- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Feature stories /

Speaking out on the stigma of mental health

Persons with psychosocial disabilities frequently face stigma, discrimination and rights violations, including within and from the medical community, which reflects broader societal stigma. One doctor relates his personal experience here and how he uses it today to challenge stigma.
When Dr Ahmed Hankir first experienced extreme psychological distress as a medical student in the United Kingdom in 2006, he delayed seeking help due to the shame and stigma of having a mental health condition.
Exacerbating his distress was the added stigma of being a man of colour and a Muslim, which, with his mental health condition, made up what he calls a “triple whammy” of stigmas that he “internalized”. It led to him feeling “dehumanised”.
The stress and strains of working low-paid jobs to support himself as a student, and an outbreak of war in Lebanon, the country of his roots and where his parents were living, made matters worse. Meanwhile, he was living in a dilapidated house in one of the most dangerous areas of Manchester.
The intersectionality of these stressors – which added a “layer upon layer” – are often overlooked at the level of the individual, he said. Racism might be passed over. “It might be there is some gaslighting... so, you know, you are not a victim of racism.”
Hankir, who was born in Belfast when his parents fled the 1982 war in Lebanon, but later returned to Lebanon as a teenager, also said he had an identity crisis. “We want to be accepted, but I wasn't treated as British in the UK and I wasn't treated as Lebanese in Lebanon.”
Stigma “rampant” in the medical profession
Yet it was in his own profession that he felt the stigma of mental health most deeply, which led to the delay in seeking help. He was “ridiculed” by fellow medical students and ostracised by his closest companions. When he sought help from the person in charge of student support, a person who had the power to have him removed from his course, he was “psychologically tortured”. He was forced to temporarily interrupt his studies.
“Stigma is rampant in the medical profession. Unless we address it, it will continue to destroy and devastate the lives of many. We’re just scratching the surface now - I don’t know an expert in stigma. There is a lot of ignorance on how to deal with mental health,” he said.
Not only is there ignorance, but there is also arrogance from health providers, some of whom look down on people with mental health conditions and psychosocial disabilities, he said.
“It takes strength to accept that you might be a source of stigma. What we need is humility. But I’ve met inspirational, humble doctors who have contributed to my recovery and continue to contribute to my resilience.”
“My lived experience is my superpower”
Today, Hankir is a psychiatrist and he draws from his past: “My lived experience is my superpower. It’s a strength, not a weakness. It makes me more insightful, empathetic and driven.
“When I'm working in frontline psychiatry and I'm providing care for a person in a mental health crisis at 2am, I often draw on my personal expertise more than my professional expertise especially when attempting to develop a rapport and 'therapeutic alliance' with the person receiving care from me.”
He believes that many of his peers have also experienced psychological distress, but have chosen to remain silent about it. “I’m honest and open about my experience of living with a mental health condition. More people are talking about it. We normalize living with mental health conditions.”

Ahmed has won multiple awards for his “Wounded Healer” presentation, including from WHO in 2022. Photo credit: WHO/ Michelle Funk
Delivering the “Wounded Healer” presentation around the world
Hankir is now renowned for his “ Wounded Healer ” presentation, which aims to debunk myths and humanize people living with mental health conditions through blending performing arts and storytelling with psychiatry.
The Wounded Healer also traces Hankir’s recovery journey. “Speaking out on stigma helps to reduce it,” he explained. More than 100,000 people in 20 countries have heard him speak. In recognition of his work, Hankir received the 2022 World Health Organization Director-General Award for Global Health, among other awards.
He welcomes WHO’s Quality Rights Initiative, which takes an approach to mental health grounded on a human rights framework that empowers, dignifies and humanizes people with mental health conditions.
“Our human rights are being violated, regardless of time and place – high income country, low income country. Too many people feel like they have been brutalized,” he said. “When care is available, there are also concerns about the quality of care.”
He continues to face negativity from some psychiatrists, some of whom are “suspicious” of his success. “They accuse me of fabricating having a severe mental health condition. It is as if people living with severe mental health conditions can’t recover or excel, and can only ever think of survival. I was miserable for many years. But now I am not just surviving, I’m thriving,” he laughed.
A version of this story first appeared in the WHO Global report on health equity for persons with disabilities.
Understanding Mental Health Stigma: 17 Ways to Reduce It

If so, you know the discomfort, shame, and dehumanization that occurs.
Labeling others separates people based on actual or perceived differences. The stigma associated with being labeled aims at one’s identity and divides us and them .
The label linked to certain assumptions lingers, impacting impressions of the individual regardless of their behavior (Yanos, 2018).
The differentiation between us and them may seem minor. However, a closer look reveals the depth it reaches to the point of eroding social capital — the strength and benefits derived through societal cohesion.
This article discusses mental health stigma, its effects, and ways to reduce it.
Before you continue, we thought you might like to download our three Positive Relationships Exercises for free . These detailed, science-based exercises will help you or your clients build healthy, life-enriching relationships.
This Article Contains
Understanding mental health stigma, 2 real-life examples and statistics, 22 effects of stigma according to research, how to reduce mental health stigma, 8 questionnaires, questions, and scales, 5 activities, worksheets, and ideas, best books to educate yourself and others, resources from positivepsychology.com, a take-home message, frequently asked questions.
The definition for the word stigma includes a brand, a mark of disgrace or infamy, and a mark of censure (Dobson & Stuart, 2021).
According to Ritzer (2021, p. 162), “stigma is a person’s characteristic that others find, define, and often label as unusual, unpleasant, or deviant.”
Labels aim to show the individual as unpredictable, unreliable, and potentially dangerous (Dobson & Stuart, 2021). A label effectively applied creates fear and distance between society and the one who is labeled.
Brief history of mental health stigma
Mental illness goes back to the earliest human writings from ancient Israel, China, and Greece, explaining it as bad luck or being cursed.
More recently, Erving Goffman’s seminal work Asylums (1961) analyzed the treatment of patients in psychiatric facilities and showed the negative impact punitive treatment had on their mental health (Dobson & Stuart, 2021).
Goffman’s work revealed that labeling and stigmatization can have enduring, if not permanent, effects on patients (Dobson & Stuart, 2021).
Mental health stigma and discrimination
According to Philip Yanos (2018, p. 10), author of Written Off: Mental Health Stigma and the Loss of Human Potential , stigmatizing labels “diminish people’s participation in community life and inhibit them from achieving their full potential as people.”
Yanos views mental health stigma as a social injustice and suggests focusing on society’s adverse reactions instead of eradicating symptoms.
Stigmatization leads to discrimination.
Discrimination became lethal in 1939 when Hitler created the heinous T-4 program to euthanize residents of private hospitals, psychiatric institutions, nursing homes, and others with psychiatric or neurological disorders (Yanos, 2018).
Sadly, discrimination toward mental illness is still in news headlines, media representations, hiring practices, and structural norms.

Approximately 43.3% of US adults with mental illness will not receive help. They may avoid seeking treatment because they fear the label, stigma, and discrimination (Evans et al., 2023).
Simone Biles
As fervor for the 2021 Tokyo Olympics grew, finalists for the various teams were announced. Simone Biles was a top US gymnast with astounding strength and skills.
Soon after the Olympics began, it became clear that Biles was struggling. Citing a case of the twisties , she pulled out of the competition to tend to her mental health.
Biles returned to competition in 2023 after a two-year hiatus to win first place in the Core Hydration Classic (Holcombe, 2023).
Aaron Hernandez
The case of Aaron Hernandez is one of tragedy and missed opportunities. Hernandez found success playing football for the New England Patriots. Unfortunately, Aaron’s behavior spiraled out of control. He was ultimately found guilty of murder in 2015.
In 2017, Aaron committed suicide in jail. Autopsy results showed he suffered from chronic traumatic encephalopathy, a neurodegenerative disease often associated with symptoms similar to dementia, violence, and depression (Gregory, 2020).
4 Mental health myths and facts
A plethora of myths abound regarding mental illness. Let’s clarify a few that were obtained from the Substance Abuse and Mental Health Services Administration (2023).
Myth – Mental health issues cannot affect me.
Fact – In the United States, 1 in 5 adults experience mental health issues in a given year.
Myth – Mental health conditions result from character flaws or personality weakness.
Fact – Various factors, including physical illness, injury, brain chemistry, trauma, abuse, and family history, contribute to mental illness.
Download 3 Free Positive Relationships Exercises (PDF)
These detailed, science-based exercises will equip you or your clients to build healthy, life-enriching relationships.
Download 3 Positive Relationships Pack (PDF)
By filling out your name and email address below.
- Email Address *
- Your Expertise * Your expertise Therapy Coaching Education Counseling Business Healthcare Other
- Email This field is for validation purposes and should be left unchanged.
Yanos (2018) identifies three primary types of stigma.
Public stigma
Public stigma refers to creating intentional chasms between us and them through the labeling process.
- Patient label – Identifying the individual as a patient requiring treatment or hospitalization.
- Pejorative labels – Labels such as crazy or insane refer disparagingly to the individual.
Discriminatory public behaviors include:
- Social isolation
- Gossiping about the individual
- Being passed over for promotion
- Concerns about reliability
This YouTube video demonstrates the public’s perception of people who have mental illness.
Self-stigma
Self-stigma happens when the labeled individual will self-handicap , self-label, and use their label as an excuse for failure, limiting their development.
The effects of self-stigma can include:
- Feeling damaged
- Feeling weak
- Feeling vulnerable
- Dressing inconspicuously to be less visible in public
- Not speaking up for themself
- Holding back from seeking positions or promotions
- Feelings of embarrassment, diminishment, and self-hatred
Discriminatory behaviors include:
- Limiting self to avoid stigma
Structural stigma
Yanos (2018, p. 3) states, “Structural stigma is again a sociological concept that identifies the inherent and intentional effects that derive from social power dynamics and the policies and practices of institutions to restrict the autonomy of people with a mental illness.”
Scenarios where this may apply include:
- Involuntary hospitalization
- Denial of insurance payments in cases of suicide
- Restriction of individuals with a history of mental illness in specific career fields
- Enacting policies that prohibit insurance claims
- Mental health screenings for specific social roles
- Restricted health care for people with mental illness
When Simone Biles withdrew from the competition, she highlighted mental health (Holcombe, 2023).
Conversation about mental illness should be omnipresent. Often, we avoid it to spare discomfort. Meanwhile, the discomfort for those suffering hits a fever pitch.
How to reduce stigma in the workplace
Harvard Business Review discusses ways managers can help create an empathetic workplace culture (O’Brien & Fisher, 2019). These can also be generalized for other uses.
1. Focus on language
Terms used in gest or casual conversion can create or add to stigmatization. Using derogatory terms such as “Mr. OCD” or “schizo” can sound like an attack to those struggling.
2. Rethink sick days
Normalizing the idea of tending to mental health using sick days can contribute toward an environment of mental and physical health.
3. Open and honest conversation
Creating a space where people can talk openly about mental health issues without fear of rejection or judgment creates psychological safety .
4. Response training
Train employees in Mental Health First Aid , a national program that helps recognize those struggling and connects them to resources that will help.
Developing lesson plans for schools
Another way to promote positive mental health is through social emotional learning (SEL) curricula. Social emotional learning enhances strategic protective factors that buffer against the risks of mental health through responsive relationships, skill development, and emotionally safe environments (Collaborative for Academic, Social, and Emotional Learning, n.d.).
In addition to bolstering mental health and wellness, SEL exercises and activities help improve attitudes about self and others and decrease risky behaviors and emotional distress.
This short TED talk explains the benefits of SEL and how to change perspectives.

