An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Chin J Cancer Res
- v.32(6); 2020 Dec 31

Cervical cancer: Epidemiology, risk factors and screening
Shaokai zhang.
1 Department of Cancer Epidemiology, Affiliated Cancer Hospital of Zhengzhou University/Henan Cancer Hospital, Henan Engineering Research Center of Cancer Prevention and Control, Henan International Joint Laboratory of Cancer Prevention, Zhengzhou 450008, China
Luyao Zhang
Youlin qiao.
2 Department of Epidemiology, National Cancer Center, Chinese Academy of Medical Sciences, School of Population Medicine and Public Health, Peking Union Medical College, Beijing 100021, China
Cervical cancer is one of the leading causes of cancer death among females worldwide and its behavior epidemiologically likes a venereal disease of low infectiousness. Early age at first intercourse and multiple sexual partners have been shown to exert strong effects on risk. The wide differences in the incidence among different countries also influenced by the introduction of screening. Although the general picture remains one of decreasing incidence and mortality, there are signs of an increasing cervical cancer risk probably due to changes in sexual behavior. Smoking and human papillomavirus (HPV) 16/18 are currently important issues in a concept of multifactorial, stepwise carcinogenesis at the cervix uteri. Therefore, society-based preventive and control measures, screening activities and HPV vaccination are recommended. Cervical cancer screening methods have evolved from cell morphology observation to molecular testing. High-risk HPV genotyping and liquid-based cytology are common methods which have been widely recommended and used worldwide. In future, accurate, cheap, fast and easy-to-use methods would be more popular. Artificial intelligence also shows to be promising in cervical cancer screening by integrating image recognition with big data technology. Meanwhile, China has achieved numerous breakthroughs in cervical cancer prevention and control which could be a great demonstration for other developing and resource-limited areas. In conclusion, although cervical cancer threatens female health, it could be the first cancer that would be eliminated by human beings with comprehensive preventive and control strategy.
Introduction
Cervical cancer is the second common female malignant tumor globally which seriously threatens female’s health. Persistent infection of high-risk human papillomavirus (HPV) has been clarified to be the necessary cause of cervical cancer ( 1 , 2 ). The clear etiology accelerated the establishment and implementation of comprehensive prevention and control system of cervical cancer. In May 2018, the World Health Organization (WHO) issued a call for the elimination of cervical cancer globally, and more than 70 countries and international academic societies acted positively immediately ( 3 - 6 ). Thereafter, in November 17, 2020, WHO released the global strategy to accelerate the elimination of cervical cancer as a public health problem to light the road of cervical cancer prevention and control in future which mean that 194 countries promise together to eliminate cervical cancer for the first time ( 7 ). At this milestone time point, we reviewed the update progress of cervical cancer prevention and control in epidemiology, risk factors and screening, in order to pave the way of cervical cancer elimination.
Epidemiology for cervical cancer
Cervical cancer is one of the leading causes of cancer death among women ( 8 ). Over the past 30 years, the increasing proportion of young women affected by cervical cancer has ranged from 10% to 40% ( 9 ). According to the WHO and International Agency for Research on Cancer (IARC) estimates, the year 2008 saw 529,000 new cases of cervical cancer globally. In developing countries, the number of new cases of cervical cancer was 452,000 and ranked second among malignancies in female patients ( 10 ). Conversely, the number of new cases of cervical cancer was 77,000 in developed countries and ranked tenth among female malignancies.
In 2018 worldwide with an estimated 570,000 cases and 311,000 deaths, cervical cancer ranks as the fourth most frequently diagnosed cancer and the fourth leading cause of cancer death in women ( 11 ). However, approximately 85% of the worldwide deaths from cervical cancer occur in underdeveloped or developing countries, and the death rate is 18 times higher in low-income and middle-income countries compared with wealthier countries ( 12 ). Cervical cancer ranks second in incidence and mortality behind breast cancer in lower Human Development Index (HDI) settings; however, it is the most commonly diagnosed cancer in 28 countries and the leading cause of cancer death in 42 countries, the vast majority of which are in Sub-Saharan Africa and South Eastern Asia ( 13 ). The highest regional incidence and mortality rates are seen in Africa ( 14 ). In relative terms, the rates are 7−10 times lower in North America, Australia/New Zealand, and Western Asia (Saudi Arabia and Iraq) ( 15 ).
In China, cervical cancer is the second largest female malignant tumor ( 11 ). According to the data from National Cancer Center in 2015, there were 98,900 new cases and 30,500 deaths of cervical cancer ( 16 ). In the past 20 years, the incidence and mortality of cervical cancer have been increasing gradually in China ( 17 ).
Between 2004 and 2007, the Chinese scientific research team, cooperated with WHO/IARC and the Cleveland Medical Center in the United States in 8 rural and urban areas (Xiangyuan county of Shanxi Province, Yangcheng county of Shanxi Province, Xinmi county of Henan Province, Hotan Prefecture of Xinjiang Uygur Autonomous Region, Shanghai City, Beijing City, Shenzhen City of Guangdong Province, and Shenyang City of Liaoning Province), carried out a population-based multicenter HPV type distribution study among females aged 15−59 years old, clarifying the dominant HPV types of rural and urban populations in China, as well as female HPV infection status and age distribution ( 18 ). Studies have confirmed that persistent infection of high-risk HPV is closely related to the occurrence of cervical cancer. There are 14 types of high-risk HPV, namely HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68 and 73. A multi-center cross-sectional survey study showed that the infection rate of high-risk HPV in China is about 14.3%, and the dominant types are HPV16 (2.9%), HPV52 (1.7%), HPV58 (1.5%), HPV33 (1%) and HPV18 (0.8%), and showed double peaks during adolescence and perimenopause ( 19 ). Globally, HPV16 has the highest infection rate, HPV18 is the second most common type, while HPV 33 is common in Asia, and HPV52 and HPV58 have relatively low infection rates. This shows that compared with the global HPV epidemiology, HPV epidemiology in China has both similarities and differences.
Subsequently, the Chinese scientific research team conducted a cross-sectional multi-center cervical cancer and precancerous HPV genotyping study based on 19 hospitals in 7 geographic regions (Northeast China, North China, Northwest China, Central China, East China, Southwest, and South China). Through the pathological laboratory procedures of strict quality control, it was found that the dominant HPV types in cervical cancer tissue were HPV16, 18, 31, 52 and 58, respectively, and that HPV16 and 18 were the most carcinogenic, which could cause more than 84.5% of cervical cancer ( 20 ). The above research on HPV dominant types from different perspectives provides solid scientific evidence and support for the future research and application of preventive HPV vaccine and in vitro diagnostic technology, epidemiological research and health economics research in the Chinese population.
Risk factors for cervical cancer
A number of risk factors for cervical cancer are linked to exposure to the HPV ( 21 , 22 ). Invasive cancer development process could prolong up to 20 years from the precursor lesion caused by sexually transmitted HPV ( 23 ). However, there are also other numerous risk factors (such as reproductive and sexual factors, behavioral factors, etc) for cervical cancers which include sexual intercourse at a young age (<16 years old), multiple sexual partners, smoking, high parity and low socio-economic level ( 24 , 25 ).
Sexually transmitted infections (STI)
The primary cause of pre-cancerous and cancerous cervical lesions is infection with a high-risk or oncogenic HPV types. Most cases of cervical cancer occur as a result of infection with HPV16 and 18. High-risk types, especially HPV16, are found to be highly prevalent in human populations ( 22 ). The infection is usually transmitted by sexual contact, causing squamous intraepithelial lesions. Most lesions disappear after 6−12 months due to immunological intervention. However, a small percentage of these lesions remain and can cause cancer.
The results of a meta-analysis showed that the highest prevalence of HPV occurs at the age of 25 years, which could be related to changes in sexual behavior ( 26 ). In a meta-analysis study, the bimodal distribution of cervical cancer in some regions has been studied. In this distribution, immediately after sexual intercourse, an outbreak of HPV can be observed, which is followed by a plateau at adult age; the second peak again is observed after 45 years old ( 27 ). Permanent infection with one of the high-risk types of HPV over time leads to the development of cervical intraepithelial neoplasia (CIN). The major mechanisms through which HPV contributes to carcinogenesis involve the activity of two viral oncoproteins, E6 and E7, which interfere with major tumor suppressor genes, P53 and retinoblastoma. In addition, E6 and E7 are associated with changes in host DNA and virus DNA methylation. Interactions of E6 and E7 with cellular proteins and DNA methylation modifications are associated with changes in key cellular pathways that regulate genetic integrity, cell adhesion, immune response, apoptosis, and cellular control ( 28 ).
Human immunodeficiency virus (HIV)
The risk of developing infection from high-risk HPV types is higher in women with HIV ( 29 ). The results of the studies on the relationship between HIV and cervical cancer suggested a higher rate of persistent HPV infection with multiple oncogene viruses, more abnormal Papanicolau (Pap) smears, and higher incidence of CIN and invasive cervix carcinoma among people with HIV ( 23 ). Women infected with HIV are at increased risk of HPV infection at an early age (13−18 years) and are at high risk of cervical cancer. Compared with non-infected women, HIV positive patients with cervical cancer are diagnosed at an earlier age (15−49 years old) ( 30 ).
Reproductive and sexual factors
Sexual partners.
Factors relating to sexual behavior have also been linked to cervical cancer. One study found that an increased risk of cervical cancer is observed in people with multiple sexual partners ( 31 ). Moreover, many studies have also suggested that women with multiple sexual partners are at high risk for HPV acquisition and cervical cancer ( 32 , 33 ). From the meta-analysis, a significant increased risk of cervical diseases was observed in individuals with multiple sexual partners compared to individuals with few partners, both in non-malignant cervical disease and in cervical cancer ( 34 ). The association remained exist even after controlling for the status of HPV infection, which is a major cause of cervical cancer. Also, early age at first intercourse is a risk factor for cervical cancer ( 35 ).
Oral contraceptive (OC) pills
OC pills are known to be a risk factor for cervical cancer. In an international collaborative epidemiological study of cervical cancer, the relative risk in current users increased with an increase in the duration of OC use. It has been reported that the use of OC for 5 years or more can double the risk of cancer ( 36 ). And in a multi-center case-control study, among women who tested positive for HPV DNA, the risk of cervical cancer increased by 3 times if they have used OC pills for 5 years or more ( 37 ). In addition, a recent systematic review & meta-analysis also suggested that OC pills use had a definite associated risk for developing cervical cancer especially for adenocarcinoma. This study concluded that use of OC pills is an independent risk factor in causing cervical cancer ( 38 ).
Cervical cancer screening
With the background of cervical cancer elimination worldwide, cervical cancer screening plays an increased role in the comprehensive prevention and control besides HPV vaccination, especially those methods that demonstrated excellent clinical performance.
Overview of cervical cancer screening methods
The screening methods for cervical cancer are mainly as following: traditional Pap smear, visual inspection with acetic acid & Lugol’s iodine (VIA/VILI), liquid-based cytology (LBC) and HPV testing. The disease burden of cervical cancer has been significantly reduced in developed countries by Pap smear, mainly in the United States, since 1950s. However, the accuracy of traditional Pap smear could be easily affected by following factors: the level of cytological room, professional technicians, sampling method, slide quality, dyeing skills, and cytological personnel experience. In developed countries with high standard experimental conditions and technical level, the sensitivity of cytology is as high as 80%−90%, in contrast, in resource-limited regions, it could be as low as 30%−40%. To overcome the limitations of traditional Pap smear in cervical cancer screening, LBC was developed and approved by Food and Drug Administration (FDA) in 1996 for clinical-use purpose. Compared with the traditional Pap smear, the sensitivity of LBC was significantly improved. Meanwhile, organized and practicable LBC screening program has also been established in developed countries which could ensure cervical cancer screening strategy is carried out continuously and effectively.
Cervical cancer screening has been facilitated since the cause clarified. HPV-based testing is a pivotal part for cervical cancer screening besides cytology-based tests.
The detection of high-risk HPV in cervical lesion biopsies and exfoliated cells has evolved from restriction endonuclease cleavage patterns and hybridization techniques to polymerase chain reaction (PCR)-based system ( 39 ) and most recently next-generation sequencing (NGS) assays ( 40 ). Currently, HPV genotyping is primarily based on the detection of individual types by various methods that utilizing the highly conserved L1 gene and PCR-based methods. These PCR methods employed consensus primers that could target and amplify different sized fragments such as 455 bp with the MY09/11|PGMY system ( 41 ), 150 bp with the GP5+/6+ system ( 42 ), or <100 bp with SPF10 ( 43 ). And another point that is worth noting is that all these techniques remained the most validated methodology to identify and characterize clinically relevant HPV ( 44 - 46 ).
Additionally, the type-specific probes are always to be used to achieve HPV genotyping, besides DNA sequencing ( 46 , 47 ). Other types of assays may be type-specific with immediate discrimination and quantitation of specific HPV types in an “onetube” assay. These methods employ real-time (RT)-PCR techniques, coupled with beta-globin detection for internal quality control utilizing specialized detection systems ( 48 ).
Cervical cancer malignant pathways are tightly correlated to the viral E6 and E7 oncoprotein activities which could also contribute to the accumulation of cellular genomic mutations and viral integration ( 47 ). Therefore, identification of HPV E6/E7 mRNA has been shown to be promising in cervical cancer screening. And most of the assays utilized reverse transcriptase PCR or nucleic acid sequence-based amplification to identify E6/E7 genome fragments ( 49 ).
Recently, the correlation between increased HPV CpG site methylation levels and high-grade cervical lesions has also been demonstrated in numerous studies and has facilitated the development of quantitative assays targeted CpG methylation ( 50 , 51 ). . Studies indicate that NGS assays can provide single-molecule CpG methylation levels to help unravel the mechanism of methylation in cervical cancer development ( 39 , 50 ).
The application of HPV detection has accelerated the transition of cervical cancer screening from morphology to molecular biology. HPV testing was initially used as a triage method for the reflex triage of population with atypical squamous cells of undetermined significance (ASC-US). In 2014, FDA approved HPV detection for the use in cervical screening. Thereafter, HPV detection plays an increasingly important role in the practice of cervical cancer screening. At present, more than 425 HPV testing has been developed worldwide, of which more than 150 is from China. To restrict and standardize HPV testing market, China released guidelines for the clinical performance evaluation for HPV testing against clinical endpoints in 2015. In other countries, it is also necessary to set similar regulations in consideration that 59.7% of HPV tests on the global market without a single peer-reviewed publication ( 49 ). To improve the coverage of cervical cancer screening, HPV testing that is rapid, simple, inexpensive could be more popular and can further promote the application in practice. In 2008, care HPV was developed in China, which demonstrated excellent performance in screening, although it was easy to use, cheap, fast and friendly to the laboratory requirements ( 52 , 53 ). In 2018, the care HPV achieved the pre-qualification certification issued by WHO, which was expected to benefit more people in developing countries and resource-poor areas such as Africa and Southeast Asia ( 54 ). In addition, the cost-effective reflex triage, referral of women, and management strategies appropriate to various resource level areas were also in evaluation ( 55 - 58 ).
In recent years, with the rapid development of science and technology, the application of artificial intelligence (AI) based products is booming. In cervical cancer prevention and control, AI also showed to be promising in cytology-based screening and colposcopy examination based on the image pattern recognition ( 59 , 60 ). These AI-based technology or system can intelligently identify lesions and assist medical staff in clinical examination and diagnosis which could alleviate difficulties in diagnosis in primary clinics.
Screening practice in China
In China, cervical cancer screening started since 1990s, although late compared with Western countries, China still achieved great breakthroughs. Common screening methods were introduced into China for the first time after clinical performance evaluation in high-risk areas which included HPV DNA detection (Hybrid Capture II, HC2), LBC and visual inspection with VIA/VILI ( 61 - 63 ). At the same time, these studies also further made it clear that “one or more HPV tests in a lifetime for cervical cancer screening could be feasible in developing countries” which had important impact on the clinical practice of cervical cancer screening in China and even in the world.
In July 2019, the State Council issued the “Healthy China Action (2019−2030)” plan, emphasizing the need to move forward the diagnosis and treatment and optimize the allocation of medical resources, from the treatment-centered to the health-centered, and to improve health level of the whole people. The program also clearly points out that cervical cancer screening coverage rate needs to reach more than 80% by 2030 ( 64 ), indicating the importance and severity of cervical cancer prevention and control.
Finally, the achievements of scientific research should be able to be developed into products and applied in practice. Based on the experience and study findings, two “National Demonstration Base for Early Diagnosis and Treatment of Cervical Cancer” were set up in Shenzhen Maternal and Child Health Hospital (City type) and Xiangyuan Maternal and Child Health Hospital (Rural type) in Shanxi Province in February 2005 ( 65 ). Thereafter, National Health and Family Planning Commission of China and China Women’s Federation launched cervical cancer and breast cancer screening program for women aged 35−64 years old in rural areas in 2009 ( 66 ), which was also one of the major public health service projects in China organized by national government. Different screening and management strategies have been set up for various resource-level regions. Up to 2017, the project has offered cervical cancer screening for 73.99 million women. Currently, the project has covered 1,501 counties ( 67 ). Meanwhile, China has developed effective cervical cancer prevention and control network which covered screening, diagnosis to treatment, follow-up and rehabilitation step by integrating government support and leadership, multi-sectors’ cooperation, professional personnel support and whole society participation. In 2017, Chinese Preventive Medicine Association released the “Guideline for Comprehensive Prevention and Control of Cervical Cancer” to further promote the standardized and development of cervical cancer prevention and control in China ( 68 ).
The priority of public health measures for cancer prevention and control reflects the government and society’s attention to public’s health, especially in resource-limited areas, and also reflects the civilization and progress of a country and society.
A large number of studies around the world have confirmed that cervical cancer could be prevented and controlled well by screening and early treatment. And it has been widely recognized if only considering the effect of cancer screening. However, the screening methods or solutions with the best effect may be not the best one. In the case of limited health resources, it is necessary to analyze and compare the input and output of different programs from the perspective of health economics which included how to scientifically determine the initial age of screening and time interval, select appropriate screening programs according to local health resources, and focus on cancer intervention in order to maximize the use of limited health resources. And then, we could determine the screening solution that not only has a good effect of disease prevention and control, but also is in line with the principle of cost-effectiveness.
Conclusions
The disease burden of cervical cancer has decreased significantly in developed countries and regions in last decades, however it is still serious in less developed countries and regions, and effective preventive measures in these areas still face serious challenges. At present, there are various available prevention and control measures that are cost-effective and scientific evidence-based to meet the needs of areas with different economic levels. It is gratifying to note that the globe has achieved a strategic consensus on the elimination of cervical cancer and also has developed and released the global strategy to accelerate the elimination of cervical cancer. Although the global elimination of cervical cancer has a long way to go, it is believed that through large-scale continuous promotion and widely use of existing effective prevention and control measures, cervical cancer will become the first cancer eliminated by human beings.
Acknowledgements
This study was supported by grants from the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (No. 2017-I2M-B&R-03 and No. 2016-I2M-1-019).
Conflicts of Interest : The authors have no conflicts of interest to declare.
Cervical Cancer Research
For some people with early-stage cervical cancer, a surgical procedure called a simple hysterectomy may be a safe and effective alternative to treatment with a radical hysterectomy, results from the SHAPE trial show.
It may be worthwhile for some individuals between ages 65 and 69 to get tested for HPV, findings from a Danish study suggest. Specifically, the testing may help prevent cervical cancer among those who haven’t had cervical cancer screening for at least 5 years.
One dose of the HPV vaccine was highly effective in protecting young women against infection from high-risk HPV types, a study in Kenya found. A single dose would make HPV vaccines more accessible worldwide, reducing cervical cancer’s global burden.
The rates of timely cervical cancer screening fell between 2005 and 2019, researchers found, and disparities existed among groups of women. The most common reason for not receiving timely screening was lack of knowledge about screening or not knowing they needed screening.
Fewer women with early-stage cervical cancer are having minimally invasive surgery, including robotic, as part of their treatment, a new study shows. The shift toward more open surgeries follows the release of results from the LACC trial in 2018.
Widespread HPV vaccine use dramatically reduces the number of women who will develop cervical cancer, according to a study of nearly 1.7 million women. Among girls vaccinated before age 17, the vaccine reduced cervical cancer incidence by 90%.
Updated cervical cancer screening guidelines from the American Cancer Society recommend HPV testing as the preferred approach. NCI’s Dr. Nicolas Wentzensen explains the changes and how they compare with other cervical cancer screening recommendations.
In a new study, an automated dual-stain method using artificial intelligence improved the accuracy and efficiency of cervical cancer screening compared with the current standard for follow-up of women who test positive with primary HPV screening.
More than a decade after vaccination, women who had received a single dose of the HPV vaccine continued to be protected against infection with the two cancer-causing HPV types targeted by the vaccine, an NCI-funded clinical trial shows.
Women with cervical or uterine cancer who received radiation to the pelvic region reported side effects much more often using an online reporting system called PRO-CTCAE than they did during conversations with their clinicians, a new study shows.
A research team from NIH and Global Good has developed a computer algorithm that can analyze digital images of the cervix and identify precancerous changes that require medical attention. The AI approach could be valuable in low-resource settings.
A new test can help to improve the clinical management of women who screen positive for HPV infection during routine cervical cancer screening, an NCI-led study has shown.
FDA has approved pembrolizumab (Keytruda) for some women with advanced cervical cancer and some patients with primary mediastinal large B-cell lymphoma (PMBCL), a rare type of non-Hodgkin lymphoma.
By comparing the genomes of women infected with a high-risk type of human papillomavirus (HPV), researchers have found that a precise DNA sequence of a viral gene is associated with cervical cancer.
Investigators with The Cancer Genome Atlas (TCGA) Research Network have identified novel genomic and molecular characteristics of cervical cancer that will aid in subclassification of the disease and may help target therapies that are most appropriate for each patient.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Global cervical cancer research: A scientometric density equalizing mapping and socioeconomic analysis
Roles Conceptualization, Investigation, Project administration, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Obstetrics and Gynecology and Division of Female Health and Preventive Medicine, Institute of Occupational Medicine, Social Medicine and Environmental Medicine, Goethe-University, Frankfurt, Germany
Roles Conceptualization, Data curation, Formal analysis, Writing – review & editing
Roles Writing – review & editing
Affiliation Department of Obstetrics and Gynecology, Keck School of Medicine of USC, Los Angeles, California, United States of America
Roles Conceptualization, Writing – review & editing
Affiliation Department of Obstetrics and Gynecology, St. Elisabeth Hospital, Loerrach, Germany
Roles Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – review & editing
Roles Conceptualization, Supervision, Writing – review & editing
- Dörthe Brüggmann,
- Kathrin Quinkert-Schmolke,
- Jenny M. Jaque,
- David Quarcoo,
- Michael K. Bohlmann,
- Doris Klingelhöfer,
- David A. Groneberg

