
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
On this page:

What is aphasia?
Who can acquire aphasia, what causes aphasia, what types of aphasia are there, how is aphasia diagnosed, how is aphasia treated, what research is being done for aphasia, where can i find additional information about aphasia.
Aphasia is a disorder that results from damage to portions of the brain that are responsible for language. For most people, these areas are on the left side of the brain. Aphasia usually occurs suddenly, often following a stroke or head injury, but it may also develop slowly, as the result of a brain tumor or a progressive neurological disease. The disorder impairs the expression and understanding of language as well as reading and writing. Aphasia may co-occur with speech disorders, such as dysarthria or apraxia of speech, which also result from brain damage.
Most people who have aphasia are middle-aged or older, but anyone can acquire it, including young children. About 1 million people in the United States currently have aphasia, and nearly 180,000 Americans acquire it each year, according to the National Aphasia Association.
Aphasia is caused by damage to one or more of the language areas of the brain. Most often, the cause of the brain injury is a stroke. A stroke occurs when a blood clot or a leaking or burst vessel cuts off blood flow to part of the brain. Brain cells die when they do not receive their normal supply of blood, which carries oxygen and important nutrients. Other causes of brain injury are severe blows to the head, brain tumors, gunshot wounds, brain infections, and progressive neurological disorders, such as Alzheimer's disease.
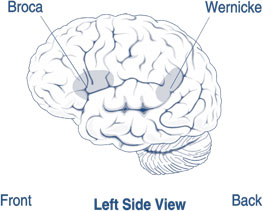
Areas of the brain affected by Broca's and Wernicke's aphasia
There are two broad categories of aphasia: fluent and nonfluent, and there are several types within these groups.
Damage to the temporal lobe of the brain may result in Wernicke's aphasia (see figure ), the most common type of fluent aphasia. People with Wernicke's aphasia may speak in long, complete sentences that have no meaning, adding unnecessary words and even creating made-up words.
For example, someone with Wernicke's aphasia may say, "You know that smoodle pinkered and that I want to get him round and take care of him like you want before."
As a result, it is often difficult to follow what the person is trying to say. People with Wernicke's aphasia are often unaware of their spoken mistakes. Another hallmark of this type of aphasia is difficulty understanding speech.
The most common type of nonfluent aphasia is Broca's aphasia (see figure ). People with Broca's aphasia have damage that primarily affects the frontal lobe of the brain. They often have right-sided weakness or paralysis of the arm and leg because the frontal lobe is also important for motor movements. People with Broca's aphasia may understand speech and know what they want to say, but they frequently speak in short phrases that are produced with great effort. They often omit small words, such as "is," "and" and "the."
For example, a person with Broca's aphasia may say, "Walk dog," meaning, "I will take the dog for a walk," or "book book two table," for "There are two books on the table." People with Broca's aphasia typically understand the speech of others fairly well. Because of this, they are often aware of their difficulties and can become easily frustrated.
Another type of aphasia, global aphasia, results from damage to extensive portions of the language areas of the brain. Individuals with global aphasia have severe communication difficulties and may be extremely limited in their ability to speak or comprehend language. They may be unable to say even a few words or may repeat the same words or phrases over and over again. They may have trouble understanding even simple words and sentences.
There are other types of aphasia, each of which results from damage to different language areas in the brain. Some people may have difficulty repeating words and sentences even though they understand them and can speak fluently (conduction aphasia). Others may have difficulty naming objects even though they know what the object is and what it may be used for (anomic aphasia).
Sometimes, blood flow to the brain is temporarily interrupted and quickly restored. When this type of injury occurs, which is called a transient ischemic attack, language abilities may return in a few hours or days.
Aphasia is usually first recognized by the physician who treats the person for his or her brain injury. Most individuals will undergo a magnetic resonance imaging (MRI) or computed tomography (CT) scan to confirm the presence of a brain injury and to identify its precise location. The physician also typically tests the person's ability to understand and produce language, such as following commands, answering questions, naming objects, and carrying on a conversation.
If the physician suspects aphasia, the patient is usually referred to a speech-language pathologist, who performs a comprehensive examination of the person's communication abilities. The person's ability to speak, express ideas, converse socially, understand language, and read and write are all assessed in detail.
Following a brain injury, tremendous changes occur in the brain, which help it to recover. As a result, people with aphasia often see dramatic improvements in their language and communication abilities in the first few months, even without treatment. But in many cases, some aphasia remains following this initial recovery period. In these instances, speech-language therapy is used to help patients regain their ability to communicate.
Research has shown that language and communication abilities can continue to improve for many years and are sometimes accompanied by new activity in brain tissue near the damaged area. Some of the factors that may influence the amount of improvement include the cause of the brain injury, the area of the brain that was damaged and its extent, and the age and health of the individual.
Aphasia therapy aims to improve a person's ability to communicate by helping him or her to use remaining language abilities, restore language abilities as much as possible, and learn other ways of communicating, such as gestures, pictures, or use of electronic devices. Individual therapy focuses on the specific needs of the person, while group therapy offers the opportunity to use new communication skills in a small-group setting.
Recent technologies have provided new tools for people with aphasia. "Virtual" speech pathologists provide patients with the flexibility and convenience of getting therapy in their homes through a computer. The use of speech-generating applications on mobile devices like tablets can also provide an alternative way to communicate for people who have difficulty using spoken language.
Increasingly, patients with aphasia participate in activities, such as book clubs, technology groups, and art and drama clubs. Such experiences help patients regain their confidence and social self-esteem, in addition to improving their communication skills. Stroke clubs, regional support groups formed by people who have had a stroke, are available in most major cities. These clubs can help a person and his or her family adjust to the life changes that accompany stroke and aphasia.
Family involvement is often a crucial component of aphasia treatment because it enables family members to learn the best way to communicate with their loved one.
Family members are encouraged to:
- Participate in therapy sessions, if possible.
- Simplify language by using short, uncomplicated sentences.
- Repeat the content words or write down key words to clarify meaning as needed.
- Maintain a natural conversational manner appropriate for an adult.
- Minimize distractions, such as a loud radio or TV, whenever possible.
- Include the person with aphasia in conversations.
- Ask for and value the opinion of the person with aphasia, especially regarding family matters.
- Encourage any type of communication, whether it is speech, gesture, pointing, or drawing.
- Avoid correcting the person's speech.
- Allow the person plenty of time to talk.
- Help the person become involved outside the home. Seek out support groups, such as stroke clubs.
Researchers are testing new types of speech-language therapy in people with both recent and chronic aphasia to see if new methods can better help them recover word retrieval, grammar, prosody (tone), and other aspects of speech.
Some of these new methods involve improving cognitive abilities that support the processing of language, such as short-term memory and attention. Others involve activities that stimulate the mental representations of sounds, words, and sentences, making them easier to access and retrieve.
Researchers are also exploring drug therapy as an experimental approach to treating aphasia. Some studies are testing whether drugs that affect the chemical neurotransmitters in the brain can be used in combination with speech-language therapy to improve recovery of various language functions.
Other research is focused on using advanced imaging methods, such as functional magnetic resonance imaging (fMRI), to explore how language is processed in the normal and damaged brain and to understand recovery processes. This type of research may advance our knowledge of how the areas involved in speech and understanding language reorganize after a brain injury. The results could have implications for the diagnosis and treatment of aphasia and other neurological disorders.
A relatively new area of interest in aphasia research is noninvasive brain stimulation in combination with speech-language therapy. Two such brain stimulation techniques, transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS), temporarily alter normal brain activity in the region being stimulated.
Researchers originally used these techniques to help them understand the parts of the brain that played a role in language and recovery after a stroke. Recently, scientists are studying if this temporary alteration of brain activity might help people re-learn language use. Several clinical trials funded by the National Institute on Deafness and Other Communication Disorders (NIDCD) are currently testing these technologies.
NIDCD-funded clinical trials are also testing other treatments for aphasia. A list of active NIDCD-funded aphasia trials can be found at ClinicalTrials.gov .
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
Use the following keywords to help you find organizations that can answer questions and provide information on aphasia:
- Speech-language pathologists
- Brain injury
For more information, contact us at:
NIDCD Information Clearinghouse 1 Communication Avenue Bethesda, MD 20892-3456 Toll-free voice: (800) 241-1044 Toll-free TTY: (800) 241-1055 Email: [email protected]
NIH Pub. No. 97-4257 December 2015
* Note: PDF files require a viewer such as the free Adobe Reader .
Jump to navigation
Find What You Need Get targeted resources quickly!

Traumatic Brain Injury: Cognitive and Communication Disorders

What are the cognitive and communication problems that result from traumatic brain injury?
Cognitive and communication problems that result from traumatic brain injury vary from person to person. These problems depend on many factors which include an individual's personality, preinjury abilities, and the severity of the brain damage.
The effects of the brain damage are generally greatest immediately following the injury. However, some effects from traumatic brain injury may be misleading. The newly injured brain often suffers temporary damage from swelling and a form of "bruising" called contusions. These types of damage are usually not permanent and the functions of those areas of the brain return once the swelling or bruising goes away. Therefore, it is difficult to predict accurately the extent of long-term problems in the first weeks following traumatic brain injury.
Focal damage, however, may result in long-term, permanent difficulties. Improvements can occur as other areas of the brain learn to take over the function of the damaged areas. Children's brains are much more capable of this flexibility than are the brains of adults. For this reason, children who suffer brain trauma might progress better than adults with similar damage.
In moderate to severe injuries, the swelling may cause pressure on a lower part of the brain called the brainstem, which controls consciousness or wakefulness. Many individuals who suffer these types of injuries are in an unconscious state called a coma. A person in a coma may be completely unresponsive to any type of stimulation such as loud noises, pain, or smells. Others may move, make noise, or respond to pain but be unaware of their surroundings. These people are unable to communicate. Some people recover from a coma, becoming alert and able to communicate.
In conscious individuals, cognitive impairments often include having problems concentrating for varying periods of time, having trouble organizing thoughts, and becoming easily confused or forgetful. Some individuals will experience difficulty learning new information. Still others will be unable to interpret the actions of others and therefore have great problems in social situations. For these individuals, what they say or what they do is often inappropriate for the situation. Many will experience difficulty solving problems, making decisions, and planning. Judgment is often affected.
Language problems also vary. Problems often include word-finding difficulty, poor sentence formation, and lengthy and often faulty descriptions or explanations. These are to cover for a lack of understanding or inability to think of a word. For example, when asking for help finding a belt while dressing, an individual may ask for "the circular cow thing that I used yesterday and before." Many have difficulty understanding multiple meanings in jokes, sarcasm, and adages or figurative expressions such as, "A rolling stone gathers no moss" or "Take a flying leap." Individuals with traumatic brain injuries are often unaware of their errors and can become frustrated or angry and place the blame for communication difficulties on the person to whom they are speaking. Reading and writing abilities are often worse than those for speaking and understanding spoken words. Simple and complex mathematical abilities are often affected.
The speech produced by a person who has traumatic brain injury may be slow, slurred, and difficult or impossible to understand if the areas of the brain that control the muscles of the speech mechanism are damaged. This type of speech problem is called dysarthria. These individuals may also experience problems swallowing. This is called dysphagia. Others may have what is called apraxia of speech, a condition in which strength and coordination of the speech muscles are unimpaired but the individual experiences difficulty saying words correctly in a consistent way. For example, someone may repeatedly stumble on the word "tomorrow" when asked to repeat it, but then be able to say it in a statement such as, "I'll try to say it again tomorrow."
How are the cognitive and communication problems assessed?
The assessment of cognitive and communication problems is a continual, ongoing process that involves a number of professionals. Immediately following the injury, a neurologist (a physician who specializes in nervous system disorders) or another physician may conduct an informal, bedside evaluation of attention, memory, and the ability to understand and speak. Once the person's physical condition has stabilized, a speech-language pathologist may evaluate cognitive and communication skills, and a neuropsychologist may evaluate other cognitive and behavioral abilities. Occupational therapists also assess cognitive skills related to the individual's ability to perform "activities of daily living" (ADL) such as dressing or preparing meals. An audiologist should assess hearing. All assessments continue at frequent intervals during the rehabilitative process so that progress can be documented and treatment plans updated. The rehabilitative process may last for several months to a year.
How are the cognitive and communication problems treated?
The cognitive and communication problems of traumatic brain injury are best treated early, often beginning while the individual is still in the hospital. This early therapy will frequently center on increasing skills of alertness and attention. They will focus on improving orientation to person, place, time, and situation, and stimulating speech understanding. The therapist will provide oral-motor exercises in cases where the individual has speech and swallowing problems.
Longer term rehabilitation may be performed individually, in groups, or both, depending upon the needs of the individual. This therapy often occurs in a rehabilitation facility designed specifically for the treatment of individuals with traumatic brain injury. This type of setting allows for intensive therapy by speech-language pathologists, physical therapists, occupational therapists, and neuropsychologists at a time when the individual can best benefit from such intensive therapy. Other individuals may receive therapy at home by visiting therapists or on an outpatient basis at a hospital, medical center, or rehabilitation facility.
The goal of rehabilitation is to help the individual progress to the most independent level of functioning possible. For some, ability to express needs verbally in simple terms may be a goal. For others, the goal may be to express needs by pointing to pictures. For still others, the goal of therapy may be to improve the ability to define words or describe consequences of actions or events.
Therapy will focus on regaining lost skills as well as learning ways to compensate for abilities that have been permanently changed because of the brain injury. Most individuals respond best to programs tailored to their backgrounds and interests. The most effective therapy programs involve family members who can best provide this information. Computer-assisted programs have been successful with some individuals.
What research is being done for the cognitive and communication problems caused by traumatic brain injury?
Researchers are studying many issues related to the special cognitive and communication problems experienced by individuals who have traumatic brain injuries. Scientists are designing new evaluation tools to assess the special problems that children who have suffered traumatic brain injuries encounter. Because the brain of a child is vastly different from the brain of an adult, scientists are also examining the effects of various treatment methods that have been developed specifically for children. These new strategies include the use of computer programs. In addition, research is examining the effects of some medications on the recovery of speech, language, and cognitive abilities following traumatic brain injury.
Where can I get more information?
NIDCD maintains a directory of organizations that can answer questions and provide printed or electronic information on traumatic brain injury. Please see the list of organizations at www.nidcd.nih.gov/directory .
NIH Pub. No. 98-4315 July 1998 Contact information updated February 2002
National Institute on Deafness and Other Communication Disorders. www.nidcd.nih.gov .
- Add new comment

