
- Schools & departments


Case Study: supporting a visually impaired student
Case study highlighting the support that can be implemented for a visually impaired student
Fiona is a new international postgraduate student who commenced her undergraduate studies in the College of Science and Engineering at the University in September. Having obtained exceptional grades at school, Fiona was able to gain admission as a direct entrant into the second year of her BSc degree.
Fiona has a number of eye conditions which result in her having extremely limited vision in both eyes. She made contact with the Student Disability Service at the beginning of her first semester, and it was clear that, in addition to the provision of a range of support/adjustments, Fiona would also benefit from the provision of assistive technology in order to enable her to be able to access all elements of her studies.
Although the advisory staff within the Disability and Learning Support Service are skilled and trained in the use and application of a very broad range of assistive technology and software, there are occasions when even more specialist knowledge and expertise are required. Consequently, the Service worked with the Royal National Institute for Blind People (RNIB), and referred Fiona to them for a detailed assessment of need. This also allowed her to trial equipment which the Service did not have available.
As a non-UK student, Fiona was not eligible for state funding for any support requirements through Disabled Students’ Allowance (DSA). Therefore, any recommendations for equipment, software or technology that arose from her RNIB assessment would be funded through the allocation that the University makes available in the form of the Disabled Students Support Fund (DSSF).
Fiona met with RNIB staff in October and they were able to let her try out a range of equipment which had practical benefits for her studies. On the basis of her feedback on ease of use and application in the academic context, the Service agreed to purchase a number of items, using finance from the DSSF, up to a total cost of £2,000. These included a digital voice recorder to record lectures, a laptop with Windows and MS Office and a ZoomText magnifier, optical magnifier and monocular telescope. This equipment enables the student to enlarge and adjust text size and utilise text to speech functions, which also minimise the need for human support and enables the student to maximise her capacity for independent learning.
Fiona has settled into her studies and is making effective use of the equipment, which she will be able to utilise for the duration of her studies. On completion of her degree, much of the equipment will be returned to Disability and Learning Support Service so that it may be used by other students in future.
Emerging Technologies for Blind and Visually Impaired Learners: A Case Study
- First Online: 31 May 2023
Cite this chapter

