- Search by keyword
- Search by citation
Page 1 of 27

Redesign of a virtual reality basic life support module for medical training – a feasibility study
Healthcare providers, including medical students, should maintain their basic life support (BLS) skills and be able to perform BLS in case of cardiac arrest. Research shows that the use of virtual reality (VR)...
- View Full Text
Assessment of the effectiveness of hospital external disaster functional drills on health care receivers’ performance, using standardized patients and mass cards simulation: a pilot study from Saudi Arabia
Given the increasing frequency of disasters globally, it is critical that healthcare systems are prepared for these mass casualty events. The Saudi health system’s preparedness for mass casualty incidents need...
The impact of ketamine on emergency rapid sequence intubation: a systematic review and meta-analysis
Rapid sequence intubation (RSI) is a crucial step in the resuscitation process for critically ill patients, and the judicious use of sedative drugs during RSI significantly influences the clinical outcomes of ...
Characteristics of trauma patients treated by Helicopter Emergency Medical Service and transported to the hospital by helicopter or ambulance
Trauma patients treated by the Helicopter Emergency Medical Services (HEMS) can be transported to the hospital either by helicopter or by ambulance, in both cases accompanied by the HEMS physician. The objecti...
Behind the scenes: a qualitative study on threats and violence in emergency medical services
The increasing prevalence of threats and violence against ambulance clinicians is a critical issue that has not been adequately studied. These incidents pose significant challenges to the provision of prehospi...
Valued technical and non-technical skills among disaster responders: a cross sectional study of disaster responders involved in the earthquake in Türkiye and Syria January 2023
Disaster responders are an important part of disaster response. However, despite large efforts to train disaster responders, there is a limited scientific knowledge regarding which competences and skills such ...
Length of stay and associated factors among pediatric patients in the pediatric emergency unit of the Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia
Length of stay in the emergency department is used as a quality indicator to gauge the overall efficiency of emergency care. The performance measure was used to evaluate the quality of care provided in the eme...
Hybrid emergency care at the home for patients – A multiple case study
Healthcare systems worldwide are facing numerous challenges, such as an aging population, reduced availability of hospital beds, staff reductions and closure of emergency departments (ED). These issues can exa...
Evaluation of stabbing assault injuries in a tertiary emergency department: a retrospective observational study
Approximately 458,000 victims were deceased from intentional violence in 2021. A stabbing assault causes 25% of homicides. The study aims to evaluate injury patterns, trauma scores, radiological findings, type...
Factors affecting neurological outcomes of patients with sudden cardiac arrest in the emergency department
Little is known about patients with sudden cardiac arrest in the emergency department (ED). This study aimed to identify factors affecting the prognosis of patients with cardiac arrest in the ED.
Redirection of low-acuity emergency department patients to nearby medical clinics using an electronic medical support system: effects on emergency department performance indicators
Overcrowded emergency departments (EDs) are associated with higher morbidity and mortality and suboptimal quality-of-care. Most ED flow management strategies focus on early identification and redirection of lo...
Prevalence, predictors and outcomes of self-reported feedback for EMS professionals: a mixed-methods diary study
Providing feedback to healthcare professionals and organisations on performance or patient outcomes may improve care quality and professional development, particularly in Emergency Medical Services (EMS) where...
Prehospital neurological emergencies– a survey on the state of prehospital neurological assessment by emergency medical professionals
Neurological emergencies are one of the major diagnosis groups in the Emergency Medical Services (EMS) with the highest rate of misdiagnosis. Despite the knowledge of time sensitivity and the importance of pre...
Comparing NEWS2, TRISS, and RTS in predicting mortality rate in trauma patients based on prehospital data set: a diagnostic study
In the recent years, National Early Warning Score2 (NEWS2) is utilized to predict early on, the worsening of clinical status in patients. To this date the predictive accuracy of National Early Warning Score (N...
Violent encounters on the front line: Sequential explanatory mixed-methods investigation of physical violence factors in the prehospital setting
Workplace violence (WPV) is an important issue in prehospital care, especially for emergency medical technicians ( EMTs) who are at increased risk of physical violence due to the nature of their work. This stu...
Comparison of Modified Early Warning Score (MEWS), Simplified Acute Physiology Score II (SAPS II), Sequential Organ Failure Assessment (SOFA), and Acute Physiology and Chronic Health Evaluation II (APACHE II) for early prediction of septic shock in diabetic patients in Emergency Departments
Sepsis is a severe medical condition that can be life-threatening. If sepsis progresses to septic shock, the mortality rate increases to around 40%, much higher than the 10% mortality observed in sepsis. Diabe...
Place of telemedicine in the organization of emergency care: feasibility and benefits
Telemedicine encompasses all medical practices that allow patients to be remotely cared for through new information and communication technologies. This study aims to assess the remote management of patients c...
Exploring the challenges of emergency medical service providers in the initial phase of the COVID-19 pandemic: a qualitative content analysis
As the COVID-19 pandemic continues to unfold, there has been a substantial increase in the demand for prehospital services. Emergency medical service (EMS) providers have encountered a myriad of challenges tha...
Emergency pediatric patients and use of the pediatric assessment triangle tool (PAT): a scoping review
We conducted a scoping review of the evidence for the use of the Pediatric Assessment Triangle (PAT) tool in emergency pediatric patients, in hospital and prehospital settings. We focused on the psychometric p...
Quality and safety in prehospital airway management – retrospective analysis of 18,000 cases from an air rescue database in Germany
Prehospital airway management remains crucial with regard to the quality and safety of emergency medical service (EMS) systems worldwide. In 2007, the benchmark study by Timmermann et al. hit the German EMS co...
The challenges of delivery in pre-hospital emergency medical services ambulances in Iran: a qualitative study
Although unplanned deliveries in ambulances are uncommon, Emergency Medical Services (EMS) providers may encounter this situation before reaching the hospital. This research aims to gather insights from Emerge...
Take-home naloxone administered in emergency settings: feasibility of intervention implementation in a cluster randomized trial
Opioids kill more people than any other class of drug. Naloxone is an opioid antagonist which can be distributed in kits for peer administration. We assessed the feasibility of implementing a Take-home Naloxon...
Negotiating grey areas: an interview-based analysis of paramedic uncertainty and decision-making in cardiac arrest events
Paramedics are responsible for critical resuscitation decisions when attending Out of Hospital Cardiac Arrests (OHCA). Existing research indicates that a range of clinical and non-clinical factors moderate the...
The impact of surge capacity enhancement training for nursing managers on hospital disaster preparedness and response: an action research study
Hospitals as the main providers of healthcare services play an essential role in the management of disasters and emergencies. Nurses are one of the important and influential elements in increasing the surge ca...
Paramedics’ experiences and observations: work-related emotions and well-being resources during the initial months of the COVID-19 pandemic—a qualitative study
As first responders, paramedics are an extremely important part of the care chain. COVID-19 significantly impacted their working circumstances. We examined, according to the experiences and observations of par...
Psychometric properties of the Farsi version of the Disaster Nursing Readiness Evaluation Index (F-DNREI)
Considering the vital role of nurses in responding to disasters, it is essential to measure their readiness with a valid and reliable tool. The present study aimed to assess the psychometric properties of the ...
Severe hyperlactatemia in the emergency department: clinical characteristics, etiology and mortality
Severe hyperlactatemia (lactate level ≥ 10 mmol/L) is associated with high mortality rates in critically ill patients. However, there is limited data on emergency department (ED) patients. We aimed to investig...
Identification of avoidable patients at triage in a Paediatric Emergency Department: a decision support system using predictive analytics
Crowding has been a longstanding issue in emergency departments. To address this, a fast-track system for avoidable patients is being implemented in the Paediatric Emergency Department where our study is condu...
Establishing a common ground: the future of triage systems
Triage systems, crucial for Emergency Departments, face unresolved doubts and issues that have not been addressed, coupled with increasing fragmentation due to a growing body of new evidence. International col...
Abated crowding by fast-tracking the Throughput component of the ED for patients in no need of hospitalization with competency managed personnel
Emergency department (ED) crowding is a major patient safety concern and has a negative impact on healthcare systems and healthcare providers. We hypothesized that it would be feasible to control crowding by e...
Oxygen accumulation and associated dangers in rescue helicopters
At the time of the COVID-19 pandemic, devastating incidents increased due to frequent oxygen administration to patients. The dangers associated with the use of oxygen, especially through local enrichments and ...
Correction: Systemic review of age brackets in pediatric emergency medicine literature and the development of a universal age classification for pediatric emergency patients - the Munich Age Classification System (MACS)
The original article was published in BMC Emergency Medicine 2023 23 :77
Validation of a checklist to facilitate serious illness conversations in adult emergency in China: a single-centre pilot study
Advances in emergency and critical care have improved outcomes, but gaps in communication and decision-making persist, especially in the emergency department (ED), prompting the development of a checklist to a...
A retrospective analysis of the need for on-site emergency physician presence and mission characteristics of a rural ground-based emergency medical service
This study aimed to address the challenges faced by rural emergency medical services in Europe, due to an increasing number of missions and limited human resources. The primary objective was to determine the n...
Emergency department visits as a potential opportunity to promote primary care attachment and modify utilization patterns – results of a pilot study in Berlin, Germany
Utilization by low acuity patients contributes to emergency department (ED) crowding. Both knowledge deficits about adequate care levels and access barriers in primary care are important promoters of such pres...
Blood pressure variability and prognostic significance in traumatic brain injury: analysis of the eICU-CRD database
Preliminary evidence demonstrates that visit-to-visit systolic blood pressure (SBP) variability is a prognostic factor of TBI. However, literature regarding the impact of initial blood pressure management on t...
Out of hospital cardiac arrest - new insights and a call for a worldwide registry and guidelines
Out of hospital cardiac arrest (OHCA) is a major public health problem with substantial mortality rates worldwide. Genetic diseases and primary electrical disorders are the most common etiologies at younger ag...
Unveiling the performance of the prehospital Rapid Emergency Medicine Score (pREMS): How the predictive score impacts in-hospital outcomes in traumatic brain injury (TBI): A retrospective observational cohort study
This study aimed to evaluate the predictive accuracy of the prehospital rapid emergency medicine score (pREMS) for predicting the outcomes of hospitalized patients with traumatic brain injury (TBI) who died, w...
Magnitude and outcome of road traffic accidents among patients admitted in dessie town governmental hospitals, Northeast Amhara, Ethiopia, 2022
Road traffic accidents(RTA) are a major public health problem worldwide, accounting for almost 1.24 million deaths per year and it is the number one cause of death among those aged group 15–29 years. Even thou...
A novel learner driver first aid eLearning program: a mixed-method pre-post pilot test and evaluation
Approximately 1.35 million people worldwide are killed in road accidents every year. Mandatory first aid training for learner drivers has been introduced in some European countries but no such requirements are...
Implementation of major trauma app: usability and data completeness
The current UK standard for major trauma patients is to record notes in a paper trauma booklet. Through an innovative collaboration between a major trauma centre and a digital transformation industry partner, ...
Identifying the key characteristics, trends, and seasonality of pedestrian traffic injury at a major trauma center in Saudi Arabia: a registry-based retrospective cohort study, 2017–2022
Pedestrian traffic injuries are a rising public health concern worldwide. In rapidly urbanizing countries like Saudi Arabia, these injuries account for a considerable proportion of trauma cases and represent a...
Emergency department utilization before and during the COVID-19 pandemic among individuals with sickle cell disease
The emergency department (ED) is a vital source of healthcare for individuals living with sickle cell disease (SCD). Prior research indicates that during the COVID-19 pandemic some individuals with SCD avoided...
Emergency preparedness in the central sterile supply department: a multicenter cross-sectional survey
To investigate the current situation of emergency preparation and emergency drill in the CSSD, and analyze its influence on the nurses’ emergency attitude and ability.
Fracture pain in children in the emergency department: the impact of a new pain management procedure
To compare compliance with the French national guidelines before and after the implementation (in 2018) of a new protocol on acute fracture pain management in the pediatric emergency department of a French uni...
Development and psychometric testing of a scale to measure effective rural emergency transfer (RET)
The process of transferring patients from small rural primary care facilities to referral facilities impacts the quality of care and effectiveness of the referral healthcare system. The study aimed to develop ...
New Trauma Score versus Kampala Trauma Score II in predicting mortality following road traffic crash: a prospective multi-center cohort study
Mortality due to injuries disproportionately impact low income countries. Knowledge of who is at risk of poor outcomes is critical to guide resource allocation and prioritization of severely injured. Kampala T...
The prevalence of physical and verbal violence among emergency medicine physicians in military hospitals vs non-military hospitals, Jeddah, Saudi Arabia: multi-center cross-sectional study
In healthcare settings, physical and verbal attacks are commonly encountered in the workplace among healthcare providers. Patients and patients’ relatives and friends have been reported to be the perpetrators ...
Comparison of prognosis between extracorporeal CPR and conventional CPR for patients in cardiac arrest: a systematic review and meta-analysis
Compared to the conventional cardiopulmonary resuscitation (CCPR), potential benefits of extracorporeal cardiopulmonary resuscitation (ECPR) for patients with cardiac arrest (CA) are still controversial. We ai...
Designing a model of emergency medical services preparedness in response to mass casualty incidents: a mixed-method study
Emergency medical services preparedness in mass casualty incidents is one of the most important concerns in emergency systems. A mass casualty incident is a sudden event with several injured individuals that o...
Important information
Editorial board
For authors
For editorial board members
For reviewers
- Manuscript editing services
Annual Journal Metrics
Citation Impact 2023 Journal Impact Factor: 2.3 5-year Journal Impact Factor: 2.5 Source Normalized Impact per Paper (SNIP): 0.936 SCImago Journal Rank (SJR): 0.745 Speed 2023 Submission to first editorial decision (median days): 14 Submission to acceptance (median days): 164 Usage 2023 Downloads: 1,251,999 Altmetric mentions: 586
- More about our metrics
Peer-review Terminology
The following summary describes the peer review process for this journal:
Identity transparency: Single anonymized
Reviewer interacts with: Editor
Review information published: Review reports. Reviewer Identities reviewer opt in. Author/reviewer communication
More information is available here
- Follow us on Twitter
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]
- Search by keyword
- Search by citation
Page 1 of 23
Red blood cell transfusion in a tertiary Haitian hospital’s emergency department: patient characteristics and availability challenges
Red blood cell (RBC) transfusions are essential for many patients admitted to emergency departments (ED). However, accessibility to red cell transfusions is often limited, especially in low-income countries su...
- View Full Text
Predictors of nursing home conveyances to emergency department
With increasing rates of patient conveyances from nursing homes to emergency departments worldwide, we aim to examine factors causing high rates of conveyances from nursing homes to the emergency department (E...
Development of decision tree classification algorithms in predicting mortality of COVID-19 patients
The accurate prediction of COVID-19 mortality risk, considering influencing factors, is crucial in guiding effective public policies to alleviate the strain on the healthcare system. As such, this study aimed ...
Virtual reality for assessing emergency medical competencies in junior doctors – a pilot study
The teaching and assessment of clinical-practical skills in medical education face challenges in adequately preparing students for professional practice, especially in handling emergency situations. This study...
A 26 years old primigravida woman presented with abdominal cutaneous entrapment syndrome: a case report
Abdominal cutaneous nerve entrapment syndrome (ACNES) is characterized by severe, mostly refractory, chronic pain due to the entrapment of the cutaneous branches of the lower torso intercostal nerves at the la...
Characteristics and outcomes of emergency department patients across health care systems: an international multicenter cohort study
A wide variation of emergency medical system configurations across countries has limited the value of comparison of quality and performance measures in the past. Furthermore, lack of quantitative data on EDs p...
Case series: star anise toxicity presenting to the emergency department in Eastern Regional Referral Hospital in Bhutan
Star anise fruit has been used in spice in Asian cuisine, ingredient for traditional medicines, component for antiviral drugs and as parts of tea and beverage across the globe. Toxicity from these plants has b...
Provider perception of presentations with nonspecific back pain in the emergency department and primary care practices: a semi-structured interview study
Increasing numbers of patients treated in the emergency departments pose challenges to delivering timely and high-quality care. Particularly, the presentation of patients with low-urgency complaints consumes r...
Surviving a classic heat stroke/hyperthermia > 42 °C – a case report
Classic heat stroke is a severe trauma which can lead to multi-organ dysfunctions and is associated with a high mortality.
Emergency department service utilisation of older patients with urgent conditions: a cross-sectional observational study
As with many countries worldwide, Singapore is experiencing a rapidly ageing population. Presentation of older persons for urgent but non-emergent conditions to the Emergency Department (ED) represents a growi...
Posterior reversible encephalopathy syndrome (PRES) on the second postpartum day: learning experience from a case report and literature review
Posterior reversible encephalopathy syndrome (PRES) is an uncommon neurological disorder which is characterised by variable symptoms. The transient clinical condition may be underestimated and misdiagnosed as ...
Aortoesophageal fistula with hemorrhagic shock successfully treated with resuscitative endovascular balloon occlusion of the aorta
Aortoesophageal fistula (AEF) is a rare cause of upper gastrointestinal hemorrhage. Despite diagnostic and therapeutic advances, the mortality rate in AEF patients remains high because of its fulminant course,...
Evaluation of advanced multi-purpose trauma moulage-based training on clinical skills for dealing with trauma-affected individuals in undergraduate nursing students
Simulation-based training courses have been developed and widely accepted.The use of simulators can prevent bitter consequences that may sometimes put human lives in danger. Increasing the skill of nursing stu...
Cervical epidural hematoma: a case series highlighting uncommon causes
Cervical epidural hematoma (CEH) is a rare but potentially devastating condition, characterized by the accumulation of blood within the epidural space of the cervical spine, leading to spinal cord compression ...
Decrease of haemoconcentration reliably detects hydrostatic pulmonary oedema in dyspnoeic patients in the emergency department – a machine learning approach
Haemoglobin variation (ΔHb) induced by fluid transfer through the intestitium has been proposed as a useful tool for detecting hydrostatic pulmonary oedema (HPO). However, its use in the emergency department (...
Management of gunshot injury to the abdominal aorta and inferior vena cava: a case report of a combat patient wounded in the Russo-Ukrainian war
Russo-Ukrainian war is associated with severe traumas, including injuries to the major vessels. Penetrating aortic injury remains one of the most difficult injuries; the mortality rate is 90–100% in case of gu...
Entrustable professional activities, emergency medicine and medical education: a systematic review
Entrustable professional activities (EPAs) are one way to assess competencies, and are designed to bridge the gap between theoretical competencies and real world clinical practice.
Unexpected Grave’s-induced acute myocardial infarction in a young female, a literature review based on a case report
Myocardial ischemia can occur due to several causes, which result in an imbalance between the supply and demand of oxygen to cardiac muscles. One potential reason for this condition is the overwork of the hear...
Utility of pelvic examination in assessing women with bleeding in early pregnancy: a multicenter Canadian emergency department study
Bleeding in early pregnancy is a common emergency department (ED) presentation. Although variability in approaches has been demonstrated, research is relatively uncommon on practices and outcomes. This study i...
Emergency care via video consultation: interviews on patient experiences from rural community hospitals in northern Sweden
Delivering emergency care in rural areas can be challenging, but video consultation (VC) offers opportunities to make healthcare more accessible. The communication and relationship between professionals and pa...
An unsuspected extracranial internal carotid pseudoaneurysm following dog bites: a case report and review of literature
Extracranial internal carotid artery (ICA) pseudoaneurysm is a rare condition that can be caused either by penetrating or blunt trauma, including dog bites, which is an uncommon occurrence. Together with the p...
Vaping-associated illness: a reassessment
In 2019, there was widespread presentation of respiratory distress as well as other organ system involvement in patients with a history of vaping. There continue to be reports of vaping-associated illness (VAI...
Cytokine release syndrome following COVID-19 infection during treatment with nivolumab for cancer of esophagogastric junction carcinoma: a case report and review
Cytokine release syndrome (CRS) is an acute systemic inflammatory syndrome characterized by fever and multiple organ failure, which is triggered by immunotherapy or certain infections. Immune checkpoint inhibi...
Incidence, characteristics, and prehospital outcomes of out-of-hospital cardiac arrest in Qatar: a nationwide gender-based investigation
Research on incidence and characteristics of Out-of-Hospital Cardiac Arrest (OHCA) in the Middle East is limited. We assessed the incidence, prehospital characteristics, and outcomes of OHCA in Qatar, a Middle...
Neuraxial anesthesia for non-neurological emergency surgery in a patient with acute ischemic stroke: a case report
The recent guidelines recommend delaying elective non-neurological surgery after an index stroke, but there is a lack of consensus regarding emergency surgery in patients with a recent stroke. Impaired cerebra...
Safety of adenosine for pediatric tachyarrhythmia treatment in the emergency department: a multi-hospital 10-year cross-sectional study
Supraventricular tachycardia is the most common dysrhythmia in children. Initial vagal maneuvers are successful less than half of the time. Adenosine, a potent AV nodal blocker with a short half-life, is recom...
Rupture of a calcified right ventricle to pulmonary artery homograft by balloon dilation– emergency rescue by venus P-Valve
Percutaneous pulmonary valve implantation (PPVI) is a recognized alternative treatment to surgery for patients with dysfunctional right ventricular outflow tracts. Patient selection is essential to avoid serio...
U-shaped correlation of lymphocyte count with all-cause hospital mortality in sepsis and septic shock patients: a MIMIC-IV and eICU-CRD database study
In sepsis, the relationship between lymphocyte counts and patient outcomes is complex. Lymphocytopenia and lymphocytosis significantly influence survival, illustrating the dual functionality of lymphocytes in ...
Diagnostic laparoscopy with indocyanine green fluorescence test for the evaluation of intestinal perfusion in abdominal blunt injury: a case report
The indocyanine green (ICG) fluorescence test has become a standard test in surgical procedures, facilitating the assessment of blood perfusion in real-time. While its utility in emergency surgeries for evalua...
Extended reality training for mass casualty incidents: a systematic review on effectiveness and experience of medical first responders
Mass casualty incidents (MCI) are unforeseeable and complex events that occur worldwide, therefore enhancing the training that medical first responders (MFRs) receive is fundamental to strengthening disaster p...
IFEM model curriculum: emergency medicine learning outcomes for undergraduate medical education
The International Federation for Emergency Medicine (IFEM) published its model curriculum for medical student education in emergency medicine in 2009. Because of the evolving principles of emergency medicine a...
Mortality and morbidity associated with new onset acute kidney injury in critically ill COVID-19 infection patients
The recent global pandemic due to severe acute respiratory syndrome coronavirus-2 resulted in a high rate of multi-organ failure and mortality in a large patient population across the world. As such, a possibl...
The MINUTES bundle for the initial 30 min management of undifferentiated circulatory shock: an expert opinion
Acute circulatory shock is a life-threatening emergency requiring an efficient and timely management plan, which varies according to shock etiology and pathophysiology. Specific guidelines have been developed ...
Catecholamine concentration as a predictor of mortality in emergency surgical patients
Trauma and emergency surgery are major causes of morbidity and mortality. The objective of this study was to determine whether serum levels of epinephrine and norepinephrine are associated with aging and morta...
A diagnostic dilemma: distinguishing a sulfasalazine induced DRESS hypersensitivity syndrome from a CD30 + lymphoma in a young patient
Drug reaction with eosinophilia and systemic symptoms (DRESS) is a severe hypersensitivity reaction characterized by cutaneous rash, lymphadenopathy, fever, eosinophilia, leukocytosis, and life-threatening org...
Comparing online and onsite simulation modules for improving knowledge and confidence in disaster preparedness among undergraduate medical students
Disaster preparedness is one of the critical strategies for effectively managing disasters and has been an area of high focus in the healthcare sector over the past few decades. The current Indian medical unde...
“Iliacus muscle abscess as an unexpected cause of posterior hip pain in a healthy young adult female”: a case report
Iliacus muscle abscess is an uncommon but potentially life-threatening condition that can present with nonspecific symptoms, posing diagnostic challenges. This case report highlights the importance of consider...
Dabigatran accumulation in acute kidney injury: is more better than less to prevent bleeding? A case report
Dabigatran is an oral anticoagulant that is mainly renally excreted. Despite its efficacy in preventing thromboembolic events, concerns arise regarding bleeding complications in patients with acute kidney inju...
Airway breathing circulation dengue: a case of multifactorial shock due to major trauma and severe dengue infection
Dengue is the most common arboviral illness reported globally, endemic to most tropical and sub-tropical regions of the world. Dengue Shock Syndrome is a rare complication of severe Dengue infection resulting ...
Treatment strategy for compartment syndrome at multiple regions due to injuries caused by a tree fall: a case report
Compartment syndrome commonly occurs in patients with forearm and lower leg fractures. Compartment syndromes of the gluteal and thigh muscles are less common. It is imperative that compartment syndrome be diag...
Early colonic-preparation and salvage laparoscopic appendectomy (ECSLA)- innovative protocol for the management of magnets ingestion
Ingestion of magnets carries risks for significant morbidity. We propose a new protocol designed to reduce the need for surgery, shorten length of stay, and decrease morbidity.
Successful management of a delayed presentation of traumatic descending thoracic aorta pseudoaneurysm: a literature review based on a case report
Blunt traumatic aortic injury (BTAI) is the second leading cause of death due to traumas in young patients. The primary presentation might be chest or interscapular pain, difficulty in breathing, and, in sever...
Do-not-attempt-resuscitation decision making: physicians’ recommendations differ from the GO-FAR score predictions
In-hospital cardiac arrest (IHCA) is a major cause of mortality globally, and over 50% of the survivors will require institutional care as a result of poor neurological outcome. It is important that physicians...
Severe COVID-19 multisystem inflammatory syndrome versus severe dengue in children from Indonesia: a cross-sectional study
Severe multisystem inflammatory syndrome in children (MIS-C) and severe dengue are challenging to identify during the COVID-19 pandemic in dengue-endemic areas. Fever, multiorgan involvement, and shock charact...
Creating a master training rotation schedule for emergency medicine residents and challenges in using artificial intelligence
The allocation of resident physicians to clinical rotations presents a complex challenge that requires balancing multiple objectives with the goals of providing optimal patient care, maintaining adequate depar...
Violence in the emergency department: a quantitative survey study of healthcare providers in India
Workplace violence (WPV) in Emergency Departments (EDs) is an increasingly recognized challenge healthcare providers face in low-resource settings. While studies have highlighted the increased prevalence of WP...
Low-dose tenecteplase during cardiopulmonary resuscitation in massive pulmonary embolism
We report the case of an 18-year-old male who presented to the Emergency Department with sudden onset dyspnea. The patient was intubated on arrival, but suffered a cardiac arrest soon after. Point-of-care echo...
Paracetamol overdose causing acute kidney injury without hepatotoxicity: a case report
Paracetamol is a widely used analgesic and antipyretic. Paracetamol-induced hepatotoxicity is well known, but nephrotoxicity without hepatotoxicity is rarely seen.
The wolf in sheep’s clothing: vasovagal syncope in acute aortic dissection
The presentation of acute aortic dissection can pose a challenge for emergency physicians, as it may occur without pain. Atypical presentations can lead to significant delays in diagnosis and increased mortali...
A potentially lifesaving error: unintentional high-dose adrenaline administration in anaphylaxis-induced cardiac arrest; a case report
Cardiopulmonary resuscitation is a crucial skill for emergency medical services. As high-risk-low-frequency events pose an immense mental load to providers, concepts of crew resource management, non-technical ...
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
- Follow us on Twitter
Annual Journal Metrics
Citation Impact 2023 Journal Impact Factor: 2.0 5-year Journal Impact Factor: 2.3 Source Normalized Impact per Paper (SNIP): 1.157 SCImago Journal Rank (SJR): 0.700 Speed 2023 Submission to first editorial decision (median days): 27 Submission to acceptance (median days): 134 Usage 2023 Downloads: 985,950 Altmetric mentions: 682
- More about our metrics
- ISSN: 1865-1380 (electronic)
- ISSN: 1865-1372 (print)
International Journal of Emergency Medicine
ISSN: 1865-1380
- General enquiries: [email protected]
- Frontiers in Disaster and Emergency Medicine
- Resuscitation and Cardiac Emergency Medicine
- Research Topics
Recent Advances in Emergency Medicine
Total Downloads
Total Views and Downloads
About this Research Topic
Since the start of basic and advanced life support seminars, medicine has evolved throughout the centuries and especially in the recent years, providing not only new insights regarding pathophysiology of medical emergencies but also new treatment strategies. All medical specialties and departments, from ...
Keywords : Emergency Medicine, Emergency, Medical Emergency, Surgical Emergency, recent advances, cardiopulmonary resuscitation, acute medicine
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.

Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.

- Journal of Emergency Medicine
- Recommended Events
- About Joint CME Providership with AAEM
- AAEM CME Online
- AAEM25 Scientific Program
- Speaker Development Group
- Claim CME for AAEM24
- Become an Examiner
- AAEM Qualifying Exam Review Course
- ED Operations Certificate Course (EDOCC)
- Claim CME for MEMC23
- Leadership Academy
- Claim CME for Past Events
- Common Sense Submissions
- Common Sense Advertising
- Western Journal of Emergency Medicine
- Insights Advertising
- AAEM Book Store
- Connect With Peers (MyAAEM)
- Chapter Divisions
- Interest Groups
- Join or Renew
- Group Membership
- Membership Justification Toolkit
- Refer a Colleague to AAEM
- AAEM Merchandise
- Envision Lawsuit
- Press Coverage
- Support Lawsuit
- AAEM Past Presidents
- Residency Visits
- Award Recipients
- Code of Ethics
- AAEM Foundation
- AAEM LEAD-EM
- Collaborating Organizations
The Journal of Emergency Medicine ( JEM ) is the official journal of the American Academy of Emergency Medicine (AAEM). JEM is an international, peer-reviewed publication featuring original contributions of interest to both the academic and practicing emergency physician. JEM features research papers, clinical studies, and articles that emphasize the education of emergency physicians and the practice of emergency medicine. AAEM actively encourages its members to contribute editorial material for publication in JEM . As AAEM’s official journal, an online subscription to JEM is included in the membership dues of each member.*
The AAEM membership list is private, however, in order to receive this member benefit, your name and address are provided to Elsevier, the publisher of the JEM . If you would prefer not to receive this member benefit, please email us at [email protected] .
* Note: There is no discount on your membership dues should you decide to opt out of this member benefit.
The Journal of Emergency Medicine Audio Summary
Monthly audio podcast summary of important articles from the Journal of Emergency Medicine, the official journal of AAEM, and discussion of emergency medicine board review topics.

