We’re fighting to restore access to 500,000+ books in court this week. Join us!

Internet Archive Audio

- This Just In
- Grateful Dead
- Old Time Radio
- 78 RPMs and Cylinder Recordings
- Audio Books & Poetry
- Computers, Technology and Science
- Music, Arts & Culture
- News & Public Affairs
- Spirituality & Religion
- Radio News Archive

- Flickr Commons
- Occupy Wall Street Flickr
- NASA Images
- Solar System Collection
- Ames Research Center

- All Software
- Old School Emulation
- MS-DOS Games
- Historical Software
- Classic PC Games
- Software Library
- Kodi Archive and Support File
- Vintage Software
- CD-ROM Software
- CD-ROM Software Library
- Software Sites
- Tucows Software Library
- Shareware CD-ROMs
- Software Capsules Compilation
- CD-ROM Images
- ZX Spectrum
- DOOM Level CD

- Smithsonian Libraries
- FEDLINK (US)
- Lincoln Collection
- American Libraries
- Canadian Libraries
- Universal Library
- Project Gutenberg
- Children's Library
- Biodiversity Heritage Library
- Books by Language
- Additional Collections

- Prelinger Archives
- Democracy Now!
- Occupy Wall Street
- TV NSA Clip Library
- Animation & Cartoons
- Arts & Music
- Computers & Technology
- Cultural & Academic Films
- Ephemeral Films
- Sports Videos
- Videogame Videos
- Youth Media
Search the history of over 866 billion web pages on the Internet.
Mobile Apps
- Wayback Machine (iOS)
- Wayback Machine (Android)
Browser Extensions
Archive-it subscription.
- Explore the Collections
- Build Collections
Save Page Now
Capture a web page as it appears now for use as a trusted citation in the future.
Please enter a valid web address
- Donate Donate icon An illustration of a heart shape
Cases in pediatric occupational therapy : assessment and intervention
Bookreader item preview, share or embed this item, flag this item for.
- Graphic Violence
- Explicit Sexual Content
- Hate Speech
- Misinformation/Disinformation
- Marketing/Phishing/Advertising
- Misleading/Inaccurate/Missing Metadata
![[WorldCat (this item)] [WorldCat (this item)]](https://archive.org/images/worldcat-small.png)
plus-circle Add Review comment Reviews
103 Previews
5 Favorites
Better World Books
DOWNLOAD OPTIONS
No suitable files to display here.
PDF access not available for this item.
IN COLLECTIONS
Uploaded by station24.cebu on July 12, 2023
SIMILAR ITEMS (based on metadata)
Copyright © 2024 OccupationalTherapy.com - All Rights Reserved
Pediatric Case Study: Child with Oculomotor and Perceptual Challenges
Nicole quint, dr.ot, otr/l.
- Early Intervention and School-Based
- Neurological and Physical Disabilities
To earn CEUs for this article, become a member.
unlimit ed ceu access | $129/year
Case introduction.
Thank you so much for having me. I want to introduce you to our case.
- Patrick: 7 y.o. male in 2nd grade that has difficulties with reading, completing homework, and the following instruction during school occupations. He does not finish copying things from the board and tends to have difficulty with writing, coloring, and ball sports. He uses his finger to read, loses his place, and often complains he can’t find things in his books. He is slow with dressing routines, buttons and fasteners are a “nightmare”, and cleaning his room is tough.
- He lives with his mother and father and two siblings. He is a shy child who loves dinosaurs, football, and Avengers. He says he wants to be a firefighter when he grows up, like his father.
- Patrick was a normal delivery without complications. Mom reports he was a fussy baby with colic. She also indicates that he was slow with some developmental motor milestones, particularly balance-related and object manipulation. She said he has always had difficulty following directions and struggles with ADLs. She calls him “clumsy”.
- Patrick also has a history of ear infections and adenoid removal. He is on his second round of ear tubes.
Today, I am doing a case study format. I want to give you a conceptual way to think about how to intervene with a child who has visual challenges that are affecting school performance, ADL performance, or play performance. Patrick is a seven-year-old male in second grade. He has difficulties with reading, completing his homework, and following instructions during his school occupation. He does not finish copying things from the board and tends to have difficulty with writing, coloring, and ball sports. He uses his finger to read, loses his place, and often complains that he cannot find things in his book. He is slow with dressing routines, and buttons and fasteners are a nightmare. He also has a tough time cleaning his room. He lives with his mother, father, and two siblings. He is a shy child who loves dinosaurs, football, and Avengers and says he wants to be a firefighter when he grows up just like his dad. Patrick was a normal delivery without complications, but mom reports he was a fussy baby with colic. She also indicates that he was slow with some developmental milestones related to motor, particularly balance-related ones, and object manipulation. She said that he has always had difficulty following directions and struggles with his ADLs. She calls him clumsy. Patrick has a history of ear infections and adenoid removal, and he is on the second round of ear tubes. This scenario might sound familiar to many of you. This is typical of a lot of the kids that I see. These are "clumsy kids" who have some difficulty in school, and it can often be misconstrued as behavioral. And, if you know Patrick, he is a really sweet kid and he is not behavioral at all.
- Extract, organize info from environment
- AKA: oculomotor skills, visual motor skills
- Interpretation of what is seen
- AKA: visual perceptual skills, visual cognitive skills
I want to start out with defining vision. It is the total process of receiving information and then processing it cognitively. It a very complicated process. How we receive information is related to sensory functions. We have to extract information from the environment. For example, in order for you to take a picture, you have to move your phone camera to the right spot. With a selfie, you might realize that you are cutting off people's heads. You have to angle it the right way to get everyone in the picture. That is an example of reception. You have to make sure that you can actually receive that information. We also refer to this as oculomotor skills or visual-motor skills. This is especially true with vision. Cognition, on the other hand, is the mental functions involved with vision. This is interpreting what is seen and that becomes much more subjective. We could call these visual perceptual skills or visual cognitive skills. Back to our picture metaphor, we look at the picture on our phone in order to process it. These are two different things, but they are very much dependent on each other. Part of the challenge I think in our profession when trying to assess someone is that they use a lot of things synonymously.
- Anatomic, physiologic
- Oculomotor, vestibulo-ocular control
- Visual perceptual skills
- Visual-motor integration
- THEN…Integrate the above functions in occupations
When we think about visual function, this is talking about visual acuity, visual fields, contrast sensitivity, etc. These are the basic functions of vision. However, you can also talk about "functional vision." Functional vision is how we use it. This focuses on ocular motor skills and how we use the two eyes together. Not only do we have to move each eye, but we also need to be able to move them together. On top of that, we have to be able to accommodate or adjust the eyes for near and far stimuli. Accommodation is sort of separate from traditional oculomotor skills because accommodation requires the integration of your lens and your ciliary muscle. Thus, when I am talking about oculomotor skills, I am not talking about accommodation. For me, the only way to really make a change in accommodation is vision therapy. When I have kids that have accommodation issues, I send them straight to vision therapy because the ciliary muscle is smooth muscle, and it is much more challenging to affect change in that. The oculomotor skills that I am talking about are things like convergence, divergence, saccades, tracking, and smooth pursuits.
What are the five functions of a mature visual system? It starts with basic anatomy and physiology. Then, we have to have oculomotor and vestibulo-ocular control. Can I move both my head and my eyes to collect that data? Sometimes the eyes move with the head, and sometimes the eyes move by themselves and do more subtle movements. Some of our kids might struggle with that operation and need to use their whole body to move with their eyes because they have difficulty with that dissociation. Next, we need to effectively interpret visual information. This is where we start to move into the cognitive piece or visual perceptual skills. We then respond to visual cues by moving our limbs for visual-motor integration. Finally, all of this is integrated into occupations. There is a hierarchy of development. Visual-motor integration is extremely complex and a lot of times our kids are missing some of these lower-level functions.
Visual Development
Here is a great link on visual development to review on your own. It is a really cool video.
Skeffington's Model
I also want to introduce to you Skeffington's model shown in Figure 1.
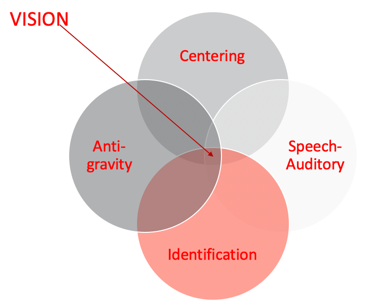
Figure 1. Skeffington's model.
I do not know how many of you are familiar with Skeffington's Model. When I started working at the university, I did program development over at the middle school. My background is in brain injury. Now I work with kids who have similar issues with visual abilities and function as well as some struggles with attention in school. I have always worked with optometrists and have had an interest in vision. Optometrists introduced me to Skeffington's model, and it helped me to understand why some of the things that I had been taught and was using with my clients was not working.
- Internal balance
- Attention and orientation
- Directing body, head, eyes toward an area in space
- Gathering meaning from areas of selected attention in external space
- Relationships between details (discrimination and differentiation)
- Analysis and communication of what is seen
Among these four circles, not one is more important than the other. They all need to be balanced. First is the antigravity system or the vestibular system. You cannot think about vision without thinking about the vestibular system. We need an internal balance for postural control. And, postural control is really essential to attending to our environment. There is also a huge relationship between the vestibular system and eye movements. The vestibular ocular reflex helps the body moves to right itself.
Centering is the idea of using attention and orientation to direct your body, head, and eyes towards something in space so you can receive information. Do I have the control to orient to something, attend to it, and dissociate as I need? There has to be underlying proprioceptive function, as well as strength, to be able to do something. The strength either needs to be internal or via external supports.
Identification was one of the pieces I was missing when I was doing a lot of the visual work in the past. Identification is gathering meaning from whatever you are attending to in space and starting to appreciate the relationships between the details. This becomes really important when processing information. These visual perceptual skills help to discriminate and differentiate between things. We are not just talking about being able to label something but label it in a way where you can tell the differences and the little nuances between things that lead to higher-level thinking and awareness.
The speech and auditory area is the ability to analyze and communicate what I am seeing. This is more of a cognitive language piece. This requires the parietal lobe functioning to bring in spatial relation or position in space. I really cannot do that functionally if I do not know that I have two sides of my body or that the right and left sides can do two different things at the same time or together. Can I cross the midline? These things inform my position in space and spatial relations. If I do not understand right versus left on myself or with a person sitting across from me who is giving me directions, I have a problem. I cannot really discriminate and differentiate how to get there from my own perspective, much less yours. This starts to make sense why this is extremely important for visual processing.
Skeffington's model tells us that we see with our whole body.
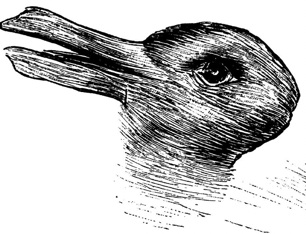
Figure 2. Optical illusion.
Figure 2 is an example of an optical illusion. Some of you might see one animal, while some of you might see another. I will give you a second to see if you can figure it out. Some of you might see both rather quickly, while others only see the one animal. some of you might struggle to see both the rabbit and the duck. Identification informs our visual perceptual skills to be somewhat subjective.
Second Grade Occupations
Our friend Patrick is in second grade. What is expected of a second-grader? Figure 3 is an overview.
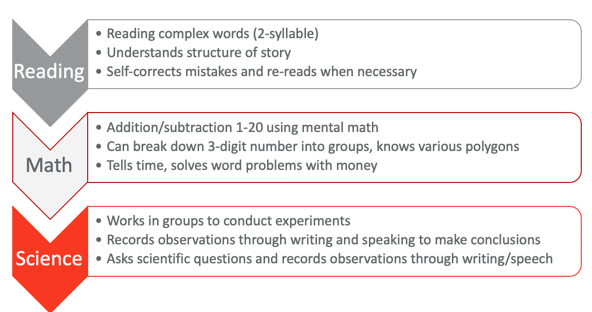
Figure 3. Overview of 2nd-grade occupations.
These are the universal standards for second grade. They should be able to read complex words which means two-syllable words, understand the structure of a story, self-correct mistakes, and reread when necessary. Those are pretty high-level reading skills. In math, they should be able to add and subtract one through 20 using mental math. I know some adults that struggle with that. They can break down three-digit numbers into groups into ones, tens, or hundreds. They also know various polygons, which would then indicate that they have some awareness of visual discrimination and form constancy starting to develop. They can tell time with an analog clock. You can put an asterisk next to that just from societal changes with technology. They still should be able to in theory to read a clock. They should be able to solve word problems with money, start to manipulate money and coins with some basic adding, and things like that. From a science perspective, they should be able to work in groups to conduct simple experiments. They should also be able to record their observations through writing and speaking to make conclusions about what they have observed. They should also be able to ask scientific questions and record observations throughout the process, not just at the end. What is kind of interesting here about the science piece is that this is universal. This scientific inquiry could be used for other topics as well.
From a visual development standpoint, I cannot emphasize enough how important this hierarchy is in Figure 4.
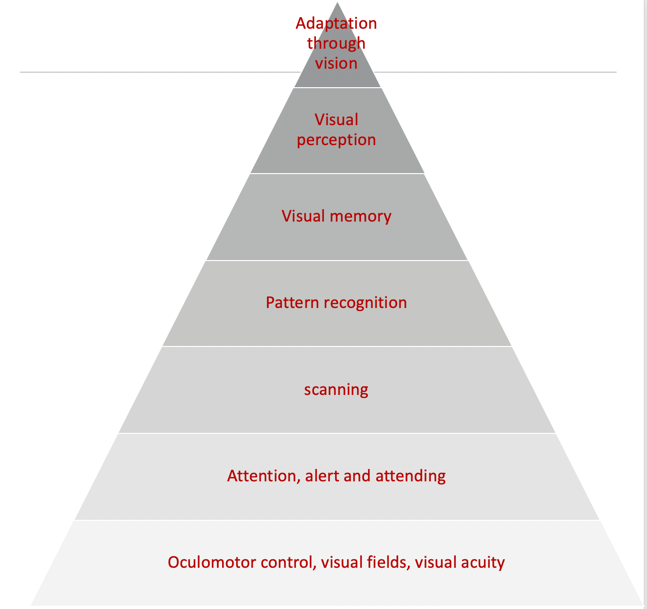
Figure 4. Visual hierarchy.
I am going to go through it rather quickly, but I want to point out the base of it all is oculomotor control. Once the oculomotor control is there, then there is visual attention as well as vigilance or a persistence toward it. If I am really looking at something to figure it out, I have to have some persistence. Once I can attend to something, the next levels are scanning and pattern recognition. Visual memory starts to kick in once patterns are recognized. With visual memories, this becomes functional visual perception. These are perceptual skills like visual closure, discrimination, spatial relations, position in space, figure-ground, and topographical orientation. These are all higher-level visual perceptual skills that we all test all the time. Once you get through all these levels, the final area is adaptation through vision.
I always use this analogy because in Florida we have hurricanes. One of the big things down here is to get hurricane windows. Hurricane windows are great because they can withstand the impact of debris flying around during a hurricane. So, if you have a strong foundation and hurricane windows, you are kind of safe from the storm or even a tornado. However, if you have a mobile home or a tiny house, even if you add hurricane windows, the whole house will blow away during the storm without a proper foundation. I think about this with our kids as well. Many of our tools are related to visual perception. Back in the day, I would start treatment with something like mazes for visual perception or handwriting for visual-motor integration without going back and appreciating that the child was missing a foundational element. We want to make sure that they have those foundational pieces.
Case Assessment Results
- Assessments: M-FUN, DTVP-3, Beery VMI, oculomotor screening,
- School reports: Below age range in reading, above age range in math, handwriting difficulties, sits in front due to difficulty following directions, no significant behavior concerns but slow with work and often doesn’t complete assignments
- Dislikes PE, but enjoys music, art, and science
For Patrick, I used the M-FUN (Miller Function and Participation Scales), the DTVP-3 (Developmental Test of Visual Perception), the Beery VMI (Beery-Buktenica Developmental Test of Visual-Motor Integration), and oculomotor screening. I also completed the SFA, which is the School Function Assessment. I used these because I wanted to get some information about vestibular functioning. I also wanted to a sensory profile and take a look at his motor and visual skills as well as non-motor and visual skills (DTVP-3). Oculomotor testing is also important. I often just do tracking kinds of things. I love the King-Devick Test for saccades. There is also the Developmental Eye Movement Test, the DEM, which is also very helpful. I do not know what you have access to, but you can do oculomotor testing just through the basic screenings that you do.
From his school reports, I saw that he was below the age range in reading, which we kind of suspected anyway, but he was above age range in math. He had some handwriting difficulties according to the teacher. She felt that he was slow, and it took him a long time and a lot of effort. She had him sitting in the front because he had such a hard time following directions. He was always kind of behind. His teacher did not feel that he had behavior concerns, but again he was slow with his work and he often did not complete assignments. She felt he was often tired.
According to the teacher, he disliked PE class, but he seemed to enjoy music and art class and he liked science. She did say he liked math too but sometimes he had a hard time copying the math problems from the board and getting his math finished. So, even though he was good at mental math, the copying of the problems was very difficult for him. Figure 5 shows the assessment results.
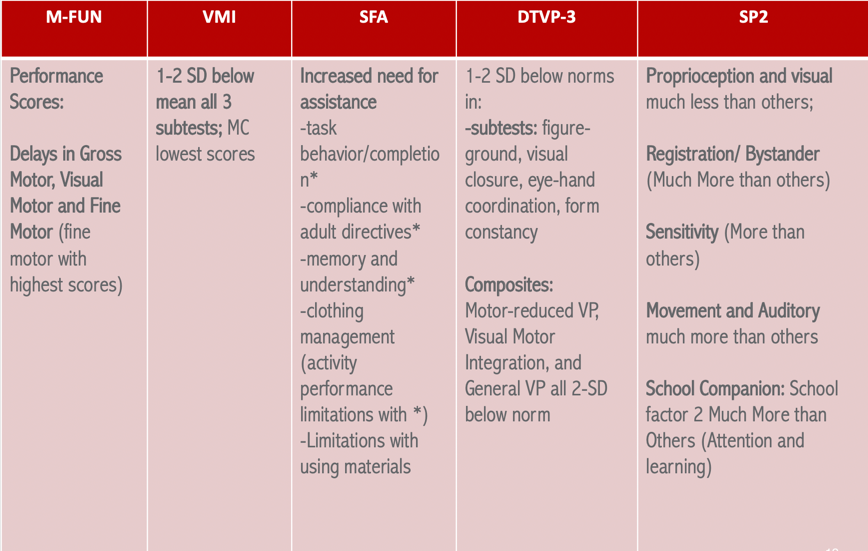
Figure 5. Assessment results.
The M-FUN results are not surprising because we knew he had some motor issues. Gross motor, visual motor and fine motor all came back as delayed. However, his fine motor had higher scores which means that they were not quite as involved as his gross motor and the visual motor functioning. On the VMI, he scored one to two standard deviations below the mean on all three subtests. However, motor coordination had the lowest scores, and that is the activity where you connect the dots. This makes sense as this one requires some motor control. I started to get a hypothesis as he was lacking the control for this subtest and that score was lower than the drawing one. I began to wonder about his oculomotor skills. The SFA said that he had an increased need for assistance on-task behavior and compliance with adult directives. These results are very similar to the teacher's report. He also had issues with memory and understanding, and clothing management. From the DTVP-3, which measures figure-ground visual closure, eye-hand coordination, form constancy, and all those visual perceptual things, he was below the norm by one to two standard deviations. He was also two standard deviations below the norm for motor-reduced VP, visual-motor integration, and general visual perception. What you are beginning to see is that it does not really make a difference if there is a motor component involved (like using a pencil to follow a track) or just using his eyes. This is a red flag that there is something going on at those lower hierarchal levels of development with respect to ocular motor functioning as well as attention. Finally, Sensory Profile 2 (SP2) showed that proprioception and visual were much less than others. He was showing low registration for those, but he also had sensitivity more than others. He also showed much more registration/bystander tendencies. And then for movement and auditory areas, these were much more than others. We are starting to see a picture here of vestibular challenges, proprioceptive challenges, visual challenges, and attention and learning using the SPSC (Sensory Profile School Companion). These results support that he was most likely missing some of those lower-level skills.
When I did the screening to test this by asking him to track and scan and tested functional saccades, I do not think it will be a surprise to tell you that this was all difficult for him. Saccades were really the area of dysfunction as well as cognitive loading with smooth pursuit. To assess cognitive loading was smooth pursuits, you have them follow an object in nice smooth patterns about 10 inches from their face. Then, you start asking them very basic questions that are long term memory kinds of things like, what did you like for breakfast? Or, who is your favorite TV character? What is your dog's name? If you see a huge discrepancy between their smooth pursuits and the cognitive loading, you will then know that there are some significant oculomotor control issues, and they are going to affect school performance. All of this information aligns with not only things we heard from school but also concerns the mom had as well.
Assessment Research
I wanted to give you just a little bit of information from the research on assessments so that this can inform your clinical reasoning (see Figure 6). Some of this is older but it is quite interesting.
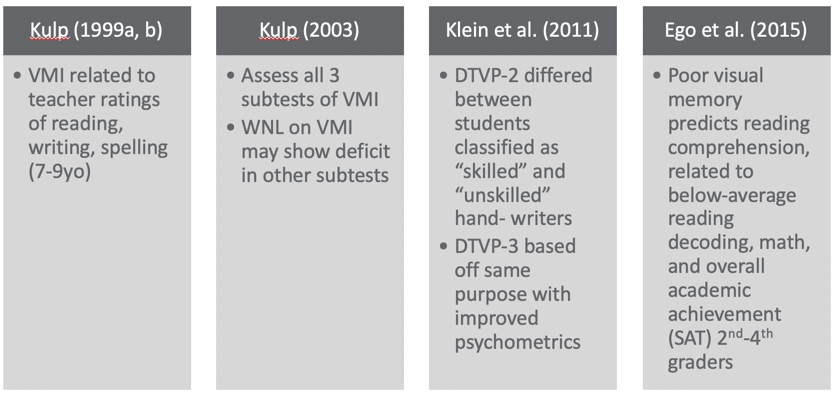
Figure 6. Overview of assessments.
The VMI is commonly used, and it is cheap and easy. In this study by Kulp (1999), it was related to teachers' ratings of reading, writing, and spelling. I think a lot of people use VMI for handwriting. It is not an effective tool to identify handwriting issues, but rather it is more effective at showing us writing, reading, and spelling challenges for ages seven to nine. This is why I chose it for Patrick. Another study, by Kulp (2003), showed that all three subtests of the VMI are really important instead of just doing one. This is because you might get "within normal limits" on one, but you might get that result on another one. For example, the blue subtest focuses on visual discrimination and if they can match a picture. Thus, it does not really give you a lot of information on other areas. Thus, Kulp recommends doing all three subtests. This is very interesting about the DTVP-2 in a study by Klein et al. (2011). The results actually differed between students classified as skilled and unskilled hand writers. So, if you want to look for handwriting challenges and figure out where the difficulties are coming from, the DTVP-3, the new version, is based on the same purpose as it just has better psychometrics. They tightened up the validity of the reliability scores in the newer version. Lastly, poor visual memory predicts reading comprehension (Ego et al., 2015). Kids who have poor visual memory also will have below-average reading, poor math decoding, and academic achievement scores for second to fourth graders. Visual memory becomes very important for this age group if they are struggling in school. This is why I use the DTVP. The TVPS (Test of Visual Perceptual Skills) is okay too but it does not capture the composite of motor versus non-motor.
EBP Remediation: Skeffington’s Model
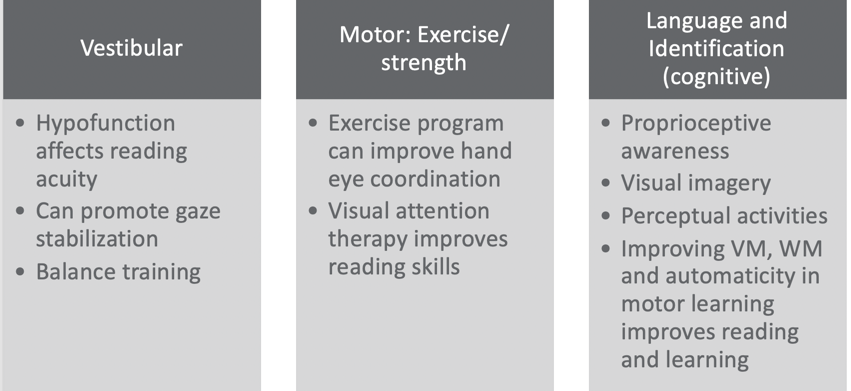
Figure 7. EBP remediation using Skeffington's Model. (Christy, 2019; Shelly-Tremblay et al., 2012; Gibson et al., 2015; Garje Mona et al. 2015; Jamal et al. 2019; Grisham et al., 2007; Sweeney et al., 2014; Mast et al., 2014, Gaymard et al., 2017; Van Hecke et al., 2019.)
Using a Skeffington's Model approach (see Figure 7), if we look at the vestibular function of Patrick, we start to realize that if you have an under-responsive vestibular system, it can affect reading acuity. Vestibular promotes gaze stabilization and balanced training related to your vestibular function for vision. He actually seemed to have a hypo functioning vestibular system according to the SP2; however, he had some over responsiveness when you looked at his post-rotary nystagmus. For the centering or motor area, exercise programs can improve hand-eye coordination. From multiple studies, the reasoning is that as the kids start to have better posture, strength, and endurance, they begin to be more aware of their bodies. Body scheme or kinesthetic awareness can also improve. They also found that visual attention therapy improves reading skills, and that visual attention therapy could result from exercise and strength programs. We also know that if someone can sustain sitting upright for a while and has postural control, they also will have better cognitive attention. However, visual attention really relies more on staying upright and sustaining a gaze on something, then there will be improved visual attention. It makes sense that if I have more postural strength and dissociation, I can do that.
Then, I combined language and identification together as the cognitive components of vision. What is very cool about this one is that proprioceptive awareness becomes very important per the research. The more proprioceptively aware you are, the higher the level of visual perceptual skills. They seem to correlate. Visual imagery became extremely important within this. You have to have some visual imagery and that involves the retina. The vestibular system interacts with the visual system as well as the proprioceptive system to provide stability within your environment. As we negotiate, through our activities, it allows for an image to be obtained by the retina and this happens as you are also moving your head to access things. Your body then integrates it. It starts to get really complicated very quickly. If I put all these things together, I start to become someone who has this dynamic ability to hone in on something, look at it, get that retinal involvement, and then start that whole processing procedure. We need the whole body in order to see. Studies also show that perceptual activities become extremely important. And if you improve visual memory (VM) and working memory (WM), as well as automaticity in motor learning, you will see improved reading and learning. This one I think really speaks to us as OTs. We might not necessarily think that that correlates to reading and learning skills, but it really does fit in this language and identification piece. If you think about it, with visual memory you now have a bank of things from which to pull, and then you can start moving up the hierarchal ladder. Working memory is being able to utilize your functional memory at the moment, and that does require visual memory as well as auditory memory. Automaticity is saying that my motor learning ability has moved beyond the skill level, and I am not in the cognitive learning level of motor learning. I have moved into the third level of motor learning which is that autonomous level where I can do something without really making a lot of errors and having to think about it. If we can get a child to the autonomous level, we will see that reading and learning flourish. This is really focusing on handwriting for the most part because that is often the tool that we use (written communication in our school occupations). If a child is focused on writing, it is really going to be hard for them to do anything else. And, when we are stuck in the motor learning cognitive phase, it can frustrating, exhausting, and hard. If we can get them beyond that level to where they are more automatic, it is much more functional for learning. A child cannot learn if they are dividing their attention. Figure 8 reinforces what we just talked about.
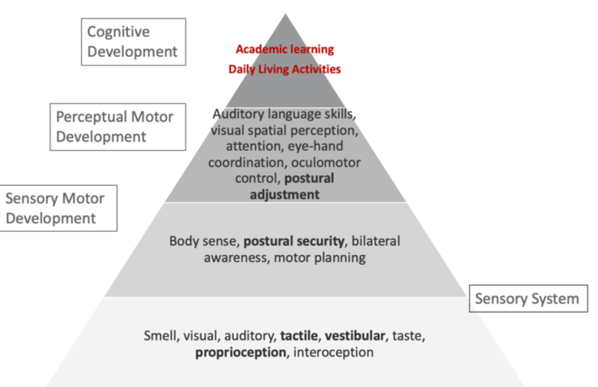
Figure 8. Sensory, motor, and cognitive development (Hk playgroup, n.d.).
The bottom part of this triangle is the very basic sensory system. The next one is the sensory-motor development. This includes body sense, postural security, bilateral awareness, and motor planning. This 2nd tier has been informed by the sensory system. Once this is pretty good, you start to develop more perceptual-motor development which is auditory language skills, visual-spatial skills, eye-hand coordination, oculomotor control, and postural adjustment. You start to see how this developmental pattern starts to make sense with vision and cognition. The top tier is academic learning, daily living activities, and the occupations that we focus on. They need a lot of these underlying skills to be able to do it. The foundation or the sensory piece is so important to vision, but all of these sensory pieces inform our subjective processing of visual information.
Remediation Approaches
Let's now see some of the remediation approaches that were used with Patrick (see Figure 9).

