Call/Text/Whatsapp:
+1 (888-687-4420)
24/7/365 Available
- College Essay
- Argumentative Essay
- Expository Essay
- Narrative Essay
- Descriptive Essay
- Scholarship Essay
- Admission Essay
- Reflective Essay
- Nursing Essay
- Economics Essay
Assignments
- Term Papers
- Research Papers
- Case Studies
- Dissertation
- Presentation
- Editing Help
- Cheap Essay Writing
- How to Order
Persuasive Essay Guide
Persuasive Essay About Covid19

How to Write a Persuasive Essay About Covid19 | Examples & Tips
14 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
A Catalogue of 300 Best Persuasive Essay Topics for Students
Persuasive Essay Outline - A Complete Guide
30+ Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
How To Write A Persuasive Essay On Abortion
Learn to Write a Persuasive Essay About Business With 5 Best Examples
Check Out 14 Persuasive Essays About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About COVID-19
- 3. Examples of Persuasive Essay About COVID-19 Vaccine
- 4. Examples of Persuasive Essay About COVID-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
| "COVID-19 vaccination mandates are necessary for public health and safety." |
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
| The COVID-19 pandemic has presented an unprecedented global challenge, and in the face of this crisis, many countries have debated the implementation of vaccination mandates. This essay argues that such mandates are essential for safeguarding public health and preventing further devastation caused by the virus. |
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
| COVID-19, caused by the novel coronavirus SARS-CoV-2, emerged in late 2019 and quickly spread worldwide, leading to millions of infections and deaths. Vaccination has proven to be an effective tool in curbing the virus's spread and severity. |
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences , evidence, and analysis. Here's an example:
| One compelling reason for implementing COVID-19 vaccination mandates is the overwhelming evidence of vaccine effectiveness. According to a study published in the New England Journal of Medicine, the Pfizer-BioNTech and Moderna vaccines demonstrated an efficacy of over 90% in preventing symptomatic COVID-19 cases. This level of protection not only reduces the risk of infection but also minimizes the virus's impact on healthcare systems. |
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
| Some argue that vaccination mandates infringe on personal freedoms and autonomy. While individual freedom is a crucial aspect of democratic societies, public health measures have long been implemented to protect the collective well-being. Seatbelt laws, for example, are in place to save lives, even though they restrict personal choice. |
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
| In conclusion, COVID-19 vaccination mandates are a crucial step toward controlling the pandemic, protecting public health, and preventing further loss of life. The evidence overwhelmingly supports their effectiveness, and while concerns about personal freedoms are valid, they must be weighed against the greater good of society. It is our responsibility to take collective action to combat this global crisis and move toward a safer, healthier future. |
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About COVID-19
When writing a persuasive essay about the COVID-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
|
Here is another example explaining How COVID-19 has changed our lives essay:
The COVID-19 pandemic, which began in late 2019, has drastically altered the way we live. From work and education to social interactions and healthcare, every aspect of our daily routines has been impacted. Reflecting on these changes helps us understand their long-term implications.
COVID-19, caused by the novel coronavirus SARS-CoV-2, is an infectious disease first identified in December 2019 in Wuhan, China. It spreads through respiratory droplets and can range from mild symptoms like fever and cough to severe cases causing pneumonia and death. The rapid spread and severe health impacts have led to significant public health measures worldwide.
The pandemic shifted many to remote work and online education. While some enjoy the flexibility, others face challenges like limited access to technology and blurred boundaries between work and home.
Social distancing and lockdowns have led to increased isolation and mental health issues. However, the pandemic has also fostered community resilience, with people finding new ways to connect and support each other virtually.
Healthcare systems have faced significant challenges, leading to innovations in telemedicine and a focus on public health infrastructure. Heightened awareness of hygiene practices, like handwashing and mask-wearing, has helped reduce the spread of infectious diseases.
COVID-19 has caused severe economic repercussions, including business closures and job losses. While governments have implemented relief measures, the long-term effects are still uncertain. The pandemic has also accelerated trends like e-commerce and contactless payments.
The reduction in travel and industrial activities during lockdowns led to a temporary decrease in pollution and greenhouse gas emissions. This has sparked discussions about sustainable practices and the potential for a green recovery.
COVID-19 has reshaped our lives in numerous ways, affecting work, education, social interactions, healthcare, the economy, and the environment. As we adapt to this new normal, it is crucial to learn from these experiences and work towards a more resilient and equitable future. |
Let’s look at another sample essay:
The COVID-19 pandemic has been a transformative event, reshaping every aspect of our lives. In my opinion, while the pandemic has brought immense challenges, it has also offered valuable lessons and opportunities for growth. One of the most striking impacts has been on our healthcare systems. The pandemic exposed weaknesses and gaps, prompting a much-needed emphasis on public health infrastructure and the importance of preparedness. Innovations in telemedicine and vaccine development have been accelerated, showing the incredible potential of scientific collaboration. Socially, the pandemic has highlighted the importance of community and human connection. While lockdowns and social distancing measures increased feelings of isolation, they also fostered a sense of solidarity. People found creative ways to stay connected and support each other, from virtual gatherings to community aid initiatives. The shift to remote work and online education has been another significant change. This transition, though challenging, demonstrated the flexibility and adaptability of both individuals and organizations. It also underscored the importance of digital literacy and access to technology. Economically, the pandemic has caused widespread disruption. Many businesses closed, and millions lost their jobs. However, it also prompted a reevaluation of business models and work practices. The accelerated adoption of e-commerce and remote work could lead to more sustainable and efficient ways of operating in the future. In conclusion, the COVID-19 pandemic has been a profound and complex event. While it brought about considerable hardship, it also revealed the strength and resilience of individuals and communities. Moving forward, it is crucial to build on the lessons learned to create a more resilient and equitable world. |
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About COVID-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of COVID-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the COVID-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About COVID-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get an idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
- Choose a Specific Angle: Narrow your focus to a specific aspect of COVID-19, like vaccination or public health measures.
- Provide Credible Sources: Support your arguments with reliable sources like scientific studies and government reports.
- Use Persuasive Language: Employ ethos, pathos, and logos , and use vivid examples to make your points relatable.
- Organize Your Essay: Create a solid persuasive essay outline and ensure a logical flow, with each paragraph focusing on a single point.
- Emphasize Benefits: Highlight how your suggestions can improve public health, safety, or well-being.
- Use Visuals: Incorporate graphs, charts, and statistics to reinforce your arguments.
- Call to Action: End your essay conclusion with a strong call to action, encouraging readers to take a specific step.
- Revise and Edit: Proofread for grammar, spelling, and clarity, ensuring smooth writing flow.
- Seek Feedback: Have someone else review your essay for valuable insights and improvements.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You’ve explored great sample essays and picked up some useful tips. You now have the tools you need to write a persuasive essay about Covid-19. So don’t let doubts hold you back—start writing!
If you’re feeling stuck or need a bit of extra help, don’t worry! MyPerfectWords.com offers a professional persuasive essay writing service that can assist you. Our experienced essay writers are ready to help you craft a well-structured, insightful paper on Covid-19.
Just place your “ do my essay for me ” request today, and let us take care of the rest!
Frequently Asked Questions
What is a good title for a covid-19 essay.
A good title for a COVID-19 essay should be clear, engaging, and reflective of the essay's content. Examples include:
- "The Impact of COVID-19 on Global Health"
- "How COVID-19 Has Transformed Our Daily Lives"
- "COVID-19: Lessons Learned and Future Implications"
How do I write an informative essay about COVID-19?
To write an informative essay about COVID-19, follow these steps:
- Choose a specific focus: Select a particular aspect of COVID-19, such as its transmission, symptoms, or vaccines.
- Research thoroughly: Gather information from credible sources like scientific journals and official health organizations.
- Organize your content: Structure your essay with an introduction, body paragraphs, and a conclusion.
- Present facts clearly: Use clear, concise language to convey information accurately.
- Include visuals: Use charts or graphs to illustrate data and make your essay more engaging.
How do I write an expository essay about COVID-19?
To write an expository essay about COVID-19, follow these steps:
- Select a clear topic: Focus on a specific question or issue related to COVID-19.
- Conduct thorough research: Use reliable sources to gather information.
- Create an outline: Organize your essay with an introduction, body paragraphs, and a conclusion.
- Explain the topic: Use facts and examples to explain the chosen aspect of COVID-19 in detail.
- Maintain objectivity: Present information in a neutral and unbiased manner.
- Edit and revise: Proofread your essay for clarity, coherence, and accuracy.

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading

Persuasive Essay Writing
Persuasive Essay About Covid 19

Top Examples of Persuasive Essay about Covid-19
Published on: Jan 10, 2023
Last updated on: Jan 29, 2024

People also read
How to Write a Persuasive Essay: A Step-by-Step Guide
Easy and Unique Persuasive Essay Topics with Tips
The Basics of Crafting an Outstanding Persuasive Essay Outline
Ace Your Next Essay With These Persuasive Essay Examples!
Persuasive Essay About Gun Control - Best Examples for Students
Learn How To Write An Impressive Persuasive Essay About Business
Learn How to Craft a Compelling Persuasive Essay About Abortion With Examples!
Make Your Point: Tips and Examples for Writing a Persuasive Essay About Online Education
Learn How To Craft a Powerful Persuasive Essay About Bullying
Craft an Engaging Persuasive Essay About Smoking: Examples & Tips
Learn How to Write a Persuasive Essay About Social Media With Examples
Craft an Effective Argument: Examples of Persuasive Essay About Death Penalty
Share this article
In these recent years, covid-19 has emerged as a major global challenge. It has caused immense global economic, social, and health problems.
Writing a persuasive essay on COVID-19 can be tricky with all the information and misinformation.
But don't worry! We have compiled a list of persuasive essay examples during this pandemic to help you get started.
Here are some examples and tips to help you create an effective persuasive essay about this pandemic.
On This Page On This Page -->
Examples of Persuasive Essay About Covid-19
The coronavirus pandemic has everyone on edge. You can expect your teachers to give you an essay about covid-19. You might be overwhelmed about what to write in an essay.
Worry no more!
Here are a few examples to help get you started.
| The spread of covid-19 pandemic has greatly impacted how people work, with many companies and organizations adapting to remote working arrangements to stay afloat. While there may be certain benefits of remote working that have emerged due to the pandemic, it is undeniable that it also presents numerous challenges. One of the main positive impacts of the pandemic on remote working is greater flexibility. Many companies have implemented flexible hours, which allow employees to work at times that best suit their schedule. This has proven beneficial for employers and employees, reducing stress levels and improving productivity. It also allows people with limited access to transportation or childcare solutions to still participate in the workforce. On the other hand, the pandemic has also brought about several negative impacts for remote workers. Isolation is one of the biggest issues, as many people lack access to social contact daily, which can lead to feelings of loneliness and depression. Working from home can also be more difficult for those who do not have a quiet workspace. Additionally, many workers may not have access to the same resources as their office-based counterparts, such as ergonomic chairs and computers with high-speed internet connections. Overall, it can be said that while there are certain positives associated with remote working due to the pandemic, it also presents numerous negatives which cannot be ignored. Companies and organizations should strive to ensure that their remote workers are given the necessary tools, resources, and support to succeed in their roles from home. Additionally, employers should prioritize employee well-being by ensuring all employees have access to social contact, even if it is only virtually. If these measures are taken, remote working due to the pandemic can be seen more positively. In conclusion, while the COVID-19 pandemic has presented certain benefits of remote working, it is also important to recognize numerous challenges associated with this arrangement. Companies and organizations should take steps to ensure that their employees have all the necessary resources and support to be able to work from home effectively. |
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
Check out some more persuasive essay examples to get more inspiration and guidance.
Examples of Persuasive Essay About the Covid-19 Vaccine
With so much uncertainty surrounding the Covid-19 vaccine, it can be challenging for students to write a persuasive essay about getting vaccinated.
Here are a few examples of persuasive essays about vaccination against covid-19.
Check these out to learn more.
Persuasive essay on the covid-19 vaccine
Tough Essay Due? Hire a Writer!

Examples of Persuasive Essay About Covid-19 Integration
Writing a persuasive essay on Covid-19 integration doesn't have to be stressful or overwhelming.
With the right approach and preparation, you can write an essay that will get them top marks!
Here are a few samples of compelling persuasive essays. Give them a look and get inspiration for your next essay.
Integration of Covid-19 Persuasive essay
Integration of Covid-19 Persuasive essay sample
Examples of Argumentative Essay About Covid-19
Writing an argumentative essay can be a daunting task, especially when the topic is as broad as the novel coronavirus pandemic.
Read the following examples of how to make a compelling argument on covid-19.
Argumentative essay on Covid-19
Argumentative Essay On Covid-19
Examples of Persuasive Speeches About Covid-19
Writing a persuasive speech about anything can seem daunting. However, writing a persuasive speech about something as important as the Covid-19 pandemic doesnât have to be difficult.
So let's explore some examples of perfectly written persuasive essays.
Persuasive Speech About Covid-19 Example
Tips to Write a Persuasive Essay
Here are seven tips that can help you create a strong argument on the topic of covid-19.
Check out this informative video to learn more about effective tips and tricks for writing persuasive essays.
1. Start with an attention-grabbing hook:
Use a quote, statistic, or interesting fact related to your argument at the beginning of your essay to draw the reader in.
2. Make sure you have a clear thesis statement:
A thesis statement is one sentence that expresses the main idea of your essay. It should clearly state your stance on the topic and provide a strong foundation for the rest of your content.
3. Support each point with evidence:
To make an effective argument, you must back up each point with credible evidence from reputable sources. This will help build credibility and validate your claims throughout your paper.
4. Use emotional language and tone:
Emotional appeals are powerful tools to help make your argument more convincing. Use appropriate language for the audience and evokes emotion to draw them in and get them on board with your claims.
5. Anticipate counterarguments:
Use proper counterarguments to effectively address all point of views.
Acknowledge opposing viewpoints and address them directly by providing evidence or reasoning why they are wrong.
6. Stay focused:
Keep your main idea in mind throughout the essay, making sure all of your arguments support it. Donât stray off-topic or introduce unnecessary information that will distract from the purpose of your paper.
7. Conclude strongly:
Make sure you end on a strong note. Reemphasize your main points, restate your thesis statement, and challenge the reader to respond or take action in some way. This will leave a lasting impression in their minds and make them more likely to agree with you.
Writing an effective persuasive essay is a piece of cake with our guide and examples. Check them out to learn more!

Tough Essay Due? Hire Tough Writers!
We hope that you have found the inspiration to write your next persuasive essay about covid-19.
However, If you're overwhelmed by the task, don't worry - our professional essay writing service is here to help.
Our expert and experienced persuasive essay writer can help you write a persuasive essay on covid-19 that gets your readers' attention.
Our professional essay writer can provide you with all the resources and support you need to craft a well-written, well-researched essay. Our essay writing service offers top-notch quality and guaranteed results.
Frequently Asked Questions
How do you begin a persuasive essay.
To begin a persuasive essay, you must choose a topic you feel strongly about and formulate an argument or position. Start by researching your topic thoroughly and then formulating your thesis statement.
What are good topics for persuasive essays?
Good topics for persuasive essays include healthcare reform, gender issues, racial inequalities, animal rights, environmental protection, and political change. Other popular topics are social media addiction, internet censorship, gun control legislation, and education reform.
What impact does COVID-19 have on society?
The COVID-19 pandemic has had a major impact on society worldwide. It has changed the way we interact with one another. The pandemic has also caused economic disruption, forcing many businesses to close or downsize their operations.
Cathy A. (Literature, Education)
For more than five years now, Cathy has been one of our most hardworking authors on the platform. With a Masters degree in mass communication, she knows the ins and outs of professional writing. Clients often leave her glowing reviews for being an amazing writer who takes her work very seriously.
Paper Due? Why Suffer? That’s our Job!
Keep reading