This program is made possible in part by a grant from the Bob Woodruff Foundation, which is dedicated to ensuring that impacted post-9/11 veterans, service members, and their families are thriving long after they return home.
BrainLine is a national service of WETA-TV, the flagship PBS station in Washington, D.C.
BrainLine, WETA Public Television 3939 Campbell Ave. Arlington, VA 22206 E-mail | Phone: 703.998.2020
© 2023 WETA All Rights Reserved | Contact Us
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Apraxia of Speech?
A Challenging Language Disorder
Apraxia of speech is a language impairment that occurs due to brain damage. The underlying causes of apraxia of speech are usually different for children than for adults. Speech apraxia is difficult to cope with, and speech therapy can help improve communication.
Diagnosis of the underlying cause is crucial, both to help direct treatment for speech difficulties and to treat and prevent further neurological problems.
Illustration by Zoe Hansen for Verywell Health
Apraxia of Speech Symptoms
Speech apraxia leads to significant difficulties in communicating. This condition usually causes persistent symptoms and typically doesn't change.
People with apraxia of speech are cognitively and physically able to produce words and sentences. Language comprehension should not be affected by apraxia of speech, and words are not slurred in apraxia of speech.
Features of apraxia of speech include the following:
- Distortion of sounds : The sounds of words and phrases are often wrong in speech apraxia. For example, the vowels or consonants might be drawn out for too long.
- Inconsistency in pronouncing words and sounds : The mispronunciation of words with speech apraxia is not necessarily consistent. For example, you could have difficulty with the first part of a word, and the next time you say that word, you might have difficulty with the middle or the end.
- Struggling for words : If you have apraxia of speech, you will work hard to say the words you want to say.
- Errors in speech : You might use the wrong words and phrases if you have apraxia of speech, despite knowing what you mean to say.
Other cognitive or physical problems can often occur with speech apraxia, depending on the underlying cause.
Apraxia vs. Other Speech and Language Disorders
Apraxia of speech is a type of language disorder. Aphasia is the most common language impairment, and dysarthria is a speech impairment caused by difficulty with motor speech function. Apraxia is distinct from these disorders, although they may share some similarities. Common speech disorders include:
- Receptive aphasia : Usually referred to as Wernicke’s aphasia, this type of language impairment is characterized by fluid speech that usually doesn’t make sense, often with word substitutions. Language comprehension is typically impaired with Wernicke’s aphasia.
- Impaired fluency : Often described as Broca’s aphasia , this is a language problem that causes people to have choppy speech without a normal rhythm. Usually, speech comprehension is not substantially affected by Broca’s aphasia.
- Conduction aphasia : In conduction aphasia, the problem is the ability to repeat a short sentence. Expression and comprehension of speech are spared.
- Dysarthria : This condition is characterized by slurred speech or difficulty making certain sounds. Usually, people with dysarthria without aphasia can understand language and may know which words they want to say but have difficulty pronouncing them.
Speech apraxia is caused by damage to regions in the brain that mediate communication between language regions in the brain and between the left and right hemispheres of the brain.
This can occur with developmental conditions, such as autism, or it may result from harm to the brain, such as from head trauma.
Conditions associated with apraxia of speech include:
- Autism spectrum disorder
- Cerebral palsy
- Head trauma
- Brain tumors
- Brain surgery
These conditions are not always associated with apraxia of speech. But they can sometimes cause damage or dysfunction to regions of the brain that allow communication between the right and left hemispheres—and then they could be associated with speech apraxia.
Speech apraxia is diagnosed based on a clinical evaluation, usually by a physician or a speech therapist . A detailed examination of speech and cognitive abilities is necessary to define apraxia of speech and to rule out other disorders that can cause similar speech and language patterns, such as dysarthria and aphasia.
Speech patterns noted in apraxia of speech include the following:
- Phonemic error frequency : This involves assessment of the frequency of mistakes while pronouncing words.
- Distortion error frequency : This is a count of how often sounds are altered during speech.
- Word syllable duration : This involves assessment of the extra time in saying a word, usually due to struggling.
The Apraxia of Speech Rating Scale (ASRS) is one of the ways that speech apraxia can be defined. Healthcare providers can use this scale to communicate with each other and follow the improvement of apraxia of speech with therapy. The ASRS includes 16 components, such as repetition of sounds or inaccurate sounds, that are rated on a scale from zero to four.
If you’ve been diagnosed with speech apraxia or any communication problem, healthcare providers will work to determine the underlying cause. Issues such as childhood neurodevelopmental problems, stroke, brain tumors, or damage from a head injury need to be identified and treated.
Diagnostic testing may include:
- Brain imaging tests : These tests can help identify common causes of apraxia of speech, such as a stroke or head trauma.
- Cognitive testing : These tests may be used as part of the assessment for autism, dementia, or psychiatric conditions, which may be related to speech challenges.
- Blood tests : Medical problems such as infections, electrolyte disturbances , or organ failure may cause communication difficulties.
In addition to diagnosing speech apraxia, your healthcare providers will also work to determine whether you have other neurological deficits that could be caused by the underlying issue causing your speech apraxia. These can include learning difficulties, behavioral problems, or body weakness.
Apraxia of speech is treated with speech therapy . This type of therapy will follow patterns of treatment that are well-established for improving speech and will also provide an individualized treatment plan.
Therapy may need to be ongoing, and the frequency and specific exercises used during your therapy can be adjusted as you improve. For example, if your speech improves substantially, you might be able to work with your speech therapist less frequently, or you may be able to do some speech exercises at home, as directed by your therapist.
It’s not possible to predict with absolute certainty whether a person will recover from apraxia of speech and how much they might improve. However, there are some diagnostic clues that can help in anticipating the extent of recovery.
If you or a loved one has apraxia of speech, it can help to know that the ability to participate in speech therapy can lead to better outcomes. If your cognitive function is not affected or is only mildly impaired, this can help you take an active role in your therapy.
Research About Prognosis and Treatment
Stronger connectivity between certain areas of the right and left hemispheres of the brain is associated with better recovery.
For example, one research study showed that early connectivity of the inferior frontal gyrus (an area that processes speech and language) within two weeks after a stroke may be a strong predictor of recovery of apraxia of speech.
And at six months, lower severity of speech apraxia was associated with stronger connectivity of the anterior insula (which supports subjective feelings) on the right and left hemispheres and the ventral premotor cortex (which is involved in grasping and manipulating objects) of the right and left hemispheres.
This type of connectivity can be identified with metabolic brain testing, which is time-consuming and often impractical. However, this research can help scientists learn about ways to improve treatment for people with apraxia of speech.
Living with a language impairment can be difficult. Communication challenges interfere with relationships and day-to-day life. This can require extra effort from family, friends, and everybody else who interacts with a person who has apraxia of speech.
Patience is essential to managing this communication difficulty. It is important to work with your speech therapist in order to identify ways to communicate as you work to recover. This can include using pictures, gestures, and other ways of expressing your needs.
Apraxia of speech is a type of language impairment that is caused by damage to the brain, either during fetal development, childhood, or adulthood. This condition can occur along with other neurological deficits that are associated with damage to the brain.
There are many different causes, and a diagnosis of the cause is essential for a comprehensive treatment of speech apraxia, as well as any associated physical and cognitive deficits. Speech therapy is the treatment for the speech impairment seen in this condition.
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Vogindroukas I, Stankova M, Chelas EN, Proedrou A. Language and speech characteristics in autism . Neuropsychiatr Dis Treat . 2022;18:2367-2377. doi:10.2147/NDT.S331987
Haley KL, Jacks A. Three-dimensional speech profiles in stroke aphasia and apraxia of speech . Am J Speech Lang Pathol. 2023:1-10. doi:10.1044/2022_AJSLP-22-00170
Hybbinette H, Östberg P, Schalling E, et al. Longitudinal changes in functional connectivity in speech motor networks in apraxia of speech after stroke . Front Neurol. 2022;13:1013652. doi:10.3389/fneur.2022.1013652
Duffy JR, Martin PR, Clark HM, et al. The apraxia of speech rating scale: reliability, validity, and utility . Am J Speech Lang Pathol. 2023;32(2):469-491. doi:10.1044/2022_AJSLP-22-00148
Zhao J, Li Y, Zhang X, et al. Alteration of network connectivity in stroke patients with apraxia of speech after tDCS: a randomized controlled study . Front Neurol. 2022;13:969786. doi:10.3389/fneur.2022.969786
By Heidi Moawad, MD Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Types of Speech Impediments
Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
:max_bytes(150000):strip_icc():format(webp)/SanjanaGupta-d217a6bfa3094955b3361e021f77fcca.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

What is aphasia?
Aphasia is a language disorder that affects how you communicate. It's caused by damage in the area of the brain that controls language expression and comprehension. Aphasia leaves a person unable to communicate effectively with others. A person with aphasia may have trouble understanding, speaking, reading, or writing.
Many people have aphasia after a stroke. Both men and women are affected equally. Aphasia can occur at any age. It is most commonly seen in those over 65 years of age.
There are many types of aphasia. These are usually diagnosed based on which area of the language-dominant side of the brain is affected. Also on the extent of the damage. For example:
People with Broca aphasia have damage to the front part of the language-dominant side of the brain.
People with Wernicke aphasia have damage to the side of the language-dominant part of the brain.
People with global aphasia have damage to a large part of the brain that controls language.
What causes aphasia?
Aphasia is caused by damage to the language-dominant side of the brain, usually the left side. It may be brought on by:
Head injury
Brain tumor
Brain infection
Dementia or Alzheimer disease
It's currently not known if aphasia causes the complete loss of language structure, or if it causes problems in how language is accessed and used.
What are the symptoms of aphasia?
The symptoms of aphasia depend on which type a person has.
Broca aphasia is sometimes called an expressive aphasia. People with this type of aphasia may eliminate the words "and" and "the" from their language, for example. They may speak in short, but meaningful, sentences. They usually can understand some speech of others. People with Broca aphasia often have right-sided weakness or paralysis of the arm and leg.
Wernicke aphasia is sometimes called a receptive aphasia. People with this type of aphasia may speak in long confusing sentences, add unnecessary words, or create new words. They usually have trouble understanding the speech of others.
People with global aphasia have trouble with speaking or understanding language.
How is aphasia diagnosed?
Aphasia can be diagnosed using language tests done by a speech-language pathologist. These tests include studying speech, naming, repetition, comprehension, reading, and writing. Making a diagnosis may also include the use of imaging procedures to look at the brain, such as:
CT scan. This imaging test uses X-rays and a computer to make detailed images of the body. A CT scan shows details of the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
MRI scan. This test uses large magnets, radio frequencies, and a computer to make detailed images of organs and structures in the body without the use of X-rays.
Positron emission tomography. This computer-based imaging method uses radioactive substances to examine body processes.
How is aphasia treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how bad the condition is.
The goal of treatment is to improve the ability to communicate through methods that may include:
Speech-language therapy
Nonverbal communication therapies, such as computers or pictures
Group therapy for patients and their families
Living with aphasia
Some people with aphasia fully recover without treatment. But for most people, some amount of aphasia typically remains. Speech therapy can often help recover some speech and language functions over time. But many people continue to have problems communicating. This can sometimes be difficult and frustrating both for the person with aphasia and for family members. It's important for family members to learn the best ways to communicate with their loved one. Speech therapists can often help with this. Suggestions might include:
Include the person with aphasia in conversations
Simplify language by using short, simple sentences
Repeat key words or write them down to clarify meaning as needed
Use a natural conversational manner at an adult level
Encourage all types of communication, including speech, gestures, pointing, or drawing
Don’t correct the person's speech
Give the person plenty of time to express themselves
Help the person become involved outside the home, such as through support groups
For some people, computers can be helpful for both communicating and improving language abilities.
Key points about aphasia
Aphasia is a language disorder caused by damage to parts of the brain that control speech and understanding of language.
Depending on which areas of the brain are affected, a person might have different levels of ability to speak, read, write, and understand others.
Aphasia might get better over time, but many people are left with some loss of language skills. Speech therapy can often be helpful, as can other tools, such as computers that can help people communicate.
Aphasia can be difficult and frustrating for both the person with aphasia and family members. It's hard but important for family members to be patient and learn the best ways to communicate with their loved one.
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are and when they should be reported.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your healthcare provider if you have questions, especially after office hours or on weekends.
Find a Doctor
Specializing In:
- Cerebrovascular Diseases
- Acute Stroke Care
- Disorders of Executive Function
- Brain Injury
- Brain Hemorrhage
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Stroke Center at the Johns Hopkins Hospital
- Intracerebral Hemorrhage Center
- Stroke Center at Johns Hopkins Bayview Medical Center
- Neurology and Neurosurgery
- Pediatric Stroke Program (Johns Hopkins All Children's Hospital)
- Cerebrovascular Center
Find Additional Treatment Centers at:

Request an Appointment

Shaken Baby Syndrome
Related Topics
- Patient Care & Health Information
- Diseases & Conditions
Stuttering is a speech condition that disrupts the normal flow of speech. Fluency means having an easy and smooth flow and rhythm when speaking. With stuttering, the interruptions in flow happen often and cause problems for the speaker. Other names for stuttering are stammering and childhood-onset fluency disorder.
People who stutter know what they want to say, but they have a hard time saying it. For example, they may repeat or stretch out a word, a syllable, or a consonant or vowel sound. Or they may pause during speech because they've reached a word or sound that's hard to get out.
Stuttering is common among young children as a usual part of learning to speak. Some young children may stutter when their speech and language abilities aren't developed enough to keep up with what they want to say. Most children outgrow this type of stuttering, called developmental stuttering.
But sometimes stuttering is a long-term condition that remains into adulthood. This type of stuttering can affect self-esteem and communicating with other people.
Children and adults who stutter may be helped by treatments such as speech therapy, electronic devices to improve speech fluency or a form of mental health therapy called cognitive behavioral therapy.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Stuttering symptoms may include:
- Having a hard time starting a word, phrase or sentence.
- Stretching out a word or sounds within a word.
- Repeating a sound, syllable or word.
- Brief silence for certain syllables or words, or pausing before or within a word.
- Adding extra words such as "um" if expecting to have problems moving to the next word.
- A lot of tension, tightness or movement of the face or upper body when saying a word.
- Anxiety about talking.
- Not being able to communicate well with others.
These actions may happen when stuttering:
- Rapid eye blinks.
- Trembling of the lips or jaw.
- Unusual face movements, sometimes called facial tics.
- Head nodding.
- Tightening of fists.
Stuttering may be worse when the person is excited, tired or under stress, or when feeling self-conscious, hurried or pressured. Situations such as speaking in front of a group or talking on the phone can be especially hard for people who stutter.
But most people who stutter can speak without stuttering when they talk to themselves and when they sing or speak along with someone else.
When to see a doctor or speech-language pathologist
It's common for children between the ages of 2 and 5 years to go through periods when they may stutter. For most children, this is part of learning to speak, and it gets better on its own. But stuttering that continues may need treatment to improve speech fluency.
Call your healthcare professional for a referral to a specialist in speech and language called a speech-language pathologist. Or you can contact the speech-language pathologist directly for an appointment. Ask for help if stuttering:
- Lasts more than six months.
- Happens along with other speech or language problems.
- Happens more often or continues as the child grows older.
- Includes muscle tightening or physically struggling when trying to speak.
- Affects the ability to effectively communicate at school or work or in social situations.
- Causes anxiety or emotional problems, such as fear of or not taking part in situations that require speaking.
- Begins as an adult.
Researchers continue to study the underlying causes of developmental stuttering. A combination of factors may be involved.
Developmental stuttering
Stuttering that happens in children while they're learning to speak is called developmental stuttering. Possible causes of developmental stuttering include:
- Problems with speech motor control. Some evidence shows that problems in speech motor control, such as timing, sensory and motor coordination, may be involved.
- Genetics. Stuttering tends to run in families. It appears that stuttering can happen from changes in genes passed down from parents to children.
Stuttering that happens from other causes
Speech fluency can be disrupted from causes other than developmental stuttering.
- Neurogenic stuttering. A stroke, traumatic brain injury or other brain disorders can cause speech that is slow or has pauses or repeated sounds.
- Emotional distress. Speech fluency can be disrupted during times of emotional distress. Speakers who usually do not stutter may experience problems with fluency when they are nervous or feel pressured. These situations also may cause speakers who stutter to have greater problems with fluency.
- Psychogenic stuttering. Speech difficulties that appear after an emotional trauma are uncommon and not the same as developmental stuttering.
Risk factors
Males are much more likely to stutter than females are. Things that raise the risk of stuttering include:
- Having a childhood developmental condition. Children who have developmental conditions, such as attention-deficit/hyperactivity disorder, autism or developmental delays, may be more likely to stutter. This is true for children with other speech problems too.
- Having relatives who stutter. Stuttering tends to run in families.
- Stress. Stress in the family and other types of stress or pressure can worsen existing stuttering.
Complications
Stuttering can lead to:
- Problems communicating with others.
- Not speaking or staying away from situations that require speaking.
- Not taking part in social, school or work activities and opportunities for success.
- Being bullied or teased.
- Low self-esteem.
- Stuttering. American Speech-Language-Hearing Association. https://www.asha.org/public/speech/disorders/stuttering/. Accessed Feb. 2, 2024.
- Fluency disorders. American Speech-Language-Hearing Association. https://www.asha.org/practice-portal/clinical-topics/fluency-disorders/. Accessed Feb. 2, 2024.
- Childhood-onset fluency disorder (stuttering). In: Diagnostic and Statistical Manual of Mental Disorders DSM-5-TR. 5th ed. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed Feb. 2, 2024.
- Stuttering. National Institute on Deafness and Other Communication Disorders. https://www.nidcd.nih.gov/health/stuttering. Accessed Feb. 2, 2024.
- Sander RW, et al. Stuttering: Understanding and treating a common disability. American Family Physician. 2019;100:556.
- Laiho A, et al. Stuttering interventions for children, adolescents and adults: A systematic review as part of the clinical guidelines. Journal of Communication Disorders. 2022; doi:10.1016/j.jcomdis.2022.106242.
- 6 tips for speaking with someone who stutters. The Stuttering Foundation. https://www.stutteringhelp.org/6-tips-speaking-someone-who-stutters-0. Accessed Feb. 2, 2024.
- 7 tips for talking with your child. The Stuttering Foundation. https://www.stutteringhelp.org/7-tips-talking-your-child-0. Accessed Feb. 2, 2024.
- Clark HM (expert opinion). Mayo Clinic. Feb. 11, 2024.
Associated Procedures
- Cognitive behavioral therapy
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Improving life after brain injury Need to talk? 0808 800 2244
- What happens in a TBI?
- How severe is the brain injury?
- Mild head injury and concussion
- Brain aneurysm
- Brain haemorrhage
- Brain tumour
- Carbon monoxide poisoning
- Encephalitis
- Hydrocephalus
- Hypoxic and anoxic brain injury
- Behavioural effects of brain injury
- Cognitive effects of brain injury
- Glasgow Coma Scale
- Language impairment (aphasia)
- Speech difficulties
- Cognitive communication difficulties
- Emotional effects of brain injury
- Executive dysfunction
- Fatigue after brain injury
- Hormonal imbalances
- Memory problems
- Physical effects of brain injury
- Post-traumatic amnesia
- At the hospital after brain injury
- Early rehabilitation after brain injury
- Discharge from hospital after brain injury
- How to support a family dealing with brain injury
- I'm calling about Chris
- Rehabilitation
- The rehabilitation team
- Continuing care
- What is self-directed support?
- How to get self-directed support
- Making a support plan
- Managing your support
- Further help with self-directed support
- Safeguarding information
- Driving after brain injury
- Returning to work after brain injury
- Returning to education
- Holidays and travel
- Support through the cost-of-living crisis
- Navigating the Cost of Living
- Appealing a welfare benefits decision
- Attendance Allowance
- Carer's Allowance
- Employment and Support Allowance (ESA)
- Personal Independence Payment (PIP)
- Preparing for welfare benefits assessments
- Statutory Sick Pay
- Tips for completing benefits application forms
- Universal Credit
- How brain injury affects relationships
- Sex and sexuality
- How brain injury affects friendships
- Parenting and supporting children
- How brain injury affects partners
- Carer support groups
- Family reaction to a brain injury
- Supporting people to make decisions
- Information library
- "But you don't look disabled"
- Shana Lewis
- Robert Ashton
- Laura Bailey 2015
- Jane Allberry
- Ian Litchfield
- Debi Pullen
- David Thomas
- Alison Winterburn
- Mel Lightfoot
- Annette Henry
- Denise Johnson
- Codey Sharp
- Keith Emmanuel
- Lizzie Smart
- Gwen and Natalie Milham
- Terisha Burge
- Maria Knights
- Joanne Davis
- Sarah Whitchurch
- Amy Perring
- Jane Clarke
- Peter Holmes
- Luke Flavell
- Lindsay Lapham
- Nic O'Leary
- Angus Swanson
- Samuel Bishop
- Phil Broxton
- Nell Gregory
- Jamie Gailer
- Kate and John Bosley
- Gary Winters
- Kathryn Edgington
- Charlie and Jake Korving
- Bruno Muratori
- Kerry Jeffs
- Mike McCall
- James Piercy
- Andy Nicholson
- Warren McKinlay
- Lauren and Claire Cowlishaw
- Sarah McKinlay
- David Horner
- Arthur Moore
- Mike Palmer
- Sarah Tomlinson
- Paul Leyland
- Warwick Jarvis
- Jackie and John Mills
- Adrian Ellis
- Kieran Wallis
- Eleanor Simcox
- Jack Rutter
- Daniel Lingard
- Bernie Bambury
- Lorraine and Kevin Pratt
- Melanie Whittaker
- John Holbrook
- Jackie Alton
- Irvine Phair
- Rebecca Grant
- Rachel Atkinson
- Marco Gambi
- Brenda and Julian
- Callum Maclean
- A simple solution
- Lost in a crowd
- Caring for carers
- Dear my new brain
- Holiday from brain injury
- The new me and my Jumbledbrain blog
- The old me is not the new me
- I see Headway as the pit stop
- Riding my horse Johnny keeps me focused
- Headway is a haven
- Brain injury didn't steal my future
- Never give up
- Fiona Grant-MacDonald
- Kiran Higgins
- Jetting off alone
- Matt Brammeier
- Brain injury vs family
- The Face of Brain Injury With Dee Snider
- Mourning lost relationships
- A mother's perspective
- Pathological laughter - it's no joke
- Polly Williamson
- Writing a book after brain injury
- Michael Mabon
- A day in the life of a carer
- "Kerry the HATS nurse was my guardian angel"
- Don't struggle alone
- Harriet Barnsley
- I don't want anyone to feel as alone as I did
- Amanda Horton
- A helping hand
- Donnie McHarg
- Shona Green
- Jenny Joppa
- Philippa Taylor
- Debra Jones
- John Dougan
- "No memory of the day that changed my life"
- Jean Parker
- My experience of parenting after brain injury
- Sue McIntyre
- Daniel Mole
- Kerry Reynolds
- Keely McGhee
- Paula Stanford
- Relationships after brain injury – Imogen’s story
- Jules Pring
- Dr Amy Izycky's Headway Exhibition
- Nicola Brown
- Rod Maxwell
- Doing it the Head way
- Carer vacancy. Unpaid. Full time. No experience required.
- Joe Sandford
- My Brain Injury ID Card
- Matthew Nichols
- Heather Pollard
- Noelle Robinson
- Giles Hudson
- Q&A - ‘Be in the moment. This is all you have.’
- Q&A – “I would be the Happiness Fairy, I’ve sprinkled Happy Dust on you, now smile.”
- Nature's Way: Gardening after brain injury
- The debilitating impact of social isolation
- Joanne Wood - Who
- David Greer
- Lynne O'Grady
- Clair Bennett
- Danielle's story - returning home
- Anne Johnston
- Q&A: Cat
- How I overcame panic attacks
- Q&A with Zalehka Price-Davies
- Philippa-Anne Dewhirst
- After my brain injury I kept questioning, 'what if I have lost my ability to be creative?'
- Chris Bryant
- Busting the myths around brain injury and sex
- I swear, he knew he was helping me
- Hannah Brandon
- Keith Poultney
- Joanna Darmody
- Terry Slade
- Tamara Bond
- Kavita Basi
- Learning to live again
- David Wheeler
- Jessica Stevens
- Andrew Plowright
- Steve Borland
- Financial fraud: a risk you can't afford to ignore
- Dating after brain injury
- Max Muteliso
- Q&A: Roger Merriman
- Parenting with a brain injury
- Kieran Broadfield
- Louise Lane
