An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Nutrition education: linking research, theory, and practice
Affiliation.
- 1 Program in Nutrition, Department of Health and Behavior Studies, Teachers College Columbia University, New York, NY 10027, USA. [email protected]
- PMID: 18296331
The increase in obesity and chronic diseases such as diabetes and heart disease worldwide reflects the complex interactions of biology, personal behaviour and environment. Consequently there has been a greater recognition of the importance of nutrition education. An analysis of the evidence from 300+ studies shows that nutrition education is more likely to be effective when it focuses on behaviour/ action (rather than knowledge only) and systematically links theory, research and practice. There are three essential components to nutrition education: 1. A motivational component, where the goal is to increase awareness and enhance motivation by addressing beliefs, attitudes through effective communication strategies. 2. An action component, where the goal is to facilitate people's ability to take action through goal setting and cognitive self-regulation skills. 3. An environmental component, where nutrition educators work with policymakers and others to promote environmental supports for action. Each component needs to be based on appropriate theory and research. The procedure for program design can use the logic model: Inputs are the resources needed as well as the needs analysis process. The outputs are the activities within the three components of nutrition education described above. Here the behavioural focus is selected and theory and research are used to design appropriate educational strategies to achieve the targeted behaviours. The outcomes are the short, medium or long-term impacts of the nutrition program. These are evaluated through the use of appropriate designs and instruments. Nutrition education programs that link research, theory, and practice are more likely to be effective.
PubMed Disclaimer
Similar articles
- Nutrition communication in the Pacific. White L, Saweri W. White L, et al. Pac Health Dialog. 2007 Sep;14(2):71-5. Pac Health Dialog. 2007. PMID: 19588610
- Nutrition knowledge, attitudes and dietary restriction behaviour of Taiwanese elderly. Lin W, Lee YW. Lin W, et al. Asia Pac J Clin Nutr. 2005;14(3):221-9. Asia Pac J Clin Nutr. 2005. PMID: 16169832
- Improvement in knowledge, social cognitive theory variables, and movement through stages of change after a community-based diabetes education program. Chapman-Novakofski K, Karduck J. Chapman-Novakofski K, et al. J Am Diet Assoc. 2005 Oct;105(10):1613-6. doi: 10.1016/j.jada.2005.07.010. J Am Diet Assoc. 2005. PMID: 16183364
- Using goal setting as a strategy for dietary behavior change. Cullen KW, Baranowski T, Smith SP. Cullen KW, et al. J Am Diet Assoc. 2001 May;101(5):562-6. doi: 10.1016/S0002-8223(01)00140-7. J Am Diet Assoc. 2001. PMID: 11374350 Review.
- [Self-efficacy among health learners/self-efficacy among health educators]. Chikamoto Y. Chikamoto Y. Kango Kenkyu. 1998 Jan-Feb;31(1):3-12. Kango Kenkyu. 1998. PMID: 10437454 Review. Japanese.
- Feeding practices of caregivers with children attending early childhood development centres in Xhariep, South Africa. Carson-Porter AC, van den Berg VL, Meko NL. Carson-Porter AC, et al. Health SA. 2024 Jul 2;29:2575. doi: 10.4102/hsag.v29i0.2575. eCollection 2024. Health SA. 2024. PMID: 39114339 Free PMC article.
- Influence of health food literacy on willingness to pay for healthier foods: focus on food insecurity. Nam SJ, Suk J. Nam SJ, et al. Int J Equity Health. 2024 Apr 22;23(1):80. doi: 10.1186/s12939-024-02135-1. Int J Equity Health. 2024. PMID: 38649971 Free PMC article.
- Educational nutritional intervention to prevent loss of health-related quality of life among older adults after a surgical treatment: design of a randomised controlled trial. Hansen MC, Uhrenfeldt L, Ingstad K, Pedersen PU. Hansen MC, et al. Trials. 2024 Apr 15;25(1):262. doi: 10.1186/s13063-024-08096-8. Trials. 2024. PMID: 38622729 Free PMC article.
- Nutrition-Related Knowledge, Attitudes, Practices, and Anemia Status of Lactating Mothers in Bukavu, Democratic Republic of the Congo-A Cross-Sectional Analysis. Beitze DE, Kavira Malengera C, Barhwamire Kabesha T, Scherbaum V. Beitze DE, et al. Nutrients. 2024 Mar 17;16(6):870. doi: 10.3390/nu16060870. Nutrients. 2024. PMID: 38542781 Free PMC article.
- Effectiveness of Sports Nutrition Education Based on Self-Determination Theory for Male University Rowing Athletes: A Randomized Controlled Trial. Enatsu N, Seino J, Tsuji T, Ogata M. Enatsu N, et al. Nutrients. 2024 Mar 11;16(6):799. doi: 10.3390/nu16060799. Nutrients. 2024. PMID: 38542710 Free PMC article. Clinical Trial.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- HEC Press, Healthy Eating Club PTY LTD
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplement Archive
- Article Collection Archive
- Author Guidelines
- Submission Site
- Open Access
- Call for Papers
- Why Publish?
- About Nutrition Reviews
- About International Life Sciences Institute
- Editorial Board
- Early Career Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, acknowledgments, supporting information, factors that contribute to effective nutrition education interventions in children: a systematic review.
- Article contents
- Figures & tables
- Supplementary Data
Mary W Murimi, Ana Florencia Moyeda-Carabaza, Bong Nguyen, Sanjoy Saha, Ruhul Amin, Valentine Njike, Factors that contribute to effective nutrition education interventions in children: a systematic review, Nutrition Reviews , Volume 76, Issue 8, August 2018, Pages 553–580, https://doi.org/10.1093/nutrit/nuy020
- Permissions Icon Permissions
Establishing healthy dietary practices at an early age is crucial, as dietary behaviors in childhood track to adulthood.
The purpose of this systematic review was to identify factors associated with successful nutrition education interventions conducted in children and published between 2009 and 2016.
Using the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) guidelines, relevant studies were identified through the PubMed, Web of Science, ScienceDirect, and ERIC (Educational Resources Information Center) databases.
Studies published in English between 2009 and 2016 that included a nutrition education intervention among children aged 2 to 19 years were included. Review articles, abstracts, qualitative or cross-sectional studies, and studies targeting children with special nutritional needs were excluded.
Four authors screened and determined the quality of the studies using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) system and extracted the data from the articles.
Forty-one studies were included: 7 targeted preschool children, 26 targeted elementary school children, and 8 targeted secondary school children. A total of 46% met their primary objectives of nutrition education intervention, while the rest either partially achieved or did not achieve their stated objectives.
Successful interventions targeting school children engaged parents by means of face-to-face sessions, identified specific behaviors to be modified, and assured fidelity by training teachers or recruiting trained experts to deliver the intervention. In addition, they allowed adequate dosage, with an intervention duration of at least 6 months, and used age-appropriate activities.
Interventions with a multicomponent approach that were age appropriate and of adequate duration (≥ 6 months), that engaged parents, and that ensured fidelity and proper alignment between the stated objectives, the intervention, and the desired outcomes were more likely to succeed.
Development and growth during childhood, which sets the trajectory for lifelong health, is heavily influenced by nutritional intake. 1 A balanced and nutrient-dense diet provides children with essential nutrients for optimal growth and development, while diets with imbalanced or inadequate nutrients may lead to insufficient nutrient intake or overweight, which affects health and performance in childhood as well as in adulthood. 1 More importantly, children’s dietary practices and behaviors may track to adulthood, potentially influencing health status during adulthood. 2 , 3 Therefore, it is important to establish healthy dietary practices and behaviors at an early age, which in turn may lead to optimal growth and development and healthier dietary choices later in life. 3
Contento 4 defined nutrition education as “any combination of educational strategies, accompanied by environmental supports, designed to facilitate voluntary adoption of food choices and other food- and nutrition-related behaviors conducive to health and well-being.” Nutrition education is a critical component in the development of healthy eating practices and behaviors, 5 as it enhances the knowledge and skills children need to make healthful dietary choices. 6–8 For example, a nutrition education intervention study by Dunton et al 6 among primary school children showed significant improvement in children’s knowledge and intake of fruit and vegetables as well as decreased consumption of soda and high-energy foods post intervention. Similarly, a properly designed nutrition education program has the potential to enhance motivation and preference for eating healthful food and to facilitate the implementation of appropriate dietary practices. 8 , 9 In addition, healthy dietary practices are associated with improved academic performance. 10 , 11 For example, after attending the nutrition education intervention EatFit, which aimed to increase the frequency and quality of morning meals, the consumption of iron-rich food, and the level of physical activity, school-aged children showed significantly improved academic performance, specifically in mathematics and English. 10
Despite convincing evidence that nutrition education has the potential to influence children’s dietary choices, improve health, and enhance academic performance, the specific characteristics of effective nutrition education programs for children are not clearly defined. 12–14 Effectiveness of nutrition education for children is further complicated by the wide variance in age, physical growth, and cognitive development during childhood, which ranges from preschool age to high school age. For example, the approaches needed to capture the cognitive capability and attention span of preschool children are different from those needed for elementary or high school children. 15–18 Active parental participation might be key for effective nutrition education for one age group, but not the other. 19 , 20 It is therefore critical to identify the aspects of nutrition education that are essential for each age group and to differentiate those that are essential for all categories. The purpose of this systematic review is to identify the characteristics associated with successful nutrition education interventions in children, as evidenced by the achievement of stated objectives in 3 different age groups: preschool children, elementary school children, and secondary school students. This review followed the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) guidelines. 21
Age categorization of children
Building on the work of a prior systematic review on factors that contribute to successful intervention in nutrition education for adults, 22 this review aims to identify factors associated with successful nutrition education interventions among children. To account for the wide range in the age (2–19 years) and cognitive development of children, the review and the subsequent analysis were based on developmental stages categorized into preschool, elementary, and secondary school children in order to identify key strategies associated with successful interventions in the context of each age category.
Research team
The research team consisted of 6 members. The lead investigator and 5 graduate students conducted the search, screened the articles for quality and relevance on basis of the established criteria, and extracted information on a spreadsheet. Authors independently analyzed the findings and identified the factors that characterized successful interventions. Afterward, results were discussed and a consensus was reached.
Literature search strategy
This review followed the recommendations and criteria established in the PRISMA statement (see Appendix S1 in the Supporting Information online). 21 Articles published between 2009 and 2016 were obtained from electronic searches of 4 databases, namely PubMed, Web of Science, Science Direct, and ERIC (Education Resources Information Center) from 2009 to 2016. Keywords entered in varying combinations included “nutrition education,” “nutrition education intervention,” “children,” and “dietary behavior.”
Inclusion and exclusion criteria
PICOS criteria for inclusion and exclusion of studies a
| Category . | Inclusion . | Exclusion . |
|---|---|---|
| Participants | Children aged 2–19 y, alone or accompanied by parents and/or teachers and/or those who prepared meals | Children aged < 2 y; children with special nutritional needs; parents or caregivers only; teachers only; those who prepared meals only |
| Intervention | Face-to-face nutrition education interventions | Online nutrition education interventions |
| Comparator | With or without control group; nutrition education intervention only, physical activity intervention only; similar intervention | None |
| Outcomes | Nutrition-related outcomes such as anthropometric measurements (eg, body mass index, waist circumference, etc); biochemical measurements (eg, glycemia, lipid profile, etc); dietary intakes, knowledge, preferences, attitudes, behaviors, self-efficacy; cultural nutrition awareness factor; dietary diversity score; physical activity (time, attitudes, behaviors); or food and beverage availability at schools | No nutrition-related outcomes; outcomes measured only in children with pre-existing medical conditions |
| Study design | Meta-analyses and systematic reviews; reviews; qualitative studies; cross-sectional studies; abstracts; gray literature; book chapters |
| Category . | Inclusion . | Exclusion . |
|---|---|---|
| Participants | Children aged 2–19 y, alone or accompanied by parents and/or teachers and/or those who prepared meals | Children aged < 2 y; children with special nutritional needs; parents or caregivers only; teachers only; those who prepared meals only |
| Intervention | Face-to-face nutrition education interventions | Online nutrition education interventions |
| Comparator | With or without control group; nutrition education intervention only, physical activity intervention only; similar intervention | None |
| Outcomes | Nutrition-related outcomes such as anthropometric measurements (eg, body mass index, waist circumference, etc); biochemical measurements (eg, glycemia, lipid profile, etc); dietary intakes, knowledge, preferences, attitudes, behaviors, self-efficacy; cultural nutrition awareness factor; dietary diversity score; physical activity (time, attitudes, behaviors); or food and beverage availability at schools | No nutrition-related outcomes; outcomes measured only in children with pre-existing medical conditions |
| Study design | Meta-analyses and systematic reviews; reviews; qualitative studies; cross-sectional studies; abstracts; gray literature; book chapters |
Elaborated according to the description of PICOS criteria as provided by Liberati et al (2009). 21
A total of 351 original studies published between 2009 and 2016 on nutrition education interventions in children without preexisting medical conditions were evaluated. Of the 351 studies evaluated, 303 (86%) did not meet the inclusion criteria ( Figure 1 21 ). For the purposes of this systematic review, 48 studies qualified for inclusion.

Flow diagram of the literature search process.
Assessment of study quality and risk of bias
To minimize bias, reviewing authors were trained to assess quality on the basis of PRISMA recommendations, 21 and 2 authors independently assessed each included article. After the initial assessment, the reviewing authors exchanged the articles without sharing the results of assessment. In addition, all authors discussed each article as a group and either confirmed or added to the findings of the 2 reviewing authors. The group made the final decision on whether to include or exclude each article, and a quality score for each study was assigned by the 2 reviewing authors.
Determination of the quality of the studies was guided by the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) system of rating the quality of evidence. 23 A thorough assessment of the study’s description, design, measurements, data analysis, interpretation of results, and power and outcomes formed the basis for quality assessment. Each factor scored 0 points if the article lacked a complete description of the factor analyzed or 1 point if the article provided a complete description of such factor. The quality score was calculated by summing all the component scores. Studies were rated and categorized as having low risk of bias (5–6 points), moderate risk of bias (3–4 points), or high risk of bias (1–2 points). Once the 2 reviewing authors established the scores, the 4 research members and the leader of the research team discussed any discrepancies until consensus was reached. Of the 48 studies that met the inclusion criteria, 7 articles categorized as having a high risk of bias were excluded from this review ( Figure 1 21 ).
Approach to analysis
Nutrition education interventions at the elementary school level
| Reference . | Study sample . | Objective of intervention . | Study design . | Length and frequency of intervention . | Behavioral theory/construct . | Achievement of objectives . | Risk of bias . | Major findings . |
|---|---|---|---|---|---|---|---|---|
| Battjes-Fries et al. (2015) | 1183 children in grades 5–8 | To assess the effect of the Dutch school-based education program Taste Lessons on children’s behavioral determinants toward tasting unfamiliar foods and eating a variety of healthy foods | Quasi-experimental | One school year (2011–2012). Teachers implemented lessons in a flexible way | No theory | Partially achieved | Moderate | < 0.01). This remained significant at the second follow-up ( < 0.05) < 0.05) |
| Cunningham-Sabo & Lohse (2013) | 237 children in 4th grade | To assess the effect of CWK on students' FV preferences, cooking attitude, and cooking self-efficacy in a mostly non-Hispanic white sample that assured no previous CWK exposure | RCT | 10 wk total, with a 1-h introductory lesson, three 2-h cooking classes, and three 1-h FV tasting sessions (10 h total) | No theory | Achieved | Moderate | = 0.012). Within IG, fruit preferences were greater in those with preintervention cooking experience at both baseline and follow-up ( < 0.05) = 0.001) = 0.02) |
| Francis et al. (2010) | 579 children in 6th grade | To evaluate the effectiveness of a short-term, school-based, multicomponent education intervention on improving the knowledge, attitudes, and behavior of primary school children toward better dietary and activity habits | RCT | 1 mo (frequency not mentioned) | Bloom’s mastery learning model | Partially achieved | Moderate | There was a significant change in the proportion of students in IG reporting fruit consumption levels of ≥2 servings a day ( < 0.01). The proportion of students in IG reporting vegetable consumption within the past 24 h significantly increased from baseline to postintervention assessment ( < 0.01). Students in IG showed significant changes in their knowledge scores vs those in CG ( < 0.01). There was a significant decline in reported fried food intake in IG from baseline to post intervention ( < 0.01). The proportion of students reporting regular PA at school at least 3 times per week significantly increased in IG ( < 0.01) |
| Gallotta et al. (2016) | 230 children aged 8–11 y | To assess the effect of a 5-mo PE and NE intervention on body composition, PA level, time spent on sedentary activities, and eating habits of primary school children | Cluster RCT | 5 mo total. NE administrated once per month. Fruit or vegetable provided once per week. 1-h PA session administered twice per week | No theory | Partially achieved | Low | < 0.0001). Sedentary time significantly decreased in children in all groups, from 565.7 to 492.1 min/wk ( < 0.0001). < 0.05) and fruits (4.30 vs 4.85, < 0.05) post intervention. Consumption of bread significantly decreased post intervention in children with normal fat (4.72 times/wk vs 4.08 times/wk, < 0.05), while the consumption of snacks significantly decreased post intervention in both children with normal fat (3.20 times/wk vs 1.94 times/wk) and in obese children (3.07 times/wk vs 2.24 times/wk) |
| Gibbs et al. (2013) | 764 children in grades 3–6 | To evaluate the achievement of the SAKG Program in increasing children’s appreciation of diverse, healthy foods | Pre-post | 2.5 y total, with 45–60 min of gardening class and 90 min of kitchen class administered every week | SEM and principles of effective health promotion | Achieved | Moderate | At follow-up, after adjusting for baseline and grade, children showed a significant increase in willingness to try new foods if they had never tried it (OR = 1.95; 95%CI, 1.06–3.58; = 0.03), if they had cooked it (OR = 2.37; 95%CI, 1.45–3.90; = 0.001), and if they had grown it (OR = 2.25; 95%CI, 1.47–3.47; < 0.001) |
| Herbert et al. (2013) | 104 children aged 7–11 y | To evaluate the effectiveness of the Energize program for changing dietary and PA habits compared with a CG of children not participating in the program | Quasi-experimental | 1-h weekly session for 12 wk | SCT, TRA, and HBM | Partially achieved | Low | There was a significant difference between groups in the post-test score for consumption of french fries and chips after controlling for the pre-test score ( = 0.044). The Energize group consumed significantly less french fries and chips compared with the CG. A marginally significant ( < 0.10) increase in vegetable consumption was detected for the Energize group as compared with the CG over time ( = 0.068). PA habits were not significantly different between the Energize and CG groups at post-test follow-up ( >0.05) |
| Katz et al. (2011) | 1180 children aged 7–9 y, grades 2–4 | To enhance the ability of both students and their parents to distinguish more healthful from less healthful options among a wide variety of food choices | RCT | Five 20-min lessons | SEM | Partially achieved | Low | Nutrition knowledge in both students and the parents of students in IG improved significantly (18.1% ± 26.9%; < 0.01; and 7.9% ± 19.9%; < 0.01) compared with baseline. No statistically significant improvements observed in dietary patterns from baseline between the IG and CG of both students and parents in terms of calories, protein, total fat, carbohydrates, iron, saturated fat, monounsaturated fat, polyunsaturated fat, cholesterol, sodium, or folate intake |
| Keihner et al. (2011) | 1154 children aged 8–12 y | To encourage children to eat the recommended amount of FVs and get at least 60 min of PA daily in order to promote healthful growth, development, and academic achievement | RCT | One 50-min lesson per week for 8 wk | Resiliency Theory and SCT | Achieved | Low | Children in IG were significantly more likely than those in CG to improve their knowledge about the total number of daily servings of FVs ( < 0.05) and the number of daily servings of vegetables needed for good health ( < 0.001), as well as the vitamin C obtained from eating FVs ( < 0.05). In both 4th and 5th grades, children in IG showed improvements in FV asking and shopping self-efficacy ( = 0.04) and in FV eating self-efficacy ( < 0.001). They were significantly more likely than CG children to improve their knowledge about the number of minutes of PA needed daily for good health ( < 0.001) and the health benefits of PA ( < 0.01) |
| Kipping et al. (2014) | 2242 children aged 9–10 y | To investigate the effectiveness of a school-based intervention to increase PA, reduce sedentary behavior, and increase FV consumption in children | Cluster RCT | 16 lessons over a period of 6–7 mo. Teachers implemented lessons in a flexible way | SCT | Not achieved | Moderate | None of the 3 primary outcomes (time spent per day in MVPA, time spent in sedentary behavior, and servings of FVs) differed between children in schools allocated to IG and those allocated to CG. The intervention was effective for 3 of 9 secondary outcomes after multiple testing was taken into account: self-reported time spent in screen viewing on weekends (−21 min/d [95%CI, −37 to −4; = 0.01]), self-reported servings of snacks (−0.22/d [95%CI, −038 to −0.05; = 0.01]), and servings of high-energy drinks (−0.26/d [95%CI, −0.43 to −0.10; = 0.002]) were all reduced |
| Kristjansdottir et al. (2010) | 265 children aged 7–9 y | To increase FV intake in the IG by at least 20% | Pre-post | 2 y (frequency not mentioned) | No theory | Achieved | Moderate | At follow-up, intakes of raw vegetables ( < 0.001), cooked vegetables ( < 0.05), and total vegetables ( < 0.001) and total intake of FVs ( < 0.05) and fish ( < 0.001) were higher in IG compared with CG, and intake of candy was lower ( < 0.05). Percentage of energy from MUFAs ( = 0.029) and the intakes of fiber ( = 0.013), potassium ( = 0.005), magnesium ( = 0.012), copper ( = 0.035), and β-carotene increased significantly in IG compared with CG, and increase in vitamin C intake was of borderline significance ( = 0.056) |
| Mittman et al. (2016) | 1376 children and adolescents aged 7–14 y | To investigate the effects of the Cancer Society of Lower Saxony's school-based NE program “5-a-Day for kids,” designed to increase children's FV consumption | Pre-post | 135 min for 1 time | No theory | Not achieved | Low | No steady increase could be observed for intake of FVs throughout the day, neither at follow-up 1 nor at follow-up 2. In contrast, intakes of vegetables and fruit juice, as well as total intake of fruit/vegetables/juice, showed a significant decline between baseline and follow-up 1 and between baseline and follow-up 2. Only fruit consumption rose temporarily between baseline and follow-up 2, though not significantly |
| Morgan et al. (2010) | 127 children aged 11–12 y | To measure the effects of a garden-based NE program on FV knowledge, willingness to taste, food preferences, and perceived quality of school life in upper primary school children vs in a control group | Quasi-experimental | Three 1-h NE sessions over 10 wk and one 45-min session 4 times per week | SCT | Partially achieved | Moderate | < 0.001). = 0.02) in FV knowledge between NE&G group and CG, but only among those students who started with lower FV knowledge. For willingness to taste, there was a significant between-group difference for 4 vegetables: capsicum ( = 0.04), broccoli ( = 0.01), tomatoes ( < 0.001), and peas ( = 0.02), with NE&G students being significantly more willing to taste these than students in NE group or CG |
| Moss et al. (2013) | 65 children in 3rd grade | To introduce the CATCH nutrition curriculum and Farm to School program to assess nutrition knowledge of 3rd-grade students, and increase their FV consumption behavior | Quasi-experimental | Two 30-min NE lessons and a 2-h farm tour over a 4-wk period | SEM | Partially achieved | Moderate | Significant differences in knowledge of fiber were found ( < 0.001). Differences in knowledge of vitamins and minerals, reported vegetable consumption behavior at school, and farm exposure were also significant ( < 0.05). No significant relationships were found between self-reported FV consumption and participation in the farm tour |
| Muros et al. (2015) | 134 children aged 10–11 y | To investigate the effects of 4 experimental conditions and 1 CG on health-related parameters, such as the lipid, physiological, and anthropometric profiles of children | Pre-post | 6-mo intervention, with 60-min sessions of PA twice a week, 2 1-h NE classes for children, and 6 2-h NE classes for parents | No theory | Achieved | Low | Students in groups receiving PA reduced their fat percentage ( ≤0.05) and increased their muscle mass post intervention ( ≤0.05). The lipid profile improved in all IGs post intervention. The proportion of macronutrients and dietary cholesterol improved ( ≤0.001) in groups receiving NE. The post-test comparison showed significantly lower fat percentage, sum of skinfolds, waist circumference, and PA in NE group relative to CG |
| Parmer et al. (2009) | 115 children in 2nd grade | To examine the effects of a school garden on children’s FV knowledge, preference, and consumption | Pre-post | 28 wk, with a biweekly 1-h sessions of NE and biweekly 1-h sessions of gardening | No theory | Achieved | Low | Participants in NE&G and NE groups exhibited significantly greater improvements in nutrition knowledge and taste ratings than those in CG ( ≤0.001). Moreover, NE&G group was more likely to choose and consume vegetables in a lunchroom setting post assessment than either the NE group or the CG ( ≤0.01) |
| Prelip et al. (2012) | 399 children aged 9–11 y | To assess the impact of a multicomponent NE program on student knowledge, attitudes, and behaviors related to consumption of FVs | Quasi-experimental | One school year. Teachers had freedom to develop their own lesson plans but were required to complete at least 10 h over a 3-mo period | SCT and TPB | Partially achieved | Moderate | The intervention with 4 components (program, nutrition curriculum, teacher training, and parent workshop) resulted in a positive change in knowledge ( < 0.05) and in attitudes and beliefs toward vegetables ( < 0.01). There were significant effects of teacher influence on students' FVs attitudes in both the intervention with 4 components and the intervention with 2 components (program and teacher’s training) ( < 0.05). However, there was no significant increase in students’ FV consumption |
| Rosário et al. (2012) | 464 children in grades 1–4 | To assess the impact of a 6-mo nutrition program, delivered and taught by classroom teachers with in-service nutrition training, on prevention of overweight and obesity among children in grades 1–4 | RCT | Twelve 3-h NE sessions over a 6-mo period | HPM and SCT | Partially achieved | Moderate | In IG, the increase in BMI score was significantly lower than that in CG ( = 0.009); fewer proportion of children became overweight in IG vs CG (5.6% vs 18.4%; = 0.037). Significantly fewer children in IG (5.6%) than in CG (18.4%) became overweight after the intervention. After controlling for confounders, the predicted odds of overweight incidence were 75% lower for IG (OR = 0.25; 95%CI, 0.07–0.92; < 0.05) |
| Rosi et al. (2016) | 8165 children in grades 3–5 | To improve nutritional knowledge of children participating to the Giocampus Program | Pre-post | Three 3-h NE classes over 2 academic years | No theory | Achieved | Moderate | Children’s nutritional knowledge significantly increased ( < 0.001) in all school grades. The integrated “learning through playing” approach, which included educational figures, tools, and games, was successful in improving children’s nutritional knowledge |
| Safdie et al. (2013) | 830 children in grades 4–5 | To evaluate the effectiveness of an ecologically based program aimed at promoting healthy eating and PA in selected Mexico City schools to optimize to overall energy balance in childhood as a strategy for obesity prevention | RCT | 18-mo intervention (frequency not mentioned) | No theory | Partially achieved | Low | In intervention schools, availability of healthy foods increased with a concomitant decrease in availability of unhealthy foods ( < 0.05). Food intake showed the same trend, but the difference was not statistically significant. In intervention schools, children did not engage in more MVPA during PE class or recess but increased their number of steps taken |
| Saraf et al. (2015) | 2384 children in grades 6–7 | To assess the effectiveness of a multicomponent school-based intervention in improving knowledge and behavioral practices related to diet, PA, and tobacco use in middle school children of rural Ballabgarh, North India | RCT | 45-min NE sessions and a 20-min flip-chart demonstration over a 9-mo period. Frequency not mentioned | No theory | Achieved | Low | Knowledge about PA, diet, and tobacco improved significantly ( < 0.05) in IG vs CG. Proportion of students attending PT classes for ≥5 d/wk increased significantly (17.8%; < 0.01) in IG vs CG. Proportion of students consuming fruits increased (10%; < 0.01) in IG vs CG. Pre-post decrease in prevalence of current smoking was significantly greater (7.7%; < 0.01) in IG vs CG |
| Sevinç et al. (2011) | 6771 children and adolescents aged 7–13 y | To (1) determine the effect of applying both PA and healthy nutrition programs vs a healthy nutrition program only for preventing obesity in primary school students in Denizli, Turkey; (2) to determine the relationship of this effect with possible variables; and (3) to construct an obesity-control program aimed at the students | RCT | 8-mo intervention. 3-h PE sessions per week plus NE program for students, parents, and teachers. Frequency and duration of NE session not mentioned | No theory | Achieved | Low | = 0.000) higher than that in both the intervention 1 (0.37 ± 1.08) and the intervention 2 (0.35 ± 1.13) groups. However, there was no significant difference between the intervention groups = 0.000) |
| Shah et al. (2010) | 3128 children and adolescents aged 8–18 y | To assess the impact of a controlled educative intervention on health- and nutrition-related knowledge and behavior of urban Asian Indian children and adolescents | Pre-post | Weekly 60-min lesson over a 6-mo period | No theory | Achieved | Low | After the intervention, knowledge and behavior scores improved in all children except 15- to 18-year-olds from private schools ( < 0.001). A significantly higher improvement in knowledge and behavior was observed in younger children (aged 8–11 y) vs those aged 12–18 y, in females vs males, and in government schools vs private schools ( < 0.05 for all) |
| Steyn et al. (2015) | 998 children in grades 4–6 | To promote healthy eating habits and regular PA in learners, parents, and educators and to promote the development of a school environment that would foster a healthy lifestyle via an HK intervention | RCT | 3-y intervention. Frequency not mentioned | No theory | Not achieved | Moderate | The intervention effect was not significant in consumption of food items (fried potato chips, fried food, pies, potato crisps, take-away foods, processed meat, table sugar, chocolate, sweets, cakes/biscuits, squashes/cordials) at follow-up 1 or at follow-up 2. Moreover, in intervention schools, there was a >10% increase in children who consumed potato crisps, processed meat, sweets, and carbonated beverages between 2009 and 2011. The mean DDS for intervention schools increased from 4.56 in 2009 to 5.03 in 2010 to 4.91 in 2011. There were no significant intervention effects at either of the 2 time points (2009, 2011) for DDS, fat intake score, and sugar intake score |
| Toruner et al. (2015) | 1105 children in grades 3–7 | To evaluate the effectiveness of a school-based healthy life program on healthy life habits (eating breakfast and exercising), knowledge, BMI, and blood pressure | RCT | Four 40-min sessions over a 6-mo period | No theory | Partially achieved | Moderate | >0.05). The percentage of children who reported daily exercise duration as ≥1 h increased from 58.8% to 67.8% ( = 0.006) = 0.001). No statistically significant ( >0.05) difference was observed in the initial or the final BMI or in the blood pressure of IG children |
| Wall et al. (2012) | 2231 children in 4th grade | To assess impact of a classroom-based, standardized intervention to address limited vegetable consumption | Pre-post | 3–5 wk | No theory | Achieved | Moderate | Students in IG improved in vegetable-related attitude, self-efficacy, preference, and knowledge scores ( < 0.001) |
| Zhou et al. (2013) | 1023 children in grades 5–8 | To assess the effectiveness of a school-based nutrition and food-safety education program among primary school and junior high school students in China. The assessment focused on change in scores for nutrition and food safety knowledge, attitude, and practices (KAP) at pre-post intervention and at 9-mo follow-up | Pre-post | 50-min sessions. Neither total duration of intervention nor frequency of sessions was mentioned | No theory | Partially achieved | Moderate | < 0.01). The long-term knowledge score in IG was 12.35, which was lower than the score immediately after the intervention ( < 0.01) but higher than the baseline score ( < 0.01) and higher than the baseline and long-term scores in CG ( < 0.01) < 0.05) < 0.01) than those of the CG both preintervention and at 9-mo follow-up |
| Reference . | Study sample . | Objective of intervention . | Study design . | Length and frequency of intervention . | Behavioral theory/construct . | Achievement of objectives . | Risk of bias . | Major findings . |
|---|---|---|---|---|---|---|---|---|
| Battjes-Fries et al. (2015) | 1183 children in grades 5–8 | To assess the effect of the Dutch school-based education program Taste Lessons on children’s behavioral determinants toward tasting unfamiliar foods and eating a variety of healthy foods | Quasi-experimental | One school year (2011–2012). Teachers implemented lessons in a flexible way | No theory | Partially achieved | Moderate | < 0.01). This remained significant at the second follow-up ( < 0.05) < 0.05) |
| Cunningham-Sabo & Lohse (2013) | 237 children in 4th grade | To assess the effect of CWK on students' FV preferences, cooking attitude, and cooking self-efficacy in a mostly non-Hispanic white sample that assured no previous CWK exposure | RCT | 10 wk total, with a 1-h introductory lesson, three 2-h cooking classes, and three 1-h FV tasting sessions (10 h total) | No theory | Achieved | Moderate | = 0.012). Within IG, fruit preferences were greater in those with preintervention cooking experience at both baseline and follow-up ( < 0.05) = 0.001) = 0.02) |
| Francis et al. (2010) | 579 children in 6th grade | To evaluate the effectiveness of a short-term, school-based, multicomponent education intervention on improving the knowledge, attitudes, and behavior of primary school children toward better dietary and activity habits | RCT | 1 mo (frequency not mentioned) | Bloom’s mastery learning model | Partially achieved | Moderate | There was a significant change in the proportion of students in IG reporting fruit consumption levels of ≥2 servings a day ( < 0.01). The proportion of students in IG reporting vegetable consumption within the past 24 h significantly increased from baseline to postintervention assessment ( < 0.01). Students in IG showed significant changes in their knowledge scores vs those in CG ( < 0.01). There was a significant decline in reported fried food intake in IG from baseline to post intervention ( < 0.01). The proportion of students reporting regular PA at school at least 3 times per week significantly increased in IG ( < 0.01) |
| Gallotta et al. (2016) | 230 children aged 8–11 y | To assess the effect of a 5-mo PE and NE intervention on body composition, PA level, time spent on sedentary activities, and eating habits of primary school children | Cluster RCT | 5 mo total. NE administrated once per month. Fruit or vegetable provided once per week. 1-h PA session administered twice per week | No theory | Partially achieved | Low | < 0.0001). Sedentary time significantly decreased in children in all groups, from 565.7 to 492.1 min/wk ( < 0.0001). < 0.05) and fruits (4.30 vs 4.85, < 0.05) post intervention. Consumption of bread significantly decreased post intervention in children with normal fat (4.72 times/wk vs 4.08 times/wk, < 0.05), while the consumption of snacks significantly decreased post intervention in both children with normal fat (3.20 times/wk vs 1.94 times/wk) and in obese children (3.07 times/wk vs 2.24 times/wk) |
| Gibbs et al. (2013) | 764 children in grades 3–6 | To evaluate the achievement of the SAKG Program in increasing children’s appreciation of diverse, healthy foods | Pre-post | 2.5 y total, with 45–60 min of gardening class and 90 min of kitchen class administered every week | SEM and principles of effective health promotion | Achieved | Moderate | At follow-up, after adjusting for baseline and grade, children showed a significant increase in willingness to try new foods if they had never tried it (OR = 1.95; 95%CI, 1.06–3.58; = 0.03), if they had cooked it (OR = 2.37; 95%CI, 1.45–3.90; = 0.001), and if they had grown it (OR = 2.25; 95%CI, 1.47–3.47; < 0.001) |
| Herbert et al. (2013) | 104 children aged 7–11 y | To evaluate the effectiveness of the Energize program for changing dietary and PA habits compared with a CG of children not participating in the program | Quasi-experimental | 1-h weekly session for 12 wk | SCT, TRA, and HBM | Partially achieved | Low | There was a significant difference between groups in the post-test score for consumption of french fries and chips after controlling for the pre-test score ( = 0.044). The Energize group consumed significantly less french fries and chips compared with the CG. A marginally significant ( < 0.10) increase in vegetable consumption was detected for the Energize group as compared with the CG over time ( = 0.068). PA habits were not significantly different between the Energize and CG groups at post-test follow-up ( >0.05) |
| Katz et al. (2011) | 1180 children aged 7–9 y, grades 2–4 | To enhance the ability of both students and their parents to distinguish more healthful from less healthful options among a wide variety of food choices | RCT | Five 20-min lessons | SEM | Partially achieved | Low | Nutrition knowledge in both students and the parents of students in IG improved significantly (18.1% ± 26.9%; < 0.01; and 7.9% ± 19.9%; < 0.01) compared with baseline. No statistically significant improvements observed in dietary patterns from baseline between the IG and CG of both students and parents in terms of calories, protein, total fat, carbohydrates, iron, saturated fat, monounsaturated fat, polyunsaturated fat, cholesterol, sodium, or folate intake |
| Keihner et al. (2011) | 1154 children aged 8–12 y | To encourage children to eat the recommended amount of FVs and get at least 60 min of PA daily in order to promote healthful growth, development, and academic achievement | RCT | One 50-min lesson per week for 8 wk | Resiliency Theory and SCT | Achieved | Low | Children in IG were significantly more likely than those in CG to improve their knowledge about the total number of daily servings of FVs ( < 0.05) and the number of daily servings of vegetables needed for good health ( < 0.001), as well as the vitamin C obtained from eating FVs ( < 0.05). In both 4th and 5th grades, children in IG showed improvements in FV asking and shopping self-efficacy ( = 0.04) and in FV eating self-efficacy ( < 0.001). They were significantly more likely than CG children to improve their knowledge about the number of minutes of PA needed daily for good health ( < 0.001) and the health benefits of PA ( < 0.01) |
| Kipping et al. (2014) | 2242 children aged 9–10 y | To investigate the effectiveness of a school-based intervention to increase PA, reduce sedentary behavior, and increase FV consumption in children | Cluster RCT | 16 lessons over a period of 6–7 mo. Teachers implemented lessons in a flexible way | SCT | Not achieved | Moderate | None of the 3 primary outcomes (time spent per day in MVPA, time spent in sedentary behavior, and servings of FVs) differed between children in schools allocated to IG and those allocated to CG. The intervention was effective for 3 of 9 secondary outcomes after multiple testing was taken into account: self-reported time spent in screen viewing on weekends (−21 min/d [95%CI, −37 to −4; = 0.01]), self-reported servings of snacks (−0.22/d [95%CI, −038 to −0.05; = 0.01]), and servings of high-energy drinks (−0.26/d [95%CI, −0.43 to −0.10; = 0.002]) were all reduced |
| Kristjansdottir et al. (2010) | 265 children aged 7–9 y | To increase FV intake in the IG by at least 20% | Pre-post | 2 y (frequency not mentioned) | No theory | Achieved | Moderate | At follow-up, intakes of raw vegetables ( < 0.001), cooked vegetables ( < 0.05), and total vegetables ( < 0.001) and total intake of FVs ( < 0.05) and fish ( < 0.001) were higher in IG compared with CG, and intake of candy was lower ( < 0.05). Percentage of energy from MUFAs ( = 0.029) and the intakes of fiber ( = 0.013), potassium ( = 0.005), magnesium ( = 0.012), copper ( = 0.035), and β-carotene increased significantly in IG compared with CG, and increase in vitamin C intake was of borderline significance ( = 0.056) |
| Mittman et al. (2016) | 1376 children and adolescents aged 7–14 y | To investigate the effects of the Cancer Society of Lower Saxony's school-based NE program “5-a-Day for kids,” designed to increase children's FV consumption | Pre-post | 135 min for 1 time | No theory | Not achieved | Low | No steady increase could be observed for intake of FVs throughout the day, neither at follow-up 1 nor at follow-up 2. In contrast, intakes of vegetables and fruit juice, as well as total intake of fruit/vegetables/juice, showed a significant decline between baseline and follow-up 1 and between baseline and follow-up 2. Only fruit consumption rose temporarily between baseline and follow-up 2, though not significantly |
| Morgan et al. (2010) | 127 children aged 11–12 y | To measure the effects of a garden-based NE program on FV knowledge, willingness to taste, food preferences, and perceived quality of school life in upper primary school children vs in a control group | Quasi-experimental | Three 1-h NE sessions over 10 wk and one 45-min session 4 times per week | SCT | Partially achieved | Moderate | < 0.001). = 0.02) in FV knowledge between NE&G group and CG, but only among those students who started with lower FV knowledge. For willingness to taste, there was a significant between-group difference for 4 vegetables: capsicum ( = 0.04), broccoli ( = 0.01), tomatoes ( < 0.001), and peas ( = 0.02), with NE&G students being significantly more willing to taste these than students in NE group or CG |
| Moss et al. (2013) | 65 children in 3rd grade | To introduce the CATCH nutrition curriculum and Farm to School program to assess nutrition knowledge of 3rd-grade students, and increase their FV consumption behavior | Quasi-experimental | Two 30-min NE lessons and a 2-h farm tour over a 4-wk period | SEM | Partially achieved | Moderate | Significant differences in knowledge of fiber were found ( < 0.001). Differences in knowledge of vitamins and minerals, reported vegetable consumption behavior at school, and farm exposure were also significant ( < 0.05). No significant relationships were found between self-reported FV consumption and participation in the farm tour |
| Muros et al. (2015) | 134 children aged 10–11 y | To investigate the effects of 4 experimental conditions and 1 CG on health-related parameters, such as the lipid, physiological, and anthropometric profiles of children | Pre-post | 6-mo intervention, with 60-min sessions of PA twice a week, 2 1-h NE classes for children, and 6 2-h NE classes for parents | No theory | Achieved | Low | Students in groups receiving PA reduced their fat percentage ( ≤0.05) and increased their muscle mass post intervention ( ≤0.05). The lipid profile improved in all IGs post intervention. The proportion of macronutrients and dietary cholesterol improved ( ≤0.001) in groups receiving NE. The post-test comparison showed significantly lower fat percentage, sum of skinfolds, waist circumference, and PA in NE group relative to CG |
| Parmer et al. (2009) | 115 children in 2nd grade | To examine the effects of a school garden on children’s FV knowledge, preference, and consumption | Pre-post | 28 wk, with a biweekly 1-h sessions of NE and biweekly 1-h sessions of gardening | No theory | Achieved | Low | Participants in NE&G and NE groups exhibited significantly greater improvements in nutrition knowledge and taste ratings than those in CG ( ≤0.001). Moreover, NE&G group was more likely to choose and consume vegetables in a lunchroom setting post assessment than either the NE group or the CG ( ≤0.01) |
| Prelip et al. (2012) | 399 children aged 9–11 y | To assess the impact of a multicomponent NE program on student knowledge, attitudes, and behaviors related to consumption of FVs | Quasi-experimental | One school year. Teachers had freedom to develop their own lesson plans but were required to complete at least 10 h over a 3-mo period | SCT and TPB | Partially achieved | Moderate | The intervention with 4 components (program, nutrition curriculum, teacher training, and parent workshop) resulted in a positive change in knowledge ( < 0.05) and in attitudes and beliefs toward vegetables ( < 0.01). There were significant effects of teacher influence on students' FVs attitudes in both the intervention with 4 components and the intervention with 2 components (program and teacher’s training) ( < 0.05). However, there was no significant increase in students’ FV consumption |
| Rosário et al. (2012) | 464 children in grades 1–4 | To assess the impact of a 6-mo nutrition program, delivered and taught by classroom teachers with in-service nutrition training, on prevention of overweight and obesity among children in grades 1–4 | RCT | Twelve 3-h NE sessions over a 6-mo period | HPM and SCT | Partially achieved | Moderate | In IG, the increase in BMI score was significantly lower than that in CG ( = 0.009); fewer proportion of children became overweight in IG vs CG (5.6% vs 18.4%; = 0.037). Significantly fewer children in IG (5.6%) than in CG (18.4%) became overweight after the intervention. After controlling for confounders, the predicted odds of overweight incidence were 75% lower for IG (OR = 0.25; 95%CI, 0.07–0.92; < 0.05) |
| Rosi et al. (2016) | 8165 children in grades 3–5 | To improve nutritional knowledge of children participating to the Giocampus Program | Pre-post | Three 3-h NE classes over 2 academic years | No theory | Achieved | Moderate | Children’s nutritional knowledge significantly increased ( < 0.001) in all school grades. The integrated “learning through playing” approach, which included educational figures, tools, and games, was successful in improving children’s nutritional knowledge |
| Safdie et al. (2013) | 830 children in grades 4–5 | To evaluate the effectiveness of an ecologically based program aimed at promoting healthy eating and PA in selected Mexico City schools to optimize to overall energy balance in childhood as a strategy for obesity prevention | RCT | 18-mo intervention (frequency not mentioned) | No theory | Partially achieved | Low | In intervention schools, availability of healthy foods increased with a concomitant decrease in availability of unhealthy foods ( < 0.05). Food intake showed the same trend, but the difference was not statistically significant. In intervention schools, children did not engage in more MVPA during PE class or recess but increased their number of steps taken |
| Saraf et al. (2015) | 2384 children in grades 6–7 | To assess the effectiveness of a multicomponent school-based intervention in improving knowledge and behavioral practices related to diet, PA, and tobacco use in middle school children of rural Ballabgarh, North India | RCT | 45-min NE sessions and a 20-min flip-chart demonstration over a 9-mo period. Frequency not mentioned | No theory | Achieved | Low | Knowledge about PA, diet, and tobacco improved significantly ( < 0.05) in IG vs CG. Proportion of students attending PT classes for ≥5 d/wk increased significantly (17.8%; < 0.01) in IG vs CG. Proportion of students consuming fruits increased (10%; < 0.01) in IG vs CG. Pre-post decrease in prevalence of current smoking was significantly greater (7.7%; < 0.01) in IG vs CG |
| Sevinç et al. (2011) | 6771 children and adolescents aged 7–13 y | To (1) determine the effect of applying both PA and healthy nutrition programs vs a healthy nutrition program only for preventing obesity in primary school students in Denizli, Turkey; (2) to determine the relationship of this effect with possible variables; and (3) to construct an obesity-control program aimed at the students | RCT | 8-mo intervention. 3-h PE sessions per week plus NE program for students, parents, and teachers. Frequency and duration of NE session not mentioned | No theory | Achieved | Low | = 0.000) higher than that in both the intervention 1 (0.37 ± 1.08) and the intervention 2 (0.35 ± 1.13) groups. However, there was no significant difference between the intervention groups = 0.000) |
| Shah et al. (2010) | 3128 children and adolescents aged 8–18 y | To assess the impact of a controlled educative intervention on health- and nutrition-related knowledge and behavior of urban Asian Indian children and adolescents | Pre-post | Weekly 60-min lesson over a 6-mo period | No theory | Achieved | Low | After the intervention, knowledge and behavior scores improved in all children except 15- to 18-year-olds from private schools ( < 0.001). A significantly higher improvement in knowledge and behavior was observed in younger children (aged 8–11 y) vs those aged 12–18 y, in females vs males, and in government schools vs private schools ( < 0.05 for all) |
| Steyn et al. (2015) | 998 children in grades 4–6 | To promote healthy eating habits and regular PA in learners, parents, and educators and to promote the development of a school environment that would foster a healthy lifestyle via an HK intervention | RCT | 3-y intervention. Frequency not mentioned | No theory | Not achieved | Moderate | The intervention effect was not significant in consumption of food items (fried potato chips, fried food, pies, potato crisps, take-away foods, processed meat, table sugar, chocolate, sweets, cakes/biscuits, squashes/cordials) at follow-up 1 or at follow-up 2. Moreover, in intervention schools, there was a >10% increase in children who consumed potato crisps, processed meat, sweets, and carbonated beverages between 2009 and 2011. The mean DDS for intervention schools increased from 4.56 in 2009 to 5.03 in 2010 to 4.91 in 2011. There were no significant intervention effects at either of the 2 time points (2009, 2011) for DDS, fat intake score, and sugar intake score |
| Toruner et al. (2015) | 1105 children in grades 3–7 | To evaluate the effectiveness of a school-based healthy life program on healthy life habits (eating breakfast and exercising), knowledge, BMI, and blood pressure | RCT | Four 40-min sessions over a 6-mo period | No theory | Partially achieved | Moderate | >0.05). The percentage of children who reported daily exercise duration as ≥1 h increased from 58.8% to 67.8% ( = 0.006) = 0.001). No statistically significant ( >0.05) difference was observed in the initial or the final BMI or in the blood pressure of IG children |
| Wall et al. (2012) | 2231 children in 4th grade | To assess impact of a classroom-based, standardized intervention to address limited vegetable consumption | Pre-post | 3–5 wk | No theory | Achieved | Moderate | Students in IG improved in vegetable-related attitude, self-efficacy, preference, and knowledge scores ( < 0.001) |
| Zhou et al. (2013) | 1023 children in grades 5–8 | To assess the effectiveness of a school-based nutrition and food-safety education program among primary school and junior high school students in China. The assessment focused on change in scores for nutrition and food safety knowledge, attitude, and practices (KAP) at pre-post intervention and at 9-mo follow-up | Pre-post | 50-min sessions. Neither total duration of intervention nor frequency of sessions was mentioned | No theory | Partially achieved | Moderate | < 0.01). The long-term knowledge score in IG was 12.35, which was lower than the score immediately after the intervention ( < 0.01) but higher than the baseline score ( < 0.01) and higher than the baseline and long-term scores in CG ( < 0.01) < 0.05) < 0.01) than those of the CG both preintervention and at 9-mo follow-up |
Abbreviations : BMI, body mass index; CATCH, Coordinated Approach to Child Health; CG, control group; CWK, Cooking with Kids; DDS, dietary diversity score; HBM, Health Belief Model; HK, Healthy Kick; HPM, Health Promotion Model; IG, intervention group; FV, fruit and vegetable; MUFAs, monounsaturated fatty acids; MVPA, moderate to vigorous physical activity; NE, nutrition education; NE&G, nutrition education and gardening; OR, odds ratio; PA, physical activity; PE, physical education; PT, physical training; RCT, randomized control trial; SAKG, Stephanie Alexander Kitchen Garden; SCT, Social Cognitive Theory; SEM, Socio-Ecological Model; TPB, Theory of Planned Behavior; TRA, Theory of Reasoned Action.
