- Introduction
- Conclusions
- Article Information
BMI indicates body mass index; SES, socioeconomic status.
a Variables smoking status, SES, drinking pattern, former drinker bias only, occasional drinker bias, median age, and gender were removed.
b Variables race, diet, exercise, BMI, country, follow-up year, publication year, and unhealthy people exclusion were removed.
eAppendix. Methodology of Meta-analysis on All-Cause Mortality and Alcohol Consumption
eReferences
eFigure 1. Flowchart of Systematic Search Process for Studies of Alcohol Consumption and Risk of All-Cause Mortality
eTable 1. Newly Included 20 Studies (194 Risk Estimates) of All-Cause Mortality and Consumption in 2015 to 2022
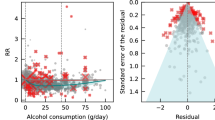
eFigure 2. Funnel Plot of Log-Relative Risk (In(RR)) of All-Cause Mortality Due to Alcohol Consumption Against Inverse of Standard Error of In(RR)
eFigure 3. Relative Risk (95% CI) of All-Cause Mortality Due to Any Alcohol Consumption Without Any Adjustment for Characteristics of New Studies Published between 2015 and 2022
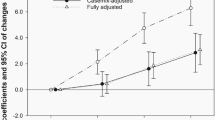
eFigure 4. Unadjusted, Partially Adjusted, and Fully Adjusted Relative Risk (RR) of All-Cause Mortality for Drinkers (vs Nondrinkers), 1980 to 2022
eTable 2. Statistical Analysis of Unadjusted Mean Relative Risk (RR) of All-Cause Mortality for Different Categories of Drinkers for Testing Publication Bias and Heterogeneity of RR Estimates From Included Studies
eTable 3. Mean Relative Risk (RR) Estimates of All-Cause Mortality Due to Alcohol Consumption up to 2022 for Subgroups (Cohorts Recruited 50 Years of Age or Younger and Followed up to 60 Years of Age)
Data Sharing Statement
- Errors in Figure and Supplement JAMA Network Open Correction May 9, 2023