- Regina Kaplan-Rakowski 9 &
- Tania Heap 9
Part of the book series: Educational Communications and Technology: Issues and Innovations ((ECTII))
214 Accesses
Blind and visually impaired (BVI) people frequently encounter challenges in their daily lives. With the COVID-19 pandemic, some of those challenges decreased, but some became more evident. The goal of this chapter is two-fold. First, we present the findings of a qualitative case study of a blind student sharing reflections of his daily barriers with online learning during the COVID-19 pandemic, his success strategies, and his impressions of using emerging technologies. Second, we discuss guidelines on using traditional and innovative technologies to assist BVI individuals. The chapter has practical implications not only for the BVI population but also for all students, applying principles of Universal Design for Learning (UDL) and illustrating the responsibility of stakeholders for inclusive policies on the implementation of assistive technologies and accessible learning experiences.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Throughout this chapter, the authors will use both person-first language, which places the person before their characteristic (e.g., people with disabilities) and identity-first language, which leads with the person’s characteristic (e.g., blind user). There are pros and cons to using either approach, but when the opportunity presents, a good practice is to ask each individual which language they prefer.
Aisami, R. S. (2015). Learning styles and visual literacy for learning and performance. Procedia-Social and Behavioral Sciences, 176 , 538–545.
Article Google Scholar
Alobaid, A. (2021). ICT multimedia learning affordances: Role and impact on ESL learners' writing accuracy development. Heliyon, 7 (7), e07517.
An, Y., Kaplan-Rakowski, R., Yang, J., Conan, J., Kinard, W., & Daughrity, L. (2021). Examining K-12 teachers’ feelings, experiences, and perspectives regarding online teaching during the early stage of the COVID-19 pandemic. Educational Technology Research and Development, 69 (2), 2589–2613. https://doi.org/10.1007/s11423-021-10008-5
Bartolic, S., Matzat, U., Tai, J., Burgess, J. L., Boud, D., Craig, H., Archibald, A., De Jaeger, A., Kaplan-Rakowski, R., Lutze-Mann, L., Polly, P., Roth, M., Heap, T., Agapito, J., & Guppy, N. (2022). Student vulnerabilities and confidence in learning in the context of the COVID-19 pandemic. Studies in Higher Education, 47 , 1–13.
Baumgartner, E., Hartshorne, R., Kaplan-Rakowski, R., Mouza, C., & Ferdig, R. E. (Eds.). (2022). A Retrospective of teaching, technology, and teacher education during the COVID-19 pandemic . Association for the Advancement of Computing in Education (AACE).
Google Scholar
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3 , 77–101.
Brown, S. E. (2008). Breaking barriers: The pioneering disability students services program at the University of Illinois, 1948–1960. In The history of discrimination in US education (pp. 165–192). Palgrave Macmillan.
Buetow, S. (2010). Thematic analysis and its reconceptualization as saliency analysis. Journal of Health Services Research and Policy, 15 (2), 123–125.
Burgstahler, S. (2020). Creating inclusive learning opportunities in higher education: A universal design toolkit (pp. 47–48). Harvard Education Press.
Burgstahler, S., & Crawford, L. (2020). The development of accessibility recommendations for online learning researchers. In S. Burgstahler (Ed.), Universal design in higher education: Promising practices . DO-IT, University of Washington. Retrieved from: www.uw.edu/doit/UDHE-promisingpractices/preface.html
Caldwell, B., Cooper, M., Reid, L. G., Vanderheiden, G., Chisholm, W., Slatin, J., & White, J. (2008). Web content accessibility guidelines (WCAG) 2.0. WWW Consortium (W3C), 290, 1–34.
CAST. (2018). Universal design for learning guidelines version 2.2 . Retrieved from: http://udlguidelines.cast.org
Crossland, M. D., Starke, S. D., Wolffsohn, J. S., & Webster, A. R. (2019). Benefit of an electronic head-mounted low vision aid. Ophthalmic & Physiological Optics, 39 (6), 422–431.
Crutchfield, B., & Haugh, J. (2018). Accessibility in the virtual/augmented reality space. CSUN 2018 Assistive Technology Conference, San Diego, CA, March 22.
Enoch, J., McDonald, L., Jones, L., Jones, P. R., & Crabb, D. P. (2019). Evaluating whether sight is the most valued sense. JAMA Ophthalmology, 137 (11), 1317–1320.
Ferdig, R. E., Baumgartner, E., Hartshorne, R., Kaplan-Rakowski, R., & Mouza, C. (2020). Teaching, technology, and teacher education during the COVID-19 pandemic: Stories from the field . Association for the Advancement of Computing in Education (AACE). Retrieved from: https://www.learntechlib.org/p/216903/
Ferdig, R. E., Baumgartner, E., Mouza, C., Kaplan-Rakowski, R., & Hartshorne, R. (2021). Editorial: Rapid publishing in a time of COVID-19: How a pandemic might change our academic writing practices. Contemporary Issues in Technology and Teacher Education, 21 (1).
Hartshorne, R., Baumgartner, E., Kaplan-Rakowski, R., Mouza, C., & Ferdig, R. E. (2020). Special issue editorial: Preservice and inservice professional development during the COVID-19 pandemic. Journal of Technology and Teacher Education, 28 (2), 137–147. https://www.learntechlib.org/primary/p/216910/
Huber, E., Chang, K., Alvarez, I., Hundle, A., Bridge, H., & Fine, I. (2019). Early blindness shapes cortical representations of auditory frequency within auditory cortex. Journal of Neuroscience, 39 (26), 5143–5152.
Kaplan-Rakowski, R. (2021). Addressing students’ emotional needs during the COVID-19 pandemic: A perspective on text versus video feedback in online environments. Educational Technology Research and Development, 69 (1), 133–136. https://doi.org/10.1007/s11423-020-09897-9
Kent, M., Ellis, K., Latter, N., & Peaty, G. (2018). The case for captioned lectures in Australian higher education. TechTrends, 62 (2), 158–165.
King, A. J. (2014). What happens to your hearing if you are born blind? Brain, 137 (1), 6–8.
Kriemeier, J., & Götzelmann, T. (2020). Two decades of touchable and walkable virtual reality for blind and visually impaired people: A high-level taxonomy. Multimodal Technologies and Interaction, 4 (4), 79. https://doi.org/10.3390/mti4040079
Kuri, N. P., & Truzzi, O. M. S. (2002). Learning styles of freshmen engineering students. In Proceedings of the International Conference on Engineering Education (ICEE 2002).
Lavrakas, P. J. (2008). Encyclopedia of survey research methods . Sage Publications.
Book Google Scholar
Lee, D., & Cho, J. (2022). Automatic object detection algorithm-based braille image generation system for the recognition of real-life obstacles for visually impaired people. Sensors (Basel), 22 (4), 1601, 1–22. Retrieved from:. https://doi.org/10.3390/s22041601
Longhurst, G. J. (2021). Teaching a blind student anatomy during the Covid-19 pandemic. Anatomical Sciences Education, 14 (5), 586–589.
Lueders, K., Perla, F., Maffit, J., Vasile, E., Jay, N., Kaplan, J., & Hanuschock, W. E., III. (2020). Remote instruction for students who are blind or visually impaired: Experiences of preservice interns. In R. E. Ferdig, E. Baumgartner, R. Hartshorne, R. Kaplan-Rakowski, & C. Mouza (Eds.), Teaching, technology, and teacher education during the COVID-19 pandemic: Stories from the field . Association for the Advancement of Computing in Education (AACE).
Mayer, R. E. (2009). Multimedia learning (2nd ed.). Cambridge University Press.
McBride, C. R. (2020). Critical issues in education for students with visual impairments: Access to mathematics and the impact of the Covid-19 pandemic [Unpublished doctoral dissertation] University of Georgia.
McDonnall, M. C., & Sui, Z. (2019). Employment and unemployment rates of people who are blind or visually impaired: Estimates from multiple sources. Journal of Visual Impairment & Blindness, 113 (6), 481–492.
Mills, A. J., Durepos, G., & Wiebe, E. (2010). Reflexivity. Encyclopediaof case study research. SAGE Publications, Inc. https://doi.org/10.4135/9781412957397
Morgan, H. (2022). Alleviating the challenges with remote learning during a pandemic. Education Sciences, 12 (2), 109, 1–12, Retrieved from:. https://doi.org/10.3390/educsci12020109
Mouza, C., Hartshorne, R., Baumgartner, E., & Kaplan-Rakowski, R. (2022). Special issue editorial: A 2025 vision for technology and teacher education. Journal of Technology and Teacher Education, 30 (2), 107–115.
Paivio, A. (1986). Mental representations: A dual-coding approach . Oxford University Press.
Rodríguez, A., Boada, I., & Sbert, M. (2018). An Arduino-based device for visually impaired people to play videogames. Multimedia Tools and Applications, 77 (15), 19591.
Rose, D. (2000). Universal design for learning. Journal of Special Education Technology, 15 (3), 45–49.
Russ, S., & Hamidi, F. (2021, April). Online learning accessibility during the COVID-19 pandemic. In Proceedings of the 18th International Web for All Conference (pp. 1–7).
Siu, A. F., Sinclair, M., Kovacs, R., Ofek, E., Holz, C., & Cutrell, E. (2020). Virtual reality without vision: A haptic and auditory white cane to navigate complex virtual worlds. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, April 25–30 .
Sooraj, V. S., Magadum, H. J., & Alluri, L. (2021, December). iTouch–blind assistance smart glove. In 2021 10th International Conference on System Modeling & Advancement in Research Trends (SMART) (pp. 172–175). IEEE.
Tellis, W. (1997). Introduction to case study. The Qualitative Report, 3 (2).
U.S. Bureau of Labor Statistics. (2022). Persons with a disability: Labor force characteristics summary . Retrieved from: https://bit.ly/2Rt9rgm
WHO. (n.d.). Assistive technology . World Health Organization : Health Topics. Retrieved from: https://www.who.int/health-topics/assistive-technology#tab=tab_1
Zhao, Y., Bennett, C. L., Benko, H., Cutrell, E., Holz, C., Morris, M. R., & Sinclair, M. (2018, April). Enabling people with visual impairments to navigate virtual reality with a haptic and auditory cane simulation. In Proceedings of the 2018 CHI conference on human factors in computing systems (pp. 1–14).
Download references
Author information
Authors and affiliations.
University of North Texas, Denton, TX, USA
Regina Kaplan-Rakowski & Tania Heap
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Regina Kaplan-Rakowski .
Editor information
Editors and affiliations.
Deborah Cockerham
Regina Kaplan-Rakowski
Wellesley Foshay
Michael J. Spector
Interview Questions to Jarrod
Online learning
What aspects of online learning work well for you?
What aspects of online learning do not work well for you?
How did the shift to online learning due to the COVID-19 pandemic impacted you?
How did the shift to online learning due to the COVID-19 pandemic impacted your community?
What support did you receive?
What support did you wish you had received?
How has the shift to online learning due to COVID-19 informed your opinion about the future of digital accessibility?
What does not work well for you? How accurate is dictation? Do you feel it is improving?
What can be done differently or better?
What technologies have you been using that are helpful to you?
What innovative technologies are you aware of that you think could be helpful to you?
What about screen readers?
What about smart speakers?
As an assistive technology user and an experienced gamer, what advice do you have for game designers and professors using gaming in their courses?
An additional question:
How much understanding of your situation do you think the sighted people have?
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Kaplan-Rakowski, R., Heap, T. (2023). Emerging Technologies for Blind and Visually Impaired Learners: A Case Study. In: Cockerham, D., Kaplan-Rakowski, R., Foshay, W., Spector, M.J. (eds) Reimagining Education: Studies and Stories for Effective Learning in an Evolving Digital Environment. Educational Communications and Technology: Issues and Innovations. Springer, Cham. https://doi.org/10.1007/978-3-031-25102-3_16
Download citation
DOI : https://doi.org/10.1007/978-3-031-25102-3_16
Published : 31 May 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-25101-6
Online ISBN : 978-3-031-25102-3
eBook Packages : Education Education (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Research article
- Open access
- Published: 12 November 2015
Visual impairment, coping strategies and impact on daily life: a qualitative study among working-age UK ex-service personnel
- Sharon A. M. Stevelink 1 ,
- Estelle M. Malcolm 1 &
- Nicola T. Fear 1 , 2
BMC Public Health volume 15 , Article number: 1118 ( 2015 ) Cite this article
26 Citations
4 Altmetric
Metrics details
Sustaining a visual impairment may have a substantial impact on various life domains such as work, interpersonal relations, mobility and social and mental well-being. How to adjust to the loss of vision and its consequences might be a challenge for the visually impaired person. The purpose of the current study was to explore how younger male ex-Service personnel cope with becoming visually impaired and how this affects their daily life.
Semi-structured interviews with 30 visually impaired male ex-Service personnel, all under the age of 55, were conducted. All participants are members of the charity organisation Blind Veterans UK. Interviews were analysed thematically.
Younger ex-Service personnel applied a number of different strategies to overcome their loss of vision and its associated consequences. Coping strategies varied from learning new skills, goal setting, integrating the use of low vision aids in their daily routine, to social withdrawal and substance misuse. Vision loss affected on all aspects of daily life and ex-Service personnel experienced an on-going struggle to accept and adjust to becoming visually impaired.
Conclusions
Health care professionals, family and friends of the person with the visual impairment need to be aware that coping with a visual impairment is a continuous struggle; even after a considerable amount of time has passed, needs for emotional, social, practical and physical support may still be present.
Peer Review reports
Becoming visually impaired can be a life changing experience and is likely to have far reaching consequences for the person affected [ 1 – 3 ]. Persons acquiring a visual impairment express a variety of emotional, cognitive, behavioural and social responses to this significant loss. The model of grief proposed by Kübler-Ross, originally used to describe coping in terminally ill persons, has shown to be useful in a variety of settings in which persons face a significant crisis, change or loss, such as acquiring a visual impairment [ 4 , 5 ]. People affected will mourn their loss of vision and associated losses including their job, leisure activities and independence and may go through various phases of grief, which include denial, anger, depression, bargaining and acceptance [ 6 ]. Positive or negative mechanisms of adjustment, also termed coping strategies, can help individuals to master their impairment. Broadly speaking, we can distinguish between adaptive coping strategies such as seeing a counsellor and goal setting or maladaptive coping strategies including social withdrawal and substance misuse [ 7 , 8 ].
Service personnel are at a higher risk of becoming visually impaired than civilians as a result of deployment experiences. A decrease in combat-related mortality has been reported during the recent deployments to Iraq and Afghanistan compared to other conflicts; this can be explained by technological and medical advances in medical care, body armour and casualty evacuation [ 9 ]. However, more Service personnel return home with combat-related trauma such as shrapnel wounds, extremity amputations, head injury and vision loss [ 9 – 12 ].
Recently, a study reviewing the prevalence of mental health problems among (ex-) service personnel with an irreversible impairment (e.g. hearing, vision, but predominantly physical) concluded that common mental health disorders such as post-traumatic stress disorder, anxiety, psychological distress and depression, were frequently reported, but levels varied widely across study populations. Nevertheless these levels appeared to be higher than found in comparable samples of civilian and military populations without an impairment [ 13 ].
This study utilised a sample of younger (ex-) Service personnel who are members of Blind Veterans UK (55 years of age or below). Blind Veterans UK is a charity organisation, formerly known as St Dunstan’s, which provides support and care for (ex-) Service personnel who have a visual impairment in both eyes, regardless of the cause. The majority of the members of Blind Veterans UK are 65 years and older, however, due to military operations in Iraq and Afghanistan, the charity has seen an influx in younger members over the last decade. Therefore Blind Veterans UK commissioned the King’s Centre for Military Health Research at King’s College London to examine the mental health and social well-being of their younger members. We explored how ex-Service men adjust to their loss of vision, which coping strategies they use and how their loss of vision and its consequences has impacted on their daily life.
Setting and design
A cross-sectional study was conducted using a mixed methods approach. Phase 1 of the study consisted of telephone interviews with male and female (ex-) Service personnel whereby clinical screening measures for mental health were used. A subsample of the phase 1 participants was invited to join phase 2 of the study. Phase 2 consisted of semi-structured in-depth face to face interviews, covering various topics including the impact of becoming visually impaired on various domains of life and coping strategies. The current paper will report on male participants included in phase 2 of the study.
Participants
All participants were members of Blind Veterans UK and were under 55 years of age at recruitment. Male participants who took part in phase 1 of this study ( n = 74) were asked if they would be interested in taking part in a qualitative interview. Sixty-six participants indicated their willingness to do the face-to-face interview. We were especially interested in those who became visually impaired due to their deployment to Iraq or Afghanistan ( n = 10). They were prioritised in the selection process for phase 2 after which other participants were invited. Thirty male ex-Service personnel were approached and two declined. Therefore, an additional two male members were invited and they agreed to participate. We deemed 30 face-to-face interviews sufficient to reach data saturation based on previous experiences and the literature [ 14 ]. The data collection period was closely monitored to ensure that the data collected was rich and descriptive and no new information seemed to emerge whilst approaching the set interview target.
A semi-structured interview schedule was used consisting of 11 open-ended questions covering different aspects of how a visual impairment can have an impact on life, difficulties experienced because of being visually impaired and how ex-Service men adjusted to life with a visual impairment (Additional file 1 ). These questions were developed in collaboration with Blind Veterans UK, to ensure they met the remit of the work commissioned and were appropriate for use in the target population. The draft interview guide was piloted by E.M.M. and S.A.M.S. among two members of Blind who just exceeded the age threshold off 55 years. Feedback from the participants suggested that the questions were received well, easy to follow and comprehensive. Therefore no changes were made to the interview guide. Socio-demographic data obtained during phase 1 were linked to the participants who were included in phase 2 of the study.
Interviews took place between December 2012 and May 2013. Prior to the interview, participants received an information package explaining the study and a detailed signposting booklet (in accessible formats) providing information about various sources of help and advice that might be useful for the participant, such as the Veterans UK helpline.
Participants were interviewed by two researchers (E.M.M. and S.A.M.S.) who were trained and experienced in using the qualitative interview schedule. The majority of the interviews took place in the participant’s home environment after verbal informed consent was given. Procedures were in place for participants who were distressed or at risk and required a call back from a Community Psychiatric Nurse. All interviews were recorded with a Dictaphone. Interviews lasted 35–105 min. At the end of the interview participants were thanked for their time and received £20 in cash.
The interviews were transcribed in full to include all spoken words and non-verbal utterances such as sighs and laughter. Recordings were listened to and transcripts were read and re-read by E.M.M. and S.A.M.S. Both independently coded five different transcripts each using NVivo as an organisational tool. Once five transcripts were independently coded, E.M.M. and S.A.M.S. met to compare and discuss. The initial coding framework was grounded in the content of the data (inductive). Data were analysed thematically [ 15 ]. Throughout the first stages of the analysis process the coding framework was revised and further developed. E.M.M. and S.A.M.S. independently read and coded three additional transcripts to ensure the coding framework reflected the data. Any disagreement about codes between the two researchers were discussed and resolved. Once the coding frame was finalised, E.M.M. independently coded all of the transcripts (Additional file 2 ). Intra-coder agreement was established by E.M.M. by coding three interviews at two time points which were one month apart. An intra-coder agreement of 84.5 % was found, indicating good agreement. Once all transcripts were coded, the codes were put into broader themes and associated sub-themes. The main themes identified for the current paper were coping (strategies) and the impact of vision loss on daily life. Pseudonyms are used when presenting the data.
Ethical approval
Ethical approval for this study was granted by the Social Care Research Ethics Committee (12-IEC08-0032).
Out of the 30 younger ex-Service men, 27 were below 45 years of age; 15 were employed at the time of the interview; four were still serving but were waiting to be medically discharged. Of those who had left the Armed Forces, 13 out of 30 had left over 10 years ago and just over half (17 out of 30) were married or in a long term relationship. The great majority (26 out of 30) had served in the Army.
Twelve men had a combat-related visual impairment, of which 10 sustained the impairment during deployment to Iraq or Afghanistan. 12 out of the 30 sustained their impairment less than 5 years ago. Genetic causes of visual impairment were the most common causes of visual impairment ( n = 7) among those with a non-combat-related visual impairment followed by ocular medical conditions (e.g. age-related macular degeneration, glaucoma) ( n = 4) and environmental causes ( n = 4) (e.g. toxic or injury related). The overwhelming majority of ex-Service personnel used low vision aids (28 out of 30); four had a guide dog, 17 used talking books and 19 used a white stick. Approximately one in three participants screened positive for probable depression, probable anxiety or probable Post-Traumatic Stress Disorder (Stevelink et al., (2015) http://bjo.bmj.com/content/early/2015/04/23/bjophthalmol-2014-305986.full .
In the next section the findings of the two themes identified for the current paper, specifically ‘coping (strategies)’ and ‘impact of vision loss on daily life’, are combined to describe how vision loss affected the person from the time directly after becoming visually impaired and how this changed subsequently.
Coping with a visual impairment and impact on daily life
Directly after becoming visually impaired, younger male ex-Service personnel thought “life is over” and they “ [didn’t] want to carry on” . Their confidence was undermined, they felt sorry for themselves and had the feeling there was no way out.
Phil (non-combat-related visual impairment, age 35–44 years) : “Well initially straightaway it [loss of vision] stopped me from going out straightaway. I went in for the first two years, first year and a half at least, I was very depressed. Very sorry for myself and thought that was it (…). (…) I didn’t think there was anything I could do so yeah, dread, full of dread and fear and all that lot did come into it.”
These feelings and experiences were reinforced by other losses that were experienced as a result of their loss of vision such as losing their job, experiencing relationship difficulties and an increased dependence on others.
In most cases, if personnel suffered a deterioration of their sight whilst in Service, they were medically discharged and as a result had to confront the issue of changing their career. This was similar amongst those who had left the Service and had started a civilian job. This forced change of career was generally experienced as a “regression” leading into a cascade of accompanying consequences such as experiencing financial hardship if living on benefits, different family dynamics due to for example family members taking on the role of carer and, above all, impaired self-esteem. Ex-Service men felt that by no longer being the breadwinner in the household and a highly trained professional, they were set back to square one as said by Alan (combat-related visual impairment, age 25–34 years):
“(…) it’s like all that experience, all that knowledge… shoved right back in your face (…). (…) You’re a broken toy now. What happens to broken toys… goes to the tip doesn’t it? (…). You know you’re a broken toy they don’t want to know you.”
Denial of the consequences of vision loss resulted in ex-Service men trying to do the things they were used to do; this resulted in feelings of frustration and irritation as illustrated by Richard (non-combat-related visual impairment, age 45–54 years):
“(…) at first it [loss of vision] made me really down and depressed and … . Because I’d known for quite a while before that there was something wrong. And I went through not accepting it. So at first I wouldn’t accept it and then when I first finished work obviously I had to walk everywhere. I got quite narky with people. If I was out with my stick and they’d bump into me. I’d get quite angry with them… because it was everybody else’s fault for getting in my way. So I went through like a stage of denial, I suppose and then being angry.”
The emotional turmoil personnel went through whilst adjusting, adversely affected their relationship with their partner. Those who were in a relationship at the time of becoming visually impaired suggested that their impairment put a strain on that relationship. Personnel experienced increased dependence on their partner resulting in changing relationship dynamics. Both the partner and the person affected needed time to adapt to this new situation. In a few cases, participants divorced or ended their relationship with their partner, but the dominant view was that the impairment was a contributing factor but not the main reason for breaking up.
Charlie (non-combat-related visual impairment, age 35–44 years): “ But it [loss of vision] very nearly I think cost us my wife and I our marriage, because I was quite unpleasant on more than one occasion. But thankfully we’re coming through the other side so yeah it’s been a difficult journey.”
Members who became visually impaired in combat were proud about the circumstances that led to their loss of vision ( “serving Queen and Country” ), whereas those with a non-combat-related visual impairment struggled with the question ‘why me?’ and even felt guilty, ashamed or embarrassed. Some personnel expressed the hope that their vision would improve over time or were looking into potential treatment options. Personnel were mourning about what they had lost and what they could have done if they had not sustained a visual impairment.
Harry (combat-related visual impairment, 35–44 years): “You know the doctors are going to say to you at some point you don’t need to come and see us anymore, and that’s when it will sink in and that’s what you’ve got for the rest of your life, that’s what you’re stuck with. And at that point you need to just accept it, just get on with it because the longer you kid yourself it’s going to get better, or there’s going to be some miracle surgery, the longer it ‘ll take you to adapt.”
The visual impairment not only affected the domain of work and interpersonal relationships but also other areas as illustrated by Nick (non-combat related, age 25–34 years):
“ (…) you do have a bad impact on your day to day life especially from washing up to having food or to prepare a meal. Then taking medication and also you know dress yourself, and also you can’t actually go out on your own all the time. So your movement is quite restricted although it can be done with some training outside, but there is the danger off (…) colliding with something or someone or some obstruction.”
As time passed, ex-Service personnel were able to “ change [their] head around ” and tried to adjust to their visual impairment and its consequences, by applying various coping strategies. The ‘military ethos’ of “crack on” and “adapt and overcome the situation” helped them to overcome any problems they experienced. However, for some personnel it acted as a barrier because they were reluctant to ask for help and struggled through with their visual impairment (defined by the researchers as coping at a cost).
Other reasons for coping at a cost were that younger ex-Service personnel felt ashamed, lacked confidence or were too proud to ask for help. They did not want to be seen as a burden on others. Coping at a cost was enforced by reactions from the public. For example, Max (non-combat-related visual impairment, 35–44 years) was assaulted when using his cane on public transport after accidently bumping into someone; they did not believe he was visually impaired so from that moment on he decided not to use a cane anymore.
The unavailability of support and resources influenced how younger members coped with their loss. Ex-Service personnel tried ‘to escape’ by, for example, substance abuse or made a non-fatal suicide attempt.
Tom (non-combat-related visual impairment, 25–34 years): “ When I first lost my eyesight I never had that emotional support. I never had it and I dealt with it on my own. My way was hitting the drinks and hitting the drugs and going crazy .”
Other examples of maladaptive behaviour included isolation and social withdrawal from family and friends, acting aggressively or in an unfriendly manner.
Besides the use of maladaptive coping strategies, several adaptive coping strategies were applied. One of these was termed by the researchers as ‘downward comparison’. Younger ex-Service personnel pointed out that they were aware of other people being worse off than themselves such as soldiers with serious brain injury, cancer patients or if they still had some vision left those who were completely blind. Others made a comparison with vision impaired members who managed to carry on successfully. By making a downward comparison or by comparing themselves with people who had faced the same problems, coping was facilitated as members got inspired and motivated to “crack on with life”.
Oliver (non-combat-related visual impairment, 35–44 years): “They [members of Blind Veterans UK] proved that there are other people in the same situation as me and even not worse, and that you know you can still do day to day tasks and you can still do a lot of varied things if you put your mind to it. You know and it’s just challenging your mind to being able to do these things.”
People’s favourite leisure activities and interests changed substantially because they were no longer able to undertake them due to their loss of vision. Driving a car was missed tremendously, followed by sporting activities and reading. Personnel tried to get around these barriers by adopting a problem-focused approach (e.g. use of low vision aids, retrain, find other activities they were able to do). Also accepting or asking for (social) support from family, friends, charities or seeking professional support, helped ex-Service personnel to adjust and carry on.
Just after becoming visually impaired, personnel needed a lot of help and relied heavily on others. Once they started to adapt, people learned new skills and strategies, resulting in increased confidence and less reliance on others. This had a positive impact on the mental well-being of the person with the visual impairment and facilitated the process of accepting their loss of vision and its consequences. Further personnel learned what they are still able to do and what not, thereby reflecting on and adapting to the restrictions their visual impairment imposed. However, the dependence on others played a limiting role and new activities such as taking up different hobbies like disability sports were not always experienced as that satisfying.
Andrew (combat-related visual impairment, 25–34 years): “You have to accept that sort of thing as part of the hard bit in the beginning. (…) once you’ve accepted it [loss of vision] you get used to it and just move on from then. Then obviously you have achievement from there and then you put yourself to whatever you need to achieve.”
Achievement was often mentioned as a next step. Younger ex-Service personnel decided to set a particular goal such as starting a new course or degree, or signed up for a sporting challenge. By working towards a particular goal, personnel got back in a daily routine, their confidence increased as well as their self-worth. This impacted positively on their mental well-being. Reflecting on the different experiences of the participants it becomes apparent that coping with loss of vision is a dynamic long-term process. Even after years, people may struggle as new situations, challenges or life events come by.
Jack (combat-related visual impairment, 25–34 years): “It’s been [amount of years] now and there was a time I thought I’d accepted what had happened to me, but you know that was temporary. And yeah I don’t think I’ve fully accepted what’s happened to me. There [are] good periods and bad periods and you know they come and go quite randomly and yeah they affect me for different amounts of time and I can get quite negative sometimes and quite self-deprecating.”
Younger ex-Service men suggested that becoming visually impaired had turned their life upside down; the accompanying consequences had adverse effects on a variety of life domains and adjusting was experienced as a tough journey. Personnel struggled with an increased level of dependence on others, a loss of freedom, a lack of confidence and impaired feelings of self-worth. Various coping strategies were applied by younger ex-Service men and these enabled them to adjust to their loss and overcome challenges they faced down the line. Coping was an on-going and dynamic process with ex-Service personnel experiencing good and bad times, even after many years since sustaining their impairment.
The Kübler-Ross model was initially developed to describe how people cope with death and dying following a distinct 5 stage model (denial, anger, depression, bargaining and acceptance) [ 6 ]. We used this model as an example in the introduction to describe how people may deal with facing a significant loss, such as sustaining a visual impairment. However, over the years this model has been critiqued widely [ 16 – 18 ].
When reflecting on our results, it became clear that ex-Service men experienced a far wider range of emotions and behaviours; in some cases these emotions occurred simultaneously. Instead of a stage like pattern of response, the data showed coping was more dynamic, highly interactive and a unique journey for every individual. Whereas the individual affected plays a central role in Kübler-Ross’ model, we found that other factors played an important role as well as to how people adjust, including the availability of social support, use of low vision aids, presence of public attitudes, family composition and other situational factors [ 19 ]. The variety of positive or negative mechanisms of adjustment helped the individual to master their impairment and should be referred to as forms of coping strategies [ 18 ]. Acceptance is described as the closing stage of the grief process by Kübler-Ross. However, as pointed out by Murray and colleagues (2010), and reflected in our data, we found coping to be a long-term process, whereby the person affected will apply different strategies depending on the changes or new situations they encounter [ 20 ]. Therefore, acceptance may occur temporarily but will interact with new periods of adjustment and the grief process can be characterised as ‘a chronic recurrent but episodic process’ [ 20 ]. This has been illustrated earlier with a quote from Jack (combat-related visual impairment, 25–34 years): he interchangeably experiences periods of acceptance vs. rejection, despite the fact that a considerable amount of time has passed by since he became visually impaired.
Personnel tried to adjust using various strategies, including a strategy termed by the researchers as ‘coping at a cost’. Underlying reasons such as feeling too embarrassed to ask for help, not wanting to burden others or wanting to ‘crack on’ alone. Participants suggested that asking for help would impede on their sense of self-pride and self-respect [ 19 , 21 – 24 ]. This attitude of ‘cracking on’ is a key element of the work ethic of the British Army and encourages pro-activity over passivity and contemplation [ 25 ]. A different strategy was comparing themselves with others they classified as worse off [ 26 , 27 ]. This downward comparison motivated and inspired people to life their live to the fullest. For ex-Service personnel with a combat-related visually impairment, feelings of being grateful to still be around were apparent. Analysis of the quantitative data of the current study suggested that the prevalence of mental health problems was not substantially different between personnel with a combat-related visual impairment (25.0 %) compared to those with a non-combat-related visual impairment (29.6 %) (Ref).
Impact of visual impairment on life domains
Various quantitative studies have examined the impact of vision loss on the psychological well-being of elderly populations [ 3 ]. A review summarizing qualitative evidence of seventeen studies on the impact of and coping with vision loss suggested that people relied more heavily on others to perform their daily activities [ 7 ]. Further, they reported the loss of leisure activities and hobbies. In addition, a negative impact on mental well-being was described such as the onset of depression, impaired self-esteem, being less socially active and experiencing challenges with regards to interpersonal relationships and communication [ 7 ]. Despite the review summarizing studies among the elderly, the findings correspond well with those from the current study. However, the researchers would like to highlight that while the actual barriers and changes due to the loss of vision and its related consequences may be unique for each person, they impede on the same highly valued core concepts of (in) dependence, autonomy, self-esteem, control, confidence, freedom and identity.
A different review synthesised the findings of quantitative studies about the psychosocial impact of vison loss in adults aged 18–59 years [ 2 ]. They concluded that the general mental health, social functioning and quality of life were adversely affected. However, this was not consistent for the impact of visual impairment on the prevalence of depression [ 2 ]. The association between depression and visual impairment appears to be more evident among elderly [ 1 , 24 ].
Limitations
This study had various limitations. First, all participants were members of the charity organisation Blind Veterans UK and had served in the UK Armed Forces. In what way these findings can be extrapolated to different visually impaired populations such as civilians, elderly, women and people who are not involved in a charity organisation remains uncertain. Second, the research team asked sensitive questions related to how personnel coped with their visual impairment. They could have given socially acceptable answers because they did not feel confident, did not trust the interviewer or did not want to appear as ‘weak’. This issue was addressed by informing them what to expect, building good rapport and providing the opportunity to ask the team questions. An important strength of this qualitative study is the substantial sample size ( n = 30). Therefore, we are confident that we captured a wide range of views and experiences.
Implications
Clinicians, ophthalmologists and other health care providers as well as partners, the wider family and friends need to be aware that coping is an on-going process and that even after a considerable amount of time, needs for emotional, social, practical and physical support may still be present. Functional training and psychosocial support should be offered enabling personnel to regain their confidence, feelings of self-worth and independence.
Our findings suggest that sustaining a visual impairment is a life changing event that has important effects on various domains of life. Adjusting to loss of vision and its related consequences can be described as a long-term and difficult journey whereby ex-Service personnel apply various coping strategies to overcome the challenges they face later on in their lives. Future research should be directed into how positive coping can be facilitated and how factors such as the duration of the visual impairment and perceived social support, influence coping processes.
Horowitz A. The prevalence and consequences of vision impairment in later life. Top Geriatr Rehabil. 2004;20(3):185–95.
Article Google Scholar
Nyman SR, Gosney MA, Victor CR. Psychosocial impact of visual impairment in working-age adults. Br J Ophthalmol. 2010;94(11):1427–31.
Article CAS PubMed Google Scholar
Pinquart M, Pfeiffer JP. Psychological well-being in visually impaired and unimpaired individuals: a meta-analysis. Br J Vis Impair. 2011;29(1):27–45.
Schilling OK, Wahl HW. Modeling late-life adaptation in affective well-being under a severe chronic health condition: the case of age-related macular degeneration. Psychol Aging. 2006;21(4):703–14.
Article PubMed Google Scholar
Bergeron CM, Wanet-Defalque M. Psychological adaptation to visual impairment: the traditional grief process revised. Br J Vis Impair. 2013;31(1):20–31.
Kübler-Ross E. On death & dying. New York: Scribner; 1969.
Google Scholar
Nyman SR, Dibb B, Victor CR, Gosney MA. Emotional well-being and adjustment to vision loss in later life: a meta-synthesis of qualitative studies. Disabil Rehabil. 2012;34(12):971–81.
Hodge S, Barr W, Bowen L, Leeven M, Knox P. Exploring the role of an emotional support and counselling service for people with visual impairments. Br J Vis Impair. 2013;31(1):5–19.
Fazal TM. Dead wrong? Battle deaths, military medicine and exaggerated reports of war’s demise. Int Secur. 2014;39(1):95–125.
Blood CG, Puyana JC, Pitlyk PJ, Hoyt DB, Bjerke HS, Fridman J, et al. An assessment of the potential for reducing future combat deaths through medical technologies and training. J Trauma. 2002;53(6):1160–5.
Eastridge BJ, Jenkins D, Flaherty S, Schiller H, Holcomb JB. Trauma system development in a theater of war: Experiences from operation Iraqi freedom and operation enduring freedom. J Trauma. 2006;61(6):1366–72. discussion 1372–1363.
Bellamy RF. A note on American combat mortality in Iraq. Mil Med. 2007;172(10):1023.
Stevelink SA, Malcolm EM, Mason C, Jenkins S, Sundin J, Fear NT. The prevalence of mental health disorders in (ex-)military personnel with a physical impairment: a systematic review. Occup Environ Med. 2014;72:243–51.
Article PubMed PubMed Central Google Scholar
Fugard AJB, Potts HWW. Supporting thinking on sample sizes for thematic analyses: a quantitative tool. Int J Soc Res Methodol. 2015;18(6):669–84.
Ritchie J, Lewis J, McNaughton Nicholls C, Ormston R. Qualitative Research Practice: a guide for social science students & researchers. 2nd ed. London: SAGE; 2014.
Brewer BW. Review and critque of models of psychological adjustment to athletic injury. J Appl Sport Psychol. 1994;6(1):87–100.
Copp G. A review of current theories of death and dying. J Adv Nurs. 1998;28(2):382–90.
Corr CA. Coping with dying-lessons that we should and should not learn from the work of Kublerross, Elisabeth. Death Stud. 1993;17(1):69–83.
Weber JA, Wong KB. Older adults coping with vision loss. Home Health Care Serv Q. 2010;29(3):105–19.
Murray SA, McKay RC, Nieuwoudt JM. Grief and needs of adults with acquired visual impairments. Br J Vis Impair. 2010;28(2):78–89.
Wong EYH, Guymer RH, Hassell JB, Keeffe JE. The experience of age-related macular degeneration. J Vis Impair Blind. 2004;98(10):629–40.
Ivanoff SD, Sjostrand J, Klepp KI, Lind LA, Lindqvist BL. Planning a health education programme for the elderly visually impaired person—a focus group study. Disabil Rehabil. 1996;18(10):515–22.
Brouwer DM, Gaynor S, Winding K, Hanneman M. Limitations in mobility: experiences of visually impaired older people. Br J Occup Ther. 2008;71(10):414–21.
Mitchell J, Bradley C. Quality of life in age-related macular degeneration: a review of the literature. Health Qual Life Outcomes. 2006;4:97.
King A. Why we’re getting it wrong in Afghanistan. In: Prospect. 2009.
Teitelman J, Copolillo A. Psychosocial issues in older adults’ adjustment to vision loss: findings from qualitative interviews and focus groups. Am J Occup Ther. 2005;59(4):409–17.
Thurston M, Thurston A, McLeod J. Socio-economic effects of the transition from sight to blindness. Br J Vis Impair. 2010;28(2):90–112.
Download references
Acknowledgements
We would like to thank Professor Christopher Dandeker based at the Department of War Studies, King’s College London, for his useful comments on an earlier draft of the paper.
Author information
Authors and affiliations.
King’s Centre for Military Health Research, King’s College London, Weston Education Centre, 10 Cutcombe Road, SE5 9RJ, London, United Kingdom
Sharon A. M. Stevelink, Estelle M. Malcolm & Nicola T. Fear
Academic Department of Military Mental Health, King’s College London, Weston Education Centre, 10 Cutcombe Road, SE5 9RJ, London, United Kingdom
Nicola T. Fear
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sharon A. M. Stevelink .
Additional information
Competing interests.
S.A.M.S., E.M.M. and N.T.F. are based at King’s College London, which receives funding from the UK Ministry of Defence (MoD). S.A.M.S. and E.M.M. receive funding from Blind Veterans UK to carry out the Blind Veterans UK study. The authors were not directed in any way by the charity or the MoD in relation to this publication.
Authors’ contribution
SAMS was involved in the planning of the study, in developing the data analysis strategy for this paper, participated in data collection, undertook the data analyses and wrote the paper. EMM was involved in developing the data analysis strategy for this paper, participated in data collection, undertook the data analyses, contributed to and commented on the paper. NTF was the principal investigator for this study, was involved in the design, planning and data analysis strategy development of the study and commented extensively on the paper. All authors read and approved the final manuscript.
Additional files
Additional file 1:.
Coding framework with the two main themes identified for the current paper. (DOCX 15 kb)
Additional file 2:
Semi-structured interview guideline. (DOCX 14 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Stevelink, S.A.M., Malcolm, E.M. & Fear, N.T. Visual impairment, coping strategies and impact on daily life: a qualitative study among working-age UK ex-service personnel. BMC Public Health 15 , 1118 (2015). https://doi.org/10.1186/s12889-015-2455-1
Download citation
Received : 27 October 2014
Accepted : 26 October 2015
Published : 12 November 2015
DOI : https://doi.org/10.1186/s12889-015-2455-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health-related quality of life
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.36(3); 2022 Mar
Association of visual impairment with disability: a population-based study
John m. nesemann.
1 Francis I Proctor Foundation, University of California San Francisco, San Francisco, CA USA
Ram P. Kandel
2 Seva Foundation, Berkeley, CA USA
Raghunandan Byanju
3 Bharatpur Eye Hospital, Bharatpur, Nepal
Bimal Poudyal
Gopal bhandari, sadhan bhandari, kieran s. o’brien.
4 Division of Epidemiology, School of Public Health, University of California Berkeley, Berkeley, CA USA
Valerie M. Stevens
Jason s. melo, jeremy d. keenan.
5 Department of Ophthalmology, University of California San Francisco, San Francisco, CA USA
Associated Data
The data that support the findings of this study are available on request from the corresponding author, JMN.
To determine the relationship between visual impairment and other disabilities in a developing country.
In this cross-sectional ancillary study, all individuals 50 years and older in 18 communities in the Chitwan region of Nepal were administered visual acuity screening and the Washington Group Short Set (WGSS) of questions on disability. The WGSS elicits a 4-level response for six disability domains: vision, hearing, walking/climbing, memory/concentration, washing/dressing, and communication. The association between visual impairment and disability was assessed with age- and sex-adjusted logistic regression models.
Overall, 4719 of 4726 individuals successfully completed visual acuity and disability screening. Median age of participants was 61 years (interquartile range: 55–69 years), and 2449 (51.9%) were female. Participants with vision worse than 6/60 in the better-seeing eye were significantly more likely to be classified as having a disability in vision (OR 18.4, 95% CI 9.9–33.5), walking (OR 5.3, 95% CI 2.9–9.1), washing (OR 9.4, 95% CI 4.0–21.1), and communication (OR 5.0, 95% CI 1.7–13.0), but not in hearing (OR 0.6, 95% CI 0.006–2.2) or memory (OR 2.2, 95% CI 0.7–5.1).
Conclusions
Visually impaired participants were more likely to self-report disabilities, though causality could not be ascertained. Public health programs designed to reduce visual impairment could use the WGSS to determine unintended benefits of their interventions.
Introduction
Globally at least 2.2 billion people have visual impairment. Of these, at least 1 billion have visual impairment that has yet to be addressed or could have been prevented [ 1 ]. The 2017 Global Burden of Diseases, Injuries, and Risk Factors study, which estimated years lived with disability to provide context about the burden of nonfatal diseases, found vision loss to be the third leading impairment for both sexes [ 2 ]. Moreover, the burden of visual impairment is forecast to increase substantially by 2050 as large portions of the global population age and life expectancy improves [ 3 ]. The high burden of visual impairment extends to the economic realm as well, leading to billions of dollars in productivity losses [ 4 ].
The burden of visual impairment is not distributed evenly. For example, the prevalence of distance visual impairment in low- and middle-income countries is estimated to be four times higher than that of high-income regions [ 5 ]. Furthermore, older individuals, women, and rural residents have also been found to have a higher risk of visual impairment [ 6 – 8 ]. Disabilities unrelated to vision are also thought to be associated with visual impairment, although supporting data are relatively sparse [ 1 ].
Disability refers to the impairments, limitations and restrictions that a person faces while interacting with their environment—physical, social, or attitudinal [ 1 ]. The importance of disability has received increased attention in recent years, but data on the relationship between visual impairment and disability are scant [ 9 ]. Several previous studies have examined the relationships between visual function, visual disability, and activities of daily living in high-income countries, and one study assessed self-reported disability and visual impairment using the World Health Organization Disability Assessment Schedule in six lower- and middle-income countries [ 10 – 13 ]. The results from these studies suggest an association between disability and visual impairment, but data from other settings would add confidence to the findings.
In the present study, we evaluated the relationship between visual impairment and self-reported disability using a standardized disability questionnaire developed by the United Nations Washington Group (WG) on Disability Statistics and recommended by the World Bank for household surveys [ 14 ]. We conducted the study in a resource-limited setting in Nepal, where the burden of both visual impairment and disability would be expected to be relatively high [ 5 ]. We hypothesized that visual impairment would be associated with higher self-reported disability.
Materials and methods
Study design and settings.
The study took place in the Chitwan district of Nepal from 16 January, 2018 to 22 December, 2019. At the time, the district was divided into numerous village development committees (VDC), which were in turn subdivided such that each VDC consisted of nine wards. As part of a cluster-randomized trial, 36 wards from 6 VDCs in the Chitwan district were randomized to receive a community-based eye disease screening intervention or no screening intervention. Screening visits were performed by the same screening team in a central area of the community. The present report is an ancillary cross-sectional study conducted only in the 18 communities randomized to the screening intervention; this ancillary study compares the results of a visual acuity assessment and a disability questionnaire completed during the screening visit. The study adhered to the Strengthening of the Reporting of Observational Studies in Epidemiology guidelines.
Participants
All individuals aged 50 years or older who were found to be residing within the randomized communities on a door-to-door census conducted 1–4 weeks prior to the screening visit were invited to participate in the study. All consenting participants reported to a central location in the community to undergo visual acuity screening and a fill out a disability questionnaire.
Visual acuity
Each eye was tested separately using a visual acuity screening card developed by Nepal Netra Jyoti Sangh (Kathmandu, Nepal); the foldable card had four faces, three of which contained a single tumbling E optotype of a different size (i.e., corresponding to visual acuities of 6/60, 6/18, and 6/9 when tested at 6 m). Each optotype size was presented at 6 m in four arbitrary directions at the discretion of the tester, with a successful effort requiring a correct answer for all four directions. Testing was conducted in a well-lit environment outside of direct sunlight. The right eye was tested first with the left eye occluded and then the left eye was tested with the right eye occluded. Participants were tested with spectacle correction, if any was available (i.e., the WHO’s definition of presenting visual acuity), followed by pinhole occlusion. Visual acuity was defined at the person level as the smallest optotypes that could be read in the better-seeing eye, either with spectacle correction if available (i.e., presenting visual acuity) or through a pinhole occluder (i.e., pinhole acuity).
The Washington Group Short Set of questions on disability (WGSS) was translated into Nepali and administered verbally to each participant [ 15 ]. This questionnaire elicits a 4-level response (i.e., “no difficulty,” “some difficulty,” “a lot of difficulty,” or “cannot do at all”) for disabilities in six domains: vision, hearing, walking/climbing, memory/concentration, washing/dressing, and communication (Supplementary Fig. 1 ). The questionnaire was administered verbally to each participant.
Statistical considerations
The exposure of interest was presenting visual acuity in the better-seeing eye, dichotomized at three different thresholds (i.e., 6/9, 6/18, and 6/60—the three thresholds screened with the visual acuity card) indicating the ability versus the inability to see that line of vision. The outcome of interest was the presence of disability for each domain, with disability defined as “a lot of difficulty” or “cannot do at all” in at least one domain on the WGSS, as recommended by the Washington Group on Disability Statistics [ 16 , 17 ]. Logistic regression models were constructed for each disability domain outcome and adjusted for the potential confounders of sex, age in years, and presence of self-reported diabetes mellitus (i.e., an indicator of systemic co-morbidity), with separate models to assess each of the visual acuity thresholds. Individuals with missing data were excluded from the analysis. In a secondary analysis, the prevalence of disability and visual impairment was calculated for each community, and community-level associations assessed with a linear regression weighted by the number of respondents per community. Intraclass correlation coefficients (ICC) were calculated to determine the degree to which disability and visual impairment clustered within communities [ 18 ]. The sample size was based on the underlying clinical trial, and therefore, fixed; we planned to enrol at least 4500 people across the 18 communities. Assuming a 2% prevalence of blindness based on a prior study from Nepal [ 19 ], a 5% prevalence of disability in people without visual impairment, and an alpha of 0.05, then this sample size would provide ~80% power to estimate a 7.5% greater prevalence of disability in the visually impaired group. Centre values for descriptive statistics are reported as medians and all odds ratios (ORs) are presented with their corresponding 95% confidence intervals (CIs). The data met underlying assumptions for logistic regression models. Analyses were performed with R version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria) [ 20 ].
The study received Institutional Review Board approval from the University of California San Francisco, and ethical approval from Nepal Netra Jyoti Sangh, and the Nepali Health Research Council. The study adhered to the guidelines of the Declaration of Helsinki. Verbal informed consent was obtained for all participants; verbal consent was approved by ethical committees due to the high levels of illiteracy in the study area. No stipend was provided.
A total of 4726 individuals aged 50 years or older presented for examination, of which 4719 successfully completed visual acuity and disability screening. The median age of participants successfully completing screening was 61 years (interquartile range: 55–69 years), and 2449 (51.9%) were female.
The best presenting visual acuity in the better-seeing eye was 6/9 in 3101 (65.7%) participants, 6/18 in 1148 (24.3%) participants, 6/60 in 369 (7.8%) participants, and worse than 6/60 in 101 (2.1%) participants. When disability was defined using the WG recommendation of “a lot of difficulty” or “inability” in at least one domain, 233 people (5.0%) reported having a disability. When disability was defined as “some difficulty” or worse in one or more domains, 842 people (17.8%) reported having a disability. Age- and sex-stratified results of the vision screening and disability questionnaire are summarized in Table 1 . As depicted in Fig. 1 , both visual impairment and the number of reported disabilities became significantly more prevalent with advanced age but did not differ substantially by sex. The proportion of people with a disability increased as presenting vision in the better-seeing eye worsened, regardless of whether the threshold for disability was defined as “some” difficulty or “a lot” of difficulty (Fig. 2 ).
Age- and sex-stratified disability and vision results.
The Washington Group Short Set disability questionnaire has four possible responses (no difficulty, some difficulty, a lot of difficulty, and cannot do at all) over six disability domains (vision, hearing, walking/climbing, memory/concentration, washing/dressing, and communication).
a Disability from the Washington Group Short Set, defined using two thresholds: (1) a lot of disability or worse (as recommended by the Washington Group), and (2) some disability or worse (since this definition has been used in other research). Values represent the number of individuals with a disability in (1) one or more of the six domains, and (2) two or more of the domains.
b Best presenting visual acuity of the three tested optotype sizes (i.e., 6/9, 6/18, and 6/60), in the better-seeing eye.