- EMResident Archives
- Publications
- Submit an Article

Critical Care
- Health Policy Journal Club
- Program Director Interviews
Greatest Hits in Emergency Medicine Research: 2023
Keeping abreast of all the high-impact papers in em is no easy feat..
EMRA’s Research Committee, in partnership with other EMRA committees, has compiled a quick review of some of the most practice-affirming or practice-changing papers recently published. This is by no means a definitive list, but our summaries of these noteworthy papers will be good to know for your next shift!
Effect of Intravenous or Intraosseous Calcium vs Saline on Return of Spontaneous Circulation in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial.
Review by Sierra F. Williams, MS, OMS-IV
This double-blind, randomized clinical trial sought to determine whether administration of calcium during out-of-hospital cardiac arrest (OHCA) improves return of spontaneous circulation (ROSC) in adults. In this trial, 397 adult patients were randomized to receive up to 2 intravenous or intraosseous doses of 5 mmol of calcium chloride (n = 197) or saline (n = 200). A dose of calcium chloride or saline was administered immediately following a dose of epinephrine. The primary outcome of the study was sustained ROSC (defined as ROSC without need for further CPR for 20 minutes), while the secondary outcome included survival and a favorable neurological outcome at 30 and 90 days, with a modified Rankin Scale score of 0-3. The trial was stopped early due to concerns of harm in the calcium group. Sustained ROSC was achieved in 19% of patients in the calcium group and 27% in the saline group (risk ratio, 0.72 [95% CI, 0.49 to 1.03]; risk difference, −7.6% [95% CI, −16% to 0.8%]; p=0.09). At 30 days, 5.2% of patients in the calcium group survived compared to 9.1% of patients in the saline group (risk ratio, 0.57 [95% CI, 0.27 to 1.18]; risk difference, −3.9% [95% CI, −9.4% to 1.3%]; p=0.17). 3.6% of patients in the calcium group reached a favorable neurological outcome compared to 7.6% of patients in the saline group (risk ratio, 0.48 [95% CI, 0.20 to 1.12]; risk difference, −4.0% [95% CI, −8.9% to 0.7%]; p=0.12). The study showed that administration of calcium during OHCA in adults did not improve sustained ROSC and can potentially cause harm.
Critique and Implications for Practice Prior to the COCA trial, evidence regarding the use of calcium in OHCA has been conflicting and lacking. However, guidelines often continue to recommend its use. There is sufficient evidence to support the use of calcium in select patient populations that were not included in this study, such as hyperkalemia, hypocalcemia, and CCB toxicity. Although the results were not statistically significant due to the low power of the study, the use of calcium in OHCA appears to be correlated with patient harm that cannot be ignored. This indicates that calcium in OHCA is not suitable for all patients and should not be used routinely. It is also important to keep in mind that there has been no study to date to demonstrate that a single medication administered during cardiac arrest made a difference in survival with a favorable neurological outcome. Early, high-quality CPR in addition to early defibrillation in the appropriate patients are the only 2 treatments that have shown improvement in these outcomes.*
*Referenced First10EM and Salim Rezaie EBM review during ResusX 2022 conference
Prehospital & Disaster Medicine, Health Systems
Using the Centers for Disease Control and Prevention’s National Syndromic Surveillance Program Data to Monitor Trends in U.S. Emergency Department Visits for Firearm Injuries, 2018 to 2019
Review by Muhammad Waseem, MD, MS & David Gordon, MS3
The authors utilized a retrospective analysis of the CDC National Syndromic Surveillance Program dataset to analyze near-real time data between January 2018 and December 2019, capturing 215 million ED visits. The study used a set of ICD-9 and ICD-10 diagnosis codes and chief complaint keywords to filter for firearm injury records. Of those visits, 132,767 were firearm related (61.6 per 100,000 ED visits). This study revealed that males aged 15-24 had higher firearm injury-related ED visit rates relative to other demographic age groups. Overall, the rate of fire-arm related injury increased for all age groups between 15 and 64 years over the interval studied. Analyzed by region, the rate of ED visits for firearm injury significantly increased in the northeast, southeast, and southwest regions. These results are consistent with other studies but were able to be reported with less lag due to the study’s near real time surveillance methods.
Critique and Implications for Practice Firearm-related injury is a major public health issue, but there is lag between when ED visits relating to firearm injury occur and when traditional reports for firearm injury are captured. This study highlights the epidemiology of firearm-related visits to the emergency department, raising awareness of the problem and noting the need for prevention strategies. The rate of firearm-related injury and presentation to the ED is only increasing. Awareness of the epidemiology of firearm injury can help target community-based public health violence prevention, facilitate training, and guide rapid response strategies. On a systems level, this method analysis can also inform resource allocation, particularly identifying where firearm visits make up a substantial portion of ED visits. In contrast to a typical 2-year data lag from traditional ED surveillance systems used to monitor firearm injury ED visits, this study utilized near-real time electronic medical record national surveillance data. Where data is available, incorporating methods that leverage real-time surveillance could provide further insight into other clinical applications as well.
Critical Care, Airway Management
Effect of Use of a Bougie vs Endotracheal Tube with Stylet on Successful Intubation on the First Attempt Among Critically Ill Patients Undergoing Tracheal Intubation: A Randomized Clinical Trial
Review by Elisa Quince DO, MS
This multicenter, randomized clinical trial assessed if utilizing a bougie or an endotracheal tube with stylet would increase the likelihood of success on the first attempt. In this study, referred to as the “BOUGIE” trial, 1,102 critically ill adults who required tracheal intubation were randomly assigned the utilization of a bougie or endotracheal tube with a stylet. The study found an 80% success rate with the utilization of the bougie versus 83% with a stylet. Overall, the study found that using a bougie did not significantly increase the incidence of successful intubation on the first attempt compared to using an endotracheal tube with a stylet.
Critique and Implications for Practice This study challenges the perception that a provider should primarily use a bougie during difficult intubations. This perception was shaped by previous observational studies and 1 RCT concluding that using a bougie was associated with increased incidence of first-attempt intubation. It encourages providers to focus more on utilizing the method the operator is most comfortable with at that time. When comparing the BEAM trial to this study, one difference is that the BEAM trial was limited to one single emergency department in Hennepin County Medical Center, while the BOUGIE trial received data from 7 different emergency departments and 8 ICUs in the United States. Differences in training styles and experiences can lead to the differences seen in the results of these studies but can lead to the implication that for difficult intubations, how one is trained can dictate comfort level, and comfort level can lead to successful intubation on the first attempt.
Pediatric EM
Effect of Amoxicillin Dose and Treatment Duration on the Need for Antibiotic Re-treatment in Children with Community-Acquired Pneumonia: The CAP-IT Randomized Clinical Trial
Review by David Leon, MD
This study is a multi-center 2x2 RCT with children who required amoxicillin for community-acquired pneumonia (CAP), randomized to receive either 35-50 mg/kg/d or 70-90 mg/kg/d of amoxicillin for a treatment duration of 3 or 7 days. The primary outcome was if it was clinically indicated to re-treat with antibiotics for respiratory infection within 28 days after randomization. There was no significant difference between the high- and low-dose groups, nor the 3-day vs 7-day groups. The secondary outcomes addressed CAP-related symptom severity. Cough duration was slightly prolonged in the 3-day course group. No significant interaction was noted between dose and duration groups. Outpatient treatment of CAP in children with a lower dose of amoxicillin was noninferior to traditional high-dose amoxicillin, and 3-days of antibiotics was noninferior to 7-days, with respect to the need for antibiotic retreatment within a month.
Critique and Implications for Practice For children with mild to moderate CAP who are not in need of significant support, such as those appropriate for discharge or only requiring overnight observation, it seems adequate to treat with both lower dose and shorter course of antibiotics. However, this data may not be applicable to children with severe CAP. Local antibiogram and resistance must be considered given that the study only included amoxicillin. This is of particular interest as there was a nationwide shortage of amoxicillin this year.
CT or Invasive Coronary Angiography in Stable Chest Pain
Review by Sandra Gad, MSc
Randomly assigned 3,561 patients (56.2% female), follow-up was complete for 3523 (98.9%). Major adverse cardiovascular events occurred in 2.1% in the CT group and in 3% of the ICA group (hazard ratio, 0.70; 95% confidence interval [CI], 0.46 to 1.07; P=0.10). Major procedure-related complications occurred in 0.5% of the CT group and in 1.9% of the ICA group (hazard ratio, 0.26; 95% CI, 0.13 to 0.55). Angina during the final four weeks of follow-up was reported in 8.8% of the patients in the CT group and 7.5% of those in the ICA group (odds ratio, 1.17; 95% CI, 0.92 to 1.48). The DISCHARGE trial group found that the incidence of major adverse cardiovascular events did not differ between the CT group and the invasive coronary angiography group in patients with stable chest pain.
Critique and Implications for Practice CT can be a reliable option with similar diagnostic abilities to ICA when diagnosing CAD in patients with stable chest pain. Using CT can significantly reduce patients’ concerns regarding the invasive nature of ICA, as well as alleviate the financial burden associated with ICA. Further, CT can speed up diagnosis and ensure timely treatment.
Sodium Bicarbonate Use During Pediatric Cardiopulmonary Resuscitation: A Secondary Analysis of the ICU-RESUScitation Project Trial
Review by Nathan Dreyfus, MD
This multi-center, retrospective cohort analysis compared the outcomes of pediatric in-hospital cardiac arrest cases (p-IHCA) between patients who received intra-resuscitation sodium bicarbonate and those who did not. Children analyzed were those who received chest compressions between ages =>37 weeks post-conceptual age and <= 18 years between October 2016 to March 2021. Various child characteristics including their Pediatric Risk of Mortality score (PRISM) and Vasoactive Inotropic Score (VIS) were collected across 10 clinical sites. The main outcome of investigation was the duration of survival to hospital discharge. Other outcomes included ROSC, neurological outcomes, and presence of new morbidity. It was shown that sodium bicarbonate was used more in children with cardiac diagnoses, increased severity of illness and longer CPR duration. Of 1,100 CPR events, use of sodium bicarbonate was associated with lower rates of survival to hospital discharge and discharge with favorable neurologic outcomes.
Critique and Implications for Practice While the propensity-weighted model in this study omits several potential confounders, the results echo similar recent papers in adult populations providing evidence against the routine or indiscriminate use of sodium bicarbonate for cardiac arrest. One limitation is that sodium bicarbonate use was more common in medical and surgical cardiac patients than non-cardiac patients, as well as with children with higher PRISM and VIS scores which could contribute to the poorer outcomes seen. Intra-arrest lab values such as pH were not analyzed so it is unknown how sodium bicarbonate would play a role for severe intra-arrest metabolic acidosis. Also, the time to first sodium bicarbonate administration was not analyzed which could pose limitations. Although sodium bicarbonate remains a part of the ACLS and PALS guidelines for cardiac arrest, its utility is not evidence-based per this study as well as per other studies. I will be thoughtful about when I choose to administer sodium bicarbonate during code situations, as this study suggests there might even be harm in doing so.
Prehospital & Disaster Medicine, Critical Care
One and Done Epinephrine in Out-of-Hospital Cardiac Arrest? Outcomes in a Multiagency United States Study
Review by Luke Wohlford, MD, MPH
A pre- and post-intervention study investigating patient outcomes when comparing the existing protocol of epinephrine every 3-5 minutes in non-traumatic cardiac arrest to a 1-time epinephrine dosing protocol. Adults included in this study among 5 North Carolina EMS agencies were assessed for survival to hospital discharge and ROSC pre- and post-implementation. After controlling for patient factors, the single-dose approach demonstrated comparable survival to discharge rates (adjusted odds ratio 0.88, 95% confidence interval 0.77–1.29), but with lower rates of ROSC (adjusted odds ratio 0.58, 95% confidence interval 0.47–0.72). With neurological outcomes as the more patient-centered outcome, an argument can be made about the validity of a 1-time epinephrine dosing protocol.
Critique and Implications for Practice Further work and additional studies may need to be done to further elucidate neurological outcomes among those with survival to hospital discharge, this study demonstrates equipoise with a 1-time epinephrine dosing protocol that may allow higher proportions of time spent on CPR during resuscitations and free up more resources for high-quality cardiac arrest care.
Performance of the Paracetamol-Aminotransferase Multiplication Product in Risk Stratification After Paracetamol (Acetaminophen) Poisoning: A Systematic Review and Meta-Analysis
Review by Mason Jackson, MD
This systematic review and meta-analysis evaluated the acetaminophen cross-product as a marker of hepatotoxicity. The cross product is calculated by multiplying the higher of the aminotransferases (AST or ALT) by the acetaminophen concentration and can be used to determine hepatotoxicity risk in scenarios excluded by the original acetaminophen overdose studies, which primarily looked at single dose, acute and timed overdoses. Target measurements were a lower threshold of 1,500 and upper threshold of 10,000. When used as a diagnostic predictor of hepatotoxicity, and hepatotoxicity in staggered ingestions, and ingestions older than 8 hours, the cross product produced a lower limit OR of 31 to 85 and a higher limit OR of 99 to 367. This demonstrates that the acetaminophen cross product is a strong diagnostic tool that can aid the emergency physician in acute acetaminophen overdose alongside the Rumack-Mathew nomogram, generating profound changes in diagnostic certainty.
Critique and Implications for Practice In patients presenting with staggered overdoses or delayed presentation of an acetaminophen overdose, utilization of the cross product will help decide the need for N-acetyl cysteine in the ED. It serves as a useful marker for intensivists and toxicologists caring for these patients on inpatient services as well.
Medical Education
Communicating Diagnostic Uncertainty at Emergency Department Discharge: A Simulation-Based Mastery Learning Randomized Trial
Review by Hannah Seyller, MD , and Kay Nicole Tipton, DO, MS
This multi-center randomized control trial examined the ability of resident physicians to communicate diagnostic uncertainty through simulated patient encounters. Though many patients leave the ED without a formal diagnosis, residents have little training communicating diagnostic uncertainty to their patients.
In this trial, 109 residents participated in a simulation-based learning curriculum that included online modules, a mobile learning application, and 3 simulated telehealth practice sessions with a standardized patient. Participants were divided into immediate and delayed intervention groups, which did not receive the intervention curriculum until after the second patient encounter. The primary outcome was each physician’s “mastery” of communicating diagnostic uncertainty after the second encounter based on the Uncertainty Communication Checklist.
Regardless of training site or stage of training, residents in the immediate access group showed an increased mastery compared to the delayed group, who had not yet received the intervention. Two-thirds of participants felt the curriculum increased their communication skills, and 60-65% said they applied skills they learned to their clinical practice. Limitations include unblinded participants and internal development of the objective scoring tool used to determine mastery.
Critique and Implications for Practice Residents are often not properly trained on how to communicate diagnostic uncertainty with patients. This article provides a framework that can be implemented in current or future practice within residencies to improve communication at discharge when the exact cause of patients’ symptoms remains unknown. Although the article did demonstrate a difference between early and late intervention groups within the measurement of the study, it did not show a difference when translated to clinical practice. Further studies will need to be performed to evaluate how this framework and others can affect clinical practice in emergency departments.
Effect of Moderate vs. Mild Therapeutic Hypothermia on Mortality and Neurologic Outcomes in Comatose Survivors of Out-of-Hospital Cardiac Arrest. The CAPITAL CHILL Randomized Clinical Trial
Review by Charles Sanky, MD, MPH
This single-center, double-blinded, stratified, randomized-controlled, clinical superiority trial was the first study to compare hypothermia at 31°C with 34°C in survivors of out-of-hospital cardiac arrest. It sought to determine whether this difference in moderate versus mild hypothermia improved clinical outcomes in comatose survivors of out-of-hospital cardiac arrest. Patients were randomly assigned to temperature management with a target body temperature of 31 °C (n = 193) or 34 °C (n = 196) for a period of 24 hours. Outcomes included all-cause mortality, ICU length of stay, neurological outcome, and adverse effects. This study found no significant difference in the composite of mortality and poor neurological outcome, occurring in 48.4% (31°C group) and 45.4% (34°C group), 95% CI, −7.2% to 13.2%; P = 0.56. However, the 31°C group had a 3-day longer median length of stay in the ICU (10 vs. 7 days; 95% CI -1.2 to 4.1; P=0.004).
Critique and Implications for Practice Numerous studies have suggested that going beyond the targeted temperature management of 32 to 36 degrees, the updated post-cardiac arrest TTM guidelines. Studies have consequently attempted to determine what the optimal temperature might be, including the much larger TTM trial in 2021, which did not find a difference in normothermia versus hypothermia. Still, the impact on ICU length of stay is concerning, possibly reflecting that moderate hypothermia could mask fevers that otherwise would have received treatment. This study may not change my practice yet but is worth considering in the wake of new ACLS guidelines regarding TTM.