See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Zhao J , Stockwell T , Naimi T , Churchill S , Clay J , Sherk A. Association Between Daily Alcohol Intake and Risk of All-Cause Mortality : A Systematic Review and Meta-analyses . JAMA Netw Open. 2023;6(3):e236185. doi:10.1001/jamanetworkopen.2023.6185
Manage citations:
© 2024
- Permissions
Association Between Daily Alcohol Intake and Risk of All-Cause Mortality : A Systematic Review and Meta-analyses
- 1 Canadian Institute for Substance Use Research, University of Victoria, Victoria, British Columbia, Canada
- 2 Department of Psychology, University of Portsmouth, Portsmouth, Hampshire, United Kingdom
- Correction Errors in Figure and Supplement JAMA Network Open
Question What is the association between mean daily alcohol intake and all-cause mortality?
Findings This systematic review and meta-analysis of 107 cohort studies involving more than 4.8 million participants found no significant reductions in risk of all-cause mortality for drinkers who drank less than 25 g of ethanol per day (about 2 Canadian standard drinks compared with lifetime nondrinkers) after adjustment for key study characteristics such as median age and sex of study cohorts. There was a significantly increased risk of all-cause mortality among female drinkers who drank 25 or more grams per day and among male drinkers who drank 45 or more grams per day.
Meaning Low-volume alcohol drinking was not associated with protection against death from all causes.
Importance A previous meta-analysis of the association between alcohol use and all-cause mortality found no statistically significant reductions in mortality risk at low levels of consumption compared with lifetime nondrinkers. However, the risk estimates may have been affected by the number and quality of studies then available, especially those for women and younger cohorts.
Objective To investigate the association between alcohol use and all-cause mortality, and how sources of bias may change results.
Data Sources A systematic search of PubMed and Web of Science was performed to identify studies published between January 1980 and July 2021.
Study Selection Cohort studies were identified by systematic review to facilitate comparisons of studies with and without some degree of controls for biases affecting distinctions between abstainers and drinkers. The review identified 107 studies of alcohol use and all-cause mortality published from 1980 to July 2021.
Data Extraction and Synthesis Mixed linear regression models were used to model relative risks, first pooled for all studies and then stratified by cohort median age (<56 vs ≥56 years) and sex (male vs female). Data were analyzed from September 2021 to August 2022.
Main Outcomes and Measures Relative risk estimates for the association between mean daily alcohol intake and all-cause mortality.
Results There were 724 risk estimates of all-cause mortality due to alcohol intake from the 107 cohort studies (4 838 825 participants and 425 564 deaths available) for the analysis. In models adjusting for potential confounding effects of sampling variation, former drinker bias, and other prespecified study-level quality criteria, the meta-analysis of all 107 included studies found no significantly reduced risk of all-cause mortality among occasional (>0 to <1.3 g of ethanol per day; relative risk [RR], 0.96; 95% CI, 0.86-1.06; P = .41) or low-volume drinkers (1.3-24.0 g per day; RR, 0.93; P = .07) compared with lifetime nondrinkers. In the fully adjusted model, there was a nonsignificantly increased risk of all-cause mortality among drinkers who drank 25 to 44 g per day (RR, 1.05; P = .28) and significantly increased risk for drinkers who drank 45 to 64 and 65 or more grams per day (RR, 1.19 and 1.35; P < .001). There were significantly larger risks of mortality among female drinkers compared with female lifetime nondrinkers (RR, 1.22; P = .03).
Conclusions and Relevance In this updated systematic review and meta-analysis, daily low or moderate alcohol intake was not significantly associated with all-cause mortality risk, while increased risk was evident at higher consumption levels, starting at lower levels for women than men.
The proposition that low-dose alcohol use protects against all-cause mortality in general populations continues to be controversial. 1 Observational studies tend to show that people classified as “moderate drinkers” have longer life expectancy and are less likely to die from heart disease than those classified as abstainers. 2 Systematic reviews and meta-analyses of this literature 3 confirm J-shaped risk curves (protective associations at low doses with increasing risk at higher doses). However, mounting evidence suggests these associations might be due to systematic biases that affect many studies. For example, light and moderate drinkers are systematically healthier than current abstainers on a range of health indicators unlikely to be associated with alcohol use eg, dental hygiene, exercise routines, diet, weight, income 4 ; lifetime abstainers may be systematically biased toward poorer health 5 ; studies fail to control for biases in the abstainer reference group, in particular failing to remove “sick quitters” or former drinkers, many of whom cut down or stop for health reasons 2 ; and most studies have nonrepresentative samples leading to an overrepresentation of older White men. Adjustment of cohort samples to make them more representative has been shown to eliminate apparent protective associations. 6 Mendelian randomization studies that control for the confounding effects of sociodemographic and environmental factors find no evidence of cardioprotection. 7
We published 2 previous systematic reviews and meta-analyses that investigated these hypotheses. The first of these focused on all-cause mortality, 8 finding negligible reductions in mortality risk with low-volume alcohol use when study-level controls were introduced for potential bias and confounding, such as the widespread practice of misclassifying former drinkers and/or current occasional drinkers as abstainers (ie, not restricting reference groups to lifetime abstainers). 8 Our alcohol and coronary heart disease (CHD) mortality meta-analysis of 45 cohort studies 9 found that CHD mortality risk differed widely by age ranges and sex of study populations. In particular, young cohorts followed up to old age did not show significant cardio-protection for low-volume use. Cardio-protection was only apparent among older cohorts that are more exposed to lifetime selection biases (ie, increasing numbers of “sick-quitters” in the abstainer reference groups and the disproportionate elimination of drinkers from the study sample who had died or were unwell).
The present study updates our earlier systematic review and meta-analysis for all-cause mortality and alcohol use, 8 including studies published up to July 2021 (ie, 6.5 years of additional publications). The study also investigated the risk of all-cause mortality for alcohol consumption according to (1) median ages of the study populations (younger than 56 years or 56 years and older), replicating the methods of Zhao et al 9 ; (2) the sex distribution of the study populations, and (3) studies of cohorts recruited before a median age of 51 years of age and followed up in health records until a median age of at least 60 years (ie, with stricter rules to further minimize lifetime selection biases). Because younger cohorts followed up to an age at which they may experience heart disease are less likely to be affected by lifetime selection biases, 9 we hypothesized that such studies would be less likely to show reduced mortality risks for low-volume drinkers. Finally, we reran the analyses using occasional drinkers (<1 drink per week) as the reference, for whom physiological health benefits are unlikely. Occasional drinkers are a more appropriate reference group, given evidence demonstrating that lifetime abstainers may be biased toward ill health. 10
The present study updates the systematic reviews and meta-analyses described above 8 by including studies published up to July 2021 to investigate whether the risk differed for subgroups. The study protocol was preregistered on the Open Science Framework. 11 Inclusion criteria, search strategy, study selection, data extraction, and statistical analytical methods of the study are summarized in later sections (see eAppendix in Supplement 1 for more details).
The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline. 12 The review sought cohort studies of all-cause mortality and alcohol consumption. We identified all potentially relevant articles published up to July 31, 2021, regardless of language, by searching PubMed and Web of Science, through reference list cross-checking of previous meta-analyses (eFigure 1 in Supplement 1 ). There were 87 studies identified by Stockwell et al. 8 After inclusion of 20 new studies meeting inclusion criteria, there were a total of 107 cohort studies (eTable 1 in Supplement 1 ). 13 - 32
Three coders (J. Z., F. A., and J. C.) reviewed all eligible studies to extract and code data independently from all studies fulfilling the inclusion criteria. Data extracted included (1) outcome, all-cause mortality; (2) measures of alcohol consumption; (3) study characteristics, including cohort ages at recruitment and follow-up; (4) types of misclassification error of alcohol consumers and abstainers; (5) controlled variables in individual studies. Alcoholic drinks were converted into grams per day according to country-specific definitions if not otherwise defined. 33 , 34
We also assessed publication bias, heterogeneity, and confounding of covariates that might potentially affect the association of interest using several statistical approaches. 35 - 41 Relative risk (RR), including hazard ratios or rate ratios, were converted to natural log-transformed formats to deal with skewness. Publication bias was assessed through visual inspection of the funnel plot of log-RR of all-cause mortality due to alcohol consumption against the inverse standard error of log-RR 42 and Egger’s linear regression method. 36 We also plotted forest graphs of log-RR of all-cause mortality for any level of drinking to assess heterogeneity among studies. 42 The between-study heterogeneity of RRs were assessed using Cochran Q 37 and the I 2 statistic. 38 If heterogeneity was detected, mixed-effects models were used to obtain the summarized RR estimates. Mixed-effects regression analyses were performed in which drinking groups and control variables were treated as fixed-effects with a random study effect because of significant heterogeneity. 43
All analyses were weighted by the inverse of the estimated variance of the natural log relative risk. Variance was estimated from reported standard errors, confidence intervals, or number of deaths. The weights for each individual study were created using the inverse variance weight scheme and used in mixed regression analysis to get maximum precision for the main results of the meta-analysis. 42 In comparison with lifetime abstainers, the study estimated the mean RR of all-cause mortality for former drinkers (ie, now completely abstaining), current occasional (<9.1 g per week), low-volume (1.3-24.0 g per day), medium-volume (25.0-44.0 g per day), high-volume (45.0-64.0 g) and highest-volume drinkers (≥65.0 grams per day). The analyses adjusted for the potential confounding effects of study characteristics including the median age and sex distribution of study samples, drinker biases, country where a study was conducted, follow-up years and presence or absence of confounders. Analyses were also repeated using occasional drinkers as the reference group. We used t tests to calculate P values, and significance was set at .05. All statistical analyses were performed using SAS version 9.4 (SAS Institute) and the SAS MIXED procedure was used to model the log-transformed RR. 44 Data were analyzed from September 2021 to August 2022.
There were 724 estimates of the risk relationship between level of alcohol consumption and all-cause mortality from 107 unique studies 13 - 32 , 45 - 131 , including 4 838 825 participants and 425 564 deaths available for the analysis. Table 1 describes the sample characteristics of the metadata. Of 39 studies 13 , 15 , 18 , 21 , 23 - 26 , 29 , 31 , 45 - 47 , 49 , 50 , 52 - 54 , 57 - 59 , 62 , 64 , 70 , 80 , 81 , 85 , 87 , 91 , 94 , 96 , 100 , 104 , 107 , 118 , 124 , 125 , 127 , 130 reporting RR estimates for men and women separately, 33 14 , 17 , 48 , 51 , 61 , 63 , 66 , 68 , 69 , 72 , 76 , 79 , 83 , 84 , 86 , 88 , 90 , 92 , 93 , 97 , 98 , 101 , 103 , 105 , 109 - 111 , 113 - 115 , 119 , 120 , 128 were for males only, 8 16 , 65 , 73 , 99 , 102 , 108 , 112 , 123 for females only, and 30 13 , 19 - 22 , 26 - 30 , 32 , 55 , 56 , 67 , 71 , 74 , 75 , 77 , 78 , 82 , 84 , 89 , 95 , 106 , 116 , 117 , 121 , 122 , 126 , 129 for both sexes. Twenty-one studies 13 , 17 , 19 , 21 , 22 , 26 , 27 , 45 - 58 (220 risk estimates) were free from abstainer bias (ie, had a reference group of strictly defined lifetime abstainers). There were 50 studies 14 - 16 , 18 , 20 , 23 - 25 , 29 , 59 - 99 (265 risk estimates) with both former and occasional drinker bias; 28 studies 28 , 30 - 32 , 100 - 122 , 130 (177 risk estimates) with only former drinker bias; and 8 studies 123 - 129 , 131 (62 risk estimates) with only occasional drinker bias.
Unadjusted mean RR estimates for most study subgroups categorized by methods/sample characteristics showed markedly or significantly higher RRs for alcohol consumers as a group vs abstainers. Exceptions were for studies with less than 10 years of follow-up and those with some form of abstainer bias ( Table 1 ). Bivariable analyses showed that mortality risks for alcohol consumers varied considerably according to other study characteristics, such as quality of the alcohol consumption measure, whether unhealthy individuals were excluded at baseline, and whether socioeconomic status was controlled for ( Table 1 ).
No evidence of publication bias was detected either by inspection of symmetry in the funnel plot of log-RR estimates and their inverse standard errors (eFigure 2 in Supplement 1 ) or by Egger linear regression analysis (eTable 2 in Supplement 1 , all P > .05 for each study group). Significant heterogeneity was observed across studies for all drinking categories confirmed by both the Q statistic ( Q 723 = 5314.80; P < .001) and I 2 estimates (all >85.87%). (See eFigure 3 in Supplement 1 for forest plot of unadjusted risk estimates of mortality risks for the 20 newly identified studies).
Pooled unadjusted estimates (724 observations) showed significantly higher risk for former drinkers (RR, 1.22; 95% CI, 1.11-1.33; P = .001) and significantly lower risk for low-volume drinkers (RR, 0.85; 95% CI, 0.81-0.88; P = .001) compared with abstainers as defined in the included studies ( Table 2 ; eFigure 4 in Supplement 1 ). In the fully adjusted model, mortality RR estimates increased for all drinking categories, becoming nonsignificant for low-volume drinkers (RR, 0.93; 95% CI, 0.85-1.01; P = .07), occasional drinkers (>0 to <1.3 g of ethanol per day; RR, 0.96; 95% CI, 0.86-1.06; P = .41), and drinkers who drank 25 to 44 g per day (RR, 1.05; 95% CI, 0.96-1.14; P = .28). There was a significantly increased risk among drinkers who drank 45 to 64 g per day (RR, 1.19; 95% CI, 1.07-1.32; P < .001) and 65 or more grams (RR, 1.35; 95% CI, 1.23-1.47; P < .001). The Figure shows the changes in RR estimates for low-volume drinkers when removing each covariate from the fully adjusted model. In most cases, removing study-level covariates tended to yield lower risk estimates from alcohol use.
Table 2 presents the RR estimates when occasional drinkers were the reference group. In fully adjusted models, higher though nonsignificant mortality risks were observed for both abstainers and medium-volume drinkers (RR, 1.04; 95% CI, 0.94-1.16; P = .44 and RR, 1.09; 95% CI, 0.96-1.25; P = .19, respectively). There were significantly elevated risks for both high and higher volume drinkers (RR, 1.24; 95% CI, 1.07-1.44; P = .004 and RR, 1.41; 95% CI, 1.23-1.61; . P = 001, respectively).
As hypothesized, there was a significant interaction between cohort age and mortality risk ( P = .02; F 601 = 2.93) and so RR estimates for drinkers were estimated in analyses stratified by median age of the study populations at enrollment ( Table 3 ). In unadjusted and partially adjusted analyses, older cohorts displayed larger reductions in mortality risk associated with low-volume consumption than younger cohorts. However, in fully adjusted analyses with multiple covariates included for study characteristics, these differences disappeared. Younger cohorts also displayed greater mortality risks than older cohorts at higher consumption levels. Among studies in which participants were recruited at age 50 years or younger and followed up to age 60 years (ie, there was likely reduced risk of lifetime selection bias) higher RR estimates were observed for all drinking groups vs lifetime abstainers. These differences were significant in all drinking groups except low-volume drinkers (eTable 3 in Supplement 1 ).
Across all levels of alcohol consumption, female drinkers had a higher RR of all-cause mortality than males ( P for interaction = .001). As can be seen in Table 4 , all female drinkers had a significantly increased mortality risk compared with female lifetime nondrinkers (RR, 1.22; 95% CI, 1.02-1.46; P = .03). Compared with lifetime abstainers, there was significantly increased risk of all-cause mortality among male drinkers who drank 45 to 64 g per day (RR, 1.15; 95% CI, 1.03-1.28; P = .01) and drank 65 or more (RR, 1.34; 95% CI, 1.23-1.47; P < .001), and among female drinkers who drank 25 to 44 g per day (RR, 1.21; 95% CI, 1.08-1.36; P < .01), 45 to 64 g (RR, 1.34; 95% CI, 1.11-1.63; P < .01) and 65 or more grams (RR, 1.61; 95% CI, 1.44-1.80; P = .001).
In fully adjusted, prespecified models that accounted for effects of sampling, between-study variation, and potential confounding from former drinker bias and other study-level covariates, our meta-analysis of 107 studies found (1) no significant protective associations of occasional or low-volume drinking (moderate drinking) with all-cause mortality; and (2) an increased risk of all-cause mortality for drinkers who drank 25 g or more and a significantly increased risk when drinking 45 g or more per day.
Several meta-analytic strategies were used to explore the role of abstainer reference group biases caused by drinker misclassification errors and also the potential confounding effects of other study-level quality covariates in studies. 2 Drinker misclassification errors were common. Of 107 studies identified, 86 included former drinkers and/or occasional drinkers in the abstainer reference group, and only 21 were free of both these abstainer biases. The importance of controlling for former drinker bias/misclassification is highlighted once more in our results which are consistent with prior studies showing that former drinkers have significantly elevated mortality risks compared with lifetime abstainers.
In addition to presenting our fully adjusted models, a strength of the study was the examination of the differences in relative risks according to unadjusted and partially adjusted models, including the effect of removing individual covariates from the fully adjusted model. We found evidence that abstainer biases and other study characteristics changed the shape of the risk relationship between mortality and rising alcohol consumption, and that most study-level controls increased the observed risks from alcohol, or attenuated protective associations at low levels of consumption such that they were no longer significant. The reduced RR estimates for occasional or moderate drinkers observed without adjustment may be due to the misclassification of former and occasional drinkers into the reference group, a possibility which is more likely to have occurred in studies of older cohorts which use current abstainers as the reference group. This study also demonstrates the degree to which observed associations between consumption and mortality are highly dependent on the modeling strategy used and the degree to which efforts are made to minimize confounding and other threats to validity.
It also examined risk estimates when using occasional drinkers rather than lifetime abstainers as the reference group. The occasional drinker reference group avoids the issue of former drinker misclassification that can affect the abstainer reference group, and may reduce confounding to the extent that occasional drinkers are more like low-volume drinkers than are lifetime abstainers. 2 , 8 , 132 In the unadjusted and partially adjusted analyses, using occasional drinkers as the reference group resulted in nonsignificant protective associations and lower point estimates for low-volume drinkers compared with significant protective associations and higher point estimates when using lifetime nondrinkers as the reference group. In the fully adjusted models, there were nonsignificant protective associations for low-volume drinkers whether using lifetime abstainers or occasional drinkers as the reference group, though this was only a RR of 0.97 for the latter.
Across all studies, there were few differences in risk for studies when stratified by median age of enrollment above or below age 56 years in the fully adjusted analyses. However, in the subset of studies who enrolled participants aged 50 years or younger who were followed for at least 10 years, occasional drinkers and medium-volume drinkers had significantly increased risk of mortality and substantially higher risk estimates for high- and higher-volume consumption compared with results from all studies. This is consistent with our previous meta-analysis for CHD, 9 in which younger cohorts followed up to older age did not show a significantly beneficial association of low-volume consumption, while older cohorts, with more opportunity for lifetime selection bias, showed marked, significant protective associations.
Our study also found sex differences in the risk of all-cause mortality. A larger risk of all-cause mortality for women than men was observed when drinking 25 or more grams per day, including a significant increase in risk for medium-level consumption for women that was not observed for men. However, mortality risk for mean consumption up to 25 g per day were very similar for both sexes.
A number of limitations need to be acknowledged. A major limitation involves imperfect measurement of alcohol consumption in most included studies, and the fact that consumption in many studies was assessed at only 1 point in time. Self-reported alcohol consumption is underreported in most epidemiological studies 133 , 134 and even the classification of drinkers as lifetime abstainers can be unreliable, with several studies in developed countries finding that the majority of self-reported lifetime abstainers are in fact former drinkers. 135 , 136 If this is the case, the risks of various levels of alcohol consumption relative to presumed lifetime abstainers are underestimates. Merely removing former drinkers from analyses may bias studies in favor of drinkers, since former drinkers may be unhealthy, and should rightly be reallocated to drinking groups according to their history. However, this has only been explored in very few studies. Our study found that mortality risk differed significantly by cohort age and sex. It might be that the risk is also higher for other subgroups, such as people living with HIV, 137 a possibility future research should investigate.
The number of available studies in some stratified analyses was small, so there may be limited power to control for potential study level confounders. However, the required number of estimates per variable for linear regression can be much smaller than in logistic regression, and a minimum of at least 2 estimates per variable is recommended for linear regression analysis, 138 suggesting the sample sizes were adequate in all models presented. It has been demonstrated that a pattern of binge (ie, heavy episodic) drinking removes the appearance of reduced health risks even when mean daily volume is low. 139 Too few studies adequately controlled for this variable to investigate its association with different outcomes across studies. Additionally, our findings only apply to the net effect of alcohol at different doses on all-cause mortality, and different risk associations likely apply for specific disease categories. The biases identified here likely apply to estimates of risk for alcohol and all diseases. It is likely that correcting for these biases will raise risk estimates for many types of outcome compared with most existing estimates.
This updated meta-analysis did not find significantly reduced risk of all-cause mortality associated with low-volume alcohol consumption after adjusting for potential confounding effects of influential study characteristics. Future longitudinal studies in this field should attempt to minimize lifetime selection biases by not including former and occasional drinkers in the reference group, and by using younger cohorts (ie, age distributions that are more representative of drinkers in the general population) at baseline.
Accepted for Publication: February 17, 2023.
Published: March 31, 2023. doi:10.1001/jamanetworkopen.2023.6185
Correction: This article was corrected on May 9, 2023, to fix errors in the Figure and Supplement.
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Zhao J et al. JAMA Network Open .
Corresponding Author: Jinhui Zhao, PhD, Canadian Institute for Substance Use Research, University of Victoria, PO Box 1700 STN CSC, Victoria, BC V8Y 2E4, Canada ( [email protected] ).
Author Contributions: Drs Zhao and Stockwell had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Zhao, Stockwell, Naimi, Churchill, Sherk.
Acquisition, analysis, or interpretation of data: Zhao, Stockwell, Naimi, Clay.
Drafting of the manuscript: Zhao, Stockwell, Clay.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Zhao, Churchill.
Obtained funding: Zhao, Stockwell, Sherk.
Administrative, technical, or material support: Zhao, Stockwell, Naimi.
Supervision: Zhao, Stockwell, Naimi.
Conflict of Interest Disclosures: Dr Stockwell reported receiving personal fees from Ontario Public Servants Employees Union for expert witness testimony and personal fees from Alko outside the submitted work. Dr Sherk reported receiving grants from Canadian Centre on Substance Use and Addiction (CCSA) during the conduct of the study. No other disclosures were reported.
Funding/Support: This study was partly funded by the CCSA as a subcontract for a Health Canada grant to develop guidance for Canadians on alcohol and health.
Role of the Funder/Sponsor: Health Canada had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. CCSA staff conducted a preliminary search to identify potentially relevant articles but did not participate in decisions about inclusion/exclusion of studies, coding, analysis, interpretation of results or approving the final manuscript.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: We gratefully acknowledge contributions by Christine Levesque, PhD (CCSA), and Nitika Sanger, PhD (CCSA), who conducted a preliminary literature search for potentially relevant articles. We also acknowledge the leadership of Drs Catherine Paradis, PhD (CCSA), and Peter Butt, MD (University of Saskatchewan), who cochaired the process of developing Canada’s new guidance on alcohol and health, a larger project which contributed some funds for the work undertaken for this study. We are grateful to Fariha Alam, MPH (Canadian Institute for Substance Use and Research), for her help coding the studies used in this study. None of them received any compensation beyond their normal salaries for this work.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
- Alcohol or alcoholic beverages contain ethanol, a psychoactive and toxic substance that can cause dependence.
- Worldwide, around 2.6 million deaths were caused by alcohol consumption in 2019. Of these, 1.6 million deaths were from noncommunicable diseases, 700 000 deaths from injuries and 300 000 deaths from communicable diseases.
- The alcohol-attributable mortality was heaviest among men, accounting for 2 million deaths compared to 600 000 deaths among women, in 2019.
- An estimated 400 million people, or 7% of the world’s population aged 15 years and older, lived with alcohol use disorders. Of this, 209 million people (3.7% of the adult world population) lived with alcohol dependence.
- Alcohol consumption, even at low levels can bring health risks, but most alcohol related harms come from heavy episodic or heavy continuous alcohol consumption.
- Effective alcohol control interventions exist and should be utilized more, at the same time it is important for people to know risks associated with alcohol consumption and take individual actions to protect from its harmful effects.
Alcohol and alcoholic beverages contain ethanol, which is a psychoactive and toxic substance with dependence-producing properties. Alcohol has been widely used in many cultures for centuries, but it is associated with significant health risks and harms.
Worldwide, 2.6 million deaths were attributable to alcohol consumption in 2019, of which 2 million were among men and 0.6 million among women. The highest levels of alcohol-related deaths per 100 000 persons are observed in the WHO European and African Regions with 52.9 deaths and 52.2 deaths per 100 000 people, respectively.
People of younger age (20–39 years) are disproportionately affected by alcohol consumption with the highest proportion (13%) of alcohol-attributable deaths occurring within this age group in 2019.
The data on global alcohol consumption in 2019 shows that an estimated 400 million people aged 15 years and older live with alcohol use disorders, and an estimated 209 million live with alcohol dependence.
There has been some progress; from 2010 to 2019, the number of alcohol-attributable deaths per 100 000 people decreased by 20.2% globally.
There has been a steady increase in the number of countries developing national alcohol policies. Almost all countries implement alcohol excise taxes. However, countries report continued interference from the alcohol industry in policy development.
Based on 2019 data, about 54% out of 145 reporting countries had national guidelines/standards for specialized treatment services for alcohol use disorders, but only 46% of countries had legal regulations to protect the confidentiality of people in treatment.
Access to screening, brief intervention and treatment for people with hazardous alcohol use and alcohol use disorder remains very low, as well as access to medications for treatment of alcohol use disorders. Overall, the proportion of people with alcohol use disorders in contact with treatment services varies from less than 1% to no more than 14% in all countries where such data are available.
Health risks of alcohol use
Alcohol consumption is found to play a causal role in more than 200 diseases, injuries and other health conditions. However, the global burden of disease and injuries caused by alcohol consumption can be quantified for only 31 health conditions on the basis of the available scientific evidence for the role of alcohol use in their development, occurrence and outcomes.
Drinking alcohol is associated with risks of developing noncommunicable diseases such as liver diseases, heart diseases, and different types of cancers, as well as mental health and behavioural conditions such as depression, anxiety and alcohol use disorders.
An estimated 474 000 deaths from cardiovascular diseases were caused by alcohol consumption in 2019.
Alcohol is an established carcinogen and alcohol consumption increases the risk of several cancers, including breast, liver, head and neck, oesophageal and colorectal cancers. In 2019, 4.4% of cancers diagnosed globally and 401 000 cancer deaths were attributed to alcohol consumption.
Alcohol consumption also causes significant harm to others, not just to the person consuming alcohol. A significant part of alcohol-attributable disease burden arises from injuries such as road traffic accidents. In 2019, of a total of 298 000 deaths from alcohol-related road crashes, 156 000 deaths were caused by someone else’s drinking.
Other injuries, intentional or unintentional, include falls, drowning, burns, sexual assault, intimate partner violence and suicide.
A causal relationship has been established between alcohol use and the incidence or outcomes of infectious diseases such as tuberculosis and HIV.
Alcohol consumption during pregnancy increases the risk of having a child with fetal alcohol spectrum disorders (FASDs), the most severe form of which is fetal alcohol syndrome (FAS), which is associated with developmental disabilities and birth defects. Alcohol consumption during pregnancy can also increase the risk of pre-term birth complications including miscarriage, stillbirth and premature delivery.
Younger people are disproportionately negatively affected by alcohol consumption, with the highest proportion (13%) of alcohol-attributable deaths in 2019 occurring among people aged between 20 and 39 years.
In the long term, harmful and hazardous levels of alcohol consumption can lead to social problems including family problems, issues at work, financial problems, and unemployment.
Factors affecting alcohol consumption and alcohol-related harm
There is no form of alcohol consumption that is risk-free. Even low levels of alcohol consumption carry some risks and can cause harm.
The level of risk depends on several factors, including the amount consumed, frequency of drinking, the health status of the individual, age, sex, and other personal characteristics, as well as the context in which alcohol consumption occurs.
Some groups and individuals who are vulnerable or at risk may have a higher susceptibility to the toxic, psychoactive and dependence-inducing properties of alcohol. On the other hand, individuals who adopt lower-risk patterns of alcohol consumption may not necessarily face a significantly increased likelihood of negative health and social consequences.
Societal factors which affect the levels and patterns of alcohol consumption and related problems include cultural and social norms, availability of alcohol, level of economic development, and implementation and enforcement of alcohol policies.
The impact of alcohol consumption on chronic and acute health outcomes is largely determined by the total volume of alcohol consumed and the pattern of drinking, particularly those patterns which are associated with the frequency of drinking and episodes of heavy drinking. Most alcohol related harms come from heavy episodic or heavy continuous alcohol consumption.
The context plays an important role in the occurrence of alcohol-related harm, particularly as a result of alcohol intoxication. Alcohol consumption can have an impact not only on the incidence of diseases, injuries and other health conditions, but also on their outcomes and how these evolve over time.
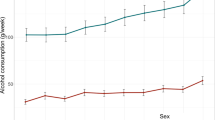
There are gender differences in both alcohol consumption and alcohol-related mortality and morbidity. In 2019, 52% of men were current drinkers, while only 35% of women had been drinking alcohol in the last 12 months. Alcohol per capita consumption was, on average, 8.2 litres for men compared to 2.2 litres for women. In 2019, alcohol use was responsible for 6.7% of all deaths among men and 2.4% of all deaths among women.
WHO response
The Global alcohol action plan 2022–2030, endorsed by WHO Member States, aims to reduce the harmful use of alcohol through effective, evidence-based strategies at national, regional and global levels. The plan outlines six key areas for action: high-impact strategies and interventions, advocacy and awareness, partnership and coordination, technical support and capacity-building, knowledge production and information systems, and resource mobilization.
Implementation of global strategy and action plan will accelerate global progress towards attaining alcohol-related targets under the Sustainable Development Goal 3.5 on strengthening the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
Achieving this will require global, regional and national actions on the levels, patterns and contexts of alcohol consumption and the wider social determinants of health, with a particular focus on implementing high-impact cost effective interventions.
It is vital to address the determinants that drive the acceptability, availability and affordability of alcohol consumption through cross-sectoral, comprehensive and integrated policy measures. It is also of critical importance to achieve universal health coverage for people living with alcohol use disorders and other health conditions due to alcohol use by strengthening health system responses and developing comprehensive and accessible systems of treatment and care that for those in need.
The SAFER initiative, launched in 2018 by WHO and partners, supports countries to implement the high-impact, cost-effective interventions proven to reduce the harm caused by alcohol consumption.
The WHO Global Information System on Alcohol and Health (GISAH) presents data on levels and patterns of alcohol consumption, alcohol-attributable health and social consequences and policy responses across the world.
Achieving a reduction in the harmful use of alcohol in line with the targets included in the Global alcohol action plan, the SDG 2030 agenda and the WHO Global monitoring framework for noncommunicable diseases, requires concerted action by countries and effective global governance.
Public policies and interventions to prevent and reduce alcohol-related harm should be guided and formulated by public health interests and based on clear public health goals and the best available evidence.
Engaging all relevant stakeholders is essential but the potential conflicts of interest, particularly with the alcohol industry, must be carefully assessed before engagement. Economic operators should refrain from activities that might prevent, delay or stop the development, enactment, implementation and enforcement of high-impact strategies and interventions to reduce the harmful use of alcohol.
By working together, with due diligence and protection from conflicts of interest, the negative health and social consequences of alcohol can be effectively reduced.
Global status report on alcohol and health and treatment of substance use disorders
Global strategy to reduce the harmful use of alcohol
Global Alcohol Action Plan 2022–2030
SAFER Alcohol Control Initiative
More on alcohol
Appointments at Mayo Clinic
- Nutrition and healthy eating
Alcohol use: Weighing risks and benefits
Drinking alcohol is a health risk regardless of the amount.
Research on alcohol suggests a sobering conclusion: Drinking alcohol in any amount carries a health risk. While the risk is low for moderate intake, the risk goes up as the amount you drink goes up.
Many people drink alcohol as a personal preference, during social activities, or as a part of cultural and religious practices. People who choose not to drink make that choice for the same reasons. Knowing your personal risk based on your habits can help you make the best decision for you.
The evidence for moderate alcohol use in healthy adults is still being studied. But good evidence shows that drinking high amounts of alcohol are clearly linked to health problems.
Here's a closer look at alcohol and health.
Defining moderate alcohol use
Moderate alcohol use may not mean the same thing in research studies or among health agencies.
In the United States, moderate drinking for healthy adults is different for men and women. It means on days when a person does drink, women do not have more than one drink and men do not have more than two drinks.
Examples of one drink include:
- 12 fluid ounces (355 milliliters) of regular beer
- 5 fluid ounces (148 milliliters) of wine
- 1.5 fluid ounces (44 milliliters) of hard liquor or distilled spirits
Health agencies outside the U.S. may define one drink differently.
The term "moderate" also may be used differently. For example, it may be used to define the risk of illness or injury based on the number of drinks a person has in a week.
Risks of moderate alcohol use
The bottom line is that alcohol is potentially addictive, can cause intoxication, and contributes to health problems and preventable deaths. If you already drink at low levels and continue to drink, risks for these issues appear to be low. But the risk is not zero.
For example, any amount of drinking increases the risk of breast cancer and colorectal cancer. As consumption goes up, the risk goes up for these cancers. It is a tiny, but real, increased risk.
Drinking also adds calories that can contribute to weight gain. And drinking raises the risk of problems in the digestive system.
In the past, moderate drinking was thought to be linked with a lower risk of dying from heart disease and possibly diabetes. After more analysis of the research, that doesn't seem to be the case. In general, a healthy diet and physical activity have much greater health benefits than alcohol and have been more extensively studied.
Risks of heavy alcohol use
Heavy drinking, including binge drinking, is a high-risk activity.
The definition of heavy drinking is based on a person's sex. For women, more than three drinks on any day or more than seven drinks a week is heavy drinking. For men, heavy drinking means more than four drinks on any day or more than 14 drinks a week.
Binge drinking is behavior that raises blood alcohol levels to 0.08%. That usually means four or more drinks within two hours for women and five or more drinks within two hours for men.
Heavy drinking can increase your risk of serious health problems, including:
- Certain cancers, such as colorectal cancer, breast cancer and cancers of the mouth, throat, esophagus and liver.
- Liver disease.
- Cardiovascular disease, such as high blood pressure and stroke.
Heavy drinking also has been linked to intentional injuries, such as suicide, as well as accidental injury and death.
During pregnancy, drinking may cause the unborn baby to have brain damage and other problems. Heavy drinking also may result in alcohol withdrawal symptoms.
When to avoid alcohol
In some situations, the risk of drinking any amount of alcohol is high. Avoid all alcohol if you:
- Are trying to get pregnant or are pregnant.
- Take medicine that has side effects if you drink alcohol.
- Have alcohol use disorder.
- Have medical issues that alcohol can worsen.
In the United States, people younger than age 21 are not legally able to drink alcohol.
When taking care of children, avoid alcohol. And the same goes for driving or if you need to be alert and able to react to changing situations.
Deciding about drinking
Lots of activities affect your health. Some are riskier than others. When it comes to alcohol, if you don't drink, don't start for health reasons.
Drinking moderately if you're otherwise healthy may be a risk you're willing to take. But heavy drinking carries a much higher risk even for those without other health concerns. Be sure to ask your healthcare professional about what's right for your health and safety.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Rethinking drinking: Alcohol and your health. National Institute on Alcohol Abuse and Alcoholism. https://www.rethinkingdrinking.niaaa.nih.gov/. Accessed Jan. 8, 2024.
- 2020-2025 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov. Accessed Jan. 8, 2024.
- Scientific Report of the 2020 Dietary Guidelines Advisory Committee. Alcoholic beverages. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov/2020-advisory-committee-report. Accessed Jan. 8, 2024.
- Canada's guidance on alcohol and health. Canadian Centre on Substance Use and Addiction. https://www.ccsa.ca/canadas-guidance-alcohol-and-health. Accessed Jan. 9, 2024.
- Science around moderate alcohol consumption. Centers for Disease Control and Prevention. https://www.cdc.gov/alcohol/fact-sheets/moderate-drinking.htm. Accessed Jan. 9, 2024.
- Alcohol use and your health. Centers for Disease Control and Prevention. https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm. Accessed Jan. 9, 2024.
Products and Services
- Available Health Products from Mayo Clinic Store
- A Book: The Mayo Clinic Diet Bundle
- The Mayo Clinic Diet Online
- A Book: Live Younger Longer
- A Book: Cook Smart, Eat Well
- A Book: Mayo Clinic on High Blood Pressure
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Guide to Home Remedies
- A Book: Mayo Clinic on Digestive Health
- Health foods
- Alkaline water
- Artificial sweeteners and other sugar substitutes
- Autism spectrum disorder and digestive symptoms
- Breastfeeding nutrition: Tips for moms
- Caffeine: How much is too much?
- Is caffeine dehydrating?
- Calorie calculator
- Can whole-grain foods lower blood pressure?
- Carbohydrates
- Chart of high-fiber foods
- Cholesterol: Top foods to improve your numbers
- Coconut water: Is it super hydrating?
- Coffee and health
- Diet soda: How much is too much?
- Dietary fats
- Dietary fiber
- Prickly pear cactus
- Does soy really affect breast cancer risk?
- Don't get tricked by these 3 heart-health myths
- High-protein diets
- How to track saturated fat
- Is there a special diet for Crohn's disease?
- Monosodium glutamate (MSG)
- Nuts and your heart: Eating nuts for heart health
- Omega-3 in fish
- Omega-6 fatty acids
- Phenylalanine
- Portion control
- Taurine in energy drinks
- Underweight: Add pounds healthfully
- Daily water requirement
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Alcohol use Weighing risks and benefits
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 June 2023
Alcohol consumption and risks of more than 200 diseases in Chinese men
- Pek Kei Im ORCID: orcid.org/0000-0002-2624-9766 1 ,
- Neil Wright ORCID: orcid.org/0000-0002-3946-1870 1 ,
- Ling Yang ORCID: orcid.org/0000-0001-5750-6588 1 , 2 ,
- Ka Hung Chan ORCID: orcid.org/0000-0002-3700-502X 1 , 3 ,
- Yiping Chen ORCID: orcid.org/0000-0002-4973-0296 1 , 2 ,
- Huaidong Du ORCID: orcid.org/0000-0002-9814-0049 1 , 2 ,
- Xiaoming Yang 1 ,
- Daniel Avery ORCID: orcid.org/0000-0002-9823-9575 1 ,
- Shaojie Wang 5 ,
- Canqing Yu ORCID: orcid.org/0000-0002-0019-0014 6 , 7 ,
- Jun Lv 6 , 7 ,
- Robert Clarke ORCID: orcid.org/0000-0002-9802-8241 1 ,
- Junshi Chen 8 ,
- Rory Collins 1 ,
- Robin G. Walters ORCID: orcid.org/0000-0002-9179-0321 1 , 2 ,
- Richard Peto 1 ,
- Liming Li ORCID: orcid.org/0000-0001-5873-7089 6 , 7 na1 ,
- Zhengming Chen ORCID: orcid.org/0000-0001-6423-105X 1 , 2 na1 ,
- Iona Y. Millwood ORCID: orcid.org/0000-0002-0807-0682 1 , 2 na1 &
China Kadoorie Biobank Collaborative Group
Nature Medicine volume 29 , pages 1476–1486 ( 2023 ) Cite this article
31k Accesses
25 Citations
824 Altmetric
Metrics details
- Epidemiology
- Genetics research
- Risk factors
Alcohol consumption accounts for ~3 million annual deaths worldwide, but uncertainty persists about its relationships with many diseases. We investigated the associations of alcohol consumption with 207 diseases in the 12-year China Kadoorie Biobank of >512,000 adults (41% men), including 168,050 genotyped for ALDH2 - rs671 and ADH1B - rs1229984 , with >1.1 million ICD-10 coded hospitalized events. At baseline, 33% of men drank alcohol regularly. Among men, alcohol intake was positively associated with 61 diseases, including 33 not defined by the World Health Organization as alcohol-related, such as cataract ( n = 2,028; hazard ratio 1.21; 95% confidence interval 1.09–1.33, per 280 g per week) and gout ( n = 402; 1.57, 1.33–1.86). Genotype-predicted mean alcohol intake was positively associated with established ( n = 28,564; 1.14, 1.09–1.20) and new alcohol-associated ( n = 16,138; 1.06, 1.01–1.12) diseases, and with specific diseases such as liver cirrhosis ( n = 499; 2.30, 1.58–3.35), stroke ( n = 12,176; 1.38, 1.27–1.49) and gout ( n = 338; 2.33, 1.49–3.62), but not ischemic heart disease ( n = 8,408; 1.04, 0.94–1.14). Among women, 2% drank alcohol resulting in low power to assess associations of self-reported alcohol intake with disease risks, but genetic findings in women suggested the excess male risks were not due to pleiotropic genotypic effects. Among Chinese men, alcohol consumption increased multiple disease risks, highlighting the need to strengthen preventive measures to reduce alcohol intake.
Similar content being viewed by others
A burden of proof study on alcohol consumption and ischemic heart disease
Effect of alcohol consumption on kidney function: population-based cohort study
Genomic prediction of alcohol-related morbidity and mortality
Alcohol consumption is a major risk factor for poor physical and mental health, accounting for about 3 million deaths and over 130 million disability-adjusted life years worldwide in 2016 (ref. 1 ). Since the 1990s, alcohol consumption has increased in many low- and middle-income countries, including China, where it almost exclusively involves men 2 , 3 . Among Chinese men, those who reported alcohol consumption in the past 12 months increased from 59% to 85% and yearly per-capita alcohol consumption increased from 7.1 to 11.2 l between 1990 and 2017 and these have been predicted to increase in future years 2 .
Previous epidemiological studies conducted in mainly western populations have provided consistent evidence about the hazards of alcohol drinking for several major diseases, including several types of cancers and cardiovascular diseases (CVDs), liver cirrhosis, infectious diseases (for example tuberculosis and pneumonia) and injuries 4 , 5 , 6 , 7 , 8 , 9 . Large western cohort studies with linkage to hospital records have also investigated the associations of alcohol with risks of several less-common or non-fatal disease outcomes (for example certain site-specific cancers 10 , 11 , 12 , dementia 13 , falls 14 and cataract surgery 15 ). For some (for example stomach cancer), there was suggestive evidence of weak positive associations with heavy drinking 10 , 11 , whereas for others (for example cataract) the limited available evidence has been contradictory 10 , 12 , 13 , 15 ; however, the evidence from western populations, even for diseases known to be associated with alcohol, may not be generalizable to Chinese populations, where the prevalence and types of alcohol drinking (mainly spirits), patterns of diseases (for example high stroke rates) and differences in the ability to metabolize alcohol 8 , 9 , 16 differ markedly from those in western populations 4 , 17 .
For many diseases, including those considered by the World Health Organization (WHO) 4 to be alcohol-related (for example ischemic heart disease (IHD) and diabetes), uncertainty remains about the causal relevance of these associations, which can be assessed in genetic studies using a Mendelian randomization (MR) approach 18 . In such studies, genetic variants can be used as instruments for alcohol consumption to investigate the potential causal relevance of alcohol drinking for diseases, which can limit the biases of confounding and reverse causality common in conventional observational studies 18 . Such studies are particularly informative in East Asian populations where two common genetic variants ( ALDH2 - rs671 and ADH1B - rs1229984 ), which are both rare in western populations, greatly alter alcohol metabolism and strongly affect alcohol intake 19 . Several studies have explored the causal relevance of alcohol consumption with CVD risk factors and morbidity 19 , 20 , 21 , 22 and cancer 16 using these genetic variants, yet findings remain inconclusive for certain diseases (for example IHD) and evidence for other diseases is sparse.
To address these questions, we conducted analyses using observational and genetic approaches to evaluate the associations between alcohol consumption and the risks of a wide range of disease outcomes in the prospective China Kadoorie Biobank (CKB).
Among the 512,724 participants (Supplementary Fig. 1 ), the mean age at baseline was 52 (s.d. 10.7) years, 41% were men and 56% lived in rural areas. Among men, 33% reported drinking alcohol regularly (at least once a week) at baseline (current drinkers), consuming on average 286 g of alcohol per week, mainly from spirits (Supplementary Tables 1 and 2 ). Non-drinkers and ex-drinkers were older and more likely to report poor self-rated health or previous chronic diseases, compared to occasional or current drinkers (Table 1 ). Compared to moderate drinkers (<140 g per week), heavier drinkers were more likely to be rural residents, had received lower education and had more unhealthy lifestyle factors (for example smoking and infrequent fresh fruit intake), higher mean blood pressure and longer duration of drinking (Supplementary Table 3 ). Among male current drinkers, 62% reported drinking daily and 37% engaging in heavy episodic drinking (Supplementary Table 2 ). Among women, only 2% drank alcohol at least weekly (mean intake 116 g per week), but there were similar associations with other baseline characteristics (Table 1 and Supplementary Tables 3 and 4 ) compared to those in men.
During a median of 12.1 (interquartile range 11.1–13.1) years of follow-up, 134,641 men (44,027 drinkers) and 198,430 women (4,420 drinkers) experienced at least one reported hospitalization event or death at age-at-risk 35–84 years, involving a total of 1,111,495 hospitalization episodes. Among men, there were 333,541 (107,857 in current drinkers) recorded events from 207 diseases across 17 International Classification of Diseases Tenth Revision (ICD-10) chapters studied that had at least 80 cases each among current drinkers (Table 2 ), while among women there were 476,986 (11,773) events from 48 diseases across 18 ICD-10 chapters (Supplementary Table 5 ).
Observational associations of alcohol with disease risks
Among men, alcohol drinking was significantly associated with higher risks of 61 disease outcomes from 15 ICD-10 chapters based on two separate analyses, (1) comparing ever-regular versus occasional drinkers and (2) dose–response among current drinkers (Table 2 and Extended Data Fig. 1 ). In each of the analyses in men, there were significant associations of alcohol consumption with 42 diseases (or outcomes), of which 23 were significant in both analyses and the remainder were directionally consistent with one exception (transient cerebral ischemic attacks, ICD-10 code G45) (Fig. 1 ). In further analyses covering all alcohol consumption categories, there were typical U-shaped or J-shaped associations, with excess risks in male ex-drinkers and non-drinkers compared to occasional or moderate drinkers for most of these diseases (Supplementary Table 6 ). Among male ex-drinkers, the overall excess morbidity risks were more considerable for alcohol-associated diseases than for other diseases, but these excess risks were lower with increasing duration after stopping drinking (Extended Data Fig. 2 ).
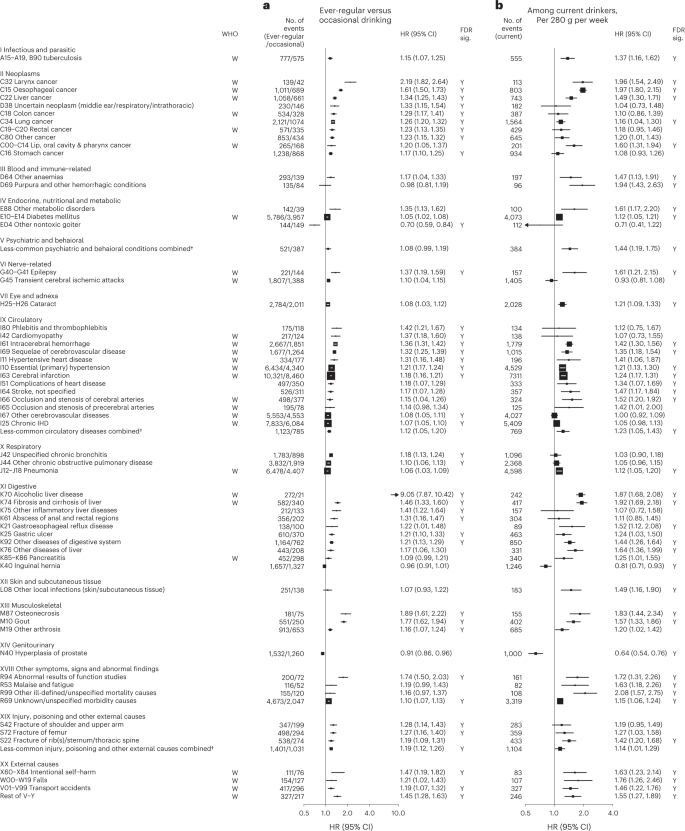
Cox models ( a ) comparing ever-regular drinkers with occasional drinkers or ( b ) assessing the dose–response per 280 g per week higher usual alcohol intake within current drinkers, were stratified by age at risk and study area and were adjusted for education and smoking. Each solid square represents HR with the area inversely proportional to the variance of the log HR. The horizontal lines indicate 95% CIs. Diseases considered to be alcohol-related by the WHO are indicated with ‘W’ under the ‘WHO’ column. The individual diseases listed included all that showed FDR-adjusted significant associations with alcohol (FDR-adjusted P < 0.05, indicated with ‘Y’ under the ‘FDR sig.’ column) and WHO alcohol-related diseases that showed nominally significant associations with alcohol ( P < 0.05). All P values are two-sided. † Included less-common ICD-10 codes within the corresponding ICD-10 chapter that were not individually investigated in the present study. ‘Less-common psychiatric and behavioral conditions’ consisted of ICD-10 codes F00–F99, excluding F32, F33 and F99. ‘Less-common circulatory diseases’ consisted of ICD-10 codes I00–I99, excluding I10, I11, I20, I21, I24, I25, I27, I42, I46, I48–I51, I60–I67, I69, I70, I80 and I83. ‘Less-common injury, poisoning and other external causes’ consisted of ICD-10 codes S00–T98, excluding S06, S09, S22, S32, S42, S52, S62, S72, S82, S92 and T14.
Of the 61 diseases positively associated with alcohol intake in male participants, 28 were considered by the WHO to be alcohol-related diseases, including tuberculosis (A15–A19 and B90), six site-specific cancers including cancers in the larynx (C32), esophagus (C15), liver (C22), colon (C18), rectum (C19 and C20) and lips, oral cavity and pharynx (C00–C14), diabetes (E10–E14), epilepsy (G40 and G41), several hypertensive diseases (I10 and I11) and cerebrovascular diseases (I61, I63, I65, I66, I67, I69 and G45), chronic IHD (I25), cardiomyopathy (I42), pneumonia (J12–J18), alcoholic liver disease (K70) and liver cirrhosis (K74), pancreatitis (K85 and K86) and external causes including self-harm (X60–X84), falls (W00–W19), transport accidents (V01–V99) and other external causes (rest of V–Y) (Fig. 1 and Extended Data Fig. 3 ). Of these 28 diseases, 22 showed significant dose–response associations with alcohol intake. The hazard ratios (HRs) per 280 g per week higher intake for the aggregated WHO alcohol-related diseases were 1.22 (95% confidence interval (CI) 1.19–1.25) (Supplementary Table 7 for detailed outcome classification), ranging from 1.12 (1.05–1.20) for pneumonia to 1.97 (1.80–2.15) for esophageal cancer.
The 33 other diseases showing false discovery rate (FDR)-adjusted significant positive associations with alcohol drinking in men included lung (C34) and stomach (C16) cancers, cataract (H25 and H26), six digestive diseases such as gastroesophageal reflux disease (K21) and gastric ulcer (K25), three musculoskeletal conditions, including gout (M10), three fracture types (S22, S42 and S72), and the aggregates of less-common psychiatric and behavioral conditions and circulatory diseases (Fig. 1 and Extended Data Fig. 4 ). Of these 33 diseases, 22 showed significant dose–response associations, with HRs per 280 g per week higher intake ranging from 1.16 (95% CI 1.04–1.30) for lung cancer to 1.94 (1.43–2.63) for purpura and other hemorrhagic conditions (D69) and 1.20 (1.16–1.24) for the aggregated CKB new alcohol-associated diseases. In contrast, three diseases showed FDR-adjusted significant inverse associations with alcohol drinking (other nontoxic goiter (E04), hyperplasia of prostate (N40) and inguinal hernia (K40)). Overall, for all-cause morbidity, the HR per 280 g per week higher intake was 1.12 (1.10–1.14) in male current drinkers.
Supplementary Figs. 2 – 4 show the dose–response associations for all disease outcomes investigated in male current drinkers. For alcohol-associated diseases and for total morbidity, the dose–response associations were unaltered after additional covariate adjustments or excluding participants with poor baseline health conditions (Supplementary Fig. 5 and Supplementary Table 8 ). Moreover, the associations were similar across various male population subgroups, but seemed to be stronger in younger men, urban residents and higher socioeconomic groups for new alcohol-associated diseases (Supplementary Fig. 6 ).
Among male current drinkers, drinking daily, heavy episodic drinking and drinking spirits were each associated with higher risks for alcohol-related diseases, but most of these associations were attenuated to the null after adjusting for total alcohol intake (Extended Data Fig. 5 ); however, for a given total alcohol intake among male current drinkers, drinking daily was associated with 30–40% higher risks of alcohol-related cancers (1.30, 1.17–1.45) and liver cirrhosis (1.39, 1.13–1.72), compared to non-daily drinking. Similarly, heavy episodic drinking was associated with higher risks of diabetes (1.23, 1.12–1.34) and IHD (1.11, 1.03–1.19), whereas drinking outside of meals was associated with 49% (1.49, 1.19–1.86) higher risk of liver cirrhosis than drinking with meals. The risks of all major alcohol-associated diseases were higher with longer duration of alcohol consumption in men (Extended Data Fig. 6 ).
Among women, due to few reported current drinkers there was a lack of statistical power to detect any associations of self-reported alcohol intake with disease risks (Supplementary Table 5 , Extended Data Fig. 7 and Supplementary Fig. 7 ).
Genetic associations of alcohol with disease risks
A genetic instrument for alcohol intake was derived using ALDH2 - rs671 (G > A) and ADH1B - rs1229984 (G > A) genotypes. The overall A-allele frequency was 0.21 for ALDH2 - rs671 and 0.69 for ADH1B - rs1229984 , with both A-alleles being more common in southern than northern study areas (Supplementary Table 9 ). Both ALDH2 - rs671 and, to a lesser extent, ADH1B - rs1229984 were strongly associated with alcohol drinking in men, but much less so in women (Supplementary Table 10 ). In men, the derived genetic instrument predicted a >60-fold difference (range 4–255 g per week, C1 to C6) in mean alcohol intake, whereas in women mean alcohol intake remained low (<10 g per week) across genetic categories (Supplementary Table 11 ). Both variants and the derived instrument were not associated with smoking or other major self-reported baseline characteristics, except for a small difference in fresh fruit intake by ALDH2 - rs671 genotype in men.
Among men, genotype-predicted mean alcohol intake was positively associated with higher risks of CKB WHO alcohol-related (HR per 280 g per week higher genotype-predicted mean male alcohol intake: 1.14, 95% CI 1.09–1.20) and CKB new alcohol-associated (1.06, 1.01–1.12) diseases (Fig. 2 ), both of which were slightly weaker than the conventional associations. For certain diseases, however, the genetic associations were stronger, with HRs of 1.38 (1.27–1.49) for stroke, 2.30 (1.58–3.35) for liver cirrhosis and 2.33 (1.49–3.62) for gout, in men (Fig. 3 and Extended Data Fig. 8 ). For individual genetic variants, the associations were directionally consistent (Extended Data Figs. 9 and 10 ). Conversely, there were no significant dose–response genotypic associations with IHD, inguinal hernia or hyperplasia of prostate in men. For other alcohol-associated diseases, higher genotype-predicted mean male alcohol intake was significantly associated with higher risks of esophageal cancer, cataract, occlusion and stenosis of cerebral arteries, sequelae of cerebrovascular disease, essential primary hypertension and fractures of ribs, sternum or thoracic spine. There were also suggestive positive genotypic associations with several digestive tract cancer types (liver, colon and stomach) and circulatory and digestive diseases, and significant inverse associations with lung cancer and other chronic obstructive pulmonary disease (J44) in men (Extended Data Figs. 8 – 10 ). Sensitivity analyses using different analytical methods to adjust for confounding by study area, or a two-stage least-squares MR approach, did not alter the main genetic findings in men (Supplementary Table 12 ). In contrast, genotypes that increased alcohol intake in men were not adversely associated with most alcohol-related disease risks among women (for example HR 1.00 (0.97–1.04) for all morbidity among female non-drinkers; Supplementary Fig. 7 and Extended Data Figs. 8 – 10 ).
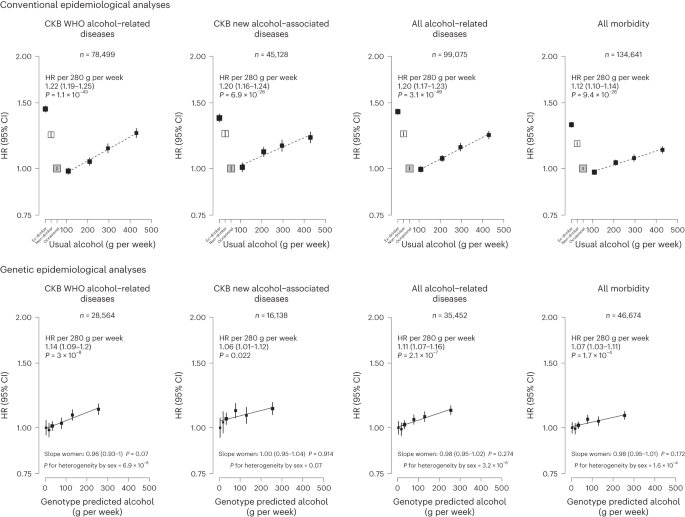
Each box represents HR with the area inversely proportional to the variance of the group-specific log hazard within subplot. The vertical lines indicate group-specific 95% CIs. Conventional epidemiological analyses relate self-reported drinking patterns to risks of diseases (reference group is occasional drinkers), using Cox models stratified by age at risk and study area and adjusted for education and smoking. Within current drinkers, HRs were plotted against usual alcohol intake and were calculated per 280 g per week higher usual alcohol intake. Genetic epidemiological analyses relate genetic categories to risks of diseases (reference group is the genotype group with lowest genotype-predicted mean male alcohol intake), using Cox models stratified by age at risk and study area and adjusted for genomic principal components. The HR per 280 g per week higher genotype-predicted mean male alcohol intake was calculated from the inverse-variance-weighted mean of the slopes of the fitted lines in each study area. The corresponding slopes in women were summarized in text and the slopes of the fitted line by sex were compared and assessed for heterogeneity using chi-squared tests (indicated by P for heterogeneity by sex). All P values are two-sided. Analyses of these aggregated outcomes were based on first recorded event of the aggregate during follow-up and participants may have had multiple events of different types of diseases. ‘All alcohol-related diseases’ includes the first recorded event from ‘CKB WHO alcohol-related diseases’ or ‘CKB new alcohol-associated diseases’ during follow-up.
Each box represents HR with the area inversely proportional to the variance of the group-specific log hazard within subplot. The vertical lines indicate group-specific 95% CIs. Conventional epidemiological analyses relate self-reported drinking patterns to risks of diseases (reference group is occasional drinkers), using Cox models stratified by age at risk and study area and adjusted for education and smoking. Within current drinkers, HRs were plotted against usual alcohol intake and were calculated per 280 g per week higher usual alcohol intake. Genetic epidemiological analyses relate genetic categories to risks of diseases (reference group is the genotype group with lowest genotype-predicted mean male alcohol intake), using Cox models stratified by age at risk and study area and adjusted for genomic principal components. The HR per 280 g per week higher genotype-predicted mean male alcohol intake was calculated from the inverse-variance-weighted mean of the slopes of the fitted lines in each study area. The corresponding slopes in women were summarized in text and the slopes of the fitted line by sex were compared and assessed for heterogeneity using chi-squared tests (indicated by P for heterogeneity by sex). All P values are two-sided. Corresponding ICD-10 codes, IHD (I20–I25); stroke (I60, I61, I63 and I64); liver cirrhosis (K70 and K74); gout (M10); inguinal hernia (K40); hyperplasia of prostate (N40).
Hospitalizations associated with alcohol drinking
Among men, ever-regular drinkers had higher numbers of hospitalizations for any causes than occasional drinkers, particularly for cancer hospitalizations, and these differences increased with increasing age at risk, except for CVD hospitalizations (Supplementary Fig. 8 ).
This prospective study provides a comprehensive assessment of the impact of alcohol consumption on a very wide range of disease outcomes in Chinese adults. Among men, alcohol consumption was associated with significantly higher risks of 61 diseases, including 33 not previously reported as alcohol-related diseases by the WHO, and higher risks of hospitalizations for any causes. For a given total amount, drinking daily, heavy episodic drinking and drinking outside of meals exacerbated the risks of four major diseases in Chinese men. Moreover, most of these associations in Chinese men were confirmed in genetic analyses, at least when assessed collectively, and are likely to reflect the effects alcohol consumption itself rather than any pleiotropic effects of the genetic instruments.
Based primarily on observational findings in western populations, alcohol consumption has been considered by the WHO 4 and the Global Burden of Disease (GBD) study 23 to be related to about 20 distinct disease categories, involving chronic diseases and cancers largely in the gastrointestinal system, several CVD types, infectious diseases and injuries. The observational analyses largely confirmed these known associations (Supplementary Table 13 ), but also provided insights into additional hazards of certain drinking patterns suggested by previous studies 8 , 9 , 24 , 25 . Moreover, this study discovered 33 additional alcohol-associated diseases across various body systems in Chinese men that had not been previously reported by the WHO. For these 33 disease outcomes, their associations with alcohol intake were confirmed in genetic analyses, at least collectively as well as for certain specific diseases (for example gout), as was the case for a similar number of WHO alcohol-related diseases. The somewhat smaller relative (but not absolute) risks of alcohol drinking with major diseases at older than younger age in men from observational analyses were consistent with previous studies of other risk factors (for example blood pressure 26 and smoking 27 ), which could be driven by a number of factors such as selection bias 27 and comorbidities.
For certain major WHO alcohol-related diseases, particularly IHD and ischemic stroke, observational studies, including this study, have consistently reported J-shaped associations, with those who drank moderately (for example 1–2 units a day) having the lowest risks 6 , 28 ; however, these apparent protective effects of moderate drinking probably largely reflect residual confounding (for example non-drinkers having worse health and socioeconomic profiles than occasional drinkers) and uncontrolled reverse causation (for example sick-quitter effect where pre-existing poor health or changes in health conditions lead to alcohol cessation), including the difficulty in defining abstainers (for example ex-drinkers may be reported as non-drinkers) as the reference group in many previous studies 3 , 29 . In this study, we used occasional drinkers rather than non-drinkers as the reference group, which, together with separate dose–response analyses among current drinkers, helped to reduce but not eliminate any such biases, which could largely be mitigated in genetic analyses using an MR approach.
To date the existing MR studies for alcohol have focused mainly on CVD types 30 , 31 , 32 and cancers 33 , 34 , 35 , with limited data for other diseases. Moreover, previous studies mainly involved European-ancestry populations and hence were constrained by availability of relatively weak genetic instruments. Using genetic instruments specific to East Asian populations that predicted >60-fold difference in alcohol consumption, we previously reported evidence for the causal relevance and apparent dose–response effects of alcohol consumption on upper-aerodigestive tract cancers 16 and stroke 19 . These findings were further corroborated by subsequent European ancestry-based MR studies 30 , 32 , 36 and the analyses presented in this study with additional follow-up data. In contrast to stroke, we found no reliable genetic evidence for a cardioprotective, nor harmful, effect of moderate drinking on risk of IHD in men, consistent with findings in other MR studies 30 , 32 . The present study also demonstrated a log-linear genetic association of alcohol with liver cirrhosis and suggestive positive associations for several WHO alcohol-related digestive tract cancers in men. Moreover, separate genetic analyses among women suggests that the excess risks observed among men were due chiefly to alcohol per se rather than to potential pleiotropic effects of the alcohol-related genotypes. Further larger genetic studies are required to confirm and elucidate the potential causal relevance for each of the other WHO alcohol-related diseases individually.
For the new alcohol-associated diseases identified in this study, the available prospective epidemiological evidence has been sparse and mostly confined to western populations. For gout, previous western prospective studies have reported positive associations 37 , 38 and an MR study of 8,000 Korean men has also reported positive associations of alcohol consumption with hyperuricemia, a risk factor for gout 39 . The present study provides genetic evidence that alcohol drinking increases the risk of gout. Consistent with the present study, previous European-ancestry-based observational studies 40 , 41 and one MR study 42 also reported positive associations of alcohol intake with risks of several fracture types. The available prospective evidence on associations between alcohol drinking and risk of cataract has been conflicting 15 , 43 and one European-ancestry-based MR study reported no genetic associations 44 . We found a significant dose–response association between alcohol and risk of cataract among Chinese men in observational analyses, which was supported by the present genetic analyses.
For several other diseases (for example gastroesophageal reflux disease and gastric ulcer), the observational findings provide additional evidence to the existing literature 5 , 45 , 46 , 47 , but the supporting genetic evidence is still constrained by limited statistical power. Similarly, our observational findings for lung and stomach cancers were generally consistent with evidence provided by previous prospective studies 7 , 11 , 48 , 49 ; however, the causal relevance of these associations remains to be elucidated in future larger MR studies with appropriate consideration of the potential gene–environment interactions between ALDH2 - rs671 and alcohol intake (the effect of alcohol intake on cancer risks being modified by ALDH2 - rs671 genotype due to excessive acetaldehyde) 16 and other aldehyde exposures 50 in cancer risks, which might similarly affect the genetic associations for respiratory diseases and other potential acetaldehyde-related diseases. In observational analyses, we found significant inverse associations for inguinal hernia, prostate hyperplasia and other nontoxic goiter, but not for several other diseases previously inversely associated with alcohol drinking, including non-Hodgkin lymphoma 48 , kidney cancer 48 , thyroid cancer 48 and gallstones 51 . The genetic analyses, albeit with limited power, did not provide reliable evidence supporting the inverse associations with these outcomes. Future well-powered genetic investigations are warranted for less-common diseases in different populations.
The strengths of this study include the prospective design, large sample size, detailed information on alcohol consumption and drinking patterns, completeness of follow-up and a wide range of morbidity outcomes analyzed. We were also able to assess the potential causal relevance of the associations using two powerful East Asian genetic variants. Moreover, the extremely low drinking prevalence in women (regardless of their genotypes) enabled assessment for potential pleiotropy, further supporting the genetic findings among men.
Nevertheless, the study also has limitations. First, it is still possible that heavy drinking was under-reported, which could have underestimated the hazards of heavy episodic drinking. Second, as in many population-based cohort studies, extreme problematic drinkers and certain alcohol-related disease events may be under-represented, but this should not affect the assessment of the associations of alcohol with most disease outcomes. Third, while the repeated measures of alcohol consumption available in the re-survey subsets allowed us to estimate long-term usual mean alcohol intake at the group level to account for regression dilution bias, we were unable to study the effects of longitudinal alcohol drinking trajectories on health. Fourth, we were unable or underpowered to study diseases that do not normally require hospitalization (for example dementia and depression), nor alcohol-related diseases only affecting women, given the low proportion of female drinkers (for example <70 cases of breast cancer in female drinkers). While the low female drinking prevalence in CKB was consistent with findings in a nationwide survey 52 , it is possible that women may be more likely to under-report drinking than men for cultural and social reasons. Hence our null findings in women should be interpreted with caution and not be taken as a lack of alcohol-related harms in women in general, especially in the context of rising alcohol consumption among Asian women 2 . Fifth, as spirits were the main beverage type and our genetic instrument did not distinguish between beverage types, we were unable to assess beverage-specific effects on disease risks, including wine consumption, which is uncommon in China 17 and has been proposed as potentially cardioprotective due to other non-alcoholic components in red wine 53 . Sixth, although our genetic analyses allowed comparison of the overall genetic effects of negligible, moderate and high mean alcohol intake levels for major and overall morbidities, we had limited power to confidently clarify any small threshold effects in the low consumption end, especially for individual diseases. Finally, the genetic analyses lacked statistical power to assess the associations with several individual alcohol-associated diseases so these findings should still be viewed as hypothesis-generating.
In recent decades, several studies have estimated the alcohol-attributable disease burden, involving predominantly WHO alcohol-related diseases. These estimates were based mainly on observational evidence and included the potentially biased U- or J-shaped associations with IHD and ischemic stroke 1 , 23 , 54 . We have demonstrated in both conventional and genetic analyses that alcohol drinking is associated with hazards in a dose–response manner with a much wider range of disease outcomes than previously considered by the WHO 4 and the GBD study 23 and do not find any evidence for protective effects for IHD or stroke, suggesting that the actual alcohol-attributable disease burden is likely to be much greater than widely believed.
Overall, the present study demonstrated substantial hazards of alcohol consumption with a wide range of disease outcomes among Chinese men. The findings reinforce the need to lower population mean levels of alcohol consumption as a public health priority in China. Future estimation of the alcohol-attributable disease burden worldwide and in specific regions should incorporate new genetic evidence from the present and any future studies about the likely causal relevance of alcohol consumption for a broad range of disease outcomes.
Study population
Details of the CKB study design and methods have been previously reported 55 . Briefly, 512,724 adults aged 30–79 years were recruited from ten geographically diverse (five rural and five urban) areas across China during 2004–2008. At local study assessment clinics, trained health workers administered a laptop-based questionnaire recording sociodemographic factors, lifestyle (for example alcohol drinking, smoking, diet and physical activity) and medical history; undertook physical measurements (for example blood pressure and anthropometry); and collected a blood sample for long-term storage. Two resurveys of ~5% randomly selected surviving participants were subsequently conducted in 2008 and 2013–2014 using similar procedures.
Ethics approval
Ethical approval was obtained from the Ethical Review Committee of the Chinese Centre for Disease Control and Prevention (Beijing, China, 005/2004) and the Oxford Tropical Research Ethics Committee, University of Oxford (UK, 025-04). All participants provided written informed consent.
Assessment of alcohol consumption
Detailed questionnaire assessment of alcohol consumption has been described previously 3 , 17 , 56 . In the baseline questionnaire, participants were asked how often they had drunk alcohol during the past 12 months (never or almost never, occasionally, only at certain seasons, every month but less than weekly or usually at least once a week). Those who had not drunk alcohol at least weekly in the past 12 months were asked whether there was a period of at least a year before that when they had drunk some alcohol at least once a week. Based on their past and current drinking history, participants were classified into: non-drinkers (had never drunk alcohol in the past year and had not drunk in most weeks in the past); ex-drinkers (had not drunk alcohol in most weeks in the past year but had done so in the past); occasional drinkers (had drunk alcohol but less than weekly in the past year and had not drunk alcohol in most weeks in the past); and current drinkers (had drunk alcohol on a weekly basis (regularly) in the past year).
Current drinkers were asked further questions about their drinking patterns, including frequency, beverage type (beer, grape wine, rice wine, weak spirits with <40% alcohol content and strong spirits with ≥40% alcohol content) and amount consumed on a typical drinking day, mealtime drinking habits, age started drinking in most week and their experience of flushing or dizziness after drinking.
Alcohol intake level was estimated based on the reported frequency (taken as the median of the reported frequency intervals; 1.5 for 1–2 d per week, 4 for 3–5 d per week, 6.5 for 6–7 d per week), beverage type and amount consumed, assuming the following alcohol content by volume (v/v) typically seen in China: beer 4%, grape wine 12%, rice wine 15%, weak spirits 38% and strong spirits 53% 57 . Among current drinkers, men were grouped into four consumption categories (<140, 140–279, 280–419 and 420+ g per week) and women into three categories (<70, 70–139 and 140+ g per week), broadly based on the recommended cutoffs for alcohol categories by the WHO 58 and national drinking guidelines. Heavy episodic drinking was defined as consuming >60 g of alcohol on a typical drinking occasion for men and >40 g per occasion for women 58 . Drinking outside of meals was defined as usually drinking between or after meals or having no regular patterns (versus usually drinking with meals). Duration of drinking was derived by the difference in years between age at baseline and age started drinking.
Ex-drinkers were asked how long (in years) ago they had stopped drinking in most weeks. Ex-drinkers were grouped with current drinkers as ‘ever-regular drinkers’.
Follow-up for mortality and morbidity
The vital status of participants was obtained periodically from local death registries, supplemented by annual active confirmation through local residential, health insurance and administrative records. Additional information on morbidity was collected through linkage with disease registries (for cancer, stroke, IHD and diabetes) and the national health insurance system, which record any episodes of hospitalization and almost has universal coverage. All events were coded with ICD-10 codes, blinded to the baseline information. By 1 January 2019, 56,550 (11%) participants had died, 311,338 (61%) were ever hospitalized, but only 4,028 (<1%) were lost to follow-up.
Outcome measures
To enable a ‘phenome-wide’ investigation, all recorded diseases and injuries (referred to as ‘diseases’ for simplicity) coded by three-character ICD-10 codes were reviewed. ICD-10 codes were combined (where appropriate) based on disease characteristics and their potential relationships with alcohol consumption 4 , 8 , 10 , 59 . Disease end points were curated based on diseases considered to be causally impacted by alcohol by the WHO 4 , 59 and major diseases previously shown to be related to alcohol in CKB and other large prospective cohort studies 8 , 10 , while retaining maximal granularity. Diseases with at least 80 cases recorded during follow-up among current drinkers, separately by sex, were analyzed individually to capture a wide range of specific conditions while ensuring reasonable statistical power (around 60–80% power to detect a HR of 2.00 per 280 g per week higher usual alcohol intake at P < 0.01 and P < 0.05, respectively). Within each ICD-10 chapter, diseases with <80 events were grouped into a ‘less-common’ category. Several ICD-10 chapters considered not directly relevant in this population (for example perinatal-origin diseases (chapter XVI) and congenital conditions (XVII); pregnancy-related diseases (XV) in men) were excluded.
Major diseases defined by the WHO as likely to be causally related with alcohol consumption 4 , including several cancers (mouth and throat, esophagus, colon-rectum, liver and female breast), diabetes mellitus, IHD, stroke, liver cirrhosis and external causes, were also selected a priori for detailed analyses of associations with drinking patterns (daily drinking, heavy episodic drinking, mealtime habit, spirit drinking and drinking duration). Similarly, diseases that were significantly and adversely associated with alcohol in the ‘phenome-wide’ investigations (either with ever-regular versus occasional drinking or in dose–response associations with amounts consumed) were further categorized as ‘CKB WHO alcohol-related diseases’ and ‘CKB new alcohol-associated diseases’ respectively for genetic investigation of causality. Detailed outcome classifications are reported in Supplementary Table 7 .
Genotyping and alcohol genetic instruments
The two East Asian genetic variants ( ALDH2 - rs671 and ADH1B - rs1229984 ) were genotyped in 168,050 participants (151,347 randomly selected, 16,703 selected as part of nested case–control studies of CVD and chronic obstructive pulmonary disease, which were only included in analyses of relevant outcomes; Supplementary Fig. 1 ) using Affymetrix Axiom ( n = 100,396) or custom Illumina GoldenGate ( n = 93,125) arrays at BGI (Shenzhen, China), with some overlap between them. Among 25,471 participants genotyped with both arrays, the concordance was >99.9% for both variants. Where discordant, genotypes obtained from the Affymetrix Axiom array were used.
The genetic instrument for alcohol was derived from ALDH2 - rs671 and ADH1B - rs1229984 and ten study areas from the random genotyped subset of male participants to avoid potential selection bias, using a previously developed method in CKB 19 . Briefly, nine genotype combinations were defined based on the genotypes for each of the two variants (each AA, AG or GG). As alcohol use varies greatly by study area, among men, mean alcohol intake was calculated for each of these nine genotype across ten study areas (that is a total of 90 genotype-area combinations) to reflect a wide range of alcohol consumption, assigning an intake of 5 g per week to occasional drinkers and excluding ex-drinkers from the calculation. Ex-drinkers were excluded from the calculation of mean alcohol intake as their baseline intake did not reflect their long-term intake; nevertheless, they were included in subsequent genetic analyses once they had been assigned a genetic group. These 90 combinations were then grouped into six categories (C1–C6) according to their corresponding mean intake values, at cutoff points of 10, 25, 50, 100 and 150 g per week, selected to facilitate investigation of the causal effects of alcohol across a wide range of mean alcohol intakes while allowing adequate sample size in each category for reliable comparisons. In this way participants (including ex-drinkers) were classified only based on their genotypes and study area, but not on individual self-reported drinking patterns. Comparisons of these six genetic categories can, where analyses are stratified by area, be used to estimate the genotypic effects on disease risks.
To facilitate the comparison of genotypic effects between sexes (pleiotropic effects), women were classified into the same six categories as men based on their genotypes and study area, regardless of female alcohol intake. This allowed comparison of genotypic effects between men (where genotype were strongly associated with alcohol intake) and women (where alcohol intake was low in all genotypic categories) (Supplementary Tables 10 and 11 ).
Statistical analysis
Given the extremely low alcohol use among women 3 , 17 , the analyses were conducted separately by sex but focused chiefly on men. All CKB participants and the genotyped subset with genomic principal components (PCs; derived from genome-wide genotyping array data and were informative for CKB population structure) 60 were included in conventional and genetic analyses, respectively (Supplementary Fig. 1 ). Means and percentages of baseline characteristics were calculated by self-reported alcohol consumption patterns and by genotype categories, adjusted for age (in 10-year intervals), ten study areas and (for genetic analysis) genomic PCs 60 to control for differences in genetic distribution due to population stratification, as appropriate.
For conventional observational analyses, Cox proportional hazard models were used to estimate HRs for individual diseases associated with different alcohol consumption categories (in three broad categories: occasional drinkers, ever-regular drinkers, non-drinkers; and in 6–7 detailed categories: occasional drinkers, ex-drinkers, non-drinkers, 3–4 further current drinker groups defined by alcohol intake level) and among current drinkers with continuous levels of alcohol intake (per 280 g per week in men, per 100 g per week in women) or with categories of alcohol intake (<140, 140–279, 280–419 and 420+ g per week in men; <70, 70–139 and 140+ g per week in women). The Cox models were stratified by age at risk (5-year groups between 35–84 years) and ten areas and adjusted for education (four groups: no formal school, primary school, middle or high school and technical school/college or above) and smoking status (six groups in men: never, occasional, ex-regular, current <15, current 15–24, current ≥25 cigarettes equivalent per day; four groups in women: never, occasional, ex-regular and current). Smoking data have been previously validated against exhaled carbon monoxide 61 . Competing risks from all-cause mortality for disease events were handled by censoring participants at death from any cause to estimate cause-specific HRs comparing event rates in participants who were alive and free of the disease of interest 62 . To reduce biases from residual confounding and uncontrolled reverse causation related to the choice of using non-drinkers (for example sick-quitter effect, pre-existing poor health or social disadvantages leading to alcohol cessation or abstinence) as the reference group 3 , 29 , we used occasional drinkers as the reference group, together with separate dose–response analyses among current drinkers. To account for within-person variation of alcohol intake over the follow-up period, repeat alcohol measures for participants who attended the two resurveys were used to estimate usual alcohol intake (Supplementary Table 1 ) and correct for regression dilution bias 9 , 63 . The shapes of dose–response associations between alcohol and disease risks were assessed among current drinkers by plotting the HRs of predefined baseline consumption categories against the corresponding mean usual alcohol intake. Log HR estimates and the corresponding standard errors for baseline alcohol intake, modeled as a continuous variable, were divided by the regression dilution ratio (0.53 for both men and women; calculated using the McMahon–Peto method 64 ) to obtain estimated HRs per 280 g per week higher usual alcohol intake among male current drinkers and HRs per 100 g per week among female current drinkers. For analyses involving drinking patterns, additional adjustments were conducted for total alcohol intake (continuous) and baseline age (continuous; for drinking duration analysis) where appropriate.
Sensitivity analyses were performed by (1) additional adjustments for further covariates (household income (<10,000, 10,000–19,999, 20,000–34,999 and ≥35,000 yuan per year), fresh fruit intake (4–7 d per week and ≤3 d per week), physical activity (continuous, in metabolic equivalent of task per hour per day), body mass index (<22, 22–24.9, 25–26.9 and ≥27 kg m 2 ); and (2) excluding individuals with poor self-reported health or previous major chronic diseases (including self-reported coronary heart diseases, stroke, transient ischemic attack, tuberculosis, emphysema or bronchitis, liver cirrhosis or chronic hepatitis, peptic ulcer, gallstone or gallbladder disease, kidney disease, rheumatoid arthritis, cancer and diabetes) at baseline. For all aggregated end points (for example CKB WHO alcohol-related, CKB new alcohol-associated and all morbidity), subgroup analyses were conducted by baseline age (<55, 55–64 and ≥65 years), area (urban and rural), education (primary school or below, middle school, high school or above), household income (<10,000, 10,000–19,999 and 20,000+ yuan per year) and smoking status (ever-regular and never-regular), with heterogeneity or trend assessed by chi-squared tests 65 . HRs for diseases associated with years of stopping among ex-drinkers compared to occasional drinkers were also estimated.
In genetic analyses, Cox regression, stratified by age at risk and study area and adjusted for 11 genomic PCs 60 , were used to estimate HRs for major alcohol-related diseases associated with the six genetic categories (C1–C6). Log HRs were plotted against the genotype-predicted mean male alcohol intake in the six categories. To control for potential confounding by population structure, similar analyses were repeated within each study area using age-at-risk-stratified and genomic PC-adjusted Cox models. A line of best fit was fitted through the log HRs against genotype-predicted mean male alcohol intake in the genetic categories present in the corresponding study area, using meta-regression. These within-area slopes (each reflecting purely genotypic effects) were combined by inverse-variance-weighted meta-analysis to yield the overall area-stratified genotypic associations, which controlled for any potential bias resulted from variations due to population structure, summarized as HR per 280 g per week higher genotype-predicted mean male alcohol intake. For total morbidity and aggregated alcohol-associated outcomes, sensitivity analyses were performed by (1) using age-at-risk- and area-stratified and genomic PC-adjusted Cox models to estimate HR per 280 g per week (area-adjusted genotypic associations); and (2) using a two-stage least-squares approach 66 .
Genotypic analyses in women were conducted not to assess the health effects of alcohol in women, but to investigate the extent to which the genotypes studied in men had pleiotropic effects (genotypic effects not mediated by drinking patterns). As few women consumed alcohol, any genotypic effects of the six genetic categories that are mediated by drinking alcohol should be much smaller in women than in men, but any other pleiotropic genotypic effects should be similar in both sexes. Hence, among women, we used the same genetic categories as in men and related the genotypic effects in women to the mean male alcohol intake in these six categories, which allows comparisons of genetic findings by sex and assessment of potential pleiotropy. To further remove the small genotypic effects on alcohol use in women (Supplementary Tables 10 and 11 ), we restricted the genetic analyses to female non-drinkers in sensitivity analyses.
The genotypic associations of individual genetic variants ( rs671 , rs1229984 ; GG versus AG genotype) with alcohol-related disease risks were also assessed using a similar area-stratified approach.
The proportional hazards assumption was tested using scaled Schoenfeld residuals for the pre-specified major diseases (no clear evidence of violation was found). For analyses involving more than two exposure categories, the floating absolute risks were used to estimate group-specific 95% CIs for all categories including the reference group 9 , 19 , 67 . All P values were two-sided. Statistical significance (at the 5% level) was evaluated using both FDR-adjusted P values applied within ICD-10 chapters to correct for multiple testing in the ‘phenome-wide’ investigation 68 , 69 , 70 and conventional P values for hypothesis testing for observational analyses of WHO alcohol-related diseases, analyses of drinking patterns and genetic analyses.
To assess the cumulative burden of alcohol consumption, the total number of hospitalizations were estimated for ever-regular versus occasional drinkers using the mean cumulative count, which does not assume independence between hospitalizations and all-cause mortality 71 , 72 , 73 . All analyses used R software (v.4.0.5).
Ethics and inclusion statement
In accordance with the Nature Portfolio journals’ editorial policies, the research has included local researchers from China throughout the research process, including study design, study implementation, data ownership and authorship. The roles and responsibilities were agreed among collaborators ahead of the research and capacity-building plans, including data collection and study implementation skills for local researchers, were discussed and delivered. This research is locally relevant to the studied country and included local collaborative partners in all aspects of the study, thus, will provide local and regional organizations with epidemiological evidence on the health impacts of alcohol consumption to inform public health policies.
This research was not restricted nor prohibited in the setting of the researchers. The study was approved by local ethics review committee. The research raised no risks related to stigmatization, incrimination, discrimination, animal welfare, the environment, health, safety, security or other personal or biorisks. No biological materials, cultural artifacts or associated traditional knowledge has been transferred out of the country. In preparing the manuscript, the authors have reviewed and cited local and regional relevant studies.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The CKB is a global resource for the investigation of lifestyle, environmental, blood biochemical and genetic factors as determinants of common diseases. The CKB study group is committed to making the cohort data available to the scientific community in China, the United Kingdom and worldwide to advance knowledge about the causes, prevention and treatment of disease. For detailed information on what data are currently available to open access users, how to apply for them and the timeline for data access (12–16 weeks), please visit the CKB website: https://www.ckbiobank.org/data-access . Researchers who are interested in obtaining the raw data from the CKB study that underlines this paper should contact [email protected]. A research proposal will be requested to ensure that any analysis is performed by bona fide researchers and, where data are not currently available to open access researchers, is restricted to the topic covered in this paper. Further information is available from the corresponding authors upon request.
Code availability
The codes used for the data analyses in this study can be made available by contacting the corresponding authors. Access to codes will be granted for requests for academic use within 4 weeks of application.
Shield, K. et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public Health 5 , e51–e61 (2020).
PubMed Google Scholar
Manthey, J., Shield, K. D., Rylett, M., Hasan, O. S. M., Probst, C. & Rehm, J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet 393 , 2493–2502 (2019).
Im, P. K. et al. Patterns and trends of alcohol consumption in rural and urban areas of China: findings from the China Kadoorie Biobank. BMC Public Health 19 , 217 (2019).
PubMed PubMed Central Google Scholar
World Health Organization. Global Status Report on Alcohol and Health 2018 (World Health Organization, 2018).
Corrao, G., Bagnardi, V., Zambon, A., La & Vecchia, C. A meta-analysis of alcohol consumption and the risk of 15 diseases. Prev. Med. 38 , 613–619 (2004).
Ferrari, P. et al. Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. BMJ Open 4 , e005245 (2014).
Yang, L. et al. Alcohol drinking and overall and cause-specific mortality in China: nationally representative prospective study of 220,000 men with 15 years of follow-up. Int. J. Epidemiol. 41 , 1101–1113 (2012).
Im, P. K. et al. Alcohol drinking and risks of total and site-specific cancers in China: a 10-year prospective study of 0.5 million adults. Int J. Cancer 149 , 522–534 (2021).
CAS PubMed PubMed Central Google Scholar
Im, P. K. et al. Alcohol drinking and risks of liver cancer and non-neoplastic chronic liver diseases in China: a 10-year prospective study of 0.5 million adults. BMC Med. 19 , 216 (2021).
Allen, N. E. et al. Moderate alcohol intake and cancer incidence in women. J. Natl Cancer Inst. 101 , 296–305 (2009).
Jayasekara, H. et al. Lifetime alcohol intake, drinking patterns over time and risk of stomach cancer: a pooled analysis of data from two prospective cohort studies. Int J. Cancer 148 , 2759–2773 (2021).
Botteri, E. et al. Alcohol consumption and risk of urothelial cell bladder cancer in the European prospective investigation into cancer and nutrition cohort. Int J. Cancer 141 , 1963–1970 (2017).
CAS PubMed Google Scholar
Sabia, S. et al. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 362 , k2927 (2018).
Tan, G. J. al. The relationship between alcohol intake and falls hospitalization: results from the EPIC-Norfolk. Geriatr. Gerontol. Int. https://doi.org/10.1111/ggi.14219 (2021).
Chua, S. Y. L. et al. Alcohol consumption and incident cataract surgery in two large UK cohorts. Ophthalmology https://doi.org/10.1016/j.ophtha.2021.02.007 (2021).
Im, P. K. et al. Alcohol metabolism genes and risks of site-specific cancers in Chinese adults: an 11-year prospective study. Int. J. Cancer 150 , 1627–1639 (2022).
Millwood, I. Y. et al. Alcohol consumption in 0.5 million people from 10 diverse regions of China: prevalence, patterns and socio-demographic and health-related correlates. Int. J. Epidemiol. 42 , 816–827 (2013).
Davey Smith, G. & Hemani, G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum. Mol. Genet. 23 , R89–R98 (2014).
Millwood, I. Y. et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet 393 , 1831–1842 (2019).
Au Yeung, S. L. et al. Moderate alcohol use and cardiovascular disease from Mendelian randomization. PLoS ONE 8 , e68054 (2013).
Shin, M. J., Cho, Y., Davey & Smith, G. Alcohol consumption, aldehyde dehydrogenase 2 gene polymorphisms, and cardiovascular health in Korea. Yonsei Med J. 58 , 689–696 (2017).
Taylor, A. E. et al. Exploring causal associations of alcohol with cardiovascular and metabolic risk factors in a Chinese population using Mendelian randomization analysis. Sci. Rep. 5 , 14005 (2015).
Griswold, M. G. et al. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392 , 1015–1035 (2018).
Google Scholar
Simpson, R. F. et al. Alcohol drinking patterns and liver cirrhosis risk: analysis of the prospective UK Million Women Study. Lancet Public Health 4 , e41–e48 (2019).
Roerecke, M. & Rehm, J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Med. 12 , 182 (2014).
Lacey, B. et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0.5 million adults in China: a prospective cohort study. Lancet Glob. Health 6 , e641–e649 (2018).
Hernán, M. A., Alonso, A. & Logroscino, G. Cigarette smoking and dementia: potential selection bias in the elderly. Epidemiology 19 , 448–450 (2008).
Rehm, J., Rovira, P., Llamosas-Falcón, L. & Shield, K. D. Dose-response relationships between levels of alcohol use and risks of mortality or disease, for all people, by age, sex, and specific risk factors. Nutrients 13 , 2652 (2021).
Rehm, J., Irving, H., Ye, Y., Kerr, W. C., Bond, J. & Greenfield, T. K. Are lifetime abstainers the best control group in alcohol epidemiology? On the stability and validity of reported lifetime abstention. Am. J. Epidemiol. 168 , 866–871 (2008).
Lankester, J., Zanetti, D., Ingelsson, E. & Assimes, T. L. Alcohol use and cardiometabolic risk in the UK Biobank: a Mendelian randomization study. PLoS ONE 16 , e0255801 (2021).
Rosoff, D. B., Davey Smith, G., Mehta, N., Clarke, T.-K. & Lohoff, F. W. Evaluating the relationship between alcohol consumption, tobacco use, and cardiovascular disease: a multivariable Mendelian randomization study. PLoS Med. 17 , e1003410 (2020).
Larsson, S. C., Burgess, S., Mason, A. M. & Michaelsson, K. Alcohol consumption and cardiovascular disease: a Mendelian randomization study. Circ. Genom. Precis. Med. 13 , e002814 (2020).
Larsson, S. C. et al. Smoking, alcohol consumption, and cancer: a mendelian randomisation study in UK Biobank and international genetic consortia participants. PLoS Med. 17 , e1003178 (2020).
Zhou, X. et al. Alcohol consumption, DNA methylation and colorectal cancer risk: results from pooled cohort studies and Mendelian randomization analysis. Int. J. Cancer https://doi.org/10.1002/ijc.33945 (2022).
Zhou, X. et al. Alcohol consumption, blood DNA methylation and breast cancer: a Mendelian randomisation study. Eur. J. Epidemiol. 37 , 701–712 (2022).
Biddinger, K. J. et al. Association of habitual alcohol intake with risk of cardiovascular disease. JAMA Netw. Open 5 , e223849 (2022).
Wang, M., Jiang, X., Wu, W. & Zhang, D. A meta-analysis of alcohol consumption and the risk of gout. Clin. Rheumatol. 32 , 1641–1648 (2013).
Neogi, T., Chen, C., Niu, J., Chaisson, C., Hunter, D. J. & Zhang, Y. Alcohol quantity and type on risk of recurrent gout attacks: an internet-based case-crossover study. Am. J. Med 127 , 311–318 (2014).
Jee, Y. H., Jung, K. J., Park, Y. B., Spiller, W. & Jee, S. H. Causal effect of alcohol consumption on hyperuricemia using a Mendelian randomization design. Int J. Rheum. Dis. 22 , 1912–1919 (2019).
Berg, K. M. et al. Association between alcohol consumption and both osteoporotic fracture and bone density. Am. J. Med. 121 , 406–418 (2008).
Søgaard, A. J. et al. The association between alcohol consumption and risk of hip fracture differs by age and gender in Cohort of Norway: a NOREPOS study. Osteoporos. Int. 29 , 2457–2467 (2018).
Yuan, S., Michaëlsson, K., Wan, Z. & Larsson, S. C. Associations of smoking and alcohol and coffee intake with fracture and bone mineral density: a Mendelian randomization study. Calcif. Tissue Int. 105 , 582–588 (2019).
Gong, Y., Feng, K., Yan, N., Xu, Y. & Pan, C.-W. Different amounts of alcohol consumption and cataract: a meta-analysis. Optom. Vis. Sci. 92 , 471–479 (2015).
Yuan, S., Wolk, A. & Larsson, S. C. Metabolic and lifestyle factors in relation to senile cataract: a Mendelian randomization study. Sci. Rep. 12 , 409 (2022).
Pan, J., Cen, L., Chen, W., Yu, C., Li, Y. & Shen, Z. Alcohol consumption and the risk of gastroesophageal reflux disease: a systematic review and meta-analysis. Alcohol Alcohol. 54 , 62–69 (2019).
Strate, L. L., Singh, P., Boylan, M. R., Piawah, S., Cao, Y. & Chan, A. T. A prospective study of alcohol consumption and smoking and the risk of major gastrointestinal bleeding in men. PLoS ONE 11 , e0165278 (2016).
Yuan, S. & Larsson, S. C. Adiposity, diabetes, lifestyle factors and risk of gastroesophageal reflux disease: a Mendelian randomization study. Eur. J. Epidemiol. 37 , 747–754 (2022).
Bagnardi, V. et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose–response meta-analysis. Br. J. Cancer 112 , 580–593 (2015).
Shen, C., Schooling, C. M., Chan, W. M., Xu, L., Lee, S. Y. & Lam, T. H. Alcohol intake and death from cancer in a prospective Chinese elderly cohort study in Hong Kong. J. Epidemiol. Community Health 67 , 813–820 (2013).
Kuroda, A. et al. Effects of the common polymorphism in the human aldehyde dehydrogenase 2 (ALDH2) gene on the lung. Respir. Res. 18 , 69 (2017).
Cha, B. H., Jang, M. J. & Lee, S. H. Alcohol consumption can reduce the risk of gallstone disease: a systematic review with a dose–response meta-analysis of case–control and cohort studies. Gut Liver 13 , 114–131 (2019).
Ma, G. S., Xhu, D. H., Hu, X. Q., Luan, D. C., Kong, L. Z. & Yang, X. Q. The drinking practice of people in China. Acta Nutrimenta Sin. 27 , 362–365 (2005).
Arranz, S., Chiva-Blanch, G., Valderas-Martínez, P., Medina-Remón, A., Lamuela-Raventós, R. M. & Estruch, R. Wine, beer, alcohol and polyphenols on cardiovascular disease and cancer. Nutrients 4 , 759–781 (2012).
Bryazka, D. et al. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the Global Burden of Disease Study 2020. Lancet 400 , 185–235 (2022).
Chen, Z. et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int. J. Epidemiol. 40 , 1652–1666 (2011).
Im, P. K. et al. Problem drinking, wellbeing and mortality risk in Chinese men: findings from the China Kadoorie Biobank. Addiction 115 , 850–862 (2020).
Cochrane, J., Chen, H., Conigrave, K. M. & Hao, W. Alcohol use in China. Alcohol Alcohol. 38 , 537–542 (2003).
World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm (World Health Organization, 2000).
Rehm, J. et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction 112 , 968–1001 (2017).
Walters, R. G. et al. Genotyping and population structure of the China Kadoorie Biobank. Preprint at medRxiv https://doi.org/10.1101/2022.05.02.22274487 (2022).
Zhang, Q. et al. Exhaled carbon monoxide and its associations with smoking, indoor household air pollution and chronic respiratory diseases among 512,000 Chinese adults. Int. J. Epidemiol. 42 , 1464–1475 (2013).
Lau, B., Cole, S. R. & Gange, S. J. Competing risk regression models for epidemiologic data. Am. J. Epidemiol. 170 , 244–256 (2009).
Clarke, R., Shipley, M. & Lewington, S. et al. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am. J. Epidemiol. 150 , 341–353 (1999).
MacMahon, S., Peto, R. & Cutler, J. et al. Blood pressure, stroke, and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 335 , 765–774 (1990).
Early Breast Cancer Trialists’ Collaborative Group. Section 5: Statistical Methods. Treatment of Early Breast Cancer. Worldwide Evidence, 1985–1990 (Oxford University Press, 1990).
Burgess, S. et al. Guidelines for performing Mendelian randomization investigations. Wellcome Open Res. 4 , 186 (2019).
Easton, D. F., Peto, J. & Babiker, A. G. Floating absolute risk: an alternative to relative risk in survival and case-control analysis avoiding an arbitrary reference group. Stat. Med. 10 , 1025–1035 (1991).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. B 57 , 289–300 (1995).
Braun, J. M., Kalloo, G., Kingsley, S. L. & Li, N. Using phenome-wide association studies to examine the effect of environmental exposures on human health. Environ. Int. 130 , 104877 (2019).
Glickman, M. E., Rao, S. R. & Schultz, M. R. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J. Clin. Epidemiol. 67 , 850–857 (2014).
Cook, R. J. & Lawless, J. F. Marginal analysis of recurrent events and a terminating event. Stat. Med. 16 , 911–924 (1997).
Dong, H., Robison, L. L., Leisenring, W. M., Martin, L. J., Armstrong, G. T. & Yasui, Y. Estimating the burden of recurrent events in the presence of competing risks: the method of mean cumulative count. Am. J. Epidemiol. 181 , 532–540 (2015).
Ghosh, D. & Lin, D. Y. Nonparametric analysis of recurrent events and death. Biometrics 56 , 554–562 (2000).
Download references
Acknowledgements
The chief acknowledgment is to the participants, the project staff and the China National Centre for Disease Control and Prevention (CDC) and its regional offices for assisting with the fieldwork. We thank J. Mackay in Hong Kong; Y. Wang, G. Yang, Z. Qiang, L. Feng, M. Zhou, W. Zhao. and Y. Zhang in China CDC; L. Kong, X. Yu and K. Li in the Chinese Ministry of Health; and S. Clark, M. Radley and M. Hill in the CTSU, Oxford, for assisting with the design, planning, organization and conduct of the study. A complete list of members of the China Kadoorie Collaborative Group is provided in the Supplementary Information. The CKB baseline survey and the first re-survey were supported by the Kadoorie Charitable Foundation in Hong Kong. The long-term follow-up of the CKB study has been supported by Wellcome grants to Z.C. at Oxford University (212946/Z/18/Z, 202922/Z/16/Z, 104085/Z/14/Z, 088158/Z/09/Z) and grants to L.L. from the National Natural Science Foundation of China (82192901, 82192904 and 82192900) and from the National Key Research and Development Program of China (2016YFC0900500). DNA extraction and genotyping was supported by grants to Z.C. from GlaxoSmithKline and the UK Medical Research Council (MC-PC-13049, MC-PC-14135). The UK Medical Research Council (MC_UU_00017/1, MC_UU_12026/2, MC_U137686851), Cancer Research UK (C16077/A29186; C500/A16896) and the British Heart Foundation (CH/1996001/9454) provide core funding to the CTSU and Epidemiological Studies Unit at Oxford University for the project. P.K.I. is supported by an Early Career Research Fellowship from the Nuffield Department of Population Health, University of Oxford. K.H.C. acknowledges support from the British Heart Foundation Centre of Research Excellence, University of Oxford (RE/18/3/34214). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. For the purpose of Open Access, the author has applied a CC-BY public copyright license to any author accepted manuscript version arising from this submission.
Author information
These authors jointly supervised this work: Liming Li, Zhengming Chen, Iona Y. Millwood.
Authors and Affiliations
Clinical Trial Service Unit and Epidemiological Studies Unit (CTSU), Nuffield Department of Population Health, University of Oxford, Oxford, UK
Pek Kei Im, Neil Wright, Ling Yang, Ka Hung Chan, Yiping Chen, Huaidong Du, Xiaoming Yang, Daniel Avery, Robert Clarke, Rory Collins, Robin G. Walters, Richard Peto, Zhengming Chen, Iona Y. Millwood, Maxim Barnard, Derrick Bennett, Ruth Boxall, Johnathan Clarke, Ahmed Edris Mohamed, Hannah Fry, Simon Gilbert, Andri Iona, Maria Kakkoura, Christiana Kartsonaki, Hubert Lam, Kuang Lin, James Liu, Mohsen Mazidi, Sam Morris, Qunhua Nie, Alfred Pozarickij, Paul Ryder, Saredo Said, Dan Schmidt, Becky Stevens, Iain Turnbull, Baihan Wang, Lin Wang & Pang Yao
Medical Research Council Population Health Research Unit (MRC PHRU), Nuffield Department of Population Health, University of Oxford, Oxford, UK
Ling Yang, Yiping Chen, Huaidong Du, Robin G. Walters, Zhengming Chen, Iona Y. Millwood, Derrick Bennett, Ruth Boxall & Christiana Kartsonaki
Oxford British Heart Foundation Centre of Research Excellence, University of Oxford, Oxford, UK
Ka Hung Chan
Fuwai Hospital, Chinese Academy of Medical Sciences, Beijing, China
NCD Prevention and Control Department, Qingdao CDC, Qingdao, China
Shaojie Wang, Liang Cheng, Ranran Du, Ruqin Gao, Feifei Li, Shanpeng Li, Yongmei Liu, Feng Ning, Zengchang Pang, Xiaohui Sun, Xiaocao Tian, Yaoming Zhai & Hua Zhang
Department of Epidemiology and Biostatistics, School of Public Health, Peking University, Beijing, China
Canqing Yu, Jun Lv, Liming Li & Dianjianyi Sun
Peking University Center for Public Health and Epidemic Preparedness & Response, Beijing, China
Canqing Yu, Jun Lv, Liming Li, Xiao Han, Can Hou, Qingmei Xia, Chao Liu, Pei Pei & Dianjianyi Sun
China National Center for Food Safety Risk Assessment, Beijing, China
- Junshi Chen
WHO Collaborating Center for Tobacco Cessation and Respiratory Diseases Prevention, China-Japan Friendship Hospital, Beijing, China
Institute of Respiratory Medicine, Chinese Academy of Medical Sciences, Beijing, China
NCD Prevention and Control Department, Guangxi Provincial CDC, Nanning, China
Naying Chen, Duo Liu & Zhenzhu Tang
NCD Prevention and Control Department, Liuzhou CDC, Liubei, Liuzhou, China
Ningyu Chen, Qilian Jiang, Jian Lan, Mingqiang Li, Yun Liu, Fanwen Meng, Jinhuai Meng, Rong Pan, Yulu Qin, Ping Wang, Sisi Wang, Liuping Wei & Liyuan Zhou
NCD Prevention and Control Department, Gansu Provincial CDC, Lanzhou, China
Caixia Dong, Pengfei Ge & Xiaolan Ren
NCD Prevention and Control Department, Maijixiang CDC, Maijixiang, Tianshui, China
Zhongxiao Li, Enke Mao, Tao Wang, Hui Zhang & Xi Zhang
NCD Prevention and Control Department, Hainan Provincial CDC, Haikou, China
Jinyan Chen, Ximin Hu & Xiaohuan Wang
NCD Prevention and Control Department, Meilan CDC, Meilan, Haikou, China
Zhendong Guo, Huimei Li, Yilei Li, Min Weng & Shukuan Wu
NCD Prevention and Control Department, Heilongjiang CDC, Harbin, China
Shichun Yan, Mingyuan Zou & Xue Zhou
NCD Prevention and Control Department, Nangang CDC, Harbin, China
Ziyan Guo, Quan Kang, Yanjie Li, Bo Yu & Qinai Xu
NCD Prevention and Control Department, Henan Provincial CDC, Zhengzhou, China
Liang Chang, Lei Fan, Shixian Feng, Ding Zhang & Gang Zhou
NCD Prevention and Control Department, Huixian CDC, Huixian, China
Yulian Gao, Tianyou He, Pan He, Chen Hu, Huarong Sun & Xukui Zhang
NCD Prevention and Control Department, Hunan Provincial CDC, Changsha, China
Biyun Chen, Zhongxi Fu, Yuelong Huang, Huilin Liu, Qiaohua Xu & Li Yin
NCD Prevention and Control Department, Liuyang CDC, Liuyang, China
Huajun Long, Xin Xu, Hao Zhang & Libo Zhang
NCD Prevention and Control Department, Jiangsu Provincial CDC, Nanjing, China
Jian Su, Ran Tao, Ming Wu, Jie Yang, Jinyi Zhou & Yonglin Zhou
NCD Prevention and Control Department, Wuzhong CDC, Wuzhong, Suzhou, China
Yihe Hu, Yujie Hua, Jianrong Jin, Fang Liu, Jingchao Liu, Yan Lu, Liangcai Ma, Aiyu Tang & Jun Zhang
NCD Prevention and Control Department, Licang CDC, Qingdao, China
Wei Hou, Silu Lv & Junzheng Wang
NCD Prevention and Control Department, Sichuan Provincial CDC, Chengdu, China
Xiaofang Chen, Xianping Wu, Ningmei Zhang & Xiaoyu Chang
NCD Prevention and Control Department, Pengzhou CDC, Pengzhou, Chengdu, China
Xiaofang Chen, Jianguo Li, Jiaqiu Liu, Guojin Luo, Qiang Sun & Xunfu Zhong
NCD Prevention and Control Department, Zhejiang Provincial CDC, Hangzhou, China
Weiwei Gong, Ruying Hu, Hao Wang, Meng Wang & Min Yu
NCD Prevention and Control Department, Tongxiang CDC, Tongxiang, China
Lingli Chen, Qijun Gu, Dongxia Pan, Chunmei Wang, Kaixu Xie & Xiaoyi Zhang
You can also search for this author in PubMed Google Scholar
- , Zhengming Chen
- , Robert Clarke
- , Rory Collins
- , Liming Li
- , Chen Wang
- , Richard Peto
- , Robin G. Walters
- , Daniel Avery
- , Maxim Barnard
- , Derrick Bennett
- , Ruth Boxall
- , Ka Hung Chan
- , Yiping Chen
- , Johnathan Clarke
- , Huaidong Du
- , Ahmed Edris Mohamed
- , Hannah Fry
- , Simon Gilbert
- , Pek Kei Im
- , Andri Iona
- , Maria Kakkoura
- , Christiana Kartsonaki
- , Hubert Lam
- , Kuang Lin
- , James Liu
- , Mohsen Mazidi
- , Iona Y. Millwood
- , Sam Morris
- , Qunhua Nie
- , Alfred Pozarickij
- , Paul Ryder
- , Saredo Said
- , Dan Schmidt
- , Becky Stevens
- , Iain Turnbull
- , Baihan Wang
- , Neil Wright
- , Ling Yang
- , Xiaoming Yang
- , Qingmei Xia
- , Dianjianyi Sun
- , Canqing Yu
- , Naying Chen
- , Zhenzhu Tang
- , Ningyu Chen
- , Qilian Jiang
- , Mingqiang Li
- , Fanwen Meng
- , Jinhuai Meng
- , Ping Wang
- , Sisi Wang
- , Liuping Wei
- , Liyuan Zhou
- , Caixia Dong
- , Pengfei Ge
- , Xiaolan Ren
- , Zhongxiao Li
- , Hui Zhang
- , Jinyan Chen
- , Xiaohuan Wang
- , Zhendong Guo
- , Huimei Li
- , Shukuan Wu
- , Shichun Yan
- , Mingyuan Zou
- , Ziyan Guo
- , Quan Kang
- , Yanjie Li
- , Liang Chang
- , Shixian Feng
- , Ding Zhang
- , Gang Zhou
- , Yulian Gao
- , Tianyou He
- , Huarong Sun
- , Xukui Zhang
- , Biyun Chen
- , Zhongxi Fu
- , Yuelong Huang
- , Huilin Liu
- , Qiaohua Xu
- , Huajun Long
- , Hao Zhang
- , Libo Zhang
- , Jinyi Zhou
- , Yonglin Zhou
- , Yujie Hua
- , Jianrong Jin
- , Jingchao Liu
- , Liangcai Ma
- , Aiyu Tang
- , Jun Zhang
- , Liang Cheng
- , Ranran Du
- , Ruqin Gao
- , Feifei Li
- , Shanpeng Li
- , Yongmei Liu
- , Feng Ning
- , Zengchang Pang
- , Xiaohui Sun
- , Xiaocao Tian
- , Shaojie Wang
- , Yaoming Zhai
- , Hua Zhang
- , Junzheng Wang
- , Xiaofang Chen
- , Xianping Wu
- , Ningmei Zhang
- , Xiaoyu Chang
- , Jianguo Li
- , Jiaqiu Liu
- , Guojin Luo
- , Qiang Sun
- , Xunfu Zhong
- , Weiwei Gong
- , Ruying Hu
- , Meng Wang
- , Lingli Chen
- , Dongxia Pan
- , Chunmei Wang
- , Kaixu Xie
- & Xiaoyi Zhang
Contributions
P.K.I., I.Y.M., L.Y. and Z.C. contributed to the conception of this paper. P.K.I., N.W., K.H.C., I.Y.M. and Z.C. planned the statistical analysis. P.K.I. analyzed the data and drafted the manuscript. P.K.I., I.Y.M. and Z.C. contributed to the interpretation of the results and the revision of manuscript. R. Collins, R.P., J.C., L.L. and Z.C. designed the study. L.L., Z.C., I.Y.M., L.Y., Y.C., Y.G., H.D., S.W., C.Y., J.L., J.C., R. Collins, R. Clarke and R.G.W. contributed to data acquisition and general study management. X.Y. and D.A. provided administrative and technical support. All authors critically reviewed the manuscript and approved the final submission.
Corresponding authors
Correspondence to Zhengming Chen or Iona Y. Millwood .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Medicine thanks Shiu Lun Au Yeung, Yan-Bo Zhang and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Ming Yang, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended data fig. 1 adjusted hrs for icd−10 chapter−specific morbidities associated with ever-regular drinking and with usual alcohol intake, in men..
Cox models comparing ever-regular drinkers with occasional drinkers, or assessing the dose–response per 280 g/week higher usual alcohol intake within current drinkers, were stratified by age-at-risk and study area and adjusted for education and smoking. Each solid square or diamond represents HR with the area inversely proportional to the variance of the log HR. The horizontal lines indicate 95% CIs. CI, confidence interval; HR hazard ratio; ICD-10, International Classification of Diseases, 10th Revision.
Extended Data Fig. 2 Adjusted HRs for different aggregated and all-cause morbidities associated with years after stopping drinking, in men.
Cox models comparing ex-drinker groups with occasional drinkers were stratified by age-at-risk and study area and were adjusted for education and smoking. Each box represents HR with the area inversely proportional to the variance of the group-specific log hazard within subplot. The vertical lines indicate group-specific 95% CIs for various ex-drinker groups. The shaded strip indicate the group-specific 95% CIs for occasional drinkers. The numbers above the error bars are point estimates for HRs. CI, confidence interval; HR hazard ratio; CKB, China Kadoorie Biobank; WHO, World Health Organization.
Extended Data Fig. 3 Associations of alcohol consumption with risks of 28 diseases previously defined as alcohol-related by the WHO, in male current drinkers.
Cox models were stratified by age-at-risk and study area and were adjusted for education and smoking. HRs were plotted against usual alcohol intake and were calculated per 280 g/week higher usual alcohol intake. All specific diseases displayed were significantly associated with alcohol intake (ever-regular drinking or per 280 g/week higher usual alcohol intake) after multiple testing correction (FDR-adjusted p<0.05), except transient cerebral ischemic attacks and related syndromes (ICD-10 code: G45), occlusion and stenosis of precerebral arteries (I65) and pancreatitis (K85-K86) which showed statistical significance at nominal level (p<0.05). Each box represents HR with the area inversely proportional to the variance of the group-specific log hazard within subplot. The vertical lines indicate group-specific 95% CIs. The numbers above the error bars are point estimates for HRs and the numbers below are number of events. All P values are two-sided. CI, confidence interval; HR hazard ratio; CKB, China Kadoorie Biobank; FDR, false discovery rate; ICD-10, International Classification of Diseases, 10th Revision; WHO, World Health Organization.
Extended Data Fig. 4 Associations of alcohol consumption with risks of 36 diseases not previously defined as alcohol-related, in male current drinkers.
Cox models were stratified by age-at-risk and study area and were adjusted for education and smoking. HRs were plotted against usual alcohol intake and were calculated per 280 g/week higher usual alcohol intake. All specific diseases displayed were significantly associated with alcohol intake (ever-regular drinking or per 280 g/week higher usual alcohol intake) after multiple testing correction (FDR-adjusted p<0.05). Each box represents HR with the area inversely proportional to the variance of the group-specific log hazard within subplot. The vertical lines indicate group-specific 95% CIs. The numbers above the error bars are point estimates for HRs and the numbers below are number of events. All P values are two-sided. CI, confidence interval; HR hazard ratio; CKB, China Kadoorie Biobank; FDR, false discovery rate.
Extended Data Fig. 5 Adjusted HRs for major diseases associated with drinking patterns, in male current drinkers.
Cox models were stratified by age-at-risk and study area and were adjusted for education and smoking and for total alcohol intake where indicated. Each solid square or diamond represents HR with the area inversely proportional to the variance of the log HR. The horizontal lines indicate 95% CIs. CI, confidence interval; HR hazard ratio; HED, heavy episodic drinking; CKB, China Kadoorie Biobank; WHO, World Health Organization.
Extended Data Fig. 6 Adjusted HRs for major diseases associated with duration of drinking, in male current drinkers.
Cox models were stratified by age-at-risk and study area and were adjusted for education, smoking, total alcohol intake and baseline age in (A). (B) had the same model specifications as (A) plus further adjustments for income, physical activity, fruit intake and body mass index. (C) had the same model specifications as (A) and excluded participants with poor self-reported health or prior chronic disease at baseline. Each box represents HR with the area inversely proportional to the variance of the group-specific log hazard. The horizontal lines indicate group-specific 95% CIs. All P values are two-sided. CI, confidence interval; HR hazard ratio; CKB, China Kadoorie Biobank; WHO, World Health Organization.
Extended Data Fig. 7 Adjusted HRs for ICD−10 chapter−specific morbidities associated with ever-regular drinking and with usual alcohol intake, in women.
Cox models comparing ever-regular drinkers with occasional drinkers, or assessing the dose–response per 100 g/week higher usual alcohol intake within current drinkers, were stratified by age-at-risk and study area and adjusted for education and smoking. Each solid square or diamond represents HR with the area inversely proportional to the variance of the log HR. The horizontal lines indicate 95% CIs. CI, confidence interval; HR hazard ratio; ICD-10, International Classification of Diseases, 10th Revision.
Extended Data Fig. 8 Adjusted HRs per 280 g/week higher genotype-predicted mean male alcohol intake for specific alcohol-associated diseases by ICD-10 chapters, in men and women.
Cox modes, stratified by age-at-risk and adjusted for genomic principal components, were used to relate genetic categories to risks of diseases within each study area. The HR per 280 g/week higher genotype-predicted mean male alcohol intake was calculated from the inverse-variance-weighted mean of the slopes of the fitted lines in each study area. Each solid square or diamond represents HR per 280 g/week higher genetically-predicted mean male alcohol intake, with the area inversely proportional to the variance of the log HR. The horizontal lines indicate 95% CIs. Diseases considered to be alcohol-related by the WHO are indicated with ‘Y’ under the ‘WHO’ column. The ‘RC’ column indicates the number of study areas that contributed to the overall area-stratified genotypic associations, as for certain less common diseases some study areas may not have enough number of cases to contribute to the inverse-variance-weighted meta-analysis. The ‘P het’ column indicates the p-value from a \(\chi\) 2 test for heterogeneity between sexes. All P values are two-sided. † Included less common ICD-10 codes within the corresponding ICD-10 chapter which were not individually investigated in the present study. CI, confidence interval; HR hazard ratio; ICD-10, International Classification of Diseases, 10th Revision; WHO, World Health Organization.
Extended Data Fig. 9 Adjusted HRs associated with GG versus AG genotype of ALDH2 - rs671 for specific alcohol-associated diseases by ICD-10 chapters, in men and women.
Area-specific genotypic effects (GG vs. AG genotype) were estimated within each study area (thus each reflecting the purely genotypic effects) using age-at-risk-stratified and genomic principal components-adjusted Cox models and were combined by inverse-variance-weighted meta-analysis to yield the overall area-stratified genotypic associations. Each solid square represents HR for GG vs. AG genotype, with the area inversely proportional to the variance of the log HR. The horizontal lines indicate 95% CIs. Diseases considered to be alcohol-related by the WHO are indicated with ‘Y’ under the ‘WHO’ column. The ‘RC’ column indicates the number of study areas that contributed to the overall area-stratified genotypic associations, as for certain less common diseases some study areas may not have enough number of cases to contribute to the inverse-variance-weighted meta-analysis. The ‘P het’ column indicates the P value from a \(\chi\) 2 test for heterogeneity between sexes. All P values are two-sided. † Included less common ICD-10 codes within the corresponding ICD-10 chapter which were not individually investigated in the present study. CI, confidence interval; HR hazard ratio; ICD-10, International Classification of Diseases, 10th Revision; WHO, World Health Organization.
Extended Data Fig. 10 Adjusted HRs associated with GG versus AG genotype of ADH1B - rs1229984 for specific alcohol-associated diseases by ICD-10 chapters, in men and women.
Supplementary information, supplementary information.
Supplementary Figs. 1–8 and Supplementary Tables 1–13.
Reporting Summary
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Im, P.K., Wright, N., Yang, L. et al. Alcohol consumption and risks of more than 200 diseases in Chinese men. Nat Med 29 , 1476–1486 (2023). https://doi.org/10.1038/s41591-023-02383-8
Download citation
Received : 16 December 2022
Accepted : 02 May 2023
Published : 08 June 2023
Issue Date : June 2023
DOI : https://doi.org/10.1038/s41591-023-02383-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Uncovering newly identified aldehyde dehydrogenase 2 genetic variants that lead to acetaldehyde accumulation after an alcohol challenge.
- Freeborn Rwere
- Joseph R. White
- Eric R. Gross
Journal of Translational Medicine (2024)
Alcohol consumption may be a risk factor for cerebrovascular stenosis in acute ischemic stroke and transient ischemic attack
- Xiaoyan Guo
BMC Neurology (2024)
Western diets and chronic diseases
- Timon E. Adolph
- Herbert Tilg
Nature Medicine (2024)
Mapping multimorbidity progression among 190 diseases
Communications Medicine (2024)
The aldehyde dehydrogenase 2 rs671 variant enhances amyloid β pathology
Nature Communications (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Alcohol facts and statistics.

