liberal Arts
- Social Sciences
- Computer Science
- Admissions Overview
- Tuition and Financial Aid
- Incoming Freshman and Graduate Students
- Transfer Students
- Military Students
- International Students
- Early Access Program
- About Maryville
- Our Faculty
- Our Approach
- Our History
- Accreditation
- Tales of the Brave
- Student Support Overview
- Online Learning Tools
- Infographics
Home / Blog
Speech Impediment Guide: Definition, Causes, and Resources
December 8, 2020

Tables of Contents
What Is a Speech Impediment?
Types of speech disorders, speech impediment causes, how to fix a speech impediment, making a difference in speech disorders.
Communication is a cornerstone of human relationships. When an individual struggles to verbalize information, thoughts, and feelings, it can cause major barriers in personal, learning, and business interactions.
Speech impediments, or speech disorders, can lead to feelings of insecurity and frustration. They can also cause worry for family members and friends who don’t know how to help their loved ones express themselves.
Fortunately, there are a number of ways that speech disorders can be treated, and in many cases, cured. Health professionals in fields including speech-language pathology and audiology can work with patients to overcome communication disorders, and individuals and families can learn techniques to help.

Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual’s ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
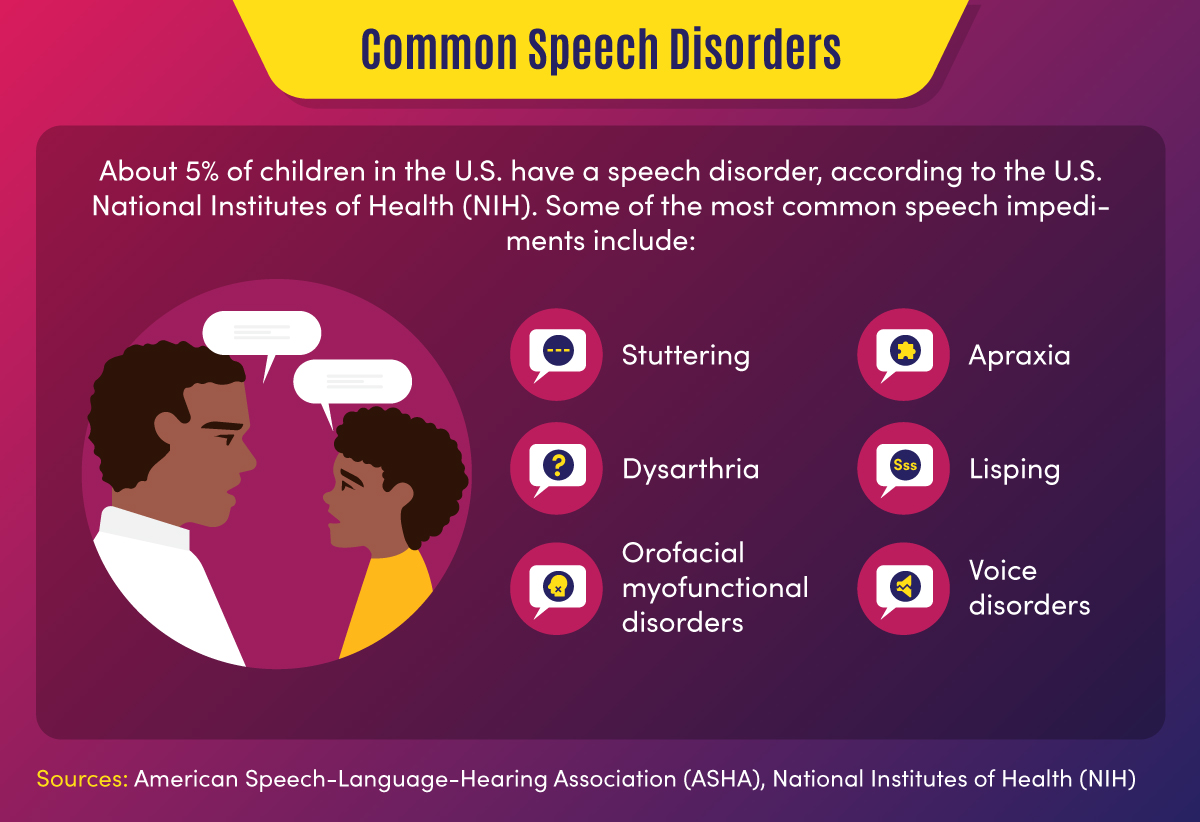
Some 7.7% of U.S. children — or 1 in 12 youths between the ages of 3 and 17 — have speech, voice, language, or swallowing disorders, according to the National Institute on Deafness and Other Communication Disorders (NIDCD). About 70 million people worldwide, including some 3 million Americans, experience stuttering difficulties, according to the Stuttering Foundation.
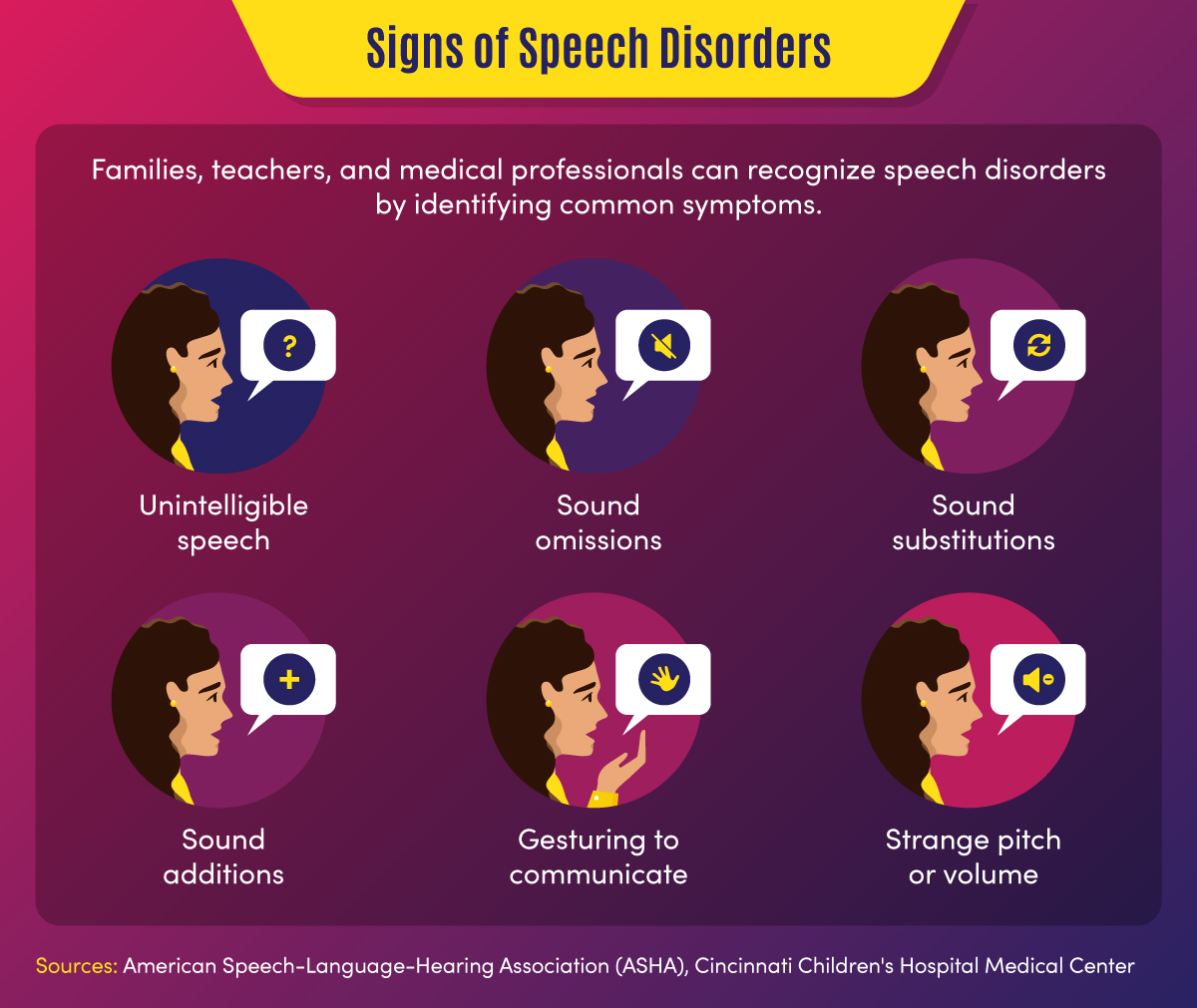
Common signs of a speech disorder
There are several symptoms and indicators that can point to a speech disorder.
- Unintelligible speech — A speech disorder may be present when others have difficulty understanding a person’s verbalizations.
- Omitted sounds — This symptom can include the omission of part of a word, such as saying “bo” instead of “boat,” and may include omission of consonants or syllables.
- Added sounds — This can involve adding extra sounds in a word, such as “buhlack” instead of “black,” or repeating sounds like “b-b-b-ball.”
- Substituted sounds — When sounds are substituted or distorted, such as saying “wabbit” instead of “rabbit,” it may indicate a speech disorder.
- Use of gestures — When individuals use gestures to communicate instead of words, a speech impediment may be the cause.
- Inappropriate pitch — This symptom is characterized by speaking with a strange pitch or volume.
In children, signs might also include a lack of babbling or making limited sounds. Symptoms may also include the incorrect use of specific sounds in words, according to the American Speech-Language-Hearing Association (ASHA). This may include the sounds p, m, b, w, and h among children aged 1-2, and k, f, g, d, n, and t for children aged 2-3.
Back To Top
Categories of Speech Impediments
Speech impediments can range from speech sound disorders (articulation and phonological disorders) to voice disorders. Speech sound disorders may be organic — resulting from a motor or sensory cause — or may be functional with no known cause. Voice disorders deal with physical problems that limit speech. The main categories of speech impediments include the following:
Fluency disorders occur when a patient has trouble with speech timing or rhythms. This can lead to hesitations, repetitions, or prolonged sounds. Fluency disorders include stuttering (repetition of sounds) or (rapid or irregular rate of speech).
Resonance disorders are related to voice quality that is impacted by the shape of the nose, throat, and/or mouth. Examples of resonance disorders include hyponasality and cul-de-sac resonance.
Articulation disorders occur when a patient has difficulty producing speech sounds. These disorders may stem from physical or anatomical limitations such as muscular, neuromuscular, or skeletal support. Examples of articulation speech impairments include sound omissions, substitutions, and distortions.
Phonological disorders result in the misuse of certain speech sounds to form words. Conditions include fronting, stopping, and the omission of final consonants.
Voice disorders are the result of problems in the larynx that harm the quality or use of an individual’s voice. This can impact pitch, resonance, and loudness.
Impact of Speech Disorders
Some speech disorders have little impact on socialization and daily activities, but other conditions can make some tasks difficult for individuals. Following are a few of the impacts of speech impediments.
- Poor communication — Children may be unable to participate in certain learning activities, such as answering questions or reading out loud, due to communication difficulties. Adults may avoid work or social activities such as giving speeches or attending parties.
- Mental health and confidence — Speech disorders may cause children or adults to feel different from peers, leading to a lack of self-confidence and, potentially, self-isolation.
Resources on Speech Disorders
The following resources may help those who are seeking more information about speech impediments.
Health Information : Information and statistics on common voice and speech disorders from the NIDCD
Speech Disorders : Information on childhood speech disorders from Cincinnati Children’s Hospital Medical Center
Speech, Language, and Swallowing : Resources about speech and language development from the ASHA
Children and adults can suffer from a variety of speech impairments that may have mild to severe impacts on their ability to communicate. The following 10 conditions are examples of specific types of speech disorders and voice disorders.
1. Stuttering
This condition is one of the most common speech disorders. Stuttering is the repetition of syllables or words, interruptions in speech, or prolonged use of a sound.
This organic speech disorder is a result of damage to the neural pathways that connect the brain to speech-producing muscles. This results in a person knowing what they want to say, but being unable to speak the words.
This consists of the lost ability to speak, understand, or write languages. It is common in stroke, brain tumor, or traumatic brain injury patients.
4. Dysarthria
This condition is an organic speech sound disorder that involves difficulty expressing certain noises. This may involve slurring, or poor pronunciation, and rhythm differences related to nerve or brain disorders.
The condition of lisping is the replacing of sounds in words, including “th” for “s.” Lisping is a functional speech impediment.
6. Hyponasality
This condition is a resonance disorder related to limited sound coming through the nose, causing a “stopped up” quality to speech.
7. Cul-de-sac resonance
This speech disorder is the result of blockage in the mouth, throat, or nose that results in quiet or muffled speech.
8. Orofacial myofunctional disorders
These conditions involve abnormal patterns of mouth and face movement. Conditions include tongue thrusting (fronting), where individuals push out their tongue while eating or talking.
9. Spasmodic Dysphonia
This condition is a voice disorder in which spasms in the vocal cords produce speech that is hoarse, strained, or jittery.
10. Other voice disorders
These conditions can include having a voice that sounds breathy, hoarse, or scratchy. Some disorders deal with vocal folds closing when they should open (paradoxical vocal fold movement) or the presence of polyps or nodules in the vocal folds.
Speech Disorders vs. Language Disorders
Speech disorders deal with difficulty in creating sounds due to articulation, fluency, phonology, and voice problems. These problems are typically related to physical, motor, sensory, neurological, or mental health issues.
Language disorders, on the other hand, occur when individuals have difficulty communicating the meaning of what they want to express. Common in children, these disorders may result in low vocabulary and difficulty saying complex sentences. Such a disorder may reflect difficulty in comprehending school lessons or adopting new words, or it may be related to a learning disability such as dyslexia. Language disorders can also involve receptive language difficulties, where individuals have trouble understanding the messages that others are trying to convey.
Resources on Types of Speech Disorders
The following resources may provide additional information on the types of speech impediments.