- Published: January 6, 2022
- https://doi.org/10.1371/journal.pone.0261503
- Reader Comments
Cervical cancer has caused substantial morbidity and mortality for millions of women over the past decades. While enormous progress has been made in diagnosis, prevention and therapy, the disease is still fatal for many women—especially in low-income countries. Since no detailed studies are available on the worldwide research landscape, we here investigated the global scientific output related to this cancer type by an established protocol. The “New Quality and Quantity Indices in Science” platform assessed all relevant cervical cancer research published in the Web of Science since 1900. A detailed analysis was conducted including country-specific research productivity, indicators for scientific quality, and relation of research activity to socioeconomic and epidemiologic figures. Visualization of data was generated by the use of density equalizing map projections. Our approach identified 22,185 articles specifically related to cervical cancer. From a global viewpoint, the United States of America was the dominating country in absolute numbers, being followed by China and Japan. By contrast, the European countries Sweden, Austria, and Norway were positioned first when the research activity was related to the population number. When the scientific productivity was related to annual cervical cancer cases, Scandinavian countries (Finland #1, Sweden #4, Norway #5, Denmark #7), the Alpine countries Austria (#2) and Switzerland (#6), and the Netherlands (#3) were leading the field. Density equalizing mapping visualized that large parts of Africa and South America were almost invisible regarding the global participation in cervical cancer research. Our data documented that worldwide cervical cancer research activity is continuously increasing but is imbalanced from a global viewpoint. Also, the study indicated that global and public health aspects should be strengthened in cervical carcinoma research in order to empower more countries to take part in international research activities.
Citation: Brüggmann D, Quinkert-Schmolke K, Jaque JM, Quarcoo D, Bohlmann MK, Klingelhöfer D, et al. (2022) Global cervical cancer research: A scientometric density equalizing mapping and socioeconomic analysis. PLoS ONE 17(1): e0261503. https://doi.org/10.1371/journal.pone.0261503
Editor: Amir Radfar, University of Central Florida, UNITED STATES
Received: October 28, 2020; Accepted: December 3, 2021; Published: January 6, 2022
Copyright: © 2022 Brüggmann et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data used in the study are owned by the Web of Science, we are not allowed to share the downloaded datasets publicly or privately. But any researcher can obtain a license ( http://apps.webofknowledge.com/WOS_GeneralSearch_input.do?product=WOS&search_mode=GeneralSearch&SID=C2F5xMA57aI8oMJ8QZE&referencesSaved= ) to gain access to the Web of Science and enter the search term described in the paper to download the respective data set. The authors had no special access privileges to the data others would not have.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
As stated by recent reviews, cervical cancer is a largely preventable female malignancy that accounts for over 300,000 worldwide deaths with more than half a million women being diagnosed every year [ 1 , 2 ]. Around 85% of cervical cancers cases and 90% of related deaths occur in low- and middle-income economy settings [ 3 ]. The disease has massive global and public health implications since these countries often lack formalized HPV vaccination and cervical screening [ 1 , 4 ]. The efficacy of cervical cancer screening to lower the disease burden in high-income countries is demonstrated by its impact on key epidemiology data [ 1 ]. Both, cervical cancer incidence and mortality, have decreased over the past decades beginning with the implementation of prevention programs [ 1 , 4 ].
Since the malignancy is highly preventable, availability and accessibility to well-trained health care professionals are associated with a low likelihood for women to fall ill, suffer and die from cervical cancer sequelae [ 5 ]. Given the fact that the related mortality is 18 times higher in low- and middle-income compared to developed countries, the geographical location where a woman lives translates into significant regional and global disparities regarding cancer detection, treatment and related morbidity and mortality [ 1 , 6 ]. This circumstance is unacceptable. Hence, the WHO released an ambitious worldwide call-to-action in May 2018 aiming to eliminate cervical cancer as a public health problem [ 7 ].
The discrepancy between efficient cervical cancer prevention leading to better survival in high-income countries and dramatic mortality in low- and middle-income countries [ 2 , 8 ] suggests that related past and present scientific trends need to be interpreted in a global context. However, there is no concise worldwide analysis of cervical cancer scientific efforts of the past decades, which could help guide future research and funding strategies. In this study, the global output of cervical cancer research, which was published in the Web of Science since 1900, was investigated in the context of the NewQIS (New Quality and Quantity Indices in Science) project. This technology allows objective, precise and reliable scientometric analyses and provides the visualization of global research trends by geographic cartographs. The objectives of this study encompassed (1) an in-depth assessment of the global cervical cancer research activity by using classical publication output parameters and in terms of geographical and chronological developments, (2) the visualization of international research networks and (3) the relation of national cervical cancer research activities to socio-economic figures and cervical cancer epidemiology.
NewQIS technology
For this study, we used the previously established NewQIS computing platform [ 9 , 10 ], which was founded in 2007/2008 at the Humboldt-University Berlin Charité by a multidisciplinary and international team of scientists. Since then, about 100 peer-reviewed studies were published using this methodology [ 11 ]. Topics ranged from infectious diseases to public and global health or gynecology and obstetrics [ 11 ]. Generally, we perform our searches employing the NewQIS computing platform according to a standardized protocol. Hence, the data obtained in this particular study can be compared to formerly published studies on other biomedical entities (e.g. ovarian and endometrial cancer) that were also based on the NewQIS platform.
Data source
As data source, we used the Web of Science (WoS core collection, Clarivate Analytics) to analyze the world scientific productivity as represented by the body of cervical cancer research articles. This database was preferred to the PubMed search engine due to its unique WoS Citation Report [ 12 ].
Cervical cancer search algorithm
In order to specifically assess publications related to cervical cancer, a “title” search was performed for the time period of 1900 to 2015. The search term (cervical OR cervix) AND (neoplasm* OR cancer* OR carcinom*) was used. The time after 12-31-2015 was excluded to avoid incomplete data acquisition due to the cited half-life phenomenon. Typically, the citated half-life in the field of biomedical research is 6–8 years ( https://jcr.clarivate.com/jcr/browse-category-list ), which leads to a dramatic decrease in citations after 2015. Therefore, the period thereafter is not suitable for valid interpretation.
On the Advanced Search interface of the Web of Science Core Collection, we restricted the analysis to the category of “articles” by setting the specific filter function to “article” [ 10 ]. This approach was chosen in order to limit the analysis to original cervical cancer research and to exclude published news, reviews or other potentially non-peer-reviewed material.
Data analysis and categorization
As stated in previous NewQIS studies, a range of different parameters was assessed. For example, we analyzed the publication year, author, country of origin, language, subject categories, and citations. The country-specific assignment of articles was based on the affiliations the authors reported in the publications and according to the present country territories. 251 “countries” we analyzed for their productivity, which included sovereign states as well as autonomous regions. Of all analyzed countries, 154 countries contributed to the identified articles on cervical cancer. Papers that were published in a collaboration between authors affiliated with different countries were counted for each affiliated country; this circumstance was considered in the collaboration analysis. Also, modified Hirsch-indices were calculated as proxy measures for scientific quality. The Hirsch-index was created by Jorge Hirsch to measure the recognition of research performance in the scientific community. Since we did not relate the index to single authors but to countries it was termed modified H-index (Hi). Here, a Hi of x describes the number of x papers, which authors affiliated with a specific country published and that have been cited at least x times. Also, country-specific citation rates (CR, total country-specific citations numbers per total numbers cervical cancer publications) were computed [ 13 ].
Socio-economic and epidemiologic analysis
A novel focus of NewQIS is the introduction of socioeconomic benchmarking among countries [ 14 ]. Cervical cancer research productivity was related to each country’s economic and demographic capabilities and cervical cancer burden. We used the following parameters for the analyses: (1) population sizes of countries (numbers of inhabitants), (2) the total economic power index gross domestic product (GDP, based on the purchasing power parity) per 1000 billion current international dollar US-$ and (3) the GDP per capita. The figures were retrieved from the CIA World Factbook edition of 2016 [ 15 ]. The CIA world factbook publishes population data based on the estimates from the US Bureau of the Census. They define population as people, male and female, child and adult living in a given geographical area, i. e. inhabitants ( https://www.cia.gov/the-world-factbook/field/population ). The number of inhabitants is used as a proxy measure for the human resources, specifically for the researchers available in a particular country, who are potentially able to generate the articles on cervical cancer. This calculation aims to compare the research output of countries in relation to the number of potential researchers in a specific field so a comparison between countries with different human resources is feasible.
In order to be able to compare categories of countries, we used the following definitions provided by the World Bank. The definitions have been based on the Gross National Income per capita in 2015, were calculated using the World Bank Atlas method ( https://datahelpdesk.worldbank.org/knowledgebase/articles/906519 ) and included low-income economies (per capita income < 1.045 US-$), high-income economies (≥ 12.736 US-$), lower-middle-income economies (1.046–4.125 US-$) and upper-middle-income economies (4.126–12.735 US-$). To calculate ratios of publication output and R&D expenditures, we used Gross domestic expenditure on R&D (GERD) provided by the UIS UNESCO Institute of Statistics: Science, technology and innovation [ 16 ]. To assess the relative cervical cancer research activity with regard to epidemiologic data, the estimated number of new cases of cervical cancer per year for each country was used, supplied by the GLOBOCAN 2020 project of the IARC/WHO [ 17 ].
International cervical cancer networks of research
We investigated international collaborative networks of cervical cancer research based on the main affiliations the authors stated on the published articles. A circle diagram was generated for improved visualization. Here, vectors indicate established scientific collaborations between authors from different countries; their width and shade of grey quantify the number of collaborations.
Density equalizing map projections
A key feature of the NewQIS method is the unique visualization of the computed results [ 18 ]. Therefore, density equalizing map projections (DEMP) were calculated for the different cervical carcinoma-specific parameters resulting in a variety of anamorphic maps. The algorithm used for the DEMP creation was invented by Gastner and Newman in 2004 [ 19 ]. In this process, metadata were transferred into a Microsoft® Access® database and used for all analyses. We employed the software “ArcGIS Cartogram”geoprocessing tool ( https://www.arcgis.com ) to build anamorphic maps. In these cartograms, the areas of the countries were resized in proportion to the selected criteria of interest (i.e. the total number country-specific articles).
General parameters of cervical cancer research
In total, global cervical cancer research activity between 1900 and 2015 produced a number of 22,185 original articles listed in the WoS. Of those, 20,717 (93%) were published in English, 634 (less than 3%) in German, 375 in French (1.7%), 159 in Russian (less than 1%), 119 in Spanish (less than 1%), 44 in Polish (less than 1%), 42 in Portuguese (less than 1%), 25 in Italian (less than 1%), 24 in Japanese (less than 1%), 14 in Chinese (other: N = 32).
Concerning the chronological development of the research activities on cervical cancer, we found only minor scientific productivity from 1900 until the 1970s. Less than 100 articles were published per year. The global research activities grew visibly in the beginning of the 1980s, when global publication activities increased to more than 200 annual articles. From 2012 on, more than 1000 papers were issued per year with a maximum number in 2015 ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Chronological development of the amount of published items per year.
https://doi.org/10.1371/journal.pone.0261503.g001
Cervical cancer country-specific analysis
We identified the United States of America (USA) as the country with the highest scientific productivity related to cervical cancer research; affiliated authors generated 5,640 original articles (n), which account for a quarter of all research in the investigated time period. China was ranked second (n = 1,997, 9%) and followed by Japan (n = 1,561, 7%). The most active European countries included the United Kingdom (UK; n = 1,199, 5%), Germany (n = 1,175, 5%) and France (n = 925). In total, 10 out of the 20 most active nations were European countries. In South America , Brazil was the most productive nation with 336 articles. Columbia (n = 101) and Argentina (n = 74) ranked second and third. In Asia , China and Japan were followed by South Korea (N = 896), India (n = 844), and Taiwan (n = 595). Africa ´s most active countries were South Africa (n = 227), Nigeria (n = 69), and Kenia (n = 51). As visualized by DEMP cartography, we found a visible North-South divide regarding cervical cancer publication output ( Fig 2 ).
Density equalizing, colours and territorial sizes indicate numbers of related articles per country.
https://doi.org/10.1371/journal.pone.0261503.g002
Cervical cancer citation analysis
We analyzed three citation parameters, which included the number of citations, average citation rates and the country-specific modified Hirsch-indices (Hi). After analysis of the metadata the results were transferred to DEMP for visualization. The citation numbers largely followed the pattern of the identified publication activities. The USA was leading the field. Articles published by US-American authors gained 174,754 citations (c). The European countries UK (c = 43.424 citations), France (c = 34.564) and Germany (c = 31.210) were ranked in second, third and fourth positions. This finding illustrates that cervical cancer studies originating from these particular countries received a higher level of recognition in the scientific community than the articles from Japan and China, which achieved 27.173 and 17.999 citations, respectively ( Fig 3A ).
A) Total numbers of citations that articles from a respective country received. B) Density Equalizing Map of the citation rates (cr). C) Country-specific Hirsch-indices were calculated for all identified cervical cancer-specific articles.
https://doi.org/10.1371/journal.pone.0261503.g003
A complete different global landscape emerged when the average citation rates were analyzed (threshold for countries to be included in this analysis were at least 30 cervical cancer specific articles). Here, the East Asian country of the Philippines was ranked first with 134.8 citations per article (cr), followed by Costa Rica (cr = 118.59) and the African country of Uganda (cr = 81.105). The three South American countries of Columbia (cr = 66.08), Chile (cr = 61.53), and Argentina (cr = 60.09) were ranked in forth, fifth and sixth position ( Fig 3B ). Among high-income countries, the articles of the following countries received the highest citation counts per article: Spain with a citation rate of cr = 55.35 (position 7), the Netherlands (cr = 43.07, position 9), and France (cr = 37.36, position 10). The North American countries Canada (position 12) and the USA (position 16) had citation rates of cr = 35.36 and cr = 30.98, respectively.
As third citation parameter, the country-specific modified Hirsch-indices (Hi) were calculated for the present set of 22,185 cervical cancer-specific articles ( Fig 3C ): The USA had by far the highest (Hi = 146). It was followed by the UK (Hi = 95), and France (Hi = 87). Seven out of the 10 leading nations were Western European counties and included the UK (Hi = 95), France (Hi = 87), Germany (Hi = 79), Sweden (HI = 63), the Netherlands (Hi = 75), Italy (Hi = 57) and Austria (Hi = 55). All of them reached a Hi above 50. Canada was ranked in 6 th position (Hi = 74). As representatives for the Asian continent, Japan (Hi = 70) was ranked 7 th followed by China (Hi = 53) ranked 13th. We identified South Africa (Hi = 30) as the African country with the highest modified Hi while Brazil (Hi = 31) was the leading country in South America . By comparison, Eastern European countries such as Slovenia (Hi = 11), Serbia (Hi = 10), Bulgaria (Hi = 7), Ukraine (Hi = 6) and Bosnia-Herzegovina (Hi = 5) were in the lower midfield of all analyzed countries. In total, we found a Hi greater than 20 for 35 countries and further 24 countries had a Hi greater or equal 10.
Cervical cancer socio-economic analysis
To add more interesting facets to our analysis, we related cervical cancer research activity to epidemiologic and socio-economic figures in order to assess the relative contribution of countries with regard to their socio-economic and demographic power as well as their burden of disease.
We assessed the correlation between the country-specific number of research articles and the population represented by the number of inhabitants, which is a proxy measure for the human resources available in a particular country (Q1 = article number (n) / number of inhabitants in millions). The following three countries were ranked closely together: Sweden with 49.70 articles per inhabitants in millions (Q1), Austria (Q1 = 47.07), and Norway (Q1 = 48.29). 9 out of 10 leading countries were European nations with only Canada (Q1 = 25.48) in 10 th position being non-European. Only three Asian countries—South Korea (Q1 = 17.60) and Singapore (Q1 = 13.49) and Japan (Q1 = 12.32)—were among the 20 highest ranked nations. The USA published 17.41 articles per inhabitants in millions. China had a Q1 of only 1.45. As a result, the focus of leading nations shifted towards the North/Western European countries and particularly the Scandinavian countries ( Table 1 ).
https://doi.org/10.1371/journal.pone.0261503.t001
In a next step, cervical cancer research was related to the gross domestic product (GDP) in 1000 billion (bn) US-$ (quotient Q2, Table 1 ). This benchmarking indicator considers the total economic power of the country and therefore gauges possible national spending in the research sector. In this ranking, Slovenia (Q2 = 1050.00) was in leading position, followed by Sweden (Q2 = 1044.88) and Austria (Q2 = 1025). One out of the first six countries did not belong to the category of high-income countries (Costa Rica, Q2 = 871.43). Denmark (Q2 = 1267.14) and Finland (Q2 = 1207,14) were listed in position 4 and 5. In total, 11 different countries had a calculated Q2 of greater or equal 500 cervical cancer articles per GDP (in 1000 bn US-$). Out of these, 3 countries were located on the Eastern European and 1 on the South American continent ( Table 1 ).
We also assessed the ratio of number of articles to the GDP per capita , which should represent the number of articles in relation to the economic strength of every individual. Here, China (Q3 = 154.8) and India (Q3 = 145.5) as upper-middle- (UMI), and lower-middle-income economy (LMI) countries were ranked before the USA. With China, India, Japan (Q3 = 41.2) and South Korea (Q3 = 25.3), four countries out of the top ten were Asian countries. This leading role of countries located on the Asian continent was a remarkable finding. To capture the ratio of publications output to research and development activities, the indicator Gross Expenditure on Research and Development (GERD) was used ( Table 2 ). In this approach Uganda, Cost Rica, Peru, Serbia and Columbia were listed in the top five.
https://doi.org/10.1371/journal.pone.0261503.t002
At last, an epidemiologic figure, we calculated the Q4 ratio relating the number of published articles to annual new cervical cancer cases in 1000 ( Table 3 , Fig 4 ). In this ratio, Scandinavian countries (Finland #1, Sweden #4, Norway #7, Denmark #6), the Alpine countries Austria (#2) and Switzerland (#5), and the Netherlands (#3) were ranked among the seven leading countries. The leader in the field, Finland, published 1140.54 articles per annual new cervical cancer in 1000 cases whereas the USA and China were visibly less active with only 416.39 and 18.20 articles per annual new cervical cancer cases in 1000, respectively ( Table 3 ).
DEMP of research activity measured in cervical cancer-related articles per estimated annual new cases of cervical cancer in 1000.
https://doi.org/10.1371/journal.pone.0261503.g004
https://doi.org/10.1371/journal.pone.0261503.t003
Network analysis of international cervical cancer research
2,069 cervical cancer articles and therefor the majority originated from bilateral scientific collaborations. Trilateral cooperative studies produced 363 publications. Collaborative efforts by four countries generated 108 articles, 70 papers were issued by authors affiliated with five countries. 1,325 collaborations involved US-American authors, followed by cooperations (number of collaborative articles = n coop ) by scientists from the UK (n coop = 360), France (n coop = 331), China (n coop = 324), Germany (n coop = 319), and Canada (n coop = 264) ( Fig 5 ).
Collaborating countries with ≥ 10 joint bilateral articles. Values in brackets: number of articles / number of collaborating articles. Thickness of bars corresponds to number of bilateral collaborations between linked countries.
https://doi.org/10.1371/journal.pone.0261503.g005
Cervical cancer research area analysis
Important information can be drawn from the subject category analysis of published cervical cancer research. Here, the leading field in cervical cancer research was attributed to Oncology (9,962 publications, n). This finding was not surprising. The second most articles were found in the subject area Obstetrics & Gynecology (6.579 articles). After a large gap, the ranking continued with areas such as Radiology , Nuclear Medicine & Medical Imaging (n = 2,343), General & Internal Medicine (n = 1,612), Public , Environmental & Occupational Health (n = 1,280), and Pathology (n = 1,186). The analysis of the relative share of specific subject areas in the total publication output over the time demonstrated that there was a continuous increase in the field of Oncology until the time period from 1996 to 2000. Since then, 40–50% of articles on cervical cancer remain attributed to this predominant area. During the period from 2011 until 2015, the field of Obstetrics & Gynecology was relatively unpopular in comparison to earlier periods. Among the subject areas with more than 1,000 publications, the field of Public , Environmental & Occupational Health (n = 1,280) had the strongest relative increase over the past periods ( Fig 6A ).
A) Relative proportion of the most assigned subject areas in 5-year intervals. B) Proportion of the most assigned subject areas of cervical cancer research.
https://doi.org/10.1371/journal.pone.0261503.g006
Lastly, a subject area analysis with regard to the ten most active countries was performed to deduce country-specific research interests. The fields Oncology followed by Obstetrics & Gynecology were among the most popular scientific areas. Both areas dominated with varying shares, e.g. in Norway, more than 60% of all articles were related to Oncology whereas in in the UK, only about 40% of articles were related to this field ( Fig 6B ).
From the viewpoint of epidemiology, cervical carcinoma can be characterized as being “Janus-faced” . A substantial decline of cervical carcinoma mortality and incidence was associated with newly implemented population-based screening programs in particular regions of the world such as Australia (e.g. New South Wales) [ 20 ]. On the other hand, cancer incidence and mortality rates in low-income countries without screening programs and novel therapeutic options remain high. This good and ill facet of cervical cancer demonstrates the necessity for a global approach to this topic. But how are worldwide scientific efforts distributed in this particular area of gynecologic oncology? To depict the global research landscape, this NewQIS project aimed to analyze all relevant articles in cervical cancer research. Scientometric data were related to socioeconomic figures and results were visualized using density equalizing map projections, which were established by Newman and Gastner in 2004 [ 19 ]. In order to overcome a too simplistic bibliometric approach, we calculated Hirsch-indices [ 13 ] on the basis of the citations numbers articles of each country gained and related research productivity to relevant socio-economic figures.
We identified 22,185 cervical cancer articles published between 1900 and 2015 by a specific search term that was present in the title of each identified article. In order to consider only scientific studies, the analysis was focused on original articles and excluded reviews, letters and other potentially non-peer-reviewed publications. The data acquisition was based on the Web of Science. This particular database was chosen because it includes only curated high-quality publications after a rigorous selection process ensuring a high level of scientific integrity.
Although the total output on cervical cancer continuously increased since 1900 a large imbalance of research activities was identified; most scientific activities were generated in countries located in the Northern hemisphere—specifically on the Northern American and the European continent. Nations with a high cancer burden and mortality such as Latin American, or African countries play almost no visible role among the research power players in the field and were rarely part of productive research collaborations. This observation corresponds with the extremely high mortality women face in these countries and represents a major health related social disparity. This represents a need to be addressed. Involving non-high-income countries into scientific collaborations could represent an opportunity for the transfer of ideas, knowledge or epidemiological data and therefore used to mutual advantage. Furthermore, this study underlines that particular countries, e.g. the Scandinavian nations, successfully address the public cancer burden by fostering research in the respective field. In our socioeconomic analyses, they were leading the field by publishing many research articles related to their population, GDP and cervical cancer cases–indicating an effective public health strategy.
