

Hydrocephalus Clinical Presentation
- Author: Stephen L Nelson, Jr, MD, PhD, FAACPDM, FAAN, FAAP, FANA; Chief Editor: Jasvinder Chawla, MD, MBA more...
- Sections Hydrocephalus
- Practice Essentials
- Pathophysiology
- Mortality/Morbidity
- Epidemiology
- Patient Education
- Complications
- Laboratory Studies
- Imaging Studies
- Other Tests
- Histologic Findings
- Medical Care
- Surgical Care
- Consultations
- Medication Summary
- Carbonic anhydrase inhibitors
- Loop diuretics
- Questions & Answers
- Media Gallery
Clinical features of hydrocephalus are influenced by the following:
Patient's age
Location of obstruction
Rapidity of onset
Symptoms in infants include the following:
Poor feeding
Irritability
Reduced activity
Symptoms in children include the following:
Slowing of mental capacity
Headaches (initially in the morning) that are more significant than in infants because of skull rigidity
Neck pain suggesting tonsillar herniation
Vomiting, more significant in the morning
Blurred vision: This is a consequence of papilledema and later of optic atrophy
Double vision: This is related to unilateral or bilateral sixth nerve palsy
Stunted growth and sexual maturation from third ventricle dilatation: This can lead to obesity and to precocious puberty or delayed onset of puberty.
Difficulty in walking secondary to spasticity: This affects the lower limbs preferentially because the periventricular pyramidal tract is stretched by the hydrocephalus.
Symptoms in adults include the following:
Cognitive deterioration: This can be confused with other types of dementia in the elderly.
Headaches: These are more prominent in the morning because cerebrospinal fluid (CSF) is resorbed less efficiently in the recumbent position. This can be relieved by sitting up. As the condition progresses, headaches become severe and continuous. Headache is rarely if ever present in normal pressure hydrocephalus (NPH).
Neck pain: If present, neck pain may indicate protrusion of cerebellar tonsils into the foramen magnum.
Nausea that is not exacerbated by head movements
Vomiting: Sometimes explosive, vomiting is more significant in the morning.
Blurred vision (and episodes of "graying out"): These may suggest serious optic nerve compromise, which should be treated as an emergency.
Double vision (horizontal diplopia) from sixth nerve palsy
Difficulty in walking
Incontinence (urinary first, fecal later if condition remains untreated): This indicates significant destruction of frontal lobes and advanced disease.
Symptoms of NPH include the following:
Gait disturbance is usually the first symptom and may precede other symptoms by months or years. Magnetic gait is used to emphasize the tendency of the feet to remain "stuck to the floor" despite patients’ best efforts to move them.
Dementia should be a late finding in pure (shunt-responsive) NPH. It presents as an impairment of recent memory or as a "slowing of thinking." Spontaneity and initiative are decreased. The degree can vary from patient to patient.
Urinary incontinence may present as urgency, frequency, or a diminished awareness of the need to urinate.
Other symptoms that can occur include personality changes and Parkinsonism. Seizures are extremely rare and should prompt consideration for an alternative diagnosis.
Physical findings in infants include the following:
Head enlargement: Head circumference is at or above the 98 th percentile for age. or an increase rapidly across percentiles on the head growth curve.
Dysjunction of sutures: This can be seen or palpated.
Dilated scalp veins: The scalp is thin and shiny with easily visible veins.
Tense fontanelle: The anterior fontanelle in infants who are held erect and are not crying may be excessively tense.
Setting-sun sign: In infants, it is characteristic of increased intracranial pressure (ICP). Ocular globes are deviated downward, the upper lids are retracted, and the white sclerae may be visible above the iris.
Increased limb tone: Spasticity preferentially affects the lower limbs. The cause is stretching of the periventricular pyramidal tract fibers by hydrocephalus.
Physical findings in children include the following:
Papilledema: If the raised ICP is not treated, this can lead to optic atrophy and vision loss. The absence of papilledema does not rule out increased intracranial pressure, since it does not develop acutely.
Failure of upward gaze: This is due to pressure on the tectal plate through the suprapineal recess. The limitation of upward gaze is of supranuclear origin. When the pressure is severe, other elements of the dorsal midbrain syndrome (ie, Parinaud syndrome) may be observed, such as light-near dissociation, convergence-retraction nystagmus, and eyelid retraction (Collier sign).
Macewen sign: A "cracked pot" sound is noted on percussion of the head.
Unsteady gait: This is related to spasticity in the lower extremities.
Large head: Sutures are closed, but chronic increased ICP will lead to progressive macrocephaly.
Unilateral or bilateral sixth nerve palsy is secondary to increased ICP. Children with ventriculoperitoneal (VP) shunts may be more likely to have congenital esotropia. [ 11 ]
Physical findings in adults include the following:
Papilledema: If raised ICP is not treated, it leads to optic atrophy.
Failure of upward gaze and of accommodation indicates pressure on the tectal plate. The full Parinaud syndrome is rare.
Unsteady gait is related to truncal and limb ataxia. Spasticity in legs also causes gait difficulty.
Large head (macrocephaly): The head may have been large since childhood.
Unilateral or bilateral sixth nerve palsy is secondary to increased ICP. Children with ventricular-peritoneal shunts may be more likely to have congenital esotropia.
The following are physical findings found in NPH:
Muscle strength is usually normal. No sensory loss is noted.
Reflexes may be increased, and the Babinski response may be found in one or both feet. These findings should prompt search for vascular risk factors (causing associated brain microangiopathy or vascular Parkinsonism), which are common in NPH patients.
Difficulty in walking varies from mild imbalance to inability to walk or to stand. The classic gait impairment consists of short steps, wide base, externally rotated feet, and lack of festination (hastening of cadence with progressively shortening stride length, a hallmark of the gait impairment of Parkinson disease ). These abnormalities may progress to the point of apraxia. Patients may not know how to take steps despite preservation of other learned motor tasks.
Frontal release signs such as sucking and grasping reflexes appear in late stages.
Congenital causes in infants and children include the following: [ 8 ]
Brainstem malformation causing stenosis of the aqueduct of Sylvius: This is responsible for 10% of all cases of hydrocephalus in newborns.
Dandy-Walker malformation: This affects 2-4% of newborns with hydrocephalus.
Arnold-Chiari malformation type 1 and type 2
Agenesis of the foramen of Monro
Congenital toxoplasmosis
Bickers-Adams syndrome: This is an X-linked hydrocephalus accounting for 7% of cases in males. It is characterized by stenosis of the aqueduct of Sylvius, severe intellectual disability, and in 50% by an adduction-flexion deformity of the thumb.
Acquired causes in infants and children include the following:
Mass lesions: Mass lesions account for 20% of all cases of hydrocephalus in children. These are usually tumors (eg, medulloblastoma , astrocytoma ), but cysts, abscesses, or hematoma also can be the cause. [ 12 ]
Hemorrhage: Intraventricular hemorrhage can be related to prematurity , head injury, or rupture of a vascular malformation.
Infections: Meningitis (especially bacterial) and, in some geographic areas, cysticercosis can cause hydrocephalus.
Increased venous sinus pressure: This can be related to achondroplasia, some craniostenoses, or venous thrombosis.
Iatrogenic: Hypervitaminosis A, by increasing secretion of CSF or by increasing permeability of the blood-brain barrier, can lead to hydrocephalus. As a caveat, hypervitaminosis A is a more common cause of idiopathic intracranial hypertension, a disorder with increased CSF pressure but small rather than large ventricles.
Causes of hydrocephalus in adults include:
Subarachnoid hemorrhage (SAH) causes one third of these cases by blocking the arachnoid villi and limiting resorption of CSF. However, communication between ventricles and subarachnoid space is preserved. [ 13 ]
Idiopathic hydrocephalus represents one third of cases of adult hydrocephalus.
Head injury, through the same mechanism as SAH, can result in hydrocephalus.
Tumors can cause blockage anywhere along the CSF pathways. The most frequent tumors associated with hydrocephalus are ependymoma, subependymal giant cell astrocytoma, choroid plexus papilloma, craniopharyngioma, pituitary adenoma, hypothalamic or optic nerve glioma, hamartoma, and metastatic tumors.
Prior posterior fossa surgery may cause hydrocephalus by blocking normal pathways of CSF flow.
Congenital aqueductal stenosis causes hydrocephalus but may not be symptomatic until adulthood. Special care should be taken when attributing new neurological deficits to congenital hydrocephalus, as its treatment by shunting may not correct these deficits.
Meningitis, especially bacterial, may cause hydrocephalus in adults.
All causes of hydrocephalus described in infants and children are present in adults who have had congenital or childhood-acquired hydrocephalus.
Causes of NPH may include the following (Most cases are idiopathic and are probably related to a deficiency of arachnoid granulations.):
Head trauma
Complications related to progression of hydrocephalus include the following:
