Benefits of Raising Your Own Fruits and Vegetables Research Paper
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment

Introduction
Raising your own fruits and vegetables in a personal garden provides one with a very satisfying experience. The taste of the home-grown fruits and vegetables is incomparable to those that are sold in the supermarket and such organic produce is even healthier since there no use of pesticides or herbicides is made. Also, most of the vegetables lose some of the healthy nutrients in them after they have been picked (Bruning & Lierberman 22); growing your own greens means that you can have them right after gathering them, thus obtaining the maximum possible health benefits from them.
This is certainly a great advantage to the vegetable gardeners. However it is not the sole one. Home grown fruits and vegetables are popular due to other reasons as well. One such is that gardening offers with a wide variety of benefits to your body. The fresh air and the exercise together make a perfect combination for a perfect health. In addition, it is said that working in natural surroundings leads to reduced stress and increased wellness (Francis & Hester 6).
Another major benefit of home grown fruits and vegetables happens to be the financial savings that result due to this; this is more the case if the home garden is planned to be for a long term. The prices of food have been rising (Geneflow 28) and at such a moment the best option could be to grow your own fruits and vegetables. Home vegetable and fruit gardens have become extremely popular now, that is during the recession.
There is an opposing view that home gardening does not lead to any economic benefits. The argument for this is that although you are working hard in order to grow your very own fruits and vegetables, you can easily get the very same items in the market and even at a lower cost. This is certainly possible since the professional growers would be having their huge farms on which they produce on a large scale. The result is the same products as yours but at a reduced price.
Although the above argument has some weight in it, there are various factors that prove otherwise.
Caring for your very own vegetable garden would certainly allow you to save money. Such a garden should be growing all kinds of vegetables and fruits that you require in everyday use. All you would need to do is to buy the variety that you want and you can simply cultivate that in your personal garden. This would result in a whole harvest of vegetables and fruits which you might want. The money spent for the purchase of the seeds will be only a small percentage of the money that you would spend for buying the same products in a market. You can produce huge amounts of fruits and vegetables, all in your backyard. The extra can be distributed or sold, or you can even get it canned for later use. That again means less purchasing of items from supermarkets.
Apart from this, it is much cheaper if you buy a packet of seeds and grow the plants yourself. For example, you will be spending less if you purchase lettuce seeds as compared to if you purchase a head of lettuce. Seeds certainly are cheaper than the fully grown plants.
A varying point here can be that there are expenses other than just the seeds in home gardening. For example, there have to be purchases made of certain other things, like tools and the gardening clothes. Plus, there has to be some planning done and effort is required for the job.
Although all these above mentioned factors may lead to the view that home gardening is more expensive than simply buying the required items from the market, it is not wholly true. In spite of these factors there is a belief that producing your own fruits and vegetables does result in substantial amounts of savings. The tools only have to be bought once and if you find them too expensive there is always the choice of second hand stores from where quality implements would be available at a cheaper cost. Plus, these would last for at least a couple of years and so the cost of them would not need to be repeated every often, which is again a benefit. Therefore, it is rightly said that home gardens lead to advantages in the financial area.
One such saving is in the transportation. If you have your garden you can obtain the required food whenever you wish, and without even going far or spending money. In the case of no garden you would have to go to the market and make the purchases. This would result in spending on transportation as well. Thus, one economic benefit of home gardens is savings from transport. This is a hidden saving and it might possibly seem to be inconsequential but if you go ahead and add up the costs that incur due to transportation only then you would realize the savings that you can make by travelling less in this era when the fuel prices are soaring higher and higher.
It is possible that initial expenses of home gardening are high but once a person gets into it he can save a lot. For example, seeds from the tomatoes can be saved and used instead of buying packets of seeds before each season. Also, there is no requirement of chemicals for the plants and the produce would be free from herbicides and pesticides; another advantage for good health, and this means that you would be healthier plus saving money. When you would be growing such “organic” food you would be saving even more since the cost of organic food in the markets is much higher than that of non organic produce.
There can be the expenses of soil builders. However, this can also be avoided by using manure instead of fertilizers; the former being cheaper as well as more environmentally friendly. Manure can even be obtained free of cost if you look around and see if there are any pets (for example, guinea pigs) in the neighbourhood. Or compost can be built using just anything at all, like the kitchen waste that includes egg shells, tea bags, peels of fruits, apple cores, etc. Then there is the option of heaping up leaves in the autumn season and allowing them to rot. This could then be used later. Thus, you would be getting your soil better which would allow for better quality of your fruits and vegetables, and this for no payment at all.
Also, water would be required for the gardening of fruits and vegetables and that would also lead to an expense. Although this would be the case in spite of it there would be savings. Water can be easily obtained. In the case where a person has no issues with having inorganic food, he can even use the water from washing to irrigate his fruits and vegetables. Apart from saving water expense, this would also allow for the soil to become more fertile due to the detergents in the water from washing. Probably there would also be no additional need of fertilizers or manure and this would again result in savings, since there would be no need to spend on fertilizers.
There are direct and indirect cost savings from having a home garden. The direct ones have been mentioned above; that you would not have to spend on transport to get the required items nor would you need to spend much to get the food. Apart from this you would also save because now you wouldn’t be paying the price for the transport of those fruits and vegetables from farms to the grocery shop, or for the salaries of the drivers who transported the produces from the farm.
Another way of saving up would be to offer your pet rabbit or guinea pig with the vegetables from your garden instead of going out and buying special food for them. This would not mean that you do not care for your pets. In fact, the natural and home grown fruits and vegetables would turn out to be healthier than the canned food that you might have been previously buying for them.
The more indirect savings involve issues like health. Since you would be having home grown fruits and vegetables you would eat more of natural foods as compared to the industrialized ones. This would lead to improved health and there will be savings since you would not need to visit a doctor, or to purchase medications for matters like heart disease, stroke, and obesity. This would also be due to the fact that you would be having organic foods, absent of any chemicals which are normally present in the market items.
Recently there had been a book published which deals with a study conducted regarding the choice of food that people normally make and how it affects them (Pollan 2008). The author of the book also presents a conclusion, stating that we only need to change our eating habits in minor ways and we would be much healthier. Some of his suggestions include eating more of leaves rather than seeds, eating more of organic instead of the processed and industrialized foods, and eating more of grass-fed rather than corn-fed when considering meat. The first two suggestions can easily be complied with if one has a home garden where he grows fruits and vegetables himself.
Also, consuming more of natural food, and specifically fruits and vegetables, allows for a person to reduce his weight. He does not need to waste his money at slimming centres neither pay a doctor to suggest him a controlled diet that would allow him to lose weight. His medication would be right there in front of his house, and without any hassle.
Taking into consideration all the factors discussed above it can be said that home grown food certainly allows for substantial savings and helps in the tougher economic times. Also, it is fun and easy, making it all the more attractive.
Bruning, Nancy Pauling & Lierberman, Shari. The Real Vitamin and Mineral Book: The Definitive Guide to Designing Your Personal Supplement Program. 4 th ed. United States: Penguin Press, 2007.
Francis, Mark & Hester, Randolph T. The Meaning of Gardens. Massachusetts: The MIT Press, 1992.
“Nutritional Security and Biodiversity: Meet the Women who strengthen the Link.” Geneflow: A Magazine about Agricultural Biodiversity. 2008: 28-, Bioversity International. Web.
Pollan, Michael. In Defence of Food: An Eater’s Manifesto. United States: Penguin Press, 2008.
- How One Man’s Contribution Transformed American Society
- Agro-Food Geographies: Food, Nature, Farmers and Agency
- Marketing an Earth-Friendly Breakthrough in Lawn Mowers
- "A Garden Still Life with a Kitten" Painting by Rosa Mayreder
- Analysis of Lando's Business Plan
- Neolithic Revolution and Climate Change
- The Debate on Conventional vs. Alternative Agricultural Approaches
- Sugar Cane Bio-Diesel in Brazil
- Experiment: Growing Tomato Plants Under Light
- Going Public: IPO Capital and Execution Strategy
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, November 13). Benefits of Raising Your Own Fruits and Vegetables. https://ivypanda.com/essays/benefits-of-raising-your-own-fruits-and-vegetables/
"Benefits of Raising Your Own Fruits and Vegetables." IvyPanda , 13 Nov. 2021, ivypanda.com/essays/benefits-of-raising-your-own-fruits-and-vegetables/.
IvyPanda . (2021) 'Benefits of Raising Your Own Fruits and Vegetables'. 13 November.
IvyPanda . 2021. "Benefits of Raising Your Own Fruits and Vegetables." November 13, 2021. https://ivypanda.com/essays/benefits-of-raising-your-own-fruits-and-vegetables/.
1. IvyPanda . "Benefits of Raising Your Own Fruits and Vegetables." November 13, 2021. https://ivypanda.com/essays/benefits-of-raising-your-own-fruits-and-vegetables/.
Bibliography
IvyPanda . "Benefits of Raising Your Own Fruits and Vegetables." November 13, 2021. https://ivypanda.com/essays/benefits-of-raising-your-own-fruits-and-vegetables/.
Grow. Play. Every Day!