Pivotal milestones in cervical cancer research and publication of national guidelines can spark interest and drive related scientific productivity. The identification of HPV as a causative agent for cervical cancer in 1975 [ 21 ] laid the groundwork for formalized cancer screening programs, HPV-based diagnostics and vaccines. Hence, the decades from 1980 to 2010 were characterized by the translation of novel research findings into relevant public health measures. For example, the ACOG and the American Cancer Society published the first joint consensus statement regarding formalized cervical cancer screening in 1988 [ 22 ]. In 1988 the first HPV-test was approved in the USA, after 2006 HPV vaccines were licensed in the USA and Canada for primary prevention [ 23 ]. In this study, analysis of chronological developments in the cervical cancer research output reflects these pivotal milestones: A striking increase in the number of annual publications was documented after 1975. Here, the output more than doubled to 180–300 articles on cervical cancer per year. Also, 6 of the 20 most cited articles were published in the ´80s, and in 1999 the most cited article of all times -“Human papillomavirus is a necessary cause of invasive cervical cancer worldwide”- was issued by Walboomers et al. [ 24 ]. In 2000 until 2011—the period of established HPV-based testing and vaccination—the number of published articles doubled again from 494 to nearly 1000 per year documenting a profound global interest in cervical cancer related research.
To estimate whether a number of 22,185 cervical cancer articles corresponds to a high or low activity from a global viewpoint, it was compared to published data on other gynecological cancers, such as breast [ 25 ], ovarian [ 26 ] and endometrial cancer [ 27 ]. When contrasting the present approach to the study of Glynn et al. on breast cancer , three large differences appear to be important: 1) breast cancer has a differing epidemiology and therefore we should expect different research activities, 2) the study of Glynn et al. covered only the years from 1945 to 2008, which is a notably shorter time period, and 3) the authors performed a broader “topic” search. Therefore, in terms of overall research activity it is not justified to compare the total number of 180,126 publications related to breast cancer to the identified 22,185 articles on cervical cancer. However, looking at chronological trends in the scientific productivity it can be stated that researchers in breast cancer demonstrated a steep increase in their output since 1945 with the USA as the leading force, followed by the UK, Germany, Italy and Japan. A similar pattern was seen in the field of cervical cancer where the global scientific output has been rising for the last 115 years (particularly since 1945) and countries such as the USA, Japan, the UK and Germany also occupy outstanding positions in the respective research community.
The previously published data on ovarian cancer research productivity [ 26 ] reported a number of 23,378 articles and is more similar in terms of the underlying methodology. This study covered the years from 1900 to 2014, so the period was shorter by only one year. Also, the search was restricted to articles as document types and to title words. With the difference of one year– 1332 articles related to cervical cancer were published in 2015 –we may compare the overall data: From 1900 to 2014, 20,855 cervical cancer articles represent 89.2% of the global ovarian carcinoma research activity (n = 23,378). If we relate these numbers to the estimated annual new cases of both cancer types, i.e. in the USA for the year 2014 (n = 12,722 for cervical cancer and n = 21,495 for ovarian cancer, https://gis.cdc.gov/Cancer/USCS/DataViz.html ) we find a ratio of 0.59. So, nearly 1.7-times more ovarian cancer cases than cervical cancer cases occur in the USA per year. Hence, it can be deduced, that the ratio between annual cases of both cancers is not reflected by the ratio between respective scientific research productivities. This observation may lead to the assumption that scientific efforts on cervical cancer might be over-supported compared to those on ovarian cancer. In 2012, Carter and Nguyen made a statement that points in the same direction [ 28 ]. The authors concluded that cervical cancer is an overfunded condition when incidence, mortality and “Years of Life Lost" were considered. However, when the specific US-American research activity in both entities is considered (5,640 cervical cancer articles versus 9,312 ovarian cancer articles) and not the global numbers, a ratio of 60.6% can be calculated, which is very similar to the ratio of new cases. Therefore, we might come to the conclusion that US-American research activities are very much balanced towards the comparative epidemiology and public cancer burden of both female cancer types. The next question points to the direction of country-specific differences in ovarian versus cervical cancer research activities. If we compare both cancer types ( Table 4 ) it is obvious that the research on cervical cancer is more balanced and globally more evenly distributed. In this respect, the top ten countries account for 76.62% of all articles in ovarian cancer research while they only account for 65.46% of all articles in cervical cancer research. However, focusing on the specific participation of developing countries in ovarian and cervical cancer research a similar pattern was found for both entities. Whereas strong output was generated in countries located in North America, Europe as well as in China, Japan and Australia only minor productivity was documented in countries on the South American continent and in Africa. Particularly, women in South America experience an exceptional burden due to both cancers. Besides the striking burden related to cervical cancer, South American women also face an intermediate age-adjusted incidence rate of 5,8 per 100,000 for ovarian cancer [ 29 ]. Hence, the low local research productivity and the rare involvement in international collaborations regarding both cancer types call for improvement. So South American countries could strengthen their scientific efforts for locally relevant cancers—like they already have in other biomedical fields such as toxoplasmosis research [ 14 ].
https://doi.org/10.1371/journal.pone.0261503.t004
Endometrial cancer is a third female carcinoma that may be compared to the presented study [ 27 ]. Within the same time period (1900–2015) and a similar search structure–identification of endometrial cancer articles by title word search—a total of 9,141 articles were found in the WoS. This corresponds to less than 50% of the identified cervical cancer research output. Among the global research power players on endometrial cancer, the USA dominated the field with more than a third of the worldwide research productivity since 1900 (n = 3,191). This equals only 56.6% of cervical cancer research issued by US-American authors (n = 5,640) during the same time period. At position 2 and 3, Japan (n = 1,074) and Chinas are listed (n = 611) for endometrial cancer, pointing to a similar pattern of the most active countries in both fields [ 27 ]. When compared to endometrial cancer, it becomes apparent that cervical cancer research is firmly established in the subject area of “Public Health”. A dramatic decrease in “Public Health” research related to endometrial cancer was documented since 1966 whereas cervical cancer articles attributed to this area achieved the strongest increase over the past decades. Thus, a solid foundation has been established, which can be used by clinicians and researchers to answer the WHO’s call-to-action aiming at the elimination of cervical cancer.
Additionally, one might also compare the present data to research on benign female neoplasms such as uterine fibroids/myomas [ 18 ]: This analysis covered the identical time span from 1900 to 2015; a title search was performed. However, it was not restricted to articles but included all other publications. Therefore, it is difficult to compare the data. Re-analysis showed that 4,293 of the 6,176 uterine fibroid-related publications were articles. This number might be related to the presently identified 22,185 cervical cancer-related articles and clearly indicates that global research activities on this benign disease were much lower. Lower scientific productivity was also present when socioeconomic ratios were taken into account, i.e. in the country-specific uterine myoma ranking concerning the population size, the highest activity was assessed for Finland with 12.55 publications per million inhabitants, followed by Israel (Q1 = 10.36), Sweden (Q1 = 7.92), and Belgium (Q1 = 6.90). In contrast, calculated ratios of cervical cancer article number per million inhabitants were by far higher in Sweden, Austria and Norway reaching a ratio of about 50 cervix cancer articles.
It would be reasonable to compare the global scientific productivity on HPV research [ 30 ] to data on cervical cancer output. But this comparison has several limitations. Firstly, the analysis of scientific activity on HPV covered a shorter period (1900 to 2009) and the search was broader because it was performed in abstract, title and keywords (“topic search”). Secondly, when country-specific research patterns on HPV were contrasted to cervical cancer, China seems under-represented in the field of HPV. This result has to be seen critically since the analysis stopped in 2009 and China has dramatically increased publication output in various fields of medicine ever since [ 31 – 33 ].
It is a unique strength of this study to depict the global scientific productivity on cervical cancer over a period of 115 years. Some limitations can be identified in this study: The WoS data bank focuses mainly on publications written in English and presents publications related to the search term in a curated way. Hence, we acknowledge that our search cannot identify all articles published on cervical cancer since 1900. Further, we must assume an underrepresentation of non-English literature in this analysis although we identified numerous articles in other languages than English. However, we deem this bias as limited since English is considered as the “language of science” and also not-native speakers publish their high-quality science in English journals. We also acknowledge that other platforms such as EMBASE or Google Scholar catalogue journal articles published in the medical field. Hence, these search engines could identify a different set of articles related to the search terminus. But these other platforms cover different time periods, show inconsistent accuracy in the citation analysis [ 34 ] and do not offer unique tools such as the Journal Citation Reports so we refrained from using them. Further, we tried to gauge scientific quality by citation parameters, which might be difficult since citations represent recognition of scientific activities in the research community and could be skewed by phenomena such as the Matthew effect or self-citations. Lastly, a relation of the country-specific research output since 1900 to the GDP in 2015 aimed to account for the economic capabilities to invest in research and related infrastructure. Here, it has to be acknowledged that the GDP of certain countries changed dramatically during the last decades. Since there is a positive relationship between the GDP and the scientific output in developed and developing countries [ 35 ] we consider the impact of these GDP changes over time as insignificant for the scientific value of the analysis.
Conclusions
Our study on cervical cancer research activity documented a continuous worldwide increase in scientific productivity since 1900. The results documented a striking global asymmetry with the Southern hemisphere being underrepresented in the scientific community although the public burden of cervical cancer remains high in these countries. Scandinavian countries were identified as effective in their research endeavors since they published high article numbers related to the local cervical cancer burden and human resources. Still, many research needs remain worldwide and have to be addressed defying geopolitical, cultural and environmental challenges. Researchers will be more successful embedded in international collaborations, which need to be facilitated by funding programs. So, health disparities will be diminished when countries are empowered to improve prevention, diagnosis and treatment of cervical cancer according to their capabilities.
Acknowledgments
We thank B. Kloft and C. Scutaru for their pioneering work for NewQIS. This study is part of a MD/PhD thesis project (KQS).
- View Article
- PubMed/NCBI
- Google Scholar
- 3. WHO. Cervical cancer: WHO; 2021 [cited 2021 2021-07-23]. Available from: http://www.who.int/cancer/prevention/diagnosis-screening/cervical-cancer/en/ .
- 7. WHO. WHO Director-General calls for all countries to take action to help end the suffering caused by cervical cancer 2018 [02-24-2021]. Available from: https://www.who.int/reproductivehealth/call-to-action-elimination-cervical-cancer/en/ .
- 12. Clarivate. Web of Science Core Collection: The Citation Report & The h-index 2021 [cited 2021 01-21-2021]. Available from: https://clarivate.libguides.com/woscc/citationreport .
- 15. Anonymus. World Economic Outlook Database: International Monetary Fund; 2013 [updated 2013]. Available from: https://www.imf.org/en/Publications/SPROLLs/world-economic-outlook-databases#sort=%40imfdate%20descending
- 16. (UIS) UIfS. Science, technology and innovation. Research and experimental development.: UNESCO; 2021 [cited 2021 2021-07-23]. Available from: URL: http://data.uis.unesco.org/Index.aspx?DataSetCode=SCN_DS&lang=en .
- 17. IARC. http://gco.iarc.fr/today/online-analysis-multi-bars?v=2018&mode=population&mode_population=countries&population=900&populations=908&key=total&sex=2&cancer=23&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=10&group_cancer=1&include_nmsc=1&include_nmsc_other=1&type_multiple=%257B%2522inc%2522%253Atrue%252C%2522mort%2522%253Afalse%252C%2522prev%2522%253Afalse%257D&orientation=horizontal&type_sort=0&type_nb_items=%257B%2522top%2522%253Atrue%252C%2522bottom%2522%253Afalse%257D&population_group_globocan_id=#collapse-group-0-4 . GLOBOCAN 2018. 2019.
- Open access
- Published: 07 April 2023
An overview of cervical cancer epidemiology and prevention in the Baltic States
- Una Kojalo 1 ,
- Anna Tisler 2 ,
- Kersti Parna 2 ,
- Anda Kivite-Urtane 1 ,
- Jana Zodzika 1 ,
- Mindaugas Stankunas 3 ,
- Nicholas Baltzer 4 ,
- Mari Nygard 4 &
- Anneli Uuskula 2
BMC Public Health volume 23 , Article number: 660 ( 2023 ) Cite this article
4503 Accesses
3 Citations
Metrics details
To inform future Baltic States-specific policy analyses, we aimed to provide an overview of cervical cancer epidemiology and existing prevention efforts in Estonia, Latvia and Lithuania.
A structured desk review: we compiled and summarized data on current prevention strategies, population demography and epidemiology (high risk human papillomavirus (HPV) prevalence and cervical cancer incidence and mortality over time) for each Baltic State by reviewing published literature and official guidelines, performing registry-based analyses using secondary data and having discussions with experts in each country.
We observed important similarities in the three Baltic States: high burden of the disease (high incidence and mortality of cervical cancer, changes in TNM (Classification of Malignant Tumors) stage distribution towards later stage at diagnosis), high burden of high-risk HPV in general population and suboptimal implementation of the preventive strategies as low screening and HPV vaccination coverage.
Conclusions
Cervical cancer remains a substantial health problem in the region and the efforts in addressing barriers by implementing a four-step plan for elimination cervical cancer in Europe should be made. This goal is achievable through evidence-based steps in four key areas: vaccination, screening, treatment, and public awareness.
Peer Review reports
For cervical cancer, effective primary and secondary prevention approaches, vaccination and screening respectively, have been successful in reducing incidence and mortality [ 1 ]. Accordingly, for the first time in history, eliminating a specific cancer from the globe is an attainable objective [ 2 ]. Improvements in cervical cancer screening programs, particularly switching to primary human papillomavirus (HPV) based testing, is considered crucial for accelerating cervical cancer elimination in studies using data from Norway [ 3 ], Australia [ 4 ], USA (United States of America) [ 5 ], and Britain [ 6 ]. Additional questions towards cervical cancer elimination are: when could elimination be achieved, and how is this timeline modified by the secondary prevention strategies selected by different countries? Depending on national cervical cancer prevention policies large variations are expected in terms of when cervical cancer will be eliminated. Mathematical models predict Australia to be on-track to eliminate cervical cancer by 2028 [ 4 ] and USA between 2038 and 2046 [ 5 ], while many countries without existing screening programs are unlikely to be cervical cancer-free this century. Detailed knowledge of the epidemiology of a disease, and prevention strategies implemented, contribute to fill the knowledge gaps.
In Europe, cervical cancer ranks as the 9th most frequent cancer among women and the 2nd most common for cancer deaths in women aged 15 to 44 years [ 7 ].. Europe is characterised by considerable disparities in incidence and mortality of cervical cancer. The Baltic States are among those European countries with the highest incidence and mortality from cervical cancer [ 8 , 9 ].
The aim of this article is to provide an overview of the epidemiology of cervical cancer as well as ongoing prevention strategies in the Baltic States and to outline the steps to accelerate the trend towards cervical cancer elimination.
A structured desk review was conducted with the documents related to cervical cancer prevention policies, protocols, practice guidelines, evaluation reports, and others, issued/published by the countries’ relevant authorities. This was complemented with other pertinent documents (including peer-reviewed journal publications) identified by the working group of experts. This review was undertaken by national experts from Estonia, Latvia and Lithuania. We selected the key performance indicators - screening intensity, screening test performance, diagnostic assessment, treatment, and post-treatment follow-up of screening and vaccination programmes [ 10 ].
The most recent data regarding cervical cancer epidemiology and prevention measures in the Baltic States are presented. The data on number of cervical cancer (International Classification of Diseases tenth edition [ICD-10] code C53) cases and deaths for the period of 1990–2018 originated from the population-based cancer and death registries in Latvia, Estonia, and Lithuania. For each country, data on the size of the female population at the screening age, size of female birth cohort, and the life expectancy for women were retrieved [ 11 , 12 , 13 ].
We summarized the current status of cervical cancer prevention in these countries in order to identify areas of consistent findings, gaps in practice, and necessary next steps for research and public health practice.
Statistical analysis
The age-standardized incidence (ASIRs) and mortality (AMIRs) rates per 100,000 were computed (using World population) [ 14 ]. The 95% confidence intervals (CIs) were computed by assuming Poisson distribution for incident and mortality counts. Joinpoint regression program [ 15 ] was used to model the rates and calculate the estimated annual percent change (APC) with 95% CI. We computed the average age at cervical cancer diagnosis and death as the weighted mean age using the mid-age of each 5-year age group for the period of 2014–2018 for Estonia and Latvia and for the period of 2014–2015 for Lithuania. Union for International Cancer Control version 7 of the TNM classification for malignant tumours was used to categorise stage. The TNM stage was obtained from the cancer registry and was available for cases diagnosed from 2005 and forward. The distribution by TNM stage is presented for the time periods 2005–2009 and 2014–2018 (Lithuania 2014–2015).
Population demography
In 2020 the proportion of female population in three Baltic States was similar, the total population in Estonia was 1,331,057 (52.6% women), in Latvia 1,901,548 (53.9% women), and in Lithuania 2,794,700 (53.7% women) [ 16 ]. The female population life expectancy at birth has increased to over 80 years over the last three decades. The largest increase from 1990 to 2019 was reported in Estonia from 74.8 to 82.8, then Latvia from 74.6 to 79.9 and Lithuania from 76.2 to 81.0 [ 17 ].
In 2019, the size of the female screening population ranged from 233,226 in Estonia (aged 30–55 years) to 636,528 in Lithuania (aged 29–59 years), and annual female birth cohorts ranged from 6,734 in Estonia to 14,672 in Lithuania (10,197 in Latvia) (Table 1 ).
HPV prevalence
A subnational study conducted in 2006 in Estonia reported an overall prevalence of 38.6% for HPV DNA in a random sampling of women with unknown cytology aged 18–35 years. High and low risk HPV prevalence was 21.3% (95% CI 16.4–26.8) and 10.1% (95% CI 7.2–14.3) respectively. HPV 16 was detected most frequently (6.4%; 95% CI 4.0-9.8%) followed by HPV 53 (4.3%; 95% CI 2.3–7.2) and HPV 66 (2.8%; 95% CI 1.3–5.2) [ 18 ].
A study from 2007 including data from Latvia reported a high-risk HPV (hrHPV) DNA (deoxyribonucleic acid) prevalence of 26.2% (9 hrHPV types tested) with a convenient sampling from three sources: women aged 15–85 attending screening, gynecologist consultation, or a sexually transmitted disease clinic. HPV 16 was the most common type (16.0%) detected. The prevalence of hrHPV when excluding women with abnormal cervical cytology findings was 21.5% [ 19 ].
From Lithuania data are available from a two region gynaecology clinic attendees-based samples from mid 2000s, that yielded hrHPV test positivity among women aged 18–50 of 25.0% (13 types hrHPV tested) [ 20 ].
In Latvia, the prevalence of HPV 16/18 among women with low-grade squamous intraepithelial lesions / cervical intraepithelial neoplasia grade 1 (LSIL/CIN-1) is the highest among the Baltic States at 35.1%, while Estonia is slightly lower at 30.6% and Lithuania differing significantly at 6.7% [ 21 ].
HPV in cervical precancerous lesions and cervical cancer
In Lithuania, 74.2% women with CIN2/3 and 85.6% of women with cervical cancer, were hrHPV positive. HPV 16 was the most prevalent subtype, detected in 50% of cervical cancers and CIN 2/3 cases, followed by ~ 10% prevalence of HPV 18 and HPV 33 in both disease groups [ 22 ]. Estonian data is closely mirroring these results – with prevalence of 55%, 12% and 8% for HPV 16, 33 and 31 respectively among women with high grade cervical lesions [ 23 ].
According to the study from Latvia by Silins et al. (2004), the most common HPV DNA type found in cervical samples of the cervical cancer patients was HPV 16 (60.6%), followed by HPV 18 (9.0%), HPV 31 (5.4%), HPV 45 (3.2%), and HPV33 (2.7%). Overall, 82.8% (183/ 221) of examined samples were HPV-positive [ 24 , 25 ].
Cervical cancer - primary prevention
There are organized population-based HPV vaccination programmes in all three Baltic States. Vaccination of the target population is free of charge and includes 12-18-year-old girls in Latvia, 12-14-year-old girls in Estonia, and 11-year-old girls in Lithuania. School-based vaccination is performed in Estonia and Lithuania, but in Latvia vaccination is provided by general practitioners (Table 1 ).
Cervical cancer - secondary prevention
In the three countries opportunistic and organised screening coexist. For example, in Estonia, about 90% of all Pap tests (Papanicolaou cytological staining) are performed in Estonia every year outside of organized screening [ 26 ]. Organized nation-wide cervical cytology-based screening programmes in the Baltic States have been in operation for over 10 years (Table 1 ).
Until 2020, cytology was the primary screening test in all three Baltic States. Pap test and Bethesda classification, recommended by the European guidelines [ 27 ], used in Estonia and Lithuania prior to this, and Giemsa stain with Leishman modification test (historical tradition from former Soviet Union cytology practice) in Latvia [ 28 ]. In 2021 Latvia switched to liquid-based cytology using Bethesda classification as a primary screening test, and Estonia to HPV DNA test.
In 2006, a nation-wide programme of the screening with the five-year interval was initiated and organized via screening cabinets in clinics that participated in the programme with specially trained midwives taking Pap test [ 29 ]. The National Health Insurance Fund under the Ministry of Social Affairs finances the programme. Since 2015, the Registry of Cancer Screening is responsible for sending invitations and monitoring the process. Women are invited for organised screening using individual invitation letters sent by e-mail, by post, or via the media information campaigns (the exact methodology of invitation differs by year). In January 2021 Estonia implemented new guidelines recommending primary HPV DNA testing for a wider age range (30 to 65 years) of women with a five-year interval [ 30 ].
In Latvia, organized cervical cancer screening started in 2009 for women aged 25–70 years using cytology test (a modified Leishman Giemsa staining). All eligible women are invited by the National Health Service to attend a screening appointment every 3 years. Invitations letters are mailed to women’s declared addresses. Screening tests are usually performed at a gynaecological clinic, general practitioners rarely take Pap smears and nurses or midwives are not involved. Although primary care practitioners are not actively involved in the screening programme, they can monitor whether their female patients have attended screening. NHS collects results of the screening tests, but ongoing follow up and monitoring of the system is not provided.
The Lithuanian National Cervical Cancer Screening Programme was launched in 2004, which is financed by the National Health Insurance Fund under the Ministry of Health of Lithuania offering a free Pap smear test every 3 years to all women aged 25–60 years.
Primary health care practitioners are responsible for inviting and screening women. Usually, personal invitations are not sent out by mail and primary practitioners (GP) tend to rely on informing women about the screening when they attend their primary health care centre [ 31 , 32 ]. Thou, programme still carries opportunistic features as it is strongly dependent on the frequency of visits to the GP and the activity of the GP in providing information about screening [ 33 ]. Data on the exact coverage of screened women are currently not available. Research projects testing the efficacy of personal invitation letters conducted in 2011 and 2014 in Lithuania yielded response rates (coverage) ranging from 22% [ 31 ] to 25% [ 32 ].
Cervical cancer screening registries are established in Latvia (2009), and Estonia (2015) [ 34 ] but not in Lithuania [ 35 ]. All three countries lack comprehensive screening test quality control systems.
Cervical cancer incidence
ASIRs are shown in Fig. 1 for women of all ages (0+) from the beginning of the observation period in 1990 until the end of the observation in 2018 (or in the last available year before 2018). During the period of 2014–2018, the average ASIR for cervical cancer in the three Baltic States were as follows − 14.4 per 100,000 women in Estonia, 15.4 per 100,000 women in Latvia, and 15.5 per 100,000 women in Lithuania (2014–2015). In all countries, ASIR increased starting from 1990 to peak between 2006 and 2014. In Estonia, ASIR increased from 1990 to 2013 by APC = 1.0% (95% CI 0.4–1.6) with the highest cervical cancer ASIR of 20.3 and 19.4 per 100,000 women in 2009 and 2012. From 1990 to 2014, Latvia witnessed a steep increase of cervical cancer incidence (APC = 2.8, 95% CI 2.3–3.4) with the peak ASIR of 17.7 per 100,000 women in 2014. SIR in Lithuania increased from 1990 to 2006 by APC = 2.7 (95% CI 2.0–3.5), with the highest rates observed in 2004 (23.0 per 100,000 women) and 2006 (21.5 per 100,000 women).
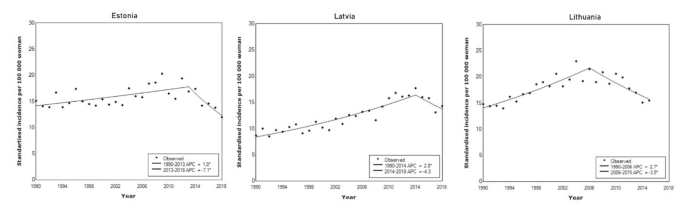
Standardised cervical cancer incidence between 1990–2018 in three Baltic States
By the end of observation period, we had seen a decrease in ASIR in all three countries: by APC = -3.5 (95% CI − 1.8 – -5.2) in Lithuania, by APC = -4.3 (95% CI − 11.5–3.4) in Latvia, and by APC = -7.1 (95% CI -1.7 – -12.2) in Estonia (Fig. 1 ; Table 1 ).
For the period of 2014–2018 average age-specific cervical cancer incidence rates were estimated (Fig. 2 ). In Estonia, the highest rates were observed for women aged 50–54 years (41.4 per 100,000 women) and 55–59 years (38.2 per 100,000 women). In Latvia, the highest rate occurred with women aged 45–49 years at 46.5 cases per 100,000 women. In Lithuania, highest age-specific incidence rates were observed in age groups 45–49 years (43.0 per 100,000 women), 50–54 years (49.0 per 100,000 women), and 55–59 years (44.5 per 100,000 women).

