Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Office of the Surgeon General (OSG). The Surgeon General’s Call to Action to Improve Maternal Health [Internet]. Washington (DC): US Department of Health and Human Services; 2020 Dec.


The Surgeon General’s Call to Action to Improve Maternal Health [Internet].
4 strategies and actions: improving maternal health and reducing maternal mortality and morbidity.
Given the importance of maternal health for our families, communities, and nation, addressing the unacceptable rates of maternal mortality and severe maternal morbidity calls for a comprehensive approach that addresses health from well before to well after pregnancy. A singular focus on the perinatal period would ignore upstream health factors associated with chronic conditions as well as other environmental and social factors that contribute to poor outcomes. 3 HHS has laid the framework by providing recommendations for preventive services that promote optimal women’s health. 79 , 80 , 81 The strategies and actions in this document are based on these recommendations as well as consensus statements and recommendations from other organizations. The following sections outline specific actions for addressing the conditions and risk factors outlined above as well as other factors that may impact maternal health. The opportunity for action exists across the spectrum of women and families; states, tribes, and local communities; healthcare professionals; healthcare systems, hospitals and birthing facilities; payors; employers; innovators, and researchers. Individuals, organizations and communities should select and implement actions as applicable to their needs. Regardless of organization or group, everyone can help to improve maternal health in the U.S.
EVERYONE CAN
- Recognize the need to address mental and physical health across the life course—starting with young girls and adolescents and extending through childbearing age. 3
- Support healthy behaviors that improve women’s health, such as breastfeeding, 82 smoking cessation, 83 and physical activity. 84
- Recognize and address factors that are associated with overall health and well-being, including those related to social determinants of health. 22
- Understand that maternal health disparities exist in the U.S., including geographic, racial and ethnic disparities ( Figures 3 – 7 ), and work to address them.
- Acknowledge that maternal age and chronic conditions, such as hypertension, obesity, and diabetes are risk factors for poor maternal health outcomes (See prior sections “ Differences in Maternal Mortality and Morbidity ” and “ Risks to Maternal Health ”).
- Learn about early ‘warning signs’ of potential health issues (such as fever, frequent or severe headaches, or severe stomach pain, to name a few 85 ) that can occur at any time during pregnancy or in the year after delivery.
- Work collaboratively to recognize the unique needs of women with disabilities and include this population of women in existing efforts to reduce maternal health disparities. 26 , 27 , 28
- WOMEN AND FAMILIES
Women can play a critical role in promoting, achieving, and maintaining their health and well-being, often with the support of fathers, partners, and other family members. Preventive health and wellness visits can provide women with screenings, risk factor assessment, support for family planning, immunizations, counseling, and education to promote optimal health. 79 Women can engage in healthy practices, monitor their overall health, and address conditions they may have such as hypertension, diabetes and obesity. Many resources in the form of books, mobile applications, social media, and guides provide information about what to expect before, during and after pregnancy as well as information on important health behaviors, preventive care, medications, and potential risks.
Prenatal appointments provide the opportunity for healthcare professionals to monitor pregnancy, perform prenatal screening tests, 85 discuss questions and concerns that women may have, including plans for delivery and infant feeding, and provide recommendations to promote a healthy pregnancy. 86 A statewide study of all live births in Pennsylvania and Washington showed that starting prenatal appointments in the second trimester instead of the first, or attending fewer prenatal appointments, was associated with a higher risk of unhealthy behaviors and adverse outcomes, including low gestational weight gain, prenatal smoking, and pregnancy complications. 87 Data also show disparities in initiating and/or receiving prenatal care, with non-Hispanic white (82.5 percent) and Asian women (81.8 percent) more likely to receive prenatal care in the first trimester than all other racial and ethnic groups, including Hispanic (72.7 percent), non-Hispanic black (67.1 percent), AI/AN (62.6 percent), and Native Hawaiian or Pacific Islander women (51.0 percent). 17
Women should also be supported after delivery to reduce the risk of adverse maternal and infant outcomes. For example, breastfeeding has demonstrated benefits for infants and can also be beneficial to mothers, including decreased bleeding after delivery and reduced risks of hypertension, type 2 diabetes, breast and ovarian cancer. 88 Black mothers are less likely to initiate breastfeeding than white or Hispanic mothers (74.0 percent versus 86.6 percent and 82.9 percent, respectively). 89 These data suggest opportunities for understanding and addressing these disparities.
WOMEN AND FAMILIES CAN
Focus on improving overall health 90.
Try to engage in healthy behaviors and practices by participating in regular physical activity, 84 eating healthy, 91 getting adequate sleep, 92 , 93 and getting ongoing preventive care that includes immunizations 57 and dental care. 94 Recognize that oral health is part of overall health and that pregnant mothers may be prone to gingivitis and cavities. 95 Abstain from tobacco 96 and other potentially harmful substances, including marijuana, 97 prior to and during pregnancy. As there is no amount of alcohol known to be safe during pregnancy or while trying to become pregnant, women should consider stopping all alcohol use when planning to become pregnant. 98 Follow medical advice for chronic health conditions such as diabetes and hypertension, learn family medical history, and adopt or maintain healthy lifestyles. Women who are planning or may become pregnant should take a daily folic acid supplement. 99 For women who are entering pregnancy at a later age or with chronic diseases or disorders, learn how to minimize associated risks through ongoing preventive and appropriate prenatal care.
PROMOTE POSITIVE INVOLVEMENT OF MEN AS FATHERS/PARTNERS DURING PREGNANCY, CHILDBIRTH, AND AFTER DELIVERY
Promote men’s positive involvement as partners and fathers. 100 Include men in decision-making to support the woman’s health, to the extent that it promotes and facilitates women’s choices and their autonomy in decision-making. 101
ATTEND HEALTH CARE APPOINTMENTS 79
Women should attend primary care, prenatal, postpartum, and any recommended specialty care visits and provide health information, including pregnancy history and complications, to their health care providers during all medical care visits, even in the years following delivery. 101 , 102 Know health numbers, such as blood pressure and body weight, and record them at each visit. If recommended, continue to monitor and record blood pressure in-between visits. 103 Those with diabetes should check and record your blood sugar regularly. 104
COMMUNICATE WITH HEALTHCARE PROFESSIONALS
Ask questions and talk to healthcare professionals about health concerns, including any symptoms you experience, past health problems, or concerns about potentially sensitive issues, such as IPV and substance use. 105 Be persistent or seek second opinions if a healthcare professional is not taking concerns seriously (See the Joint Commission “Speak Up” guide for ways patients can become active in their care 106 ).
LEARN HOW TO IDENTIFY PHYSICAL AND MENTAL WARNING SIGNS DURING AND AFTER PREGNANCY
Utilize resources that provide information about the changes that occur with a healthy pregnancy and how to recognize the warning signs 85 for complications that may need prompt medical attention. The CDC’s Hear Her campaign seeks to raise awareness of warning signs, empower women to speak up and raise concerns, and encourage their support systems and providers to engage with them in life-saving conversations. 107 Learn to recognize the symptoms of postpartum depression such as feelings of sadness, anxiety, or despair, especially those that interfere with daily activities, and seek support. 108
ENGAGE IN HEALTHY BEHAVIORS IN THE POSTPARTUM PERIOD
If electing to breastfeed, seek support as needed. Resources include healthcare providers, lactation consultants, lactation counselors, peer counselors, and others. Attend postpartum visits as they are the best way to assess physical, social, and psychological well-being and identify any new or unaddressed health issues that could affect future health. 109 Continue engaging in healthy behaviors after pregnancy, such as managing chronic disease and living a healthy lifestyle.
- STATES, TRIBES AND LOCAL COMMUNITIES
States, tribes, and local communities can create environments that are supportive of women’s health and tailored to local needs and challenges. They can create the infrastructure needed to engage in healthier lifestyles and to ensure access to high quality medical care.
Healthy People provides national goals to guide health promotion and disease prevention efforts in the U.S. and highlights the importance of creating social and physical environments that promote good health for all. 22 Often referred to as social determinants of health, the conditions into which people are born, live, work, play, worship, and age can strongly influence their overall health. 22 Examples of social determinants include access to educational opportunities, availability of resources to meet daily needs (e.g., healthy food options), public safety and exposure to crime. 22 Examples of physical determinants include natural and built environments (e.g., green space, sidewalks, bike lanes), and housing and community design, and exposure to physical hazards. 22 Case studies have demonstrated that health outcomes can be improved where there is a concerted and coordinated effort involving both healthcare systems and communities where their patients live. 110 , 111 , 112
Perinatal regionalization or risk-appropriate care 113 is a promising approach for improving maternal safety as it has been shown to be an effective strategy for improving neonatal outcomes, 114 though more research is needed to assess its impact on maternal health outcomes. States can explore this approach as well as other strategies to increase access to quality care, such as the adoption of telemedicine, and the review of the scope of practice laws (what health care professionals are authorized to do), licensure and recruitment policies. Perinatal Quality Collaboratives (PQCs) are state or multi-state networks of multidisciplinary teams that work to improve maternal and infant outcomes by advancing evidence-informed clinical practice through quality improvement initiatives. 115
States, tribes and local health agencies play a role in providing essential services to protect the health and promote the well-being of their communities through education, prevention, and treatment. They provide support for community-driven initiatives and evidence-based practices that address topics such as emerging infections (e.g., COVID-19), sexually transmitted infections, and immunizations. The role of public health is changing due to increased demands from chronic disease, new economic forces, and changing policy environment. 116 The National Consortium for Public Health Workforce released a Call to Action addressing the need for strategic skills in the public health workforce to enable collaboration across sectors to address the social and economic factors that drive health. 117
MMRCs Multidisciplinary committees that perform comprehensive reviews of deaths among women during and within a year of the end of pregnancy
Surveillance data can help to monitor trends and focus efforts to reduce maternal morbidity and mortality. States, tribes, and communities have the opportunity to assess maternal deaths, injuries and illnesses and identify strategies for preventing these adverse outcomes. The Centers for Disease Control and Prevention (CDC) supports states in establishing MMRCs to perform comprehensive reviews of deaths among women during pregnancy or within a year after birth, obtain better data on the circumstances and root causes surrounding each death, and develop recommendations for the prevention of these deaths. 117 However, MMRC reviews can lag by several years, and some states have not yet created MMRCs. Ensuring that MMRCs collect uniform data, such as through the Maternal Mortality Review Information Application (MMRIA), 118 will provide comprehensive national data on maternal mortality and result in more timely and detailed reporting to inform prevention efforts.
Representative population-based data on pregnancy and disability are lacking. 118 State health departments, researchers, and other stakeholders can work together to address gaps in surveillance and identify best practices for reducing health disparities, including among pregnant women with disabilities.
STATES, TRIBES, AND LOCAL COMMUNITIES CAN
Create social and physical environments that promote good health 22.
Improve factors that are associated with health and wellness, including safe communities, clean water and air, stable housing, access to affordable healthy food, public transportation, parks and sidewalks, and other social determinants of health. Support prevention of domestic violence and abuse. Consider addressing areas recognized as “food deserts” (areas with little access to affordable, nutritious food) or “food swamps” (areas with an abundance of fast food and junk food outlets). Encourage healthy eating initiatives tailored to the community such as community gardens, farmer’s markets, school programs, businesses’ support of healthy foods, as well as participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) for eligible women.
PROVIDE BREASTFEEDING SUPPORT AT THE INDIVIDUAL AND COMMUNITY LEVELS
Establish policies to support women’s abilities to breastfeed, to reach their breastfeeding goals once they return to their communities and worksites, and thus achieve full health benefits of breastfeeding for their babies and themselves. 119 , 120
STRENGTHEN PERINATAL REGIONALIZATION AND QUALITY IMPROVEMENT INITIATIVES
Consider adopting a classification system for maternal care that ensures women and infants receive risk-appropriate care in every region utilizing national-level resources, such as the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) joint consensus document on levels of maternal care, 121 and other state-level guidelines. Develop coordinated regional systems for risk-appropriate care that address maternal health needs.
PROMOTE COMMUNITY-DRIVEN INITIATIVES 101 AND WORKFORCE DEVELOPMENT
Pursue promising community-driven initiatives, such as the Health Resources and Services Administration’s (HRSA) Maternal and Child Health Bureau’s Healthy Start program 122 and the Best Babies Zone Initiative, 123 funded by the W.K. Kellogg Foundation, that aim to reduce disparities in short-term (e.g., access to maternal healthcare), medium-term (e.g., breastfeeding and postpartum visits), and/or long-term outcomes (e.g., premature births and low birth weight infants). Develop or recruit a workforce that supports the maternal health needs of the community. Incentivize healthcare professionals with obstetric training to serve in rural, remote or underserved areas. 124
ENSURE A BROAD SET OF OPTIONS FOR WOMEN TO ACCESS QUALITY CARE
Examine scope of practice and telehealth laws to maximize women’s access to a variety of healthcare professionals, 125 especially in rural regions and underserved areas, 125 while ensuring procedures are in place to address obstetric emergencies. Engage and collaborate with federal and tribal health systems within states to avoid duplication of services and support access to a full range of care. Support partnerships between academic medical centers and rural hospitals for staff education and training and improved coordination and continuity of care. Support state and regional PQCs in their efforts to improve the quality of care and outcomes for mothers and infants.
SUPPORT EVIDENCE-BASED PROGRAMS TO ADDRESS HEALTH RISKS BEFORE, DURING AND AFTER PREGNANCY
Provide funding for local implementation of evidence-based programs, such as home-visiting, substance use disorder treatment, tobacco cessation, mental health services and other programs as recommended by the Community Preventive Services Task Force. 126 Support local efforts to prevent family violence and provide support for women experiencing IPV. Educate the public about risk factors for high-risk pregnancies, pregnancy-related warning signs, risk-reducing behaviors, and the importance of prenatal and postpartum care.
IMPROVE THE QUALITY AND AVAILABILITY OF DATA ON MATERNAL MORBIDITY AND MORTALITY
Address challenges with vital statistics and data reporting, 127 , 128 such as racial misclassification, 129 and misclassification and documentation of the causes of death, and improve the accuracy of maternal mortality and morbidity reporting for national comparison and analysis. Enhance data and monitoring of racial and ethnic disparities. Expand and strengthen MMRCs to review and assess all pregnancy-associated deaths (the death of a woman while pregnant or within one year of the termination of pregnancy, regardless of the cause) 130 and identify opportunities for prevention.
- HEALTHCARE PROFESSIONALS
While states, tribes, and local communities help to ensure infrastructure and programmatic support for maternal health, individual healthcare professionals provide education, support, and care for women before, during, and after pregnancy.
The full range of healthcare professionals and teams should understand factors that contribute to women’s overall health and work to identify and mitigate potential pregnancy risks. Every medical appointment or interaction with health care professionals is an opportunity to ensure that standards of care and the full needs of women are being met. Given the vast diversity in geography, economy, and racial and ethnic make-up of communities across the U.S., healthcare professionals can ensure that the care they provide is scientifically-sound and culturally appropriate to the individual and their respective community. 101
Fragmented care across healthcare settings may inhibit providers from having a full understanding of a patient’s medical condition(s) and risks. 131 , 132 Many opportunities exist across providers to improve communication, including through care coordination, adoption of mobile applications, and enhanced interoperability of electronic health records (EHRs). Even healthcare professionals who do not normally care for pregnant women play a role in reducing maternal morbidity and mortality. Engaging and coordinating care among a diverse set of healthcare professionals, such as primary care providers, emergency department providers, dentists, cardiologists, endocrinologists, psychologists, and social workers, can be challenging, but strengthens the ability to identify, address, and prevent harm.
Various professional associations play a key role in developing standards of care to provide guidance on screenings, preventive care, prenatal and postpartum care, and management of obstetric emergencies. Associations are valuable resources for developing evidence-based guidelines on areas important to maternal health.
HEALTHCARE PROFESSIONALS CAN
Ensure quality preventive healthcare for all women, children, and families.
Increase knowledge, awareness, and utilization of clinical practice tools such as those associated with recommendations from the USPSTF; 133 the Women’s Preventive Services Guidelines; 79 Bright Futures Guidelines for Health Supervision of Infants, Children and Adolescents; 134 and the CDC. Use preventive health care and wellness visits to conduct screenings, assess risk factors, provide support for family planning, offer immunizations, and provide education and counseling to promote optimal health. Include such topics as folic acid supplementation for all women who are planning or capable of pregnancy, 100 breastfeeding, nutrition, physical activity, sleep, oral health, substance use, and injury and violence prevention. 91
ADDRESS DISPARITIES SUCH AS RACIAL, SOCIOECONOMIC, GEOGRAPHIC, AND AGE, AND PROVIDE CULTURALLY APPROPRIATE CARE 110 IN CLINICAL PRACTICES
Increase self and situational awareness of and attention to disparities. Participate in research to determine if provider training may improve patient-provider interactions. Learn how to identify and work to address inequities within health systems, processes, and clinical practices using standardized protocols. Provide culturally and linguistically appropriate services that respect and respond to individual needs and preferences. 135
HELP PATIENTS TO MANAGE CHRONIC CONDITIONS
Reduce the burden of chronic conditions, such as hypertension, diabetes, and obesity, as well as mental health and substance use disorders (See prior section “ Risks to Maternal Health ”) on women’s health across the lifespan by helping them to manage these conditions. For example, refer women at risk to diabetes educators, nutritionists, and mental health professionals. Conduct cardiovascular risk evaluation, to include history of hypertensive disorders of pregnancy and gestational diabetes, 136 and provide risk reduction strategies for women of childbearing age before, during, and after pregnancy.
COMMUNICATE WITH WOMEN AND THEIR FAMILIES ABOUT PREGNANCY
Listen to women and their family members’ concerns before, during, and after delivery. Engage the family in creating a supportive environment. Discuss and make available options for traditional practices that may vary by culture and personal preferences. Educate about warning signs 85 during pregnancy and the postpartum period. 137 Use culturally acceptable and easily understandable methods of communication. 138 Link women with a substance use disorder to family-centered treatment approaches. 139
FACILITATE TIMELY RECOGNITION AND INTERVENTION OF EARLY WARNING SIGNS DURING AND UP TO ONE YEAR AFTER PREGNANCY
Track patient vital signs (e.g., blood pressure) across healthcare visits, including prenatal, initial hospital admission, and postpartum visits. Learn to recognize and react to signs and symptoms associated with hemorrhage, pre-eclampsia, hypertension, cardiomyopathy, infection, embolism, substance use, and mental health issues. Use screenings and tools to identify warning signs early so women can receive timely treatment. Coordinate care across obstetrician-gynecologists and primary care providers and consult with specialists, as needed.
IMPROVE HEALTHCARE SERVICES DURING THE POSTPARTUM PERIOD AND BEYOND
Communicate the importance of postpartum visits, including the ACOG recommendation for an initial assessment within the first 3 weeks postpartum followed by ongoing care as needed and a comprehensive visit within 12 weeks after delivery. 110 Non-obstetric providers can have an important role to play. For example, pediatricians could screen for maternal mental health during well-baby visits utilizing validated tools, such as the Edinburgh Postnatal Depression scale. 140 Other non-obstetric providers should ask about prior pregnancies when taking medical history and be aware of pregnancy-related morbidities that can occur up to one year post-delivery and those that raise life-time risks, such as gestational diabetes, 141 gestational hypertension, and preeclampsia, 34 , 35 , 36 , 37 and follow recommended guidelines. 102 , 103
PARTICIPATE IN QUALITY IMPROVEMENT AND SAFETY INITIATIVES TO IMPROVE CARE
Engage with state and/or national quality collaboratives and patient safety initiatives to improve maternal health. (See section “ Health Systems, Hospitals, and Birthing Facilities ”). Consider using resources, such as the Agency for Healthcare Research and Quality’s Toolkit for Improving Perinatal Safety 142 which includes patient safety bundles, TeamSTEPPS® (team strategies and techniques to enhance performance and patient safety 143 ) and simulation training.
- HEALTH SYSTEMS, HOSPITALS, AND BIRTHING FACILITIES
Health systems provide comprehensive care for the full range of women’s health before, during, and after pregnancy. Within these systems, hospitals provide the vast majority of delivery services. In 2018, approximately 98 percent of all live births occurred in hospital settings. 17 Over the past two decades, many rural counties have lost their hospital-based obstetric services. 144 In these areas, women are more likely to have out-of-hospital births and to deliver in hospitals without obstetric units, as compared to those living in rural counties that maintained hospital-based obstetric services. 145 Additionally, in rural or underserved areas, access to maternal care in the prenatal and postpartum period may be limited. 125
Hospitals and health systems can address this through strategies such as telemedicine and linking facilities that do not offer planned childbirth services with those that do, and facilitating prompt consultation and safe transportation to the appropriate level of maternal care. The designation of levels of care, as outlined in the ACOG/SMFM Levels of Maternal Care, helps to ensure that women receive care at facilities that are best equipped to address their needs. 122 The CDC developed the Levels of Care Assessment Tool (LOCATe) to assist states and other jurisdictions in assessing and monitoring levels of care. 146
Quality improvement strategies, such as participation in PQCs 116 and implementation of maternal “safety bundles,” may help hospitals and health systems to reduce maternal morbidity and mortality. 147 A safety bundle is a set of practices and policies designed to identify appropriate and timely actions the health care staff can take in response to maternal complications. The Alliance for Innovation on Maternal Health (AIM) is a maternal safety and quality improvement initiative that addresses preventable causes of maternal morbidity and mortality through the implementation of bundles to identify and swiftly respond to common pregnancy-related complications. 148 The President’s FY 2021 Budget proposes $15 million to expand the AIM Program. Adoption of safety bundles by hospitals requires leadership and clinical team commitment, as well as training and implementation support.
Offering diverse provider types for maternal care, such as family physicians, midwives and support personnel (e.g., doulas) in hospitals and other healthcare settings may support women’s preferences. Midwifery care is provided in hospital settings, birth centers, and home settings, and can be a valuable part of women’s health care. 148
Medical history associated with pregnancy and delivery does not always travel with women in their future medical records or across different types of providers. Addressing this is key to ensuring coordinated care across providers within and between health systems.
HEALTH SYSTEMS, HOSPITALS AND BIRTHING FACILITIES CAN
Ensure availability of risk-appropriate care across the healthcare system.
Ensure staff, equipment, and services are available to address the health needs of women with both low- and high-risk pregnancies. Implement guidelines for levels of maternal care at all birthing hospitals and facilities and work with states to adopt standardized criteria and uniform definitions for levels of maternal care (See prior section, “ States, Tribes and Local Communities ”).
IMPROVE ACCESS TO CARE AND COMMUNICATION WITH PATIENTS
Adopt methods for improving access to care and communication, especially in rural or underserved areas or when conditions limit face-to-face interactions, while ensuring patient safety and quality of care. These methods can include telehealth and remote monitoring, among others. Work with health insurers to address gaps in access to medical facilities, equipment, information, and transportation for women with disabilities. 149
IMPROVE THE QUALITY AND SAFETY OF PERINATAL CARE
Provide evidence-based clinical practice, including utilization of standardized protocols related to pregnancy, delivery, and the postpartum period. Consider other resources, such as the Agency for Healthcare Research and Quality’s Toolkit for Improving Perinatal Safety. 143 Participate in state, or regional PQCs to implement quality improvement efforts and monitor progress with standardized data. Consider routine surveillance and monitoring of “near misses” and other SMM events.
PROVIDE COMPREHENSIVE DISCHARGE INSTRUCTIONS
Ensure discharge processes include education for women and families about warning signs (e.g., Association of Women’s Health, Obstetrics and Neonatal Nurses’ Save Your Life discharge instructions 150 ), and the importance of postpartum visits. 110
TRAIN HEALTHCARE PROFESSIONALS IN NON-OBSTETRIC SETTINGS ABOUT OBSTETRIC EMERGENCIES
Standardize protocols and training to respond to obstetric emergencies in the emergency department 8 and other non-obstetric settings, to include transportation to the most appropriate facility for care. Train non-obstetric clinicians to consider and seek recent pregnancy history when assessing patients. 8
ENCOURAGE OBSTETRIC CARE-TRAINED PROVIDERS TO SERVE IN RURAL, REMOTE AND UNDERSERVED AREAS 125
Support additional training in obstetric care in residencies for family physicians, especially those who will practice in rural, remote or underserved areas.
OFFER A VARIETY OF HEALTHCARE PROVIDER AND SUPPORT OPTIONS TO FIT MATERNAL PREFERENCES AND NEEDS
Leverage and incorporate midwives into hospital obstetric care and other community programs. 126 Support maternal-infant home visiting and away-from-home programs/pre-maternal homes (where pregnant women from remote areas can stay before the birth of their child 101 ) to support care.
ADDRESS DISPARITIES AND PROVIDE CULTURALLY APPROPRIATE CARE IN HEALTHCARE SETTINGS
Provide education and training on disabilities. Identify and work to address inequities within health systems, processes, and clinical practices. Ensure the availability of culturally and linguistically appropriate services that respect and respond to individual needs and preferences. 136
SUPPORT BREASTFEEDING PRACTICES
Implement hospital or birthing center initiatives, such as the Baby Friendly Hospital Initiative, to help women successfully initiate and continue breastfeeding their infants. 151 Ensure access to lactation support providers for breastfeeding women.
COORDINATE WITH COMMUNITY RESOURCES
Consider coordination with resources, such as group prenatal programs, 152 WIC, 153 home visiting programs, 154 and others that address social determinants of health. Consider alternative approaches to expanding access and education, to include use of community health workers. 155
ENHANCE COMMUNICATION WITHIN AND ACROSS HEALTHCARE SETTINGS
Adopt methods to ensure the seamless transition of information between providers along the care continuum, including strengthening communication and care coordination among obstetrician-gynecologists and other health care professionals.
Health insurance coverage is a key determinant of health care access and utilization. 156 Payors – including private health insurers, state-based Medicaid and the Children’s Health Insurance Program (CHIP) -- can play a key role in addressing maternal health by helping to ensure affordability of and access to high quality preconception, prenatal, delivery, and postpartum care. 157 , 158
Reimbursement for, and access to, comprehensive care, such as preventive services recommended by the USPSTF (A or B rating), 134 Women’s Preventive Services Initiative, 79 and Bright Futures Guidelines for Health Supervision of Infants, Children and Adolescents, 135 can ensure women and children receive recommended services. These services may include preventive screening (e.g., blood pressure, weight status, diabetes, infectious diseases, sexually transmitted infections, cancer) and vaccinations, breastfeeding support, mental health support, substance use screening and treatment, and screening for intimate partner and family violence.
Ensuring a wide range of healthcare professionals are included in a health plan’s network may broaden women’s access to comprehensive services that address the full spectrum of care. Coverage of programs, such as those that fund transportation to appointments, or technology, such as applications that facilitate chronic condition management and timely and convenient communication, can reduce barriers to care.
Overall, while there are many strategies that payors can consider for helping to improve maternal health, including those outlined below, more research is needed to assess the impact of these actions on maternal health outcomes.
PROMOTE ACCESS AND PAYMENT FOR WOMEN’S HEALTH SERVICES ACROSS THE LIFESPAN
Develop services and networks to provide care before, during, and after pregnancy, including pre-pregnancy counseling. Reimburse time spent with healthcare professionals to discuss healthy lifestyles, family planning, optimal management of chronic conditions (e.g., diabetes, hypertension, obesity), substance use disorders, and mental health conditions. Reduce cost barriers and ensure payment options are understood by women and their families.
ALIGN FINANCIAL INCENTIVES WITH THE FULL RANGE OF PERINATAL CARE
Provide financial reimbursement and quality incentives related to improving maternal care for women of all races and ethnicities and implementing standards of care. Implement value-based payment incentives for innovative ways of delivering high quality care. Support efforts to reduce barriers that patients may face when accessing healthcare, such as transportation, language needs, or geographic isolation. Promote telehealth, as appropriate, for women in underserved, rural or remote areas or under conditions that limit face-to-face interaction and support remote monitoring of highly prevalent and harmful conditions like hypertension and diabetes.
ENSURE A WIDE RANGE OF HEALTHCARE PROFESSIONALS ARE INCLUDED IN A HEALTH PLAN’S NETWORK
Also, consider coverage for supportive services, such as doulas, lactation support, and home visiting programs.
MONITOR POPULATION-LEVEL TRENDS AND IDENTIFY OPPORTUNITIES FOR IMPROVEMENT
Utilize data to inform strategies for improving maternal health and support provider participation in quality improvement efforts in states and local communities, such as PQCs. Track trends in quality of care and health care utilization and develop approaches that may reduce identified disparities.
Employers play a key role in establishing norms and expectations around the support of working mothers, including paid family leave and workplace policies.
The postpartum period is a crucial time for women to recover from birth, bond with their new infant(s), and firmly establish breastfeeding practices. Lawmakers have been working to prioritize parental leave for the American people. In 1993, the Family and Medical Leave Act (FMLA) 159 was signed into law to provide certain employees up to 12 weeks of unpaid leave, including after the birth or adoption of a child. 160 FMLA applies to public agencies (local, state, or federal government agencies), public and private elementary and secondary schools, and private-sector employers with 50 or more employees. 161 FMLA covers more than half of the workforce, however, some eligible women may be unable to take this unpaid leave for financial reasons. 161
In December 2019, Congress passed and the President signed into law a major improvement in the compensation and benefits package for the government’s 2.1 million Federal civilian employees as part of the National Defense Authorization Act (NDAA). 162 The Act provides Federal civilian employees with up to 12 weeks of paid parental leave to care for a new child, whether through birth, adoption, or foster care, beginning in October 2020.
In addition to parental leave, other federal worker protection laws have been enacted, such as the Fair Labor Standards Act (FLSA), which ensures that American workers receive a minimum wage. 163 In 2010, the FLSA was amended to require employers to provide reasonable break time and a space for an employee to express breast milk for her nursing child for one year after the child’s birth. 164
Employers have an opportunity to play a key role in supporting women during their pregnancies and in the postpartum period. Due to the recognized health and economic benefits, ACOG endorses paid parental leave, including full benefits and 100% of pay for at least six weeks after delivery. 165 In addition to paid leave 166 in the postpartum period, other family-friendly benefits such as flexible work schedules, preventive medical care, and childcare for sick children may improve recruitment of potential employees and greater retention of current employees.
Employers who offer health insurance are in a position to advocate for comprehensive care coverage to support maternal health. Effective workplace programs and policies can also reduce health risks and improve the quality of life for workers, including women and their families. 167
Overall, there are many strategies that employers can consider that may help to improve maternal health, including those outlined below, however, more research is needed to assess the impact of these actions on maternal health outcomes.
EMPLOYERS CAN
Adopt and support family-friendly policies.
Consider paid family leave 168 and other family-friendly policies, such as flexible work schedules and on-site or easy-to-access high quality childcare. These policies may also help with recruitment and retention of valuable employees. 167
SUPPORT BREASTFEEDING
Provide lactation spaces for breastfeeding mothers, including for those who do not qualify under the FLSA. 166 Consider going beyond what is required in the FLSA 164 (e.g., break time, private rooms) by providing hospitable and welcoming environments, including access to refrigerators, comfortable chairs, sinks and microwaves, for applicable employees.
ENSURE ROBUST MATERNAL CARE THROUGH EMPLOYER-SPONSORED COVERAGE
Negotiate with health insurers on behalf of employees for comprehensive care, including expanding options for receiving care (e.g., telehealth), reducing out-of-pocket costs, and implementing innovative approaches to monitor and manage risk factors (See prior section, “ Payors ”).
DEVELOP A WORKPLACE HEALTH PROGRAM
Develop or adopt workplace programs and policies that promote healthy behaviors, such as ready access to local fitness facilities, healthy vending or cafeteria options, tobacco-free environments and work settings free of environmental threats. Provide worksite blood pressure screening, health education, and lifestyle counseling to help employees control their blood pressure. 169
Innovative approaches across the health care arena can improve maternal health outcomes through policies, technology, systems, products, services, delivery methods, and models of care.
For example, while diabetes educators and nutritionists may already be included in some models of obstetric care, the inclusion of hypertension educators may be an innovative approach to further enhance comprehensive care in the obstetric setting. Technological innovation, such as mobile or computer-based applications, may help to monitor and/or manage women’s health during and beyond pregnancy. This could include mobile applications or monitoring systems that can help to manage conditions, such as diabetes or hypertension. For example, HRSA’s Remote Pregnancy Monitoring Challenge supports innovative-technology-based solutions to help providers remotely monitor the health of pregnant women while empowering these women to monitor their own health and healthcare. 170
Improvements and innovations in EHR technology offer an opportunity for improving maternal health. Interoperability between systems can allow providers to have a more complete view of a woman’s health by incorporating information from various clinical settings and systems. However, the demands of the current EHR systems may take time away from direct patient-provider communication. EHR systems should be improved to ensure they are provider-friendly and valuable to health care professionals. They should also incorporate improvements such as recommended care guidelines and clinical decision support tools, and facilitate linkage of maternal health records with infant health records.
Finally, innovation in delivery methods can address access issues for women who have barriers to care, such as those living in rural or underserved areas, or with limited transportation, or when conditions limit face-to-face interactions. Telehealth innovators can help states and providers identify opportunities for connecting women with a broad range of services to meet their needs. This could include providing remote access to obstetricians, maternal-fetal medicine and other specialists.
Listed below are some topic areas for innovators to consider that may improve maternal health. Innovations should be evaluated to assess their impact on maternal health outcomes.
INNOVATORS CAN
Improve communication between providers and women.
Decrease burden of EHRs on providers to allow more time for communication with patients. Develop mobile applications to facilitate communications during and after pregnancy so that women can conveniently raise issues or concerns to providers and providers can remotely monitor key vital signs. Such applications can focus on various aspects of prenatal and postpartum care and can involve a team of healthcare professionals. Consider developing applications tailored to a variety of cultures, health literacy levels, and racial and ethnic populations and incorporating human-centered design in the development of these applications.
PROMOTE COORDINATION OF CARE ACROSS HEALTHCARE PROFESSIONALS
Help to address a fragmented system by facilitating communication across different providers using innovative approaches.
DEVELOP AND/OR PARTICIPATE IN NEW MODELS OF MATERNAL CARE
Consider models of care that address maternal health risk factors, such as hypertension, diabetes, unhealthy weight, substance use disorders, mental health conditions, and IPV, to name a few. For example, the Center for Medicare and Medicaid Innovation’s Maternal Opioid Misuse (MOM) Model supports the coordination of care and integration of critical health services for pregnant and postpartum Medicaid beneficiaries with opioid use disorder. This, and other innovative payment and delivery models have the potential to improve quality of care for mothers and infants. 171
EXPAND DELIVERY METHODS FOR ACCESSING SPECIALTY CARE
For example, telehealth companies can better meet maternal health needs by designing technology that connects women to needed specialty care providers (e.g., obstetricians, maternal-fetal medicine specialists, cardiologists, endocrinologists, pulmonologists, nephrologists, nutritionists, and mental health professionals) and services.
- RESEARCHERS
A critical component of developing solutions and monitoring their impact is the ability to glean information from reliable and comprehensive data; however, there are substantial data limitations and gaps in existing research on maternal health. Further, clinical studies often exclude pregnant women due to an increased risk or concern for adverse outcomes in this population, particularly in research for therapeutic products. Researchers have opportunities to advance this area by adding to the field of evidence on clinical outcomes and by improving the quality of data that are available for analysis.
In clinical arenas, more outcomes-based research would be valuable for understanding the interaction of comorbidities during and after pregnancy and the effectiveness of selected interventions on improving maternal health. More research is needed on disease processes and clinical interventions, protective factors, demographic risk factors, racial disparities, and health system factors. 172
Research is also needed to fill clinical gaps in knowledge related to the defining and treating medical conditions that are known risk factors for maternal mortality, including preeclampsia, cardiovascular disease, peripartum cardiomyopathy, and hemorrhage. 173 , 174 , 175 Research on screening algorithms, risk assessments, and diagnosis involving biomarkers could help to improve timeliness of the identification of women with these conditions and their referral to treatment. 175 , 176 The National Institutes of Health (NIH) supports research addressing many aspects of maternal health.
Evidence has been provided throughout this document for many strategies and actions, however, more research is needed for others, particularly those in the “ Payors ” and “ Employers ” section. Researchers should consider examining those areas, as well as those listed below.
RESEARCHERS CAN
Identify biological, environmental, and social factors that affect maternal health.
Consider analyzing data from NIH’s PregSource®, a crowdsourcing research project designed to improve the understanding of pregnancy by gathering information directly from pregnant women via confidential online questionnaires. 177 The Pregnancy Risk Assessment and Monitoring System (PRAMS) 178 and the National Health and Nutrition Examination Survey (NHANES) 179 are examples of publicly available data sources that can be used for analysis. The Transformed Medicaid Statistical Information System (T-MSIS) also has data and research-ready files specific to Medicaid and CHIP information. 180
ADVANCE A RESEARCH AGENDA, SUCH AS DISCUSSED IN THE HHS ACTION PLAN 181 , TO IDENTIFY EFFECTIVE, EVIDENCE-BASED CLINICAL BEST PRACTICES AND HEALTHCARE SYSTEM FACTORS, INCLUDING RESEARCH ON REDUCING DISPARITIES
Conduct research to identify, develop, and rigorously test clinical interventions to address risk factors; identify healthcare factors (e.g., quality of care); and provide insights into healthcare delivery approaches (e.g., care coordination, innovative models of care) for improving access to high-quality maternal health care. Support research to understand, prevent, and reduce adverse maternal health outcomes among racial and ethnic minority women, those who are socioeconomically disadvantaged, and those in rural, remote and/or underserved areas. This should include exploring the potential effects of inequities within health systems, processes, and clinical practices on maternal health outcomes.
EXPAND RESEARCH TO DEVELOP SUFFICIENT EVIDENCE ON MEDICATIONS AND TREATMENT
Adopt recommendations made by the HHS Task Force on Research Specific to Pregnant Women and Lactating Women (PRGLAC), 182 to increase research for therapeutic products already in use by pregnant or lactating women and for existing therapeutic products not currently licensed for use during pregnancy, but with potential benefit for pregnant women and their infants, and to increase discovery and development of new therapeutic products for these populations.
ENHANCE MATERNAL HEALTH SURVEILLANCE BY IMPROVING THE ACCURACY, QUALITY, CONSISTENCY, SPECIFICITY, TRANSPARENCY, TIMELINESS, AND STANDARDIZATION OF EPIDEMIOLOGICAL DATA ON MATERNAL HEALTH
Improve data quality and timeliness; enhance data and monitoring of racial, ethnic and geographic disparities, and disparities among women with disabilities; and assess strategies to leverage and harmonize national data systems for monitoring maternal health.
Unless otherwise noted in the text, all material appearing in this work is in the public domain and may be reproduced without permission. Citation of the source is appreciated.
- Cite this Page Office of the Surgeon General (OSG). The Surgeon General’s Call to Action to Improve Maternal Health [Internet]. Washington (DC): US Department of Health and Human Services; 2020 Dec. 4, STRATEGIES AND ACTIONS: IMPROVING MATERNAL HEALTH AND REDUCING MATERNAL MORTALITY AND MORBIDITY.
- PDF version of this title (15M)
In this Page
Other titles in this collection.
- Publications and Reports of the Surgeon General
Recent Activity
- STRATEGIES AND ACTIONS: IMPROVING MATERNAL HEALTH AND REDUCING MATERNAL MORTALIT... STRATEGIES AND ACTIONS: IMPROVING MATERNAL HEALTH AND REDUCING MATERNAL MORTALITY AND MORBIDITY - The Surgeon General’s Call to Action to Improve Maternal Health
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Maternal and Child Health (MCH) Handbook and Its Effect on Maternal and Child Health Care: A Systematic Review and Meta-Analysis