Wilderness Medicine
A New Multi-Disciplinary Approach Supported by Accident and Field Test Data to Optimize Survival Chances in Rescue and First Aid of Avalanche Patients
Review by Chelsea McAuslan, MS4
This retrospective analysis of 1070 full avalanche burials from accident databases and large prospective field test datasets were used to develop evidence-based algorithms exclusively for the avalanche rescue environment. AvaLife provides a holistic and tailor-made tool for avalanche first aid with its consideration of adapted sequence of actions, inclusion of rescue tactical considerations, advice for cases with multiple burials where there is a shortage of resources, considerations of using recovered subjects as a resource in the ongoing rescue, the adapted definition of “injuries incompatible with life,” reasoning behind the importance of rescue breaths, and the updated BLS iCPR algorithm.
Critique and Implications for Practice This study highlights the method AvaLife in the rescue and treatment of patients trapped from the effects of an avalanche. It provides ALS and BLS providers with the methods of triage to allow for the best chances of survival for patients who undergo entrapment. The principle of the “greatest good for the greatest number” is shown crucial in these cases of situational resource shortage. Rescuers must analyze the environment, take into consideration the forces that could prolong excavation, and proceed with appropriate survival techniques according to AvaLife Protocol in patients with injuries resulting from avalanche and burial.
Admin & Operations
The use of the word "quiet" in the emergency department is not associated with patient volume: A randomized controlled trial
Review by David Gordon, MS3
This randomized control trial evaluates if hearing the word “quiet” bears any change in patient volume and perception of the business of an ED shift. In this trial, 506 staff surveys were collected over a sample of 47 shifts. For each, a researcher approached staff members with a greeting. If the day were randomized to the intervention, the researcher asked, “Has it been quiet in here?” Three hours later, the researcher returned to the staff member to administer the survey, which assessed crowdedness of ED, feelings toward patient volume entering ED, and the belief that the word quiet affects business of the day. There was no association between the word “quiet” and increased patient volumes. However, staff members who perceived that the word “quiet” influenced patient volumes reported a perception of a more crowded ED with more patients after hearing the word “quiet.” Some staff members provided qualitative responses that shifts had “worsened” following hearing the word “quiet,” citing acutely ill patient cases they were managing.
Critique and Implications for Practice Throughout an ED shift, someone might approach an ED staff member and ask if the day is a “quiet” day. ED providers care for patients as they enter the department, but the word “quiet” does not influence patient volume. Though this study was conducted at a single site, the methodology of the study provides a robust analysis to address a common concern among emergency department staff. Staff members who feel as though there is an increase in ED volume and business following hearing the word “quiet” likely have a preconceived belief that this is true. A staff member’s initial preconceived notions of factors that trigger business within the ED may contribute to their perceptions of the ED shift. Generalizing on the study’s results, if staff adopts a mindset that the word “quiet” does not affect patient volumes, they may perceive decreased business over the course of the shift.
Any papers we missed? Let the EMRA Research Committee know a nd we can discuss it at an upcoming journal club!
This list was compiled and edited by EMRA Research Committee members Charles Sanky, MD, MPH; David Gordon, MS3; Kristina Pagano, MS3; and Nathan Roberts, MD, PhD.
Related Articles
Getting started in em research: lessons from rising stars, rapid research review: power, all articles.
- Administration and Operations Committee 2
- Critical Care Committee 4
- Education Committee 10
- Government Services 4
- Health Policy Committee 8
- Informatics Committee 3
- Medical Student Council 7
- Pediatrics Committee 4
- Research Committee 6
- Simulation Committee 3
- Social EM Committee 7
- Wilderness Committee 5
- International Committee 8
- Prehospital and Disaster Medicine Committee 5
- Simulation Division 2
- Sports Medicine Committee 5
- Advancement of EM 110
- Administration & Operations 57
- Admin Ops Literature Review 8
- Diversity and Inclusion 18
- Research 31
- Rapid Research Review 9
- Attending 2
- Award Winners 20
- Educational Courses 2
- Residency Leadership 2
- Travel Scholarships 3
- ACEP Member Benefits 2
- Career Planning 78
- Board Certification 7
- Interviewing 5
- Job Search 3
- Practice Environments 25
- Community 2
- International 10
- Locum Tenens 2
- Clinical 981
- Addiction Medicine 4
- Surgical Airway 1
- Behavioral Health 5
- Cardiology 154
- ECG Challenge 47
- Consult Corner 5
- Critical Care 227
- Critical Care Alert 103
- Critical Care Devices 11
- Critical Care Roadblock 3
- Critical Care Ultrasound 14
- Deep Dive in CritCare 9
- Ventilator Management 6
- Dermatology 8
- Disaster Medicine 12
- Prehospital Care 21
- Endocrinology 11
- Event Medicine 2
- Gastroenterology 15
- Geriatrics 4
- Hematology 19
- Immunology 1
- Infectious Disease 131
- COVID-19 80
- Informatics 19
- Telemedicine 3
- International EM 25
- Nephrology 14
- Neurology 50
- Ophthalmology 16
- Orthopedics 26
- Osteopathic 3
- Pain Management 24
- Palliative Care 14
- Patient Interactions 18
- Pediatric EM 99
- Psychiatry 9
- Mental Health 3
- Pulmonary 17
- Radiology 7
- Rheumatology 1
- Simulation 13
- Social EM 52
- Space Medicine 3
- Sports Medicine 11
- Toxicology 98
- Medications 12
- Recreational Drugs 10
- Penetrating 1
- Traumatic Brain Injury 2
- Ultrasound 84
- Guided Procedures 5
- POCUS For the Win 7
- Undersea and Hyperbaric 2
- Visual Diagnosis 20
- Wilderness Medicine 25
- Editorial 129
- Editor's Forum 54
- Heart of EM 12
- Opinion-Editorial 13
- Leadership Reports 77
- ACEP Representative 2
- ACGME RC-EM 11
- President's Message 48
- Speaker Report 8
- Treasurer's Report 3
- Membership 3
- Events & Activities 21
- ACEP Scientific Assembly 6
- CORD Academic Assembly 2
- EM Wellness Week 1
- EMRA MedWAR 3
- Leadership and Advocacy Conference 6
- Fellowships 12
- Education Fellowships 2
- Global EM Fellowships 2
- Health Policy Fellowships 1
- Pediatric Fellowships 2
- Health Equity 3
- Health Policy 146
- Advocacy 45
- Affordable Care Act 7
- Health Policy Journal Club 78
- Legislation 9
- Regulatory 2
- Leadership 181
- Committees and Divisions 4
- EMRA Board of Directors 40
- EMRA Spotlight 127
- Representative Council 9
- Medical Education 80
- Board Review 2
- Questions 1
- Med Ed Fellowship Director Interview Series 10
- Medical Students 199
- Advising 60
- Away Rotations 8
- Dual Degree Programs 1
- ERAS & Residency Application 3
- Military Advising 2
- Program Director Interviews 83
- Rank List 1
- Residents Program Interviews 4
- Medical Student Council 29
- Mentorship 4
- Non Clinical 64
- Health Care Administration 35
- Otolaryngology 5
- Resuscitation 5
- Wellness 130
- Compassion Fatigue 9
- Financial 10
- Insurance 2
- Loan Refinancing 2
- Personal Finance 4
- Medico Legal 32
- Medical Liability 2
- Risk Management Pitfalls 23
- Personal 14
- Workplace 21
- Med Student 46
- Advertise with us
- Submit an article
- Connect with us
© 2021 Emergency Medicine Residents' Association | Privacy Policy | Website Links Policy | Social Media Policy
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Emergency medicine: past, present, and future challenges
Wei, Shujian a,b,c,d,e,∗
a Department of Emergency Medicine and Chest Pain Center, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
b Clinical Research Center for Emergency and Critical Care Medicine of Shandong Province, Institute of Emergency and Critical Care Medicine of Shandong University, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
c Key Laboratory of Emergency and Critical Care Medicine of Shandong Province, Key Laboratory of Cardiopulmonary-Cerebral Resuscitation Research of Shandong Province, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
d Key Laboratory of Cardiovascular Remodeling and Function Research, Chinese Ministry of Education, Chinese Ministry of Health and Chinese Academy of Medical Sciences, State and Shandong Province Joint Key Laboratory of Translational Cardiovascular Medicine, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
e Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China.
∗Corresponding author. Address: Department of Emergency Medicine and Chest Pain Center, Qilu Hospital, Cheeloo College of Medicine, Shandong University, No. 107, Wenhuaxi Road, Jinan, Shandong, 250012, China. E-mail address: [email protected] (S. Wei).
How to cite this article: Wei S. Emergency medicine: past, present, and future challenges. Emerg Crit Care Med. 2021;1:49–52. doi: 10.1097/EC9.0000000000000017
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal. http://creativecommons.org/licenses/by-nc-nd/4.0
Origin and history of emergency medicine
The term “emergency,” first used in the 1630s, is derived from the Latin word emergere , meaning unforeseen events that require immediate attention. The term “emergency medicine” can be traced to the French Revolution (1789–1799). In 1792, Dominique Jean Larrey, a military medical surgeon, gained a position in the Army of the Rhine and left for Strasbourg, where he witnessed great mobility of the horse artillery and then suggested that General Adam Philippe de Custine have the medical staff use this method to speed up transport of the wounded. The general approved Larrey's proposal. Larrey's “ambulance” was a simple carriage, despite the exposure to enemy fire. In 1797, during the first Italian campaign, Larrey created a complete rescue system with an active medical team in the battlefield. In contrast to previous rescue methods, Larrey transported critically wounded patients to the rescue station and operated on them as soon as possible, instead of delaying the operation after the battle. The timely rescue system created by him enabled every wounded soldier to be treated within 24 hours, which significantly reduced the mortality rate. Therefore, Larrey has often been referred to as “the father of emergency medical services.” [1]
Medicine, as a professional field, dates back to the early 19th century, while emergency medicine can only be traced back to 50 years ago, making it the most recently developed major field in medicine. Before the 1960s, staff in hospital emergency departments usually worked in rotation with family doctors, general surgeons, physicians, and other specialists. In many small emergency departments, nurses conducted the triage of patients, and specialty doctors were called in based on the type of injury or disease. Many pioneers of emergency medicine were family doctors and other specialists, who believed that extra training in first aid was necessary. A group of doctors left their professional positions and devoted themselves to education. In 1952, Maurice Ellis was appointed as the first “first aid consultant” at Leeds General Infirmary in England. In 1967, the Casualty Surgeons Association was founded, with Maurice Ellis as its president. [2,3] In 1961, in the United States, Dr James DeWitt Mills, along with 4 assistant physicians, established 24/7 emergency care at Alexandria Hospital in Alexandria, Virginia; it was later known as the Alexandria Plan. [4] In 1970, the University of Cincinnati launched the first emergency resident physician program in the world. In 1971, the University of Southern California became the first American medical school to establish a department of emergency medicine. [5] History was made in 1979, when the American Board of Medical Specialties voted to make emergency medicine a recognized medical specialty in the United States. [5]
In China, emergency medicine started relatively late. The Ministry of Health issued “Suggestions on Strengthening First Aid Work in the City” and “On the Release of the Construction Plan of Hospital Emergency Departments (Trial)” on October 30, 1980 and June 11, 1984, respectively. These 2 documents stipulated the work direction, scope, and tasks of the emergency department; thereby, laying the foundation for the construction of emergency departments in China. In 1985, Peking Union Medical College Hospital established the first postgraduate program in emergency medicine. [6–8]
Current state of emergency medicine
Emergency medicine mainly involves the rapid assessment, treatment, and triage of critically ill patients, and has transformed from the emergency room to the emergency department or emergency center. Hospitals typically set up a relatively complete emergency medical system of “out-of-hospital emergency medical services, in-hospital emergency medical services, and critical care.” Numerous emergency diagnostic and treatment technologies, such as cardiopulmonary resuscitation, emergency percutaneous coronary intervention, continuous renal replacement therapy, left ventricular assistive devices, and extracorporeal membrane oxygenation, are applied in emergency medicine. Moreover, a growing number of qualified physicians have devoted themselves to emergency medicine, and several academic platforms have been established, which facilitate knowledge exchange.
With the continuous reform of the medical system and the comprehensive implementation and promotion of hierarchical diagnostic and treatment systems from medical reform, the development of emergency medicine is confronted with rare opportunities and more challenges. For example, the construction of emergency systems varies across nations and regions. Practitioners in emergency services have the vital task of establishing a complete emergency diagnosis and treatment system to maintain the daily health of the public and to satisfy the emergency demands of major public health events. It is necessary to move the front of first aid forward, carry out multidisciplinary cooperation, treat all types of critically ill patients, deal with public health emergencies, and boost hierarchical diagnosis and treatment work. Amid the rapid growth of modern medicine, advanced technology and innovative drugs continue to emerge. In many cases of emergency work, it is the timely, orderly, and efficient application of these technologies and drugs to the early treatment of critically ill patients that matters. Therefore, “process optimization and early treatment” is an important direction in emergency medicine research.
With the development of a medical discipline, each medical specialty is more characterized, and even some single diseases tend to form specialties. [9] Following the law of medical development, emergency medicine also gives full play to specialty characteristics and the development of subspecialties. [10] For example, in areas with a high incidence of cardiovascular diseases, emergency centers have subspecialty focus areas for cardiovascular diseases, and in rural areas with a common occurrence of acute poisoning, emergency departments of primary hospitals establish a subspecialty for the treatment of acute poisoning. In developing subspecialties, emergency medicine focuses on the advancement of diagnostic and treatment technologies for life-threatening diseases and integration with other subspecialties. The construction of high-quality subspecialties in emergency medicine is conducive to the development of new diagnostic and treatment equipment and technology.
Future of emergency medicine
The coronavirus disease pandemic has brought huge challenges to medical systems, especially emergency medicine. [11] Elevating the capability of early identification, appropriate treatment, and life support for severe or critical patients will always be the core topics of emergency medicine.
Emergency medicine in the future will be characterized by continuous advances in practices, research, technologies, and so forth. In terms of clinical practices, problems such as inefficiency and crowding may arise and cause tension in emergency departments. The development of emergency medicine is still in its primary stage and is extremely uneven between rural and urban areas. The resolution of such issues and optimization of processes in emergency medicine can be realized by implementing an increasing number of equipment configurations, improving the structure of emergency medical personnel, and establishing a closer linkage between out-of-hospital and in-hospital emergency services. In essence, “process optimization and early treatment” manifests as an influential component in the development of emergency medicine. In the optimization of the emergency process, the stability of emergency medical professionals is a valuable resource. Upgrading clinical emergency care competence, including rapid response, effectiveness, and service attitude, and improving the skills of medical professionals in the emergency department are of great importance.
The demands for technology are certain to direct the course of emergency services, as the need for timely diagnosis and treatment of patients continues to grow. Information technology can be used to tap available resources and collect information on patients and disease management to aid emergency staff in real time via telemedicine. Specifically, in the absence of specialists or general practitioners on site, the vital signs of patients and critical information can be wirelessly transmitted to experts who can provide remote guidance that may be critical to saving lives. [12] In addition, remote monitoring also enables hospitals to grasp the condition of patients at the earliest time, formulate emergency plans in advance, and ensure a seamless connection between out-of-hospital emergency and in-hospital treatment. By virtue of networks, the real-time transmission of medical devices that monitor information, ambulances’ positioning information, and video footage from inside and outside ambulances can facilitate remote consultation and guidance. Moreover, the collection, processing, storage, transmission, and sharing of out-of-hospital emergency information can fully enhance treatment efficiency and service quality, thereby optimizing the process and mode of service.
Big data technology can fully explore medical information to aid in the management and decision-making of emergency care. [13] One of the applications of big data in the medical field is the establishment of a cloud platform for emergency and critical care information management. Such a platform would collect the diagnosis-, examination-, and treatment-related information of patients from databases, such as an emergency logbook, a hospital information system, a picture archiving and communication system, a microbial detection and management system, and a pathology information system. Next, the data were classified, cleaned, extracted, and explored in depth using the platform. Based on this information, a teaching management system can be obtained, including a multidisciplinary triage management system, a critical care score and grading management system, and an early warning system for serious emergencies. The application of big data technology in emergency medicine provides medical practitioners with access to various information databases for each individual and possible treatment options, which will greatly improve teaching efficiency and the ability to diagnose and treat related diseases.