A The proportion with disabilities in each age group and B the proportion in each visual acuity group, defined by best presenting acuity.

Presenting acuity results were classified into four ordered groups based on the best visual acuity line successfully read. Bars show the distribution of disability scores within each vision group. Note limit of the y -axis is set to 40% so as to better visualize the distribution of disability scores within each vision group.
Participants with worse presenting visual acuity were more likely to self-report a disability, with greater magnitudes of association for those with more advanced vision loss (Fig. 3 ). For example, compared to those with better vision, participants whose presenting vision was worse than 6/60 in the better-seeing eye were more likely to be classified as having a disability in the vision (OR 18.4, 95% CI 9.9–33.5), walking (OR 5.3, 95% CI 2.9–9.1), washing (OR 9.4, 95% CI 4.0–21.1), and communication (OR 5.0, 95% CI 1.7–13.0) domains. In contrast, disabilities in the hearing and memory domains had weaker associations with visual impairment (OR 0.6, 95% CI 0.06–2.2 and OR 2.2, 95% CI 0.7–5.1, respectively). Conclusions did not change when analyses were repeated with pinhole-corrected visual acuity (Supplementary Fig. 2 ).

Each dot represents the odds ratio from an age- and sex-adjusted logistic regression that models the presence of disability as a function of a dichotomous visual acuity exposure variable; bars represent 95% confidence intervals. Visual acuity groups indicate the best presenting visual acuity achieved (relative to those not achieving the respective acuity). The horizontal dashed line represents an odds ratio of 1.
The community prevalence of visual impairment (i.e., visual acuity worse than 6/60) did not significantly correlate with the community prevalence of disability (i.e., “a lot of difficulty” or “unable to do” in at least one domain of the WGSS), with each 10 percentage-point increase in the prevalence of visual impairment corresponding to a 3.1 percentage-point reduction (95% CI 25.6-point reduction to 19.4-point increase) in the prevalence of disability ( P = 0.77, regression weighted by a number of respondents per community; Fig. 4 ). Other thresholds of visual acuity impairment and disability were likewise not statistically significant. The magnitude of within-community clustering, as assessed by the ICC, was estimated to be 0.007 (95% CI 0–0.17) for the presence of at least one disability and 0.06 (95% CI 0–0.42) for presenting visual acuity impairment worse than 6/60.

Disability was defined as “a lot of difficulty” or “unable to do” in one or more domains of the disability questionnaire and visual impairment as best presenting acuity worse than 6/60. Each point represents a study community, sized proportional to the number of community members tested. The best-fit line from a linear regression of community-level data is shown as a dashed line.
This study’s principal finding was that people with visual impairment were more likely to have other self-reported disabilities. The likelihood of an association was strengthened by the observation of a dose response, with greater odds of disability for worsening states of visual impairment (Fig. 3 ).
We found that ~2.1% of the population 50 years or older in this region of Nepal had a presenting visual acuity worse than 6/60 in the better-seeing eye. Although the visual acuity thresholds and age groups of this study differ somewhat from prior studies, the extent of visual impairment observed here was generally in line with previous estimates of visual impairment in Nepal and indicates a relatively large burden of visual impairment in this region of Nepal [ 19 , 21 , 22 ].
Several previous studies found lower estimates of social and physical functioning in those with visual impairment, but these studies used a variety of measurement tools and did not focus specifically on disability [ 12 , 23 – 27 ]. For example, one study using data collected from 2007 to 2010 in six lower- and middle-income countries found an association between visual impairment and self-reported disability as assessed by the World Health Organization Disability Assessment Schedule 2.0 [ 13 ]. In the years since this study was completed, consensus has grown to support the United Nations WGSS of disability questions, a relatively quick 6-item questionnaire [ 28 ]. Use of this instrument in the present study enhances its generalizability and provides valuable, internationally comparable data. It was simple to incorporate into the study, added little time to fieldwork, and will help provide context to the main results of the clinical trial. We recommend its use by other research groups.
We found that approximately 5% of participants 50 years and older reported a lot of difficulty or inability in at least one of the tested disability domains, with rapidly increasing prevalence as the population aged (Fig. 1A ). Of the queried domains, self-reported difficulty with vision was most common. Reduced visual acuity was significantly associated with self-reported disabilities in walking, washing, and communication, but not hearing or memory (Fig. 3 ). Although this study cannot assess causality, it is reasonable to speculate that difficulty with vision would make walking and washing more challenging and could also hamper the ability to initiate and maintain communication. In contrast, vision has a less plausible direct causal impact on hearing loss, although both are associated with age. Of note, prior work has shown a longitudinal association between vision loss and cognitive decline [ 29 – 31 ]. The lack of an association between vision loss and memory in the present study could be due to several factors, including inadequate sample size, inability of a single question to accurately assess cognition when compared to the neuro-psychiatric tests used in other studies, and difficulty obtaining accurate responses from those who suffer severe deficits in cognition.
Despite the inability to assess causality in the present study, it is tempting to speculate whether interventions to improve visual acuity in a population could also reduce other perceived disabilities, especially since vision correction is likely a more easily modifiable risk factor than others for the disabilities elicited in this study. Future randomized trials of interventions that specifically target visual impairment, but not other disabilities, might consider including disability assessments as secondary outcomes.
The present study found that 5.0% of participants 50 years or older reported at least 1 disability when the threshold for a disability was set to “a lot” of difficulty (i.e., the cutoff recommended by the WG), and 17.8% when the threshold was defined as “some” difficulty in one or more domains (the definition employed by some other groups). These estimates are relatively consistent with population-based studies from Peru, Morocco, and Uganda, although the study definitions and/or reporting of outcomes are not exactly the same between the studies, making a direct comparison difficult [ 32 – 34 ]. These previous studies have found visual disability to be either the most common or second most common disability among the six tested domains, and have found an increasing prevalence of disability with age—each of which was also confirmed in the present study.
We found that community-level estimates of visual impairment did not correlate strongly with community-level disability prevalence, and that the magnitude of within-community clustering was minimal. This suggests that studies based on cluster sampling that seek to investigate the relationship between visual impairment and disability would likely be better off using an individual-level rather than community-level outcome.
Several limitations of the present study should be noted. Visual acuity was tested at only three acuity levels, limiting the granularity of the data and thus the statistical power. As stated above, the observational nature of the study precluded conclusions about causality. Ordinal multi-category data on disability and visual acuity impairment were dichotomized, a simplification that reduced statistical power but also made for more parsimonious regression models that were easier to interpret. While the regression models were adjusted for self-reported diabetes, data on other potential confounders of the relationship between vision and disability were not collected, preventing a more detailed multivariable analysis. Finally, while the inclusion of a random set of communities increased the study’s generalizability within this region of Nepal, the generalizability of the findings outside of Nepal is not clear: it is possible that visual impairment has a stronger magnitude of association with other disabilities in a place like Nepal with limited access to health services.
In summary, we found a significant association between visual impairment and disabilities in seeing, walking, washing, and communication, with higher odds of disability for groups with more advanced visual impairment in this area of Nepal. The causality of this association remains unclear. Incorporation of the WGSS into a community-based study of a blindness prevention program was quick and easy, and well accepted by the study participants. Inclusion of disability questions could be worthwhile for future studies of interventions for visual impairment, either to provide context about the characteristics of the study population or as a secondary outcome.
What was known before
- Disabilities unrelated to vision are thought to be associated with visual impairment although data is scarce.
What this study adds
- A population-based sample of adults 50 years and older in Nepal had visual acuity testing and answered a standardized disability questionnaire developed by the United Nations Washington Group on Disability Statistics and recommended by the World Health Organization.
- Individuals with vision worse than 6/60 in the better-seeing eye were more likely to report disabilities in vision, walking, washing, and communication but not hearing or memory.
- The questionnaire was easy to implement and may provide information on unintended benefits of public health programs intended to reduce visual impairment.
Supplementary information
Author contributions.
Concept and design: JDK, KSO, JSM, and VMS. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: JMN and JDK. Critical revision of the manuscript for important intellectual content: All Authors. Administrative, technical, or material support: RPK, RB, BP, HB, SB, KSO, VMS, and JSM. Supervision: JDK.
The study was supported by the National Eye Institute and the Fogarty International Center of the National Institutes of Health (NIH) [Award Number D43TW009343] as well as the University of California Global Health Institute (UCGHI) in the form of a Fogarty grant to JMN and grants from That Man May See, the Fortisure Foundation, the Harper-Inglis Memorial for Eye Research, the Peierls Foundation, the Alta California Eye Research Foundation, the Bofinger Glaucoma Research Fund, and Research to Prevent Blindness. The authors held no agreement with the funders that may have limited their ability to complete the research as planned and have full control of all primary data.
Data availability
Compliance with ethical standards.
The authors declare no competing interests.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The online version contains supplementary material available at 10.1038/s41433-021-01498-x.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 May 2024
How do I manage functional visual loss
- Neil Ramsay ORCID: orcid.org/0000-0003-3179-8126 1 ,
- Justin McKee 2 ,
- Gillian Al-Ani 2 &
- Jon Stone 3
Eye ( 2024 ) Cite this article
29 Altmetric
Metrics details
- Rehabilitation
Functional visual loss is a subtype of functional neurological disorder (FND) and is a common cause of visual impairment seen in both general and neuro-ophthalmological practice. Ophthalmologists can generally diagnose functional visual loss reasonably confidently but often find it harder to know what to say to the patient, how to approach, or even whether to attempt, treatment. There is little evidence-based treatment despite studies showing up to 60% of adults having impactful symptoms on long-term follow-up. The last 20 years has seen large changes in how we understand, approach, and manage FND more widely. In this article, we set out our practical approach to managing functional visual loss which includes : 1) Make a positive diagnosis based on investigations that demonstrate normal vision in the presence of subjectively impaired vision, not just because tests or ocular exam is normal; 2) Explain and label the condition with an emphasis on these positive diagnostic features, not reassurance; 3) Consider eye or brain comorbidities such as migraine, idiopathic intracranial hypertension or amblyopia; 4) Consider working with an orthoptist using diagnostic tests in a positive way to highlight the possibility of better vision; 5) Develop simple treatment strategies for photophobia; 6) Consider psychological factors and comorbidity as part of assessment and therapy, but keep a broader view of aetiology and don’t use this to make a diagnosis; 7) Other treatment modalities including hypnotherapy, transcranial magnetic stimulation and more advanced forms of visual feedback are promising candidates for functional visual loss treatment in the future.
功能性视力损失是功能性神经障碍(FND)的一种亚型, 也是综合眼科和神经眼科常见的视力损害原因。眼科医生通常可以十分自信地诊断功能性视力损失, 但往往难以弄清如何向患者解释, 如何处理, 甚至是否尝试治疗。
尽管研究显示高达60%的成年人在长期随访中出现症状, 但几乎没有循证治疗。过去的20年里, 我们在更广泛地理解、处理和管理FND方面发生了巨大变化。本文阐述了功能性视觉损失的管理的实用方法, 包括: 1)在主观视力受损的情况下, 根据显示视力正常的检查做出阳性诊断, 而非仅因为眼科检查提示正常;2)强调用阳性诊断特征来向患者解释和标记病情, 而不是口头上的保证;3)需考虑眼或脑的合并症, 如偏头痛、特发性高颅压或弱视;4)需考虑与斜视医生的合作, 积极使用诊断测试, 以突出改善视力的可能性;5)针对畏光症制定简单的治疗措施;6)评估和治疗时应考虑心因性疾病, 但要从更广泛的角度看待病因, 不要依此诊断;7)其他治疗方式包括催眠疗法、经颅磁刺激和更高级的视觉反馈形式, 未来有望成为治疗功能性视力损失的备选方案。
Similar content being viewed by others
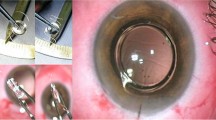
Implantable vision-enhancing devices and postoperative rehabilitation in advanced age-related macular degeneration
How do different lighting conditions affect the vision and quality of life of people with glaucoma? A systematic review
Delphi methodology for symptomatology associated with visual dysfunctions
Introduction.
Functional visual loss like other subtypes of functional neurological disorder (FND) involve the subjective experience of visual impairment in the presence of findings that demonstrate that visual pathways in the eye and brain are structurally intact, sometimes called internal inconsistency [ 1 ]. The brain of the person with functional visual loss won’t let them have the visual experience that they ought to be able to have.
In the ophthalmology literature, there is often an incorrect assumption that functional visual loss, in which the person experiences the symptoms, and simulated or malingered visual loss, where the person deliberately pretends to have symptoms, are strongly overlapping phenomena. Feigned, factitious or malingered factitious visual loss does also occur and is discussed below but is much rarer than functional visual loss.
A recent survey of 119 UK ophthalmologists found that 26% did not feel comfortable diagnosing functional visual loss, 59% felt they would not be confident in discussing functional visual loss and 58% felt they would struggle to discuss associated psychological factors if present [ 2 ]. It highlighted ambivalent attitudes to management with 37% stating that patients should not be able to claim disability benefits because it may prevent recovery. Many felt they lacked the space and time to provide treatment as well as concerns about accessing appropriate psychological input.
Most articles in this area have focused on diagnosis and the means to provide positive evidence of visual tract function despite symptomatic visual loss. Descriptions of treatment often involve simple reassurance from the ophthalmologist or referral to a psychiatrist.
This review aims for something different in providing a practical approach to the management of the patient once the diagnosis has been made. We have focused especially on management that ophthalmologists or neuro-ophthalmologists can get involved with, including using tests as part of the explanation and potential therapies to improve visual function. We have restricted ourselves to functional visual loss only and do not discuss functional disorders of eye movement, or visual hyperphenomena such as visual snow. We have provided two case vignettes (Box 1 and 2 ).
Box 1 Migraine and bilateral functional visual loss
A 19-year-old female presented with progressive photophobia and severe migraine with visual aura [43]. After two weeks she experienced persistent blurred vision in her right eye followed by her left. She spent most of her time in her bedroom in the dark because of migraine. One day she woke and had no vision apart from a faint glow. Migraine improved. She was told that she had functional blindness because of the normal investigations and that it was a psychological problem but was not persuaded this was correct.
Six months later she was referred for another opinion. We were able to demonstrate normal optokinetic nystagmus and asked her mother to use this at home to show the rest of the family how her brain could be made to respond to visual stimuli. We formulated her headache as a consequence of migraine and photophobia, her brain had shut down visual input to try to protect her from headache. We encouraged the family to look for occasions when the patient could see things and feed this back to her. Three sessions of transcranial magnetic stimulation were received positively by the patient who was surprised at the visual experience of phosphenes that it gave her. The patient also found four sessions of hypnotherapy helpful and considered they had ‘stirred something’ in her, although there was no immediate improvement. About 1 month later she found that she started to see more light with patterns of spots and after another month woke up to discover she had normal vision. Complete recovery has persisted at 5 year follow up.
Box 2 Functional visual loss with other types of FND
A 16-year-old male presented with a history of visual impairment since the age of 12. He had been diagnosed 6 months earlier with a post fracture complex regional pain syndrome affecting the left leg with redness, swelling, dystonia and weakness. He also had anxiety, PTSD and was being assessed for autism spectrum disorder. He was put on Pregabalin and experienced visual blurring and dizziness and visual blurring that was initially intermittent but gradually became permanent. He reported being able to see colours and shapes but not letters. Vision is worse for moving objects. MRI brain, ERG, OCT and VEPs were normal and visual acuity was demonstrated as transiently normal using a prism examination.
He didn’t need much persuading that the diagnosis was functional visual loss having read already about the connection between CRPS and FND but was desperate to have improved vision. We experimented with reading words on paper that he couldn’t see at all, and he had to guess what they were. ‘Dog’ was guessed as ‘Cat’ and ‘Round’ was guessed as ‘Circle’ and we were able to reflect on how that indicated that there was a route from her eye to her brain that he wasn’t aware of. We also discussed times when he was able to read signs and tended to get a headache and how those indicated that we were challenging the block in his brain. He reported feeling very positive with the consultation. He found a discussion about the film Inside Out especially helpful. He is currently having hypnotherapy as well as psychotherapy for PTSD and visual acuity has improved. We have had frank conversations about how he might explain recovery of visual function to friends and family who might be surprised that he had improved.
How common is functional visual loss and when does it need treatment?
Functional visual loss, and especially functional visual signs are common. One of the best studies found that it accounted for 12% ( n = 133) of 1108 new neuro-ophthalmology patients to a centre in Oregon [ 3 ] with 57% female and 14% younger than 18 years old. The same study found that 53% had co-existent eye or brain disease that led to comorbid neuro-ophthalmological findings. 14% had experienced head or eye trauma within the past month and 14% had experienced a recent surgical procedure.
A 2016 systematic review of the prognosis of functional visual loss included 5 studies (between 1966 and 1989) with 132 patients, mostly adults, with a follow up over several years. Between 46 and 78% of patients had improved or remitted at follow up [ 4 ]. A further study of 8 cases in children showed that 25% had recovered in 1 month [ 5 ].
Our own experience is that only a proportion of patients with functional visual signs actually want or need further treatment for associated difficulties with acuity or visual fields. A patient’s poor performance during a test may not correlate with their difficulties day to day, which may indeed be partly how the diagnosis is made. For example, a patient with idiopathic intracranial hypertension who has spiralled visual fields but doesn’t complain of much in the way of visual symptoms does not need a detailed explanation or management of functional visual loss.
Understanding aetiology and mechanism to enable explanation of functional visual loss
A clinician cannot be expected to be able to manage or explain a condition if they don’t have some understanding of it themselves. For many ophthalmologists, functional disorders are a ‘black box’ that they haven’t had training in where simplistic ideas (i.e. that it’s a purely psychological problem) pervade. This can lead clinicians to feel that it’s ‘not my problem’, or conversely to try to approach the problem in a way that doesn’t capture what we know about the complexity of what causes these symptoms.
Figure 1 indicates a more nuanced way to think about the aetiology and mechanism of functional visual loss. There are a range of possible aetiological risk factors which include eye and brain comorbidities as well as psychological risk factors such as adverse experience. Many of these can operate as predisposing, precipitating and perpetuating factors. Several studies have highlighted how commonly functional visual loss co-exists with neurological conditions such as migraine and idiopathic intracranial hypertension (IIH) and as well as other eye conditions (i.e. diabetic retinopathy or glaucoma). In one small series, 25% of patients had another neurological condition [ 6 ]. This comorbidity of other eye and brain conditions with functional symptoms and signs is often called ‘functional overlay’. We prefer the term ‘functional disorder comorbidity’, or dual diagnosis to emphasise the positive identification of a separate comorbidity with a different range of treatment. We don’t after all talk about ‘depression overlay’.
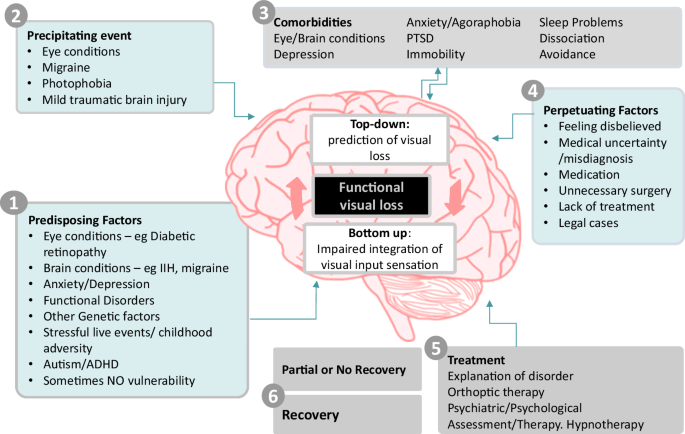
A predisposing, precipitating and perpetuating model of aetiology can combine with a mechanistic understanding of functional visual loss at the level of the brain.
Studies in FND generally have indicated that there is a higher frequency of adverse experience, especially emotional neglect in people with the condition [ 7 ], although data in people with functional visual loss is sparse. One study of 36 patients found that only 20% had experienced a recent stressful event [ 6 ], although there are also examples of functional blindness occurring in clusters related to stress, for example in refugees from the Cambodian war [ 8 ]. Adverse childhood experience can lead to an amplified dissociative response to threat or may be associated with difficulty labelling emotions that could lead later to bodily sensations of distress not being recognized and being amplified. Recent research has highlighted autism spectrum disorder and attention deficit hyperactivity disorder (ADHD) as risk factors for FND. Autism is also associated with increased sensory sensitivity which may be especially important in promoting a ‘shut down’ response of the visual brain in response to threat.
There are only very limited studies of neural correlates in functional visual loss. A functional MRI study of five patients with functional visual loss and seven controls found reduced activation in visual cortices but increased activation in left frontal cortex, insula, bilateral striatum, left limbic structures and left posterior cingulate cortex [ 9 ]. Wider studies of people with motor FND are beginning to find convergent evidence of abnormalities in several brain networks, especially those related to the sense of agency (i.e., the parts of the brain that give you the sense that you are the agent of your own actions and sensations), attention (i.e., ability to respond to stimuli), and emotion) [ 10 ].
Another useful way to think about FND is a disorder of the predictive brain [ 11 ]. A wide range of evidence suggests that the brain works on a day-to-day basis by predicting action and sensation and then, after the event, checking whether sensory input matches the prediction. Most of the time it matches very well, and we have a seamless experience of agency. However, a range of disorders, especially in neurology and psychiatry make sense as disorder of this predictive processing. For example, in phantom limb phenomena, the brain predicts that a limb is still there, even though there is ‘bottom-up’ sensory input telling the brain otherwise. The prediction is so strong that it overrides sensory input. Similarly, in functional visual loss, it may be that the brain is predicting visual loss so strongly that it ignores visual input that should be updating that prediction.
Strong predictions are not necessarily ‘beliefs’ about blindness, they are neural models that may arise for maladaptive reasons, for example, to shut down visual input when it’s not wanted, for example because of photophobia.
Feigning remains a notable concern in ophthalmology, perhaps more so than in other disciplines. This may be because the tests so definitely prove that vision is present when the patient says it is not. Feigning and malingering does occur, especially in legal scenarios, but remains rare in clinical practice. A recent review article explained the numerous clinical and neuroscience reasons why feigning is such a poor explanation for the majority of FND symptoms that present in clinical practice [ 12 ]. James Paget’s 1873 quote about a female patient with ‘hysterical paralysis’; – ‘ She says I cannot, it looks like I will not, but it is I cannot will’ – has not been bettered. In other words, functional neurological symptoms may look wilfully exaggerated, but they are instead a disorder of higher volitional control and agency of movement and sensation.
Diagnosis by inclusion – treats not tricks
The method of diagnosis depends on the severity of the visual impairment and whether monocular or binocular. Assessment of patients should be tailored to each situation. Assessment by an experienced orthoptist can be invaluable.
Examples of tests are shown in Table 1 . Other reviews go through the details of these diagnostic tests in more detail, and many will be familiar to experienced ophthalmologists or neuro-ophthalmologists [ 13 , 14 ].

It can be explained to the patient as evidence that the brain is ‘suppressing’ vision to match an internal model. Reprinted from Stone et al. [ 18 ].
We share them here to help the reader think about the therapeutic opportunities that some of these tests afford, in sharing the diagnosis, explaining the mechanism of symptoms and what might be done to improve vision.
Ophthalmology affords more techniques to make a firm diagnosis of FND than for any other motor or sensory symptom. Ophthalmologists will be aware that these tests are mostly based on ‘trickery’– which the patient usually never finds out about. One important advance in the FND field more generally has been a recognition that explaining these ‘tricks’ (see Table 1 ) can be therapeutic. For example, Hoover’s sign of FND-related limb weakness (weakness of hip extension which returns to normal during contralateral hip flexion), or the tremor entrainment sign in functional tremor (cessation or entrainment of tremor with contralateral externally cued movements), is one of the best ways of helping people to understand and have confidence in their diagnosis. This was reflected in an article entitled ‘ Trick or Treat’ describing this process in relation to motor FND assessment [ 15 , 16 ].
Investigations – to look for comorbidity, not to make a diagnosis of exclusion
In addition to slit lamp examination, most patients will require some degree of further investigation to look for eye, retinal or neurological pathology, including optical coherence tomography, retinal imaging and autofluorescence and MRI brain and orbits with contrast. MRI is the modality of choice as CT will miss some cerebral pathologies such as demyelination. MRI is also more helpful for looking for changes compatible with conditions like posterior cortical atrophy. These tests are typically regarded as essential to ‘excluding’ other pathology which can also give the incorrect impression that the diagnosis of functional visual loss is also a diagnosis of exclusion.
In the presence of clear positive features of functional visual loss we recommend reframing investigations as a search for comorbidity, which we know is common in functional visual loss. However, even if something is found, if the patient has evidence of better vision than they are aware of, unless it’s cortical visual loss/blindsight, then this also means they have functional visual loss.
Try explaining to your patient, at the earliest opportunity that you have found evidence of functional visual loss, but that you need to do further investigations to make sure there is nothing else going on.
Many clinicians are reluctant to bring up the possibility of functional visual loss until every test has been completed. But by that stage, several consultations may have occurred, and a significant amount of time may have lapsed. Introducing a functional visual loss diagnosis at a late stage is harder. The patient may reasonably wonder why the clinician hadn’t mentioned it earlier or whether other things are being kept from them. Trust and transparency are an essential element in any doctor-patient relationship and should be no different for people with functional disorders.
Better management of functional visual loss involves the clinician normalising it as a condition and treating it the same way as any other neuro-ophthalmological diagnosis, which includes discussing it early as a differential when appropriate.
Optical Coherence Tomography (OCT) scanning
OCT scanning can reveal retinal pathology in eyes which appear normal on slit lamp fundal examination. Particular attention should be paid to the outer segments of the photoreceptors, ellipsoid zone, and retinal pigment epithelium to look for subtle disruption that can be seen in occult or early retinopathy. Careful assessment of both the peripapillary retinal nerve fibre layer thickness and the macular ganglion cell layer may be especially important.
Supplementing OCT with wide-field fundus photography and autofluorescence can add further confidence that no subtle outer retinal pathology is being missed.
Electrophysiological testing
Electrophysiological testing, which is discussed extensively in another article in this issue of Eye is often important to look for other retinal comorbidities in functional visual loss [ 17 ].
We recommend an MRI brain and orbits with contrast in all patients with significant or long-lasting diagnoses of functional visual loss. It’s particularly important to consider whether your patient may have a structural cause of cortical visual loss such as stroke, multiple sclerosis, or tumour. A particular catch are patients with neurodegenerative diseases, especially posterior cortical atrophy, which can present with variable visual field deficits that may vary between assessments and not necessarily be obvious on MRI emphasising the importance of the clinical history and examination.

Explaining functional visual loss to a patient – “do what you normally do” and “don’t be weird”
There is consensus that patient’s confidence in the diagnosis of FND and motivation to engage with rehabilitation therapy is essential for successful treatment [ 18 ]. Conversely, if a patient rejects the diagnosis, perhaps because it’s poorly explained, or because information is hard to access or understand, rehabilitation often fails. A successful explanation about FND to a patient is therefore a vital first step to allow successful treatment. In some cases, a well communicated diagnostic explanation can be, in of itself, therapeutic.
In general, what tends to go wrong in the explanations of functional visual loss, and FND more widely, is that clinicians behave and talk in a way that is at variance with their normal practice. In essence, they do things that are ‘weird’ and are perceived as such by the patient. To correct this, all that needs to happen is for the clinicians to explain this disorder in the same way as they do any other condition in neuro-ophthalmology.
Normally when a clinician explains a diagnosis, they start by naming the condition (i.e., idiopathic intracranial hypertension), give an explanation of why they think that diagnosis is correct (fulfils the diagnostic criteria), perhaps some discussion of mechanism (there is a problem with CSF overproduction) and then finally, when the time is right, a discussion of why it may have happened (metabolic disease in association with weight gain). There may be a discussion of what conditions the patient doesn’t have, especially if they had a concern about brain tumour, but those typically follow on after the identification of the actual diagnosis.
A recent US review of functional visual loss warned against “confronting” a patient with their diagnosis of functional visual loss as it is ‘rarely helpful given its aggressive and negative connotation’ [ 19 ]. Instead, management with reassurance that symptoms are likely to improve is suggested as the default option by many authors and the American Academy of Ophthalmology [ 19 , 20 ]. Another recent review suggested that patients should be diagnosed with functional visual loss but should be told that their symptoms ‘do not have any anatomic or physiologic basis’ [ 21 ].
In the UK we suspect patients with functional visual loss are more frequently given a diagnosis, but even here, clinicians have traditionally often started by explaining that all the tests are normal, and that there is no reason for the visual symptoms in the eye or brain. As discussed in ‘investigations’ above, this often occurs after a long period of testing in which the patient may have an expectation that an answer is going to finally be found. There may then be an awkward moment where the patient is thinking ‘OK but what is it then?’. The clinician may then venture that these kinds of problems can occur in relation to psychological issues or stress or are ‘non-organic’. This kind of approach generally leads to a patient believing that the doctors are saying their symptoms are ‘all in their head’ or ‘imagined’, because their tests have failed to pick up a problem. When a physical symptom such as visual loss is attributed to psychological factors, most patients, as well as doctors, have ambiguity about whether that is a genuine problem, or whether its potentially feigned. The patient who has the experience of being unable to see, is understandably going to be upset and angry at the implication that they have something they might have control over, when their experience is the opposite, that they have no control over it.
What has gone wrong here is breaking of the normal rules of explanation. The clinician has not named the condition, has only explained what the patient doesn’t have, and jumped to conclusions about ‘why’ they have the problem without going through the expected stages of communication including evidence for the diagnosis and explanation of mechanism.
To correct this our primary recommendation is for clinicians to ‘do what you normally do’ when it comes to explanation of functional visual loss, the caveat being that you may not be used to giving the condition a name or explaining the nature of your testing.
Provide a name
Diagnostic labels are signposts to information and to treatment. They can also be a burden to patients. Usually someone should only be told they have functional visual loss if they are clearly symptomatic from that or may benefit from treatment.
Be careful with the use of the term functional neurological disorder (FND). Not everyone wants or needs to have a ‘disorder’. Some people just want to know what is causing their symptoms. The name you choose should sit comfortably with you and be consistent with the information provided. Functional visual loss is, in our view, the least worst term that we currently have. It emphasises a problem with function, rather that structure of the nervous system, promoting a less dualistic framework of understanding that leaves room for multiple aetiological factors. It is however a broad term which can be confusing for patients. In contrast, psychogenic visual loss, conversion disorder and somatisation, suggest a narrow psychological aetiology for functional visual loss. This is not in keeping with broader understanding of FND which clearly does involve the brain, as well as recognising the importance that comorbid eye and brain disease play in predisposing and precipitating functional visual loss. The term non-organic should, in our view, be abandoned since human beings are wholly organic and cannot have disorders that are not based at some level on “organic” processes.
Explain why you are making the diagnosis
In Table 1 we have outlined how nearly all the diagnostic procedures used to make a diagnosis of functional visual loss can be turned into opportunities for explanation and discussion with the patient.
The principal here is of transparency between clinician and patient, that may come as a relief to both of them. Instead of the diagnosis being handed down by the MRI scanner, OCT or electrophysiology, the process is brought back to the bedside. When successful our experience is that this is the key part of the diagnostic explanation. Demonstration of vision which is better when distracted or automatic compared to when the person is attending to or “voluntarily” seeing, has several immediate implications. It shows that there is a possibility of improvement, it indicates that the problem must be in the brain rather than the eye, and that changing attentional focus may play a role in treatment. It also helps the patient see that as a clinician you still believe they have a problem, even though you both now know that vision can be better than it appears to be.
In addition to the specific explanations around tests above we have provided some further ideas for ways to explain functional visual loss in general, as well as phrases that are often not helpful or misinterpreted in Table 2 .
The use of metaphor may be helpful. The brain is not a computer and ultimately every change in function must have some change in structure, but analogies to software malfunctioning (or a piano or car out of tune for those that don’t understand software) may help. For some people we have found it helpful to refer to the 2015 Pixar film ‘ Inside Out’ in which there are different characters in charge of different brain functions. In functional visual loss it is as if the character in control of vision has decided to go on strike.
Instead of jumping to a discussion of aetiological risk factors, we recommend starting with a discussion about the mechanism of symptoms first, for example a clinician may say “Your eyes are sending visual signals to the brain, but the brain is not letting you experience them” – see Table 2 . This is what ophthalmologists and neurologists are used to doing. For example, you wouldn’t try to explain to a patient why they had developed multiple sclerosis or Parkinson’s disease without first explaining that these are conditions associated with inflammation of the brain or loss of dopamine.
Making referrals to other specialists should also be done with care. If the basic problem is the brain not working, then it’s important to consider a wide range of techniques that might help the brain work better again. This may include psychological assessment and therapy, based on the model of what we think causes functional visual loss or other treatments like hypnotherapy that may need some careful explanation to avoid misunderstanding about what’s being suggested.
A concern many ophthalmologists may have in discussing functional visual loss is that any consultation may be consumed by discussing psychological factors or adverse life events which they may feel they lack the skills or time for. As outlined in Fig. 1 adverse life events or mental health diagnoses can be seen as risk factors and not the cause of the visual loss. Given limitations on time and the distress that comes with discussing these topics there is often no need to discuss these aspects in detail especially in the first diagnostic consultation and especially if the patient is not keen to do so. The priority in initial consultations is to reach a diagnosis based on clinical evidence and explore mechanisms of symptoms with patients. Integrating that with more complex risk factors where present takes time, should occur at the patient’s own pace and is often a goal of treatment, rather than something that can be ‘solved’ at the first appointment.
Providing written materials and onward signposting can be helpful for people. Copying your letter to the patient is another way of promoting transparency and educating the patient. At present, there aren’t detailed materials for people with functional visual loss, but they could be signposted to FND resources such as neurosymptoms.org (made by JS one of the authors), or patient-led organisations such as FND Hope, FND Action. The MyFND app can also be appreciated by patients. Be careful however, not to simply recommend a whole FND resource if the patient has only visual symptoms. It may be frightening for them to read about seizures or paralysis. Instead, direct them to the specific resources about functional visual symptoms. There is also now an international FND Society for health professionals, all of which lends legitimacy to the condition (fndsociety.org).
Following up the patient and triaging for treatment
Many patients report bewilderment at being given a complex diagnosis such as FND and then being immediately discharged. Again, is this what you would normally do for someone with visual loss due to a structural condition? A follow-up visit allows the neuro-ophthalmologist to see if the patient agrees with the diagnosis given and whether now is the correct time for treatment. Is the patient actually troubled by their visual loss? Do they want further treatment at this time?
If the diagnosis has been raised at the first visit, then there may be investigations to review anyway at the time of a follow up. If treatment is being attempted then experience more broadly with FND suggests that therapists notice greatly enhanced treatment responses if the diagnosing clinician or a health professional who can explain the method of diagnosis, remains involved [ 22 ].
Further Management
The lack of research into the management of functional visual loss is striking. A study of 10 patients used transcranial magnetic stimulation with improvement in 9 patients [ 23 ]. A case series of 33 paediatric patients reported that 28 recovered with suggestion therapy [ 24 ]. The Edinburgh FND research group published a detailed description of the more multi-faceted approach, describing visual recovery in two individuals with complete functional visual loss, with a focus on explanatory models, combined with transcranial magnetic stimulation and hypnotherapy [ 25 ]. This does not provide an evidence base on which to recommend treatment so what we have written here is based on experience.
While we advocate for ophthalmologists to stay involved, treatment of FND including functional visual loss should be a multidisciplinary endeavour.
The predictive processing model of functional visual loss described earlier opens the possibility for newer treatments for functional visual loss (Fig. 3 ), some of which may be enhanced by education and techniques at the bedside.

A model of functional visual loss highlighting the mismatch between “top-down predications” and “bottom-up” visual input and how potential therapies can target this.
Encouraging the patient and carers to look out for evidence of briefly better vision
Instead of ‘glossing over’ the variability of vision seen in functional visual loss, we have found it helpful to ask patients and carers to look out for instances of better vision. In most cases these have already been noticed, especially by carers. For example, a recent patient of ours went into a shop and saw a t-shirt of the cartoon character ‘Bluey’ that she thought would look lovely on their baby. Instead of feeling bewildered or worried that people might think she was making up her symptoms, she and her partner had been encouraged to see this as a sign of visual pathways working better at a moment when she was thinking about someone external, and something to reflect and feel positive about.
Orthoptic therapy using diagnostic tests as treatment
Our early experience using diagnostic tests to help patients and their carers glimpse normal vision has been positive. Based on other forms of FND it seems likely that this can form the basis of an initial approach to therapy that can be started by neuro-ophthalmologists but delivered most effectively by orthoptists. Essentially the overweighted strong ‘prediction’ of visual loss which is not challenged by normal visual input can be challenged by the kind of visual input created during testing. Orthoptists bring a combination of knowledge of the visual system, understanding of the mechanisms of testing but also the ability to carry out a longer assessment and begin to integrate other elements of treatment.
Some examples of this may include:
Swapping between phone font vision and test vision to see if better test vision can be achieved.
Testing visual acuity using single letter optotype and comparing to acuity when letters are together.
Repeat the fogging test, but therapeutically until the patient is seeing out of their “bad” eye and then provide positive feedback or carry out visual tasks.
Using an app like ‘peekaboo vision’ (see Fig. 4 ) to see if the patient can become aware of their own visual choices. Ask the patient to guess where to tap the screen, even if they don’t perceive it and provide feedback about accuracy. Some individuals may show below chance performance which is also an opportunity to discuss that the brain must be seeing something in order to choose the opposite response.