Figure 9. Motor approaches.
If I am going to treat oculomotor skills to try to build visual attention, I need to focus on postural strength, endurance, postural control, and head eye association. Now, all of a sudden, they become little visual receptors. They can receive information while moving within their environment. What does that look like in therapy? These can be all sorts of cool activities that really work on improving that strength like yoga and crawling around doing things to get stronger. It is important to have this postural strength and control for tracking and adequate vision for learning. I want to explain to you a little bit more about prone extension and supine flexion. I want you to take your fingers and put them on the back of your neck. In the middle of your neck, lightly palpate while your eyes are tracking laterally or horizontally. I want you to feel what is happening in the back of your neck as you are scanning. You should feel a contraction. There is a direct relationship between your lateral or horizontal tracking and your posterior or extensor neck muscles. This is the same if you go into the front of your neck. This is a little trickier to find. Lightly palpate the front of your neck during vertical tracking, and you should also feel a very slight contraction. These areas can facilitate improved tracking if you can strengthen them.
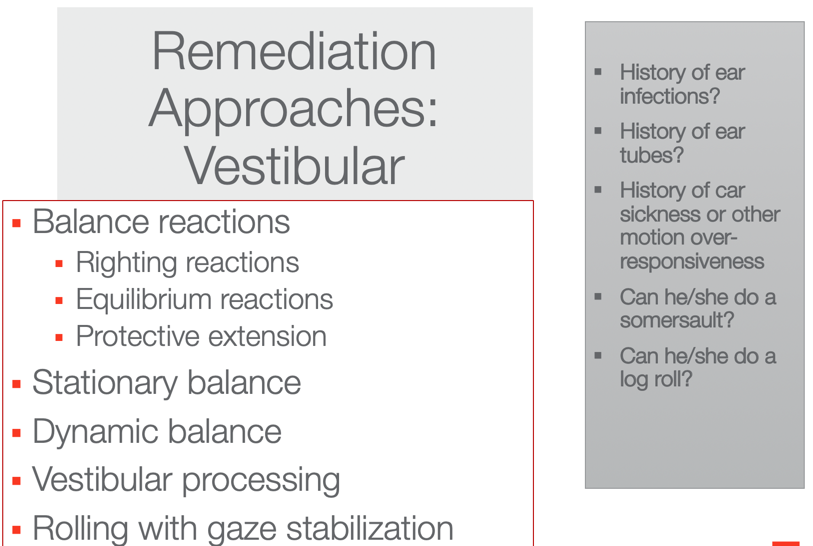
Figure 10. Vestibular approaches.
We want to determine a history of ear infections, ear tubes, or car sickness. Can they somersault? Can they log roll? These can tell us how their vestibular system is working. And, these are activities that we want to work on with these kids to really get that antigravity circle of Skeffington's Model working. I also want to make sure that their balance reactions are working. I like to use an onion swing for this kind of thing. Another activity is rolling with gaze stabilization. When they are ready and are not getting nauseous from these movements, we can have them log roll or somersault forward or backward and then have them stop and practice gaze stabilization on something. Then, we can have them roll again, stop, focus their gaze, and so on. There are a million ways to do it that can be fun. With these types of approaches, you are going to see a huge change in the function of the saccades.
Case Application: Patrick
- Perform top-down occupational analysis and find a discrepancy
- Identify and incorporate occupation-based practice to address discrepancies
- Final occupation-based activity mimics real activity in context
- Incorporate adaptations as needed (including education and consulting)
- Embed vestibular, motor, and cognitive-perceptual based upon visual hierarchy and discrepancies
Let's apply a top-down approach to our friend Patrick. During this top-down occupational analysis, we want to incorporate occupation-based practice to address those discrepancies as we do not function without occupation. Thus, the final occupation-based activity should mimic a real activity in context. We want to incorporate adaptations as needed including educating the parents and the teachers. We also want to embed vestibular, antigravity, motor, centering and cognitive-perceptual activities. This is where it can get a little tricky. What I want you to appreciate here is that if you see a deficit, like pattern recognition, you treat one level below. You do not start at the level of dysfunction in the hierarchal development, but you always start one level below.
If I find that Patrick's issue is at the lowest level, there really is not anything lower to go so that is where we are going to start. I would send them to optometry anyway to make sure visual acuity is okay. If I had a kid whose issue was visual memory and that was the deficit that really stuck out to me on whatever assessments I did, I would start with pattern recognition. Again, it is important to go one level below.
Figure 11 shows this top-down approach that I was just talking about.
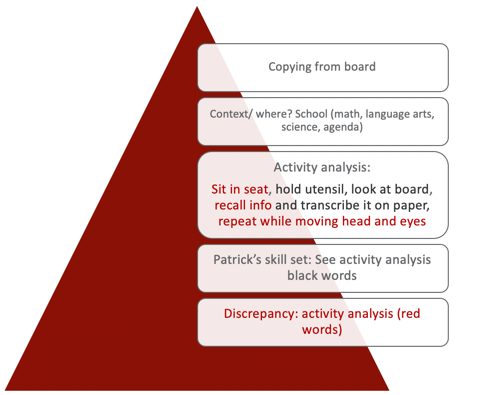
Figure 11. Top-down analysis 1.
If the goal if for Patrick to copy from the board, we want Patrick to be able to copy from the board. In his class, he had to copy a journal topic, math problems, and spelling words from the board. I could have gotten a little more focused on this pyramid, but I kept it general. What is the context? Where does it happen? This activity happens in school during math, language arts, science, and also his agenda. The next thing we would do is an activity analysis. As OTs, this is our special sauce. This is what makes us really unique. I realized this the more I do presentations to other disciplines. We really know how to do an activity or occupational analysis. I did a very basic one here but he has to sit in his seat, hold the utensil, look at the board, recall the information, transcribe it on the paper, and then repeat that as he moves his head and eyes until he gets everything copied. The next level of the process is looking at Patrick's skill set. Those are the black words in the activity analysis. He could hold the utensil, he could look at the board, and he could transcribe it. If this is true, what is the discrepancy between the activity analysis and Patrick's skills? This information is the red text. Sitting in the seat, recalling the information, and then repeating it over and over while moving his head and eyes was difficult for him. Right away that tells me that he has difficulty with centering, vestibular function, and probably something to do with the language like the recalling or identification of the information. I suspect this is because he has difficulty with proprioception. The focus of my treatment then is getting towards a sustained posture, working on the association of head and eyes with gaze stabilization, and visual memory. Activities that I could do in our therapy sessions would be things like Mad Libs. Some of you might have done these as kids. I love Mad Libs and the kids really enjoy them. Secret decoding is another fun one. Other activities I use are scavenger hunts and obstacle courses. I can then embed the things that I need a child to work on like vestibular gaze stabilization and postural strengthening. We used to do something called "Patrick Olympics" which was where we would just come up with different activities. I would pick some and he would pick some. He would try to do all of the activities to get a gold medal. Here's another one in Figure 12.
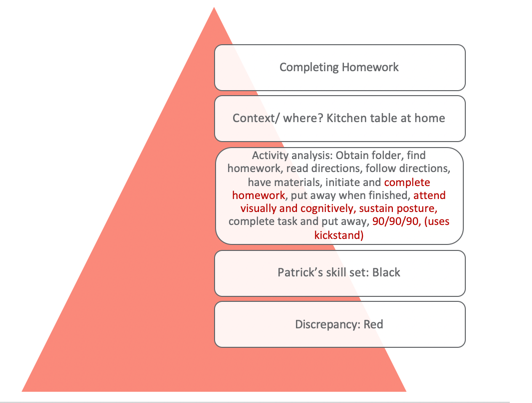
Figure 12. Top-down analysis 2.
This one is for completing homework. You can see in the activity analysis the different steps involved. Again, Patrick's skills are the ones that are in black and then the discrepancies are those in red. Our focus is going to be completing the task which requires sustained attention, postural and bilateral integration, and environmental supports, which I am going to get to in a second. Activities we used included Mad Libs and fantasy football. For the fantasy football activity, we had to come up with something that would be similar to completing a homework assignment. I made it second grade appropriate but it had football charts and plays as he is really into that. He loved that because he got to draw up these little football charts and he got to teach them to me. The goal was that he had to finish the assignment. He also loved to mimic a fireman so I had him "stop, drop and roll" through an obstacle course. This tapped into his vestibular system. Figure 13 looks at buttoning and zipping his pants.
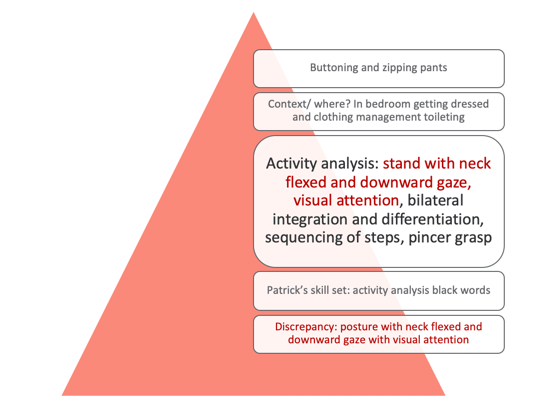
Figure 13. Top-down analysis 3.
Again, you can see in the activity analysis that his skill set is in black and the discrepancies are in red. With this one, I am focusing on his posture with sustained neck flexion and downward gaze with sustained visual attention. This can be a very hard task for kids. For occupations, we did mini golf which was great for this posture. We also did an egg game. The egg game is where you have to carry an egg in a little pouch. While you are walking, you have to watch the egg with a downward gaze and go very slow or the egg will fall out. If it breaks, you lose. It is silly but kids love it. Crab soccer is another great one as it facilitates that neck flexion in sustained pattern. We also did a game called fire rescue. This was done on a scooter board in supine. He had to find "fires" throughout the environment, and he had to keep his neck in a flexed position. Again, it is important to embed some of these activities that align with the Skeffington model approach.
Evidence-Based Approaches: Adaptive Approaches
Figure 14 shows some adaptive approaches.
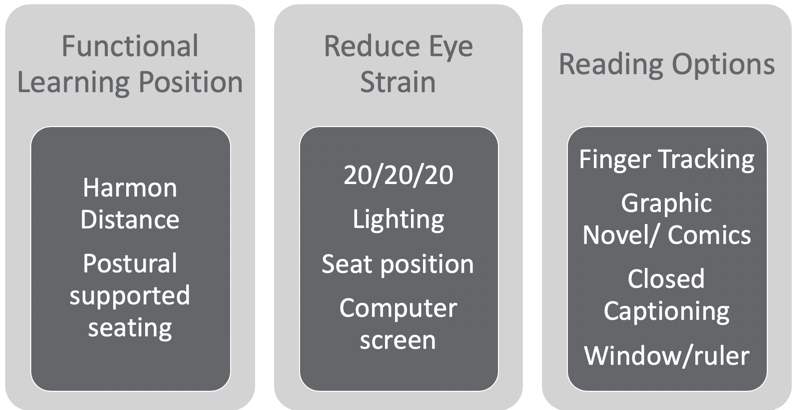
Figure 14. Adaptive approaches.
The functional learning position is really important and this is called the Harmon distance. The Harmon distance is the distance from your fist resting on your cheek to your elbow. This is an evidence-based approach for maximizing visual learning. We also need to look at postural supported seating. If somebody is struggling, we want to make sure that they are supported. This is not news to any of you but really making sure that the desk and the table fit the kid. You know that in the school system or even at home, that is not always the case.
Another approach is to reduce eye strain. A great tip is the 20/20/20 rule. Every 20 minutes, you stare at an object 20 feet away for 20 seconds to recalibrate your eyes and relax the tension. You also want to make sure the lighting is good, and fluorescent lights are not ideal. Again, the seated position is important. We want to make sure that they are not somewhere where they constantly have to strain. For computer use, they really should take a break every 20 minutes from the computer screen. And, if you can get them on a black background with a white font instead of white with black, it's better. The other thing with reading on the computer is that there is no point of reference. For example, on a post-it note or piece of paper, there are four corners of orientation. If I turn it to the backside, again, there are four corners of orientation. There is a sequence to how you read with the boundaries. This does not happen when you are reading a book on a Kindle or on a computer. You lose those corners of orientation. You and I know how to read so we do not need those corners of orientation as our skills are already intact. However, kids are still learning and gaining skills. They need those corners of orientation for reading comprehension, sequencing of events, and trying to find things. It really sort of happens in a vacuum when you are in a Kindle or an online book. Some of you might have even experienced that when you are unable to find a passage or page. Researchers are starting to find that reading online is not good for learning to read or for school development.

Figure 15. Adaptive approaches.
If kids use their fingers to read, let them. It helps them so do not take that approach away. Graphic novels and comics are fantastic. They give them a visual supplement to the reading, and the text is usually not as dense. Closed captioning is probably one of the best ways to help. You can have them watch videos and have the closed captioning at the bottom. This has been shown to cause parts of the brain for reading to light up in a functional MRI. That also works really well for kids with dyslexia. I also like using the window method or a ruler to help with reading. This can be used to block out whatever is below and helps them to focus.
Patrick tends to use a kickstand, or his arm to support his head. Can we set up his desk to achieve the Harmon distance (see Figure 15) and give him proper support? We already know that Patrick is using his finger so we would want to let him keep doing that. I also think the closed captioning would be great. I could recommend that his mom use closed captioning for tv and movies. I could also investigate if he would like to read graphic novels or comics.
- https://www.trianglevisions.com/blog/your-childs-vision-development/
- https://www.aao.org/eye-health/tips-prevention/children-vision-development
- http://www.healthofchildren.com/E-F/Eye-and-Vision-Development.html
- VERA vision screening program https://visualscreening.com/
- https://www.covd.org
- AMAZING blog with lots of sections: https://visionhelp.wordpress.com/
Here are some helpful resources. VERA is a free vision screening program, and they invite occupational therapists to join in. It is awesome, and I highly recommend you check it out. I also love the VisionHelp blog on the bottom. There are a bunch of sections to help you learn some in-depth stuff about vision. The developmental optometrist on there is amazing, and he explains everything. COVD is a group of vision folks that come together so that is a good one as well.
Alenizi, M. A. K. (2019). Effectiveness of a program based on a multi-sensory strategy in developing visual perception of primary school learners with learning disabilities: A contextual study of Arabic learners. International Journal of Educational Psychology, 8 (1), 72-104.
Bense, M. S. (2016). The effect of an oculomotor-vestibular-proprioceptive sensory stimulation programme on reading skills in children aged 8 to 12 years 11 months (Doctoral dissertation).
Chokron, S., & Dutton, G. N. (2016). Impact of cerebral visual impairments on motor skills: implications for developmental coordination disorders. Frontiers in psychology, 7 , 1471.
Christy, J. (2019). Use of vestibular rehabilitation in the pediatric population. Perspectives of the ASHA Special Interest Groups, 4 (6), 1399-1405.
Cohen, D., & Xavier, J. (2017). Oculomotor impairments in developmental dyspraxia. The Cerebellum, 16 (2), 411-420.
Ego, A., Lidzba, K., Brovedani, P., Belmonti, V., Gonzalez‐Monge, S., Boudia, B., ... & Cans, C. (2015). Visual–perceptual impairment in children with cerebral palsy: A systematic review. Developmental Medicine & Child Neurology, 57 , 46-51.
Garje Mona, P., Dhadwad, V., Yeradkar, M. R., Adhikari, A., & Setia, M. (2015). Study of visual perceptual problems in children with a learning disability. Indian Journal of Basic and Applied Medical Research, 4 (3), 492-97.
Gaymard, B., Giannitelli, M., Challes, G., Rivaud-Péchoux, S., Bonnot, O., Cohen, D., & Xavier, J. (2017). Oculomotor impairments in developmental dyspraxia. The Cerebellum, 16 (2), 411-420.
Klein, S., Guiltner, V., Sollereder, P., & Cui, Y. (2011). Relationships between fine-motor, visual-motor, and visual perception scores and handwriting legibility and speed. Physical & Occupational Therapy in Pediatrics, 31 (1), 103-114.
Kulp, M. T., & Sortor, J. M. (2003). Clinical value of the Beery visual-motor integration supplemental tests of visual perception and motor coordination. Optometry & Vision Science, 80 (4), 312-315.
KULP, M. T., Edwards, K. E., & Mitchell, G. L. (2002). Is visual memory predictive of below-average academic achievement in second through fourth graders? Optometry & Vision Science, 79 (7), 431-434.
Jamal, K., Leplaideur, S., Leblanche, F., Raillon, A. M., Honoré, T., & Bonan, I. (2019). The effects of neck muscle vibration on postural orientation and spatial perception: A systematic review. Neurophysiologie Clinique .
Mast, F. W., Preuss, N., Hartmann, M., & Grabherr, L. (2014). Spatial cognition, body representation, and affective processes: The role of vestibular information beyond ocular reflexes and control of posture. Frontiers in integrative neuroscience, 8 , 44.
Quaid, P., & Simpson, T. (2013). Association between reading speed, cycloplegic refractive error, and oculomotor function in reading disabled children versus controls. Graefe's Archive for Clinical and Experimental Ophthalmology, 251 (1), 169-187.
Sales, R., & Colafêmina, J. F. (2014). The influence of eye movement and the vestibularocular reflex in reading and writing. Revista CEFAC, 16 (6).
Solan, H. A., Shelley-Tremblay, J., & Larson, S. (2007). Vestibular function, sensory integration, and balance anomalies: A brief literature review. Optometry and Vision Development, 38(1), 13.
Van Hecke, R., Danneels, M., Dhooge, I., Van Waelvelde, H., Wiersema, J. R., Deconinck, F. J., & Maes, L. (2019). Vestibular function in children with neurodevelopmental disorders: A systematic review. Journal of Autism and Developmental Disorders , 1-23.
Quint, N. (2020) . Pediatric case study: Child with oculomotor and perceptual challenges. OccupationalTherapy.com , Article 5120. Retrieved from http://OccupationalTherapy.com

Nicole Quint has been an occupational therapist for over 15 years, currently serving as an Associate Professor in the Occupational Therapy Department at Nova Southeastern University, teaching in both the Masters and Doctoral programs. She provides outpatient pediatric OT services, specializing in children and adolescents with Sensory Processing Disorder and concomitant disorders. She also provides consultation services for schools, professional development, and special education services. She provides continuing education on topics related to SPD, pediatric considerations on the occupation of sleep, occupational therapy and vision, reflective therapist, executive functions, leadership in occupational therapy and social emotional learning.
What is Pediatric Occupational Therapy? Scenarios of OT for Kids
by Niagara Therapy, LLC | September 12, 2022

