- Open access
- Published: 01 May 2022

Interventions in hypertension: systematic review and meta-analysis of natural and quasi-experiments
- Tong Xia ORCID: orcid.org/0000-0001-7136-8361 1 ,
- Fan Zhao ORCID: orcid.org/0000-0002-1261-5841 1 &
- Roch A. Nianogo ORCID: orcid.org/0000-0001-5932-6169 1 , 2
Clinical Hypertension volume 28 , Article number: 13 ( 2022 ) Cite this article
9418 Accesses
12 Citations
3 Altmetric
Metrics details
Hypertension is an urgent public health problem. Consistent summary from natural and quasi-experiments employed to evaluate interventions that aim at preventing or controlling hypertension is lacking in the current literature. This study aims to summarize the evidence from natural and quasi-experiments that evaluated interventions used to prevent or control hypertension.
We searched PubMed, Embase and Web of Science for natural and quasi-experiments evaluating interventions used to prevent hypertension, improve blood pressure control or reduce blood pressure levels from January 2008 to November 2018. Descriptions of studies and interventions were systematically summarized, and a meta-analysis was conducted.
Thirty studies were identified, and all used quasi-experimental designs including a difference-in-difference, a pre-post with a control group or a propensity score matching design. Education and counseling on lifestyle modifications such as promoting physical activity (PA), promoting a healthy diet and smoking cessation consultations could help prevent hypertension in healthy people. The use of computerized clinical practice guidelines by general practitioners, education and management of hypertension, the screening for cardiovascular disease (CVD) goals and referral could help improve hypertension control in patients with hypertension. The educating and counseling on PA and diet, the monitoring of patients’ metabolic factors and chronic diseases, the combination of education on lifestyles with management of hypertension, the screening for economic risk factors, medical needs, and CVD risk factors and referral all could help reduce blood pressure. In the meta-analysis, the largest reduction in blood pressure was seen for interventions which combined education, counseling and management strategies: weighted mean difference in systolic blood pressure was − 5.34 mmHg (95% confidence interval [CI], − 7.35 to − 3.33) and in diastolic blood pressure was − 3.23 mmHg (95% CI, − 5.51 to − 0.96).
Conclusions
Interventions that used education and counseling strategies; those that used management strategies; those that used combined education, counseling and management strategies and those that used screening and referral strategies were beneficial in preventing, controlling hypertension and reducing blood pressure levels. The combination of education, counseling and management strategies appeared to be the most beneficial intervention to reduce blood pressure levels.
Cardiovascular diseases (CVD) represent the leading cause of death, accounting for one in three deaths in the United States (US) and worldwide [ 1 , 2 , 3 ]. One of their most potent risk factors, hypertension (also known as high blood pressure), is a common risk factor for CVD [ 3 , 4 ]. Approximately 40% of adults aged 25 and over had elevated blood pressure in 2008 [ 3 ]. What is more, hypertension is responsible for at least 45% of deaths due to heart diseases and 51% of deaths due to stroke worldwide [ 3 , 4 ]. In the US alone, the direct medical and indirect expenses from CVDs were estimated at approximately $329 billion in 2013 to 2014 [ 5 ]. Effective large-scale interventions to prevent or treat hypertension are therefore urgently needed to reverse this trend. Yet, as new and promising interventions are surfacing every day, the need for rigorous evaluation of these interventions to inform evidence-based policies and clinical practice is ever growing.
To this effect, several randomized clinical trials (RCT) have been conducted to evaluate interventions used to prevent hypertension or improve its control [ 6 , 7 , 8 ]. However, although RCTs represent the gold standard for evaluating the efficacy (i.e., impact under ideal conditions) of most health interventions because of their high internal validity [ 9 , 10 ], they are not always feasible, appropriate or ethical for the evaluation of certain types of interventions. Furthermore, results from RCTs are not always generalizable to populations or settings of interest due to the highly selected sample and because the intervention is generally conducted under more stringent conditions ( low external validity ) [ 11 ]. To evaluate the effectiveness of an intervention (i.e., impact under real conditions) and to increase the uptake and implementation of evidence-based health interventions in the communities of interests, other types of experimental designs have been proposed. One such example is natural and quasi-experiments. The terms “natural experiments” and “quasi-experiments” are sometimes used interchangeably. In this study, and as described by others [ 12 ], we will distinguish these two concepts. Natural and quasi-experiments are similar in that, in both cases, there is no randomization of treatments or exposures (i.e., no random assignment). They differ, however, in that, natural experiments are those that involve naturally occurring or unplanned events (e.g., a national policy, new law), while quasi-experiments involve intentional or planned interventions implemented (typically for the purpose of research/evaluation) to change a specific outcome of interest (e.g., a community intervention program). Furthermore, in natural experiments, the investigator does not have control over the treatment assignment whereas in quasi-experiments, the investigator has control over the treatment assignment [ 12 ]. These experiments include difference-in-difference (DID) designs, synthetic controls and regression discontinuity designs to name a few [ 13 , 14 , 15 ].
As utilization of natural and quasi-experiments is increasing in public health and in the biomedical field [ 13 , 14 , 15 ], more natural and quasi-experiments are being conducted to evaluate interventions targeted to prevent or control hypertension [ 16 , 17 , 18 , 19 ]. This could be due to recent development or the reframing of classical approaches for determining causality in natural and quasi- experiments [ 13 , 14 , 15 , 20 ]. However, unlike RCTs of interventions aiming to prevent hypertension or improve its control [ 6 , 7 , 8 ], consistent summary and synthesis of evidence from natural and quasi- experiments is lacking in the current literature. The primary aim of the current systematic review is to summarize the evidence from natural and quasi-experiments that have evaluated interventions used to prevent, control hypertension or reduce blood pressure levels. A secondary aim of this study is to conduct a meta-analysis to summarize intervention effectiveness.
Data sources and strategy
We searched PubMed, Embase and Web of Science from January 2008 to November 2018. This time frame was selected to encompass studies that would have likely benefited from recent development and improvement in natural and quasi- experiments [ 13 , 20 ]. Briefly, the search strategy consisted in intersecting keywords related to the study methods (e.g., natural experiments, quasi-experiments, DID, synthetic control, interrupted time series, etc.) with the environment or settings (e.g., community, nation, organization, etc.) and the outcome (e.g., hypertension, elevated blood pressure, etc.). The full search strategy is described in Table S 1 . This systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement [ 21 ] (Fig. 1 ).
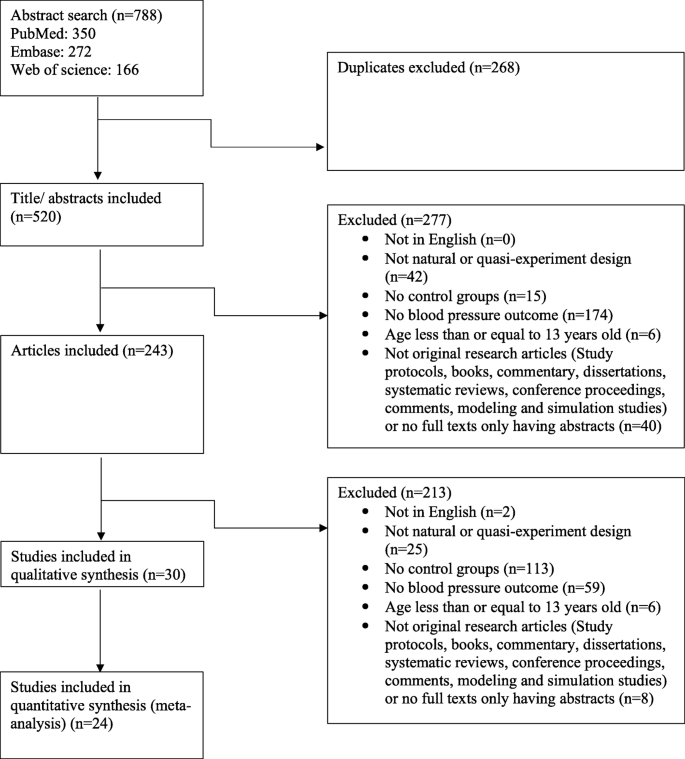
Study search and selection flow
Study selection
Two trained members (TX, FZ) screened abstracts and full-text articles. Disagreements were decided by a third member (RN). We included studies that used natural and quasi-experiments to evaluate interventions aimed at preventing hypertension, controlling hypertension or reducing blood pressure levels. The outcome measures were prevalence of hypertension and changes in mean blood pressure. Studies were excluded if they were not in English, were not a natural experiment or a quasi-experimental design, did not include a control group (as it has higher risk to internal validity due to the absence of comparison to adjust for time trends and confounding) [ 22 ], did not include blood pressure or hypertension as their outcome or included participants that were 13 years old or younger. In addition, we excluded studies that were not original research articles (e.g., study protocol, books, commentary, dissertations, conference proceedings, comments, systematic reviews, modeling and simulation studies), or had no full text available.
Data extraction and quality assessment
The following information was extracted: study design, sample size, study duration, data source, geographic location, participants’ socio-demographic characteristics, intervention types, intervention levels (e.g., individuals, community, school, clinic and national levels as suggested by the socio-ecological model [ 23 ]), behavior targeted and outcome measures (prevalence of hypertension or mean blood pressure change) (Table 1 , Table S 2 ).
The interventions were classified by strategies into four types:
Education and counseling: This subcategory includes strategies that aim at educating and providing knowledge and counseling to participants on lifestyle modifications (e.g., increasing physical activity (PA), eating better, avoiding or stopping smoking, etc.).
Management: This subcategory includes strategies that aim at monitoring patients’ metabolic factors and chronic diseases (e.g., blood pressure, cholesterol level, etc.) as well as patients’ adherence to medication. These strategies are generally done or facilitated by physicians, general practitioners (e.g., by assessing computerized clinical guidelines in the electronic health record management system), nurses, other staffs, or patients themselves.
Education, counseling and management: This subcategory combines education and counseling strategies with management strategies as described above.
Screening and referral for management: This subcategory includes strategies that aim at screening for (i.e., checking for the presence of) economic risk factors, medical needs, and CVD risk factors, followed by the referral of participants who screened positive to professionals who specialize in the management of those needs.
We also classified the interventions by settings into (1) community level; (2) health center level (i.e., primary care center or general practices), (3) organization level and (4) nationwide. In addition, we have classified the intervention by duration of the study into short-term (i.e., participants were followed for less than 12 months) and long-term (i.e., participants were followed for longer than or equal to 12 months).
We implemented the Cochrane Risk of Bias Tool for risk of bias and used the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach to assess the quality of the evidence for mean blood pressure change outcome [ 50 ], since the meta-analysis focused on this outcome. The risk of bias for studies included in this review could be found in Table S 3 and the quality of studies has also been summarized in Table S 4 .
Meta-analysis
To summarize the effectiveness of interventions on mean blood pressure changes, we also conducted a meta-analysis. Due to the high heterogeneity in the studies and interventions, we undertook a random-effects model and only summarized the effectiveness of intervention strategies by subgroup defined by intervention types, settings and duration. We estimated the weighted mean difference (WMD) of blood pressure and 95% confidence intervals (CIs). The studies included in the meta-analysis were only those whose outcomes were mean differences (MDs) in blood pressure ( n = 27) [ 16 , 19 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ] as these studies provided the data needed for performing the meta-analysis. Three studies [ 38 , 39 , 43 ] were excluded as they did not provide enough information to compute the standard errors (SEs). To estimate the average effect of the intervention when not directly provided, we subtracted the before-and-after change in the intervention group from that in the control group or subtracted the intervention-to-control difference at follow-up to that at baseline (pre-post design with a control group). Methods to calculate intervention impact and SEs were outlined in the appendix (Figs. S 1 , S 2 , Table S 5 ).
We presented the meta-analysis results using forest plots (Table 2 , Fig. 2 , Figs. S 3 , S 4 ). We assessed the heterogeneity by using the I 2 (Table 2 , Fig. 2 , Figs. S 3 , S 4 ). We did not perform meta-regression as it is not recommended when the number of studies is small (< 10 studies per covariate) [ 51 ]. We assessed publication bias by using funnel plots of SEs (Figs. S 5 , S 6 , S 7 ). To test the robustness of our results, we performed sensitivity analyses by removing one study at a time from the pool of studies to assess its impact on the findings (Tables S 6 , S 7 , S 8 , Figs. S 8 , S 9 , S 10 ). Data were analyzed with Stata 15.1 (StataCorp LLC, College Station, TX, USA).
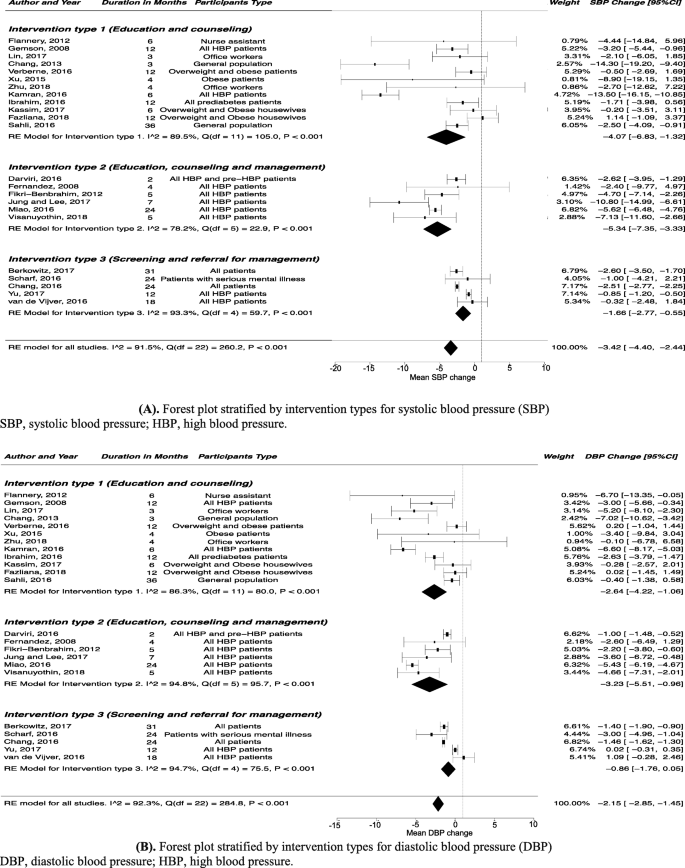
Forest plot stratified by intervention types for blood pressure. A Forest plot stratified by intervention types for systolic blood pressure (SBP). B Forest plot stratified by intervention types for diastolic blood pressure (DBP)
Overall, 788 titles of potentially relevant studies were identified and screened. In total, 545 were excluded and 243 full papers were retrieved, then 30 studies were included in the final sample ( Fig. 1 ) .
Study characteristics
Of the 30 studies included in this review [ 16 , 17 , 18 , 19 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ], three studies reported changes in hypertension prevalence, among which one study reported preventing hypertension in the general population [ 24 ] and two studies reported blood pressure control in patients with hypertension [ 17 , 18 ]; 25 studies reported mean blood pressure changes [ 16 , 19 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]; two studies reported both outcome measures (changes in hypertension prevalence and mean blood pressure changes) [ 25 , 26 ]. Thirteen studies used education and counseling intervention strategies [ 24 , 25 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ]; four studies used management intervention strategies [ 18 , 19 , 38 , 39 ]; seven studies combined education, counseling and management intervention strategies [ 26 , 40 , 41 , 42 , 43 , 44 , 45 ]; and six studies used screening and referral for management intervention strategies [ 16 , 17 , 46 , 47 , 48 , 49 ]. Fourteen studies followed participants for less than 12 months (i.e., short-term interventions) [ 17 , 26 , 27 , 29 , 30 , 32 , 33 , 34 , 36 , 40 , 41 , 42 , 43 , 45 ]. Twelve studies were conducted in the US [ 16 , 17 , 19 , 24 , 27 , 28 , 32 , 33 , 39 , 41 , 43 , 46 ] and most studies included both genders [ 16 , 17 , 18 , 19 , 24 , 25 , 26 , 28 , 29 , 30 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ] and all racial/ethnic groups [ 16 , 17 , 18 , 19 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]. We found no natural experiments according to the definition used in this study (Table 1 , Table S 2 ).
Quality ratings
According to the Cochrane Risk of Bias Tool, most studies included in this review were found to have a high risk of bias ( Table S 3 ). This was so because the Cochrane Risk of Bias Tool was mostly designed for RCTs. Studies included in this review only used quasi-experiment designs and as such did not use randomization, allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. Using the GRADE approach, the quality of evidence was deemed of low quality for the mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) change outcome (Table S 4 ).
Studies that reported prevalence of hypertension in the general population or changes in the prevalence of controlled blood pressure in hypertension patients after intervention
Outcome of interest: prevention of hypertension in healthy people, education and counseling intervention strategies.
Two studies evaluated the education and counseling intervention strategies, and both found that those strategies could help prevent hypertension in healthy people [ 24 , 25 ]. One study in the US found that nutritional education and giving access to fruits and vegetables through community gardens helped reduce hypertension prevalence (61.0% vs. 45.0%; P < 0.01), whereas the prevalence of hypertension in the control group did not change (46.7% vs. 49.8%; P = 0.39) [ 24 ]. The other study in Africa showed that an education strategy which promoted PA and healthy diet and combined with free smoking cessation consultations could help reduce the prevalence of hypertension (22.8% vs. 16.2%; P = 0.01), compared to that in control group (14.0% vs. 15.1%; P = 0.52) [ 25 ].
Outcome of interest: improvement of hypertension control in patients with hypertension
Management intervention strategies.
A study in the US showed that patients whose general practitioners accessed the computerized clinical practice guideline at least twice a day improved their hypertension control compared to the patients whose general practitioners never accessed the computerized clinical practice guideline ( P < 0.001) [ 18 ].
Education, counseling and management intervention strategies
A study in the US found that patients who received education about hypertension and did home blood pressure monitoring had a better control of their hypertension compared to the control group ( P = 0.03) [ 26 ].
Screening and referral for management intervention strategies
A study in the US showed that for White patients, interventions which involved a coordinator who identified and reached out to patients not meeting CVD goals and linked them to management programs could improve the odds of blood pressure control (odds ratio, 1.13; 95% CI, 1.05 to 1.22) compared to no intervention [ 17 ].
Studies that reported mean blood pressure changes after intervention
Outcome of interest: reduction in mean blood pressure.