Age-specific cervical cancer incidence during 2014–2018 in Estonia and Latvia and 2014–2015 in Lithuania
The cumulative incidence of cervical cancer by age 75 was 1.4 in Estonia, 1.5 in Latvia, and 1.5 in Lithuania. The one-year relative survival ranged from 74.6% in Latvia to 86% in Estonia, and five-year relative survival ranged from 51.0% in Latvia to 67% in Estonia (Table 1 ).
Cervical cancer stage distribution at the time of diagnosis
Across the countries and years, about one third of cervical cancer cases have been diagnosed at stage I. In Estonia and Lithuania, TNM stage distribution shifted towards later stages at diagnosis from 2005 to 2009 to 2014–2018. The proportion of stage I cases decreased from 39.3 to 32.5% while stage IV cases increased from 10.3 to 16.9% in Estonia. In Lithuania stage I cases went from 40.8 to 32.8% and stage IV cases increased from 7.7 to 9.1% (Fig. 3 ).
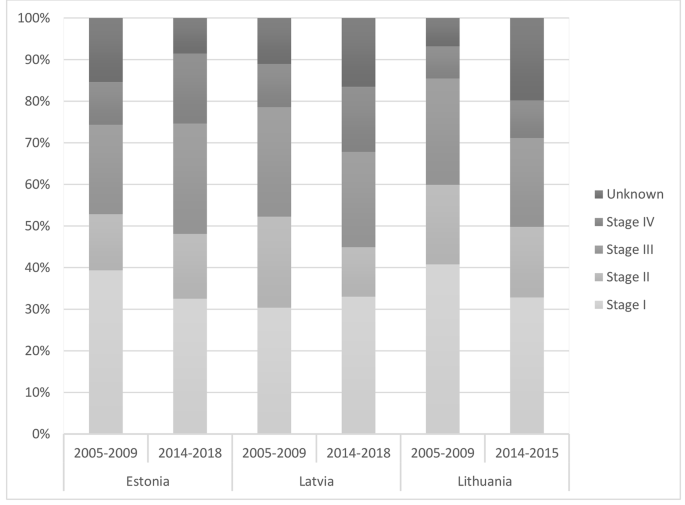
TNM stage distribution of cervical cancer cases in Baltic States
Cervical cancer mortality
In Estonia, the AMIRs declined throughout the period under analysis by APC= -1.5 (95% CI -0.9 – -2.1). In 2018, cervical cancer AMIR was 3.9 per 100,000 women. In contrast, in Latvia, the AMIR increased (APC= 1.5, 95% CI 0.8–2.1), and in 2018 cervical cancer AMIR was 6.4 per 100,000. In Lithuania, age-standardised mortality was stable until 2002 (APC = 1.3, 95% CI -0.2–2.8), and declined thereafter (APC= -2.2, 95% CI -0.8 – -3.5) (Fig. 4 ).
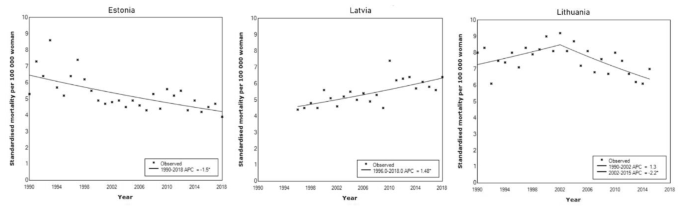
Standardised cervical cancer mortality during 1990–2018 in Baltic States
We have provided a comprehensive overview of the trends in cervical cancer incidence and mortality, and an update of the cervical cancer prevention efforts in the Baltic States. In parallel to the increase in life expectancy over the last three decades, cervical cancer remains a substantial health problem in the region. We observed important similarities among the three countries: high burden of the disease (high incidence and mortality of cervical cancer, changes in TNM stage distribution towards later stage at diagnosis (in Lithuania and Estonia), high burden of hrHPV in general population and suboptimal implementation of the preventive strategies (low screening and HPV vaccination coverage).
Disease burden
Among general population women, the prevalence of hrHPV in Estonia and Lithuania is higher than that reported from central and western European countries and is comparable to former Soviet Union countries [ 18 , 20 , 25 , 36 , 37 ]. This tendency might be explained by the influence of the primary prevention (insufficient sexual education at schools as well as the limited effect of HPV vaccination – it has been introduced in 2018 in Estonia for girls aged 12–14 years (12 years since 2020) and in 2016 in Lithuania for girls aged 11 years, but the coverage seems to be insufficient (31.3% in Estonia in 2019, no data for Lithuania), cultural and regional relations from Soviet Union times but also can be attributed to the differences in study design and use of different HPV testing methods [ 38 ].
In comparison to neighbouring Scandinavian countries, cervical cancer incidence in the Baltic States is higher and the decline of the incidence rate has been delayed for about 50 years. Over two thirds of the period of observation, the cervical cancer incidence increased, and has only started a downward trend in more recent years. The highest age-specific incidence is also similar in Baltic States – among women aged 50–59 years, with Latvia in the slightly younger age group of 45–49 years. A slight peak is also observed after the age of 70.
Cervical cancer mortality in the Baltic countries exceeds that in neighbouring Scandinavian or Western European countries by more than two times [ 39 ]. There are some differences in cervical cancer mortality trends in the Baltic States. While the absolute mortality rates differ, in Estonia and Lithuania the mortality is declining. In Latvia, it is gradually increasing. Whether or not the decline in mortality can be attributed to screening effect is debatable. A very worrisome sign is shifting the cancer into later stages at cervical cancer diagnosis in Estonia and Lithuania [ 40 ].
Cervical cancer prevention
Data from other countries have shown that vaccination effectively reduces the prevalence of HPV, cervical high-grade precancerous lesions, and cancer [ 41 , 42 ].
Vaccination against HPV has been introduced among teenage girls in all Baltic States, but the vaccination coverage is suboptimal. Studies have shown, that the main barriers to HPV vaccination are the lack of HPV awareness among the general public, lack of provider recommendation, concerns about HPV vaccination [ 43 ]. Young adults need parental consent for the vaccination and the acceptance of the HPV vaccine is highly dependent on the knowledge, perceptions, and approval of their parents. ‘Fake news’ about vaccination safety generally and HPV vaccination specifically has been associated with rapid fall in uptake in Europe [ 44 ]. There is a clear need to improve public knowledge about the value and the safety of vaccination. The possible solutions are increasing health literacy, professional awareness of HPV and the dissemination of emotive stories of patient advocates [ 45 ].
While the organised cervical cancer screening programmes in the Baltic States differ in some relevant details (target age groups, screening interval), the underlying principles (being population-based with repeated screening episodes over an extended period) and problems, barriers (low coverage, inadequately working screening test, lacking / inconsistent quality control system) are universal. Screening at the population level every three to five years can reduce cervical cancer incidence up to 80% [ 27 ]. Low attendance and lack of assured high-quality of screening programmes in all Baltic States potentially contribute to high cervical cancer incidence, and mortality. Several factors are recognized to impact screening attendance rate in the Baltic States, including personal (fear to give a Pap-smear, did not like the physician who took the sample, lack of time) and organizational (long waiting list for an appointment, distant location of the clinic [ 46 , 47 ]. Local research has postulated that besides inadequate screening uptake, also the insufficient quality of the Pap-smear based screening program as drives behind the failure of cervical cancer prevention [ 48 ]. The introduction of primary HPV screening is strongly recommended to decrease cervical cancer incidence [ 49 ]. HPV testing has several advantages as a primary screening strategy, including equivalent or higher sensitivity than Pap-smears, ability to predict women at high risk for future disease, lower technician skill level needed when compared to cytology, and having the potential for self-collection [ 50 ].
Special efforts are needed to increase screening attendance in general and among high-risk women. Potentially, multiple components culturally tailored cervical cancer screening intervention combining education, and navigation, in addition to no-cost screening for all women, are needed to significantly increase cervical cancer screening uptake and to alleviate cervical cancer health disparities.
Importantly, we were unable to locate data on screening test performance, diagnostic assessment, treatment efficiency, and post-treatment follow-up. Scarcity of these data potentially indicates on weakness of organised screening programmes in Baltic States. Quality management processes distinguish organised screening programmes from opportunistic screening. Quality is an integral part of screening programmes, and proactive approach to quality improvement is required to achieve the vision, strategic outcomes [ 51 ].
No studies have been conducted to determine the practice of cervical cancer prevention and adherence to cervical cancer screening and treatment guidelines among healthcare professionals in Baltic countries within the last 10 years. There is a lack of information in regard to the knowledge on barriers to comply. According to a qualitative study conducted by Estonian health insurance fund, the delivery of cervical cancer prevention programs can vary among screening and treatment providers. The focus group participants have indicated that education of health professionals on cervical cancer preventative clinical practices should be continuous and regular [ 52 ].
Cervical cancer elimination depends strongly on contextual factors. The evidence is there - through cost-effective, evidence-based interventions, including improving public and professional awareness and education about HPV, universal HPV vaccination, high level uptake of the screening and treatment of precancerous lesions according to best practice guidelines, and assuring access to diagnosis and treatment of invasive cancers, cervical cancer as a public health problem is amenable for elimination. We see the most important factors that should be acted upon in Baltic States: (i) a political decision to accelerate activities; (ii) ownership and the performance of the national screening programs; and (iii) their adaptability to new interventions.
High cervical cancer incidence and mortality urge not only the use of well-validated methods in screening but also the introduction of systematic monitoring, evaluation, and quality assurance in the programme and other related services. To do this, a collaboration between cervical cancer screening programmes in other countries is required. The goal of cervical cancer free future in Baltic States could be achieved through realistic investment and evidence-based steps improving vaccination and screening coverage, public and professional awareness and treatment outcomes.
Data availability
The datasets generated and analysed during the current study are not publicly available due to the fact that no primary data are used in the study; only anonymized secondary data from population-based registries are used (aggregated data), but they are available from the corresponding author on reasonable request.
Abbreviations
age-standardized mortality rate
annual percent change
age-standardized incidence rate
confidence interval
cervical intraepithelial neoplasia grade 1
cervical intraepithelial neoplasia grades 2/3
deoxyribonucleic acid
European Economic Area
primary practitioner
high risk human papillomavirus
high-risk HPV
International Classification of Diseases tenth edition
low-grade squamous intraepithelial lesions
Papanicolaou cytological staining
Classification of Malignant Tumors
United States of America
Vaccarella S, Lortet-Tieulent J, Plummer M, et al. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013;49:3262–73.
Article PubMed Google Scholar
World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. https://www.who.int/publications/i/item/9789240014107 (2020, accessed 6th April 2022)
Portnoy A, Pedersen K, Trogstad L, et al. Impact and cost-effectiveness of strategies to accelerate cervical cancer elimination: a model-based analysis. Prev Med. 2021;144:106276.
Hall MT, Simms KT, Lew JB, et al. The projected timeframe until cervical cancer elimination in Australia: a modelling study. The Lancet Public health. 2019;4:19–27.
Article Google Scholar
Burger EA, Smith MA, Killen J, et al. Projected time to elimination of cervical cancer in the USA: a comparative modelling study. Lancet Public Health. 2020;5:213–22.
Castanon A, Rebolj M, Sasieni P. Is a delay in the introduction of human papillomavirus-based cervical screening affordable? J Med Screen. 2019;26:44–9.
Bruni L, Albero G, Serrano B et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World.Summary Report October2021
Wojtyla C, Ciebiera M, Kowalczyk D, et al. Cervical Cancer mortality in East-Central European Countries. Int J Environ Res Public Health. 2020;17:4639.
Article PubMed PubMed Central Google Scholar
Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. The Lancet Global health. 2020;8:191–203.
Publication Office of the European Union. European guidelines for quality assurance in cervical cancer screening. https://op.europa.eu/en/publication-detail/-/publication/a41a4c40-0626-4556-af5b-2619dd1d5ddc (accessed 6th April 2022)
Central Statistical Bureau of Latvia. Population number and characteristics, https://data.stat.gov.lv/pxweb/en/OSP_PUB/START__POP__IR / (2021, accessed 6th January 2021)
Statistics Estonia. https://andmed.stat.ee/en/stat (2021, accessed 12 January 2021)
Statistics Lithuania. https://osp.stat.gov.lt/lietuvos-gyventojai-2020/mirtingumas/vidutine-tiketina-gyvenimo-trukme (2021, accessed 12 January 2021)
Bray F, Colombet M, Mery L, et al. Cancer incidence in five continents, vol. XI (electronic version). Lyon: International Agency for Research on Cancer; 2017.
Google Scholar
National Cancer Institute. Joinpoint trend analysis software. https://surveillance.cancer.gov/joinpoint/ (2022, accessed December 1st, 2021)
The Wolrd Bank. Population total Estonia, Latvia, Lithuania. https://data.worldbank.org/indicator/SP.POP .TOTL?locations=EE-LV-LT%20Female:%20https://data.worldbank.org/indicator/SP.POP.TOTL.FE.IN?locations=EE-LV-LT%20 (2022, accessed 18 March 2022)
The World Bank. Life expectancy at birth. https://data.worldbank.org/indicator/SP.DYN.LE00.FE.IN?locations=EE LV-LT(2022, accessed 18 March 2022)
Uusküla A, Kals M, Kosenkranius L, et al. Population-based type-specific prevalence of high-risk human papillomavirus infection in Estonia. BMC Infect Dis. 2010;10:63.
Kulmala SM, Shabalova IP, Petrovitchev N, et al. Prevalence of the most common high-risk HPV genotypes among women in three new independent states of the former Soviet Union. J Med Virol. 2007;79:771–81.
Kliucinskas M, Nadisauskiene RJ, Minkauskiene M. Prevalence and risk factors of HPV infection among high-risk rural and urban lithuanian women. Gynecol Obstet Invest. 2006;62:173–80.
HPV Information Centre. https://hpvcentre.net/datastatistics.php (2021, accessed 12 Janury 2021)
Gudleviciene Z, Kanopiene D, Didziapetriene J, et al. Differences on the prevalence of cervical HPV between Lithuania and Belarus. Cent Eur J Med. 2014;9:285–91.
Padrik L, Raud T, Kriisa L et al. HPV DNA prevalence in Estonian women with high-grade Lesions. European Federation for Colposcopy. Berlin 27–29 May 2010
Silins I, Wang X, Tadesse A, et al. A population-based study of cervical carcinoma and HPV infection in Latvia. Gynecol Oncol. 2004;93:484–92.
Poljak M, Seme K, Maver PJ, et al. Human papillomavirus prevalence and Type-Distribution, Cervical Cancer Screening Practices and current status of vaccination implementation in Central and Eastern Europe. Vaccine. 2013;31:59–70.
Koreinik L, EMAKAKAELAVÄHI SÕELUURINGUS OSALEMIST MÕJUTAVAD TEGURID, EESTIS. (2019) https://dspace.ut.ee/handle/10062/66725 (accessed 07 April 2022)
Arbyn M, Anttila A, Jordan J et al. European Guidelines for Quality Assurance in Cervical Cancer Screening. Second edition. IARC, 2008
Viberga I, Engele L, Baili P. Past, present and future of the cervical cancer screening in Latvia. Tumori. 2010;96:529–37.
Partanen V, Antilla A, Heinävaara S et al. NordScreen: Performance indicators on cancer screening in the Nordic countries, https://nordscreen.org/wp-content/uploads/2017/07/cervix-fact-sheet-estonia-2017.pdf (2019, accessed 01.09 2020)
National Health Insurance Fund. Screenings for women https://haigekassa.ee/soeluuring (2022, accessed 31 January 2022)
Kurtinaitienė R, Rimienė J, Labanauskaitė I, et al. Increasing attendance in a cervical cancer screening programme by personal invitation: experience of a lithuanian primary health care centre. Acta Med Lituanica. 2016;23:180–4.
Paulauskiene J, Ivanauskiene R, Skrodeniene E, Petkeviciene J. Organised Versus Opportunistic Cervical Cancer Screening in Urban and Rural Regions of Lithuania. Medicina. 2019;55(9):570.
Maver PJ, Seme K, Korać T et al. Cervical cancer screening practices in central and eastern Europe in 2012. Acta dermatovenerologica Alpina, Pannonica, et Adriatica 2013; 22: 7–19
National institute for health development.Cancer screening registries, https://tai.ee/et/tegevused/registrid/vahi-soeluuringute-register (2021, accessed 13 January 2021)
Vale DB, Anttila A, Ponti A, et al. Invitation strategies and coverage in the population-based cancer screening programmes in the European Union. Eur J Cancer Prev. 2019;28:131–40.
Rogovskaya SI, Shabalova IP, Mikheeva IV, et al. Human papillomavirus prevalence and type-distribution, cervical cancer screening practices and current status of vaccination implementation in Russian Federation, the western countries of the former Soviet Union, Caucasus region and Central Asia. Vaccine. 2013;7:46–58.
Bosch FX, Broker TR, Forman D, et al. Comprehensive control of human papillomavirus infections and related diseases. Vaccine. 2013;7:1–31.
Wang W, Kothari S, Baay M, et al. Real-world impact and effectiveness assessment of the quadrivalent HPV vaccine: a systematic review of study designs and data sources. Expert Rev Vaccines. 2022;21:227–40.
Article CAS PubMed Google Scholar
European Cancer Information System. Series of Cancer Fact Sheets EU 27 countries. https://ecis.jrc.ec.europa.eu/factsheets.php (2020, accessed 12 January 2021)
Everatt R, Intaite B. Trends in cervical cancer mortality rates in Lithuania, 1987–2016. Cancer Epidemiol. 2018;57:85–9.
Drolet M, Bénard É, Pérez N, et al. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet. 2019;394:497–509.
Lei J, Ploner A, Elfström KM, et al. HPV Vaccination and the risk of Invasive Cervical Cancer. N Engl J Med. 2020;383:1340–8.
Cartmell KB, Young-Pierce J, McGue S, et al. Barriers, facilitators, and potential strategies for increasing HPV vaccination: a statewide assessment to inform action. Papillomavirus Res. 2018;5:21–31.
Suppli CH, Hansen ND, Rasmussen M, et al. Decline in HPV-vaccination uptake in Denmark – the association between HPV-related media coverage and HPV-vaccination. BMC Public Health. 2018;18:1360.
European Cancer Organisation. A four step plan for eliminating HPV cancers in Europe. https://www.europeancancer.org/resources/159:viral-protection-achieving-the-possible-a-four-step-plan-for-eliminating-hpv-cancers-in-europe.html (2020, accessed 1 February 2022)
Zodzika J, Krumina K, Jermakova I, et al. Post-reproductive aged women: a lost generation in the cervical cancer screening programme. Eur J Contracept Reprod Health Care. 2021;26:23–8.
Kivistik A, Lang K, Baili P, et al. Women’s knowledge about cervical cancer risk factors, screening, and reasons for non-participation in cervical cancer screening programme in Estonia. BMC Womens Health. 2011;11:43.
Ojamaa K, Innos K, Baburin A, et al. Trends in cervical cancer incidence and survival in Estonia from 1995 to 2014. BMC Cancer. 2018;18:1075.
Anttila A, Lönnberg S, Ponti A, et al. Towards better implementation of cancer screening in Europe through improved monitoring and evaluation and greater engagement of cancer registries. Eur J Cancer. 2015;51:241–51.
Mandelblatt JS, Lawrence WF, Womack SM, et al. Benefits and costs of using HPV testing to screen for cervical cancer. JAMA. 2002;287(18):2372–81.
World Health Organization. Screening programmes: a short guide. Increase effectiveness, maximize benefits and minimize harms. https://www.euro.who.int/en/publications/abstracts/screening-programmes-a-short-guide.-increase-effectiveness,-maximize-benefits-and-minimize-harm-2020 (2020, accessed 1 March 2022)
Ental H, Aavik HM, Lubi K, Plešs N. Estonian Cervical Cancer Screening – an opportunity that should not be missed. Road project report 2021. Estonian health insurance fund. 2021.
European Cancer Registry. Survival of cancer patients in Europe. http://www.eurocare.it/ (2021, accessed 12 January 2021)
Download references
Acknowledgements
Not applicable.
This work was supported through grant EMP416 from the EEA (European Economic Area) and Norway Grants.
Author information
Authors and affiliations.
Institute of Public Health, Riga Stradins University, Riga, Latvia
Una Kojalo, Anda Kivite-Urtane & Jana Zodzika
Institute of Family Medicine and Public Health, University of Tartu, Tartu, Estonia
Anna Tisler, Kersti Parna & Anneli Uuskula
Department of Health Management, Lithuanian University of Health Sciences, Kaunas, Lithuania
Mindaugas Stankunas
Cancer Registry of Norway, Oslo, Norway
Nicholas Baltzer & Mari Nygard
You can also search for this author in PubMed Google Scholar
Contributions
UK elaborated the conceptual framework of the article, carried out the calculations, drafted the text, AT elaborated the conceptual framework of the article, requested the data from national registries, drafted the text, KP elaborated the conceptual framework of the article, drafted the text, AKU requested the data from national registries, drafted and reviewed the text, JZ elaborated the conceptual framework of the article, drafted the text, MS requested the data from national registries, reviewed the text, NB elaborated the conceptual framework of the article, reviewed the text, MN elaborated the conceptual framework of the article, reviewed the text, AU elaborated the conceptual framework of the article, drafted and reviewed the text.
Corresponding author
Correspondence to Anda Kivite-Urtane .
Ethics declarations
Ethics approval and consent to participate.
Consent to participate - not applicable as no primary data are used in the study; only anonymized secondary data from population-based registries are used (aggregated data). Ethics approval - approved by Research Ethics Committee of the University of Tartu (protocols 300/T-17 20.01.2020, 332/M-7 21.12.2020), Estonian Committee on Bioethics and Human Research (protocol 1.1–12/660, 14.01.2021), Research Ethics Committee of Riga Stradins University (decision No 6 − 1/07/33, 25.06.2020).
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kojalo, U., Tisler, A., Parna, K. et al. An overview of cervical cancer epidemiology and prevention in the Baltic States. BMC Public Health 23 , 660 (2023). https://doi.org/10.1186/s12889-023-15524-y
Download citation
Received : 06 July 2022
Accepted : 25 March 2023
Published : 07 April 2023
DOI : https://doi.org/10.1186/s12889-023-15524-y