- Garden of Eatin'
Why You Should Grow Your Own Food: 8 Research-Backed Reasons
Ever wondered whether it’s worth the time and effort (not to mention money) to grow your own food when it’s so easy and convenient to just buy what you need at the grocery store? I did—but after more than 14 years of growing my own food under a variety of challenging conditions, I can confidently say it’s always worth it.
Written by Linda Ly

Ever wondered whether it’s worth the time and effort (not to mention money) to grow your own food when it’s so easy and convenient to just buy what you need at the grocery store? Especially if you live in a challenging climate, don’t have a lot of space, or work a full-time job on top of family obligations?
I did—and I’ve dealt with all those scenarios. But after more than 12 years of growing my own food (in two vastly different climate zones, from a small second-story deck to now an acre homestead, and with two kids underfoot while running a business from home), I can confidently say it’s always worth it.
Here are eight reasons—all backed by research—you should seriously consider growing an edible garden this year.
Disclosure: If you shop from my article or make a purchase through one of my links, I may receive commissions on some of the products I recommend.
1. Growing food can save you money.

With the current state of affairs in the world, the cost of groceries has jumped more than 7 percent since January 2021. More specifically, the fruit and vegetable index rose 0.9 percent over January 2022 and price surges are still happening due to inflation.
So it stands to reason that growing your own food can save some money on groceries, but let’s be real: Some people go all out on their gardens and the amount of money they’re actually saving is debatable.
Like any financial investment, your potential return (and long-term success) largely depends on what you choose to grow. Not all crops have the same monetary value, but knowing what to grow can offer significant savings over supermarket purchases.
What kind of crops are worth your time? It helps to start with how much they cost at the market. Prices tend to fluctuate based on the season, geographic location, and environmental factors like drought or disease, but generally, these items are the most expensive to buy organic:
- Bell peppers
- Leaf lettuce (and other leafy greens like kale and chard)
- Summer squash (including zucchini)
- Beans (you can get more bang for the buck by growing pole beans up a trellis, thereby maximizing your garden space)
One of the reasons I don’t include root vegetables like carrots, turnips, or radishes on my list of high-value crops to grow is because they’re what I call “one and done” crops. That is, you plant them once, harvest them once, the end.
It takes a little more effort to keep these crops going through succession planting, and unless you’re looking for specialty varieties (like black radishes ), it’s generally more cost-effective to buy them in the store.
On the other hand, a single tomato plant can yield upwards of 35 pounds of tomatoes. Bell peppers (the organic ones go for $2.50 each in my local grocer) continue to grow all season long until the first freeze, giving you several harvests from a healthy plant.
When you implement an organic, closed-loop garden that uses natural systems to sustain itself (a method that I teach in Lazy Gardening Academy ), you’ll have more productive crops that require fewer outside resources to thrive. And that means more savings in your pocket.
2. Growing your own food results in less waste.

This is a topic I covered extensively in my book, The No-Waste Vegetable Cookbook , and it’s a topic I’m passionate about. In the United States, we waste a considerable amount of produce not only in our homes, but in our supply chains (waste that totals roughly half of the US produce supply ).
There are many edible and delicious parts of vegetables that never make it to market because:
- Industrial farming is hard on the plants due to fertilizers, pesticides, and mechanical harvesting—you know this if you’ve ever bought carrots or radishes with limp, dingy greens.
- They won’t survive transit, at least not without looking a little ragged (which ultimately leads to waste since consumers are wary of imperfect produce).
- People just don’t know what to do with them because they’re not widely used in this country (but are, in fact, staples in other countries).
That doesn’t mean things like pea shoots, broccoli leaves , squash leaves, and sweet potato leaves are any less nutritious or palatable than their more commonly known “vegetable parts” (in fact, they sometimes pack even more nutrients than the pods, flower buds, fruits, and tubers).
It simply means we, as a culture, need to open ourselves to “new” foods and strive to make vegetables a larger portion of our meals.
Read more: 11 Vegetables You Grow That You Didn’t Know You Could Eat
When you grow your own food, you not only minimize waste, you double the amount of food in your garden (without having to plant more plants) because you can harvest and use the entire vegetable from top to tail. (And that goes back to the first reason: growing food can save you money, sometimes in unexpected ways).
(Pssst… I have an entire guide inside Lazy Gardening Academy that details all the edible parts of common vegetables you buy or grow, so you always know what’s safe to eat and how to prepare it.)
3. Food you grow is guaranteed to be fresh.

About 30 percent of fresh vegetables and 55 percent of fresh fruits sold in the United States come from overseas , and those numbers continue to grow. That means they traveled many hundreds or thousands of miles to reach your grocery store, in trucks, trains, and ships.
How fresh do you think all that produce really is by the time it lands on your table?
Yeah, probably not so fresh—especially when a lot of vegetables (for example, tomatoes) are harvested when they’re still green and forced to ripen in produce distributors’ warehouses by artificial exposure to ethylene gas.
This is why your red, supposedly-ripe supermarket tomatoes are still rock hard when you buy them and taste kind of like styrofoam. (Honestly, you’re probably better off buying canned tomatoes if you intend to cook them.)
Related: 4 Easy Ways to Ripen Your Tomatoes on the Vine
No one can argue that your own yard is as fresh and local as it gets. And since your food is just steps away, you can pick your vegetables at peak ripeness (and peak nutrition) in the proper season, with flavors and textures that surpass those of commercially grown produce.
4. Homegrown produce doesn’t get recalled.

So, all the vegetables and fruits I just mentioned that are shipped from overseas? Turns out, less than 1 percent of imported foods are physically inspected by the FDA.
When you grow your own food, you control your growing environment. And that means you don’t need to worry about E. coli, salmonella, or listeria outbreaks, as long as you keep a tidy garden and have a clean water source.
5. Commercially grown produce often lacks nutrients.

Despite (or because of) scientific advances and modern farming practices, the vegetables of today have fewer vitamins, minerals, and phytonutrients than the vegetables our grandparents and great-grandparents ate. Research has shown up to a 40 percent decline in nutritional content in fruits and vegetables since the 1940s.
Agricultural researchers attribute this decline to two causes :
Environmental dilution effect. The yield increases resulting from fertilization, irrigation, and other environmental means used in industrial farming tend to decrease the concentrations of minerals in those plants. So while farmers can get greater yields from their crops (at more affordable costs), it comes at the expense of lower-quality food.
Genetic dilution effect. This is the result of scientists breeding high-yielding crops without a focus on broad nutrient content, and it’s why heirloom tomatoes are far more flavorful and nutritious than conventional tomatoes .
Much of the food grown commercially comes from hybrid plants that were bred for “desirable” characteristics such as pest and disease resistance, uniformity in appearance, and high yields in a short span of time. While all of this makes it easier for industrial farmers to reliably produce vast amounts of perfect-looking food, nutritional value sometimes suffers.
6. You know exactly what goes in (and on) your food.

There’s another reason conventional supermarket produce looks so perfect: pesticides.
Not all pesticides are equal, as some are relatively benign while others are more concerning (especially to children and other vulnerable people). But, it’s always wise to reduce or moderate your consumption of fruits and vegetables that are known to be vigorously treated with pesticides.
The numbers are fairly shocking if you’ve never thought about it. For example:
- Strawberries may contain as many as 45 pesticide residues .
- Celery may contain as many as 64 pesticide residues .
- Cucumbers may contain as many as 86 pesticide residues .
- Sweet (bell) peppers may contain as many as 53 pesticide residues .
- Spinach may contain as many as 54 pesticide residues .
EWG has a handy guide for what it calls the “Dirty Dozen” (that is, plants you should probably grow yourself to avoid contaminants) and the “Clean 15” (plants that are least likely to contain pesticide residue).
In my garden, even natural or organic pesticides (like neem oil or insecticidal soap ) are a last resort.
Rather, I rely on biological controls, crop rotation, interplanting, and soil building to manage pests effectively, and these are methods I teach inside Lazy Gardening Academy . (It might sound complicated, but I named my course Lazy Gardening for a reason!)
7. Growing your own food makes you happier.