Common Speech Disorders: A guide to the most common speech impediments from GreatSpeech
Speech impairment in adults: Descriptions of common adult speech issues from MedlinePlus
Stuttering Facts: Information on stuttering indications and causes from the Stuttering Foundation
Speech disorders may be caused by a variety of factors related to physical features, neurological ailments, or mental health conditions. In children, they may be related to developmental issues or unknown causes and may go away naturally over time.
Physical and neurological issues. Speech impediment causes related to physical characteristics may include:
- Brain damage
- Nervous system damage
- Respiratory system damage
- Hearing difficulties
- Cancerous or noncancerous growths
- Muscle and bone problems such as dental issues or cleft palate
Mental health issues. Some speech disorders are related to clinical conditions such as:
- Autism spectrum disorder
- Down syndrome or other genetic syndromes
- Cerebral palsy or other neurological disorders
- Multiple sclerosis
Some speech impairments may also have to do with family history, such as when parents or siblings have experienced language or speech difficulties. Other causes may include premature birth, pregnancy complications, or delivery difficulties. Voice overuse and chronic coughs can also cause speech issues.
The most common way that speech disorders are treated involves seeking professional help. If patients and families feel that symptoms warrant therapy, health professionals can help determine how to fix a speech impediment. Early treatment is best to curb speech disorders, but impairments can also be treated later in life.
Professionals in the speech therapy field include speech-language pathologists (SLPs) . These practitioners assess, diagnose, and treat communication disorders including speech, language, social, cognitive, and swallowing disorders in both adults and children. They may have an SLP assistant to help with diagnostic and therapy activities.
Speech-language pathologists may also share a practice with audiologists and audiology assistants. Audiologists help identify and treat hearing, balance, and other auditory disorders.
How Are Speech Disorders Diagnosed?
Typically, a pediatrician, social worker, teacher, or other concerned party will recognize the symptoms of a speech disorder in children. These individuals, who frequently deal with speech and language conditions and are more familiar with symptoms, will recommend that parents have their child evaluated. Adults who struggle with speech problems may seek direct guidance from a physician or speech evaluation specialist.
When evaluating a patient for a potential speech impediment, a physician will:
- Conduct hearing and vision tests
- Evaluate patient records
- Observe patient symptoms
A speech-language pathologist will conduct an initial screening that might include:
- An evaluation of speech sounds in words and sentences
- An evaluation of oral motor function
- An orofacial examination
- An assessment of language comprehension
The initial screening might result in no action if speech symptoms are determined to be developmentally appropriate. If a disorder is suspected, the initial screening might result in a referral for a comprehensive speech sound assessment, comprehensive language assessment, audiology evaluation, or other medical services.
Initial assessments and more in-depth screenings might occur in a private speech therapy practice, rehabilitation center, school, childcare program, or early intervention center. For older adults, skilled nursing centers and nursing homes may assess patients for speech, hearing, and language disorders.
How Are Speech Impediments Treated?
Once an evaluation determines precisely what type of speech sound disorder is present, patients can begin treatment. Speech-language pathologists use a combination of therapy, exercise, and assistive devices to treat speech disorders.
Speech therapy might focus on motor production (articulation) or linguistic (phonological or language-based) elements of speech, according to ASHA. There are various types of speech therapy available to patients.
Contextual Utilization — This therapeutic approach teaches methods for producing sounds consistently in different syllable-based contexts, such as phonemic or phonetic contexts. These methods are helpful for patients who produce sounds inconsistently.
Phonological Contrast — This approach focuses on improving speech through emphasis of phonemic contrasts that serve to differentiate words. Examples might include minimal opposition words (pot vs. spot) or maximal oppositions (mall vs. call). These therapy methods can help patients who use phonological error patterns.
Distinctive Feature — In this category of therapy, SLPs focus on elements that are missing in speech, such as articulation or nasality. This helps patients who substitute sounds by teaching them to distinguish target sounds from substituted sounds.
Core Vocabulary — This therapeutic approach involves practicing whole words that are commonly used in a specific patient’s communications. It is effective for patients with inconsistent sound production.
Metaphon — In this type of therapy, patients are taught to identify phonological language structures. The technique focuses on contrasting sound elements, such as loud vs. quiet, and helps patients with unintelligible speech issues.
Oral-Motor — This approach uses non-speech exercises to supplement sound therapies. This helps patients gain oral-motor strength and control to improve articulation.
Other methods professionals may use to help fix speech impediments include relaxation, breathing, muscle strengthening, and voice exercises. They may also recommend assistive devices, which may include:
- Radio transmission systems
- Personal amplifiers
- Picture boards
- Touch screens
- Text displays
- Speech-generating devices
- Hearing aids
- Cochlear implants
Resources for Professionals on How to Fix a Speech Impediment
The following resources provide information for speech therapists and other health professionals.
Assistive Devices: Information on hearing and speech aids from the NIDCD
Information for Audiologists: Publications, news, and practice aids for audiologists from ASHA
Information for Speech-Language Pathologists: Publications, news, and practice aids for SLPs from ASHA
Speech Disorder Tips for Families
For parents who are concerned that their child might have a speech disorder — or who want to prevent the development of a disorder — there are a number of activities that can help. The following are tasks that parents can engage in on a regular basis to develop literacy and speech skills.
- Introducing new vocabulary words
- Reading picture and story books with various sounds and patterns
- Talking to children about objects and events
- Answering children’s questions during routine activities
- Encouraging drawing and scribbling
- Pointing to words while reading books
- Pointing out words and sentences in objects and signs
Parents can take the following steps to make sure that potential speech impediments are identified early on.
- Discussing concerns with physicians
- Asking for hearing, vision, and speech screenings from doctors
- Requesting special education assessments from school officials
- Requesting a referral to a speech-language pathologist, audiologist, or other specialist
When a child is engaged in speech therapy, speech-language pathologists will typically establish collaborative relationships with families, sharing information and encouraging parents to participate in therapy decisions and practices.
SLPs will work with patients and their families to set goals for therapy outcomes. In addition to therapy sessions, they may develop activities and exercises for families to work on at home. It is important that caregivers are encouraging and patient with children during therapy.
Resources for Parents on How to Fix a Speech Impediment
The following resources provide additional information on treatment options for speech disorders.
Speech, Language, and Swallowing Disorders Groups: Listing of self-help groups from ASHA
ProFind: Search tool for finding certified SLPs and audiologists from ASHA
Baby’s Hearing and Communication Development Checklist: Listing of milestones that children should meet by certain ages from the NIDCD
If identified during childhood, speech disorders can be corrected efficiently, giving children greater communication opportunities. If left untreated, speech impediments can cause a variety of problems in adulthood, and may be more difficult to diagnose and treat.
Parents, teachers, doctors, speech and language professionals, and other concerned parties all have unique responsibilities in recognizing and treating speech disorders. Through professional therapy, family engagement, positive encouragement and a strong support network, individuals with speech impediments can overcome their challenges and develop essential communication skills.
Additional Sources
American Speech-Language-Hearing Association, Speech Sound Disorders
Identify the Signs, Signs of Speech and Language Disorders
Intermountain Healthcare, Phonological Disorders
MedlinePlus, Speech disorders – children
National Institutes of Health, National Institutes on Deafness and Other Communication Disorders, “Quick Statistics About Voice, Speech, Language”
Bring us your ambition and we’ll guide you along a personalized path to a quality education that’s designed to change your life.
Take Your Next Brave Step
Receive information about the benefits of our programs, the courses you'll take, and what you need to apply.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Types of Speech Impediments
Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
:max_bytes(150000):strip_icc():format(webp)/SanjanaGupta-d217a6bfa3094955b3361e021f77fcca.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
- Follow Us On:

- What is the CPIR?
- What’s on the Hub?
- CPIR Resource Library
- Buzz from the Hub
- Event Calendar
- Survey Item Bank
- CPIR Webinars
- What are Parent Centers?
- National RAISE Center
- RSA Parent Centers
- Regional PTACs
- Find Your Parent Center
- CentersConnect (log-in required)
- Parent Center eLearning Hub
Select Page
Speech and Language Impairments

- En español | In Spanish
- See fact sheets on other disabilities
Table of Contents
A Day in the Life of an SLP
Christina is a speech-language pathologist. She works with children and adults who have impairments in their speech, voice, or language skills. These impairments can take many forms, as her schedule today shows.
First comes Robbie. He’s a cutie pie in the first grade and has recently been diagnosed with childhood apraxia of speech—or CAS. CAS is a speech disorder marked by choppy speech. Robbie also talks in a monotone, making odd pauses as he tries to form words. Sometimes she can see him struggle. It’s not that the muscles of his tongue, lips, and jaw are weak. The difficulty lies in the brain and how it communicates to the muscles involved in producing speech. The muscles need to move in precise ways for speech to be intelligible. And that’s what she and Robbie are working on.
Next, Christina goes down the hall and meets with Pearl in her third grade classroom. While the other students are reading in small groups, she works with Pearl one on one, using the same storybook. Pearl has a speech disorder, too, but hers is called dysarthria. It causes Pearl’s speech to be slurred, very soft, breathy, and slow. Here, the cause is weak muscles of the tongue, lips, palate, and jaw. So that’s what Christina and Pearl work on—strengthening the muscles used to form sounds, words, and sentences, and improving Pearl’s articulation.
One more student to see—4th grader Mario , who has a stutter. She’s helping Mario learn to slow down his speech and control his breathing as he talks. Christina already sees improvement in his fluency.
Tomorrow she’ll go to a different school, and meet with different students. But for today, her day is…Robbie, Pearl, and Mario.
Back to top
There are many kinds of speech and language disorders that can affect children. In this fact sheet, we’ll talk about four major areas in which these impairments occur. These are the areas of:
Articulation | speech impairments where the child produces sounds incorrectly (e.g., lisp, difficulty articulating certain sounds, such as “l” or “r”);
Fluency | speech impairments where a child’s flow of speech is disrupted by sounds, syllables, and words that are repeated, prolonged, or avoided and where there may be silent blocks or inappropriate inhalation, exhalation, or phonation patterns;
Voice | speech impairments where the child’s voice has an abnormal quality to its pitch, resonance, or loudness; and
Language | language impairments where the child has problems expressing needs, ideas, or information, and/or in understanding what others say. ( 1 )
These areas are reflected in how “speech or language impairment” is defined by the nation’s special education law, the Individuals with Disabilities Education Act, given below. IDEA is the law that makes early intervention services available to infants and toddlers with disabilities, and special education available to school-aged children with disabilities.
Definition of “Speech or Language Impairment” under IDEA
The Individuals with Disabilities Education Act, or IDEA, defines the term “speech or language impairment” as follows:
Development of Speech and Language Skills in Childhood
Speech and language skills develop in childhood according to fairly well-defined milestones (see below). Parents and other caregivers may become concerned if a child’s language seems noticeably behind (or different from) the language of same-aged peers. This may motivate parents to investigate further and, eventually, to have the child evaluated by a professional.
______________________
More on the Milestones of Language Development
What are the milestones of typical speech-language development? What level of communication skill does a typical 8-month-old baby have, or a 18-month-old, or a child who’s just celebrated his or her fourth birthday?
You’ll find these expertly described in How Does Your Child Hear and Talk? , a series of resource pages available online at the American Speech-Language-Hearing Association (ASHA): http://www.asha.org/public/speech/development/chart.htm
Having the child’s hearing checked is a critical first step. The child may not have a speech or language impairment at all but, rather, a hearing impairment that is interfering with his or her development of language.
It’s important to realize that a language delay isn’t the same thing as a speech or language impairment. Language delay is a very common developmental problem—in fact, the most common, affecting 5-10% of children in preschool. ( 2 ) With language delay, children’s language is developing in the expected sequence, only at a slower rate. In contrast, speech and language disorder refers to abnormal language development. ( 3 ) Distinguishing between the two is most reliably done by a certified speech-language pathologist such as Christina, the SLP in our opening story.
Characteristics of Speech or Language Impairments
The characteristics of speech or language impairments will vary depending upon the type of impairment involved. There may also be a combination of several problems.
When a child has an articulation disorder , he or she has difficulty making certain sounds. These sounds may be left off, added, changed, or distorted, which makes it hard for people to understand the child.
Leaving out or changing certain sounds is common when young children are learning to talk, of course. A good example of this is saying “wabbit” for “rabbit.” The incorrect articulation isn’t necessarily a cause for concern unless it continues past the age where children are expected to produce such sounds correctly. ( 4 ) ( ASHA’s milestone resource pages , mentioned above, are useful here.)
Fluency refers to the flow of speech. A fluency disorder means that something is disrupting the rhythmic and forward flow of speech—usually, a stutter. As a result, the child’s speech contains an “abnormal number of repetitions, hesitations, prolongations, or disturbances. Tension may also be seen in the face, neck, shoulders, or fists.” ( 5 )
Voice is the sound that’s produced when air from the lungs pushes through the voice box in the throat (also called the larnyx), making the vocal folds within vibrate. From there, the sound generated travels up through the spaces of the throat, nose, and mouth, and emerges as our “voice.”
A voice disorder involves problems with the pitch, loudness, resonance, or quality of the voice. ( 6 ) The voice may be hoarse, raspy, or harsh. For some, it may sound quite nasal; others might seem as if they are “stuffed up.” People with voice problems often notice changes in pitch, loss of voice, loss of endurance, and sometimes a sharp or dull pain associated with voice use. ( 7 )
Language has to do with meanings, rather than sounds. ( 8 ) A language disorder refers to an impaired ability to understand and/or use words in context. ( 9 ) A child may have an expressive language disorder (difficulty in expressing ideas or needs), a receptive language disorder (difficulty in understanding what others are saying), or a mixed language disorder (which involves both).