Seven [ 25 , 27 , 28 , 29 , 30 , 34 , 35 ] of twelve [ 25 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ] (58.3%) studies showed that the education and counseling intervention strategies could help reduce mean blood pressure compared to the control group. Education and counseling interventions targeting lifestyle modifications (e.g., diet and PA) have been found effective in reducing blood pressure in the workplace. A study in US female nursing assistants found that combining education and continuing motivation (e.g., counseling on questions of interventions and receiving feedback) on diet and PA led to more reduction in DBP compared to the control group who only received the education (MD, − 6.70 mmHg; 95% CI, − 13.35 to − 0.05) [ 27 ]. Two other studies also found that multi-component lifestyle interventions in the workplace including sharing health information by messages, putting up posters, using pedometers, and giving education on PA could help healthy employees or employees with hypertension lower blood pressure [ 28 , 29 ]. Besides the workplace, interventions implemented in a community setting also appeared to work in reducing blood pressure. A study that included participants age 55 years or more in Asia found that people who attended 60-min Tai Chi three times per week for 12 weeks had a larger reduction in SBP (MD, − 14.30 mmHg; 95% CI, − 19.20 to − 9.40) and in DBP (MD, − 7.02 mmHg; 95% CI, − 10.62 to − 3.42) compared to people maintaining usual daily activities [ 30 ]. Another study among patients with hypertension in Asia found that education about the nutritional behavior and guidelines from dietary approaches to stop hypertension (DASH) approach could help reduce blood pressure more in the intervention group compared to the control group who only received the instruction booklets used in intervention group (SBP: MD, − 13.50 mmHg; 95% CI, − 16.15 to − 10.85; DBP: MD, − 6.60 mmHg; 95% CI, − 8.17 to − 5.03) [ 34 ]. One study in Africa also showed that education on promoting PA and healthy diet, combined with free smoking cessation consultations could help reduce SBP in the intervention group [ 25 ].
Two [ 19 , 39 ] of three [ 19 , 38 , 39 ] (66.7%) studies showed that the management intervention strategies could help reduce mean blood pressure compared to the control group. A study in the US showed that supporting diabetes patients’ self-management of hypertension by team-based chronic models (e.g., proactive patient outreach, depression screening, and health coaching) could decrease more DBP over a 6-month period compared to the usual care (MD, − 1.13 mmHg; 95% CI, − 2.23 to − 0.04) [ 19 ]. A study among hypertension patients in Asia showed that improving the social health insurance system by increasing outpatient expenditure reimbursement ratio could help reduce more SBP (MD, − 2.9 mmHg; P = 0.01) compared to outpatient expense not covered [ 38 ]. The other study among diabetes patients in the US also showed that team-based treatment with trained staff on medical management and self-management helped lower SBP (MD, − 0.88 mmHg; P = 0.01), but it did not compare the MD between treatment and control group [ 39 ].
Six [ 26 , 40 , 42 , 43 , 44 , 45 ] of seven [ 26 , 40 , 41 , 42 , 43 , 44 , 45 ] (85.7%) studies showed that the combination of education, counseling and management intervention strategies led to more blood pressure reduction compared to the control group. One study among hypertension patients in Europe found that management of stress by biofeedback-assisted relaxation and lifestyle counseling on diet and PA reduced more SBP (MD, − 2.62 mmHg; 95% CI, − 3.96 to − 1.29) and DBP (MD, − 1.00 mmHg; 95% CI, − 1.90 to − 0.93) compared to the control group [ 40 ]. One study among hypertension patients in the US also found that education about hypertension and home blood pressure monitoring could help reduce more SBP (MD, − 4.70 mmHg; 95% CI, − 7.14 to − 2.26) and DBP (MD, − 2.20 mmHg; 95% CI, − 3.80 to − 0.60) compared to controls [ 26 ]. A study among 65-year-and-older hypertension patients in Asia found that the intervention group who received education on hypertension management, community-based eHealth monitoring, and monthly telephone counseling had more reduction in SBP (MD, − 10.80 mmHg; 95% CI, − 14.99 to − 6.61) compared to the control group who only received a poster about hypertension management [ 42 ]. A study among hypertension patients in the US also showed that interventions on lifestyle modifications, and nutritional, pharmacological therapies as well as medication adherence lowered SBP and DBP compared to the control group [ 43 ]. A study among hypertension patients in Asia found that integration of preventive-curative services delivery and cooperation among village-town-county physicians for education on lifestyle modifications, taking blood pressure drugs regularly and monitoring the blood pressure could help reduce blood pressure more in the intervention group [ 44 ]. The other study in Asia also found that integrated program with health education on home blood pressure monitoring and hypertension measurement skills could help reduce blood pressure more in the intervention group [ 45 ].
Four [ 16 , 46 , 47 , 48 ] of five [ 16 , 46 , 47 , 48 , 49 ] (80.0%) studies showed that the screening and referral for management intervention strategies could help reduce more blood pressure compared to the control group. Screening for medical or economic needs followed by offering treatment and resources has been found helpful. One study in the US found that screening for unmet needs in primary care and offering those who screened positive some resources could reduce SBP (MD, − 2.6 mmHg; 95% CI, − 3.5 to − 1.7]) and DBP (MD, − 1.4 mmHg; 95% CI, − 1.9 to − 0.9) in patients [ 16 ]. The other study among patients with serious mental illness in the US also found that using registry for general medical needs and outcomes, screening and referral for general medical illness prevention and treatment could help reduce more DBP compared to controls (MD, − 3.00 mmHg; 95% CI, − 4.96 to − 1.04) [ 46 ]. Assessing and screening CVD risk followed by a management program has also been found beneficial to reduce blood pressure. A study in Europe showed that participating in CVD risk assessment and management program, including screening and tailored strategies for lifestyle advice on CVD risk factors could reduce more SBP (MD, − 2.51 mmHg; 95% CI, − 2.77 to − 2.25) and DBP (MD, − 1.46 mmHg; 95% CI, − 1.62 to − 1.29) compared to controls [ 47 ]. A study among hypertension patients in Asia also found that a standardized CVD-risk assessment, a hypertension complication screening and adherence to medications could help reduce more blood pressure compared to the usual care [ 48 ].
Meta-analysis of the effectiveness of interventions on mean blood pressure change
Intervention type sub-group analysis.
The largest blood pressure reduction (SBP: WMD, − 5.34 mmHg; 95% CI, − 7.35 to − 3.33; DBP: WMD, − 3.23 mmHg; 95% CI, − 5.51 to − 0.96) was seen for interventions that combined education, counseling and management intervention strategies (Table 2 , Fig. 2 ).
Intervention setting sub-group analysis
Participants who experienced interventions implemented in community settings (WMD, − 3.77 mmHg; 95% CI, − 6.17 to − 1.37) and in health center settings (WMD, − 3.77 mmHg; 95% CI, − 5.78 to − 1.76) had large SBP reduction. Participants experienced interventions implemented in organization settings had large DBP reduction (WMD, − 3.92 mmHg; 95% CI, − 5.80 to − 2.04) (Table 2 , Fig. S 3 ).
Intervention duration sub-group analysis
Participants who were followed for less than 12 months (i.e., short-term interventions) had a large reduction in blood pressure (SBP: WMD, − 6.25 mmHg; 95% CI, − 9.28 to − 3.21; DBP: WMD, − 3.54 mmHg; 95% CI, − 5.21 to − 1.87) and participants who were followed for longer than or equal to 12 months (i.e., long-term interventions) had a moderate reduction in blood pressure (SBP: WMD, − 1.89 mmHg; 95% CI, − 2.80 to − 0.97; DBP: WMD, − 1.33 mmHg; 95% CI, − 2.11 to − 0.55) (Table 2 , Fig. S 4 ).
We summarized the evidence from quasi-experiments that have evaluated interventions used to (1) prevent hypertension in the general population, (2) improve hypertension control in patients with hypertension or (3) reduce blood pressure levels in both the general population and patients.
In this systematic review, we found that the intervention strategies such as (1) education and counseling, (2) management, (3) education, counseling and management and (4) screening and referral for management were beneficial in preventing, controlling hypertension or reducing blood pressure levels. In particular, we found that education and counseling on lifestyle modifications (i.e., promoting PA, healthy diet, smoking cessation consultations) could help prevent hypertension in healthy people. The use of computerized clinical practice guidelines by general practitioners, education and management of hypertension, screening for CVD goals and referral to management could help improve hypertension control in patients with hypertension. The education and counseling on lifestyle modifications, the monitoring of patients’ metabolic factors and chronic diseases (e.g., blood pressure, cholesterol level, etc.) as well as patients’ adherence to medication, the combined education and management of hypertension, the screening for economic risk factors, medical needs, and CVD risk factors, followed by the referral to management all could help reduce blood pressure levels. Our study is one of the few systematic reviews that have summarized the evidence from quasi-experiments on hypertension prevention and control. A previous systematic review [ 52 ] which summarized evidence from cluster-randomized trials and quasi-experimental studies had been conducted and found that education, counseling and management strategies were also beneficial in controlling hypertension and reducing blood pressure. It showed that educating healthcare providers and patients, facilitating relay of clinical data to providers, promoting patients’ accesses to resources were associated with improved hypertension control and decreased blood pressure [ 52 ]. Another systematic review which summarized evidence from RCTs found that several interventions including blood pressure self-monitoring, educational strategies, improving the delivery of care, and appointment reminder systems could help control hypertension and reduce blood pressure [ 6 ]. Another study also found that community-based health workers interventions including health education and counseling, navigating the health care system, managing care, as well as giving social services and support had a significant effect on improving hypertension control and decreasing blood pressure [ 53 ]. A review from observational studies and RCT evidence from the US Preventive Services Task Force found that office measurement of blood pressure could effectively screen adults for hypertension [ 7 ].
Our review did not find natural experiments studies according to the definition used in this study. Quasi-experimental designs included DID, propensity score matching and pre-post designs with a control group (PPCG). While PPCG designs generally involve two groups (intervention and control) and two different time points (before and after the intervention), DID designs generally involve two or more intervention and control groups and multiple time points [ 13 ]. In this review, we did not include pre-post without a control group design because of its higher risk to internal validity due to the absence of comparison to adjust for time trends and confounding [ 22 ]. The findings in this review, highlight that, quasi-experiments are increasingly used to evaluate the effectiveness of health interventions for hypertension management when RCTs are not feasible or appropriate. For instance, several studies included in our systematic review often indicated that RCTs would have been difficult to be implemented given that the intervention was conducted in a particular setting such as a pragmatic clinical setting [ 16 , 43 , 45 , 48 ], a community setting [ 24 , 35 , 36 , 42 ], or a real-world organizational setting [ 33 ] because of ethical concerns and human resources issues. Another reason why quasi-experiments were chosen had to do with the need for translation and generalizability of the evidence in a specific community setting [ 32 ]. In fact, RCTs are not always generalizable to the communities or settings of interests [ 11 ]. The growing interest in and hence the increase in the use of natural and quasi-experiments in public health may be due to the recognition and realization of its usefulness in evaluating health interventions [ 14 , 54 ].
Given that there was high heterogeneity in the studies included in this systematic review, we have performed a random effects model and have only presented the subgroup analysis by intervention types, settings and duration of the study. Overall, our study suggested that interventions that combined education, counseling and management strategies appeared to show a relatively large beneficial effect for reducing blood pressure. However, our finding should be interpreted with caution due to the high-risk of bias and lower quality of evidence given the quasi-experimental nature of the designs (as opposed to evidence from randomized experiments). Nevertheless, the findings here can give us some insights on the benefit of interventions such as education, counseling and management, especially given that our findings are in line with previous studies [ 6 , 8 , 52 , 55 ]. Given that RCTs are not always feasible or appropriate, scientists should develop more rigorous methods to increase the internal validity of non-randomized studies. Compared to previous studies, one systematic review with meta-analysis including cluster-randomized trials and quasi-experiment studies showed that multi-component interventions which incorporated education of health care providers and patients, facilitating relay of clinical data to providers, and promoting patients’ accesses to resources could reduce more blood pressure compared to controls [ 52 ]. A recent systematic review with meta-analysis of RCTs also reported that interventions which included blood pressure self-monitoring, appointment reminder systems, educational strategies, and improving the delivery of care showed beneficial effects on lowering blood pressure [ 6 ]. Another systematic review and meta-analysis of RCTs also showed that self-measured blood pressure monitoring lowered SBP by 3.9 mmHg and DBP by 2.4 mmHg at 6 months compared to the usual care group [ 8 ]. One systematic review and meta-analysis of RCTs found that diet improvement, aerobic exercise, alcohol and sodium restriction, and fish oil supplements reduced blood pressure as well [ 55 ].
Limitations
This review has some limitations. First, the definition of natural and quasi-experiments is not consistent across fields. Second, the main limitation in most if not all the quasi-experimental study designs noted in this review was the potential for unobserved and uncontrolled confounding, which is a threat to internal validity and could lead to biased findings. Third, our findings may not be generalizable to all countries and settings as we only included studies published in the English language in this review. Fourth, as is the case in most other reviews, we could have missed relevant studies despite our best attempt to conduct a thorough search of the literature. Fifth, we found that most studies included in this study had a high risk of bias. It might be because we used the Cochrane Risk of Bias Tool to assess bias which was designed for examining RCTs. Studies in this review only used quasi-experiment designs and did not have randomization, allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. Sixth, studies generally reported the measure of intervention impact differently across studies, making it difficult to combine the findings. In addition, studies were highly heterogeneous in terms of the types of individuals included in the study (e.g., healthy individuals and patients). We conducted the subgroup meta-analysis to reduce the heterogeneity, but the high heterogeneity still existed. Therefore, the results from meta-analysis need to be interpreted with caution. The individual impact reported for each individual study and the results from systematic review should be given more consideration.
In this systematic review, interventions that used education and counseling strategies; those that used management strategies; those that combined education, counseling and management strategies and those that used screening and referral for management strategies were beneficial in preventing, controlling hypertension and reducing blood pressure levels. The combination of education, counseling and management strategies appeared to be the most beneficial intervention to reduce blood pressure levels. The findings in this review, highlight that, a number of interventions that aim at preventing, controlling hypertension or reducing blood pressure levels are being evaluated through the use of quasi-experimental studies. Given that RCTs are not always feasible or appropriate, scientists should develop more rigorous methods to increase the internal validity of such quasi-experimental studies.
Availability of data and materials
The data supporting the conclusions of this article is included within the article and the additional file.
Abbreviations
Confidence interval
Cardiovascular disease
Dietary approaches to stop hypertension
Diastolic blood pressure
Difference-in-difference
Grading of Recommendations, Assessment, Development, and Evaluation
Mean difference
Physical activity
Pre-post designs with a control group
Randomized clinical trial
Systolic blood pressure
Standard error
United States
Weighted mean difference
National Center for Health Statistics & Heron, M. Deaths: Leading Causes for 2018. Atlanta: CDC; 2021.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524–32.
Article PubMed Google Scholar
World Health Organization (WHO). A global brief on hypertension: silent killer, global public health crisis: World Health Day 2013. Geneva: WHO; 2013.
Sun D, Liu J, Xiao L, Liu Y, Wang Z, Li C, et al. Recent development of risk-prediction models for incident hypertension: an updated systematic review. PLoS One. 2017;12:e0187240.
Article PubMed PubMed Central Google Scholar
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–492.
Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010;3:CD005182.
Google Scholar
Sheridan S, Pignone M, Donahue K. Screening for high blood pressure: a review of the evidence for the U.S. preventive services task force. Am J Prev Med. 2003;25:151–8.
Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–94.
de Simone G, Izzo R, Verdecchia P. Are observational studies more informative than randomized controlled trials in hypertension? Pro side of the argument. Hypertension. 2013;62:463–9.
Li DZ, Zhou Y, Yang YN, Ma YT, Li XM, Yu J, et al. Acupuncture for essential hypertension: a meta-analysis of randomized sham-controlled clinical trials. Evid Based Complement Alternat Med. 2014;2014:279478.
Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291:2720–6.
Article CAS PubMed Google Scholar
Remler DK, Van Ryzin GG. Research methods in practice: strategies for description and causation. 2nd ed. SAGE: Los Angeles; 2014.
Handley MA, Lyles CR, McCulloch C, Cattamanchi A. Selecting and improving quasi-experimental designs in effectiveness and implementation research. Annu Rev Public Health. 2018;39:5–25.
Basu S, Meghani A, Siddiqi A. Evaluating the health impact of large-scale public policy changes: classical and novel approaches. Annu Rev Public Health. 2017;38:351–70.
Craig P, Katikireddi SV, Leyland A, Popham F. Natural experiments: an overview of methods, approaches, and contributions to public health intervention research. Annu Rev Public Health. 2017;38:39–56.
Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244–52.
James A, Berkowitz SA, Ashburner JM, Chang Y, Horn DM, O’Keefe SM, et al. Impact of a population health management intervention on disparities in cardiovascular disease control. J Gen Intern Med. 2018;33:463–70.
Comin E, Catalan-Ramos A, Iglesias-Rodal M, Grau M, Del Val JL, Consola A, et al. Impact of implementing electronic clinical practice guidelines for the diagnosis, control and treatment of cardiovascular risk factors: a pre-post controlled study. Aten Primaria. 2017;49:389–98.
Panattoni L, Hurlimann L, Wilson C, Durbin M, Tai-Seale M. Workflow standardization of a novel team care model to improve chronic care: a quasi-experimental study. BMC Health Serv Res. 2017;17:286.
Bor J. Capitalizing on natural experiments to improve our understanding of population health. Am J Public Health. 2016;106:1388–9.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Ho AM, Phelan R, Mizubuti GB, Murdoch JAC, Wickett S, Ho AK, et al. Bias in before-after studies: narrative overview for anesthesiologists. Anesth Analg. 2018;126:1755–62.
Bronfenbrenner U. The ecology of human development: experiments by nature and design. Cambridge: Harvard University Press; 1979.
Barnidge EK, Baker EA, Schootman M, Motton F, Sawicki M, Rose F. The effect of education plus access on perceived fruit and vegetable consumption in a rural African American community intervention. Health Educ Res. 2015;30:773–85.
Article CAS PubMed PubMed Central Google Scholar
Sahli J, Maatoug J, Harrabi I, Ben Fredj S, Dendana E, Ghannem H. Effectiveness of a community-based intervention program to reduce hypertension prevalence among adults: results of a quasiexperimental study with control group in the region of Sousse. Tunisia Glob Heart. 2016;11:131–7.