Nutrition education interventions at the secondary school level
| Reference . | Study sample . | Objective of intervention . | Study design . | Length and frequency of intervention . | Behavioral theory/construct . | Achievement of objectives . | Risk of bias . | Major findings . |
|---|---|---|---|---|---|---|---|---|
| Campos Pastor et al. (2012) | 263 children and adolescents aged 12–16 y | To assess the repercussion of an NE program on anthropometric variables, eating habits, and metabolic syndrome components in adolescents | Pre-post | 45-min session every 2 wk for a school year | No theory | Achieved | Moderate | At end of school year, the percentage of male and female adolescents with overweight or obesity in IG was significantly lower (overweight from 31.5% to 21.3% in males and 21.7% to 14% in females ( < 0.001); obesity from 7.9% to 5.5% in males and 4.7% to 3.9% in females ( < 0.001). Percentage of students with biochemical data suggestive of metabolic syndrome was significantly lower (32.2% vs 19.7%, < 0.001) |
| Dehdari et al. (2014) | 100 girls aged 13 y | To examine the effect of an NE intervention based on Pender's HPM in improving the frequency and nutrient content of breakfast among female Iranian students | Quasi-experimental | Weekly 60-min session for 4 wk | Pender’s HPM | Achieved | Moderate | IG reported a significant increase ( < 0.05) in perceived benefit, self-efficacy, positive activity-related effect, interpersonal influences, situational influences, commitment to a plan of action, and weekly frequency of breakfast consumption compared with CG. There were significant reductions ( < 0.05) in immediate competing demands and preferences, perceived barriers, and negative activity-related effect constructs in IG compared with CG |
| Maatoug et al. (2015) | 4003 children and adolescents aged 11–16 y | To evaluate the effectiveness of Schools in Health, a school-based PA and nutritional behavior intervention, in reducing rates of overweight and obesity among school children in Sousse, Tunisia | Quasi-experimental | No theory | Partially achieved | Low | < 0.001). = 0.03), while it decreased significantly in CG, from 40.2% to 35.0% ( = 0.001) = 0.01) | |
| Murimi et al. (2015) | 233 children and adolescents aged 11–19 y | To examine the effects of a school-based point-of-testing counseling and NE intervention on age- and gender-specific BMI percentile, blood lipid profile, and blood pressure among students in grades 6–12 in a rural community and to examine changes in students’ nutrition knowledge over a 3-y period | Longitudinal | No theory | Partially achieved | Moderate | High-density lipoprotein levels significantly increased between the 2nd and 4th visits ( < 0.05). Participants who attended the intervention at least 4 times showed stabilized or improved blood values and anthropometric measurements. Significant increases in nutrition knowledge were documented for students in grades 7 and 8 but not for those in other grades ( < 0.01) | |
| Rani et al. (2013) | 181 adolescents in grades 8–9 | To assess the knowledge and practices of high school students with respect to healthy diets before and after an NE program | Pre-post | Weekly 1-h session for 10 wk | HBM | Partially achieved | Moderate | < 0.001). Similarly, students showing a positive attitude toward healthy diet increased from 18% to 40% ( < 0.001) < 0.01), and consumption of fast food items through fast food restaurants declined significantly |
| Singhal et al. (2010) | 510 adolescents aged 15–17 y | To assess the effectiveness of a school-based low-cost nutrition and lifestyle education intervention on behavior modification and risk profile of Asian Indian adolescents in a metropolitan city in North India | RCT | No theory | Achieved | Low | Significant increase seen in proportion of IG having knowledge of the following: simple and complex carbohydrates ( = 0.003), concept of empty calories ( < 0.001), sources and adverse effects of fats ( < 0.001), high-fat milk products ( = 0.002), refined cereals ( = 0.003), importance of fiber in the diet ( = 0.02), and causes and types of diabetes ( < 0.001). Significantly lower proportion of IG consumed aerated drinks ( < 0.001) and energy-dense unhealthy foods such as burgers, pizzas, and french fries at follow-up ( = 0.03). Significant decrease in mean waist circumference ( = 0.02), sagittal abdominal diameter ( < 0.001), waist-to-hip ratio ( = 0.02), and fasting blood glucose ( = 0.05) in IG compared with CG | |
| Somsri et al. (2016) | 131 adolescents aged 16 y | To examine and compare the effectiveness of a CCBNEd program and an HCBNEd program on the promotion of FV consumption | Quasi-experimental | Weekly 50-min NE session for 4 wk | SCT | Achieved | Low | < 0.001) in all 3 groups post test < 0.01). Post test, an increase in eating FVs was observed in CCBNEd. Amounts of FVs consumed increased significantly ( < 0.001) in CCBNEd, 3-fold (from 40 g to 120 g) for fruit and 2-fold (from 65 g to 123 g) for vegetables, compared with baseline values |
| Viggiano et al. (2014) | 3110 children and adolescents aged 9–19 y | To confirm the effectiveness of Kaledo (a board game) in improving nutrition knowledge and in promoting long-term healthy dietary behavior in a large cohort study | Cluster RCT | Weekly 30-min session for 20 wk | No theory | Achieved | Moderate | At first postintervention assessment (6 mo), IG had significantly higher scores than CG (14.4 vs 10.9, < 0.001) on AFHC |
| In addition, there was a significant difference between IG and CG in mean values of nutritional knowledge adjusted for score at baseline (6.5 vs 4.6, < 0.001). At the same assessment, for the section “healthy and unhealthy diet and food,” there was a significant difference between IG and the CG in mean values adjusted for score at baseline (11.2 vs 10.4, < 0.001). There was a significantly higher moderator effect difference between IG and CG in high schools (11.8 vs 10.4, = 0.023) compared with middle schools (10.7 vs 10.9, = 0.571) |
| Reference . | Study sample . | Objective of intervention . | Study design . | Length and frequency of intervention . | Behavioral theory/construct . | Achievement of objectives . | Risk of bias . | Major findings . |
|---|---|---|---|---|---|---|---|---|
| Campos Pastor et al. (2012) | 263 children and adolescents aged 12–16 y | To assess the repercussion of an NE program on anthropometric variables, eating habits, and metabolic syndrome components in adolescents | Pre-post | 45-min session every 2 wk for a school year | No theory | Achieved | Moderate | At end of school year, the percentage of male and female adolescents with overweight or obesity in IG was significantly lower (overweight from 31.5% to 21.3% in males and 21.7% to 14% in females ( < 0.001); obesity from 7.9% to 5.5% in males and 4.7% to 3.9% in females ( < 0.001). Percentage of students with biochemical data suggestive of metabolic syndrome was significantly lower (32.2% vs 19.7%, < 0.001) |
| Dehdari et al. (2014) | 100 girls aged 13 y | To examine the effect of an NE intervention based on Pender's HPM in improving the frequency and nutrient content of breakfast among female Iranian students | Quasi-experimental | Weekly 60-min session for 4 wk | Pender’s HPM | Achieved | Moderate | IG reported a significant increase ( < 0.05) in perceived benefit, self-efficacy, positive activity-related effect, interpersonal influences, situational influences, commitment to a plan of action, and weekly frequency of breakfast consumption compared with CG. There were significant reductions ( < 0.05) in immediate competing demands and preferences, perceived barriers, and negative activity-related effect constructs in IG compared with CG |
| Maatoug et al. (2015) | 4003 children and adolescents aged 11–16 y | To evaluate the effectiveness of Schools in Health, a school-based PA and nutritional behavior intervention, in reducing rates of overweight and obesity among school children in Sousse, Tunisia | Quasi-experimental | No theory | Partially achieved | Low | < 0.001). = 0.03), while it decreased significantly in CG, from 40.2% to 35.0% ( = 0.001) = 0.01) | |
| Murimi et al. (2015) | 233 children and adolescents aged 11–19 y | To examine the effects of a school-based point-of-testing counseling and NE intervention on age- and gender-specific BMI percentile, blood lipid profile, and blood pressure among students in grades 6–12 in a rural community and to examine changes in students’ nutrition knowledge over a 3-y period | Longitudinal | No theory | Partially achieved | Moderate | High-density lipoprotein levels significantly increased between the 2nd and 4th visits ( < 0.05). Participants who attended the intervention at least 4 times showed stabilized or improved blood values and anthropometric measurements. Significant increases in nutrition knowledge were documented for students in grades 7 and 8 but not for those in other grades ( < 0.01) | |
| Rani et al. (2013) | 181 adolescents in grades 8–9 | To assess the knowledge and practices of high school students with respect to healthy diets before and after an NE program | Pre-post | Weekly 1-h session for 10 wk | HBM | Partially achieved | Moderate | < 0.001). Similarly, students showing a positive attitude toward healthy diet increased from 18% to 40% ( < 0.001) < 0.01), and consumption of fast food items through fast food restaurants declined significantly |
| Singhal et al. (2010) | 510 adolescents aged 15–17 y | To assess the effectiveness of a school-based low-cost nutrition and lifestyle education intervention on behavior modification and risk profile of Asian Indian adolescents in a metropolitan city in North India | RCT | No theory | Achieved | Low | Significant increase seen in proportion of IG having knowledge of the following: simple and complex carbohydrates ( = 0.003), concept of empty calories ( < 0.001), sources and adverse effects of fats ( < 0.001), high-fat milk products ( = 0.002), refined cereals ( = 0.003), importance of fiber in the diet ( = 0.02), and causes and types of diabetes ( < 0.001). Significantly lower proportion of IG consumed aerated drinks ( < 0.001) and energy-dense unhealthy foods such as burgers, pizzas, and french fries at follow-up ( = 0.03). Significant decrease in mean waist circumference ( = 0.02), sagittal abdominal diameter ( < 0.001), waist-to-hip ratio ( = 0.02), and fasting blood glucose ( = 0.05) in IG compared with CG | |
| Somsri et al. (2016) | 131 adolescents aged 16 y | To examine and compare the effectiveness of a CCBNEd program and an HCBNEd program on the promotion of FV consumption | Quasi-experimental | Weekly 50-min NE session for 4 wk | SCT | Achieved | Low | < 0.001) in all 3 groups post test < 0.01). Post test, an increase in eating FVs was observed in CCBNEd. Amounts of FVs consumed increased significantly ( < 0.001) in CCBNEd, 3-fold (from 40 g to 120 g) for fruit and 2-fold (from 65 g to 123 g) for vegetables, compared with baseline values |
| Viggiano et al. (2014) | 3110 children and adolescents aged 9–19 y | To confirm the effectiveness of Kaledo (a board game) in improving nutrition knowledge and in promoting long-term healthy dietary behavior in a large cohort study | Cluster RCT | Weekly 30-min session for 20 wk | No theory | Achieved | Moderate | At first postintervention assessment (6 mo), IG had significantly higher scores than CG (14.4 vs 10.9, < 0.001) on AFHC |
| In addition, there was a significant difference between IG and CG in mean values of nutritional knowledge adjusted for score at baseline (6.5 vs 4.6, < 0.001). At the same assessment, for the section “healthy and unhealthy diet and food,” there was a significant difference between IG and the CG in mean values adjusted for score at baseline (11.2 vs 10.4, < 0.001). There was a significantly higher moderator effect difference between IG and CG in high schools (11.8 vs 10.4, = 0.023) compared with middle schools (10.7 vs 10.9, = 0.571) |
Abbreviations: AFHC, Adolescent Food Habit Checklist; BMI, body mass index; CCBNEd, Cosmetic Content-Based Nutrition Education; CG, control group; FV, fruit and vegetable; HCBNEd, Health Content-Based Nutrition Education; HBM, Health Belief Model; HPM, Health Promotion Model; IG, intervention group; NE, nutrition education; PA, physical activity; RCT, randomized controlled trial; SCT, Social Cognitive Theory.
Nutrition education interventions at the preschool level
| References . | Study sample . | Objective of nutrition education . | Study design . | Length and frequency of intervention . | Behavioral theory/construct . | Achievement of objectives . | Risk of bias . | Major findings . |
|---|---|---|---|---|---|---|---|---|
| De Bock et al. (2012) | 377 children aged 3–6 y | To assess the effects of a preschool-based nutritional intervention on both behavioral outcomes, such as children's FV and water consumption, and anthropometric measures | Cluster randomized | 15 sessions, 2 h each, over a 6-mo period | Pandura’s social learning theory and Zajonc’s exposure effect | Partially achieved | Moderate | Significant change from baseline in FV intake ( < 0.05 and < 0.01): mean increase from baseline of 0.17 point on the 6-point ordinal scale ( < 0.05) for fruit consumption frequency and 0.22 point ( < 0.01) for vegetable consumption frequency. Intervention had no significant effect on daily water intake, consumption of high-energy drinks, BMI, waist-to-height ratio, or total body fat |
| Gao et al. (2016) | 1819 preschool children aged 4–6 y | To examine the effect of NE on children’s breakfast patterns | RCT | Monthly lecture and activities for 8 mo (2 semesters in a kindergarten) | Cognitive Behavioral Change Theory | Achieved | Moderate | = 0.02) < 0.001) < 0.001) |
| Hoffman et al. (2011) | 297 children in kindergarten and 1st grade | To examine the effects of a multicomponent, theory-based, 2.5-y intervention on children's FV consumption, FV preferences, FV knowledge, and BMI | Randomized, multiyear intervention | Daily or most of the days during the school year | SCT and SLT | Partially achieved | Moderate | < 0.0001 and < 0.005, respectively) compared with children in CG < 0.0005 and < 0.05, respectively) compared with children in CG < 0.05) < 0.05) < 0.05) |
| Hu et al. (2010) | 1819 children aged 4–6 y | To evaluate the impact of NE in kindergartens and to promote healthy dietary habits in children | RCT | Once monthly for 8 mo | No theory | Partially achieved | Low | < 0.05) < 0.05). Mean scores for nutritional knowledge among IG parents rose significantly from pre test (10.5 points) to post test (11.9 points) ( < 0.0001) |
| Lerner-Geva et al. (2015) | 204 children aged 4–6 y | To assess the effectiveness of an intervention program to improve kindergarten children’s eating and leisure habits in Israel | Cluster RCT with 3 groups: full intervention (NE plus PA), intervention (only NE), and CG | One lesson per week for 10 wk | No theory | Partially achieved | Moderate | Significant association between level of nutritional knowledge and age ( < 0.01). In the initial analysis adjusted for baseline measures, significant reduction in daily energy intake was seen in entire IG with entire intervention (NE and PA), from 5239 kJ at baseline to 4709 kJ at follow-up ( = 0.03). Group with intervention (only NE) significantly increased nutritional knowledge ( = 0.03). No changes in BMI, time spent watching television or playing computer games, exercise, and sleep observed after the intervention |
| Peñalvo et al. (2013) | 2062 children aged 3–5 y | To evaluate the efficacy of the Program SI! in improving indicators of the acquisition of healthy behaviors in children aged 3–5 y | Cluster RCT | During 1 academic year: 20 h of instruction per program component (diet, PA, and human body) and 10 h of instruction for managing emotions | SCT and trans-theoretical models in health promotion | Partially achieved | Low | After 1 school year, the intervention increased children’s knowledge, attitudes, and habits scores, both overall (3.45; 95%CI, 1.84–5.05) and component specific (diet: 0.93; 95%CI, 0.12–1.75; PA: 1.93; 95%CI, 1.17–2.69; human body: 0.65; 95%CI: 0.07–1.24) score. However, no effect on the school environment or on overall scores for parents or teachers was found |
| Witt & Dunn (2012) | 263 preschool children aged 4–5 y | To determine whether CMH, an interactive nutrition and PA program for preschool children, increases FV consumption | Intervention study with IG and CG | Weekly sessions of 15–30 min for 6 wk | No theory | Achieved | Moderate | Children who received CMH significantly increased their consumption of fruit snacks by approximately 20.8% ( < 0.001) and their consumption of vegetable snacks by approximately 33.1% ( < 0.01) between baseline assessment and the assessment conducted 3 mo after completion of CMH program |
| References . | Study sample . | Objective of nutrition education . | Study design . | Length and frequency of intervention . | Behavioral theory/construct . | Achievement of objectives . | Risk of bias . | Major findings . |
|---|---|---|---|---|---|---|---|---|
| De Bock et al. (2012) | 377 children aged 3–6 y | To assess the effects of a preschool-based nutritional intervention on both behavioral outcomes, such as children's FV and water consumption, and anthropometric measures | Cluster randomized | 15 sessions, 2 h each, over a 6-mo period | Pandura’s social learning theory and Zajonc’s exposure effect | Partially achieved | Moderate | Significant change from baseline in FV intake ( < 0.05 and < 0.01): mean increase from baseline of 0.17 point on the 6-point ordinal scale ( < 0.05) for fruit consumption frequency and 0.22 point ( < 0.01) for vegetable consumption frequency. Intervention had no significant effect on daily water intake, consumption of high-energy drinks, BMI, waist-to-height ratio, or total body fat |
| Gao et al. (2016) | 1819 preschool children aged 4–6 y | To examine the effect of NE on children’s breakfast patterns | RCT | Monthly lecture and activities for 8 mo (2 semesters in a kindergarten) | Cognitive Behavioral Change Theory | Achieved | Moderate | = 0.02) < 0.001) < 0.001) |
| Hoffman et al. (2011) | 297 children in kindergarten and 1st grade | To examine the effects of a multicomponent, theory-based, 2.5-y intervention on children's FV consumption, FV preferences, FV knowledge, and BMI | Randomized, multiyear intervention | Daily or most of the days during the school year | SCT and SLT | Partially achieved | Moderate | < 0.0001 and < 0.005, respectively) compared with children in CG < 0.0005 and < 0.05, respectively) compared with children in CG < 0.05) < 0.05) < 0.05) |
| Hu et al. (2010) | 1819 children aged 4–6 y | To evaluate the impact of NE in kindergartens and to promote healthy dietary habits in children | RCT | Once monthly for 8 mo | No theory | Partially achieved | Low | < 0.05) < 0.05). Mean scores for nutritional knowledge among IG parents rose significantly from pre test (10.5 points) to post test (11.9 points) ( < 0.0001) |
| Lerner-Geva et al. (2015) | 204 children aged 4–6 y | To assess the effectiveness of an intervention program to improve kindergarten children’s eating and leisure habits in Israel | Cluster RCT with 3 groups: full intervention (NE plus PA), intervention (only NE), and CG | One lesson per week for 10 wk | No theory | Partially achieved | Moderate | Significant association between level of nutritional knowledge and age ( < 0.01). In the initial analysis adjusted for baseline measures, significant reduction in daily energy intake was seen in entire IG with entire intervention (NE and PA), from 5239 kJ at baseline to 4709 kJ at follow-up ( = 0.03). Group with intervention (only NE) significantly increased nutritional knowledge ( = 0.03). No changes in BMI, time spent watching television or playing computer games, exercise, and sleep observed after the intervention |
| Peñalvo et al. (2013) | 2062 children aged 3–5 y | To evaluate the efficacy of the Program SI! in improving indicators of the acquisition of healthy behaviors in children aged 3–5 y | Cluster RCT | During 1 academic year: 20 h of instruction per program component (diet, PA, and human body) and 10 h of instruction for managing emotions | SCT and trans-theoretical models in health promotion | Partially achieved | Low | After 1 school year, the intervention increased children’s knowledge, attitudes, and habits scores, both overall (3.45; 95%CI, 1.84–5.05) and component specific (diet: 0.93; 95%CI, 0.12–1.75; PA: 1.93; 95%CI, 1.17–2.69; human body: 0.65; 95%CI: 0.07–1.24) score. However, no effect on the school environment or on overall scores for parents or teachers was found |
| Witt & Dunn (2012) | 263 preschool children aged 4–5 y | To determine whether CMH, an interactive nutrition and PA program for preschool children, increases FV consumption | Intervention study with IG and CG | Weekly sessions of 15–30 min for 6 wk | No theory | Achieved | Moderate | Children who received CMH significantly increased their consumption of fruit snacks by approximately 20.8% ( < 0.001) and their consumption of vegetable snacks by approximately 33.1% ( < 0.01) between baseline assessment and the assessment conducted 3 mo after completion of CMH program |
Abbreviations: BMI, body mass index; CG, control group; CMH, Color Me Healthy; FV, fruit and vegetable; IG, intervention group; NE, nutrition education; PA, physical activity; RCT, randomized controlled trial; SCT, Social Cognitive Theory; SLT, Social Learning Theory; tbsp, tablespoon; tsp, teaspoon.
A semiquantitative approach was used to summarize the findings from nutrition education interventions. Results from nutrition education interventions were dichotomized on the basis of whether they reported a statistically significant ( P < 0.05) improvement in dietary intakes, physical activity, or other related risk factors for obesity and diet-related chronic diseases. This approach was used to allow for the diverse range of reported statistics, outcomes, and measurement units. 63
A total of 41 studies describing nutrition education interventions focused on children and published between 2009 and 2016 were assessed for their effectiveness on the basis of reported evidence that the interventions met their stated primary research objectives. A majority of the studies (73%; n = 30) were conducted outside the United States, while slightly more than one-fourth of the studies (27%; n = 11) were conducted within the United States. Most of the studies (63%; n = 26) targeted elementary school children ( Table 2 ), while 8 (20%) targeted secondary school children ( Table 3 ) and 7 (17%) targeted preschool children ( Table 4 ).
A total of 19 studies (46%) met their primary research objectives, as evidenced by their reported results, while another 19 studies (46%) partially met their stated objectives and 3 studies (7%) did not meet their stated objectives. Seventeen of the 41 studies were informed by theory but were not theory driven. There was no convincing difference between the studies that used theory as compared with those that did not use theory.
Successful nutrition education interventions in elementary schools
Successful interventions targeting elementary school children engaged parents by means of face-to-face sessions, identified specific behaviors to be modified, and assured fidelity by training teachers or recruiting trained experts to deliver the intervention. In addition, they allowed adequate dosage, with an intervention duration of at least 6 months, and used age-appropriate activities.
Parental engagement.
Although engaging parents in the interventions was a common factor in both successful and unsuccessful interventions, half of the successful interventions engaged parents on a face-to-face basis instead of simply sending information to parents. 28 , 33 , 37 , 42–44 For example, Muros et al 37 conducted 6 nutrition classes for parents in addition to the activities provided for children in the 3 groups that received nutrition education (nutrition education, nutrition education plus physical activity, and nutrition education plus physical activity plus provision of 2 L of extra virgin olive oil per week so that parents could substitute olive oil for the usual oil consumed). After the intervention, the children’s cholesterol intake was significantly decreased in all 3 groups ( P = 0.000, P = 0.001, and P = 0.000, respectively), bringing the cholesterol values closer to the stated recommendations of less than 300 mg/d. In contrast, studies that engaged parents remotely by providing websites, assigning homework, or sending written materials such as newsletters did not report achieving their objectives. 24 , 27 , 32 , 35 For example, the study by Morgan et al 35 provided 3 series of newsletters that focused on the health benefits of eating fruits and vegetables and included strategies for increasing fruit and vegetable intake at home. This intervention did not succeed in increasing either vegetable or fruit consumption ( P = 0.22 and P = 0.23, respectively). Similarly, 8 (57%) of the studies that targeted elementary school students but did not engage parents at all were not successful in achieving their objectives. 3 , 29 , 34 , 36 , 39 , 41 , 45 , 46 For example, Moss et al 36 conducted an intervention that aimed to increase knowledge and consumption of fruit and vegetables among 3rd-grade students. They reported improved knowledge of fiber ( P < 0.001) and vitamins and minerals ( P < 0.05), but they did not find a significant change in consumption of fruit and vegetables.
Specific and measurable behavioral outcomes.
Similarly, identification of a specific desired behavioral outcome was critical in achieving stated objectives. 25 , 28 , 31 , 33 , 37 , 38 , 40 , 43 , 44 , 47 For example, Kristjansdottir et al 33 aimed to increase fruit and vegetable intake in the intervention group by at least 20%. Participants in this study increased their intake of fruits and vegetables by 54%. Other common behavioral outcomes identified were to improve fruit and vegetable preferences 25 , 28 , 38 ; to increase knowledge about nutrition 38 , 42 , 44 and physical activity 31 , 42 , 44 ; and to improve health-related parameters such as physiological and/or anthropometric measurements. 42 , 43 In contrast, interventions designed with broad goals that were not specific to a behavior were not successful in achieving their objectives. 24 , 27 , 29 , 30 , 35 , 39 , 41 , 45 , 46 For instance, the intervention by Steyn et al 45 aimed to promote physical activity and healthy eating habits among the participants. Although dietary diversity increased, physical activity and fruit and vegetable consumption did not. The intervention was not specific to the desired behavioral outcomes of increased physical activity and improved eating habits.
Fidelity of interventions.
The importance of implementing the interventions as intended by using a standardized protocol to ensure fidelity was critical among successful interventions targeting elementary school children. Successful interventions either trained existing teachers or engaged nutrition experts in the implementation of the intervention. 26 , 28 , 33 , 37 , 38 , 40 , 42–44 , 47 For example, in the study by Cunningham-Sabo and Lohse, 25 food educators received for 30 hours of training to teach cooking and tasting lessons for the intervention. This study significantly increased the preferences of fruits and vegetables ( P = 0.012 and P = 0.001, respectively) and improved attitudes toward cooking ( P =0.02). Conversely, interventions that lacked proper training for the implementers compromised fidelity and were unsuccessful. 8 , 24 , 35 , 34 , 39 , 41 For instance, although the study by Battjes-Fries et al 24 provided an introductory workshop as well as manuals and materials for the teachers, a standardized protocol for implementation to ensure fidelity was lacking. Teachers were given options to implement the intervention over 2 weeks, 1 week, or even a semester. As a result of the lack of a standardized implementation plan, only one-third of the intervention was implemented, leaving the other two-thirds of the intervention uncompleted and, therefore, unsuccessful.
Adequate duration of intervention (at least 6 months).
In addition to fidelity, an adequate nutrition education dosage or intervention period of 6 months or more was predictive of success for most of the successful interventions (67%; n = 8). 28 , 33 , 37 , 38 , 40 , 42–44 For example, the intervention carried out by Parmer et al 38 focused on increasing fruit and vegetable knowledge, preferences, and consumption among 2nd-grade children for a duration of 7 months. The results showed significant improvement in nutrition knowledge ( P < 0.01) and taste ratings ( P < 0.001) in the intervention group compared with the control group. In contrast, the 8 studies (57%) that spent less than 6 months on the intervention did not meet or only partially met their stated objectives. 3 , 27 , 29 , 30 , 34–36 , 46 For example, a 1-time (135 min) intervention study by Mittman et al 34 among 7- to 14-year-old children and their parents did not achieve its stated objective of increasing fruit and vegetable intake in any of the assessment periods. Instead, fruit and vegetable intake showed a significant decline between baseline and the 2 follow-up assessments.
Age-appropriate activities.
Finally, successful interventions targeting elementary school children used age-appropriate activities. 25 , 26 , 28 , 31 , 37 , 38 , 40 , 42 , 44 , 47 Age-appropriate activities at the elementary school level included cooking and/or tasting sessions 25 , 28 , 47 ; a learning-through-playing approach based on age or grade 40 , 44 , 47 ; gardening sessions 28 , 38 ; training classes in physical activity 37 , 42 ; the use of posters, masks, and songs 31 , 44 ; and the use of vocabulary and mathematics questions based on nutrition-related issues. 26 , 31 In particular, the intervention carried out by Keihner et al 31 designed different activities based on grade level. For example, 4th-grade students were asked to search for a nutrition-related word and write a composition about its qualities and health benefits, while the 5th-grade students completed a word scramble and prepared a group oral report about food qualities and health benefits. This study significantly increased students’ knowledge of fruits and vegetables ( P < 0.05) and self-efficacy toward eating fruits and vegetables ( P < 0.001), while interventions that implemented a single intervention within a wide age range without discriminating according to age were not successful in achieving their objectives. 3 , 8 , 24 , 27 , 29 , 30 , 34 , 39 , 46 For example, Herbert et al 29 evaluated the effectiveness of their intervention in changing behavior and physical activity habits among children aged 7 to 11 years. This intervention, which included a 15-minute lecture on different nutrition topics, a 10-minute physical activity warm-up, and a 35-minutes aerobic exercise and fitness game, provided the same activities for all age groups. Although the intervention group showed a significant reduction in the consumption of french fries and chips, there was no significant increase in either the consumption of vegetables or physical activity in comparison with the control group.
Successful nutrition education interventions in secondary schools
The successful nutrition education interventions that targeted secondary school children added policy and environmental changes to the intervention, used age-appropriate activities that included technology, identified specific behaviors, aligned activities with their stated objectives, offered the intervention frequently (such as weekly or biweekly), engaged parents on a face-to-face basis, and trained implementers to ensure fidelity.
Environmental and policy changes.
Change of environment was a factor in 3 of the 8 successful interventions in this category. 48 , 50 , 53 It was effective in increasing healthy food choices, changing attitudes, or reducing weight as measured by body mass index (BMI). For example, an intervention by Campos Pastor et al 48 provided a daily balanced breakfast composed of a dairy product, fruits, cereals, nuts, and a sandwich with protein content; a prescribed well-balanced diet; and lessons on dietary and lifestyle recommendations for students, family members, and teachers. After the intervention, the authors observed decreases in the prevalence of overweight and obesity ( P < 0.001) and the prevalence of metabolic syndrome ( P < 0.001). Similarly, a study by Singhal et al 53 that introduced environmental and policy-level change in the school cafeterias replaced soft drinks and high-calorie foods with healthful Indian foods. At the 6-month follow-up assessment, a significant reduction was found in the proportion of children who consumed soft drinks (from 26.3% to 11.2%; P < 0.001) and energy-dense unhealthy foods (from 16.1% to 7.2%; P = 0.03). Likewise, Maatoug et al 50 encouraged the snack stores in schools to replace sugary snacks with healthful snacks and encouraged students to include fruit, vegetables, or dairy products in their meals by offering incentives. After the intervention, students in the intervention group significantly increased their intake of fruit and vegetables ( P = 0.04).
Similar to the interventions conducted among elementary school children, interventions that used age-appropriate activities among secondary school children were more likely to achieve their objectives. Age-appropriate activities in secondary school included role play, peer-led discussions, student health fairs, sports games, the use of cosmetic content–based nutrition education, and the use of technology, such as surfing the internet or using a multimedia CD. 49 , 50 , 54 , 55 For example, the intervention developed by Dehdari et al 49 focused on frequency and nutrient intake during breakfast, using the theory of Pender’s Health Promotion Model. Students were divided into small groups to surf the internet, design posters, or create role play about aspects of breakfast consumption. Other activities included strategies to overcome the perceived barriers to eating a healthy breakfast. The results of the intervention showed significant increases in perceived benefit, perceived self-efficacy, positive activity-related affect, interpersonal influences, situational influences, commitment to a plan of action, and weekly frequency of breakfast consumption in the intervention group compared with the control group ( P < 0.05). In addition, the use of age-appropriate topics relevant to secondary school children was effective in changing behavior. For instance, Somsri et al 54 compared the effectiveness of a cosmetic content–based nutrition education with that of a health content–based nutrition education in promoting fruit and vegetable consumption. After the intervention, knowledge scores, attitude scores, and the amount and variety of fruits and vegetables consumed in the cosmetic content–based nutrition education group significantly increased compared with baseline ( P < 0.001).
Aligning objectives with activities.
Alignment of intervention activities with the stated objectives and the desired outcome was critical for the success of interventions among secondary school children. 48 , 49 , 53–55 For example, the intervention developed by Viggiano et al 55 assessed the effectiveness of the game Kaledo in improving nutrition knowledge and in promoting long-term healthy dietary behavior in adolescents. The intervention focused on the use of Kaledo, a board game that represents a journey through daily meals of the Mediterranean diet. After 6 months of the intervention, the results showed a significant improvement in the children’s nutrition knowledge, physical activity, food habits, and BMI z score in the intervention group compared with the control group ( P < 0.001).
Adequate duration of intervention (at least 6 months).
Adequate dosage and frequency of exposure were important factors among successful secondary school interventions. Six of the 8 successful interventions provided weekly or biweekly sessions that lasted between 30 and 60 minutes. 48 , 49 , 52–55 For instance, Campos Pastor et al 48 designed a 45-minute program that was implemented biweekly for 1 academic year. Significant decreases in the percentage of students who were overweight ( P < 0.001) and who improved their glucose and triglyceride levels ( P < 0.001) were observed in the intervention group.
Similar to findings in effective elementary school interventions, 4 of the 8 successful interventions involved face-to-face interaction with parents. 48–50 , 53 For instance, the study by Singhal et al 53 engaged parents by providing a day-long health camp led by a trained nutritionist. At the 6-month follow-up assessment, significantly more students from the intervention group brought lunch from home that included fruit ( P < 0.001) as compared with the control group.
As noted with the elementary school interventions, accurate implementation of interventions is critical to ensure fidelity. Among the secondary school interventions, all 8 interventions were implemented by trained nutritionists, researchers, or teachers and reported using a standardized format. 48–55
Successful nutrition education interventions in preschools
Successful nutrition interventions in preschoolers targeted specific behaviors, aligned activities with the stated objectives and expected behaviors, engaged parents on a face-to-face basis, and provided hands-on activities. Similar to successful interventions in the other age groups, effective preschool interventions included age-appropriate activities, ensured fidelity by providing training to teachers, and offered short but frequent sessions to accommodate the short concentration span of preschoolers.
Targeting specific behaviors to modify was one of the characteristics commonly observed among the successful interventions. 56–58 , 62 For example, Hoffman et al 58 planned a 2.5-year intervention that included knowledge, preference, and consumption of fruits and vegetables. More specifically, their results showed a significant increase in fruit and vegetable intake, ie, 1.5 tablespoons of fruit ( P < 0.0001) and 1.5 teaspoons of vegetables during lunch ( P = 0.005) for the duration of the project.
Successful interventions strongly aligned their objectives with the activities implemented. 57 , 58 , 60 , 61 For instance, Gao et al 57 examined the effect of nutritional education on children’s breakfast patterns. The intervention included teaching parents the benefits of breakfast for children and the methods of breakfast preparation. The lessons were accompanied by visual aids such as pictures and food models of breakfast items and an illustrated book for children. Parents received brochures with example of breakfast meals. This intervention resulted in a significant increase in both the frequency of breakfast intake ( P = 0.02) and the selection of more nutrient-dense breakfast meals ( P < 0.001) in the intervention group compared with the control group. In contrast, 2 interventions that partially met their objectives did not align their stated objectives with the activities. 56 , 59 For example, De Bock et al 56 conducted an intervention aimed to improve fruit, vegetable, and water consumption and to decrease anthropometric measurements such as BMI, waist circumference, waist-to-height ratio, and total body fat. The intervention activities were focused on fruits and vegetables as snacks and the importance of drinking water. Although the intervention significantly increased the intake of fruits and vegetables ( P < 0.05 and P < 0.01, respectively), there was no significant change in daily water consumption, BMI, waist-to-height ratio, or total body fat.
As observed among successful interventions in elementary and secondary schools, 5 of 7 studies that targeted preschoolers in this review included parental engagement on face-to-face basis, with hands-on activities in addition to lectures. 56 , 57 , 59–61 For example, De Bock et al 56 created hands-on activities in which parents and children interacted in activities such as preparing fruit and vegetable snacks. These strategies significantly increased the intake of fruits ( P < 0.05) and vegetables ( P < 0.01).
To ensure fidelity, all successful nutrition education interventions provided training to teachers 58 , 60–62 or health professionals 56 , 57 , 59 to implement the interventions. For instance, Lerner-Geva et al 60 provided training for teachers. By the end of the intervention, children showed significantly increased nutritional knowledge ( P = 0.03).
Although age-appropriate interventions were important in all age groups, they were critical in the preschooler age group. 56–60 , 62 Age-appropriate activities in preschool included learning through a story book 57 , 59 ; using role models through play acting, posters, or videos 56 , 58 ; exploring with the senses 62 ; and playing games or coloring sheets with peers. 60 For instance, the intervention conducted by Witt and Dunn 62 consisted of hands-on, 30-minute weekly lessons. It included the use of music, exploration of the senses, colors, and imaginary trips to promote the consumption of fruits and vegetables. The intervention was delivered in short but frequent sessions to accommodate the short concentration span of preschoolers. As a result, there was a significant increase between baseline and the 3-month follow-up in the consumption of fruit snacks (by approximately 20.8%; P < 0.001) and vegetables snacks (by approximately 33.1%; P < 0.01). In contrast, a study by Peñalvo et al 61 designed to promote healthy behaviors in preschool children included activities to teach correct management of emotions to develop protective behaviors against abuse of tobacco, alcohol, and drugs. At the end of the intervention, no significant improvement in this component was observed. In the current systematic review, the discussion of tobacco, alcohol, and drugs was not considered age-appropriate for preschool children.