Some characteristics of language disorders include:
- improper use of words and their meanings,
- inability to express ideas,
- inappropriate grammatical patterns,
- reduced vocabulary, and
- inability to follow directions. ( 10 )
Children may hear or see a word but not be able to understand its meaning. They may have trouble getting others to understand what they are trying to communicate. These symptoms can easily be mistaken for other disabilities such as autism or learning disabilities, so it’s very important to ensure that the child receives a thorough evaluation by a certified speech-language pathologist.
What Causes Speech and Language Disorders?
Some causes of speech and language disorders include hearing loss, neurological disorders, brain injury, intellectual disabilities, drug abuse, physical impairments such as cleft lip or palate, and vocal abuse or misuse. Frequently, however, the cause is unknown.
Of the 6.1 million children with disabilities who received special education under IDEA in public schools in the 2005-2006 school year, more than 1.1 million were served under the category of speech or language impairment. ( 11 ) This estimate does not include children who have speech/language problems secondary to other conditions such as deafness, intellectual disability, autism, or cerebral palsy. Because many disabilities do impact the individual’s ability to communicate, the actual incidence of children with speech-language impairment is undoubtedly much higher.
Finding Help
Because all communication disorders carry the potential to isolate individuals from their social and educational surroundings, it is essential to provide help and support as soon as a problem is identified. While many speech and language patterns can be called “baby talk” and are part of children’s normal development, they can become problems if they are not outgrown as expected.
Therefore, it’s important to take action if you suspect that your child has a speech or language impairment (or other disability or delay). The next two sections in this fact sheet will tell you how to find this help.
Help for Babies and Toddlers
Since we begin learning communication skills in infancy, it’s not surprising that parents are often the first to notice—and worry about—problems or delays in their child’s ability to communicate or understand. Parents should know that there is a lot of help available to address concerns that their young child may be delayed or impaired in developing communication skills. Of particular note is the the early intervention system that’s available in every state.
Early intervention is a system of services designed to help infants and toddlers with disabilities (until their 3rd birthday) and their families. It’s mandated by the IDEA. Through early intervention, parents can have their young one evaluated free of charge, to identify developmental delays or disabilities, including speech and language impairments.
If a child is found to have a delay or disability, staff work with the child’s family to develop what is known as an Individualized Family Services Plan , or IFSP . The IFSP will describe the child’s unique needs as well as the services he or she will receive to address those needs. The IFSP will also emphasize the unique needs of the family, so that parents and other family members will know how to support their young child’s needs. Early intervention services may be provided on a sliding-fee basis, meaning that the costs to the family will depend upon their income.
To identify the EI program in your neighborhood | Ask your child’s pediatrician for a referral to early intervention or the Child Find in the state. You can also call the local hospital’s maternity ward or pediatric ward, and ask for the contact information of the local early intervention program.
Back to top
Help for School-Aged Children, including Preschoolers
Just as IDEA requires that early intervention be made available to babies and toddlers with disabilities, it requires that special education and related services be made available free of charge to every eligible child with a disability, including preschoolers (ages 3-21). These services are specially designed to address the child’s individual needs associated with the disability—in this case, a speech or language impairment.
Many children are identified as having a speech or language impairment after they enter the public school system. A teacher may notice difficulties in a child’s speech or communication skills and refer the child for evaluation. Parents may ask to have their child evaluated. This evaluation is provided free by the public school system.
If the child is found to have a disability under IDEA—such as a speech-language impairment—school staff will work with his or her parents to develop an Individualized Education Program , or IEP . The IEP is similar to an IFSP. It describes the child’s unique needs and the services that have been designed to meet those needs. Special education and related services are provided at no cost to parents.
There is a lot to know about the special education process, much of which you can learn at the Center for Parent Information and Resources (CPIR). We offer a wide range of publications and resource pages on the topic. Enter our special education information at: http://www.parentcenterhub.org/repository/schoolage/
Educational Considerations
Communication skills are at the heart of the education experience. Eligible students with speech or language impairments will want to take advantage of special education and related services that are available in public schools.
The types of supports and services provided can vary a great deal from student to student, just as speech-language impairments do. Special education and related services are planned and delivered based on each student’s individualized educational and developmental needs.
Most, if not all, students with a speech or language impairment will need speech-language pathology services . This related service is defined by IDEA as follows:
(15) Speech-language pathology services includes—
(i) Identification of children with speech or language impairments;
(ii) Diagnosis and appraisal of specific speech or language impairments;
(iii) Referral for medical or other professional attention necessary for the habilitation of speech or language impairments;
(iv) Provision of speech and language services for the habilitation or prevention of communicative impairments; and
Thus, in addition to diagnosing the nature of a child’s speech-language difficulties, speech-language pathologists also provide:
- individual therapy for the child;
- consult with the child’s teacher about the most effective ways to facilitate the child’s communication in the class setting; and
- work closely with the family to develop goals and techniques for effective therapy in class and at home.
Speech and/or language therapy may continue throughout a student’s school years either in the form of direct therapy or on a consultant basis.
Assistive technology (AT) can also be very helpful to students, especially those whose physical conditions make communication difficult. Each student’s IEP team will need to consider if the student would benefit from AT such as an electronic communication system or other device. AT is often the key that helps students engage in the give and take of shared thought, complete school work, and demonstrate their learning.
Tips for Teachers
— Learn as much as you can about the student’s specific disability. Speech-language impairments differ considerably from one another, so it’s important to know the specific impairment and how it affects the student’s communication abilities.
— Recognize that you can make an enormous difference in this student’s life! Find out what the student’s strengths and interests are, and emphasize them. Create opportunities for success.
—If you are not part of the student’s IEP team, a sk for a copy of his or her IEP . The student’s educational goals will be listed there, as well as the services and classroom accommodations he or she is to receive.
— Make sure that needed accommodations are provided for classwork, homework, and testing. These will help the student learn successfully.
— Consult with others (e.g., special educators, the SLP) who can help you identify strategies for teaching and supporting this student, ways to adapt the curriculum, and how to address the student’s IEP goals in your classroom.
— Find out if your state or school district has materials or resources available to help educators address the learning needs of children with speech or language impairments. It’s amazing how many do!
— Communicate with the student’s parents . Regularly share information about how the student is doing at school and at home.
Tips for Parents
— Learn the specifics of your child’s speech or language impairment. The more you know, the more you can help yourself and your child.
— Be patient. Your child, like every child, has a whole lifetime to learn and grow.
— Meet with the school and develop an IEP to address your child’s needs. Be your child’s advocate. You know your son or daughter best, share what you know.
— Be well informed about the speech-language therapy your son or daughter is receiving. Talk with the SLP, find out how to augment and enrich the therapy at home and in other environments. Also find out what not to do!
— Give your child chores. Chores build confidence and ability. Keep your child’s age, attention span, and abilities in mind. Break down jobs into smaller steps. Explain what to do, step by step, until the job is done. Demonstrate. Provide help when it’s needed. Praise a job (or part of a job) well done.
— Listen to your child. Don’t rush to fill gaps or make corrections. Conversely, don’t force your child to speak. Be aware of the other ways in which communication takes place between people.
— Talk to other parents whose children have a similar speech or language impairment. Parents can share practical advice and emotional support. See if there’s a parent nearby by visiting the Parent to Parent USA program and using the interactive map.
— Keep in touch with your child’s teachers. Offer support. Demonstrate any assistive technology your child uses and provide any information teachers will need. Find out how you can augment your child’s school learning at home.
Readings and Articles
We urge you to read the articles identified in the References section. Each provides detailed and expert information on speech or language impairments. You may also be interested in:
Speech-Language Impairment: How to Identify the Most Common and Least Diagnosed Disability of Childhood http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2491683/
Organizations to Consult
ASHA | American Speech-Language-Hearing Association Information in Spanish | Información en español. 1.800.638.8255 | [email protected] | www.asha.org
NIDCD | National Institute on Deafness and Other Communication Disorders 1.800.241.1044 (Voice) | 1.800.241.1055 (TTY) [email protected] | http://www.nidcd.nih.gov/
American Cleft Palate and Craniofacial Association (ACPA) 1.800.242.5338 | https://acpacares.org/
Childhood Apraxia of Speech Association of North America | CASANA http://www.apraxia-kids.org
National Stuttering Foundation 1.800.937.8888 | [email protected] | http://www.nsastutter.org/
Stuttering Foundation 1.800.992.9392 | [email protected] | http://www.stuttersfa.org/
1 | Minnesota Department of Education. (2010). Speech or language impairments . Online at: http://education.state.mn.us/MDE/EdExc/SpecEdClass/DisabCateg/SpeechLangImpair/index.html
2 | Boyse, K. (2008). Speech and language delay and disorder . Retrieved from the University of Michigan Health System website: http://www.med.umich.edu/yourchild/topics/speech.htm
4 | American Speech-Language-Hearing Association. (n.d.). Speech sound disorders: Articulation and phonological processes . Online at: http://www.asha.org/public/speech/disorders/speechsounddisorders.htm
5 | Cincinnati Children’s Hospital. (n.d.). Speech disorders . Online at: http://www.cincinnatichildrens.org/health/s/speech-disorder/
6 | National Institute on Deafness and Other Communication Disorders. (2002). What is voice? What is speech? What is language? Online at: http://www.nidcd.nih.gov/health/voice/pages/whatis_vsl.aspx
7 | American Academy of Otolaryngology — Head and Neck Surgery. (n.d.). About your voice . Online at: http://www.entnet.org/content/about-your-voice
8 | Boyse, K. (2008). Speech and language delay and disorder . Retrieved from the University of Michigan Health System website: http://www.med.umich.edu/yourchild/topics/speech.htm
9 | Encyclopedia of Nursing & Allied Health. (n.d.). Language disorders . Online at: http://www.enotes.com/nursing-encyclopedia/language-disorders
10 | Ibid .
11 | U.S. Department of Education. (2010, December). Twenty-ninth annual report to Congress on the Implementation of the Individuals with Disabilities Education Act: 2007 . Online at: http://www2.ed.gov/about/reports/annual/osep/2007/parts-b-c/index.html

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Speech and Language Impairments
The Individuals with Disabilities Education Act, or IDEA, defines the term “speech or language impairment” as follows:
“(11) Speech or language impairment means a communication disorder, such as stuttering, impaired articulation, a language impairment, or a voice impairment, that adversely affects a child’s educational performance.” [34 CFR §300.8(c)(11]
(Parent Information and Resources Center, 2015)
Table of Contents

What is a Speech and Language Impairment?
Characteristics of speech or language impairments, interventions and strategies, related service provider-slp.
- A Day in the Life of an SLP
Assistive Technology
Speech and language impairment are basic categories that might be drawn in issues of communication involve hearing, speech, language, and fluency.
A speech impairment is characterized by difficulty in articulation of words. Examples include stuttering or problems producing particular sounds. Articulation refers to the sounds, syllables, and phonology produced by the individual. Voice, however, may refer to the characteristics of the sounds produced—specifically, the pitch, quality, and intensity of the sound. Often, fluency will also be considered a category under speech, encompassing the characteristics of rhythm, rate, and emphasis of the sound produced.
A language impairment is a specific impairment in understanding and sharing thoughts and ideas, i.e. a disorder that involves the processing of linguistic information. Problems that may be experienced can involve the form of language, including grammar, morphology, syntax; and the functional aspects of language, including semantics and pragmatics.
(Wikipedia, n.d./ Speech and Language Impairment)
*It’s important to realize that a language delay isn’t the same thing as a speech or language impairment. Language delay is a very common developmental problem—in fact, the most common, affecting 5-10% of children in preschool. With language delay, children’s language is developing in the expected sequence, only at a slower rate. In contrast, speech and language disorder refers to abnormal language development. Distinguishing between the two is most reliably done by a certified speech-language pathologist. (CPIR, 2015)
The characteristics of speech or language impairments will vary depending upon the type of impairment involved. There may also be a combination of several problems.
When a child has an articulation disorder , he or she has difficulty making certain sounds. These sounds may be left off, added, changed, or distorted, which makes it hard for people to understand the child.
Leaving out or changing certain sounds is common when young children are learning to talk, of course. A good example of this is saying “wabbit” for “rabbit.” The incorrect articulation isn’t necessarily a cause for concern unless it continues past the age where children are expected to produce such sounds correctly
Fluency refers to the flow of speech. A fluency disorder means that something is disrupting the rhythmic and forward flow of speech—usually, a stutter. As a result, the child’s speech contains an “abnormal number of repetitions, hesitations, prolongations, or disturbances. Tension may also be seen in the face, neck, shoulders, or fists.”
Voice is the sound that’s produced when air from the lungs pushes through the voice box in the throat (also called the larnyx), making the vocal folds within vibrate. From there, the sound generated travels up through the spaces of the throat, nose, and mouth, and emerges as our “voice.”
A voice disorder involves problems with the pitch, loudness, resonance, or quality of the voice. The voice may be hoarse, raspy, or harsh. For some, it may sound quite nasal; others might seem as if they are “stuffed up.” People with voice problems often notice changes in pitch, loss of voice, loss of endurance, and sometimes a sharp or dull pain associated with voice use.
Language has to do with meanings, rather than sounds. A language disorder refers to an impaired ability to understand and/or use words in context. A child may have an expressive language disorder (difficulty in expressing ideas or needs), a receptive language disorder (difficulty in understanding what others are saying), or a mixed language disorder (which involves both).
Some characteristics of language disorders include:
- improper use of words and their meanings,
- inability to express ideas,
- inappropriate grammatical patterns,
- reduced vocabulary, and
- inability to follow directions.
Children may hear or see a word but not be able to understand its meaning. They may have trouble getting others to understand what they are trying to communicate. These symptoms can easily be mistaken for other disabilities such as autism or learning disabilities, so it’s very important to ensure that the child receives a thorough evaluation by a certified speech-language pathologist.
(CPIR, 2015)
- Use the (Cash, Wilson, and DeLaCruz, n.d) reading and/or the [ESU 8 Wednesday Webinar] to develop this section of the summary.