Updated: 2024
Learn up-to-date facts and statistics on alcohol consumption and its impact in the United States and globally. Explore topics related to alcohol misuse and treatment, underage drinking, the effects of alcohol on the human body, and more.
Find up-to-date statistics on lifetime drinking, past-year drinking, past-month drinking, binge drinking, heavy alcohol use, and high-intensity drinking.
Learn how many people ages 12 to 20 engage in underage alcohol misuse in the United States and the impact it has.
Explore how many people ages 18 to 25 engage in alcohol misuse in the United States and the impact it has.
Find out how many people have alcohol use disorder in the United States across age groups and demographics.
Discover how many people with alcohol use disorder in the United States receive treatment across age groups and demographics.
Discover the effects that alcohol consumption has on the human body such as increased risk for diseases and injuries.
Learn statistics about alcohol use during pregnancy.
Discover the impact alcohol has on children living with a parent or caregiver with alcohol use disorder.
Explore statistics on alcohol-related deaths and emergency visits in the United States.
Learn more about the financial impact of alcohol misuse in the United States.
Learn more about impacts of alcohol misuse globally.
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
- Share full article
Advertisement
Supported by
Even a Little Alcohol Can Harm Your Health
Recent research makes it clear that any amount of drinking can be detrimental. Here’s why you may want to cut down on your consumption beyond Dry January.