Yanos (2018, p. 41) describes microaggressions as “subtle communications of prejudice toward individuals based upon memberships in marginalized social groups.”
Microaggressions include comments that are rude and insensitive. The comments may exclude or nullify one’s experiences.
Yanos and his colleague Lauren Gonzales (as cited in Yanos, 2018) used the Mental Illness Microaggression Scale-Perpetrator version to measure microaggressions. They found that 62% of respondents endorsed patronizing behavior with mentally ill individuals by talking to them more slowly. Furthermore, 81% of respondents reported frequently reminding them to take their medication.
Mental health quiz
Prejudice comprises preconceived negative attitudes, feelings, and beliefs toward members of a marginalized group. These notions come from unsubstantiated opinions or stereotypes (Ritzer, 2021).
One way to combat prejudice and subsequent stigma is to learn more about the targeted group.
The following 10-question quiz will help dispel harmful attitudes and misunderstandings regarding mental illness. Dispelling myths can help reduce stigma, creating an environment of inclusiveness.
Take this mental health quiz from the Centers for Disease Control and Prevention.
Questions to ponder
- How does segregating groups of people in society impact your values?
- What do you stand to lose if you stand up for someone with mental illness? What would you gain?
- How does it make you feel when you hear about an individual with mental illness being stigmatized?
- What is the underlying fear surrounding mental illness stigma?
- What resources do you need to make a change?
- What is mental health stigma costing society?
While on the subject of interesting questions to ponder, you may find this article helpful as well: 72 Mental Health Questions for Counselors and Patients .
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
Many people are uncertain about starting a conversation on mental illness and stigma. Below are ideas for getting started.
1. SAFE: Mental health facts for families
Because many veterans struggle with mental illness, Michelle Sherman and the Oklahoma Veterans Affairs Medical Center created the SAFE Program : Mental health facts for families.
The acronym SAFE stands for Support and Family Education. Each session provides questions and materials for a class or group.
In particular, session 18 helps families understand the stigma around mental illness (Sherman, 2008). The program includes facts about the impact of stigma on the family’s experience of mental illness and prompts compelling questions, such as:
- What has been the most significant consequence of your loved one’s mental illness?
- What kept them from seeking treatment?
This invaluable program and others like it help families and the diagnosed realize they are not alone, provide insightful information, and build empathy and compassion for their loved ones.
2. Discussion starter
This simple handout, Stigma Discussion Starters , analyzes what stigma looks like and means and asks questions about what it would feel like to have mental illness and experience stigma.
This handout can be used as a template for discussions in college classrooms, in the workplace, and in medical settings to create a deeper understanding of what mental health stigma looks and feels like.
3. Interactive website
The wonderfully interactive website Make It OK provides resources to help educate people about mental illness and videos on language to avoid. It provides various podcasts, questions, and interactions. For example, you can scroll down to take a quiz and also sign a pledge to do your part to erase stigma.
The site is also aimed at helping those struggling with mental illness, as it provides relatable stories and resources.
4. Helpful group activities
Mental health stigma has wide-ranging effects on those labeled and society. Dialogue is essential to effect change.
Talking circles
Talking circles are integral to restorative justice and help people connect with each other and themselves.
In Heart of Hope , Carolyn Boyes-Watson and Kay Pranis state (2010, p. 170), “Chronic conditions of unmet needs for dignity, respect, and basic necessities can induce the trauma response.” Unmet needs can lead to acting-out behaviors that can disconnect individuals from their true selves.
Boyes-Watson and Pranis (2010, p. 170) go on to say, “Acknowledging the harm of these structures and having an opportunity to tell the story of the harms in one’s life are essential in promoting resilience in the face of the harmful impacts.”
Talking circles are one way to listen and speak about societal injustices like mental illness stigma. Circles are used within the justice system, schools, and other contexts.
The process includes inviting members of the community and those harmed to sit together while they share personal stories and listen to the stories of others.
In order to address mental health stigma, the circle keeper could approach various topics such as respect, dimensions of identity, or empathy.
In this YouTube video, Kay Pranis captures the essence of talking circles and outlines the origins, objectives, and process.
Empathy Bingo
The Empathy Bingo worksheet provides an opportunity to demonstrate the difference between showing empathy and other responses. This activity works great in a therapeutic setting and other settings such as a classroom or the workplace.
The facilitator reads one of the 12 prepared scenarios and corresponding responses. Participants decide if the response exemplifies empathy or other choices provided, such as one-upping, correcting, or fixing it.
This exercise is a creative way to become aware of how our responses can be interpreted and how to build empathy, which is vital for reducing stigma.
The following books provide resources to understand mental illness and its stigma.
1. Written Off: Mental Health Stigma and the Loss of Human Potential – Philip T. Yanos
Written by Philip T. Yanos, the book conveys how the pervasive nature of stigma impacts those with mental illness, profoundly affecting their lives.
Yanos approaches the topic of stigma from the standpoint of social injustice, believing that when stigma prohibits mentally ill individuals from participating in society, it is not just a personal loss, but a communal one.
Yanos discusses negative attitudes and behaviors toward mental illness, community participation of those diagnosed, and ideas for changing perceptions.
Find the book on Amazon .
2. Another Kind of Madness: A Journey Through the Stigma and Hope of Mental Illness – Stephen P. Hinshaw
Written by Stephen P. Hinshaw, it is a biographical depiction of his journey through his father’s mental illness.
After 18 years of silence, the life-changing revelation of his father’s mental illness came during a spring break from college.
Jolting as it was, it helped explain his father’s ups and downs and extended absences. It also awakened his journey to becoming a clinical and developmental psychologist and professor.
One way to internalize a lesson is through activities and exercises. Below are examples of both that can help formulate the building blocks of empathy and healing.
Positive Relationships Masterclass
Healthy relationships are crucial to individual wellbeing. The Positive Relationships Masterclass© is a coaching masterclass to help others build and maintain healthy relationships.
Participants will learn why positive relationships are crucial markers of wellbeing, the types of support needed, the benefits of building social capital resulting in stronger communities, perceptions about relationships, and how to manage relationships.
Learning to create and negotiate healthy relationships provides insight into relationship dynamics and helps change how individuals see and interact with others.
Recommended reading
If you too are intrigued by mental wellness, we have a great selection of articles that you will find interesting. Here is a short list of must-read articles:
- 19 Mental Health Exercises & Interventions for Wellbeing
- The Benefits of Mental Health According to Science
- 28 Mental Health Games, Activities & Worksheets (& PDF)
2 Worksheets
Telling an Empathy Story is a worksheet used in dyads or groups to build empathy through storytelling. Participants can use someone else’s story or a biography. The storyteller uses art to help convey emotions and then shares it with another or a group, thus learning empathy and allowing for self-expression through art.
The Compassion Formulation exercise encourages psychological and emotional wellbeing by bolstering self-compassion and compassion for others. Participants will explore aspects of past influences, primary fears, protective behaviors, and unintended outcomes.
An activity for kids
This class exercise called Group Circle allows kids to show kindness and enjoy its benefits through talking circles. Participants can experience empathy by talking about a time they felt different.
Positive relationship tools
If you’re looking for more science-based ways to help others build healthy relationships, check out this collection of 17 validated positive relationship tools for practitioners. Use them to help others form healthier, more nurturing, and life-enriching relationships.
17 Exercises for Positive, Fulfilling Relationships
Empower others with the skills to cultivate fulfilling, rewarding relationships and enhance their social wellbeing with these 17 Positive Relationships Exercises [PDF].
Created by experts. 100% Science-based.
The butterfly effect posits that positive shifts could ultimately create global waves of change.
This blog post presents a challenge and an opportunity. It contains questions, books, resources, and ideas to change perspectives on mental illness.
We can create a space for those struggling with mental illness to feel accepted, understood, and validated.
This change also transforms us by opening our minds and hearts and building empathy muscles. In addition, it builds social capital through communities where empathy trumps fear.
We hope you enjoyed reading this article. Don’t forget to download our three Positive Relationships Exercises for free .
Stigma affects those struggling with mental health, as it
- Limits participation in society
- Creates obstacles to seeking treatment
- Inhibits the ability to be authentic
Stigma is most often caused by:
- Lack of knowledge and understanding
- Lack of empathy
- Negative media portrayals
- Pejorative terms
If faced with stigma, the best way to cope is to:
- Seek professional help
- Find a supportive community
- Use coping mechanisms to reduce stress and anxiety
- Public stigma: “Patient” labeling and pejorative labeling
- Self-stigma: Feeling damaged, weak, or vulnerable; holding back from sticking up for yourself
- Structural stigma: Built into societal institutions
- Boyes-Watson, C., & Pranis, K. (2010). Heart of hope resource guide: Using peacemaking circles to develop emotional literacy, promote healing and build healthy relationships . Center for Restorative Justice at Suffolk University.
- Collaborative for Academic, Social, and Emotional Learning. (n.d.). SEL and mental health. Retrieved September 17, 2023, from https://casel.org/fundamentals-of-sel/how-does-sel-support-your-priorities/sel-and-mental-health/.
- Dobson, K., & Stuart, H. L. (Eds.). (2021). The stigma of mental illness: Models and methods of stigma reduction . Oxford University Press.
- Evans, L., Chang, A., Dehon, J., Streb, M., Bruce, M., Clark, E., & Handal, P. (2023). The relationships between perceived mental illness prevalence, mental illness stigma, and attitudes toward help-seeking. Current Psychology , 1–10.
- Goffman, E. (1961). Asylums . Doubleday & Company.
- Gregory, H. (2020). Making a murderer: Media renderings of brain injury and Aaron Hernandez as a medical and sporting subject. Social Sciences & Medicine , 244 .
- Holcombe, M. (2023, August 9). What we can learn from Simone Biles’ mental health break . CNN. Retrieved September 8, 2023, from https://www.cnn.com/2023/08/09/health/biles-mental-health-break-wellness/index.html.
- Kessler, R. C., Angermeyer, M., Anthony, J. C., De Graaf, R., Demyttenaere, K., Gasquet, I., De Girolamo, G., Gluzman, S., Gureje, O., Haro, J. M., Kawakami, M., Karam, A., Levinson, D., Medina Mora, M. E., Oakley Browne, M. A., Posada-Villa, J., Stein, D. J., Adley Tsang, C. H., Aguilar-Gaxiola, S., … Bedirhan Ustun, T. (2007). Life-time prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s Mental Health Survey Initiative. World Psychiatry, 6 (3), 168–176.
- O’Brien, D., & Fisher, J. (2019, February 19). 5 ways bosses can reduce the stigma of mental health at work . Harvard Business Review. Retrieved September 12, 2023, from https://hbr.org/2019/02/5-ways-bosses-can-reduce-the-stigma-of-mental-health-at-work.
- Ritzer, G. (2021). Essentials of sociology (4th ed.). SAGE.
- Sherman, M. D. (2008, April). Support and family education: Mental health facts for families . University of Oklahoma Health Sciences Center. Retrieved September 17, 2023, from https://www.ouhsc.edu/safeprogram/index.html.
- Substance Abuse and Mental Health Services Administration. (2023, April 24). Mental health myths and facts. Retrieved September 8, 2023, from https://www.samhsa.gov/mental-health/myths-and-facts.
- Yanos, P. T. (2018). Written off: Mental health stigma and the loss of human potential . Cambridge University Press.
Share this article:
Article feedback
Let us know your thoughts cancel reply.
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

High-Functioning Autism: 23 Strengths-Based Daily Worksheets
Autism diagnoses are rising exponentially. A study by Russell et al. (2022) reported a 787% increase in UK diagnoses between 1998 and 2018. Similarly, 1 [...]

Treating Phobias With Positive Psychology: 15 Approaches
Phobophobia is a fear of phobias. That is just one in our list of 107 phobias. Clearly a person suffering from phobophobia has a lot [...]

How to Fuel Positive Change by Leveraging Episodic Memory
Some researchers believe that our memory didn’t evolve for us to only remember but to imagine all that might be (Young, 2019). Episodic memory is [...]
Read other articles by their category
- Body & Brain (52)
- Coaching & Application (39)
- Compassion (23)
- Counseling (40)
- Emotional Intelligence (22)
- Gratitude (18)
- Grief & Bereavement (18)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (16)
- Mindfulness (40)
- Motivation & Goals (41)
- Optimism & Mindset (29)
- Positive CBT (28)
- Positive Communication (23)
- Positive Education (37)
- Positive Emotions (32)
- Positive Leadership (16)
- Positive Parenting (14)
- Positive Psychology (21)
- Positive Workplace (35)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (39)
- Self Awareness (20)
- Self Esteem (37)
- Strengths & Virtues (29)
- Stress & Burnout Prevention (33)
- Theory & Books (42)
- Therapy Exercises (37)
- Types of Therapy (54)

Download 3 Free Positive Psychology Tools Pack (PDF)
3 Positive Psychology Tools (PDF)

Mental Health Stigma
How the stigma of mental illness has evolved over time, anthropologist roy richard grinker explores the roots of stigma in his new book..
Posted January 12, 2021

Though progress has been made in recent years, mental illness remains highly stigmatized—the mentally ill are often victims of shame , marginalization, or outright mistreatment. In his upcoming book Nobody's Normal: How Culture Created the Stigma of Mental Illness, George Washington University anthropologist Roy Richard Grinker explores the roots of mental illness stigma around the world and highlights the cultural changes that have, he argues, brought us to the cusp of reimagining our relationship with neurodiversity and mental illness.
How does culture create stigma?
Evolutionary biologists would say that it’s natural for us to be afraid of some people. But what we are afraid of varies from society to society.
Most of the world doesn’t blame the individual for their suffering. Most of the world blames the family at large, God, a malevolent spirit, karma, or the stress of war, poverty, or an abusive relationship. It’s culture that teaches us how to seek blame, and how to explain differences. And if we explain differences in this very American way, that the individual is responsible for everything they succeed and fail in, it’s no surprise that people don’t want to seek care for certain conditions, especially conditions that threaten the ideals of being independent and achieving—the ideal American.
What’s an example of a condition that’s treated differently in different cultures?
I’ll give you an example of something that’s treated completely differently in the same location by a medical doctor and by his community. A man I’ll call Tamzo, who lives in rural Namibia, has what we would call schizophrenia. He walks 20 kilometers to the village once a month to get antipsychotic medicine. The Western doctor there writes down his diagnosis as schizophrenia. But at home he is thought to be the victim of a curse that somebody placed on their village that settled randomly on Tamzo. In his family and his village, as long as he is not hearing voices, he’s not considered at all to be sick. Whereas in the clinic, it’s “once labeled, always labeled.”
Your book discusses the relationship between capitalism and stigma. How has it informed beliefs about mental illness?
When capitalism took hold, we started to value individual autonomy and productivity for everybody. Before that, we didn’t hold a person responsible for all of their differences and all of their successes and failures. One of the things that characterized the first asylums in the 1700s, particularly in England and France, were that they were for people who violated the goals of productivity. They were idle, they didn’t work, or they were criminals. The asylums didn’t separate people into these different categories; they were all just the idle. It was only after humanitarian reformers sought to separate out the criminals from the non-criminals that you finally had people with mental illness (what was called insanity) by themselves, and then scientists could see them.
One of the problems for people with disabilities in general is what Alexis de Tocqueville observed in the early 1800s: In the U.S., the hero is the individual. People with disabilities aren’t necessarily always able to be independent. By the very nature of capitalism, the person who depends on others, who lives with others, or who isn’t an efficient worker is considered to be a failure.
How might that manifest today?
Something that really affects people is the idea that they can’t live up to capitalist values. We learn that certain occupations are valued more than others. In the book, I tell a story about my daughter with autism , Isabel. She loves to clean, and she’s very good at it. She got an internship at CVS, so the employer and my wife and I went over her duties. Isabel said, “When I get here in the morning, I’m a cleaning lady.” The employer snapped at her and said, “You are not a cleaning lady—you are a retail associate!”
It was a perfect example of how we learn that some ways of being are more valued than others. Until that moment, Isabel hadn’t realized that there was anything wrong with calling yourself a cleaning lady. There is nothing wrong with that.
The book also discusses the influence of war. How have wars altered the way people think of mental illnesses?
Wars can lead to massive transformations in all areas of life, including how we think about human behavior. The whole field of psychological testing derives from World War I and World War II. Various kinds of therapies that we take for granted, like community therapy , milieu therapy, and many other therapeutic techniques and medical technologies, all have their origins in wars.
The other thing is that each war creates new symptoms. In the Civil War, people experienced stress by having “soldier’s heart” or nostalgia . There was shell shock in World War I, war neurosis in World War II, and PTSD after Vietnam. These ideas come to fruition within the wars, but then they generalize to the community at large. Wars say that you can be strong, the ideal patriotic masculine warrior—and you’re still a human being that is going to be distressed by trauma .

Are we at a transition point in eradicating stigma?
I hope so. There’s been a real increase in the number of people who want to become psychiatrists and clinical psychologists. And I have a sense that, especially among young people, it’s expected to talk openly about things that people used to be ashamed of. Celebrities and athletes have been coming forward, like Lady Gaga, Bruce Springsteen, Jane Fonda, and Metta Sandiford-Artest.
But my real heroes are the people like my students who, on the first day of class, tell everyone, “I have Tourette syndrome, so please don’t be too upset when I say something that is inappropriate. I’m trying to control it, but sometimes I’ll say a swear word.” Or the student who says, “Getting diagnosed with ADHD was one of the best days of my Freshman year. For the first time, somebody saw that I wasn’t lazy or stupid. I just needed support.”
I’m not as optimistic about the most serious conditions. Things like schizophrenia and substance abuse threaten the ideals of capitalist society, that we should always be in control and masters of ourselves.
What led to this transition point?
So many things have changed the way we view human suffering and disability in general. You can take a particular case, like autism, and see how much our changing views of autism have come about because of our changing economies. The people who used to be denigrated for being "computer nerds" are now our heroes.
We’re also appreciating remote work. We’re starting to value stay-at-home parents more, and stay-at-home dads, which used to be considered weird. Why is that important? Being able to value a stay-at-home dad is to say that you are not necessarily disabled if you are not engaged in wage labor. You’re not a bad person if you’re not the sole breadwinner. The person with the disability who lives with their family, who doesn’t move out at the arbitrary age of 18, isn’t seen as violating some set of social rules. The disability rights movement, which includes the rights of people to have new identities, is also expanding the view that we all exist on a spectrum and that we can change over time. Being human means having some fluidity and change. Our views of mental illness are following that as well. It’s this openness and fluidity that I see as the tide that’s raising all boats.
Which is not to say that people aren’t suffering or discriminated against due to societal beliefs. But we’re more aware that that’s a form of suffering that we can eventually have control over. Because culture created it. If culture created it, we can change it.
How can people continue striving to eliminate stigma?
One of the things that bothers me is how much effort has been put toward eradicating stigma through education and awareness, like public service announcements and commercials. There’s nothing wrong with that, but Patrick Corrigan at the University of Illinois wrote a book called The Stigma Effect, in which he’s pretty clear that those things don’t work very well.
So, what does work? When we have interactions. We can get all the education we want, but if we don’t have proximity and interaction with networks and family who have mental illness and talk about them, we’re not going to get where we want to go.
One substitute for proximity is cinematic and television depictions. When I started working on autism in South Korea in the early 2000s, nobody would talk about mental illnesses. On autism, they would say, “Oh we don’t have that here,” or “We do, but it’s very rare.” If I heard somebody had a friend or colleague with autism, they would say, “They have autism, but you can’t talk to them because I never mentioned that I know.” It was so secretive. Today we’re seeing change in South Korea led in part by cinematic and television depictions. The Good Doctor, for example, was invented in Korea. It showed autism in a way that it had never been depicted before.
LinkedIn image: Rawpixel.com/Shutterstock