Cash, A, Wilson, R. and De LaCruz, E.(n,d.) Practical Recommendations for Teachers: Language Disorders. https://www.education.udel.edu/wp-content/uploads/2013/01/LanguageDisorders.pdf
[ESU 8 Wednesday Webinar] Speech Language Strategies for Classroom Teachers.- video below
Video: Speech Language Strategies for Classroom Teachers (15:51 minutes)’
[ESU 8 Wednesday Webinars]. (2015, Nov. 19) . Speech Language Strategies for Classroom Teachers. [Video FIle]. From https://youtu.be/Un2eeM7DVK8
Most, if not all, students with a speech or language impairment will need speech-language pathology services . This related service is defined by IDEA as follows:
(15) Speech-language pathology services include—
(i) Identification of children with speech or language impairments;
(ii) Diagnosis and appraisal of specific speech or language impairments;
(iii) Referral for medical or other professional attention necessary for the habilitation of speech or language impairments;
(iv) Provision of speech and language services for the habilitation or prevention of communicative impairments; and
(v) Counseling and guidance of parents, children, and teachers regarding speech and language impairments. [34 CFR §300.34(c)(15)]
Thus, in addition to diagnosing the nature of a child’s speech-language difficulties, speech-language pathologists also provide:
- individual therapy for the child;
- consult with the child’s teacher about the most effective ways to facilitate the child’s communication in the class setting; and
- work closely with the family to develop goals and techniques for effective therapy in class and at home.
Speech and/or language therapy may continue throughout a student’s school years either in the form of direct therapy or on a consultant basis.
A Day in the Life of an SLP
Christina is a speech-language pathologist. She works with children and adults who have impairments in their speech, voice, or language skills. These impairments can take many forms, as her schedule today shows.
First comes Robbie. He’s a cutie pie in the first grade and has recently been diagnosed with childhood apraxia of speech—or CAS. CAS is a speech disorder marked by choppy speech. Robbie also talks in a monotone, making odd pauses as he tries to form words. Sometimes she can see him struggle. It’s not that the muscles of his tongue, lips, and jaw are weak. The difficulty lies in the brain and how it communicates to the muscles involved in producing speech. The muscles need to move in precise ways for speech to be intelligible. And that’s what she and Robbie are working on.
Next, Christina goes down the hall and meets with Pearl in her third grade classroom. While the other students are reading in small groups, she works with Pearl one on one, using the same storybook. Pearl has a speech disorder, too, but hers is called dysarthria. It causes Pearl’s speech to be slurred, very soft, breathy, and slow. Here, the cause is weak muscles of the tongue, lips, palate, and jaw. So that’s what Christina and Pearl work on—strengthening the muscles used to form sounds, words, and sentences, and improving Pearl’s articulation.
One more student to see—4th grader Mario , who has a stutter. She’s helping Mario learn to slow down his speech and control his breathing as he talks. Christina already sees improvement in his fluency.
Tomorrow she’ll go to a different school, and meet with different students. But for today, her day is…Robbie, Pearl, and Mario.
Assistive technology (AT) can also be very helpful to students, especially those whose physical conditions make communication difficult. Each student’s IEP team will need to consider if the student would benefit from AT such as an electronic communication system or other device. AT is often the key that helps students engage in the give and take of shared thought, complete school work, and demonstrate their learning. (CPIR, 2015)
Project IDEAL , suggests two major categories of AT computer software packages to develop the child’s speech and language skills and augmentative or alternative communication (AAC).
Augmentative and alternative communication ( AAC ) encompasses the communication methods used to supplement or replace speech or writing for those with impairments in the production or comprehension of spoken or written language. Augmentative and alternative communication may used by individuals to compensate for severe speech-language impairments in the expression or comprehension of spoken or written language. AAC can be a permanent addition to a person’s communication or a temporary aid.
(Wikipedia, (n.d. /Augmentative and alternative communication)
Center for Parent Information and Resources (CPIR) (2015), Speech and Language Impairments, Newark, NJ, Author, Retrieved 4.1.19 from https://www.parentcenterhub.org/speechlanguage/
Wikipedia (n.d.) Augmentative and alternative communication. From https://en.wikipedia.org/wiki/Augmentative_and_alternative_communication
Wikipedia, (n.d.) Speech and Language Impairment. From https://en.wikipedia.org/wiki/Speech_and_language_impairment
Updated 8.8.23
Understanding and Supporting Learners with Disabilities Copyright © 2019 by Paula Lombardi is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Healthy Habits
- Data and Statistics
- Resources for Child Development
- Positive Parenting Tips
- Keeping Children with Disabilities Safe
Developmental Disability Basics
What to know.
- Developmental disabilities are a group of conditions due to an impairment in physical, learning, language, or behavior areas.
- These conditions begin during the child's developmental period, may impact day-to-day functioning, and usually last throughout a person's lifetime.
- Most developmental disabilities begin before a baby is born, but some can happen after birth because of injury, infection, or other factors.

Causes and risk factors
Most developmental disabilities are thought to be caused by a complex mix of factors. These factors include genetics; parental health and behaviors (such as smoking and drinking) during pregnancy; complications during birth; infections the mother might have during pregnancy or the baby might have very early in life; and exposure of the mother or child to high levels of environmental toxins, such as lead. For some developmental disabilities, such as fetal alcohol syndrome, which is caused by drinking alcohol during pregnancy, we know the cause. But for most, we don’t.
Following are some examples of what we know about specific developmental disabilities:
- At least 25% of hearing loss among babies is due to maternal infections during pregnancy, such as cytomegalovirus (CMV) infection ; complications after birth; and head trauma.
- Some of the most common known causes of intellectual disability include fetal alcohol syndrome disorder ; genetic and chromosomal conditions, such as Down syndrome and fragile X syndrome ; and certain infections during pregnancy.
- Children who have a sibling with autism spectrum disorder are at a higher risk of also having autism spectrum disorder.
- Low birthweight , premature birth, multiple birth, and infections during pregnancy are associated with an increased risk for many developmental disabilities.
- Untreated newborn jaundice (high levels of bilirubin in the blood during the first few days after birth) can cause a type of brain damage known as kernicterus. Children with kernicterus are more likely to have cerebral palsy, hearing and vision problems, and problems with their teeth. Early detection and treatment of newborn jaundice can prevent kernicterus.
The Study to Explore Early Development (SEED) is a multiyear study funded by CDC. It is currently the largest study in the United States to help identify factors that may put children at risk for autism spectrum disorders and other developmental disabilities.
Who is affected
Developmental disabilities occur among all racial, ethnic, and socioeconomic groups. Recent estimates in the United States show that about 1 in 6, or about 17%, of children aged 3 through 17 years have one or more developmental disabilities, such as
- Autism spectrum disorder
- Cerebral palsy
- Hearing loss
- Fragile X syndrome
- Tourette syndrome
- and other developmental disabilities 1
For more than a decade, CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network has been tracking the number and characteristics of children with autism spectrum disorder, cerebral palsy, and intellectual disability in several diverse communities throughout the United States.
Healthy living for people with disabilities
Children and adults with disabilities need health care and health programs for the same reasons anyone else does—to stay well, active, and a part of the community.
Having a disability does not mean a person is not healthy or that he or she cannot be healthy. Being healthy means the same thing for all of us—getting and staying well so we can lead full, active lives. That includes having the tools and information to make healthy choices and knowing how to prevent illness. Some health conditions, such as asthma, gastrointestinal symptoms, eczema and skin allergies, and migraine headaches, have been found to be more common among children with developmental disabilities. Thus, it is especially important for children with developmental disabilities to see a health care provider regularly.
CDC does not study education or treatment programs for people with developmental disabilities, nor does it provide direct services to people with developmental disabilities or to their families. However, CDC has put together a list of resources for people affected by developmental disabilities.
Don't Wait!
- Zablotsky B, Black LI, Maenner MJ, et.al. Prevalence and Trends of Developmental Disabilities among Children in the US: 2009–2017 . Pediatrics. 2019; 144(4):e20190811.
Child Development
The early years of a child’s life are very important for their health and development. Parents, health professionals, educators, and others can work together as partners to help children grow up to reach their full potential.
- Open access
- Published: 13 May 2024
Neuropsychological profile associated with KAT6A syndrome: Emergent genotype-phenotype trends
- Rowena Ng ORCID: orcid.org/0000-0001-7193-4300 1 , 2 ,
- Allison J Kalinousky 3 &
- Jacqueline Harris 1 , 3 , 4 , 5
Orphanet Journal of Rare Diseases volume 19 , Article number: 196 ( 2024 ) Cite this article
117 Accesses
2 Altmetric
Metrics details
KAT6A (Arboleda-Tham) syndrome is a Mendelian disorder of the epigenetic machinery caused by pathogenic variants in the lysine acetyltransferase 6 A ( KAT6A ) gene. Intellectual disability and speech/language impairment (e.g., minimally verbal) are common features of the disorder, with late-truncating variants associated with a more severe form of intellectual disability. However, much of the cognitive phenotype remains elusive given the dearth of research.
Participants and methods
This study examined non-verbal and social skills of 15 individuals with molecularly-confirmed diagnoses of KAT6A syndrome (Mean age = 10.32 years, SD = 4.12). Participants completed select subtests from the DAS-II, the NEPSY-II, and the Beery Buktenica Developmental Test of Visual Motor Integration 6th Edition, and their caregivers completed an assortment of behavior rating inventories.
Findings suggest global cognitive impairment with nonverbal cognition scores similar to those for receptive language. Autism-related features, particularly restricted interests and repetitive behaviors, and broad adaptive deficits were common in our sample juxtaposed with a relatively strong social drive and low frequency of internalizing and externalizing behavioral problems. A general trend of lower performance scores on nonverbal and receptive language measures was observed among those with protein-truncating variants vs. missense variants; however, no effect was observed on caregiver rating inventories of daily behaviors. Late and early truncating variants yielded comparable neuropsychological profiles.
Conclusions
Overall, study results show the cognitive phenotype of KAT6A syndrome includes equally impaired nonverbal cognition and receptive language functioning, paired with relatively intact social drive and strengths in behavior regulation. Emergent genotype-phenotype correlations suggest cognition may be more affected in protein-truncating than missense mutations although similar neurobehavioral profiles were observed.
Introduction
KAT6A syndrome (Arboleda-Tham syndrome; MIM: 616,268) is a rare Mendelian disorder of epigenetic machinery (MDEM), a class of relatively newly defined neurodevelopmental disorders that result from mutations in genes dedicated to encoding epigenetic regulators [ 1 ]. KAT6A syndrome is caused by a pathogenic variant in histone K lysine acetyltransferase KAT6A (Arboleda et al., 2015), a gene that belongs to the MYST family of histone acetyltransferases that facilitates histone acetylation and regulation of transcription. The prevalence rate of this syndrome is not clear although 500 cases of KAT6A and KAT6B disorders have been reported through the patient-driven KAT6 Foundation ( www.kat6a.org ). Individuals with KAT6A syndrome, like other MDEMs, share some overlapping traits including intellectual disability, hypotonia, and congenital heart defects [ 2 , 3 ]. Other cardinal features of KAT6A disorder include microcephaly, unique facial dysmorphology, vision defects like strabismus and ptosis, oromotor dysfunction, hypotonia, gastrointestinal issues, congenital cardiac malformation, and sleep disturbance Arboleda et al., 2015 [ 2 , 3 , 4 , 5 ].
The neuropsychological profile of KAT6A syndrome remains relatively unknown although intellectual disability and/or global developmental delay is almost universally seen among affected individuals [ 6 ]. Language is severely affected, with nearly 75% of affected individuals presenting with minimally verbal skills [ 6 ]. Previously, receptive language or comprehension of language was reported to be more preserved [ 2 ], however, recent findings have shown receptive language is similarly affected in those with this syndrome [ 6 ]. Investigations on genotype-phenotype correlations in cognition and neurobehavioral functioning in KAT6A syndrome have yielded mixed results. Late truncating variants (exons 16–17) as compared to early truncating (exons 1–15) have been associated with more severe intellectual disability based on clinician-ratings or documented diagnoses based on medical records [ 2 , 6 ] and greater difficulties in receptive communication, socialization, and daily living skills based on parent-rating inventories [ 6 ]. Other prospective behavioral studies did not observe differences in internalizing, externalizing, and adaptive behaviors based on truncating variant [ 4 ]. Notably, a vast majority of studies focused on KAT6A syndrome rely on retrospective review of medical charts and/or clinician- or caregiver-rating measures rather than performance-based testing. Other than language [ 6 ], it remains unclear the extent other cognitive domains may be affected in these individuals. Likewise, it is possible the documented rates of intellectual disability associated with KAT6A syndrome may largely reflect verbal/language deficits whereby nonverbal skills are more preserved.
Accordingly, this study aimed to prospectively characterize nonverbal cognition and neurobehavioral functioning in those with KAT6A syndrome. Genotype-phenotype correlations (truncating vs. missense variants) were examined. To our knowledge, this study is the first in the literature to define the neuropsychological phenotype of KAT6A syndrome utilizing a combination of standardized performance-based and caregiver-report measures. Given the exploratory nature of this investigation, we had no a priori hypotheses.
Participants
A total of 15 individuals with KAT6A syndrome participated in this study (8 F, Mean age = 10.32 years, SD = 4.12, range = 4–20). Our sample was largely non-Hispanic, White (80%). As shown in Table 1 , demographic background was similar between those with truncating vs. missense variant. All participants were recruited through the KAT6 Foundation via their website or social media platforms (Twitter, Facebook).
A physician at the authors’ institute reviewed genetic test records shared by caregivers to confirm the variant in KAT6A . Of the 15 participants, 12 had a truncating variant (2 with early truncating variants in exons 1 to 15, 10 with late truncating variants in exon 16 and 17), and three had missense variants. The majority of the sample were diagnosed through whole exome sequencing (73.33%) while the remainder were diagnosed from genetic panel testing. Most were classified as a pathogenic variant (86.67%). One had a variant of uncertain significance but has been examined by an author on this paper and the clinical phenotype is consistent with KAT6A syndrome, and another possessed a likely pathogenic variant. Most variants were de novo (73.33%), while three had unknown inheritance as parents were not tested. Figure 1 illustrates the KAT6A variants in our clinical sample.