By Dana G. Smith
Sorry to be a buzz-kill, but that nightly glass or two of wine is not improving your health.
After decades of confusing and sometimes contradictory research (too much alcohol is bad for you but a little bit is good; some types of alcohol are better for you than others; just kidding, it’s all bad), the picture is becoming clearer: Even small amounts of alcohol can have health consequences.
Research published in November revealed that between 2015 and 2019, excessive alcohol use resulted in roughly 140,000 deaths per year in the United States. About 40 percent of those deaths had acute causes, like car crashes, poisonings and homicides. But the majority were caused by chronic conditions attributed to alcohol, such as liver disease, cancer and heart disease.
When experts talk about the dire health consequences linked to excessive alcohol use, people often assume that it’s directed at individuals who have an alcohol use disorder. But the health risks from drinking can come from moderate consumption as well.
“Risk starts to go up well below levels where people would think, ‘Oh, that person has an alcohol problem,’” said Dr. Tim Naimi, director of the University of Victoria’s Canadian Institute for Substance Use Research. “Alcohol is harmful to the health starting at very low levels.”
If you’re wondering whether you should cut back on your drinking, here’s what to know about when and how alcohol impacts your health.
How do I know if I’m drinking too much?
“Excessive alcohol use” technically means anything above the U.S. Dietary Guidelines ’ recommended daily limits. That’s more than two drinks a day for men and more than one drink a day for women.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
The Effects of Alcohol Consumption on Academic Performance: A Literature Review
- February 2023
- Volume 5(Issue 2):77-84

- Polytechnic College of Botolan

- Polytechnic College of Botoaln

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Lyvonne Tume

- Int J Environ Res Publ Health

- Chiedu Eseadi

- Scott T. Leatherdale

- Brian Pittman

- Jenna McClintock
- Cent Eur J Publ Health

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Skip to main content
- Skip to main navigation
New Research Examines Morning-After Effects of Alcohol on the Body’s Cardiovascular Response
Researchers in Baylor’s Robbins College use microneurography to assess sympathetic nervous system control of blood pressure after simulated binge drinking

Baylor University researchers in the Robbins College of Health and Human Sciences used an innovative combination of advanced physiological measurement techniques in their study of sympathetic nervous system control of blood pressure the morning after simulated binge drinking. (Matthew Minard/Baylor University)
Contact: Lori Fogleman , 254-709-5959 Follow us on X (Twitter): @BaylorUMedia
While a general link between alcohol consumption and cardiovascular disease is well known, Baylor University researchers are digging into the “why” behind this detrimental association – especially after a night of binge drinking – in a study published in the American Heart Association’s Hypertension journal .
The research – led by Jason R. Carter, Ph.D. , dean of Baylor’s Robbins College of Health and Human Sciences; Jeremy Bigalke, Ph.D. , assistant research scientist in the Department of Health, Human Performance and Recreation; and their collaborators – used an innovative combination of advanced physiological measurement techniques to demonstrate the negative impacts of alcohol on sympathetic nervous system control of blood pressure the morning after simulated binge drinking.
Fight or flight
The sympathetic nervous system – best known for driving the “fight-or-flight” response – helps regulate heart rate, blood pressure, digestion, urination, sweating and other functions outside of conscious control. Carter, Bigalke and their team evaluated the sympathetic nervous system using a technique known as microneurography.

In this procedure as part of a randomized, fluid-controlled study of 26 healthy adults, an acupuncture-sized electrode was inserted into the fibular nerve in the lower leg to measure sympathetic nerve activity to blood vessels. It is the only technique able to directly measure the sympathetic nervous system in humans – and Baylor’s Autonomic Function Laboratory , where Carter and Bigalke conduct their research, has the equipment and expertise to use it.
“The technique of microneurography is truly a gold-standard approach to assessing the sympathetic nervous system in humans,” Carter said. “There are very few studies that have used this approach as it relates to alcohol research, and no studies that have employed it in conjunction with overnight laboratory sleep assessments.”
In their study, Carter, Bigalke and team found that otherwise healthy adults – who underwent simulated binge drinking – experienced the same level of sympathetic nervous activity the following morning compared with a control group. However, the blood pressure response resulting from that nervous system activity was elevated. In other words, for those who experienced the simulated binge drinking, the cardiovascular response (in this case, a change in blood pressure) was more sensitive to surges of sympathetic nerve activity than the individual’s standard response.
Multiplying the risk
The researchers said this implies that alcohol is not affecting the sympathetic nerve activity directly, but instead, the impact occurs at the intersection of sympathetic nervous activity and the cardiovascular system – like when the nervous system signals a blood pressure increase. Carter and Bigalke’s research shows that this increase for someone who engaged in binge drinking the previous evening could be exaggerated, therefore multiplying the risk for cardiovascular disease.