Observing saccades towards the striated target enables examiner and carer to infer the patient has seen it, even if the patient reports they do not see it. In addition, the patient can be asked to guess where the target is by touching the screen even when they can’t see it. This can help gauge/ prove to the patient whether their ‘brain’ can still see, even if they don’t have visual experience.
Explaining to patients that seeing a “saltire” cross in Bagolini glasses indicates that both eyes are receiving vision even if one eye is blocked in normal circumstances.
Following tests of stereoscopic function such as the Frisby stereo test, explore whether patients would wish to practice with 3-D picture books, stereograms or even 3-D films to build confidence that both eyes are functioning.
There is a large potential here for innovative therapies that use these principles, in a similar way to what has successfully been described for physiotherapy in functional motor disorders [ 26 , 27 ]. They could become automated using gaze tracking or mobile phone technology.
Managing eye and brain co-morbidity
Optimising these comorbidities can have the effect of improving functional visual comorbidity by improving ‘bottom up’ visual input and also improving confidence and optimism in vision.
Migraine is commonly co-morbid with FND and can often improve if migraine is better treated. Although ophthalmologists are not headache specialists, it’s important to recognise that migraine is often undertreated. For example, is the patient taking appropriate acute migraine treatment? (i.e., a combination of high dose NSAID, anti-emetic and a triptan). Is the patient overusing analgesia? (i.e., use of painkiller >10 days per month, with particular focus on overuse of codeine). If they are having frequent headache days, is the patient on an appropriate preventative for migraine at the correct dose? Botulinum toxin injections, CGRP monoclonal antibodies and CGRP receptor antagonists or “gepants” have greatly expanded potential therapies for migraine [ 28 ].
Other types of functional neurological disorder (for example, functional movement disorder or seizures) and functional disorders (for example irritable bowel syndrome or fibromyalgia) are more common in patients with functional visual loss [ 29 ]. An integration of these conditions as having overlapping mechanism is usually helpful in management [ 6 ].
Management of photophobia
Photophobia is common in functional visual loss. A study looking at 34 consecutive patients who wear sunglasses in clinic found that 79% had functional visual loss, with nearly all of them citing photophobia and/or headache [ 30 ]. The authors of the paper suggested this might be a phenomenon designed to emphasise visual loss or copy famous individuals with blindness such as Stevie Wonder. These authors considered use of sunglasses was not ‘reasonable’ in this group. However, in our experience, the behaviour develops primarily because of photophobia which can become extreme, for example sitting in a darkened room because taking the glasses off is uncomfortable. The use of sunglasses is therefore reasonable to the patient and has short term benefits, although in the longer term makes things worse. We recommend starting by explaining that the brain is sensitive, but the more you wear sunglasses the more sensitive it becomes. Management involves graded sensitisation to light which may involve a structured plan to have reductions in opacity of sunglasses or spend longer and longer without sunglasses. This kind of graded exposure is generically familiar territory for clinical psychology, for example in relation to insect or flying phobia, but they may need support to understand that this approach can also work for photophobia. A clinical psychologist may be helpful but is not always essential to help people wean themselves off sunglasses in our experience.
Psychological assessment and therapy
More detailed psychiatric assessment, typically from a liaison or neuropsychiatrist familiar with FND, can be valuable in assessing for risk factors and comorbidities. Treatment of common psychiatric comorbidity such as anxiety, depression, PTSD or obsessive-compulsive disorder with psychological therapy or medication can sometimes help to improve or resolve FND symptoms. Assessment for developmental differences such as autism, ADHD or emotionally unstable personality traits may be an important part of reaching a formulation. Psychologists can also assist with graded exposure for those wearing sunglasses who have photophobia (as above) and integrate psychological experiences and symptoms into their experience of functional visual symptoms. Individuals with trauma may benefit from a trauma focused approach to therapy that helps explain their brains tendency to dissociate in response to threat and find different ways to respond to medically or psychologically threatening sensations. Approach to psychological treatment here can borrow from what we have learnt about the approach to other FND symptoms, such as seizures and limb weakness [ 31 ].
Our experience with patients who do recover vision is that it helps to prepare them for how they are going to explain a recovery to others. Some patients worry that if they recover people will think they were “making up their symptoms all along”. Most people are aware that visual impairment is hard to treat unless you have an operation or medical treatment. We advise our patients to tell friends and family that a truthful statement they are undergoing therapy which aims to “retrain the brain” and improve vision is helpful in advance.
Hypnotherapy, suggestion and relaxation during education
Suggestion and relaxation techniques are components of many therapies including mindfulness, eye movement desensitization and reprocessing (EMDR) therapy and hypnotherapy. They may all enhance the process of ‘altering brain predictions’ about vision, perhaps during a visual task such as eye tracking.
Hypnotherapy and suggestion have been tested in over 30 studies in the FND literature including 5 randomised controlled trials [ 32 ]. In most of these studies patients showed benefit. Some of these studies had mixed patients with functional visual loss [ 33 ] or where single case reports so are hard to draw conclusions from. One study in particular focused on a suggestion technique in 8 consecutive patients with functional visual loss (2 of whom were over 16). The patients were given a lengthy but non-specific visual task to carry out at home along with a strong suggestion of improvement [ 34 ], with most reporting improvement or having evidence of improvement on testing. It’s likely that the outcome in a younger group like this would have been better anyway.
Our own experience is that hypnotherapy, in the right hands, can be helpful but it is essential that the practitioner understand the principles of diagnosis of functional visual loss to integrate this into their approach.
Other novel treatments
Transcranial magnetic stimulation (tms).
TMS has been trialled by researchers treating motor FND. It can undoubtedly be helpful, although it appears that cranial TMS is just as effective as spinal TMS suggesting the effect is more about demonstrating movement in a limb that is paralysed rather than neuromodulation [ 35 ]. Occipital TMS generates a visual experience of phosphenes. Our experience is that it can be a useful adjunct to support treatment, especially for bilateral visual loss [ 25 ]. The phosphenes provide evidence that the visual cortex can produce visual experience when stimulated. It also likely has a strong suggestive value but even that can be discussed transparently.
Therapeutic sedation
Using sedation and anaesthesia has a history of treatment in FND going back over a century. One of the authors (JS) described a case series of patients with functional paralysis, dystonia, coma and other symptoms with resolution of symptoms in some [ 36 ]. We have not used this for functional blindness, but it is a technique that would be reasonable if others failed and if the patient had a good relationship with the treating clinician.
Other management issues
Managing paediatric patients.
The literature consistently demonstrates better outcomes for children and young people compared to adults with FND. In younger children, especially if the problem is recent onset, an explicit diagnosis may not be so necessary and reassurance that things are likely to improve may be reasonable depending on the family and school situation. In teenagers the management is usually quite similar to adults. Liaison with school at an early stage often helps with management.
Register visually impaired or not?
In the UK survey of 119 ophthalmologists mentioned earlier, 22% considered that those with functional visual loss should not be registered as visually impaired. This is not a black and white issue and is a similar question to whether people with severe disability from motor forms of FND ought to be provided with wheelchairs and disability aids. A consensus view occupational therapy guideline concluded that for individuals with persistent disability (who were not in active treatment) that quality of life should be maximised and likely benefit and gain greater independence with disability aids such as a wheelchair [ 37 ]. Similarly, if someone has persistent visual loss then it is likely to be helpful to be registered blind or partially sighted. However, if the history is quite short and they are engaged in treatment, it may be counterproductive to be encouraged to rely on visually impaired aids or to be registered blind.
Unusual functional visual agnosias
We have seen a number of unusual visual symptoms in people with FND which have not been well documented in the literature. This includes a 14-year-old who couldn’t see letters or numbers but could see symbols. A 26-year-old whose vision became black and white at the same time as she became severely depersonalised, and a 15 year old who developed a problem reading individual lines of text or graphs but could do so if they were isolated from other text. These agnosias, and possibly functional visual apraxia presentations deserve further study. There is overlap between these acquired visual symptoms and developmental visual symptoms.
Functional visual loss is a relatively common clinical issue for a neuro-ophthalmologist. The diagnosis is usually relatively straightforward for an experienced clinician, but the management has not been well described. With greater experience of wider functional neurological disorder subtypes, the time is now ripe to apply similar principals to patients with functional visual loss. A conventional approach to labelling, explaining the method of diagnosis and mechanism of symptoms to people with functional visual loss works much better than one which emphasises the normality of tests or psychological risk factors. There are promising avenues to develop new types of treatments and multidisciplinary therapy for functional visual loss.
Hallett M, Aybek S, Dworetzky BA, McWhirter L, Staab JP, Stone J. Functional neurological disorder: new subtypes and shared mechanisms. Lancet Neurol. 2022;21:537–50.
Article CAS PubMed PubMed Central Google Scholar
Laginaf M, Costello H, Price G. How do ophthalmologists manage functional visual symptoms? A UK survey of ophthalmologists’ experience. Graefe’s Arch Clin Exp Ophthalmol. 2022;260:1307–13.
Article Google Scholar
Scott JA, Egan RA. Prevalence of organic Neuro-ophthalmologic disease in patients with functional visual loss. Am J Ophthalmol. 2003;135:670–5.
Article PubMed Google Scholar
Gelauff J, Stone J. Prognosis of functional neurologic disorders. Handb Clin Neurol. 2016;139:523–41.
Article CAS PubMed Google Scholar
Daniel MC, Coughtrey A, Heyman I, Dahlmann-Noor AH. Medically unexplained visual loss in children and young people: An observational single site study of incidence and outcomes. Eye (Basingstoke). 2017;31:1068–73.
CAS Google Scholar
O’Leary ÉD, McNeillis B, Aybek S, Riordan-Eva P, David AS. Medically unexplained visual loss in a specialist clinic: A retrospective case-control comparison. J Neurol Sci. 2016;361:272–6.
Ludwig L, Pasman JA, Nicholson T, Aybek S, David AS, Tuck S, et al. Stressful life events and maltreatment in conversion (functional neurological) disorder: systematic review and meta-analysis of case-control studies. Lancet Psychiatry. 2018;5:307–20.
Hustvedt S. I wept for four years and when I stopped I was blind. Neurophysiologie Clin. 2014;44:305–13.
Article CAS Google Scholar
Werring DJ, Weston L, Bullmore ET, Plant GT, Ron MA. Functional magnetic resonance imaging of the cerebral response to visual stimulation in medically unexplained visual loss. Psychol Med. 2004;34:583–9.
Perez DL, Nicholson TR, Asadi-Pooya AA, Bègue I, Butler M, Carson AJ, et al. Neuroimaging in Functional Neurological Disorder: State of the Field and Research Agenda. Neuroimage Clin. 2021;30:102623.
Article PubMed PubMed Central Google Scholar
Jungilligens J, Paredes-Echeverri S, Popkirov S, Barrett LF, Perez DL. A new science of emotion: implications for functional neurological disorder. Brain. 2022;145:2648–63.
Edwards MJ, Yogarajah M, Stone J. Why functional neurological disorder is not feigning or malingering. Nat Rev Neurol. 2023;19:246–56.
Dattilo M, Biousse V, Bruce BB, Newman NJ. Functional and simulated visual loss. In: Handbook of Clinical Neurology. Hallett M, Stone J, Elsevier; 2016. 329–49.
Pula J. Functional vision loss. Curr Opin Ophthalmol. 2012;23:460–5.
Stone J, Edwards M. Trick or treat? Showing patients with functional (psychogenic) motor symptoms their physical signs. Neurology. 2012;79:282–4.
Stone J. Functional symptoms and signs in neurology: assessment and diagnosis. J Neurol Neurosurg Psychiatry. 2005;76:i2–12.
Calcagni A, Neveu MM, Jurkute N, Rosbon AG. Electrodiagnostic tests of the visual pathway and applications in neuro-ophthalmology. Eye. 2024; In press
Stone J, Carson A, Hallett M. Explanation as treatment for functional neurologic disorders. In: Handbook of Clinical Neurology. 2016. 543–53.
Tao BKL, Xie JS, Margolin E. Functional vision disorder: a review of diagnosis, management and costs. Br J Ophthalmol. 2024;bjo-2023-324856.
Sverdlichenko I, Brossard-Barbosa N, Micieli JA, Margolin E. Characteristics of 110 Patients With Functional Visual Loss. Am J Ophthalmol. 2023;250:171–6.
Raviskanthan S, Wendt S, Ugoh PM, Mortensen PW, Moss HE, Lee AG. Functional vision disorders in adults: a paradigm and nomenclature shift for ophthalmology. Surv Ophthalmol. 2022;67:8–18.
Bennett K, Diamond C, Hoeritzauer I, Gardiner P, McWhirter L, Carson A, et al. A practical review of functional neurological disorder (FND) for the general physician. Clin Med, J R Coll Physicians Lond. 2021;21:28–36.
Google Scholar
Parain D, Chastan N. Large-field repetitive transcranial magnetic stimulation with circular coil in the treatment of functional neurological symptoms. Neurophysiologie Clin/Clin Neurophysiol. 2014;44:425–31.
Abe K, Suzuki T. Functional Visual Loss in Childhood and Suggestibility. Clin Child Psychol Psychiatry. 2000;5:239–46.
Yeo JM, Carson A, Stone J. Seeing again: treatment of functional visual loss. Pr Neurol. 2019;19:168–72.
Nielsen G, Stone J, Matthews A, Brown M, Sparkes C, Farmer R, et al. Physiotherapy for functional motor disorders: a consensus recommendation. J Neurol Neurosurg Psychiatry. 2015;86:1113–9.
Nielsen G, Buszewicz M, Stevenson F, Hunter R, Holt K, Dudziec M, et al. Randomised feasibility study of physiotherapy for patients with functional motor symptoms. J Neurol Neurosurg Psychiatry. 2017;88:484–90.
Ferrari MD, Goadsby PJ, Burstein R, Kurth T, Ayata C, Charles A, et al. Migraine. Nat Rev Dis Prim. 2022;8:1–20.
Lawlor M, Huynh B, Humphreys K, Ogunbowale L, Kopelman MD, Plant GT. Observational cohort study of 100 patients presenting with functional visual loss: clinical characteristics and comparison with other functional neurologic disorders. Can J Ophthalmol. 2024. https://doi.org/10.1016/j.jcjo.2024.02.018
Bengtzen R, Woodward M, Lynn MJ, Newman NJ, Biousse V. The ‘sunglasses sign’ predicts nonorganic visual loss in neuro-ophthalmologic practice. Neurology. 2008;70:218–21.
Gutkin M, McLean L, Brown R, Kanaan RA. Systematic review of psychotherapy for adults with functional neurological disorder. J Neurol Neurosurg Psychiatry. 2021;92:36–44.
Connors MH, Quinto L, Deeley Q, Halligan PW, Oakley DA, Kanaan RA. Hypnosis and suggestion as interventions for functional neurological disorder: A systematic review. Gen Hosp Psychiatry. 2024;86:92–102.
Mousavi SG, Rahimi J, Afshar H. Comparison of four different treatment options in the management of acute conversion disorder. Iran J Psychiatry Behav Sci. 2008;2:21–5.
Pula JH, Fischer M, Yuen CA, Kattah JC. Using the theories of Joseph Babinski to manage functional vision loss. Cogn Behav Neurol. 2015;28:46–52.
Garcin B, Mesrati F, Hubsch C, Mauras T, Iliescu I, Naccache L, et al. Impact of transcranial magnetic stimulation on functional movement disorders: Cortical modulation or a behavioral effect? Front Neurol. 2017;8:1–7.
Stone J, Hoeritzauer I, Brown K, Carson A. Therapeutic sedation for functional (psychogenic) neurological symptoms. J Psychosom Res. 2014;76:165–8.
Nicholson C, Edwards MJ, Carson AJ, Gardiner P, Golder D, Hayward K, et al. Occupational therapy consensus recommendations for functional neurological disorder. J Neurol Neurosurg Psychiatry. 2020;91:1037–45.
Download references
JS is supported by an NRS Career Fellowship from the Chief Scientist Office.
Author information
Authors and affiliations.
Institute of Neurological Sciences, Queen Elizabeth University Hospital, Glasgow, UK
Neil Ramsay
Dept Ophthalmology, Royal Infirmary of Edinburgh and Princess Alexandra Eye Pavilion, Edinburgh, UK
Justin McKee & Gillian Al-Ani
Centre for Clinical Brain Sciences, University of Edinburgh, Edinburgh, UK
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation: JS and NR. Writing –original draft: NR and JS. Writing–review and editing: JMcK, GA, JS and NR. Supervision: JS.
Corresponding author
Correspondence to Jon Stone .
Ethics declarations
Competing interests.
JS royalties from UpToDate and carries out expert witness work in relation to FND; runs a free website for people with FND, www.neurosymptoms.org ; and is on the FND Society board. The other authors have no conflicts of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ramsay, N., McKee, J., Al-Ani, G. et al. How do I manage functional visual loss. Eye (2024). https://doi.org/10.1038/s41433-024-03126-w
Download citation
Received : 21 February 2024
Revised : 25 April 2024
Accepted : 02 May 2024
Published : 22 May 2024
DOI : https://doi.org/10.1038/s41433-024-03126-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Share on twitter
- Share on facebook
Sight loss should not mean a fading academic career
With the right support, academics with visual impairments are prospering, but barriers to true inclusivity remain, says kate armond, while a lecturer reflects on how practice on reasonable adjustments can fall short of policy.
- Share on linkedin
- Share on mail

Six months ago, Ghana’s University of Cape Coast appointed its first visually-impaired lecturer , Carruthers Tetteh, to teach law. A month later, in January’s Australia Day Honours list, Paul Harpur, a professor at the University of Queensland’s Law School, was awarded a Medal of the Order of Australia , to add to his success as a Paralympian and champion of human rights. Last month, lecturer Yusufi Kapadiya made headlines for his work supporting and educating blind children in rural areas of India, where their disability is viewed as a curse, and some are abandoned by their parents or beaten and starved to drive out evil spirits.
Passionate, charismatic, blind from childhood, these lecturers and their stories suggest a changing world of inspiration, influence and inclusivity. My own research into the careers and experiences of sight-impaired lecturers has revealed a much quieter, more private and diffident presence within the academy and enduring problems that cause many talented individuals to struggle or leave.
My research began in an informal way 20 years ago, when, as a sight-impaired UK undergraduate, I listened to a lecture delivered by an academic with multiple sclerosis. He arrived in the ground floor lecture theatre in his wheelchair, spoke with some difficulty, but always with enthusiasm for his subject, and welcomed conversation afterwards. He held our respect and our attention, and he was the first academic to speak to me about sight loss and working in higher education. Even at that early stage, I knew that I wanted to teach university students, and he made me feel it would be possible.
Without my sense of him as encouraging, talking about his work with humour and honesty, I might have been overwhelmed with doubt at many stages of my academic career. In the past five years, my formal research has expanded to engage with the organisations that support sight-impaired employees and advocate for equality so that I can balance recording experiences with offering the right advice and potential solutions.
While many enlightened universities are busy anticipating reasonable adjustments and creating accessible environments, I have heard from academics who are still reluctant to share the details of their disability or to follow up requests for reasonable adjustments when the adjustments are not forthcoming.
Campus resource: How to create an inclusive learning environment for visually impaired students
I completely understand this. When I began lecturing and teaching as a PhD student, I shared the details of my sight impairment with just three people: my primary PhD supervisor, the university’s disability adviser and one friend. Rachel, my PhD supervisor, is the best example of a supportive colleague. She accepted without fuss or questions what I wanted to share about my sight problems, and she would talk me through work that she had read, marked or collaborated on as an instinctive response to my situation, rather than overloading me with emails and text. She let me make voice recordings of our meetings if I wanted to.
I did not apply for reasonable adjustments with my other teaching tasks, however. I worked at the weekend rather than unsettle deadlines. I endured the dread of manoeuvring in the Stygian gloom of the lecture theatre. And I presented as more than usually anxious when delivering lectures as moving my eyes from large-print notes to the faces in front of me made refocusing impossible. The module leader would insist “You need to look up more!” and I would blush and feel disheartened and frustrated.
I moved absurdly slowly with my tray in the staff canteen and I used my long, telescopic monocular surreptitiously as I scanned the titles on the top shelves in the library – not dissimilar to Johnny Depp’s telescope use in Pirates of the Caribbean . I reasoned and sometimes argued with obstinate, sighted students who refused to relinquish their place at the assisted-technologies computers in the university library and religiously avoided social events. Like so many employees with sight impairments, I was cautious and lacking in confidence, worried about being seen as a problem or creating extra work, and I was not well informed about disability and law.
My knowledge about inclusivity and equality in the workplace has improved slowly. Particularly supportive have been the UK’s Royal National Institute of Blind People (RNIB), the Equality and Human Rights Commission, the support charity Scope and the Equality Advisory and Support Service. Understanding that employers have a legal duty to provide reasonable adjustments for disabled employees under the Equality Act of 2010 was life-changing. I realised that it is my responsibility to ask for these adjustments and to explain how my sight impairment impacts my working life, not just for my own benefit and so that I can do my job well, but to familiarise universities with this process. Workplace adjustments are the single most important factor in helping disabled people remain in work. For your blind or partially-sighted colleague, emailing in a bold simple typeface, arranging meetings in accessible rooms or producing module information in Braille, large-print or audio formats not only allows them to work with confidence and ease, it also registers respect and goodwill.
Many people with sight loss choose not to have a guide dog or use a cane, and some academics are further bewildered when their blind or partially-sighted peers experience fluctuations in their sight; I was registered as blind in 2000. My vision later improved after surgery but is now deteriorating again. Rather than remain enigmas, however, partially-sighted academics can help colleagues with simple, factual explanations of their visual difficulties at the beginning of working relationships. I have moved from using similes in which the world becomes a fairground hall of mirrors to drawing images of a loss of visual field.
Sight loss can impact an academic career at any age. During my research, lecturers as young as 22 have contacted me to discuss diagnoses that will prove degenerative in terms of their vision. Diabetes, thyroid problems, cancer, the side-effects of cancer treatment, multiple sclerosis, benign tumours, accidents and contact sports: all of these have led to visual impairments for academics in the UK.
Feedback and case studies have also helped me to understand the effects of ocular diseases such as glaucoma, macular degeneration, retinal detachment and retinitis pigmentosa. The more lecturers there are who reach out for adjustments and stay in post, the more adept universities will become at integrating this spectrum of sensory disability into the fabric of higher education.
Even if you have been in post for some time, it is still essential to get clear, written confirmation of all of your duties for planning and securing reasonable adjustments; ask well in advance for reading lists, a breakdown of when each topic will be taught and your lecturing responsibilities. Similarly, it’s important to have this information before accepting any new post. On one occasion, a senior academic talked me through my teaching and pastoral responsibilities and I naively felt confident in accepting the job. During the first week of term, however, a lecturer from another department appeared at my office door to inform me that I also had to produce an additional four lectures for some of his modules that term, on subjects that had nothing to do with my work, discipline or research. My meticulously planned and prepared work schedule for the next 10 weeks capsized.
When I appeared hesitant, his response was that he hoped I was going to “cooperate”. Suddenly, a disorganised stranger had turned me into a difficult individual who was “not getting off to a good start”. Sadly, my research has revealed that he is not the only academic to translate the vulnerability of visually impaired colleagues into pressure to prove ourselves to be capable and “team players” while overburdening us.
Whether you are a new member of staff or an established employee, having the right evidence of your visual impairment is also helpful. A consultant ophthalmologist will provide certification of a diagnosis, and the patient will be recorded as severely sight-impaired (blind) or sight-impaired (partially sighted). Although some lecturers have secured support without official documents, this certificate is the gateway to protection under the 2010 Equality Act. Your most important ally and point of contact is your line manager: they will then contact the university’s occupational health team, who have the expertise to assess needs and implement accessing technology such as video magnifiers and software. Discussing your disability with human resources if you are new to the university is also an option, and the RNIB offers work-related assessments, makes recommendations and communicates these directly to your manager.
Having a list of your professional responsibilities can also help you to focus in a positive way on what you could do once the right reasonable adjustments are in place. Share what you love about your subject, your role and your institution when negotiating for adjustments, and be prepared to be flexible and realistic about where you struggle. One of the most heartening details of my research has been learning about a readiness to exchange responsibilities within job descriptions among co-workers. And sensitive decisions around timetabling have allowed me and other sight-impaired lecturers to leave before rush hour, pace our working day and structure contact time with students to enable more working in the home environment if this is helpful.
With our sector under huge financial pressure, however, many academics are worried about the financial cost of asking for support. Beyond ensuring fair and predictable workloads, reasonable adjustments can include altered lighting, tactile signage and alternative formats and software for reading work-related documents – all of which are the responsibility of the university.
The government’s Access to Work scheme can fund far more. These grants are available to lecturers living and working in England, Scotland and Wales and are not affected by how much an individual earns; the only negative is there can be a waiting list. This scheme has enabled visually impaired academics to employ support workers, note takers or workplace mentors. It can also fund practical changes to offices or equipment and the development of hybrid working, as well as cover travel or training costs. For those considering a move away from the pressures of full-time positions, the grant also covers internships, placements and part-time employment.
These alterations are both appreciated and essential for sight-impaired scholars, but some believe this paradigm of “adjustments” is unambitious and, ultimately, inadequate. Instead of persisting with the ableist narratives and structures of higher education, the “authoring with integrity” initiative suggests that the sector’s practices should begin with accessibility as their premise rather than helicoptering in “adjustments” as an occasional afterthought.
This idea is currently engaging and unsettling academics in equal measure. In the past year, I have attended academic conferences, research seminars and online forums where it has provoked strong emotions, including controversial and, at times, offensive counterarguments, as well as really intelligent and informed discussion. Authoring with integrity has been received variously as positive discrimination gone mad, a rational and fair way to ensure inclusivity or a pipe dream.
In this space, authoring is not restricted to writing about equality: it extends to include designing, instructing and innovating. Those with a disability should write, advise, teach, interview, regulate, conduct professional development courses and preside at the highest levels within universities, but there are so many flawed or inadequate interventions, however well-intentioned, made by those who do not have the lived experiences and the diagnoses themselves.
If you want to see authoring with integrity in action, turn to Channel Five’s Mixmups , a groundbreaking and enchanting children’s programme launched last November about a sight-impaired bear, a disabled cat and an able-bodied rabbit. Its sight- and hearing-impaired creator, Rebecca Atkinson, had become frustrated at the lack of realistic representations of disability in children’s toys. She has also ensured that disabled actors and newcomers voice the parts. Fairy dust and magic spoon aside, the Mixmups’ adventures are presided over by the Lucky Loover Bird. Its watchwords – “there’s always another way” – greet situations where disability presents difficulties, and the programme is already winning awards and fostering a remarkable culture of inclusivity in our youngest generation.
My students think this is compulsive viewing for everyone. It is ironic that in the same month that the last of my feedback sheets from sight-impaired lecturers were returned, some containing upsetting examples of discrimination, my youngest nephew and his peers are busy making Mixmup-style participation for their disabled friend the premise for all of their games, parties and school activities.
Kate Armond has taught literature and international modernism at the University of East Anglia and the University of Essex . She is now senior lecturer in literature and critical theory. The research for this article was made possible thanks to the Royal National Institute of Blind People (RNIB) and the Equality and Human Rights Commission.

Making work work: Ask for adjustments and be prepared to help yourself
If there is anything more central to my job than reading and writing, I’m not sure what it is. I spend most of every day reading, mainly on a computer: reading articles for my teaching and research; preparing lectures and seminars; delivering teaching. So it’s immensely frustrating to be unable to see properly – especially when other people are usually completely unaware of my difficulties.
I first experienced problems with my vision in 2010, when I suffered an attack of optic neuritis in one eye. This left me with a patch of vision that was partially obscured. Subsequently, I was diagnosed with multiple sclerosis and had further relapses, involving sensation and mobility. Having recovered from these and got used to life with MS, I experienced a second bout of optic neuritis last year, in my “good” eye, leaving me with both eyes affected. I was devastated and (impotently) angry. It’s unusual for both eyes to be affected, though not unheard of; I found myself wondering why I had to have this particular profile of symptoms, rather than any other, given the importance of good vision for my work. But who doesn’t need to be able to see well? And what would be a “good” symptom profile to have? Mobility issues? Spasms and incontinence? Cognitive dysfunction?
I started to get used to the impairment and how to manage it. Damage caused by optic neuritis is particularly sensitive to heat (both body and environmental heat). This means I have to make some odd requests, which can be met initially with bemused responses from my department. Why do I need access to a freezer at work? Because drinking iced water is one way for me to recover my vision more quickly. Why is the lecture room I’ve been assigned not adequate? Because it’s overcrowded, is at the top of six flights of stairs and has no windows I can open when I've climbed them because the lift is out of order. So I cannot cool down and cannot read my notes to deliver my teaching.
On a recent visit as an external examiner, I got so hot and flustered finding my way to the right room that I couldn’t see when I got there. Luckily, I had explained in advance what issues might arise, so they provided me with iced water and a cool room, and I was able to cool down and do the job I was there for.
I have (eventually) been assessed by occupational health, and a report was issued listing any adjustments needed. Actually getting these put in place, though, is another matter. Though the freezer access I asked for was at one point in train, it got lost in changes in admin personnel and I’ve given up asking. Now, I just go and buy myself an iced drink from the nearest cafe. At £3.50 or so a time, this goes against my policy of saving money on lunches and drinks by bringing my own, but needs must.
I need a new laptop as mine is on its last legs. It is possible to borrow one from IT services, but they are all 14-inch screens (too small for me to enlarge and read documents easily), and when I enquired if a larger one could be loaned (not given) to me, I was told that I didn’t need one since I have been given a monitor in my office and at home. But most of my job is teaching, so the times when I am not in my office or working from home, what then? Again, I have given up asking, especially since I am on a temporary contract so feel awkward making a fuss.
Probably the main thing I have learned through having experienced this disability is that you have to do a lot of legwork yourself. You have to keep asking, keep pushing, even if the right boxes have been ticked – for example, occupational health devolves to departments the responsibility for determining what is a “reasonable adjustment”. Sometimes it’s easier just to muddle through and find your own solutions.
The author is a social sciences lecturer at a Russell Group university.
POSTSCRIPT:
Print headline: Academic life with sight loss
Register to continue
Why register?
- Registration is free and only takes a moment
- Once registered, you can read 3 articles a month
- Sign up for our newsletter
Or subscribe for unlimited access to:
- Unlimited access to news, views, insights & reviews
- Digital editions
- Digital access to THE’s university and college rankings analysis
Already registered or a current subscriber? Login
Related articles

Stammering: higher education’s ‘invisible disability’ must be tackled
On International Stammering Awareness Day, two academics who stammer explain why higher education must do more to support those with this ‘invisible disability’

‘An intellect stripped down to its essentials’
Blindness gave the late politics professor Roger Williams a unique ability to focus on the structure and coherence of what was being said to him. And though his interrogations could be exacting, Lincoln Allison wishes more sighted academics shared his talent
Reader's comments (4)
You might also like.

‘Use of AI in research widespread but distrust still high’ – OUP
Poll finds most researchers are using AI but only a tiny number trust technology companies on data privacy

Gender-critical scholars claim discrimination over BMJ rejections
Researchers say emails suggest disapproval of social media posts on transgender issues contributed to rejections

DSA outsourcing ‘put targets before disabled applicants’
MPs hear concerns about quality of assessment process under new suppliers Capita and Study Tech

The OfS’ free speech guidance for English universities goes too far
The regulator’s example scenarios fail to acknowledge the harm that even lawful speech can cause on campus, say Naomi Waltham-Smith and James Murray
Featured jobs

- Free Case Studies
- Business Essays
Write My Case Study
Buy Case Study
Case Study Help
- Case Study For Sale
- Case Study Service
- Hire Writer
Case study on Visual Impairment
Visual impairment case study:.
Visual impairment is the condition of the serious loss of vision because of various factors. The characteristic feature of visual impairment is that it is impossible to restore the person’s vision, as all the operations and lenses are helpless. Visual impairment occurs because of the impact of various factors, like physical damage of eyes, genetic problems, cataracts, diabetes, glaucoma, psychological disorders and problems with the central nervous system. Visual impairment is becoming a serious problem of the human society, because the number of the people who have problems with vision is constantly increasing.
Very soon more than 10% of all the people of the developed countries will have serious problems with eyesight and it will be impossible to cure them. The main reason of this fact is that the people of the developed countries exhaust their eyes rapidly being under the constant impact of stress and digital devices, like laptops, PCs, smart phones, pads, etc.When visual impairment is met at the educational institutions, the educational process should be conformed to the needs of such people. If students are partially sighted, it will be enough to increase the size of the print during the classes and reduce the use of the visual appliances. When the students have more serious problems, the methods of education should be far more different and focus on the use of the audio techniques. Totally blind people use the print of Braille and other means to read information.
We Will Write a Custom Case Study Specifically For You For Only $13.90/page!
Visually impaired people have the same rights to live in the human society normally and it is important to provide them with the means which can make their life easier (books with the print of Braille, sound notification systems, etc).Visual impairment is a serious problem of the modern society and it is surely worth attention. A successful visual impairment case study should explain the problem from all sides and dwell on the types and risk factors of visual impairment and define the importance and relevance of the problem. The student who is investigating the case is obliged to collect many trustworthy facts about the problem, get to know about the cause and effect of the problem and think over the most helpful solutions to the problem.In order to cope with a case study the student can use the pluses of the Internet and read a free example case study on visual impairment composed by the professional writer. Due to the advantages of a free sample case study on visually impaired children a student can learn about the best manner of the research of the problem, the methodology of paper writing and the general norms of formatting and logical composition of the paper.
Related posts:
- Eagle Impairment Case
- Case Study on Visual Merchandising
- Visual Arguments
- Visual Perception
- Visual Analysis
- Effective Visual Communication
- State School Visual Analysis
Quick Links
Privacy Policy
Terms and Conditions
Testimonials
Our Services
Case Study Writing Service
Case Studies For Sale
Our Company
Welcome to the world of case studies that can bring you high grades! Here, at ACaseStudy.com, we deliver professionally written papers, and the best grades for you from your professors are guaranteed!
[email protected] 804-506-0782 350 5th Ave, New York, NY 10118, USA
Acasestudy.com © 2007-2019 All rights reserved.

Hi! I'm Anna
Would you like to get a custom case study? How about receiving a customized one?
Haven't Found The Case Study You Want?
For Only $13.90/page
- Search Menu
- Sign in through your institution
- Advance Articles
- Special Issues
- Supplements
- Virtual Collection
- Online Only Articles
- International Spotlight
- Free Editor's Choice
- Free Feature Articles
- Author Guidelines
- Submission Site
- Calls for Papers
- Why Submit to the GSA Portfolio?
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About The Gerontologist
- About The Gerontological Society of America
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- GSA Journals
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Aging concerns, challenges, and everyday solution strategies study, research design and methods, conflict of interest, data availability, acknowledgments.
- < Previous
Everyday Challenges for Individuals Aging With Vision Impairment: Technology Implications
- Article contents
- Figures & tables
- Supplementary Data
Elena T Remillard, Lyndsie M Koon, Tracy L Mitzner, Wendy A Rogers, Everyday Challenges for Individuals Aging With Vision Impairment: Technology Implications, The Gerontologist , Volume 64, Issue 6, June 2024, gnad169, https://doi.org/10.1093/geront/gnad169
- Permissions Icon Permissions
There are growing numbers of older adults with long-term vision impairment who are likely to experience everyday activity challenges from their impairment in conjunction with age-related changes. Technology has potential to support activity engagement. To develop effective technologies and interventions, we need to understand the context of activity challenges and identify unmet support needs.
The Aging Concerns, Challenges, and Everyday Solution Strategies (ACCESS) study is a mixed-method approach to explore everyday challenges of people aging with long-term disabilities. Participants included 60 adults aging with long-term vision impairment (63% female; M age = 67, SD = 4.6) who completed in-depth, structured interviews exploring the nature of everyday challenges and their unmet support needs for activity engagement. We conducted a content analysis using a deductive and inductive approach to build a detailed coding scheme of challenge codes and subcodes.
The analyses provided detailed insights about the nature of challenges people aging with vision impairment experience when performing specific instrumental activities of daily living (IADLs) in the context of home maintenance, transportation, shopping/finance, and managing health. Vision-related challenges and participation restrictions were identified for several activities that require reading, navigation, and identification (e.g., shopping, medication management, public transportation). Emergent challenge themes for performing IADLs included personal limitations (e.g., physical, cognitive, financial) and environmental barriers (e.g., accessibility, technology, transportation).
Contextual examples of IADL challenges among individuals aging with vision impairment highlight opportunities for technology design and innovation to support participation in everyday activities.
Vision impairment can create barriers to engaging in everyday activities, which may inhibit one’s independence, community participation, and overall well-being. The term vision impairment is an umbrella term to describe eyesight that cannot be corrected to a normal level, from mild vision impairment to total blindness, due to a variety of eye conditions or diseases ( National Academies of Sciences Engineering and Medicine, 2016 ; World Health Organization, 2019 ). A recent framework conceptualized how vision impairment can affect older adults’ functional ability in multiple domains, including physical, cognitive, and psycho-social abilities ( Swenor et al., 2020 ). In line with the International Classification of Functioning, Disability and Health (ICF; World Health Organization, 2001 ), Swenor et al. indicated that the impact of vision impairment on one’s ability to perform daily activities is dependent on several contextual factors, including the characteristics of the vision impairment (e.g., cause, degree, functional limitations), personal factors (e.g., comorbidities), and environment (e.g., social supports). There is heterogeneity among people aging with vision impairment in terms of activity challenges and support needs ( Remillard et al., 2020 ). Technology provides an opportunity to address these challenges, thereby facilitating activity engagement, performance, and independence ( Harrington et al., 2015 ).
The 2019 U.S. Census American Community Survey estimated that 6% of older Americans (over age 65) have a vision impairment, with prevalence increasing to 9% for Americans over age 75 ( Erickson et al., 2022 ). A recent analysis of the 2021 National Health and Aging Trends (NHATS) study, which incorporated objective measures of visual functioning, estimated the prevalence to be higher, with over 1 in 4 U.S. older adults (ages 71+) having vision impairment ( Killeen et al., 2023 ). The number of older Americans with vision impairment is expected to grow with the aging of the U.S. population ( Varma et al., 2016 ). In contrast to younger counterparts, older adults with vision impairment are likely to have a greater number of comorbid health conditions, such as stroke, hypertension, arthritis, and diabetes ( Crews et al., 2017 ; Steinman, 2016 ). They may also experience a variety of normative age-related declines (e.g., mobility, hearing, cognitive; Czaja et al., 2019 ). Collectively, these factors can exacerbate functional limitations for older adults with vision impairment ( Swenor et al., 2020 ).
Among this population, a subset of individuals has long-term vision impairment due to vision conditions or eye injuries acquired earlier in life. These individuals are subject to the unique circumstance of managing their long-term vision impairment, as well as age-related conditions, that together can create significant barriers to activity performance and increase risk of disability ( Mitzner et al., 2018 ). There are known socioeconomic disadvantages for people aging with long-term disabilities, including employment and lower income, as well as greater likelihood of poor health behaviors (e.g., sedentary lifestyle; Clarke & Latham, 2014 ).
Although vision impairment can affect a wide range of activities, certain types of activities tend to be more affected than others. Basic activities of daily living (ADLs; Katz et al., 1970 ), such as bathing and eating, may be generally less affected by visual impairment, as they are fundamental tasks ingrained in everyday routines and often occur in the familiar home environment, which can facilitate adaptations ( Hochberg et al., 2012 ). In contrast, instrumental activities of daily living (IADLs), which represent key tasks for independent living, are more complex and visually demanding ( Berger & Porell, 2008 ; Lawton & Brody, 1969 ). Common IADLs include cooking, cleaning, managing finances, managing medications, using the telephone, and transportation ( Graf, 2008 ; Lawton & Brody, 1969 ). The visual abilities required to perform IADLs vary by specific activity, but include reading, identifying and manipulating items, navigating spaces, using fine motor movements, and lifting objects.
Home-based IADLs, such as housework, meal preparation, medication management, and money management, have been reported as particularly difficult among older adults with vision impairment ( Hochberg et al., 2012 ; Peres et al., 2017 ; Steinman, 2016 ). Vision impairment can contribute to mobility challenges among older adults, including limitations with walking, navigation, and physical activity, as well as fear of falling ( Bayles et al., 2022 ; National Academies of Sciences Engineering and Medicine, 2016 ). Community-based activities that involve outdoor mobility and transportation, such as going to appointments or shopping, have also been documented as difficult activities ( Cimarolli et al., 2012 ; Hochberg et al., 2012 ). Moreover, given that many individuals with vision impairment do not drive, they often experience issues with transportation availability, accessibility, and affordability ( Bleach et al., 2020 ; Crudden et al., 2015 ). Research has identified activities that are difficult for people aging with vision impairment, but little is known about the context of their challenges.
Functional limitations with everyday activities can lead to a loss of independence and have negative psychological and social health consequences. Indeed, people with vision impairment are at greater risk for depression, anxiety, and poor quality of life ( Demmin & Silverstein, 2020 ; National Academies of Sciences Engineering and Medicine, 2016 ; Nyman et al., 2012 ; Renaud & Bédard, 2013 ). Activity and participation restrictions in the home and community are associated with loneliness and social isolation, which are prevalent among older adults with vision impairment ( Brunes et al., 2019 ; Coyle et al., 2017 ). Hence, supports are critically needed to assist with IADL engagement, thereby supporting aging-in-place, functional independence, quality of life, and well-being.
Innovative technology solutions have the potential to improve the lives of those aging with long-term vision impairments by providing needed support for daily activities. In the past two decades, there has been rapid evolution and growth in development of assistive technology (AT) for people with vision impairment ( Bhowmick & Hazarike, 2017 ). Assistive technology refers to a variety of supports, including equipment, devices, and systems to help users engage in daily activities, such as housework or shopping. Common examples of vision AT are screen readers, magnifiers, scanners, and navigational canes. Accessibility tools for people with vision loss are also integrated into modern personal computing devices (e.g., smart phones, computers, tablets), such as enlarged text, enhanced contrast, and voice to text. Emerging technologies include robots to support wayfinding (e.g., Liu et al., in press ).
Technology supports will only be helpful if they are successfully adopted. However, many assistive technologies are underused by older adults with vision impairment. Technology adoption among older adults with vision loss may be influenced by number of factors including usefulness, ease of use/usability, accessibility, cost, safety, and compatibility with the user’s attitudes, behaviors, and environment ( Kim, 2021 ; McGrath & Corrado, 2019 ). Perceived usefulness and ease of use are two of the most significant predictors of technology adoption ( Mitzner et al., 2016 ). Hence, to facilitate the use of technology supports developers must design technologies to support unmet needs and research must explore usability challenges of existing technologies.
People aging with long-term vision impairment have been navigating challenges with everyday activities for an extended period, for some, most, or all, of their lives. These individuals offer a unique opportunity to investigate persisting activity challenges (i.e., unmet support needs) as well as technology experiences. The objective of this study was to explore the nature and context of challenges experienced by adults aging with long-term vision impairment when performing IADLs and the specific factors contributing to their challenges. These rich insights can be used to drive the design and development of innovative technologies ( Harrington et al., 2015 ; Mitzner et al., 2018 ).
The Aging Concerns, Challenges, and Everyday Solution Strategies study (hereafter ACCESS) is a mixed-method exploration of everyday challenges of people aging with disabilities ( Koon et al., 2020 ; Remillard et al., 2018 ). Covering a wide range of everyday activities in the home and community, ACCESS investigated the breadth and depth of activity-specific challenges as well as the strategies and solutions employed to manage the challenges. Participants were 180 adults with long-term disabilities: 60 with mobility impairment, 60 with vision impairment, and 60 who were deaf. The current paper focuses on the vision group.
The interviews provided detailed insights about the challenges people aging with vision impairment experience performing IADLs, which are key to independent living. ACCESS covered a broad range of IADLs, including activities from the original scale developed by Lawton and Brody (1969) , as well as from extended scales that capture a broader range of activities ( Fieo et al., 2014 ; LaPlante, 2010 ). Specific aspects of IADLs were assessed. For example, instead of focusing on the high-level category of “transportation” as an activity in and of itself, participants were asked about a variety of transportation modes (e.g., getting a ride from a friend or family member; using a taxi/Uber/Lyft; flying on an airplane). Similarly, different methods for shopping (i.e., in-person or online) were explored.
The primary research questions were twofold. First, what is the nature of challenges (e.g., type, frequency, context) people aging with vision impairment experience in performing a broad range of IADLs? Second, what are unmet support needs for IADL performance among people aging with vision impairment? The findings provide guidance for technology design and innovation to support activity participation and independence among this population.
Participants
ACCESS was conducted at the University of Illinois Urbana-Champaign and the Georgia Institute of Technology with Institutional Review Board approval from each university. Participants were recruited through outreach to local and national organizations for persons who were blind or had visual impairments, through flyer distribution, social media postings, and word-of-mouth referrals. Eligible participants were age 60–79, who self-identified as having a long-term vision impairment (serious difficulty seeing, even when wearing glasses or contact lenses) that began prior to the age of 50, fluent in English, and resided in the United States.
There were 60 participants with vision impairment (M = 67; SD = 4.6), 38 females and 22 males. Causes of vision impairment were diverse with the most common being retinal damage/condition (e.g., retinitis pigmentosa, macular degeneration; 40% of sample), followed by congenital condition or abnormality (e.g., morning glory syndrome, congenital rubella syndrome; 26%), and nerve damage/condition (e.g., glaucoma, optic nerve atrophy; 24%). Other causes, each representing 3% of the sample, included: chronic eye inflammation, cataracts, and other eye injury or damage (e.g., gunshot wound, computer vision syndrome). The mean age of onset of vision impairment was 12 years ( SD = 14.2), ranging from birth to age 49. The mode for age of vision impairment onset was 0 years (i.e., from birth; n = 24). For duration of having a vision impairment, the mean was 56 years ( SD = 15.4), the mode was 65 ( n = 4), and range was 16 to 76 years.
Table 1 provides information about participants’ socioeconomic and health characteristics. The majority had some college education, were predominately White/Caucasian (59%) and married (42%), with an annual income of less than $25,000 (41%). In addition, the majority rated their health as good (51%) or very good (27%).
Participant Characteristics
Note: Data were missing for one participant, so the cells sum to 59.
ACCESS method details are in Remillard et al. (2018) and Koon et al. (2020) . To summarize, after telephone screening eligible participants completed two questionnaires (45–60 min) via online survey, mailed paper copies, or phone to assess demographics, health, and vision impairment. Interviews (60–90 min) were conducted by phone or in-person by trained research team members, including: 1 research scientist who is a gerontologist (author), 1 postdoc with a background in sport and exercise science (author), and 5 graduate students with fields of study including: engineering psychology, community health, and biomedical engineering. See technical report for complete interview guide ( Remillard et al., 2018 ). All participants provided verbal informed consent and received $30 compensation. Interviews were audio-recorded and transcribed verbatim.
The structured interviews covered six broad activity categories: Outside the Home; Around the Home; Shopping/Finances; Transportation; Health; and Basic Activities. For each category, participants were asked about 5–8 specific activities that were guided by the literature and findings from subject matter expert interviews ( Preusse et al., 2016 ). Participants rated their difficulty with specific activities (1 = not at all difficult, 2 = a little difficult, 3 = very difficult, or not applicable). For their most difficult activity in each category, participants answered open-ended follow-up questions probing the specific aspect of the activity that created the most challenge for them and how they managed that challenge (e.g., assistance from others, tools or technologies, own methods, or other strategies; Table 2 ).
Follow-up Interview Questions for the Activity Identified as ‘Most Difficult’ in Each Category
Data Analysis
We conducted a content analysis ( Erlingsson & Brysiewicz, 2012 ; Vaismoradi & Snelgrove, 2019 ; Vaismoradi et al., 2013 ) with four members of the research team using both deductive ( Harrington et al., 2015 ; Preusse et al., 2016 ; Remillard et al., 2019 ; Rogers et al., 1998 ) and inductive approaches ( Elo & Kyngas, 2008 ). We iteratively developed a coding scheme that included challenge codes, subcodes, definitions, and example participant quotes. We discussed and revised the coding scheme with the entire research team until consensus was reached (see Koon et al., 2019 , 2020 ). Transcript coding was conducted using the qualitative software program MAXQDA. All four researchers coded a sample transcript until independent coding reliability and agreement were met ( r = 0.85). This process was repeated for four additional sample transcripts to ensure reliability across coders; as needed, the team modified definitions and added examples to improve clarity of the coding scheme. Each transcript ( N = 60) was coded by one of the four researchers (random assignment). See Supplementary Material for complete coding scheme.
The coding scheme was applied to the units of analysis, defined as participants’ responses to the question, “What aspect or part of this activity creates the most challenge for you?” for the following IADL activity categories: Household Tasks; Shopping and Finances; Transportation; and Health Management (see Figure 1 for activities). The category “Household Tasks” includes IADLs in the “Around the Home” ACCESS study category. The activity of “Driving” was excluded, as most of the participants in the sample did not drive.