There’s certainly a feeling of accomplishment when you harvest something you grew with your own hands, but that natural high isn’t merely pride: It’s also the result of mood-altering soil bacteria entering your bloodstream.
Read next: Getting Stoned on Soil: How to Dose Yourself With Nature’s Happy Drug
No need to panic though. The feel-good bacterium, Mycobacterium vaccae , is harmless and present in all living soils.
By working in your garden or running your hands through soil, you inadvertently inhale M. vaccae (or get it through a cut), which (according to a 2019 study ) has anti-inflammatory, immunoregulatory, and stress resilience properties.
In other words, M. vaccae bacteria works like nature’s Prozac, giving you a serotonin boost and improving your mood and performance every time you come in contact with the earth.
8. Gardening is simply good for your health.

So you know the mental benefits of gardening, but how about the physical benefits?
Just the simple act of getting outside and doing some light physical activity like mulching , mowing, or raking can reduce cardiovascular mortality by 19 percent. (And according to this study , all it takes is 15 minutes a day of moderate exercise. I don’t know about you, but I get that just from moving bags of compost around the yard!)
Science has proven many times over that gardening has positive effects on your overall health and body by contributing to longevity , reducing heart disease and stroke , reducing risk of death from respiratory illnesses (thanks to improved air quality), warding off dementia , reducing obesity , improving your sleep , and boosting vitamin D levels (which in turn help prevent chronic diseases ).
All that—without ever stepping foot in a gym, and with all the joy of feeding yourself and your family fresh, nutrient-dense food while doing good for the earth, too.
Learn how to grow more food with less work—using my tried-and-true Lazy Gardening techniques.
View the Web Story on research-backed reasons you should grow your own food .
I'm a plant lover, passionate road-tripper, and cookbook author whose expert advice and bestselling books have been featured in Time, Outside, HGTV, and Food & Wine. The National Parks Cookbook is my latest book. Garden Betty is where I write about modern homesteading, farm-to-table cooking, and outdoor adventuring—all that encompass a life well-lived outdoors. After all, the secret to a good life is... Read more »
Leave a Reply Cancel reply
Your email address will not be published. All fields are required.
Save my name and email in this browser for the next time I comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Recommended Reads
- Garden of eatin’
- House & Home

What I Always Plant Midsummer for an Epic Fall Harvest

How (Not) to Fertilize Your Plants This Summer

How to Pollinate Squash by Hand (and Why Your Plants Have Lots of Flowers but No Fruits)

The Best Time to Pick Tomatoes for Peak Quality (It’s Not What You Think!)

What You Should Know Before Buying Land (My Real-Life Tips)

Construction Loans: What I Wish I’d Known As a First-Time Borrower

Dark Room? 9 Actually Low-Light Plants That Don’t Need a Lot of Sun

Getting Rid of Fungus Gnats: 11 Remedies That Really Work

Easy Peasy Homemade Tomato Sauce (No Peeling Required)

This Is the Best Way to Freeze Fresh Tomatoes

Fiery Fermented Hot Sauce: 3 Simple Variations

Spicy Fermented Salsa: Take Tomatoes to the Next Level
Want to level up your garden this year.
Sign up for my free, never-boring newsletter and every week you’ll get the game-changing emails you wish you’d gotten sooner.
- About Linda Ly
- What’s In My Garden
- Lazy Gardening Academy
- Sponsorships
- Site Policies

Back to the top
Disclosure: Garden Betty independently selects products to feature on this site. I may receive a commission when you buy something through one of my links. As an Amazon Associate, I earn from qualifying purchases.
© 2024 Garden Betty. All Rights Reserved.

Want to grow your own food? 9 tips to help you get started
By Mary Halton on June 15, 2020 in News + Updates

Whether it’s as a hobby while people are stuck at home or a way to get fresh produce without going to stores, vegetable and fruit gardening is having a bit of a renaissance right now.
But if you’ve been killing houseplants for years or aren’t sure where to start, it’s not all that complicated, says Stephen Ritz , New York City educator and founder of the Green Bronx Machine . He’s been growing food with kids in classrooms for years in the South Bronx, an area considered to be a food desert , where access to supermarkets — and fresh, healthy food — is limited.
Here are his tips for growing your own food:
1. Choose plants that match your experience level
There are a lot of plants that are easy for first-time growers. “I call them the unders and the overs,” explains Ritz. “There are some things that grow over the ground, like lettuces, spinach and scallions, and you can’t go wrong with them. And then there are things that grow under the ground, like radishes, carrots, green onions, that are real easy. Parsley, oregano, other herbs — these are more things you can’t go wrong with. Tomatoes are also really easy plants to grow.” ( Editor’s note: If you are trying to grow any plants indoors, you must have a spot that gets a lot of direct sun — at least 4 – 6 hours a day for vegetables and 8 – 10 hours a day for fruit. )
Besides ease, it’s also good to choose plants you can continue to enjoy, instead of ones you just harvest once, says Ritz. “Things that you can clip and continually eat like collard greens and mustard greens. Mint is so cool to grow at home. I think the best mint to grow is chocolate mint, because the leaves are broad and really fragrant. But spearmint, peppermint, lemon balm are great, too — herbs like these have a smell good, look good and flower.”
2. Use what you have at home
You don’t need to buy fancy planters or special window boxes. There are probably dozens of things already in your home that your plants will live quite happily in, says Ritz. “Coffee cans, yogurt containers, you name it. Old fish tanks … anything ceramic. You can use virtually anything, and that’s the beauty of gardening. Some of my favorite containers to grow in are two-liter soda bottles. You cut them in half. With yogurt containers, you can hang them vertically on a terrace, fire escape or outdoor space with fishing line or good twine. Be creative, have fun, make it decorative.”
“A lot of things are fun to grow if you have enough space for their roots to spread,” he explains. “You can actually grow potatoes in a reusable IKEA bag or reusable grocery bag. If you cut a hole in it, then you can pull the potatoes right out of the bottom [when it’s time to harvest]. It’s really cool. Same thing with carrots and radishes.”
3. Plant placement is key
Make sure you give your plants the best start in life. If you’re beginning from seed, ample sun will influence how strong and healthy your plant will become, says Ritz. A south-facing exposure is usually the best spot. “When the seedlings get long and leggy, it’s because they’re chasing light. That’s not good.”
His other advice for indoor gardeners: “Avoid drafts and excessive heat. Don’t put them on the radiator; those plants will heat up and you’ll just disintegrate the seed. A windowsill is great. Lots of sun, warmth, little bit of moisture, and a covering [that lets light through], a lot of love, good conversation — you’re all good.”
4. Use food scraps to grow new plants and avoid food waste
Regrowing your leftover scraps — like celery, scallions, leeks and more — is another doable project, says Ritz. “It’s a great way to avoid food waste and continue to perpetuate the food cycle. Ultimately, things do need soil once the roots start coming off, because you don’t want to drown them. You could take the remains of a head of celery, stick it in a plate of water. Leave it for a week or two, you’ll have roots, and then plant it in soil.”
5. Your home is its own unique microclimate
The best way to learn what grows well there is by trying it out yourself. “The most important thing to remember is there’s only one place that has the perfect plant: A picture. I’ve killed a lot more things than I’ve grown, but I only take pictures of the living ones,” laughs Ritz.
6. Don’t overpack or overwater
There are a few common pitfalls to steer clear of, according to Ritz. “Don’t overpack soil in your containers. People think they should jam it down, but basically you end up creating cement. Plants’ roots like to spread, so keep the soil loose. The biggest mistake, really, is overwatering plants. One of the easiest things you could do is put a little gravel or a little charcoal at the bottom [of the pot] or sometimes even a bottle cap, so there’s space for drainage. If you do overwater, the water will sit in the bottom.”
7. Choose the right plants for the space you have
If you’re growing larger plants, pick varieties that won’t engulf your space. For example, you might think that cherry tomatoes will be a manageable size, but that’s actually not the case, says Ritz. “You want to grow San Marzano or Roma tomatoes, or dwarf tomatoes. If you’re limited in space, you definitely want to stay away from cherry tomatoes. You’ll get a huge crop, but manicuring those plants — it can be like a jungle. They can be six feet tall sometimes!”
“One plant that I recommend as a not-to-grow — but could be a wonderful thing to grow for beginners — is zucchini. The problem is they’re very invasive; they can take over the garden. On the one hand, it’s wonderful that you can’t go wrong; on the other hand, it’s a bit of a bully. But if you want success and you want to see something big, go with a zucchini.”
If you’re not sure whether anything can grow in your low-light apartment, try these robust plants. “Oregano and mint do really well in shady areas,” says Ritz. “Lettuces do well in normal house light. The better the light, the quicker you’ll grow. You can also get a cheap full-spectrum grow light for anywhere from $10 to $20, including the fixture.”
8. Grow what you know you like to eat
While it’s tempting to grow things that are easy, Ritz says, it’s important that your time, effort and energy go into creating food you like so it doesn’t contribute to food waste. If COVID-19 restrictions mean you can’t easily give away food or you’ve had a bumper crop, try preserving methods like canning, pickling or drying so you can consume them later.
9. Most importantly — enjoy yourself!
Ritz has seen urban farming change the lives of his students. There’s no reason you can’t experience that in your own home, no matter where you are. “What I really want people to do is have fun,” he says. “I think growing food is a whole new maker space. The food system and hacking growing should be fun. I still marvel that you take this little teeny tiny seed, and 60 days later, you can have a big bounty to eat.”
For people who are at home with their families now, growing can be a wonderful way to connect. Grow with your kids, or get your parents involved. Ritz says, “I believe food is the language through which society reveals itself, and how we grow it and share it is critical for this and future generations.”
Watch his TED Talk here:
ABOUT THE AUTHOR
Mary Halton is Assistant Ideas Editor at TED, and a science journalist based in the Pacific Northwest.
This post was originally published on TED Ideas . It’s part of the “How to Be a Better Human” series, each of which contains a piece of helpful advice from someone in the TED community; browse through all the posts here.