Legal & Policies
- Privacy Policy
- Cookies Policy
- Terms of Use
- Refunds & Cancellations
- Our Writers
- Success Stories
- Our Guarantees
- Affiliate Program
- Referral Program
- AI Essay Writer
Disclaimer: All client orders are completed by our team of highly qualified human writers. The essays and papers provided by us are not to be used for submission but rather as learning models only.
Help inform the discussion
- X (Twitter)
Presidential Speeches
September 9, 2021: remarks on fighting the covid-19 pandemic, about this speech.
September 09, 2021
As the Delta variant of the Covid-19 virus spreads and cases and deaths increase in the United States, President Joe Biden announces new efforts to fight the pandemic. He outlines six broad areas of action--implementing new vaccination requirements, protecting the vaccinated with booster shots, keeping children safe and schools open, increasing testing and masking, protecting our economic recovery, and improving care of those who do get Covid-19.
- Download Full Video
- Download Audio
THE PRESIDENT: Good evening, my fellow Americans. I want to talk to you about where we are in the battle against COVID-19, the progress we’ve made, and the work we have left to do.
And it starts with understanding this: Even as the Delta variant 19 [sic] has—COVID-19—has been hitting this country hard, we have the tools to combat the virus, if we can come together as a country and use those tools.
If we raise our vaccination rate, protect ourselves and others with masking and expanded testing, and identify people who are infected, we can and we will turn the tide on COVID-19.
It will take a lot of hard work, and it’s going to take some time. Many of us are frustrated with the nearly 80 million Americans who are still not vaccinated, even though the vaccine is safe, effective, and free.
You might be confused about what is true and what is false about COVID-19. So before I outline the new steps to fight COVID-19 that I’m going to be announcing tonight, let me give you some clear information about where we stand.
First, we have cons—we have made considerable progress
in battling COVID-19. When I became President, about 2 million Americans were fully vaccinated. Today, over 175 million Americans have that protection.
Before I took office, we hadn’t ordered enough vaccine for every American. Just weeks in office, we did. The week before I took office, on January 20th of this year, over 25,000 Americans died that week from COVID-19. Last week, that grim weekly toll was down 70 percent.
And in the three months before I took office, our economy was faltering, creating just 50,000 jobs a month. We’re now averaging 700,000 new jobs a month in the past three months.
This progress is real. But while America is in much better shape than it was seven months ago when I took office, I need to tell you a second fact.
We’re in a tough stretch, and it could last for a while. The highly contagious Delta variant that I began to warn America about back in July spread in late summer like it did in other countries before us.
While the vaccines provide strong protections for the vaccinated, we read about, we hear about, and we see the stories of hospitalized people, people on their death beds, among the unvaccinated over these past few weeks.
This is a pandemic of the unvaccinated. And it’s caused by the fact that despite America having an unprecedented and successful vaccination program, despite the fact that for almost five months free vaccines have been available in 80,000 different locations, we still have nearly 80 million Americans who have failed to get the shot.
And to make matters worse, there are elected officials actively working to undermine the fight against COVID-19. Instead of encouraging people to get vaccinated and mask up, they’re ordering mobile morgues for the unvaccinated dying from COVID in their communities. This is totally unacceptable.
Third, if you wonder how all this adds up, here’s the math: The vast majority of Americans are doing the right thing. Nearly three quarters of the eligible have gotten at least one shot, but one quarter has not gotten any. That’s nearly 80 million Americans not vaccinated. And in a country as large as ours, that’s 25 percent minority. That 25 percent can cause a lot of damage—and they are.
The unvaccinated overcrowd our hospitals, are overrunning the emergency rooms and intensive care units, leaving no room for someone with a heart attack, or pancreitis [pancreatitis], or cancer.
And fourth, I want to emphasize that the vaccines provide very strong protection from severe illness from COVID-19. I know there’s a lot of confusion and misinformation. But the world’s leading scientists confirm that if you are fully vaccinated, your risk of severe illness from COVID-19 is very low.
In fact, based on available data from the summer, only one of out of every 160,000 fully vaccinated Americans was hospitalized for COVID per day.
These are the facts.
So here’s where we stand: The path ahead, even with the Delta variant, is not nearly as bad as last winter. But what makes it incredibly more frustrating is that we have the tools to combat COVID-19, and a distinct minority of Americans –supported by a distinct minority of elected officials—are keeping us from turning the corner. These pandemic politics, as I refer to, are making people sick, causing unvaccinated people to die.
We cannot allow these actions to stand in the way of protecting the large majority of Americans who have done their part and want to get back to life as normal.
As your President, I’m announcing tonight a new plan to require more Americans to be vaccinated, to combat those blocking public health.
My plan also increases testing, protects our economy, and will make our kids safer in schools. It consists of six broad areas of action and many specific measures in each that—and each of those actions that you can read more about at WhiteHouse.gov. WhiteHouse.gov.
The measures—these are going to take time to have full impact. But if we implement them, I believe and the scientists indicate, that in the months ahead we can reduce the number of unvaccinated Americans, decrease hospitalizations and deaths, and allow our children to go to school safely and keep our economy strong by keeping businesses open.
First, we must increase vaccinations among the unvaccinated with new vaccination requirements. Of the nearly 80 million eligible Americans who have not gotten vaccinated, many said they were waiting for approval from the Food and Drug Administration—the FDA. Well, last month, the FDA granted that approval.
So, the time for waiting is over. This summer, we made progress through the combination of vaccine requirements and incentives, as well as the FDA approval. Four million more people got their first shot in August than they did in July.
But we need to do more. This is not about freedom or personal choice. It’s about protecting yourself and those around you—the people you work with, the people you care about, the people you love.
My job as President is to protect all Americans.
So, tonight, I’m announcing that the Department of Labor is developing an emergency rule to require all employers with 100 or more employees, that together employ over 80 million workers, to ensure their workforces are fully vaccinated or show a negative test at least once a week.
Some of the biggest companies are already requiring this: United Airlines, Disney, Tysons Food, and even Fox News.
The bottom line: We’re going to protect vaccinated workers from unvaccinated co-workers. We’re going to reduce the spread of COVID-19 by increasing the share of the workforce that is vaccinated in businesses all across America.
My plan will extend the vaccination requirements that I previously issued in the healthcare field. Already, I’ve announced, we’ll be requiring vaccinations that all nursing home workers who treat patients on Medicare and Medicaid, because I have that federal authority.
Tonight, I’m using that same authority to expand that to cover those who work in hospitals, home healthcare facilities, or other medical facilities–a total of 17 million healthcare workers.
If you’re seeking care at a health facility, you should be able to know that the people treating you are vaccinated. Simple. Straightforward. Period.
Next, I will sign an executive order that will now require all executive branch federal employees to be vaccinated—all. And I’ve signed another executive order that will require federal contractors to do the same.
If you want to work with the federal government and do business with us, get vaccinated. If you want to do business with the federal government, vaccinate your workforce.
And tonight, I’m removing one of the last remaining obstacles that make it difficult for you to get vaccinated.
The Department of Labor will require employers with 100 or more workers to give those workers paid time off to get vaccinated. No one should lose pay in order to get vaccinated or take a loved one to get vaccinated.
Today, in total, the vaccine requirements in my plan will affect about 100 million Americans—two thirds of all workers.
And for other sectors, I issue this appeal: To those of you running large entertainment venues—from sports arenas to concert venues to movie theaters—please require folks to get vaccinated or show a negative test as a condition of entry.
And to the nation’s family physicians, pediatricians, GPs—general practitioners—you’re the most trusted medical voice to your patients. You may be the one person who can get someone to change their mind about being vaccinated.
Tonight, I’m asking each of you to reach out to your unvaccinated patients over the next two weeks and make a personal appeal to them to get the shot. America needs your personal involvement in this critical effort.
And my message to unvaccinated Americans is this: What more is there to wait for? What more do you need to see? We’ve made vaccinations free, safe, and convenient.
The vaccine has FDA approval. Over 200 million Americans have gotten at least one shot.
We’ve been patient, but our patience is wearing thin. And your refusal has cost all of us. So, please, do the right thing. But just don’t take it from me; listen to the voices of unvaccinated Americans who are lying in hospital beds, taking their final breaths, saying, “If only I had gotten vaccinated.” “If only.”
It’s a tragedy. Please don’t let it become yours.
The second piece of my plan is continuing to protect the vaccinated.
For the vast majority of you who have gotten vaccinated, I understand your anger at those who haven’t gotten vaccinated. I understand the anxiety about getting a “breakthrough” case.
But as the science makes clear, if you’re fully vaccinated, you’re highly protected from severe illness, even if you get COVID-19.
In fact, recent data indicates there is only one confirmed positive case per 5,000 fully vaccinated Americans per day.
You’re as safe as possible, and we’re doing everything we can to keep it that way—keep it that way, keep you safe.
That’s where boosters come in—the shots that give you even more protection than after your second shot.
Now, I know there’s been some confusion about boosters. So, let me be clear: Last month, our top government doctors announced an initial plan for booster shots for vaccinated Americans. They believe that a booster is likely to provide the highest level of protection yet.
Of course, the decision of which booster shots to give, when to start them, and who will give them, will be left completely to the scientists at the FDA and the Centers for Disease Control.
But while we wait, we’ve done our part. We’ve bought enough boosters—enough booster shots—and the distribution system is ready to administer them.
As soon as they are authorized, those eligible will be able to get a booster right away in tens of thousands of site across the—sites across the country for most Americans, at your nearby drug store, and for free.
The third piece of my plan is keeping—and maybe the most important—is keeping our children safe and our schools open. For any parent, it doesn’t matter how low the risk of any illness or accident is when it comes to your child or grandchild. Trust me, I know.
So, let me speak to you directly. Let me speak to you directly to help ease some of your worries.
It comes down to two separate categories: children ages 12 and older who are eligible for a vaccine now, and children ages 11 and under who are not are yet eligible.
The safest thing for your child 12 and older is to get them vaccinated. They get vaccinated for a lot of things. That’s it. Get them vaccinated.
As with adults, almost all the serious COVID-19 cases we’re seeing among adolescents are in unvaccinated 12- to 17-year-olds—an age group that lags behind in vaccination rates.
So, parents, please get your teenager vaccinated.
What about children under the age of 12 who can’t get vaccinated yet? Well, the best way for a parent to protect their child under the age of 12 starts at home. Every parent, every teen sibling, every caregiver around them should be vaccinated.
Children have four times higher chance of getting hospitalized if they live in a state with low vaccination rates rather than the states with high vaccination rates.
Now, if you’re a parent of a young child, you’re wondering when will it be—when will it be—the vaccine available for them. I strongly support an independent scientific review for vaccine uses for children under 12. We can’t take shortcuts with that scientific work.
But I’ve made it clear I will do everything within my power to support the FDA with any resource it needs to continue to do this as safely and as quickly as possible, and our nation’s top doctors are committed to keeping the public at large updated on the process so parents can plan.
Now to the schools. We know that if schools follow the science and implement the safety measures—like testing, masking, adequate ventilation systems that we provided the money for, social distancing, and vaccinations—then children can be safe from COVID-19 in schools.
Today, about 90 percent of school staff and teachers are vaccinated. We should get that to 100 percent. My administration has already acquired teachers at the schools run by the Defense Department—because I have the authority as President in the federal system—the Defense Department and the Interior Department—to get vaccinated. That’s authority I possess.
Tonight, I’m announcing that we’ll require all of nearly 300,000 educators in the federal paid program, Head Start program, must be vaccinated as well to protect your youngest—our youngest—most precious Americans and give parents the comfort.
And tonight, I’m calling on all governors to require vaccination for all teachers and staff. Some already have done so, but we need more to step up.
Vaccination requirements in schools are nothing new. They work. They’re overwhelmingly supported by educators and their unions. And to all school officials trying to do the right thing by our children: I’ll always be on your side.
Let me be blunt. My plan also takes on elected officials and states that are undermining you and these lifesaving actions. Right now, local school officials are trying to keep children safe in a pandemic while their governor picks a fight with them and even threatens their salaries or their jobs. Talk about bullying in schools. If they’ll not help—if these governors won’t help us beat the pandemic, I’ll use my power as President to get them out of the way.
The Department of Education has already begun to take legal action against states undermining protection that local school officials have ordered. Any teacher or school official whose pay is withheld for doing the right thing, we will have that pay restored by the federal government 100 percent. I promise you I will have your back.
The fourth piece of my plan is increasing testing and masking. From the start, America has failed to do enough COVID-19 testing. In order to better detect and control the Delta variant, I’m taking steps tonight to make testing more available, more affordable, and more convenient. I’ll use the Defense Production Act to increase production of rapid tests, including those that you can use at home.
While that production is ramping up, my administration has worked with top retailers, like Walmart, Amazon, and Kroger’s, and tonight we’re announcing that, no later than next week, each of these outlets will start to sell at-home rapid test kits at cost for the next three months. This is an immediate price reduction for at-home test kits for up to 35 percent reduction.
We’ll also expand—expand free testing at 10,000 pharmacies around the country. And we’ll commit—we’re committing $2 billion to purchase nearly 300 million rapid tests for distribution to community health centers, food banks, schools, so that every American, no matter their income, can access free and convenient tests. This is important to everyone, particularly for a parent or a child—with a child not old enough to be vaccinated. You’ll be able to test them at home and test those around them.
In addition to testing, we know masking helps stop the spread of COVID-19. That’s why when I came into office, I required masks for all federal buildings and on federal lands, on airlines, and other modes of transportation.
Today—tonight, I’m announcing that the Transportation Safety Administration—the TSA—will double the fines on travelers that refuse to mask. If you break the rules, be prepared to pay.
And, by the way, show some respect. The anger you see on television toward flight attendants and others doing their job is wrong; it’s ugly.
The fifth piece of my plan is protecting our economic recovery. Because of our vaccination program and the American Rescue Plan, which we passed early in my administration, we’ve had record job creation for a new administration, economic growth unmatched in 40 years. We cannot let unvaccinated do this progress—undo it, turn it back.
So tonight, I’m announcing additional steps to strengthen our economic recovery. We’ll be expanding COVID-19 Economic Injury Disaster Loan programs. That’s a program that’s going to allow small businesses to borrow up to $2 million from the current $500,000 to keep going if COVID-19 impacts on their sales.
These low-interest, long-term loans require no repayment for two years and be can used to hire and retain workers, purchase inventory, or even pay down higher cost debt racked up since the pandemic began. I’ll also be taking additional steps to help small businesses stay afloat during the pandemic.
Sixth, we’re going to continue to improve the care of those who do get COVID-19. In early July, I announced the deployment of surge response teams. These are teams comprised of experts from the Department of Health and Human Services, the CDC, the Defense Department, and the Federal Emergency Management Agency—FEMA—to areas in the country that need help to stem the spread of COVID-19.
Since then, the federal government has deployed nearly 1,000 staff, including doctors, nurses, paramedics, into 18 states. Today, I’m announcing that the Defense Department will double the number of military health teams that they’ll deploy to help their fellow Americans in hospitals around the country.
Additionally, we’re increasing the availability of new medicines recommended by real doctors, not conspir-—conspiracy theorists. The monoclonal antibody treatments have been shown to reduce the risk of hospitalization by up to 70 percent for unvaccinated people at risk of developing sefe-—severe disease.
We’ve already distributed 1.4 million courses of these treatments to save lives and reduce the strain on hospitals. Tonight, I’m announcing we will increase the average pace of shipment across the country of free monoclonal antibody treatments by another 50 percent.
Before I close, let me say this: Communities of color are disproportionately impacted by this virus. And as we continue to battle COVID-19, we will ensure that equity continues to be at the center of our response. We’ll ensure that everyone is reached. My first responsibility as President is to protect the American people and make sure we have enough vaccine for every American, including enough boosters for every American who’s approved to get one.
We also know this virus transcends borders. That’s why, even as we execute this plan at home, we need to continue fighting the virus overseas, continue to be the arsenal of vaccines.
We’re proud to have donated nearly 140 million vaccines over 90 countries, more than all other countries combined, including Europe, China, and Russia combined. That’s American leadership on a global stage, and that’s just the beginning.
We’ve also now started to ship another 500 million COVID vaccines—Pfizer vaccines—purchased to donate to 100 lower-income countries in need of vaccines. And I’ll be announcing additional steps to help the rest of the world later this month.
As I recently released the key parts of my pandemic preparedness plan so that America isn’t caught flat-footed when a new pandemic comes again—as it will—next month, I’m also going to release the plan in greater detail.
So let me close with this: We have so-—we’ve made so much progress during the past seven months of this pandemic. The recent increases in vaccinations in August already are having an impact in some states where case counts are dropping in recent days. Even so, we remain at a critical moment, a critical time. We have the tools. Now we just have to finish the job with truth, with science, with confidence, and together as one nation.
Look, we’re the United States of America. There’s nothing—not a single thing—we’re unable to do if we do it together. So let’s stay together.
God bless you all and all those who continue to serve on the frontlines of this pandemic. And may God protect our troops.
Get vaccinated.
More Joe Biden speeches
- Login / Sign Up
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
- Recommendations
Most Popular
- Sign up for Vox’s daily newsletter
- 7 questions — and zero conspiracy theories — about the allegations against Sean “Diddy” Combs
- The ugly reality behind Tim Walz’s farm-friendly image
- One chart shows how Hurricane Helene turned into a monstrous storm
- Take a mental break with the newest Vox crossword
Today, Explained
Understand the world with a daily explainer plus the most compelling stories of the day.
This is the title for the native ad
More in Culture

The aesthetic of Cybertrucks, energy drinks, and MMA, explained.

Everything we know about the growing case against the music mogul.

In defense of the supremely useful and unfairly maligned word.

The toxic stans aren’t the problem, it’s fan culture itself.

Kids love to eat them. Parents love to fight about them.

In the deeply-felt Intermezzo, the celebrity novelist plays chess with God.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 26 October 2022
Mastering the art of persuasion during a pandemic
- Elizabeth Svoboda 0
Elizabeth Svoboda is a science writer in San Jose, California.
You can also search for this author in PubMed Google Scholar
Credit: Sam Falconer
When Robb Willer looks back on the early days of the COVID-19 pandemic — when leaders still had a chance to stop the virus from bringing the world to a halt — there’s a fateful moment that stands out. In February 2020, global health authorities spoke in one voice, advising the public not to wear masks to prevent infection.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 610 , S34-S36 (2022)
doi: https://doi.org/10.1038/d41586-022-03354-8
This article is part of Nature Outlook: Pandemic preparedness , an editorially independent supplement produced with the financial support of third parties. About this content .
Cure, L. & Van Enk, R. Am. J. Infect. Control 43 , 917–921 (2015).
Article PubMed Google Scholar
Milkman, K. L. et al. Proc. Natl Acad. Sci. USA 118 , e2101165118 (2021).
Law, A. C. et al. JAMA Intern Med. 182 , 235–237 (2022).
Brewer, N. T. et al. Lancet Reg. Health Am. 8 , 100205 (2022).
PubMed Google Scholar
Milkman, K. L. et al. Nature Hum. Behav . https://doi.org/10.1038/s41562-022-01437-0 (2022).
Article Google Scholar
Pfattheicher, S. et al. Psychol Sci. 31 , 1363–1373 (2020).
Galasso, V. et al. NBER Working Paper 29741 https://doi.org/10.3386/w29741 (2022).
Basol, M., Roozenbeek, J. & van der Linden, S. J. Cogn. 3 , 2 (2020).
Larsen, B. et al. NBER Working Paper 29896 https://doi.org/10.3386/w29896 (2022).
Barari, S. et al. Preprint at medRxiv https://doi.org/10.1101/2020.03.27.20042820 (2020).
Krpan, D. et al. Behav. Public Policy. 5 , 153–179 (2021).
COVID-19 National Preparedness Collaborators Lancet 399 , 1489–1512 (2022).
Download references
Related Articles

Sponsor feature: Enabling rapid responses to infectious diseases
Sponsor feature: How to build an mRNA arsenal for pandemic prevention
- Public health
- Human behaviour

COVID pandemic started in Wuhan market animals after all, suggests latest study
News 20 SEP 24

Tackling the reality of noma
Outlook 19 SEP 24
Is bird flu spreading among people? Data gaps leave researchers in the dark
News 19 SEP 24

UK university departments on the brink as higher-education funding crisis deepens
Career Feature 25 SEP 24

Universities are not just businesses, but an investment in future generations
Editorial 25 SEP 24
More measures needed to ease funding competition in China
Correspondence 24 SEP 24

How ‘green’ electricity from wood harms the planet — and people
News Feature 20 AUG 24

The science of protests: how to shape public opinion and swing votes
News Feature 26 JUN 24