2017, Journal of Community Medicine & Public Health
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Search by keyword
- Search by citation
Page 1 of 4
National chlorhexidine coverage and factors associated with newborn umbilical cord care in Bangladesh and Nepal: a cross-sectional analysis using household data
Preventable newborn deaths are a global tragedy with many of these deaths concentrated in the first week and day of life. A simple low-cost intervention, chlorhexidine cleansing of the umbilical cord, can prev...
- View Full Text
Racial and ethnic differences in the risk of recurrent preterm or small for gestational age births in the United States: a systematic review and stratified analysis
The risk of recurrent adverse birth outcomes has been reported worldwide, but there are limited estimates of these risks by social subgroups such as race and ethnicity in the United States. We assessed racial ...
Hydrocolpos causing bowel obstruction in a preterm newborn: a case report
Imperforate hymen is the most common congenital defect of the female urogenital tract. The spectrum of clinical manifestations is broad, ranging from mild cases undiagnosed until adolescence to severe cases of...
Neonatal blood pressure by birth weight, gestational age, and postnatal age: a systematic review
Blood pressure is a vital hemodynamic marker during the neonatal period. However, normative values are often derived from small observational studies. Understanding the normative range would help to identify i...
Assessing the agreement of chronic lung disease of prematurity diagnosis between radiologists and clinical criteria
Chronic lung disease of prematurity (CLD) is the most prevalent complication of preterm birth and indicates an increased likelihood of long-term pulmonary complications. The accurate diagnosis of this conditio...
Perinatal dengue and Zika virus cross-sectional seroprevalence and maternal-fetal outcomes among El Salvadoran women presenting for labor-and-delivery
Despite maternal flavivirus infections’ linkage to severe maternal and fetal outcomes, surveillance during pregnancy remains limited globally. Further complicating maternal screening for these potentially tera...
Examination of risk factors for high Edinburgh postnatal depression scale scores: a retrospective study at a single university hospital in Japan
Perinatal mental health, such as postpartum depression, is an important issue that can threaten the lives of women and children. It is essential to understand the risk factors in advance and intervene before t...
Evaluating mean platelet volume and platelet distribution width as predictors of early-onset pre-eclampsia: a prospective cohort study
Platelets are pivotal players in the pathophysiology of pre-eclampsia, with observed lower counts in affected individuals compared to normotensive counterparts. Despite advancements, the elusive cause of pre-e...
Association between social relationship of mentors and depressive symptoms in first-time mothers during the transition from pregnancy to 6-months postpartum
First-time motherhood is characterized by high psychosocial distress, which untreated, has serious consequences. Informal social support provided by specially trained mentors may be protective against postpart...
Dietary supplement use among lactating mothers following different dietary patterns – an online survey
Breastfeeding is important for the healthy growth and development of newborns, and the nutrient composition of human milk can be affected by maternal nutrition and supplementation. In Germany, iodine supplemen...
Unconditional cash transfers for preterm neonates: evidence, policy implications, and next steps for research
To address socioeconomic disparities in the health outcomes of preterm infants, we must move beyond describing these disparities and focus on the development and implementation of interventions that disrupt th...
That head lag is impressive! Infantile botulism in the NICU: a case report
Infantile botulism (IB) is a devastating and potentially life-threatening neuromuscular disorder resulting from intestinal colonization by Clostridium botulinum and the resultant toxin production. It can present ...
Maternal education and its association with maternal and neonatal adverse outcomes in live births conceived using medically assisted reproduction (MAR)
To examine the association between maternal education and adverse maternal and neonatal outcomes in women who conceived using medically assisted reproduction, which included fertility medications, intrauterine...
The use of projected autonomy in antenatal shared decision-making for periviable neonates: a qualitative study
In this study, we assessed the communication strategies used by neonatologists in antenatal consultations which may influence decision-making when determining whether to provide resuscitation or comfort measur...
Sub-optimal maternal gestational gain is associated with shorter leukocyte telomere length at birth in a predominantly Latinx cohort of newborns
To assess in utero exposures associated with leukocyte telomere length (LTL) at birth and maternal LTL in a primarily Latinx birth cohort.
Maternal and perinatal outcomes of women with vaginal birth after cesarean section compared to repeat cesarean birth in select South Asian and Latin American settings of the global network for women’s and children’s health research
Our objective was to analyze a prospective population-based registry including five sites in four low- and middle-income countries to observe characteristics associated with vaginal birth after cesarean versus...
Expressed breast milk and maternal expression of breast milk for the prevention and treatment of neonatal hypoglycemia: a systematic review and meta-analysis
Worldwide, many guidelines recommend the use of expressed breast milk (EBM) and maternal expression of breast milk for the prevention and treatment of neonatal hypoglycemia. However, the impact of both practic...
Maternal healthcare use by women with disabilities in Rajasthan, India: a secondary analysis of the Annual Health Survey
Women with disabilities face a number of barriers when accessing reproductive health services, including maternal healthcare. These include physical inaccessibility, high costs, transportation that is not acce...
Intravenous immunoglobulin treatment of congenital parvovirus B19 induced anemia - a case report
Parvovirus is a common childhood infection that could be very dangerous to the fetus, if pregnant women become infected. The spectrum of effects range from pure red blood cell aplasia with hydrops fetalis to m...
Benzylpenicillin concentrations in umbilical cord blood and plasma of premature neonates following intrapartum doses for group B streptococcal prophylaxis
Dutch obstetrics guideline suggest an initial maternal benzylpenicillin dose of 2,000,000 IU followed by 1,000,000 IU every 4 h for group-B-streptococci (GBS) prophylaxis. The objective of this study was to ev...
What are the barriers preventing the screening and management of neonatal hypoglycaemia in low-resource settings, and how can they be overcome?
Over 25 years ago, the World Health Organization (WHO) acknowledged the importance of effective prevention, detection and treatment of neonatal hypoglycaemia, and declared it to be a global priority. Neonatal ...
Correction to: Congenital pleuropulmonary blastoma in a newborn with a variant of uncertain significance in DICER1 evaluated by RNA-sequencing
The original article was published in Maternal Health, Neonatology and Perinatology 2023 9 :4
Benefits of maternally-administered infant massage for mothers of hospitalized preterm infants: a scoping review
Infant massage (IM) is a well-studied, safe intervention known to benefit infants born preterm. Less is known about the benefits of maternally-administrated infant massage for mothers of preterm infants who of...
Burden of intestinal parasitic infections and associated factors among pregnant women in East Africa: a systematic review and meta-analysis
The ultimate goal of preventing intestinal parasites among pregnant women is to reduce maternal and newborn morbidity and mortality. Numerous primary studies were conducted in East Africa presented intestinal ...
Congenital pleuropulmonary blastoma in a newborn with a variant of uncertain significance in DICER1 evaluated by RNA-sequencing
Pleuropulmonary blastoma (PPB) is a rare mesenchymal malignancy of the lung and is the most common pulmonary malignancy in infants and children. Cystic PPB, the earliest form of PPB occurring from birth to app...
The Correction to this article has been published in Maternal Health, Neonatology and Perinatology 2023 9 :7
Association of maternal nationality with preterm birth and low birth weight rates: analysis of nationwide data in Japan from 2016 to 2020
The rate of low birth weight or preterm birth is known to vary according to the birth place of mothers. However, in Japan, studies that investigated the association between maternal nationalities and adverse b...
Systemic vasculitis diagnosed during the post-partum period: case report and review of the literature
The vasculitis diagnosed specifically in the post-partum period are less well known. We report here such a case followed by a descriptive review of the literature.
Addressing ethical issues related to prenatal diagnostic procedures
For women of advanced maternal age or couples with high risk of genetic mutations, the ability to screen for embryos free of certain genetic mutations is reassuring, as it provides opportunity to address age-r...
Retraction Note: Prevalence and associated factors of early initiation of breastfeeding among women delivered via Cesarean section in South Gondar zone hospitals Ethiopia, 2020
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1186/s40748-020-00121-3.
Non-invasive sensor methods used in monitoring newborn babies after birth, a clinical perspective
Reducing the global new-born mortality is a paramount challenge for humanity. There are approximately 786,323 live births in the UK each year according to the office for National Statistics; around 10% of thes...
Analysis of association between low birth weight and socioeconomic deprivation level in Japan: an ecological study using nationwide municipal data
Several international studies have indicated an association between socioeconomic deprivation levels and adverse birth outcomes. In contrast, those investigating an association between socioeconomic status and...
Case report of congenital methemoglobinemia: an uncommon cause of neonatal cyanosis
Methemoglobinemia can be an acquired or congenital condition. The acquired form occurs from exposure to oxidative agents. Congenital methemoglobinemia is a rare and potentially life-threatening cause of cyanos...
Prenatal exposure to tobacco and adverse birth outcomes: effect modification by folate intake during pregnancy
Fetal exposure to tobacco increases the risk for many adverse birth outcomes, but whether diet mitigates these risks has yet to be explored. Here, we examined whether maternal folate intake (from foods and sup...
Nasolabial and distal limbs dry gangrene in newborn due to hypernatremic dehydration with disseminated intravascular coagulation: a case report
Gangrene is the death of an organ or tissue due to lack of blood supply or bacterial infection. In neonates, gangrene is usually caused by sepsis, dehydration, maternal diabetes, asphyxia, or congenital antico...
Evidence based recommendations for an optimal prenatal supplement for women in the US: vitamins and related nutrients
The blood levels of most vitamins decrease during pregnancy if un-supplemented, including vitamins A, C, D, K, B1, B3, B5, B6, folate, biotin, and B12. Sub-optimal intake of vitamins from preconception through...
Effects of inter-pregnancy intervals on preterm birth, low birth weight and perinatal deaths in urban South Ethiopia: a prospective cohort study
Preterm birth, low birth weight and perinatal deaths are common adverse perinatal outcomes that are linked with each other, and a public health problems contributing to neonatal mortality, especially in develo...
Prematurity and low birth weight: geospatial analysis and recent trends
Prematurity and low birth weight are of concern in neonatal health. In this work, geospatial analysis was performed to identify the existence of statistically significant clusters of prematurity and low birth ...
CNS Malformations in the Newborn
Structural brain anomalies are relatively common and may be detected either prenatally or postnatally. Brain malformations can be characterized based on the developmental processes that have been perturbed, ei...
Outcomes of multiple gestation births compared to singleton: analysis of multicenter KID database
The available data regarding morbidity and mortality associated with multiple gestation births is conflicting and contradicting.
Outcomes of neonatal hypothermia among very low birth weight infants: a Meta-analysis
Neonatal admission hypothermia (HT) is a frequently encountered problem in neonatal intensive care units (NICUs) and it has been linked to a higher risk of mortality and morbidity. However, there is a disparit...
Incidence and determinants of perinatal mortality among women with obstructed labour in eastern Uganda: a prospective cohort study
In Uganda, the incidence and determinants of perinatal death in obstructed labour are not well documented. We determined the incidence and determinants of perinatal mortality among women with obstructed labour...
The risk of diabetes after giving birth to a macrosomic infant: data from the NHANES cohort
Gestational diabetes (GDM) increases the risk of developing type 2 diabetes and thus warrants earlier and more frequent screening. Women who give birth to a macrosomic infant, as defined as a birthweight great...
Methods for exploring the faecal microbiome of premature infants: a review
The premature infant gut microbiome plays an important part in infant health and development, and recognition of the implications of microbial dysbiosis in premature infants has prompted significant research i...
Determinants of stillbirths among women who gave birth at Hawassa university comprehensive specialized hospital, Hawassa, Sidama, Ethiopia 2019: a case-control study
Globally over 2.6 million pregnancy ends with stillbirth annually. Despite this fact, only a few sherds of evidence were available about factors associated with stillbirth in Ethiopia. Therefore, the study aim...
Traditional medicine utilisation and maternal complications during antenatal care among women in Bulilima, Plumtree, Zimbabwe
As part of the expectation enshrined in the Sustainable Development Goals, countries are expected to ensure maternal health outcomes are improved. It follows that under ideal circumstances, pregnant women shou...
Prevalence of rhesus D-negative blood type and the challenges of rhesus D immunoprophylaxis among obstetric population in Ethiopia: a systematic review and meta-analysis
Transplacental or fetomaternal hemorrhage (FMH) may occur during pregnancy or at delivery and lead to immunization to the D antigen if the mother is Rh-negative and the baby is Rh-positive. This can result in ...
Antibiotic exposure and growth patterns in preterm, very low birth weight infants
Antibiotic exposure in term infants has been associated with later obesity. Premature, very-low-birth-weight (birth weight ≤ 1500 g) infants in the neonatal intensive care unit frequently are exposed to antibi...
A case study of the first pregnant woman with COVID-19 in Bukavu, eastern Democratic Republic of the Congo
Vertical transmission of covid-19 is possible; its risk factors are worth researching. The placental changes found in pregnant women have a definite impact on the foetus.
Effects of timing of umbilical cord clamping on preventing early infancy anemia in low-risk Japanese term infants with planned breastfeeding: a randomized controlled trial
Japanese infants have relatively higher risk of anemia and neonatal jaundice. This study aimed to assess the effects of delayed cord clamping (DCC) on the incidence of anemia during early infancy in low-risk J...