Precision medicine is a medical model that fully considers individual differences in the genes, environment, and lifestyle of patients to achieve the most effective treatment and prevention of diseases. The emergency department is the first critical link in the clinical diagnosis and treatment of critical illnesses and infectious diseases, and individualized accurate assessment and prevention of disease susceptibility is a valuable research direction for precision emergency medicine. [14] Acute infectious diseases are among the most common diseases in the emergency department. However, given the complexity of diseases, lag in detection technology, and lack of multidimensional clinical information integration technology, the diagnosis and treatment of common diseases such as community-acquired pneumonia remain stagnant. In addition, the emergence of drug-resistant pathogens and emerging microorganisms poses a challenge to empirical therapy protocols. Identifying pathogenic microorganisms quickly and accurately is critical for initiating individualized treatment plans and is also the core component of precision emergency medicine systems. The ideal method of monitoring the outbreak of drug-resistant pathogenic microorganisms in communities or hospitals is to analyze the genetic ancestry of pathogenic microorganisms through genome technology. One of the essential tasks of emergency medicine is to use clinical information to provide individualized diagnosis and treatment for cases without a clear etiology. To some extent, it is necessary to establish etiological diagnoses through emergency treatment processes. In addition to molecular etiology diagnoses based on pathogenic specimens (eg, throat swabs, sputum, and body fluids), diagnostic techniques based on omics information have also seen rapid advances, which will improve precision emergency treatment services. For the differential diagnosis of emergency and critical care illnesses, precision emergency medicine can enhance diagnostic effectiveness significantly with the help of multidimensional and omics data, thus creating the ideal conditions for individualized diagnosis and treatment.
With the combination of big data and precision medicine, information technology can promote the growth of scientific research and clinical work in emergency medicine, such as sequencing, information construction, data integration, and analysis, and improve the use of big data in emergency medicine. Under these circumstances, it is possible to achieve breakthroughs in the development of targeted drugs for precision therapy, complete the closed-loop service of precision emergency medicine, and establish a disciplinary system for precision emergency medicine in China.
Artificial intelligence can promote the growth of emergency medicine. [15] Equipped with capabilities in prediction, analysis, and response, artificial intelligence systems can aid emergency staff in diagnosis and treatment. When artificial intelligence tools execute instructions, they can learn from big data through image recognition, speech recognition, human–computer interaction, physical sensing, and other means. After finishing examinations quickly, artificial intelligence tools can formulate a relatively accurate diagnosis and individualized medicine. In addition, artificial intelligence can assist in locating potential risks and threats in advance. In some emergency events, artificial intelligence can assess the situation and predict the required medical services. Another example of artificial intelligence is the use of medical robots. Apart from their application during complex surgeries, medical robots can deliver objects to patients in quarantine and help avoid human contact during virus epidemics. In short, the use of artificial intelligence will undoubtedly benefit emergency medicine in the future.
As more countries are improving their emergency medical systems, the global scale of information exchange is empowering international emergency medicine. Promoting the quality of academic exchange among countries is a priority in the development of international emergency medicine. Moreover, the variety and complexity of emergency diseases pose challenges to timely and accurate emergency medical treatment, and require emergency medical staff to possess rich medical knowledge and accurate judgment.
Although the development of emergency medicine is confronted with quite a few challenges, it has entered the era of communication among various schools of thought. This journey provides opportunities to the field of emergency medicine. With the joint efforts and hard work of stakeholders worldwide, emergency medicine will accomplish more historic advancements.
Conflict of interest statement
Shujian Wei is the Executive Editor of Emergency and Critical Care Medicine . The author declares no conflicts of interest.
Author contributions
Shujian Wei wrote the article.
Ethical approval of studies and informed consent
Acknowledgements.
- Cited Here |
- Google Scholar
- PubMed | CrossRef |
- View Full Text | PubMed | CrossRef |
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Bioinformatics analysis of sars-cov-2 infection-associated immune injury and..., emergency medicine and covid-19: now and next year, new problems and countermeasures in the prevention and control of covid-19, expert consensus by qilu hospital of shandong university on the diagnosis,..., treatment of acute pulmonary edema by blocking vegf-induced vascular leakage.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- West J Emerg Med
- v.21(5); 2020 Sep
Resident Research in Emergency Medicine: An Introduction and Primer
James h. paxton.
* Wayne State University, Department of Emergency Medicine, Detroit, Michigan
Anne M. Messman
Nicholas e. harrison, adrienne n. malik.
† Kansas University Medical Center, Department of Emergency Medicine, Kansas City, Kansas
Raina J. Burke
‡ Wheeling Hospital, Department of Emergency Medicine, Wheeling, West Virginia
Phillip D. Levy
Training in research methodology represents an important aspect of emergency medicine (EM) resident education, but best methods for design, implementation, and dissemination of resident research remain elusive. Here we describe recommendations and best practices from the existing literature on EM resident research, including helpful tips on how to best implement a resident research program.
INTRODUCTION
When René Laënnec, a French physician in 1816, failed to adequately percuss the thorax of a young woman with heart disease, he improvised. Laënnec wrote, “I rolled a quire of paper into a sort of cylinder and applied one end of it to the region of the heart and the other to my ear.” 1 After numerous revisions, his invention was revealed to the medical community, and quickly caught on. Within a few years, primitive stethoscopes could be found in medical shops throughout Paris. Had Laënnec stopped with that rolled-up piece of paper, his one-time improvisation would have been lost to the annals of history. Fortunately, he chose to build upon his initial discovery and, crucially, to share his breakthrough with the world. Laënnec’s journey charts an enduring and fundamental trajectory of medical innovation: from observation, through inspiration, refinement and testing, to dissemination.
Development of a research project can be especially daunting to physicians already engaged in an emergency medicine (EM) residency training program. But execution of a research project during residency remains a worthwhile experience, allowing participants to meaningfully contribute to medical knowledge and develop an investigative spirit. 2 Residents participating in research appear to attain greater job satisfaction, 3 and can objectively frame everyday questions and methodically seek answers 3 to problems including (among others) staffing issues, wait times, and communication barriers. 4 – 5
The Accreditation Council for Graduate Medical Education Residency Review Committee for EM recognizes the importance of these efforts, mandating resident completion of a “scholarly project” prior to graduation. Their requirement cites the following as examples of qualifying activities: “…the preparation of a scholarly paper such as a collective review or case report, active participation in a research project or formulation and implementation of an original research project.” 6 These activities should include problem identification, data collection, analysis, and conclusion. 7 Performance and documentation of these projects are vital to the acceptance of a scholarly project, whether a case report, community project, development of medical software, or traditional research project. 7 Recent reports from within the EM community have emphasized the importance of scholarly activity to EM resident education. 8 – 9
Advancing the state of scientific knowledge is not a requirement for success in resident research, but it is a potential benefit of this exercise. It is the responsibility and privilege of those involved in residency administration to facilitate the training of EM resident researchers in the development and execution of research projects that support not only the professional careers of residents but also the advancement of our specialty. 8 – 9
What is Resident Research?
It has been suggested that “resident research” is, “research where a resident has a principal role in the implementation and completion of the project.” 10 We suggest that the resident research experience be defined by the engagement of the resident learner in the research process, focusing upon the educational value of the project rather than the resident’s official role or involvement in the design and execution of the project. Research studies are intended to create new generalizable knowledge that can be applied to other populations and settings. 11 Consequently, we propose that “resident research” be defined as any systematic investigation designed to yield new information that actively engages the resident-learner and facilitates the acquisition of a greater understanding of the scientific method. This is in distinction to quality improvement projects, which seek to apply existing knowledge to improve healthcare outcomes within a local healthcare institution or setting. 12
Setting Realistic Expectations
One purpose of resident research is to expose residents to the methods by which research is conducted, creating “educated consumers” of the medical literature. However, residencies hoping to establish a resident research program de novo must recognize the additional workload that resident research projects impose upon faculty. Mentors should be primarily responsible for guiding and supervising resident research, but should be adequately vetted to ensure that the research experience yields a positive result for all involved. Research directors should provide guidance relating to funding opportunities, deadlines for abstract submission to key research conferences, important institutional and federal regulations, and departmental resources. 13 Departmental leadership should create an environment in which research is actively promoted, providing appropriate funding and protected time for mentors and other research faculty. 13
Getting Started
Clinical experiences, journal club articles, or experiences with different teaching modalities may generate an appropriate resident research topic including relevant clinical or educational questions. 2 , 14 – 15 Additional ideas may come from the resident’s personal interests or experiences.
Learning Research Methodology
Most programs will offer training through didactic presentations, journal clubs or evidence-based literature discussions. However, a focused educational effort specifically targeting research methodologies has been shown to correlate with improved resident skills, knowledge, and research productivity. 16 Nearly one in four EM training programs offers a fixed rotation in research. 5 , 17 A more feasible format for the busy trainee might be the Advanced Research Methodology Evaluation and Design video series available from the Society of Academic Emergency Medicine (SAEM), including “how-to” webinars and podcasts produced by senior researchers. 18
The Research Question
A general research question must be formulated, which will generate a testable hypothesis. 3 , 19 All possible outcomes should be considered, and at least one of them must be worthwhile. 20 The FINER criteria may be used to assess the relative merits of the proposal: 14 – 15 , 21
Can the project be completed within the time allotted using the given resources? Can the proposed investigation enroll enough patients to demonstrate a difference in the proposed outcome measures?
Is the topic engaging enough to be worth the effort?
Is the proposed investigation different enough from what has been done before to add knowledge on the subject?
Does the proposed investigation respect the morals of the community, the patient, and the profession?
Are the results likely to be applicable to many patients? Will the results be useful and contribute to the greater good?
Formulating a Hypothesis
A suitably refined and meaningful research question will help in generating a hypothesis, providing a clear delineation of what the investigation will attempt to prove. Investigation of a well-designed hypothesis will be interesting even if a negative result is found.
A mentor experienced in the resident’s area of research interest can be an invaluable resource by offering hints at project scope, helping with setbacks, and tailoring the learning experience to the resident’s needs. 22 Most often, the mentor is an established researcher within the department but could include a specialist in another field, or even a non-physician investigator. 5 , 23 – 24 Goals and expectations should be discussed early on, to avoid frustration for both parties. 5 Terregino has shown that, in general, EM residents are relatively unfamiliar with what resources are available to them, which can lead to significant amounts of time wasted. 25 Most hospitals provide research support that is invisible to the outside observer, including project coordinators, departmental research directors, and biostatisticians. 25 The mentor should be aware of all available institutional resources.
The Literature Search
A valid research project must be informed by past work. Most literature reviews will begin with a search of PubMed.gov , the database of the National Library of Medicine, or OVID.org , which includes textbooks as well as journals. 26 Search terms used must be carefully selected, and the proper Boolean operators assigned. One study has shown physicians to be especially inept at crafting effective search strings. 27 Any doubts about the literature search process or its results should be referred to a librarian.
Each paper identified from the literature review should be thoroughly read. Investigators should avoid citing abstracts alone, as they are often incomplete in their data presentation. This process is labor-intensive but necessary to form a strong foundation for the research project. All references cited within each article should be assessed for relevance. The selected literature should be reviewed to better understand the subject matter and to develop context for the proposed work. If adequate data from existing sources are uncovered, one may consider a retrospective evaluation of prior results including a meta-analysis. 2 , 28 – 29
Research Design
The novice researcher should look to the existing medical literature for guidance in how to properly design a new study. Selection of the proper research methodology will depend upon multiple factors, including the research question, hypothesis, and predetermined outcome measures. A timeline should be implemented to ensure that all tasks are achievable within the allotted time. Resident physicians should develop a team approach, incorporating input from the faulty mentor as well as a staff epidemiologist or biostatistician. The required sample size will depend upon a variety of factors, including the acceptable level of significance, power of the study, expected effect size, underlying event rate in the population, and standard deviation in the population. 30 – 31 Efforts should be made to collect an inclusive and truly random sampling, to avoid convenience selection bias. 32 Early consultation with the biostatistician will also inform the researcher’s decisions on the most appropriate methods for the statistical analysis of data derived from the study. For further information about study design specifics, the reader is referred to several existing publications. 2 , 4 , 13 , 33 – 34
The Institutional Review Board
Any research project that involves human participants or their data requires submission to the local institutional review board (IRB). Research protocols submitted to the IRB can fall into one of three categories: full submission; expedited; or exempt. Research involving greater than minimal risk to human subjects will require a thorough review by the IRB and development of an informed consent document. Prospective projects involving only minimal risk may be approved via the expedited process, where a single reviewer may approve the work in lieu of the convened board. Studies that include only retrospective data from the electronic health record may be exempt from IRB review, but this determination should be made by the IRB, rather than by the investigator. Investigators should confer with their local IRB to confirm what level of IRB review is required before beginning data collection.
Conducting the Study
After the research protocol has been IRB-approved or exempted, data collection can commence. Prior development of a data collection tool will greatly enhance the efficiency of this process, facilitating both IRB approval and the subsequent data analysis. Subject enrollment can also be improved with use of a trained research assistant. This problem may be circumvented through creation of an “academic associate program,” which integrates EM research with undergraduate education. 35
Research Funding
Resident research projects usually require little external funding. On occasion, additional costs may be incurred to help pay for statistical analysis, or the purchase of required equipment. 36 Internal sources, as well as the Emergency Medicine Foundation 37 and the SAEM Foundation 38 represent potential sources for funding.
Presentation and Publication
Once the data have been collected and analyzed, the researcher should consider how the results will be disseminated. The annual meeting of SAEM, the Research Forum at the American College of Emergency Physicians’ annual scientific assembly, and the Annual Assembly of the Council of Residency Directors in Emergency Medicine (CORD) represent the premier locales for presentation of EM research. 39
Ideally, the resident research experience should lead to a manuscript, although the lack of immediate publication must not be interpreted as failure. Only 40% of EM abstracts go on to become full article publications. 15 , 40 Most manuscripts are published 1–2 years after initial presentation. 17 Appropriate journal selection for submission enhances the likelihood of success, as does a thorough understanding of manuscript preparation techniques and review criteria. 41 – 43
While any research resultant from a resident’s scholarly project is unlikely to have the impact of Laënnec’s stethoscope, EM residents may still gain much from engaging in clinical research. For some, it will light an investigative fire that will burn for an entire career. At the least, resident research projects can provide an opportunity to explore issues central to the practice of EM, helping the resident to become a more well-rounded physician.
Section Editor: Whitney Johnson, MS, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest : By the West JEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.