Abigail Fagan is a Senior Associate Editor at Psychology Today .
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- Introduction
- Conclusions
- Article Information
Changes shown on attributions (A), preferences for social distance (B), and perceptions of dangerousness (C), by condition. Significant changes ( P < .05) from one wave to the next (eg, 1996 to 2006) are indicated with heavy lines. Changes that were significant across the full time period (ie, 1996-2018), but not across successive waves, are indicated with a dashed line. All estimates are weighted. Data collected from the US National Stigma Studies. 12
The solid line provides the estimated trend across age groups (A), over time (B), and across cohorts (C). The shaded areas around the lines represent CIs, from light (95%) to dark (75%). Estimated cohort trends, which represent cohort-specific deviations from age and period trends, were obtained by averaging over all of the age-by-period combinations for a given cohort. For convenience, cohorts are indexed according to the first birth year in the birth cohort. The 1907 and 1917 cohorts were pooled to increase cell sizes. In all cases, higher values indicate a preference for greater social distance; lower values indicate the reverse. All estimates are weighted and adjust for respondents’ educational level, sex, and race and ethnicity, as well as the education, sex, and race and ethnicity of the person described in the vignette. Data collected from the US National Stigma Studies.
eMethods. Materials and Methods
eTable 1. Unadjusted Survey Year Differences
eTable 2. Adjusted Survey Year Differences
eTable 3. Model Fit of Candidate Models in APC Analyses
eTable 4. Deviation Magnitude Tests
eTable 5. Average Cohort Deviation Across Periods
eTable 6. Age and Period Main Effects
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Pescosolido BA , Halpern-Manners A , Luo L , Perry B. Trends in Public Stigma of Mental Illness in the US, 1996-2018. JAMA Netw Open. 2021;4(12):e2140202. doi:10.1001/jamanetworkopen.2021.40202
Manage citations:
© 2024
- Permissions
Trends in Public Stigma of Mental Illness in the US, 1996-2018
- 1 Department of Sociology, Indiana University, Bloomington
- 2 Department of Sociology, Pennsylvania State University, University Park
Question What changes in the prejudice and discrimination attached to mental illness have occurred in the past 2 decades?
Findings In this survey study of 4129 adults in the US, survey data from 1996 to 2006 showed improvements in public beliefs about the causes of schizophrenia and alcohol dependence, and data from a 2018 survey noted decreased rejection for depression. Changes in mental illness stigma appeared to be largely associated with age and generational shifts.
Meaning Results of this study suggest a decrease in the stigma regarding depression; however, increases and stabilized attributions regarding the other disorders may need to be addressed.
Importance Stigma, the prejudice and discrimination attached to mental illness, has been persistent, interfering with help-seeking, recovery, treatment resources, workforce development, and societal productivity in individuals with mental illness. However, studies assessing changes in public perceptions of mental illness have been limited.
Objective To evaluate the nature, direction, and magnitude of population-based changes in US mental illness stigma over 22 years.
Design, Setting, and Participants This survey study used data collected from the US National Stigma Studies, face-to-face interviews conducted as 1996, 2006, and 2018 General Social Survey modules of community-dwelling adults, based on nationally representative, multistage sampling techniques. Individuals aged 18 years or older, including Spanish-speaking respondents, living in noninstitutionalized settings were interviewed in 1996 (n = 1438), 2006 (n = 1520), and 2018 (n = 1171). The present study was conducted from July 2019 to January 2021.
Main Outcomes and Measures Respondents reacted to 1 of 3 vignettes (schizophrenia, depression, alcohol dependence) meeting Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition , criteria or a control case (daily troubles). Measures included beliefs about underlying causes (attributions), perceptions of likely violence (danger to others), and rejection (desire for social distance).
Results Of the 4129 individuals interviewed in the surveys, 2255 were women (54.6%); mean (SD) age was 44.6 (16.9) years. In the earlier period (1996-2006), respondents endorsing scientific attributions (eg, genetics) for schizophrenia (11.8%), depression (13.0%), and alcohol dependence (10.9%) increased. In the later period (2006-2018), the desire for social distance decreased for depression in work (18.1%), socializing (16.7%), friendship (9.7%), family marriage (14.3%), and group home (10.4%). Inconsistent, sometimes regressive change was observed, particularly regarding dangerousness for schizophrenia (1996-2018: 15.7% increase, P = .001) and bad character for alcohol dependence (1996-2018: 18.2% increase, P = .001). Subgroup differences, defined by race and ethnicity, sex, and educational level, were few and inconsistent. Change appeared to be consistent with age and generational shifts among 2 birth cohorts (1937-1946 and 1987-2000).
Conclusions and Relevance To date, this survey study found the first evidence of significant decreases in public stigma toward depression. The findings of this study suggest that individuals’ age was a conservatizing factor whereas being in the pre–World War II or millennial birth cohorts was a progressive factor. However, stagnant stigma levels for other disorders and increasing public perceptions of likely violence among persons with schizophrenia call for rethinking stigma and retooling reduction strategies to increase service use, improve treatment resources, and advance population health.
Stigma, the prejudice and discrimination attached to devalued conditions, has been consistently cited as a major obstacle to recovery and quality of life among people with psychiatric disorders. 1 - 3 Stigma has been implicated in worsening outcomes for people with serious mental illness, 4 , 5 with nearly 40% of this population reporting unmet treatment needs despite available effective treatments. 6 , 7 Although some psychiatrists claim that stigma has decreased 8 or is irrelevant, 9 stigma remains concerning to health care professionals, patients, advocacy groups, and policy makers. Research has not supported claims of a decrease in stigma. 3 Moreover, national levels of public stigma have been associated with treatment-seeking intentions and experiences of discrimination reported by people with mental illness. 10 , 11 Findings on antistigma interventions also reflect the persistence of stigma 3 , 12 , 13 ; the unclear, limited, or short-term effectiveness of both large-scale messaging and small-scale interventions 12 - 16 ; and the lack of scalability of many such programs. Herein, we examine US public stigma over a 22-year period to provide a detailed assessment of changes in the nature and magnitude of public stigma over 2 decades for major mental health disorders.
The US National Stigma Studies (US-NSSs) use the General Social Survey (GSS), a biannual, household-based, multistage, cluster-sampled interview project providing nationwide, representative data on adults (age ≥18 years) living in noninstitutionalized settings in the continental US. 12 Face-to-face interviews for the US-NSSs were conducted by trained interviewers using the pencil/paper mode in 1996 (n = 1444; response rate, 76.1%) and computer-assisted personal interview format in 2006 (n = 1522; response rate, 71.2%) and 2018 (n = 1173; response rate, 59.5%). The GSS follows the American Association for Public Opinion Research ( AAPOR ) reporting guideline, which the present study followed. Mode effects, tested between 1996 and 2006, were minimal 17 and analyses to identify potential biases resulting from changing response rates did not identify problems. 18 Weights are provided and used where appropriate. Respondents receive an information page in English/Spanish and are asked for their consent to begin the interview. Institutional review board approval for the GSS and this study is held at NORC and at Indiana University. The present study was conducted from July 2019 to January 2021.
The US-NSSs used a survey experimental design using vignettes describing a fictitious person with behaviors meeting Diagnostic & Statistical Manual of Mental Disorders, Fourth Edition 19 criteria for schizophrenia, major depression, alcohol dependence, and a daily troubles control (eMethods in the Supplement ). 20 , 21 This vignette strategy avoids identifying the nature of the problem, allowing for data collection on knowledge, recognition, and labeling by respondents. 20 , 21 The vignette character’s psychiatric condition as well as their self-reported sex (man or woman), race (African American, Hispanic, or White), and educational level (eighth grade, high school, or college) were randomly varied and assigned as experimental characteristics in the stimulus. These data were not reported or collected in the interview. One vignette per respondent was read aloud by the interviewer and printed on a card given to the respondent who was then asked a series of questions.
Three sets of dependent variables operationalized stigma. First, attributions targeted respondents’ evaluation of likely scientific causes (chemical imbalance and genetics) as well as their recognition of the situation as a mental illness. Other potential moral/social explanations (bad character, God’s will, ups and downs of life, and way raised [all coded 1 if very/somewhat likely; 0 otherwise]) were also included. Second, dangerousness asked about the likelihood that the vignette person would do something violent toward others (coded 1 if very/somewhat likely; 0 otherwise). Third, social distance, the most common measure of stigma, measured respondents’ unwillingness to work closely with the vignette person on a job, live next door to them, spend an evening socializing with them, marry into their family, make friends with them, or live near a group home (categories collapsed into not willing/do not know [1] or willing [0]); details are reported in eTable 1 in the Supplement . Additional analyses used an overall social distance, factor-analytic scale for depression (1-factor solution, factor loadings ranging between 0.47 and 0.80, Cronbach α = .85).
Statistical analyses evaluated changes across years. Because data were weighted, a design-based F statistic that used the second-order Rao and Scott 22 correction was used to test the equality of raw percentages. To adjust for possible sociodemographic shifts between survey years and examine disparities, logistic regression models were fit. Differences in the estimated probabilities for outcomes were calculated, holding control variables at sample-specific means. The delta method was used to determined 95% CIs. To explore subgroup differences in trends, we fit a series of regression models that included interactions between time periods and respondents’ sociodemographic characteristics. Model estimates were used to calculate estimated probabilities of preferring social distance at each time point (1996, 2006, and 2018) and for each group (eg, men vs women), as well as group-specific changes over time and group differences in trends. Owing to the population representation of racial and ethnic groups in the US population, African American and Hispanic groups were collapsed into a non-White category in the subgroup analysis to avoid estimation problems within the vignette-specific analyses. Variance estimates were again obtained via the delta method. In addition, an exploratory age, period, and cohort analysis applied the age-period cohort (APC)–I method of Luo and Hodges 23 to assess the unique contribution of birth cohorts to overall trends in the preferences of US residents for social distance. Aligned with Ryder’s view that a cohort’s meaning is “implanted in the age-time specification,” 24 [p861] this approach quantifies cohort associations as the differential outcomes of time periods depending on age groups (eMethods in the Supplement ). Different from conventional APC models that assume cohort associations occur independently of period and age, the APC-I approach acknowledges the association of age, period, and cohort, as originally proposed by Ryder, which makes the approach useful for identifying factors that might be attributed to cohort membership. The total sample size of the individual-level APC analysis is 4134, with the number of participants per age-period combination ranging between 126 and 345. Hypothesis tests were all 2 sided. The APC analysis was carried out using R, version 3.6.2 (R Foundation for Statistical Analysis). The rest of the analysis—including data cleaning and variable transformations—was performed using Stata, version 16 (StataCorp LLC). Findings at P < .05 were considered significant.
Table 1 provides the sociodemographic profile of US NSS respondents across the 3 survey periods: 1996 (n = 1438), 2006 (n = 1520), and 2018 (n = 1171). Representation of age, sex, race and ethnicity, and educational level were roughly in line with US Census Bureau data (1996: men, 642 [44.6%]; women, 796 [55.4%]; mean [SD] age, 44.7 [17.0] years; 2006: men, 666 [43.8%]; women, 854 [56.2%]; mean [SD] age, 46.7 [17.0] years; men, 566 [48.3%]; women, 605 [51.7%]; mean [SD] age, 49.0 [17.4] years). The slight overrepresentation of women across time has been commonly seen in interview studies. The GSS did not collect specific ethnicity data until 2000; from then, race and ethnicity categories comprised non-White (2006: 425 [28.0%]; 2018: 322 [27.5%]) and White (2006: 1095 [72.0%]; 2018: 849 [72.5%]) individuals. Overall mean (SD) age was 44.6 (16.9) years.
Figure 1 depicts unadjusted changes across survey waves. Adjusted changes reveal few differences compared with unadjusted results and are reported here (eTable 2 in the Supplement ). Scientific attributions (chemical imbalance, genetics) were high and selected by increasing percentages of US residents, with the major increase occurring in the first period (1996-2006). Overall, in the earlier period (1996-2006), scientific attributions (eg, genetics) for schizophrenia (11.8%), depression (13.0%), and alcohol dependence (10.9%) increased. The only case in which public endorsement was lower than 50%, but still substantial, was for the control situation: daily troubles ( Figure 1 A; eTable 1 in the Supplement ). These results may suggest a medicalization of life problems. However, this early significant increase in the category of chemical imbalance was followed by a decrease later.
Although problem recognition increased only for schizophrenia in the first period and for alcohol dependence only in the second period, the levels were high for all mental illnesses. No change was documented for depression, with recognition already high, or for the control, in which depression was considered not warranted, signaling a distinct difference in the public response to nonclinical problems ( Figure 1 A).
Social and moral attributions were endorsed by relatively few respondents with little change over time ( Figure 1 A). Significantly fewer respondents cited ups and downs as a cause of depression or selected God’s will. The latter choice decreased significantly in the first period for daily troubles, even as the way an individual was raised increased significantly later. Alcohol dependence, however, was increasingly stigmatized, marked by significant change in respondents simultaneously citing bad character (18.2%) and ups and downs of life (11.3%) (eTable 2 in the Supplement ). Overall, trends suggest increasing mental health literacy, including distinguishing between daily problems and mental illness.
Social distance showed little change over time, except for depression ( Figure 1 B). In the later period (2006-2018), the desire for social distance decreased for depression in work (18.1%), socializing (16.7%), friendship (9.7%), family marriage (14.3%), and group home (10.4%) (eTable 2 in the Supplement ). For depression, the decreases were statistically significant and substantial. Reductions occurred in the later period, spanning all domains except neighbor, which was already low. Other minor changes in a direction indicating a higher stigma were in evidence early. This change included an increase in social distance for schizophrenia as neighbor and having the vignette person marry into the family ( Figure 1 B; eTable 2B in the Supplement ).
Inconsistent, sometimes regressive change, was observed, particularly regarding dangerousness for schizophrenia ( Figure 1 C) (1996-2018: 15.7% increase, P ≤ .001) and bad character for alcohol dependence (1996-2018: 18.2% increase, P ≤ .001).
The similarity between unadjusted and adjusted results suggests that sociodemographic characteristics offer little power in explaining stigma. Table 2 reports the results of analyses of subgroup factors for race and ethnicity, sex, age, and educational attainment (vignette person characteristics controlled). There were no significant differences in the overall time trends for sociodemographic groups, but a few associations were observed within periods. More men endorsed stigma (ie, in the most recent period for socializing, in the middle period for neighbor, and in the earliest period for friendship and group home support) compared with women. More respondents who self-reported race as non-White desired social distance from individuals with depression as neighbors in the most recent period.