- Adam Nicke - Q&A
- Hitting the High Street at Headway's Hinckley shop
- Hitting the high street at headway hinckley
- London Marathon Runners
- Rebecca Hutchings
- Joanne Wood
- Paws for Thought
- Jake Elliott
- Growing Together with Headway Cambridgeshire
- Lauren Walkington Q&A
- Daniel Parslow
- Alex Murphy
- Matt Masson
- Alphabet Brains
- Pete Bourne
- David Yabbacome
- Julie Sadler
- Lottie Butler
- Candice Ridley
- Belinda Medlock
- Unravelling the mystery of fatigue
- Lara Newson: Head Smash
- Robert Courtnell
- Hipatia Preis
- Stewart Gray
- Mary's Story
- Hannah O'Dowd
- Victoria Wicks
- Carol Smith
- ABI Week across the UK
- Rebecca Ivatts
- Nicola Evans
- 'Writing gives me meaning'
- The perils of gambling after brain injury
- Fit for purpose: The benefits of being active after brain injury
- Festival fun after brain injury
- 6 strategies for getting back to work after brain injury
- Matt Rhodes
- Stop the bus! A guide to public transport
- Brain injury: To tell or not to tell?
- 5 ways to cope with taste and smell problems after brain injury
- The uneasy relationship between alcohol and brain injury
- 9 ways to help with planning problems after brain injury
- 7 top tips for managing visual problems after brain injury
- 10 ways to cope with depression after brain injury
- Supporting children: visiting a parent in hospital
- Supporting children after a parent's brain injury: when a parent comes home
- Donna Siggers
- How to manage memory problems after brain injury
- Hot weather after brain injury: tips for keeping cool
- Stefan Leader
- A picture speaks a thousand words
- Andrew Purnell
- Ruth Berkoff
- David Aston
- Katherine McKinstry
- Chloé Briffa
- Socialising after brain injury
- Shane Booth
- Theme parks: accessibility after brain injury
- William Windle
- Rebecca Jones
- Sarah Scott
- Pregnancy after brain injury
- Music after brain injury
- Emma Martins
- Dancing after brain injury
- Scottie Elliott
- Let's talk tech
- Lorna Lancaster
- Carol Evans
- John Wrathall
- Fiona Baker-Holden
- Ryan Goodenough
- Christmas after brain injury
- Cecilia Danielsson
- Saturday Night Fever
- Anthony Hewson
- Q&A: Julian Earl
- Fireworks after brain injury
- Coping with Christmas in hospital
- Eleanor Brander
- Beccy Young
- Veronica Woods
- 10 things not to say to someone with a brain injury
- Tracey Newman
- Lauren Gilligan
- Louis McGuire
- Fighting the bear
- David Macdonald
- Yvette Lumley
- Christina Sweeney
- Charlotte Warhurst
- Cindy Hollingsworth
- Spencer Senior
- Q&A: Steven Kelly
- I am a firm believer in not just speaking of the change, but actively searching to be part of it.
- Carwyn Wooldridge
- Charli Skinner
- Lucy Rogoff
- Bryony Wilshaw
- David Wozny
- Sarah Allwood
- "We're all going on an assisted holiday"
- Anne's top tips for self-isolation
- Sammy's top tips for managing mental health problems during self-isolation
- Kavita's tips for self-isolation
- Belinda’s story: Isolation after brain injury
- Mikey Smithson
- Let’s talk continence problems after brain injury
- Mark Kennedy
- Gary Younge
- Mindfulness and me
- Life in lockdown: Alison's story
- John Beaumont
- Catherine Erdal
- Lyndsey Anderson
- Rock painting by Deborah Johnston
- Q&A: Hollie-Blue Huntsman
- Donna Davies
- Caroline Spiers
- More than my brain injury: Danielle Grant
- Brain Injury Sunblock and the Infernal Birdsong
- Sandra Liddell
- Brain Injury And Covid: Jane Hallard
- Brain Injury And Covid: Jean Parker
- A day in the life of a Headway helpline consultant
- Brain injury and Covid: Tom Harris
- Brain Injury And Covid: Michael Perry
- Rebekah Nesbitt
- The Headway helpline: You're not alone
- The price of a punch
- David Baker
- Donna Harris
- 7 signs of executive dysfunction after brain injury
- My poetry: Joseph McAloon
- Angela Lewis
- Daniel Sutherland
- Andrew Brown
- Sarah McGrath
- Dan Goldstraw
- In her own words: Emma Davey
- My poetry: John Marshall
- Disinfectant by Sarah-Louise Lennon
- Karen Whitehead
- In his own words: Max Bongard
- Karl Hargreaves
- Samuel Moore
- Animation: Memory loss after brain injury
- How to cope with memory problems after brain injury
- Q&A: George Mitchell
- Michelle Hay
- Q&A: Alan Heal
- Lucy Hunter
- Cara's story
- Q&A: Rosemary Shaw
- Mental health and brain injury
- Emma Chivers
- Q&A: Terence Berritt
- Q&A: Emma Linnell
- Tai Chi After Brain Injury with Dr Giles Yeates
- In her own words: Emma Lindsay
- Phillip Cragg
- Paintings by Hannah Jenkins
- Q&A: Alison Rockall
- Imogen Cauthery
- Alex Danson-Bennett MBE
- My poetry: Helen Wilson
- Haydn Garrod
- Podcast: Life with no filter
- Overcoming challenges after brain injury
- Creative Expression: Mark and Jules Kennedy
- Eleanor Furneaux
- Creative Expression: Lucy Pugh
- Claire Bullimore
- My artwork: Sandra E Ball
- Blue Mundane Monday Mix by Glen Stephenson
- Nicola Cross
- Survival is a Team Dream by Philippa Bateman
- Brain Attack Music by Andy Dovey
- Top tips for coping with parenting through lockdown
- Pauline O'Connor
- Duncan Boak
- Gill and Terry Oliver
- Jelly Brain documentary: A gift to mum
- In her own words: Jodie Bacon
- Monica Petrosino
- Josh Rawson
- What triggers anger after brain injury?
- Gerald Heffernan
- Back behind the wheel: Paula Barlow
- Back behind the wheel: Driving FAQs
- Elizabeth Wilkins
- My poetry: Sam Norris
- Alex Richardson
- Emerging from lockdown: Tips for brain injury survivors
- My podcast by Nikki Webber MBE
- Isolation and loneliness: Life with no filter podcast
- A life of lockdown? Belinda's story
- A life of lockdown? Derek's story
- A life of lockdown? Melanie's story
- A life of lockdown? Elizabeth's story
- Mindfulness Training after Brain Injury with Dr Niels Detert
- Fresh Start by the Headway Glasgow Writing Group
- 'I've Made It!' by Becki York
- Lucy O'Donovan
- Top tips for coping with headaches
- Helena Breslin
- Sue Williams
- Reflections of Chair-Man Eason
- Ceara's story
- Tracy Dickson
- Julie Mueller
- Thomas Leeds
- Headaches: The whats, whys and hows
- My photography: Rob Dinwoodie
- Nick Henderson
- Lenka Brunclikova
- Emma Doherty
- Planting a seed of thought - Natalie Parr
- 'My Broken Brain' by Sam Hedges
- Sally Smith
- Catherine Jessop - Pulling Through
- My poetry: Sam Moore
- Exploring your dreams
- Sweet dreams? Getting a good night's sleep after brain injury
- Mindfulness after brain injury
- Amy Streather
- Eleanor May Blackburn
- Paul Wilkins
- Barry Cusack: My body and mind
- Our relationship reality: Love after brain injury
- Love after brain injury: Thalia and Matt
- Tisha's story
- Executive dysfunction explained
- Let’s talk about sex...
- When Catwalks are Barbed
- Hope by Angela Webb
- Headway gets creative!
- From a child's mind to centre stage
- Bernadette Bendall
- Zoe Rainaki
- What did you not see? By Stef Harvey
- A Windy Moment by Nick Fletcher
- Helen and Liz
- The Sound of Recovery
- A family united to support life after brain injury
- See the Hidden Me: Iona's story
- See the Hidden Me: Annette's story
- See the Hidden Me: John's story
- See the Hidden Me: Christine's story
- The Brain Injury Cookbook
- Raj Gataora
- Marco Gambi: A passion for food
- Celebrating 10,000 Brain Injury ID Cards
- 'Rehabilitation rather than incarceration'
- Theresa Malcom
- Tim Richens
- Visual problems: A closer look
- Dusty Zeisberger – 24-hour treadmill challenge
- A conversation with... Ian Scott-Logan
- Ways to help cope at Christmas: tips for survivors, families, friends, and carers
- World’s first ABI Games a huge success!
- Steven Lomas
- Memory systems
- Stevie Ward
- Five Years On by Clare Jones
- The Penny Drops
- Stephen Evans
- Don’t get bitten by the sharks!
- Jonathan Hiron
- Finding your superpower...
- Post-traumatic growth after brain injury
- Nick Blackwell
- Heads, Hats and Healing: Making and Creating Silver Linings
- Nigel and Paula's story
- Joseph's story
- John's story
- How to manage isolation after brain injury
- Managing anxiety after brain injury
- Simon and Marc's story
- Sandi's story
- Relearning life skills
- "A charity of love"
- Dawn, Headway volunteer
- Pat Griffiths, Chair of Trustees for Headway Meirionnydd
- Creative writing sessions: Laura Bailey
- Creative writing sessions: Sam Moore
- Creative writing sessions: Helen Davies
- Nicola Bird Blunt
- In her own words: Lynn Boyle
- My brother was killed by one punch: Aaron Matcham
- Completing my life-long dream of running the Brighton Marathon: Adam Clarke
- Drained by fatigue? Try these 8 ways to cope after brain injury
- 8 ways to manage a lack of insight after brain injury
- How to help someone with a brain injury: Top tips for friends and family
- Balance problems after brain injury
- Safe travels! Your holiday tips
- Early warning signs of fatigue
- Keeping your relationship healthy after brain injury
- Carers: Try these 4 ways to care for yourself
- 7 tips for volunteering after brain injury
- 10 top tips for coping with stress after brain injury
- Top 10 tips for staying safe online
- In memory of much-loved partner and dad
- 10 ways to manage anger: tips for brain injury survivors
- Managing impulsivity and disinhibition following brain injury
- Friends: 5 ways to support someone with a brain injury
- Diet after brain injury: Healthy body, healthy mind?
- Top tips for a good night's sleep
- An awfully big row: Giles Johnson
- Jurate Ardour
- Dean Osborne
- Iain Millar: Rising from Adversity to Find Purpose on the Golf Course
- Finding Hope on the Fairway, Anthony Roberts' Journey of Resilience and Inspiration
- James Heather
- Andy Southey
- From one punch victim to Headway Hero: A Half Marathon triumph
- Mark Winterbourne
- World Mental Health Day
- Thanking Our Fundraiser: Sahara Trek Triumphm
- Sisters’ challenge inspired by ‘hero’ sibling’s brain injury
- The devastating consequences of one punch
- Get to know – Jen, Director of Fundraising
- Putting the ‘I’ in identity after brain injury
- Coping with winter blues
- Making returning to work, work for you
- Alan's story
- Get to know – Sarah, Trust and Foundations Manager
- Give up, or focus tremendously on rehabilitation
- What really counts?
- Laura Macfarlane
- The role art can play in positive change
- World Poetry Day
- Poem: TBI Survivor
- Adapting to life after brain injury: Returning to work
- Meet the volunteer - Roger Beattie
- We are family! Siblings run for Headway in support of their mum
- The impact of brain injury on a family
- A craniotomy – ‘the last resort’
- David's story A Life Re-written
- Andrew's story A Life Re-written
- Alison's story A Life Re-written
- Liz and Justina's story A Life Re-written
- Registration process
- Who can apply?
- What constitutes a Unit?
- Why is accreditation important?
- Summary of standards to be assessed
- Criminal Justice System Professionals
- Headway Annual Awards
- Clinical guidelines
- Supporting carers
- Resources for GPs
- Headway Head Injury Solicitors Directory
- Headway services
- Life after acquired brain injury: Coping with anxiety and depression
- Diet and nutrition after brain injury
- Smell and taste disorders after brain injury
- Nature’s benefit after brain injury
- Managing sleep and fatigue after brain injury
- Understanding MY brain injury
- Navigating life after brain injury
- An introduction to brain injury
- Understanding brain injury
- Effective communication strategies
- Understanding behaviours that challenge
- Goals training
- Brain Injury Solicitors training
- Understanding brain injury training for criminal justice professionals
- Intimate partner violence (IPV) and brain injury
- Headway group training sessions
- About the brain
- Choosing the right solicitor
- The claim process
- Meeting your solicitor
- Questions to ask your solicitor
- Headway personal injury lawyers code of conduct
- Complaints and disclaimer
- Find a solicitor
- Find an approved care provider
- Common brain injury terms
- Useful organisations
- Buy Headway publications

Stories of life after brain injury
- Channel Islands
- Headway Cambridge and Peterborough - Chesterton
- Headway Cambridge and Peterborough - Peterborough
- East Midlands
- Northern Ireland
- Isle of Wight
- Headway Birmingham and Solihull - Headway House
- Headway Birmingham and Solihull - Sutton House
- National solicitors
- Approved care providers
- Charity shops
- Brain injury and the criminal justice system
- Headway Emergency Fund
- Headway’s Justice Programme
- Online communities
- Keeping family and friends updated
- I recently sustained a brain injury
- I'm living with a brain injury
- Someone I know has a brain injury