Schematic diagram of the pathogenic variants identified in our clinical sample. Note . Participant #4 has both variants p.N621S and p.P1651L
Prior to the assessment appointment, all caregivers completed a research intake questionnaire that inquired about their child’s developmental history, intervention history (i.e., current and past engagement in therapies), and diagnostic history of intellectual disability, autism spectrum disorder, and attention deficit/hyperactivity disorder (ADHD). One parent did not complete the form in full and thus diagnoses were not documented. Cognitive testing was completed at the annual KAT6 Foundation Conference held in Boston, USA ( N = 9), or at the Department of Neuropsychology at Kennedy Krieger Institute ( N = 6). Parents of participants completed additional standardized caregiver-report questionnaires at the time of testing.
Parent-rating inventories
All inventories (outlined below) are rated on a Likert-scale with responses normed by age and sex, when available. The Behavior Rating Inventory of Executive Functioning 2nd Edition (BRIEF-2) [ 8 ], Preschool version (BRIEF-P) [ 7 ] or Adult version (BRIEF-A) [ 11 ] were administered to index daily executive functioning. The inventories provide several subscales of executive functions – those that overlap across the three versions include Inhibit, Emotional Control, Working Memory, Planning/Organize, and Shift. Inhibit refers to impulse control and behavior disengagement, while Working Memory represents the ability to hold information and/or manipulate it in goal-directed behaviors. Emotional Control indexes emotion regulation and Shift represents flexibility in problem-solving or transitioning between activities. Planning/Organize refers to the ability to develop a plan, set objectives, and work towards the targeted goal. All three versions also yield a Global Executive Composite that daily problems with executive functioning. Of note, only one participant was an adult and thus her parent completed the BRIEF-A. On the BRIEF, T-Scores ≥ 70 represent clinically significant problems in the domain, and scores of 60–69 denote areas at risk.
The Social Responsiveness Scale 2nd Edition (SRS-2) [ 15 ] is an inventory often used to screen for behaviors related to autism spectrum disorder (ASD). The five domains indexed by the SRS-2 include Social Awareness, Social Cognition, Social Communication, Social Motivation, and Restricted Interests and Repetitive Behaviors (RRB); and these together yield the SRS-2 Total Composite. Social Awareness represents ones’ sensitivity to detect social cues while Social Cognition indexes the extent one can interpret social cues. Social Communication represents reciprocal communication in interactions, and Social Motivation measures day-to-day motivation to engage in social interactions with others. RRB refers to observed stereotypies and highly restricted interests. T-scores of 60–65 indicate mild difficulty, 66–75 indicate moderate difficulty, and 76 or above indicates severe challenges.
The Child Behavior Checklist (CBCL) is a rating measure used to assess behavioral problems [ 18 , 19 , 20 ]. This measure yields Internalizing and Externalizing Behaviors scales, as well as a Social Problems subscale. Internalizing Behaviors scale consists of items about anxious/low mood and withdrawn behaviors, while Externalizing Behaviors scale includes noncompliant, aggressive and rule-breaking tendencies. Social Problems subscales index daily challenges in peer interactions and relationships. T-Scores ≥ 70 represent clinically significant problems in the area.
Daily adaptive behaviors were assessed by the Adaptive Behavior Assessment 3rd Edition (ABAS-3) [ 9 ]. The ABAS-3 requires caregivers to rate their child’s adaptive behaviors across three domains (Conceptual, Social, Practical). The Conceptual domain comprises of Functional Communication, Functional Academics, and Self-Direction. The Social domain includes both Social and Leisure scales. The Practical domain is computed by the following scales Community Use, Home Living, Health and Safety, and Self-Care. All scales are needed to yield the General Adaptive Composite (GAC), a measure of overall adaptive functioning. Domains that yield standard scores < 70 are extremely low or impaired.
Of note, standard scores and T-scores have means of 100 and 50, and standard deviations of 15 and 10 respectively. Elevated T-scores across the BRIEF, CBCL, and SRS-2 are indicative of more difficulty in the behavioral domain, whereas lower standard scores on the ABAS-3 reflect more challenges in the adaptive skill area.
Performance-based cognitive measures
The following cognitive tests were selected to form a brief test battery that could be administered within 1.5 hours at an annual family conference for those affected by KAT6A syndrome (KAT6 Conference). Initially, test measures were selected for school- to adolescent-age youth. One adult participant later enrolled as the study recruitment continued after the conference. DAS-II and NEPSY-II were not administered to that individual given she was out of the available age norms for the tests.
Based on the participant’s age at testing, the Early Years or School-Age versions of the Differential Ability Scale 2nd Edition (DAS-II) [ 17 ] was administered. Those between 7 years to 8 years, 11 months were administered the Early Years version given the low performance on receptive language measures. Past studies have highlighted severe expressive language difficulties among individuals with KAT6A syndrome with most presenting with limited to minimally verbal skills [ 6 ], as such, non-verbal cognition was emphasized in this study. Both versions offer a Special Nonverbal Composite based on performance across four subtests. In the Early Years version, this composite was comprised of Pattern Construction, Picture Similarities, Matrices and Copying subtests. In the School-Age version. Pattern Construction, Matrices, Recall of Designs and Sequential and Quantitative Reasoning subtests were the main non-verbal measures.
Based on the participant’s age, Arrows and Comprehension of Instructions subtests from the Developmental Neuropsychological Assessment (NEPSY-II) [ 14 ] were used to assess visuospatial perception and receptive language respectively. These subtests were included in our test battery as these they do not require verbal responses. Participants are allowed to point or touch pictures to answer test items. NEPSY-II can be used to assess children between age 3 to 16, although specific subtests vary in available age-based norms. In line with the test manual, NEPSY-II Comprehension of Instructions was given to individuals aged 3 to 16 years, while NEPSY-II Arrows was administered to those aged 5 to 16 years.
To measure visuomotor and visual perceptual skills, the Beery-Buktenica Developmental Test of Visual-Motor Integration 6th Edition (VMI-6) [ 12 ] was included in the research assessment. This test can be administered to individuals aged 2 years and older. The Visual Perceptual and Visual-Motor Integration subtests were selected to examine visual matching of geometric shapes and eye-hand coordination when copying illustrations of shapes of increasing complexity.
Finally, the Peabody Picture Vocabulary Test 5th Edition (PPVT-5) [ 16 ], which assesses receptive vocabulary in individuals aged 2.5 years and older, was included in testing. All performance raw scores were converted to standard scores using age norms provided in test manuals. Lower standard scores reflect more difficulty in the cognitive measure.
Data strategy
Descriptive analyses were used to examine the proportion of participants with a diagnosis of intellectual disability, ASD, and ADHD; and current or prior participation in interventions (speech/language, occupational, physical, behavioral therapies).
With caregiver-report measures, we examined the proportion of our sample with impairment in behavioral functioning (standard score of < 70 on the ABAS-3, T-score > 70 on the BRIEF, SRS-2, or CBCL). Friedman test was used to determine within-group differences across BRIEF, ABAS, CBCL, and SRS-2 Scales in the whole sample to identify areas of relative strengths/weaknesses. Pairwise comparisons with Bonferroni correction were subsequently applied given multiple tests. Although our sample of participants with missense variants is small, Mann-Whitney U-test was utilized to provide preliminary findings on genotype-phenotype associations across behavioral domains, which can be used to inform future investigations.
With cognitive assessment measures, we similarly applied Friedman Test to determine within-group differences in performance across DAS-II Special Nonverbal Composite, PPVT-5, and NEPSY-II Comprehension of Instruction. VMI-6 was not included in this analysis given the DAS-II subtests that comprise the Special Nonverbal Composite measure some similar constructs (e.g., VMI-6 Visual-Motor Integration and DAS-II Copying both assess ones’ ability to draw or copy simple designs). NEPSY-II Arrows was also not included in this analysis, as we were selective in choosing cognitive tests given the limited sample size. Mann-Whitney U-test was repeated to identify any effect of truncating variants on cognitive domains. Of note, given limited individuals with early truncating variants, we first examined broad differences in behavioral and cognitive functioning between those with truncating vs. missense variants. Areas that yielded significant effect of truncating variants (truncating vs. missense variants) were then subject to Kruskal-Wallis test with three groups (early truncating, late truncating, missense variant).
Finally, given a relatively high number of individuals who were unable to participate in testing across measures due to limited comprehension skills (e.g., unable to demonstrate understanding of task instructions with practice items and feedback), we examined the extent these participants were comprised of those with late/early truncating vs. missense variant.
Diagnostic history
Of the 14 parents who completed the diagnostic history section of our research intake questionnaires, 12 reported their child has a diagnosis of intellectual disability (85.71%), 4 with ASD (28.57%), and 4 with ADHD (28.57%). All 14 participants had at least one of these three diagnosis. Those with a truncating vs. missense variants did not show significant difference in diagnostic history for the neurodevelopmental disorders (Table 1 ).
Intervention history
The entire sample reported a history of occupational and speech language therapy, and most have a history of physical therapy (86.67%). In contrast, only 26.67% reported a history of behavior therapy. The proportion of the participants with a history of behavior therapy was slightly more robust in those with missense variants than those with truncating variants (Table 1 ).
Table 2 outlines mean ratings and proportion of our whole sample that reached clinical significance on behavioral measures, which was defined as two standard deviations from the normative mean. Table 3 shows the average ratings across inventory among those with truncating/missense variants. No effect of variant type (truncating, missense variant) was observed across inventories.
Child behavior checklist (CBCL)
Wilcoxon signed rank test showed caregivers provided more elevated ratings for Internalizing than Externalizing behaviors (Z=-3.08, p = 0.002). Despite this trend, on average, our sample was rated within broad typical range for Internalizing and Externalizing behaviors, and Social Problems – a pattern that was observed across truncating and missense variants (Table 3 ). Approximately 15% of the sample was rated to present with clinical level of Internalizing behaviors or Social Problems, but no participant met clinical cut-off for Externalizing behaviors.
Behavior rating inventory of executive functioning (BRIEF-P, BRIEF-2, BRIEF-A)
Overall executive functioning, indexed by BRIEF Global Executive Composite, was in the at-risk range (Table 2 ) with 36% of individuals in the clinical range for global executive composite problems. Within-group comparisons indicate executive functions are differentially affected in those with KAT6A syndrome (χ 2 (4) = 19.83, p < 0.001). Emotional Control yielded less elevated ratings than Inhibit ( p = 0.05), Shift ( p = 0.006), or Working Memory ( p = 0.002). Across subscales, Working Memory was the only area that met clinical level of difficulty, and while Emotional Control was the one executive function that was within typical range. Over 70% of the sample present with significant difficulties in Working Memory, whereas none of the participants was rated to show challenges with Emotional Control. A sizeable proportion of our sample also demonstrates clinical level of problems with Shift, or the ability to problem solve flexibly (45%).
Social Responsiveness Scale 2nd Edition (SRS-2)
Per parent ratings, our sample of individuals with KAT6A syndrome present with moderate severity of ASD-related features (Table 2 ). Within-group comparisons revealed lower scores in Social Motivation in our sample than Social Communication ( p = 0.07) and Restricted Interests/Repetitive Behavior (RRB)( p = 0.005)(χ 2 (4) = 13.67, p = 0.008). Specifically, Social Motivation was rated in the mild severity range whereas all other domains were rated in the moderate level. Likewise, while 20% of our sample yielded Social Motivation scores that were two standard deviations above the normative mean, over twice as many participants were rated to demonstrate prominent problems in other domains (Social Cognition, Social Communication, Social Awareness, RRB). In contrast, two-thirds of our sample met this cut-off for RRB. In brief, lack of social drive is a less common feature in this syndrome, whereas RRB may be a prominent disease characteristic.
Adaptive Behavior Assessment 3rd Edition (ABAS-3)
General Adaptive Composite was very low in our sample. Although, Conceptual, Social and Practical domains were all rated in the very low range, individuals with KAT6A syndrome show different levels of challenge across these areas (χ 2 (2) = 12.31, p = 0.002) (Table 2 ). Conceptual and Practical domains were rated lower than Social domain ( p = 0.003 and 0.04 respectively). Approximately half our sample was rated over two standard deviations below the normative mean for the Social domain compared to over 70% in Practical and Conceptual domains.
In summary, across rating inventories, those with truncating vs. missense variants generally presented with similar behavioral profiles. Areas that are of relative strength for those with KAT6A syndrome include emotion control, behavior regulation, and an affinity for socially interacting with others.
Cognitive testing
Table 4 outlines the average performance across cognitive measures. In the whole sample of individuals with KAT6A syndrome, participants performed significantly below normative mean (> 2 standard deviations) across virtually all measures with the exception of NEPSY-II Arrows which assesses spatial perception. Friedman test did not reveal differences in performance scores across cognitive measures, suggesting non-verbal cognition is similarly affected as receptive language skills (χ 2 (2) = 3.80, p = 0.15).
Descriptive analyses also generally show a trend towards higher performance across nearly all cognitive measures among those with a missense variant vs. a protein-truncating variant. However, with inferential statistics, limited cognitive tests yielded an effect of variant type. Those with a truncating variant yielded lower DAS-II Special Nonverbal Composite, which represents non-verbal skills broadly (Table 4 ) (Fig. 2 ) largely due to their low performance scores on the DAS-II Pattern Construction subtest, which assesses visuomotor skills (Fig. 2 ). A marginal effect of variant type was found in performance scores on the DAS-II Pattern Construction (χ 2 (2) = 4.64, p = 0.09) with a trend of stronger visuomotor skills in those with a missense variant than late truncating variant (Table 4 ). As shown in Table 5 , compared to the early truncating and missense groups, a large proportion of those with late truncating variants were unable to complete cognitive test measures due to comprehension difficulties (e.g., unable to demonstrate understanding of task instructions with practice items and feedback or modified directions).