‘It can feel like there’s no way out’ — political scientists face pushback on their work
News Feature 19 JUN 24
The recruitment for Earth Science High-talent in IDSSE, CAS
Seeking global talents in the field of Earth Science and Ocean Engineering.
Sanya, Hainan, China
Institute of Deep-sea Science and Engineering, Chinese Academy of Sciences
Locum Chief Editor, Nature Structural & Molecular Biology
Job Title: Locum Chief Editor, Nature Structural & Molecular Biology Location: New York or Milan Closing date: Friday, October 18th This job is of...
New York City, New York (US)
Springer Nature Ltd
Postdoc Fellow in Cardiology
Looking for postdoctoral fellow to study immunometabolic derangements associated with heart failure sterile inflammation.
University of Washington, Seattle
University of Washington - Cardiology
Faculty(Group Leaders or Principal Investigators) and Postdoc positions
Faculty and Postdoc positions are open all year.
Hangzhou, Zhejiang, China
The Stomatology Hospital, School of Stomatology, Zhejiang University School of Medicine(ZJUSS)
Tenure-track Assistant Professor in Modelling Plant Stress Responses
Become a tenure-track Assistant Professor focusing on modelling plant stress responses at Umeå Plant Science Centre and IceLab, Umeå University!
Umeå (Stad), Västerbotten (SE)
Umeå University (KBC)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
The Science of Persuasion Offers Lessons for COVID-19 Prevention
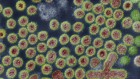
Hand washing, mask wearing, social distancing—experts agree these protective behaviors are key to stemming coronavirus disease 2019 (COVID-19). But how should leaders encourage their uptake?
Look to the science of persuasion, says communications professor Dominique Brossard, PhD. Brossard is part of a new National Academies of Science, Engineering, and Medicine group called the Societal Experts Action Network, or SEAN, whose recent report lays out research-based strategies to encourage COVID-19–mitigating behaviors.
Brossard says the changes must feel easy to do—and to repeat, which helps to form habits. Past public health campaigns also suggest it’s wise to know and understand one’s target audience, and to tailor messages and messengers accordingly.
“It’s difficult to change people’s behavior at the massive level,” Brossard, chair of the life sciences communications department at the University of Wisconsin-Madison, said in a recent interview with JAMA. The following is an edited version of that conversation.
JAMA: You and your coauthors write that simply explaining the science of COVID-19 and its risks will rarely translate to a change in attitudes and behaviors, even if people understand and accept the facts. Why isn’t it enough to explain the science if you want to change health behaviors?
Dr Brossard: Because human beings rely more on the psychological dimensions of the risk than the quantitative aspect of the risk. If experts measure risk in numbers, such as the probability of getting harmed by something, human beings in general—you and me included—look at what we call the qualitative aspect of that risk: the potential magnitude of the effect, the potential dread, how much it may impact people [close] to us, and so on. So, psychological dimensions.
JAMA: How does that translate to people’s unwillingness to change their attitudes and behaviors?
Dr Brossard: If we’re asked to do something new, that will impact our willingness to do it for a variety of reasons. It might be because people around us, our social network, the norms around us tell us that this is something that’s not acceptable. It might be because it’s a little inconvenient. It might be because we forget about it. At the end of the day, when we perform certain behaviors, rarely do we think about the science that tells us why we shouldn’t do it and why this might be dangerous. We do it because, as social animals, we pay attention to cues that our minds tell us to pay attention to and our community and people around us tell us to pay attention to. Therefore, our behavior is really based on the psychological components rather than more quantifiable aspects.
JAMA: Your report recommends 5 habit-promoting strategies: make the behavior easy to start and repeat; make the behavior rewarding to repeat; tie the behavior to an existing habit; alert people to behaviors that conflict with existing habits and provide alternative behaviors; and provide specific descriptions of desired behaviors. How can these strategies be applied today?
Dr Brossard: People are more likely to act in healthy ways when it’s easy for them to perform that behavior. So let’s think in terms of hand washing, for example. It will be very important to have hand washing stations and hand sanitizer easily accessible to people. Making the behavior very easy to start and to repeat is very important. If you put a mask next to your front door, and it’s easy to grab when you go out the door, that’s going to be easy to implement and you may be more likely to actually do it again. If you want to encourage people to physically distance from other people around them, having signs on the floor is actually something that works. They don’t have to calculate in their mind: what does it mean to be physically distanced? How far am I from other people? They simply stand where the mark tells them. It makes the behavior easy to repeat and easy to perform.
JAMA: So you’re trying to take away any barriers to the behaviors?
Dr Brossard: Exactly. The idea is if you take away as many barriers as possible, you encourage people to repeat the behavior. And then you end up creating a habit.
JAMA: In your report you mentioned that having many hand sanitizer stations sets the norm—that it’s normal to hand sanitize.
Dr Brossard: Mask wearing and physically distancing are new habits we’re creating from scratch. As social animals, that’s not something we do, in general. However, hand washing is a habit that we would have hoped the population already had. The problem is it hasn’t been really implemented. People do it very inconsistently. If you have hand sanitizers everywhere, it’s very easy. As a matter of fact, in supermarkets, when you have the hand sanitizer at the door, people line up and do it. So it’s that idea of the social norm and making it sound like, this is something you do, it’s widely available, other people do it as well, and therefore, this is socially acceptable and highly encouraged, and we should just all do it.
JAMA: The report also discusses 10 strategies for communicating risk, like using clear, consistent, and transparent messaging. It feels like that’s the opposite of what we’ve had. What’s your take on the federal government’s messaging around COVID-19 mitigation?
Dr Brossard: I think that in this case what’s really crucial is the messaging at the local level. At the state level vs county level vs town level, having a consistent strategy, consistent messages, is very important. It’s clear that for public health–related issues, really what makes a difference is the action of local leaders. It’s really the community-based action that can change people’s behavior. At the local level people trust the doctors, the public health officials.
JAMA: Masks unfortunately have become politicized. Is it too late for universal masking to be accepted or do you think minds can still be changed?
Dr Brossard: You will always have extremes on both ends. The vast majority of the population will be somewhere in between. People that are extremely set on the attitude not to wear a mask, which is, by the way, a very, very small minority, are unlikely to change their views. However, all the others can change their views. People are reasonable in the sense that they want to protect their own, they want to protect the community, they want to have the economy reopen, and so on. So I would say, yes, there’s still hope. And we see it. Every week, our group at the SEAN Network publishes a summary of all the polls that address [COVID-19–related] behaviors. We see that mask wearing is increasing. It’s not yet at the level that we would like to make sure that we are protected, but it’s indeed increasing.
JAMA: You reported that highlighting crowded beaches or people who aren’t wearing masks can be counterproductive. Why? And what’s a better approach?
Dr Brossard: They end up thinking that it’s a more prevalent behavior than it actually is. Or it may actually prompt them to think, “Oh, I wish I was on the beach.” You want to highlight good behavior and make it sound like this is socially acceptable rather than highlighting undesirable behavior and making it sound like it’s more frequent than it actually is.
JAMA: So local leaders should emphasize that mask wearing is increasing, for example?
Dr Brossard: Exactly. The research on social norms is extremely, extremely important here. We tend to get cues based on the people around us. Human beings have something that we call fear of isolation. We don’t like to be the lonely person that is the only one doing a certain thing when the vast majority around us are doing another thing. So it’s very important to actually show, “Look, this is going in this direction. Political leaders from both sides of the spectrum are doing it.” To show that the desirable behavior is something that’s becoming prevalent and that this is the direction society is taking.
JAMA: One lesson in your report is that it’s important to concede uncertainty. Why should leaders say things like, “Based on what we know today…”?
Dr Brossard: This is a really key message of risk communication. If you highlight something as being certain and then the science changes and suddenly you say, “Well, wait a minute, actually this was wrong, and now it is this,” you destroy trust. Science evolves, particularly in the context of COVID-19. We are all discovering this virus. The social sciences have shown that acknowledging uncertainty will actually increase trust, much more than painting things as certain. So it’s very important to say, “Based on the science of today, this is what we should do.” It’s very important to show that it’s a work in progress.
JAMA: What about the messengers themselves? Have we tapped into social media influencers enough? And who are community influencers that have the power to change our collective behaviors?
Dr Brossard: It makes us think of the AIDS community, where the leaders of the communities were messengers in helping promote protective behaviors. Using messengers that are trusted by the target audiences and relying on social media is extremely important. And as far as influencers in the communities, this will depend from one community to the other. Let’s take Wisconsin, for example. Football is a sport that people enjoy regardless of their political ideology, age, and so on. So the [Green Bay] Packers are messengers that transcend potential barriers there. It’s important to find trusted messengers that can connect with the audience on social media but also face-to-face. That can be a trusted local business leader, for example.
JAMA: What have we learned from past public health campaigns, like antismoking and wearing seatbelts, that can be applied now?
Dr Brossard: In the ’70s, we had social marketing approaches that suggested that we needed to stop trying to educate people and actually adapt a marketing technique to social issues. The antismoking Truth campaign, as it was called, was a successful application of social marketing techniques. The idea that you need to segment your audience and tailor the message specifically to that audience is something that the Truth campaign very well illustrated. A specific audience that needed to be targeted was adolescents and teenagers, and one thing that adolescents do is rebel against authority. They don’t like people to force them to do things. So the Truth campaign tried to appeal to their drive for autonomy by showing them that the tobacco industry was taking advantage of the adolescent population. That was extremely powerful. The problem is that a mass media campaign like that can be extremely, extremely expensive. That’s why it’s very important also to rely on what we think of as organic dissemination of messaging through social media, which we couldn’t do when the Truth campaign was put together.
JAMA: How can physicians apply these strategies of persuasion with patients, in their communities, or on social networks?
Dr Brossard: We are all tempted to correct misinformation. And right now, we see it everywhere, right? However, we need to be careful because by repeating the misinformation itself, we make it more prevalent. When physicians want to communicate about COVID-19, it’s better to actually communicate the right information without repeating the misinformation itself. I think it’s very important to remember that all of us are part of the solution by making sure that those right behaviors get communicated to as many people as we can. I think physicians have a really, really big part to play in this organic dissemination.
JAMA: How will these strategies apply once we have a COVID-19 vaccine?
Dr Brossard: It goes back to that idea of targeting and audience segmentation to understand who has issues with the vaccine—in this case potentially COVID-19—and why. We actually do not know why people think the way they do. What we do know is that there’s no wrong concern. If people are concerned, they’re concerned. We need to listen and try to understand why and then address that.
See More About
Abbasi J. The Science of Persuasion Offers Lessons for COVID-19 Prevention. JAMA. 2020;324(13):1271–1272. doi:10.1001/jama.2020.15139
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

COVID-19 public health messages have been all over the place – but researchers know how to do better
Assistant Professor of Life Sciences Communication, University of Wisconsin-Madison
Professor and Chair of Life Sciences Communication, University of Wisconsin-Madison
Postdoctoral Fellow in Life Sciences Communication, University of Wisconsin-Madison
Disclosure statement
Nothing to disclose.
Dominique Brossard and Todd Newman do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
University of Wisconsin–Madison provides funding as a member of The Conversation US.
View all partners
Persuading people to get a COVID-19 vaccine remains a challenge even as more than a 120 million people in the U.S. have received at least one dose.
Public health officials have struggled to find persuasive and accessible approaches throughout the pandemic, from explaining where COVID-19 originated to how the virus spreads among individuals , along with steps to prevent its transmission, its inequitable impacts on people’s lives, and now relevant risks and benefits information about vaccines.
COVID-19 is not just a medical issue. It is also a social justice, economic and political issue. That makes it hard to figure out how best to share information about it, especially since messages come from a range of communicators – including elected officials, journalists, scientists, physicians and community leaders – and are delivered to diverse audiences.
And the science itself has been uncertain and evolving. New information can change what’s known almost daily , making clear, accurate communication a “ moving target .”
As researchers focused on the science of science communication , we can suggest several communication strategies , based on a July 2020 report from the National Academies for Science, Engineering and Medicine, that encourage protective behaviors related to COVID-19.
Clear and open, even about uncertainty
Decades of research in risk communication show that people’s perception of their own risk is key to motivating them to take preventive measures. For that to work, public health messages must be clear, consistent and transparent.
One way to ensure that, especially for issues that have high uncertainty, like the pandemic, is for science and health messages to include context that connects the news to people’s concerns and prior experiences. What does risk or uncertainty about how the virus is transferred mean for the audience? How can they act on that information in their own lives? The “so what” of the message has to feel relevant. One approach, for example, is to emphasize how adoption of preventive behaviors – such as mask-wearing and hand-washing – leads to local businesses reopening and faster economic recovery.
Ensuring consistency in messaging, even for a rapidly changing issue, also means considering context – the bigger-picture processes shaping the issue. In other words, where do both the information and the uncertainty come from? What do scientists, policymakers and health care workers know or not know at this point? Then, most crucially, what are people doing to address that uncertainty and what can audiences still do to act in the face of it?

Tap into a crowd mentality
At various points during the pandemic, public health officials needed to persuade people to change aspects of their daily lives. To do this effectively, it helps to remember that people change their behavior and beliefs to better match what they perceive other people are doing – especially those they most identify with. It’s human nature to want to go along with social norms .
Health messages should avoid putting a spotlight on “bad” behaviors, since that can actually exacerbate the problem . Disproportionate attention paid to vaccine hesitancy or people refusing to wear masks, for example, gives the impression that these behaviors are more common than they actually are. Rather, attention to “good” behaviors, such as small business successfully implementing social distancing practices, can be more effective.

But even well-intended efforts to promote social norms, such as vaccination selfies, may provoke significant backlash , including jealousy, anger and feelings of injustice.
One way to avoid unintended backlash is to consider, before sharing, who is likely to see this message beyond the intended audiences. Are those who might see the message able to act on this information? If people can’t sign up for their own vaccination yet, a photo of a happy newly vaccinated person may make them feel angry and trigger negative feelings about systemic unfairness and resentment toward those who do have access.
Balancing the good news with the bad
The fear of a threat can motivate action . But a fear-based message often leads to people feeling helpless unless it’s paired with clear actions they can take to mitigate the threat.
Alternatively, hope is a powerful motivator , much more so and more consistently than fear or anger in many cases. Fortunately, for science communication in particular, surveys find that the majority of Americans remain hopeful about the promise of science to improve people’s lives.
Communicating hope can happen implicitly, through highlighting what does work and the benefits of actions. For example, clients following mask-wearing policies permitted many small businesses like hair salons to remain safely open.
What tends to be more common, especially in news coverage, is an emphasis on the negative – both in the current situation and in hypothetical futures and risks that could come if people don’t change course. You can see this focus in the coverage of gatherings that violate health regulations, like crowded beaches during spring break.
The weight of constant bad news reduces how equipped individuals feel to deal with a problem or avoid a risk . And this negative tendency can paint an unrealistic picture of an issue that has both wins and losses to report.
Without a fuller picture of the good news – what does work and what people are doing right – it becomes very difficult to envision how the world could look any different, or what anyone can do to move forward to a better place.
[ Understand new developments in science, health and technology, each week. Subscribe to The Conversation’s science newsletter .]
- Science communication
- Public health campaigns
- Social norms
- Coronavirus
- Science journalism
- Risk perception
- Health messages
- Science of science communication

Economics Editor

Deputy Vice-Chancellor (Indigenous Strategy and Services)