Get support near you

Legal advice
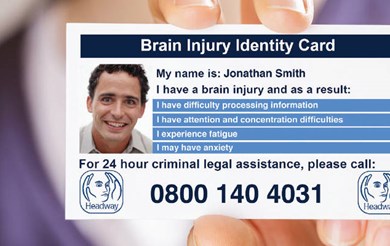
Brain Injury Identity Card
- Latest news and updates
- Real life stories
- Share your story
- Headway News magazine
- Media centre
- A Life Re-written - brain injury survey
- Brain Drain: Wake up to fatigue!
- Budget for brain injury
- Concussion guides
- Cycle safety
- Every 90 seconds
- Memory Loss: A campaign to remember
- See the hidden me
- You, me, and brain injury
- Creative expression
- Right First Time
- Second Hand September
- ABI Week: A life re-written

Headway News spring 2024
- Hats for Headway Day
- Headway Charity Golf Day
- Mince Pie Morning
- Friends of Headway
- Superhero Series
- Ultra Challenge Series
- Bournemouth Marathon Festival (5K, 10K, Half Marathon)
- Edinburgh 5K and 10K (part of the Edinburgh Marathon Series)
- Great Bristol Run 10K
- Great Bristol Run Half Marathon
- Great Manchester Run 10K
- Great Manchester Run Half Marathon
- Great North Run Half Marathon
- Great North Run 10K
- Great North Swim Weekend
- Great South Run
- Hackney Half Marathon
- Paris Marathon
- Robin Hood Half Marathon
- TCS London Marathon
- Great Scottish Run Half Marathon
- Great Scottish Run 10K
- Paris Half Marathon
- Three Peaks Challenge
- Yorkshire Three Peaks Challenge
- Payroll Giving
- Organising your own event?
- Download your fundraising pack
- Easy ways to support us
- Head Injury Solicitors Directory
- Fund the Headway Helpline
- Corporate events
- Charity Partnerships
- Corporate Membership
- Trusts and foundations
- Our fundraising principles
- A gift in your will
- A gift in memory
- Celebrations
- Donate your unwanted items
- Local groups and branches
- Headway UK offices
- Featured stories
- Video and audio
- The written word
- Living with brain injury
- Headway Heroes
Brain injury and me

- Headway training courses
- Headway webinar series
- Hard Hat Awareness Week
- BABICM Annual conference - 2 Day
- East of England stroke forum conference
- Headway Lincolnshire's Annual Brain Injury Conference
- Carers Week: Putting Carers on the Map
- Volunteers' Week
- Aims and objectives
- The history of Headway
- Headway supporters
- Parliamentary Champions
- Headway UK staff
- Headway trustees
- Publications
- Merchandise

Help us continue our work
For individuals, for professionals, further information, related resources.
Sometimes brain injury causes communication difficulties by impairing the physical ability to speak, rather than the ability to understand and express language.
The two main speech disorders are:
Dyspraxia of speech
Dysarthria occurs when there is damage to parts of the nervous system involved in the control of muscles used for speech. It can also occur because of injury or weakness more directly affecting the muscles themselves. Dysarthria results in reduced control and clarity of speech.
When dysarthria occurs in isolation, a person's ability to speak will be impaired, but their ability to understand language and construct sentences will be intact. However, in practise there are often elements of both aphasia and dysarthria present.
Features may include:
- Reduced movement (range or strength) of the lips, tongue, and soft palate
- Problems controlling the flow of air from the lungs when speaking
- Difficulty in producing varied and controlled changes in the volume of speech
- Difficulty in producing varied and controlled patterns in the tone of speech
- Slurring of speech
Dyspraxia is a disorder of planned and co-ordinated movement. It occurs because of injury to areas of the brain responsible for conscious movement, mainly situated in the frontal lobes.
Dyspraxia of speech causes people to have difficulty saying what they are consciously thinking about saying. However, some individuals may be able to speak perfectly normally when not thinking about it, for example, if someone asks them a question and they have to respond spontaneously. Long words tend to be more difficult to say then short words for some people with dyspraxia of speech.
The disorder can range from mild in some people to very severe in others.
A Speech and Language Therapist will be able to identify and assess dysarthria and dyspraxia of speech. Recovery and degree of difficulties will depend upon the severity of the initial brain injury. However, for a variety of reasons (e.g. presence of other difficulties), individuals may respond differently to therapy. Some people will make more progress than others, despite having had a similar injury.
In severe cases, those with speech difficulties may be unable to achieve recognisable speech. In such cases, they may benefit from the use of an Augmentative Aid to Communication (AAC). Headway's booklet Coping with communication problems after brain injury contains a section on communication aids which explains this in more detail.
Communication problems
Communication problems after brain injury are very common. This section goes into detail about some of the communication issues that may arise after brain injury.
Injury to language centres of the brain leads to a condition called aphasia. Find out about receptive aphasia, reading problems, expressive aphasia and writing problems after brain injury.
Communication is a complex process, which involves many aspects of thinking and social skills. If brain injury impairs any of these skills then it can affect the ability to communicate successfully.
Effects of brain injury
Find out about some of the main difficulties that arise after brain injury, together with some suggestions as to how to deal with them.
Share this page

Supporting you

Headway in your area
Friends of Headway Individual membership Join/Renew
Contact Us t: 0115 924 0800 e: [email protected]
Help us improve life after brain injury.
Improving life after brain injury 0808 800 2244.
Call our free helpline 9am - 5pm, Monday to Friday. Or email [email protected]
Join our online Community
- Corporate policies
- Terms & Conditions
- Accessibility
- Resource centre
- Find a Headway
- Complaints and compliments
- Join our mailing list
Headway - the brain injury association is registered with the Charity Commission for England and Wales (Charity no. 1025852) and the Office of the Scottish Regulator (Charity no. SC 039992). Headway is a company limited by guarantee, registered in England no. 2346893.
© Copyright Headway 2024 - Site designed and developed by MEDIAmaker
Our sponsors:

- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 16, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Neuroplasticity study shows how singing rehabilitates speech production in post-stroke aphasia
by University of Helsinki
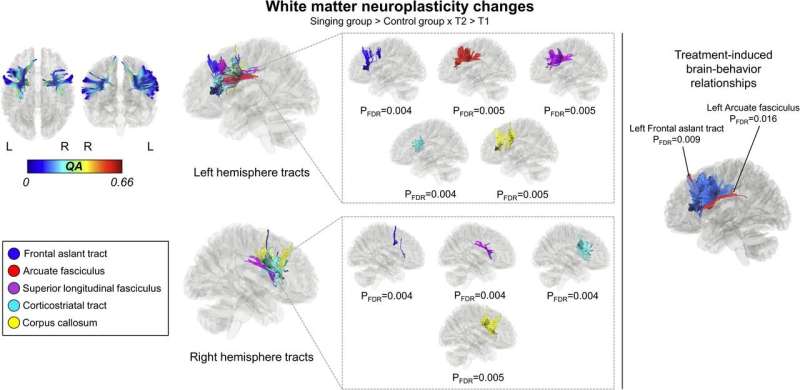
Cerebrovascular accidents, or strokes, are the most common cause of aphasia, a speech disorder of cerebral origin. People with aphasia have a reduced ability to understand or produce speech or written language. An estimated 40% of people who have had a stroke have aphasia. As many as half of them experience aphasia symptoms even a year after the original attack.
Researchers at the University of Helsinki previously found that sung music helps in the language recovery of patients affected by strokes. Now, the researchers have uncovered the reason for the rehabilitative effect of singing. The recently completed study was published in eNeuro .
According to the findings, singing repairs the structural language network of the brain. The language network processes language and speech in our brain. In patients with aphasia, the network has been damaged.
"For the first time, our findings demonstrate that the rehabilitation of patients with aphasia through singing is based on neuroplasticity changes, that is, the plasticity of the brain," says University Researcher Aleksi Sihvonen from the University of Helsinki.

Singing improves language network pathways
The language network encompasses the cortical regions of the brain involved in the processing of language and speech, as well as the white matter tracts that convey information between the different end points of the cortex.
According to the study results, singing increased the volume of gray matter in the language regions of the left frontal lobe and improved tract connectivity especially in the language network of the left hemisphere, but also in the right hemisphere.
"These positive changes were associated with patients' improved speech production ," Sihvonen says.
A total of 54 aphasia patients participated in the study, of whom 28 underwent MRI scans at the beginning and end of the study. The researchers investigated the rehabilitative effect of singing with the help of choir singing, music therapy and singing exercises at home.
Singing is a cost-effective treatment
Aphasia has a wide-ranging effect on the functional capacity and quality of life of affected individuals and easily leads to social isolation.
According to Sihvonen, singing can be seen as a cost-effective addition to conventional forms of rehabilitation, or as rehabilitation for mild speech disorders in cases where access to other types of rehabilitation is limited.
"Patients can also sing with their family members , and singing can be organized in health care units as a group-based, cost-efficient rehabilitation ," Sihvonen says.
Explore further
Feedback to editors

New technique detects novel biomarkers for kidney diseases with nephrotic syndrome
May 25, 2024

In experiments, mice get ill from raw milk carrying bird flu virus
May 24, 2024

Understanding a broken heart—study finds link between stress and recurrent heart failure

Genetic cause of rare childhood immune disorders discovered

New surgical tool moves tiny bioparticles with robotics and acoustic energy

The link between defective autophagy and pancreatitis could point to new treatments

Possible association between tattoos and lymphoma revealed

Walkability in neighborhoods linked to health, study of siblings shows

Scientists uncover new treatment pathway for rare 'spider web' childhood brain tumors

How COVID-19 'breakthrough' infections alter your immune cells
Related stories.

Novel information on the neural origins of speech and singing
Aug 10, 2023

Singing found to support stroke rehabilitation
Dec 29, 2022

Investigating the loss of musical ability
Mar 27, 2024

Listening to vocal music boosts the recovery of language functions after stroke
Jul 9, 2021

Can conventional speech therapy combined with singing address voice problems in individuals with Parkinson's disease?
Jun 7, 2023

Neurologist explains aphasia
Feb 28, 2024
Recommended for you

Scientists show that serotonin activates brain areas influencing behavior and motivation

Scientists leverage machine learning to decode gene regulation in the developing human brain

Study connects genetic risk for autism to changes observed in the brain

Researchers develop new light-controlled 'off switch' for brain cells

How neurons build a 3D vascular structure to keep the retina healthy
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Dysarthria Speech Disorder Assessment Using Genetic Algorithm (GA)-Based Layered Recurrent Neural Network
- Conference paper
- First Online: 24 May 2024
- Cite this conference paper