Research & Innovation
Leading in the advancement of emergency medicine through innovation and scientific discovery..
Emergency Medicine is a rapidly-developing field, and Stanford is leading research in many facets of care. The department benefits from collaboration with other disciplines at Stanford, within local Silicon Valley, and across the globe.
Stanford is leading research efforts to transform health care for all through Precision EM. Precision Emergency Medicine utilizes information and technology to effectively, efficiently, and authentically deliver acute care for our patients and our communities.
RESEARCH AREAS INCLUDE: Pre-hospital Care; AI; Telehealth; Informatics; Medical Education; Pediatric EM; Global EM; Population Health; Wilderness Medicine; Ultrasound; Wellness; and Diagnostics.

Join us for StEMI X 2024 on October 17!
Our fourth annual symposium on emergency medicine innovation is free and open to all! Learn more

Stanford Emergency Medicine Magazine
Download PDF

PROFILES IN INNOVATION
Take a deeper dive into select emergency medicine research initiatives at Stanford, from informatics, to diagnostics, to education. More
PUBLISHED RESEARCH
Browse through our online database of recent publications

FACULTY LABS & CENTERS
Precision Education and Assessment Research Lab (PEARL)
Global Pediatric Emergency Equity Lab
Emergency Care Health Services Research Data Coordinating Center
The Bennett Lab

Stanford Department of Emergency Medicine Seed Grants
Since 2020 Stanford University’s Department of Emergency Medicine has awarded seed grants that encourage early-career physician-scientists in the department to explore new territories in emergency medicine. Read about the recipients
Quick Links
- Stanford Clinical Trials Directory
- National Institutes of Health
- Society for Academic Emergency Medicine
- American College of Emergency Physicians
- American Academy of Emergency Medicine
- Wilderness Medical Society
- Annals of Emergency Medicine
- Academic Emergency Medicine
- American Journal of Emergency Medicine
- Journal of Emergency Medicine
- Emergency Medicine Journal
- European Journal of Emergency Medicine
SUPPORT EMERGENCY Medicine RESEARCH

2024-2025 Research Topics
EMF funds groundbreaking EM research to advance our specialty. To explore the 2024-2025 funding priorities, see the visualization below. For a full list of current grantees and their projects, visit here .
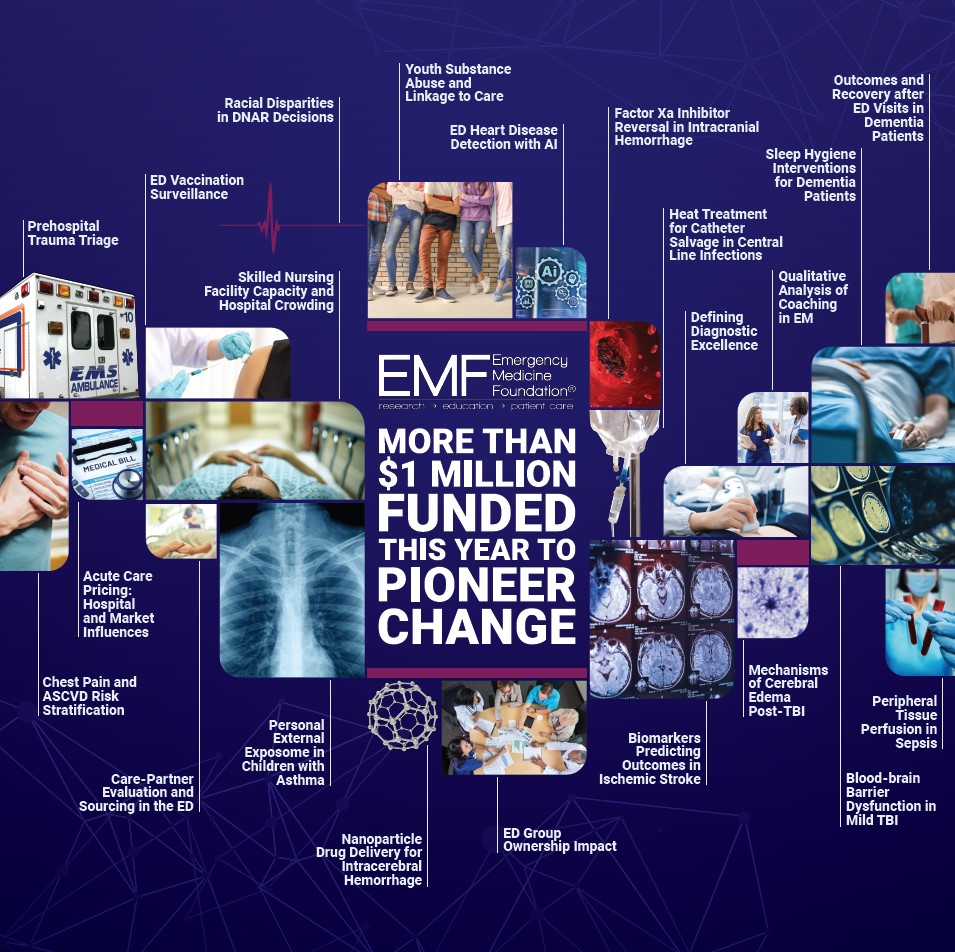
- News & Events
- EM Diversity Committee
- Visiting Program for Underrepresented Students
- Past Newsletter Issues
- Informatics
- Emergency Department Clinical Sites
- Critical Care Transport
- Trauma Center
- Stroke Center
- Yale Program in Addiction Medicine
- Crisis Intervention Unit
- Chest Pain Center
- Behavioral Health & Chronic Illness
- Clinical Trials
- Digital Health
- Faculty, Staff & Trainees
- Workshops and Events
- Healthcare Simulation
- Health Policy and Services
- Observational Studies
- Substance Use Disorders (Prevention and Treatment)
- Abujarad's Digital Health Lab
- Current Research
- Melnick Lab
- Venkatesh Lab
Publications
- Faculty by MESH Keywords
Research Faculty
Research administration.
- Training and Education
- Faculty & Fellows
- GEOHealth-MENA
- Resident Education
- Academic Career Development
- Framework of Structured Mentorship
- Promotion metrics and timeline
- The Faculty Development Series
- Topics of Importance
- Calendar and Resources
- All Faculty
- Area of Concentration (AoC)
- Electives & Research
- Compensation & Benefits
- Hospital Profiles
- Past Residents
- Living in New Haven
- Application
- Program Overview
- Application Process
- Current Fellows
- Publications by Fellows
- Previous Fellows
- Drug Abuse, Addiction, and HIV Research Scholars
- Emergency Ultrasound
- Medical Simulation
- Wilderness Medicine
- In the News
- YES Residents and Alumni
- Medical Students
- Alumni & Giving
INFORMATION FOR
- Residents & Fellows
- Researchers
Emergency medicine research at Yale has unparalleled depth and breadth of expertise, but what really sets us apart is the collaborative environment of discovery, learning, and growth.
Our Mission
Our mission is to Advance the Science and Practice of Emergency Medicine. In 2021, the department ranked first in the nation in research dollars awarded by the National Institutes of Health—a demonstration of our commitment to our mission, as we continue to push the envelope of science and advocate for our patients and communities.
EM research is an interdisciplinary field that addresses multiple subjects and medical specialties, ranging from acute critical care to improving public health. Our faculty are nationally recognized experts in their fields of study, dedicated to creating new knowledge and providing residents with exceptional opportunities to advance academic careers and individual research interests. Our work is supported by NIH, AHRQ, SAMHSA, CDC, EMF, and RWJF, among others. We encourage you to explore the spectrum of research content foci in our department.
Partner With Us
Areas of focus.
Quick Links
- UW HR Resources

We are dedicated to promoting excellence in the practice of emergency medicine through collaborative efforts to discover, develop, and disseminate strategies for improving care of acutely ill and injured patients.
Nathan White Vice Chair of Research [email protected]
Nate Ashford Research Operations Manager [email protected]
The University of Washington provides an exceptional environment for research and is considered a top-funded public research institution, receiving over one billion dollars each year in research funding. UW resources and infrastructure provide unparalleled opportunities for investigation and collaboration.
Within our department, our investigators are engaging in scientific inquiry, promoting evidence-based research, and advancing education and training on a variety of topics. Research is being conducted by our faculty in a broad range of topics, including basic and translational trials.
Areas of research
- Cardiac Arrest and Prehospital Care
- Trauma and Hemorrhage Control
- Medical Education Research
- Health Care Policy and Services
- Opiate Use & Substance Use Disorder
- Sepsis and ARDS
- International Healthcare Delivery
- Environmental Health and Climate Change
- Development and Evaluation of Health Systems
- Point-of-Care Ultrasound (POCUS)
- Novel Ultrasound Technology, Techniques, and Applications
- Workplace and Provider Safety
- Emergency Care Delivery and Quality of Care

Active Research Projects
Learn more about our department's projects.

Research Team
Meet the 30+ members that make up our department's team.

Critical Care & Resuscitation Science
Advancing the care of critically ill and injured patients in the emergency department and beyond.

Quality and Safety
Patient and provider safety is our top priority, and we are dedicated to quality improvement work through both research and education.

Population Health Research
Promoting the health of populations and the environment worldwide.

Ultrasound Research
Putting cutting-edge ultrasound technology and knowledge into practice to enhance patient care and safety.