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cervical cancer
- Human papillomavirus
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
ORIGINAL RESEARCH article
Immune cell infiltration and prognostic index in cervical cancer: insights from metabolism-related differential genes.

- Department of Obstetrics and Gynecology, Xijing Hospital, Fourth Military Medical University, Xi'an, China
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Background: Cervical cancer remains a significant gynecologic malignancy in both China and the United States, posing a substantial threat to women's lives and health due to its high morbidity and mortality rates. Altered energy metabolism and dysregulated mitochondrial function play crucial roles in the development, growth, metastasis, and recurrence of malignant tumors. In this study, we aimed to predict prognosis and assess efficacy of anti-tumor therapy in cervical cancer patients based on differential genes associated with mitochondrial metabolism.Methods: Transcriptomic data and clinical profiles of cervical cancer patients were retrieved from the TCGA and GEO databases. Differential gene-related cellular pathways were identified through GO, KEGG, and GSEA analyses. Prognostic indices were constructed using LASSO regression analysis. Immune cell infiltration was assessed using CIBERSORT and ssGSEA, and the correlation between immune checkpoint inhibitor genes and differential genes was examined. Tumor mutation load (TMB) and its association with prognostic indices were analyzed using nucleotide variant data from the TCGA database. Patient response to immunotherapy and sensitivity to antitumor drugs were determined using the TIDE algorithm and the oncoPredic algorithm, respectively.Results: A prognostic index based on metabolism-related differential genes was developed to predict the clinical outcome of cervical cancer patients, enabling their classification into two distinct subtypes. The prognostic index emerged as an independent risk factor for unfavorable prognosis. The high-index group exhibited a significantly worse overall prognosis, along with elevated tumor mutation burden (TMB), increased immune cell infiltration, and lower TIDE scores, indicating a potential benefit from immunotherapy. Conversely, the low-index group demonstrated increased sensitivity to metabolism-related antitumor agents, specifically multikinase inhibitors.The aim of this study was to develop a prognostic index based on differential genes associated with mitochondrial metabolism, which could be used to predict cervical cancer patients' prognoses. When combined with TIDE and TMB analyses, this prognostic index offers insights into the immune cell infiltration landscape, as well as the potential efficacy of immunotherapy and targeted therapy. Our analysis suggests that the Iron-Sulfur Cluster Assembly Enzyme (ISCU) gene holds promise as a biomarker for cervical cancer immunotherapy.
Keywords: mitochondrion, Energy Metabolism, cervical cancer, immune, IscU
Received: 02 Apr 2024; Accepted: 08 May 2024.
Copyright: © 2024 Ma, Ren, Yin, Zhao, Li and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Jia Li, Department of Obstetrics and Gynecology, Xijing Hospital, Fourth Military Medical University, Xi'an, China Hong Yang, Department of Obstetrics and Gynecology, Xijing Hospital, Fourth Military Medical University, Xi'an, China
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Português Br
- Journalist Pass
Mayo Clinic Q&A: What to know about cervical cancer
Susan Barber Lindquist
Share this:

DEAR MAYO CLINIC: My mom had a pap smear recently, and the results came back as abnormal. After further testing, we were shocked when she was diagnosed with cervical cancer. She didn't have any symptoms. Now, her healthcare team is discussing surgery and medications. What should I know about her illness? As her daughter, should I be worried about myself? Most importantly, how I can support her during treatment?
ANSWER: I commend you for finding ways to support your mom through her cervical cancer diagnosis. Gathering reliable information about her illness and treatment is a great start.
Part of the reproductive system, the cervix connects the vagina to the uterus, also known as the womb. By collecting cervical cells (called the Pap smear after the scientist who pioneered the screening test in the mid-1900s), cancer can be detected even at an early stage.
While cervical cancer may cause symptoms of bleeding or pain, it often does not cause any symptoms, especially in early stages. That's why Pap smears typically are recommended every three years for women ages 21 to 65. For women who are 30 and up, Pap smears may be recommended every five years, combined with testing for HPV infection . Pelvic examination with assessment of the cervix and other gynecologic structures, such as the vagina, vulva, urethra, anus, uterus and ovaries, can be easily performed in years when a Pap smear is not due.
HPV is the most common cause of cervical cancer. It is a frequent viral infection transmitted sexually through skin-to-skin contact. To help protect from cancer in the future, an HPV vaccine is available for males and females starting at ages 9 to 11. The vaccine is approved by the Food and Drug Administration (FDA) for people ages 9 to 45.
Treatment for cervical cancer will depend on many factors. For early-stage cervical cancer, a surgery called a total hysterectomy to remove the cervix and uterus may be considered. A hysterectomy may be performed through a cut in the lower part of the belly. Or a hysterectomy can be done through a cut in the vagina. Minimally invasive procedures, such as with robotic-assisted or laparoscopic surgery using long, thin surgical instruments passed through small cuts in the belly also are options.
However, removing the uterus means pregnancy no longer is possible. Some surgical procedures, such as a trachelectomy (cervix removal), can preserve the uterus and fertility options.
For cervical cancer that has advanced but has not spread to other parts of the body, chemotherapy and radiation — delivered internally, externally or both — are typically recommended.
Medications are available for advanced cervical cancer that is continuing, keeps coming back or has spread. Targeted therapy called bevacizumab often is used in combination with other medicines. For patients who test positive for PD-L1 — a type of protein that stops the immune system from attacking cancer — an immunotherapy called pembrolizumab also may be used.
So-called "second-line treatments," such as tisotumab vedotin-tftv, given after earlier treatments have been unsuccessful, also are available and showing improved overall response rate.
While all treatments have benefits and risks, these treatments hold promise for enhanced long-term outcomes for patients with advanced and recurrent cervical cancer.
No matter what treatment plan your mom pursues with her care team, you can help in a variety of ways, such as doing household chores like cooking or cleaning. Your mom may appreciate you going to her medical appointments to ask questions, take notes or be another person to process all the information.
Don't forget prevention measures to reduce your risk of developing cervical cancer:
- Ask your healthcare team about an appropriate Pap test routine for you depending on your age and individual factors.
- Consider the HPV vaccine. The HPV vaccine is approved by the FDA to age 45. Are you up to date on your vaccines?
- If you are sexually active, practice safe sex by using condoms and limiting sexual partners.
- If you smoke, work hard to quit . Your healthcare team can point you to a variety of resources to stop tobacco use. Research shows women who smoke are twice as likely to get cervical cancer.
Kristina Butler, M.D. , Obstetrics and Gynecology, Mayo Clinic, Phoenix
- Mayo Clinic Q & A: Going plant-based: Exploring the myths, health benefits Mayo Clinic, Nemours Children’s Health, Jacksonville collaborate for pediatric care, medical education, research
Related Articles