- M. Usha 9
Part of the book series: Communications in Computer and Information Science ((CCIS,volume 2121))
Included in the following conference series:
- International Conference on Intelligent Computing for Sustainable Development
A speech issue known as dysarthria occurs because of muscular weakness and nerve damage following a stroke, an infection in the brain, or a brain injury. Many Speech Therapies are involved in assisting people with Dysarthria Speech Disorder. Dysarthria is also said to have an influence on the comprehensive potentiality, speech accessibility and a specific persons’ capability to unite and interconnect in day to day chores. The Purpose of this work is for the early detection of speech disorder hence would have a positive influence on the quality of life. An effective new approach for Dysarthria speech recognition requires optimization and learning patterns to get better accuracy measurements. In this, Cuckoo Search Optimization Technique is used for better accuracy results. Genetic Algorithm (GA)-based Layered Recurrent Neural Network Improved Cuckoo Search Optimization (GALRNN-ICSO) method is used for Dysarthria Speech Recognition. The suggested GALRNN-ICSO method's primary goal is to improve test-accuracy measurement via accuracy rate as well as the precision and RMSE rate while recognizing Dysarthria Speech. The objective is to increase the accuracy and cuts down the time required for Dysarthria Speech recognition. From the experimental result, proposed GALRNN-ICSO method ensures more accuracy with precise assessment of disorder compared to existing state-of-the-art methods.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Borrie, S.A., McAuliffe, M.J., Liss, J.M.: Perceptual learning of dysarthric speech: a review of experimental studies. J. Speech Langu. Hearing Res. 55 (1), 290–305 (2012)
Article Google Scholar
D. Rodrigues, L.A.M.P., Souza, A.N., Ramos, C.C., Yan, X.: Binary Cuckoo search: a binary cuckoo search algorithm for feature selection. In: IEEE International Symposium on Circuits and Systems (ISCAS), pp. 465–468 (2013)
Google Scholar
Kim, M., Cao, B., An, K., Wang, J.: Dysarthric speech recognition using convolutional LSTM neural network. Proc. Interspeech 2018 , 2948–2952 (2018)
Kadia, K.L., Selouani, S.A., Boudraa, B., Boudraa, M.: Fully automated speaker identification and intelligibility assessment in dysarthria disease using auditory knowledge. Biocybern. Biomed. Eng. 36 (1), 233–247 (2016)
Becerra, A., de la Rosa, J.I., Gonzalez, E.: Speech recognition in a dialog system: from conventional to deep processing. Multimedia Tools Appl. 77 , 15875–15911 (2018)
Gill, J., et al.: Adaptive neuro-fuzzy inference system (ANFIS) approach for the irreversibility analysis of a domestic refrigerator system using LPG/TiO2 nanolubricant. Energy Rep. 6 , 1405–1417 (2020)
Yakoub, M.S., Selouani, S., Zaidi, B.-F., Bouchair, A.: Improving dysarthric speech recognition using empirical mode decomposition and convolutional neural network. EURASIP J. Audio Speech Music Process. 2020 (1), 1–7 (2020)
Umapathy, S., Rachel, S., Thulasi, R.: Automated speech signal analysis based on feature extraction and classification of spasmodic dysphonia: a performance comparison of different classifiers. Int. J. Speech Technol. 21 , 9–18 (2018)
Rudzicz, F.: Articulatory knowledge in the recognition of dysarthric speech. IEEE Trans. Audio Speech Lang. Process. 19 (4), 947–960 (2011)
Copaci, D., Flores, A., Rueda, F., Alguacil, I., Blanco, D., Moreno, L.: Wearable elbow exoskeleton actuated with shape memory alloy. In: Ibáñez, J., González-Vargas, J., Azorín, J.M., Akay, M., Pons, J.L. (eds.) Converging Clinical and Engineering Research on Neurorehabilitation II. BB, vol. 15, pp. 477–481. Springer, Cham (2017). https://doi.org/10.1007/978-3-319-46669-9_79
Chapter Google Scholar
Chita-Tegmark, M., Scheutz, M.: Assistive robots for the social management of health: a framework for robot design and human–robot interaction research. Int. J. Soc. Robot. 1–21 (2020)
Nehaniv, C.L., Dautenhahn, K.: Imitation and Social Learning in ROBOTS, HUMANS and Animals: Behavioural, Social and Communicative Dimensions. Cambridge University Press, Cambridge (2007)
Book Google Scholar
Kennedy, J., Baxter, P., Belpaeme, T.: Nonverbal immediacy as a characterisation of social behaviour for human-robot interaction. Int. J. Soc. Robot. 9 , 109–128 (2017)
Takayanagi, K., Kirita, T., Shibata, T.: Comparison of verbal and emotional responses of elderly people with mild/moderate dementia and those with severe dementia in responses to seal robot, PARO. Front. Aging Neurosci. 6 , 257 (2014)
Bartlett, M.S., Littlewort, G., Frank, M., Lainscsek, C., Fasel, I., Movellan, J.: Recognizing facial expression: machine learning and application to spontaneous behavior. In: 2005 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR'05), San Diego, CA, USA, pp. 568–573 (2005)
Sun, Y., Chen, Y., Wang, X., Tang, X.: Deep learning face representation by joint identification-verification. In: Proceedings of the 27th International Conference on Neural Information Processing Systems. NIPS’14, vol. 2, Cambridge, MA, USA, pp. 1988–1996, MIT Press (2014)
Altman, N.S.: An introduction to kernel and nearest-neighbor nonparametric regression. Am. Stat. 46 (3), 175–185 (1992)
Article MathSciNet Google Scholar
Download references
Author information
Authors and affiliations.
Department of Information Technology, KG College of Arts and Science College, Coimbatore, Tamil Nadu, India
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to M. Usha .
Editor information
Editors and affiliations.
Anurag University, Hyderabad, Telangana, India
S. Satheeskumaran
University of Leicester, Leicester, UK
Yudong Zhang
Aurel Vlaicu University of Arad, Arad, Romania
Valentina Emilia Balas
National University of Kaohsiung, Kaohsiung, Taiwan
Tzung-pei Hong
University of Teramo, Teramo, Italy
Danilo Pelusi
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper.
Usha, M. (2024). Dysarthria Speech Disorder Assessment Using Genetic Algorithm (GA)-Based Layered Recurrent Neural Network. In: Satheeskumaran, S., Zhang, Y., Balas, V.E., Hong, Tp., Pelusi, D. (eds) Intelligent Computing for Sustainable Development. ICICSD 2023. Communications in Computer and Information Science, vol 2121. Springer, Cham. https://doi.org/10.1007/978-3-031-61287-9_22
Download citation
DOI : https://doi.org/10.1007/978-3-031-61287-9_22
Published : 24 May 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-61286-2
Online ISBN : 978-3-031-61287-9
eBook Packages : Computer Science Computer Science (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Paralysis can rob people of their ability to speak. Now researchers hope to give it back

When Jaimie Henderson was 5 years old, his father was in a devastating car crash. The accident left his father barely able to move or speak. Henderson remembers laughing at his dad's jokes, though he never could understand the punchlines. "I grew up wishing I could know him and communicate with him."
That early experience drove his professional interest in helping people communicate.
Now, Henderson's an author on one of two papers published Wednesday showing substantial advances toward enabling speech in people injured by stroke, accident or disease.
Although still very early in development, these so-called brain-computer interfaces are five times better than previous generations of the technology at "reading" brainwaves and translating them into synthesized speech. The successes suggest it will someday be possible to restore nearly normal communication ability to people like Henderson's late father.
"Without movement, communication is impossible," Henderson said, referencing the trial's participant who has amyotrophic lateral sclerosis, or ALS , which robs people of their ability to move. "We hope to one day tell people who are diagnosed with this terrible disease that they will never lose the ability to communicate."
Both the technologies, developed at Stanford and nearby at the University of California, San Francisco , enabled a volunteer to generate 60 to 80 words per minute. That's less than half the pace of normal speech, which typically ranges from 150 to 200 words per minute, but substantially faster than previous brain-computer interfaces. The new technologies can also interpret and produce a much broader vocabulary of words, rather than simply choosing from a short list.
At Stanford, researchers chose to decode signals from individual brain cells. The resolution will improve as the technology gets better at allowing recording from more cells, Henderson said.
"We're sort of at the era of broadcast TV, the old days right now," he said in a Tuesday news conference with reporters. "We need to increase the resolution to HD and then on to 4K so that we can continue to sharpen the picture and improve the accuracy."
The two studies "represent a turning point" in the development of brain-computer interfaces aimed at helping paralyzed people communicate, according to an analysis published in the journal Nature along with the papers .
"The two BCIs represent a great advance in neuroscientific and neuroengineering research, and show great promise in boosting the quality of life of individuals who have lost their voice as a result of paralysing neurological injuries and diseases," wrote Dutch neurologist Nick Ramsey and Johns Hopkins University School of Medicine neurologist Nathan Crone.
Paralyzed patients walking in minutes: New electrode device a step forward in spinal injury care
Two different approaches to communication, both work
At UCSF, researchers chose to implant 253 high-density electrodes across the surface of a brain area involved in speech.
The fact that the different approaches both seem to work is encouraging, the two teams said Tuesday.
It's too early to say whether either will ultimately prove superior or if different approaches will be better for different types of speech problems. Both teams implanted their devices into the brains of just one volunteer each, so it's not yet clear how challenging it will be to get the technology to work in others.
The UCSF team also personalized the synthesized voice and created an avatar that can recreate the facial expressions of the participant, to more clearly reeplicate natural conversation. Many brain injuries, like ALS and stroke also paralyze the muscles of the face, leaving the person unable to smile, look surprised, or offer concern.
Ann, the participant in the USCF trial, had a brain stem stroke 17 years ago and has been participating in the research since last year. Researchers identified her only by her first name to protect her privacy.
The electrodes intercepted brain signals that, if not for Ann's stroke, would have gone to muscles in her, tongue, jaw and larynx, as well as her face, according to UCSF. A cable, plugged into a port fixed to her head, connected the electrodes to a bank of computers.
For weeks, she and the team trained the system’s artificial intelligence algorithms to recognize her distinctive brain signals by repeating phrases over and over again.
Instead of recognizing whole words, the AI decodes words from phonemes, according to UCSF. “Hello,” for example, contains four phonemes: “HH,” “AH,” “L” and “OW."
Researchers used video from Ann's wedding to create a computer-generated voice that sounds much like her own did and to create an avatar that can make facial expressions similar to the ones she made before her stroke.
Advances in machine learning have made such technologies possible, said Sean Metzger, a bioengineering graduate student who helped lead the research. " Overall, I think this work represents accurate and naturalistic decoding of three different speech modalities, text, synthesis and an avatar to hopefully restore fuller communication experience for our participant," he told reporters.
The healing power of a good beat: Neurologic music therapy helps kids with brain injuries
Stanford approach: Tiny sensors on the brain
The Stanford trial relied on volunteer Pat Bennett, now 68, a former human resources director, who was diagnosed with ALS in 2012.
“When you think of ALS, you think of arm and leg impact,” Bennett wrote in an interview with Stanford staff conducted by email and provided to the media. “But in a group of ALS patients, it begins with speech difficulties. I am unable to speak.”
On March 29, 2022, neurosurgeons at Stanford placed two tiny sensors each on the surface of two regions of Bennett's brain involved in speech production. About a month later, she and a team of Stanford scientists began twice-weekly, four-hour research sessions to train the software that was interpreting her speech.
She would repeat in her mind sentences chosen randomly from telephone conversations, such as: “It’s only been that way in the last five years.” Another: “I left right in the middle of it.”
As she recited these sentences, her brain activity was translated by a decoder into a stream of "sounds" and then assembled into words. Bennett repeated 260 to 480 sentences per training session. Initially, she was restricted to a 50-word vocabulary, but then allowed to choose from 125,000 words, essentially, all she would ever need.
After four months, she was able to generate 62 words per minute on a computer screen merely by thinking them.
“For those who are nonverbal, this means they can stay connected to the bigger world, perhaps continue to work, maintain friends and family relationships,” she wrote.
The technology made a lot of mistakes. About 1 out of every 4 words was interpreted incorrectly even after this training.
Frank Willett, the research scientist who helped lead the Stanford work, said he hopes to improve accuracy in the next few years, so that only 1 out of 10 words will be wrong.
Edward Chang, the senior researcher on the UCSF paper, said he hopes his team's work will "really allow people to interact with digital spaces in new ways," communicating beyond simply articulating words.
All four researchers said restoring communication abilities to Ann and Bennett during the trial was a highlight in their professional careers.
"It was quite emotional for all of us to see this work," said Chang, a member of the UCSF Weill Institute for Neuroscience.
"I felt like I'd come full circle from wishing I could communicate with my dad as a kid to seeing this actually work," Henderson added. "It's indescribable."
Contact Karen Weintraub at [email protected].
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input .
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- What do we know about...
What do we know about covid-19’s effects on the brain?
- Related content
- Peer review
- Katharine Lang , freelance journalist
- lang.kathj26{at}gmail.com
Katharine Lang investigates how SARS-CoV-2 infection can affect the brain, how it might have these effects, and what can be done to minimise the risk
What are the neurological symptoms of covid-19?
Covid may be primarily a respiratory infection, but a common symptom is “brain fog”—problems with memory or concentration—which can persist for weeks or months as part of long covid. 1 And it’s not the only neurological effect.
Giovanni Schifitto, professor of neurology at the University of Rochester Medical School in New York, explains that neurological symptoms are widespread. “In the acute phase, common things like lack of smell, changes in taste, increase in headaches, cognitive dysfunction, and strokes have been reported, and there are effects on the peripheral nervous system,” he says.
Although these complications are more likely in people with severe covid—a 2021 study found that 80% of people admitted to hospital with covid-19 experienced neurological symptoms 2 —they can also affect people who experience only mild covid symptoms. 3 These neurological symptoms were also found to be more likely in people who were older, male, or white and in people with pre-existing neurological disorders.
The most common neurological symptoms are loss of smell (anosmia) and loss of taste (ageusia). Studies have suggested that during a bout of covid as many as 68% of people experience loss of smell and 44% lose their sense of taste. 4 5 But no evidence suggests that these effects are due to the virus entering the brain.
Other studies have reported a range of neurological symptoms alongside general fatigue. These symptoms are much like those experienced after a “mild traumatic brain injury” (as defined in one study 6 ) or from concussion—including dizziness, headaches, seizures, stroke, delirium, and balance disturbances.
The UK Covid and Cognition study (Covcog, from the University of Cambridge) reported cognitive dysfunction in some 70% of people with signs of long covid (or “post-covid condition,” 7 although it’s worth noting that there are no agreed international diagnostic criteria for long covid), and brain fog and difficulty concentrating were found to be more common than lasting respiratory symptoms. 8 The Covcog study found that the severity of lasting symptoms was related to the severity of symptoms during acute covid.
Data from the UK Coronavirus (Covid-19) Infection Survey from March 2023 9 showed that difficulty concentrating was the second most common symptom in long covid (after fatigue) and was experienced by 51% of respondents. More recently, a community based study used online assessments to evaluate cognitive impairment after covid infection. 10 Participants who had been infected showed measurable long term cognitive deficits not evident in the no-covid group.
What causes these symptoms? Is it the virus entering the brain?
This is a complex issue and the subject of much debate. In vitro studies have found that the virus disrupts the blood-brain barrier, although this was seen only with the original wild-type SARS-CoV-2 and omicron variants. 11 This research also found that the virus may affect the function of cells in the central nervous system.
Because loss of smell is a common symptom, some researchers have suggested that the virus may enter the brain through the olfactory system. Stephen Griffin, virologist at the University of Leeds, notes that the UK Biobank study 12 recorded “reduced grey matter thickness—comprised of the main cellular ‘bodies’ of neurons, rather than their tendril-like projections—in parts of the brain linked with olfactory sensing, namely the limbic system and primary olfactory cortex,” which could be evidence for this route of entry.
However, there’s little other evidence that the virus enters cells in the brain. Schifitto says, “There’s been one report suggesting the virus gets into astrocytes 13 ; others have not really found the virus in specific cells.”
But he adds, “The virus can cause damage without infecting cells. If it’s activating other cells in the brain that cause inflammation, you don’t need the virus to be there to cause problems. The amount of cytokines in the blood could activate, for example, microglia, a classical cell type involved in chronic neuroinflammation.”
Does inflammation play a role?
The consensus is that inflammation, rather than invasion by the virus, is highly likely to be responsible for the neurological symptoms seen in both acute and long covid. One 2023 study found raised levels of brain injury markers and inflammatory mediators during the acute phase of covid. 14
Daniel Altmann, professor of immunology at Imperial College London, says, “Many ideas have been put forward, but just as there can be immunopathology in any other organ—for example, through excessive inflammatory cytokines—so it is for the brain.”
He cites a 2022 study in mice and people 15 that showed lasting post-covid cytokine activity, particularly CCL11 (eotaxin 1) in the central nervous system. CCL11 is known to play a role both in allergic conditions and in brain disorders. 16 Studies in mice revealed that, as well as elevated cytokines/chemokines in the cerebrospinal fluid, the myelin on nerve cells was damaged, which could be one explanation for cognitive issues. Little evidence suggests that demyelination has been seen in people after covid.
Another study, published in October 2023, has proposed an alternative theory: that peripheral serotonin reduction after covid impedes the vagus nerve—impairing the responses of the hippocampus, which is involved in learning, memory, and emotion. 17
What about microbleeds and strokes associated with covid-19?
Many people have reported microbleeds and strokes after infection. Schifitto says that the virus often infects endothelial cells anywhere in the body, including those in the brain vessels. He explains, “It’s not surprising, if something is affecting the endothelial cells, that this may predispose people to small strokes, large strokes, or dysregulation of the blood-brain barrier, which then could predispose to additional inflammation coming from the bloodstream into the brain.”
Altmann says, “There is massive evidence for this. Many mechanisms have been demonstrated for endothelial, prothrombotic effects of the virus, so the effect is fairly easily rationalised.”
What’s the effect of covid-19 on dementia?
Schifitto expresses concern that covid may lead to an increase in dementias, telling The BMJ that dementias are “almost always a mix with vascular disease included—so if SARS-CoV-2 has had an impact on the microcirculation, we may see an increase in vascular disease in the brain, which may contribute to earlier or more aggressive dementia. That’s a concern, but there’s no evidence so far.”
Benedict Michael, professor of neuroscience at the University of Liverpool, says that this risk may well not apply to the whole population but could potentially increase the likelihood of dementia in people already at increased risk of neurodegenerative disease.
Schifitto adds, “Most dementias do not progress rapidly, so it would be unlikely that we’d see a surge within a few years.” He’s currently investigating neuroimaging biomarkers to see if these might give early warning of small vessel disease or microcirculation problems in people who have had covid.
Can vaccination help reduce the neurological effects of covid-19?
The only way to avoid neurological symptoms during and after infection is to avoid catching covid in the first place, says Altmann. But vaccination could also reduce the risk.
Griffin points to preclinical studies 18 indicating that vaccination can prevent SARS-CoV-2 from damaging the brain in some experimental models. He adds, “Plus, we know that vaccination is one of the few things that reduce the risk of long covid.”
Griffin warns that the long term consequences of covid aren’t being considered enough when planning vaccination and other prevention strategies in the UK—“which would seem most unwise given the accumulating evidence of long term harm in neurological and indeed other tissues.”
Competing interests: None declared.
Provenance and peer review: Commissioned; peer reviewed.
This article is made freely available for personal use in accordance with BMJ's website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
- McCorkell L ,
- GCS-NeuroCOVID Consortium and ENERGY Consortium
- Fastenberg JH ,
- Granholm AC
- ↵ World Health Organization. Post-covid 19 condition (long covid). 7 Dec 2022. https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition
- Benito Ballesteros A ,
- ↵ Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (covid-19) infection in the UK: 30 March 2023. 30 Mar 2023. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/30march2023
- Hampshire A ,
- Atchison C ,
- Skorniewska Z ,
- PHOSP-COVID Study Collaborative Group
- Alfaro-Almagro F ,
- Michael BD ,
- Needham EJ ,
- ISARIC4C Investigators ,
- COVID-CNS Consortium
- Fernández-Castañeda A ,
- Geraghty AC ,
- Ivanovska M ,
- Murdjeva M ,
- Devason AS ,
- Villadiego J ,
- García-Arriaza J ,
- Ramírez-Lorca R ,
Communication Sciences and Disorders
Sharice clough rejoins csd, this time as assistant professor.