What is Pediatric Occupational Therapy? Pediatric OT Scenarios
Occupational therapy is a form of physical and mental rehabilitation that focuses on performing activities required in daily life. In the case of pediatric occupational therapy, this generally focuses on getting children to engage in play, school, and peer interactions. Pediatric occupational therapy helps children develop skills including vision, perception, coordination, strength, sensory processing, writing, emotional management, and social interaction.
The overall goal of occupational therapy is to improve a child’s ability to effectively interact with and learn from the environment in order to develop skills necessary for daily function. Often this simply looks like play to a bystander, but play is the way children learn! An occupational therapist can use many fun materials or even games to encourage development of new skills in a fun and creative way.
What Specific Areas Can OT Address?
Occupational therapy can help children with many different aspects of life. For example, it can help children with using appropriate social skills and regulating emotions. Being able to dress oneself and having the appropriate self care fine motor skills to use utensils, pencils, button a button or zip up a zipper, are all areas of focus in occupational therapy. Many children have difficulty with knowing left from right, which can affect the ability to orient clothing for dressing, scan to read a book or know how to tie shoes. Occupational therapy can address this left/right awareness or “laterality” in daily activities.
Sensory integration is another area that occupational therapy can address. Improved sensory integration is often achieved by expanding the variety of textures and tastes in a child’s diet and improving tolerance to various clothing textures. An OT could help develop a sensory “diet” with the goal to improve attention or transitions between tasks that are necessary in the school setting.
Many times kids will present with difficulty with visual perception and ocular motor skills . OT can provide exercises and activities to improve these skills which can affect school and homework activities as well as participation in many sporting activities. OT can also address gross motor skills, motor planning and executive function.
There are times children exhibit symptoms of retained primitive reflexes in their function. Primitive reflexes are involuntary motions that often help to protect infants. Typically these are integrated into more mature and voluntary responses; however, if not integrated, these reflexive patterns can create functional concerns. Retained reflexes can look like difficulty paying attention, anxiety, impaired fine or gross motor coordination, difficulty with balance or reading, difficulty with left-right awareness or a multitude of other concerns. Occupational therapy can provide guidance to integrate primitive reflexes. With this developmental foundation, children can improve the skills needed to make daily function more efficient.
There are times that the most effective way for a child to complete a task is to utilize adaptive equipment. Some examples of adaptive equipment are adapted eating utensils or pencil grips, slant boards, wheelchairs or crutches, and splints. An OT will also often recommend sensory equipment for the home or school setting as well.
Does My Child Need Occupational Therapy?
Occupational therapy can be helpful for a wide variety of challenges that children face, and can help children improve skills related to school, play, and daily life in general. Occupational may be helpful for your child if they are dealing with any of the following:
- Sensory integration difficulties or limited emotional management
- Limited diet and food sensitivity
- Weak and uncoordinated movements
- Poor handwriting
- Difficulty focusing in school
- Difficulty reading
- Difficulty tying shoes, buttoning, and dressing
- Spasms/Muscle Cramps/Spasticity
- Needing specialty equipment (writing, eating, sensory tools, etc.)
Feel free to get in touch with us to learn more about how our team of expert occupational therapists can help your child reach their maximum potential.
Common Scenarios and Case Studies of Pediatric Occupational Therapy
Niagara Therapy’s team of occupational therapists has helped many children over the years. We’ve outlined some common scenarios to help give you a better understanding of what occupational therapy looks like in the real world.
JH is a 6 year old girl who has a difficult time playing on the playground. Her teacher noticed that she falls frequently and seems clumsy. She loves the social aspect of tee ball, but has a hard time connecting the bat to the ball.
She was referred to occupational therapy, and we noted that she had difficulty with visual perception, using both hands together, and had a hard time crossing midline in activity. Each of these areas is vital when trying to swing a bat or catch a ball. She also had some retained primitive reflexes that have affected development of these skills.
We determined that occupational therapy intervention would be helpful for JH. Treatment would focus on improving visual perception, bimanual use, midline crossing, and primitive reflex integration.
Scenario 2
PR is really struggling with handwriting and copying his assignments from the board at school. His OT found that he has hand weakness and poor fine motor skills as well as limited core strength affecting sitting posture and balance. He also demonstrates difficulty with visual perception and ocular motor skills which contribute to the challenge of handwriting.
We determined that occupational therapy services would help to improve core strength, fine motor skills, and address visual concerns. By regularly completing tasks or exercises as recommended by an OT, PR should gain skills to improve his abilities in these areas, and his parents and teachers should see improvements in school work.
HC is an 8 year old who cannot tie his shoes or button a shirt. He also requires some assistance to put on his clothing and has trouble crossing midline in activity. In OT, he demonstrates impaired hand strength and fine motor skills as well as some retained primitive reflexes.
We determined that occupational therapy can help him learn left/right and spatial awareness to
improve his ability to orient clothing. He is also given exercises and activities to do at home to improve strength and fine motor skills that would allow him to more easily tie a shoe or button a button. Reflex integration can also develop underlying skills to help to make these tasks easier.
YG sustained a concussion, has been experiencing headaches, and has difficulty organizing schoolwork or cleaning her room. When evaluated in OT she was found to have ocular motor and visual perceptual impairments that are contributing to headaches and difficulty with reading.
We determined that occupational therapy can help to improve visual deficits and address executive function.
Scenario 5
KL is unable to tolerate wearing various textures of clothing and is a very picky eater. This has made getting ready for school and mealtimes very frustrating for everyone in the house.
Our occupational therapist had KL’s caregiver complete a sensory profile to evaluate the various areas of sensory processing in order to determine how those sensory abilities affect daily function. The OT also observed and interacted with the child to determine how to plan the best intervention for KL. We evaluated sensory preferences and assisted in exploring strategies to make these areas less stressful for both the child and parent.
What Do All of These Children Have in Common?
Each of these children has some observable functional difficulties with underlying causes that can be addressed in occupational therapy! As you can see, OT addresses a variety of areas. Undeveloped or underdeveloped skills can make everyday tasks challenging. Determining and addressing these areas is crucial for improved function. An occupational therapist will look at the big picture to help determine what skills may need improved to ultimately affect function.
Pediatric Occupational Therapy with Niagara Therapy
Your kids are important to us at Niagara Therapy, and we love to get to know them and their interests in order to help them enjoy every moment and be as independent as possible every day. We utilize tools and techniques that are not available anywhere else in the region. Interactive Metronome and Brain beats are computerized programs that can help improve coordination and attention as well as auditory processing. The Neuro Sensoriomotor Integrator or NSI is a fun & interactive technological tool we can use to improve letter and number recognition as well as ocular motor and visual perceptual skills. Our therapists use various programs to improve body awareness, visual perception, handwriting, emotional regulation and explore new foods.
We offer speech, physical and occupational therapies at Niagara Therapy and use a team approach driven by your goals. We offer sessions between 7 AM and 7 PM and focus on only one client at each session. If your child is experiencing difficulties with independent function or meeting developmental milestones, call us at 814-464-0627.
Quick Links
- PT for Kids
- PT for Adults
- OT for Kids
- OT for Adults
- Speech Therapy for Kids
- Speech Therapy for Adults
Mon- Fri: 7 AM – 7 PM
- Meet The Team
- How To Get Started
- Advanced Therapies in Erie, PA
- Pediatric Physical Therapy
- Pediatric Occupational Therapy
- Pediatric Speech Therapy
- Physical Therapy
- Occupational Therapy
- Speech Therapy
EMAIL [email protected] PHONE 814-464-0627 ADDRESS 2631 W 8th St Erie, Pennsylvania 16505
Let us know what’s on your mind!
Occupational Therapy Interventions for Children and Youth Ages 5 to 21 Years
- Standard View
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Stephanie Beisbier , Susan Cahill; Occupational Therapy Interventions for Children and Youth Ages 5 to 21 Years. Am J Occup Ther July/August 2021, Vol. 75(4), 7504390010. doi: https://doi.org/10.5014/ajot.2021.754001
Download citation file:
- Ris (Zotero)
- Reference Manager
Evidence Connection articles provide a clinical application of practice guidelines developed in conjunction with the American Occupational Therapy Association’s (AOTA’s) Evidence-Based Practice Program. Each article in the series summarizes the evidence from the published reviews on a given topic and presents an application of the evidence to a related clinical case. The articles illustrate how the research evidence from the practice guidelines can be used to inform and guide clinical decision making. In this Evidence Connection article, we describe a case report of a child receiving occupational therapy services and summarize the evaluation and intervention processes for supporting sleep, activities of daily living, and social participation. The practice guideline on this topic was published in the July/August 2020 issue of the American Journal of Occupational Therapy ( Cahill & Beisbier, 2020 ).
Occupational therapy practitioners work with children and families to identify meaningful goals for performance and participation and to make decisions about the types of intervention that will be used as well as the context in which services will be provided. In using child- and family-centered care principles, occupational therapy practitioners incorporate the priorities and perspectives of both the child and the family. Occupational therapy practitioners provide habilitative services that promote skill acquisition and participation in meaningful daily life activities.
- Self-Care Routines
Children often receive occupational therapy services to address issues with participation and performance in activities of daily living (ADLs) typical for their age group. Successful completion of self-care routines helps them to build confidence and autonomy. Significant positive outcomes are associated with the use of functional tasks to improve children’s performance of self-care routines ( Laverdure & Beisbier, 2021 ). Explicit skills training in ADLs and structured practice, including tasks with graded difficulty provided in natural contexts, is effective in supporting development and engagement in self-care skills. Caregiver and family involvement is critical to providing occupational therapy services to children, and increased family involvement allows occupational therapy practitioners to model strategies to encourage the child’s participation and leads to skill mastery. Caregiver coaching and feedback are particularly effective in promoting children’s independence with ADL tasks and reducing the need for caregiver assistance ( Laverdure & Beisbier, 2021 ).
- Play and Social Participation
Play is an important occupation of children. Statistically significant positive outcomes are associated with the use of play-based interventions to increase the skills associated with children’s social participation ( Cahill & Beisbier, 2020 ). Play-based activities that involve peers and support the child’s use of intrinsic motivation are effective for increasing playfulness. Coaching, peer modeling, and instruction on how and when to use specific skills (e.g., showing empathy) are effective in increasing collaborative play and play engagement ( Laverdure & Beisbier, 2021 ). Caregiver and family involvement is also critical to the development of play and the skills associated with sustained social participation ( Cahill & Beisbier, 2020 ).
Sleep is a factor in overall health, and it can affect the daily functioning of children and their caregivers. Consideration of sleep quality and sleep routines should be part of each child’s occupational profile. The use of rigorous exercise as an intervention should include guided practice for the child and caregiver and follow-up to assess effectiveness and considerations for modification to the exercise and activity plan ( Cahill & Beisbier, 2020 ). Interventions that include coaching of caregivers and focus on building sleep routines and healthy sleep habits can have a significant impact on overall quality of sleep and daily functioning for both the child and members of the household ( Cahill & Beisbier, 2020 ).
- Clinical Case
Jacob is a 9-yr-old boy who is in third grade and attends a public elementary school, where he has an Individualized Education Program and receives special education instruction for math as well as school-based occupational therapy and speech-language pathology services. Jacob lives with his father, his younger sister, and his paternal grandmother in a three-bedroom home. Jacob’s father works full time and commutes approximately an hour to and from work. Jacob’s grandmother helps Jacob get ready for school in the morning and greets him when the bus drops him off at home at the end of the day.
Jacob’s favorite pastime is reading comic books and graphic novels alone in his room. He also enjoys being outdoors and doing a weekly swimming activity with his father and sister. Jacob remembers to put dirty dishes in the sink after meals and clean up his toys at the end of the day. Jacob is quiet and slow to warm to strangers, including children his own age. Although Jacob likes to be at the park, he does not try to interact with other children and seems fearful when they approach to ask him to play. His grandmother has noticed that he has difficulty completing self-care tasks that other children his age perform independently, such as brushing his teeth and dressing himself. Jacob also has trouble falling asleep and sleeping through the night. Jacob was referred to occupational therapy by his pediatrician with a diagnosis of delayed milestone in childhood (Code R62.0; International Classification of Diseases and Related Health Problems, 10th Revision; World Health Organization, 1992 ) after receiving low scores on a developmental screening checklist.
Occupational Therapy Assessment and Findings
In advance of the evaluation session and on the basis of the referral, the occupational therapist provided Jacob’s father with a sleep tracking document and the Children’s Sleep Habits Questionnaire ( Owens et al., 2000 ) to complete at home. On the day of the evaluation session, the occupational therapist met the family at their home. The occupational therapist began the initial evaluation by interviewing Jacob, his father, and his grandmother to develop an occupational profile ( American Occupational Therapy Association [AOTA], 2021 ). During the interview, the occupational therapist learned about Jacob’s occupational history and gained important information about Jacob’s interests and values, strengths, performance patterns, and performance skills. The occupational therapist was also able to ask questions about how Jacob performed occupations in different contexts and identified contextual aspects that supported and inhibited his engagement. During the interview, Jacob and his father and grandmother identified barriers and challenges related to Jacob’s initiating and performing ADLs, following and maintaining sleep routines, and sustaining peer interactions.
The occupational therapist also completed the Waisman Activities of Daily Living Scale ( Maenner et al., 2013 ) and reviewed the sleep record with Jacob and his family. The occupational therapist walked with Jacob and his father to the local playground and used the Test of Playfulness in observing Jacob ( Skard & Bundy, 2008 ). Table 1 summarizes the evaluation findings.
Goal Setting and Priorities for Intervention
Jacob and his family reviewed the evaluation findings with the occupational therapist and identified priorities for intervention. The occupational therapist learned that Jacob’s sleep routine (or sleep pattern) has a significant impact on the family. Jacob and his family identified getting to sleep and getting enough hours of consecutive sleep as the main barriers to his occupational performance and daily routine. Jacob expressed pride in being able to prepare a cold snack and help with dishes after dinner. However, he expressed a desire to brush his teeth and hair and get dressed independently. Jacob’s grandmother would also like him to be able to blow his nose without support. Jacob and his family recognized his relative strength in social interaction with family members and expressed a desire to increase Jacob’s opportunities to play with peers and initiate social interactions.
Occupational Therapy Intervention
The occupational therapist used a combination of practice experience, information from current literature, and the unique client context to collaborate with Jacob and his family to develop an intervention plan that was informed by evidence and would maximize Jacob’s strengths and leverage his current support systems. The occupational therapist used the Occupational Therapy Practice Guidelines for Children and Youth Ages 5–21 Years ( Cahill & Beisbier, 2020 ) as a tool to guide decision making and considered Jacob’s presentation in relation to the diagnoses addressed in the practice guidelines. The occupational therapist then reviewed the practice guidelines, paying special attention to the information in the clinical recommendations table and the implications specific to outcomes that were aligned with Jacob’s priorities.
The occupational therapist found
strong strength of evidence for the use of functional tasks and cognitive-based interventions to improve performance and engagement in self-care activities and routines;
strong strength of evidence for the use of play-based interventions to improve social participation; and
moderate strength of evidence for education, coaching, and cognitive strategies to improve sleep.
Evidence from the practice guideline, Jacob’s interests, and the family’s preferences informed the occupational therapy intervention plan. Sessions were conducted in the natural environment (i.e., home, playground, and community swimming pool) and included training, coaching, and consultation during the occupations of play, self-care, and social participation. Sleep was addressed through a coaching and consultation model. Family-centered, community-based sessions occurred 2 times per week over 8 wk.
Intervention 1: Self-Care
The occupational therapist collaborated with Jacob and his family to address grooming and dressing and establish a plan that included graded introduction of more complex tasks and shaping, thought restructuring, and parent involvement ( Drahota et al., 2011 ). For example, during dressing, the occupational therapist first introduced a short-sleeved pullover t-shirt. Once Jacob demonstrated independent performance with the short-sleeved t-shirt, a long-sleeved t-shirt was introduced and then, finally, a button-down shirt. The occupational therapist challenged Jacob’s negative statements (e.g., “My grandma won’t ever help me again”) and supported positive thought restructuring (e.g., “My grandma will still help me if I need it, but I can try to do this on my own”). Jacob’s grandmother was coached to support his attempts at mastery and to provide feedback and praise. Shaping, or providing positive reinforcement when Jacob’s performance approximated the desired performance, was used to encourage him to complete tasks independently and in accordance with established social norms (i.e., using own toothbrush rather than a family member’s and blowing his nose with a tissue instead of a hand towel). The occupational therapist used the shaping technique when praising Jacob as he made attempts at mastery or completed a small component of a task, such as putting his arm through a sleeve, even when he was unsuccessful at fully donning the shirt.
Intervention 2: Social Participation
The occupational therapist formed an after-school play group for same-age peers with the purpose of providing opportunities for all the children to develop relationships, practice social communication skills, and expand play repertoires ( Wolfberg et al., 2015 ). The group included five children with varying levels of communication and interaction skills and used a consistent routine, which included a greeting activity, peer-mediated play choices, and a closing activity. Visual supports, such as activity choice boards, were provided, and all participants were encouraged to engage in spontaneous and flexible play with others.
The occupational therapist facilitated Jacob’s play initiations by encouraging him to speak to children who appeared to capture his interest and helped peers interpret the ways in which Jacob expressed interests and enjoyment, such as squeezing his hands together while jumping up and down. The occupational therapist challenged all the play group participants to extend their play by systematically adjusting the amount of adult support needed and encouraged them to gain one another’s attention and engagement in reciprocal play during games such as catch. The therapist provided parent-friendly information that outlined the importance of peer interaction for developing skills associated with meaningful social participation. The therapist actively coached Jacob’s father as they used problem-solving strategies to identify appropriate games and activities to maximize interaction with peers and assisted them in determining the appropriate level and timing of support to provide Jacob ( Kretzman et al., 2015 ).
Intervention 3: Daily Routines Promoting Sleep
After each 30-min playground session, the family (Jacob, Jacob’s father, and his sister) and the occupational therapist went to the nearby community swimming pool. Swimming is part of the family’s weekly routine. The therapist coached the family through a 45- to 60-min aquatic activity sequence ( Oriel et al., 2016 ). The aquatic sequence included warm-up movements, such as arm circles and marching, and a cardio segment with options such as jogging and performing jumping jacks in the pool. The warm-up activities were followed by a series of pool games that involved the family members and willing peers. The games included tag and other imaginative and action-oriented games (e.g., “hot and cold” and “sharks and minnows”). The last two elements of the aquatic sequence included time for unstructured play or swimming and a cool-down activity.
The occupational therapist provided Jacob and his family with encouragement to remain active and brainstormed other activities that could be done in the pool. Each night, Jacob’s father logged Jacob’s sleep behaviors to share with the occupational therapist. Jacob’s family and the occupational therapist discussed the difference in Jacob’s sleep patterns and noted improvements when he had the opportunity to go to the pool compared with days when he engaged in less physical activity. To support Jacob on days when the pool visit is not feasible, the therapist used sleep coaching strategies ( Sciberras et al., 2011 ) aimed at building consistent bedtime routines and habits. The family actively identified unhealthy bedtime habits and problem solved ways to shift to healthy practices.
Occupational Therapy Outcomes
After 8 wk, Jacob demonstrated significant progress and achieved the outcomes that were established at the beginning of occupational therapy intervention. Jacob began initiating and performing ADLs, following and maintaining sleep routines, and sustaining peer interactions. Jacob fell asleep, on average, within 20 min of going to bed and slept for an average of 7 hr. His grandmother reported improved daily functioning for the family (i.e., less conflict) because the sleep quality of everyone in the home had improved. Jacob’s ratings on the Waisman Activities of Daily Living Scale ( Maenner et al., 2013 ) increased from “does with help” to “does independently” for dressing and grooming. Jacob initiated play with two peers on the playground within 10 min and engaged in parallel play (e.g., swinging on swings and singing with a peer) and cooperative play (e.g., playing tag) without adult assistance.
Occupational therapy practitioners use child- and family-centered care principles to provide services to children in their natural environments. The child’s natural or typical context provides opportunities to practice skills while contending with unique and sometimes unanticipated factors. Such occasions encourage problem solving and collaboration among the occupational therapy practitioner, the child, and the child’s family members. Occupational therapy practitioners should collaborate with family to design interventions to address self-care, sleep, and social participation through the use of functional tasks, play-based activities, education, coaching, and cognitive strategies.

- Previous Article
- Next Article

Data & Figures
Evaluation Findings
| Assessment Tool | Results |
| Occupational Profile ( ) | exploring environments, expressing emotions, showing preferences, making choices, and following transitions with adult support difficulty initiating and performing activities of daily living, following and maintaining sleep routines, sustaining peer interactions Jacob’s priorities are to feel more comfortable playing with other children and to dress without his grandmother’s assistance. |
| Children’s Sleep Habits Questionnaire ( ) | unafraid of the dark, unafraid of sleeping alone, no presence of parasomnias (e.g., grinding teeth, sleep walking, or night terrors) amount of time to fall asleep, amount of sleep per night, restless sleep, and tired upon awakening |
| Sleep record completed by father for 7 consecutive days | >90 min time to sleep 5 of 7 days. 60–75 min time to sleep 2 of 7 days. Sleep duration 4–5 consecutive hours of sleep 7 of 7 days. |
| Waisman Activities of Daily Living Scale ( ) | independent with toileting, eating, drinking, bathing, putting away toys, preparing a cold snack, and clearing table after dinner inconsistent and below-age expectations for performance with brushing teeth and hair, dressing, and nose blowing because of limited motor and process skills |
| Test of Playfulness ( ) | appears to feel safe during play and is beginning to incorporate people into play. Two incidences of peer social engagement (responded to peer’s question) after parent prompt; one incident of cooperative play on playground equipment with parent directive and ongoing support limited communication and interaction skills for cooperative play, responding to other’s facial or body cues, and engaging in challenges. Does not independently initiate peer play in 30 min in familiar setting with familiar peers; 2 additional attempts for cooperative play on playground with parent directive failed. Demonstrates onlooker play behaviors. Does not try to overcome obstacles or barriers to play. |
Supplements
- Occupational Therapy Practice Guidelines for Children and Youth Ages 5–21 Years
Citing articles via
Email alerts.
- Special Collections
- Conference Abstracts
- Browse AOTA Taxonomy
- AJOT Authors & Issues Series
- Online ISSN 1943-7676
- Print ISSN 0272-9490
- Author Guidelines
- Permissions
- Privacy Policy
- Cookie Policy
- Accessibility
- Terms of Use
- Copyright © American Occupational Therapy Association, Inc.
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Occupational Therapy Pediatric Case Study Examples
Select the pediatric case for study, review child's diagnosis and medical history, set up an initial meeting with the child and parents or guardians, prepare a detailed initial assessment plan, conduct initial assessment on physical, cognitive and emotional capabilities of the child, record observations during the initial assessment, evaluate child's clinical reports, develop an occupational therapy treatment plan based on findings, approval: treatment plan.
- Develop an occupational therapy treatment plan based on findings Will be submitted
Prepare necessary therapy materials and equipment
Conduct therapy sessions.
- 1 Sensory integration activities
- 2 Fine motor skill exercises
- 3 Hand-eye coordination games
- 4 Social skills building exercises
- 5 Cognitive tasks
Monitor and record the child's progress during each therapy session
Provide feedback and recommendations to parents or guardians, regularly update the treatment plan based on child's progress, re-evaluate the child's capabilities periodically, prepare a comprehensive final report based on case study, approval: final report.
- Prepare a comprehensive final report based on case study Will be submitted
Discuss final report and future recommendations with parents or guardians
Final Report and Future Recommendations - {{form.Meeting_Date}}
We are pleased to share the comprehensive final report on {{form.Child_Name}} 's occupational therapy case study. The report highlights the assessment findings, progress, and specific recommendations for future interventions.
We kindly request your presence at a scheduled meeting on {{form.Meeting_Date}} to discuss the report and address any questions or concerns you may have. Your active participation is essential in shaping the child's therapy journey.
We look forward to fruitful and collaborative discussions.
Best regards,
The Occupational Therapy Team
Close the case study
Take control of your workflows today., more templates like this.

Understanding and Supporting Interoception in Occupational Therapy: Case Studies
Interoception, often referred to as the “eighth sense,” plays a crucial role in how individuals perceive and respond to their internal bodily signals. This sense is essential for self-regulation, emotional awareness, and overall well-being. For occupational therapy practitioners, understanding interoception and its impact on daily functioning is vital for providing effective interventions, particularly in pediatric populations. This comprehensive guide delves into the science of interoception, its relevance in occupational therapy, and evidence-based strategies to support individuals with interoceptive challenges.
What is Interoception?
Interoception is the sensory process that allows individuals to perceive internal bodily sensations, such as hunger, thirst, heart rate, respiration, and the need to use the bathroom. These internal signals are conveyed to the brain via the autonomic nervous system and the insular cortex, which then interprets them and triggers appropriate responses (Craig, 2015). Interoception is fundamental for maintaining homeostasis and is linked to emotional experiences and self-regulation (Critchley & Garfinkel, 2018).
The Role of Interoception in Daily Life
Interoceptive awareness allows individuals to recognize and respond to bodily needs, which is essential for survival and well-being. It also plays a significant role in emotional regulation, as bodily sensations often inform emotional states. For instance, an increased heart rate may signal anxiety, while a relaxed breathing pattern may indicate calmness (Schulz & Vögele, 2015).
Interoception and Emotional Regulation
Emotional regulation relies heavily on the ability to accurately perceive and interpret internal signals. Research suggests that individuals with better interoceptive awareness have more effective emotional regulation skills (Mehling et al., 2012). This connection highlights the importance of interoception in managing stress, anxiety, and other emotional responses.
Interoception and Self-Regulation
Self-regulation involves the ability to manage one’s behavior, emotions, and thoughts in response to external demands. Interoceptive signals provide critical feedback that informs self-regulatory actions. For example, recognizing the physical signs of hunger can prompt an individual to eat, thus preventing irritability and maintaining focus (Füstös et al., 2013).
Interoception is intricately linked to several brain regions, including the insular cortex, anterior cingulate cortex, and the somatosensory cortex. The insular cortex is particularly important as it integrates internal bodily signals and contributes to emotional awareness and self-regulation. Studies using functional magnetic resonance imaging (fMRI) have shown that individuals with heightened interoceptive awareness exhibit increased activation in these brain areas when processing internal stimuli (Craig, 2015).
Interoception and Mental Health
Interoception is not only crucial for physical and emotional regulation but also has significant implications for mental health. Poor interoceptive awareness is associated with various mental health conditions, including anxiety, depression, and eating disorders. For instance, individuals with anxiety disorders may misinterpret normal bodily sensations, such as an increased heart rate, as signs of impending danger, exacerbating their anxiety symptoms (Khalsa et al., 2018). Enhancing interoceptive awareness through therapeutic interventions can therefore play a critical role in mental health treatment.
Interoceptive Awareness and Learning Disabilities
Children with learning disabilities often face challenges beyond academic skills, including difficulties with interoceptive awareness. These children may struggle with recognizing when they are tired, hungry, or need a break, which can impact their ability to focus and learn effectively. Addressing interoceptive awareness in occupational therapy can help these children better understand their bodily needs, leading to improved attention and learning outcomes (Mahler, 2017).
Interoception and Physical Health
Interoception also plays a significant role in maintaining physical health. For example, accurate interoceptive awareness is essential for managing chronic conditions such as diabetes, where individuals need to recognize signs of low or high blood sugar levels. Improving interoceptive skills can help individuals with chronic illnesses better monitor and manage their health, leading to more effective disease management and better overall health outcomes (Herbert et al., 2012).
Interoceptive Awareness in Adolescents
Adolescence is a critical period for the development of interoceptive awareness. As the body undergoes significant changes during puberty, adolescents must learn to navigate new and sometimes confusing bodily signals. Enhancing interoceptive awareness during this stage can support better emotional regulation and mental health, helping adolescents manage stress and anxiety more effectively (Price & Hooven, 2018). Occupational therapists can play a key role in supporting adolescents through targeted interventions that promote body awareness and emotional resilience.
Interoception and Occupational Performance
Interoceptive awareness significantly impacts occupational performance in various daily activities, including eating, sleeping, and engaging in physical activities. For instance, children with poor interoceptive awareness might have difficulty recognizing when they are full, leading to overeating, or might struggle with sleep hygiene because they cannot identify when they are tired. Occupational therapy interventions that enhance interoceptive awareness can improve these daily routines, contributing to better health and well-being (Miller et al., 2012).
Family and Caregiver Involvement
Involving families and caregivers in interventions for interoceptive awareness is crucial. Educating parents about interoception and its impact can help them understand their child’s behaviors and provide appropriate support. Caregivers can be trained to use specific strategies at home, such as creating consistent routines and using visual aids, to reinforce the skills being developed in therapy. Collaborative efforts between therapists and families can enhance the effectiveness of interventions and support the child’s overall development (Schaaf et al., 2014).
Integrating Technology in Interoceptive Training
The integration of technology in occupational therapy offers new opportunities for enhancing interoceptive awareness. Wearable devices that monitor physiological signals, such as heart rate and skin conductance, can provide real-time feedback to individuals and therapists. Biofeedback and virtual reality (VR) are emerging tools that can help individuals visualize and understand their internal bodily signals, making interoceptive training more engaging and effective (Khalsa et al., 2018).
Interoception Across the Lifespan
Interoceptive awareness is important at all stages of life, not just in childhood. Adults and older adults can also benefit from interventions aimed at improving interoception. For instance, older adults may experience diminished interoceptive awareness due to aging, which can impact their ability to manage chronic conditions and maintain overall health. Occupational therapists can tailor interventions to support interoceptive awareness across the lifespan, ensuring that individuals can continue to respond effectively to their bodily needs (Herbert et al., 2012).
Future Directions in Interoceptive Research
Ongoing research in the field of interoception continues to uncover its complexities and implications for health and well-being. Future studies are needed to explore the most effective interventions for enhancing interoceptive awareness and to understand the neural mechanisms underlying interoceptive processing. As our knowledge expands, occupational therapy practitioners will be better equipped to develop innovative and evidence-based strategies to support individuals with interoceptive challenges (Critchley & Garfinkel, 2018).
Interoception in Pediatric Populations
In pediatric populations, particularly those with developmental conditions such as autism spectrum disorder (ASD) and sensory processing disorder (SPD), interoceptive awareness can be significantly impaired. These impairments can lead to challenges in recognizing and responding to bodily needs, contributing to difficulties in self-regulation and emotional management (Mahler, 2017).
Interoception and Autism Spectrum Disorder
Children with ASD often exhibit atypical interoceptive processing, which can manifest as challenges in recognizing hunger, thirst, or the need to use the bathroom. These difficulties can exacerbate behavioral issues and impact overall functioning. Studies indicate that interventions targeting interoceptive awareness can improve self-regulation and reduce anxiety in children with ASD (Schaaf et al., 2014).
Interoception and Sensory Processing Disorder
SPD is characterized by difficulties in processing sensory information, including interoceptive signals. Children with SPD may struggle to interpret bodily sensations, leading to issues such as overeating, dehydration, or poor toileting habits. Addressing interoceptive awareness in therapy can help these children develop better self-regulation and body awareness (Miller et al., 2012).
Assessment of Interoception
Assessing interoceptive awareness is a critical step in developing effective interventions. Various tools and methods can be used to evaluate interoceptive processing in children.
Self-Report Measures
Self-report measures, such as the Body Perception Questionnaire (BPQ) and the Multidimensional Assessment of Interoceptive Awareness (MAIA), can provide insights into an individual’s interoceptive awareness. These tools are useful for older children and adults who can articulate their internal experiences (Mehling et al., 2012).