Mean non-verbal composite scores across participants with variants in KAT6A
In brief, individuals with KAT6A syndrome present with global cognitive challenges that encompass both non-verbal skills and receptive language. Limited differences were observed between those with truncating and missense variants, albeit our low sample size reduces the statistical power to detect more nuanced effects (See Fig. 3 ).

Mean performance scores across visuomotor, visual-spatial processing, receptive language, and social cognitive measures as a function of KAT6A variants
To our knowledge, this study is the first study to use performance-based cognitive measures to characterize the neuropsychological phenotype of KAT6A syndrome. Main findings from our clinical sample highlight non-verbal cognition among those with KAT6A syndrome may be impaired akin to receptive language. Caregiver ratings also indicate global deficits in adaptive behaviors and high rates of inflexible behaviors in the context of relative strengths in emotion regulation and their desire to interact with others. Based on review of descriptive results, a trend of lower performance scores was observed among those with protein-truncating variants compared to those with missense variants albeit, when non-parametric tests were applied, this effect of variant type reached statistical significance on a very limited subset of the cognitive measures.
Among individuals with KAT6A syndrome, non-verbal reasoning skills and receptive language are not spared and similarly affected. While our abbreviated test battery did not include expressive language measures for comparison, our findings combined with recent findings on language communication skills in KAT6A syndrome [ 6 ] suggest global cognitive challenges, highlighting the central regulatory role KAT6A has on neurodevelopmental processes [ 21 ]. Clinicians who provide care management for those with KAT6A syndrome should consider interventions to support daily functioning for affected individuals beyond speech/language impairment.
Consistent with Smith and Harris [ 4 ], our sample of individuals with KAT6A syndrome demonstrate low rates of behavioral problems and relatively strong social drive, juxtaposed with adaptive deficits and significant restricted interests and repetitive behaviors. Those with truncating and missense variants shared this common neurobehavioral phenotype as well as similar participation in intervention services (speech/language, occupational, physical therapies). It is possible frontal-limbic neural networks may be differentially impacted by mutations in KAT6A compared to other neural systems, particularly given the frontal lobe undergoes protracted development postnatally. Longitudinal investigations that incorporate both cognitive testing and neurobiological methods (e.g., electroencephalogram, functional magnetic resonance imaging, magnetic resonance imaging) are necessary to determine if the function of the gene may impact specific neural substrates differentially. These efforts may aid in understanding the long-term regulatory impact this gene has on both structural and functional brain development.
Our study results, with small sample sizes, provided initial clues that truncating variants causing KAT6A syndrome may be associated with more difficulty in a measure of visuomotor skills than those with a missense variant. Notably, the performance scores across the vast majority of cognitive tests were higher in those with missense than protein-truncating mutations, although these additional measures did not reach statistical significance. Those with late truncating variants represented most of the participants who could not complete cognitive testing secondary to severe comprehension challenges. It is important to highlight our small sample sizes significantly limited our ability to ascertain more moderate effects in performance scores across truncating and missense groups, which may explain the few significant findings resultant from inferential analyses in spite of the consistent descriptive patterns. In brief, taken together, these observations offer initial clues that protein-truncating variants may be associated with more cognitive difficulties as compared to non-truncating variants. Given extremely small sample sizes in the early truncating and missense variant groups and lack of effects seen in all other visuomotor measures (e.g., Beery Visual Motor Integration), it is not possible to make conclusions on how genotype correlates with non-verbal cognition, but further investigations are warranted given the very low statistical power.
Interestingly, those with late truncating, early-truncating, and missense variants demonstrate comparable adaptive functioning deficits (Table 3 ). Although those with protein truncating variants yielded lower mean performance scores than those with missense variants, those with late and early truncating variants performed similarly across most cognitive tests. Overall, these patterns are in contrast with findings reported in Kennedy et al. [ 2 ] and St. John et al. [ 6 ], both suggesting severity of intellectual disability differs between those with late and early truncating variants in KAT6A . It should be noted that both studies measured intellectual disability by a review of medical records and/or clinician ratings. In addition, the rating criterion were not provided in the original published study. In all, severity of impairment was operationalized in a heterogeneous manner. Moreover, these studies did not provide detail in the manner intellectual functioning was determined. Given severe expressive language impairment commonly seen in individuals with KAT6A syndrome, if intelligence was assessed by full-scale intellectual quotient (FSIQ), which incorporates both verbal and non-verbal reasoning skills, IQ may be disproportionately affected by low performance scores on measures requiring verbal responses. Consequently, discrepancies between our results with prior investigations may stem from study design. Future investigations with a comprehensive cognitive test battery (e.g., including measures for expressive language), more robust participant recruitment, and integration of neurobiological metrics will be important to identify genotype-phenotype associations in KAT6A syndrome, particularly in neurocognition. Alternative methods to index cognitive functions (e.g., eye gaze) should be considered given higher rates of sensorimotor impairment among affected persons.
Study limitations and future directions
Despite the novel contribution our study findings add to the sparse literature on neurocognition and KAT6A syndrome, future research should consider our methodological limitations in their study design. Caregivers provided diagnostic history in our study. Our intake form did not require parents to document the type of assessor (e.g., pediatrician, neurologist, neuropsychologist) or evaluation that yielded the diagnoses, and as such, heterogeneous clinical approaches were likely used in the classification of the developmental disorders. As evidenced by the number of participants who were unable to engage in select measures, more sensitive measurement tools that capture a wider range of cognition are needed. Other than traditional paper and pencil neuropsychological tests, use of eye-tracking and other methodological approaches that reduces motor demands may be important to consider, particularly when working with clinical populations with more medical complexities and significant hypotonia like KAT6 disorders. Our sample had a wide age range due to challenges with participant recruitment of ultra-rare diseases like KAT6A syndrome. Ideally, future studies should consider focusing on a cohort around the same developmental period. Finally, cross-syndrome research that compares neuropsychological profiles between those with KAT6A syndrome with other MDEMs with similar affected proteins (e.g., KAT6B disorders) or epigenetic machinery more broadly (disorder of the histone machinery such as Kabuki syndrome) will shed light on shared pathogenic pathways and downstream effects on neurodevelopment. Given animal models of MDEMs of the histone machinery like Rubinstein-Taybi syndrome have shown promise in the amelioration of cognitive dysfunction [ 13 ], detailed characterization of the phenotype associated with KAT6A syndrome and shared features with other MDEMS are critical steps towards determining outcome markers in designing clinical trials. From a clinical standpoint, these efforts will inform professionals who work with affected individuals to offer disease-specific care management and behavioral interventions.
In summary, study results highlight the neuropsychological profile of KAT6A syndrome includes equally impaired nonverbal cognition similar to receptive language, high rates of inflexible behaviors, and global adaptive deficits, combined with relative strengths in emotion regulation and strong appetitive social drive. A preliminary review of genotype-phenotype trends showed nonverbal cognition, particularly visuomotor skills, may be slightly stronger among those with missense than protein-truncating variants, but investigations with larger samples are necessary to draw conclusive interpretations. Those with early vs. late truncating variants were comparable across behavioral and cognitive measures. Cross-syndrome investigations that apply interdisciplinary methodological approaches are warranted to uncover the disease-causing processes in which epigenetic regulators of the histone machinery impact neurodevelopment (See Appendix Table 6 ).
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Fahrner JA, Bjornsson HT. Mendelian disorders of the epigenetic machinery: tipping the balance of chromatin states. Annu Rev Genom Hum Genet. 2014;15:269–93.
Article CAS Google Scholar
Kennedy, J., Goudie, D., Blair, E., Chandler, K., Joss, S., McKay, V., … Newbury-Ecob,R. (2019). KAT6A Syndrome: genotype–phenotype correlation in 76 patients with pathogenic KAT6A variants. Genetics in Medicine , 21 (4), 850–860.
Tham E, Lindstrand A, Santani A, Malmgren H, Nesbitt A, Dubbs HA, Nordgren A. Dominant mutations in KAT6A cause intellectual disability with recognizable syndromic features. Am J Hum Genet. 2015;96(3):507–13.
Article CAS PubMed PubMed Central Google Scholar
Smith C, Harris J. Sleep, behavior, and adaptive function in KAT6A syndrome. Brain Sci. 2021;11(8):966.
Urreizti R, Lopez-Martin E, Martinez-Monseny A, Pujadas M, Castilla-Vallmanya L, Pérez-Jurado LA, Balcells S. Five new cases of syndromic intellectual disability due to KAT6A mutations: widening the molecular and clinical spectrum. Orphanet J Rare Dis. 2020;15(1):1–14.
Article Google Scholar
St John M, Amor DJ, Morgan AT. Speech and language development and genotype–phenotype correlation in 49 individuals with KAT6A syndrome. Am J Med Genet Part A. 2022;188(12):3389–400.
Article CAS PubMed Google Scholar
Gioia GA, Espy KA, Isquith PK. Behavior rating inventory of executive function - preschool version. Odessa, FL: Psychological Assessment Resources; 2003.
Google Scholar
Gioia GA, Isquith PK, Guy SC, Kenworthy L. BRIEF-2: behavior rating inventory of executive function. Lutz, FL: Psychological Assessment Resources; 2015.
Harrison PL, Oakland T. ABAS-3: adaptive behavior assessment system. Los Angeles, CA: Western Psychological Services; 2015.
KAT6 Foundation. KAT6 Known Cases. Retrieved August 3. 2023 from https://www.kat6a.org/ .
Roth RM, Isquith PK, Gioia GA. Behavioral rating inventory of executive function—adult version. Lutz, FL: Psychological Assessment Resources, Inc.; 2005.
Beery KE, Beery NA. The Beery-Buktenica Developmental Test of Visual-Motor Integration: Administration, Scoring, and Teaching Manual. 6th ed. Minneapolis, MN: NCS Pearson; 2010.
Bourtchouladze R, Lidge R, Catapano R, Stanley J, Gossweiler S, Romashko D, Tully T. A mouse model of Rubinstein-Taybi syndrome: defective long-term memory is ameliorated by inhibitors of phosphodiesterase 4. Proc Natl Acad Sci. 2003;100(18):10518–22.
Brooks BL, Sherman EM, Strauss E. NEPSY-II: a developmental neuropsychological assessment. Child Neuropsychol. 2009;16(1):80–101.
Constantino JN, Gruber CP. Social Responsiveness Scale: SRS-2. Torrance, CA: Western Psychological Services; 2012.
Dunn DM. Peabody Picture Vocabulary Test. 5th ed. Bloomington, MN: NCS Pearson; 2019.
Elliott CD, Salerno JD, Dumont R, Willis JO. (2007). Differential ability scales, Second edition. San Antonio, TX .
Achenbach TM, Rescorla L. Manual for the ASEBA Adult forms & profiles: for ages 18–59: adult Self-Report, adult Behavior Checklist. ASEBA: Burlington, VT; 2003.
Achenbach TM, Rescorla L. (2000). Manual for the ASEBA Preschool Forms & Profiles: An Integrated System of Multi-Informant Assessment ASEBA: Burlington, VT.
Achenbach TM, Rescorla L. (2001). Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant Assessment ASEBA: Burlington, VT.
Wiesel-Motiuk N, Assaraf YG. The key roles of the lysine acetyltransferases KAT6A and KAT6B in physiology and pathology. Drug Resist Updates. 2020;53:100729.
Download references
Acknowledgements
We would like to thank the patients and their families who participated in this study, as well as acknowledging the support of the KAT6 Foundation.
R.N. is supported by grants from the Wiedemann-Steiner Syndrome Foundation and KAT6 Foundation. J.H. receives support from the Kabuki Syndrome Foundation, Rubinstein-Taybi Syndrome Children’s Foundation, Sekel-Bredenstein Fund, and the National Institute of Child Health and Development (K23HD101646). This study was also supported by NIH P50HD103538 and UL1 TR003098.
Author information
Authors and affiliations.
Department of Neuropsychology, Kennedy Krieger Institute, 1750 E. Fairmount Ave, Baltimore, USA
Rowena Ng & Jacqueline Harris
Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, USA
Department of Genetic Medicine, Johns Hopkins University School of Medicine, Baltimore, USA
Allison J Kalinousky & Jacqueline Harris
Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, USA
Jacqueline Harris
Department of Neurology, Johns Hopkins University School of Medicine, Baltimore, USA
You can also search for this author in PubMed Google Scholar
Contributions
R.N. and J.H. conceived the study and designed the project. R.N. wrote the first draft of the manuscript with feedback from A.K. and J.H. All authors read, edited and approved the final manuscript.
Corresponding author
Correspondence to Rowena Ng .
Ethics declarations
Ethics approval.
The institutional review board at Johns Hopkins Medicine approved study procedures.
Consent for publication
Not applicable.
Competing interests
Dr. Harris receives research funding from Oryzon Genomics.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ng, R., Kalinousky, A.J. & Harris, J. Neuropsychological profile associated with KAT6A syndrome: Emergent genotype-phenotype trends. Orphanet J Rare Dis 19 , 196 (2024). https://doi.org/10.1186/s13023-024-03175-0
Download citation
Received : 21 November 2023
Accepted : 30 March 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s13023-024-03175-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Genetics/Genetic disorders
- Histone machinery
- Social functioning
Orphanet Journal of Rare Diseases
ISSN: 1750-1172
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
What's in this year's federal budget? Here are all of the announcements we already know about
Treasurer Jim Chalmers will hand down his third budget on Tuesday night, but has been tempering expectations for weeks in the lead-up, warning Australians not to expect a "cash splash".
Inflation remains a key challenge for the government, and we already have a pretty good idea of how Mr Chalmers plans to use his budget to provide cost-of-living relief while also trying to jump-start a slowing economy and navigate growing uncertainty overseas.
Here are the measures we already know about before the treasurer reveals all at 7:30pm AEST.