The most consistent sociodemographic association was noted with age. Older individuals in each period were significantly more unwilling to have the vignette person marry into the family. This response did not change over time. In addition, more individuals with lower levels of education endorsed stigma in the most recent period (neighbor) and the middle period (marriage into the family).
In Figure 2 , a composite social distance scale depicts possible explanations of the stigma decrease for depression (eTables 3-6 in the Supplement ). Age and social distance appeared to be conservatizing factors ( Figure 2 A). Distinct period responses were noted, especially from 2006 to 2018, when stigma toward depression decreased significantly (Figure 2B). Two cohorts were more likely than expected to report lower stigma—the Silent Generation (part of the 1937-1946 birth cohort, after the Greatest Generation but before the Baby Boomers) and Millennials (1987-2000 birth cohort) ( Figure 2 C). The average deviation for the 1937-1946 birth cohort was −0.12 (SE, 0.05) ( P = .02), and the average deviation for the 1987-2000 birth cohort was−0.21 (SE, 0.08) ( P = .01) (eTable 5 in the Supplement ).
Our analyses identified both stability and change in stigma over the 22-year period from 1996 to 2018. Five robust and clear patterns emerged. First, the period around the turn of the century (1996-2006) saw a substantial increase in the public acceptance of biomedical causes of mental illness. Survey participants were more likely to recognize problems as mental illness and draw a line between daily troubles and diagnosable conditions. These changes mark greater scientific beliefs and a decrease in stigmatizing attributions, but no reduction in social rejection. Overall, trends suggest increasing mental health literacy, including distinguishing between daily living problems and mental illness, aligning with earlier research. 25 , 26 Second, the more recent period (2006-2018) documented, to our knowledge, the first significant, substantial decrease in stigma, albeit for one mental illness diagnosis: major depression. Fewer survey respondents expressed a desire for social distance from people with depression across nearly all domains, including work and family. Considered in the context of previous research, these decreases are statistically significant, substantively large, and persist in the presence of controls. Other disorders did not see reductions in social distance, and public perceptions of dangerousness for schizophrenia and moral attributions for alcohol dependence increased.
Third, respondents’ sociodemographic characteristics offered little insight into stigma, generally, or into observed decreases for depression. What is unusual about these findings is the absence of subgroup differences, suggesting a broad shift in the respondents’ thinking about depression. This absence of sociodemographic differences may be unexpected, but it supports findings from earlier NSSs. 10 , 27
Fourth, change over time may be associated with age as a conservatizing factor, 28 , 29 a cohort process in which older, more conservative individuals are replaced by younger, more liberal US residents, 29 , 30 and/or a period outcome stemming from broad shifts that are uniformly seen regarding social distance discriminatory predispositions across age and cohort. Although prior research tended to assume the observed trends primarily reflect a period-based process, we used the APC-I method to explore unique cohort patterns in public stigma of mental illness. Disaggregating the effects of age, period, and cohort revealed age as a conservatizing factor also seen in a parallel German study, 12 and a liberalizing tendency among both pre-WWII birth cohorts (referred to by demographers as the Silent Generation) and the most recent birth cohorts (Millennials), and a recent period outcome.
Fifth, although findings for depression are notable, other results may raise concerns. For schizophrenia, there has been a slow shift toward greater belief of dangerousness. Although not statistically significant in either of the time periods, the increase was substantial and relatively large over the entire period (approximately 13%), a finding analyzed in detail elsewhere. 31 The results for alcohol dependence are similarly mixed. Although there was an increase in the selection of alcohol dependence as a mental illness with chemical and genetic roots, the problem was also trivialized as ups and downs. Moreover, we observed a return to a moral attribution of bad character in the first period that remain stable into the second period.
This study has limitations. Responses to survey vignettes reflect attitudes, beliefs, and predispositions—not behavior. The lack of importance of sociodemographic characteristics may signal insensitivity in a vignette approach or in stigma measurement. 32 - 34 Although subgroup differences are widely believed to exist, such research is rare and often not generalizable. Yet, although our estimates of sociodemographic outcomes are somewhat inefficient owing to sample size constraints, power analyses indicate that they are adequately powered to detect very small effects overall (Cohen h = 0.12), and small to moderate associations within vignette condition (Cohen h = 0.25) (eMethods in the Supplement ). In addition, our vignettes are designed to capture public perceptions of behavior changes that typically occur with the onset of mental illness. Public response might differ if the vignettes included information about help-seeking and eventual recovery. Research that specifically targeted this limitation revealed a small but statistically significant lowering of public stigma when vignette persons were described as being in treatment or recovery. 35
Other limitations must also be considered. Decreasing response rates present a challenge to researchers who seek to model trends over time in attitudes or behaviors. As noted, GSS response rates decreased approximately 16% over the 22-year period in question. If GSS respondents were somehow increasingly selected on tolerance for individuals with mental illness, finding stigma change would be likely even in the absence of actual change. This explanation seems unlikely given our results. We found respondents’ attitudes toward mental illness were more accepting in some cases (eg, depression), but less accepting in others (eg, schizophrenia). Even for depression, in which change was found across social venues, the degree to which that happens varied greatly. If findings were an artifact of a simple sample selection process, we would not expect to observe this level of complexity. Trends over time would be more consistent across conditions, and differences between social domains would be less pronounced.
Equally important, although it may be tempting to associate the changes in mental health literacy in the earlier period with the stigma reduction for depression in the latter period, doing so would be premature. These data cannot support claims about lag effects owing to the GSS’s cross-sectional design. In addition, previous work, which examined this issue in detail in the earlier period alone, could document neither individual nor aggregate associations between accepting scientific attributions for mental illness and stigma levels. 10
Despite limitations, these findings have important implications for research and treatment as well as antistigma program and policy efforts. First and foremost, the results of this study suggest that public stigma can change. To our knowledge, this study is one of the first indications that revise the larger cultural climate of prejudice and discrimination without the coordinated, translational, and research-monitored program of stigma reduction used in other Western nations. 3 , 12 , 13 Research and antistigma efforts require content retooling to make use of what is known and address the most problematic and unique aspects of stigma. In the US, controversial and structural aspects of mental illness stigma have rarely been addressed. Not only are perceptions of violence increasing for schizophrenia, individuals with schizophrenia likely face the greatest resistance in dismantling public, legal, policy, treatment, and resource barriers. Furthermore, calls for tailoring efforts to diverse or specialized populations may be limited by a thin, unrepresentative, and contradictory scientific base. 36 , 37 Data gaps in our analysis signal the need for novel stigma targets in research, whether new measures or populations widely believed to hold distinct ideas about mental illness and stigma. Our results also raise questions on how the progress reported herein can be accelerated and regressive shifts reversed. These results suggest that we must be realistic because societies change slowly and change efforts must be persistent and sustainable. Randomized clinical trial–based antistigma research often reports positive findings in typical inoculation-style programs but confronts effects that are extinguished over time. 3 , 38
The NSSs have served as the de facto primary data source about public stigma in the US for the past 2 decades. In this analysis of 22 years of survey data, we found a significant decrease in public stigma toward major depression and increased scientific attribution for schizophrenia, major depression, and alcohol dependence. Our findings are consistent with the claims of Braslow et al 5 that what the public believes and knows often aligns with science (ie, increasing agreement with scientific attributions) but may fail to influence their attitudes and behavior (ie, desire for social distance from individuals with mental illness, except depression). The societal and individual effects of stigma are broad and pervasive. Stigma translates into individual reluctance to seek care, mental health professional shortages, and societal unwillingness to invest resources into the mental health sector. Yet, the research, teaching, and programming resources targeted to redress prejudice and discrimination remain a low priority, small in scale, and individually focused. 39 With indications that the level of stigma may be reducing, strategies to identify factors associated with the decrease in stigma for depression, to address stagnation or regression in other disorders, and to reach beyond current scientific limits are essential to confront mental illness’s contribution to the global burden of disease and improve population health.
Accepted for Publication: October 27, 2021.
Published: December 21, 2021. doi:10.1001/jamanetworkopen.2021.40202
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2021 Pescosolido BA et al. JAMA Network Open .
Corresponding Author: Bernice A. Pescosolido, PhD, Department of Sociology, Indiana University, 1022 E Third St, Bloomington, IN 47401 ( [email protected] ).
Author Contributions: Drs Pescosolido and Halpern-Manners had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Pescosolido, Halpern-Manners, Luo.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Pescosolido, Halpern-Manners.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Halpern-Manners, Luo.
Obtained funding: Pescosolido, Perry.
Administrative, technical, or material support: Pescosolido, Perry.
Supervision: Pescosolido.
Conflict of Interest Disclosures: Dr Luo reported receiving grants from the National Institutes of Health outside the submitted work. No other disclosures were reported.
Funding/Support: Support for the study was provided by the Brain & Behavior Research Foundation (formerly National Alliance for Research on Schizophrenia & Depression) Distinguished Investigator Award and from Indiana University Network Science Institute (Dr Pescosolido), and base support and supplement from the National Science Foundation to the National Opinion Research Center (NORC) for the General Social Survey (GSS) and the National Stigma Studies.
Role of the Funder/Sponsor: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Information: All GSS data are available from NORC ( https://gss.norc.org ) and the GSS data explorer ( https://gssdataexlporer.norc.org ).
Additional Contributions: We thank Alejandra Laszlo Capshew, MS (Indiana Consortium for Mental Health Services Research), who assisted with project management; the College of Arts and Sciences and the Sociomedical Sciences Research Institute at Indiana University provided infrastructural support; and Tom W. Smith, PhD, and Jaesok Son, PhD (NORC at the University of Chicago), provided project assistance as key members of the NORC GSS Team. No financial compensation was provided.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Challenging the Public Stigma of Mental Illness: A Meta-Analysis of Outcome Studies
Information & authors, metrics & citations, view options, conclusions, three approaches to change, past reviews.
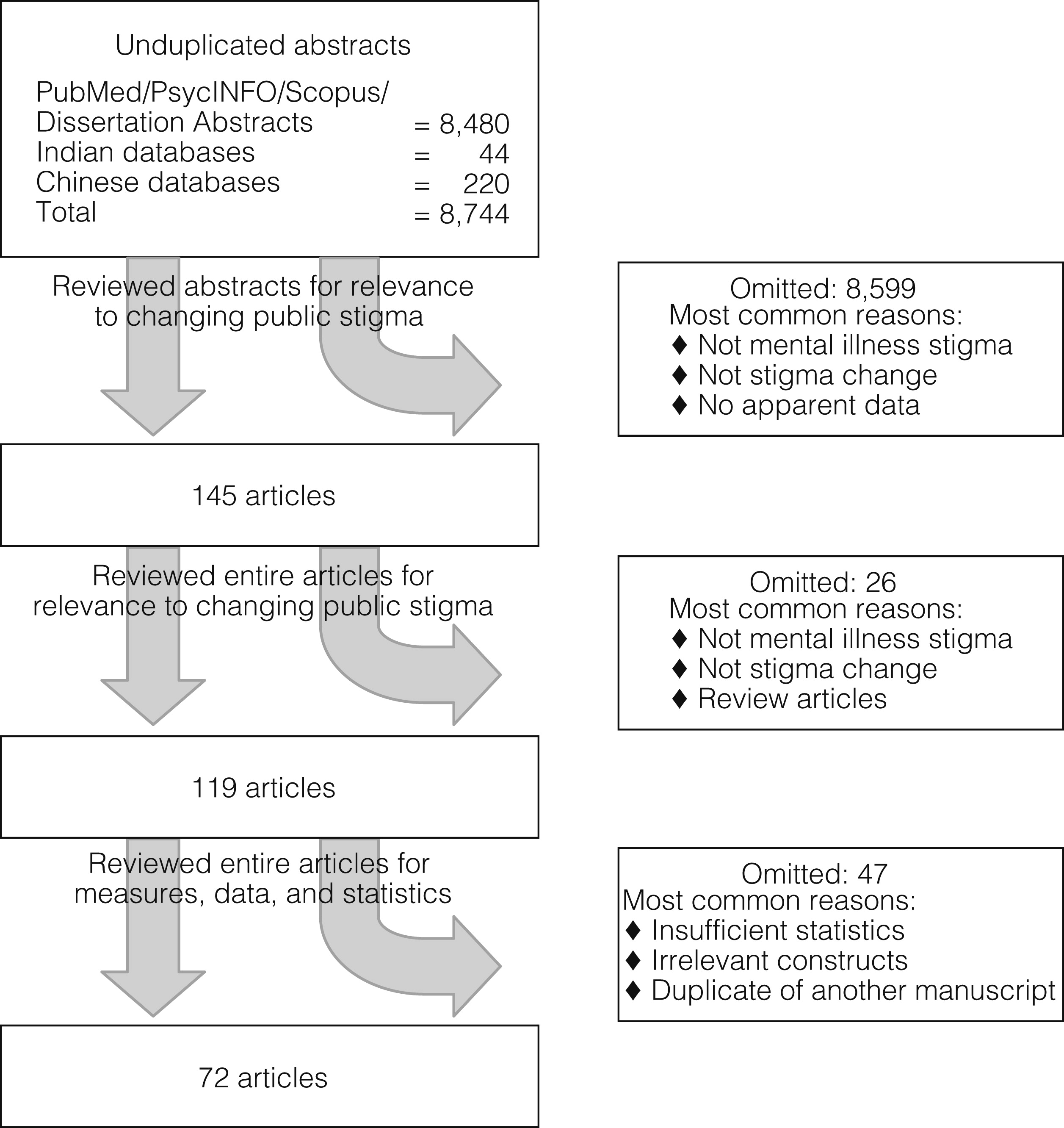
Effect size analysis
| Characteristic | Frequency (%) | Range (%) |
|---|---|---|
| Research participants | ||
| Age (M±SD) | 27.7±10.4 | 15–49 |
| Female | 58.7±18.4 | 3–100 |
| Ethnicity | ||
| European or European American | 61.1±27.1 | 0–95 |
| African or African American | 21.1±29.8 | 0–100 |
| Asian or Asian American | 6.1±12.9 | 0–52 |
| Hispanic or Hispanic American | 5.6±9.4 | 0–37 |
| Other | 7.8±12.5 | 0–52 |
| Marital status | ||
| Married | 22.1±25.9 | 0–66 |
| Single | 70.8±33.7 | 18–100 |
| Divorced | 3.5±3.6 | 0–9 |
| Widowed | 3.6±8.6 | 0–23 |
| Employment status | ||
| Full-time | 27.8±42.8 | 0–100 |
| Part-time | 1.7±8.3 | 0–47 |
| Student | 69.0±45.2 | 0–100 |
| Unemployed | 1.9±5.8 | 0–29 |
| Educational attainment | ||
| Less than high school | 31.6±47.0 | 0–100 |
| High school diploma or GED | 5.8±13.6 | 0–59 |
| Some college | 46.0±46.9 | 0–100 |
| 4-year degree | 11.8±24.0 | 0–100 |
| Graduate degree | 5.2±15.0 | 0–67 |
| Target of stigma change | ||
| College students | 27.2 | |
| Children under 12 | .8 | |
| Adolescents | 24.1 | |
| Adults (>18) | 26.5 | |
| Professionals | 4.7 | |
| Family members | .3 | |
| Students in professional programs | 8.5 | |
| Criminal justice professionals | 7.2 | |
| Quality of antistigma program | ||
| Antistigma manual (% yes) | 40.1 | |
| Manual training (% yes) | 14.2 | |
| Outcome measure | ||
| Attitudes | ||
| Competence | 4.2 | |
| Dangerousness | 6.5 | |
| Empowerment | 1.0 | |
| Poor prognosis | 4.2 | |
| Responsibility | 4.2 | |
| Benevolence | 2.1 | |
| Negative perceptions | 1.0 | |
| Personality | .3 | |
| Credibility | .3 | |
| Affect | ||
| Anger | 1.6 | |
| Fear | 2.8 | |
| Pity | 1.5 | |
| Shame | .8 | |
| Behavioral intentions | ||
| Avoidance | 10.9 | |
| Coercion | 2.4 | |
| Help | 2.4 | |
| Segregation | 2.9 | |
| Authoritarian | 2.1 | |
| Community health ideology | 1.6 | |
| Social restrictiveness | 2.4 | |
| Interpersonal ideology | .8 |
Effects of contact and education on public stigma change
| Antistigma approach | Overall | Attitudes | Affect | Behavioral intentions | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| d | SE | SD | K | Qw | d | SE | SD | K | Qw | d | SE | SD | K | Qw | d | SE | SD | K | Qw | |
| All studies | ||||||||||||||||||||
| Protest | .099 | .284 | .096 | 4 | .006 | 0 | 0 | 0 | ||||||||||||
| Education | .286 | .023 | .304 | 431 | 335.5 | .310 | .026 | .291 | 280 | 209.8 | .144 | .067 | .261 | 24 | 27.2 | .251 | .048 | .363 | 127 | 106.7 |
| Contact | .282 | .036 | .583 | 177 | 261.1 | .406 | .046 | .611 | 93 | 156.2 | –.030 | .077 | .197 | 17 | 14.4 | .189 | .068 | .616 | 66 | 80.3 |
| Randomized controlled trials (N=13) | ||||||||||||||||||||
| Education | .153 | .034 | .158 | 116 | 28.8 | .207 | .054 | .118 | 50 | 19.1 | .103 | .046 | .170 | 55 | 33.8 | |||||
| Contact | .363 | .069 | .443 | 71 | 145.8 | .626 | .146 | .631 | 27 | 69.9 | .268 | .060 | .358 | 33 | 56.6 | |||||
Video versus in-person effects
| Antistigma approach | Overall | Attitudes | Behavioral intentions | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean d | SE | SD | K | Qw | Mean d | SE | SD | K | Qw | Mean d | SE | SD | K | Qw | |
| All studies (N=79) | |||||||||||||||
| Contact in person | .516 | .060 | .473 | 58 | 81.6 | .656 | .086 | .513 | 34 | 34.5 | .397 | .075 | .462 | 22 | 16.3 |
| Contact by video | .155 | .048 | .211 | 83 | 54.2 | .296 | .122 | .087 | 44 | 60.3 | .197 | .063 | .177 | 26 | 26.7 |
| Studies focusing on adolescents (N=19) | |||||||||||||||
| Education | .392 | .056 | .262 | 78 | 98.7 | .453 | .065 | .364 | 50 | 50.1 | .302 | .133 | .214 | 22 | 33.4 |
| Contact | .244 | .061 | .177 | 68 | 46.1 | .242 | .068 | .213 | 46 | 43.0 | .303 | .150 | .281 | 18 | 5.0 |
| In person | .401 | .090 | .338 | 23 | 12.7 | .371 | .120 | .377 | 15 | 8.3 | .457 | .131 | .342 | 8 | 3.3 |
| By video | .166 | .060 | .155 | 45 | 51.5 | .183 | .080 | .143 | 31 | 34.9 | .172 | .098 | .121 | 10 | 11.7 |
Effects on adolescents
Acknowledgments and disclosures, supplementary material.
- View/Download
Information
Published in.


Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - Psychiatric Services
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Appointments at Mayo Clinic
Mental health: overcoming the stigma of mental illness.
False beliefs about mental illness can cause significant problems. Learn what you can do about stigma.
Stigma is when someone views you in a negative way because you have a distinguishing characteristic or personal trait that's thought to be, or actually is, a disadvantage (a negative stereotype). Unfortunately, negative attitudes and beliefs toward people who have a mental health condition are common.
Stigma can lead to discrimination. Discrimination may be obvious and direct, such as someone making a negative remark about your mental illness or your treatment. Or it may be unintentional or subtle, such as someone avoiding you because the person assumes you could be unstable, violent or dangerous due to your mental illness. You may even judge yourself.
Some of the harmful effects of stigma can include:
- Reluctance to seek help or treatment
- Lack of understanding by family, friends, co-workers or others
- Fewer opportunities for work, school or social activities or trouble finding housing
- Bullying, physical violence or harassment
- Health insurance that doesn't adequately cover your mental illness treatment
- The belief that you'll never succeed at certain challenges or that you can't improve your situation
Steps to cope with stigma
Here are some ways you can deal with stigma:
- Get treatment. You may be reluctant to admit you need treatment. Don't let the fear of being labeled with a mental illness prevent you from seeking help. Treatment can provide relief by identifying what's wrong and reducing symptoms that interfere with your work and personal life.
- Don't let stigma create self-doubt and shame. Stigma doesn't just come from others. You may mistakenly believe that your condition is a sign of personal weakness or that you should be able to control it without help. Seeking counseling, educating yourself about your condition and connecting with others who have mental illness can help you gain self-esteem and overcome destructive self-judgment.
- Don't isolate yourself. If you have a mental illness, you may be reluctant to tell anyone about it. Your family, friends, clergy or members of your community can offer you support if they know about your mental illness. Reach out to people you trust for the compassion, support and understanding you need.
- Don't equate yourself with your illness. You are not an illness. So instead of saying "I'm bipolar," say "I have bipolar disorder." Instead of calling yourself "a schizophrenic," say "I have schizophrenia."
- Join a support group. Some local and national groups, such as the National Alliance on Mental Illness (NAMI), offer local programs and internet resources that help reduce stigma by educating people who have mental illness, their families and the general public. Some state and federal agencies and programs, such as those that focus on vocational rehabilitation and the Department of Veterans Affairs (VA), offer support for people with mental illness.
- Get help at school. If you or your child has a mental illness that affects learning, find out what plans and programs might help. Discrimination against students because of a mental illness is against the law, and educators at primary, secondary and college levels are required to accommodate students as best they can. Talk to teachers, professors or administrators about the best approach and resources. If a teacher doesn't know about a student's disability, it can lead to discrimination, barriers to learning and poor grades.
- Speak out against stigma. Consider expressing your opinions at events, in letters to the editor or on the internet. It can help instill courage in others facing similar challenges and educate the public about mental illness.
Others' judgments almost always stem from a lack of understanding rather than information based on facts. Learning to accept your condition and recognize what you need to do to treat it, seeking support, and helping educate others can make a big difference.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- StigmaFree me. National Alliance on Mental Illness. https://www.nami.org/Get-Involved/Take-the-stigmafree-Pledge/StigmaFree-Me. Accessed April 25, 2017.
- What is stigma? Why is it a problem? National Alliance on Mental Illness. https://www.nami.org/stigmafree. Accessed April 25, 2017.
- Stigma and mental illness. Centers for Disease Control and Prevention. https://www.cdc.gov/mentalhealth/basics/stigma-illness.htm. Accessed April 25, 2017.
- Sickel AE, et al. Mental health stigma: Impact on mental health treatment attitudes and physical health. Journal of Health Psychology. http://journals.sagepub.com/doi/pdf/10.1177/1359105316681430. Accessed April 25, 2017.
- Americans with Disabilities Act and mental illness. Womenshealth.gov. https://www.womenshealth.gov/mental-health/your-rights/americans-disability-act.html. Accessed April 25, 2017.
- Picco L, et al. Internalized stigma among psychiatric outpatients: Associations with quality of life, functioning, hope and self-esteem. Psychiatric Research. 2016;246:500.
- The civil rights of students with hidden disabilities under Section 504 of the Rehabilitation Act of 1973. U.S. Department of Education. https://www2.ed.gov/about/offices/list/ocr/docs/hq5269.html. Accessed May 2, 2017.
- Wong EC, et al. Effects of stigma and discrimination reduction trainings conducted under the California Mental Health Services Authority. Rand Health Quarterly. 2016;5:9.
Products and Services
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Family Health Book
- Abdominal pain
- Alcohol use disorder
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- Antidepressants: Side effects
- Antidepressants: Selecting one that's right for you
- Antidepressants: Which cause the fewest sexual side effects?
- Are you thinking about suicide? How to stay safe and find treatment
- Atypical antidepressants
- Clinical depression: What does that mean?
- DBS for Tremor
- Deep brain stimulation
- Depression and anxiety: Can I have both?
- Depression, anxiety and exercise
- What is depression? A Mayo Clinic expert explains.
- Depression in women: Understanding the gender gap
- Depression (major depressive disorder)
- Depression: Supporting a family member or friend
- Electroconvulsive therapy (ECT)
- How opioid use disorder occurs
- How to tell if a loved one is abusing opioids
- Intervention: Help a loved one overcome addiction
- Kratom: Unsafe and ineffective
- Kratom for opioid withdrawal
- Male depression: Understanding the issues
- MAOIs and diet: Is it necessary to restrict tyramine?
- Marijuana and depression
- Mental health providers: Tips on finding one
- Mental health
- Mental illness
- Mental illness in children: Know the signs
- Monoamine oxidase inhibitors (MAOIs)
- Natural remedies for depression: Are they effective?
- Nervous breakdown: What does it mean?
- Opioid stewardship: What is it?
- Pain and depression: Is there a link?
- Passive-aggressive behavior
- Prescription drug abuse
- Psychotherapy
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Suicide: What to do when someone is thinking about suicide
- Suicide and suicidal thoughts
- Tapering off opioids: When and how
- Integrative approaches to treating pain
- Nutrition and pain
- Pain rehabilitation
- Self-care approaches to treating pain
- Thyroid scan
- Transcranial magnetic stimulation
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Vagus nerve stimulation
- Video: Vagus nerve stimulation
- Violinist Still Making Music After DBS Surgery
- Vitamin B-12 and depression
- What are opioids and why are they dangerous?
- Mayo Clinic neurosurgeon Kendall H. Lee, M.D., Ph.D., describes deep brain stimulation research
- Mayo Clinic Minute: Do not share pain medication
- Mayo Clinic Minute: Avoid opioids for chronic pain
- Mayo Clinic Minute: Be careful not to pop pain pills
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Mental health Overcoming the stigma of mental illness
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(5); 2023 May
- PMC10220277