Fikri-Benbrahim N, Faus MJ, Martínez-Martínez F, Alsina DG, Sabater-Hernandez D. Effect of a pharmacist intervention in Spanish community pharmacies on blood pressure control in hypertensive patients. Am J Health Syst Pharm. 2012;69:1311–8.
Flannery K, Resnick B, Galik E, Lipscomb J, McPhaul K, Shaughnessy M. The worksite heart health improvement project (WHHIP): feasibility and efficacy. Public Health Nurs. 2012;29:455–66.
Gemson DH, Commisso R, Fuente J, Newman J, Benson S. Promoting weight loss and blood pressure control at work: impact of an education and intervention program. J Occup Environ Med. 2008;50:272–81.
Lin YP, Lin CC, Chen MM, Lee KC. Short-term efficacy of a “sit less, walk more” workplace intervention on improving cardiometabolic health and work productivity in office workers. J Occup Environ Med. 2017;59:327–34.
Chang MY, Yeh SC, Chu MC, Wu TM, Huang TH. Associations between Tai chi Chung program, anxiety, and cardiovascular risk factors. Am J Health Promot. 2013;28:16–22.
Verberne LD, Hendriks MR, Rutten GM, Spronk I, Savelberg HH, Veenhof C, et al. Evaluation of a combined lifestyle intervention for overweight and obese patients in primary health care: a quasi-experimental design. Fam Pract. 2016;33:671–7.
Xu F, Letendre J, Bekke J, Beebe N, Mahler L, Lofgren IE, et al. Impact of a program of Tai chi plus behaviorally based dietary weight loss on physical functioning and coronary heart disease risk factors: a community-based study in obese older women. J Nutr Gerontol Geriatr. 2015;34:50–65.
Zhu W, Gutierrez M, Toledo MJ, Mullane S, Stella AP, Diemar R, et al. Long-term effects of sit-stand workstations on workplace sitting: a natural experiment. J Sci Med Sport. 2018;21:811–6.
Kamran A, Sharifirad G, Heydari H, Sharifian E. The effect of theory based nutritional education on fat intake, weight and blood lipids. Electron Physician. 2016;8:3333–42.
Ibrahim N, Ming Moy F, Awalludin IA, Mohd Ali Z, Ismail IS. Effects of a community-based healthy lifestyle intervention program (co-HELP) among adults with prediabetes in a developing country: a quasi-experimental study. PLoS One. 2016;11:e0167123.
Kassim MSA, Manaf MRA, Nor NSM, Ambak R. Effects of lifestyle intervention towards obesity and blood pressure among housewives in Klang Valley: a quasi-experimental study. Malays J Med Sci. 2017;24:83–91.
PubMed PubMed Central Google Scholar
Fazliana M, Liyana AZ, Omar A, Ambak R, Mohamad Nor NS, Shamsudin UK, et al. Effects of weight loss intervention on body composition and blood pressure among overweight and obese women: findings from the MyBFF@home study. BMC Womens Health. 2018;18(Suppl 1):93.
Miao Y, Gu J, Zhang L, He R, Sandeep S, Wu J. Improving the performance of social health insurance system through increasing outpatient expenditure reimbursement ratio: a quasi-experimental evaluation study from rural China. Int J Equity Health. 2018;17:89.
Scanlon DP, Hollenbeak CS, Beich J, Dyer AM, Gabbay RA, Milstein A. Financial and clinical impact of team-based treatment for medicaid enrollees with diabetes in a federally qualified health center. Diabetes Care. 2008;31:2160–5.
Darviri C, Artemiadis AK, Protogerou A, Soldatos P, Kranioutou C, Vasdekis S, et al. A HEALth promotion and STRESS management program (HEAL-STRESS study) for prehypertensive and hypertensive patients: a quasi-experimental study in Greece. J Hum Hypertens. 2016;30:397–403.
Fernandez S, Scales KL, Pineiro JM, Schoenthaler AM, Ogedegbe G. A senior center-based pilot trial of the effect of lifestyle intervention on blood pressure in minority elderly people with hypertension. J Am Geriatr Soc. 2008;56:1860–6.
Jung H, Lee JE. The impact of community-based eHealth self-management intervention among elderly living alone with hypertension. J Telemed Telecare. 2017;23:167–73.
Hussain T, Franz W, Brown E, Kan A, Okoye M, Dietz K, et al. The role of care management as a population health intervention to address disparities and control hypertension: a quasi-experimental observational study. Ethn Dis. 2016;26:285–94.
Miao Y, Zhang L, Sparring V, Sandeep S, Tang W, Sun X, et al. Improving health related quality of life among rural hypertensive patients through the integrative strategy of health services delivery: a quasi-experimental trial from Chongqing. China Int J Equity Health. 2016;15:132.
Visanuyothin S, Plianbangchang S, Somrongthong R. An integrated program with home blood-pressure monitoring and village health volunteers for treating poorly controlled hypertension at the primary care level in an urban community of Thailand. Integr Blood Press Control. 2018;11:25–35.
Scharf DM, Schmidt Hackbarth N, Eberhart NK, Horvitz-Lennon M, Beckman R, Han B, et al. General medical outcomes from the primary and behavioral health care integration grant program. Psychiatr Serv. 2016;67:1226–32.
Chang KC, Lee JT, Vamos EP, Soljak M, Johnston D, Khunti K, et al. Impact of the National Health Service Health Check on cardiovascular disease risk: a difference-in-differences matching analysis. CMAJ. 2016;188:E228–38.
Yu EY, Wan EY, Wong CK, Chan AK, Chan KH, Ho SY, et al. Effects of risk assessment and management programme for hypertension on clinical outcomes and cardiovascular disease risks after 12 months: a population-based matched cohort study. J Hypertens. 2017;35:627–36.
van de Vijver S, Oti SO, Gomez GB, Agyemang C, Egondi T, Moll van Charante E, et al. Impact evaluation of a community-based intervention for prevention of cardiovascular diseases in the slums of Nairobi. the SCALE-UP study Glob Health Action. 2016;9:30922.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Wiley-Blackwell: Hoboken; 2020.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: John Wiley & Sons; 2009.
Book Google Scholar
Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–57.
Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. 2016;106:e3–28.
Rehkopf DH, Basu S. A new tool for case studies in epidemiology-the synthetic control method. Epidemiology. 2018;29:503–5.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33.
Download references
Acknowledgments
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Epidemiology, Fielding School of Public Health, University of California, Los Angeles (UCLA), 650 Charles E. Young Drive South, Los Angeles, CA, 90095, USA
Tong Xia, Fan Zhao & Roch A. Nianogo
California Center for Population Research (CCPR), 337 Charles E. Young Drive East, Los Angeles, CA, 90095, USA
Roch A. Nianogo
You can also search for this author in PubMed Google Scholar
Contributions
TX participated in the study conception, design and analysis and wrote the initial first draft of the article. FZ participated in the study conception, design and reviewed the first draft of the article. RN conceived and supervised the design and analysis, finalized the first draft and critically reviewed and revised the manuscript. All authors provided critical input and insights into the development and writing of the article and approved the final manuscript as submitted.
Corresponding author
Correspondence to Roch A. Nianogo .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table s1..
Search words. Table S2. Summary of the characteristics of the studies included in this review ( n = 30). Table S3. Risk of Bias Tool Assessments Across Studies (n = 30). Table S4. GRADE Evidence Profiles Across Studies in Meta-analysis ( n = 24). Table S5. Estimates and parameters in studies that reported on the mean difference in blood pressure ( n = 27). Table S6. Sensitivity analysis for systolic blood pressure (SBP) and diastolic blood pressure (DBP) in meta-analysis stratified by intervention type. Table S7. Sensitivity analysis for systolic blood pressure (SBP) and diastolic blood pressure (DBP) in meta-analysis stratified by intervention setting. Table S8. Sensitivity analysis for systolic blood pressure (SBP) and diastolic blood pressure (DBP) in meta-analysis stratified by intervention duration. Fig. S1. Methods to calculate mean differences (MD). Fig. S2. Methods to calculate standard errors (SE). Fig. S3. Forest plot stratified by intervention settings for blood pressure. (A) Forest plot stratified by intervention settings for systolic blood pressure (SBP). (B) Forest plot stratified by intervention settings for diastolic blood pressure (DBP). Fig. S4. Forest plot stratified by intervention duration for blood pressure. ( A) Forest plot stratified by intervention duration for systolic blood pressure (SBP). ( B) Forest plot stratified by intervention duration for diastolic blood pressure (DBP). Fig. S5. Funnel plot of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention types. Fig. S6. Funnel plot of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention settings. Fig. S7. Funnel plot of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention duration. Fig. S8. Sensitivity analysis of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention types. Fig. S9. Sensitivity analysis of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention settings. Fig. S10. Sensitivity analysis of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention duration
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Xia, T., Zhao, F. & Nianogo, R.A. Interventions in hypertension: systematic review and meta-analysis of natural and quasi-experiments. Clin Hypertens 28 , 13 (2022). https://doi.org/10.1186/s40885-022-00198-2
Download citation
Received : 19 February 2021
Accepted : 21 January 2022
Published : 01 May 2022
DOI : https://doi.org/10.1186/s40885-022-00198-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Non-randomized controlled trials as topic
- Comparative effectiveness research
Clinical Hypertension
ISSN: 2056-5909
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Endocrine causes of hypertension: literature review and practical approach
Affiliations.
- 1 Hypertension Unit, AP-HP, Hôpital Européen Georges Pompidou, F-75015, Paris, France. [email protected].
- 2 Université Paris Cité,, F-75015, Paris, France. [email protected].
- 3 Hypertension Unit, AP-HP, Hôpital Européen Georges Pompidou, F-75015, Paris, France.
- 4 Université Paris Cité,, F-75015, Paris, France.
- PMID: 37821565
- DOI: 10.1038/s41440-023-01461-1
Hypertension (HTN) affects more than 30% of adults worldwide. It is the most frequent modifiable cardiovascular (CV) risk factor, and is responsible for more than 10 million death every year. Among patients with HTN, we usually distinguish secondary HTN, that is HTN due to an identified cause, and primary HTN, in which no underlying cause has been found. It is estimated that secondary hypertension represents between 5 and 15% of hypertensive patients [1]. Therefore, routine screening of patients for secondary HTN would be too costly and is not recommended. In addition to the presence of signs suggesting a specific secondary cause, screening is based on specific criteria. Identifying secondary HTN can be beneficial for patients in certain situations, because it may lead to specific treatments, and allow better control of blood pressure and sometimes even a cure. Besides, it is now known that secondary HTN are more associated with morbidity and mortality than primary HTN. The main causes of secondary HTN are endocrine and renovascular (mainly due to renal arteries abnormalities). The most frequent endocrine cause is primary aldosteronism, which diagnosis can lead to specific therapies. Pheochromocytoma and Cushing syndrome also are important causes, and can have serious complications. Other causes are less frequent and can be suspected on specific situations. In this article, we will describe the endocrine causes of HTN and discuss their treatments.
Keywords: Aldosteronism; Hypertension; Pheochromocytoma; Secondary hypertension..
© 2023. The Author(s), under exclusive licence to The Japanese Society of Hypertension.
PubMed Disclaimer
Similar articles
- How to Explore an Endocrine Cause of Hypertension. de Freminville JB, Amar L. de Freminville JB, et al. J Clin Med. 2022 Jan 14;11(2):420. doi: 10.3390/jcm11020420. J Clin Med. 2022. PMID: 35054115 Free PMC article. Review.
- Hypertensive Conditions: Secondary Causes of Hypertension in Adults. Daly PL, Goodwin ET, Kipnis CM, Smith DK. Daly PL, et al. FP Essent. 2022 Nov;522:13-17. FP Essent. 2022. PMID: 36374634
- The evaluation and treatment of endocrine forms of hypertension. Velasco A, Vongpatanasin W. Velasco A, et al. Curr Cardiol Rep. 2014 Sep;16(9):528. doi: 10.1007/s11886-014-0528-x. Curr Cardiol Rep. 2014. PMID: 25119722
- Secondary Arterial Hypertension: From Routine Clinical Practice to Evidence in Patients with Adrenal Tumor. Grasso M, Boscaro M, Scaroni C, Ceccato F. Grasso M, et al. High Blood Press Cardiovasc Prev. 2018 Dec;25(4):345-354. doi: 10.1007/s40292-018-0288-6. Epub 2018 Nov 10. High Blood Press Cardiovasc Prev. 2018. PMID: 30415425 Review.
- Evaluation and Management of Endocrine Hypertension During Pregnancy. Corsello SM, Paragliola RM. Corsello SM, et al. Endocrinol Metab Clin North Am. 2019 Dec;48(4):829-842. doi: 10.1016/j.ecl.2019.08.011. Epub 2019 Sep 19. Endocrinol Metab Clin North Am. 2019. PMID: 31655779 Review.
- Effects of sodium intake, age, gender, blood sampling time on distribution of plasma aldosterone, renin activity, deoxycorticosterone, cortisol, cortisone, and 24 h urinary aldosterone levels in normotensive individuals based on LC-MS/MS. Zhang Q, Zhao Z, Cheng W, Zhang Y, Li Z, Liu H, Xu C, Wang K. Zhang Q, et al. Endocrine. 2024 Aug;85(2):947-954. doi: 10.1007/s12020-024-03899-w. Epub 2024 Jun 4. Endocrine. 2024. PMID: 38833202
- Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35:1245–54.
- Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37. - PubMed - PMC
- Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global Burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317:165–82. - PubMed
- de Freminville J-B, Amar L. How to explore an endocrine cause of hypertension. JCM. 2022;11:420. - PubMed - PMC
- Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–57. - PubMed
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Nature Publishing Group
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Introduction
- Conclusions
- Article Information
A and B, Included are 56 387 residents across 1157 neighborhoods. C, The sample was limited to the 20 863 patients with diagnosed hypertension. Cut points for antihypertensive use and percentages of blood pressure control and Black patients were comparable with observed quartiles within Cuyahoga County, Ohio. White lines demarcate Cleveland city limits, and black lines denote major highways. White shaded areas have sparse or no residential population (ie, airports, industrial districts). ADI indicates area deprivation index.
eTable 1. Demographic, Neighborhood, and Clinical Variables Between the Analyzed Cohort and Cohorts Excluded for Missing Data or Limited Sample Sizes of Self-Reported Race Categories
eTable 2. Performance Characteristics of Sex-Stratified Conditional Autoregressive Poisson Regressions
eTable 3. Sensitivity Analysis of Hypertension Prevalence and Odds Ratios (ORs) of Hypertension Diagnosis Derived From Multivariable Logistic Regression With Interaction Among Sex, Race, and ADI Quintile Derived From the Wisconsin Neighborhood Atlas
eTable 4. Sensitivity Analysis of Hypertension Prevalence Ratios Derived From Sex-Stratified Conditional Autoregressive (CAR) Poisson Rate Models Incorporating ADI Quintile Associated With Patients’ Census Block Group of Residence
eFigure. ADI Deciles for US Census Block Groups in Cuyahoga County, Ohio, Derived From Sociome and Neighborhood Atlas
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Blazel MM , Perzynski AT , Gunsalus PR, et al. Neighborhood-Level Disparities in Hypertension Prevalence and Treatment Among Middle-Aged Adults. JAMA Netw Open. 2024;7(8):e2429764. doi:10.1001/jamanetworkopen.2024.29764
Manage citations:
© 2024
- Permissions
Neighborhood-Level Disparities in Hypertension Prevalence and Treatment Among Middle-Aged Adults
- 1 Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, Ohio
- 2 Center for Healthcare Research and Policy, Case Western Reserve University/MetroHealth Medical Center, Cleveland, Ohio
- 3 Quantitative Health Sciences, Lerner Research Institute, Cleveland Clinic, Cleveland, Ohio
- 4 Cleveland Clinic Value-Based Operations, Cleveland Clinic, Cleveland, Ohio
- 5 Center for Value-Based Care Research, Cleveland Clinic, Cleveland, Ohio
Question Are there disparities in hypertension burden and treatment across neighborhoods by socioeconomic disadvantage and racial and ethnic composition?
Findings In this cross-sectional study of geocoded electronic health record data for 56 387 middle-aged adults, a disproportionate burden of hypertension prevalence and treatment was found in socioeconomically disadvantaged and predominantly Black neighborhoods.
Meaning These findings suggest the presence of neighborhood-level disparities in hypertension and treatment, indicating a need to investigate how to address these disparities at a structural level.
Importance Hypertension in middle-aged adults (35-50 years) is associated with poorer health outcomes in late life. Understanding how hypertension varies by race and ethnicity across levels of neighborhood disadvantage may allow for better characterization of persistent disparities.
Objective To evaluate spatial patterns of hypertension diagnosis and treatment by neighborhood socioeconomic position and racial and ethnic composition.
Design, Setting, and Participants In this cross-sectional study of middle-aged adults in Cuyahoga County, Ohio, who encountered primary care in 2019, geocoded electronic health record data were linked to the area deprivation index (ADI), a neighborhood disadvantage measure, at the US Census Block Group level (ie, neighborhood). Neighborhoods were stratified by ADI quintiles, with the highest quintile indicating the most disadvantage. Data were analyzed between August 7, 2023, and June 1, 2024.
Exposure Essential hypertension.
Main Outcomes and Measures The primary outcome was a clinician diagnosis of essential hypertension. Spatial analysis was used to characterize neighborhood-level patterns of hypertension prevalence and treatment. Interaction analysis was used to compare hypertension prevalence by racial and ethnic group within similar ADI quintiles.
Results A total of 56 387 adults (median [IQR] age, 43.1 [39.1-46.9] years; 59.8% female) across 1157 neighborhoods, which comprised 3.4% Asian, 31.1% Black, 5.5% Hispanic, and 60.0% White patients, were analyzed. A gradient of hypertension prevalence across ADI quintiles was observed, with the highest vs lowest ADI quintile neighborhoods having a higher hypertension rate (50.7% vs 25.5%) and a lower treatment rate (61.3% vs 64.5%). Of the 315 neighborhoods with predominantly Black (>75%) patient populations, 200 (63%) had a hypertension rate greater than 35% combined with a treatment rate of less than 70%; only 31 of 263 neighborhoods (11.8%) comprising 5% or less Black patient populations met this same criterion. Compared with a spatial model without covariates, inclusion of ADI and percentage of Black patients accounted for 91% of variation in hypertension diagnosis prevalence among men and 98% among women. Men had a higher prevalence of hypertension than women across race and ADI quintiles, but the association of ADI and hypertension risk was stronger in women. Sex prevalence differences were smallest between Black men and women, particularly in the highest ADI quintile (1689 [60.0%] and 2592 [56.0%], respectively).
