Communication in Nursing: Documentation and Reporting
Effective communication is the cornerstone of nursing, fostering strong nurse -client relationships and ensuring high-quality patient care . As nurses navigate their roles, they must adeptly manage various phases of communication , from establishing initial connections to executing interventions and ultimately concluding the therapeutic relationship . This article delves into the critical guidelines and phases of nursing communication , offering insights into best practices for documentation, maintaining confidentiality, and overcoming barriers to effective interaction.

Table of Contents
Communication in nursing, purpose of communication, elements of communication, steps in the communication process, auditory channels, visual channels, kinesthetic channels, verbal communication, nonverbal communication, characteristics of good communication, factors influencing communication, clients who cannot speak clearly (aphasia, dysarthria, muteness), clients who are cognitively impaired, clients who are unresponsive, clients with hearing impairments, clients who do not speak english, barriers to effective communication, orientation phase, working phase, termination phase, reports in healthcare, confidentiality, guidelines for quality documentation and reporting, legal guidelines for recording.
Communication is the process of sharing information and generating meanings between individuals or groups. It involves conveying meanings through mutually understood signs, symbols, and semiotic rules. As the foundation of human interaction, communication is essential for personal well-being and fulfilling psychosocial needs like love, affection, and recognition. It is a fundamental component of human relationships and is particularly crucial in the field of nursing.
Communication serves as the foundation for establishing a helping-healing relationship. It plays a critical role in influencing behavior and achieving successful outcomes in nursing interventions . Effective communication is essential for the following reasons:
- Establishing Therapeutic Relationships. Communication is the primary means through which nurses build therapeutic relationships with their patients.
- Influencing Behavior. It enables nurses to influence patient behavior positively, leading to improved health outcomes.
Communication is fundamental to human interaction and serves several vital purposes.
- Gathering Information . Collecting data and insights to make informed decisions.
- Validating Information . Confirming the accuracy and relevance of the collected information.
- Sharing Information . Disseminating knowledge, ideas, and updates to others.
- Building Relationships . Developing trust and rapport through meaningful interactions.
- Expressing Feelings . Conveying emotions to connect on a personal level.
- Imagining . Sharing creative and conceptual thoughts to foster innovation and understanding.
- Influencing . Persuading and guiding others to align with certain ideas or actions.
- Meeting Social Expectations . Fulfilling societal norms and engaging in appropriate interactions.
Effective communication relies on six essential elements that ensure clarity and understanding.
- Referent or Stimulus . The motivation behind communication, such as an objective, emotion, or need that prompts an individual to communicate.
- Sender or Encoder . The individual who initiates the message, converting thoughts into communicable information.
- Message . The content of the communication, including the information, ideas, or feelings being conveyed.
- Channel . The medium through which the message is transmitted, such as auditory (spoken words), visual (written text, images), or tactile ( touch ).
- Receiver or Decoder . The person who receives the message and interprets its meaning.
- Feedback . The response from the receiver that indicates whether the message was understood as intended, completing the communication loop.
The communication process in nursing involves several critical steps to ensure clear and effective interaction between nurses and patients. Each step plays a vital role in the successful exchange of information, facilitating better patient care and outcomes.
- Thinking . The communication process begins with formulating the idea or message. The nurse identifies what needs to be communicated, such as instructions for a medication regimen or an update on a patient’s condition. For example, a nurse decides to explain the importance of taking prescribed antibiotics to a patient recovering from surgery .
- Encoding . In this step, the nurse translates thoughts into communicable forms, such as spoken words, written text, or gestures. This involves choosing the right words and communication methods that the patient will understand. For example, the nurse might use simple language and supportive gestures to explain the antibiotic regimen to an elderly patient who may have difficulty understanding complex medical terms.
- Transmitting . The nurse sends the encoded message through a chosen channel, such as face-to-face conversation, a written note, or a digital message. The choice of channel depends on the situation and the patient’s needs. For instance, the nurse might sit down with the patient and verbally explain the medication instructions while also providing a written handout for reference.
- Perceiving . The receiver (patient) perceives the message through their senses, such as hearing the nurse’s words, reading the written instructions, or observing the nurse’s gestures. The patient listens to the nurse’s explanation and reads the provided handout, absorbing the information through auditory and visual channels.
- Decoding . The patient interprets the message by processing the received information to make sense of it. This step involves the patient’s cognitive abilities and background knowledge. For example, the patient thinks about the nurse’s instructions and relates them to their own understanding of medication schedules.
- Understanding . The final step is when the patient comprehends the intended message, fully grasping the nurse’s instructions or information. Effective understanding ensures that the patient knows what is expected and can follow through appropriately. For instance, the patient understands the necessity of taking antibiotics at specific times and the importance of completing the course to prevent infection .
Channels of Communication
Effective communication utilizes various channels to convey messages clearly and ensure understanding. In nursing, these channels are particularly important for providing comprehensive care to patients.
- Hearing . Perceiving sounds such as conversations, alarms, or equipment beeps. For example, a nurse might hear a patient’s call bell and respond promptly to their needs.
- Listening . Actively interpreting and understanding spoken messages. In a clinical setting, this might involve listening to a patient’s description of their symptoms during an audio conference with other healthcare professionals to ensure accurate diagnosis and treatment.
- Sight . Observing visual elements like signs, body language, and visual aids. For instance, a nurse might notice a patient’s non-verbal cues, such as grimacing, which indicates pain .
- Reading . Decoding written symbols such as medical charts, letters, or memos. For example, a nurse reads a patient’s medical history and care plan to ensure appropriate interventions.
- Observation . Gaining information through careful observation, such as monitoring vital signs or patient behavior. For instance, a nurse observes a patient’s wound healing process to assess the effectiveness of treatment.
- Perception . Becoming aware of something through the senses, which can include sight, hearing, and touch. For example, a nurse perceives changes in a patient’s condition through a combination of visual inspection and listening to their complaints.
- Procedural Touch . Used in medical assessments and interventions. For example, a nurse uses touch to locate a vein for an intravenous injection or to palpate an abdomen to assess for tenderness.
- Caring Touch . Used for comfort and emotional support. For example, a nurse might place a reassuring hand on a patient’s shoulder to provide comfort during a stressful procedure.
Modes of Communication
Communication in nursing can be verbal or nonverbal, each with its own set of principles and techniques to ensure effective information exchange.
Verbal communication involves the use of spoken or written words. Effective verbal communication in nursing encompasses several key principles:
- Pace and Intonation . The manner of speech, including the pace and intonation, significantly influences the impact of the message. For instance, speaking slowly and softly to an excited client can help calm them.
- Simplicity. Using commonly understood words, brevity, and completeness is crucial. Nurses should select appropriate and understandable terms based on the client’s age, knowledge, culture, and education. For example, instead of saying, “The nurses will be catheterizing you tomorrow for a urinalysis,” it is more appropriate to say, “Tomorrow we need to get a sample of your urine by putting a small tube into your bladder .”
- Clarity and Brevity. Direct and simple messages are more effective. Clarity involves saying precisely what is meant, and brevity involves using the fewest words necessary. To ensure clarity, nurses should speak slowly and enunciate carefully.
- Timing and Relevance. The timing of the message is crucial to ensure it is heard and understood. This involves being sensitive to the client’s needs and concerns. For example, a client who is anxious about cancer may not be receptive to explanations about unrelated procedures.
- Adaptability. What the nurse says and how it is said must be individualized and carefully considered. For instance, if a nurse who typically greets clients cheerfully notices a distressed client, they should modify their tone and expression to convey concern.
- Credibility. Credibility involves being worthy of belief, trustworthy, and reliable. Nurses build credibility by being consistent, dependable, and honest. They should convey confidence and acknowledge their limitations, such as saying, “I don’t know the answer to that, but I will find someone who does.”
- Humor. Humor can be a powerful tool in the nurse-client relationship but must be used with care. It is important to consider the client’s perception of what is humorous to ensure it is appropriate and beneficial.
Nonverbal communication involves the use of gestures, facial expressions, posture, gait, body movements, physical appearance, and body language to convey messages. These nonverbal cues are critical in understanding and interpreting the feelings and attitudes of others.
- Personal Appearance. The way a person dresses and presents themselves often reflects their feelings and state of well-being. For instance, changes in grooming habits among acutely ill clients, such as a man requesting a shave or a woman asking for a shampoo and makeup, can indicate improvement in their condition. When the symbolic meaning of an object or attire is unfamiliar, nurses can inquire about its significance to foster rapport with the client.
- Posture and Gait. The way people walk and carry themselves can be reliable indicators of their self-concept, mood, and health. Erect posture and a purposeful stride suggest well-being, while slouched posture and a shuffling gait may indicate depression or physical discomfort. Nurses can clarify the meaning of observed behaviors by saying, for example, “You look like it really hurts you to move. I’m wondering how your pain is and if you might need something to make you more comfortable.”
- Facial Expression. The face is the most expressive part of the body, capable of conveying a wide range of emotions. While genuine emotions are often reflected in facial expressions, it is also possible to control these expressions to some extent. When the message is unclear, nurses should seek feedback to ensure the intended expression is understood. Nurses must be aware of their own facial expressions and what they communicate to others, especially in sensitive situations. Eye contact is another crucial element, as it can convey attentiveness and sincerity.
- Gestures. Hand and body gestures can emphasize and clarify spoken words or communicate specific feelings and signals independently of speech. For example, a thumbs-up can indicate approval, while crossed arms might suggest defensiveness. These gestures can significantly enhance the clarity and impact of verbal communication.
Electronic Communication
In modern healthcare, many agencies are transitioning to electronic medical records (EMRs) to document assessments and nursing care. This shift enhances efficiency, accuracy, and accessibility of patient information.
Email is a widely used form of electronic communication in healthcare due to its speed, efficiency, legibility, and ability to provide a documented record of messages sent and received. However, it poses confidentiality risks and is not suitable for urgent information, highly confidential details (such as HIV status, mental health issues, or chemical dependency), or abnormal lab data. To mitigate these risks, healthcare agencies establish standards and guidelines to ensure privacy, security, and effective communication, safeguarding patient information and maintaining professional protocols.
Effective communication is essential in healthcare, enabling nurses to interact successfully with patients and colleagues. The following characteristics are key to ensuring clear and impactful communication:
- Simplicity. Effective communication uses commonly understood words and is brief and complete. This ensures the message is easily comprehensible. For example, instead of saying, “We need to obtain a sample of cerebrospinal fluid via lumbar puncture ,” a nurse might say, “We need to take a small amount of fluid from your back to check for an infection.”
- Clarity. Clear communication involves articulating exactly what is meant. Nurses should speak slowly and enunciate well to ensure the message is understood. As an example, when explaining medication instructions, the nurse could say, “Take one pill every morning with breakfast,” rather than, “Take this daily,” to avoid any confusion .
- Timing and Relevance. Effective communication requires choosing the appropriate time to convey a message and considering the client’s interests and concerns. It’s important to ask one question at a time and wait for a response before proceeding. For example, if a patient is anxious about surgery , the nurse should wait until after addressing their immediate concerns before discussing post-operative care.
- Adaptability. Good communication involves adjusting the message and delivery based on the client’s mood and behavior. This personalization ensures the message is received positively and effectively. For example, if a usually cheerful patient seems distressed, the nurse might adopt a more gentle tone and approach, saying, “I see you’re upset today. Is there something specific that’s bothering you?”
- Credibility. Credible communication is trustworthy and reliable. Nurses must have adequate knowledge about the topic, provide accurate information, and convey confidence and certainty in their messages.
Effective communication is influenced by various factors that shape how messages are sent, received, and interpreted. Understanding these factors can help enhance interactions and build stronger relationships.
- Development. Language, psychosocial, and intellectual development progress through different stages across the lifespan, affecting how individuals communicate and understand information. For example, a nurse may use simpler language and visual aids when explaining a procedure to a young child, compared to a more detailed explanation given to an adult.
- Gender. Communication styles can vary by gender. People often use language to seek confirmation, minimize differences, and establish intimacy, while others may use language to assert independence and negotiate status within a group.
- Values and Perception. Values are the standards that guide behavior, and perceptions are individual interpretations of events. Both significantly influence how messages are understood and responded to. A patient’s cultural background might affect how they perceive pain management suggestions, and a nurse must consider these values when communicating treatment options.
- Personal Space . Personal space refers to the physical distance preferred during interactions. The nurse should be aware of personal space preferences, such as standing closer to a patient when providing emotional support (personal distance) and stepping back during a public health presentation (public distance).
- Territoriality . Territoriality involves the space and objects individuals consider their own. Respecting these boundaries is crucial for effective communication. For example, the should respect a patient’s personal items and space in their hospital room, asking for permission before moving belongings.
- Roles and Relationships. The choice of words, sentence structure, and tone of voice can vary significantly depending on roles and relationships, such as between a nursing student and instructor, a client and primary care provider, or a parent and child. A nursing student might use more formal language and structure when speaking to an instructor, while using a more relaxed tone with peers.
- Environment. People communicate most effectively in comfortable environments. Factors such as noise, privacy, and physical comfort can enhance or hinder communication. A nurse might choose a quiet, private room to discuss sensitive health information with a patient to ensure they feel comfortable and heard.
- Congruence. Congruence refers to the alignment between verbal and nonverbal messages. A nurse teaching a client how to care for a colostomy should ensure their facial expressions and body language convey confidence and reassurance to match their words.
- Interpersonal Attitudes. Attitudes convey beliefs, thoughts, and feelings about people and events. Caring and warmth create a sense of emotional closeness, while respect emphasizes the worth and individuality of others. Acceptance involves receiving another person’s honest feelings without judgment, fostering an open and trusting communication environment. A nurse demonstrates respect and acceptance by listening openly to a patient’s concerns about their treatment plan, even if the nurse has a different opinion.
Communicating with Clients Who Have Special Needs
Effective communication with clients who have special needs requires patience, empathy, and appropriate strategies to ensure their needs are met and understood. Here are tailored approaches for different situations:
When communicating with clients who have difficulty speaking clearly, it’s essential to adapt your communication style to facilitate understanding.
- Listen attentively , be patient, and do not interrupt.
- Ask simple questions that require “yes” or “no” answers.
- Allow time for understanding and response.
- Use visual cues such as words, pictures, and objects.
- Allow only one person to speak at a time to avoid confusion .
- Do not shout or speak too loudly; maintain a calm tone.
- Use communication aids such as a pad and felt-tipped pen, magic slate, pictures denoting basic needs, or call bells.
For clients with cognitive impairments, creating a supportive environment and simplifying communication can enhance understanding.
- Reduce environmental distractions while conversing.
- Get the client’s attention before speaking.
- Use simple sentences and avoid long explanations.
- Ask one question at a time and wait for a response.
- Be an attentive listener to gauge understanding and comfort.
- Include family and friends in conversations, especially about familiar subjects.
Communicating with unresponsive clients requires maintaining respect and providing orientation to help them stay connected.
- Call the client by name during interactions.
- Communicate verbally and by touch to provide comfort and presence.
- Explain all procedures and sensations to keep them informed.
- Provide orientation to person, place, and time regularly.
- Avoid talking about the client to others in their presence.
- Avoid saying things the client should not hear.
To communicate effectively with clients who have hearing impairments, ensure clarity and reduce environmental noise.
- Establish a method of communication such as pen/paper or sign language.
- Pay attention to the client’s non-verbal cues for understanding.
- Decrease background noise such as television or radio.
- Always face the client when speaking to facilitate lip-reading.
- Consult with family on the best ways to communicate with the client.
- Contact appropriate resources for further assistance with communication aids.
When communicating with clients who do not speak English, use translation aids and maintain a respectful tone.
- Speak in a normal tone of voice ; shouting can be perceived as anger.
- Establish a method for the client to signal a desire to communicate (e.g., call light or bell).
- Provide an interpreter or translator as needed.
- Avoid using family members , especially children, as interpreters to maintain professionalism and accuracy.
- Develop communication boards , pictures, or cards to aid understanding.
- Have a dictionary available if the client can read in their language (e.g., English/Spanish).
Several barriers can hinder communication:
- Giving an Opinion. This takes decision-making away from the client. It inhibits spontaneity, stalls problem-solving, and creates doubt.
- Offering False Reassurances. This involves twisting the truth into something that sounds reassuring but is indefinite enough that it could mean anything.
- Being Defensive. Defensive behaviors are usually harmful to both the person doing them and those on the receiving end.
- Showing Approval or Disapproval. Expressing approval can be as harmful to both parties as stating disapproval. Offering unnecessary approval on the other hand implies that the behavior being praised is the only acceptable one.
- Stereotyping. Making assumptions about someone because of factors like race, status, beliefs, etc. The use of stereotypes inhibits communication and threatens the relationship between both parties.
- Changing the Subject Matter Inappropriately. This approach shows lack of empathy. Changing the subject halts the progress of the communication process.
- Language barrier. Conflicting language might occur and the communicators might not be able to understand each other. This can happen in any setting because everyone has their own mother tongue language as well as their own understanding of certain words and phrases.
- Time Barrier. Choosing when to approach an individual to talk to about something is very significant because if you do not choose the appropriate time, the person whom you are trying to convey the message might not be engaged in listening to you.
- Lack of knowledge on the topic . Lack of understanding of the topic would make communication complicated for both the sender and the receiver. Normally, people communicate easier when the topic is something that both of them are familiar with.
- Information overload. Processing information takes time and if communication does not go at a pace where both parties can have sufficient time to carry out their thought process, then it will cause communication breakdown as concentration and attention might be haltered.
Phases of Communication
Effective communication in nursing progresses through distinct phases, each essential for establishing, maintaining, and concluding the nurse-client relationship. Understanding these phases helps nurses provide comprehensive and empathetic care.
During the orientation phase, the tone and guidelines for the relationship between the nurse and client are established. Despite being strangers, each individual brings preconceptions based on previous experiences, attitudes, and beliefs. The parameters of the relationship, such as the place of meeting, length, frequency, roles, confidentiality, and duration, are clearly defined. Trust, respect, honesty, and effective communication are foundational principles at this stage, as the nurse and client begin to know and trust each other as partners in the therapeutic process. For example, a nurse might explain the purpose of a hospital stay, outline daily routines, and ensure the patient understands their rights and responsibilities.
The working phase is the longest phase, where most nursing interventions take place. During this time, problems and issues are identified, and plans to address them are put into action. Positive changes may occur, though they may alternate with resistance or lack of change. Interaction is crucial in this phase, with the nurse validating the client’s thoughts, feelings, and behaviors. The nurse assists the client in exploring their views of self, others, and their environment, as well as feelings of grief , anger, mistrust, and sadness, and behaviors like promiscuity, aggression, withdrawal , and hyperactivity . Although the content to be explored is chosen by the client, the nurse facilitates the process and continues assessment throughout the relationship. Further problems and needs may arise, requiring the nurse to advocate for the client’s perspectives and priorities in the plan of care. The interactions are designed to ensure the achievement of mutually agreed-upon goals and objectives. For instance, a nurse might help a patient with diabetes manage their condition by setting goals for diet and exercise, monitoring blood sugar levels, and providing education on insulin administration.
The termination phase, or resolution phase, is the final stage of the nurse-client relationship. This phase occurs when the initial agreement’s conclusion is acknowledged. After addressing the client’s problems or issues, the relationship must be completed before it can be terminated. The ending is based on mutual understanding and a celebration of goals that have been met, resulting in growth for both the nurse and the client. Termination may bring uncertainty, and both parties must recognize that loss can accompany the end of a relationship. Sharing feelings related to the ending of the therapeutic relationship is important, and validating plans for the future can be a useful strategy. Increased autonomy for both the client and the nurse is recognized during this phase. For example, a nurse might review the progress made during care, ensure the patient knows how to manage their health independently, and provide a summary of follow-up plans before discharge.
Reports are essential exchanges of information among caregivers , ensuring continuity and quality of patient care . They can be oral, written, or audio-recorded. Below are common types of reports used in healthcare:
- Change-of-Shift Report . A comprehensive update provided during shift changes to ensure seamless patient care. This report includes patient status, treatment plans, and any significant events that occurred during the previous shift.
- Telephone Report . Information exchanged via phone, often used for updates or consultations. This type of report is crucial for timely communication between healthcare providers who are not in the same location.
- Telephone or Verbal Orders . Only registered nurses (RNs) are authorized to accept telephone orders, ensuring accuracy and compliance . These orders are typically used in urgent situations and must be documented immediately in the patient’s medical record.
- Transfer Report . Details provided when a patient is transferred from one department or facility to another. This report includes the patient’s current condition, recent treatments, and any specific instructions for continued care.
- Incident Report . Documentation of any unusual or adverse events, such as patient falls or medication errors , to improve future safety and care. These reports are used to analyze incidents and implement measures to prevent recurrence.
Documentation in Nursing
Documentation encompasses any written or printed material relied upon as a record or proof for authorized personnel. It is a vital component of nursing practice , ensuring that patient care is accurately and thoroughly recorded. Effective documentation is characterized by several key attributes.
Accuracy is paramount in documentation, requiring precise and exact recording of patient information. This ensures that every detail of patient care is correctly captured, which is crucial for making informed clinical decisions.
Comprehensiveness in documentation means including all necessary details, from patient history and current condition to treatments administered and patient responses. This thorough approach helps in building a complete picture of the patient’s health status and care needs.
Flexibility is another important aspect, allowing healthcare professionals to retrieve critical data, maintain continuity of care, track patient outcomes , and reflect current standards of nursing practice . Flexible documentation systems adapt to various clinical situations and support efficient information management.
Effective documentation is essential for ensuring continuity of care, saving time, and minimizing the risk of errors. Nurses, as integral members of the healthcare team, must communicate patient information accurately and promptly. Proper documentation prevents fragmented care, reduces task repetition, and avoids delays or omissions in therapy.
Confidentiality is a cornerstone of nursing practice , rooted in both legal and ethical obligations. All recorded, reported, or communicated data must be handled with utmost confidentiality to protect patient privacy and comply with legal and ethical standards. Nurses must safeguard sensitive information, ensuring that only authorized personnel have access. Here are the key principles nurses must follow to maintain client confidentiality:
- Legal and Ethical Obligation . Nurses are required by law and professional ethics to keep all client information confidential.
- Restricted Information Sharing . Nurses must not discuss a client’s examination, observation, conversation, or treatment with anyone not directly involved in the client’s care.
- Access to Records . Only staff members who are directly involved in a specific client’s care have legitimate access to their records.
- Client Rights . Clients have the right to request and read copies of their medical records. Nurses must facilitate this process while ensuring privacy.
- Protection of Records . Nurses are responsible for safeguarding records from unauthorized access. This includes both physical and electronic records.
- Authorized Use. When using records for data gathering, research, or continuing education, nurses and other healthcare professionals must obtain appropriate authorization according to agency policy.
- Professional Behavior . Maintaining confidentiality is essential to professional conduct. Nurses must protect sensitive and private information diligently.
- Prohibition of Gossip . Sharing personal information or gossiping about clients violates nursing ethical codes and practice standards. Such behavior undermines trust and damages interpersonal relationships .
Effective documentation and reporting are essential in nursing to ensure accurate communication, continuity of care, and legal compliance . Here are key guidelines to follow with relevant nursing examples:
- Factual. Quality documentation must be based on descriptive, objective information about what a nurse observes through sight, hearing, touch, and smell . Avoid vague terms like “appears,” “seems,” and “apparently,” as they imply subjective opinions rather than facts. For example, instead of writing, “The client seems anxious,” document specific observations such as, “The client is wringing their hands, has a furrowed brow, and is breathing rapidly at 22 breaths per minute.”
- Accurate. Accuracy involves the use of exact measurements and clear, concise data. This precision helps in providing a clear understanding of the client’s condition and care needs. For example, document “Client’s temperature is 101.4°F (38.6°C)” rather than “Client has a fever ” to provide a precise measurement.
- Complete. Complete documentation includes all relevant and essential information within each recorded entry. Ensure that all necessary details are provided to give a full picture of the client’s condition and care. For example, “The client verbalizes sharp, throbbing pain localized along the lateral side of the right ankle, beginning approximately 15 minutes ago after twisting their foot on the stair. Client rates pain as 8 on a scale of 0-10. Administered 500 mg of acetaminophen orally. Client reports pain reduced to 4 on a scale of 0-10 after 30 minutes.”
- Current. Timeliness is crucial in documentation. Record entries promptly to ensure they reflect the current status of the client and reduce the risk of errors and duplications. For example, immediately document after administering medication: “Administered 2 mg morphine IV at 14:00 for pain rated at 7/10. Client reports pain relief to 3/10 by 14:30.”
- Organized. Organized documentation presents information in a logical and systematic order. This clarity helps in understanding the sequence of events and interventions. For example, an organized note might describe the client’s pain, followed by the nurse’s assessment , the interventions taken, and the client’s response: “Client reports sharp, constant abdominal pain at 8/10. Assessed abdomen, noted rigidity and rebound tenderness in the right lower quadrant. Informed physician, who ordered an abdominal CT scan . Administered 4 mg ondansetron IV for nausea . Client reports pain reduced to 5/10 after 30 minutes, and nausea subsided.”
Adhering to legal guidelines in nursing documentation is crucial for ensuring accuracy, accountability, and patient safety . Here are the key principles to follow, with relevant examples:
- Correcting Errors . Draw a single line through any error, write “error” above it, and sign your name or initials. Then, record the correct information. For example, if you mistakenly document a patient’s heart rate as 80 bpm when it is 90 bpm, draw a line through “80,” write “error,” initial it, and then write “90 bpm.”
- Professional Language. Avoid retaliatory or critical comments about the client or other healthcare professionals. Documentation should remain professional and focused on the facts. For instance, instead of writing “The doctor was rude and unhelpful,” document “Discussed treatment options with Dr. Smith.”
- Objective Descriptions. Enter only objective descriptions of the client’s behavior. For example, quote the client’s exact words when documenting their comments to ensure accuracy. An example is writing, “Client stated, ‘I feel dizzy and can’t keep my balance,'” rather than “Client seems unsteady.”
- Prompt Corrections. Correct all errors promptly to prevent misinterpretation that could lead to errors in treatment. For example, if you realize a mistake in dosage documentation, correct it immediately: “Administered 5 mg morphine at 1400 hrs, not 50 mg.”
- Accurate Charting. Avoid rushing when completing charting . Ensure all information is accurate and thoroughly documented. For instance, take time to accurately document vital signs, medications administered, and patient responses rather than hastily summarizing.
- No Blank Spaces. Do not leave blank spaces in the nurse’s notes. Chart consecutively, line by line. If space is left, draw a line horizontally through it and sign your name at the end to prevent tampering. For example, if there is a blank space at the end of a note, draw a line through it and sign your name.
- Legible Entries. Record all entries legibly and in black ink. Never use pencil or felt pen, as black ink is more legible when records are photocopied or transferred to microfilm. This may vary from agency.
- Clarification of Orders. If an order is questioned, document that clarification was sought. This demonstrates diligence and attention to detail. For example, write, “Clarified with Dr. Jones regarding the dosage of insulin ; confirmed to administer 10 units instead of 100 units.”
- Accountability. Chart only for yourself and never for someone else. You are accountable for the information you enter into the chart. For instance, do not document for a colleague; ensure entries reflect your own observations and actions: “Wound dressing changed by J. Smith, RN .”
- Specific Descriptions. Avoid using generalized, empty phrases such as “status unchanged” or “had a good day.” Provide specific details about the client’s condition and any changes. For example, instead of “Had a good day,” write, “Client ambulated 50 feet with minimal assistance, reported pain level of 2/10.”
- Timeliness. Begin each entry with the time and end with your signature and title. Do not wait until the end of your shift to record important changes that occurred several hours earlier. Sign each entry to authenticate it. For example, “1300 hrs: Administered 500 mg acetaminophen for headache. J. Smith, RN.”
- Computer Documentation. Keep your computer documentation password secure and never share it. Maintain security and confidentiality by not leaving the computer screen unattended once logged in. For example, log out of the electronic health record system if you need to step away, even briefly, to ensure patient information remains secure.
1 thought on “Communication in Nursing: Documentation and Reporting”
Good and well defined notes
Leave a Comment Cancel reply
30 Top Therapeutic Communication Techniques in Nursing + How to Use Them

Nurses interact with people every day. Whether you talk with patients, family members, nurses, or other healthcare providers, it is vital for nurses to develop effective communication skills that promote favorable outcomes for patients and the healthcare team. Therapeutic communication should be at the core of every nurse-patient, nurse-caregiver, or interdisciplinary team relationship. Perhaps you are wondering, “What is therapeutic communication in nursing?” In this article, I will answer that question and provide you with examples of how to develop therapeutic communication skills. As you continue reading, you will find the 30 top therapeutic communication techniques in nursing + how to use them.
What is Therapeutic Communication in Nursing?
What is the difference between therapeutic and non-therapeutic communication in nursing, when do nurses engage in therapeutic communication, 5 reasons why therapeutic communication is important in nursing, what are the five 5 essential components of therapeutic communication in nursing, 1. respect for the patient’s values and beliefs:, 3. patience:, 4. honesty:, 5. compassion:, 6 key skills required to successfully engage in nursing therapeutic communication, 1. verbal communication:, 2. nonverbal communication:, 3. written communication:, 4. patient education:, 5. make personal connections:, 6. learn to be culturally aware:, what are the top therapeutic communication techniques in nursing, technique #1: using active listening, why this technique works:, how to use this technique:, technique #2: seek clarification, technique #3: give broad openings and use open-ended sentences, technique #4: use time and/or sequence, technique #5: know when to be silent, technique #6 : give the patient recognition, technique #7: use observation skills, technique #8: encourage the patient to use comparisons, technique #9: focus, technique #10: summarize, technique #11: reflect, technique #12: use touch, technique #13: confronting, technique #14: be available, technique #15: offer hope, technique #16: find and share humor, technique #17: voice doubt, when appropriate, technique #18: encourage patients to describe their feelings, technique #19: suggest options (not medical advice), technique #20: use general leads, technique #21: offer acceptance, technique #22: exploration, technique #23: rephrase what the patient says, technique #24: verify impressions of what the patient says, technique #25: present reality, technique #26: share personal experiences, technique #27: asking patients to describe their perception of a situation/event, technique #28: attempt to translate what the patient says in the form of his feelings, technique #29: show empathy, technique #30: encourage participation in care planning, 15 non-therapeutic communication techniques nurses should avoid, 1. asking irrelevant personal questions:, 2. using stereotypical comments or cliches:, 3. giving unsolicited personal opinions:, 4. changing the subject:, 5. pressuring the patient:, 6. imposing the nurse’s approval or disapproval about a patient’s choice:, 7. arguing with the patient:, 8. using passive responses:, 9. giving aggressive or defensive responses:, 10. questioning the patient “why”:, 11. imposing sympathy:, 12. underloading:, 13. making the patient feel like what he is saying is not important:, 14. offering false reassurances:, 15. incongruence:, 7 most-common barriers to therapeutic communication in nursing and how to overcome them, barrier #1: physical barriers, about the barrier:, how to overcome:, barrier #2: language barriers, barrier #3: information overload, barrier #4: avoiding eye contact, barrier #5: talking too much, barrier #6: not being prepared, barrier #7: allowing personal conflicts to affect your outlook, bonus 5 expert tips to help nurses improve their therapeutic communication skills, 1. learn to use nonverbal signs to show you are listening:, 2. become a reader:, 3. learn to use your peripheral vision:, 4. be aware of how you demonstrate nonverbal communication:, 5. respect your patient's decisions:, my final thoughts, frequently asked questions answered by our expert, 1. what is the main goal of therapeutic communication in nursing, 2. is nursing therapeutic communication an intervention, 3. what is constructive criticism in nursing therapeutic communication, 4. is therapeutic communication necessary for all types of nurses, 5. which nurse would most likely be the best therapeutic communicator, 6. how do nursing schools teach therapeutic communication, 7. how does body language play a role in therapeutic communication in nursing, 8. how does therapeutic communication affect patient care, 9. how do nurses communicate therapeutically with alcoholic patients, 10. how to therapeutically communicate with pediatric patients, 11. is empathy a nursing therapeutic communication technique, 12. which communication technique is demonstrated when the nurse connects with a patient on a social level, 13. are there any disadvantages of therapeutic communication in nursing, 14. what happens when nursing therapeutic communication fails.