The purpose of this systematic review was to identify factors characterizing studies published between 2009 and 2016 that were successful in achieving their stated objectives in nutrition interventions among children. In order to capture age-based strategies, studies were grouped and reviewed according to their targeted age groups: preschool, elementary, and secondary school children. Seven overarching factors emerged as critical to successful nutrition education among children: (1) a multicomponent (involving teachers and parents), multilevel (including the schools and the home) approach; (2) adequate duration of intervention and frequency of exposure; (3) parental engagement; (4) age-appropriate, hands-on experiences; (5) fidelity as ensured by training of the implementers and standardization of the protocol among all groups; (6) environmental change to impact knowledge (upstream outcome) and then behavior (midstream outcome); and (7) proper alignment between the stated objectives, the intervention, and the desired outcome, which is needed to affect weight or BMI (downstream outcome). The findings of the current systematic review are based on critical analysis of these factors. The use of behavior theories in the studies reviewed was not associated with success of interventions, perhaps because other factors mentioned above were more critical or because the majority of the studies that used theory were informed by theory but were not theory driven. However, a review by Murimi et al 22 that looked at factors associated with successful interventions among adults found that interventions were more likely to succeed if they were theory driven. Theory-driven studies use the specific theory constructs in the methodology, intervention, and assessment, while theory-informed studies might identify the theory that informs their studies but may not use all its constructs throughout the study. 4
Multicomponent and multilevel interventions
Effective nutrition education is a complex undertaking that calls for a systematic and comprehensive assessment of the determinants of—as well as the barriers to—the desired outcome to inform the intervention. 64 This review found that nutrition education interventions with a comprehensive, multicomponent, and multilevel approach were more likely to achieve their stated objectives in all age groups. For example, a majority of the preschool interventions that were successful utilized both teachers and nutrition experts to implement the interventions in school settings and engaged the parents to extend the intervention to the home. 56–62 In addition to incorporating multiple components, they included several levels of intervention, such as knowledge, tasting sessions, and skills building. 56 , 60 , 61 , 62 These findings confirm the finding of a systematic review by Colquitt et al, 65 who concluded that multicomponent interventions in preschool children were associated with a reduction in overweight or obesity. Similarly, the current review found that nutritional interventions in elementary schools were more likely to meet their objectives when they were multifaceted, had a high frequency of exposure, were delivered by nutritionists or trained teachers, and engaged parents. This confirms the findings of a review by Van Cauwenberghe et al, 66 namely that multicomponent interventions that include improved availability of fruit and vegetables, a nutrition education curriculum delivered by teachers, and at least some parental involvement can improve intake of fruits and vegetables.
Duration and frequency of exposure
Health-related behavior change is a complex process that includes new behaviors to learn and undesired behaviors to reduce. This process often requires time to learn new skills, identify resources, practice the new behavior, and identify support to sustain the new behavior. 67 In addition to including multiple levels and multiple components, this current review found that reviewed interventions were more likely to meet their stated objectives when they were implemented for more than 6 months and offered frequent exposures, such as weekly or biweekly. This finding was in agreement with the results of a systematic review performed by Murimi et al 22 on nutrition education for adults, which found that interventions implemented for more than 5 months were more likely to meet their stated goals. Similarly, a systematic review by Ling et al 68 found that increasing the length of an intervention or including a long-term follow-up of at least 12 months might help to identify a delayed intervention effect.
Parental engagement
Although most school children spend most of their day time at school, significant health and dietary behaviors are acquired long before school age and are enforced daily either by parental modeling, feeding style, or availability of the desired food choices during breakfast or dinner. 69 It is therefore critical for interventions targeting children to incorporate both the school and the home environment to be effective in promoting a sustainable healthy lifestyle. 70 This systematic review found parental engagement in all 3 age groups to be critical for successful interventions aimed at modifying dietary behavior or weight loss. The majority (n = 21) of the studies did not engage parents, and other studies engaged parents by passive methods (n = 6) such as providing them with written information or directing them to a website. 24 , 27 , 31 , 32 , 35 , 62 Successful studies were more likely to engage parents actively, ie on a face-to-face basis, by offering them nutrition classes 33 , 37 , 49 , 59 , 60 or health fairs 42 , 50 , 53 , 61 ; requiring them to accompany their children during cooking, tasting, or nutrition education sessions 43 , 48 , 56 , 57 ; or allowing them to be part of the program’s staff. 28 , 44 This was especially critical in the interventions that targeted preschool students. 56 , 57 , 59–61 These findings are congruent with the results of a meta-analysis performed by Ling et al, 68 who concluded that interventions providing skills training and behavioral change strategies aimed at parents were associated with improvement of children’s BMI in preschool. Similarly, a systematic review by Loveman et al 71 demonstrated that, when interventions with multiple components (ie, diet, physical activity, and behavior) were delivered to the parents of elementary school children, children’s body weight improved by significantly decreasing an average of 0.1 in BMI z score at the longest follow-up period (9–12 months) ( P = 0.04). Similarly, Meiklejohn et al 72 found significant changes in anthropometric measures among adolescents when parents were engaged. More importantly, active parental engagement compensated for short intervention durations, as demonstrated by a review conducted by Neimeier et al, 19 who found that children and adolescents’ actual BMI reductions were greater in interventions that engaged parents, even when controlling for the duration of interventions. In addition, the duration of interventions and parent participation both contributed independently to intervention success rates. 19
Age-appropriate and experiential learning
The pool of interventions in the current review represented a wide age range, from preschool to high school age. The wide difference in age implies a wide difference in cognition, abstract thinking, and skills, among others. 15–18 It was therefore critical for this review to assess the design of the interventions on the basis of age appropriateness. The results of this assessment showed that interventions applying age-appropriate and/or experiential activities were more likely to be successful. For example, Hoffman et al 58 and Witt and Dunn 62 designed studies to increase the consumption of fruits and vegetables among preschoolers by implementing age-appropriate activities such as the use of role models (cartoons, teachers, coaches) and activity-based lessons that included tasting, imagining, and color associations with fruits and vegetables. Hoffman et al 58 significantly increased the consumption of fruits and vegetables, and Witt and Dunn 62 significantly increased the consumption of fruit and vegetable snacks. The findings of this systematic review concur with those of Dudley et al, 73 who concluded that experiential learning strategies were associated with the largest effects across studies that reported outcomes of reduced food consumption or energy intake, increased fruit and vegetable consumption or preference, and increased nutritional knowledge. Similarly, all elementary school interventions that met their stated objective applied interactive education and hands-on experiences in teaching physical activity and healthy eating behaviors. 25 , 26 , 28 , 31 , 33 , 37 , 38 , 40 , 42–44 , 47 Among secondary school children, age-appropriate activities that led to successful interventions included the use of topics important to adolescents. For example, the cosmetic content–based nutrition intervention by Somsri et al 54 (a nutrition education intervention that explained the benefits of fruit and vegetable consumption for the skin, body shape, body weight, and other aspects of body image) was more effective in increasing fruit and vegetable consumption than the health-based intervention.
Fidelity of interventions
Fidelity in intervention ensures that all intervention activities are executed as planned in the methods. In this review, studies that had high fidelity were more likely to succeed in achieving their stated objectives, ie, approximately 82% (n = 31) of the interventions that met or partially met their objectives trained existing teachers or engaged nutrition and physical activity experts in the implementation of the interventions. These findings are in agreement with a review by Ross et al 74 and Ling et al, 68 who found that providing preschool teachers with a health promotion opportunity to enhance their health knowledge increased healthy behaviors, reduced stress, and increased the fidelity and quality of the intervention.
Environmental changes for upstream and midstream outcomes
The results of this review found that environmental changes were critical in achieving stated objectives among interventions that targeted secondary school students. For example, 3 of the 7 successful interventions 48 , 50 , 53 were effective in increasing positive attitudes toward increasing fruit and vegetable consumption and reducing either weight as measured by BMI or unhealthy food choices such as carbonated drinks, burgers, pizzas, and french fries. Environmental changes included providing a standardized breakfast for students during the duration of the intervention and prescribing a well-balanced diet. These resulted in a significant decrease in the prevalence of overweight and obesity ( P < 0.001) and metabolic syndrome ( P <0.001). 48 Similarly, a study by Singhal et al 53 that implemented an environmental and policy-level intervention by replacing sugar-added beverages with healthful Indian foods was successful in reducing the consumption of sugar-added beverages and increasing the consumption of healthful alternatives. Other systematic reviews have found environmental and/or policy interventions to be effective in changing behavior. For example, a systematic review by Silveira et al 75 showed that school environmental change to ensure an uninterrupted supply of fruits and vegetables in schools allowed children and adolescents to have access to these foods, thereby increasing the feasibility of incorporating fruits and vegetables in their diet. Similarly, a systematic review by Mercado et al 76 found studies that addressed the school or community environment were successful in decreasing the BMI of participants. Examples of environmental strategies included modification of food served in schools and creation of safe walking routes to schools. Another environmental strategy, the Delicious and Nutritious Garden intervention, included cooking and taste testing reported a significant increase in the number of fruits and vegetables ever eaten, in vegetable preferences, and in fruit and vegetable asking behavior at home.
Activities based on stated objectives and targeted expected outcomes
The importance of setting realistic objectives and planning activities aligned with the objectives and the desired behavior was critical in studies that were successful in achieving their objectives. Nutrition education interventions that succeeded had clear alignment between the stated objectives, the desired outcome, and the implemented activities. For example, in the study by Gao et al, 57 the objective of the program was to promote consumption of a healthy breakfast for children. To achieve their objectives, the authors addressed both the children, who had a role in consuming the breakfast, and the parents, who had a role in preparing the breakfast. The intervention included educating children about the benefits of eating breakfast and educating parents about the methods of breakfast preparation. This intervention resulted in a significant increase in the number of times children ate breakfast and the selection of more nutrient-dense breakfast choices in the intervention group. Another example is provided by Singhal et al, 53 whose study among adolescents focused on the benefits of physical activity and healthy foods such as fruits, vegetables, and dairy and the harmful effects of junk foods. The study promoted healthy lifestyles among the adolescents by engaging them in activities such as planning their own lunch, planning healthy diets daily by themselves, and listing healthy alternatives to high-calorie foods. The intervention significantly lowered the consumption of carbonated drinks and energy-dense foods and significantly increased fruit intake during lunch. Other systematic reviews found similar findings. For example, a review by Murimi et al 22 found that studies whose objectives, activities, and desired outcomes were aligned were more likely to be successful. Similarly, a systematic review by Silveira et al 75 concluded that interventions using structured activities aligned with specific objectives to provide knowledge about the benefits of maintaining a healthy diet were more likely to be successful.
This review has 2 limitations. First, only articles published in English were considered. Therefore, it is possible that some recent and important findings published in languages other than English were left out. Second, this review was limited by a lack of adequate information in the methods and results of some articles. This hindered the ability to properly evaluate the contributions and effectiveness of specific components of nutrition education interventions, including the use of theory and the dosage of interventions (frequency and duration). Despite these limitations, the strength of the current review lies in its analysis of several factors that contributed to the success of various types of interventions. This is different from previous reviews that focused primarily on the analysis of a single type of intervention and the related outcome.
This review indicates that nutrition education interventions are more likely to be successful in achieving their objectives when experiential activities such as gaming, gardening, and cooking demonstrations are incorporated and when specific dietary behaviors are targeted for modification. In addition, interventions that engaged parents through face-to-face interaction and delivered extensive training for external experts and teachers to enhance fidelity were more likely to achieve their objectives. While all the successful interventions reported an increase in participants’ knowledge, interventions were more likely to be successful in changing behavior when the duration of the intervention was more than 6 months.
Studies that delivered interventions within a period of less than 6 months, used intervals of more than 2 weeks between lessons, or delivered a single-dose educational intervention were less likely to be successful in achieving their objectives. Similarly, interventions that delivered passive education programs for parents, such as providing a web link or written material, did not benefit from that component of parental involvement. In addition, interventions were less likely to meet their stated objectives if they broadly promoted healthy eating in general without targeting a specific behavior or did not ensure fidelity but just provided tool kits without specific guidance on the usage of the material instead of training the teachers directly. While most interventions were successful in improving knowledge, attitudes, and behavioral measures, downstream variables such as BMI, waist circumference, and percent body fat, when used as outcome measures, did not show any meaningful improvement without the use of multiple components and long durations.
This systematic review demonstrates the importance of designing an age-appropriate intervention of adequate duration (at least 6 months) to change behavior in all age groups of school children. Researchers planning to implement interventions among preschool children are encouraged to design short but frequent sessions to accommodate the short attention span of preschoolers, to include hands-on activities, and to work with parents, preferably on a face-to-face basis. A combination of adequate dose (duration of at least 6 months) and trained implementers is critical for elementary school children, while the use of technology and age-appropriate topics is important for secondary school children. Although the use of theory did not determine the success of the interventions analyzed in this review, it is important to note that most of the interventions were only informed by a theory but were not designed and driven by theory. As indicated by a previous systematic review on nutrition education in adults, theory-driven interventions are more likely to be successful. 22
Author contributions . M.W.M. conceptualized the systematic review. M.W.M., A.F.M-C., B.N., S.S., and R.A. conducted the literature search, screened the selected articles, and assessed the quality and extracted the information of the included articles. B.N. and S.S. wrote the introduction. M.R.A. wrote the methods section. M.W.M., A.F.M-C., and V.N. analyzed the articles. M.W.M. and A.F.M-C. wrote the results section. M.W.M. and V.N. wrote the discussion and conclusion and provided critical revision of the manuscript. A.F.M-C. edited the manuscript. M.W.M. approved the final version of the manuscript.
Funding/support . No external funds supported this work.
Declaration of interest . The authors have no relevant interests to declare.
The following Supporting Information is available through the online version of this article at the publisher’s website.
Appendix S1 PRISMA checklist
World Health Organization . Diet, Nutrition and the Prevention of Chronic Diseases . http://apps.who.int/iris/bitstream/10665/42665/1/WHO_TRS_916.pdf? ua=1 . Published 2003. Accessed October 23, 2017. WHO Technical Report Series 916.
Cohen DA , Sturm R , Scott M et al. , . Not enough fruit and vegetables or too many cookies, candies, salty snacks, and soft drinks? Public Health Rep. 2010 ; 125 : 88 – 95 .
Google Scholar
Zhou WJ , Xu XL , Li G et al. , . Effectiveness of a school-based nutrition and food safety education program among primary and junior high school students in Chongqing, China . Glob Health Promot. 2016 ; 23 : 37 – 49 .
Contento IR. Nutrition Education: Linking Research, Theory, and Practice . 3rd ed. Burlington, MA : Jones & Bartlett Learning ; 2016 .
Google Preview
Grabauskas V , Petkeviciene J , Kriaucioniene V et al. , . Health inequalities in Lithuania: education and nutrition habits . Medicina (Kaunas) 2004 ; 40 : 875 – 883 .
Dunton GF , Liao Y , Grana R et al. , . State-wide dissemination of a school-based nutrition education programmme: a RE-AIM (Reach, Efficacy, Adoption, Implementation, Maintenance) analysis . Public Health Nutr. 2012 ; 17 : 422 – 430 .
Turconi G , Guarcello M , Maccarini L et al. , . Eating habits and behaviors, physical activity, nutritional and food safety knowledge and beliefs in an adolescent Italian population . J Am Coll Nutr . 2008 ; 27 : 31 – 43 .
Prelip M , Kinsler J , Le Thai C et al. , . Evaluation of a school-based multicomponent nutrition education program to improve young children’s fruit and vegetable consumption . J Nutr Educ Behav . 2012 ; 44 : 310 – 318 .
Shariff ZM , Bukhari SS , Othman N et al. , . Nutrition education intervention improves nutrition knowledge, attitude and practices of primary school children: a pilot study . Int J Health Educ . 2008 ; 11 : 119 – 123 .
Shilts MK , Lamp C , Horowitz M et al. , . Pilot study: EatFit impacts sixth graders’ academic performance on achievement of mathematics and English education standards . J Nutr Edu Behav . 2009 ; 41 : 127 – 131 .
Pucher KK , Boot NMWM , De Vries NK. Systematic Review: School health promotion interventions targeting physical activity and nutrition can improve academic performance in primary- and middle-school children . Health Educ . 2013 ; 113 : 372 – 391 .
Black AP , D’Onise K , McDermott R et al. , . How effective are family-based and institutional nutrition interventions in improving children’s diet and health? A systematic review . BMC Public Health . 2017 ; 17 : 1-19 . doi:10.1186/s12889-017-4795-5
Horodyska K , Luszczynska A , Van Den Berg M et al. , . Good practice characteristics of diet and physical activity interventions and policies: an umbrella review . BMC Public Health . 2015 ; 15 : 19. doi: 10.1186/s12889-015-1354-9
Diep CS , Chen TA , Davies VF et al. , . Influence of behavioral theory on fruit and vegetable intervention effectiveness among children: a meta-analysis . J Nutr Edu Behav . 2014 ; 46 : 506 – 546 .
Centers for Disease Control and Prevention . Child development: preschoolers (3-5 years of age). https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/preschoolers.html . Updated January 3, 2017. Accessed October 10, 2017.
Centers for Disease Control and Prevention . Child development: middle childhood (6-8 years of age). https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle.html . Updated January 3, 2017. Accessed October 10, 2017.
Centers for Disease Control and Prevention . Child development middle childhood (9-11 years of age). https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle2.html . Updated March 15, 2016. Accessed October 10, 2017.
Centers for Disease Control and Prevention . Child development: young teens (12-14 years of age). https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/adolescence.html . Updated January 3, 2017. Accessed October 10, 2017.
Niemeier BS , Hektner JM , Enger KB. Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis . Prev Med . 2012 ; 55 : 3 – 13 .
Hingle MD , O’Connor TM , Dave JM et al. , . Parental involvement in interventions to improve child dietary intake: a systematic review . Prev Med. 2010 ; 51 : 103 – 111 .
Liberati A , Altman DG , Tetzlaff J et al. , . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration . PLoS Med . 2009 ; 6 : e1000100. doi:10.1371/journal.pmed.1000100
Murimi MW , Kanyi M , Mupfudze T et al. , . Factors influencing efficacy of nutrition education interventions: a systematic review . J Nutr Educ Behav. 2017 ; 49 : 142 – 165 .
Ryan R , Hill S. How to GRADE the quality of the evidence. Version 3.0. Cochrane Consumers and Communication Group, London, UK. http://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/how_to_grade_revising_1_december_2016.pdf . Published December 2016. Accessed July 20, 2017.
Battjes-Fries MC , Haveman-Nies A , Renes RJ et al. , . Effect of the Dutch school-based education programme ‘Taste Lessons’ on behavioural determinants of taste acceptance and healthy eating: a quasi-experimental study . Public Health Nutr. 2015 ; 18 : 2231-2241. doi:10.1017/S1368980014003012
Cunningham-Sabo L , Lohse B. Cooking with kids positively affects fourth graders’ vegetable preferences and attitudes and self-efficacy for food and cooking . Child Obes . 2013 ; 9 : 549 – 556 .
Francis M , Nichols SS , Dalrymple N. The effects of a school-based intervention programme on dietary intakes and physical activity among primary-school children in Trinidad and Tobago . Public Health Nutr. 2010 ; 13 : 738 – 747 .
Gallotta MC , Iazzoni S , Emerenziani GP et al. , . Effects of combined physical education and nutritional programs on schoolchildren’s healthy habits . Peer J 2016 ; 4e1880. doi:10.7717/peerj.1880
Gibbs L , Staiger PK , Johnson B et al. , . Expanding children’s food experiences: the impact of a school-based kitchen garden program . J Nutr Educ Behav. 2013 ; 45 : 137 – 146 .
Herbert PC , Lohrmann DK , Seo DC et al. , . Effectiveness of the Energize elementary school program to improve diet and exercise . J School Health. 2013 ; 83 : 780 – 786 .
Katz DL , Katz CS , Treu JA et al. , . Teaching healthful food choices to elementary school students and their parents: the Nutrition Detectives™ program . J Sch Health . 2011 ; 81 : 21 – 28 .
Keihner AJ , Meigs R , Sugerman S et al. , . The Power Play! Campaign’s School Idea & Resource Kits improve determinants of fruit and vegetable intake and physical activity among fourth- and fifth-grade children . J Nutr Educ Behav . 2011 ; 43 : S122 – S129 .
Kipping RR , Howe LD , Jago R et al. , . Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for Life Year 5 (AFLY5) school based cluster randomized controlled trial . BMJ. 2014 ; 348 : g3256. doi:10.1136/bmj.g3256
Kristjansdottir AG , Johannsson E , Thorsdottir I. Effects of a school-based intervention on adherence of 7–9-year-olds to food-based dietary guidelines and intake of nutrients . Public Health Nutr. 2010 ; 13 : 1151 – 1161 .
Mittmann S , Austel A , Ellrott T. Behavioural effects of a short school-based fruit and vegetable promotion programme: 5-a-Day for kids . Health Educ . 2016 ; 116 : 222 – 237 .
Morgan PJ , Warren JM , Lubans DR et al. , . The impact of nutrition education with and without a school garden on knowledge, vegetable intake and preferences and quality of school life among primary-school students . Public Health Nutr. 2010 ; 13 : 1931 – 1940 .
Moss A , Smith S , Null D et al. , . Farm to school and nutrition education: positively affecting elementary school-aged children’s nutrition knowledge and consumption behavior. Child Obes 2013 ; 9 : 51 – 56 .
Muros JJ , Zabala M , Oliveras-López MJ et al. , . Effect of physical activity, nutritional education, and consumption of extra virgin olive oil on lipid, physiological, and anthropometric profiles in a pediatric population . J Phys Act Health . 2015 ; 12 : 1245 – 1252 .
Parmer SM , Salisbury-Glennon J , Shannon D et al. , . School gardens: an experiential learning approach for a nutrition education program to increase fruit and vegetable knowledge, preference, and consumption among second-grade students . J Nutr Educ Behav . 2009 ; 41 : 212 – 217 .
Rosário R , Oliveira B , Araújo A et al. , . The impact of an intervention taught by trained teachers on childhood overweight . Int J Environ Res Public Health . 2012 ; 9 : 1355 – 1367 .
Rosi A , Brighenti F , Finistrella V et al. , . Giocampus school: a “learning through playing” approach to deliver nutritional education to children . Int J Food Sci Nutr. 2016 ; 67 : 207 – 215 .
Safdie M , Jennings-Aburto N , Lévesque L et al. , . Impact of a school-based intervention program on obesity risk factors in Mexican children . Salud Publica Mex. 2013 ; 55 : S374 – S387 .
Saraf DS , Gupta SK , Pandav CS et al. , . Effectiveness of a school based intervention for prevention of non-communicable diseases in middle school children of rural North India: a randomized controlled trial . Indian J Pediatr. 2015 ; 82 : 354 – 362 .
Sevinç Ö , Bozkurt AI , Gündoğdu M et al. , . Evaluation of the effectiveness of an intervention program on preventing childhood obesity in Denizli, Turkey . Turk J Med Sci . 2011 ; 41 : 1097 – 1105 .
Shah P , Misra A , Gupta N et al. , . Improvement in nutrition-related knowledge and behaviour of urban Asian Indian school children: findings from the ‘Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ (MARG) intervention study . Br J Nutr. 2010 ; 104 : 427 – 436 .
Steyn NP , de Villiers A , Gwebushe N et al. , . Did HealthKick, a randomised controlled trial primary school nutrition intervention improve dietary quality of children in low-income settings in South Africa? BMC Public Health . 2015 ; 15 : 948 . doi:10.1186/s12889-015-2282-4
Toruner EK , Ayaz S , Altay N et al. , . Efficacy of a school-based healthy life program in Turkey . Child Health Care . 2015 ; 44 : 69 – 86 .
Wall DE , Least C , Gromis J et al. , . Nutrition education intervention improves vegetable‐related attitude, self‐efficacy, preference, and knowledge of fourth‐grade students . J Sch Health. 2012 ; 82 : 37 – 43 .
Campos Pastor MM , Serrano Pardo MD , Fernández Soto ML et al. , . Impact of a ‘school-based’ nutrition intervention on anthropometric parameters and the metabolic syndrome in Spanish adolescents . Ann Nutr Metab. 2012 ; 61 : 281 – 288 .
Dehdari T , Rahimi T , Aryaeian N et al. , . Effect of nutrition education intervention based on Pender’s Health Promotion Model in improving the frequency and nutrient intake of breakfast consumption among female Iranian students . Public Health Nutr. 2014 ; 17 : 657 – 666 .
Maatoug J , Msakni Z , Zammit N et al. , . School-based intervention as a component of a comprehensive community program for overweight and obesity prevention, Sousse, Tunisia, 2009–2014 . Prev Chronic Dis. 2015 ; 12 : E160 . doi:10.5888/pcd12.140518
Murimi MW , Chrisman MS , Hughes K et al. , . Effects of school-based point-of-testing counselling on health status variables among rural adolescents . Health Educ J . 2015 ; 74 : 557 – 567 .
Rani MA , Shriraam V , Zachariah R et al. , . Does a nutrition education programme change the knowledge and practice of healthy diets among high school adolescents in Chennai, India? Health Educ J . 2013 ; 72 : 733 – 741 .
Singhal N , Misra A , Shah P et al. , . Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India . Eur J Clin Nutr. 2010 ; 64 : 364 – 373 .
Somsri P , Satheannoppakao W , Tipayamongkholgul M et al. , . A cosmetic content–based nutrition education program improves fruit and vegetable consumption among grade 11 Thai students . J Nutr Educ Behav. 2016 ; 48 : 190 – 198 .
Viggiano A , Viggiano E , Di Costanzo A et al. , . Kaledo, a board game for nutrition education of children and adolescents at school: cluster randomized controlled trial of healthy lifestyle promotion . Eur J Pediatr. 2015 ; 174 : 217 – 228 .
De Bock F , Breitenstein L , Fischer JE. Positive impact of a pre-school-based nutritional intervention on children’s fruit and vegetable intake: results of a cluster-randomized trial . Public Health Nutr. 2012 ; 15 : 466 – 475 .
Gao Y , Cai C , Sun W et al. , . Nutritional intervention and breakfast behavior of kindergartens . Iran J Public Health . 2016 ; 45 : 297 – 304 .
Hoffman JA , Thompson DR , Franko DL et al. , . Decaying behavioral effects in a randomized, multi-year fruit and vegetable intake intervention . Prev Med . 2011 ; 52 : 370 – 375 .
Hu C , Ye D , Li Y et al. , . Evaluation of a kindergarten-based nutrition education intervention for pre-school children in China . Public Health Nutr. 2010 ; 13 : 253 – 260 .
Lerner-Geva L , Bar-Zvi E , Levitan G et al. , . An intervention for improving the lifestyle habits of kindergarten children in Israel: a cluster-randomised controlled trial investigation . Public Health Nutr. 2015 ; 18 : 1537 – 1544 .
Peñalvo JL , Sotos-Prieto M , Santos-Beneit G et al. , . The Program SI! intervention for enhancing a healthy lifestyle in preschoolers: first results from a cluster randomized trial . BMC Public Health . 2013 ; 13 : 1208. doi: 10.1186/1471-2458-13-1208
Witt KE , Dunn C. Increasing fruit and vegetable consumption among preschoolers: evaluation of Color Me Healthy . J Nutr Educ Behav . 2012 ; 44 : 107 – 113 .
Ammerman AS , Lindquist CH , Lohr KN et al. , . The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence . Prev Med . 2002 ; 35 : 25 – 41 .
Baranowski T , Cerin E , Baranowski J. Steps in the design, development and formative evaluation of obesity prevention-related behavior change trials . Int J Behav Nutr Phys Act. 2009 ; 6 : 6. doi:10.1186/1479-5868-6-6
Colquitt JL , Loveman E , O’Malley C et al. , . Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years . Cochrane Database Syst Rev . 2016 ;( 3) : CD02105. doi:10.1002/14651858.CD012105.
Van Cauwenberghe E , Maes L , Spittaels H et al. , . Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: systematic review of published and “grey” literature . Br J Nutr. 2010 ; 103 : 781 – 797 .
Glanz K , Rimer BK , Viswanath K. Health Behavior: Theory, Research, and Practice . 5th ed. San Francisco, CA : Jossey-Bass ; 2015 .
Ling J , Robbins LB , Wen F. Interventions to prevent and manage overweight or obesity in preschool children: a systematic review . Int J Nurs Stud. 2016 ; 53 : 270 – 289 .
Kunin-Batson AS , Seburg EM , Crain AL et al. , . Household factors, family behavior patterns, and adherence to dietary and physical activity guidelines among children at risk for obesity . J Nutr Educ Behav . 2015 ; 47 : 206 – 215 .
Østbye T , Malhotra R , Stroo M et al. , . The effect of the home environment on physical activity and dietary intake in preschool children . Int J Obes (Lond). 2013 ; 37 : 1314 – 1321 .
Loveman E , Al-Khudairy L , Johnson RE et al. , . Parent-only interventions for childhood overweight or obesity in children aged 5 to 11 years . Cochrane Database Syst Rev . 2015 ;( 12) : CD012008 . doi:10.1002/14651858.CD012008.
Meiklejohn S , Ryan L , Palermo C. A systematic review of the impact of multi-strategy nutrition education programs on health and nutrition of adolescents . J Nutr Educ Behav. 2016 ; 48 : 631 – 646 .
Dudley DA , Cotton WG , Peralta LR. Teaching approaches and strategies that promote healthy eating in primary school children: a systematic review and meta-analysis . Int J Behav Nutr Phys Act. 2015 ; 12 : 28 . doi:10.1186/s12966-015-0182-8
Ross SW , Romer N , Horner RH. Teacher well-being and the implementation of school-wide positive behavior interventions and supports . J Posit Behav Interv . 2012 ; 14 : 118 – 128 .
Silveira JA , Taddei JA , Guerra PH et al. , . Effectiveness of school-based nutrition education interventions to prevent and reduce excessive weight gain in children and adolescents: a systematic review . J Pediatr (Rio J). 2011 ; 87 : 382 – 392 .
Mercado J , Aufa’l ARAM , Belyeu-Camacho T et al. , . A review of promising multicomponent environmental child obesity prevention intervention strategies by the Children’s Healthy Living Program . J Environ Health . 2016 ; 79 : 18 – 26 .
- science of nutrition
- elementary schools
- secondary schools
Supplementary data
| Month: | Total Views: |
|---|---|
| May 2018 | 52 |
| June 2018 | 104 |
| July 2018 | 96 |
| August 2018 | 93 |
| September 2018 | 95 |
| October 2018 | 364 |
| November 2018 | 385 |
| December 2018 | 232 |
| January 2019 | 94 |
| February 2019 | 90 |
| March 2019 | 82 |
| April 2019 | 101 |
| May 2019 | 58 |
| June 2019 | 50 |
| July 2019 | 41 |
| August 2019 | 33 |
| September 2019 | 44 |
| October 2019 | 60 |
| November 2019 | 100 |
| December 2019 | 69 |
| January 2020 | 71 |
| February 2020 | 89 |
| March 2020 | 113 |
| April 2020 | 87 |
| May 2020 | 45 |
| June 2020 | 75 |
| July 2020 | 183 |
| August 2020 | 685 |
| September 2020 | 804 |
| October 2020 | 543 |
| November 2020 | 385 |
| December 2020 | 295 |
| January 2021 | 321 |
| February 2021 | 339 |
| March 2021 | 364 |
| April 2021 | 385 |
| May 2021 | 376 |
| June 2021 | 317 |
| July 2021 | 274 |
| August 2021 | 196 |
| September 2021 | 344 |
| October 2021 | 516 |
| November 2021 | 441 |
| December 2021 | 327 |
| January 2022 | 286 |
| February 2022 | 402 |
| March 2022 | 484 |
| April 2022 | 553 |
| May 2022 | 382 |
| June 2022 | 401 |
| July 2022 | 282 |
| August 2022 | 275 |
| September 2022 | 455 |
| October 2022 | 598 |
| November 2022 | 551 |
| December 2022 | 396 |
| January 2023 | 326 |
| February 2023 | 325 |
| March 2023 | 421 |
| April 2023 | 506 |
| May 2023 | 422 |
| June 2023 | 321 |
| July 2023 | 305 |
| August 2023 | 282 |
| September 2023 | 418 |
| October 2023 | 526 |
| November 2023 | 455 |
| December 2023 | 383 |
| January 2024 | 385 |
| February 2024 | 369 |
| March 2024 | 534 |
| April 2024 | 605 |
| May 2024 | 539 |
| June 2024 | 331 |
| July 2024 | 379 |
| August 2024 | 352 |
| September 2024 | 322 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1753-4887
- Print ISSN 0029-6643
- Copyright © 2024 International Life Sciences Institute
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Our systems are now restored following recent technical disruption, and we’re working hard to catch up on publishing. We apologise for the inconvenience caused. Find out more: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert
- > Journals
- > Journal of Nutritional Science
- > Volume 12
- > A scoping review of nutrition education interventions...

Article contents
Introduction, a scoping review of nutrition education interventions to improve competencies, lifestyle and dietary habits of medical students and residents.
Published online by Cambridge University Press: 02 March 2023
We reviewed the available research and gave an overview of the effects of nutrition education interventions (NEIs) on medical students’ and residents’ knowledge of nutrition, attitudes towards nutrition care, self-efficacy, dietary practices and readiness to offer nutrition care. From 28 May through 29 June 2021, we searched Google Scholar, PubMed, ProQuest, Cochrane and ProQuest to retrieve 1807 articles. After conducting de-duplication and applying the eligibility criteria and reviewing the title and abstract, 23 papers were included. The data were descriptively and narratively synthesised, and the results were displayed as frequencies, tables and figures. Twenty-one interventions were designed to increase participants’ knowledge of nutrition-related topics, and eighteen studies found that nutrition knowledge had significantly improved post-intervention. Only four of the eleven studies that reported on attitudes about nutrition post-intervention showed a meaningful improvement. The self-efficacy of participants was examined in more than half of the included studies ( n 13, 56⋅5 %), and eleven of these studies found a significant increase in the participants’ level of self-efficacy to offer nutrition care post-intervention. At the post-intervention point, seven interventions found that dietary and lifestyle habits had significantly improved. The review demonstrated the potential of NEIs to enhance participants’ dietary habits and nutrition-related knowledge, attitudes and self-efficacy. Reduced nutrition knowledge, attitude and self-efficacy scores during the follow-up, point to the need for more opportunities for medical students and residents to learn about nutrition after the intervention.
Morbidity and death in all age groups are considerably increased by poor diets. One in five fatalities worldwide are caused by poor nutrition. In 2017, 11 million deaths were attributable to dietary risk factors, with 3 million deaths each due to high salt intake and poor whole grain intake, and 2 million due to low fruit intake ( Reference Murray 1 ) .
Promoting healthy eating habits is a recognised strategy to lessen the impact of malnutrition. Since doctors are usually the gatekeepers in the healthcare system, they play an important role in encouraging people to eat healthy and live a healthy lifestyle. Doctors can assist individuals by giving nutrition counselling, nutrition assessments or identifying and recommending patients to seek professional dietetic care, all of which are referred to as nutrition care.
Doctors are typically seen as trustworthy sources of nutrition by the general public and are expected to provide nutrition care. The Behavioural Risk Factor Surveillance System study revealed a roughly threefold increase in patients’ attempts to treat their nutrition issues following physician advice ( Reference Rutledge, Groesz and Linke 2 ) . Thus, it should come as no surprise that the majority of professional bodies in a number of countries list nutrition care as one of the responsibilities that doctors should take on when delivering healthcare ( Reference Crowley, Ball and Hiddink 3 ) .
Nonetheless, physicians worldwide continue to underutilise this opportunity to render nutrition care to their clients. Doctors struggle to provide nutrition care due to a lack of training in nutrition counselling, limited expertise and low confidence ( Reference Crowley, Ball and Hiddink 3 , Reference Mogre, Stevens and Aryee 4 ) . The vast majority of practicing doctors, medical students and incoming interns frequently report being dissatisfied and unwilling to counsel patients with nutritional issues ( Reference Mogre, Stevens and Aryee 4 , Reference Hark, Deen and Morrison 5 ) .
Some nutrition education interventions (NEIs) have been carried out over the years to improve medical students’ nutrition education experiences, with results published in the literature, in order to promote effective nutrition care provision. However, there has been a scarcity of critical systematic reviews of the literature to help inform the design and development of these interventions on the competencies and dietary habits of medical students and residents. There have been three previous reviews of this phenomenon ( Reference Crowley, Ball and Hiddink 3 , Reference Mogre, Scherpbier and Stevens 6 , Reference Sunguya, Poudel and Mlunde 7 ) . Mogre et al. ( Reference Mogre, Scherpbier and Stevens 6 ) conducted a realist review of the literature to determine what types of educational interventions work, how, for whom, why and under what conditions to improve doctors’ and other healthcare professionals’ competencies and nutrition care delivery. Crowley et al. ( Reference Crowley, Ball and Hiddink 3 ) conducted a critical review of the literature in 2019 and reported on the types of nutrition education provided to medical students, but did not report on their impact on medical students’ and residents’ competencies. Sunguya et al. ( Reference Sunguya, Poudel and Mlunde 7 ) reported on the effectiveness of in-service nutrition training programmes on health workers’ nutrition knowledge, counselling skills and child undernutrition management practices. Although the review by Mogre et al. ( Reference Mogre, Scherpbier and Stevens 6 ) reported on the impact of NEIs on medical students’ competencies, it did not extensively evaluate the impact of NEIs on medical students’ own dietary habits, only included studies published until 2014, and has not been updated since. Crowley et al. ( Reference Crowley, Ball and Hiddink 3 ) conducted a review that included both interventional and non-interventional studies, as well as studies published up to 2018.
This scoping review aims to map current literature and provide a summary of the impact of NEIs on nutrition care competencies, self-efficacy and dietary habits of medical students and residents as a prelude to conducting a comprehensive systematic review and meta-analysis of the literature. This will provide information that both academics and practitioners may find useful.
The study followed the scoping review guidelines proposed by Arksey and O'Malley ( Reference Arksey and O'Malley 8 ) and the recommendations of Levac et al . ( Reference Levac, Colquhoun and O'Brien 9 ) . We used these guidelines to screen data from existing databases and then reported in accordance with the PRISMA extension for scoping review ( Reference Tricco, Lillie and Zarin 10 ) .
Eligibility criteria
Studies were chosen based on the following eligibility criteria.
Participants: Medical students and residents.
Outcomes: Eligible studies included those that reported on nutrition knowledge, attitudes towards nutrition care, self-efficacy, nutrition counselling skills, dietary and lifestyle practices, and readiness to provide nutrition care. Intervention studies aimed at changing the dietary and lifestyle habits of medical students and residents were also considered.
Study design: Randomised control trials, quasi-experimental studies and prospective studies.
Time frame: From January 2010 to June 2021. Only published studies were considered.
Language: Only English-language publications were considered.
Exclusion criteria
All systematic reviews and one-time studies were excluded. Interventions aimed at medical doctors or family physicians were also excluded from the study. Furthermore, commentaries, case studies, conference proceedings, non-peer-reviewed papers, opinion pieces, letters to the editor and abstracts were not accepted.
Information sources and search strategy
We searched four electronic databases, including PubMed, ProQuest, Cochrane and Google Scholar, to find relevant literature (for grey literature). From 28 May 2021 to 29 June 2021, the literature was searched, and email alerts were set up to notify of newly published articles. BYA developed the search strategy based on the study's main research question, which was then reviewed by VM. Keywords and databases pertinent to the study were identified by BYA, VM and a librarian. Appropriate MESH terms as well as free text of keywords were identified and used as needed. Keywords included ‘nutrition care’, ‘nutrition care competency’, ‘knowledge’, ‘attitudes’, ‘nutrition counselling’, ‘nutrition education’ and ‘medical students’ (undergraduate students or trainees or future doctors). The appropriate Boolean operators were used. The search strategy was developed first for PubMed and then applied to the other databases.
Selection of relevant studies
All search results were exported into EndNote X9 reference manager for de-duplication and selection. BYA and VM independently screened the titles and abstracts against the eligibility criteria. Full-text screening was used for articles with insufficient information in the title and abstract to justify their inclusion. BYA and VM discussed the results of the screening process with the rest of the review team, highlighting areas of disagreement that were resolved through discussion. The reference list of the selected articles was searched for additional relevant articles to include.
Data extraction/charting
We extracted data on population (i.e. medical students or interns or residents or student doctor or trainee doctor), sample size, study design, focus or objective of the study, educational level of participants, methods of teaching and learning, type of intervention (e.g. workshop, curriculum design), duration of intervention, outcome of intervention and study location. Components of the data extraction form was based on previous research ( Reference Mogre, Scherpbier and Stevens 6 , Reference Steinert, Mann and Centeno 11 ) . Each full text was reviewed using this format, and the data were extracted into an Excel spreadsheet. BYA extracted the data, and the results were discussed with VM and the other team members. We did not assess the methodological quality of the included studies because we were scoping the literature for a more comprehensive systematic review.
Data analysis and synthesis
The data were analysed in Microsoft Excel 2013. Descriptive analysis was performed and presented in the form of frequencies, percentages and narrative format. Furthermore, we classified the included studies based on the type of outcomes reported, NEI and study designs.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans for this study.
The four databases yielded 1807 articles. After de-duplication, there were 1787 articles left for screening. After removing 1750 studies based on title and abstract screening, the remaining 37 studies were subjected to full-text screening, with 23 articles found eligible and included in the analysis. The flowchart of the selection process is shown in Fig. 1 .