“The sympathetic nervous system represents a key physiological mechanism that can contribute to increased cardiovascular risk associated with binge drinking,” Bigalke said. “Understanding how these mechanisms work within the body is important in developing therapeutic strategies and targets to reduce alcohol-related cardiovascular disease.”
The knowledge gained through Carter and Bigalke’s research reinforces and strengthens targeted public health messaging around the negative impact of excessive alcohol consumption, particularly as it relates to cardiovascular disease. Understanding that the adverse effects of alcohol are still present the following morning – and are tied to the bodies’ “fight-or-flight” responses – can help encourage healthy lifestyle choices and informed decisions around alcohol use.
“It is important to understand that these ‘fight-or-flight’ responses in the body can linger well beyond the actual drinking episode,” Carter said. “And given the higher likelihood of negative cardiovascular events in the morning hours, we need to stay attentive to the adverse impact of binge drinking hours beyond the actual consumption.”
The study was funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health (NIH).
ABOUT THE RESEARCHERS

Jason R. Carter, Ph.D. , is dean of Baylor University’s Robbins College of Health and Human Sciences, which offers undergraduate, graduate and doctoral programs with a common purpose of improving health, well-being and quality of life for individuals, families, communities and environments. Carter is an active researcher focusing on neural control of the cardiovascular system in humans and the role of sleep in cardiovascular disease. He has been the principal investigator or co-PI on more than $74 million in external research awards, including two active NIH R01 grants. He has more than 100 peer-reviewed journal publications and currently serves as associate editor for the American Journal of Physiology – Heart and Circulatory Physiology . Carter was elected Fellow of the National Academy of Kinesiology in 2017 and received the Jerry R. Thomas Distinguished Leadership Award from the American Kinesiology Association, the society’s top peer-reviewed award, in 2021.

Jeremy Bigalke, Ph.D. , is an a ssistant research scientist in the D epartment of Health, Human Performance and Recreation at Baylor University’s Robbins College of Health and Human Sciences. He received his Bachelor of Science in Physiology from Michigan State University, a Master of Science in Kinesiology from Michigan Technological University and his Ph.D. in Psychological Science from Montana State University. Bigalke’s research investigates the intersection between sleep, stress and cardiovascular health, specifically through function of the autonomic nervous system.
ABOUT ROBBINS COLLEGE OF HEALTH AND HUMAN SCIENCES AT BAYLOR UNIVERSITY
The Robbins College of Health and Human Sciences at Baylor University seeks to prepare leaders in health and quality of life through science, scholarship and innovation. Together, the departments housed within the Robbins College – Communication Sciences and Disorders; Health, Human Performance and Recreation; Human Sciences and Design; Occupational Therapy; Physical Therapy; Public Health; and a number of Army-Baylor graduate programs – promote a team-based approach to transformational education and research, establishing interdisciplinary research collaborations to advance solutions for improving quality of life for individuals, families and communities. For more information, visit the Robbins College website .
ABOUT BAYLOR UNIVERSITY
Baylor University is a private Christian University and a nationally ranked Research 1 institution. The University provides a vibrant campus community for more than 20,000 students by blending interdisciplinary research with an international reputation for educational excellence and a faculty commitment to teaching and scholarship. Chartered in 1845 by the Republic of Texas through the efforts of Baptist pioneers, Baylor is the oldest continually operating University in Texas. Located in Waco, Baylor welcomes students from all 50 states and more than 100 countries to study a broad range of degrees among its 12 nationally recognized academic divisions.
Media and Public Relations
Baylor University One Bear Place #97024 Waco, TX 76798
- General Information
- Academics & Research
- Administration
- Gateways for ...
- About Baylor
- Give to Baylor
- Social Media
- Strategic Plan
- College of Arts & Sciences
- Diana R. Garland School of Social Work
- George W. Truett Theological Seminary
- Graduate School
- Hankamer School of Business
- Honors College
- Louise Herrington School of Nursing
- Research at Baylor University
- Robbins College of Health and Human Sciences
- School of Education
- School of Engineering & Computer Science
- School of Music
- University Libraries, Museums, and the Press
- More Academics
- Compliance, Risk and Safety
- Human Resources
- Marketing and Communications
- Office of General Counsel
- Office of the President
- Office of the Provost
- Operations, Finance & Administration
- Senior Administration
- Student Life
- University Advancement
- Undergraduate Admissions
- Graduate Admissions
- Baylor Law School Admissions
- Social Work Graduate Programs
- George W. Truett Theological Seminary Admissions
- Online Graduate Professional Education
- Virtual Tour
- Visit Campus
- Alumni & Friends
- Faculty & Staff
- Prospective Faculty & Staff
- Prospective Students
- Anonymous Reporting
- Annual Fire Safety and Security Notice
- Cost of Attendance
- Digital Privacy
- Legal Disclosures
- Mental Health Resources
- Web Accessibility

Drinking alcohol before conceiving a child could accelerate their aging – new research in mice
Professor of Physiology, Texas A&M University
Disclosure statement
Michael Golding receives funding through a Medical Research Grant from the W. M. Keck Foundation and a research grant from the NIH through the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Texas A&M University provides funding as a founding partner of The Conversation US.
View all partners
The conditions within a person’s home, family and community affect their ability to stay healthy. Scientists studying these social determinants of health are trying to understand whether nature or nurture has a stronger effect on a person’s ability to fight disease.
I am a developmental physiologist studying the ways that drinking affects fetal development and lifelong health. Although researchers have long recognized that a father’s alcohol abuse negatively affects his children’s mental health and social development , it hasn’t been clear if paternal drinking has any lasting biological effects on his offspring’s physical health.
My lab’s recently published research shows that chronic alcohol use from both parents has an enduring effect on the next generation by causing their offspring to age faster and become more susceptible to disease.
Fetal alcohol spectrum disorders
According to the National Institutes of Health, nearly 11% of adults in the U.S. have an alcohol use disorder. Heavy drinking causes multiple health issues , including liver disease, heart problems, declining cognitive function and accelerated aging .
Parents may pass these health problems on to their children. Fetal alcohol spectrum disorders refer to a wide range of alcohol-related physical, developmental and behavioral deficits that affect as many as 1 in 20 U.S. schoolchildren .

Children with fetal alcohol spectrum disorders experience an early onset of adult diseases , including type 2 diabetes and heart disease. Cardiovascular disease first appears during adolescence for people with these disorders, while the rest of the population is affected typically in their 40s and 50s. Children with fetal alcohol spectrum disorders are also more likely to be hospitalized and have lifespans that are 40% shorter than children without these conditions.
However, it has been unclear whether these health problems are because of life circumstances – people with fetal alcohol spectrum disorders have high rates of psychiatric disorders , which cause stress that makes them more susceptible to aging and disease – or if their parents’ substance use directly causes lasting negative effects to their health. In other words, can a parent’s alcohol abuse before conception directly influence their offspring’s physical health and lifespan?
Mom and dad drinking
In our study, my colleagues and I used a mouse model to measure the effects that alcohol use by mom, dad or both parents around the time of conception have on their offspring aging and chronic disease. The mice chose when and how much alcohol to drink.
We found that paternal and maternal drinking both cause harmful changes to their offspring’s mitochondria . Mitochondria – often called the battery of the cell – control many aspects of aging and health . Like a cellphone battery, mitochondria deteriorate over time and cause cells to lose their ability to repair damage and control metabolism.
Our experiments in mice show that dad’s drinking causes a defect in mitochondrial function that first emerges during fetal development and persists into adult life , causing the offspring to age faster. For example, paternal alcohol exposure caused a twofold increase in age-related liver disease, suggesting that parental alcohol use – particularly by the father – could have significant implications on aging and age-related diseases.
Importantly, we found that when both parents drank, the effects on their offspring were worse than when only one parent consumed alcohol. For example, we observed a threefold increase in age-related liver scarring when both parents consumed alcohol.
Treating fetal alcohol syndrome
People with fetal alcohol syndrome face lifelong challenges , including problems with hand-eye coordination and difficulties with memory and attention.
Early educational interventions for children with fetal alcohol spectrum disorders, like using visual and auditory materials instead of print, can provide additional structure to help facilitate learning.
Although my team and I examined chronic alcohol exposure, we do not know if moderate alcohol use also causes mitochondrial problems. We also don’t know if these same effects emerge in people who haven’t been diagnosed with fetal alcohol spectrum disorders but whose parents drank heavily. Whether paternal drinking influences human embryonic development is still unclear, although emerging studies are beginning to suggest it does.
The next step is to explore if interventions that focus on mitochondrial health, such as exercise and specific diets , can improve health outcomes for people with fetal alcohol spectrum disorders.
- Fetal development
- Alcohol abuse
- Fetal Alcohol Spectrum Disorder
- Fetal Alcohol Syndrome
- New research
- STEEHM new research

Manager, Regional Training Hub

Head of Evidence to Action

Supply Chain - Assistant/Associate Professor (Tenure-Track)

OzGrav Postdoctoral Research Fellow

Casual Facilitator: GERRIC Student Programs - Arts, Design and Architecture
Exploring what works, what doesn’t, and why.

As drinking habits shift, global alcohol industry fights to stay ahead
- Share on LinkedIn
- Share on Twitter
- Share on Facebook
- Share on WhatsApp
- Share through Email
This story was reported by The Examination , a nonprofit newsroom that investigates global health threats. Sign up to get The Examination ’s newsletter in your inbox.
For a growing number of American and European youth, drinking simply isn’t as cool as it once was.
Young people—increasingly aware of the myriad physical and mental health issues linked to alcohol—are shunning drinking in favor of healthier lifestyle choices. The rise of mocktails , nonalcoholic beer, and legal weed offer plenty of alternatives.
That’s encouraging for public health experts, since alcohol is one of the world’s most significant preventable causes of death: Excess drinking kills 2.6 million people each year, according to a status report the World Health Organization published in June , accounting for one in every 21 deaths worldwide.
But the alcohol industry is doing everything it can to stay relevant. In pursuit of new profit centers, booze, beer, and wine makers are marketing to demographics they’ve historically underserved, including women, and looking to new markets in the Global South, where burgeoning economies with young populations offer growth opportunities. Conveniently, many of these countries also place few or no limitations on how alcohol is sold and marketed.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
- Email address By clicking “Subscribe,” you agree to receive email communications from Harvard Public Health.
- Email This field is for validation purposes and should be left unchanged.
During an investor meeting last year, a representative from Heineken, the Dutch brewer, said the company’s fastest-growing markets were in Asia Pacific and Africa. A slide deck titled “Africa drives global beer growth” showed the volume of Heineken sales on the continent had quadrupled in the last 20 years.
“Africa is the next frontier of growth,” Roland Pirmez, president of Heineken’s Africa, Middle East, and Eastern European region, said in a slide deck from the presentation, citing the continent’s growing population, rapid urbanization, and increasing prosperity.
Jürgen Rehm, a professor at the University of Toronto and senior scientist at the Centre for Addiction and Mental Health in Canada, said that industry marketing had led people in Asia and Africa to begin drinking at younger ages than prior generations who had grown up with different norms and less discretionary income.
“The overall concern is that alcohol consumption is normalized globally and that a majority of the world’s adults may be drinkers 10 years from now,” Rehm wrote in an email. This result will have “serious consequences” for alcohol-related disease and economic prosperity, he said.
Heineken did not respond to questions from The Examination about these concerns.
Changing demographics
The harms of excessive drinking have been well known for centuries, but science measuring the risks is becoming more precise. In the last decade, numerous studies have suggested that even “moderate” levels of consumption—as little as two drinks per day for men and one for women—increase the risk of heart disease and cancer. That knowledge has begun to sink in. In the West, drinking is no longer an unquestioned rite of passage for young people: European and American adolescents are drinking less compared with a generation ago. A study of drinking habits in 28 European countries found that weekly use among adolescents peaked in 2007 and has since declined.
Boys, in particular, who historically drank more than girls, are cutting back. A recent WHO survey from Europe, Central Asia, and Canada found that girls, for the first time, were more likely than boys to have tried alcohol by age 15.
Adults are also picking up the slack. In the U.S., millennials are consuming more alcohol than previous generations in their 30s and 40s. The uptick has been particularly pronounced among women, especially those with a college education .
Katherine Keyes, a professor of epidemiology at Columbia University, published a review of several studies and found binge drinking and alcohol-related hospitalizations have been rising fastest among U.S. women 26 to 35 and 45 to 64.
“What we’ve seen is this shift where drinking declines during adolescence but then the acceleration of drinking during the transition to adulthood is getting faster,” Keyes said.
The COVID-19 pandemic exacerbated dangerous drinking habits. Between 2020 and 2021, women aged 40 to 64 experienced significant increases in urgent complications from alcoholic liver disease, according to an analysis of insurance claims data published in the Journal of the American Medical Association .
From a man’s drink to “mommy juice”
This shift in drinking behavior didn’t occur by chance. Alcohol companies that once alienated women with ads suffused with sexist imagery are now marketing directly and more effectively to women, according to a 2020 report by investment research and brokerage firm Bernstein Research.
Diageo, one of the world’s largest spirit conglomerates, regularly participates in the United Nation’s annual International Women’s Day, and has wrapped itself in its messaging . Recent advertising campaigns by 20 alcohol makers frame drinking as post-feminist —adopting language like “girl power” and “strong women” while also reinforcing gender norms by dousing their campaigns in pink—and as a way for mothers to destress and briefly escape the burdens of parenting. In one social media campaign by Bailey’s Nigeria, the company celebrated Mother’s Day by asking drinkers to comment on “why your mum deserves a Baileys Treat from us.”
Companies are also pivoting to products that appeal to women. Beer makers, which historically struggled to attract female consumers, have eagerly invested in ready-to-drink beverages like hard seltzers—a product category that appeals equally to both genders . Soda companies also have leaped into the fray , producing alcoholic offerings of their own.
Lawmakers attempting to rein in excess drinking are up against a tsunami of spending. Alcohol makers spend billions to market their products. AB InBev—which produces Budweiser and Corona, among hundreds of other labels—spent $6.8 billion on advertising in 2022, according to Marketing Week .
Unlike tobacco companies, which since the 1998 Tobacco Master Settlement Agreement have been prohibited from exempting the money they spend on advertising from their U.S. taxes, the alcohol industry is under no such restrictions. That meant the 10 largest alcohol producers could write off taxes on $1.5 billion in advertising expenses in 2017, according to the public health advocacy organization Vital Strategies . Whereas the majority of developed countries restrict beer advertising on television and radio, most of the countries with no advertising restrictions are in Africa and Central and South America, according to the WHO. A third of countries have a total or partial ban on beer company sponsorships at sporting events, but in many developing economies there are no restrictions.
Raising taxes
Economists and scientists say one of the most effective ways to curb excess drinking is to raise taxes on alcohol. Taxes are “best buy” interventions for reducing noncommunicable diseases , according to the WHO, as they are highly cost-effective and relatively easy to implement.
Taxes have been crucial to curbing drinking rates in Eastern Europe—a region once home to some of the world’s heaviest drinkers. Since 2002, former Soviet states Estonia, Latvia, and Lithuania have raised taxes on alcohol and seen alcohol-attributable deaths fall . Lithuania later implemented additional excise tax increases and saw an extra three percent decline in mortality by any cause.
Countries have experimented with other pricing policies, too. In Russia, after the government set a minimum price per unit for spirits, alcohol consumption per capita fell by 26 percent from 2010 to 2016. A similar policy In Scotland reduced alcohol sales by three percent and cut hospital admissions and deaths from chronic diseases, according to an independent review.
Although global alcohol companies like Diageo preach “the importance of moderation,” this shifts the responsibility for excess alcohol use onto the drinker. Meanwhile, companies fiercely oppose measures shown to reduce excess drinking, such as raising alcohol taxes. Diageo has lobbied to cut taxes on its products in Mexico; Anheuser-Busch and other alcohol businesses have largely funded efforts to kill alcohol tax bills in New Mexico and Oregon .
Recent advertising campaigns by 20 alcohol makers frame drinking as post-feminist—adopting language like “girl power” and “strong women.”
Politicians have listened. In the U.S., state alcohol taxes have fallen more than 30 percent in real terms since 1990 . In 2020, a bipartisan group of federal lawmakers awarded permanent tax cuts to many alcohol sellers. As of August 1, the alcohol industry had 280 registered lobbyists in Washington, D.C.
Asked for comment, a Diageo spokesperson responded, “We are committed to changing the way people drink for the better,” citing the company’s educational website DrinkIQ and its growing portfolio of nonalcoholic beverages. “The right information empowers consumers to make the right choices.”
Global health policymakers have not made combatting excessive drinking a priority. Governments and philanthropic organizations spend $4.17 on alcohol policy for each death due to excessive drinking, compared with $11,000 for each death caused by HIV/AIDS, according to a recent analysis .
The WHO has set an ambitious goal to cut drinking by 20 percent by 2030, but member states have done little to further it . Its recent status report found that nearly half of reporting countries have no alcohol policies in place.
Warning labels add cancer to the list of risks
Where governments have hesitated to limit alcohol sales practices by other means, health advocates have turned to a new weapon: information. A growing number of countries are requiring labels warning drinkers about alcohol’s potential health impacts, which a recent systematic review in The Lancet shows have the potential to raise awareness and reshape behaviors. And alcohol makers are struggling to argue why consumers shouldn’t be fully informed about the products they are buying.
The efforts are a patchwork so far but could be gaining steam. Last fall, Australia and New Zealand began enforcing a requirement for stronger pregnancy warning labels on alcoholic beverages . Ireland went a step further, mandating that in 2026, beverages carry labels informing drinkers that alcohol causes cancer . And this spring in Alaska, lawmakers passed a new requirement that bars post signs warning patrons about the link between alcohol and cancer. The fight can still be an uphill battle. In 2015, after Thailand proposed adding stronger warning labels to alcohol products, other countries with large alcohol export industries disputed the measure in the World Trade Organization, and Thailand ultimately withdrew it. (The government recently rebooted the effort but is again facing fierce opposition from businesses .)
Setting global standards to rein in alcohol makers
Some have called for a global treaty to protect people from alcohol-related harms, modeled after the WHO’s Framework Convention on Tobacco Control . The 20-year-old treaty signed by countries with 90 percent of the world’s population has helped curb smoking rates in many places. It includes many of the same strategies public health experts recommend for regulating alcohol, such as raising taxes and regulating marketing.
One of the most striking parts of the FCTC is that it explicitly excludes tobacco companies from policy negotiations, said Ben Hawkins, a researcher at the University of Cambridge. In contrast, the alcohol industry often has a seat at the table during policy negotiations.
Maristela Monteiro, a retired senior adviser on alcohol at the Pan American Health Organization, said alcohol companies are in dire need of regulation.
“They’re stronger than the tobacco corporations,” she said. “They learned from the tobacco case, and they know that they need to be ahead of the game.”
Image: bodnarphoto / Adobe Stock

More in Policy & Practice
Is alcohol good or bad for you? Yes.

NYC is working to help residents live longer, healthier lives

Families in states with bans on trans care are finding hope across state lines
New research shows even moderate drinking isn't good for your health
A new analysis of over 100 studies debunks beliefs about benefits of alcohol.
Drinking a glass of wine a day will not help you live longer, according to a new analysis of alcohol research that debunks a longstanding belief about the possible health benefits of drinking alcohol moderately.
The analysis, published recently in JAMA Network Open , looked at over 100 studies with nearly 5 million participants in all.
It found not only no significant health benefit to moderate alcohol consumption, but also that drinking a daily serving of alcohol of less than 1 ounce for women and around 1.5 ounces for men increased the risk of death.
"When you talk about risk versus benefit, it's one thing to say there is no benefit," said Dr. Jennifer Ashton, a board-certified OB-GYN and ABC News chief medical correspondent, who was not involved in the research. "It's another thing, at certain levels, to find a risk, and that's what this new research found."
For women, a moderate alcohol intake per week is defined as seven servings of alcohol or less. For men, it is 14 servings of alcohol or less per week, according to the U.S. Centers for Disease Control and Prevention .
Heavy drinking is typically defined as consuming eight drinks or more per week, according to the CDC.
One serving of alcohol is defined as 5 ounces for wine and just 1 1/2 ounces for hard alcohol, far less than what is typically served in bars, restaurants and people's homes.
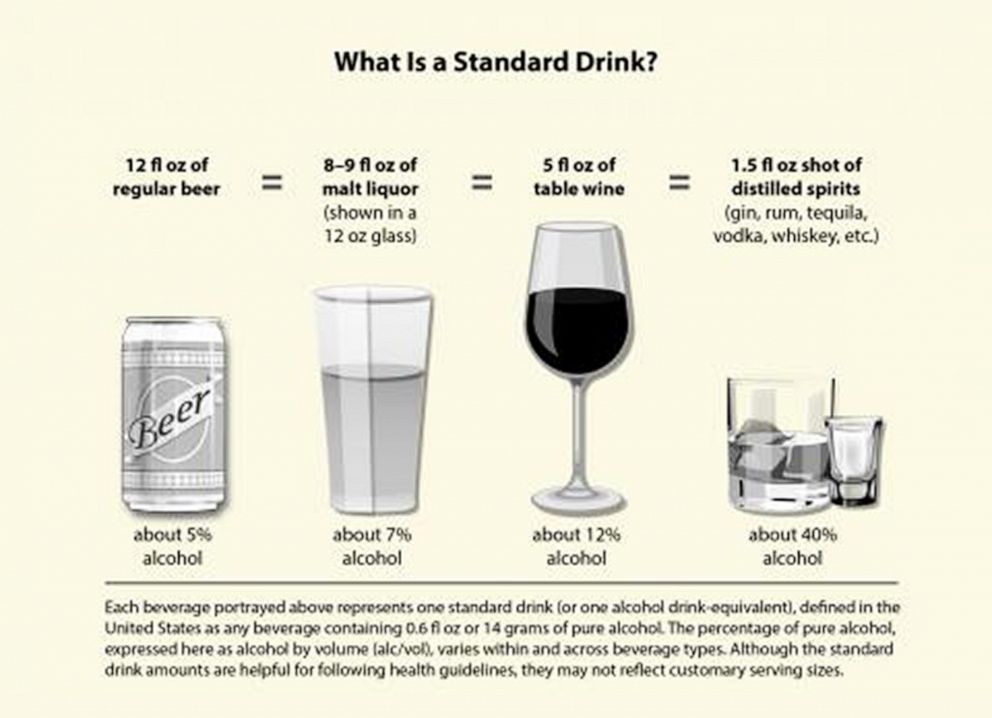
The new analysis found that people who drank more than 2 ounces of alcohol a day had the highest risk of death, about 35% higher than people who drank more moderately.
The risk of death was also found to be greater for women, with a 61% increased risk for women who drink more than 2 ounces of alcohol per day.
Editor’s Picks

Alcohol linked to greater risk of cancer in women: What to know

4 unexpected benefits of giving up alcohol for Dry January

New cancer prevention guidelines call for no alcohol consumption
More: dry weddings become increasingly popular. what to know about the nonalcoholic trend.
Previous research has already shown that just as women metabolize alcohol differently than men, they also face more serious health consequences.
Women are more susceptible to alcohol-related heart disease than men; alcohol misuse produces brain damage more quickly in women than in men; women may be more susceptible than men to alcohol-related blackouts, or gaps in memory; and women who regularly misuse alcohol are more likely than men who drink the same amount to develop alcoholic hepatitis, a potentially deadly condition, according to the National Institute on Alcohol Abuse and Alcoholism.
Data shows that even casual drinkers face a greater risk of cancer , most commonly liver and throat cancers but also colon and head and neck cancers, in addition to breast cancer.
Drinking alcohol is listed by the Department of Health and Human Services as a known human carcinogen.

In 2020, the American Cancer Society updated its guidelines to say that cutting alcohol out of a person's diet completely is best for cancer reduction and prevention.
MORE: Taking a one-time pill may help curb binge drinking, study finds
Ashton said that it's important for people to talk to their healthcare providers about their alcohol consumption to make the most informed decisions.
"Alcohol is a known carcinogen. We know it's associated with an increased risk of cancer," Ashton said. "But it's also part of our social fiber and our culture, so it's not an easy decision."
Ashton also noted though that the data is "crystal clear" that abstaining completely from alcohol is best for a person's overall health.
For questions and concerns about alcohol use, SAMHSA , the Substance Abuse and Mental Health Services Administration, has a 24/7 free and confidential helpline available at 1-800-662-HELP (4357), and online at samhsa.gov/find-help/national-helpline .
Related Topics
Popular reads.

Trump charged in Jan. 6 superseding indictment
- Aug 27, 6:25 PM

Ex-MLB star's daughter found after going missing
- Aug 27, 8:43 AM

Female student at Rice University killed
- Aug 27, 12:11 AM

Body of endangered man found under home
- Aug 27, 12:32 PM

Pilot who tried to shut down engines shares story
- Aug 23, 6:10 AM
ABC News Live
24/7 coverage of breaking news and live events
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Alcohol consumption and awareness of its effects on health among secondary school students in Nigeria
Editor(s): Kufa., Tendesayi
a Department of Home Economics and Hospitality Management Education, Faculty of Vocational and Technical Education, University of Nigeria
b Department of Food Science and Technology, Ebonyi State University Abakaliki, Ebonyi State
c Department of Educational Foundations, Faculty of Education, University of Nigeria, Nsukka, Enugu State
d Department of Home Economics Education, Ebonyi State University Abakaliki, Ebonyi State
e Department of Human Kinetics and Health Education, Faculty of Education, University of Nigeria, Nsukka, Enugu State, Nigeria.
Correspondence: Amaka Bibian Ezeanwu, Department of Home Economics and Hospitality Management Education, Faculty of Vocational and Technical Education, University of Nigeria, Nsukka, P.M.B. 410001, Enugu State, Nigeria (e-mail: [email protected] ).
Abbreviations: % = Percentage, ADCQSSS = Alcoholic Drinks Consumption Questionnaire for Secondary School Students, CI = confidence interval, DNC = does not consume, EA = extremely aware, HC = highly consume, M ± SD = means and standard deviation, MA = moderately aware, MC = moderately consume, NA = not aware, RC = rarely consume, SA = slightly aware, t = t test statistic.
Authorship: NME, CE, UCU, and HAN conceived the study. NME, BNA, HAN, CE, JIO, and BAE designed the study procedure. All the authors were involved in the data collection. CE, BNA, UCU, NME, JIO, and BAE carried out the analysis and interpretation of these data. NME, CE, UCU, HAN, BNA, JIO, and BAE drafted the manuscript. CE, HAN, BNA, NME, JIO, UCU, and BAE critically revised the manuscript for intellectual content. All authors read and approved the final manuscript.
The authors report no conflicts of interest.
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms. http://creativecommons.org/licenses/by-nc-sa/4.0
Received June 23, 2017
Received in revised form November 4, 2017
Accepted November 8, 2017
Alcohol consumption among secondary school students is a major public health issue worldwide; however, the extent of consumption among secondary school students and their understanding of its effects on human health remain relatively unknown in many Nigerian States. This study aimed to determine the extent of alcohol consumption and of the awareness of its negative effects on human health among secondary school students.
The study used a cross-sectional survey design. Self-report questionnaire developed by the researchers was administered to representative sample (N = 1302) of secondary school students in the study area. The data collected from the respondents were analyzed using means and t test.
The results showed that male secondary school students moderately consumed beer (55.2%) and local cocktails (51.5%), whereas their female counterparts reported rare consumption of these 2 alcoholic drinks (44.8%; 48.5% respectively). The findings also indicated rare consumption of distilled spirits among both male and female students in the investigated area, whereas wine, liquor, local spirits, and palm wine were consumed moderately, regardless of gender. Finally, male and female secondary school students differed significantly in their awareness of the negative effects of alcohol consumption on health.
There is a need to intensify efforts to further curtail the extent of alcohol consumption and increase awareness of the negative effects of alcohol use on human health among secondary school students.
1 Introduction
Alcohol consumption is a serious public health challenge worldwide, including in Nigeria. Although the level of alcohol consumption differs widely around the world, the burden of disease and death remains significant in most regions, with Europe and America having the highest alcohol attributable fractions at 6.5% and 5.6%, respectively. [1] Recent evidence also indicates that alcohol consumption is now the world's third largest risk factor for disease and disability; almost 4% of all deaths globally are attributed to alcohol. [2] However, alcohol is the most commonly used psychoactive drug in both young people and adults in Nigeria. [3–5] Some of the factors contributing to alcohol consumption among Nigerians include the absence of alcohol policies, easy access to alcoholic drinks, and lack of implementation of a minimum drinking age by both the government and the brewers. [6]
According to Bada and Adebiyi, [7] it is not rare for Nigerian secondary school students to consume alcoholic drinks; this consumption could be due to their curiosity as adolescents, an irresistible urge, emotional disturbances such as anxiety, the subculture, and the influence of advertisements. Several previous studies have shown the prevalence of alcohol consumption among the Nigerian population, but they did not explore adolescent students’ understanding of its negative health effects. For instance, Lasebikan and Ola [8] found that the prevalence of lifetime alcohol use was 57.9% and that of current alcohol use was 27.3% among a sample of Nigerian semirural community dwellers. Through in-person interviews with Nigerian adults, previous research by Gureje et al [3] revealed that the lifetime prevalence of alcohol consumption was 56%. A recent study by Alex-Hart et al [9] showed that the prevalence of current alcohol consumption among a sample of Nigerian secondary school students was 30.6% and that 38.1% of current drinkers had also been drunk in the past 30 days, with 17.2% being drunk very frequently.
Alcohol consumption negatively affects human health across the lifespan. Previous studies show that alcohol consumption is associated with a burden of diseases such as cancer, [10] pancreatitis, liver cirrhosis, tuberculosis, pneumonia, diabetes mellitus, alcohol use disorder, malignancies, psychiatric morbidity, and injury. [11] Although 18 years of age is the legal limit for alcohol consumption per policy in many parts of the world, sociocultural influences [12,13] seem to hinder strict adherence to this public health policy in Nigerian society. The objective of the present study was therefore to investigate the level of alcohol consumption and knowledge of its negative effects on health among secondary school students in Nigeria. Specifically, the study sought to determine the responses of secondary school students regarding the extent of their alcohol consumption and the extent to which students are aware of the negative health effects of alcohol consumption.
2.1 Ethical consideration
Ethical committee approval was obtained by the authors for this study (Ethical Approval Number: VTE/ERA/0023). Furthermore, parents of the selected participants signed an informed consent form to indicate their approval. School principals of the selected students provided informed consent and conveyed their approval to the researchers in writing. Participants were informed that they were free to participate or to decline participation in the study.
2.2 Study design
The current study adopted a cross-sectional survey design.
2.3 Study setting
This study was conducted in public secondary schools in Ebonyi and Enugu States, Nigeria.
2.4 Study participants
The participants comprised 1302 senior secondary school students who were purposively selected to participate in the study. The study sample size was determined using G*Power 3.1 software [14,15] based on a statistical power of 0.95. Brown [16] stated that if the observed statistical power is large enough (≥0.80), the sample size can be considered adequate for the study. Figure 1 shows the results of the sample size determination. Table 1 summarizes the characteristics of the participants.