Conclusions and Relevance These findings show an association between neighborhood deprivation and hypertension prevalence, with disparities observed particularly among Black patients, emphasizing a need for structural interventions to improve community health.
More than 116 million US adults have hypertension, which is the top modifiable individual-level risk factor for cardiovascular disease. 1 - 3 A decrease in systolic blood pressure by 10 mm Hg is estimated to reduce the risk of a cardiovascular event by 20% to 30%. 3 Middle age (35-50 years) is a critical time for intervention, as midlife hypertension has implications for poor cardiovascular health in subsequent decades 4 and is associated with cognitive decline and dementia risk. 5 , 6 The disproportionate burden of uncontrolled hypertension in non-Hispanic Black adults is a key contributor to existing disparities in stroke, cardiovascular disease, and mortality. 7 , 8 Due to historical redlining, Black individuals have been systematically housed in neighborhoods that experienced disinvestment. 9 Furthermore, where a person lives, including local resources and social environment, has been associated with hypertension risk. 10 , 11
Critically, place-based interventions have shown positive outcomes and are necessary to target existing health inequities. 12 - 14 Many reports of hypertension prevalence use national databases, such as the National Health and Nutrition Examination Survey (NHANES), that provide nationally representative estimates of disease at the population level. 15 - 17 Few studies have reported small area–level hypertension rates, 4 , 18 and none have evaluated to what extent neighborhoods connect the association between race and ethnicity and hypertension among midlife adults. In this report, we evaluate whether spatial patterns of hypertension diagnosis and treatment are associated with neighborhood socioeconomic position and racial and ethnic composition.
In this cross-sectional study, we analyzed electronic health record (EHR) data of adults aged 35 to 50 years who resided in Cuyahoga County, Ohio, and had 1 or more primary care appointments within the Cleveland Clinic Health System or MetroHealth System in 2019. The first primary care appointment attended in 2019 for each patient was classified as their index visit. The study was approved by the Cleveland Clinic Institutional Review Board (No. 22-896). Informed consent was waived due to institutional review board determination of minimal risk and that the research could not practicably be performed otherwise. Our report follows the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We derived area deprivation index (ADI) values in Ohio from 2015 to 2019 American Community Survey 5-year data at the US Census Block Group level using the R package sociome. 19 The ADI includes measures of income, education, housing, and occupation on a scale of 40 to 160, where a higher score indicates greater disadvantage. We used a local representation of the ADI due to technical limitations of the University of Wisconsin Neighborhood Atlas, described elsewhere 20 , 21 (eFigure in Supplement 1 ).
Our primary outcome was a clinician diagnosis of essential hypertension on or prior to the index visit. We defined essential hypertension as at least 1 International Statistical Classification of Diseases and Related Problems, Tenth Revision code in the Clinical Classification Software 98 diagnostic group. Our secondary outcome was hypertension treatment, which we defined as an antihypertensive medication prescribed on or up to 365 days prior to the index visit among patients with a hypertension diagnosis. In neighborhood-level analyses, we used the variable treatment rate, or the percentage of patients per neighborhood with hypertension who were prescribed an antihypertensive medication.
We grouped patients into neighborhoods based on their address at the time of their primary care visit. We then created ADI quintiles derived from all Ohio census block groups (ie, neighborhoods). We calculated the percentage of Black patients residing in each neighborhood and performed analyses using categories comparable with observed quartiles of our study sample within Cuyahoga County (≤5%, 5.1%-25.0%, 25.1%-75.0%, and >75.0%). This variable was included in models as the percentage of Black patients.
We obtained patient age, sex, and race and ethnicity from the EHR. Patients self-reported race as American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, White, or multiracial and self-reported ethnicity as Hispanic or not Hispanic. Due to sample size limitations, we analyzed the following combined racial and ethnic categories: Asian, Hispanic, non-Hispanic Black (hereafter Black), and non-Hispanic White (hereafter White). We excluded patients who identified as American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and multiracial as well as patients with missing race and ethnicity, sex, or geographic identifiers.
To characterize patient health, we obtained body mass index and common comorbidities documented on or before the patients’ index visit. We considered patients to have a comorbidity if they had at least 1 International Statistical Classification of Diseases, Tenth Revision code for each of the following diseases: type 2 diabetes, lipid or metabolic disorders, coronary artery disease, chronic kidney disease, cerebrovascular disease, depression disorders, anxiety disorders, tobacco use, alcohol use, and substance abuse.
We descriptively compared patient demographics, comorbidities, and antihypertensive prescribing across ADI quintiles using frequencies and percentages for categorical variables and medians and IQRs for continuous variables. We estimated the prevalence of essential hypertension in middle-aged adults by ADI quintile and race and ethnicity and stratified results by sex because hypertension prevalence rates differ across men and women. 22 As a sensitivity analysis, we used the ADI from Kind and Buckingham 23 via the 2015 Wisconsin Neighborhood Atlas. The statistical analysis for this report was conducted between August 7, 2023, and June 1, 2024.
We conducted a spatial analysis for a deeper understanding of neighborhood-level patterns of hypertension prevalence and treatment. We developed map visualizations to compare hypertension prevalence with the percentage of Black patients across neighborhoods, ADI, and antihypertensive medication prescribing rates among those with hypertension. We estimated area-level correlation measures using Pearson correlation coefficients and Moran I statistics to identify the strength of the association among our variables of interest.
To characterize neighborhood-level hypertension rates while accounting for potential spatial correlation between neighboring block groups, we used sex-stratified bayesian conditional autoregressive (CAR) Poisson rate models. We developed 3 models: (1) a null model with no covariates (ie, random and spatial effects only), (2) a model accounting for ADI quintile to characterize hypertension prevalence across socioeconomic position, and (3) a model accounting for the interaction of ADI quintile and the percentage of Black patients per neighborhood to understand the overall degree of neighborhood-level variability in hypertension accounted for by these 2 factors.
We developed an interaction model to compare hypertension prevalence by racial and ethnic group within similar ADI quintiles. We conducted a multivariable logistic regression with a 3-way interaction among sex, race and ethnicity, and ADI quintile. Interaction terms were selected a priori to investigate the heterogeneity of hypertension across racial and ethnic groups in each ADI quintile, stratified by sex. 22 Odds ratios (ORs) from this model are displayed with the hypertension prevalence of each subgroup analyzed.
All analyses were performed using R, version 4.3.1 statistical software (R Foundation for Statistical Computing) within the Posit Workbench–integrated development environment, version 2023.09.0 + 463 (Posit Software, PBC). Bayesian estimates are reported as posterior mean (95% credible interval [CrI]), and frequentist estimates are reported as maximum likelihood estimate (95% CI).
A total of 60 546 patients met the inclusion criteria. We removed 3130 unique patients due to missing race or ethnicity (n = 3120), missing sex (n = 4), or addresses that could not be geocoded to a US Census Block Group (n = 7). We removed 1029 patients in race categories with small sample sizes (113 American Indian or Alaska Native, 27 Native Hawaiian or Pacific Islander, and 889 multiracial) (eTable 1 in Supplement 1 ). Our final analytic sample included 56 387 adults who resided in 1157 Cuyahoga County neighborhoods (block groups). The number of neighborhoods per quintile was as follows: quintile 1, 259; quintile 2, 176; quintile 3, 159; quintile 4, 187; and quintile 5, 376.
Among the 56 387 patients analyzed, the median (IQR) age was 43.1 (39.1-46.9) years, 59.8% were female, and 40.2% were male. Overall, 21.6% of patients lived in the highest (least resources) ADI quintile, and 31.2% lived in the lowest (most resources) ADI quintile. The cohort racial and ethnic background included, 1944 Asian (3.4%), 17 557 Black (31.1%), 3089 Hispanic (5.5%), and 33 797 White (60.0%) patients. The racial background of the population differed across quintiles; in the lowest ADI quintile, 1229 patients (7.0%) were Black and 15 146 (86.1%) were White compared with 7436 Black patients (61.2%) and 3006 White patients (24.6%) in the highest ADI quintile. We found a socioeconomic gradient for most comorbidities, including cerebrovascular disease, obesity, and coronary artery disease. Patients residing in neighborhoods in the highest ADI quintile had a higher prevalence of hypertension (50.7% vs 25.5%) and lower treatment rates (61.3% vs 64.5%) ( Table 1 ).
We observed a gradient in hypertension prevalence across ADI quintiles for almost all racial and ethnic groups ( Table 2 ). Across ADI quintiles, men consistently had higher rates of hypertension than women, though prevalence differences were smallest between Black men and women, particularly in the highest ADI quintile (1689 of 2833 [65.0%] and 2592 of 4630 [56.0%], respectively). For all quintiles combined, Black men and women had the highest prevalence of hypertension compared with all other racial and ethnic groups (men, 3644 of 6446 [56.5%]; women, 5715 of 11 111 [51.4%]).
We found a high degree of spatial clustering for hypertension rates (Moran I = 0.58; P < .001) and a small but significant degree of spatial clustering for antihypertensive prescribing (Moran I = 0.05; P = .002). Higher neighborhood-level prevalence of hypertension was correlated with a higher ADI quintile ( r = 0.73; P < .001) ( Figure , A) and a higher percentage of Black patients ( r = 0.64; P < .001) ( Figure , B). Neighborhoods with a greater percentage of Black patients tended to have a higher ADI score ( r = 0.62; P < .001). We assessed how groups of neighborhoods compared with national hypertension prevalence (33% based on a cutoff of 140/90 mm Hg) and treatment prevalence (73%) estimated using NHANES data by Aggarwal et al. 24 Among the 315 neighborhoods with predominantly Black (>75%) patient populations, 200 neighborhoods (63%) had hypertension rates of greater than 35% combined with antihypertensive prescription rates of less than 70% ( Figure , C). Of those 200 neighborhoods, 80% were in the highest ADI quintile. In comparison, only 31 of the 263 neighborhoods (11.8%) in which Black patients comprised 5% or less of the population had hypertension rates of greater than 35% combined with treatment rates of less than 70%.
In the CAR Poisson rate model incorporating ADI quintile (model 1), men living in neighborhoods in the highest ADI quintile had a 58% increased prevalence of hypertension compared with the lowest ADI quintile (posterior mean, 1.58; 95% CrI, 1.46-1.70) ( Table 3 ). In the women’s CAR model incorporating ADI quintile only, neighborhoods in the highest quintile had twice the prevalence of hypertension compared with the lowest ADI quintile (posterior mean, 2.08; 95% CrI, 1.91-2.25). Compared with a null CAR model (no covariates), ADI quintile accounted for 85% of neighborhood-level variation in men and 78% in women. The CAR model incorporating an interaction between ADI quintile and percentage of Black patients per neighborhood accounted for 91% of spatial variation in hypertension prevalence in men and 98% in women compared with the null model (performance characteristics shown in eTable 2 in Supplement 1 ).
In our interaction model, which included a 3-way interaction among sex, race and ethnicity, and ADI quintile, the odds of hypertension in the highest vs lowest ADI quintile were higher for White men (OR, 1.77; 95% CI, 1.57-2.00; P < .001) and White women (OR, 2.88; 95% CI, 2.58-3.21; P < .001) compared with Black men (OR. 1.46; 95% CI, 1.20-1.77; P < .001) and Black women (OR, 1.68; 95% CI, 1.44-1.96; P < .001) ( Table 2 ). Hispanic women had significantly increased odds of hypertension with increasing neighborhood disadvantage (quintile 5 vs quintile 1: OR, 2.49; 95% CI, 1.56-4.15; P < .001), while higher ADI quintiles were comparatively not associated with higher odds of hypertension within Hispanic men. Asian women had relatively smaller (compared with other women) but significant increases in hypertension odds across most ADI quintiles (quintile 2: OR, 1.58 [95% CI, 1.03-2.39; P = .03]; quintile 3: OR, 1.89 [95% CI, 1.10-3.16; P = .02]; quintile 4: OR, 2.04 [95% CI, 1.21-3.36; P = .006]). Among Asian men, we found increased odds of hypertension only for patients in the highest ADI quintile neighborhoods compared with those in the lowest ADI quintile neighborhoods (OR, 2.01; 95% CI, 1.11-3.56; P = .02).
We conducted a sensitivity analysis of our spatial analysis and interaction analysis using ADI quintiles from the 2015 Wisconsin Neighborhood Atlas. 23 We excluded 99 patients who resided in a block group with suppressed ADI due to a high group quarter population. Results of the spatial analysis were similar overall (eTable 3 in Supplement 1 ). In the interaction analysis, ORs for hypertension were lower across Wisconsin Neighborhood Atlas–derived ADI quintiles for Hispanic women as in our primary analysis; results were otherwise comparable (eTable 4 in Supplement 1 ).
In this cross-sectional study, we found corresponding increases in hypertension prevalence as neighborhood disadvantage and the percentage of Black patients residing in a neighborhood increased. We identified a higher burden of midlife hypertension in Black adults compared with other racial and ethnic groups that persisted across levels of socioeconomic disadvantage. We also found that living in socioeconomically disadvantaged neighborhoods was associated with higher hypertension rates among people of all racial and ethnic backgrounds.
A growing body of evidence suggests that midlife hypertension increases the risk for heart failure, coronary heart disease, cognitive decline, and all-cause mortality. 5 , 6 , 25 , 26 In alignment with prior epidemiologic research, we found that men had a greater prevalence of hypertension than women. 27 - 29 However, the association of worsening neighborhood socioeconomic status and hypertension risk was more pronounced among Black, Hispanic, and White women. These findings are concordant with the existing literature, including a longitudinal cohort that showed the steepest annual growth in systolic blood pressure for women living in more socioeconomically vulnerable areas. 30 , 31 Thus, given the long-term consequences for health and mortality, midlife is a key time for optimization of cardiovascular risk factors. To our knowledge, our study is the first to describe the composition of neighborhood-level disparities in hypertension prevalence and treatment using the intersection of racial and ethnic composition and socioeconomic position.
In the spatial analyses, interactions between ADI and the percentage of Black patients per neighborhood accounted for nearly all the spatial variation in hypertension rates, beyond that accounted for by ADI alone in our models. This finding aligns with the history of racial residential segregation—including 20th century redlining practices that systematically excluded Black individuals from housing opportunities 9 —in Cuyahoga County, Ohio, which remains one of the most segregated areas in the US. In this study, we conceptualized race and ethnicity as socially constructed variables representing exposure to racism at interpersonal and structural levels. 9 , 32 - 34 In a robust regional population similar to our cohort, measures of structural racism were associated with a higher burden of hypertension and other chronic conditions. 35 Our stratified analysis revealed that White patients who lived in the highest ADI quintile were also diagnosed with hypertension at high rates. This finding suggests that neighborhood disinvestment and economic decline may be associated with health measures of all who live there, regardless of their racial and ethnic background.
Importantly, we found significant treatment disparities among neighborhoods that geographically corresponded to patterns of historical racial residential segregation and neighborhood disadvantage. 36 There were lower antihypertensive medication treatment rates within socioeconomically disadvantaged, predominately Black neighborhoods than in more resourced neighborhoods, suggesting that national estimates may mask nuanced variation in treatment across small areas. Despite reported national disparities in hypertension prevalence, previous estimates have also found that antihypertensive treatment rates for Black individuals in the US are comparable with those for White individuals. 8 , 24 , 27 , 37 Yet, at the neighborhood level, treatment varies across neighborhood resource level and racial and ethnic composition, suggesting that localized disparities persist.
Ongoing systemic racism has been independently associated with an increased risk of high blood pressure for both Black and Hispanic individuals. 38 In a prior cross-sectional analysis using NHANES and US Census data, Black adults had higher odds of hypertension regardless of individual or neighborhood poverty level, while only White adults living in low-income neighborhoods had higher odds of hypertension. 17 , 35 In Cuyahoga County, we report that Black men and women in midlife have hypertension prevalence rates of 57% and 51%, respectively, which are comparable with the highest national estimates within Black adults, depending on the definitions used. 7 , 24 , 39 In our analysis, nearly two-thirds of predominately (>75% population) Black neighborhoods in Cuyahoga County simultaneously exceeded the national average hypertension prevalence and were below average in antihypertensive treatment rates. Furthermore, 80% of these neighborhoods were characterized by a lack of socioeconomic resources. Hence, our study shows an intersectionality of race and place in the context of disparities in midlife hypertension, which is a critical factor in determining health and longevity later in the life course.
Our findings extend prior research on the association between neighborhoods and hypertension outcomes. 40 , 41 Successful place-based efforts have included using barber shops and salons to screen patients for hypertension who might otherwise not access primary care. 42 Place-based interventions that are more ecologically focused include setting up farmers’ markets and attracting grocery stores to food deserts to support access to healthy food. 11
Larger-scale approaches have included improving housing to ensure that it is free from lead (a known risk factor for hypertension). 43 Access to safe housing may reduce stress, another risk factor for hypertension. 44 , 45 Health system interventions, such as screening for and addressing health-related social needs that are inequitably distributed across neighborhoods, may improve blood pressure control, as well as large-scale hypertension-focused quality improvement programs. Most health system efforts are focused on the individual patient care setting 46 and are effective overall, but they do not address the disparities in blood pressure control across diverse patient populations. 47 , 48 The utility of our approach is not only that we used the ADI—a measure of income, education, housing, and employment resources, which are related to place-based interventions—but also that we demonstrate in the Figure how spatial analysis could be used to identify specific neighborhoods in which to place these interventions.
Our study has several limitations. Our population is limited to patients who interact with the health care system and obtain primary care services. Thus, the hypertension estimates provided are not the true neighborhood-level prevalence of hypertension, as only individuals who can access care are represented. It is also possible that patients may have had undiagnosed hypertension, thus making the prevalence estimates more conservative than the true estimates. We were also unable to determine whether the patients who had been prescribed an antihypertensive medication were taking the medication to treat hypertension, since antihypertensive medications are a broad category and are used to treat other conditions. Other indications for antihypertensive medication may have resulted in an overestimate of the number of patients being treated pharmacologically. Additionally, while race and ethnicity in the EHR are intended to be self-reported, we cannot exclude the possibility that this information was documented by another party without adequate verification. Finally, we focused on a single county for our analysis, with recognized limitations in generalizability of findings. However, the redlining and downstream structural racism that created the residential segregation in Cuyahoga County are widespread in the US. 9 , 49 Since racial segregation among neighborhoods is found in many large US cities, further research should investigate place-based disparities to promote equitable hypertension care in other locales.