Case report: necrotizing enterocolitis with a transverse colonic perforation in a 2-day old term neonate and literature review
Necrotizing enterocolitis (NEC), while classically discussed in preterm and low birth weight neonates, also occurs in the term infant and accounts for 10% of all NEC cases. Despite there being fewer reported c...
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2023 Speed 11 days submission to first editorial decision for all manuscripts (Median) 111 days submission to accept (Median)
2023 Usage 303,952 downloads 71 Altmetric mentions
- More about our metrics
Maternal Health, Neonatology and Perinatology
ISSN: 2054-958X
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 05 June 2024
Key barriers to the provision and utilization of maternal health services in low-and lower-middle-income countries; a scoping review
- Yaser Sarikhani 1 ,
- Seyede Maryam Najibi 2 &
- Zahra Razavi 1
BMC Women's Health volume 24 , Article number: 325 ( 2024 ) Cite this article
61 Accesses
Metrics details
The preservation and promotion of maternal health (MH) emerge as vital global health objectives. Despite the considerable emphasis on MH, there are still serious challenges to equitable access to MH services in many countries. This review aimed to determine key barriers to the provision and utilization of MH services in low- and lower-middle-income countries (LLMICs).
In this scoping review, we comprehensively searched four online databases from January 2000 to September 2022. In this study, the approach proposed by Arksey and O’Malley was used to perform the review. Consequently, 117 studies were selected for final analysis. To determine eligibility, three criteria of scoping reviews (population, concept, and context) were assessed alongside the fulfillment of the STROBE and CASP checklist criteria. To synthesize and analyze the extracted data we used the qualitative content analysis method.
The main challenges in the utilization of MH services in LLMICs are explained under four main themes including, knowledge barriers, barriers related to beliefs, attitudes and preferences, access barriers, and barriers related to family structure and power. Furthermore, the main barriers to the provision of MH services in these countries have been categorized into three main themes including, resource, equipment, and capital constraints, human resource barriers, and process defects in the provision of services.
Conclusions
The evidence from this study suggests that many of the barriers to the provision and utilization of MH services in LLMICs are interrelated. Therefore, in the first step, it is necessary to prioritize these factors by determining their relative importance according to the specific conditions of each country. Consequently, comprehensive policies should be developed using system modeling approaches.
Peer Review reports
Maternal care encompasses a series of interventions aimed at mitigating the effects of risk factors, managing illnesses, and ultimately safeguarding the well-being of both women and children. Maternal health (MH) services are concerned with maintaining the health of women before and during pregnancy, during childbirth, and in the postnatal period. Maternal care, which involves a broad spectrum of services including screening, early disease detection, prompt treatment, and health education, plays a vital role in decreasing mortality rates and improving women’s health outcomes [ 1 ]. Despite the advancements in medical science and the provision of guidelines and operational instructions, health policymakers have consistently prioritized the maintenance and improvement of MH. This concern is especially prominent in low-income countries, where addressing the issue remains a top priority [ 2 ]. The significance of maternal mortality extends beyond being a mere indicator of poor health conditions; it also represents a formidable challenge for healthcare systems [ 3 ].
Annually, over 500,000 women across the globe lose their lives due to pregnancy and childbirth-related complications. It is noteworthy that developing countries experience an alarming 99% of maternal deaths, underscoring the pressing need for targeted interventions to address this issue [ 4 ]. Despite the particular focus on MH, the maternal mortality rate in 2019 was 145 per 100,000 live births worldwide. Meanwhile, in developing countries, this ratio is estimated at 276 deaths for every 100,000 live births [ 5 ]. Studies also show that maternal mortality decreased from 11.2 to 5.01 per 100,000 population worldwide between 1999 and 2019. In low-income countries, this index fell from 43.31 to 21.10. Moreover, from 1999 to 2019, the rate of disability-adjusted life years (DALYs) in the 100,000 population due to maternal disorders decreased from 695 to 394 globally and from 2,536 to 1,262 in low-income countries [ 6 ]. Consequently, even though the global maternal mortality rates are decreasing, there remains a substantial disparity between the average global rates and those observed in low-income countries. This emphasizes the critical need to prioritize MH services in numerous nations.
According to available reports, the main direct factors associated with maternal death and injury are heavy bleeding, infections, hypertension, and unsafe abortion, while the main indirect causes are anemia, malaria, and heart disease [ 4 ]. Meanwhile, the goal of maternal care standards is to improve access to effective services, make the efficient use of available resources to achieve desired outcomes, help healthcare providers improve the quality of services, improve people’s satisfaction, and promote the use of services [ 7 ]. Nonetheless, even with the considerable attention given to maternal care, numerous obstacles hinder the successful implementation of maternal care programs. These challenges are present at both the level of mothers as recipients of services and the level of service providers. Numerous research from different parts of the world have investigated the barriers to accessing MH care services. In 2020, Shibata et al. showed that prenatal care utilization was significantly associated with geographic location, household income, and education level [ 8 ]. Transportation to access health facilities [ 9 , 10 , 11 ], high cost of services [ 12 , 13 ], and lack of competence of health professionals [ 10 , 11 , 12 , 13 ] were also among the barriers mentioned in different studies.
Effective MH care is vital for reaching the health-related Sustainable Development Goals (SDGs). In this context, adopting comprehensive strategies is essential for the provision of suitable MH services and the reduction of maternal mortality rates globally [ 14 ]. Identifying key obstacles to the provision and utilization of MH services can provide policymakers with insights to develop the necessary strategies to address and overcome these obstacles. In light of this matter, it is feasible to provide communities with timely and high-quality services to address the pressing challenges of reducing maternal mortality. This is especially vital for low-income countries [ 15 ], as it can substantially contribute to the improvement of public health. Therefore, this study aims to determine the main barriers to the provision and utilization of MH services in low- and lower-middle-income countries (LLMICs), using a scoping review approach.
We used a scoping review method to identify barriers to the provision and utilization of MH services. A comprehensive review was conducted, resulting in the creation of an evidence map associated with the topic. The provision of mental health services is largely determined by the socioeconomic conditions of communities. Therefore, this study investigated these factors in LLMICs to leverage the findings for policy interventions in countries with similar contexts. The classification of countries is based on the information provided by the World Bank. Countries with a gross national income (GNI) per capita of less than US$1,045 were classified as low-income countries using the Atlas method. Additionally, countries where the above index ranged from $1046 to $4095 were classified as lower-middle-income countries [ 16 ].
A scoping review is used in this study because this type of review provides the possibility of involving studies with different designs and sampling methods [ 17 ]. This type of research also allows for the identification of key components of a topic to provide a map of evidence and reveal the research gap in the considered area [ 18 ]. In this study, the approach proposed by Arksey and O’Malley was used to perform a scoping review. This approach involves five separate steps: 1- determining the research question, 2- finding and extracting studies, 3- selecting relevant studies, 4- tabulating data, and 5- summarizing information, analyzing themes, and presenting results [ 17 ].
Determining the research question
The scope and extent of a review study is usually determined by the research question. However, because scoping research has a continuous and iterative process of searching, selecting articles, and modifying the research question, the research question of this review study was finalized during the study process. In this study, barriers to the provision and utilization of MH services in LLMICs were considered as the expected result. This research was conducted to answer the question: “What are the main barriers to the provision and utilization of MH services in LLMICs?”
Finding and extracting studies
Before conducting a comprehensive search, the research team searched the Cochrane database and other databases to ensure that there were no comparable reviews. Subsequently, four main databases were searched systematically for articles published between January 2000 and September 2022. These databases are PubMed, Scopus, Web of Science, and ScienceDirect. The Google Scholar search engine and scientific society websites were also searched for reports and other publications. To retrieve related articles, relevant words were searched in three fields, including title, abstract, and keywords. According to the initial review of similar studies and to perform a more precise search, the keywords have been divided into 2 groups and according to the methodology of the scoping review, these groups were modified and completed during the study. The keywords and phrases in each group were combined with the logical operator “OR”, and the search results from each group were combined with other groups with the logical operator “AND”. The search keywords were determined by reviewing the keywords indexed in the MeSH and Emtree databases, as well as the corresponding entry terms associated with these databases. Table 1 shows the search strategy of the review. In this study, Endnote 20 software was used to manage references.
Selecting relevant studies
To select articles related to the review objective, the research team conducted a three-step iterative assessment process. In this procedure, the three stages involved are scanning the title, abstract, and full text, respectively. At each step, the search strategy was modified, and new articles were searched for and assessed.
In all three phases, the assessment was performed in parallel and independently by two members of the research team. To become more familiar with the different steps of the study, two researchers conducted a preliminary pilot study. we used three criteria of scoping reviews to develop the research question, as well as at all steps of the assessment. Accordingly, mothers, barriers to the provision and utilization of MH services, and LLMICs were considered as “population, concept, and context” (PCC), respectively. Within the scope of this study, healthcare provision is characterized as the process of providing health interventions through the integration of resources such as funds, personnel, facilities, and medications to meet health requirements. Moreover, healthcare utilization pertains to the degree to which individuals make use of healthcare services, which is influenced by their level of awareness, the availability, and accessibility of these services, as well as their satisfaction with the quality of care provided. Finally, the concept of maternal care encompasses the provision of services and support to women before and during pregnancy, at the time of childbirth, and in the postpartum period, with the primary objective of ensuring the overall well-being of both the mother and the child.
To improve the validity of the results, the quality of the selected articles was assessed using standard checklists. To do this, we used two tools, including the strengthening the reporting of observational studies in epidemiology (STROBE) checklist [ 19 ] and the critical appraisal skills program (CASP) checklists [ 20 ]. At all stages of the evaluation, cases of disagreement were reviewed by the third researcher, and the final decision was made.
Due to limitations related to the translation of the texts, only articles with the full text in English were selected. Moreover, given that changes in socio-economic status impact the utilization and provision of MH services, articles published since 2000 were selected for analysis to examine the most recent research in this field. We only included original studies and debate articles, so review articles and articles published in the form of letters to the editor and commentaries were not included in the analysis.
Tabulating data
To extract data from the selected articles, we created a data charting form. For each article retrieved, this form contains information, including the author’s name, article title, year of publication, publishing journal, research design, and the main results of the article. To this end, the researchers participated in the previous phases, jointly extracted the data and continuously filled in the data charting form. The data charting form is provided as Additional file 1.
Summarizing information, analyzing themes, and presenting results
To synthesize and analyze the extracted data, we used the method proposed for this purpose, namely qualitative content analysis [ 21 ]. Two researchers independently analyzed the data and then compared the results so that cases of agreement were determined and confirmed and cases of disagreement were identified and resolved. In the first phase of the thematic analysis, two researchers became familiar with the data by reading the texts several times and then extracted the primary codes according to the research objectives. In the next step, the researchers interpreted the primary codes and determined the categories, sub-themes, and main themes. Sub-themes and main themes were then evaluated and reviewed by two researchers. In the final phase, the research team held a joint meeting, where the themes were revised and if necessary, they were combined, separated, or deleted, and finally, the themes were named according to their conceptual context. The results of the qualitative themes analysis are presented in the form of a table. Tables related to thematic analysis are provided in Additional file 2. To allow a better understanding of the extent of the evidence, the table of themes also includes information on the number of articles used to develop each theme. Finally, the thematic network resulting from the analysis was designed as a conceptual framework of evidence to provide a more comprehensive insight into the topic.
To ensure the trustworthiness and rigor of the results, the criteria proposed by Guba and Lincoln were used, including credibility, confirmability, dependability, and transferability. To enhance the credibility of the findings, we have benefited from long-term engagement with the texts and the use of peer checks in the analyses. To improve confirmability, we asked two experts in the field of qualitative research to confirm the accuracy of the data analysis process. To achieve dependability, the study process was explained clearly and in detail. In this regard, four external reviewers assessed the study protocol. Finally, to enhance transferability, comprehensive details of the study process are provided to allow replication by other similar studies [ 22 ].
Our search in various databases resulted in the extraction of 12,719 articles. After removing the duplicates, 6814 articles entered the analysis phase. In the first review phase, we scanned the titles and 849 articles entered the second review stage. In the second phase, the article abstracts were reviewed and the items that did not match the scope of the study were removed. Based on this, we selected 293 articles for further analysis. In the third step, the full text of the remaining articles was assessed and 117 articles were selected for final analysis [ 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 ]. In Fig. 1 , the article selection process is outlined through a PRISMA flowchart. Table 2 presents the characteristics of the articles used in the thematic analysis. Of the selected articles, 57 (49%) focused on utilization challenges, 17 (14%) on provision barriers, and 43 (36%) explored both types of barriers. The highest number of articles published per year was from 2016 to 2022 with an average of more than 12 articles per year. More than 66% ( N = 78) of the studies were conducted in Africa, with Ethiopia and Nigeria having the highest number of articles with 27 (23%) and 16 (13.6%) studies, respectively. Among Asian countries, India had the most articles ( N = 6, 5.1%).

PRISMA flowchart of the study
The thematic analysis led to the identification of four main themes and eight sub-themes regarding the barriers to the utilization of MH services, the results of which are presented in Table 3 . Additionally, three main themes and eight sub-themes related to challenges in the provision of MH service were identified, and presented in Table 4 . The conceptual framework of evidence resulting from thematic analysis is presented in Fig. 2 .