Behavioral Observations
For younger children or those with limited communication skills, behavioral observations can be an effective assessment method. Observing how a child responds to internal cues, such as hunger or the need to use the bathroom, can provide valuable information about their interoceptive awareness (Mahler, 2017).
Physiological Measures
Physiological measures, such as heart rate variability and skin conductance, can also be used to assess interoceptive processing. These measures provide objective data on how the body responds to internal signals and can be particularly useful in research settings (Critchley & Garfinkel, 2018).
Evidence-Based Interventions for Interoceptive Awareness
Occupational therapy practitioners can employ various evidence-based interventions to support interoceptive awareness in children. These interventions aim to enhance the ability to recognize and respond to internal bodily signals, thereby improving self-regulation and emotional management.
Mindfulness-Based Interventions
Mindfulness practices, such as body scans and mindful breathing, can enhance interoceptive awareness by encouraging individuals to focus on internal sensations. Research indicates that mindfulness interventions can improve interoceptive accuracy and emotional regulation in children and adults (Fissler et al., 2016).
Body Scan Meditation
Body scan meditation involves focusing attention on different parts of the body, noticing sensations without judgment. This practice can help children become more aware of internal signals and improve their ability to interpret and respond to these signals appropriately (Mehling et al., 2012).
Mindful Breathing
Mindful breathing exercises encourage individuals to focus on their breath, noticing the sensations of inhaling and exhaling. This practice can enhance awareness of respiratory sensations and promote relaxation and emotional regulation (Schulz & Vögele, 2015).
Sensory Integration Therapy
Sensory integration therapy (SIT) aims to improve the brain’s ability to process and integrate sensory information, including interoceptive signals. This approach involves providing controlled sensory experiences to help children develop more accurate sensory processing and regulation skills (Schaaf et al., 2014).

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley Open Access Collection

Effectiveness of paediatric occupational therapy for children with disabilities: A systematic review
1 Cerebral Palsy Alliance, Discipline of Child and Adolescent Health, The University of Sydney, Camperdown North South Wales, Australia
Associated Data
Introduction.
Paediatric occupational therapy seeks to improve children's engagement and participation in life roles. A wide variety of intervention approaches exist. Our aim was to summarise the best‐available intervention evidence for children with disabilities, to assist families and therapists choose effective care.
We conducted a systematic review (SR) using the Cochrane methodology, and reported findings according to PRISMA. CINAHL, Cochrane Library, MEDLINE, OTSeeker, PEDro, PsycINFO were searched. Two independent reviewers: (i) determined whether studies met inclusion: SR or randomised controlled trial (RCT); an occupational therapy intervention for children with a disability; (ii) categorised interventions based on name, core components and diagnostic population; (iii) rated quality of evidence and determined the strength of recommendation using GRADE criteria; and (iv) made recommendations using the Evidence Alert Traffic Light System.
129 articles met inclusion ( n = 75 (58%) SRs; n = 54 (42%)) RCTs, measuring the effectiveness of 52 interventions, across 22 diagnoses, enabling analysis of 135 intervention indications. Thirty percent of the indications assessed ( n = 40/135) were graded ‘do it’ (Green Go); 56% (75/135) ‘probably do it’ (Yellow Measure); 10% ( n = 14/135) ‘probably don't do it’ (Yellow Measure); and 4% ( n = 6/135) ‘don't do it’ (Red Stop). Green lights were: Behavioural Interventions; Bimanual; Coaching; Cognitive Cog‐Fun & CAPS; CO‐OP; CIMT; CIMT plus Bimanual; Context‐Focused; Ditto; Early Intervention (ABA, Developmental Care); Family Centred Care; Feeding interventions; Goal Directed Training; Handwriting Task‐Specific Practice; Home Programs; Joint Attention; Mental Health Interventions; occupational therapy after toxin; Kinesiotape; Pain Management; Parent Education; PECS; Positioning; Pressure Care; Social Skills Training; Treadmill Training and Weight Loss ‘Mighty Moves’.
Evidence supports 40 intervention indications, with the greatest number at the activities‐level of the International Classification of Function. Yellow light interventions should be accompanied by a sensitive outcome measure to monitor progress and red light interventions could be discontinued because effective alternatives existed.
Occupational therapy intervention for children promotes engagement and participation in children's daily life roles (Mandich & Rodger, 2006 ). Children's roles include, developing personal independence, becoming productive and participating in play or leisure pursuits (Roger et al .). Inability to participate because of disease, disability or skill deficits, can cause marginalisation, social isolation and lowered self‐esteem (Mandich & Rodger, 2006 ). Occupational therapists select interventions for children based upon an analysis of the child's performance of daily life roles, how their performance is affected by their disability, and how their environment supports or constrains their performance (Mandich & Rodger, 2006 ).
The practices of paediatric occupational therapists have evolved and changed based on research and theory (Rodger, Brown & Brown, 2005 ), such as family centred care and the World Health Organisation's (WHO) International Classification of Functioning, Disability and Health (ICF; World Health Organisation, 2001 ). These frameworks have led many occupational therapists to move away from impairment‐based interventions at the body structures and functions level aimed at remediating the child's deficits (known as ‘bottom‐up’ interventions), and instead to focus on improving functional activity performance and participation (‘top‐down’ interventions) (Weinstock‐Zlotnick & Hinojosa, 2004 ), as well as partnering with parents to deliver therapy embedded within daily life.
Clinicians will always have different expertise and preferences, but there are financial and ethical ramifications of delivering interventions. Ensuring the latest research findings are easily accessible to families and clinicians is vital. Occupational therapists positively embrace evidence‐based practice, but on the ground, implementation can lag (Flores‐Mateo & Argimon, 2007 ; Upton, Stephens, Williams & Scurlock‐Evans, 2014 ). Systematic reviews (SR) indicate that the translation of the latest evidence into routine clinical care lags 10–20 years in all countries and specialities ( Flores‐Mateo & Argimon ), which for paediatric patients is an entire childhood. Multiple paediatric occupational therapy interventions exist to address children's specific goals. In partnership with parents, it is the therapist's role to choose and tailor the intervention choices to match the child and parent's goals, preferences and potential for improvement based upon their diagnosis. Staying up‐to‐date is time‐consuming. Furthermore, appraising evidence and up skilling in new interventions requires reallocation of time and resources.
The aim of this paper is to systematically describe current intervention options available to paediatric occupational therapists across different child diagnostic populations, rating the quality and recommendations for use of each intervention, using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (Guyatt et al ., 2008 ) and the Evidence Alert Traffic Light System (Novak & McIntyre, 2010 ). The purpose of reviewing and rating the entire evidence‐base is to provide a ‘one‐stop’ access guide for clinicians and policy‐makers, allow for the easy comparison of interventions, encourage the uptake of evidence‐based interventions, to confer better outcomes for children. We sought to answer the following ‘PICOs’ question: What is the effectiveness of occupational therapy intervention for children with disabilities? P opulation = children with a disability (including arthrogyposis OR attention deficit hyperactivity disorder OR autism spectrum disorder OR behaviour disorders OR brachial plexus OR brain injury OR burns OR cerebral palsy OR cancer OR chronic pain OR developmental coordination disorder OR developmental disability OR down syndrome OR fetal alcohol spectrum disorder OR learning disability OR mental health OR muscle diseases; OR intellectual disability OR obesity OR preterm infants OR physical disability OR rheumatoid arthritis OR spina bifida); I ntervention = occupational therapy (including all specific named occupational therapy techniques); C omparison = none specified; O utcome = all outcomes accepted; and S tudy Design = SR OR randomised controlled trials (RCTs).
Study design
A SR of reviews was conducted, to provide an overview of the best available evidence. RCTs not included within the SRs were also appraised.
Search strategy
This review was carried out according to the Cochrane Collaboration methodology (Higgins & Green, 2011 ), incorporating the recommended quality features for conducting SRs of reviews (Smith, Devane, Begley & Clarke, 2011 ), and is reported according to the PRISMA statement (Moher, Liberati, Tetzlaff & Altman, 2010 ). Relevant articles were identified by searching: CINAHL (1983–2016); Cochrane Database of Systematic Reviews ( http://www.cochrane.org ); Database of Reviews of Effectiveness (DARE); EMBASE (1980–2016); ERIC; Google Scholar; MEDLINE (1956–2014); OTSeeker ( http://www.otseeker.com ); and PsycINFO (1935–2016). Searches were supplemented by hand searching and retrieval of any additional articles meeting eligibility criteria that were cited in reference lists. The search of all published studies was performed in March 2014 and updated in August 2018. Interventions and keywords for investigation were identified using the contributing authors’ knowledge.
Inclusion criteria
Published studies fulfilling the following criteria were included: (i) Type of study: All SRs and RCTs meeting inclusion criteria were appraised. SRs were preferentially sought since they provide a summary of large bodies of evidence and help to explain differences amongst studies. Plus, SRs limit bias. We also included RCTs not included within the SRs, because they are the gold standard design for measuring the effectiveness of interventions. Lower levels of evidence were only included if: the SR reviewed lower levels of evidence; (ii) Types of interventions: Studies that involved the provision of any type of occupational therapy intervention; and (iii) Types of participants: Studies that explicitly involved humans in which 100% of the participants were children of any childhood disability diagnosis.
Exclusion criteria
(i) Studies about typically developing children or adults; (ii) diagnostic studies OR prognostic studies OR about outcome measure psychometrics OR about theoretical frameworks NOT intervention; (iii) interventions that primarily fall under the skillset of another profession, for example pharmacotherapies, psychotherapy, speech therapies, etc. (iv) a second publication of the same study (Note: RCTs that met inclusion criteria but were also cited within included SRs, were treated as duplicates and not reported on twice); (v) studies were unpublished or non‐peer reviewed; and (vi) full‐text was not available in English.
Data abstraction
A data abstraction form was devised based on the Cochrane's recommendations (Higgins & Green, 2011 ). Abstracts identified from searches were screened by two independent raters. Both independent raters reviewed full‐text versions of the articles and articles were retained if they met inclusion criteria. Agreement on inclusion and exclusion assignment was unanimous. Data extracted from included studies comprised: authors and date of study; type of intervention (if named), core components and diagnostic population; who delivered the intervention; location of where the intervention was carried out; intensity of the intervention; study design and original authors’ conclusions about efficacy across study outcomes (Table S1 ). In addition, based on intervention description and ICF definitions, reviewers assigned an ICF domain to each intervention outcome sought by study authors (World Health Organisation, 2001 ). Where multiple SRs or RCTs existed, we noted when the older research was superseded by newer evidence. Interventions with the same name and/or similar core components, and that were administered to the same diagnostic populations, were grouped together. All data required to answer the study questions were published within the papers, so no contact with authors was necessary. All the supporting data are included with Table S1 .
Quality of the evidence
Quality ratings were assigned by two independent raters for each publication using GRADE (Guyatt et al ., 2008 ), which is endorsed by the World Health Organization. Within GRADE randomised trials are initially rated high, observational studies low; and other levels of evidence very low. However, high quality evidence is downgraded if methodological flaws exist, and low quality evidence is upgraded when high rigor and large effect sizes exist ( Guyatt et al . ). Ultimately, a high score indicates ‘further research is unlikely to change our confidence in the estimate of effect’; moderate scores indicate ‘further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate’; low scores indicate ‘further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate’; and very low scores indicate ‘any estimate of effect is very uncertain’ ( Guyatt et al . ).
Strength of recommendation
Unlike SR frameworks, the GRADE framework does not solely examine effect size to determine efficacy of intervention. Instead, effect size makes up just one component when weighing up the benefits and harms of each intervention. In line with the GRADE framework, the following factors were considered by both independent raters when evaluating the body of evidence for the intervention and arriving at a strength of recommendation for each diagnostic group: (i) methodological quality regarding likely benefits vs. likely risks; (ii) inconvenience; (iii) importance of the outcome that the intervention prevents; (iv) magnitude of intervention effect (effect size); (v) precision of estimate of effect; (vi) burdens; (vii) costs; and (viii) varying clinician and family values (Guyatt et al ., 2008 ).
The Evidence Alert Traffic Light System (Novak & McIntyre, 2010 ) was then applied based on the strength of recommendations by both independent raters. The Evidence Alert Traffic Light System is a GRADE‐complementary knowledge translation tool designed to assist clinicians and families to obtain easily readable, clinically useful answers within minutes (Campbell, Novak, McIntyre & Lord, 2013 ), because the alert uses a simple, three‐level colour coding that recommends a course of action. Green signifies ‘go’ because high quality evidence indicates effectiveness; red signifies ‘stop’ because high quality evidence indicates harm or ineffectiveness; and yellow signifies ‘measure’ because insufficient evidence exists to be certain about whether the child will benefit. Yellow can be assigned in three scenarios: (i) promising evidence (weak positive), (ii) unknown effectiveness because no research exists, or (iii) evidence suggests possibly no effect (weak negative).
Ethics and data
The study did not involve contact with humans, so the need for ethical approval was waived by the Cerebral Palsy Alliance's National Health and Medical Council Human Research Ethics Committee. This SR was not registered.
3138 citations were identified using the search strategy, of which 129 articles met the inclusion criteria for review. Of the 129 included articles, 58% ( n = 75/129) were SRs; 42% ( n = 54/129) were RCTs. Note, more than 54 RCTs exist in the paediatric occupational therapy evidence base, but we treated any RCT that was cited within an included SR as a duplicate. Flow of information is presented in the PRISMA diagram (Fig. 1 ).

PRISMA Flow Diagram
The results are now presented using PICO question format headings.
P opulation (Participants)
Included studies were across the following childhood disability diagnoses: arthrogyposis; attention deficit hyperactivity disorder (ADHD); autism spectrum disorder (ASD); behaviour disorders; brachial plexus injury; brain injury (BI); burns; cerebral palsy (CP); cancer; chronic pain; developmental coordination disorder (DCD); developmental disability (DD); Down syndrome; foetal alcohol spectrum disorder; learning disability (LD); mental health; intellectual disability (ID); obesity; preterm infants; physical disability; rheumatoid arthritis; and spina bifida. Some studies included samples from a variety of the aforementioned diagnoses. Consistent with childhood disability population incidence data, more research existed about ASD ( n = 32/135; 24%), ADHD ( n = 8/135; 6%), CP ( n = 38/135; 28%) and DCD ( n = 9/135; 7%), than other conditions.
Paediatric occupational therapy involves working with the child, the parent and the family unit: The child was the primary client for 87% ( n = 45/52) of the interventions, i.e. therapy focussed on improving the child outcomes (e.g. an orthotic worn by the child to improve hand function), whereas the parent was the primary client for 13% ( n = 7/52) for the interventions (e.g. parent education, aiming to improve knowledge, skills and confidence).
I nterventions
Included studies, researched the effectiveness of 52 occupational therapy intervention groups: (1) Acupuncture; (2) Assistive Devices; (3) Assistive Technology; (4) Behavioural Interventions including Applied Behavioural Analysis (ABA) and Positive Parenting Program (Triple P); (5) Bimanual Training; (6) Biofeedback; (7) Coaching; (8) Cognitive Interventions including CogFun, CogMed, (9) Cognitive Orientation to Occupational Performance (CO‐OP); (10) Conductive Education; (11) Constraint Induced Movement Therapy (CIMT); (12) CIMT &/or Bimanual; (13) Context Focused; (14) Ditto™ (hand held education & distraction device for burns patients); (15) Early Intervention, including a Developmental Approach, Neurodevelopmental Therapy (NDT) and Goals Activity and Motor Enrichment (GAME); (16) Electrical Stimulation (ES); (17) Family Centred Care; (18) Feeding Interventions; (19) Goal Directed Training, including Task Specific Training, Functional Training, Neuromotor Task Training (NTT) and Motor Imagery; (20) Handwriting Interventions; (21) Hippotherapy [Therapeutic Horse Riding]; (22) Home Programs; (23) Joint Attention; (24) Massage; (25) Meditation and/or Mindfulness; (26) Mental Health Interventions; (27) Neuro‐Developmental Therapy (NDT); (28) Occupational Therapy after BoNT; (29) Orthotics; (30) Pain Management; (31) Parent Counselling; (32) Parent Education/Parent Training; (33) Picture Exchange Communication System (PECS); (34) Play Therapy; (35) Positioning; (36) Pressure Care; (37) School Therapy; (38) Self‐Management; (39) Sensation Training; (40) Sensory Approach, including brushing, therapy balls, weighted vests, warm‐ups, sensory stimulation; (41) Sensory Integration, including sensory diets, swinging, brushing, therapy balls, weighted vests, body socks; (42) Skills Training via Mental Imagery; (43) Sleep Interventions; (44) Social Skills Training; (45) Stretching, including passive: self‐administered, therapist‐administered and device‐administered; (46) Treatment and Education of Autistic and Communication Handicapped Children (TEACCH); (47) Therapeutic Listening; (48) Treadmill Training; (49) Visual Motor Interventions; (50) Weight Loss; (51) Whole Body Vibration; and (52) Yoga.
Of the 12 included articles, authors measured the effectiveness of 52 occupational therapy interventions, across 22 diagnoses. From this, 136 intervention outcome indicators were identified, whereby an intervention, with an individual target outcome was administered to specific diagnostic groups. Insufficient data was available for analysis on one of these outcome indicators (number 74 in Table S1 , where the SR authors found no publish data examining the effectiveness of hand orthotics in children with brain injury and therefore no recommendations could be made), (Jackman, Novak & Lannin, 2014 ) resulting in 135/136 intervention outcome indicators available for analysis.
Of the 135 intervention outcome indications: 30% ( n = 40/135) were graded ‘do it’ (Green Go) (Arbesman, Bazyk & Nochajski, 2013 ; Bellows et al ., 2011 ; Bleyenheuft, Arnould, Brandao, Bleyenheuft & Gordon, 2015 ; Brown, Kimble, Rodger, Ware & Cuttle, 2014 ; Chang & Yu, 2014 ; Chen, Pope, Tyler & Warren, 2014c ; Chen et al ., 2014b ; Christmas, Sackley, Feltham & Cummins, 2018 ; Crompton et al ., 2007 ; Estes et al ., 2014 ; Fehlings et al ., 2010 ; Frolek Clark & Schlabach, 2013 ; Hechler et al ., 2014 ; Heinrichs, Kliem & Hahlweg, 2014 ; Hoare & Imms, 2004 ; Hoare, Imms, Carey & Wasiak, 2007 ; Hoare et al ., 2010 ; Hoy, Egan & Feder, 2011 ; Huang, Fetters, Hale & McBride, 2009 ; Inguaggiato, Sgandurra, Perazza, Guzzetta & Cioni, 2013 ; Kamps et al ., 2015 ; Kasari et al ., 2016 ; Kaya Kara et al ., 2015 ; Kurowski et al ., 2014 ; Lannin, Scheinberg & Clark, 2006 ; Lidman, Nachemson, Peny‐Dahlstrand & Himmelmann, 2015 ; Lin & Wuang, 2012 ; Madlinger‐Lewis et al ., 2014 ; Maeir et al ., 2014 ; Novak, 2014a ; Park, Maitra, Achon, Loyola & Rincón, 2014 ; Speth et al ., 2015 ; Spittle, Orton, Anderson, Boyd & Doyle, 2012 ; Spittle, Orton, Doyle & Boyd, 2007 ; Stavness, 2006 ; Stickles Goods, Ishijima, Chang & Kasari, 2013 ; Vroland‐Nordstrand, Eliasson, Jacobsson, Johansson & Krumlinde‐Sundholm, 2016 ; Zwaigenbaum et al ., 2015 ); 56% (75/135) were graded ‘probably do it’ (Yellow Measure) (Armstrong, 2012 ; Au et al ., 2014 ; Auld, Russo, Moseley & Johnston, 2014 ; Bialocerkowski, Kurlowicz, Vladusic & Grimmer, 2005 ; Bodison & Parham, 2018 ; Cameron et al ., 2017a , 2017b; Chacko et al ., 2014 ; Chantry & Dunford, 2010 ; Chen, Lee & Howard, 2014a ; Chiu, Ada & Lee, 2014 ; Cole, Harris, Eland & Mills, 1989 ; Copeland et al ., 2014 ; Dagenais et al ., 2009 ; De Vries, Beck, Stacey, Winslow & Meines, 2015 ; Duncan et al ., 2012 ; Fedewa, Davis & Ahn, 2015 ; Grynszpan, Weiss, Perez‐Diaz & Gal, 2014 ; Hahn‐Markowitz, Berger, Manor & Maeir, 2017 ; Hammond, Jones, Hill, Green & Male, 2014 ; Huang et al ., 2014 ; Jackman et al ., 2018 ; James, Ziviani, Ware & Boyd, 2015 ; Janeslätt, Kottorp & Granlund, 2014 ; Jones et al ., 2014 ; Krisanaprakornkit, Ngamjarus, Witoonchart & Piyavhatkul, 2010 ; Lannin, Novak & Cusick, 2007 ; Malow et al ., 2014 ; Maskell, Newcombe, Martin & Kimble, 2014 ; Mast et al ., 2014 ; Matute‐Llorente, González‐Agüero, Gómez‐Cabello, Vicente‐Rodríguez & Mallén, 2014 ; McLean et al ., 2017 ; Meany‐Walen, Bratton & Kottman, 2014 ; Miller‐Kuhaneck & Watling, 2018 ; Montero & Gómez‐Conesa, 2014 ; Morgan, Novak, Dale & Badawi, 2015 ; Morgan et al ., 2016a ; Morgan, Novak, Dale, Guzzetta & Badawi, 2016b ; Pfeiffer B & Arbesman, 2018 ; Polatajko & Cantin, 2010 ; Reeuwijk, van Schie, Becher & Kwakkel, 2006 ; Schaaf, Dumont, Arbesman & May‐Benson, 2018 ; Smith et al ., 2014 ; Snider, Majnemer & Darsaklis, 2010 ; Storebø et al ., 2011 ; Tatla et al ., 2013 ; Tatla, Sauve, Jarus, Virji‐Babul & Holsti, 2014 ; Vargas & Lucker, 2016 ; Westendorp et al ., 2014 ; Whalen & Case‐Smith, 2012 ; Xu, He, Mai, Yan & Chen, 2015 ; Zadnikar & Kastrin, 2011 ; Ziviani, Feeney, Rodger & Watter, 2010 ; Zwicker & Mayson, 2010 ); 10% ( n = 14/130) were graded ‘probably don't do it’ (Yellow Measure) (Wallen & Gillies, 2006 ; Wells, Marquez & Wakely, 2018 ); and 4% ( n = 6/135) were graded ‘don't do it’ (Red Stop) (Gringras et al ., 2014 ; Katalinic et al ., 2010 ).
The 40 green light ‘do it’ interventions indications included: (1) Behavioural Intervention using ABA for children with ASD; (2) Behavioural Intervention using Triple P for children behaviour disorders; (3) Behavioural Intervention using token economy contracts for children with a brain injury; (4) Bimanual Training for children with hemiplegic CP; (5) Coaching for parents of children at risk of disability to promote development; (6) Coaching for parents of children with ASD to promote function and behaviour; (7) CAPS cognitive intervention for children with brain injury to improve long term executive function; (8) Cog‐Fun intervention for children with attention deficit disorder to improve executive function; (9) CO‐OP for children with DCD for functional motor task performance; (10) CIMT for children with CP to improve hand function; (11) CIMT plus Bimanual for children with CP to improve hand function; (12) Context Focused intervention for children with CP for functional motor task performance; (13) Ditto hand held devices for children with burns to provide procedural distraction and self‐management education; (14) Early Intervention using ABA for children with ASD; (15) Early Intervention using Developmental Care for preterm infants; (16) Family Centred Care for children with brain injury or CP, to improve children's function; (17) Parent education feeding intervention for children with disability to improve feeding competency and growth; (18) Physiological feeding intervention for children with disability; (19) Goal Directed Training for children with CP, to improve functional task performance; (20) Goal Directed Training for children with DCD, to improve functional task performance; (21) Handwriting Task‐Specific Practice for children with DCD; (22) Home Programs for children with CP, to improve functional task performance; (23) Home Programs for children with ID, to improve functional task performance; (24) Joint Attention for children with ASD to improve social interactions; (25) Mental Health interventions for children with ASD; (26) Mental Health interventions for children with developmental delay; (27) Mental Health interventions for children with mental health disorders; (28) Occupational therapy after botulinum toxin injections for children with CP to promote hand function; (29) Kinesiotape for children with CP to improve hand function; (30) Pain Management for children with chronic pain secondary to physical disability and or chronic health conditions; (31) Parent Education using mindfulness for parents of children with ASD to reduce parental stress; (32) Parent Education using problem solving for parents of children with ASD to reduce parental stress; (33) Parent Education for children with disabilities to promote parenting confidence; (34) Parent Education for children with behaviour disorders to improve parent well‐being; (35) PECS for children with ASD to promote communication; (36) Positioning in NICU for preterm infants to promote normal movement development; (37) Pressure Care for children with CP using mattresses and cushions; (38) Social Skills Training mediated by peers for children with ASD; (39) Treadmill training for children with Down Syndrome to accelerate the onset of independent walking; (40) Weight loss using a family education and activity program called ‘Mighty Moves’ for children with obesity.
We assigned an ICF category to the primary and secondary intervention outcome of each intervention. Using the primary ICF level code, we mapped the profile of the paediatric OT evidence base to the ICF framework (Fig. 2 ). Green light effective interventions existed at the body structures and function ICF level ( n = 14/74 indications (19%)), the activity level ( n = 14/27 indications (52%)) and the environment level ( n = 12/34 indications (35%)). When we compared the proportions of green light to yellow light to red light interventions by ICF levels, the activity level contained the largest number of green lights. At the activity level where there was 27 indications, green lights outweighed the number of yellow and red lights (Gree n = 14/27; Yellow = 13/27; Red = 0/27), meaning the most common traffic code at the activity level was green, which we illustrated by green shading in Figure 2 . At the body structures and function ICF level, the most common traffic code was yellow, which we illustrated by yellow shading in Figure 2 . All the red lights within the evidence base existed at the body structures and function level. At the environmental level, the most common traffic code was also yellow, which we illustrated by yellow shading in Figure 2 . Two intervention's primary ICF code was at the participation level (Willis et al., 2010 ) and none at the personal level, indicating gaps in the occupational therapy evidence base, which we illustrated using grey shading in Figure 2 . The two participation codes were weak positive, but these were based on trials that used activity‐based interventions and assumed an upstream participation gain, which was not well‐supported.