Total hysterectomy versus radical hysterectomy in neuroendocrine cervical cancer: a SEER-database analysis
- Open access
- Published: 06 May 2024
- Volume 150 , article number 236 , ( 2024 )
Cite this article
You have full access to this open access article

- Feitianzhi Zeng 1 ,
- Peng Guo 1 ,
- Meng Xia 1 &
- Mian He 1
194 Accesses
Explore all metrics
We conducted this study to evaluate the efficacy of total hysterectomy versus radical hysterectomy in the treatment of neuroendocrine cervical cancer (NECC).
Eligible NECC patients were identified from the Surveillance, Epidemiology and End Results (SEER) database. Demographic characteristics, clinical treatment and survival of the patients were collected. The overall survival (OS) and cancer-specific survival (CSS) were estimated by Kaplan–Meier analysis with log-rank test.
A total of 286 patients were included, with 104 patients undergoing total hysterectomy and 182 patients undergoing radical hysterectomy. The 5-year OS were 50.8% in the total hysterectomy group and 47.5% in the radical hysterectomy group (p = 0.450); and the corresponding 5-year CSS were 51.6% and 49.1% (p = 0.494), respectively. Along with surgery, radiotherapy was given to 49.0% of patients in the total hysterectomy group and 50.5% in the radical hysterectomy group; and chemotherapy was administered to 77.9% of patients in the total hysterectomy group and 85.7% in the radical hysterectomy group. Unexpectedly, in patients who received adjuvant radiotherapy with or without chemotherapy, the OS was superior in the total hysterectomy group compared with the radical hysterectomy group (p = 0.034). While in patients who received chemotherapy alone and those who received neither radiotherapy nor chemotherapy, the OS still remained comparable between the total hysterectomy and radical hysterectomy group.
Compared with radical hysterectomy, total hysterectomy was not associated with compromised survival prognosis in patients with NECC. Total hysterectomy has the potential to be a surgical alternative in the multimodal management of NECC.
Similar content being viewed by others

Survival impact of adjuvant concurrent chemoradiotherapy after radical hysterectomy in FIGO stage IIIC1 cervical adenocarcinoma

Survival benefit of surgery with postoperative radiotherapy in locally advanced cervical adenocarcinoma: a population-based analysis