Conceptual framework of evidence on key barriers to the utilization and provision of MH services in LLMICs
A) barriers to the utilization of MH services
A-1- knowledge barriers.
This theme explains the barriers to the utilization of MH services related to the weakness of general and specific health knowledge among women.
Weakness of specific knowledge on MH
The results of this review showed that women’s poor knowledge of MH is the most frequent barrier (N: 56, 47.86%) to the utilization of MH services in LLMICs. The low level of specific knowledge on MH is reflected in three areas, including a lack of awareness of risk factors and danger signs [ 89 , 90 , 106 ], failure to receive special care and information in previous stages of care [ 26 , 87 , 138 ] and lack of awareness of available health services [ 27 , 55 , 122 ].
Weakness of general health knowledge
The results showed that the lack of general health knowledge among women is a major barrier to the use of MH services. Lack of awareness of health needs [ 100 , 113 ] and limited access to media and information [ 55 , 84 , 124 ] are two key challenges in this area.
A-2- barriers related to beliefs, attitudes, and preferences
This theme represents the barriers to the use of MH services related to perceptual and cultural aspects of women in LLMICs.
Negative attitude towards the service delivery system
The results show that women’s negative attitudes towards the health system in LLMICs can be seen as a barrier to the optimal use of MH services. This challenge can be explained in three categories including, negative attitudes toward services [ 78 , 129 ], negative attitudes towards the competence of service providers [ 31 , 49 ], and negative experiences from past services [ 81 , 91 ].
Cultural barriers
The findings of the review showed that cultural aspects can be powerful barriers to the use of MH services. The results of the thematic analysis led to the explanation of five challenges in this area, namely Self-treatment tendencies [ 92 , 111 ], cultural and traditional customs barriers [ 36 , 74 ], preferences for using traditional services [ 108 , 128 ], sense of shame and fear [ 81 , 82 ], and communication barriers [ 31 , 92 ].
A-3- Access barriers
This theme represents the barriers that limit the accessibility of MH services. The main challenges explained in this theme were the financial and physical barriers.
Economic barriers
The results of the current study revealed that poor insurance coverage [ 30 , 73 ] and financial restrictions [ 63 , 66 ] are two major economic challenges that hinder the use of maternal care services in LLMICs.
Physical access barrier
This challenge explains the limitations of the transportation system [ 95 , 100 , 118 ]. This problem is particularly significant for the residents of remote and rural areas.
A-4- barriers related to family structure and power
This theme expresses the barriers that prevent women from accessing MH services due to discriminatory power structures within the family. The challenges of autonomy and decision-making as well as support issues are explained in this theme.
Challenges of autonomy and independence in decision-making
The results indicate that this challenge was the second most frequent problem in the studies analyzed. The results of the thematic analysis showed that limited autonomy and low decision-making power [ 31 , 32 ] as well as dependence on spouses in decision-making [ 88 , 100 ] are two main barriers related to women’s decision-making power that prevent them from using MH services in LLMICs.
Lack of support
This review revealed that a lack of support from relatives can be a barrier to the utilization of MH services. This challenge can be divided into two categories including, lack of support from family members [ 44 , 67 ] and lack of spousal support [ 70 ].
B) barriers to the provision of MH services
B-1- resource, equipment, and capital constraints.
This theme explains the barriers to the provision of MH services related to the lack of medical equipment and medicines, financial resources, and physical capital.
Shortage of medical equipment and supplies
The results of this review showed that in more than 13% of studies conducted in LLMICs, the problem of lack of equipment [ 98 , 114 ] and medicines [ 66 , 104 ] was mentioned as the challenge of providing MH services.
Restrictions on the physical space of the services
This challenge explains the barriers that limit service due to physical space issues. in this context, three categories were determined, namely limitations of service delivery space [ 76 , 93 ], insufficient infrastructure [ 24 , 75 ], and inappropriate service delivery environment [ 35 , 72 ].
Limitation of resources
The results of the study indicated that the limited financial resources [ 58 , 100 ] and shortage of physical capital [ 93 ] are two barriers to the provision of optimal MH services in LLMICs.
B-2- human resource barriers
This theme explains the problems in the provision of MH services caused by the shortage of health human resources and the low competency and efficiency of health professionals.
Shortage of health workforce
The results of this study showed that the shortage of qualified health workers [ 42 , 66 ] and the consequent limitation of working hours [ 86 , 100 ] are among the most important obstacles to the provision of MH services in LLMICs.
Weakness of scientific and practical capabilities of the health workforce
The findings of this study indicated that the weakness of scientific and practical capabilities of the health workforce was the second most frequent challenge in the provision of MH services. This challenge can be divided into four categories including, the negative attitude of the health workforce [ 66 , 96 ], incompetence of health professionals [ 58 , 103 ], inadequate knowledge of service providers [ 35 , 113 ], and Insufficient motivation of service providers [ 58 , 76 ].
B-3- process defects in the provision of services
This theme explains barriers to the provision of MH services that arise due to defects in management processes, non-compliance with standard policies, and inability to deliver necessary services.
Challenges in providing standards-compliant services
The results of this review indicated that the shortage of appropriate guidelines [ 42 , 103 ] and the low quality of services [ 49 , 127 ] are two important challenges in the provision of MH services in LLMICs.
Defects in the service management system
This review revealed that lack of integrity in the service provision system [ 113 , 135 ], weakness of managerial processes [ 67 , 76 ], poor management of the information system [ 58 ], and political restrictions [ 58 ] are four categories of this challenge.
Weakness in providing adequate essential services
The findings of this review indicated that the weakness in providing adequate essential services was the barrier most frequently mentioned in the studies carried out in LLMICs (N:31, 26,49%). This challenge was divided into two categories including, lack of availability of necessary services [ 73 , 127 , 129 , 134 ] and long waiting list [ 118 , 123 ].
Preserving the health of mothers and children is a fundamental objective in global health agendas [ 140 ] given that insufficient access to MH care can contribute to elevated maternal mortality rates [ 141 ]. The SDGs highlight the importance of achieving equitable access to maternal and child health care services globally. Despite the setting of goals and action plans, 94% of maternal deaths still take place in low-and middle-income countries, which are often preventable [ 142 ]. Research on the determinants that impact mothers’ health reveals that MH is a social construct with various effects that are influenced by contextual factors [ 143 ]. This highlights the need for comprehensive evidence to ensure the provision of effective services. Accordingly, this study aimed to explain the challenges associated with providing and utilizing MH services in LLMICs. Numerous studies have emphasized the impact of some demographic factors, such as education and income, on the use of MH services. The final analysis of this study did not include demographic characteristics, as the focus was on elucidating the fundamental and systemic obstacles linked to the underutilization of MH services. The analysis resulted in the identification of four main themes and eight sub-themes regarding the barriers to the utilization of MH services. Moreover, three main themes and eight sub-themes regarding challenges in the provision of MH service were identified. The research findings are discussed in this section, categorized by each theme and sub-theme.
Barriers to the utilization of MH services
The findings of this review indicate that the most frequent barrier to the utilization of MH services in LLMICs is the knowledge barrier. Earlier studies have shown that low levels of education in low-income countries have an impact on women’s awareness of the advantages of MH care and can occasionally discourage them from using services even when those services are easily accessible [ 144 , 145 ]. This is because being able to utilize a service and having knowledge of its existence does not always indicate that a woman has a thorough understanding of its purpose [ 120 ]. Furthermore, the continued use of MH care is an important issue related to women’s level of knowledge and education [ 146 , 147 ], so that educated women have better health-seeking behavior and more knowledge about MH services [ 148 ]. The issue of limited access to education and scarce opportunities for health information is particularly prevalent in rural communities. Women residing in these areas face significant challenges in obtaining knowledge about maternal and general health, which further exacerbates the problem [ 149 ]. In light of this matter, it is crucial to prioritize the empowerment of women through education and enhance their understanding of MH by employing culturally sensitive communication strategies [ 8 ]. The development of educational strategies should consider the contextual nuances of rural and urban communities, incorporate community-based health promotion programs, and follow the basic literacy levels of the residents [ 25 ]. It is also necessary to use the capacity of the media to keep MH services fully informed [ 146 ] because women exposed to the media have better knowledge and attitudes toward the danger signs of pregnancy and childbirth, which will lead to increased use of MH services [ 150 ].
Barriers related to family structure and power are among the other barriers to the utilization of MH services, which are mentioned in 35% of the studies included in this review. In this theme, the lack of independence and autonomy and the lack of support for mothers are issues that have been explained as barriers to the use of MH services. Decision-making about MH services and reproductive rights depends on the interaction between women, their partners, and other family members. Restricting these opportunities can hinder access to MH services [ 50 ]. In this regard, studies show that women’s independence in decision-making or joint decision-making by husband and wife increases the likelihood of using MH care [ 151 , 152 ]. Although the concept of women’s autonomy is intricate and challenging to measure, there is no widely agreed-upon definition or method for its evaluation [ 153 ], previous studies show that women’s limitation in decision-making is related to several underlying factors, such as women’s educational attainment [ 50 , 153 ], family socioeconomic status [ 50 ], age [ 153 , 154 ], urbanity [ 154 ], monthly income [ 155 , 156 ], and patriarchal culture in some societies [ 157 , 158 ]. In a meta-analysis study, Natnael estimated decision autonomy for MH services in low- and middle-income countries at 55.16% [ 154 ]. Meanwhile, Tiruneh’s study found that, among many other factors, women’s decision-making power was the strongest predictor of increased use of MH services [ 159 ]. For this reason, the 2030 SDGs consider women’s empowerment and gender inequality as essential components of public health interventions [ 154 ]. Therefore, there should be more strategies to encourage men’s participation in MH-related activities through couple counseling to increase utilization of MH services [ 157 ]. It is also suggested to expand women’s access to education to improve their skills and self-confidence, which in turn increases women’s ability to make decisions about health care and personal development [ 154 ].
Barriers related to beliefs, attitudes, and preferences are among other barriers to the utilization of MH services, which include cultural barriers and challenges related to negative attitudes towards the service provision system. To overcome cultural barriers, community-based dialogue and consultation are needed to understand concerns about MH care utilization, as well as specific reasons for avoiding or delaying care [ 25 ]. In addition, measures such as cultural adaptation of maternity care, increasing men’s involvement in MH care, community mobilization and involvement, launching health education campaigns, and challenging social beliefs and practices that limit access and use of MH services, are also suggested in this area [ 160 ].
Economic and physical access barriers were among the other challenges in using MH services explained in our study. Direct and indirect costs of services are among the major barriers to MH care utilization, which have been mentioned repeatedly in the studies included in this review. In low-income countries, families with low socioeconomic status face high out-of-pocket expenses and indirect costs, such as transportation expenditures to access health services, which can lead to financial hardship [ 161 ]. Even though low-income countries experience a large share of the global burden of diseases, they allocate only a small part of their budget to the healthcare sector [ 162 ]. Consequently, governments in low-income countries must make adequate investments to eliminate impediments to both economic and physical access to healthcare services [ 9 ].
Barriers to the provision of MH services
While social, economic, and cultural factors play a role in determining the utilization of MH services, it is essential to address barriers on the service provider side to enhance MH outcomes [ 163 ].
Among the studies analyzed in this review, process defects in the provision of services emerged as the most prevalent obstacle to the provision of MH services. This theme explains weaknesses in providing adequate essential services, challenges in providing standards-compliant services, and defects in the service management system. The lack of comprehensive and integrated services, a poor referral system, and the lack or poor implementation of guidelines are among the main barriers to the provision of MH care in LMICs, making it difficult to deliver high-quality services. Referral plays a crucial role in the healthcare system by facilitating the transfer of women to an appropriate healthcare facility, thereby ensuring the provision of quality services and reducing the risk of maternal mortality. This is even though some maternal mortality is attributed to non-standard care at the referral level [ 164 ]. An effective referral system requires adequate coordination and communication between the different levels of care. However, according to previous studies, the communication cycle between referral levels is often problematic in low-income countries due to the lack of an appropriate transport system [ 58 , 98 , 115 , 165 ]. Consequently, due to the importance of the referral system in the development of quality and integrated services in low-income countries, the availability of a reliable transportation system plays an important role in the timely delivery of MH services and facilitates referrals between different levels of care [ 58 ].
This review led to the explanation of human resource barriers and resource, equipment, and capital constraints as other key challenges to MH service provision. Healthcare providers like physicians, midwives, and nurses play a crucial role in maternal and child health services, and numerous deficiencies within the healthcare system stem from the constraints of existing services and the scarcity of proficient health professionals [ 166 ]. Insufficient allocation of resources towards health human resources, medical equipment, and medicines, coupled with inadequate infrastructure including roads, electricity, and water, along with deficiencies in the referral system, will greatly impede the delivery of services in low-income countries [ 12 ]. On the other hand, health professionals in low-income countries work in challenging environments with limited systemic support, such as poor management and coordination of staff, lack of motivation due to low wages, and lack of infrastructure such as electricity or water supply. Additionally, the dearth of supervision and training opportunities can impact the quality of services and the performance of professionals [ 76 , 167 ]. The development of training modules, the improvement of the payment system, and the consideration of non-financial incentives can be used as strategies to enhance the motivation of health professionals, resulting in increased staff performance and the quality of MH services. Moreover, the lack of modern medical equipment in some low-income countries reduces the effectiveness of maternal care providers. As a result, while promoting local investment, the governments of these nations need to collaborate with international organizations to secure funding for medical equipment and medicines, as well as to implement practical strategies to enhance sustainable supply chain management [ 168 ].
Knowledge gap
The examination of available literature in this review has brought to light a significant trend, indicating that the majority of studies conducted during the specified time frame focused on identifying barriers to achieving equitable access to MH services in African nations. Conversely, a limited number of studies were dedicated to investigating these pertinent issues in Asian and Latin American countries. Consequently, due to the specific socioeconomic context of each region, it is essential for future research in these countries to meticulously investigate the associated challenges and solutions. Moreover, considering the scarce resources available in low-income countries, there is a dearth of thorough investigations examining the relative importance and weight of each factor that affects equitable access to MH services. Determining the weight and significance of these factors can assist in prioritizing them for interventions, thus enabling the provision of more precise evidence to inform related policies and actions. A meticulous evaluation of the findings of this study suggests a complex interdependence among many of the barriers to equitable access to MH services within a systemic structure. Therefore, in light of the importance of systems thinking, the World Health Organization has emphasized employing this approach to solve health system issues. Accordingly, it is necessary to conduct studies using system modeling to provide a holistic approach to all key factors influencing equitable access to MH services, taking into account their interrelationships, through the development of causal models, and thus provide optimal solutions.
Limitations of the study
One significant limitation of this study was the exclusion of studies written in languages other than English, mainly because of translation challenges. Moreover, the diverse range of MH services and the publication of articles and reports with widely dispersed titles and keywords made it difficult to search, evaluate, and choose articles for this study. Accordingly, despite the extensive attention devoted to the review process, certain studies may have been omitted.
Based on the findings of this review, the main challenges in the utilization of MH services in LLMICs are explained under four main themes including, knowledge barriers, barriers related to beliefs, attitudes and preferences, access barriers, and barriers related to family structure and power. Financial barriers, lack of support, cultural obstacles, and deficiencies in general and specialized knowledge are the main issues within this domain. Furthermore, the main barriers to the provision of MH services in these countries have been categorized into three main themes including, resource, equipment, and capital constraints, human resource barriers, and process defects in the provision of services. This area is confronted with several critical problems, including a problematic medicine and equipment supply chain, a weak management system, inadequate financial and physical resources, and an inefficient human resource management system. The conclusions drawn from this study reveal that research efforts in the subject of this review have been unevenly distributed among LLMICs, highlighting the potential for additional research in many nations. The evidence from this study suggests that many of the factors identified in this review are interrelated. Therefore, in the first step, it is necessary to prioritize these factors by determining their relative importance according to the specific conditions of each country. Consequently, comprehensive policies should be developed using system modeling approaches.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
Critical appraisal skills program
Disability-adjusted life year
Gross national income
Low-and lower-middle-income countries
- Maternal health
Strengthening the reporting of observational studies in epidemiology
Sustainable development goals
WHO. WHO recommendations on maternal health: guidelines approved by the WHO Guidelines Review Committee. Geneva: World Health Organization; 2017.
Google Scholar
Crear-Perry J, Correa-de-Araujo R, Lewis Johnson T, McLemore MR, Neilson E, Wallace M. Social and structural determinants of health inequities in maternal health. J Women’s Health. 2021;30(2):230–5.
Article Google Scholar
Pierre AS, Zaharatos J, Goodman D, Callaghan WM. Challenges and opportunities in identifying, reviewing, and preventing maternal deaths. Obstet Gynecol. 2018;131(1):138.
WHO. Maternal mortality: fact sheet: to improve maternal health, barriers that limit access to quality maternal health services must be identified and addressed at all levels of the health system. Geneva: World Health Organization; 2014.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Global Burden of Disease Study 2019. (GBD 2019) Results [Internet]. Institute for Health Metrics and Evaluation (IHME). 2023 [cited 1/8/2023]. https://vizhub.healthdata.org/gbd-results/ .
WHO. Standards for maternal and neonatal care. Geneva: World Health Orgnization; 2007.
Milkowska-Shibata MA, Aye TT, Yi SM, Oo KT, Khaing K, Than M, et al. Understanding barriers and facilitators of maternal health care utilization in Central Myanmar. Int J Environ Res Public Health. 2020;17(5):1464.
Article PubMed PubMed Central Google Scholar
Dahab R, Sakellariou D. Barriers to accessing maternal care in low income countries in Africa: a systematic review. Int J Environ Res Public Health. 2020;17(12):4292.
Miteniece E, Pavlova M, Rechel B, Groot W. Barriers to accessing adequate maternal care in Central and Eastern European countries: a systematic literature review. Soc Sci Med. 2017;177:1–8.
Article PubMed Google Scholar
Miteniece E, Pavlova M, Rechel B, Rezeberga D, Murauskienė L, Groot W. Barriers to accessing adequate maternal care in Latvia: a mixed-method study among women, providers and decision-makers. Health Policy. 2019;123(1):87–95.
Sumankuuro J, Crockett J, Wang S. Perceived barriers to maternal and newborn health services delivery: a qualitative study of health workers and community members in low and middle-income settings. BMJ open. 2018;8(11):e021223.
Miteniece E, Pavlova M, Shengelia L, Rechel B, Groot W. Barriers to accessing adequate maternal care in Georgia: a qualitative study. BMC Health Serv Res. 2018;18(1):1–12.
Akselrod S, Banerjee A, Collins TE, Acharya S, Artykova N, Askew I, et al. Integrating maternal, newborn, child health and non-communicable disease care in the sustainable development goal era. Front Public Health. 2023;11:1183712.
Solnes Miltenburg A, Kvernflaten B, Meguid T, Sundby J. Towards renewed commitment to prevent maternal mortality and morbidity: learning from 30 years of maternal health priorities. Sex Reprod Health Matters. 2023;31(1):2174245.
World Bank Country and Lending Groups [Internet]. The World Bank Group. 2023 [cited 1/8/2023]. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
CASP. Critical Appraisal Skills Programme checklists. Oxford: Critical Appraisal Skills Programme. 2022 [ https://casp-uk.net/casp-tools-checklists/ .
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):1–10.
Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handb Qualitative Res. 1994;2(163–194):105.
Wegene MA, Gejo NG, Bedecha DY, Kerbo AA, Hagisso SN, Damtew SA. Utilization of preconception care and associated factors in Hosanna Town, Southern Ethiopia. PLoS ONE. 2022;17(1):e0261895.
Article CAS PubMed PubMed Central Google Scholar
Nuryana D, Viwattanakulvanid P, Romadlona NA. Maternal health services utilization and its contributing factors among adolescent mothers. Int J Public Health Sci. 2022;11(1):77–87.
Marquis A, O’Keeffe J, Jafari Y, Mulanda W, Carrion Martin AI, Daly M, et al. Use of and barriers to maternal health services in southeast Chad: results of a population-based survey 2019. BMJ Open. 2022;12(3):e048829.
Amaje E, Fikrie A, Utura T. Utilization of preconception care and its associated factors among pregnant women of West Guji zone, Oromia, Ethiopia, 2021: a community-based cross-sectional study. Health Serv Res Manag Epidemiol. 2022;9:23333928221088720.
PubMed PubMed Central Google Scholar
Aksünger N, De Sanctis T, Waiyaiya E, van Doeveren R, van der Graaf M, Janssens W. What prevents pregnant women from adhering to the continuum of maternal care? Evidence on interrelated mechanisms from a cohort study in Kenya. BMJ Open. 2022;12(1):e050670.
Zeleke LB, Wondie AT, Tibebu MA, Alemu AA, Tessema MT, Shita NG, Khajehei M. Postnatal care service utilization and its determinants in East Gojjam Zone, Northwest Ethiopia: a mixed-method study. PLoS ONE. 2021;16(8):e0256176.
Yoseph S, Dache A, Dona A. Prevalence of early postnatal-care service utilization and its associated factors among mothers in Hawassa Zuria District, Sidama Regional State, Ethiopia: a cross-sectional study. Obstet Gynecol Int. 2021;2021:5596110.
Woldeamanuel BT, Aga MA. Trends, regional inequalities and determinants in the utilization of prenatal care and skilled birth attendant in Ethiopia: a multilevel analysis. Clin Epidemiol Glob Health. 2021;11:100771.
Udenigwe O, Okonofua FE, Ntoimo LFC, Imongan W, Igboin B, Yaya S. Perspectives of policymakers and health providers on barriers and facilitators to skilled pregnancy care: findings from a qualitative study in rural Nigeria. BMC Pregnancy Childbirth. 2021;21(1):1–14.
Tsegaye B, Shudura E, Yoseph A, Tamiso A. Predictors of skilled maternal health services utilizations: a case of rural women in Ethiopia. PLoS ONE. 2021;16(2):e0246237.
Tsegaye B, Amare B, Reda M. Prevalence and factors associated with Immediate postnatal care utilization in Ethiopia: analysis of Ethiopian Demographic Health Survey 2016. Int J Womens Health. 2021;13:257–66.
Singh A, Palaniyandi S, Palaniyandi A, Gupta V, Panika RK, Mahore RK, Goel PK. A cross-sectional study to assess the utilization pattern of maternal health services and associated factors in aspirational district of Haryana, India. J Family Med Prim Care. 2021;10(8):2879–85.
Shahzaib N, Ali TS, Pradhan NA, Abrejo F, Shahid S, Samnani AA. Factors affecting maternal-care during labour at maternity centres of Karachi, Pakistan: exploratory study. J Pak Med Assoc. 2021;71(8):2061–4.
PubMed Google Scholar
Oyovwe P, Woolhead G. Exploring health care professionals’ and women’s perspectives on the barriers to maternal health services: a qualitative study in Eku Town of Delta State, Nigeria. AIMS Public Health. 2021;8(1):154–71.
Okemo JK, Kamya D, Mwaniki AM, Temmerman M. Determinants of preconception care among pregnant women in an urban and a rural health facility in Kenya: a qualitative study. BMC Pregnancy Childbirth. 2021;21(1):752.
Ojifinni OO, Munyewende PO, Ibisomr L. Exploring the perception of and attitude towards preconception care service provision and utilisation in a south western Nigerian community – a qualitative study. Etude De La Popul Africaine. 2021;35(1):5230–42.
Konje ET, Hatfield J, Sauve R, Kuhn S, Magoma M, Dewey D. Late initiation and low utilization of postnatal care services among women in the rural setting in Northwest Tanzania: a community-based study using a mixed method approach. BMC Health Serv Res. 2021;21(1):635.
Habte A, Gebiremeskel F, Shewangizaw M, Dessu S, Glagn M. Uptake of complete postnatal care services and its determinants among rural women in Southern Ethiopia: community-based cross-sectional study based on the current WHO recommendation. PLoS ONE. 2021;16(2):e0246243.
Habte A, Dessu S, Haile D. Determinants of practice of preconception care among women of reproductive age group in southern Ethiopia, 2020: content analysis. Reprod Health. 2021;18(1):100.
Elhady GW, Tawfik TA, Hussein EA, Magdy S, Salem MR. Postnatal care in rural Egypt: perspectives of women and health care providers. Open Access Macedonian J Med Sci. 2021;9(E):328–35.
Doyle K, Kazimbaya S, Levtov R, Banerjee J, Betron M, Sethi R, et al. The relationship between inequitable gender norms and provider attitudes and quality of care in maternal health services in Rwanda: a mixed methods study. BMC Pregnancy Childbirth. 2021;21(1):156.
David R, Evans R, Fraser HS. Modelling prenatal care pathways at a Central Hospital in Zimbabwe. Health Serv Insights. 2021;14:11786329211062742.
Amatya R, Tipayamongkholgul M, Suwannapong N, Tangjitgamol S. Factors influencing inequitable access to maternal health services in Morang district, Nepal. J Public Health Dev. 2021;19(2):1–13.
Ahuru BRR, Okungbowa OG, Iseghohi JO, Akpojubaro EH. Non-utilization of Primary Healthcare Centres for skilled pregnancy care among women in rural communities in delta State, Southern Nigeria: perspectives from mothers, fathers, and healthcare providers. J Int Women’s Stud. 2021;22(9):142–59.
Tolera H, Gebre-Egziabher T, Kloos H. Risk factors for women’s non-utilization of decentralized primary health care facilities for postnatal care in rural western Ethiopia. Ther Adv Reprod Health. 2020;14:2633494120928340.
Teshome F, Kebede Y, Abamecha F, Birhanu Z. Why do women not prepare for pregnancy? Exploring women’s and health care providers’ views on barriers to uptake of preconception care in Mana District, Southwest Ethiopia: a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):504.
Tesfaye G, Chojenta C, Smith R, Loxton D. Delaying factors for maternal health service utilization in eastern Ethiopia: a qualitative exploratory study. Women Birth. 2020;33(3):e216–26.
Rizkianti A, Afifah T, Saptarini I, Rakhmadi MF. Women’s decision-making autonomy in the household and the use of maternal health services: an Indonesian case study. Midwifery. 2020;90:102816.
Pindani M, Phiri C, Chilinda I, Chikazinga W, Botha J, Chorwe-Sungani G. Health Surveillance Assistants’ Practices of Postnatal Care in Lilongwe District, Malawi. Afr J Nurs Midwifery. 2020;22(2):1−12.
Mochache V, Wanje G, Nyagah L, Lakhani A, El-Busaidy H, Temmerman M, Gichangi P. Religious, socio-cultural norms and gender stereotypes influence uptake and utilization of maternal health services among the Digo community in Kwale, Kenya: a qualitative study. Reprod Health. 2020;17(1):71.
Manote M, Gebremedhin T. Determinants of postnatal care non-utilization among women in Demba Gofa rural district, southern Ethiopia: a community-based unmatched case-control study. BMC Pregnancy Childbirth. 2020;20(1):546.
Manang F, Yamauchi C. The impact of access to health facilities on maternal care use, travel patterns, and health status: evidence from longitudinal data from Uganda. Econ Dev Cult Change. 2020;69(1):405–51.
Khankhell RMK, Ghotbi N, Hemat S. Factors influencing utilization of postnatal care visits in Afghanistan. Nagoya J Med Sci. 2020;82(4):711–23.
Gebrehiwot TG, Mekonen HH, Gebru TH, Kiros KG, Gebresilassie B, Teklu G, et al. Prevalence and associated factors of early postnatal care service use among mothers who had given birth within the last 12 months in Adigrat town, Tigray, northern Ethiopia, 2018. Int J Women’s Health. 2020;12:869–79.
Chauhan PA, Bhalani KD. Evaluation of maternal health services being provided to the high-risk mothers of Bhavnagar District, Gujarat. Indian J Community Med. 2020;45(1):18–22.
Cagayan MSFS, Ang-Bon RM, Garcia FB, Juan FSS, Llave CL, Banwell C, Llamas-Clark EF. Barriers to an effective maternal health service delivery network: a qualitative study among health providers in Legazpi City, Albay. Acta Med Philippina. 2020;54(5):462–71.
Atuoye KN, Barnes E, Lee M, Zhang LZ. Maternal health services utilisation among primigravidas in Uganda: what did the MDGs deliver? Global Health. 2020;16(1):40.
Yaya S, Okonofua F, Ntoimo L, Udenige O, Bishwajit G. Gender inequity as a barrier to women’s access to skilled pregnancy care in rural Nigeria: a qualitative study. Int Health. 2019;11(6):551–60.
Upadhyai N, Gupta SK. Utilization of postnatal care services and factors affecting it among women of urban slums in Dehradun, Uttarakhand. Indian J Community Health. 2019;31(4):470–6.
Sharma Gautam D, Hearn G. No time, no money, no luck: barriers to prenatal care among dalit women in rural Nepal. Health Care Women Int. 2019;40(7–9):914–30.
Ntoimo LFC, Okonofua FE, Igboin B, Ekwo C, Imongan W, Yaya S. Why rural women do not use primary health centres for pregnancy care: evidence from a qualitative study in Nigeria. BMC Pregnancy Childbirth. 2019;19(1):1−13.
Kim ET, Singh K, Speizer IS, Angeles G, Weiss W. Availability of health facilities and utilization of maternal and newborn postnatal care in rural Malawi. BMC Pregnancy Childbirth. 2019;19(1):503.
Kassa A, Human S, Gemeda H. Level of Healthcare Providers’ Preconception Care (PCC) practice and factors associated with non-implementation of PCC in Hawassa, Ethiopia. Ethiop J Health Sci. 2019;29(1):903–12.
Fantaye AW, Okonofua F, Ntoimo L, Yaya S. A qualitative study of community elders’ perceptions about the underutilization of formal maternal care and maternal death in rural Nigeria. Reprod Health. 2019;16(1):164.
Diba F, Ichsan I, Muhsin M, Marthoenis M, Sofyan H, Andalas M, et al. Healthcare providers’ perception of the referral system in maternal care facilities in Aceh, Indonesia: a cross-sectional study. BMJ Open. 2019;9(12):e031484.
Demisse TL, Aliyu SA, Kitila SB, Tafesse TT, Gelaw KA, Zerihun MS. Utilization of preconception care and associated factors among reproductive age group women in Debre Birhan town, North Shewa, Ethiopia. Reprod Health. 2019;16(1):96.
Berhe A, Bayray A, Berhe Y, Teklu A, Desta A, Araya T, et al. Determinants of postnatal care utilization in Tigray, Northern Ethiopia: a community based cross-sectional study. PLoS ONE. 2019;14(8):e0221161.
Asresu TT, Hailu D, Girmay B, Abrha MW, Weldearegay HG. Mothers’ utilization and associated factors in preconception care in northern Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. 2019;19(1):347.
Ali Khan RE, Ahmad TI, Noreen S, Ejaz A. Quantity of prenatal care (PNC) services use in Southern Punjab: a case study of Bahawalpur. J Pak Med Assoc. 2019;69(1):64–7.
Patel SB, Sharma A, Vati J. A mixed method study on utilization of maternal health services and barriers among women of reproductive age in Gujarat state-pilot study. Indian J Public Health Res Dev. 2018;9(11):159–64.
Patel P, Das M, Das U. The perceptions, health-seeking behaviours and access of scheduled caste women to maternal health services in Bihar, India. Reprod Health Matters. 2018;26(54):114–25.
Okonofua F, Ntoimo L, Ogungbangbe J, Anjorin S, Imongan W, Yaya S. Predictors of women’s utilization of primary health care for skilled pregnancy care in rural Nigeria. BMC Pregnancy Childbirth. 2018;18(1):1–15.
Odetola TD, Fakorede EO. Assessment of Perinatal Care satisfaction amongst mothers attending postnatal care in Ibadan, Nigeria. Ann Glob Health. 2018;84(1):36–46.
Mugo NS, Dibley MJ, Damundu EY, Alam A. Barriers faced by the Health Workers To Deliver Maternal Care Services and their perceptions of the factors preventing their clients from receiving the services: a qualitative study in South Sudan. Matern Child Health J. 2018;22(11):1598–606.
Mon AS, Phyu MK, Thinkhamrop W, Thinkhamrop B. Utilization of full postnatal care services among rural Myanmar women and its determinants: a cross-sectional study. F1000Res. 2018;7:1167.
Mohamed-Ahmed R, Aziz MA, Walker R. Antenatal care in Sudan: a qualitative study into accessibility and quality of maternal health services in Khartoum. Int J Childbirth. 2018;8(2):77–86.
Mafuta EM, Buning TD, Lolobi DL, Mayala PM, Mambu TNM, Kayembe PK, Dieleman MA. Factors influencing the capacity of women to voice their concerns about maternal health services in the Muanda and Bolenge Health Zones, Democratic Republic of the Congo: a multi-method study. BMC Health Serv Res. 2018;18:1–14.
Kibusi SM, Sunguya BF, Kimunai E, Hines CS. Health insurance is important in improving maternal health service utilization in Tanzania - Analysis of the 2011/2012 Tanzania HIV/AIDS and malaria indicator survey. BMC Health Serv Res. 2018;18(1).
Kea AZ, Tulloch O, Datiko DG, Theobald S, Kok MC. Exploring barriers to the use of formal maternal health services and priority areas for action in Sidama Zone, southern Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):96.
Kane S, Rial M, Kok M, Matere A, Dieleman M, Broerse JEW. Too afraid to go: fears of dignity violations as reasons for non-use of maternal health services in South Sudan. Reprod Health. 2018;15(1):51.
Gebrehiwot G, Medhanyie AA, Gidey G, Abrha K. Postnatal care utilization among urban women in northern Ethiopia: cross-sectional survey. BMC Womens Health. 2018;18(1):78.
Gebre E, Worku A, Bukola F. Inequities in maternal health services utilization in Ethiopia 2000–2016: magnitude, trends, and determinants. Reprod Health. 2018;15(1):119.
Ekem NN, Lawani LO, Onoh RC, Iyoke CA, Ajah LO, Onwe EO, et al. Utilisation of preconception care services and determinants of poor uptake among a cohort of women in Abakaliki Southeast Nigeria. J Obstet Gynaecol. 2018;38(6):739–44.
Chol C, Hunter C, Debru B, Haile B, Negin J, Cumming RG. Stakeholders’ perspectives on facilitators of and barriers to the utilisation of and access to maternal health services in Eritrea: a qualitative study. BMC Pregnancy Childbirth. 2018;18(1):35.
Angore BN, Tufa EG, Bisetegen FS. Determinants of postnatal care utilization in urban community among women in Debre Birhan Town, Northern Shewa, Ethiopia. J Health Popul Nutr. 2018;37(1):10.
Akter MK, Yimyam S, Chareonsanti J, Tiansawad S. The challenges of prenatal care for Bangladeshi women: a qualitative study. Int Nurs Rev. 2018;65(4):534–41.
Article CAS PubMed Google Scholar
Abota TL, Atenafu NT. Postnatal care utilization and associated factors among Married women in Benchi-Maji Zone, Southwest Ethiopia: a community based cross-sectional study. Ethiop J Health Sci. 2018;28(3):267–76.
Abebo TA, Tesfaye DJ. Postnatal care utilization and associated factors among women of reproductive age Group in Halaba Kulito Town, Southern Ethiopia. Archives Public Health. 2018;76:1–10.
Sacks E, Masvawure TB, Atuyambe LM, Neema S, Macwan’gi M, Simbaya J, Kruk M. Postnatal Care experiences and barriers to care utilization for home- and facility-delivered newborns in Uganda and Zambia. Matern Child Health J. 2017;21(3):599–606.
Probandari A, Arcita A, Kothijah K, Pamungkasari EP. Barriers to utilization of postnatal care at village level in Klaten District, central Java Province, Indonesia. BMC Health Serv Res. 2017;17(1):541.
Nguyen THT, Wilson A, McDonald F. Health workers’ perspectives on infrastructure to support maternal health services in rural areas of Vietnam. Asia Pac J Health Manage. 2017;12(2):55–61.
Makate M, Makate C. Prenatal care utilization in Zimbabwe: examining the role of community-level factors. J Epidemiol Glob Health. 2017;7(4):255–62.
Machira K, Palamulen M. Rural-urban differences in the use of postnatal care services in Malawi. J Egypt Public Health Assoc. 2017;92(1):1–10.
Elkhoudri N, Baali A, Amor H. Postnatal care: levels and determinants in Morocco. Iran J Public Health. 2017;46(2):242–8.
Banke-Thomas A, Banke-Thomas O, Kivuvani M, Ameh CA. Maternal health services utilisation by Kenyan adolescent mothers: analysis of the Demographic Health Survey 2014. Sex Reprod Healthc. 2017;12:37–46.
Nnebue CC, Ebenebe UE, Duru CB, Egenti NB, Emelumadu OF, Ibeh CC. Availability and continuity of care for maternal health services in the Primary Health Centres in Nnewi, Nigeria (January - March 2010). Int J Prev Med. 2016;7:44.
Limenih MA, Endale ZM, Dachew BA. Postnatal Care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos Town, Northwestern Ethiopia: a community-based cross-sectional study. Int J Reprod Med. 2016;2016:7095352.
King R, Jackson R, Dietsch E, Hailemariam A. Utilisation of maternal health services in Ethiopia: a key informant research project. Dev Pract. 2016;26(2):158–69.
Dehury RK, Samal J. Health system competency for maternal health services in Balasore District and Jaleswar Block, Balasore, Odisha, India: an assessment. J Clin Diagn Res. 2016;10(8):Ic01–5.
Browne JL, Kayode GA, Arhinful D, Fidder SAJ, Grobbee DE, Klipstein-Grobusch K. Health insurance determines antenatal, delivery and postnatal care utilisation: evidence from the Ghana Demographic and Health Surveillance data. BMJ Open 2016;6(3):e008175.
Bayrami R, Roudsari RL, Allahverdipour H, Javadnoori M, Esmaily H. Experiences of women regarding gaps in preconception care services in the Iranian reproductive health care system: a qualitative study. Electron Physician. 2016;8(11):3279–88.
Arnold J, Samson M, Schechter J, Goodwin AS, Braganza S, Sesso GC, et al. Getting there: overcoming barriers to reproductive and maternal health services access in Northern Togo—a qualitative study. World Med Health Policy. 2016;8(3):223–44.
Alam N, Chowdhury ME, Kouanda S, Seppey M, Alam A, Savadogo JR, et al. The role of transportation to access maternal care services for women in rural Bangladesh and Burkina Faso: a mixed methods study. Int J Gynaecol Obstet. 2016;135(Suppl 1):S45–50.
Agho KE, Ezeh OK, Issaka AI, Enoma AI, Baines S, Renzaho AM. Population attributable risk estimates for factors associated with non-use of postnatal care services among women in Nigeria. BMJ Open. 2016;6(7):e010493.
Adhikari R. Effect of Women’s autonomy on maternal health service utilization in Nepal: A cross sectional study. BMC Womens Health. 2016;16(1):1–7.
Yiran GSA, Teye JK, Yiran GAB. Accessibility and Utilisation of Maternal Health Services by migrant female head porters in Accra. J Int Migration Integr. 2015;16(4):929–45.
Sultana N, Shaikh BT. Low utilization of postnatal care: searching the window of opportunity to save mothers and newborns lives in Islamabad capital territory, Pakistan. BMC Res Notes. 2015;8:645.
Chi PC, Bulage P, Urdal H, Sundby J. A qualitative study exploring the determinants of maternal health service uptake in post-conflict Burundi and Northern Uganda. BMC Pregnancy Childbirth. 2015;15(1):1−14.
Alenoghena IO, Isah EC, Isara AR. Maternal health services uptake and its determinants in public primary health care facilities in edo state, Nigeria. Niger Postgrad Med J. 2015;22(1):25–31.
Tesfahun F, Worku W, Mazengiya F, Kifle M. Knowledge, perception and utilization of postnatal care of mothers in Gondar Zuria District, Ethiopia: a cross-sectional study. Matern Child Health J. 2014;18(10):2341–51.
Sarfraz M, Hamid S. Challenges in delivery of skilled maternal care - experiences of community midwives in Pakistan. BMC Pregnancy Childbirth. 2014;14:59.
Nnebue CC, Ebenebe UE, Adogu PO, Adinma ED, Ifeadike CO, Nwabueze AS. Adequacy of resources for provision of maternal health services at the primary health care level in Nnewi, Nigeria. Niger Med J. 2014;55(3):235–41.
Donmozoun TS, Sombie I, Meda N. What prevent women for a sustainable use of maternal care in two medical districts of Burkina Faso? A qualitative study. Pan Afr Med J. 2014;18:1−6.
Babalola SO. Factors associated with use of maternal health services in Haiti: a multilevel analysis. Rev Panam Salud Publica. 2014;36(1):1–9.
Abrokwah SO, Moser CM, Norton EC. The effect of social health insurance on prenatal care: the case of Ghana. Int J Health Care Finance Econ. 2014;14(4):385–406.
Kumbani L, Bjune G, Chirwa E, Malata A, Odland J. Why some women fail to give birth at health facilities: a qualitative study of women’s perceptions of perinatal care from rural Southern Malawi. Reprod Health. 2013;10:9.
King S, Passey M, Dickson R. Perceptions and use of maternal health services by women in rural coastal Madang Province. P N G Med J. 2013;56(1–2):5–13.
Idris SH, Sambo MN, Ibrahim MS. Barriers to utilisation of maternal health services in a semi-urban community in northern Nigeria: the clients’ perspective. Niger Med J. 2013;54(1):27–32.
Hou XH, Ma N. The effect of women’s decision-making power on maternal health services uptake: evidence from Pakistan. Health Policy Plann. 2013;28(2):176–84.
Abel Ntambue ML, Françoise Malonga K, Dramaix-Wilmet M, Donnen P. Determinants of maternal health services utilization in urban settings of the Democratic Republic of Congo–a case study of Lubumbashi City. BMC Pregnancy Childbirth. 2012;12:66.
Kambala C, Morse T, Masangwi S, Mitunda P. Barriers to maternal health service use in Chikhwawa, southern Malawi. Malawi Med J. 2011;23(1):1–5.
Islam MR, Odland JO. Determinants of antenatal and postnatal care visits among indigenous people in Bangladesh: a study of the Mru community. Rural Remote Health. 2011;11(2):1672.
CAS PubMed Google Scholar
Choudhury N, Ahmed SM. Maternal care practices among the ultra poor households in rural Bangladesh: a qualitative exploratory study. BMC Pregnancy Childbirth. 2011;11:15.
Bhusal CL, Singh SP, Bc RK, Dhimal M, Jha BK, Acharya L, et al. Effectiveness and efficiency of Aama Surakshya Karyakram in terms of barriers in accessing maternal health services in Nepal. J Nepal Health Res Counc. 2011;9(2):129–37.
Yakong VN, Rush KL, Bassett-Smith J, Bottorff JL, Robinson C. Women’s experiences of seeking reproductive health care in rural Ghana: challenges for maternal health service utilization. J Adv Nurs. 2010;66(11):2431–41.
Titaley CR, Hunter CL, Heywood P, Dibley MJ. Why don’t some women attend antenatal and postnatal care services? A qualitative study of community members’ perspectives in Garut, Sukabumi and Ciamis districts of West Java Province, Indonesia. BMC Pregnancy Childbirth. 2010;10:61.
Matsuoka S, Aiga H, Rasmey LC, Rathavy T, Okitsu A. Perceived barriers to utilization of maternal health services in rural Cambodia. Health Policy. 2010;95(2–3):255–63.
Mrisho M, Obrist B, Schellenberg JA, Haws RA, Mushi AK, Mshinda H, et al. The use of antenatal and postnatal care: perspectives and experiences of women and health care providers in rural southern Tanzania. BMC Pregnancy Childbirth. 2009;9:10.
Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria - looking beyond individual and household factors. BMC Pregnancy Childbirth. 2009;9:43.
Nyamtema AS, Urassa DP, Massawe S, Massawe A, Mtasiwa D, Lindmark G, van Roosmalen J. Dar es Salaam perinatal care study: needs assessment for quality of care. East Afr J Public Health. 2008;5(1):17–21.
Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, Mwakipa H. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth. 2007;7:29.
Dhakal S, Chapman GN, Simkhada PP, van Teijlingen ER, Stephens J, Raja AE. Utilisation of postnatal care among rural women in Nepal. BMC Pregnancy Childbirth. 2007;7:19.
Pettersson KO, Johansson E, Pelembe MDFM, Dgedge C, Christensson K. Mozambican midwives’ views on barriers to quality perinatal care. Health Care Women Int. 2006;27(2):145–68.
Gage AJ, Guirlène Calixte M. Effects of the physical accessibility of maternal health services on their use in rural Haiti. Popul Stud (Camb). 2006;60(3):271–88.
Hotchkiss DR, Krasovec K, El-Idrissi M, Eckert E, Karim AM. The role of user charges and structural attributes of quality on the use of maternal health services in Morocco. Int J Health Plann Manage. 2005;20(2):113–35.
Alexandre PK, Saint-Jean G, Crandall L, Fevrin E. Prenatal care utilization in rural areas and urban areas of Haiti. Rev Panam Salud Publica. 2005;18(2):84–92.
Matsumura M, Gubhaju B. Women’s status, household structure and the utilization of maternal health services in Nepal. Asia-Pacific Popul J. 2001;16(1):23–44.
Harahap NC, Handayani PW, Hidayanto AN. Barriers and technologies of maternal and neonatal referral system in developing countries: a narrative review. Inf Med Unlocked. 2019;15:100184.
Lewis G. Maternal mortality in the developing world: why do mothers really die? Obstetric Med. 2008;1(1):2–6.
UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Trends in maternal mortality 2000 to 2017: estimates by WHO. Geneva: World Health Organization; 2019. p. 9241516488. Report No.
Sanneving L, Trygg N, Saxena D, Mavalankar D, Thomsen S. Inequity in India: the case of maternal and reproductive health. Global Health Action. 2013;6(1):19145.
Dako-Gyeke P, Aikins M, Aryeetey R, Mccough L, Adongo PB. The influence of socio-cultural interpretations of pregnancy threats on health-seeking behavior among pregnant women in urban Accra, Ghana. BMC Pregnancy Childbirth. 2013;13(1):1–12.
Sumankuuro J, Crockett J, Wang S. The use of antenatal care in two rural districts of Upper West Region, Ghana. PLoS ONE. 2017;12(9):e0185537.
Alamneh TS, Teshale AB, Yeshaw Y, Alem AZ, Ayalew HG, Liyew AM, et al. Barriers for health care access affects maternal continuum of care utilization in Ethiopia; spatial analysis and generalized estimating equation. PLoS ONE. 2022;17(4):e0266490.
Hamed A, Mohamed E, Sabry M. Egyptian status of continuum of care for maternal, newborn, and child health: Sohag Governorate as an example. Int J Med Sci Public Health. 2018;7(6):1.
Mainuddin A, Begum HA, Rawal LB, Islam A, Islam SS. Women empowerment and its relation with health seeking behavior in Bangladesh. J Family Reprod Health. 2015;9(2):65.
Saxena D, Vangani R, Mavalankar D, Thomsen S. Inequity in maternal health care service utilization in Gujarat: analyses of district-level health survey data. Global Health Action. 2013;6(1):19652.
Wulandari RD, Laksono AD. Determinants of knowledge of pregnancy danger signs in Indonesia. PLoS ONE. 2020;15(5):e0232550.
Moinuddin M, Christou A, Hoque DME, Tahsina T, Salam SS, Billah SM, et al. Birth preparedness and complication readiness (BPCR) among pregnant women in hard-to-reach areas in Bangladesh. PLoS ONE. 2017;12(12):e0189365.
Awoleye AF, Victor C, Alawode OA. Women autonomy and maternal healthcare services utilization among young ever-married women in Nigeria. Int J Nurs Midwifery. 2018;10(6):62–73.
Kassahun A, Zewdie A. Decision-making autonomy in maternal health service use and associated factors among women in Mettu District, Southwest Ethiopia: a community-based cross-sectional study. BMJ open. 2022;12(5):e059307.
Gebeyehu NA, Gelaw KA, Lake EA, Adela GA, Tegegne KD, Shewangashaw NE. Women decision-making autonomy on maternal health service and associated factors in low-and middle-income countries: systematic review and meta-analysis. Women’s Health. 2022;18:17455057221122618.
CAS PubMed PubMed Central Google Scholar
Osamor PE, Grady C. Women’s autonomy in health care decision-making in developing countries: a synthesis of the literature. Int J Women’s Health. 2016;8:191.
Ghose B, Feng D, Tang S, Yaya S, He Z, Udenigwe O, et al. Women’s decision-making autonomy and utilisation of maternal healthcare services: results from the Bangladesh Demographic and Health Survey. BMJ open. 2017;7(9):e017142.
Imo CK. Influence of women’s decision-making autonomy on antenatal care utilisation and institutional delivery services in Nigeria: evidence from the Nigeria Demographic and Health Survey 2018. BMC Pregnancy Childbirth. 2022;22(1):1–12.
Islam N, Islam MT, Yoshimura Y. Practices and determinants of delivery by skilled birth attendants in Bangladesh. Reprod Health. 2014;11(1):1–7.
Tiruneh FN, Chuang KY, Chuang YC. Women’s autonomy and maternal healthcare service utilization in Ethiopia. BMC Health Serv Res. 2017;17(1):1–12.
Ganle J. Addressing socio-cultural barriers to maternal healthcare in Ghana: perspectives of women and healthcare providers. J Womens Health Issues Care. 2014;6:2.
Lu C, Schneider MT, Gubbins P, Leach-Kemon K, Jamison D, Murray CJ. Public financing of health in developing countries: a cross-national systematic analysis. Lancet. 2010;375(9723):1375–87.
Gottret PE, Schieber G. Health financing revisited: a practitioner’s guide. Washington, D.C.: World Bank Group; 2006.
Book Google Scholar
Knight HE, Self A, Kennedy SH. Why are women dying when they reach hospital on time? A systematic review of the ‘third delay’. PLoS ONE. 2013;8(5):e63846.
Jahn A, Dar Iang M, Shah U, Diesfeld H. Maternity care in rural Nepal: a health service analysis. Tropical Med Int Health. 2000;5(9):657–65.
Article CAS Google Scholar
Oladapo OT, Iyaniwura CA, Sule-Odu AO. Quality of antenatal services at the primary care level in southwest Nigeria. Afr J Reprod Health. 2008;12(3):71−92.
WHO. A Universal Truth. No health without a workforce. Geneva: World Health Organisation; 2013.
Chandler CI, Chonya S, Mtei F, Reyburn H, Whitty CJ. Motivation, money and respect: a mixed-method study of Tanzanian non-physician clinicians. Soc Sci Med. 2009;68(11):2078–88.
Tayelgn A, Zegeye DT, Kebede Y. Mothers’ satisfaction with referral hospital delivery service in Amhara Region, Ethiopia. BMC Pregnancy Childbirth. 2011;11(1):1–7.
Download references
No funding was received for this study.
Author information
Authors and affiliations.
Research Center for Social Determinants of Health, Jahrom University of Medical Sciences, Jahrom, Iran
Yaser Sarikhani & Zahra Razavi
Research Center for Traditional Medicine and History of Medicine, Department of Persian Medicine, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
Seyede Maryam Najibi
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the design of the study. YS and SMN Gathered the data. All authors contributed to the analysis of the data. YS and SMN were the major contributors in writing the manuscript. ZR write some parts of the article and critically revised it. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Seyede Maryam Najibi .
Ethics declarations
Ethics approval and consent to participate.
The protocol of this study was approved by the Ethics Committee of Jahrom University of Medical Sciences under the code IR.JUMS.REC.1400.112.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sarikhani, Y., Najibi, S.M. & Razavi, Z. Key barriers to the provision and utilization of maternal health services in low-and lower-middle-income countries; a scoping review. BMC Women's Health 24 , 325 (2024). https://doi.org/10.1186/s12905-024-03177-x
Download citation
Received : 25 November 2023
Accepted : 30 May 2024
Published : 05 June 2024
DOI : https://doi.org/10.1186/s12905-024-03177-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Maternal Health Services
- Utilization
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Triple Billion
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment case
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Health topics /
Maternal health
Maternal health refers to the health of women during pregnancy, childbirth and the postnatal period.
Each stage should be a positive experience, ensuring women and their babies reach their full potential for health and well-being.
Although important progress has been made in the last two decades, about 287 000 women died during and following pregnancy and childbirth in 2020. This number is unacceptably high.
The most common direct causes of maternal injury and death are excessive blood loss, infection, high blood pressure, unsafe abortion, and obstructed labour, as well as indirect causes such as anemia, malaria, and heart disease.
Most maternal deaths are preventable with timely management by a skilled health professional working in a supportive environment.
Ending preventable maternal death must remain at the top of the global agenda. At the same time, simply surviving pregnancy and childbirth can never be the marker of successful maternal health care. It is critical to expand efforts reducing maternal injury and disability to promote health and well-being.
Every pregnancy and birth is unique. Addressing inequalities that affect health outcomes, especially sexual and reproductive health and rights and gender, is fundamental to ensuring all women have access to respectful and high-quality maternity care.
About 140 million births take place every year and the proportion attended by skilled health personnel has increased: from 58% in 1990 to 81% in 2019. This is mostly due to larger numbers of births taking place at a health facility.
Deaths from complications during pregnancy, childbirth, and the postnatal period have declined by 38% in the last two decades, but at an average reduction of just under 3% per year, this pace of progress is far too slow.
It also hides vast inequalities within and across countries.
More than half of maternal deaths occur in fragile and humanitarian settings. Sub-Saharan Africa and Southern Asia share the greatest burden of maternal deaths, 86% of the global total in 2017.
The Sustainable Development Goals (SDGs) offers an opportunity for the international community to work together and accelerate progress to improve maternal health for all women, in all countries, under all circumstances.
SDG targets for maternal health include 3.1, aiming for an average global ratio of less than 70 deaths per 100 000 births by 2030, and 3.8, calling for the achievement of universal health coverage. These cannot be achieved without reproductive, maternal, newborn and child health coverage for all.
Improving maternal health is one of WHO’s key priorities, grounded in a human rights approach and linked to efforts on universal health coverage.
WHO advocates for health planning where women’s values and preferences are at the centre of their own care. Meaningful engagement and empowerment of women, families, communities, and providers is essential for quality improvement initiatives.
Promoting health along the whole continuum of pregnancy, childbirth and postnatal care is also crucial. This includes good nutrition, detecting and preventing diseases, ensuring access to sexual and reproductive health and supporting women who may be experiencing intimate partner violence.
It is WHO’s responsibility to monitor progress towards the global goal for reducing maternal death (SDG target 3.1). WHO generates data, research, clinical guidelines and programmatic tools to support achievement of global targets and evidence-based strategies for ending preventable maternal mortality (EPMM) and improving maternal health and well-being.
WHO supports Member States as they implement plans to promote access to quality health services for all. Strong partnerships are crucial, such as The Network for Improving Quality of Care for Maternal, Newborn and Child Health, launched by WHO and UNICEF.
- Adolescent pregnancy
- Maternal mortality
- WHO Statement on Caesarean Section Rates
- Maternal death data
- Maternal, newborn, child and adolescent health data portal
- WHA72.2 Primary health care
- WHA72.3 Community health workers delivering primary health care: opportunities and challenges
- Maternal Health Unit
- Maternal, Newborn, Child, Adolescent health and Ageing department
- Department of Sexual and Reproductive Health and Research including the UN cosponsored Special Research Programme in Human Reproduction (HRP)
- Maternal and perinatal health (SRH)
Experts warn of serious health impacts from climate change for pregnant women, children, and older people
Awards for outstanding contributions to public health presented during the Seventy-seventh World Health Assembly
Countries commit to recover lost progress in maternal, newborn & child survival
New series highlights the importance of a positive postnatal experience for all women and newborns
Latest publications