Emergency Medical Services Research
A global leader in prehospital emergency medical services research across a broad range of topics from resuscitation science to the management of critically ill and injured patents in the air medical transport setting.
Research resources
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Volume 19, Issue 3
- Clinical research in emergency medicine: putting it together
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- A M T Good 1 ,
- P Driscoll 2
- 1 Accident and Emergency Department, Royal Liverpool University Hospital, Liverpool, UK
- 2 Accident and Emergency Department, Hope Hospital, Salford, UK
- Correspondence to: Dr A M T Good, Accident and Emergency Department, Royal Liverpool University Hospital, Prescot Street, Liverpool L7 8XP, UK; Anthony.Good{at}rlbuh-tr.nwest.nhs.uk
The difficulties in conducting good clinical research in emergency medicine can be overcome. This article will begin by identifying the main difficulties faced by the emergency medicine researcher. It will then discuss some solutions through the development and application of the research protocol. Finally, recommendations will be made with regard to writing for publication.
- clinical research
https://doi.org/10.1136/emj.19.3.242
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
The top 100 cited articles published in emergency medicine journals
Affiliations.
- 1 Division of Emergency Radiology, Department of Radiology and Imaging Sciences, Emory University Hospital, Atlanta, GA; Department of Emergency Medicine, Hospital General de la Plaza de Salud, Santo Domingo, Dominican Republic. Electronic address: [email protected].
- 2 Department of Clinical Epidemiology and Public Health, Universidad Autónoma de Santo Domingo, Santo Domingo, Dominican Republic.
- 3 Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan.
- 4 Department of Emergency Medicine, Hospital General de la Plaza de Salud, Santo Domingo, Dominican Republic.
- 5 Department of Emergency Medicine, New York Methodist Hospital, Brooklyn, NY.
- PMID: 25979301
- DOI: 10.1016/j.ajem.2015.04.047
Introduction: Our objective was to identify trends and examine the characteristics of the top 100 cited articles in emergency medicine (EM) journals.
Methods: Scopus Library database was queried to determine the citations of the top 100 EM articles. A second database (Google Scholar) was used to gather the following information: number of authors, publication year, journal name, impact factor, country of origin, and article type (original article, review article, conference paper, or editorial). The top 100 cited articles were selected and analyzed by 2 independent investigators.
Results: We identified 100 top-cited articles published in 6 EM journals, led by Annals of Emergency Medicine (65) and American Journal of Emergency Medicine (15). All top-cited articles were published between 1980 and 2009. The common areas of study were categorized as cardiovascular medicine, emergency department administration, toxicology, pain medicine, pediatrics, traumatology, and resuscitation. A statistically significant association was found between the journal impact factor and the number of top 100 cited articles (P < .005).
Conclusion: The top-cited articles published in EM journals help us recognize the quality of the works, discoveries, and trends steering EM. Our analysis provides an insight to the prevalent areas of study being cited within our field of practice.
Copyright © 2015 Elsevier Inc. All rights reserved.
PubMed Disclaimer
- Am J Emerg Med. 2015 Dec;33(12):1837-8
- Top cited articles and journal impact factors. Lee CH. Lee CH. Am J Emerg Med. 2015 Dec;33(12):1837. doi: 10.1016/j.ajem.2015.09.023. Epub 2015 Sep 21. Am J Emerg Med. 2015. PMID: 26458535 No abstract available.
- The author replies. Shuaib W. Shuaib W. Am J Emerg Med. 2015 Dec;33(12):1837-8. Am J Emerg Med. 2015. PMID: 27010044 No abstract available.
Similar articles
- Top-cited articles in emergency medicine. Tsai YL, Lee CC, Chen SC, Yen ZS. Tsai YL, et al. Am J Emerg Med. 2006 Oct;24(6):647-54. doi: 10.1016/j.ajem.2006.01.001. Am J Emerg Med. 2006. PMID: 16984831
- Bibliometric analysis of the top 100 cited cardiovascular articles. Shuaib W, Khan MS, Shahid H, Valdes EA, Alweis R. Shuaib W, et al. Am J Cardiol. 2015 Apr 1;115(7):972-81. doi: 10.1016/j.amjcard.2015.01.029. Epub 2015 Jan 15. Am J Cardiol. 2015. PMID: 25670637 Review.
- An Analysis of the Top-cited Articles in Emergency Medicine Education Literature. Munzer BW, Love J, Shipman BL, Byrne B, Cico SJ, Furlong R, Khandelwal S, Santen SA. Munzer BW, et al. West J Emerg Med. 2017 Jan;18(1):60-68. doi: 10.5811/westjem.2016.10.31492. Epub 2016 Nov 23. West J Emerg Med. 2017. PMID: 28116010 Free PMC article.
- The 100 top-cited articles published in psychiatric journals. Mazhari S. Mazhari S. J Psychiatr Pract. 2013 Jul;19(4):327-38. doi: 10.1097/01.pra.0000432604.06835.da. J Psychiatr Pract. 2013. PMID: 23852109
- Top-cited articles in endodontic journals. Fardi A, Kodonas K, Gogos C, Economides N. Fardi A, et al. J Endod. 2011 Sep;37(9):1183-90. doi: 10.1016/j.joen.2011.05.037. Epub 2011 Jul 20. J Endod. 2011. PMID: 21846531 Review.
- A Bibliometric Analysis of the Top 100 Cited Papers in Retinal Detachment. Asahi MG, Pakhchanian H, Doepker C, Raiker R, Gallemore RP. Asahi MG, et al. J Vitreoretin Dis. 2021 May 18;5(6):467-478. doi: 10.1177/24741264211007378. eCollection 2021 Nov-Dec. J Vitreoretin Dis. 2021. PMID: 37007181 Free PMC article.
- A bibliometric analysis of systematic reviews and meta-analyses in ophthalmology. Fu Y, Mao Y, Jiang S, Luo S, Chen X, Xiao W. Fu Y, et al. Front Med (Lausanne). 2023 Mar 2;10:1135592. doi: 10.3389/fmed.2023.1135592. eCollection 2023. Front Med (Lausanne). 2023. PMID: 36936241 Free PMC article.
- Global trends of dalbavancin: A bibliometric analysis. Monteagudo-Martínez N, Solís García Del Pozo J, Ikuta I, Galindo MF, Jordán J. Monteagudo-Martínez N, et al. J Clin Pharm Ther. 2022 Sep;47(9):1299-1311. doi: 10.1111/jcpt.13719. Epub 2022 Jun 23. J Clin Pharm Ther. 2022. PMID: 35735062 Free PMC article. Review.
- The latest research trends in primary biliary cholangitis: a bibliometric analysis. Zhao Y, Yin Z, Du H, Huang K, Zhang F, Chen H. Zhao Y, et al. Clin Exp Med. 2023 Jun;23(2):347-355. doi: 10.1007/s10238-022-00825-0. Epub 2022 Apr 7. Clin Exp Med. 2023. PMID: 35389157
- Endodontic Microbiology: A Bibliometric Analysis of the Top 50 Classics. Karobari MI, Maqbool M, Ahmad P, Abdul MSM, Marya A, Venugopal A, Shaik GM, Scardina GA, Messina P, Noorani TY. Karobari MI, et al. Biomed Res Int. 2021 Jun 1;2021:6657167. doi: 10.1155/2021/6657167. eCollection 2021. Biomed Res Int. 2021. PMID: 34746305 Free PMC article. Review.
- Search in MeSH
LinkOut - more resources
Full text sources.
- ClinicalKey
- Elsevier Science
- Ovid Technologies, Inc.
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Research Priorities
- Research Strategy
- James Lind Alliance
RCEM Research Strategy 2020
Top research priorities in emergency medicine.
RCEM, in partnership with the James Lind Alliance (JLA), has conducted a Research Priority Setting Partnership with the aim of including patients, carers and clinicians in a process to establish the top research priorities in emergency medicine.
James Lind Alliance Emergency Medicine Priority Setting Partnership Refresh 2022
We’re excited to share that after the success of the original PSP, the Royal College of Emergency Medicine have recently completed a refresh of the Emergency Medicine research priorities for the next five years. This will ensure that priorities are current and representative of today’s patients, carers, and clinicians. The new top 10 research priorities in Emergency Medicine can be found below.
In January 2017 the JLA Emergency Medicine Priority Setting Partnership (EM PSP) published its first list of research priorities, providing guidance on the research, learning and development in the field of emergency medicine. Since then, our world and the landscape of emergency medicine have changed significantly, and some of the original priorities have been addressed through funded research studies .
Emergency Medicine is a broad, dynamic subject area and includes a variety of different medical areas such as acute medical emergencies, minor illness and injury, major trauma, acute mental health problems and the management of elderly patients with complex co-morbidities and social problems (not to mention the current challenges posed by COVID-19). Defining research priorities for such a diverse speciality and large potential patient base is a significant but rewarding challenge, driving innovation in the field. What’s more the EM PSP refresh will help to connect researchers and funders with real world experience.
The process involved research questions being collected, screened and added to a long list in survey format so that individuals that wished to take part in the survey were able to rank each of the research questions. The survey was open over summer of 2022 and closed in early September. The results of the survey allowed us to develop a short-list of the top 26 ranked research questions which were brought to the final workshop at the end of September.
The aim of the workshop was to review and agree the top 10 questions for research into Emergency Medicine. This will help researchers focus on finding answers to questions which will make the most difference to people who need to use an Emergency Medicine Department, and to those who work there. Workshop participants included individuals with lived experience, and health and care professionals who work within this area. Participants discussed in small and larger groups the short-list of 26 questions and decided together about which 10 research questions that they believed should be prioritised.
The James Lind Alliance (JLA) is a not-for-profit organisation, working to bring patients, carers and clinicians together in Priority Setting Partnerships (PSP) to identify and prioritise the Top 10 unanswered questions or evidence uncertainties that they agree are the most important.
This was our second time around collaborating with the JLA, and we were delighted to be partnering with them again.
You can find out more about the JLA here , and you can find the EM PSP here .
Related Pages

Research Advice and Resources

Research Awards and Fellowships

RCEM Research Grants and Awards

- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
The Glass Ceiling—Racial Disparities Among Emergency Medicine Chief Residents
- 1 Harvard Medical School, Boston, Massachusetts
- 2 Stanford University School of Medicine, Stanford, California
- Original Investigation Race and Sex Disparities Among Emergency Medicine Chief Residents Jennifer W. Tsai, MD, MEd; Mytien Nguyen, MS; Sarah N. Dudgeon, MPH; William McDade, MD, PhD; Jung G. Kim, PhD, MPH; Pooja Agrawal, MD, MPH; Dowin Boatright, MD, MBA, MHS JAMA Network Open
The role of a chief resident extends beyond a mere title; it is a gateway to opportunities and a stepping stone to leadership roles in both academic and community emergency medicine (EM) settings. Within the department, a chief resident signals to faculty and trainees that the title-bearer is clinically excellent, organized, thorough, and well-respected. It is often considered an unspoken metric for fellowship trainee positions, medical directorships, and other leadership-oriented roles. Although this title denotes increased academic responsibilities, it is also tethered to social capital capable of launching a successful career in EM.
However, this coveted position may not be equally accessible to all. Data from Tsai et al 1 suggest that women underrepresented in medicine (URIM; a category that included residents identified as Black, Hispanic, American Indian or Alaskan Native, and Native Hawaiian or Other Pacific Islander) were least likely to be selected for chief promotion, and 50% as likely to be selected for chief resident compared with White men. This is corroborated by other studies demonstrating that URIM physicians, particularly Black women, are less likely to occupy executive leadership roles (commonly referred to as the “c-suite”) or departmental leadership roles (ie, department chair, vice chair, program director). 2 , 3 This disparity systematically distances URIM physicians from career trajectories that could lead to significant social and economic capital.
Some consider facets such as individual popularity, likability, and on-shift performance to be driving forces in the selection process for chief residents. Although the selection criteria are thought to be objective, there is an inherent subjectivity to nomination, ranking, and voting. This perception may provide insight into the true state of department and residency culture in the US. Furthermore, it raises the question: Are the requirements for becoming a chief intrinsically and structurally biased? If so, this could suggest that the standards and requirements for these roles may need to be reevaluated to ensure fairness and inclusivity.
Chief residents have line of sight to both residency and departmental operations. As a function of proximity and open communication, chiefs can build close relationships with faculty and administration during this formative year. Under their tutelage, significant growth occurs and produces enduring mentorship and sponsorship threads; this serves as an inflection point in career trajectory. The overlay of mentorship and sponsorship, or the lack thereof, can widen the opportunity gap in professional development.
The downstream implications of this disparity in representation are profound. Some programs select their fellows from the pool of chief residents, and some groups and departments only hire chief residents. The skill set development that chief residents undergo is attractive to employers and directly translates into administrative and leadership roles in EM. Thus, the lack of URIM physicians in these roles can limit their career advancement opportunities.
One counterargument has been the floor effect; in other words, the selection pool of URIM residents is inherently low, which contributes to the scarcity of URIM chief residents. However, the recruitment of URIM physicians partly hinges on representation at leadership levels; among those ranks are chief residents. Fewer URIM chiefs can translate to fewer persons with voting privileges advocating on behalf of URIM applicants. For active URIM residents, it reinforces the notion of a glass ceiling—that is, a systemic barrier of access to leadership roles within medicine and health care.
As health care has pivoted toward precision medicine, monitoring outcomes, and cost-savings models, value has been placed on leadership that can influence these factors. And although not explicitly stated, chief residents are in this leadership pipeline—which makes the selection process even more critical. To date, there are no studies that link the presence (or absence) of URIM chiefs to health outcomes. However, for the most vulnerable populations concordance literature does reflect improved clinical outcomes, greater adherence, reduced utilization, and lower health care expenditures (all metrics of interest) when clinicians come from URIM backgrounds. 4 Despite the seemingly natural alignment in goals, a dearth of URIM chiefs exists, as evidenced by this study.
Tsai et al 1 underscores the value of continued implicit bias and microaggression training. It also highlights a significant area of ignorance in the recruitment, advancement, and sponsorship of URIM physicians in leadership roles within the EM workforce. Furthermore, it indirectly elevates a dialogue about the connection between leadership and equitable health outcomes. These dynamics impact health outcomes for diverse patients and represent a branching point where intervention can be targeted. 5
Association of American Medical Colleges and American Medical Association both support diversity, equity, and inclusion (DEI) in medicine; American College of Emergency Physicians, American Academy of Emergency Medicine, Society for Academic Emergency Medicine, and Emergency Medicine Residents’ Association all support DEI within emergency medicine. 5 , 6 Unfortunately, there is also an overarching, concerted effort to dismantle DEI initiatives. Some irony lies in the fact that many of the targets have been Black women newly hired in leadership roles, despite its benefit being skewed toward White women. 7 This article provides additional evidence for why these efforts are both necessary and urgent.
The underrepresentation of URIM physicians in leadership roles, such as chief residents, is a pressing issue that needs to be addressed. It is crucial for the medical community to recognize this disparity and take proactive steps to ensure equal opportunities for all, regardless of their race, ethnicity, and gender. This will not only enrich the diversity of leadership in emergency medicine but also enhance the quality of patient care and health outcomes.
Published: September 24, 2024. doi:10.1001/jamanetworkopen.2024.32606
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Landry AM et al. JAMA Network Open .
Corresponding Author: Alden M. Landry, MD, MPH, DICP, 164 Longwood Ave, 2nd Floor, Boston, MA 02215 ( [email protected] ).
Conflict of Interest Disclosures: Dr Brown reported receiving consulting fees from GSK outside the submitted work. No other disclosures were reported.
See More About
Landry AM , Brown I. The Glass Ceiling—Racial Disparities Among Emergency Medicine Chief Residents. JAMA Netw Open. 2024;7(9):e2432606. doi:10.1001/jamanetworkopen.2024.32606
Manage citations:
© 2024
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Emergency Medicine Topics
- Antibiotic Resistance
- Bioterrorism and Disaster Medicine
- Cardiac Emergencies
- Clostridium difficile Infection
- Coronavirus (COVID-19)
- Emerging and Reemerging Infectious Diseases
- Methicillin-Resistant Staphylococcus aureus (MRSA)
- Pain Management
- Stroke/Cerebrovascular Disease
- Wound Management
All Medscape Topics
- Acute Coronary Syndromes (ACS)
- Acute Leukemia
- Adolescent Medicine
- Aesthetic Medicine
- Affordable Care Act (ACA)
- Alzheimer's Disease
- AMD and Retinal Disease
- Antiretroviral Therapy
- Anxiety Disorders
- Arrhythmia & EP
- Arthroplasty
- Atopic Dermatitis
- Atrial Fibrillation
- Bariatric Surgery
- Barrett's Esophagus
- Bioterrorism/Disaster Medicine
- Bipolar Disorder
- Bladder Cancer
- Bone and Mineral Disorders
- Benign Prostatic Hyperplasia (BPH)
- Brain Cancer
- Breast Cancer
- C. difficile
- Cardiovascular Risk Reduction
- Cataract and Refractive Surgery
- Celiac Disease
- Child and Adolescent Psychiatry
- Chronic Kidney Disease
- Chronic Leukemia
- Colorectal Cancer
- Cornea and External Disease
- Cosmetic Dermatology
- Critical Care Nursing
- Crohn's Disease
- CVD Prevention
- Cystic Fibrosis
- Dental and Oral Health
- Diabetic Microvascular Complications
- Eating Disorders
- Electronic Health Records
- End-Stage Renal Disease
- Erectile Dysfunction
- Exercise and Sports Medicine
- Fibromyalgia
- Gallbladder and Biliary Disease
- Genomic Medicine
- Geriatrics-Palliative Care
- GI/Colorectal Cancer
- GI/Noncolorectal Cancer
- GU/Prostate Cancer
- Head and Neck Cancer
- Health Diversity
- Healthcare Reform & the ACA
- Heart Failure
- Hepatitis B
- Hepatitis C
- HIV Transmission & Prevention
- Hodgkin's Lymphoma
- Hospital Medicine
- HPV and Cervical Cancer
- Hypertension
- Hypogonadism
- IBS and Chronic Constipation
- Immunization
- Infertility
- Inflammatory Bowel Disease
- Insulin Therapy
- Integrative Medicine
- Interventional Cardiology & Surgery
- Joint Disorders
- Kidney & Pancreas Transplant
- Lipids & Metabolic
- Liver & Intestine Transplant
- Lung Cancer
- Lyme Disease
- Mechanical Ventilation
- Medical Lifestyle
- Medical Malpractice and Legal Issues
- Medical Practice Management
- Mental Health and Psychiatric Nursing
- Metastatic Breast Cancer
- Minimally Invasive Gastrointestinal Surgery (MIGS)
- Moderate to Severe Asthma
- Multiple Myeloma
- Multiple Sclerosis
- Neonatal Medicine
- Neurosurgery
- Non-Hodgkin's Lymphoma
- Novel Coronavirus
- Nurse Career and Education
- Nurse Practitioners
- OB/GYN and Women's Health Nursing
- Obesity and Weight Management
- Osteoarthritis
- Osteoporosis
- Otitis Media
- Otolaryngology
- Ovarian Cancer
- Palliative Care
- Pancreatitis
- Parenteral and Enteral Nutrition
- Parkinson's Disease
- Patient Safety
- Pediatric Dermatology
- Pediatrics/Neonatal Care Nursing
- Pediatric Ophthalmology
- Peptic Ulcer Disease
- Perioperative Nursing
- Preclinical Studies
- Prostate Cancer
- Psoriatic Arthritis
- Pulmonary Arterial Hypertension
- Rare Diseases
- Reimbursement and Quality
- Renal Cell Carcinoma
- Reproductive Endocrinology
- Restless Legs Syndrome
- Rheumatoid Arthritis
- Schizophrenia
- Science and Technology
- Sjögren's Syndrome
- Skin Cancer
- Sleep Disorders
- Social Determinants of Health
- Spinal Disorders
- Substance Abuse and Addiction
- Systemic Lupus Erythematosus
- Thyroid Cancer
- Thyroid Disease
- Type 1 Diabetes
- Type 2 Diabetes
- Ulcerative Colitis
- Urinary Incontinence & OAB
- Women's Sexual Health
Featured Topics