Director and Chief of Staff, Indigenous Portfolio

Chief People & Culture Officer
Lecturer / senior lecturer in construction and project management.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Examining persuasive message type to encourage staying at home during the COVID-19 pandemic and social lockdown: A randomized controlled study in Japan
- • We examined persuasive message types in terms of a narrator encouraging self-restraint.
- • Messages from a governor, an expert, a physician, a patient, and a resident were compared.
- • The message from a physician increased intention to stay at home the most.
- • The physician’s message conveyed the crisis of collapse of the medical system.
Behavioral change is the only prevention against the COVID-19 pandemic until vaccines become available. This is the first study to examine the most persuasive message type in terms of narrator difference in encouraging people to stay at home during the COVID-19 pandemic and social lockdown.
Participants (n = 1,980) were randomly assigned to five intervention messages (from a governor, a public health expert, a physician, a patient, and a resident of an outbreak area) and a control message. Intention to stay at home before and after reading messages was assessed. A one-way ANOVA with Tukey’s or Games–Howell test was conducted.
Compared with other messages, the message from a physician significantly increased participants’ intention to stay at home in areas with high numbers of people infected (versus a governor, p = .002; an expert, p = .023; a resident, p = .004).
The message from a physician―which conveyed the crisis of overwhelmed hospitals and consequent risk of people being unable to receive treatment―increased the intent to stay at home the most.
Practice implications
Health professionals and media operatives may be able to encourage people to stay at home by disseminating the physicians’ messages through media and the internet.
1. Introduction
The outbreak of the coronavirus disease 2019 (COVID-19) has emerged as the largest global pandemic ever experienced [ 1 ]. Experts have proposed that social lockdown will lead to improvements such as controlling the increase in the number of infected individuals and preventing a huge burden on the healthcare system [ [2] , [3] , [4] ]. Governments of many countries across the world have declared local and national social lockdown [ 4 , 5 ]. In April 2020, the Japanese government declared a state of emergency, which allows prefectural governors to request residents to refrain from unnecessary and nonurgent outings from home [ 6 ]. However, despite such governor declarations, people in various countries have resisted and disregarded calls to stay at home [ [7] , [8] , [9] ]. Because social lockdown is the only existing weapon for prevention of the pandemic until vaccines becomes available to treat COVID-19, behavioral change in individuals regarding staying at home is crucial [ 3 , 4 ]. Many news articles about COVID-19 are published daily by the mass media and over the internet. Such articles convey messages from governors, public health experts, physicians, COVID-19 patients, and residents of outbreak areas, encouraging people to stay at home. This is the first study to examine which narrator’s message is most persuasive in encouraging people to do so during the COVID-19 pandemic and social lockdown.
2.1. Participants and design
Participants were recruited from people registered in a survey company database in Japan. The eligibility criterion was men and women aged 18–69 years. Exclusion criteria were individuals who answered screening questions by stating: that they cannot go out because of illness or disability; that they have been diagnosed with a mental illness; or/and that they or their family members have been infected with COVID-19. A total of 1,980 participants completed the survey from May 9–11, 2020, when the state of emergency covered all prefectures in Japan. Participants were included according to the population composition ratio in Japan nationwide by gender, age, and residential area. Participants were randomly assigned either to a group that received an intervention message (i.e., from a governor, a public health expert, a physician, a patient, and a resident of the outbreak area) or to one that received a control message. The study was registered as a University Hospital Medical Information Network Clinical Trials Registry (number: UMIN000040286) on May 1, 2020. The methods of the present study adhered to CONSORT guidelines. The protocol was approved by the ethical review committee at the Graduate School of Medicine, University of Tokyo (number: 2020032NI). All participants gave written informed consent in accordance with the Declaration of Helsinki.
2.2. Intervention and control messages
We searched news articles about COVID-19 using Yahoo! JAPAN News ( https://news.yahoo.co.jp ), the largest Japanese news portal site. We also searched videos posted by residents of outbreak areas such as New York using YouTube ( https://www.youtube.com/user/YouTubeJapan ). By referring to these articles and videos, we created five intervention messages from a governor, a public health expert, a physician, a patient, and a resident of an outbreak area. The content of each message encouraged readers to stay at home. We included threat and coping messages in each intervention message based on protection motivation theory (PMT) [ 10 , 11 ]. Appendix A shows the five intervention messages used in this study, translated into English for this report. For a control message we obtained textual information about bruxism from the website of the Ministry of Health, Labour and Welfare ( https://www.e-healthnet.mhlw.go.jp/ ).
2.3. Measures
The primary outcome was intention to stay at home. The secondary outcomes were PMT constructs (i.e., perceived severity, vulnerability, response efficacy, and self-efficacy). Participants responded to two or three questions for each measure (see Appendix B ). These measures were adapted and modified from previous studies [ [12] , [13] , [14] , [15] ]. All primary and secondary outcomes were measured before and after the participants read intervention or control messages, and mean scores were calculated. Higher scores indicated greater intention and perception. All participants were asked for their sociodemographic information before they read intervention or control messages.
2.4. Sample size
Based on the effect size in a previous randomized controlled study [ 16 ], we estimated a small effect size (Cohen’s d = .20) in the current study. We conducted a power analysis at an alpha error rate of .05 (two-tailed) and a beta error rate of .20. The power analysis indicated that 330 participants were required in each of the intervention and control groups.
2.5. Statistical analysis
A one-way analysis of variance (ANOVA) was conducted with the absolute change in mean values for each measure before and after intervention as the dependent variable and the group assignment as the independent variable. For multiple comparisons, Tukey’s test was conducted on significant main effects where appropriate. The Games–Howell test was performed when the assumption of homogeneity of variances was not satisfied. Additionally, we conducted subgroup analyses including only participants who lived in 13 “specified warning prefectures,” where the number of infected individuals showed a marked increase [ 17 ]. A p value of <.05 was considered significant in all statistical tests. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 21.0 (IBM, Armonk, NY, USA).
Table 1 shows the participants’ characteristics. Table 2 , Table 3 present a comparison among the five intervention groups using one-way ANOVA and multiple comparisons when including all prefectures and only participants who lived in the specified warning prefectures, respectively. More significant differences between intervention messages were found in the specified warning prefectures compared with all prefectures. In Table 3 , the Games–Howell test indicates that the message from a physician increased participants’ intention to stay at home significantly more than other narrators’ messages (versus a governor, p = .002; an expert, p = .023; a resident, p = .004). Multiple comparisons demonstrated that the message from a physician increased participants’ perceived severity (versus a governor, p = .015), response efficacy (versus a resident, p = .014), and self-efficacy (versus a governor, p = .022; a patient, p = .009) significantly more than other narrators’ messages.
Participants’ sociodemographic information.
| Governor (n = 330) | Expert (n = 330) | Physician (n = 330) | Patient (n = 330) | Resident (n = 330) | Control (n = 330) | Total (N = 1,980) | |
|---|---|---|---|---|---|---|---|
| 49.7 | 49.7 | 49.7 | 49.7 | 49.7 | 49.7 | 49.7 | |
| 18–29 | 16.1 | 16.1 | 16.1 | 16.1 | 16.1 | 16.1 | 16.1 |
| 30–39 | 18.5 | 18.5 | 18.5 | 18.5 | 18.5 | 18.5 | 18.5 |
| 40–49 | 23.6 | 23.6 | 23.6 | 23.6 | 23.6 | 23.6 | 23.6 |
| 50–59 | 20.6 | 20.6 | 20.6 | 20.6 | 20.6 | 20.6 | 20.6 |
| 60–69 | 21.2 | 21.2 | 21.2 | 21.2 | 21.2 | 21.2 | 21.2 |
| Hokkaido | 4.8 | 4.8 | 4.8 | 4.8 | 4.8 | 4.8 | 4.8 |
| Tohoku | 7.9 | 7.9 | 7.9 | 7.9 | 7.9 | 7.9 | 7.9 |
| Kanto | 32.4 | 32.4 | 32.4 | 32.4 | 32.4 | 32.4 | 32.4 |
| Hokuriku and Chubu | 17.9 | 17.9 | 17.9 | 17.9 | 17.9 | 17.9 | 17.9 |
| Kinki | 16.7 | 16.7 | 16.7 | 16.7 | 16.7 | 16.7 | 16.7 |
| Chugoku and Shikoku | 8.8 | 8.8 | 8.8 | 8.8 | 8.8 | 8.8 | 8.8 |
| Kyushu and Okinawa | 11.5 | 11.5 | 11.5 | 11.5 | 11.5 | 11.5 | 11.5 |
| 16.8 | 17.3 | 16.2 | 16.3 | 17.8 | 15.5 | 64.3 | |
| Less than high school | 1.5 | 1.8 | 1.2 | 3.0 | 1.8 | 0.6 | 1.7 |
| High school graduate | 29.1 | 25.2 | 24.2 | 23.0 | 27.0 | 27.6 | 26.0 |
| Some college | 21.5 | 24.5 | 28.2 | 22.7 | 26.4 | 21.5 | 24.1 |
| College graduate | 43.6 | 39.1 | 38.2 | 42.1 | 36.7 | 44.5 | 40.7 |
| Graduate school | 4.2 | 9.4 | 8.2 | 9.1 | 8.2 | 5.8 | 7.5 |
| Less than 2 million yen | 7.9 | 9.7 | 8.8 | 9.4 | 8.2 | 11.5 | 9.2 |
| 2–6 million yen | 42.7 | 43.3 | 40.0 | 46.1 | 45.5 | 46.1 | 43.9 |
| More than 6 million yen | 41.8 | 34.5 | 42.1 | 35.2 | 36.1 | 33.6 | 37.2 |
| Unknown | 7.6 | 12.4 | 9.1 | 9.4 | 10.3 | 8.8 | 9.6 |
Comparison of amount of change before and after intervention among groups when including all prefectures (N = 1,980).
| Governor (n = 330) | Expert (n = 330) | Physician (n = 330) | Patient (n = 330) | Resident (n = 330) | Control (n = 330) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | Change | Before | After | Change | Before | After | Change | Before | After | Change | Before | After | Change | Before | After | Change | ||
| Intention | 4.72 (0.73) | 4.89 (0.74) | 0.17 (0.13–0.22) | 4.81 (0.75) | 5.00 (0.74) | 0.19 (0.14–0.24) | 4.74 (0.71) | 5.01 (0.76) | 0.27 (0.21–0.32) | 4.69 (0.79) | 4.91 (0.82) | 0.22 (0.16–0.27) | 4.78 (0.74) | 4.96 (0.74) | 0.18 (0.14–0.23) | .098 | 4.71 (0.74) | 4.77 (0.75) | 0.06 (0.01–0.09) |
| Severity | 4.42 (0.79) | 4.48 (0.84) | 0.06 (0.01–0.12) | 4.34 (0.84) | 4.51 (0.85) | 0.17 (0.10–0.24) | 4.25 (0.86) | 4.42 (0.87) | 0.17 (0.10–0.24) | 4.24 (0.93) | 4.57 (0.90) | 4.37 (0.88) | 4.51 (0.88) | 0.14 (0.09–0.21) | <.001 | 4.34 (0.84) | 4.27 (0.86) | −0.07 (−.14 to −0.00) | |
| Vulnerability | 3.04 (0.88) | 3.19 (0.86) | 0.15 (0.07–0.22) | 3.10 (0.97) | 3.24 (1.00) | 0.14 (0.06–0.23) | 3.09 (0.89) | 3.21 (0.97) | 0.12 (0.04–0.20) | 3.05 (0.96) | 3.46 (1.00) | 3.16 (0.90) | 3.58 (0.92) | <.001 | 3.10 (0.86) | 3.13 (0.82) | 0.029 (−0.04–0.10) | ||
| Response efficacy | 4.42 (0.85) | 4.67 (0.75) | 0.25 (0.18–0.31) | 4.47 (0.84) | 4.79 (0.82) | 0.33 (0.26–0.39) | 4.40 (0.80) | 4.76 (0.82) | 0.36 (0.29–0.43) | 4.42 (0.86) | 4.71 (0.88) | 0.29 (0.22–0.37) | 4.50 (0.83) | 4.74 (0.83) | 0.24 (0.18–0.30) | .065 | 4.43 (0.76) | 4.52 (0.81) | .09 (0.04–0.15) |
| Self-efficacy | 4.67 (0.73) | 4.85 (0.75) | 0.18 (0.12–0.23) | 4.72 (0.78) | 4.94 (0.75) | 0.22 (0.15–0.28) | 4.67 (0.73) | 4.95 (0.75) | 0.28 (0.22–0.34) | 4.67 (0.77) | 4.85 (0.81) | 0.17 (0.12–0.23) | 4.72 (0.78) | 4.92 (0.75) | 0.20 (0.15–0.26) | .089 | 4.65 (0.71) | 4.73 (0.75) | .08 (0.03–0.12) |
Comparison of amount of change before and after intervention among groups when including only the “specified warning prefectures” (N = 1,274).
| Governor (n = 214) | Expert (n = 220) | Physician (n = 207) | Patient (n = 208) | Resident (n = 227) | Control (n = 198) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | Change | Before | After | Change | Before | After | Change | Before | After | Change | Before | After | Change | Before | After | Change | ||
| Intention | 4.72 (0.72) | 4.89 (0.75) | 0.17 (0.11.22) | 4.88 (0.72) | 5.07 (0.69) | 0.19 (0.13–0.25) | 4.75 (0.71) | 5.08 (0.70) | 4.72 (0.79) | 4.92 (0.84) | 0.21 (0.14–0.27) | 4.81 (0.76) | 4.99 (0.74) | 0.17 (0.12–0.23) | .003 | 4.68 (0.76) | 4.79 (0.73) | 0.11 (0.05–0.16) | |
| Severity | 4.40 (0.79) | 4.46 (0.82) | 0.06 (−0.00–0.12) | 4.29 (0.84) | 4.51 (0.84) | 4.21 (0.86) | 4.45 (0.85) | 4.26 (0.90) | 4.56 (0.91) | 4.35 (0.90) | 4.45 (0.90) | 0.10 (0.03–0.18) | <.001 | 4.37 (0.81) | 4.30 (0.82) | –0.08 (−0.16–0.00) | |||
| Vulnerability | 3.07 (0.84) | 3.23 (0.86) | 0.16 (0.07–0.25) | 3.12 (0.98) | 3.24 (1.04) | 0.12 (0.02–0.22) | 3.14 (0.88) | 3.24 (0.99) | 0.10 (0.00–0.19) | 3.11 (0.94) | 3.49 (0.95) | 3.14 (0.90) | 3.56 (0.92) | <.001 | 3.09 (0.88) | 3.17 (0.87) | .09 (−0.01–0.19) | ||
| Response efficacy | 4.46 (0.80) | 4.69 (0.74) | 0.23 (0.16–0.30) | 4.49 (0.84) | 4.85 (0.81) | 4.41 (0.78) | 4.78 (0.80) | 4.41 (0.86) | 4.69 (0.91) | 0.28 (0.19–0.37) | 4.54 (0.88) | 4.73 (0.88) | 0.19 (0.12–0.26) | .005 | 4.42 (0.77) | 4.52 (0.81) | .10 (0.04–0.17) | ||
| Self-efficacy | 4.68 (0.75) | 4.85 (0.75) | 0.17 (0.11–0.23) | 4.81 (0.77) | 5.00 (0.74) | 0.19 (0.11–0.28) | 4.68 (0.68) | 5.01 (0.71) | 4.70 (0.76) | 4.86 (0.85) | 0.16 (0.09–0.23) | 4.74 (0.81) | 4.94 (0.76) | 0.21 (0.14–0.27) | .008 | 4.65 (0.70) | 4.73 (0.75) | .08 (0.03–0.14) | |
4. Discussion and conclusion
4.1. discussion.
As Appendix A shows, the message from a physician specifically communicated the critical situation of hospitals being overwhelmed and the consequent risk of people being unable to receive treatment. Depiction of the crisis of overwhelmed hospitals may have evoked heightened sensation that elicited sensory, affective, and arousal responses in recipients. Social lockdown presumably evoked psychological reactance in many individuals [ 18 ]. Psychological reactance is considered one of the factors that impedes individuals’ staying at home during a pandemic [ 18 ]. Studies of psychological reactance have indicated that heightened sensation is the feature of a message that reduces psychological reactance [ 19 , 20 ]. Additionally, in Japan recommendations by physicians have a strong influence on individuals’ decision making owing to the remnants of paternalism in the patient–physician relationship [ 21 ]. These may constitute the reasons for the message from a physician generating the greatest impact on recipients’ protection motivation.
Public health professionals, governors, media professionals, and other influencers should use messages from physicians and disseminate relevant articles through the media and social networking services to encourage people to stay at home. It is important that health professionals and media have a network and collaborate with one another [ 22 ]. To build relationships and provide reliable resources, health professionals are expected to hold press conferences and study meetings with journalists. Through such networking, journalists can acquire accurate information in dealing with the pandemic, such as using messages from physicians to encourage people to stay at home. Consequently, journalists should disseminate such messages. It is also important that governments, municipalities, medical associations, and other public institutions convey messages from physicians and that the media effectively spread those messages. Owing to the advances of Web 2.0 [ 23 ], health professionals’ grassroots communication with journalists and citizens via social media may provide opportunities for many people to access persuasive messages from physicians.
4.1.1. Limitations
First, the content of the intervention messages in this study may not represent voices of all governors, public health experts, physicians, patients, and residents of outbreak areas. Second, it is not clear from this study which sentences in the intervention message made the most impact on recipients and why. Third, this study assessed intention rather than actual behavior. Finally, it is unclear as to what extent the present findings are generalizable to populations other than the Japanese participants in this study.
4.2. Conclusion
In areas with high numbers of infected people, the message from a physician, which conveyed the crisis of hospitals being overwhelmed and the consequent risk of people being unable to receive treatment, increased the intention to stay at home to a greater extent than other messages from a governor, a public health expert, a patient with COVID-19, and a resident of an outbreak area.
4.3. Practice implications
Governors, health professionals, and media professionals may be able to encourage people to stay at home by disseminating the physicians’ messages through media such as television and newspapers as well as social networking services on the internet.
This work was supported by the Japan Society for the Promotion of Science KAKENHI (grant number 19K10615).
CRediT authorship contribution statement
Tsuyoshi Okuhara: Conceptualization, Methodology, Formal analysis, Investigation, Writing - original draft, Funding acquisition. Hiroko Okada: Methodology, Investigation, Writing - review & editing. Takahiro Kiuchi: Supervision, Writing - review & editing.
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
Acknowledgement
We thank Hugh McGonigle, from Edanz Group ( https://en-author-services.edanzgroup.com/ac ), for editing a draft of the manuscript.
Appendix A.
Intervention: the message from a governor.
The following is a message from the governor of your local area.
| “As the novel coronavirus spreads, now is a crucial time in deciding whether we will see an explosive growth in the number of cases. The same epidemic and overwhelmed hospitals that have occurred in cities abroad can occur here. Unless absolutely essential, please refrain from going out unnecessarily and stay at home. Please do not go to these three high-density places: closed spaces with poor ventilation, crowded places where many people gather together, and intimate spaces where you would have conversations in close proximity. As for commuting, please work from home or stagger commuting times where possible to reduce contact with other people. The action taken by all of us will be the most effective remedy in overcoming this disease and ending the coronavirus epidemic quickly. We will do our utmost to improve our healthcare provision system, prevent the spread of infection, and mitigate the impacts on the local economy. Let us all work together to overcome this difficult situation.” |
Please avoid leaving your house as much as possible.
Staying at home can save lives and prevent the spread of infection.
Intervention: The message from an expert
The following is a message from an infectious disease control expert.
| “One characteristic of the novel coronavirus is that it is difficult to notice that you are infected. As a result, it is possible that you could feel healthy but pass the virus on to 2–3 people within a week. Those individuals could then each pass the virus on to a further 2–3 people, and those in turn could then pass the virus on to another 2–3 people. Two will become 4, 4 will become 8, 8 will become 16, 16 will become 32, and so on, and the number of infected people will keep doubling. Unless contact between people decreases, it is estimated that about 850,000 people will become seriously ill in Japan and about 420,000 people will die. However, if everybody stops going out and stays at home, and if we are able to reduce our contact with people by 80 %, we will be able to prevent the spread of infection. For example, stop meeting with your friends, stop going shopping, and work from home. If we can reduce the number of people infected, we can reduce the burden on doctors and nurses and prevent hospitals being overwhelmed.” |
Intervention: The message from a physician
The following is a message from an emergency medical care doctor.
| “The beds and intensive care units at my hospital have all been filled by patients who have the novel coronavirus, and we can no longer accept new patients. The overwhelming of hospitals and collapse of the healthcare system that happened in Italy and New York is already under way in Japan. Doctors and nurses are being fully mobilized for treatment, but they lack masks and protective clothing. We have cut plastic folders with scissors to make face shields to cover our faces. We use the same mask for 3 days. With the high risk of infection, we are being pushed to the limit. It is not uncommon for infection to occur within the hospital. Even if only one of the doctors or nurses gets infected, many co-workers have to isolate themselves at home and are unable to continue providing treatment. This means that, if any one of you becomes infected and their condition becomes critical, there may be no treatment available. We are staying in the hospitals and continuing to provide treatment. So please, stay at home. If you do your part, we will be able to do ours.” |
Intervention: The message from a patient
The following is a message from a patient who is infected with the novel coronavirus.
| “I had a 40-degree fever and a headache that felt like someone was stomping on my head. I could not stop coughing, and the pain felt as though I was inhaling broken glass. I really thought that I was going to die. I have no pre-existing conditions, do not smoke, and was perfectly healthy, but now I cannot breathe without a breathing tube. I have a drip and a catheter stuck into both of my hands. Right now, I feel ten times better than I did when I was at my worst, and I am able to talk about my condition. But my fever refused to go down even after I had taken medication, and I do not know how many days have passed since I was hospitalized. I do not know where I was infected. I do not know the route of infection, whether it was my workplace, somewhere I had visited for work, or when I was out shopping. Afterward, the rest of my family also tested positive. I had passed it to them. You do not know where you can be infected. Do not assume that you will be okay because you are young or healthy. The virus does not pick and choose. Please stop going out. Stay at home.” |
Intervention: The message from a resident
The following is a message from an individual who lives in an area where an outbreak of novel coronavirus has occurred.
| “In the beginning, I did not really feel a sense of crisis. Of course I thought ‘Coronavirus is scary; better be careful,’ but nothing more. However, in the area where I live, the number of those infected has increased tenfold from 1500 to 15,000 in just one week. It is a real outbreak. The number of infected people increased all at once and overwhelmed the hospitals. They are lacking beds and ventilators. Some doctors and nurses are infected, and there are not enough hospital staff. Because of the healthcare system collapse, even if you are infected with coronavirus you will be unable to receive a test or treatment. If I or my family are infected and our condition becomes critical, we will likely die. I am scared to go grocery shopping. I always disinfect my purchases with alcohol, but soon my alcohol will run out. If you continue to go out, the number of those infected could jump to the tens of thousands, and the situation in your area will be the same as it is here. Please stop going out. Stay at home.” |
A control message
According to the traditional definition, grinding one’s teeth is when somebody makes a sound by strongly grinding the teeth together, usually unconsciously or while asleep. Nowadays, it is often referred to as ‘teeth grinding,’ a term which also covers various actions that we do while awake.
Whether you are sleeping or awake, the non-functional biting habit of grinding one’s teeth dynamically or statically, or clenching one’s teeth, can also be referred to as bruxism (sleep bruxism if it occurs at night). Bruxism can be categorized into the movements of: sliding the upper and lower teeth together like mortar and pestle (grinding); firmly and statically engaging the upper and lower teeth (clenching); and dynamically bringing the upper and lower teeth together with a tap (tapping).
Bruxism is difficult to diagnose, as it often has no noticeable symptoms. Stress and dentition are thought to be causes of bruxism, but it is currently unclear and future research is anticipated.
Splint therapy, which involves the use of a mouthpiece as an artificial plastic covering on one’s teeth, and cognitive behavioral therapy are being researched as treatments for bruxism.
Appendix B.
| (Cronbach’s α 0.863) |
| (1) Would you like to cancel or postpone plans such as “meeting people,” “eating out,” and “attending events” because of the new coronavirus infection? |
| (2) Would you like to reduce the time you spend shopping in stores outside your home because of the new coronavirus infection? |
| (3) Would you like to avoid crowded spaces because of the new coronavirus infection? |
| (Cronbach’s α 0.480) |
| (1) How serious do you think your health will be if you are infected with the new coronavirus? |
| (2) How serious do you think the social situation will be if the new coronavirus spreads? |
| (Cronbach’s α 0.875) |
| (1) How likely are you to be infected with the new coronavirus? |
| (2) How likely are you to be infected with the new coronavirus when compared with someone of the same sex and age as you? |
| (Cronbach’s α 0.921) |
| (1) Do you think that you can save your life from the new coronavirus infection and prevent the spread of infection …by canceling or postponing your appointments such as “meeting people,” “eating out,” and “attending events”? |
| (2) …by reducing the time you spend shopping at stores outside your home? |
| (3) …by avoiding crowded spaces? |
| (Cronbach’s α 0.853) |
| (1) Do you think that you can cancel or postpone your appointments such as “meeting people,” “eating out,” and “attending events” because of the new coronavirus infection? |
| (2) Do you think you can reduce the time you spend shopping in stores outside your home because of the new coronavirus infection? |
| (3) Do you think you can avoid the crowded spaces because of the new coronavirus infection? |
All questions above were on a scale of 1–6, ranging from “extremely unlikely” to “unlikely,” “a little unlikely,” “a little likely,” “likely,” and “extremely likely.”