Occupational Therapy Interventions and the International Classification of Function
C omparisons
In the included papers, consistent with conventional beliefs about it being unethical to withhold early intervention from children, rarely did researchers design studies where the control group received no intervention. In most studies, the controlled comparison was usual care. Some researchers carried out short duration studies using a wait‐list control design, where the control group received the experimental intervention after study completion.
CIMT for children with CP, was the only intervention comprehensively and empirically compared to other intervention options, using head‐to‐head RCT comparisons identified in our search strategy. CIMT was: (i) compared head‐to‐head with Bimanual Training showing no difference between the approaches (Sakzewski et al ., 2015 ; Tervahauta, Girolami & Øberg, 2017 ); and (ii) combined with Bimanual Training and/or Botulinum toxin A, showing no additive benefits occurred from a combined intervention approach (Hoare et al ., 2013 ). These researcher's concluded ‘intensity’ of practice was the key ingredient of these effective CP approaches ( Sakzewski et al . ; Tervahauta et al ., 2017 ).
A meta‐analysis of intervention options for children with DCD compared the relative effect of DCD motor interventions by calculating and comparing effect sizes (Smits‐Engelsman et al ., 2013 ). The authors calculated that ‘top‐down’ approaches (effect size = 0.89) were more effective than ‘bottom‐up’ approaches (effect size = 0.12).
To assist with comparative clinical decision‐making across the paediatric occupational therapy evidence base, we created bubble charts. We mapped the 52 identified paediatric occupational therapy interventions, across 22 diagnoses, spanning 135 intervention indications, which sought to provide analogous outcomes, by diagnosis, into separate bubbles. In the bubble charts, the size of the bubble indicated the volume of published evidence, which was calculated by counting the number of published studies on the topic. The location of the bubble on the y ‐axis of the graph corresponded to the GRADE system rating. The colour of the bubble denoted the Traffic Light Evidence Alert System rating (Fig. 3 ).