The journey of Dr. Sharice Clough (MA-SLP, 2018) from a student to a professional in her field, and soon-to-be faculty member, speaks volumes about CSD’s bragging rights that they’re a department dedicated to cultivating leaders in the field of communication sciences and disorders.
“I’m excited and confident that Sharice will bring fresh perspectives, innovative ideas, and a deep commitment to excellence in her new role,” said Eric Hunter, Department Executive Officer and Harriet B. and Harold S. Brady Chair in Liberal Arts and Sciences.
After completing her master’s degree in Speech-Language Pathology at Iowa, Clough embarked on doctoral studies in Hearing and Speech Sciences at Vanderbilt University, followed by interdisciplinary post-doctoral training in the Multimodal Language Department at the Max Planck Institute for Psycholinguistics in Nijmegen, The Netherlands.
She will join us as an assistant professor in CSD at Iowa in Fall 2026.
Clough investigates acquired neurogenic communication disorders, such as traumatic brain injury, aphasia, and dementia in adults. More specifically, she strives to know more about how people use and comprehend language in rich and dynamic contexts, like those we encounter in daily life.
Real-world communication is interactive , involving a collaborative exchange between individuals. It is also multimodal , containing a variety of communicative cues like speech, gesture, facial expressions, and eye gaze. Her goal is to better understand how these flexible and social language abilities are disrupted by brain injury.
For example, in a recent behavioral experiment, she examined how adults with and without traumatic brain injury adapted their speech, gesture, and eye gaze behavior when talking to groups of listeners with different levels of knowledge based on their prior interactions. These types of social skills underlie the ability to design our communication appropriately and efficiently for different audiences (e.g., talking to a friend versus a group of coworkers).
"Although people with traumatic brain injury can have difficulty with social communication, we tend to assess language in very controlled and isolated contexts in both the clinic and lab," she said. “It’s critical that we incorporate these dynamic and rich properties of language into our practices to create assessments that sensitively detect communication difficulties and treatments that generalize beyond the clinic room into the real world.”
Clough uses a variety of methods to study the cognitive and neural systems that underlie neurogenic communication disorders, such as behavioral testing, eye-tracking, motion tracking, neuropsychological testing, and lesion mapping. In addition to advancing our understanding of the communication abilities of people with acquired brain injury, combining these methods allows her to learn more about the links between language and the brain.
“Iowa CSD is the perfect place to grow my research program and lab. My experiences as a master’s student in the department opened many doors for me and ignited a passion for science and discovery that I’m excited to pass on to future students. Iowa has all the right ingredients and an incredible community of scholars who I’m thrilled to be joining,” she said.
Hunter says he’s eager to see the research, academic, and leadership impacts Clough will undoubtedly have on the CSD program and its students.
“ Iowa CSD leans into its mission to foster a culture of growth and discovery. Our graduates –such as Sharice -- go on to achieve great things, and it’s doubly-fulfilling when those individuals return to give back to the community that supported them,” he said.
NOTICE: The University of Iowa Center for Advancement is an operational name for the State University of Iowa Foundation, an independent, Iowa nonprofit corporation organized as a 501(c)(3) tax-exempt, publicly supported charitable entity working to advance the University of Iowa. Please review its full disclosure statement.
To sound like a hockey player, speak like a Canadian
American athletes tend to signal their identity as hockey players through canadian english-like accents.
As a hockey player, Andrew Bray was familiar with the slang thrown around the "barn" (hockey arena). As a linguist, he wanted to understand how sport-specific jargon evolved and permeated across teams, regions, and countries. In pursuit of the sociolinguistic "biscuit" (puck), he faced an unexpected question.
"It was while conducting this initial study that I was asked a question that has since shaped the direction of my subsequent research," said Bray. "'Are you trying to figure out why the Americans sound like fake Canadians?'"
Canadian English dialects are stereotypically represented by the vowel pronunciation, or articulation, in words like "out" and "about," borrowed British terms like "zed," and the affinity for the tag question "eh?" Bray, from the University of Rochester, will present an investigation into American hockey players' use of Canadian English accents Thursday, May 16, as part of a joint meeting of the Acoustical Society of America and the Canadian Acoustical Association, running May 13-17 at the Shaw Centre located in downtown Ottawa, Ontario, Canada.
Studying how hockey players talk required listening to them talk about hockey. To analyze unique vowel articulation and the vast collection of sport-specific slang terminology that players incorporated into their speech, Bray visited different professional teams to interview their American-born players.
"In these interviews, I would ask players to discuss their career trajectories, including when and why they began playing hockey, the teams that they played for throughout their childhood, why they decided to pursue collegiate or major junior hockey, and their current lives as professionals," said Bray. "The interview sought to get players talking about hockey for as long as possible."
Bray found that American athletes borrow features of the Canadian English accents, especially for hockey-specific terms and jargon, but do not follow the underlying rules behind the pronunciation, which could explain why the accent might sound "fake" to a Canadian.
"It is important to note that American hockey players are not trying to shift their speech to sound more Canadian," said Bray. "Rather, they are trying to sound more like a hockey player."
Players from Canada and northern American states with similar accents have historically dominated the sport. Adopting features of this dialect is a way hockey players can outwardly portray their identity through speech, called a linguistic persona. Many factors influence this persona, like age, gender expression, social category, and as Bray demonstrated, a sport.
Going forward, Bray plans to combine his recent work with his original quest to investigate if Canadian English pronunciation and the hockey linguistic persona are introduced to American players through the sport's signature slang.
- Brain Injury
- Language Acquisition
- Racial Issues
- Relationships
- Child Development
- Neuroscience
- Game theory
- Great Ape language
- Self-concept
- Milgram experiment
- Stress (medicine)
Story Source:
Materials provided by Acoustical Society of America . Note: Content may be edited for style and length.
Cite This Page :
Explore More
- Charge Your Laptop in a Minute?
- Caterpillars Detect Predators by Electricity
- 'Electronic Spider Silk' Printed On Human Skin
- Engineered Surfaces Made to Shed Heat
- Innovative Material for Sustainable Building
- Human Brain: New Gene Transcripts
- Epstein-Barr Virus and Resulting Diseases
- Origins of the Proton's Spin
- Symbiotic Bacteria Communicate With Plants
- Birdsong and Human Voice: Same Genetic Blueprint
Trending Topics
Strange & offbeat.