Coronavirus Disease 2019
The coronavirus speech i’d give, realistic reasons for hope..
Posted March 21, 2020 | Reviewed by Jessica Schrader
- Take our Your Mental Health Today Test
- Find a therapist near me

Updated: Apr. 24, 2020
The media’s core message on the coronavirus is that even if we behave, coronavirus will change life as we know it for years to come: massive job loss, disease, and yes, death, rivaling the Spanish Flu, which killed 50 to 100 million people.
Perhaps a perspective from someone with little to gain from sensationalism nor from political blaming might replace some of the fear with realistic hope.
There are at least three reasons for realistic hope that the coronavirus problem will be satisfactorily addressed than is feared:
1. A simpler, faster test is here: Abbott Laboratories have developed a COVID-19 test that produces the results in five minutes, onsite, and the FDA has just authorized the first at-home swab test.
2. As of April 6, there were more than 200 coronavirus vaccines and treatments in development. It would seem that with some of the world's greatest minds working tirelessly, one will be developed, again, sooner than later. The WHO says that an effective treatment is likely just weeks or months away.
3. Social distancing works and in the U.S. compliance has risen to over 90 percent as of April 15, and since then, subjectively, I've noted ever greater compliance.
So live your life. Sure, practice social distancing, wear a mask in stores, and wash your hands often, but also take advantage of the slowed economy to do things you had wished you had time to do: Speak with friends, do a hobby, do volunteer work by phone or on the internet. Upgrade your skills and networking connections so when the economy and job market improves, you'll be ready. Love more.
Society will survive the coronavirus pandemic, not just because of improved preparedness for an epidemic but because we’ll live with a greater sense of perspective and appreciation of life’s small pleasures: from that first bite of food to the beauty of your loved ones to more present conversations with friends and family. Don’t let coronavirus deprive you of life's wonders. Live.
For some silver linings in the coronavirus situation, you might want to read my previous post, " My Shelter Diary ," including the excellent comment by "Your Reader in Pennsylvania."
I read this aloud on YouTube.

Marty Nemko, Ph.D ., is a career and personal coach based in Oakland, California, and the author of 10 books.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Testing persuasive messaging to encourage COVID-19 risk reduction
Roles Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing
Affiliations Institution for Social and Policy Studies, Yale University, New Haven, Connecticut, United States of America, Center for the Study of American Politics, Yale University, New Haven, Connecticut, United States of America
Roles Conceptualization, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Institution for Social and Policy Studies, Yale University, New Haven, Connecticut, United States of America, Center for the Study of American Politics, Yale University, New Haven, Connecticut, United States of America, Department of Political Science, Yale University, New Haven, Connecticut, United States of America
Roles Conceptualization, Writing – original draft, Writing – review & editing
Affiliations Institute for Global Health, Yale University, New Haven, Connecticut, United States of America, Department of Internal Medicine, Infectious Diseases, Yale School of Medicine, New Haven, Connecticut, United States of America
Roles Conceptualization, Funding acquisition, Writing – review & editing
Affiliations Institute for Global Health, Yale University, New Haven, Connecticut, United States of America, Department of Internal Medicine, Infectious Diseases, Yale School of Medicine, New Haven, Connecticut, United States of America, Yale School of Public Health, New Haven, Connecticut, United States of America
- Scott E. Bokemper,
- Gregory A. Huber,
- Erin K. James,
- Alan S. Gerber,
- Saad B. Omer