3.1 Therapeutic Communication
Learning objectives.
By the end of this section, you will be able to:
- Describe the process of therapeutic communication in nursing
- Identify characteristics of effective therapeutic communication
- Recognize how to evaluate therapeutic communication
Effective patient communication generates an increase in positive outcomes. These positive outcomes may include but are not limited to improvements in a patient’s compliance with medical plans, self-regulation of diet and medications, and coping mechanisms. These outcomes improve the patient's functional status after treatment.
For example, chronic diseases are especially impacted by improved patient relationships and communication with healthcare providers, due to the complex nature of chronic diseases and the need for extensive treatment. High blood pressure, or hypertension , is a chronic illness that requires scheduled follow up visits. A patient who considers themself healthy, eats a balanced diet, and works out regularly might be very disheartened with this diagnosis. This patient will need to have a solid relationship with their nurse to navigate disease management, lifestyle adjustments, and possible mental health issues they might develop from feeling like “their body betrayed them.” Furthermore, this and every patient who receives a chronic diagnosis or life-altering health news depends on their nurse to serve as a healthcare guide. This role requires effective patient communication.
The specific techniques and strategies nurses use to establish a therapeutic relationship with patients and promote the patient’s well-being is referred to as therapeutic communication . Therapeutic communication techniques used by nurses have roots going back to Florence Nightingale , who insisted on the importance of building trusting relationships with patients and believed in the therapeutic healing that resulted from nurses’ presence with patients. Since then, several professional nursing associations have highlighted therapeutic communication as one of the most vital elements in nursing.
Therapeutic communication is a vital skill in nursing for multiple reasons. It can help establish a trusting patient-nurse relationship, prevent misunderstandings and errors, promote patient-centered care, improve patient satisfaction, and improve outcomes (Slade & Sergent, 2023). Nurses should understand and practice various therapeutic techniques as part of providing the best possible nursing care.
Process of Therapeutic Communication in Nursing
Establishing the therapeutic nurse-patient relationship is vital in nursing care. Nurses engage in compassionate, supportive, professional relationships with their patients as part of the art of nursing. This is especially true in psychiatric care, where the therapeutic relationship is considered the foundation of patient care and healing. The nurse-patient relationship establishes trust and rapport with a specific purpose; it facilitates therapeutic communication and engages the patient in decision-making regarding their plan of care.
Therapeutic nurse-patient relationships vary in depth, length, and focus. Brief therapeutic encounters might last only a few minutes and focus on the patient’s immediate needs, current feelings, or behaviors. For example, in the emergency department setting, a nurse may therapeutically communicate with a patient in crisis who recently experienced a situational trauma. During longer periods of time, such as inpatient care, nurses work with patients in setting short-term goals and outcomes that are documented in the nursing care plan and evaluated regularly. In long-term care settings, such as residential facilities, the therapeutic nurse-patient relationship may last several months, or even years, and include frequent interactions focusing on behavior modification. Whether the relationship is brief or longer-term, each therapeutic interaction is built on the same basic framework.
Clinical Safety and Procedures (QSEN)
Qsen competency: patient communication.
See the competency checklist for Patient Communication. You can find the checklists on the Student resources tab of your book page on openstax.org.
Develop Communication Goals
Developing communication goals is a crucial first step in establishing a therapeutic relationship with a patient. Part of developing communication goals is assessing the patient's communication needs. This may involve reviewing the patient's medical history, identifying any communication barriers, and assessing the patient's emotional and cognitive status.
Based on the patient's needs, specific communication goals can be established. When developing these communication goals, think of the acronym SMART . SMART stands for specific, measurable, attainable, relevant, and timely ( Figure 3.2 ). For example, a nurse may have as a general goal to spend more time with their patients. A SMART goal would be “I will spend an extra 15 minutes with Mrs. Cabrillo this morning and ask her three questions about her home environment in order to determine what kind of support system she has there.”
Create the Message
Once the nurse has identified goals, they can develop a plan to achieve them. The nurse must create a message to present to the patient in a way that benefits the therapeutic communication process and the patient. The message is the thought or content that someone wishes to convey. This involves selecting the appropriate communication techniques based on the patient’s language or other factors that may affect their ability to receive information, such as with a hearing, sensory, or vision impairment. Communication strategies may be based on the patient’s cognitive abilities, educational levels, cultural preferences, or other factors. It is the responsibility of the nurse to know as much as possible about these details in advance of the interaction with the patient.
Deliver the Message
Delivering the message is a key aspect of therapeutic communication. It involves conveying information in a clear, supportive, and respectful manner, using appropriate verbal and nonverbal communication skills. The verbal communication involves the use of words to deliver a message. On the other hand, nonverbal communication refers to conveying a message without the use of words ( Figure 3.3 ). Nonverbal communication can involve such qualities as facial expression, body language, tone of voice, and personal space.
To deliver the message effectively, nurses should use a clear tone and plain language, be mindful of the patient’s body language, use the patient’s preferred language so they understand, actively listen to the patient, and demonstrate patience and respect throughout the conversation. Additional considerations may be needed to reiterate and reinforce key points. Nurses should use visuals (as applicable), demonstrate empathy , encourage active two-way communication, and adapt the communication style to be culturally appropriate. When verbal communication signals match nonverbal communication signals, it can help increase the level of trust and comfort between the patient and nurse. As the nurse conducts a conversation, it is important for them to continually practice and evaluate the communication techniques being used.
Listen to the Response
Therapeutic communication is not a one-way process; delivering the message is only part of the task. The nurse must also listen to the patient, seeking feedback in the form of both verbal and nonverbal communication. This may involve asking directly for feedback from the patient or observing their nonverbal responses to different techniques used during the conversation.
Seek Clarification of the Response
The nurse should clarify any indirect, unclear, or ambiguous responses with the patient when possible. For example, a nurse may ask a patient if they eat a special diet when they are performing the admission assessment, and the patient responds “no,” but their tone sounds angry and they suddenly become quiet. A question such as “I noticed that your arms are crossed and you have stopped talking; are you upset?” can help clarify nonverbal communication from the patient. Based on the feedback received, adjust the plan as needed to better meet the patient's communication needs and achieve the established goals.
Characteristics of Effective Therapeutic Communication
Effective therapeutic communication is crucial to delivering high-quality healthcare. It is a skilled approach to caring for patients that requires training and education. There are numerous strategies that can be classified as either therapeutic or nontherapeutic approaches to communication.
Therapeutic communication requires respect, trust, empathy, and a nonjudgmental culturally aware approach from the nurse. Other key characteristics of therapeutic communication include active listening , clarity and simplicity, openness and honesty, encouragement, a supportive environment, a patient-centered approach, positive reinforcement, and appropriate use of silence. Nurses who incorporate these elements in their communication style can enhance patient outcomes and provide better quality care.
Patient Conversations
A therapeutic conversation with a nervous patient.
Scenario: The nurse enters the patient’s room to complete their morning assessment and notices nonverbal communication from the patient.
Nurse: Good morning, Ali. How are you feeling today?
Patient: Not so good, my pain is still bothering me.
Nurse: I’m sorry to hear that. Can you tell me more about your pain?
Patient: It’s a sharp pain in my lower back, and it gets worse when I try to move. It’s about a 7 out of 10.
Nurse: I see. Have you been taking your pain medication that the doctor ordered?
Patient: No, I don’t like the way it makes me feel.
Nurse: I understand. Can you tell me what it is that you don’t like?
Patient: They make me feel dizzy and sleepy.
Nurse: Hm. Well let’s see if we can try some other strategies to help manage your pain. Have you tried any relaxation techniques, like deep breathing or meditation?
Patient: No, I haven’t.
Nurse: Well, those techniques can be really helpful for managing pain. I can show you some exercises that might work for you. And we can also talk to your doctor about adjusting your medication if necessary.
Patient: Okay, that sounds good.
Nurse: Great. Let’s start with some breathing exercises. I’ll guide you through them, and you can let me know how it feels.
Patient: Okay, thank you.
Build Trust Through Honesty
A trusting nurse-patient relationship can lead to increased adherence to the treatment plan and improved outcomes. Also, a patient who trusts their interviewer is more likely to communicate personal and private information regarding themselves and their lifestyle. The nurse can build a trusting relationship through admitting mistakes/errors, honoring patient’s autonomy and choices, finding unknown answers and following up to close the loop, providing realistic expectations, building rapport, demonstrating consistent behavior, and encouraging open communication.
Another way to create a safe and trusting space for patients is by being transparent. Having transparency means being open and honest with the patient about their health conditions, treatment options, and potential outcomes. It also involves educating the patient on these issues and options in plain language that is readily understandable by the patient, including using a translator if necessary.
Keeping promises is another way to build trust through honesty with patients. For example, if the nurse tells the patient they will return in one hour with their pain medication, they should try their best to keep their promise to their patient in order to foster a pattern of trust.
Active Listening
Listening is obviously an important part of communication. There are three main types of listening: competitive, passive, and active. During competitive listening we are focused on sharing our own point of view instead of listening to someone else. During passive listening we are not interested in listening to the other person and we assume we understand what the person is communicating, without verifying the other person’s message . During active listening , we are communicating verbally and nonverbally that we are interested in what the other person is saying while also actively verifying with the speaker that we understand. For example, an active listening technique is to restate what the person said and then verify our understanding is correct. This feedback process is the main difference between passive listening and active listening.
Active listening involves fully focusing on and understanding the message being conveyed by the speaker. It requires paying close attention to both verbal and nonverbal cues, such as tone of voice, body language, and facial expressions, and responding appropriately to the speaker’s message. Active listening involves withholding judgment and providing feedback, without interruption to the speaker, that shows the speaker that they have been heard and understood. This technique is important in building and maintaining effective communication and relationships, as it helps to create an environment where individuals feel heard, valued, and understood.
Non verbal communication is an important component of active listening. SOLER is a mnemonic for establishing good nonverbal communication with patients. SOLER stands for the following:
- S: Sitting and squarely facing the patient
- O: Using open posture (such as avoiding crossing arms)
- L: Leaning toward the patient to indicate interest in listening
- E: Maintaining good eye contact
- R: Maintaining a relaxed posture
Link to Learning
This brief video shows examples of active listening as well as strategies for demonstrating the skill.
Respect the Patient’s Values and Beliefs
According to the American Nurses Association (ANA) Code of Ethics (2015), nurses must practice with cultural humility and inclusiveness (ANA, 2015). Cultural humility is a lifelong process where one examines their own cultural beliefs and practices as well as adopts a humble and respectful attitude while learning about individuals of other cultures. Culture is constantly changing and evolving, so true cultural competence requires a lifetime of learning and adapting to these changes. It is important for the nurse to accept their own cultural beliefs, as well as their patient’s when building a trusting relationship.
There are both intrapersonal and interpersonal components to cultural humility (Hughes et al., 2020). The intrapersonal component consists of a personal awareness of one’s own limited knowledge of the patient’s culture. The interpersonal component involves a respect for the patient’s culture and openness to their beliefs and experiences. By focusing on developing partnerships with patients, the nurse can create a space that encourages learning and appreciation for other cultures. It is a patient-centered way of providing culturally sensitive care.
Cultural Awareness
An individual’s cultural background influences their beliefs, feelings, and attitudes toward health care. Their culture determines how they view health and illness, which in turn shapes how they view healthcare providers and how receptive they are to their treatment plans. Culture also determines who receives care and the quality of their care. Certain cultures experience higher rates of disease due to genetics or health disparities caused by socioeconomic factors. Various cultures have their own traditional healing practices and beliefs, and many people still use these practices, either alongside or in place of Western medicine. Nurses face patients from different cultures with their own beliefs and practices. Cultural awareness is the recognition of the characteristics of one’s own culture and other people’s, and of the differences between cultures. It is important that nurses be respectful of these individual differences in order to counteract any biases so that patients can receive the best possible care.
To ensure patients feel respected and heard, healthcare professionals should actively listen to their patients, respect cultural practices, ask open-ended questions, and use nonjudgmental language. They should also be aware of their own biases and avoid imposing their beliefs or values on patients.
Cultural Context
Providing culturally sensitive care.
One way the nurse can show cultural sensitivity is by safely incorporating elements of the patients’ culture into their care. The nurse will speak with the patient and try to identify a cultural norm that can be safely integrated into the patients’ prescribed plan of care. An example of this could be in allowing the patients’ newborn baby to be wrapped in a special blanket that does not have animals on it. Another example might be the nurse showing respect of the Judaism practice of waiting until the eighth day of life for circumcision to take place. This allows the patient to feel safe that their baby’s soul will not be stolen by the animals. While this practice might seem confusing to the nurse, a culturally sensitive nurse will see this as an opportunity to safely incorporate the patients’ belief into their care.
Show Compassion
In addition to the therapeutic techniques listed in Table 3.1 , nurses should genuinely communicate with empathy . Communicating honestly, genuinely, and authentically is powerful. It opens the door to creating true connections with others. Communicating with empathy has also been described as communicating with emotion. Research has demonstrated that when healthcare teams communicate with empathy, there is improved patient healing, reduced symptoms of depression, and decreased medical errors.
| Techniques | Description |
|---|---|
| Using Silence | At times, it’s useful to not speak at all. Deliberate silence can give both nurses and patients an opportunity to think through and process what comes next in the conversation. It may give patients the time and space they need to broach a new topic. |
| Accepting | Sometimes it is important to acknowledge a patient’s message and affirm that they’ve been heard. Acceptance isn’t necessarily the same thing as agreement; it can be enough to simply make eye contact and say, “Yes, I hear what you are saying.” Patients who feel their nurses are listening to them and taking them seriously are more likely to be receptive to care. |
| Giving Recognition | Recognition acknowledges a patient’s behavior and highlights it. For example, saying something such as “I noticed you took all of your medications today” draws attention to the action and encourages it. |
| Offering Self | Hospital stays can be lonely and stressful at times. When nurses are present with their patients, it shows patients they value them and are willing to give them time and attention. Offering to simply sit with patients for a few minutes is a powerful way to create a caring connection. |
| Giving Broad Openings/ Open-Ended Questions | Therapeutic communication is often most effective when patients direct the flow of conversation and decide what to talk about. To that end, giving patients a broad opening such as “What’s on your mind today?” or “What would you like to talk about?” can be a good way to allow patients an opportunity to discuss what’s on their mind. |
| Seeking Clarification | Similar to active listening, asking patients for clarification when they say something confusing or ambiguous is important. Saying something such as “I’m not sure I understand. Can you explain it to me?” helps nurses ensure they understand what’s actually being said and can help patients process their ideas more thoroughly. |
| Placing the Event in Time or Sequence | Asking questions about when certain events occurred in relation to other events can help patients (and nurses) get a clearer sense of the whole picture. It forces patients to think about the sequence of events and may prompt them to remember something they otherwise wouldn’t. |
| Making Observations | Observations about the appearance, demeanor, or behavior of patients can help draw attention to areas that may indicate a problem. Observing that they look tired may prompt patients to explain why they haven’t been getting much sleep lately, or making an observation that they haven’t been eating much may lead to the discovery of a new symptom. |
| Encouraging Descriptions of Perception | For patients experiencing sensory issues or hallucinations, it can be helpful to ask about these perceptions in an encouraging, nonjudgmental way. Phrases such as “What do you hear now?” or “What does that look like to you?” give patients a prompt to explain what they’re perceiving without casting their perceptions in a negative light. |
| Encouraging Comparisons | Patients often draw upon previous experiences to deal with current problems. By encouraging them to make comparisons to situations they have coped with before, nurses can help patients discover solutions to their problems. |
| Summarizing | It is often useful to summarize what patients have said. This practice demonstrates to patients that the nurse was listening and allows the nurse to verify information. Ending a summary with a phrase such as “Does that sound correct?” gives patients explicit permission to make corrections if they’re necessary. Reflecting patients often ask nurses for advice about what they should do about particular problems. Nurses can ask patients what they think they should do, which encourages patients to be accountable for their own actions and helps them come up with solutions themselves. |
| Focusing | Sometimes during a conversation, patients mention something particularly important. When this happens, nurses can focus on the important statement, prompting patients to discuss it further. Patients don’t always have an objective perspective on what is relevant to their case, but as impartial observers, nurses can more easily pick out the topics on which to focus. |
| Confronting | Nurses should only apply this technique after they have established trust. In some situations, it can be vital to the care of patients to disagree with them, present them with reality, or challenge their assumptions. Confrontation, when used correctly, can help patients break destructive routines or understand the state of their current situation. |
| Voicing Doubt | Voicing doubt can be a gentler way to call attention to incorrect or delusional ideas and perceptions of patients. By expressing doubt, nurses can force patients to examine their assumptions. |
| Offering Hope and Humor | Because hospitals can be stressful places for patients, sharing hope that patients can persevere through their current situation and lightening the mood with humor can help nurses establish rapport quickly. This technique can keep patients in a more positive state of mind. However, it is important to tailor humor to the patient’s sense of humor. |
Nontherapeutic Communication
Communication patterns or techniques that have negative effects on the development of a therapeutic relationship are referred to as nontherapeutic communication . It can also have negative effects on the patient’s well-being. Nontherapeutic communication can include behaviors such as interrupting the patient, giving personal opinions or advice without being asked, using judgmental or dismissive language, being insensitive to cultural or individual differences, or failing to provide adequate emotional support. These communication patterns may lead to misunderstandings, increased anxiety, decreased trust, and diminished patient satisfaction. Nurses must be aware of these types of potential barriers to communication. There are several nontherapeutic responses to avoid. Table 3.2 lists responses that often block the patient’s communication of their feelings or ideas.
| Response | Why It Is Nontherapeutic |
|---|---|
| Asking Personal Questions | Asking personal questions that are not relevant to the situation is not professional or appropriate. Don’t ask questions just to satisfy your curiosity. For example, asking, “Why have you and Mary never married?” is not appropriate. A more therapeutic question would be, “How would you describe your relationship with Mary?” |
| Giving Personal Opinions | Giving personal opinions takes away the decision-making from the patient. Effective problem-solving must be accomplished by the patient, not the nurse. For example, stating, “If I were you, I’d put your father in a nursing home” is not therapeutic. Instead, it is more therapeutic to say, “Let’s talk about what options are available to your father.” |
| Changing the Subject | Changing the subject when someone is trying to communicate with you demonstrates a lack of empathy and blocks further communication. It seems to say that you don’t care about what the person is sharing. For example, stating, “Let’s not talk about your insurance problems; it’s time for your walk now” is not therapeutic. A more therapeutic response would be, “After your walk, let’s talk some more about what’s going on with your insurance company.” |
| Stating Generalizations and Stereotypes | Generalizations and stereotypes can threaten nurse-patient relationships. For example, it is not therapeutic to state the stereotype, “Older adults are often confused.” It is better to focus on the patient’s concern and ask, “Tell me more about your concerns about your father’s confusion.” |
| Providing False Reassurances | When a patient is seriously ill or distressed, the nurse may be tempted to offer hope with statements such as, “You’ll be fine” or “Don’t worry; everything will be all right.” These comments tend to discourage further expressions of feelings by the patient. Here is a more therapeutic response: “It must be difficult not to know what the surgeon will find. What can I do to help?” |
| Showing Sympathy | Sympathy focuses on the nurse’s feelings rather than the patient’s. A statement like, “I’m so sorry about your amputation; I can’t imagine losing a leg.” shows pity rather than trying to help the patient cope with the situation. A more therapeutic response would be, “The loss of your leg is a major change; how do you think this will affect your life?” |
| Asking “Why” Questions | A nurse may be tempted to ask the patient to explain “why” they believe, feel, or act in a certain way. However, patients and family members may interpret “why” questions as accusations and become defensive. It is best to phrase a question by avoiding the word “why.” For example, instead of asking, “Why are you so upset?” it is better to rephrase the statement as, “You seem upset. What’s on your mind?” |
| Approving or Disapproving | Nurses should not impose their own attitudes, values, beliefs, and moral standards on others while in the professional nursing role. Judgmental messages contain terms such as “should,” “shouldn’t,” “ought to,” “good,” “bad,” “right,” or “wrong.” Agreeing or disagreeing sends the subtle message that nurses have the right to make value judgments about the patient’s decisions. Approving implies that the behavior being praised is the only acceptable one, and disapproving implies that the patient must meet the nurse’s expectations or standards. Instead, the nurse should help the patient explore their own beliefs and decisions. For example, it is nontherapeutic to state, “You shouldn’t consider elective surgery; there are too many risks involved.” A more therapeutic response would be, “So you are considering elective surgery. Tell me more about it.” This gives the patient a chance to express their ideas or feelings without fear of being judged. |
Evaluating the Effectiveness of Therapeutic Communication
As discussed previously, therapeutic communication is defined as the specific techniques and strategies nurses use to establish a therapeutic relationship with patients and promote the patient’s well-being. Therefore, the general goal of every therapeutic interaction between a nurse and patient is the mutual exchange of information that leads to a new understanding on the part of the patient. After every therapeutic communication, the nurse must evaluate the interaction for its effectiveness in order to determine if more education or assistance is needed. Sometimes, specific phrases are encouraged for use at the end of the conversation. “Is there anything else I can do for you? I have the time.” is one such phrase that is encouraged. It allows the patient to ask for any additional assistance while showing that the nurse is present and available. The hope is that patients feel heard and attended to by their healthcare providers.
Reflect on Response
Nonverbal cues such as the patient’s general mood can be an indicator of how they are feeling about an interaction. If the patient’s body language indicates that they might be angry, scared, or upset, ask them about it. Using therapeutic techniques, talk to the patient and try to find out why they are feeling negatively about the interaction.
If the goal of the conversation has been met, seek feedback directly from the patient. Ask if the conversation was helpful for them. Specific questions to ask patients might include:
- What concerns do you have about your plan of care?
- What questions do you have about your medications?
- Did I answer your question(s) clearly or is there additional information you would like?
Listen closely for feedback from patients. Feedback provides an opportunity to improve patient understanding, improve the patient-care experience, and provide high-quality care.
Compare Response to Desired Communication Goals
The best way to determine patient understanding of the conversation is to use the teach-back method . In order to judge their level of understanding, have the patient re-state to you, in their own words, your original message . Then, compare the patient’s understanding of the therapeutic communication with the original communication goals. Remember that a SMART goal should be set prior to a therapeutic communication in order to provide specific details to guide the interaction ( Table 3.3 ). This goal will not always be met, even if the nurse and patient get along and communicate well. The important thing is to determine if the goal was met, and if not, what prevented it.
| SMART Goal | Action/Response | Met/Not Met |
|---|---|---|
| The patient will notify the nurse promptly for pain intensity level that is greater than their comfort-function goal throughout shift. | The patient called for pain management for a pain level of 4/10 during the shift. | Met |
| The patient’s blood pressure and heart rate will return to baseline levels by the end of the shift. | During last round of shift, patients’ vital signs included: Heart Rate 104 B/P 114/74 | Met |
| The patient will identify and perform preferred actions to ensure adequate sleep by discharge. | The patient verbalized techniques for healthy sleep promotion, including decreasing stimulation by turning TV off and using soft ambient lights. | Not Met- Patient identified actions to promote quality sleep but did not perform these actions. At midnight the patient had overhead room lights on, the TV was loud, and four friends were at the bedside. |
| The patient will demonstrate appropriate use of adaptive equipment (e.g., a walker) for safe ambulation by the end of the shift. | Patient demonstrated use of walker to ambulate to bedside chair and again when returning to bed. | Met |
QSEN Competency: Using the Teach-Back Method
See the competency checklist for Using the Teach-Back Method. You can find the checklists on the Student resources tab of your book page on openstax.org.
This Use the Teach-Back Method sheet describes how nurses can incorporate plain language, teach-back, and coaching to promote consistent use of teach-back when educating patients.
Revise Message if Communication Ineffective
If the therapeutic communication proves ineffective, the first step is to attempt to determine why. It could be due to nontherapeutic communication techniques from the nurse or an emotional response from the patient. Explore and address any communication barriers, as well as any patient concerns. If necessary, revise and redeliver the goal message .
An example of a nurse encountering a therapeutic barrier is when the nurse asks the patient about their pain control. “Are you in pain? What about when you’re walking around? The medication should help you with that.” The nurse asks these questions while typing on the computer and looking at the screen. The patient responds, “No it’s fine. I’ll be all right.” The nurse should realize that they have met a communication barrier. They asked several questions without waiting for a response; they also suggested a response for the patient, and they did not make eye contact with the patient. In order to fix this, the nurse can close the computer screen and sit at the patient’s bedside; make eye contact; ask one question at a time; and wait for the patient’s response before continuing. This scenario shows that sometimes it is necessary for the nurse to rephrase their questions or messages and deliver them in a different way to elicit a more detailed patient response.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/clinical-nursing-skills/pages/1-introduction
- Authors: Christy Bowen
- Publisher/website: OpenStax
- Book title: Clinical Nursing Skills
- Publication date: Jun 26, 2024
- Location: Houston, Texas
- Book URL: https://openstax.org/books/clinical-nursing-skills/pages/1-introduction
- Section URL: https://openstax.org/books/clinical-nursing-skills/pages/3-1-therapeutic-communication
© Jun 25, 2024 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
3.2 Communication
Effective communication is a vital component of effective assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA). [1]
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1 for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
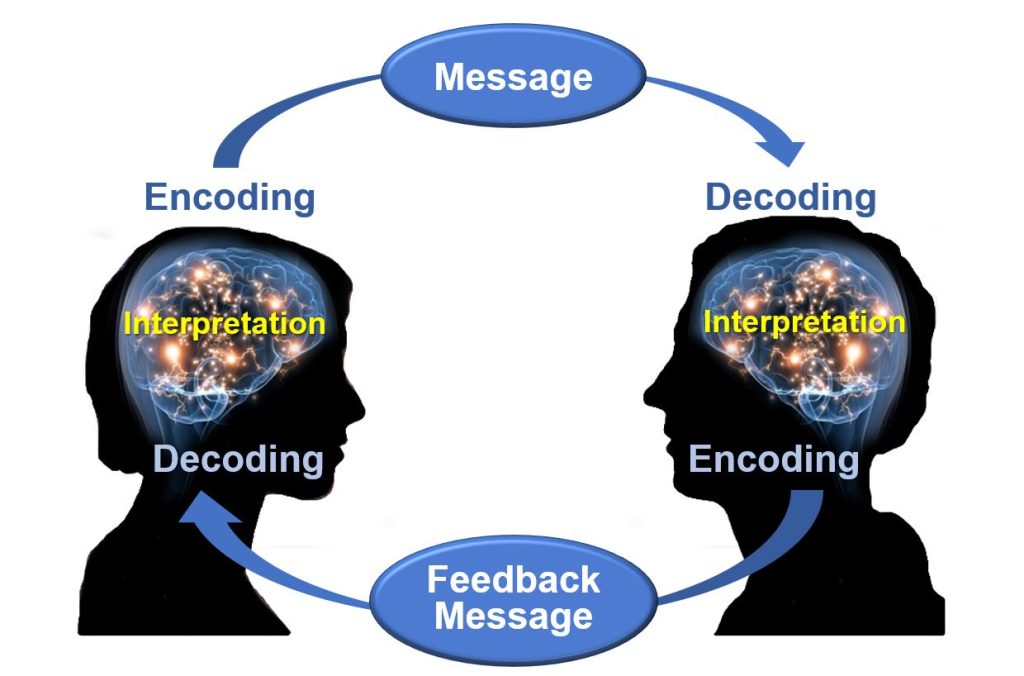
Closed-loop communication is vital for communication among health care team members to avoid misunderstanding that can cause unsafe client care. According to the HIPAA Journal , poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.” [2] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. Expressing clarity when providing direction is integral. A lack of clarity will lead to misunderstanding, unfinished tasks, incomplete care, and medical errors. [3]
Effective communication is at the heart of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and patients’ needs often change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift:
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task but excessive or irrelevant information should be avoided. Excessive or irrelevant information can confuse the listener and waste precious time.
- Correct: Correct communication is not cloudy or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act.
- Complete: Complete instructions leave no room for doubt. Assuming a nursing team member knows what to do and how to do it, along with what information to report and when, can create havoc and frustration for both staff and clients. [4]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider during a medical emergency. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN carrying out the order confirms hearing, understanding, and completing the order by repeating back, “Epinephrine 1 mg/mL IV push was given now.” Health care team members participating in this verbal exchange of information ensure unit functioning while also focusing on achieving desired client outcomes.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- HIPAA Journal. (n.d.). Effects of poor communication in healthcare. https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/ ↵
- LaCharity, L. A., Kumagai, C. K., & Bartz, B. (2019). Prioritization, delegation and assignment (4th ed.). Mosby, p. 6. ↵
A process that enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly.
Leadership and Management of Nursing Care Copyright © 2022 by Kim Belcik and Open Resources for Nursing is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book

3.2 Communication
Effective communication is a vital component of proper assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA). [1] Research has identified that new graduate nurses are more susceptible to stress and isolation within their job roles due to poor communication and teamwork within the interdisciplinary team. [2] Strong communication skills foster a supportive work environment and colleagial relationships that benefit both clients and nursing staff.
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1 [3] for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
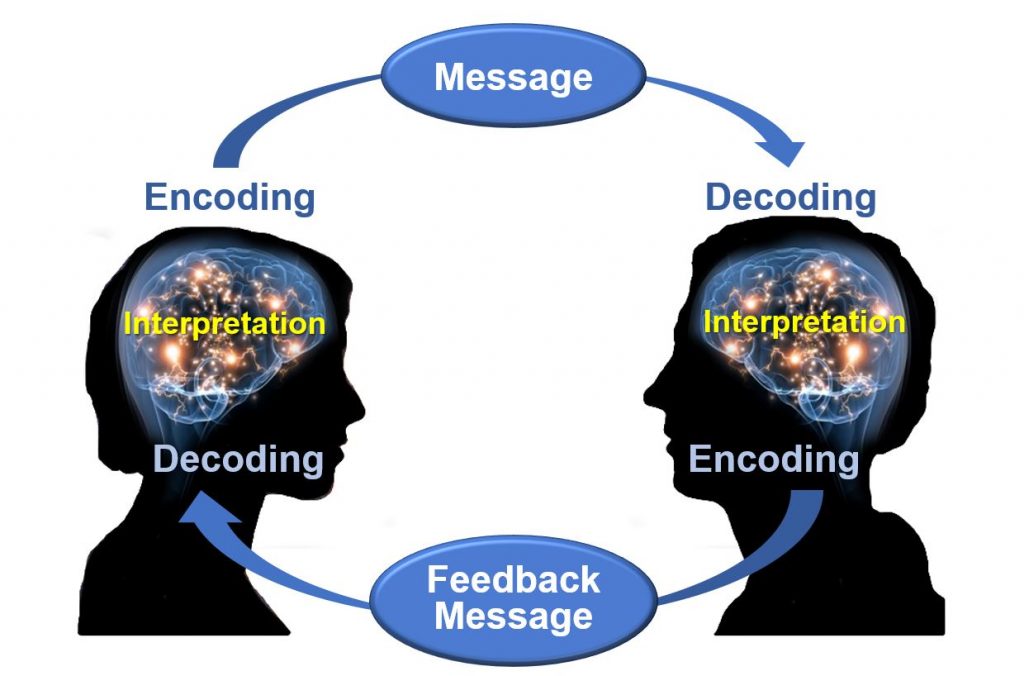
Closed-loop communication is vital for communication among health care team members to avoid misunderstandings that can cause unsafe client care. According to the HIPAA Journal , poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.” [4] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. It is imperative for the RN to provide clear, complete, concise instructions when delegating. A lack of clarity can lead to misunderstanding, unfinished tasks, incomplete care, and/or medical errors. [5]
Effective communication is at the core of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and clients’ needs change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift. These communication characteristics can be remembered by using the mnemonic the “4 Cs”:
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task, but excessive or irrelevant information should be avoided because it can confuse the listener and waste precious time.
- Correct: Correct communication is not vague or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act and other state regulations.
- Complete: Complete instructions leave no room for doubt. Always ask if further information or clarification is needed, especially regarding tasks that are infrequently performed or include unique instructions. [6]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN confirms correct understanding of the order by repeating back, “I will prepare Epinephrine 1 mg/mL to be given IV push now.” After the provider confirms the verbal order and the task is completed, the nurse confirms completion of the task by stating, “Epinephrine 1 mg/mL IV push was administered.”
In addition to using closed-loop communication, a common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of I ntroduction, S ituation, B ackground, A ssessment, R equest/Recommendations, and R epeat Back. ISBARR and other communication strategies are discussed in more detail in the “ Interprofessional Communication ” section of the “Collaboration Within the Interprofessional Team” chapter.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Leonard, J.C., Whiteman, K., Stephens, K., Henry, C., Swanson-Bieaman, B. (2022). Imporving communication and collaboration skills in graduate nurses: An evidence-based approach. The Online Journal of Issues in Nursing, 27 (2), 3. https://www.doi.org/10.3912/OJIN.Vol27No02Man03 ↵
- “Osgood-Schramm-model-of-communication.jpg” by Jordan Smith at eCampus Ontario is licensed under CC BY 4.0 . Access for free at https://ecampusontario.pressbooks.pub/communicationatwork/chapter/1-3-the-communication-process/ ↵
- HIPAA Journal. (n.d.). Effects of poor communication in healthcare. https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/ ↵
- LaCharity, L. A., Kumagai, C. K., & Bartz, B. (2019). Prioritization, delegation and assignment (4th ed.). Mosby, p. 6. ↵
A process that enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly.
Nursing Management and Professional Concepts 2e Copyright © by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Nursing
Effective Communication in Nursing
Submitted: 27 October 2017 Reviewed: 06 February 2018 Published: 21 March 2018
DOI: 10.5772/intechopen.74995
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Edited by Nilgun Ulutasdemir
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
13,007 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Nurses are critical in the delivery of essential health services and are core in strengthening the health system. They bring people-centred care closer to the communities where they are needed most, thereby helping improve health outcomes and the overall cost-effectiveness of services. Nurses usually act as first responders to complex humanitarian crises and disasters; protectors and advocates for the community and communicators and co-ordinators within teams. Communication is a core component of sound relationships, collaboration and co-operation, which in turn are essential aspects of professional practice. The quality of communication in interactions between nurses and patients has a major influence on patient outcomes. Increases in nursing communication can lessen medical errors and make a difference in positive patient outcomes. This chapter explores how effective communication and interpersonal skills can enhance professional nursing practice and nursing relationships with various stakeholders. It explains principles of communication, communication process, purpose of communication, types of communication, barriers to effective communication, models of communication and strategies of improving communication and guidelines for successful therapeutic interactions.
- communication
- communication skills
- non-verbal communication
- nurse–patient relationship
- nursing verbal communication
Author Information
Maureen nokuthula sibiya *.
- Durban University of Technology, Durban, South Africa
*Address all correspondence to: [email protected]
1. Introduction
Nurses are critical in the delivery of essential health services and are core in strengthening the health system [ 1 , 2 ]. They bring people-centred care closer to the communities where they are needed most, thereby helping improve health outcomes and the overall cost-effectiveness of services [ 3 ]. Nurses usually act as first responders to complex humanitarian crises and disasters; protectors and advocates for the community and communicators and co-ordinators within teams. Communication skills for nurses are essential but may be difficult to master. Communication is the exchange of information between people by sending and receiving it through speaking, writing or by using any other medium. Clear communication means that information is conveyed effectively between people. To be a successful nurse, excellent communication skills are required [ 4 ]. Nurses speak to people of varying educational, cultural and social backgrounds and must do so in an effective, caring and professional manner, especially when communicating with patients and their families [ 5 ]. The quality of communication in interactions between nurses and patients has a major influence on patient outcomes. This influence can play a very important role in areas such as patient health, education and adherence [ 6 ]. Good communication plays an important role in the organization’s effective functioning [ 7 , 8 , 9 ]. A nurse must therefore, continuously try to improve his/her communication skills as poor communication can be dangerous and lead to confusion.
2. Principles of communication
Communication is a process;
Communication is not linear, but circular;
Communication is complex;
Communication is irreversible; and
Communication involves the total personality [ 5 ].
3. Communication process
A clear message; and
A receiver [ 12 ].
4. Purpose of communication
To convey information/opinion, for example, “I have headache” or “I am here to give you medication”.
To request information/opinion/behavior, for example, “Are you allergic to penicillin?” or “Tell me more about the injury”.
To give social acknowledgement, for example, “Hello” or “Good morning”.
These three primary types of messages can be combined in many ways so that they form an interaction (conversation). The goals of the interaction can be comprehensive. Nurses strive to make all their communication with patients therapeutic, that is, their communication is purposefully and consciously planned to promote the patient’s health and wellbeing.
5. Types of communication
Verbal and non-verbal communications are the two main types of communication used by human beings.
5.1. Verbal communication
Verbal communication is associated with spoken words and is vitally important in the healthcare context. Members of the multi-disciplinary healthcare team communicate verbally with one another and with patients as well as family members.
5.2. Verbal communication
Bodily contact
Direction of gaze
Emotive tone in speech
Facial and gestural movements
Physical appearance
Speech errors
Timing of speech [ 5 , 8 , 9 , 10 ].
6. Communication process
The communication process may be explained by means of a linear model of communication, interactive model of communication or transactional model of communication [ 11 ].
6.1. Linear model of communication
Linear model of communication entails a sender, a message, a receiver and noise ( Figure 1 ).