Understanding and Addressing Mental Health Stigma Across Cultures for Improving Psychiatric Care: A Narrative Review
Ahmed a ahad.
1 Psychiatry and Behavioral Sciences, Florida International University, Herbert Wertheim College of Medicine, Miami, USA
Marcos Sanchez-Gonzalez
2 Health Services Administration, Lake Erie College of Osteopathic Medicine, Bradenton, USA
Patricia Junquera
Stigma, characterized by negative stereotypes, prejudice, and discrimination, is a significant impediment in psychiatric care, deterring the timely provision of this care and hindering optimal health outcomes. Pervasive in all aspects of psychiatric care, stigma leads to delayed treatment, increased morbidity, and diminished quality of life for those with poor mental health. Hence, better understanding the impact of stigma across different cultural contexts is critically essential, aiming to inform culturally nuanced strategies to minimize its consequences and contribute to a more equitable and effective psychiatric care system. The purpose of the present literature review is twofold (i) to examine the existing research on the stigma surrounding psychiatry across different cultural contexts and (ii) to identify the commonalities and differences in the nature, magnitude, and consequences of this stigma in different cultures in the psychiatry field. In addition, potential strategies for addressing stigma will be proposed. The review covers a range of countries and cultural settings, emphasizing the importance of understanding cultural nuances to combat stigma and promote mental health awareness globally.
Introduction and background
Stigma, characterized by societal prejudice and discrimination, profoundly influences psychiatric care, creating barriers to the timely recognition and treatment of mental health disorders [ 1 ]. Deeply embedded in societal norms, stigma is a multifaceted issue permeating every level of psychiatric care, leading to delayed treatment, increased morbidity, and a diminished quality of life for patients.
The importance of addressing stigma in psychiatry cannot be overstated as stigma impacts individuals seeking care, their families, healthcare professionals, and broader society. At the individual level, stigma can lead to fear and avoidance of mental health services, causing delays in seeking help even when a patient is in dire need. Delays in seeking care can exacerbate mental health conditions leading to worse outcomes and reduced quality of life [ 2 ]. For families, the stigma can lead to shame and isolation, making seeking necessary support and resources more difficult. Interestingly, in healthcare professionals, stigma can lead to burnout and demoralization, reducing the quality and provision of care. Stigmatization can also create barriers between healthcare providers and patients, complicating matters to establishing trustful and therapeutic relationships, which are essential for effective care [ 1 ]. For society at large, stigma can result in the misallocation of resources, with mental health services often being underfunded and overlooked [ 3 ]. Hence stigma has profound effects at personal and societal levels, negatively impacting multiple levels of the psychotic care continuum.
Addressing the stigma surrounding mental health can significantly enhance the effectiveness of psychiatric care. To this end, developing programs and strategies that foster a culture of understanding and acceptance may encourage more individuals to seek help when they need it, improving early detection and intervention, which are crucial for better health outcomes. Furthermore, challenging and changing stigmatizing attitudes can improve the therapeutic relationship between healthcare providers and patients, leading to more personalized and effective treatment strategies.
Stigma, however, is not a monolithic entity but varies across cultures, influenced by distinct societal norms, values, and beliefs. Understanding these cultural variations is essential for developing effective, culturally sensitive interventions. Therefore, this literature review aims to examine the manifestation and impacts of stigma across different cultural contexts, laying the foundation for tailored strategies to combat this healthcare barrier.
Stigma as a psychological construct
In the literature, there have been several attempts at creating instruments to measure and understand stigma as a psychological construct in the context of mental health. In this vein, the Internalized Stigma of Mental Illness (ISMI) scale and the Perceived Devaluation-Discrimination Scale, among others, seek to quantify stigma more objectively [ 4 , 5 ] . The ISMI scale, as defined by Ritsher et al. (2003), measures the subjective experience of stigma, including the internalization of negative stereotypes and beliefs about mental illness [ 4 ]. It includes five subscales: Alienation, Stereotype Endorsement, Discrimination Experience, Social Withdrawal, and Stigma Resistance. These subscales were further defined as follows: (i) Alienation: The feeling of being less than a full member of society due to one's mental illness, (ii) Stereotype Endorsement: The extent to which the individual agrees with common negative stereotypes about people with mental illness, (iii) Discrimination Experience: Personal experiences of rejection or exclusion due to mental illness, (iv) Social Withdrawal: The extent to which the individual avoids social situations for fear of being stigmatized, and (v) Stigma Resistance: The individual's ability to resist or counteract stigma. The Perceived Devaluation-Discrimination Scale, as described by Link (1987), measures the extent to which individuals believe that most people will devalue or discriminate against someone with a mental illness [ 5 ]. It focuses on the individual's perceptions of societal attitudes, rather than their personal experiences with stigma. Overall, while the ISMI scale can give insights into the internalization and personal experience of stigma, the Perceived Devaluation-Discrimination Scale can provide a view of societal attitudes and perceived discrimination. The above are crucial to understanding the full landscape of stigma in psychiatry across different cultures by helping identify where interventions might be most needed and most effective, whether at the level of societal attitudes, personal beliefs, or both. The pervasive nature of stigma presents a daunting challenge to psychiatry, necessitating a rigorous and nuanced approach to its understanding and mitigation. However, despite recent awareness campaigns, the field still struggles with the barriers that stigma imposes on patient care, necessitating additional analysis of the effects.
Individual and societal impact of stigma
Stigmatization of mental illness across cultures is a significant barrier to psychiatric care. The stigma can lead to delayed diagnosis and treatment-seeking behaviors, reduced quality of life, and an increased risk of social exclusion and discrimination [ 2 ]. Furthermore, mental illness stigma often intersects with other forms of stigma, such as gender, race, and socio-economic status, leading to further marginalization of already vulnerable populations making it challenging to provide equitable, culturally sensitive, and effective psychiatric care to individuals with mental illness. Accumulating research suggests that stigma toward mental illness is common in various cultures, which can affect mental illness diagnosis, treatment, and management [ 6 ]. Furthermore, some studies reveal that mental health stigma manifests differently across cultures and can be influenced by cultural beliefs, attitudes, and values [ 7 ]. The stigma surrounding psychiatry and mental health disorders has numerous detrimental effects on individuals and communities, including:
1. Delayed Treatment-Seeking Behavior
Stigma plays a significant role in delaying treatment-seeking behavior for individuals struggling with mental health issues. The fear of being labeled, ostracized, or misunderstood due to their condition often deters individuals from seeking help promptly. According to a study by Clement et al. (2015), stigma was associated with an increased likelihood of delaying or avoiding seeking help for mental health concerns [ 8 ]. Consequently, symptoms may worsen over time, escalating the condition's severity and making treatment and prospective recovery more challenging. Healthcare delays can also lead to decreased self-esteem and increased depressive symptoms, creating a vicious cycle of self-blame, isolation, and hopelessness. Prolonged untreated mental health issues can further impair an individual's functionality in various life domains, including work, relationships, and self-care, thus reducing their overall quality of life [ 9 ].
2. Social Isolation and Discrimination
Stigma can lead to social isolation and discrimination for those affected by mental health issues. Brohan and Thornicroft (2010) found that individuals with mental health disorders often face discrimination in multiple life domains, including employment and interpersonal relationships [ 2 ]. The negative stereotypes and misconceptions surrounding mental illness often result in a lack of understanding and empathy from others, leading to social exclusion [ 10 ]. Individuals with mental health issues might face discrimination in various aspects of life, including the workplace, where they might encounter bias in hiring, job retention, and career advancement. Furthermore, to complicate matters, discrimination can further strain personal relationships, as friends and family may distance themselves due to discomfort, fear, or misunderstanding, exacerbating feelings of isolation and loneliness [ 9 ].
3. Reduced Treatment Adherence
Stigma can significantly impact adherence to mental health treatments. Sirey et al. (2001) found that perceived stigma predicted treatment discontinuation in older adults with depression [ 11 ]. People living with mental health conditions may avoid or discontinue treatment due to fear of being identified as a mental health patient. This fear could stem from concerns about the stigma associated with visiting mental health facilities, taking psychiatric medications, or being seen engaging in therapeutic activities [ 12 ]. Non-adherence to treatment regimens can lead to suboptimal treatment outcomes, hinder recovery, and increase the risk of relapse or worsening symptoms. Furthermore, stigma can diminish self-efficacy, making individuals less likely to actively engage in their treatment process, which is crucial for successful recovery.
4. Perpetuation of Misconceptions
Stigmatizing attitudes towards mental illness contribute to the perpetuation of harmful stereotypes and misinformation. AsCorrigan and Watson (2007) discussed, stereotypes such as appearing dangerous, unpredictable, or culpable for their illness can make people with mental illness perceived inaccurately as dangerous or to blame for their condition, both internally and externally [ 12 ]. Stereotyping, deeply embedded in societal attitudes, can foster a culture of fear, rejection, and discrimination against individuals with mental health conditions. Misconceptions often result in people with mental health issues being perceived inaccurately as dangerous, unpredictable, or responsible for their condition. In addition, misinformation can hinder public understanding and acceptance of mental illness, exacerbating stigma while negatively influencing policy and legislation, leading to inadequate funding and support for mental health services.
5. Influence of Gender on Stigma
The impact of stigma on individuals with mental illness is known to vary across different social and demographic categories, including gender. Research evidence indicates that the experience of stigma related to mental illness can be significantly different for men and women, and these differences can be further influenced by cultural context.
In some societies, women seem to face higher levels of stigma related to mental health issues compared with men. A study by Al Krenawi et al. (2006) conducted in the Bedouin-Arab community found that women experienced a significantly higher degree of stigma associated with mental illness than their male counterparts [ 13 ]. This may be due to traditional gender roles and societal expectations, which often place women in a more subordinate position and associate mental illness with weakness or vulnerability. Women with mental illnesses may therefore face dual discrimination - first for their gender and then for their mental health condition. This can make women less likely to seek help for mental health issues, further exacerbating their condition and creating a vicious cycle of stigma and untreated mental illness.
However, the influence of gender on stigma is not uniform across all cultures. Ayalon and Areán's (2004) study on older adults in an Arab cultural context found that men reported higher levels of perceived stigma related to mental illness than women [ 14 ]. This discrepancy might be rooted in traditional masculine norms prevalent in many Arab societies, which value strength, stoicism, and emotional control. Mental illness, which is often erroneously perceived as a sign of emotional weakness or lack of control, can be particularly stigmatizing for men in these contexts. Furthermore, the expectation for men to be the primary earners and providers in the family can make the potential economic impacts of mental illness, such as unemployment or reduced productivity, particularly stigmatizing.
These findings underscore the importance of considering gender and cultural context in understanding and addressing stigma related to mental illness. It is crucial to develop and implement culturally sensitive strategies that consider these differences in the experience of stigma. This might involve, for example, promoting mental health literacy, challenging harmful gender norms, and providing gender-specific mental health services. We can move toward a more equitable and effective mental health care system by acknowledging and addressing the unique stigma-related challenges different groups face.
Ethnic and cultural variations in stigma
The stigma surrounding psychiatry, as research suggests, manifests differently across cultures due to various factors [ 7 ]. This stigma operates at various levels, including individuals, families, healthcare providers, and society, and cultural norms, religious beliefs, and social attitudes influence its manifestations and implications.
At the individual level, mental health issues may be internalized differently depending on cultural background. For instance, some Asian cultures may view mental health issues as a sign of personal weakness or a failure of self-control [ 15 ]. The internalization of stigma can significantly influence an individual's self-perception and willingness to seek help. In the family context, cultural beliefs also play a significant role in shaping attitudes toward mental health. A study by Yang and Kleinman (2008) found that in Chinese culture, mental illness is often attributed to social and interpersonal factors, such as family conflict [ 16 ]. Such attributions can contribute to a sense of shame or blame within the family, exacerbating the stigma experienced by the individual with mental illness.
Healthcare providers are not immune to these cultural beliefs and they can influence their practice. In some cultures, mental illnesses are viewed through a supernatural lens rather than a medical one. Girma et al. (2013) found that in Ethiopian culture, mental illness is commonly associated with supernatural causes, such as evil spirits or curses [ 17 ]. This widely held belief can influence healthcare providers' approach and potentially limit the provision of evidence-based psychiatric care.
Lastly, at the societal level, these cultural perceptions and beliefs can contribute to the broader social stigma surrounding mental health, leading to discrimination and social exclusion. Differences in societal perceptions across cultures can lead to distinct forms of discrimination, further compounding the challenges faced by individuals with mental health issues. Hence, understanding and addressing cultural stigma in psychiatry involves a multifaceted approach that considers individual, family, healthcare providers, and societal levels. Each level offers potential avenues for stigma reduction and improved mental health outcomes.
Asian Cultures
In many Asian societies, mental health issues are often perceived as a sign of personal weakness or a failure of self-control. The concept of 'face' is significantly influential, and the stigma associated with mental illness can be seen as bringing shame to the family [ 15 ]. For instance, a strong cultural emphasis on academic and professional achievement in South Korea contributes to stigmatizing attitudes toward mental illness, which may discourage individuals from seeking help [ 18 ].
African Cultures
Mental illnesses in some African cultures are often attributed to spiritual or supernatural causes such as curses or possession by evil spirits. This understanding can contribute to high levels of stigma and deter individuals from seeking psychiatric help [ 19 ]. In Ethiopia, the belief in supernatural causes of mental illness has been reported, leading to the stigmatization of affected individuals [ 17 ].
Arab Cultures
Mental illness in Arab societies is frequently viewed as a form of divine punishment. Religious belief perpetuating mental health stigma can lead to delayed or avoided treatment as individuals may resort to religious or spiritual interventions [ 20 ].
Latin American Cultures
In some Latin American cultures, mental illness is often attributed to personal weakness or lack of willpower. This perspective could stigmatize individuals with mental health disorders and discourage them from seeking psychiatric care [ 21 ].
Western Cultures
In Western societies, stigma often stems from misconceptions about mental illness, including the belief that individuals with mental health disorders are dangerous or unpredictable. While mental illness is recognized more as a health issue, stigma still exists, often resulting in social exclusion and discrimination [ 12 ].
Additionally, culture-bound syndromes, defined here as a combination of psychiatric and somatic symptoms that are considered to be a recognizable disease within specific cultures or societies, are a critical component of a discussion on cultural stigma in psychiatry. That is to say, culture-bound syndromes refer to unique mental health conditions closely tied to specific cultures or ethnic groups. For instance, among the Latino community, 'Ataque de Nervios,' characterized by uncontrollable shouting, crying, trembling, and sometimes aggressive behavior, is a recognized condition often associated with a stressful event such as a panic attack [ 21 ].
Hence, a clinician's awareness and understanding of such culture-bound syndromes can enhance their diagnostic and therapeutic effectiveness. In fact, a study conducted by Hughes and Wintrob (1995) in New York discovered a significant improvement in therapeutic relationships when clinicians were knowledgeable about culture-bound syndromes prevalent in their patients' cultures, such as 'Qigong Psychotic Reaction' in Chinese immigrants, a condition associated with overdoing Qigong, a type of spiritual martial art [ 22 ].
Furthermore, cultural competence, which includes knowledge about culture-bound syndromes, has a substantial impact on treatment outcomes. Culturally competent care, defined by an understanding and respect for cultural differences, can improve patient satisfaction and adherence to treatment. A systematic review by Truong et al. (2014) demonstrated the positive effect of cultural competence on healthcare outcomes, including in a Native American population suffering from 'Ghost Sickness,' a culture-bound syndrome characterized by feelings of terror, weakness, and a sense of impending doom, often linked to the perceived presence of the supernatural [ 23 ].
Simultaneously, addressing culture-bound syndromes can influence and reduce mental health stigma across cultures. Misinterpretation of these syndromes can contribute to stigma, as individuals might be wrongly diagnosed or misunderstood. For instance, Kirmayer's (2012) study on cultural variations in depression and anxiety found that misunderstanding culture-bound syndromes, such as 'Taijin Kyofusho,' a Japanese syndrome characterized by an intense fear that one's body or bodily functions are displeasing to others, could lead to misdiagnosis and increase stigma [ 24 ]. Practices that raise awareness of culture-bound syndromes offer a deeper, richer perspective on cultural influences on mental health. Awareness and understanding of these syndromes can enhance diagnostic and treatment approaches, optimize patient outcomes, and potentially contribute to reducing mental health stigma across various cultures.
Taken together, these studies highlight the importance of understanding cultural contexts when addressing the stigma surrounding mental health disorders and psychiatric care. The cultural beliefs and attitudes towards mental health disorders, summarized below in Table Table1, 1 , influence how stigma is manifested and the approaches needed to reduce it effectively. By acknowledging cultural variations, more culturally appropriate and effective strategies can be developed to combat stigma and improve mental health care across different societies worldwide.
| Authors | Cultural Group | Perception of Mental Illness | Impact on Stigma |
| Chen & Mak, 2008 [ ] | Asian | Seen as a sign of personal weakness or failure of self-control | Stigma leads to family shame, discourages help-seeking |
| Girma et al., 2013 [ ] | African | Attributed to spiritual or supernatural causes | High stigma levels, deter individuals from seeking psychiatric help |
| Karam et al., 2008 [ ] | Arab | Viewed as a form of divine punishment | Significant stigma, leads to delayed or avoided treatment |
| Alegria et al., 2002 [ ] | Latin American | Attributed to personal weakness or lack of willpower | Stigmatizes individuals, discourages them from seeking psychiatric care |
| Corrigan & Watson, 2007 [ ] | Western | Misconceptions about danger or unpredictability | Results in social exclusion and discrimination |
Strategies for addressing mental health stigma
Several strategies have been proposed in the literature to address the stigma surrounding psychiatry across cultures:
1. Public Awareness Campaigns
Awareness campaigns can be instrumental in dismantling misconceptions and fostering understanding of mental health disorders. Public awareness campaigns can dispel myths, reduce stigma, and encourage empathy towards affected individuals by promoting accurate information about mental illnesses, their prevalence, and the possibilities for recovery. For instance, a study by Pinfold et al., (2003) showed that public campaigns using direct social contact with people with mental illness could significantly improve public attitudes towards mental health [ 25 ]. The study by Pinfold et al., (2003) implemented educational interventions in UK secondary schools, consisting of video presentations and direct social contact with individuals who had personal experiences with mental illness [ 25 ]. The UK campaign's goal was to challenge common myths about mental illness and replace them with accurate information. The results showed that students exposed to this intervention demonstrated less fear and avoidance of people with mental health problems and were more likely to see them as individuals rather than defining them by their illness.
2. Cultural Competency Training for Healthcare Professionals
Medical education can equip healthcare providers with the necessary knowledge and skills to understand and respect their patients' cultural backgrounds and experiences, which is critical for reducing stigma in healthcare settings. Research indicates that healthcare providers who lack cultural competence may inadvertently contribute to stigma, further deterring patients from seeking help [ 26 ]. A study by Kirmayer (2012) found that cultural competence training improved healthcare providers' understanding of cultural influences on health behaviors and led to more effective patient-provider communication, thereby reducing perceived stigma [ 24 ]. For instance, a study in Australia provided cultural competency training to healthcare providers and found that their understanding of Indigenous Australians' health needs significantly improved [ 24 ]. They were able to better respect and incorporate Indigenous perspectives in treatment, which led to increased trust and better patient-provider relationships.
3. Peer Support Programs
People with lived experiences of mental health disorders who share their stories, can normalize mental health issues and challenge stigma. By providing real-life examples of individuals living with and managing their mental health disorders, peer-to-peer advocacy programs may debunk myths and reduce the perceived 'otherness' of mental illness. A study by Pitt et al. (2013) showed that peer support reduced self-stigma and improved self-esteem and empowerment among individuals with mental health disorders [ 27 ]. The study focused on "consumer-providers," individuals who had personally experienced mental health issues and were now providing support services to others. The findings demonstrated that consumer-providers significantly reduced self-stigma among service users, while also improving self-esteem and feelings of empowerment.
4. Community-Based Mental Health Services
Integrating mental health care into primary care and community settings can reduce the stigma associated with seeking psychiatric help. This emphasis on integrating measures for mental well-being along with other routine and standard primary care protocols allows mental health care to be more accessible and less intimidating, encouraging individuals to seek help when needed. A study by Thornicroft et al. (2015) found that community-based mental health services can reduce stigma and discrimination and improve mental health outcomes [ 28 ]. For instance, a program in India called the MANAS project integrated mental health services into primary care and community settings [ 28 ]. This approach not only made mental health services more accessible but also more 'normal' and less stigmatizing. The project reported a significant increase in the utilization of mental health services and a decrease in the experience of stigma among service users.
5. Evidence-Based Approach
Another approach to overcoming the barriers created by stigma is to use evidence-based methods to reduce mental illness stigma. A meta-analysis by Corrigan et al. (2016) found that various evidence-based interventions, including education and contact-based interventions, can effectively reduce mental illness stigma across cultures [ 9 ]. Contact-based interventions involve interaction between people with mental illness and members of the public to challenge negative attitudes and beliefs. Education-based interventions aim to increase knowledge and awareness of mental illness and reduce negative stereotypes. Educational interventions can be delivered in a variety of formats, such as in-person workshops, online courses, and mass media campaigns.
The role of the healthcare provider in ameliorating stigma cannot be overlooked. Moreover, a review by Ayalon and Areán (2004) suggests that mental health providers can play a critical role in reducing mental illness stigma by engaging in culturally sensitive practices [ 14 ]. For instance, mental health providers can develop cultural competence, which refers to the ability to provide effective services to individuals from diverse cultural backgrounds. Cultural competence involves understanding and respecting cultural differences, tailoring treatment to meet diverse populations' unique needs, and integrating cultural factors into treatment planning.
Research also highlights that stigma towards mental illness has significant implications for treating and managing mental health conditions. For example, several studies suggest that stigma can lead to delayed diagnosis and treatment-seeking behaviors [ 13 , 16 ]. This is concerning because early intervention is critical for managing mental illness and improving outcomes for individuals living with these conditions. Considering the documented impact of stigma on timely diagnosis and treatment-seeking behaviors, strategies such as public awareness campaigns, cultural competency training for healthcare professionals, peer support programs, community-based mental health services, and an evidence-based approach can play a crucial role in combating cultural stigma in psychiatry. These measures collectively contribute to improved awareness, understanding, and acceptance of mental health conditions, thus facilitating early intervention and better management of mental illnesses across diverse cultural contexts.
Conclusions
Stigma surrounding mental health and psychiatric care is a complex and multifaceted issue that varies across ethnic and cultural contexts. To effectively address and reduce stigma in mental healthcare settings, developing culturally sensitive interventions and promoting understanding and acceptance of mental health issues is crucial. By doing so, we can work towards improving access to mental health care and promoting the well-being of individuals and communities across the globe.
Overall, the literature suggests that stigma is a complex and pervasive issue that affects individuals with mental illness across cultures. The studies reviewed reveal that mental illness stigma is influenced by cultural beliefs, attitudes, and values, and can manifest in different ways across cultures. It is important to understand these cultural differences to develop more effective interventions to reduce mental illness stigma and improve outcomes for individuals living with mental illness. Furthermore, stigma across cultures impacts psychiatric care in various ways and can create significant barriers to effective treatment. Evidence-based interventions, including education, contact-based interventions, and culturally sensitive practices can help overcome these barriers. Mental health providers should strive to develop cultural competence and deliver culturally sensitive interventions to meet the needs of diverse populations. Research to understand the impact of stigmatization of mental health patients and its impact in providing services is warranted. Reducing mental illness stigma is critical to providing equitable, effective, and compassionate psychiatric care to individuals with mental illness.
The authors have declared that no competing interests exist.
Confronting the Challenge of Mental Health Stigma: A New Report and a New National Initiative
- October 14, 2022
- Public awareness
In a report issued Oct. 9, The Lancet Commission on Ending Stigma and Discrimination in Mental Health issues a call to action to “act now to stop stigma and to start inclusion.” The report summarizes extensive research around the world, highlights the results of an international survey, and provides recommendations for actions by a range of stakeholders.
"People with lived experience of mental health conditions are the key change agents for stigma reduction." The Lancet Commission
Importantly, the report incorporates and highlights the voices and perspectives of people with lived experience of mental health conditions. The report was the work of more than 50 people led by Graham Thornicroft, Ph.D., and was published online in The Lancet* in early October. “It is time to end all forms of stigma and discrimination against people with mental health conditions, for whom there is double jeopardy: the impact of the primary condition and the severe consequences of stigma,” the report urges.
Harmful Effects of Stigma
The report summarizes the negative impact of stigma and discrimination which “contravene basic human rights and have severe, toxic effects on people with mental health conditions that exacerbate marginalization and social exclusion, for example by reducing access to mental and physical health care and diminishing educational and employment opportunities.”
The report also points to the role of the media in both perpetuating and potentially decreasing stigma. The media contributes to further stigmatization, for example, by reinforcing stereotypes such as the dangerousness of people with mental illness. The media can also play a positive role, for example, when following accepted guidance on how to report on suicides. p
Addressing Stigma
Based on an umbrella review of more than 200 articles, the Commission found that stigma is most effectively addressed through interventions based on social contact — including in-person, virtual or indirect — that have been adapted for the culture and context. Anti-stigma programs were most effective when
- They involve people with lived experience of mental health conditions in all aspects.
- Target groups are consulted on content and delivery.
- Efforts are sustained over the long term.
The report proposes a series of goals and recommendations for action by different sectors, each with specific targets and indicators. They are:
- International non-governmental organizations should issue guidance that all forms of stigma and discrimination towards people with mental health conditions are unacceptable.
- Governments of all nations should implement policies to support the end of stigma and discrimination against people with mental health conditions.
- Employers should ensure that stigma and discrimination against people with mental health conditions in the workplace are eradicated.
- Healthcare and social-care sectors should include mandatory sessions (co-delivered by people with lived experience) on the needs and rights of people with mental health conditions in national professional and vocational training curricula.
- Media organizations should systematically remove stigmatizing content.
- People with lived experience and local communities should be strongly supported to reduce stigma and discrimination.
New National Anti-Stigma Initiative