Bubble Charts Comparing the Effectiveness of Different Occupational Therapy Indications for Different Diagnoses
We set out to systematically summarise the current intervention options available to paediatric occupational therapists across different childhood disability populations. We found 40 interventions that received a ‘strong’ recommendation for use, indicating a high‐quality evidence base with more benefits than harms. These ‘green light’ interventions included: Behavioural Interventions (including ABA, Triple P and Token Economies); Bimanual; Coaching; Cognitive Cog‐Fun and CAPS; CO‐OP; CIMT; CIMT plus Bimanual; Context‐Focused; Ditto; Early Intervention (including ABA and Developmental Care); Family Centred Care; Feeding interventions (including coaching and physiologic); Goal Directed Training; Handwriting Task‐Specific Practice; Home Programs; Joint Attention; Mental Health Interventions; occupational therapy after BoNT; Kinesiotape; Pain Management; Parent Education; PECS; Positioning in NICU; Pressure Care; Social Skills Training Peer Mediated; Treadmill training and Weight loss ‘Mighty Moves’.
The paediatric occupational therapy evidence base is under immense growth and expansion. The SRs and trials greater than 10 years old were predominantly about CP with one study about Brachial Plexus and DD. Almost always these older studies showed that the ‘bottom‐up’ interventions were ineffective with no difference between the experimental and control groups.
Clinical Implications
Occupational therapists working with children and their parents have several evidence based interventions to choose from. The strength of this paper is that it provides a systematic, clear and concise summary of all the available interventions by diagnosis with an easy to interpret summary of efficacy. There are some important learnings:
A. Parent partnership within occupational therapist intervention is effective and worthwhile
Occupational Therapists embrace the principles of family centred care (Hanna & Rodger, 2002 ) where the parent is the decision‐maker and the expert in knowing their child and the therapist is a technical resource to the family. We found that 13% of paediatric occupational therapy interventions are directed at the parent, so parents can deliver intervention at home within daily parenting. Evidence suggests that parent‐delivered intervention is equally effective to therapist‐delivered intervention (Baker et al ., 2012 ), which is not surprising given parent's knowledge of their children's preferences and engagement style, and the volume of caregiving they carryout (Smith, Cheater & Bekker, 2015 ). In the diagnoses studied (ADHD, ASD, At risk, Behavioural Disorders, BI, CP, DD, LD, obesity), it was very clear that parents respond well to parent education and training (Antonini et al ., 2014 ; Barlow, Smailagic, Huband, Roloff & Bennett, 2012 ; Case‐Smith & Arbesman, 2008 ; Dykens, Fisher, Taylor, Lambert & Miodrag, 2014 ; Feinberg et al ., 2014 ; Hanna & Rodger, 2002 ; Howe & Wang, 2013 ; Kuhaneck, Madonna, Novak & Pearson, 2015 ; Lawler, Taylor & Shields, 2013 ; Tanner, Hand, O'toole & Lane, 2015 ; Zwi, Jones, Thorgaard, York & Dennis, 2011 ), consistent with family centred philosophy about parents’ aspirations of parenting well, to help their children (Hanna & Rodger, 2002 ). Moreover, parents and children carry out intervention effectively at home, and therefore home programs (Novak & Berry, 2014b ; Novak et al ., 2013 ; Sakzewski, Ziviani & Boyd, 2013 ; Sakzewski et al ., 2015 ; Wuang, Ho & Su, 2013 ) and self‐management programs (Lindsay, Kingsnorth, Mcdougall & Keating, 2014 ; Moola, Faulkner, White & Kirsh, 2014 ) are an effective method for increasing the intensity of therapy.
When carrying out parent education, literature tells us that parents need and want: knowledge of the condition and intervention options; help accessing support services; and advice about coping strategies, via a collaborative partnership (Smith et al ., 2015 ). Even though family centred practice has existed since the 1990s, parents still experience some resistance to their input from health professionals ( Smith et al . ). Unclear expectations about roles further elevate parental stress (Coyne, 2015 ). Occupational therapists therefore need to be mindful of parent's experiences and aim to clearly communicate information and coach parents to guide care, to optimise family outcomes ( Coyne ).
B. Activities‐based, ‘top‐down’ interventions deliver bigger gains
Numerous occupational therapy interventions exist, aiming to improve motor, behavioural and functional outcomes (Fig. 3 ), affording a lot of choice to families and clinicians. The greatest number of effective green light interventions was at the activity level of the ICF, indicating that daily life skills training using a ‘top‐down’ approach is a strength of the occupational therapy profession. Examples include: Bimanual Training; CIMT; CO‐OP; GAME; Goal‐Directed Training; Handwriting Task Training; Home Programs using Goal‐Directed Training; Social Skills Training; and Task Training. Consistent with current knowledge about the conditions for inducing neuroplasticity (Kleim & Jones, 2008 ), the green light, ‘top‐down’, activity level interventions all have the following key ingredients in common: (i) begin with the child's goal, to optimise motivation and saliency of practice; (ii) practice of real‐life activities in natural environments to optimise the child's learning and the variability of the practice; (iii) intense repetitions to activate plasticity, including home‐based practice; and (iv) scaffolded practice to the ‘just right challenge’ to enable success under self‐generated problem‐solving conditions, to optimise enjoyment.
In contrast, some of the most established paediatric occupational therapy interventions NDT/Bobath and SI were originally developed as ‘bottom‐up’ interventions. NDT/Bobath and SI originated in an era of medicine when intervention aimed to remediate the child's body structural deficits, thinking function would emerge (Rodger et al ., 2005 ; Rodger et al ., 2006). However, over time the NDT/Bobath and SI approaches have been broadened to also accommodate use of ‘top‐down’ functional training approaches. Fidelity to the original NDT/Bobath and SI approach therefore varies greatly (Mayston, 2016 ), and as such, a leading Bobath expert has recently stated that Bobath ‘no longer stands for a valid universal therapy approach’ (Mayston, 2016 , p. 994). This means that interpreting the meaning of historical NDT/Bobath and SI research evidence about efficacy within the context of contemporaneous clinical practice is challenging. The efficacy of both NDT/Bobath and SI have been critiqued within SRs (Boyd & Hays, 2001 ; Brown & Burns, 2001 ; Case‐Smith & Arbesman, 2008 ; Case‐Smith, Clark & Schlabach, 2013 ; Case‐Smith, Weaver & Fristad, 2015 ; Lang et al ., 2012 ; May‐Benson & Koomar, 2010 ; Novak et al ., 2013 ; Sakzewski, Ziviani & Boyd, 2009 ; Sakzewski et al ., 2013 ; Steultjens et al ., 2004 ; Watling & Hauer, 2015 ; Weaver, 2015 ) and these data mostly relate to older trials. SR authors have concluded that NDT/Bobath and SI rarely confer motor gains superior to no intervention, but the RCTs contain so many methodological flaws that recommendations for use or discontinuation of use within practice cannot be made with certainty (Boyd & Hays, 2001 ; Brown & Burns, 2001 ; Case‐Smith & Arbesman, 2008 ; Case‐Smith et al ., 2013 ; Case‐Smith et al ., 2014; Lang et al ., 2012 ; May‐Benson & Koomar, 2010 ; Novak et al ., 2013 ; Sakzewski et al ., 2009 , 2013 ; Steultjens et al ., 2004 ; Watling & Hauer, 2015 ; Weaver, 2015 ). Some therapists have interpreted the uncertainty of the NDT/Bobath and SI systematic evidence as justification of continuance, whereas others in the profession recommend discontinuance because of the growing body of ‘top‐down’ evidence that offer effective alternatives (Rodger et al ., 2006). A Bobath expert has recommended that the common‐sense way forward for the profession is to choose interventions that promote activity and participation outcomes (Mayston, 2016 ) and to use consistent language to describe intervention options. For example, describing interventions by clear uniform terminology (i.e. ‘splitting’) might be more helpful than ‘clumping’ interventions into expanded NDT/Bobath umbrella terms.
We analysed the breakdown of the effectiveness of motor interventions, above and below the worth it line (Fig. 3 ), in terms of ‘bottom‐up’ vs. ‘top‐down’, and a trend favouring ‘top‐down’ emerged. Of the seven motor intervention indications below the ‘worth it line’, coded on GRADE as weak negative or strong negative (red), 7/7 (100%) were ‘bottom‐up’ approaches. Of the 22 motor intervention indications above the ‘worth it line’ eight were green and 14 were yellow: 8/8 (100%) green indications (strong positive) were ‘top‐down’. A similar trend emerged in the comparative effectiveness analysis of functional interventions. Of the seven functional intervention indications above the ‘worth it line’, coded on GRADE as strong positive (green), 4/4 (100%) were ‘top‐down’. There were a small number of studies using SI and the sensory approach to improve function coded on GRADE as weak positive, but the studies had a high risk of bias and SR authors recommended interpreting the positive results with caution (Case‐Smith et al ., 2014; Case‐Smith et al ., 2015 ; Watling & Hauer, 2015 ).
Research Implications
The following areas of the evidence‐base would benefit from more research: (i) Parent Education : None of the parent education approaches were ineffective. Thus, more research is worthwhile exploring parent's preferred learning styles and levels of support required to manage the stress of raising a child with a disability. There are potential financial gains to the health system by thoroughly understanding effective parent interventions, because parent‐delivered intervention is equally effective and less expensive; (ii) Head‐to‐head comparisons : Head‐to‐head comparisons of different interventions aiming to achieve the same outcomes, in well‐controlled trials with cost‐effectiveness data, would enable determinations about best practice to be made from good evidence, and thus inform parent and policy‐maker's decision‐making; (iii) ‘Dose’ comparison studies : ‘Dose’ comparison studies using well controlled intensity trials would enable occupational therapists to better inform parents about ‘how much’ intervention is enough; and (iv) Participation Interventions : There is a clear gap in the evidence‐base about interventions that directly improve a child's participation in life and should be the focus of future RCTs and other rigorous methodologies. CIMT, Bimanual and Home Program occupational therapy interventions were measured to confirm whether or not they conferred participation gains, and the clinical trials demonstrated no between group differences (Adair, Ullenhag, Keen, Granlund & Imms, 2015 ). These results indicate that there is a clear need to develop interventions that specifically target participation, rather than anticipating activities‐based interventions will confer upstream participation gains. Changes in participation are multifactorial and involve individual factors, contextual factors, the nature of the participation activity and the environment in which the activity is being performed (Imms et al ., 2017 ). Any new participation intervention invented, will need to address all of these factors to be successful.
Limitations
Our review has several limitations. First, we only included SRs and RCTs because we aimed to analyse best‐available evidence, but means some intervention approaches will have been excluded and overlooked because no trials or reviews existed. Second, this was an analysis of secondary data sources and reporting bias and publication bias may be in operation, because positive findings have a higher chance of being published. This evidence may exist suggesting some interventions are ineffective which we were unable to review. Third, our search terms included ‘occupational therapy’ and thus will have excluded other effective interventions used by occupational therapists, but not invented or published by occupational therapists e.g. ‘Triple P’ for children with CP. Fourth, our paper was designed to provide an overview for clinicians indicating which interventions are effective, however, it does not provide enough detail about any one intervention to guide administration or training in any specific intervention. Clinicians need to refer directly to the cited article and more widely in the published literature for this information. Our findings must be interpreted within the context of our study limitations.
Conclusions
This review provides a high‐level summary of effective paediatric occupational therapy interventions. Thirty‐nine effective intervention indications exist, offering both families and clinicians many choices to match their preferences and expertise. The paediatric occupational therapy evidence base suggests a growing trend towards activities‐level, ‘top‐down’ approaches and parent education, over and above ‘bottom‐up’ approaches. There are important ethical implications of translating these effective evidence‐based occupational therapy intervention options into clinical practice to give children the best chance at achieving their goals.
Key points for occupational therapy
- Collaboration with parents is effective and worthwhile.
- Activities‐based, top‐down interventions confer larger clinical gains, than bottom‐up approaches, when aiming to improve a child's function.
All authors declare that this is original work and that they meet the criteria for authorship. Iona Novak designed the study, extracted the data, conducted the analyses and wrote the manuscript. Ingrid Honan conducted the analyses and wrote the manuscript. All authors read and approved the final manuscript.
The study was unfunded and there are no competing financial disclosures.
Conflict of interest
The authors have no conflicts of interest to disclose.
Supporting information
Table S1. Main results table.
- Adair, B. , Ullenhag, A. , Keen, D. , Granlund, M. & Imms, C. (2015). The effect of interventions aimed at improving participation outcomes for children with disabilities: A systematic review . Developmental Medicine & Child Neurology , 57 ( 12 ), 1093–1104. 10.1111/dmcn.12809. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Antonini, T. N. , Raj, S. P. , Oberjohn, K. S. , Cassedy, A. , Makoroff, K. L. , Fouladi, M. et al (2014). A pilot randomized trial of an online parenting skills program for pediatric traumatic brain injury: Improvements in parenting and child behavior . Behavior Therapy , 45 ( 4 ), 455–468. 10.1016/j.beth.2014.02.003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Arbesman, M. , Bazyk, S. & Nochajski, S. M. (2013). Systematic review of occupational therapy and mental health promotion, prevention, and intervention for children and youth . American Journal of Occupational Therapy , 67 ( 6 ), e120–e130. 10.5014/ajot.2013.008359. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Armstrong, D. (2012). Examining the evidence for interventions with children with developmental coordination disorder . British Journal of Occupational Therapy , 75 ( 12 ), 532–540. 10.4276/030802212X13548955545413. [ CrossRef ] [ Google Scholar ]
- Au, A. , Lau, K. M. , Wong, A. H. C. , Lam, C. , Leung, C. , Lau, J. et al (2014). The efficacy of a group Triple P (Positive Parenting Program) for Chinese parents with a child diagnosed with ADHD in Hong Kong: A pilot randomised controlled study . Australian Psychologist , 49 ( 3 ), 151–162. 10.1111/ap.12053. [ CrossRef ] [ Google Scholar ]
- Auld, M. L. , Russo, R. , Moseley, G. L. & Johnston, L. M. (2014). Determination of interventions for upper extremity tactile impairment in children with cerebral palsy: A systematic review . Developmental Medicine & Child Neurology , 56 ( 9 ), 815–832. 10.1111/dmcn.12439. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baker, T. , Haines, S. , Yost, J. , DiClaudio, S. , Braun, C. & Holt, S. (2012). The role of family‐centered therapy when used with physical or occupational therapy in children with congenital or acquired disorders . Physical Therapy Reviews , 17 ( 1 ), 29–36. 10.1179/1743288X11Y.0000000049. [ CrossRef ] [ Google Scholar ]
- Barlow, J. , Smailagic, N. , Huband, N. , Roloff, V. & Bennett, C . (2012). Group‐based parent training programmes for improving parental psychosocial health . Cochrane Database of Systematic Reviews , 6 , CD002020 10.1002/14651858.cd002020.pub4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bellows, L. , Silvernail, S. , Caldwell, L. , Bryant, A. , Kennedy, C. , Davies, P. et al (2011). Parental perception on the efficacy of a physical activity program for preschoolers . Journal of Community Health , 36 ( 2 ), 231–237. 10.1007/s10900-010-9302-1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bialocerkowski, A. , Kurlowicz, K. , Vladusic, S. & Grimmer, K. (2005). Effectiveness of primary conservative management for infants with obstetric brachial plexus palsy . International Journal of Evidence‐Based Healthcare , 3 ( 2 ), 27–44. 10.1111/j.1479-6988.2005.00020.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bleyenheuft, Y. , Arnould, C. , Brandao, M. B. , Bleyenheuft, C. & Gordon, A. M. (2015). Hand and Arm Bimanual Intensive Therapy Including Lower Extremity (HABIT‐ILE) in children with unilateral spastic cerebral palsy: A randomized trial . Neurorehabilitation and Neural Repair , 29 ( 7 ), 645–657. 10.1177/1545968314562109. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bodison, S. C. & Parham, L. D. (2018). Specific sensory techniques and sensory environmental modifications for children and youth with sensory integration difficulties: A systematic review . American Journal of Occupational Therapy , 72 ( 1 ), 7201190040p1–7201190040p11. 10.5014/ajot.2018.029413 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bonnechere, B. , Jansen, B. , Omelina, L. , Degelaen, M. , Wermenbol, V. , Rooze, M. et al (2014). Can serious games be incorporated with conventional treatment of children with cerebral palsy? A review. Research in Developmental Disabilities , 35 ( 8 ), 1899–1913. 10.1016/j.ridd.2014.04.016. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boyd, R. N. & Hays, R. M. (2001). Current evidence for the use of botulinum toxin type A in the management of children with cerebral palsy: A systematic review . European Journal of Neurology , 8 , 1–20. 10.1046/j.1468-1331.2001.00034.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown, G. T. & Burns, S. A. (2001). The efficacy of neurodevelopmental treatment in paediatrics: A systematic review . British Journal of Occupational Therapy , 64 ( 5 ), 235–244. 10.1177/030802260106400505. [ CrossRef ] [ Google Scholar ]
- Brown, N. J. , Kimble, R. M. , Rodger, S. , Ware, R. S. & Cuttle, L. (2014). Play and heal: Randomized controlled trial of Ditto™ intervention efficacy on improving re‐epithelialization in pediatric burns . Burns , 40 ( 2 ), 204–213. 10.1016/j.burns.2013.11.024. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cameron, D. , Craig, T. , Edwards, B. , Missiuna, C. , Schwellnus, H. & Polatajko, H. J. (2017). Cognitive Orientation to daily Occupational Performance (CO‐OP): A new approach for children with cerebral palsy . Physical & Occupational Therapy in Pediatrics , 37 ( 2 ), 183–198. 10.1080/01942638.2016.1185500. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Campbell, L. , Novak, I. , McIntyre, S. & Lord, S. (2013). A KT intervention including the evidence alert system to improve clinician's evidence‐based practice behavior—A cluster randomized controlled trial . Implementation Science , 8 ( 1 ), 132 10.1186/1748-5908-8-132. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Case‐Smith, J. & Arbesman, M. (2008). Evidence‐based review of interventions for autism used in or of relevance to occupational therapy . The American Journal of Occupational Therapy , 62 ( 4 ), 416 10.5014/ajot.62.4.416. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Case‐Smith, J. , Clark, G. J. F. & Schlabach, T. L. (2013). Systematic review of interventions used in occupational therapy to promote motor performance for children ages birth–5 years . American Journal of Occupational Therapy , 67 ( 4 ), 413–424. 10.5014/ajot.2013.005959. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Case‐Smith, J. , Weaver, L. L. & Fristad, M. A. (2015). A systematic review of sensory processing interventions for children with autism spectrum disorders . Autism , 19 ( 2 ), 133–148. https://doi.org/10.1177%2F1362361313517762 . [ PubMed ] [ Google Scholar ]
- Chacko, A. , Bedard, A. C. , Marks, D. J. , Feirsen, N. , Uderman, J. Z. , Chimiklis, A. et al (2014). A randomized clinical trial of Cogmed Working Memory Training in school‐age children with ADHD: A replication in a diverse sample using a control condition . Journal of Child Psychology and Psychiatry , 55 ( 3 ), 247–255. 10.1111/jcpp.12146. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chang, S. H. & Yu, N. Y. (2014). The effect of computer‐assisted therapeutic practice for children with handwriting deficit: A comparison with the effect of the traditional sensorimotor approach . Research in Developmental Disabilities , 35 ( 7 ), 1648–1657. 10.1016/j.ridd.2014.03.024. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chantry, J. & Dunford, C. (2010). How do computer assistive technologies enhance participation in childhood occupations for children with multiple and complex disabilities? A review of the current literature . British Journal of Occupational Therapy , 73 ( 8 ), 351–365. https://doi.org/10.4276%2F030802210X12813483277107 [ Google Scholar ]
- Chen, Y. P. , Lee, S. Y. & Howard, A. M. (2014a). Effect of virtual reality on upper extremity function in children with cerebral palsy: A meta‐analysis . Pediatric Physical Therapy , 26 ( 3 ), 289–300. 10.1097/PEP.0000000000000046. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen, H. C. , Chen, C. L. , Kang, L. J. , Wu, C. Y. , Chen, F. C. & Hong, W. H. (2014b). Improvement of upper extremity motor control and function after home‐based constraint induced therapy in children with unilateral cerebral palsy: Immediate and long‐term effects . Archives of Physical Medicine and Rehabilitation , 95 ( 8 ), 1423–1432. 10.1016/j.apmr.2014.03.025. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen, Y. P. , Pope, S. , Tyler, D. & Warren, G. L. (2014c). Effectiveness of constraint‐induced movement therapy on upper‐extremity function in children with cerebral palsy: A systematic review and meta‐analysis of randomized controlled trials . Clinical Rehabilitation , 28 ( 10 ), 939–953. https://doi.org/10.1177%2F0269215514544982 [ PubMed ] [ Google Scholar ]
- Chiu, H. C. , Ada, L. & Lee, H. M. (2014). Upper limb training using Wii Sports Resort™ for children with hemiplegic cerebral palsy: A randomized, single‐blind trial . Clinical Rehabilitation , 28 ( 10 ), 1015–1024. https://doi.org/10.1177%2F0269215514533709 [ PubMed ] [ Google Scholar ]
- Christmas, P. M. , Sackley, C. , Feltham, M. G. & Cummins, C. (2018). A randomized controlled trial to compare two methods of constraint‐induced movement therapy to improve functional ability in the affected upper limb in pre‐school children with hemiplegic cerebral palsy: CATCH TRIAL . Clinical Rehabilitation , 32 ( 7 ), 909–918. https://doi.org/10.1177%2F0269215518763512 [ PubMed ] [ Google Scholar ]
- Cole, K. N. , Harris, S. R. , Eland, S. F. & Mills, P. E. (1989). Comparison of two service delivery models: In‐class and out‐of‐class therapy approaches . Pediatric Physical Therapy , 1 ( 2 ), 49–54. [ Google Scholar ]
- Copeland, L. , Edwards, P. , Thorley, M. , Donaghey, S. , Gascoigne‐Pees, L. , Kentish, M. et al (2014). Botulinum toxin A for nonambulatory children with cerebral palsy: A double blind randomized controlled trial . The Journal of Pediatrics , 165 ( 1 ), 140–146. 10.1016/j.jpeds.2014.01.050 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coyne, I. (2015). Families and health‐care professionals’ perspectives and expectations of family‐centred care: Hidden expectations and unclear roles . Health Expectations , 18 ( 5 ), 796–808. 10.1111/hex.12104. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crompton, J. , Imms, C. , McCoy, A. T. , Randall, M. , Eldridge, B. , Scoullar, B. et al (2007). Group‐based task‐related training for children with cerebral palsy: A pilot study . Physical & Occupational Therapy in Pediatrics , 27 ( 4 ), 43–65. 10.1080/J006v27n04_04. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dagenais, L. M. , Lahay, E. R. , Stueck, K. A. , White, E. , Williams, L. & Harris, S. R. (2009). Effects of electrical stimulation, exercise training and motor skills training on strength of children with meningomyelocele: A systematic review . Physical & Occupational Therapy in Pediatrics , 29 ( 4 ), 445–463. 10.3109/01942630903246018. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Vries, D. , Beck, T. , Stacey, B. , Winslow, K. & Meines, K. (2015). Music as a therapeutic intervention with autism: A systematic review of the literature . Therapeutic Recreation Journal , 49 ( 3 ), 220. [ Google Scholar ]
- Duncan, B. , Shen, K. , Zou, L. P. , Han, T. L. , Lu, Z. L. , Zheng, H. et al (2012). Evaluating intense rehabilitative therapies with and without acupuncture for children with cerebral palsy: A randomized controlled trial . Archives of Physical Medicine and Rehabilitation , 93 ( 5 ), 808–815. 10.1016/j.apmr.2011.12.009. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dykens, E. M. , Fisher, M. H. , Taylor, J. L. , Lambert, W. & Miodrag, N. (2014). Reducing distress in mothers of children with autism and other disabilities: A randomized trial . Pediatrics , 134 , e454–e463. 10.1542/peds.2013-3164. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Estes, A. , Vismara, L. , Mercado, C. , Fitzpatrick, A. , Elder, L. , Greenson, J. et al (2014). The impact of parent‐delivered intervention on parents of very young children with autism . Journal of Autism and Developmental Disorders , 44 ( 2 ), 353–365. 10.1007/s10803-013-1874-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fedewa, A. , Davis, M. A. & Ahn, S. (2015). Effects of stability balls on children's on‐task behavior, academic achievement, and discipline referrals: A randomized controlled trial . American Journal of Occupational Therapy , 69 , 6902220020p1–p9. 10.5014/ajot.2015.014829 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fehlings, D. , Novak, I. , Berweck, S. , Hoare, B. , Stott, N. S. & Russo, R. N. (2010). Botulinum toxin assessment, intervention and follow‐up for paediatric upper limb hypertonicity: International consensus statement . European Journal of Neurology , 17 , 38–56. 10.1111/j.1468-1331.2010.03127.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Feinberg, E. , Augustyn, M. , Fitzgerald, E. , Sandler, J. , Suarez, Z. F. C. , Chen, N. et al (2014). Improving maternal mental health after a child's diagnosis of autism spectrum disorder: Results from a randomized clinical trial . JAMA Pediatrics , 168 ( 1 ), 40–46. 10.1001/jamapediatrics.2013.3445. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flores‐Mateo, G. & Argimon, J. M. (2007). Evidence based practice in postgraduate healthcare education: A systematic review . BMC Health Services Research , 7 ( 1 ), 119 10.1186/1472-6963-7-119. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frolek Clark, G. J. & Schlabach, T. L. (2013). Systematic review of occupational therapy interventions to improve cognitive development in children ages birth–5 years . American Journal of Occupational Therapy , 67 ( 4 ), 425–430. 10.1186/1472-6963-7-119. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gringras, P. , Green, D. , Wright, B. , Rush, C. , Sparrowhawk, M. , Pratt, K. et al (2014). Weighted blankets and sleep in autistic children—A randomized controlled trial . Pediatrics , 134 , 298–306. 10.1542/peds.2013-4285. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grynszpan, O. , Weiss, P. L. , Perez‐Diaz, F. & Gal, E. (2014). Innovative technology‐based interventions for autism spectrum disorders: A meta‐analysis . Autism , 18 ( 4 ), 346–361. https://doi.org/10.1177%2F1362361313476767 [ PubMed ] [ Google Scholar ]
- Guyatt, G. H. , Oxman, A. D. , Vist, G. E. , Kunz, R. , Falck‐Ytter, Y. , Alonso‐Coello, P. et al (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations . BMJ , 336 , 924–926. 10.1136/bmj.39489.470347.ad. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hahn‐Markowitz, J. , Berger, I. , Manor, I. & Maeir, A. (2017). Impact of the Cognitive–Functional (Cog–Fun) intervention on executive functions and participation among children with attention deficit hyperactivity disorder: A randomized controlled trial . American Journal of Occupational Therapy , 71 ( 5 ), 7105220010p1–9. 10.5014/ajot.2017.022053 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hammond, J. , Jones, V. , Hill, E. L. , Green, D. & Male, I. (2014). An investigation of the impact of regular use of the WiiFit to improve motor and psychosocial outcomes in children with movement difficulties: A pilot study . Child: Care, Health and Development , 40 ( 2 ), 165–175. 10.1111/cch.12029 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hanna, K. & Rodger, S. (2002). Towards family‐centred practice in paediatric occupational therapy: A review of the literature on parent–therapist collaboration . Australian Occupational Therapy Journal , 49 ( 1 ), 14–24. 10.1046/j.0045-0766.2001.00273.x. [ CrossRef ] [ Google Scholar ]
- Hechler, T. , Ruhe, A. K. , Schmidt, P. , Hirsch, J. , Wager, J. , Dobe, M. et al (2014). Inpatient‐based intensive interdisciplinary pain treatment for highly impaired children with severe chronic pain: Randomized controlled trial of efficacy and economic effects . Pain , 155 , 118–128. 10.1016/j.pain.2013.09.015. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heinrichs, N. , Kliem, S. & Hahlweg, K. (2014). Four‐year follow‐up of a randomized controlled trial of Triple P group for parent and child outcomes . Prevention Science , 15 ( 2 ), 233–245. 10.1007/s11121-012-0358-2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Higgins J. & Green S. (Eds.). (2011). Cochrane handbook for systematic reviews of interventions . 5th ed West Sussex: John Wiley & Sons Ltd. [ Google Scholar ]
- Hoare, B. J. & Imms, C. (2004). Upper‐limb injections of botulinum toxin‐A in children with cerebral palsy: A critical review of the literature and clinical implications for occupational therapists . American Journal of Occupational Therapy , 58 ( 4 ), 389–397. 10.5014/ajot.58.4.389. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoare, B. , Imms, C. , Carey, L. & Wasiak, J. (2007). Constraint‐induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy: A Cochrane systematic review . Clinical Rehabilitation , 21 ( 8 ), 675–685. 10.1002/14651858.cd004149.pub2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoare, B. , Imms, C. , Villanueva, E. , Rawicki, H. B. , Matyas, T. & Carey, L. (2013). Intensive therapy following upper limb botulinum toxin A injection in young children with unilateral cerebral palsy: A randomized trial . Developmental Medicine & Child Neurology , 55 ( 3 ), 238–247. 10.1111/dmcn.12054. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoare, B. J. , Wallen, M. A. , Imms, C. , Villanueva, E. , Rawicki, H. B. & Carey, L. (2010). Botulinum toxin A as an adjunct to treatment in the management of the upper limb in children with spastic cerebral palsy (UPDATE) . Cochrane Database of Systematic Reviews , 1 , CD003469 10.1002/14651858.cd003469.pub4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Howe, T. H. & Wang, T. N. (2013). Systematic review of interventions used in or relevant to occupational therapy for children with feeding difficulties ages birth–5 years . American Journal of Occupational Therapy , 67 ( 4 ), 405–412. 10.5014/ajot.2013.004564. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoy, M. M. , Egan, M. Y. & Feder, K. P. (2011). A systematic review of interventions to improve handwriting . Canadian Journal of Occupational Therapy , 78 ( 1 ), 13–25. 10.2182/cjot.2011.78.1.3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang, H. H. , Fetters, L. , Hale, J. & McBride, A. (2009). Bound for success: A systematic review of constraint‐induced movement therapy in children with cerebral palsy supports improved arm and hand use . Physical Therapy , 89 ( 11 ), 1126–1141. 10.2522/ptj.20080111. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang, J. S. , Dillon, L. , Terrones, L. , Schubert, L. , Roberts, W. , Finklestein, J. et al (2014). Fit4Life: A weight loss intervention for children who have survived childhood leukemia . Pediatric Blood & Cancer , 61 ( 5 ), 894–900. 10.1002/pbc.24937. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Imms, C. , Granlund, M. , Wilson, P. H. , Steenbergen, B. , Rosenbaum, P. L. & Gordon, A. M. (2017). Participation, both a means and an end: A conceptual analysis of processes and outcomes in childhood disability . Developmental Medicine & Child Neurology , 59 , 16–25. 10.1111/dmcn.13237. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Inguaggiato, E. , Sgandurra, G. , Perazza, S. , Guzzetta, A. & Cioni, G. (2013). Brain reorganization following intervention in children with congenital hemiplegia: A systematic review . Neural Plasticity . 10.1155/2013/356275 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jackman, M. , Novak, I. & Lannin, N. (2014). Effectiveness of hand splints in children with cerebral palsy: A systematic review with meta‐analysis . Developmental Medicine & Child Neurology , 56 ( 2 ), 138–147. 10.1111/dmcn.12205. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jackman, M. , Novak, I. , Lannin, N. , Froude, E. , Miller, L. & Galea, C. (2018). Effectiveness of Cognitive Orientation to daily Occupational Performance over and above functional hand splints for children with cerebral palsy or brain injury: A randomized controlled trial . BMC Pediatrics , 18 ( 1 ), 248 10.1186/s12887-018-1213-9. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- James, S. , Ziviani, J. , Ware, R. S. & Boyd, R. N. (2015). Randomized controlled trial of web‐based multimodal therapy for unilateral cerebral palsy to improve occupational performance . Developmental Medicine & Child Neurology , 57 ( 6 ), 530–538. 10.1111/dmcn.12705. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Janeslätt, G. , Kottorp, A. & Granlund, M. (2014). Evaluating intervention using time aids in children with disabilities . Scandinavian Journal of Occupational Therapy , 21 ( 3 ), 181–190. 10.3109/11038128.2013.870225. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jones, D. J. , Forehand, R. , Cuellar, J. , Parent, J. , Honeycutt, A. , Khavjou, O. et al (2014). Technology‐enhanced program for child disruptive behavior disorders: Development and pilot randomized control trial . Journal of Clinical Child & Adolescent Psychology , 43 ( 1 ), 88–101. 10.1080/15374416.2013.822308. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kamps, D. , Thiemann‐Bourque, K. , Heitzman‐Powell, L. , Schwartz, I. , Rosenberg, N. , Mason, R. et al (2015). A comprehensive peer network intervention to improve social communication of children with autism spectrum disorders: A randomized trial in kindergarten and first grade . Journal of Autism and Developmental Disorders , 45 ( 6 ), 1809–1824. 10.1007/s10803-014-2340-2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kasari, C. , Dean, M. , Kretzmann, M. , Shih, W. , Orlich, F. , Whitney, R. et al (2016). Children with autism spectrum disorder and social skills groups at school: A randomized trial comparing intervention approach and peer composition . Journal of Child Psychology and Psychiatry , 57 ( 2 ), 171–179. 10.1111/jcpp.12460. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Katalinic, O. M. , Harvey, L. A. , Herbert, R. D. , Moseley, A. M. , Lannin, N. A. & Schurr, K. (2010). Stretch for the treatment and prevention of contractures . Cochrane Database of Systematic Reviews , 9 ( 9 ). 10.1002/14651858.cd007455.pub2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaya Kara, O. , Atasavun Uysal, S. , Turker, D. , Karayazgan, S. , Gunel, M. K. & Baltaci, G. (2015). The effects of Kinesio Taping on body functions and activity in unilateral spastic cerebral palsy: a single‐blind randomized controlled trial . Developmental Medicine & Child Neurology , 57 ( 1 ), 81–88. 10.1111/dmcn.12583. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kleim, J. A. & Jones, T. A. (2008). Principles of experience‐dependent neural plasticity: Implications for rehabilitation after brain damage . Journal of Speech, Language, and Hearing Research , 51 ( 1 ), S225–S239. 10.1044/1092-4388(2008/018). [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krisanaprakornkit, T. , Ngamjarus, C. , Witoonchart, C. & Piyavhatkul, N. (2010). Meditation therapies for attention‐deficit/hyperactivity disorder (ADHD) . Cochrane Database of Systematic Reviews , 6 , CD006507 10.1002/14651858.cd006507.pub2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuhaneck, H. M. , Madonna, S. , Novak, A. & Pearson, E . (2015). Effectiveness of interventions for children with autism spectrum disorder and their parents: A systematic review of family outcomes . American Journal of Occupational Therapy , 69 ( 5 ), 6905180040p1–6905180040p14. 10.5014/ajot.2015.017855 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kurowski, B. G. , Wade, S. L. , Kirkwood, M. W. , Brown, T. M. , Stancin, T. & Taylor, H. G. (2014). Long‐term benefits of an early online problem‐solving intervention for executive dysfunction after traumatic brain injury in children: A randomized clinical trial . JAMA Pediatrics , 168 ( 6 ), 523–531. 10.1001/jamapediatrics.2013.5070. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lang, R. , O'Reilly, M. , Healy, O. , Rispoli, M. , Lydon, H. , Streusand, W. et al (2012). Sensory integration therapy for autism spectrum disorders: A systematic review . Research in Autism Spectrum Disorders , 6 ( 3 ), 1004–1018. 10.1016/j.rasd.2012.01.006. [ CrossRef ] [ Google Scholar ]
- Lannin, N. , Scheinberg, A. & Clark, K. (2006). AACPDM systematic review of the effectiveness of therapy for children with cerebral palsy after botulinum toxin A injections . Developmental Medicine and Child Neurology , 48 ( 6 ), 533–539. 10.1111/j.1469-8749.2006.tb01309.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lannin, N. A. , Novak, I. & Cusick, A. (2007). A systematic review of upper extremity casting for children and adults with central nervous system motor disorders . Clinical Rehabilitation , 21 ( 11 ), 963–976. 10.1177/0269215507079141. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lawler, K. , Taylor, N. F. & Shields, N. (2013). Outcomes after caregiver‐provided speech and language or other allied health therapy: A systematic review . Archives of Physical Medicine and Rehabilitation , 94 ( 6 ), 1139–1160. 10.1016/j.apmr.2012.11.022. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lidman, G. , Nachemson, A. , Peny‐Dahlstrand, M. & Himmelmann, K. (2015). Botulinum toxin A injections and occupational therapy in children with unilateral spastic cerebral palsy: a randomized controlled trial . Developmental Medicine & Child Neurology , 57 ( 8 ), 754–761. 10.1111/dmcn.12739. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lin, H. C. & Wuang, Y. P. (2012). Strength and agility training in adolescents with Down syndrome: A randomized controlled trial . Research in Developmental Disabilities , 33 ( 6 ), 2236–2244. 10.1016/j.ridd.2012.06.017. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lindsay, S. , Kingsnorth, S. , Mcdougall, C. & Keating, H. (2014). A systematic review of self‐management interventions for children and youth with physical disabilities . Disability and Rehabilitation , 36 ( 4 ), 276–288. 10.3109/09638288.2013.785605. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Madlinger‐Lewis, L. , Reynolds, L. , Zarem, C. , Crapnell, T. , Inder, T. & Pineda, R. (2014). The effects of alternative positioning on preterm infants in the neonatal intensive care unit: A randomized clinical trial . Research in Developmental Disabilities , 35 ( 2 ), 490–497. 10.1016/j.ridd.2013.11.019. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Maeir, A. , Fisher, O. , Bar‐Ilan, R. T. , Boas, N. , Berger, I. & Landau, Y. E. (2014). Effectiveness of Cognitive‐Functional (Cog–Fun) occupational therapy intervention for young children with attention deficit hyperactivity disorder: A controlled study . American Journal of Occupational Therapy , 68 ( 3 ), 260–267. 10.5014/ajot.2014.011700. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Malow, B. A. , Adkins, K. W. , Reynolds, A. , Weiss, S. K. , Loh, A. , Fawkes, D. et al (2014). Parent‐based sleep education for children with autism spectrum disorders . Journal of Autism and Developmental Disorders , 44 ( 1 ), 216–228. 10.1007/s10803-013-1866-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mandich, A. & Rodger, S. (2006). Doing, being and becoming: their importance for children. Occupational therapy with children: understanding children's occupations and enabling participation . Oxford, UK: Blackwell Publishing Ltd, 123–125. [ Google Scholar ]
- Maskell, J. , Newcombe, P. , Martin, G. & Kimble, R. (2014). Psychological and psychosocial functioning of children with burn scarring using cosmetic camouflage: A multi‐centre prospective randomised controlled trial . Burns , 40 ( 1 ), 135–149. 10.1016/j.burns.2013.04.025. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mast, J. E. , Antonini, T. N. , Raj, S. P. , Oberjohn, K. S. , Cassedy, A. , Makoroff, K. L. et al (2014). Web‐based parenting skills to reduce behavior problems following abusive head trauma: A pilot study . Child Abuse & Neglect , 38 ( 9 ), 1487–1495. 10.1016/j.chiabu.2014.04.012. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Matute‐Llorente, Á. , González‐Agüero, A. , Gómez‐Cabello, A. , Vicente‐Rodríguez, G. & Mallén, J. A. C. (2014). Effect of whole‐body vibration therapy on health‐related physical fitness in children and adolescents with disabilities: A systematic review . Journal of Adolescent Health , 54 ( 4 ), 385–396. 10.1016/j.jadohealth.2013.11.001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- May‐Benson, T. A. & Koomar, J. A. (2010). Systematic review of the research evidence examining the effectiveness of interventions using a sensory integrative approach for children . American Journal of Occupational Therapy , 64 ( 3 ), 403–414. 10.5014/ajot.2010.09071. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mayston, M. (2016). Bobath and neurodevelopmental therapy: What is the future? Developmental Medicine & Child Neurology , 58 ( 10 ), 994 10.1111/dmcn.13221. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McLean, B. , Taylor, S. , Blair, E. , Valentine, J. , Carey, L. & Elliott, C. (2017). Somatosensory discrimination intervention improves body position sense and motor performance in children with hemiplegic cerebral palsy . American Journal of Occupational Therapy , 71 ( 3 ), 7103190060p1–9. 10.5014/ajot.2016.024968 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Meany‐Walen, K. K. , Bratton, S. C. & Kottman, T. (2014). Effects of Adlerian play therapy on reducing students’ disruptive behaviors . Journal of Counseling & Development , 92 ( 1 ), 47–56. 10.1002/j.1556-6676.2014.00129.x. [ CrossRef ] [ Google Scholar ]
- Miller‐Kuhaneck, H. & Watling, R. (2018). Parental or teacher education and coaching to support function and participation of children and youth with sensory processing and sensory integration challenges: A systematic review . American Journal of Occupational Therapy , 72 ( 1 ), 7201190030p1–11. 10.5014/ajot.2018.029017 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moher, D. , Liberati, A. , Tetzlaff, J. & Altman, D. G. (2010). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement . International Journal of Surgery , 8 ( 5 ), 336–341. 10.1371/journal.pmed.1000097. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Montero, S. M. & Gómez‐Conesa, A. (2014). Technical devices in children with motor disabilities: A review . Disability and Rehabilitation: Assistive Technology , 9 ( 1 ), 3–11. 10.3109/17483107.2013.785034. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moola, F. J. , Faulkner, G. E. J. , White, L. & Kirsh, J. A . (2014). The psychological and social impact of camp for children with chronic illnesses: A systematic review update . Child: Care, Health and Development , 40 ( 5 ), 615–631. 10.1111/cch.12114 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morgan, C. , Novak, I. , Dale, R. C. & Badawi, N. (2015). Optimising motor learning in infants at high risk of cerebral palsy: A pilot study . BMC Pediatrics , 15 ( 1 ), 30 10.1186/s12887-015-0347-2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morgan, C. , Darrah, J. , Gordon, A. M. , Harbourne, R. , Spittle, A. , Johnson, R. et al (2016a). Effectiveness of motor interventions in infants with cerebral palsy: A systematic review . Developmental Medicine & Child Neurology , 58 ( 9 ), 900–909. 10.1111/j.1365-2214.2008.00921_2.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morgan, C. , Novak, I. , Dale, R. C. , Guzzetta, A. & Badawi, N. (2016b). Single blind randomised controlled trial of GAME (Goals‐Activity‐Motor Enrichment) in infants at high risk of cerebral palsy . Research in Developmental Disabilities , 55 , 256–267. 10.1186/s12883-014-0203-2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Novak, I. (2014a). Evidence to practice commentary new evidence in coaching interventions . Physical & Occupational Therapy in Pediatrics , 34 ( 2 ), 132–137. 10.3109/01942638.2014.903060. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Novak, I. & Berry, J. (2014b). Home program intervention effectiveness evidence . Physical & Occupational Therapy in Pediatrics , 34 ( 4 ), 384–389. 10.3109/01942638.2014.964020. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Novak, I. & McIntyre, S. (2010). The effect of education with workplace supports on practitioners’ evidence‐based practice knowledge and implementation behaviours . Australian Occupational Therapy Journal , 57 ( 6 ), 386–393. 10.1111/j.1440-1630.2010.00861.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Novak, I. , Mcintyre, S. , Morgan, C. , Campbell, L. , Dark, L. , Morton, N. et al (2013). A systematic review of interventions for children with cerebral palsy: State of the evidence . Developmental Medicine & Child Neurology , 55 ( 10 ), 885–910. 10.1111/dmcn.12246. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Park, H. Y. , Maitra, K. , Achon, J. , Loyola, E. & Rincón, M. (2014). Effects of early intervention on mental or neuromusculoskeletal and movement‐related functions in children born low birthweight or preterm: A meta‐analysis . American Journal of Occupational Therapy , 68 ( 3 ), 268–276. 10.5014/ajot.2014.010371. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pfeiffer B, Clark GF & Arbesman, M. (2018). Effectiveness of cognitive and occupation‐based interventions for children with challenges in sensory processing and integration: A systematic review . American Journal of Occupational Therapy , 72 ( 1 ), 7201190020p1–7201190020p9. 10.5014/ajot.2018.028233 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Polatajko, H. J. & Cantin, N. (2010). Exploring the effectiveness of occupational therapy interventions, other than the sensory integration approach, with children and adolescents experiencing difficulty processing and integrating sensory information . American Journal of Occupational Therapy , 64 ( 3 ), 415–429. 10.5014/ajot.2010.09072. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reeuwijk, A. , van Schie, P. E. , Becher, J. G. & Kwakkel, G. (2006). Effects of botulinum toxin type A on upper limb function in children with cerebral palsy: A systematic review . Clinical Rehabilitation , 20 ( 5 ), 375–387. 10.1191/0269215506cr956oa. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rodger, S. , Brown, G. T. & Brown, A. (2005). Profile of paediatric occupational therapy practice in Australia . Australian Occupational Therapy Journal , 52 ( 4 ), 311–325. 10.1111/j.1440-1630.2005.00487.x. [ CrossRef ] [ Google Scholar ]
- Sakzewski, L. , Ziviani, J. & Boyd, R. (2009). Systematic review and meta‐analysis of therapeutic management of upper‐limb dysfunction in children with congenital hemiplegia . Pediatrics , 123 ( 6 ), e1111–e1122. 10.1542/peds.2008-3335. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sakzewski, L. , Ziviani, J. & Boyd, R. N. (2013). Efficacy of upper limb therapies for unilateral cerebral palsy: A meta‐analysis . Pediatrics , 133 , e175–e204. 10.1542/peds.2013-0675. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sakzewski, L. , Miller, L. , Ziviani, J. , Abbott, D. F. , Rose, S. , Macdonell, R. A. et al (2015). Randomized comparison trial of density and context of upper limb intensive group versus individualized occupational therapy for children with unilateral cerebral palsy . Developmental Medicine & Child Neurology , 57 ( 6 ), 539–547. 10.1111/dmcn.12702. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schaaf, R. C. , Dumont, R. L. , Arbesman, M. & May‐Benson, T. A. (2018). Efficacy of occupational therapy using Ayres Sensory Integration®: A systematic review . American Journal of Occupational Therapy , 72 ( 1 ), 7201190010p1–10. 10.5014/ajot.2018.028431 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith, V. , Devane, D. , Begley, C. M. & Clarke, M. (2011). Methodology in conducting a systematic review of systematic reviews of healthcare interventions . BMC Medical Research Methodology , 11 ( 1 ), 15 10.1186/1471-2288-11-15. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith, T. O. , Bacon, H. , Jerman, E. , Easton, V. , Armon, K. , Poland, F. et al (2014). Physiotherapy and occupational therapy interventions for people with benign joint hypermobility syndrome: A systematic review of clinical trials . Disability and Rehabilitation , 36 ( 10 ), 797–803. 10.3109/09638288.2013.819388. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith, J. , Cheater, F. & Bekker, H. (2015). Parents’ experiences of living with a child with a long‐term condition: A rapid structured review of the literature . Health Expectations , 18 ( 4 ), 452–474. 10.1111/hex.12040. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smits‐Engelsman, B. C. , Blank, R. , van der Kaay, A. C. , Mosterd‐Van Der Meijs, R. , Vlugt‐Van Den Brand, E. , Polatajko, H. J. et al (2013). Efficacy of interventions to improve motor performance in children with developmental coordination disorder: A combined systematic review and meta‐analysis . Developmental Medicine & Child Neurology , 55 ( 3 ), 229–237. 10.1111/dmcn.12008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Snider, L. , Majnemer, A. & Darsaklis, V. (2010). Virtual reality as a therapeutic modality for children with cerebral palsy . Developmental Neurorehabilitation , 13 ( 2 ), 120–128. 10.3109/17518420903357753. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Speth, L. , Janssen‐Potten, Y. , Rameckers, E. , Defesche, A. , Winkens, B. , Becher, J. et al (2015). Effects of botulinum toxin A and/or bimanual task‐oriented therapy on upper extremity activities in unilateral cerebral palsy: A clinical trial . BMC Neurology , 15 ( 1 ), 143 10.1186/s12883-015-0404-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spittle, A. , Orton, J. , Doyle, L. W. & Boyd, R. (2007). Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants . Cochrane Database of Systematic Reviews , ( 2 ), CD005495 10.1002/14651858.cd005495.pub2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spittle, A. , Orton, J. , Anderson, P. , Boyd, R. & Doyle, L. W. (2012). Early developmental intervention programmes post‐hospital discharge to prevent motor and cognitive impairments in preterm infants . Cochrane Database of Systematic Reviews , ( 12 ), CD005495 10.1002/14651858.cd005495.pub3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stavness, C. (2006). The effect of positioning for children with cerebral palsy on upper‐extremity function: A review of the evidence . Physical & Occupational Therapy in Pediatrics , 26 ( 3 ), 39–53. 10.1300/j006v26n03_04. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Steultjens, E. M. , Dekker, J. , Bouter, L. M. , Van De Nes, J. C. , Lambregts, B. L. & van den Ende, C. H. (2004). Occupational therapy for children with cerebral palsy: A systematic review . Clinical Rehabilitation , 18 ( 1 ), 1–14. 10.1002/14651858.cd004490. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stickles Goods, K. , Ishijima, E. , Chang, Y. C. & Kasari, C. (2013). Preschool based JASPER intervention in minimally verbal children with autism: Pilot RCT . Journal of Autism and Developmental Disorders , 43 ( 5 ), 1050–1056. 10.1007/s10803-012-1644-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Storebø, O. J. , Skoog, M. , Damm, D. , Thomsen, P. H. , Simonsen, E. & Gluud, C. (2011). Social skills training for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years . Cochrane Database of Systematic Reviews , 12 , CD008223 10.1002/14651858.cd008223.pub2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tanner, K. , Hand, B. N. , O'toole, G. & Lane, A. E . (2015). Effectiveness of interventions to improve social participation, play, leisure, and restricted and repetitive behaviors in people with autism spectrum disorder: A systematic review . American Journal of Occupational Therapy , 69 ( 5 ), 6905180010p1–6905180010p12. 10.5014/ajot.2015.017806 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tatla, S. K. , Sauve, K. , Virji‐Babul, N. , Holsti, L. , Butler, C. & Van Der Loos, H. F. M. (2013). Evidence for outcomes of motivational rehabilitation interventions for children and adolescents with cerebral palsy: An American Academy for Cerebral Palsy and Developmental Medicine systematic review . Developmental Medicine & Child Neurology , 55 ( 7 ), 593–601. 10.1111/dmcn.12147. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tatla, S. K. , Sauve, K. , Jarus, T. , Virji‐Babul, N. & Holsti, L. (2014). The effects of motivating interventions on rehabilitation outcomes in children and youth with acquired brain injuries: A systematic review . Brain Injury , 28 ( 8 ), 1022–1035. 10.3109/02699052.2014.890747. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tervahauta, M. H. , Girolami, G. L. & Øberg, G. K. (2017). Efficacy of constraint‐induced movement therapy compared with bimanual intensive training in children with unilateral cerebral palsy: A systematic review . Clinical Rehabilitation , 31 ( 11 ), 1445–1456. 10.1177/0269215517698834. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Upton, D. , Stephens, D. , Williams, B. & Scurlock‐Evans, L. (2014). Occupational therapists’ attitudes, knowledge, and implementation of evidence‐based practice: A systematic review of published research . British Journal of Occupational Therapy , 77 ( 1 ), 24–38. 10.4276/030802214x13887685335544. [ CrossRef ] [ Google Scholar ]
- Vargas, S. & Lucker, J. R. (2016). A quantitative summary of The Listening Program (TLP) efficacy studies: What areas were found to improve by TLP intervention? Occupational Therapy International , 23 ( 2 ), 206–217. 10.1002/oti.1425. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vroland‐Nordstrand, K. , Eliasson, A. C. , Jacobsson, H. , Johansson, U. & Krumlinde‐Sundholm, L. (2016). Can children identify and achieve goals for intervention? A randomized trial comparing two goal‐setting approaches . Developmental Medicine & Child Neurology , 58 ( 6 ), 589–596. 10.1111/dmcn.12925. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wallen, M. M. & Gillies, D. (2006). Intra‐articular steroids and splints/rest for children with juvenile idiopathic arthritis and adults with rheumatoid arthritis . Cochrane Database of Systematic Reviews , 1 , CD002824 10.1002/14651858.cd002824.pub2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Watling, R. & Hauer, S. (2015). Effectiveness of Ayres Sensory Integration ® and sensory‐based interventions for people with autism spectrum disorder: A systematic review . American Journal of Occupational Therapy , 69 ( 5 ), 1–12. 10.5014/ajot.2015.018051. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weaver, L. L . (2015). Effectiveness of work, activities of daily living, education, and sleep interventions for people with autism spectrum disorder: A systematic review . American Journal of Occupational Therapy , 69 ( 5 ), 6905180020p1–6905180020p11. 10.5014/ajot.2015.017962 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weinstock‐Zlotnick, G. & Hinojosa, J. (2004). Bottom‐up or top‐down evaluation: Is one better than the other? American Journal of Occupational Therapy , 58 ( 5 ), 594–599. 10.5014/ajot.58.5.594. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wells, H. , Marquez, J. & Wakely, L. (2018). Garment therapy does not improve function in children with cerebral palsy: A systematic review . Physical & Occupational Therapy in Pediatrics , 38 , 395–416. 10.1080/01942638.2017.1365323. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Westendorp, M. , Houwen, S. , Hartman, E. , Mombarg, R. , Smith, J. & Visscher, C. (2014). Effect of a ball skill intervention on children's ball skills and cognitive functions . Medicine and Science in Sports and Exercise , 46 , 414–422. 10.1249/mss.0b013e3182a532b3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whalen, C. N. & Case‐Smith, J. (2012). Therapeutic effects of horseback riding therapy on gross motor function in children with cerebral palsy: A systematic review . Physical & Occupational Therapy in Pediatrics , 32 ( 3 ), 229–242. 10.3109/01942638.2011.619251. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Willis, C. , Nyquist, A. , Girdler, S. , Jahnsen, R. , Reid, S. , Rosenberg, M. et al (2016). Identifying and operationalising the active ingredients of a participation intervention for children with disabilities: Staff perspectives . Developmental Medicine & Child Neurology , 58 , 42–43. [ Google Scholar ]
- World Health Organisation . (2001). ICF: International classification of functioning, disability and health (9241545429) . Geneva, Switzerland: World Health Organisation; 10.4135/9781412950510.n454. [ CrossRef ] [ Google Scholar ]
- Wuang, Y. P. , Ho, G. S. & Su, C. Y. (2013). Occupational therapy home program for children with intellectual disabilities: A randomized, controlled trial . Research in Developmental Disabilities , 34 ( 1 ), 528–537. 10.1016/j.ridd.2012.09.008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Xu, K. , He, L. , Mai, J. , Yan, X. & Chen, Y. (2015). Muscle recruitment and coordination following constraint‐induced movement therapy with electrical stimulation on children with hemiplegic cerebral palsy: A randomized controlled trial . PLoS ONE , 10 ( 10 ), e0138608 10.1371/journal.pone.0138608. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zadnikar, M. & Kastrin, A. (2011). Effects of hippotherapy and therapeutic horseback riding on postural control or balance in children with cerebral palsy: A meta‐analysis . Developmental Medicine & Child Neurology , 53 ( 8 ), 684–691. 10.1111/j.1469-8749.2011.03951.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ziviani, J. , Feeney, R. , Rodger, S. & Watter, P. (2010). Systematic review of early intervention programmes for children from birth to nine years who have a physical disability . Australian Occupational Therapy Journal , 57 ( 4 ), 210–223. 10.1111/j.1440-1630.2010.00850.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zwaigenbaum, L. , Bauman, M. L. , Choueiri, R. , Kasari, C. , Carter, A. , Granpeesheh, D. et al (2015). Early intervention for children with autism spectrum disorder under 3 years of age: Recommendations for practice and research . Pediatrics , 136 ( Suppl 1 ), S60–S81. 10.1542/peds.2014-3667E. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zwi, M. , Jones, H. , Thorgaard, C. , York, A. & Dennis, J. A . (2011). Parent training interventions for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years . Cochrane Database of Systematic Reviews , 12 , CD003018 10.4073/csr.2012.2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zwicker, J. G. & Mayson, T. A. (2010). Effectiveness of treadmill training in children with motor impairments: An overview of systematic reviews . Pediatric Physical Therapy , 22 ( 4 ), 361–377. 10.1097/pep.0b013e3181f92e54. [ PubMed ] [ CrossRef ] [ Google Scholar ]
Sign Up for a FREE Physical Therapy / Occupational Therapy Documentation Cheat Sheet!!
- How Can We Help
Treatments and Documentation
Copyright © 2020 The Note Ninjas LLC - All Rights Reserved.
Powered by GoDaddy
- Email Subscribe
- Privacy Policy
- Terms and Conditions
- Subscription
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.
Grab Your FREE Skilled Care and Documentation Cheat Sheet!
For PTs, OTs, Assistants, and Students
Enhance Patient Outcomes, Streamline Documentation, and Prevent Burnout!
- Skip to main navigation