Linear model of communication.
6.2. Interactive model of communication
Interactive model of communication gives a slightly more complex explanation of the communication process. Communication is seen as a process in which the listener gives feedback or responds to a message after a process of interpretation. A communicator creates and interprets a message with a personal field of expertise and/or a frame of reference Figure 2 ).

Interactive model of communication.
6.3. Transactional model of communication
Transactional model of communication acknowledges and gives emphasis to the dynamic nature of interpersonal communication and the multiple roles of the communicators. Features such as time, messages, noise, fields of experience, frames of reference, meanings, shared systems of communicators and personal systems all pay a role in the process of communication. Communicators often participate simultaneously (sending, receiving and interpreting). The unique interpretive and perceptual processes of individuals thus play an essential role in the communication process.
7. Barriers to effective communication
Effective communication skills and strategies are important for nurses. Clear communication means that information is conveyed effectively between the nurse, patients, family members and colleagues. However, it is recognized that such skills are not always evident and nurses do not always communicate well with patients, family members and colleagues. The message sent may not be the message received. The meaning of a message depends on its literal meaning, the non-verbal indicators accompanying it and the context in which it is delivered. It is therefore, easy to misinterpret the message, or to interpret it correctly, but to decide not to pursue its hidden meaning this leads to obstruction to communication. Continuous barriers to effective communication brings about a gradual breakdown in relationships. The barriers to effective communication outlined below will help nurses to understand the challenges [ 8 ].
7.1. Language barrier
Language differences between the patient and the nurse are another preventive factor in effective communication. When the nurse and the patient do not share a common language, interaction between them is strained and very limited [ 9 , 10 , 11 ]. Consequently, a patient may fail to understand the instructions from a nurse regarding the frequency of taking medication at home.
7.2. Cultural differences
Culture is another hindrance. The patient’s culture may block effective nurse–patient interactions because perceptions on health and death are different between patients [ 12 , 13 , 14 ]. The nurse needs to be sensitive when dealing with a patient from a different culture [ 9 , 15 , 16 ]. What is acceptable for one patient may not be acceptable for another. Given the complexity of culture, no one can possibly know the health beliefs and practices of every culture. The nurse needs check with the patient whether he/she prefers to be addressed by first name or surname. The use of eye contact, touching and personal space is different in various cultures and rules about eye contact are usually complex, varying according to race, social status and gender. Physical contact between sexes is strictly forbidden in some cultures and can include handshakes, hugging or placing a hand on the arm or shoulder. A ‘yes’ does not always mean ‘yes’. A smile does not indicate happiness, recognition or agreement. Whenever people communicate, there is a tendency to make value judgements regarding those perceived as being different. Past experiences can change the meaning of the message. Culture, background and bias can be good if they allow one to use past experiences to understand something new; it is when they change meaning of the message that they interfere with the communication process [ 12 ]. It is important for nurses to think about their own experiences when considering cultural differences in communication and how these can challenge health professionals and service users.
7.3. Conflict
Conflict is a common effect of two or more parties not sharing common ground. Conflict can be healthy in that it offers alternative views and values. However, it becomes a barrier to communication when the emotional ‘noise’ detracts from the task or purpose. Nurses aim for collaborative relationships with patients, families and colleagues.
7.4. Setting in which care is provided
The factors in care setting may lead to reduction in quality of nurse–patient communication. Increased workload and time constraints restrict nurses from discussing their patients concerns effectively [ 16 ]. Nurses work in busy environments where they are expected to complete a specific amount of work in a day and work with a variety of other professionals, patients and their families. The roles are hard, challenging and tiring. There is a culture to get the work done. Some nurses may consider colleagues who spend time talking with patients to be avowing the ‘real’ work and lazy. Nurses who might have been confident in spending time with patients in an area where this was valued, when faced with a task-orientated culture have the dilemma of fitting into the group or being outside the group and spending time engaging with patients. Lack of collaboration between the nurses and the doctors in information sharing also hinder effective communication. This leads to inconsistencies in the information given to patients making comprehension difficult for the patient and their families.
7.5. Internal noise, mental/emotional distress
Internal noise has an impact on the communication process. Fear and anxiety can affect the person’s ability to listen to what the nurse is saying. People with feelings of fear and anger can find it difficult to hear. Illness and distress can alter a person’s thought processes. Reducing the cause of anxiety, distress, and anger would be the first step to improving communication.
7.6. Perception
If a healthcare professional feels that the person is talking too fast, not fluently, or does not articulate clearly etc., he/she may dismiss the person. Our preconceived attitudes affect our ability to listen. People tend to listen uncritically to people of high status and dismiss those of low status.
7.7. Difficulty with speech and hearing
People can experience difficulty in speech and hearing following conditions like stroke or brain injury. Stroke or trauma may affect brain areas that normally enable the individual to comprehend and produce speech, or the physiology that produces sound. These will present barriers to effective communication.
7.8. Medication
Medication can have a significant effect on communication for example it may cause dry mouth or excess salivation, nausea and indigestion, all of which influence the person’s ability and motivation to engage in conversation. If patients are embarrassed or concerned that they will not be able to speak properly or control their mouth, they could be reluctant to speak.
Equipment or environmental noise impedes clear communication. The sender and the receiver must both be able to concentrate on the messages they send to each other without any distraction.
8. Improving communication
Listen without interrupting the sender.
Show empathy at all times and try to understand.
Try to stay focused on the conversation. Do not however, force the patient to continue if he/she becomes anxious or seems to wish to change the subject.
Use the body language that indicates your interest and concern. Touch the patient if it seems appropriate. Lean forward, listen intently and maintain eye contact if it culturally acceptable.
Offer factual information. This relieves anxiety. Do not offer your personal opinion. Assure the patient that you have professional discretion.
Try to reflect the feelings and thoughts the patient is expressing by rephrasing questions and comments using their own words.
Avoid unclear or misleading messages.
Avoid giving long explanations.
Give your co-workers your full attention when communicating with them.
Ask questions to clarify unclear messages.
Do not interrupt until the sender has completed the message.
Provide a quiet environment without distractions.
Be convincing wen communicating [ 17 ].
9. Communicating with patients
Be open, respectful and gracious in all your interactions with the patient and keep his/her cultural preferences in mind.
Answer nurses’ bells promptly.
Make sure you have the patients’ attention when communicating.
Use words that are non-threatening – explain what you would like to do and do not give orders to the patient.
Use simple, understandable phrases, not medical terms as most patients do not understand these terms.
Speak clearly and courteously.
Use a pleasant and normal tone of voice to the hard of hearing.
Always stand so that the patient can see the nurse’s face when communicating, as lip reading is part of all normal hearing.
Use body language that is appropriate.
Explain facts and procedures before donning a mask that covers the wearer’s mouth and lower face.
Be alert to the patient’s needs. Allow time for answers to your requests and to answer patient’s questions [ 17 ].
10. Communicating by phone
Always speak clearly into the mouthpiece of the phone.
Offer a greeting for example, good morning or good afternoon.
Identify the unit or place of work.
Identify yourself by indicating who you are and where you are phoning from.
Identify the person to whom you are speaking.
Politely listen to the message and make notes if you think you may not remember all the information.
If you are asked to call another person, note the date, time, caller’s name and telephone number together with the message.
Date and sign the message [ 17 ].
11. Assertive communication
Content – where the rights of the people involved are embedded gently in the statement. This could be done by using an explanation, empathy for the listener, and praise for the listener, an apology for the consequence for the listener or a compromise that is favorable to both people.
Covert elements – where the speaker is able to recognize their rights and the rights of the listener in the communication process. These include respect, expressing feelings, having your own priorities, being able to say ‘no’, being able to make mistakes and choosing to say nothing.
Process – concerned with how people express themselves assertively. Is their body language, intonation and choice of language reflective of a confident assertive person? Are the processes that make up communication congruent, in keeping with what is being said? The process also involves managing the setting so that people are not embarrassed, or the noise levels are kept to a minimum. Increasing the likelihood of assertive communication happening again involves feedback to the listener to show that their accomplishment is appreciated.
Non-verbal cues – gesture, touch, proxemics and posture – also need to reflect confidence, regard and respect for self and others.
12. Therapeutic interactions
Assess a patient : The nurse wants to know more about a patient to identify his/her problems. This type of conversation can be a structured interview using an interview schedule. The purpose of this conversation is always a better understanding of the patient.
Instruct a patient : Patient instruction may vary from an informal conversation during which few facts are conveyed to an elaborate instruction session.
Problem solving : If a patient discuss his/her problems with a nurse, the nurse helps the patient to analyze the problem, consider possible alternative ways of handling it and how to decide which way is the best. Problem solving is done with the patients and not for them.
Give emotional support : The presence of an empathetic nurse, that is, one who can enter into the patient’s shoes and understand the patient’s experience, is immensely supportive of the patient. Emotional support alleviates the loneliness of the patient’s experience of illness and increases his/her dignity [ 17 ].
13. Guidelines for successful therapeutic interactions
After the purpose of the therapeutic interaction has been established, the following guidelines assist in conducting a successful interaction:
13.1. Maintaining a low-authority profile
The nurse must strive to maintain a low-authority profile at the beginning of the conversation. As the conversation progresses, the nurse can use more directive techniques to find out specific information. There are usually differences in age, sex, occupation, cultural background, moral and religious convictions between the nurse and the patient. These differences make it impossible for the nurse to fully understand the patient’s behavior and reactions. It is therefore, important for the nurse to understand and accept differences in patients’ cultures and beliefs. When in doubt, check with the patient. If trust is established, patient will be willing to teach the nurse.
13.2. Use of understandable language
The nurse should determine the patient’s level of understanding and if necessary change the use of language, comments and questions. Using the terminology which the patient does not understand can also frighten the patient and make him/her think that he/she has a more serious problem than he/she originally wanted help for. At the same time, the patient could give incorrect information because due to confusion, he/she may give affirmative answers to questions about symptoms that he/she has not actually experienced [ 18 ]. Nurses should share their aims with patients before expecting them to participate in the interaction. They should understand that there is a mutual understanding of each other’s point of departure. In an assessment interview, the nurse can, for instance, say: “Mr Jones, I would like to give you information on how to lose weight so as to bring down you high blood pressure, but I first need to find out what you already know about the condition”. It is not only important that the patients understand what nurses expect from the conversation; it is also essential that nurses understand the patients and convey this understanding before they participate in the conversation. When providing emotional support, this understanding is often all that is necessary. For nurses to understand patients, they must encourage them to talk – not just about facts, but also about their feelings. The nurse must listen more than speak, both to what the patient is saying verbally and what is being said non-verbally. Having listened carefully, the nurse then concentrates and responds empathetically to the patients’ feelings. Only when the nurse has a reasonably complete understanding of the patient’s situation and has communicated this understanding, can she proceed to interventions, such as giving information or solving a problem.
13.3. Tailor the message to the totality of the person
Saying something does not necessary mean that the message has been received and understood. It is the responsibility of the nurse to ensure that the person with whom he/she is conversing understands the message. To ensure this, the message has to be adapted to the language, culture and socio-economic status of the patient. The emotional or physical condition of patients may also make it difficult for them to receive long of complicated messages or even any message. There may also be other disturbances in the immediate environment for example, noise that can make the patient not to hear or understand the message. The message must also be adapted to the age of the patient [ 10 ].
13.4. Validate the interpretation with the patient
Validation means that you ask the patient whether your interpretation is correct or not. You therefore, ask him/her to confirm your understanding of what he/she said. Many misunderstandings arise because people interpret other people’s words without checking their interpretation. The nurse should try to eliminate misunderstandings in the conversations by checking meaning with the patient.
13.5. Active listening
Is the eye contact maintained with the person who is speaking?
Are the body and face turned towards the speaker?
Are there regular verbal responses, even if these consist only of encouraging sounds?
Does the response indicate understanding, not only of the facts, but also of the feelings and the implications of the facts?
It is much easier to speak than to listen. Nurses are, in general, very active people, who want help b acting quickly. To ‘just listen’ without expressing opinions or offering advice is therefore, often not in their nature. Active listening is a valuable skill to acquire [ 10 , 17 , 18 ].
13.6. Evaluate own communication
Simplicity : Say what you want to say concisely and without using difficult or unfamiliar terms.
Clarity : Say precisely what you want to say without digressing, and support your verbal message with non-verbal indicators.
Relevance : Make sure that your message suits the situation, the time and the person you are speaking to.
Adaptability : Adapt your response to the clues the patient that the patient gives you.
Respect : Always show respect for the individuality and dignity of the person you are speaking to [ 17 ].
14. Therapeutic communication techniques
Table 1 gives an overview of therapeutic communication techniques and provides examples of each technique [ 10 , 13 ].
| General area of issue | Therapeutic communication techniques | Rationale | Examples |
|---|---|---|---|
| To obtain information | Make broad opening remarks | This gives the patient the freedom to choose what he/she wishes to talk about | “Please tell me more about yourself” |
| Use open-ended questions | This type of question allows the patient to talk about his/her views about the subject. In this way, what the patient sees as important, what his/her intellectual capacity is and how well-orientated he/she is, becomes clear. This encourages the patient to say more and does not limit answers to a ‘yes’ or ‘no’ | “How did you experience the pain?” “You say you felt dizzy, and then…” “Tell me more about that” | |
| Share observations and thoughts | This shows that you are aware of what is happening to the patient and encourages him/her to talk about it | “You seem to be upset” | |
| Confrontation | This entails confronting the patient with an observation you have made and assess his/her reaction to it. This technique is useful when verbal and non-verbal communication do not match | “You say that your ankle is very painful, but you do not react when I bend the ankle. How is it possible?” | |
| Reflection | This means that you repeat what the patient said in the same or different words. This shows you are involved in what the patient is saying and that he/she should talk more about a specific point, or explain further | Patient: “It is sore”. Nurse: “Very painful?” | |
| Encourage description | This is used to obtain more information about patient’s views and feelings | “Tell me how it happened” | |
| Validate what is being said | This is to make sure that you understand the patient correctly | “Do I understand you correctly when you say…” | |
| Offer your presence | The nurse offers his/her attention and interest without making demands | “I will be with you until they come to fetch you for the operation in theater” | |
| Summarizing | By organizing and checking what the patient has said, especially after a detailed discussion. This technique is used to indicate that a specific part of the discussion is coming to an end and that if the patient wishes to say any more, she should do so | “You went for a walk and then you felt the sharp chest pains, which radiated down your arm” | |
| Use of interpretation | Draw a conclusion from the information you have gathered and discuss it with your patient to see whether it is true. The patient can then disagree with it, or confirm that your conclusions are true | “You must have been exhausted after walking a long distance from home to the hospital” | |
| To give support | Supportive remarks | Make supportive remarks to encourage the patient to participate in the conversation. Show that you are listening | “Yes….” “Mmmm…” “Go on, I am listening” |
| Appropriately touch the patient | Touch can assure the patient that the nurse cares and is present | Hold his/her hand. Consider the cultural belief and comfort of the patient before touching | |
| Paraphrasing | This conveys understanding of the patient’s basic message | “It sounds as though the most important problem is the diet” | |
| To assist in analysis and problem solving | Acknowledge the person | This promotes a sense of dignity | “Good morning Mr. Jones” |
| Sequencing | This helps the patient to see the connection between the parts of an occurrence. To effectively assess the patient’s needs, the nurse often needs to know the time frame within which symptom sand /or problems developed or occurred | “Did you experience this sharp pain before or after eating?” | |
| Ask for clarification | This helps the nurse to understand and the patient to communicate more clearly | “What do you mean by everybody?” | |
| Ask for alternatives | This stimulates creative thought and promotes finding solutions | “What else can you try?” | |
| Use of transition | This is used to guide the conversation to another subject, without losing the continuity of the conversation | “It seems to me that you have solved the problem of poor appetite, but I would like to hear more about your diabetes. How long have you been aware of this illness?” | |
| Comparison | Use of examples and comparisons to concrete objects. In this way, a vague or abstract concept can be more easily explained | “Does the pain feel like a sharp or a blunt object that hits you?” | |
| Use silence | This gives the patient the chance to think, and/or to his/her organize thoughts. Silence also give a nurse an opportunity to observe the patient. However, the nurse should avoid silences that last too long because they can make the patient anxious | ||
| To instruct the patient | Give information | This explains information and puts it at the patient’s disposal | “After the operation, you will have a drainage tube” |
| Orientate the patient towards reality | When the patient interprets something incorrectly, the nurse draws his/her attention to reality | “I am not your daughter, I am Nurse Jones” | |
| Query what the patient says | The patient’s observation is called into question without belittling him/her, or arguing about it | Are you sure about that?” | |
| Withhold social reward | Do not give social approval to wrong behavior so as not to encourage a repeat of the wrong behavior | Do not smile, nod or agree when the patient jeopardizes his/her recovery with wrong behavior | |
| Give social reward | Reward behavior that promotes health to encourage a repeat of the correct behavior | Nod is approval at a patient with a weight problem who declines to eat a heavy meal |
Therapeutic communication techniques.
15. Counter-productive communication techniques
There are certain counter-productive communication techniques that the nurse should avoid as they do not assist in the recovery of the patient and do not have any therapeutic value. Table 2 shows counter-productive communication techniques, explains why these should be avoided and gives examples [ 10 , 18 ].
| Non-therapeutic techniques | Rationale | Examples |
|---|---|---|
| Inappropriate reassurance | The nurse attempts to brush aside the patient’s aside the patient’s worry by acting as though it is unnecessary or inappropriate. Reassurance is not based on fact or real certainty. This helps the nurse more than it helps the patient | “Do not worry; everything will be fine” |
| Passing judgment | The nurse passes judgment on the patient’s behavior, thoughts or feelings and in doing so, places herself in the position of an adversary or a person who knows better and more | “As a Christian, I do not think you should terminate this pregnancy” |
| Giving advice | The nurse tells the patient how he/she ought to feel, think or act. This implies that she has the correct information and knows better than the patient. This is particularly problematic when the advice is based on limited assessment and knowledge of the patient and the situation | “I think you must…” |
| Closed questions | These questions require only a single word as an answer when specific information is needed. If this type of question is used often, the patient are less inclined to give the information and may be interpreted as an interrogation | “Do you feel any pain in your arm?” |
| ‘Why’ questions | These questions demand that the patient explains behavior, feelings or thoughts that he/she often does not understand himself or herself. These questions are often asked early in a conversation when the nurse cannot even be certain that the patient wants to explain himself of herself to the nurse | “Why are you upset?” |
| Offering platitudes | This is stereotyped expression of something the patient is in any case aware of and which, therefore, helps little. This is similar to giving advice | “Everybody goes through this in life” |
| Defensiveness | The nurse tries to defend someone or something the patient criticized. This places the nurse and the patient on opposite sides and does not promote further openness on the part of the patient | “We are very short-staffed; so we cannot help everyone at the same time” |
Non-therapeutic communication techniques that should be avoided.
16. Conclusion
Promoting effective communication in health care is demanding and challenging because of the nature of the work environment. Nurses who have received training in communication skills communicate effectively and show increased confidence in communicating with patients. Many nurses choose to work in other countries, providing an opportunity to broaden their experience and knowledge. However, it is important that nurses who have the opportunity to work in other countries develop communication skills, cultural awareness and sensitivity before arriving. For example, in China talking about death is taboo [ 19 ]. In South Africa, maintaining eye during communication may be regarded as being disrespectful by Black people [ 11 ]. This article provides a reflective account of the experiences of one of the authors of working overseas. This chapter provides the effective communication and interpersonal skills that enhance professional nursing practice and nursing relationships by explaining principles of communication, communication process, purpose of communication, types of communication, barriers to effective communication, models of communication and strategies of improving communication and guidelines for successful therapeutic interactions.
Acknowledgments
The author wishes to acknowledge the Durban University of Technology for funding this book chapter.
Conflict of interest
The author declares that there is no conflict of interest in this chapter.
- 1. World Health Organization (WHO). Global strategic directions for strengthening nursing and midwifery 2016-2020. 2016. Geneva: WHO
- 2. Mokoka KE, Ehlers VJ, Oosthuizen MJ. Factors influencing the retention of registered nurses in the Gauteng Province of South Africa. Curationis. 2011; 34 (1):1-9
- 3. Mokoka E, Oosthuizen MJ, Ehlers VJ. Retaining professional nurses in South Africa: Nurse managers’ perspectives. Health SA Gesondheid. 2010; 15 (1):1-9
- 4. Neese B. Effective Communication in Nursing: Theory and Best Practices. [Internet]. 2015. Available from: http://online.seu.edu/effective-communication-in-nursing/ [Accessed: December 28, 2017]
- 5. Bush H. Communication Skills for Nurses. [Internet]. 2016. Available from: https://www.ausmed.com/articles/communication-skills-for-nurses/ [Accessed: December 28, 2017]
- 6. O’Hagan S, Manias E, Elder C, Pill J, Woodward-Kron R, McNamara T, Webb G, McColl G. What counts as effective communication in nursing? Evidence from nurse educators’ and clinicians’ feedback on nurse interactions with simulated patients. Journal of Advanced Nursing. 2013:1344-1355
- 7. Sibiya MN. People management. In: Booyens S, Jooste K, Sibiya N, editors. Introduction to Health Services Management for the Unit Manager. 4th ed. Claremont: Juta and Company (Pty) Ltd; 2015. pp. 194-205. ISBN: 978-0-70218-866-4
- 8. van Niekerk V. Relationship, helping and communication skills. In: van Rooyen, D, Jordan PJ, editors. Foundations of Nursing Practice: Fundamentals of Holistic Care. African Edition. 2nd ed. Edinburgh: Mosby Elsevier; 2016. pp. 181-207. ISBN: 978-0-7020-6628-3
- 9. Jooste K. Effective leadership communication. In: Jooste K, editor. Leadership in Health Services Management. 2nd ed. Claremont: Juta and Company (Pty) Ltd; 2011. pp. 205-220. ISBN: 9-780702-180347
- 10. Uys L. Interpersonal needs. In: Uys L, editor. Integrated Fundamental Nursing. 2nd ed. Cape Town: Pearson; 2017. pp. 453-571. ISBN: 978-1-775-95450-7
- 11. du Plessis E, Jordaan EJ, Jali MN. Communication in a health care unit. In: Jooste K, editor. The Principles and Practice of Nursing and Health Care. Pretoria: Van Schaik Publishers; 2010. pp. 205-220. ISBN: 9-780627-027857
- 12. Kai J, Beavan J, Faull C. Challenges of mediated communication, disclosure and patient autonomy in cross-cultural cancer care. British Journal of Cancer. 2011; 105 (7):918-924
- 13. McCarthy J, Cassidy I, Margaret MG, Tuohy D. Conversations through barriers of language and interpretation. Bristish Journal of Nursing. 2013; 22 (6):335-340
- 14. Tay LH, Ang E, Hegney D. Nurses’ perceptions of the barriers in effective communication with inpatient cancer adults in Singapore. Journal of Clinical Nursing. 2012; 21 (17-18):2647-2658
- 15. Aslakson RA, Wyskiel R, Thornton I, Copley C, Shaffer D, Zyra M, Pronovost PJ. Nurse-perceived barriers to effective communication regarding prognosis and optimal end-of-life care for surgical ICU patients: A qualitative exploration. Journal of Palliative Medicine. 2012; 15 (8):910-915
- 16. Helft PR, Chamness A, Terry C, Uhrich M. Oncology nurses’ attitudes toward prognosis-related communication: A pilot mailed survey of oncology nursing society members. Oncology Nursing Forum. 2011; 38 (4):468-474
- 17. Booyens L, Erasmus I, van Zyl M. The Auxiliary Nurse. 3rd ed. Cape Town: Juta and Company Ltd; 2013. 504 p. ISBN: 978-0-702 19-794-9
- 18. Viljoen MJ, Sibiya N. History Taking and Physical Examination. 2nd ed. Cape Town: Pearson Education South Africa (Pty) Ltd; 2009. ISBN: 978-1-86891-976-5
- 19. Zheng RS, Guo QH, Dong FQ, Owens RG. Chinese oncology nurses’ experience on caring for dying patients who are in their final days: A qualitative study. International Journal of Nursing Studies. 2015; 52 (1):288-296
© 2018 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Published: 19 September 2018
By Vasfiye Bayram Değer
3781 downloads
By Mayumi Uno
1346 downloads
By Nilgun Ulutasdemır
1526 downloads
IntechOpen Author/Editor? To get your discount, log in .
Discounts available on purchase of multiple copies. View rates
Local taxes (VAT) are calculated in later steps, if applicable.
Support: [email protected]

University Administration
- Careers @ USA
- For Current Students
- Request Information
- Master of Occupational Therapy (MOT)
- Doctor of Occupational Therapy (OTD)
- Post-Professional Doctor of Occupational Therapy (PPOTD)
- Master of Health Administration (MHA)
- Doctor of Education (EdD)
- Graduate Certificates
- Clinical Orthopedic Residency (OCS)
- Orthopaedic Manual Physical Therapy Fellowship (OMPT)
- Continuing Professional Education (CPE)
- Doctor of Physical Therapy (DPT)
- Non-Degree Physical Therapy Online Courses
- Master of Science in Speech-Language Pathology (MS-SLP)
- Post-Graduate Nursing Certificates
- Master of Science in Nursing (MSN)
- Doctor of Nursing Practice (DNP)
- Browse All Degree-Programs
- Admissions & Aid Home
- Scholarships & Grants
- How to Apply
- Cost of Attendance
- Financial Aid
- Application Deadlines
- Academic Calendar
- Financial Aid FAQ
- Admissions FAQs
- Catalog/Handbook
- Our History
- Accreditation
- B Corp Certified
- Change of Ownership
- Student Achievement Data
- Institutional Learning Outcomes (ILOs)
- Diversity & Inclusion
- San Marcos, California
- St. Augustine, Florida
- Miami, Florida
- Austin, Texas
- Dallas, Texas
- Our Faculty
- Board of Directors

Nursing MSN & DNP
| 20 May 2024
The Importance of Effective Communication in Nursing

To be a successful healthcare provider, clinical nurse or nurse leader, you need exceptional communication skills—and you need to be able to use them during high-stress situations.
Why Is Communication Important in Nursing?
Having good communication skills is essential to collaborating on teams with your fellow nurses and colleagues from other disciplines. It’s also important to patient-centered care.
Nurses who take the time to listen and understand the concerns of each of their patients are better prepared to address issues as they arise, resulting in better patient outcomes.
On the other hand, poor communication, or lack of communication in healthcare , can lead to patients misunderstanding directions and failing to follow treatment protocols. It can also lead to workflow breakdowns on the team, resulting in a medical error . A report by the Joint Commission found that poor communication in healthcare during patient transfers contributed to 80% of serious medical errors.
Additionally, patients who have established an open and secure dialogue with a nurse or healthcare provider are more likely to disclose the true extent of their symptoms. According to the book Interpersonal Relationships: Professional Communication for Nurses by Arnold and Boggs , healthcare communication competency offers a primary means for establishing a trusting, collaborative relationship with patients and families. Interpersonal communication skills influence the quality of decisions made, as well as the level of patient motivation to follow treatment protocols and achieve desired clinical outcomes.
10 Effective Communication Skills for Nurses