- Published: March 23, 2022
- https://doi.org/10.1371/journal.pone.0264782
- Reader Comments
What types of public health messages are effective at changing people’s beliefs and intentions to practice social distancing to slow the spread of COVID-19? We conducted two randomized experiments in summer 2020 that assigned respondents to read a public health message and then measured their beliefs and behavioral intentions across a wide variety of outcomes. Using both a convenience sample and a pre-registered replication with a nationally representative sample of Americans, we find that a message that reframes not social distancing as recklessness rather than bravery and a message that highlights the need for everyone to take action to protect one another are the most effective at increasing beliefs and intentions related to social distancing. These results provide an evidentiary basis for building effective public health campaigns to increase social distancing during flu pandemics.
Citation: Bokemper SE, Huber GA, James EK, Gerber AS, Omer SB (2022) Testing persuasive messaging to encourage COVID-19 risk reduction. PLoS ONE 17(3): e0264782. https://doi.org/10.1371/journal.pone.0264782
Editor: Camelia Delcea, Bucharest University of Economic Studies, ROMANIA
Received: October 20, 2021; Accepted: February 16, 2022; Published: March 23, 2022
Copyright: © 2022 Bokemper et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Replication materials have been uploaded to Harvard Dataverse, https://doi.org/10.7910/DVN/VUKNOQ .
Funding: The authors acknowledge support from the Yale Institution for Social and Policy Studies, the Center for the Study of American Politics, and the Yale Institute for Global Health for funding this research.
Competing interests: The authors have declared that no competing interests exist.
Governments and public health officials have emphasized the importance of social (physical) distancing and other related measures in mitigating the spread of COVID-19. Given ongoing vaccine hesitancy, that vaccines are not fully effective in preventing COVID-19 infections, and the lack of vaccine access in certain parts of the world, the need for interventions that cause individuals to take actions that reduces the risk of infection remain essential. In practice, many messaging and communication strategies have been observed. However, despite these widespread and varied efforts, we lack a robust evidentiary basis for understanding the messages that are effective at increasing individuals’ willingness to embrace actions that reduce the spread of COVID-19.
We conducted two experiments to examine how different public health messages affect people’s beliefs about the efficacy of social distancing, their intentions to practice social distancing, and their attitudes about enforcing social norms, such as persuading others to practice social distancing and negatively judging those who do not. Experiment 1 was exploratory in nature and tested a large number of messages that combined elements from different conceptual frameworks discussed below in an effort to find messages that increased respondents’ intentions to practice social distancing and willingness to encourage others to do so.
In Experiment 2, we take the two most successful messages from Experiment 1 and conduct a preregistered trial using a nationally-representative sample of American adults against both a Baseline Informational control similar to that used in Experiment 1 and a placebo-treated control group that is not exposed to any information about COVID-19 risk reduction. In our second study, in light of ongoing discussions about other practices to reduce the spread of COVID-19, we also examined mask wearing, willingness to self-isolate if exposed to COVID-19, and cooperation with government contact tracing. In both studies, we examine the possibility that certain messages are more effective among specific segments of the population.
This paper offers three important contributions. First, we conduct a large-scale multi-message study of different messages designed to encourage COVID-19 risk reduction actions with multiple outcomes followed by a replication study of the most promising messages. Testing a large number of messages means we can directly assess the relative effectiveness of different messages, decompose compound messages into their component parts to understand which elements of those messages make them effective, and address concerns that prior studies testing individual messages and finding them effective are driven by false positives. Our repeat testing of promising messages also allows us to understand whether messages that are initially effective remain effective, helping to further rule out sampling variability and understand the durability of apparently effective messages in light of changing public rhetoric about COVID-19 [ 1 ]. Finally, our focus on multiple outcomes means that we can understand both whether messages are effective only for the targeted individual’s own risk reduction behavior or also affect their likelihood of encouraging others to undertake these protective behaviors.
Second, we test a large number of different messages, drawn from three broad and theoretically relevant categories. First, we test messages that differ in whether they frame social distancing as a self- or other-regarding action and whether they highlight reciprocity in producing desirable outcomes. While several other papers have considered other-regarding messages, we also explicitly test whether it is easier to promote other-regarding behavior when highlighting reciprocity—that is how the other-regarding behavior of other individuals is also helping to protect the person targeted for persuasion. Second, we test a set of messages we characterize as “values consistent.” These are messages that try to frame social distancing in terms of values individuals likely hold, so that individuals who might otherwise be resistant to the behavior undertake it. We also test messages observed in public health and political rhetoric at the time these studies were fielded. In all cases, we test these messages relative to both a pure control that does not provide any COVID-19 relevant content and to a baseline public health message that provides a simple informational basis for social distancing as well as an injunctive appeal for doing so. This latter comparison provides further leverage in isolating the effects of any novel persuasive rhetoric.
Finally, these messaging studies provide an important window into the efficacy and limitations of efforts to promote COVID-19 risk reduction in the early stages of the pandemic in the United States and as it later evolved. Existing work on public health messaging has demonstrated behavioral change in response to specific messages about tobacco use, consumption of sugary beverages, high risk sexual behavior, and vaccination uptake [ 2 – 6 ]. Messages used in past work often target one or a very small number of behaviors at a time. However, successful public health strategies that address the COVID-19 pandemic require large numbers of people to change a broad range of daily behaviors, such as how they interact with friends and relatives, whether they wear face coverings in public, and cooperation with government efforts to identify infectious individuals. This suggests that a more fruitful messaging strategy needs to change attitudes towards social distancing more broadly rather than targeted messaging to increase the prevalence of a specific action. Changes in attitudes could also increase the willingness of individuals to encourage others to engage in these behaviors—that is, to reinforce desired behaviors through social norms [ 7 – 9 ]. Importantly, unlike other health behaviors, many individuals are at a relatively low risk of serious COVID-19 complications, but their behavior is nonetheless important for reducing the risk to individuals who are more vulnerable as the disease continues to spread throughout the general population.
Before proceeding, we note that we use the term social distancing rather than physical distancing as it reflects the language at the time the experiments were fielded. As has been noted by other researcher, the term physical distancing may be more appropriate [ 10 – 14 ].
The emergence of COVID-19 created an urgent need for governments and public health officials around the globe to induce behavioral change among people in society writ large. While formal restrictions, like closing schools, prohibiting large gatherings, and restricting travel, can quickly produce behavioral change, slowing the spread of infectious diseases also requires voluntary action by individuals like working from home, avoiding dining inside restaurants, and refraining from socializing with friends and family. An important challenge for public health officials is persuading people to change a large number of behaviors that cause a significant disruption to daily routines.
Given the novelty of social distancing in the United States early in the pandemic and the large number of people being told to distance to keep themselves, their families, and their community safe, it was not clear ex ante what types of messaging strategies would be effective at increasing people’s willingness to dramatically change their daily lives. While considerable work on public health messaging has been produced during the pandemic, in the early stages it was important to understand whether any component of the “kitchen sink” messages observed being used could be effective at increasing people’s beliefs about the importance of social distancing and their intentions to engage in the behavior.
The large number of messages we tested were motivated by different approaches in behavioral science. Specifically, we combined appeals about 1) social norms, 2) self-interest vs. other-regarding motives, 3) individual vs. collective action, and 4) values reframing, to better understand whether attitudes toward social distancing could be changed with written persuasive messages.
Social norms and health behaviors
Public health campaigns often invoke social norms to encourage the public to practice positive health behaviors, like wearing sunscreen [ 15 , 16 ], quitting smoking [ 17 ], and using condoms [ 18 ] (see also [ 19 ]). Beliefs about social norms have been shown to be powerful motivators of health behavior (for review, see [ 20 ]). Unsurprisingly, social norms theory has been applied to understanding people’s behaviors during the COVID-19, such as the decision to wear a mask [ 7 , 8 ] and whether to practice social distancing [ 9 , 21 – 23 ]. Social norms can be classified as either descriptive , i.e. what most people do, or injunctive , i.e. people’s beliefs about what they should do or what is believed to be the morally acceptable thing to do [ 24 ].
Early in the pandemic, public health experts had to rely on appealing to injunctive norms, emphasizing what most people should be doing to stay safe. Prior to COVID-19 infection becoming widespread in the United States, most people were not engaging in social distancing making it difficult to credibly appeal to descriptive norms as a way to increase the prevalence of the behavior. An appropriate baseline for comparison of messaging strategies about social distancing is therefore one that includes an appeal to injunctive norms, an approach that was relatively common at the beginning of the pandemic. Our baseline message therefore explains that public health officials believe individuals ought to socially distance to end the COVID-19 pandemic and details the specific health behaviors that people should undertake.
However, as social distancing became more widespread in the early months of the pandemic, public health messaging could also emphasize descriptive norms in conjunction with injunctive norms. For both social distancing and mask wearing, people report being more likely to engage in a public health promoting behavior when they report that others around them are doing so as well [ 7 , 9 ]. Descriptive social norms may also play a causal role in the decision to wear a mask. In a vignette-based experiment, respondents in the United States and Italy were more likely to report that they would wear a mask or ask someone to wear theirs properly when other people were described as wearing masks compared to when they were not [ 8 ]. This positive effect has also been observed when accounting for local ordinances and has been shown to be stronger when people also endorse the injunctive norm that social distancing is the morally correct behavior [ 25 ]. Thus, the combination of an injunctive norm with a descriptive norm may be especially likely to increase people’s willingness to engage in social distancing.
Self-interest vs. prosocial concern for social distancing
Descriptive social norms provide information about the prevalence of a behavior in a group of people, but this does not provide information as to why others are engaging in the behavior per se. That is, people may be practicing social distancing to protect themselves from contracting COVID-19, or they may also be practicing social distancing to protect others. It could also be that people are motivated by some combination of both motives. Past research has observed that both a concern for one’s own health and a concern for the health of others are motivations for social distancing behavior. In a survey of adults in North America and Europe, over 80% of respondents reported that they practice social distancing to protect themselves and to protect others [ 26 ]. Both motivations were also shown to be predictive of social distancing behavior in a computer-based scenario experiment in which participants reported their social distancing behavior in common daily situations, like meeting a friend or going to a grocery store [ 27 ]. Regarding concern for one’s own health, people who believe that they are more vulnerable to the disease are more likely to report higher levels of social distancing behavior [ 28 – 30 ]. Survey research has also examined the correlation between individual differences in personality and values has found that people who are more concerned about the well-being of others are more likely to engage in social distancing [ 31 – 34 ] and that this concern for others may be more predictive of behavior than concern for oneself [ 35 ]. Further, people who were less willing to place risk on others in an incentivized experiment were more likely to report engaging in social distancing than those who placed another individual at greater risk [ 36 ].
While both self-interested and prosocial motives are present in people’s decisions to engage in social distancing, research on persuasion and public health messaging has produced mixed results for the effectiveness of appealing to either motive on behavioral intentions related to social distancing. Posters highlighting an “identifiable victim” or the spread of the disease to many others have been shown to decrease the willingness to engage in behaviors that were thought to spread COVID-19, like meeting with a friend or relative in their house [ 37 ]. Other work has found that inducing empathy for someone who is particularly vulnerable to COVID-19 can increase social distancing intentions [ 38 ]. Jordan, Rand, and Yoeli [ 39 ] observed that a prosocial framing of social distancing on a flier, i.e. avoid spreading coronavirus, was more effective than a self-interested frame, i.e. avoid getting coronavirus, in March 2020, although the prosocial frame was no more effective than the self-interested frame in a related experiment fielded a month later. Prosocial and empathy-inducing messages delivered as text have also been shown to be no more effective than the informational control to which they were added [ 40 ]. Thus, it is not clear whether persuasive messaging that appeals to protecting oneself or protecting others consistently produces the intended behavioral change beyond simply providing people with information.
Individual action vs. collective action
Descriptive social norms also do not convey how individual actions produce a benefit. Fundamentally, an outcome can be produced by individual or collective action, and the nature of a cooperative production function can differ substantially. In the case of individual production, public health campaigns could emphasize that each individual’s action produces a benefit. This approach aligns with past work on how beliefs about self-efficacy, an individual’s belief that they have the ability to perform an action to bring about a specific outcome, are an important determinant of whether an individual will perform a positive health behavior [ 41 , 42 ]. Beliefs about self-efficacy have been associated with intentions to practice social distancing in response to COVID-19 [ 43 , 44 ] and a hypothetical flu pandemic [ 45 ]. Thus, public health messaging may emphasize the importance of individual action as a means of protecting oneself and protecting others against COVID-19.
Alternatively, public health appeals could instead emphasize that the overall success of social distancing depends on collective action. Social distancing can be thought of as a collective action problem in which people have to work together to produce a group benefit. These types of cooperation dilemmas are widespread in human society and they vary in how the successful provision of a collective benefit is achieved [ 46 ]. One important feature of arguments that combine cooperative production with descriptive norms is that they invoke notions of reciprocity, the idea that one’s (costly) actions are being reciprocated by others in society, a factor that is shown to increase a willingness to undertake costly action [ 47 – 49 ].
The mapping between cooperative actions and outcomes may also vary. For one, social distancing to reduce the spread of COVID-19 could be thought of as a linear public good in which each individual’s social distancing provides an additional benefit to others. In this view, even if many people do not practice social distancing, those who do will still provide some benefit, although the fact each person’s actions matter may also encourage free-riding. Alternatively, social distancing could be thought of as a threshold public good in which the benefits are not realized until a critical mass of individuals engage in the behavior [ 50 ]. In this case, the possibility of not reaching a critical threshold may counteract the tendency to free-ride, although if the number of individuals falls short of the threshold, the benefit of social distancing is not produced and so one’s willingness to act may depend on believing enough other people are doing so.
Values reframing
One limitation of norm based approaches for policymakers and public health officials is that some people believe that COVID-19 does not pose a threat [ 27 , 51 ] or that social distancing violates another value they care about, such as displaying bravery rather than living in fear, an argument that appeared in the rhetoric of then President Donald Trump [ 52 , 53 ]. Rather than attempting to convince people with these beliefs about the threat posed by COVID-19, it may instead be effective when trying to persuade them to social distance to instead frame the action of social distancing as aligning with a value that they already hold [ 54 ]. For instance, bravery and risk-taking are generally viewed as attractive traits across a variety of cultures [ 55 – 57 ]. And indeed, many individuals, like medical professionals and emergency responders, demonstrated these desirable traits during the COVID-19 pandemic. Is reframing the act of social distancing as demonstrating an individual’s strength and bravery an effective strategy? A values-based approach has been shown to be effective at increasing attitudes toward masking among American conservatives when messaging appealed to loyalty moral values [ 58 ]. More broadly, other work has considered how metaphors can be useful ways to frame responses to the pandemic in ways that people can easily relate to [ 59 ].
The present experiments
We present results from two experiments that combined elements of the theoretical approaches describe above to assess the efficacy of persuasive messages to increase people’s willingness to practice social distancing.
In Experiment 1, we tested the efficacy of a large number of messages against a Baseline Informational control message that defined social distancing and stated that public health experts believe it would reduce the spread of COVID-19. We note that this message also invoked an injunctive norm because it states public health experts believe people ought to be social distancing. This was a more conservative approach than testing against an untreated control group, which we chose because we were searching for promising messages that could outperform the baseline content most similar to extant public health outreach and to which they were added in the experimental context. Our focus in Experiment 1 is to examine whether any message outperforms that Baseline Informational content to which it was added.
In Experiment 2, we re-tested the two most promising messages from Experiment 1 on a nationally-representative sample of Americans against the Baseline Informational control and a separate placebo control message.
Experiment 1
Participants were randomly assigned to read a Baseline Informational message or to one of ten intervention messages. Due to the number of comparisons that utilize the baseline message, we assigned participants to this message with a 3/13 chance, while the remaining ten intervention messages each had a 1/13 chance of assignment. The survey was administered using Qualtrics survey software. Both experiments presented here were fielded under an exemption granted by the Yale IRB and written consent was obtained before participants could begin the study.
Study sample
We used a self-service online platform provided by the survey firm Lucid to recruit a sample of American adults ( n = 3,184). Lucid provides a diverse sample of respondents that more closely matches demographic characteristics of nationally representative samples than other survey platforms like Amazon Mechanical Turk [ 60 ]. Approximately 81% of respondents assigned to an intervention completed the survey. Attrition was lower among those assigned to most of the intervention messages apart from the Baseline Informational message, by up to 8 percentage points. We did not find that pre-treatment covariates that explain outcomes differentially predicted attrition. The final analyzed sample was 2,568 respondents.
Participants were randomly assigned to read a Baseline Informational message that defined social distancing and stated that public health experts believe it would reduce the spread of COVID-19 or to one of ten intervention messages grouped into three categories. Each intervention message was added to the Baseline Informational message that included an injunctive norm statement. Table 1 shows the full text of the treatment messages and displays which parts of each tap into various theoretical constructs.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0264782.t001
The first category of messages varied the beneficiary of social distancing behaviors and whether individual or collective action was needed to produce these benefits. In all of these messages, descriptive social norms were invoked by describing others as already social distancing (“Many other people are already social distancing.”). The beneficiary of social distancing was either the individual (“you could get sick and die”) or others (“members of your family and community could get sick and die”). We combined manipulation of the beneficiary with what was necessary to produce this benefit. Specifically, social distancing was framed as providing a benefit if an individual practiced it (individual action, “when you practice social distancing you reduce the risk”), if enough other people practiced it (threshold collective action, “if enough people practice social distancing then we can reduce the risk”), or for each additional person who practiced (linear collective action, “every person who practices social distancing reduces the risk”). As we note above, the latter two frames about collective production also emphasized norms of reciprocity in that they linked others’ behaviors to outcomes relevant for the respondent. Crossing these two dimensions of manipulation produced the six total intervention messages in this category.
The second category of messages were efforts at value reframing and stated that people who believe they are being brave by continuing with their daily routines despite the threat of the virus are actually being reckless. Theses message start with an example of people who are being brave during the pandemic, e.g. firefighters, and then takes a seemingly desirable action as incompatible with a value and reframes it instead as selfish and unattractive (“people who don’t practice social distancing… aren’t brave, they are reckless”). The message also emphasizes that by not social distancing, people are placing others at risk, i.e. the opposite of true bravery. This reframing was either presented alone (Reframing Bravery) or with language about how people who spread COVID-19 pollute the environment around them (Reframing Bravery + Pollution).
The final category of messages invoked the idea that practicing social distancing would facilitate returning to “normal” life before the COVID-19 pandemic (“Social distancing now means we can more quickly return to our normal way of life”) or that doing so involved adapting to an unavoidable “new normal” (“we are adapting to the ‘new normal’ necessary because of COVID-19”). These two messages were designed to mirror rhetoric being used by political leaders and in the media and were added to the Other-regarding, Linear Cooperation message.
We form four mean scales as outcome measures, with all scales ranging from 0 to 1 with 1 indicating behaviors or beliefs associated with reducing the spread of COVID-19. The four scales were: 1) a BELIEFS/norms scale that assesses agreement with beliefs about social distancing being important for your health and others people’s health and whether an individual would feel guilty for not practicing social distancing, 2) a social distancing (DISTANCING) scale that captures people’s intended willingness to social distance, avoid attending gatherings, forego elective medical procedures, and wear a mask, 3) a FOOD behavior scale that assesses people’s willingness to avoid high-risk food related behavior like going to a restaurant, and 4) a persuade/evaluate OTHERS scale that measures whether people would persuade others to social distance, report a business for violating rules, and negatively judge non-compliers. Several items in the DISTANCING and FOOD scales had previously been shown to be affected by rhetoric focusing on selfish and prosocial motivations for social distancing [ 39 ]. All of the outcomes were coded such that higher values corresponded to attitudes and behavioral intentions consistent with greater social distancing. The internal consistency of the scales was generally good with the exception of the FOOD scale, which had a Cronbach’s Alpha of 0.65. Full text of outcome measures and scaling information appears in S1 Appendix .
We analyze our data using OLS regression comparing outcomes to the Baseline Informational message using indicators for each treatment and including pre-treatment demographic covariates to improve efficiency. Two messages appear particularly promising compared to the Baseline Informational message, with all treatment effect estimates plotted in Fig 1 . (Underlying regression analysis and distribution of scale outcomes appears in the S2 Appendix ). Among the messages that appear most effective, the Other-regarding, Linear Cooperation message also performs well relative to the Baseline Informational condition. For all four scales, the estimated effects of this message are positive. For the social distancing scale, the effect is .034 (95% CI: .002, .067) or 14.7% of a standard deviation. Respondents’ beliefs about the importance of social distancing also increase with an estimated effect of .040 (95% CI: -.002, .084) on the BELIEFS scale. The effect on the FOOD scale is .038 (95% CI: -.003, .079). The latter two effects are not statistically significant at the conventional 5% level, but do provide evidence that the Other-regarding, Linear Cooperation message broadly moved beliefs relevant to practicing social distancing.
Estimates displayed with 95% confidence intervals. Each panel shows the effect of each treatment message relative to the Baseline Informational condition for a primary outcome scale. All outcomes scales were coded such that higher values indicate more positive attitudes or intentions toward social distancing.
https://doi.org/10.1371/journal.pone.0264782.g001
The Reframing Bravery message increases all four scale outcomes. The estimated effect on the OTHERS scale is .058 (95% CI: .023, .092), indicating that respondents who read the Reframing Bravery message report more willingness to enforce norms to promote social distancing. We also observe suggestive evidence that this message affects both the BELIEFS scale and the own social distancing scale. For the BELIEFS scale the estimate is .037 (95% CI: -.005, .079) or about 12.8% of a standard deviation, while the effect for the DISTANCING scale is .030 (95% CI: -.004, .064) or about 13% of a standard deviation. The estimated effect for the FOOD scale is positive, but imprecise.
It is also interesting that two messages appear, on average, less effective than the Baseline Informational content and the Other-regarding, Linear Cooperation message to which they are added. While no coefficient estimates are individually statistically significant, both the Return to Normal and New Normal messages are generally less effective than the content to which they were added across our primary outcome measures.
We also conduct a number of exploratory analyses for heterogeneous treatment effects by age, gender, partisanship, and geographic location and do not uncover large differences in average treatment effectiveness across these groups ( S3 Appendix ). Due to the rhetoric among the public and political elites surrounding the degree to which measures to address the spread of COVID-19 infringe upon people’s liberties, we elicited people’s adoption of a liberty moral foundation that captures their belief about the role of government in society [ 61 ]. We found evidence that intervention effectiveness varies by endorsement of liberty values. Compared to respondents below the mean in their adoption of liberty values, respondents who are above the mean in their adoption of liberty are more responsive to the Reframing Bravery message than to the Baseline Informational condition on the BELIEFS scale (p = .05) and OTHERS scale (p < .01), with weaker evidence for the DISTANCING scale (p = .14). The effects of the Reframing Bravery message are uniformly statistically insignificant for those low in liberty.
The two most promising messages were the Other-regarding, Linear Cooperation message and the Reframing Bravery message. Both were the highest performing messages on at least two of the four outcome scales when compared to the baseline content to which they were added. Given this, these messages were the ones that were selected to be re-tested on a nationally representative sample of Americans to discern whether they are more effective than the Baseline Informational content to which they were added. Additionally, we believe there was value in retesting the most effective messages at a later point in the time in the pandemic when attitudes about social distancing may have become more crystallized, perhaps making people harder to persuade.
Experiment 2