- Talk to us:
- Call: 0330 223 0888
- Email: office@otforkids.co.uk

Show all / Hide all
- Who are we?
- What is paediatric OT?
- Our processes
- Information Gathering
- Problem Formulation
- Goal Setting
- Therapy Intervention Planning
- Regular Reviews
- Outcome measurement
- Final Review
- Our Mission
- Our Promises
- Our Clinics
- Assessments
- Autistic Spectrum Disorder Assessment
- Dyspraxia Assessment
- Movement ABC
- Detailed Assessment of Speed of Handwriting (DASH)
- Handwriting Assessment
- Functional Assessment
- Equipment Assessment
- Sensory Assessment
- Risk Assessment
- Autistic Spectrum Disorder Report
- DCD/Dyspraxia Report
- Sensory Modality Assessment and Rehabilitation Technique (SMART) Report
- Equipment Report
- Functional Assessment Report
- OT Programme Report
- Medico-legal Report
- SEN Statement Report
- Case Manager Report
- Risk Assessment and Management Report
- Wheelchair Assessment Report
- Access Audit Report
- Home Assessment Report
- Adaptive Equipment
- Sensory Integration Therapy
- Fine Motor Improvement Therapy
- Concentration and Memory Improvement Therapy
- Gross Motor Activity Training
- Handwriting Improvement Therapy
- Confidence Improvement Therapy
- One on One Treatment
- Home Visits
- School Visits
- Hydrotherapy
- Consultancy
- OT Groups for schools
- Concentration Group
- Fine Motor Group
- Handwriting Group
- Movement Group
- Organisation Group
- School Consultancy
- Experiencing Differences Day
- Teacher Training
- Seminar and Conference talks
- Sloped Writing Boards
- OT Assistant Classroom and Home Support
- In Clinic Groups
- OT Groups for Schools
- Autistic Spectrum Disorder (ASD)
- Acquired Head/Brain injury
- Attention Deficit (Hyperactivity) Disorder (ADD/ADHD)
- Asperger's Syndrome
- Childhood Cancer
- Cerebral Palsy
- Dyspraxia or Developmental Co-ordination Disorder (DCD)
- Developmental Delay
- Down's Syndrome
- Hydrocephalus (Child)
- Multiple Sclerosis (Child)
- Muscular Dystrophy
- Rett Syndrome
- Sensory Processing Disorder (SPD)
- Spina Bifida
- Problems we help
- Delayed Milestones
- Early Development (0-12 months)
- Toddler and Early Infancy (1 to 3 years)
- Infancy (3 to 5 years)
- Child (5 to 10 years)
- Developing into Teenage Years (10 to 15 years)
- Teenager (15 years plus)
- Poor Handwriting
- Difficulty Concentrating
- Fine Motor Difficulties
- Visual Perception Difficulties
- Gross Motor Difficulties
- Sensory Regulation Difficulties
- Low Confidence and Social Difficulties
- Who we work with
- Case Managers
- Organisations
- Testimonials

- Case Studies
Jimmy is 10 years old, he enjoys playing football and wants to do well at school. Jimmy has dyspraxia, or developmental co-ordination disorder. Dyspraxia is a well known condition, however the association between the condition and how it can affect a child at school is not so well understood. Dyspraxia affects a child's planning, processing, and motor co-ordination, which dramatically impacts upon a child's performance in school.
Jimmy struggles to ride a bike, he is never picked for the school football team, and the teachers at his school are expressing concerns regarding his writing. Jimmy tries very hard to keep up with the class when he is copying from the board, however he just can't keep up. He has to concentrate so hard on making his writing neat and legible, that he often misses the information being taught and the objectives for the lesson.
Jimmy came to our clinic and received an initial assessment and ongoing monthly treatment. Alongside his ongoing treatment, Jimmy and his parents worked through a home programme of activities to improve his skills, and Caroline, his Occupational Therapist, visited his school to improve his environment and increase his learning opportunities.
Over time, Jimmy's writing became legible and he was able to kick a football with good accuracy and he even managed to get his way onto the school football team! Both Jimmy and his parents were extremely pleased with the support, advice and expert help they received from OT for Kids in helping Jimmy achieve his goals.
All of our assessments and treatments are centred around the patient.
We believe that together we achieve more.

- 0330 223 0888
- office@otforkids.co.uk
- 2 Hagley Rd, Salford M5 3EY [ map ]
Testimonials »
Why choose us.
- Caring and Professional Service
- Variety of services available
- First class Occupational Therapists
- Modern clinics
- Saturday and Sunday appointments available
- Able to see you at home, in school or in one of our clinics
- Registered with the Health Professions Council and the British Association of Occupational Therapy
Useful Links »
- Our services
Clinics »
- Manchester Clinic
- Sale Clinic

Get in Touch
- 2 Hagley Rd, Salford M5 3EY[ map ]
We're registered...

Groups »
We run a range of Groups for children aged 0-18 years.

Want to find out more?
We've put together a handy brochure that will cover everything you need to know!

- What Is Paediatric OT?
- Treatment We Provide
- Attention Deficit Disorder (ADD/ADHD)

- Confidentiality
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Occupational therapy in pediatric rehabilitation
Affiliation.
- 1 Research and Therapy Services, Great Falls, Va.
- PMID: 2259681
Occupational therapy in pediatric rehabilitation focuses on the effects of diseases and of the environment on a child's abilities to function successfully in daily life settings (home, school and playground) and roles (family member, student, etc.). In this paper, the process of pediatric occupational therapy, from assessment to discharge planning, is briefly described. Pediatric occupational therapy intervention strategies including treatment, environmental adaptation, and systems change are presented and illustrated. Three case studies highlighting occupational therapy intervention are discussed.
PubMed Disclaimer
Similar articles
- Functional assessment and intervention in occupational therapy. Brown C. Brown C. Psychiatr Rehabil J. 2009 Winter;32(3):162-70. doi: 10.2975/32.3.2009.162-170. Psychiatr Rehabil J. 2009. PMID: 19136348
- Contemporary trends and practice strategies in pediatric occupational and physical therapy. Jirikowic T, Stika-Monson R, Knight A, Hutchinson S, Washington K, Kartin D. Jirikowic T, et al. Phys Occup Ther Pediatr. 2001;20(4):45-62. Phys Occup Ther Pediatr. 2001. PMID: 11382205
- Physical and occupational therapy. Case-Smith J, Rogers S. Case-Smith J, et al. Child Adolesc Psychiatr Clin N Am. 1999 Apr;8(2):323-45. Child Adolesc Psychiatr Clin N Am. 1999. PMID: 10202593 Review.
- Pediatric occupational therapy in the home. Hinojosa J, Anderson J, Strauch C. Hinojosa J, et al. Am J Occup Ther. 1988 Jan;42(1):17-22. doi: 10.5014/ajot.42.1.17. Am J Occup Ther. 1988. PMID: 3281464 Review.
- Pediatric physical therapy in a rehabilitation setting. Eigsti H, Aretz M, Shannon L. Eigsti H, et al. Pediatrician. 1990;17(4):267-77. Pediatrician. 1990. PMID: 2259680 Review.
Publication types
- Search in MeSH
LinkOut - more resources
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 28 June 2024
Developing an entrustable professional activity for providing health education and consultation in occupational therapy and examining its validity
- Chung-Pei Fu 1 ,
- Ching-Kai Huang 2 ,
- Yi-Chiun Yang 3 ,
- Wei-Sheng Liao 4 ,
- Shih-Min Huang 5 ,
- Wei-Di Chang 6 ,
- Yi-Ju Chen 7 ,
- Ming-Wei Li 5 ,
- Yi-Ju Lin 8 ,
- Chin-Lung Wu 8 ,
- Hsin-Yu Chi 5 ,
- Chia-Yi Lee 9 ,
- Fu-Mei Chiang 10 ,
- Yu-Lan Chen 11 ,
- Ching-Fen Tsou 9 ,
- Tzu-Hung Liu 12 , 13 ,
- Chia-Ting Su 1 ,
- Ai-Lun Yang 14 ,
- Nung-Chen Kuo 15 &
- Wan-Ying Chang 16
BMC Medical Education volume 24 , Article number: 705 ( 2024 ) Cite this article
174 Accesses
Metrics details
Entrustable Professional Activities (EPA)-based assessment is easily and intuitively used in evaluating the learning outcomes of competency-based medical education (CBME). This study aimed to develop an EPA for occupational therapy focused on providing health education and consultation (TP-EPA3) and examine its validity.
Nineteen occupational therapists who had completed online training on the EQual rubric evaluation participated in this study. An expert committee identified six core EPAs for pediatric occupational therapy. TP-EPA3 was developed following the EPA template and refined through consensus meetings. The EQual rubric, a 14-item, five-point criterion-based anchor system, encompassing discrete units of work (DU), entrustable, essential, and important tasks of the profession (EEIT), and curricular role (CR), was used to evaluate the quality of TP-EPA3. Overall scores below 4.07, or scores for DU, EEIT, and CR domains below 4.17. 4.00, and 4.00, respectively, indicate the need for modifications.
The TP-EPA3 demonstrated good validity, surpassing the required cut-off score with an average overall EQual score of 4.21 ( SD = 0.41). Specific domain scores for DU, EEIT, and CR were 3.90 ( SD = 0.69), 4.46 ( SD = 0.44), and 4.42 ( SD = 0.45), respectively. Subsequent revisions clarified observation contexts, enhancing specificity and focus. Further validation of the revised TP-EPA3 and a thorough examination of its reliability and validity are needed.
The successful validation of TP-EPA3 suggests its potential as a valid assessment tool in occupational therapy education, offering a structured approach for developing competency in providing health education and consultation. This process model for EPA development and validation can guide occupational therapists in creating tailored EPAs for diverse specialties and settings.
Peer Review reports
Introduction
Competency-based medical education (CBME) represents a strategic evolution in the methodology of medical training, emphasizing the development of specific competencies essential for effective clinical practice [ 1 , 2 ]. Although competency frameworks have been developed by the Accreditation Council for Graduate Medical Education (ACGME) and Canadian Medical Education Directives for Specialists (CanMEDS), their implementation in clinical practice has been limited. Entrustable professional activities (EPAs) and milestones have emerged to bridge the gap between competency frameworks and assessment and training in clinical practices [ 3 , 4 , 5 ].
EPAs are discrete clinical activities that require the integration of various competencies and represent an activity associated with a specific clinical event [ 6 , 7 ], whereas milestones refer to observable markers along a continuum of progress [ 8 ]. However, the application of milestones as evaluative tools for trainees’ competency faces challenges due to their sheer number, the extensive and complex training required, and the necessity for full participation in the learning process [ 9 ]. Therefore, EPA-based assessment is easier and more intuitive to use in evaluating the learning outcomes of the CBME [ 10 , 11 ].
EPAs have been well developed in many medical professions, such as medicine of various specialties [ 12 , 13 , 14 , 15 , 16 , 17 , 18 ], dentistry [ 19 ], nursing [ 20 ], pharmacy [ 21 , 22 ], radiology [ 23 , 24 , 25 ], physical therapy [ 26 ], and occupational therapy [ 27 , 28 ]. While EPAs tailored to occupational therapy have been established in Singapore, they primarily focus on undergraduate education during the earlier years of study, emphasizing fundamental professional activities crucial for early-stage clinical education. However, it is crucial to develop EPAs specific to the final year of undergraduate clinical training and post-graduate clinical training. During this phase, occupational therapy students are exposed to four major domains: physical, mental, pediatric, and community. Each domain encompasses unique core competencies and professional activities. Thus, developing EPAs tailored to each domain of occupational therapy is essential. Accordingly, the purpose of this study was to delineate the process of developing an EPA in pediatric occupational therapy, using the EPA3 Providing Health Education and Consultation in occupational therapy (TP-EPA3) serving as an example, and to examine its validity. While we developed six EPAs in pediatric occupational therapy, this study focuses exclusively on TP-EPA3 as a representative example due to its broad applicability across the four major domains of occupational therapy: physical, mental, pediatric, and community.
This study was approved by the institutional review boards of Fu Jen Catholic University (C110093) and Taipei Hospital, Ministry of Health and Welfare (TH-IRB-0022–0027).
Participants
Nineteen occupational therapists (11 females, 8 males), who had completed online training on the EQual rubric evaluation, rated the 6 core EPAs in pediatric occupational therapy on the EQual rubric. Their age distribution was as follows: 21.1% were aged 31–40 years; 63.2%, 41–50 years; and 15.8%, 51–60 years. Their workplaces were medical centers (42.1%), regional teaching hospitals (47.4%), and district teaching hospitals (5.3%). Their positions were chiefs of occupational therapy (26.3%), chiefs of pediatric occupational therapy (15.8%), teaching directors of occupational therapy (26.3%), clinical teachers (57.9%), and university teachers. The average duration of their work experience was 20.2 years ( SD = 6.7), whereas that as clinical teachers was 15.6 years ( SD = 7.8).
This study comprised two stages: the development of TP-EPA3, and an examination of the structure and quality of TP-EPA3.
In the first stage, six topics for the core EPAs were identified by expert committee using the nominal group technique and survey questionnaires distributed to 131 teaching hospitals in Taiwan [ 29 ]. The expert committee included two university teachers from departments of occupational therapy, 24 clinical teachers of pediatric occupational therapy in teaching hospitals, and one external expert developing EPAs in family medicine in Taiwan. The nominal group technique and survey questionnaires were chosen to ensure a comprehensive and systematic collection of expert opinions and have been detailed in previous studies [ 30 , 31 ]. The survey was distributed to 131 teaching hospitals in Taiwan, providing a broad basis for the identification of core EPAs [ 29 ].
The Taiwan Occupational Therapy Association made only minor textual refinements to the titles of the six core EPAs: EPA1, “Providing evaluations in occupational therapy”; EPA2, “Providing interventions in occupational therapy”; EPA3, “Providing health education and consultation” (TP-EPA3); EPA4, “Writing occupational therapy medical records”; EPA5, “Providing transdisciplinary collaboration healthcare”; and EPA6, “Providing services of splints or assistive devices”, without altering the core competencies or the content of the EPAs themselves. The draft of TP-EPA3 was written by two pediatric occupational therapy clinical teachers (corresponding and co-corresponding authors) from two teaching hospitals within the expert committee, based on the EPA template [ 11 ]. Following three rounds of consensus meetings, the expert committee finalized the description of TP-EPA3, as shown in Appendix 1.
In the second stage, 16 committee members from the stage one expert committee, along with 3 non-committee occupational therapy experts with EPA experience, rated TP-EPA3. All raters had completed the online training of the EQual rubric evaluation and assessed TP-EPA3 according to the EQual rubric.
The EQual rubric is a 14-item evaluation utilized to assess the quality of EPAs [ 32 ]. This rubric measures the constructs of EPAs across 3 domains, including discrete units of work (DU) (items 1–6), entrustable, essential, and important tasks of the profession (EEIT)(items 7–10), and curricular role (CR) (items 11–14) [ 32 ]. Each item is scored using a five-point criterion-based anchor system [ 32 ], and an online training video is available for scoring [ 33 ]. A cut-off score of 4.07 determines whether a given EPA requires modification, with an average overall EQual score below 4.07 indicating that it does [ 32 ]. Moreover, the cutoff scores for the DU, EEIT, and CR domains are 4.17, 4.00, and 4.00, respectively [ 34 ]. The EQual rubric evaluation has been found to be reliable, valid and useful in EPA development [ 32 , 34 , 35 ].
Data analysis
Data analyses were performed in Microsoft Excel 16.75 for Mac. We calculated mean and standard deviation for the EQual rubric score and three domain scores to determine whether the EPA needs modification. The EQual rubric score represented the average of all 14 items, and domain scores for DU, EEIT, and CR were calculated from items 1–6, 7–10, and 11–14, respectively [ 32 , 34 , 35 ]. Additionally, the scatter plot was used to examine the dispersion of scores across the three domains.
Development of EPA3, providing health education and consultation (TP-EPA3)
The description of TP-EPA3 is shown in Appendix 1. The EPA comprises 8 parts: title; specifications and limitations; potential risks in case of failure; most relevant competency domains; required knowledge, skills, attitude and experiences; assessment information sources to assess progress and ground a summative entrustment decision; entrustment for which level of supervision is to be reached at which stage of training; and expiration date.
The entrustment and supervision scale for TP-EPA3 adopted Chen’s entrustment and supervision scale [ 36 ]. Specifically, clinical teachers were asked to assess the trainee's level of entrustment using the following question: "If you were to supervise this trainee again in a similar professional task and situation, which of the following statements aligns with how you would assign the task?" This question was used to guide the clinical teachers' entrustment decisions. The entrustment and supervision scale comprised 5 levels, with level 1 and level 2 being further divided into two sublevels, and level 3 being divided into three sublevels (Appendix 2). The definition of level 1a was “Not allowed to observe practicing the EPA”. Level 1b was “Not allowed to practice the EPA; allowed to observe”. Level 2a was "Allowed to practice the EPA only under proactive, full supervision as co-activity with supervisor”. Level 2b was “Allowed to practice the EPA only under proactive, full supervision with supervision in room ready to step in as needed”. Level 3a was “Allowed to practice the EPA only under reactive/on-demand supervision with supervisor immediately available, all findings double-checked”. Level 3b was “Allowed to practice the EPA only under reactive/on-demand supervision with supervision immediately available, key findings double-checked”. Level 3c was “Allowed to practice the EPA only under reactive/on-demand supervision with supervisor distantly available, findings reviewed”. Level 4 was “Allowed to practice the EPA unsupervised”. Level 5 was “Allowed to supervise others in practice of the EPA”.
Results of the EQual rubric
Eighteen occupational therapists rated the TP-EPA3 according to the EQual rubric. The response rate was 94.7%. The EQual item, domain, and overall scores for the TP-EPA3 are listed in Table 1 . The average scores of the individual items on the Equal rubric ranged from 3.17 to 4.83. The average overall EQual score was 4.21 ( SD = 0.41), which was higher than the cut-off score, 4.07. The domain scores for DU, EEIT, and CR were 3.90 ( SD = 0.69), 4.46 ( SD = 0.44), and 4.42 ( SD = 0.45), respectively. Only the domain score for DU (3.90) was lower than the domain cut-off score (4.17). The scatter plot of the three domain scores of the EQual is shown in Fig. 1 .