A new national initiative, launched by Huntsman Mental Health Institute in collaboration with many other organizations, aims to end the stigma of mental illness and substance use disorders. On World Mental Health Day, October 10, more than 180 leaders from across the country gathered in Utah to develop strategic actions for the 10-year Stop Stigma Together campaign. The goal of the effort is “to pose a grand challenge to our friends, family, employers, health care providers and governments to end the stigma around mental health and substance-use disorders to establish true well-being.” It will involve:
- Establishing metrics and sustainable funding models.
- Building infrastructure to coordinate and communicate evidence-based best practices.
- Creating outreach plans to connect to hard-to-reach and underserved communities and populations.
- Hosting pilot projects and gathering evidence to identify new success models.
* The Lancet is a two-century-old widely respected medical journal. Its commissions, made up of global experts, publish research and comments on important issues in medicine.
Medical leadership for mind, brain and body.
Mobile menu.
- Psychiatrists
- Residents & Medical Students
- Patients and Families
- Advocacy & APAPAC
- Diversity & Health Equity
- Research & Registry
- Meetings & Events
- Search Directories & Databases
- International
- Medical Students
- What is Psychiatry?
- Find a Psychiatrist
- Addiction and Substance Use Disorders
- Dementia and Alzheimer's Disease
- Alcohol Use Disorder
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder
- Bipolar Disorders
- Climate Change and Mental Health Connections
- Coping After Disaster
- Disruptive, Impulse-Control and Conduct Disorders
- Dissociative Disorders
- Domestic Violence
- Eating Disorders
- E-Cigarettes and Vaping
- Gambling Disorder
- Gender Dysphoria
- Helping a Loved One Cope with Mental Illness
- Hoarding Disorder
- Integrated Behavioral Healthcare
- Intellectual Disability
- Internet Gaming
- Obsessive-Compulsive Disorder
- Opioid Use Disorder
- Perinatal Depression (formerly Postpartum)
- Personality Disorders
- Posttraumatic Stress Disorder (PTSD)
- Prolonged Grief Disorder
- Schizophrenia
- Seasonal Affective Disorder (SAD)
- Sleep Disorders
- Somatic Symptom Disorder
- Specific Learning Disorders
- Stigma, Prejudice and Discrimination Against People with Mental Illness
- Suicide Prevention
- Technology Addictions: Social Media, Online Gaming, and More
- Warning Signs of Mental Illness
- Electroconvulsive Therapy (ECT)
- What is Mental Illness?
- What is Psychotherapy?
- What is Telepsychiatry?
- La Salud Mental
- Childhood Disorders: Medication Guides for Parents
- Lifestyle to Support Mental Health
- Member Benefits
- Honorary Fellowship (FAPA & DFAPA)
- Awards & Leadership Opportunities
- Get Involved
- Directories, Contact Info & FAQs
- District Branches
- APA's Vision, Mission, Values, and Goals
- Meet Our Organization
- Read APA Organization Documents and Policies
- Work At APA
- About APA's Headquarters
- Policy Finder
- News Releases
- Messages from the APA President
- Reporting on Mental Health Conditions
- Goldwater Rule
- Annual Meeting Press Registration + Guidelines
- APA Public Opinion Polls
- Reporter Toolkit: Recommendations on Covering the AAPI Community
- Comunicados de prensa en español
- APA Annual Meeting
- APA Communities
- APA Foundation
- APA JobCentral
- APA Learning Center
- APA Publishing
- Center for Workplace Mental Health
- Melvin Sabshin, M.D. Library & Archives
- Psychiatric News
- Psychiatry Online
- Annual Meeting
- APA On Demand
- At the APA Educational Series
- Books and Journals
- Certification and Licensure
- Diversity and Health Equity Education Resources
- Meeting Submission and Guidelines
- Mental Health Innovation Zone
- The Mental Health Services Conference
- The Virtual Immersive
- Virtual Paid Courses
- Clinical Practice Guidelines
- Covid-19 / Coronavirus
- Digital Mental Health
- Helping Patients Access Care
- Media and Communications
- Mental Health Apps
- Mental Health Parity
- Practice Management
- Professional Interests
- Quality Improvement
- Risk Management
- Social Media
- Sunshine Act
- Telepsychiatry
- The Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program
- Transition to Practice and Early Career Resources
- Well-being and Burnout
- Mental Health and Faith Community Partnership
- Mental Health Equity Looking Beyond Series
- Minority and Underrepresented (M/UR) Caucuses
- Moore Equity in Mental Health Initiative
- News and Updates
- Striving for Excellence Series
- SAMHSA Minority Fellowship Program
- AMNet: Addiction Medicine Practice Based Research Network
- PsychPRO: APA's Mental Health Registry
- Research Colloquium for Junior Psychiatrist Investigators
- Perinatal Mental Health Toolkit
- Psychiatric Bed Crisis Report
- Advocacy Action Center
- Congressional Advocacy Network
- Election Resource Center
- Federal Affairs
- State Affairs
- Implementing 9-8-8
- Advocacy Update Webinars
- 2025 Annual Meeting
- The 2024 Mental Health Services Conference
- Addressing Structural Racism Town Hall Series
- APA Meetings App
- Governance Meetings
- Mental Health Equity Fireside Chat Series
- Moore Equity in Mental Health 5K
- Policy & Practice Insights Series
- September Component Meetings
- Social Determinants of Mental Health Town Hall Series
- Amicus Briefs
- Assembly Directory
- Component Directory
- Conference Publications
- Library and Archive
- Member Directory
- Member Obituaries
- Practice Guidelines
- Resource Documents
- International Trainees
- International Humanitarian Opportunities
- Global Mental Health
- International Medical Graduates Resources
- Residents' Journal
- Featured Publications
- APAF Fellowships
- External Fellowships and Awards
- Helping Residents Cope with a Patient Suicide
- Vacant Resident Positions
- Leadership Positions
- SET for Success
- Apply for Psychiatric Residency
- Choosing a Career in Psychiatry
- Building a Career in Psychiatry
- Medical Student Programs
- Resident-Fellow Census
- Transitioning to Residency During COVID-19
- What Is a Substance Use Disorder?
- Expert Q&A: Addiction and Substance Use Disorders
- What Are Dementia and Alzheimer’s Disease?
- Expert Q&A: Dementia and Alzheimer's Disease
- What are Anxiety Disorders?
- Expert Q&A: Anxiety Disorders
- What is ADHD?
- Expert Q&A: ADHD
- What Is Autism Spectrum Disorder?
- Expert Q&A: Autism Spectrum Disorder
- What Are Bipolar Disorders?
- Expert Q&A: Bipolar Disorder
- How Extreme Weather Events Affect Mental Health
- Who Is Affected by Climate Change?
- What Is Depression?
- Expert Q&A: Depression
- What are Disruptive, Impulse Control and Conduct Disorders?
- Expert Q&A: Disruptive, Impulse Control and Conduct Disorders
- What Are Dissociative Disorders?
- Expert Q&A: Dissociative Disorders
- What are Eating Disorders?
- Expert Q&A: Eating Disorders
- What is Gambling Disorder?
- Expert Q&A: Gambling Disorder
- What is Gender Dysphoria?
- Expert Q&A: Gender Dysphoria
- What is Hoarding Disorder?
- Expert Q&A: Hoarding Disorder
- What is Intellectual Disability?
- Expert Q&A: Intellectual Disability
- What Is Obsessive-Compulsive Disorder?
- Expert Q&A: Obsessive-Compulsive Disorder
- What is Perinatal Depression (formerly Postpartum)?
- Expert Q&A: Perinatal Depression
- What are Personality Disorders?
- Expert Q&A: Personality Disorders
- What is Posttraumatic Stress Disorder (PTSD)?
- Expert Q&A: Posttraumatic Stress Disorder (PTSD)
- What is Schizophrenia?
- Expert Q&A: Schizophrenia
- What are Sleep Disorders?
- Expert Q&A: Sleep Disorders
- What is Somatic Symptom Disorder?
- Expert Q&A: Somatic Symptom Disorder
- What Are Specific Learning Disorders?
- Expert Q&A: Specific Learning Disorders
- What is Technology Addiction?
- Expert Q&A: Technology Addiction
- Cigarrillos electrónicos y vapeo
- Trastorno del espectro autista
- Trastorno por consumo de alcohol
- Trastorno por consumo de opioides
- Trastorno de estrés postraumático (TEPT)
- Adicción a la tecnología: redes sociales, juegos en línea, y más
- ¿Qué es la psiquiatría?
- Conexiones entre el cambio climático y la salud mental
- Más temas de salud mental
- General Members
- Early Career Psychiatrists
- Residents and Fellows
- International Resident-Fellows
- Semi-Retired and Retired
- View Your Profile
- Resident-Fellow Members
- Fellow of the APA
- Distinguished Fellow of the APA
- International Fellow of the APA
- International Distinguished Fellow of the APA
- 2024 Class of Honorary Fellows
- 2025 APA National Elections
- Councils, Committees and Components
- Resident-Fellow Leadership Opportunities
- Volunteer Leadership Opportunities
- Advocacy and APAPAC
- APA/APAF Fellowships
- APA Insider Sessions
- APA Specialty Interest Caucuses, Listservs & Communities
- Leadership, Equity and Diversity Institute
- Mentorship Program for APA/APAF Fellows
- Research Colloquium
- Contact Your Membership Specialist
- Contact Your District Branch
- Membership FAQs
- Semi-Retired and Retired FAQs
- Lump Sum Dues
- 2025 APA Dues Rate Changes FAQs
- District Branch Resources
- District Branch Dues for General Members
- District Branch Dues for Residents and Fellows
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
How the Stigma of Mental Health Is Spread by Mass Media
xavierarnau / iStock
What Is Stigmatization?
- Trivialization
- Depictions in Film
- Why It's Damaging
- What's Accurate In Media Portayals?
- Impact of Media Portrayals
What Can Be Done?
In the aftermath of an unconscionable act of random violence, many people are inclined to label the perpetrator “crazy.” Although the criminal may have a mental illness , automatically assigning the label “crazy” does a great disservice to people who live with mental illness every day.
In reality, somebody with mental illness is much more likely to be a victim—rather than a perpetrator—of violence. Calling a violent offender “crazy” spreads a dangerous stereotype and belies the complex relationship between criminality and mental illness.
The media teaches us about people with whom we do not routinely interact. This constant flow of data gives us incessant social cues about the nature of other groups of people—including which groups of people should be praised or scorned.
Media portrayals of those with mental illness often skew toward either stigmatization or trivialization. Consequently, all forms of media—including television, film, magazines, newspapers, and social media—have been criticized for disseminating negative stereotypes and inaccurate descriptions of those with mental illness.
Stigma involves negative beliefs, attitudes, and behaviors directed toward people based on some distinguishing characteristics. In the case of mental health stigma, it involves the presence of mental health symptoms or a mental health diagnosis.
In other cases, stigma can also involve health conditions, disabilities, gender, race, sexuality, culture, religion, and sexuality.
Stigma happens when some person is viewed as an “other.” A person considered an "other" is denied full social acceptance.
The impact of mental health stigma is serious. Evidence suggests that it is linked to worse mental health outcomes because it reduces the likelihood that a person will seek help, receive adequate care, and adhere to their treatment plan.
Stigmatization of Mental Illness By the Media
Stigmatization of mental illness in media is abundant. For example, certain mental health conditions, such as schizophrenia are seen as being so disruptive that people with those conditions must be isolated from society.
The stigmatization of mental illness is so entwined with the media that researchers have used newspaper articles as a proxy metric for stigma in society.
Media accounts tend to focus on the individual with mental illness rather than framing mental illness as a societal issue. Consequently, media consumers are more likely to blame an individual for the illness.
Mental Illness Is Overgeneralized
People with mental illness can also suffer from overgeneralization in media portrayals. Every person with a specific mental health condition is expected to display the same characteristics or symptoms.
For instance, common depictions are that all people with depression are suicidal , and all people with schizophrenia hallucinate. In reality, 60% and 80% of people with schizophrenia experience auditory hallucinations . An even smaller number of people experience visual hallucinations.
It's also not uncommon for media portrayals to discount that many people with mental illness don’t need to disclose their condition to everyone around them.
Instead, mental illness often goes unrecognized (whether by intention or not). The portrayals in the media tend to present situations where everyone in a character's life knows about their mental illness.
Perhaps most concerning, the media often portrays mental illness as untreatable or unrecoverable.
Trivialization of Mental Illness By the Media
The media can also trivialize mental illness, either by promoting mental illness as not being severe or being less severe than it really is.
For instance, many people with eating disorders such as anorexia nervosa feel that their condition is made out to be less severe than it really is. This is in part because people with the condition portrayed in the media often minimize its seriousness and hide the severe consequences of the disease.
The truth is, the death rate for people with anorexia is high. In reality, anorexia has one of the highest mortality rates of any mental health condition. Research suggests the risk of dying is 10 times higher for people who have anorexia nervosa.
Mental illness can also be oversimplified by the media. For instance, a person with obsessive-compulsive disorder (OCD) is often depicted as being overly concerned with cleanliness and perfectionism. However, the obsessive thoughts that drive their compulsions are overlooked or absent.
The symptoms of mental illness are sometimes portrayed as being beneficial. For example, in the popular television series Monk , the protagonist is a detective with OCD. The fact that he pays close attention to detail helps him solve crimes and advance his career.
People who do not have disabilities can use media channels to mock people who do have disabilities, such as by appropriating mental-illness terminology. For instance, the hashtag OCD (#OCD) is commonly used on Twitter to describe one's attention to cleanliness or organization.
Depictions of Schizophrenia in Film
Probably the most disparaging stigmatizations of mental illness in media lie in the film portrayals of antagonists with mental illness. In particular, when characters with schizophrenia are presented as “homicidal maniacs” in “slasher” or “psycho killer” movies.
Inaccurate portrayals of mental illness in the media disseminate misinformation about the symptoms, causes, and treatment of schizophrenia and other forms of severe mental illness. Unfortunately, popular movies and tv shows can exert potent influences on attitude formation.
In one study, researchers analyzed 41 movies that had been released between 1990 and 2010 for depictions of schizophrenia.
Based on the findings of the analysis, researchers drew several conclusions.
- Most of the characters displayed "positive" symptoms of schizophrenia, with delusions being featured most frequently, followed by auditory and visual hallucinations.
- The majority of characters displayed violent behavior toward themselves or others.
- Nearly one-third of violent characters engaged in homicidal behavior.
- About one-fourth of the characters committed suicide.
- The cause of schizophrenia was infrequently noted. However, in about one-fourth of the movies it was implied that a traumatic life event for the character had been a significant causative factor.
- Of the movies that alluded to or showed mental illness treatment, psychotropic medications were most commonly portrayed.
Research has also found that 75% of depictions of mental illness in popular video games are negative or stereotyped.
Why Such Portrayals Are Damaging
These portrayals are not only incorrect but damaging—and for several reasons.
They Spread Myths About Mental Illness
The portrayals of schizophrenia often focus on symptoms such as visual hallucinations, bizarre delusions, and disorganized speech, and present them as commonplace. In reality, symptoms like decreased motivation, poverty of speech, and flat affect are more common.
They Link Mental Illness to Violence
Several movies have spread the false stereotype that people with schizophrenia are prone to violence and unpredictable behavior. Some films even presented people with schizophrenia as being “possessed.”
These violent stereotypes influence viewers and engender harsh negative attitudes toward people with mental illness.
They Exaggerate Suicide Risk
While suicide is a significant concern for people with schizophrenia, the research on media portrayals of schizophrenia found that this risk is often exaggerated in film and tv representations. In one study, 24% of the characters with schizophrenia committed suicide.
In reality, estimates suggest that between 4% and 13% of people with schizophrenia die by suicide, and approximately 18% to 55% attempt suicide at some point in their lifetime.
They Misrepresent Who Is Affected
Demographics is another aspect of mental illness that is often misrepresented by media portrayals of mental illness.
For example, characters with schizophrenia are frequently depicted as being white males, but schizophrenia disproportionately affects African Americans. It also affects men and women almost equally.
They Spread Myths About Causes of Mental Illness
In a few movies, schizophrenia was depicted as being secondary to traumatic life events or curable by love—both of which are misrepresentations of the condition's causes and treatment.
Press Play for Advice On Navigating Mental Health Advice on Social Media
This episode of The Verywell Mind Podcast points out the bad mental health advice you may find on social media. Click below to listen now.
Follow Now : Apple Podcasts / Spotify / Google Podcasts / Amazon Music
What's Accurate In Media Portayals?
Not all the information presented about schizophrenia was found to be incorrect, misleading, or stigmatizing. For example, in more than half of the movies that researchers analyzed, the use of psychiatric medications was depicted or alluded to.
Nearly half the characters with schizophrenia were depicted as being poor, which aligns with epidemiological data suggesting that schizophrenia is diagnosed less frequently in people of higher socioeconomic standing.
Even when some movies get it right, the negative media portrayals—especially those that are violent—of people with schizophrenia and other severe forms of mental illness still contribute to stigmatization, stereotyping, discrimination, and social rejection.
Impact of the Media on Mental Health
The impact of mental health stigmatization by the media can contribute to a number of different effects.
- Self-stigma : Media portrayals can contribute to self-stigma, which refers to feelings of internalized shame, negative beliefs, and negative attitudes that people have about their own mental health condition.
- Incorrect information : Because of media portrayals of mental illness, people often get incorrect ideas about the symptoms of mental health conditions. It can also lead people to develop inaccurate ideas about how mental illness is diagnosed and treated.
- Barriers to treatment : Media messages can also create barriers to treatment. Because people internalize stigmatized attitudes about mental illness, they may be less likely to seek out help or treatment when they experience symptoms.
- Poor treatment adherence : People are more likely to adhere to their treatment if they have social support and encouragement from others. Negative attitudes toward mental illness and stereotypes portrayed in the media may contribute to worse attitudes about mental health treatments and poorer adherence.
- Self-diagnosis : People might also be more likely to self-diagnose themselves based on viral social media posts seen on Tik Tok and Instagram. Such information is often shared by people who are not mental health professionals and is often inaccurate.
We need a better understanding of how these messages are disseminated by the media before we can rectify them. There is limited research looking at how media promotes mental-illness stereotypes, stigmatization, and trivialization.
Nevertheless, certain suggestions have been made on how to improve the depiction of people with mental illness in the media, such as:
- Analyzing mass-media production procedures to better understand screenwriters, producers, and journalists' current practices, needs, values, and economic realities (for instance, understanding the balance between being newsworthy or emotionally arousing and verifiable).
- Implementing a mental health short course when training journalists.
- Including expert input from psychiatrists during a film's production.
- Preferring non-individualized descriptions of mental illness and instead focusing on the societal aspects.
- Presenting mental illness only when relevant to the story.
- Using mental-health terminology with precision, fairness, and expertise.
As individuals who consume copious amounts of mass media and engage with social media, the best thing we can do is stop using words like “crazy” and “deranged” in a derogatory or flippant fashion. We also need to remember that it's best to avoid making a psychiatric diagnosis outside of a clinical setting.
A Word From Verywell
Only a specialist can make a diagnosis of OCD , depression , bipolar disorder , schizophrenia, and other mental health conditions. When we give someone the label of being mentally ill without clinical evidence, we hurt people who live with mental illness on a daily basis.
Thornicroft G. People with severe mental illness as the perpetrators and victims of violence: time for a new public health approach . The Lancet Public Health . 2020;5(2):e72-e73. doi:10.1016/S2468-2667(20)30002-5
Rössler W. The stigma of mental disorders: A millennia-long history of social exclusion and prejudices . EMBO Rep . 2016;17(9):1250-1253. doi:10.15252/embr.201643041
McGinty EE, Kennedy-Hendricks A, Choksy S, Barry CL. Trends in news media coverage of mental illness in the United States: 1995-2014 . Health Aff (Millwood) . 2016;35(6):1121-1129. doi:10.1377/hlthaff.2016.0011
Waters F, Collerton D, Ffytche DH, Jardri R, Pins D, Dudley R, Blom JD, Mosimann UP, Eperjesi F, Ford S, Larøi F. Visual hallucinations in the psychosis spectrum and comparative information from neurodegenerative disorders and eye disease . Schizophr Bull . 2014;40 Suppl 4(Suppl 4):S233-45. doi:10.1093/schbul/sbu036
Fichter MM, Quadflieg N. Mortality in eating disorders - results of a large prospective clinical longitudinal study . Int J Eat Disord . 2016;49(4):391-401. doi:10.1002/eat.22501
Kubrak T. Impact of films: Changes in young people's attitudes after watching a movie . Behav Sci (Basel) . 2020;10(5):86. doi:10.3390/bs10050086
Owen PR. Portrayals of schizophrenia by entertainment media: a content analysis of contemporary movies . Psychiatr Serv . 2012;63(7):655-659. doi:10.1176/appi.ps.201100371
Buday J, Neumann M, Heidingerová J, et al. Depiction of mental illness and psychiatry in popular video games over the last 20 years . Front Psychiatry . 2022;13:967992. doi:10.3389/fpsyt.2022.967992
Sher L, Kahn RS. Suicide in schizophrenia: An educational overview . Medicina (Kaunas) . 2019;55(7):361. doi:10.3390/medicina55070361
Olbert CM, Nagendra A, Buck B. Meta-analysis of Black vs. White racial disparity in schizophrenia diagnosis in the United States: Do structured assessments attenuate racial disparities ? J Abnorm Psychol . 2018;127(1):104-115. doi:10.1037/abn0000309
Luo Y, Zhang L, He P, Pang L, Guo C, Zheng X. Individual-level and area-level socioeconomic status (SES) and schizophrenia: cross-sectional analyses using the evidence from 1.9 million Chinese adults . BMJ Open . 2019;9(9):e026532. doi:10.1136/bmjopen-2018-026532
Babić D, Babić R, Vasilj I, Avdibegović E. Stigmatization of mentally ill patients through media . Psychiatr Danub . 2017 Dec;29(Suppl 5):885-889. PMID: 29283984.
Kamaradova D, Latalova K, Prasko J, et al. Connection between self-stigma, adherence to treatment, and discontinuation of medication . Patient Prefer Adherence . 2016;10:1289-1298. doi:10.2147/PPA.S99136
Maiorano A, Lasalvia A, Sampogna G, Pocai B, Ruggeri M, Henderson C. Reducing stigma in media professionals: Is there room for improvement? Results from a systematic review . Can J Psychiatry . 2017;62(10):702-715. doi:10.1177/0706743717711172
By Naveed Saleh, MD, MS Naveed Saleh, MD, MS, is a medical writer and editor covering new treatments and trending health news.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Stigma?
Views of Mental Health, Physical Disabilities, and More
A stigma is a negative attitude or idea about a mental, physical, or social feature of a person or group of people that implies social disapproval. Stigmas are a major concern because they can lead to poor treatment of groups of people, impaired mental and physical health of those groups, and other negative effects such as discrimination.
While there are many different kinds of social stigmas, mental health stigma tends to be very common. It can be strong, and it can impact both mental and physical health outcomes in serious ways. Some impacts of stigma include social withdrawal or isolation, compromised employment and financial security, physical violence, and more.
This article will discuss what stigma is and examples and types of stigma. It also addresses the impacts and how to cope.
Martin Dimitrov / Getty Images
Examples of Stigma
Signs of stigma may be obvious, or they may be so subtle that they go unnoticed. For example, a stigma can be presented as a joke that not everyone recognizes as a negative view. Even when stigmas go unnoticed, the effects can be damaging.
Examples of stigma include:
- Using slang or labels to exclude people or groups of people
- Assuming that someone with a mental illness is dangerous
- Believing that people with physical health conditions are unable to contribute to society
- Jokes about a physical or mental health condition or race, ethnicity, religion, etc.
- Halloween costumes that portray people or groups of people in a negative way
- Assumptions made about a person's intelligence or behavior based on a physical or mental health condition or race, ethnicity, religion, etc.
- People of certain groups repeatedly being shown in the media in a negative way
- Different treatment that is either isolating or harmful because of a mental, physical, or social feature of a person or group of people
- Laws or institutional regulations that isolate or negatively impact certain groups of people
What Causes Stigma?
A few different theories try to explain why some people stigmatize others. These include:
- Labeling: Labeling a person as "good" or "bad" is a natural way to avoid the effort involved in trying to understand someone else's challenges or experiences.
- Social identity: People base their identities on the specific groups they belong to, and therefore perceive members of other groups less favorably. Stigmatizing members of other groups can be a way to justify privilege, exploit others for personal gain, or boost a person's perceived importance.
- Terror management: People are naturally fearful of developing a mental illness or disability. If the stigmatized person can be blamed for their own condition, it may ease fears that the condition could happen to anyone.
Types of Stigma
There are three primary types of stigma. They were first described in 1963 by sociologist Erving Goffman, though Goffman's types were slightly different than those identified today.
The three types of stigma include mental illness stigma, physical deformation stigma, and race, ethnicity, religion, ideology, etc., stigma. Within these categories, there are additional types of stigmas.
You may have also heard the expression "stigma in health," which can relate to physical health, mental health, or both. It occurs when someone with a physical or mental health concern is viewed negatively because of that health challenge.
Mental Health Stigma
Mental health stigma is a negative attitude or idea about a mental health feature of a person or group of people. It relates to social disapproval of the person or group based on the mental health feature.
The negative beliefs can come from a variety of sources, including the person with that mental health feature. For example, stigmas are often associated with mental illnesses such as depression . This stigma may prevent people with depression from pursuing educational and career goals due to a belief of being less capable than people without depression.
Types of mental health stigma include:
- Social stigma or public stigma : When society or the general public share negative thoughts or beliefs about a person or group of people with a mental health condition
- Structural stigma or institutional stigma : Systemic stigma of mental illness at a higher level of government or organization that impacts policies or decision-making
- Self-perceived stigma or self-stigma : When a person with a mental health condition has negative thoughts or beliefs about themselves based on that mental illness
- Health practitioner stigma : When the care of a person is negatively impacted by stereotypes, thoughts, or associations of the provider about mental illness
- Associative stigma or courtesy stigma : A stigma that impacts people connected with someone with a mental health condition, such as friends or family members
Stigma Associated With Physical Deformation
Physical deformation stigma is a negative attitude or idea about a feature of a person or group of people related to a physical difference or disability. It relates to social disapproval of the person or group based on the physical feature or condition. This can lead to serious negative effects.
Like mental health stigma, there are different types of physical deformation stigma. Examples of this type of stigma include negative associations with deafness and blindness , or stigma associated with certain health conditions like HIV or sexually transmitted infections (STIs).
Stigma Associated With Race, Ethnicity, Religion, Ideology, etc.
Stigma associated with race, ethnicity, religion, ideology, etc., is a negative attitude or idea about one of these, or similar, features of a person or group of people. It relates to social disapproval of the person or group based on the feature or features.
Like mental health stigma, there are different types of race, ethnicity, religion, ideology, etc., stigma. This type of stigma can impact generations and has influenced laws and politics throughout history.
For example, the United States continued to enforce "separate but equal" laws for decades after the abolition of slavery, and in the 1980s, laws criminalizing sexual activity between same-sex couples were upheld as constitutional by the Supreme Court.
Effects of Stigma
Social stigma, or public stigma, occurs when society or the general public shares negative thoughts or beliefs about a person or group of people. For example, a mental health social stigma may be an association between mental illness and danger or a belief that people with mental illness lose control and hurt others.
People who are experiencing stigma and discrimination as a result of stigma can be harmed in multiple ways, both psychologically and in their daily lives. For example, someone who has been stigmatized may:
- Experience feelings of distress and loss of hope
- Develop a low sense of self-esteem
- Experience a worsening of psychiatric symptoms
- Stop treatment or decide not to seek treatment
They may also experience difficulties in their work or personal life, such as:
- Trouble maintaining social relationships
- Difficulty maintaining employment or problems at work
- Social isolation, exclusion from social activities
- Discrimination when seeking housing or employment
- Bullying and harassment
- Health insurance that isn't adequate to treat the condition
Social stigma can also have larger problems that go beyond impacts on the individual. For example, people who have been stigmatized may become homeless or develop substance use disorders. Some may become victims of violent crime.
Stigma Can Create a Stereotype
This type of stigma and the negative effects can harm the people with the condition, people close to them such as friends, family, caregivers, community members, and people who share attributes with them but do not have the condition. It is often seen in the form of stereotypes and discrimination of those with the condition and others.
For example, in addition to someone with depression being discriminated against, someone who is going through a hard time and is sad, but does not have depression, may also be discriminated against. Despite the challenges, there are ways to cope with stigmas.
Coping With Stigma
It is important to understand how to cope when you are facing stigma but also how to avoid stigmatizing others.
Coping With Stigma From Others
It's important to first take care of your own health by seeking treatment for any mental health concerns you may be experiencing as a result of the stigmatizing behavior of others. You can also:
- Find out if your employer offers Employee Assistance Programs (EAPs) to support employees with work and life concerns including stigmas, discrimination, and issues that negatively impact mental and emotional well-being.
- Look for support from community or school resources.
- Join a support group for those with similar mental health conditions who may also be experiencing the effects of stigma.
Preventing Stigma
There are some steps you can take to support people who are experiencing stigma, to avoid stigmatizing others, and/or to avoid spreading stigmatizing ideas:
- Notice signs of social withdrawal and reach out to family, friends, and health professionals.
- Talk openly about the facts and realities of mental illness.
- Understand that mental health conditions are illnesses like physical health conditions.
- Be careful with word choices to remain sensitive to others.
- Bring awareness to language and actions that represent stigmas so they can be changed.
- Educate others to help destigmatize mental illness.
- Choose to believe and show others that stigmas are not accurate.
A stigma is a negative attitude or idea about a mental, physical, or social feature of a person or group of people that involves social disapproval. This issue is a significant concern for people with mental health conditions and for society as a whole. It can lead to discrimination and negatively impact mental health and overall wellbeing.
Mental illness stigma, physical deformation stigma, and race, ethnicity, religion, ideology, etc., stigma are the three primary types of stigma. Despite the negative effects of stigma, there are strategies to help cope with and overcome these challenges.
American Psychological Association. Stigma .
Hart J, Richman S. Why do we joke about killing ourselves? Suicide, stigma, and humor . Modern Psychological Studies . 2020;25(2).
Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic . Front Public Healt h. 2021;8:577018. doi:10.3389/fpubh.2020.577018
Harvard University. Stigma .
Dilkov D, Dimitrova M, Marinova Y, Ulchar M. Investigation of attitudes/stigma/towards people with mental illness and opportunities to access psychiatric health care . Int J Surg Med . 2020;6(6):42-. doi:10.5455/ijsm.stigma-mental-illness
National Alliance on Mental Illness. Overcoming stigma .
White S. From Bowers to Obergefell: The US Supreme Court’s erratic, yet correct, jurisprudence on gay rights . J Philos Polit Econ. 2022;4(1):111-125.
Yanos PT, DeLuca JS, Roe D, Lysaker PH. The impact of illness identity on recovery from severe mental illness: A review of the evidence . Psychiatry Res . 2020;288:112950. doi:10.1016/j.psychres.2020.112950
American Psychiatric Association. Stigma, prejudice and discrimination against people with mental illness .
Wogen J, Restrepo MT. Human rights, stigma, and substance use . Health Hum Rights . 2020;22(1):51-60.
World Health Organization. A guide to preventing and addressing social stigma associated with COVID-19 .
By Ashley Olivine, Ph.D., MPH Dr. Olivine is a Texas-based psychologist with over a decade of experience serving clients in the clinical setting and private practice.

IMAGES
VIDEO
COMMENTS
Speaking out on the stigma of mental health. 2 December 2022. Persons with psychosocial disabilities frequently face stigma, discrimination and rights violations, including within and from the medical community, which reflects broader societal stigma. One doctor relates his personal experience here and how he uses it today to challenge stigma.
Stigma around mental illness is especially an issue in some diverse racial and ethnic communities, and it can be a major barrier to people from those cultures accessing mental health services. ... Brief video interventions to reduce self-, public, and affiliate stigma among/toward young individuals with psychosis. Presentation at APA 2023 ...
The following books provide resources to understand mental illness and its stigma. 1. Written Off: Mental Health Stigma and the Loss of Human Potential - Philip T. Yanos. Written by Philip T. Yanos, the book conveys how the pervasive nature of stigma impacts those with mental illness, profoundly affecting their lives.
Mental health stigma refers to negative beliefs people may hold about those with mental illness, which can lead to stereotypes, prejudice, and discrimination. Public awareness and literacy have ...
NAMI Ending the Silence presentations include two leaders: one who shares an informative presentation and a young adult with a mental health condition who shares their journey of recovery. Audience members can ask questions and gain understanding of an often-misunderstood topic. Through dialogue, we can help grow the movement to end stigma.
Anthropologist Roy Richard Grinker explores the roots of stigma in his new book. Though progress has been made in recent years, mental illness remains highly stigmatized—the mentally ill are ...
Stigma, the prejudice and discrimination attached to devalued conditions, has been consistently cited as a major obstacle to recovery and quality of life among people with psychiatric disorders. 1-3 Stigma has been implicated in worsening outcomes for people with serious mental illness, 4,5 with nearly 40% of this population reporting unmet ...
Many people with mental illness experience shame, ostracism, and marginalisation due to their diagnosis, and often describe the consequences of mental health stigma as worse than those of the condition itself. Interventions to address stigma educate about mental illness and overcome the stereotypes that underlie prejudicial reactions. Along with pharmacological and psychological therapies ...
The Lancet Commission on ending stigma and discrimination in mental health had six aims (panel 1). From traditional definitions of stigma, we have developed four main components to consider in this report: self-stigma (or internalised stigma), which occurs when people with mental health conditions are aware of the negative stereotypes of others ...
Stigma and Mental Health. Stigma is a growing public health concern. Internationally. WPA. Open-the-Doors Global Network (1996) Stigma and Mental Disorder Section (2005) Task force on the destigmatization of psychiatry and psychiatrists (2009) ... PowerPoint Presentation - Slide 1
Stigma associated with mental illness has malignant effects on the lives of people with serious mental illnesses. Many strategies have been used to combat public stigma—the prejudice and discrimination endorsed by the general population. To identify the most effective approaches, researchers conducted a meta-analysis of data from 72 outcome studies in 14 countries. Overall, strategies that ...
The stigma attached to mental illness is ubiquitous. There is no country, society or culture where people with mental illness have the same societal value as people without a mental illness. In a survey that included respondents from 27 countries, nearly 50% of persons with schizophrenia reported discrimination in their personal relationships.
1. Introduction. The stigma of living with a mental health condition has been described as being worse than the experience of the illness itself [].The aversive reactions that members of the general population have towards people with mental illness is known as public stigma and can be understood in terms of (i) stereotypes, (ii) prejudice, and (iii) discrimination [].
Stigma is when someone views you in a negative way because you have a distinguishing characteristic or personal trait that's thought to be, or actually is, a disadvantage (a negative stereotype). Unfortunately, negative attitudes and beliefs toward people who have a mental health condition are common. Stigma can lead to discrimination ...
Introduction and background. Stigma, characterized by societal prejudice and discrimination, profoundly influences psychiatric care, creating barriers to the timely recognition and treatment of mental health disorders [].Deeply embedded in societal norms, stigma is a multifaceted issue permeating every level of psychiatric care, leading to delayed treatment, increased morbidity, and a ...
In a report issued Oct. 9, The Lancet Commission on Ending Stigma and Discrimination in Mental Health issues a call to action to "act now to stop stigma and to start inclusion." The report summarizes extensive research around the world, highlights the results of an international survey, and provides recommendations for actions by a range of stakeholders.
Common examples of stigma related to mental health. We often use the word "stigma" to describe the overarching experience that people have. However, there are actually three types of stigma ...
Stigma involves negative beliefs, attitudes, and behaviors directed toward people based on some distinguishing characteristics. In the case of mental health stigma, it involves the presence of mental health symptoms or a mental health diagnosis. In other cases, stigma can also involve health conditions, disabilities, gender, race, sexuality ...
Coping. A stigma is a negative attitude or idea about a mental, physical, or social feature of a person or group of people that implies social disapproval. Stigmas are a major concern because they can lead to poor treatment of groups of people, impaired mental and physical health of those groups, and other negative effects such as discrimination.
Young prostitutes in São Paulo, 2019. The Impact of prostitution on mental health refers to the psychological, cognitive, and emotional consequences experienced by individuals involved in prostitution.These consequences include a wide range of mental health issues and difficulties in emotional management and interpersonal relationships.Prostitution is closely linked to various psychological ...