2.5 Assumptions about the sample size calculations
We conducted an a priori analysis to determine the study sample size based on the assumptions that a required sample size can be computed as a function of user-specified values for the required significance level α , the desired statistical power 1– β , and the to-be-detected population effect size. [14,15,17,] According to Uzoagulu, [18] researchers should endeavor to make use of statistical technique to determine sample size, and should be aware that the fewer a sample size is, the greater the possibility of sampling error. Thus, the assumptions underlying the use of a priori analysis for sample size calculations were considered appropriate for the current study.
2.6 Sampling strategy
Before sampling, the researchers and assistants purposively visited 40 secondary schools each in the surveyed States to seek for the school principals’ approval, and to explain to them the purpose of the study, and possibility of being included or excluded from the study later on due to certain criteria. All the school principals visited gave their informed consent, and their schools were therefore qualified for sampling. Through multistage sampling technique, the researchers selected the current study sample. First, the simple random sampling technique (balloting without replacement) was used to select only 31 school secondary schools from each State, making a total of 62 secondary schools surveyed. This technique was used in order to give each of the secondary schools the opportunity of being selected and thus eliminate selection bias. Furthermore, 21 senior students from each of the selected schools in the 2 States were selected to participate in the study through stratified random sampling. The samples were stratified by gender (male, n = 651, 50%; female, n = 651, 50%) and other demographics as summarized in Table 1 . Both the schools and their students were selected on the basis of certain inclusion criteria set by the researchers.
2.7 Inclusion and exclusion criteria
The inclusion criteria included that the school principal must provide informed consent in writing; the respondent (student) must be in senior secondary school class two or three, agree to participate freely, inform their parents/guardians about the study, and provide a letter of consent from them. A participant must also be at least 16 years of age and above. Those who did not meet these criteria were excluded from the current study.
2.8 Measures
The Alcoholic Drinks Consumption Questionnaire for Secondary School Students (ADCQSSS) is a structured questionnaire developed by the researchers based on previous literature. [2,8,19] The ADCQSSS consists of 22 items divided into 2 major sections (A and B). Section A assesses respondents’ personal data (age, gender, religion, socioeconomic background, and educational class level). Section B has 2 parts; part one contains 7 items that evaluate the extent to which students consume alcohol with regard to a variety of alcoholic drinks (i.e., Beer, Distilled Spirits, Wine, Liquor, Local Spirits, Local Cocktails, and Palm Wine), and part two contains 15 items that ask respondents about their awareness of the negative effects of alcoholic drinks on human health. The ADCQHSS has a 5-point rating scale from Do not consume/Not aware (0) to Highly Consume/Extremely aware (4). The ADCQSSS was validated by 2 experts in Home Economics and Hospitality Management Education and 2 other independent experts in Educational Research, Measurement, and Evaluation. Cronbach alpha reliability coefficient of the ADCQSSS was 0.72 for part one, 0.76 for part two, and 0.85 for the entire scale, based on data from the current study sample.
2.9 Data collection
To overcome the challenges of participant attrition and nonretrieval of instruments, which are common to many cross-sectional surveys, the questionnaires were distributed and retrieved from each respondent on the spot with the help of 4 research assistants. Respondents met with the researchers and assistants in school halls to complete the questionnaire during long break periods in school. The respondents were guided appropriately and given sufficient time (15–20 minutes) to avoid incomplete responses. Respondents were encouraged to call the attention of any of the researchers or assistants if they need additional clarification on any item or how to complete the questionnaire. Given these measure, responses and return rates were 100%.
2.10 Data entry, management procedure, and analysis
The data collected from the respondents were analyzed using means, percentage, and t test. Item scores were included as the dependent variables and sex as the independent variables. Using purposively determined mean benchmark values, the item scores for the first part of the ADCQHSS section B (the extent to which students consumed alcoholic drinks) were interpreted as follows: Highly Consume (HC) = 3.50 to 4.00; Moderately Consume (MC) = 3.00 to 3.49; Rarely Consume (RC) = 2.50 to 2.99; and Does Not Consume (DNC) = 1.00 to 2.49. Using similarly purposively set mean benchmark values, the item scores for the second part of the ADCQHSS section B (awareness of the negative effects of alcoholic drinks on health) were interpreted as follows: Extremely Aware (EA) = 3.50 to 4.00; Moderately Aware (MA) = 3.00 to 3.49; Slightly Aware (SA) = 2.50 to 2.99; and Not Aware (NA) = 1.00 to 2.49. The t test was used to examine the differences between male and female students at a 0.05 level of significance. To perform the t tests, item scores were treated as test variables, whereas sex was used as the grouping variable. During coding, the numerical value of 1 was used as the label for male students, whereas the value of 2 was applied for female students. Before performing the t tests, the normality of the distribution of the data was assessed using Shapiro–Wilks normality test. The data were found to be normally distributed ( P = .95). Furthermore, we described the percentage (%) of students scoring below or above given thresholds ( see Tables 2 and 3 ). A database created from Microsoft Excel was used for data management, which involved compiling, organizing, defining, and managing data. Thereafter, the statistical software used for analysis was the Statistical Package for the Social Sciences (SPSS) version 21 (IBM Corp., Chicago, IL). [20] To assure quality, we checked for missing data and violation of assumptions using the IBM SPSS statistical software. There were no missing data.

The results in Table 2 reveal the extent of participants’ consumption of alcoholic drinks by gender. Male secondary school students (55.2%) in this study reported moderate consumption of beer (M ± SD = 3.17 ± .83), while females (44.8%) reported rare consumption of beer (2.57 ± .57). In addition, distilled spirits (male=50.3%; female=49.7%) were rarely consumed by both genders, whereas wine, liquors, local spirits, and palm wine were moderately consumed by both (see Table 2 ). These results imply that secondary school students in the study area consumed different types of alcoholic beverages. In addition, the results in Table 2 reveal a significant difference between male and female students in their extent of consumption of beer [ t = -15.25, P = .000, 95% confidence interval (95% CI) -0.676 to 0.522] and local cocktails ( t = -3.92, P = .000, 95% CI -0.263 to -0.088) at 1300 degrees of freedom, as the corresponding P values were lower than the chosen level of significance (.05). This finding means that male and female students in the investigated area consumed these alcoholic drinks unequally due to gender. Male secondary school students moderately consumed beer and local cocktails, whereas their female counterparts were rare consumers of these 2 alcoholic drinks (see Table 2 ).
Furthermore, the results in Table 2 reveal nonsignificant differences between male and female students in the extent to which they consume distilled spirits ( t = -0.991, P = .322, 95% CI -0.109 to 0.036], wine ( t = -0.268, P = .789, 95% CI -0.089 to 0.068), liquor ( t = -0.846, P = .398, 95% CI -0.138 to 0.055), local spirits ( t = -0.098, P = .922, 95% CI -0.097 to 0.088), and palm wine ( t = -0.066, P = .947, 95% CI -0.094 to 0.088), given that the P values for all t tests ranged from .32 to .95 at 1300 degrees of freedom and were therefore higher than the chosen level of significance (.05). This finding suggests that male and female students in the investigated area consumed these alcoholic drinks similarly regardless of gender (see Table 2 ).
Table 3 summarizes the extent to which students were aware of the negative effects of alcohol consumption on health. The results show that male and female students differed significantly in their awareness of the following negative effects of alcohol consumption on human health: excessive drinking can cause alcoholic hepatitis ( t = 39.39, P = .000, 95% CI 1.347–1.488); heavy alcohol intake increases the risk of many forms of cancers ( t = 12.92, P = .000, 95% CI 0.526–0.715); excessive alcohol intake can result in sleep disturbances ( t = -5.01, P = .000, 95% CI -0.329 to 0.144); alcohol abuse can increase the risk of injuries and accidents ( t = -2.65, P = .008, 95% CI -0.193 to 0.029); alcohol abuse can cause liver disease ( t = 3.38, P = .001, 95% CI 0.059–0.221); alcohol abuse can damage the salivary glands ( t = -4.14, P = .000, 95% CI -0.215–0.077); alcohol abuse can lead to gum disease and tooth decay ( t = 6.23, P = .000, 95% CI 0.201–0.386); people who abuse alcohol suffer from malnutrition ( t = 32.98, P = .000, 95% CI 0.972–1.095); excessive alcohol intake can cause a woman to stop menstruating and become infertile ( t = 6.44, P = .000, 95% CI 0.179–0.337); an immune system weakened by alcohol abuse has difficulty fighting off illness ( t = -7.66, P = .000, 95% CI -0.382 to 0.226); and heavy drinking can cause damage to the heart ( t = -15.46, P = .000, 95% CI -0.748 to 0.579) (see Table 3 ).
Finally, the results in Table 3 further show that male and female students were similarly aware of the following effects of alcohol on human health, in that no significant differences were found: excessive alcohol intake can affect coordination, interfering with balance and the ability to walk ( t = 0.70, P = .484, 95% CI -0.055 to 0.117); heavy alcohol use can result in alcohol dependence ( t = 0.00, P = .998, 95% CI -0.088 to 0.088); alcohol use can make people with depression feel worse ( t = -0.86, P = .388, 95% CI -0.121 to 0.047); and erectile dysfunction is a side effect of alcohol abuse in men ( t = 1.66, P = .097, 95% CI -0.009 to 0.104) (see Table 3 ).
4 Discussion
The current study determined the extent of alcoholic drink consumption and of awareness of its negative effects on human health among secondary school students in Nigeria. First, our findings showed that male secondary school students moderately consume beer and local cocktails, whereas their female counterparts were rare consumers of these 2 alcoholic drinks. These findings support those of Lasebikan and Ola, [8] who found that current alcohol drinking was highly related to male gender. In addition, the current study showed that both male and female students in the investigated area rarely consumed distilled spirits, whereas wine, liquor, local spirits, and palm wine were consumed moderately by the students regardless of their gender. According to the authors, more than two-thirds of the current drinking population are moderate drinkers. [8] Bada and Adebiyi [7] noted that it is not difficult to identify Nigerian secondary school students who consume alcohol. Despite what literature might suggest as reasons for students’ alcohol consumption, Cox et al [21] indicate that negative reasons for alcohol consumption are stronger determinants of drinking problems than are positive reasons among both secondary-level school students. Sociocultural factors may also explain the reason for the differences as well as similarities on the extent of alcoholic drink consumption in Nigerian population. [12,13]
Furthermore, the present study showed that male and female secondary school students differed significantly in their awareness of the following negative effects of alcohol consumption on health: excessive drinking can cause alcoholic hepatitis; heavy alcohol intake increases the risk of many forms of cancers; excessive alcohol intake can result in sleep disturbances; alcohol abuse can increase the risk of injuries and accidents; alcohol abuse can cause liver disease; alcohol abuse can damage the salivary glands; alcohol abuse can lead to gum disease and tooth decay; people who abuse alcohol suffer from malnutrition; excessive alcohol intake can cause a woman to stop menstruating and become infertile; an immune system weakened by alcohol abuse has difficulty fighting off illness; and heavy drinking can cause damage to your heart. Finally, our findings also showed that male and female students had similar levels of awareness of the following effects of alcohol on human health, as no significant differences were found: excessive alcohol intake can affect coordination, interfering with balance and the ability to walk; heavy alcohol use can result in alcohol dependence; alcohol use can make people with depression feel worse; and erectile dysfunction is a side effect of alcohol abuse in men. These outcomes support previous studies, [1,9] which show that alcohol increases the risk of numerous diseases and all injury outcomes. According to the WHO, [2] alcohol consumption is now the world's third largest risk factor for disease and disability, with almost 4% of all global deaths attributed to alcohol.
5 Limitations
Our study has several limitations. First, this study used a cross-sectional survey design, which does not enable conclusions regarding causality. However, a cross-sectional survey was considered necessary because previous studies did not investigate the extent of alcohol consumption or of awareness of its negative effects on human health among secondary school students. In the future, longitudinal studies are needed to determine the causal relationship between alcoholic drink consumption and awareness of its negative effects on students’ health. Second, all participants were recruited from secondary schools in 2 States in Nigeria. This approach may have limited the ability to generalize these findings to other populations. Third, our study used self-reported assessments. The instrument showed good validity; however, future research may need to use observational assessments and interview.
6 Implications
If no further research or action is implemented to determine the extent of alcohol consumption and awareness of its negative effects on human health among secondary school students in Nigeria, in other parts of the country in particular, then alcohol consumption among adolescent students may be associated with increased school-based violence, student neglect and abuse, and absenteeism in school, among other social issues. In addition, policy interventions and other actions to reduce the patterns of alcohol use among the student population may not be realistic. Therefore, further research is needed to examine the patterns and prevalence of alcohol consumption and of awareness of its negative effects on human health among secondary school students across the globe.
7 Conclusion
The present study suggests that male secondary school students moderately consume beer and local cocktails, whereas their female counterparts are slight consumers of these 2 alcoholic drinks. Furthermore, both male and female students in the investigated area slightly consumed distilled spirits, whereas wine, liquor, local spirits, and palm wine were consumed moderately by students regardless of gender. Finally, male and female secondary school students significantly differed in their awareness of some of the negative effects of alcohol consumption on health. Overall, secondary school students are not very aware of some of the negative effects of alcohol on human health. Accordingly, health education teachers, school health counselors, and school administrators should combine their professional experiences to promote health education interventions and health counseling programs aimed at reducing students’ engagement in alcohol consumption. Schools should organize seminars for students to provide education on the health-related issues surrounding alcohol consumption. Addiction counselors should also organize awareness campaigns to orient Nigerian secondary school students to the damages caused by alcohol consumption. Parents should properly monitor and counsel their adolescent students on matters relating to alcohol consumption and its effect on their health.
Acknowledgments
We would like to thank the editor and anonymous reviewers for their constructive remarks regarding this work. We also are thankful to AuthorAID and American Journal Experts (AJEs) for their editing support. We are very much grateful to the research assistants and all the schooling adolescents who made this study a success.
alcohol; consumption; health; Nigeria; secondary school; students
- + Favorites
- View in Gallery
Drinking Alcohol Before Conceiving A Child Could Accelerate Their Aging

The conditions within a person’s home, family and community affect their ability to stay healthy. Scientists studying these social determinants of health are trying to understand whether nature or nurture has a stronger effect on a person’s ability to fight disease.
I am a developmental physiologist studying the ways that drinking affects fetal development and lifelong health. Although researchers have long recognized that a father’s alcohol abuse negatively affects his children’s mental health and social development , it hasn’t been clear if paternal drinking has any lasting biological effects on his offspring’s physical health.
My lab’s recently published research shows that chronic alcohol use from both parents has an enduring effect on the next generation by causing their offspring to age faster and become more susceptible to disease.
Fetal Alcohol Spectrum Disorders
According to the National Institutes of Health, nearly 11% of adults in the U.S. have an alcohol use disorder. Heavy drinking causes multiple health issues , including liver disease, heart problems, declining cognitive function and accelerated aging .
Parents may pass these health problems on to their children. Fetal alcohol spectrum disorders refer to a wide range of alcohol-related physical, developmental and behavioral deficits that affect as many as 1 in 20 U.S. schoolchildren .
Children with fetal alcohol spectrum disorders experience an early onset of adult diseases , including type 2 diabetes and heart disease. Cardiovascular disease first appears during adolescence for people with these disorders, while the rest of the population is affected typically in their 40s and 50s. Children with fetal alcohol spectrum disorders are also more likely to be hospitalized and have lifespans that are 40% shorter than children without these conditions.
However, it has been unclear whether these health problems are because of life circumstances – people with fetal alcohol spectrum disorders have high rates of psychiatric disorders , which cause stress that makes them more susceptible to aging and disease – or if their parents’ substance use directly causes lasting negative effects to their health. In other words, can a parent’s alcohol abuse before conception directly influence their offspring’s physical health and lifespan?
Mom And Dad Drinking
In our study, my colleagues and I used a mouse model to measure the effects that alcohol use by mom, dad or both parents around the time of conception have on their offspring aging and chronic disease. The mice chose when and how much alcohol to drink.
We found that paternal and maternal drinking both cause harmful changes to their offspring’s mitochondria . Mitochondria – often called the battery of the cell – control many aspects of aging and health . Like a cellphone battery, mitochondria deteriorate over time and cause cells to lose their ability to repair damage and control metabolism.
Our experiments in mice show that dad’s drinking causes a defect in mitochondrial function that first emerges during fetal development and persists into adult life , causing the offspring to age faster. For example, paternal alcohol exposure caused a twofold increase in age-related liver disease, suggesting that parental alcohol use – particularly by the father – could have significant implications on aging and age-related diseases.
Importantly, we found that when both parents drank, the effects on their offspring were worse than when only one parent consumed alcohol. For example, we observed a threefold increase in age-related liver scarring when both parents consumed alcohol.
Treating Fetal Alcohol Syndrome
People with fetal alcohol syndrome face lifelong challenges , including problems with hand-eye coordination and difficulties with memory and attention.
Early educational interventions for children with fetal alcohol spectrum disorders, like using visual and auditory materials instead of print, can provide additional structure to help facilitate learning.
Although my team and I examined chronic alcohol exposure, we do not know if moderate alcohol use also causes mitochondrial problems. We also don’t know if these same effects emerge in people who haven’t been diagnosed with fetal alcohol spectrum disorders but whose parents drank heavily. Whether paternal drinking influences human embryonic development is still unclear, although emerging studies are beginning to suggest it does.
The next step is to explore if interventions that focus on mitochondrial health, such as exercise and specific diets , can improve health outcomes for people with fetal alcohol spectrum disorders.
This article by Michael Golding originally appeared on The Conversation .
Related Stories

Children Can Inherit Early Aging Symptoms From Parents Who Abuse Alcohol, Researchers Find
These accelerated aging effects include high cholesterol, heart problems, arthritis and early onset dementia.

Texas A&M Researcher Says Men Should Abstain From Drinking At Least Three Months Prior To Conceiving
In examining the effects of paternal alcohol consumption on fetal alcohol syndrome, a groundbreaking new study reveals that it can take over a month for negative alcohol effects to wear off.

Father’s Alcohol Consumption Before Conception Linked To Brain And Facial Defects In Offspring
Fetal alcohol syndrome-related craniofacial differences could be seen in offspring born to fathers who regularly consumed as little alcohol as the legal limit.
Recent Stories

From Turfgrass To Touchdowns
Go behind the scenes to see how Aggie turfgrass science students keep Kyle Field game day ready.

Texas A&M Teams Up To Advance Robotic Dexterity
A&M joins a Northwestern University-led center to bring highly skilled, affordable robotic assistance to the workforce and beyond.

25 By 25 Goal Achieved In Fall 2023
The College of Engineering initiative expanded engineering education access to meet rising demand for engineers in Texas and beyond.

Subscribe to the Texas A&M Today newsletter for the latest news and stories every week.
Kia ora - welcome to our new website. We've tried to ensure old links will redirect to the correct pages, but some links may no longer work. Find out more .
About us Mō mātou
About the Ministry of Health and the New Zealand health system.
Quick links
- Consultations
New Zealand’s health system
- Government Policy Statement
- Health system roles and organisations
- Overview and statutory framework
- Vote Health
Organisation and leadership
- Chief clinical officers
- Executive Governance Team
- Ministry directorates
- Public Health Agency
- Statutory roles
Corporate publications
- Annual reports
- Briefings to incoming Ministers
- Health and Independence reports
- Mental health annual reports
- Strategic intentions
- Current vacancies
- Employee benefits
- Information for job applicants
Regulation & legislation Ngā here me ngā ture
Health providers and products we regulate, and laws we administer.
- Legislation we administer
- Rest home audit reports
Assisted dying
Certification of health care services, drug checking, health practitioners competence assurance act, medicinal cannabis, medicines control, mental health and addiction, notifiable diseases, pharmacy licensing, psychoactive substances, smoked tobacco, vaping, herbal smoking and smokeless tobacco, strategies & initiatives he rautaki, he tūmahi hou.
How we’re working to improve health outcomes for all New Zealanders.
Health strategies
- New Zealand Health Strategy
- Health of Disabled People Strategy
- Pae Tū: Hauora Māori Strategy
- Rural Health Strategy
- Te Mana Ola: The Pacific Health Strategy
- Women’s Health Strategy
Programmes and initiatives
- Gambling harm
- Health workforce
- Mental health, addiction and suicide prevention
- Pacific health
- Smokefree 2025
Māori health Hauora Māori
Increasing access to health services, achieving equity and improving outcomes for Māori.
- Subscribe for Māori health updates
Ao Mai te Rā anti-racism initiative
Māori health models, te tiriti o waitangi framework, wai 2575 health services and outcomes inquiry, whakamaua: māori health action plan, statistics & research he tatauranga, he rangahau.
Data and insights from our health surveys, research and monitoring.
- New Zealand Health Survey
- Health targets
System monitoring
- Mental health and addiction targets
- Planning and performance data
- New Zealand Gambling Survey
- Past surveys
Statistics and data sets
- Māori health data and statistics
- Mental health data and statistics
- Obesity data and statistics
- Suicide data and statistics
- Tobacco data and statistics
- COVID-19 and immunisation research projects
- Gambling harm research and evaluation
- Our role in health research
Alcohol use data and statistics
Statistical publications and data sets on alcohol use.
Health data in New Zealand
Since 2022, Health New Zealand – Te Whatu Ora has been responsible for collecting and publishing data on most health topics in New Zealand.
Data and statistics – Health New Zealand
The Ministry of Health continues to produce the New Zealand Health Survey .
Publications
Mental health and problematic substance use data explorer.
The New Zealand Health Survey (NZHS) included a module on mental health and problematic substance use (including tobacco, alcohol and illicit substance use) in 2016/17, 2021/22 and 2022/23. The Mental Health and Problematic Substance Use Data Explorer presents data from that module and covers topics such as mental health, risk of problematic substance use, informal help-seeking and access to mental health and addictions services for adults and children.

Mental Health and Problematic Substance Use
The New Zealand Health Survey (NZHS) included a module on mental health and problematic substance use (including tobacco, alcohol and illicit substance use) in 2016/17, 2021/22 and 2022/23. This report presents information and key results from the mental health and problematic substance use module.
Annual Update of Key Results 2022/23: New Zealand Health Survey
The Annual Data Explorer presents results from the 2022/23 New Zealand Health Survey, with comparisons to earlier surveys where possible. Results are available by gender, age group, ethnic group, neighbourhood deprivation and disability status.

Annual Update of Key Results 2021/22: New Zealand Health Survey
The Annual Data Explorer presents results from the 2021/22 New Zealand Health Survey, with comparisons to earlier surveys where possible. Results are available by gender, age group, ethnic group, neighbourhood deprivation and disability status.

Annual Update of Key Results 2020/21: New Zealand Health Survey
The Annual Data Explorer presents results from the 2020/21 New Zealand Health Survey, with comparisons to earlier surveys where possible. Results are available by gender, age group, ethnic group, neighbourhood deprivation and disability status.
Annual Update of Key Results 2017/18: New Zealand Health Survey
This Annual Data Explorer presents the 2017/18 results from the New Zealand Health Survey, for both adults and children. The Annual Data Explorer includes information on health behaviours and risk factors, health conditions and access to health services
Annual Update of Key Results 2016/17: New Zealand Health Survey
This Annual Data Explorer presents the 2016/17 results from the New Zealand Health Survey, for both adults and children. The Annual Data Explorer includes information on health behaviours and risk factors, health conditions and access to health services.
Annual Update of Key Results 2015/16: New Zealand Health Survey
This report presents the 2015/16 results from the New Zealand Health Survey, for both adults and children. The reports includes information on health behaviours and risk factors, health conditions and access to health services.
Alcohol Use 2012/13: New Zealand Health Survey
This report presents information on patterns of alcohol consumption, alcohol use by pregnant women, and alcohol availability and use in 2012/13.

Alcohol factsheets
These alcohol factsheets outline New Zealand’s drinking patterns and alcohol-related health, crime and violence, and drink driving.
The 2007/08 New Zealand Alcohol and Drug Use Survey: Online data tables
All NZADUS results presented in this report and some additional results are available in Excel format.
Drug Use in New Zealand: Key results of the 2007/08 New Zealand Alcohol and Drug Use Survey
This report presents the key findings about drug use and drug-related harm among New Zealand adults, from the 2007/08 New Zealand Alcohol and Drug Use Survey (NZADUS). The survey measured alcohol and drug use among over 6,500 New Zealanders aged 16–64 years from August 2007 to April 2008.
Alcohol Use in New Zealand, Key results of the 2007/08 New Zealand Alcohol and Drug Use Survey
This report presents the key findings about alcohol use and alcohol-related harm among New Zealand adults, from the 2007/08 New Zealand Alcohol and Drug Use Survey. The survey measured alcohol and drug use among over 6,500 New Zealanders aged 16–64 years from August 2007 to April 2008.
Related areas
- Alcohol and Drug Use Survey
- email Email
- print Print
- chat Feedback
© Ministry of Health – Manatū Hauora
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Newsletters
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Balance transfer cards
- Cash back cards
- Rewards cards
- Travel cards
- Online checking
- High-yield savings
- Money market
- Home equity loan
- Personal loans
- Student loans
- Options pit
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
New on Yahoo
- Privacy Dashboard
Drinking alcohol before conceiving a child could accelerate their aging – new research in mice
The conditions within a person’s home, family and community affect their ability to stay healthy. Scientists studying these social determinants of health are trying to understand whether nature or nurture has a stronger effect on a person’s ability to fight disease.
I am a developmental physiologist studying the ways that drinking affects fetal development and lifelong health. Although researchers have long recognized that a father’s alcohol abuse negatively affects his children’s mental health and social development , it hasn’t been clear if paternal drinking has any lasting biological effects on his offspring’s physical health.
My lab’s recently published research shows that chronic alcohol use from both parents has an enduring effect on the next generation by causing their offspring to age faster and become more susceptible to disease.
Fetal alcohol spectrum disorders
According to the National Institutes of Health, nearly 11% of adults in the U.S. have an alcohol use disorder. Heavy drinking causes multiple health issues , including liver disease, heart problems, declining cognitive function and accelerated aging .
Parents may pass these health problems on to their children. Fetal alcohol spectrum disorders refer to a wide range of alcohol-related physical, developmental and behavioral deficits that affect as many as 1 in 20 U.S. schoolchildren .
Children with fetal alcohol spectrum disorders experience an early onset of adult diseases , including type 2 diabetes and heart disease. Cardiovascular disease first appears during adolescence for people with these disorders, while the rest of the population is affected typically in their 40s and 50s. Children with fetal alcohol spectrum disorders are also more likely to be hospitalized and have lifespans that are 40% shorter than children without these conditions.
However, it has been unclear whether these health problems are because of life circumstances – people with fetal alcohol spectrum disorders have high rates of psychiatric disorders , which cause stress that makes them more susceptible to aging and disease – or if their parents’ substance use directly causes lasting negative effects to their health. In other words, can a parent’s alcohol abuse before conception directly influence their offspring’s physical health and lifespan?
Mom and dad drinking
In our study, my colleagues and I used a mouse model to measure the effects that alcohol use by mom, dad or both parents around the time of conception have on their offspring aging and chronic disease. The mice chose when and how much alcohol to drink.
We found that paternal and maternal drinking both cause harmful changes to their offspring’s mitochondria . Mitochondria – often called the battery of the cell – control many aspects of aging and health . Like a cellphone battery, mitochondria deteriorate over time and cause cells to lose their ability to repair damage and control metabolism.
Our experiments in mice show that dad’s drinking causes a defect in mitochondrial function that first emerges during fetal development and persists into adult life , causing the offspring to age faster. For example, paternal alcohol exposure caused a twofold increase in age-related liver disease, suggesting that parental alcohol use – particularly by the father – could have significant implications on aging and age-related diseases.
Importantly, we found that when both parents drank, the effects on their offspring were worse than when only one parent consumed alcohol. For example, we observed a threefold increase in age-related liver scarring when both parents consumed alcohol.
Treating fetal alcohol syndrome
People with fetal alcohol syndrome face lifelong challenges , including problems with hand-eye coordination and difficulties with memory and attention.
Early educational interventions for children with fetal alcohol spectrum disorders, like using visual and auditory materials instead of print, can provide additional structure to help facilitate learning.
Although my team and I examined chronic alcohol exposure, we do not know if moderate alcohol use also causes mitochondrial problems. We also don’t know if these same effects emerge in people who haven’t been diagnosed with fetal alcohol spectrum disorders but whose parents drank heavily. Whether paternal drinking influences human embryonic development is still unclear, although emerging studies are beginning to suggest it does.
The next step is to explore if interventions that focus on mitochondrial health, such as exercise and specific diets , can improve health outcomes for people with fetal alcohol spectrum disorders.
This article is republished from The Conversation , a nonprofit, independent news organization bringing you facts and trustworthy analysis to help you make sense of our complex world. It was written by: Michael Golding , Texas A&M University
Your favorite drink can cause breast cancer – but most women in the US aren’t aware of alcohol’s health risks
What links aging and disease? A growing body of research says it’s a faulty metabolism
Job supervisors with disabilities can boost productivity, new research shows
Michael Golding receives funding through a Medical Research Grant from the W. M. Keck Foundation and a research grant from the NIH through the National Institute on Alcohol Abuse and Alcoholism (NIAAA).

Feeling Judged When You Opt for a Mocktail? You're Not Alone
Research uncovers why those abstaining can make drinkers uncomfortable..
Posted August 26, 2024 | Reviewed by Jessica Schrader
- What Is Alcoholism?
- Find a therapist to overcome addiction
- People who choose not to drink alcohol in social situations where others are drinking often feel judged.
- Research points to three common reasons why drinkers may feel uncomfortable when others choose to abstain.
- Leveraging social support and being mindful of the reasons you're choosing not to drink can be helpful.

Just as alcoholism is a stigmatized health condition, being a non-drinker also carries a stigma . According to research , abstaining from alcohol can lead to negative social consequences, and can even be viewed as “deviant” or unusual behavior, especially in situations where other people are drinking. Choosing not to drink in a social drinking environment takes courage, whether you have a drinking problem or are simply deciding to abstain to optimize your health.
Studies show that those who opt for a non-alcoholic beverage in social situations where drinking is an option often feel the need to “legitimize” their decision or provide reasons that other people will accept as “valid,” such as religious or health-related restrictions. Some cope with the stigma attached to being a non-drinker by hiding the fact that they’re not drinking, for example by ordering mocktails, while others might avoid situations where there could be social pressure to drink.
Why are people who drink judgmental toward those who choose not to?
Scientists interviewed drinkers about their attitudes and feelings toward people who abstained from alcohol in social situations, and they found that there were three themes that summarized the way non-drinkers were perceived:
- Threat to fun : Drinkers felt that those who weren’t drinking might judge them negatively, making them feel self-conscious. This would detract from the fun social vibe shared amongst those who were drinking.
- Threat to connection: Drinkers found it difficult to connect socially with those who were not drinking. This could create an unpleasant awkward feeling.
- Threat to self: Being around a non-drinker prompted those who were drinking to engage in “unwanted self-reflection” about problematic aspects of their own drinking.
In other words, when people are drinking, being around individuals who aren’t can make them feel self-conscious about their own relationship with alcohol, and that can kill some of the fun.
Stand firm and do what you need to stay healthy, regardless of the “sober stigma"
If you or a loved one is actively trying to reduce or stop drinking alcohol completely, remember that it is normal to feel a little uncomfortable when you’re turning down someone who offers you a drink in a social situation. Remind yourself that the reasons someone might react in a way that appears judgmental when you don’t join in and drink with them is because of how it makes them feel about themselves.
Manage self-disclosure
You don’t have to explain yourself and your decisions about drinking to everyone you socialize with. According to one study, non-drinkers had the best experience with self-disclosure when the benefits of sharing that they were intentionally abstaining from alcohol outweighed the risks. These benefits, when being open with certain people, included: (1) inspiring other people, (2) maintaining one’s sobriety, and (3) building close relationships.
Don’t do it alone
For people who avoid or withdraw from situations where there might be social pressure to drink, the lifestyle changes involved with reducing or quitting drinking can feel very lonely or isolating. For this, among other reasons, having a strong social support system is an important part of the addiction recovery process, and studies have shown that people with support have increased chances of long- term success.
I cover this important topic in more depth on my podcast and in my new book, Addiction: What Everyone Needs to Know .