Short on time?
There's been no shortage of announcements in the lead-up to the budget. If you're interested in a specific topic, tap on the links below to take you there:
Cost-of-living relief
Education, training and hecs changes, tax changes, future made in australia, health and aged care, paid parental leave, domestic violence, defence and foreign affairs, environment, infrastructure, additional announcements.
Is your area of interest not covered?
- Tell us what other cost-of-living measures you're hoping to see included in this year's budget .
The bottom line
Will the budget be in surplus or deficit?
- The budget will deliver a surplus of $9.3 billion for the 2023-24 financial year, making it the second consecutive budget surplus in almost two decades
- That said, the following three financial years are all forecasted to have larger deficits than previously expected in December, but the size of each deficit is not yet known
- Overall, the treasurer says Australia's total debt has been reduced by $152 billion in the 2023-24 financial year, and the budget will benefit by a $25 billion boost in revenue upgrades
What does the budget mean for inflation and interest rates?
- The treasurer has repeatedly said he's kept inflation in mind when crafting this year's budget, and is confident that the measures won't contribute to it
- In fact, Treasury predicts inflation will fall to 2.75 per cent by December — well before the Reserve Bank's most recent forecast for the end of 2025 — due to yet-to-be-announced budget measures taking pressure off inflation
- For what it's worth, RBA governor Michele Bullock wasn't too concerned about the upcoming budget last Tuesday, saying she would wait to see its impact first , but she said the treasurer reassured her that he was focused on curbing inflation
The reworked stage 3 tax cuts form the centrepiece of the government's budget. They were announced in January, legislated in February and come into effect on July 1.
The changes to tax cuts originally legislated by the Morrison government mean that all Australian taxpayers who earn more than $18,200 (that is, more than the tax-free threshold) will get a tax cut.
Before Labor's changes, the original stage 3 tax cuts were skewed more heavily to higher-income earners .
A person with a taxable income between $45,000 and $120,000 will receive a tax cut of $804 more come July 1 under the revised stage 3 changes compared to the Morrison government's tax plan.
However, the government has hinted at other cost-of-living measures, with the treasurer calling the tax cuts the "foundation stone" of broader assistance.
Among those measures appears to be energy bill relief (in addition to what some states have already announced), with the treasurer pointing out that last year's measure curbed living costs and eased inflation.
Adjustments to rent assistance also seem likely, as do increases to JobSeeker and the aged pension.
Back to top
The biggest announcement in this area is the wiping out of $3 billion worth of HECS debts triggered by last year's indexation of 7.1 per cent.
It means student debts will be lowered for more than 3 million Australians, with the average student receiving an indexation credit of about $1,200 for the past two years.
The debt relief will also apply for apprentices who owe money through the VET Student Loan program or the Australian Apprenticeship Support Loan.
Speaking of university, the government is aiming to tackle "placement poverty" by providing financial support to students to help make ends meet while they complete practical hands-on training as part of their course.
Under the scheme, those studying nursing, teaching or social work will receive a Commonwealth Prac Payment of up to $319.50 a week, but they will be subjected to means testing.
Similarly, apprentices willing to learn clean energy skills as part of their trade will be eligible to receive up to $10,000 in payments . The scheme already exists, but the government has broadened the eligibility to include apprentices in the automotive, electrical, housing and construction sectors based on industry feedback.
Universities will also be required to stop a surge in the number of international students, as part of the government's broader plans to cut annual migration levels back to 260,000 a year — much to the concern of peak education bodies .
Another $90 million will be put towards 15,000 fee-free TAFE and VET places to get more workers into the housing construction sector , with an extra 5,000 pre-apprenticeship places provided from 2025.
While we can expect to hear more about the stage 3 tax cuts, it seems likely that the government will unveil other changes to tax in the budget to encourage business investment.
One such change will be the extension of the government's instant asset write-off scheme for small businesses for another year, allowing businesses with a turnover of less than $10 million to claim $20,000 from eligible assets.
However, the same measure from last year's budget is still yet to pass parliament — and businesses are urgently calling on them to pass the measure before it expires on June 30 .
In addition to spending more to attract skilled workers in the housing and construction sectors, the government is also tipping billions of dollars into building new homes across the country .
It's estimated the government will be putting roughly $11.3 billion towards housing, as the government works to deliver its promised 1.2 million new homes by 2030.
$1 billion will be spent on crisis and transitional accommodation for women and children fleeing family violence and youth through the National Housing Infrastructure Facility, which is re-allocated funding.
The government has also committed to providing $9.3 billion to states and territories under a new five-year agreement to combat homelessness, assist in crisis support, and to build and repair social housing — including $400 million of federal homelessness funding each year, matched by the states and territories.
Another $1 billion will be given to states and territories to build other community infrastructure to speed up the home-building process, including roads, sewerage, energy and water supplies.
The government has also committed to consulting with universities to construct more purpose-built student accommodation.
Overall, the funding announcements for housing build on the $25 billion already committed to new housing investments, with $10 billion of that in the Housing Australia Future Fund, which is designed to help build 30,000 social and affordable rental homes.
The government says the housing funding measures will also help take the pressure off the private rental market, which is experiencing record-low vacancy rates and surging growth in weekly rent prices.
Aside from the revised stage 3 tax cuts, the revival of local manufacturing is the other centrepiece of the government's budget this year.
The Future Made in Australia Act (which is often referred to without the "act" on the end) is bringing together a range of new and existing manufacturing and renewable energy programs under one umbrella, totalling in excess of $15 billion.
In other words, the government is putting serious taxpayer money towards supporting local industry and innovation, especially in the renewable energy space.
A number of measures have already been announced (or re-announced), including:
- $1 billion for the Solar SunShot program to increase the number of Australian-made solar panels
- $2 billion for its Hydrogen Headstart scheme to accelerate the green hydrogen industry
- $470 million to build the world's first "fault-tolerant" quantum computer in Brisbane , matching the Queensland government's contribution
- $840 million for the Gina Rinehart-backed mining company Arafura to develop its combined rare earths mine and refinery in Central Australia
- $230 million for WA lithium hopeful Liontown Resources , which is also partly owned by Gina Rinehart
- $566 million over 10 years for Geoscience Australia to create detailed maps of critical minerals under Australia's soil and seabed
- $400 million to create Australia's first high-purity alumina processing facility in Gladstone
- $185 million to fast-track Renascor Resources' Siviour Graphite Project in South Australia
- A $1 billion export deal to supply Germany with 100 infantry fighting vehicles , manufactured at Rheinmetall's facility in Ipswich
All up, the government is spending an extra $8.5 billion on health and Medicare in this year's federal budget, with $227 million of that put towards creating another 29 urgent care clinics.
Millions of dollars are also being poured into medical research, including $20 million for childhood brain cancer research , and a $50 million grant for Australian scientists developing the world's first long-term artificial heart .
Another $49.1 million is being invested to support people who have endometriosis and other complex gynaecological conditions such as chronic pelvic pain and polycystic ovarian syndrome. The funding will allow for extended consultation times and increased rebates to be added to the Medicare Benefits Schedule.
As for aged care, the government hasn't announced anything specific for the sector, nor has it outlined its response to the Aged Care Taskforce report that was delivered in March.
Parents accessing the government-funded paid parental leave scheme will be paid superannuation in addition to their payments from next July .
Under the current program, a couple with a newborn or newly adopted child can access up to 20 weeks of paid parental leave at the national minimum wage — however that figure will continue to rise until it reaches 26 weeks in July 2026 .
The plan, which Labor will take to the next election, would see superannuation paid at 12 per cent of the paid parental leave rate, which is based on the national minimum wage of $882.75 per week.
The cost to the budget is not yet known, however a review commissioned by the former government estimated that paying super on top of paid parental leave would cost about $200 million annually.
About 180,000 families access the government paid parental leave payments each year.
The federal government has pledged almost $1 billion to combat violence against women , including permanent funding to help victim-survivors leave violent relationships, and a suite of online measures to combat online misogyny and prevent children from viewing pornography.
The $925.2 million will go towards permanently establishing the Leaving Violence Program over five years, after it was established as a pilot program in October 2021 known as the Escaping Violence Program.
The program will provide eligible victim-survivors with an individualised support package of up to $1,500 in cash and up to $3,500 in goods and services, plus safety planning, risk assessment and referrals to other essential services for up to 12 weeks.
While the funding has been broadly welcomed, survivors and advocates want to see more investment .
The package also includes funding to create a pilot of age verification technology to protect children from harmful content, including the "easy access to pornography" online, which the government says will tackle extreme online misogyny that is "fuelling harmful attitudes towards women".
The federal government is planning to spend an extra $50 billion on defence over the next decade , meaning Australia's total defence spend will be equivalent to 2.4 per cent of its gross domestic product (GDP) within 10 years.
All up, the government is planning to invest a total of $330 billion through to 2033-34, which includes the initial cost for the AUKUS initiative to purchase nuclear-powered submarines.
Part of that $50 billion will be spent on upgrading defence bases across northern Australia, with $750 million to be allocated in the budget for the "hardening" of its bases in the coming financial year.
More than $1 billion of that funding will also be spent on an immediate boost on long-range missiles and targeting systems.
In the Pacific, Australia has committed $110 million to fund development initiatives in Tuvalu , including an undersea telecommunications cable and direct budget support.
The government has also pledged $492 million to the Asian Development Bank to provide grants to vulnerable countries in the Asia-Pacific.
The only dedicated announcement for the environment so far is the scrapping of the waste export levy , also known as a "recycling tax".
The proposed $4 per tonne levy was first legislated by the Morrison government in 2020 in a bid to reduce and regulate waste exports, after China announced it would no longer handle Australian rubbish.
Waste industry players had been concerned that once the levy was introduced in July, it would have caused more waste to be sent to landfill instead of being recycled.
The scrapping of the waste export levy is part of Australia's broader move to manage its own waste.
A slew of funding commitments have been made around the country, including a $1.9 billion funding commitment for upgrades in Western Sydney, ranging from road improvements to planning projects and train line extensions.
The government is also putting $3.25 billion towards Victoria's North East Link, which is being built between the Eastern Freeway and M80 Ring Road in Melbourne.
Ahead of the Brisbane Olympics in 2032, the government is also chipping in $2.75 billion to fund a Brisbane to Sunshine Coast rail link , matching the amount promised by Queensland Premier Steven Miles. (That said, $1.6 billion had been previously announced by the federal government.)
Also in Queensland, the Bruce Highway will receive $467 million for upgrades, while Canberra will receive $50 million to extend its light rail.
A proposed high-speed train line between Sydney and Newcastle will also receive $78.8 million to deliver a business case for the project.
The government will also put $21 million towards the creation of a national road safety data hub.
There are several other funding commitments the government has made in the lead-up to the budget that don't fit neatly into the categories above.
The government will spend $161.3 million on creating a national firearms register , which will give police and other law-enforcement agencies near real-time information on firearms and who owns them across the states and territories.
The money will be spent over four years to establish the register, and comes after state and territory leaders agreed to set up the register in December last year. The government has described the register as the biggest change to Australia's firearm management systems in almost 30 years.
Another $166.4 million will be spent on expanding anti-money-laundering reporting obligations , requiring real estate agents, lawyers and accountants to report dodgy transactions in a move that will bring Australia in line with the rest of the developed world.
And ahead of the 2032 Brisbane Olympic Games, the government has given the Australian Institute of Sport (AIS) a $249.7 million funding boost to upgrade its facilities to support local athletes.
The government has also committed to a $107 million support package for farmers, after announcing it will end Australia's live sheep export trade by 2028 .
Farmers and regional communities will also benefit from a $519.1 million funding boost to the government's Future Drought Fund.
- X (formerly Twitter)
- Business, Economics and Finance
- Cost of Living
- Economic Growth
- Economic Trends
- Federal Government
- Money and Monetary Policy
- Overview An introduction to the IHRA organization
- Member Countries The countries that are IHRA members
- Permanent International Partners How we work with intergovernmental organizations
- People leading the IHRA Those leading and managing our work
- Our structure How our organization and the Permanent Office is set up
- Careers Current vacancies and working here
- Overview An introduction to the work we do or support
- Focus areas The eight subject areas we are working in
- Our work Current projects, campaigns and activities
- IHRA Grant Program Our grant program, what we fund and how to apply
- Statements Official statements issued by our Chairs or the Membership
- Annual report Recent highlights, achievements and key decisions
- For Memorial & Museum Professionals Information that helps museums, memorials and similar organizations
- For Education Professionals Information that helps Education professionals who are teaching about the Holocaust
- For Policymakers Information that helps governmental organizations and people in the Government
- For Scholars & Researchers Information that helps people in academic organizations
- All Resources Explore our working definitions and other tools
- News & Events
Working definition of antisemitism
Read the full text of the IHRA’s non-legally binding working definition of antisemitism and learn more about this important tool with FAQs.
Read the full text of the IHRA’s non-legally binding working definition of antisemitism and learn more about this important tool with the FAQs below.
Our working definitions are available in multiple languages. While we try to ensure the accuracy of all of our translations, in the event of any discrepancies, the English translation takes precedence.
In the spirit of the Stockholm Declaration that states: “With humanity still scarred by …antisemitism and xenophobia the international community shares a solemn responsibility to fight those evils” the committee on Antisemitism and Holocaust Denial called the IHRA Plenary in Budapest 2015 to adopt the following working definition of antisemitism.
On 26 May 2016, the Plenary in Bucharest decided to:
Adopt the following non-legally binding working definition of antisemitism: “Antisemitism is a certain perception of Jews, which may be expressed as hatred toward Jews. Rhetorical and physical manifestations of antisemitism are directed toward Jewish or non-Jewish individuals and/or their property, toward Jewish community institutions and religious facilities.”