Oncologic outcomes of patients with FIGO 2014 stage IB-IIA cervical adenocarcinoma who underwent radical surgery
Avoid common mistakes on your manuscript.
Introduction
NECC is a rare type of cervical malignancy, comprising 1–1.5% of all cases(Tempfer et al. 2018 ). Due to its aggressive biological behavior, NECC often leads to lymph node and widespread hematogenous metastasis. Previous studies have indicated that 31.5–49.5% of NECC patients had lymph nodal involvement, and 4–13% had distant metastasis at initial diagnosis(Cohen et al. 2010 ; Stecklein et al. 2016 ; Castelnau-Marchand et al. 2018 ; Zhang et al. 2019 ). The prognosis for NECC patients remains poor even in the early stage, with a 5-year survival rate of only 31.6–36.8%, compared with up to 87% for common cervical cancer(Chan et al. 2003 ; Cohen et al. 2010 , 2019 ).
Radical hysterectomy with regional lymphadenectomy is recommended as a primary treatment option for patients with early-stage NECC(Gardner et al. 2011 ; Satoh et al. 2014 ; National Comprehensive Cancer Network 2022 ). Compared with total hysterectomy, radical hysterectomy is characterized by extended resection of the parametrium, upper vagina and partial uterosacral ligaments. The purpose of radical hysterectomy for cervical cancer includes removing potential micro-metastasis in the soft tissue surrounding the cervix to prevent pelvic recurrence, and providing pathological information of the parametrium as an indicator for adjuvant treatment(Wright et al. 2007 ). However, due to the clinical aggressiveness of NECC, adjuvant radiation and chemotherapy are almost routinely considered for NECC patients, regardless of their pathological risk factors(Salvo et al. 2019 ; National Comprehensive Cancer Network 2022 ). Therefore, the question whether radical hysterectomy is necessary for NECC patients has been raised(Salvo et al. 2021 ).
On the other hand, in comparison to total hysterectomy, radical hysterectomy has a higher risk of surgery related complications, such as urinary, nerve and vascular injury(Obermair et al. 2020 ; Kim et al. 2021 ; Plante et al. 2023 ). The incidence of postoperative urinary incontinence and urinary retention is 11.0% and 9.9%, respectively, in patients receiving radical hysterectomy, compared to 4.7% and 0.6%, respectively, in patients undergoing total hysterectomy(Plante et al. 2023 ). Thus, avoidance of radical hysterectomy may reduce surgical morbidity and improve postoperative quality of life.
Notwithstanding, it remains unclear whether the substitution of total hysterectomy for radical hysterectomy in the multimodal treatment of NECC would compromise the survival prognosis of the patients. Therefore, we conducted this retrospective study to compare the efficacy of total hysterectomy and radical hysterectomy in the treatment of NECC using data from the SEER database.
Patients selection
The research data for this study was obtained from the SEER database, using the SEER*Stat software (version 8.4.0; National Cancer Institute, USA). According to the International Classification of Diseases for Oncology, Third Edition (ICD-O-3), we identified patients with NECC using the primary site codes of C53.0-C53.1, C53.8-C53.9 and the histology codes of 8012, 8013, 8014, 8041, 8043, 8240, 8246 and 8249. Patients diagnosed between 1998 and 2017, aged 20–84 years, and treated with total or radical hysterectomy were eligible for this study. Patients with unavailable survival data were excluded.
Data collection
Demographic and clinical characteristics of the patients were collected, including age at diagnosis, histology, stage, tumor size, lymph node status, distant metastasis, surgery of primary site, radiotherapy, chemotherapy and survival status. The primary endpoints of this study were OS and CSS, which were defined as the time interval from diagnosis to death from any cause and from cancer, respectively.
Statistical analysis
The t-test was used to compare the differences in continuous variables, and the χ 2 test or Fisher’s exact test was used for categorial variables. OS and CSS were estimated by the Kaplan–Meier analysis with log-rank test. The Cox regression analysis was used for multivariate analysis to estimate the effect of potential prognostic factors. P-value < 0.05 was considered as statistically significant. The IBM SPSS Statistics for Windows, version 26.0 (IBM Corp, Armonk, NY) and GraphPad Prism version 5.0 for Windows (GraphPad Software, San Diego, CA) were used for statistical analysis.
Demographic characteristics
A total of 286 patients who met the inclusion criteria were identified from the SEER database. Among them, 104 patients underwent total hysterectomy and the other 182 patients underwent radical hysterectomy. Demographic characteristics of patients in both groups, including age at diagnosis, histology, tumor size, stage, lymph node status, and distant metastasis, were summarized in Table 1 . The proportion of patients who diagnosed at age 45 years or older was significantly higher in the total hysterectomy group than in the radical hysterectomy group (55.8% vs 36.3%, p = 0.002). Regarding lymph node metastasis, 36.6% and 31.7% of patients in the total hysterectomy group were found to be negative and with unknown status, respectively, while the corresponding ratios in the radical hysterectomy group were 56.0% and 7.7% (p < 0.001). All other demographic characteristics were comparable between the total hysterectomy group and the radical hysterectomy group.
The treatments administered to patients in each group were presented in Table 2 , including surgery for regional lymph node and distant metastatic lesion, radiotherapy, and chemotherapy.
74.2% of patients in the radical hysterectomy group received regional lymph node resection and 17.6% received lymph node biopsy. Whereas in the total hysterectomy group, the corresponding ratios were 59.6% and 4.8%, respectively. In both groups, fewer than 5% of patients had their distant metastatic lesions resected. Radiotherapy was given to 49.0% of patients in the total hysterectomy group and 50.5% in the radical hysterectomy group. In patients who had radiotherapy, 92.2% in the total hysterectomy group and 94.6% in the radical hysterectomy group received external beam radiation with or without brachytherapy. Chemotherapy was administered to 77.9% of patients in the total hysterectomy group and 85.7% in the radical hysterectomy group. However, information on the chemotherapy regimen and number of chemotherapy cycles were not available in the database.
Furthermore, patients in the total hysterectomy group were found to receive neoadjuvant therapy more often than those in the radical hysterectomy group. 29.4% of patients in the total hysterectomy group underwent preoperative radiotherapy and 21.0% of them underwent preoperative chemotherapy, both higher than the corresponding rates in the radical hysterectomy group of 8.7% (p = 0.002) and 10.2% (p = 0.061), respectively.
Survival analysis
The 5-year OS rate were 50.8% in the total hysterectomy group and 47.5% in the radical hysterectomy group (Fig. 1 A); and the corresponding 5-year CSS rate were 51.6% and 49.1%, respectively (Fig. 1 B). There’s no statistically significant difference in either OS ( P = 0.450; HR, 0.881; 95% CI, 0.633–1.227) or CSS ( P = 0.494; HR, 0.887; 95% CI, 0.627–1.255) between the two groups.
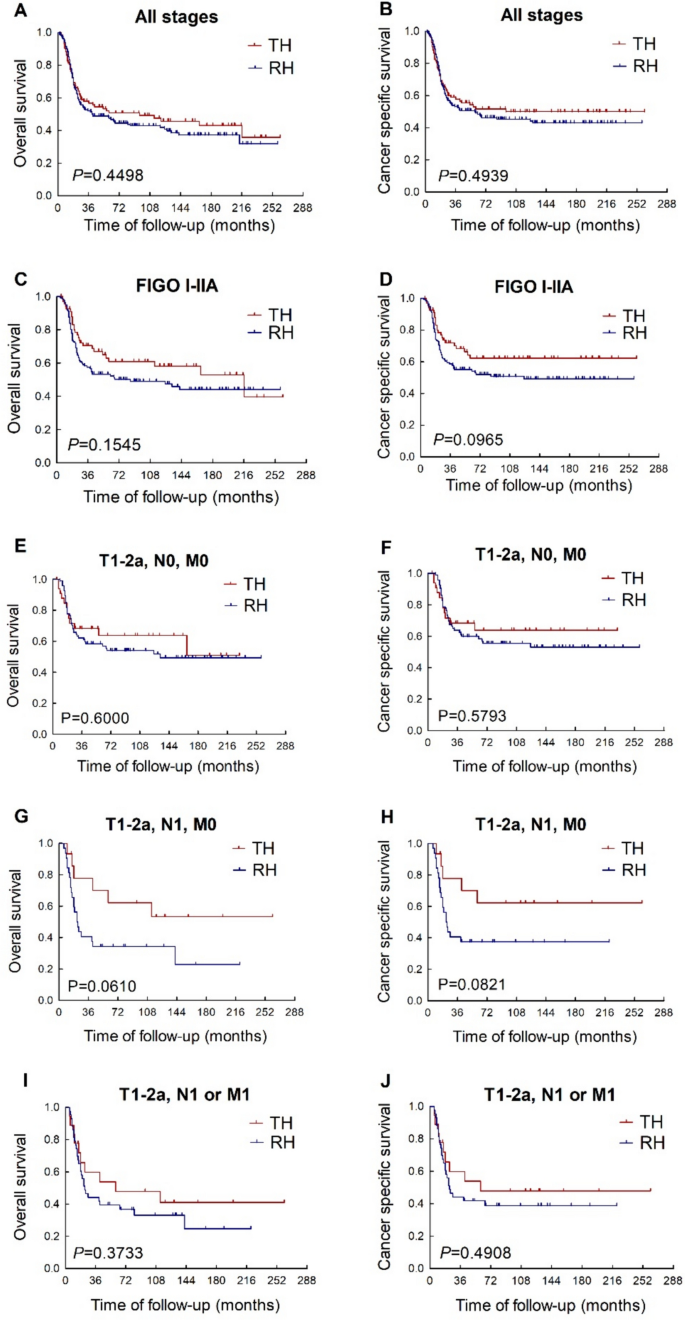
Comparison of total hysterectomy and radical hysterectomy in NECC patients in different stages. TH total hysterectomy. RH : radical hysterectomy
Patients with FIGO stage I-IIA cervical cancer are considered as candidates for radical surgery according to most clinical guidelines. In the subset of patients with FIGO stage I-IIA NECC (Fig. 1 C, D), it’s unexpected that the survival prognosis appeared to be better in the total hysterectomy group than in the radical hysterectomy group, although the difference in both OS (p = 0.154; HR, 0.735; 95% CI, 0.482–1.123) and CSS (p = 0.096; HR, 0.686; 95% CI, 0.440–1.070) between the total hysterectomy group and the radical hysterectomy group didn’t reach statistical significance.
To investigate the impact of lymph node status, we further divided patients with FIGO stage I-IIA NECC into two subsets, namely patients with lymph node metastasis (T1-2a/N1/M0) and without lymph node metastasis (T1-2a/N0/M0). In the subset of T1-2a/N0/M0 patients (Fig. 1 E, F), both OS (p = 0.600; HR, 0.848; 95% CI, 0.458–1.571) and CSS (p = 0.579; HR, 0.834; 95% CI, 0.440–1.583) were comparable between the total hysterectomy group and the radical hysterectomy group. While in the subset of T1-2a/N1/M0 patients (Fig. 1 G, H), the superiority of survival prognosis in patients underwent total hysterectomy to those underwent radical hysterectomy seemed to be further improved, but the difference in both OS (p = 0.061; HR, 0.475; 95% CI, 0.218–1.035) and CSS (p = 0.082; HR, 0.480; 95% CI, 0.210–1.098) between these two groups still didn’t reach statistical significance.
Due to the aggressiveness of NECC, patients may present with distant metastatic lesions while the primary lesion remains confined to the cervix and upper vagina (T1-2a/N1 or M1), which is considered as resectable. In the subset of patients with T1-2a/N1 or M1 disease (Fig. 1 I, J, the OS (p = 0.373; HR, 0.734; 95% CI, 0.371–1.450) and CSS (p = 0.491; HR, 0.775; 95% CI, 0.376–1.599) were still comparable between the total hysterectomy group and the radical hysterectomy group.
A multivariate Cox regression was conducted to assess the impact of potential prognostic factors, including age, lymph node status, FIGO stage, main surgery type, radiotherapy, and chemotherapy. The analysis revealed that age older than 45, lymph node metastasis and advanced stage were identified as risk factors for both OS and CSS (Supplementary Table 1).
The effects of adjuvant treatments
Adjuvant therapy was given to 85.3% of patients in this study. Among them, 127 patients received both adjuvant chemotherapy and radiotherapy, 110 patients received adjuvant chemotherapy alone and 7 patients received adjuvant radiotherapy alone. The addition of adjuvant radiotherapy with or without chemotherapy (Fig. 2 A) yielded significantly better OS (p = 0.034; HR, 0.598; 95% CI, 0.372–0.963) in the total hysterectomy group compared with the radical hysterectomy group. Similar result was found in patients receiving both adjuvant radiotherapy and chemotherapy (Fig. 2 B). However, there was no statistically significant difference in OS between the total hysterectomy and radical hysterectomy groups among patients who received adjuvant chemotherapy alone (Fig. 2 C) or adjuvant chemotherapy with or without radiotherapy (Fig. 2 D). The OS in patients who received neither adjuvant radiotherapy nor chemotherapy (Fig. 2 E) was also comparable between the two groups.
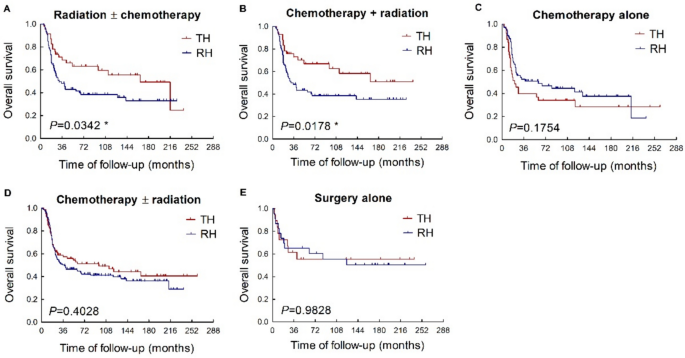
Comparison of total hysterectomy and radical hysterectomy in NECC patients receiving different adjuvant therapies. TH : total hysterectomy. RH : radical hysterectomy
Similar results were also observed in the subgroup of patients with FIGO stage I-IIA NECC. When adjuvant radiotherapy with or without chemotherapy was administered, the patients undergoing total hysterectomy exhibited significantly improved CSS compared to those undergoing radical surgery (Supplementary Fig. 1C; p = 0.047; HR, 0.552; 95% CI, 0.307–0.993). While in patients who received adjuvant chemotherapy alone or no adjuvant treatment, CSS remained comparable between the total and radical hysterectomy groups (Supplementary Fig. 1A, D).
Furthermore, our study showed that patients in the radical hysterectomy group were less likely to benefit from adjuvant treatments. In the total hysterectomy group (Fig. 3 A), the CSS in patients with FIGO stage I-IIA NECC was comparable between those who received adjuvant radiotherapy and those who didn’t receive any form of adjuvant treatment. While in the radical hysterectomy group (Fig. 3 B), the CSS in patients with FIGO stage I-IIA NECC was deteriorated when adjuvant radiotherapy and chemotherapy was administered, although statistical significance was not reached.
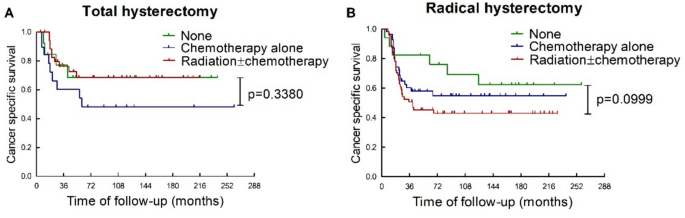
Influence of adjuvant therapies on the efficacy of total hysterectomy and radical hysterectomy in patients with FIGO stage I-IIA NECC
In this study, we found that total hysterectomy didn’t compromise the OS or CSS in patients with NECC compared with radical hysterectomy. Furthermore, our study showed that when adjuvant radiotherapy was administered, total hysterectomy could even provide a better survival prognosis than radical hysterectomy in NECC patients.
In the NeCTuR study that evaluated 100 patients with early-stage NECC who underwent upfront radical surgery, 95% of patients met the criteria for adjuvant therapy based on pathological risk factors (Salvo et al. 2021 ). Parametrial involvement was found in 10% of patients in the NeCTuR study, while all of these patients had other coexisting indications for adjuvant therapy (Salvo et al. 2021 ). Given the poor prognosis of NECC, most clinical guidelines recommend the combination of surgery, chemotherapy and radiotherapy as a multimodal management, regardless of pathological risk factors (Salvo et al. 2019 ; National Comprehensive Cancer Network 2022 ). Therefore, the question has been raised whether radical surgery can be replaced by simple hysterectomy in the multimodal treatment of NECC to minimize postoperative morbidity and improve quality of life.
The finding in our study demonstrated that the efficacy of total hysterectomy might not be inferior to radical hysterectomy in NECC. It could be explained by the fact that early-stage patients might already have distant micro-metastasis, due to the aggressive nature of NECC. In our study, 21% of the patients presented with positive lymph nodes and/or distant metastasis while their cervical lesions were still in the early stages. As shown in the ABRAX trial, completion of radical hysterectomy didn’t improve the survival compared with definitive chemoradiation in cervical cancer patients with lymph node metastasis, regardless of histological type (Cibula et al. 2021 ). Removal of the primary cervical lesion and the potential regional metastatic lesion by radical hysterectomy may not be efficient enough if there has been distant micro-metastasis.
Besides, the recurrence pattern may also provide an explanation for why patients with NECC benefit less from radical hysterectomy. Previous studies have shown that 60–70% of NECC patients experience a recurrence outside the pelvis, with the lung and liver being the most common sites of recurrence (Stecklein et al. 2016 ; Ishikawa et al. 2018 ; Salvo et al. 2021 ; Pan et al. 2022 ). Radical hysterectomy is mainly aimed at preventing pelvic recurrence. Therefore, extensive resection of the local lesion may not be the primary prognostic factor for recurrence of NECC. Moreover, theoretically, there’s a greater chance that cancer cells will disseminate from the primary cervical lesion during a radical surgery, due to the longer duration of operation and the larger extent of resection (Suhail et al. 2019 ). Nevertheless, it remains unclear whether radical hysterectomy is associated with an increased risk of distant recurrence in NECC in our study, since data on the pattern of recurrence is not available from the SEER database.
Adjuvant radiotherapy is used as a local treatment to prevent pelvic recurrence and control positive regional lymph nodes in common cervical cancer patients with postoperative pathological high risk factors, including lymph node involvement, parametrium metastasis and positive surgical margins (National Comprehensive Cancer Network 2022 ). However, the role of adjuvant radiotherapy in NECC is controversial. A meta-analysis by Kim et al. showed that patients with early-stage NECC who received radical surgery with postoperative radiotherapy had lower pelvic recurrence rate than those who didn’t receive radiotherapy (12.5% vs 24.3%, p = 0.09), but the OS rate was not improved by postoperative radiotherapy (34.8% vs 35.2%, p = 0.66), because of the high incidence of distant recurrence in both groups (Kim et al. 2023 ). Kim’s study also found that the rate of distant recurrence was significantly higher in patients who received postoperative radiotherapy (33.3% vs 9.2%, p = 0.007), although the mechanism remains unclear (Kim et al. 2023 ). On the other hand, a SEER-based study by Dong et al. found that surgery with adjuvant radiotherapy was associated with significantly improved OS in NECC patients with metastasis comparing with surgery alone (median OS: 80.9 months vs 44.6 months, p = 0.004) (Dong et al. 2021 ). This finding indicated that NECC patients with distant metastasis may still potentially benefit from intensive local treatments containing adjuvant radiotherapy. In our study, when adjuvant radiotherapy was given, patients who underwent total hysterectomy had better survival than those who had radical hysterectomy. This intriguing finding may also be associated with the ineffectiveness of adjuvant radiation in preventing distant recurrence.
Chemotherapy is a common systematic treatment for NECC. The most widely used regimen for NECC is platinum combined with etoposide (Sundstrøm et al. 2002 ). The study of Seino et al. demonstrated that in patients with stage IB2 and T1N1M0 NECC, those who received surgery followed by chemotherapy had superior OS compared with those who received surgery followed by radiotherapy (Seino et al. 2023 ). Ishikawa’s study also showed that adjuvant chemotherapy after surgery could reduce the risk of recurrence in patients with stage I-II NECC (Ishikawa et al. 2018 ). In addition, previous studies have highlighted the importance of the number of adjuvant chemotherapy cycles as a prognostic factor, with patients receiving four or more cycles of adjuvant chemotherapy having significantly improved survival prognosis compared to those receiving fewer cycles (Ishikawa et al. 2019 ; Wang et al. 2022 ). In our study, over 80% of NECC patients had received chemotherapy, but adjuvant chemotherapy was not associated with improved OS, irrespective of whether they underwent total hysterectomy or radical hysterectomy. Nonetheless, we’re not able to further investigate the effect of chemotherapy on NECC in this study, because the detailed information on chemotherapy, such as regimens and number of cycles, was not available in the SEER database.
NECC is known to have a poor prognosis. Our study showed that age older than 45, lymph node metastasis and advanced stage were associated with worse survival prognosis in NECC patients. Several recent studies have also sought to identify potential prognostic factors and to construct prognostic models to improve the prediction of the oncological outcomes for NECC patients (Chen et al. 2023 ; Yu et al. 2024 ). Yu’s study identified larger tumor size, metastasis, advanced tumor stages, and chemotherapy as independent prognostic factors of OS (Yu et al. 2024 ). Yu et al. subsequently constructed a prognostic nomogram based on these four factors, demonstrating a C-index of 0.724, an area under the receiver operating characteristic curve (AUC) of 0.769 and 0.766 for the prediction of 3-year and 5-year OS, respectively(Yu et al. 2024 ). The construction of prognostic prediction models has the potential to facilitate the identification of NECC patients with high risk and the development of individualized treatment strategy.
To the best of our knowledge, our study is the first to compare the clinical outcomes of total hysterectomy and radical hysterectomy in patients with NECC. Our study has enrolled 286 NECC cases from the SEER database, the sample size of which is larger than most previous clinical studies on NECC. The results of our study indicate that total hysterectomy may be a potential surgical option in the multimodal management of NECC. However, due to the methodology and retrospective nature of this study, it has several limitations. We’re not able to compare the effect of total hysterectomy and radical hysterectomy on progression-free survival in this study, since the data of recurrence are not available in the database. Similarly, the detailed information of chemotherapy and radiotherapy, such as chemotherapy regimen, radiation therapy technique and dose, are not recorded in the database either. Non-standardized adjuvant treatment would also result in bias in this study. Therefore, future multicenter studies are needed to further evaluate the role of total hysterectomy in NECC.
Our study showed that the survival prognosis in patients with NECC receiving total hysterectomy was not inferior to those undergoing radical hysterectomy, particularly when combined with adjuvant radiotherapy. Total hysterectomy may be considered as a surgical alternative in the multimodal management of NECC.
Data availability
The research data for this study was available in the SEER database: https://seer.cancer.gov/ .
Castelnau-Marchand P, Pautier P, Genestie C et al (2018) Multimodal management of locally advanced neuroendocrine cervical carcinoma: a single institution experience. Int J Gynecol Cancer 28:1013–1019. https://doi.org/10.1097/IGC.0000000000001242
Article PubMed Google Scholar
Chan JK, Loizzi V, Burger RA et al (2003) Prognostic factors in neuroendocrine small cell cervical carcinoma. Cancer 97:568–574. https://doi.org/10.1002/cncr.11086
Chen X, Shi W, Wang C, Zhu H (2023) Personalized prognostic prediction tool for high-grade neuroendocrine cervical cancer: a SEER database analysis and single-center validation. J Cancer Res Clin Oncol 149:17395–17404. https://doi.org/10.1007/s00432-023-05414-6
Article PubMed PubMed Central Google Scholar
Cibula D, Dostalek L, Hillemanns P et al (2021) Completion of radical hysterectomy does not improve survival of patients with cervical cancer and intraoperatively detected lymph node involvement: ABRAX international retrospective cohort study. Eur J Cancer 143:88–100. https://doi.org/10.1016/j.ejca.2020.10.037
Article CAS PubMed Google Scholar
Cohen JG, Kapp DS, Shin JY et al (2010) Small cell carcinoma of the cervix: treatment and survival outcomes of 188 patients. Am J Obstet Gynecol 203:347.e1-347.e6. https://doi.org/10.1016/j.ajog.2010.04.019
Cohen PA, Jhingran A, Oaknin A, Denny L (2019) Cervical cancer. Lancet 393:169–182. https://doi.org/10.1016/S0140-6736(18)32470-X
Dong M, Gu X, Ma T et al (2021) The role of radiotherapy in neuroendocrine cervical cancer: SEER-based study. Sci Prog 104:003685042110093. https://doi.org/10.1177/00368504211009336
Article CAS Google Scholar
Gardner GJ, Reidy-Lagunes D, Gehrig PA (2011) Neuroendocrine tumors of the gynecologic tract: a Society of gynecologic oncology (SGO) clinical document. Gynecol Oncol 122:190–198. https://doi.org/10.1016/j.ygyno.2011.04.011
Ishikawa M, Kasamatsu T, Tsuda H et al (2018) Prognostic factors and optimal therapy for stages I–II neuroendocrine carcinomas of the uterine cervix: a multi-center retrospective study. Gynecol Oncol 148:139–146. https://doi.org/10.1016/j.ygyno.2017.10.027
Ishikawa M, Kasamatsu T, Tsuda H et al (2019) A multi-center retrospective study of neuroendocrine tumors of the uterine cervix: prognosis according to the new 2018 staging system, comparing outcomes for different chemotherapeutic regimens and histopathological subtypes. Gynecol Oncol 155:444–451. https://doi.org/10.1016/j.ygyno.2019.09.018
Kim H, Jeong HJ, Kim BW, Hwang JH (2021) The incidence of urologic complications requiring urologic procedure in radical hysterectomy and difference between abdominal radical hysterectomy and laparoscopic radical hysterectomy. J Gynecol Oncol. https://doi.org/10.3802/jgo.2021.32.e84
Kim C, Salvo G, Ishikawa M et al (2023) The role of postoperative radiation after radical hysterectomy for women with early-stage neuroendocrine carcinoma of the cervix: a meta-analysis. Gynecol Oncol 170:328–332. https://doi.org/10.1016/j.ygyno.2023.01.036
National Comprehensive Cancer Network (2022) NCCN clinical practice guidelines in oncology (NCCN Guidelines ® ) for cervical cancer. Version 1:2023
Google Scholar
Obermair A, Asher R, Pareja R et al (2020) Incidence of adverse events in minimally invasive vs open radical hysterectomy in early cervical cancer: results of a randomized controlled trial. Am J Obstet Gynecol 222:249.e1-249.e10. https://doi.org/10.1016/j.ajog.2019.09.036
Pan B, Wan T, Jiang Y et al (2022) Impact of the initial site of metastases on post-recurrence survival for neuroendocrine cervical cancer. BMC Cancer 22:655. https://doi.org/10.1186/s12885-022-09737-4
Plante M, Kwon JS, Ferguson S et al (2023) An international randomized phase III trial comparing radical hysterectomy and pelvic node dissection (RH) vs simple hysterectomy and pelvic node dissection (SH) in patients with low-risk early-stage cervical cancer (LRESCC): a gynecologic cancer intergro. J Clin Oncol 41:LBA5511–LBA5511. https://doi.org/10.1200/JCO.2023.41.17_suppl.LBA5511
Article Google Scholar
Salvo G, Gonzalez Martin A, Gonzales NR, Frumovitz M (2019) Updates and management algorithm for neuroendocrine tumors of the uterine cervix. Int J Gynecol Cancer 29:986–995. https://doi.org/10.1136/ijgc-2019-000504
Salvo G, Ramalingam P, Flores Legarreta A et al (2021) Role of radical hysterectomy in patients with early-stage high-grade neuroendocrine cervical carcinoma: a NeCTuR study. Int J Gynecol Cancer 31:495–501. https://doi.org/10.1136/ijgc-2020-002213
Satoh T, Takei Y, Treilleux I et al (2014) Gynecologic cancer InterGroup (GCIG) consensus review for small cell carcinoma of the cervix. Int J Gynecol Cancer 24:S102–S108. https://doi.org/10.1097/IGC.0000000000000262
Seino M, Nagase S, Ohta T et al (2023) Impact of adjuvant chemotherapy on the overall survival of patients with resectable bulky small cell neuroendocrine cervical cancer: a JSGO-JSOG joint study. J Gynecol Oncol. https://doi.org/10.3802/jgo.2023.34.e4
Stecklein SR, Jhingran A, Burzawa J et al (2016) Patterns of recurrence and survival in neuroendocrine cervical cancer. Gynecol Oncol 143:552–557. https://doi.org/10.1016/j.ygyno.2016.09.011
Suhail Y, Cain MP, Vanaja K et al (2019) Systems biology of cancer metastasis. Cell Syst 9:109–127. https://doi.org/10.1016/j.cels.2019.07.003
Article CAS PubMed PubMed Central Google Scholar
Sundstrøm S, Bremnes RM, Kaasa S et al (2002) Cisplatin and etoposide regimen is superior to cyclophosphamide, epirubicin, and vincristine regimen in small-cell lung cancer: results from a randomized phase iii trial with 5 years’ follow-up. J Clin Oncol 20:4665–4672. https://doi.org/10.1200/JCO.2002.12.111
Tempfer CB, Tischoff I, Dogan A et al (2018) Neuroendocrine carcinoma of the cervix: a systematic review of the literature. BMC Cancer 18:530. https://doi.org/10.1186/s12885-018-4447-x
Wang R, Xiao Y, Ma L et al (2022) Exploring a better adjuvant treatment for surgically treated high-grade neuroendocrine carcinoma of the cervix. Gynecol Obstet Invest 87:398–405. https://doi.org/10.1159/000527661
Wright JD, Grigsby PW, Brooks R et al (2007) Utility of parametrectomy for early stage cervical cancer treated with radical hysterectomy. Cancer 110:1281–1286. https://doi.org/10.1002/cncr.22899
Yu C, Wu X, Zhang S et al (2024) Prognostic model for survival in patients with neuroendocrine carcinomas of the cervix: SEER database analysis and a single-center retrospective study. PLoS ONE 19:e0296446. https://doi.org/10.1371/journal.pone.0296446
Zhang X, Lv Z, Lou H (2019) The clinicopathological features and treatment modalities associated with survival of neuroendocrine cervical carcinoma in a Chinese population. BMC Cancer 19:22. https://doi.org/10.1186/s12885-018-5147-2
Download references
This study was supported by Guangzhou Municipal Science and Technology Bureau-Basic and Applied Basic Research Scheme (No. 2023A04J2220).
Author information
Authors and affiliations.
Department of Gynecology, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, Guangdong, China
Feitianzhi Zeng, Peng Guo, Meng Xia & Mian He
You can also search for this author in PubMed Google Scholar
Contributions
Study design and original manuscript preparation were performed by Feitianzhi Zeng. Data collection and analysis were performed by Peng Guo and Meng Xia. Supervision of the study and manuscript revision were performed by Mian He. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mian He .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethics approval
This study was exempt from ethics committee review, because all data are anonymous and publicly available.
Informed consent
Patient consent was not required due to the retrospective nature of this study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 187 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Zeng, F., Guo, P., Xia, M. et al. Total hysterectomy versus radical hysterectomy in neuroendocrine cervical cancer: a SEER-database analysis. J Cancer Res Clin Oncol 150 , 236 (2024). https://doi.org/10.1007/s00432-024-05773-8
Download citation
Received : 29 February 2024
Accepted : 30 April 2024
Published : 06 May 2024
DOI : https://doi.org/10.1007/s00432-024-05773-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Neuroendocrine cervical cancer
- Radical hysterectomy
- Total hysterectomy
- Find a journal
- Publish with us
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 30 January 2024
Cervical cancer kills 300,000 people a year — here’s how to speed up its elimination
- Lynette Denny 0 ,
- Ishu Kataria 1 ,
- Lisa Huang 2 &
- Kathleen M. Schmeler 3
Lynette Denny is a professor of special projects in the Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa.
You can also search for this author in PubMed Google Scholar
Ishu Kataria is a senior public-health researcher at the Center for Global Noncommunicable Diseases at RTI International, New Delhi, India.
Lisa Huang is director of the SUCCESS project at Expertise France, Abidjan, Côte d’Ivoire.
Kathleen M. Schmeler is a professor of gynaecological oncology and associate vice-president of the Global Oncology Program, MD Anderson Cancer Center, Houston, Texas.
You have full access to this article via your institution.
Cervical cancer can be prevented through vaccination and be cured if diagnosed early. Yet it still kills more than 300,000 people worldwide each year. Globally, only around 21% of women have had a vaccine against the human papillomaviruses (HPVs) that cause the disease.

Cervical cancer could be eliminated: here’s how
That number needs to rise to 90% by 2030, if cervical cancer is to be eliminated in the next century — as the World Health Organization (WHO) plans . Screening and treatment should also become routine worldwide, with 70% of people with a cervix checked by the age of 35 and again at 45, and 90% of those with signs of cervical cancer treated.
The world is not on track to meet any of these targets. A step change is urgently needed. The tools to vaccinate, screen and treat people are available, and effective. But a lack of funding, staffing and infrastructure — coupled with vaccine hesitancy — are major obstacles. Here, four specialists highlight pockets of good practice that can help to buck the trend.
LYNETTE DENNY: Target schools for vaccination programmes

Oncologist Lynette Denny has spent 29 years working in the field of cervical cancer prevention. Credit: Lynette Denny
Schools are the most effective place to roll out national HPV vaccination programmes. As long as enrolment levels in education are high, it’s easier to reach young people at school than in health-care settings. Political will is crucial, as is collaboration between a government’s health and education departments — and close communication with schools.
I’ve seen the benefits of school-based vaccination at first hand. In 2013, I helped to run a pilot project targeting girls in 31 primary schools in South Africa, in regions where poverty and lack of health-care provision are typically obstacles to high vaccination rates. Our pilot provided 97.8% of eligible girls with what was then the full course of three vaccines 1 . (In December 2022, the WHO advised that a single dose is sufficient to protect against cervical cancer.) Similar results were seen in other pilots, including in Bolivia, Uganda and Vietnam.
Scaling these up to country-wide programmes requires determination. But lessons can be learnt from countries around the world. Take Rwanda. In 2011, it became the first low-income country to implement a national HPV immunization programme for girls in the sixth grade (mostly aged 11–12 years). By 2018, more than one million girls had received a vaccination — 98% of the target population 2 .
Women’s health research lacks funding — these charts show how
To do this, Rwanda had to overcome a lack of resources — a common problem in low- and middle-income countries (LMICs) — and put cervical cancer at the apex of its health agenda. Merck provided free vaccines for three years and helped to prepare for the national roll-out. Later funding came from GAVI, the Vaccine Alliance — an international organization focused on providing vaccines for children in LMICs. Multiple government departments 3 collaborated to set up committees that would oversee all aspects of the programme. Together, these partners organized and delivered school-based vaccinations, rigorously monitored vaccination coverage and ran awareness campaigns 4 . Girls not enrolled in schools, or absent on vaccination days, were tracked by community health workers and vaccinated at health-care facilities instead.
As Rwanda shows, strong, trustworthy and reliable collaboration between all stakeholders is key. We’ve found the same ingredients to be essential in South Africa, where we invested more than six months in regular meetings between health-care workers, education providers, technology specialists and the government to ensure that the roll-out was well coordinated.
High-income countries, which typically have more resources and fewer barriers to introducing vaccination programmes, would do well to learn from Sweden. In 2012, the country rolled out a free, school-based HPV vaccination programme for girls as young as 10 — alongside a successful screening and treatment programme. Here again, planning and stakeholder cooperation was essential. By 2021, 90% of girls in the country had received one vaccine dose by age 15, and 84% had received two.
Going forward, governments around the world must place prevention of cervical cancer high on the health agenda. Health and education departments must cooperate, and must allocate funding to all aspects of HPV vaccination — from vaccine procurement to infrastructure, awareness campaigns to human resources. Without this focus, roll-out will fail.
ISHU KATARIA: Bust myths through communication campaigns

Ishu Kataria surveyed physicians in India to understand their hesitancy around the HPV vaccine. Credit: Ishu Kataria
People in India are generally not hesitant about vaccines, especially for children. Yet, the Indian government has not included the HPV vaccine in its national immunization programme — even though one person dies from cervical cancer every eight minutes here.
In 2019, I interviewed 32 physicians in Kolkata, to try and understand the hesitancy surrounding HPV vaccination 5 . The physicians’ foremost reason was that many parents associate HPV vaccination with promiscuity. Because HPV is transmitted through sexual intercourse, parents often assume that giving a young child the vaccine will be viewed in the community as a sign that they are sexually active.
Physicians were also unclear about the benefits of recommending the HPV vaccine before a child becomes sexually active, and they did not want to risk their reputation by making a recommendation that could be controversial. Similar concerns and misunderstandings are common elsewhere, including in Eastern Mediterranean countries 6 .