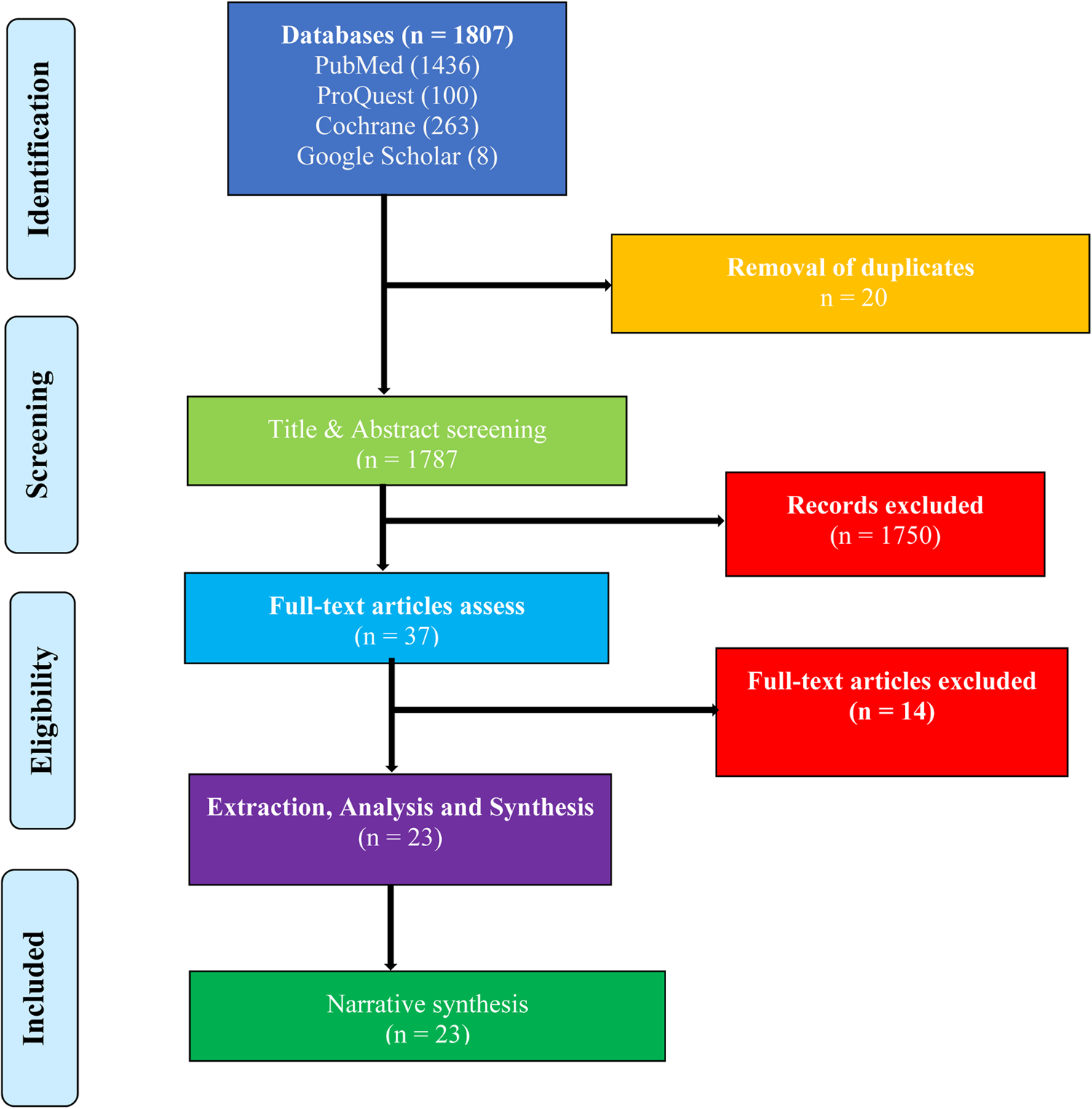
Fig. 1. A PRISMA flowchart of the study selection process.
Eighteen of the studies (78⋅3 %) were conducted in the United States of America (USA), while the remaining articles were conducted in the Netherlands, Indonesia, Iran, New Zealand and Portugal (shown in Table 1 ).
Table 1. Characteristics of the included studies ( n 23)
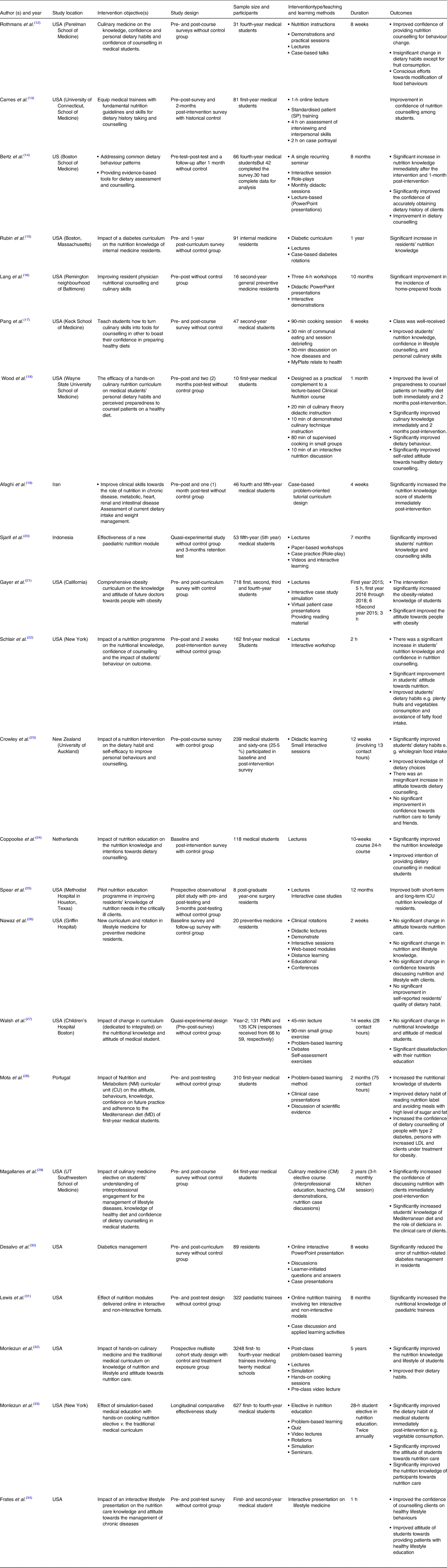
Table 2 summarises the study designs, methodological approaches and the format of intervention of the included studies. The articles used a variety of study designs, with the majority ( n 15, 65⋅2 %) using a quasi-experimental design. The included studies had a total sample size of 6621 participants (median = 81 participants; interquartile range (IQR): 25⋅5 and 252⋅5). The studies with integrated participation (a combination of preclinical and clinical year students) had the largest sample size (median = 718, IQR: 672⋅5 and 1983). Slightly more than three-quarters of the studies ( n 18, 78⋅3 %), used only survey questionnaires and a few studies ( n 5, 21⋅7 %) combined surveys and open-ended questions. The majority of the surveys ( n 14, 60⋅9 %) were conducted using validated questionnaires adapted from previous research. Eighteen (78⋅3 %) of the studies used a quantitative method, while the remaining ( n 5, 21⋅7 %) used mixed methods (quantitative and qualitative methods combined). Mixed method approaches were used in studies that reported on participants’ feedback about the intervention ( n 5, 21⋅7 %). The interventions were delivered through a variety of methods, including problem-based learning sessions, demonstrations, interactive case presentations, interactive case studies, interactive workshops, paper-based workshops, debates, hands-on experience self-assessment, visual patient presentation, culinary sessions, case-based presentations, video lecture and rotations in lifestyle medicine.
Table 2. Study designs, format of intervention and data collection methods
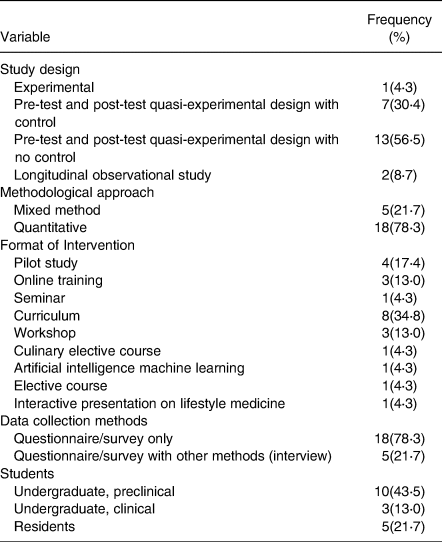
Nutrition-related knowledge
Almost all the studies ( n 21, 91⋅3 %) assessed changes in study participants’ nutrition-related knowledge ( Reference Rothman, Bilici and Mergler 12 , Reference Berz, Donovan and Eyllon 14 – Reference Mota, Castelo and Morais 28 , Reference Lewis, Frank and Nagel 31 – Reference Magallanes, Sen and Siler 35 ) . Eighteen of these studies (85⋅7 %) ( Reference Rothman, Bilici and Mergler 12 , Reference Berz, Donovan and Eyllon 14 – Reference Spear, Sim and Moore 25 , Reference Mota, Castelo and Morais 28 , Reference Lewis, Frank and Nagel 31 – Reference Monlezun, Leong and Joo 33 , Reference Magallanes, Sen and Siler 35 ) found a significant positive change in knowledge immediately following intervention. Three studies ( n 3, 14⋅3 %) reported no change in knowledge or improvement without specifying whether the change was statistically significant ( Reference Nawaz, Petraro and Via 26 , Reference Walsh, Ziniel and Delichatsios 27 , Reference Frates, Xiao and Simeon 34 ) . Nawaz et al. found a slight but insignificant increase in residents’ knowledge on various lifestyle components after following a lifestyle medicine curriculum that included didactics, distance learning, educational conferences and a newly developed lifestyle medicine rotation programme in a study of twenty preventive medicine residents ( Reference Nawaz, Petraro and Via 26 ) .
The qualitative feedback of study participants demonstrates that students learned about nutrition-related disorders, and how to encourage the adoption of healthy dietary practices ( Reference Rothman, Bilici and Mergler 12 ) . Except for four studies ( Reference Berz, Donovan and Eyllon 14 , Reference Wood, Gleit and Levine 18 , Reference Sjarif, Yuliarti and Wahyuni 20 , Reference Spear, Sim and Moore 25 ) , which had a two-time measurement and a follow-up (or third time measurement) assessment post-intervention, all the studies had two-time measurements (i.e. baseline and post-intervention). Two of these studies reportedly conducted a 3-month follow-up assessment ( Reference Sjarif, Yuliarti and Wahyuni 20 , Reference Spear, Sim and Moore 25 ) . One study each, included 1-month ( Reference Berz, Donovan and Eyllon 14 ) and 2-month ( Reference Wood, Gleit and Levine 18 ) post-intervention follow-up measurements. Except for one study, all the studies that had follow-up assessments reported a decrease in the mean knowledge scores of the participants at follow-up compared with immediately post-intervention but higher than the baseline score. For example, Wood et al. ( Reference Wood, Gleit and Levine 18 ) discovered that first-year medical students’ baseline mean knowledge score was 5⋅3 out of a possible 10⋅0 points, which increased significantly ( P = 0⋅001) to 8⋅8 points immediately following the intervention and declined to 6⋅9 points 2 months later ( Reference Wood, Gleit and Levine 18 ) . In addition, Berz et al. ( Reference Berz, Donovan and Eyllon 14 ) discovered a baseline score of 4⋅3 that significantly increased to 5⋅8 immediately post-intervention but declined to 5⋅2 at the 1-month follow-up assessment. In an observational prospective study, Spear et al. ( Reference Spear, Sim and Moore 25 ) implemented nutrition education among surgery residents, with mean knowledge scores increasing from 45 % at baseline to 82 % immediately post-intervention and declining by 65 % 3 months later. Sjarif et al. ( Reference Sjarif, Yuliarti and Wahyuni 20 ) found a knowledge score of 23⋅7 % at baseline that increased to 61⋅7 % post-intervention and 63 % at 3-months post-intervention using a quasi-experimental design.
Attitude towards nutrition care
Of the twenty-three studies, 47⋅8 % ( n 11) investigated changes in study participants’ attitudes. Four (36⋅4 %) studies ( Reference Gayer, Weiss and Clearfield 21 , Reference Schlair, Hanley and Gillespie 22 , Reference Monlezun, Dart and Vanbeber 32 , Reference Monlezun, Leong and Joo 33 ) reported a significant change in attitude after the intervention, while seven (63⋅6 %) studies ( Reference Lang, Jennings and Lam 16 , Reference Wood, Gleit and Levine 18 , Reference Coppoolse, Seidell and Dijkstra 24 , Reference Nawaz, Petraro and Via 26 – Reference Mota, Castelo and Morais 28 ) reported no significant change. Schlair et al. ( Reference Schlair, Hanley and Gillespie 22 ) observed medical students developing the attitude that patients are more likely to lose weight if they are counselled by physicians about weight and obesity management immediately following the intervention compared with baseline. Two studies found statistically significant increases in the odds of medical students reporting that nutrition counselling should be made a routine practice in medical care ( Reference Monlezun, Dart and Vanbeber 32 , Reference Monlezun, Leong and Joo 33 ) , as well as the belief that physician counselling could increase the odds of patients wanting to improve their diet ( Reference Monlezun, Leong and Joo 33 ) . A study conducted in the United States with 718 first- to fourth-year medical students discovered a significant reduction in their perception of obese people having low intelligence and sexual attractiveness after intervention when compared with baseline ( Reference Gayer, Weiss and Clearfield 21 ) . Another study found that after intervention, participants’ attitudes towards reading and understanding nutrition labels for healthy food choices improved ( Reference Mota, Castelo and Morais 28 ) . The seven studies that did not report a significant change in attitude post-intervention reported positive attitudes towards nutrition at baseline that were maintained post-intervention. Wood et al. ( Reference Wood, Gleit and Levine 18 ) discovered that at baseline, participants were both highly motivated (mean = 8⋅2 points) and excited (mean = 8⋅2 points) to counsel patients on healthy lifestyle choices, which was sustained post-intervention. Similarly, at the outset of three other studies ( Reference Coppoolse, Seidell and Dijkstra 24 , Reference Nawaz, Petraro and Via 26 , Reference Frates, Xiao and Simeon 34 ) , almost all students believed that talking to patients about healthy lifestyles was important, and some believed that nutritional counselling could lead to improved dietary behaviours.
Self-efficacy in nutrition care
More than half of the studies ( n 13, 56⋅5 %) examined study participants’ self-efficacy ( Reference Rothman, Bilici and Mergler 12 – Reference Berz, Donovan and Eyllon 14 , Reference Lang, Jennings and Lam 16 – Reference Wood, Gleit and Levine 18 , Reference Schlair, Hanley and Gillespie 22 – Reference Coppoolse, Seidell and Dijkstra 24 , Reference Nawaz, Petraro and Via 26 , Reference Mota, Castelo and Morais 28 , Reference Frates, Xiao and Simeon 34 , Reference Magallanes, Sen and Siler 35 ) . Immediately following the intervention, eleven of the included studies found a significant improvement in participants’ self-efficacy to provide nutrition care ( Reference Rothman, Bilici and Mergler 12 – Reference Berz, Donovan and Eyllon 14 , Reference Lang, Jennings and Lam 16 – Reference Wood, Gleit and Levine 18 , Reference Schlair, Hanley and Gillespie 22 , Reference Coppoolse, Seidell and Dijkstra 24 , Reference Mota, Castelo and Morais 28 , Reference Frates, Xiao and Simeon 34 , Reference Magallanes, Sen and Siler 35 ) . The aspects that were improved were increased efficacy in using the plate dietary method, making appropriate referrals, and confidence in providing dietary counselling in the treatment of people with obesity, elevated LDL-cholesterol and type 2 diabetes. Following a qualitative approach, Rothmans et al. reported that some of the students who participated in their intervention commented that, unlike before, they are now confident in their dietary care prowess and thus willing to provide nutrition care ( Reference Rothman, Bilici and Mergler 12 ) . In terms of follow-up assessments, Berz et al. reported a 1-month follow-up self-efficacy assessment, and while the score decreased from 4⋅1 to 3⋅9, it remained higher than the baseline score of 3⋅3.
The two studies that did not report significant improvements in self-efficacy either reported a significant decrease in participants’ confidence in providing nutrition care and health-related counselling to family/friends ( Reference Crowley, Ball and Leveritt 23 ) or reported a non-significant increase in confidence in discussing lifestyle issues with patients ( Reference Nawaz, Petraro and Via 26 ) . Crowley et al. explained that students’ confidence dropped as a result of the intervention's emphasis on the physiological aspects of nutrition rather than behaviour counselling ( Reference Crowley, Ball and Leveritt 23 ) .
Dietary and lifestyle habits of medical students and residents participating in NEIs
Nine (39⋅1 %) of the included studies ( Reference Rothman, Bilici and Mergler 12 , Reference Wood, Gleit and Levine 18 , Reference Schlair, Hanley and Gillespie 22 , Reference Crowley, Ball and Leveritt 23 , Reference Nawaz, Petraro and Via 26 , Reference Mota, Castelo and Morais 28 , Reference Monlezun, Dart and Vanbeber 32 , Reference Monlezun, Leong and Joo 33 , Reference Magallanes, Sen and Siler 35 ) ) looked at the impact of nutrition education on the dietary and lifestyle habits of medical students and residents. Except for one ( Reference Nawaz, Petraro and Via 26 ) , all of these studies ( n 8, 89 %) improved participants’ dietary habits post-intervention ( Reference Rothman, Bilici and Mergler 12 , Reference Wood, Gleit and Levine 18 , Reference Schlair, Hanley and Gillespie 22 , Reference Crowley, Ball and Leveritt 23 , Reference Mota, Castelo and Morais 28 , Reference Monlezun, Dart and Vanbeber 32 , Reference Monlezun, Leong and Joo 33 , Reference Magallanes, Sen and Siler 35 ) . Some of the improvements included increased fruit consumption, increased consumption of homemade food over restaurant and pre-prepared meals, avoidance of fatty foods, increased frequency of wholegrain food intake and decreased consumption of processed meat, avoiding the consumption of high sugar and fat foods, decreased odds of daily soft drink consumption and decreased odds of believing that healthy eating is expensive and time-consuming. The remaining study, Nawaz et al. , reported an insignificant change in the eating habits of their study participants with a statistically significant improvement in their ability to manage their own stress ( Reference Nawaz, Petraro and Via 26 ) .
Preparedness of medical students and residents to provide nutrition care
Three studies looked into how prepared participants were to provide nutrition care ( Reference Lang, Jennings and Lam 16 , Reference Wood, Gleit and Levine 18 , Reference Mota, Castelo and Morais 28 ) . In the study by Woods et al ., participants’ self-rated level of preparedness increased significantly both immediately post-intervention (coefficient = 2⋅8 points; 95 % CI 1⋅6, 4⋅0 points; P = 0⋅001) and 2 months later (M: 2⋅2, 95 % CI 1⋅0, 3⋅4, P = 0⋅002). Mota et al. investigated the proportion of medical students who believed they could provide dietary counselling as a preventive measure before and after taking a nutrition and metabolism course during a semester. The authors discovered that the percentage of students who agreed they felt capable of providing dietary counselling increased significantly from 31⋅6 % at baseline to 73⋅3 % immediately post-intervention ( Reference Mota, Castelo and Morais 28 ) . Lang et al. ( Reference Lang, Jennings and Lam 16 ) examined preventive medicine residents’ self-rated level of feeling as a competent cook and discovered that 50 % perceived themselves as competent cooks, which increased significantly to 67 % immediately post-intervention.
Participants’ assessments of NEIs
Bert et al. and Rothmans et al. reported in their evaluation of participants’ experiences with the interventions that participants identified the need for the intervention to be extended to all medical students, the nutrition education programme being their best experience over their 4 years of medical education, and rating of the programme as their most preferred course since coming to medical school ( Reference Rothman, Bilici and Mergler 12 , Reference Berz, Donovan and Eyllon 14 ) .
We conducted a scoping review of the literature and summarised the effects of NEIs on the nutrition-related knowledge, attitude, self-efficacy, dietary and lifestyle habits, and preparedness to provide nutrition care among medical students and residents. We examined twenty-three studies that reported various interventions to improve the nutrition education experiences of medical students and residents, with significant improvements in the outcome variables reported. NEIs, in particular, were effective in improving participants’ nutrition-related knowledge, attitudes and self-efficacy following intervention. Furthermore, as reported in a number of the included studies, the personal dietary and lifestyle habits of medical students and residents improved post-intervention. Finally, the NEIs improved medical students’ and residents’ readiness to provide effective nutrition care in the future. These findings show that by implementing appropriate NEIs, it is possible to address the problem of inadequate nutrition education in the medical curriculum.
The twenty-three included studies in this review demonstrate the growing recognition of the need to improve medical students’ nutrition education experiences. Furthermore, critical stakeholders such as medical educators and researchers are showing an interest in finding solutions to the long-standing issue of inadequate nutrition education in the medical curriculum. It is also worth noting that almost all the interventions were designed to improve important competency outcomes such as nutrition-related knowledge, self-efficacy and attitudes, and personal dietary habits, all of which are required competencies for medical students and residents to provide effective nutrition care.
Nutrition-related knowledge is an important component of providing effective nutrition care, but it is not the only factor or attribute required. It is thus commonplace to find that twenty-one of the included studies designed studies aimed at improving participants’ nutrition-related knowledge, with more than 70 % ( n 18) of those studies reporting significant improvements. This finding is consistent with the findings of the realist review reported by Mogre et al. ( Reference Mogre, Scherpbier and Stevens 6 ) , in which the majority of the included studies reported improvements in participants’ nutrition-related knowledge. Similarly, Sunguya et al. ( Reference Sunguya, Poudel and Mlunde 7 ) discovered in their systematic review that eighteen of the twenty-five included studies reported significant post-nutrition training improvements in health workers’ nutrition knowledge. Despite these gains in knowledge, it is important to note that increased nutrition knowledge alone is insufficient to promote effective nutrition care delivery. This is supported by the findings of Mogre et al. ( Reference Mogre, Scherpbier and Stevens 6 ) who found that interventions aimed solely at increasing knowledge were less likely to change nutrition practice behaviour.
Another significant finding of this scoping review was that the included studies demonstrated that medical students and residents had a positive attitude towards nutrition education and saw nutrition care as an important responsibility prior to intervention. The majority of the reviewed studies did not report significant changes in participants’ attitudes towards nutrition care because the authors of the included studies reported that the participants already had positive and favourable attitudes towards nutrition care at the baseline measurements. It is commendable that the NEIs maintained the participants’ positive attitudes, as this is an important determinant of doctors’ ability to provide effective nutrition care ( Reference Crowley, Ball and Hiddink 3 , Reference Mogre, Scherpbier and Stevens 6 ) .
Self-efficacy is an important predictor of nutrition care, so it is not surprising that some of the interventions were designed to improve participants’ nutrition self-efficacy. Previous reviews also discovered a substantial number of included studies that designed interventions to improve this phenomenon or conducting cross-sectional surveys to investigate this phenomenon ( Reference Crowley, Ball and Hiddink 3 , Reference Mogre, Scherpbier and Stevens 6 ) . Eleven of the thirteen studies that looked into this phenomenon found that participants’ nutrition self-efficacy improved significantly after the intervention. This is generally laudable, given that increased self-efficacy is likely to result in increased nutrition care provision. Mogre et al. ( Reference Mogre, Scherpbier and Stevens 6 ) reported in their realist review of identifying the mechanisms that demonstrate why some NEIs succeed in improving nutrition care practice that interventions were more likely to result in improving nutrition care practice if they reportedly improved the participants’ nutrition self-efficacy.
In a realist review, Mogre et al. ( Reference Mogre, Scherpbier and Stevens 6 ) discovered that doctors will feel more at ease and more likely to provide nutrition care if they themselves practice healthy dietary and lifestyle habits. Several studies included in this review also investigated this concept. Following this concept, nine of the included studies designed interventions to improve the participants’ personal dietary and lifestyle habits, with the majority of them reporting post-intervention improvements in this phenomenon. These findings highlight the importance of improving nutrition education, as it will not only improve the competencies of medical students and residents, but will also help them change their dietary habits, lowering their risk of developing non-communicable diseases.
We also discovered that studies with post-intervention follow-up assessments/measurements found a decrease in knowledge and self-efficacy. This finding is concerning because the majority of the interventions included in this scoping review were single required courses delivered as a one-time event primarily during the preclinical level (some as early as the first and second years of medical school) with no opportunity for reinforcement ( Reference Schlair, Hanley and Gillespie 22 ) . Even though these interventions reported significant changes of the outcomes, the sustainability of these acquired competencies till practice will be difficult in the absence of opportunities for reinforcement. Furthermore, as demonstrated in a previous review, the majority of these interventions focused on increasing participants’ knowledge, which does not always translate into practice ( Reference Mogre, Scherpbier and Stevens 6 ) . Nutrition self-efficacy and nutrition care expectations, as noted by Schlair et al . ( Reference Schlair, Hanley and Gillespie 22 ) may be difficult to address in the early preclinical years due to a lack of clinical exposure. Integration of nutrition content throughout the entire medical programme, with opportunities for clinical exposure and reinforcement, may be more effective and should be recommended.
Except for one, all the included studies used multiple teaching and learning strategies to achieve the interventions’ intended outcomes. This is consistent with the findings of the systematic reviews published by Mogre et al. ( Reference Mogre, Scherpbier and Stevens 6 ) and Sunguya ( Reference Sunguya, Poudel and Mlunde 7 ) . The use of multiple teaching and learning strategies is most likely informed by the fact that the studies had multiple outcomes that necessitated the use of various approaches. There is also evidence that interventions that used multiple approaches to meet participants’ educational needs were more likely to report significant changes ( Reference Mogre, Scherpbier and Stevens 6 ) . In the findings of a previous review ( Reference Mogre, Scherpbier and Stevens 6 ) , the use of multiple, non-traditional teaching and learning strategies was found to improve nutrition care competencies as well as nutrition practice behaviour ( Reference Mogre, Stevens and Aryee 4 ) . Simulated patient cases, group work, role-plays, hands-on demonstrations, group practice, panel discussions, case-based learning, problem-based learning tutorials, computer or web-based cases, student-led debates, self-assessment exercises, interactive lectures and clinical case presentations were some of the non-traditional approaches used in the included studies in this scoping review.
Culinary medicine is a new and innovative approach to nutrition education that has gained popularity in recent years. Six of the included studies used this teaching model, which resulted in significant improvements in students’ confidence in nutrition counselling, home meal preparation, nutrition-related knowledge, personal cooking skills and dietary behaviour ( Reference Rothman, Bilici and Mergler 12 , Reference Lang, Jennings and Lam 16 , Reference Wood, Gleit and Levine 18 ) . Its success may be due to its ability to provide hands-on, experiential learning opportunities that encourage active participation and strong interprofessional collaboration ( Reference Aspry, Van Horn and Carson 36 , Reference Crawford and Aspry 37 ) . Thus, culinary medicine adds to the toolbox of approaches that could be used to improve the nutrition education experience of medical students and residents.
The strength of this review lies in the use of a comprehensive and extensive search strategy to identify relevant nutrition education interventional studies to provide an evidence account of the impact of the interventions. Despite its strengths, there are some significant limitations to consider. The majority of the included studies provided a limited description of the processes of intervention implementation relating to the ‘what’, ‘why’ and ‘how’ outcomes of the interventions were achieved, making it difficult for successful interventions to be repeated and adopted in other contexts and settings. Furthermore, because we only included articles in English, articles in other languages that may contain very rich information relevant to the purpose of this study may be overlooked. Only a few of the studies included studies had follow-up surveys, which provided limited information about the long-term impact of nutrition education on participants’ competencies, dietary and lifestyle habits.
We found a diverse range of NEIs that used a variety of teaching and learning approaches, as well as a relatively large number of studies that could support a systematic review and meta-analysis, while taking into account the various designs and instruments, and advocating for nutrition education researchers to develop uniform instruments for assessing intervention outcomes. Despite this, the interventions showed promise in improving nutrition-related knowledge, self-efficacy, attitudes and preparedness to provide nutrition care among medical students and residents. The interventions also demonstrated their potential for improving the personal dietary and lifestyle habits of medical students and residents, which is required to potentially provide them with confidence to support individuals in adopting healthy dietary practices. Future NEIs should aim to follow-up with doctors beyond medical school, in order to assess how they use the acquired nutrition care competencies and skills in patient care to improve clinical outcomes.
Acknowledgements
The authors would like to thank the University Library for assisting them in locating relevant databases.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
B. Y. A. conceptualised and managed the project, collected, curated, analysed and visualised the data, and wrote the original and revised drafts. V. M. is the supervisor, who accepts full responsibility for the work and/or the study's conduct, has access to the data, and has final say on whether to publish. P. K. G. designed the project and reviewed the draft.
The authors declare no conflict of interest.
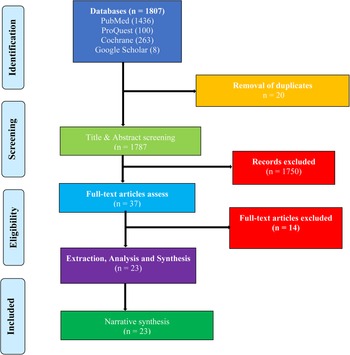
This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Victor Mogre (a1) , Bright Yammaha Amoore (a1) and Patience Kanyiri Gaa (a2)
- DOI: https://doi.org/10.1017/jns.2023.16
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
- Open access
- Published: 11 July 2017
Systematic review of control groups in nutrition education intervention research
- Carol Byrd-Bredbenner 1 ,
- FanFan Wu 1 ,
- Kim Spaccarotella 2 ,
- Virginia Quick ORCID: orcid.org/0000-0002-4338-963X 1 ,
- Jennifer Martin-Biggers 1 &
- Yingting Zhang 1
International Journal of Behavioral Nutrition and Physical Activity volume 14 , Article number: 91 ( 2017 ) Cite this article
11k Accesses
39 Citations
7 Altmetric
Metrics details
Well-designed research trials are critical for determining the efficacy and effectiveness of nutrition education interventions. To determine whether behavioral and/or cognition changes can be attributed to an intervention, the experimental design must include a control or comparison condition against which outcomes from the experimental group can be compared. Despite the impact different types of control groups can have on study outcomes, the treatment provided to participants in the control condition has received limited attention in the literature.
A systematic review of control groups in nutrition education interventions was conducted to better understand how control conditions are described in peer-reviewed journal articles compared with experimental conditions. To be included in the systematic review, articles had to be indexed in CINAHL, PubMed, PsycINFO, WoS, and/or ERIC and report primary research findings of controlled nutrition education intervention trials conducted in the United States with free-living consumer populations and published in English between January 2005 and December 2015. Key elements extracted during data collection included treatment provided to the experimental and control groups (e.g., overall intervention content, tailoring methods, delivery mode, format, duration, setting, and session descriptions, and procedures for standardizing, fidelity of implementation, and blinding); rationale for control group type selected; sample size and attrition; and theoretical foundation.
The search yielded 43 publications; about one-third of these had an inactive control condition, which is considered a weak study design. Nearly two-thirds of reviewed studies had an active control condition considered a stronger research design; however, many failed to report one or more key elements of the intervention, especially for the control condition. None of the experimental and control group treatments were sufficiently detailed to permit replication of the nutrition education interventions studied.
Conclusions
Findings advocate for improved intervention study design and more complete reporting of nutrition education interventions.
A major goal of nutrition education research is to elucidate factors that enable individuals to improve diet-related behaviors and/or cognitions associated with better health and greater longevity. These factors can then be incorporated in educational and health promotion interventions which, in turn, can be evaluated to determine whether the intervention effects change behaviors and/or cognitions among those assigned to the intervention vs. those in a control condition.
Well-designed research trials are critical for determining the efficacy and effectiveness of new interventions [ 1 ]. The basic components of educational research intervention trials include experimental variables, such as a novel curriculum; strong, measurable research questions or hypotheses; valid and reliable instruments for documenting change in behavior and/or cognitions; a strong data analysis plan; and an experimental design that minimizes threats to internal validity. To determine whether behavioral and/or cognition changes can be attributed to the intervention, the experimental design must include a control or comparison condition against which outcomes from the experimental group can be compared [ 2 , 3 , 4 , 5 ]. The randomized controlled trial (RCT) is typically considered the “gold standard” for ascertaining intervention efficacy and effectiveness [ 2 ].
Experts emphasize that to robustly minimize biases and variability of factors that may influence intervention trial outcomes, the control and experimental conditions must: 1) contain randomly assigned participants; 2) occur simultaneously to ensure both conditions experience the same history (i.e., external events, such as political change, natural disasters, scientific discoveries) and maturation (i.e., internal events, such as physical growth, memory decline with aging); 3) be structurally equivalent on as many non-specific factors as possible (i.e., factors other than the “active” ingredients in the experimental condition, such as participant time commitment, format and timeline of activities and data collection, and extent of attention and support from research staff) [ 5 ]; and 4) offer equal value, attractiveness, credibility, and outcome expectations to keep participants blind to their condition assignment and thereby avoid novelty effects, differential dropout rates, disappointment arising from assignment to the control group, and/or efforts by control group participants to seek an alternate source of the treatment offered to the experimental group [ 1 , 3 , 4 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 ]. The control condition also must not modify the intervention’s specific factors (i.e., behavior and/or cognitions targeted in the experimental condition) [ 4 , 7 ].
To reduce the risk of a Type 1 error (acceptance of an ineffective intervention) [ 1 , 9 , 17 ], treatment received by control condition participants should differ from those in the experimental condition only in the non-receipt of the “active ingredient” of the intervention hypothesized to affect study outcomes [ 4 , 6 ]. Rigorous control of non-specific factors, however, tends to increase intervention research costs because a plausible control intervention must be developed and implemented. Additionally, as the stringency of control exerted over non-specific factors increases, the risk of understating the effectiveness of the intervention rises because effect size is inversely associated with rigor of non-specific factor control [ 9 , 17 , 18 , 19 ]. Therefore, to demonstrate statistically meaningful differences, larger sample sizes are needed to avoid Type 2 errors (failure to recognize an intervention is effective) and detect treatment effects when the control and experimental group treatments are structurally equivalent than when a less equivalent control treatment is used [ 1 , 9 , 17 ].
A key challenge to nutrition education researchers is selecting a suitable treatment for the control condition that is congruent with the research question, study resources, availability of standard treatment/usual care, and ethical considerations [ 7 , 9 , 10 , 12 , 20 , 21 ]. Control condition participants may receive treatment ranging from nothing at all to extensive treatment in an alternate “active” control condition unrelated to the experimental condition. As indicated in Table 1 , the type of control condition selected can have important effects on study resources, participants, internal validity, and outcomes. For instance, resource investment in the treatment for the control condition can range from zero for the inactive control to considerable for active control. Ethical issues may be more highly problematic in inactive control conditions when participants in need of the intervention are denied treatment, but ethical issues are lessened when a standard or usual treatment can be offered. Preventing disappointed control group participants from seeking alternate sources of the treatment may not be possible, which weakens internal validity and undermines a true evaluation of the intervention’s effect. Even in active control conditions where participants receive a contemporaneous intervention equal to the treatment condition in all aspects, except the “active ingredient”, researchers may inadvertently treat control participants differently. Those delivering the intervention (e.g., research staff, educators) also may dislike being in the control condition [ 22 ] and seek opportunities to provide participants with treatment like that being given to the experimental group.
Clearly, the efficacy and “effectiveness of the experimental condition inherently depends as much on the control condition as on the experimental condition” [ 1 ],p.276. Despite the impact different types of control groups can have on study outcomes [ 23 ], the treatment provided to participants in the control condition has received limited attention in the literature [ 1 , 7 , 12 , 17 , 20 , 24 , 25 , 26 ] and sometimes is not even described in research designs [ 27 , 28 ]; yet in the words of Mohr et al. with regard to psychological interventions, “inappropriate control conditions can overestimate the effectiveness of a treatment, or kill off a potentially useful treatment” [ 1 ],p.283. Thus, a systematic review of control groups in nutrition education interventions was conducted with the goal of better understanding how control conditions are described in peer-reviewed primary outcomes journal articles in comparison with experimental conditions. An additional goal of this investigation is to open discussions among colleagues as to how best to improve reporting of control and experimental condition treatments in intervention evaluation studies to facilitate advancement of the field.
A systematic literature search was conducted after review of guidance from the Nutrition Education Systematic Review Project [ 29 ]. The study team then identified databases to use in the systematic review, search terms, and inclusion and exclusion criteria.
Search strategies
Search strategies were formulated according to the PRISMA guidelines [ 30 ]. Subject headings or search terms unique to each database were identified and searched in combination with keywords derived from the major concepts of “nutrition education intervention” and “control groups” or “study design”. Table 2 shows the final search strategy for the selected databases (i.e., CINAHL, PubMed, PsycINFO, WoS, and ERIC). Searches were conducted in winter 2016.
To be included in the systematic review, the articles had to report primary research findings of controlled nutrition education intervention trials from peer-reviewed journals. Included studies could address content other than nutrition, but nutrition had to be a key component. Additionally, included interventions had to focus on health promotion and disease prevention and have an education component. Inclusion criteria also required that interventions consist of more than one session and be conducted in the United States with free-living consumer populations. All included articles were published in English between January 2005 and December 2015. In cases where more than one article from the same study was located, only primary outcomes paper was included in the review to prevent over-representation of the type of control group used.
Excluded articles were studies reporting pilot, feasibility, cross-sectional, follow-up, or secondary analysis findings and those lacking a control or comparison group. Studies that focused on weight loss or disease management/treatment and those lacking an education component (e.g., those solely manipulating environmental factors) also were excluded. Additionally, all studies targeting professionals (e.g., health care, child care) or individuals recruited due to a pre-existing disease, such as diabetes, eating disorders, and obesity, or hospitalization, were excluded.
Data management
Citations for the 1164 articles returned by the systematic literature search were entered in a citation management tool (Fig. 1 ). After removal of duplicates ( n = 46) and publications that were not complete primary research articles (e.g., commentaries, viewpoints, editorials, letters, survey studies, abstracts, review articles, n = 50), two members of the study team independently conducted an initial screening of all article titles to identify those congruent with the study purpose. The title review yielded 195 articles that appeared to meet inclusion criteria. Next, article abstracts were independently reviewed by the same team members and 83 were identified as congruent with study purposes. Four team members scanned the articles and identified 53 articles meeting inclusion criteria. During data extraction, 10 additional articles were eliminated because they did not meet inclusion criteria thereby yielding a total of 43 reviewed articles.
Flow chart of literature search results for controlled research studies reporting (e.g., not secondary analysis or pilot, feasibility, or follow-up studies) results of nutrition education primary-prevention (e.g., not part of treatment for disease or weight loss) interventions consisting of more than one session conducted with free-living individuals in the United States
Data collection and analysis
After scrutinizing guidance from the Nutrition Education Systematic Review Project [ 29 ] and Cochrane Collaboration [ 31 , 32 ] as well as previously published systematic reviews [ 33 , 34 , 35 ], data extraction tables were designed by the study team. These tables were iteratively pilot-tested and refined.
Data were extracted by one team member and independently checked for accuracy by two other team members. As shown in Table 3 , the factors extracted included treatment provided to the experimental and control groups, overall intervention content, procedures used to tailor the intervention to participants, intervention delivery mode (e.g., group, individual), intervention format (e.g., curriculum, website, brochure) and duration, intervention setting, individual intervention session description (e.g., number of sessions or interactions, session duration, session frequency, content of each session, time allotment for each session component, overall duration of the intervention), procedures for standardizing intervention across multiple sites/practitioners, procedures for assessing fidelity of implementation across multiple sites, and procedures for blinding (masking) participants and/or intervention staff to participant group assignment, rationale for control group type selected, as well as sample size, attrition rate, and theoretical foundation. The goal of the factors extracted was to document the explicit presence or absence of each factor reported in the article. Additionally, only the 43 articles identified in the search were reviewed; extracting additional data from bibliographical references to previous developmental work cited in articles was beyond the scope of this study. A written narrative describing the treatment groups was prepared for each study. Extraction tables were content analyzed by team members to identify themes used to prepare a narrative synthesis of findings.
The treatment provided to the experimental and control conditions in the studies meeting the inclusion criteria are described in Table 4 . For accuracy, these descriptions used verbiage from the original research inasmuch as possible [ 36 ]. More than one-third of the 43 studies in the review had an inactive control condition; that is, the control group received no treatment or delayed-treatment (or wait-list). Because a key goal of this study was to compare how control and experimental conditions are described in peer-reviewed literature, results will focus on the 28 studies that had an active control condition. Of these studies, 7 had a usual or standard treatment for the control group, 12 offered an alternative active treatment to control participants, and 9 were dismantling (or additive) component active controls (2 of the 9 were mixed in that control groups received an alternative active treatment whereas the experimental groups received additive treatments).
Factors extracted in reviewed articles
Additional file 1 Table S5 compares the presence of factors extracted in the systematic review of articles. Each factor is described below, citing examples of studies demonstrating the factor
Description of overall intervention content
Reviewed articles commonly included a description of the overall intervention content provided. Content tended to focus on increasing fruit and/or vegetable intake, lowering fat intake, and healthy eating in general. The extensiveness of the overall content description for experimental groups ranged from only naming the general topic area (e.g., fruits and vegetables) [ 37 ] to listing topics and content addressed [ 38 , 39 ] to reporting content and participant activities [ 40 , 41 , 42 ] and teaching strategies [ 43 , 44 , 45 , 46 ].
Descriptions of the overall content for the control conditions tended to provide much less detail compared to experimental conditions. For example, among those employing usual or standard treatment, one study indicated only that “control classrooms did not receive vegetable-related instruction” [ 40 ],p.39 whereas another study reported that health education with no nutrition content was given [ 43 ], with neither indicating what control group participants received. Other descriptions of the control condition of usual treatment studies were equally vague indicating these participants received “traditional”, “regular”, or “normal” lessons [ 37 , 38 , 41 , 47 ]. Descriptions of treatment provided to the control groups in some alternative active treatment studies also were vague (e.g., control received pamphlet on fruits and vegetables [ 48 ], “packet of 5 printed commercially available booklets [ 49 ],” videos on sleep disorders [ 50 ]). However, several alternative active treatment investigations were more informative, including content similar in detail to the experimental group [ 46 , 49 , 51 , 52 , 53 ]. Dismantling studies tended to provide the greatest detail about the control condition largely because most experimental conditions were additive to the base formed by the control.
Description of how the intervention was tailored
Unless a goal of an investigation was to determine the effects of tailoring, little information on this factor was reported for experimental or control conditions regardless of whether a usual or other active control condition was used. In usual treatment control conditions, only one study mentioned tailoring for the experimental group [ 37 ]. A few alternative active treatment control condition studies tailored experimental and control treatments to demographic characteristics (e.g., older adult learners, African American women) [ 51 , 52 ]. Some investigations tailored treatments for experimental groups by allowing participants to choose topics or materials [ 45 , 49 ], with one study giving both experimental and control groups the ability to select topics [ 51 ]. The aim of most dismantling studies was to assess the effects of tailoring (experimental groups) vs not tailoring (control group); thus, tailoring descriptions for the control group generally were not applicable. On the other hand, the relative importance of the tailoring method to study aims made reasonably complete descriptions of this process requisite to report for experimental groups. Gans et al. reported [ 54 ] that tailoring was based on participant’s fat, fruit, and vegetable intake and related behaviors, self-identified needed behavior changes, personal motivators, barriers, and other psychosocial issues associated with healthy eating, needs, and interests. Resnicow et al.’s [ 53 ] report is notable in that these authors provided a table describing messages and graphic images used to tailor study newsletters.
Description of intervention delivery mode, material type used, duration, and setting
Across all types of control conditions, investigators consistently reported the intervention delivery mode, with the most common being group sessions or online. Descriptions for experimental conditions tended to express delivery mode in explicit terms whereas for control conditions, it was often left to the reader to decide on the mode using implicit clues. This was particularly the case when the control group received a “usual” treatment without further clarification [ 40 , 41 , 43 , 47 , 55 ].
The type of material that provided intervention content directed to participants tended to be printed (e.g., brochures, pamphlets, manuals, newsletters) and online (e.g., websites, videos). Interventions delivered by instructors to groups used mostly curricula and “lessons.” Some of the reviewed articles gave bibliographical references, internet links, or other means for obtaining intervention materials, with sources for instructional materials more commonly given for experimental than control groups [ 38 , 40 , 41 , 42 , 43 , 47 , 55 , 56 , 57 , 58 , 59 ]. An examination by control group type found that references for resources used to deliver usual treatment to control groups were not included. Among alternative active treatment studies, the material types used with both experimental and control groups had comparably detailed descriptions [ 39 , 42 , 51 , 60 ], with some exceptions where great detail about the materials used by the experimental group was provided while giving only limited descriptions of those intended for the control group [ 44 , 48 ]. Material type descriptions tended to be more even across dismantling studies.