Insight and inspiration in turbulent times.

- All Latest Articles
- Environment
- Food & Water
- Featured Topics
- Editor’s Picks
- Get Started
- Online Course
- Holding the Fire
- What Could Possibly Go Right?
- About Resilience
- Fundamentals
- Submission Guidelines
- Commenting Guidelines
- All Articles
- Log in / Sign Up
Act: Inspiration
The year in which i grow our food: an introduction.
By Jocelyn Siegel , originally published by Medium
September 27, 2022

It started as a challenge, as well as a necessity.
I have been growing food for my family and myself for many years, at first only because I wanted us to eat better food, but then later because I could smell on the wind what was coming and wanted a bit of insulation against it. I had tinkered with food production for years — growing a garden, planting fruit trees, raising animals — all of which would yield quite a bit, depending on how much I put into it. But I could never put into it 100% of my time. So what would happen if I did?
As things looked to get much worse very rapidly a few years ago, I started to buckle down and focus on how to improve the systems I already had in place. Last year, when things really got dodgy and this year looked to be the start of things becoming terrible for the near future, I bit the bullet. I stayed home to raise the food we would eat. This little journal will be the accounting of what that looks like.
So…some quick facts to start with:
1. I am doing this almost entirely by myself. I have a family, but none of them are interested in doing what I do. My husband works. My adult children are in college. That leaves me and two Corgis to do all the work, and believe me, the Corgis are no flipping help at all.
2. I do this work by hand — I don’t have any equipment. Unless you count a wheelbarrow. (Do you count a wheelbarrow?) Oh, and a chain saw and some small power tools. No forklifts or backhoes, though. Me and a shovel.
3. I am a middle-aged woman. Honestly, this fact means nothing at all. Being a woman just means I’m a hell of a lot tougher than a man, and being middle aged just means that my back and knees hurt. I provide this fact in case you needed some creds. There they are.
4. Please note that I say that this is the year in which I grow our food, but I did NOT say that I grow ALL our food. It is out of the grasp of most of us to grow ALL our own food. Even if you have all the space, money, time, and equipment in the world, you can still have a bad year and things might die, leaving you without. I don’t have all the space, money, time, or equipment in the world, so it’s a non-starter. However, I can grow quite a lot of food, and make a huge dent in our grocery needs. That’s still very worth doing, especially nowadays.
5. I am not an expert. What I am is highly skilled, with many years of experience. I can do many things, and I can do them well (because of years of practice). Possibly others can do things better. Are they experts, then? I don’t know. What does that even mean?
6. I know that very few or none of you are going to stop working to grow your own food. I’m not trying to convince you to. What I am trying to show you is what is behind doing something like this — growing and making what you eat. This way, you might be inspired to try a little something. Then if you like that, you might do a little something more. Believe me; doing a little something now is a very, very good idea.
**In case you need a little extra convincing, or are afraid that this is very hard work: I have raised food for my family while caring for two small children, while caring for two small children and working part time, and while caring for two slightly larger children (who STILL needed a lot of attention and time) while working full time. Yes, it really can be done. I’m not the only one who’s done it, either. **
Slide Anything shortcode error: A valid ID has not been provided
And now some background info:
I grew up on suburban/urban Long Island, where I was not interested in plants or gardening at all until I became a teenager (I was a weird teenager, obviously), and then the bug bit hard. At that point I was relegated to houseplants, but I brought home many, made shelves for them in my room where I could, and just enjoyed being around them. Years later, I started gardening in earnest at our first house. I loved putting things in the ground wherever I felt like it, and watching them grow.
Fast-forward quite a bit, and I had been gardening everywhere we lived, and the edible food garden became an obsession. When the 2008 whirlwind disaster had departed, it left me with two small kids and a husband without his very lucrative job. Our house was sold out of desperation, and we had begun looking for another much smaller place to live. One with some property, though, that was the caveat. We had lived in houses with smaller pieces, but I wanted some land to grow some things and raise some chickens. When we found it, after driving the realtor completely insane, all I can say is that I stepped into the backyard, looked at the woods, and my gut said “ Yup ”. That was that. Luckily, the nondescript house was in pretty decent shape, because I hadn’t even bothered to look. We bought it, a little house on about 4 acres in a field of grass. However, it was bordered by two streams and woods all around. It was a place to start.
And start I did. Since that day 12 years ago, I have built two chicken coops, duck and goose housing, a greenhouse, two goat houses, a few arbors because they are pretty and I like hammocks, I hand-dug a pond (it’s small, don’t get excited), put in a large vegetable garden, planted an orchard, and gardened the crap out of all of that stupid grass. It is a very non-suburban home in what is a demi-suburban area, and it does provide quite a lot of the food we eat. Most of the land is not cleared, and never will be. I work with what is probably equivalent to an acre and a half of cleared land. Of this, most is gardened as permaculture. The vegetable garden is the exception to this rule. Due to heavy deer predation, it is fenced and orderly. The rest of the yard is a profusion of plants on top of plants on top of plants. It is either beautiful, or unruly, depending on your point of view. I can go either way, sometimes.
That’s my story. As I said, this will be a journal of what this year looked like/looks like when you try to produce as much of your own food as you can. It won’t go in any chronological order, but I’ll tell you what the processes looks like for the things I do.
Why read it? I’ve been told I’m funny. I know I’m very sarcastic, so maybe that works for you. In addition, you will get to see some cute Corgi pictures, and Corgis are adorable (though a HANDFUL). There you go, plenty of reasons.

Adorable Corgi picture #1. This is Elin.
See you next time!
Jocelyn Siegel
Related articles.