For nurses, good communication in healthcare means approaching every patient interaction with the intention to understand the patient’s concerns, experiences, and opinions. This includes using verbal and nonverbal communication skills, along with active listening and patient teach-back techniques. Below, we explore 10 communication skills that are important for nurses.
1. Verbal Communication
Excellent verbal communication is key. Aim to always speak with clarity, accuracy, and honesty. It’s also important to know your audience and speak appropriately according to the person’s age, culture, and level of health literacy. If you are feeling stressed out or frustrated, be aware of your tone of voice and don’t let these emotions leak into your patient interaction. You can:
- Encourage patients to communicate by asking open questions like, “Can you tell me a bit more about that?”
- Avoid condescending pet names like “honey” or “sweetie” and instead use the patient’s first name or name of choice.
- Speak in clear, complete sentences and avoid technical jargon.
2. Nonverbal Communication
Using elements of nonverbal communication—such as facial expressions, eye contact, body language, gestures, posture, and tone of voice—is also essential in creating rapport. Simply smiling can go a long way. You can also:
- Show interest in what the patient is saying by maintaining eye contact and nodding your head.
- Smile, but don’t stare.
- Sit down when you can, and lean forward to show you’re engaged.
- Use nonthreatening body language that conveys openness.
3. Active Listening
“Active listening” means listening in order to understand the other person’s experience. The highest and most effective form of listening requires complete attention and engagement. This skill is important not only for clinical nurses but also for nurse executives and other healthcare providers as a tool for building trust and commitment with their staff. Active listening includes both verbal and nonverbal communication skills. For example:
- Nod your head, but never interrupt.
- Lean forward and maintain eye contact to let the person know you’re engaged.
- Include minimal verbal encouragement, such as “I understand,” and “go on.”
4. Written Communication
Written communication skills are also essential for effective nurse-to-nurse communication. As a nurse, you will be responsible for creating and updating the patient ’s medical record . It is critical that the medical record is accurate and current so your patients can receive the best care possible. Also, remember to protect patient confidentiality. Some tips:
- Make notes immediately following patient care so you do not forget anything.
- Write legibly and clearly, using simple language.
- Be sure to note accurate dates and times.
5. Presentation Skills
Effective presentation skills are most applicable during “handover”—when you are transferring patient care to another nurse or other healthcare providers . These skills will also help you demonstrate your knowledge and expertise clearly in a variety of workplace settings, such as presenting at conferences, participating in job interviews, giving case reports to physicians, and more. It’s a good idea to:
- Plan out your presentation and practice.
- Pay attention to both your verbal communication and body language.
- Add visuals to your presentation for a better explanation.
- Understand your audience and know what they want and need from the presentation.
6. Patient Education (Patient Teach-Back)
Nurses are in charge of most of the communication between the healthcare team and patients. This includes informing patients and family members of health conditions, diagnoses, treatment plans, and medication protocols. This skill is especially important for family nurse practitioners who work with patients and families to provide health and education counseling.
Patient teach-back is an effective communication strategy where providers ask patients to repeat the information back to them. This method improves patient understanding and encourages adherence to care instructions. Poor understanding of information can cause patients and their family members to feel anxious or become defensive. For example, you can say:
- “We’ve gone over a lot of information. Now I’d like you to repeat it back to me to make sure you remember everything.”
- “Can you repeat the instructions for taking this medicine back to me?”
- “Let’s review what we just discussed. Can you explain it to me in your own words?”
7. Making Personal Connections
It’s important to get to know the person behind the patient. Patient-centered relationships are critical in helping patients feel safe and comfortable. Creating meaningful connections with patients can improve outcomes and trust. Some ideas:
- Spend a couple of extra minutes every day with each patient getting to know them.
- Find out a fun fact about each patient.
- Show interest in their lives and share stories of your own.
It’s important for healthcare professionals to inspire trust in patients by listening actively and taking every complaint and concern seriously. Building trust takes time. Healthcare settings are scary for some patients. It’s important to make them feel as comfortable as possible.
Trust is something that nurse educators and leaders should also cultivate as they work to develop the next generation of nurses. To inspire trust, nurse leaders and educators should:
- Always tell the truth.
- Share information openly.
- Be willing to admit mistakes.
9. Cultural Awareness
You will likely work with people every day who come from a wide range of social, cultural, and educational backgrounds. Every patient and coworker is unique, and it’s important to be aware and sensitive. For example, gauge the patient’s fluency with English and grade your vocabulary accordingly or bring in a translator if necessary and possible. With trans and gender nonbinary patients, be sure to use their preferred name and pronoun.
10. Compassion
Conveying compassion is an essential communication skill in healthcare. According to the Journal of Compassionate Healthcare , “studies show that compassion can assist in prompting fast recovery from acute illness, enhancing the management of chronic illness, and relieving anxiety.” You can deliver compassionate nursing care by putting yourself in the patient’s shoes and understanding their needs and expectations.
How to Overcome Communication Barriers in Nursing
Sometimes the message sent is not always received the way it was desired. Communication barriers in nursing result in weak patient-nurse interactions and relationships. To overcome these, we must first understand the types of communication barriers that nurses face. In the article “ Communication and Language Needs ,” Dawn Weaver identifies three common communication barriers in nursing: physical, social, and psychological.
Physical Barriers
The environment in which you communicate with a patient can make a huge difference in effective communication. Busy, loud, and distracting settings can increase patient stress. To create a safe and comfortable environment, try closing doors, opening blinds, and mitigating outside noises whenever you can.
Social Barriers
Social barriers include differences in language, religion, culture, age, and customs. Understanding each patient’s cultural background can help nurses avoid prejudice and communicate clearly. It’s a good idea to tailor your communication strategies depending on the patient’s age, as well: A 12-year-old and a 70-year-old will have very different ideas of what health and healthcare mean to them.
Psychological Barriers
For many patients, a trip to the doctor is anxiety-inducing. Anxiety and stress are psychological barriers, as are dementia and other cognitive conditions. To help reduce their influence, it helps to take extra time to listen, empathize, and be supportive. Such psychosocial care has been proven to improve patient health outcomes and quality of life.
Nurses may also need to overcome their own psychological barriers. Speaking to patients and family members about death, disease, and other sensitive topics can be distressing. A study in the Journal of Advanced Nursing explored the fact that many nurses experience feelings of anxiety when discussing patient medical needs and conditions.
Get Started Developing Crucial Communication Skills Today
Learning these and other communication skills should be part of your education, whether you’re enrolled in undergraduate nursing school or a graduate nursing program . They are also easy to practice on the job, as you will get plenty of opportunities for communicating with patients and your colleagues. Put your favorite idea into practice today!
The University of St. Augustine for Health Sciences (USAHS) offers Master of Science in Nursing (MSN), Doctor of Nursing Practice (DNP), and Post-Graduate Nursing Certificates designed for working nurses. Our degrees are offered online, with optional on-campus immersions* and an annual interprofessional trip abroad. Role specialties include Family Nurse Practitioner (FNP), Nurse Educator (MSN only) , and Nurse Executive . The MSN has several options to accelerate your time to degree completion. Complete coursework when and where you want—and earn your advanced nursing degree while keeping your work and life in balance.
*The FNP track includes two required hands-on clinical intensives as part of the curriculum.
The Joint Commission. “Joint Commission Center for Transforming Healthcare Releases Targeted Solutions Tool for Hand-Off Communications.” Joint Commission Perspectives 32, no. 8 (August 2012): 1, 3. https://pubmed.ncbi.nlm.nih.gov/22928243/. Accessed: January 26, 2022
Agency for Healthcare Research and Quality. “Use the Teach-Back Method: Tool #5.” Last reviewed September 2020. https://www.ahrq.gov/health-literacy/quality-resources/tools/literacy-toolkit/healthlittoolkit2-tool5.html. Accessed: January 26, 2022
Chen, Cassandra Siyun, Sally Wai-Chi Chan, Moon Fai Chan, Suk Foon Yap, Wenru Wang, and Yanika Kowitlawakul. “Nurses’ Perceptions of Psychosocial Care and Barriers to Its Provision: A Qualitative Study.” The Journal of Nursing Research 25, no. 6 (2017): 411–418. doi:10.1097/JNR.0000000000000185.
ARE YOU INSPIRED?
There could be an article about you here one day. Take charge of your own life-story!
Take charge of your own life-story
More Nursing MSN & DNP Articles

Dr. Elisabeth McGee Discusses USAHS’ Driving Role in Future-Focused Healthcare

Nurse Practitioner vs. Physician Assistant: Key Differences
85 Nursing Quotes: Words of Wisdom for Nurses
Upcoming nursing msn & dnp events.

Post Professional Doctor of Occupational Therapy (OTD) Webinar - September 10 | USAHS

Occupational Therapy Programs (OTD, OTD Flex, MOT, & MOT Flex) - Admissions Webinar - September 16 | USAHS

Doctor of Physical Therapy (DPT) - Admissions Webinar - September 17 @ 4:00 pm PDT

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
MODULE 7: THERAPEUTIC COMMUNICATION
Therapeutic communication.
This module aligns with key elements of APNA’s “Communication Theory and Interpersonal Skills” (American Psychiatric Nurses Association Education Council, Undergraduate Branch, 2022).
Module Outline
- Therapeutic Communication
- Non-Therapeutic Communication
Module Learning Outcomes
- Summarize therapeutic communication techniques
- Summarize non-therapeutic communication techniques
This module will review therapeutic communication techniques for non-therapeutic communication techniques. Nurses use therapeutic communication and empathy to cultivate rapport and a therapeutic relationship with patients. Below is an overview of therapeutic versus non-therapeutic communication strategies.
See Sharma and Gupta (2022) for further reading.
Therapeutic Communication Strategies
Sharma and Gupta (2022) summarize therapeutic communication strategies . These include:
- Open-ended questions -ask open ended questions to learn more about the patient and enable a free-flow of information exchange; closed-ended questions can be used to focus on specific information
- Active listening -active listening involves behaviors such as making eye-contact and nodding
- Non-verbal indicators -be mindful of non-verbal indicators such as looking frequently at the clock/watch, toe-tapping, having an open body stance
- Silence -sitting with a patient during a difficult time and listening without interruption can be therapeutic
- Reflecting -the nurse repeats the patient’s communication back to them; encourages the patient to reflect on their feelings
Non-Therapeutic Communication Strategies
Summarization of Sharma and Gupta’s (2022) non-therapeutic communication include:
- Value judgements/Approval/Disapproval -avoid interjecting one’s biases and judgements, providing approval or disapproval of the patient’s thoughts or actions
- Negative body language -avoid crossing arms, appearing distracting, and standing over the patient during engagement/conversation
- Advice- avoid providing a patient advice on recommended action(s)
- False reassurance- avoid false reassurance; can lead to mistrust, especially in the case that an expected outcome is not realized
Level Up RN. (2022). Nurse/client relationship, therapeutic communication-psychiatric mental health nursing [Video]. YouTube. https://youtube.com/watch?v=t_59thyrje8&si=EnSIkaIECMiOmarE
Key Takeaways
You should have learned the following in this section:
- Use of therapeutic communication techniques and empathy helps the nurse build rapport and a therapeutic relationship with the patient
- Non-therapeutic communication actions can erode a therapeutic relationship
Empathy is putting yourself into the patient's shoes to allow the nurse's understanding of the situation from the patient's point of view.
MENTAL HEALTH IS A VERB Copyright © 2023 by Jake Bush and Jill Van Der Like is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
Career Advice > Professional Development > Bosses and Coworkers > How to Use Assertive Communication in Nursing
How to Use Assertive Communication in Nursing
Search resource center.

Historically, nursing has been known as a submissive profession. Gone are the days when nurses simply “follow the doctor’s orders.” Today, nursing education is more rigorous and arduous, nurses are more autonomous, and their responsibilities and areas of practice are more extensive.
These changes have resulted in the need for assertive communication in nursing. Ideally, all team members, regardless of assumed hierarchy or profession, are active participants in patient care discussions. Your communication style can enable or inhibit this process.
Eager to learn how to use this effective method of communication? We’ll explain what assertive communication is, why it’s important, and give you examples of how to use it in common nursing scenarios.
What Is Assertive Communication?
Assertive communication is a communication style that is direct, clear, concise, honest , confident, and respectful. It entails expressing thoughts, feelings, and opinions in a considerate way that respects others.
It is meant to foster and maintain healthy relationships, rectify conflicts, and prevent resentment due to unexpressed needs. This element of respect and directness is what separates assertiveness from passive-aggressive communication in nursing.
Aggressive vs. Assertive
Assertive communication is not being rude, blunt, or malicious, nor does it give you permission to say whatever you want. Respect is still alive and well here. The intent of assertiveness is to be straightforward and concise — not to be condescending, superior, or violent.
Aggressive communication, on the other hand, also allows you to express yourself and your opinions, but it violates the rights of others at the same time. Aggressiveness goes beyond being direct — it involves tactics to dominate, appear superior, and belittle others. Essentially, with aggressive communication the goal is to be “right” at any cost.
When to Use Assertive Communication
Assertiveness is needed in many situations. Nurses communicate time-sensitive, medically important information. These scenarios require direct, honest, and mutually respectful communication. Common examples include:
- Providing nursing feedback (i.e., performance reviews, evaluating a preceptee)
- Calling a doctor
- Correcting or interrupting a colleague providing unsafe care
- Multidisciplinary team rounding
- Setting boundaries with patients’ family members
- Rejecting a patient assignment
Why Is Assertive Communication in Nursing Important?
Effective communication is an essential skill in nursing. Think about it — being able to speak up when a provider orders an incorrect dose for a medication can prevent a devastating medication error. Not only does assertive communication positively impact patient safety and care, but it can also improve a nurse’s job satisfaction .
A lack of assertiveness in nursing can also lead to misunderstandings, resentment, overwork and burnout, increased staff turnover, distrust from patients and colleagues, irritation, and mistakes. Remember, nurses are communicating serious matters. Being able to speak concisely and candidly saves everyone time. The importance of assertive communication in nursing truly cannot be emphasized enough.
Benefits of Assertiveness in Nursing
Assertiveness helps you advocate for yourself and enables you to cope effectively with workplace stressors. Some benefits of assertive communication include:
- Builds trust and rapport
- Aids in conflict resolution
- Boosts self-empowerment
- Improves stress management
What Are the Components of Assertive Communication?
Communicating assertively means that you respect both yourself and others . To make it simple, think of these three C’s: clear, confident, and controlled.
Clear: Your message is easy to understand.
Confident: You are composed and believe in your ability to navigate this situation.
Controlled: You are self-regulating, calm, and level-headed.
Additional components include:
- Advocacy (for yourself and your patient)
- Using “I” statements
- Making requests
- High self-confidence and self-esteem
Examples of Assertive Communication in Nursing
1. rejecting a patient assignment.
Scenario: You arrive in the intensive care unit (ICU), go to check the assignment sheet, and get report. You notice that your second patient is in the OR for an open heart surgery and will be arriving later. You have not been trained on immediate post-op care for open heart surgery patients and you don’t feel equipped.
You find your charge nurse and say, “I cannot accept this assignment. I do not have the necessary training to care for this patient undergoing open heart surgery. Who can swap assignments with me?”
Takeaway: This gets straight to the point, uses “I” statements, includes a request, and firmly communicates the rejection of the assignment.
2. Setting Boundaries With Family
Scenario: You are caring for a patient with multiple IV infusions. You hear the IV pump alarming from the nurse’s station. As you enter the room, you notice the alarm has stopped. You ask the patient’s family member if another nurse came in the room. They say, “Oh no — I saw the nurse this morning hit this button to make the alarm quiet, so I hit it for you. I know how busy you are.”
You respond, “I appreciate your desire to help. It’s important for me to observe the pump, IV and tubing, and the IV site when this alarms so I can be sure no harm is done. Please do not turn off any alarms or touch the equipment.”
Takeaway: The nurse directly addresses the problem, makes a clear request, and provides the rationale in a respectful manner. Had the nurse ignored the situation, the family member may have innocently continued to silence the alarm and complications may have occurred as a result.
3. Correcting a Colleague
Scenario: Your colleague requested a witness for a medication administration. Their patient is receiving insulin. The nurse reports their blood glucose, says they need 4 units of insulin, and shows you the amount in the syringe. You observe 4 units, but per the orders, the patient should receive 6 units.
You say, “Yes, this is 4 units, however, this order states they need 6 units for a blood glucose in that range. Would you like me to go with you to the Pyxis and witness there?”
Takeaway: The nurse advocates for the patient and explicitly states the discrepancy observed in a respectful, objective way. The nurse also makes an offer to continue helping the nurse as a witness (which, as you know, can be a challenge when you are short staffed). This approach fosters a healthy workplace and assertive communication in nursing.
4. Multidisciplinary Team Rounding
Scenario: You are in the middle of rounding on your patient in room 9. The attending physician, dietitian, pharmacist, physical therapy, speech therapist, and respiratory therapist are present. The physical therapist says, “Let’s get the patient up to the chair twice today. They’re ready for it.” You know that today you are working short staffed and will have a busy morning.
You say, “That’s a great goal. My morning is very busy and we are short staffed, so I will need someone else to step in to make it happen. Are you or someone else on your team available to assist with transfers?”
Takeaway: This is straightforward, plainly stated, and makes a request. By stating the need, the nurse honors their boundaries and does not take on extra stress on top of a full workload.
Should Nurses Use Assertive Communication With Patients?
Yes — absolutely. In addition to being assertive with colleagues, nurses need to speak clearly and candidly to patients when providing education, such as how to take their medication. They need to speak confidently when answering questions to foster trust. They also need to set boundaries and make requests when a patient is behaving inappropriately.
Ready to Implement These Skills?
You’ve learned how to use assertive communication in nursing — are you ready to apply it? Start advocating for yourself now by selecting a job that fits your life. Take control of your career and find your best job match on IntelyCare today.
Related Articles
Is there a chain of command in nursing, 10 things to know when dating a nurse, can nurses smoke weed, the critical importance of autonomy in nursing, incivility in nursing: how today’s nurses can respond, related jobs.

- Online DNP Overview
- BSN to DNP-AGACNP
- BSN to DNP-FNP
- BSN to DNP-PMHNP
- DNP Careers
- Online MSN Overview
- MSN Careers
- Online PMC Overview
- Micro-Credentials
- Tuition and Fees

10 Effective Nursing Communication Skills for Nurse Leaders
August 29, 2023
View all blog posts under Articles

Through advanced education, such as earning a Doctor of Nursing Practice , nurse leaders can develop crucial communication techniques that facilitate the optimal delivery of care. Verbal, nonverbal, and technological communication, as well as rapport-building skills, such as active listening and compassion, are among 10 nursing communication skills that aim to improve medical care.
Organizational Nursing Communication Skills
The ability to communicate efficiently and effectively can have serious and long-lasting effects. Between health care professionals, communication often involves critical information such as a patient's care, medication, or standards of procedure, making accuracy essential. To ensure information is relayed properly, a few key nursing communication skills optimize delivery among staff, organizational leaders, and stakeholders.
1. Verbal Communication
Effective communicators are assertive in their approach. Using calm, measured speech and a respectful tone, nurse leaders can minimize the risk of miscommunication and ensure information is not lost in medical jargon. Nurses can support each other and improve patient care by cultivating an environment of reciprocal respect through open communication.
2. Nonverbal Communication
Nonverbal cues play a large role in interpersonal communication. Something as simple as crossed arms or slumped posture can greatly affect the way an individual interprets an interaction. The implications and meanings of certain motions such as eye contact or hand gestures may vary among cultures, so nurse leaders must be culturally competent and aware of what their nonverbal cues may be communicating.
3. Written Communication
Maintaining accurate and well-formatted medical information is fundamental for effective communication. Correct grammar, spelling, and diction are all integral parts of proper written conduct and remaining professional.
4. Presentation Skills
During advanced degree programs, graduate students learn to build nursing communication skills necessary for a compelling presentation. Nurse leaders can tailor data and visual aids to fit their target audience and streamline the delivery of new information, critical knowledge, and policies to groups, organizations, or staff.
Rapport-Building Nursing Communication Skills
Developing a relationship of trust and respect between health care professionals and their patients is crucial to the proper delivery of care. By acknowledging individuals’ varying circumstances, experiences, and beliefs, nurse leaders can build open and thoughtful rapports with patients.
5. Active Listening
According to a study published in Medical Care concerning perceived discrimination during a health care visit, the majority of non-white participants reported experiencing perceived racism or classism and felt like their providers did not listen to them. To prevent communication breakdowns and establish an open rapport, many nurse leaders utilize active listening.
Both a nonverbal and verbal skill, active listening is the act of giving one’s undivided attention to another individual. Using culturally appropriate cues and affirmations, the listener shows that they are invested in the conversation, which can encourage patients to speak openly.
6. Compassion
Compassion is a sympathetic desire to help, allowing nurses to make a patient feel cared for while conserving their own energy. It is an extremely valuable nursing communication skill for interactions with patients as well as colleagues, as it entails conveying kindness while maintaining some emotional distance for the care provider. For nurse leaders, it is crucial to not only be compassionate but to recognize when they or the nurses they oversee face compassion fatigue.
At some point in their career, nurses may deal with some level of compassion fatigue. While the symptoms may be similar to burnout, it is an occupational hazard that occurs due to the challenging and traumatic situations nurses encounter, and can affect their worldview or ability to feel compassion for others. Nurse leaders who can provide a supportive environment that encourages awareness and self-care can improve the lives of nurses and their patients.
Empathy allows someone to understand another person’s feelings, creating a safe environment for open communication. Patients who feel empathy from their health care providers may be more willing to divulge the root cause of an issue, leading to more accurate and effective care and an increased likelihood of medical plan compliance.
Contextual Nursing Communication Skills
The goal of culturally competent health care is equal and consistent quality of care regardless of cultural, ethnic, racial, or religious backgrounds. Upholding this practice requires that providers take the time to understand a patient’s beliefs, motivations, and circumstances. By acknowledging and understanding each patient’s unique lived experience, nurse leaders can form context-specific and effective treatment plans for each individual.
8. Cultural Competency
The integration of cultural intelligence into health care allows nurse leaders to work in tandem with patients and their families. Adapting treatment plans, hiring interpreters, and consulting with a patient’s family and loved ones are ways nurses can accommodate and be cognizant of cultural beliefs. Through higher education and mindful learning, nurses pursuing an advanced degree have the opportunity to specialize in awareness training and transcultural care delivery.
9. Religious Beliefs
Religion and spirituality can impact any number of medical decisions, including dietary restrictions, medication, and willingness to pursue care. Encouraging open communication helps to reduce patient anxiety and helps nurses elect appropriate treatments that are sensitive to patients’ religious beliefs and increase the likelihood of care compliance.
10. Education
A new medical care plan may involve significant shifts in a patient’s daily life, so patients need to understand the reasoning behind these lifestyle changes. Educating patients on both the processes and rationale behind their treatment is crucial to care compliance and achieving positive change. Depending on a patient’s comfort level and knowledge of the care required, nurses must be able to modify explanations to ensure patients fully comprehend their situation.
Between nurse leaders and the nurses they oversee, opportunities for education involve both teaching new skills to nurses starting out in their careers and mentoring them on best practices when educating patients.
Develop Better Communication Skills to Provide Better Care
With strong nursing communication skills, nurse leaders can build a rapport with patients and develop an environment of trust and positivity in health care. For patients, being able to trust providers leads to greater compliance in care. Effective communication within health care teams also decreases the likelihood of mistakes and miscommunications, creating more positive medical outcomes.
In the true spirit of aloha — "kindness, grace, unity, humility, and patience" — Hawai‘i Pacific University’s MSN to Doctor of Nursing Practice is rooted in holistic care and designed to help you succeed. Featuring 100% online coursework, small classes with accessible faculty members, and dedicated student support from first contact through graduation, HPU is passionate about preparing you for leadership opportunities. Discover the difference you can make by pursuing an MSN to DNP with Hawai‘i Pacific University.
Recommended Readings:
The Benefits of Advanced Nursing: What Is the Expected MSN Salary Range?
Careers in Advanced Nursing: What Is a Family Nurse Practitioner?
How Family Nurse Practitioners Can Play a Major Role in Addressing the Growing Physician Shortage in the U.S.
The Balance Careers, "Important Active Listening Skills and Techniques"
Healthcare , "The Role of Empathy in Health and Social Care Professionals"
HIPAA Journal , "Communication in Nursing"
Houston Chronicle , "The Role of a Nurse Leader in Communication"
Journal of the Royal Society of Medicine , "Effects of Empathic and Positive Communication in Healthcare Consultations: A Systematic Review and Meta-Analysis"
Medical Care , "Impact of Perceived Discrimination in Health Care on Patient-Provider Communication"
Medical Care , "Perceived Discrimination in Healthcare and Mental Health/Substance Abuse Treatment Among Blacks, Latinos, and Whites"
Movement, Health & Exercise Journal , "Avoiding Medication Errors Through Effective Communication in Healthcare Environment"
Nurse & Midwife Support, "Communication Skills"
StatPearls, "Cultural Religious Competence in Clinical Practice"
Do More With HPU
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Abdolrahimi M, Ghiyasvandian S, Zakerimoghadam M, Ebadi A. Therapeutic communication in nursing student: a Walker and Avant concept analysis. Electron Physician.. 2017; 9:(8)4968-4977 https://doi.org/10.19082/4968
Communication skills 1: benefits of effective communication for patients. 2017. https://tinyurl.com/y3nzu222 (accessed 10 August 2020)
Communication skills 3: non-verbal communication. 2018. https://tinyurl.com/y5ay4uhd (accessed 10 August 2020)
Bandura A. Self-efficacy: toward a unifying theory of behavior change. Psychol Rev.. 1977; 84:191-215 https://doi.org/10.1016/0146-6402(78)90002-4
Barratt J. Developing clinical reasoning and effective communication skills in advanced practice. Nurs Stand.. 2019; 34:(2)37-44 https://doi.org/10.7748/ns.2018.e11109
Bergdahl E, Berterö CM. Concept analysis and the building blocks of theory: misconceptions regarding theory development. J Adv Nurs.. 2016; 72:(10)2558-2566 https://doi.org/10.1111/jan.13002
Bloomfield J, Pegram A. Care, compassion and communication. Nurs Stand.. 2015; 29:(25)45-50 https://doi.org/10.7748/ns.29.25.45.e7653
Bramhall E. Effective communication skills in nursing practice. Nurs Stand.. 2014; 29:(14)53-59 https://doi.org/10.7748/ns.29.14.53.e9355
Brown R. An analysis of loneliness as a concept of importance for dying persons. In: McKenna H, Cutcliffe J (eds). Philadelphia (PA): Elsevier Churchill Livingstone; 2005
Burley D. Better communication in the emergency department. Emerg Nurse.. 2011; 19:(2)32-36 https://doi.org/10.7748/en2011.05.19.2.32.c8509
Cambridge University Press. Effective. 2018. https://tinyurl.com/y7dqcypc (accessed 10 August 2020)
Campbell JD, Lavallee LF. Who am I? The role of self-concept confusion in understanding the behavior of people with low self-esteem. In: Baumeister RF (ed). New York (NY): Plenum Press; 1993
Carment DW, Miles CG, Cervin VB. Persuasiveness and persuasibility as related to intelligence and extraversion. Br J Soc Clin Psychol.. 1965; 4:(1)1-7 https://doi.org/10.1111/j.2044-8260.1965.tb00433.x
Casey A, Wallis A. Effective communication: principle of nursing practice E. Nurs Stand.. 2011; 25:(32)35-37 https://doi.org/10.7748/ns2011.04.25.32.35.c8450
Daly L. Effective communication with older adults. Nurs Stand.. 2017; 31:(41)55-62 https://doi.org/10.7748/ns.2017.e10832
Department of Health and Social Care. Essence of care 2010: benchmarks for the fundamental aspects of care. 2010. https://tinyurl.com/y3z8grqe (accessed 10 August 2020)
Dithole KS, Thupayagale-Tshweneagae G, Akpor AO, Moleki MM. Communication skills intervention: promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs.. 2017; 16:(74)1-6 https://doi.org/10.1186/s12912-017-0268-5
Draper P. A critique of concept analysis. J Adv Nurs.. 2014; 70:(6)1207-1208 https://doi.org/10.1111/jan.12280
Duldt BW, Giffin K, Patton BR. Interpersonal communication in nursing: a humanistic approach.Philadelphia (PA): FA Davis; 1983
Fakhr-Movahedi A, Salsali M, Negharandeh R, Rahnavard Z. Exploring contextual factors of the nurse-patient relationship: a qualitative study. Koomesh.. 2011; 13:(1)23-34
Fleischer S, Berg A, Zimmermann M, Wuste K, Behrens J. Nurse-patient interaction and communication: a systematic literature review. J Public Health.. 2009; 17:339-353 https://doi.org/10.1007/s10389-008-0238-1
Foley A, Davis A. A guide to concept analysis. Clin Nurse Spec.. 2017; 31:(2)70-73 https://doi.org/10.1097/NUR.0000000000000277
Gadamer HG. Philosophical hermeneutics. Translated by DE Linge.Berkeley (CA): University of California Press; 1976
Gallagher L. Continuing education in nursing: a concept analysis. Nurse Educ Today.. 2007; 27:(5)466-473 https://doi.org/10.1016/j.nedt.2006.08.007
Ghafouri R, Rafii F, Oskouie F, Parvizy S, Mohammadi N. Nursing professional regulation: Rodgers' evolutionary concept analysis. Int J Med Res Health Sci. 2016; 5:(9S)436-442
Griffiths J. Person-centred communication for emotional support in district nursing: SAGE and THYME model. Br J Community Nurs.. 2017; 22:(12)593-597 https://doi.org/10.12968/bjcn.2017.22.12.593
Hazzard A, Harris W, Howell D. Taking care: practice and philosophy of communication in a critical care follow-up clinic. Intensive Crit Care Nurs.. 2013; 29:(3)158-165 https://doi.org/10.1016/j.iccn.2013.01.003
Jevon P. Clinical examination skills.Chichester: Wiley-Blackwell Publications; 2009
Jones A. The foundation of good nursing practice: effective communication. J Renal Nurs.. 2012; 4:(1)37-41 https://doi.org/10.12968/jorn.2012.4.1.37
Kelton D, Davis C. The art of effective communication. Nurs Made Incred Easy.. 2013; 11:(1)55-56 https://doi.org/10.1097/01.NME.0000423378.98763.96
Kourkouta L, Papathanasiou IV. Communication in nursing practice. Mater Sociomed.. 2014; 26:(1)65-67 https://doi.org/10.5455/msm.2014.26.65-67
McCabe C. Nurse patient communication: an exploration of patients' experiences. J Clin Nurs.. 2004; 13:41-49 https://doi.org/10.1111/j.1365-2702.2004.00817.x
McCabe C, Timmins F. Communication skills for nursing practice, 2nd edn. Basingstoke: Palgrave; 2013
McCarthy DM, Buckley BA, Engel KG, Forth VE, Adams JG, Cameron KA. Understanding patient-provider conversations: what are we talking about?. Acad Emerg Med.. 2013; 20:(5)441-448 https://doi.org/10.1111/acem.12138
McCroskey JC, Richmond VP. Willingness to communicate: differing cultural perspectives. South Commun J.. 1990; 56:(1)72-77 https://doi.org/10.1080/10417949009372817
McCuster M. Apathy: who cares? A concept analysis. Ment Health Nurs.. 2015; 36:693-697 https://doi.org/10.3109/01612840.2015.1022844
McKenna HP. Nursing theories and models.London: Routledge; 1997
McKinnon J. The case for concordance: value and application in nursing practice. Br J Nurs.. 2013; 22:(13)16-21 https://doi.org/10.12968/bjon.2013.22.13.766
Miller L. Effective communication with older people. Nurs Stand.. 2002; 17:(9)45-50 https://doi.org/10.7748/ns2002.11.17.9.45.c3298
Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital settings: a qualitative systematic review protocol. JBI Database System Rev Implement Rep.. 2015; 13:(1)76-87 https://doi.org/10.11124/jbisrir-2015-1072
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci.. 2016; 8:(6)65-74 https://doi.org/10.5539/gjhs.v8n6p65
Nuopponen A. Methods of concept analysis: a comparative study. LSP.. 2010; 1:(1)4-12
Nursing and Midwifery Council. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. 2018. https://tinyurl.com/zy7syuo (accessed 10 August 2020)
O'Hagan S, Manias E, Elder C What counts as effective communication in nursing? Evidence from nurse educators' and clinicians' feedback on nurse interactions with simulated patients. J Adv Nurs.. 2013; 70:(6)1344-1355 https://doi.org/10.1111/jan.12296
Orem DE. Nursing: concepts of practice, 4th edn. St. Louis (MO): Mosby-Year Book; 1991
Oxford University Press. Communication. 2018. https://tinyurl.com/y7k22yxb (accessed 10 August 2020)
Communication barriers. 2016. https://tinyurl.com/y3sn342h (accessed 10 August 2020)
Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf.. 2014; 23:(8)678-689 https://doi.org/10.1136/bmjqs-2013-002437
Rodgers BL. Concepts, analysis and the development of nursing knowledge: the evolutionary cycle. J Adv Nurs.. 1989; 14:(4)330-335 https://doi.org/10.1111/j.1365-2648.1989.tb03420.x
Rodgers BL, Knafi KA. Concept development in nursing: foundations, techniques and applications, 2nd edn. Philadelphia (PA): WB Saunders; 2000
Royal College of Nursing. Communication-end of life care. 2015. https://tinyurl.com/go28vsm (accessed 10 August 2020)
Schirmer JM, Mauksch L, Lang F Assessing communication competence: a review of current tools. Fam Med.. 2005; 37:(3)184-192
Skär L, Söderberg S. Patients' complaints regarding healthcare encounters and communication. Nurs Open.. 2018; 5:(2)224-232 https://doi.org/10.1002/nop2.132
Snowden A, Martin C, Mathers B, Donnell A. Concordance: a concept analysis. J Adv Nurs.. 2014; 70:(1)46-59 https://doi.org/10.1111/jan.12147
Tay LH, Ang E, Hegney D. Nurses' perceptions of the barriers in effective communication with inpatient cancer adults in Singapore. J Clin Nurs. 2011; 21:(17-18)2647-2658 https://doi.org/10.1111/j.1365-2702.2011.03977.x
Thompson CJ. Nursing theory and philosophy terms: a guide.South Fork (CO): CJT Consulting and Education; 2017
Tofthagen R, Fagerstrøm LM. Rodgers' evolutionary concept analysis – a valid method for developing knowledge in nursing science. Scand J Caring Sci. 2010; 24:21-31 https://doi.org/10.1111/j.1471-6712.2010.00845.x
Nursing, admission assessment and examination. 2018. https://tinyurl.com/y4ykv2uo (accessed 10 August 2020)
Walker LO, Avant KC. Strategies for theory construction in nursing, 5th edn. Norwalk (CT): Appleton and Lange; 2011
Webb L. Exploring the characteristics of effective communicators in healthcare. Nurs Stand.. 2018; 33:(9)47-51 https://doi.org/10.7748/ns.2018.e11157
Wikström B, Svidén G. Exploring communication skills training in undergraduate nurse education by means of a curriculum. Nurs Rep.. 2011; 1:(1) https://doi.org/10.4081/nursrep.2011.e7
Effective communication between nurses and patients: an evolutionary concept analysis
Dorothy Afriyie
Student Nurse, University of West London, Brentford
View articles · Email Dorothy