Total duration of the intervention delivered to the experimental group was explicitly stated in nearly all studies reviewed. For control groups, total duration was less likely to be clearly described and frequently had to be deduced from a review of the study timeline (e.g., when the baseline and post-test was administered) and comparison to statements made about the experimental group. The setting where group sessions were delivered normally was overtly indicated (e.g., school, community center). Interventions directed to individuals who received mailed materials or used websites generally only implied the setting as being home or worksite [ 49 , 50 , 56 , 57 ] and did not report where participants generally used intervention materials.
Description of individual intervention sessions
Across all types of control groups, the number of sessions or interactions (e.g., newsletters) usually was explicitly stated for both treatment groups. The duration of individual sessions or length of materials was more commonly reported for experimental than usual treatment control groups; for other types of control groups, duration was somewhat more consistently reported for both treatment groups [ 48 , 61 ]. Reporting of frequency of sessions was fairly even across experimental and control groups in all types of control conditions except usual treatment, where this information was rarely included.
Reports of the content of individual sessions/interactions were provided in about half the active control articles reviewed with most descriptions being abbreviated for the experimental group and virtually non-existent for the control group. In a few cases, researchers provided a table or figure listing concepts/topics/objectives addressed in each session/interaction for the experimental group [ 40 , 41 , 54 , 61 , 62 ]. Only 2 studies provided a table describing the content of both the experimental and control treatments [ 46 , 49 ]. Descriptions of the duration of each main component of individual sessions/interactions were rare. The exceptions were Ratcliffe et al. [ 61 ] who stated “[e]ach hour-long session consisted of approximately 20 min of instruction followed by 40 min of hands-on garden experiences”p.38, Herbert et al. [ 38 ] who reported “Energize engages children in 1, 60-minute class once a week … by involving them in 15 minutes of nutrition education, a 10-minute warm-up … and 35 minutes of aerobic exercise activities and fitness games”p.781, and Pobocik et al. [ 41 ] who indicated “[a]pproximately 20 minutes of the 45-minute class were allotted to presenting information … remaining time … for testing, activities, and demonstrations”p.22. Comparable descriptions for control groups were not included.
Procedures for standardization across centers/practitioners
Procedures for standardizing the experimental condition intervention delivery across centers/practitioners took several forms, including training instructors [ 38 , 40 , 43 , 45 , 47 , 52 , 55 ] and utilizing pre-established curricula (instructional lessons and protocols) [ 38 , 40 , 41 , 43 , 47 , 55 ] and/or instructional materials (e.g., printed materials, videos, websites) [ 37 , 48 , 49 , 50 , 56 , 57 ]. Standardization procedures were similarly addressed across types of interventions for the experimental group. In contrast, little information related to standardization of implementation of control group treatments was provided for usual treatment control conditions. In alternative and dismantling active treatment studies, the procedures for standardizing control group treatment were frequently addressed and mostly took the form of pre-established instructional materials [ 39 , 49 , 50 , 52 , 53 , 54 , 56 , 57 , 59 , 63 , 64 , 65 ].
Procedures for assessing fidelity of implementation
Only about half of active control studies addressed fidelity of adherence to procedures, with most of these including information about procedures for both the experimental and control conditions. Methods used to establish fidelity of implementation for both experimental and control groups in active control studies where teachers or instructors delivered the treatment included detailed/scripted presentations [ 43 , 46 ], frequent meetings with researchers [ 38 , 46 , 47 ], random observation/videotaping of instructors [ 43 , 46 , 55 ], teaching/feedback logs [ 43 , 52 ], and audiotaping [ 57 ]. Methods used in active control group studies in which participants self-directed their engagement with pre-established treatments (e.g., web-based, printed materials) included completing forms documenting usage of treatment materials immediately after use [ 50 , 64 , 65 ], self-report posttest survey items that gauged extent of treatment use [ 53 , 58 ], and website tracking data [ 59 ].
The vast majority of active control studies provided little detail about fidelity procedures. One notable exception was McCaughtry et al. [ 43 ], who described fidelity procedures as including “very detailed (nearly scripted) lessons in the curriculum…a research assistant [who] conducted randomized school visits to observe each health education teacher’s instruction to guarantee that the control teachers were not teaching nutrition content and that the intervention teachers were implementing the curriculum with fidelity,”p.279. Another noteworthy example was provided by Wolf et al.: “Treatment fidelity checks were conducted on 200 (41%) of the intervention calls. Trained raters listened to audio recordings of the calls and completed a checklist documenting whether specific points were covered and whether the interventionist spoke at an appropriate pace, responded to questions with clear answers and probed at appropriate times” [ 57 ],p.34.
Procedures for blinding participants and researchers to treatment group assignment
Limited attention was given to the issue of blinding participants or researchers in the reviewed articles. In many cases, it was not clear whether participants were blinded (or aware there was a control vs experimental group), although this is a typical component of informed consent procedures. None of the studies providing the control group with usual treatment addressed participant blinding. Two articles blinded participants to group assignment by explaining that they were getting one of two programs or using alternate names for “control” or “experimental” groups. In specific, McCarthy et al. stated “A portion of the script used by project staff read … This is a cancer prevention study to compare two programs designed to help black women reduce their risk of cancer and improve their appearance. The first program involves 8 weekly 2-h sessions on diet and exercise. The second program involves 8 weekly 2-h sessions on current health topics of interest to black women, such as breast cancer and menopause. Both programs will be conducted by black women physicians and other professionals. We'll decide which group you'll be assigned to randomly, for example, by flipping a coin…” [ 51 ], p.247. In McClelland et al.’s crossover design study, these researchers assigned participants “to either the Apples Group (n=6) with the treatment curriculum … delivered first or the Beans Group (n=7) with the control curriculum … delivered first” [ 42 ], p.2. Another study reported that participant blinding efforts may not have worked. These researchers stated that “[g]irls, mothers, and troop leaders were masked to their group membership assignment;” but went on to say “because the project was called the Osteoporosis Prevention Project, some individuals in the control troops may have determined their status owing to the generic health focus of the sessions” [ 46 ],p.158.
The issue of blinding research staff likely is less important when interventions are automated and participant exposure to staff is minimal or non-existent. However, even when there was significant interaction with staff (e.g., in interventions delivering in-person or phone-based treatments), studies rarely addressed staff blinding. A few investigators reported using different instructors for experimental and control conditions [ 51 , 52 ], whereas others indicated that instructors were not blind to condition due to the nature of the intervention [ 46 , 55 , 57 ]. Blinding also would have been difficult in some of the dismantling studies where part of the treatment for only one of multiple experimental groups involved live interactions with staff [ 59 , 63 ]. In a few cases, articles reported that study evaluators were kept blind to participant study group assignment [ 57 , 58 , 64 ].
Rationale for selection of control group type
Reviewed studies seldom provided a rationale for the type of control group used and for those that did, various reasons were cited. These included convenience and comparability (e.g., “Three comparison [college] courses … were selected because they also were upper-level Human Biology courses, were delivered the same quarter, and were taught by experienced health promotion researchers and focused on a health message” [ 44 ], p.544) and relative strength (e.g., “Control group participants received fewer follow-up mailings … [that] resulted in a difference in “attention” between treatment arms, it is nonetheless a stronger design than a no-treatment control group” [ 60 ], p.62). Appropriateness to setting and participants also was considered (e.g., “Employees … were … assigned to the Web-based … or the print condition. It was recognized that the print materials could also be effective instruments of health behavior improvement (unlike a no-treatment control group) and could be a challenge as a control group … [and] would be a likely workplace alternative to an online program; therefore, the print group was thought to be an appropriate control group for the study” [ 49 ], p.e17). Yet, after finding both interventions yielded similar improvements, the article added to the control group rationale by stating… “[b]ecause it was originally thought that the print materials would form a relatively weak intervention compared to the Web program, a no-treatment control was not included in the design” [ 49 ],p.e17. Only 3 studies indicated the rationale for the control group was to control for non-specific effects (i.e.,“[t]he control group provided an intervention of identical intensity and program delivery format as the experimental group, ruling out “attention” effects in the experimental group” [ 52 ],p.386, “we used an attention control group to take into account the effect of participation” [ 65 ],p.37, and “[t]he purpose of this group was to control for any nonspecific effects from being educated about healthy lifestyles and from contact time and number of sessions … with professionals [ 46 ],p.158.”
Behavior change theory use
Nearly one-quarter of all reviewed studies did not indicate whether a theory was used to guide the intervention. Of those that indicated application of a behavior change theory, more than half used the social cognitive theory and about one-quarter used the transtheoretical model. Most studies named the theory used with little additional explanation of how it was operationalized. The most explicit reporting of theory application was by Pobocik et al. [ 41 ], who included a table listing social cognitive theory constructs, definition of the construct, and an example of how the construct was operationalized in the Do Dairy intervention. Of those reporting how theories were applied, several used the stage of change construct for tailoring materials [ 48 , 63 , 66 ] and/or selecting assessment scales [ 40 , 48 , 50 , 54 , 64 ]. Particularly illustrative of theory use in assessment were the tables Wall et al. [ 40 ] and Elder et al. [ 64 ] provided that listed theory constructs and corresponding evaluation items.
Comparison across control condition types
In the 7 investigations using a usual or standard active control condition, consisting of “traditional” or “regular” instruction, participants tended to be children enrolled in school or participants in government sponsored programs—perhaps because these systems have an ongoing program available for comparison. Articles gave fairly complete descriptions of the intervention provided to the experimental group, which were mostly curriculum based. They tended not to indicate if or how interventions were tailored and rarely provided information on the content of each session/interaction or how time was apportioned in each session, although this information may be available in the curricula referenced. With regard to the control group intervention, other than the overall intervention content, delivery (individual or group), and setting, little other information was provided. In most cases, too little information was provided about the usual treatment to determine whether the control group’s treatment was comparable on non-specific factors to that received by the experimental group [ 38 , 40 , 41 , 47 , 55 ]. Descriptions in one study, which compared differences in teaching strategies (e.g., traditional vs. tailored online) indicated fairly similar attention to non-specific factors [ 37 ].
In the 12 studies providing an alternative active treatment to the control group, investigators included a fairly even description of the treatments given to both experimental and control groups—a notable exception for both groups was a lack of specificity regarding the amount of time in each session devoted to the main components of the treatment. Additionally, many of the interventions were mail- or web-based and did not explicitly indicate the intervention setting. A comparison of the intensity of the treatments offered indicates that in some studies, the control group received “lighter” treatment doses than the experimental group (e.g., control group received a single pamphlet whereas the experimental group received tailored monthly magazines for 8 months [ 48 ], packet of printed booklets vs. highly interactive web-based program [ 49 ], manual vs manual coupled with coaching calls, tailored newsletters, and personalized feedback [ 56 ]). Many studies appeared comparable across a range of non-specific factors that could affect study outcomes [ 42 , 51 , 52 ]. One example of comparable treatment is Wolf et al. [ 57 ] who provided both experimental and control groups with a brochure (different topics) and tailored telephone education. Healy et al. [ 39 ] offers a second example in which both groups received a treatment that was the same length of time (7 50-min sessions over 1.5 weeks), used similar teaching strategies (i.e., lecture, discussion, question/answer, group activities), and differed only on content taught.
The 7 dismantling (additive) component active control studies tended to have 2 or more experimental groups. Interestingly, in all but one of these studies, the differences between the experimental and control treatments hinged on tailoring [ 61 ]. The control, or comparison, group in nearly all of these studies received less personalized and less intensive treatment than the experimental group [ 54 , 59 , 61 , 63 , 64 ]. In one study, for example, 3 groups of women either received non-tailored newsletters, tailored newsletters, or tailored newsletters and visits with lay health advisors [ 64 ]. Because of the derivative nature and increasing intensity of treatment provided by most dismantling studies [ 54 , 59 , 61 , 63 , 64 ], there was an imbalance in non-specific factors between/among study groups. The in-person and frequent phone contact received by one experimental group vs ongoing access to the project website and automated individual risk profiling given to a second experimental group vs printed materials provided one time to control participants demonstrated the imbalanced attention across study groups [ 59 ]. Among dismantling studies, the greatest balance in non-specific effects was achieved by Resnicow et al. [ 53 ] in that both experimental and control groups received the same newsletters except the tailoring of the experimental newsletters was more specific.
An additional two dismantling studies were classified as “mixed” [ 46 , 65 ] because the control participants received an alternate treatment that was not a derivative of the experimental group but was similar to treatment provided to control participants in alternative active treatment conditions. For instance, control condition participants in one study received 2 45-min web sessions on anatomy whereas those in the 2 experimental groups received 2 45-min web sessions on nutrition or 2 45-min web sessions plus a 45-min booster session [ 65 ]. The comparability of treatment provided to control groups in these 2 mixed dismantling active control studies tended to be more balanced on non-specific factors than the other 7 dismantling studies that did not have an alternative treatment.
Other findings
Reports of sample size and attrition were uneven. Some studies provided a complete description of total numbers recruited and retained, by treatment group, at each phase of the study [ 55 , 67 ], with several including CONSORT diagrams [ 48 , 53 , 54 , 55 , 57 , 58 , 59 , 63 , 65 , 66 , 68 , 69 ]. However, other studies only reported sample sizes at baseline [ 70 ], posttest [ 43 , 71 , 72 ], those completing both pretest and posttest [ 22 , 45 ], or sample sizes and/or attrition rates for both groups combined [ 41 , 73 ].
More than 3 out of 4 studies reviewed had random assignment of participants or intact groups (e.g., classrooms). Of the 10 non-randomized trials, half had no treatment control conditions. Of the remainder, one did not address randomization [ 41 ], one indicated the experimental group was comprised of students in classrooms with teachers who volunteered to participate [ 38 ], and another involving college students used intact classes and did not randomize the classes [ 44 ]. Two studies offered more explanation. One that was offered in WIC clinics indicated randomization was impractical and stated that “the practicality of being able to actually study comparisons of nutrition education intervention modalities in a typical clinic setting overcompensated for the lack in ability to develop a randomized design” [ 37 ],p.754. Authors of the second study offered this rationale, “The high cost and limited availability of randomized controlled trials in community settings highlight a need to evaluate and report on nonrandomized interventions that can be implemented in existing community settings” [ 45 ],p. 265.
Terminology used to describe control groups was not always consistent with definitions in Table 1 . For example, two papers referred to control groups who received usual instruction as no treatment controls [ 37 , 43 ]. Another provided an alternative active treatment, yet referred to it as a standard treatment [ 48 ]. Still another referred to the alternative active treatment control group as an attention placebo group [ 65 ]. A placebo should have no effect on a person, however because learning likely occurred in this and other alternate education-related control conditions, the term placebo does not accurately describe the control condition.
The goal of this study was to conduct a systematic review of control groups in nutrition education interventions and describe how control conditions are reported in peer-reviewed primary outcomes journal articles in comparison with experimental conditions. The findings of this systematic review indicate that the articles sampled focused on a wide array of controlled nutrition education intervention studies. Most addressed fruits and vegetables, fat intake, and healthy eating and tended to target school children as well as limited resource youth and families enrolled in government sponsored programs. Overall, descriptions of experimental conditions, regardless of type of active control condition, tended to be far more complete than descriptions of control conditions. Studies tended to report nearly all key factors (i.e., intervention content, delivery mode, material type, total duration, setting, individual session/interaction components [e.g.,, number, duration or length, frequency, content], standardization procedures, procedures for assessing fidelity of implementation, references for materials, theoretical underpinnings, and randomization) for the experimental condition. However, descriptions of the experimental group commonly lacked procedures for blinding and tailoring (except when the study was comparing differences in the effect of tailoring). In contrast, control conditions lacked descriptions of many key factors, with the most commonly omitted factors being individual sessions/interactions (e.g., number, duration, frequency, content of individual sessions), procedures for standardization, procedures for assessing implementation fidelity, blinding procedures, rationale for the type of control group selected, and references for instructional materials. Additionally, the factors that were reported for control conditions tended to be less explicit and included fewer details than provided for the experimental condition. In many cases, too little information was provided to determine the comparability of the control group vis-à-vis non-specific factors. Overall, the descriptions of both control and experimental group treatments became more complete as the type of active control became stronger and more complex; that is, alternative active treatments and dismantling studies provided the most detailed descriptions of the control group condition whereas usual or standard control conditions provided the least detail.
One-third of the 43 reviewed studies had inactive control conditions (i.e., no treatment or delayed treatment), a research design that is considered weak [ 7 , 17 ]. The Food and Drug Administration instructs that a no-treatment control be used only when investigation outcomes are entirely objective and cannot be biased by lack of blinding [ 74 ]—although this advice is directed at drug trials, it can be reasonably applied to education trials using inactive controls. For instance, in one delayed treatment study, researchers stated that a lack of blinding among those teaching the educational intervention was problematic (i.e., they “generally did not like to be randomized to the control condition [ 22 ],p.31”). Failure to implement procedures to prevent differential treatment, commitment, and engagement of both experimental and control condition instructors has the potential to confound results [ 75 ]. Likely many researchers conducting the 43 reviewed studies had implemented appropriate blinding procedures for participants, instructors, and researchers; however descriptions of procedures for blinding and/or prevention of differential treatment were not reported in most studies.
Active control conditions, considered a stronger research design than inactive [ 7 ], were used in two-thirds of the reviewed studies. In this and other studies [ 76 ], usual treatment was considered an active control whereas some researchers categorize usual treatment as inactive (or passive) because it typically is not structurally equivalent on non-specific factors to the experimental condition [ 6 , 7 , 24 , 32 , 76 ]. All usual treatment conditions in reviewed studies offered control groups traditional or regular instruction that did not include content offered to the experimental group. As Street and Luoma point out, it usually is not possible to equalize all non-specific factors (particularly credibility and outcome expectations) when using education about an unrelated topic as the usual treatment [ 6 ]. The limited information about the usual treatment given to control participants negated the possibility of confidently affirming equivalency of intensity and structure of control and experimental treatments.
A hallmark of evidence building is replicability. Similar to findings by researchers in other fields [ 12 , 26 ], none of the experimental and control group treatments were sufficiently detailed to permit replication of the nutrition education interventions studied. About half of the experimental treatment descriptions included a reference for the intervention materials and a third of the control treatment descriptions included this information; these materials may mitigate replication issues associated with missing information in the reviewed article. Another alternative is to contact authors to obtain intervention details. When Glasziou et al. contacted authors who published non-pharmacological medical treatment intervention outcomes, treatment descriptions improved significantly; however one-third of the studies they reviewed still had insufficient detail, in part because study authors did not respond despite repeated attempts or were unwilling to provide additional information [ 26 ].
Standardization and fidelity procedures are equally important for control and experimental conditions—without these procedures, either group may receive more or less than the research protocol intended which likely will confound outcomes [ 75 , 77 , 78 ]. The limited reporting of standardization procedures (e.g., use of manuals, standard operating procedures) and process evaluation activities in the reviewed studies, and noted by others in psychological therapy research [ 77 ], indicates that either reports are incomplete or these procedures were not implemented—neither of which are helpful when trying to weigh the value of the study outcomes and determine whether treatment groups received differential treatment from unblinded research staff.
Random assignment is considered critical to minimizing biases in trial outcomes and maximizing accuracy of analysis of intervention effects. One-quarter of the reviewed studies did not randomly assign participants, and likely suffered from at least some selection bias [ 79 ]. Compounding the lack of randomization is that many of these same studies did not address participant or researcher blinding and/or procedures for assessing intervention implementation fidelity, all of which impair internal validity [ 79 ].
Reporting sample size seems like a fairly straightforward task, regardless of how complex an intervention design may be. Indeed, CONSORT flow diagrams [ 80 ] make reporting changes in sample size at each stage of the study clear and easy to report. Yet, many of the studies reviewed lacked key sample size information, a phenomenon noted by others [ 81 , 82 ]. In some cases, sample size was not declared in tables reporting data [ 38 , 47 , 51 , 72 ].
It is interesting that so few articles provided a justification for the type of control condition used, especially given this is a conscious decision made during study planning. A systematic review of psychosocial interventions with substance use disorders also found studies gave little justification for control group choice or considerations for how this choice may have affected study outcomes [ 24 ].
The classic work of Campbell and Stanley identifies the Solomon 4 group design as offering the greatest internal and external validity checks [ 5 ]. This design includes these groups: experimental (pretest-intervention-posttest), no pretest experimental (intervention-posttest), control (pretest-posttest), no pretest control (posttest). Comparison of posttest scores across the 4 groups reveals whether changes are the result of the intervention and/or learning from the test [ 5 , 79 ]. None of the reviewed studies had non-pretested comparison groups. This lack of control for testing may have important implications; indeed researchers note that repeated measurements may encourage control condition participants to reflect on behaviors and initiate the behavior targeted in the experimental condition [ 83 , 84 ]. Another research group suggested that the research design for psychosocial treatments that most closely equates to a double-blind design is one that compares “two bona fide interventions … delivered by advocates for those interventions” [ 24 ],p. 426–427. In the reviewed studies, just one study met these criteria [ 57 ]. That is, Wolf et al. reported that immigrant men were given either a fruit/vegetable or prostate cancer prevention brochure [ 57 ]. Both groups received 2 tailored telephone education calls that could be considered to be delivered by an “advocate” because callers use a standardized telephone protocol and were audiotaped as a check for fidelity of delivery (however, no mention was made as to whether different callers were used for each treatment). Still another research group felt that to disentangle effects of the “active ingredient” from effects of non-specific factors, studies should include 3 groups: wait list control, attention control, and experimental group [ 85 ]. Many of the reviewed studies had 2 of these groups, but none had all 3.
Dismantling designs make it possible to separately account for the effects of each intervention component. However, the reviewed dismantling studies were mostly additive—that is, the treatment groups received increasingly intensive treatments thereby making it impossible to ascertain whether it was the greater dose of the additive treatment that contributed to changes or just the additional element [ 46 , 54 , 58 , 63 , 65 ]. For instance, one had a control group who received 12 weekly non-tailored newsletters by mail, an experimental group received 12 weekly tailored newsletters by mail, and another experimental group received the 12 weekly tailored newsletters plus weekly home visits from a promotora (lay health advisor/counselor) [ 64 ]. There was not a group who received only promotora visits, thus differentiating between intensity and independent effects of the promotora was not possible.
In the words of Montgomery et al., “[p]oor reporting limits the ability to replicate interventions, synthesise evidence in systematic reviews, and utilise findings for evidence-based policy and practice. The lack of guidance for reporting the specific methodological features of complex intervention RCTs contributes to poor reporting” [ 86 ],p.99. To improve reporting, the CONSORT extension underway for randomized controlled trials of social and psychological interventions may be appropriate and/or adaptable for health and nutrition education and promotion programs [ 86 ]. Methods for overcoming deficiencies in reporting design and execution of both control and experimental conditions reported by others may serve as models for reporting nutrition education interventions [ 7 , 87 ]. One research group has even suggested creating a repository of treatment descriptions, citing the Centers for Disease Control and Prevention’s Replicating Effective Programs ( https://www.cdc.gov/hiv/research/interventionresearch/rep/index.html ) as an example, and establishing a detailed checklist of characteristics to be included in intervention descriptions [ 26 ]. In fact, the supplementary table published by Greaves and colleagues is an excellent reporting method that ensures all salient elements are included [ 87 ]. Table 3 in this paper is another tool for ensuring key information is reported in nutrition education outcomes papers.
Strengths of this review lie in the large number of papers included and the extensive extraction of data contributing to this comprehensive description of control groups in nutrition education interventions and how they and experimental conditions are recounted in peer-reviewed journals. Additionally, it is the first study to explore control conditions in nutrition education and is among the first in any field to examine this critically important research intervention study design and reporting component [ 7 , 26 , 85 ]. This study is, however, limited to studies conducted in the United States. Furthermore, the studies reviewed likely included at least some of the extracted factors reported as missing in Additional file 1 : Table S5, but did not explicitly report them in the published paper. Also, no attempt was made to examine cited sources, which may supplement the information provided in the reviewed papers. Examination of the appropriateness of outcome measures, adequacy of sample sizes, and effect of control condition on study outcomes were beyond the scope of this review, but are important targets for future investigations.
Calls for more transparency and detail in reporting interventions have occurred sporadically since at least 1991, yet little has changed [ 77 , 88 ]. In this day and age of ever constricting research funding, coupled with the dire need for interventions that effectively improve nutritional status and associated outcomes, it is imperative that intervention research use more robust study designs that permit us to understand the effects of each component of the intervention [ 26 , 85 ]. Additionally, researchers and journal editors should assume the responsibility for ensuring that practitioners can easily access the details needed to implement effective interventions with fidelity. The key historic barrier to reporting this data in printed form has been overcome with electronic publishing [ 26 , 89 ]. Clearly there is a great deal of opportunity to improve intervention study design and reporting—seizing this opportunity can only help to advance the field and improve consumer health. A goal set at the outset of the investigation reported here is to open a dialogue among nutrition education researchers that leads to improved reporting of control and experimental condition treatments in intervention evaluation studies to promote advancement and impact of our work.
Mohr D, Spring B, Freedland K, Beckner V, Arean P, Hollon S, Ockene J, Kaplan R. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. 2009;78:275–84.
Article PubMed Google Scholar
Sullivan G. Getting off the "gold standard": randomized controlled trials and education research. J Grad Med Ed. 2011;3:285–9.
Article Google Scholar
Fogg L, Gross D. Threats to validity in randomized clinical trials. Research in Nursing & Health. 2000;23:79–87.
Article CAS Google Scholar
Beal CC, Stuifbergen A, Volker D, Becker H. Women's experiences as members of attention control and experimental intervention groups in a randomized controlled trial. Can J Nurs Res. 2009;41(4):16–31.
PubMed Google Scholar
Campbell D, Stanley J. Experimental and quasi-experimental designs for research. Chicago: Rand McNally College Publishing Company; 1963.
Google Scholar
Street L, Louma J. Control groups in psychosocial intervention research: ethical and methodological issues. Ethics & Behavior. 2002;12:1–30.
Lindquist R, Wyman J, Talley K, Findorff M, Gross C. Design of control-group conditions in clinical trials of behavioral interventions. J Nurs Scholarsh. 2007;39:214–21.
Avenell A, Grant AM, McGee M, McPherson G, Campbell MK, McGee MA. The effects of an open design on trial participant recruitment, compliance and retention--a randomized controlled trial comparison with a blinded, placebo-controlled design. Clin Trials. 2004;1(6):490–8.
Rethorst CD, Greer TL, Grannemann B, Ring KM, Marcus BH, Trivedi MH. A health education intervention as the control condition in the CTN-0037 STRIDE multi-site exercise trial: rationale and description. Ment Health Phys Act. 2014;7(1):37–41.
Schwartz C, Chesney M, Irvine M, Keefe F. The control group dilemma in clinical research: applications for psychosocial and behavioral medicine trials. Psychosom Med. 1997;59:362–71.
Article CAS PubMed Google Scholar
Solomon P, Cavanaugh M, Draine J. Randomized controlled trials: design and implementation for community-based psychosocial interventions. Oxford: Oxford University Press, Inc; 2009.
Book Google Scholar
Kinser P, Robins J. Control group design: enhancing rigor in research of mind-body therapies for depression. Evid BasedComplement Alternat Med. 2013;2013:140467.
Vickers A, de Craen A. Why use placebos in clinical trials? A narrative review of the methodological literature. J Clin Epidemiol. 2000;53:157–61.
Engel R, Schutt R. Fundamentals of social work research. 2nd ed. Thousand Oaks, CA: SAGE Publications; 2014.
Wiersma W. Research methods in education. 7th ed. Boston: Allyn and Bacon; 2000.
Petersen S, Zoffmann V, Kjaergaard J, Steensballe L, Greisen G. Disappointment and adherence among parents of newborns allocated to the control group: a qualitative study of a randomized clinical trial. Trials. 2014;15:126.
Freeland K. Demanding attention: reconsidering the role of attention control groups in behavioral intervention research. Psychosom Med. 2013;75:100–2.
Kazdin A, Bass D. Power to detect differences between alternative treatments in comparitive psychotherapy outcome research. J Consult Clin Psychol. 1989;57:138–47.
Freedland K, Mohr D, Davidson K, Schwartz J. Usual and unusual care: existing practice control groups in randomized controlled trials of behavioral interventions. Psychosom Med. 2011;73:323–35.
Article PubMed PubMed Central Google Scholar
Au D, Castro M, Krishnan J. Selection of controls in clinical trials. Proc Am Thorac Soc. 2007;4:567–9.
European Medicines Agency: ICH Topic E 10, Choice of control group in clinical trials; Step 5; Note for guidance on choice of control group in clinical trials (CPMP/ICH/364/96). In. London; 2001. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002925.pdf .
Townsend MS, Johns M, Shilts MK, Farfan-Ramirez L. Evaluation of a USDA nutrition education program for low-income youth. J Nutr Educ Behav. 2006;38(1):30–41.
Cuijpers P, Van Straten A, Warmerdam L, Smits N. Characteristics of effective psychological treatments of depression: a meta regression analysis. Psychother Res. 2009;18:225–36.
Karlsson P, Bergmark A. Compared with what? An analysis of control-group types in Cochrane and Campbell reviews of psychosocial treatment efficacy with substance abuse disorders. Addiction. 2014;110:420–8.
de Bruin M, Viechtbauer W, Hospers H, Schaalma H, Kok G. Standard care quality determines treatment outcomes in control groups of HAART-adherence intervention studies: implications for the interpretation of comparision of intervention effects. Health Psychol. 2009;28:668–74.
Glasziou P, Meats E, Heheghan C, Shepperd S. What is missing from descriptions of treatment in trials and reviews. BMJ Open. 2008;336:1472–4.
Glanz K, Sorensen G, Farmer A. The health impact of worksite nutrition and cholesterol intervention programs. Am J Health Promot. 1995;10:453–70.
Glaziou P. What is missing from descriptions of treatment in trials and reviews. BMJ Open. 2008;336:1472–4.
Nutrition education systematic review project: methodology. https://www.cnpp.usda.gov/nutrition-evidence-library-systematic-review-projects . Accessed 20 Sept 2015.
Moher D, Liberati A, Tetzlaff J, Altman D, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Armstrong R, Waters E, Jackson N, Oliver S, Popay J, Shepherd J, Petticrew M, Anderson L, Bailie R, Brunton G, et al. Guidelines for systematic reviews of health promotion and public health interventions, version 2. In. London: The Cochrane Collaboration; 2007.
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions, version 5.1.0. In. London: The Cochrane Collaboration; 2011.
Oldroyd J, Burns C, Lucas P, Haikerwal A, Waters E. The effectiveness of nutrition interventions on dietary outcomes by relative social disadvantage: a systematic review. J Epidemiol Comm Health. 2008;62(7):573–9.
Ajie WN, Chapman-Novakofski KM. Impact of computer-mediated, obesity-related nutrition education interventions for adolescents: a systematic review. J Adolesc Health. 2014;54(6):631–45.
Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, Johnson DB, Buchanan LR, Archer WR, Chattopadhyay S, Kalra GP, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med. 2009;37(4):340–57.
Glenton C, Underland V, Kho M, Pennick V, Oxman A. Summaries of findings, descriptions of interventions, and information about adverse effects would make reviews more informative. J Clin Epidemiol. 2006;59:770–8.
Bensley RJ, Anderson JV, Brusk JJ, Mercer N, Rivas J. Impact of internet vs traditional special supplemental nutrition program for women, infants, and children nutrition education on fruit and vegetable intake. J Am Diet Assoc. 2011;111(5):749–55.
Herbert PC, Lohrmann DK, Seo DC, Stright AD, Kolbe LJ. Effectiveness of the energize elementary school program to improve diet and exercise. J School Health. 2013;83(11):780–6.
Healy N, Joram E, Matvienko O, Woolf S, Knesting K. Impact of an intuitive eating education program on high school Students' eating attitudes. Health Educ. 2015;115:214–28.
Wall DE, Least C, Gromis J, Lohse B. Nutrition education intervention improves vegetable-related attitude, self-efficacy, preference, and knowledge of fourth-grade students. J School Health. 2012;82(1):37–43.
Pobocik RS, Haar CM, Dawson EE, Coleman P, Bakies K. Curriculum for junior high school students: dairy food consumption self-efficacy. J Fam Consumer Sci. 2009;101(4):20–6.
McClelland JW, Jayaratne KSU, Bird CL. Nutrition education brings behavior and knowledge change in limited-resource older adults. J Extension. 2013;51(2):Article 2FEA1.
McCaughtry N, Fahlman M, Martin JJ, Shen B. Influences of constructivist-oriented nutrition education on urban middle school Students' nutrition knowledge, self-efficacy, and behaviors. Am J Health Educ. 2011;42(5):276–85.
Hekler EB, Gardner CD, Robinson TN. Effects of a college course about food and society on students' eating behaviors. Am J Prev Med. 2010;38(5):543–7.
Devine CM, Farrell TJ, Hartman R. Sisters in health: experiential program emphasizing social interaction increases fruit and vegetable intake among low-income adults. J Nutr Educ Behav. 2005;37(5):265–70.
Ievers-Landis CE, Burant C, Drotar D, Morgan L, Trapl ES, Colabianchi N, Kwoh K. A randomized controlled trial for the primary prevention of osteoporosis among preadolescent girl scouts: 1-year outcomes of a behavioral program. J Pediatric Psychol. 2005;30(2):155–65.
Hopper CA, Munoz KD, Gruber MB, Nguyen KP. The effects of a family fitness program on the physical activity and nutrition behaviors of third-grade children. Res Q Exerc Sport. 2005;76(2):130–9.
Nitzke S, Kritsch K, Boeckner L, Greene G, Hoerr S, Horacek T, Kattelmann K, Lohse B, Oakland M, Phillips B, et al. A stage-tailored multi-model intervention increases fruit and vegetable intakes of low-income young adults. Am J Health Promot. 2007;22:6–14.
Cook RF, Billings DW, Hersch RK, Back AS, Hendrickson A. A field test of web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: randomized controlled trial. J Med Internet Res. 2007;9(2):1–14.
Clifford D, Anderson J, Auld G, Champ J. Good grubbin': impact of a TV cooking show for college students living off campus. J Nutr Educ Behav. 2009;41(3):194–200.
McCarthy WJ, Yancey AK, Harrison GG, Leslie J, Siegel JM. Fighting cancer with fitness: dietary outcomes of a randomized, controlled lifestyle change intervention in healthy African-american women. Prev Med. 2007;44(3):246–53.
Mitchell RE, Ash SL, McClelland JW. Nutrition education among low-income older adults: a randomized intervention trial in congregate nutrition sites. Health Educ Behav. 2006;33(3):374–92.
Resnicow K, Davis R, Zhang N, Tolsma D, Alexander G, Wiese C, Cross WE Jr, Anderson JP, Calvi J, Strecher V. Tailoring a fruit and vegetable intervention on ethnic identity: results of a randomized study. Health Psychol. 2009;28(4):394–403.
Gans K, Risica P, Dulin-Keita A, Mello J, Dawood M, Strolla L, Harel O. Innovative video tailoring for dietary change: final results of the good for you! Cluster randomized trial. Int J Behav Nutr Phys Act. 2015;12:130.
Dzewaltowski DA, Rosenkranz RR, Geller KS, Coleman KJ, Welk GJ, Hastmann TJ, Milliken GA. HOP'N after-school project: an obesity prevention randomized controlled trial. Int J Behav Nutr Phys Act. 2010;7:90.
Greene GW, Fey-Yensan N, Padula C, Rossi SR, Rossi JS, Clark PG. Change in fruit and vegetable intake over 24 months in older adults: results of the SENIOR project intervention. Gerontologist. 2008;48(3):378–87.
Wolf RL, Lepore SJ, Vandergrift JL, Basch CE, Yaroch AL. Tailored telephone education to promote awareness and adoption of fruit and vegetable recommendations among urban and mostly immigrant black men: a randomized controlled trial. Prev Med. 2009;48(1):32–8.
Gans KM, Risica PM, Strolla LO, Fournier L, Kirtania U, Upegui D, Zhao J, George T, Acharyya S. Effectiveness of different methods for delivering tailored nutrition education to low income, ethnically diverse adults. Int J Behav Nutr Phys Act. 2009;6:24.
Hughes SL, Seymour RB, Campbell RT, Shaw JW, Fabiyi C, Sokas R. Comparison of two health-promotion programs for older workers. Am J Public Health. 2011;101(5):883–90.
Glanz K, Hersey J, Cates S, Muth M, Creel D, Nicholls J, Fulgoni V, Zaripeh S. Effect of a nutrient rich foods consumer education program: results from the nutrition advice study. J Acad Nutr Diet. 2012;112:56–63.
Ratcliffe MM, Merrigan KA, Rogers BL, Goldberg JP. The effects of school garden experiences on middle school-aged students’ knowledge, attitudes, and behaviors associated with vegetable consumption. Health Promot Pract. 2011;12(1):36–43.
Dollahite JS, Pijai EI, Scott-Pierce M, Parker C, Trochim W. A randomized controlled trial of a community-based nutrition education program for low-income parents. J Nutr Educ Behav. 2014;46(2):102–9.
Alexander GL, McClure JB, Calvi JH, Divine GW, Stopponi MA, Rolnick SJ, Heimendinger J, Tolsma DD, Resnicow K, Campbell MK, et al. A randomized clinical trial evaluating online interventions to improve fruit and vegetable consumption. Am J Public Health. 2010;100(2):319–26.
Elder JP, Ayala GX, Slymen DJ, Arredondo EM, Campbell NR. Evaluating psychosocial and behavioral mechanisms of change in a tailored communication intervention. Health Educ Behav. 2009;36(2):366–80.
Franko DL, Cousineau TM, Trant M, Green TC, Rancourt D, Thompson D, Ainscough J, Mintz LB, Ciccazzo M. Motivation, self-efficacy, physical activity and nutrition in college students: randomized controlled trial of an internet-based education program. Prev Med. 2008;47(4):369–77.
Kattelmann KK, Byrd-Bredbenner C, White AA, Greene G, Hoerr S, Kidd T, Colby S, Horacek TM, Phillips BW, Koenings MM, et al. The effects of young adults eating and active for health (YEAH): a theory-based web-delivered intervention. J Nutr Educ Behav. 2014;46:S28–42.
Backman D, Scruggs V, Atiedu AA, Bowie S, Bye L, Dennis A, Hall M, Ossa A, Wertlieb S, Foerster SB. Using a toolbox of tailored educational lessons to improve fruit, vegetable, and physical activity behaviors among African american women in California. J Nutr Educ Behav. 2011;43(4):S75–85.
Wilcox S, Parrott A, Baruth M, Laken M, Condrasky M, Saunders R, Dowda M, Evans R, Addy C, Warren TY, et al. The faith, activity, and nutrition program: a randomized controlled trial in African-american churches. Am J Prev Med. 2013;44(2):122–31.
Alaimo K, Carlson J, Pfeiffer K, Eisenmann J, Paek H, Bets H, Thompson T, Wen Y, Norman G. Project FIT: a school, community and social marketing intervention improves healthy eating among low-income elementary school children. J Commun Health. 2015;40:815–26.
Katz DL, Katz CS, Treu JA, Reynolds J, Njike V, Walker J, Smith E, Michael J. Teaching healthful food choices to elementary school students and their parents: the nutrition detectives[TM] program. J School Health. 2011;81(1):21–8.
Powers AR, Struempler BJ, Guarino A, Parmer SM. Effects of a nutrition education program on the dietary behavior and nutrition knowledge of second-grade and third-grade students. J School Health. 2005;75(4):129.
Kemirembe OMK, Radhakrishna RB, Gurgevich E, Yoder EP, Ingram PD. An evaluation of nutrition education program for low-income youth. J Extension. 2011;49(3):3.
Bogart LM, Cowgill BO, Elliott MN, Klein DJ, Hawes-Dawson J, Uyeda K, Elijah J, Binkle DG, Schuster MA. A randomized controlled trial of students for nutrition and eXercise: a community-based participatory research study. J Adolesc Health. 2014;55(3):415–22.
United States Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research: Guidance for Industry. E 10 choice of control group and related issues in clinical trials. In. Washington, DC; 2001. https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm073139.pdf .
Castongay L. Controlling is not enough: the importance of measuring the process and specific effectiveness of psychotherapy treatment and control conditions. Ethics Behav. 2002;12:31–42.
Ferri M, Amato L, Davoli M. Alcoholics anonymous and other 12-step programmes for alcohol dependence. Cochrane Database Syst Rev. 2006;3:CD005032.
Moncher F, Prinz R. Treatment fidelity in outcome studies. Clin Psychol Rev. 1991;11:247–66.
Gearing R, El-Bassel N, Ghesquiere A, Baldwin S, Gillies J, Ngeow E. Major ingredients of fidelity: a review and scientific guide to improving quality of intervention research implemention. Clin Psychol Rev. 2011;31:79–88.
Schutt R. Investigating the social world. The process and practices of research. 7th ed. Thousand Oaks, CA: Sage Publications, Inc; 2012.
CONSORT Transparent Reporting of Trials, CONSORT 2010 Flow Diagram http://www.consort-statement.org/consort-statement/flow-diagram . Accessed 20 Augt 2015.
Mikkelsen M, Husby S, Skov L, Perez-Cueto J. A systematic review of types of health eating interventions in preschools. Nutr J. 2014;13:56.
Bond M, Wyatt K, Lloyd J, Welch K, Taylor R. Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report. Health Technol Assessment. 2009;13(61):1–75.
Waters L, Reeves M, Fjeldsoe B, Eakin E. Control group improvements in physical activity intervetnion trials and possible explanatory factors: a systematic review. J Phys Act Health. 2012;9:884–95.
van Sluijs E, van Poppel M, Twisk J, van Mechelen W. Physical activity measurements affected participants' behavior in a randomized controlled trial. J Clin Epidemiol. 2006;59:404–11.
Jensen P, Weersing R, Hoagwood K, Goldman E. What is the evidence for evidence-based treatments? A hard look at our soft underbelly. Ment Health Serv Res. 2005;7:53–74.
Montgomery P, Grant S, Hopewell S, Macdonald G, Moher D, Michie S, Mayo-Wilson E. Protocol for CONSORT-SPI: an extension for social and psychological interventions. Implementation Sci. 2013;8:99.
Greaves C, Gillison F, Stathi A, Bennett P, Reddy P, Dunbar J, Perry R, Messom D, Chandler R, Francis M, et al. Waste the waist: a pilot randomized controlled trial of a primary care based interventino to support lifestyle change in people with igh cardiovascular disease. Int J Behav Nutr Phys Act. 2015;12:1.
Mayo-Wilson E. Reporting implementation in randomized trials.: proposed additions to the consolidated standars of reporting trials statement. Am J Public Health. 2007;97:630–3.
Chalmers I, Altman D. How can medical journals help prevent poor medical research? Some opportunities presented by electronic publishing. Lancet. 1999;353:490–3.
Arean P, Alvidrez J. Ethical considerations in psychotherapy effectiveness research: choosing the comparison group. Ethics Behav. 2002;12:63–73.
Pagoto SL, McDermott M, Reed G, Greenland P, Mazor K, Ockene J, Whited M, Schneider K, Appelhans B, Leung K, et al. Can attention control conditions have detrimental effects in behavioral medicine randomized trials? Psychosom Med. 2013;75:137–43.
Waters E, de Silva-Sanigorski A, Burford B, Brown T, Cambell K, Gao Y, Armstrong R, Prosser L, Summerbell C. Interventions for preventing obesity in children. Cochrane Database Syst Reviews. 2011;12:CD001871.