Will science and technology save us?
By Gunnar Rundgren , Garden Earth
My point is certainly not that science as such is bad, but that we should not put it too high on the pedestal and in that process disregard other ways to understand what it is to be human and how we should live.
September 3, 2024

Newsflash No.2: manufactured food update
By Chris Smaje , Small Farm Future
Given the basically non-existent ‘transition’ into clean energy outlined in my previous post which is failing to meet even existing needs for energy, the vast increase in renewable electricity generation that would be required to fund the additional energy demands of manufactured food if it’s to play any major part in a sustainable future makes this technology a non-starter as a mass food approach.
August 29, 2024

Feeding the birds
By Eliza Daley , By my solitary hearth
Because the birds you attract to a habitat — rather than just a feeder — will be eating a varied diet — including those mosquitos. And you will also be creating space for other mosquito predators, like frogs, bats, mantises, turtles and more. You are rebuilding the balanced world a little bit at a time.
- Secondary School
Essay on let's grow our own food

COMMON ! LET 'S GROW OUR OWN FOOD !
Explanation:
these days our food is also being imported from other countries even though ours is an agriculture based country. For importing the food from others, we need to exchange some or the other valuable product of ours with them. in turn we are even losing the valuable resource of ours.
So, if we try to grow our own food and use it sufficiently, we no need to lose anything for us and we can even feel independent to eat ours....
we can even take necessary measures while growing that doesn't affect our health i.e growing them carefully without leading to the unhealthy issues. we can grow the food that enhances our health.

is the own food which was grow our health

New questions in English
The Benefits of Growing Your Own Food
| --> Growing fruits and vegetables seems overwhelming to most people, but it’s actually much simpler than it sounds. (Plus, you don’t have to trade in your suburban or urban lifestyle in the name of self-sufficiency or savings.) All you need is a few square feet of the great outdoors, a water source, and a little time. Consider these benefits of backyard gardening: Eating more fresh fruits and vegetables is one of the most important things you and your family can do to stay healthy. When they’re growing in your backyard, you won’t be able to resist them, and their vitamin content will be at their highest levels as you bite into them straight from the garden. Parents, take note: A study published in the found that preschool children who were almost always served homegrown produce were more than twice as likely to eat five servings of fruits and vegetables a day—and to like them more—than kids who rarely or never ate homegrown produce. Your grocery bill will shrink as you begin to stock your pantry with fresh produce from your backyard. A packet of seeds can cost less than a dollar, and if you buy heirloom, non-hybrid species, you can save the seeds from the best producers, dry them and use them next year. If you learn to dry, can or otherwise preserve your summer or fall harvest, you’ll be able to feed yourself even when the growing season is over. Backyard gardening helps the planet in many ways. If you grow your food organically, without pesticides and herbicides, you’ll spare the earth the burden of unnecessary air and water pollution, for example. You’ll also reduce the use of fossil fuels and the resulting pollution that comes from the transport of fresh produce from all over the world (in planes and refrigerated trucks) to your supermarket. Planting, weeding, watering and harvesting add purposeful physical activity to your day. If you have kids, they can join in, too. Be sure to lift heavy objects properly, and to stretch your tight muscles before and after strenuous activity. Gardening is also a way to relax, de-stress, center your mind and get fresh air and sunshine. Fresh food is the best food! How long has the food on your supermarket shelf been there? How long did it travel from the farm to your table? Comparing the flavor of a homegrown tomato with the taste of a store-bought one is like comparing apples to wallpaper paste. If it tastes better, you’ll be more likely to eat the healthy, fresh produce that you know your body needs. Watching a seed blossom under your care to become food on your and your family’s plates is gratifying. Growing your own food is one of the most purposeful and important things a human can do—it's work that directly helps you thrive, nourish your family and maintain your health. Caring for your plants and waiting as they blossom and "fruit" before your eyes is an amazing sense of accomplishment. With recalls on peanut butter, spinach, tomatoes and more, many people are concerned about food safety in our global food marketplace. When you responsibly grow your own food, you don't have to worry about contamination that may occur at the farm, manufacturing plant or transportation process. This means that when the whole world is avoiding tomatoes, for example, you don't have to go without—you can trust that your food is safe and healthy to eat. Americans throw away about $600 worth of food each year! It's a lot easier to toss a moldy orange that you paid $0.50 for than a perfect red pepper that you patiently watched ripen over the course of several weeks. When it's "yours," you will be less likely to take it for granted and more likely to eat it (or preserve it) before it goes to waste. Even if you don't have a big backyard—or any yard for that matter—you can still grow food. Consider container gardening if you have a sunny balcony or patio or an indoor herb garden on a windowsill. You’ll be amazed at how many tomatoes or peppers can grow out of one pot. Or find out if your city has a community garden, where you can tend to your very own plot. Check out to locate a community garden near you. Whatever your motivation for breaking ground on your own backyard garden, chances are good that you’ll take pleasure in this new healthy hobby, and that your wallet, the environment, your body and your taste buds will thank you. |
Related Content


45,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Healthy Food Essay 150 and 300 Words in English for Students

- Updated on
- Apr 4, 2024

Eating healthy food is important for a healthy and disease-free life. A person who eats healthy food means he/ she is taking good care of his/ her body and overall well-being. From childhood, we are told to eat healthy food, which includes green vegetables, fruits, dry fruits, dairy products, etc. On this page, we will be discussing healthy food essay 150 and 300 words for school students.
Table of Contents
- 1 Healthy Food Essay 150 Words
- 2 Essay on Healthy Food in 300 Words
- 3 10 Healthy Food Essay Lines
Quick Read: Essay on Good Habits
Healthy Food Essay 150 Words
‘Healthy food means food that is good for our physical growth and overall well-being. From an early age, we are told to eat healthy foods, ones that are rich in protein, fiber, and calcium. There are five types of healthy foods: Fruit and vegetables; starchy food; dairy products; proteins and fats.
Food is essential for growth and development, and when we talk about healthy food, it means better growth and a healthy lifestyle. Taking care of our bodies is our responsibility, and it all starts with eating healthy food.
Today, India is the largest producer of milk and pulses, and the second largest producer of rice, wheat, sugarcane, groundnut, vegetables, and fruit. The country not only sustains its 1.4 billion population with healthy food but also exports a large amount of it.
Our health is our responsibility, which can only be achieved by eating healthy food and exercising. There is a saying in sports, ‘ Your performance is determined by the type of fuel you provide to your body.’ So, let’s all live a healthy and happy life with healthy food.’
Quick Read: 200+ English Essay Topics
Essay on Healthy Food in 300 Words
‘Food is a source of energy for every living being. Even plants require food in the form of sunlight, water, and minerals from the soil. As humans, we all want to eat our favorite and most delicious food, which is mostly unhealthy. Healthy food, on the other hand, is not preferred by all, as some people don’t consider it tasty. Healthy food is known for its rich fiber and protein content. There are several benefits of eating healthy food, which are very important for our growth, body functioning and to live a sustained life.’
‘A healthy diet is generally a balanced diet of proteins, carbohydrates, fats, minerals and vitamins. Proteins and fats are required for energy, carbohydrates support our bodily functions and physical activity, and vitamins and minerals help boost the immune system, and support normal growth and development.’
‘India is one of the largest producers of healthy foods. In India, the Northern Plains, the Central Highlands, and the coastal areas are known for their rich production of healthy and nutritious food. Uttar Pradesh is the leading producer of sugarcane and wheat, West Bengal of rice, Karnataka for coffee, and Rajasthan of millet. We are surrounded by so many natural and healthy food resources, which can help lead a healthy and sustained life.’
‘Healthy food helps maintain a good body weight. It’s all about balancing what we eat and drink with the energy we burn. Sure, filling our plates with good food is important, but watching how much we take helps too.’
‘Eating healthy food is not just advice to live a healthy life. It’s a way of life that we all must adhere to. Adding fruits, vegetables, and dairy products to our diets will help us maintain good body weight, boost our immune system, and enhance our cells and body functioning.’
10 Healthy Food Essay Lines
Here are 10 healthy food essay lines for students:
- Eating healthy food is very important for a healthy and happy life.
- We get all the important nutrients and minerals from healthy food.
- Vegetables, fruits, dairy products, and dry fruits are part of healthy food.
- Dairy products such as milk, eggs, ghee, butter, and cotton cheese are rich sources of protein.
- Healthy food keeps our mind and body fit.
- Avoiding junk food and switching to healthy food can help us live a healthier life.
- World Health Day is celebrated on April 7 every year to promote a healthy lifestyle and healthy food.
- Healthy food makes us agile and increases body functioning.
- Healthy food can help boost our immune system and digestion.
- Healthy food can uplift our mood and make us feel good.
Ans: ‘Healthy food means food that is good for our physical growth and overall well-being. From an early age, we are told to eat healthy foods, ones that are rich in protein, fiber, and calcium. There are five types of healthy foods: Fruit and vegetables; starchy food; dairy products; proteins and fats.’ ‘Food is essential for growth and development, and when we talk about healthy food, it means better growth and a healthy lifestyle. Taking care of our body is our responsibility and it all starts with eating healthy food.’
Ans: Food is a source of energy for every living being. Even plants require food in the form of sunlight, water, and minerals from the soil. As humans, we all want to eat our favourite and delicious food, which is mostly unhealthy. Healthy food, on the other hand, is not preferred by all, as some people don’t consider it tasty. Healthy food is known for its rich fiber and protein content. There are several benefits of eating healthy food, which are very important for our growth, body functioning, and living a sustained life.
Ans: ‘Healthy food helps in maintaining a good body weight It’s all about balancing what we eat and drink with the energy we burn. Sure, filling our plates with good food is important, but watching how much we take helps too. Healthy food makes us agile and increases body functioning. Healthy food can help boost our immune system and digestion. Healthy food can uplift our mood and make us feel good.
Popular Essay Topics for Students
For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Shiva Tyagi
With an experience of over a year, I've developed a passion for writing blogs on wide range of topics. I am mostly inspired from topics related to social and environmental fields, where you come up with a positive outcome.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
45,000+ students realised their study abroad dream with us. take the first step today..