Binge drinking is a growing public health crisis − a neurobiologist explains how research on alcohol use disorder has shifted
Assistant Professor of Biology, Biomedical Engineering and Pharmacology, Penn State
Disclosure statement
Nikki Crowley receives funding from The National Institutes of Health, The Brain and Behavior Research Foundation, and the Penn State Huck Institutes of the Life Sciences endowment funds.
Penn State provides funding as a founding partner of The Conversation US.
View all partners
With the new Amy Winehouse biopic “Back to Black ” in U.S. theaters as of May 17, 2024, the late singer’s relationship with alcohol and drugs is under scrutiny again. In July 2011, Winehouse was found dead in her flat in north London from “death by misadventure” at the age of 27. That’s the official British term used for accidental death caused by a voluntary risk.
Her blood alcohol concentration was 0.416%, more than five times the legal intoxication limit in the U.S. – leading her cause of death to be later adjusted to include “alcohol toxicity” following a second coroner’s inquest.
Nearly 13 years later, alcohol consumption and binge drinking remain a major public health crisis , not just in the U.K. but also in the U.S.
Roughly 1 in 5 U.S. adults report binge drinking at least once a week, with an average of seven drinks per binge episode . This is well over the amount of alcohol thought to produce legal intoxication, commonly defined as a blood alcohol concentration over 0.08% – on average, four drinks in two hours for women, five drinks in two hours for men.
Among women, days of “heavy drinking” increased 41% during the COVID-19 pandemic compared with pre-pandemic levels , and adult women in their 30s and 40s are rapidly increasing their rates of binge drinking , with no evidence of these trends slowing down. Despite efforts to comprehend the overall biology of substance use disorders, scientists’ and physicians’ understanding of the relationship between women’s health and binge drinking has lagged behind.
I am a neurobiologist focused on understanding the chemicals and brain regions that underlie addiction to alcohol . I study how neuropeptides – unique signaling molecules in the prefrontal cortex , one of the key brain regions in decision-making, risk-taking and reward – are altered by repeated exposure to binge alcohol consumption in animal models.
My lab focuses on understanding how things like alcohol alter these brain systems before diagnosable addiction, so that we can better inform efforts toward both prevention and treatment.
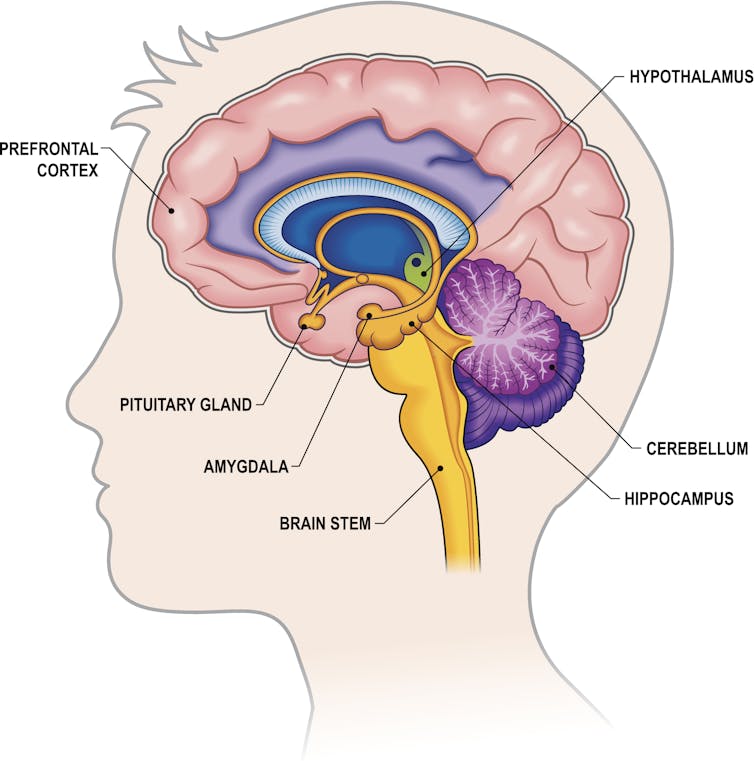
The biology of addiction
While problematic alcohol consumption has likely occurred as long as alcohol has existed, it wasn’t until 2011 that the American Society of Addiction Medicine recognized substance addiction as a brain disorder – the same year as Winehouse’s death. A diagnosis of an alcohol use disorder is now used over outdated terms such as labeling an individual as an alcoholic or having alcoholism.
Researchers and clinicians have made great strides in understanding how and why drugs – including alcohol, a drug – alter the brain. Often, people consume a drug like alcohol because of the rewarding and positive feelings it creates, such as enjoying drinks with friends or celebrating a milestone with a loved one. But what starts off as manageable consumption of alcohol can quickly devolve into cycles of excessive alcohol consumption followed by drug withdrawal.
While all forms of alcohol consumption come with health risks, binge drinking appears to be particularly dangerous due to how repeated cycling between a high state and a withdrawal state affect the brain. For example, for some people, alcohol use can lead to “ hangxiety ,” the feeling of anxiety that can accompany a hangover.
Repeated episodes of drinking and drunkenness, coupled with withdrawal, can spiral, leading to relapse and reuse of alcohol. In other words, alcohol use shifts from being rewarding to just trying to prevent feeling bad.
It makes sense. With repeated alcohol use over time, the areas of the brain engaged by alcohol can shift away from those traditionally associated with drug use and reward or pleasure to brain regions more typically engaged during stress and anxiety .
All of these stages of drinking, from the enjoyment of alcohol to withdrawal to the cycles of craving, continuously alter the brain and its communication pathways . Alcohol can affect several dozen neurotransmitters and receptors , making understanding its mechanism of action in the brain complicated.
Work in my lab focuses on understanding how alcohol consumption changes the way neurons within the prefrontal cortex communicate with each other. Neurons are the brain’s key communicator, sending both electrical and chemical signals within the brain and to the rest of your body.
What we’ve found in animal models of binge drinking is that certain subtypes of neurons lose the ability to talk to each other appropriately. In some cases, binge drinking can permanently remodel the brain. Even after a prolonged period of abstinence, conversations between the neurons don’t return to normal .
These changes in the brain can appear even before there are noticeable changes in behavior . This could mean that the neurobiological underpinnings of addiction may take root well before an individual or their loved ones suspect a problem with alcohol.
Researchers like us don’t yet fully understand why some people may be more susceptible to this shift, but it likely has to do with genetic and biological factors, as well as the patterns and circumstances under which alcohol is consumed.
Women are forgotten
While researchers are increasingly understanding the medley of biological factors that underlie addiction, there’s one population that’s been largely overlooked until now: women.
Women may be more likely than men to have some of the most catastrophic health effects caused by alcohol use, such as liver issues, cardiovascular disease and cancer . Middle-aged women are now at the highest risk for binge drinking compared with other populations.
When women consume even moderate levels of alcohol, their risk for various cancers goes up, including digestive, breast and pancreatic cancer , among other health problems – and even death. So the worsening rates of alcohol use disorder in women prompt the need for a greater focus on women in the research and the search for treatments.
Yet, women have long been underrepresented in biomedical research.
It wasn’t until 1993 that clinical research funded by the National Institutes of Health was required to include women as research subjects. In fact, the NIH did not even require sex as a biological variable to be considered by federally funded researchers until 2016. When women are excluded from biomedical research, it leaves doctors and researchers with an incomplete understanding of health and disease, including alcohol addiction.
There is also increasing evidence that addictive substances can interact with cycling sex hormones such as estrogen and progesterone . For instance, research has shown that when estrogen levels are high, like before ovulation, alcohol might feel more rewarding , which could drive higher levels of binge drinking. Currently, researchers don’t know the full extent of the interaction between these natural biological rhythms or other unique biological factors involved in women’s health and propensity for alcohol addiction.

Looking ahead
Researchers and lawmakers are recognizing the vital need for increased research on women’s health. Major federal investments into women’s health research are a vital step toward developing better prevention and treatment options for women.
While women like Amy Winehouse may have been forced to struggle both privately and publicly with substance use disorders and alcohol, the increasing focus of research on addiction to alcohol and other substances as a brain disorder will open new treatment avenues for those suffering from the consequences.
For more information on alcohol use disorder, causes, prevention and treatments, visit the National Institute on Alcohol Abuse and Alcoholism .
- Amy Winehouse
- Binge drinking
- Neurobiology
- Intoxication
- Alcohol consumption
- Alcohol use
- Alcohol use disorder
- COVID-19 pandemic

Research Fellow

Senior Research Fellow - Women's Health Services

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

IMAGES
VIDEO
COMMENTS
A speech impediment, or speech disorder, is a condition that makes it hard for you to communicate. There are many types of speech impediments, and anyone can develop one. In some cases, children are born with conditions that affect speech. Other times, people have conditions or injuries that affect speech. Speech therapy can help.
TBI is a brain injury that can happen from a bump or blow to the head or when an object goes through the skull and into the brain. No matter what type of TBI you have, damage to your brain happens right away. Later, you may develop seizures or brain swelling. Doctors treat these medical problems. TBI can cause speech, language, thinking, and ...
Aphasia is caused by damage to one or more of the language areas of the brain. Most often, the cause of the brain injury is a stroke. A stroke occurs when a blood clot or a leaking or burst vessel cuts off blood flow to part of the brain. Brain cells die when they do not receive their normal supply of blood, which carries oxygen and important ...
Right hemisphere damage (RHD; also known as "right hemisphere disorder" and "right hemisphere brain damage") is an acquired brain injury—usually secondary to stroke or TBI—that causes impairments in language and other cognitive domains that affect communication.
The speech produced by a person who has traumatic brain injury may be slow, slurred, and difficult or impossible to understand if the areas of the brain that control the muscles of the speech mechanism are damaged. This type of speech problem is called dysarthria. These individuals may also experience problems swallowing. This is called dysphagia.
Types of speech disorder include stuttering, apraxia, and dysarthria. Learn more about speech disorders here. ... Apraxia is a general term referring to brain damage that impairs a person's ...
Right hemisphere brain damage, or RHD, is damage to the right side of the brain. Our brains have two sides, or hemispheres. In most people, language skills are in the left side of the brain. The right side controls attention, memory, reasoning, and problem solving. RHD may lead to problems with these important thinking skills.
A speech impediment describes speaking difficulties, such as stuttering and child apraxia. Learn how therapy, games, and guided treatment can help. ... often resulting in toxic damage to organs; Brain tumor: A growth that may damage areas of the brain, including those that control speech or language;
The American Speech-Language-Hearing Association (ASHA), in conjunction with a multidisciplinary panel of subject matter experts, has developed evidence-based clinical practice recommendations for the management of cognitive dysfunction associated with acquired brain injury (ABI) based on a systematic review and meta-analysis of 112 studies published between 1980 and 2020.
There are three general categories of speech impairment: Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production. Voice disorder. A voice ...
Dysarthria is a motor speech disorder where damage to your nervous system causes the muscles that produce speech to become paralyzed or weakened. The damage may make it difficult to control your tongue or voice box, causing you to slur words. ... Traumatic brain injury: Some 10% to 65% of people with traumatic brain injury have dysarthria ...
Summary. Apraxia of speech is a type of language impairment that is caused by damage to the brain, either during fetal development, childhood, or adulthood. This condition can occur along with other neurological deficits that are associated with damage to the brain. There are many different causes, and a diagnosis of the cause is essential for ...
A speech impediment, also known as a speech disorder, is a condition that can affect a person's ability to form sounds and words, ... Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington's disease, multiple sclerosis, muscular dystrophy, Huntington's disease ...
Causes. The most common cause of aphasia is brain damage resulting from a stroke — the blockage or rupture of a blood vessel in the brain. Loss of blood to the brain leads to brain cell death or damage in areas that control language. Brain damage caused by a severe head injury, a tumor, an infection or a degenerative process also can cause ...
Aphasia is a language disorder that affects how you communicate. It's caused by damage in the area of the brain that controls language expression and comprehension. Aphasia leaves a person unable to communicate effectively with others. A person with aphasia may have trouble understanding, speaking, reading, or writing.
Unlike aphasia that happens because of a brain injury, dysarthria is a speech disorder. It may happen if the muscles used to speak become weak, injured, or paralyzed. Causes can include damage to ...
Speech fluency can be disrupted from causes other than developmental stuttering. Neurogenic stuttering. A stroke, traumatic brain injury or other brain disorders can cause speech that is slow or has pauses or repeated sounds. Emotional distress. Speech fluency can be disrupted during times of emotional distress.
3) Use Speech Therapy Apps. The key to learning how to speak again after brain injury is to practice as much as possible. While participating in speech therapy is effective, individuals also need to practice speech exercises at home to optimize their recovery. An excellent way to do this is to download speech therapy apps onto your phone or tablet.
Aphasia is a brain disorder where a person has trouble speaking or understanding other people speaking. This happens with damage or disruptions in parts of the brain that control spoken language. It often happens with conditions like stroke. Aphasia is often treatable, and speech therapy can still help people who have this condition permanently.
Dysarthria is a motor speech disorder. This happens when brain or nerve damage changes the way your muscles work. It can be mild to severe. Children and adults can have dysarthria. There are many reasons people have trouble talking. Dysarthria can happen with other speech and language problems.
Dyspraxia is a disorder of planned and co-ordinated movement. It occurs because of injury to areas of the brain responsible for conscious movement, mainly situated in the frontal lobes. Dyspraxia of speech causes people to have difficulty saying what they are consciously thinking about saying. However, some individuals may be able to speak ...
The recently completed study was published in eNeuro. According to the findings, singing repairs the structural language network of the brain. The language network processes language and speech in ...
Wikimedia Commons. In a remarkable feat of neuroscience and assistive technology, researchers at the California Institute of Technology (Caltech) have successfully developed brain implants that ...
Dysarthria one of the types of Neuro-motor speech disorder, is referred to as the recurrent indication of several neurological disorders with stroke, Parkinsonism, and traumatic brain injury. Dysarthria is also said to have an influence on the comprehensive potentiality, speech accessibility and a specific persons' capability to unite and ...
On March 29, 2022, neurosurgeons at Stanford placed two tiny sensors each on the surface of two regions of Bennett's brain involved in speech production. About a month later, she and a team of ...
Katharine Lang investigates how SARS-CoV-2 infection can affect the brain, how it might have these effects, and what can be done to minimise the risk Covid may be primarily a respiratory infection, but a common symptom is "brain fog"—problems with memory or concentration—which can persist for weeks or months as part of long covid.1 And it's not the only neurological effect. Giovanni ...
Real-world communication is interactive, involving a collaborative exchange between individuals. It is also multimodal, containing a variety of communicative cues like speech, gesture, facial expressions, and eye gaze. Her goal is to better understand how these flexible and social language abilities are disrupted by brain injury.
Acoustical Society of America. "To sound like a hockey player, speak like a Canadian." ScienceDaily. ScienceDaily, 16 May 2024. <www.sciencedaily.com / releases / 2024 / 05 / 240516122636.htm ...
Singer Amy Winehouse died from alcohol toxicity in 2011, the same year that the American Society of Addiction Medicine publicly recognized addiction as a brain disorder.
A Jewish teenager was pelted with stones by a gang of youths who chased him along a north London street in the middle of the day. The suspected attack is the latest in a growing number of anti ...