Instrumental activities of daily living (IADL) categories. Some participants reported more than one category as “Most Difficult” yielding 183 total response.
We present frequencies of challenge codes reported across the four IADL activities. For each category, we highlight challenges for specific activities and present illustrative participant quotes about the context of these challenges. Quotes are not exhaustive but rather provide rich, descriptive information about activity challenges specific to adults aging with vision impairment.
IADL Challenges
Figure 1 shows the distribution of the most difficult IADLs. For the Household Tasks category, the most frequently discussed activity was repairing and maintaining home; for Shopping and Finances, it was managing finances; for Transportation it was flying on an airplane; and for Managing Health it was exercising.
Figure 2 provides a treemap visualization of the data, which highlights recurrent challenges across activities. For example, financial challenges were mentioned nine times across five activities, including: repairing/maintaining home, managing finances, monitoring health, exercising, and flying on an airplane. The five most frequently reported challenges included: visual, need for assistance from others, technology, accessibility, and transportation. The treemap also reveals the types of challenges reported for a specific activity. For example, with exercising (weightlifting icon), nine different challenges were reported, including: visual, need for assistance from others, technology, accessibility, transportation, physical, financial, other, and environmental. In contrast, managing medication (pill icon) had only two different types of challenges reported (i.e., visual, accessibility).