Cancer will cost the world $25 trillion over next 30 years
A campaign run by national health departments is needed to instil confidence in the vaccine among physicians. It should make clear that vaccination is most effective between the ages of 9 and 14, because that is when it produces the most robust immune response. The campaign should highlight that the vaccine is extremely safe. It should provide guidance on communicating the benefits to parents in a culturally sensitive way — as a vaccine to prevent cancer, rather than against a sexually transmitted infection.
Raising general awareness — among schoolteachers, parents, children and adolescents — is also crucial.
The campaign run by the health department for the northeastern state of Sikkim when it first rolled out the HPV vaccine in 2018 provides a blueprint for others to follow. Sikkim’s six-month-long campaign educated physicians, community leaders, government officials, the media and the public through workshops, written materials and television and radio broadcasts. It resulted in 97% HPV vaccine uptake among eligible girls 7 .
Indian states cannot afford to roll out the vaccine unless it is part of the national immunization programme (in which case the government covers the cost of the vaccine). The launch of an affordable, cost-effective, India-manufactured vaccine by the Serum Institute in September 2022 has put pressure on the Indian government to fund the HPV vaccine, with a decision expected after this year’s election. States should now lay the groundwork for roll-out, following Sikkim’s lead. Key first steps include communication with physicians and parents, along with logistical planning.
LISA HUANG: Integrate screening into health-care systems

Public-health expert Lisa Huang. Credit: Expertise France
There is no one-size-fits-all approach to rolling out cervical cancer screening programmes. For LMICs, the best strategies focus on maximizing efficiency — and thereby reducing costs — for resource-poor countries.
This can be achieved by integrating screening and treatment programmes into existing health-care systems and facilities. The SUCCESS project, of which I am a director, is trialling such an approach in Burkina Faso, Côte d’Ivoire, Guatemala and the Philippines.
Performing screens in existing health-care settings minimizes the need for extra medical workers, who are scarce in LMICs. Screening programmes can be run in primary health-care settings, gynaecology clinics, family-planning services and — importantly — HIV clinics. The last is essential because the 20 million women living with HIV are six times more likely than other women to develop cervical cancer.

African scientists call for research equity as a cancer crisis looms
Local contexts need to be considered. In many countries, staff members will need to be trained in screening, and supply chains and inventory management systems will need to be set up. Digital health-information systems are crucial, allowing patient information to be passed between departments and between health workers to aid follow-up.
In the SUCCESS project, we’ve seen the benefits of such digital solutions. In Burkina Faso and Côte d’Ivoire we’ve made use of the DHIS2 Tracker, an app available as part of DHIS2 — an open-source health-information management platform widely used in LMICs. Using a tablet, a health-care worker can input patient information into the tracker along with information about any follow-up needed, which the patient can be told of either by instant messaging or when visiting another health centre.
Although it is challenging to collect digital data in LMICs, I am confident that tracking screening will save lives. Governments should aim to implement tracking technologies as soon as possible. People often resist complex changes, so engagement with health-care workers is an essential first step in a move towards digitization, to gain support for the switch. Investment from local and international funders is key, and time must be taken to understand each country’s health-care ecosystem and ensure that new digital solutions are interoperable with those already in use.
KATHLEEN M. SCHMELER: Use international mentors to train doctors

Kathleen Schmeler helps to train medical graduates in Mozambique. Credit: Sarah Berger
LMICs face a shortage of medical providers. Just 4% of the global medical workforce is in Africa, for instance — yet the continent shoulders one-quarter of the global disease burden 8 . Most LMICs have no formal training programmes for cancer specialists, particularly surgeons. In these countries, more specialized nurses and physicians are urgently needed to diagnose and treat cervical cancer.
Global collaboration can help to meet the need for training, as demonstrated by two international projects in which I’ve been involved. Both focused on Mozambique, a country that has no organized screening programme and few trained medical providers. In Mozambique, 39 of every 100,000 women die from cervical cancer, compared with the global average of 7.2.
First, I co-lead a collaboration between the Mozambique Ministry of Health, the MD Anderson Cancer Center in Houston, Texas, and five institutes in Brazil. The collaboration — which was initiated in 2014 at the request of the First Lady of Mozambique — aims to build capacity in Mozambique by teaching the nation’s medical providers to treat ‘pre-cancerous’ cells. Specialists from Texas and Brazil travel to Mozambique three or four times a year to provide lectures, hands-on training and mentoring to trainee doctors and nurses. We train 30–40 participants each time. Ongoing support is provided through monthly video conferences.
Second, I co-chair a global gynaecological oncology fellowship run by the International Society of Gynecologic Cancer (see go.nature.com/4b6edzk ) for institutions in LMICs that lack formal training in cancer care. The fellowship site is paired with a partner institute in a high-income country. Fellows — recently, graduates in obstetrics and gynaecology — spend two years undertaking a comprehensive education and training programme, mainly in their home country, but with a few months at the mentor institution. Maputo Central Hospital in Mozambique was a pilot site when the programme first began in 2017. There are now fellowship sites in 22 countries.
Each of these projects initially required a handful of very motivated international mentors. But training and mentoring is now being performed, at least in part, by programme graduates living in Mozambique.
To scale up these efforts, institutes in high-income countries must coordinate with one another, and enhance collaborations with health ministries and training institutions in LMICs. Funding for our work has come from small grants, philanthropic, institution and foundation budgets, and often from the volunteers themselves. These types of donation can fund individual projects, but investment from governments, United Nations agencies and industry partners is needed to make the approach work on a global scale.
Nature 626 , 30-32 (2024)
doi: https://doi.org/10.1038/d41586-024-00241-2
Moodley, I., Tathiah, N., Mubaiwa, V. & Denny, L. S. Afr. Med. J. 103 , 318–321 (2013).
Article Google Scholar
Sayinzoga, F. et al. Vaccine 38 , 4001–4005 (2020).
Article PubMed Google Scholar
Binagwaho, A. et al. Bull. World Health Org. 90 , 623–628 (2012).
Kabakama, S. et al. BMC Public Health 16 , 834 (2016).
Kataria, I. et al. Vaccine X 12 , 100228 (2022).
Hakimi, S., Lami, F., Allahqoli, L., Alkatout, I. J. Turk. Ger. Gynecol. Assoc. 24 , 48–56 (2023).
Sankaranarayanan, R. et al. Lancet Oncol. 20 , e637–e644 (2019).
Boniol, M. et al. BMJ Glob. Health. 7 , e009316 (2022).
Download references
Reprints and permissions
Competing Interests
The authors declare no competing interests.
Related Articles

- Public health

Decoding the interplay between genetic and non-genetic drivers of metastasis
Review Article 15 MAY 24

Engineered CD47 protects T cells for enhanced antitumour immunity
Article 15 MAY 24

Mapping genotypes to chromatin accessibility profiles in single cells
Article 08 MAY 24

Neglecting sex and gender in research is a public-health risk
Comment 15 MAY 24
Interpersonal therapy can be an effective tool against the devastating effects of loneliness
Correspondence 14 MAY 24

Is the Internet bad for you? Huge study reveals surprise effect on well-being
News 12 MAY 24
Imprinting of serum neutralizing antibodies by Wuhan-1 mRNA vaccines

Vaccine-enhancing plant extract could be mass produced in yeast
News & Views 08 MAY 24

UTIs make life miserable — scientists are finding new ways to tackle them
News 02 MAY 24
PhD/master's Candidate
PhD/master's Candidate Graduate School of Frontier Science Initiative, Kanazawa University is seeking candidates for PhD and master's students i...
Kanazawa University
Senior Research Assistant in Human Immunology (wet lab)
Senior Research Scientist in Human Immunology, high-dimensional (40+) cytometry, ICS and automated robotic platforms.
Boston, Massachusetts (US)
Boston University Atomic Lab
Postdoctoral Fellow in Systems Immunology (dry lab)
Postdoc in systems immunology with expertise in AI and data-driven approaches for deciphering human immune responses to vaccines and diseases.
Global Talent Recruitment of Xinjiang University in 2024
Recruitment involves disciplines that can contact the person in charge by phone.
Wulumuqi city, Ürümqi, Xinjiang Province, China
Xinjiang University
Tenure-Track Assistant Professor, Associate Professor, and Professor
Westlake Center for Genome Editing seeks exceptional scholars in the many areas.
Westlake Center for Genome Editing, Westlake University
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
FDA Approves First Self-Test Collection Kit for HPV
By Dennis Thompson HealthDay Reporter

WEDNESDAY, May 15, 2024 (HealthDay News) -- The U.S. Food and Drug Administration has approved a kit that will allow women to collect their own vaginal sample for HPV screening, a move that could increase early detection in those at risk for cervical cancer .
Women will be able to swab themselves in privacy at a doctor’s office, clinic or pharmacy, and the sample will then be sent off for analysis.
More than half of U.S. women diagnosed with cervical cancer have never been screened or screened only infrequently for the virus, the kit’s maker Roche said in a news release announcing the approval on Wednesday.
“With vaccinations, innovative diagnostic tools and screening programs, achieving the WHO’s goal of eliminating cervical cancer by 2030 is within reach,” Roche Diagnostics CEO Matt Sause said. “Our HPV self-collection solution helps support this goal by reducing barriers and providing access to HPV screening by allowing people to privately collect their own sample for HPV testing.”
U.S. Cities With the Most Homelessness

Each year, about 11,500 U.S. women are diagnosed with cervical cancer and about 4,000 women die from it, according to the U.S. Centers for Disease Control and Prevention.
HPV is the known cause of more than 95% of cervical cancers, Roche added.
“Almost all cervical cancers are caused by persistent infection with certain types of HPV,” Dr. Karen Knudsen , CEO of the American Cancer Society (ACS), said in a statement. “Self-collection can expand access to screening and reduces barriers, which will give more people the opportunity to detect, treat and ultimately survive cancer.”
Most primary care doctors don’t test for HPV. Instead, women are most often screened by gynecologists during a pelvic exam, a procedure to which some don’t have access and others find too intrusive and embarrassing.
“Roche’s self-collection solution can help reduce these barriers by offering an alternative to clinician collection procedures, while also providing accurate and reliable results,” Roche said.
The HPV test itself is already covered by private insurance, Medicare and Medicaid, Roche told the Washington Post .
“This literally just opens up another option for a different demographic of people that might not feel comfortable, that might not have access [and] may not have time” to get tested otherwise, Irene Aninye , chief science officer for the Society for Women’s Health Research, told the Post .
The ACS recommends that cervical cancer screening begin at age 25, and that women ages 25 to 65 have an HPV test every five years.
Studies done for the past two decades have found that self-collection for HPV testing is feasible and acceptable, and that women can collect samples as well as their physicians, the ACS said.
“Self-collection was not FDA-approved at the time our current guideline was released, but we now expect a minor update to the guideline to note that primary HPV testing via clinician-collected sample or self-collection is acceptable,” said ACS Chief Scientific Officer Dr. William Dahut .
“We anticipate self-collection will play an increasingly prominent role in cervical cancer screening once regulatory and clinical prerequisites are in place and as supporting evidence continues to accumulate,” Dahut added.
The approval could also open the door for at-home collection of samples.
Teal Health received FDA breakthrough designation last week for an at-home cervical cancer screening device called the Teal Wand. Women would collect their own sample at home, then send it to a lab to be tested for HPV.
The designation grants Teal Health priority status from regulators when clinical trials wrap up and the data is submitted to the FDA.
“No more stirrups, no more speculum,” the Teal Health website promises. “The Teal Wand replaces the need for an in-office pap smear using stirrups, a speculum and a hard plastic brush or broom. With self-collect, you are in control.”
More information
The National Cancer institute has more on cervical cancer .
SOURCE: Roche, news release, May 15, 2024; American Cancer Society, statement, May 15, 2024; Washington Post
Copyright © 2024 HealthDay . All rights reserved.
Join the Conversation
Tags: sexually transmitted diseases , cancer
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Who Is Prime Minister Robert Fico?
Laura Mannweiler May 15, 2024

Biden and Trump Agree to Debate
Lauren Camera May 15, 2024

Biden Muddies Message on Israel
Aneeta Mathur-Ashton May 15, 2024

Consumers Get a Break From Inflation
Tim Smart May 15, 2024

Trump Team Gets Its Shot at Cohen
Lauren Camera May 14, 2024

New China Tariffs: What to Know
Cecelia Smith-Schoenwalder May 14, 2024


IMAGES
COMMENTS
Epidemiology for cervical cancer. Cervical cancer is one of the leading causes of cancer death among women ().Over the past 30 years, the increasing proportion of young women affected by cervical cancer has ranged from 10% to 40% ().According to the WHO and International Agency for Research on Cancer (IARC) estimates, the year 2008 saw 529,000 new cases of cervical cancer globally.
The burden of cervical cancer remains high in many parts of the world, and in most countries, the incidence and mortality of the disease remain much higher than the threshold set by the WHO initiative on cervical cancer elimination. We identified substantial geographical and socioeconomic inequalities in cervical cancer globally, with a clear gradient of increasing rates for countries with ...
Cervical cancer, the second most prevalent cancer affecting women, arises from abnormal cell growth in the cervix, a crucial anatomical structure within the uterus. The significance of early ...
Each year, more than half a million women are diagnosed with cervical cancer and the disease results in over 300 000 deaths worldwide. High-risk subtypes of the human papilloma virus (HPV) are the cause of the disease in most cases. The disease is largely preventable. Approximately 90% of cervical cancers occur in low-income and middle-income countries that lack organised screening and HPV ...
Globally, cervical cancer is the fourth most common female cancer after breast, colorectal, and lung cancer and accounts for 600 000 new cases and 340 000 deaths annually [ 1, 3, 4 ]. Importantly, approximately 83% of all new cervical cancer cases and 88% of all deaths occur in LMICs [ 3, 4 ]. Indeed, cervical cancer is the leading cause of ...
This article reviews recent evidence from the International Agency for Research on Cancer on the best methods of screening for cervical cancer, including by means of conventional cytology, visual i...
The Cancer Genome Atlas Research Network now reports the genomic and molecular characterization of 228 primary cervical cancers. ... Cervical cancer is one of the main causes of cancer-related ...
Cervical cancer articles from across Nature Portfolio. Cervical cancer is a disease in which the cells of the cervix become abnormal and start to grow uncontrollably. Approximately 90% are ...
Among Swedish girls and women 10 to 30 years old, quadrivalent HPV vaccination was associated with a substantially reduced risk of invasive cervical cancer at the population level. (Funded by the ...
Find research articles on cervical cancer, which may include news stories, clinical trials, blog posts, and descriptions of active studies. ... The rates of timely cervical cancer screening fell between 2005 and 2019, researchers found, and disparities existed among groups of women. The most common reason for not receiving timely screening was ...
Despite decreases in incidence in the twentieth century, cervical cancer continues to be a highly morbid disease in the United States. For those diagnosed with locally advanced disease, single-agent cisplatin-based chemotherapy concurrent with radiation remains the mainstay of treatment. For patients with metastatic, progressive, and recurrent disease, treatment typically consists of ...
Cervical cancer pathogenesis. Cervical cancer (CC) remains a public health problem and ranks fourth in cancer mortality in women worldwide ().The main etiologic factor for CC development is a persistent infection with high-risk (HR) human papillomavirus (HPV), responsible for almost 100% of all CC cases ().However, some studies report that between 5 and 8% of CC cases are HPV-negative ...
With the difference of one year- 1332 articles related to cervical cancer were published in 2015 -we may compare the overall data: From 1900 to 2014, 20,855 cervical cancer articles represent 89.2% of the global ovarian carcinoma research activity (n = 23,378).
Globally, 570 000 cases of Cervical Cancer and 311000 deaths from the disease occurred in 2018. Cervical Cancer is the fourth most common cancer in women, ranking after breast cancer (2.1 million cases), colorectal cancer (0.8 million) and lung cancer (0.7 million). 1 It is the 2nd most leading cause of female cancer among women aged 15-44 years in India.
The Cancer Genome Atlas Research Network recently published the most comprehensive, multi-omic molecular characterization of cervical cancers performed to date.
For cervical cancer, effective primary and secondary prevention approaches, vaccination and screening respectively, have been successful in reducing incidence and mortality [].Accordingly, for the first time in history, eliminating a specific cancer from the globe is an attainable objective [].Improvements in cervical cancer screening programs, particularly switching to primary human ...
Globally, cervical cancer is the fourth most common cancer in women, with around 660 000 new cases in 2022. In the same year, about 94% of the 350 000 deaths caused by cervical cancer occurred in low- and middle-income countries. The highest rates of cervical cancer incidence and mortality are in sub-Saharan Africa (SSA), Central America and ...
Dear editor. We have read a research article entitled Survival Status and Predictors Among Women with Advanced Stage of Cervical Cancer" by Teshome, Citation 1 recently published in International Journal of Women's Health. We congratulate the authors on this successful article and make some contributions.
In this study, we aimed to predict prognosis and assess efficacy of anti-tumor therapy in cervical cancer patients based on differential genes associated with mitochondrial metabolism.Methods: Transcriptomic data and clinical profiles of cervical cancer patients were retrieved from the TCGA and GEO databases.
HPV is the most common cause of cervical cancer. It is a frequent viral infection transmitted sexually through skin-to-skin contact. To help protect from cancer in the future, an HPV vaccine is available for males and females starting at ages 9 to 11. The vaccine is approved by the Food and Drug Administration (FDA) for people ages 9 to 45.
Purpose We conducted this study to evaluate the efficacy of total hysterectomy versus radical hysterectomy in the treatment of neuroendocrine cervical cancer (NECC). Methods Eligible NECC patients were identified from the Surveillance, Epidemiology and End Results (SEER) database. Demographic characteristics, clinical treatment and survival of the patients were collected. The overall survival ...
Kathleen M. Schmeler. Cervical cancer can be prevented through vaccination and be cured if diagnosed early. Yet it still kills more than 300,000 people worldwide each year. Globally, only around ...
"Almost all cervical cancers are caused by persistent infection with certain types of HPV," Dr. Karen Knudsen, CEO of the American Cancer Society (ACS), said in a statement. "Self-collection ...
New research centers on the use of engineered autologous T cells to reinforce the immune system and allow it to directly target ovarian cancer cells. ... "This is a novel type of immunotherapy that has shown some promise, and in cervical cancer adoptive immunotherapy has earned breakthrough designation by the FDA," says Peter Rose, MD, a ...