Preventing unplanned pregnancies: implementation review and planning guide: outpatient family planning...
Frontline health workers are critical to the provision of effective counselling about family planning and support to women on the correct use of contraceptives....

Engaging the private sector in delivering quality maternal, newborn and child health services
The purpose of this workbook is to assist ministries of health, health managers and practitioners in engaging with the private sector on delivery of quality...

Report of the eighth meeting of the Strategic and Technical Advisory Group of Experts for Maternal, Newborn,...
The eighth meeting of the Strategic and Technical Advisory Group of Experts (STAGE) for maternal, newborn, child and adolescent health and nutrition...

Improving the health and wellbeing of children and adolescents: guidance on scheduled child and adolescent...
To survive and thrive, children and adolescents need good health, adequate nutrition, secure, safe and a supportive clean environment, and opportunities...
Prioritizing quality of care in maternal health
Strengthening health systems and communities
Raising the importance of postnatal care
Making childbirth a positive experience
Promoting healthy pregnancy
Strengthening home-based records implementation
Robust monitoring of maternal health data
Strengthening quality midwifery for all mothers and newborns
10th Meeting of the Strategic and Technical Advisory Group of Experts (STAGE) for Maternal, Newborn, Child and Adolescent Health and Nutrition (MNCAHN)
New Lancet Series: Maternal health in the perinatal period and beyond, Western Africa
New Lancet Series: Maternal health in the perinatal period and beyond, Latin America

Infographics

Supporting women, parents and families for a positive postnatal experience

More than one-third of women experience long-term health problems after childbirth

Inequalities across borders and within countries threaten newborn health

Every 7 seconds, a woman or newborn dies, or a baby is lost to stillbirth

Sexual and Reproductive Health and Rights: Film Festival panel discussion at ECTMIH

Maternal Sepsis: Working towards an end in Malawi

WHO Labour Care Guide to support intrapartum care for a positive birth experience

Maternal & Perinatal Health - Dr Femi Oladapo: HRP@50 Expert Series
Related health topics
Breastfeeding
Newborn health
Nursing and midwifery
Sexual health
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Thursday, August 17, 2023
NIH establishes Maternal Health Research Centers of Excellence
Initiative to support research to reduce pregnancy-related complications and deaths and promote maternal health equity.
The National Institutes of Health has awarded $24 million in first-year funding to establish Maternal Health Research Centers of Excellence. Part of NIH’s Implementing a Maternal Health and Pregnancy Outcomes Vision for Everyone (IMPROVE) initiative , the centers will develop and evaluate innovative approaches to reduce pregnancy-related complications and deaths and promote maternal health equity. The grants are expected to last seven years and total an estimated $168 million, pending the availability of funds.
Compared to other high-income countries, the United States has a high rate of maternal deaths, with more than 1,200 such deaths occurring in 2021, the most recent year for which data are available. Each year tens of thousands more Americans experience severe pregnancy-related complications, which can raise the risk of future health concerns, including high blood pressure, diabetes and mental health conditions. There are stark disparities in these maternal health outcomes by racial and ethnic group, age, education, socioeconomic status and geographic region.
“The magnitude and persistence of maternal health disparities in the United States underscore the need for research to identify evidence-based solutions to promote health equity and improve outcomes nationwide,” says Diana W. Bianchi, M.D., director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). “Through collaborations with community partners and others, the Maternal Health Research Centers of Excellence will generate critical scientific evidence to help guide clinical care and reduce health disparities during and after pregnancy.”
NICHD, the NIH Office of Research on Women’s Health and the National Institute of Nursing Research co-lead the IMPROVE initiative, with involvement from several other components at NIH .
The centers of excellence include 10 research centers, a data innovation and coordinating hub and an implementation science hub. Together, these institutions will work to design and implement research projects to address the biological, behavioral, environmental, sociocultural and structural factors that affect pregnancy-related complications and deaths. They will focus on populations that experience health disparities, including racial and ethnic minorities, socioeconomically disadvantaged populations, those living in underserved rural areas, sexual and gender minority populations and people with disabilities.
Research centers will partner with community collaborators, such as state and local public health agencies, community health centers and faith-based organizations. Additionally, the research centers will support training and professional development of maternal health researchers, including those from backgrounds underrepresented in the biomedical research workforce.
Funding for the centers was awarded after a competitive peer review process. The following institutions, listed alphabetically along with project name and contact principal investigator, will participate as research centers:
- Avera McKennan Hospital, Sioux Falls, South Dakota Maternal American-Indian Rural Community Health (MARCH) Principal investigator: Amy J. Elliott, Ph.D.
- Columbia University, New York City NY Community-Hospital-Academic Maternal Health Equity Partnerships (NY-CHAMP) Principal investigator: Uma Reddy, M.D.
- Jackson State University, Jackson, Mississippi Delta Mississippi Center of Excellence in Maternal Health Principal investigator: Mary D. Shaw, Ph.D.
- Medical College of Wisconsin, Milwaukee Addressing Key Social-Structural Risk Factors for Racial Disparities in Maternal Morbidity in Southeastern Wisconsin (ASCEND WI) Principal investigator: Anna Palatnik, M.D.
- Michigan State University, East Lansing Maternal Health Multilevel Intervention/s for Racial Equity (MIRACLE) Center Principal investigator: Cristian Ioan Meghea, Ph.D.
- Morehouse School of Medicine, Atlanta Center to Advance Reproductive Justice and Behavioral Health among Black Pregnant/Postpartum Women and Birthing People (CORAL) Principal investigator: Natalie Dolores Hernandez, Ph.D.
- Stanford University, Stanford, California Stanford PRIHSM: Preventing Inequities in Hemorrhage-related Severe Maternal Morbidity Principal investigator: Yasser Y. El-Sayed, M.D.
- Tulane University, New Orleans Southern Center for Maternal Health Equity Principal investigator: Emily Wheeler Harville, Ph.D.
- University of Oklahoma Health Sciences Center, Oklahoma City Center for Indigenous Resilience, Culture, and Maternal Health Equity Principal investigator: Karina M. Shreffler, Ph.D.
- University of Utah, Salt Lake City ELEVATE Center: Reduction of Maternal Morbidity from Substance Use Disorder in Utah Principal investigator: Torri D. Metz, M.D.
Johns Hopkins University, Baltimore, will serve as the data innovation and coordinating hub. Led by principal investigator Andreea Creanga, M.D., Ph.D., this hub will support data collection, ensure high data quality and provide data science expertise. The University of Pennsylvania, Philadelphia, will serve as the implementation science hub. Under the direction of principal investigator Meghan Brooks Lane-Fall, M.D., this hub will help to promote the integration of research findings and evidence into public health, clinical practice and community settings.
About the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD): NICHD leads research and training to understand human development, improve reproductive health, enhance the lives of children and adolescents, and optimize abilities for all. For more information, visit https://www.nichd.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Connect with Us
- More Social Media from NIH
Maternal Health
Maternal health refers to the well-being of women during pregnancy, childbirth, and the postpartum period. It is an essential aspect of global health, as it directly affects the health and survival of both the mother and the newborn. Healthy maternal outcomes depend on a plethora of factors, including access to quality healthcare, skilled health providers during pregnancy, well-equipped facilities for safe deliveries, the mother's nutrition, and education levels, amongst others. Inadequate maternal health care is a crucial contributor to preventable deaths of women during and after childbirth worldwide. Effective interventions that can save the lives of mothers during and after childbirth include access to skilled antenatal care (ANC) services, effective labour and delivery care, and access to postnatal care. ANC is vital in preventing, detecting, and managing pregnancy complications early on while delivery care encompasses skilled attendance, thus reducing the risks of childbirth. Postnatal care is also integral to monitoring and managing any complications of delivery. To improve maternal health outcomes and reduce maternal mortality rates worldwide, as well as the mortality rates of newborns, WHO recommends increasing funding to support maternal health programs, improving the quality of maternal health care services, and implementing policies that improve access to healthcare for women at all stages of life. Additionally, increasing women's education and empowerment through advocacy, capacity building, and grassroots partnerships are critical for achieving and sustaining good maternal health.
Related Topics
Health Policy
Related Article For "Maternal Health"
About (131) results
Full-text HTML
Download as PDF
Download as XML
- UNC Chapel Hill