Treemap displaying proportion of challenge codes ( n = 257) reported across 17 activities. Data are presented in nested rectangles that each represent distinct challenge codes, proportional in size to the number of times the challenge was reported across activities. Within each rectangle (1) the frequency of each challenge type is listed below the name of each challenge and (2) the presence of an activity icon indicates the challenge type was reported for that activity (challenge codes reported fewer than three times excluded from figure).
To provide context on the lived experience of these activity challenges, Tables 3 – 6 highlight challenges for specific activities along with illustrative, example quotes from participants across the four categories.
Household tasks
Table 3 shows Household tasks. For repairing and maintaining the home, many reported challenges shared the common theme of outsourcing tasks that are difficult, time-consuming, or potentially unsafe. Participants described concerns about the cost of services and trusting service providers. Some participants reported no longer doing certain desired home improvement activities, such as gardening. For housekeeping, challenges were primarily related to the inability to see things that need to be cleaned up (e.g., messes, stains) and lacking spatial awareness for tasks, such as avoiding obstacles while vacuuming.
Household Tasks Category: Example Challenges and Quotes
Shopping and finances
Table 4 depicts Shopping and finances. For managing finances, several participants reported not being able to independently complete tasks, such as banking and signing receipts. This reliance on others to engage in tasks was primarily due to vision limitations, specifically with reading, but some attributed their need for assistance to physical limitations (e.g., carpal tunnel) or limited technology familiarity.
Shopping and Finances Category: Example Challenges and Quotes
Distinct challenges were reported for in-person shopping compared to online shopping. Many in-person shopping challenges were attributed to visual limitations, such as identifying items and reading labels. Participants described using AT, such as magnifiers and barcode readers, to shop in-person, yet these devices were reported as being tedious and time-consuming to use, especially when shopping for numerous items. Shopping for clothes was described by some as particularly difficult, given the wide array of colors, sizes, and styles. Participants expressed challenges in obtaining helpful descriptive information about the items from informational tags as well as other people. One individual shared their experience of being perceived as being suspected of stealing by store employees when using their strategies for clothes shopping, such as using a magnifier and holding items closely.
Online shopping challenges were related to the use and accessibility of technology. For some, the challenge was simply not knowing how to use a computer or smart phone for shopping. Among participants who were familiar with online shopping, website accessibility was a common issue. Several participants described being unable to use certain shopping websites because the content was not “screen-reader friendly.” Screen readers are designed to read aloud the text on a screen, yet participants reported that many shopping websites were not compatible with their screen reading software. Example issues include websites not providing image descriptions (i.e., alternative text) or appropriate headers to support content navigation. One participant, who used computer screen magnification, described how it was difficult to navigate the online shopping process, from browsing to checkout, because the text on their screen was so large that relevant information on the website could not be seen.
Transportation
Challenges were reported for all modes of transportation we evaluated ( Table 5 ). For flight travel, participants reported difficulty navigating the airport. One participant described how it is often the standard protocol of airport staff to put customers who need assistance in a wheelchair and push them, although it was noted that most would prefer someone to walk with them as a sighted guide. Challenges with walking were primarily related to navigation. Participants described safety concerns, namely tripping and falling, especially when walking on uneven sidewalks or landscapes. Some individuals discussed challenges using wayfinding technologies, such as smartphone maps and apps. One participant who used a wayfinding app designed for individuals with visual impairment found that, although the app read aloud helpful information, it often gave too much detail, which was distracting and inhibited other critical observations (e.g., auditory crosswalk signals). Physical challenges associated with walking as a pedestrian (e.g., fatigue, limited stamina) were also reported.
Transportation Category: Example Challenges and Quotes
Challenges with getting a ride from family or friends were related to the availability and reliability of others. Some participants expressed emotional challenges with getting a ride, such as feeling burdensome and vulnerable. For riding a train or subway, challenges included vision limitations, lack of knowledge about the system, and unfamiliar environments. One participant described their fear of falling onto the tracks, whereas others described negative experiences navigating crowds on trains and subway systems. Safety concerns about falling were reported for using the bus, especially when getting on and off, and preparing for stops when the bus is in motion. For taxi and ride-share services, participants reported issues related to not knowing how to use the technology and limited availability of drivers. Additionally, participants shared concerns about having to trust a stranger to drive them around because they cannot see what the driver looks like or what route they are taking.
Managing health
Table 6 highlights challenges for Managing Health. Accessibility was the most reported challenge for exercising. Participants described how many exercise machines (e.g., treadmills) are not accessible to them because they often feature touchscreen interfaces without tactile buttons, and only provide visual, rather than audio, feedback. Group exercise classes were also described as inaccessible, as many instructors rely on visually demonstrating movements without adequately describing the movement (e.g., direction, specific body parts engaged). Other exercise challenges included transportation to fitness centers and personal limitations (e.g., physical declines, lack of motivation).
Managing Health Category: Example Challenges and Quotes
For managing diet and nutrition, participants discussed challenges in reading information, such as food labels or recipes. Many reported having issues with assistive devices that were intended to support these activities (e.g., handheld readers unable to read contents on the back of a product due to the font size). For managing and monitoring health, some participants mentioned struggling with making healthy meals at home due to the high cost of fresh food, as well as safety concerns using the stove. Participants described barriers to accessing healthcare information, as processes have shifted to being mostly online with limited opportunities to speak with a representative for support. Some noted that their healthcare and insurance provider websites were not screen reader accessible. One participant described their difficulty keeping track of online portals, account information, and passwords.
Transportation challenges getting to/from healthcare appointments and the pharmacy were discussed. Participants described how healthcare monitoring devices are often not accessible to people with vision impairment. For example, two individuals described issues with talking blood glucose monitors, devices intended to help users with vision impairment manage diabetes; they reported trouble lining up the test strip with the blood sample (due to visual challenges) and the phone application for the meter only providing visual infographics (e.g., photos of scales) instead of text information that could be read aloud by a screen reader.
Regarding medication, participants described challenges reading labels on prescriptions and over-the-counter medicines to ensure they are taken at the correct dosage and time. Issues remembering to take medications were also reported. For going to healthcare appointments, challenges were associated with having to rely on other people, both for transportation and navigating healthcare facilities.
This qualitative study explored challenges with a broad range of IADLs in the home and community among people aging with vision impairment. Participants discussed a wide range of IADL challenges that are most difficult for them personally. Across participants, the most difficult, and therefore most frequently discussed, activities were repairing and maintaining the home (Household Tasks), managing finances (Shopping and Finances), flying on an airplane (Transportation), and exercising (Managing Health). The details they described highlighted many themes but most frequently the nature of the challenges related to visual limitations, need for assistance from others, technology issues, lack of accessibility, and transportation barriers. These data provide insights for technology design and innovation to support activity participation for this population.
Visual Challenges
Not surprisingly, challenges explicitly related to visual ability were the most frequently reported type of IADL challenge and included reading fine print (e.g., medication labels), distance vision (e.g., in-person shopping, identifying messes or spills), and outdoor mobility (e.g., navigating public transportation systems). These findings are consistent with prior research ( Cimarolli et al., 2012 ; Lamoureux et al., 2004 ). Previous findings have shown that poorer visual ability (in terms of acuity, contrast sensitivity, and useful field of view) is independently related to longer times for completing certain IADL tasks among older adults ( Owsley et al., 2001 ). We found that people aging with vision impairment reportedly experience a broad array of challenges with IADLs, that go beyond visual limitations, including both personal factors (e.g., physical, cognitive, emotional) and environmental factors (e.g., accessibility, financial, transportation). Design of supportive solutions for people aging with vision impairment must consider that users may experience a combination of challenges that can affect their ability to engage in an activity and/or effectively utilize a service or device.
Relying on Assistance From Others
Participants frequently reported struggles associated with getting or requiring assistance from others for IADLs. Key issues included: being dependent on others to complete tasks and challenges with hiring help (e.g., cost, trust, reliability). Our findings suggest people aging with vision impairment want to perform activities as independently as possible, consistent with prior research that identified loss of independence as the most challenging adjustment to vision impairment ( Nyman et al., 2012 ). People aging with vision impairment are accustomed to using their voice to support everyday tasks and could benefit greatly from the growing market of voice-controlled technologies ( Bhowmick & Hazarike, 2017 ). Voice-activated digital assistants (e.g., Alexa, Siri, Google Home) have tremendous potential to support independence in IADLs, from making and reading grocery lists, to delivering medication reminders, to controlling various smart home devices (e.g., smart light bulbs and vacuums). However, for these devices and skills to be effective, they must be intuitive to set up, learn, and use, and must be designed to accommodate users with diverse abilities ( Kadylak et al., 2022 ).
Transportation Challenges
Transportation was reportedly a challenging aspect of activities outside the home and a challenging IADL in and of itself. This largely nondriving population could benefit greatly from accessible public and private transportation. It cannot be assumed that they can rely on rides from family or friends, as this option may not be available, convenient, or desired. Participants’ desire to use public transportation was coupled with a need for navigational technology that facilitates spatial awareness, safety, and ease in using these systems. Mobile apps that offer real-time transit information and step-by-step wayfinding information in an accessible format hold great promise to enhance independent community mobility for this population. Insights from participants suggest the need for customizable transportation and wayfinding apps that enable users to pick and choose what and how information is relayed. For example, we found that if pedestrian wayfinding apps provide too much auditory information, they can create cognitive overload for people with vision impairment, as they also rely on observing sound cues in their environment. These results also identify an opportunity for app-based ridesharing services, like Uber and Lyft, to increase safety, trust, and confidence for users with vision impairment by providing accessible information that confirms their driver and route progress.
Technology and Accessibility Challenges
Many technology challenges were interconnected with accessibility issues (e.g., inaccessible devices, applications, and websites), so these key challenges are discussed collectively here. Insights from people aging with vision impairment demonstrated how the internet can be involved in supporting all IADLs, either directly (e.g., online banking) or indirectly (e.g., a website for finding home repair professionals). Our findings suggest that website accessibility, or lack thereof, is a central issue facing people aging with vision impairment. There are known solutions to make online content accessible for users who are visually impaired, such as minimum contrast standards, text resizing capabilities, and screen reader-accessible content (e.g., describing images using alternative text; using headers to aid in page and website navigation). The Web Content Accessibility Guidelines are generally accepted as the accessibility standards for webpages and mobile applications and provide instructions for website and app owners to ensure that their platforms are accessible to, and do not discriminate against, users with varying disabilities ( W3C Web Accessibility Initiative, 2022 ). Recently, the Americans with Disabilities Act (ADA) specified that websites and mobile applications are considered “places of public accommodation,” and therefore, state and local governments as well as businesses open to the public must provide accessible web content ( ADA.gov, 2022 ). However, there is clearly a gap between this requirement and current practice. In fact, an increasing number of lawsuits confirm the requirement of public businesses to provide accessible web content ( Palmer & Palmer, 2018 ).
Despite reported challenges with web accessibility, most participants described using personal computing devices (e.g., laptops, smart phones, and tablets) to carryout IADLs, from shopping, to banking, to accessing healthcare information. For these personal devices, participants mentioned using a wide variety of applications and software designed for users with vision impairment (e.g., bar code scanners, color identifiers, screen readers) as well as built-in accessibility features (e.g., magnification, large text). These devices hold great potential to support this population, as they offer the benefit of an integrated platform that is mainstream, unobtrusive, and lacks the stigma of separate AT ( Hakobyan et al., 2013 ). Moreover, digital interfaces are dynamic and adaptable for users with a wide range of abilities, which can facilitate the implementation of universal design principles ( Sanford & Remillard, 2021 ). In line with prior research, some reported technology challenges were related to a lack of structured, accessible training oriented toward people with vision impairment, which can play an important role in technology adoption ( Piper et al., 2017 ; Tapu et al., 2020 ).
This study identified a few key opportunities for technology innovation that are activity-specific. First, given the extensive challenges reported for in-person shopping, there is a critical need to make online shopping accessible for people aging with vision impairment so they can obtain everyday goods, from groceries to clothing, from the convenience of home. To do so, online retailers must provide comprehensive product information on their websites in an accessible format so visually impaired users can make informed purchases.
With regard to healthcare, our findings suggest that, in addition to making healthcare communication and portals accessible, providers should maintain some capacity for phone support to be inclusive of individuals who are less familiar with the internet, or unable to navigate the website due to accessibility issues. Participants described instances where healthcare devices and applications did not provide feedback that was useful and usable, indicating the need for devices to be designed with intuitive cueing and facilitate comprehensive audio description. For exercising, participants described barriers to engaging in in-person classes and utilizing fitness facilities (e.g., transportation access, inaccessible classes, and equipment). Results indicate the need for technology-based exercise equipment to be multimodal (e.g., audio input/output, tactile buttons), as touchscreen interfaces alone are not inclusive of users with vision impairment. Exercise programs delivered remotely via tele-technologies like videoconferencing (e.g., Zoom) can be especially impactful for this population as they offer the convenience of participating from home and utilize the user’s personal computer or smart phone, which they can adjust to their accessibility needs and preferences. Moreover, these telewellness programs can expand access to accessible exercise programs that provide sufficient verbal cueing and instructors who are sensitive to the needs of people with vision impairment ( Mitzner et al., 2022 ).
Limitations
There are a few limitations of this study to note. The convenience sample was majority White/Caucasian with high education and high self-perceptions of health. Activity challenges might be greater among racial/ethnic minority populations and those with lower education due to known disparities in access to transportation, healthcare, and technology ( Kaye et al., 2022 ; Meade et al., 2015 ). Causes of vision impairment were not strategically sampled, but represent a variety of conditions, diseases, injuries, and abnormalities that were congenital or acquired at an early age. Nevertheless, the diversity of the sample in terms of degree, functional limitations, and cause of vision impairment is a strength of this study, as the population aging with vision impairment is diverse and is likely to have unique experiences that are important to consider to develop effective solutions ( Bhowmick & Hazarike, 2017 ).
The interviews were structured to elicit conversations from participants regarding their most difficult activity(ies) in each category. That is not to say they did not experience difficulties with other activities that were not the focus of the discussion. The current paper focused on challenges with IADLs and not participants’ strategies/solutions for managing activity challenges, which are captured in the ACCESS data set. To effectively support activity performance of people aging with vision impairment with technology interventions, there is a need to understand more about what works, what does not, and if/how new emerging technology is being adopted and used long-term. Such knowledge is necessary to inform the design of effective products and services for this understudied population and is an important area of future exploration.
Implications
Our findings highlight many opportunities for design and technology innovation to support activity participation and independence among older adults with vision impairment. Two promising types of technologies to support IADL performance for the challenges noted include (1) voice-activated digital assistants and (2) apps for smart phones and personal computing devices, which have digital interfaces that are adaptable for users with a wide range of abilities. There is a clear need to make existing technologies accessible for people with vision impairment with the most pressing issue being websites that are not compatible with screen readers. Our findings emphasize the need for broader mandates and policies that both enforce and incentivize the development and maintenance of accessible web content. There is also a need to make nontechnology items (e.g., price tags, food, and clothing labels) more accessible to AT devices, such as scanners. Given that technology has become ubiquitous in everyday life (e.g., ATMs, shopping, healthcare portals, rideshare apps), technology training for these everyday technologies that is targeted at people with vision impairment is necessary. Vision rehabilitation centers, which offer a variety of resources to help individuals with vision impairment engage in IADLs (e.g., community mobility training, AT matching, and training), are ideal for delivering such training but require dedicated, sufficient funding to offer these services on an ongoing basis.
This work was supported by a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR, grant numbers 90REGE0006-01-00, 90RE5016-01-00) under the auspices of the Rehabilitation Engineering Research Center on Technologies to Support Aging-in-Place for People with Long-Term Disabilities (TechSAge; www.TechSAgeRERC.org ). NIDILRR is a Center within the Administration for Community Living, Department of Health and Human Services.
Data are not publicly available. Researchers interested in analyzing the ACCESS data set can contact the study team to explore opportunities for archival analyses in partnership with the research team. Study methods, assessments, and the coding scheme are detailed in technical reports available from the authors ( Remillard et al., 2018 ). Preregistration is not applicable given the nature of the study.
The authors thank Maurita Harris, Jordan Hartley, and Jenny Singleton for their contributions on the project, as well as Lisa Le for her assistance with data visualizations. We also acknowledge Susan Primo and Johan Rempel for subject matter expert consultation on conducting and reporting research with older adults with vision impairment.
ADA.gov . ( 2022 ). Guidance on web accessibility and the ADA . https://www.ada.gov/resources/web-guidance/
Bayles , M. A. , Kadylak , T. , Liu , S. , Hasan , A. , Liang , W. , Hong , K. , Driggs-Campbell , K. , & Rogers , W. A. ( 2022 ). An interdisciplinary approach: Potential for robotic support to address wayfinding barriers among persons with visual impairments . Proceedings of the Human Factors and Ergonomics Society Annual Meeting , 66 ( 1 ), 1164 – 1168 . https://doi.org/10.1177/1071181322661384
Berger , S. , & Porell , F. ( 2008 ). The association between low vision and function . Journal of Aging and Health , 20 ( 5 ), 504 – 525 . https://doi.org/10.1177/0898264308317534
Bhowmick , A. , & Hazarike , S. M. ( 2017 ). An insight into assistive technology for the visually impaired and blind people: State-of-the-art and future trends . Journal on Multimodal User Interfaces , 11 , 1 – 24 . https://doi.org/10.1007/s12193-016-0235-6
Bleach , K. , Fairchild , N. , Rogers , P. , & Rosenblum , L. P. ( 2020 ). improving transportation systems for people with vision loss . American Foundation for the Blind .
Google Scholar
Google Preview
Brunes , A. , Hansen , M. B. , & Heir , T. ( 2019 ). Loneliness among adults with visual impairment: Prevalence, associated factors, and relationship to life satisfaction . Health and Quality of Life Outcomes , 17 ( 24 ), 1 – 7 . https://doi.org/10.1186/s12955-019-1096-y
Cimarolli , V. R. , Boerner , K. , Brennan-Ing , M. , Reinhardt , J. P. , & Horowitz , A. ( 2012 ). Challenges faced by older adults with vision loss: A qualitative study with implications for rehabilitation . Clinical Rehabilitation , 26 ( 8 ), 748 – 757 . https://doi.org/10.1177/0269215511429162
Clarke , P. , & Latham , K. ( 2014 ). Life course health and socioeconomic profiles of Americans aging with disability . Disability and Health Journal , 7 ( 1 Suppl ), S15 – 23 . https://doi.org/10.1016/j.dhjo.2013.08.008
Coyle , C. E. , Steinman , B. A. , & Chen , J. ( 2017 ). Visual acuity and self-reported vision status: Their associations with social isolation in older adults . Journal of Aging and Health , 29 ( 1 ), 128 – 148 . https://doi.org/10.1177/0898264315624909
Crews , J. E. , Chou , C. -F. , Sekar , S. , & Saaddine , J. B. ( 2017 ). The prevalence of chronic conditions and poor health among people with and without vision impairment, aged >65 years, 2010–2014 . American Journal of Opthalmology , 182 , 18 – 30 . https://doi.org/10.1016/j.ajo.2017.06.038
Crudden , A. , McDonnall , M. C. , & Hierholzer , A. ( 2015 ). Transportation: An electronic survey of persons who are blindor have low vision . Journal of Visual Impairment & Blindness , 109 ( 6 ), 445 – 456 . https://doi.org/10.1177/0145482x1510900603
Czaja , S. J. , Boot , W. R. , Charness , N. , & Rogers , W. A. ( 2019 ). Designing for older adults: Principles and creative human factors approaches (3rd. ed.) . CRC Press .
Demmin , D. L. , & Silverstein , S. M. ( 2020 ). Visual impairment and mental health: Unmet needs and treatment options . Clinical ophthalmology , 14 , 4229 – 4251 . https://doi.org/10.2147/OPTH.S258783
Elo , S. , & Kyngas , H. ( 2008 ). The qualitative content analysis process . Journal of Advanced Nursing , 62 ( 1 ), 107 – 115 . https://doi.org/10.1111/j.1365-2648.2007.04569.x
Erickson , W. , Lee , C. , & von Schrader , S. ( 2022 ). Disability statistics from the American Community Survey (ACS) . Cornell University and Yang-Tan Institute (YTI) . www.disabilitystatistics.org
Erlingsson , C. L. , & Brysiewicz , P. ( 2012 ). Orientation among multiple truths: An introduction to qualitative research . African Journal of Emergency Medicine , 3 ( 2 ), 92 – 99 . https://doi.org/10.1016/j.afjem.2012.04.005
Fieo , R. , Manly , J. J. , Schupf , N. , & Stern , Y. ( 2014 ). Functional status in the young-old: Establishing a working prototype of an extended-instrumental activities of daily living scale . Journals of Gerontology, Series A: Biological Sciences and Medical Sciences , 69 ( 6 ), 766 – 772 . https://doi.org/10.1093/gerona/glt167
Graf , C. ( 2008 ). The Lawton instrumental activities of daily living scale . American Journal of Nursing , 108 ( 4 ), 52 – 62 . https://doi.org/10.1097/01.NAJ.0000314810.46029.74
Hakobyan , L. , Lumsden , J. , O’Sullivan , D. , & Bartlett , H. ( 2013 ). Mobile assistive technologies for the visually impaired . Survey of Ophthalmology , 58 ( 6 ), 513 – 528 . https://doi.org/10.1016/j.survophthal.2012.10.004
Harrington , C. N. , Mitzner , T. L. , & Rogers , W. A. ( 2015 ). Understanding the role of technology for meeting the support needs of older adults in the USA with functional limitations . Gerontechnology , 14 ( 1 ), 21 – 31 . https://doi.org/10.4017/gt.2015.14.1.004.00
Hochberg , C. , Maul , E. , Chan , E. S. , Landingham , S. V. , Ferrucci , L. , Friedman , D. S. , & Ramulu , P. Y. ( 2012 ). Association of vision loss in glaucoma and age-related macular degeneration with IADL disability . Investigative Ophthamology and Visual Science , 53 ( 6 ), 3201 – 3206 . https://doi.org/10.1167/iovs.12-9469
Kadylak , T. , Blocker , K. A. , Kovac , C. E. , & Rogers , W. A. ( 2022 ). Understanding the potential of digital home assistant devices for older adults through their initial perceptions and attitudes . Gerontechnology , 21 ( 1 ), 1 – 10 . https://doi.org/10.4017/gt.2022.21.1.486.06
Katz , S. , Downs , T. D. , Cash , H. R. , & Grotz , R. C. ( 1970 ). Progress in development of the index of ADL . Gerontologist , 10 ( 1 ), 20 – 30 . https://doi.org/10.1093/geront/10.1_part_1.20
Kaye , H. S. , Yeager , P. , & Reed , M. ( 2022 ). Disparities in usage of assistive technology among people with disabilities . Assistive Technology , 20 ( 4 ), 194 – 203 . https://doi.org/10.1080/10400435.2008.10131946 .
Killeen , O. J. , De Lott , L. B. , Zhou , Y. , Hu , M. , Rein , D. , Reed , N. , Swenor , B. K. , & Ehrlich , J. R. ( 2023 ). Population prevalence of vision impairment in US adults 71 years and older: TheNational Health and Aging Trends Study . JAMA Ophthalmology , 141 ( 2 ), 197 – 204 . https://doi.org/10.1001/jamaophthalmol.2022.5840
Kim , H. N. ( 2021 ). Characteristics of technology adoption by older adults with visual disabilities . International Journal of Human–Computer Interaction , 37 ( 13 ), 1 – 13 . https://doi.org/10.1080/10447318.2021.1876359
Koon , L. M. , Remillard , E. T. , Hartley , J. Q. , Harris , M. T. , Mitzner , T. L. , & Rogers , W. A. ( 2019 ). Coding scheme for the Aging Concerns, Challenges, and Everyday Solution Strategies (ACCESS) Study: Adults aging with mobility or vision disability (TechSAge-TR-1902) .
Koon , L. M. , Remillard , E. T. , Mitzner , T. L. , & Rogers , W. A. ( 2020 ). Aging Concerns, Challenges, and Everyday Solution Strategies (ACCESS) for adults aging with a long-term mobility disability . Disability and Health Journal , 13 ( 4 ), 100936 . https://doi.org/10.1016/j.dhjo.2020.100936
Lamoureux , E. L. , Hassell , J. B. , & Keeffe , J. E. ( 2004 ). The determinants of participation in activities of daily living in people with impaired vision . American Journal of Ophthalmology , 137 ( 2 ), 265 – 270 . https://doi.org/10.1016/j.ajo.2003.08.003
LaPlante , M. P. ( 2010 ). The classic measure of disability in activities of daily living is biased by age but an expanded IADL/ADL measure is not . Journals of Gerontology, Series B: Psychological Sciences and Social Sciences , 65 ( 6 ), 720 – 732 . https://doi.org/10.1093/geronb/gbp129
Lawton , M. P. , & Brody , E. M. ( 1969 ). Assessment of older people: Self-maintaining and instrumental activities of daily living . Gerontologist , 9 ( 3 ), 179 – 186 . https://doi.org/10.1093/geront/9.3_Part_1.179
Liu , S. , Hasan , A. , Hong , K. , Wang , R. , Chang , P. , Mizrachi , Z. , Lin , J. , McPherson , D. L. , Rogers , W. A. , & Driggs-Campbell , K. R. ( in press ). DRAGON: A dialogue-based robot for assistive navigation with visual language grounding . Proceedings of the 7th Annual Conference on Robot Learning.
McGrath , C. , & Corrado , A. M. ( 2019 ). The environmental factors that influence technology adoption for older adults with age-related vision loss . British Journal of Occupational Therapy , 82 ( 8 ), 493 – 501 . https://doi.org/10.1177/0308022618813247
Meade , M. A. , Mahmoudi , E. , & Lee , S. Y. ( 2015 ). The intersection of disability and healthcare disparities: A conceptual framework . Disability and Rehabilitation , 37 ( 7 ), 632 – 641 . https://doi.org/10.3109/09638288.2014.938176
Mitzner , T. L. , Remillard , E. T. , & Mumma , K. T. ( 2022 ). Research-driven guidelines for delivering group exercise programs via videoconferencing to older adults . International Journal of Environmental Research and Public Health , 19 ( 13 ), 7562 – 15 . https://doi.org/10.3390/ijerph19137562
Mitzner , T. L. , Rogers , W. A. , Fisk , A. D. , Boot , W. R. , Charness , N. , Czaja , S. J. , & Sharit , J. ( 2016 ). Predicting older adults’ perceptions about a computer system designed for seniors . Universal Access in the Information Society , 15 ( 271 ), 271 – 280 . https://doi.org/10.1007/s10209-014-0383-y .
Mitzner , T. L. , Sanford , J. A. , & Rogers , W. A. ( 2018 ). Closing the capacity-ability gap: Using technology to support aging with disability . Innovation in Aging , 2 ( 1 ), igy008 . https://doi.org/10.1093/geroni/igy008
National Academies of Sciences Engineering and Medicine . ( 2016 ). Making eye health a population health imperative: Vision for tomorrow . The National Academies Press (US) .
Nyman , S. R. , Dibb , B. , Victor , C. R. , & Gosney , M. A. ( 2012 ). Emotional well-being and adjustment to vision loss in later life: A meta-synthesis of qualitative studies . Disability and Rehabilitation , 34 ( 12 ), 971 – 981 . https://doi.org/10.3109/09638288.2011.626487
Owsley , C. , McGwin , G. Sloane , M. E. , Stalvey , B. T. , & Wells , J. ( 2001 ). Timed instrumental activities of daily living tasks: Relationship to visual function in older adults . Optometry and Vision Science , 78 ( 5 ), 350 – 359 . https://doi.org/10.1097/00006324-200105000-00019
Palmer , Z. B. , & Palmer , R. H. ( 2018 ). Legal and ethical implications of website accessibility . Business and Professional Communication Quarterly , 81 ( 4 ), 399 – 420 . https://doi.org/10.1177/2329490618802418
Peres , K. , Matharan , F. , Daien , V. , Nael , V. , Edjolo , A. , Bourdel-Marchasson , I. , Ritchie , K. , Tzourio , C. , Delcourt , C. , & Carriere , I. ( 2017 ). Visual loss and subsequent activity limitations in the elderly: The French three-city cohort . American Journal of Public Health , 107 ( 4 ), 564 – 569 . https://doi.org/10.2105/AJPH.2016.303631
Piper , A. M. , Brewer , R. , & Cornejo , R. ( 2017 ). Technology learning and use among older adults with late-life vision impairments . Universal Access in the Information Society , 16 , 699 – 711 . https://doi.org/10.1007/s10209-016-0500-1
Preusse , K. , Gonzalez , E. , Singleton , J. , Mitzner , T. , & Rogers , W. ( 2016 ). Understanding the needs of individuals ageing with impairment . International Journal of Human Factors and Ergonomics , 4 , 144 . https://doi.org/10.1504/IJHFE.2016.082246
Remillard , E. T. , Fausset , C. B. , & Fain , W. B. ( 2019 ). Aging with long-term mobility impairment: Maintaining activities of daily living via selection, optimization, and compensation . Gerontologist , 59 ( 3 ), 559 – 569 . https://doi.org/10.1093/geront/gnx186
Remillard , E. T. , Griffiths , P. C. , Mitzner , T. L. , Sanford , J. A. , Jones , B. D. , & Rogers , W. A. ( 2020 ). The TechSAge minimum battery: A multidimensional and holistic assessment of individuals aging with long-term disabilities . Disability and Health Journal , 13 ( 3 ), 1 – 9 . https://doi.org/10.1016/j.dhjo.2019.100884
Remillard , E. T. , Mitzner , T. L. , Singleton , J. L. , Koon , L. M. , & Rogers , W. A. ( 2018 ). Developing the Aging Concerns, Challenges, and Everyday Solution Strategies (ACCESS) Study (TechSAge-TR-1801) .
Renaud , J. , & Bédard , E. ( 2013 ). Depression in the elderly with visual impairment and its association with quality of life . Clinical Interventions in Aging , 8 , 931 – 943 . https://doi.org/10.2147/CIA.S27717
Rogers , W. A. , Meyer , B. , Walker , N. , & Fisk , A. D. ( 1998 ). Functional limitations to daily living tasks in the aged: A focus group analysis . Human Factors , 40 ( 1 ), 111 – 125 . https://doi.org/10.1518/001872098779480613
Sanford , J. A. , & Remillard , E. T. ( 2021 ). Design for one is design for all: The past, present and future of universal design as a strategy for aging-in-place with disability . In M. Putnam & C. Bigby (Eds.), Handbook on ageing with disability . Taylor & Francis/Routledge . https://www.taylorfrancis.com/chapters/edit/10.4324/9780429465352-15/design-one-design-jon-sanford-elena-remillard
Steinman , B. A. ( 2016 ). Health outcomes associated with self-reported vision impairment in older adults . Journal of Visual Impairment & Blindness , 110 ( 6 ), 385 – 398 . https://doi.org/10.1177/0145482x1611000602
Swenor , B. K. , Lee , M. J. , Varadaraj , V. , Whitson , H. E. , & Ramulu , P. Y. ( 2020 ). Aging with vision loss: A framework for assessing the impact of visual impairment on older adults . Gerontologist , 60 ( 6 ), 989 – 995 . https://doi.org/10.1093/geront/gnz117
Tapu , R. , Mocanu , B. , & Zaharia , T. ( 2020 ). Wearable assistive devices for visually impaired: A state of the art survey . Pattern Recognition Letters , 137 , 37 – 52 . https://doi.org/10.1016/j.patrec.2018.10.031
Vaismoradi , M. , & Snelgrove , S. ( 2019 ). Theme in qualitative content analysis and thematic analysis . Forum Qualitative Social Research , 20 ( 3 ), 1 – 14 . https://doi.org/10.17169/fqs-20.3.3376
Vaismoradi , M. , Turunen , H. , & Bondas , T. ( 2013 ). Content analysis and thematic analysis: Implications for conducting a Qualitative Descriptive Study . Nursing & Health Sciences , 15 ( 3 ), 398 – 405 . https://doi.org/10.1111/nhs.12048
Varma , R. , Vajaranant , T. S. , Burkemper , B. , Wu , S. , Torres , M. , Hsu , C. , Choudhury , F. , & McKean-Cowdin , R. ( 2016 ). Visual impairment and blindness in adults in the United States: Demographic and geographic variations from 2015 to 2050 . JAMA Ophthalmology , 134 ( 7 ), 802 – 809 . https://doi.org/10.1001/jamaophthalmol.2016.1284
W3C Web Accessibility Initiative . ( 2022 ). W3C accessibility standards overview . https://www.w3.org/WAI/standards-guidelines/
World Health Organization . ( 2001 ). International classification of functioning, disability and health: ICF . https://iris.who.int/handle/10665/42407
World Health Organization . ( 2019 ). World report on vision . https://iris.who.int/handle/10665/328717
- visual impairment
- transportation
- instrumental activities of daily living
Supplementary data
Email alerts, citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1758-5341
- Copyright © 2024 The Gerontological Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
VIDEO
COMMENTS
Case study highlighting the support that can be implemented for a visually impaired student. Fiona is a new international postgraduate student who commenced her undergraduate studies in the College of Science and Engineering at the University in September. Having obtained exceptional grades at school, Fiona was able to gain admission as a ...
Report included: Luke is a 12 month old infant with a history of epilepsy, right-sided limb weakness and delayed development of uncertain aetiology. He is under the ongoing care of ophthalmology and receives regular occupational and physiotherapy input. His seizures are currently well controlled and mum reports a reduction in the roving eye ...
experiences. A case study approach was used to gather the data in a naturalistic setting. In this case study, all student participants were individuals with visual impairments along the spectrum of being legally blind. Findings of this study revealed four emerging themes that produced evidence of the unique participant's experiences.
The purpose of the case study that is presented in this article was to consider the social and psychological experiences of students with visual impairments by examining the psychosocial development of Eric (a pseudonym), a sixth-grade student with low vision.
The present study examines the perceptions of visually impaired individuals towards inclusive education in Malaysia, including the challenges faced. The impact on their social lives was also ...
This was a systematic review on the inclusive education of students with visual impairment. This study focused on two of the most addressed topics: the perceptions of general education teachers and challenges faced by students with visual impairment in accessing academic subjects.
The participants in the study included Sarah and Madison, two students who are visually impaired; Sarah's father and Madison's mother; 10 general education teachers; and 2 teachers of students with visual impairments (both the former and current teacher of visually impaired students). All 12 teachers were bilingual and biliterate, but the ...
Our chapter describes a case study of a blind student who shared his daily experience with online learning, highlighting both the encountered struggles and the type of assistance received during the pandemic. The discussion on the future use of emerging technologies for the BVI concludes our chapter.
This research was carried out as part of an Erasmus + project called "Visually Impaired Mentally Sighted" targeting to improve the conditions and materials used in the educational environment and to develop personal and professional skills of the school staff. This qualitative study employed descriptive case study design.
The purpose of his study is to investigate the experiences of the students with visual impairment in online learning environment with regards to instructional media (text, visual, audio, and multimedia) with the purpose of developing suggestions for accessible online course design.
Abstract and Figures. Blind and visually impaired (BVI) people frequently encounter challenges in their daily lives. With the COVID-19 pandemic, some of those challenges decreased, but some became ...
The visual factors, physical environmental factors, and human-environment interactive factors that significantly impact the spatial cognition of visually impaired people were discussed. Conclusions: (1) visual acuity affects the spatial cognition of the visually impaired in familiar environments; (2) the spatial cognition of the visually ...
This scoping study sought to establish a baseline for how well the needs of children with cortical visual impairment (CVI) who use augmentative and alternative communication (AAC) are currently aligned with the services available to them. CVI is the most common cause of visual impairment in children today, and AAC methods rely heavily on vision. Yet, the prevalence of CVI in children who use ...
This study was conducted at one of the secondary school located in southern part of the country. It employed qualitative case study design using four (4) general teachers teaching in classes having students with visual impairments. Data collection was done using semi-structured interviews and participant- observation methods.
An exploratory study on smartphone use among people with visual impairment shows that more than 90% of respondents used their smartphones for activities such as calls, sending and receiving ...
WHO fact sheet on blindness and visual impairment providing key facts, definitions, causes, who is at risk, global and WHO response.
Background Sustaining a visual impairment may have a substantial impact on various life domains such as work, interpersonal relations, mobility and social and mental well-being. How to adjust to the loss of vision and its consequences might be a challenge for the visually impaired person. The purpose of the current study was to explore how younger male ex-Service personnel cope with becoming ...
A 55-year-old right-handed woman presented with a 3-year history of cognitive changes. Early symptoms included mild forgetfulness—for example, forgetting where she left her purse or failing to remember to retrieve a take-out order her family placed—and word-finding difficulties. Problems with depth perception affected her ability to back her car out of the driveway. When descending stairs ...
The burden of visual impairment is not distributed evenly. For example, the prevalence of distance visual impairment in low- and middle-income countries is estimated to be four times higher than that of high-income regions [ 5 ].
Functional visual loss is a subtype of functional neurological disorder (FND) and is a common cause of visual impairment seen in both general and neuro-ophthalmological practice.
The findings showed that students with visual impairment experience. five main challenges in higher education regarding financial, public stigma, accessibility, peer- to -. peer acceptance and ...
This study focused on two of the most addressed topics: the perceptions of general education teachers and challenges faced by students with visual impairment in accessing academic subjects.
With the right support, academics with visual impairments are prospering, but barriers to true inclusivity remain, says Kate Armond, while a lecturer reflects on how practice on reasonable adjustments can fall short of policy. Six months ago, Ghana's University of Cape Coast appointed its first visually-impaired lecturer, Carruthers Tetteh ...
Visual impairment is the condition of the serious loss of vision because of various factors. The characteristic feature of visual impairment is that it is impossible to restore the person's vision, as all the operations and lenses are helpless. Visual impairment occurs because of the impact of various factors, like physical damage of eyes ...
For example, two individuals described issues with talking blood glucose monitors, devices intended to help users with vision impairment manage diabetes; they reported trouble lining up the test strip with the blood sample (due to visual challenges) and the phone application for the meter only providing visual infographics (e.g., photos of ...
Visual impairment (VI) is a condition of reduced visual performance that cannot be r emedied. by refractive correction (spectacles or contact lenses), surgery or medical methods. Consequently, it ...
Human visual experience is increasingly mediated. As technology facilitates the sharing of diverse images, understanding the world through photography and videos is crucial. However, visuality affects the digital existence of communities with visual impairments. Focusing on the short-video consumption of individuals with visual impairments, this study examines their media experiences in a ...