Communication can be considered as the basis of the nurse-patient relationship and is an essential element in building trust and comfort in nursing care. Effective communication is a fundamental but complex concept in nursing practice. This concept analysis aims to clarify effective communication and its impact on patient care using Rodgers's (1989) evolutionary framework of concept analysis. Effective communication between nurses and patients is presented along with surrogate terms, attributes, antecedents, consequences, related concepts and a model case. Effective communication was identified to be a multifactorial concept and defines as a mutual agreement between nurses and patients. This influences the nursing process, clinical reasoning and decision-making. Consequently, promotes high-quality nursing care, positive patient outcome and patient's and nurse's satisfaction of care.
Communication is an essential element of building trust and comfort in nursing, and it is the basis of the nurse–patient relationship ( Dithole et al, 2017 ). Communication is a complex phenomenon in nursing and is influenced by multiple factors, such as relationship, mood, time, space, culture, facial expression, gestures, personal understanding and perception ( McCarthy et al, 2013 ; Kourkouta and Papathanasiou, 2014 ). Effective communication has been linked to improved quality of care, patient satisfaction and adherence to care, leading to positive health outcomes ( Burley, 2011 ; Kelton and Davis, 2013 ; Ali, 2017 ; Skär and Söderberg, 2018 ). It is an important part of nursing practice and is associated with health promotion and prevention, health education, therapy and treatment as well as rehabilitation ( Fakhr-Movahedi et al, 2011 ). The Nursing and Midwifery Council (NMC) (2018) emphasised effective communication as one of the most important professional and ethical nursing traits. Nonetheless, communication remains a complicated phenomenon in nursing, and most patient-reported complaints in healthcare are around failed communication ( Reader et al, 2014 ). The aim of the present concept analysis is to explore and clarify the complexity of establishing effective communication between nurses and patients in practice.
Concept analysis
Concept analysis is the foundation and preparatory phase of nursing research ( Walker and Avant, 2011 ). Concept analysis aids in clarifying concepts in nursing by using simpler elements to reduce ambiguity and identify all aspects of a concept ( Nuopponen, 2010 ; Foley and Davis, 2017 ). Draper (2014) criticised concept analysis as being methodologically weak and philosophically dubious, further arguing that there is no evidence of its contribution to patient care. However, concept analysis facilitates the review of literature on a concept of interest, thereby enabling a thorough examination of the concept ( Bergdahl and Berterö, 2016 ). This helps in understanding the concept and, therefore, applying it appropriately. Correspondingly, understanding key concepts in nursing practice enables the nurse to identify strategic interventions that could benefit patients. Although McKenna (1997) argued that there is no definite meaning of a concept because they are experienced and perceived differently by people, Walker and Avant (2011) highlighted that the ability of the nurse to describe concepts in an exploratory way is an important means to demonstrate evidence base in practice. Nursing is an evidence-based practice; hence it is the responsibility of the nurse to keep up-to-date with quality evidence and demonstrate it in practice ( Thompson, 2017 ). Therefore, it is paramount for nurses to understand concept analysis and be able to analyse key concepts in nursing.
This concept analysis aims to clarify the concept of effective communication and address the gap in knowledge using Rodgers's (1989) theoretical framework. The evolutionary method of concept analysis was chosen because it adopts a systematic approach with focused phases ( Tofthagen and Fagerstrøm, 2010 ). Rodgers's (1989) method is perceived as a simultaneous task approach, which does not seek boundaries to restrict a concept and considers its application within multiple contexts ( Gallagher, 2007 ). However, the framework will be used because it facilitates an exploration and deep comprehension of a concept ( McCuster, 2015 ). Additionally, the framework offers an alternative to a positivist approach to concepts, allowing different findings depending on the situation ( Ghafouri et al, 2016 ). Moreover, the framework provides an opportunity to identify attributes and related features in a manner that minimises bias ( McCuster, 2015 ). Effective communication between patients and nurses was analysed using the seven phases of Rodgers's (1989) evolutionary method ( Box 1A ). Further, the following four questions were addressed ( Box 1B ).
Box 1A.Rodgers's method of analysis (1989)
| Stage 1: Identify and name the concept of interest |
| Stage 2: Identify surrogate terms and relevant uses of the concept |
| Stage 3: Identify and select an appropriate realm (sample) for data collection |
| Stage 4: Identify the attributes of the concept |
| Stage 5: Identify the references, antecedents, and consequences of the concept, if possible |
| Stage 6: Identify concepts that are related to the concept of interest |
| Stage 7: Identify a model case of the concept |
Box 1B.Rationale for the four focused questionsThe focus questions were driven by the Rodgers's (1989) framework of concept analysis; the four questions are aimed at analysing the concept of effective communication using the seven stages of the framework in a systematic manner to engender an understanding of effective communication
- What is effective communication?
- What are the surrogate terms and related use of the concept of effective communication?
- What attributes, antecedents and consequences apply to the concept of effective communication?
- Who benefits from effective communication between nurses and patients?
Identifying the appropriate realm for data collection
As endorsed by Brown (2005) , a comprehensive review of the literature was conducted for this analysis. Explicit inclusion and exclusion criteria were used to select relevant articles, as recommended by Tofthagen and Fagerstrøm (2010) . Two electronic databases-Cumulative Index for Nursing and Allied Health (CINAHL) and MEDLINE (Ovid)-were searched using the keywords ‘effective communication’ and ‘nurses’ and ‘patients’. The inclusion criteria allowed selection of only peer-reviewed academic journals written in the English language. Studies exploring or analysing effective communication among nurses and patients with underlying communication difficulties and cognitive disabilities were excluded, because it is likely that such patients or nurses represent a special challenge in communicating. Only articles exploring effective communication and factors that influence communication between nurses and patients were considered. A total of 2086 articles were retrieved from the databases, and these articles were screened for relevance by reading the abstract. Finally, 30 articles were determined to meet the inclusion criteria for the analysis ( Figure 1 ). The articles selected were published between 1965 and 2019.
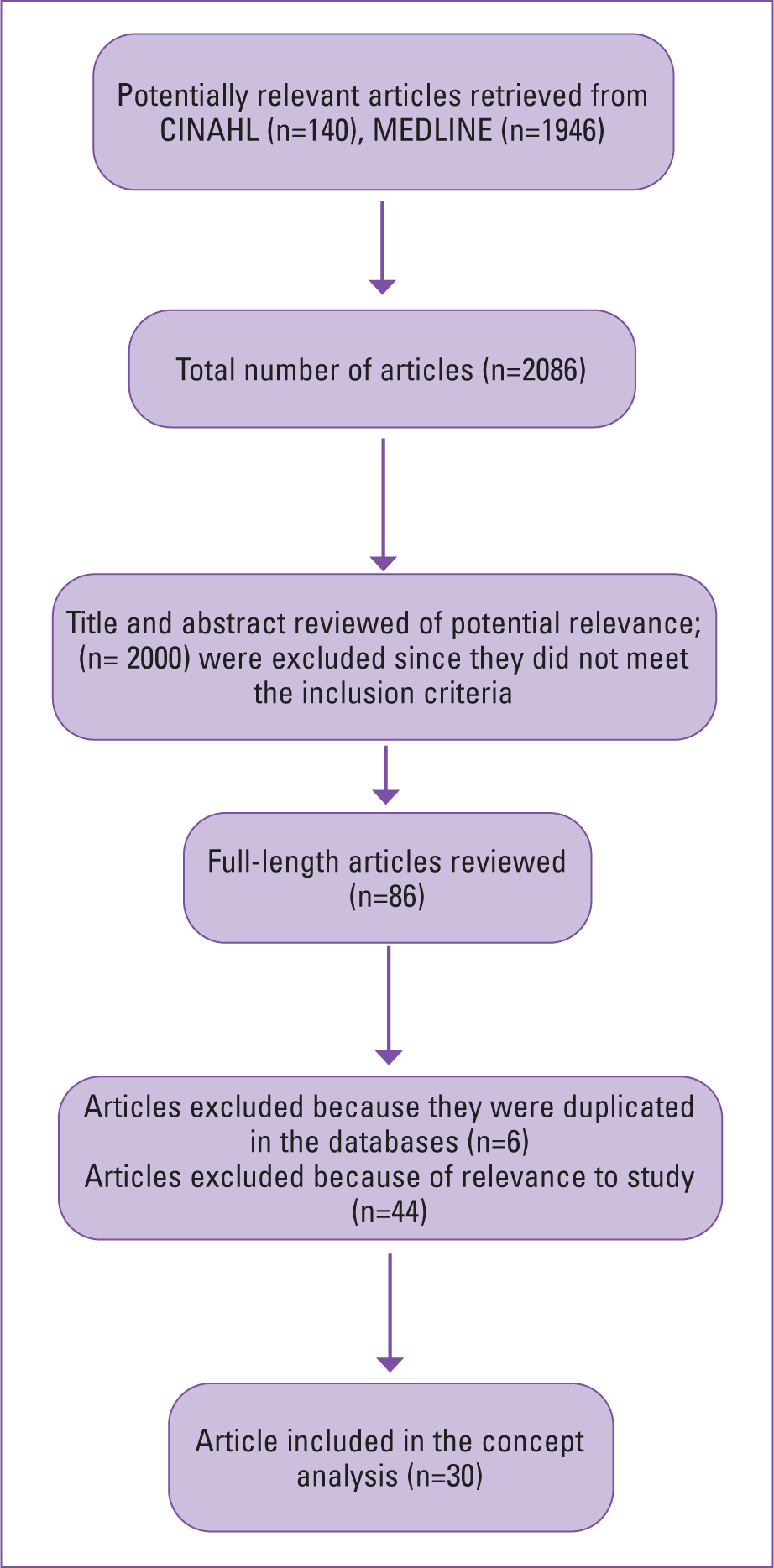
Defining effective communication
The Cambridge English dictionary defines ‘effective’ as ‘successful or achieving the results that you want’ ( Cambridge University Press, 2018 ). According to the Oxford English Dictionary, communication is ‘imparting or exchanging information by speaking, writing or using some other medium’ ( Oxford University Press, 2018 ). The Department of Health and Social Care (2010) described communication as the meaningful exchange of facts, needs, opinions, thoughts, feelings or other information between two or more people. Further, communication can be face-to-face, over the phone or by written words. McCabe and Timmins (2013) also described communication as a cyclical and dynamic process, involving transmission, receiving and interpretation of information between people using verbal or non-verbal means. Rani (2016) simply described communication as ‘sharing meaning’.
Interestingly, Hazzard et al (2013) described communication as a primary condition of human consciousness. They further explained that people always identify themselves in a communicative state. This would imply that people are always exchanging information. The authors, however, described communication as the actions taken after speaking to someone; this highlights communication as responsive. This may be the action and reaction people adopt after a communicated request or statement. Nonetheless, Gadamer (1976) , a twentieth-century philosopher, highlighted communication as what we are and not just what we do. Kourkouta and Papathanasiou (2014) defined communication as the use of speech or other means to exchange information, thoughts and feelings among people. Therefore, effective communication may be classified as exchanging information, thoughts and feelings using either verbal or non-verbal expressions to successfully produce a desired or intended result.
Effective communication between nurses and patients may be analysed from both the nurse's and the patient's perspective. McCabe (2004) identified that the patients' perspective of effective communication entails patient-centred interaction. On the other hand, O'Hagan et al (2013) found that nurses' perspective of effective communication revolves around time, task, rapport and patients' agreement on what has been communicated. Although both perspectives appear to differ, they are both driven by the expectations of the patient and nurse. A nurse may ultimately identify effective communication as the ability to engage with patients and to achieve clinical goals. Similarly, patients may be influenced by their expectation regarding their management outcome ( Schirmer et al, 2005 ). Therefore, effective communication between nurses and patients may be defined as mutual agreement and satisfaction with care (provided and received).
Surrogate terms and relevant uses
The terms most commonly serving a manifestation of effective communication include: therapeutic communication, interpersonal relationship, intercommunication, interpersonal communication and concordance. From a literature search, these terms appear frequently, highlighting their close usage with the concept of effective communication ( Fleischer et al, 2009 ; Casey and Wallis, 2011 ; Jones, 2012 ; Bloomfield and Pegram, 2015 ; Daly, 2017 ). For example, through intercommunication or interpersonal communication, a nurse can encourage a patient to participate in their care decision-making. However, a patient's acceptance to engage in shared decision-making regarding care and agree with a negotiated care plan could reflect effective communication. This act of mutual agreement through negotiation and shared decision-making suggests concordance ( Mckinnon, 2013 ; Snowden et al, 2014 ). Abdolrahimi et al (2017) pointed out that therapeutic communication is the basis for effective communication. They highlighted therapeutic communication as an important means for establishing interpersonal relationships. These concepts are different from effective communication; however, these notions express an idea of the concept of effective communication and highlight an understanding of effective communication as emphasised by Rodgers (1989) .
Daly (2017) described communication as dynamic and cyclical, because it involves a process of transmission, receiving and interpretation through verbal or non-verbal means. This reflects the complexity of communication, which involves speaking, being heard, listening, understanding or being accepted, as well as being seen and acknowledged. Hence, assessing factors that could affect communication, such as noise or interference, is always crucial for effective communication ( McCabe and Timmins, 2013 ; Webb, 2018 ). Daly (2017) explained that other skills for effective communication, which are consciousness, compassion, competence, professionalism and person-centredness, are all important concepts in nursing studies and practice. This indicates that communication is intentional in nature, so the purpose and perspective of individuals involved should be valued and respected ( Jones, 2012 ). In the case of the nurse–patient relationship, a nurse must consider a patient's perspective, background and concerns when communicating. It is important for a nurse to be competent, ethical and professional and exhibit an individualised approach in communicating with patients ( Bramhall, 2014 ; Bloomfield and Pegram, 2015 ). For example, when communicating with a patient with no medical background, medical terms should be explained further or avoided. This promotes person-centredness, which is a determinant for effective communication for patients.
A nurse must respect human rights and be professional ( NMC, 2018 ). However, it can be challenging when communicating with a patient who does not want to communicate about their health, which reflects their right to autonomy. Nonetheless, it is paramount for a nurse to identify the purpose of communication and the difficulties, so that they can mitigate them as part of their professional and ethical duties ( Royal College of Nursing, 2015 ; NMC, 2018 ). This can be done by reassuring and encouraging patients. Correspondingly, this act of communication features in Duldt et al's (1983) theory of humanistic nursing communication. This theory is reflected in Bramhall (2014) and Kourkouta and Papathanasiou's (2014) exploration on communication in nursing. The theory explains the need for comprehensive and exclusive communication among nurses and clients as well as colleagues. The focus of the theory is on interpersonal communication and emphasises the need for humanistic approaches to help improve professional communication. These approaches include empathy, deeper respect, encouragement and interpersonal relationship. For example, listening to people, providing privacy when communicating, giving patients ample time, using kind and courteous words such as ‘please’ and ‘thank you’, as well as being frank and honest when communicating. All these approaches may promote effective communication between nurses and patients ( Jevon, 2009 ; Bramhall, 2014 ; Bloomfield and Pegram, 2015 ).
Further, Miller (2002) , Burley (2011) , Casey and Wallis (2011) , Jones (2012) Bloomfield and Pegram (2015) and Daly (2017) demonstrated how effective communication is key in the assessment, planning and implementation of personalised nursing care. Holistic assessment in nursing includes history-taking, general appearance, physical examination, vital signs and documentation ( Toney-Butler and Unison-Pace, 2018 ). Patient assessment aids in identifying the communication needs of a patient in order to promote person-centred care ( Toney-Butler and Unison-Pace, 2018 ). Moreover, non-verbal cues such as general appearance or posture are vital in communication, and understanding them could help in the assessment process. General appearance such as facial expressions, dressing, hair or skin integrity may convey information that may be helpful in the nursing assessment process. Although not ideal, however, appearance can be a powerful transmitter of intentional or unintentional messages ( Ali, 2018 ). For instance, a nurse may sense neglect or abuse when a patient appears physically unkempt, with bruises or sores. This may inform the nurse on appropriate questions to ask during history-taking in order to ascertain the patient's situation and safeguard, signpost or refer them for support if necessary. Nurses' ability to identify these concerns may aid in providing the best necessary care for their patients. This promotes person-centredness, which is perceived as a means of effective communication by patients ( McCabe, 2004 ).
Effective communication promotes comprehensive history-taking. History-taking involves communicating with patients to collect subjective data and using this information to determine management plans ( Jevon, 2009 ). In history-taking, inaccurate information may be collected when communication is not effective ( Burley, 2011 ; Jones, 2012 ; Daly, 2017 ). However, it is important for nurses to establish good personal relationships with patients, so the latter can feel comfortable in sharing their complaints ( Casey and Wallis, 2011 ). It needs to be noted that, since patients are experts in their own lives, the nurse's ability to make patients feel comfortable may encourage patients to share valuable information, as well as their expectations, concerns and fears. Effective communication is important if nurses are to implement their roles effectively with regard to holistic assessment, considering the subjective experience and characteristics of their patient. Further, a well-informed collaborative assessment through effective communication may contribute to positive patient management outcomes ( Kourkouta and Papathanasiou, 2014 ). For instance, a patient may convey all necessary information to a nurse during assessment, and this may inform the nurse and patient of the necessary examination and investigations to aid in evidence-based nursing diagnosis and a collaborative management plan. The ability to establish a mutual agreement for the nursing process suggests effective communication for both parties.
Effective communication aids in planning and implementing personalised care. It helps patients to set realistic goals and choose preferred management for better outcomes. Communication is a bidirectional process in which a sender becomes a receiver and vice versa ( Kourkouta and Papathanasiou, 2014 ). Therefore, there is a need for both patients and nurses to realise that they are partners in communicating care planning and implementation ( Bloomfield and Pegram, 2015 ). This realisation may promote the patient's dignity and may also influence patients' desire to adhere to their plan when they feel involved in decision-making ( Casey and Wallis, 2011 ). Conversely, patients may be reluctant and unhappy if they feel dictated to or patronised. Most importantly, involving patients through effective communication can empower them to have full control over their health and wellbeing. This is reflected in the self-care theory proposed by Orem (1991) and the theory of self-efficacy proposed by Bandura (1977) . These theories focus on the role of the individual in initiating and sustaining change and healthy behaviours. Orem (1991) reinforced the importance of communication, as self-care is learned through communication and interpersonal relationships.
Attributes of effective communication
Certain attributes can be used to develop a definition of effective communication that is more realistically reflective of how patients and nurses use the term in healthcare settings ( Rodgers and Knafi, 2000 ). The most common attributes identified in the literature include: effective communication as ‘a building foundation for interpersonal-relationship’, ‘a determinant of promoting respect and dignity’, ‘a precedent of achieving concordance’, ‘an important tool in empowering self-care in patient’, ‘a significant tool in planning and implementing person-centred care’ and ‘a determinant of clinical reasoning and the nursing process’ ( Casey and Wallis, 2011 ; Jones, 2012 ; McCabe and Timmins, 2013 ; Bramhall, 2014 ; Bloomfield and Pegram, 2015 ; Daly, 2017 ; Webb, 2018 ; Barratt, 2019 ). These attributes make it possible to identify situations that can be categorised under the concept of effective communication.
Antecedents of effective communication
According to the literature, antecedents to effective communication include: personality trait, perceived communication competence and level of education on communication. Personality traits were linked with communication in early research. Carment et al (1965) demonstrated that people who are introverts are less likely to communicate well compared with extroverts. McCroskey and Richmond (1990) also indicated that people with low self-esteem are less willing to communicate. This is because they are more sensitive to environmental cues ( Campbell and Lavallee, 1993 ). Additionally, McCroskey and Richmond (1990) asserted that people who perceived themselves as poor communicators may be less willing to communicate. Nonetheless, people who may be very capable of communicating may not be willing to, due to low self-esteem, anxiety or fear. As a result, such people may have low communication efficacy despite having high actual competence ( McCroskey and Richmond, 1990 ). Therefore, it is important for nurses to consider these factors when communicating with patients in order to identify their communication needs and manage them accordingly ( Daly, 2017 ). Furthermore, Dithole et al (2017) and Norouzinia et al (2016) highlighted that the nurse's level of education on communication may influence the ability to communicate effectively. Thus, incorporation of targeted communication skills education in the training curriculum and on-the-job training will empower nurses to communicate effectively with their patients.
Consequences of effective communication
The consequences of effective communication can be classified into patient–nurse-related and healthcare system-related outcomes. Skär and Söderberg (2018) mentioned that effective communication ensures a good healthcare encounter for patients. In the community settings, effective communication empowers patients to talk about their concerns and expectations ( Griffiths, 2017 ). Further, effective communication promotes a pleasant and comfortable hospital experience for patients as well as their families; this can also be reflected in the community settings, where patients may report pleasant and comfortable nursing care ( Newell and Jordan, 2015 ; Barratt, 2019 ). Kourkouta and Papathanasiou (2014) and Wikström and Svidén (2011) pointed out that the success of a nurse mostly depends on how effectively they can communicate with their patient. Conversely, ineffective communication may lead to unsuccessful outcomes. For example, a patient may convey their fears, signs and symptoms to a nurse and how the nurse decodes and applies the information may influence the intervention given ( Kourkouta and Papathanasiou, 2014 ). Likewise, a nurse may convey a piece of information to a patient, but the patient's understanding of the information will determine their action. Therefore, how the message is understood determines the action taken ( Kourkouta and Papathanasiou, 2014 ). Additionally, through effective communication, a patient may be empowered to have full control over their health and wellbeing ( Newell and Jordan, 2015 ) and may not require extended care. Clearly, effective communication can lead to positive and cost-saving consequences for patients, nurses and the healthcare system.
The final phase of Rodgers's (1989) method of analysis highlights an application of the concept in an exploratory case scenario. A model case for effective communication between a nurse and a patient is given in Box 2 . This case portrays effective communication between a nurse and a patient, revealing some surrogate terms, defining attributes, antecedents and consequences of the concept. The case model highlighted Audrey's positive engagement in her care decision-making when the nurse Dani communicated effectively. Dani visited Audrey in her home, where Audrey had spatial and environmental control, but she was reluctant to engage in her own care. Audrey perceived that other nurses did not involve her in her care decision-making. This indicates ineffective communication and may be attributed to factors such as age difference, generational gap, gender and culture and ethnic differences between Audrey and the other nurses ( Tay et al, 2011 ; Norouzinia et al, 2016 ).
Box 2.Model caseAudrey, a 90-year-old housebound patient with bilateral leg ulcers was visited by Dani, a 45-year-old community staff nurse working in a diverse multicultural district nursing team. On arrival, Dani introduced herself in a suitable tone, maintaining eye contact. Audrey responded in a low tone, without maintaining eye contact. Audrey appeared to be quiet and in a low mood; Dani identified this nonverbal cue and was determined to engage Audrey in conversation. Dani knew from her experience that leg ulcer treatment can affect a person's mental health, causing low self-esteem, fear and anxiety. Dani asked how Audrey felt and if there was something she could help her with. Audrey mentioned she was fine; her carers had visited and supported her with personal care, breakfast and medication, she had been waiting for the nurse's visit. Dani asked Audrey about her ulcers and how she felt about her dressings; Audrey mentioned she was fine, but expressed concerns about the ulcers not healing. Dani reassured Audrey, explained leg ulcers to her and advised Audrey about some effective practice to promote the healing process.Dani asked Audrey ‘How best can I help you, and how do you want your care to be delivered?’. Audrey responded, ‘You are the nurse, you know better’. Dani took ample time to explain to Audrey how she understands her own body better than any other person. Dani also reassured and encouraged Audrey that her opinions mattered, as this helped empower her, promoted her dignity and informed the nurse on how to care for her. Audrey then expressed to Dani that her other nurses, who are much younger than Dani, never ask her opinion regarding the ulcer management; hence, she was not willing to speak. Audrey mentioned that those nurses came in to re-dress her ulcers and they spoke to her about the care plan, but she did not feel involved in decision-making about her care. Audrey then mentioned that she did not mean to create problems or report anyone. Dani reassured Audrey that there would be no trouble, so she should not be afraid to speak up. Audrey thought that having an honest communication about her needs and views could create problems for her or for the nurses if it seemed that she had reported them.Dani then reassured and encouraged Audrey that the situation will be addressed in a professional manner, and none of the other nurses would feel they had been reported; however, they would involve her in her care and decision-making, which is the expectation. Audrey was then comfortable, communicated in a suitable tone and maintained eye contact with Dani. She asked Dani if she could bandage her right leg first, as she tends to be in pain for a long time when the left one is dressed first. Dani gained consent from Audrey, explained the procedure and advised Audrey to stop her whenever she experienced pain. Dani also asked Audrey a bit more about her pain and her analgesia. Dani identified that Audrey's analgesia had not been reviewed for over 3 years. Dani explained to Audrey that she would be making a referral to her GP about this matter. Audrey was very pleased and indicated she was happy with how Dani had communicated with her; she felt she could trust her. Dani was also pleased, because she could provide the best care for Audrey.
Another important factor that can affect effective communication is the environmental factor. Norouzinia et al (2016) revealed that the hospital environment is a barrier to effective communication for patients. Additionally, Tay et al. (2011) indicated the possibility of unilateral communication due to the hierarchical structure of the hospital environment. Conversely, although nurses may feel quite comfortable in the hospital or inpatient setting, they might feel relatively intimidated when visiting a patient's home. Therefore, an awareness of the contextual discomfort and how it may affect communication is important and should be considered when planning for effective two-way communication between the nurse and patient during home visits. Although all these factors are important in communication, a full discussion of these is beyond the scope of this paper and should be the focus of another complete work.
In the model case described in Box 2 , the nurse acknowledged that she was privileged to be a guest in Audrey's home, and she tailored her strategy to gain Audrey's perspective. The nurse's aim was to get Audrey involved in her care decision-making since Audrey knows herself best. Additionally, Audrey's participation in the decision-making made it possible for her to receive her preferred care. This shows that effective communication is bidirectional, and both partners (nurse and patient) must work together to achieve their desired outcomes, in this case, the patient's satisfaction with care and the nurse's ability to provide the best care.
Effective communication in nursing is clearly a complex, multidimensional and multifactorial concept. Factors such as emotions, general appearance, personality trait, mood and level of education on communication may influence the practice and outcome of effective communication. However, effective communication is an ultimate determinant of success for a nurse. Effective communication was defined as a mutual agreement and satisfaction of care for both patients and nurses. It has been linked to precede the achievement of concordance in patients, and in nurses, it influences clinical reasoning and the nursing process. This aids in implementing compassionate person-centred care and, when successful, it promotes positive patient outcomes and satisfaction with nursing care. Thus, effective communication is an important concept to prioritise in nursing education and practice. For this reason, engaging nurses in communication skills and on-the-job training will empower them to communicate effectively with their patients. As endorsed by Rodgers's (1989) , the outcome of this analysis is not the endpoint of the concept but should direct the future exploration of effective communication. Therefore, a systematic study of effective communication between nurses and patients as well as a systematic review considering effective communication among nurses and patients with underlying communication difficulties, cognitive disabilities and intercultural perspectives can ultimately enhance nursing science.
- Effective communication is a key component of nursing practice
- Effective communication is intentional in nature and can be improved through direct actions taken by the nurse
- Communication is a complex phenomenon and is an essential element of building trust and comfort in nursing
- Concept analysis is the basic way of understanding complex concepts and developing different meanings and perceptions
CPD REFLECTIVE QUESTIONS
- How might concept analysis be relevant in nursing studies or practice?
- What does effective communication mean to you?
- What are some challenges nurses face in communicating effectively?
- How can an interpersonal relationship between nurses and patients influence effective communication?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Educational Interventions for Nursing Students to Develop Communication Skills with Patients: A Systematic Review
Introduction: Nursing students establish therapeutic relationships with their patients and as future nursing professionals, they should be trained to be effective communicators. The objective of this systematic review was to know the impact of educational interventions on nursing students to develop their communication skills with patients. Methods: A systematic review of literature was carried out. The following databases were consulted: CINAHL, PubMed (Ovid Medline), SCOPUS and Web of Science. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guided this review. As for inclusion criteria, published articles in English from 2000 to 2020 were included. The methodological rigor of the included articles was evaluated with the JBI Critical Appraisal Checklist for Randomized Controlled Trial or Quasi-Experimental Studies. Changes in communication skills with the patient after the implementation of an intervention were analyzed. Results: Of the included studies in this systematic review (N = 19), two studies were randomized controlled trials, others were single group quasi-experimental studies (N = 11) and two group quasi-experimental studies (n = 6). The majority of the studies were carried out in the USA (n = 7). The most frequent educational intervention was simulation (n = 11). As for the improvement of communication skills, 13 of the 19 articles found statistically significant differences in patient-centered communication skills of nursing students. Conclusions: This systematic review provides preliminary evidence of the effectiveness of interventions used to train nursing students in patient-centered communication. Although all the interventions obtained significant results in communication skills, it has not yet been determined which methodology is more effective.
1. Introduction
Therapeutic communication (TC) is defined as the process of using verbal and nonverbal communication to connect with patients [ 1 ]. TC is holistic, patient-centered and involves aspects of the physiological, psychological, environmental and spiritual care of the patient [ 2 ]. It is based on understanding and addressing the patient’s situation, including life circumstances, beliefs, perspectives, relevant concerns and needs in order to plan adequate patient care [ 3 , 4 ]. TC between the nurse and patient is considered one of the most significant clinical methods of communication and the basis of nursing care [ 5 ].
The TC that nurses establish with their patients has been explored in various clinical areas. In particular, with psychiatric patients, it has shown improved health outcomes and decreased clinical anxiety and depression [ 6 ]. In the case of chronically ill patients, it has contributed to an increase in adherence to treatment [ 7 ], and therefore, an improvement in the self-management of their disease [ 8 ]. Additionally, in palliative care, communication skills are essential to provide the patient with effective symptom management, psychosocial and spiritual support and advance care planning [ 9 ].
A nurse’s ability to communicate in an effective way is essential for developing therapeutic relationships with their patients and obtain greater patient satisfaction. It also minimizes treatment errors and improves the quality of nursing care [ 10 , 11 ]. Patients and their caregivers positively value professionals who attentively listen, the depth of conversation, the moment of delivering information and communicating in an empathetic way [ 12 ]. However, various studies have shown that nurses lack communication skills due to inadequate training or a failure to appreciate the importance of patient-centered communication [ 7 , 13 ]. For this reason, nursing professors must find active and effective ways to foster communication skills in the education of nursing students [ 14 ].
Teaching and training how to effectively communicate can be complicated due to the variety of potentially difficult conversations that nursing students may face in clinical settings [ 15 ]. This situation constitutes a challenge for university professors in charge of educating nursing students [ 15 , 16 ]. Nursing students establish therapeutic relationships with their patients, and as future nursing professionals, they should be trained to be effective communicators [ 17 ]. Therefore, the concept of TC should be emphasized in the nursing curriculum to meet the educational needs of the students, as well as the needs of the patients [ 18 , 19 , 20 ]. However, most interventions aimed at improving patient-centered communication have been for doctors [ 21 , 22 ]. Given the above, the question was posed as to whether nursing students that receive educational interventions could improve their communication skills with patients. Therefore, the objective of this systematic review was to know the impact of educational interventions on nursing students to develop their communication skills with patients.
2.1. Search Strategy
A systematic review was carried out from September 2019 to January 2020. For this purpose, a critical evaluation of all related evidence was conducted, following a widely documented methodology, in order to answer the specific research question [ 23 ]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was used as a guide for the search and presentation of the results [ 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ].
An initial search was conducted to obtain information on the breadth of publications and identify the words contained in the titles and abstracts on Google Scholar. A search was then made in the PubMed database (see Box 1 ) through the US National Library of Medicine in order to identify the Medical Subjects Headings (MeSH). However, the term MeSH ‘therapeutic communication’ and similar terms found were not linked to any educational subgroup in the search tree. Subsequently, a systematic search was performed using all the keywords identified in the following databases: CINAHL, PubMed (Ovid Medline), SCOPUS and Web of Science.
Example of search strategy conducted in PubMed.
(((((((("students, nursing"[MeSH Terms] AND prelicensure[Title/Abstract]) OR undergraduate[Title/Abstract]) AND intervention[Title/Abstract]) OR effectiveness[Title/Abstract]) AND therapeutic communication[Title/Abstract]) OR nurse-patient communication[Title/Abstract]) OR patient-centered communication[Title/Abstract]) OR interpersonal communication[Title/Abstract]) AND English[Language]
A systematic strategy was used derived from the terms ‘nursing students’ (population); ‘education’ or ‘teaching’ and ‘therapeutic communication’ (intervention); ‘undergraduate’ or ‘prelicensure’ or ‘university’ (context); and ‘effectiveness’ or ‘impact’ (outcome). Finally, manual searches were conducted in the references lists of recent studies and reviews in search of eligible articles that could have been previously lost.
As for inclusion criteria, the review included quantitative studies whose design were Randomized Clinical Trials (RCT) and quasi-experimental trials published in English from January 2000 to January 2020. Regarding the participants, studies were included with participants that were undergraduate (or pre-licensure) nursing students, regardless of their age, sex or country of origin. With respect to the types of intervention, the review included studies of TC training or patient-centered training. In regards to the types of measured results, the review considered any objectively measured or self-reported quantitative data reporting on therapeutic communication outcomes.
2.2. Data extraction
A total of 5,845 articles were identified in the initial search. All citations and abstracts identified in the search strategy were downloaded to Mendeley. The first author (LG) assessed the titles of the articles obtained from the search in the databases. The search yielded 612 articles after eliminating duplicates (see the systematic review flow diagram in Figure 1 ). The abstracts were reviewed and studies were excluded if: (a) the intervention was not aimed at TC or patient-centered; (b) if the intervention was not aimed at nursing students; (c) articles that were systematic reviews, meta-analysis, qualitative studies, case studies, doctoral thesis or conference abstracts; (d) articles not written in English. Of the 86 abstracts reviewed, 27 articles were selected by the first author for revision of the full text. From the manual search, 10 relevant articles were identified for inclusion in the review. Both reviewers independently analyzed the 27 articles taking the preestablished criteria into account.

Systematic review flow diagram.
Data from the included articles were reviewed by two independent reviewers (LG and VM), using the JBI-MAStARI data extraction tool. The reviewers extracted information from each of the articles including data on design, theoretical framework, participants, intervention, outcome measures and results. The most relevant characteristics of the studies included in the review are summarized in Table 1 . Due to variations in the intervention methods and outcome measures, it was not possible to carry out a meta-analysis.
Main characteristics of the selected studies.
| Order Number | 1st Author, Date (Country) | MAStARI | Participants | Objetives | Study Design |
|---|---|---|---|---|---|
| 1 | Becker et al. 2006 [ ] (USA) 1C | 10 | n = 147 nursing students enrolled in a psychiatric nursing course (IG = 58; CG = 89). | To evaluate knowledge of depression and therapeutic communication skills SP. | Desing: randomized control group. pre-test, post-test. |
| 2 | Baghcheghi et al. 2011 [ ] (Iran) 2C | 7 | N = 34 sophomore nursing students (16 IG; 18 CG). | To evaluate the effect of tradicional learning and cooperative learning methods on nursing students´communication with patients. | Design: Experimental, observer-blinder two groups study. Data collection: pre-test, post-test. |
| 3 | Kim et al. 2012 [ ] (Korea) 2C | 7 | n = 70 sophomores nursing students enrolled in a theoretical course in maternity. | To determine the effect of simulation-based education on the communication skill and clinical competence of nursing students in maternity nursing practicum. | Design: quasi-experimental study, two gropup study. Data Collection: pre-test, post-test. |
| 4 | Wittenberg-Lyles et al. 2012 [ ] (USA) 2D | 7 | n = 32 nursing students. | To assess the effects of communication training for the practical nurse. | Design: quasi-experimental pilot study. Data collection: pre-test, post-test. |
| 5 | Jo and An 2013 [ ] (Korea) 2C | 7 | n = 39 nursing students (19 IG; 20 GC) from two universities. | To examine the effects of a humanistic end-of-life care course on South Korean undergraduate nursing students’ attitudes toward death, death anxiety, and communication skills. | Design: quasi-experimental two group study. Data collection: Pre-test, post-test. |
| 6 | Lau and Wang 2013 [ ] (China) 2D | 7 | n = 62 fourth-year nursing students enrolled CST course. | To develop a learner-centered Communication Skills Training (CST) course; (2) to evaluate the course by comparing scores for communication skills, clinical interaction, interpersonal dysfunction, and social problem-solving ability. | Design: quasi-experimental single group study, two-phase mixed methods Data collection: pre-test, post-test. |
| 7 | Lin et al. 2013 [ ] (Taiwan) 1C | 9 | n = 26 first year nursing students (14 IG; 12 CG). | To examine the effectiveness of using SP with SP feedback and group discussion to teach Interpersonal and communication skills (IPCS) in nursing education. | Desing: Randomized Controlled Study two group. Data collection: pre-tets, post-test. |
| 8 | Lau and Wang 2014 [ ] (China) 2D | 7 | n = 59 fourth-year nursing students attended the summer camp program. | To develop a learner-centered educational summer camp program for nursing students and to evaluate the effectiveness of the camp program on enhancing the participants’ communication skills. | Design: quasi-experimental single group study, two-phase mixed methods. Data collection: pre-test, post-test. |
| 9 | Webster 2014 [ ] (USA) 2D | 7 | n = 89 senior baccalaureate nursing students enrolled in a psychiatric clinical course. | To determine the effectiveness of SPEs as a teaching modality to improve nursing students’ use of therapeutic communication skills with individuals with mental illness. | Design: quasi-experimental, one group study. Data Collection: pre-test, post-test. |
| 10 | Bloomfield et al. 2015 [ ] (UK) 2D | 6 | n = 28 second-year nursing students and fourth-year medical students from a population of N = 180 nursing students and N = 450 medical students. | To design, implement, and evaluate an educational intervention employing simulated patient actors to enhance students’ abilities to communicate with dying patients and their families. | Design: quasi-experimental single group study, two-phase mixed methods. Data Collection: pre-test, post-test. |
| 11 | Yoo and Park 2015 [ ] (Korea) 2C | 7 | n = 143 (72 IG; 71 CG) sophomore undergraduate nursing student enrolled in a mandatory health communication course from a population of N = 151. | To evaluate the effectiveness of Case-based learning on undergraduate nursing students in the health communication course. | Design: quasi-experimental two group study. Data collection: pre-test, post-test. |
| 12 | Lai 2016 [ ] (Taiwan) 2D | 7 | n = 50 quasi-experimental single group study. | To implement an online video peer assessment system to scaffold their communication skills and to examine the effects and validity of the peer assessment. | Desing: quasi-experimental single group study. Data collection: pre-test, post-test. |
| 13 | Martin and Chanda 2016 [ ] (USA) 2D | 8 | n = 28 prelicensure nursing students enrolled in a mental health nursing theory and clinical course. | To introduce therapeutic communication simulations with emphasis on symptoms related to psychiatric disorders as a part of mental health theory and clinical courses. | Design: quasi-experimental, one group. Data collection: pre-test, post-test. |
| 14 | Taghizadeh et al. 2017 [ ] (Iran) 2D | 8 | n = 66 last year nursing students and n = 132 patients. | To determine the impact of teaching communication skills to nurse students on the quality of care given by nursing students. | Design: quasi-experimental single group study. Data collection: pre-test, post- test. |
| 15 | Shorey et al. 2018 [ ] (China) 2D | 8 | n = 124 first-year undergraduate nursing students enrolled in the nursing course. | To evaluate the effectiveness of blended learning pedagogy in a redesigned communication module among nursing undergraduates in enhancing their satisfaction levels and attitudes towards learning communication module as well as self-efficacy in communication. | Design: quasi-experimental single group study. Data Collection: pre-test, post-test. |
| 16 | Blake and Blake 2019 [ ] (USA) 2D | 5 | n = 32 nursing students in their capstone course from a population of N = 35. | To examine the effects of a nursing lab simulation used to increase the self-efficacy of nursing students with their ability to use effective communication. | Design: quasi-experimental single group. Data collection: pre-test, post-test. |
| 17 | Donovan and Mullen 2019 [ ] (USA) 2D | 7 | n = 116 undergraduate nursing students registered for three successive mental health nursing courses during academic year from a population of N = 160 (RR 72.5%). | To examine the efficacy of learned classroom therapeutic communication techniques applied to a standardized patient mental health simulated experience. | Design: quasi-experimental single group study. Data collection: pre-test, post-test. |
| 18 | Gaylle 2019 [ ] (USA) 2C | 7 | n = 65 senior students enrolled in a psychiatric clinical rotation at a public university from a population of N = 67 (RR 97%). (IG = 32; CG = 33). | To explored the effects of in-simulation and postsimulation debriefing on students’ knowledge, performance, anxiety, and perceptions of the debriefing process. | Design: quasi-experimental, two group study. Data collection: pre-test, post-test. |
| 19 | Ok et al. 2019 [ ] (Turkey) 2C | 6 | n = 85 third-year nursing students enroled in a course on mental health and psychiatric at two different universities from a population of N = 103 (RR 82.5%). (IG = 52; CG = 33) | To measure the impact of using standardized patient simulation (SPS) prior to clinical practice on the anxiety levels and communication skills. | Design: quaxi-experimental two group Data collection: pre-test, post-test |
IG, Intervention Group; CG, Control Group; SP, Standardized Patient; CST, Communication Skills Training; IPCS, Interpersonal Communication Skills; SPEs, Standardized Patient Experiences; SPS, Standardized Patient Simulation.
2.3. Quality appraisal
The selected articles were independently evaluated by two reviewers (GA and VG), before being included in this review. The methodological validity was evaluated using the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument standardized critical appraisal instrument (JBI MAStARI). For the RCTs, the JBI MAStARI for RCTs was used. This checklist is made up of thirteen items. The possible answers to the items are yes, no, unclear or not applicable. If “yes” is answered, a point is obtained. For the study to be included, it had to obtain a score equal to or greater than seven. In the quasi-experimental studies, JBI MASTARI for quasi-experimental studies was used. This checklist is made up of nine items that can be rated yes, no, unclear or not applicable. If “yes” is chosen for the item, a point is obtained. For the study to be included in the systematic review, it had to obtain a score equal to or greater than five. This process enabled an increase in methodological rigor and evaluated possible biases and threats to the validity [ 25 ]. The discrepancies between the reviewers of the articles that were to be included in the review were discussed until a consensus was reached. After review, evaluation and discussion, eight articles were excluded that were not based on TC interventions, as defined in the inclusion criteria, or for methodological reasons. Finally, 19 articles were included after confirmation by both reviewers.
3.1. Characteristics of the study
The overall sample size of the studies included in this review was N = 1,295 participants. In the included studies, there was a great deal of variation in the sample size, ranging from 26 to 147 (median, n = 62). Although the literature search was conducted from the year 2000, the first study included in this review was from 2006. Ninety percent of the studies (n = 18) were carried out in the last ten years and more than fifty percent (n = 10) were conducted in the last five years. Most studies (n = 9) were in mental health. The other areas represented were end-of-life and maternity. As for the study designs, the majority were quasi-experimental studies (n = 17) followed by RCTs (n = 2). In all of the included studies, pre-test and post-test measurements were performed (N = 19) ( Table 1 ).
3.2. Theoretical frameworks
Only two of the 19 studies included in this systematic review included a description of a theoretical framework. Donova and Mullen [ 26 ] used the Constructivist Learning Theory by Merriam, Cafferella and Baumgartner [ 27 ]. While Shorey et al. [ 28 ] used a combination of the two frameworks (a) the Self-Efficacy Theory [ 29 ]; and (b) the Authentic Learning Concept [ 30 ].
3.3. Intervention characteristics
Eleven studies used simulation as the intervention. The majority of them (n = 8) used SP to facilitate learning [ 26 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ] and three studies used simulation to aid in the assessment of communication skills, performed by a faculty member [ 38 ], peer [ 39 ], or both [ 40 ]. Nine were carried out through simulation using Standardized Patients (SP) [ 26 , 31 , 32 , 33 , 36 , 37 , 38 , 40 ]. One study used simulation through role playing [ 39 ] and with high-fidelity patient (n = 1) [ 34 ]. Three studies used innovative educational methodologies, such as a blended learning environment [ 28 ], cooperative learning methods [ 41 ], and Case-Based learning [ 42 ]. Five studies focused their intervention on the development of courses [ 43 , 44 , 45 , 46 , 47 ], and four of the courses indicated the included activities.
Regarding the contexts of the interventions, nine studies focused on mental health [ 26 , 31 , 33 , 35 , 36 , 37 , 38 , 39 , 40 ], three studies on end-of-life [ 32 , 43 , 47 ], one focused on maternity [ 34 ], and six studies focused on general patient-centered communication skills [ 28 , 41 , 42 , 44 , 45 , 46 ]. As for the duration of the interventions, it varied from one hour to one semester ( Table 2 ).
Intervention characteristics.
| Order Number | 1st Author, Date (Country) | Participants | Study Design | Theoretical Framework | Intervention | Quantitative Measures |
|---|---|---|---|---|---|---|
| 1 | Becker et al. 2006 [ ] (USA) | n = 147 nursing students enrolled in a psychiatric nursing course (IG = 58; CG = 89). | Design: randomized control group. Data collection: pre-test, post-test. | Not mentioned. | Simulation—using Standardized Patient (SP). Lectures on therapeutic communication and nursing care of clients with depression (both group), Interview SP, debriefing, videotape self-analysis with accompanying handbook. Duration: once a week, 7 weeks. Interview SP (30 min), debriefing (30 min), videotape self-analysis (after 1 week of the SP encounter). CG - usual classroom lecture format. | Students: Communication Knowledge Test (CKT), developed by the authors for this study. Student Self-Evaluation of SP Encounter (SSPE), developed by the authors for this study. Patients: SP checklist, developed by the authors for this study. Standardized Patient Interpersonal Ratings (SPIR), developed by the authors for this study. |
| 2 | Baghcheghi et al. 2011 [ ] (Iran) | N = 34 sophomore nursing students (16 IG; 18 CG). | Design: Experimental, observer-blinder two groups study. Data collection: pre-test, post-test. | Not mentioned. | Cooperative learning methods. (work in group) Activities included in lectures: Socratic questioning, paired discussion of homework assignments, paired pop quizzes, small group discussion of case scenarios, paired concept-map generation exercises, student identification of examples for concepts being discussed, and think-pair-share exercises. Each group would be responsible for presenting a 15 to 20-minute review of information from their particular content category to the class. Throughout the semester the group members evaluated each other with a weekly evaluation tool; feedback. Duration: one semester. CG—usual classroom lecture format. | Nursing Students’ communication with patient scale. |
| 3 | Kim et al. 2012 [ ] (Korea) | n = 70 sophomores nursing students enrolled in a theoretical course in maternity. | Design: quasi-experimental study, two group study. Data Collection: pre-test, post-test. | Not mentioned | Simulation—using high-fidelity patient simulator. Duration: 9 h over three weeks (briefing, simulation lab, debriefing). CG—usual classroom lecture format. | Communication Skills Tool. Clinical Competence Tool (CCT). |
| 4 | Wittenberg-Lyles et al. 2012 [ ] (USA) | n = 32 nursing students. | Design: quasi-experimental pilot study. Data collection: pre-test, post-test. | Not mentioned | COMFORT communication and consulting course. interactive, educational training session and taught students using a combination of PowerPoint lectures, case studies, small group discussions, and exercises. Students were exposed to concepts including narrative clinical practice, person-centered messages, the task and relational components in all interactions, and participated in 3 encounters using these concepts. Duration: 3h. | Course Experience Questionnarie (CEQ) created by authors for this study. Perceived Importance of Medical Communication (PIMC). Communication Skill Attitude Scale (CSAS). Caring Self-Efficacy Scale (CES). |
| 5 | Jo and An 2013 [ ] (Korea) | n = 39 nursing students (19 IG; 20 GC) from two universities. | Design: quasi-experimental two group study. Data collection: Pre-test, post-test. | Not mentioned. | End-of-life- Care course teaching included uses humanistic educational methods such as lectures, group discussion, watching a movie, analysis of novel and poem, appreciation of music, and collage art, role-play, and sharing personal experiences. Duration: 2h x 16 weeks. CG—usual classroom lecture format. | Attitudes toward death. Death Anxiety Scale (DAS). Communication Assessment Tool (CAT). |
| 6 | Lau and Wang 2013 [ ] (China) | n = 62 fourth-year nursing students enrolled CST course. | Design: quasi-experimental single group study, two-phase mixed methods Data collection: pre-test, post-test. | Not mentioned. | Communication Skills Training (CST) course. Included theoretical lectures and practical components (Immediate feedback; Role Playing; Group discussion; didactical games). Duration: two day, 8 h per day. | Communication Ability Scale (CAS) Clinical Interaction Scale (CIS). Interpersonal Dysfunction Checklist (IDC). Social Problem Solving Inventory-Revised (C-SPSI-R). |
| 7 | Lin et al. 2013 [ ] (Taiwan) | n = 26 first year nursing students (14 IG; 12 CG). | Design: Randomized Controlled Study two group. Data collection: pre-test, post-test. | Not mentioned. | Simulation - using SP. Briefing; scenario demonstration; role-playing. Duration: 2-day (SP assessments with SP feedback and group discussion). CG—usual classroom lecture format. | Interpersonal Communication Skills (IPCS) assessment tool. Student Learning Satisfaction (SLS) Scale. |
| 8 | Lau and Wang 2014 [ ] (China) | n = 59 fourth-year nursing students attended the summer camp program. | Design: quasi-experimental single group study, two-phase mixed methods. Data collection: pre-test, post-test. | Not mentioned | Educational Summer Camp Program on Communication Skills—three sharing sessions and five experimental learning games. Sharing sessions on self-exploration, teambuilding, and clinical interaction. Experiential learning games were used as learning strategies (icebreaker, self-discovery, team building, problem solving, and communication). Duration: 3 days | Communication Ability Scale (CAS) Clinical Interaction Scale (CIS). Interpersonal Dysfunction Checklist validated Chinease (IDC). Social Problem Solving Inventory-Revised (SPSI-R). |
| 9 | Webster 2014 [ ] (USA) | n = 89 senior baccalaureate nursing students enrolled in a psychiatric clinical course. | Design: quasi-experimental, one group study. Data Collection: pre-test, post-test. | Not mecioned. | Simulation—using SP, simulations were video-recorded, watched their video and conducted a self-reflection of strengths and areas for improvement; debriefing conducted by faculty using a problem-based learning approach. Duration: Two SPEs, one at the beginning of the semester and one at the end of the semester. 15–20 min sessions. | The effectiveness of the use of SPEs to teach therapeutic communication skills in psychiatric nursing ckecklist created by author for this study. Feedback from faculty ckecklist created by author for this study. |
| 10 | Bloomfield et al. 2015 [ ] (UK) | n = 28 second-year nursing students and fourth-year medical students from a population of N = 180 nursing students and N = 450 medical students. | Design: quasi-experimental single group study, two-phase mixed methods. Data Collection: pre-test, post-test. | Not mentioned. | Simulation—using SP (two scenarios), pre-briefing; simulation; debrief. Duration: 45 min including pre-brief, simulation and debrief. | students’ perceived levels of confidence, competence, and concern when communicate with dying patients and their families questionnaire created by authors for this study. |
| 11 | Yoo and Park 2015 [ ] (Korea) | n = 143 (72 IG; 71 CG) sophomore undergraduate nursing student enrolled in a mandatory health communication course from a population of N = 151. | Design: quasi-experimental two group study. Data collection: pre-test, post-test. | Not mencioned. | Case-Based Learning (CBL) - as teaching activity in a course. Five authentic cases of patient-nurse communication. (Stage of each 5-Cases: Case presentation; Student´s case analysis individually; group discussion and analysis; finding proper solution by group; group presentation of the cases). Duration: 28 h. CG –traditional lecture-based learning. | Communication Assessment Tool (CAT). Problem-Solving Inventory (PSI). Instructional Materials Motivation Scale (IMMS). |
| 12 | Lai 2016 [ ] (Taiwan) | n = 50 quasi-experimental single group study. | Design: quasi-experimental single group study. Data collection: pre-test, post-test. | Not mentioned. | Simulation—using SP an online video peer assessment system. Recorded therapeutic consultation with a SP and uploaded to YouTube; peer assessment and feedback through a web-based assessment system; expert evaluation (two rounds; different scenarios). Duration: SP twice; once in the mid-term exam week and the other in the final exam week. Duration not stated. | Interpersonal Communication Assessment Scale (ICAS). |
| 13 | Martin and Chanda 2016 [ ] (USA) | n = 28 prelicensure nursing students enrolled in a mental health nursing theory and clinical course. | Design: quasi-experimental, one group. Data collection: pre-test, post-test. | Not mentioned. | Simulation using SP (three stations; two simulation sessions). Briefing; simulation with two standardized patients and a case study; debriefing. Duration: 40-50 min simulation followed by an hour debriefing. | Confidence with Communication Skill Scale. Therapeutic communication and nontherapeutic communication techniques, checklist created by authors, with the purpose of evaluating skills that would occur during the SP encounters. |
| 14 | Taghizadeh et al. 2017 [ ] (Iran) | n = 66 last year nursing students and n = 132 patients. | Design: quasi-experimental single group study. Data collection: pre-test, post- test. | Not mentioned. | Communication Training Course. lectures and workshops using educational equipment and technology. Duration: 6 h. | Student´s Communication skills checklist created by the authors for this study. Quality of Care Questionnaire for Patients. |
| 15 | Shorey et al. 2018 [ ] (China) | n = 124 first-year undergraduate nursing students enrolled in the nursing course. | Design: quasi-experimental single group study. Data Collection: pre-test, post-test. | Bandura´s self-efficacy theory (1997). | Blended learning environment face-to-face each week for tutorials (Role-playing and problem-based learning); lecture materials online (breeze presentations, PowerPoints slides, and multi-media components, delivered) online quizzes, discussion forums, and reflection exercises; assessment (analyzing real life clinical scenarios by creating online videos; interview with SP). Duration: 13 weeks. Four modular credit x 10 h (2–3 h for face-to-face tutorial or lecture and 7–8 h for the self-directed learning). | Blended Learning Satisfaction Scale (BLSS). Communication Skills Attitude Scale (CSAS). Communication Skills subscale of the Nursing Students Self-Efficacy Scale (C-NSSES). |
| 16 | Blake and Blake 2019 [ ] (USA) | n = 32 nursing students in their capstone course from a population of N = 35. | Design: quasi-experimental single group. Data collection: pre-test, post-test. | Not mentioned. | Simulation—role-playing, debriefing Duration: a week. | Self-efficacy related to therapeutic communication, developed by the authors for this study. A rubric for therapeutic and nontherapeutic statements or actions developed by the authors for this study. |
| 17 | Donovan and Mullen 2019 [ ] (USA) | n = 116 undergraduate nursing students registered for three successive mental health nursing courses during academic year from a population of N = 160 (RR 72.5%). | Design: quasi-experimental single group study. Data collection: pre-test, post-test. | Constructivist learning theory (Merriam et al. 2012). | Simulation—using SP. Lectures on therapeutic communication techniques, which included readings, video clips with discussion; simulation; debriefing. Duration: 60 min including briefing, simulation and debriefing. | Confidence Simulation, with a dimension about level of confidence of learned therapeutic communication skills. |
| 18 | Gaylle 2019 [ ] (USA) | n = 65 senior students enrolled in a psychiatric clinical rotation at a public university from a population of N = 67 (RR 97%). (IG = 32; CG = 33). | Design: quasi-experimental, two group study. Data collection: pre-test, post-test. | Not mentioned. | Simulation—using SP (four scenarios) briefing; simulation; In simulation-debriefing. Duration: one week. CG - briefing, simulation, postsimulation debriefing. | Students’ knowledge of psychiatric assessment. Therapeutic communication checklist created by author. Students’ perceived anxiety related to a psychiatric clinical practicum created by author. Perceptions of the debriefing experience checklist created by author for this study. |
| 19 | Ok et al. 2019 [ ] (Turkey) | n = 85 third-year nursing students enrolled in a course on mental health and psychiatric at two different universities from a population of N = 103 (RR 82.5%). (IG = 52; CG = 33) | Design: quasi-experimental two group Data collection: pre-test, post-test | Not mentioned. | Simulation—using SP theoretical lecture on communication skills and schizophrenia; simulation using SP, debriefing. Duration: 5 hours theoretical lectures, 10–12 min simulation, 30–35 min debriefing. CG—Theoretical lectures and clinical practices. | Communicational Skills Inventory (CSI) State-Trait Anxiety Inventory (STAI) |
IG, Intervention Group; CG, Control Group; SP, Standardized Patient; CKT, Communication Knowledge Test; SSPE, Student Self-Evaluation of Standardized Patient Encounter; SPIR, Standardized Patient Interpersonal Ratings; CST, Communication Skills Training; CCT, Clinical Competence Tool; CEQ, Course Experience Questionnarie; PIMC, Perceived Importance of Medical Communication; CSAS, Communication Skill Attitude Scale; CES, Caring Self-Efficacy Scale; DAS, Death Anxiety Scale; CAT, Communication Assessment Tool; CAS, Communication Ability Scale; CIS, Clinical Interaction Scale; IDC, Interpersonal Dysfunction Checklist; C-SPSI-R, Social Problem Solving Inventory Revised; IPCS, Interpersonal Communication Skills; SLS, Student Learning Satisfaction; SPEs, Standardized Patient Experiences; CBL, Case-Based Learning; PSI, Problem-Solving Inventory; IMMS, Instructional Materials Motivation Scale; ICAS, Interpersonal Communication Assessment Scale; BLSS, Blended Learning Satisfaction Scale; C-NSSES, Communication Skills subscale of the Nursing Students Self-Efficacy Scale; CSI, Communicational Skills Inventory; STAI, State-Trait Anxiety Inventory.
3.4. Outcome measures
The included studies reported 19 different instruments of patient-centered communication. Most of the studies provided data on the reliability and validity of the instruments, either in previous studies or calculated for the study they carried out. However, several authors designed the instruments themselves to evaluate interpersonal communication. For six instruments, no validity data was provided [ 31 , 32 , 33 , 36 , 38 , 39 ].
3.5. Intervention impact on outcomes
Of the articles included in the review, thirteen determined a statistically significant improvement in the results. More than fifty percent (n = 11) of the studies used simulation as part of the training of patient-centered communication skills. Several studies that used simulation found no statistically significant differences between the groups [ 33 , 35 , 37 ]. However, they did determine an improvement in the patient-centered communication skills of the intervention group (IG) with respect to the control group (CG) [ 33 , 35 , 37 ] (see Table 3 ).
Main results and conclusions.
| Order Number | 1st Author, Date (Country) | Findings | Conclusions |
|---|---|---|---|
| 1 | Becker et al. 2006 [ ] (USA) | No significant differences were found between the two groups on measures of interpersonal skills, therapeutic communication skills, and knowledge of depression. | Further research is needed, this study support the use of SPs in nursing education for communication skills training. |
| 2 | Baghcheghi et al. 2011 [ ] (Iran) | The results showed that no significant difference between the two groups in students’ communication skills scores before the teaching intervention (p > 0.05), but did show a significant difference between the two groups in the interaction skills and problem follow up sub-scales scores after the teaching intervention (p < 0.05). | This study provides evidence that cooperative learning is an effective method for improving and increasing communication skills of nursing students especially in interactive skills and follow up the problems sub-scale, thereby it is recommended to increase nursing students’ participation in arguments by applying active teaching methods which can provide the opportunity for increased communication skills. |
| 3 | Kim et al. 2012 [ ] (Korea) | The communication skill score of the experimental group that participated in simulation-based education increased 0.58 points and the control group increased 0.09 points, indicating a significant difference between the two groups (p = 0.020). The clinical competence score of the experimental group that participated in simulation-based education increased 0.63 points, and the score for the control group increased 0.15 points, indicating a significant difference between the two groups (p = 0.009). | Simulation-based education in maternity is effective in promoting communication skill and clinical competence. |
| 4 | Wittenberg-Lyles et al. 2012 [ ] (USA) | The practical nurses’ exposure to the COMFORT communication training allowed students to see its benefits, resulting in more positive attitudes to communication skills learning as measured by the CSAS (p < 0.000). The COMFORT communication curriculum also increased perceptions of the importance of communication in nurse training as assessed by the PIMC (p < 0.009). In addition, COMFORT training resulted in an increase in practical nurses’ reported self-efficacy in using communication skills with patients and families, although no statistically differences were found (p = 0.052). | This study shows promise for the feasibility and use of the CONFORT curriculum for nursing students communication training. |
| 5 | Jo and An 2013 [ ] (Korea) | Attitudes toward death (p = 0.027) and communication skills (p = 0.008) appeared to have significantly increased in the experimental group. However, death anxiety (p = 0.984) did not significantly differ between the two groups after intervention. | The course is effective in reducing negative attitudes toward death and increasing the communication skills of nursing students. |
| 6 | Lau and Wang 2013 [ ] (China) | There were significantly increase between students: the mean pre-test and post-test scores for communication ability (p = 0.015). there were improvement in the scores for content of communication and handling of communication barriers (p < 0.001). In addition, the training was practically important, as indicated by the effect size of 2.39 in the score for the handling of communication barriers. Although the scales of communication ability, clinical interaction, interpersonal dysfunction, and social problem solving were improved, they were not statistically significant (p >.05). | The course was effective in improving communication skills in nursing students. |
| 7 | Lin et al. 2013 [ ] (Taiwan) | All participants expressed high SLS (94.44%) and showed significant (p ≤ 0.025) improvements on IPCS total scores, interviewing, and counseling. However, there were no significant differences between groups (p = 0.374). | Using SPs to teach IPCS to nursing students produced a high SLS, but future studies are needed to confirm the effectiveness of SP feedback and group discussions. |
| 8 | Lau and Wang 2014 [ ] (China) | The analysis showed a significant difference between the mean pretest and posttest scores of the subscales (p = 0.003) and total communication skills scores (p < 0.0001). There was a statistically significant increase in the cognition of communication scores from pre-test to post-test (p < 0.0001), content of communication (p = 0.009), and handling of communication barriers (p < 0.001). The mean pretest and posttest CIS total scores increased (p < 0.0001), sympathetic consideration (p < 0.0001), active listening (p = 0.001), and taking the initiative in care subscales (p = 0.009). The scores of positive problem orientation subscale of the SPSI-R improved (p = 0.037). | The Educational Summer Camp Program was effective in improving nursing students´communication skills. |
| 9 | Webster 2014 [ ] (USA) | The students did not demonstrate significant improvement on 2 of the 14 evaluation criteria -approaching client with a nonthreatening body stance (p = 0.218) and introducing self (p = 0.74)- although there was improvement noted for the two evaluation criteria. There was improvement noted in anxiety, students’ ability to establish eye contact, to engage in efforts to put the patient at ease, safety assessments, the ability to set limits on inappropriate behavior (p < 0.05). In building a therapeutic relationship, Improvements were also noted in all three of these areas (using therapeutic communication techniques; responding appropriately to verbal statements and responding appropriately to nonverbal behavior), (p < 0.05). The ability to validate the meaning of a patient’s response increased significantly. Last, the appropriate termination were increase significantly for these two areas (summarizing content of interaction, terminating appropriately), (p < 0.05). | This study suggests that the use of SPEs is an effective methodology for promoting therapeutic communication skills in nursing students. |
| 10 | Bloomfield et al. 2015 [ ] (UK) | After the simulation, self-perceived confidence levels when communicating with the family and friends of dying patients increased significantly (p < 0.05). The majority of students reported increased levels of competence when talking with the family of dying patients (p < 0.05). | Simulation was found to be an effective means of preparing nursing students to communicate with dying patients and their families. |
| 11 | Yoo and Park 2015 [ ] (Korea) | A significant increase in the communication skills score of the intervention group was observed (p < 0.001) while a slight increase was observed for the control group (p < 0.001). There was a significant difference in the communication skills of the two groups (p < 0.001). A significant decrease in the problem solving ability score of the intervention group was observed (p < 0.001), whereas an increase was observed in the control group (p < 0.001). A significant improvement was observed for the problem-solving ability of the intervention group, as compared to the control group (p < 0.001). Finally, scores for learning motivation showed a significant increase (p < 0.001), for the intervention group, whereas a decrease (p > 0.05), was observed for the control group. Moreover, a significant difference was found in the learning motivation scores of the two groups (p < 0.001). | This finding suggests that case-based learning is an effective learning and teaching method. |
| 12 | Lai 2016 [ ] (Taiwan) | The scores given by the peers were significatly corelated with those given by experts (r = 0.36, p<0.05). In relation, students’ attitudes toward the peer assessment activities. Overall, the mean scores of each item were greater than 4 (agree) which means the students were satisfied with the peer assessment learning activities. | The nursing students had improved their skills in therapeutic communication as a result of the networking peer assessment. Expert evaluation scores showed that students’ communication performance, when involved in peer assessments, significantly improved. |
| 13 | Martin and Chanda 2016 [ ] (USA) | There was significant improvement (p = 0.000), in student’s self-reported confidence with their communication skills and knowledge following a mental health simulation experience using standardized patients. | A therapeutic communication mental health simulation give before students participating in their clinical experience should be integrated into undergraduate nursing education. |
| 14 | Taghizadeh et al. 2017 [ ] (Iran) | The results showed that there was a significant difference between the mean quality of patients’ care prior to and following the intervention (p≤0.001). Also, there was a significant difference between the means for nursing student’s’ communication skills before and after the intervention (p≤0.001). Moreover, there was a significant correlation between mean scores of students and the quality of care and communication skills (p≤0.001). | The course was effective in improving communication skills in nursing students. |
| 15 | Shorey et al. 2018 [ ] (China) | There was a statistically significant increase in the BLSS scores from pre-test to post-test (p = 0.012). Similarly, a statistically significant increase in the CSAS scores were seen from pre-test to post-test (p = 0.042). There was also a statistically significant increase in the C-NSSES scores from pre-test to post-test (p = 0.003). | Participants had enhanced satisfaction levels with blended learning pedagogy, better attitudes in learning communication skills, and improved communication self-efficacies at posttest. |
| 16 | Blake and Blake 2019 [ ] (USA) | An improvement in student self-efficacy in therapeutic communication skills after the course simulation as indicated by the five questions were all significant with p < 0.01. | The lab simulation was helpful in improving students regarding their therapeutic communication skills. |
| 17 | Donovan and Mullen 2019 [ ] (USA) | The pre/post results suggest the standardized simulated experience enhanced nursing student confidence p < 0.001. These results suggest that the student nurse confidence in therapeutic communication with a mental health patient had increased. | Simulation with SPs promoted an active learning environment that highlighted individualized confidence in therapeutic communication skills through a realistic application process. |
| 18 | Gaylle 2019 [ ] (USA) | The overall change from pretest to posttest for therapeutic communication for both groups combined was statistically significant and practically important with a large effect size of 1.34 (Cohen d). On average, both groups showed statistically significant improvement (p < 0.05). The in-simulation group demonstrated a greater increase in therapeutic-communication techniques and a larger decrease in nontherapeutic communication than their peers in the post-simulation group. Differences in means between the in-simulation and the post-simulation groups for therapeutic communication (mean, 1.39 and 0.83) but there are not statistically differences significant between groups. | In simulation debriefing is an effective tool for teaching therapeutic communication to nursing students. |
| 19 | Ok et al. 2019 [ ] (Turkey) | There are differences between the students who received and who did not receive SPS in terms of the scores obtained from the STAI-S (p = 0.01), STAI-T (p = 0.046), but there are not statistically differences in CSI (p = 0.09), except for the subscale cognitive of the CSI (p = 0.043). The comparison of the scores obtained by the intervention group prior to and after the SPS shows a statistically meaningful decrease in the anxiety levels (p = 0.001; p = 0.009) and a statistically meaningful increase in the communication skills of the intervention group after the simulation exercise (p = 0.001), except for the emotional subscale (p = 0.074). | Simulation with SPs may help nursing students gain experience and increase communication skills with patients. |
SP, Standardized Patient; SLS, Student Learning Satisfaction; CIS, Clinical Interaction Scale; IPCS, Interpersonal Communication Skills; SPSI-R, Social Problem Solving Inventory Revised; SPEs, Standardized Patient Experiences; BLSS, Blended Learning Satisfaction Scale; CSAS, Communication Skill Attitude; C-NSSES, Communication Skills subscale of the Nursing Students Self-Efficacy Scale; SPS, Standardized Patient Simulation; CSI, Communicational Skills Inventory; STAI, State-Trait Anxiety Inventory
3.6. Quality assessment
Based on JBI criteria for the effectiveness of experimental designs, the two RCTs included were evaluated at level 1C (See Table 1 ). The quasi-experimental studies (n = 6) with two groups reported a level of evidence of 2C and the experimental studies with a single group (n = 11) reported evidence at level 2D for effectiveness, according to the criteria of evidence levels of JBI [ 25 ] ( Table 4 and Table 5 ).
Results of critical appraisal for quasi-experimental studies.
| Order Number | MAStARI Question | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Baghcheghi et al. 2011 [ ] (Iran) | Yes | Yes | Unclear | Yes | Yes | No | Yes | Yes | Yes | 7 |
| 2 | Kim et al. 2012 [ ] (Korea) | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | 7 |
| 3 | Wittenberg-Lyles et al. 2012 [ ] (USA) | Yes | Unclear | Yes | No | Yes | Yes | Yes | Yes | Yes | 7 |
| 4 | Jo and An 2013 [ ] (Korea) | Yes | Yes | Unclear | Yes | Yes | Unclear | Yes | Yes | Yes | 7 |
| 5 | Lau and Wang 2013 [ ] (China) | Yes | Yes | Yes | No | Yes | Unclear | Yes | Yes | Yes | 7 |
| 6 | Lau and Wang 2014 [ ] (China) | Yes | Yes | Yes | No | Yes | Unclear | Yes | Yes | Yes | 7 |
| 7 | Webster 2014 [ ] (USA) | Unclear | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 7 |
| 8 | Bloomfield et al. 2015 [ ] (UK) | Yes | Yes | Yes | No | Yes | Yes | Yes | Unclear | Unclear | 6 |
| 9 | Yoo and Park 2015 [ ] (Korea) | Yes | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | 7 |
| 10 | Lai 2016 [ ] (Taiwan) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | 7 |
| 11 | Martin and Chanda 2016 [ ] (USA) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 8 |
| 12 | Taghizadeh et al. 2017 [ ] (Iran) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 8 |
| 13 | Shorey et al. 2018 [ ] (China) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 8 |
| 14 | Blake and Blake 2019 [ ] (USA) | Yes | Yes | Yes | No | Yes | No | Yes | No | No | 5 |
| 15 | Donovan and Mullen 2019 [ ] (USA) | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | 7 |
| 16 | Gaylle 2019 [ ] (USA) | Unclear | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 7 |
| 17 | Ok et al. 2019 [ ] (Turkey) | Yes | No | Unclear | Yes | Yes | Yes | No | Yes | Yes | 6 |
Results of critical appraisal for Randomized Controlled Trials.
| Order Number | MAStARI Question | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Becker et al. 2006 [ ] (USA) | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10 |
| 2 | Lin et al. 2013 [ ] (Taiwan) | Yes | Unclear | Unclear | Yes | Unclear | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | 9 |
4. Discussion
This systematic review provides an overview of the research carried out on nursing students in order to develop communication skills with the patient. The objective of this systematic review was to identify, critically evaluate and synthesize the evidence of the impact of educational interventions on nursing students to develop their communication skills with patients. Despite the various educational pedagogies used to develop communication skills with the patient. All research agrees on the importance of developing interventions to improve communication skills with the patient in nursing students. From the main findings, it can be indicated that the majority of the analyzed studies used simulation as the methodology for communication skills training, obtaining statistically significant results. Regarding the countries in which they have carried out the studies, it is worth noting that the majority have been carried out in the USA, these data coincide with those reported in previous research on the analysis of scientific communication publications [ 48 , 49 ]. Regarding theoretical and conceptual frameworks to guide the intervention studies, only two studies used theoretical frameworks to guide the intervention [ 26 , 28 ]. However, the theoretical and conceptual frameworks are essential to develop experimental studies allowing the variables and the relationship between them to be established, described in previous studies. The conceptual frameworks provide information about the subjects, the way of collecting and statistical analysis of the data, making it possible to guide the interventions in the experimental studies and helping the interpretation of the data [ 50 ].
However, measuring patient-centered communication can be difficult due to the numerous definitions that exist to refer to this type of communication such as TC, nurse–patient communication or interpersonal communication. In addition, there are numerous aspects of communication with the patient that must be considered, as reflected in, for example, the conceptual framework of interpersonal relationships [ 2 ]. The instruments used must prove to be valid and reliable. However, only fourteen of the articles reviewed provided data on the validity and reliability of the tool [ 26 , 28 , 34 , 35 , 36 , 37 , 40 , 42 , 43 , 44 , 45 , 46 , 47 ]. These issues suggest that researchers should consider the relevance of instruments to assess patient-centered communication before using them. In addition to considering the validity and reliability of the instruments, if they were developed in previous studies, psychometric tests should be performed for the study population. In the case that these instruments were developed by the researchers of the study, they should report the psychometric properties of them. On the other hand, previous studies have indicated the need to develop and validate instruments to assess patient-centered communication skills of nursing students [ 51 , 52 ]. The development of validated instruments to assess communication skills with patients would allow evaluating the impact of the interventions developed on nursing students and determining which interventions are more effective.
Regarding interventions to improve patient-centered communication skills of nursing students, it was observed that the majority focused on simulation, using SP (e.g., [ 26 , 32 , 33 ]), role-playing [ 39 ] or high-fidelity patient [ 34 ], to either facilitate learning or evaluate communication skills. Previous studies indicate the importance of incorporating simulation in communication skills training. In particular, simulation provides realistic scenarios that allow nursing students to practice and evaluate TC with patients, without putting real patients at risk [ 53 ]. In addition, various studies indicate that the simulation with SP offers nursing students the opportunity to practice TC before clinical practices, being able to improve communication with the patient in the clinical setting [ 54 , 55 ]. Simulation using SP can be effective in teaching patient-centered clinical skills [ 53 , 56 ]. On the other hand, previous studies have shown the training of individuals to treat patients in realistic situations provides an opportunity to improve the competencies of nursing students through human interaction and feedback [ 57 , 58 ]. In this review, all of the studies that implemented simulation conducted feedback with the nursing students. The process of providing feedback during or after the simulation sessions allowed them to address their strengths and weaknesses in order to improve their performance [ 57 , 58 ]. In conclusion, previous research indicates that the implementation of simulation in clinical skills training programs could be useful to improve nurses’ communication skills and the ability to interact with patients [ 6 , 52 ]. In relation to the application of innovative educational pedagogies, various studies have indicated the need to implement new active learning pedagogies that involve students in their training in order to improve their clinical skills [ 59 , 60 ]. Regarding the use of courses as an intervention to improve communication skills with the patient, they have been shown to be effective in some of the included studies. However, the development of courses based on master classes is not recommended as the only educational resource in the training of nursing students and should be combined with other educational pedagogies [ 61 ]. In short, previous studies indicate that the new generation of students prefer self-directed, immediate, exciting and immersive experiences [ 62 ]. They encourage nurse educators to superimpose the dissonances between traditional teaching and generational learning needs, based on active learning, simulations, reflective learning and educational games [ 63 , 64 ]. Hence, most studies are based on simulation or innovative pedagogies, to encourage student participation in the acquisition of skills.
Following the analysis of the included articles, the contexts were mainly based on mental health [ 26 , 31 , 33 , 35 , 36 , 37 , 38 , 39 , 40 ], end-of-life [ 32 , 43 , 47 ] and maternity [ 34 ]. Six studies focused on general patient-centered communication skills [ 28 , 41 , 42 , 44 , 45 , 46 ]. Previous studies have indicated that interventions to teach nurse-patient communication skills target the most challenging clinical interactions [ 52 ]. These data are consistent with the studies included in this review. In particular, previous studies indicate that nursing students feel challenged and anxious when they have to talk and interact with mental health patients [ 65 , 66 ]; hence, it is one of the most predominant clinical areas in this review. In addition a review indicated that further studies are needed to improve the available evidence on the clinical practice of nursing students with mental health patients [ 67 ]. However, the communication skills involved in everyday conversation with patients are equally important, especially given the perception that nurses lack the time to communicate with patients [ 68 ] or with chronically ill patients [ 7 , 8 ], and this was not addressed in the nursing students. Regarding the year that the nursing students were enrolled in, statistically significant improvements were observed in both the students enrolled in their first year [ 28 , 32 , 34 , 35 , 42 ] and those in their last year of the nursing degree [ 33 , 37 , 38 , 39 , 44 , 45 , 46 ]. In addition, several studies indicate that communication skills training should be incorporated into the nursing degree curriculum every year. Therefore, the students learn and practice various communication skills before beginning their clinical practices in different clinical areas [ 15 , 68 ].
In this systematic review, in which 19 quantitative studies on patient-centered communication interventions in nursing students were reviewed, half of them were found, specifically thirteen [ 26 , 28 , 32 , 34 , 36 , 38 , 39 , 40 , 42 , 44 , 45 , 46 , 47 ], to be effective in improving patient-centered communication skills. The differences between the obtained results may be due to the study design, as there was a lot of variability in the designs, sampling, teaching interventions, duration and sample size. In addition, several studies indicated improvements in patient-centered communication skills, although the results were not statistically significant in some of them (e.g., [ 33 , 35 , 37 ]). On the other hand, only one study evaluated the long-term impact of intervention on nursing students, finding statistically significant differences [ 38 ]. It would be necessary for future studies to evaluate the long-term impact of the interventions in order to improve their communication skills with patients and to determine the effectiveness over time.
A longitudinal study design is recommended to assess the stability and long-term influence of the improvements in communication skills observed in this study. Specifically, observational studies are needed to assess student performance in clinical areas.
Strengths and limitations
This review includes the following limitations. First, articles that were not in English were excluded, which may constitute a bias by not considering other languages. Most of the included studies used self-report measures to identify the results and few studies used more objective measures. Furthermore, the heterogeneity of the intervention methods and measurements of the studies’ results prevented a synthesis of results through meta-analysis. The studies need more evidence to address the possibility of bias due to the use of self-report measures and other potential forms of bias [ 69 ]. For example, the inclusion of quasi-experimental studies without randomization presents a selection bias. This aspect tends to overestimate the effects of intervention, even though a rigorous methodology and relevant data are presented. The studies of a single group that evaluate the impact of intervention, based on differences between pre-test and post-test measures, can interfere with internal validity by not being compared with students of the same cohort who were not exposed to the intervention. The studies where training was carried out over a period of time can lead to biases, as it is not possible to prove whether changes were due to the intervention or other academic activities. Another risk of bias in the studies is that the instructors who performed the interventions were not blinded due to the nature of the educational intervention studies. On the other hand, it is also important to consider that almost 50% of the studies were carried out within the context of mental health, as communication is a key element of the nurse-patient relationship in this area. However, it would be interesting in future research to be able to deepen the analysis of communication skills learning within the nursing curriculum and the subjects or areas in which it is involved.
This systematic review had some strengths. First, a broad search was performed using MeSH terms and keywords that addressed the communication of nursing students with the patient; and this search was performed in multiple databases. Despite this, research methods have been systematically applied in this review following the guidelines established for systematic review. In addition, a two-person review of what studies to include and the assessment of their quality increased the rigor of the findings. Therefore, the results obtained expand and update what was known thus far about patient-centered communication interventions for nursing students.
More research is needed to develop instruments that evaluate all aspects that interfere with patient-centered communication in order to improve patient-centered communication skills of nursing students through more effective educational strategies, guided by theoretical frameworks, in a more consistent way. In addition, studies should be carried out that report the perspective of the patient in regards to communication established with the nursing students.
5. Conclusions
This systematic review provides preliminary evidence of the effectiveness of interventions used to train nursing students in patient-centered communication. Although all the interventions obtained significant results in communication skills, it has not yet been determined which methodology is more effective. The majority of the analyzed studies used simulation as the methodology for communication skills training, obtaining statistically significant results. This methodology could be combined with other educational strategies that have indicated improved communication of nursing students with their patients.
Author Contributions
Conceptualization, L.G.-P. and V.V.M.-H.; Methodology, L.G.-P., V.V.M.-H., V.G.-P., G.A.-M.; Writing—Original Draft Preparation, L.G.-P., V.V.M.-H., and G.A.-M.; Writing—Review & Editing, V.G.-P. and G.G.-G.; Supervision: L.G.-P., V.V.M.-H.,V.G.-P., G.G.-G., G.A.-M. All authors have read and agreed to the published version of the manuscript.
This research received no external funding
Conflicts of Interest
The authors declare no conflict of interest.
- Click here - to use the wp menu builder