Research Topic: Maternal and Fetal Health
| Or search for anything: | |||
| ', html:true, content:function(){ return jQuery('#'+jQuery(this).data('contentwrapper')).html(); } }).on('shown.bs.popover', function () { jQuery( '.popover.oscitas-bootstrap-container' ).attr( 'aria-hidden', 'false'); jQuery( '.popover.oscitas-bootstrap-container .popover-title' ).focus(); jQuery(document).on('keydown', function(event) { if (event.key == 'Escape') { jQuery('.osc_popover_new').popover('toggle') } }); }).on( 'hidden.bs.popover', function() { jQuery( '.popover.oscitas-bootstrap-container' ).attr( 'aria-hidden', 'true'); }); }); | |||
Gillings School of Global Public Health > Department of Maternal and Child Health > Division: None
Alison Stuebe is interested in modifiable risk factors for metabolic disease in the perinatal period, gestational diabetes, pregnancy-associated weight gain, maternal health effects of lactation, effects of postpartum depression on breastfeeding physiology, the role of subclinical infection in breast pain, and the etiology of racial and ethnic disparities in breastfeeding, breastfeeding difficulties, and postpartum depression. (Keywords: Asymptomatic infection, breastfeeding, breastfeeding (complications), ethnic disparities (etiology), gestational diabetes, lactation (health aspects), maternal health, metabolic diseases, metabolic diseases (risk factors), perinatology, postpartum depression, postpartum depression (epidemiology), pregnant women (weight gain in), race disparities (etiology))
School of Medicine > Department of Obstetrics and Gynecology > Division: Global Women's Health
Jennifer Tang is interested in family planning, maternal neonatal health, and global women’s health. (Keywords: Family planning, global women’s health, maternal health, neonatal health)
School of Medicine > Department of Cell Biology and Physiology > Division: None
Kathleen Caron is interested in mouse models of fetal growth restriction and preeclampsia. (Keywords: Fetal growth restriction, mouse models, preeclampsia)
School of Medicine > Department of Obstetrics and Gynecology > Division: Maternal-Fetal Medicine (MFM)
Kim Boggess is interested in infection and inflammation in pregnancy outcomes. (Keywords: Infection, inflammation, pregnancy outcome)
Neeta Vora is interested in reproductive genetics and prenatal diagnosis as they pertain to maternal obesity, fetal neurodevelopment, preterm labor, and growth parameters. (Keywords: Fetal neurodevelopment, growth, maternal obesity, prenatal diagnosis, preterm labor, reproductive genetics)
Tracy Manuck is interested in preterm labor, cervical insufficiency, preterm premature rupture of membranes, multiple gestations, and caring for pregnancies complicated by fetal chromosomal or structural anomalies. (Keywords: Human chromosomes (abnormalities), multiple pregnancy, obstetric labor complications, pregnancy care, pregnancy complications (chromosomal), preterm labor, uterine cervical incompetence)
- Introduction
- Conclusions
- Article Information
eTable 1. Comparison of women included in the study sample and women excluded for missing information on anesthesia care.
eTable 2. ICD - 9 - CM and ICD - 10 - CM codes used in this study.
eTable 3. Variables included in the propensity score.
eFigure 1. Distribution of the stabilized weights.
eFigure 2. The unified interaction and mediation analysis framework.
eFigure 3. Flowchart of the study.
eTable 4. Comparison of women who did not receive neuraxial analgesia for vaginal delivery and those who did, before and after propensity-score matching.
eTable 5. Odds ratios of postpartum hemorrhage associated with neuraxial analgesia for vaginal delivery with the successive addition of patient and hospital characteristics in the propensity score used for weighting.
eTable 6. Odds ratios of postpartum hemorrhage associated with neuraxial analgesia for vaginal delivery with the individual addition of each of the hospital characteristics to the propensity score used for weighting.
- Neuraxial Labor Analgesia for Vaginal Delivery and Severe Maternal Morbidity JAMA Network Open Invited Commentary February 22, 2022 Evelina Pankiv, MD; Alan Yang, MSc; Kazuyoshi Aoyama, MD, PhD
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Guglielminotti J , Landau R , Daw J , Friedman AM , Chihuri S , Li G. Use of Labor Neuraxial Analgesia for Vaginal Delivery and Severe Maternal Morbidity. JAMA Netw Open. 2022;5(2):e220137. doi:10.1001/jamanetworkopen.2022.0137
Manage citations:
© 2024
- Permissions
Use of Labor Neuraxial Analgesia for Vaginal Delivery and Severe Maternal Morbidity
- 1 Department of Anesthesiology, Columbia University Vagelos College of Physicians and Surgeons, New York, New York
- 2 Department of Health Policy and Management, Columbia University Mailman School of Public Health, New York, New York
- 3 Division of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Columbia University Vagelos College of Physicians and Surgeons, New York, New York
- 4 Department of Epidemiology, Columbia University Mailman School of Public Health, New York, New York
- Invited Commentary Neuraxial Labor Analgesia for Vaginal Delivery and Severe Maternal Morbidity Evelina Pankiv, MD; Alan Yang, MSc; Kazuyoshi Aoyama, MD, PhD JAMA Network Open
Question Is use of labor neuraxial analgesia for vaginal delivery associated with decreased risk of severe maternal morbidity?
Findings In this cross-sectional study of 575 524 women with vaginal delivery in New York hospitals from 2010 to 2017, use of neuraxial analgesia was associated with a 14% decrease in risk of severe maternal morbidity.
Meaning Increasing the access to and utilization of labor neuraxial analgesia may help reduce severe maternal morbidity and improve maternal health outcomes.
Importance Addressing severe maternal morbidity (SMM) is a public health priority in the US. Use of labor neuraxial analgesia for vaginal delivery is suggested to reduce the risk of postpartum hemorrhage (PPH), the leading cause of preventable severe maternal morbidity.
Objective To assess the association between the use of labor neuraxial analgesia for vaginal delivery and SMM.
Design, Setting, and Participants In this population-based cross-sectional study, women aged 15 to 49 years undergoing their first vaginal delivery were included. Data were taken from hospital discharge records from New York between January 2010 and December 2017. Data were analyzed from November 2020 to November 2021.
Exposures Neuraxial analgesia (ie, epidural or combined spinal-epidural) vs no neuraxial analgesia.
Main Outcomes and Measures The primary outcome was SMM, as defined by the US Centers for Disease Control and Prevention, and the secondary outcome was PPH. Adjusted odds ratios (aORs) and 95% CIs of SMM associated with neuraxial analgesia were estimated using the inverse propensity score–weighting method and stratified according to race and ethnicity (non-Hispanic White vs racial and ethnic minority women, including non-Hispanic Asian or Pacific Islander, non-Hispanic Black, Hispanic, and other race and ethnicity) and to the comorbidity index for obstetric patients (low-risk vs high-risk women). The proportion of the association of neuraxial analgesia with the risk of SMM mediated through PPH was estimated using mediation analysis.
Results Of 575 524 included women, the mean (SD) age was 28 (6) years, and 46 065 (8.0%) were non-Hispanic Asian or Pacific Islander, 88 577 (15.4%) were non-Hispanic Black, 104 866 (18.2%) were Hispanic, 258 276 (44.9%) were non-Hispanic White, and 74 534 (13.0%) were other race and ethnicity. A total of 400 346 women (69.6%) were in the low-risk group and 175 178 (30.4%) in the high-risk group, and 272 921 women (47.4%) received neuraxial analgesia. SMM occurred in 7712 women (1.3%), of which 2748 (35.6%) had PPH. Before weighting, the incidence of SMM was 1.3% (3486 of 272 291) with neuraxial analgesia compared with 1.4% (4226 of 302 603) without neuraxial analgesia (risk difference, −0.12 per 100; 95% CI, −0.17 to −0.07). After weighting, the aOR of SMM associated with neuraxial analgesia was 0.86 (95% CI, 0.82-0.90). Decreased risk of SMM associated with neuraxial analgesia was similar between non-Hispanic White women and racial and ethnic minority women and between low-risk and high-risk women. More than one-fifth (21%; 95% CI, 14-28) of the observed association of neuraxial analgesia with the risk of SMM was mediated through the decreased risk of PPH.
Conclusions and Relevance Findings from this study suggest that use of neuraxial analgesia for vaginal delivery is associated with a 14% decrease in the risk of SMM. Increasing access to and utilization of labor neuraxial analgesia may contribute to improving maternal health outcomes.
In 2020, addressing severe maternal morbidity (SMM) was defined as a public health priority by the US Department of Health and Human Services. 1 , 2 Indeed, the reported incidence of SMM has more than doubled between 1999 and 2017, affecting approximately 1 in 60 women in 2017. 3 Of concern, the risk of SMM is up to 3-fold increased for racial and ethnic minority women compared with non-Hispanic White women. 4 - 7 As of 2021, postpartum hemorrhage (PPH) remains the leading cause of preventable SMM and maternal mortality. 8 - 11
Labor neuraxial analgesia (ie, epidural or combined spinal-epidural analgesia) is the most effective technique to alleviate labor pain and is used in 70% of birthing women in the US. 12 , 13 Use of neuraxial analgesia has been associated with reduced risk of severe PPH. One study analyzing vaginal births between 2004 and 2006 in France reported a 47% decreased risk of severe PPH, defined as a decrease in postpartum hemoglobin concentration greater than 4 g/dL (to convert to grams per liter, multiply by 10), for women who received labor neuraxial analgesia compared with those who did not. 14 The proposed mechanism is that the presence of the epidural catheter allows immediate and effective management of PPH because interventions to stop the bleeding require anesthesia (eg, manual removal of a retained placenta). Timely management of obstetric hemorrhage after a vaginal delivery prevents escalation into severe hemorrhage, with potentially superimposed coagulation defects (eg, disseminated intravascular coagulation). Replication of the association identified in the French study is important, given advances in obstetric and anesthesia care practices since the study was conducted, and the marked differences in the health care systems and maternal health outcomes between the US and France. 15 - 18 For instance, the maternal mortality ratio in the US is twice the maternal mortality ratio in France and other high-income countries. 16 , 17 Using data from a large cohort of vaginal deliveries in New York hospitals, the objective of this study was to assess the association between labor neuraxial analgesia and SMM.
The study protocol was granted exemption under 45 Code of Federal Regulation 46 (not human subjects research) by the Institutional Review Board of Columbia University Irving Medical Center. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
Data for this study came from the New York State Inpatient Database (SID), collected as part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality. 19 The SID includes patient characteristics, diagnoses, and procedure codes for all inpatient discharges from nonfederal acute care community hospitals. This analysis was limited to New York, as it is the only Healthcare Cost and Utilization Project–participating state also providing information on anesthesia care. 20 , 21
The study sample included hospitalizations for vaginal delivery among women aged 15 to 49 years between January 1, 2010, and December 31, 2017. Vaginal delivery cases were identified using previously published algorithms. 22 , 23 If a woman had more than 1 delivery during the study period, only the first was included. Women were excluded if (1) information on anesthesia care was missing or did not correspond to no neuraxial analgesia or to neuraxial analgesia, (2) the hospital American Hospital Association identifier or hospital Federal Information Processing Standards county code were missing, (3) the hospital had no labor and delivery unit, and (4) the hospital had less than 10 annual deliveries. Women requiring general anesthesia for urgent cesarean delivery after neuraxial analgesia was placed were excluded.
The exposure of interest was labor neuraxial analgesia (ie, epidural or combined spinal-epidural) compared with no neuraxial analgesia. In SID data, anesthesia care is reported as a categorical variable with values corresponding to no anesthesia care, local anesthesia, general anesthesia, regional anesthesia (ie, neuraxial), other anesthesia, and missing. For the purpose of the study, the study sample was limited to discharges recording no anesthesia care or regional (neuraxial) analgesia. Because of the high proportion of discharges excluded for missing information on anesthesia care (189 825 of 950 649 [19.9%] hospitalizations for first vaginal delivery), we conducted a sensitivity analysis including these discharges and handling missing values for anesthesia care with multiple imputation. The comparison of women excluded because of missing information on anesthesia care and women included in the study sample is presented in eTable 1 in the Supplement .
The primary outcome was SMM according to the US Centers for Disease Control and Prevention definition, which includes 16 maternal complications (eg, heart failure) and 5 procedures (eg, hysterectomy). 24 The Centers for Disease Control and Prevention definition has a sensitivity of 77% and specificity of 99%, using individual medical record analysis as the criterion standard. 25 The secondary outcome was PPH ( International Classification of Diseases, Ninth Revision, Clinical Modification [ ICD - 9 - CM ] diagnosis codes 666.0 to 666.2 and ICD - 10 - CM codes O72.0 to O72.2).
Women characteristics were recorded directly from the SID, including age (19 years and younger, 20 to 29 years, 30 to 39 years, and 40 years and older), race and ethnicity, residence (rural or urban), health insurance (Medicaid, Medicare, private, self-pay, or other), and admission day (weekday or weekend). In the SID, race and ethnicity includes 7 mutually exclusive categories: non-Hispanic Asian or Pacific Islander, non-Hispanic Black, Hispanic, Native American, non-Hispanic White, other race and ethnicity, and missing. Because of the low number of Native American women in the study sample, these women were included in the other race and ethnicity group. Individual comorbidities were summarized using the comorbidity index for obstetric patients (CMI-OB; categorized into low risk [CMI-OB = 0] vs high risk [CMI-OB of 1 or greater]). 26 , 27 This index includes maternal age and 20 maternal conditions (eg, severe preeclampsia) that are predictive of maternal end-organ injury or death during the delivery hospitalization through 30 days postpartum. Possible contraindications to neuraxial analgesia and obstetrical characteristics were identified using ICD - 9 - CM and ICD - 10 codes (eTable 2 in the Supplement ).
For each hospital, the following characteristics were calculated for each year of the study period among all deliveries using SID data: volume of delivery, cesarean delivery rate, proportion of induced labor, proportion of racial and ethnic minority women, proportion of women who are safety net patients (Medicaid or Medicare beneficiaries and uninsured), proportion of women with an CMI-OB score of 1 or greater, proportion of admissions during a weekend, proportion of neuraxial analgesic or anesthetic techniques in deliveries, and coding intensity (mean number of diagnosis and procedure codes per discharge). The number of labor and delivery units in the hospital, hospital location (rural or urban), and teaching status were abstracted from the American Hospital Association Annual Survey Database. 28 The numbers of obstetrician and gynecologists, physician anesthesiologists, and certified registered nurse anesthetist per 1000 in-hospital births were abstracted at the hospital county level from the Area Health Resources Files. 29
Using the inverse propensity score–weighting method and mediation analysis, this retrospective cross-sectional study of vaginal delivery cases examined whether labor neuraxial analgesia was associated with decreased risk of SMM and the mediating role of PPH. Two stratified analyses were planned a priori according to (1) race and ethnicity (non-Hispanic White vs racial and ethnic minority women) and (2) the CMI-OB (low-risk women vs high-risk women).
Statistical analysis was performed with R version 3.6.2 (The R Foundation) and specific packages ( mice for multiple imputations, Matching for matching, and survival for conditional logistic regression). Mediation analysis was performed using SAS version 9.4 (SAS Institute). 30
Comparisons of characteristics between women with and without neuraxial analgesia used the absolute standardized mean difference (SMD), with a value greater than 10% used to define a clinically important imbalance. The incidence of SMM and PPH was calculated in women with and without neuraxial analgesia overall, according to race and ethnicity (non-Hispanic White vs racial and ethnic minority women), and according to CMI-OB value (low risk vs high risk). The risk difference was calculated as the difference in SMM or PPH incidence between women with and without neuraxial analgesia. The 95% CI for the risk difference was estimated using bootstrap with replacement (B = 2000) and the percentile method.
Crude odds ratios (ORs) of SMM and PPH associated with labor neuraxial analgesia were estimated using univariate logistic regression models overall, according to race and ethnicity, and according to CMI-OB value. Adjusted ORs were estimated using the inverse propensity score–weighting method and stabilized weights (eFigure 1 in the Supplement ). The propensity score estimated the individual probability of receiving neuraxial analgesia. It was calculated using a fixed-effect logistic regression model, with neuraxial analgesia as the dependent variable and the 37 patient-level and hospital-level characteristics listed in eTable 3 in the Supplement as the independent variables. Interaction terms and quadratic terms were included in the propensity score. A complete case analysis was performed because less than 1% of discharges (n = 4967) had missing values for variables included in the propensity score. Balance after weighting was assessed using the SMD. Adjusted ORs for SMM and PPH associated with neuraxial analgesia were estimated using weighted logistic regression models overall, according to race and ethnicity, and according to CMI-OB value and with further adjustment for variables with a persistent imbalance after weighting.
To assess the robustness of the main analysis, the following sensitivity analyses were performed. First, the adjusted OR of SMM associated with neuraxial analgesia was estimated using stabilized weights truncated at 1% and at 99%. Second, we used the propensity score–matching method. Matching used the nearest-neighbor approach with a caliper of 0.2 and 1 case matched to 1 control. Adjusted OR of SMM associated with neuraxial analgesia were estimated using conditional logistic regression models, with further adjustment for variables with persistent imbalance after matching (eTable 4 in the Supplement ). Third, discharges with missing information on anesthesia care were included and handled using multiple imputation and adjusted OR of SMM associated with neuraxial analgesia estimated using the inverse propensity score–weighting method and stabilized weights, as previously described.
We used the unified interaction and mediation analysis framework to decompose the association of labor neuraxial analgesia with the risk SMM into a direct association and an indirect association (eFigure 2 in the Supplement ). 31 The direct association corresponds to the association of neuraxial analgesia with the risk of SMM in the absence of PPH and the indirect association to the association of labor neuraxial analgesia with the risk of SMM mediated through PPH. The mediation analysis was performed using propensity score–matched data and variables with persistent imbalance after matching were included in the models.
Because there is no validated solution to estimate the required sample size or study power using the inverse propensity score–weighting method, we do not provide such estimates. 32
During the study period, 575 524 women with vaginal delivery were included and analyzed (eFigure 3 in the Supplement ). The mean (SD) age was 28 (6) years, and 46 065 (8.0%) were non-Hispanic Asian or Pacific Islander, 88 577 (15.4%) were non-Hispanic Black, 104 866 (18.2%) were Hispanic, 258 276 (44.9%) were non-Hispanic White, and 74 534 (13.0%) were other race and ethnicity. A total of 400 346 women (69.6%) were in the low-risk group and 175 178 (30.4%) in the high-risk group, and 272 921 women (47.4%) received neuraxial analgesia.
Compared with women without labor neuraxial analgesia, women with labor neuraxial analgesia were more likely to be non-Hispanic White, have private health insurance, premature rupture of membranes, an induced labor, or fetal heart rhythm abnormalities ( Table 1 ). Women with neuraxial labor analgesia were also likely to give birth in a high-volume teaching hospital, with a higher utilization of neuraxial techniques, and with a higher number of obstetrician and gynecologists, physician anesthesiologists, or nurse anesthetists.
SMM occurred in 7712 women (1.3%; 95% CI, 1.31-1.37), of which 2748 (35.6%) had PPH. Before weighting, the incidence of SMM among women with labor neuraxial analgesia was 1.3% (3486 of 272 291) vs 1.4% (4226 of 302 603) among women without, yielding a risk difference of −0.12% (95% CI, −0.17 to −0.07) and a crude OR of 0.91 (95% CI, 0.87-0.96) ( Table 2 ). Conversely, the incidence of PPH was significantly higher in women with neuraxial analgesia compared with women without neuraxial analgesia ( Table 2 ).
After weighting, the risk difference for SMM between women with and without neuraxial analgesia was −0.21% (95% CI, −0.30 to −0.12) and the adjusted OR for SMM associated with labor neuraxial analgesia 0.86 (95% CI, 0.82-0.90) ( Table 3 ). The decreased risk of SMM was similar between non-Hispanic White women and racial and ethnic minority women and between low-risk and high-risk women. Contrary to the unadjusted analysis, labor neuraxial analgesia was associated with a decreased risk of PPH (adjusted OR, 0.91; 95% CI, 0.88-0.94). A post hoc analysis identified hospital characteristics as the factors accounting for the inversion of the OR of PPH (eTable 5 in the Supplement ), particularly the hospital utilization of neuraxial techniques (eTable 6 in the Supplement ).
In the sensitivity analyses ( Table 4 ), the adjusted OR of SMM associated with labor neuraxial analgesia was 0.90 (95% CI, 0.85-0.94) with stabilized weights truncated at 1% and 99%, 0.91 (95% CI, 0.83-0.99) with the propensity score–matching method, and 0.91 (95% CI, 0.87-0.95) with handling discharges with missing information on anesthesia care using multiple imputations ( Table 4 ).
Of the observed association of neuraxial analgesia with the risk of SMM, 79% (95% CI, 64-94) was ascribed to the direct association and 21% (95% CI, 14-28) to the indirect association (ie, mediated through the decreased risk of PPH).
In this study of vaginal delivery cases in New York hospitals, labor neuraxial analgesia was associated with a decreased risk of SMM, which was partially mediated through a decreased risk of PPH. Decreased risk of SMM was consistent across racial and ethnic groups and across risk groups.
Our study found the suggested association between labor neuraxial analgesia and decreased risk of PPH and extends it to decreasing the risk of SMM. 14 Early evaluation and management of the third stage of labor should avoid escalation of PPH into severe PPH and may prevent the development of potentially superimposed coagulation defects, kidney failure, and SMM. However, decreased risk of PPH accounted for only 21% of the protective association of labor neuraxial analgesia with the risk of SMM, indicating that there are other mechanisms linking labor neuraxial analgesia to the decreased risk of SMM. Other possible mechanisms may include sustained intrapartum hemodynamic monitoring of parturient women with neuraxial analgesia, which enhances maternal monitoring and early detection of blood loss immediately after delivery; adequate intravenous access and fluid resuscitation; and continuous anesthesia availability and oversight of the process of labor and delivery and preparedness for acute events. 33
Lower labor neuraxial analgesia utilization has been repeatedly reported among racial and ethnic minority, uninsured, and low-income obstetric patients. 13 , 34 - 40 While approximately 80% of non-Hispanic White women receive labor neuraxial analgesia nationwide, 70% of non-Hispanic Black women receive labor neuraxial analgesia and only 65% of Hispanic women; approximately 75% of pregnant women with a health insurance receive labor neuraxial analgesia but only 50% of uninsured pregnant women do. 13 Several interventions can be suggested to increase access and higher utilization of labor neuraxial analgesia for these patients. First, implementation of language-concordant educational programs have been associated with decreased misconceptions about neuraxial analgesia and increased neuraxial analgesia utilization among racial and ethnic minority women. 41 These programs facilitate patient participation in medical decision-making by making the risks and benefits associated with treatment alternatives more understandable. Second, cost may represent a financial obstacle to receive labor neuraxial analgesia for low-income patients without health insurance coverage. The mean cost of a labor neuraxial analgesia in the US is approximately $2100, which corresponds to a monthly income of 150% of the Federal Poverty Level for a single pregnant woman. Labor neuraxial analgesia is one of the most frequent surprise bills for childbirth. 42 Up to 13% of pregnant women are uninsured in the month of delivery. 43 - 45 Federal policies aiming at increasing insurance coverage for low-income pregnant people may help remove this financial barrier. For example, the 2014 Medicaid expansion under the Affordable Care Act has decreased the proportion of uninsured pregnant people, but its effect on labor neuraxial analgesia utilization and maternal health outcomes has been insufficiently investigated. 46 , 47 Last, continuous availability of an in-house obstetric anesthesia team is required to provide uninterrupted access to labor neuraxial analgesia. Continuous in-house coverage of obstetric anesthesia services is available in approximately 86% of hospitals with more than 1500 annual deliveries, 41% of hospitals with 500 to 1500 annual deliveries, and 15% of hospitals with less than 500 annual deliveries. 40 Approximately 60% of childbirths in the US occur in hospitals with less than 1000 deliveries, suggesting that creating continuous in-house coverage of obstetric anesthesia services in low-volume and intermediate-volume hospitals could substantially increase access to and utilization of labor neuraxial analgesia. 48
Our study has limitations. First, our study is observational in nature, and the associations between neuraxial analgesia and SMM are not necessarily causal. Second, we did not specifically assess the risk of SMM in each racial and ethnic minority group (eg, Black women) because of the low number of cases in some of these groups. Since the incidence of SMM and severe PPH is higher in American Indian and Black women compared with both White women and other racial and ethnic minority women, 4 , 7 , 11 we cannot exclude a greater effect of labor neuraxial analgesia in American Indian or Black women. Third, our data do not contain detailed information on the type of neuraxial analgesia precluding the analysis of the association of the neuraxial techniques (epidural or combined spinal-epidural) with SMM. 49 , 50 Fourth, we used the number of physicians and nurses at the hospital-county level as a proxy for the number of physicians and nurses at the individual hospital level because no current data system provides this information. 20 While this approach may be accurate for counties with only 1 hospital, it may not be accurate for counties with more than 1 hospital. Fifth, we did not include women with labor neuraxial analgesia who later required an intrapartum cesarean delivery. The benefits of labor neuraxial analgesia in such context might have been a reduction in the utilization rate of general anesthesia and risks associated with avoidable general anesthesia, rather than a decreased risk of PPH. 51 Sixth, identification of SMM cases was limited to the delivery hospitalization period and did not account for SMM occurring after discharge that account for approximately 15% of SMM cases. 52
In this study, use of labor neuraxial analgesia for vaginal delivery was associated with a decreased risk of SMM. Our findings suggest that increasing access to and higher utilization of labor neuraxial analgesia might help decrease severe maternal morbidity and improve maternal health outcomes in the US.
Accepted for Publication: December 21, 2021.
Published: February 22, 2022. doi:10.1001/jamanetworkopen.2022.0137
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 Guglielminotti J et al. JAMA Network Open .
Corresponding Author: Jean Guglielminotti, MD, PhD, Department of Anesthesiology, Columbia University Vagelos College of Physicians and Surgeons, 622 W 168th St, PH5-505, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Guglielminotti had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design : Guglielminotti, Daw, Li.
Acquisition, analysis, or interpretation of data : Guglielminotti, Landau, Friedman, Chihuri, Li.
Drafting of the manuscript : Guglielminotti, Landau, Friedman, Li.
Critical revision of the manuscript for important intellectual content : Guglielminotti, Landau, Daw, Chihuri, Li.
Statistical analysis : Guglielminotti, Daw, Chihuri, Li.
Obtained funding : Li.
Administrative, technical, or material support : Friedman, Li.
Study supervision : Li.
Conflict of Interest Disclosures: Dr Guglielminotti has received grants from the National Institute On Minority Health And Health Disparities outside the submitted work. No other disclosures were reported.
Meeting Presentation: This work was presented virtually at the Best Paper Session of the 53rd Meeting of the Society of Obstetric Anesthesia and Perinatology; May 16, 2021.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
research@BSPH
The School’s research endeavors aim to improve the public’s health in the U.S. and throughout the world.
- Funding Opportunities and Support
- Faculty Innovation Award Winners
Conducting Research That Addresses Public Health Issues Worldwide
Systematic and rigorous inquiry allows us to discover the fundamental mechanisms and causes of disease and disparities. At our Office of Research ( research@BSPH), we translate that knowledge to develop, evaluate, and disseminate treatment and prevention strategies and inform public health practice. Research along this entire spectrum represents a fundamental mission of the Johns Hopkins Bloomberg School of Public Health.
From laboratories at Baltimore’s Wolfe Street building, to Bangladesh maternity wards in densely packed neighborhoods, to field studies in rural Botswana, Bloomberg School faculty lead research that directly addresses the most critical public health issues worldwide. Research spans from molecules to societies and relies on methodologies as diverse as bench science and epidemiology. That research is translated into impact, from discovering ways to eliminate malaria, increase healthy behavior, reduce the toll of chronic disease, improve the health of mothers and infants, or change the biology of aging.
120+ countries
engaged in research activity by BSPH faculty and teams.
of all federal grants and contracts awarded to schools of public health are awarded to BSPH.
citations on publications where BSPH was listed in the authors' affiliation in 2019-2023.
publications where BSPH was listed in the authors' affiliation in 2019-2023.
Departments
Our 10 departments offer faculty and students the flexibility to focus on a variety of public health disciplines
Centers and Institutes Directory
Our 80+ Centers and Institutes provide a unique combination of breadth and depth, and rich opportunities for collaboration
Institutional Review Board (IRB)
The Institutional Review Board (IRB) oversees two IRBs registered with the U.S. Office of Human Research Protections, IRB X and IRB FC, which meet weekly to review human subjects research applications for Bloomberg School faculty and students
Generosity helps our community think outside the traditional boundaries of public health, working across disciplines and industries, to translate research into innovative health interventions and practices
Introducing the research@BSPH Ecosystem
The research@BSPH ecosystem aims to foster an interdependent sense of community among faculty researchers, their research teams, administration, and staff that leverages knowledge and develops shared responses to challenges. The ultimate goal is to work collectively to reduce administrative and bureaucratic barriers related to conducting experiments, recruiting participants, analyzing data, hiring staff, and more, so that faculty can focus on their core academic pursuits.