Suzette Glasner, Ph.D., is a licensed clinical psychologist and an Associate Professor in the Department of Psychiatry and Biobehavioral Sciences at UCLA.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Alcohol Res
- v.38(1); 2016

Social and Cultural Contexts of Alcohol Use
Alcohol use and misuse account for 3.3 million deaths every year, or 6 percent of all deaths worldwide. The harmful effects of alcohol misuse are far reaching and range from individual health risks, morbidity, and mortality to consequences for family, friends, and the larger society. This article reviews a few of the cultural and social influences on alcohol use and places individual alcohol use within the contexts and environments where people live and interact. It includes a discussion of macrolevel factors, such as advertising and marketing, immigration and discrimination factors, and how neighborhoods, families, and peers influence alcohol use. Specifically, the article describes how social and cultural contexts influence alcohol use/misuse and then explores future directions for alcohol research.
The alcohol research literature is overwhelmingly focused on risk factors, from the societal level down to the individual. Worldwide, 3.3 million deaths were attributed to alcohol misuse in 2012 ( World Health Organization 2014 ). Excessive alcohol use is the third leading cause of death in the United States, accounting for 88,000 deaths per year ( Centers for Disease Control and Prevention 2014 ). Globally, alcohol-attributable disease and injury are responsible for an estimated 4 percent of mortality and 4 to 5 percent of disability-adjusted life-years (DALYs) ( Rehm et al. 2009 ). The harmful effects of alcohol misuse are far reaching and range from accidents and injuries to disease and death, as well as consequences for family, friends, and the larger society. Economic costs attributed to excessive alcohol consumption are considerable. In the United States alone, the costs of excessive alcohol use were estimated at $223.5 billion in 2006, or $746 per person ( Bouchery et al. 2011 ). Much of these costs result from a loss in workplace productivity as well as health care expenses, criminal justice involvement, and motor vehicle crashes ( Rehm et al. 2009 ).
This article reviews some of the cultural and social influences on alcohol use and places individual alcohol use within the contexts and environments where people live and interact. This is not an exhaustive review but aims to show the wide range of contexts that may shape alcohol use.
Disparities in and Influences on Alcohol Use: A Social–Ecological Framework
Alcohol consumption varies across gender and race/ethnicity. Across the world, men consume more alcohol than women, and women in more developed countries drink more than women in developing countries ( Rehm et al. 2009 ). American men are much more likely than women to use alcohol (56.5 percent vs. 47.9 percent, respectively), to binge drink (30.4 percent vs. 16 percent, respectively), and to report heavy drinking (9.9 percent vs. 3.4 percent, respectively) ( Substance Abuse and Mental Health Services Administration [SAMSHA] 2013 ). (Binge drinking is defined here as the number of instances in the past 12 months that women drank 4 or more drinks and men drank 5 or more drinks within a 2-hour period.) Among racial and ethnic groups, Whites report the highest overall alcohol use among persons age 12 and over (57.4 percent). American Indian/Alaska Natives report the highest levels of binge drinking (30.2 percent), followed by Whites (23.9 percent), Hispanic/Latinos (23.2 percent), African Americans (20.6 percent), and Asians (12.7 percent) ( SAMHSA 2013 ). Alarmingly, according to two nationally representative samples, trends in alcohol misuse increased among both men and women and African-American and Hispanic youth over the decade between 1991–1992 and 2001–2002. Rates of dependence also increased among men, young Black women, and Asian men during the same time period ( Grant et al. 2004 ).
Given these trends, it is clear that a better understanding of the underlying social and cultural factors contributing to these disparities is needed. For example, socioeconomic status (SES) indicators (i.e., education, income, and occupation) usually are strong predictors of health behaviors and outcomes and tend to be positively associated with health. People with higher SES tend to drink more frequently than others ( Huckle et al. 2010 ). Among drinkers, low-SES groups tend to drink larger quantities of alcohol ( Huckle et al. 2010 ).
Like other health issues, alcohol use can be linked to a complex array of factors ranging from individual-level (i.e., genetics) to population-level (i.e., cultural and societal factors) characteristics ( Berkman et al. 2000 ; Krieger 2001 ; Link and Phelan 1995 ). On a population level, emerging research has documented the relationship between social determinants and health ( Berkman and Kawachi 2000 ; Berkman et al. 2000 ) and, specifically, the social epidemiology of alcohol use ( Bernstein et al. 2007 ; Galea et al. 2004 ). Social capital theory suggests that social networks and connections influence health ( Berkman et al. 2000 ). Individuals who have higher levels of social support and community cohesion generally are thought to be healthier because they have better links to basic health information, better access to health services, and greater financial support with medical costs. ( Berkman and Kawachi 2000 ).
This article examines these population-level as well as individual influences through a social–ecological framework, which posits that human health and development occur across a spectrum—from the individual to the macro or societal level ( Bronfenbrenner 1994 ). In the context of alcohol use, individuals are nested within their microsystem (their home, work, and school environments), which is nested itself within the larger community. Macrolevel factors, such as exposure to advertising, may influence family and peer network attitudes and norms, which ultimately affect individual attitudes and behaviors (see figure ).

A social–ecological framework for explaining influences on alcohol use. Individual-level factors that influence alcohol use are nested within home, work, and school environments, which are nested within the larger community. Macro-level factors, such as exposure to advertising, may influence family and peer network attitudes and norms, which ultimately affect individual attitudes and behaviors.
Societal Influences: Advertising, Marketing, and Social Media
Media exposure helps influence social norms about alcohol through advertising, product placements, and stories in a wide range of sources, including movies, television, social media, and other forms of entertainment. Although alcohol sales and marketing are highly regulated, people are exposed to a wide variety of alcohol and liquor advertisements, especially in the United States. Whether these advertisements directly result in an increase in consumption has been the topic of many public policy debates and much alcohol and consumer research. Recent studies have used robust methodological designs in order to assess the effects of advertisements on alcohol consumption ( Grenard et al. 2013 ; Koordeman et al. 2012 ). Although longitudinal studies have found that alcohol commercials particularly affected younger adolescents’ propensity to consume alcohol ( Grenard et al. 2013 ), an experimental design randomly assigning college students to alcohol advertisements demonstrated no differences compared with the control group ( Koordeman et al. 2012 ). It is likely that the effects of advertisement differ across age groups and races. The alcohol industry uses complex targeted marketing strategies that focus on African Americans, Latinos, and American Indians, among other demographic groups, such as youth and other ethnic minorities ( Alaniz and Wilkes 1998 ; Moore et al. 2008 ). Empirical studies show that targeted alcohol marketing results in individuals developing positive beliefs about drinking, and creating and expanding environments where alcohol use is socially acceptable and encouraged ( Alaniz and Wilkes 1998 ; Hastings et al. 2005 ; McKee et al. 2011 ). These factors can result in the onset of drinking and binge drinking, and in increased alcohol consumption ( Tanski et al. 2015 ).
Since the introduction of flavored alcoholic beverages in the 1980s, the alcohol industry has engaged in targeted marketing efforts toward youth in general, and especially young women ( Mosher and Johnsson 2005 ). Products with sweet fruity flavors, colorful appearance and packaging, as well as lower alcohol content are designed to appeal to young women. Fruity drinks mask the taste of traditional alcoholic beverages with the sugary flavors of soft drinks ( Mosher and Johnsson 2005 ), making them more palatable for this consumer market. Although the alcohol industry claims that its marketing strategies target adults ages 21–29, products like flavored alcoholic beverages remain attractive to younger drinkers.
Research estimates that 38.5 percent of high school students have used alcohol in the past month, and 20.5 percent of teenagers started drinking before age 13 ( Eaton et al. 2012 ). Approximately 75 percent of high school seniors and 64 percent of high school 10th graders report having experimented with alcohol ( Kann et al. 2014 ). Youth under age 21 see and hear marketing for flavored alcoholic beverages disproportionally on a per capita basis compared with adults ( Jernigan et al. 2005 ), and a disproportionate number of youth consume alcoholic beverages ( Mosher and Johnsson 2005 ). Furthermore, youth exposed to alcohol advertisements tend to drink more on average than their peers who were exposed to less intensive alcohol-related marketing ( Snyder et al. 2006 ). Specifically, the authors found that each additional advertisement viewed by youth increased the reported number of drinks consumed by 1 percent.
Alcohol marketing also can lead to youth and young adults developing alcohol brand preferences ( Albers et al. 2014 ; Ross et al. 2015 ), which can influence their reports of alcohol consumption ( Roberts et al. 2014 ). For example, youth reported on average 11 more drinks per month when responding to an online survey that used brand-specific measures compared with a survey using more general alcohol measures ( Roberts et al. 2014 ). The relationship between alcohol brand receptivity and alcohol brand consumption also has been linked to whether and when adolescents begin to binge drink ( Morgenstern et al. 2014 ).
Increased use of social media for alcohol marketing has paralleled changes in communication methods among adolescents and college-age youth ( Hoffman et al. 2014 ). Marketing techniques for a wide range of products reflect studies that online platforms are likely to influence adolescent behaviors ( Cook et al. 2013 ). Social media venues are most widely used by youth, with 92 percent of teens reporting being online daily and 24 percent online “almost constantly” ( Lenhart 2015 ). Social-networking sites such as Twitter, Instagram, and Facebook feature alcohol-related marketing. One study found that by 2012, there were more than 1,000 alcohol-related sites on Facebook alone ( Nhean et al. 2014 ). Alcohol use increases with the number of online peer ties and greater peer density, a measure of interconnectedness in the social network ( Cook et al. 2013 ). Despite self-imposed regulations aimed at preventing underage youth from accessing alcohol advertisements on social media, more than two-thirds of advertisements on YouTube are accessible to youth under the legal drinking age ( Barry et al. 2015 ).
Racial and ethnic minorities, especially those living in African-American communities, are likewise exposed to targeted alcohol beverage advertisements ( Wilson and Till 2012 ). African Americans account for 13 percent of the U.S. population, but they purchase 67 percent of all malt liquor sold ( Miller Brewing Company 2000 ). Malt liquor generally has higher alcohol content, is less expensive, and is sold in larger volumes than other beers and ales, and African Americans are exposed to more malt liquor advertisements than other groups. Billboards and other advertisements for malt liquor are disproportionately found in neighborhoods with higher percentages of African Americans, and rap music lyrics frequently mention malt liquor ( Herd 2013 ; McKee et al. 2011 ). When examining alcohol advertising in newspapers, Cohen and colleagues (2006) found that there were more alcohol-related ads in newspapers targeted to African-American readers compared with newspapers with a more general readership. Kwate and Meyer (2009) found a correlation between problem drinking among African-American women and exposure to alcohol advertisements, suggesting that as ad exposure increased, so did alcohol consumption.
These findings, however, must be interpreted with caution, as it is difficult to determine whether advertisements directly result in increased alcohol consumption. To begin with, a variety of marketing strategies including distribution, product development, pricing, and targeted marketing all may affect links between advertising and consumption ( Alaniz and Wilkes 1998 ; Roberts et al. 2014 ). For example, Molloy (2015) found that after controlling for targeting, only moderate advertising effects are seen, despite the strong correlations between alcohol advertising and drinking among youth. It also is unclear which aspects of online social media advertisements are related to the observed correlations. Research shows that drinkers like advertising about alcohol more than nondrinkers do, respond neurologically to the advertising more intensively than nondrinkers do, and may recall the advertising more clearly ( Snyder et al. 2006 ), making it harder to distinguish among the specific mechanisms behind the observed relationships. As a result, making causal statements about alcohol use and marketing is problematic because the temporal order between using alcohol and seeing advertisements is not frequently established ( Snyder et al. 2006 ).
Despite these challenges, it is important to develop new strategies to systematically examine the impact of advertising and marketing on alcohol use among different populations. For example, researchers might continue to compare marketing and advertising strategies within specific neighborhoods to more fully understand targeted marketing’s influence on alcohol use. Further research and evaluation studies also are needed that can help establish whether and how advertising and marketing can lead to alcohol use in vulnerable and disadvantaged populations.
Influences From Discrimination
A number of social and cultural factors predict increased alcohol use, including discrimination and its related stigma. The role of discrimination and stress in health-related risk behaviors, including alcohol use, is well established ( Dawson et al. 2005 ; Hatzenbuehler 2009 ; Paradies 2006 ). The stress and coping framework frequently is applied to explain the influence of discrimination and stigma on health ( Krieger 1999 ; Pascoe and Smart Richman 2009 ; Walters et al. 2002 ). This long-held theory posits that people consume alcohol to cope with the stress of their daily lives, including work-related stressors and racial and ethnic discrimination ( Conger 1956 ).
Discrimination is seen as a key social stressor that elicits a physiological response, including elevated blood pressure and release of stress hormones ( Williams and Mohammed 2009 ), which may have lifelong deleterious effects, including increased alcohol use ( Pascoe and Smart Richman 2009 ). Self-reported unfair treatment and racial discrimination has been linked to higher alcohol use among Asian Americans ( Chae et al. 2008 ; Gee et al. 2007 ; Yoo et al. 2010 ) and Latinos ( Mulia et al. 2008 ).
The picture is less clear among African Americans. Although similar positive associations have been found between level of discrimination and alcohol use in this population ( Boynton et al. 2014 ; Gibbons et al. 2004 ; Mulia et al. 2008 ), other recent studies ( Kwate and Meyer 2009 ) among African-American adults have found no relationship between high levels of racial discrimination and heavy and episodic drinking. However, Borrell and colleagues (2007) did report an association between discrimination and past-year alcohol use. The mixed results among African Americans may relate more to SES than to discrimination. Past studies suggest that African Americans with higher levels of education were more likely to report experiencing discrimination, whereas the opposite was true among Whites ( Borrell et al. 2007 ; Krieger et al. 1998 ). This may be because better educated African Americans find themselves in situations in which they may be exposed to discrimination, or they may be more acutely aware of how subtly it can be expressed. Whites of lower SES may be in the minority and therefore may be more likely to report experiencing discrimination. This may explain the mixed results found in this particular population segment, as socioeconomic position actually may mute the effects of discrimination on alcohol use. Further research is needed to examine these potential mechanisms and other underlying factors that interact with racial discrimination to influence and alcohol use and misuse among minorities.
Another group that may be at particular risk for alcohol problems stemming from their experiences with discrimination are those in the lesbian, gay, bisexual, and transgender (LGBT) community, who experience high levels of discrimination related to sexual orientation and gender identification ( Krieger and Sidney 1997 ). One study found that more than two-thirds of LGBT adults experienced discrimination, and individuals who reported discrimination based on race, gender, and sexual orientation were almost four times more likely to use alcohol and other substances ( McCabe et al. 2010 ). This suggests that future studies and public health interventions should focus not only on racial and gender discrimination, but also sexual orientation and gender identification.
Immigration-Related Influences
Societal influences can shape drinking behavior among immigrants to the United States. In 2010, nearly 40 million people, or 13 percent of the U.S. population, had been born in another country—the largest absolute number of U.S. immigrants ever and the highest proportion who are foreign born since the 1920s ( Grieco et al. 2012 ). With wide diversity among immigrants in terms of national origin, language, religion, and social class, and with even more reasons for and processes of migration than ever before ( Dubowitz et al. 2010 ), it is no surprise that the evidence on alcohol consumption among immigrants is similarly complex.
Immigration may influence alcohol consumption and its consequences in at least two ways. The first theory suggests that immigrants encounter difficulties and hardships as they transition into a new society and culture ( Berry 1997 ). Hardships include the stress of experiencing new environments and cultures; living in poor neighborhoods; finding good, secure jobs in safe work environments; encountering few opportunities to enhance income or wealth; and engaging with fewer and smaller social networks that may otherwise offer instrumental and emotional support. It also is possible that immigrants may not become fully integrated into American society because of experiences with discrimination and obstacles in social mobility ( Unger et al. 2014 ). Because these factors are associated with alcohol consumption and problems, immigrants may consume more alcohol ( Unger et al. 2014 ). As they become settled in the new society, this consumption pattern decreases ( Bui 2012 ). A second hypothesis posits that alcohol consumption increases the longer immigrants live in a new location ( Lee et al. 2013 ). Over time, immigrants may learn the behaviors and adapt the lifestyles often associated with alcohol consumption in American society (i.e. experience acculturation) ( Caetano 1987 ; Vaeth et al. 2012 ).
Strong evidence indicates that norms in countries of origin have long-term effects on the drinking patterns of immigrants ( Cook et al. 2014 ). Recent immigrants generally have lower rates of alcohol consumption and excessive drinking than other U.S. residents ( Brown et al. 2005 ; Szaflarski et al. 2011 ). Available reviews find that acculturation leads to more alcohol consumption among immigrants, including Latinos ( Valencia and Johnson 2008 ; Zemore 2007 ). Higher acculturation is associated with higher odds of drinking and heavier drinking among Latino women ( Zemore 2007 ). The findings for Latino men appear less clear cut, with high acculturation tied to greater likelihood of drinking but not a definitive pattern for problem drinking.
Studies are beginning to recognize the importance of premigration factors, including levels of alcohol use before migration as well as the cultural influences of countries of origin ( Sanchez et al. 2014 ; Walsh et al. 2014 ). One study ( Sanchez et al. 2014 ) among Latinos found that Latino men had higher levels of alcohol use before immigration, with steeper declines postmigration compared with Latino women. This finding suggests that future studies may need to focus on trajectories of alcohol use to address alcohol prevention efforts. Moreover, retaining culture of origin also has been shown to have protective influences for alcohol use ( Schwartz et al. 2012 ), including protective family and traditional values.
Timing also may be critical in understanding how immigration is associated with alcohol consumption. Age at immigration can be seen as the developmental context of people’s experiences when they first arrive in the United States. This context helps to shape language use, heterogeneity of social networks, and schooling. The social institutions that affect people’s lives vary by age of immigration ( Fuligni 2004 ; Rumbaut 2004 ). The number of social groups and institutions, such as schools, clubs, friendship networks, and family ties, geared toward supporting children to integrate into their new society is far greater than those available for adults ( Takeuchi et al. 2007 ). These social groups, in turn, offer children greater access to the opportunity structures in a new culture. Conversely, immigrant children may have a larger set of social groups available to them than older immigrants. As a result, they also could experience a greater amount of negative stressors and influences that could lead to detrimental social and health outcomes as they mature. Immigrants who move to the United States at younger ages may be at risk for behaviors like alcohol use and misuse because they have the potential to be involved in social networks that may offer greater access and opportunity to engage in these behaviors, as well as lower levels of parental attachment ( Hahm et al. 2003 ; Vaeth et al. 2012 ).
A recent study found that Mexican immigrants who come to the United States before age 14 have higher alcohol consumption rates than those who are older when they immigrate ( Reingle et al. 2014 ). Immigrants who come at a younger age have alcohol consumption patterns similar to their U.S.-born counterparts. The study by Reingle and colleagues also shows that immigrants who arrive when they are younger than 14 and who live beyond the U.S.–Mexico border region have much higher rates of alcohol use than immigrants in the border region. This particular finding suggests that where immigrants live is another social context worth further investigation.
Community Influences
The literature on community influences on alcohol use focuses primarily on environmental aspects, such as neighborhood characteristics and opportunities for alcohol purchasing and consumption. For example, one study found that individuals who lived in a neighborhood with a poorly built environment, characterized by inferior building conditions, housing, and water and sanitation indicators, were 150 percent more likely to report heavy drinking compared with those living in better built environments ( Bernstein et al. 2007 ). Other studies have examined the spatial epidemiology of neighborhoods regarding alcohol availability, individual consumption, and community disorganization and violence ( Cohen et al. 2006 ; LaVeist and Wallace 2000 ; Scribner et al. 2000 ; Shimotsu et al. 2013 ; Theall et al. 2011 ). Spatial relations between alcohol outlets and individual consumption also may be a key to explaining differential rates in alcohol use across racial/ethnic groups. A number of studies suggest that minority communities have higher concentrations of liquor stores than White communities ( Alaniz and Wilkes 1998 ; LaVeist and Wallace 2000 ; Pollack et al. 2005 ; Romley et al. 2007 ; Treno et al. 2000 ), potentially increasing access to alcohol among minority populations ( Freisthler et al. 2015 ; Scribner et al. 2000 ). Moreover, living in a disadvantaged neighborhood at an early age has long-term effects. Childhood exposure to violence leads to increased exposure to delinquent peers and alcohol use ( Trucco et al. 2014 ). In another study, realizing how easy it is to get alcohol, witnessing neighborhood drug dealing, and seeing peers drink were all associated with increased alcohol use ( Chung et al. 2014 ).
Relating neighborhood characteristics to alcohol use risk is useful for public health program planning because it allows policymakers and programmers to understand how changing structural-level factors of the built environment may affect health risk behaviors, including alcohol use. However, methodological challenges remain when analyzing the impact of complex community factors on individual behaviors. Such factors include social stratification (i.e., the probability of living in certain neighborhoods, which is higher for certain types of persons) and social selection (i.e., the probability that drinkers are more likely to move to certain types of neighborhoods). It remains unclear whether neighborhood disadvantage causes alcohol problems, and whether frequent drinkers are in fact usually more attracted to certain neighborhoods (i.e., self-selection). These challenges limit the interpretation of research on community-level effects. Some studies have attempted to address these issues using propensity matching and time-sensitive indicators ( Ahern et al. 2008 ). Future studies should take these challenges into consideration and address subgroup differences in alcohol use norms across race/ethnicity and gender.
Cultural Norms
Cultural norms and beliefs are strong predictors of both current drinking and frequent heavy drinking ( Brooks-Russell et al. 2013 ; Caetano and Clark 1999 ; LaBrie et al. 2012 ; O’Grady et al. 2011 ; Paschall et al. 2012 ). Across race and ethnicity, African Americans and Latinos report more conservative attitudes toward drinking compared with Whites ( Caetano and Clark 1999 ; LaBrie et al. 2012 ). These more conservative norms may be associated with lower drinking rates among African Americans and Latinos compared with Whites ( SAMHSA 2013 ). Few studies have examined diversity within racial and ethnic groups such as Latinos, Blacks, and Asians, limiting our ability to meet the needs of specific subpopulations. Some studies suggest that alcohol-related problems differ substantially across Latino subgroups, including higher rates of alcohol abuse and dependence among Mexican-American and Puerto Rican men compared with Cuban Americans and Central and South Americans ( Caetano et al. 2008 ). These findings may best be explained by considerable differences in cultural norms, especially the cultural beliefs regarding appropriate alcohol use ( Greenfield and Room 1997 ; LaBrie et al. 2012 ). For example, some scholars explain heavy-drinking patterns among Latino men through the concept of machismo , which has been a significant cultural influence for generations and remains integral to Latino male identity ( Dolezal et al. 2000 ). Machismo suggests that Latino men attempt to appear strong and masculine because of cultural values, and drinking greater amounts of alcohol further exemplifies their masculinity. More recently, scholars have commented that concepts like machismo cannot account for the complexity of Latino drinking behavior ( Caetano 1990 ).
Asians, on the other hand, generally are thought to have higher abstention rates compared with other racial and ethnic groups, especially when they are integrated within their ethnic cultures ( Cook et al. 2012 ). One measure of the retention of ethnic values and cultural norms is generation status. That is, the longer immigrants have lived in the United States, the more likely they are to acculturate to the cultural norms of their destination community ( Berry et al. 2006 ). Lower levels of ethnic identity may be one explanation for these differences across Asian subgroups. Japanese Americans, Filipino Americans, and Korean Americans often have been in the United States longer than other Asian subgroups, such as Cambodians, Thais, and Vietnamese, and also report higher levels of alcohol use compared with other Asian Americans and Asian immigrants ( Iwamoto et al. 2012 ). Ethnic identity may promote stronger family values and traditional ties, leading to lower levels of alcohol use. Moreover, Asian-American adolescents who have a high attachment to family or who share their family’s negative attitudes toward drinking are less likely to consume alcohol ( Hahm et al. 2003 ).
Cultural norms also vary by context and place. Some alcohol researchers have used multilevel approaches to distinguish among the causal effects of individual and neighborhood-level norms. For example, Ahern and colleagues (2008) found that neighborhood norms against drunkenness were a more robust and stronger predictor of binge drinking than permissive beliefs about it held either by the individual or family and friends. If an individual lived in a neighborhood that frowns on binge drinking, that individual was less likely to drink, even if he or she believed it acceptable to do so. This was particularly true for women, suggesting gender norms around alcohol use may be a factor.
Specifically, past studies found that gender differences in alcohol use may reflect the greater social stigma directed at women who drink. This seems to be more pronounced in certain cultures. Caetano and Clark (1999) , for example, found stronger gender norms related to alcohol use in Latino cultures compared with the United States ( Kulis et al. 2012 ). This results in greater gender differences in alcohol use among Latinos compared with other U.S. populations, with recent trends suggesting similar levels of binge drinking between men and women in Western cultures ( Iwamoto et al. 2012 ). This may reflect changing beliefs about gender and social status. Although traditionally perceived as a “masculine” behavior, binge drinking is now more acceptable among women in certain cultures that foster more balanced gender roles ( Lyons and Willott 2008 ).
Family and Peer Influences on Adolescent and Young Adult Drinking
Some of the strongest influences on adolescent drinking behavior come from the people that youth spend the most time with: family and friends. Studies have found that higher levels of alcohol use among parents and peers is associated with increased alcohol use among adolescents and young adults ( Cruz et al. 2012 ; Dawson 2000 ; Mares et al. 2011 ; Osgood et al. 2013 ; Trucco et al. 2014 ; Varvil-Weld et al. 2014 ; Wallace et al. 1999 ; Walsh et al. 2014 ; Williams and Smith 1993 ). Developmentally, people’s social contexts shift from the family unit during childhood to focus more on their peers and their schools during adolescence. Reflecting this, parental alcohol use seems to exert a greater influence before age 15 and diminishes over time ( Dawson 2000 ).
Conversely, family support, bonding, and parental monitoring is associated with lower alcohol use ( Bahr et al. 1995 ; White et al. 2006 ) and social networks and social support also have protective effects ( Ramirez et al. 2012 ). For example, one study that assessed the effects of leaving home and attending college found that although the transition overall was associated with higher levels of alcohol use, young people with fewer friends who use alcohol reported higher levels of religiosity. Higher parental monitoring also protected against alcohol and marijuana use ( White et al. 2006 ). Moreover, higher levels of familism (values that place family needs over individual needs) and being in a nuclear family served as protective factors among adolescents ( Ewing et al. 2015 ).
Peer norms play an important role at this life stage ( Jackson et al. 2014 ). By the late adolescent period, parental influences related to alcohol use are small compared with peer influences ( Schwinn and Schinke 2014 ; Zehe and Colder 2014 ). Much of the focus on peer influences has highlighted the risk networks associated with alcohol use. Peer pressure ( Studer et al. 2014 ), peer alcohol norms ( Varvil-Weld et al. 2014 ), and socializing with substance-using peers ( Patrick et al. 2013 ) were associated with alcohol misuse and binge drinking. Studies note that leaving the home environment, entering college, and joining Greek organizations increased alcohol use as a result of more socially permissive norms around drinking ( Scott-Sheldon et al. 2008 ; White et al. 2006 ).
More recent studies have attempted to assess the synergistic influence of peers and families. Whereas the majority of studies on peers have focused on the negative consequences of social networks, research shows that greater parental support and monitoring can lead to prosocial peer affiliations ( Williams et al. 2015 ). One study found that protective influences in parental domains can moderate the negative effects of negative peer influences among Latino college students ( Varvil-Weld et al. 2014 ). In particular, maternal communication resulted in less alcohol use; conversely, maternal permissive norms and peer norms were associated with more alcohol use. Greater parental disapproval toward alcohol use is associated with lower involvement in peer networks that use alcohol, less peer influence to use, and greater self-efficacy and stronger negotiation skills to avoid alcohol ( Nash et al. 2005 ). Interventions aimed at establishing and fostering conservative peer norms were found to be more effective than individual resistance training ( Hansen and Graham 1991 ), whereas multilevel interventions incorporating peers, families, and communities are known to be effective among adolescents ( Chapman et al. 2013 ; Perry et al. 2002 ; Toumbourou et al. 2013 ).
Existing successful interventions to reduce alcohol use include incorporating culturally sensitive delivery models, such as employing community health workers among Latino populations (Ornelas et al. 2014) and using Web-based interventions to change norms ( Patrick et al. 2014 ). In a recent review, Familias: Preparando la Nueva Generación, a culturally grounded intervention for parents to support Mexican-heritage youth, showed reductions in parental drinking ( Williams et al. 2015 ). Because past studies show that parents may potentially moderate negative peer influence, fostering synergistic solutions between multiple contexts should be a priority ( Ewing et al. 2015 ).
Directions for Future Research
This article highlights examples of how societal factors, cultural norms, neighborhoods, and social contexts may be associated with alcohol misuse. Certain gaps in the literature clearly remain. Methodologically, these findings should be interpreted with caution, because it is difficult to distinguish between and among societal and community-level influences. Future studies should use advanced statistical methods such as multilevel modeling techniques, based on theoretical and conceptual approaches in population health. In addition, longitudinal data will help support causal hypotheses and relationships.
Risk and protective factors, prosocial peer affiliations, and synergistic relationships between social contexts are worth further research. Among immigrants, retaining the cultural values of the country of origin has shown to have protective influences on alcohol use, and this finding should be incorporated into future interventions for immigrant populations. Focusing on risk and protective factors will help inform future programs addressing alcohol initiation, specifically helping parents and communities understand how they may influence alcohol use among adolescents and young adults.
Alcohol research should also more actively acknowledge new social contexts among youth culture. A better understanding of the influence online social networking sites and new media have on alcohol use is particularly important among adolescent populations, and this should be explored more fully in future studies.
Developmentally appropriate strategies are needed to delay initiation of alcohol use, because the family environment may be less influential compared with the influence of peers, social norms, and media among older adolescents and young adults. Future interventions should focus on multiple levels of societal environments, from the community to the individual level.
Finally, given the changing demographic landscape of the United States, including a larger and more diverse immigrant population, interventions and treatment options should also reflect the growing needs of certain groups. However, studies have found that focusing only on changing social norms is insufficient, and that broader interventions that influence multiple levels of an individual’s environment, such as family and schools, may have greater impact. Alcohol education programs need to also address individual intent and motivations while offering personalized feedback and protective behavioral strategies ( Patrick et al. 2014 ). Public health and treatment programs need to be culturally sensitive, paying particular attention to cultural factors such as ethnic identification and orientation.
Financial Disclosure
The authors declare that they have no competing financial interests.
- Ahern J, Galea S, Hubbard A, et al. “Culture of drinking” and individual problems with alcohol use. American Journal of Epidemiology. 2008; 167 (9):1041–1049. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alaniz ML, Wilkes C. Pro-drinking messages and message environments for young adults: The case of alcohol industry advertising in African American, Latino, and Native American communities. Journal of Public Health Policy. 1998; 19 (4):447–472. [ PubMed ] [ Google Scholar ]
- Albers AB, DeJong W, Naimi TS, et al. The relationship between alcohol price and brand choice among underage drinkers: Are the most popular alcoholic brands consumed by youth the cheapest? Substance Use & Misuse. 2014; 49 (13):1833–1843. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bahr SJ, Marcos AC, Maughan SL. Family, educational and peer influences on the alcohol use of female and male adolescents. Journal of Studies on Alcohol. 1995; 56 (4):457–469. [ PubMed ] [ Google Scholar ]
- Barry AE, Johnson E, Rabre A, et al. Underage access to online alcohol marketing content: A YouTube case study. Alcohol and Alcoholism. 2015; 50 (1):89–94. [ PubMed ] [ Google Scholar ]
- Berkman LF, Kawachi I. Social Epidemiology. 1st ed. New York: Oxford University Press; 2000. [ Google Scholar ]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000; 51 (6):843–857. [ PubMed ] [ Google Scholar ]
- Bernstein KT, Galea S, Ahern J, et al. The built environment and alcohol consumption in urban neighborhoods. Drug and Alcohol Dependence. 2007; 91 (2–3):244–252. [ PubMed ] [ Google Scholar ]
- Berry JW. Immigration, acculturation, and adaptation. Applied Psychology. 1997; 46 (1):5–34. [ Google Scholar ]
- Berry JW, Phinney JS, Sam DL, Vedder P. Immigrant youth: Acculturation, identity, and adaptation. Applied Psychology. 2006; 55 (3):303–332. [ Google Scholar ]
- Borrell LN, Jacobs DR, Jr, Williams DR, et al. Self-reported racial discrimination and substance use in the Coronary Artery Risk Development in Adults Study. American Journal of Epidemiology. 2007; 166 (9):1068–1079. [ PubMed ] [ Google Scholar ]
- Bouchery EE, Harwood HJ, Sacks JJ, et al. Economic costs of excessive alcohol consumption in the U.S., 2006. American Journal of Preventive Medicine. 2011; 41 (5):516–524. [ PubMed ] [ Google Scholar ]
- Boynton MH, O’Hara RE, Covault J, et al. A mediational model of racial discrimination and alcohol-related problems among African American college students. Journal of Studies on Alcohol and Drugs. 2014; 75 (2):228–234. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bronfenbrenner U. International Encyclopedia of Education. 2nd ed. Oxford, UK: Elsevier; 1994. Ecological models of human development; pp. 1643–1647. [ Google Scholar ]
- Brooks-Russell A, Simons-Morton B, Haynie D, et al. Longitudinal relationship between drinking with peers, descriptive norms, and adolescent alcohol use. Prevention Science. 2013; 15 (4):497–505. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown JM, Council CL, Penne MA, Gfroerer JC. Immigrants and substance use: Findings from the 1999–2001 National Surveys on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration (SAMHSA); 2005. (DHHS Publication No. SMA 04-3909, Analytic Series A-23) [ Google Scholar ]
- Bui HN. Racial and ethnic differences in the immigrant paradox in substance use. Journal of Immigrant and Minority Health. 2012; 15 (5):866–881. [ PubMed ] [ Google Scholar ]
- Caetano R. Acculturation and drinking patterns among U. S. Hispanics. British Journal of Addiction. 1987; 82 (7):789–799. [ PubMed ] [ Google Scholar ]
- Caetano R. Hispanic drinking in the US: Thinking in new directions. British Journal of Addictions. 1990; 85 :1231–1236. [ PubMed ] [ Google Scholar ]
- Caetano R, Clark CL. Trends in situational norms and attitudes toward drinking among whites, blacks, and Hispanics: 1984–1995. Drug and Alcohol Dependence. 1999; 54 (1):45–56. [ PubMed ] [ Google Scholar ]
- Caetano R, Ramisetty-Milker S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): Rates and predictors of alcohol abuse and dependence across Hispanic national groups. Journal of Studies on Alcohol and Drugs. 2008; 69 (3):441–448. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention (CDC) CDC—Data, Trends and Maps—Alcohol. Atlanta: CDC; 2014. [Accessed June 22, 2015]. Available at: http://www.cdc.gov/alcohol/data-stats.htm . [ Google Scholar ]
- Chae DH, Takeuchi DT, Barbeau EM, et al. Alcohol disorders among Asian Americans: Associations with unfair treatment, racial/ethnic discrimination, and ethnic identification (the national Latino and Asian Americans study, 2002–2003. Journal of Epidemiology and Community Health. 2008; 62 (11):973–979. [ PubMed ] [ Google Scholar ]
- Chapman RL, Buckley L, Sheehan M, Shochet I. School-based programs for increasing connectedness and reducing risk behavior: A systematic review. Educational Psychology Review. 2013; 25 (1):95–114. [ Google Scholar ]
- Chung T, Pedersen SL, Kim KH, et al. Racial differences in type of alcoholic beverage consumed during adolescence in the Pittsburgh Girls Study. Alcoholism: Clinical and Experimental Research. 2014; 38 (1):285–293. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cohen DA, Ghosh-Dastidar B, Scribner R, et al. Alcohol outlets, gonorrhea, and the Los Angeles civil unrest: A longitudinal analysis. Social Science & Medicine. 2006; 62 (12):3062–3071. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Conger JJ. Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956; 17 (2):296–305. [ PubMed ] [ Google Scholar ]
- Cook SH, Bauermeister JA, Gordon-Messer D, Zimmerman MA. Online network influences on emerging adults’ alcohol and drug use. Journal of Youth and Adolescence. 2013; 42 (11):1674–1686. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cook WK, Karriker-Jaffe KJ, Bond J, Lui C. Asian American problem drinking trajectories during the transition to adulthood: Ethnic drinking cultures and neighborhood contexts. American Journal of Public Health. 2014; 105 (5):1020–1027. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cook WK, Mulia N, Karriker-Jaffe K. Ethnic drinking cultures and alcohol use among Asian American adults: Findings from a national survey. Alcohol and Alcoholism. 2012; 47 (3):340–348. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cruz JE, Emery RE, Turkheimer E. Peer network drinking predicts increased alcohol use from adolescence to early adulthood after controlling for genetic and shared environmental selection. Developmental Psychology. 2012; 48 (5):1390–1402. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dawson DA. The link between family history and early onset alcoholism: Earlier initiation of drinking or more rapid development of dependence? Journal of Studies on Alcohol. 2000; 61 (5):637–646. [ PubMed ] [ Google Scholar ]
- Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: Modifying effects of gender and vulnerability. Alcohol and Alcoholism. 2005; 40 (5):453–460. [ PubMed ] [ Google Scholar ]
- Dolezal C, Carballo-Diéguez A, Nieves-Rosa L, Díaz F. Substance use and sexual risk behavior: Understanding their association among four ethnic groups of Latino men who have sex with men. Journal of Substance Abuse. 2000; 11 (4):323–336. [ PubMed ] [ Google Scholar ]
- Dubowitz T, Bates LM, Acevedo-Garcia D. The Latino health paradox: Looking at the intersection of sociology and health. In: Bird CE, Conrad P, Fremont AM, editors. Handbook of Medical Sociology. 6th ed. Nashville, TN: Vanderbilt University Press; 2010. [Accessed June 22, 2015]. pp. 106–123. Available at: http://www.rand.org/pubs/external_publications/EP50222.html . [ Google Scholar ]
- Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2011. Morbidity and Mortality Weekly Report Surveillance Summaries. 2012; 61 (4):1–162. [ PubMed ] [ Google Scholar ]
- Ewing BA, Osilla KC, Pedersen ER, et al. Longitudinal family effects on substance use among an at-risk adolescent sample. Addictive Behaviors. 2015; 41 :185–191. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Freisthler B, Lipperman-Kreda S, Bersamin M, Gruenewald PJ. Tracking the when, where, and with whom of alcohol use: Integrating ecological momentary assessment and geospatial data to examine risk for alcohol-related problems. Alcohol Research: Current Reviews. 2015; 36 (1):29–38. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fuligni AJ. Convergence and divergence in the developmental contexts of immigrants to the United States. In: Schaie W, Elder G, editors. Historical Influences on Lives and Aging. New York: Springer; 2004. pp. 89–98. [ Google Scholar ]
- Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiologic Reviews. 2004; 26 (1):36–52. [ PubMed ] [ Google Scholar ]
- Gee GC, Delva J, Takeuchi DT. Relationships between self-reported unfair treatment and prescription medication use, illicit drug use, and alcohol dependence among Filipino Americans. American Journal of Public Health. 2007; 97 (5):933–940. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gibbons FX, Gerrard M, Cleveland MJ, et al. Perceived discrimination and substance use in African American parents and their children: A panel study. Journal of Personality and Social Psychology. 2004; 86 (4):517–529. [ PubMed ] [ Google Scholar ]
- Grant BF, Dawson DA, Stinson FS, et al. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004; 74 (3):223–234. [ PubMed ] [ Google Scholar ]
- Greenfield TK, Room R. Situational norms for drinking and drunkenness: trends in the US adult population, 1979–1990. Addiction. 1997; 92 (1):33–47. [ PubMed ] [ Google Scholar ]
- Grenard JL, Dent CW, Stacy AW. Exposure to alcohol advertisements and teenage alcohol-related problems. Pediatrics. 2013; 131 (2):e369–e379. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grieco EM, Acost YD, de la Cruz GP, et al. The Foreign-born Population in the United States: 2010, American Community Survey Reports. Washington, DC: U.S. Bureau of the Census; 2012. [Accessed June 22, 2015]. Available at: http://www.census.gov/prod/2012pubs/acs-19.pdf . [ Google Scholar ]
- Hahm HC, Lahiff M, Guterman NB. Acculturation and parental attachment in Asian-American adolescents’ alcohol use. Journal of Adolescent Health. 2003; 33 (2):119–129. [ PubMed ] [ Google Scholar ]
- Hansen WB, Graham JW. Preventing alcohol, marijuana, and cigarette use among adolescents: Peer pressure resistance training versus establishing conservative norms. Preventive Medicine. 1991; 20 (3):414–430. [ PubMed ] [ Google Scholar ]
- Hastings G, Anderson S, Cooke E, Gordon R. Alcohol marketing and young people’s drinking: A review of the research. Journal of Public Health Policy. 2005; 26 (3):296–311. [ PubMed ] [ Google Scholar ]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin. 2009; 135 (5):707–730. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Herd D. Changes in the prevalence of alcohol in rap music lyrics 1979–2009. Substance Use & Misuse. 2013; 49 (3):333–342. [ PubMed ] [ Google Scholar ]
- Hoffman EW, Pinkleton BE, Weintraub Austin E, Reyes-Velázquez W. Exploring college students’ use of general and alcohol-related social media and their associations with alcohol-related behaviors. Journal of American College Health. 2014; 62 (5):328–335. [ PubMed ] [ Google Scholar ]
- Huckle T, You RQ, Casswell S. Socio-economic status predicts drinking patterns but not alcohol-related consequences independently. Addiction. 2010; 105 (7):1192–1202. [ PubMed ] [ Google Scholar ]
- Iwamoto D, Takamatsu S, Castellanos J. Binge drinking and alcohol-related problems among U.S.-born Asian Americans. Cultural Diversity & Ethnic Minority Psychology. 2012; 18 (3):219–227. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jackson KM, Roberts ME, Colby SM, et al. Willingness to drink as a function of peer offers and peer norms in early adolescence. Journal of Studies on Alcohol and Drugs. 2014; 75 (3):404–414. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jernigan DH, Ostroff J, Ross C. Alcohol advertising and youth: A measured approach. Journal of Public Health Policy. 2005; 26 (3):312–325. [ PubMed ] [ Google Scholar ]
- Kann L, Kinchen S, Shanklin S, et al. Atlanta: Centers for Disease Control and Prevention (CDC); 2014. [Accessed June 22, 2015]. Youth Risk Behavior Surveillance—United States, 2013. (Morbidity and Mortality Weekly Report). Available at: http://www.cdc.gov/mmwr/pdf/ss/ss6304.pdf?utm_source=rss&utm_medium=rss&utm_campaign=youth-risk-behavior-surveillance-united-states-2013-pdf . [ Google Scholar ]
- Koordeman R, Anschutz DJ, Engels RCME. The effect of alcohol advertising on immediate alcohol consumption in college students: An experimental study. Alcoholism: Clinical and Experimental Research. 2012; 36 (5):874–880. [ PubMed ] [ Google Scholar ]
- Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services: Planning, Administration, Evaluation. 1999; 29 (2):295–352. [ PubMed ] [ Google Scholar ]
- Krieger N. Theories for social epidemiology in the 21st century: An ecosocial perspective. International Journal of Epidemiology. 2001; 30 (4):668–677. [ PubMed ] [ Google Scholar ]
- Krieger N, Sidney S. Prevalence and health implications of anti-gay discrimination: A study of black and white women and men in the CARDIA cohort. Coronary Artery Risk Development in Young Adults. International Journal of Health Services: Planning, Administration, Evaluation. 1997; 27 (1):157–176. [ PubMed ] [ Google Scholar ]
- Krieger N, Sidney S, Coakley E. Racial discrimination and skin color in the CARDIA study: Implications for public health research. Coronary Artery Risk Development in Young Adults. American Journal of Public Health. 1998; 88 (9):1308–1313. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kulis S, Marsiglia FF, Nagoshi JL. Gender roles and substance use among mexican american adolescents: A relationship moderated by acculturation? Substance Use & Misuse. 2012; 47 (3):214–229. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kwate NOA, Meyer IH. Association between residential exposure to outdoor alcohol advertising and problem drinking among African American women in New York City. American Journal of Public Health. 2009; 99 (2):228–230. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- LaBrie JW, Atkins DC, Neighbors C, et al. Ethnicity specific norms and alcohol consumption among Hispanic/Latino/a and Caucasian students. Addictive Behaviors. 2012; 37 (4):573–576. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- LaVeist TA, Wallace JM., Jr Health risk and inequitable distribution of liquor stores in African American neighborhood. Social Science & Medicine. 2000; 51 (4):613–617. [ PubMed ] [ Google Scholar ]
- Lee CS, Colby SM, Rohsenow DJ, et al. Acculturation stress and drinking problems among urban heavy drinking Latinos in the Northeast. Journal of Ethnicity in Substance Abuse. 2013; 12 (4):308–320. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lenhart A. Teens, Social Media and Technology Overview 2015. Washington, DC: Pew Research Center; 2015. [ Google Scholar ]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995; 35 :80–94. [ PubMed ] [ Google Scholar ]
- Lyons AC, Willott SA. Alcohol consumption, gender identities and women’s changing social positions. Sex Roles. 2008; 59 (9–10):694–712. [ Google Scholar ]
- Mares SHW, van der Vorst H, Engels RCME, Lichtwarck-Aschoff A. Parental alcohol use, alcohol-related problems, and alcohol-specific attitudes, alcohol-specific communication, and adolescent excessive alcohol use and alcohol-related problems: An indirect path model. Addictive Behaviors. 2011; 36 (3):209–216. [ PubMed ] [ Google Scholar ]
- McCabe SE, Bostwick WB, Hughes TL, et al. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health. 2010; 100 (10):1946–1952. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McKee P, Jones-Webb R, Hannan P, Pham L. Malt liquor marketing in inner cities: the role of neighborhood racial composition. Journal of Ethnicity in Substance Abuse. 2011; 10 (1):24–38. [ PubMed ] [ Google Scholar ]
- Miller Brewing Company. Behavioral Tracking Study 2000. Milwaukee, WI: Miller Brewing Company; 2000. [ Google Scholar ]
- Molloy E. This ad is for you: Targeting and the effect of alcohol advertising on youth drinking. Health Economics. 2015 Jan 9; [Epub ahead of print] [ PubMed ] [ Google Scholar ]
- Moore H, Jones-Webb R, Toomey T, Lenk K. Alcohol advertising on billboards, transit shelters, and bus benches in inner-city neighborhoods. Contemporary Drug Problems. 2008; 35 (2/3):509. [ Google Scholar ]
- Morgenstern M, Sargent JD, Sweeting H, et al. Favourite alcohol advertisements and binge drinking among adolescents: A cross-cultural cohort study. Addiction. 2014; 109 (12):2005–2015. [ PubMed ] [ Google Scholar ]
- Mosher JF, Johnsson D. Flavored alcoholic beverages: An international marketing campaign that targets youth. Journal of Public Health Policy. 2005; 26 (3):326–342. [ PubMed ] [ Google Scholar ]
- Mulia N, Ye Y, Zemore SE, Greenfield TK. Social disadvantage, stress, and alcohol use among Black, Hispanic, and White Americans: Findings from the 2005 U.S. National Alcohol Survey. Journal of Studies on Alcohol and Drugs. 2008; 69 (6):824–833. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nash SG, McQueen A, Bray JH. Pathways to adolescent alcohol use: Family environment, peer influence, and parental expectations. Journal of Adolescent Health. 2005; 37 (1):19–28. [ PubMed ] [ Google Scholar ]
- Nhean S, Nyborn J, Hinchey D, et al. The frequency of company-sponsored alcohol brand-related sites on Facebook TM —2012. Substance Use & Misuse. 2014; 49 (7):779–782. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- O’Grady MA, Cullum J, Tennen H, Armeli S. Daily relationship between event-specific drinking norms and alcohol use: A four-year longitudinal study. Journal of Studies on Alcohol and Drugs. 2011; 72 (4):633–641. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ornelas IJ, Allen C, Vaughan C, et al. Vida PURA: A cultural adaptation of screening and brief intervention to reduce unhealthy drinking among Latino day laborers. Substance Abuse. 2015; 36 (3):264–271. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Osgood DW, Ragan DT, Wallace L, et al. Peers and the emergence of alcohol use: Influence and selection processes in adolescent friendship networks. Journal of Research on Adolescence. 2013; 23 (3):500–512. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006; 35 (4):888–901. [ PubMed ] [ Google Scholar ]
- Paschall MJ, Grube JW, Thomas S, et al. Relationships between local enforcement, alcohol availability, drinking norms, and adolescent alcohol use in 50 California cities. Journal of Studies on Alcohol and Drugs. 2012; 73 (4):657–665. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009; 135 (4):531–554. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Patrick ME, Lee CM, Neighbors C. Web-based intervention to change perceived norms of college student alcohol use and sexual behavior on spring break. Addictive Behaviors. 2014; 39 (3):600–606. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Patrick ME, Schulenberg JE, Martz ME, et al. Extreme binge drinking among 12th-grade students in the United States: Prevalence and predictors. JAMA Pediatrics. 2013; 167 (11):1019–1025. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Perry CL, Williams CL, Komro KA, et al. Project Northland: Long-term outcomes of community action to reduce adolescent alcohol use. Health Education Research. 2002; 17 (1):117–132. [ PubMed ] [ Google Scholar ]
- Pollack CE, Cubbin C, Ahn D, Winkleby M. Neighbourhood deprivation and alcohol consumption: Does the availability of alcohol play a role? International Journal of Epidemiology. 2005; 34 (4):772–780. [ PubMed ] [ Google Scholar ]
- Ramirez R, Hinman A, Sterling S, et al. Peer influences on adolescent alcohol and other drug use outcomes. Journal of Nursing Scholarship. 2012; 44 (1):36–44. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009; 373 (9682):2223–2233. [ PubMed ] [ Google Scholar ]
- Reingle JM, Caetano R, Mills BA, Vaeth PAC. The role of immigration age on alcohol and drug use among border and non-border Mexican Americans. Alcoholism: Clinical and Experimental Research. 2014; 38 (7):2080–2086. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Roberts SP, Siegel MB, DeJong W, Jernigan DH. A comparison between brand-specific and traditional alcohol surveillance methods to assess underage drinkers’ reported alcohol use. American Journal of Drug and Alcohol Abuse. 2014; 40 (6):447–454. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Romley JA, Cohen D, Ringel J, Sturm R. Alcohol and environmental justice: The density of liquor stores and bars in urban neighborhoods in the United States. Journal of Studies on Alcohol and Drugs. 2007; 68 (1):48–55. [ PubMed ] [ Google Scholar ]
- Ross CS, Maple E, Siegel M, et al. The relationship between population-level exposure to alcohol advertising on television and brand-specific consumption among underage youth in the US. Alcohol and Alcoholism. 2015; 50 (3):358–364. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rumbaut RG. Ages, life stages, and generational cohorts: Decomposing the immigrant first and second generations in the United States. International Migration Review. 2004; 38 (3):1160–2105. [ Google Scholar ]
- Sanchez M, De La Rosa M, Blackson TC, et al. Pre- to postimmigration alcohol use trajectories among recent Latino immigrants. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2014; 28 (4):990–999. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schwartz SJ, Unger JB, Des Rosiers SE, et al. Substance use and sexual behavior among recent Hispanic immigrant adolescents: Effects of parent- adolescent differential acculturation and communication. Drug and Alcohol Dependence. 2012; 125 (Suppl 1):S26–34. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schwinn TM, Schinke SP. Alcohol use and related behaviors among late adolescent urban youth: Peer and parent influences. Journal of Child & Adolescent Substance Abuse. 2014; 23 (1):58–64. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scott-Sheldon LAJ, Carey KB, Carey MP. Health behavior and college students: Does Greek affiliation matter? Journal of Behavioral Medicine. 2008; 31 (1):61–70. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scribner RA, Cohen DA, Fisher W. Evidence of a structural effect for alcohol outlet density: A multilevel analysis. Alcoholism: Clinical and Experimental Research. 2000; 24 (2):188–195. [ PubMed ] [ Google Scholar ]
- Shimotsu ST, Jones-Webb RJ, MacLehose RF, et al. Neighborhood socioeconomic characteristics, the retail environment, and alcohol consumption: A multilevel analysis. Drug and Alcohol Dependence. 2013; 132 (3):449–456. [ PubMed ] [ Google Scholar ]
- Snyder LB, Milici FF, Slater M, et al. Effects of alcohol advertising exposure on drinking among youth. Archives of Pediatrics & Adolescent Medicine. 2006; 160 (1):18–24. [ PubMed ] [ Google Scholar ]
- Studer J, Baggio S, Deline S, et al. Peer pressure and alcohol use in young men: A mediation analysis of drinking motives. International Journal on Drug Policy. 2014; 25 (4):700–708. [ PubMed ] [ Google Scholar ]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Rockville, MD: SAMHSA, Center for Behavioral Health Statistics and Quality; 2013. [Accessed June 22, 2015]. National Survey on Drug Use and Health, 2011 and 2012. Available at: http://media.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/DetTabs/NSDUH-DetTabsSect2peTabs1to42-2012.htm#Tab2.1A . [ Google Scholar ]
- Szaflarski M, Cubbins LA, Ying J. Epidemiology of alcohol abuse among US immigrant populations. Journal of Immigrant and Minority Health. 2011; 13 (4):647–658. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Takeuchi DT, Hong S, Gile K, Alegría M. Developmental contexts and mental disorders among Asian Americans. Research in Human Development. 2007; 4 (1):49. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tanski SE, McClure AC, Li Z, et al. Cued recall of alcohol advertising on television and underage drinking behavior. JAMA Pediatrics. 2015; 169 (3):264–271. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Theall KP, Lancaster BP, Lynch S, et al. The neighborhood alcohol environment and at-risk drinking among African-Americans. Alcoholism: Clinical and Experimental Research. 2011; 35 (5):996–1003. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Toumbourou JW, Gregg MED, Shortt AL, et al. Reduction of adolescent alcohol use through family–school intervention: A randomized trial. Journal of Adolescent Health. 2013; 53 (6):778–784. [ PubMed ] [ Google Scholar ]
- Treno AJ, Alaniz ML, Gruenewald PJ. The use of drinking places by gender, age and ethnic groups: An analysis of routine drinking activities. Addiction. 2000; 95 (4):537–551. [ PubMed ] [ Google Scholar ]
- Trucco EM, Colder CR, Wieczorek WF, et al. Early adolescent alcohol use in context: How neighborhoods, parents, and peers impact youth. Development and Psychopathology. 2014; 26 (2):425–436. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Unger JB, Schwartz SJ, Huh J, et al. Acculturation and perceived discrimination: Predictors of substance use trajectories from adolescence to emerging adulthood among Hispanics. Addictive Behaviors. 2014; 39 (9):1293–1296. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vaeth PAC, Caetano R, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): The association between acculturation, birthplace and alcohol consumption across Hispanic national groups. Addictive Behaviors. 2012; 37 (9):1029–1037. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Valencia EY, Johnson V. Acculturation among Latino youth and the risk for substance use: Issues of definition and measurement. Journal of Drug Issues. 2008; 38 (1):37–68. [ Google Scholar ]
- Varvil-Weld L, Turrisi R, Hospital MM, et al. Maternal and peer influences on drinking among Latino college students. Addictive Behaviors. 2014; 39 (1):246–252. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wallace JM, Jr, Forman TA, Guthrie BJ, et al. The epidemiology of alcohol, tobacco and other drug use among black youth. Journal of Studies on Alcohol. 1999; 60 (6):800–809. [ PubMed ] [ Google Scholar ]
- Walsh SD, Djalovski A, Boniel-Nissim M, Harel-Fisch Y. Parental, peer and school experiences as predictors of alcohol drinking among first and second generation immigrant adolescents in Israel. Drug and Alcohol Dependence. 2014; 138 :39–47. [ PubMed ] [ Google Scholar ]
- Walters KL, Simoni JM, Evans-Campbell T. Substance use among American Indians and Alaska natives: Incorporating culture in an “indigenist” stress-coping paradigm. Public Health Reports. 2002; 117 (Suppl 1):S104–S117. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- White HR, McMorris BJ, Catalano RF, et al. Increases in alcohol and marijuana use during the transition out of high school into emerging adulthood: The effects of leaving home, going to college, and high school protective factors. Journal of Studies on Alcohol. 2006; 67 (6):810–822. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009; 32 (1):20–47. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams JG, Smith JP. Alcohol and other drug use among adolescents: Family and peer influences. Journal of Substance Abuse. 1993; 5 (3):289–294. [ PubMed ] [ Google Scholar ]
- Williams LR, Marsiglia FF, Baldwin A, Ayers S. Unintended effects of an intervention supporting Mexican-heritage youth: Decreased parent heavy drinking. Research on Social Work Practice. 2015; 25 :181–189. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wilson RT, Till BD. Targeting of outdoor alcohol advertising: A study across ethnic and income groups. Journal of Current Issues & Research in Advertising. 2012; 33 (2):267–281. [ Google Scholar ]
- World Health Organization (WHO) WHO Global Status Report on Alcohol and Health 2014. Geneva: WHO; [Accessed August 18, 2015]. Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/en/ [ Google Scholar ]
- Yoo HC, Gee GC, Lowthrop CK, Robertson J. Self-reported racial discrimination and substance use among Asian Americans in Arizona. Journal of Immigrant and Minority Health/Center for Minority Public Health. 2010; 12 (5):683–690. [ PubMed ] [ Google Scholar ]
- Zehe JM, Colder CR. A latent growth curve analysis of alcohol-use specific parenting and adolescent alcohol use. Addictive Behaviors. 2014; 39 (12):1701–1705. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zemore SE. Acculturation and alcohol among Latino adults in the United States: A comprehensive review. Alcoholism: Clinical and Experimental Research. 2007; 31 (12):1968–1990. [ PubMed ] [ Google Scholar ]