Experiment 2 retested the two most successful interventions in Experiment 1 (Reframing Bravery, and Other-regarding Linear Cooperation and the Baseline Informational compared to an untreated Control message about an unrelated topic (bird feeding)). Experiment 2 was a pre-registered trial fielded between mid-July and early August 2020, a time when the COVID-19 outbreak in the United States had become far more widespread than during Experiment 1 [ 62 ]. We allocated respondents with equal probability to each intervention and written consent was obtained prior to participation.
We used the survey firm YouGov to recruit a nationally-representative sample of American adults. Respondents completed the study on their personal electronic devices. Power calculations indicated greater than 80% power to detect treatment effects 75% as large as in Experiment 1 with an N of 3,000 assuming scale distributions were the same as observed in Experiment 1. The study was fielded twice because of an implementation error in programming by the vendor for survey content that followed the items analyzed here for the first fielding (the error was for items for an unrelated project that was not about COVID-19, and which followed all of the items analyzed here). Consequently, the vendor re-fielded the entire survey resulting in a sample that was approximately twice as large as the sample described in our pre-registration document ( n = 3,000 pre-registered, n = 6,079 in final analysis dataset). YouGov does not provide data for respondents who decline to participate or drop out during the study.
The Baseline Informational treatment message was slightly modified from Experiment 1 to reflect changing guidance during the pandemic. It read:
To end the COVID-19 pandemic, public health officials believe we should practice social distancing. Social distancing means that you should:
- Work from home when possible
- Wear a mask that covers your nose and mouth when outside of your home around other people
- Stay at least 6 feet away from others if you need to go out in public, for example to shop for food or medicine
- Avoid large gatherings, especially indoors
- Stay home except to seek medical care if you are sick or have recently had close contact (closer than 6 feet for at least 15 minutes) with a person with COVID-19
- Avoid pooled rides or rides where multiple passengers are picked up who are not in the same household
The additional content added to this baseline for the Other-regarding, Linear Cooperation and the Reframing Bravery messages was unchanged from how they appear in Table 1 .
We made incremental changes to the four scales (BELIEFS, DISTANCING, FOOD, and OTHERS) used in Experiment 1 to reflect changing policies and circumstances. Given that contemporary discourse around social distancing had changed, we included new items that reflected what people were likely thinking about in their daily lives. We added items to the DISTANCING scale about attendance at religious services, participation in political events, self-isolation following COVID-19 exposure, and alerting public health authorities if diagnosed with COVID-19. For the OTHERS scale we added an item about cooperating in contact tracing. In the months between our studies, the behaviors we added to the scales had become salient in public discourse about COVID-19 risk reduction. We also included a new MASK scale composed of items about wearing a face covering in six circumstances, as well as relative willingness to shop at a store that requires rather than prohibits face masks. These additional items (and perhaps the passage of time) increased the reliability of the four scales that were used in Experiment 1 with the FOOD scale having the lowest reliability (Cronbach’s alpha of 0.78). The modified outcome text and scale reliability appears in S4 Appendix .
At the time this experiment was fielded, messaging outside of the experimental context about the importance of items in our DISTANCING scale had become far more widespread, although mask wearing remained a contested policy tool. It was therefore unclear whether messaging would be similarly effective in this new context.
We find baseline increases in scores on the BELIEFS and DISTANCING scales over time (i.e., averages for these outcomes in the bird feeding Control message in Experiment 2 are greater than the averages in the Baseline Informational condition in Experiment 1). Fig 2 plots main effects of message efficacy compared to the Control message for all outcomes (underlying regression analysis and distribution of scale outcomes appears in S5 Appendix ). The Baseline Informational message is associated with increased BELIEFS and DISTANCING scores (p < .05, one-sided, in both cases) relative to the bird feeding message. The Reframing Bravery and Other-regarding, Linear Cooperation messages appear to be more effective, however. Each is associated with a statistically significant increase in four outcomes: the BELIEFS, DISTANCING, OTHERS, and MASKS scales, with p-values < .05, one-sided, in all cases. The magnitudes of these effects are approximately 0.1 standard deviation for each measure. None of the messages have large or statistically precise effects on the FOOD scale.
Compared to the placebo control, the Baseline Informational message, the Reframing Bravery message, and the Other-regarding, Linear Cooperation increase beliefs and reported behavioral intentions to practice social distancing. These are OLS regression coefficient estimates for each primary outcome by treatment compared to the placebo control with 90% confidence intervals. The dashed vertical line represents the effect of the Baseline Informational Message on an outcome. All outcomes scales were coded such that higher values indicate more positive attitudes or intentions toward social distancing.
https://doi.org/10.1371/journal.pone.0264782.g002
There is less clear evidence that these messages are incrementally more effective that the Baseline Informational content to which they are added. For the BELIEFS, DISTANCING, OTHERS, and MASKS scales, both the Reframing Bravery and Other-regarding, Linear Cooperation messages are associated with effects that are always larger than the Baseline Informational message, with the magnitudes of these differences ranging from 22% to 88% and averaging 50%. Because effect sizes are still modest, however, these differences are not generally statistically distinguishable at p < .05, two-sided, with the notable exception of the Reframing Bravery message which has an effect 88% larger than the Baseline Informational message on the OTHERS scale.
Differences in effects for those who endorse liberty values partially confirm Study 1 (See S6 Appendix ). Compared to the Control message, the Reframing Bravery message is more effective among those who endorse liberty for encouraging social distancing—it increases DISTANCING measure by .027 units (90% CI: .009, .043), an effect that is 70% larger than the effect for those who do not endorse liberty values. This difference is not significant, however, and the estimates for the other outcomes are inconsistently signed. If we instead focus on the relative effectiveness of the Reframing Bravery message compared to the Baseline Informational message, a test that accounts for the fact that those who endorse liberty values may respond differently to the baseline content, we uncover more evidence that those who endorse liberty values respond more to the Reframing Bravery treatment. In particular, for those who endorse liberty values, the Reframing Bravery message is between 20% and 125% more effective than the Baseline message for the five primary outcomes. The largest difference is for the DISTANCING scale outcome, where the difference is .014 (90% CI: -.004, .033).
In addition to our scale outcomes, we also examine results for several individual items of particular interest, including the three measures of compliance with government policies to reduce the spread of COVID-19 discussed above: Self-isolation for those exposed, alerting authorities if testing positive, and cooperation with authorities in contact tracing. These items are included in the DISTANCING behavior index, but are also individually of interest because they are areas where governments have reported difficulty obtaining compliance. Fig 3 show that the Reframing Bravery message is associated with a statistically significant increase in self-isolation and willingness to alert authorities, effects that are larger than and statistically distinguishable from the effects of the Baseline Informational message. (Underlying regression results appear in S5 Appendix ) Similarly, the Other-regarding, Linear Cooperation message is associated with a statistically significant increase in self-isolation and willingness to cooperate in contact tracing, effects that are larger than and statistically distinguishable from the effects of the Baseline Informational message.
The Reframing Bravery and Other-regarding, Linear Cooperation message increase respondents reported intentions to not engage in key behaviors to reduce the spread of COVID-19 and to cooperate with government officials, even compared to the Baseline Informational message. This figure shows OLS regression coefficient estimates compared to the Control message with 95% confidence intervals. All outcomes scales were coded such that higher values indicate more positive attitudes or intentions toward social distancing.
https://doi.org/10.1371/journal.pone.0264782.g003
Second, we also examine effects for three isolated behaviors, attendance at religious gatherings and inside visits to a friend and family member’s house. Religious gatherings emerged as sources of conflict over prohibitions on group meetings ( 18 ), while private indoor meetings are thought to be vehicles by which asymptomatic individuals expose those who are at more serious risk for infection. Once again, these items are individually in the DISTANCING behavior index. Results appear in Fig 3 . The Reframing Bravery Message is associated with statistically significant increases in all three outcomes, while the Other-regarding, Linear Cooperation message is associated with changes in both the family and friend small gathering outcomes. The Reframing Bravery effect for attendance at religious services is statistically distinguishable from the effect of the Baseline Informational message (p < .05). The Other-regarding, Linear Cooperation effect for each type of private gatherings is also statistically larger than the effect of the Baseline Informational message (p < .03 and .05, respectively).
In Experiment 2 we find that the Baseline Informational message, the Other-regarding Linear Cooperation message, and the Reframing Bravery message outperform the placebo control message on the primary outcome scales, with the exception of the FOOD scale. Moreover, this experiment replicates the finding from Experiment 1 that respondents who are high in liberty values are more responsiveness to the Reframing Bravery message.
General discussion
The results presented here show that public health messaging can increase behavioral intentions and beliefs about social distancing that helps reduce the spread of COVID-19. Specifically, we observed that an Other-regarding, Linear Cooperation message that 1) focused people on protecting others, 2) increased the salience of risk presented by COVID-19, 3) emphasized that other people were social distancing, and 4) stated that every person who practices social distancing protects others was effective at increasing attitudes and behavioral intentions related to social distancing. We also found that a Reframing Bravery message that 1) gave examples of bravery, 2) reframe not social distancing as not being brave, but being reckless, and 3) emphasized that not social distancing is not attractive and places others at risk was effective. Importantly, these messages are effective in both an initial study fielded in May 2020 and in a replication study fielded in August 2020, and this efficacy is in comparison to a Baseline Informational message communicating the factual basis for social distancing behavior and instructing others to do so. We observe these effects for measures of a respondent’s own intended social distancing activities as well as for how individuals are likely to behave toward others who do not social distance.
It is also worth noting that a simple Baseline Informational message that invoked an injunctive norm that people should be social distancing and explained what social distancing was outperformed a placebo-control condition in Experiment 2. This suggests that relatively early in the pandemic simply providing people with information and emphasizing that doing these things is the correct behavior may be enough to increase attitudes toward social distancing and behavioral intentions to do so.
Moral foundations theory, [ 61 , 63 ] which postulates that humans have several underlying common values that are differentially emphasized by various individuals, has been used to explain health behaviors such as vaccination [ 64 ]. Increasingly, opposition to public health measures is grounded in the language of personal freedoms [ 64 ] and, indeed, concerns about government infringement on personal freedoms have arisen during the COVID-19 pandemic [ 65 , 66 ]. We find that emphasis on liberty value modifies the impact of the Reframing Bravery intervention indicating that such messages are particularly powerful for those for whom personal freedoms are important.
A potential avenue future research could explore how messaging strategies interact with people’s motivation for social distancing. Past research has found that many people engage in social distancing to protect themselves and to protect others [ 26 ]. However, other work has observed that people who endorsed conspiracy theories were more concerned about themselves and were also less likely to report intentions to practice social distancing [ 67 ]. Given heterogeneity in people’s motivations to protect themselves or to protect others, some messaging strategies, like the Other-regarding, Linear Cooperation message, may have different effects depending on whether it aligns with the motivation that a given individual holds. More broadly, future work should consider how people’s concern for themselves and concern for others interact with how receptive they are to specific public health campaigns.
This work has several limitations that should be considered alongside the results. First, while we observe robust attitudinal change in response to persuasive messaging, we do not observe actual behavioral change. Given the relatively small effect sizes, approximately 0.1 standard deviation increases on the primary outcomes in Experiment 2, these treatment messages as written communication may be insufficient to push people to change their behavior. Second, we utilized compound treatments that invoked many different constructs that are thought to produce attitude and behavioral change. Future work should focus on disentangling whether specific elements of the messages are particularly effective at promoting social distancing. Third, policymakers and public health experts had repeatedly emphasized the importance of social distancing and survey respondents may have over-reported their intentions to social distance due to social desirability concerns, though past work has found that reported behavioral intentions correlate with actual behavior [ 68 ] and people’s self-reported behavior is not affected by social desirability bias [ 69 ]. Third, as the COVID-19 pandemic has rapidly evolved and different behaviors, like masking or vaccination, have become more salient in public discourse, the messages that we find to be effective in summer 2020 may not be as effective as the pandemic has progressed. Finally, we only measured attitudes and behavioral intentions at a single point in time so we cannot make claims about the duration of the effects that we observe.
Our findings can inform both mass public health messaging initiatives (e.g. those deployed on social and electronic media) as well as interpersonal communication strategies such as healthcare provider-level communication and persuasion. While this work shows robust attitudinal changes in response to public health messaging, additional research is necessary to determine which specific elements of the treatments produced these changes.
Supporting information
S1 appendix. experiment 1 outcomes..
https://doi.org/10.1371/journal.pone.0264782.s001
S2 Appendix. Regression results for Fig 1 and distribution of outcomes for Experiment 1.
https://doi.org/10.1371/journal.pone.0264782.s002
S3 Appendix. Subgroup analyses for Experiment 1.
https://doi.org/10.1371/journal.pone.0264782.s003
S4 Appendix. Experiment 2 outcome measures.
https://doi.org/10.1371/journal.pone.0264782.s004
S5 Appendix. Regression results for Figs 2 and 3 and distribution of outcomes for Experiment 2.
https://doi.org/10.1371/journal.pone.0264782.s005
S6 Appendix. Liberty endorsement subgroup analysis for Experiment 2.
https://doi.org/10.1371/journal.pone.0264782.s006
- View Article
- Google Scholar
- PubMed/NCBI
- 10. Abel T, McQueen D. The COVID-19 pandemic calls for spatial distancing and social closeness: not for social distancing!: Springer; 2020. p. 231–.
- 20. Reid AE, Cialdini RB, Aiken LS. Social norms and health behavior. Handbook of behavioral medicine: Springer; 2010. p. 263–74.
- 46. Ostrom E. Governing the commons: The evolution of institutions for collective action: Cambridge university press; 1990.
- 52. Huppke R. Column: Trump wants ‘warrior’ Americans to face COVID-19 and reopen the country. You first, Mr. President.: Chicago Tribune; 2020 [cited 2021 October 18]. Available from: https://www.chicagotribune.com/columns/rex-huppke/ct-coronavirus-trump-warrior-economy-reopen-businesses-huppke-20200506-dmg7iwujc5fovdeurnv2xjjp4q-story.html .
- 53. Cathey L. ’I had to do it’: Trump suggests he got virus as act of political courage: ABC News; 2020 [cited 2021 October 18]. Available from: https://abcnews.go.com/Politics/trump-suggests-virus-act-political-courage/story?id=73452023 .
- 62. Huber GA. Encouraging Behavior to Reduce the Spread of COVID-19: Experimental Analysis.: OSF; 2020. Available from: osf.io/vpafh.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- News & Events
- Speeches by FDA Officials
- Remarks by Commissioner Stephen Hahn, M.D. — The COVID-19 Pandemic — Finding Solutions, Applying Lessons Learned - 06/01/2020
Speech | Virtual
Event Title Remarks by Commissioner Stephen Hahn, M.D. — The COVID-19 Pandemic — Finding Solutions, Applying Lessons Learned June 1, 2020
The COVID-19 Pandemic — Finding Solutions, Applying Lessons Learned
(Remarks as prepared for delivery. The text and video of this speech are slightly, though not substantively different from the version presented by Dr. Hahn on June 1 to the Alliance for a Stronger FDA, via audio broadcast only. Because of evolving scheduling challenges, it was not clear whether Dr. Hahn would be able to present the speech live and so it was recorded by video earlier. Ultimately, he did give the speech live to the Alliance, but only via an audio link. Given the minimal changes in the live version, we are posting the video version and the accompanying text.)
One of the most frustrating challenges each of us can face is the inability to control the events that affect our lives. Often, we are thrust into situations not of our own making. It’s no surprise that one of the most familiar adages concerns the best laid plans of mice and men going awry.
And yet, to borrow another often-used saying, necessity is the mother of invention. History teaches us that crises often lead to accelerated change and innovations and new discoveries.
This dynamic has been on my mind a great deal recently. It wasn’t too long ago – last December, to be exact -- that I had the distinction of being confirmed as the 24th Commissioner of the Food and Drug Administration.
This is the greatest honor of my life. I have long cherished the critical role the FDA plays in protecting and promoting the public health, and I’ve relied on the Agency’s expertise throughout my professional life.
So, I eagerly embraced my new responsibilities and the chance to make a real difference in public health. I was especially conscious that we live in a time of extraordinary scientific achievement, especially in oncology, with unprecedented opportunities to help make the lives of American patients and consumers healthier and safer.
I quickly immersed myself in the Agency’s broad and complex responsibilities, seizing every opportunity to learn about the FDA, both those areas with which I’d previously had minimum involvement, such as food policy, and those with which I had more familiarity, like cancer treatments and innovative clinical trial design.
I began to work with, and learn from, the agency’s extraordinary leadership team. I learned very quickly that the principles that have guided me throughout my life, such as my commitment to relying only on the best medical science and most rigorous data in support of advancing innovation and discovery, and my fundamental belief in promoting integrity and transparency in the scientific process, are the same principles that guide the FDA in both science and regulation.
So, I was in the midst of transitioning from being Chief Medical Executive at MD Anderson Cancer Center to being Commissioner of FDA when our entire world was turned upside down with the appearance of the novel COVID-19 coronavirus.
I certainly did not anticipate a public health emergency of this magnitude when I joined the agency. And I could not have imagined how significantly my new role would change and be shaped by this pandemic. I definitely could not have known that discussions about personal protective equipment (or PPE) or face masks or nasal swabs would be central to my work as Commissioner.
One thing was apparent: I would need to manage this evolving situation even as I was still learning about FDA.
From the very start I knew that even in a crisis situation – or perhaps especially because we are in a crisis situation – it is imperative that we maintain FDA’s high standards for evaluating products and making sure that the benefits outweigh potential harms.
To maintain our standard, I pledged to myself and emphasized to my new colleagues at FDA that our decisions would always be rooted in science. Having spent my entire career as a physician and scientist caring for patients with cancer, I’ve always valued highly a commitment to good data and sound science. I feel comfortable working with the scientists at FDA because I know they not only share that value, that commitment, but that they will tolerate nothing less. So, it was critical to me, as the pandemic escalated that this be reinforced as the guidepost for all of our decisions.
It may have been trial by fire, but I have the good fortune to work with an enormous number of talented individuals and teams who are helping guide us through this crisis. Every day they show extraordinary expertise, commitment, and resilience.
I also was able to call on many from outside the agency, including former FDA leaders as well as colleagues from the medical community.
What struck me was the uniformity of their advice. Those who formerly worked at FDA urged me to rely upon the FDA staff, many of whom have the experience to help manage a pandemic. My friends from outside the agency urged that we move quickly to make decisions, set direction and to be transparent about what we are doing. I have tried to follow all of this excellent advice.
Protecting the Food Supply
Since this crisis and the actions of the FDA have evolved so rapidly, let me summarize what we have done. I am confident that the FDA has measured up to this unprecedented challenge.
I want to start with the first word in the FDA’s name – food. Most of us take food safety for granted. But it takes a lot of hard work to maintain a safe food supply. This was true even before the COVID-19 pandemic but is especially challenging during an ongoing international crisis.
During the pandemic, through the collaboration of the FDA, the food industry and our federal and state partners, we have been able to maintain the safety of the nation’s food supply. Our Coordinated Outbreak Response and Evaluation team remained on the job, monitoring for signs of foodborne illness outbreaks and prepared to take action when needed.
And along with our federal partners, including CDC and USDA, we also have provided best practices for food workers, industry, and consumers on how to stay safe and keep food safe.
Diagnosing and Developing Treatments
On the medical side, we immediately committed to facilitating efforts to develop diagnostic tests, treatments and vaccines for the disease. We have helped facilitate increases in our national testing capacity, have helped ensure continued access to necessary medical products, and have sought to prevent the sale of fraudulent products.
If there’s one thing that’s been reaffirmed during this crisis, it’s the essential role of medical devices, including diagnostics, to countering this pandemic.
From the earliest days of our response, we worked to ensure that we had the essential medical devices, including personal protective equipment, to help treat those who are ill and to ensure that health care workers and others on the front line are properly protected.
To be sure, there were bumps along the road, but today we have an adequate supply of the devices that have been in unprecedented high demand such as PPE, ventilators, and others.
We’ve reviewed and issued emergency use authorizations for medical devices for COVID-19 at an incredibly fast pace.
And we’ve worked closely with many companies that don’t regularly make medical products but wanted to pitch in by making hand sanitizer, ventilators, or PPE.
There was a special focus on the development and availability of accurate and reliable COVID-19 tests. We need to know who has the disease and who has had it. This is essential if we are to understand this virus and return to a more normal lifestyle.
Since January, we’ve worked with hundreds of test developers, many of whom have submitted emergency use authorization requests to FDA for tests that detect the virus or antibodies to the virus.
As you have seen reported, early in the crisis we provided regulatory flexibility for developers with validated tests as outlined in our policies because public health needs dictated that we do as much testing as possible. But as the process has matured, we have helped increase the number of authorized tests, and we have adapted some of our policies to best serve the public need.
Today, if evidence arises that raises questions about a particular test’s reliability, we will take appropriate action to protect consumers from inaccurate tests. This is a dynamic process that is continually being informed by new data and evidence.
We’ve used a similar dynamic process in the search for therapeutic treatments and vaccines.
We are working closely with partners throughout the government and academia, and with drug and vaccine developers to explore, expedite, and incentivize the development of these products.
More than 90 drugs are being studied, and FDA is actively working with numerous vaccine sponsors, including three sponsors who have announced they have vaccine candidates that are now in clinical trials in the U.S. More than 144 clinical trials have been initiated for therapeutic agents, with hundreds more in the pipeline. We don’t have a cure or vaccine yet, but we’re on our way, at unprecedented speed.
Ultimately, of course, the way we’ll eventually defeat this virus is with a vaccine. FDA is working closely to provide technical assistance to federal partners, vaccine developers, researchers, manufacturers, and experts across the globe and exploring all possible options to advance the most efficient and timely development of vaccines, while at the same time maintaining regulatory independence.
Communicating and Educating
There is much more to do going forward, and that includes research, exploration and discovery, and communicating what we know.
As the country starts to reopen, it’s essential that the public understands what they need to do to continue to protect themselves. There has been a proliferation of information, and misinformation, on the internet and in other sources. Consumers need to understand that this virus is still with us and that we, as individuals and communities working together, need to take steps to continue to contain its spread.
The FDA has an important part to play in communicating public information to all populations in the U.S. FDA has increased outreach by developing and disseminating COVID-19 health education materials for consumers in multiple languages to diverse communities and the public overall. Everyone should have a clear understanding of why hand-washing and social distancing remain essential. Consumers need to think about how to shop for food safely. People need to know when to call their doctors and when to ask about getting tested. Health care professionals need to know how to manage their patients in this new environment, and how best to apply telemedicine, the use of which is rapidly accelerating.
I want the FDA to serve as a national resource for the public and health care community. I regard educating the public and providing accurate, reliable, up-to-date information as not just an Agency priority, but one of my own personal responsibilities as Commissioner. I will be out in public and in the media talking about how individuals can help us contain and conquer this virus.
I believe my personal experience with being self-quarantined will make me a better communicator. Being quarantined for 14 days in May was certainly no fun, but because we at FDA were already functioning very effectively virtually, I was able to continue to be fully engaged, and provide direction and leadership. And it made me even more focused on making sure consumers have all the information they need about self-protection.
We now need to look forward. A major strength of the FDA is not just in our response to a crisis, but in our ability to learn from the work we do and apply that experience in the future.
As this pandemic evolved, it was clear that some FDA processes needed to be adjusted to accommodate the urgency of the pandemic. I think the entire FDA team has now seen first-hand that we need to look at some of our processes and policies. I have instructed my staff to identify the lessons learned from this pandemic and what adjustments may be needed, not just to manage this or future emergencies, but to make FDA itself more efficient in carrying out our regulatory responsibilities.
I am committed to making sure that some of the lessons learned from managing this pandemic will lead to permanent improvements at the FDA in processes and policies.
For example, in facilitating the development of new treatments, we streamlined some of our processes.
We have taken a fresh look at how clinical trials should be designed and conducted. In a pandemic we knew we needed to get answers more quickly. For instance, early on, the FDA, National Institutes of Health, and industry worked together to facilitate the implementation of a “master protocol” that can be used in multiple clinical trials and allows for the study of more than one promising new drug for COVID-19 at a time. And we have used expanded access to meet the needs of patients who are not eligible or who are unable to participate in randomized clinical trials.
Many of the permanent changes that we will implement really represent an acceleration of where we were headed before. For example, the concept of decentralized clinical trials, in which trial procedures are conducted near the patient’s home and through use of local health care providers or local laboratories has been discussed before, and laid the foundation for some of the trials for COVID-19 products.
Another area where our pre-COVID work has informed our response to the pandemic involves the use of Real World Evidence (RWE).