Visual changes
Occlusion of posterior cerebral arteries secondary to downward transtentorial herniation
Chronic papilledema injuring the optic disc
Dilatation of the third ventricle with compression of optic chiasm
Cognitive dysfunction
Incontinence
Gait changes
Complications related to medical treatment include the following:
Electrolyte imbalance
Metabolic acidosis
Complications related to surgical treatment include the following:
Signs and symptoms of increased intracranial pressure (ICP) can be a consequence of undershunting or shunt obstruction or disconnection.
Subdural hematoma or hygroma is secondary to overshunting. Headache and focal neurological signs are common.
Treat seizures with antiepileptic drugs.
Shunt infection occasionally can be asymptomatic. In neonates, it manifests as alteration of feeding, irritability, vomiting, fever, lethargy, somnolence, and a bulging fontanelle. Older children and adults present with headache, fever, vomiting, and meningismus. With ventriculoperitoneal (VP) shunts, abdominal pain may occur.
Shunts can act as a conduit for extraneural metastases of certain tumors (eg, medulloblastoma).
Hardware erosion through the skin occurs in premature infants with enlarged heads and thin skin who lie on 1 side of the head.
VP shunt complications include peritonitis, inguinal hernia, perforation of abdominal organs, intestinal obstruction, volvulus, and CSF ascites.
Ventriculoatrial (VA) shunt complications include septicemia, shunt embolus, endocarditis, and pulmonary hypertension.
Lumboperitoneal shunt complications include radiculopathy and arachnoiditis.
Rekate HL. A contemporary definition and classification of hydrocephalus. Semin Pediatr Neurol . 2009 Mar. 16(1):9-15. [QxMD MEDLINE Link] .
Kahlon B, Annertz M, Stahlberg F, Rehncrona S. Is aqueductal stroke volume, measured with cine phase-contrast magnetic resonance imaging scans useful in predicting outcome of shunt surgery in suspected normal pressure hydrocephalus?. Neurosurgery . 2007 Jan. 60(1):124-9; discussion 129-30. [QxMD MEDLINE Link] .
Hattingen E, Jurcoane A, Melber J, Blasel S, Zanella FE, Neumann-Haefelin T. Diffusion tensor imaging in patients with adult chronic idiopathic hydrocephalus. Neurosurgery . 2010 May. 66(5):917-24. [QxMD MEDLINE Link] .
Hamilton MG. Treatment of hydrocephalus in adults. Semin Pediatr Neurol . 2009 Mar. 16(1):34-41. [QxMD MEDLINE Link] .
Kuruvilla LC. Benign enlargement of sub-arachnoid spaces in infancy. J Pediatr Neurosci . 5/9/2014. 9:129-31. [QxMD MEDLINE Link] . [Full Text] .
Woodworth GF, McGirt MJ, Williams MA, Rigamonti D. Cerebrospinal fluid drainage and dynamics in the diagnosis of normal pressure hydrocephalus. Neurosurgery . 2009 May. 64(5):919-25; discussion 925-6. [QxMD MEDLINE Link] .
Lacy M, Oliveira M, Austria E, Frim MD. Neurocognitive outcome after endoscopic third ventriculocisterostomy in patients with obstructive hydrocephalus. J Int Neuropsychol Soc . 2009 May. 15(3):394-8. [QxMD MEDLINE Link] .
Garne E, Loane M, Addor MC, Boyd PA, Barisic I, Dolk H. Congenital hydrocephalus - prevalence, prenatal diagnosis and outcome of pregnancy in four European regions. Eur J Paediatr Neurol . 2009 Apr 30. [QxMD MEDLINE Link] .
Partington MD. Congenital hydrocephalus. Neurosurg Clin N Am . 2001 Oct. 12(4):737-42, ix. [QxMD MEDLINE Link] .
Vinchon M, Rekate HL, Kulkarni AV. Pediatric hydrocephalus outcomes: a review. Fluids Barriers CNS . 2012 Aug 27. 9(1):18. [QxMD MEDLINE Link] .
DeBenedictis CN, Rubin SE, Kodsi SR. Esotropia in Children with Ventricular-Peritoneal Shunts. Strabismus . 2015 Sep. 23 (3):117-20. [QxMD MEDLINE Link] .
Chauvet D, Sichez JP, Boch AL. [Early epidural hematoma after CSF shunt for obstructive hydrocephalus]. Neurochirurgie . 2009 Jun. 55(3):350-3. [QxMD MEDLINE Link] .
Oertel JM, Mondorf Y, Baldauf J, Schroeder HW, Gaab MR. Endoscopic third ventriculostomy for obstructive hydrocephalus due to intracranial hemorrhage with intraventricular extension. J Neurosurg . 2009 May 8. [QxMD MEDLINE Link] .
Espay AJ, Narayan RK, Duker AP, Barrett ET Jr, de Courten-Myers G. Lower-body parkinsonism: reconsidering the threshold for external lumbar drainage. Nat Clin Pract Neurol . 2008 Jan. 4(1):50-5. [QxMD MEDLINE Link] .
[Guideline] Dormont D, Seidenwurm DJ, Davis PC. Dementia and movement disorders. American College of Radiology (ACR) . 2007. [Full Text] .
Larsson A, Moonen M, Bergh AC, Lindberg S, Wikkelso C. Predictive value of quantitative cisternography in normal pressure hydrocephalus. Acta Neurol Scand . 1990 Apr. 81(4):327-32. [QxMD MEDLINE Link] .
Walchenbach R, Geiger E, Thomeer RT, Vanneste JA. The value of temporary external lumbar CSF drainage in predicting the outcome of shunting on normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry . 2002 Apr. 72(4):503-6. [QxMD MEDLINE Link] .
Lee JH, Back DB, Park DH, Cha YH, Kang SH, Suh JK. Increased Vascular Endothelial Growth Factor in the Ventricular Cerebrospinal Fluid as a Predictive Marker for Subsequent Ventriculoperitoneal Shunt Infection : A Comparison Study among Hydrocephalic Patients. J Korean Neurosurg Soc . 2012 Jun. 51(6):328-33. [QxMD MEDLINE Link] . [Full Text] .
Black PML. Hydrocephalus in adults. Youmans JR, ed. Neurological Surgery . Philadelphia: WB Saunders Company; 1996. 927-44.
Chang CC, Kuwana N, Noji M, Tanabe Y, Koike Y, Ikegami T. Cerebral blood flow in patients with normal pressure hydrocephalus. Nucl Med Commun . 1999 Feb. 20(2):167-9. [QxMD MEDLINE Link] .
Colak A, Albright AL, Pollack IF. Follow-up of children with shunted hydrocephalus. Pediatr Neurosurg . 1997 Oct. 27(4):208-10. [QxMD MEDLINE Link] .
Czosnyka M, Pickard JD. Monitoring and interpretation of intracranial pressure. J Neurol Neurosurg Psychiatry . 2004 Jun. 75(6):813-21. [QxMD MEDLINE Link] .
Damasceno BP, Carelli EF, Honorato DC, Facure JJ. The predictive value of cerebrospinal fluid tap-test in normal pressure hydrocephalus. Arq Neuropsiquiatr . 1997 Jun. 55(2):179-85. [QxMD MEDLINE Link] .
du Plessis AJ. Posthemorrhagic hydrocephalus and brain injury in the preterm infant: dilemmas in diagnosis and management. Semin Pediatr Neurol . 1998 Sep. 5(3):161-79. [QxMD MEDLINE Link] .
Frim DM, Scott RM, Madsen JR. Surgical management of neonatal hydrocephalus. Neurosurg Clin N Am . 1998 Jan. 9(1):105-10. [QxMD MEDLINE Link] .
Garvey MA, Laureno R. Hydrocephalus: obliterated perimesencephalic cisterns and the danger of sudden death. Can J Neurol Sci . 1998 May. 25(2):154-8. [QxMD MEDLINE Link] .
Goumnerova LC, Frim DM. Treatment of hydrocephalus with third ventriculocisternostomy: outcome and CSF flow patterns. Pediatr Neurosurg . 1997 Sep. 27(3):149-52. [QxMD MEDLINE Link] .
Hoppe-Hirsch E, Laroussinie F, Brunet L, et al. Late outcome of the surgical treatment of hydrocephalus. Childs Nerv Syst . 1998 Mar. 14(3):97-9. [QxMD MEDLINE Link] .
Libenson MH, Kaye EM, Rosman NP, Gilmore HE. Acetazolamide and furosemide for posthemorrhagic hydrocephalus of the newborn. Pediatr Neurol . 1999 Mar. 20(3):185-91. [QxMD MEDLINE Link] .
Mercuri E, Faundez JC, Cowan F, Dubowitz L. Acetazolamide without frusemide in the treatment of post-haemorrhagic hydrocephalus. Acta Paediatr . 1994 Dec. 83(12):1319-21. [QxMD MEDLINE Link] .
Poca MA, Mataro M, Del Mar Matarin M, Arikan F, Junque C, Sahuquillo J. Is the placement of shunts in patients with idiopathic normal-pressure hydrocephalus worth the risk? Results of a study based on continuous monitoring of intracranial pressure. J Neurosurg . 2004 May. 100(5):855-66. [QxMD MEDLINE Link] .
Sainte-Rose C. Hydrocephalus in childhood. Youmans JR, ed. Neurological Surgery . Philadelphia: WB Saunders Company; 1996. 890-926.
Sansone JM, Iskandar BJ. Endoscopic cerebral aqueductoplasty: a trans-fourth ventricle approach. J Neurosurg . 2005 Nov. 103(5 Suppl):388-92. [QxMD MEDLINE Link] .
Shbeeb MI, O'Duffy JD, Michet CJ Jr, O'Fallon WM, Matteson EL. Evaluation of glucocorticosteroid injection for the treatment of trochanteric bursitis. J Rheumatol . 1996 Dec. 23(12):2104-6. [QxMD MEDLINE Link] .
Tanaka A, Kimura M, Nakayama Y, Yoshinaga S, Tomonaga M. Cerebral blood flow and autoregulation in normal pressure hydrocephalus. Neurosurgery . 1997 Jun. 40(6):1161-5; discussion 1165-7. [QxMD MEDLINE Link] .
Vogel TW, Bahuleyan B, Robinson S, Cohen AR. The role of endoscopic third ventriculostomy in the treatment of hydrocephalus. J Neurosurg Pediatr . 2013 Jul. 12(1):54-61. [QxMD MEDLINE Link] .
Williams MA, Razumovsky AY, Hanley DF. Comparison of Pcsf monitoring and controlled CSF drainage diagnose normal pressure hydrocephalus. Acta Neurochir Suppl . 1998. 71:328-30. [QxMD MEDLINE Link] .
- Noncommunicating obstructive hydrocephalus caused by obstruction of the foramina of Luschka and Magendie. This MRI sagittal image demonstrates dilatation of lateral ventricles with stretching of corpus callosum and dilatation of the fourth ventricle.
- Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates dilatation of the lateral ventricles.
- Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates fourth ventricle dilatation.
- Communicating hydrocephalus with surrounding "atrophy" and increased periventricular and deep white matter signal on fluid-attenuated inversion recovery (FLAIR) sequences. Note that apical cuts (lower row) do not show enlargement of the sulci, as is expected in generalized atrophy. Pathological evaluation of this brain demonstrated hydrocephalus with no microvascular pathology corresponding with the signal abnormality (which likely reflects transependymal exudate) and normal brain weight (indicating that the sulci enlargement was due to increased subarachnoid cerebrospinal fluid [CSF] conveying a pseudoatrophic brain pattern).

Contributor Information and Disclosures
Stephen L Nelson, Jr, MD, PhD, FAACPDM, FAAN, FAAP, FANA Professor of Pediatrics, Neurology, Neurosurgery, and Psychiatry, Medical Director, Tulane Center for Autism and Related Disorders, Tulane University School of Medicine; Pediatric Neurologist and Epileptologist, Ochsner Hospital for Children; Professor of Neurology, Louisiana State University School of Medicine Stephen L Nelson, Jr, MD, PhD, FAACPDM, FAAN, FAAP, FANA is a member of the following medical societies: American Academy for Cerebral Palsy and Developmental Medicine , American Academy of Neurology , American Academy of Pediatrics , American Epilepsy Society , American Medical Association , American Neurological Association , The Society of Federal Health Professionals (AMSUS) , Child Neurology Society , Southern Pediatric Neurology Society Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Received salary from Medscape for employment. for: Medscape.
Jasvinder Chawla, MD, MBA Chief of Neurology, Hines Veterans Affairs Hospital; Professor of Neurology, Loyola University Medical Center Jasvinder Chawla, MD, MBA is a member of the following medical societies: American Academy of Neurology , American Association of Neuromuscular and Electrodiagnostic Medicine , American Clinical Neurophysiology Society , American Medical Association Disclosure: Nothing to disclose.
Anthony M Murro, MD Professor, Laboratory Director, Department of Neurology, Medical College of Georgia, Georgia Regents University Anthony M Murro, MD is a member of the following medical societies: American Academy of Neurology , American Epilepsy Society Disclosure: Nothing to disclose.
Alberto J Espay, MD, MSc Associate Professor, Director of Clinical Research, Gardner Family Center for Parkinson's Disease and Movement Disorders, University of Cincinnati College of Medicine
Alberto J Espay, MD, MSc is a member of the following medical societies: American Academy of Neurology and Movement Disorders Society
Disclosure: Abbott Consulting fee Consulting; Chelsea therapeutics Consulting fee Consulting; Novartis Honoraria Speaking and teaching; TEVA Consulting fee Consulting; NIH Grant/research funds K23 Career Development Award; Eli Lilly Consulting fee Consulting; Great Lakes Neurotechnologies Other; Michael J Fox Foundation Grant/research funds Other; Lippincott Williams & Wilkins Royalty Book; American Academy of Neurology Honoraria Speaking and teaching
Eugenia-Daniela Hord, MD Instructor, Departments of Anesthesia and Neurology, Massachusetts General Hospital Pain Center, Harvard Medical School
Eugenia-Daniela Hord, MD is a member of the following medical societies: American Academy of Neurology and American Pain Society
Disclosure: Nothing to disclose.
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- Hydrocephalus
- Neurosurgery for Hydrocephalus
- Posttraumatic Hydrocephalus
- Spina Bifida Hydrocephalus and Shunts
- Normal Pressure Hydrocephalus Imaging
- Normal Pressure Hydrocephalus
- Subarachnoid Hemorrhage

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 2002326411-overviewDiseases & Conditions Diseases & Conditions Posttraumatic Hydrocephalus

- Upload Ppt Presentation
- Upload Pdf Presentation
- Upload Infographics
- User Presentation
- Related Presentations

The Treatment And Management of Eczema
By: JenniferDwayne Views: 1775

Nutrition and training plans to alter body composition
By: JenniferDwayne Views: 947

Pediatric Radiology
By: JenniferDwayne Views: 3961

Osteoporosis Update-Advances in Treatment
By: JenniferDwayne Views: 994

Pharmacology Basics
By: JenniferDwayne Views: 1101

By: mjosedp Views: 1548

Neurological Emergencies-Stroke
By: KhushbuSG Views: 830

Structure of the Nervous System
By: drdwayn Views: 888

Coordination and Control
By: drdwayn Views: 1274

Synaptic Transmission
By: JenniferDwayne Views: 1285

- About : Professor, College of Nursing and Health Sciences
- Occupation : Medical Professional
- Specialty : MD
- Country : United States of America
HEALTH A TO Z
- Eye Disease
- Heart Attack
- Medications
CASE PRESENTATION HYDROCEPHALUS PRESENTED BY:
Aug 08, 2014
970 likes | 8.78k Views
CASE PRESENTATION HYDROCEPHALUS PRESENTED BY: EDDELYN UPANTO(NICU). DEMOGRAPHIC DATA case #: 190*** age: 21 days sex: male diagnosis: severe hydrocephalus ward: nicu. PHYSICAL ASSESSMENT General Appearance Weak in appearance Restless With OGT F5
Share Presentation
- shunt infection
- performance iq
- blood stream
- hemorrhagic events
- ineffective tissue perfusion

Presentation Transcript
CASE PRESENTATION HYDROCEPHALUS PRESENTED BY: EDDELYN UPANTO(NICU)
DEMOGRAPHIC DATA • case #: 190*** • age: 21 days • sex: male • diagnosis: severe hydrocephalus • ward: nicu
PHYSICAL ASSESSMENT • General Appearance • Weak in appearance • Restless • With OGT F5 • Wt.=2.46kg, Lt.=42cm, HC=34.5cm
SKIN • Pinkish • Warm to touch • Slightly dry • Scaly • Thin
HEAD AND NECK • Bulging Fontanels • Facial symmetry • Iris is black, pupils are equal, round reactive to light • Cloudy cornea • Conjunctiva are pale • No inflammation and discharges noted • Has both patent and equal nosetrills
DISCUSSION OF THE DECEASE: Hydrocephalus also known as "water on the brain," is a medical condition in which there is an abnormal accumulation of cerebrospinal fluid (CSF) in the ventricles, or cavities, of the brain. This may cause increased intracranial pressure inside the skull and progressive enlargement of the head, convulsion, tunnel vision, and mental disability. Hydrocephalus can also cause death. The name derives from the Greek words (hydro-) "water", and (kephalos) "head".
CLASSIFICATION Based on its underlying mechanisms, hydrocephalus can be classified into communicating and non-communicating (obstructive). Both forms can be either congenital or acquired. • Communicating • Communicating hydrocephalus, also known as non-obstructive hydrocephalus, is caused by impaired cerebrospinal fluid resorption in the absence of any CSF-flow obstruction between the ventricles and subarachnoid space. Various neurologic conditions may result in communicating hydrocephalus, including subarachnoid/intraventricular hemorrhage, meningitis and congenital absence of arachnoid villi. Scarring and fibrosis of the subarachnoid space following infectious, inflammatory, or hemorrhagic events can also prevent resorption of CSF, causing diffuse ventricular dilatation.]
NON-COMMUNICATING • Non-communicating hydrocephalus, or obstructive hydrocephalus, is caused by a CSF-flow obstruction ultimately preventing CSF from flowing into the subarachnoid space (either due to external compression or due to intraventricular mass lesions).
CONGENITAL • The cranial bones fuse by the end of the third year of life. For head enlargement to occur, hydrocephalus must occur before then. The causes are usually genetic but can also be acquired and usually occur within the first few months of life, which include: • 1) Intraventricular matrix hemorrhages in premature infants, • 2) Infections • 3) Type II Arnold-Chiari malformation • 4) Aqueduct Atresia and stenosis • 5) Dandy-Walker malformation
ACQUIRED • This condition is acquired as a consequence of CNS infections, meningitis, brain tumors, head trauma, intracranial hemorrhage (subarachnoid or intraparenchymal) and is usually extremely painful.
ANATOMY AND PHYSIOLOGY
PATHOPHYSIOLOGY OF HYDROCEPHALUS • If there is obstruction in the ventricular system or the subarachnoid space, dilated cerebral ventricles, causing ventricular surface wrinkle, and tearing ependymal lines. White mater below it will atrophy and reduced to a thin ribbon. In the gray matter there is maintenance that is selective, so that although ventricular enlargement gray matter has been experiencing a disruption. Dilation process can be a sudden process / acute and can also selectively depending on the position of the blockage. The process was a case of acute emergency. In infants and small children cranial suture folds and widened to accommodate increased cranial mass. If the anterior fontanela not closed then it will not expand and feel tight in touch. Stenosis aquaductal (family illness / adrift offspring sex) causes dilation of the ventricles laterasl point and center, this dilation causes the appearance of distinctive shaped head protruding forehead is dominant (dominant frontal blow). Syndroma dandy walkker would happen if there is obstruction at the foramina outside the IV ventricle. Fourth ventricle dilated and prominent posterior fossae meet most of the space under the tentorium. Clients with type hydrocephalus above will have an enlarged cerebrum which is symmetric and disproportionately small face. • In older people, cranial sutures had closed thus limiting the expansion of the brain, as the result showed the symptoms: increase in ICP before the cerebral ventricles, becomes greatly enlarged. Damage in the absorption and circulation of CSF in hydrocephalus incomplete. CSF exceeds the normal capacity of the ventricular system, every 6-8 hours and the total absence of absorption will cause death. • In ventricular dilation causes tearing of the line normal ependyma, which allows an increase in the wall cavity absorption. If the route collateral sufficient to prevent further ventricular dilatation there will be a state of compensation.
ETIOLOGY • Blockage of cerebrospinal fluid (CSF) can be caused by a variety of conditions such as: spina bifida and other birth defects of the brain; certain brain infections like meningitis (pus can cause a blockage); hemorrhage within or around the brain, usually due to prematurity or a ruptured aneurysm; and brain trauma, or tumouhyrors. The blockage can occur within the ventricles themselves (obstructive hydrocephalus), or outside the brain in the areas where the spinal fluid is reabsorbed back into the blood stream (communicating hydrocephalus). • The term congenital refers to cases where hydrocephalus is present at birth, but without any genetic factors. In cases of congenital hydrocephalus, it is usually not possible to determine the cause, and this is referred to as 'idiopathic'. In these cases, one assumes that the condition arose before birth, in the form of developmental problems due to infections, problems with blood supply, etc.
SIGNS AND SYMPTOMS • Signs and symptoms of infant with severe hydrocephalus: • Eyes that appear to gaze downward • Irritability • Seizures • Separated sutures • Sleepiness • Vomiting • Symptoms that may occur in older children can include: • Brief, shrill, high-pitched cry • Changes in personality, memory, or the ability to reason or think • Changes in facial appearance and eye spacing • Crossed eyes or uncontrolled eye movements • Difficulty feeding • Excessive sleepiness • Headache • Irritability, poor temper control • Loss of bladder control (urinary incontinence) • Loss of coordination and trouble walking • Muscle spasticity (spasm) • Slow growth (child 0–5 years) • Slow or restricted movement • Vomiting
EFFECTS • Because hydrocephalus can injure the brain, thought and behavior may be adversely affected. Learning disabilities including short-term memory loss are common among those with hydrocephalus, who tend to score better on verbal IQ than on performance IQ, which is thought to reflect the distribution of nerve damage to the brain. However the severity of hydrocephalus can differ considerably between individuals and some are of average or above-average intelligence. Someone with hydrocephalus may have motion and visual problems, problems with coordination, or may be clumsy. They may reach puberty earlier than the average child. About one in four develops epilepsy.
TREATMENT • Hydrocephalus treatment is surgical, generally creating various types of cerebral shunts. It involves the placement of a ventricular catheter (a tube made of silastic), into the cerebral ventricles to bypass the flow obstruction/malfunctioning arachnoidal granulations and drain the excess fluid into other body cavities, from where it can be reabsorbed. Most shunts drain the fluid into the peritoneal cavity (ventriculo-peritoneal shunt), but alternative sites include the right atrium (ventriculo-Atrial shunt), pleural cavity (ventriculo-pleural shunt), and gallbladder. A shunt system can also be placed in the lumbar space of the spine and have the CSF redirected to the peritoneal cavity (Lumbar-peritoneal shunt). An alternative treatment for obstructive hydrocephalus in selected patients is the endoscopic third ventriculostomy (ETV), whereby a surgically created opening in the floor of the third ventricle allows the CSF to flow directly to the basal cisterns, thereby shortcutting any obstruction, as in aqueductal stenosis. This may or may not be appropriate based on individual anatomy.
SHUNT COMPLICATIONS • Examples of possible complications include shunt malfunction, shunt failure, and shunt infection, along with infection of the shunt tract following surgery (the most common reason for shunt failure is infection of the shunt tract). Although a shunt generally works well, it may stop working if it disconnects, becomes blocked (clogged), infected, or it is outgrown. If this happens the cerebrospinal fluid will begin to accumulate again and a number of physical symptoms will develop (headaches, nausea, vomiting, photophobia/light sensitivity), some extremely serious, like seizures. • Another complication can occur when CSF drains more rapidly than it is produced by the choroid plexus, causing symptoms -listlessness, severe headaches, irritability, light sensitivity, auditory hyperesthesia (sound sensitivity), nausea, vomiting, dizziness, vertigo, migraines, seizures, a change in personality, weakness in the arms or legs, strabismus, and double vision - to appear when the patient is vertical.
NURSING PROBLEM PRIORITIZATION • Acute pain • Delayed growth and development • Imbalanced nutrition: Less than body requirements • Gas exchange • Ineffective tissue perfusion: Cerebral. • Interrupted family processes. • Infant Behavior, risk for disorganized. • Risk For Infection
NURSING CARE PLAN
REFERENCE: • ^http://www.nlm.nih.gov/medlineplus/ency /article/001571.htm Accessed 19 June 2010 • ^ abcd Alfred Aschoff, Paul Kremer, BahramHashemi, Stefan Kunze (October 1999). "The scientific history of hydrocephalus and its treatment". Neurosurgical Review (Springer) 22 (2–3): 67–93 [67]. doi:10.1007/s101430050035. ISSN1437-2320 • ^ "The scientific history of hydrocephalus and its treatment.".United States National Library of Medicine. • ^"Hydrocephalus Fact Sheet", National Institute of Neurological Disorders and Stroke. (August 2005). • ^ Cabot, Richard C. (1919) Physical diagnosis , William Wood and company, New York, 7th edition, 527 pages, page 5. (Google Books) • ^Yadav YR, Mukerji G, Shenoy R, Basoor A, Jain G, Nelson A (2007). "Endoscopic management of hypertensive intraventricular haemorrhage with obstructive hydrocephalus". BMC Neurol7: 1. doi:10.1186/1471-2377-7-1. PMC1780056. PMID17204141. http://www.biomedcentral.com/1471-2377/7/1. • ^ Greenberg, Mark S (2010-02-15). Handbook of Neurosurgery. ISBN9781604063264. http://books.google.com/?id=0TC9Cns4Qz8C&pg=PA307&lpg=PA307&dq=Greenberg+handbook+of+neurosurgery+external+hydrocephalus#v=onepage&q&f=false. • ^wwww.spinabifidamoms.com • ^http://www.hydroassoc.org/media/stats • ^ Warf, Benjamin C. (2005). "Comparison of 1-year outcomes for the Chhabra and Codman-Hakim Micro Precision shunt systems in Uganda: a prospective study in 195 children". J Neurosurg (Pediatrics 4)102 (4 Suppl): 358–362. doi:10.3171/ped.2005.102.4.0358. PMID15926385. http://thejns.org. http://thejns.org/doi/pdf/10.3171/ped.2005.102.4.0358 • ^"Man with Almost No Brain Has Led Normal Life", Fox News (2007-07-25). Also see "Man with tiny brain shocks doctors", NewScientist.com (2007-07-20); "Tiny Brain, Normal Life", ScienceDaily (2007-07-24). • ^"Man Lives Normal Life Despite Having Abnormal Brain". The Globe and Mail. July 19, 2007. Archived from the original on August 28, 2007. http://web.archive.org/web/20070828013153/http://www.theglobeandmail.com/servlet/story/RTGAM.20070719.wbrain0719/BNStory/Science/home. Retrieved July 15, 2012. • ^"Man with tiny brain shocks doctors", New Scientist online, 20 July, 2007 • ^ Brain of a white-collar worker. Feuillet, L., Dufour, H. & Pelletier, J., et al. The Lancet, Volume 370, Issue 9583, Page 262, 21 July 2007 pmid=17658396 • ^http://www.startribune.com/entertainment/books/11435616.html
- More by User
Support for Creation of an ICD-9 Code for Normal Pressure Hydrocephalus (NPH)
Support for Creation of an ICD-9 Code for Normal Pressure Hydrocephalus (NPH) Michael A. Williams, M.D. Adult Hydrocephalus Program Departments of Neurology and Neurosurgery Johns Hopkins Hospital Baltimore, MD Disclosure In the last 12 months:
975 views • 23 slides
Endodontic Case Presentation
Endodontic Case Presentation. PRESENTED BY AHMAD S. ALQAHTANI [SSC-Dent(Endo)], R3 27 jan 2010. FIRST CASE. Patient personal data. Age: 29 year-old Sex: male Nationality :- Saudi Date started: 10 /Nov/2009 Date finished: 17 /Nov/2009. Chief complaint.
6.82k views • 35 slides
Anemia Case Presentation
Anemia Case Presentation. Presented by Hanadi Basha 6 th year Med student Damascus Uni. 58 y/o Male presented with general fatigue, palpitation for 2 months duration with no other complaints.
1.24k views • 22 slides
CASE PRESENTATION
CASE PRESENTATION. « Doctor my pupils are dilated » Richard Plantive R3 Emergency Medicine November 17, 2004. CASE PRESENTATION. ID: 41 year old female PMHx: renal cysts Meds: none. CASE PRESENTATION. HPI Blurry vision Near vision more blurry than far
1.85k views • 48 slides
Case Presentation
Case Presentation. Said Al Mazroui. On 11/10/09. 5 months child presented with 5 days history of loose motion. for 3-4 times daily (normal 1-2 times/day). the diarrhea was associated with low grade fever ( not ducomented ) 2 times vomiting only .
884 views • 52 slides
Case presentation
Case presentation. Torsade de Pointes. C15 Case. Mr X presented to ED from Bosbokrandt (Nelspruit area) visiting in CPT. He is previously well 28yr old who looks acutely ill. History from family
632 views • 35 slides
BEACON FOUNDATION’S CASE PRESENTATION CONTEST 2006
BEACON FOUNDATION’S CASE PRESENTATION CONTEST 2006. A CASE OF CEREBRO- VASCULAR ACCIDENT PRESENTED BY DR. NIRANJAN PAI M.D. PART –2 DEPARTMENT OF MEDICINE M.L.D.M.H.I. PALGHAR. Preliminary Data: Mr. P. G, 50yrs/ Male 20/8/05.
420 views • 25 slides
Hydrocephalus
Hydrocephalus. Hydrocephalus is a condition where there is an imbalance between the production of cerebrospinal fluid and its absorption over the surface of the brain and into the circulatory system . Cerebrospinal fluid is constantly produced to protect the brain and spinal cord.
985 views • 35 slides


Case for Just In Case Inventory
Case for Just In Case Inventory . Presented by Philip E. Quigley, CFPIM, PMP Sylvan D. Finestone, MBA, PMP . Presented to Orange County APICS- 8/19/2009. Overview. The case for Just-In-Time (JIT) inventory, or lean, has been made for many years now
248 views • 23 slides
Case Presentation. Abdullah Almaghraby, MBBS. History. A 16 year old male with Cystic Fibrosis has End stage lung disease on O2. Pancreatic insufficiency. On PEG tube for feeding. Presented to ER with epigastric pain,vomiting and no bowel motion for 2 days. History.
571 views • 46 slides
HYDROCEPHALUS
HYDROCEPHALUS. Dr. VASHDEV KHIMANI ASSISTANT PROFESSOR DEPT. OF NEUROSURGERY LUMHS JAMSHORO. Definition. Hydrocephalus derived from Greek word means water on brain. It is an abnormal accumulation of CSF in ventricles or cavities of brain. Functions of CSF. 1. Shock absorber
1.2k views • 36 slides
Case Presentation. 48 yo Black female with well controlled HTN, h/o borderline hyperthyroidism No specific complaints or concerns Meds: HCTZ for BP control FHx remarkable for HTN, DM, no other endocrine D/O’s, no known AIDz SHx unremarkable. Case Presentation.
384 views • 4 slides
Case Presentation Presented by: Dr.Safaa fadhl Supervised by: Dr.Kamal Marghani
Case Presentation Presented by: Dr.Safaa fadhl Supervised by: Dr.Kamal Marghani. 29 yrs male presented to ED at 1:40pm complaining of cough , S OB, and fever. At triage :. Pt was admitted to room A at 2:00pm
600 views • 41 slides
2009 December Featured Case and 2009 IDSA Fellows' Day Case Presentation
Case Presentation. 2009 December Featured Case and 2009 IDSA Fellows' Day Case Presentation. M Haghighi MD Shahid Beheshti univesity of medical science. This case was originally presented at the Annual Meeting of the Infectious Diseases Society of America 2009 (IDSA, 47th meeting).
616 views • 40 slides
Case Presentation THR ,B/L TKR and LCP Fixation
Case Presentation THR ,B/L TKR and LCP Fixation. Dr.R.K.Pandey Sr. Consultant Orthopeadic Orthonova Hospital ,& Rockland Hospital New Delhi ,India. Case Study. Mrs.Parvati 70 years female. Presented with Neglected Fracture Neck of Femur.
866 views • 25 slides
A CASE PRESENTATION OF A PATIENT WITH DIABETIC KETOACIDOCIS (DKA)
A CASE PRESENTATION OF A PATIENT WITH DIABETIC KETOACIDOCIS (DKA). Prepared by: Tristan Villanueva Arcibal BSN-RN Presented on: July 16, 2013. DEMOGRAPHIC DATA. Name : Mr. X Case no . :201--- Age : 28 y/o Gender : Male Nationality : Saudi Admission date : 11-4-2013
7.16k views • 41 slides
CASE PRESENTATION PREECLAMPSIA
CASE PRESENTATION PREECLAMPSIA. PRESENTED BY : Avneep Aggarwal MODERATOR : Anjan Trikha. www.anaesthesia.co.in [email protected]. HISTORY. Name: Savita Age: 27 yrs Resident of New delhi Date of admission 11/08/08 Presenting complaint : Missed periods for 8 months.
5.03k views • 44 slides
Nephrology Case Presentation
Nephrology Case Presentation. Douglas A. Stahura 24 January 2002. Case Presentation. 48 y/o WM presents with back pain Sharp, over L side/ribs Intermittent but severe 8/10 No radiation No recent injury, lifting, straining etc Nothing like this ever happened before. Case Presentation.
866 views • 31 slides
Show case Presentation
Show case Presentation. Presented by T hamsanqa Ncube (I.T LECTURER). Teaching methodologies Development Plan Portfolio showcase Scholarship of Teaching and Learning Challenges during 2013. The presentation will focus on:. Teaching methodologies implemented in 2013.
225 views • 11 slides
Radiology Case Presentation
Radiology Case Presentation. David R. Beckert, MS-4 11/8/05. Case Background. Clinical History: 22 y.o. female presented to Neuro angio for imaging of AVM, which was discovered at OSH, in order to proceed to interventional radiology for gamma knife ablation procedure.
855 views • 13 slides
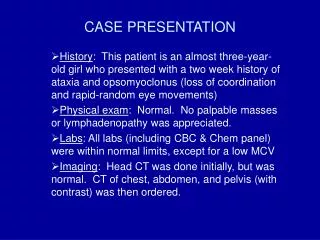
CASE PRESENTATION. History : This patient is an almost three-year-old girl who presented with a two week history of ataxia and opsomyoclonus (loss of coordination and rapid-random eye movements) Physical exam : Normal. No palpable masses or lymphadenopathy was appreciated.
435 views • 5 slides
Hydrocephalus & Shunts
Hydrocephalus & Shunts. Sean’s Story. What is hydrocephalous?. Hydrocephalus is the medical term for a condition that is commonly called “ water on the brain .” It is a combination of the Greek word “hydro,” which means water and “cephalus” which means head .
740 views • 30 slides
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Asian J Neurosurg
- v.16(4); Oct-Dec 2021

Evaluation of Pediatric Hydrocephalus: Clinical, Surgical, and Outcome Perspective in a Tertiary Center
Rahul singh.
Department of Neurosurgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India
Ravi Shankar Prasad
Ramit chandra singh, adarsh trivedi.
1 Department of Neurosurgery, Shri Shankracharya Institute of Medical Sciences, Bhilai, Madhya Pradesh, India
Kulwant Singh Bhaikhel
Anurag sahu.
Pediatric hydrocephalus (PH) results in significant clinical and psychosocial morbidity in pediatric population.
The aims of the study are to evaluate clinical, surgical, and outcome perspective of PH patients of age <12 years.
Settings and Design:
This is a retrospective cohort study.
Materials and Methods:
This study includes 117 pediatric patients (age ≤12 years) of hydrocephalus due to various etiology admitted in our department between September 2018 and December 2020. Demographic profile, etiology, clinical presentation, management, complications and postoperative outcome characteristics were evaluated. Survival analysis was done with respect to etiology and age group.
Statistical Analysis Used:
P < 0.05 was considered statistically significant. Unpaired t -test and Chi-square test were used. Kaplan–Meier curve plotting and survival analysis were also done.
Male-to-female ratio was 1.3:1. Most frequent etiology of PH was postinfectious (35%). Posterior fossa pilocytic astrocytoma (34.2%) was the most common neoplastic etiology. Surgical procedure performed for PH was ventriculoperitoneal shunting ( n = 103), Ommaya reservoir ( n = 2) placement, and endoscopic third ventriculostomy (ETV) ( n = 8). Mortality was significantly ( P = 0.0139) more in patients of neoplastic etiology. Cognitive deficits and delayed developmental milestones were significantly ( P < 0.05) more in congenital hydrocephalus etiology. There was a nonsignificant difference in survival between age groups ( P = 0.1971). However, a significant survival difference was evident ( P = 0.0098) for etiology.
Conclusions:
Disease-specific mortality is main cause of mortality in PH. Neoplastic etiology PH has poor survival when compared to others. Life-long routine controls are required to avoid future possible complications and enhance better rehabilitation of the child.
Introduction
Pediatric hydrocephalus (PH) (namely, congenital, prematurity germinal matrix bleed, postinfectious, and neoplastic) when compared to adult patients of hydrocephalus is more complicated and has significantly more developmental and cognitive morbidities. Hydrocephalus may be defined as “an active dilatation of the ventricles resulting from imbalance between cerebrospinal fluid (CSF) production in ventricles and its absorption to systemic circulation.“[ 1 ]
Hydrocephalus in pediatric population is having high morbidity and mortality. The prevalence of hydrocephalus in pediatric population varies from 30 to 423 per 100,000 pediatric population in various reported studies[ 2 , 3 , 4 , 5 ] with prevalence been higher in developing nations in comparison to developed world. Congenital hydrocephalus contains heterogenous etiology comprising of primary aqueductal stenosis (PAS), Dandy–Walker malformation (DWM), germinal matrix hemorrhage (GMH) and intrauterine infections leading to gliosis, intraventricular space-occupying lesions, X-linked hydrocephalus and Chiari malformations, neural tube defects, and many other syndromic and genetic disorders.[ 6 , 7 ]
Acquired hydrocephalus in pediatric population is commonly attributed to intracranial infections, intracranial hemorrhage (especially intraventricular hemorrhage [IVH] and subarachnoid bleed), benign and neoplastic lesions.[ 6 ]
Computed tomography (CT) and magnetic resonance imaging (MRI) of brain are the common radiological modalities for evaluating and diagnosing PH [ Figure 1 ]. Measuring ventricle size on MRI or CT is quite helpful in cases of diagnostic dilemma.[ 8 ] MRI is superior for evaluating ventricle size, etiological diagnosis, endoscopic third ventriculostomy (ETV) patency, and parenchymal changes. Sensitivity of CT scan when compared to MRI is more for catheter tip localization[ 9 ] if it is used as an adjunct with neuronavigation.

Noncontrast computed tomography scan axial sections of brain of a child showing. (a) Posterior fossa tumor compressing 4 th ventricle leading to hydrocephalus; (b) Postinfectious hydrocephalus with dilatation of all ventricles; (c) Dandy–Walker malformation with large posterior fossa cyst communicating with 4 th ventricle and hydrocephalus; (d) Primary aqueductal stenosis with dilatation of third and lateral ventricles but normal 4 th ventricle
Surgical modalities such as ventriculoperitoneal (VP) shunt, ETV, and Ommaya reservoir (in selected cases) depend on surgeon's preference and indications.
In this study, we aim to evaluate clinical, surgical, and outcome perspective of PH patients of age <12 years. This study will hopefully serve the purpose of analyzing hydrocephalus in pediatric population and its effects on pediatric age groups.
Materials and Methods
This retrospective cohort study consisted of 117 pediatric patients (age ≤12 years) of hydrocephalus due to various etiologies admitted in our department between September 1, 2018, and December 30, 2020.
This retrospective cohort study was done in two phases: a cross-sectional phase where the patients included in the sample were evaluated for the following described variables and a follow-up phase at hospital discharge and at subsequent outpatient department (OPD) visits by the patient. Each patient was evaluated in terms of demographic profile, etiology of hydrocephalus, clinical presentation, management, CSF diversion procedures used, complications, and postoperative outcome characteristics. Survival analysis was also done with respect to etiology and age group of PH.
Medical and surgical records submitted in medical record section of our institute were used to collect data of these 117 patients retrospectively. Follow-up data were collected from OPD records.
Cerebrospinal fluid diversion procedure
We used medium pressure VP shunt (Chhabra shunt) either bacterial resistant (silver impregnated) or nonmedicated for VP shunting. Ommaya reservoir was used in few patients of septic meningitis and IVH with HCP which was converted to permanent shunt after resolution of IVH and CSF infection. ETV was done in some patient of PAS, neoplasm, and postinfectious hydrocephalus. Choice of CSF diversion procedure was decided by senior author preferences. All procedures were done under general anesthesia under neuronavigation guidance. CSF collected during the surgery was sent for analysis. Assessment of shunt function was done by history (headache, vomiting, convulsions), neurological examination (vision, motor, and sensory), local examination (inspection and palpation of shunt system and testing of shunt pump for refill), and CT/MRI scans. Shunt complications were managed accordingly.
Statistical analysis
The data were summarized using medians/mean and counts and percentages. Differences of significance were evaluated by unpaired t -test and Chi-square test. Kaplan–Meier curve was plotted for survival analysis with respect to age group and etiology of PH. Survival analysis was done using Log-rank (Mantel-Cox) test (MCT), Log-rank test for trends (LTT), and Gehan–Breslow-Wilcoxon test (GBW). Values with P < 0.05 were considered statistically significant. GraphPad Prism software was used for statistical analysis.
A total of 117 pediatric patients (age ≤12 years) were admitted during the study period. Out of these patients, 50 patients were female and 67 patients were males and male-to-female ratio was 1.3:1. Number of pediatric patients with age ≤1 year was 23, between 1 and 6 years was 51 and between 6 and 12 years was 43. Most common etiology of PH was postinfectious (35%) (septic –9.4%; tubercular–25.6%) followed by neoplasm (32.5%) and aqueductal stenosis (12.8%) [ Table 1 ]. Among neoplastic etiologies, posterior fossa pilocytic astrocytoma (13, 34.2%) was most common followed in succession by medulloblastoma (11, 28.9%), craniopharyngioma (6, 15.8%), intraventricular tumor (4, 10.5%), and brainstem glioma (4, 10.5%). Out of all patients, 12 patients of neoplasm, 14 patients of posttuberculous meningitis hydrocephalus, and 6 patients of shunt block were operated on emergency basis due to rapid neurological deterioration and features of raised intracranial tension. Emergency VP shunting was done in all of them.
Etiology of pediatric (<12 years) hydrocephalus ( n =117)
| Etiology | Number of patients, (%) |
|---|---|
| Neoplasm | 38 (32.5) |
| Aqueductal stenosis | 15 (12.8) |
| Dandy-Walker malformation | 5 (4.3) |
| Postinfectious | 41 (35) |
| Septic | 11 (9.4) |
| Tubercular | 30 (25.6) |
| Posttraumatic | 3 (2.6) |
| GMH in premature infants | 3 (2.6) |
| Failed shunt | 11 (9.4) |
| Spina bifida with HCP | 1 (0.9) |
HCP – Hydrocephalus; GMH – Germinal matrix hemorrhage
Most common symptoms were general irritability (52.1%) and headache (49.6%) [ Table 2 ]. Most common signs were progressive increase in head circumference (31.6%), bradycardia (27.3%), and hypertension (27.3%) [ Table 2 and Figure 2 ].
Clinical presentation
| Clinical presentation | Number of patients, (%) |
|---|---|
| Poor feeding | 31 (26.5) |
| Vomiting/nausea | 43 (36.7) |
| General irritability | 61 (52.1) |
| Drowsiness | 44 (37.6) |
| Seizure | 27 (23.1) |
| Impaired eye movements | 4 (3.4) |
| Bradycardia | 32 (27.3) |
| Hypertension | 32 (27.3) |
| Prominent scalp veins | 29 (24.8) |
| Loss of vision | 17 (14.5) |
| Headache | 58 (49.6) |
| Double vision | 2 (1.7) |
| Loss of bladder control | 6 (5.1) |
| Personality changes | 3 (2.6) |
| Loss of memory | 13 (11.1) |
| Progressive increase in head circumference | 37 (31.6) |
| Bulging of the fontanels | 26 (22.2) |
| Neck pain | 12 (10.3) |
| Transient blurring of vision | 10 (8.5) |
| Spastic weakness of lower limbs | 6 (5.1) |
| Failure of upward gaze | 31 (26.5) |
| Sunset sign | 31 (26.5) |
| Cranial nerve VI palsy | 2 (1.7) |
VI – Abducens nerve

(a) A child with progressive hydrocephalus showing increased head size and sunset sign; (b) Shunt migration and per rectal appearance in a child; (c) Distal ventriculoperitoneal shunt catheter extrusion in right hypochondrial region.; (d) Top view of head of an infant with shunt over drainage resulting in sunken fontanel
Of 117 patients, 114 patients (97.5%) underwent surgical intervention while three patients (2.5%) were managed conservatively (neonates with GMH leading to hydrocephalus). Most common surgical procedure performed for addressing hydrocephalus was VP shunting ( n = 103, 90.3%) followed by Omaya reservoir ( n = 2, 1.7%) and ETV ( n = 8, 7%). Mean duration of follow-up was 7.2 months with range of 1–13 months.
Surgical outcome resulted in uneventful recovery of hydrocephalus in 60.5% patients. Patients with neoplastic etiology were either operated in the same setting (13, 34.2%) or operated in second setting after CSF diversion procedure (25, 65.8%). Most common shunt related complications were shunt obstruction (11.6%) followed by shunt infection (5.8%) and shunt extrusion (4.8%) [ Table 3 and Figure Figure2b 2b - -d]. d ]. In this PH cohort, disease-specific mortality was 10.5% and shunt-related mortality was 1.7% [ Table 3 ].
Outcome of pediatric hydrocephalus management
| Outcome characteristics | Number of patients, (%) |
|---|---|
| Surgical outcome ( =114) | |
| Uneventful recovery | 69 (60.5) |
| VP shunting ( =103) | |
| Shunt obstruction | 12 (11.6) |
| Shunt infection | 6 (5.8) |
| Shunt migration | 2 (1.9) |
| Shunt extrusion | 5 (4.8) |
| Shunt kinking | 2 (1.9) |
| Shunt disconnection | 1 (1) |
| Shunt over drainage | 2 (1.9) |
| Subdural hematoma | 1 (1) |
| ETV ( =8) | |
| ETV failure | 2 (25) |
| Total mortality | |
| Disease specific | 12 (10.5) |
| Shunt related | 2 (1.7) |
| Clinical morbidity ( =117) | |
| Cognition deterioration | 13 (11.1) |
| Motor system | 9 (7.7) |
| Vision | 17 (14.5) |
| Seizure | 13 (11.1) |
| Chronic headache | 22 (18.8) |
| Neuroendocrine problem | 3 (2.6) |
| Psychosocial outcome | |
| School drop | 34 (29) |
| Social integration impairment | 23 (19.6) |
| Delayed developmental milestones | 22 (18.8) |
VP – Ventriculoperitoneal; ETV – Endoscopic third ventriculostomy
Chronic headache (18.8%), loss of vision (14.5%), seizure (11.1%), and cognition deterioration (11.1%) were common clinical morbidities that persisted after CSF diversion procedures or conservative management. Most common psychosocial outcome evident during follow-up was school drop (29%) [ Table 3 ].
On analyzing PH outcome in relation to etiology, mortality was significantly ( P = 0.0139) more in patients of neoplastic etiology. Cognitive deficits ( P = 0.0151) and delayed developmental milestones ( P < 0.0001) were significantly more in congenital hydrocephalus etiology (aqueductal stenosis and DWM). Shunt failure, shunt infection, recovery, neurological deficits, seizure, vision loss, and chronic headache were not significantly associated with etiology of PH [ Table 4 ].
Outcome analysis based on etiology
| Outcome characteristic | Neoplasm (38) | Aqueductal stenosis (15) | Postinfectious (41) | Posttraumatic (3) | DWM (5) | |
|---|---|---|---|---|---|---|
| Shunt obstruction (12) | 2 | 2 | 7 | 1 | 0 | 0.3055 |
| Shunt infection (6) | 1 | 0 | 5 | 0 | 0 | 0.3177 |
| ETV failure (2) | 0 | 1 | 1 | - | - | 0.1546 |
| Uneventful recovery (69) | 22 | 13 | 27 | 2 | 5 | 0.1596 |
| Mortality (14) | 11 | 0 | 3 | 0 | 0 | 0.0139* |
| Neurological deficit (9) | 7 | 1 | 1 | 0 | 0 | 0.1214 |
| Cognitive deficit (13) | 3 | 3 | 4 | 0 | 3 | 0.0151* |
| Seizure (13) | 9 | 1 | 2 | 1 | 0 | 0.0679 |
| Vision loss (17) | 11 | 2 | 5 | 0 | 0 | 0.1930 |
| Delayed developmental milestones (22) | 4 | 8 | 7 | 1 | 5 | <0.0001* |
| Chronic headache (22) | 11 | 1 | 8 | 1 | 1 | 0.4707 |
*Significant ( P <0.05). DWM – Walker malformation; ETV – Endoscopic third ventriculostomy
Aqueductal stenosis ( P = 0.0445), DWM ( P = 0.0022), and GMH ( P = 0.0019) as an etiology to PH were significantly more in the age group of ≤1 year [ Table 5 ]. Psychosocial morbidity was significantly ( P = 0.0015) more in age groups 1–6 years and 6–12 years [ Table 5 ]. There was no significant difference ( P > 0.05) in terms of shunt complications, ETV failure, neurological morbidity, and mortality between the three age groups [ Table 5 ].
Age distribution in relation to etiology, management, and outcome
| Patients characteristics | ≤1 year (23) | 1-6 years (51) | 6-12 years (43) | |
|---|---|---|---|---|
| Etiology | ||||
| Neoplasm (38) | 4 | 21 | 15 | 0.1353 |
| Aqueductal stenosis (15) | 6 | 7 | 2 | 0.0445* |
| DWM (5) | 4 | 1 | 0 | 0.0022* |
| Postinfectious (41) | 6 | 15 | 20 | 0.1350 |
| Posttraumatic (3) | 0 | 1 | 2 | 0.4894 |
| Germinal matrix | ||||
| Hemorrhage (3) | 3 | 0 | 0 | 0.0019* |
| Failed shunt (11) | 0 | 5 | 4 | 0.3021 |
| Spina bifida with HCP (1) | 0 | 1 | 0 | 0.5207 |
| Management | ||||
| Conservative (3) | 3 | 0 | 0 | 0.8149 |
| Surgical (114) | ||||
| Ventriculoperitoneal | ||||
| Shunt (103) | 18 | 45 | 41 | |
| Ommaya reservoir (2) | 0 | 1 | 1 | |
| ETV (8) | 2 | 5 | 1 | |
| Complications | ||||
| Shunt obstruction (12) | 1 | 6 | 5 | 0.5809 |
| Shunt infection (6) | 0 | 2 | 4 | 0.2304 |
| Shunt extrusion (5) | 1 | 3 | 2 | 0.9472 |
| Neurological morbidity (9) | 2 | 4 | 3 | 0.9679 |
| ETV failure (2) | 0 | 1 | 1 | 0.5134 |
| Mortality | ||||
| Disease specific (12) | 1 | 4 | 7 | 0.2358 |
| Shunt related (2) | 0 | 1 | 1 | 0.7725 |
| Psychosocial morbidity (34) | 0 | 16 | 18 | 0.0015* |
*Significant ( P <0.05). DWM – Walker malformation; ETV – Endoscopic third ventriculostomy; HCP – Hydrocephalus
On comparing type of shunt and its complication, shunt infection was significantly less ( P = 0.0236) in patients in whom silver-impregnated shunt was used when compared with standard shunt. No significant difference was observed with respect to shunt block, shunt extrusion, shunt disconnection, shunt migration, and shunt over drainage between the two types of shunt used [ Table 6 ].
Shunt complication analysis in relation to type of shunt catheter used
| Shunt complications | Silver impregnated shunt (51) | Standard shunt (63) | |
|---|---|---|---|
| Shunt block (12) | 5 | 7 | 0.8211 |
| Shunt infection (6) | 0 | 6 | 0.0236* |
| Shunt extrusion (5) | 2 | 3 | 0.8275 |
| Shunt disconnection (1) | 0 | 1 | 0.3662 |
| Shunt migration (2) | 1 | 1 | 0.8800 |
| Shunt over drainage (2) | 1 | 1 | 0.8800 |
*Significant ( P <0.05)
Age group in relation to mortality was plotted in Kaplan–Meier survival curve [ Figure 3a ]. There was nonsignificant survival difference between three age groups using MCT ( P = 0.1971), LTT ( P = 0.0758), and GBW test ( P = 0.4166).

Kaplan–Meier survival curve (a) Age-related survival; (b) Etiology-related survival
Etiology of PH in relation to mortality was plotted in Kaplan–Meier survival curve [ Figure 3b ]. Significant difference in survival between etiology was seen on using MCT ( P = 0.0098*), LTT ( P = 0.0035*), and GBW test ( P = 0.0254).
PH may affect normal brain development proportionate to time and duration of this pathology. HCP results in damage to ependymal layer, white matter ultrastructural changes, changes in cerebral circulation and metabolic activities, gliotic changes in the cortex, and injury to axons.[ 10 , 11 ]
In this study, male children were more commonly affected when compared with females and male-to-female ratio was 1.3:1. Various studies have reported male preponderance in cases of hydrocephalus in pediatric population.[ 12 , 13 , 14 , 15 ]
Most common causes of PH were postinfective (35%) followed by neoplasm (32.5%) in our study. Worldwide, postinfectious HCP is the most frequent etiology of neonatal and PH.[ 16 , 17 ] However, in developed countries, posthemorrhagic HCP is the most frequent etiology of neonatal HCP.[ 18 ]
HCP is present in more than half of pediatric brain tumor cases at diagnosis and as the second most common comorbidity at presentation.[ 18 ] We found that posterior fossa pilocytic astrocytoma (34.2%) was the most common neoplastic etiology causing PH followed by medulloblastoma (28.9%). Other causes of PH are ependymomas, choroid plexus tumors, pineal region tumors (also can cause aqueductal compression).[ 18 ] According to some authors, ETV is the intervention preferred for posterior fossa tumors with HCP after tumor resection. VP shunting should be done in case of ETV failure.[ 19 ] However, we prefer to do VP shunting in all posterior fossa tumors with HCP presenting in emergency before tumor resection. We do simultaneous VP shunting in elective surgery of posterior fossa tumor with HCP or ETV for HCP persisting after postfossa tumor resection depending on senior author preference.
In our study, 27.3% of patients underwent emergency VP shunting. Most common etiology implicated in emergency shunting was postinfective (43.75%) followed by neoplastic (37.5%) due to features of raised Intracranial tension (ICT). Various studies have also shown increased rates of emergency VP shunting in postinfective and neoplastic PH.[ 20 ]
More common presentations of PH in our study were irritability, headache, drowsiness, vomiting, and progressive increase in head size. Clinical manifestations depend on the status of cranial sutures and fontanels. Before their closure, the child mainly presents with progressively increasing head circumference and bulging of the fontanels. After their closure, the chief presentations are related to raise intracranial pressure levels manifesting as headache nausea/vomiting, bradycardia, hypertension, and loss of vision.[ 21 ]
In our study, we managed three patients of GMH in premature neonate conservatively which resolved spontaneously. Intraventricular hemorrhage in premature babies results in posthemorrhagic ventricular dilation. Some cases may get self-resolved and may not require any procedural intervention if resolution of IVH occurs without any secondary changes in CSF pathways. Temporary intraventricular reservoirs with intermittent CSF tapping may be used in neonates with progressively increasing HCP and IVH. Rate of conversion to VP shunting depends on the degree of posthemorrhagic PH with about 20% of grade 3 and 40% of grade 4 hemorrhage requiring VP shunting.[ 22 ]
Most common surgical intervention used in our study was VP shunting (90.3%) followed by ETV in eight patients and Ommaya reservoir in two patients. VP shunts are the most common CSF diversion devices available. Although it significantly improves the outcome of PH patients, the complication rates with resultant increased mortality or morbidity remain high at present.[ 10 , 23 , 24 ] ETV is also gaining popularity for PH. Early infancy, postinfectious hydrocephalus, and patients with partial choroid plexus cauterization (CPC) may show less favorable results to endoscopic treatment.[ 25 ] When compared with VP shunting, ETV is having higher failure with relative risk being 40% higher than VP shunting at 3-month follow-up.[ 26 ] ETV with CPC has shown decreased chance of ultimate VP shunt dependence by 26%.[ 25 ]
In our study, post-CSF diversion procedures, majority (60.5%) of patients showed uneventful resolution of hydrocephalus. Etiology of the disease process guided the ultimate outcome in these cases.
Shunt complications range from mechanical problems (namely, shunt blockage, shunt migration, shunt extrusion, and shunt disconnection); flow- related issues (CSF over drainage) resulting in subdural hematoma/hygroma, low-pressure headache, cranial deformity, slit ventricle syndrome, and secondary craniostenosis; abdominal end complications, namely ascites, pseudocyst, hydrocele, and visceral perforations; to shunt infections.[ 27 , 28 , 29 , 30 ] In our study, most common shunt complication was shunt obstruction (11.6%), followed by shunt infection (5.8%) and shunt extrusion (4.8%). Studies had reported that shunt infection rates vary from 3% to 15%.[ 31 , 32 ] Overall shunt failure rates at 1 month and 1 year are about 13% and 29%, respectively.[ 25 ]
In our study, the use of silver-impregnated shunt (BR Chhabra shunt) was having significantly less shunt infection when compared with standard shunts. However, there was no difference in terms of shunt block, shunt extrusion, shunt disconnection, shunt migration, and shunt over drainage between the two types of shunt used. Shunt catheters may be standard, silver impregnated or antibiotic impregnated. Evidence regarding their comparative effectiveness is lacking[ 33 ] and choice of shunt catheter depends on economic condition of the patient and surgeons' preferences. However, a meta-analysis had showed results favoring less shunt infection in the antibiotic-impregnated VP shunt group.[ 34 ]
In our study, mortality due to primary pathology was 10.5% and mortality due to shunt complications was 1.7%. Studies have shown overall mortality in PH to be 1.22% to 14.6%,[ 35 , 36 ] nonneoplastic mortality to be 8.6% to 13.7%,[ 37 , 38 ] and shunt-related mortality 0%–3.65%.[ 39 , 40 ] Neoplastic etiology, in our study, was significantly having more mortality as compared to others which may correlate with disease-specific mortality.
Congenital hydrocephalus patients showed significantly higher psychosocial deficits, cognitive impairment, and delayed developmental milestones. Psychosocial morbidity was significantly more in age groups 1 to 6 years and 6–12 years in our study. School drop rates (29%) and poor social interaction and integration (19.6%) were significant. Delayed developmental milestones (18.8%) in these hydrocephalus patients may be due to white matter changes in these disorders due to raised intraventricular pressure. School drops/difficulties may be more commonly due to cognitive deficit and also due to repeated hospital admissions. Ultimate outcome of PH is evident by child psychosocial outcome and community integration to lead a normal productive life in society.
On doing survival analysis, we could not find any difference in survival in these patients with respect to age groups. Patients with neoplastic etiology were having significant poor survival when compared to benign and congenital etiologies. This can be obviously attributed to higher disease-specific mortality in neoplastic etiology of PH. Life-long routine controls are required to avoid future possible complications and enhance better rehabilitation of the child. Optimization of neuropsychological support to such a child is an imperative component of the management of PH.
Conclusions
PH results in significant clinical and psychosocial morbidity. Neoplastic etiology having highest mortality rate in PH. Postinfective HCP is the most common cause of PH. Pilocytic astrocytoma and medulloblastoma are most common neoplastic etiology causing PH. Most common shunt complications are shunt obstruction, shunt infection, and shunt extrusion. BR shunts have significantly less shunt infection rates as compared to their nonmedicated shunt. Psychosocial and developmental delays are more common in congenital hydrocephalus group. Neoplastic etiology PH has poor survival when compared to other etiologies.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgment
This study was self-funded.

IMAGES
VIDEO
COMMENTS
This study reports a rare case of acute obstructive hydrocephalus following aqueductal stenosis caused by an unruptured grade IV perimesencephalic arteriovenous malformation. An 11-year-old boy admitted to the hospital with progressive headache, nausea and vomiting throughout a month. A Computerized Tomography (CT) showed an obstructive ...
Case 606 -- A 6 year old girl with hydrocephalus. CLINICAL HISTORY. A 6-years-old African American girl presented with severe headache for several days associated with vomiting, neck stiffness, fever, and unsteady gait. Physical examination was otherwise unremarkable. She was recently treated for otitis media approximately one week prior to ...
Hydrocephalus can be defined broadly as a disturbance of formation, flow, or absorption of cerebrospinal fluid (CSF) that leads to an increase in volume occupied by this fluid in the CNS. This condition also could be termed a hydrodynamic disorder of CSF.
Check out this medical presentation on Neurology, which is titled "Hydrocephalus", to know about Hydrocephalus.
INTRODUCTION: Hydrocephalus is the enlargement of the brain ventricular system due to an excess in the volume of cerebrospinal fluid (CSF). This excess of CSF maybe due to an overproduction or poor reabsorption, which results in raised intracranial pressure (ICP)1. Accumulation of CSF in the subarachnoid space is called external hydrocephalus. Multiple causes have been identified in literature ...
Introduction: Hydrocephalus is the accumulation of fluid in the cavities deep within the brain. The extra fluids cause the ventricles to expand, putting pressure on the brain. The brain and spinal ...
Sings and symptom pt case book base The term hydrocephalus is derived from the Greek words "hydro" meaning water and "cephalus" meaning head definition Physical signs • Abnormal enlargement of a toddler's head swelling of the optic disk within the eye's optic nerve • Sleepiness • Difficulty remaining awake or waking up • Poor coordination Behavioral and cognitive changes • Problems ...
Presentation Transcript. Hydrocephalus Definition-Hydrocephalus is a disorder in which the cerebral ventricular system contains an excessive amount of cerebrospinal fluid (CSF) and is dilated because of increased pressure PHYSIOLOGY CSF is produced - choroid plexus. circulates through the ventricular system & absorbed into the systemic ...
DISCUSSION OF THE DECEASE: Hydrocephalus also known as "water on the brain," is a medical condition in which there is an abnormal accumulation of cerebrospinal fluid (CSF) in the ventricles, or cavities, of the brain. This may cause increased intracranial pressure inside the skull and progressive enlargement of the head, convulsion, tunnel ...
Pediatric hydrocephalus (PH) results in significant clinical and psychosocial morbidity in pediatric population.The aims of the study are to evaluate clinical, surgical, and outcome perspective of PH patients of age <12 years.This is a retrospective ...