The findings of this cross-sectional study suggest stark racial and neighborhood disparities in hypertension prevalence and antihypertensive treatment among adults in midlife, with a significant burden of undertreated hypertension in socioeconomically disadvantaged and racially segregated communities. Using spatial analysis techniques to identify neighborhoods in need, future research might investigate structural interventions to address place-based hypertension disparities.
Accepted for Publication: June 27, 2024.
Published: August 23, 2024. doi:10.1001/jamanetworkopen.2024.29764
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Blazel MM et al. JAMA Network Open .
Corresponding Author: Jarrod E. Dalton, PhD, Quantitative Health Sciences, Lerner Research Institute, Cleveland Clinic, 9500 Euclid Ave, JJN-3, Cleveland, OH 44195 ( [email protected] ).
Author Contributions: Dr Dalton had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs Pfoh and Dalton contributed equally as co–senior authors.
Concept and design: Blazel, Perzynski, Mourany, Jones, Pfoh, Dalton.
Acquisition, analysis, or interpretation of data: Blazel, Perzynski, Gunsalus, Mourany, Gunzler, Dalton.
Drafting of the manuscript: Blazel, Pfoh, Dalton.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Blazel, Perzynski, Gunsalus, Mourany, Gunzler, Dalton.
Obtained funding: Perzynski, Dalton.
Administrative, technical, or material support: Perzynski, Jones.
Supervision: Perzynski, Jones, Pfoh, Dalton.
Conflict of Interest Disclosures: Dr Perzynski reported equity ownership in Global Health Metrics and book royalties from Springer Nature and Taylor & Francis outside the submitted work. Dr Gunzler reported receiving personal fees from BioSensics and Taylor & Francis outside the submitted work. Dr Pfoh reported receiving a Clinical Translational Science Award from the National Center for Advancing Translational Sciences to Case Western Reserve University and Cleveland Clinic. Dr Dalton reported receiving grants from the National Heart, Lung, and Blood Institute outside the submitted work. No other disclosures were reported.
Funding/Support: This work was supported by grant R01AG080486 from the National Institute on Aging (Drs Dalton and Perzynski).
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Review Series - Hypertension and Sociology
- Published: 20 July 2022
Social determinants of hypertension in high-income countries: A narrative literature review and future directions
- Atsushi Nakagomi 1 , 2 ,
- Yuichi Yasufuku 1 ,
- Takayuki Ueno 1 &
- Katsunori Kondo 1
Hypertension Research volume 45 , pages 1575–1581 ( 2022 ) Cite this article
8932 Accesses
17 Citations
4 Altmetric
Metrics details
Hypertension is a leading cause of cardiovascular disease and despite established strategies to lower blood pressure, the control of hypertension remains poor. This is true even in high-income countries with well-established welfare and medical systems. Among the social factors associated with hypertension (i.e., social determinants of hypertension, SDHT), individual socioeconomic status (SES), including education, income, and occupation, can be crucial for hypertension management (prevalence, awareness, treatment, and control). This article reviews the findings of recently published studies that examined the association between SES and hypertension management in high-income countries. It also discusses social prescribing, which targets social isolation and loneliness as modifiable SDHT to improve hypertension management.
Similar content being viewed by others
Modifiable risk factors of inequalities in hypertension: analysis of 100 million health checkups recipients

Perceptions of the determinants of health across income and urbanicity levels in eight countries
Stressful life events, neighbourhood characteristics, and systolic blood pressure in South Africa
Introduction.
High blood pressure (BP, hypertension) is a leading cause of cardiovascular disease. Between 1990 and 2015, the prevalence of elevated systolic BP (≥140 mmHg) substantially increased, and disability-adjusted life-years and deaths associated with elevated BP also increased [ 1 ]. This high prevalence of hypertension is consistent globally, regardless of a country’s income status: low, middle, or high [ 2 ]. To minimize the burden of hypertension, several guidelines emphasize the management of the hypertension cascade: development (prevalence), screening (to promote awareness), treatment, and control [ 3 , 4 , 5 ]. The control of hypertension has generally improved in recent decades [ 3 , 6 ]; however, despite the availability of low-cost and effective antihypertensive medications, the rates of controlled hypertension remain less than 50%, even in high-income countries [ 2 , 3 ].
Primordial prevention aims to avoid the establishment of social, economic, and environmental conditions that contribute to an elevated risk of disease [ 7 , 8 ]. Among these conditions, social factors, particularly individual socioeconomic status (SES) measures, including educational attainment, income level, and occupation, have been repeatedly found to be associated with hypertension (i.e., social determinants of hypertension, SDHT) (Fig. 1 ) [ 2 , 9 , 10 ]. Intermediary factors of individual SES that lead to hypertension development include material circumstances (e.g., housing and healthy food availability), behavioral factors (e.g., diet, exercise, smoking, and alcohol consumption), and psychosocial factors (e.g., stressors, social isolation, and loneliness). Individual SES can also affect hypertension control via these same factors and additional behavioral factors, such as adherence to medical guidance and medication, which can be influenced by community/state-level factors such as the level of national health systems.
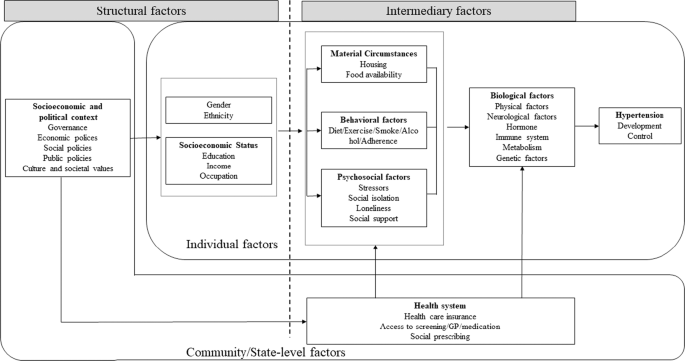
Conceptual framework of social determinants of hypertension. Based on World Health Organization (2010) [ 10 ]
This article evaluated the SDHT and hypertension management cascade (prevalence/incidence, awareness, treatment, and control). It was restricted to studies in high-income countries with well-established welfare and medical systems because the effect of these factors on hypertension management was expected to vary across various levels of national medical systems. Furthermore, this review focused on social isolation and loneliness as modifiable SDHT to improve hypertension management from the perspective of social prescribing.
SES and hypertension
A literature review of articles published between January 2000 and June 2021 was performed via the MEDLINE database to assess the influence of SES on the prevalence/incidence, awareness, treatment, and control of hypertension in high-income countries. We included the keywords “socioeconomic factors” (MeSH) or “socioeconomic factors” and “hypertension” in the title/abstract search, and added “prevalence,” “incidence,” “awareness,” “treatment,” or “control”. The titles and abstracts of the references were screened and those that were apparently irrelevant reports were excluded. We retrieved full-text articles for the remaining references and screened them to identify studies for inclusion. Our inclusion criteria were articles written in English and studies conducted in high-income countries. The Supplementary Table presents the data on the detailed study characteristics of the included studies.
Education and hypertension
The association between education and hypertension prevalence/incidence in high-income countries is relatively consistent [ 2 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 ]. A meta-analysis, for example, reported that lower educational attainment is associated with an increased prevalence/incidence of hypertension in high-income countries (odds ratio [OR] (lowest vs. highest education level category): 1.69 [95% confidential interval: 1.49 to 1.91]) [ 9 ].
In general, the role of education in improving the awareness, treatment, and control of hypertension in high-income countries seems to be small. Several studies reported a null association between education and hypertension awareness [ 2 , 11 , 16 , 21 , 30 , 31 , 32 , 33 , 34 , 35 ], treatment [ 2 , 16 , 18 , 32 , 33 , 35 , 36 ], and control [ 2 , 11 , 15 , 19 , 21 , 22 , 30 , 31 , 32 , 33 , 35 , 37 , 38 ]. A few studies have reported a significant but inconsistent association between education and hypertension awareness and treatment. For example, a study in South Korea reported an association between educational attainment and better awareness among women [ 15 ], while a study in Spain reported greater awareness among people with lower educational attainment [ 18 ]. Two studies conducted in Singapore [ 11 ] and South Korea [ 19 ] reported better treatment among people with high educational attainment, while three studies in Switzerland [ 21 ], Australia [ 39 ], and Japan [ 30 ] reported lower treatment among these people those. The reasons behind such inconsistent findings remain unclear. In some settings, highly educated people may think that they can manage their BP with a nonpharmacological approach or that a nonpharmacological approach might be presented more often by general practitioners (GPs). However, the associations, although only observed in a few studies in Spain [ 18 ], Austria [ 40 ], and France [ 41 ], between education and hypertension control are consistent. In some high-income countries, hypertension in people with high educational attainment might be better controlled than in those with low educational attainment.
Income and hypertension
The association between income and hypertension prevalence/incidence in high-income countries is relatively consistent [ 11 , 12 , 15 , 22 , 25 , 42 , 43 ]. A meta-analysis, for example, reported that lower income is associated with an increased prevalence/incidence of hypertension in high-income countries (OR (lowest vs. highest income category)): 1.36 ([1.16 to 1.59]) [ 9 ].
In general, it seems that income does not play an important role in improving the awareness, treatment, and control of hypertension in high-income countries. Several studies reported a null association between income and hypertension awareness [ 19 , 30 , 32 , 33 , 36 ], treatment [ 19 , 30 , 32 , 33 , 36 ], and control [ 11 , 15 , 19 , 30 , 32 ]. Only a few studies have reported positive associations between income level and hypertension treatment (Singapore [ 11 ] and the United States [ 44 ]) and control (the United States [ 33 , 45 ]). Income may improve the treatment and control of hypertension only in limited settings.
Occupation and hypertension
Although evidence for employment is relatively scarce compared to that for education and income, employment has been associated with lower hypertension prevalence/incidence in high-income countries [ 14 , 16 , 22 ]. A meta-analysis, for example, indicated that a lower occupational grade is associated with an increased prevalence/incidence of hypertension in high-income countries (OR (lowest vs. highest occupational grade category): 1.63 (1.27 to 2.09)) [ 9 ].
The evidence for occupation and the awareness/treatment/control of hypertension is scarce and inconclusive. Some recent studies showed a null association between employment and hypertension awareness [ 11 , 30 ], treatment [ 11 , 19 ], and control [ 30 , 37 ]. Meanwhile, a study in Finland [ 16 ] showed that retirement is associated with better awareness of hypertension than being employed, while a study in Scotland [ 35 ] showed that unemployment due to sickness is associated with better awareness than full-time employment. Two studies in Japan [ 30 ] and Australia [ 39 ] showed that unemployment is associated with better treatment compared to employment. A study in Finland [ 16 ] showed that retirement, but not unemployment, is associated with better treatment compared to employment. A study in Scotland [ 35 ] showed that those who are unemployed and seeking work undergo worse treatment than those with full-time jobs, while unemployment due to sickness was associated with better treatment than full-time employment. A few reports have shown null [ 30 , 37 ] associations between employment and hypertension control. A study in Singapore [ 11 ] showed that retirement/unemployment was associated with better control compared to employment/studying full-time. A study in Scotland [ 35 ] showed that being a homemaker or retired was associated with worse control compared to having a full-time job.
Care should be taken while interpreting the findings in this field because the situations of people with different employment statuses cannot be described simply. For example, the notion of unemployment was defined differently in the studies mentioned above. Some studies differentiated between students, homemakers, retired people, people seeking work, and people with sickness, while others did not. Even among employed people, full-time work and part-time work differently affect the hypertension care cascade because, for example, people with full-time jobs have less time to visit their general practitioner than people with part-time jobs and those who do not work.
Future directions
In high-income countries, individuals with high SES, such as those with high educational attainment, high income, and employment, are consistently associated with a low prevalence of hypertension. Several pathways can be identified, such as disparities in material circumstances, health behaviors (e.g., due to less health literacy, learned effectiveness, and personal control) [ 46 , 47 ], and psychological stressors (i.e., due to a low problem-solving ability) [ 48 , 49 ] between people with high and low SES. Closing the SES gap, as a long-term strategy, and/or reducing disparities in intermediary factors of SDHT between people with high and low SES are potential approaches to reduce disparities in hypertension prevalence in high-income countries.
However, SES is not likely to play an important role in hypertension control. This is probably because once established welfare and health care systems are achieved, these factors do not considerably change the accessibility to medical care or the affordability of antihypertensive drugs in contrast to their expected changes in low-income countries where health systems are often weak. In this context, closing the gap in SES is not considered a promising approach to improve hypertension control.
Targeting modifiable intermediary factors of SDHT: Social prescribing
A possible target of SDHT is a modifiable intermediary factor. Social prescribing, which is “a way of linking patients in primary care with sources of support within the community [ 50 ],” can be an approach to improve some psychosocial factors, such as social isolation (the objective state of having few social connections with others) and loneliness (a subjective feeling of being isolated) [ 51 , 52 ]. In response to increasing concerns about the societal and health impacts of social isolation and loneliness [ 53 , 54 ], some countries, such as the UK and Japan, have recently appointed “ministers of loneliness”.
Social isolation/loneliness and hypertension
Although evidence is limited, a few studies have reported the prevalence of an association between hypertension and social isolation, as well as loneliness and elevated BP in the U.S [ 55 , 56 ]. Possible mechanisms by which social isolation and loneliness influence BP levels and hypertension control are psychological stress [ 57 ] and social contagion: [ 58 ] behaviors spread in a social network through the diffusion of information or the transmission of behavioral norms. Health-related behaviors, such as physical activity, smoking, and medication adherence, can be adversely affected in the case of socially isolated people with a small social network [ 54 , 59 ]. However, little is known about how social isolation and loneliness are related to the awareness, treatment, and control of hypertension.
Social prescribing for hypertension
A systematic review suggested that the current evidence is insufficient to demonstrate definitive guidance for social prescribing [ 50 ]. There is little evidence for hypertension; however, some studies that focused on social participation suggest the potential of social prescribing in hypertension care. A cross-sectional study and a longitudinal study in Japan, for example, reported the association of membership in social organizations with a lower prevalence of hypertension [ 60 , 61 ]. A multilevel analysis showed a lower prevalence of hypertension among people in communities with high proportions of people participating in social organizations, suggesting a spillover effect of social participation on hypertension: [ 62 ] hypertension might be prevented only by living in communities that are rich in social participation.
A study in Sweden reported that low social participation is associated with low adherence to antihypertensive medication [ 63 ]. Although a cross-national analysis showed that membership in social organizations was associated with control in lower-middle-income/low-income countries but not in high-income/upper-middle-income countries [ 64 ], a recent study in Japan showed an association between social participation and better control of hypertension among older people [ 65 ].
The role of social prescribing in improving hypertension control is inconclusive. However, the lack of robust evidence does not necessarily mean that social prescribing is ineffective. Future studies should address the complex issue of social prescribing. Furthermore, wide variations in the nature of the interventions are required [ 51 ].
Face-to-face social interaction, which is supposed to be prescribed in social prescribing, can be restricted in specific settings, such as the ongoing COVID-19 pandemic. Social connections on the internet are a possible alternative to face-to-face social interactions in this case. The use of the internet for communication, for example, has been related to fewer feelings of loneliness [ 66 ] and the onset of depression [ 67 ], suggesting a simultaneous BP-lowering effect among people who use the internet to communicate. Although this remains unclear, social contagion might also be observed in online social connections where health-related behaviors, such as physical activity, smoking, and medication adherence, can be altered. Future studies should examine the role of online social connections in hypertension control as a new resource that is referred to in social prescribing.
Determinants of hypertension and its care are diverse and often interconnected; therefore, holistic and comprehensive approaches are required. This article highlighted the contribution of the SDHT in high-income countries. The SDHT are a crucial factor in understanding the dynamics of hypertension. Future studies should examine whether intervening in SDHT is effective in reducing hypertension prevalence and achieving optimal hypertension control. Particularly, social prescribing, which involves referring people to community resources to reduce social isolation and loneliness via face-to-face and online connections, has the potential to improve hypertension control.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317:165–82.
Article PubMed Google Scholar
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959–68.
Article CAS PubMed Google Scholar
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. Group ESD. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol. 2018;71:e127–248.
Beckman AL, Herrin J, Nasir K, Desai NR, Spatz ES. Trends in cardiovascular Health of US Adults by Income, 2005-2014. JAMA Cardiol. 2017;2:814–6.
Article PubMed PubMed Central Google Scholar
Bonita R, Beaglehole R, Kjellström T, World Health O. Basic epidemiology. 2nd ed ed. Geneva: World Health Organization; 2006.
Google Scholar
Social Determinants of Health in Non-communicable Diseases: Case Studies from Japan: Springer Nature, 2020.
Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33:221–9.
Organization WH. A Conceptual Framework for Action on the Social Determinants of Health 2010.
Liew SJ, Lee JT, Tan CS, Koh CHG, Van Dam R, Müller-Riemenschneider F. Sociodemographic factors in relation to hypertension prevalence, awareness, treatment and control in a multi-ethnic Asian population: a cross-sectional study. BMJ Open. 2019;9:e025869.
Gee ME, Bienek A, McAlister FA, Robitaille C, Joffres M, Tremblay MS, et al. Factors associated with lack of awareness and uncontrolled high blood pressure among Canadian adults with hypertension. Can J Cardiol. 2012;28:375–82.
Yip W, Wong TY, Jonas JB, Zheng Y, Lamoureux EL, Nangia V, et al. Prevalence, awareness, and control of hypertension among Asian Indians living in urban Singapore and rural India. J Hypertens. 2013;31:1539–46.
Rodrigues AP, Gaio V, Kislaya I, Graff-Iversen S, Cordeiro E, Silva AC, et al. Sociodemographic disparities in hypertension prevalence: Results from the first Portuguese National Health Examination Survey. Rev Port Cardiol (Engl Ed). 2019;38:547–55.
Article Google Scholar
Lee HY. Socioeconomic Disparities in the Prevalence, Diagnosis, and Control of Hypertension in the Context of a Universal Health Insurance System. J Korean Med Sci. 2017;32:561–7.
Sivén SS, Niiranen TJ, Aromaa A, Koskinen S, Jula AM. Social, lifestyle and demographic inequalities in hypertension care. Scand J Public Health. 2015;43:246–53.
Redondo A, Benach J, Subirana I, Martinez JM, Muñoz MA, Masiá R, et al. Trends in the prevalence, awareness, treatment, and control of cardiovascular risk factors across educational level in the 1995-2005 period. Ann Epidemiol. 2011;21:555–63.
Perez-Fernandez R, Mariño AF, Cadarso-Suarez C, Botana MA, Tome MA, Solache I, et al. Prevalence, awareness, treatment and control of hypertension in Galicia (Spain) and association with related diseases. J Hum Hypertens. 2007;21:366–73.
Cha SH, Park HS, Cho HJ. Socioeconomic disparities in prevalence, treatment, and control of hypertension in middle-aged Koreans. J Epidemiol. 2012;22:425–32.
Bann D, Fluharty M, Hardy R, Scholes S. Socioeconomic inequalities in blood pressure: co-ordinated analysis of 147,775 participants from repeated birth cohort and cross-sectional datasets, 1989 to 2016. BMC Med. 2020;18:338.
Guessous I, Bochud M, Theler JM, Gaspoz JM, Pechère-Bertschi A. 1999-2009 Trends in prevalence, unawareness, treatment and control of hypertension in Geneva, Switzerland. PLoS One. 2012;7:e39877.
Article CAS PubMed PubMed Central Google Scholar
Choi HM, Kim HC, Kang DR. Sex differences in hypertension prevalence and control: Analysis of the 2010-2014 Korea National Health and Nutrition Examination Survey. PLoS One. 2017;12:e0178334.
Article PubMed PubMed Central CAS Google Scholar
Howard G, Cushman M, Moy CS, Oparil S, Muntner P, Lackland DT, et al. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA 2018;320:1338–48.
Park CS, Ha KH, Kim HC, Park S, Ihm SH, Lee HY. The Association between Parameters of Socioeconomic Status and Hypertension in Korea: the Korean Genome and Epidemiology Study. J Korean Med Sci. 2016;31:1922–8.
Baek TH, Lee HY, Lim NK, Park HY. Gender differences in the association between socioeconomic status and hypertension incidence: the Korean Genome and Epidemiology Study (KoGES). BMC Public Health. 2015;15:852.
Pereira M, Lunet N, Paulo C, Severo M, Azevedo A, Barros H. Incidence of hypertension in a prospective cohort study of adults from Porto, Portugal. BMC Cardiovasc Disord. 2012;12:114.
Conen D, Glynn RJ, Ridker PM, Buring JE, Albert MA. Socioeconomic status, blood pressure progression, and incident hypertension in a prospective cohort of female health professionals. Eur Heart J. 2009;30:1378–84.
Dupre ME. Educational differences in health risks and illness over the life course: a test of cumulative disadvantage theory. Soc Sci Res. 2008;37:1253–66.
Vargas CM, Ingram DD, Gillum RF. Incidence of hypertension and educational attainment: the NHANES I epidemiologic followup study. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152:272–8.
Satoh A, Arima H, Ohkubo T, Nishi N, Okuda N, Ae R, et al. Associations of socioeconomic status with prevalence, awareness, treatment, and control of hypertension in a general Japanese population: NIPPON DATA2010. J Hypertens. 2017;35:401–8.
Abu-Saad K, Chetrit A, Eilat-Adar S, Alpert G, Atamna A, Gillon-Keren M, et al. Blood pressure level and hypertension awareness and control differ by marital status, sex, and ethnicity: a population-based study. Am J Hypertens. 2014;27:1511–20.
Nguyen QC, Waddell EN, Thomas JC, Huston SL, Kerker BD, Gwynn RC. Awareness, treatment, and control of hypertension and hypercholesterolemia among insured residents of New York City, 2004. Prev Chronic Dis. 2011;8:A109.
PubMed PubMed Central Google Scholar
Ostchega Y, Hughes JP, Wright JD, McDowell MA, Louis T. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens. 2008;21:159–65.
Tompkins G, Forrest LF, Adams J. Socio-economic differences in the association between self-reported and clinically present diabetes and hypertension: secondary analysis of a population-based cross-sectional study. PLoS One. 2015;10:e0139928.
Chen R, Tunstall-Pedoe H, Morrison C, Connaghan J, A’Brook R. Trends and social factors in blood pressure control in Scottish MONICA surveys 1986-1995: the rule of halves revisited. J Hum Hypertens. 2003;17:751–9.
Vallée A, Grave C, Gabet A, Blacher J, Olié V. Treatment and adherence to antihypertensive therapy in France: the roles of socioeconomic factors and primary care medicine in the ESTEBAN survey. Hypertens Res. 2021;44:550–60.
Article PubMed CAS Google Scholar
McNaughton CD, Jacobson TA, Kripalani S. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns. 2014;96:165–70.
Patel R, Lawlor DA, Whincup P, Montaner D, Papacosta O, Brindle P, et al. The detection, treatment and control of high blood pressure in older British adults: cross-sectional findings from the British Women’s Heart and Health Study and the British Regional Heart Study. J Hum Hypertens. 2006;20:733–41.
Appleton SL, Neo C, Hill CL, Douglas KA, Adams RJ. Untreated hypertension: prevalence and patient factors and beliefs associated with under-treatment in a population sample. J Hum Hypertens. 2013;27:453–62.
Rohla M, Haberfeld H, Tscharre M, Huber K, Weiss TW. Awareness, treatment, and control of hypertension in Austria: a multicentre cross-sectional study. J Hypertens. 2016;34:1432–40.
de Gaudemaris R, Lang T, Chatellier G, Larabi L, Lauwers-Cances V, Maitre A, et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension 2002;39:1119–25.
Andersen UO, Jensen GB. Gender difference and economic gradients in the secular trend of population systolic blood pressure. Eur J Intern Med. 2013;24:568–72.
Matthews KA, Kiefe CI, Lewis CE, Liu K, Sidney S, Yunis C. Socioeconomic trajectories and incident hypertension in a biracial cohort of young adults. Hypertension 2002;39:772–6.
LeBrón AM, Schulz AJ, Mentz G, Gamboa C, Reyes A. Antihypertensive Medication Use: Implications for Inequities in Cardiovascular Risk and Opportunities for Intervention. J Health Care Poor Underserved. 2018;29:192–201.
Shahu A, Herrin J, Dhruva SS, Desai NR, Davis BR, Krumholz HM, et al. Disparities in socioeconomic context and association with blood pressure control and cardiovascular outcomes in ALLHAT. J Am Heart Assoc. 2019;8:e012277.
Nowotny KM, Masters RK, Boardman JD. The relationship between education and health among incarcerated men and women in the United States. BMC Public Health. 2016;16:916.
Pampel FC, Krueger PM, Denney JT. Socioeconomic Disparities in Health Behaviors. Annu Rev Socio. 2010;36:349–70.
D’Zurilla TJ, Sheedy CF. Relation between social problem-solving ability and subsequent level of psychological stress in college students. J Personal Soc Psychol. 1991;61:841.
Manstead ASR. The psychology of social class: How socioeconomic status impacts thought, feelings, and behaviour. Br J Soc Psychol. 2018;57:267–91.
Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open. 2017;7:e013384.
Drinkwater C, Wildman J, Moffatt S. Social prescribing. BMJ 2019;364:l1285.
Reinhardt GY, Vidovic D, Hammerton C. Understanding loneliness: a systematic review of the impact of social prescribing initiatives on loneliness. Perspect Public Health. 2021;141:204–13.
Cuffee Y, Ogedegbe C, Williams NJ, Ogedegbe G, Schoenthaler A. Psychosocial risk factors for hypertension: an update of the literature. Curr Hypertens Rep. 2014;16:483.
National Academies of Sciences E, and Medicine. Social isolation and loneliness in older adults Opportunities for the health care system. Washington, DC: The National Academies Press; 2020.
Yang YC, Li T, Ji Y. Impact of social integration on metabolic functions: evidence from a nationally representative longitudinal study of US older adults. BMC Public Health. 2013;13:1210.
Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25:132–41.
Ernst JM, Cacioppo JT. Lonely hearts: psychological perspectives on loneliness. Appl Preventive Psychol. 1999;8:1–22.
Berkman LF, Kawachi I, Glymour MM. Social epidemiology. 2nd ed. New York (NY): Oxford University Press; 2014.
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–18.
Yazawa A, Inoue Y, Fujiwara T, Stickley A, Shirai K, Amemiya A, et al. Association between social participation and hypertension among older people in Japan: the JAGES Study. Hypertens Res. 2016;39:818–24.
Oshio T, Kan M. Preventive impact of social participation on the onset of non-communicable diseases among middle-aged adults: A 10-wave hazards-model analysis in Japan. Prev Med. 2019;118:272–8.
Nakagomi A, Tsuji T, Hanazato M, Kobayashi Y, Kondo K. Association between community-level social participation and self-reported hypertension in older Japanese: A JAGES multilevel cross-sectional study. Am J Hypertens. 2019;32:503–14.
Johnell K, Råstam L, Lithman T, Sundquist J, Merlo J. Low adherence with antihypertensives in actual practice: the association with social participation–a multilevel analysis. BMC Public Health. 2005;5:17.
Palafox B, Goryakin Y, Stuckler D, Suhrcke M, Balabanova D, Alhabib KF, et al. Does greater individual social capital improve the management of hypertension? Cross-national analysis of 61 229 individuals in 21 countries. BMJ Glob Health. 2017;2:e000443.
Ueno T, Nakagomi A, Tsuji T, Kondo K Association between social participation and hypertension control among older people with self-reported hypertension in Japanese communities. Hypertension Res. 2022. https://doi.org/10.1038/s41440-022-00953-w .
Szabo A, Allen J, Stephens C, Alpass F. Longitudinal analysis of the relationship between purposes of internet use and well-being among older adults. Gerontologist. 2019;59:58–68.
Nakagomi A, Shiba K, Kondo K, Kawachi I Can online communication prevent depression among older people? A longitudinal analysis. J Appl Gerontol. 2020:733464820982147.
Download references
Acknowledgements
This study was supported by the Open Innovation Platform with Enterprises, Research Institute and Academia (OPERA, JPMJOP1831) from the Japan Science and Technology (JST). The funding source had no role in the study design, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Social Preventive Medical Sciences, Center for Preventive Medical Sciences, Chiba University, Chiba, Japan
Atsushi Nakagomi, Yuichi Yasufuku, Takayuki Ueno & Katsunori Kondo
Department of Cardiology, Chiba University Hospital, Chiba, Japan
Atsushi Nakagomi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Atsushi Nakagomi .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary table, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Nakagomi, A., Yasufuku, Y., Ueno, T. et al. Social determinants of hypertension in high-income countries: A narrative literature review and future directions. Hypertens Res 45 , 1575–1581 (2022). https://doi.org/10.1038/s41440-022-00972-7
Download citation
Received : 30 September 2021
Revised : 19 January 2022
Accepted : 02 February 2022
Published : 20 July 2022
Issue Date : October 2022
DOI : https://doi.org/10.1038/s41440-022-00972-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Social determinants of health
- Socioeconomic status
- Social prescribing
This article is cited by
- Naoki Kondo
Hypertension Research (2024)
The association of body composition and fat distribution with hypertension in community-dwelling older adults: the Bushehr Elderly Health (BEH) program
- Mohammad Mehdi Khaleghi
- Ali Jamshidi
- Bagher Larijani
BMC Public Health (2023)
Treatment Intensity, Prescribing Patterns, and Blood Pressure Control in Rural Black Patients with Uncontrolled Hypertension
- Doyle M. Cummings
- Alyssa Adams
- Monika M. Safford
Journal of Racial and Ethnic Health Disparities (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Prev Cardiol
- v.2; 2020 Jun
State-of-the-Art review: Hypertension practice guidelines in the era of COVID-19
Keith c. ferdinand.
a Tulane Heart and Vascular Institute, John W. Deming Department of Medicine (KCF), USA
Thanh N. Vo
b Tulane University School of Medicine (TNV), Tulane University, New Orleans, LA, 70112, USA
Melvin R. Echols
c Cardiology Division (MRE), Department of Medicine, Morehouse School of Medicine, Atlanta, GA, 30310, USA
The global burden of hypertension (HTN) is immense and increasing. In fact, HTN is the leading risk factor for adverse cardiovascular disease outcomes. Due to the critical significance and increasing prevalence of the disease, several national and international societies have recently updated their guidelines for the diagnosis and treatment of HTN. In consideration of the COVID-19 pandemic, this report provides clinicians with the best strategies to prevent HTN, manage the acute and long-term cardiac complications of HTN, and provide the best evidence-based care to patients in an ever-changing healthcare environment. The overarching goal of the various HTN guidelines is to provide easily accessible information to healthcare providers and public health officials, which is key for optimal clinical practice. However, the COVID-19 pandemic has challenged the ability to provide safe care to the most vulnerable hypertensive populations throughout the world. Therefore, this review compares the most recent guidelines of the 2017 American College of Cardiology/American Heart Association and multiple U.S. societies, the 2018 European Society of Cardiology/European Society of Hypertension, the 2019 National Institute for Care and Health Excellence, and the 2020 International Society of Hypertension. While a partial emphasis is placed on the management of HTN in the midst of COVID-19, this review will summarize current concepts and emerging data from the listed HTN guidelines on the diagnosis, monitoring, management, and evidence-based treatments in adults.
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel coronavirus composed of a single stranded positive-sense RNA. The specifics of the detailed pathobiology and human cellular interactions have been described previously [ [1] , [2] , [3] , [4] ]. This virus binds to the angiotensin-converting enzyme 2 (ACE2), a cellular transmembrane homologue of angiotensin-converting enzyme (ACE), in order to enter most human cell lines, including pneumocytes and those in the cardiovascular system [ 4 ]. Consequently, in addition to the eponymous respiratory complications, COVID-19 is associated with increased vascular thrombosis, myocardial inflammation, arrhythmia, and potentially increased risk for adverse outcomes in patients with HTN [ 5 ]. In a recent meta-analysis of 6560 patients from 30 studies, HTN was associated with an increased composite poor outcome, which included mortality, acute respiratory disease syndrome, need for intensive care, and disease progression in patients with COVID-19 [ 6 ]. Other studies have shown similar findings of the deleterious effects of COVID-19 patients with HTN [ 7 , 8 ]. Yet it remains unclear how contemporary guideline recommendations may be impacted in the setting of the COVID-19 pandemic.
Moreover, the current public health crisis of COVID-19 has already impacted patients with HTN from multiple aspects. Approximately 1.5 million people in the U.S. lost their employment-based health insurance coverage, directly affecting patients with HTN and other chronic conditions [ 9 ]. Coverage losses are likely the steepest in states without Medicaid expansion under the Patient Protection and Affordable Care Act. Unfortunately, access to health coverage is most deficient in states with the largest racial/ethnic disparities in cardiovascular care, potentially impacting adherence and medication affordability [ 10 , 11 ]. Specifically, African Americans may suffer worse outcomes related to COVID-19 exposure, due to a variety of reasons, including socioeconomic factors and limited health access [ 12 ].
This review will compare and contrast contemporary evidence-based guidelines for the prevention and treatment of HTN: the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults; the 2018 European Society of Cardiology/European Society of Hypertension (ESC/ESH) Guidelines for the Management of Arterial Hypertension; the 2019 National Institute for Health and Care Excellence (NICE) Hypertension in Adults; and the 2020 International Society of Hypertension (ISH) Global Hypertension Practice Guidelines. Accordingly, this review will summarize current best practices in HTN management, taken into account the current COVID-19 pandemic, emerging data on diagnosis and BP monitoring, and evidence-based treatment of certain special populations, including related to race/ethnicity. Guidelines-directed medical care will provide best strategies to battle the acute and long-term cardiac complications of HTN across diverse populations in the COVID-19 era and beyond.
2. The hypertension pandemic
HTN, the most widely prevalent and potent risk factor for atherosclerosis cardiovascular disease (ASCVD) and associated microvascular complications, affects an estimated 1.4 billion people worldwide, disproportionately so in low- and middle-income countries. Globally, upwards to 1 in 4 men and 1 in 5 women have the chronic HTN [ 13 , 14 ]. Consequently, HTN is the leading global cause of mortality, accounting for 10.4 million deaths per year and a major cause of premature death worldwide [ 15 ]. Regarding systolic blood pressures (SBP), there are over 7.8 million deaths and ~140,000 million disease adjusted life years (DALYs) attributed to a SBP > 140 mmHg alone [ [13] , [14] , [15] ].
As well, there are unique considerations and persistent world-wide disparities in HTN death and morbidity in specific populations, such as related to racial/ethnicity, female sex, advanced age, and socioeconomic status. Recent data from the Centers for Disease Control and Prevention (CDC) noted a significantly higher prevalence of uncontrolled HTN among U.S. racial/ethnic minority groups compared with non-Hispanic whites [ 16 ]. The prevalence of self-reported HTN in 2017 (≥140/90 mmHg) was much higher in Non-Hispanic blacks (African Americans) and American Indians (40% vs. 37%, respectively) than the self-reported prevalence of HTN in Hispanics and whites (28% vs. 29%, respectively) [ 16 ]. After the introduction of the 2017 ACC/AHA and multi-society high blood pressure (HBP) guidelines, the prevalence of HTN increased from 32% in the U.S. to 46% using a BP threshold for HTN ≥130/80 mmHg, further disproportionately affecting blacks and older individuals [ 17 ]. Due to the increasing prevalence of HTN in younger patients, the U.S. Preventive Task Force recommendations now support office BP screening in patients 18 years of age and older [ 18 ]. Therefore, there may be further disparate prevalence among various groups with HTN as time progresses.
This review evaluates current recommended lifestyle interventions and pharmacotherapy within the major guidelines, and the ongoing efforts to combat the challenges of HTN management in the setting of COVID-19. Although recommended in evidence-based guidelines, the COVID-19 pandemic has limited physical activity secondary to social distancing, home quarantining, and fitness center shutdowns [ 19 ]. Moreover, the COVID-19 pandemic has forced the practice of medicine into a new paradigm, where telehealth technologies and self-monitoring techniques have developed more prominent roles for clinical management of HTN and ASCVD risk reduction.
3. Recent major guidelines for hypertension: similarities and differences
Current guidelines, despite major and minor differences, serve as tools for the advancement of “standard of care” recommendations in clinical practice, including specific populations, usually with a regional emphasis. The 2017 ACC/AHA recommendations for tighter BP control were supported by several sources, including several meta-analyses of observational cohorts associated with a significantly higher range of hazard ratios (1.1–1.5) for cardiovascular disease (CVD) and stroke with SBP/DBP ≥ 120–129/80-84 mmHg as compared to <120/80 mmHg [ 17 , 20 ]. Furthermore, data for the benefit of tighter BP control also emerged from the Systolic Blood Pressure Intervention Trial (SPRINT). This National Institute of Health landmark trial was a large randomized control study which evaluated the benefits of intensive BP goals (<120 mmHg) compared with standard treatment goals (<140 mmHg) [ 21 ]. As a result of an overwhelming positive effect, SPRINT was stopped early after demonstrating a 25% and 27% relative risk reduction (RRR) in the primary endpoint and all-cause mortality in the intensive BP lowering group compared to standard treatment (HR 0.75, 95% CI 0.64–0.89, HR 0.73, 95% CI 0.60–0.90, respectively). Thus, the prospect of encouraging patients and providers in the U.S. to manage HTN more intensively was recommended to decrease end-organ damage and mortality.
The 2018 ESC/ESH HTN guidelines reflected a broad scope, intended for the treatment of hypertensive individuals in countries with various socioeconomic populations [ 22 ]. The prevalence of HTN (≥140/90 mmHg) in central and Eastern Europe is approximately 30–45%, affecting over 150 million adults, with an increasing prevalence of up to 60% in adults of advanced age. Instead of focusing on tighter BP control, the ESC/ESH guidelines defined HTN as the level of BP at which the benefits of treatment, whether lifestyle interventions or medications, outweighed the risks. Recommendations were based on meta-analyses of randomized controlled trials (RCTs), in which treatment of stage I BP values of ≥140/90 mmHg were considered beneficial [ 22 ]. Moreover, utilizing older and high-risk cohort studies may increase statistical power over a shorter duration of follow-up. These differences in the type of evidence used between the 2017 ACC/AHA and the 2018 ESC/ESH guidelines may provide clarity as to why the BP thresholds for HTN vary between the reports.
Most recently published are the NICE’s ‘Hypertension in Adults’ in 2019 and the 2020 ISH report [ 23 , 24 ]. The NICE guidelines only reviewed evidence beyond the year 2000, reflecting the current use of electronic BP devices. However, both guidelines use the SBP/DBP threshold of 140/90 mmHg to define Stage I HTN. The 2020 ISH proposes HTN guidelines for global use, fit for low and high resource settings by advising essential and optimal standards, in a concise and easy to use format. Therefore, the overarching goal of contemporary HTN development is to reduce the adverse outcomes in the populations of interest and regional differences often inhibit complete uniformity.
4. Current definitions of Arterial Hypertension in adult
Although the CVD morbidity and mortality of increased BP is linear, direct, and continuous, the definition of HTN varies among guidelines ( Table 1 ). The current recommendations, in general, provide BP thresholds based on average measurements in an office setting. The rationale for these categorizations is determined primarily by in-office observational data related to the association of SBP/DBP and CVD risk, randomized-controlled trials (RCTs) of lifestyle modifications to lower BP, and RCTs of medication therapy to reduce BP [ 17 ]. The 2018 ESC/ESH HTN definition characterizes ‘optimal’ BP defined as SBP <120 mmHg and DBP <80 mmHg. On the other hand, this level of blood pressure is considered ‘normal’ by the 2017 ACC/AHA definitions [ 17 ] ( Table 1 ) .
Table 1
Guideline Definitions of Hypertension [ 17 , 22 , 24 , 29 ].
| BP Category (mmHg) | ACC/AHA 2017 | ESC/ESH 2018 | NICE 2019 | ISH 2020 |
|---|---|---|---|---|
| SBP | <120 | 120–129 | <140 | <130 |
| DBP | <80 | 80–84 | <90 | <85 |
| SBP | 120–129 | 130–139 | ∗ | 130–139 |
| DBP | <80 | 85–89 | ∗ | 85–89 |
| SBP | 130–139 | 140–159 | 140–179 | 140–159 |
| DBP | 80–89 | 90–99 | 90–119 | 90–99 |
| SBP | ≥140 | 160–179 | ≥180 | ≥160 |
| DBP | ≥90 | 100–109 | ≥120 | ≥100 |
| SBP | ∗ | ≥180 | ∗ | ∗ |
| DBP | ≥110 | ∗ | ∗ | |
BP , blood pressure; SBP , systolic blood pressure; DBP , diastolic blood pressure; ACC/AHA , American College of Cardiology/American Heart Association; ESC/ESH , European Society of Cardiology, European Society of Hypertension; NICE , National Institute for Health and Care Excellence; ISH , International Society of Hypertension.
The NICE and ISH publications use similar thresholds for the definitions of HTN (≥140/90 mmHg). The BP for a visit is determined by the average of at least two measurements in the clinic setting, at least one minute apart. If the final BP measurement is between 140/90 and 180/120 mmHg, the NICE and ISH guidelines recommend offering ambulatory blood pressure monitoring (ABPM) to confirm the diagnosis [ 23 , 24 ]. Additionally, all of the reviewed guidelines strongly recommend the utilization of out-of-office BP measurements for monitoring and/titration antihypertensive therapies. The various reports reviewed herein support the initial or concomitant use of nonpharmacological interventions for most patients, which include lifestyle modifications of dietary and activity levels, prior to medications in most individuals to reduce BP values.
5. Contemporary recommendation of blood pressure techniques and devices
The accurate measurement of in-office and out-of-office BP is crucial in HTN diagnosis and management. Although the traditional use of devices calibrated to a column of mercury is still utilized in some regions, most guidelines report recommendations from data using electronic devices for BP monitoring. All of the guidelines recommend validated devices, whether electronic or manual [ 25 , 26 ]. The US Blood Pressure Validated Device Listing (VDLTM) was the first U.S. list of blood pressure (BP) measurement devices developed to assist physicians and patients in identifying BP devices that are validated for clinical accuracy. BP devices listed on the VDLTM have specific criteria detailed as determined through independent review. Visit ValidateBP.org to view the current device listings for more information on the independent review process [ 27 ]. The ESC/ESH guidelines recommend validated devices by the Association of Medical Instrumentation [ 26 ].
As errors in BP measurements are common in most settings, the HTN guidelines all thoroughly describe protocols to obtain accurate results [ 28 ]. BP is measured in both arms to detect any differences in the first office visit. Most guidelines recommend using the arm with the higher BP reading for a subsequent visit. All of the reviewed guidelines suggest taking the BP 2–3 times, separated by at least 1 min apart, averaging at least two of the readings for the final result. The ESC/ESH and NICE guidelines also suggest measuring the standing BP at least once after standing for 1 min, to determine the likelihood of orthostatic BP changes [ 22 , 29 ]. All guidelines also suggest measuring BP in at least two separate office visits to diagnose HTN before any interventions are recommended. Expert panels of the AHA and ACC have published recent scientific statements evaluating the accuracy of BP measurements in further detail, emphasizing the need for proper and ongoing training of technicians and healthcare providers for the use of validated devices [ 28 , 30 ].
6. Guidance for out-of-office and ambulatory BP monitoring
The reviewed HTN guidelines acknowledge the benefits of ABPM and home blood pressure monitoring (HBPM) and provide strong recommendations of these techniques to confirm the diagnosis of HTN and monitor medication adjustments. HBPM is an alternative to confirm the diagnosis of HTN if ABPM is not possible. The technology for ABPM has been available for many years and is recommended by the ACC/AHA, ESH/ESC, NICE, and ISH guidelines with similar protocols suggested for use. ABPM has a stronger association with hypertension-related target-organ damage and adverse clinical outcomes [ 30 ].
The ABPM devices usually measure BP every 15–30 min during the day and every 15 min to 1 h during the night over a 24-hour period. There are BP correlate values to in-office setting BP measurements within the guidelines for HTN management to assist with HTN management ( Table 2 ). ABPM is also useful to detect certain BP phenotypes of HTN that may confer increased CVD risk. White-coat HTN occurs when individuals demonstrate higher BP measurements in the office setting when compared with measurements outside of the office. The white-coat effect is a term used to describe the same phenomenon in patients having a history of HTN and receiving antihypertensive medications [ 26 ]. Although the data are limited, there may be a modest increase in CVD risks for patients experiencing these conditions. Most studies demonstrating an increased CVD risk are in patients with other CVD risk factors that could explain the higher risk [ 31 , 32 ]. The guidelines also reference terminology of isolated office HTN and other subclasses of HTN, although these conditions are not covered extensively within this review [ 17 , 22 , 24 ].
Table 2
Hypertension Correlation of Clinic, Home, and Ambulatory Blood Pressure Monitoring [ 17 , 22 , 24 , 29 ].
| Guideline | Clinic (mmHg) | HBPM (mmHg) | Daytime ABPM (mmHg) | Nightime ABPM (mmHg) | 24-h avg ABPM (mmHg) |
|---|---|---|---|---|---|
| ≥130/80 | ≥130/80 | ≥130/80 | ≥110/65 | ≥125/75 | |
| ≥140/90 | ≥135/85 | ≥135/85 | ≥120/70 | ≥130/80 | |
| ⁺ | ≥140/90 | ≥135/85 | ≥135/85 | ∗ | ∗ |
| ≥140/90 | ≥135/85 | ≥135/85 | ≥120/70 | ≥130/80 | |
HBPM , home blood pressure monitoring; A BPM , ambulatory blood pressure monitoring; ACC/AHA , American College of Cardiology/American Heart Association; ESC/ESH , European Society of Cardiology, European Society of Hypertension; NICE , National Institute for Health and Care Excellence; ISH , International Society of Hypertension.
ABPM has also been used to detect masked HTN, which refers to individuals demonstrating a mean out-of-office BP in the hypertensive range and normal BP measurements in an office setting. The ESC/ESH guidelines suggest incorporation of nighttime BP measurements with daytime readings for this diagnosis, although most guidelines use daytime readings of ABPM [ 22 , 30 ]. Incorporation of nighttime readings also increases the detection and prevalence rates of masked HTN in blacks, associated with higher rates of declining renal function [ 33 , 34 ].
Despite the evidence supporting the use of ABPM in HTN management, several issues limit its use and availability for patients. The monitoring requires proper training of patients and providers, as well as compliance of use to provide accurate and helpful information. The reimbursement rates for the utilization of ABPM is historically low, representing <1% of Medicare beneficiary claims in some studies [ 35 ]. There are also only modest data supporting better outcomes with the treatment of white-coat or masked HTN outside of standard treatment of existing CVD risk factors. Further investigations as to whether ABPM can specify individuals requiring additional treatments to reduce CVD risk may be warranted.
As recommended in all contemporary guidelines, HBPM and self-monitored blood pressure (SMBP) outside the office are considered a more practical alternative to ABPM. The Agency for Healthcare Research and Quality (AHRQ) found strong evidence that SMBP plus additional support (defined below) was more effective than usual care in lowering blood pressure among patients with HTN [ 36 , 37 ]. SMBP protocols are likely to become much more useful in HTN control as the COVID-19 pandemic continues to direct current day medical care (see Fig. 1 ).

Feedback loop between patients and healthcare providers supporting SMBP [ 36 ].
Public health organizations have recognized the devastating effects of HTN on the US population and have developed several initiatives to utilize the techniques of SMBP to manage CVD outcomes for HTN. The Million Hearts 2022 is a national initiative to prevent 1 million heart attacks and strokes within 5 years through the implementation of evidence-based strategies that can improve cardiovascular health for all. This effort recognizes the use of out-of-office BP monitoring and recommends use of these strategies, according to the best evidence [ 36 ]. The TargetBP national initiative, formed by the AHA and the American Medical Association, also assists health care organizations and care teams, at no cost, in improving BP control rates through a quality improvement program [ 38 ]. These large-scale efforts will provide new insights into the challenges and management of adherence with BP recommendations for all populations within the US.
In general, the use of HBPM/SMBP have been recommended by several societies, and most recently as a potential means to manage HTN during the COVID-19 outbreak in conjunction with the 2020 surge in telehealth [ 13 , 18 , 39 ]. It is likely these BP measuring methods will become more useful over time as the readings outside of the office may decrease the prevalence of white-coat hypertension and inconsistent readings within office measurements. These measures, in conjunction with advancing telehealth services, have the potential to provide more responsibility for the patient’s HTN management. Thus, the increasing steps to use out of office BP monitoring and telehealth services may indirectly increase patient engagement and health literacy.
Many health centers and medical practices have quickly introduced more pronounced telehealth services into the current models of care management, which is ideal at this time. Several barriers to overcome include payment and regulatory structures, state licensing, and credentialing across health centers [ 40 ]. Yet, the use of remote patient monitoring, patient-initiated messaging, telephone visits, and video visits are within the reach of telehealth medicine should be beneficial for BP control in a large population effort. Wosik and colleagues suggest the COVID-19 pandemic will stimulate the need for telehealth services in significant shifts or phases of care. Phase I, or the initial outpatient management of conditions such as HTN with the “stay at home”, order has already begun as some health centers have increased the need for telehealth services to as much as 70% of total outpatient visits. Phase II is described as the telehealth needs during inpatient related surge, through the use of network care management and e-consultations. Phase III is considered the post-pandemic recovery period, which is still unknown at this time. The authors appropriately discuss the issues in delayed care for serious non-COVID-19 related medical conditions, such as acute coronary syndromes, which has already occurred in many communities. A “care debt” is described as well from the first two phases and will likely require intense sustained telehealth efforts [ 41 ].
In addition, mobile health services may become a preferred method of HTN management during and post the COVID-19 pandemic, particularly in poorer populations with less health care access. Mobile health interventions for HTN usually involve the use of a patient’s mobile phone, along with a validated BP measuring device, to track and communicate measurements with providers. A recent meta-analysis of eleven randomized controlled trials (4271 participants) associated significantly lower systolic and diastolic BP measurements with the use of mobile health interventions in patients with HTN [ 42 ]. These findings were consistent through study duration and treatment intervention intensity within the trials. Further investigations, involving nonpharmacologic interventions and modes of patient engagement, may increase the effectiveness of future mobile and telehealth BP interventions.
7. Evidence-based approaches to nonpharmacologic management of HTN
Therapeutic lifestyle changes are necessary to prevent poor CVD outcomes with HTN. All of the major HTN guidelines support interventions of weight-control (weight loss if necessary), sodium restriction, smoking cessation, regular physical activity, healthy diet, and limiting alcohol consumption to reduce blood pressure in all individuals ( Table 3 ) [ 17 , 22 , 29 ] . However, the Dietary Approaches to Stop Hypertension (DASH) pattern appears most effective to yield significant reductions in BP for all individuals (blacks with reductions of SBP as high as 20 mmHg) slowing the decline of renal dysfunction and for weight loss with overweight status [ [43] , [44] , [45] ].
Table 3
Blood pressure reductions of nonpharmacological interventions [ 17 ].
| Nonpharmacological Intervention | Dose | Reduction in SBP (mmHg) | |
|---|---|---|---|
| HTN | Normal BP | ||
| Weight loss | Aim for at least 1-kg reduction in body weight for most adults who are overweight. Expect ~1 mmHg reduction for every 1-kg reduction in body weight. | 5 | 2–3 |
| Diet rich in fruits, vegetables, whole grains, low-fat dairy products, with reduced content of saturated and total fat. Available at . | 11 | 3 | |
| Optimal goal <1500 mg/day. Aim for at least 1000 mg/day reduction in most adults | 5–6 | 2–3 | |
| Approximately 3500–5000 mg/day. For a list of high potassium foods, visit | 4–5 | 2 | |
| 90–150 min/week at 65–75% of max heart rate | 5–8 | 2–4 | |
| 90–150 min/week; 6 exercises, 3 sets/exercise, 10 repetitions/set | 4 | 2 | |
| 4 × 2 min (hand grip), 1 min rest between exercises; 3 sessions/week for 8–10 week duration | 5 | 4 | |
| In individuals who drink alcohol, reduce to: Men ≤ 2 drinks daily, Women ≤ 1 drink daily (~12 oz. beer, 5 oz. of wine, or 1.5 oz. distilled spirits) | 4 | 3 | |
Increased potassium intake (3500–5000 mg/day), aside from following the DASH diet, is recommended by the ACC/AHA to provide further reductions in BP (2–5 mmHg for hypertensive individuals) [ 17 ]. Dietary supplementation of potassium can help further lower blood pressure by easing tension on blood vessel walls. Behavioral therapies such as yoga and meditation, effectively reduce blood pressure [ 24 ]. Additionally, the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease and a report from the American Society of Preventive Cardiology (ASPC) support the benefits of therapeutic lifestyle interventions for BP control [ 13 , 46 ].
Additionally, Mediterranean diet (MedDiet) may have a favorable effect on the risk of HTN in contrast to unfavorable dietary patterns such as red meat, processed meat, and poultry [ 47 ]. The MedDiet or DASH diet are also likely beneficial over the Western diet (WD) in relation to COVID-19 susceptibility, as the high rate of consumption of saturated fats, sugars, and refined carbohydrates in the WD contribute to the prevalence of obesity and type 2 diabetes (T2D) potentially increasing the risk for severe COVID-19 pathology and mortality [ 48 ].
Patient engagement, in addition to nonpharmacologic interventions, will likely require more emphasis during and post COVID-19, as the prevalence of HTN could increase over time with decreased activity and attention to diet. The need for health coaching by clinicians and members of the community may increase in order to initiate or maintain adherence to nonpharmacologic BP interventions. A recent meta-analysis comparing implementation strategies for HTN control evaluated a total of 55, 920 patients, which included studies evaluating the use of patient-level health coaching. Health coaching was associated with a significant reduction in blood pressure over a minimum of 6 months (−3.9 mmHg, 95% CI -5.4 to −2.3 mmHg) [ 49 ]. Thus, multilevel interventions, including patient-level strategies, are likely to become more important in the treatment of HTN during and after the COVID-19 pandemic.
8. Impact of adherence on blood pressure control and outcomes
Nonadherence, affecting as much as 80% of patients with HTN, increases the associated risk for CVD morbidity and mortality, with approximately one of every four patients not filling their initial prescription [ 17 , 24 ]. The major HTN guidelines equally recognize the economic burden of HTN medications increasing nonadherence [ 50 ]. In a recent study, 67% of patients who do not experience financial barriers to pharmacotherapy are more likely adherent and have normal BP within the past 12 months [ [50] , [51] , [52] , [53] ]. There are promising data using highly sensitive high-performance liquid chromatography-tandem mass spectrometry biochemical measurements of drug levels in the serum or urine as a surrogate of compliance [ 54 , 55 ]. Although these measurements are now available for clinical use and covered by some insurance plans, more research is warranted for determining the effect on large populations and mainstream use.