To guide IHRA in its work, the following examples may serve as illustrations:
Manifestations might include the targeting of the state of Israel, conceived as a Jewish collectivity. However, criticism of Israel similar to that leveled against any other country cannot be regarded as antisemitic. Antisemitism frequently charges Jews with conspiring to harm humanity, and it is often used to blame Jews for “why things go wrong.” It is expressed in speech, writing, visual forms and action, and employs sinister stereotypes and negative character traits.
Contemporary examples of antisemitism in public life, the media, schools, the workplace, and in the religious sphere could, taking into account the overall context, include, but are not limited to:
- Calling for, aiding, or justifying the killing or harming of Jews in the name of a radical ideology or an extremist view of religion.
- Making mendacious, dehumanizing, demonizing, or stereotypical allegations about Jews as such or the power of Jews as collective — such as, especially but not exclusively, the myth about a world Jewish conspiracy or of Jews controlling the media, economy, government or other societal institutions.
- Accusing Jews as a people of being responsible for real or imagined wrongdoing committed by a single Jewish person or group, or even for acts committed by non-Jews.
- Denying the fact, scope, mechanisms (e.g. gas chambers) or intentionality of the genocide of the Jewish people at the hands of National Socialist Germany and its supporters and accomplices during World War II (the Holocaust).
- Accusing the Jews as a people, or Israel as a state, of inventing or exaggerating the Holocaust.
- Accusing Jewish citizens of being more loyal to Israel, or to the alleged priorities of Jews worldwide, than to the interests of their own nations.
- Denying the Jewish people their right to self-determination, e.g., by claiming that the existence of a State of Israel is a racist endeavor.
- Applying double standards by requiring of it a behavior not expected or demanded of any other democratic nation.
- Using the symbols and images associated with classic antisemitism (e.g., claims of Jews killing Jesus or blood libel) to characterize Israel or Israelis.
- Drawing comparisons of contemporary Israeli policy to that of the Nazis.
- Holding Jews collectively responsible for actions of the state of Israel.
Antisemitic acts are criminal when they are so defined by law (for example, denial of the Holocaust or distribution of antisemitic materials in some countries).
Criminal acts are antisemitic when the targets of attacks, whether they are people or property – such as buildings, schools, places of worship and cemeteries – are selected because they are, or are perceived to be, Jewish or linked to Jews.
Antisemitic discrimination is the denial to Jews of opportunities or services available to others and is illegal in many countries.
Download the IHRA working definition of antisemitism
Frequently asked questions
The IHRA is the only intergovernmental organization mandated to focus solely on Holocaust-related issues. With evidence that the scourge of antisemitism was once again on the rise, we resolved to take a leading role in combating it.
Combating antisemitism requires international cooperation among experts, governments, and civil society, which meant a mutual starting point for discussion and action was needed. Following the example of the working definition of Holocaust denial and distortion (2013), the IHRA’s experts set out to adopt a similar tool to help guide the organization’s work on combating antisemitism.
The experts in the IHRA’s Committee on Antisemitism and Holocaust Denial built international consensus around a non-legally binding working definition of antisemitism, which was then adopted by the Plenary, the IHRA’s decision-making body made up of representatives from all IHRA Member Countries. By doing so, the IHRA provided an important practical tool for its Member Countries.
The working definition of antisemitism has brought the issue once more to the attention of leaders around the world, making them aware that much work still needs to be done to address antisemitism, which is deeply rooted in our societies.
As a result, countries and organizations have developed national and regional strategies to counter antisemitism, and have appointed Special Envoys and other advisors on the issue. The working definition has helped educate and sensitize administrations, politicians, judges, police, teachers, media, and civil society.
Its broad international implementation has allowed monitoring organizations to better track antisemitism across borders, and has provided researchers and civil society organizations with a way to better moderate content online, including by training AI tools.
The working definition has helped guide countless governments, organizations, and individuals in their efforts to identify antisemitism. This practical tool has also been formally adopted or endorsed* by these groups, both at the national and organizational level.
National level
The following UN member states have adopted or endorsed the IHRA working definition of antisemitism. Beyond the 43 countries listed below, a wide range of other political entities, including a large number of regional/state and local governments, have done so as well. Depending on their domestic situation, countries may use different terminology, including adopt, endorse, embrace, recognize, support, and so on.
Albania (22 October 2020)
Argentina (4 June 2020)
Australia (13 October 2021)
Austria (25 April 2017)
Belgium (14 December 2018)
Bosnia (22 July 2022)
Bulgaria (18 October 2017)
Canada (27 June 2019)
Colombia (2 June 2022)
Croatia (20 January 2023)
Cyprus (18 December 2019)
Czech Republic (25 January 2019)
Denmark (January 2022)
Estonia (29 April 2021)
Finland (17 February 2022)
France (3 December 2019)
Germany (20 September 2017)
Greece (8 November 2019)
Guatemala (27 January 2021)
Hungary (18 February 2019)
Israel (22 January 2017)
Italy (17 January 2020)
Latvia (11 April 2023)
Lithuania (24 January 2018)
Luxembourg (10 July 2019)
Moldova (18 January 2019)
Netherlands (27 November 2018)
North Macedonia (6 March 2018)
Panama (10 May 2023)
Philippines (18 February 2022)
Poland (13 October 2021)
Portugal (28 July 2021)
Romania (25 May 2017)
Serbia (26 February 2020)
Slovakia (28 November 2018)
Slovenia (20 December 2018)
South Korea (4 August 2021)
Spain (22 July 2020)
Sweden (21 January 2020)
Switzerland (4 June 2021)
United Kingdom (12 December 2016)
United States (11 December 2019)
Uruguay (27 January 2020)
Organizations
The following international organizations have expressed support for the working definition of antisemitism:
United Nations
- Secretary General Antonio Guterres acknowledged the efforts of the IHRA Member Countries to agree on a common definition of antisemitism and underlined that it could serve as a basis for law enforcement, as well as preventive policies.
- Special Rapporteur for freedom of religion or belief Ahmed Shaheed recommended that governments use the IHRA working definition of antisemitism as a non-legally binding educational and training tool and ensure it is incorporated, together with relevant human rights standards-based guidance on protecting freedom of opinion and expression, into training and educational materials for all public officials, such as police, prosecutors, and judges, government employees, educators, and national human rights institutions, and integrated into diversity inclusion programs.
European Union
- Council and Parliament called on Member States that had not done so already to endorse the non-legally binding working definition of antisemitism employed by the International Holocaust Remembrance Alliance (IHRA) as a useful guidance tool in education and training, including for law enforcement authorities in their efforts to identify and investigate antisemitic attacks more efficiently and effectively.
- Commission highlighted the working definition of antisemitism by the International Holocaust Remembrance Alliance as the benchmark for developing a victim-centered approach and urged for its adoption.
Organization of American States
- Secretary General Luis Almagro asked every member state to adopt the working definition and announced it would be employed to guide OAS work.
Council of Europe
- European Commission against Racism and Intolerance welcomed the non-legally binding IHRA working definition of antisemitism in the sense that it aids and promotes a better understanding of antisemitism. It considered that it can be a positive tool and encouraged Council of Europe member states to take it into account, in particular in the areas of data collection, education, and awareness-raising.
- The Parliament of MERCOSUR approved a proposal endorsing the IHRA working definition of antisemitism during its LXXXIII Ordinary Session on 11 November 2022.
* Different countries and organizations will use different terminology, including adopt, endorse, embrace, recognize, support, and so on.
Related Resource
EU Handbook for the practical use of the IHRA working definition of antisemitism published
The Handbook presents the IHRA working definition of antisemitism and relates its guiding examples to the contexts of real-world antisemitic incidents and crimes.
Download the EU Handbook
Related content
Antisemitism.
We are creating a shared understanding of how antisemitism impacts our societies – and how we can fight it.
Working definition of antigypsyism/anti-Roma discrimination
Read the full text of the IHRA’s non-legally binding working definition of antigypsyism/anti-Roma discrimination and learn more about this important tool with the FAQs.

IHRA Toolkit Against Holocaust Distortion
Take steps towards recognizing and countering Holocaust distortion with the practical tools, guidance, and example activities included in this online Toolkit.
Sign up to our newsletter to receive the latest updates
By signing up to the IHRA newsletter, you agree to our Privacy Policy

IMAGES
VIDEO
COMMENTS
Speech disorders affect a person's ability to produce sounds that create words, and they can make verbal communication more difficult. ... is a rare type of learning disability that impacts a ...
A speech impediment, or speech disorder, is a condition that makes it hard for you to communicate. There are many types of speech impediments, and anyone can develop one. In some cases, children are born with conditions that affect speech. Other times, people have conditions or injuries that affect speech. Speech therapy can help.
Definition. A speech disorder is a condition in which a person has problems creating or forming the speech sounds needed to communicate with others. This can make the child's speech difficult to understand. Common speech disorders are: Articulation disorders; Phonological disorders; Disfluency Voice disorders or resonance disorders
Speech disorders, impairments, or impediments, are a type of communication disorder in which normal speech is disrupted. This can mean fluency disorders like stuttering, cluttering or lisps.Someone who is unable to speak due to a speech disorder is considered mute. Speech skills are vital to social relationships and learning, and delays or disorders that relate to developing these skills can ...
There are three general categories of speech impairment: Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production. Voice disorder. A voice ...
Common causes of childhood speech impediments include: Autism spectrum disorder: A neurodevelopmental disorder that affects social and interactive development. Cerebral palsy: A congenital (from birth) disorder that affects learning and control of physical movement. Hearing loss: Can affect the way children hear and imitate speech.
Common speech disorders are: Articulation disorders. Phonological disorders. Disfluency. Voice disorders or resonance disorders. Speech disorders are different from language disorders in children. Language disorders refer to someone having difficulty with: Getting their meaning or message across to others (expressive language)
Many disorders can affect our ability to speak and communicate. They range from saying sounds incorrectly to being completely unable to speak or understand speech. Causes include: Hearing disorders and deafness. Voice problems, such as dysphonia or those caused by cleft lip or palate. Speech problems like stuttering. Developmental disabilities.
Fluency: Your child may have problems with how their words and sentences flow. Stuttering is a fluency disorder. That's when your child repeats words, parts of words, or uses odd pauses. It's ...
Speech and language impairment are basic categories that might be drawn in issues of communication involve hearing, speech, language, and fluency. A speech impairment is characterized by difficulty in articulation of words. Examples include stuttering or problems producing particular sounds. Articulation refers to the sounds, syllables, and ...
Speech and Language Disorders. Speech is how we say sounds and words. People with speech problems may: not say sounds clearly. have a hoarse or raspy voice. repeat sounds or pause when speaking, called stuttering. Language is the words we use to share ideas and get what we want. A person with a language disorder may have problems:
Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual's ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders. There are many different types of speech impediments, including: Disfluency. Articulation errors. Ankyloglossia. Dysarthria. Apraxia. This article explores the causes, symptoms, and treatment of the different ...
IDEA is the law that makes early intervention services available to infants and toddlers with disabilities, and special education available to school-aged children with disabilities. Definition of "Speech or Language Impairment" under IDEA. The Individuals with Disabilities Education Act, or IDEA, defines the term "speech or language ...
A child with this type of speech impairment may hesitate or stutter or have blocks of silence when speaking. Language-based learning disabilities (LBLD) are very different from speech impairments. LBLD refers to a whole spectrum of difficulties associated with young children's understanding and use of spoken and written language.
Having a language or speech delay or disorder can qualify a child for early intervention (for children up to 3 years of age) and special education services (for children aged 3 years and older). Schools can do their own testing for language or speech disorders to see if a child needs intervention. An evaluation by a healthcare professional is ...
Definition of Speech Impairment. A speech impairment is a condition in which the ability to produce speech sounds that are necessary to communicate with others is impaired. Speech impairments can ...
Definition. The Individuals with Disabilities Education Act (IDEA) officially defines speech and language impairments as "a communication disorder such as stuttering, impaired articulation, a language impairment, or a voice impairment that adversely affects a child's educational performance." Each point within this official definition represents a speech and language subcategory.
A language impairment is a specific impairment in understanding and sharing thoughts and ideas, i.e. a disorder that involves the processing of linguistic information. Problems that may be experienced can involve the form of language, including grammar, morphology, syntax; and the functional aspects of language, including semantics and pragmatics.
About Learning Disabilities. A child with LD has problems with reading, spelling, and writing. These are language problems. Early speech and language problems can lead to later reading and writing problems. A child with LD may also have problems with math or social skills. LD has nothing to do with how smart your child is.
(11) Speech or language impairment means a communication disorder, such as stuttering, impaired articulation, a language impairment, or a voice impairment, that adversely affects a child's educational performance. Severe Discrepancyidea_regulations-template-default single single-idea_regulations postid-56834 wp-custom-logo wp-embed-responsive with-font-selector no-anchor-scroll footer-on ...
Developmental disabilities are a group of conditions due to an impairment in physical, learning, language, or behavior areas. These conditions begin during the child's developmental period, may impact day-to-day functioning, and usually last throughout a person's lifetime. Most developmental disabilities begin before a baby is born, but some ...
KAT6A (Arboleda-Tham) syndrome is a Mendelian disorder of the epigenetic machinery caused by pathogenic variants in the lysine acetyltransferase 6 A (KAT6A) gene. Intellectual disability and speech/language impairment (e.g., minimally verbal) are common features of the disorder, with late-truncating variants associated with a more severe form of intellectual disability.
What does the budget mean for inflation and interest rates? The treasurer has repeatedly said he's kept inflation in mind when crafting this year's budget, and is confident that the measures won't ...
Denying the fact, scope, mechanisms (e.g. gas chambers) or intentionality of the genocide of the Jewish people at the hands of National Socialist Germany and its supporters and accomplices during World War II (the Holocaust). Accusing the Jews as a people, or Israel as a state, of inventing or exaggerating the Holocaust.
Hateful references. We prohibit targeting individuals or groups with content that references forms of violence or violent events where a protected category was the primary target or victims, where the intent is to harass. This includes, but is not limited to media or text that refers to or depicts: genocides, (e.g., the Holocaust);