Department of Emergency Medicine’s Annual Research Showcase 2024 Recap

On Thursday, September 12, 2024, the Department of Emergency Medicine held its annual Research Showcase in the Trent Semans Center for Health Equity’s Great Hall. Given the new accommodations for the event, this year the planners wanted to show a broad perspective on how the faculty and students participate in the department’s research mission. And it did not disappoint.
The attendees were welcomed with coffee and a continental breakfast before Dr. Alexander Limkakeng , Vice Chair of Research, took the stage at 8 a.m. His introduction to this year’s event encapsulated both Duke’s Centennial through a generational look at academia and research in the field of Emergency Medicine and the future of the field through inspiration.
Dr. Limkakeng also introduced our hosts for the event, the current Chief Residents: Amna Nawaz, Carmen Estrada Huerta, and Sekar Novika. Dr. Novika, in turn, introduced this year’s Keynote Speaker, Theodore “Ted” Corbin, MD .
Dr. Corbin, Professor and Chairperson of the Department of Emergency Medicine at Rush University Medical Center in Chicago, presented our audience an overview of his work in solving violence in under-served youth through trauma-informed, hospital-based interventions. In his presentation, "Viewing Violence through the Lens of Trauma and Healing," Dr. Corbin touched on topics ranging from the applied tools he has found beneficial in helping young victims of interpersonal injury, to discussing his behavioral health services program. He also touched on how research, in using different methodologies, can inform new research approaches which, in turn, can inform policy change too.
Dr. Corbin set the stage for the wide-ranging, community-focused and emergency medicine field-focused research presented throughout the rest of the event.
Throughout the program of interlaced podium research and abstract presentations, those assembled learned of studies ranging from underwater hyperbaric research to medicines in space, and everything in between. One special video highlighted a GEMINI Center collaborator, Dr. Abiola Fasina , and her research entitled "Three Delays Model in Sepsis Care in Lagos, Nigeria."
Two breaks in our program schedule, centered around abstract posters on bulletin boards displayed around the Great Hall, gave attendees a chance to talk directly to project investigators (PIs) and their research.
The event closed with comments from Dr. Charles Gerardo , Professor and Chair of Duke University Department of Emergency Medicine. He reviewed the far-reaching research our faculty and students engage in and how this research touches communities far beyond Durham, North Carolina. The event adjourned with prepared lunches for the participants.

We invite you to view the 2024 Research Showcase with our on-demand stream .
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
September 27, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Period poverty research finds 1 in 3 teens lack access to menstruation products
by American Academy of Pediatrics

One in three adolescents who have visited a pediatric emergency department report difficulties in accessing menstruation products, according to research presented during the American Academy of Pediatrics 2024 National Conference & Exhibition at the Orange County Convention Center from Sept. 27–Oct. 1.
Staff Scientist Meleah Boyle, Ph.D. MPH, co-senior author of the study, said addressing period poverty, as the issue has been called, is a growing area of research in the United States
"Our study highlights the widespread nature of period poverty and the need for broad actions—both locally and nationally—to increase the affordability and accessibility of these products for youth," Boyle said.
Menstrual equity means that every person who menstruates should have equal access to affordable and quality menstrual products. Unfortunately, many people do not have access to these necessary products. In the study, researchers found that 30% of adolescents do not have the products they need with no differences based on measures of socioeconomic status, such as insurance and community opportunity, or individual differences , such as race and ethnicity.
Prior research estimates that of those who menstruate, 11.9 million struggle to find access to menstrual products. This lack of access can lead to absences from school and/or work as well as negative health outcomes such as urinary tract infections and bacterial vaginosis.
Boyle said the research highlights the need for public health programs and policy changes to ensure youth have access to the products they need to avoid negative impacts on their health and engagement.
"Ensuring access to healthy and appropriate menstrual health products should be a public health priority," Boyle said.
Study co-author Riya Metha is scheduled to present the research from 5:15–6:15 pm ET on Saturday, Sept. 28.
Explore further
Feedback to editors

New drug for schizophrenics has experts excited
4 hours ago

Distant relatedness in biobanks harnessed to identify undiagnosed genetic disease

Circadian disruption, gut microbiome changes linked to colorectal cancer progression

Hydrogel with ultrasound activation enables sustained drug release

Study finds estrogens play a hidden role in cancers, inhibiting a key immune cell
19 hours ago

Study reveals critical role of tRNA modifying enzyme in brain function
20 hours ago

Exploring how melanin influences clinical oxygen measurements

Two studies find SARS-CoV-2 virus becoming resistant to antiviral drugs used to treat patients

Circadian rhythm disruption linked to lung inflammation

Researchers discover what hinders DNA repair in patients with Huntington disease
Related stories.

Ensuring menstrual product access equity in the criminal legal system
Aug 8, 2023

Free menstrual products matter to support equity, but so do adequate facilities and sinks
Sep 17, 2024

A significant number of New Zealand teenagers are missing school because they cannot afford menstrual products
Feb 20, 2020

Ensuring women and girls have access to safe and affordable menstrual products
Aug 25, 2021

Study explores homeless women's experiences of 'period poverty'
Mar 14, 2024

Australian budget pledged $12.5 million for free menstrual products in Indigenous communities—why it's needed
May 21, 2024
Recommended for you

How changes in risk factors may be contributing to growing number of babies born prematurely
22 hours ago

Vape residue may harm unborn babies, mouse study suggests
21 hours ago

Genetic background of pregnant women can influence non-invasive prenatal test results
Sep 26, 2024

Rates of sudden unexpected infant death changed during the COVID-19 pandemic, study finds

Signs of developing asthma are evident in the first year of life, health data analysis shows

Researchers discover treatment for major cause of recurrent pregnancy loss
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
Ensitrelvir for mild to moderate COVID-19 (March 2024) Although nirmatrelvir-ritonavir reduces hospitalization and death from COVID-19,drug interactions preclude its use in some patients. Ensitrelvir is an oral protease inhibitor that prevents SARS-CoV-2 replication and has fewer drug interactions.
Y.G. Bodien and OthersN Engl J Med 2024;391:598-608. Among 241 persons with disorders of consciousness who had no observable response to commands, 25% had a verifiable response to commands on EEG ...
JAMA Network Open. Research. September 24, 2024. This cohort study of US emergency medicine residents graduating in 2017 and 2018 analyzes the selection of chief residents by race, ethnicity, and sex. Equity, Diversity, and Inclusion Health Care Workforce Health Policy Medical Education Medical Education and Training.
To investigate the current situation of emergency preparation and emergency drill in the CSSD, and analyze its influence on the nurses' emergency attitude and ability. Jiawei Liu, Fengliu Gui, Mengmeng Zhang and Hui Chen. BMC Emergency Medicine 2024 24:133. Research Published on: 29 July 2024.
Ingestion of magnets carries risks for significant morbidity. We propose a new protocol designed to reduce the need for surgery, shorten length of stay, and decrease morbidity. Ortal Schaffer, Adi Kenoshi and Osnat Zmora. International Journal of Emergency Medicine 2024 17:88. Research Published on: 15 July 2024.
It is often difficult to keep up with all of the highest impact papers in emergency medicine. The EMRA Research Committee has compiled a quick review of some of the most practice-affirming or practice-changing papers published from September 2020 to September 2021. This is by no means a definitive list, but all of these papers will likely be ...
Research education is an important component of emergency medicine training, with many programs encouraging formalized exposure to research for students, residents, and junior faculty.1, 2 Regardless of whether directly involved with research or not, a basic understanding of research methodology aids emergency clinicians in the assessment of scientific evidence and its potential relevance to ...
The goal of this Research Topic is to present the latest advances that are made during the last years in the field of emergency medicine that falls into the spectrum of both basic and clinical science. This special collection will not only present topics related to cardiopulmonary resuscitation but also emergencies that exist in all medical ...
The Official Journal of the American Academy of Emergency Medicine. The Journal of Emergency Medicine is an international, peer-reviewed publication featuring original contributions of interest to both the academic and practicing emergency physician.JEM, published monthly, contains research papers and clinical studies as well as articles focusing on the training of emergency physicians and on ...
The Journal of Emergency Medicine (JEM) is the official journal of the American Academy of Emergency Medicine (AAEM). JEM is an international, peer-reviewed publication featuring original contributions of interest to both the academic and practicing emergency physician. JEM features research papers, clinical studies, and articles that emphasize the education of emergency physicians and the ...
Prehospital & Disaster Medicine, Health Systems. Using the Centers for Disease Control and Prevention's National Syndromic Surveillance Program Data to Monitor Trends in U.S. Emergency Department Visits for Firearm Injuries, 2018 to 2019. Review by Muhammad Waseem, MD, MS & David Gordon, MS3
The emergency department is the first critical link in the clinical diagnosis and treatment of critical illnesses and infectious diseases, and individualized accurate assessment and prevention of disease susceptibility is a valuable research direction for precision emergency medicine. [14] Acute infectious diseases are among the most common ...
Since its publication in 2001, the National EMS Research Agenda has brought attention to a relative paucity of emergency medical services (EMS)-specific research and has called for an increase in funding and infrastructure to support EMS research. We investigated the trends in EMS-specific publications and National Institutes of Health (NIH)-funded research grants in the 20 years since this ...
Training in research methodology represents an important aspect of emergency medicine (EM) resident education, but best methods for design, implementation, and dissemination of resident research remain elusive. ... or experiences with different teaching modalities may generate an appropriate resident research topic including relevant clinical ...
Areas of active research focus include: Acute management of bone fractures and compartment syndrome. Allergic reactions and anaphylaxis. Bedbugs. Health policy. Management and diagnosis of acute respiratory illness. Management of corneal abrasion with a bandage contact lens. Management of COVID-19.
Emergency Medicine is a rapidly-developing field, and Stanford is leading research in many facets of care. The department benefits from collaboration with other disciplines at Stanford, within local Silicon Valley, and across the globe. Stanford is leading research efforts to transform health care for all through Precision EM.
EMERGENCY Medicine RESEARCH Donate. 2024-2025 Research Topics. EMF funds groundbreaking EM research to advance our specialty. To explore the 2024-2025 funding priorities, see the visualization below. For a full list of current grantees and their projects, visit here. SUPPORT
Our Mission. Our mission is to Advance the Science and Practice of Emergency Medicine. In 2021, the department ranked first in the nation in research dollars awarded by the National Institutes of Health—a demonstration of our commitment to our mission, as we continue to push the envelope of science and advocate for our patients and communities.
Meet the 30+ members that make up our department's team. Critical Care & Resuscitation Science. Advancing the care of critically ill and injured patients in the emergency department and beyond. Quality and Safety. Patient and provider safety is our top priority, and we are dedicated to quality improvement work through both research and education.
The difficulties in conducting good clinical research in emergency medicine can be overcome. This article will begin by identifying the main difficulties faced by the emergency medicine researcher. It will then discuss some solutions through the development and application of the research protocol. Finally, recommendations will be made with regard to writing for publication.
The top 100 cited articles were selected and analyzed by 2 independent investigators. Results: We identified 100 top-cited articles published in 6 EM journals, led by Annals of Emergency Medicine (65) and American Journal of Emergency Medicine (15). All top-cited articles were published between 1980 and 2009.
The new top 10 research priorities in Emergency Medicine can be found below. In January 2017 the JLA Emergency Medicine Priority Setting Partnership (EM PSP) published its first list of research priorities, providing guidance on the research, learning and development in the field of emergency medicine. Since then, our world and the landscape of ...
The role of a chief resident extends beyond a mere title; it is a gateway to opportunities and a stepping stone to leadership roles in both academic and community emergency medicine (EM) settings. Within the department, a chief resident signals to faculty and trainees that the title-bearer is clinically excellent, organized, thorough, and well ...
Emergency Medicine Topics. Antibiotic Resistance. Bioterrorism and Disaster Medicine. Cardiac Emergencies. Clostridium difficile Infection. Coronavirus (COVID-19) Ebola. Emerging and Reemerging ...
On Thursday, September 12, 2024, the Department of Emergency Medicine held its annual Research Showcase in the Trent Semans Center for Health Equity's Great Hall. Given the new accommodations for the event, this year the planners wanted to show a broad perspective on how the faculty and students participate in the department's research mission.
Patel, 28, is part of the UCSF Department of Emergency Medicine's Residency Program. While most often at Parnassus Heights, he also splits his time with emergency departments at Zuckerberg San Francisco General Hospital and Trauma Center and Mission Bay - experience that propelled him on the islands.
More information: Abstract Title: Prevalence of Period Poverty in a Pediatric Emergency Department Study co-author Riya Metha is scheduled to present the research from 5:15-6:15 pm ET on ...