Parshuram C, Kavanaugh B. Positive clinical trails. Understand the control group before implementing the result. Am J Respir Crit Care Med. 2004;170:223–6.
Boutron I, Moher D, Altman D, Schulz K, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2006;146:295–309.
Tolsgaard M, Ku C, Woods N, Kulasegaram K, Brydges R, Ringsted C. Quality of randomised controlled trials in medical education between 2012 and 2013: a systematic review. BMJ Open. 2014;4:e005155.
Keihner AJ, Meigs R, Sugerman S, Backman D, Garbolino T, Mitchell P. The power play! Campaign's School Idea & Resource Kits improve determinants of fruit and vegetable intake and physical activity among fourth- and fifth-grade children. J Nutr Educ Behav. 2011;43(4 Suppl 2):S122–9.
Roofe NL. Improving Families' nutrition knowledge through service learning. J Allied Health. 2011;40(4):194–8.
McCarthy E, Wolff C, Bianco-Simeral S, Crozier J, Goto K. The effects of a school-based nutrition intervention on fruit and vegetable preferences, self-efficacy, and consumption among low-income, Hispanic and white middle-school students. J Child Nutr Manage. 2012;36(2):2.
Eicher-Miller HA, Mason AC, Abbott AR, McCabe GP, Boushey CJ. The effect of food stamp nutrition education on the food insecurity of low-income women participants. J Nutr Educ Behav. 2009;41(3):161–8.
Madsen K, Linchey J, Gerstein D, Ross M, Myers E, Brown K, Crawford P. Energy balance 4 kids with play: results from a two-year cluster-randomized trial. Child Obes. 2015;11:375–83.
Download references
Acknowledgements
Not applicable.
This study is funded by the United States Department of Agriculture, National Institute of Food and Agriculture, Grant Number 2011–68001–30,170.
Availability of data and materials
Author information, authors and affiliations.
Rutgers, The State University of New Jersey, 26 Nichol Avenue, New Brunswick, NJ, 08901, USA
Carol Byrd-Bredbenner, FanFan Wu, Virginia Quick, Jennifer Martin-Biggers & Yingting Zhang
Kean University, 1000 Morris Ave, Union, NJ, 07083, USA
Kim Spaccarotella
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in the study design and contributed to the development and implementation of the study. CBB, FW, KS, VQ, JMB conducted the analysis and interpretation of the data. All authors were involved in drafting manuscript components and contributed to editing and reviewing the final manuscript. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Virginia Quick .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: table s5..
Factors extracted in systematic review of articles. (DOCX 37 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Byrd-Bredbenner, C., Wu, F., Spaccarotella, K. et al. Systematic review of control groups in nutrition education intervention research. Int J Behav Nutr Phys Act 14 , 91 (2017). https://doi.org/10.1186/s12966-017-0546-3
Download citation
Received : 13 December 2016
Accepted : 03 July 2017
Published : 11 July 2017
DOI : https://doi.org/10.1186/s12966-017-0546-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Research design
- Control group
- Experimental group
- Systematic review
- Nutrition education
International Journal of Behavioral Nutrition and Physical Activity
ISSN: 1479-5868
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.10(6); 2019 Nov
Advancing Nutrition Education, Training, and Research for Medical Students, Residents, Fellows, Attending Physicians, and Other Clinicians: Building Competencies and Interdisciplinary Coordination
Linda van horn.
1 Department of Preventive Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
Carine M Lenders
2 Department of Pediatrics, Boston University School of Medicine, Boston, MA, USA
Charlotte A Pratt
3 Division of Cardiovascular Sciences, National Institutes of Health, National Heart, Lung, and Blood Institute, Bethesda, MD, USA
Bettina Beech
4 Department of Population Health Science, University of Mississippi Medical Center, Jackson, MS, USA
Patricia A Carney
5 Department of Family Medicine; of Public Health, Oregon Health & Science University, Portland, OR, USA
William Dietz
6 Redstone Global Center for Prevention and Wellness, Milken Institute School of Public Health, George Washington University, Washington, DC, USA
Rose DiMaria-Ghalili
7 College of Nursing and Health Professions, Drexel University, Philadelphia, PA, USA
Timothy Harlan
8 Department of Medicine, Tulane University School of Medicine, New Orleans, LA, USA
Robert Hash
9 American Medical Association, Chicago, IL, USA
Martin Kohlmeier
10 Department of Nutrition, University of North Carolina-Chapel Hill, Chapel Hill, NC, USA
Kathryn Kolasa
11 Department of Family Medicine; of Pediatrics, Brody School of Medicine at East Carolina University, Greenville, NC, USA
Nancy F Krebs
12 Department of Pediatrics, University of Colorado School of Medicine, Aurora, CO, USA
Robert F Kushner
13 Department of Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
Mary Lieh-Lai
14 Accreditation Council for Graduate Medical Education, Chicago, IL, USA
Janet Lindsley
15 Department of Biochemistry, University of Utah School of Medicine, Salt Lake City, UT, USA
Susan Meacham
Holly nicastro, caryl nowson.
17 Department of Nutrition and Ageing, Institute for Physical Activity and Nutrition, School of Exercise and Nutrition Sciences, Deakin University, Geelong, Victoria, Australia

Carole Palmer
18 Division of Nutrition & Oral Health, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA
Miguel Paniagua
19 Test Materials Development, National Board of Medical Examiners, Philadelphia, PA, USA
Edward Philips
20 Department of Physical Medicine and Rehabilitation, Harvard Medical School, Boston, MA, USA
Sumantra Ray
21 Global Center for Nutrition and Health, University of Cambridge, Cambridge, United Kingdom
Suzanne Rose
22 Department of Medicine, School of Health, University of Connecticut, Farmington, CT, USA
Marcel Salive
23 Division of Geriatrics & Clinical Gerontology, National Institutes of Health, National Institute on Aging, Bethesda, MD, USA
Marsha Schofield
24 Nutrition Services Coverage, Academy of Nutrition and Dietetics, Chicago, IL, USA
Kathryn Thompson
25 Department of Biomedical Sciences, College of Osteopathic Medicine, University of New England, Biddeford, ME, USA
Jennifer L Trilk
26 Department of Biomedical Sciences, University of South Carolina School of Medicine, Greenville, SC, USA
Gwen Twillman
27 Department of Education & Development, American Society for Nutrition, Rockville, MD, USA
Jeffrey D White
28 Division of Cancer Treatment and Diagnosis, National Institutes of Health, National Cancer Institute, Bethesda, MD, USA
Giovanna Zappalà
29 Division of Geriatrics and Clinical Gerontology and Head of the Office of Nutrition, National Institutes of Health, National Institute on Aging, Bethesda, MD, USA
Ashley Vargas
30 Office of Disease Prevention, National Institutes of Health, Rockville, MD, USA
Christopher Lynch
31 Office of Nutrition Research, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, USA
Nutrition plays an important role in health promotion and disease prevention and treatment across the lifespan. Physicians and other healthcare professionals are expected to counsel patients about nutrition, but recent surveys report minimal to no improvements in medical nutrition education in US medical schools. A workshop sponsored by the National Heart, Lung, and Blood Institute addressed this gap in knowledge by convening experts in clinical and academic health professional schools. Representatives from the National Board of Medical Examiners, the Accreditation Council for Graduate Medical Education, the Liaison Committee on Medical Education, and the American Society for Nutrition provided relevant presentations. Reported is an overview of lessons learned from nutrition education efforts in medical schools and health professional schools including interprofessional domains and competency-based nutrition education. Proposed is a framework for coordinating activities of various entities using a public–private partnership platform. Recommendations for nutrition research and accreditation are provided.
Introduction
Nutrition and dietary behaviors are major contributors to the development and management of chronic diseases including obesity, cardiometabolic disease, and cancer, but healthcare providers remain inadequately trained to initiate or effect patient change ( 1–3 ). Adherence to recommended eating patterns can reduce risk and extend quality of life, but consistent and coordinated approaches to assuring the education, training, and competency of healthcare providers remain inconsistent ( 4 , 5 ).
Physicians are on the frontlines of patient care. Their combined diagnostic and patient counseling skills are vital in initiating and sustaining ongoing follow-up and facilitating patient adherence to prevention and treatment strategies. Health professionals including dietitians and nutritionists, nurse practitioners (NPs), physician assistants (PAs), pharmacists, dentists, and others also play an important role in integrating nutrition and diet interventions in a coordinated interprofessional practice model that can be applied to benefit patients throughout the healthcare spectrum.
To address these topics, the National Heart, Lung, and Blood Institute (NHLBI) of the NIH convened a workshop on the 7–8 September, 2017, that included an interdisciplinary team of over 50 clinicians and educators with expertise in medical nutrition, NIH representatives from other nutrition-related institutes, locally interested graduate and undergraduate medical students, and other healthcare professionals with expertise in academic medicine. This effort followed a 2012 NHLBI workshop that reviewed the contributions of the Nutrition Academic Award (NAA), an initiative conducted among 21 medical schools from 1998 to 2005. Curricular objectives, teaching tools, assessment methodologies, and examination questions for the National Board of Medical Examiners (NBME) were developed through the NAA ( 1 , 2 ). These accomplishments provided a good start; however, the absence of ongoing infrastructural support limited sustainability and advancements in subsequent years. Manuscripts endorsing the premise and goals of the NAA motivated renewed efforts to proceed with next steps ( 3–7 ).
The latest workshop was organized to advance the 2012 workshop goals and identify research gaps and other factors limiting progress towards successful implementation of medical nutrition education. There was further intent to formulate a framework for optimal adaptation of the NAA curriculum guide within the shifting model of education in physician training. Experts in nutrition, metabolism, and lifestyle medicine shared perspectives, deliberated on existing nutrition programs, and considered new culinary medicine interests and emerging priorities. High priorities included updating the curriculum guide, formalizing new and evolving topic areas, developing realistic models for implementing clinical nutrition care, and evaluating competencies and skills. Broader understanding of important integrative educational components and potential strategies to move a multidimensional integrated plan forward were achieved.
This paper summarizes the discussions, case studies, and the coordinated integrated effort needed to achieve workshop goals. The overall goal is to equip trainees with improved nutrition assessment and counseling skills, competencies to make referrals to appropriate providers, and increased awareness of available resources needed to optimize patient care. Research needed to compare outcomes and inform future interprofessional education and training is also summarized.
The Evolving Model of Medical Nutrition Education Then and Now: Historical Perspectives and Lessons Learned
In 1985, based on results of a survey of 45 US medical schools, the National Academy of Sciences recommended at least 25 h of nutrition education in undergraduate medical education (UME) ( 8 ). The American Society for Clinical Nutrition's [ASCN; renamed as the American Society for Nutrition (ASN)] Committee on Medical/Dental School and Residency Nutrition Education recommended a minimum of 44 h ( 9 ). Consensus on nutrition content in the medical school curriculum remains an ongoing challenge, particularly because of integrated curricula and how hours are counted, more online learning and use of class time for problem solving and discussion ( 4 ). In residency and fellowship programs, little medical nutrition education is provided. During the 1980s, the Nutrition in Medicine (NIM) program, a web-based interactive medical nutrition education teaching tool with case studies, was developed at the University of North Carolina, Chapel Hill, and offered free of charge to all US medical schools ( 10 ). In 1983, a prototype of a National Nutrition Test Item Bank was developed at the University of Alabama Birmingham in conjunction with the ASCN Committee on Nutrition Education and was deemed viable to address student assessment. Since then, several websites for health professionals have offered links to educational materials including lectures, modules, interactive videos, blogs, and books related to medical nutrition. In addition to nutrition-related societies such as the Academy of Nutrition and Dietetics, ASN, the American Association for Parenteral and Enteral Nutrition (ASPEN), the North American Society for Pediatric Gastroenterology, and The Obesity Society, other societies and institutions such as the American Academy of Pediatrics, the American Academy of Family Physicians, and the American Association of Medical Colleges (AAMC) provide access to peer-reviewed material.
Over the course of the NAA (1998–2005), the 21 funded medical schools developed educational efforts focused on advancing the diet-related guidelines of the National Cholesterol Education Program organized and developed by the NHLBI ( 2 ). The NAA schools adopted a variety of approaches ( 11 , 12 ) and different educational priorities. Common goals included: 1 ) Establish clear nutrition objectives; 2 ) Collaborate with the NBME, the AAMC, and the Accreditation Council for Graduate Medical Education (ACGME); 3 ) Identify how objectives would be nationally standardized and evaluated; and 4 ) Establish a Coordinating Center to help implement and sustain medical nutrition education.
Evolving models of education and training require a national approach to integrating nutrition across the curriculum supported by teaching faculty and medical school leadership. Pedagogies now emphasize active learning models focused on competencies such as culinary exercises, small group interactions, and hands-on community involvement. In 2006, Boston University School of Medicine (BUSM) created a novel model of medical nutrition education involving students and including student-mentored extracurricular activities to develop, evaluate, and sustain nutrition medicine education ( 13 , 14 ). Teaching hours in nutrition increased by >5-fold at BUSM, with >108 h of nutrition-related content in the curriculum in 2017–2018. Subsequently, >80% of the NAA curriculum guide was covered across 4 y of UME. Using a medical education database required for full accreditation surveys reviewed by the Liaison Committee on Medical Education (LCME), nutrition was identified in the top 5 out of 32 behavioral and socioeconomic subjects included in required courses at BUSM ( 13 ). Subscores on the United States Medical Licensing Examination (USMLE) steps I and II improved. Finally, a cross-sectional electronic survey of first-year to fourth-year medical students including 6 knowledge and 4 self-efficacy nutrition questions showed that students desired more training in counseling and referrals to other healthcare professionals and community resources. Several groups of interested medical students are now involved in extracurricular and curricular nutrition efforts in other universities, including Columbia University, University of North Carolina, Harvard University, Northwestern University, and Tufts University.
Since the 2012 NIH workshop, several professional societies reviewed program practices and provided recommendations. In 2013–2014, 2 bills advocating nutrition education of physicians were introduced into the US Congress ( 15 , 16 ). Legislative progress is limited but interest in culinary medicine, applied nutrition training, competency, and skill development has increased. Several societies and groups approached the LCME to update nutrition questions in the exams, and nutrition champions or advocates have recommended a national medical board for obesity and physician nutrition specialists ( 4 , 17 , 18 ). Needs for interprofessional education to be a component of medical education ( 18 ), the development of a coordinating center ( 4 ), and the involvement of other government centers, such as Nutrition Obesity Research Centers, in nutrition education and training ( 7 ) were also articulated. Nutrition Obesity Research Centers are primarily focused on obesity and nutrition research, but the potential to leverage these resources towards nutrition education and training were identified. The following case studies offer further examples of successful approaches towards providing medical nutrition education.
Case study 1: Brody School of Medicine, East Carolina University
The Brody School of Medicine includes nutrition education in both UME and family medicine curricula. Brody integrated nutrition into the basic science and introductory clinical courses, Family Medicine clerkships, and an elective, as championed by at least 1 physician and a registered dietitian nutritionist and supported by the senior associate dean for curriculum. The current program is under 25 h because of competing priorities, including mandates from the accrediting agency to reduce total curriculum hours. Assessment of clinical nutrition skills occurred within the objective structured clinical examination cases. Curriculum renewal resulted in consensus regarding the requirement for several recommended competencies ( 19 ) as follows:
- Perform basic nutritional assessment in the inpatient setting and recognize when patient needs to be fed.
- Perform basic nutritional assessment in the outpatient setting.
- Counsel patients on basic public health nutrition issues (e.g., obesity prevention and treatment, hypertension, cardiovascular disease, and diabetes).
- Recognize fads (nonevidence-based diets/supple-ments).
- Understand when/how to refer patients to a qualified Registered Dietitian Nutritionist (RDN) or other professional and know the content of that consultation.
- Recognize and plan for personal nutrition, physical activity, and wellness.
Case study 2: nutrition education for medical students in rural areas, University of Mississippi
Mississippi is a rural and poor state with multiple health and healthcare challenges, whose residents could benefit from changes in dietary practices and improved access to affordable healthy food. In 2016 the University of Mississippi Medical Center restarted the Department of Preventive Medicine, residing in both the School of Medicine and the John D. Bower School of Population Health. The Department of Preventive Medicine aims to transform health care into a system that values prevention over cure, effectively addresses psychosocial, behavioral, and community factors that influence health, and implements evidence-based interventions for populations as well as individuals. Central to the departmental mission is a commitment to educate medical students and residents regarding nutritional factors that predispose people to chronic diseases, particularly residents in rural, underserved areas.
Led by the Population Health Education Workgroup, nutrition education courses and experiential learning activities were added across all 4 y of UME. The revised curriculum draws from the social science literature in rural health and best practices in competency-based nutrition education, including the NIM program. Nutrition was integrated into organ system education for first-year and second-year students, use of standardized patients was employed during the third year, fourth year students participated in competitions that involved interdisciplinary clinical cases with nutrition content embedded within them. Practice opportunities were designed to increase student awareness of community-based nutrition resources and services.
Medical Education Evolution from Knowledge Acquisition to Knowledge Application: UME to GME—Role and Implementation of Entrustable Professional Activities
Changing paradigms in medical education foster high standards of learner achievement and success. These evolving concepts affect learners across the continuum of medical education and, therefore, it is important to consider the entire continuum from UME to graduate medical education (GME) and continuing medical education (CME). In 1990 Miller ( 20 ) described a pyramid of 4 stages of clinical competence showing progressive accomplishments: knows (fact gathering), knows how (interpretation/application), shows (demonstration of learning), does (performance integrated to practice). Miller's pyramid has aided educators in thinking about learner assessment where knowledge is primary in the first 2 levels, and behaviors or skills are embedded in the upper portions of the pyramid.
As the concepts of assessment tied to achievement have progressed, new nomenclature has been identified. The ACGME established 6 competencies (patient care, medical knowledge, systems-based practice, practice-based learning, professionalism, and interpersonal and communication skills). There are additional subcompetencies to further define developmental progression in specific areas.
Entrustable professional activities (EPAs) are those activities or specific tasks that define a profession or specialty related to a particular role ( 21 ). EPAs were developed across various disciplines in GME, and the AAMC has established 13 core EPAs related to the completion of UME for those entering residency ( 22 ).
All of the gastrointestinal societies (the American Association for the Study of Liver Diseases, the American College of Gastroenterology, the American Gastroenterological Association, the American Neurogastroenterology and Motility Society, the American Society for Gastrointestinal Endoscopy, and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition) in a group called the Oversight Working Network, convened to create EPAs for gastroenterology, hepatology, and nutrition. Based on the gastrointestinal Core Curriculum, it accounted for changing paradigms in medical education, health care, and technology ( 23 ). In total, 13 EPAs ( 24 ) were identified including 1 specific to nutrition: “Assess nutritional status and develop and implement nutritional therapies in health and disease” ( 25 ).
Each EPA includes the following: title, detailed description, behaviorally anchored objectives in knowledge, skills, and attitudes, a list of ACGME competencies related to the EPA, the list of reporting milestones to achieve mastery, the time expected to achieve a level of unsupervised practice, suggested assessments, identification of who will make the entrustment decision, and finally, implications of entrustment. A toolbox was created to assist evaluators of trainees to aid in tracking, evaluation, and required reporting.
Program directors can use the Nutrition EPA to tailor educational curricula to fit within a particular program's framework. Flexibility exists to create educational programming that allows trainees to achieve mastery in the patient setting, in simulated exercises, in online training, or in case-based sessions that might include interprofessional partnerships. Similarly, assessments can be designed that conform to the technological capabilities of the educational program and personalized to the program and trainee.
Examples of assessment using curricular elements include:
- clinical rotations: direct observations;
- standardized patients: 360° evaluations;
- case-based conferences: chart-stimulated recall;
- online modules: chart audit;
- national courses: in-training examination, patient surveys.
EPAs have a great advantage of being competency-based and EPAs promote individualized and personalized education. Creating EPAs across societies provided an opportunity to define the tasks of the profession. Some challenges were identified, particularly embracing change with reflection on new paradigms in education and assessment. The greatest challenge appears to be identifying the ideal assessments to evaluate learner achievement of each EPA's objectives. The ideal assessments are competency-based, and several steps must be considered: 1 ) Agreeing on what competency is required; 2 ) Setting milestones that mark progress toward competency; 3 ) Transitioning from a culture of largely norm-based assessments to criterion-based assessments; and 4 ) Addressing challenges associated with direct observations of learners ( 26 ). This is an opportunity for experts in specific areas, such as nutrition, to contribute to these efforts to ensure that learners and practitioners are skilled and demonstrate competence in these key areas. Figure 1 illustrates these concepts.

A competency-based educational model rather than knowledge alone, competency in application is prioritized. EPA, entrustable professional activity; OSCE, objective structured clinical examination. Adapted and reproduced with permission from ( 41 ).
Survey Results in US Medical Schools: What Do Medical Students Need to Know?
In 2012–2013 Adams and colleagues sent a survey to 133 accredited medical schools to identify nutrition content taught across the 4 y of medical school ( 27 ). Only 22 (18%) medical schools had a nutrition course. Nutrition taught in UME averaged <20 h, below the 25 h recommended by National Academy of Sciences and 44 h by ASCN (renamed ASN). However, several schools dedicated more time through integrated courses and clinical practice sessions. Eight (6%) medical schools offered >40 h of nutrition education. An average 6.4 h was devoted to clinical practice in only 55 (45%) medical schools that required any clinical practice sessions. Although many schools have nutrition electives, few interested students attend them. Recent unpublished data from the same group has shown no improvement in nutrition education. Thus, “many US medical schools still fail to prepare future physicians for everyday nutrition challenges in clinical practice” ( 27 ). Key challenges include the limited number of 1 ) nutrition providers (e.g., physician nutrition specialists, RDNs) that serve as role models for interprofessional collaboration; and 2 ) clinics/nutrition services that are accessible to medical students and offer a worthwhile training environment.
In response to these survey findings, the International Association for Medical Science Educators (IAMSE) recognized the need to improve nutrition training and assessment of medical students, and a Nutrition Advocates working group was formed. In 2015 they updated the NAA learning objectives ( 28 ) by reorganizing the objectives into 11 categories based on a Core Nutrition Classification proposed at the 2012 NIH workshop and published in 2014 ( 5 ). The objectives were revised and simplified, resulting in 92 amended objectives. A survey assessing whether medical students should meet specific learning objectives/outcomes by the end of UME was distributed to IAMSE members and identified nutrition educators. A total of 67 responses from a combination of basic scientists, dietitian/nutritionists, and physicians were returned. Based on these survey results, several objectives were rewritten, and 9 were deleted because of redundancy or lower importance. In addition to the final 83 learning objectives, the IAMSE Nutrition Advocates also identified 1 overarching goal to help focus future efforts: “All graduating medical students will assess nutritional status and manage the clinical encounter to facilitate a personalized nutritional approach for optimal health.” This goal and learning objectives have recently been published in Medical Science Educator ( 29 ).
ASN's Nutrition Education in Professional Schools Committee became aware of IAMSE's efforts, and in 2016 a collaboration was formed to conduct a more expansive survey encompassing multiple nutrition interest groups. The ASN survey used the same 11 categories to classify the objectives. Through committee discussion, the initial (NAA) and amended (IAMSE) objectives were reviewed and consensus gained on 101 objectives to include in the survey. Although “nutrition champions” (internal advocates within the existing medical schools) may be teaching in UME, many are not part of the official teaching faculty. In addition, many nutrition champions are members of ASN's Medical Nutrition Council and may be clinicians, educators, and/or advocates. Therefore, the questionnaire was distributed to 153 accredited US medical schools and 41 schools of osteopathic medicine champions ( n = 194) via the NIM network of nutrition champions and to members of ASN's Medical Nutrition Council ( n = 2046). Nutrition champions from accredited schools were also asked to survey medical students for feedback, including schools with student nutrition clubs. Data collected included individual age, sex, profession, role in the medical school, years in practice, years in curriculum development, and inclusion of nutrition in various years of curriculum and electives. Participants were asked whether all medical students should meet the learning objectives/outcomes within the 11 categories by the end of their UME. Institutional Review Board approval was obtained, and data were analyzed using STATA (version 12.1).
A total of 147 individuals completed the ASN and IAMSE collaborative survey. Not all participants responded to each question. Among 117 respondents, 66% were women. A total of 120 individuals provided information on their professional status (120 of 147) ( Table 1 ). Of 112 respondents, 30% were course directors, 42% were course/curriculum developers, and 82% were faculty (instructor to professor level). About 44% of 118 respondents had >20 y of practice and 33% had 5–20 y of experience with a nutrition curriculum. Only 20% of 114 respondents mentioned that nutrition was included in all years of medical school in their institution, and 17% reported that it was included in the clinical years. For each of the 11 categories used to classify the objectives, respondents recommended dropping an average of 3–7% of the nutrition objectives proposed and rewriting 1–4% of the objectives. Although the number of objectives to be retained without modification was similar between students and faculty, for some objectives, student responses varied from those of faculty. For example, counter to faculty responses, students were supportive of retaining the following objective: “Explain how the physician can be more involved in nutrition in the community.” Thus, student attitudes and opinions must be considered in any effort to modernize the education of the next generation of physicians. Feedback from this survey will inform the final NAA curriculum guide objectives and provide the basis for future competences and assessments of medical trainees. Finalized objectives are expected in 2019–2020 to support the future work of a coordinating center.
Professional status in the IAMSE survey (percentage of each survey total sample) 1
| Professional affiliation | IAMSE ( = 67) | ASN/IAMSE ( = 147) |
|---|---|---|
| MD | 20 (30%) | 27 (18%) |
| Basic sciences | 29 (43%) | 34 (23%) |
| RDN | 27 (40%) | 47 (32%) |
| Trainees | 0 (0%) | 15 (10%) |
| Other | 10 (15%) | 27 (18%) |
| No response | 4 (6%) | 27 (18%) |
Learning to Reconcile Old Dogmas with New Concepts?
A major challenge in clinical practice is reconciling the conflict between previously established knowledge and emerging information. Medical nutrition educators teach solid foundations and current guidelines while preparing learners for new concepts just over the horizon. They accomplish this by strengthening critical thinking skills, encouraging questions on both old and new claims, and illustrating the importance of lifelong learning. A key message is that best practice must constantly realign with new scientific insight and clinical evidence. In medicine this “scientific uncertainty” is met with excitement as being at the cutting edge of evidence-informed practice, an approach likewise central to the interface of nutrition and medicine.
For example, precision nutrition acknowledges that each individual has unique dietary needs, requiring the mix of new “omics” technologies (genomics, metabolomics, microbiome, and more) to match specific preventive and therapeutic strategies. There are many opportunities throughout the preclinical and clinical curriculum to better understand nutritionally relevant molecular structures, functional mechanisms, and metabolic pathways, and how they are affected by both nutrition and common genetic variants. Similarly, the community of intestinal microbes is unique in each individual and influences the individual's response to dietary changes. When trainees are introduced to these concepts early on, it simplifies their capacity to keep up with emerging findings and translate them more readily to clinical practice.
This lesson was learned from the NAA experience where medical students increased nutrition knowledge and self-efficacy over the 4 y of the NAA and the strongest predictor of the highest USMLE scores was taking a nutrition course before starting medical school ( 4 , 6 , 30 ). The workshop participants agreed this would undergird a focus on nutrition in pathophysiology, public health, precision medicine, and other specialty areas in medical school.
Developing a Competency-Based Nutrition Curriculum: Examples from the Obesity Curriculum with Local and International Approaches
A competency-based obesity curriculum to prevent and treat obesity was developed by the Bipartisan Policy Institute in collaboration with many stakeholders and partners ( 31 ). Major provider competencies include core obesity knowledge, interprofessional obesity care of patients, and patient interactions related to obesity. An analogous process to develop a competency-based nutrition curriculum could include:
- define terms, scope, and application;
- identify and engage diverse stakeholders;
- collect data;
- draft nutrition competencies for stakeholder review;
- apply the competencies, e.g., Curricular Design, Process Improvement, Program Evaluation;
- periodically review and provide updates.
Using these steps, nutrition competencies could include identification of major nutritional deficits in the US population, description of the contribution of diet to chronic diseases in the United States, use of evidence-based care for the delivery of dietary needs of inpatients and outpatients, and development of skills necessary for interprofessional collaboration for nutritional management. Existing examples of schools with UME nutrition competencies include Northwestern University Feinberg School of Medicine and at Deakin University, Australia, in collaboration with other partners.
Case study 3: UME lifestyle medicine thread, Northwestern University
Feinberg school of medicine.
Northwestern University Feinberg School of Medicine underwent curricular renewal in 2012 following the shifting focus promoted by the AAMC towards competency training ( 22 ). The traditional 4-y structure of medical education was replaced with 3 competency-based phases organized by 4 elements (science in medicine, clinical medicine, health and society, and professional development) and 5 threads (healthcare quality and patient safety, health equity and advocacy, medical decision-making, teamwork and leadership, and lifestyle medicine) ( 32 ). Lifestyle medicine, including assessment/counseling for diet/nutrition, physical activity, smoking, alcohol, stress, and weight management, became a thread as these health behaviors are primary contributors to noncommunicable diseases (NCDs) ( 33 ). The practice of lifestyle medicine requires interrelated skills and competencies to address multiple health risk behaviors. Thus, diet/nutrition was integrated throughout the curriculum as 1 component of the lifestyle medicine thread ( 34 ).
During phase 1, the first 20 mo of medical school, including 13 organ-based modules, diet/nutrition is addressed within 78 different sessions. Using this model, students are sequentially exposed to nutritional concepts that are pertinent to the basic science, clinical care, or population health aspects of the various organ systems. For example, the endocrinology module presents appetite regulation and energy balance, the method for taking a body weight history ( 35 ), and the global impact of obesity as a contributor to NCDs. As part of the thread, students also complete a personal behavior change plan, experiencing the process and principles of behavior change while striving to improve their own health ( 36 ).
Case study 4: development and future for competency-based nutrition curriculum in Australia
To address the lack of nutrition content in medical courses in Australia ( 37 ), an expert group developed a set of 9 nutrition competencies (2009–2011) specifically designed to be easily embedded into draft competency-based Standards for Assessment and Accreditation of Primary Medical Programs by the Australian Medical Council (ratified 2012) ( 38 ). These competencies (4 knowledge-based and 5 skills-based) were circulated to educators, the Royal Australian College of General Practitioners, and the Dietitians Association of Australia for feedback. As part of a national teaching award, in collaboration with Monash University, the Universities of Queensland and Tasmania, and the Dietitians Association of Australia, a web-based Nutrition Competency Implementation Toolkit was designed to embed nutrition into the medical curriculum ( 39 ). In the Toolkit, competencies were detailed to provide more information on suggested learning objectives, examples of learning activities, and assessment methods, including a bank of appropriate multiple choice examination questions.
The number of competencies was restricted, and simple language was used for easy communication. The nutrition competencies were designed to align with the existing framework required for medical course accreditation and interprofessional competency statements. Feedback indicated that the basic nutrition competencies should not be overly prescriptive and should be readily integrated within a variety of different curricula structures across the learning continuum. They need to be flexible with respect to a range of practice settings and must link to learning activities, and behavioral assessments should be developmentally appropriate for learners at different stages. A future research challenge is to develop and evaluate robust student competency evaluation tools, particularly for practical tasks, with feedback to facilitate the development of nutrition competencies throughout the different stages. Lifestyle medicine has emerged as a systematized approach for the management of chronic disease, encompassing nutrition, physical activity, and mental health. Accordingly, medical schools may be more receptive to embedding nutrition into the curriculum as a component of a cohesive lifestyle medicine program. The student competency domains related to assisting patients to address physical activity and mental health issues are similar to nutrition. There is a research gap to develop common frameworks to evaluate competencies and to assess the impact of producing “lifestyle competent” health professionals on patient lifestyle behaviors and health status. There are significant advantages in linking nutrition competencies with exercise and mental well-being professionals’ education to develop 1 common set of competencies for medical, nursing, and allied health graduates.
The Need for Nutrition Education/Innovation Program, Australia/New Zealand network (NNEdPro NZ) is a collaboration among dietitians, doctors, academics, medical and healthcare educators, researchers, students, and professional associations in the region, linked with the NNEdPro Global Centre in Cambridge, United Kingdom, to build collaborations and initiatives to advance nutrition education. An action plan was developed at a recent workshop (December 2017) ( 40 ), encouraging medical schools to map the nutrition competencies of their medical curriculum, and NNEdPro is developing a plan to evaluate the impact of nutrition educational initiatives. Coordinated efforts across the health professions to embed lifestyle competencies during training and evaluation of the impact of increased student lifestyle competencies on patients’ health are necessary to progress this area and ultimately reduce health inequalities ( 41 ).
Nutrition in Accreditation and Licensure
The role of the usmle.
Sponsored by the Federation of State Medical Boards and the NBME, the USMLE is a 3-step examination for medical licensure in the United States that assesses a physician's ability to apply knowledge, concepts, and principles, and to demonstrate fundamental patient-centered skills that are important in health and disease and that constitute the basis of safe and effective patient care. Since 2003, “nutrition” has been a reported score category on the USMLE Step I examination and was subsequently included in the subscore domain of “biochemistry” since 2016. Further, nutrition content is represented on the Step II Clinical Knowledge and Step III examinations as a cross-content area within ICD-9 coded diagnoses (e.g., feeding and nutrition issues, nutrition and digestive system disorders, foundations of independent practice domains). Nutrition content is further represented in the Step II Clinical Skills examination in the domain of “health behavior change.”
The inclusion and design of nutrition questions and how they are monitored are primarily driven by the USMLE content outline. This is the basis for the examination material created by the NBME's national faculty of medicine, a representative group of medical educators, practicing physicians, and state medical board members. On a periodic schedule, at least 2 committees critically appraise each test item or case in the USMLE. Material that performs poorly on the examination series or is outdated is discarded. Of note, nutrition-related content is specific to >10 areas of the content outlined across the lifespan and disorders. Periodically, the USMLE program grants requests to review the content of the examination series to external specialty interest groups, including those in the area of nutrition. Similarly, in 2015, the American Board of Obesity Medicine and The Obesity Society reviewed the exams for obesity-related content and made recommendations for improvement to promote more balanced testing of knowledge in obesity. Because of these recommendations and others made over the past 3 decades, the USMLE program responded by enhancing recruitment of additional test committee members with nutrition expertise and attempting to improve cross-content area representation on the exams.
The role of the LCME
The LCME is recognized by the US Department of Education as the reliable authority for the accreditation of US medical education programs leading to the Medical Doctor (MD) degree. As of 1 March, 2018, there were 151 LCME-accredited allopathic medical education programs in the United States that enrolled approximately 81,000 medical students and an additional 17 programs accredited by the LCME in Canada. Allopathic programs must be accredited by the LCME for their graduates to be eligible for postgraduate (residency) training, and medical/osteopathic licensure.
The LCME evaluates an educational program's performance against 93 Elements organized under 12 Accreditation Standards ( 42 ). For the most part, the Standards and Elements are nonprescriptive to allow programs flexibility in using resources and expertise, and tailoring the educational program to meet the strengths of the educational environment and the school's mission. The LCME does have expectations that certain topics are covered but does not explicitly specify where in the curriculum or “how much is enough.” Adequacy and effectiveness are determined by outcome measures (such as USMLE) and student satisfaction data.
Standard 7, Element 7.1, requires programs to include content from biomedical, behavioral, and socioeconomic sciences, as applicable to the health of individuals. The data collection instrument for Element 7.3 documents and assesses the location and impact of nutrition as taught in the curriculum. The LCME also queries programs about nutrition curriculum in an annual survey instrument. Data from those surveys document that nutrition content is required within preclinical and clinical courses. Neither the accreditation data collection instrument nor the annual surveys identify or define the actual content, quantity, learning objectives, or assessment measures for nutrition subject matter in the curriculum.
Potential research areas might include 1 ) student assessment methods used by schools for the nutrition curriculum, 2 ) granularity on nutrition curriculum content and methods of curriculum delivery, 3 ) measuring effectiveness of nutrition curriculum on knowledge and skills imparted by nutritional curricula, and 4 ) GME program satisfaction with postgraduate year 1 resident regarding nutrition education, and how that might relate to medical school curriculum content.
The role of the ACGME
Nutrition, dietary behavior, and societal influences are major contributors to the development of chronic diseases such as obesity. Despite rapidly increasing rates of obesity in both children and adults, many physicians and other healthcare providers do not have the skills necessary to intervene in this epidemic.
The ACGME sets standards for US GME programs and the institutions that sponsor them, and renders accreditation decisions based on compliance with the standards. Accreditation provides assurance that sponsoring institutions and programs meet the quality standards to prepare their graduates and physicians of the future to provide good patient care. The ACGME provides accreditation to 830 sponsoring institutions, including 11,214 programs with 135,326 medical residents and fellows (including fellows whose combined focus can involve clinical practice, research into public health and/or advocacy) and 176,616 faculty members. Although obesity permeates all levels of society and the entire age spectrum, and therefore all specialties, it may be best to direct initial GME training for nutrition dietary behavioral intervention and the treatment of obesity toward the primary specialties including pediatrics, family medicine, and internal medicine. As of December 2018, there were 1350 primary specialty programs, with 48,967 residents and 35,960 faculty (ACGME Data Resource Book Academic Year 2017–2018).
Common and specialty program requirements ensure that medical residents and fellows are provided with a curriculum and clinical environment that ensure sufficient exposure to the diagnostic and therapeutic methods of the specialty. In addition, programs are required to provide clinical experiences and didactic education in preventive health, acute and chronic disease management, and access to longitudinal continuity experiences. Furthermore, medical residents must demonstrate knowledge of established and evolving biomedical, clinical, epidemiological, and social-behavioral sciences, as well as the application of this knowledge to patient care. However, specialty program requirements are written in more general terms without listing every single disease state nor providing a comprehensive list of therapeutic modalities.
The proposed role of ACGME in medical residency and fellowship education in nutrition, dietary behavior and the treatment of obesity is 2-fold.
- Dissemination of knowledge through the creation of a “microsite” within the ACGME website. This mechanism successfully provided educational modules for specific topics such as physician wellness, milestones, clinical competency committee, and self-study. In addition, ACGME has a newly established Department of Distance Learning that can create learning modules, video clips and other educational activities for use by medical residents, fellows, and program faculty. This format can provide educational modules in nutrition and obesity to a wide audience.
- Creation of a new subspecialty in nutrition and obesity under the primary specialties of pediatrics, family medicine, and internal medicine. ACGME accredits programs in subspecialties that demonstrate that the clinical care of patients and their safety will be improved through accreditation of training in that discipline. Creation of this new subspecialty has several purposes including advanced training that will lead to subspecialists and leaders who will improve the care of patients with obesity, and the education of others who are involved in the care of such patients. Other benefits include focused and standardized care such that medical fellows who complete subspecialty training will share a common foundational knowledge base and skill set in the management of nutrition and obesity.
The panel recommended justification for and benefit derived from a board-certified ACGME-approved subspecialty in nutrition and stated it would advance progress in addressing many of the gaps and limitations in medical nutrition education and training. It further raises awareness regarding the importance of qualified faculty to teach, train, and grow the nutrition focus and develop new career paths. If the leadership and programs are in place, medical students, residents, and other professionals will come. An example is the University of Colorado School of Medicine where fellowship training in Pediatric Nutrition and Obesity/Lifestyle Medicine that follows ACGME guidelines has proven successful with more applicants than positions available.
Interprofessional Nutrition Education
Behavioral science competencies.
In 2004, the Institute of Medicine (IOM) summarized how UME curricula should be enhanced to address critical health issues facing the United States today ( 43 ). Approximately half of all causes of mortality in the United States are linked to social and behavioral factors such as smoking, diet, alcohol, sedentary lifestyle, and accidents ( 44 ), but <5% of the 2 trillion dollars spent on health care annually in the United States is devoted to reducing behavioral and social risk factors ( 45 , 46 ).
The IOM further reported that most US medical schools do not provide curricula sufficient to teach these behavioral and social risk factors. In response to the IOM report, the NIH awarded grants to 9 medical schools to develop, pilot test, and disseminate behavioral and social sciences integrated curricula across 6 domains: 1 ) Mind–Body Interactions in Health and Disease, 2 ) Patient Behavior, 3 ) Physician Role and Behavior, 4 ) Physician–Patient Interactions, 5 ) Social and Cultural Issues in Health Care, and 6 ) Health Policy and Economics. In all of these areas, nutrition education is vital. Collaborators and curricular innovations are described in detail elsewhere ( 47 ).
Briefly, some innovations specific to diet and exercise include: 1 ) inpatient rounds that include an assessment of nutrient needs and/or interventions associated with discharge care; 2 ) use of interprofessional teams in student-run health clinics to consistently address nutrition and exercise with every patient seen; 3 ) involving medical residents in hiking programs with children from local elementary schools and providing a healthy lunch; and 4 ) having students map neighborhoods’ fast food locations, community gardens, and exercise areas.
Research gaps include: 1 ) data documenting physician interventions and patient outcomes related to changing diet/exercise behaviors; 2 ) data comparing educational designs and dose-timing effects to document the importance of nutrition; 3 ) data resulting from novel strategies to activate physician–patient interactions; and 4 ) results derived from “collaboratories” among medical schools to study and identify best educational practices for improving patient outcomes.
Nutrition and dietetics professionals; RD/RDNs: competencies in team-based care, an interprofessional approach
Identifying potential gaps.
The Academy of Nutrition and Dietetics is the largest association of food and nutrition professionals in the United States, representing more than 100,000 RDNs, registered nutrition and dietetic technicians, and advanced-degree nutritionists, and is committed to improving the nation's health through food and nutrition across the lifecycle ( 48 ). The Academy's position is that RDNs should play a significant role in educating medical students, residents, fellows, and physicians in practice ( 30 ). Training of medical students involving interaction with RDNs develops competencies in addressing the preventive and therapeutic role of nutrition throughout the lifecycle and recognizing the importance of the MD/RDN collaborative effort. Addressing the following gaps in competencies may support interprofessional practice and better meet the nutrition needs of patients served:
- Underuse of RDNs' interprofessional education and care: despite strong evidence documenting the value of nutrition interventions/counseling provided by an RDN as part of the healthcare team in improving patient outcomes ( 49 ), RDNs remain highly underused in both interprofessional education and interprofessional care. Medical students benefit from opportunities to interact with RDNs and nutrition and dietetics students as part of their education to practice interprofessionally on graduation. The goal is not to become nutrition experts, rather, to understand the value of referral to RDNs and best to leverage their expertise as part of the healthcare team and augment the physician's care of the patient.
- Payer coverage of nutrition services provided by RDNs: medical providers often operate under an outdated, incorrect assumption that payment for nutrition services does not exist. On the contrary, Medicare coverage for patients with diabetes, nonend stage renal disease and postrenal transplant has existed since 2001, yet only 5% of the >12 million Medicare beneficiaries with diabetes are provided ( 30 ).
- Medical Nutrition Therapy: benefits of nutrition counseling have evolved, especially in the private payer world. Competency in applying these fundable and essential referrals to RDNs is a crucial skill for achieving best patient outcomes ( 30 ).
- Skills in making referrals and activating patients towards seeking RDNs: medical providers benefit from understanding the full range of RDN services to effectively prescribe for their patients the benefit and need to follow-up on referrals ( 50 ).
- Coding for nutrition services: medical providers need basic knowledge about coding for nutrition services as part of their practice management competencies.
- The role of RDNs and nutrition services in value-based payment models: medical providers who learn how to apply these models to support and pay for RDN nutrition services benefit patients. Data show financial viability in having an RDN on the team, especially in category 2, 3, and 4 payment models ( 51 ).
- Nutrition services advocacy: medical education should advocate strategies for nutrition services coverage at the patient, practice, and/or healthcare system level.
- Finding an RDN: medical education starts with recognizing the value of the RDN on the team and how best to recruit the appropriate RDN expert for the team.
Other interprofessional organizations have developed their own goals and objectives as well.
Oral health
Relations between nutrition and oral health are abundant and relevant to overall health. Oral problems including dental caries, tooth loss, and oral soft tissue and oral bone infections are major risk factors for malnutrition, choking risk, and even potentially fatal systemic infection. Research provides clear, irrefutable evidence that dietary and nutritional factors, in conjunction with oral flora, are the essential etiologic factors in dental caries (the most prevalent disease of children to age 19). New evidence of relations between systemic nutrition and oral soft tissue and bone health and disease is continuously emerging ( 52 ).
Consequently, schools of dental medicine and dental hygiene have taught nutrition in some form since the earliest recognition of relations among nutrition, oral health, and disease ( 53 ). The importance of these relations is formalized through position/policy statements from both dental and nutrition professional organizations, and through related accreditation standards. Nevertheless, ensuring that nutrition is included in dental curricula in a meaningful way has been a consistent challenge ( 53 ). Many system-wide issues contribute to this difficulty:
- Nutrition is not a traditional core subject in dental education, which now favors more general outcomes/competencies. Few practice models and curricular road maps exist. Accreditation guidelines for dental hygiene schools are more prescriptive than for dental schools, whereas guidelines for dental school outcomes relate only to basic science education requiring that the “graduate must be competent in oral health promotion and disease prevention for all age groups.” Nutrition is implied but not named.
- Faculty available and qualified to teach nutrition in dental and dental hygiene schools are rare or nonexistent. Various faculty including biochemists, oral biologists, general dentists with an interest in nutrition, and on-site dental hygiene faculty typically fill these roles, but nutrition knowledge and skills vary widely and may conflict. Ideally, an RDN with core skills in direct patient care is best suited to this role, but few nutrition professionals have training in oral health.
- For nutrition teaching to be meaningful in dental education, graduates must be able to apply their knowledge. Students need to be as “comfortable” discussing nutrition as they are discussing oral hygiene or fluoride ( 54 ).
- Incorporating nutrition into patient care requires an “applied nutrition” curriculum, including interviewing and counseling skills, as well as nutrition science ( 55 ).
Interprofessional education offers effective training in applied nutrition and an integrated curriculum including nutrition science, dental science, communication skills, applied nutrition, and clinical practice.
Physical activity
In addition to nutrition training, educating health professionals in the clinical knowledge, skills, and attitudes regarding physical activity for health benefits, a key component of Lifestyle Medicine, is essential for decreasing lifestyle-related chronic disease morbidity, mortality, and economic burden. The definition of physical activity is “any bodily movement that increases energy expenditure”; structured exercise, a subcategory of physical activity, is “planned, structured, repetitive and intentional movement intended to improve or maintain physical fitness” ( 56 ). Both physical activity and exercise may be used to maintain wellness and reduce the risk of chronic diseases.
Physical activity competencies for medical professionals should include: 1 ) physical activity assessment; 2 ) exercise prescription and implementation, 3 ) exercise counseling and behavioral strategies; and 4 ) self-care for the physician.
Physical activity assessment
To provide health benefits and lower risk of NCDs, the 2008 Physical Activity Guidelines for Americans ( 57 ) recommendation is for all adults to perform at least 150 min/wk of moderate-intensity or 75 min/wk of vigorous-intensity, aerobic activity, and moderate-intensity or high-intensity muscle-strengthening activities involving all major muscle groups on ≥2 d/wk. In addition to encouraging patients to follow these guidelines, screening for physical activity behaviors should be implemented at every patient visit through a physical activity vital sign ( 58 ).
Exercise prescription and implementation
The “FITT” Principle (frequency, intensity, time and type) is the most common and acknowledged method to effectively prescribe exercise and implement into a patient's lifestyle. Frequency: How many times per week; Intensity: low, moderate, or vigorous, Time: how long every session; and Type: walking, jogging, bicycling, etc., are ways to prescribe and implement exercise for optimal results.
Exercise counseling and behavioral strategies
Tools to implement physical activity and exercise into patients’ lifestyles include using the Transtheoretical Model Stages of Change, Motivational Interviewing, and Shared Decision-Making for both the healthy ambulatory patients and especially for patients with or at risk for chronic disease. Special conditions and populations (e.g., children and adolescents, older adults, disabled individuals, pregnancy, obesity, cancer) must be taken into consideration.
Self-care for the physician
Physician burnout is prevalent in health care, with >50% of physicians reporting symptoms of burnout. The Healthy Doc-Healthy Patient study also demonstrated that physicians who have a healthy lifestyle are also more likely to counsel their patients on adopting and maintaining a healthy lifestyle. Therefore, physical activity and exercise should be promoted by physicians and to physicians alike ( 59 ).
The University of South Carolina School of Medicine Greenville was the first medical school to require all undergraduate medical students to obtain training in nutrition, clinical exercise physiology, sleep hygiene, self-care/stress management, behavior change, and other lifestyle medicine components as part of their curriculum ( 59 ). For medical schools wishing to adopt and implement lifestyle medicine training in their schools, the Lifestyle Medicine Education Collaborative ( 60 ) offers leadership, guidance, and resources in medical schools throughout the United States and internationally.
Nursing/NPs
Nutrition is an important practice component for nurses and NPs. The present state, challenges, and opportunities in terms of nutrition education and training for nurses and NPs is well-documented ( 6 ). A socioecological framework is used to identify education and training opportunities related to nutrition for nurses and NPs, review current nutrition-related practice initiatives that impact nurses and NPs, and identify areas for further research ( 61 ).
Individual level
Knowledge, attitudes, and beliefs are key individual level factors in any socioecological model. Standalone nutrition courses are “not mandated” by accrediting bodies for nurse training at the prelicensure level, but nutrition content is integrated into the curriculum as it is testable knowledge on the National Council Licensure Examination ( 6 ). An educational action item centers on development of a standardized nutrition curriculum for the varied NP specialty programs as formal nutrition courses are not taught at the graduate level. NP programs could enhance content on nutritional assessment, the integration of nutrition with acute and chronic disease management, the diagnosis of nutritional alterations, and the prescription of appropriate nutritional therapies. Standards of nutrition care practice and professional performance for nurses and NPs were recently published by the ASPEN Nurse Standards Revision Task Force ( 62 ). These standards differentiate competencies for nurses and NPs for the nutrition support nurse specialist and nonspecialist (generalist), and could serve as a framework for updated NP curricular threads. Finally, improving one's personal attitudes and beliefs toward nutrition and a healthy lifestyle could potentially impact patient care. In 2017 the American Nurses Association initiated the Healthy Nurse, Healthy Nation Grand Challenge to empower the 3.6 million American nurses to increase their personal wellness and that of their family, community, patients, and, ultimately, the nation. Components of the program include choosing nutritious foods and maintaining an active lifestyle. Future research could identify nutrition-related knowledge, attitudes, and practice patterns of the Healthy Nurse program participants.
Interprofessional level
Hospitals are the only healthcare settings where the majority of the interprofessional healthcare team provides care, including dietitians, nurses, NPs, pharmacists, physicians, PAs, and physical therapists (PTs). Nutrition is an important component of the care delivered in the hospital setting. The Joint Commission mandates that all patients receive a nutrition screen within 24 h of admission ( 63 ). In most hospitals, the initial screen is performed by nurses ( 64 ), and dietitians conduct in-depth nutritional assessment and recommend appropriate medical nutrition therapy. Healthcare professionals have numerous opportunities to integrate nutrition into care and services across the care continuum including wellness and fitness centers, retail pharmacy, physician offices and clinics, urgent care, diagnostic imaging centers, ambulatory procedure centers, emergency departments, inpatient rehabilitation, outpatient rehabilitation, extended care facilities, skilled nursing facilities, home health, and hospices. They should incorporate essential nutrition principles into health promotion and wellness activities, as well as acute and chronic disease management. Nurses/NPs should also know when referral to RDNs is necessary ( 64 ).
Organizational level
Professional organizations play a key role in developing and implementing nutrition practice standards in alignment with their missions. For example, ASPEN focuses on reducing the incidence of hospital malnutrition; their Malnutrition Solution Center houses important interprofessional resources ( 65 ).
Community level
The transition from hospital to home represents a gap in nutrition care. Patients undergo a nutrition screen at hospital admission, but there is no mandated requirement to conduct a nutrition screen upon discharge, nor a mandated requirement for home care nurses to perform a nutrition screening in the home care setting. Postdischarge malnutrition impacts hospital readmission rates ( 66 , 67 ), but the true prevalence of malnutrition during the transition between hospital and home in the United States is unknown. Further compounding the issue is the limited number of dietitians who work in home care settings. At a recent National Academies of Science, Engineering, and Medicine workshop ( 68 ), DiMaria-Ghalili recommended that research should focus on integrating nutrition risk assessment into predictive models to determine the level of nutritional care postdischarge. Nutritional interventions in the postdischarge, community, or home care setting could be prioritized into 3 levels: high-risk nutritional interventions delivered by a registered dietitian, medium-risk interventions delivered by nurses, and low-risk nutrition interventions delivered by social workers or lay health community or home care workers. Some hospitals collaborate with home-delivered meal options to provide food postdischarge. Evaluative data are urgently needed.
Policy level
Strategic policy initiatives, such as educational program accreditation standards, credentialing or licensure standards, healthcare accreditation standards, or reimbursement regulations are badly needed. A 2015 commentary published by the ASPEN Malnutrition Committee in The Joint Commission Journal on Quality and Patient Safety called for a malnutrition-focused national goal to address the issue of disease-related malnutrition ( 69 ). Targeted messaging to key stakeholders of the importance of integrating nutrition principles in education and practice can help raise awareness, eventually impacting policy.
Osteopathic medicine, PAs, and PTs
Nutrition education in osteopathic medical schools.
Nutrition education is integral to the distinct osteopathic philosophy and osteopathic physician (DO) training even more than in allopathic medical schools. There are 33 osteopathic medical schools and more than 108,000 practicing DOs in the United States, reflecting a 68% increase in the last 10 y according to the 2017 Osteopathic Medical Profession MP Report ( 70 ). DOs are licensed in all 50 states to practice the full scope of medicine. Graduate medical education doctors from both allopathic (MD) and osteopathic (DO) schools of medicine have merged and now compete for the same residency training programs and take the same national medical licensing examination ( 71 ). DOs may choose any medical specialty and often become primary care physicians, providing much-needed health care in underserved regions ( 70 , 71 ).
The osteopathic curriculum is a 4-y postbaccalaureate program. Students learn preventive medicine, pharmacology, and surgery, with added training (>200 h) in osteopathic manipulative medicine. Nutrition education averages 25 h of lectures for allopathic preclinical curricula ( 72 ). DO nutrition curricula include strong biochemical and clinical components, reinforcing the role of nutrients in metabolism. Additional instruction includes nutritional assessment, patient education, and collaboration with credentialed RDNs.
In 2017, the Journal of the American Osteopathic Association published results of a survey of DOs (often the sole providers of patient nutrition education and counseling) stating that nutrition is often overlooked during office visits, with <10% of primary care providers offering weight loss counseling to their patients ( 73 ). Allopathic medicine has long recognized this problem and dedicated training in providing patients with nutrition awareness, especially as a component of preventive medicine. The MD and DO single graduate medical education accreditation systems provide new opportunities for curricular reform.
Nutrition education for PAs and PTs
The number of PAs graduating from 173 accredited programs is expected to increase in the United States. PAs, taught to treat the whole patient, value the importance of health promotion and disease prevention. PAs serve as partners to advocate for patient nutrition education. They receive graduate-level education in the basic sciences, and clinical skills, including initiation of nutritional assessment and diet counseling. Similar to nurses, NPs, and nursing assistants, PAs can make referrals to RDNs.
Surveys of PA students initially found that nutrition knowledge and attitudes were lower than expected ( 74 , 75 ); however, this improved progressively with each year of PA education.
There are no specified requirements for nutrition education in PA programs as set by the Accreditation Standards for Physician Assistant Education; however, 10% of the national certification examination relates to gastrointestinal and nutrition questions ( 74 ). PA training programs are typically based in academic medical centers where establishment of a medical subspecialty in Nutrition and Obesity would support multiple Advance Practice Training programs including those for PAs.
PTs complete a doctoral degree program, and nutrition is a component of their professional scope of practice. Nutrition was included as an element of PT education in 2012 and added to the guidelines of the Commission on Accreditation for Physical Therapy Education. The American Physical Therapy Association (APTA) states, “the role of the physical therapist is to screen for and provide information on diet and nutritional issues to patients, clients, and the community within the scope of physical therapist practice.” The PT profession supports helping patients understand how nutrition affects function. However, each state has its own laws and regulations regarding how PTs can fulfill that role and who can legally provide nutrition counseling. Some states permit them to give nutrition advice, but only RDNs can charge or bill insurance. Other states require licensed RDNs to give nutrition advice.
The APTA web page, Nutrition and Physical Therapy , provides resources and links to state regulations and laws and states APTA's position that it is the role of PTs to “screen for and provide information on diet and nutritional issues…within the scope of practice for PT” ( 76 ).
Culinary medicine
The nutrition-related chronic disease epidemic requires enhanced education of healthcare professionals in assisting patients with nutrition. Pilot studies demonstrate efficacy of nutrition education interventions aimed at improving competencies among medical students. Yet their generalizability is limited by a lack of control comparison ( 77–85 ), validated survey metrics ( 77 , 78 , 82 , 84 ), multiyear longitudinal follow-up ( 77 , 79 , 80 , 82–84 ), and large sample size ( 77–81 , 83 , 84 ). Past studies ( 77–84 ) also fail to incorporate the most extensively supported diet for patients, including the Dietary Approaches to Stop Hypertension (DASH) and Mediterranean diets ( 85–87 ).
Simulation-based medical education with deliberate practice (SBME-DP) has been shown to be superior for skill acquisition in mastery learning ( 88 ). Culinary medicine programming addresses this disparity using SBME-DP through hands-on cooking classes as a platform for teaching healthcare providers positive food-related messaging that they can incorporate into their patient encounters. In a large sample of medical students, a multiyear prospective observational cohort study showed superiority of SBME-DP-style hands-on cooking and nutrition education elective over traditional clinical education for preventive medicine ( 89 ).
Culinary medicine SBME-DP programming extends to multiple educational and clinical settings for students including:
- required hands-on culinary medicine programming offered at 3 medical schools;
- multiple-module hands-on culinary medicine programming offered as electives;
- standalone condition and disease-specific programming offered as optional programming;
- medical student involvement and delivery of hands-on community cooking classes.
Growth has accelerated over the last 5 y with more than 35 medical schools, 3 nursing schools, and 9 graduate medical education programs offering Culinary Medicine programs nationwide. More than 40 of these sites are using courseware focused on the Mediterranean diet with translation for the American kitchen, as well as teaching healthcare providers practical strategies to effect change in their patients.
Nutrition Research and Training Needs and the Road to Sustainability
A major NIH goal is to develop, diversify, and sustain the scientific workforce. Research training of health professionals is an integral component of its mission. Within the various NIH institutes, training through career development and fellowships has been the hallmark of their mission, and many institutes have implemented strategies to enhance their training efforts. One example of such training is the previously discussed NAA program.
To examine federal funding of training of medical professionals in nutrition as a follow-up to the NAA, we reviewed the NIH portfolios from 2006 through 2017 using the search terms “nutrition and medical school,” “nutrition and primary care,” and “nutrition and residency training,” and then manually screened grants for relevance. We excluded training awards that were awarded to individuals (e.g., K awards) or training programs that trained scientists for research careers. We found 9 NIH-funded projects over the 12-y period that addressed the topic of nutrition training for medical students and health professionals. Four of the 9 NIH-funded projects used training mechanisms. This includes 2 T35 short-term research training projects that added an optional summer course to medical students’ curricula. The NIH also funded 1 T32 institutional national research service award on nutrition and obesity research training and 1 D43 international research training grant for a training program on nutrition and metabolism in HIV. These grants, while adding important nutrition-related topics that reached a portion of medical students, did not create permanent changes in the medical training of their recipient institutions.
Three of the 9 NIH-funded relevant projects were R25 short-term education projects to increase diversity in health-related research. Two of these R25 awards aimed to provide education in nutrition and cancer to medical students, residents, and preceptors and the remaining R25 award aimed to foster opportunities for nutrition and global health. The NIH also funded 2 R13 conference grants in this time frame. These conference grants provided funds to support scientific conferences. While scientific conferences have a large potential reach because of the number of participants, a major limitation of these grants is that they are funded for only 1 y and do not provide funds to sustain a training program. These results demonstrate that nutrition research training in the health professions represents an important need and an opportunity for investigators to address.
The T32 postdoctoral training fellowship offers an important opportunity for physicians to receive research training and preparation for future careers in academic medicine with a specific focus on nutrition/obesity/metabolism. Areas of nutrition research range from basic (T1) to translational (T4) research that offer outstanding faculty development opportunities for growth.
Recently, the NIH established a Nutrition Research Task Force to coordinate and accelerate progress in nutrition research and to develop a nutrition strategic research plan to be implemented within 10 y across NIH Institutes and Centers. Through crowdsourcing across NIH and the extramural community and meetings with thought leaders across the United States, 7 research themes emerged:
- Investigate nutritional biochemistry, physiology, behavior, and the microbiome.
- Assess the role of nutrition and dietary patterns in development, health, and disease across life stages.
- Explore individual variability in response to diet to inform nutrition science, improve health, and prevent disease.
- Enhance clinical nutrition to improve treatment outcomes in patients.
- Advance research on implementation of nutrition-related programs, practices, and behaviors.
- Develop and refine research methods and tools.
- Support training to build an outstanding nutrition research workforce.
These themes have the potential to provide a strong foundation to train the next generation of researchers including medical and other health professionals in nutrition.
The following are examples of nutrition research and training interests identified by NIH staff who attended the workshop.
The National Institute on Aging's nutrition research and training agenda focuses on dietary interventions that have the potential to modulate aging changes, delay or prevent the occurrence of chronic conditions, and promote healthy aging. The National Institute on Aging's GEMSSTAR program supports training of early career physician-/dentist-scientists in aging research and/or clinical care of older adults (including diet and nutrition) using the R03 grant mechanism. The Butler-Williams Scholars Program provides training opportunities for junior faculty and researchers to gain insight about research on aging from different perspectives, including health disparities and nutrition.
The National Cancer Institute (NCI) supports preclinical and clinical research and training that covers the full range of the cancer continuum, from prevention to end of life. In fiscal year 2017 the NCI funded 377 grants and cooperative agreements involving nutrition research totaling $117 million. There are currently no targeted nutrition training solicitation programs; however, the portfolio of projects includes several grants that provide support to investigators at different stages in their careers including educational (R25) and training grants (T32) and career awards (K). Nutrition training may be provided via other mechanisms within larger research center grants (e.g., P01s, P30s, P50s). Funding opportunity announcements are available through the NCI's Division of Cancer Prevention ( 90 ).
The NHLBI is the second largest NIH funder of nutrition research. It supports basic and mechanistic nutrition research, nutrition epidemiology and population science, clinical trials, and translational research. NHLBI support of nutrition research has ranged from $221 million/y to $239 million/y over the past 10 y. The NHLBI supports academic and professional training in nutrition research as well as the development of innovative nutrition education programs for medical students, residents, attending physicians, and other healthcare professionals. Nutrition research topics of interest to the NHLBI that could form the basis for training health professionals include research that identifies the mechanisms and risk factors associated with cardiovascular-related, pulmonary-related, and blood-related diseases, nutritional assessment, nutrition interventions, and translational research ( 91 ). Applicants may use any of the existing grant mechanisms, including Educational (R25), Training (T32, T35), or Research Project Grant (R01). It is important to talk with a program officer about current funding opportunities before applying for funds.
Other organizations such as the US Preventive Services Task Force recommend that primary care physicians intervene or refer patients for intensive behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease (CVD) prevention, specifically for adults who are overweight or obese and have additional CVD risk factors. They reviewed evidence that demonstrated the effectiveness of intensive behavioral counseling interventions that often combined diet and exercise and took from 2 to 10 h in helping patients make small but important changes in health behavior and improvements in other intermediate outcomes over 1–2 y. The Task Force noted gaps in the delivery of these counseling interventions in the real world and commented that many such programs require resources that are not yet available. They suggested additional dissemination and implementation research to put these recommendations into current primary care practice. These resources are needed at all levels of primary care training from undergraduate to fellowship level ( 92 ).
Ongoing Sustainability
Nutrition education, training, and research (basic, clinical epidemiological) is a dynamic process and the need to refine mechanisms, address validated assessment methods, and formulate new guidelines is ever evolving. Achievement of this major effort requires collaboration among existing governmental and nongovernmental organizations and institutions that include strong nutrition committees/working groups specializing in specific topic areas and who publish in those areas. A few examples included in this workshop are noted below.
The AHA model: CVD diet competencies with tools, training, assessment, and applications to AHA “Simple 7” goals
The AHA routinely updates reviews of nutrition research to formulate guidelines that can be used in patient care and public health efforts ( 93–95 ). The AHA has also developed and validated the “Life's Simple 7” goals that include interprofessional efforts to facilitate adherence to a healthy diet as well as nonsmoking, physical activity behaviors, and meeting risk factor goals for blood pressure and blood cholesterol ( 96 ). The AHA has also included medical and integrative nutrition education efforts to facilitate training at the UME, GME, and CME levels ( 97 ). Taking full advantage of these activities and leveraging them to help spread the word interprofessionally can augment and strengthen the updated efforts to standardize nutrition messages across all medical specialty areas.
ASN: development of a coordinating center
For >3 decades, ASN has been advocating and publishing, as an organization and in partnership with governmental and nongovernmental organizations, on the topic of medical nutrition, metabolism, and lifestyle education and training as well as the ethics of public–private partnerships. Although there are multiple efforts in the United States and abroad to educate and train healthcare professionals in nutrition and physical activity, these efforts vary in focus and quality, are largely uncoordinated and partially redundant, and in some cases, compete. In 2014 the ASN and the NHLBI published recommendations for remodeling nutrition education ( 4 , 5 , 7 , 98 ). Establishing a mechanism to coordinate the multiple stakeholders was identified as critical to advancing the medical nutrition education agenda.
Recently, the ASN Board approved an effort to seek funding to establish a coordinating center to guide the nutrition education of healthcare professionals. A planning committee defined the effort's scope, governance structure, and timeline, and completed a gap analysis. Over the past year, meetings have been held with key stakeholders including the AAMC, the LCME, governmental agencies, the National Board of Physician Nutrition Specialists, and groups that have successfully impacted medical education. Critical to advancing medical school education are:
- Coordination of resources to collect, centralize, and distribute multidisciplinary educational resources, credentialing resources, and practice and reimbursement resources.
- Community building to establish a network of key contacts at medical schools and medical and scientific organizations to increase organization of already available educational data, educational materials, examination questions, etc.
- Confirmation of objectives with stakeholders to define provider competencies for medical schools and EPAs for residence programs.
- Development of a career path through a recognized subspecialty in nutrition.
- Capacity building to train “nutrition ambassadors” to conduct and consult on educational programs for healthcare professionals within and outside of the United States.
- Research to identify and disseminate funding opportunities.
- Advocacy for education, legislation, and/or research funding.
The September 2017 NHLBI workshop attendees acknowledged the need for improved coordination to advance a broad-based educational effort including identifying strategies to assess improvements in patient care and outcomes from coordinated activities.
Throughout the United States and abroad, interprofessional education has become an important approach advocated by various leading medical groups. Registered dietitians, nurses, NPs, PAs, pharmacists, dental hygienists, exercise physiologists, and others can positively affect patient care by providing and/or reinforcing nutrition metabolism and lifestyle education ( 6 , 99 ). An effort to establish a coordinating center on medical nutrition, metabolism, and lifestyle education training and research is a precursor to a broader effort to collaborate on the education and training of all health professionals engaged in improving nutrition-related patient outcomes.
The proposed coordinating center will be directed by a leadership structure using multidisciplinary volunteers representing various medical and scientific societies. Optimally, all medical organizations concerned with nutrition (e.g., AHA, American Diabetes Association, American Academy of Pediatrics, American Gastroenterological Association, ASPEN, Academy of Nutrition and Dietetics, AAMC, IAMSE, and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition) will be engaged. The National Board of Physician Nutrition Specialists maintains credentialing standards for assessment and certification of physicians seeking recognition as a nutrition specialist. This group is committed to the education and training of nutrition faculty in medical schools and a critical partner in this effort. A proposed structure is displayed in Figure 2 .

Proposed leadership framework for an ASN-led coordinating center. 1 Recommendations from groups such as USMLE, AAMC, societies, etc. 2 Partners (e.g., foundations, nongovernmental organizations, government, scientific and medical societies, industry, individual donors). 3 Strategic planning team includes education leaders familiar with EPAs and nutrition curriculum, administrative personnel, etc. 4 Medical education research is overseen by ASN and partners. 5 With its partners, ASN coordinates committees to develop tools to guide medical curriculum development for undergraduate and graduate medical education (e.g., EPA competencies, objectives), which are critical for interprofessional nutrition education and practice. 6 ASN coordinates CME, mentoring, and implementation phase of projects with partners (e.g., CME, train-of-trainer, media, material links, mentoring, blog). AAMC, American Association of Medical Colleges; ASN, American Society for Nutrition; CME, continuing medical education; EPA, entrustable professional activity; GME, graduate medical education; UGME, undergraduate medical education; USMLE, US Medical Licensing Examination. Created by C.M. Lenders in cooperation with the ASN Nutrition Education in Professional Schools Committee.
Funding to establish this coordinating center is being sought from government, industry, and other public and private entities. ASN developed best practices for public–private partnerships involving governmental, nongovernmental, industry, and academic partners to address food and nutrition-related research challenges ( 100 ). Grant funding from governmental and nongovernmental organizations is proposed for outcomes-based research, education, and training in nutrition, metabolism, and lifestyles.
Conclusions and Next Steps
The workshop identified major avenues to advance the implementation of medical nutrition education in the United States and abroad, and to promote interprofessional nutrition education and better achieve a collaborative and complementary outcome. Consensus among workshop participants included the need for competency-based nutrition curricula, accreditation boards, integrative nutrition education across the health professions, and focus on selected NIH institutes’ interested in funding nutrition training. A collaborative leadership framework is proposed to guide the coordination of nutrition training within the United States.
The workshop underscored the need to develop, diversify, and sustain the scientific workforce by developing curricula and educational resources for healthcare providers. To achieve these efforts, the construct of a career path in nutrition that includes a board-approved medical subspecialty in nutrition is key to attracting faculty members who will build high-quality programs and trainees who want to follow their lead. This document is a resource for organizations with representation across various disciplines, including allopathic medicine, bioinformatics, dietetics/nutrition, family medicine, internal medicine, nursing, obesity and metabolic health, oral health, pediatrics, physical activity, population health, and surgery among others ( 101 ). Leaders from the NBME, the ACGME, the LCME, and other organizations are encouraged to collaborate in support for implementation of the proposed framework to enhance medical nutrition education, training, and research.
Acknowledgments
The authors’ responsibilities were as follows—LVH, CAP, CML: decided on content and wrote the manuscript; GT: supplied the figures; and all authors: contributed summaries of their workshop presentations and read and approved the final manuscript.
Presented at the Workshop, “Advancing Nutrition Training, and Research for Medical Students, Residents, Fellows, Attending Physicians and other Clinicians” held in Bethesda, Maryland, 7–8 September, 2017.
Supported by National Institutes of Health, National Heart, Lung, and Blood Institute, National Institutes of Health, Office of Dietary Supplements, National Institutes of Health, Office of Disease Prevention, American Society for Nutrition.
Author disclosures: CML: educational/research support at the time of this activity includes the New Balance Foundation, a public–private partnership (BUSM, BioQuest Global Solutions Pvt. Ltd, & Nutrition Nestle Institute–NNI), the Robert Wood Johnson Foundation, and the Boston Nutrition Obesity Research Center (P30 DK40561); RFK: currently on the Scientific Advisory Board for WW (formally Weight Watchers); EP: Co-Director of the Lifestyle Medicine Education Collaborative (LMEd), which has received program support from Ardmore Institute of Health, American Council on Exercise, Physicians Committee for Responsible Medicine, and Josiah Macy Jr Foundation; JLT: Co-Director of the Lifestyle Medicine Education Collaborative (LMEd), which has received program support from Ardmore Institute of Health, American Council on Exercise, Physicians Committee for Responsible Medicine, and Josiah Macy Jr Foundation. All other authors report no conflicts of interest.
Disclaimer: The content expressed in this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute, the National Institute of Aging, the National Cancer Institute, the National Institutes of Health, or the US Department of Health and Human Services.
Published in a supplement to Advances in Nutrition . The Guest Editors for this supplement were LVH, CML, and CAP, and each has no disclosures. Publication costs for this supplement were defrayed in part by the payment of page charges by the National Institutes of Health, Office of Disease Prevention, and the American Society for Nutrition. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Advances in Nutrition .
The Supplement Coordinators for the supplement publication were Charlotte A Pratt, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD 20892, USA, and Gwen Twillman, American Society for Nutrition, Rockville, MD 20850, USA. Both Supplement Coordinators have no disclosures.
Abbreviations used: AAMC, American Association of Medical Colleges; ACGME, Accreditation Council for Graduate Medical Education; APTA, American Physical Therapy Association; ASCN, American Society for Clinical Nutrition; ASN, American Society for Nutrition [renamed from American Society for Clinical Nutrition (ASCN)]; ASPEN, American Association for Parenteral and Enteral Nutrition; BUSM, Boston University School of Medicine; CME, continuing medical education; CVD, cardiovascular disease; DO, osteopathic physician; EPA, entrustable professional activity; GME, graduate medical education; IAMSE, International Association for Medical Science Educators; IOM, Institute of Medicine (now called the National Academy of Medicine); LCME, Liaison Committee on Medical Education; MD, Medical Doctor; NAA, Nutrition Academic Award; NBME, National Board of Medical Examiners; NCD, noncommunicable disease; NCI, National Cancer Institute; NHLBI, National Heart, Lung, and Blood Institute; NIM, Nutrition in Medicine; NNEdPro, Need for Nutrition Education/Innovation Program; NP, nurse practitioner; PA, physician assistant; PT, physical therapist; RD, Registered Dietitian; RDN, Registered Dietitian Nutritionist; SBME-DP, simulation-based medical education with deliberate practice; UME, undergraduate medical education; USMLE, United States Medical Licensing Examination.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Journal Proposal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Journal Menu
- Nutrients Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
- arrow_forward_ios Forthcoming issue arrow_forward_ios Current issue
- Vol. 16 (2024)
- Vol. 15 (2023)
- Vol. 14 (2022)
- Vol. 13 (2021)
- Vol. 12 (2020)
- Vol. 11 (2019)
- Vol. 10 (2018)
- Vol. 9 (2017)
- Vol. 8 (2016)
- Vol. 7 (2015)
- Vol. 6 (2014)
- Vol. 5 (2013)
- Vol. 4 (2012)
- Vol. 3 (2011)
- Vol. 2 (2010)
- Vol. 1 (2009)
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
Implications of Nutrition Education for Health, Behavior and Lifestyle
Special issue editors, special issue information, benefits of publishing in a special issue.
- Published Papers
A special issue of Nutrients (ISSN 2072-6643). This special issue belongs to the section " Nutritional Policies and Education for Health Promotion ".
Deadline for manuscript submissions: closed (31 May 2021) | Viewed by 70335
Share This Special Issue

Dear Colleagues,
According to the World Health Organization, nutrition is defined as “the intake of food in relation to the body’s dietary needs”. Malnutrition is an umbrella term used for over- and under-nutrition to reflect macronutrient intake, but recently the term “hidden hunger” has emerged to underline the importance of micronutrients in the diet. An adequate, well-balanced diet is a cornerstone of good health, has a great impact on wellbeing, and is reflected by dietary intake and behavior. Diet and behavior are highly modifiable factors that can help to prevent the emergence of new cases or ameliorate their progression. Nutrition education represents the main means for training individuals and groups on the principles of good nutrition, based on their needs, making nutrition information digestible and usable in everyday life.
Currently, a wide discrepancy exists in nutrition-related advice that originates from a wide range of different sources, many of which are unreliable and scientifically invalid, further underlining the need for fitting nutrition education.
Although health professionals play a different role in educating an individual in the clinic, the community, or a long-term healthcare facility, nutrition education is not fully integrated in the training programs of most healthcare professions. This partly explains the public’s considerable confusion on what is correct nutritional advice, which is exacerbated by the discrepancy.
The aim of this Special Issue is to publish original research articles and systematic reviews that report the design and implementation of nutrition education intervention programs and their effectiveness in terms of lifestyle, health, and wellbeing. More specifically, this Special Issue aims to bring together a selection of original research articles and reviews that showcase the latest evidence on the design of nutrition education programs that target individuals or groups at different life stages and of different health statuses and their effectiveness in promoting sustainable changes in diet, lifestyle, health, and wellbeing.
We welcome the submission of design and intervention studies as well as systematic reviews and meta-analyses from a wide range of related disciplines (e.g., human nutrition and dietetics, public health, epidemiology, health promotion, and non-communicable chronic diseases).
Prof. Dr. Antonis Zampelas Dr. George Moschonis Dr. Emmanuella Magriplis Guest Editors
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website . Once you are registered, click here to go to the submission form . Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Nutrients is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
- nutrition education
- dietary behavior
- dietary intervention
- healthy eating
- behavioral changes
- prevention of chronic diseases
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- e-Book format: Special Issues with more than 10 articles can be published as dedicated e-books, ensuring wide and rapid dissemination.
Further information on MDPI's Special Issue polices can be found here .
Published Papers (15 papers)
Jump to: Research , Review
Jump to: Editorial , Review
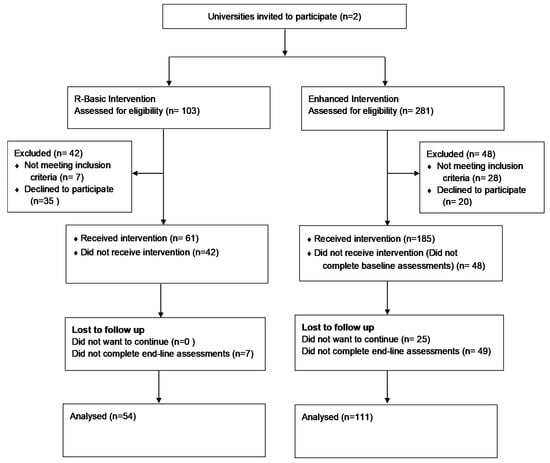
Graphical abstract
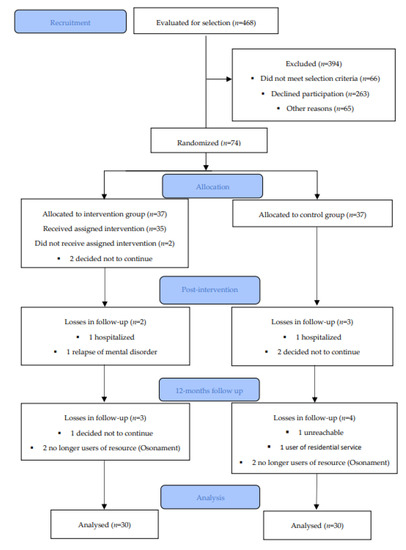
Jump to: Editorial , Research
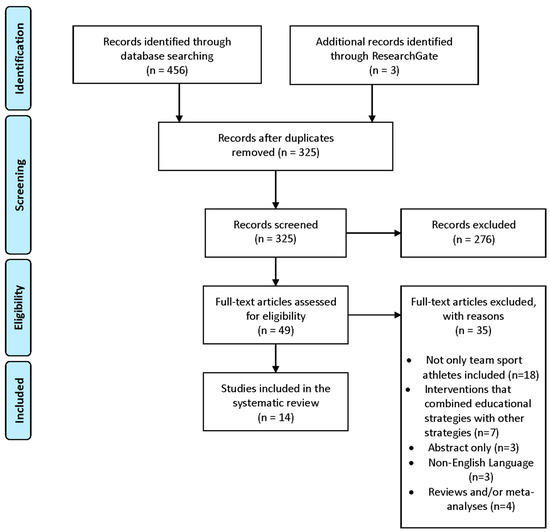
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Research article
- Open access
- Published: 12 February 2018
Why nutrition education is inadequate in the medical curriculum: a qualitative study of students’ perspectives on barriers and strategies
- Victor Mogre 1 , 2 ,
- Fred C. J. Stevens 2 ,
- Paul A. Aryee 3 ,
- Anthony Amalba 1 &
- Albert J. J. A. Scherpbier 2
BMC Medical Education volume 18 , Article number: 26 ( 2018 ) Cite this article
13k Accesses
70 Citations
33 Altmetric
Metrics details
The provision of nutrition care by doctors is important in promoting healthy dietary habits, and such interventions can lead to reductions in disease morbidity, mortality, and medical costs. However, medical students and doctors report inadequate nutrition education and preparedness during their training at school. Previous studies investigating the inadequacy of nutrition education have not sufficiently evaluated the perspectives of students. In this study, students’ perspectives on doctors’ role in nutrition care, perceived barriers, and strategies to improve nutrition educational experiences are explored.
A total of 23 undergraduate clinical level medical students at the 5th to final year in the School of Medicine and Health Sciences of the University for Development Studies in Ghana were purposefully selected to participate in semi-structured individual interviews. Students expressed their opinions and experiences regarding the inadequacy of nutrition education in the curriculum. Each interview was audio-recorded and later transcribed verbatim. Using the constant comparison method, key themes were identified from the data and analysis was done simultaneously with data collection.
Students opined that doctors have an important role to play in providing nutrition care to their patients. However, they felt their nutrition education was inadequate due to lack of priority for nutrition education, lack of faculty to provide nutrition education, poor application of nutrition science to clinical practice and poor collaboration with nutrition professionals. Students opined that their nutrition educational experiences will be improved if the following strategies were implemented: adoption of innovative teaching and learning strategies, early and comprehensive incorporation of nutrition as a theme throughout the curriculum, increasing awareness on the importance of nutrition education, reviewing and revision of the curriculum to incorporate nutrition, and involving nutrition/dietician specialists in medical education.
Though students considered nutrition care as an important role for doctors they felt incapacitated by non-prioritisation of nutrition education, lack of faculty for teaching of nutrition education, poor application of nutrition science and poor collaboration with nutrition professionals. Incorporation of nutrition as a theme in medical education, improving collaboration, advocacy and creating enabling environments for nutrition education could address some of the barriers to nutrition education.
Peer Review reports
There is ample evidence that nutrition interventions can decrease morbidity, mortality, human suffering, and medical costs [ 1 , 2 , 3 , 4 ]. Given the cost-effectiveness of disease prevention through nutrition over pharmacological treatment, the availability of practicing doctors with adequate knowledge, attitudes and skills in nutrition is very essential [ 5 ]. Studies have reported that if doctors gave nutrition advice to their patients the incidence of nutrition-related diseases will decline [ 6 , 7 ]. However, most doctors usually miss the opportunity to provide nutrition care to patients in the general practice setting and often refer patients to hospital dieticians or nutritionists, that is if these are available [ 8 , 9 ]. Research suggests that practicing doctors lack sufficient nutrition care competencies to provide dietary advice to their patients [ 10 , 11 , 12 , 13 , 14 , 15 ].
Indeed, there is an unfilled role for medical education in preparing doctors to provide nutrition care to patients [ 16 ]. Several studies investigating the situation of nutrition education in the medical curriculum have found both practicing doctors and medical students reporting inadequate nutrition education during medical school [ 14 , 17 , 18 , 19 , 20 , 21 ].
Several barriers to inadequate nutrition education have been reported largely in the form of symposiums, commentaries, essays and special articles [ 8 , 22 , 23 , 24 , 25 ]. Few studies have systematically investigated the issue [ 5 , 26 , 27 , 28 ]. These studies generally echo the perspectives of teachers or practicing doctors. A number of strategies to improving nutrition education in the medical curriculum have also been discussed by some of these studies [ 8 , 22 , 23 ]. However, the perspectives of students are unclear.
This is an important issue to investigate, as students are likely to bring unique and valuable perspectives on the inadequacy of nutrition education in their curriculum. Their views should be considered in efforts to improve nutrition education in the medical curriculum.
The study therefore aimed to explore students’ perceptions of doctors’ role in nutrition care, and barriers that prevent effective nutrition education and strategies that could potentially increase the effectiveness of nutrition education in the medical curriculum. The following research questions were investigated
What are the roles of doctors in the provision of nutrition care in the general practice setting?
Why is nutrition education inadequate in the medical curriculum?
How could nutrition education be improved in the medical curriculum?
Theoretical orientation
Our research was informed by two closely related theories [ 29 ]: social learning theory and social cognitive theory. Arguably, delivery of nutrition care by health care providers is a behaviour demonstrated in the social context of the workplace settings which is influenced by observing and modelling the behaviours, attitudes, and emotional reactions of others (e.g. superiors) [ 30 ]. Also embedded in our study is the social cognitive theory of learning which emphasizes how cognitive, behavioural, personal, and environmental factors interact to determine motivation and behaviour [ 31 ]. Nutrition education in the medical school setting is a learning process that is influenced by factors within the academic environment relating to the quantity, quality and nutrition content in the curriculum as well as the teaching and learning methods employed and the reinforcement experienced by the individual and by others.
Methodology
Our research is within the constructivists’ research paradigm. In constructivism, knowledge is socially constructed and realities are generated by the interaction of social, cultural and interpersonal factors [ 32 , 33 ]. Accordingly, there are multiple accounts of realities and meaning is realised through mutual interactions between the researcher and participants and the context of the research [ 34 ]. In this research approach, identification of the background and assumptions of the researcher and how they may influence the data collection and analysis is important and should be reflected upon by the researcher and shared with readers to facilitate interpretation of the research findings [ 35 , 36 ]. VM has a nutrition background and teaches in the medical school. His co-authors have significant experience in medical education (AJJA, FCJS), qualitative research (AJJA, FCJS), nutrition (PAA), pharmacology (AA) and also teach in the medical school (AJJA, FCJS, AA, PAA).
Setting, participants and procedures
We adopted a purposive sampling to select the study participants. All participants were selected from the University for Development Studies, School of Medicine and Health Sciences (UDS-SMHS), which runs a problem-based undergraduate medical curriculum. In the first 3 years, students are taken through the basic sciences using system-based blocks. The next year focuses on the learning of pathology and patho-physiology of diseases. Although students have some early patient encounters, the first 4 years are usually non-clinical (preclinical). In preparing students to qualify as doctors, the remaining 3 years focus on the clinical application of principles learned in the preclinical years and the creation of opportunities for students to learn from real patients at the hospital through departmental clinical rotations. The UDS-SMHS also runs a community-based education and service (COBES) programme in which students live, learn and provide service in rural communities of Ghana for a period of 4 weeks per year during year 2 to 4. It is during the preclinical years that majority of nutrition education is learned.