Guideline-recommended strategies include adherence feedback to the patient, HBPM/SBPM, linkage of behavior with daily habits, electronic aids, such as mobile phones and reduction of polypharmacy utilizing a single pill combination is possible [ 24 , 46 , 56 ] ( Table 4 ). As most patients will often require more than one antihypertensive agent to control BP, fixed-dose combinations (FDC) pills for HTN are supported by the major guidelines [ 17 , 22 , 24 ]. A recent meta-analysis of 62,481 patients with HTN reported a mean medication adherence difference of ~15% in patients receiving FDC medications vs. free separate equivalent dose pills [ 57 ]. Many common FDC HTN therapies are included in formularies at reduced co-pays and may attenuate HTN management costs during the COVID-19 pandemic and beyond.
Table 4
Guideline recommendations for adherence to antihypertensive therapies [ 17 , 22 , 24 ].
The polypill concept, including HTN and lipid drugs, may help reduce prescribing complexities for CVD prevention [ [58] , [59] , [60] ]. A recent randomized, controlled polypill (atorvastatin 10 mg, amlodipine 2.5 mg, losartan 25 mg, and hydrochlorothiazide 12.5 mg) trial, involving adults with a CVD risk of >10% demonstrated significant BP and LDL reduction at 12 months versus standard care of participants at a federally qualified community health center in Alabama [ 61 ]. The mean estimated 10-year cardiovascular risk was 12.7% for the participants, with a mean baseline blood pressure LDL cholesterol of 140/83 mmHg and 113 mg per deciliter, respectively. The monthly cost of the polypill was $26. At 12 months, polypill adherence was 86%. The mean systolic blood pressure decreased by 9 mm Hg in the polypill group, as compared with 2 mmHg in the usual-care group (difference, −7 mm Hg; 95% confidence interval [CI], −12 to −2; P = 0.003) [ 61 ].
9. Telehealth and hypertension in the COVID-19 era
As previously noted, telehealth, prior to the COVID-19 pandemic, had been heralded as a potential advancement in successful HTN and CVD risk management. Moreover, due to safety concerns, the COVID-19 pandemic required telemedicine for routine outpatient visits, significantly affecting HTN and other chronic medical condition management. Initiatives, such as Million Hearts 2022 and Target BP, have emphasized the importance of SBPM with continual patient and provider feedback. In addition, the Centers of Medicare and Medicaid Services (CMS) recently published reimbursement information for telephone and other monitoring services [ 62 ] ( See Table 5 ). As a significant amount of time and detail must be devoted to these modes of communication and assessment, it is important that providers receive adequate compensation. Therefore, CMS expanded telephone consultation payment on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act: particularly for high-risk COVID-19 beneficiaries and with widespread availability of smart phones, telehealth may become future standard medical practice [ 62 , 63 ].
Table 5
Summary of medicare telemedicine services [ 62 ].
| Type of Service | What is the Service? | HCPCS/CPT Code | Type of Patient |
|---|---|---|---|
| A visit with a provider that uses telecommunication systems between a provider and a patient | (Office or other outpatient visit) (Telehealth consultations, emergency department or initial inpatient) (Follow-up inpatient telehealth consultations furnished to beneficiaries in hospitals or SNFs) | New or Established | |
| A brief (5–10 min) check in with a patient via telephone or other telecommunications device to decide whether an office visit or other service is needed. A remote evaluation of recorded video and/or images submitted by an established patient | ∗ ∗ | Established | |
| A communication between a patient and their provider through an online patient portal | Established | ||
HCPCS, The Healthcare Common Procedure Codign System; CPT, Common Procedural Technology; SNFs , Skilled nursing facilities.
Nevertheless, the use of digital technology may further increase disparities. A recent study evaluating telehealth in cardiac clinics suggested disparate use of video encounters in low income and black patients [ 64 ]. Of the 2940 patients scheduled for a telehealth encounter during the study, 1339 (46%) completed telehealth encounters and 1601 (54%) patients had a canceled/no-show visit. On unadjusted analysis, patients with a completed telehealth visit were slightly older, more likely to be male and speak English. However, low income and black patients were less likely to video visits possibly related to insurance coverage [ 64 ]. More investigation is warranted in the future to understand the risks and benefits of video telehealth encounters to enhance cardiac care.
10. Special populations: diabetes, race/ethnicity, sex, and older age
Although each guideline provides specific comments for the management of special populations, including persons with diabetes (DM) and certain involving race/ethnicity, sex, and older age, this review will only detail various aspects of care for certain groups [ 17 , 22 , 24 , 29 , 65 ]. The vast majority of adults with DM have 10-years ASCVD risk >10% placing them in a high-risk category. However, in the most recent ADA recommendations, patients with DM and a 10-year ASCVD risk <15% should maintain a target of <140/90 mmHg, with <130/80 mmHg for the highest risk patients [ 66 ]. In ACC/AHA 2017 and other major guidelines, antihypertensive drug treatment with diabetes should be initiated at a BP of 130/80 mmHg or higher with a treatment goal of <130/80 mmHg [ 17 , 67 ]. Moreover, major guidelines recommend the addition of renin-angiotensin modulators, including an angiotensin converting enzyme inhibitor (ACE-I) or angiotensin receptor blockers (ARB) in the setting of compelling comorbid issues such as diabetes with albuminuria, renal dysfunction, or HF [ 17 , 22 , 24 , 66 , 67 ].
The ACC/AHA, ESC/ESH, and ISH guidelines discuss the significance of race/ethnicity in HTN management. In the U.S., as well as globally, black ancestry may be associated with a higher prevalence of HTN than that of Hispanic Americans, whites, Native Americans, and other groups [ 17 , 22 , 24 ]. In some parts of the world, HTN prevalence is greater than 60% among blacks [ 15 , 68 ]. In comparison to the U.S., the prevalence of HTN in the black population in Europe is higher than the non-black population. The ESC/ESH guidelines emphasize the data are scarce for the European black populations and extrapolate much of their recommendations from U.S. studies [ 22 ]. Non-Hispanic U.S. white adults are more likely to have a higher prevalence of controlled HTN when compared to other groups. The lower rates of control in Hispanic Americans are likely secondary to decreased awareness. However, American blacks have lower controlled rates due to more severe HTN and possibly to less effective treatments [ 17 ].
Thiazide-type diuretics and calcium channel blockers (CCBs) are most effective as the first step in lowering BP and stroke in blacks. Although ACE-I and ARB are less effective in blacks as monotherapy when compared to whites, combination therapy is equally effective in whites and blacks [ 51 , 69 , 70 ]. Perhaps due to suppression of the renin angiotensin aldosterone system, ACE-I and ARB may not only lower BP less effectively, but also for the prevention of heart failure and stroke [ [69] , [70] , [71] ]. ACE-I are also associated with a higher incidence of angioedema in blacks, and ARBs are recommended over an ACE-I by the ESC/ESH and ISH guidelines for HTN treatment, in combination with a diuretic or CCBs. The ACC/AHA, ESC/ESH, and ISH guidelines recommend two or more antihypertensive medications to achieve adequate BP control in blacks, with a diuretic or CCBs used as first-line agents. Patients with BP that is 20/10 mmHg above target may be considered for combination therapy at treatment onset. Given resistant hypertension (rHTN) is more common in African American patients, multidrug pharmacological therapy may be often indicated [ 17 , 22 , 24 ].
The ISH guidelines acknowledge ethnic-specific characteristics for East and South Asian populations, who have a greater likelihood of salt-sensitivity accompanied with mild obesity [ 24 ]. East Asians also have a higher prevalence of hemorrhagic stroke and nonischemic heart failure when compared to Western populations, associated with morning or nighttime HTN. Individuals from the Indian subcontinent have high risks for CVD and type 2D.
Although of considerable interest, special populations related to sex and older age are not detailed in this review, although detailed in the ACC/AHA and ESC/ESH guidelines [ 17 , 22 ]. Furthermore, the ISH guidelines also provide extensive recommendations for the treatment of HTN in pregnancy, whereas this area is covered in supplementary documents for the others [ 24 ]. Most recently, Aronow extensively reviewed the management of HTN in the elderly [ 65 ]. Overall, recognizing unique aspects in the treatment of various populations, including regional differences, is an important component for optimal care.
11. HTN and COVID-19: present and future concepts
According to the most recent data from the World Health Organization COVID-19 has infected over 11.1 million people, responsible for over 528,000 deaths worldwide [ 72 ]. Further clinical observation may be required to determine the long-term risk of COVID-19 and HTN. The devastating effects of COVID-19 have also disproportionately affected several vulnerable populations, including those with certain comorbid diseases, advanced age, and lower socioeconomic status. COVID-19 also has the potential to impact CVD outcomes via a ‘domino effect’, which is initiated by social fears and issues stemming from social distancing. Due to concerns of visiting hospital facilities, patients may not present for outpatient and emergent care needed, such as with acute coronary syndromes. Furthermore, physical inactivity and unhealthy eating due to home quarantine status, along with the social stressors related to increasing unemployment, may increase the rates of HTN, obesity, and CVD events in years to come [ 73 ].
Despite the early concern that ACEI/ARB therapy would worsen outcomes by upregulating ACE2, RAS inhibitors may actually improve the clinical status of COVID-19 patients with hypertension and may even be preferential for antihypertensive treatment [ 2 , [74] , [75] , [76] ]. In a recent study of 417 COVID-19 patients with HTN from China, the data suggest ACEI/ARB therapy attenuated the inflammatory response, potentially through the inhibition of IL-6 levels, which is consistent with the findings that ACEI and ARB therapy alleviated pneumonic injury [ 77 ]. Perhaps, ACEI/ARB therapy has a beneficial effect on the immune system by avoiding peripheral T cell depletion, thereby allowing for a better immune response to the virus in these patients.
As the standards of practice, the Heart Failure Society of America, ACC, AHA, and American Society of Preventive Cardiology currently recommend the continuation of RAS inhibitors with compelling complications such as: heart failure, hypertension, or ischemic heart disease [ 39 , 78 ]. Moreover, abrupt withdrawal of RAS inhibitors in high-risk patients, including those who have heart failure or have had recent myocardial infarction, may result in clinical instability and adverse health outcomes [ 79 ].
On the other hand, dihydropyridines CCBs (nifedipine and amlodipine) may be a benefit for the treatment of hypertensive patients with COVID-19. In a retrospective analysis, a small cohort of elderly hypertensive patients treated with a CCB during a COVID-19 infection, had a significantly higher survival rate and were much less likely to require mechanical intubation (50% vs. 14.6%, respectively) as compare to those not on CCBs [ 80 ]. Although further clinical studies are warranted, the data are promising that treatment of a CCB in hypertensive patients with COVID-19 may significantly improve outcomes.
12. Conclusion
Current guideline recommendations emphasize the importance of evidence-based care to curtail the widespread mortality and morbidity related to HTN and associated ASCVD. Additionally, the acute and long-term effects of COVID-19 may influence treatment in the hypertensive population and require further investigation. The importance of unifying recommendations that help to curve the burden of HTN may become more significant in the coming years as we learn more about new treatments and the long-term effects of the current COVID-19 crisis. The COVID-19 associated morbidity and mortality including patients with underlying HTN and CVD are likely to have profound impact for several decades due to the worldwide medical, economic, and psychological effects. However, although contemporary guidelines suggest benefits of the use of telehealth technologies and out-of-office medical management, as recently required by the cOVID-19 pandemic, these evolving techniques will be increasingly used for HTN control and CVD risk control. Ultimately, future HTN guidelines may increasingly reflect the impact of the COVID-19 pandemic and the utility of measures such as SMBP/HBMP over time.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.

COMMENTS
Hypertension Diagnosis. Once a person has been screened and found to have high blood pressure, ambulatory blood pressure monitoring (ABPM) is regarded as the most accurate way to diagnose hypertension and is recommended by guidelines to routinely to confirm elevated blood pressure readings [2, 17, 18].Ambulatory monitors typically involve portable, automated cuffs worn continuously that ...
Literature review current through: Jul 2024. This topic last updated: Jan 31, 2024. INTRODUCTION. The global prevalence of hypertension is high, and among nonpregnant adults in the United States, treatment of hypertension is the most common reason for office visits and for the use of chronic prescription medications . In addition, roughly one ...
Several important findings bearing on the prevention, detection, and management of hypertension have been reported since publication of the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline. This review summarizes and places in context the results of relevant observational studies, randomized clinical trials, and meta-analyses published between January ...
Since publication of the 2017 ACC/AHA BP Guideline, several new findings have emerged which, taken together, can better inform the approach to the prevention, detection and management of hypertension. The major findings (January, 2018-March, 2021) and their relevance to the management of hypertension are summarized in Table 7.
November 8, 2022. Treatment of Hypertension: A Review. Robert M. Carey, MD 1; Andrew E. Moran, MD 2; Paul K. Whelton, MB, MD, MSc 3. Author Affiliations Article Information. 1 Division of Endocrinology and Metabolism, Department of Medicine, University of Virginia Health System, Charlottesville. 2 Division of General Medicine, Department of ...
Hypertension is a major cause of cardiovascular disease and deaths worldwide especially in low- and middle-income countries. ... The systematic review group conducted systematic searches of the literature to identify existing systematic reviews published between 2015 and 2020 in PubMed, Embase, The Cochrane Library, and Epistemonikos that ...
Endurance training reduces BP more in persons with hypertension than in individuals with normal BP. A narrative review of 27 randomized clinical trials in individuals with hypertension showed that regular medium-intensity to high-intensity aerobic activity reduced BP by a mean of 11/5 mmHg 125. Sessions lasting 40-60 minutes performed at ...
Abstract. Several important findings bearing on the prevention, detection, and management of hypertension have been reported since publication of the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline. This review summarizes and places in context the results of relevant observational studies, randomized ...
These results suggest that AT2R is a new target for the treatment of hypertension and AT2R agonists may act as novel anti-hypertensive drugs in the future. 2.2. ACE2/Ang1-7/Mas receptor axis. In addition to the classic ACE-Ang II-ATR1 axis, the RAAS system also features the ACE2/Ang1-7/Mas axis.
Objective: To evaluate the literature regarding blood pressure control and management in older adult patient population over 70 years of age. Methods: A literature search was conducted using PubMed and capturing the data from 2006 to 2016. Terms used included MeSH headings for hypertension/therapy and antihypertension agents. A systematic review of published studies was performed.
Background Hypertension is an urgent public health problem. Consistent summary from natural and quasi-experiments employed to evaluate interventions that aim at preventing or controlling hypertension is lacking in the current literature. This study aims to summarize the evidence from natural and quasi-experiments that evaluated interventions used to prevent or control hypertension. Methods We ...
Hypertension (HTN) affects more than 30% of adults worldwide. It is the most frequent modifiable cardiovascular (CV) risk factor, and is responsible for more than 10 million death every year.
Short stature is associated with coronary heart disease: a systematic review of the literature and a meta-analysis. Eur Heart J. 2010;31:1802-9. Article PubMed Google Scholar
INTRODUCTION. Hypertension is the leading preventable risk factor for cardiovascular disease (CVD) and all-cause mortality worldwide. 1,2 In 2010, 31.1% of the global adult population (1.39 billion people) had hypertension, defined as systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg. 3 The prevalence of hypertension is rising globally owing to ageing of the population and increases in ...
Hypertension is one of the most prevalent cardiovascular diseases worldwide. However, in the population of resistant hypertension, blood pressure is difficult to control effectively. ... New drug targets for hypertension: A literature review Biochim Biophys Acta Mol Basis Dis. 2021 Mar 1;1867(3):166037. doi: 10.1016/j.bbadis.2020.166037. Epub ...
The global increase in prevalence of hypertension was consistent by sex (5.5% in men and 5.0% in women), but varied by economic development 3. From 2000 to 2010, the prevalence of hypertension ...
PDF | On Jan 1, 2019, Laxmi Narayan Goit and others published Treatment of Hypertension: A Review | Find, read and cite all the research you need on ResearchGate
Interventions in hypertension: systematic review and meta-analysis of natural and quasi-experiments. Tong Xia, 1 Fan Zhao, 1 and Roch A. Nianogo 1, 2 ... employed to evaluate interventions that aim at preventing or controlling hypertension is lacking in the current literature. This study aims to summarize the evidence from natural and quasi ...
Hypertension (HTN) affects more than 30% of adults worldwide. It is the most frequent modifiable cardiovascular (CV) risk factor, and is responsible for more than 10 million death every year. ... Endocrine causes of hypertension: literature review and practical approach Hypertens Res. 2023 Dec;46(12):2679-2692. doi: 10.1038/s41440-023-01461-1.
Treatment of hypertension: a review. JAMA. 2022;328(18):1849-1861. doi: ... These findings are concordant with the existing literature, including a longitudinal cohort that showed the steepest annual growth in systolic blood pressure for women living in more socioeconomically vulnerable areas. 30,31 Thus, given the long-term consequences ...
conducting a literature review on behalf of the Vermont Blueprint for Health and OneCare Vermont with the goal of identifying effective and scalable self-management or community-based programs to address the underlying health behaviors associated with hypertension. The criteria for the review include:
A literature review of articles published between January 2000 and June 2021 was performed via the MEDLINE database to assess the influence of SES on the prevalence/incidence, awareness, treatment ...
Hypertension is divided into two categories, stage 1: SBP = 130-139 mm Hg or DBP 80-89 mm Hg; and stage 2: SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg. Hypertension diagnosis is based on ≥ 2 BP readings at ≥ 2 visits. The same guidelines recommend a BP goal of less than 130/80 mm Hg.
The present study aims to provide an extensive literature review of emerging digital payment technologies. The authors have gathered data from different databases, which include Scopus, Web of Science, EBSCO, and Elsevier using the keywords "Digital Payments", "Internet Banking", "Mobile Banking", "E-payments", "Electronic ...
Corresponding Author. S Xiao [email protected] State Key Laboratory of Oral Diseases & National Center for Stomatology & National Clinical Research Center for Oral Diseases & Department of Periodontics, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan, China
Most recently published are the NICE's 'Hypertension in Adults' in 2019 and the 2020 ISH report [ 23, 24 ]. The NICE guidelines only reviewed evidence beyond the year 2000, reflecting the current use of electronic BP devices. However, both guidelines use the SBP/DBP threshold of 140/90 mmHg to define Stage I HTN.