Research at the Bloomberg School is a team sport.
In order to provide extensive guidance, infrastructure, and support in pursuit of its research mission, research@BSPH employs three core areas: strategy and development, implementation and impact, and integrity and oversight. Our exceptional research teams comprised of faculty, postdoctoral fellows, students, and committed staff are united in our collaborative, collegial, and entrepreneurial approach to problem solving. T he Bloomberg School ensures that our research is accomplished according to the highest ethical standards and complies with all regulatory requirements. In addition to our institutional review board (IRB) which provides oversight for human subjects research, basic science studies employee techniques to ensure the reproducibility of research.
Research@BSPH in the News
Four bloomberg school faculty elected to national academy of medicine.
Considered one of the highest honors in the fields of health and medicine, NAM membership recognizes outstanding professional achievements and commitment to service.
The Maryland Maternal Health Innovation Program Grant Renewed with Johns Hopkins
Lerner center for public health advocacy announces inaugural sommer klag advocacy impact award winners.
Bloomberg School faculty Nadia Akseer and Cass Crifasi selected winners at Advocacy Impact Awards Pitch Competition
The independent source for health policy research, polling, and news.

Health Policy Issues in Women’s Health
Published: May 28, 2024
KFF Authors:

Ivette Gomez

Laurie Sobel

Alina Salganicoff
Usha Ranji , Karen Diep , Ivette Gomez , Laurie Sobel and Alina Salganicoff
Table of Contents
Introduction.
Health care is a central element of women’s lives, shaping their ability to care for themselves and their families, to be productive members of their communities, to contribute to the workforce, and to build a base of economic security. Women’s reproductive health care needs, their central roles managing family health as parents and as family caregivers, and their longer lifespans, albeit with greater rates of chronic health problems and functional limitations than men, all shape their relationships with the health care system. While women are major consumers of health care services and play a central role as health navigators and caregivers for their families, structural factors can challenge their ability to get the health care they need. Factors, including national and state policies that shape the health care delivery system to research priorities and discriminatory economic and societal forces, can deprioritize women’s health concerns. Access challenges are greater for women who are in low-income households, who face structural and societal racism and discrimination, who struggle with complex or understudied medical conditions, or who live in states or communities that have enacted or invested in policies and programs that do not support their health needs.
In the United States, the women’s health movement gained significant traction in the 1960s and 1970s as part of a larger grassroots women’s rights movement that challenged long-standing inequities and discrimination that limited women’s economic and social opportunities. The book, “ Our Bodies, Ourselves ,” brought a wide range of women’s health concerns, ranging from abortion and sexuality to menopause and cancer, into the mainstream. Over time, federal action also began to address many of the long-standing discriminatory sex and gender-based policies that were baked into our employment, health, and research policies. The 1973 U.S. Supreme Court ruling in Roe v. Wade decriminalized and protected the right to abortion care for nearly 50 years; the Pregnancy Discrimination Act of 1978 offered workplace and insurance protections to pregnant workers; the National Institutes of Health (NIH) Revitalization Act of 1993 mandated the inclusion of women in clinical research and formally established the NIH Office of Women’s Health; and in 2010, the Affordable Care Act (ACA) banned many of the discriminatory practices that had shaped women’s coverage of and access to care.
This primer focuses on some of the key areas disproportionately affecting women today that are shaped by national and state health policies. This includes health coverage and costs, reproductive health services, maternal health, mental health, and intimate partner violence. In addition, it highlights some of the structural factors and inequities that still impact women’s health, particularly women of color and gender-expansive individuals such as those who are transgender or non-binary or otherwise gender fluid or non-conforming who are at risk of being marginalized or discriminated against by their health coverage or providers. We note that while we refer to “women” and “women’s health” throughout this chapter, some persons assigned female sex at birth do not identify as women, such as transgender men, non-binary individuals, and otherwise gender-expansive individuals. Still, many of the issues discussed in this chapter also apply to them.
What Is the Demographic Profile of Women?
More than 128 million adult women over the age of 19 live in the U.S. today, with great diversity in many demographic characteristics. A third of adult women are between the ages of 35-54 (33%) and the majority are White (60%) (Figure 1). Nearly 1 in 5 (17%) women are Hispanic, 12% are Black and 6% are Asian.
Almost two-thirds (65%) of women live in a household with at least one full-time worker, while 1 in 10 (9%) live in a household with only part-time workers, and 25% of women live in households with no workers (data not shown). Given the important role of employment in shaping health coverage, workforce participation is a significant determinant of the type of health insurance that working women or women who live in households with full-time workers can obtain.
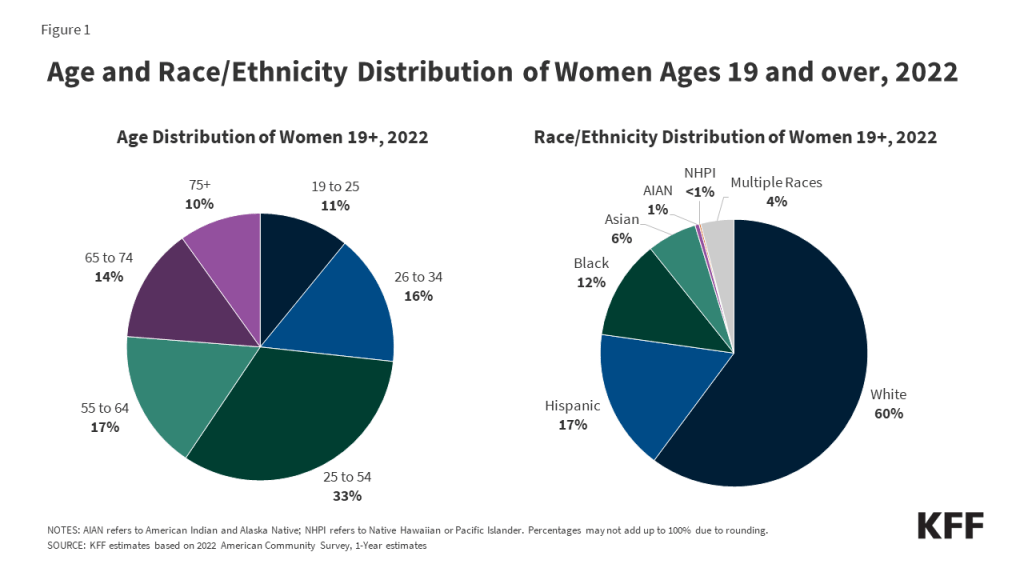
While most women in the U.S. report having good health, nearly 1 in 5 ( 18% ) women 18 and older rate their health as “fair” or “poor” and 14% report having a disability such as difficulty with vision, hearing, or walking. As women age, they are more likely to experience chronic health problems and declines in health status. These factors are highly predictive of their need for and use of health care services.
Income also plays a major role in health coverage and access to care. Income affects the resources that women have to pay for out-of-pocket health care costs and contribute to premium costs. Income also determines women’s eligibility for programs such as Medicaid or subsidies to secure coverage through the ACA Marketplace. Three in 10 (29%) adult women are part of households with low incomes (family income below 200% of the FPL was $47,112 for a family of three in 2022). Almost 4 in 10 (35%) women have completed a bachelor’s degree or higher, almost a third (27%) have a child under the age of 19 living at home, and 93% are U.S. citizens. Nearly 4 in 10 women live in the South (39%), almost a quarter (24%) live in the West, a fifth (20%) live in the Midwest, and 18% live in the Northeast (Figure 2).
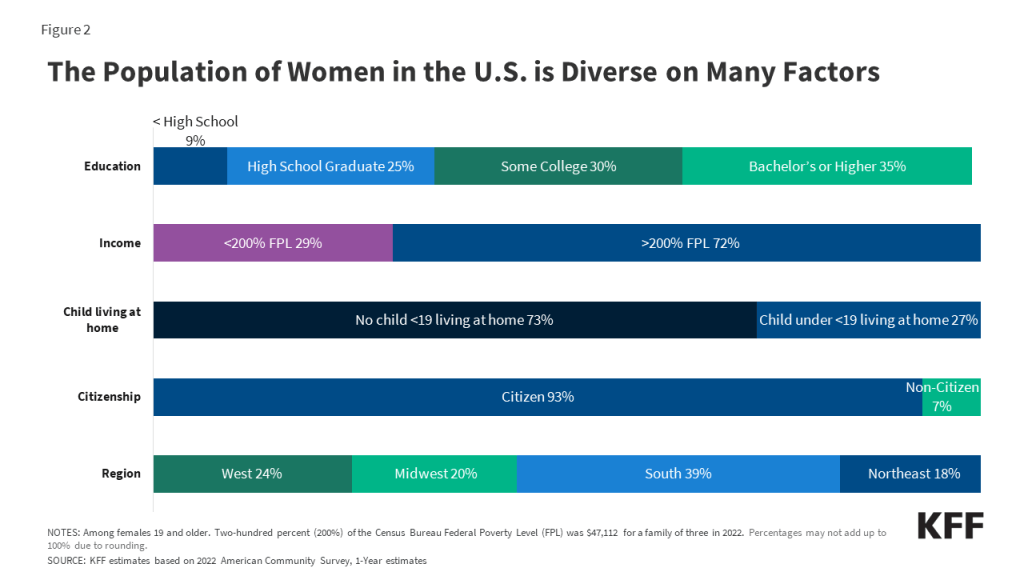
What Are the Sources of Health Insurance Coverage for Women?
While most adult women have some form of either private or public health insurance, the coverage profile for those who are under and over age 65 differs considerably. For those who are under age 65 , employer-sponsored coverage, individually purchased policies, and Medicaid—the state-federal program for people with low incomes—comprise the majority of coverage options. However, nearly 1 in 10 women in that age group are currently uninsured. Among women 65 years and older, the Medicare program plays a critical role covering nearly all seniors in the U.S., though often with considerable coverage gaps (such as hearing, vision and long-term services and supports) and cost-sharing burdens.
Employer-Sponsored Insurance
Approximately 58.3 million women aged 19-64 (60%) received their health coverage from employer-sponsored insurance in 2022 (Figure 3). Women in families with at least one full-time worker are more likely to have job-based coverage (70%) than women in families with only part-time workers (33%) or without any workers (17%).
Employer-sponsored insurance can come with substantial out-of-pocket costs based on premiums, deductibles, co-insurance, and co-payment levels. In 2022, annual insurance premiums for employer-sponsored insurance averaged $7,911 for individuals and $22,463 for families. On average, workers paid 17% of premiums for individual coverage and 28% for family coverage with the employers picking up the balance.
Non-Group Insurance
In 2022, about 9% of women ages 19 to 64 (approximately 8.3 million women) and 8% of their male counterparts purchased insurance in the non-group market. This includes individuals who purchased private policies from state-based Marketplaces established under the ACA, as well as those who purchased coverage from private insurers that operate outside of the ACA Marketplaces.
Most individuals who seek insurance policies in their state’s Marketplace qualify for assistance with the coverage costs. Individuals with incomes below $58,320 (400% of the Federal Poverty Level in 2023) can receive federal tax credits which lower premium costs.
The ACA set new standards for all individually purchased plans and eliminated many historically discriminatory practices that affected disadvantaged women in particular. Today, plans are prohibited from charging women higher premiums than men for the same level of coverage (gender rating) or from disqualifying women from coverage because they had certain pre-existing medical conditions, including pregnancy. All direct purchase plans must also cover certain “essential health benefits” ( EHBs ) that fall under 10 different categories, including maternity and newborn care, mental health, and a wide range of preventive health care services. Prior to the ACA, many individual plans excluded maternity care benefits or required policyholders to purchase costly riders to obtain maternity coverage.
Medicaid, the state-federal program for individuals with low incomes, covered 19% of adult women ages 19 to 64 in 2022, compared to 14% of men. Historically, to qualify for Medicaid, women had to have very low incomes and be in one of Medicaid ’s eligibility categories: pregnant, mothers of children 18 and younger, a person with a disability, or over 65. Women who didn’t fall into these categories typically were not eligible regardless of how low their incomes were. The ACA allowed states to broaden Medicaid eligibility to most individuals with incomes less than 138% of the FPL regardless of their family or disability status, effective January 2014. As of December 2023, 40 states and Washington, D.C. have expanded their Medicaid programs under the ACA, but 10 states have not and still base eligibility on historical categorical and income standards. For example, in Mississippi, the Medicaid income eligibility for parents is 28% of the FPL, which was approximately $6,900 for a family of three in 2023. Therefore, parents in families of three in Mississippi with incomes above this amount do not qualify for Medicaid because their income exceeds the state’s eligibility level.
Medicaid covers the poorest segment of women in the U.S. Forty-three percent of women with incomes below 200% of the FPL and 52% of women with incomes below 100% of the FPL have Medicaid coverage. By federal law, all states must provide Medicaid coverage to pregnant women with incomes up to 133% of the FPL through 60 days postpartum. However, in recent years, there has been a growing interest in expanding the length of the postpartum coverage period and, as of March 2024, nearly all states have taken steps to extend postpartum Medicaid coverage to one year.
Medicaid covers many health services that are essential for women. Medicaid financed 41% of births in the U.S. in 2021 and accounts for 75% of all publicly-funded family planning services. State Medicaid programs are prohibited from charging any cost-sharing for pregnancy-related care or family planning services. Over half of states have established programs that use Medicaid funds to cover the costs of family planning services for women with low incomes who remain uninsured, and most states have limited scope Medicaid programs to pay for breast and cervical cancer treatment for certain uninsured women with low incomes. Conversely, coverage for abortion is very limited under Medicaid as a result of the Hyde Amendment, a rider to federal appropriations that bans any federal funds from being used to pay for abortions unless the pregnancy is determined to be a result of rape or incest or poses a threat to the pregnant person’s life (more on abortion in the following section).
Uninsured Women
In 2022, approximately 10% of non-elderly women (9.5 million) were uninsured. This rate is slightly lower than that of men (13%) because, on average, women have lower incomes and have been more likely to qualify for Medicaid than men under one of Medicaid’s eligibility categories: pregnant, parent of children under 18, disability, or over 65. The ACA opened the door for states to eliminate the categorical requirements, but the gender gap in the insured rates between men and women persists.
The disadvantage uninsured individuals experience in accessing care and health outcomes is well established. Compared to women with insurance, those who are uninsured have lower use of important preventive services such as mammograms, Pap tests , and timely blood pressure checks. They are also less likely to report having a regular doctor , which is associated with better access to care and higher rates of use of recommended preventive services.
Women with lower incomes, women of color, and non-citizen women are at greater risk of being uninsured (Figure 4). One in 5 Hispanic (20%) and American Indian and Alaska Native (20%) women and 18% of women with incomes under 200% of the FPL are uninsured. A higher share of single mothers are uninsured (10%) than women in two-parent households (8%) (data not shown). Most uninsured women live in a household where someone is working; 69% are in families with at least one adult working full-time; and 82% are in families with at least one part-time or full-time worker (data not shown).
Many women who are uninsured are eligible for financial assistance with the costs of coverage. A fifth of uninsured women (20%) are eligible for Medicaid coverage but are not enrolled in the program (Figure 5) . One in 4 uninsured women (39%), about 3.7 million women, qualify for subsidies to cover the premium costs and some of the out-of-pocket costs of Marketplace plans but may not be aware of coverage options or may face barriers to enrollment. However, 7% of uninsured women live in states that have not adopted the ACA Medicaid expansion and fall into a “ coverage gap ” because their incomes are above the thresholds to qualify for Medicaid but below the levels to qualify for Marketplace tax credits (below 100% of the FPL). Approximately 1 in 3 (34%) uninsured women are not eligible for any assistance with health coverage due to their immigration status, their income, or because they have an offer of coverage from their employer.
There is considerable state-level variation in uninsured rates across the nation, ranging from 21% of women in Texas to 3% of women in Washington D.C., Massachusetts, and Vermont (Figure 6). Of the 15 states with uninsured rates above the national average (10%), nine have not adopted the ACA Medicaid expansion.
Medicare is the federal program that provides health coverage to virtually all people ages 65 and older as well as younger people with long-term disabilities. In 2020, Medicare covered 35 million women, including nearly 31 million ages 65 and older, and over 4 million under age 65 with long-term disabilities.
More than half (55%) of all Medicare beneficiaries are women and 45% are men. The population of women covered by Medicare is diverse, with varying social, economic, and health circumstances. Women live longer than men on average (79 years vs. 73 years life expectancy at birth in 2021), and many live with certain chronic illnesses, cognitive and mental impairments, and functional problems at higher rates than men. A higher share of older women than men also experience urinary incontinence, depression, osteoporosis, pulmonary disease, and Alzheimer’s/dementia. Medicare plays a key role in supporting the health and well-being of women, covering a broad range of essential services, including preventive, primary and specialty care, and prescription drugs. However, reflecting Medicare’s original role as a program to serve the medical needs of older adults, coverage of services for enrollees of reproductive age may be more limited. For example, there is no federal requirement for Medicare to cover all contraceptive services and supplies for the purpose of preventing pregnancy for younger Medicare enrollees with permanent disabilities.
Another gap in the Medicare program is the absence of coverage for long-term care services and supports (LTSS), such as nursing home stays and home care services, which many older adults need and seek but are expensive and unaffordable for some. Compared with men, women are more likely to require these services because they have more chronic conditions, have higher rates of physical and cognitive impairments, and are more likely to live alone. Medicare only covers time-limited LTSS after a hospitalization and does not cover ongoing LTSS for those with chronic conditions or functional impairments. Some older women can qualify for Medicaid for LTSS, but only if they have low incomes and, in some cases, must spend down most of their assets. Just a small share of seniors have private long-term care insurance to help cover some of the costs of LTSS. As a result, unless they have incomes low enough to qualify for Medicaid, many older people do not have any coverage for LTSS and rely on unpaid caregiving provided by family, friends, or neighbors. The majority of informal caregivers are women, who are most commonly caring for aging parents and spouses.
Women with Medicare also tend to have more modest incomes than men—a consequence of smaller lifetime savings, lower retirement income, and divorce and widowhood that result in only one income. While Medicare covers many necessary health care services, gaps in benefits, cost-sharing requirements, and spending on premiums for Medicare and supplemental coverage can translate into high out-of-pocket expenses for some people in the program. In 2020, 13% of women and 11% of men with Medicare reported that they had faced cost-related challenges in the past 12 months, such as trouble getting care due to cost or problems paying medical bills. These challenges are more common among female Medicare enrollees who are Black (22%) and Hispanic (18%), do not have a bachelor’s degree (15%), and those with annual incomes below $20,000 (20%).
How Do Health Care Costs and Scope of Benefits Affect Women’s Access to Care?
The ACA set national standards for the scope of benefits offered in private plans. As mentioned earlier, many insurance plans had adopted practices that discriminated against women that were addressed in the ACA. In addition to the broad categories of essential health benefits (EHBs) offered by Marketplace plans, all privately purchased plans must cover maternity care, which had been historically excluded from most individually purchased plans requiring the purchase of an expensive rider for that benefit to be covered. In addition, most private plans must cover preventive services without co-payments or other cost sharing. This includes screenings for breast and cervical cancers, well-woman visits (including prenatal visits), prescribed contraceptives, breastfeeding supplies and supports such as breast pumps, and several services for sexually transmitted infections (STI). Higher shares of women with private and Medicaid coverage report having had recommended preventive services such as mammograms, Pap screenings or colonoscopies compared to those who were uninsured (Figure 7).
Affordability of coverage continues to be a significant concern for many women, both for those who are uninsured as well as those with coverage. The leading reason why uninsured adults report that they have not obtained coverage is that it is too expensive . Under employer-sponsored insurance, the major source of coverage for women, 61% of all covered workers with a general annual deductible have deductibles of at least $1,000 for single coverage. Despite having coverage, many insured women (31%) report that their plans did not always cover all of their needed care or paid less than they expected (Figure 8).
What Are the Issues Affecting Women's Care and Access?
Reproductive health.
Maternity Care
In 2022, there were approximately 3.6 million births in the U.S. Childbirth is the leading reason for hospitalization, and most private insurance plans and the Medicaid program are required to cover care associated with childbirth. Medicaid covers about 4 in 10 births nationally and, in some states, more than half. The Medicaid program prohibits plans from charging out-of-pocket charges for pregnancy-related care, and coverage lasts through one year postpartum in most, but not all, states. For people with private insurance, which finances just over half of births ( 51% ), the federal Pregnancy Discrimination Act requires employer plans to cover maternity care benefits. However, even for those with private insurance, a pregnancy often comes with significant out-of-pocket health expenses that can reach thousands of dollars . A KFF analysis estimated that women enrolled in large group plans pay around $3,000 out-of-pocket for costs associated with pregnancy, childbirth, and post-partum care. On average, Caesarean section births, which account for approximately one-third of births in the U.S., are significantly more expensive than vaginal deliveries. The ACA also requires individual plans to cover maternity care and bans plans from implementing restrictions on coverage of pre-existing health conditions, including pregnancy.
In recent years, there has been growing attention to pregnancy-related quality of care and maternal health. Maternal and infant mortality rates in the U.S. are far higher than those in similarly large and developed countries, and people of color are at a considerably higher risk for poor maternal and infant health outcomes compared to their White peers. Despite continued advancements in medical care, rates of maternal mortality and morbidity and preterm birth have been rising in the U.S., characterized by stark racial disparities. Notably, rates of pregnancy-related death (deaths within one year of pregnancy) among Native Hawaiian or Pacific Islander (NHPI), Black, and American Indian and Alaska Native (AIAN) women are over four to two times higher, respectively, compared to the rate for White women (14.1 and 62.8 vs. 39.9 vs. 32 per 100,000 births) (Figure 9). The Centers for Disease Control and Prevention (CDC) has determined that many of these pregnancy-related deaths were preventable, caused by cardiac-related conditions, infection, hemorrhage, and mental health conditions , including substance use. Maternal death rates increased during the COVID-19 pandemic and racial disparities widened for Black women. Black, AIAN, and Native Hawaiian or Pacific Islander (NHPI) women also have higher shares of preterm births, low birthweight births, or births for which they received late or no prenatal care compared to White women. Infants born to Black, AIAN, and NHOPI people have markedly higher mortality rates than those born to White women.
The disparities in maternal and infant health are symptoms of broader underlying social and economic inequities that are rooted in racism and discrimination. Differences in health insurance coverage and access to care play a role, but notably, disparities in maternal and infant health persist even when controlling for certain underlying social and economic factors, such as education and income, pointing to the roles racism and discrimination play in driving disparities. Moreover, with the overturning of Roe v. Wade and the numerous states that have enacted abortion bans across the nation, increased barriers to abortion for people of color may widen the already existing large disparities in maternal and infant health.
There have been efforts at the policy level and in clinical circles to improve maternal health and address disparities. The Biden Administration issued the White House Blueprint for Addressing the Maternal Health Crisis , outlining policy priorities and strategies. These include funding to expand and diversify the perinatal workforce, enhancing training for clinicians to better listen to patient concerns, investing in maternal mental health care, and strengthening perinatal care in rural communities. At the state and local levels, multidisciplinary maternal mortality review committees and perinatal quality collaboratives have focused on data collection and reviewing the causes behind pregnancy-related deaths in their communities to try to prevent deaths in the future.
Fertility Assistance
Many people require fertility assistance to have children. These services include diagnostic services, treatment services, and fertility preservation. People seek fertility assistance for several reasons, such as if they or their partner has infertility, or because they are in a same-sex relationship or are single and desire children. Both female and male factors contribute to infertility, including problems with ovulation (when the ovary releases an egg), structural problems with the uterus or fallopian tubes, problems with sperm quality or motility, and hormonal factors. About 25% of the time, infertility is caused by more than one factor, and in about 10% of cases , infertility is unexplained. Infertility estimates, however, do not account for LGBTQ+ or single individuals who may also need fertility assistance for family building. Thus, there are varied reasons that may prompt individuals to seek fertility care.
Despite a need for fertility services, fertility care in the U.S. is inaccessible to many due to the cost. Fertility treatments are expensive and often are not covered by insurance. While some private insurance plans cover diagnostic services, there is very little coverage for costly treatment services such as intrauterine insemination, in vitro fertilization, and cryopreservation.
Most people who use fertility services must pay out of pocket, with costs often reaching thousands of dollars depending on the services received. This means that in the absence of insurance coverage, fertility care is out of reach for many people. Few states require private insurance plans to cover fertility assistance services, but these only apply to a subset of insurance plans and beneficiaries. Additionally, even fewer states have any fertility coverage requirement under Medicaid, the health coverage program for people with low incomes.
Nearly 1 in 4 women in the U.S. have an abortion in their lifetime. Starting with the 1973 landmark Supreme Court ruling in Roe v. Wade , women in the U.S. had the right to abortion up until the point of viability, regardless of where they lived. On June 24, 2022, the Supreme Court issued a ruling in Dobbs v. Jackson Women’s Health Organization that overturned the constitutional right to abortion as well as the federal standards of abortion access, established by prior decisions in the cases Roe v. Wade and Planned Parenthood v. Casey . The Dobbs decision allows states to set policies regarding the legality of abortions and establish gestational limits. Access to and availability of abortions vary widely between states , with large swaths of the country banning or restricting almost all abortions, with few exceptions, and some states enshrining and protecting abortion rights (Figure 10).
Decades of research have shown that abortion is a very safe medical service. Still, despite its strong safety profile, abortion is the most highly regulated medical service in the country and is now banned or restricted to early gestational stages in many states. In addition to bans on abortion altogether, many states impose other limitations on abortion that are not medically indicated, including waiting periods, ultrasound requirements, and parental notification and consent requirements. These restrictions typically delay receipt of services and can increase costs associated with abortion care.
Obtaining an abortion can be costly, with median costs exceeding $500 in out-of-pocket expenses for patients who self-pay. On average, the costs are higher for abortions in the second trimester than in the first trimester. People may have to travel if abortions are prohibited or not available in their area, adding costs related to travel and lodging. Given abortion bans and Hyde Amendment restrictions on payment for abortions under Medicaid and state restrictions on insurance coverage of abortion services, many people pay for abortion services out of pocket. Some people are able to receive assistance from local abortion funds if they need financial support to obtain abortion services, particularly if they have to travel out of state or have low incomes and cannot afford the costs of the abortion. For some, however, the costs of abortion services and travel will put the service out of reach and force them to have a birth that is not desired or is a risk to their health or life.
Insurance coverage for abortion services is heavily restricted in some state-regulated private insurance plans and public programs, like Medicaid and Medicare. Private insurance covers most women of reproductive age, and states can choose whether abortion coverage is included or excluded in private plans that are not self-insured. Prior to the Dobbs ruling, about half of the states had enacted private plan restrictions and banned abortion coverage from ACA Marketplace plans. Since the Dobbs ruling, some of these states have also banned the provision of abortion services altogether. However, 10 states have enacted laws that require private plans to cover abortion, typically without cost-sharing.
The Hyde Amendment has banned the use of federal funds for abortion unless the pregnancy is a result of rape, incest, or it endangers the woman’s life. States may use non-federal state-only funds to pay for abortions under other circumstances for women covered by Medicaid, which 17 states currently do. However, more than half ( 56% ) of women covered by Medicaid live in states where they have no coverage for abortion, unless they qualify for an exception.
The impact of the Dobbs decision goes far beyond abortion care. It has also affected the provision of related health care services, including management of miscarriages and pregnancy-related emergencies, treatments for cancer and other chronic illnesses , contraceptive options , and much more. Women with low incomes, women of color, sexual/gender minorities, and other pregnant people have been disproportionately affected by the sweeping impacts of this ruling, as they are less likely to have the resources to travel potentially long distances to seek care.
Since the Dobbs ruling, there has been a constant stream of legal challenges , with a plethora of cases that seek to challenge abortion bans as well as block access to abortion medication or services. While most of the litigation is in state courts, the Supreme Court is considering a case involving the FDA’s approved conditions for using mifepristone, one of the drugs used for medication abortion , as well as a case about potential conflict between state-level abortion bans and Emergency Medical Treatment and Labor Act (EMTALA), the federal law that requires hospitals to provide care to stabilize patients experiencing medical emergencies. The Supreme Court will likely issue its decision in these cases in June 2024.
Contraception
Contraceptive care is an important component of overall health care for many women and people capable of becoming pregnant. Federal and state policies shape access to and the availability of contraceptive care, but factors such as provider characteristics, as well as individual preferences and experiences also impact contraceptive choices and use. For most people, private insurance coverage and Medicaid greatly reduce or eliminate financial barriers to contraceptive care. However, access is still limited in many parts of the U.S. with more than 19 million women living in contraceptive deserts where they may not have access to a health center offering the full range of contraceptive methods. There have been more efforts to broaden contraceptive availability outside of traditional clinical settings, including through commercial apps that use telehealth platforms, state efforts to allow pharmacists to prescribe birth control, and, most recently, over-the-counter (OTC) access to contraceptives without a traditional prescription.
The importance and impact of contraceptives in women’s lives are unquestionable. The 2022 KFF Women’s Health Survey highlighted that the majority of females 18 to 64 (90%) have used contraception at some point in their reproductive years, with most reporting they have used oral contraceptives and male condoms at some point in their lives (Figure 11). Many women have used more than one contraceptive method throughout their lifetime (76%), a reflection of changing needs and preferences across the lifespan.
The ACA requires that most private plans cover contraceptive services for females without cost-sharing – this includes patient education and counseling and FDA-approved methods of contraception with a prescription. This provision has dramatically reduced cost-sharing for contraception among females with private insurance plans, though some privately insured females who are eligible for no-cost coverage are still paying some of the cost of their contraceptives (Figure 12 ) . Reasons include someone using a brand-name contraceptive that is not in the plan’s formulary or consumers unaware of or not offered a generic alternative.
Despite its far-reaching impact, the ACA’s requirement for contraceptive coverage has been challenged in the courts on multiple occasions, with three cases reaching the Supreme Court. The earlier cases, Burwell v. Hobby Lobby (2014) and Zubik v. Burwell (2016), challenged the Obama Administration's regulations implementing the contraceptive coverage requirement, contending that the requirement violated some employers’ religious rights. The most recent cases , Little Sisters of the Poor v. Pennsylvania (2020) and Trump v. Pennsylvania (2020), involved regulations issued by the Trump Administration, which currently exempt employers with religious objections from providing contraceptive coverage to their employees.
For people with lower incomes, the Medicaid program is the primary funding source for contraceptives. The federal Medicaid statute establishes minimum standards, and, for decades, has classified family planning as a mandatory benefit category that all state programs must cover. States may not charge any out-of-pocket costs for family planning services and must allow beneficiaries to see any Medicaid provider within their state for family planning care. Many states also have programs that provide Medicaid coverage just for family planning services to people who have lower incomes but do not qualify for full Medicaid benefits.
Additionally, the federal Title X family planning program, administered by the HHS Office of Population Affairs (OPA), is the only federal program specifically dedicated to supporting the delivery of family planning care for individuals who are uninsured and have lower incomes. The program provides funding to more than 4,000 health clinics, public health departments, and nonprofit agencies across the country to deliver contraceptives and other family planning services to individuals with low incomes. Title X-funded providers must follow the program’s requirements, which include offering a broad range of family planning methods for low or no cost and ensuring confidentiality for adolescents. Federal rules also require that participating clinics offer their patients non-directive pregnancy option counseling that includes abortion, adoption, and prenatal referral for those who seek those services.
While there have been numerous over-the-counter contraceptive methods available (e.g. condoms, spermicides), in July 2023, the Food and Drug Administration (FDA) approved the first over-the-counter daily oral contraceptive pill, known as Opill . FDA’s approval of Opill makes it the most effective form of contraception available OTC intended for regular use. Private insurers and Medicaid generally require a prescription to cover OTC products, so even though Opill and other OTC products are available without needing a prescription from a clinician, coverage without a prescription will be limited without federal or state action.
Mental Health
Mental health has emerged as a rapidly growing concern in recent years, with 90% of Americans saying there is a mental health crisis in a recent KFF-CNN poll. Women experience several mental health conditions such as anxiety, depression, and eating disorders more frequently than men, and some also experience mental health disorders that are unique to women, such as perinatal depression (including prenatal and postpartum depression) and premenstrual dysphoric disorders that may occur when hormone levels change.
A KFF survey found that in 2022, a significantly higher share of women (50%) than men (35%) thought they needed mental health services in the past two years. The rates were particularly higher among younger women (64% of women ages 18-25). However, barriers to accessing timely and affordable mental health services persist for many. Almost half of women who said they needed mental health services and tried to get care were able to get an appointment within a month, but more than one-third of women had to wait longer. Among those who could not get an appointment, women cite limited provider availability and cost as the main reasons they were unable to access mental health care. Significantly larger shares of women who are uninsured (60%) say they could not get an appointment due to affordability reasons, compared to those who have health insurance either through private plans (33%) or Medicaid (30%) (Figure 13).
Prior KFF research has documented the challenges some consumers with health insurance face when finding in-network mental health care. In fact, 2 in 10 privately insured women with a mental health care appointment in the past two years say their provider did not accept their insurance. The option is effectively not available to women who have low incomes or are on Medicaid and lack the financial resources to pay for out-of-network care.
Among the COVID-19 pandemic and the rise of racist attacks , the ongoing opioid epidemic is a commonly cited stressor that has exacerbated long-standing mental health issues and prompted growing demand for mental health services in the past several years. Women face unique gender and sex-related differences when it comes to substance use, including greater physical, psychological, and social harms associated with drug use. Use of certain substances in women has been linked to increased rates of depression and anxiety disorders. Studies have also shown that women who use substances are at risk for issues related to pregnancy , fertility, breastfeeding, menstrual cycle, and more. All of these factors also shape the availability of treatment and services accessible to women.
Intimate Partner Violence Against Women
Intimate partner violence (IPV), defined as sexual violence, stalking, physical violence, and psychological aggression perpetrated by a current or former intimate partner, affects nearly a third of all Americans at some point in their lives. Although IPV affects men and women of all ages, women experience IPV at higher rates. Rates are higher among some groups of women, particularly those who are young, Black, American Indian or Alaska Native, and LGBTQ. It is difficult to quantify the number of people who experience IPV, as many cases are not reported. Some studies have estimated 9 million women in the U.S. experience sexual violence, physical violence, or stalking by an intimate partner in a single year. People who experience IPV are more likely to experience a range of health problems such as chronic pain, cardiovascular problems, and neurological problems. Both the CDC and U.S. Preventive Services Task Force (USPSTF) have identified IPV as a significant public health issue in the US.
Several federal programs and laws fund health care services and supports to survivors of IPV. The Violence Against Women Act (VAWA) has a broad scope, covering domestic violence, sexual harassment, stalking, and sexual assault. VAWA provides grants to states, local governments, and other organizations to establish their own violence-related programs and protocols. While some of the focus of VAWA and other public policies is prosecution of those who commit violence, provisions in VAWA also address health care coverage and costs for people who have experienced IPV.
It is well recognized that the health care system can serve as a site of IPV screening and support, and some professional medical organizations recommend that clinicians screen women for IPV. Under the ACA, IPV screening is considered a preventive service as screening is recommended by the USPSTF and Health Resources and Services Administration (HRSA) preventive services for women. When health care providers routinely screen patients for IPV, it helps identify cases and connect survivors to resources and supports. However, this can be challenging as a KFF survey of OBGYNs found that many clinicians say they do not have sufficient resources within their practices to provide follow-up services when cases of IPV are identified. Connections to community-based services are particularly important for clinicians to be able to care for patients who disclose IPV.
Future Outlook
Women’s health has become one of the most politicized issues in society and health care. The overturning of Roe v. Wade in 2022 marked a seismic change in an important aspect of women’s health care that has implications for all pregnancy-related care and women’s economic future and well-being. The high and rising rates of maternal mortality and morbidity in the U.S. and the persistent gaps in mortality rates experienced by women of color highlight the need to address the roles that poverty, racism, and discrimination play in women’s health. Some of the key challenges that remain to be addressed in women’s health include:
- How to address and eliminate the persistent inequities in health coverage and outcomes experienced by women of color
- How to build a delivery system and develop coverage policies that is responsive to the reproductive and sexual health needs of women and other gender minorities to promote optimal health outcomes
- How to shape policies that protect women with low incomes from experiencing financial barriers to care
- Identifying and implementing policies that improve maternal health outcomes and also eliminate the structural and systemic barriers to care
- Providing access to comprehensive care to pregnant people who live in areas where abortion is unavailable due to state-level bans and restrictions
- How to provide care to women dealing with issues that are heavily stigmatized and marginalized, such as intimate partner violence and mental health challenges.
- Abortion in the United States Dashboard
- State Profiles for Women's Health
- Women's Health Insurance Coverage
- Medicaid Coverage for Women | KFF
- State Health Facts Women's Health Indicators
- 2022 Women's Health Survey reports
- State and Federal Reproductive Rights and Abortion Litigation Tracker
- Preventative Services Tracker
- A Focus on Contraception in the Wake of Dobbs
- Resources about the Title X National Family Planning Program
Ranji, Usha, Diep, Karen, Gomez, Ivette, Sobel, Laurie, & Salganicoff, Alina, Health Policy Issues in Women's Health. In Altman, Drew (Editor), Health Policy 101, (KFF, May 28, 2024) https://www.kff.org/health-policy-101-health-policy-issues-in-womens-health/ (date accessed).