IMAGES
COMMENTS
Epidemiological studies concerning the health effect of alcohol might greatly benefit from taking into consideration the patterns of alcohol drinking, which are a function of cultural differences from region to region, and country to country (e.g., British or American pub culture versus Italian or Spanish wine drinking at meals).
Alcohol Health & Research World. 1994; 18 (3):243-248. [PMC free article] [Google Scholar] Harford TC, Grant BF, Hasin DS. Effect of average daily consumption and frequency of intoxication on the occurrence of dependence symptoms and alcohol-related problems. In: Clark WB, Hilton ME, editors. Alcohol in America: Drinking Practices and Problems.
Various research studies conducted over many years clearly show the association of prolonged alcohol intake in the causation, aggravation, worsening, and deterioration of the health of its consumers. ... be it acute or chronic. Heavy alcohol drinking is shown to impact the cardiovascular system in many ways, one of the most important among them ...
Alcohol is an established carcinogen and alcohol consumption increases the risk of several cancers, including breast, liver, head and neck, oesophageal and colorectal cancers. In 2019, 4.4% of cancers diagnosed globally and 401 000 cancer deaths were attributed to alcohol consumption. Alcohol consumption also causes significant harm to others ...
In addition to negative affect and coping motives for drinking, research has focused on changes to the social context of alcohol use to understand mechanisms for changes in alcohol use during the ...
Background: Excessive alcohol consumption has negative effects not only on the drinkers' health but also on others around them. Previous studies suggest that excessive alcohol consumption can be related to a combination of factors such as age, family background, religiosity, etc. Investigating and clarifying these roots of alcohol consumption is crucial so that the right type of ...
Science-based information on alcohol from NIAAA, including alcohol's effects on the brain and body, drinking levels, alcohol use disorder, and when to get help.
We also estimated the mean risk curve and 95% UI for the relationship between alcohol consumption and IHD using only data from cohort studies. In total, 95 cohort studies - of which one was a ...
Research on alcohol suggests a sobering conclusion: Drinking alcohol in any amount carries a health risk. While the risk is low for moderate intake, the risk goes up as the amount you drink goes up. Many people drink alcohol as a personal preference, during social activities, or as a part of cultural and religious practices.
Alcohol Research Resource (R24 and R28) Awards. Resources include biological specimens, animals, data, materials, tools, or services made available to any qualified investigato r to accelerate alcohol-related research in a cost-effective manner. Current and potential alcohol research investigators and trainees are encouraged to subscribe to our ...
We investigated the associations of alcohol consumption with 207 diseases in the 12-year China Kadoorie Biobank of >512,000 adults (41% men), including 168,050 genotyped for ALDH2- rs671 and ADH1B ...
Learn up-to-date facts and statistics on alcohol consumption and its impact in the United States and globally. Explore topics related to alcohol misuse and treatment, underage drinking, the effects of alcohol on the human body, and more. Find up-to-date statistics on lifetime drinking, past-year drinking, past-month drinking, binge drinking ...
Alcohol is known to be a direct cause of seven different cancers: head and neck cancers (oral cavity, pharynx and larynx), esophageal cancer, liver cancer, breast cancer and colorectal cancer ...
Abstract. Alcohol consumption is known to be an addiction that provides negative outcomes mainly on health, excessive drinking of alcohol brings adverse effects on human health, also on activities ...
Alcohol and drug use can lead to poor decision making, like breaking the law, sexual abuse, getting in fights, etc. Of the respondents, 92.4% were white and the average age was 22.3 years. This study found that a little more than 68% reported using alcohol and/or drugs during the past year.
alcohol poisoning — many people don't realize that if you drink enough alcohol over a short period of time, it can be fatal; ... There are important limitations to research on alcohol consumption. Most rely on self-reporting, do not analyze binge drinking, do not assess alcohol consumption over a lifetime, or do not account for the fact that ...
According to a large, population-based study by the National Institute on Alcohol Abuse and Alcoholism on alcohol drinking habits in the United States (the National Epidemiological Survey on Alcohol and Related Conditions: NESARC), approximately 65% of American adults report consuming alcohol (i.e., one or more drinks in the last 12-month period).
Introduction: Heavy drinking is a considerable public health concern. There is a broad evidence-base examining the separate contributions of personality characteristics, motives and alcohol-expectancies on subsequent alcohol use to identify those at risk. However, little is known about the complex relationships by which these variables may interact to predict drinking behavior.
Contact: Lori Fogleman, 254-709-5959 Follow us on X (Twitter): @BaylorUMedia While a general link between alcohol consumption and cardiovascular disease is well known, Baylor University researchers are digging into the "why" behind this detrimental association - especially after a night of binge drinking - in a study published in the American Heart Association's Hypertension journal.
Michael Golding receives funding through a Medical Research Grant from the W. M. Keck Foundation and a research grant from the NIH through the National Institute on Alcohol Abuse and Alcoholism ...
This shift in drinking behavior didn't occur by chance. Alcohol companies that once alienated women with ads suffused with sexist imagery are now marketing directly and more effectively to women, according to a 2020 report by investment research and brokerage firm Bernstein Research.
Drinking a glass of wine a day will not help you live longer, according to a new analysis of alcohol research that debunks a longstanding belief about the possible health benefits of drinking ...
"Alcohol is a carcinogen and contributes to about 50 different types of death," said Dr. Timothy Naimi, who directs the Canadian Institute for Substance Use Research at the University of ...
the extent of alcohol consumption and of the awareness of its negative effects on human health among secondary school students. The study used a cross-sectional survey design. Self-report questionnaire developed by the researchers was administered to representative sample (N = 1302) of secondary school students in the study area. The data collected from the respondents were analyzed using ...
Understanding the relationship between teenage drinking and high school grades is pertinent given the high prevalence of alcohol use among this age cohort and recent research on adolescent brain development suggesting that early heavy alcohol use may have negative effects on the physical development of brain structure (Brown, Tapert, Granholm ...
The mice chose when and how much alcohol to drink. We found that paternal and maternal drinking both cause harmful changes to their offspring's mitochondria. Mitochondria - often called the battery of the cell - control many aspects of aging and health. Like a cellphone battery, mitochondria deteriorate over time and cause cells to lose ...
Statistics & research He tatauranga, he rangahau expand_more; Topics A to Z Ngā kaupapa A ki te Z; Close. ... These alcohol factsheets outline New Zealand's drinking patterns and alcohol-related health, crime and violence, and drink driving. The 2007/08 New Zealand Alcohol and Drug Use Survey: Online data tables.
Michael Golding receives funding through a Medical Research Grant from the W. M. Keck Foundation and a research grant from the NIH through the National Institute on Alcohol Abuse and Alcoholism ...
Key points. People who choose not to drink alcohol in social situations where others are drinking often feel judged. Research points to three common reasons why drinkers may feel uncomfortable ...
The alcohol research literature is overwhelmingly focused on risk factors, from the societal level down to the individual. Worldwide, 3.3 million deaths were attributed to alcohol misuse in 2012 (World Health Organization 2014).Excessive alcohol use is the third leading cause of death in the United States, accounting for 88,000 deaths per year (Centers for Disease Control and Prevention 2014).