This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search

Search menu
Abdolrahimi M, Ghiyasvandian S, Zakerimoghadam M, Ebadi A. Therapeutic communication in nursing student: a Walker and Avant concept analysis. Electron Physician.. 2017; 9:(8)4968-4977 https://doi.org/10.19082/4968
Communication skills 1: benefits of effective communication for patients. 2017. https://tinyurl.com/y3nzu222 (accessed 10 August 2020)
Communication skills 3: non-verbal communication. 2018. https://tinyurl.com/y5ay4uhd (accessed 10 August 2020)
Bandura A. Self-efficacy: toward a unifying theory of behavior change. Psychol Rev.. 1977; 84:191-215 https://doi.org/10.1016/0146-6402(78)90002-4
Barratt J. Developing clinical reasoning and effective communication skills in advanced practice. Nurs Stand.. 2019; 34:(2)37-44 https://doi.org/10.7748/ns.2018.e11109
Bergdahl E, Berterö CM. Concept analysis and the building blocks of theory: misconceptions regarding theory development. J Adv Nurs.. 2016; 72:(10)2558-2566 https://doi.org/10.1111/jan.13002
Bloomfield J, Pegram A. Care, compassion and communication. Nurs Stand.. 2015; 29:(25)45-50 https://doi.org/10.7748/ns.29.25.45.e7653
Bramhall E. Effective communication skills in nursing practice. Nurs Stand.. 2014; 29:(14)53-59 https://doi.org/10.7748/ns.29.14.53.e9355
Brown R. An analysis of loneliness as a concept of importance for dying persons. In: McKenna H, Cutcliffe J (eds). Philadelphia (PA): Elsevier Churchill Livingstone; 2005
Burley D. Better communication in the emergency department. Emerg Nurse.. 2011; 19:(2)32-36 https://doi.org/10.7748/en2011.05.19.2.32.c8509
Cambridge University Press. Effective. 2018. https://tinyurl.com/y7dqcypc (accessed 10 August 2020)
Campbell JD, Lavallee LF. Who am I? The role of self-concept confusion in understanding the behavior of people with low self-esteem. In: Baumeister RF (ed). New York (NY): Plenum Press; 1993
Carment DW, Miles CG, Cervin VB. Persuasiveness and persuasibility as related to intelligence and extraversion. Br J Soc Clin Psychol.. 1965; 4:(1)1-7 https://doi.org/10.1111/j.2044-8260.1965.tb00433.x
Casey A, Wallis A. Effective communication: principle of nursing practice E. Nurs Stand.. 2011; 25:(32)35-37 https://doi.org/10.7748/ns2011.04.25.32.35.c8450
Daly L. Effective communication with older adults. Nurs Stand.. 2017; 31:(41)55-62 https://doi.org/10.7748/ns.2017.e10832
Department of Health and Social Care. Essence of care 2010: benchmarks for the fundamental aspects of care. 2010. https://tinyurl.com/y3z8grqe (accessed 10 August 2020)
Dithole KS, Thupayagale-Tshweneagae G, Akpor AO, Moleki MM. Communication skills intervention: promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs.. 2017; 16:(74)1-6 https://doi.org/10.1186/s12912-017-0268-5
Draper P. A critique of concept analysis. J Adv Nurs.. 2014; 70:(6)1207-1208 https://doi.org/10.1111/jan.12280
Duldt BW, Giffin K, Patton BR. Interpersonal communication in nursing: a humanistic approach.Philadelphia (PA): FA Davis; 1983
Fakhr-Movahedi A, Salsali M, Negharandeh R, Rahnavard Z. Exploring contextual factors of the nurse-patient relationship: a qualitative study. Koomesh.. 2011; 13:(1)23-34
Fleischer S, Berg A, Zimmermann M, Wuste K, Behrens J. Nurse-patient interaction and communication: a systematic literature review. J Public Health.. 2009; 17:339-353 https://doi.org/10.1007/s10389-008-0238-1
Foley A, Davis A. A guide to concept analysis. Clin Nurse Spec.. 2017; 31:(2)70-73 https://doi.org/10.1097/NUR.0000000000000277
Gadamer HG. Philosophical hermeneutics. Translated by DE Linge.Berkeley (CA): University of California Press; 1976
Gallagher L. Continuing education in nursing: a concept analysis. Nurse Educ Today.. 2007; 27:(5)466-473 https://doi.org/10.1016/j.nedt.2006.08.007
Ghafouri R, Rafii F, Oskouie F, Parvizy S, Mohammadi N. Nursing professional regulation: Rodgers' evolutionary concept analysis. Int J Med Res Health Sci. 2016; 5:(9S)436-442
Griffiths J. Person-centred communication for emotional support in district nursing: SAGE and THYME model. Br J Community Nurs.. 2017; 22:(12)593-597 https://doi.org/10.12968/bjcn.2017.22.12.593
Hazzard A, Harris W, Howell D. Taking care: practice and philosophy of communication in a critical care follow-up clinic. Intensive Crit Care Nurs.. 2013; 29:(3)158-165 https://doi.org/10.1016/j.iccn.2013.01.003
Jevon P. Clinical examination skills.Chichester: Wiley-Blackwell Publications; 2009
Jones A. The foundation of good nursing practice: effective communication. J Renal Nurs.. 2012; 4:(1)37-41 https://doi.org/10.12968/jorn.2012.4.1.37
Kelton D, Davis C. The art of effective communication. Nurs Made Incred Easy.. 2013; 11:(1)55-56 https://doi.org/10.1097/01.NME.0000423378.98763.96
Kourkouta L, Papathanasiou IV. Communication in nursing practice. Mater Sociomed.. 2014; 26:(1)65-67 https://doi.org/10.5455/msm.2014.26.65-67
McCabe C. Nurse patient communication: an exploration of patients' experiences. J Clin Nurs.. 2004; 13:41-49 https://doi.org/10.1111/j.1365-2702.2004.00817.x
McCabe C, Timmins F. Communication skills for nursing practice, 2nd edn. Basingstoke: Palgrave; 2013
McCarthy DM, Buckley BA, Engel KG, Forth VE, Adams JG, Cameron KA. Understanding patient-provider conversations: what are we talking about?. Acad Emerg Med.. 2013; 20:(5)441-448 https://doi.org/10.1111/acem.12138
McCroskey JC, Richmond VP. Willingness to communicate: differing cultural perspectives. South Commun J.. 1990; 56:(1)72-77 https://doi.org/10.1080/10417949009372817
McCuster M. Apathy: who cares? A concept analysis. Ment Health Nurs.. 2015; 36:693-697 https://doi.org/10.3109/01612840.2015.1022844
McKenna HP. Nursing theories and models.London: Routledge; 1997
McKinnon J. The case for concordance: value and application in nursing practice. Br J Nurs.. 2013; 22:(13)16-21 https://doi.org/10.12968/bjon.2013.22.13.766
Miller L. Effective communication with older people. Nurs Stand.. 2002; 17:(9)45-50 https://doi.org/10.7748/ns2002.11.17.9.45.c3298
Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital settings: a qualitative systematic review protocol. JBI Database System Rev Implement Rep.. 2015; 13:(1)76-87 https://doi.org/10.11124/jbisrir-2015-1072
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci.. 2016; 8:(6)65-74 https://doi.org/10.5539/gjhs.v8n6p65
Nuopponen A. Methods of concept analysis: a comparative study. LSP.. 2010; 1:(1)4-12
Nursing and Midwifery Council. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. 2018. https://tinyurl.com/zy7syuo (accessed 10 August 2020)
O'Hagan S, Manias E, Elder C What counts as effective communication in nursing? Evidence from nurse educators' and clinicians' feedback on nurse interactions with simulated patients. J Adv Nurs.. 2013; 70:(6)1344-1355 https://doi.org/10.1111/jan.12296
Orem DE. Nursing: concepts of practice, 4th edn. St. Louis (MO): Mosby-Year Book; 1991
Oxford University Press. Communication. 2018. https://tinyurl.com/y7k22yxb (accessed 10 August 2020)
Communication barriers. 2016. https://tinyurl.com/y3sn342h (accessed 10 August 2020)
Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf.. 2014; 23:(8)678-689 https://doi.org/10.1136/bmjqs-2013-002437
Rodgers BL. Concepts, analysis and the development of nursing knowledge: the evolutionary cycle. J Adv Nurs.. 1989; 14:(4)330-335 https://doi.org/10.1111/j.1365-2648.1989.tb03420.x
Rodgers BL, Knafi KA. Concept development in nursing: foundations, techniques and applications, 2nd edn. Philadelphia (PA): WB Saunders; 2000
Royal College of Nursing. Communication-end of life care. 2015. https://tinyurl.com/go28vsm (accessed 10 August 2020)
Schirmer JM, Mauksch L, Lang F Assessing communication competence: a review of current tools. Fam Med.. 2005; 37:(3)184-192
Skär L, Söderberg S. Patients' complaints regarding healthcare encounters and communication. Nurs Open.. 2018; 5:(2)224-232 https://doi.org/10.1002/nop2.132
Snowden A, Martin C, Mathers B, Donnell A. Concordance: a concept analysis. J Adv Nurs.. 2014; 70:(1)46-59 https://doi.org/10.1111/jan.12147
Tay LH, Ang E, Hegney D. Nurses' perceptions of the barriers in effective communication with inpatient cancer adults in Singapore. J Clin Nurs. 2011; 21:(17-18)2647-2658 https://doi.org/10.1111/j.1365-2702.2011.03977.x
Thompson CJ. Nursing theory and philosophy terms: a guide.South Fork (CO): CJT Consulting and Education; 2017
Tofthagen R, Fagerstrøm LM. Rodgers' evolutionary concept analysis – a valid method for developing knowledge in nursing science. Scand J Caring Sci. 2010; 24:21-31 https://doi.org/10.1111/j.1471-6712.2010.00845.x
Nursing, admission assessment and examination. 2018. https://tinyurl.com/y4ykv2uo (accessed 10 August 2020)
Walker LO, Avant KC. Strategies for theory construction in nursing, 5th edn. Norwalk (CT): Appleton and Lange; 2011
Webb L. Exploring the characteristics of effective communicators in healthcare. Nurs Stand.. 2018; 33:(9)47-51 https://doi.org/10.7748/ns.2018.e11157
Wikström B, Svidén G. Exploring communication skills training in undergraduate nurse education by means of a curriculum. Nurs Rep.. 2011; 1:(1) https://doi.org/10.4081/nursrep.2011.e7
Effective communication between nurses and patients: an evolutionary concept analysis
Dorothy Afriyie
Student Nurse, University of West London, Brentford
View articles · Email Dorothy

Communication can be considered as the basis of the nurse-patient relationship and is an essential element in building trust and comfort in nursing care. Effective communication is a fundamental but complex concept in nursing practice. This concept analysis aims to clarify effective communication and its impact on patient care using Rodgers's (1989) evolutionary framework of concept analysis. Effective communication between nurses and patients is presented along with surrogate terms, attributes, antecedents, consequences, related concepts and a model case. Effective communication was identified to be a multifactorial concept and defines as a mutual agreement between nurses and patients. This influences the nursing process, clinical reasoning and decision-making. Consequently, promotes high-quality nursing care, positive patient outcome and patient's and nurse's satisfaction of care.
Communication is an essential element of building trust and comfort in nursing, and it is the basis of the nurse–patient relationship ( Dithole et al, 2017 ). Communication is a complex phenomenon in nursing and is influenced by multiple factors, such as relationship, mood, time, space, culture, facial expression, gestures, personal understanding and perception ( McCarthy et al, 2013 ; Kourkouta and Papathanasiou, 2014 ). Effective communication has been linked to improved quality of care, patient satisfaction and adherence to care, leading to positive health outcomes ( Burley, 2011 ; Kelton and Davis, 2013 ; Ali, 2017 ; Skär and Söderberg, 2018 ). It is an important part of nursing practice and is associated with health promotion and prevention, health education, therapy and treatment as well as rehabilitation ( Fakhr-Movahedi et al, 2011 ). The Nursing and Midwifery Council (NMC) (2018) emphasised effective communication as one of the most important professional and ethical nursing traits. Nonetheless, communication remains a complicated phenomenon in nursing, and most patient-reported complaints in healthcare are around failed communication ( Reader et al, 2014 ). The aim of the present concept analysis is to explore and clarify the complexity of establishing effective communication between nurses and patients in practice.
Concept analysis
Concept analysis is the foundation and preparatory phase of nursing research ( Walker and Avant, 2011 ). Concept analysis aids in clarifying concepts in nursing by using simpler elements to reduce ambiguity and identify all aspects of a concept ( Nuopponen, 2010 ; Foley and Davis, 2017 ). Draper (2014) criticised concept analysis as being methodologically weak and philosophically dubious, further arguing that there is no evidence of its contribution to patient care. However, concept analysis facilitates the review of literature on a concept of interest, thereby enabling a thorough examination of the concept ( Bergdahl and Berterö, 2016 ). This helps in understanding the concept and, therefore, applying it appropriately. Correspondingly, understanding key concepts in nursing practice enables the nurse to identify strategic interventions that could benefit patients. Although McKenna (1997) argued that there is no definite meaning of a concept because they are experienced and perceived differently by people, Walker and Avant (2011) highlighted that the ability of the nurse to describe concepts in an exploratory way is an important means to demonstrate evidence base in practice. Nursing is an evidence-based practice; hence it is the responsibility of the nurse to keep up-to-date with quality evidence and demonstrate it in practice ( Thompson, 2017 ). Therefore, it is paramount for nurses to understand concept analysis and be able to analyse key concepts in nursing.
This concept analysis aims to clarify the concept of effective communication and address the gap in knowledge using Rodgers's (1989) theoretical framework. The evolutionary method of concept analysis was chosen because it adopts a systematic approach with focused phases ( Tofthagen and Fagerstrøm, 2010 ). Rodgers's (1989) method is perceived as a simultaneous task approach, which does not seek boundaries to restrict a concept and considers its application within multiple contexts ( Gallagher, 2007 ). However, the framework will be used because it facilitates an exploration and deep comprehension of a concept ( McCuster, 2015 ). Additionally, the framework offers an alternative to a positivist approach to concepts, allowing different findings depending on the situation ( Ghafouri et al, 2016 ). Moreover, the framework provides an opportunity to identify attributes and related features in a manner that minimises bias ( McCuster, 2015 ). Effective communication between patients and nurses was analysed using the seven phases of Rodgers's (1989) evolutionary method ( Box 1A ). Further, the following four questions were addressed ( Box 1B ).
Box 1A.Rodgers's method of analysis (1989)
Box 1B.Rationale for the four focused questionsThe focus questions were driven by the Rodgers's (1989) framework of concept analysis; the four questions are aimed at analysing the concept of effective communication using the seven stages of the framework in a systematic manner to engender an understanding of effective communication
- What is effective communication?
- What are the surrogate terms and related use of the concept of effective communication?
- What attributes, antecedents and consequences apply to the concept of effective communication?
- Who benefits from effective communication between nurses and patients?
Identifying the appropriate realm for data collection
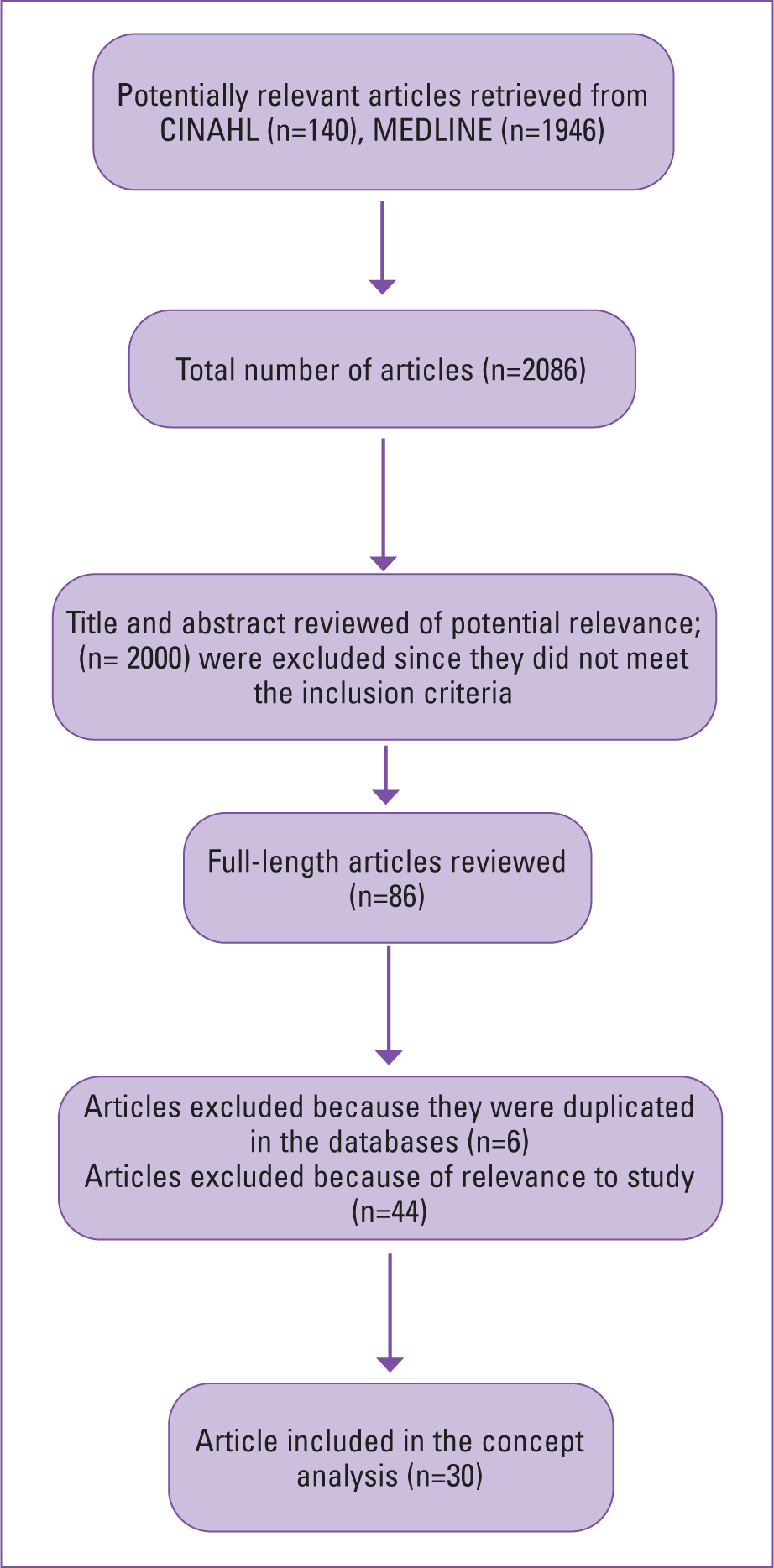
As endorsed by Brown (2005) , a comprehensive review of the literature was conducted for this analysis. Explicit inclusion and exclusion criteria were used to select relevant articles, as recommended by Tofthagen and Fagerstrøm (2010) . Two electronic databases-Cumulative Index for Nursing and Allied Health (CINAHL) and MEDLINE (Ovid)-were searched using the keywords ‘effective communication’ and ‘nurses’ and ‘patients’. The inclusion criteria allowed selection of only peer-reviewed academic journals written in the English language. Studies exploring or analysing effective communication among nurses and patients with underlying communication difficulties and cognitive disabilities were excluded, because it is likely that such patients or nurses represent a special challenge in communicating. Only articles exploring effective communication and factors that influence communication between nurses and patients were considered. A total of 2086 articles were retrieved from the databases, and these articles were screened for relevance by reading the abstract. Finally, 30 articles were determined to meet the inclusion criteria for the analysis ( Figure 1 ). The articles selected were published between 1965 and 2019.
Defining effective communication
The Cambridge English dictionary defines ‘effective’ as ‘successful or achieving the results that you want’ ( Cambridge University Press, 2018 ). According to the Oxford English Dictionary, communication is ‘imparting or exchanging information by speaking, writing or using some other medium’ ( Oxford University Press, 2018 ). The Department of Health and Social Care (2010) described communication as the meaningful exchange of facts, needs, opinions, thoughts, feelings or other information between two or more people. Further, communication can be face-to-face, over the phone or by written words. McCabe and Timmins (2013) also described communication as a cyclical and dynamic process, involving transmission, receiving and interpretation of information between people using verbal or non-verbal means. Rani (2016) simply described communication as ‘sharing meaning’.
Interestingly, Hazzard et al (2013) described communication as a primary condition of human consciousness. They further explained that people always identify themselves in a communicative state. This would imply that people are always exchanging information. The authors, however, described communication as the actions taken after speaking to someone; this highlights communication as responsive. This may be the action and reaction people adopt after a communicated request or statement. Nonetheless, Gadamer (1976) , a twentieth-century philosopher, highlighted communication as what we are and not just what we do. Kourkouta and Papathanasiou (2014) defined communication as the use of speech or other means to exchange information, thoughts and feelings among people. Therefore, effective communication may be classified as exchanging information, thoughts and feelings using either verbal or non-verbal expressions to successfully produce a desired or intended result.
Effective communication between nurses and patients may be analysed from both the nurse's and the patient's perspective. McCabe (2004) identified that the patients' perspective of effective communication entails patient-centred interaction. On the other hand, O'Hagan et al (2013) found that nurses' perspective of effective communication revolves around time, task, rapport and patients' agreement on what has been communicated. Although both perspectives appear to differ, they are both driven by the expectations of the patient and nurse. A nurse may ultimately identify effective communication as the ability to engage with patients and to achieve clinical goals. Similarly, patients may be influenced by their expectation regarding their management outcome ( Schirmer et al, 2005 ). Therefore, effective communication between nurses and patients may be defined as mutual agreement and satisfaction with care (provided and received).
Surrogate terms and relevant uses
The terms most commonly serving a manifestation of effective communication include: therapeutic communication, interpersonal relationship, intercommunication, interpersonal communication and concordance. From a literature search, these terms appear frequently, highlighting their close usage with the concept of effective communication ( Fleischer et al, 2009 ; Casey and Wallis, 2011 ; Jones, 2012 ; Bloomfield and Pegram, 2015 ; Daly, 2017 ). For example, through intercommunication or interpersonal communication, a nurse can encourage a patient to participate in their care decision-making. However, a patient's acceptance to engage in shared decision-making regarding care and agree with a negotiated care plan could reflect effective communication. This act of mutual agreement through negotiation and shared decision-making suggests concordance ( Mckinnon, 2013 ; Snowden et al, 2014 ). Abdolrahimi et al (2017) pointed out that therapeutic communication is the basis for effective communication. They highlighted therapeutic communication as an important means for establishing interpersonal relationships. These concepts are different from effective communication; however, these notions express an idea of the concept of effective communication and highlight an understanding of effective communication as emphasised by Rodgers (1989) .
Daly (2017) described communication as dynamic and cyclical, because it involves a process of transmission, receiving and interpretation through verbal or non-verbal means. This reflects the complexity of communication, which involves speaking, being heard, listening, understanding or being accepted, as well as being seen and acknowledged. Hence, assessing factors that could affect communication, such as noise or interference, is always crucial for effective communication ( McCabe and Timmins, 2013 ; Webb, 2018 ). Daly (2017) explained that other skills for effective communication, which are consciousness, compassion, competence, professionalism and person-centredness, are all important concepts in nursing studies and practice. This indicates that communication is intentional in nature, so the purpose and perspective of individuals involved should be valued and respected ( Jones, 2012 ). In the case of the nurse–patient relationship, a nurse must consider a patient's perspective, background and concerns when communicating. It is important for a nurse to be competent, ethical and professional and exhibit an individualised approach in communicating with patients ( Bramhall, 2014 ; Bloomfield and Pegram, 2015 ). For example, when communicating with a patient with no medical background, medical terms should be explained further or avoided. This promotes person-centredness, which is a determinant for effective communication for patients.
A nurse must respect human rights and be professional ( NMC, 2018 ). However, it can be challenging when communicating with a patient who does not want to communicate about their health, which reflects their right to autonomy. Nonetheless, it is paramount for a nurse to identify the purpose of communication and the difficulties, so that they can mitigate them as part of their professional and ethical duties ( Royal College of Nursing, 2015 ; NMC, 2018 ). This can be done by reassuring and encouraging patients. Correspondingly, this act of communication features in Duldt et al's (1983) theory of humanistic nursing communication. This theory is reflected in Bramhall (2014) and Kourkouta and Papathanasiou's (2014) exploration on communication in nursing. The theory explains the need for comprehensive and exclusive communication among nurses and clients as well as colleagues. The focus of the theory is on interpersonal communication and emphasises the need for humanistic approaches to help improve professional communication. These approaches include empathy, deeper respect, encouragement and interpersonal relationship. For example, listening to people, providing privacy when communicating, giving patients ample time, using kind and courteous words such as ‘please’ and ‘thank you’, as well as being frank and honest when communicating. All these approaches may promote effective communication between nurses and patients ( Jevon, 2009 ; Bramhall, 2014 ; Bloomfield and Pegram, 2015 ).
Further, Miller (2002) , Burley (2011) , Casey and Wallis (2011) , Jones (2012) Bloomfield and Pegram (2015) and Daly (2017) demonstrated how effective communication is key in the assessment, planning and implementation of personalised nursing care. Holistic assessment in nursing includes history-taking, general appearance, physical examination, vital signs and documentation ( Toney-Butler and Unison-Pace, 2018 ). Patient assessment aids in identifying the communication needs of a patient in order to promote person-centred care ( Toney-Butler and Unison-Pace, 2018 ). Moreover, non-verbal cues such as general appearance or posture are vital in communication, and understanding them could help in the assessment process. General appearance such as facial expressions, dressing, hair or skin integrity may convey information that may be helpful in the nursing assessment process. Although not ideal, however, appearance can be a powerful transmitter of intentional or unintentional messages ( Ali, 2018 ). For instance, a nurse may sense neglect or abuse when a patient appears physically unkempt, with bruises or sores. This may inform the nurse on appropriate questions to ask during history-taking in order to ascertain the patient's situation and safeguard, signpost or refer them for support if necessary. Nurses' ability to identify these concerns may aid in providing the best necessary care for their patients. This promotes person-centredness, which is perceived as a means of effective communication by patients ( McCabe, 2004 ).
Effective communication promotes comprehensive history-taking. History-taking involves communicating with patients to collect subjective data and using this information to determine management plans ( Jevon, 2009 ). In history-taking, inaccurate information may be collected when communication is not effective ( Burley, 2011 ; Jones, 2012 ; Daly, 2017 ). However, it is important for nurses to establish good personal relationships with patients, so the latter can feel comfortable in sharing their complaints ( Casey and Wallis, 2011 ). It needs to be noted that, since patients are experts in their own lives, the nurse's ability to make patients feel comfortable may encourage patients to share valuable information, as well as their expectations, concerns and fears. Effective communication is important if nurses are to implement their roles effectively with regard to holistic assessment, considering the subjective experience and characteristics of their patient. Further, a well-informed collaborative assessment through effective communication may contribute to positive patient management outcomes ( Kourkouta and Papathanasiou, 2014 ). For instance, a patient may convey all necessary information to a nurse during assessment, and this may inform the nurse and patient of the necessary examination and investigations to aid in evidence-based nursing diagnosis and a collaborative management plan. The ability to establish a mutual agreement for the nursing process suggests effective communication for both parties.
Effective communication aids in planning and implementing personalised care. It helps patients to set realistic goals and choose preferred management for better outcomes. Communication is a bidirectional process in which a sender becomes a receiver and vice versa ( Kourkouta and Papathanasiou, 2014 ). Therefore, there is a need for both patients and nurses to realise that they are partners in communicating care planning and implementation ( Bloomfield and Pegram, 2015 ). This realisation may promote the patient's dignity and may also influence patients' desire to adhere to their plan when they feel involved in decision-making ( Casey and Wallis, 2011 ). Conversely, patients may be reluctant and unhappy if they feel dictated to or patronised. Most importantly, involving patients through effective communication can empower them to have full control over their health and wellbeing. This is reflected in the self-care theory proposed by Orem (1991) and the theory of self-efficacy proposed by Bandura (1977) . These theories focus on the role of the individual in initiating and sustaining change and healthy behaviours. Orem (1991) reinforced the importance of communication, as self-care is learned through communication and interpersonal relationships.
Attributes of effective communication
Certain attributes can be used to develop a definition of effective communication that is more realistically reflective of how patients and nurses use the term in healthcare settings ( Rodgers and Knafi, 2000 ). The most common attributes identified in the literature include: effective communication as ‘a building foundation for interpersonal-relationship’, ‘a determinant of promoting respect and dignity’, ‘a precedent of achieving concordance’, ‘an important tool in empowering self-care in patient’, ‘a significant tool in planning and implementing person-centred care’ and ‘a determinant of clinical reasoning and the nursing process’ ( Casey and Wallis, 2011 ; Jones, 2012 ; McCabe and Timmins, 2013 ; Bramhall, 2014 ; Bloomfield and Pegram, 2015 ; Daly, 2017 ; Webb, 2018 ; Barratt, 2019 ). These attributes make it possible to identify situations that can be categorised under the concept of effective communication.
Antecedents of effective communication
According to the literature, antecedents to effective communication include: personality trait, perceived communication competence and level of education on communication. Personality traits were linked with communication in early research. Carment et al (1965) demonstrated that people who are introverts are less likely to communicate well compared with extroverts. McCroskey and Richmond (1990) also indicated that people with low self-esteem are less willing to communicate. This is because they are more sensitive to environmental cues ( Campbell and Lavallee, 1993 ). Additionally, McCroskey and Richmond (1990) asserted that people who perceived themselves as poor communicators may be less willing to communicate. Nonetheless, people who may be very capable of communicating may not be willing to, due to low self-esteem, anxiety or fear. As a result, such people may have low communication efficacy despite having high actual competence ( McCroskey and Richmond, 1990 ). Therefore, it is important for nurses to consider these factors when communicating with patients in order to identify their communication needs and manage them accordingly ( Daly, 2017 ). Furthermore, Dithole et al (2017) and Norouzinia et al (2016) highlighted that the nurse's level of education on communication may influence the ability to communicate effectively. Thus, incorporation of targeted communication skills education in the training curriculum and on-the-job training will empower nurses to communicate effectively with their patients.
Consequences of effective communication
The consequences of effective communication can be classified into patient–nurse-related and healthcare system-related outcomes. Skär and Söderberg (2018) mentioned that effective communication ensures a good healthcare encounter for patients. In the community settings, effective communication empowers patients to talk about their concerns and expectations ( Griffiths, 2017 ). Further, effective communication promotes a pleasant and comfortable hospital experience for patients as well as their families; this can also be reflected in the community settings, where patients may report pleasant and comfortable nursing care ( Newell and Jordan, 2015 ; Barratt, 2019 ). Kourkouta and Papathanasiou (2014) and Wikström and Svidén (2011) pointed out that the success of a nurse mostly depends on how effectively they can communicate with their patient. Conversely, ineffective communication may lead to unsuccessful outcomes. For example, a patient may convey their fears, signs and symptoms to a nurse and how the nurse decodes and applies the information may influence the intervention given ( Kourkouta and Papathanasiou, 2014 ). Likewise, a nurse may convey a piece of information to a patient, but the patient's understanding of the information will determine their action. Therefore, how the message is understood determines the action taken ( Kourkouta and Papathanasiou, 2014 ). Additionally, through effective communication, a patient may be empowered to have full control over their health and wellbeing ( Newell and Jordan, 2015 ) and may not require extended care. Clearly, effective communication can lead to positive and cost-saving consequences for patients, nurses and the healthcare system.
The final phase of Rodgers's (1989) method of analysis highlights an application of the concept in an exploratory case scenario. A model case for effective communication between a nurse and a patient is given in Box 2 . This case portrays effective communication between a nurse and a patient, revealing some surrogate terms, defining attributes, antecedents and consequences of the concept. The case model highlighted Audrey's positive engagement in her care decision-making when the nurse Dani communicated effectively. Dani visited Audrey in her home, where Audrey had spatial and environmental control, but she was reluctant to engage in her own care. Audrey perceived that other nurses did not involve her in her care decision-making. This indicates ineffective communication and may be attributed to factors such as age difference, generational gap, gender and culture and ethnic differences between Audrey and the other nurses ( Tay et al, 2011 ; Norouzinia et al, 2016 ).
Box 2.Model caseAudrey, a 90-year-old housebound patient with bilateral leg ulcers was visited by Dani, a 45-year-old community staff nurse working in a diverse multicultural district nursing team. On arrival, Dani introduced herself in a suitable tone, maintaining eye contact. Audrey responded in a low tone, without maintaining eye contact. Audrey appeared to be quiet and in a low mood; Dani identified this nonverbal cue and was determined to engage Audrey in conversation. Dani knew from her experience that leg ulcer treatment can affect a person's mental health, causing low self-esteem, fear and anxiety. Dani asked how Audrey felt and if there was something she could help her with. Audrey mentioned she was fine; her carers had visited and supported her with personal care, breakfast and medication, she had been waiting for the nurse's visit. Dani asked Audrey about her ulcers and how she felt about her dressings; Audrey mentioned she was fine, but expressed concerns about the ulcers not healing. Dani reassured Audrey, explained leg ulcers to her and advised Audrey about some effective practice to promote the healing process.Dani asked Audrey ‘How best can I help you, and how do you want your care to be delivered?’. Audrey responded, ‘You are the nurse, you know better’. Dani took ample time to explain to Audrey how she understands her own body better than any other person. Dani also reassured and encouraged Audrey that her opinions mattered, as this helped empower her, promoted her dignity and informed the nurse on how to care for her. Audrey then expressed to Dani that her other nurses, who are much younger than Dani, never ask her opinion regarding the ulcer management; hence, she was not willing to speak. Audrey mentioned that those nurses came in to re-dress her ulcers and they spoke to her about the care plan, but she did not feel involved in decision-making about her care. Audrey then mentioned that she did not mean to create problems or report anyone. Dani reassured Audrey that there would be no trouble, so she should not be afraid to speak up. Audrey thought that having an honest communication about her needs and views could create problems for her or for the nurses if it seemed that she had reported them.Dani then reassured and encouraged Audrey that the situation will be addressed in a professional manner, and none of the other nurses would feel they had been reported; however, they would involve her in her care and decision-making, which is the expectation. Audrey was then comfortable, communicated in a suitable tone and maintained eye contact with Dani. She asked Dani if she could bandage her right leg first, as she tends to be in pain for a long time when the left one is dressed first. Dani gained consent from Audrey, explained the procedure and advised Audrey to stop her whenever she experienced pain. Dani also asked Audrey a bit more about her pain and her analgesia. Dani identified that Audrey's analgesia had not been reviewed for over 3 years. Dani explained to Audrey that she would be making a referral to her GP about this matter. Audrey was very pleased and indicated she was happy with how Dani had communicated with her; she felt she could trust her. Dani was also pleased, because she could provide the best care for Audrey.
Another important factor that can affect effective communication is the environmental factor. Norouzinia et al (2016) revealed that the hospital environment is a barrier to effective communication for patients. Additionally, Tay et al. (2011) indicated the possibility of unilateral communication due to the hierarchical structure of the hospital environment. Conversely, although nurses may feel quite comfortable in the hospital or inpatient setting, they might feel relatively intimidated when visiting a patient's home. Therefore, an awareness of the contextual discomfort and how it may affect communication is important and should be considered when planning for effective two-way communication between the nurse and patient during home visits. Although all these factors are important in communication, a full discussion of these is beyond the scope of this paper and should be the focus of another complete work.
In the model case described in Box 2 , the nurse acknowledged that she was privileged to be a guest in Audrey's home, and she tailored her strategy to gain Audrey's perspective. The nurse's aim was to get Audrey involved in her care decision-making since Audrey knows herself best. Additionally, Audrey's participation in the decision-making made it possible for her to receive her preferred care. This shows that effective communication is bidirectional, and both partners (nurse and patient) must work together to achieve their desired outcomes, in this case, the patient's satisfaction with care and the nurse's ability to provide the best care.
Effective communication in nursing is clearly a complex, multidimensional and multifactorial concept. Factors such as emotions, general appearance, personality trait, mood and level of education on communication may influence the practice and outcome of effective communication. However, effective communication is an ultimate determinant of success for a nurse. Effective communication was defined as a mutual agreement and satisfaction of care for both patients and nurses. It has been linked to precede the achievement of concordance in patients, and in nurses, it influences clinical reasoning and the nursing process. This aids in implementing compassionate person-centred care and, when successful, it promotes positive patient outcomes and satisfaction with nursing care. Thus, effective communication is an important concept to prioritise in nursing education and practice. For this reason, engaging nurses in communication skills and on-the-job training will empower them to communicate effectively with their patients. As endorsed by Rodgers's (1989) , the outcome of this analysis is not the endpoint of the concept but should direct the future exploration of effective communication. Therefore, a systematic study of effective communication between nurses and patients as well as a systematic review considering effective communication among nurses and patients with underlying communication difficulties, cognitive disabilities and intercultural perspectives can ultimately enhance nursing science.
- Effective communication is a key component of nursing practice
- Effective communication is intentional in nature and can be improved through direct actions taken by the nurse
- Communication is a complex phenomenon and is an essential element of building trust and comfort in nursing
- Concept analysis is the basic way of understanding complex concepts and developing different meanings and perceptions
CPD REFLECTIVE QUESTIONS
- How might concept analysis be relevant in nursing studies or practice?
- What does effective communication mean to you?
- What are some challenges nurses face in communicating effectively?
- How can an interpersonal relationship between nurses and patients influence effective communication?
Communication Skills
- First Online: 24 January 2019
Cite this chapter
- Stephanie Fry 3 ,
- Kathryn Burrell 3 &
- Tamie Samyue 3
1721 Accesses
Communication is a vital component of the nursing role and is essential for the delivery of successful, quality healthcare. Good interpersonal communication increases the accuracy of information shared between nurse and patient and can amplify elements that are crucial in achieving positive health outcomes.
Effective and open communication is a key factor when liaising with a multidisciplinary team and can result in a collaborative and collegial approach to patient care.
Health literacy needs to be considered when communicating with patients. Knowledge of how to ensure patients understand basic health information will enable the delivery of information that is appropriate, effective and tailored to the individual’s needs.
In this chapter, the practical skills required to facilitate good communication will be reviewed and common barriers to communication explored, along with how to maintain effective communication via telephone and electronic mail. Communicating effectively within a professional capacity will also be discussed.
The importance of health literacy and the impact it has on communication with the patient will be highlighted and practical ways of providing information and education to patients explored.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Adams RL, Appleton SL, Hill CL, Dodd M, Findlay C, Wilson DH (2009) Risks associated with low functional health literacy in an Australian population. Med J Aust 191(10):530–534
PubMed Google Scholar
Australian Commission on Safety and Quality in Health Care (2014) Health literacy: taking action to improve safety and quality. ACSQHC, Sydney
Google Scholar
Balzer-Riley J (2017) Communication in nursing, 8th edn. Elsevier, Missouri
Burgoon JK, Guerrero LK, Floyd K (2016) Nonverbal communication. Routledge, New York
Book Google Scholar
Carlisle A, Jacobson KL, Di Francesco L, Parker R (2011) Practical strategies to improve communication with patients. Pharm Ther 36(9):576–589
Centre for Health Care Strategies (2013) Society of Hospital Medicine: how is health literacy identified? http://www.chcs.org/media/How_is_Low_Health_Literacy_Identified.pdf . Cited 15 Mar 2017
Crohn’s and Colitis Australia (2016) Australian IBD standards: standards of healthcare for people with inflammatory bowel disease in Australia. https://www.crohnsandcolitis.com.au/ibdqoc/ibd-audit-report/ . Cited 27 Mar 2017
del Rio-Lanza AB, Suarez-Alvarez L, Suarez-Vazquez A, Vasquez-Casielles R (2016) Information provision and attentive listening as determinants of patient perceptions of shared decision-making around chronic illness. Springerplus 5:1386
Article Google Scholar
Iedema R, Manidis M (2013) Patient-clinician communication: an overview of relevant research and policy literatures. Australian Commission on Safety and Quality in Health Care and UTS Centre for Health Communication, Sydney
Kessels R (2003) Patients’ memory for medical information. J R Soc Med 96(5):219–222
PubMed PubMed Central Google Scholar
Knox R, Cooper M (2015) The therapeutic relationship in counselling and psychotherapy. Sage, New York
Miller WR, Rollnick SR (2013) Motivational interviewing: helping people change, 3rd edn. The Guildford Press, New York
O’Connor M, Bager P, Duncan J, Gaarenstroom J, Younge L, Détré P et al (2013) N-ECCO consensus statements on the European nursing roles in caring for patients with Crohn’s disease or ulcerative colitis. J Crohn’s Colitis 7(9):744–764
O’Daniel M, Rosenstein A (2008) Professional communication and team collaboration. In: Hughes RG (ed) Patient safety and quality: an evidence-based handbook for nurses. Agency for Healthcare Research and Quality, Rockville, pp 271–284
Panes J, O’Connor M, Peyrin-Biroulet L, Irving P, Petersson J, Colombel JF (2014) Improving quality of care in inflammatory bowel disease: what changes can be made today? J Crohn’s Colitis 8:919–929
Pulvirenti M, McMillan J, Lawn S (2011) Empowerment, patient centred care and self management. Health Expect 17:303–310
Rollnick S, Miller WR, Butler CC (2008) Motivational interviewing in health care: helping patients change behaviour. The Guildford Press, New York
Watts S, Stevenson C, Adams M (2016) Improving health literacy in patients with diabetes. Nursing 47(1):24–31
Download references
Author information
Authors and affiliations.
Department of Gastroenterology, St Vincent’s Hospital (Melbourne), Fitzroy, VIC, Australia
Stephanie Fry, Kathryn Burrell & Tamie Samyue
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stephanie Fry .
Editor information
Editors and affiliations.
DRK Kliniken Berlin Westend, Department of Gastroenterology, Berlin, Germany
Andreas Sturm
Gastroenterology Level 5, John Radcliffe Hospital, Oxford, UK
Lydia White
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Fry, S., Burrell, K., Samyue, T. (2019). Communication Skills. In: Sturm, A., White, L. (eds) Inflammatory Bowel Disease Nursing Manual. Springer, Cham. https://doi.org/10.1007/978-3-319-75022-4_37
Download citation
DOI : https://doi.org/10.1007/978-3-319-75022-4_37
Published : 24 January 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-75021-7
Online ISBN : 978-3-319-75022-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Communication skills in nursing: A phenomenologically-based communication training approach
Affiliations.
- 1 Ersta Sköndal Bräcke University College, Department of Health Care Sciences, Stockholm, Sweden. Electronic address: [email protected].
- 2 Ersta Sköndal Bräcke University College, Department of Health Care Sciences, Stockholm, Sweden. Electronic address: [email protected].
- 3 Ersta Sköndal Bräcke University College, Department of Health Care Sciences, Stockholm, Sweden. Electronic address: [email protected].
- 4 Ersta Sköndal Bräcke University College, Department of Health Care Sciences, Stockholm, Sweden. Electronic address: [email protected].
- 5 Ersta Sköndal Bräcke University College, Department of Health Care Sciences, Stockholm, Sweden. Electronic address: [email protected].
- 6 Ersta Sköndal Bräcke University College, Department of Health Care Sciences, Stockholm, Sweden. Electronic address: [email protected].
- PMID: 31487674
- DOI: 10.1016/j.nepr.2019.08.011
The aim of this article is to present a communication skills training curriculum for nursing students, based upon phenomenology. Research shows that nurses have difficulty prioritizing dialogue with patients, due to lack of time, organizational and cultural factors. Like other health care professionals, nurses may also have difficulties communicating with patients due to personal fears and shortcomings. The communication training curriculum based upon phenomenology aims at systematically training students to stay focused upon patients' and relatives' narratives, allowing them to reflect upon and better understand their current situation. This approach to communication is applicable in any clinical situation where it important to provide space for the patients' experiences. The philosophical principles guiding the training are presented here as well as the practical steps in the program. Finally, the approach is compared to other common communication methods used in nursing (motivational interviewing, caring conversations, empathy training). The authors hope that the article will highlight the nurses' role as dialogue partner as well as emphasize the importance of communication skills training in nursing education. This approach can be refined, tested and modified in future research and may serve as an inspirational model for creating a generic communicative competence for nurses. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Keywords: Communication training; Nurse-patient interaction; Phenomenology.
Copyright © 2019 Elsevier Ltd. All rights reserved.
- Clinical Competence*
- Communication*
- Education, Nursing
- Nurse-Patient Relations*
- Students, Nursing
- Open access
- Published: 16 May 2024
Comparison of barriers to effective nurse-patient communication in COVID-19 and non-COVID-19 wards
- Hamed Bakhshi ORCID: orcid.org/0009-0008-7865-0149 1 ,
- Mohammad Javad Shariati ORCID: orcid.org/0009-0000-5518-698X 1 ,
- Mohammad Hasan Basirinezhad ORCID: orcid.org/0000-0002-3672-556X 2 &
- Hossein Ebrahimi ORCID: orcid.org/0000-0001-5731-7103 3
BMC Nursing volume 23 , Article number: 328 ( 2024 ) Cite this article
250 Accesses
Metrics details
Communication is a basic need of humans. Identifying factors that prevent effective nurse-patient communication allows for the better implementation of necessary measures to modify barriers. This study aims to compare the barriers to effective nurse-patient communication from the perspectives of nurses and patients in COVID-19 and non-COVID-19 wards.
Materials and methods
This cross-sectional descriptive study was conducted in 2022. The participants included 200 nurses (by stratified sampling method) and 200 patients (by systematic random sampling) referred to two conveniently selected hospitals in Shahroud, Iran. The inclusion criteria for nurses were considered having at least a bachelor’s degree and a minimum literacy level for patients to complete the questionnaires. Data were collected by the demographic information form and questionnaire with 30 and 15 questions for nurses and patients, which contained similar questions to those for nurses, based on a 5-point Likert scale. Data were analysis using descriptive indices and inferential statistics (Linear regression) in SPSS software version 18.
The high workload of nursing, excessive expectations of patients, and the difficulty of nursing work were identified by nurses as the main communication barriers. From the patients’ viewpoints, the aggressiveness of nurses, the lack of facilities (welfare treatment), and the unsanitary conditions of their rooms were the main communication barriers. The regression model revealed that the mean score of barriers to communication among nurses would decrease to 0.48 for each unit of age increase. Additionally, the patient’s residence explained 2.3% of the nurses’ barriers to communication, meaning that native participants obtained a mean score of 2.83 units less than non-native nurses, and there was no statistically significant difference between the COVID and non-COVID wards.
In this study, the domain of job characteristics was identified by nurses as the major barrier, and patients emphasized factors that were in the domain of individual/social factors. There is a pressing need to pay attention to these barriers to eliminate them through necessary measures by nursing administrators.
Peer Review reports
First observed in Wuhan, China, the COVID-19 pandemic is an acute and very severe respiratory syndrome that the World Health Organization has raised as a health problem because of its high spread rate and consequences on an international scale. The number of COVID-19 patients is increasingly on the rise [ 1 , 2 ]. Illness and hospitalization are usually stressful and associated with bad experiences for patients and their family members [ 3 ].
According to Tabandeh Sadeghi et al. (2011) “Communication is a basic need of humans. Any interaction is an opportunity to achieve effective communication and participation in understanding the issue, which leads to the achievement of mutual goals by individuals.” [ 4 ]. The three important aspects of communication that are emphasized the most are the message’s sender, the receiver, and the environment. Communicating is an interaction between the sender and the receiver of the message, and the environment affects them [ 5 , 6 ]. In the context of a hospital, these three aspects of communication can be defined as nurse, patient, and hospital environment, and all three should be considered when examining the obstacles [ 7 ]. “According to Ali Fakhr Movahedi et al. (2012)” Communication is considered a central concept in nursing and an essential part of nursing work [ 8 ]. Patients perceive interaction with nurses as the basis of their treatment [ 9 ]. Nurse-patient communication is an interpersonal process that is created between these two groups during treatment. This process generally includes the start, work, and end stages. Effective communication is an essential aspect of patient care by nurses, and many nursing tasks cannot be performed without this activity [ 10 ]. Effective communication consists of explicit transmission and receipt of message content, in which information is consciously and unconsciously produced by a person and communicated to the recipient through verbal and non-verbal patterns [ 11 ]. The non-verbal aspect of communication plays an essential role and is more important than the verbal aspect of language in emergencies. The mandatory use of face masks during the COVID-19 pandemic negatively influenced nurse-patient communication, notably because this tool significantly reduced the messages arising from non-verbal communication channels [ 12 ]. In this regard, Vitale et al. investigated wearing face masks as a communication barrier between nurses and patients. The results showed no differences in the patients’ opinions before and during the COVID-19 pandemic; patients believed that the mask was not a communication barrier, while nurses thought that wearing masks was a communication barrier [ 12 ]. Unfavorable communication can hamper the patient’s recovery and may even permanently deprive the patient of health or life.
In comparison, good communication affects the patient’s recovery more than medication. In fact, nurses will succeed in their tasks when they can communicate well with their patients [ 13 ]. Effective communication can affect pain control, adherence to a treatment regimen, and the patient’s mental health and play an important role in reducing the patient’s anxiety and fear and faster recovery [ 14 ]. During good communication, patients can disclose and express sensitive and personal information. Consequently, nurses can also transfer necessary information, attitudes, or skills [ 4 ]. Identifying factors that prevent effective nurse-patient communication allows for the better implementation of measures required to adjust obstacles [ 15 ].
The first published reports of the deaths of coronavirus-infected doctors during caring for patients indicate that the virus transmission to healthcare workers in healthcare centers is a hazardous issue [ 16 , 17 ]. Under these stressful conditions, nurses must manage long shift hours and the fear of contagion and overcome communication difficulties through layers of personal protective equipment. These problems may disrupt communication with patients and cause less focus of health workers on the psychosocial well-being of patients [ 18 , 19 ]. Baillie states that the lack of time is a clear barrier to communication between emergency nurses and patients [ 20 ]. Meehan et al. also reported that nurses mentioned the lack of time, fatigue, and workload of personnel to be the factors preventing nurse-patient interaction. In the same research, patients cited the issue of gender as a factor preventing their interaction with nurses. However, male and female patients had difficulty communicating with male nurses [ 21 ].
Identifying factors that prevent effective nurse-patient communication makes it possible to elucidate the direction of necessary measures for the planners and executives of the health sector to eliminate or modify barriers. In particular, when these barriers are identified and expressed with a realistic approach, i.e., from nurses’ and patients’ perspectives [ 22 ]. Before this, no study compared barriers to nurse-patient communication in COVID and non-COVID wards. Therefore, this research aims to compare the barriers to effective nurse-patient communication from nurses’ and patients’ perspectives in COVID-19 and NON-COVID-19 wards. Hopefully, identifying these obstacles and planning to solve them as soon as possible will make us have nurses in the future who can communicate well with patients and improve service delivery.
Study design
This cross-sectional descriptive research was conducted on 200 nurses and 200 patients at hospitals affiliated with the Shahroud University of Medical Sciences. The participants included nurses and patients from different wards of two conveniently selected hospitals in Shahroud. To sample nurses by the stratified method, the sample size was first divided by the total number of nurses in the mentioned hospitals to obtain the sampling fraction. According to Mohammadi et al. study, standard deviations reported for all subscales for barrier’s to effective communication (individual/social factors = 6.22), job characteristics = 6.74, patient’s clinical conditions = 4.22), and environmental factors = 9.09) were utilized to estimate the sample size [ 23 ]. Estimation error was considered 0.15 of standard deviation values. The confidence levels and power were considered at 0.95 and 0.8 respectively with a 15% dropout probability. Also, another sample size was calculated similarly using the standard deviation reported in Norouzinia et al. study for patient’s questionnaire equal to 1.96 [ 24 ]. Finally, among the estimated values; the largest number (200) was considered as the sample size of the present study for nurses and patients.
Considering that the total number of nurses is around 700 and the sample size calculated by the statistics consultant is 200 nurses, our sampling fraction was calculated as \(\frac{2}{7}\) . Therefore, \(\frac{2}{7}\) personnel of each department were included in the study. The patients were sampled by a systematically random method using the hospital list, file number, and dates of admission and discharge. The inclusion criteria for nurses were a bachelor’s degree or higher and a minimum literacy level for patients to complete the questionnaire. Moreover, the questionnaire contained questions about the nurses’ work experience or no experience in COVID-19 wards. The duration of working in COVID-19 wards was included in the questionnaire questions, and the duration was considered in the analysis. Data were collected using a questionnaire provided to the nurses through daily visits to various wards of the mentioned hospitals, including emergency, surgery, special care, internal medicine, gastroenterology, cardiology, urology, orthopedics, ICU, CCU, and other wards. The questionnaire was also provided to the patients hospitalized in surgery, special care, internal medicine, gastroenterology, cardiology, urology, ICU, and CCU wards, among others. Due to the reduced coronavirus spread during that period, the information on COVID-19 patients was accessed using hospital information by obtaining permission, and the questionnaire was completed through phone calls.
Measurements
Demographic information form.
It contained questions about information related to age, gender, marital status, language, and residence.
Communication barrier questionnaire
The barriers to effective nurse-patient communication were investigated using the same questionnaire designed by Anoosheh et al. This questionnaire contains 30 items for nurses and aims to evaluate nurses’ views about the barriers to effective nurse-patient communication. The response of this questionnaire is in the Likert range (completely false = 1, false = 2, I have no opinion = 3, agree = 4, and completely agree = 5). The nurses’ questionnaire contains four dimensions, and the question numbers of each dimension include individual/social factors (1–8), occupational characteristics (9–17), patient’s clinical conditions (18–21), and environmental factors (22–30). The domain of individual/social factors includes questions such as the gender difference between the patient and the nurse, age difference, aggressiveness of nurses, etc. The domain of job characteristics includes questions about the high workload of nursing, the difficulty of nursing work, the low salaries of nurses, etc. The domain of the patient’s clinical condition also includes questions such as the severity of the disease, the presence of the patient’s companion, etc. The domain of environmental factors: where communication occurs is important. The nurse and the patient should feel calm and safe in the treatment environment. This domain also includes questions such as the Lack of facilities (welfare - treatment) for patients, the unsanitary condition of the patient’s room, the High cost of treating patients, etc. A pilot study was carried out to assess the face validity among nurses. In addition, the content validity was assessed by estimation of content validity ratio and content validity index among nursing educators. The internal consistency for the present questionnaire assessed by Cronbach’s alpha coefficient equal to 0.96 [ 25 ].
The patient questionnaire contains 15 questions and aims to evaluate the patients’ views about the barriers to effective nurse-patient communication. The response of this questionnaire is in the Likert range (completely false = 1, false = 2, I have no opinion = 3, agree = 4, and completely agree = 5). No separate dimension was considered for the patient questionnaire. The reliability based on internal consistency was reported using Cronbach’s alpha equal to 0.91 [ 25 ]. The total score of the questionnaire is obtained by summing up the total scores of all questions. The score of each dimension is obtained from the sum of scores for each question of that dimension. Higher scores in each dimension indicate the greater strength of that dimension as a barrier to effective nurse-patient communication and vice versa. After completing the communication barrier questionnaire, a separate question was asked from the patients and nurses about whether or not the face mask was a communication barrier. This question was scored with a Likert scale (completely false = 1, false = 2, I have no opinion = 3, agree = 4, and completely agree = 5). The score of this question was measured separately from the nurse-patient communication barrier questionnaire.
Ethical considerations
Initially, necessary permissions were obtained from the Vice Chancellor of Research and Technology and the Research Ethics Council (code of ethics: IR.SHMU.REC.1401.140) at the Shahroud University of Medical Sciences. Necessary coordination was also made with the administrators of two conveniently selected hospitals in Shahroud. After explaining the purpose of the research and answering the questions of nurses and patients regarding the questionnaire and how to complete them, enough time was given to answer them.
Statistical analysis
Data were analyzed using descriptive statistics (frequency, percentage, mean, and standard deviation) and inferential tests (Linear regression) in SPSS software version 18. All variables with a significance level of less than 0.2 are included in the final regression model. A significance level of 0.05 was considered. Considering that one of the purposes of this study is to determine the barriers to effective nurse-patient communication based on demographic information, three participants were excluded from the data analysis due to a lack of demographic information completion.
The average ages of nurses and patients were respectively 33.28 and 38.57 years, and most nurses (85.3%) and patients (61.5%) were females and males, respectively. Other demographic characteristics are listed in Table 1 .
In this study, the mean score obtained for each domain of the barriers to nurse-patient communication was determined from the nurses’ point of view. According to these results, the highest score with an average of 32.41 ± 6.75 related to the domain of job characteristics, and the lowest score with an average of 11.76 ± 3.17 related to the domain of Patient’s Clinical Conditions. Additional information is presented in Table 2 .
The excessive patients’ expectations in the domain of individual/social factors, the high workload of nursing in the domain of job characteristics, the severity of the disease in the domain of the patient’s clinical conditions, and no appreciation for nurses by authorities in the domain of environmental factors were the major communication barriers. The patient-nurse age difference from the domain of individual/social factors, the patient’s contact with multiple nurses with different attitudes from the domain of job characteristics, previous hospitalization history from the domain of the patient’s clinical conditions, and the high cost of patient treatment from the domain of environmental factors were the least important barriers to communication from the nurses’ viewpoints. From the patients’ views, the aggressiveness of nurses and the patient-nurse age difference were the major and the minor barriers to communication, respectively. Face masks were among the minor barriers to nurse-patient communication from the viewpoints of both groups (Table 3 ); this table is placed at the end of the article.
The relationship between nurses’ age and communication barriers was investigated using a regression model. This model was first run as a univariate type, and variables with a significance of < 0.2 were introduced into a multivariate model using the backward method. Finally, the model showed that the nurses’ age variable explained 3.8% of the score variance. In other words, the regression model revealed that the mean score of nurses would decrease to 0.486 for each year of age increase, and there is no statistically significant difference between the COVID and non-COVID wards (Table 4 ).
Additionally, the patient’s residence variable explained 2.3% of the score variance, meaning that native people obtained a mean score of 2.813 units less than non-native people, and there is no statistically significant difference between the COVID and non-COVID wards (Table 5 ).
The present study aimed to determine the barriers to effective nurse-patient communication from the viewpoints of nurses and patients in COVID-19 and non-COVID-19 wards in hospitals affiliated with the Shahroud University of Medical Sciences. The results of this study showed that in the domains of barriers to effective communication, nurses reported the highest score in job characteristics and the lowest score in the patient’s clinical conditions. In a study on nursing students at Urmia Midwifery School of Nursing, Habibzadeh et al. (2017) reported the highest and the lowest mean scores for questions related to occupational characteristics and the patient’s clinical conditions [ 26 ], which corresponds to our results. Work congestion conditions increase the work pressure of nurses, leading to fatigue, a situation in which nurses lack enough time to discover the patient’s concerns [ 27 ]. Stress and pressure caused by time constraints often result in miscommunication and reduce the satisfaction of nurses and patients [ 28 ].
The results of this study showed that the high workload of nursing and excessive expectations of patients are mentioned as two major obstacles to effective communication with patients from the point of view of nurses. Anoushe et al. (2015) and Baraz Pordanjani et al. (2016) investigated barriers to effective nurse-patient communication. They reported that nurses identify their workload as a major barrier to effective patient communication [ 15 , 22 ]. However, Habibzadeh et al. (2017) claimed that nurses’ lack of information and skills in patient communication was identified as the main communication barrier [ 26 ]. A possible reason for this discrepancy might be that the current study was conducted during the COVID-19 pandemic, concurrent with the increased workload of nurses compared to the pre-pandemic period.
The difficulty of nursing work, the psychophysical fatigue of nurses, the lack of comfort facilities for nurses, and no appreciation for nurses by administrators are in the next ranks of importance. Similarly, Anoushe et al. (2005) reported the difficulty of nursing work, the lack of comfort facilities for nurses, and psychophysical fatigue among the barriers with more emphasis by nurses [ 22 ]. The notable point is that nurses do not have the opportunity to establish effective communication with patients due to their workload. Furthermore, their work type is hard and tiring, and they do not receive proper benefits or appreciation. In such a situation, one cannot expect good nurse-patient communication, and the conditions affect patients’ moods. As expressed by the patients, this issue also negatively affects the quality of their relationships with patients [ 15 ].
The aggressiveness of nurses mentioned as the main obstacle to effective communication with patients from the patients’ point of view. Likewise, Baraz Pordanjani et al. (2009) found a statistically significant difference between the aggressiveness of nurses from the perspectives of nurses and patients [ 15 ].
Regarding the communication barriers from the patient’s perspective, the lack of facilities (welfare treatment) for them and the unsanitary condition of their rooms were among the factors more emphasized by patients than by the nurses. Interestingly, Baraz Pordanjani et al. observed that nurses believed more than patients that the lack of comfort facilities for patients and the unsanitary condition of their rooms would hinder effective communication [ 15 ]. This contradictory result can result from the difference in facilities and health/treatment conditions of the studied hospitals.
The viewpoints of both nurse and patient groups show that age and class differences do not negatively influence their relationships. Since nurses are responsible for initiating and maintaining communication with patients, it can be claimed that they perform their professional tasks, including communication establishment, regardless of the social class and age of patients, who also acknowledge this issue.
The face mask also obtained a low score from the viewpoints of patients and nurses. Vitale et al. investigated the use of face masks as a communication barrier between nurses and patients. The results indicated no difference in the patients’ opinions before and during the COVID-19 pandemic; that is, patients did not consider the mask a communication barrier, which is consistent with the present study. However, nurses thought that using a mask would be a communication barrier [ 12 ].
The present results revealed a significant relationship between the age of nurses and the barriers to effective nurse-patient communication; as such, the total score of nurses decreased for each year of age increase; However, no statistically significant difference was observed in the comparison of COVID and non-COVID wards. In this regard, Gopichandran et al. (2021) aimed to determine communication barriers between doctors and patients during the COVID-19 pandemic in India. They claimed that communication barriers decreased with age [ 29 ]. Nurses gain more experience and skills with rising age. Enough experience is also a characteristic that patients consider necessary for nursing work [ 30 ]. “According to Aram Feizi et al. (2006)” Mark (2001) concluded that the experience of the nursing unit could create satisfaction in both nurses and patients [ 30 ]. The possible reason for obtaining different results could be that the COVID-19 vaccination process was carried out slowly in Iran. For this reason, the nurses, both in the COVID and non-COVID wards, considered all patients with unique viewpoints (all of the patients considered potential cases of COVID-19). For this reason, there was no statistical difference between the communication barriers of the COVID and non-COVID departments.
No statistically significant difference was observed between the scores of male and female nurses and the barriers to effective nurse-patient communication. Unlike this result, Mohammadi et al. (2013) reported a significant difference between job characteristics, patients’ clinical conditions, environmental factors, and the gender of nurses [ 23 ]. The discrepant results might be caused by the heterogeneous distribution of participants in terms of gender, as 56% of the nurses were male in the study of Mohammadi et al. In comparison, less than 20% of the participants were male nurses in the present study.
The present results showed that the patients’ residence was significantly related to the barriers to effective nurse-patient communication, and native people obtained a lower mean score than non-native people: However, there was no any no significant difference between COVID and NON-COVID wards This result might be because nurses are more informed of the accents and dialects of native patients. Caring for patients speaking different languages and accents can lead to problems in the quantity and quality of nurse-patient communication. When patients and caregivers have different cultural values and languages, communication can cause the inability to exchange information [ 27 ]. Tilki and Okoughan presented evidence that differences in spoken language could hinder effective communication [ 31 ]. On the other hand, the results of the study by Vitale et al. showed that there was no difference between the patients before and during the covid-19 pandemic, which is consistent with the results of the present study [ 12 ].
Limitations
Among the limitations of this study, we can mention the low response rate by nurses and patients, which was completed with the continuous presence of the researcher. Since this research is conducted only in public medical centers affiliated to Shahroud University of Medical Sciences, the results may not be generalizable to centers affiliated with other universities of medical sciences in Iran and non-academic centers such as private medical centers. It is recommended that future research be conducted in larger settings.
This study demonstrated that nurses identified the domain of job characteristics as the most critical barrier among the four domains of barriers to effective nurse-patient communication. Patients more emphasized factors that were in the domain of individual/social factors. There is a pressing need to pay attention to these barriers to eliminate them through necessary measures by nursing officials. Hopefully, the elimination of these barriers in the future will lead to nurses who can communicate well with patients and improve service delivery.
Implications
This research helps to identify barriers to effective communication between nurses and patients. In the field of policy and management, the results of this research can help to plan for effective nurse-patient communication. In the field of education, according to the results of this article, necessary training should be given to nurses and patients regarding communication barriers to help improve communication. There will be a basis for further, more comprehensive research in the field of research. Hopefully, these results can help nursing officials and nurses remove communication barriers and improve service delivery.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, Health Care Workers, and Health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–71.
Article CAS PubMed PubMed Central Google Scholar
WHO. Coronavirus disease (COVID-19). Situation Report– 161. 2020.[cited 2020 June 29] https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200629-covid-19-sitrep-161.pdf?sfvrsn=74fde64e_2 .
Sheldon LK, Barrett R, Ellington L. Difficult communication in nursing. J Nurs Scholarsh. 2006;38(2):141–7.
Article PubMed Google Scholar
Sadeghi T, Dehghan Nayyeri N, Karimi R. Nursing-patient relationship: a comparison between nurses and adolescents perceptions. Iran J Med Ethics History Med. 2011;4(3):69–78.
Google Scholar
Caris-Verhallen WM, De Gruijter IM, Kerkstra A, Bensing JM. Factors related to nurse communication with elderly people. J Adv Nurs. 1999;30(5):1106–17.
Article CAS PubMed Google Scholar
Kopp P. Better communication with older patients. Professional nurse (London, England). 2001;16(8):1296-9.
Aghamolaei T, Hasani L. Communication barriers among nurses and elderly patients. Hormozgan Med J. 2011;14(4):312–8.
Fakhr-Movahedi A, Negarandeh R, Salsali M. Exploring nurse-patient communication strategies. J Hayat. 2013;18(4):28–46.
Kettunen T, Poskiparta M, Gerlander M. Nurse-patient power relationship: preliminary evidence of patients’ power messages. Patient Educ Couns. 2002;47(2):101–13.
Hagerty BM, Patusky KL. Reconceptualizing the nurse-patient relationship. J Nurs Scholarsh. 2003;35(2):145–50.
Clancy CM, Farquhar MB, Sharp BA. Patient safety in nursing practice. J Nurs Care Qual. 2005;20(3):193–7.
Vitale E, Giammarinaro MP, Lupo R, Archetta V, Fortunato RS, Caldararo C, et al. The quality of patient-nurse communication perceived before and during the COVID-19 pandemic: an Italian pilot study. Acta Biomed. 2021;92(S2):e2021035.
CAS PubMed PubMed Central Google Scholar
Jan Mohamady S, Salami S, Abasi Marei F, Masror D, Nazary Jobrany M. F J. Civilization and Nursing.Tehran: Publication Salemi2002. 107-9 p.
Maskor NA, Krauss SE, Muhamad M, Nik Mahmood NH. Communication competencies of oncology nurses in Malaysia. Asian Pac J Cancer Prev. 2013;14(1):153–8.
Baraz Pordanjani S, Shariati A, Alijani H, Moein Mosavi B. Assessing barriers of nurse-patient’s effective communication in educational hospitals of Ahwaz. Iran J Nurs Res. 2010;5(16):45–52.
Bowdle A, Munoz-Price LS. Preventing infection of patients and Healthcare workers should be the New Normal in the era of Novel Coronavirus Epidemics. Anesthesiology. 2020;132(6):1292–5.
Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67(5):568–76.
Fritzsche K, Scheib P, Ko N, Wirsching M, Kuhnert A, Hick J, et al. Results of a psychosomatic training program in China, Vietnam and Laos: successful cross-cultural transfer of a postgraduate training program for medical doctors. Biopsychosoc Med. 2012;6(1):17.
Article PubMed PubMed Central Google Scholar
Eltaybani S, Igarashi A, Cal A, Lai CK, Carrasco C, Sari DW et al. Long-term care facilities’ response to the COVID‐19 pandemic: An international, cross‐sectional survey. J Adv Nurs. 2023.
Baillie L. An exploration of nurse-patient relationships in accident and emergency. Accid Emerg Nurs. 2005;13(1):9–14.
Cleary M, Edwards C, Meehan T. Factors influencing nurse–patient interaction in the acute psychiatric setting: an exploratory investigation. Aust N Z J Mental Health Nurs. 1999;8(3):109–16.
Article CAS Google Scholar
Anoosheh M, Zarkhah S. Investigating barriers to effective nurse-patient communication. Teb Tazkie. 2006;15(2):49–57.
Mohammadi I, Mozafari M, Beigi EJ, Kaikhavani S. Barriers to effective nurse- patient communication from perspective of nurses employed in Educational hospitals of Ilam. J Neyshabur Univ Med Sci. 2015;2(3):20–7.
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2015;8(6):65–74.
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009;56(2):243–9.
Habibzadeh H, Dehgannejad J, Hoseinzadeghan F, Bafandehzendeh M. Barriers to establishing Effective Communication between Nurse and Patient according to nursing students’ viewpoints Urmia nursing and midwifery Faculty. Nurs Midwifery J. 2019;17(9):696–704.
Mazhariazad F, Taghadosi M, Erami E. Challenges of nurse-patient communication in Iran: a review study. Sci J Nurs Midwifery Paramedical Fac. 2019;4(4):15–29.
Jahromi MK, Ramezanli S. Evaluation of barriers contributing in the demonstration of an effective nurse-patient communication in educational hospitals of Jahrom, 2014. Global J Health Sci. 2014;6(6):54.
Gopichandran V, Sakthivel K. Doctor-patient communication and trust in doctors during COVID 19 times-A cross sectional study in Chennai, India. PLoS ONE. 2021;16(6):e0253497.
Feizi A, Mohammadi R, Nikravesh M. Factors causing patient’s Trust in Nurse from patients’ perspective. Razi J Med Sci. 2006;13(52):177–87.
Okougha M, Tilki M. Experience of overseas nurses: the potential for misunderstanding. Br J Nurs. 2010;19(2):102–6.
Download references
Acknowledgements
The present study is a research project approved under the number 14010048 at Shahroud University of Medical Sciences. The researchers are grateful to the Vice Chancellor of Research and Technology at Shahroud University of Medical Sciences for the necessary financial support of the present study and the participating nurses and patients.
No funding.
Author information
Authors and affiliations.
Student Research Committee, School of Nursing and Midwifery, Shahroud University of Medical Sciences, Shahroud, Iran
Hamed Bakhshi & Mohammad Javad Shariati
Department of Epidemiology and Biostatistics, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Mohammad Hasan Basirinezhad
Center for Health Related Social and Behavioral Sciences Research, Shahroud University of Medical Sciences, Shahroud, Iran
Hossein Ebrahimi
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the writing of the article: design and writing of the article (HB, HE), data collection (HB, MS), analysis and interpretation of data (HB, MB), final approval of the submitted version (HE, HB).
Corresponding author
Correspondence to Hossein Ebrahimi .
Ethics declarations
Ethics approval and consent to participate.
In order to observe ethical considerations, after explaining the study objectives and method to nurses and patients, written informed consent was obtained from them. It should be noted that the principles of the Helsinki Declaration, including the right to enter the research freely, no harm or loss to participants, maintaining the right to withdraw from the study, and confidentiality of information, were observed in this study. Besides, the researchers committed themselves to adhering to the principles of the Committee on Publication Ethics (COPE) set out for the publication of the results. This cross-sectional study was approved by the ethics committee of Shahroud University of Medical Sciences with the registration number: IR.SHMU.REC.1401.140.

Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bakhshi, H., Shariati, M., Basirinezhad, M. et al. Comparison of barriers to effective nurse-patient communication in COVID-19 and non-COVID-19 wards. BMC Nurs 23 , 328 (2024). https://doi.org/10.1186/s12912-024-01947-4
Download citation
Received : 05 August 2023
Accepted : 18 April 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s12912-024-01947-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Communication barriers
- Communication
- Nurse–patient communication
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
CPD Previous Next
Effective communication skills in nursing practice, elaine bramhall managing director, consultant and trainer, effective communication matters, manchester, england.
This article highlights the importance of effective communication skills for nurses. It focuses on core communication skills, their definitions and the positive outcomes that result when applied to practice. Effective communication is central to the provision of compassionate, high-quality nursing care. The article aims to refresh and develop existing knowledge and understanding of effective communication skills. Nurses reading this article will be encouraged to develop a more conscious style of communicating with patients and carers, with the aim of improving health outcomes and patient satisfaction.
Nursing Standard . 29, 14, 53-59. doi: 10.7748/ns.29.14.53.e9355
This article has been subject to double blind peer review
Received: 18 July 2014
Accepted: 01 September 2014
communication - communication skills - active listening - non-verbal communication - nurse-patient relations
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

09 December 2014 / Vol 29 issue 14
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Effective communication skills in nursing practice
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Examining effective communication in nursing practice during COVID‐19: A large‐scale qualitative study
Shannon d. simonovich.
1 School of Nursing, College of Science & Health, DePaul University, Chicago IL, USA
Roxanne S. Spurlark
Donna badowski, susan krawczyk.
2 School of Nurse Anesthesia, NorthShore University HealthSystem, Evanston IL, USA
Cheryl Soco
Tiffany n. ponder, debi rhyner, rachel waid, elizabeth aquino, christina lattner, lucy mueller wiesemann, kashica webber‐ritchey, joseph d. tariman.
The aim of this study was to conduct a primary examination of the qualitative communication experiences of nurses during the first wave of the COVID‐19 pandemic in the United States.
Ambiguity in ever‐evolving knowledge on how to provide care during COVID‐19. Remaining safe has created a sense of urgency, which has in turn created the need for organizations to quickly alter their operational plans and protocols to support measures that increase capacity and establish a culture of safe care and clear communication. However, no known study has described communication in nursing practice during COVID‐19.
Utilizing qualitative descriptive methodology, semi‐structured interviews were conducted with 100 nurse participants from May to September 2020 and recorded for thematic analysis. The consolidated criteria for reporting qualitative studies (COREQ), a 32‐item checklist, were used to ensure detailed and comprehensive reporting of this qualitative study protocol.
Study participants shared descriptions of how effective communication positively impacted patient care and nursing practice experiences during the first wave of the COVID‐19 pandemic. The thematic network analyses identified the importance of effective communication across three levels: (1) organizational leadership, (2) unit leadership and (3) nurse‐to‐nurse communication. Within this structure, three organizing themes, essential to effective communication, were described including (a) presence, (b) education and (c) emotional support.
Examining existing crisis communication policies and procedures across healthcare organizations is imperative to maintain highly relevant, innovative, and data‐driven policies and strategies that are fundamental to preserving quality patient care and supporting optimal nursing practice.
Implications for Nursing Policy and Health Policy
Effective communication is critical to support nurses through extended periods of crisis. COVID‐19 represents a unique contemporary challenge to the nursing workforce given the high stress and prolonged strain it has created for both human and healthcare supply resources. There is value in nurses’ presence at local, unit level and organizational leadership levels to convey critical information that directly informs leadership decision‐making during unprecedented emergencies such as the COVID‐19 pandemic.
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) global pandemic has created a sense of volatility and uncertainty in communication across the healthcare arena (Eldridge et al., 2020 ). Ambiguity in ever‐evolving knowledge on how to provide care during COVID‐19 while remaining safe has created a sense of urgency, which has in turn created the need for organizations to quickly alter their operational plans and protocols to support measures that increase capacity and establish a culture of safe care and clear communication. Successful navigation during any crisis requires communication that is timely in its dissemination, purposeful in its planning and clear in its directives (Edmonson et al., 2016 ; Eldridge et al., 2020 ). Effective communication is a priority and is vital to the performance of healthcare teams (Edmonson et al., 2016 ).
Nurses are noted in the healthcare workforce as the majority of providers for patient care (AACN, 2019 ); therefore, nurses’ voices should be relied upon to promote communication in patient care that focuses on safety and optimizing clinical outcomes while decreasing uncertainty and distress. Research to date notes that enhanced communication is linked to decreased stress, burnout and fatigue among nurses (Knupp et al., 2018 ). However, no known study has described communication in nursing practice during COVID‐19. Therefore, the purpose of this study was to conduct a primary examination of the qualitative communication experiences of nurses during the first wave of the COVID‐19 pandemic in the United States.
Study design
This qualitative descriptive study was conducted utilizing methodological design principles in which interviews with study participants were conducted to interpret their lived experiences in nursing practice during the first wave of COVID‐19 (Polit & Beck, 2020 ). Semi‐structured one‐on‐one interviews were conducted by nurse researchers with 100 nurse participants from May to September 2020 and recorded utilizing two digital voice recorders with subsequent verbatim transcription for thematic analysis. COREQ guidelines were followed in the description of the study design, analysis and presentation of findings (Tong et al., 2007 ).
This study was theory‐generating in its design with subsequent analysis grounded in thematic analysis of interview content and development of a conceptual framework. Research team members trained in qualitative methodology examined nurses’ experiences during the first wave of the COVID‐19 pandemic by conducting semi‐structured one‐on‐one interviews with nurses across the United States from May 2020 to September 2020. The consolidated criteria for reporting qualitative studies (COREQ), a 32‐item checklist, were used to ensure detailed and comprehensive reporting of the 100 interviews with nurses. Consideration to ensure validity and rigour were exemplified in this study's ‘design consideration, data generation, analytic procedures, and presentation’ of finding as evident in the utilization of a self‐conscious theory‐generating design, purposive sampling techniques, the standardization of the data collection process and the thorough triangulation of data in the analysis (Cypress, 2017 ).
Ethical considerations
All data collection processes, procedures and formal documentation received proper approval from DePaul University Institutional Review Board located in Chicago, Illinois, USA, Research Protocol #SS041620NUR. All participants completed the study protocol voluntarily and received a gift card for 50 US dollars to an online retailer for their participation. All interviews were completed one‐on‐one via telephone at the participant's convenience. Participants were matched with interviewers from similar nursing background as well as racial and ethnic background as much as possible to build trust and rapport. The information sheet was read, and verbal consent was obtained from each participant before beginning the formal interview. All participants were ensured of the confidentiality of information shared during the interview. All participants were told they may skip any questions or end the interview at any time with no consequences and were given the information for the DePaul University's Institutional Review Board should they have any concerns they would like to report.
Characteristics of the research team
The principal investigator, an experienced PhD‐prepared qualitative public health nursing scientist with formal training from the University of Washington, a globally recognized nursing research institution, was responsible for building the research study team, which at completion included 14 PhD‐prepared nurse scientists and DNP‐prepared advanced practice nurses from specialities including emergency department, acute care and nursing education settings. All doctorally prepared research team members served in nursing education roles at the time of data collection and were professional contacts of the study principal investigator. The 100 interviews were conducted by 9 doctorally prepared research study team members, each trained in group and one‐on‐one training sessions by the study principal investigator. In addition, the study team included 10 graduate student research assistants who aided in participant recruitment, data cleaning and data analysis. In sum, the research team was comprised of 23 females and one male. The research team met regularly from May 2020 forward to discuss study progress and the principal investigator debriefed with the research team members conducting interviews in weekly meetings during the study's data collection phase.
Study participants
Prospective study participants were recruited utilizing various approaches, including convenience sampling, purposive sampling and distribution of a digital recruitment flyer through social media platforms. Additionally, snowball sampling was utilized asking study participants, at the end of each completed interview, to recruit colleagues who may be interested in participation. Prospective study participants were told that the study was titled ‘an examination of nursing practice during COVID‐19’ and that the reason for conducting the study was to ‘learn more about the experiences of nurses practicing during COVID‐19’ to understand how the pandemic was impacting the ‘nursing profession’ and the health of communities. The principal investigator determined the study eligibility criteria for participants based upon the following inclusion criteria: nurses, including all levels of education and areas of practice, who self‐identify as having provided nursing care during COVID‐19 and can complete the study protocol in English. Exclusion criteria included nurses unwilling to complete the screening or that do not consent to be audio‐recorded. To obtain a broad understanding of nurses’ experiences providing care during COVID‐19, the extensive research study team aided in participant recruitment and data collection, with the effort exerted to obtain participants from traditionally underrepresented groups in nursing research. Prospective participants were asked to complete a screening tool that assessed their demographic characteristics and nursing practice background before the interview was scheduled. This tool enabled the team to recruit a diverse sample of study participants. The study team received over 300 email inquiries from prospective study participants for the 100 interviews funded. With regard to non‐participation, the study did not have any participants who refused to participate in the interview after reading the information sheet; however, there were prospective participants who emailed the study team but did not move forward with scheduling an interview.
Data collection and instrument
The interview guide was primarily developed by the principal investigator. The interview guide's content validity was performed by co‐investigator (CS), a DNP‐prepared emergency department nurse practitioner with 20 years’ experience working the front line in one of the country's largest academic medical centres. The interview guide was subsequently reviewed and approved by all research team members across practice disciplines. The interview guide was intentionally developed to be broad and inclusive for utilization across nursing specialities and roles. The interview guide is presented in Figure Figure1 1 .

Nursing During COVID‐19 Semi‐Structured Interview Guide
Study participants were interviewed by research team members with whom they did not have established relationships as much as possible. All participants were interviewed by research team members with whom they do not practice clinically and all interview matches were checked for conflicts of interest or close established relationships at the time of scheduling and rescheduled with a different research team member when necessary. The data collection took place via telephone in participants’ homes. The interviews included the interviewer and interviewee, in addition to the principal investigator during training interviews or a graduate research assistant for education purposes. The research team interviewer began the telephone call by introducing themselves by their first name, identifying themselves as a nurse, and reading the information sheet verbatim. Each interview lasted from 20 to 45 min, dependent upon the study participant's length of responses. Field notes were not formally made during the interviews. No repeat interviews were carried out, and transcripts were not returned to participants for comments. Two identical audio recordings of each interview, captured with a digital recorder, were uploaded to a secure cloud‐based web application for storage. Data saturation was discussed in the research team meetings with saturation occurring by completion of the data collection period in September 2020.
Data analysis
Quantitative analysis of study participant characteristics was tabulated and analysed by the principal investigator and study coordinator (TNP) utilizing Microsoft excel and SPSS 26 statistical software. Happyscribe cloud‐based software was utilized for the automatic transcription of the audio recordings. Then, each audio recording was verified by hand by trained graduate student research assistants for accuracy. The qualitative interview data were analysed using thematic content network analyses first by hand by 10 of the study team members including seven doctorally prepared nurses and three masters student research assistants, reviewing the first 20 transcripts as a full team. Once the thematic network was approved and discussed by the team, formal coding was completed utilizing Dedoose's web‐based software platform for qualitative analysis by the three student research assistants under the guidance of the principal investigator and second author. Themes were derived from the data. There were no diverse cases departing from the major thematic findings. Study participants did not provide feedback on the findings; however, the themes identified demonstrated good face validity when presented and discussed among the full research team of 24. Participants’ quotations are presented anonymously to illustrate the themes derived from the study data. For this study, codes related to effective communication were synthesized into distinct themes.
The study participants ( n = 100) had a mean age of 37.9 years, with a range of 38, a minimum of 24 and a maximum of 62. The majority of study participants identified as female, 84, while 14 identified as male, and two identified as trans/non‐binary. The study sample racial composition included 57% reporting as White, 20% as Black, 14% as Asian, 7% as multiracial and 2% as American Indian. With regard to ethnicity, 20% of our study sample identified as Hispanic or Latinx. In total, only 37% of our sample identified as both White and non‐Hispanic, yielding a study sample composition in which the majority of nurses interviewed, 63% identified as a member of an underrepresented racial/ethnic group. A more detailed summary of the participants’ characteristics can be found in Table Table1 1 .
Demographic characteristics of study sample ( n = 100)
Overall, our semi‐structured interviews with nurses across the US revealed overarching shared descriptions of how effective communication positively impacted patient care and nursing practice experiences during the first wave of the COVID‐19 pandemic. Based on the interview data, we define effective communication as expressions that positively impact nurses’ psychosocial well‐being. Within this context of effective communication, thematic network analyses enabled our team to identify the importance of effective communication across three levels: (1) organizational leadership, (2) unit leadership and (3) nurse‐to‐nurse communication. Within this structure, three critical organizing themes present at these three aforementioned levels led to positive patient care and nursing practice experiences. These three organizing themes, essential to effective communication, include (a) presence, (b) education and (c) emotional support, presented in Figure Figure2. 2 . These three organizing themes’ illustrative quotes are detailed in Table Table2 2 .

Effective Communication During COVID‐19 Conceptual Framework
Key themes and illustrative quotes
Organizational leadership
Effective communication was necessary at the organizational leadership level during the first wave of the COVID‐19 pandemic. For this study, organizational leadership is defined as individuals and departments whose operations impact the entire healthcare organization's structure and function. Effective communication at the organizational leadership level is embodied by the three organizing themes of (a) organizational leadership presence, (b) organizational leadership education and (c) organizational leadership emotional support.
Organizational leadership: Presence
Study participants reported the importance of the presence of organizational leadership during the first wave of the COVID‐19 pandemic. One nurse interviewed described feeling ‘tons of support’ from organizational leadership such as CNOs through their visibility daily. Study participants described feeling an increased level of presence from their organizational leadership through the development of command centres, where they could see key stakeholders from throughout the organization planning as a group. One nurse manager interviewed recalled, ‘I remember driving in at 3:00 in the morning once and my regional CNO giving me a call saying, “Are you okay? I’m headed in with you. I know you're coming in.”’ Nurses interviewed spoke of the importance of presence at the highest levels of leadership, with one participant stating,
When you have a good CEO…when you have a good leader that embraces and engages with its members, it is then that you get a sense of “we” right. [Our CEO] is very inclusive of my information, my expertise, my knowledge at the table. So it’s not like I’m by myself or she’s by herself. And there’s other nurses at the table. There were many of these roundtable discussions. It’s very powerful… I have talked to other people, and you’ll hear a lot of “they” and consequently… a lot of dissatisfaction. “They” do this and “they” do that. But when you say ‘we,’ it changes this whole perspective.
Organizational leadership: Education
Nurse participants interviewed described effective communication in the ongoing education surrounding COVID‐19 offered by the organizational leadership within their institutions. As one participant recalled,
It was… all hands on deck and educating [through] daily huddles after my command center call with the hospital. I would relay that information to my triage nurse and my clinical staff, to my physician team. The guidelines changed almost daily because we were learning as we went, we have a daily huddle board. That whole huddle board became a COVID board. So, as things came from nurse education and the command center and infectious disease, I would make sure I educated all my staff but also posted all of that on the COVID board.
Nurses interviewed also described the importance of effective organizational leadership communication through online platform utilization, including developing COVID websites to enable staff to educate themselves and stay up to date on corporate communication that would impact their job function. Given the evolving nature of information during the beginning of the COVID‐19 pandemic, ongoing education offered by organizational leadership was imperative, as one participant shared, ‘there [were] a lot of things that were written… in theory that we had to kind of rewrite on the fly [through] daily meetings with the leadership’. Effective communication through organizational leadership's ongoing commitment to education for employees allowed nurses and allied health professionals to rewrite pandemic care plans in a timely fashion.
Organizational leadership: Emotional support
Study participants described the importance of organizational leadership, offering emotional support as a means of effective communication during the first wave of the COVID‐19 pandemic. Emotional support at the organizational level included ‘wellness teams’, as described by one participant, who offered both physical and emotional nourishment to nurses by rounding 24 h a day. Another participant noted creation of safe environments within her work facility, a ‘zen den’ where nurses can ‘process [their] feelings’, in addition to ongoing resiliency and spiritual care programming. Furthermore, nurses spoke of the importance of formal Employee Assistance Programmes with behavioural health services financially covered by their institutions and proper financial support for quarantined nurses. As one nurse recalled, ‘[For] staff [who have] had symptoms, [we have] financial support if they had to be quarantined. We have 14 days of pay… so that they [don't] lose income’. Both formal and informal structured that reinforced emotional support for nurses during the first wave of COVID‐19 was perceived as effective communication from organizational leadership.
Unit leadership
Effective communication was imperative at the unit leadership level during the first wave of the COVID‐19 pandemic. For this study, unit leadership is defined as individuals and groups whose operations impact structure and function at the unit level. Effective communication at the unit level is embodied by the three organizing themes of (a) unit leadership presence, (b) unit leadership education and (c) unit leadership emotional support. See Table Table2 2 for more detail.
Unit leadership: Presence
Study participants described the usefulness of unit leadership presence as a form of effective communication during the first wave of the COVID‐19 pandemic. Descriptions of unit leadership presence included leadership participating in making daily rounds, holding daily huddles, checking in daily by e‐mail and being physically present on the floor, particularly in an emergency, critical care, and COVID‐19 units across all shifts including weekends with both managers and executive directors in attendance. The frequency of unit leadership presence was crucial in describing effective unit leadership communication during the COVID‐19 crisis, with daily presence received positively, including one unit nurse who reported it helped them to feel ‘supported’. As one nurse leader interviewed shared with us, ‘We [were] getting together with groups of staff [and asking] what… can we do better to help with the next surge?’ another participant noted, ‘I just really wanted to…communicate with them and let them know what a great job they are doing and how much I appreciate it’.
Unit leadership: Education
Unit leadership providing education for nurses was described by many study participants as a form of effective communication during COVID‐19. Providing formal education to nurses on laboratories, medications for first‐line treatment, clotting issues and running mock patient scenarios were among the effective communication strategies employed by unit leadership. Evolution and adaptation for several unit training and education throughout the first wave of COVID‐19 also proved vital. Education as effective communication in unit leadership is exemplified in one participant's response as follows,
[I] think we learned a lot [of] the information that we were getting from our operations team and the department management… the administrative people were… getting a lot of information from… the World Health Organization or Centers for Disease Control to help provide guidelines. Things [were] very fluid and changing almost by the minute [and] by the hour during our shift.
Unit leadership: Emotional support
Unit leadership demonstrating emotional support for nurses was a well‐described theme surrounding effective communication during the first wave of the COVID‐19 pandemic. Unit leadership helping its staff members process the emotional challenges of working in healthcare during COVID‐19 was essential. One study participant noted, ‘[We] advocated for [debriefings] …. [from] our management [because] we were really burnt out and a lot of people weren't doing well on the unit as far as nurses processing everything that ha[s] happened’. Another participant shared, ‘[We have] been doing… debriefings and… we [have done] a remembrance… [for] the patients that we [have] lost. We actually wrote cards to our patients’ families who passed [away] too. That… obviously hurt but helped with… closure. A lot of us have much anxiety’. Emotional support, even in the form of digital updates from unit leadership including ‘feel good articles’ and ‘wellbeing resources’, were perceived as helpful communication by two nurses interviewed.
Nurse to nurse
In addition to organizational leadership and unit leadership communication, effective communication also impactful in nurse‐to‐nurse relationships during the first wave of the COVID‐19 pandemic. For this study, nurse‐to‐nurse communication is defined as communication between individuals or groups where they function in similar roles, whether within the same unit or different practice areas, and demonstrate mutual trust and validation. Effective communication at the nurse‐to‐nurse level is embodied by the three organizing themes of (a) nurse‐to‐nurse presence, (b) nurse‐to‐nurse education and (c) nurse‐to‐nurse emotional support. See Table Table2 2 for more detail.
Nurse to nurse: Presence
Nurse‐to‐nurse presence was a well‐described compelling communication theme among our study sample of 100 US nurses. Study participants described the importance of feeling other nurses’ emotional and physical presence during the first wave of the COVID‐19 pandemic. The closeness of nurses within departments was mentioned with frequency describing camaraderie, teamwork and emotional support among seasoned nurse colleagues. These sentiments were also shared between nurses changing shifts to talk about the stress of everchanging COVID nursing care. In addition, nurses articulated greater collaboration between departments, as one participant noted,
The two ICU nurses had to come [to our floor to] take care of [patients] because [the] ICU’s [were full]. The [ICU nurses] have broken the walls… There is such collaboration between the two units now, and honestly, it is so refreshing to see.
Nurse to nurse: Education
Education among nurses was a well‐described effective communication theme during the first wave of COVID‐19. Many novice nurses interviewed in our study sample described how they leaned on seasoned nurses’ guidance for educational support, such as one shared,
I asked [experienced COVID‐19 nurses] for their advice. They said… limit as much contact as possible, cluster your care and ask for help. I asked them because they had gone [to the COVID ICU] more often…so by the time it was my turn to go, I wanted to ask them… What can I expect?
Another new graduate nurse expressed that as novices, they were ‘thrown into [a] crazy world’, but were learning ‘at high speed’ due to the mentorship by experienced nurse colleagues. In addition to nurse education being effective communication for new nurses, it also proved effective for seasoned nurses as practice guidelines shifted and cross‐training among nurses became necessary. One participant described that,
We’re all cross‐training. They’re combining us, the PACU nurses, with the preop nurses and the ambulatory surgical staff. Everyone’s cross‐training. People who didn’t have ICU experience before are being sent over to the ICUs to shadow. We’re basically all being prepared to be able to perform any of the roles that fall under our giant umbrella.
Nurse to nurse: Emotional support
The effective communication theme of the nurse‐to‐nurse emotional support was well‐described by study participants. Nurses described the role the emotional support of peers played in their ability to feel supported during the first wave of COVID‐19, as one participant stated, ‘it's nice to have someone understand what you're going through’ as fellow nurses working in patient care settings during the pandemic. Another nurse interviewee shared,
Family and friends… they knew about… how harmful and severe COVID was, but only your fellow nurses and co‐workers knew exactly what you were going through. So, at lunch break, talking about what someone [was] struggling with or what can be done better. Or after a shift, calling a nurse friend that is also going through that same situation. I think talking with other fellow nurses is what helped me the most.
Emotional support at the nurse‐to‐nurse level also allowed nurses to advocate for themselves as a collective group. One participant shared that, ‘If we had a problem, we could band together and have the courage to bring it up to [a] manager or provider’. Nurse‐to‐nurse emotional support during COVID‐19 was, as one participant noted, about ‘nurses coming together… something that [will] make us stronger after the pandemic’.
This study describes that nurses value reliable communication from organizational leaders, unit leaders, and nurse colleagues in the forms of presence, education and emotional support during the first wave of the COVID‐19 pandemic. These findings reinforce the findings of previous researchers who note that during times of crisis, the non‐technical skill of communication, the foundation of thoughts and actions, is critical for resilience in healthcare workers (Paquin et al., 2018 ).
In times of crisis, effective communication is a crucial fundamental leadership skill (Eldridge et al., 2020 ). It requires an understanding of psychological and emotional barriers to promote trust and credibility (Eldridge et al., 2020 ; Tseng et al., 2005 ). Similar to prior investigations on the SARS outbreak, this study findings highlight the importance of the dissemination of accurate and timely information delivered efficiently and consistently from organizational and nursing leadership to mitigate anxiety and fear (Liu & Liehr, 2009 ; Wong et al., 2020 ). This study also reinforces previous findings that describe how effective communication can set the foundation for best practices between leadership and providers by fostering transparency and trust (Hsu et al., 2017 ).
This study also described nurses valuing presence as a form of communication in relationships with other clinical nurses and among unit and organizational leaders. Presence is the condition of being either physically or felt to be present, either in the immediate vicinity, nearby, or in spirit (Merriam Webster, 2020 ). In their publication discussing the Boston Marathon bombings, Vitello‐Cicciu and Quinn found that nurse leaders promoted their employees’ psychological and environmental safety by being present, making daily rounds and speaking individually with their staff ( 2013 ). Even in non‐crisis situations, the importance of presence has been established. Rosengren et al. described how that clinical nurses require their nurse leader's physical, mental and social presence to support their day‐to‐day practice and promote clinical excellence ( 2007 ). However, this study is the first known qualitative examination of the importance of presence during a time of prolonged crisis such as a global pandemic. In addition, nurse‐to‐nurse communication, including knowledge sharing and emotional support, significantly impacted our study participants. Collegial information sharing acted as a coping strategy and aided study participants in adapting to the stressful and uncertain circumstances surrounding providing patient care during COVID‐19. The nursing profession depends on and expects experienced nurse's guidance and expertise to empower new generations of nurses at every level of practice, in every speciality, and to contribute to the profession's depth and strength (Luis & Vance, 2020 ).
Similar to the SARS crisis, limited information about COVID‐19 was available at the initial outbreak. Technological advancements in electronic, online, virtual platforms and social media have added measures to allow rapid communication and education (Wong et al., 2020 ). This research found various communication platforms useful, including online, virtual and person‐to‐person (Raderstorf et al., 2020 ). However, despite advancements in technology, recommendations for utilizing social media for crisis communication are ongoing, given limitations in transmission, accessibility and risk reduction (Lin et al., 2016 ). Aligned with our study, an investigation by Labrague et al. found that emotional support from trusted colleagues and top organizational leaders improved healthcare professionals’ coping and resilience ( 2018 ). Organizational leaders in our findings encouraged nurses to utilize system‐wide resources such as EAP and pastoral care personnel. Unit leaders encouraged the use of debriefings and sending electronic ‘feel good’ articles. Finally, the nurse‐to‐nurses sharing of their feelings of working through this highly stressful crisis was invaluable.
IMPLICATIONS FOR NURSING POLICY AND HEALTH POLICY
Organizational and unit‐level nurse leaders must be cognizant that their physical presence reassures the staff nurses when they communicate openly, honestly, and in a timely manner. As the liaisons between the organizational and staff nurse, the unit‐level nurse leaders are positioned to model and facilitate effective communication. Organizational and unit‐level nurse leaders should work in partnership to develop and implement programmatic solutions to optimize clinical outcomes. Organizations invest in the knowledge and skill of nurse leaders because they directly impact patient outcomes. Therefore, investing resources to improve nurses’ experiences with communication should be regarded as equally important. The pandemic has unveiled an emergency juncture with both chronic high stress and high stakes for nurses. Policies that support an increased structure for effective communication across levels allow nurse leaders the ability to foster a sense of care and concern for nurses and mitigate issues as they arise.
This study is novel in its timely representation of the experiences of a diverse group of nurses during the first wave of the COVID‐19 pandemic. Limitations of this study include its cross‐sectional design, capturing each nurses’ perspective at a single point in time, limiting our ability to describe how nurses’ experiences and perspectives have shifted over the course of the pandemic. Furthermore, transcripts were not returned to participants for comments or corrections, nor did participants provide feedback on the findings. Future research may consider a longitudinal design to capture the arc of nurses’ experiences over time, or perhaps utilize survey methodology to quantify the prevalence of the qualitative themes described by the sample of 100 nurses interviewed for this study.
This qualitative examination of US nurses’ experiences providing patient care during the first wave of the COVID‐19 pandemic discusses the importance of effective communication at the organizational level, unit level, and among nurse colleagues. Nurses interviewed reported the value of communication in the form of presence, education and emotional support across these three levels. Based on these findings, organizations should understand that nurse‐to‐nurse communication provides nurses the opportunity to deliver compassion to one another. Nurse‐to‐nurse communication offers opportunities for sharing knowledge and experiences. The ability to support communication develops trust and builds collaborative relationships. Policies that improve communication can mitigate workflow breakdowns, decrease errors and attenuate the effects of ineffective treatment regimens during times of crisis. Examining existing crisis communication policies and procedures across healthcare organizations is imperative to maintain highly relevant, innovative and data‐driven policies and strategies that are fundamental to preserving quality patient care and supporting optimal nursing practice.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTIONS
Study design: SDS. Data collection: SDS, RSS, DB, SK, CS, TNP, EA, LC, LMC, KWR. Data analysis: SDS, RSS, DB, SK, CS, TNP, DR, RW, EA, SL, JDT. Study supervision: SDS, TNP. Manuscript writing: SDS, RSS, DB, SK, CS, TNP, DR, RW, SL, JDT. Critical revisions for important intellectual content: JDT, SDS.
ACKNOWLEDGMENTS
Research reported in this publication was supported by the Zeta Sigma Chapter of Sigma Theta Tau International, the Illinois Nurses Foundation, and DePaul University College of Science & Health and School of Nursing. The content is solely the responsibility of the authors and does not necessarily represent the official views of Sigma Theta Tau International, the Illinois Chapter of the American Nurses Association or DePaul University.
The authors thank Dorothy Kozlowski, PhD, Stephanie Dance‐Barnes, PhD, Kim Amer, PhD, RN, Suling Li, PhD, APRN, FNP‐BC and Jennifer Wronkiewicz, MBA, for facilitating university support for this project.
The principal investigator would like to acknowledge the steadfast support of Jordan, Charlie, William and Teddy during this extensive study as well Elena Vela for providing childcare and moral support during the COVID‐19 pandemic.
As a study team, we would like to acknowledge the nurses who were brave enough to share their vulnerability with us as we discussed their experiences on the frontlines fighting this unprecedented global pandemic. This paper and all publications and dissemination efforts related to this study are meant to communicate our collective support for you, our cherished colleagues, and are dedicated to the memory of the nurses around the world who sacrificed their lives providing care to COVID‐19 patients.
Zeta Sigma Chapter of Sigma Theta Tau International, Illinois Nurses Foundation, DePaul University College of Science and Health & School of Nursing.
- American Association of Colleges of Nursing . Nursing fact sheet . Available at: https://www.aacnnursing.org/news‐Information/fact‐sheets/nursing‐fact‐sheet [Accessed 1st December 2020].
- Cypress, B.S. (2017) Rigor or reliability and validity in qualitative research: Perspectives, strategies, reconceptualization, and recommendations . Dimensions of Critical Care Nursing , 36 ( 4 ), 253–263. 10.1097/DCC.0000000000000253 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Edmonson, C. , Sumagaysay, D. , Cueman, M. & Chappell, S. (2016) The nurse leader role in crisis management . Journal of Nursing Administration , 46 ( 9 ), 417–419. 10.1097/NNA.0000000000000367 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eldridge, C.C. , Hampton, D. & Marfell, J. (2020) Communication during crisis . Nursing Management , 51 ( 8 ), 50–53. 10.1097/01.NUMA.0000688976.29383.dc [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hsu, Y.‐C. , Chen, Y.‐L. , Wei, H.‐N. , Yang, Y.‐W. & Chen, Y.‐H. (2017) Risk and outbreak communication: lessons from Taiwan’s experiences in the post‐SARS era . Health Security , 15 ( 2 ), 165–169. 10.1089/hs.2016.0111 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Knupp, A.M. , Patterson, E.S. , Ford, J.L. , Zurmehly, J. & Patrick, T. (2018) Associations among nurse fatigue, individual nurse factors, and aspects of the nursing practice environment . The Journal of Nursing Administration , 48 ( 12 ), 642–648. 10.1097/nna.0000000000000693 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Labrague, L.J. , McEnroe‐Petitte, D.M. , Leocadio, M.C. , Van Bogaert, P. & Cummings, G.G. (2018) Stress and the ways of coping among nurse managers: an integrative review . Journal of Clinical Nursing , 27 , 1346–1359. 10.1111/jocn.14165 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lin, X. , Spence, P.R. , Sellnow, T.L. & Lachlan, K.A. (2016) Crisis communication, learning, and responding: best practices in social media . Computers in Human Behavior , 65 , 601–605. 10.1016/j.chb.2016.05.080 [ CrossRef ] [ Google Scholar ]
- Liu, H. & Liehr, P. (2009) Instructive messages from Chinese nurses’ stories of caring for SARS patients . Journal of Clinical Nursing , 18 ( 20 ), 2880–2887. 10.1111/j.1365-2702.2009.02857.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Luis, C. & Vance, C. (2020) A pandemic crisis: Mentoring, leadership, and the millennial nurse . Nursing Economics , 38 ( 3 ), 152–163. [ Google Scholar ]
- Merriam Webster . Presence . Available from: https://www.merriam‐webster.com [Accessed 1st December 2020].
- Paquin, H. , Bank, I. , Young, M. , Nguyen, L.H.P. , Fisher, R. & Nugus, P. (2018) Leadership in crisis situations: merging the interdisciplinary silos . Leadership in Health Services , 31 ( 1 ), 110–128. 10.1108/LHS-02-2017-0010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Polit, D.F. & Beck, C.T. (2020) Nursing research . Philadelphia, PA: Lippincott Williams & Wilkins. [ Google Scholar ]
- Raderstorf, T. , Barr, T.L. , Ackerman, M. & Melnyk, B.M. (2020) A guide to empowering frontline nurses and healthcare clinicians through evidence‐based innovation leadership during COVID‐19 and beyond . Worldviews on Evidence‐based Nursing , 17 ( 4 ), 254–257. 10.1111/wvn.12451 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rosengren, K. , Athlin, E. & Segesten, K. (2007) Presence and availability: staff conceptions of nursing leadership on an intensive care unit . Journal of Nursing Management , 15 ( 5 ), 522–529. 10.1111/j.1365-2834.2007.00712.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tong, A. , Sainsbury, P. & Craig, J. (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups . International Journal for Quality in Health Care , 19 ( 6 ), 349–357. 10.1093/intqhc/mzm042 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tseng, H. , Chen, T. & Chou, S. (2005) SARS: key factors in crisis management . Journal of Nursing Research , 13 ( 1 ), 58–64. [ PubMed ] [ Google Scholar ]
- Vitello‐Cicciu, J.M. & Quin, M. (2013) Looking through the eyes of nursing leaders: the Boston marathon tragedy . Journal of Nursing Administration , 43 ( 9 ), 436–437. 10.1097/NNA.0b013e3182a23be3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wong, A.S.K. , Ooi, C.C. , Leow, M.Q.H. , Kiew, Y.S. , Yeo, K.C.W. , Tan, S.G. et al. (2020) Adapting lessons from SARS for the COVID‐19 pandemic— Perspectives from radiology nursing in Singapore . Journal of Radiology Nursing , 39 ( 3 ), 164–167. 10.1016/j.jradnu.2020.06.008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
It was found that the effect of communication skills of health professionals on anxiety levels of patients was 18.2% and the highest effect on anxiety levels was found to be the nonverbal ...
Effective communication between nurses and patients is presented along with surrogate terms, attributes, antecedents, consequences, related concepts and a model case. Effective communication was identified to be a multifactorial concept and defines as a mutual agreement between nurses and patients. This influences the nursing process, clinical ...
Communication assists in the performance of accurate, consistent and easy nursing work, ensuring both the satisfaction of the patient and the protection of the health professional. When health professionals are not trained in communication skills, they face more difficulties separating work from their personal life, tending to transfer problems ...
A preceptor short of adequate interpersonal and communication skills may be able to facilitate positive interpersonal relationships with the nursing students and patients ( Martínez-Linares et al., 2019). Interpersonal and communication skills are practical skills.
Strong communication skills are essential to provide safe, quality, patient-centered care. Nurses develop therapeutic relationships with patients and family members each day to ensure that health care concerns and needs are addressed. If communication breaks down, information exchange stops and needs go unidentified. Nurses optimize communication channels with patients and families by ...
This study aims to evaluate the effectiveness of a needs-based communication skills training for nursing professionals and to derive indications for future implementation. A two-armed randomized controlled trial including components from both effectiveness and implementation research will be applied. Additionally, a comprehensive process ...
Communication is an essential element of building trust and comfort in nursing, and it is the basis of the nurse-patient relationship (Dithole et al, 2017).Communication is a complex phenomenon in nursing and is influenced by multiple factors, such as relationship, mood, time, space, culture, facial expression, gestures, personal understanding and perception (McCarthy et al, 2013; Kourkouta ...
The Journal of Advanced Nursing (JAN) is a world-leading nursing journal that contributes to the advancement of evidence-based nursing, midwifery and healthcare. Abstract Aim To examine the feedback given by nurse educators and clinicians on the quality of communication skills of nurses in interactions with simulated patients.
18.5 Conclusion. Effective communication is a key component of patient-centered care and involves a continuous process of verbal and non-verbal exchange between healthcare professionals and patients. It requires healthcare professionals to adopt a reflective and listening attitude, radiate empathy, and involvement and recognize and understand ...
The tone, pacing, wording and clarity of questioning, along with good listening skills, are some of the foundation skills of quality communication (Rollnick et al. 2008 ). Informing is the most commonly used communication skill used in healthcare. When providing information to a patient, remember: Be friendly.
It focuses on core communication skills, their definitions and the positive outcomes that result when applied to practice. Effective communication is central to the provision of compassionate, high-quality nursing care. The article aims to refresh and develop existing knowledge and understanding of effective communication skills.
Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices. ... Health communication research for nursing science and ...
A significant proportion of research is available examining the development of interpersonal and communication skills in nursing, particularly at the undergraduate level. Identifying best practices for teaching interpersonal and communication skills in nursing education can assist nurse educators in adapting such methods for preceptorship ...
Introduction. Communication plays a vital role in professional disciplines such as nursing. Usually, establishing an effective communication with patients is an essential aspect of nursing care. 1 Nurses, through communication skills, can recognize the patient's healthcare needs, as a meaningful communication with patients enable nurses aspire to enhance a thorough knowledge of individual ...
New graduate nurses (NGN) often have an idealistic view of nursing compared to the reality of providing complex patient care. NGNs may lack communication and collaborations skills needed to effectively interact with challenging patients, families, and interdisciplinary teams, leading to stress and burnout. This evidence-based quality improvement project provided NGNs an opportunity to practice ...
Research associates positive patient and staff outcomes with a leader who exhibits communication competences. Implications for Nursing Management. Assessment of current competence levels in communication in nurse managers is needed. Education for improving communication skills is also needed.
Abstract. The aim of this article is to present a communication skills training curriculum for nursing students, based upon phenomenology. Research shows that nurses have difficulty prioritizing dialogue with patients, due to lack of time, organizational and cultural factors. Like other health care professionals, nurses may also have ...
Background Communication is a basic need of humans. Identifying factors that prevent effective nurse-patient communication allows for the better implementation of necessary measures to modify barriers. This study aims to compare the barriers to effective nurse-patient communication from the perspectives of nurses and patients in COVID-19 and non-COVID-19 wards. Materials and methods This cross ...
Despite the importance of competent and effective therapeutic communication, nursing students and novice nurses often lack competency in practical communication skills. Research supports that nursing students are not only poorly prepared to be competent communicators by nursing programs (Kavanaugh & Swezda, 2017), but also lack confidence and ...
This systematic review provides an overview of the research carried out on nursing students in order to develop communication skills with the patient. The objective of this systematic review was to identify, critically evaluate and synthesize the evidence of the impact of educational interventions on nursing students to develop their ...
This article highlights the importance of effective communication skills for nurses. It focuses on core communication skills, their definitions and the positive outcomes that result when applied to practice. Effective communication is central to the provision of compassionate, high-quality nursing care. The article aims to refresh and develop ...
For example: Nod your head, but never interrupt. Lean forward and maintain eye contact to let the person know you're engaged. Include minimal verbal encouragement, such as "I understand," and "go on.". 4. Written Communication. Written communication skills are also essential for effective nurse-to-nurse communication.
Nurses need to communicate with each other to ensure patients receive quality care. A 2023 study published by the National Library of Medicine found that fostering quality communication and trust between nurses improves the standard of care and patient safety. So, the entire profession grows stronger when nurses understand how to communicate.
Research has shown that combining a machine learning tool and a single reviewer can significantly ... 15 older patients in nursing homes: Non-verbal communication (listening and touching the shoulder) ... and possession of nonverbal communication skills. Patient factors that can also influence the effectiveness of nonverbal communication ...
This is particularly true in nursing, which relies on effective communication for the optimal delivery of patient care. Research in recent years has shown that there are many different communication styles. Therefore, educators must be able to engage a variety of personalities and skills to connect with all their students.
Implications for Nursing Policy and Health Policy. Effective communication is critical to support nurses through extended periods of crisis. COVID‐19 represents a unique contemporary challenge to the nursing workforce given the high stress and prolonged strain it has created for both human and healthcare supply resources.