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out

LETS GROW OUR OWN FOODS

- Skip to main content
- Skip to secondary menu
- Skip to primary sidebar
- Skip to footer
A Plus Topper
Improve your Grades
Food Essay | Essay on Food for Students and Children in English
February 12, 2024 by Prasanna
Food Essay: Food is the basic materisal that the body needs for its survival and well-being. The human diet is not restricted to any special category of Food. The human body needs a variety of the following five nutrients – protein, carbohydrate, fat, vitamins, and minerals – which comes from the Food we eat to stay healthy, active, and productive. Firstly, protein is required to build, maintain, and restore blood, muscle, bones, and skin, and organs in the body.
There are such a wide range of cooking styles and food inclinations worked by social and ethnic foundations, topographical areas, and social classes. India is a place that is known for flavours, Africa is a mainland of sauces, Europe unveils esthetical excellence of Food and opens up new chances and innovations for the individuals who esteem.
You can also find more Essay Writing articles on events, persons, sports, technology and many more.
Long and Short Essays on Food for Students and Kids in English
We are providing students with essay samples on a long essay of 500 words and a short of 150 words on the topic of Food for reference.
Long Essay on Food 500 Words in English
Long Essay on Food is usually given to classes 7, 8, 9, and 10.
Food is the basic need for humans to stay alive. According to Abraham Maslow’s Hierarchy of Needs, a motivational psychological theory, Food is an innate physiological need along with water, warmth, and rest. This tells the importance of Food in everyone’s lives. Food is the need of every living organism. Therefore, we mustn’t waste Food.
In line with this, the human body needs a variety of the following five nutrients – protein, carbohydrate, fat, vitamins, and minerals – which comes from the Food we eat to stay healthy, active, and productive. Firstly, protein is required to build, maintain, and restore blood, muscle, bones, and skin, and organs in the body. Healthy food habits keep you healthy and keep you away from diseases. Avoid eating junk food since it affects your health, and it has few of the nutrients your body needs, and a lot of fat, sugar, and salt, which your body can easily get too much of.
Children can be trained to eat nutritious meals as well as getting plenty of exercises and adequate sleep every day. These positive health habits will help children grow strong and stay healthy, interact well with others, and lessen the tendencies that they will become overweight or obese.
Thus, all the dishes have different tastes. Everything is available from fruits to vegetables, from Dairy food to seafood. Different countries have their speciality of dishes. Therefore, some of them are below:
World-famous Cuisines are:
Italian Cuisines – Italian cuisines are one of the most popular cuisines around the world. Moreover, it is widely available in India too. Dishes like pizza, pasta, and lasagna are favourite dishes of many people, and people like them a lot. Besides, cafés like Dominos and Pizza cabin are accessible everywhere on the nation. Each dish is load with cheddar, which upgrades the flavour of these Italian dishes. Indian cuisine –Whether veg or non-veg the dishes are in curry form. Moreover, Indian cuisine has so many types of Food that further contain different branches. Also, almost every Indian loves Muglia dishes.
Chinese Cuisine – Chinese cuisine is also very popular in India. There are many Chinese theme-based restaurants here. Besides, in these cafés, Chinese are the best gourmet specialists since they can just give the ideal Chinese mix. Chinese cuisines have a wide variety of dishes.
Some Chinese cuisines are Chinese noodles, Dumplings, fried rice, etc. Dumplings have a different name here. These cuisines are some of the favourites of people in India. Moreover, these are available in most parts of the city. You can find it in any place, whether be it in five-star restaurants or at the side of the street as street foods.
There are such various cooking styles and food inclinations worked by social and ethnic foundations, topographical areas, and social classes. India is a place that is known for flavours, Africa is a mainland of sauces, Europe reveals esthetical excellence of Food and opens up new chances and innovations for the individuals who esteem and appreciate eating.
Short Essay on Food 150 Words in English
Short Essay on Food is usually given to classes 1, 2, 3, 4, 5, and 6.
Food is very important for every living being to stay alive. Food is the basic material that the body needs for its survival and well-being. There are such various cooking styles and food inclinations worked by social and ethnic foundations, topographical areas, and social classes. India is a place that is known for flavours, Africa is a mainland of sauces, Europe reveals esthetical excellence of Food and opens up new chances and innovations for the individuals who esteem and appreciate eating. The human body needs a variety of the following five nutrients – protein, carbohydrate, fat, vitamins, and minerals – which comes from the Food we eat to stay healthy, active, and productive. Firstly, protein is required to build, maintain, and restore blood, muscle, bones, and skin, and organs in the body. You should inculcate the habit of eating healthy things so that they will keep you healthy and you should avoid eating junk food since it affects your health.
10 Lines on Food Essay in English

FAQ’s on Food Essay
Question 1. How does healthy Food benefit us?
Answer: Healthy Benefit has a lot of benefits. It keeps us healthy and fit. It keeps away diseases like diabetes, cholesterol, blood pressure, etc.
Question 2. Why is junk food harmful?
Answer: Junk food is very harmful to our bodies. It contains large quantities of sugar, fats, salts, oils, and more, which is not good for health. It also causes a lot of problems like obesity and high blood pressure. Therefore, we must not have junk food more and encourage healthy eating habits.
Question 3. Which important nutrients are needed for the human body?
Answer: Human body needs a variety of the following five nutrients – protein, carbohydrate, fat, vitamins, and minerals.
Question 4. Why is junk food called junk food?
Answer: People use the term junk food to describe a food that has few of the nutrients your body needs, and a lot of fat, sugar, and salt, which your body can easily get too much of.
- Picture Dictionary
- English Speech
- English Slogans
- English Letter Writing
- English Essay Writing
- English Textbook Answers
- Types of Certificates
- ICSE Solutions
- Selina ICSE Solutions
- ML Aggarwal Solutions
- HSSLive Plus One
- HSSLive Plus Two
- Kerala SSLC
- Distance Education
Talk to our experts
1800-120-456-456
- Healthy Food Essay

Essay on Healthy Food
Food is essential for our body for a number of reasons. It gives us the energy needed for working, playing and doing day-to-day activities. It helps us to grow, makes our bones and muscles stronger, repairs damaged body cells and boosts our immunity against external harmful elements like pathogens. Besides, food also gives us a kind of satisfaction that is integral to our mental wellbeing, but there are some foods that are not healthy. Only those food items that contain nutrients in a balanced proportion are generally considered as healthy. People of all ages must be aware of the benefits of eating healthy food because it ensures a reasonably disease-free, fit life for many years.
Switching to a healthy diet doesn't have to be a one-size-fits-all approach. You don't have to be perfect, you don't have to eliminate all of your favourite foods and you don't have to make any drastic changes all at once—doing so frequently leads to straying or abandoning your new eating plan.
Making a few tiny modifications at a time is a recommended approach. Maintaining modest goals will help you achieve more in the long run without feeling deprived or overwhelmed by a very drastic diet change. Consider a healthy diet as a series of tiny, accessible actions such as including a salad in your diet once a day. You can slowly add additional healthy options as your minor modifications become habitual.
Cultivating a positive relationship with food is also crucial. Rather than focusing on what you should avoid, consider what you may include on your plate that will benefit your health such as nuts for heart-healthy, predominant fat that reduces low-density lipoprotein levels called monounsaturated fatty acids(raspberries) for fibre and especially the substances that inhibit oxidation which we call antioxidants.
Why is Healthy Food Important?
Living a healthy lifestyle has immense payback. Over time, making smart eating choices lowers your risk of cardiovascular disease, certain malignancies, type 2 diabetes, obesity, and even anxiety and depression. Daily, you will have more energy, feel better and possibly even be in a better mood.
It all boils down to how long and how good your life is. According to several surveys, A healthy diet consists of whole grains, vegetables, fruits, nuts, and fish. A higher diet of red or processed meats on the other hand doubled the chance of dying young.
Types of Healthy Food:
Following are the various types of healthy foods and their respective nutritional value:
Cereals,potatoes,bread and other root vegetables- These are the main sources of carbohydrates. The calories obtained from them enable us to do work.
Pulses, milk and milk products, eggs, bird meat, animal meat in limited quantities - these are great sources of protein. They build muscles and repair the damaged cells of our body, i.e., they are important for our immunity.
Ghee, butter, nuts and dry fruits, edible oil used in restrained quantities- These are rich sources of good fat. They provide more energy to our body than carbohydrates but should be consumed in a smaller amount.
Fresh fruits, vegetables and leafy vegetables, fish, egg, milk-these are good sources of vitamins, minerals and antioxidants are essential for normal functioning of the body. Though they are needed in small amounts, nowadays, nutrition experts prescribe their higher consumption as they help to fight lifestyle diseases like diabetes, obesity and even cancer.
Different types of healthy food when included in our daily diet in the right proportions along with water and roughage comprise a balanced diet. However, a balanced diet is not the same for all individuals considering many factors. It depends on a person’s age, gender, condition of the body-healthy or suffering from any disease and the type of work or physical activity a human does.
Benefits of Eating Healthy
Healthy food intake nourishes both our physical and mental health and helps us stay active for many years. One who break downs this broad benefit into micro-benefits will see that eating healthy:
Helps us in weight management
Makes us agile and increases our productivity
Decreases the risk of heart diseases, stroke, diabetes mellitus, poor bone density, and some cancers, etc.
Helps in uplifting mood
Improves memory
Improves digestion and appetite
Improves sleep cycle
Healthy food habits are inculcated in children by their parents early on. These habits along with the right education and physical exercise lead to an overall development of an individual which ultimately becomes the greatest resource of a country.
What is Unhealthy Food or Junk Food?
To fully understand the prominence of healthy food in our diet, we must also be aware of unhealthy food, that is, the food that we must avoid eating. These are mainly junk food items which are low in nutritional value and contain an excessive amount of salt, sugar and fats which is not healthy for a human body.
Junk food is one of the unhealthy intakes in the present day scenario. It makes us more unfit than ever before. It is high time that one realised this and adopted a healthy food habit for a sustainable lifestyle.
Steps to improve Eating Habits:
Make a detailed plan; break down the timings; kind of food to be included in each meal and keep the plan weekly and avoid making the process dull and repetitive.
Cook your food, minimise eating from outside. It helps keep the ingredients, quality and measurements in check as well as saves money.
Stock your kitchen with healthy snacks for your cravings rather than processed food so that your options are reduced to consuming unhealthy food.
Take the process slowly. You do not have to have a strict plan; ease yourself into a healthy mindset. Your mind and body will adjust gradually. Consistency is important.
Track your eating habits to understand the intake of food, items, portions etc. This motivates you to see the progress over time and make changes according to your needs.
Myths About Healthy Food:
Carrots affect eyesight: According to historic times, during World War II, there was a popular belief that eating a lot of veggies would assist maintain the pilot's eyes in good repair. In actuality, the fighter pilot's eyesight was aided by advanced technology. However, the myth has persisted since then and many parents still use this narrative to get their children to eat more veggies. Carrots are high in vitamin A and make a terrific supplement to any healthy diet, but they don't usually help you see better.
Fat-Free Food : Health foods continue to dominate grocery store shelves but it's always a good idea to look beyond the label before buying. This is especially true when it comes to "fat-free," "low-fat," and "non-fat" foods. It's generally true that anything with less fat is preferable for some dairy and meat items.
Lower fat alternatives in packaged and processed foods contain other dangerous additives as fat substitutes. Manufacturers compensate for the loss of fat in packaged cookies, for example, by adding other undesirable elements like sugar.
Protein shakes: Pre-made smoothie beverages and protein powder mixes which typically claim to contain less sugar than milkshakes, slushies and diet sodas are likely to be the popular choice among customers because of the above mentioned reason. They both have the same amount of sugar and artificial sweeteners.
However, this is not true of all pre-made protein shakes and smoothies. Many of them, particularly the plant-based mixtures, are still nutritious additions to a balanced diet. Check the nutrition label to be sure there are no added sugars or artificially sweetened mixtures.
Organic food is better: Foods that are grown organically are better for you. Nutritionists labelling a product as organic doesn't mean it's superior to non-organic foods. It's a popular misperception that organic produce is nutritionally superior to non-organic produce. Organic produce has the same caloric and nutritional value as non-organic produce since it is grown and prepared according to federal rules.

FAQs on Healthy Food Essay
1) Is sugar unhealthy?
Sugar is considered to be harmful for a healthy diet. Since it tastes so good in many foods, humans tend to increase it’s intake. It is also hidden in foods you wouldn't expect. It makes body organs fat, depresses well-being and also leads to heart diseases. However, to maintain a healthy diet, it is necessary to distinguish between natural and added sugars. Sugars are carbs that provide an essential source of energy and nourishment, nevertheless, sugar is often added to many popular dishes, which is when sugar becomes unhealthy. Natural sugars found in fruits and vegetables are regarded as healthy when consumed in moderation. Still added sugars give little nutritional benefit and contribute considerably to weight gain, compromising your healthy diet. As a result, it's critical to double-check the label.
2) What is Omega 3?
Omega-3 is the superfood of the fat group, which is particularly useful for various conditions, since the term "superfood" was coined. Omega-3 fatty acid is a medicine used in treating nutritional deficiencies. It is one of the essential nutrients with good antioxidant properties. Depression, memory loss, heart problems, joint and skin disorders and general improvement of physical and mental health and wellness are among them. Omega-3 which is abundant in fish-based diets is considered a necessary fatty acid for good health.
Subscribe : Get The Guide To Preserving Food!
Click HERE to Get Your Free Guide!

52 Reasons Why You Should Grow Your Own Food
As an Amazon Associate and member of other affiliate programs, I earn from qualifying purchases.
We all have our own reasons for growing food. Sometimes it’s to try new things and sometimes it’s because we want to provide more for our family. Everyone has a slightly unique perspective on vegetable gardening.
So I asked my favorite gardeners why they started growing their own food, and I got some really awesome answers. They allowed me to share them on the blog today in hopes of encouraging others to start their own vegetable garden .

Here are 52 reasons you should grow your own food
- To have as much organic produce as possible
- To grow in bulk and preserve to have homegrown food to eat year-round
- To know the food I feed them is safe for my kids
- Because it’s magic, fun, amazing, and a miracle.
- For my mental health .
- To be able to have a large variety of healthy food
- To have vegetables with higher nutrient content
- For freshness
- Knowing exactly what I give my family to eat.
- Having the ability to preserve it for the whole year .
- Getting to teach my girls self-sustainability.
- Getting everyone outside to help (even the teenager).
- To relieve stress
- Self-sufficiency , mostly
- Because so many of the veggies from the store (even organics) smell and taste like bleach.
- Because I love to play in the dirt and feel the sun on my shoulders.
- Because I grew up this way.
- Homegrown produce is fresher, therefore, it tastes better.
- It’s a great feeling of pride to know that I can provide food for myself
- I grow my own food to avoid pesticides and GMOs.
- Because it amazes me that I can grow things. It feels like I have a superpower, 😁 😁 😁
- Just the challenge.
- I love seeing things sprout from apparently nothing. I love watching the evolution of a plant grow.
- It inspires me, slows down life, and brings me back to what is important.
- I love cooking amazing dishes from things I created on my own back porch! Nothing better than going outside a few steps and snipping something 100% fresh for dinner.
- I l ove the whole process of planting and seeing every single plant sprout and come to life. It’s amazing!
- Affordable organic produce. That’s a blessing! 🤗
- Because I just enjoy whatever we grow!
- My family member has a serious iron deficiency
- I know it will save money in the long run
- To ease the carbon footprint ie: using less gas and plastic bags for groceries
- For better food quality
- To know where my food comes from
- For fresh veggies over week old store-bought
- It’s great exercise
- Absorbing vitamin D from the sun
- Feeling the joy of harvesting your own creation…you can’t buy that
- I love gaining knowledge every year of how to grow, what grows well and what doesn’t do well
- For better variety than the supermarket
- To make less waste in the trash
- For connecting back to nature
- A way to unplug from the phone, internet etc
- Produce free of pesticides
- To have less lawn to mow and water
- For easier access to fruits and veggies that are expensive to buy at the store
- For natural medicines
- Because my dog loves to hang out in the garden with me.
- To learn a new hobby
- For upcycling wood and discarded materials to turn into plant beds and planter.
- To give back to my community. For example, I’m growing carrots for Noah’s ark pig sanctuary
- It brought us closer to our neighbors by sharing freshly cut veggies
- To teach my kids about how the earth provides for us and it’s our responsibility to care for the earth in return.
I wasn’t surprised to find out that everyone’s reasons were a little bit different and some are a little bit the same. I think the common thread is that we all feel strongly that it’s important to have a vegetable garden. It’s a part of us, and we all feel like something would be missing if we weren’t growing our own food.
Why do you grow your own food?
Share your experience with us in the comments below!
Similar Posts
5 Reasons I Love Growing Tomatoes

Heirlooms, Hybrids, and GMOs: What they are and why you should care.

12 Ways Gardening Helps You Keep Your New Year’s Resolution
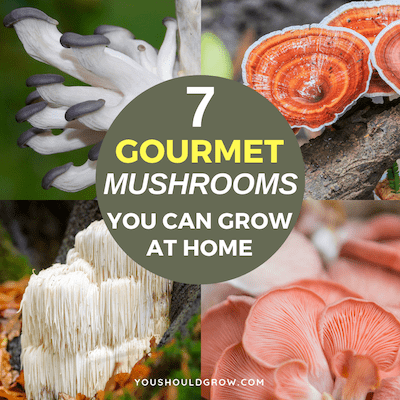
7 Gourmet Mushroom Growing Kits Anyone Can Grow

Garden Gem Tomato: A Tomato Geek’s Review

9 Fall Garden Tasks You Can’t Ignore
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
This site uses Akismet to reduce spam. Learn how your comment data is processed .

IMAGES
VIDEO
COMMENTS
This is an essay about grow our own food & explanation.
Get ready for your English exams with this fun whiteboard essay video! Learn how to describe your favourite book in one paragraph. Perfect for students who w...
1. Planting straight into the ground. This is a traditional form of gardening and it will work wonderfully if you have your own home and space for a garden. You also need to be lucky enough to have great soil. Midwesterners will likely have great soil -- especially those in Illinois, Iowa, and Indiana.
Another major benefit of home grown fruits and vegetables happens to be the financial savings that result due to this; this is more the case if the home garden is planned to be for a long term. The prices of food have been rising (Geneflow 28) and at such a moment the best option could be to grow your own fruits and vegetables.
Grace Williams, a student at Kirkwood High School in Kirkwood, Missouri, enjoys playing tennis, baking, and spending time with her family. Grace also enjoys her time as a writing editor for her school's yearbook, the Pioneer. In the future, Grace hopes to continue her travels abroad, as well as live near extended family along the sunny ...
Pick a spot with at least 6 hours of good daytime light and access to water. Use contaminant-free soil. Consider using a raised garden bed, which allows you to control the soil and nutrient blend. Talk to farmers or other backyard gardeners in your area to get a sense of what grows well in your region and when.
Homegrown produce doesn't get recalled. 5. Commercially grown produce often lacks nutrients. 6. You know exactly what goes in (and on) your food. 7. Growing your own food makes you happier. 8. Gardening is simply good for your health.
Having your own garden is like having your own personal piece of heaven. A place where you could be at peace. A place where it heals your soul, satisfies your mind, and makes your heart sing. The ...
500+ Words Essay on Healthy Food. Healthy food refers to food that contains the right amount of nutrients to keep our body fit. We need healthy food to keep ourselves fit. Furthermore, healthy food is also very delicious as opposed to popular thinking. Nowadays, kids need to eat healthy food more than ever. We must encourage good eating habits ...
Don't put them on the radiator; those plants will heat up and you'll just disintegrate the seed. A windowsill is great. Lots of sun, warmth, little bit of moisture, and a covering [that lets light through], a lot of love, good conversation — you're all good.". 4. Use food scraps to grow new plants and avoid food waste.
A Food Revolution Starts with Seed. By Sinead Fortune, originally published by Oxford Real Farming Conference. May 20, 2020. Growing your own food has seen a resurgence on a scale that has been compared to the Dig For Victory campaigns of the second world war. But with so few places selling seed, how can you take advantage of this planting ...
By Jocelyn Siegel, originally published by Medium. September 27, 2022. It started as a challenge, as well as a necessity. I have been growing food for my family and myself for many years, at first only because I wanted us to eat better food, but then later because I could smell on the wind what was coming and wanted a bit of insulation against it.
ratnach12345gmailcom. Answer: COMMON! LET 'S GROW OUR OWN FOOD! Explanation: these days our food is also being imported from other countries even though ours is an agriculture based country. For importing the food from others, we need to exchange some or the other valuable product of ours with them. in turn we are even los.
Reduce your environmental impact. Backyard gardening helps the planet in many ways. If you grow your food organically, without pesticides and herbicides, you'll spare the earth the burden of unnecessary air and water pollution, for example. You'll also reduce the use of fossil fuels and the resulting pollution that comes from the transport ...
Healthy Food Essay 150 Words. 'Healthy food means food that is good for our physical growth and overall well-being. From an early age, we are told to eat healthy foods, ones that are rich in protein, fiber, and calcium. There are five types of healthy foods: Fruit and vegetables; starchy food; dairy products; proteins and fats.
Growing our own foods is a simple solution to numerous health, environmental and economic problems. at the beginning of this year I decided to grow my own vegetables and fruits in our garden. This project was implemented at our garden. I planted numerous plants along with fruits and vegetables with the usage of organic fertilizers. I planted ...
10 Lines on Food Essay in English. 1. Food is the basic material that the body needs for its survival and well-being. 2. Food, when eaten in proper intervals and the right amount, can make children fitter. 3. Eating food that is healthy and rich in nutrients is vital for proper body functioning. 4. Food is considered healthy if it provides the ...
An Essay Let's grow our own food Growing our own food is one of the most important things that we should do. It can be a very good leisure time activity too. ... Nisan's Essential English for students-NEEfS ... Lets grow our own food essay . 2y. Ravindu Lakshan. 2y. Sanjeevaraj Sanjeevan. Tenor. 2y. Rinas Tahir. Thanks. 2y. Rinas Tahir.
500+ Words Essay on Food. Food is the basic human need to stay alive. Moreover, it is the need of every living organism. Therefore it is important that we should not waste food. Our world consists of different types of cultures. These cultures have varieties of dishes of food in them. Thus, all the dishes have different taste.
Essay on Healthy Food. Food is essential for our body for a number of reasons. It gives us the energy needed for working, playing and doing day-to-day activities. It helps us to grow, makes our bones and muscles stronger, repairs damaged body cells and boosts our immunity against external harmful elements like pathogens.
Conclusion: In conclusion, the importance of eating healthy food cannot be overstated. It extends beyond mere physical health and encompasses emotional, social, intellectual, and financial well-being. By prioritizing a balanced diet and conscious eating habits, we invest in our own well-being and happiness. Good health is nature's greatest ...
Here are 52 reasons you should grow your own food. Because it's magic, fun, amazing, and a miracle. For my mental health. Knowing exactly what I give my family to eat. Having the ability to preserve it for the whole year. Getting to teach my girls self-sustainability. Getting everyone outside to help (even the teenager).
Tools, soil, seeds, fertilizers, etc. to start. Pays off quickly. Small or big garden. ScottsMiracle-Gro Co. found the average family with a vegetable garden spends just $70 a year on it and grows an estimated $600 worth of vegetables. See full transcript.