- Privacy Policy
- Refund Policy
- Terms Of Service
- Nursing notes PDF
- Nursing Foundations
- Medical Surgical Nursing
- Maternal Nursing
- Pediatric Nursing
- Behavioural sciences
- BSC NURSING
- GNM NURSING
- MSC NURSING
- PC BSC NURSING
- HPSSB AND HPSSC
- Nursing Assignment
Types of Therapeutic Communication in Nursing
In this Types of Therapeutic Communication in Nursing article, we will explore various types of therapeutic communication techniques employed by nurses to enhance patient care.
Table of Contents
Defining Therapeutic Communication in Nursing
Therapeutic communication in nursing is a purposeful, patient-centered interaction that promotes a trusting relationship between the nurse and the patient. It involves active listening , empathy, and effective communication to address the physical and emotional needs of patients.
Importance of Therapeutic Communication in Nursing
Establishing a strong therapeutic relationship through communication is crucial in nursing. It not only improves patient satisfaction but also contributes to better health outcomes and increased adherence to treatment plans.
Explore the various types of therapeutic communication in nursing that play a pivotal role in enhancing patient care.
Verbal Therapeutic Communication
Open-ended questions.
Nurses often use open-ended questions to encourage patients to express their thoughts and feelings freely. This technique promotes a more in-depth understanding of the patient’s concerns.
Reflective Responses
Reflective responses involve paraphrasing or restating what the patient has communicated. This technique validates the patient’s feelings and shows that the nurse is actively engaged in the conversation.
Clarification
Clear communication is vital in healthcare. Nurses use clarification techniques to ensure that they understand the patient’s statements accurately, reducing the risk of misunderstandings.
Non-Verbal Therapeutic Communication
Active listening.
Active listening involves not only hearing the patient’s words but also paying attention to their non-verbal cues. Nurses use this technique to demonstrate empathy and understanding.
Eye Contact and Body Language
Maintaining appropriate eye contact and positive body language conveys attentiveness and warmth, contributing to a trusting nurse-patient relationship .
Judicious use of touch, such as a comforting hand on the shoulder, can provide emotional support and reassurance to patients.
Written Therapeutic Communication
Beyond spoken words, the written form plays a vital role. Whether it’s documenting patient information or crafting empathetic notes, nurses proficient in written therapeutic communication ensure that every aspect of patient care is well-documented and understood.
Empathetic Communication
Nurses validate patients’ feelings by acknowledging their emotions without judgment. This fosters a sense of understanding and support.
Empathetic Statements
Expressing empathy through statements like “I understand how you feel” demonstrates compassion and helps patients feel heard and supported.
Educational Therapeutic Communication
Teach-back method.
Nurses use the teach-back method to ensure patients comprehend medical information by asking them to explain it in their own words.
Providing Information
Clear and concise information about diagnoses, treatments, and care plans helps empower patients to actively participate in their healthcare.
Therapeutic Humor
Lightening the mood.
Appropriate humor can create a positive and relaxed atmosphere, easing tension and promoting a more comfortable patient experience.
Building Rapport
Sharing light moments through humor helps build rapport between nurses and patients, contributing to a more positive therapeutic relationship.
De-escalation Techniques
Calm communication.
In high-stress situations, nurses employ de-escalation techniques, such as maintaining a calm tone and using soothing words, to diffuse tension.
Redirection
Redirecting a patient’s focus from a stressful situation to a more positive or neutral topic can help de-escalate emotions.
Spiritual Therapeutic Communication
Active listening to spiritual concerns.
Nurses acknowledge and respect patients’ spiritual beliefs, actively listening to their concerns and incorporating them into the care plan.
Providing Spiritual Support
Offering spiritual support, such as facilitating visits from religious leaders or providing quiet spaces for prayer, contributes to holistic patient care.
In Types of Therapeutic Communication in Nursing conclusion, therapeutic communication in nursing involves a diverse set of techniques aimed at establishing meaningful connections with patients. Whether through verbal or non-verbal means, the goal is to create an environment that promotes trust, understanding, and collaboration in the pursuit of optimal patient care.
Why is therapeutic communication important in nursing?
Therapeutic communication in nursing is crucial for building trust, understanding patient needs, and improving overall patient outcomes.
How do nurses use empathy in their communication?
Nurses express empathy through validation, empathetic statements, and actively listening to patients’ concerns.
Why is humor considered a therapeutic communication technique in nursing?
Humor can lighten the mood, build rapport, and create a positive atmosphere, contributing to a more comfortable patient experience.
Please note that this article is for informational purposes only and should not substitute professional medical advice.
Leave a Reply Cancel reply
Recent articles, nursing informatics: the intersection of nursing and technology, patient positioning: importance, techniques, and safety considerations, hyperthermia nursing diagnosis and care plan, types of immunity system of body, home care nursing services, benefits and challenges, types of nursing courses: which one is right for you, download nursing notes pdf, mental health nursing history collection, nursing assignment on contraceptive pills, case study on appendicitis nursing assignment, male and female reproductive system pdf, nursing foundation note for bsc and gnm, staff nurse syllabus and exam pattern question bank -1, sensory system and sense organs pdf, medical surgical nursing- nursing assignment on dialysis, more like this, gifts for nursing home residents, gift ideas for nursing students, crystalloid and colloid: differences and when to use each, how to insert a catheter in a female patient -female catheterization, mental health nursing diagnosis care plan pdf, child pediatric health nursing notes -bsc nursing, mid-wifery pdf notes for nursing students, national health programmes in india pdf, reproductive system nursing notes pdf, primary health care nursing notes pdf, psychology note nursing pdf, nursingenotes.com.
- STUDY NOTES
- SUBJECT NOTES
A Digital Platform For Nursing Study Materials
Latest Articles
Most popular.
© Nursingenotes.com | All rights reserved |
COPR 640 Analytics in Crisis Communication
- Course Description
For information regarding prerequisites for this course, please refer to the Academic Course Catalog .
Course Guide
View this course’s outcomes, policies, schedule, and more.*
*The information contained in our Course Guides is provided as a sample. Specific course curriculum and requirements for each course are provided by individual instructors each semester. Students should not use Course Guides to find and complete assignments, class prerequisites, or order books.
All individuals in any organization must be armed with strategies to communicate in crisis. Analyzing historic crises will ready them for future events and aid in the overall mitigation of organization crisis.
Course Assignment
Textbook readings and lecture presentations.
No details available.
Course Requirements Checklist
After reading the Course Syllabus and Student Expectations , the student will complete the related checklist found in the Course Overview.
Video Discussion: Introduction
Video Discussions are collaborative learning experiences. Therefore, the student will complete one Video Discussion: Introduction in this course. During the first week, the student will record a short video introducing himself or herself to the class. The student should post this in the initial thread. The length of the video is up to the student (but typically 2-4 minutes). Then, the student will post a written response of 200 words to 2 other classmates’ video introductions. No scholarly sources/citations are required.
Discussions (4)
Discussions are collaborative learning experiences. Therefore, the student will complete five standard discussions within this course. The content of this course is extensive and will require the student to look at a variety of concepts in a variety of ways. The student will have to think analytically, articulate carefully, and work quickly. The student will prepare an initial thread and then respond to at least 2 of his or her peers. Each thread must be a minimum of 400 words and include 3 scholarly citations (including 1 of the textbooks) and 1 Biblical reference in current APA format. Each reply must be a minimum of 250 words and include 2 scholarly citations and 1 Biblical reference in current APA format.
Comparative Case Study Assignment
Compare and contrast the crisis communication strategies of two recent organizational crises. Analyze the effectiveness of pre-crisis planning, crisis response tactics, and post-crisis recovery efforts in each case to gain a better understanding of post-crisis success. These paper will be approximately 1,000 words in current APA format. It will include at least 8 references, including both of the course textbooks (2) and the Bible.
Analysis of Crisis Response Assignment
This assignment focuses on a critical analysis of a recent organizational crisis response and its communication strategies. The student will dissect the strengths and weaknesses of the communication approach, exploring alternative tactics that might have led to different outcomes. These paper will be approximately 1,000 words in current APA format. It will include at least 8 references, including both of the course texts (2) and the Bible.
Case Study Assignment
After reading many case studies throughout this program, this assignment challenges the student to delve into a recent crisis and analyze its impact through a case study format. These paper will be approximately 1,000 words in current APA format. It will include at least 8 references, including both of the course textbooks (2) and the Bible.
Quizzes (3)
Each quiz will cover the Learn material for the assigned Module: Week. Each quiz will be open-book/open-notes, contain 2-3 short-answer questions, and have a 1-hour time limit. The student should support his or her responses using the course textbooks and other outside sources.

Have questions about this course or a program?
Speak to one of our admissions specialists.
Inner Navigation
- Assignments
Have questions?

Are you ready to change your future?
Apply FREE This Week*
Request Information
*Some restrictions may occur for this promotion to apply. This promotion also excludes active faculty and staff, military, non-degree-seeking, DGIA, Continuing Education, WSB, and certificate students.
Request Information About a Program
Request info about liberty university online, choose a program level.
Choose a program level
Bachelor’s
Master’s
Certificate
Select a Field of Study
Select a field of study
Select a Program
Select a program
Next: Contact Info
Legal first name.
Enter legal first name
Legal Last Name
Enter legal last name
Enter an email address
Enter a phone number
Full Address
Enter an address
Apt., P.O. Box, or can’t find your address? Enter it manually instead .
Select a Country
Street Address
Enter Street Address
Enter State
ZIP/Postal Code
Enter Zip Code
Back to automated address search
Start my application now for FREE
- Open access
- Published: 05 September 2024
Bridging the generational gap between nurses and nurse managers: a qualitative study from Qatar
- Ahmad A. Abujaber 1 ,
- Abdulqadir J. Nashwan ORCID: orcid.org/0000-0003-4845-4119 1 ,
- Mark D. Santos 1 ,
- Nabeel F. Al-Lobaney 1 ,
- Rejo G. Mathew 1 ,
- Jamsheer P. Alikutty 1 ,
- Jibin Kunjavara 3 &
- Albara M. Alomari 2
BMC Nursing volume 23 , Article number: 623 ( 2024 ) Cite this article
Metrics details
The nursing workforce comprises multiple generations, each with unique values, beliefs, and expectations that can influence communication, work ethic, and professional relationships. In Qatar, the generational gap between nurses and nurse managers poses challenges to effective communication and teamwork, impacting job satisfaction and patient outcomes.
This study investigates the generational gap between nurses and nurse managers in Qatar, aiming to identify strategies to enhance collaboration and create a positive work environment.
A qualitative research design was used, involving semi-structured interviews with 20 participants, including frontline nurses and senior nurse managers. Participants were purposively sampled to represent different generations. Data were collected through face-to-face and virtual interviews, then transcribed and thematically analyzed.
Four key themes emerged: Optimizing the Work Environment : Older generations preferred transformational and situational leadership, while younger nurses valued respect, teamwork, accountability, and professionalism. Strengthening Work Atmosphere through Communication and values : Older nurses favored face-to-face communication, while younger nurses preferred digital tools. Cultivating Respect and Empathy : Younger nurses emphasized fairness in assignments and promotions, while older nurses focused on empathy and understanding. Dynamic Enhancement of Healthcare Systems : Younger nurses were more adaptable to technology and professional development, while older nurses prioritized clinical care and patient outcomes.
The study reveals significant generational differences in leadership preferences, communication styles, and adaptability to technology. Addressing these gaps through effective leadership, ongoing education, and open communication can improve job satisfaction and patient care.
Peer Review reports
Introduction
The nursing profession faces a significant challenge of a multigenerational workforce that can cause conflict and hinder effective communication, especially between nurse managers and nurses [ 1 ]. In addition, a literature review of studies conducted over the past two decades indicates that the generational gap between nurses and nurse managers is a complex phenomenon requiring concerted efforts to address it [ 2 , 3 ].
The nursing workforce comprises four generations, including the Baby Boomers (born between 1946 and 1964), Generation X (born between 1965 and 1979), Generation Y or Millennials (born between 1980 and 1994), and Generation Z (born after 1995) [ 4 ]. These generations have unique values, beliefs, attitudes, and expectations that influence their communication style, work ethic, and approach to work [ 4 ].
In 2013, Hendricks and Cope discussed the impact of generational differences on the nursing workforce and the challenges it presents for nurse managers [ 5 ]. They searched various databases electronically and found that generational diversity affects nurses’ attitudes, beliefs, work habits, and expectations. The paper suggested that accepting and embracing this diversity can lead to a more harmonious work environment and facilitate nurse retention [ 5 ].
The article focused on the cultural and work ethic differences between Baby Boomers and Generation Xers, with Baby Boomers primarily managing the workforce [ 6 ]. Baby Boomers are described as driven and dedicated, equating work with self-worth and personal fulfillment [ 6 ]. At the same time, Generation Xers have ideas of an acceptable workplace, and their terms of employment are usually non-negotiable [ 6 ]. The article summarized recent literature and studies to guide healthcare leadership in recruiting, retaining, and managing Generation X workers in the nursing field [ 6 ].
Similarly, Carver & Candela (2008) conducted a study to inform nurse managers about the generational differences among nurses and how they affect the work environment [ 7 ]. With four generations in the nursing workforce, understanding the characteristics of each generation can lead to increased job satisfaction, productivity, and decreased turnover [ 7 ]. Considering generational differences as part of an overall strategy to increase organizational commitment can improve nursing work environments and address the global nursing shortage [ 7 ]. Managers should increase their knowledge of generational diversity to tap into the strengths of each generation [ 7 ]. In addition, Younger nurses have different career expectations than their older colleagues [ 8 ]. They seek a balanced lifestyle with reasonable work hours, demand to use the latest technology, and expect to be vocal team members [ 8 ].
Managing a multigenerational workforce requires recognizing and valuing the strengths of each generation. Leaders who maximize everyone’s talents and address individual and generational needs can create synergy and improve team performance. Each generation brings unique strengths to the workforce that should be celebrated and utilized to the organization’s advantage. Meeting the needs of each employee, such as providing opportunities for advancement, work/life balance, compensation, benefits, and learning and development, can lead to higher-functioning work teams [ 9 ]. Nurse leaders should know their employees’ multigenerational characteristics and expectations and provide timely and specific feedback to manage them effectively [ 9 ]. With an appreciation of multigenerational differences and a commitment to higher-functioning work teams, leaders can improve organizational efficiency and patient care outcomes [ 9 ].
To bridge the generational gap in nursing, the SIT offers a comprehensive approach to enhancing communication, collaboration, and teamwork between nurses and nurse managers [ 5 ]. This involves acknowledging and respecting each generation’s unique characteristics, values, and experiences, which fosters a better understanding and more effective cooperation. Establishing a shared vision and goal for patient care unites nurses and nurse managers, helping to overcome any multigenerational conflicts that might arise in the workplace [ 5 ]. Additionally, encouraging multigenerational communication and mentoring is vital. This can be facilitated through programs where experienced nurses share their knowledge and skills with younger colleagues, promoting a cohesive and supportive team environment. Furthermore, providing training and development opportunities tailored to each generation’s diverse learning styles and preferences is essential for building a more skilled and competent workforce [ 10 ].
The literature indicates that the generational gap between nurses and nurse managers is a global complex phenomenon that can affect communication, work values, job satisfaction, retention, and quality of care [ 11 ]. Nursing leaders can recognize generational differences in values and behaviors as potential strengths. By gaining a deeper understanding of generational influences, these insights can be harnessed to develop effective strategies that sustain the diverse yet shrinking nursing workforce. Leveraging generational differences can also create positive work environments, enhance quality and productivity, and ultimately improve patient care. As generational differences increasingly become a critical aspect of diversity, it is essential to understand the dynamics between work engagement and meaningful work across generational cohorts to tailor approaches that align with each organization’s unique needs [ 12 , 13 ].
Understanding how to bridge the generational gap in nursing is crucial for nurses and nurse managers to work together effectively and provide better patient care, ultimately leading to improved patient outcomes. This study aims to enhance workplace communication and collaboration by identifying and addressing the factors contributing to multigenerational workplace conflicts. By doing so, nurses and nurse managers can build more cohesive and supportive teams, resulting in a more positive work environment. Finally, addressing the generational gap in nursing benefits the workplace and enables the organization to develop a more engaged and motivated workforce. Multigenerational learning and development opportunities can increase job satisfaction and retention. Recognizing and valuing the unique perspectives and experiences each generation brings is essential.
Study significance
To the best of our knowledge, no studies have been conducted in Qatar that addressed the generational gap among nurses. In line with this, the study aims to identify and compare the work engagement levels and managerial approaches among nurses and nurse managers across different generations and explore and propose effective strategies for improving communication, collaboration, and job contentment in an intergenerational work environment. The findings will contribute to the nursing profession’s knowledge and provide practical solutions for managing a diverse nursing workforce in Qatar.
This study utilized a descriptive qualitative research design. After considering the participants’ time limits, commitments, and convenience, data were collected through semi-structured interviews with nurses and nurse managers (Executive and assistant executive directors of nursing). The authors developed the interview questions for this study (Supplementary File 1). Participants were recruited from healthcare facilities within the organization through purposive sampling. The sample size was determined based on the data saturation point, where no new themes or perspectives emerged. Interviews were conducted face-to-face or virtually, depending on the participant’s preference and availability. With the participant’s permission, interviews were audio-recorded to aid in accurate transcription and were thematically analyzed.
Development of the interview guide
The interview guide was thoughtfully developed to capture participants’ experiences and insights effectively. The process began with an in-depth review of studies examining the generational gap between nurses and managers, identifying key themes such as work engagement, organizational environment, communication, and technological advancement. These themes provided the framework for creating open-ended questions to elicit detailed and reflective responses. Probing questions were also included to deepen the data collected by clarifying and expanding on participants’ initial answers. The draft questions underwent multiple rounds of review and refinement to ensure clarity, relevance, and the elimination of bias, with potential input from qualitative research experts.
Qualitative research aimed to generate a deep understanding of the generational gap between nurses and their managers. This understanding could not be answered in a quantitative approach. Several strategies were employed throughout the research process to ensure the credibility of the findings.
Firstly, to ensure the credibility of the data collected, the researcher established trust and rapport with the participants. This was achieved by being transparent about the research aims, building rapport, and showing genuine interest in the participants’ experiences. The researcher also ensured that the participants felt comfortable sharing their experiences and opinions by creating a safe and non-judgmental environment.
Secondly, data triangulation was used to enhance the credibility of the data. Data triangulation involves using multiple data sources to provide a more comprehensive understanding of the phenomenon being studied.
Thirdly, the researcher conducted member checking to validate the data collected. Member checking involved sharing the findings with the participants and asking for their feedback on whether the findings accurately represented their experiences and opinions. This process ensured that the researcher’s interpretation of the data aligned with the participants’ experiences and perceptions.
Fourthly, the researcher engaged in reflexivity throughout the research process. Reflexivity involves reflecting on the researcher’s biases, values, and assumptions that might have influenced the research process and findings. By being aware of their biases, the researcher ensured they did not influence the data collection or interpretation of the findings.
Finally, the researcher used a systematic and rigorous approach to analyze the data collected. This study used thematic analysis to identify patterns and themes in the data. The analysis was conducted using a coding scheme, and the findings were supported with quotes from the participants, enhancing the credibility of the findings.
Study population and setting
The participants were approached using a purposive sampling technique. A total of 20 participants were expected to join the study. All participants were approached based on an email from the corporate nursing mail group. The participants of this study met the following criteria: they represented diverse generations, with 3–4 from each of the subsequent generations: Generation X (1965–1980), Generation Y (1981–1996), and Generation Z (1997–2012); they had joined HMC for at least one year; and they were willing to participate in the study.
Study procedures
Before conducting the study, the researcher had obtained the consent of the participants (Research Information Sheet). Interviews were done face-to-face or virtually, depending on the participants’ preferences and availability. During the interviews, conversations were audio-recorded to facilitate transcriptions of the responses, completed within 24 h of the interview, and reviewed by two study researchers. The data saturation was determined by redundancy of information is indicated when similar patterns, themes, or categories keep appearing in the data, and no new information is being uncovered during additional interviews or data collection efforts.
The richness and depth of the data collected are critical. Saturation is considered reached when the data sufficiently explores and explains the research questions and key concepts, providing a comprehensive understanding of the phenomenon. Data saturation was reached after twenty interviews; however, two additional interviews were conducted to confirm this. Ethical principles were strictly observed, primarily explaining the nature and purpose of the study before obtaining their consent to participate. Identifiers were removed from the transcripts, and codes were used to label participants (e.g., Participants 1, 2, etc.). Participants were informed that they had the right to withdraw from the study at any time should they decide not to participate in further sessions.
Data analysis
Initially, all interviews were professionally transcribed verbatim, with pseudonyms used to anonymize participants and protect their identities. Both authors (JK and NFA) thoroughly read and re-read the transcripts multiple times to become familiar with the content and ensure the transcripts accurately reflected the audio recordings. then applied an inductive coding approach, deriving codes directly from the data rather than imposing them beforehand. This involved systematically identifying and highlighting significant quotes and segments within the transcripts that were relevant to the research questions. These initial codes were subsequently organized into potential themes by grouping together codes that shared a common essence or underlying concept. Following this, the researchers organized these initial codes into potential themes by grouping codes that shared a common essence or underlying concept.
The potential themes underwent a two-phase review and refinement process. In the first phase, the researchers reviewed the coded data extracts to ensure they coherently supported the identified themes. In the second phase, the themes were examined in relation to the entire data set to confirm that they accurately represented the data and captured the full range of participants’ experiences. Some themes were modified, combined, or discarded during this process based on their relevance and data representation.
The final step involved crafting a coherent and compelling narrative that provided a detailed account of each theme. The report included illustrative quotes from participants to substantiate the themes and vividly depict their experiences. This structured approach ensured that the analysis was thorough and that the resulting themes were deeply rooted in the data. By following Braun and Clarke’s six-step process, the study moved from raw transcripts to well-defined themes that offer meaningful insights into the generational gap among nurses and Nurse managers.
This study had a cohort of ten frontline nurses from the new generation and ten senior nurse managers from the old generation, as shown in Table 1 . The mean age of the new generation was 32.4 years (SD 4.9 years). The nurses had an average of 8.3 years of overall work experience (SD 3.09 years), specifically at Hamad Medical Corporation (HMC); they had a mean work experience of 4.7 years (SD 1.1 years). Gender distribution among the participants was 80% male and 20% female. This demographic profile reveals a well-experienced group, particularly regarding their tenure at HMC, providing a stable basis for analyzing their professional perspectives and experiences.
On the other hand, the old generation demographics: 60% were Executive Directors and 40% were Assistant Executives. Most participants belonged to Generation X (ages 44 to 59 years old), suggesting a consistent age distribution. On average, the executives had 27.9 years of overall work experience (SD 9.46 years), highlighting substantial professional tenure with considerable variability. Specifically, their mean work experience at Hamad Medical Corporation (HMC) was 17.4 years (SD 8.24 years), reflecting a diverse range of service durations at this institution. The gender distribution was evenly split, with 50% male and 50% female participants. Details on the demographic data of the old generation participants are detailed in Table 2 . Three major themes were derived from the study, as illustrated in Fig. 1 .