In recent years, the agency has taken steps to leverage modern, rigorous analyses of real-world data—such as data from electronic health records, insurance claims, patient registries and lab results.
As the pandemic brought an urgency to these efforts, the FDA advanced collaborations with public and private partners to collect and analyze a variety of real-world data sources, using our Sentinel system and other resources.
Evaluation of real-world data has the potential to provide a wealth of rapid, actionable information to better understand disease symptoms, describe and measure immunity, and use available medical product supplies to help mitigate potential shortages. These data can also inform ongoing work to evaluate potential therapies, vaccines or diagnostics for COVID-19. The more experience we have with real world evidence, the more confidence we will have in using it for product decisions.
I mention real world evidence, but in reality, we have so many examples of how lessons learned from the pandemic will affect FDA in the future.
To the extent that the innovations and adaptations we implemented during the pandemic crisis worked and would be appropriate to implement outside of a pandemic situation, we will incorporate them into standard FDA procedures. And to the extent that we identified unnecessary barriers, we will remove them. This is one of my top priorities. Permanent change where needed will take place, and will make FDA an even stronger agency.
As I mentioned before, anything that enables quicker reviews and authorizations we will seek to make permanent.
But make no mistake. We will not cut corners on safety or effectiveness. I said this before, and I say it again. Good science as the basis for decision making has been a hallmark of my career, and is a value that I hold deeply. The American public must have confidence in the products regulated by the FDA.
Speed is important, but so are safety, accuracy and effectiveness.
FDA’s commitment to good science and rigorous data is unwavering, even as we look at how we can learn from this pandemic.
I am hopeful that this is a once-in-a-lifetime experience for all of us. An unprecedented historic event that has required an unprecedented response from us and everyone around the world.
That said, I am pleased that throughout this crisis the rest of the FDA’s work has continued, with relatively few interruptions. New drugs and devices have been authorized. Our food safety surveillance has adapted and our outbreak response resources have been maintained. Our oversight of tobacco products, including e-cigarettes, has gone on. The Agency has measured up to the challenge in all ways.
And we are well positioned as we move into a new phase, that is, transitioning back to what has come to be known as the “new normal.” Our staff has done a phenomenal job of adapting to this new normal. And I am confident that they are ready to deal with any additional upcoming challenges.
I will close with something I’ve seen reaffirmed time and time again over the past few months. That is the essential role that the FDA plays in consumer protection and beyond in advancing public health.
Before coming to the FDA, I had heard about the extraordinary dedication of the agency’s workforce. Working side by side with my colleagues in response to this pandemic, I’ve seen that characterization validated over and over.
It is my great honor to serve with so many highly skilled and committed professionals. And the American people can be assured that this agency is working around the clock for them, doing whatever is necessary to fulfill our mission to protect and promote the health of the American public.
I encourage you all to stay safe, aware, and focused as we continue to respond to the challenges of this public health emergency.
- Federal Reserve Facebook Page
- Federal Reserve Instagram Page
- Federal Reserve YouTube Page
- Federal Reserve Flickr Page
- Federal Reserve LinkedIn Page
- Federal Reserve Threads Page
- Federal Reserve Twitter Page
- Subscribe to RSS
- Subscribe to Email
- Recent Postings
- Publications
Board of Governors of the Federal Reserve System
The Federal Reserve, the central bank of the United States, provides the nation with a safe, flexible, and stable monetary and financial system.
- News & Events
August 26, 2020
The Pandemic’s Effect on the Economy and Banking
Governor Michelle W. Bowman
At the Kansas Bankers Association CEO and Senior Management Forum/Annual Meeting, Topeka, Kansas (via webcast)
Good afternoon. It's great to be with you, and I look forward to our discussion. As you all know, the COVID-19 pandemic has caused significant disruption and hardship in nearly every aspect of our lives, and it continues to weigh heavily on our national economy, which is why it will be the central focus of my remarks here today. Let me set the stage for our discussion by outlining the economic effects of the pandemic most relevant to the banking sector, describing the Federal Reserve's response to the crisis, and then making some observations about conditions for smaller banks.
The Pandemic's Effects on the Economy and Banking We began this year with the economy in excellent shape—by some measures the strongest in decades. From my seat as a monetary policymaker, we appeared to be in a good position regarding both legs of our dual mandate, which are maximum employment and stable prices.
But that picture was dramatically altered with the onset of the COVID-19 pandemic. Efforts to contain the spread of the virus caused a sudden stop in economic activity during March and April. While the extent of the closures and shutdowns varied widely throughout the country, the sudden loss of employment and the contraction in output were like nothing our nation has experienced before.
The decline in activity was mostly due to temporary business closures, and the economy has bounced back noticeably in recent months as businesses reopen and fiscal support was distributed to many Americans. Even so, the economy is still far from back to normal. The future course and timing of the recovery is still highly uncertain, and its pace and intensity are likely to vary across areas of the country—heavily influenced by the decisions of state and local governments. That speaks to another aspect of this episode that is unusual—how the timing and severity of the pandemic's impact seem to differ greatly from one area to the next.
Among Kansas's major industries, oil and gas production and equipment manufacturing have been hurt by the worldwide slump in energy demand. Aviation manufacturing has been hit hard by the downturn and by the uncertainty over the recovery in air travel. Agriculture continues to face challenges but is faring somewhat better than many sectors of the economy. Ag producers are still facing tough financial conditions, including the low commodity price environment. While most indications are that agriculture land prices continue to hold fairly steady, I have seen some reports that less-productive land has been showing some hints of cracks in valuations.
Turning to employment, nationwide, we know that the initial job losses were heavily concentrated among the most financially vulnerable, including lower-wage workers, young people, women, and minority groups. According to the Fed's latest Report on The Economic Well-Being of U.S. Households , 20 percent of people surveyed in April reported a recent job loss. Among those surveyed who live in households with annual incomes below $40,000, the reported job loss was nearly double that, at around 40 percent. 1 That said, both of those figures are likely to include a number of layoffs due to pandemic-related shutdowns of businesses that were hopefully only temporary.
Households were in a generally strong financial position at the beginning of this year, but the restrictions implemented to fight COVID-19 resulted in an unprecedented spike in unemployment, which likely led to a number of families finding it difficult to keep up with their payment obligations. That is especially true for lower-income households, which may have had much less of a financial cushion before the onset of the crisis. Along with our monetary policy actions, stimulus checks and enhanced unemployment benefits provided in the CARES Act have been a substantial and timely source of financial support to households during this difficult time.
Understanding the financial stress this could place on many borrowers, the Fed and other federal regulators implemented guidance to encourage banks to work with their borrowers. By mid-July, only around 8 percent of outstanding residential mortgage loans were in forbearance, well below what many industry observers had feared. It remains possible that the economic challenges will persist beyond the forbearance time period provided in the CARES Act, and if so, we would almost certainly see some of these loans transition into longer-term delinquency status or enter into renewed deferment periods. Thus far, however, the data have been encouraging.
Turning to the impact on businesses, we know the effects have been most severe in the services sector, especially travel, leisure, and hospitality. To give some sense of the losses, employment in the leisure and hospitality sectors nationwide was down nearly 40 percent in the 12 months through May and still down about 25 percent through July. Retail employment fell 15 percent over March and April, though it has recovered substantially since then, and in July it was 6 percent below the pre-COVID level.
It is encouraging to see that even those sectors most heavily affected by the crisis are finding ways to innovate. Stores are adjusting hours and ramping up delivery, restaurants are changing menus and creating outdoor space, distilleries shifted from making bourbon to hand sanitizers, and independent businesses that hadn't previously relied heavily on technology are now using it to stay connected to customers and regulate workflow.
Timely and supportive fiscal and monetary policy measures also have helped, but with the progress of the recovery still tentative, I expect that many businesses will continue to fight for survival in the months ahead, with the support of their lenders and communities.
Looking ahead, the economic outlook will continue to evolve quickly. We experienced a pronounced and very welcome bounceback in national retail spending and housing activity over the early summer months. We also saw positive news on progress toward a vaccine and in the effective treatment of patients. Even so, positive cases and hospitalizations have risen in some areas and continue to weigh on some regions and the overall economy. As Chair Powell has noted, the timeline for the recovery is highly uncertain and will depend heavily on the course of the pandemic. We must therefore recognize that progress toward a full recovery in economic activity may well be slow and uneven
The Fed's Response to the Pandemic Now let me turn to the Federal Reserve's role in the government's response to the pandemic. During the initial phase of the crisis, we took a number of actions to stabilize financial markets that came under intense stress, including purchasing sizable amounts of Treasury and mortgage-backed securities. To support households and businesses, the Fed quickly lowered our target for the federal funds rate, which has helped to lower borrowing costs but created a different challenge for financial institutions—depressed net interest margins. The Fed has also supported actions by Congress and the administration by creating a number of new emergency lending programs. These programs were designed to restore and sustain proper functioning in certain financial markets that had seized up in March and to facilitate the continued flow of credit from banks to households and businesses.
One federal stimulus program that relied heavily on the participation and expertise of community bankers is the Paycheck Protection Program (PPP). Working through banks, the PPP program has delivered more than $500 billion to small businesses to help them weather the storm. Community bankers played a crucial role in getting these funds to businesses that needed it, showing once again how essential community banks are to the customers they serve. And in response to feedback we received from a number of community bankers, the Fed created the PPP lending facility to alleviate balance-sheet capacity issues for banks that otherwise would not have been able to provide PPP loans to their small-business customers.
The PPP was created to help small businesses keep their employees on staff, and the Main Street Lending program is designed to support lending to mid-sized businesses through the recovery. The Federal Reserve has not engaged in lending directly to businesses before, but it was a step that seemed appropriate considering the breadth and depth of the challenges we face. We continue to solicit feedback and make adjustments to the program based on the suggestions received from bankers and other stakeholders, and we continue to welcome your thoughts and ideas on how we can make Main Street more effective. I would be interested to visit with those who may already have experience with this new loan program, and I would also be interested to hear about how you plan to use it to meet the needs of your business customers.
Together, these policy actions have helped stabilize financial markets, boost consumer and business sentiment, and assist millions of households and thousands of businesses harmed by the response to the pandemic. Credit markets, which had seized up earlier this year, have resumed functioning.
In our other role as a prudential regulator and bank supervisor, the Federal Reserve took several steps intended to reduce burden on banks and help them focus on the needs of their customers and communities.
Together, with our fellow federal regulators, we delayed the impact of the CECL accounting standard in our capital rules and temporarily eased the leverage ratio requirement for community banks. We also delayed reporting dates for Call Reports and other data collections. In addition, to address concerns about real estate appraisal delays, we provided temporary relief from certain appraisal requirements.
From a supervisory perspective, beginning in late March the Fed paused examinations for most small banks and took steps to lengthen remediation timeframes for outstanding issues. We considered the exam pause an important step to provide bankers time to adjust operations to protect the health of customers and employees, to prioritize the financial needs of their customers and communities, and to play an essential and vital role in implementing critical relief programs like the PPP.
As we continue to support the recovery and work to ensure that supervision and examination is as effective and efficient as possible, I think it's important to hear directly from you, who are actually working in the economy, about the conditions facing your communities and any challenges impeding your ability to meet the needs of your customers. In addition to my regular outreach to community banks, I am currently engaged in an effort to speak with every CEO of the more than 650 community banks supervised by the Fed. I want to hear directly from bankers about what you are seeing and your thoughts and ideas about the recovery. These conversations are incredibly valuable to me as a bank regulator and policymaker. They give context to the mountains of data we analyze and a unique perspective with real-world local examples to a complex and dynamic economic picture. For those of you from Fed member banks who I have not yet had the opportunity to meet or speak with by phone in these times of COVID, I look forward to our conversation. Your local Reserve Bank will be in contact to find a convenient time for us to meet.
Conditions for Smaller Banks This audience knows better than most that smaller banks entered the pandemic in strong condition. At the end of 2019, over 95 percent of community and regional banks supervised by the Fed were rated a 1 or 2 under the CAMELS rating system. After coming through the last financial crisis in generally stronger condition than larger banks, smaller institutions had strengthened their capital positions and substantially improved asset quality in the years since, leaving them better positioned to deal with the current stress related to the pandemic. Likewise, credit concentrations, especially in construction and commercial real estate, were lower for smaller banks than at the outset of the last financial crisis, and risk management of concentrations improved over the last decade. Smaller banks also entered the pandemic with high levels of liquidity, and this liquidity has further improved with deposit inflows associated with pandemic-related stimulus programs.
Overall, community and regional banks remain well positioned to continue to extend credit and play an essential role in supporting our nation's recovery from the effects of COVID-19.
With this in mind, on June 15 the Federal Reserve announced our plan to resume bank examinations. We recognize the unique and challenging conditions under which the industry has been operating, and we will certainly consider that as we resume examinations. Our initial focus will be to assess higher risk banks, particularly those with credit concentrations in higher risk or stressed industries. Finally, we will continue to be sensitive to the capacity of each bank to participate in examinations and strive to prevent undue burden on banks struggling with crisis-related operational challenges.
The Road Ahead Like many native Kansans, I am an eternal optimist, so let me end my formal remarks on a hopeful note. While the road ahead is highly uncertain, and we don't yet know when the economy will return to its previous strength, America will recover from this crisis, as it has from all of our past challenges. Our economic fundamentals are strong, and we have the solid foundation of the entrepreneurial spirit and resiliency of the American people. For its part, the Federal Reserve will continue to monitor progress and respond promptly and flexibly to support the recovery. We will closely watch economic and financial conditions, and we will use our monetary policy tools to respond as appropriate to pursue our dual mandate of maximum employment and price stability. We will also remain open to further adjustments to supervisory schedules and expectations, as needed.
Thank you for the opportunity to speak with you today. I look forward to our discussion.
1. Board of Governors of the Federal Reserve System, Report on the Economic Well-Being of U.S. Households in 2019 - May 2020 (Washington: Board of Governors, May 2020). Return to text
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Persuasive messaging to increase COVID-19 vaccine uptake intentions
Affiliations.
- 1 Yale Institute for Global Health, New Haven, CT, USA; Department of Internal Medicine, Section of Infectious Diseases, Yale School of Medicine, New Haven, CT, USA.
- 2 Institution for Social and Policy Studies, Yale University, New Haven, CT, USA; Center for the Study of American Politics, Yale University, New Haven, CT, USA.
- 3 Institution for Social and Policy Studies, Yale University, New Haven, CT, USA; Center for the Study of American Politics, Yale University, New Haven, CT, USA; Department of Political Science, Yale University, New Haven, CT, USA.
- 4 Yale Institute for Global Health, New Haven, CT, USA; Department of Internal Medicine, Section of Infectious Diseases, Yale School of Medicine, New Haven, CT, USA; Department of Epidemiology of Microbial Diseases, Yale School of Public Health, New Haven, CT, USA; Yale School of Nursing, West Haven, CT, USA.
- 5 Institution for Social and Policy Studies, Yale University, New Haven, CT, USA; Center for the Study of American Politics, Yale University, New Haven, CT, USA; Department of Political Science, Yale University, New Haven, CT, USA. Electronic address: [email protected].
- PMID: 34774363
- PMCID: PMC8531257
- DOI: 10.1016/j.vaccine.2021.10.039
Widespread vaccination remains the best option for controlling the spread of COVID-19 and ending the pandemic. Despite the considerable disruption the virus has caused to people's lives, many people are still hesitant to receive a vaccine. Without high rates of uptake, however, the pandemic is likely to be prolonged. Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective action problem and highlighting the prosocial benefit of vaccination or the reputational costs that one might incur if one chooses not to vaccinate. Another subgroup of messages built on contemporary concerns about the pandemic, like issues of restricting personal freedom or economic security. We find that persuasive messaging that invokes prosocial vaccination and social image concerns is effective at increasing intended uptake and also the willingness to persuade others and judgments of non-vaccinators. We replicate this result on a nationally representative sample of Americans and observe that prosocial messaging is robust across subgroups, including those who are most hesitant about vaccines generally. The experiments demonstrate how persuasive messaging can induce individuals to be more likely to vaccinate and also create spillover effects to persuade others to do so as well. The first experiment in this study was registered at clinicaltrials.gov and can be found under the ID number NCT04460703 . This study was registered at Open Science Framework (OSF) at: https://osf.io/qu8nb/?view_only=82f06ecad77f4e54b02e8581a65047d7.
Copyright © 2021 Elsevier Ltd. All rights reserved.
PubMed Disclaimer
Conflict of interest statement
Declaration of Competing Interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Experiment 1. Messages that frame…
Experiment 1. Messages that frame vaccination as a cooperative action to protect others…
Experiment 2. The Not Bravery,…
Experiment 2. The Not Bravery, Community Interest, and Community Interest + Embarrassment messages…
Similar articles
- The Efficacy of a Brief, Altruism-Eliciting Video Intervention in Enhancing COVID-19 Vaccination Intentions Among a Population-Based Sample of Younger Adults: Randomized Controlled Trial. Zhu P, Tatar O, Griffin-Mathieu G, Perez S, Haward B, Zimet G, Tunis M, Dubé È, Rosberger Z. Zhu P, et al. JMIR Public Health Surveill. 2022 May 30;8(5):e37328. doi: 10.2196/37328. JMIR Public Health Surveill. 2022. PMID: 35544437 Free PMC article. Clinical Trial.
- Video-based messages to reduce COVID-19 vaccine hesitancy and nudge vaccination intentions. Jensen UT, Ayers S, Koskan AM. Jensen UT, et al. PLoS One. 2022 Apr 6;17(4):e0265736. doi: 10.1371/journal.pone.0265736. eCollection 2022. PLoS One. 2022. PMID: 35385505 Free PMC article.
- Information From Same-Race/Ethnicity Experts Online Does Not Increase Vaccine Interest or Intention to Vaccinate. Gadarian SK, Goodman SW, Michener J, Nyhan B, Pepinsky TB. Gadarian SK, et al. Milbank Q. 2022 Jun;100(2):492-503. doi: 10.1111/1468-0009.12561. Epub 2022 Mar 22. Milbank Q. 2022. PMID: 35315950 Free PMC article. Clinical Trial.
- Effect of persuasive messaging about COVID-19 vaccines for 5- to 11-year-old children on parent intention to vaccinate. Kaufman J, Steffens MS, Hoq M, King C, Marques MD, Mao K, Bullivant B, Danchin M. Kaufman J, et al. J Paediatr Child Health. 2023 Apr;59(4):686-693. doi: 10.1111/jpc.16374. Epub 2023 Feb 18. J Paediatr Child Health. 2023. PMID: 36807943 Clinical Trial.
- International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Robinson E, Jones A, Lesser I, Daly M. Robinson E, et al. Vaccine. 2021 Apr 8;39(15):2024-2034. doi: 10.1016/j.vaccine.2021.02.005. Epub 2021 Feb 6. Vaccine. 2021. PMID: 33722411 Free PMC article. Review.
- The power of the family in times of pandemic: Cross-country evidence from 93 countries. Gu M. Gu M. SSM Popul Health. 2024 Jul 4;27:101698. doi: 10.1016/j.ssmph.2024.101698. eCollection 2024 Sep. SSM Popul Health. 2024. PMID: 39139826 Free PMC article.
- Unraveling Herpes Zoster Vaccine Hesitancy, Acceptance, and Its Predictors: Insights From a Scoping Review. Wang X, Shang S, Zhang E, Dai Z, Xing Y, Hu J, Gao Y, Fang Q. Wang X, et al. Public Health Rev. 2024 Jul 24;45:1606679. doi: 10.3389/phrs.2024.1606679. eCollection 2024. Public Health Rev. 2024. PMID: 39113825 Free PMC article. Review.
- Behavioral nudges in social media ads show limited ability to encourage COVID-19 vaccination across countries. Çat O, Chang J, Hlatky R, Li H, Nielson DL. Çat O, et al. PNAS Nexus. 2024 Aug 6;3(8):pgae189. doi: 10.1093/pnasnexus/pgae189. eCollection 2024 Aug. PNAS Nexus. 2024. PMID: 39108305 Free PMC article.
- Presidents and vaccines: head of state inoculation as a tool for vaccine promotion. Collart L, Lunanga E, Stoop N, Verpoorten M. Collart L, et al. Front Public Health. 2024 May 14;12:1364927. doi: 10.3389/fpubh.2024.1364927. eCollection 2024. Front Public Health. 2024. PMID: 38808000 Free PMC article.
- Assessment of COVID-19 Messaging Strategies to Increase Testing for Students With Intellectual and Developmental Disabilities. Walsh TJ, Kalb LG, Gemmell M, Liu J, Caburnay CA, Gurnett CA, Newland JG; COMPASS‐T Study Group. Walsh TJ, et al. J Sch Health. 2024 Jun;94(6):551-561. doi: 10.1111/josh.13448. Epub 2024 Mar 29. J Sch Health. 2024. PMID: 38551064 Clinical Trial.
- Funk C., Tyson A. (Pew Research Center Science & Society); 2020. Intent to get a COVID-19 vaccine rises to 60% as confidence in research and development process increases.
- Bauch C.T., Galvani A.P., Earn D.J.D. Group interest versus self-interest in smallpox vaccination. Proc Natl Acad Sci. 2003;100(18):10564–10567. - PMC - PubMed
- Bauch C.T., Earn D.J.D. Vaccination and the theory of games. Proc Natl Acad Sci. 2004;101(36):13391–13394. - PMC - PubMed
- Böhm R., Betsch C., Korn L. Self-rational non-vaccination: Experimental evidence from an interactive vaccination game. J Econ Behav Organ. 2016;131:183–195.
- Böhm R., Betsch C., Korn L., Holtmann C. Exploring and promoting prosocial vaccination: a cross-cultural experiment on vaccination of health care personnel. Biomed Res Int:6870984. 2016;2016:1–9. - PMC - PubMed
Publication types
- Search in MeSH
Associated data
- Search in ClinicalTrials.gov
Related information
Grants and funding.
- UL1 TR001863/TR/NCATS NIH HHS/United States
LinkOut - more resources
Full text sources.
- ClinicalKey
- Elsevier Science
- Europe PubMed Central
- PubMed Central
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
VIDEO
COMMENTS
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus. Check out some examples of persuasive speeches on Covid-19:
Examples of Persuasive Speeches About Covid-19. Writing a persuasive speech about anything can seem daunting. However, writing a persuasive speech about something as important as the Covid-19 pandemic doesnâ t have to be difficult. So let's explore some examples of perfectly written persuasive essays.
Drawing inspiration from Boin, Stern and Sundelius', work on persuasive narratives, this study shows the ways that Solberg's posts about COVID-19 exhibit all five identified frame functions.
Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective action problem and highlighting the prosocial benefit of vaccination or the ...
COVID-19: Social distancing Olivia Gray Overview Introduction 1. Thematic statement 2. How social distancing and safety precautions help decrease amount of cases 3. Protests against social distancing and masks, the impact on economy and the people 4. How the United States should
DOI: 10.1001/JAMA.2020.7308. The author discusses the economic and healthcare crisis the COVID-19 pandemic created. The projections drawn in the paper predict a 10 to 25% contraction of the US economy in the second quarter. The writer asserts that the United States has entered a COVID-19 recession.
COVID-19 and the Economy. Chair Jerome H. Powell. At the Hutchins Center on Fiscal and Monetary Policy, The Brookings Institution, Washington, D.C. (via webcast) Watch Live. Good morning. The challenge we face today is different in scope and character from those we have faced before. The coronavirus has spread quickly around the world, leaving ...
About this speech. Joe Biden. ... As the Delta variant of the Covid-19 virus spreads and cases and deaths increase in the United States, President Joe Biden announces new efforts to fight the pandemic. He outlines six broad areas of action--implementing new vaccination requirements, protecting the vaccinated with booster shots, keeping children ...
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
During the COVID-19 pandemic, disinformation played a major part in sowing division and undermining the authority of health officials, Gauri says. That paved the way for fast viral spread and low ...
Look to the science of persuasion, says communications professor Dominique Brossard, PhD. Brossard is part of a new National Academies of Science, Engineering, and Medicine group called the Societal Experts Action Network, or SEAN, whose recent report lays out research-based strategies to encourage COVID-19-mitigating behaviors.. Brossard says the changes must feel easy to do—and to repeat ...
Published: April 14, 2021 8:38am EDT. X (Twitter) Persuading people to get a COVID-19 vaccine remains a challenge even as more than a 120 million people in the U.S. have received at least one dose ...
19 Response and Vaccination. Program. 1:41 P.M. EDT. THE PRESIDENT: Good afternoon. Today, the Vice President and I would like to lay out our plan for June, to counter — continue, I should say ...
Such articles convey messages from governors, public health experts, physicians, COVID-19 patients, and residents of outbreak areas, encouraging people to stay at home. This is the first study to examine which narrator's message is most persuasive in encouraging people to do so during the COVID-19 pandemic and social lockdown.
The severity of Covid-19 symptoms varies widely. Symptoms aren't always present. The typical symptoms are high temperatures, a dry cough, and difficulty breathing. Covid - 19 individuals also exhibit other symptoms such as weakness, a sore throat, muscular soreness, and a diminished sense of smell and taste.
The media's core message on the coronavirus is that even if we behave, coronavirus will change life as we know it for years to come: massive job loss, disease, and yes, death, rivaling the ...
Biden on Fighting the COVID-. 19. Pandemic. Briefing Room. Speeches and Remarks. East Room. 4:31 P.M. EDT. THE PRESIDENT: Good afternoon. I'd like to make an important announcement today in our ...
What types of public health messages are effective at changing people's beliefs and intentions to practice social distancing to slow the spread of COVID-19? We conducted two randomized experiments in summer 2020 that assigned respondents to read a public health message and then measured their beliefs and behavioral intentions across a wide variety of outcomes. Using both a convenience sample ...
19. Pandemic. Briefing Room. Speeches and Remarks. 5:02 P.M. EDT. THE PRESIDENT: Good evening, my fellow Americans. I want to talk to you about where we are in the battle against COVID-19, the ...
The COVID-19 Pandemic — Finding Solutions, Applying Lessons Learned (Remarks as prepared for delivery. The text and video of this speech are slightly, though not substantively different from the ...
Speeches and Remarks. South Court Auditorium. Eisenhower Executive Office Building. 12:54 P.M. EDT. THE PRESIDENT: Good afternoon. I've just been briefed by my COVID-19 team on the progress we ...
But that picture was dramatically altered with the onset of the COVID-19 pandemic. Efforts to contain the spread of the virus caused a sudden stop in economic activity during March and April. While the extent of the closures and shutdowns varied widely throughout the country, the sudden loss of employment and the contraction in output were like ...
Without high rates of uptake, however, the pandemic is likely to be prolonged. Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective ...