Myocardial Infarction (MI) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial

Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Definition of Myocardial Infarction (MI)
Myocardial infarction, commonly known as a heart attack, is a critical medical event that occurs when the blood supply to the heart muscle is severely reduced or completely blocked. It is a leading cause of death worldwide and a significant public health concern.
Introduction to Myocardial Infarction (MI)
This nursing case study aims to provide a comprehensive understanding of myocardial infarction by delving into its various aspects, including its pathophysiology, risk factors, clinical presentation, diagnostic methods, and management strategies. Through the exploration of a fictional patient’s journey, we will shed light on the intricate nature of this life-threatening condition and highlight the importance of early recognition and intervention.
Background and Significance of Myocardial Infarction
Myocardial infarction is a sudden and often catastrophic event that can have profound consequences on an individual’s health and well-being. Understanding its underlying mechanisms and risk factors is essential for healthcare professionals, as timely intervention can be life-saving. This case study not only serves as a learning tool but also emphasizes the critical role of medical practitioners in identifying and managing myocardial infarctions promptly.
Pathophysiology of Myocardial Infarction
A crucial aspect of comprehending myocardial infarction is exploring its pathophysiology. We will delve into the intricate details of how atherosclerosis, the buildup of plaque in coronary arteries, leads to the formation of blood clots and the subsequent interruption of blood flow to the heart muscle. This disruption in blood supply triggers a cascade of events, ultimately resulting in the death of cardiac cells.
Risk Factors of Myocardial Infarction
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental in developing effective strategies for prevention and risk reduction.
Clinical Presentation Myocardial Infarction
Recognizing the signs and symptoms of myocardial infarction is crucial for timely intervention. We will present a fictional patient’s experience, illustrating the typical clinical presentation, which often includes chest pain or discomfort, shortness of breath, nausea, lightheadedness, and diaphoresis. Through this patient’s journey, we will highlight the importance of accurate symptom assessment and prompt medical attention.
Diagnostic Methods for Myocardial Infarction
Modern medicine offers various diagnostic tools to confirm a myocardial infarction swiftly and accurately. This case study will explore these diagnostic methods, such as electrocardiography (ECG), cardiac biomarkers, and imaging techniques like coronary angiography. By understanding these diagnostic modalities, healthcare professionals can make informed decisions and initiate appropriate treatments promptly.
Management Strategies for Myocardial Infarction
The management of myocardial infarction involves a multidisciplinary approach, including medication, revascularization procedures, and lifestyle modifications. We will discuss the fictional patient’s treatment plan, emphasizing the importance of reestablishing blood flow to the affected heart muscle and preventing further complications.
Nursing Case Study for Myocardial Infarction (MI)
Having established a foundational understanding of myocardial infarction, we will now delve deeper into Mr. Salazar’s case, tracing his journey through diagnosis, treatment, and recovery. This in-depth examination will shed light on the real-world application of the principles discussed in the introduction, providing valuable insights into the clinical management of myocardial infarction and its impact on patient outcomes.
Mr. Salazar, a 57-year-old male, arrives at the Emergency Department (ED) with complaints of chest pain that began approximately one hour after dinner while he was working. He characterizes the discomfort as an intense “crushing pressure” located centrally in his chest, extending down his left arm and towards his back. He rates the pain’s severity as 4/10. Upon examination, Mr. Salazar exhibits diaphoresis and pallor, accompanied by shortness of breath (SOB).
What further nursing assessments need to be performed for Mr. Salazar?
- Heart Rate (HR): The number of heartbeats per minute.
- Blood Pressure (BP): The force of blood against the walls of the arteries, typically measured as systolic (during heartbeats) and diastolic (between heartbeats) pressure.
- Respiratory Rate (RR): The number of breaths a patient takes per minute.
- Body Temperature (Temp): The measurement of a patient’s internal body heat.
- Oxygen Saturation (SpO2): The percentage of oxygen in the blood.
- S1: The first heart sound, often described as “lub,” is caused by the closure of the mitral and tricuspid valves.
- S2: The second heart sound, known as “dub,” results from the closure of the aortic and pulmonic valves.
- These sounds provide important diagnostic information about the condition of the heart.
- Clear: Normal, healthy lung sounds with no added sounds.
- Crackles (Rales): Discontinuous, often high-pitched sounds are heard with conditions like pneumonia or heart failure.
- Wheezes: Whistling, musical sounds often associated with conditions like asthma or chronic obstructive pulmonary disease (COPD).
- Pulses refer to the rhythmic expansion and contraction of arteries with each heartbeat. Common pulse points for assessment include the radial artery (wrist), carotid artery (neck), and femoral artery (groin). Evaluating pulses helps assess the strength, regularity, and rate of blood flow.
- Edema is the abnormal accumulation of fluid in body tissues, leading to swelling. It can occur in various body parts and may indicate underlying conditions such as heart failure, kidney disease, or localized injury. Edema assessment involves evaluating the degree of swelling and its location.
- Skin condition (temperature, color, etc.)
What interventions do you anticipate being ordered by the provider?
- Oxygen therapy involves administering oxygen to a patient to increase the level of oxygen in their blood. It is used to treat conditions such as respiratory distress, and hypoxia (low oxygen levels), and to support patients with breathing difficulties.
- Nitroglycerin is a medication used to treat angina (chest pain) and to relieve symptoms of heart-related conditions. It works by relaxing and widening blood vessels, which improves blood flow to the heart, reducing chest pain.
- Aspirin is a common over-the-counter medication and antiplatelet drug. In the context of myocardial infarction (heart attack), it is often administered to reduce blood clot formation, potentially preventing further blockage in coronary arteries.
- A 12-lead EKG is a diagnostic test that records the electrical activity of the heart from 12 different angles. It provides information about the heart’s rhythm, rate, and any abnormalities, helping diagnose conditions like arrhythmias, heart attacks, and ischemia.
- Cardiac enzymes are proteins released into the bloodstream when heart muscle cells are damaged or die, typically during a heart attack. Measuring these enzymes, such as troponin and creatine kinase-MB (CK-MB), helps confirm a heart attack diagnosis and assess its severity.
- A chest X-ray is a diagnostic imaging procedure that creates images of the chest and its internal structures, including the heart and lungs. It is used to identify issues like lung infections, heart enlargement, fluid accumulation, or fractures in the chest area.
- Possibly an Echocardiogram
Upon conducting a comprehensive assessment, it was observed that the patient exhibited no signs of jugular vein distention (JVD) or edema. Auscultation revealed normal heart sounds with both S1 and S2 present, while the lungs remained clear, albeit with scattered wheezes. The patient’s vital signs were recorded as follows:
- BP 140/90 mmHg SpO 2 90% on Room Air
- HR 92 bpm and regular Ht 173 cm
- RR 32 bpm Wt 104 kg
- Temp 36.9°C
The 12-lead EKG repor t indicated the presence of “Normal sinus rhythm (NSR) with frequent premature ventricular contractions (PVCs) and three- to four-beat runs of ventricular tachycardia (VT).” Additionally, there was ST-segment elevation in leads I, aVL, and V2 through V6 (3-4mm), accompanied by ST-segment depression in leads III and aVF.
Cardiac enzyme levels were collected but were awaiting results at the time of assessment. A chest x-ray was also ordered to provide further diagnostic insights.
In response to the patient’s condition, the healthcare provider prescribed the following interventions:
- Aspirin: 324 mg administered orally once.
- Nitroglycerin: 0.4 mg administered sublingually (SL), with the option of repeating the dose every five minutes for a maximum of three doses.
- Morphine: 4 mg to be administered intravenously (IVP) as needed for unrelieved chest pain.
- Oxygen: To maintain oxygen saturation (SpO2) levels above 92%.
These interventions were implemented to address the patient’s myocardial infarction (heart attack) and alleviate associated symptoms, with a focus on relieving chest pain, improving oxygenation, and closely monitoring vital signs pending further diagnostic results.
What intervention should you, as the nurse, perform right away? Why?
- Apply oxygen – this can be done quickly and easily and can help to prevent further complications from low oxygenation.
- Oxygen helps to improve oxygenation as well as to decrease myocardial oxygen demands.
- Often it takes a few minutes or more for medications to be available from the pharmacy, so it makes sense to take care of this intervention first.
- ABC’s – breathing/O 2 .
What medication should be the first one administered to this patient? Why? How often?
- Nitroglycerin 0.4mg SL – it is a vasodilator and works on the coronary arteries. The goal is to increase blood flow to the myocardium. If this is effective, the patient merely has angina. However, if it is not effective, the patient may have a myocardial infarction.
- Aspirin should also be given, but it is to decrease platelet aggregation and reduce mortality. While it can somewhat help prevent the worsening of the blockage, it does little for the current pain experienced by the patient.
- Morphine should only be given if the nitroglycerin and aspirin do not relieve the patient’s chest pain.
What is the significance of the ST-segment changes on Mr. Salazar's 12-lead EKG?
- ST-segment changes on a 12-lead EKG indicate ischemia (lack of oxygen/blood flow) or infarction (death of the muscle tissue) of the myocardium (heart muscle).
- This indicates an emergent situation. The patient’s coronary arteries are blocked and need to be reopened by pharmacological (thrombolytic) or surgical (PCI) intervention.
- Time is tissue – the longer the coronary arteries stay blocked, the more of the patient’s myocardium that will die. Dead heart tissue doesn’t beat.
Mr. Salazar’s chest pain was unrelieved after three (3) doses of sublingual nitroglycerin (NTG). Morphine 5 mg intravenous push (IVP) was administered, as well as 324 mg chewable baby aspirin. His pain was still unrelieved at this point
Mr. Salazar’s cardiac enzyme results were as follows:
Troponin I 3.5 ng/mL
Based on the results of Mr. Salazar's labs and his response to medications, what is the next intervention you anticipate? Why?
- Mr. Salazar needs intervention. He will either receive thrombolytics or a heart catheterization (PCI).
- Based on the EKG changes, elevated Troponin level, and the fact that his symptoms are not subsiding, it’s possible the patient has a significant blockage in one or more of his coronary arteries.
- It seems as though it may be an Anterior-Lateral MI because ST elevation is occurring in I, aVL, and V 2 -V 6 .
Mr. Salazar was taken immediately to the cath lab for a Percutaneous Coronary Intervention (PCI). The cardiologist found a 90% blockage in his left anterior descending (LAD) artery. A stent was inserted to keep the vessel open.
What is the purpose of Percutaneous Coronary Intervention (PCI), also known as a heart catheterization?
- A PCI serves to open up any coronary arteries that are blocked. First, they use contrast dye to determine where the blockage is, then they use a special balloon catheter to open the blocked vessels.
- If that doesn’t work, they will place a cardiac stent in the vessel to keep it open.[ /faq]
[faq lesson="true" blooms="Application" question="What is the expected outcome of a PCI? What do you expect to see in your patient after they receive a heart catheterization?"]
- Blood flow will be restored to the myocardium with minimal residual damage.
- The patient should have baseline vital signs, relief of chest pain, normal oxygenation status, and absence of heart failure symptoms (above baseline).
- The patient should be able to ambulate without significant chest pain or SOB.
- The patient should be free from bleeding or hematoma at the site of catheterization (often femoral, but can also be radial or (rarely) carotid.
Mr. Salazar tolerated the PCI well and was admitted to the cardiac telemetry unit for observation overnight. Four (4) hours after the procedure, Mr. Salazar reports no chest pain. His vital signs are now as follows:
- BP 128/82 mmHg SpO 2 96% on 2L NC
- HR 76 bpm and regular RR 18 bpm
- Temp 37.1°C
Mr. Salazar will be discharged home 24 hours after his arrival to the ED and will follow up with his cardiologist next week.
What patient education topics would need to be covered with Mr. Salazar?
- He should be taught any dietary and lifestyle changes that should be made.
- Diet – low sodium, low cholesterol, avoid sugar/soda, avoid fried/processed foods.
- Exercise – 30-45 minutes of moderate activity 5-7 days a week, u nless instructed otherwise by a cardiologist. This will be determined by the patient’s activity tolerance – how much can they do and still be able to breathe and be pain-free?
- Stop smoking and avoid caffeine and alcohol.
- Medication Instructions
- Nitroglycerin – take one SL tab at the onset of chest pain. If the pain does not subside after 5 minutes, call 911 and take a second dose. You can take a 3rd dose 5 minutes after the second if the pain does not subside. Do NOT take if you have taken Viagra in the last 24 hours.
- Aspirin – take 81 mg of baby aspirin daily
- Anticoagulant – the patient may be prescribed an anticoagulant if they had a stent placed. They should be taught about bleeding risks.
- When to call the provider – CP unrelieved by nitroglycerin after 5 minutes. Syncope. Evidence of bleeding in stool or urine (if on anticoagulant). Palpitations, shortness of breath, or difficulty tolerating activities of daily living.
Linchpins for Myocardial Infarction Nursing Case Study
In summary, Mr. Salazar’s case highlights the urgency of recognizing and responding to myocardial infarction promptly. The application of vital signs, EKG, cardiac enzymes, and medications like aspirin, nitroglycerin, and morphine played a pivotal role in his care. Diagnostic tools like echocardiography and chest X-rays contributed to a comprehensive evaluation.
Nurses must remain vigilant and compassionate in such emergencies. This case study emphasizes the importance of adhering to best practices in the assessment, diagnosis, and management of myocardial infarction, with the ultimate goal of achieving favorable patient outcomes.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Patient presentation.
Mr. Smith is a 60-year-old Caucasian male, who presents with 8/10 chest pain after working out. He just quit smoking and started a new workout and diet program after recently retiring. He has noticed some chest and shoulder discomfort with working out that usually resolves with rest, but decided to come to the emergency department because this episode was unrelenting and more severe. Mr. Smith describes his current pain as severe and sharp, and also complains of nausea and shortness of breath. Vital signs are HR: 110 BP: 150/90 RR: 30 Temp 97.6 O2 Sat: 92% on 2L nasal cannula, EKG shows ST segment elevation in leads II, III and AVf. Labs were drawn, including an elevated troponin (4.23 ng/ml), and slightly elevated white blood cell count (13.6 × 10 9 /L) .
Past Medical History
Type II diabetes (age 47), dyslipidemia (age 33), atherosclerosis (age 52), hypertension (age 49), obesity (age 33), viral pneumonia (age 29), hiatal hernia (age 28), peptic ulcer disease (age 41)
Family Medical History
Mother (deceased) – atrial fibrillation (diagnosed at age 45), died of MI (age 65)
Father (83) – obesity, type II diabetes (diagnosed at 50), COPD (diagnosed at 55)
Social History
Smoker (20 pack years), worked in an office sitting at a desk his whole career (35 years), recently began working out at his local gym since retiring this year.

- My presentations

Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
Case study 1: acute myocardial infarction
Published by Shanon Hunter Modified over 9 years ago
Similar presentations
Presentation on theme: "Case study 1: acute myocardial infarction"— Presentation transcript:
Cardiovascular Diseases
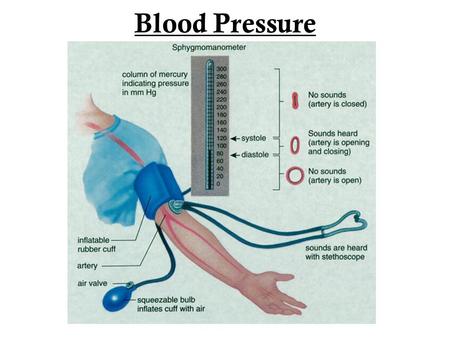
Blood Pressure.
Why is Physical Education so Important?. Benefits of Exercise Gives you more energy Reduces risk of Heart Failure Improves your Fitness Level Helps cope.
How can you prevent cardiovascular disease?. A disease that is not transmitted by another person, vector, or the environment Habits and behaviors.
The Healthy Heart Figure 14.1.
What You Will Do Identify changeable risk factors that can lead to diseases of the heart and lungs. Explain diseases that can result from certain lifestyles.
Mosby items and derived items © 2006 by Mosby, Inc. Slide 1 Chapter 19 Coronary Heart Disease and Hypertension.
By: Chelsea Eckel I’m too young to worry about heart disease. I’d know if I had high blood pressure because there are warning signs. I’ll know when I’m.
What is Diabetes? A disease in which there are high levels of sugar in the blood. Three types of Diabetes: Type 1 Type 2 Gestational Diabetes affects.
By Cyneetha Strong, MD May 19, Diseases and conditions pertaining to the heart and vascular (blood vessels) system Primarily includes heart.
Lifesaving information on Heart Attacks Presented to: Members of Virtua’s Health Systems Presented by: Rachel Zeilman.

The force of blood pushing against the walls of the arteries as the heart pumps blood High Blood Pressure is when the force of the blood against your.
What is Coronary Heart Disease? Who is at Risk for Coronary Heart Disease? Signs and Symptoms of Coronary Heart Disease. How Is Coronary Heart.
Hypertension and Nutrition Haley Aimone What Is HYPERTENSION Chronic medical condition Blood pressure in arteries are elevated Can lead to heart disease,
Transports nutrients and removes waste from the body. Supplies blood and oxygen to the body.
Risks & Prevention for Young Adults Cardiovascular Disease Kristen Hinners.

HEART HEALTH. LET’S SEE WHAT YOU KNOW ABOUT THE HUMAN HEART!
Angina and MI.
Lifestyle Diseases.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

- Upload Ppt Presentation
- Upload Pdf Presentation
- Upload Infographics
- User Presentation
- Related Presentations

GERD Case Study
By: missmani Views: 2590

Gastroesophageal Reflux Disease
By: missmani Views: 1028
Asexual Reproduction
By: missmani Views: 2380

Amnesia Aphasia and Prosopagnosia
By: missmani Views: 672

Monkeypox Outbreak in the US
By: missmani Views: 1922

Hemorrhagic stroke
By: JenniferDwayne Views: 2283

Congestive Heart Failure
By: Anto Views: 4135

Arteriosclerosis and Coronary Heart Disease-CHD
By: FrankMarco Views: 640

Le traitement pharmacologique
By: djalilthinker Views: 1376

Vascular Trauma
By: ekasaraswti Views: 1048

- About : I am medical student part of such a reputated institute
- Occupation : Medical Professional
- Specialty : NP Students
- Country : India
HEALTH A TO Z
- Eye Disease
- Heart Attack
- Medications
Acute Myocardial Infarction
Oct 15, 2014
720 likes | 1.99k Views
Acute Myocardial Infarction. Willis E. Godin D.O., FACC. Acute Myocardial Infarction. Definition: Decreased delivery of oxygen and nutrients to the myocardium Myocardial tissue necrosis causing irreparable tissue/cell death. Pathophysiology.
Share Presentation
- coronary artery
- smoking cessation
- myocardial infarction
- left coronary artery
- left circumflex artery lcx

Presentation Transcript
Acute Myocardial Infarction Willis E. Godin D.O., FACC
Acute Myocardial Infarction • Definition: • Decreased delivery of oxygen and nutrients to the myocardium • Myocardial tissue necrosis causing irreparable tissue/cell death
Pathophysiology • The most frequent cause of an acute MI is a disruption in the vascular endothelium that is associated with myocardial plaque • Plaque occurs over a period of years to decades • This combination causes the development of an intra-coronary thrombus, which causes the coronary artery to occlude • Within 20-40 minutes of an occlusion, irreversible myocardial cell damage/death occurs
Pathophysiology • 2 primary characteristics of plaque development are 1) a fibromuscular cap and 2) an underlying lipid rich core. • The overall loss of structural stability of the plaque usually occurs at the junction between the fibromuscular cap and the vessel wall (shoulder region) • Thrombus develops (due to the platelet-mediated activation of the coagulation cascade) and partial or complete occlusion occurs causing an acute myocardial infarction.
Pathophysiology • The severity of an MI depends on three factors • 1) The level of the occlusion in the coronary artery • Generally, the more proximal the coronary occlusion, the more extensive the amount of myocardium that will be at risk of necrosis • 2) The length of time of the occlusion • The longer the period of vessel occlusion, the greater the chances of irreversible myocardial damage distal to the occlusion • 3) The presence or absence of collateral circulation
Pathophysiology • STEMI • “complete” blockage of a coronary artery • NSTEMI • “near-complete” blockage of a coronary artery
Pathophysiology • Left Coronary Artery • Left Anterior Descending Artery (LAD) • “widow maker” • Anterior MI • Lateral MI • Left Circumflex Artery (LCx) • Lateral MI • Posterior MI • Right Coronary Artery • Inferior MI • RV MI
Prevalence • Myocardial Infarction is the leading cause of death in the United States • Approximately 450,000 people in the US die from coronary disease per year • 50% of all acute MI’s in the US occur in people under the age of 65 • No longer considered a “disease of the elderly”
Risk Factors • Dyslipidemia • Diabetes Mellitus • Hypertension • Tobacco use • Family History • Male gender
Diagnosis • Symptoms (gained by an accurate history) • Electrocardiogram (ECG) • Laboratory Tests • CK • CK-MB • Troponin • Echocardiogram
Symptoms • Chest pain described as a pressure sensation, fullness, or squeezing in the midportion of the thorax • Radiation of chest pain into the jaw or teeth, shoulder, arm, and/or back • Associated dyspnea or shortness of breath • Associated epigastric discomfort with or without nausea and vomiting • Associated diaphoresis or sweating • Syncope or near syncope without other cause • Impairment of cognitive function without other cause
Electrocardiogram • ST elevation myocardial infarction (STEMI) • > 1mm ST elevations in contiguous leads • Non-ST elevation myocardial infarction (NSTEMI) • ST depression • T wave inversions • No obvious ECG changes
ECG - STEMI
ECG -NSTEMI
ECG - NSTEMI
Cardiac Enzymes • Serial blood draws • Every 4 hours x 4 sets • Myoglobin peaks first (detectable in 1-4 hrs) • Troponin • peaks last (detectable in 3-12 hrs) • most specific • remains detectable in serum the longest
Cardiac Enzymes
Imaging (Echocardiography) • An echocardiogram can be performed to assess areas of the left ventricle that are not contracting normally as compared to areas that are contracting normally • After normal blood flow is interrupted, the area of the myocardium affected by the occluded artery will not function normally. • This abnormal wall motion can be detected by echocardiography
Treatment • Antiplatelets • Supplemental oxygen • Nitrates • Pain control • Beta Blockers • Statin Therapy • Heparin (unfractionated / low-molecular-weight heparin) • Fibrinolytics • Angiotensin-Converting Enyme Inhibitors / Angiotensin Receptor Blockers • Glycoprotein Iib/IIIa Antagonists • Aldosterone Antagonists
Other Treatment Options • Percutaneous Coronary Intervention • PCI / coronary stenting • Surgical Revascularization • CABG • Implantable Cardiac Defibrillators • AICD
Treatment Outcomes • Long-term medications • Smoking cessation • Cardiac Rehabilitation
Long-Term Medications • Most oral medications instituted in the hospital at the time of acute MI will be continued long term • Aspirin, beta blockade, and statin therapy is continued indefinitely in all patients • ACE inhibitors are continued indefinitely in patients with CHF, left ventricular dysfunction, hypertension, or diabetes • Diet modification, regular exercise
Smoking Cessation • Smoking is a major risk factor for coronary artery disease and MI • For patients who have undergone an MI, smoking cessation is essential to recovery, long-term health, and prevention of re-infarction • In one study, the risk of recurrent MI decreased by 50% after 1 year of smoking cessation
Smoking Cessation • All STEMI and NSTEMI patients with a history of smoking should be advised to quit and offered smoking cessation resources • Nicotine replacement therapy • Pharmacologic therapy • Referral to behavioral counseling or support groups • Smoking cessation counseling should begin in the hospital, at discharge, and during follow up
Cardiac Rehabilitation • Provides a venue for continued education, reinforcement of lifestyle modification, and adherence to a comprehensive prescription of therapies for recovery from MI including exercise training • Participation in cardiac rehabilitation programs after MI is associated with decreases in subsequent cardiac morbidity and mortality • Other benefits include improvements in quality of life, functional capacity, and social support
Summary • MI results from myocardial ischemia and cell death, most often because of an intra-arterial thrombus superimposed on an ulcerated or unstable atherosclerotic plaque • Despite advances in therapy, MI remains the leading cause of death in the United States. • MI risk factors include hyperlipidemia, diabetes, hypertension, male gender, and tobacco use. • Diagnosis is based on the clinical history, ECG, and blood test results, especially creatinephosphokinase (CK), CK-MB fraction, and troponin I and T levels.
Summary • Outcome following an MI is determined by the infarct size and location, and by timely medical intervention. • Aspirin, nitrates, and beta blockers are critically important early in the course of MI for all patients. • Post-discharge management requires ongoing pharmacotherapy and lifestyle modification.
- More by User
Acute Myocardial Infarction. Christopher Powe, PhD (c), ACNP Trauma & Surgical Critical Care University of Mississippi Medical Center. Acute MI.
1.93k views • 81 slides
Acute Coronary Syndrome (ACS). Refers to the array of clinical signs and symptoms produced by acute myocardial ischemiaUnstable anginaNon-ST-segment-elevation MIST-segment-elevation MIEach condition shares common pathophysiologic origins related to the instability and rupture of artherosclerotic
1.38k views • 59 slides
Acute Myocardial Infarction (Heart Attack)
Acute Myocardial Infarction (Heart Attack). Committee Membership: B. Majcher, APRN C. Mulhall, APRN M. Cichon, DO, Director of Emergency Department F. Leya MD, Director Cardiac Cath lab/Interventional Cardiology D. Wilber MD, Director C.V. Institute, Chief Cardiology
666 views • 13 slides
MYOCARDIAL INFARCTION AND ACUTE CORONARY SYNDROME
CHART LIBRARY POWERPOINT TOOL The best way to find out what information a particular CHART library can give you, is to take a look at the summary sheet. To do this, simply click on one of the libraries below. MYOCARDIAL INFARCTION AND ACUTE CORONARY SYNDROME. SAFER PRESCRIBING.
998 views • 70 slides
Complications of Acute Myocardial Infarction
Overview. Recurrent Ischemia/InfarctionCongestive Heart Failure/LV FailureCardiogenic ShockInterventricular Septal RuptureFree Wall RuptureAcute Mitral RegurgitationRight Ventricular InfarctionArrhythmiasPericardial Effusion and Pericarditis. Recurrent Ischemia and Infarction. Incidence of p
1.93k views • 46 slides
Management of Acute Myocardial Infarction
Management of Acute Myocardial Infarction. Sivanandam Vasudevan . Management of Acute Myocardial Infarction. Pre Hospital Phase ER CCU Step-down - Telemetry Post Hospital Phase. Complications of Acute Myocardial Infarction. Arrhythmic Complications Mechanical Complications
713 views • 24 slides
Defibrillator in Acute Myocardial Infarction Trial
DINAMIT. Defibrillator in Acute Myocardial Infarction Trial. Presented at American College of Cardiology Scientific Sessions 2004 Presented by Drs. Stewart Connelly and Stefan H. Hohnloser . DINAMIT.
144 views • 5 slides
Acute Myocardial Infarction (Heart Attack). Committee Membership:
307 views • 10 slides
Acute Myocardial Infarction. Dr. Meg- angela Christi Amores. one of the most common diagnoses in hospitalized patients mortality rate from AMI is ~30 % more than half of these deaths occurring before the stricken individual reaches the hospital. Acute MI.
1.03k views • 14 slides
Acute Myocardial Infarction (Acute MI)
Acute Myocardial Infarction (Acute MI). Prof. Arthur Pollak, M.D. Director, Acute Cardiac Care Center Director of Clinical Research Heart Institute Hadassah – Hebrew University Medical Center. Atherosclerosis is a Generalized Disease.
1.52k views • 52 slides
Acute Myocardial Infarction. Laura Kay M.D. EMS Medical Director. Worldwide Statistics. Each year: > 4 million patients are admitted with unstable angina and acute MI > 900,000 patients undergo PTCA with or without stent. Cumulative 6-month mortality from ischemic heart disease.
2.19k views • 66 slides
ACUTE MYOCARDIAL INFARCTION
ACUTE MYOCARDIAL INFARCTION. AMI. Myocardial Infarction. Occurs when there is a sudden and total occlusion or near-occlusion of blood flowing through an affected coronary artery to an area of heart muscle
3.03k views • 73 slides
Case study 1: acute myocardial infarction
Case study 1: acute myocardial infarction. Megan Fuchs Good Sam Dietetic Intern January 5, 2012. Patient Profile Personal Information. 46 year old white male Lives in Cincinnati, OH with wife, daughter, and grandson Leads a physically active lifestyle
1.5k views • 31 slides
LV aneurysm after acute myocardial infarction
LV aneurysm after acute myocardial infarction. 울산의대 서울아산병원 흉부외과. 주 석 중. Historical background. Baily. 1954 년 최초로 좌심실류 절제술에 성공함 . Cooley. 1958 년 최초로 심폐기하에서 좌심실류 repair 에 성공 (Plication/ Linear repair) Lillehei, Stoney, Daggett, Dor, Jatene, Cooley 등에 의해서 계속 발전됨.
735 views • 37 slides
Acute Myocardial Infarction. Willis E. Godin, D.O. South Jersey Heart Group Lourdes Cardiology Services. Acute Coronary Syndrome (ACS). Refers to the array of clinical signs and symptoms produced by acute myocardial ischemia Unstable angina Non-ST-segment-elevation MI
1.6k views • 55 slides
Milestones in Acute Myocardial Infarction
1. Milestones in Acute Myocardial Infarction. Celebrating 10 Years of Insights from the National Registry of Myocardial Infarction. Cardiovascular Disease: Problems/Opportunities. 58 million Americans have one or more types of cardiovascular disease
1.61k views • 115 slides
Safer Healthcare Now! Acute Myocardial Infarction
Safer Healthcare Now! Acute Myocardial Infarction. Presented by Amanda Thompson, Safer Healthcare Now Facilitator. Safer Healthcare Now! Background. Largest patient safety initiative in Canadian history Adopted form IHI Over 600 teams registered across Canada
519 views • 32 slides
SGD 1: Acute Myocardial Infarction
SGD 1: Acute Myocardial Infarction. PATHOLOGY. Chest Pain. An unpleasant sensation in the anterior wall of the thorax actual or potential tissue damage mediated by specific nerve fiber to the brain - conscious appreciation may be modified by various factors.
906 views • 19 slides
Arrhythmias Complicating Acute Myocardial Infarction
Arrhythmias Complicating Acute Myocardial Infarction. Sinus Bradycardia. Most common arrhythmia occurring during the early hours after MI and may occur in up to 40% of inferior and posterior infarcts. May be related to autonomic imbalance or to atrial and sinus node ischemia or both.
441 views • 27 slides
Improved Acute Myocardial Infarction (AMI) Guidelines
ICD-10-CM implementation brought several significant changes to the OCG (Official Guidelines for Coding and Reporting) with regard to Chapter 9 (Diseases of the Circulatory System) I.C.9.e Acute myocardial infarction (AMI). Preparing yourself for coding updates based on MI type is not sufficient. You also must learn how to apply these new codes using OGC for Coding and Reporting.
56 views • 3 slides
Practical Electrocardiography – Myocardial Ischemia and Acute Myocardial Infarction
Practical Electrocardiography – Myocardial Ischemia and Acute Myocardial Infarction. Scott Ewing, D.O. Cardiology Fellow August 30, 2006. Assess Initial 12-Lead ECG Findings. Classify patients with acute ischemic chest pain. ST elevation or new or presumably new LBBB:
578 views • 49 slides
Practical Electrocardiography – Myocardial Ischemia and Acute Myocardial Infarction. Scott Ewing, D.O. Cardiology Fellow August 30, 2006. Assess Initial 12-Lead EKG Findings. Classify patients with acute ischemic chest pain. ST elevation or new or presumably new LBBB:
637 views • 49 slides

IMAGES
VIDEO
COMMENTS
This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental in developing effective strategies for prevention and risk reduction. Clinical Presentation Myocardial Infarction
Pathophysiology of Myocardial Infarction Myocardial infarction occurs due to the obstruction of coronary arteries, typically from atherosclerosis. This obstruction leads to ischemia and necrosis of heart muscle, causing impaired function and potentially fatal outcomes. Risk
STEMI comprises 25-40% of myocardial infarction presentations. In-hospital mortality 5-6%. One year mortality 7-18% has significantly decreased with appropriate care including primary PCI and GDMT. Benjamin EJ, et al. Heart Disease and Stroke Statistics 2017 Update, Report From The AHA.
An Image/Link below is provided (as is) to download presentation Download Policy: ... Case study 1: acute myocardial infarction. Case study 1: acute myocardial infarction. Megan Fuchs Good Sam Dietetic Intern January 5, 2012. Patient Profile Personal Information. 46 year old white male Lives in Cincinnati, OH with wife, daughter, and grandson ...
Patient Presentation. Mr. Smith is a 60-year-old Caucasian male, who presents with 8/10 chest pain after working out. He just quit smoking and started a new workout and diet program after recently retiring. He has noticed some chest and shoulder discomfort with working out that usually resolves with rest, but decided to come to the emergency ...
Download ppt "Case study 1: acute myocardial infarction". Patient Profile Personal Information 46 year old white male Lives in Cincinnati, OH with wife, daughter, and grandson Leads a physically active lifestyle Works in maintenance - constant movement Lifts weights and swims regularly No ethnic or religious considerations.
Slide 2-. Myocardial infarction (MI) or acute myocardial infarction (AMI), commonly known as a heart attack, is the interruption of blood supply to part of the heart, causing some heart cells to die. Either one of the following criteria satisfies the diagnosis for an acute, evolving, or recent myocardial infarction: 1.
Presentation Transcript. Case study 1: acute myocardial infarction Megan Fuchs Good Sam Dietetic Intern January 5, 2012. Patient ProfilePersonal Information • 46 year old white male • Lives in Cincinnati, OH with wife, daughter, and grandson • Leads a physically active lifestyle • Works in maintenance - constant movement • Lifts ...
CHART LIBRARY POWERPOINT TOOL The best way to find out what information a particular CHART library can give you, is to take a look at the summary sheet. To do this, simply click on one of the libraries below. ... Case study 1: acute myocardial infarction. Case study 1: acute myocardial infarction. Megan Fuchs Good Sam Dietetic Intern January 5 ...