COMMENTS
Given the importance of maternal health for our families, communities, and nation, addressing the unacceptable rates of maternal mortality and severe maternal morbidity calls for a comprehensive approach that addresses health from well before to well after pregnancy. A singular focus on the perinatal period would ignore upstream health factors associated with chronic conditions as well as ...
of maternal mortality and morbidity, reducing the disparities in maternal health outcomes, and improving the overall experience of pregnancy, birth, and postpartum for people across the country.
Reproductive Health and Research (SRH) conducted the global SRMNCAH policy survey in 2018-2019. This survey is the fifth such survey on maternal, newborn, child and adolescent health since 2009-2010, and it is the first to include sexual and reproductive health and to align with the SDGs and the Global Strategy for
Why is maternal, newborn and child health a focus area for 2021-2025? Dramatic reductions have been achieved in maternal, newborn and child health in recent decades. Yet deep inequities remain between and within countries, which are being exacerbated by COVID-19. For instance,
Section 1: Background and rationale for review. The Maternal Mortality working group have recently presented new estimates of MMR, reporting a total of 536,000 maternal deaths in 2005 thus an average of 402 deaths per 100,000 live births, with 50% occurring in SS Africa (900/100,000 live births) and 45% in Asia.
Health Research to Improve Women's and Maternal Health Outcomes Improving maternal health before, during, and after pregnancy is among the nation's most pressing public health priorities. The Centers for Disease Control and Prevention (CDC) estimates 17.4 maternal deaths occurred per 100,000 live births in 2018, 2, 3. and an estimated 25,000
Abbreviationsiv Introduction1. Promote, prevent and protect maternal and perinatal health 3. 1. Antenatal care 3 Nutritional supplements 3 Maternal and fetal assessment 4 Preventive measures 6 Interventions for common physiological symptoms 7 Health systems interventions 8 2. Prevention of pre-eclampsia and eclampsia 9 3.
and Adolescence at the Department of Reproductive Health and Research, WHO (1994- 2009), independent consultant on sexual and reproductive health and rights (2009-2014). Estzer Kismödi, Human Rights Adviser, Department of Reproductive Health and Research, WHO (2002-2012), independent consultant for WHO (2012-2014).
Journal of Community Medicine & Public Health Bhuiyan S, et al. J Community Med Public Health: CMPH-109. Research Article DOI: 10.29011/CMPH-109/100009 Maternal and Child Health (MCH) Handbook and Its Effect on Maternal and Child Health Care: A Systematic Review and Meta-Analysis Shafi Bhuiyan1,2*, Housne Begum2,3, Deena2, Sabeen Ehsan2, Syed Jamal Shah2, Rabia Shariff2, Vanessa Linton2,3 ...
Maternal and child health. This brief summarizes the contributions of Kaiser Permanente Research since 2007 on the topic of maternal and child health, including prepregnancy risk factors and a variety of risks and outcomes occurring both during and following childbirth. According to the Centers for Disease Control and Prevention (CDC), Kaiser ...
To assess in utero exposures associated with leukocyte telomere length (LTL) at birth and maternal LTL in a primarily Latinx birth cohort. Apurva Prasad, Jue Lin, Laura Jelliffe-Pawlowski, Kimberley Coleman-Phox, Larry Rand and Janet M Wojcicki. Maternal Health, Neonatology and Perinatology 2023 9 :14.
Maternal Health. Healthy mothers, healthy babies: taking stock of maternal health. UNICEF, 2019. This brief provides a general overview and data on the causes of pregnancy-related complications and a call for action. Maternal mortality fact sheet. WHO, 2019. This fact sheet includes critical data, key facts
Background The preservation and promotion of maternal health (MH) emerge as vital global health objectives. Despite the considerable emphasis on MH, there are still serious challenges to equitable access to MH services in many countries. This review aimed to determine key barriers to the provision and utilization of MH services in low- and lower-middle-income countries (LLMICs). Methods In ...
WHO develops guidelines on a broad array of clinical, public health, health system, health promotion and implementation strategies. These interventions are often highly context-specific, with multiple factors that directly and indirectly impact the health and societal outcomes, and as part of these strategies, to identify key research priorities that could accelerate improvement in maternal ...
Maternal health. Maternal health refers to the health of women during pregnancy, childbirth and the postnatal period. Each stage should be a positive experience, ensuring women and their babies reach their full potential for health and well-being. Although important progress has been made in the last two decades, about 287 000 women died during ...
maternal mental health. During the meeting, experts and stakeholders discussed maternal mental health and specifi cally focused on the perinatal period. The discussion addressed topics such as risk factors, bar-riers to mental health care, areas in need of research, and potential policy interventions. The authors of this
study, and research on significant issues in health policy. Established in 1918, Childbirth Connection (formerly Maternity Center Association) is a national not-for-profit voice for the needs and interests of childbearing families. Its mission is to improve the quality of maternity care through research, education, advocacy, and policy.
Theories and Models applicable in Maternal and Child Health Nursing. May 2014. In book: Essentials Concepts and Issues in Nursing (pp.246-261) Publisher: Samdavies. Authors:
Maternal health refers to the health of women before and during pregnancy, at childbirth and during the postpartum period (2). 2 The European Region has made substantial progress in improving maternal health, with an average official reported maternal mortality rate of 11 per 100 000 live births in 2014. However,
The National Institutes of Health has awarded $24 million in first-year funding to establish Maternal Health Research Centers of Excellence. Part of NIH's Implementing a Maternal Health and Pregnancy Outcomes Vision for Everyone (IMPROVE) initiative, the centers will develop and evaluate innovative approaches to reduce pregnancy-related ...
Maternal health refers to the well-being of women during pregnancy, childbirth, and the postpartum period. It is an essential aspect of global health, as it directly affects the health and survival of both the mother and the newborn. Healthy maternal outcomes depend on a plethora of factors, including access to quality healthcare, skilled ...
Research Topic: Maternal and Fetal Health $ Don't forget to check out funding opportunities! $ Explore research topics Browse by... Or search for anything: ... Center for Women's Health Research at UNC 104B Market Street, CB#7521 Chapel Hill, NC 27599-7521 P: 919-843-7720 F: 919-843-7364
The COVID-19 pandemic challenged health systems across the world and may have played a role in limiting women's access to health care. 6 The increase in maternal deaths in several countries during the pandemic may have been due to a rise in respiratory or viral conditions directly related to COVID or to conditions worsened by the virus, such ...
In 2020, addressing severe maternal morbidity (SMM) was defined as a public health priority by the US Department of Health and Human Services. 1,2 Indeed, the reported incidence of SMM has more than doubled between 1999 and 2017, affecting approximately 1 in 60 women in 2017. 3 Of concern, the risk of SMM is up to 3-fold increased for racial ...
Jenn Leiferman, Ph.D., chair and professor in the Department of Community and Behavioral Health at the University of Colorado-Denver, focuses her research on maternal and child mental health. Mental health conditions, including perinatal or maternal depression that occurs during pregnancy and up to a year after delivery, are a leading ...
The Department of Population, Family and Reproductive Health is dedicated to improving health throughout the life course worldwide. We train research scientists, public health leaders, and health professionals to excel in careers related to a broad spectrum of population, family, and reproductive health issues.
The WHO Departments of Maternal, Newborn, Child and Adolescent Health and Ageing (MCA), Mental Health . and Substance Use (MSD), Nutrition and Food Safety (NFS), and Sexual and Reproductive Health and Research (SRH) gratefully acknowledge the contributions that many individuals and organizations have made to the . development of this guideline.
Systematic and rigorous inquiry allows us to discover the fundamental mechanisms and causes of disease and disparities. At our Office of Research (research@BSPH), we translate that knowledge to develop, evaluate, and disseminate treatment and prevention strategies and inform public health practice.Research along this entire spectrum represents a fundamental mission of the Johns Hopkins ...
This Health Policy 101 chapter explores how national and state policies shape coverage and access to care for women, with a focus on recent policy and legal developments that affect women's health.