The major themes and Sub-Themes derived from the study
Optimizing the working environment
Healthy work environments that maximize the health and well-being of nurses are essential in achieving good patient and societal outcomes, as well as optimal organizational performance. This theme consisted of three sub-themes: Influencing leadership style, Patient outcome and nurse satisfaction, and Adaptation of technological advancement.
Influential leadership styles
When investigating the leadership style, all older generations consistently agreed to prefer the transformational one because of its capacity to inspire and motivate frontline staff. However, to respond to specific situational demands, the older generation in our study modified and combined aspects of situational and democratic leadership.
Which type of leadership I’m following is transformational leadership. But sometimes , we can take that democratic leadership in some situations , but not all of it. We can say situational leadership at the same time. But any leadership style you will follow should be , I can tell , a combination of some practice and attitude toward your staff”. (Participant 17).
On the other hand, the new generation perceives leadership style by retrieving the inner values of their leaders, such as respect, teamwork, accountability, and professionalism.
“Actually , our leaders primarily lead by maintaining a good relationship , and he is making sense of decreasing the distance between the higher and lower positions. So , I can say that I share the same attitudes and values with my senior managers , but it might differ from one person to another.” ( Participant 1).
Enhanced patient outcomes and nurses’ satisfaction
The older generation perceived the working environment as a motivator for enhancing patient outcomes. Mainly, they are putting serving humanity at the top of their priority, which might be achieved through creativity, collaboration, and compassion. As articulated by Participant 7, “I believe that exerting the best effort in one’s job demonstrates ownership and respect for the profession. Serving humanity , I prioritize creativity , collaboration , and compassion in my work”.
This quote demonstrates the deep values held by this group, highlighting their strategy of combining individual achievement with a wider humanitarian influence.
The new generation views the working environment as a vital element in improving nurses’ satisfaction, considering many contributing factors, such as the current status of the global economy and the opportunities for nurses to work and move abroad. As elaborated by Participant 13,
“I think we can see a difference between the young and the old generation , and I think the way they look at nursing as a profession. There is a big difference between all the new generations , and I can see how the old generation looks at it. The older generation is looking at ways to help people. It is a way to provide support for older people. Unfortunately , I think the new generation has started looking at it as a job—more than a way of helping people. And I believe there are many different reasons for this. I think about the economic status around the world , and the other thing that you know is that I believe the world is open nowadays for nurses to travel around. Therefore , it’s started becoming a job more than a profession. Unfortunately , that’s why people start looking at it in a completely different way , which is not something good.” (Participant 13).
Adaptation to technological advancements
When examining the technological aspects, the older generation acknowledges the presence of the gab. Most of them believe the gap exists because they adhere to the old practices they learned previously.
“There is a noticeable difference between the younger and older generations of nurses , primarily due to advancements in technology and medical knowledge. Younger nurses are often more up-to-date with the latest care techniques and medical research , as they can access various modern resources. Older nurses , however , may adhere to practices they learned earlier in their careers , which might not incorporate recent technological changes”. (Participant 16)
On the other hand, the new generation views new technologies as an easy-to-adopt opportunity. They like to use the new potentials that come with AI. For example, the new generation is becoming more dependent on technology due to the greater benefits it provides compared to traditional approaches in terms of diagnosis and treatment.
“Technology is a significant factor for us , being part of the newer generation. It’s very important in our year of nursing. We use computers , advanced machines , and electronic documentation , which differ from past practices.”(participant 10) . “The younger generation is adapting more easily to new technologies and software , like using EMR for documentation. The older generation , who are used to manual documentation , find it harder to adapt to this new system in patient care. I’ve also heard that some facilities are using GPS and AI systems to assist in diagnoses and results. So , artificial intelligence is becoming a part of nursing , and younger generations are adapting more easily to it. It will take time for the older generation to adapt because they are accustomed to different practices”. (Participant 8)
Strengthening the work atmosphere through communication and values
Effective communication enhances working relationships and knowledge translation and reduces conflict responsible for errors, improving patient safety. This theme consisted of three sub-themes, diverse and practical communication approaches, positive work atmosphere cultivation, and emphasis on shared values across teams.
Diverse and effective communication approaches
The older generation emphasizes the importance of training sessions on communication skills and advanced technologies to bridge the gap with the new generation. Moreover, they believe the new generation needs to be more skilled in direct interpersonal communication.
“Effective communication strategies that bridge generational gaps should be promoted. This could include training on communication best practices and the use of technology for older nurses and encouraging younger nurses to develop strong interpersonal skills for face-to-face interactions”. (Participant 20) “The older generations , always think of , they are more of insightful , in terms of , in the meetings they will be able to translate or interpret the information much differently. And that’s how I see.”( Participants − 18) .
According to the new generation, effective and direct communication without any mediator can enhance the work atmosphere and ease professional communication with older generations. It can help the new generation have more chances to interact with the old generation.
“Certainly , open and direct communication is helpful. As previously said , it is crucial to have someone who can assist in communicating with my manager in my home country. Establishing a direct line of communication with my management and developing a robust professional connection without intermediaries is vital. I appreciate the older generation’s facilitation of an open-door policy , as it cultivates a direct and efficient communication atmosphere.” (Participant 1).
Positive work atmosphere cultivation
When examining the intergenerational dynamics in the workplace, the findings indicated that differences in experience, training, and access to technology significantly impact the work environment and the level of collaboration among employees. As one participant articulated,
“The work atmosphere impacts collaboration. I think it does impact that and impacts these differences from one generation to another. It’s not about good and bad , but it’s rather about the differences in the experiences , differences in the training , and differences in the work environment as well as the availability of technology. So , I would say that there is a difference.” (Participant 19). However, the new generation focuses on the technological aspect and how that might affect the work atmosphere positively.
Emphasis on shared values across teams
Conflicts arise when older generations rely on experience while new generations prefer evidence-based practices. This affects workplace shared values.
“For instance , there might be a conflict over a non-scientifically backed common practice. The older generation might argue that they’ve been doing it for years without issues. However , from a knowledge-based perspective , the practice might be incorrect. Overall , the older generation’s viewpoint is based on their experience , where they haven’t seen negative outcomes. Conversely , the new generation would argue based on scientific principles and current best practices. The older generation might resist changing to these new practices. So , conflicts like these might arise from differing viewpoints on practices and approaches.” (Participant 9) .
The new generations perceive shared values as part of the staff-manager relationship and can’t isolate it. When the old generation leads, the staff investigates the old generation’s way of leading, which will affect the new generation’s attitudes and values. Consequently, the new generation still takes the old generation as an example to be followed. This meaning can be found in Participant 1 answers. “Actually , our leaders primarily lead by maintaining a good relationship , and he is making sense of decreasing the distance between the higher and lower positions. So , I can say that I share the same attitudes and values with my senior managers , but it might differ from one person to another.” ( Participant 1) .
Cultivating respect and empathy
This theme focuses on two subthemes: commitment to fairness and fostering a sense of purpose among staff.
Commitment to fairness
The results of the older generation highlight the importance of fostering empathy in the workplace. Participant 20 suggests promoting understanding by encouraging the new generation to consider their colleagues’ perspectives and motivations, enhancing mutual respect and cooperation.
“Encourage Empathy: Foster empathy among employees by encouraging them to put themselves in each other’s shoes. Encouraging individuals to consider the motivations and experiences of their colleagues can lead to better understanding” (Participant 20). “They can challenge you as a leader and they can challenge each other. That’s how you build a better workplace to have a conversation , a clear professional conversation. If you want to build a professional conversation , the two respect the critiques to respect the differences. So those differences are not conflicts. Differences are differences of opinion due to the experiences everybody can brings in.”(Participants 18) .
However, the new generation demands that older generations be more open to work-related discussions, assignments, and promotion opportunities. They believe the new generation has a greater chance to be promoted if they get a fair chance as they are equipped and well-educated. This was clear by Participant 9.“ Compared to the older generation , the new generation of nurses has more opportunities for service and promotion based on education. In the past , nurses often held diplomas or auxiliary nursing qualifications , with the attitude focused primarily on patient care. Now , there’s a trend towards having more knowledgeable nurses capable of providing advanced care”( Participant 9).
Fostering a sense of purpose among staff
A sense of purpose plays a crucial role in developing cohesive nursing teams by promoting transparent communication and mutual learning, as emphasized by Participant 18.
“The most effective way that I felt worked during this period is the mentorship , working closely with the people and letting them have open communication all the time , providing the proper support , and providing the platform to share the experience and knowledge while you are learning or why they are learning from , and this learning process will be from both. So , this sharing of information through a clear mentorship , in one way or another , will create a culture of mutual respect , and this will end with time; this is not just easy; it takes time. But eventually , if it is done appropriately from the beginning , it will formulate a more cohesive nursing team.“(Participant 18).
The sense of purpose was more obvious among the new generation’s responses, as can be seen in Participant 7’s response: “ Our teamwork is initially built on collaboration , where each nurse supports and enhances the work of others.”
Dynamic enhancement of healthcare systems
The new generation is more adaptable to technological changes and modern healthcare systems. They often embrace new approaches and value work-life balance and a more collaborative approach to patient care. Older nurses have been exposed to a traditional healthcare system and may have had to adapt to technological changes later in their careers.
Continuous education and professional development
The new generation is involved in all nursing and patient care areas. They are advancing in roles such as nurse advocates and nurse researchers. So, the new generation is expanding into new fields and trying to improve the nursing career by pursuing education and professional development. In contrast, the older generation focuses more on clinical areas and patient outcomes.
“There are more options available now , especially for the younger generations. Previously , options were limited. You would start at a hospital or a specific department and stay there. With education and different pathways , you can work in patient care or move into education or other areas. This variety of options makes it easier for the younger generations.” (Participant:8) . “The other thing that when you are dealing with the old generation , you’ll find the love to be with the patient , patient bedside dealing with the patient day today.” (Participant:13) .
Promotion of organizational openness and transparency
The old generation perceived transparency as the need for the new and old generations to openly discuss changes, address concerns, and collaboratively adapt to evolving practices, fostering a transparent and supportive environment in the nursing profession. “Create an environment where nurses and nurse managers can openly discuss changes in the profession , address concerns , and work together to adapt” (Participant 20).
The new generation perceives transparency as a valuable key to promoting change. Participant No. 1’s answers reveal this meaning: “By open communication , that will help. Straight communication and effective communication indeed will help in preparing for the change. As I mentioned before , I need some help or someone to communicate with my manager in my home country. Also , by ensuring that there is no second person between you and your manager , maintain good relationships.”(Participant:1).
This study assessed the generational gap between the new and the old generation. We have identified four main themes: optimizing the working environment, strengthening the work atmosphere through communication and values, cultivating respect and empathy, and dynamic enhancement of healthcare systems. Overall, the results of this study identify the generational gap between these two generations. Moreover, the findings of this research shed light on significant subthemes that highlight the evolving dynamics within the nursing profession, particularly the differences and similarities between new and old generations. The demographic data provided a clear understanding of the structure of both generations, with a notable representation of male staff nurses in the new generation and a diverse range of experiences in healthcare.
Working environment
Perceiving the work environment was evident as a generational gap in our study; the leadership style and other subthemes were also identified. This study discovered that the older generation significantly promotes effective leadership styles, including transformational and situational leadership. These styles enhance teamwork, promote autonomy, and ensure a supportive work environment. This is consistent with the findings of Cummings et al. (2018), who highlighted that transformational leadership positively impacts nurse satisfaction and patient outcomes by fostering a supportive and communicative work environment [ 14 ]. Furthermore, situational leadership is vital for the older generation in dynamic critical care units, offering flexibility to address staff readiness levels effectively [ 15 ].
On the other hand, the new generation stressed the importance of inner values such as respect, teamwork, accountability, and professionalism rather than the leadership style of the old generation. The new generation’s focus on internal values suggests a potential shift in organizational culture that prioritizes individual integrity and an attitude of collaboration over traditional hierarchical leadership approaches. This trend indicates that future healthcare entities’ strategies may incrementally prioritize cultivating an environment where ethical behaviors, mutual respect, and collective responsibility play crucial roles in achieving organizational success. This result is consistent with another study done by Boamah et al. (2018), who found that supportive leadership practices enhance nurses’ work engagement and patient care quality, emphasizing the need for recognition and acknowledgment strategies to boost job satisfaction [ 16 ].
In addition, our study evidently shows generational differences in adaptation to technological advancements, with the new generation demonstrating a higher ability to adopt new technologies into their practice. This finding is supported by Lera et al. (2020), who noted that the new generation is more comfortable with modern digital tools and evidence-based practices than the old generation [ 17 ].
Strengthening work atmosphere through communication and values
The current study has found that generational differences in communication preferences exist, with the new generation leveraging technology for more accessible communication. In contrast, the old generation prefers face-to-face interactions for clearer understanding. This aligns with the findings of Rosi et al. (2019), who noted that younger healthcare professionals are more likely to use digital communication tools, whereas the older generation favors traditional methods [ 18 ]. Effective communication strategies that bridge these generational gaps are crucial. Training on communication best practices and the use of technology for the old generation, as well as encouraging the new generation to develop strong interpersonal skills for face-to-face interactions, are crucial [ 19 ].
Regular feedback mechanisms are crucial for identifying and addressing concerns related to the work atmosphere. Boamah et al. (2018) suggest that understanding and addressing generational differences in work preferences can improve team cohesion and reduce conflicts, ultimately leading to better patient care [ 16 ]. The study participants also emphasized the importance of feedback in creating a positive work environment, consistent with the findings of Lin et al. (2021), who stressed the value of input in fostering a supportive workplace [ 20 ]. The current study found that creating a work culture where debate is encouraged, disagreements are respectful, and active listening helps build a team-oriented mindset. This finding aligns with research by Flores et al. (2023), who noted that promoting shared values and respectful communication enhances team cohesion and collaboration [ 21 ].
The current study has found another generational gap in respect and empathy. The new generation emphasizes the importance of having fair assignments, work-related discussions, and promotion opportunities [ 22 ]. Choi et al. (2018), consistent with our study, reported that fair clinical assignments will enhance staff satisfaction, improve nurses’ working conditions, and positively impact patient outcomes [ 23 ].
Professional self-concept is crucial to staff satisfaction, retention, and well-being [ 24 ]. The sense of purpose is part of the nurse’s professional self-concept; hence, the old generation, especially the leaders, must promote staff well-being by considering their purpose and fostering an environment of mutual benefit [ 25 ]. This finding aligns with the current study, which revealed that the new generation views a sense of purpose as fundamental to their professional needs.
The healthcare system is generally considered a significant influence on nursing careers. Regardless of generation, the healthcare system affects nurses and healthcare providers as it is continuously changed, modified, and developed, creating new challenges and opportunities for healthcare providers.
The progression of nursing practice has been significantly influenced by advancements in education and professional development, leading to a shift in roles and opportunities for nurses. The new generation, who are more adaptable to technological changes and evidence-based practices, are increasingly moving into diverse roles beyond traditional clinical settings. They are now prominent in fields such as nurse advocacy, research, and education, reflecting a broadening of the nursing profession and ultimately enhancing healthcare systems. This shift contrasts with the experiences of the older generation who have primarily focused on direct patient care within clinical environments. Recent studies support this trend. For instance, a study found that new nurses are more likely to engage in continuous education and seek roles that allow for more incredible professional growth and diversification than older nurses [ 26 ].
Our study revealed that creating an environment that promotes openness and transparency is essential for fostering effective communication and collaboration between different generations of nurses. Fostering mentorship and knowledge sharing bridges the generational gap and ensures the transmission of valuable experiences and practices. An open dialogue between nurses and nurse managers about changes in the profession, concerns, and adaptation strategies is critical for cohesive teamwork. These findings are consistent with Bragadóttir et al. (2022), which indicate that organizational transparency and open communication channels significantly enhance teamwork and job satisfaction among nursing staff [ 24 ].
This study highlights the evolving dynamics within the nursing profession, focusing on generational differences and similarities. The new generation is more skillful at integrating technology and embracing diverse roles beyond traditional clinical settings, whereas the old generation brings valuable experience and historical perspectives. Effective leadership, continuous education, and open communication are critical for optimizing the work environment, enhancing nurse satisfaction, and improving patient outcomes. Bridging the generational gap through mentorship and fostering a culture of respect and empathy are essential for a cohesive and resilient healthcare system.
Recommendations
Future research should explore strategies to effectively bridge the generational gap in nursing by integrating leadership styles, communication preferences, and technology adoption across different generations. Longitudinal studies could examine how generational dynamics evolve as new generations enter the workforce and older generations transition out, providing insights into the sustainability of organizational changes. Additionally, expanding research to diverse healthcare settings and cultural contexts would enhance the generalizability of findings. At the same time, intervention studies could test the effectiveness of tailored mentorship programs, continuous education initiatives, and organizational transparency in fostering intergenerational collaboration and improving patient care outcomes.
The study’s methodology, including potential sampling bias due to purposive selection, interviewer bias, and the subjective nature of data saturation, could also influence the results. Additionally, the context-specific nature of the study and the use of virtual interviews might limit the depth and transferability of the findings. Finally, time constraints may have restricted the comprehensiveness of the data collected.
Implications for nursing management
Nurse managers should adopt a multi-faceted leadership approach, embracing both transformational and situational styles, to meet the diverse needs of a multigenerational workforce. Implementing targeted communication training and fostering an environment of respect and empathy can improve team cohesion and patient outcomes. Investing in continuous professional development and technological training will further support the integration of new and experienced nurses.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Stanley D. Multigenerational workforce issues and their implications for leadership in nursing. J Nurs Manag. 2010;18(7):846–52.
Article PubMed Google Scholar
Rudolph CW, Rauvola RS, Zacher H. Leadership and generations at work: a critical review. Leadersh Q. 2018;29(1):44–57.
Article Google Scholar
Santos SR, Cox K. Workplace adjustment and intergenerational differences between matures, boomers, and xers. Nurs Econ. 2000;18(1):7–13.
CAS PubMed Google Scholar
Blythe J, Baumann A, Zeytinoglu IU, Denton M, Akhtar-Danesh N, Davies S, et al. Nursing generations in the contemporary workplace. Public Personnel Manage. 2008;37(2):137–59.
Hendricks JM, Cope VC. Generational diversity: what nurse managers need to know. J Adv Nurs. 2013;69(3):717–25.
Cordeniz JA. Recruitment, retention, and management of generation X: a focus on nursing professionals. J Healthc Manag/Am Coll Healthc Exec. 2002;47(4):237–49.
Google Scholar
Carver L, Candela L. Attaining organizational commitment across different generations of nurses. J Nurs Manag. 2008;16(8):984–91.
Greene J. What nurses want. Different generations. Different expectations. Hosp Health Networks. 2005;79(3):34–840.
Outten MK. From veterans to nexters: managing a multigenerational nursing workforce. Nurs Manage. 2012;43(4):42–7.
Rollan Oliveira S, Siles González J. Nursing professionals within the intergenerational context during the 20th and 21st centuries: an integrative review. Investigacion Y Educ en enfermeria. 2021;39(3).
Wolff AC, Ratner PA, Robinson SL, Oliffe JL, Hall LM. Beyond generational differences: a literature review of the impact of relational diversity on nurses’ attitudes and work. J Nurs Manag. 2010;18(8):948–69.
Arslan A, Ahokangas P, Haapanen L, Golgeci I, Tarba SY, Bazel-Shoham OJTF et al. Generational differences in organizational leaders: an interpretive phenomenological analysis of work meaningfulness in the nordic high-tech organizations. 2022;180:121717.
Tan SHE, Chin GFJB. Generational effect on nurses’ work values, engagement, and satisfaction in an acute hospital. 2023;22(1):88.
Cummings GG, Tate K, Lee S, Wong CA, Paananen T, Micaroni SP et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. 2018;85:19–60.
Dorgham SR. SJIJoN Al-Mahmoud 2013 Leadership styles and clinical decision making autonomy among critical care nurses: a comparative study. Sci H 1 4 71–83.
Boamah SA, Laschinger HKS, Wong C, Clarke, SJNo. Effect of transformational leadership on job satisfaction and patient safety outcomes. 2018;66(2):180–9.
Lera M, Taxtsoglou K, Iliadis CK, Frantzana AA, Kourkouta LJAPINJ. Nurses’ Attitudes toward Lifelong Learn via new Technol. 2020;5(2):89.
Bridges D, Davidson RA, Soule Odegard P, Maki IV. Tomkowiak JJMeo. Interprofessional Collaboration: Three best Pract Models Interprofessional Educ. 2011;16(1):6035.
Chan PG, Schaheen LW, Chan EG, Cook CC, Luketich JD, D’Cunha JJJoSE. Technology-enhanced simulation improves trainee readiness transitioning to cardiothoracic training. 2018;75(5):1395–402.
Lin L-C, Huang Y-C, Carter P, Zuniga JJANR. Resilience among nurses in long term care and rehabilitation settings. 2021;62:151518.
Flores IF, Dator WLT, Olivar JJ, Gaballah MK, editors. Congruence of Effective Leadership values between nurse leaders and staff nurses in a Multicultural Medical City in Saudi Arabia: a sequential mixed-methods study. Healthcare: MDPI; 2023.
Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S, editors. The role of empathy in health and social care professionals. Healthcare: MDPI; 2020.
Mlambo M, Silén C, McGrath CJB. Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature. 2021;20:1–13.
Bragadóttir H, Kalisch BJ, Flygenring BG, Tryggvadóttir GBJSON. The relationship of nursing teamwork and job satisfaction in hospitals. 2023;9:23779608231175027.
Allobaney NF, Eshah NF, Abujaber AA, Nashwan AJJJ. Professional self-concept and self-confidence for nurses dealing with COVID-19 patients. 2022;12(2):134.
Choi J, Miller PJJNS. Registered nurse perception of patient assignment linking to working conditions and outcomes. 2018;50(5):530–9.
Download references
Acknowledgements
The authors would like to acknowledge the nurses and nurse managers who participated in the study.
This study was funded by the Medical Research Center at Hamad Medical Corporation (MRC-01-23-206).
Author information
Authors and affiliations.
Department of Nursing, Hazm Mebaireek General Hospital, Hamad Medical Corporation, Doha, Qatar
Ahmad A. Abujaber, Abdulqadir J. Nashwan, Mark D. Santos, Nabeel F. Al-Lobaney, Rejo G. Mathew & Jamsheer P. Alikutty
University of Doha for Science & Technology, P.O. Box 3050, Doha, Qatar
Albara M. Alomari
Nursing and Midwifery Research Department, Hamad Medical Corporation, Doha, Qatar
Jibin Kunjavara
You can also search for this author in PubMed Google Scholar
Contributions
AAA, AJN: Conceptualization. NFA, MDS, JK: Formal analysis.AAA, AJN, MDS, NFA, RGM, JPA, JK, AMA: Methodology, Data curation, Manuscript writing (draft and final review). All authors read and approved the final manuscript.
Corresponding author
Correspondence to Abdulqadir J. Nashwan .
Ethics declarations
Ethical approval.
This study was approved by the Medical Research Center of Hamad Medical Corporation (MRC-01-23-206). The study has been conducted in accordance with the ethical standards noted in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consents were obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Abujaber, A.A., Nashwan, A.J., Santos, M.D. et al. Bridging the generational gap between nurses and nurse managers: a qualitative study from Qatar. BMC Nurs 23 , 623 (2024). https://doi.org/10.1186/s12912-024-02296-y
Download citation
Received : 29 June 2024
Accepted : 26 August 2024
Published : 05 September 2024
DOI : https://doi.org/10.1186/s12912-024-02296-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Generational gap
- Nursing leadership
- Multigenerational workforce
- Workplace communication
- Nurse manager relationships
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Strong communication skills are essential to provide safe, quality, patient-centered care. Nurses develop therapeutic relationships with patients and family members each day to ensure that health care concerns and needs are addressed. If communication breaks down, information exchange stops and needs go unidentified. Nurses optimize communication channels with patients and families by ...
Effective verbal communication in nursing encompasses several key principles: Pace and Intonation. The manner of speech, including the pace and intonation, significantly influences the impact of the message. For instance, speaking slowly and softly to an excited client can help calm them. Simplicity.
1. Therapeutic communication in nursing helps establish strong nurse-patient relationships. 2. Nursing therapeutic communication is an essential part of interdisciplinary relationships, promoting effective and efficient collaboration among team members to promote positive patient outcomes. 3.
Nurses engage in compassionate, supportive, professional relationships with their clients as part of the "art of nursing." [1] This chapter will review the nurse-client relationship, therapeutic communication, and motivational interviewing. It will also introduce teletherapy and telehealth.
To begin with, let's look at the following two definitions of communication: A process by which information is exchanged between individuals through a common system of symbols, signs, or behavior. 3 Communication is giving, receiving or exchanging ideas, information, signals or messages through appropriate media, enabling individuals or groups to persuade, to seek information, to give ...
Therapeutic communication is a vital skill in nursing for multiple reasons. It can help establish a trusting patient-nurse relationship, prevent misunderstandings and errors, promote patient-centered care, improve patient satisfaction, and improve outcomes (Slade & Sergent, 2023). Nurses should understand and practice various therapeutic ...
Effective communication is a vital skill for nursing assistants. Nursing assistants communicate professionally with patients and other health care team members throughout every shift. This chapter will review the communication process, discuss strategies for adapting communication based on the needs of the client and health care team, and introduce guidelines for documentation and reporting.
3.2 Communication Effective communication is a vital component of effective assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA). [1] Consider the fundamentals of good communication practices.
3.2 Communication Effective communication is a vital component of proper assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA). [1] Research has identified that new graduate nurses are more susceptible to stress and isolation within their job roles due to poor communication and teamwork within ...
What is Communication in Nursing. Effective communication in nursing refers to the exchange of information, thoughts, and feelings between healthcare professionals, patients, and their families. It serves as the cornerstone of quality healthcare and encompasses various dimensions, including verbal and non-verbal communication, active listening ...
Effective communication is the bedrock of exceptional nursing care. It goes beyond mere information exchange; it's about establishing trust, alleviating anxiety, and cultivating healing partnerships. In the intricate realm of healthcare, where emotions and decisions intertwine, a nurse's proficiency in communication becomes a powerful tool.
Nurses are critical in the delivery of essential health services and are core in strengthening the health system. They bring people-centred care closer to the communities where they are needed most, thereby helping improve health outcomes and the overall cost-effectiveness of services. Nurses usually act as first responders to complex humanitarian crises and disasters; protectors and advocates ...
Strategies for Success in a Nursing Program 10: Communicating 10.6: Barriers to Effective Communication ... Meredith waited impatiently the entire class session for Anvi to ask about the assignment. With class time almost up, Meredith spoke up, telling the instructor in front of the class that Anvi had a question about the assignment ...
For example: Nod your head, but never interrupt. Lean forward and maintain eye contact to let the person know you're engaged. Include minimal verbal encouragement, such as "I understand," and "go on.". 4. Written Communication. Written communication skills are also essential for effective nurse-to-nurse communication.
Sharma and Gupta (2022) summarize therapeutic communication strategies. These include: Open-ended questions -ask open ended questions to learn more about the patient and enable a free-flow of information exchange; closed-ended questions can be used to focus on specific information. Active listening -active listening involves behaviors such as ...
Examples of Assertive Communication in Nursing 1. Rejecting a Patient Assignment. Scenario: You arrive in the intensive care unit (ICU), go to check the assignment sheet, and get report. You notice that your second patient is in the OR for an open heart surgery and will be arriving later.
2. PRINCIPLES OF COMMUNICATION. Communication can be defined as a transaction and message creation. The entire process occurs in a context consisting of physical space, cultural and social values and psychological conditions ().Communication assists in the performance of accurate, consistent and easy nursing work, ensuring both the satisfaction of the patient and the protection of the health ...
3. Written Communication. Maintaining accurate and well-formatted medical information is fundamental for effective communication. Correct grammar, spelling, and diction are all integral parts of proper written conduct and remaining professional. 4. Presentation Skills.
The Four Cs of Communication in Nursing. Patient care can suffer and relationships lose trust when communication is not clear. Interactions with colleagues, patients, and families are dependent on quality communication. When evaluating your communication habits, try focusing on the four Cs - keep things Clear, Concise, Correct, and Complete.
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients' and caregivers' needs ...
Communication is an essential element of building trust and comfort in nursing, and it is the basis of the nurse-patient relationship (Dithole et al, 2017).Communication is a complex phenomenon in nursing and is influenced by multiple factors, such as relationship, mood, time, space, culture, facial expression, gestures, personal understanding and perception (McCarthy et al, 2013; Kourkouta ...
Utilizing the therapeutic & non-therapeutic techniques handouts, list 2 specific examples of non-verbal therapeutic communication that were utilized by the nurse in the videos. Division of Nursing- N Therapeutic Communication Assignment. Personal Appearance- the nurse looked professional in wrinkle-free clean looking scrubs and lab coat.
1. Introduction. Therapeutic communication (TC) is defined as the process of using verbal and nonverbal communication to connect with patients [].TC is holistic, patient-centered and involves aspects of the physiological, psychological, environmental and spiritual care of the patient [].It is based on understanding and addressing the patient's situation, including life circumstances, beliefs ...
Defining Therapeutic Communication in Nursing. Therapeutic communication in nursing is a purposeful, patient-centered interaction that promotes a trusting relationship between the nurse and the patient. It involves active listening, empathy, and effective communication to address the physical and emotional needs of patients.
Communication skills are essential for nurses collaborating on teams and providing efficient medical care. They tell patients about diagnostics, treatments, prevention, prognosis and rehabilitation. They also write accurate health records and descriptions of patients' conditions. Some nursing programs require aspiring nurses to take ...
Case Study Assignment. After reading many case studies throughout this program, this assignment challenges the student to delve into a recent crisis and analyze its impact through a case study format.
The nursing profession faces a significant challenge of a multigenerational workforce that can cause conflict and hinder effective communication, especially between nurse managers and nurses [].In addition, a literature review of studies conducted over the past two decades indicates that the generational gap between nurses and nurse managers is a complex phenomenon requiring concerted efforts ...