Our participants were therefore clinical level students, who had covered over 50% of the curriculum. Our choice of participants and sampling procedure was informed by our aim to select participants who will provide rich information [ 36 , 37 ] regarding nutrition education in the medical curriculum.
VM contacted all prospective participants through face-to-face meetings after usual lectures. During such meetings, the purpose of the study was explained and participants were also informed that the interview will be audio-recorded. They were assured of the confidentiality of the recordings. Participation was voluntary and both written and verbal informed consent was obtained from all participants who agreed to participate in the study. The institutional review board of the Navrongo Health Research Institute approved the research protocol.
Semi-structured interviews
All data was collected using semi-structured individual interviews. Semi-structured interviews are frequently used in healthcare and provide the researcher the opportunity to have guidance on areas to explore while allowing for some flexibility to enable discovery or elaboration [ 38 , 39 ]. All interviews were conducted by VM to ensure uniformity. Interviews were informed by open ended questions to explore values, attitudes, experiences, opinions, and behaviours of participants regarding nutrition education in the medical curriculum (See Appendix for interview guide). Interviews provided time and scope for participants to give detail and in depth about their opinions regarding nutrition education in the medical curriculum, allowing for their understanding and point of view rather than assuming generalizations. The questions were derived from the literature [ 27 , 40 ]. During the interviews VM probed and sought for clarification or elaboration of participants’ responses as needed. Opportunities were provided for participants to voice out unsolicited opinions and experiences.
The questions were evaluated by all members of the team who have varying levels of experience in qualitative research, medical education and nutrition. We pilot tested the semi-structured interviews on a group of 8 students to ensure clarity and understanding of the questions. During this process participants provided feedback regarding the structure of the questions and also identified areas that needed clarification. AA observed these pilot interview sessions, providing the opportunity to train and give feedback. The data generated from the pilot sessions were not included into the main data analysis.
Data analysis
All interviews were transcribed verbatim without identifying information by a trained research assistant, and entered into MAXQDA (version 12), a qualitative data analysis software. All subsequent data analyses were conducted using a comparative strategy [ 41 , 42 ]. Coding was performed by VM, who initially applied as many codes as needed for each transcript and inductively renamed, reorganised and redefined codes as required within categories. Another member of the team, AA went through the same process to evaluate VM’s categorisation. VM and AA then compared and discussed their findings until a consensus was achieved. Disagreements were resolved through discussions and adjudication by AA or FCJS if needed. To raise the analytic level from categorical to conceptual, axial coding was performed to identify dominating themes and to explore relationship among these themes. All members of the research team discussed the results of the analysis process until a consensus was established. Data collection and analysis were conducted simultaneously until thematic saturation was realised.
Twenty-three students participated in semi-structured interviews lasting 10 to 20 min each during the study period, July to September, 2015. This number was arrived at after the point of saturation and further data collection and/or analysis was unnecessary. Table 1 presents the demographic characteristics of the participants.
Four main themes emerged from the data: role of doctors in nutrition care, adequacy of nutrition education, barriers to nutrition education, and strategies to increase and improve nutrition education. Illustrative quotes are provided to substantiate each of these themes. Statements represent the views of students and not the authors.
Theme 1: The role of doctors and nutrition care
The majority of the students felt that doctors had an important role to play in providing nutrition care to patients although they recognised that nutritionists and dieticians were trained to perform such functions. They considered the role of the doctor to be one that is supportive or complementary to that of the nutritionist/dietician. The main roles identified by the students are shown in list 1.
List 1: Roles doctors could play in nutrition care
Nutrition advice/education
Supporting patients to follow healthful diets
Collaborating with nutritionists/dieticians
Monitoring progress of nutrition care
Nutrition diagnosis
Referring patients to nutritionists
Advocating for nutrition care
“They [doctors] should also play a part in the health education of the patient. So when they see a patient of any kind they have to advise them on their nutrition, diet and other behaviours that affect their nutrition and all of that.”
Students believed that the doctor should be the first to provide basic nutrition care and refer the patient to a nutritionist/dietician for specialised care if need be.
“When they [patients] come to the hospital, the doctor has the first encounter with them. The doctor could begin to provide nutrition care based on his/her minimal knowledge in nutrition. Then afterwards if he/she sees that there is still more to be done, then he/she can refer the patient to the nutritionist or the dietician who are specially trained to provide nutrition care.”
In order to assess whether medical students considered themselves to be responsible for the nutrition care of their patients when they become doctors, they were asked a hypothetical question about how they will react if a diabetic patient sought dietary advice from them in the general practice setting. All of the students said they will feel obligated and enthusiastic to provide such dietary advice to the patient.
“Oh I will feel happy to assist the patient. As such I will tell the patient the causes of diabetes and what to do to avoid [prevent] it. I will advise the patient to avoid excessive intake of sugar.”
Theme 2: Adequacy of nutrition education
Although students felt that nutrition care was important and felt obligated to provide it to patients, majority of them felt unconfident in their ability to provide such care to their patients.
“Well I think it is the right thing to find out how they [patients] manage their nutrition based on their condition. But looking at the kind of training that we [students] also have, you realize that much attention is not given to nutrition. So if a patient should ask me at this moment about nutritional status or let’s say about their nutritional situation, I might not feel adequate enough to answer.”
In addition, almost all the students considered the quality and quantity of their nutrition education to be inadequate.
“For me I think… even though we have done something very little concerning nutrition, it is as if we [students] have not done anything. We [students] have been given very little training when it comes to nutrition.”
It is thus unsurprising that students felt they required further education in nutrition although they were in the senior years of their medical education.
“I think there is more to be done because we [students] have not really had more lectures on it. We [students] have not been taken through a lot on nutrition; it is just a little bit of everything like small, small, small. So I think it would be better if we [students] are given more education on nutrition before we are able to come out.”
In order to gain more knowledge and skills in nutrition some students undertook self-directed learning and also consulted nutrition departments at the hospital on their own volition to acquire knowledge and skills in nutrition care.
“Because we [students] realized that our nutrition education was inadequate, when we [students] came here we had to go to the nutrition department to kind of like talk to them to take us through how they managed their [nutrition department] malnutrition cases”.
Theme 3: Barriers to adequate nutrition education
Students identified a number of barriers contributing to the inadequacy in their nutrition education. These barriers were classified into three subthemes: personal, interpersonal and environmental barriers as shown in Table 2 . In accordance with the descriptions of Williams et al. [ 43 ], personal barriers refers to factors related to the individual, whiles interpersonal barriers are attributable to relationship between two or more individuals. Contextual factors that may influence nutrition education are described as environmental barriers. Next we describe further some of these barriers.
Poor translation of nutrition science to clinical practice
Most students felt that the application of nutrition science to clinical practice was poor in most of the already limited nutrition lectures they received, especially during their preclinical training. The apparent lack of application of nutrition science to clinical practice made it difficult for them to appreciate the relationship between nutrition and health and to apply nutrition during their clinical training.
“Though at the preclinical level we [students] were given a little bit knowledge about nutrition it was not practical. It was like kind of raw information. You come here [clinical training] then you realize that there is no correlation. Not correlation as such but here [clinical training] you realize that it demands you to apply.”
Another student adds that “the practical aspect of nutrition education has not really been taught or we are not exposed to it”.
Perception that nutrition care is not the responsibility of doctors
Another important barrier identified by the students was the perception of faculty and curricula planners that nutrition care may not be the responsibility of doctors and as such did not see the need to include adequate content of nutrition education into the curriculum. According to the students, faculty and curricula planners considered nutrition care to be the role of nutritionists and thus the medical curriculum should concentrate on how to treat diseases.
“May be the authorities’ feel it’s not an essential part of medical training. I don’t know but that is the way I see it”.
“May be the focus of the whole medical training is more on treating diseases.”
“I think because there are nutritionist who are specially trained to provide nutrition care”.
Poor collaboration with nutrition professionals in medical education
Students were concerned that their nutrition education did not involve nutrition professionals thus presenting limited opportunities to collaborate to learn about nutrition. The poor collaboration made it difficult for them to appreciate the role of nutrition care in improving the clinical outcomes of patients and also do not foster inter-professional training to promote multidisciplinary care required in patient care.
“If there can be more integration. For instance when we [students] have cases that are nutrition related, it is still being managed by medical professionals and doctors. I mean once in a while dieticians come but it is like off record or something. So if those who are directly involved in the nutrition sector can be integrated more. May be it will help. But right now they are separated, nutrition is on one side and medicine is on the other. So maybe if there is a problem that will be the area it is.”
Students identified that nutrition professional were not involved in their training because they were not available i.e. they were in short supply.
Lack of priority for nutrition education
Majority of the students felt that the medical curriculum concentrates largely on anatomy, physiology and pathology with a little attention for nutrition. The students felt strongly that nutrition has not been given the needed attention and priority that it deserved.
“Like we have anatomy, physiology and the other basic sciences incorporated, we don’t actually have a course on nutrition incorporated into the courses that we do. I think that is the major issue”.
“It’s also because nutrition is not a priority in the medical program and hence have been given less attention.”
According to the students, the lack of priority for nutrition education has resulted in the limited contact hours allocated for nutrition, inadequate content for nutrition in the medical curriculum and poor integration of nutrition education as a theme throughout the entire medical curriculum.
Lack of faculty to teach nutrition
Students were also concerned about the lack of trained faculty to provide nutrition education.
“May be it could also be that we don’t have the people around to actually, I mean teach us or take us through nutrition.”
“I think sometimes the lecturers may not be available to give a lecture on that [nutrition].”
A number of students also felt that faculty does not have the needed knowledge and skills to provide students with the required nutrition education.
“May be I think it is….Because those taking you, they themselves they don’t have the clinical knowledge. It is like they just read raw nutrition [theoretical aspect of nutrition] and that’s how they also passed it on to you.”
Theme 4: Strategies to improve nutrition education
Having recognized the inadequacy of their nutrition education and the contributing barriers, students provided several important and insightful recommendations that could improve nutrition education.
Increase lectures, tutorials and self-study time for nutrition education
To increase the contact hours and nutrition content in the curriculum students suggested that more lecture topics on nutrition should be included into the curriculum.
“Not really as in a full course but may be some few lectures in nutrition. I don’t think we need so much but some few things that you need on the job that to help you, that is very important. I think that aspect could be incorporated into the training, it will help.”
Others also suggested that nutrition training could be improved by incorporating nutrition topics into their tutorials to promote self-directed learning.
“I think that we can also introduce them into our tutorial topics because sometimes for most of the students tutorials really help. You read a lot before you come so you can introduce some of them into our tutorial topics”.
Concerning the promotion of self-directed learning and to cater for the overcrowded curriculum, students suggested that articles on nutrition could be given to them to read to promote their understanding of nutrition concepts. The self-study time for students could also be increased to grant students the opportunity to read further on nutrition. In addition, students suggested the organization of symposiums on nutrition in which research papers in nutrition could be presented in order to increase their interest and understanding of nutrition.
“Well it’s very dicey because there is time issue and stuff. But if we could get articles or make symposiums where we can teach nutrition courses and make it lively because nutrition is kind of like difficult. So if we make it motivational they will be able to come out and get the knowledge about nutrition so that they can educate the people.”
Early incorporation of nutrition as a theme and throughout the entire curriculum
As evidenced by the following code, students felt that their knowledge and skills in nutrition could be improved if nutrition as a theme was incorporated early in their training and maintained throughout the entire curriculum.
“Looking at the early [preclinical] aspect of the training, they can incorporate nutrition subjects there, nutritional modules or topics and things like that especially at the very early aspects of it. So that people [students] will take interest in that and probably might grow their knowledge as they go along the PBL training.”
Increasing awareness on the importance of nutrition education in the medical curriculum
Some students opined that nutrition education will be improved if those in charge were educated on the importance and need for nutrition education. Students believed that if faculty and curriculum planners could be convinced of the fact that nutrition is an important role of the doctor, this might change their perception regarding nutrition and increase attention and priority for nutrition. An increase in attention and priority for nutrition education may result in an increase in the content and contact hours for nutrition.
“I think if they can realize that it is also very very important then they can increase the amount of time that is spent on that [nutrition education]”.
Reviewing and revision of the curriculum to incorporate nutrition
Students believed that for nutrition education to be improved there is the need for faculty and curriculum planners to review the entire curriculum to identify students nutrition educational needs and how and where those needs could be met and incorporated into the curriculum. Students recognised that such revisions could not be effected during their time in the medical school but could be beneficial to those in the succeeding years in medical school.
“That is what I previously stated that they should revise our curriculum and find a place to put nutrition so that at least we [students] will have knowledge about it. At least at this level I should have had enough knowledge about nutrition. So if they put it there those following us can benefit. Right now if they can add it to our curriculum, I think it will be enough.”
Involving nutrition/dietician specialists
Students opined that nutritionists or dieticians should be actively involved in their training. This should take the following forms:
Clinical sessions in which nutritionists/dieticians will present nutrition cases
Opportunities to consult nutritionist/dieticians for relevant nutrition topics/content
Including the nutrition department into clinical rotations
Seminars and lectures presented by nutritionists/dieticians
“It [nutrition education] should be added to the medical school’s curriculum and we [students] should actually...ehmm if they have a nutrition department, we should actually be exposed to nutrition” “Even in the hospital we [students] can have nutritionist being involved in our training on the ward especially when we [students] are managing patients so that we can have more time with the nutritionist”.
General discussion and doctors’ roles in nutrition care
Undergraduate clinical level medical students believed medical doctors have a responsibility to provide nutrition care to their patients in the general practice setting. They believe doctors’ role regarding nutrition care should be one of identifying patients in need of nutrition care, providing first line nutrition management, advocating nutrition care for patients, referring patients to nutritionists/dieticians for specialist care and reinforcing nutrition care provided by nutritionists/dieticians. These students felt their current nutrition education was inadequate due to barriers such as lack of priority for nutrition education, poor application of nutrition to clinical practice, an already overcrowded medical curriculum, lack of faculty trained in nutrition and poor collaboration with nutrition professionals in the teaching and learning of nutrition. Students recognised the need to increase awareness on the relevance and need for nutrition education in the medical curriculum among faculty and curriculum planners and to undertake a revision of the medical curriculum to identify nutrition educational needs and avenues to meet such needs as well as recognising the need to involve nutritionists/dieticians in their training.
Student’s views that medical doctors have an important role to play regarding nutrition care are similar to those expressed by medical educators, practicing doctors [ 27 , 44 ] and students [ 45 ] of previous studies from other parts of the world.
Barriers to nutrition education and suggested strategies
Consistent with previous findings, students were concerned that their nutrition education was inadequate [ 17 , 45 , 46 , 47 , 48 , 49 , 50 ].
Although an already overcrowded curriculum and inadequate contact hours/content for nutrition education were frequently described as barriers to effective nutrition education, some of the students believed that this was more an issue of low priority and attention for nutrition education. According to these students if nutrition was considered an important responsibility of the medical doctor, faculty and curriculum planners will find avenues within the curriculum to include nutrition. There is thus the need to increase faculty and curriculum planners’ awareness on the relevance and need for nutrition education in the medical curriculum.
Students’ suggestion of integrating nutrition as a theme throughout the entire curriculum to cater for barriers such as inadequate contact hours/content for nutrition and overcrowded curriculum is consistent with best practices for improving nutrition education [ 5 , 51 ]. Integration of nutrition as a theme in the medical curriculum has been shown to be effective in reducing students’ perception of the inadequacy of the amount of nutrition taught to them and improving nutrition clinical skills as assessed by Objectively Structured Clinical Examination (OSCE) scores [ 52 ]. The integration of nutrition as a theme throughout the curriculum should be comprehensive including the early stages of preclinical training up to clinical training and continued to postgraduate medical education [ 5 , 8 , 24 , 53 ].
Fundamental to the feasibility of integrating nutrition as a theme throughout the medical curriculum is the need to undertake a review of the entire curriculum. This provides opportunities to look into the formal and informal/hidden curriculum to identify gaps and avenues to integrate nutrition education and improve the learning environment [ 5 , 54 ].
Given that multidisciplinary teaching is a key focus of education guidelines for future health professionals [ 55 ] it is consistent that students’ recognized poor collaboration with nutrition and other health professionals in their nutrition education as an important barrier. The apparent poor collaboration may not give students the opportunity to realise the multidisciplinary nature of nutrition care [ 56 ] and will hinder inter-professional development and collaboration required for clinical care [ 57 ]. The identification and integration of nutrition content into the curriculum may also be hampered if nutrition professionals are not involved in the planning and development of the medical curricula. Collaborating with nutrition and other relevant health professionals has been found to be effective in improving the status of nutrition education in the medical curriculum [ 56 ]. Reflecting on the success of a nutrition education initiative at the University of Cambridge, Ball et al. [ 56 ] asserts that the multidisciplinary nature of the programme contributed to its success. The multidisciplinary team included medical practitioners, dieticians, nutritionists, and nurses in the delivery and evaluation of nutrition education sessions. This multidisciplinary nature was recognized at two levels: during the development of the intervention and implementation of the teaching and learning strategies of the intervention. This approach has also been widely encouraged by other institutions to model the contribution of health professionals in addressing nutrition in patient practice [ 58 , 59 ].
The students suggestion of providing them with nutrition articles and the organisation of nutrition symposiums and seminars to address the barriers of overcrowded and inadequate curriculum are widely accepted innovative teaching and learning strategies of improving nutrition education [ 60 , 61 ]. These strategies are more likely to be adopted by students and could result in improved nutrition education given that they perceive nutrition to be important to their future practice as medical doctors.
The lack of faculty for nutrition education is an important barrier that has been identified in previous findings [ 5 , 8 , 24 ]. Closely linked to this barrier is faculty’s lack of interest in nutrition education. These barriers are fundamental to the effectiveness of nutrition education in the sense that if faculty trained in nutrition are lacking, increases in contact hours and nutrition content and integration of nutrition as a theme in the curriculum may not yield the needed results. The availability of faculty trained in nutrition may facilitate identification of appropriate nutrition content, coordination of teaching and learning activities in nutrition, promotion of active participation in nutrition education activities by both faculty and students, translation of nutrition science to clinical practice, and promotion of role modelling of nutrition care at the hospital [ 52 , 61 , 62 , 63 , 64 ].
Strengths and limitations
This is the first study to qualitatively explore students’ perceptions of nutrition education, barriers and strategies as far as we know. It adds to the existing literature that nutrition education is inadequate and several barriers are contributing to the current situation. Also, the findings identify a number of strategies that could be relied upon to improve nutrition education. An important novelty of the methods of this study is the reliance on students’ perspectives that hitherto may not be considered as obvious sources of information regarding this topic. The students provided important barriers and strategies that are comparable to those reported by medical educators and practicing doctors. It is yet additional evidence supporting the widely accepted recognition of students as important stakeholders of the curriculum who could be relied upon to improve the learning environment.
This study is not without limitations. Our adoption of non-probability and convenience sampling may result in the recruitment of students with an interest in nutrition, generating a potential source of sampling bias. However, this potential bias can be described as a strength rather than a limitation in qualitative research that propagates for the collection of data from individuals considered as rich sources of information [ 27 ]. We recruited students from only one medical school, thus limiting the generalizability of our findings. The opinions expressed by these students, only grant one aspect of the situation of nutrition education in the medical curriculum and may be insufficient in providing a holistic and complete understanding of the situation. Nevertheless, following a constructivists approach, that aims to develop a comprehensive understanding of the situation of nutrition education, their opinions are valuable insights. As a measure to reduce interviewer’ bias that may influence students’ opinions during the semi-structured interviews, we limited the interviews to questions and clarifications, where necessary and avoided expression of interviewer opinion. Our study explored students’ opinions regarding nutrition education but did not evaluate whether improving nutrition education will result in improved nutrition practice behaviour or enhance clinical outcomes.
Implications and future research
The findings of this study provide data that could inform the planning and design of educational interventions to improve nutrition education. Future studies should investigate whether the removal of the identified barriers could result in improved nutrition education. It will be important for studies to evaluate the effectiveness of the strategies suggested by the students to improve nutrition education in the medical curriculum. In addition, future studies should investigate the influence of improved nutrition education on nutrition practice behaviour in the clinical setting.
Students perceived nutrition care to be an important role and responsibility of medical doctors. They considered their current nutrition education to be inadequate due to personal, interpersonal and environmental barriers. A number of important strategies have been suggested by these students including incorporation of nutrition as a theme in the medical curriculum, collaboration, and advocacy and creating enabling environments for nutrition education.
Abbreviations
and UDS-SMHS
University for Development Studies, School of Medicine and Health Sciences
Navrongo Health Research Centre Institutional Review Board
Problem-based learning/Community-based Education and Service
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the national VA surgical risk study. Arch Surg. 1999;134:36–42.
Article Google Scholar
Halsted CH. Clinical nutrition education - relevance and role models. Am J Clin Nutr. 1998;67:192–6.
Montgomery DL, Splett PL. Economic benefit of breast-feeding infants enrolled in WIC. J Am Diet Assoc. 1997;97:379–85.
van Weel C. Morbidity in family medicine: the potential for individual nutritional counseling, an analysis from the Nijmegen continuous morbidity registration. Am J Clin Nutr. 1997;65:1928S–32S.
St Jeor ST, Krenkel JA, Plodkowski RA, Veach TL, Tolles RL, Kimmel JH. Medical nutrition: a comprehensive, school-wide curriculum review. Am J Clin Nutr. 2006;83:963S–7S.
Google Scholar
Eckel R, Jakicic J, Ard J, Miller N, Hubbard V, Nonas C, de Jesus J, Sacks F, Lee I, Lichtenstein A. AHAe/ACC guideline on lifestyle management to reduce cardiovascular risk. A report of the ACC/AHA task force on Practiceguideline. Circulation. 2013;63:1524–4539.
Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Rep. 2012;61:1–52.
Kris-Etherton PM, Akabas SR, Bales CW, Bistrian B, Braun L, Edwards MS, Laur C, Lenders CM, Levy MD, Palmer CA. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am J Clin Nutr. 2014;99:1153S–66S.
Wynn K, Trudeau JD, Taunton K, Gowans M, Scott I. Nutrition in primary care: current practices, attitudes, and barriers. Can Fam Physician. 2010;56:e109–16.
Tziraki C, Graubard BI, Manley M, Kosary C, Moler JE, Edwards BK. Effect of training on adoption of cancer prevention nutrition-related activities by primary care practices: results of a randomized, controlled study. J Gen Intern Med. 2000;15:155–62.
Glanz K, Gilboy MB. Physicians, preventive care, and applied nutrition: selected literature. Acad Med. 1992;67:776–81.
Krause T, Fox H. Nutritional knowledge and attitudes of physicians. J Am Diet Assoc. 1977;70:607–9.
Soltesz KS, Price JH, Johnson LW, Telljohann SK. Perceptions and practices of family physicians regarding diet and cancer. Am J Prev Med. 1994;11:197–204.
Crowley J, Ball L, Han DY, Arroll B, Leveritt M, New Zealand WC. Medical students have positive attitudes and moderate confidence in providing nutrition care: a cross-sectional survey. J Biomed Educ. 2014.
Winick M. Nutrition education in medical schools. Am J Clin Nutr. 1993;58:825–7.
Chisholm A, Mann K, Peters S, Hart J. Are medical educators following general medical council guidelines on obesity education: if not why not? BMC Med Educ. 2013;13:53.
Mihalynuk TV, Coombs JB, Rosenfeld ME, Scott CS, Knopp RH. Survey correlations: proficiency and adequacy of nutrition training of medical students. J Am Coll Nutr. 2008;27:59–64.
Adams KM, Lindell KC, Kohlmeier M, Zeisel SH. Status of nutrition education in medical schools. Am J Clin Nutr. 2006;83:941S–4S.
Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine: nutrition education for medical students and residents. Nutr Clin Prac. 2010;25:471–80.
Chung M, van Buul V, Wilms E, Nellessen N, Brouns F. Nutrition education in European medical schools: results of an international survey. Eur J Clin Nutr. 2014;68:844–6.
Gramlich LM, Olstad DL, Nasser R, Goonewardene L, Raman M, Innis S, Wicklum S, Duerksen D, Rashid M, Heyland D. Medical students' perceptions of nutrition education in Canadian universities. Appl Physiol Nutr Metab. 2010;35:336–43.
Schulman J. Nutrition education in medical schools: trends and implications for health educators. Med Educ Online. 1999;4:4307.
Walker WA. Innovative teaching strategies for training physicians in clinical nutrition: an overview. J Nutr. 2003;133:541S–3S.
Touger-Decker R. Nutrition education of medical and dental students: innovation through curriculum integration. Am J Clin Nutr. 2004;79:198–203.
Intersociety Professional Nutrition Education Consortium. Bringing physician nutrition specialists into the mainstream: rationale for the intersociety professional nutrition education consortium. Am J Clin Nutr. 1998;68:894–8.
Levine BS, Wigren MM, Chapman DS, Kerner J, Bergman R, Rivlin R. A national survey of attitudes and practices of primary-care physicians relating to nutrition: strategies for enhancing the use of clinical nutrition in medical practice. Am J Clin Nutr. 1993;57:115–9.
Ball LE, Hughes RM, Leveritt MD. Nutrition in general practice: role and workforce preparation expectations of medical educators. Aust J Prim Health. 2010;16:304–10.
Wong V, Millen BE, Geller AC, Rogers AE, Maury J-J, Prout MN. What's in store for medical students? Awareness and utilization of expert nutrition guidelines among medical school preceptors. Prev Med. 2004;39:753–9.
Mogre V, Scherpbier A, Dornan T, Stevens F, Aryee PA, Cherry MG. A realist review of educational interventions to improve the delivery of nutrition care by doctors and future doctors. Syst Rev. 2014;3:148.
Bandura A, McClelland DC. Social learning theory. Oxford: Prentice Hall; 1977.
Crothers LM, Hughes TL, Theory MKA. Cases in school-based consultation: a resource for school psychologists, school counselors, special educators, and other mental health professionals. Boca Raton: CRC Press; 2008.
Guba EG, Lincoln YS. Competing paradigms in qualitative research. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. London: Sage; 1994. p. 105–17.
Crotty M. The foundations of social research: meaning and perspective in the research process. London: Thousand Oaks, Sage Publications; 1998.
McLellan L, Yardley S, Norris B, de Bruin A, Tully MP, Preparing DT. To prescribe: how do clerkship students learn in the midst of complexity? Adv Health Sci Educ Theory Pract. 2015;20:1339–54.
Mills J, Bonner A, Francis K. The development of constructivist grounded theory. Int J Qual Methods. 2006;5:25–35.
Watling C, Driessen E, Vleuten CP, Vanstone M, Music LL. Lessons: revealing medicine's learning culture through a comparison with that of music. Med Educ. 2013;47:842–50.
Watling CJ, Grounded LL. Theory in medical education research: AMEE guide no. 70. Med. Teacher. 2012;34:850–61.
Gill P, Stewart K, Treasure E, Chadwick B. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J. 2008;204:291–5.
Britten N. Qualitative research: qualitative interviews in medical research. BMJ. 1995;311:251–3.
Martin L. De van der Schueren MA, Blauwhoff-Buskermolen S, Baracos V, Gramlich L. identifying the barriers and enablers to nutrition care in head and neck and esophageal cancers: an international qualitative study. JPEN J Parenter Enteral Nutr. 2016;40:355–66.
Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd ed. London: Thousand Oaks, Sage Publications; 2008.
Book Google Scholar
Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: Thousand Oaks, Sage Publications; 2006.
Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83:257–64.
Crowley J, Ball L, Han DY, McGill A-T, Arroll B, Leveritt M, Wall C. Doctors' attitudes and confidence towards providing nutrition care in practice: comparison of New Zealand medical students, general practice registrars and general practitioners. J Prim Health Care. 2015;7:244–50.
Crowley J, Ball L, Han DY, Arroll B, Leveritt M, Wall C. New Zealand medical students have positive attitudes and moderate confidence in providing nutrition care: a cross-sectional survey. J Biomed Educ. 2015:259653.
Spencer EH, Frank E, Elon LK, Hertzberg VS, Serdula MK, Predictors GDA. Of nutrition counseling behaviors and attitudes in US medical students. Am J Clin Nutr. 2006;84:655–62.
Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in US medical schools: latest update of a national survey. Acad Med. 2010;85:1537–42.
Walker WA. Advances in nutrition education for medical students - overview. Am J Clin Nutr. 2000;72:865S–7S.
Weinsier RL, Boker JR, Feldman EB, Read MS, Brooks CM. Nutrition knowledge of senior medical students: a collaborative study of southeastern medical schools. Am J Clin Nutr. 1986;43:959–68.
Hyska J, Mersini E, Mone I, Bushi E, Sadiku E, Hoti K, Bregu A. Assessment of knowledge, attitudes and practices about public health nutrition among students of the University of Medicine in Tirana, Albania. SEEJPH. 2015;1:1.
Lo C. Integrating nutrition as a theme throughout the medical school curriculum. Am J Clin Nutri 2000;72:882s-889s.
Taren DL, Thomson CA, Koff NA, Gordon PR, Marian MJ, Bassford TL, Fulginiti JV, Ritenbaugh CK. Effect of an integrated nutrition curriculum on medical education, student clinical performance, and student perception of medical-nutrition training. Am J Clin Nutr. 2001;73:1107–12.
Krebs NF, Primak LE. Comprehensive integration of nutrition into medical training. Am J Cli Nutr. 2006;83:945S–50S.
Hafferty FW. Beyond curriculum reform: confronting medicine's hidden curriculum. Acad Med. 1998;73:403–7.
Hughes L. Creating an interprofessional workforce: an education and training framework for health and social care in England. London: Dept of Health/CAIPE; 2007.
Ball L, Crowley J, Laur C, Rajput-Ray M, Gillam S, Ray S. Nutrition in medical education: reflections from an initiative at the University of Cambridge. J Multidiscip Healthc. 2014;7:209.
Bridges DR, Davidson RA, Odegard PS, Maki IV, Tomkowiak J. Interprofessional collaboration: three best practice models of interprofessional education. Med Educ online. 2011;16:16.
Friedman G, Kushner R, Alger-Mayer S, Bistrian B, Gramlich L, Marik PE. Proposal for medical school nutrition education topics and recommendations. JPEN J Parenter Enteral Nutr. 2010;34:40S–6S.
Pearson TA, Stone EJ, Grundy SM, McBride PE, Van Horn L, Tobin BW. Translation of nutritional sciences into medical education: the nutrition academic award program. Am J Clin Nutr. 2001;74:164–70.
Hillenbrand KM, Larsen PG. Effect of an educational intervention about breastfeeding on the knowledge, confidence, and behaviors of pediatric resident physicians. Pediatrics. 2002;110:e59.
Mogre V, Scherpbier AJ, Stevens F, Aryee P, Cherry MG, Dornan T. Realist synthesis of educational interventions to improve nutrition care competencies and delivery by doctors and other healthcare professionals. BMJ Open. 2016;6:e010084.
Buchowski MS, Plaisted C, Fort J, Zeisel SH. Computer-assisted teaching of nutritional anemias and diabetes to first-year medical students. Am J Clin Nutr. 2002;75:154–61.
Maiburg BHJ, Rethans JE, Schuwirth LWT, Mathus-Vliegen LMH, van Ree JW. Controlled trial of effect of computer-based nutrition course on knowledge and practice of general practitioner trainees. Am J Clin Nutr. 2003;77:1019S–24.
Carson JAS, Gillham MB, Kirk LM, Reddy ST, Battles JB. Enhancing self-efficacy and patient care with cardiovascular nutrition eduction. Am J Prev Med. 2002;23:296–302.
Download references
Acknowledgements
Authors wish to thank all students who agreed and consented to participate in the study. In addition, authors wish to acknowledge the efforts of Kwaku Appiah-Kubi of the Department of Applied Biology of the University for Development Studies for his assistance in editing the English language of the manuscript.
Not applicable
Availability of data and materials
Data is available upon request from the corresponding author.
Author information
Authors and affiliations.
Department of Health Professions Education and Innovative Learning, School of Medicine and Health Sciences, University for Development Studies, P. O. Box TL, 1883, Tamale, Ghana
Victor Mogre & Anthony Amalba
School of Health Professions Education, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, The Netherlands
Victor Mogre, Fred C. J. Stevens & Albert J. J. A. Scherpbier
Department of Nutritional Sciences, School of Allied Health Sciences, University for Development Studies, Tamale, Ghana
Paul A. Aryee
You can also search for this author in PubMed Google Scholar
Contributions
VM conceived and designed the study; collected and performed data analysis and interpretation, and drafting of manuscript. FCJS, PAA, AA and AJJAS jointly undertook critical revision of the manuscript. All authors approved the manuscript for publication.
Corresponding author
Correspondence to Victor Mogre .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was granted by the Navrongo Health Research Centre Institutional Review Board (NHRCIRB) (Ethics Approval ID: NHRCIRB209), Ghana. Students gave a written consent prior to participating in the study. The data was handled in an anonymously and confidentially. Participation was voluntary and both written and verbal informed consent was obtained from all participants who agreed to participate in the study.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Interview guide
- Medical students
What is your level in medical school?
In your opinion, what is the role of doctors in providing nutrition care in the general practice setting?
In your opinion, which professionals have a role in giving nutrition care to patients? Probe further for reasons.
How would you feel if a patient suffering from diabetes asked you for nutrition advice in the general practice setting?
Could you tell me your experience of patients requesting for nutrition advice in the general practice?
In what ways might patient care be affected if all doctors were able to give nutrition advice for routine care?
How will you describe the status of nutrition education in your medical curriculum? Probe further
In what ways have you learned about nutrition, if at all? Probe further
What is responsible for the current status of nutrition in your medical curriculum? Probe further
In what ways do you think your medical program needs improvement in nutrition? Probe further
In what ways could nutrition be improved in your medical program? Probe further
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Mogre, V., Stevens, F.C.J., Aryee, P.A. et al. Why nutrition education is inadequate in the medical curriculum: a qualitative study of students’ perspectives on barriers and strategies. BMC Med Educ 18 , 26 (2018). https://doi.org/10.1186/s12909-018-1130-5
Download citation
Received : 11 February 2017
Accepted : 24 January 2018
Published : 12 February 2018
DOI : https://doi.org/10.1186/s12909-018-1130-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nutrition education
- Qualitative research
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
| Property | Value |
|---|---|
| Status | |
| Version | |
| Ad File | |
| Disable Ads Flag | |
| Environment | |
| Moat Init | |
| Moat Ready | |
| Contextual Ready | |
| Contextual URL | |
| Contextual Initial Segments | |
| Contextual Used Segments | |
| AdUnit | |
| SubAdUnit | |
| Custom Targeting | |
| Ad Events | |
| Invalid Ad Sizes |

- Submit Member Login
Access provided by
Strengthening Nutrition Education and Behavior Research for Academicians and Practitioners
- Karen Chapman-Novakofski
Download started
- Add to Mendeley
- nutrition education
- behavioral research
- nutrition training

Get full text access
Log in, subscribe or purchase for full access.
Article metrics
Related articles.
- Download Hi-res image
- Download .PPT
- Access for Developing Countries
- Articles & Issues
- Articles In Press
- Current Issue
- List of Issues
- Supplements
- For Authors
- Author Guidelines
- Submit Your Manuscript
- Statistical Methods
- Guidelines for Authors of Educational Material Reviews
- Permission to Reuse
- About Open Access
- Researcher Academy
- For Reviewers
- General Guidelines
- Methods Paper Guidelines
- Qualitative Guidelines
- Quantitative Guidelines
- Questionnaire Methods Guidelines
- Statistical Methods Guidelines
- Systematic Review Guidelines
- Perspective Guidelines
- GEM Reviewing Guidelines
- Journal Info
- About the Journal
- Disclosures
- Abstracting/Indexing
- Impact/Metrics
- Contact Information
- Editorial Staff and Board
- Info for Advertisers
- Member Access Instructions
- New Content Alerts
- Sponsored Supplements
- Statistical Reviewers
- Reviewer Appreciation
- New Resources
- New Resources for Nutrition Educators
- Submit New Resources for Review
- Guidelines for Writing Reviews of New Resources for Nutrition Educators
- Podcast/Webinars
- New Resources Podcasts
- Press Release & Other Podcasts
- Collections
- Society News
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

Society Member Access
SNEB Members, full access to the journal is a member benefit. Login via the SNEB Website to access all journal content and features.
- Institutional Access: Log in to ScienceDirect
- Existing Subscriber: Log in
- New Subscriber: Claim access with activation code. New subscribers select Claim to enter your activation code.
Academic & Personal
Corporate r&d professionals.
- Full online access to your subscription and archive of back issues
- Table of Contents alerts
- Access to all multimedia content, e.g. podcasts, videos, slides

IMAGES
VIDEO
COMMENTS
Despite research showing that schools can make a positive impact on children's nutritional outcomes, it is also reported that schools and teaching staff note many barriers that restrict nutritional education programming and delivery. First, nutrition education is often seen as unnecessary because the content is not included on standardized tests.
The Journal of Nutrition Education and Behavior has a special interest in research related to Nutrition Literacy, Nutrition Education Programs, Nutrition Education and Psychosocial Correlates, and Technology in Nutrition Education and Behavior. View all calls for papers for special issues.
The Journal of Nutrition Education and Behavior (JNEB), the official peer-reviewed journal of the Society for Nutrition Education and Behavior Opens in new window , since 1969, serves as a global resource to advance nutrition education and behavior related research, practice, and policy. JNEB publishes original research, as well as papers ...
Materials and Methods. Articles were identified through relevant databases (i.e., Medline, Science Direct, CINAHL [EBSCOhost], and Google Scholar) from 1990 until 2011 using the following keywords: nutrition education, effectiveness, college/university students, and dietary habits.. The keyword-based screening strategy alone generated 52 articles, but only 14 met the specified inclusion ...
The aim of the Nutrients Special Issue "Implications of Nutrition Education, for Health, Behavior, and Lifestyle" is to publish original research articles and reviews that report the design and implementation of nutrition education intervention programs and their effectiveness in terms of lifestyle, health, and wellbeing. The importance of exploring this field in depth is highlighted in ...
Quantitative nutrition education research assists nutrition educators first, by helping them understand the factors that influence dietary behavior, and second, by providing a systematic method of investigating the most effective methods for influencing dietary behavior to promote health. This paper discusses four broad categories of factors influencing dietary behavior: physiological factors ...
Education. Food and nutrition education has a critical role in enabling access to sufficient quality and quantity of foods for households and communities. Educational seminars and resources in food and nutrition have been shown to positively affect individuals' food choices. Nutrition and food systems education can be focused on a number of ...
An analysis of the evidence from 300+ studies shows that nutrition education is more likely to be effective when it focuses on behaviour/ action (rather than knowledge only) and systematically links theory, research and practice. There are three essential components to nutrition education: 1. A motivational component, where the goal is to ...
The need for evidence-based, outcomes-driven nutrition education programming has never been more important, as it is central to improving well-being and reducing the risk of chronic disease, obesity, and malnutrition worldwide. 2-6 In the context of this position paper and its associated competencies, SNEB—an organization specifically dedicated to advancing the field of nutrition education ...
Research articles were evaluated using the PICOS (Population, Intervention, Comparators, Outcome, and Study design) model . 21 The following inclusion criteria were applied: (1) studies were published between 2009 and 2016, (2) publications were available in English, and (3) articles described nutrition education interventions conducted among ...
We reviewed the available research and gave an overview of the effects of nutrition education interventions (NEIs) on medical students' and residents' knowledge of nutrition, attitudes towards nutrition care, self-efficacy, dietary practices and readiness to offer nutrition care.
DISCUSSION Describing Nutrition Education Researchers. In general, NEB researchers hold postbaccalaureate degrees. 9, 10, 11 Not only are they employed in academic settings, NEB researchers work within public health, health care, governmental, and nongovernmental organizations, not-for-profit entities and the private sector. 9, 10, 11 There is no 1 uniform curriculum for training the nutrition ...
Aims & Scope. The Journal of Nutrition Education and Behavior (JNEB), the official peer-reviewed journal of the Society for Nutrition Education and Behavior, since 1969, serves as a global resource to advance nutrition education and behavior related research, practice, and policy. JNEB publishes original research, as well as papers focused on ...
To evaluate the effectiveness of nutrition education for the public. More specifically, to address two key questions: (1) Does nutrition education work? If so, what are the successful elements across interventions? (2) What are the implications of the findings for nutrition education programme implementation, research, and policy?
Background Well-designed research trials are critical for determining the efficacy and effectiveness of nutrition education interventions. To determine whether behavioral and/or cognition changes can be attributed to an intervention, the experimental design must include a control or comparison condition against which outcomes from the experimental group can be compared. Despite the impact ...
A scoping review was conducted utilizing PubMed, Cochrane Library and CINAHL to identify research articles from 2009 to 2024, resulting in 2568 articles total. Inclusion criteria consisted of a middle school population, primary research, and measured outcomes of nutrition knowledge or nutrition-related behaviors.
Philadelphia, September 11, 2023 - Research published in the Journal of Nutrition Education and Behavior determined the effect of Food Sensations for Adults on food literacy behaviors and selected dietary behaviors. Determining the Effectiveness of an Adult Food Literacy Program Using a Matched Control Group.
The article by DiMaria-Ghalili et al describes the importance of implementing nutrition across the continuum of medical and health profession education, training, and research. The article presents opportunities and challenges that confront the individual health care professions and highlights the need for the development of interprofessional ...
Nutrition education, training, and research (basic, clinical epidemiological) is a dynamic process and the need to refine mechanisms, address validated assessment methods, and formulate new guidelines is ever evolving. Achievement of this major effort requires collaboration among existing governmental and nongovernmental organizations and ...
Nutrition education represents the main means for training individuals and groups on the principles of good nutrition, based on their needs, making nutrition information digestible and usable in everyday life. ... Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract ...
Full length article Volume 124, Supplement 9 1820S-1822S September 1994. Community-Based Nutrition Education 1. Janet Usinger-Lesquereux. Presented at the "W.O. Atwater Centennial Celebration Symposium" held June 2-4, 1993 in Washington, D.C. The symposium was sponsored by the U.S. Department of Agriculture, the International Life Sciences ...
Nutrition education is any combination of educational strategies, accompanied by environmental supports, designed to facilitate voluntary adoption of food choices and other food- and nutrition-related behaviors conducive to health and well-being. Nutrition education is delivered through multiple venues and involves activities at the individual ...
Background The provision of nutrition care by doctors is important in promoting healthy dietary habits, and such interventions can lead to reductions in disease morbidity, mortality, and medical costs. However, medical students and doctors report inadequate nutrition education and preparedness during their training at school. Previous studies investigating the inadequacy of nutrition education ...
Materials and methods. The journal list for this review was obtained from SCImago Journal Rankings, in the category "Nutrition and Dietetics" for the most recent complete year, 2022 (SCImago Citation 2024).The SCImago Journal Rank (SJR) indicator is a journal size-independent indicator of scientific journal prestige, which accounts for both the number of citations received by a journal and ...
Nutrition education and behavior research is essential for translating scientific nutrition-related evidence into actionable strategies at the individual, family, community, and policy levels. To enhance the impact of nutrition educators and researchers' efforts, there is a need for continued and directed support to sustain the rigor of research. It is the perspective of this paper that the ...