Scatter plot of the three EQual domain scores of TP-EPA3: Providing Health Education and Consultation in pediatric occupational therapy in Taiwan. Note: EPA = entrustable professional activity. DU = Discrete units of work. EEIR = Entrustable, essential, and important tasks of the profession. CR = Curricular role
To the best of our knowledge, this study was the first to illustrate the development process of EPAs in pediatric occupational therapy, specifically tailored for use in the final year of undergraduate clinical training and post-graduate clinical training in the pediatric domain. The EPAs developed in this study can complement those developed in Singapore [ 27 , 28 ], which are utilized during the earlier years of undergraduate education. Early exposure to EPAs in undergraduate education can enhance students' understanding of the EPA concept, increase clinical engagement, foster a stronger sense of professional identity, bridge the gap between theoretical knowledge and clinical practice, and facilitate comprehension of future practice expectations during conditional registration [ 28 , 37 , 38 ]. Using EPAs in pediatric occupational therapy during the final year of undergraduate clinical training and post-graduate clinical training can assess students' advanced clinical skills in pediatric occupational therapy domain, enable students to engage in self-directed learning to address their weakness, as well as determine their readiness to become independent pediatric occupational therapists [ 39 , 40 ].
The overall EQual score of TP-EPA3 (4.21), being higher than the cut-off score of 4.07, indicated good validity and quality. However, the EQual domain score for DU (3.90), below the cut-off score of 4.17, indicated a need for further revisions of the items within this domain. The scatter plot revealed greater variability in EQual domain scores for DU than for the other domains. Notably, the average scores for item 1 (“This EPA has a clearly defined beginning and end”) and item 3 (“This EPA is specific and focused”) were the lowest (Table 1 ). In pediatric occupational therapy, health education and consultations frequently occurred during various interactions with parents, such as following screenings, assessments, interventions, cessation of interventions, or even during casual conversations about the child's recent behaviors or challenges. Therapists often used these opportunities to recommend home program, activity adjustments, environmental modifications, or changes in parenting strategies. Due to the nature of these interactions, it would be challenging to identify a clear beginning and end for providing consultations and health education. This might explain why items 1 and 3 received lower scores. Consequently, the observation contexts of TP-EPA3 were refined to focus on four specific contexts: after screening, after evaluation, after intervention, and intervention discontinuation. These specifications were revised in alignment with the definitions, sequences, and crucial observation points related to providing health education and consultation. The revised version of the TP-EPA3 is provided in Appendix 3.
The TP-EPA3 presented in this paper may not be universally applicable to all occupational therapy fields, such as physical, mental, and community settings, or at different levels of hospitals or community agencies, or in all countries. However, occupational therapists can employ the EPA topic development process [ 29 ] and EPA content development process in this paper to develop their core EPAs tailored to their respective fields, hospitals or community agencies, or countries. In cases where occupational therapy units provide specialized services or interventions, specialized EPAs may also be developed by following this EPA development process. For instance, if an occupational therapy unit specializes in telemedicine or screening, specialized EPAs can be developed. Moreover, if only certain components of the professional tasks of the EPAs can be performed due to the size or other constraints, nested EPAs [ 11 ], which are smaller units of the original EPA, can be considered.
The assessment information sources utilized in evaluating progress and grounding a summative entrustment decision for the TP-EPA3, as presented in this study, encompass all the assessment methods typically employed to evaluate trainees’ capabilities. Occupational therapy clinical teachers can select the assessment methods they already utilize from those provided in the TP-EPA3. The key point in determining the summative entrustment and supervision levels for EPAs is to thoroughly consider the outcomes of multiple assessment methods and assessments. This approach prevents trainees from being unfairly labeled as “under proactive” based solely on one performance or poor performance on severe patients [ 41 ].
Since our EPAs were designed to evaluate both UGY and PGY trainees, Chen’s prospective entrustment and supervision scale [ 36 ] was adopted for two main reasons. First, the prospective nature of Chen’s scale could reduce the influence of contextual factors such as time of observation and work load, as well as task factors such as complexity of patient’s conditions [ 41 ]. Second, Chen’s scale expands the lower levels of the scale to include finer gradation of supervision, making it more suitable for assessing the performances of UGY trainees [ 36 ]. Thus, the scale offers a more comprehensive framework for evaluating the trainees’ performances at different stages of training, allowing more detailed analysis of their progress.
Limitations and suggestions
This study had four major limitations. First, although the overall EQual score of the initial TP-EPA3 indicated acceptable content validity, the revised TP-EPA3 still needs to be examined to determine whether the DU domain score has been improved. Second, since only the content validity of TP-EPA3 was examined, its inter-rater and intra-rater reliability, convergent and discriminant validity, and responsiveness should be further investigated. Third, the target entrustment and supervision levels of UGY and PGY trainees were recommended by the expert committee. Future studies should investigate the perspectives of occupational therapy clinical teachers on these target levels. Fourth, a potential limitation of our study is the overlap of committee members across the development and evaluation phases of TP-EPA3. Sixteen of the nineteen experts who assessed TP-EPA3 using the EQual rubric evaluation were involved in the initial development. Despite all raters being trained using the EQual rubric, their prior involvement could introduce unintentional rater bias, potentially influencing the impartiality of their assessments.
EPAs provide a time-efficient, feedback-oriented, and workplace-based assessment for evaluating whether trainees can perform clinical professional tasks competently without supervision. The EPA development process outlined in this study can help occupational therapists develop core EPAs, specialized EPAs, or nested EPAs tailored to their specific fields, hospitals or community agencies, or countries. In conclusion, EPAs are not only easy and intuitive for assessing the learning outcomes of CBME but also support clinical teachers in evaluating trainee independence in significant clinical professional activities and in curriculum design. Furthermore, EPAs help trainees prepare for clinical professional activities. Specifically, the TP-EPA3, which focus on providing health education and consultation in pediatric occupational therapy in Taiwan, has been validated using the EQual rubric, paving the way for the development of additional core EPAs using the process described.
Availability of data and materials
Data is available upon reasonable request from corresponding author. The e-mail of the corresponding author is [email protected] and [email protected] .
Abbreviations
- Entrustable Professional Activity
- Competency-based medical education
EPA3 for occupational therapy focused on providing health education and consultation
Discrete units of work
Entrustable, essential, and important tasks of the profession
Curricular role
Accreditation Council for Graduate Medical Education
Canadian Medical Education Directives for Specialists
Undergraduate year
Post-graduate year
Association of American Medical Colleges. Competency-Based Medical Education (CBME). Available from: https://www.aamc.org/about-us/mission-areas/medical-education/cbme .
Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–45.
Article Google Scholar
Carraccio C, Burke AE. Beyond competencies and milestones: adding meaning through context. J Grad Med Educ. 2010;2(3):419–22.
Jones MD Jr, Rosenberg AA, Gilhooly JT, Carraccio CL. Perspective: competencies, outcomes, and controversy–linking professional activities to competencies to improve resident education and practice. Acad Med. 2011;86(2):161–5.
van Loon KA, Driessen EW, Teunissen PW, Scheele F. Experiences with EPAs, potential benefits and pitfalls. Med Teach. 2014;36(8):698–702.
ten Cate O. Entrustability of professional activities and competency-based training. Med Educ. 2005;39(12):1176–7.
ten Cate O, Scheele F. Competency-based postgraduate training: can we bridge the gap between theory and clinical practice? Acad Med. 2007;82(6):542–7.
Royal College of Physicians and Surgeons of Canada. EPAs and Milestones 2017. 2017. Available from: http://www.royalcollege.ca/rcsite/cbd/implementation/cbd-milestones-epas-e .
Lin HJ, Wu JH, Chen CY. Competency-based medical education and milestones assessment. J Int Med Taiwan. 2020;31(2):115–21.
Google Scholar
Shorey S, Lau TC, Lau ST, Ang E. Entrustable professional activities in health care education: a scoping review. Med Educ. 2019;53(8):766–77.
Ten Cate O, Chen HC, Hoff RG, Peters H, Bok H, van der Schaaf M. Curriculum development for the workplace using Entrustable Professional Activities (EPAs): AMEE Guide No. 99. Med Teach. 2015;37(11):983–1002.
Hauer KE, Kohlwes J, Cornett P, Hollander H, Ten Cate O, Ranji SR, et al. Identifying entrustable professional activities in internal medicine training. J Grad Med Educ. 2013;5(1):54–9.
Kearse LE, Schmiederer IS, Anderson TN, Dent DL, Payne DH, Korndorffer JR Jr. American board of surgery entrustable professional activities (EPAs): assessing graduating residents’ perception of preoperative entrustment. J Surg Educ. 2021;78(6):e183–8.
McCloskey CB, Domen RE, Conran RM, Hoffman RD, Post MD, Brissette MD, et al. Entrustable professional activities for pathology: recommendations from the college of american pathologists graduate medical education committee. Acad Pathol. 2017;4:2374289517714283.
Mallow M, Baer H, Moroz A, Nguyen VQ. Entrustable professional activities for residency training in physical medicine and rehabilitation. Am J Phys Med Rehabil. 2017;96(10):762–4.
Royal College of Physicians and Surgeons of Canada. Entrustable professional activities for internal medicine. 2019.
Shaughnessy AF, Sparks J, Cohen-Osher M, Goodell KH, Sawin GL, Gravel J Jr. Entrustable professional activities in family medicine. J Grad Med Educ. 2013;5(1):112–8.
Young JQ, Hasser C, Hung EK, Kusz M, O’Sullivan PS, Stewart C, et al. Developing end-of-training entrustable professional activities for psychiatry: results and methodological lessons. Acad Med. 2018;93(7):1048–54.
Ramaswamy V, Fitzgerald M, Danciu T, Nalliah R, de Peralta T, Munz SM, Murdoch-Kinch CA. Entrustable professional activities framework for assessment in predoctoral dental education, developed using a modified Delphi process. J Dent Educ. 2021;85(8):1349–61.
Zhou W, Poh CL, Chan HL, Shorey S. Development of entrustable professional activities for advanced practice nurses education. Nurse Educ Today. 2022;116:105462.
Lockman K, Lowry MF, DiScala S, Lovell AG, Uritsky TJ, Kematick BS, et al. Development of entrustable professional activities for specialist hospice and palliative care pharmacists. J Pain Symptom Manage. 2022;64(1):37–48.
Pittenger AL, Chapman SA, Frail CK, Moon JY, Undeberg MR, Orzoff JH. Entrustable professional activities for pharmacy practice. Am J Pharm Educ. 2016;80(4):57.
Deitte LA, Gordon LL, Zimmerman RD, Stern EJ, McLoud TC, Diaz-Marchan PJ, Mullins ME. Entrustable professional activities: ten things radiologists do. Acad Radiol. 2016;23(3):374–81.
Royal College of Physicians and Surgeons of Canada. Entrustable professional activities for diagnostic radiology 2022. Available from: https://Users/medot/Downloads/epa-diagnostic-radiology-v1-e.pdf .
Tu CY, Huang KM, Cheng CH, Lin WJ, Liu CH, Yang CW. Development, implementation, and evaluation of entrustable professional activities (EPAs) for medical radiation technologists in Taiwan: a nationwide experience. BMC Med Educ. 2024;24(1):95.
Zainuldin R, Tan HY. Development of entrustable professional activities for a physiotherapy undergraduate programme in Singapore. Physiotherapy. 2021;112:64–71.
Zainuldin R, Tan HY. Entrustable professional activities developed for allied health entry-level programs across a national level training standards framework in Singapore. J Allied Health. 2023;52(2):104–12.
Zainuldin R, Tan HSK. Entrustable professional activities implementation in undergraduate allied health therapy programs. Asia Pac Schol. 2024;9(1):42–8.
Fu CP, Chiang FM, Lee CY, Chi HY, Wu CL, Lin YJ, et al. Developing the topics of entrustable professional activities in pediatric occupational therapy in Taiwan: a pilot study. Taiwan J Occup Ther. 2023;41(2):1–20.
Tsai SL, Chang SC, Ho MJ. Defining the core competencies of medical humanities education through the nominal group technique. J Med Educ. 2008;12(2):70–6.
Chiu HY. Survey research methods. Taipei: San Min Book Co., Ltd.; 2007.
Taylor DR, Park YS, Egan R, Chan MK, Karpinski J, Touchie C, et al. EQual, a novel rubric to evaluate entrustable professional activities for quality and structure. Acad Med. 2017;92((11S association of American medical colleges learn serve lead: proceedings of the 56th annual research in medical education sessions)):S110–7.
Department of Medicine Queen’s University. EQual rubric training video for EPA evaluation. Available from: https://www.youtube.com/watch?v=yQZuWdzkQKM .
Meyer EG, Taylor DR, Uijtdehaage S, Durning SJ. EQual rubric evaluation of the association of american medical colleges’ core entrustable professional activities for entering residency. Acad Med. 2020;95(11):1755–62.
Chen JW, Hsu WC. Developing a competency-based medical education for Taiwan otolaryngology-head and neck surgery resident physician training-an integrated entrustable professional activities model. J Taiwan Otolaryngol Head Neck Surg. 2022;57(2):110–22.
Chen HC, van den Broek WE, ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90(4):431–6.
Kuehl SE, Spicer JO. Using entrustable professional activities to better prepare students for their postgraduate medical training: a medical student’s perspective. Perspect Med Educ. 2022;11(6):359–64.
Bramley AL, McKenna L. Entrustable professional activities in entry-level health professional education: a scoping review. Med Educ. 2021;55(9):1011–32.
Stephan A, Cheung G, van der Vleuten C. Entrustable professional activities and learning: the postgraduate trainee perspective. Acad Psychiatry. 2023;47(2):134-42.
de Graaf J, Bolk M, Dijkstra A, van der Horst M, Hoff RG, Ten Cate O. The implementation of entrustable professional activities in postgraduate medical education in the netherlands: rationale, process, and current status. Acad Med. 2021;96(7S):S29–35.
Hauer KE, Ten Cate O, Boscardin C, Irby DM, Iobst W, O’Sullivan PS. Understanding trust as an essential element of trainee supervision and learning in the workplace. Adv Health Sci Educ Theory Pract. 2014;19(3):435–56.
Download references
Acknowledgements
We gratefully appreciate the Taiwan Occupational Therapy Association, the President, Dr. Ching-Yi Wu, the Chair of the Professional Quality Committee, Dr. I-Ping Hsueh, and Yi-Fang Wu for their support of our research. We also acknowledge the non-committee occupational therapy experts for their help in examining the validity of the EPAs.
This study was supported by research grants from the Taipei Hospital, Ministry of Health and Welfare (Project No. 202315).
Author information
Authors and affiliations.
Department of Occupational Therapy, College of Medicine, Fu Jen Catholic University, New Taipei City, Taiwan
Chung-Pei Fu & Chia-Ting Su
Department of Rehabilitation, Occupational Therapy, Linkuo Chang Gung Memorial Hospital, Taoyuan, Taiwan
Ching-Kai Huang
Department of Rehabilitation, Lotung Poh-Ai Hospital, Yilan, Taiwan
Yi-Chiun Yang
Department of Rehabilitation, Taipei Medical University Hospital, Taipei, Taiwan
Wei-Sheng Liao
Department of Rehabilitation, Sijhih Cathay General Hospital, New Taipei City, Taiwan
Shih-Min Huang, Ming-Wei Li & Hsin-Yu Chi
Department of Rehabilitation, Mackay Memorial Hospital, Taipei, Taiwan
Wei-Di Chang
Department of Rehabilitation, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan
Department of Rehabilitation, Changhua Christian Hospital, Changhua, Taiwan
Yi-Ju Lin & Chin-Lung Wu
Department of Rehabilitation, Cathay General Hospital, Taipei, Taiwan
Chia-Yi Lee & Ching-Fen Tsou
Department of Physical Medicine and Rehabilitation, National Taiwan University Hospital, Taipei, Taiwan
Fu-Mei Chiang
Department of Physical Medicine and Rehabilitation, Taipei Veterans General Hospital, Taipei, Taiwan
Yu-Lan Chen
Department of Family Medicine, Taipei Tzu Chi Hospital, New Taipei City, Taiwan
Tzu-Hung Liu
School of Medicine, Tzu Chi University, Hualien City, Taiwan
Institute of Sports Sciences, University of Taipei, Taipei, Taiwan
Ai-Lun Yang
Department of Occupational Therapy, Taoyuan General Hospital, Ministry of Health and Welfare,, No. 1492, Zhongshan Rd.,Taoyuan Dist., Taoyuan, 330, Taiwan
Nung-Chen Kuo
Department of Physical Medicine and Rehabilitation, Taipei Hospital, Ministry of Health and Welfare, No. 127, Su-Yuan Rd., Hsin-Chung Dist., New Taipei City, Taiwan
Wan-Ying Chang
You can also search for this author in PubMed Google Scholar
Contributions
C.P.F: co-principal investigator, wrote manuscript, designed research, collected and analyzed data, one of the expert committee members. C.K.H., Y.C.Y., W.S.L., S.M.H., W.D.C., Y.J.C., M.W.L., YJ.L., C.L.W., H.Y.C., C.Y.L., F.M.C., Y.L.C., C.F.T.: expert committee members, assisted in research execution, EPAs lead authors. T.H.L.: Taught the concepts and framework of competency-based medical education and entrustable professional activities to the expert committee, guided the occupational therapy expert committee to develop EPAs, assisted in designing research, assisted in writing manuscripts, shared EPAs developmental experiences in family medicine. C.T.S.: edited manuscripts, one of the expert committee members. A.L.Y.: shared EPAs development experiences in physical therapy, external experts, edited manuscripts. Corresponding author N.C.K.: lead author of the TP-EPA3 for providing health education and consultation in occupational therapy, which is presented in this manuscript, one of the expert committee members, assisted in research execution. Co-corresponing author W.Y.C.: principal investigator, lead author of the TP-EPA3 which is presented in this manuscript, one of the expert committee members, assisted in research execution.
Corresponding authors
Correspondence to Nung-Chen Kuo or Wan-Ying Chang .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the institutional review boards of Fu Jen Catholic University (C110093) and Taipei Hospital, Ministry of Health and Welfare (TH-IRB-0022–0027). Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fu, CP., Huang, CK., Yang, YC. et al. Developing an entrustable professional activity for providing health education and consultation in occupational therapy and examining its validity. BMC Med Educ 24 , 705 (2024). https://doi.org/10.1186/s12909-024-05670-1
Download citation
Received : 03 February 2024
Accepted : 18 June 2024
Published : 28 June 2024
DOI : https://doi.org/10.1186/s12909-024-05670-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Occupational therapy education
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
List initial occupational theories or models that might guide the occupational therapy process: Person-Environment-Occupation (PEO) (Case-Smith & O'Brien, 2015, p. 31): Focus on child's performance and the environmental influences that enable a child's engagement and participation in activities. Health is supported and maintained when ...
Utilizing developmental approaches and the Skeffington model, participants will learn both remediative and adaptive strategies to promote occupational performance. auditory, textual, visual 129 USD Subscription Unlimited COURSE Access for $129/year OnlineOnly OccupationalTherapy.com www.occupationaltherapy.com Pediatric Case Study: Child with ...
xviii, 183 pages : 28 cm "Cases in Pediatric Occupational Therapy: Assessment and Intervention is designed to provide a comprehensive collection of case studies that reflects the scope of current pediatric occupational therapy practice."--Publisher's website
The first article described a case report of occupational therapy provided to a child with a diagnosis of autism spectrum disorder and challenges in sensory integration in a clinic setting (Parham et al., 2019). This article describes the same child's occupational therapy service delivery by the occupational therapist working in the school ...
Today, I am doing a case study format. I want to give you a conceptual way to think about how to intervene with a child who has visual challenges that are affecting school performance, ADL performance, or play performance. Patrick is a seven-year-old male in second grade. He has difficulties with reading, completing his homework, and following ...
Cases in Pediatric Occupational Therapy: Assessment and Intervention is designed to provide a comprehensive collection of case studies that reflects the scope of current pediatric occupational therapy practice. Drs. Susan Cahill and Patricia Bowyer, along with more than 50 contributors, begin each section with an introduction to the practice setting and direct instructors and students to ...
For this case report, we focus on identifying and highlighting the distinct value of occupational therapy in the treatment of a pediatric patient with COVID-19 and MIS-C in an acute care hospital setting. This case study was completed in accordance with our institution's policy and did not require institutional review board review.
Pediatric OT Scenarios. Occupational therapy is a form of physical and mental rehabilitation that focuses on performing activities required in daily life. In the case of pediatric occupational therapy, this generally focuses on getting children to engage in play, school, and peer interactions. Pediatric occupational therapy helps children ...
OCCUPATIONAL THERAPY CASE STUDY Situation: Sam began occupational therapy to address oral motor challenges at age 2. He ingested all of his calories from formula bottle feedings. His weight was very low for his age. Sam demonstrated oral defensiveness and rejected, spit out and pushed away food when it was o˜ered to him. Sam demonstrated high ...
Cases in pediatric occupational therapy : assessment and intervention Authors : Susan M. Cahill ( Editor ) , Patricia Bowyer ( Editor ) Summary : "Cases in Pediatric Occupational Therapy: Assessment and Intervention is designed to provide a comprehensive collection of case studies that reflects the scope of current pediatric occupational ...
The occupational therapist used the Occupational Therapy Practice Guidelines for Children and Youth Ages 5-21 Years (Cahill & Beisbier, 2020) as a tool to guide decision making and considered Jacob's presentation in relation to the diagnoses addressed in the practice guidelines. The occupational therapist then reviewed the practice ...
In pediatric occupational therapy, there is insufficient evidence examining assessment tool selection by occupational therapists and how assessment tools contribute to occupation-based practice. To examine the perceptions of occupation-based assessment tool selection by pediatric occupational therapists, a phenomenological research study was ...
1. Select the pediatric case for study. Review child's diagnosis and medical history. Set up an initial meeting with the child and parents or guardians. Prepare a detailed initial assessment plan. Conduct initial assessment on physical, cognitive and emotional capabilities of the child. Record observations during the initial assessment.
Introduction. Occupational therapy intervention for children promotes engagement and participation in children's daily life roles (Mandich & Rodger, 2006).Children's roles include, developing personal independence, becoming productive and participating in play or leisure pursuits (Roger et al.).Inability to participate because of disease, disability or skill deficits, can cause marginalisation ...
Schaaf RC, Nightlinger KM. Occupational therapy using a sensory integrative approach: A case study of effectiveness. American Journal of Occupational Therapy. 2007; 61:239-246. [Google Scholar] Shoener RF, Kinnealey M, Koenig KP. You can know me now if you listen: Sensory, motor, and communication issues in a nonverbal person with autism.
For occupational therapy practitioners, understanding interoception and its impact on daily functioning is vital for providing effective interventions, particularly in pediatric populations. This comprehensive guide delves into the science of interoception, its relevance in occupational therapy, and evidence-based strategies to support ...
Pediatric occupational therapy practitioners frequently provide interventions for children with differences in sensory processing and integration. ... position sense, and endurance. For example, two case studies have demonstrated the benefits of a supervised strength-training intervention for children with DCD (Kaufman & Schilling, 2007; Menz ...
Including a relationship-focus in pediatric occupational therapy interventions requires practitioners to modify the way in which initial appointments, case history taking, and interventions occur. ... and that this translated across activities without a direct focus on these activities during therapy sessions. While this case study demonstrates ...
The client will be able to exhibit receptive and expressive communication skills - alert and responding to simple questions, at the end of 15 sessions. The client will be able to perform all ADL task with 1-2 verbal prompts and cues per task, after 5 sessions. The client will have established a daily routine for self-care, after 10 sessions.
Introduction. Occupational therapy intervention for children promotes engagement and participation in children's daily life roles (Mandich & Rodger, 2006).Children's roles include, developing personal independence, becoming productive and participating in play or leisure pursuits (Roger et al.).Inability to participate because of disease, disability or skill deficits, can cause marginalisation ...
A physical and occupational therapist providing you with evidence-based treatments and examples of documentation to show your skill. Case Study for Pediatric Occupational Therapy. Sign Up for a FREE Physical Therapy / Occupational Therapy Documentation Cheat Sheet!! The Note Ninjas
Abstract. The purpose of this qualitative constructivist grounded theory study was to develop a model to explain potential mechanisms of change in the nature-based pediatric occupational therapy process, based on analysis of the perspectives of occupational therapy practitioners currently engaging in nature-based practice with children.
Case Studies Meet Jimmy. Jimmy is 10 years old, he enjoys playing football and wants to do well at school. Jimmy has dyspraxia, or developmental co-ordination disorder. Dyspraxia is a well known condition, however the association between the condition and how it can affect a child at school is not so well understood.
Rehabilitation / methods*. Occupational therapy in pediatric rehabilitation focuses on the effects of diseases and of the environment on a child's abilities to function successfully in daily life settings (home, school and playground) and roles (family member, student, etc.). In this paper, the process of pediatric occupation ….
Entrustable Professional Activities (EPA)-based assessment is easily and intuitively used in evaluating the learning outcomes of competency-based medical education (CBME). This study aimed to develop an EPA for occupational therapy focused on providing health education and consultation (TP-EPA3) and examine its validity. Nineteen occupational therapists who had completed online training on the ...