Ultimate Guide to Nurse Charting, Documentation, and Notes


Table of Contents
“Clear, accurate, and accessible documentation is an essential element of safe, quality, evidence-based nursing practice.”
Thus begins the American Nurses Association’s (ANA’s) Principles for Nursing Documentation . Discover the six principles outlined by the ANA, types of nursing notes, and tips for effective charting in this ultimate guide to nurse documentation.
What Is Medical Charting?

Also called a medical record, health record, or patient chart, a medical chart refers to documentation that includes a patient’s medical history and clinical data. This record or chart encompasses treatment plans, surgeries, medications, vital signs, diagnoses, and other information relevant to the patient’s healthcare.
Many healthcare professionals, such as physicians, radiological technicians, laboratory technicians, and, of course, nurses, may be involved in creating and managing medical records. Likewise, nurse charts or nursing record systems refer to the documentation of care that nurses or other healthcare professionals plan and provide to individual patients. These records constitute all the available information about nursing care after treatment has been provided. How healthcare providers document this information has varied over time and may also vary from one setting to another.
Importance of Nurse Charting
Quality nursing care is dependent on clear and accurate documentation. Nurses must obtain and use this information to provide and coordinate care with other healthcare team members. Furthermore, this record allows care to continue uninterrupted when nurses change shifts and can guide future care. For example, if a patient returns to a hospital months after initial treatment, documentation of the patient’s symptoms and treatments can inform current diagnoses and care plans.
Nurse documentation has the following uses:
- Communicating with other members of the healthcare team: Through electronic health records (EHRs) , members of the healthcare team can stay informed of assessments, clinical problems, medication records, patient responses and outcomes, and other essential information, all in real-time.
- Communicating with other professionals: Nurses must also document care for several other purposes, including compliance , credentialing, legal, research, reimbursement, regulation and legislation, and quality process and performance improvement.
Even if nurses do their best to provide quality patient care, malpractice lawsuits are always possible. Therefore, not only is documentation an essential aspect of providing quality care, but it’s also a protection for clinicians and facilities. Through proper documentation, nurses can demonstrate compliance with federal, state, third-party payer, and other regulations.
6 Principles of Nursing Documentation
According to ANA policy documents, state nurse practice acts, government regulations, and organizational policies and procedures—documentation is essential to nursing practice. Therefore, nurses must know how to document correctly, and hospitals and other healthcare facilities must provide the necessary resources for nurses to be able to chart safely and effectively. According to the American Nurses Association, the following are six fundamentals of medical record documentation:
1. Documentation Characteristics
Regardless of the method used to record nursing care, nurse charts must have the following characteristics:
- Accessible and retrievable
- Accurate, relevant, and consistent
- Clear, concise, and complete
- Legible/readable
- Timely, contemporaneous, and sequential
- Reflective of the nursing process
2. Education and Training
Hospitals and other facilities must provide nurses with sufficient training in the technical elements of documentation. Nurses must be competent in using computers and their supporting hardware and proficient in using charting software systems.
3. Policies and Procedures
Nurses must be familiar with organizational policies and procedures related to documentation and follow these as part of their nursing practice.
4. Protection Systems
In accordance with industry standards, governmental mandates, accrediting agencies, and organizational policies and procedures, documentation systems must guarantee the following protections:
- Security of data
- Protection of patient identification
- Confidentiality of patient, clinician, and organizational information
5. Documentation Entries
All documentation, including entries into organization documents or health records, must meet the following requirements:
- Accurate, valid, and complete
- Authenticated (the authors identify themselves and guarantee that the information is truthful and that nothing has been added or inserted)
- Dated and time-stamped by the persons who create the entries
- Legible/readable
- Using standardized terminology
6. Standardized Terminologies
Documentation should utilize standardized terminologies, including acronyms and symbols, to describe the planning, delivery, and evaluation of the patient’s nursing care.
What Types of Nursing Documentation Are There?
The following are a few examples of methods for charting nursing notes:
Narrative Nursing Notes
As the name indicates, this type of documentation narrates the nurses’ actions and observations. This note-taking method is straightforward and easily understood by others. However, nurses’ notes may be unnecessarily long and repetitive, and descriptions may be subjective. Many nurse charting systems include a section for “additional nursing notes,” but it is often optional and used only when a nurse’s findings don’t fit into other parts of the charting system.
SOAP Charting in Nursing
The acronym SOAP stands for “subjective,” “objective,” “assessment,” and “plan.” Some nurses prefer the acronym SOAP(IER) to include “intervention,” “evaluation,” and “revision.” Each word is a reminder of a step in the charting process.
- Subjective: This part includes the patient’s medical history, encompassing any information provided by the patient or family members.
- Objective: This includes the vital signs, laboratory results, and any other data obtained during the patient’s treatment at the healthcare facility.
- Assessment: This step refers to evaluating the previously obtained subjective and objective data to reach a diagnosis.
- Plan: After obtaining a diagnosis, the healthcare team must create a care plan, including treatments, instructions for the patient, follow-up appointments, etc.
- Interventions: Nurses must document everything they do for patients, including administering medications, providing education and instructions, etc.
- Evaluation: This step is an assessment of the results of interventions based on subjective and objective data. For example, is the patient reporting a decrease in pain?
- Revision: This section indicates whether any changes in the care plan are necessary.
Since this type of documentation is comprehensive, it is also time-consuming, which explains why its use is becoming less prevalent.

Charting by Exception
The main advantage of this charting system is that nursing notes are shorter and less time-consuming since nurses only need to document what is outside the norm. However, this method requires nurses to know what is typical for particular patients. Furthermore, with this system, it is impossible to determine whether clinicians performed specific procedures, and it may be more challenging to evaluate the evolution of the patient’s condition. Although the specifics of this type of documentation vary, many settings use checklists and flow sheets to document patient information. Therefore, documentation simply requires nurses to check a few boxes or sign their initials.
Dos and Don’ts of Nursing Documentation
Of course, you want to document accurately and clearly and contribute to providing the best possible patient care. However, despite your best intentions, mistakes are possible. Here are a few tips to help you avoid errors or omissions in your notes.
6 Dos of Nurse Charting
Follow these tips to ensure complete and accurate documentation:
- Chart in the right place: This may seem obvious, but you may take notes in the wrong patient’s health record if you don’t double-check the spelling of names and birth dates.
- Be objective: Include your interventions, observations, and information provided by the patients but not opinions or any inappropriate comments about patients, family members, or other members of the care team.
- Include test results and consultation reports: All information relevant to patient care must be available to the healthcare team.
- Record patient communication: Nurses should document any education or instructions provided to patients as well as patient complaints, questions, and other concerns, including the steps taken to address patient concerns.
- Record instances of non-adherence: In addition to documenting interventions that do occur , nurses should report what doesn’t occur , including missed appointments, refusal to provide information, and rejection of treatment recommendations.
- Protect your patients’ healthcare information: Follow your organization’s information security practices to ensure you do not lose patient information and unauthorized individuals do not access it.
4 Don’ts of Nurse Charting
Make sure you don’t fall into the following common charting mistakes:
- Don’t delay charting: Do your best to record your interventions or observations immediately. You could leave out important information if you wait until the end of your shift.
- Don’t routinely copy-paste: It is easy to copy-paste the wrong information. Therefore, it is ideal to document manually or double-check the copy-pasted information.
- Don’t attempt to alter the patient record: If you make a mistake, you must correct it, but you cannot modify your original entry. Mark any corrections or modifications as late entries.
- Don’t forget delegated tasks: Even if you delegate a task, you must verify and document whether those under your direction and supervision completed that task.
Is There an End to Charting in Sight?
There is no way around it: Charting is an essential part of the nursing practice, and it’s not going anywhere. You might change the way you take notes. Handwritten notes may be a thing of the past, and your facility may have moved on to digital checklists. Regardless, as a nurse, you must document—the quality of the care you provide your patients depends on it.
The quality of your nursing care also depends on your assessment skills. Hone your nursing skills by reviewing what a head-to-toe nursing assessment involves.
Additional Sources:
- National Library of Medicine: Nursing record systems: effects on nursing practice and healthcare outcomes
- National Library of Medicine: Keeping good nursing records: a guide
- BMC Nursing: Nursing documentation and its relationship with perceived nursing workload: a mixed-methods study among community nurses

Laila is a contributing copywriter and editor at Nursa who specializes in writing compelling long-form content about nursing finances, per diem job locations, areas of specialization, guides, and resources that help nurses navigate their career paths.
Sign Up with Nursa and Request PRN Jobs near You
Related blog posts.
.webp)
Choose Multiple PRN Shifts on Your Schedule
Nursa isn't just about finding a job ; it's about crafting your ideal work schedule by selecting shifts. Once you create a Nursa profile, you will experience the convenience of scheduling shifts in real-time.
See More Shifts and Apply Now
Explore and find where you would like to work
Pick Up a Job Today
Find per diem PRN job opportunities in your area . High paying CNA, LPN and RN and many more are now available now.
Post Your Jobs Today
Facilities who use Nursa fill 3 times as many open per diem shifts , on average, compared to trying to fill the shifts themselves.
Download the App Now
Lecturio Nursing
Cheat Sheets
Nursing Knowledge
Nursing Charting & Medical Records
Table of contents, what is charting in nursing .
Charting in nursing is the systematic documentation of a patient’s medical history, care provided, observations, interventions, responses, and any other important information around their care. It forms an integral part of the medical record.
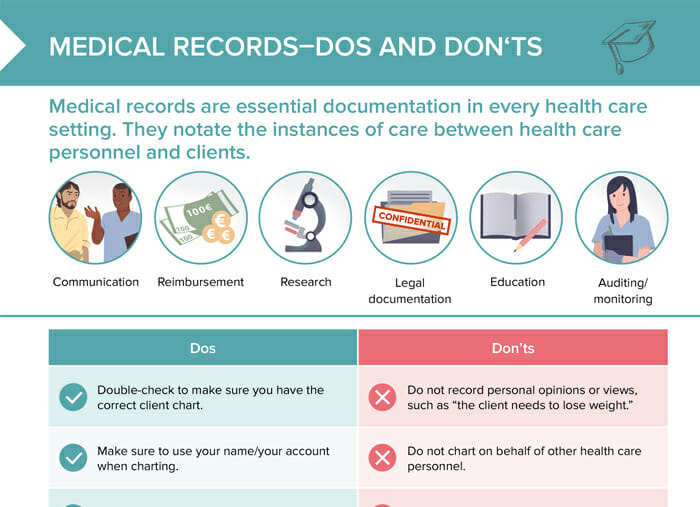
What are medical records?
Medical records, often referred to as health records or medical charts, are systematic documentation of a patient’s medical history and care over time.
Many medical records have transitioned from paper-based systems to Electronic Health Records (EHRs), which offer greater accessibility, interoperability, and efficiency.
Medical record template
How medical records are set up varies between facilities. This is an example of what the content outline of a medical record could look like:
Table: Example of a medical record template
| Patient data | Name, age, gender, address, contacts |
| Responsible primary care provider | Contact information |
| Insurance information | Provider and policy |
| Known allergies | Medications, food, environmental |
| Medication plan | With dosage, frequency and indication |
| Medical/surgical and family history | Include relation and dates of diagnosis |
| Social history | Smoking, alcohol, other drugs, occupation and relationships |
| Visit documentation | Date, reason, findings, treatment |
| Lab and imaging results |
How long do medical records need to be kept?
The duration for which medical records need to be saved depends on local regulations, patient age, type of record, and other factors. In general, adult medical records in the United States need to be retained for at least 6–10 years after the last interaction with the patient. For minors, records need to be kept until the patient reaches the age of majority plus the required retention time frame for adults.
Nursing charting systems
Nursing charting systems are methods that nurses can apply to make their patient care documentation more structured and consistent. Examples are:
- Narrative charting: comprehensive and chronological account in full sentences that is good for giving context, but quite time-consuming
- POMR: problem-oriented medical record, organizes all information sorted by patient problems
- SOAPIE charting: follows the template Subjective – Objective – Assessment – Plan – Evaluation, moving from the patient’s subjective feelings to test and exam results, to the nurse’s clinical judgment and the interventions + how the patient responded.
- Focus charting: following patient issues in three steps, data – action – response
- Charting by exception: charting only deviations from the standard or norm
- Checklists: pre-written sets of interventions for specific scenarios that eliminate the need for everything to be written from scratch; the relevant items are only checked off
Nursing charting example
An example of focus charting could look as follows:
Focus: shortness of breath
Date:
Time:
Data: Patient reports difficulty in breathing since morning. Oxygen saturation measured at 88% on room air.
Action: Positioned patient in a high Fowler’s. Administered 2L oxygen through a nasal cannula and provided a nebulizer treatment.
Response: After intervention, the patient’s breathing became less labored to respirations at 18/min, with oxygen saturation increasing to 94%. Patient verbalized relief, stating, “I can breathe easier now.”
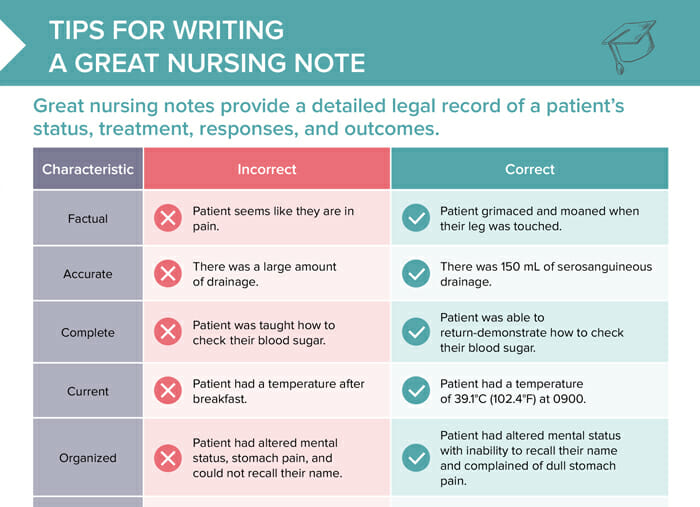
Tips for medical records
Tips for writing professional medical records.
- Double-check to make sure you have the correct client chart.
- Make sure to use your name/your account when charting.
- Keep your password safe and secure.
- Chart in real time or as soon as possible after taking care of a client.
- Chart facts, such as “the client ambulated 100 steps today.”
- Chart interactions with other healthcare personnel, such as calls to health care providers or orders from the lab.
What to avoid in medical records
- Do not record personal opinions or views, such as “the client needs to lose weight.”
- Do not chart on behalf of other health care personnel.
- Do not share your login information.
- Do not chart ahead of time, as situations can change.
- Do not alter prior charts.
- Do not copy and paste information from other sections in someone’s chart.
- Do not chart interactions that are not relevant to your client care, such as “awaiting voicemail” or “orders pending.”
RELATED TOPIC:
Nursing Notes Template
FREE CHEAT SHEET
Free Download
Nursing Cheat Sheet
Master the topic with a unique study combination of a concise summary paired with video lectures.
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
User Reviews
Get premium to test your knowledge.
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
#1 Duquesne University Graduate School of Nursing is Ranked #1 for Veterans by Militaryfriendly.com for 7 years running

- Adult-Gerontology Acute Care Nurse Practitioner
- Executive Nurse Leadership and Health Care Management
- Family Nurse Practitioner
- Forensic Nursing
- Nursing Education and Faculty Role
- Psychiatric-Mental Health Nurse Practitioner
- Clinical Leadership
- Admissions & Aid
- About Duquesne
- Why Duquesne Online?

Tips for Patient Charting
April 6, 2020
View all blog posts under Articles | View all blog posts under Master of Science in Nursing

Accurate and concise patient charting is an important part of a nurse’s job. Through charting, nurses communicate vital information to the entire healthcare team. A patient chart is also a legal document that describes all aspects of a patient’s care, including medications administered, services provided and procedures performed.
Because the charting process is so essential, nurses should take the time to accurately and concisely document patient care before moving on to the next patient.
Many healthcare providers understand how time-consuming patient charting can be, and so many are moving toward implementing and refining Electronic Health Records (EHRs) to help streamline the process. Among the proponents is HCA Healthcare, a network of 185 hospitals and 119 freestanding surgery centers in the U.S. and the U.K.
As Sarah Michel, MBA, BSN, RN, NE-BC, director of nursing Innovation at HCA, told MEDITECH, “we recently implemented a redesigned EHR system across 170 facilities in 20 states, following an evidence-based design that aligns minimum documentation requirements with ideal workflow. As a result, we’ve saved up to two hours spent on documentation per nurse, per shift.”
Even nurses who work for providers with less advanced technology can take a page from HCA’s approach by using standardized terminology in their charting, and by using evidence-based nursing care plans.
These nurse charting tips can help save time and improve patient outcomes:
Use Evidence-Based Care Plans
The use of care plans encourages good documentation practices and provide a continuity of care across healthcare teams. As RN Central, an information and education portal for prospective nurses, explains, care plans specifically, “outline which observations to make, what nursing actions to carry out, and what instructions the client or family members require.”
Document Patient Care Using Standard Medical Terminology
The use of standard terminology helps healthcare teams communicate accurately and appropriately with one another. Using standardized terminology in a patient’s chart also reduces the risk of medical error.
“Nurses from different units, hospitals, geographic areas, or countries will be able to use commonly understood terminology to identify the specific problem or intervention implied and the outcome observed,” Marjorie A. Rutherford, RN, MA, explained in the Online Journal of Issues in Nursing.
Avoid Using Restricted Abbreviations in Patient Charting
The use of abbreviations in patient charting has been found to lead to medical error. As such, all healthcare providers should familiarize themselves with the Joint Commission’s “Do Not Use” list of abbreviations, and use this list religiously.
The “Do Not Use” list was developed to help prevent medical error by avoiding common misunderstandings and misinterpretations when reading a patient’s chart. When following these guidelines, nurses are prompted to write complete words, rather than abbreviations. For example, using “unit” instead of “u.”
Save Time by Integrating Technology
The widespread use of EHRs has revolutionized patient charting. Nurses can save time and improve charting accuracy by using their EHRs at a patient’s bedside and documenting observations, the administration of medication and practices performed in real time. The effective use of EHRs in charting can also improve communication between team members , helping nursing teams save time and avoid mistakes.
Use the HER’s Dictation Functionality
The dictation functionality included in many EHRs enable healthcare professionals to record their notes by speaking. This is one way that nurses can save time while recording pertinent details while at the patient’s bedside. When using dictation in the medical chart, nurses should always review the information recorded to ensure accuracy.
Document to Medical Necessity
The medical chart is a record of care. As such, the chart should include all pertinent details from a nurse’s contact with the patient. This includes all care provided, including patient education and relevant family interactions. Everything should be documented to medical necessity in order to provide a thorough record of care.
Remember that Medical Charts are Legal Documents
At the end of the day, the medical chart is a legal document. The medical chart can be a resource in payment disputes and in medical malpractice lawsuits. For this reason, nurses should always be objective, accurate and clear when charting. Doing so will protect all members of the nursing team as well as the healthcare provider.
Avoid Common Mistakes
Nurses still charting on paper can avoid common mistakes by writing clearly and legibly , drawing lines through blank spaces, and documenting actions as they occur. Doing so will help save time in the long run, while also preventing costly mistakes.
About Duquesne University’s Online MSN Program
Duquesne University’s MSN degree program prepares RNs for careers in leadership and to set new standards of care. The university’s online MSN and Post-Master’s Certificate degree programs allow nurses to continue their careers and personal lives while earning an advanced education. The school offers programs in Family (Individual Across a Life Span) Nurse Practitioner, Forensic Nursing and Nursing Education and Faculty Role.
Duquesne University provides one-on-one faculty support to encourage success at every step. Graduates are eligible to sit for certification boards, including the American Academy of Nurse Practitioners Certification Board (AANPCP) and American Nurses Credentialing Center (ANCC) Family Nurse Practitioner certification examinations. For more information, contact Duquesne University today .
How evidence-based clinical documentation gives time back to nurses: Meditech
What Is A Nursing Care Plan and Why is it Needed?: RNCentral.com
Standardized Nursing Language: What Does It Mean for Nursing Practice?: OJIN
Do Not Use List: Joint Commission
The Impact of Abbreviations on Patient Safety: Joint Commission Journal
Reducing unsafe abbreviations: NCBI
8 common charting mistakes to avoid: NSO
Documentation: You’ve got a lot to lose: American Nurse Today
Nurse Charting: 7 Tips And Tricks That Will Make Your Life Easier: Onward Healthcare
Getting Your Notes Done on Time: FPM Journal
| 1. | What is your highest level of education? |
| 2. | Do you currently hold an unencumbered RN license? |
| 3. | Which are you interested in? |
| 4. | Who is this brochure for? |
Patient Charting and Health Information – Tips for Nurses
- Request Info
Patient care involves a lot of moving parts, especially in critical situations. Nurses must think on their feet, make quick decisions and be confident those decisions are correct. Even in lower-stress provider-patient interactions, such as a routine checkup, certain steps are crucial to optimize patient care.
One imperative process is charting.
What Is Charting and Why Is It so Important?
In simple terms, charting is documentation to have a record of patient status, medical services and more. It may include test results, medication history, health history and any procedures the patient has undergone throughout their lifetime.
These data points allow everyone attending to the patient to provide the highest level of care. Other nurses, physicians and specialists rely on good charting to fully understand the patient’s needs. This information is essential when it comes to medication use. Many medications interact , so it’s vital that medical professionals document every drug in the patient’s records.
In some cases, charting has legal or insurance purposes which provides even more incentive for nurses to be highly skilled in their documentation practices. The following are five tips on how nurses can make charting easier and better for patient outcomes overall.
1) Consistency Is Key
Have you ever jotted down a note with a symbol or abbreviation to save time, only to not remember what it signified when you really needed it? Identifying a consistent charting system for your own purposes removes potential confusion when the information matters most.
Fortunately, nurses do have some guidance in this regard. The Joint Commission has created a “Do Not Use” list that clarifies which abbreviations and terminology they prefer regarding medication-related documentation.
2) Technology Is Your Friend!
Some people prefer pen and paper. However, an increasing number of healthcare institutions are migrating to digital documentation, and nurses can use that to their advantage. Keyboard shortcuts expedite the charting process. Digital documentation also eliminates the potential for illegible penmanship.
One word of caution: Avoid copying and pasting information. It might save time, but there’s also more room for error.
3) When In Doubt, Over-Chart
You don’t want to be redundant, but you need to capture every piece of relevant information about the patient. Remember, not everyone is as intimately involved with your patient as you are. Lawyers, insurance adjusters and outside specialists assume that everything they need to make decisions is in the chart.
Rule of thumb: If information is important now, or might be necessary for the future, include it.
4) Try to Chart in Real Time
Our memories inevitably fail us from time to time. Therefore, the sooner you can record patient details, the better. One suggestion is to use a voice memo to quickly record the most important information between patients. At the very least, carry a pen and small notebook to jot down highly pertinent information that may jog your memory when you can sit down and document in full.
5) Keep It Neutral
As professionals in healthcare, nurses know they need to have an unbiased perspective. Yet, the compassion and advocacy aspect of patient care is also a strong motivator. Nurses can still do their job well without voicing a subjective opinion or speculative information via the patient’s chart. In fact, the best approach you can take for your patients is to be as objective and patient-focused as possible.
Not All Charting Is Equal
There are many different “types” of charting , such as:
- Narrative Notes
- Charting By Exception (CBE)
- SOAP(IER) for subjective, objective, assessment, plan, intervention, evaluation, revision
- PIE for problems, interventions, evaluations
- Focus (DAR) for data, action, response
Each type of charting has its advantages and disadvantages. For example, CBE only documents things that are outside the “norm.” But how can outside parties know what is normal for any individual patient? As a nurse, you may not get to choose which system you prefer if there’s a standard in place. The best course is to rise to an expert level of charting, no matter your assignment.
The good news is, you don’t have to figure that all out on your own. Charting is a vital part of nursing education. Registered nurses (RNs) pursuing higher education with their Bachelor of Science in Nursing (BSN) degree have access to a fully holistic approach to the nursing profession. With a BSN, you’ll have the knowledge and skills to serve your patients in the best way possible.
Learn more about Mississippi College’s online RN to BSN program .
Related Articles
200 S. Capitol Street, Clinton, MS 39056 601.925.3000
Nursing Notes: How to write them (with Examples)

Although nursing documentation may at times seem overwhelming, it is a key part of nursing practice. Colloquially known as “charting,” nursing documentation provides a record of nursing care provided to a patient, family, or community. Charting and, more specifically, nursing notes, allow nurses to demonstrate that the care they provided was ethical, safe, and informed by relevant nursing knowledge.
In this article:
- Nursing Notes vs. Charting
- How Are Nursing Notes Used?
- How to Write Good Nursing Notes (What’s included)
- SOAPIE Example
- DAR Example
- General Advice on Writing Nursing Notes
Charting is a nursing process that includes all the documentation required from nurses. This might include legal, professional, and institution-specific requirements. Some examples of charting include documenting medications administered, vital signs, physical assessments, and interventions provided. Nursing notes are a narrative written summary of a given nursing care encounter. This might include a description of a nursing visit, a specific care event, or a summary of care. A nurse’s note is a form of charting that describes the nurse’s decision-making process regarding the nursing care provided.
Nursing notes are an important part of high-quality nursing documentation because they provide an opportunity for nurses to demonstrate their nursing knowledge and communicate the nursing process to other team members of the patient’s interprofessional care team.
A clear and comprehensive nursing note serves several purposes in nursing practice, both in patient care and to provide legal protection to the nurse writing the note. Reasons to write high-quality nursing notes include:
- Contributing to continuity of care for patients. Continuous care requires that the care provided to the patient is well-organized and that there is cooperative communication between nurses and other interdisciplinary team members. Continuous care contributes to patient-centered and safe care. Nursing notes allow all people on the care team to understand the patterns of patient care. 1
- Communicating care goals. Nursing notes are one place where the nurse can share the plan of care with team members. Nursing notes also allow others to see what interventions have been performed so far and what the outcome of those interventions were.
- Demonstrating the nurse’s knowledge as required by professional regulators. Nursing notes are useful for demonstrating the knowledge, skill, and judgment required by the nurse’s professional regulators, such as their college. In addition, if there is ever a concern about a nurse’s license, nursing notes can be used as evidence of competent and safe practice in line with professional standards of practice.
- Contribute to quality improvement. Quality improvement projects across nursing settings may include a review of charts to understand the care process. Nursing notes that accurately and comprehensively reflect care delivered allow for more precise quality improvement initiatives.
- Contribute to nursing research. Nursing research projects may include a review of the chart. Similar to quality improvement initiatives, nursing notes that accurately reflect the care provided allow accurate research data to be collected.
- Legal protection. Nursing notes are included in the patient/client’s permanent medical record. In the case of legal action related to care that a nurse provided or was involved in, nursing notes demonstrating that ethical and competent nursing care was delivered provide legal protection to the nurse.
- Reimbursing insurance claims. In some jurisdictions, insurance or other healthcare payers may directly reimburse nursing care. The nursing note may describe the rationale for reimbursable nursing activities in this case.
These are just a few key reasons nurses should spend time and effort writing high-quality nursing notes.
Different work settings may have an expected format or even templates for nursing notes. However, all nursing notes should include evidence of the nursing process. There are different templates for what should be included in a nursing note. Institutional or hospital policies may be in place on what should be included in the nursing note. However, it is the individual nurse’s responsibility and a demonstration of nursing knowledge and judgment to decide what information is relevant or irrelevant for the nursing note.
Nurses’ notes usually include subjective (what the patient tells you) and objective (assessment/analysis) data. However, the nurse should be careful not to include judgements or their own opinion in nursing notes. It is important to include subjective data. However, subjective data should be written in quotation marks as statements made by the patient rather than objective facts.
Two common templates for nursing notes use the mnemonics DAR and SOAPIE . Rather than absolute rules that describe how a nursing note should be structured, these two mnemonics are to be used as guidelines and to help the nurse remember what information should be included in their note.
SOAPIE: subjective (what the patient tells you), objective (the nurse’s assessment), analysis (interpretation of data), plan (what the nurse plans to do), implementation (what was done) and evaluation (how did the intervention work?)
DAR: Data (both subjective and objective), action (what was done), response (how did the patient respond?
There are other acceptable templates for nursing notes. The nurse should check with their institution if there is a preferred or institution-specific policy regarding what should be included in the nursing note. Overall, what must be included in the nursing note is the nurse’s own name, the name of the patient/client, the date and time of the note, and a demonstration of the appropriate nursing process. Nursing notes should also be made in chronological order.
When writing a nursing note regarding a consultation with another healthcare provider, the nurse should include the name and designation of the other healthcare provider in addition to other components of the nursing note.
Nursing Note Examples
In the following section you will find nursing note examples for the SOAPIE as well as for the DAR format.
Patient: Jane Doe Date: January 30, 2023
13:17: Patient reports pain to lower abdomen, rates pain at 7/10. She states that the pain has been increasing over the past half hour after her return from PACU. Mrs. Doe describes the pain as a “dull ache.” ( Subjective ) Abdominal dressing is dry and intact. Bowel sounds are hypoactive X4. Most recent vital signs BP 114/82, HR 88, respiration 18, Sp02 94% on room air. ( Objective ) Patient experiencing post-operative pain related to recent hernia operation. ( Analysis ) Writer will offer patient education regarding PCA usage. ( Plan )
13:26: Writer reminded the patient about how to use the button on her PCA to control her pain. Writer educated patient on the importance of managing post-surgical pain early to maintain comfort. ( Intervention )
13:57 Reassessed patient pain after PCA education. Patient now describes that her pain is “subsiding.” When rating her pain on the pain scale, patient now describes her pain as 2/10 which is acceptable to her. ( Evaluation )
This note includes all elements of the SOAPIE note and also is written at the time in which the activity was performed so there is a clear sequence of events.
Patient: Jill Doe Date: January 30, 2023
0927: On assessment patient described increased shortness of breath related to her chronic asthma. Patient stated that she “uses her inhaler at home when I get short of breath.” Patient respiration rate 22, Sa02 92% on room air, wheeze audible on auscultation of lungs. ( Data ) Writer administered 2 puffs (34 mcg) of patient’s Ipratropium PRN inhaler. ( Action ) Patient states that shortness of breath now resolved. ( Response )
Writing high-quality nursing notes is a skill like any other nursing skill that takes time and focused effort to improve. With practice, nursing notes will become second nature as one pillar of safe and effective clinical practice. Here are a few quick practice pointers to improve your nursing notes.
- If you are using paper charting, ensure that the writing is legible . Illegible charting does not accomplish the goal of communicating care to the team and will not legally protect the nurse.
- Include both subjective and objective data . Including both subjective and objective data in the nursing note creates a comprehensive clinical picture.
- Remember to document significant interactions with family members, significant others, or substitute decision-makers. This might include interactions such as a family member describing the patient’s medical history when the patient is unable to do so themselves.
- Limit your use of abbreviations. If you do use abbreviations, ensure that they are allowed for your institution
- Document as soon as possible after the care interaction. It is preferable to document the care interaction as soon as possible. If the nurse waits to document, they may forget important details.
- If an error is made in documentation, do not delete, white-out, or attempt to erase the error. Instead, document that the first entry was made in error by drawing a line through and initialing for paper charting or following the correct procedure for the electronic medical record.
- For paper charting, use only black or blue ink , which is accepted in legal proceedings and is the easiest to read.
- Read other documentation on the patient! This could include other members of the interprofessional team or nurses’ notes on the patient. These notes may include helpful information that may inform your care of the patient. However, a word of caution is that the nurse should never rely on another’s assessment . Always double check the details of the patient’s history and make your own assessment.
To ensure high-quality nursing notes, the nurse might ask themselves if their note adequately answers the following question: “If another nurse were to take over this assignment, without a verbal handover, is there enough information here that they could provide safe and continuous care for this patient?” 2 If the answer is no, the nurse might consider that more detail ought to be provided.
- College of Nurses of Ontario. Documentation, Revised 2008. Published online 2008. Accessed January 28, 2023. https://www.cno.org/globalassets/docs/prac/41001_documentation.pdf
- College of Registered Nurses of Manitoba. Documentation Guidelines for Registered Nurses. Accessed January 28, 2023. https://crnm.mb.ca/wp-content/uploads/2022/01/Documentation-Guidelines-for.pdf


Getting clear on the new coding rules can help you eliminate bloated documentation and improve reimbursement to reflect the value of your visits.
THOMAS WEIDA, MD, FAAFP, AND JANE WEIDA, MD, FAAFP
Fam Pract Manag. 2022;29(1):26-31
Author disclosures: no relevant financial relationships.

In 2021, significant changes were adopted for the documentation guidelines for outpatient evaluation and management (E/M) visit codes. Most notably, medical decision making or time became primary drivers of visit level selection, rather than the number of history and physical exam bullets.
In this article, we review the context for these changes, describe them briefly, and offer a quick reference tool to help physicians apply the new rules in practice.
The revisions to the E/M outpatient visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements.
Code level selection is now simplified — based on either medical decision making or total time.
The authors' one-page coding reference tool can help simplify the new rules.
HOW WE GOT HERE
In the 2019 Medicare physician fee schedule final rule, released in November 2018, the Centers for Medicare & Medicaid Services (CMS) adopted revisions to the outpatient E/M codes in order to reduce administrative burden. (See https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year .) Originally scheduled for implementation in 2021, these changes would have combined visit levels 2–4 into a blended payment rate (e.g., one rate for 99202-99204 and one rate for 99212-99214), among other changes.
In response, the American Medical Association (AMA) convened a joint CPT Editorial Board and Relative Value Scale Update Committee (RUC) workgroup to build on the changes and propose some alternatives. The workgroup's goals were to decrease administrative burden, payer audits, and unnecessary medical record documentation while ensuring that payment of E/M services is resource-based.
The workgroup approved significant revisions to the outpatient office visit E/M codes. Code 99201 was deleted. The history and/or physical examination and the counting of bullets were eliminated as components for code selection (although history and/or physical examination documentation should still be performed as medically appropriate). Medical decision making (MDM) or time could be used for code level selection. Changes were made to the code descriptors for 99202-99205 and 99211-99215, the definition of medical decision making, and the calculation of time, and a shorter prolonged services add-on code was created. CMS adopted these new E/M coding guidelines. As a result of the changes to medical decision making and time-based coding, the RUC revised the 2021 relative value units (RVUs) for office visit E/M codes. Most of the values increased, yielding an overall increase of more than 10%.
CODING BASED ON MEDICAL DECISION MAKING
For outpatient E/M coding, medical decision making now has three components:
Number and complexity of problems addressed at the encounter,
Amount and/or complexity of data to be reviewed and analyzed,
Risk of complications and/or morbidity or mortality of patient management.
There are four levels of decision making for each of these components: straightforward, low complexity, moderate complexity, and high complexity.
To determine the level of code for a visit, two of the three components must meet or exceed that level of coding. ( See the table .) For example, if the patient has multiple problems addressed at the encounter, but the data is limited and the risk of complications is low, then the level of medical decision making would be low. New patient codes 99202-99205 and established patient codes 99212-99215 use the same components and levels of decision making for code selection.
| Straightforward | Minimal | Minimal or none | Minimal |
| Low | Low | Limited | Low |
| Moderate | Moderate | Moderate | Moderate |
| High | High | Extensive | High |
Determining medical decision making usually starts with identifying the number and complexity of problems addressed and then determining the data or risk components that support that medical decision making. If a second component does not meet or exceed the problem component, then a lower level of decision making is appropriate. The set of tables below illustrate the essential concepts of these code levels. Each level has specific criteria for each component.
Straightforward medical decision making: Codes 99202 and 99212 include one self-limited or minor problem with minimal or no data and minimal risk.
An example of a 99202 or 99212 is an otherwise healthy patient with cough and congestion due to the common cold.
Low complexity medical decision making: Codes 99203 and 99213 include two or more self-limited or minor problems, one stable chronic illness, or one acute uncomplicated illness or injury.
The data component requires one of two categories to establish the level. Category 1 data requires at least two items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, or each unique test ordered. Tests include imaging, laboratory, psychometric, or physiologic data. A clinical lab panel, such as a complete blood count, is a single test. Of note, if a test is ordered, the review of that test is included with the ordering, even if the review is done at a subsequent visit. Tests ordered outside of an encounter may be counted in the encounter in which they are analyzed. Category 2 data includes significant history given by an independent historian. Parents giving the history for their child is a typical example.
The risk component is low. There is low risk of morbidity from additional diagnostic testing or treatment.
An example of a 99203 or 99213 is a sinus infection treated with an antibiotic. Although the prescription makes the risk component moderate, the one acute uncomplicated illness is a low-complexity problem, and there are no data points.
Moderate complexity medical decision making: Codes 99204 and 99214 include two or more stable chronic illnesses, one or more chronic illnesses with exacerbation, progression, or side effects of treatment, one undiagnosed new problem with uncertain prognosis, one acute illness with systemic symptoms, or one acute complicated injury. A patient who is not at a treatment goal, such as a patient with poorly controlled diabetes, is not stable. Systemic general symptoms such as fever or fatigue in a minor illness (e.g., a cold with fever) do not raise the complexity to moderate. More appropriate would be fever with pyelonephritis, pneumonitis, or colitis.
The data component requires one of three categories to establish the level. Category 1 data requires at least three items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, each unique test ordered, or independent historian involvement. Physicians cannot count tests that they or someone of the same specialty and same group practice are interpreting and reporting separately (e.g., electrocardiogram, X-ray, or spirometry). Category 2 data includes the independent interpretation of a test performed by another physician/other qualified health care professional (QHP) (not separately reported). For instance, if a chest X-ray was ordered and the ordering clinician included the interpretation in the visit documentation, this would qualify for data point Category 2. However, if the ordering clinician bills separately for the interpretation of the X-ray, then that cannot be used as an element in this category and would be an element for Category 1. Category 3 data includes discussion of management or test interpretation with an external physician/QHP (not separately reported).
The risk component may include prescription drug management, a decision for minor surgery with patient or procedure risk factors, a decision for elective major surgery without patient or procedure risk factors, or social determinants of health (SDOH) that significantly limit diagnostic or treatment options, such as food or housing insecurity. For prescription drug management, renewing pre-existing chronic medications would qualify. Documentation that the physician is managing the patient for the condition for which the medications are being prescribed would help establish validity in the use of this criterion for MDM.
An example of a 99204 or 99214 is a patient being seen for follow-up of hypertension and diabetes, which are well-controlled. An example using SDOH would be a patient with chronic knee pain and a positive anterior drawer test who needs imaging of the knee but cannot afford this care. Documenting that the patient cannot afford to obtain an MRI of the knee at this time, which significantly limits your ability to confirm the diagnosis and recommend treatment, adds to the risk component.
High complexity medical decision making: Codes 99205 and 99215 include one or more chronic illnesses with a severe exacerbation, progression, or side effects of treatment, or one acute or chronic illness or injury that poses a threat to life or bodily function.
The data component requires two of three categories to establish the level. These data categories are the same as those for 99204 and 99214, and they follow the same rules.
The risk component may include drug therapy requiring intensive monitoring for toxicity. Decisions regarding elective major surgery with patient or procedure risk, emergency major surgery, hospitalization, or “do not resuscitate” orders are also high risk. Intensive prescription drug monitoring is typically supported by a laboratory test, physiologic test, or imaging, and is done to evaluate for complications of the treatment. It may be short-term or long-term. Long-term monitoring is at least quarterly. An example would be monitoring for cytopenia during antineoplastic therapy. Monitoring the therapeutic effect of a treatment, such as glucose monitoring during insulin therapy, is not considered intensive prescription drug monitoring.
An example of a 99205 or 99215 is a patient with severe exacerbation of chronic heart failure who is admitted to the hospital.
CODING OUTPATIENT E/M VISITS
| Minimal or none | Minimal risk of morbidity from additional diagnostic testing or treatment |
| 99202 | 15–29 | 99212 | 10–19 |
| 99203 | 30–44 | 99213 | 20–29 |
| 99204 | 45–59 | 99214 | 30–39 |
| 99205 | 60–74 | 99215 | 40–54 |
| 99205 + G2212 | 89–103 | 99215 + G2212 | 69–83 |
| 99205 + G2212 X 2 | 104–118 | 99215 + G2212 X 2 | 84–98 |
| 99205 + G2212 X 3 or more for each 15 minutes | 119 or more | 99215 + G2212 X 3 or more for each 15 minutes | 99 or more |
| 99205 + 99417 | 75–89 | 99215 + 99417 | 55–69 |
| 99205 + 99417 X 2 | 90–104 | 99215 + 99417 X 2 | 70–84 |
| 99205 + 99417 X 3 or more for each additional 15 minutes | 105 or more | 99215 + 99417 X 3 or more for each additional 15 minutes | 85 or more |
TIME-BASED CODING
An alternative method to determine the appropriate visit level is time-based coding. A major change is that total time now includes both face-to-face and non-face-to-face services personally performed by the physician/QHP on the day of the visit. Additionally, time-based coding is no longer restricted to counseling services. Instead, it includes the following:
Preparing to see the patient (e.g., reviewing external test results),
Obtaining and/or reviewing separately obtained history,
Performing a medically appropriate examination and/or evaluation,
Counseling and educating the patient, family, or caregiver,
Ordering medications, tests, or procedures,
Referring and communicating with other health care professionals (when not separately reported),
Documenting clinical information in the electronic or other health record,
Independently interpreting results (not separately reported with a CPT code) and communicating results to the patient, family, or caregiver.
Care coordination (not separately reported with a CPT code).
Time spent by clinical staff cannot count toward total time. However, time spent by another physician/QHP (not a resident physician) in the same group can be included. If a nurse practitioner performs the initial intake and the physician provides the assessment and plan, both of those times can be counted, although only one person's time can be counted while they are discussing the case with each other. The visit should be billed under the clinician who provided the substantive portion (more than half) of the time, although both clinicians need to be identified in the medical record. Time spent must be documented in the note. It is advisable to specifically document the time spent and the activities performed both face-to-face and non-face-to-face.
The amount of total time required for each level of coding changed under the new time-based coding guidelines. (See the “Total time ” table.)
PROLONGED VISIT CODES
When time on the date of service extends beyond the times for codes 99205 or 99215, prolonged visit codes can be used. The AMA CPT committee developed code 99417 for prolonged visits, and Medicare developed code G2212. These are added in 15-minute increments in addition to codes 99205 or 99215. Code G2212 can be added once the maximum time for 99205 or 99215 has been surpassed by a full 15 minutes, whereas code 99417 can be added once the minimum time for 99205 or 99215 has been surpassed by a full 15 minutes. Less than 15 minutes is not reportable. Multiple units can be reported. Prolonged visit codes cannot be used with the shorter E/M levels, i.e., 99202-99204 and 99212-99214. (See “Prolonged services ” tables.) Clinicians should consult with individual payers to determine which code to use — G2212 or 99417.
SIMPLIFIED CODING AND DOCUMENTATION
The revisions to the outpatient E/M visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements. Only medically appropriate documentation is required. Code level selection is simplified — based on either medical decision making or total time. By applying these changes, primary care clinicians can eliminate bloated documentation and improve reimbursement reflecting the value of the visit.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2022 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

Printable Caregiver Daily Log Sheet, Checklist, Template for Elderly
Table of Contents
What are Caregiver daily logs used for?
What is a nursing assessment, what is adl and iadl, who can use a caregiver daily log sheet, when should a caregiver daily log be used, what’s included in a caregiver daily log, how do i create a caregiver daily log, how can the careclinic app help keep a caregiver daily log, is there a printable pdf spreadsheet that can be used, does a caregiver logbook help with medicine reminders and symptom tracking, which other logs can be beneficial for patients to print and use, what are some other things that can be tracked in careclinic, how do i log a dependent’s health in careclinic as a caregiver, collaborative at-home patient documentation.
Caregiver daily logs can be used to track the progress of an individual over time and to identify any areas in which their needs are not being met. They can also be used to help plan future care by providing a record of what has been done in the past and what has been found to be effective.
As an example, if a caregiver daily log shows that an individual has been particularly agitated in the evening hours, this may be used to inform the care plan for the following day. The log may also be reviewed by other members of the care team, such as doctors or nurses, to get a better understanding of the individual’s needs.
A nursing assessment is a key component of the nursing process. It is an opportunity for nurses to gather information about their patients to develop a plan of care. The assessment should be comprehensive and include all aspects of the patient’s health, including physical, psychological, social, and spiritual needs. A patient assessment is usually conducted at the beginning of the nurse-patient relationship, but it can also be done at any time when there is a change in the patient’s condition. A nurse report sheet is a form that is used by nurses to document assessment data.
What is SBAR?
SBAR is an acronym that stands for Situation, Background, Assessment, and Recommendation. It is a tool that can be used to improve communication between healthcare providers. SBAR can be used in any situation where clear and concise communication is needed, such as during handoffs or when calling a doctor for consultation. SBAR can be used to improve communication between healthcare providers; however, it is not necessarily used on a caregiver log sheet.
There are many different ways to measure ADL and IADL. One way is to use the Lawton and Brody Scale, which rates activities from 0 (unable to do) to 8 (independent). Another way is to use the Katz Index of Independence in Activities of Daily Living, which rates activities from 0 (dependent) to 4 (independent).
The type of help someone needs with ADLs or IADLs can vary from person to person. Some people may need help with only one activity, while others may need help with several activities. Some people may need help only occasionally, while others may need help on a daily basis. If you are a caregiver, you may be wondering how to best assist someone with ADLs or IADLs. One option is to provide hands-on help, such as helping someone get dressed or taking them to appointments. Another option is to provide guidance and support, such as showing someone how to use a microwave or teaching them how to budget their money.

No matter what type of help you provide, it is important to be patient, respectful, and flexible. ADLs and IADLs can be frustrating for both the person who is struggling to do them and the caregiver who is trying to help. Remember to take breaks when needed, and ask for help from friends or family members if you are feeling overwhelmed.
It is not just for patients or clients. It can be used by teens, elderly, or anyone with a chronic condition that is being managed. It is most commonly used to track medical appointments, medications, and other treatments. However, it can also be used to document behaviors or changes in mood, sleep patterns, eating habits, and any other notable changes. It is particularly useful for those with Alzheimer’s disease, dementia, or other cognitive impairments.
A caregiver daily log should be used whenever there is a need to track the progress of an individual over time. This may be on a daily, weekly, or monthly basis, depending on the individual’s needs.
The contents of a caregiver daily log will vary depending on the type of care being provided and the needs of the individual. However, common information that may be recorded in a caregiver’s daily log includes:
- The date and time of each task or activity performed
- A description of the task or activity performed
- The duration of the task or activity
- Any special instructions for performing the task or activity
- Any observations made about the individual during the course of the day
- Insurance details
- Notes from doctor appointments
A caregiver daily log can replace the need for individual medication log books, or disease-specific log books for diabetes, hypertension and allergies if you are managing a dependents’ health.
There are some basic steps that can be followed to get started:
- Decide what information you want to include in the log.
- Choose a format for recording the information. This could be a paper notebook, an electronic spreadsheet, or a specialized app like CareClinic.
- Set up a system for recording the information. This may involve assigning specific tasks to different caregivers, setting up times during the day when the log will be updated, or both.
- Train caregivers on how to use the system and what information should be included in the log.
- Begin recording information in the log daily.
- Review the log regularly to ensure that it is being used effectively and that all relevant information is being captured.
- If necessary, make changes to the system based on your observations.
Can a caregiver’s daily log be used for any type of patient?
A caregiver daily log can be used for any type of patient, including those receiving in-home care, those in a hospice or nursing home setting, and those in a hospital. It is common to use for in-home care patients, as it can be difficult for family members to keep track of all the tasks and activities being performed by the caregiver. However, any type of patient can benefit from having a daily log kept of their care.
If you are a caregiver, consider keeping a daily log to document the care you provide. This can be a valuable tool for tracking the individual’s progress and communicating information to other members of the care team. It can also help you to reflect on your own practice and identify areas in which you may need more training or support.
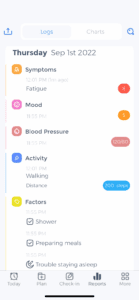
The CareClinic app is designed to help caregivers track the care they provide. It includes features such as:
- A customizable care plan for each individual
- The ability to record tasks, activities, and observations in a daily log
- Notes section for recording additional information
- The option to share logs with other members of the care team
- Reminders and alerts to help keep on track
If you are looking for a way to keep a caregiver daily log, the CareClinic app may be a good option for you. It can help you to stay organized and ensure that all relevant information is recorded. Plus, it’s free to download and easy to use. Try it today!
Yes, there is a printable PDF spreadsheet that can be used to keep a caregiver daily log. This can be found here:
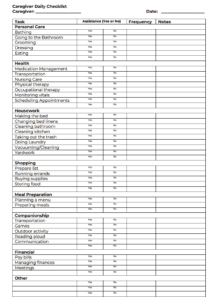
⤵️ Printable caregiver daily checklist template
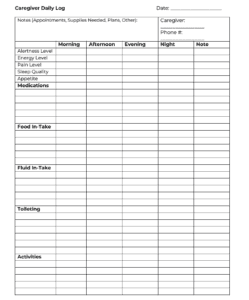
⤵️ Printable caregiver daily log
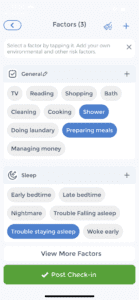

⤵️ Try Factors Check-list in App
⤵️ View Caregiver Logs in App
The spreadsheet includes columns for the date, time, task or activity performed, duration, special instructions, and observations. There is also a notes section where additional information can be recorded. This can be helpful if you want to track specific details about the individual’s progress or care. However, it is recommended that you try the app as it can keep all caregivers or families in the loop about a dependent that is being cared for.
This information can be shared with other members of the care team, which can be helpful in determining the best course of treatment. Finally, many apps also offer features like goal setting and progress tracking. This can be beneficial for both the caregiver and the individual receiving care.
There are a variety of other logs that can be beneficial for patients to print and use. These include Blood pressure , pulse log, blood sugar , heart rate, pain journal, sleep log, diet diary, activity tracker, symptom tracker and a body temperate log . It may also make sense to simply buy a workbook if you feel like a digital solution or printing sheets one by one is not the right solution for you, you can find these by clicking here.
In addition to tracking medication and symptoms, the CareClinic app can also be used to track:
- Appointments and other plans for tomorrow
- Any other health concerns in notes
- Immunizations and allergies
- Vital signs such as blood pressure, blood oxygen, heart rate
- For infants: Weight and height measurements
- Diet including fluid in-take at different times of the day
- Exercise and or any other physical therapy or activity
- Sleep patterns, naps, times woken up and why
- Bathroom/stool log
- Mood and behavior
- Supplies needed soon
- Alertness, happiness, pain levels, or any measurement that is required
- CareClinic also comes with over 50 health assessments, tests and surveys built directly into the app for many health conditions
This information can help understand the individual’s overall health and well-being. It can also be useful in identifying any trends or patterns that may be emerging. If you are looking for a way to track all of this information in one place, CareClinic may be a good option for you. Try it today!
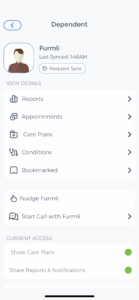
Easily Share All Details and Review Medical History
A benefit of using the app is that you can still print out all details to share with caregivers on a day-to-day basis and to share with other health care providers. The App provides pre-set trackers for each patient so there is no time wasted in thinking about what to log, how to log it, and adding new items to a care plan as the App comes with a built-in database of medications, supplements, symptoms, measurements (with units), activities, therapies, and other trackers for stool and sleep monitoring.
Improved Patient Visit Notes
Another key benefit provided by CareClinic is that you can spot patterns easily with automated charting, correlations, and logs within the App. This is not possible with a physical logbook. Another benefit is that at-home caregivers are much more inclined to quickly tap items on a screen rather than handwrite notes for patients due to time or other constraints.
CareClinic is cross-platform and works online-offline, and what that means is that the App may be left open for caregivers to quickly make check-ins for a patient as most entries will involve tapping and sliding different values. This leads to fewer mistakes, and improved communication from the caregiver filling out the details, and you are able to access it from anywhere at any time to share with anyone you may need to share it with.
The CareClinic app can be used to keep track of a wide range of caregiving tasks and activities. It is customizable to meet the needs of each individual, and it offers the ability to share logs with other members of the care team.
Plus, it’s free to download and easy to use. Try it today! It is particularly useful when there are many caregivers and everyone needs to remain updated on how a dependent is doing and what the next tasks are. This way no mistakes are made, and everything is private and can be shared safely.
- Recent Posts
- How to Tell if Nausea is from Anxiety
- Keeping a Kidney Stone Log: A Comprehensive Guide
- The Pinch Method for Diabetes: Reduce High Blood Sugar Levels
- Printable Blood Pressure Tracking Chart & Pulse Log
- 99 Gratitude Journal Prompts for Daily Reflection
- Bipolar Mood Tracker and Journaling: 3 Tips for…
- Printable Blood Sugar Log: Free PDF Sheets to…
- The Role of SIBO in Chronic Fatigue
- Medication Log Sheet Printable
Registered Nurse RN
Registered Nurse, Free Care Plans, Free NCLEX Review, Nurse Salary, and much more. Join the nursing revolution.
Nursing Report Sheet Templates | Free Report Sheets for Nurses
Nursing report sheets are premade templates of paper used by nurses to help them keep track of their patients. A nursing report sheet is started at the beginning of the nurses shift while she/he is getting report from the leaving nurse who is giving them nursing report. This nursing report sheet should not be confused with the SBAR tool which is a tool used as a guide for giving nursing report.
Why Do Nurses Use Nursing Report Sheets?
Nurse report sheets are very handy because they contain tidbits of vital information concerning your patient’s diagnosis, history, allergies, attending doctor,consults, things that need to be done on your shift, medication times, vital signs, lab results etc. The report sheet has other usage as well. Other usages of the nursing report sheet include but are not limited to:
- Keeping track of telephone orders received from doctors
- Critical Lab values called to you from lab
- Helps you keep track of intake and output
- Helps you keep track of blood sugars and insulin coverage
- Nursing notes to remind yourself of things you need to do for the patient or chart on
- Notes to yourself on things you want to remind the next shift
Most nurses who use report sheets consider their report sheet to be their “brain,” and panic when they misplace them. Nurses who use them tend to keep them folded in their scrub pocket or on their clip board for easy access.
Always make sure to get a good report on your patients before starting a new shift. Learn more about questions to ask when getting report .
Video on How to Give Nursing Shift Report
Benefits of a Nursing Report Sheet
- Fast access to patient information. If you are asked by a doctor what a particular patient’s INR was you could simply look at your report sheet to find out. You won’t have fumble around and try to remember which patient he/she was talking about.
- Helps you keep track of things you need to get done before your shift is over.
- Helps you differate between each patient. When you have a 6 to 7 patient load, patient diagnosis and histories can run together and you may get them confused.
- Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do. Again with 6 to 7 patients things tend to run together.
Nursing Report Sheets (Templates)

Remember to always shred your report sheet at the end of your shift. Never take your report sheet home with you!
Please Share:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Anonymous says
May 24, 2015 at 3:26 am
Ur just too good n doing a praiseworthy job.thank u so much.god bless
S.L. Page says
May 24, 2015 at 4:24 am
I just wanted to thank you personally for this comment. Comments like these are very encouraging and motivating. Thank you again for taking the time to comment these kind words.
Disclosure and Privacy Policy
Important links, follow us on social media.
- Facebook Nursing
- Instagram Nursing
- TikTok Nurse
- Twitter Nursing
- YouTube Nursing
Copyright Notice
5 Nursing Narrative Note Examples + How to Write

One of the most important lessons nursing students learn is the importance of documentation. Whether you are a nursing student or a seasoned nurse, knowing how to create accurate nurses' notes is vital. Narrative nurses' notes are one of the most popular forms of nursing documentation. Perhaps you are wondering how to write a nursing narrative note? In this article, I will share 5 nursing narrative note examples + how to write them and discuss the importance of accurate charting.
What Is A Nursing Narrative Note?
What is the purpose of writing a nursing narrative note, what is the difference between a nursing narrative note and a nursing progress note, 3 advantages of nursing narrative notes, 3 disadvantages of nursing narrative notes, what elements should be included in a nursing narrative note, • date and time:, • the patient’s name:, • subjective data:, • objective data:, • assessment:, • interventions:, • evaluation:, what elements should not be included in a nursing narrative note, 1. symptoms without intervention:, 2. speculations:, 3. non-descriptive or non-precise terminology:, 4. premature charting:, 5. personal information about the patient’s family or loved ones:, featured online msn programs, how to write a nursing narrative note, 1. stay on point and be specific, 2. state the facts, 3. note presentation, 4. note objective data, 5. record subjective data, 6. make notes regarding your assessment, 7. record any medication you administer or treatment you perform, 8. did you have to include interdisciplinary team members, 9. don’t forget to sign each entry of your note with your name and credentials, what are some excellent examples of nursing narrative notes, example #1: head-to-toe admission assessment narrative note for patient admitted with recent cerebrovascular accident (cva), example #2: assessment of nursing home resident, example #3: nursing narrative note example for patient recently admitted and found on hospital floor, example #4: patient with complaints of left knee pain, example #5: patient complaint of nausea, prn medication administered, bonus 6 expert tips for writing an excellent nursing narrative note, 1. document nursing actions immediately., 2. keep documentation descriptive., 3. be objective., 4. add new information anytime it is necessary., 5. convey enough information to get your point across., 6. make sure your handwriting is legible., my final thoughts, frequently asked questions answered by our expert, 1. who can write a nursing narrative note, 2. when to write a nursing narrative note, 3. can i use abbreviations in a nursing narrative note, 4. what tense do you write a nursing narrative note, 5. are nursing narrative notes handwritten or printed, 6. how to sign off a nursing narrative note, 7. what happens if i forget to write a narrative note in the time it should have been written, 8. should i write about a patient crying in my nursing narrative note, 9. how to note pulses on a nursing narrative note, 10. how to describe lab results in a nursing narrative note, 11. can a nursing student write a nursing narrative note, 12. what are the common mistakes nurses make when writing narrative notes.


A new patient-acuity tool promotes equitable nurse-patient assignments
Have you ever struggled to classify a patient’s acuity level? If so, you’re not alone. Have you ever looked at your patient assignments and wondered, “Why are the assignments so unfair? How will I care for all my patients effectively?” Again, you’re not alone.
Most nurses expect patient assignments to be equitable, with each nurse bearing a fair share of the workload so all patients can receive excellent care.
Nurses’ job satisfaction depends partly on their workload and their perceived ability to deliver high quality care. Nurse-sensitive indicators (including pressure ulcers, falls, medication errors, nosocomial infections, pain management, and patient satisfaction) depend largely on nursing care and are affected by nurses’ ability to recognize and intervene when a patient’s condition changes. Nursing workloads directly influence a nurse’s ability to assess thoroughly and promote excellent patient outcomes. When patient assignments aren’t equitable, nurses may feel inadequate and frustrated.
Problems also can arise when all nurses are assigned the same number of patients without regard for acuity levels. Yet determining patients’ acuity to promote more equitable assignments can be challenging. Some hospitals or nursing units use an established acuity tool. Others rely on charge nurses’ judgments of patient acuity.
Our nurses were getting restless
At Indiana University Health Ball Memorial Hospital in Muncie, we moved our progressive care unit (PCU) to a newly constructed area of our regional medical center. A short time later, we noticed increases in patient volumes, comorbidities, device support, and overall acuity. The patients’ nursing-care requirements varied widely, so assigning the same number of patients to all nurses would mean unequal assignments.
Although were using an acuity assessment tool, our increasingly dissatisfied nurses deemed it ineffective. It called for nurses to rank each patient as a 1, 2, or 3 based on their individual perception of the patient’s status or difficulty of care required. But the tool wasn’t providing useful information because nurses’ perceptions varied; also the cultural norm tends to make nurses rate most patients a 2. In addition, when more staff nurses were needed, we lacked an objective measure to make a case for obtaining additional staff. When our hospital tested a new nurse-satisfaction survey, nurses’ discontent with their workload became apparent.
Then a PCU direct-care nurse approached the unit-based council (UBC) and asked for an evaluation of our acuity tool. The nurse manager and UBC agreed that equitable patient assignments and adequate unit staffing could be addressed by improving the tool. Following the Iowa model of evidence-based practice (EBP), the UBC formed a team of staff nurses, charge nurses, unit manager, clinical nurse specialist, and nurse researcher to explore the inquiry.
What the evidence told us
The team’s literature review found a limited amount of research pertaining to acuity tools for PCUs, even though hospital expenses decrease and high-quality nursing care increases when leaders are empowered with better, more detailed knowledge of patient acuity and nursing workloads. A recurrent theme in the literature: nurses’ voices add value to processes and nurses should be involved in assessing their own workloads and making decisions about resources. Evidence also suggested that involving staff in developing an acuity assessment tool would yield a valued, more efficient instrument that could improve nurse satisfaction and job retention.
Formulating a plan
During our literature review, we found a tool to adapt for our adult PCU. On a flip chart in the nurses’ lounge, we displayed our existing tool alongside the new tool we’d revised from the literature search. Staff viewed both tools and provided input into what made a patient’s care difficult, time-consuming, or complex. This gave us a better picture of PCU patients and helped us ensure all tasks were represented, from the least to the most time-consuming. Brainstorming meetings clarified key elements of acuity that guided continued evolution of the new tool.
Tool-development strategies
In our new tool, criteria categories included complicated procedures, education, psychosocial/therapeutic interventions, number of oral medications, and complicated I.V. drugs and other medications. Rating options on the tool run from 1 through 4, with 1 indicating low acuity and 4 indicating high acuity. Ratings are based on nursing time needed to complete a task, emotional and physical energy expenditure required, expertise required, frequency of tasks and interventions, and follow-up assessments related to a specific task. Ratings for all five criteria categories are summed up to obtain a total acuity score for each patient, ranging from 1 to 60. Then the total scores are clustered into acuity category scores, which range from 1 to 4, with 1 being the lowest acuity and 4 being the highest. (See Acuity criteria categories .)
Now we were ready to test the new tool. Initially, charge nurses from each shift tested it with the same patients on different shifts. When we found that scores between shifts weren’t congruent, we tested the tool again, with charge nurses on the same shift assessing the same patients separately. This trial yielded an inter-rater reliability of 85%—an acceptable congruency level across nurse raters.
This trial provided insight into acuity differences between shifts and helped determine how to use the tool. With our previous acuity tool, tasks and procedures of the rater’s shift determined acuity, with no consideration of upcoming tasks or procedures for the next shift. So for the new tool, the team and staff agreed nurses would proactively score acuity for the oncoming shift by calculating current and projected needs and medications.
Measuring outcomes
We identified three outcome measures as indicators of the effectiveness of the new acuity approach.
- First, the team developed an eight-item survey to measure nurse satisfaction with the new acuity assessment process, which nurses completed 1 month before the new process began and then 1 month, 6 months, and 12 months later.
- Next, the team identified items on the standardized annual employee engagement and satisfaction survey, specifically targeting workload and perception of quality of care delivered.
- Finally, we tracked nurse sensitive indicators affected by workload, including falls and hospital-acquired pressure ulcers.
Translating scores into patient assignments
To translate acuity scores into equitable patient assignments, charge nurses collected the acuity tools that direct-care nurses completed for each patient, and calculated total acuity scores and acuity category scores near the end of their shift. Then the charge nurses designed nurse-patient assignments by considering both the category score from 1 to 4 and the total acuity score of 0 to 60 for each patient, aiming to keep category scores balanced across nurses. Charge nurses also considered the geographic location of rooms on the unit, need for continuity of care, and congruency between nurses’ expertise and patient needs. (See Current acuity tool on last page .)
Unit-wide rollout
Before we rolled out the new tool, direct-care nurses on our team provided education to all PCU nurses. Teaching strategies included showing video clips of patient scenarios, presenting case studies so nurses could practice using the tool, and playing a game-show exercise to stimulate discussion of the benefits of acuity scoring. Nurses voiced favorable responses to the new tool, specifically the benefits of empowerment, assurance of quality care, patient safety and satisfaction, nurse retention, and equitable assignments. The team encouraged staff to provide feedback on the new process and expect revisions to ensure its effectiveness and sustainability.
To hardwire the new acuity assessment process, team members rounded on nurses each shift for 1 week and then three times monthly. The team answered questions, audited acuity scores, and coached nurses to achieve a highly standardized approach to scoring. During orientation, preceptors trained newly hired nurses to use the acuity assessment tool.
Charge nurses kept a log of assignments, acuity scores, and overall unit activities, overtime, and informal comments on workload. In huddles held daily for the first week, charge nurses and the nurse manager reviewed acuity scores and the process. A numerical benchmark emerged as an indicator for requesting more staffing, based on total acuity scores and acuity category scores of all patients on the unit.
Evaluation and sustainability
At the end of the first month, scores on surveys of nurse satisfaction with the new acuity assessment process showed marked improvement in nurses’ reports of the equity of patient assignments (7% satisfaction before rollout, 55% satisfaction after) and the consistency with which the acuity assessment process occurred (21% consistency before rollout, 89% consistency after). Almost 80% of nurses reported that completing the new acuity tool wasn’t a waste of time. The team implemented suggestions for refining the process and set a target goal of 85% nurse satisfaction by the 6-month evaluation.
The sustainability plan for year 1 calls for quarterly reevaluation of the acuity assessment process and semiannual reevaluation thereafter, including scoring processes, staffing level benchmarks, nurse satisfaction per survey, and nurse-sensitive outcomes. It also calls for nurses to review reports of outcome data regularly during staff meetings. When revisions are indicated, the team will provide additional education.
As the process of creating ideal nurse-patient assignments evolves, the team will explore the benefits of the synergy model, which matches nurses’ strengths and competencies with patient and family characteristics. The team may conduct qualitative research studies to better understand the complex judgments charge nurses make when creating nurse patient assignments, with the goal of standardizing the process for sustainability and optimal outcomes.
In evaluating the overall projects experience, team members listed lessons learned and captured key ideas to use in future projects. (See Acuity tool: Lessons learned by clicking the PDF icon above). The team validated usefulness of the Iowa model in developing the tool and process, and recommended adopting a model for translating evidence into practice. Nurses on the team reflected that a highly satisfying aspect of the project was identifying a clinical issue and playing an active role in addressing it as valued partners in the change process.
Selected references
Choi J, Choi JE, Fucile JM. Power up your staffing model with patient acuity. Nurs Manage . 2011;42(9):40-3.
Duffield C, Diers D, O’Brien-Pallas L, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl Nurs Res . 2011;24(4):244-55.
Fram N, Morgan B. Ontario: linking nursing outcomes, workload and staffing decisions in the workplace: the Dashboard Project. Nurs Leadersh (Tor Ont). 2012;25(Spec No 2012): 114-25.
Hardin SR, Kaplow R, eds. Synergy for Clinical Excellence: The AACN Synergy Model for Patient Care . Sudbury, MA: Jones and Bartlett; 2005.
Harper K, McCully C. Acuity systems dialogue and patient classification system essentials. Nurs Adm Q . 2007;31(4):284-99.
Titler MG, Kleiber C, Steelman VJ, et al. The IOWA model of evidence-based practice to promote quality care. Crit Care Nurs Clin North Am. 2001;13(4):497-509.
The authors work at Indiana University Health Ball Memorial Hospital in Muncie. Michelle Kidd is a critical care clinical nurse specialist. Kimberly Grove, Melissa Kaiser, and Brandi Swoboda are direct- care nurses in the progressive care unit (PCU). Ann Taylor is nurse manager in the PCU.
29 Comments .
Hello, I would like to request permission to utilize the patient acuity tool in my DNP project.
Hello, I would like to request permission to use this tool as a reference in my BSN assignment.
Hello Kaitlynn, The authors of the article are happy to grant others permission to use the tool. Please be sure to credit the source. Best, Cheryl Mee MSN, MBA, RN, FAAN, Executive Editorial Director, American Nurse Journal
Would like permission to use this tool for our Acute Care Floor in northern MN. Having a lot of the same issues discuss prior to your implementing…. Assignment and staffing inconsistencies, teams of 5 plus, multiple unsafe staffing scenarios. Think this would be a huge help! Thank you!
Hi, Our unit (surgical unit) are currently doing brain storming and gathering ideas on how to improve our nurse:patient assignment. We are trying to develop a patient acuity tool which would suit our patient care environment. Hoping we could reference and use your tools with your permission.
Very much appreciated.
can you share your acuity tool. We are also trying to come up with a solution instead of the admin. staffing by census…..
Can you email me at [email protected] please to discuss? Thanks!
Yes, you may.
Hi, I would love to use this as a reference to adapt an appropriate acuity tool for the medical surgical unit at our hospital. I am hoping to be granted permission to use , with appropriate citations.
Dear Micaela,
The authors of the article are happy to grant others permission to use the tool. Please be sure to credit the source.
Cynthia Saver, MS, RN
Firstly, we would like to congratulate the authors of the New Tool and we wish to be granted to use the tool with citation of the authors. What about Chemotherapy, is it under the complicated IV drugs but it is not specified? Hope to be clarified about it. Thank you.
Ruhaina Ladja,
Thank you for your interest in the acuity tool. I would venture to say chemotherapy would be included in complicated IV drugs, but in the units for which we first developed this tool the nurses did not administer chemotherapy.
Thanks again, Michelle J Kidd, MS, APRN, ACNS-BC, CCRN-K
Hi there, I am seeking permission to utilize this patient acuity tool for our evidence-based project on our IMU/ICU unit. Thank you so much.
The authors of the article are happy to grant others permission to use the tool. Please be sure to credit the source. Cynthia Saver, MS, RN, Editorial director for American Nurse Journal
Does anyone have the contact information for the authors of this tool? I would like to use this tool for my DNP project and need permission to use.
I would like to request fro your permission to utilize this tool for a pilot project initiative in my department.
The authors of the article are happy to grant others permission to use the tool. Please be sure to credit the source. Cynthia Saver, MS, RN, Editorial director for American Nurse Journal.
I am requesting permission to use this tool Thank you
I am requesting permission to use this tool on my Med/Surg floor
Thank you, Tiffany Brisken, BSN, RN, PHN
I would love to use your tool on my floor which is cardiac. I am researching and hoping this will work for us.
Wendee, the author of the article is happy to grant permission for you to use the tool.
Cynthia Saver, MS, RN, Editorial director for American Nurse Journal.
Looking to obtain permission to use tool for QI project. Please let me know who to contact.
We did contact the authors, and they gave permission for the use of the tool. Thank you for your inquiry!
-Lydia Kim, Digital Content Editor at American Nurse Today
Hello Can you help me get an acuity tool that helps nurses?
Hello Ms. Kidd,
Can I get permission to use your acuity tool for my research? Hoping for your favorable response.
Kathy Carandang
I agree! I would love to see a follow up!
Any chance to see this “patient-acuity” tool? I am working on developing one for my unit.
Awesome, this is a HUGE help.
Would love to see the follow up on this article! The results only discuss nurse satisfaction after 1 month. What happened to the results from the other nurse-sensitive indicators discussed?
I would like to use your tool for my DNP project, how would I go about contacting the right person(s) to get permission? I would appreciate your feedback.
Comments are closed.

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

From the Midwest to the Middle East

Increasing diversity in nursing with support from Nurses on Boards Coalition

Adventures in lifelong learning

The power of language

Making peace with imperfection

When laws and nursing ethics collide

Taking on health disparities

Oncology nursing: Clinical assistant onboarding

Medication safety and pediatric health

Confidence is in

Tailored falls prevention plans

Men in nursing

Chylothorax: A stepwise approach to care

Aortic dissection

FAQs: AI and prompt engineering
CNA Report Sheet
Discover Carepatron's free CNA Report Sheet template. Use the free resource to streamline your daily patient reporting.

By Ericka Pingol on Jun 20, 2024.
Fact Checked by Nate Lacson.

What is a CNA Report Sheet Template?
Certified Nursing Assistants (CNAs) are integral players in healthcare, providing vital support to registered nurses and other medical staff. They work closely with patients, assisting with daily bathing, eating, and mobility.
In addition to these tasks, CNAs often take on an emotional support role, offering comfort and companionship to patients. Their contribution enables the smooth running of healthcare facilities and enhances the quality of patient care.
To better streamline their workflows, CNAs can use a CNA Report Sheet Template and document relevant patient information. This can include vital signs, medication schedules, and other important details that must be monitored closely.
These report sheets also serve as a tool for CNAs to communicate with other healthcare team members, ensuring that all necessary tasks are completed and patients receive the best care possible.
Printable CNA Report Sheet
Download this CNA Report Sheet to document relevant patient information and streamline their workflows.
How does it work?
Our printable CNA Report Sheet Template lets you create well-organized reports in minutes. It is fully digital and user-friendly, making clinical documentation a breeze. Follow the steps below to start using the template:
Step 1: Obtain a copy of the template
Download the free CNA Report Sheet Template using the link on this page. You can also get it from the Carepatron app or our resources library.
Step 2: Fill in the patient's details
Once you have opened the template, fill in the patient's name, room number, and other necessary information. This will help to identify the report when it is reviewed.
Step 3: Record vital signs and other observations
Use the designated sections on the report sheet to record essential measurements such as blood pressure, pulse rate, temperature, and respiratory rate. You can also add any observations or notes that may be relevant to the patient's condition.
Step 4: Document medication schedules
In this section, you can list all the medications prescribed for the patient and their corresponding schedule. This will help CNAs track when medications need to be administered and avoid errors.
Step 5: Include other important information
The report sheet also has sections for recording daily activities, dietary requirements, and any special instructions from the healthcare team. This ensures that all necessary tasks are completed and patients receive the best care possible.
Step 6: Save and share
Once you have completed filling in the report sheet, save it digitally or print a hard copy to share with other healthcare team members.
CNA Report Sheet example (sample)
Our team has written a sample CNA Report Sheet Template PDF to show you how it should be completed. This sample includes all the necessary sections and is designed to make the reporting process as easy and efficient as possible. You can view the sample here or download a PDF copy.
Download the free CNA Report Sheet example:

When would you use this template?
You can use this CNA Report Sheet Template in various healthcare settings, including hospitals, nursing homes, and home health care. It can also document patients' progress and communicate important information to other healthcare team members during a shift change or patient handoff.
Some other situations where this template can be helpful are:
When a new patient is admitted
Our free CNA Report Sheet Template can be used as an admission form for new patients. You can use it to collect all the necessary information about a patient, such as their medical history, current medications, and any specific care instructions from the healthcare team.
During rounds or check-ins
CNAs are responsible for monitoring patients' health and well-being throughout their shift. Our report sheet template can help you keep track of essential details, such as vital signs, changes in condition, and any concerns or observations you have made during rounds or check-ins.
When transferring a patient to another unit or facility
It is crucial to provide accurate and detailed information about their care needs if a patient is being transferred to another unit or healthcare facility. Our report sheet template can be a transfer form, helping you communicate essential information to the receiving healthcare team.
For end-of-shift reporting
As your shift ends, our report sheet template can assist you in providing a thorough and detailed report of your patient's conditions. This will help the incoming CNA have all the necessary information to provide continuity of care.
Benefits of using Carepatron's free CNA Report Sheet
Our printable CNA Report Sheet can streamline your documentation and make it easy to keep on top of your electronic health records. Here are some of the benefits of the template:
Easy to customize
Our template is fully customizable, allowing you to add or remove sections according to your facility's needs. You can also edit the categories and headings to suit your documentation style better.
Efficient and time-saving
Our CNA Report Sheet Template lets you quickly record vital signs, observations, concerns, and other essential details in one convenient location. This ensures that all necessary information is recorded accurately and saves you time from flipping through multiple pages.
Improved communication
Effective communication is crucial in the healthcare setting, especially regarding patient care. Our report sheet template makes it easy to transfer vital information and updates to other healthcare team members, promoting better coordination and quality patient care.
100% digital
Our CNA Report Sheet Template is a digital document accessed from any computer or device with internet access. This eliminates the need to carry physical copies or worry about lost documentation.
Tips for writing an effective CNA Report Sheet
To ensure that your CNA Report Sheet accurately reflects the patient's condition and helps with continuity of care, here are some tips to keep in mind:
● Use clear and concise language to avoid confusion or misinterpretation.
● Include only necessary information and avoid irrelevant details.
● Double-check for accuracy before submitting the report sheet.
● Keep the report sheet updated and communicate any changes or updates to the healthcare team.
● Use standard abbreviations and symbols for consistency and efficiency.
● Prioritize important information, such as allergies, current medications, and critical observations.
● Avoid using vague terms or subjective language.
● Remember to protect patient privacy by only sharing necessary information with authorized individuals.
● Seek guidance or clarification from a supervisor if unsure about any aspect of the report sheet.
Why use Carepatron as your CNA Report Sheet app?
Make the smart choice today - choose Carepatron, a comprehensive practice management software designed to streamline your healthcare processes.
With Carepatron, you can effortlessly manage patient records, appointments, billing, and communication, all within a single, easy-to-use interface. Our CNA Report Sheet Template app boasts advanced features such as automated reminders, intuitive scheduling, and secure online payments. Our HIPAA-compliant platform ensures your patient data remains confidential and safe.
Carepatron stands out from other CNA Report Sheet Template software because we focus on customization and flexibility. We understand that every healthcare practice has unique needs, and we strive to cater to those specific requirements. Our platform allows easy customization of templates, workflows, and reports, giving you complete control over your practice management processes.
Join the growing community of healthcare professionals who have chosen Carepatron as their go-to practice management software. Take the leap today and see the difference!
Commonly asked questions
CNAs use CNA Report Sheet Templates to document important patient information and provide a quick overview of their condition. These templates are used during shift changes, allowing for continuity of care and effective communication between CNAs.
A CNA Report Sheet typically includes patient demographics, vital signs, intake/output measurements, prescribed medication and treatment details, and any notes or observations made by the CNA during their shift.
Yes, with Carepatron, you can customize templates and workflows easily to meet your specific practice requirements. This ensures that your CNA Report Sheet Templates accurately reflect the information and data that is most important for your practice.
Related Templates
.jpeg)
Popular Templates

Join 10,000+ teams using Carepatron to be more productive

IMAGES
VIDEO
COMMENTS
4) PIE Charting. Similar to SOAP (IER), PIE is a simple acronym you can use to document specific problems (P), as well as their related interventions (I) and evaluations (E). Nurses write down their assessment on a separate form or flow sheet in the patient's chart and assign each individual problem a number.
Proper nurse charting skills are essential for compliance. Also called a medical record, health record, or patient chart, a medical chart refers to documentation that includes a patient's medical history and clinical data. This record or chart encompasses treatment plans, surgeries, medications, vital signs, diagnoses, and other information ...
Nursing Cheat Sheet. Medical records are essential documentation in every health care setting. They notate the instances of care between health care personnel and clients. These records serve multiple functions: they guide clinical decisions, act as a legal reference, are important for reimbursement, education, and auditing.
Enhanced patient care. With the assignment sheet, elevate your patient care strategies. This resource facilitates detailed documentation of vital signs, medications, and patient status, enabling nursing assistants to prioritize tasks effectively, resulting in a higher quality of care and improved outcomes. Collaborative workflow
The patient acuity tool. Each patient is scored on a 1-to-4 scale (1, stable patient; 2, moderate-risk patient; 3, complex patient; 4, high-risk patient) based on the clinical patient characteristics and the care involved (workload.) Each nurse scores his or her patients, based on acuity, for the upcoming shift and relays this information to ...
NOTE: Student-Patient or Student-Nurse assignments are required to be made with the Charge Nurse or Supervisor in advance of the clinical start time. ... and co-validating documentation. PLEASE LEAVE THIS SHEET POSTED FOR A COMPLETE DAY SO THAT PATIENTS WILL NOT BE ASSIGNED TO A SECOND NURSING STUDENT IN THE SAME DAY.
Tips for Patient Charting. Accurate and concise patient charting is an important part of a nurse's job. Through charting, nurses communicate vital information to the entire healthcare team. A patient chart is also a legal document that describes all aspects of a patient's care, including medications administered, services provided and ...
Patient Charting Assignment Sheet PART I-INSTRUCTIONS Interpret or translate the following charting entries into common English and medical terms as if you were reading it to another person. If you have completed the prescription exercises, translate the Rx as well or refer to Skill Sheet; if that Mod has not been completed, Rx may be omitted per instructor's instructions.
In simple terms, charting is documentation to have a record of patient status, medical services and more. It may include test results, medication history, health history and any procedures the patient has undergone throughout their lifetime. These data points allow everyone attending to the patient to provide the highest level of care. Other ...
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
Nursing notes are a narrative written summary of a given nursing care encounter. This might include a description of a nursing visit, a specific care event, or a summary of care. A nurse's note is a form of charting that describes the nurse's decision-making process regarding the nursing care provided. Nursing notes are an important part of ...
Clinical documentation refers to the creation of medical records that pertain to pati e nt healthcare. These documents may contain symptoms, diagnosis, assessment, treatment, and testing information. While there is no straightforward or universal standard for clinical documents, they are used by over 90% of health practitioners in the US and ...
Decide on the process. Now that you've gathered the information you need, you're ready to develop your plan for assigning nurses. This step usually combines the unit layout with your patient flow. Nurses typically use one of three processes—area, direct, or group—to make assignments. (See Choose your process.)
In 2021, significant changes were adopted for the documentation guidelines for outpatient evaluation and management (E/M) visit codes. Most notably, medical decision making or time became primary ...
A caregiver daily log is a written record of the tasks and activities performed by a caregiver during the course of a day. The log may be used to document the care provided to a patient or client, as well as to communicate information about the individual's needs and progress to other members of the care team. Table of Contents.
Step 1: Patient identification and chief complaint. Begin by obtaining the patient's identifying information, including name, date of birth, and gender. Prompt the patient to state their chief complaint, the primary reason for their visit, which guides subsequent assessment and treatment decisions.
Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do. Again with 6 to 7 patients things tend to run together. Nursing Report Sheets (Templates) Below are free for your to download nursing report sheet templates. You can print ...
1. A nursing narrative note allows nurses to give a detailed account of their patient's status, including changes in body systems and responses to treatments. 2. Narrative nurses' notes are easily combined with other types of documentation, such as graphs and flow sheets. 3.
Patient Charting Assignment-Victoria Day PART I - INSTRUCTIONS Interpret or translate the following charting entries into common English and medical terms as if you were reading it to another person.If you have completed the prescription exercises, translate the Rx as well or refer to Skill Sheet; if that Mod has not been completed, Rx may be omitted per instructor's instructions.
The Patient Tracking worksheet is where you will enter data related to patient contacts. The Caseload Overview worksheet provides a summary view of that data which can be used to identify and sort patients for psychiatric case review. On the Patient Tracking worksheet, some cells are shaded, and some are white. Enter information only
Then a PCU direct-care nurse approached the unit-based council (UBC) and asked for an evaluation of our acuity tool. The nurse manager and UBC agreed that equitable patient assignments and adequate unit staffing could be addressed by improving the tool. Following the Iowa model of evidence-based practice (EBP), the UBC formed a team of staff ...
History/Interview Sheet Interview to obtain: Patient's demographic data Medical and surgical history Family and social history Fill out interview sheets with the information provided. Scan interview sheet into the patient's EMR Review the charted information with the patient. √ √ A digital questionnair e filled in chronologic al order 2 ...
It can also document patients' progress and communicate important information to other healthcare team members during a shift change or patient handoff. Some other situations where this template can be helpful are: When a new patient is admitted. Our free CNA Report Sheet Template can be used as an admission form for new patients.